- Mayo Clinic Libraries
- Evidence Synthesis Guide
- Risk of Bias by Study Design

Evidence Synthesis Guide : Risk of Bias by Study Design
- Review Types & Decision Tree
- Standards & Reporting Results
- Materials in the Mayo Clinic Libraries
- Training Resources
- Review Teams
- Develop & Refine Your Research Question
- Develop a Timeline
- Project Management
- Communication
- PRISMA-P Checklist
- Eligibility Criteria
- Register your Protocol
- Other Resources
- Other Screening Tools
- Grey Literature Searching
- Citation Searching
- Minimize Bias
- GRADE & GRADE-CERQual
- Data Extraction Tools
- Synthesis & Meta-Analysis
- Publishing your Review
Risk of Bias of Individual Studies

““Assessment of risk of bias is a key step that informs many other steps and decisions made in conducting systematic reviews. It plays an important role in the final assessment of the strength of the evidence.” 1
Risk of Bias by Study Design (featured tools)
- Systematic Reviews
- Non-RCTs or Observational Studies
- Diagnostic Accuracy
- Animal Studies
- Qualitative Research
- Tool Repository
- AMSTAR 2 The original AMSTAR was developed to assess the risk of bias in systematic reviews that included only randomized controlled trials. AMSTAR 2 was published in 2017 and allows researchers to identify high quality systematic reviews, including those based on non-randomised studies of healthcare interventions. more... less... AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews)
- ROBIS ROBIS is a tool designed specifically to assess the risk of bias in systematic reviews. The tool is completed in three phases: (1) assess relevance(optional), (2) identify concerns with the review process, and (3) judge risk of bias in the review. Signaling questions are included to help assess specific concerns about potential biases with the review. more... less... ROBIS (Risk of Bias in Systematic Reviews)
- BMJ Framework for Assessing Systematic Reviews This framework provides a checklist that is used to evaluate the quality of a systematic review.
- CASP Checklist for Systematic Reviews This CASP checklist is not a scoring system, but rather a method of appraising systematic reviews by considering: 1. Are the results of the study valid? 2. What are the results? 3. Will the results help locally? more... less... CASP (Critical Appraisal Skills Programme)
- CEBM Systematic Reviews Critical Appraisal Sheet The CEBM’s critical appraisal sheets are designed to help you appraise the reliability, importance, and applicability of clinical evidence. more... less... CEBM (Centre for Evidence-Based Medicine)
- JBI Critical Appraisal Tools, Checklist for Systematic Reviews JBI Critical Appraisal Tools help you assess the methodological quality of a study and to determine the extent to which study has addressed the possibility of bias in its design, conduct and analysis.
- NHLBI Study Quality Assessment of Systematic Reviews and Meta-Analyses The NHLBI’s quality assessment tools were designed to assist reviewers in focusing on concepts that are key for critical appraisal of the internal validity of a study. more... less... NHLBI (National Heart, Lung, and Blood Institute)
- RoB 2 RoB 2 provides a framework for assessing the risk of bias in a single estimate of an intervention effect reported from a randomized trial, rather than the entire trial. more... less... RoB 2 (revised tool to assess Risk of Bias in randomized trials)
- CASP Randomised Controlled Trials Checklist This CASP checklist considers various aspects of an RCT that require critical appraisal: 1. Is the basic study design valid for a randomized controlled trial? 2. Was the study methodologically sound? 3. What are the results? 4. Will the results help locally? more... less... CASP (Critical Appraisal Skills Programme)
- CONSORT Statement The CONSORT checklist includes 25 items to determine the quality of randomized controlled trials. Critical appraisal of the quality of clinical trials is possible only if the design, conduct, and analysis of RCTs are thoroughly and accurately described in the report. more... less... CONSORT (Consolidated Standards of Reporting Trials)
- NHLBI Study Quality Assessment of Controlled Intervention Studies The NHLBI’s quality assessment tools were designed to assist reviewers in focusing on concepts that are key for critical appraisal of the internal validity of a study. more... less... NHLBI (National Heart, Lung, and Blood Institute)
- JBI Critical Appraisal Tools Checklist for Randomized Controlled Trials JBI Critical Appraisal Tools help you assess the methodological quality of a study and to determine the extent to which study has addressed the possibility of bias in its design, conduct and analysis.
- ROBINS-I ROBINS-I is a tool for evaluating risk of bias in estimates of the comparative effectiveness… of interventions from studies that did not use randomization to allocate units to comparison groups. more... less... ROBINS-I (Risk Of Bias in Non-randomized Studies – of Interventions)
- NOS This tool is used primarily to evaluate and appraise case-control or cohort studies. more... less... NOS (Newcastle-Ottawa Scale)
- AXIS Cross-sectional studies are frequently used as an evidence base for diagnostic testing, risk factors for disease, and prevalence studies. The AXIS tool focuses mainly on the presented study methods and results. more... less... AXIS (Appraisal tool for Cross-Sectional Studies)
- NHLBI Study Quality Assessment Tools for Non-Randomized Studies The NHLBI’s quality assessment tools were designed to assist reviewers in focusing on concepts that are key for critical appraisal of the internal validity of a study. • Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies • Quality Assessment of Case-Control Studies • Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group • Quality Assessment Tool for Case Series Studies more... less... NHLBI (National Heart, Lung, and Blood Institute)
- Case Series Studies Quality Appraisal Checklist Developed by the Institute of Health Economics (Canada), the checklist is comprised of 20 questions to assess the robustness of the evidence of uncontrolled case series studies.
- Methodological Quality and Synthesis of Case Series and Case Reports In this paper, Dr. Murad and colleagues present a framework for appraisal, synthesis and application of evidence derived from case reports and case series.
- MINORS The MINORS instrument contains 12 items and was developed for evaluating the quality of observational or non-randomized studies. This tool may be of particular interest to researchers who would like to critically appraise surgical studies. more... less... MINORS (Methodological Index for Non-Randomized Studies)
- JBI Critical Appraisal Tools for Non-Randomized Trials JBI Critical Appraisal Tools help you assess the methodological quality of a study and to determine the extent to which study has addressed the possibility of bias in its design, conduct and analysis. • Checklist for Analytical Cross Sectional Studies • Checklist for Case Control Studies • Checklist for Case Reports • Checklist for Case Series • Checklist for Cohort Studies
- QUADAS-2 The QUADAS-2 tool is designed to assess the quality of primary diagnostic accuracy studies it consists of 4 key domains that discuss patient selection, index test, reference standard, and flow of patients through the study and timing of the index tests and reference standard. more... less... QUADAS-2 (a revised tool for the Quality Assessment of Diagnostic Accuracy Studies)
- JBI Critical Appraisal Tools Checklist for Diagnostic Test Accuracy Studies JBI Critical Appraisal Tools help you assess the methodological quality of a study and to determine the extent to which study has addressed the possibility of bias in its design, conduct and analysis.
- STARD 2015 The authors of the standards note that essential elements of diagnostic accuracy study methods are often poorly described and sometimes completely omitted, making both critical appraisal and replication difficult, if not impossible. The Standards for the Reporting of Diagnostic Accuracy Studies was developed to help improve completeness and transparency in reporting of diagnostic accuracy studies. more... less... STARD 2015 (Standards for the Reporting of Diagnostic Accuracy Studies)
- CASP Diagnostic Study Checklist This CASP checklist considers various aspects of diagnostic test studies including: 1. Are the results of the study valid? 2. What were the results? 3. Will the results help locally? more... less... CASP (Critical Appraisal Skills Programme)
- CEBM Diagnostic Critical Appraisal Sheet The CEBM’s critical appraisal sheets are designed to help you appraise the reliability, importance, and applicability of clinical evidence. more... less... CEBM (Centre for Evidence-Based Medicine)
- SYRCLE’s RoB Implementation of SYRCLE’s RoB tool will facilitate and improve critical appraisal of evidence from animal studies. This may enhance the efficiency of translating animal research into clinical practice and increase awareness of the necessity of improving the methodological quality of animal studies. more... less... SYRCLE’s RoB (SYstematic Review Center for Laboratory animal Experimentation’s Risk of Bias)
- ARRIVE 2.0 The ARRIVE 2.0 guidelines are a checklist of information to include in a manuscript to ensure that publications on in vivo animal studies contain enough information to add to the knowledge base. more... less... ARRIVE 2.0 (Animal Research: Reporting of In Vivo Experiments)
- Critical Appraisal of Studies Using Laboratory Animal Models This article provides an approach to critically appraising papers based on the results of laboratory animal experiments, and discusses various bias domains in the literature that critical appraisal can identify.
- CEBM Critical Appraisal of Qualitative Studies Sheet The CEBM’s critical appraisal sheets are designed to help you appraise the reliability, importance and applicability of clinical evidence. more... less... CEBM (Centre for Evidence-Based Medicine)
- CASP Qualitative Studies Checklist This CASP checklist considers various aspects of qualitative research studies including: 1. Are the results of the study valid? 2. What were the results? 3. Will the results help locally? more... less... CASP (Critical Appraisal Skills Programme)
- Quality Assessment and Risk of Bias Tool Repository Created by librarians at Duke University, this extensive listing contains over 100 commonly used risk of bias tools that may be sorted by study type.
- Latitudes Network A library of risk of bias tools for use in evidence syntheses that provides selection help and training videos.
References & Recommended Reading
1. Viswanathan, M., Patnode, C. D., Berkman, N. D., Bass, E. B., Chang, S., Hartling, L., ... & Kane, R. L. (2018). Recommendations for assessing the risk of bias in systematic reviews of health-care interventions . Journal of clinical epidemiology , 97 , 26-34.
2. Kolaski, K., Logan, L. R., & Ioannidis, J. P. (2024). Guidance to best tools and practices for systematic reviews . British Journal of Pharmacology , 181 (1), 180-210
3. Fowkes FG, Fulton PM. Critical appraisal of published research: introductory guidelines. BMJ (Clinical research ed). 1991;302(6785):1136-1140.
4. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed). 2017;358:j4008.
5.. Whiting P, Savovic J, Higgins JPT, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. Journal of clinical epidemiology. 2016;69:225-234.
6. Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed). 2019;366:l4898.
7. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. Journal of clinical epidemiology. 2010;63(8):e1-37.
8.. Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical research ed). 2016;355:i4919.
9. Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ open. 2016;6(12):e011458.
10. Guo B, Moga C, Harstall C, Schopflocher D. A principal component analysis is conducted for a case series quality appraisal checklist. Journal of clinical epidemiology. 2016;69:199-207.e192.
11. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ evidence-based medicine. 2018;23(2):60-63.
12. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ journal of surgery. 2003;73(9):712-716.
13. Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of internal medicine. 2011;155(8):529-536.
14. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ (Clinical research ed). 2015;351:h5527.
15. Hooijmans CR, Rovers MM, de Vries RBM, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE's risk of bias tool for animal studies. BMC medical research methodology. 2014;14:43.
16. Percie du Sert N, Ahluwalia A, Alam S, et al. Reporting animal research: Explanation and elaboration for the ARRIVE guidelines 2.0. PLoS biology. 2020;18(7):e3000411.
17. O'Connor AM, Sargeant JM. Critical appraisal of studies using laboratory animal models. ILAR journal. 2014;55(3):405-417.
- << Previous: Minimize Bias
- Next: GRADE & GRADE-CERQual >>
- Last Updated: Aug 30, 2024 2:14 PM
- URL: https://libraryguides.mayo.edu/systematicreviewprocess
- Geoffrey R. Weller Library
View complete hours
- Subject Guides
Knowledge Synthesis Guide
- Critical Appraisal
- What is Knowledge Synthesis?
- Developing your question
- Consider Eligibility Criteria
- Grey Literature
- Create Search Terms for Each Concept
- Identify Controlled Vocabulary for Each Concept
- Building Your Search
- Translating a Search Strategy
- Run Your Searches
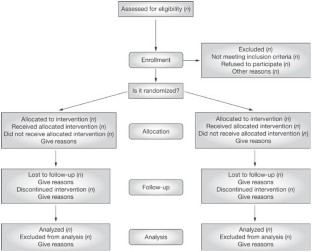
- Reporting Your Results with PRISMA
- Utilize a Screening Tool
- Data Extraction
- Information About Publishing This link opens in a new window
Tools for Critical Appraisal
Critical appraisal is the careful analysis of a study to assess trustworthiness, relevance and results of published research. Here are some tools to guide you.
- JBI Critical Appraisal
- CASP Checklists
- The AACODS checklist
Appraisal Resources - Grey Literature
Appraising Grey Literature:
- Guide to Appraising Grey Literature ( Public Health Ontario)
- << Previous: Utilize a Screening Tool
- Next: Data Extraction >>
- Last Updated: Sep 19, 2024 4:47 PM
- URL: https://libguides.unbc.ca/KnowledgeSynthesis
Geoffrey R. Weller Library University of Northern British Columbia 3333 University Way Prince George, B.C. V2N 4Z9
Circulation: (250) 960-6613 Reference: (250) 960-6475 Regional Services: 1-888-440-3440 (toll free within 250 area code)
- Suggestions Form
- Planning & Policies
- Staff Directory
- Frequently Called Numbers
- Citation Management
- Course Reserves
- Faculty Services
- Interlibrary Loans
- Open Access
- Data & Statistics
- Maps & Photos
- Research Help
Medicine: A Brief Guide to Critical Appraisal
- About this guide
- First Year Library Essentials
- Literature Reviews and Data Management
- Systematic Search for Health This link opens in a new window
- Guide to Using EndNote This link opens in a new window
- A Brief Guide to Critical Appraisal
- Manage Research Data This link opens in a new window
- Articles & Databases
- Point of Care Tools
- Anatomy & Radiology
- Drugs and Medicines
- Diagnostic Tests & Calculators
- Health Statistics
- Multimedia Sources
- News & Public Opinion
Have you ever seen a news piece about a scientific breakthrough and wondered how accurate the reporting is? Or wondered about the research behind the headlines? This is the beginning of critical appraisal: thinking critically about what you see and hear, and asking questions to determine how much of a 'breakthrough' something really is.
The article " Is this study legit? 5 questions to ask when reading news stories of medical research " is a succinct introduction to the sorts of questions you should ask in these situations, but there's more than that when it comes to critical appraisal. Read on to learn more about this practical and crucial aspect of evidence-based practice.
What is Critical Appraisal?
Critical appraisal forms part of the process of evidence-based practice. “ Evidence-based practice across the health professions ” outlines the fives steps of this process. Critical appraisal is step three:
- Ask a question
- Access the information
- Appraise the articles found
- Apply the information
Critical appraisal is the examination of evidence to determine applicability to clinical practice. It considers (1) :
- Are the results of the study believable?
- Was the study methodologically sound?
- What is the clinical importance of the study’s results?
- Are the findings sufficiently important? That is, are they practice-changing?
- Are the results of the study applicable to your patient?
- Is your patient comparable to the population in the study?
Why Critically Appraise?
If practitioners hope to ‘stand on the shoulders of giants’, practicing in a manner that is responsive to the discoveries of the research community, then it makes sense for the responsible, critically thinking practitioner to consider the reliability, influence, and relevance of the evidence presented to them.
While critical thinking is valuable, it is also important to avoid treading too much into cynicism; in the words of Hoffman et al. (1):
… keep in mind that no research is perfect and that it is important not to be overly critical of research articles. An article just needs to be good enough to assist you to make a clinical decision.
How do I Critically Appraise?
Evidence-based practice is intended to be practical . To enable this, critical appraisal checklists have been developed to guide practitioners through the process in an efficient yet comprehensive manner.
Critical appraisal checklists guide the reader through the appraisal process by prompting the reader to ask certain questions of the paper they are appraising. There are many different critical appraisal checklists but the best apply certain questions based on what type of study the paper is describing. This allows for a more nuanced and appropriate appraisal. Wherever possible, choose the appraisal tool that best fits the study you are appraising.
Like many things in life, repetition builds confidence and the more you apply critical appraisal tools (like checklists) to the literature the more the process will become second nature for you and the more effective you will be.
How do I Identify Study Types?
Identifying the study type described in the paper is sometimes harder than it should be. Helpful papers spell out the study type in the title or abstract, but not all papers are helpful in this way. As such, the critical appraiser may need to do a little work to identify what type of study they are about to critique. Again, experience builds confidence, but understanding the typical features of common study types certainly helps.
To assist with this, the Library has produced a guide to study designs in health research .
The following selected references will help also with understanding study types but there are also other resources in the Library’s collection and freely available online:
- The “ How to read a paper ” article series from The BMJ is a well-known source for establishing an understanding of the features of different study types; this series was subsequently adapted into a book (“ How to read a paper: the basics of evidence-based medicine ”) which offers more depth and currency than that found in the articles. (2)
- Chapter two of “ Evidence-based practice across the health professions ” briefly outlines some study types and their application; subsequent chapters go into more detail about different study types depending on what type of question they are exploring (intervention, diagnosis, prognosis, qualitative) along with systematic reviews.
- “ Translational research and clinical practice: basic tools for medical decision making and self-learning ” unpacks the components of a paper, explaining their purpose along with key features of different study designs. (3)
- The BMJ website contains the contents of the fourth edition of the book “ Epidemiology for the uninitiated ”. This eBook contains chapters exploring ecological studies, longitudinal studies, case-control and cross-sectional studies, and experimental studies.
Reporting Guidelines
In order to encourage consistency and quality, authors of reports on research should follow reporting guidelines when writing their papers. The EQUATOR Network is a good source of reporting guidelines for the main study types.
While these guidelines aren't critical appraisal tools as such, they can assist by prompting you to consider whether the reporting of the research is missing important elements.
Once you've identified the study type at hand, visit EQUATOR to find the associated reporting guidelines and ask yourself: does this paper meet the guideline for its study type?
Which Checklist Should I Use?
Determining which checklist to use ultimately comes down to finding an appraisal tool that:
- Fits best with the study you are appraising
- Is reliable, well-known or otherwise validated
- You understand and are comfortable using
Below are some sources of critical appraisal tools. These have been selected as they are known to be widely accepted, easily applicable, and relevant to appraisal of a typical journal article. You may find another tool that you prefer, which is acceptable as long as it is defensible:
- CASP (Critical Appraisal Skills Programme)
- JBI (Joanna Briggs Institute)
- CEBM (Centre for Evidence-Based Medicine)
- SIGN (Scottish Intercollegiate Guidelines Network)
- STROBE (Strengthing the Reporting of Observational Studies in Epidemiology)
- BMJ Best Practice
The information on this page has been compiled by the Medical Librarian. Please contact the Library's Health Team ( [email protected] ) for further assistance.
Reference list
1. Hoffmann T, Bennett S, Del Mar C. Evidence-based practice across the health professions. 2nd ed. Chatswood, N.S.W., Australia: Elsevier Churchill Livingston; 2013.
2. Greenhalgh T. How to read a paper: the basics of evidence-based medicine. 5th ed. Chichester, West Sussex: Wiley; 2014.
3. Aronoff SC. Translational research and clinical practice: basic tools for medical decision making and self-learning. New York: Oxford University Press; 2011.
- << Previous: Guide to Using EndNote
- Next: Manage Research Data >>
- Last Updated: Sep 16, 2024 1:27 PM
- URL: https://deakin.libguides.com/medicine
Cookies on this website
We use cookies to ensure that we give you the best experience on our website. If you click 'Accept all cookies' we'll assume that you are happy to receive all cookies and you won't see this message again. If you click 'Reject all non-essential cookies' only necessary cookies providing core functionality such as security, network management, and accessibility will be enabled. Click 'Find out more' for information on how to change your cookie settings.

