Genetic Testing: Advantages and Disadvantages Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
The issue of genetic testing is a highly controversial one, as its advantages and disadvantages present various dilemmas. It is still not clear if genetic testing should or should not become a common procedure that all people undergo regularly. I believe that it is an extremely personal decision to make. There are certain limitations and concerns that a diagnosed person can face, especially when they are diagnosed with untreatable and lethal disorders (Norrgard, 2008). Knowing about conditions like that may significantly decrease the quality of life and even lead to depression and anxiety.
At the same time, I acknowledge all the benefits that genetic testing can bring in terms of diagnosing a wide range of diseases and conditions. Fearing that they might discover hereditary predispositions to some untreatable diseases, many people choose not to get tested. However, I believe that deep inside, they still think about it and have concerns; I would if my family had a history of genetic conditions. That is why some people may even feel relieved when they undergo testing and have to face difficult results. At least they can know for sure that they are predisposed to certain conditions and focus on ways to improve their lives (Kurian et al., 2019). After all, genes are believed to be malleable; a positive approach, holistic nutritional program, and avoiding environmental toxins will not harm any person whose genetic testing results show a predisposition to certain diseases.
In the end, I do not think there is a universal answer to this question. Each person’s choice has to be authentic because they are the ones who will have to live their lives with this knowledge. I do believe, though, that scientific and health communities might focus more on raising awareness about genome sequencing, with particular reference to conditions that can be caught in the early stages, such as different types of cancer.
Kurian, A. W., Ward, K. C., Howlader, N., Deapen, D., Hamilton, A. S., Mariotto, A., Miller, D., Penberthy, L. S., & Katz, S. J. (2019). Genetic testing and results in a population-based cohort of breast cancer patients and ovarian cancer patients . Journal of Clinical Oncology , 37 (15), 1305-1315.
Norrgard, K. (2008). Genetic testing and family planning | Learn science at Scitable . Scitable.
- Discussion of Editing Human Embryos and Adults
- Should Cloning Be 100% Legal or Illegal?
- Next-Generation and Traditional Sequencing Methods
- Infectious Bacterial Identification From DNA Sequencing
- Whole-Genome Sequencing for Identification and Gene Function Prediction of Bacterial Genomes
- Genetic Modification and Cloning
- Gene Modification: Building Baby From the Genes Up
- "Ghost in the Genes" Video Review
- Editing the Genome of Human Embryos: Pros and Cons
- Down Syndrome: Congenital Heart Disease and Prenatal Testing
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, November 8). Genetic Testing: Advantages and Disadvantages. https://ivypanda.com/essays/genetic-testing-advantages-and-disadvantages/
"Genetic Testing: Advantages and Disadvantages." IvyPanda , 8 Nov. 2022, ivypanda.com/essays/genetic-testing-advantages-and-disadvantages/.
IvyPanda . (2022) 'Genetic Testing: Advantages and Disadvantages'. 8 November.
IvyPanda . 2022. "Genetic Testing: Advantages and Disadvantages." November 8, 2022. https://ivypanda.com/essays/genetic-testing-advantages-and-disadvantages/.
1. IvyPanda . "Genetic Testing: Advantages and Disadvantages." November 8, 2022. https://ivypanda.com/essays/genetic-testing-advantages-and-disadvantages/.
Bibliography
IvyPanda . "Genetic Testing: Advantages and Disadvantages." November 8, 2022. https://ivypanda.com/essays/genetic-testing-advantages-and-disadvantages/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
- Building for the Future
- Honors & Awards
- Our Global REACH
- Community Health Services
- Arts in Health
- Community Health Planning & Investment
- Life-Saving Donations
- Osher Lifelong Learning Institute (OLLI)
- Sponsorship
- House Officer & Faculty Programs
- Office for Health Equity and Inclusion
- Patient & Community Support
- Professional Development Training
- Students & Pathways
- Workforce Diversity
- Areas to Support
- Ways to Give
- Get Involved
- Fundraising Events
- Resources for Faculty and Staff
- About the Office of Development
- Medicine at Michigan
- Michigan Answers
- Michigan Medicine Podcast Network
- About Community Health Services
- Our Services
- Volunteer & Give
- Get Involved with Friends
- Apply for Funding
- About Housing Bureau for Seniors
- Make a Gift
- Programs and Services
- Senior Living Week
- About Immunization & Health Screening
- PMCH Services
- Regional Alliance for Healthy Schools
- About Volunteer Services
- Current Volunteers
- New Volunteers
- Pre-Approved Volunteers
- Returning Volunteers
- What Is Arts in Health
- Our Mission & History
- Our Team & Partners
- Exhibit or Perform
- Make Art Now
- Watch a Concert Now
- Permanent Art Collection
- Art Purchase
- Community Art
- Gallery Diagrams & Info
- Art Cart Posters
- Bedside Art Program
- Bedside Music Program
- Bedside Story Studio
- Coloring Books
- Comfort Legacy Kits
- Hamsa Hands
- Music Resources
- Nature Resources
- About the Life Sciences Orchestra
- Give to the Life Sciences Orchestra
- Join the Life Sciences Orchestra
- About Community Health Planning and Investment
- Community Health Investments
- Community Health Needs Assessment (CHNA)
- Community Outreach and Engagement Programs
- Donate Blood
- Share Your Story
- Become a Volunteer
- About Osher Lifelong Learning Institute
- Donate Now to OLLI
- OLLI Programs and Activities
- OLLI Volunteer Roles
- Frequently Asked Questions About Sponsorship
- Health Equity and Quality Scholars Program
- Anti-Racism Oversight Committee
- K-12 Programs
- Health Equity Leadership Program
- Health Equity Visiting Clerkship
- Leadership and Enrichment for Academic Diversity (LEAD)
- Undergraduate Programs
- DEI Mini Grants
- DEI Resource Groups
- Medical School Scholarships
- Rogel Cancer Center
- A. Alfred Taubman Medical Research Institute
- Alumni Class Giving
- Anesthesiology
- Ann Arbor Meals on Wheels
- Biological Chemistry
- Biomedical Engineering
- C.S. Mott Children's Hospital
- Cardiac Surgery
- Cell & Developmental Biology
- Chad Carr Pediatric Brain Tumor Center
- Computational Medicine & Bioinformatics
- Congenital Heart Center
- Dermatology
- Eisenberg Family Depression Center
- Elizabeth Weiser Caswell Diabetes Institute
- Emergency Medicine
- Family Medicine
- Fast Forward Medical Innovation
- Forbes Institute for Cancer Discovery
- Frankel Cardiovascular Center (CVC)
- Heinz C. Prechter Bipolar Research Program
- Human Genetics
- Institute for Healthcare Policy & Innovation
- Allergy and Clinical Immunology
- Pulmonary and Critical Care Medicine
- Rheumatology
- Gastroenterology/Hepatology
- General Medicine
- Genetic Medicine
- Geriatric and Palliative Medicine
- Infectious Diseases
- Hematology/Oncology
- Hospital Medicine
- Kellogg Eye Center
- Kresge Hearing Research Institute
- Learning Health Sciences
- Mary H. Weiser Food Allergy Center
- Medical School Student Programs
- Michigan Alzheimer's Disease Center
- Michigan Neuroscience Institute
- Molecular & Integrative Physiology
- Neuroscience Graduate Program
- Neurosurgery
- Obstetrics & Gynecology
- Office of Graduate and Postdoctoral Studies
- Ophthalmology and Visual Sciences
- Orthopaedic Surgery
- Otolaryngology-Head and Neck Surgery
- Pharmacology
- Physical Medicine & Rehabilitation
- Radiation Oncology
- Ronald Weiser Center for Prostate Cancer
- Social Work
- Transplant Center
- Von Voigtlander Women's Hospital
- Annual & Recurring Gifts
- Corporate and Foundation Gifts
- Endowments that Empower
- Estate & Planned Gifts
- In-Kind Gifts
- Memorial or Tribute Gifts
- Sponsorship Opportunities
- Storytellers
- Sponsorship and Ticket Info
- Sponsorships & Foursomes
- 2024 Sponsors
- Sponsorships & Tickets
- Committee Members
- Sponsorship Levels
- Contact Information
- Alumni Stories
- Faculty Stories
- Featured Stories
- Student Stories
- Past Issues
- Share Your Michigan Answer
- Breaking Down Mental Health
- Health Lab Podcast
- Michigan Medicine Presents
- Michigan Medicine Surgery Sessions
- Minding Memory
- Clips for Broadcast Media
- Contact the Media Team
- Patient Privacy and HIPAA
- Research News
Genetic testing, when appropriate, is a powerful tool to gauge a patient’s risk for disease. A Michigan Medicine genetic counselor explains the process.
December 8, 2017 7:00 AM
Author | Kevin Joy