Critical Appraisal tools
Critical appraisal worksheets to help you appraise the reliability, importance and applicability of clinical evidence.
Critical appraisal is the systematic evaluation of clinical research papers in order to establish:
- Does this study address a clearly focused question ?
- Did the study use valid methods to address this question?
- Are the valid results of this study important?
- Are these valid, important results applicable to my patient or population?
If the answer to any of these questions is “no”, you can save yourself the trouble of reading the rest of it.
This section contains useful tools and downloads for the critical appraisal of different types of medical evidence. Example appraisal sheets are provided together with several helpful examples.
Critical Appraisal Worksheets
- Systematic Reviews Critical Appraisal Sheet
- Diagnostics Critical Appraisal Sheet
- Prognosis Critical Appraisal Sheet
- Randomised Controlled Trials (RCT) Critical Appraisal Sheet
- Critical Appraisal of Qualitative Studies Sheet
- IPD Review Sheet
Chinese - translated by Chung-Han Yang and Shih-Chieh Shao
- Systematic Reviews Critical Appraisal Sheet
- Diagnostic Study Critical Appraisal Sheet
- Prognostic Critical Appraisal Sheet
- RCT Critical Appraisal Sheet
- IPD reviews Critical Appraisal Sheet
- Qualitative Studies Critical Appraisal Sheet
German - translated by Johannes Pohl and Martin Sadilek
- Systematic Review Critical Appraisal Sheet
- Diagnosis Critical Appraisal Sheet
- Prognosis Critical Appraisal Sheet
- Therapy / RCT Critical Appraisal Sheet
Lithuanian - translated by Tumas Beinortas
- Systematic review appraisal Lithuanian (PDF)
- Diagnostic accuracy appraisal Lithuanian (PDF)
- Prognostic study appraisal Lithuanian (PDF)
- RCT appraisal sheets Lithuanian (PDF)
Portugese - translated by Enderson Miranda, Rachel Riera and Luis Eduardo Fontes
- Portuguese – Systematic Review Study Appraisal Worksheet
- Portuguese – Diagnostic Study Appraisal Worksheet
- Portuguese – Prognostic Study Appraisal Worksheet
- Portuguese – RCT Study Appraisal Worksheet
- Portuguese – Systematic Review Evaluation of Individual Participant Data Worksheet
- Portuguese – Qualitative Studies Evaluation Worksheet
Spanish - translated by Ana Cristina Castro
- Systematic Review (PDF)
- Diagnosis (PDF)
- Prognosis Spanish Translation (PDF)
- Therapy / RCT Spanish Translation (PDF)
Persian - translated by Ahmad Sofi Mahmudi
- Prognosis (PDF)
- PICO Critical Appraisal Sheet (PDF)
- PICO Critical Appraisal Sheet (MS-Word)
- Educational Prescription Critical Appraisal Sheet (PDF)
Explanations & Examples
- Pre-test probability
- SpPin and SnNout
- Likelihood Ratios
CASP Checklists
- How to use our CASP Checklists
- Referencing and Creative Commons
- Online Training Courses
- CASP Workshops
- What is Critical Appraisal
- Study Designs
- Useful Links
- Bibliography
- View all Tools and Resources
- Testimonials
Critical appraisal tools and resources
CASP has produced simple critical appraisal checklists for the key study designs. These are not meant to replace considered thought and judgement when reading a paper but are for use as a guide and aide memoire. All CASP checklists cover three main areas: validity , results and clinical relevance.
What is Critical Appraisal?
Critical Appraisal is the process of carefully and systematically examining research to judge its trustworthiness, and its value and relevance in a particular context. It is an essential skill for evidence-based medicine because it allows people to find and use research evidence reliably and efficiently.
Learn more about what critical appraisal is, why we need it and more
A complete list (published & unpublished) of articles and research papers about CASP and other critical appraisal tools and approaches, covering from 1993-2012.
- CASP Checklist
Need more information?
- Online Learning
- Privacy Policy

Critical Appraisal Skills Programme
Critical Appraisal Skills Programme (CASP) will use the information you provide on this form to be in touch with you and to provide updates and marketing. Please let us know all the ways you would like to hear from us:
We use Mailchimp as our marketing platform. By clicking below to subscribe, you acknowledge that your information will be transferred to Mailchimp for processing. Learn more about Mailchimp's privacy practices here.
Copyright 2024 CASP UK - OAP Ltd. All rights reserved Website by Beyond Your Brand
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Critical Appraisal Tools and Reporting Guidelines for Evidence-Based Practice
Affiliations.
- 1 Professor, School of Nursing & Health Professions, University of San Francisco, San Francisco, CA, USA.
- 2 Reference Librarian and Primary Liaison, School of Nursing & Health Professions, Gleeson Library, Geschke Center, University of San Francisco, San Francisco, CA 94117, USA.
- PMID: 28898556
- DOI: 10.1111/wvn.12258
Background: Nurses engaged in evidence-based practice (EBP) have two important sets of tools: Critical appraisal tools and reporting guidelines. Critical appraisal tools facilitate the appraisal process and guide a consumer of evidence through an objective, analytical, evaluation process. Reporting guidelines, checklists of items that should be included in a publication or report, ensure that the project or guidelines are reported on with clarity, completeness, and transparency.
Purpose: The primary purpose of this paper is to help nurses understand the difference between critical appraisal tools and reporting guidelines. A secondary purpose is to help nurses locate the appropriate tool for the appraisal or reporting of evidence.
Methods: A systematic search was conducted to find commonly used critical appraisal tools and reporting guidelines for EBP in nursing.
Rationale: This article serves as a resource to help nurse navigate the often-overwhelming terrain of critical appraisal tools and reporting guidelines, and will help both novice and experienced consumers of evidence more easily select the appropriate tool(s) to use for critical appraisal and reporting of evidence. Having the skills to select the appropriate tool or guideline is an essential part of meeting EBP competencies for both practicing registered nurses and advanced practice nurses (Melnyk & Gallagher-Ford, 2015; Melnyk, Gallagher-Ford, & Fineout-Overholt, 2017).
Results: Nine commonly used critical appraisal tools and eight reporting guidelines were found and are described in this manuscript. Specific steps for selecting an appropriate tool as well as examples of each tool's use in a publication are provided.
Linking evidence to action: Practicing registered nurses and advance practice nurses must be able to critically appraise and disseminate evidence in order to meet EBP competencies. This article is a resource for understanding the difference between critical appraisal tools and reporting guidelines, and identifying and accessing appropriate tools or guidelines.
Keywords: critical appraisal tools; evidence-based nursing; evidence-based practice; reporting guidelines.
© 2017 Sigma Theta Tau International.
PubMed Disclaimer
Similar articles
- Differences Between Magnet and Non-Magnet-Designated Hospitals in Nurses' Evidence-Based Practice Knowledge, Competencies, Mentoring, and Culture. Melnyk BM, Zellefrow C, Tan A, Hsieh AP. Melnyk BM, et al. Worldviews Evid Based Nurs. 2020 Oct;17(5):337-347. doi: 10.1111/wvn.12467. Epub 2020 Oct 6. Worldviews Evid Based Nurs. 2020. PMID: 33022875
- Endorsement and Validation of the Essential Evidence-Based Practice Competencies for Practicing Nurses in Finland: An Argument Delphi Study. Saunders H, Gallagher-Ford L, Vehviläinen-Julkunen K. Saunders H, et al. Worldviews Evid Based Nurs. 2019 Aug;16(4):281-288. doi: 10.1111/wvn.12377. Epub 2019 Jun 4. Worldviews Evid Based Nurs. 2019. PMID: 31162823
- Evidence-Based Practice Competencies for RNs and APNs: How Are We Doing? Bell SG. Bell SG. Neonatal Netw. 2020 Aug 1;39(5):299-302. doi: 10.1891/0730-0832.39.5.299. Neonatal Netw. 2020. PMID: 32879046
- Facilitating interprofessional evidence-based practice in paediatric rehabilitation: development, implementation and evaluation of an online toolkit for health professionals. Glegg SM, Livingstone R, Montgomery I. Glegg SM, et al. Disabil Rehabil. 2016;38(4):391-9. doi: 10.3109/09638288.2015.1041616. Epub 2015 Apr 29. Disabil Rehabil. 2016. PMID: 25924019 Review.
- A systematic review of how studies describe educational interventions for evidence-based practice: stage 1 of the development of a reporting guideline. Phillips AC, Lewis LK, McEvoy MP, Galipeau J, Glasziou P, Hammick M, Moher D, Tilson JK, Williams MT. Phillips AC, et al. BMC Med Educ. 2014 Jul 24;14:152. doi: 10.1186/1472-6920-14-152. BMC Med Educ. 2014. PMID: 25060160 Free PMC article. Review.
- Exploring measurement tools used to assess knowledge, attitudes, and perceptions of pregnant women toward prenatal screening: A systematic review. Sacca L, Zerrouki Y, Burgoa S, Okwaraji G, Li A, Arshad S, Gerges M, Tevelev S, Kelly S, Knecht M, Kitsantas P, Hunter R, Scott L, Reynolds AP, Colon G, Retrouvey M. Sacca L, et al. Womens Health (Lond). 2024 Jan-Dec;20:17455057241273557. doi: 10.1177/17455057241273557. Womens Health (Lond). 2024. PMID: 39206551 Free PMC article.
- Barriers and Facilitators of Physical Activity in People Living With HIV: A Systematic Review of Qualitative Studies. Song D, Hightow-Weidman L, Yang Y, Wang J. Song D, et al. J Int Assoc Provid AIDS Care. 2024 Jan-Dec;23:23259582241275819. doi: 10.1177/23259582241275819. J Int Assoc Provid AIDS Care. 2024. PMID: 39155592 Free PMC article.
- Promoting patient-centered care in CAR-T therapy for hematologic malignancy: a qualitative meta-synthesis. Xie C, Duan H, Liu H, Wang Y, Sun Z, Lan M. Xie C, et al. Support Care Cancer. 2024 Aug 16;32(9):591. doi: 10.1007/s00520-024-08799-3. Support Care Cancer. 2024. PMID: 39150486 Free PMC article. Review.
- Clinical Evaluation of Artificial Intelligence-Enabled Interventions. Hogg HDJ, Martindale APL, Liu X, Denniston AK. Hogg HDJ, et al. Invest Ophthalmol Vis Sci. 2024 Aug 1;65(10):10. doi: 10.1167/iovs.65.10.10. Invest Ophthalmol Vis Sci. 2024. PMID: 39106058 Free PMC article. Review.
- Acceptability, Effectiveness, and Roles of mHealth Applications in Supporting Cancer Pain Self-Management: Integrative Review. Wu W, Graziano T, Salner A, Chen MH, Judge MP, Cong X, Xu W. Wu W, et al. JMIR Mhealth Uhealth. 2024 Jul 18;12:e53652. doi: 10.2196/53652. JMIR Mhealth Uhealth. 2024. PMID: 39024567 Free PMC article. Review.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Searching with critical appraisal tools
Glasofer, Amy DrNP(c), MSN, RN, ONC
Amy Glasofer is a senior educator for Virtua Center for Learning in Mt. Laurel, N.J.
CATs help journal club members rate the quality of research
The author has disclosed that she has no financial relationships related to this article.
Nurses rank feeling unable to judge the quality of research as one of the greatest hurdles to using research in practice. Participation in a journal club improves members' ability to critically appraise the quality of research.

Critical appraisal is “the process of assessing and interpreting evidence by systematically considering its validity, results and relevance to an individual's work.” 1 Nurses rank feeling incapable of assessing the quality of research as one of the greatest barriers to using research in practice. 2 Participation in a journal club (JC) can improve members' abilities to critically appraise the quality of research. 3,4 The use of a formalized critical appraisal tool (CAT) during JC facilitates improvement in appraisal skills. 3,4 The purpose of this article is to review the literature on selecting a CAT.
Literature review
CATs are designed to help readers rate the quality of research. 5 In reference to research, quality is the extent to which a study has minimized biases in the selection of subjects and measurement of outcomes, as well as minimized influence of anything outside of the factors being studied on the results. 6 CATs are superior to informal appraisal in bringing readers with different levels and types of knowledge to a similar conclusion about a research paper. 5 Their utility in a JC seems obvious; however, selecting a CAT isn't a simple task.
As a component of the Healthcare Research and Quality Act of 1999, Congress charged the Agency for Healthcare Research and Quality (AHRQ) with developing methods to ensure that reviews of healthcare literature are scientifically and clinically sound. 6 To fulfill this charge, the AHRQ commissioned a study to describe systems that rate the quality of evidence and to provide guidance on best practices. This report analyzed over 120 published CATs. 6 The AHRQ review, and others published since, have come to the same conclusions: there's no “gold standard” CAT for any specific study design, there's no generic tool that can be applied equally across study designs, and users of CATs should be careful about the CAT they select and how they use it. 6–8
The AHRQ developed standard categories that any CAT should address to adequately rate specific research designs (see AHRQ critical rating categories for CATs by research design ). 6 Based on these criteria, they put forth 19 recommended CATs depending on research design (see AHRQ recommended CATs ). Aside from being potentially outdated, the AHRQ-recommended CATs may be difficult to use in a nursing JC. Although different research designs require varying criteria for appraisal, it would be simpler to use CATs of similar formats across designs. Additionally, the CATs put forth by the AHRQ aren't inclusive of some forms of research and nonresearch evidence that JCs might wish to cover, including qualitative research, meta-synthesis, clinical practice guidelines, consensus or position statements, literature reviews, expert opinions, organizational experience, or case reports. 28 Lastly, all of the CATs recommended by the AHRQ were developed for appraising medical literature. These tools may not translate easily for use in a nursing JC.
Selecting our CAT
For these reasons, the JC at our institution opted to evaluate additional CATs. One of the JC facilitators who was completing her doctoral coursework took on this task. Several resources were utilized including searching academic databases and the Internet, and consulting with mentors and evidence-based practice texts. Ultimately, the CATs selected for our JC came from the Johns Hopkins Model for Evidence Based Practice. 28 This reference contains two tools for appraising individual articles. The first is for appraising research evidence (randomized control trials, quasi-experimental studies, nonexperimental studies, qualitative studies, systematic reviews, and systematic reviews with meta-analysis or meta-synthesis). All of the categories considered critical for systematic reviews, randomized control trials, and observational studies by the AHRQ are covered in this CAT, with the exception of assessing for funding or sponsorship. The AHRQ allowed for the absence of funding criteria in recommended CATs as this category was so often not addressed. 6 The second Johns Hopkins CAT is for evaluating nonresearch articles. 28 There's less guidance available for evaluating a nonresearch CAT. However, the Johns Hopkins tool is based on established criteria for appraising nonresearch evidence. 28–30

There are some limitations to the Johns Hopkins CATs. First, the research appraisal tool applies a single set of questions across multiple research designs and depends on the user to determine if the question is appropriate. The AHRQ cautioned that utilizing such a generalized tool could weaken the analysis. Although our JC had received education on critical appraisal and the use of the tools, members did struggle initially with determining which questions applied to the study they were critiquing. As they grew more comfortable with the CAT, with various research designs, and with research terminology, JC members did become more fluent with utilizing the tool. Additionally, the research appraisal tool doesn't contain the AHRQ-recommended criteria for evaluating research on a diagnostic study, such as the reliability and validity of a new blood test. This hasn't yet been an issue for our JC because the group hasn't selected any diagnostic studies for review. We would have to choose a different CAT should this ever occur. Finally, when our JC formed, we weren't utilizing the most current version of the Johns Hopkins CATs. 31 These older versions rely on the user to determine if the study is a research study versus a quality improvement project, for example. At the onset of our JC, members had difficulty in naming the study design. However, the CATs from the second edition include an algorithm to assist the user in defining the research design and selecting the appropriate CAT. 28 This feature would be very helpful to novice JC members.
Aside from these few limitations, the Johns Hopkins CATs have proven to be excellent tools for critical appraisal in our JC. Having only two forms to choose from, members were quickly able to select the appropriate CAT for each study and readily grew accustomed to the tool formats. It also eased the logistics of ensuring that each participant had the necessary forms. Though conversation in JC initially focused on summaries of the article and whether participants liked the article or not, content shifted to truly being an analysis of the quality of the research and its applicability to practice as members became more skilled in critical appraisal. Surveys of participants' perceptions of barriers to research utilization were conducted at baseline, at 6 months, and at 2 years after initiation of the JC. 33 Participant perception of their own research values, skills, and awareness as barriers to research utilization decreased by 18% at 6 months, and 22% after the JC had been established for 2 years. During an unrelated meeting regarding a practice change, one clinical nurse remarked that she had recently read a randomized controlled trial on the topic, and that she actually understood what that meant thanks to JC. Participation in a JC, utilizing a formalized CAT, can help nurses feel more capable of assessing the quality of research, an important step in promoting the use of research in practice.
- Cited Here |
- PubMed | CrossRef
- View Full Text | PubMed | CrossRef
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Determining the level of evidence: experimental research appraisal, caring for hospitalized patients with alcohol withdrawal syndrome, a guide to critical appraisal of evidence, the roper-logan-tierney model of nursing.
Justice Studies Research: Critical Appraisal
- APA 7th edition
Critical Appraisal
Video: get lit: the literature review.
Critical Thinker Mind Map

Doing a Literature Review
There are many different resources to help you conduct a thorough literature review. A good one is available from the University of Toronto Library .
How to read a Journal Article from the University of Michigan .
Thinking Critically
Critically appraising articles is vital to evaluating best practice for your population. There are many resources and checklists that can be used to critically appraise for clinical significance such as these Cochrane appraisal tools.
Common questions to ask when critically appraising an article:
- Is my research question clear and concise?
- Are the articles supporting my argument I am articulating in my research question?
- Was the sample size large enough for you to make some general results?
- Are the results statistically significant?
- Are the results clinically significant?
- Did the authors address potential bias in the study?
- Did the researchers identify confounding variables? If so, explain how they authors use control factors.
In addition to appraising the research methodology and quality of your research, social workers should also consider the clinical application to their individual client and client population. Consider the following while you read through your research:
Before reading
- Do I have everything I need about the client’s history, culture, priorities
- Am I making assumptions or bringing forward any personal bias?
- Is my searching accurate to describe the context and history of my clients’ problems? (e.g., “racism AND health” or “structural racism AND mental health” or “racial discrimination AND mental health”)
- Am I really prepared to assess the research?
- Am I using a broad range of knowledge sources and strategies for ways of knowing about a client?
During reading
- Document any questions that I have.
- Is each article/policy really showing the client’s experience and supporting what I my research question?
- Am I noting any structural racism or health inequities in the practices proposed in this policy or article?
- Does the intervention include any internalized scripts of racial, gender or other superiority and inferiority?
- Are there cultural or power contexts that need to be considered?
After reading
- Have I considered using multiple perspectives/disciplines to better understand the problem?
- Do I still need to learn more about my client's language, customs, history or context to better understand the problem?
- If I act on the evidence, am I contributing to dismantling structural racism, power inequities?
- If I move forward with these practices, am I contributing to create conditions where my client can thrive?
Once you have considered all these questions, you are ready to begin writing your paper.
Resource: NASW Evidence-based practice https://www.socialworkers.org/News/Research-Data/Social-Work-Policy-Research/Evidence-Based-Practice
- << Previous: APA 7th edition
- Last Updated: Sep 17, 2024 10:41 AM
- URL: https://libraryguides.nau.edu/justicestudies

- Critical Appraisal Tools
- Introduction
- Related Guides
- Getting Help
Critical Appraisal of Studies
Critical appraisal is the process of carefully and systematically examining research to judge its trustworthiness, and its value/relevance in a particular context by providing a framework to evaluate the research. During the critical appraisal process, researchers can:
- Decide whether studies have been undertaken in a way that makes their findings reliable as well as valid and unbiased
- Make sense of the results
- Know what these results mean in the context of the decision they are making
- Determine if the results are relevant to their patients/schoolwork/research
Burls, A. (2009). What is critical appraisal? In What Is This Series: Evidence-based medicine. Available online at What is Critical Appraisal?
Critical appraisal is included in the process of writing high quality reviews, like systematic and integrative reviews and for evaluating evidence from RCTs and other study designs. For more information on systematic reviews, check out our Systematic Review guide.
- Next: Critical Appraisal Tools >>
- Last Updated: Nov 16, 2023 1:27 PM
- URL: https://guides.library.duq.edu/critappraise
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 27, Issue Suppl 2
- 12 Critical appraisal tools for qualitative research – towards ‘fit for purpose’
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Veronika Williams 1 ,
- Anne-Marie Boylan 2 ,
- Newhouse Nikki 2 ,
- David Nunan 2
- 1 Nipissing University, North Bay, Canada
- 2 University of Oxford, Oxford, UK
Qualitative research has an important place within evidence-based health care (EBHC), contributing to policy on patient safety and quality of care, supporting understanding of the impact of chronic illness, and explaining contextual factors surrounding the implementation of interventions. However, the question of whether, when and how to critically appraise qualitative research persists. Whilst there is consensus that we cannot - and should not – simplistically adopt existing approaches for appraising quantitative methods, it is nonetheless crucial that we develop a better understanding of how to subject qualitative evidence to robust and systematic scrutiny in order to assess its trustworthiness and credibility. Currently, most appraisal methods and tools for qualitative health research use one of two approaches: checklists or frameworks. We have previously outlined the specific issues with these approaches (Williams et al 2019). A fundamental challenge still to be addressed, however, is the lack of differentiation between different methodological approaches when appraising qualitative health research. We do this routinely when appraising quantitative research: we have specific checklists and tools to appraise randomised controlled trials, diagnostic studies, observational studies and so on. Current checklists for qualitative research typically treat the entire paradigm as a single design (illustrated by titles of tools such as ‘CASP Qualitative Checklist’, ‘JBI checklist for qualitative research’) and frameworks tend to require substantial understanding of a given methodological approach without providing guidance on how they should be applied. Given the fundamental differences in the aims and outcomes of different methodologies, such as ethnography, grounded theory, and phenomenological approaches, as well as specific aspects of the research process, such as sampling, data collection and analysis, we cannot treat qualitative research as a single approach. Rather, we must strive to recognise core commonalities relating to rigour, but considering key methodological differences. We have argued for a reconsideration of current approaches to the systematic appraisal of qualitative health research (Williams et al 2021), and propose the development of a tool or tools that allow differentiated evaluations of multiple methodological approaches rather than continuing to treat qualitative health research as a single, unified method. Here we propose a workshop for researchers interested in the appraisal of qualitative health research and invite them to develop an initial consensus regarding core aspects of a new appraisal tool that differentiates between the different qualitative research methodologies and thus provides a ‘fit for purpose’ tool, for both, educators and clinicians.
https://doi.org/10.1136/ebm-2022-EBMLive.36
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Read the full text or download the PDF:
Your web browser is outdated and may be insecure
The RCN recommends using an updated browser such as Microsoft Edge or Google Chrome
Critical Appraisal
Use this guide to find information resources about critical appraisal including checklists, books and journal articles.
Key Resources
- This online resource explains the sections commonly used in research articles. Understanding how research articles are organised can make reading and evaluating them easier View page
- Critical appraisal checklists
- Worksheets for appraising systematic reviews, diagnostics, prognostics and RCTs. View page
- A free online resource for both healthcare staff and patients; four modules of 30–45 minutes provide an introduction to evidence based medicine, clinical trials and Cochrane Evidence. View page
- This tool will guide you through a series of questions to help you to review and interpret a published health research paper. View page
- The PRISMA flow diagram depicts the flow of information through the different phases of a literature review. It maps out the number of records identified, included and excluded, and the reasons for exclusions. View page
- A useful resource for methods and evidence in applied social science. View page
- A comprehensive database of reporting guidelines. Covers all the main study types. View page
- A tool to assess the methodological quality of systematic reviews. View page
Book subject search
- Critical appraisal
Journal articles
- View article
Shea BJ and others (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions or both, British Medical Journal, 358.
- An outline of AMSTAR 2 and its use for as a critical appraisal tool for systematic reviews. View article (open access)
- View articles
Editor of this guide
RCN Library and Museum
Upcoming events relating to this subject guide

Stay up to date with online journals
Learn how RCN members can stay up to date with online journals quickly and easily using our fantastic BrowZine tool.

Easy referencing ... in 45 minutes
Learn how to generate quick references and citations using free, easy to use, online tools.

Introduction to RCN Library Services
Discover the library service for RCN members

Know How to Search CINAHL
Learn about using the CINAHL database for literature searches at this event for RCN members.

Know How to Reference Accurately
Learn how to use the Harvard referencing style and why referencing is important at this event for RCN members.
Learn how to generate quick references and citations using a free, easy to use, online tool.

Library essentials: finding books and articles online
Learn how to find and access online books and articles using the RCN library search tool.

Know How to Evaluate Healthcare Information
This workshop is led by RCN librarians, who will help you develop the important skill of evaluating healthcare information.
Page last updated - 17/09/2024
Your Spaces
- RCNi Profile
- Steward Portal
- RCN Foundation
- RCN Library
- RCN Starting Out
Work & Venue
- RCNi Nursing Jobs
- Work for the RCN
- RCN Working with us
Further Info
- Manage Cookie Preferences
- Modern slavery statement
- Accessibility
- Press office
Connect with us:
© 2024 Royal College of Nursing
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 20 January 2009

How to critically appraise an article
- Jane M Young 1 &
- Michael J Solomon 2
Nature Clinical Practice Gastroenterology & Hepatology volume 6 , pages 82–91 ( 2009 ) Cite this article
52k Accesses
99 Citations
446 Altmetric
Metrics details
Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article in order to assess the usefulness and validity of research findings. The most important components of a critical appraisal are an evaluation of the appropriateness of the study design for the research question and a careful assessment of the key methodological features of this design. Other factors that also should be considered include the suitability of the statistical methods used and their subsequent interpretation, potential conflicts of interest and the relevance of the research to one's own practice. This Review presents a 10-step guide to critical appraisal that aims to assist clinicians to identify the most relevant high-quality studies available to guide their clinical practice.
Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article
Critical appraisal provides a basis for decisions on whether to use the results of a study in clinical practice
Different study designs are prone to various sources of systematic bias
Design-specific, critical-appraisal checklists are useful tools to help assess study quality
Assessments of other factors, including the importance of the research question, the appropriateness of statistical analysis, the legitimacy of conclusions and potential conflicts of interest are an important part of the critical appraisal process
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Making sense of the literature: an introduction to critical appraisal for the primary care practitioner

How to appraise the literature: basic principles for the busy clinician - part 2: systematic reviews and meta-analyses