On the surface, the concept seems like a no-brainer: A sample of blood or saliva can offer clues to your body's genetic defects, a road map to predicting future problems ranging from Alzheimer's disease to cancer.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
But put into practice, genetic testing is more nuanced.
The results, after all, might not be what patients want to hear — especially because they could reveal an inherited mutation that puts themselves or their kids at risk. And since each parent contributes 50 percent to a child's DNA, two siblings may have different test results.
"The science is easy to process; the emotional component is not," says Rajani Aatre, M.S., M.Sc., a genetic counselor at the University of Michigan Frankel Cardiovascular Center .
"Let's say you find out your kid got something because you passed it down. No matter how much you intellectualize it, you can't ever discount that the feeling of responsibility or guilt won't affect you."
Still, she says, there is power in knowledge: It allows recipients to be proactive about their own health — and to help determine if other family members are at risk.
And as awareness of genetic mutations grows , testing mechanisms have become quicker, cheaper and more precise.
"It's just exploded," says Aatre. "The kind of tests we have today weren't even possible 20 years ago."
But the decision to get a test, she notes, shouldn't be made lightly. It's why most people first need a recommendation from their primary care physician.
They'll also meet with a certified genetic counselor to explain the process and the many considerations that come with getting the detailed analysis.
"Most people, once they've understood that, want to do it," says Aatre, who explained some of the pros and cons of genetic testing she discusses with patients:

Pros of genetic testing
It offers insight: With genetic testing, "we're targeting the coding part of the gene that is relevant to your particular disease," Aatre says. That, she notes, involves reading a DNA sequence from start to finish to see if there are any "interruptions/disruptions" — mutations associated with the disease in question — that stop the gene from making normal proteins.
Uncertainty is lessened: Worried about a future ailment? Knowing that a particular mutation is absent can help people ease anxiety about their own health and that of their children. "A big part of genetic testing is trying to determine who else in the family is at risk ," Aatre says. "But you're also providing reassurance."
SEE ALSO: Collecting a Family's Cancer History: What You Should Ask
You can take action: A clearer portrait of risk can guide medical care. "Certain genes are associated with more severe diseases," Aatre says. "Some genes respond to certain medications and treatments better." That, depending on circumstance, might lead to additional diagnostic testing or monitoring, healthful lifestyle shifts or getting family members tested.
Discrimination is (mostly) protected: Genetic testing results will appear on your medical record. That's why several anti-discrimination laws protect recipients, notably the Genetic Information Nondiscrimination Act of 2008, which prohibits employers using that data to hire, fire or promote and health insurance companies from using it as a pre-existing condition. Notable exceptions: Disability, life and long-term care insurance could be affected.

Cons of genetic testing
Not everyone is eligible: To get tested, a loved one must already have been affected by a disease or disorder — and been genetically tested, too. The reason? "You need to know what to go after," Aatre says. Everyone's body has seven to 10 nonworking/altered genes, she notes, so family and clinical history must dictate when and where to focus attention (and avoid unnecessary anxiety).
SEE ALSO: Should Young People Get a Colon Cancer Screening? It Depends on Their Risk
It isn't a full-body review: Testing is targeted: "When someone walks in my door, I'm not going to screen them for everything on the planet," Aatre says. "Without clear markers, you're opening Pandora's box." A patient whose parent was tested for a genetic heart condition , for example, wouldn't be a candidate for BRCA 1 or 2 testing to determine breast cancer risk.
Testing can be costly: The price of genetic testing ranges from a few hundred dollars to several thousand dollars. "They're cheaper than they used to be but are still very expensive," Aatre says. Still, insurance typically covers such tests for newborns and expectant mothers, as well as patients with a documented personal or family history or a physician's recommendation.
Results may trigger emotions: Finding out that a gene mutation is absent can offer a deep sense of relief. And others who find out that they are carriers can take comfort in having more control. Still, says Aatre: "This crystal ball, all of a sudden, can pop in front of you." That may spark deep feelings of guilt (regardless of findings) or difficult decisions.
For more information or to make an appointment for genetic counseling or testing at the Frankel Cardiovascular Center, call 888-287-1082 .