How to appraise the literature: basic principles for the busy clinician - part 1: randomised controlled trials
Druss BG and Marcus SC (2005) Growth and decentralisation of the medical literature: implications for evidence-based medicine. J Med Libr Assoc 93 : 499–501
PubMed PubMed Central Google Scholar
Glasziou PP (2008) Information overload: what's behind it, what's beyond it? Med J Aust 189 : 84–85
PubMed Google Scholar
Last JE (Ed.; 2001) A Dictionary of Epidemiology (4th Edn). New York: Oxford University Press
Google Scholar
Sackett DL et al . (2000). Evidence-based Medicine. How to Practice and Teach EBM . London: Churchill Livingstone
Guyatt G and Rennie D (Eds; 2002). Users' Guides to the Medical Literature: a Manual for Evidence-based Clinical Practice . Chicago: American Medical Association
Greenhalgh T (2000) How to Read a Paper: the Basics of Evidence-based Medicine . London: Blackwell Medicine Books
MacAuley D (1994) READER: an acronym to aid critical reading by general practitioners. Br J Gen Pract 44 : 83–85
CAS PubMed PubMed Central Google Scholar
Hill A and Spittlehouse C (2001) What is critical appraisal. Evidence-based Medicine 3 : 1–8 [ http://www.evidence-based-medicine.co.uk ] (accessed 25 November 2008)
Public Health Resource Unit (2008) Critical Appraisal Skills Programme (CASP) . [ http://www.phru.nhs.uk/Pages/PHD/CASP.htm ] (accessed 8 August 2008)
National Health and Medical Research Council (2000) How to Review the Evidence: Systematic Identification and Review of the Scientific Literature . Canberra: NHMRC
Elwood JM (1998) Critical Appraisal of Epidemiological Studies and Clinical Trials (2nd Edn). Oxford: Oxford University Press
Agency for Healthcare Research and Quality (2002) Systems to rate the strength of scientific evidence? Evidence Report/Technology Assessment No 47, Publication No 02-E019 Rockville: Agency for Healthcare Research and Quality
Crombie IK (1996) The Pocket Guide to Critical Appraisal: a Handbook for Health Care Professionals . London: Blackwell Medicine Publishing Group
Heller RF et al . (2008) Critical appraisal for public health: a new checklist. Public Health 122 : 92–98
Article Google Scholar
MacAuley D et al . (1998) Randomised controlled trial of the READER method of critical appraisal in general practice. BMJ 316 : 1134–37
Article CAS Google Scholar
Parkes J et al . Teaching critical appraisal skills in health care settings (Review). Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: cd001270. 10.1002/14651858.cd001270
Mays N and Pope C (2000) Assessing quality in qualitative research. BMJ 320 : 50–52
Hawking SW (2003) On the Shoulders of Giants: the Great Works of Physics and Astronomy . Philadelphia, PN: Penguin
National Health and Medical Research Council (1999) A Guide to the Development, Implementation and Evaluation of Clinical Practice Guidelines . Canberra: National Health and Medical Research Council
US Preventive Services Taskforce (1996) Guide to clinical preventive services (2nd Edn). Baltimore, MD: Williams & Wilkins
Solomon MJ and McLeod RS (1995) Should we be performing more randomized controlled trials evaluating surgical operations? Surgery 118 : 456–467
Rothman KJ (2002) Epidemiology: an Introduction . Oxford: Oxford University Press
Young JM and Solomon MJ (2003) Improving the evidence-base in surgery: sources of bias in surgical studies. ANZ J Surg 73 : 504–506
Margitic SE et al . (1995) Lessons learned from a prospective meta-analysis. J Am Geriatr Soc 43 : 435–439
Shea B et al . (2001) Assessing the quality of reports of systematic reviews: the QUORUM statement compared to other tools. In Systematic Reviews in Health Care: Meta-analysis in Context 2nd Edition, 122–139 (Eds Egger M. et al .) London: BMJ Books
Chapter Google Scholar
Easterbrook PH et al . (1991) Publication bias in clinical research. Lancet 337 : 867–872
Begg CB and Berlin JA (1989) Publication bias and dissemination of clinical research. J Natl Cancer Inst 81 : 107–115
Moher D et al . (2000) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUORUM statement. Br J Surg 87 : 1448–1454
Shea BJ et al . (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology 7 : 10 [10.1186/1471-2288-7-10]
Stroup DF et al . (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283 : 2008–2012
Young JM and Solomon MJ (2003) Improving the evidence-base in surgery: evaluating surgical effectiveness. ANZ J Surg 73 : 507–510
Schulz KF (1995) Subverting randomization in controlled trials. JAMA 274 : 1456–1458
Schulz KF et al . (1995) Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 273 : 408–412
Moher D et al . (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology 1 : 2 [ http://www.biomedcentral.com/ 1471-2288/1/2 ] (accessed 25 November 2008)
Rochon PA et al . (2005) Reader's guide to critical appraisal of cohort studies: 1. Role and design. BMJ 330 : 895–897
Mamdani M et al . (2005) Reader's guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ 330 : 960–962
Normand S et al . (2005) Reader's guide to critical appraisal of cohort studies: 3. Analytical strategies to reduce confounding. BMJ 330 : 1021–1023
von Elm E et al . (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335 : 806–808
Sutton-Tyrrell K (1991) Assessing bias in case-control studies: proper selection of cases and controls. Stroke 22 : 938–942
Knottnerus J (2003) Assessment of the accuracy of diagnostic tests: the cross-sectional study. J Clin Epidemiol 56 : 1118–1128
Furukawa TA and Guyatt GH (2006) Sources of bias in diagnostic accuracy studies and the diagnostic process. CMAJ 174 : 481–482
Bossyut PM et al . (2003)The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med 138 : W1–W12
STARD statement (Standards for the Reporting of Diagnostic Accuracy Studies). [ http://www.stard-statement.org/ ] (accessed 10 September 2008)
Raftery J (1998) Economic evaluation: an introduction. BMJ 316 : 1013–1014
Palmer S et al . (1999) Economics notes: types of economic evaluation. BMJ 318 : 1349
Russ S et al . (1999) Barriers to participation in randomized controlled trials: a systematic review. J Clin Epidemiol 52 : 1143–1156
Tinmouth JM et al . (2004) Are claims of equivalency in digestive diseases trials supported by the evidence? Gastroentrology 126 : 1700–1710
Kaul S and Diamond GA (2006) Good enough: a primer on the analysis and interpretation of noninferiority trials. Ann Intern Med 145 : 62–69
Piaggio G et al . (2006) Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. JAMA 295 : 1152–1160
Heritier SR et al . (2007) Inclusion of patients in clinical trial analysis: the intention to treat principle. In Interpreting and Reporting Clinical Trials: a Guide to the CONSORT Statement and the Principles of Randomized Controlled Trials , 92–98 (Eds Keech A. et al .) Strawberry Hills, NSW: Australian Medical Publishing Company
National Health and Medical Research Council (2007) National Statement on Ethical Conduct in Human Research 89–90 Canberra: NHMRC
Lo B et al . (2000) Conflict-of-interest policies for investigators in clinical trials. N Engl J Med 343 : 1616–1620
Kim SYH et al . (2004) Potential research participants' views regarding researcher and institutional financial conflicts of interests. J Med Ethics 30 : 73–79
Komesaroff PA and Kerridge IH (2002) Ethical issues concerning the relationships between medical practitioners and the pharmaceutical industry. Med J Aust 176 : 118–121
Little M (1999) Research, ethics and conflicts of interest. J Med Ethics 25 : 259–262
Lemmens T and Singer PA (1998) Bioethics for clinicians: 17. Conflict of interest in research, education and patient care. CMAJ 159 : 960–965
Download references
Author information
Authors and affiliations.
JM Young is an Associate Professor of Public Health and the Executive Director of the Surgical Outcomes Research Centre at the University of Sydney and Sydney South-West Area Health Service, Sydney,
Jane M Young
MJ Solomon is Head of the Surgical Outcomes Research Centre and Director of Colorectal Research at the University of Sydney and Sydney South-West Area Health Service, Sydney, Australia.,
Michael J Solomon
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jane M Young .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Young, J., Solomon, M. How to critically appraise an article. Nat Rev Gastroenterol Hepatol 6 , 82–91 (2009). https://doi.org/10.1038/ncpgasthep1331
Download citation
Received : 10 August 2008
Accepted : 03 November 2008
Published : 20 January 2009
Issue Date : February 2009
DOI : https://doi.org/10.1038/ncpgasthep1331
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Emergency physicians’ perceptions of critical appraisal skills: a qualitative study.
- Sumintra Wood
- Jacqueline Paulis
- Angela Chen
BMC Medical Education (2022)
An integrative review on individual determinants of enrolment in National Health Insurance Scheme among older adults in Ghana
- Anthony Kwame Morgan
- Anthony Acquah Mensah
BMC Primary Care (2022)
Autopsy findings of COVID-19 in children: a systematic review and meta-analysis
- Anju Khairwa
- Kana Ram Jat
Forensic Science, Medicine and Pathology (2022)
The use of a modified Delphi technique to develop a critical appraisal tool for clinical pharmacokinetic studies
- Alaa Bahaa Eldeen Soliman
- Shane Ashley Pawluk
- Ousama Rachid
International Journal of Clinical Pharmacy (2022)
Critical Appraisal: Analysis of a Prospective Comparative Study Published in IJS
- Ramakrishna Ramakrishna HK
- Swarnalatha MC
Indian Journal of Surgery (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Clin Res
- v.12(2); Apr-Jun 2021
Critical appraisal of published research papers – A reinforcing tool for research methodology: Questionnaire-based study
Snehalata gajbhiye.
Department of Pharmacology and Therapeutics, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India
Raakhi Tripathi
Urwashi parmar, nishtha khatri, anirudha potey.
1 Department of Clinical Trials, Serum Institute of India, Pune, Maharashtra, India
Background and Objectives:
Critical appraisal of published research papers is routinely conducted as a journal club (JC) activity in pharmacology departments of various medical colleges across Maharashtra, and it forms an important part of their postgraduate curriculum. The objective of this study was to evaluate the perception of pharmacology postgraduate students and teachers toward use of critical appraisal as a reinforcing tool for research methodology. Evaluation of performance of the in-house pharmacology postgraduate students in the critical appraisal activity constituted secondary objective of the study.
Materials and Methods:
The study was conducted in two parts. In Part I, a cross-sectional questionnaire-based evaluation on perception toward critical appraisal activity was carried out among pharmacology postgraduate students and teachers. In Part II of the study, JC score sheets of 2 nd - and 3 rd -year pharmacology students over the past 4 years were evaluated.
One hundred and twenty-seven postgraduate students and 32 teachers participated in Part I of the study. About 118 (92.9%) students and 28 (87.5%) faculties considered the critical appraisal activity to be beneficial for the students. JC score sheet assessments suggested that there was a statistically significant improvement in overall scores obtained by postgraduate students ( n = 25) in their last JC as compared to the first JC.
Conclusion:
Journal article criticism is a crucial tool to develop a research attitude among postgraduate students. Participation in the JC activity led to the improvement in the skill of critical appraisal of published research articles, but this improvement was not educationally relevant.
INTRODUCTION
Critical appraisal of a research paper is defined as “The process of carefully and systematically examining research to judge its trustworthiness, value and relevance in a particular context.”[ 1 ] Since scientific literature is rapidly expanding with more than 12,000 articles being added to the MEDLINE database per week,[ 2 ] critical appraisal is very important to distinguish scientifically useful and well-written articles from imprecise articles.
Educational authorities like the Medical Council of India (MCI) and Maharashtra University of Health Sciences (MUHS) have stated in pharmacology postgraduate curriculum that students must critically appraise research papers. To impart training toward these skills, MCI and MUHS have emphasized on the introduction of journal club (JC) activity for postgraduate (PG) students, wherein students review a published original research paper and state the merits and demerits of the paper. Abiding by this, pharmacology departments across various medical colleges in Maharashtra organize JC at frequent intervals[ 3 , 4 ] and students discuss varied aspects of the article with teaching faculty of the department.[ 5 ] Moreover, this activity carries a significant weightage of marks in the pharmacology university examination. As postgraduate students attend this activity throughout their 3-year tenure, it was perceived by the authors that this activity of critical appraisal of research papers could emerge as a tool for reinforcing the knowledge of research methodology. Hence, a questionnaire-based study was designed to find out the perceptions from PG students and teachers.
There have been studies that have laid emphasis on the procedure of conducting critical appraisal of research papers and its application into clinical practice.[ 6 , 7 ] However, there are no studies that have evaluated how well students are able to critically appraise a research paper. The Department of Pharmacology and Therapeutics at Seth GS Medical College has developed an evaluation method to score the PG students on this skill and this tool has been implemented for the last 5 years. Since there are no research data available on the performance of PG Pharmacology students in JC, capturing the critical appraisal activity evaluation scores of in-house PG students was chosen as another objective of the study.
MATERIALS AND METHODS
Description of the journal club activity.
JC is conducted in the Department of Pharmacology and Therapeutics at Seth GS Medical College once in every 2 weeks. During the JC activity, postgraduate students critically appraise published original research articles on their completeness and aptness in terms of the following: study title, rationale, objectives, study design, methodology-study population, inclusion/exclusion criteria, duration, intervention and safety/efficacy variables, randomization, blinding, statistical analysis, results, discussion, conclusion, references, and abstract. All postgraduate students attend this activity, while one of them critically appraises the article (who has received the research paper given by one of the faculty members 5 days before the day of JC). Other faculties also attend these sessions and facilitate the discussions. As the student comments on various sections of the paper, the same predecided faculty who gave the article (single assessor) evaluates the student on a total score of 100 which is split per section as follows: Introduction –20 marks, Methodology –20 marks, Discussion – 20 marks, Results and Conclusion –20 marks, References –10 marks, and Title, Abstract, and Keywords – 10 marks. However, there are no standard operating procedures to assess the performance of students at JC.
Methodology
After seeking permission from the Institutional Ethics Committee, the study was conducted in two parts. Part I consisted of a cross-sectional questionnaire-based survey that was conducted from October 2016 to September 2017. A questionnaire to evaluate perception towards the activity of critical appraisal of published papers as research methodology reinforcing tool was developed by the study investigators. The questionnaire consisted of 20 questions: 14 questions [refer Figure 1 ] graded on a 3-point Likert scale (agree, neutral, and disagree), 1 multiple choice selection question, 2 dichotomous questions, 1 semi-open-ended questions, and 2 open-ended questions. Content validation for this questionnaire was carried out with the help of eight pharmacology teachers. The content validity ratio per item was calculated and each item in the questionnaire had a CVR ratio (CVR) of >0.75.[ 8 ] The perception questionnaire was either E-mailed or sent through WhatsApp to PG pharmacology students and teaching faculty in pharmacology departments at various medical colleges across Maharashtra. Informed consent was obtained on E-mail from all the participants.