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
[email protected]
734-764-2220
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!

We transform lives through bold discovery, compassionate care and innovative education.
- Diversity, Equity & Inclusion
- News & Stories
- Find a Doctor
- Conditions & Treatments
- Patient & Visitor Guide
- Patient Portal
- Clinical Trials
- Research Labs
- Research Centers
- Cores and Resources
- Programs & Admissions
- Our Community
- Departments, Centers & Offices
- About the Medical School
Global Footer Secondary Navigation
- Branches of Biology
- Importance of Biology
- Domain Archaea
- Domain Eukarya
- Biological Organization
- Biological Species Concept
- Biological Weathering
- Cellular Organization
- Cellular Respiration
- Types of Plants
- Plant Cells Vs. Animal Cells
- Prokaryotic Cells Vs. Eukaryotic Cells
- Amphibians Vs. Reptiles
- Anatomy Vs. Physiology
- Diffusion vs. Osmosis
- Mitosis Vs. Meiosis
- Chromosome Vs. Chromatid
- History of Biology
- Biology News

- Pros and Cons
12 Pros and Cons of Genetic Testing

- shares
Pros and Cons of Genetic Testing : The human body is composed of millions of cells , which are considered as the “basic units of life”. Inside each cell lies the genetic material or the DNA (Deoxyribonucleic Acid).
Short sections of DNA are called together as the gene. The gene is also dubbed as the “basic unit of heredity” as it contains the information and instructions that dictate how the body should develop and function. Also, the gene is important in the expression of inheritable characters and traits.

- TOP-SELLING CONSUMER DNA TEST: From your origins in over 2,600 global regions to the most connections to living relatives, no other DNA test kit delivers an experience as unique and interactive as AncestryDNA
Previously we’ve seen disadvantages of genetically modified foods and genetic engineering pros & cons . In this article, we’ll explore the pros and cons of genetic testing .
What Is Actually Genetic Testing?
Genetic testing is a type of health program that involves the identification of any changes in genes, chromosomes , and proteins .
Do you have a family history of acquiring a specific disease? Or are you planning to have a child but afraid that he/she might inherit a trait you wouldn’t want to? Genetic testing is the solution to all of these questions. The results of a genetic test confirm and eliminate the possibility of any suspected genetic disorder. Such results will be highly advantageous for the early treatment and prevention of diseases.
How Is Genetic Testing Done?

There are a lot of types of genetic testing depending on what you want to test. Genetic testing can range from biochemical tests, molecular approach, or simply family history questionnaires. To perform a genetic test, a tissue from any organ that usually develops during pregnancy can be obtained. Examples of such are the placenta, amniotic fluid (pregnant woman’s water), bone marrow, or blood .
Pros and Cons of Genetic Testing
Now we will explore the pros and cons of genetic testing. First, let’s focus on pros.
Advantages of Genetic Testing
There are a lot of potential advantages which can arise as a result of genetic testing. The following are some of them.
1. Early prevention and treatment of disease

As with any disease, early diagnosis of the disease will greatly help in faster treatment. The results of genetic testing can also help your healthcare provider in predicting the likelihood and deciding about the management of the disorder. In addition, the results of the test can also help one to learn more about the genetic disease and how it may possibly affect them and their relatives as well.
2. Peace of mind

For some people, finding out that they do not have the gene for a certain disease can become a blessing. They may feel a lot more peace because of the fact that they have not passed any gene abnormality to their children. In addition, because they no longer require the same type of medical treatment as with people who have the gene, the resources can be allotted to those who have the risk of having the disease.
3. Can determine parenthood

Genetic tests can be helpful in establishing evidence for the parenthood of a person for a case like child custody and support. The results of genetic test can also be used as a support for placing a parent’s name on the birth certificate of a child. Depending upon the country/state where you live in, DNA testing can be ordered by the judge for settling disputes in child custody laws.
4. The results can aid decisions in the future

For instance, if there is a low probability of passing a certain unwanted genetic condition, couples can have be assured that they can have children free of the disorder. On the other hand, a positive result may give the couple an idea of deciding not to have children because doing so may result to a high risk of their child developing the condition.
5. Can examine developmental delays in children

Like how it can determine parenthood, being genetically tested can be helpful is determining and interpreting developmental delays in children. Reasons for significant lags in physical, mental, and emotional growth can be determined.
Also if a woman has two or more miscarriages or pregnancy over age 34, genetic testing will be helpful for early diagnosis which can help identify the appropriate treatment options.
Disadvantages & Limitations of Genetic Testing
While the process has great advantages, indeed, several disadvantages that a person who wishes to undergo testing should be aware of. The following are some of them.
1. Physical risks

The physical risks associated with most genetic tests are indeed very small as some tests only require mere blood or tissue samples. However, some tests can be really destructive. As an example, the methods for prenatal testing involves the acquisition of amniotic fluid around the fetus. Such practice can be really dangerous because the mother may suffer from miscarriage.
2. May cause emotional and psychological stress

As alluded to earlier, the results of genetic testing can provide freedom from any uncertainty. However, in some cases, the results of genetic testing may create an emotional trauma for the person who finds out that he/she has a certain disease. It can lead to an increased anxiety to the individual as he might blame himself for possessing a gene that causes the disorder and potentially passing it onto their children.
3. May cause tension among family members
About this, the results of these tests may also create tension among family members when information about a family member is revealed. Having a negative test can cause emotional distress because it gives him/her the feeling of “survivor guilt” from being unaffected by the disease while his/her sibling is at risk.
4. Genetic discrimination may happen

Genetic discrimination is the condition wherein a person feels and gets discriminated due to the fact that he/she possesses a genetic abnormality that increases the chances of him/her developing a certain genetic disorder. And because the results of genetic tests are included in a person’s medical history, the fact that he/she has this abnormality becomes known to employers and other people in the workplace. As a result, people may treat him/her differently.
5. The information is very limited

While it is true that some tests can be very specific about the genetic disorder, these test often cannot tell the severity of the manifestation of the disease. Also, a negative result may not be conclusive because it is not possible for a single test to identify all the genetic changes and abnormalities in a certain disorder. Because of this, additional tests may be necessary. Another thing is that while most genetic disorders can be easily diagnosed using these tests, there are still potentially millions of genetic mutations which are still not understood. Furthermore, treatment strategies are still lacking.
6. Gene products (from tissue samples) are unstable

For instance, one disadvantage of using biochemical test as a genetic test is that proteins from the tissue samples are more unstable that the gene itself. Easy deterioration of samples means a higher chances of inaccuracy in the results. Therefore, they should be properly stored and analyzed immediately after obtaining.
7. Tests can be costly

Basically, the price of having genetic test will depend on various factors including the type of test and the clinic you visit. According to the National Human Genome Research Institute , the average cost of genetic testing in the US can range from less than $100 to $2,000! And as mentioned above, a single test may not be able to determine all genetic abnormalities so additional tests may be advised. The expensive price of genetic testing is only suitable for a small groups of patients because only those who can afford it can be tested.
The Accuracy of Genetic Testing
It is important to note that not all tests have the same predictability. The accuracy of any result would be, of course, depend on whether the disorder is caused by an abnormality of the gene and chromosome or just a mere result of acquisition from the environment.
What’s Next?
According to a study by the Harvard School of Public Health , a large majority of Americans are not into adopting this kind of genetic technology. In fact, only 6 percent of adults said that they had undergone genetic testing. While genetic testing is not compulsory, just like any medical intervention, this technique aims to do good than to harm.
However, some consequences of the process are inevitable. Therefore, to avoid such complications, it is vital to have counseling before and after genetic testing. In this way, individuals are free to choose whether they want to or don’t want to undergo testing. And if needed, they could have extra support.
So if you’re planning to be genetically tested, you might want to ponder this question: Is having genetic testing a mere trend that offers unproven hope, or does it represent the first sign of treatment for affected patients? What do you think?
Cite This Page
Related articles more from author.