Graphical representation of the percentage of students/teachers who agreed that critical appraisal of research helped them improve their knowledge on various aspects of research, perceived that faculty participation is important in this activity, and considered critical appraisal activity beneficial for students. The numbers adjacent to the bar diagrams indicate the raw number of students/faculty who agreed, while brackets indicate %
Part II of the study consisted of evaluating the performance of postgraduate students toward skills of critical appraisal of published papers. For this purpose, marks obtained by 2 nd - and 3 rd -year residents during JC sessions conducted over a period of 4 years from October 2013 to September 2017 were recorded and analyzed. No data on personal identifiers of the students were captured.
Statistical analysis
Marks obtained by postgraduate students in their first and last JC were compared using Wilcoxon signed-rank test, while marks obtained by 2 nd - and 3 rd -year postgraduate students were compared using Mann–Whitney test since the data were nonparametric. These statistical analyses were performed using GraphPad Prism statistical software, San Diego, Calfornia, USA, Version 7.0d. Data obtained from the perception questionnaire were entered in Microsoft Excel sheet and were expressed as frequencies (percentages) using descriptive statistics.
Participants who answered all items of the questionnaire were considered as complete responders and only completed questionnaires were analyzed. The questionnaire was sent through an E-mail to 100 students and through WhatsApp to 68 students. Out of the 100 students who received the questionnaire through E-mail, 79 responded completely and 8 were incomplete responders, while 13 students did not revert back. Out of the 68 students who received the questionnaire through WhatsApp, 48 responded completely, 6 gave an incomplete response, and 14 students did not revert back. Hence, of the 168 postgraduate students who received the questionnaire, 127 responded completely (student response rate for analysis = 75.6%). The questionnaire was E-mailed to 33 faculties and was sent through WhatsApp to 25 faculties. Out of the 33 faculties who received the questionnaire through E-mail, 19 responded completely, 5 responded incompletely, and 9 did not respond at all. Out of the 25 faculties who received the questionnaire through WhatsApp, 13 responded completely, 3 were incomplete responders, and 9 did not respond at all. Hence, of a total of 58 faculties who were contacted, 32 responded completely (faculty response rate for analysis = 55%). For Part I of the study, responses on the perception questionnaire from 127 postgraduate students and 32 postgraduate teachers were recorded and analyzed. None of the faculty who participated in the validation of the questionnaire participated in the survey. Number of responses obtained region wise (Mumbai region and rest of Maharashtra region) have been depicted in Table 1 .
Region-wise distribution of responses
| Students ( =127) | Faculty ( =32) | |
|---|---|---|
| Mumbai colleges | 58 (45.7) | 18 (56.3) |
| Rest of Maharashtra colleges | 69 (54.3) | 14 (43.7) |
Number of responses obtained from students/faculty belonging to Mumbai colleges and rest of Maharashtra colleges. Brackets indicate percentages
As per the data obtained on the Likert scale questions, 102 (80.3%) students and 29 (90.6%) teachers agreed that critical appraisal trains the students in doing a review of literature before selecting a particular research topic. Majority of the participants, i.e., 104 (81.9%) students and 29 (90.6%) teachers also believed that the activity increases student's knowledge regarding various experimental evaluation techniques. Moreover, 112 (88.2%) students and 27 (84.4%) faculty considered that critical appraisal activity results in improved skills of writing and understanding methodology section of research articles in terms of inclusion/exclusion criteria, endpoints, and safety/efficacy variables. About 103 (81.1%) students and 24 (75%) teachers perceived that this activity results in refinement of the student's research work. About 118 (92.9%) students and 28 (87.5%) faculty considered the critical appraisal activity to be beneficial for the students. Responses to 14 individual Likert scale items of the questionnaire have been depicted in Figure 1 .
With respect to the multiple choice selection question, 66 (52%) students and 16 (50%) teachers opined that faculty should select the paper, 53 (41.7%) students and 9 (28.1%) teachers stated that the papers should be selected by the presenting student himself/herself, while 8 (6.3%) students and 7 (21.9%) teachers expressed that some other student should select the paper to be presented at the JC.
The responses to dichotomous questions were as follows: majority of the students, that is, 109 (85.8%) and 23 (71.9%) teachers perceived that a standard checklist for article review should be given to the students before critical appraisal of journal article. Open-ended questions of the questionnaire invited suggestions from the participants regarding ways of getting trained on critical appraisal skills and of improving JC activity. Some of the suggestions given by faculty were as follows: increasing the frequency of JC activity, discussion of cited articles and new guidelines related to it, selecting all types of articles for criticism rather than only randomized controlled trials, and regular yearly exams on article criticism. Students stated that regular and frequent article criticism activity, practice of writing letter to the editor after criticism, active participation by peers and faculty, increasing weightage of marks for critical appraisal of papers in university examinations (at present marks are 50 out of 400), and a formal training for research criticism from 1 st year of postgraduation could improve critical appraisal program.
In Part II of this study, performance of the students on the skill of critical appraisal of papers was evaluated. Complete data of the first and last JC scores of a total of 25 students of the department were available, and when these scores were compared, it was seen that there was a statistically significant improvement in the overall scores ( P = 0.04), as well as in the scores obtained in methodology ( P = 0.03) and results section ( P = 0.02). This is depicted in Table 2 . Although statistically significant, the differences in scores in the methodology section, results section, and overall scores were 1.28/20, 1.28/20, and 4.36/100, respectively, amounting to 5.4%, 5.4%, and 4.36% higher scores in the last JC, which may not be considered educationally relevant (practically significant). The quantum of difference that would be considered practically significant was not decided a priori .
Comparison of marks obtained by pharmacology residents in their first and last journal club
| Section | Marks obtained by pharmacology residents in their first journal club ( =25) | Marks obtained by pharmacology residents in their last journal club ( =25) | Wilcoxon signed-rank test | ||
|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | value | |
| Introduction (maximum: 20 marks) | 13.48±2.52 | 14 (12-16) | 14.28±2.32 | 14 (13-16) | 0.22 |
| Methodology (maximum: 20 marks) | 13.36±3.11 | 14 (12-16) | 14.64±2.40 | 14 (14-16.5) | 0.03* |
| Results and conclusion (maximum: 20 marks) | 13.60±2.42 | 14 (12-15.5) | 14.88±2.64 | 15 (13.5-16.5) | 0.02* |
| Discussion (maximum: 20 marks) | 13.44±3.20 | 14 (11-16) | 14.16±2.78 | 14 (12.5-16) | 0.12 |
| References (maximum: 10 marks) | 7.12±1.20 | 7 (6.5-8) | 7.06±1.28 | 7 (6-8) | 0.80 |
| Title, abstract, and keywords (maximum: 10 marks) | 7.44±0.92 | 7 (7-8) | 7.78±1.12 | 8 (7-9) | 0.17 |
| Overall score (maximum: 100 marks) | 68.44±11.39 | 72 (64-76) | 72.80±11.32 | 71 (68-82.5) | 0.04* |
Marks have been represented as mean±SD. The maximum marks that can be obtained in each section have been stated as maximum. *Indicates statistically significant ( P <0.05). IQR=Interquartile range, SD=Standard deviation
Scores of two groups, one group consisting of 2 nd -year postgraduate students ( n = 44) and second group consisting of 3 rd -year postgraduate students ( n = 32) were compared and revealed no statistically significant difference in overall score ( P = 0.84). This is depicted in Table 3 . Since the quantum of difference in the overall scores was meager 0.84/100 (0.84%), it cannot be considered practically significant.
Comparison of marks obtained by 2 nd - and 3 rd -year pharmacology residents in the activity of critical appraisal of research articles
| Section | Marks obtained by 2 -year pharmacology students ( =44) | Marks obtained by 3 -year pharmacology students ( =32) | Mann-Whitney test, value | ||
|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | ||
| Introduction (maximum: 20 marks) | 14.09±2.41 | 14 (13-16) | 14.28±2.14 | 14 (13-16) | 0.7527 |
| Methodology (maximum: 20 marks) | 14.30±2.90 | 14.5 (13-16) | 14.41±2.24 | 14 (13-16) | 0.8385 |
| Results and conclusion (maximum: 20 marks) | 14.09±2.44 | 14 (12.5-16) | 14.59±2.61 | 14.5 (13-16) | 0.4757 |
| Discussion (maximum: 20 marks) | 13.86±2.73 | 14 (12-16) | 14.16±2.71 | 14.5 (12.5-16) | 0.5924 |
| References (maximum: 10 marks) | 7.34±1.16 | 8 (7-8) | 7.05±1.40 | 7 (6-8) | 0.2551 |
| Title, abstract, and keywords (maximum: 10 marks) | 7.82±0.90 | 8 (7-8.5) | 7.83±1.11 | 8 (7-8.5) | 0.9642 |
| Overall score (maximum: 100 marks) | 71.50±10.71 | 71.5 (66.5-79.5) | 72.34±10.85 | 73 (66-79.5) | 0.8404 |
Marks have been represented as mean±SD. The maximum marks that can be obtained in each section have been stated as maximum. P <0.05 was considered to be statistically significant. IQR=Interquartile range, SD=Standard deviation
The present study gauged the perception of the pharmacology postgraduate students and teachers toward the use of critical appraisal activity as a reinforcing tool for research methodology. Both students and faculties (>50%) believed that critical appraisal activity increases student's knowledge on principles of ethics, experimental evaluation techniques, CONSORT guidelines, statistical analysis, concept of conflict of interest, current trends and recent advances in Pharmacology and trains on doing a review of literature, and improves skills on protocol writing and referencing. In the study conducted by Crank-Patton et al ., a survey on 278 general surgery program directors was carried out and more than 50% indicated that JC was important to their training program.[ 9 ]
The grading template used in Part II of the study was based on the IMRaD structure. Hence, equal weightage was given to the Introduction, Methodology, Results, and Discussion sections and lesser weightage was given to the references and title, abstract, and keywords sections.[ 10 ] While evaluating the scores obtained by 25 students in their first and last JC, it was seen that there was a statistically significant improvement in the overall scores of the students in their last JC. However, the meager improvement in scores cannot be considered educationally relevant, as the authors expected the students to score >90% for the upgrade to be considered educationally impactful. The above findings suggest that even though participation in the JC activity led to a steady increase in student's performance (~4%), the increment was not as expected. In addition, the students did not portray an excellent performance (>90%), with average scores being around 72% even in the last JC. This can be probably explained by the fact that students perform this activity in a routine setting and not in an examination setting. Unlike the scenario in an examination, students were aware that even if they performed at a mediocre level, there would be no repercussions.
A separate comparison of scores obtained by 44 students in their 2 nd year and 32 students in their 3 rd year of postgraduation students was also done. The number of student evaluation sheets reviewed for this analysis was greater than the number of student evaluation sheets reviewed to compare first and last JC scores. This can be spelled out by the fact that many students were still in 2 nd year when this analysis was done and the score data for their last JC, which would take place in 3 rd year, was not available. In addition, few students were asked to present at JC multiple times during the 2 nd /3 rd year of their postgraduation.
While evaluating the critical appraisal scores obtained by 2 nd - and 3 rd -year postgraduate students, it was found that although the 3 rd -year students had a mean overall score greater than the 2 nd -year students, this difference was not statistically significant. During the 1 st year of MD Pharmacology course, students at the study center attend JC once in every 2 weeks. Even though the 1 st -year students do not themselves present in JC, they listen and observe the criticism points stated by senior peers presenting at the JC, and thereby, incur substantial amount of knowledge required to critically appraise papers. By the time, they become 2 nd -year students, they are already well versed with the program and this could have led to similar overall mean scores between the 2 nd -year students (71.50 ± 10.71) and 3 rd -year students (72.34 ± 10.85). This finding suggests that attentive listening is as important as active participation in the JC. Moreover, although students are well acquainted with the process of criticism when they are in their 3 rd year, there is certainly a scope for improvement in terms of the mean overall scores.
Similar results were obtained in a study conducted by Stern et al ., in which 62 students in the internal medicine program at the New England Medical Center were asked to respond to a questionnaire, evaluate a sample article, and complete a self-assessment of competence in evaluation of research. Twenty-eight residents returned the questionnaire and the composite score for the resident's objective assessment was not significantly correlated with the postgraduate year or self-assessed critical appraisal skill.[ 11 ]
Article criticism activity provides the students with practical experience of techniques taught in research methodology workshop. However, this should be supplemented with activities that assess the improvement of designing and presenting studies, such as protocol and paper writing. Thus, critical appraisal plays a significant role in reinforcing good research practices among the new generation of physicians. Moreover, critical appraisal is an integral part of PG assessment, and although the current format of conducting JCs did not portray a clinically meaningful improvement, the authors believe that it is important to continue this activity with certain modifications suggested by students who participated in this study. Students suggested that an increase in the frequency of critical appraisal activity accompanied by the display of active participation by peers and faculty could help in the betterment of this activity. This should be brought to attention of the faculty, as students seem to be interested to learn. Critical appraisal should be a two-way teaching–learning process between the students and faculty and not a dire need for satisfying the students' eligibility criteria for postgraduate university examinations. This activity is not only for the trainee doctors but also a part of the overall faculty development program.[ 12 ]
In the present era, JCs have been used as a tool to not only teach critical appraisal skills but also to teach other necessary aspects such as research design, medical statistics, clinical epidemiology, and clinical decision-making.[ 13 , 14 ] A study conducted by Khan in 2013 suggested that success of JC program can be ensured if institutes develop a defined JC objective for the development of learning capability of students and also if they cultivate more skilled faculties.[ 15 ] A good JC is believed to facilitate relevant, meaningful scientific discussion, and evaluation of the research updates that will eventually benefit the patient care.[ 12 ]
Although there is a lot of literature emphasizing the importance of JC, there is a lack of studies that have evaluated the outcome of such activity. One such study conducted by Ibrahim et al . assessed the importance of critical appraisal as an activity in surgical trainees in Nigeria. They reported that 92.42% trainees considered the activity to be important or very important and 48% trainees stated that the activity helped in improving literature search.[ 16 ]
This study is unique since it is the first of its kind to evaluate how well students are able to critically appraise a research paper. Moreover, the study has taken into consideration the due opinions of the students as well as faculties, unlike the previous literature which has laid emphasis on only student's perception. A limitation of this study is that sample size for faculties was smaller than the students, as it was not possible to convince the distant faculty in other cities to fill the survey. Besides, there may be a variation in the manner of conduct of the critical appraisal activity in pharmacology departments across the various medical colleges in the country. Another limitation of this study was that a single assessor graded a single student during one particular JC. Nevertheless, each student presented at multiple JC and thereby came across multiple assessors. Since the articles addressed at different JC were disparate, interobserver variability was not taken into account in this study. Furthermore, the authors did not make an a priori decision on the quantum of increase in scores that would be considered educationally meaningful.
Pharmacology students and teachers acknowledge the role of critical appraisal in improving the ability to understand the crucial concepts of research methodology and research conduct. In our institute, participation in the JC activity led to an improvement in the skill of critical appraisal of published research articles among the pharmacology postgraduate students. However, this improvement was not educationally relevant. The scores obtained by final-year postgraduate students in this activity were nearly 72% indicating that there is still scope of betterment in this skill.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge the support rendered by the entire Department of Pharmacology and Therapeutics at Seth GS Medical College.
- Open access
- Published: 20 September 2024
Dementia Friendly communities (DFCs) to improve quality of life for people with dementia: a realist review
- Stephanie Craig ORCID: orcid.org/0000-0003-0783-4975 1 ,
- Peter O’ Halloran ORCID: orcid.org/0000-0002-0022-7331 1 ,
- Gary Mitchell ORCID: orcid.org/0000-0003-2133-2998 1 ,
- Patrick Stark ORCID: orcid.org/0000-0003-2659-0865 1 &
- Christine Brown Wilson ORCID: orcid.org/0000-0002-7861-9538 1
BMC Geriatrics volume 24 , Article number: 776 ( 2024 ) Cite this article
Metrics details
Currently, there are more than 55 million people living with dementia worldwide. Supporting people with dementia to live as independently as possible in their communities is a global public health objective. There is limited research exploring the implementation of such interventions in the community context. The aim of the review was to create and refine programme theory – in the form of context mechanism-outcome configurations – on how the characteristics of dementia-friendly communities (DFCs) as geographical locations interact with their social and organisational contexts to understand what works for whom and why.
This realist review sourced literature from 5 electronic databases: Cochrane Library, CINAHL, Medline, Scopus, PsychINFO and Google Scholar, as well as relevant websites such as Alzheimer’s Society to identify grey literature. Methodological rigour was assessed using the Joanna Briggs Institute critical appraisal tool.
Seven papers were included in this realist review that focused on DFCs in a geographical context The implementation of DFC interventions emerged as a process characterised by two pivotal implementation phases, intricately linked with sub-interventions. The first intervention, termed Hierarchy Commitment (I1a/b), involves the formalisation of agreements by businesses and organizations, along with the implementation of dementia-friendly action plans. Additionally, Educational Resources (I1c) play a significant role in this phase, engaging individuals with dementia and their caregivers in educational initiatives. The second phase, Geographical/Environmental Requirements (I2), encompasses the establishment of effective dementia-friendly signage, accessible meeting places, and community support.
Conclusions
This realist review highlighted a theoretical framework that might guide the development of dementia-friendly communities to enhance the experiences of individuals with dementia and their caregivers within DFCs. Emphasising the need for a theoretical framework in developing geographical DFCs, the review outlines contextual elements, mechanisms, and outcomes, providing a foundation for future studies. The ultimate goal is to establish a robust body of evidence for the sustainable implementation of dementia-friendly communities, thereby improving the quality of life for those with dementia.
Study registration
This study is registered as PROSPERO 2022 CRD42022317784.
Peer Review reports
Introduction
Currently, there are more than 55 million people living with dementia worldwide [ 1 ]. It is estimated that this number will rise to 139 million by 2050. Dementia is the seventh leading cause of death and one of the major causes of disability and dependence among older people globally, resulting in reduced quality of life for people with dementia and their care partners, with associated social and financial consequences [ 1 ].
Neurological changes that occur with dementia cause the individual to experience impairments; however, it is increasingly recognised that it is the intersection of these impairments with the physical and social environments encountered that creates the experience of disability for the person with dementia [ 2 ]. Since most people who have dementia live in communities, the structure and culture of those communities are likely to have an impact on how dementia is perceived [ 3 ]. In response to this, the World Health Organisation, Dementia Alliance International, and Alzheimer’s Disease International have created programmes that promote a community model of social participation [ 4 ].
People with dementia, as well as their families and carers, value meaningful connections [ 5 , 6 ] and need to be active participants in their social networks to maintain meaningful social connections [ 7 ]. Supporting people with dementia and their carers to live as independently as possible in their communities by providing social and emotional support is a global public health objective [ 8 ]. The worldwide action plan on the public health response to dementia was adopted by the World Health Organisation (WHO) in May 2017 [ 8 , 9 ]. The plan suggests that increasing public awareness and understanding of dementia and making the environment dementia-friendly will enable people with dementia to maximise their autonomy through improved social participation [ 10 ].
ADI [ 3 ] define a dementia-friendly community (DFC) as a place or culture in which people with dementia and their care partners can feel empowered, supported, and included in society- Table 1 identifies the main elements of a DFC.
While a community is typically characterised by its geographic location, communities can also be made up of people who have similar hobbies, religious affiliations, or ethnic backgrounds e.g., organisations with a specific focus of dementia- friendliness [ 3 ]. According to Lin and Lewis [ 11 ], the idea of dementia-friendly communities focuses on the lived experiences of individuals with dementia and is most pertinent to addressing both their needs and the needs of those who live with and support them. According to Mitchell, Burton, and Raman [ 12 ], dementia-friendly communities are likely to be all-inclusive and promote community engagement for everyone, not only those who have dementia.
Several models and frameworks have been developed to operationalise DFCs. The Dementia Friends USA Framework [ 13 ] focuses on raising awareness and understanding of dementia across various sectors. The Alzheimer’s Society in the UK [ 14 ] has a model emphasising awareness, participation, and stakeholder involvement. The Community Engagement Model prioritises the involvement of people with dementia and their caregivers in developing DFC initiatives. Social Inclusion Strategies aim to improve social inclusion through supportive environments and community education [ 15 ]. The Multi-Sector Collaboration Model promotes cooperation among local governments, healthcare providers, businesses, and other organisations to support people with dementia comprehensively.
The DFC concept is inspired by the World Health Organisation’s Age-Friendly Cities initiative [ 15 , 16 ], which aims to create inclusive environments supporting active and healthy aging [ 17 , 18 ]. Both dementia-friendly and age-friendly approaches emphasise empowering local stakeholders to enhance social inclusion, reduce stigma, and remove barriers in physical and social environments [ 19 ].
Despite its potential, the DFC concept faces challenges and criticisms. Swaffer [ 20 ] highlights that the language around dementia often perpetuates stigma, negatively impacting those affected. Swaffer [ 20 ] and Rahman & Swaffer [ 21 ] criticise many DFC initiatives as tokenistic, often failing to genuinely include people with dementia in decision-making. They advocate for an assets-based approach, recognising and leveraging the strengths of individuals with dementia. Shakespeare et al. [ 22 ] emphasise the need for a human rights framework to ensure dignity, respect, and full inclusion for people with dementia. Effective DFCs should go beyond superficial friendliness to ensure authentic inclusion, empowerment, and adherence to a rights-based approach.
Person-centered care is a foundational approach that emphasises treating individuals with dementia with respect, valuing their uniqueness, and understanding their behaviours as meaningful communication [ 23 ]. The bio-psychosocial approach provides a holistic framework [ 24 ], recognising dementia as influenced by biological, psychological, and social factors, guiding comprehensive care strategies. Attachment theory [ 25 ] offers insights into the behaviours and relationships of individuals with dementia based on their attachment histories. The need-driven dementia-compromised behaviour model [ 26 ] shifts focus to addressing underlying needs behind behavioural symptoms rather than merely managing them. Thijssen and colleagues’ work on social health and dementia-friendly communities [ 27 ] aligns well with these person-centered and psychosocial approaches, emphasising social participation, autonomy, and environmental adaptation. Key principles for dementia-friendly communities derived from these theories include recognising individuality, fostering supportive environments, promoting autonomy and meaningful engagement, interpreting behaviours as expressions of needs, and prioritising holistic health and positive relationships. Implementing these principles can enhance inclusivity and support for people with dementia, with ongoing evaluation and adaptation crucial for sustained effectiveness of dementia-friendly initiatives [ 28 , 29 ].
The existing body of evidence offers support for the effectiveness of DFCs, with previous research exploring various dimensions of their establishment. One perspective underscores the significance of a robust policy framework and an enhanced support infrastructure [ 30 , 31 ]. Alternatively, other studies delve into the priorities of individuals with dementia and their caregivers, emphasising factors such as fostering social connections and promoting acceptance of dementia within the community [ 4 , 15 , 32 , 33 ]. Additionally, investigations into the experiences of people with dementia residing in DFCs, including their awareness of living in such a community, have been conducted [ 34 ].
Despite extensive efforts to evaluate DFCs, their effectiveness remains challenging to ascertain due to the multifaceted and complex nature of the intervention. The evaluation process is further complicated by the diverse needs and preferences of individuals with dementia, variations in resources and support across different communities, and the dynamic nature of dementia care and research. A recent rapid-realist review by Thijssen et al. [ 27 ] comprehensively examined how dementia-friendly initiatives (DFIs) function for people with dementia and their caregivers. While some studies have reviewed dementia-friendly hospital settings, such as Lin [ 35 ] and a realist review by Handley [ 36 ] Thijssen et al.‘s [ 27 ] rapid realist review primarily focused on initiatives often serving as building blocks in DFC development. These initiatives are typically activity-based and on a smaller scale compared to larger communities. Despite these valuable insights, there remains a limited understanding of how geographical DFCs specifically contribute to improving the quality of life for individuals living with dementia.
Dementia-friendly communities are complex interventions. Understanding what works, why and what factors help or hinder their effectiveness can optimise the design and implementation of DFCs for the benefit of individuals with dementia and their caregivers [ 37 ], thus contributing to the development of robust and impactful DFC interventions [ 38 ].
DFCs are often understood primarily as geographical communities, which has several important implications [ 30 ]. Defining DFCs geographically allows for a localised approach tailored to specific towns, cities, or regions, enabling initiatives to address the unique needs and characteristics of particular areas [ 39 ]. Geographical DFCs aim to transform entire villages, towns, cities, or regions to become more inclusive and supportive of people with dementia, potentially impacting all aspects of community life [ 2 ]. This approach emphasises the importance of adapting the physical and built environment to be more accessible and navigable for people with dementia, including clear signage, rest areas, and dementia-friendly urban design. A geographical focus also encourages involvement from various local stakeholders, such as businesses, public services, and residents, fostering a collective effort to support people with dementia. Countries like England have incorporated geographically defined DFCs into national policy [ 30 ], setting targets for their creation and establishing recognition systems, allowing for more structured implementation and evaluation. Different geographical areas may adopt diverse strategies based on their specific demographics, resources, and needs, allowing for innovation and context-specific solutions. Additionally, geographical DFCs can facilitate increased social and cultural engagement for people with dementia within their local area, helping them remain active and valued community members [ 34 ]. Defining DFCs geographically enables more straightforward evaluation of their impact on the lives of people affected by dementia within a specific area [ 40 ]. While some DFCs are also defined as communities of interest, focusing on specific groups or shared experiences rather than physical location, the geographical approach remains significant due to its comprehensive nature and ability to create tangible changes in the everyday environments where people with dementia live and interact.
This realist review will therefore offer a novel and unique contribution to the existing literature enabling a greater understanding of geographical DFCs and enable the identification of relevant interventions related to outcomes.
Aim and objectives
The aim of this review is to create and refine a programme theory – in the form of context-mechanism-outcome (CMO) configurations – that explains how the characteristics of geographical Dementia-Friendly Communities (DFCs) interact with their social and The aim of this review is to create and refine a programme The aim of this review is to create and refine a programme The aim of this review is to create and refine a programme.
To identify the dominant programme theories on how geographical DFCs can be successful in improving the quality of life for people with dementia.
To determine the characteristics of geographical DFCs, and the social and organisational contexts that may aid or hinder their effectiveness in providing individual benefits for people with dementia.
Study design
A project protocol was registered with PROSPERO in March 2022 [ 41 ] with the review conducted between April 2022- February 2024. This review followed RAMESES (Realist and Meta-narrative Evidence Syntheses Evolving Standards) guidelines [ 42 ], aiming to create and refine programme theory in the form of context-mechanism-outcome (CMO) configurations.
Step 1: scoping the literature
The first step in the review process was to define the scope of the review. This phase offered the framework and structure for examining and synthesising a variety of study findings [ 43 ]. To understand broad implementation strategies, an initial exploratory literature search was conducted. This included combining worldwide research literature to ensure a comprehensive view, grey literature such as reports and theses for practical insights, and pertinent policy papers to understand real-world applications and guidelines. Implementation strategies aim to identify and understand various methods used to implement changes effectively.
Step 2: search methods for the review
The search strategy was developed in consultation with a subject librarian at Queen’s University Belfast. The databases searched included Cochrane Library, CINAHL, Medline, Scopus, PsychINFO and Google Scholar, as well as relevant websites such as Alzheimer’s Society to identify grey literature. The reference lists of all articles included in this review were also searched. An example of the search strategy used is shown in table 2 .
Step 3: Selection and appraisal of articles
Covidence software [ 44 ] was utilised for the selection of articles, which automatically removed duplicate papers. All articles were reviewed by SC. PS/GM reviewed 50% of each of the articles. This ensured that two people independently and blindly reviewed each script. Any conflicts were resolved as a three-way discussion between all reviewers. The selection of articles was based on inclusion/exclusion criteria (Table 3 ) alongside how well they informed the programme theory. No temporal limits were applied to initial searches, however, we only searched for papers written in English language. Traditionally, realist reviews do not assess methodological quality. However, this aspect was included in this review to provide the reader with an understanding of the strength of the evidence underpinning the conclusions. The methodological quality of all included studies was assessed using JBI appraisal tools [ 45 ].
Step 4: data extraction
A data extraction form based on the RAMESES recommendations for realist synthesis and previously used in realist reviews [ 46 , 47 , 48 ] was used to extract data from the included full-text papers [ 42 ] in the following areas: theoretical foundation of the intervention, participant characteristics, type of DFC intervention, how the intervention was intended to function, implementation characteristics, and contextual issues that facilitated or hindered implementation of the DFC intervention.
The review focused on theoretical foundations such as community social capital, social contagion, empowerment of PLWD, lessons from global best practices, culturally competent approaches, economic and social benefits, stakeholder involvement, and flexible adaptation of DFC models were integral. The review was also guided by strategic policies supporting DFC development and sustainability. Context-Mechanism-Outcome (CMO ) configurations were utilised to identify contexts that enabled or hindered DFC initiatives, the processes or resources activated by DFCs ( mechanisms ), and the outcomes for people with dementia and their caregivers. Key aspects of DFCs, including physical environment adaptations, social and cultural initiatives and education and awareness programs, were systematically analysed. Implementation strategies, stakeholder engagement processes, barriers, and facilitators were also explored. The review further examined the experiences and perspectives of people living with dementia and caregivers, the impact of DFCs on caregivers, policies supporting DFCs, cultural adaptations of DFC concepts, and evaluation frameworks used to assess DFC effectiveness.
Step 5: synthesising the evidence and drawing conclusions
Identification of candidate theories.
A realist review focuses on the discovery, articulation, and analysis of underlying programme theories to determine if these theories are supported by the evidence [ 49 ]. Following data extraction, candidate theories were formulated, debated and reviewed with the study team. Few papers explain their programme theory; therefore, implicit theories were presumed from components of the interventions. Identifying contextual factors that aided or impeded implementation further developed each candidate theory. Candidate theories from each paper were written in the C-M-O configurations by identifying contextual factors that aid or hinder implementation.
Synthesis of candidate theories
The initial candidate theories were synthesised and grouped into themes relating to the context (C), mechanism (M), outcome (O), and intervention (I). All members of the research team and the study’s expert reference group discussed the relevance of the synthesised candidate theories as the programme theory was developed. The synthesised theories were combined into an overarching programme theory to indicate how geographically bounded DFC interventions may be successfully implemented in the community for people with dementia and their carers (Fig. 2 ).
Study selection
The search identified 2,861 records in total (Fig. 1 ). After duplicates were removed a total of 2,516 papers were left. Titles and abstracts were reviewed together by S.C, P.S and G.M. Following this stage S.C. reviewed all full-text articles while P.S and G.M reviewed 50% of full-text papers. Full-text screening resulted in 68 articles for full-text review, 61 papers were excluded This was resulting in 7 papers for data extraction. Reasons for exclusion are documented in Fig. 1 .