Top 10 Genetics News of 2020

Top 10 BEST Genetics Discoveries of 2019
Top 12 Best Genetics Textbooks

Top 25 Most Recent Genetic Discoveries in 2018

Top 20 Biomass Energy Pros and Cons

Top 34 Gene Therapy Pros and Cons
great sight
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.
By using this form you agree with the storage and handling of your data by this website. *
Recent Posts

Top 25 Colorful Tulips: A Rainbow in Your Garden

The Top 25 Bicolor Flowers: Nature’s Two-Toned Wonders

Top 18 Amazon Rainforest Plants

Top 26 Best Hawaiian Flowers

25 Must-See Colorful Orchids

What Do Peacocks Eat?
- Privacy Policy
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
- What are the benefits of genetic testing?
Genetic testing has potential benefits whether the results are positive or negative for a gene mutation. Test results can provide a sense of relief from uncertainty and help people make informed decisions about managing their health care. For example, a negative result can eliminate the need for unnecessary checkups and screening tests in some cases. A positive result can direct a person toward available prevention, monitoring, and treatment options. Some test results can also help people make decisions about having children. Newborn screening can identify genetic disorders early in life so treatment can be started as early as possible.
Topics in the Genetic Testing chapter
- What is genetic testing?
- What are the different types of genetic tests?
- What are the uses of genetic testing?
- How is genetic testing done?
- What is informed consent?
- How can I be sure a genetic test is valid and useful?
- What do the results of genetic tests mean?
- What is the cost of genetic testing, and how long does it take to get the results?
- Will health insurance cover the costs of genetic testing?
- What are the risks and limitations of genetic testing?
- What is genetic discrimination?
- Can genes be patented?
- How are genetic screening tests different from genetic diagnostic tests?
- How does genetic testing in a research setting differ from clinical genetic testing?
- What are whole exome sequencing and whole genome sequencing?
- What are secondary findings from genetic testing?
- What is noninvasive prenatal testing (NIPT) and what disorders can it screen for?
- What is circulating tumor DNA and how is it used to diagnose and manage cancer?
Other chapters in Help Me Understand Genetics