PRISMA flow diagram
Study characteristics (table 4 )
The seven studies employed a range of methodological designs. Three studies used cross-sectional study designs [ 50 , 51 , 52 ]. Three articles used qualitative methodology [ 53 , 54 , 55 ] and one study was a mixed-methods design [ 56 ].
Methodological quality
The methodological quality of the empirical evidence in each of the seven papers included in this review was critically appraised using Joanna Briggs Institute critical appraisal tools [ 45 ]. Using the JBI tool, Goodman et al. [ 56 ] was assessed as strong, two articles were accessed as moderate [ 51 , 52 ] and four were accessed as weak [ 50 , 53 , 54 , 55 ].
Main objectives of the studies
The included studies had three main sets of objectives: to explore the experiences of living/ working within a DFC [ 51 , 56 ] and to understand how a community can become dementia-friendly [ 50 , 52 , 53 , 55 ]. The third objective focused on the perception of residents on building a DFC in a minority area [ 54 ].
Study populations
The studies described different types of DFCs across four continents; Asia [ 51 ] Oceania [ 52 ] North America [ 50 , 54 ] and Europe [ 53 , 55 , 56 ]. Two studies collected data from people with dementia ( n = 35) [ 54 , 56 ]. Three studies from caregivers/ family care partners ( n = 152) [ 50 , 54 , 55 ]. Four of the studies collected data from additional participants ( n = 454). For example, community workers [ 52 , 53 , 54 , 55 ]. Tsuda et al. [ 51 ] categorised their participants ( n = 2633) as older adults living in an apartment block with a mean age of 77.4, 45.7% living alone and 7.7% reported living with impaired cognitive function. Participants with a diagnosis of dementia did not disclose the clinical stage of their diagnosis.
Characteristics of DFC interventions
All studies explored the use of dementia-friendly programmes within the community. DFC programmes involve the implementation of various person-centred approaches to the community environment to support people with dementia. The programmes identified in this realist review are not standardised interventions and do not involve a single intervention but rather a collective of different community activities interventions aided by members of the public/policymakers with ongoing input from dementia charities e.g., Alzheimer’s Society or Alzheimer’s Disease International. These programmes focus on improving the places in which people with dementia interact and live in their daily lives.
Characteristics of DFC outcomes
DFC interventions have been shown to yield a variety of positive outcomes. These interventions have led to increased social interaction [ 51 ] among individuals living with dementia, fostering a sense of belonging and reducing social isolation [ 52 ]. Moreover, interventions promoting the involvement of people with dementia within the community have resulted in improved quality of life for people with dementia [ 52 , 54 ]. DFC intervention results in improved community capacity to deliver dementia-friendly services, such as support groups and workshops, these interventions have also positively impacted caregivers by reducing depression and promoting healthy outcomes for carers [ 50 ]. Additionally, DFC interventions support people with dementia’s independence and ability to continue living in their own homes [ 55 ]. Small-scale initiatives developed by PWD and their caregivers, such as the EndAge Day and Memory Bank projects, have further enriched community engagement and encouraged participation in meaningful activities [ 53 ]. The interventions have also led to greater access to public amenities, which promotes a greater quality of life which contributes to active participation in the community and people with dementia living longer in their own homes [ 56 ].
Candidate theories
The preliminary scoping of the literature did not identify any explicit theory underlying the implementation of DFCs for people living with dementia or their caregivers. However, common sense implicit theories were identified. It was evident that providing dementia awareness information in the community is a key component of a DFC [ 51 , 52 , 53 , 54 , 56 ]. If dementia awareness is raised within the community, further support can be provided for people living with dementia and their caregivers which can contribute to positive changes within the environment [ 51 , 54 , 55 ] and government policies [ 51 ]. This will likely encourage people with dementia and their caregivers to engage in DFCs as they will feel supported and confident in the community [ 51 , 52 , 53 , 54 , 56 ]. In addition, this will improve the quality of life for people with dementia [ 56 ]. However, one study identified how hierarchy commitment is necessary for a business/ organisation to become dementia friendly [ 55 ]. This indicates a strong organisational commitment from the top-down of a business/ organisation. This commitment involves leaders and decision-makers at varying levels endorsing and actively participating in efforts to make the organisations more supportive of people living with dementia. This involves the business/ organisation formalising agreements to become dementia-friendly and implementing dementia-friendly action plans. This is reinforced by another study which states that communities need to prioritise an action plan when implementing a dementia friendly community [ 54 ].
Contextual factors that help or hinder the implementation of DFC interventions
Several contextual factors were identified that help or hinder the implementation of DFC interventions for people living with dementia. The issue of having a recognisable geographical boundary for a DFC remains one of the most significant contextual factors that help the implementation of DFC interventions [ 51 , 52 , 54 , 56 ]. However, one study states that dementia-friendly communities are not defined by a geographical boundary, they are locations where people with dementia can find their way around and feel safe in their locality/ community/ city where they can maintain their social networks, so they feel they still belong in the community [ 53 ].
Dementia-friendly communities thrive in rural areas where there is often a smaller population and a strong sense of community [ 52 , 54 ] and it may be easier to engage local stakeholders [ 55 ]. Close-knit communities where people know each other well can foster greater understanding and support for people living with dementia and their caregivers, and also allow a greater opportunity for tailored and personalised interventions [ 54 , 55 ].
Existing resources e.g., advisory groups, awareness activities, diagnostic and treatment centres, community and family caregiver education and care services and political support are crucial facilitators in the successful implementation of dementia-friendly communities [ 50 , 52 , 53 , 54 , 55 , 56 ]. The presence of ample resources [ 50 , 51 , 52 , 54 ] coupled with robust political endorsement [ 56 ], constitutes a pivotal framework for the success of such initiatives. Governmental bodies, as exemplified, play a crucial role by furnishing financial support for community projects and endorsing policies, thereby enabling a comprehensive approach to assist individuals with dementia and their caregivers (However, a range of factors that both facilitated or hindered these DFCs was also identified – for example, DFCs exhibit notable success in rural settings, as evidenced by their thriving presence in such areas [ 50 , 52 , 53 , 54 , 55 , 56 ]. Sufficient funding is imperative for sustaining programs and services, and financial backing from governmental entities, philanthropic organisations, and local authorities becomes instrumental in meeting the expenses associated with the implementation of DFC interventions [ 53 , 54 ]. Financial constraints can limit the availability of resources, services and infrastructure needed to create and sustain dementia-friendly communities [ 53 , 54 ]. Political support extends beyond mere financial contributions; it catalyses the development and implementation of policies conducive to dementia-friendly practices, addressing issues like anti-discrimination measures and caregiver support. This, in turn, fosters collaboration among stakeholders [ 54 , 55 ]. The establishment of policies also catalyses public awareness campaigns, aimed at mitigating associated stigmas [ 52 , 54 , 56 ]. By leveraging existing resources and garnering political support, communities can cultivate an environment where individuals with dementia are comprehended, esteemed, and supported. This concerted effort leads to the achievement of dementia-friendly communities, ultimately enhancing the overall quality of life for both individuals living with dementia and their caregivers.
Factors identified as hindering implementation can include the younger population’s involvement due to lack of awareness, or lack of involvement or understanding, and can indeed present some challenges in the implementation of a DFC [ 52 , 55 ]. While typically younger individuals may not directly experience dementia first-hand themselves, their attitudes, understanding, and engagement in the community play a significant role in shaping the overall dementia-friendly environment. The gender of people living with dementia can also influence the implementation of dementia-friendly interventions through the concept of social contagion and the existing differences in social networks between men and women. The existing gender differences in social networks can impact the effectiveness of a DFC intervention because typically women already have stronger social networks than men [ 51 ]. Negative cultural stereotypes can also hinder implementation due to the lack of culturally appropriate services, and a lack of understanding of dementia [ 50 ]. Disparities in Alzheimer’s disease and Alzheimer’s Disease-related dementia’s create significant obstacles to the adoption of dementia-friendly communities across all communities, particularly those of colour [ 54 ].
This section explains the intervention (I), mechanism (M), and contexts (C) that are thought to produce the outcome (O) of improved quality of life (QOL) for people living with dementia, increased social interactions, support and inclusivity for people with dementia and their carers. The aim of this synthesis was to create and refine programme theory on how DFCs’ characteristics interact with their social and organisational contexts to produce desired outcomes. Figure 2 depicts the theoretical paradigm for how DFC interventions are expected to work.
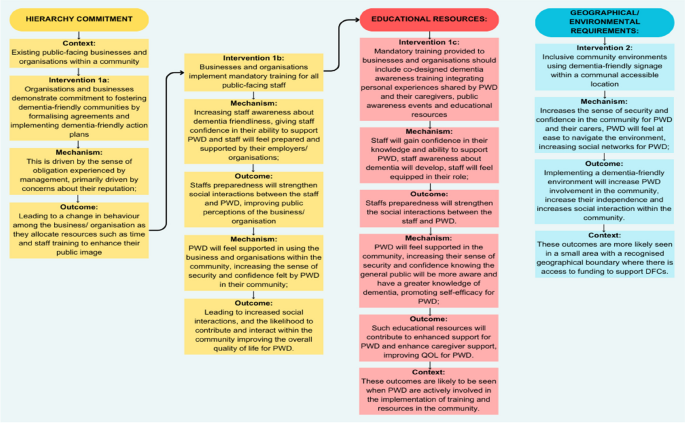
A theoretical model of how DFC interventions for people with dementia are thought to work. Legend: Theoretical model of the Context +Mechanism = Outcome (CMO) configuration. Context is shown as either helping (C+) or hindering (C-) implementation. The intervention is divided into two phases, facilitation (I1) and display (I2), activating underlying mechanisms (M) that result in improved outcomes (O)
The implementation of DFC interventions appeared to involve two crucial implementation phases: Hierarchy commitment (I 1a/b )interlinked with educational resources (I 1c ) and Geographical/ environmental requirements (I 2 ). Hierarchy commitment involves two sub-interventions, which are seen in existing public-facing businesses and organisations within a community (C). Organisations and businesses demonstrate a commitment to fostering dementia-friendly communities by formalising agreements and implementing dementia-friendly action plans (I 1a ). This is driven by the sense of obligation experienced by management, primarily driven by concerns about their reputation (M); leading to a change in behaviour among the business/ organisation as they allocate resources such as time and staff training to enhance their public image (O). This leads to businesses and organisations implementing mandatory training for all public-facing staff (I 1b ), which increases staff awareness about dementia friendliness (M), giving staff confidence in their ability to support PWD (M) and staff will feel prepared and supported by their employers/ organisations (M); Staffs preparedness will strengthen social interactions between the staff and PWD, improving public perceptions of the business/ organisation (O). By the same intervention, PWD will feel supported in using the business and organisations within the community (M), increasing the sense of security and confidence felt by PWD in their community (M); leading to increased social interactions, and likelihood to contribute and interact within the community improving the overall quality of life for PWD (O).
Mandatory training provided to businesses and organisations should include co-designed dementia awareness training integrating personal experiences shared by PWD and their caregivers, public awareness events and educational resources (I 1C ), staff will gain confidence in their knowledge and ability to support PWD (M), staff awareness about dementia will develop (M), staff will feel equipped in their role (M); Staffs preparedness will strengthen the social interactions between the staff and PWD (O). By the same intervention, PWD will feel supported in the community (M) increasing their sense of security and confidence knowing the general public will be more aware and have a greater knowledge of dementia (M), promoting self-efficacy for PWD (M); such educational resources will contribute to enhanced support for PWD and enhance caregiver support, improving QOL for PWD (O). These outcomes are likely to be seen when PWD are actively involved in the implementation of training and resources in the community (C).
Secondly, dementia-friendly signage creates inclusive community environments within a communal accessible location (I2) to increase the sense of security and confidence in the community for PWD and their carers (M). Further, PWD will feel at ease to navigate the environment (M), increasing social networks for PWD (M); therefore, implementing a dementia- friendly environment will increase PWD involvement in the community, increase their independence and social interaction within the community (O). These outcomes are more likely seen in a small area with a recognised geographical boundary where there is access to funding to support DFCs (C).
This realist review elucidates the underlying mechanisms that drive the success of DFC interventions in diverse community settings. The realist approach, rooted in understanding the interactions between contexts, mechanisms, and outcomes, allowed this review to identify the complexities of DFC interventions. The initial candidate theory emerging from the synthesis of the literature emphasised the importance of creating dementia-friendly communities to support those affected by dementia [ 50 , 51 , 52 , 53 , 54 , 55 , 56 ]. This theoretical model builds upon this by explicitly identifying the context and mechanisms involved in successful DFC implementation in geographical locations.
The theoretical model posits that hierarchical commitment, educational resources, and geographical/environmental requirements [ 50 , 51 , 52 , 54 , 56 ] are pivotal interventions leading to positive outcomes for individuals living with dementia. These findings extend those of the DEMCOM study’s logic model [ 56 ] by highlighting the critical role of cultural appropriateness and community structures in the success of DFCs. For instance, DFCs thrive in rural settings due to strong community ties and the utilisation of existing resources, which stimulate localised services for people with dementia [ 57 ]. However, these supports may be weakened when younger family members move away [ 7 ]. Moreover, governmental support and utilisation of existing resources significantly contribute to the facilitation of DFCs [ 4 ]. This suggests that while the DEMCOM logic model provides a robust framework, it may benefit from a more explicit integration of cultural and geographical factors. These findings challenge some conclusions of the DEMCOM study by showing that political support and financial backing, while necessary, are not sufficient on their own. The presence of culturally appropriate services and strong community engagement are equally vital. For example, the use of culturally sensitive language and involvement of community leaders were found to be critical in the API community, which was not a primary focus in the DEMCOM logic model.
The combination of context and mechanisms in this review provides an explanation as to why DFC interventions were successfully implemented. For example, recognisable geographical boundaries and rural areas [ 51 , 52 , 54 , 56 ] facilitate the accessibility of dementia-friendly communities for people living with dementia and their carers. Government support is critical in providing resources in such areas that enable appropriate signage and environmental changes that enable engagement within this geographical boundary [ 50 , 52 , 53 , 55 , 56 ]. Effective signage tailored to individuals can create a positive environment for people living with dementia, overall improving the environment [ 58 ]. Training for the public and businesses to generate awareness with their staff supports the sustainability of dementia-friendly communities as it facilitates a widespread understanding of the disease and fosters inclusivity. Staff will also feel an increase in confidence in supporting people living with dementia in businesses within DFCs, which fosters an inclusive community that empowers people living with dementia to maintain their independence and improve their quality of life. It is acknowledged that people with dementia need to be appropriately supported and empowered to remain part of their community [ 59 ].
There are notable gaps in the evidence regarding the long-term impacts of DFCs on different demographic groups. While this study identified several immediate benefits, such as increased social engagement and reduced stigma, more longitudinal research is needed to understand the sustained impact on the quality of life and mental health outcomes for people with dementia. Additionally, there is limited evidence on the specific mechanisms through which DFCs benefit caregivers. Furthermore, factors such as the outmigration of younger individuals to larger urban areas and gender dynamics can hinder the implementation of DFCs, as evidenced by Wiersma and Denton [ 7 ] and Herron and Rosenberg [ 60 ], respectively.
This study indicates that DFCs primarily benefit people with dementia and their caregivers by enhancing social inclusion, reducing stigma, and providing culturally relevant support. In rural settings, the entire community benefits from increased awareness and support structures, contributing to a more inclusive and supportive environment for all residents. However, these findings also suggest that not all groups benefit equally. For example, in urban areas with diverse populations, the lack of culturally tailored services can limit the effectiveness of DFCs. Therefore, for DFCs to be truly effective, they must be designed with the specific needs and characteristics of the target communities in mind. According to Phillipson et al. [ 52 ], creating a model that satisfies everyone’s needs is challenging. According to Turner and Cannon [ 61 ], given their commonalities and the possibility that certain groups will have overlapping interests, it might be beneficial if projects were collaborative rather than parallel. According to research on age-friendliness in rural areas, there is variation both within and between rural communities. While younger people may leave some communities, others may see an influx of relatively wealthy retirees, which may marginalise older residents who have lived in poverty for a longer period of time [ 62 ].
The WHO [ 63 ] toolkit for dementia-friendly initiatives (DFIs) provides a valuable framework for understanding the foundational components necessary for the successful implementation of DFCs. Although our review primarily focuses on geographical DFCs, the toolkit’s recommendations can be relevant as they highlight the importance of establishing strong partnerships, engaging key stakeholders, and creating structured, well-planned initiatives that serve as the building blocks for DFCs [ 17 , 27 , 64 ]. DFIs and DFCs are closely related since DFIs are a part of DFCs and their results are essential to DFC support. The toolkit offers detailed guidance on how to set up DFIs, which can be seen as essential precursors to the broader goal of developing inclusive and supportive communities for individuals living with dementia.
While the research available offers significant insights into the theoretical aspects of DFC interventions, it is important to acknowledge the current lack of concrete evidence on their efficacy. Nonetheless, the realist review methodology enables us to consider the diverse perspectives of participants and stakeholders, leading to a more comprehensive understanding of the complex interplay between interventions, mechanisms, and outcomes. To ensure the sustainability of DFCs, future research should focus on the long-term impacts of existing interventions and the perspectives of decision-makers and programme creators, such as the Alzheimer’s Society. By applying the realist lens to these investigations, we can further refine our theoretical framework and identify the critical elements needed for the continued success of DFC initiatives. The realist review methodology has been instrumental in shaping a theoretical framework for the implementation of dementia-friendly communities. By acknowledging the specific contexts, identifying underlying mechanisms, and exploring outcomes, this approach moves beyond conventional systematic reviews and offers a more nuanced understanding of how DFC interventions work. While evidence on their effectiveness may still be evolving, the insights gained from this realist review contribute significantly to the growing body of knowledge, guiding the development of sustainable and effective dementia-friendly communities that truly enhance the quality of life for individuals living with dementia and their caregivers.
Strengths and limitations
This realist review has contributed to an ever-growing evidence- base on the creation of a theoretical framework for the implementation of dementia-friendly communities, and it includes both the elements required for implementation and the underlying mechanisms that might affect outcomes. However, there was no advice on how to carry out these interventions. There is also little understanding of how the interplay between the intervention, mechanism, and setting affects people with dementia or their caregivers because DFCs were developed in various contexts and ways.
Further research looking into the sustainability of existing dementia-friendly communities is urgently needed. Future studies should also consider the lessons learned from the implementation of complex DFC interventions from people living with dementia in/and people working/volunteering within dementia-friendly communities. In acknowledging the limitations of this study, it is important to note that the existing body of literature is limited. The scarcity of relevant studies in this area may impact the generalisability of our findings and the overall programme theory. Due to the nature of the review, we could only screen English papers and therefore there may have been key literature missed. Additionally, another limitation to this study is that this review focuses solely on geographical DFCs. However, this helped to narrow the focus of this review amongst the literature.
This realist review has illuminated a theoretical framework that might guide the development of geographical dementia-friendly communities for those with dementia and their caregivers. However, it has highlighted a gap in the existing literature, specifically the lack of a realist approach that explicitly theorises the specific contexts, intervention components, and resulting mechanisms. The review’s aim is to create and refine a programme theory on how to improve the experiences of living in dementia-friendly communities, which is significant for both individuals living with dementia and their caregivers. Moreover, there is a need to apply this theoretical framework to the development of geographical dementia-friendly communities, enhancing the quality of life for people living with dementia. This realist review outlines significant contextual elements, mechanisms, and outcomes in relation to geographical dementia-friendly communities which can guide future studies (Fig. 2 ). Future research should concentrate on building a robust body of evidence to support the sustainable implementation of dementia-friendly communities, further improving the quality of life for those diagnosed with dementia.
Availability of data and materials
No datasets were generated or analysed during the current study.
Reference list
World Health Organization. Dementia. 2022. https://www.who.int/news-room/fact-sheets/detail/dementia .
Dementia Alliance International. Human rights for people living with dementia: From rhetoric to reality. Dementiaallianceinternational.org. 2016. Available from: https://dementiaallianceinternational.org/assets/2016/05/Human-Rights-for-People-Living-with-Dementia-Rhetoric-to-Reality.pdf .
Alzheimer’s Disease International. Dementia Friendly Communities. 2022. (Online). Available at: https://www.alzint.org/what-we-do/policy/dementia-friendly-communities/ ].
Novak LS, Horne E, Brackett JR, Meyer K, Ajtai RM. Dementia-friendly communities: A review of current literature and reflections onimplementation. Curr Geriatr Rep. 2020;9:176–82.
Article Google Scholar
Phinney A, Chaudhury H, O’Connor DL. Doing as much as I can do: the meaning of activity for people with dementia. Aging Ment Health. 2007;11:384–93.
Article PubMed Google Scholar
Phinney A, Kelson E, Baumbusch J, et al. Walking in the neighbourhood: performing social citizenship in dementia. Dementia. 2016;15:381–94.
Wiersma EC, Denton A. From social network to safety net: dementia-friendly communities in rural Northern Ontario. Dementia. 2016;15:51–68.
World Health Organization. Global action plan on the public health response to dementia 2017–2025. 2017. https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025
Alzheimer’s Disease International. WHO Global action plan on dementia. 2022. Available at: https://www.alzint.org/what-we-do/partnerships/world-health-organization/who-global-plan-on-dementia/ .
Alzheimer’s Disease International. Dementia-Friendly Communities: Global Developments 2nd Edition. https://www.alzint.org/u/dfc-developments.pdf . (2017). Accessed 28 June 2024.
Lin SY, Lewis FM. Dementia friendly, dementia capable, and dementia positive: concepts to prepare for the future. Gerontologist. 2015;55(2):237–44.
Article PubMed PubMed Central Google Scholar
Mitchell L, Burton E, Raman S. Dementia-friendly cities: designing intelligible neighbourhoods for life. J Urban Des. 2004;9(1):89–101.
Dementia Friendly America. Dementia Friends USA [Online] Dementia Friendly America. 2024. https://dfamerica.org/overview-and-5-key-messages/
Alzheimer’s Society. What is a dementia friendly community? Alzheimer’s Society. 2024. https://www.alzheimers.org.uk/get-involved/dementia-friendly-resources/what-dementia-friendly-community .
Hung L, Hudson A, Gregorio M, Jackson L, Mann J, Horne N, Berndt A, Wallsworth C, Wong L, Phinney A. Creating dementia-friendly communities for social inclusion: a scoping review. Gerontol Geriatric Med. 2021;7:p23337214211013596.
Ogilvie K, And Eggleton A. Standing Senate Committee on Social Affairs, Science and Technology. Dementia in Canada: a national strategy for dementia-friendly communities; 2016.
Google Scholar
Hebert CA, Scales K. Dementia friendly initiatives: a state of the science review. Dementia. 2019;18(5):1858–95. https://doi.org/10.1177/1471301217731433 .
Webster D. Dementia-friendly communities Ontario: a Multi-sector collaboration to improve quality of life for people living with dementia and Care Partners Ontario. The Alzheimer Society of Ontario; 2016.
Grogan C. Doing dementia friendly communities locally: Tensions in committee practices and micro-processes. Diss. Queensland University of Technology; 2022.
Swaffer K. Dementia: stigma, language, and dementia-friendly. Dementia (London). 2014;13(6):709–16. https://doi.org/10.1177/1471301214548143 .
Rahman S, Swaffer K. Assets-based approaches and dementia-friendly communities. Dementia (London). 2018;17(2):131–7. https://doi.org/10.1177/1471301217751533 .
Shakespeare T, Zeilig H, Mittler P. Rights in mind: thinking differently about dementia and disability. Dement (London). 2019;18(3):1075–88. https://doi.org/10.1177/1471301217701506 .
Fazio S, Pace D, Flinner J, Kallmyer B. The fundamentals of person-centered care for individuals with dementia. The Gerontologist. 2018;58(Issue suppl_1):S10–9. https://doi.org/10.1093/geront/gnx122 .
Spector A, Orrell M. Using a biopsychosocial model of dementia as a tool to guide clinical practice. Int Psychogeriatr. 2010;22(6):957–65.
Miesen B. Attachment theory and dementia. Care-giving in Dementia. Routledge; 2014. pp. 38–56.
Kovach CR, Noonan PE, Schlidt AM, Wells T. A model of consequences of need-driven, dementia‐compromised behavior. J Nurs Scholarsh. 2005;37(2):134–40.
Thijssen M, Daniels R, Lexis M, Jansens R, Peeters J, Chadborn N, Nijhuis‐van der Sanden MW, Kuijer‐Siebelink W, Graff M. How do community based dementia friendly initiatives work for people with dementia and their caregivers, and why? A rapid realist review. Int J Geriatr Psychiatry. 2022;37(2).
Thijssen M, Graff MJ, Lexis MA, Nijhuis-van der Sanden MW, Radford K, Logan PA, Daniels R, Kuijer-Siebelink W. Collaboration for developing and sustaining community dementia-friendly initiatives: a realist evaluation. Int J Environ Res Public Health. 2023;20(5):4006.
Thijssen M, Kuijer-Siebelink W, Lexis MA, Nijhuis-Van Der Sanden MW, Daniels R, Graff M. What matters in development and sustainment of community dementia friendly initiatives and why? A realist multiple case study. BMC Public Health 2023 23(1):296.
Buckner S, Mattocks C, Rimmer M, Lafortune L. An evaluation tool for age-friendly and dementia friendly communities. Work Older People. 2018;22(1):48–58. https://doi.org/10.1108/WWOP-11-2017-0032 .
Shannon K, Bail K, Neville S. Dementia-friendly community initiatives: an integrative review. J Clin Nurs. 2019;28(11–12):2035–45.
Smith K, Gee S, Sharrock T, Croucher M. Developing a dementia-friendly Christchurch: Perspectives of people with dementia. Australas J Ageing. 2016;35(3):188–92.
Wu SM, Huang HL, Chiu YC, Tang LY, Yang PS, Hsu JL, Liu CL, Wang WS, Shyu YIL. Dementia-friendly community indicators from the perspectives of people living with dementia and dementia-family caregivers. J Adv Nurs. 2019;75(11):2878–9.
Darlington N, Arthur A, Woodward M, et al. A survey of the experience of living with dementia in a dementia-friendly community. Dementia. 2021;20(5):1711–22.
Lin SY. ‘Dementia-friendly communities’ and being dementia friendly in healthcare settings. Curr Opin Psychiatry. 2017;30(2):145.
Handley M, Bunn F, Goodman C. Dementia-friendly interventions to improve the care of people living with dementia admitted to hospitals: a realist review. BMJ open. 2017;7(7):e015257.
Singh NS, Kovacs RJ, Cassidy R, Kristensen SR, Borghi J, Brown GW. A realist review to assess for whom, under what conditions and how pay for performance programmes work in low-and middle-income countries. Soc Sci Med. 2021;270:113624.
Haynes A, Gilchrist H, Oliveira JS, Tiedemann A. Using realist evaluation to understand process outcomes in a COVID-19-impacted yoga intervention trial: a worked example. Int J Environ Res Public Health. 2021;18(17):p9065.
European Foundations on Dementia. Mapping Dementia- Friendly Communities Across Europe. 2016. [PDF] https://www.dataplan.info/img_upload/5c84ed46aa0abfec4ac40610dde11285/mapping_dfcs_across_europe_final_v2.pdf .
Craig S, Mitchell G, Halloran PO, et al. Exploring the experiences of people living with dementia in Dementia Friendly communities (dfcs) in Northern Ireland: a realist evaluation protocol. BMC Geriatr. 2023;23:361. https://doi.org/10.1186/s12877-023-04090-y .
Craig S, Wilson B, O’Halloran C. P., Mitchell G, Stark P. How do people with dementia and their caregivers experience Dementia Friendly communities (dfcs) and how are these sustained over time: a realist review. 2022.
Wong G, Greenhalgh T, Westhorp G, Et al. RAMESES publication standards: realist syntheses. BMC Med. 2013;11:21. https://doi.org/10.1186/1741-7015-11-21 .
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1suppl):21–34.
Covidence systematic review software. Veritas Health Innovation, Melbourne, Australia. 2022. Available at www.covidence.org .
The Joanna Briggs Institute. Critical appraisal tools. The Joanna Briggs Institute. 2017. Retrieved June 16, 2022, from https://jbi.global/critical-appraisal-tools .
Morton T, Wong G, Atkinson T, et al. Sustaining community-based interventions for people affected by dementia long term: the SCI-Dem realist review. BMJ Open. 2021;11:e047789. https://doi.org/10.1136/bmjopen-2020-047789 .
O’Halloran P, Scott D, Reid J, Porter S. Multimedia psychoeducational interventions to support patient self-care in degenerative conditions: a realist review. Palliat Support Care. 2015;13(5):1473–86. https://doi.org/10.1017/S1478951514001229 .
McGrath D, O’Halloran P, Prue G, Brown M, Millar J, O’Donnell A, McWilliams L, Murphy C, Hinds G, Reid J. Exercise interventions for women with ovarian cancer: a realist review. Healthcare. 2022;10(4):720.
Rycroft-Malone J, mccormack B, Hutchinson AM, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci. 2012;7:33. https://doi.org/10.1186/1748-5908-7-33 .
Kally Z, Cherry DL, Howland S, And Villarruel M. Asian Pacific Islander dementia care network: a model of care for underserved communities. J Gerontol Soc Work. 2014;57(6–7):710–27.
Tsuda S, Inagaki H, Okamura T, Sugiyama M, Ogawa M, Miyamae F, Edahiro A, Ura C, Sakuma N, Awata S. Promoting cultural change towards dementia friendly communities: a multi-level intervention in Japan. BMC Geriatr. 2022;22(1):1–13.
Phillipson L, Hall D, Cridland E, Fleming R, Brennan-Horley C, Guggisberg N, Frost D, Hasan H. Involvement of people with dementia in raising awareness and changing attitudes in a dementia friendly community pilot project. Dementia. 2019;18(7–8):2679–94.
Dean J, Silversides K, Crampton JA, Wrigley J. Evaluation of the York Dementia Friendly Communities Programme. York: Joseph Rowntree Foundation; 2015a.
Bergeron CD, Robinson MT, Willis FB, Albertie ML, Wainwright JD, Fudge MR, Parfitt FC, Lucas JA. Creating a dementia friendly community in an African American neighborhood: perspectives of people living with dementia, care partners, stakeholders, and community residents. J Appl Gerontol. 2023;42(2):280–9.
Heward M, Innes A, Cutler C, Hambidge S. Dementia-friendly communities: challenges and strategies for achieving stakeholder involvement. Health Soc Care Commun. 2017;25(3):858–67.
Goodman C, Arthur A, Buckner S, Buswell M, Darlington N, Dickinson A, Killett A, Lafortune L, Mathie E, Mayrhofer A, Reilly P, Skedgel C, Thurman J, Woodward M. The DEMCOM study: a national evaluation of Dementia Friendly communities. National Institute for Health Research Policy Research (NIHR); 2019. https://uhra.herts.ac.uk/handle/2299/23477 .
Marshall F, Basiri A, Riley M, et al. Scaling the Peaks Research Protocol: understanding the barriers and drivers to providing and using dementia-friendly community services in rural areas—a mixed methods study. BMJ Open. 2018;8:e020374. https://doi.org/10.1136/bmjopen-2017-020374 .
Gresham M, Taylor L, Keyes S, Wilkinson H, McIntosh D, Cunningham C. Developing evaluation of signage for people with dementia. Hous Care Support. 2019;22(3):153–61.
Quinn C, Hart N, Henderson C, Litherland R, Pickett J, Clare L. Developing supportive local communities: perspectives from people with dementia and caregivers participating in the IDEAL programme. J Aging Soc Policy. 2022;34(6):839–59.
Herron RV, Rosenberg MW. “Not there yet”: Examining community support from the perspective of people with dementia and their partners in care. Soc Sci Med. 2017;173:81–7.
Article CAS PubMed Google Scholar
Turner N, Cannon S. Aligning age-friendly and dementia‐ friendly communities in the UK. Working Older People. 2018;22(1):9–19. https://doi.org/10.1108/WWOP-12-2017-0036 .
Keating N, Eales J, Phillips JE. Age-friendly rural com‐ munities: conceptualizing ‘best‐fit’. Can J Aging/La Revue Canadienne Du Vieillissement. 2013;32(4):319–32. https://doi.org/10.1017/S0714980813000408 .
World Health Organization. WHO launches new toolkit to promote dementia inclusive societies [Internet]. 2021. Available from: https://www.who.int/news/item/06-08-2021-who-launches-new-toolkit-to-promote-dementia-inclusive-societies.
Williamson T. Mapping Dementia-Friendly Communities Across Europe. European Foundations’ Initiative on Dementia, Brussels. 2016. https://ec.europa.eu/eip/ageing/sites/eipaha/files/results_attachments/mapping_dfcs_across_europe_final.pdf .
Download references
Acknowledgements
Not applicable.
This research is fully funded by the Department for Education (DfE) in Northern Ireland.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Queen’s University Belfast, Belfast, Northern, Ireland
Stephanie Craig, Peter O’ Halloran, Gary Mitchell, Patrick Stark & Christine Brown Wilson
You can also search for this author in PubMed Google Scholar
Contributions
CBW, GM, POH, and PS are co-investigators and led on the design of the study. SC led the write-up of this manuscript, and all authors made comments and approved the final manuscript.
Corresponding author
Correspondence to Stephanie Craig .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Craig, S., Halloran, P.O., Mitchell, G. et al. Dementia Friendly communities (DFCs) to improve quality of life for people with dementia: a realist review. BMC Geriatr 24 , 776 (2024). https://doi.org/10.1186/s12877-024-05343-0
Download citation
Received : 19 February 2024
Accepted : 29 August 2024
Published : 20 September 2024
DOI : https://doi.org/10.1186/s12877-024-05343-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Realist review
- Realist synthesis
- Dementia-friendly communities
- Dementia friends
- Quality of Life
BMC Geriatrics
ISSN: 1471-2318
- General enquiries: [email protected]

COMMENTS
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179-187 ... Sears K, Klugar M, Tufanaru C, Leonardi-Bee J, Aromataris E, Munn Z. The revised JBI critical appraisal tool for the assessment of risk of bias for ...
Critical appraisal is not complete without a specific recommendation. Each of the phases is explained in more detail below. Phase 1: Rapid critical appraisal. Rapid critical appraisal involves using two tools that help clinicians determine if a research study is worthy of keeping in the body of evidence.
JBI Critical appraisal tools have been developed by the JBI and collaborators and approved by the JBI Scientific Committee following extensive peer review. Although designed for use in systematic reviews, JBI critical appraisal tools can also be used when creating Critically Appraised Topics (CAT), in journal clubs and as an educational tool.
Critical appraisal of published research: introductory guidelines. BMJ (Clinical research ed). 1991;302(6785):1136-1140. 4. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed). 2017;358 ...
JBI Critical Appraisal Tools All systematic reviews incorporate a process of critique or appraisal of the research evidence. The purpose of this appraisal is to assess the methodological quality of a study and to determine the extent to which a study has addressed the possibility of bias in its design, conduct and analysis. All papers
Tools for Critical Appraisal. Critical appraisal is the careful analysis of a study to assess trustworthiness, relevance and results of published research. Here are some tools to guide you. JBI Critical Appraisal. CASP Checklists. The AACODS checklist. Appraisal Resources - Grey Literature.
Critical appraisal forms part of the process of evidence-based practice. " Evidence-based practice across the health professions " outlines the fives steps of this process. Critical appraisal is step three: Critical appraisal is the examination of evidence to determine applicability to clinical practice. It considers (1):
Critical appraisal is the course of action for watchfully and systematically examining research to assess its reliability, value and relevance in order to direct professionals in their vital clinical decision making [1]. Critical appraisal is essential to: Continuing Professional Development (CPD).
Clarity on the types of research under scrutiny helps reviewers match suitable critical appraisal criteria and tools to the investigations they are assessing. Steps 2 and 3 warrant separation because different types of primary research are often included in a review, and investigators may need to use multiple critical appraisal criteria and tools.
This section contains useful tools and downloads for the critical appraisal of different types of medical evidence. Example appraisal sheets are provided together with several helpful examples. Critical Appraisal Worksheets. English. Systematic Reviews Critical Appraisal Sheet; Diagnostics Critical Appraisal Sheet; Prognosis Critical Appraisal ...
Critical appraisal. ' The process of carefully and systematically examining research to judge its trustworthiness, and its value and relevance in a particular context '. -Burls A [1] The objective of medical literature is to provide unbiased, accurate medical information, backed by robust scientific evidence that could aid and enhance ...
Critical Appraisal is the process of carefully and systematically examining research to judge its trustworthiness, and its value and relevance in a particular context. It is an essential skill for evidence-based medicine because it allows people to find and use research evidence reliably and efficiently. Learn more about what critical appraisal ...
Critical appraisal tools facilitate the appraisal process and guide a consumer of evidence through an objective, analytical, evaluation process. Reporting guidelines, checklists of items that should be included in a publication or report, ensure that the project or guidelines are reported on with clarity, completeness, and transparency. Purpose ...
In Brief. Figure. Critical appraisal is "the process of assessing and interpreting evidence by systematically considering its validity, results and relevance to an individual's work." 1 Nurses rank feeling incapable of assessing the quality of research as one of the greatest barriers to using research in practice. 2 Participation in a ...
Schondelmeyer A. C., Bettencourt A. P., Xiao R., Beidas R. S., Wolk C. B., Landrigan C. P., Brady P. W., Brent C. R., Parthasarathy P., Kern-Goldberger A. S., Sergay ...
The Infection Prevention and Control Guidelines Critical Appraisal Tool Kit was developed in response to needs for training in critical appraisal, assessing evidence from a wide variety of research designs, and a method for going from assessing individual studies to characterizing the strength of a body of evidence. Clinician researchers ...
Critical Appraisal. Critically appraising articles is vital to evaluating best practice for your population. There are many resources and checklists that can be used to critically appraise for clinical significance such as these Cochrane appraisal tools. Common questions to ask when critically appraising an article:
What are critical appraisal tools? Historically, critical appraisal tools were educational instruments used by clinicians and researchers to evaluate the quality of research papers. They have been adopted for use in systematic reviews and facilitate the assessment of a research study's limitations. One domain of critical appraisal involves ...
JBI Critical Appraisal Tools All systematic reviews incorporate a process of critique or appraisal of the research evidence. The purpose of this appraisal is to assess the methodological quality of a study and to determine the extent to which a study has addressed the possibility of bias in its design, conduct and analysis. All papers selected for
Critical Appraisal of Studies. Critical appraisal is the process of carefully and systematically examining research to judge its trustworthiness, and its value/relevance in a particular context by providing a framework to evaluate the research. During the critical appraisal process, researchers can: Decide whether studies have been undertaken ...
Qualitative research has an important place within evidence-based health care (EBHC), contributing to policy on patient safety and quality of care, supporting understanding of the impact of chronic illness, and explaining contextual factors surrounding the implementation of interventions. However, the question of whether, when and how to critically appraise qualitative research persists ...
Buccheri RK and Sharifi C (2017) Critical appraisal tools and reporting guidelines for evidence‐based practice, Worldviews on Evidence‐Based Nursing, 14 (6), pp. 463-472. View article. Connelly LM (2016) Trustworthiness in qualitative research. (Understanding research), MedSurg Nursing, 25 (6), pp.435-436.
Key Points. Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article. Critical appraisal provides a basis for decisions on whether to use the ...
INTRODUCTION. Critical appraisal of a research paper is defined as "The process of carefully and systematically examining research to judge its trustworthiness, value and relevance in a particular context."[] Since scientific literature is rapidly expanding with more than 12,000 articles being added to the MEDLINE database per week,[] critical appraisal is very important to distinguish ...
The methodological quality of the empirical evidence in each of the seven papers included in this review was critically appraised using Joanna Briggs Institute critical appraisal tools . Using the JBI tool, Goodman et al. was assessed as strong, two articles were accessed as moderate [51, 52] and four were accessed as weak [50, 53,54,55].