Genetics Home Reference has merged with MedlinePlus. Genetics Home Reference content now can be found in the "Genetics" section of MedlinePlus. Learn more
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
- Patient Care & Health Information
- Tests & Procedures
- Genetic testing
Genetic testing involves examining your DNA, the chemical database that carries instructions for your body's functions. Genetic testing can reveal changes (mutations) in your genes that may cause illness or disease.
Although genetic testing can provide important information for diagnosing, treating and preventing illness, there are limitations. For example, if you're a healthy person, a positive result from genetic testing doesn't always mean you will develop a disease. On the other hand, in some situations, a negative result doesn't guarantee that you won't have a certain disorder.
Talking to your doctor, a medical geneticist or a genetic counselor about what you will do with the results is an important step in the process of genetic testing.
Genome sequencing
When genetic testing doesn't lead to a diagnosis but a genetic cause is still suspected, some facilities offer genome sequencing — a process for analyzing a sample of DNA taken from your blood.
Everyone has a unique genome, made up of the DNA in all of a person's genes. This complex testing can help identify genetic variants that may relate to your health. This testing is usually limited to just looking at the protein-encoding parts of DNA called the exome.
Products & Services
- A Book: Mayo Clinic Family Health Book
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Genetic testing plays a vital role in determining the risk of developing certain diseases as well as screening and sometimes medical treatment. Different types of genetic testing are done for different reasons:
- Diagnostic testing. If you have symptoms of a disease that may be caused by genetic changes, sometimes called mutated genes, genetic testing can reveal if you have the suspected disorder. For example, genetic testing may be used to confirm a diagnosis of cystic fibrosis or Huntington's disease.
- Presymptomatic and predictive testing. If you have a family history of a genetic condition, getting genetic testing before you have symptoms may show if you're at risk of developing that condition. For example, this type of test may be useful for identifying your risk of certain types of colorectal cancer.
- Carrier testing. If you have a family history of a genetic disorder — such as sickle cell anemia or cystic fibrosis — or you're in an ethnic group that has a high risk of a specific genetic disorder, you may choose to have genetic testing before having children. An expanded carrier screening test can detect genes associated with a wide variety of genetic diseases and mutations and can identify if you and your partner are carriers for the same conditions.
- Pharmacogenetics. If you have a particular health condition or disease, this type of genetic testing may help determine what medication and dosage will be most effective and beneficial for you.
- Prenatal testing. If you're pregnant, tests can detect some types of abnormalities in your baby's genes. Down syndrome and trisomy 18 syndrome are two genetic disorders that are often screened for as part of prenatal genetic testing. Traditionally this is done looking at markers in blood or by invasive testing such as amniocentesis. Newer testing called cell-free DNA testing looks at a baby's DNA via a blood test done on the mother.
- Newborn screening. This is the most common type of genetic testing. In the United States, all states require that newborns be tested for certain genetic and metabolic abnormalities that cause specific conditions. This type of genetic testing is important because if results show there's a disorder such as congenital hypothyroidism, sickle cell disease or phenylketonuria (PKU), care and treatment can begin right away.
- Preimplantation testing. Also called preimplantation genetic diagnosis, this test may be used when you attempt to conceive a child through in vitro fertilization. The embryos are screened for genetic abnormalities. Embryos without abnormalities are implanted in the uterus in hopes of achieving pregnancy
More Information
Genetic testing care at Mayo Clinic
- Angelman syndrome
- Atypical genitalia
- Brugada syndrome
- Cavernous malformations
- Cerebral palsy
- Charcot-Marie-Tooth disease
- Choroid plexus carcinoma
- Colon polyps
- Congenital adrenal hyperplasia
- Craniosynostosis
- Cystic fibrosis
- Diabetes insipidus
- DiGeorge syndrome (22q11.2 deletion syndrome)
- Dilated cardiomyopathy
- Down syndrome
- Ehlers-Danlos syndrome
- Epidermolysis bullosa
- Factor V Leiden
- Gaucher disease
- Hemochromatosis
- Huntington's disease
- Hypertrophic cardiomyopathy
- Infertility
- Klinefelter syndrome
- Long QT syndrome
- Low sperm count
- Lynch syndrome
- Male infertility
- Marfan syndrome
- Muscular dystrophy
- Myelofibrosis
- Noonan syndrome
- Paraganglioma
- Phenylketonuria (PKU)
- Pheochromocytoma
- Polycythemia vera
- Prader-Willi syndrome
- Pulmonary hypertension
- Rett syndrome
- Schwannomatosis
- Thalassemia
- Thoracic aortic aneurysm
- Triple X syndrome
- Turner syndrome
- Wilson's disease
Generally genetic tests have little physical risk. Blood and cheek swab tests have almost no risk. However, prenatal testing such as amniocentesis or chorionic villus sampling has a small risk of pregnancy loss (miscarriage).
Genetic testing can have emotional, social and financial risks as well. Discuss all risks and benefits of genetic testing with your doctor, a medical geneticist or a genetic counselor before you have a genetic test.
How you prepare
Before you have genetic testing, gather as much information as you can about your family's medical history. Then, talk with your doctor or a genetic counselor about your personal and family medical history to better understand your risk. Ask questions and discuss any concerns about genetic testing at that meeting. Also, talk about your options, depending on the test results.
If you're being tested for a genetic disorder that runs in families, you may want to consider discussing your decision to have genetic testing with your family. Having these conversations before testing can give you a sense of how your family might respond to your test results and how it may affect them.
Not all health insurance policies pay for genetic testing. So, before you have a genetic test, check with your insurance provider to see what will be covered.
In the United States, the federal Genetic Information Nondiscrimination Act of 2008 (GINA) helps prevent health insurers or employers from discriminating against you based on test results. Under GINA, employment discrimination based on genetic risk also is illegal. However, this act does not cover life, long-term care or disability insurance. Most states offer additional protection.
What you can expect
Depending on the type of test, a sample of your blood, skin, amniotic fluid or other tissue will be collected and sent to a lab for analysis.
- Blood sample. A member of your health care team takes the sample by inserting a needle into a vein in your arm. For newborn screening tests, a blood sample is taken by pricking your baby's heel.
- Cheek swab. For some tests, a swab sample from the inside of your cheek is collected for genetic testing.
- Amniocentesis. In this prenatal genetic test, your doctor inserts a thin, hollow needle through your abdominal wall and into your uterus to collect a small amount of amniotic fluid for testing.
- Chorionic villus sampling. For this prenatal genetic test, your doctor takes a tissue sample from the placenta. Depending on your situation, the sample may be taken with a tube (catheter) through your cervix or through your abdominal wall and uterus using a thin needle.
The amount of time it takes for you to receive your genetic test results depends on the type of test and your health care facility. Talk to your doctor, medical geneticist or genetic counselor before the test about when you can expect the results and have a discussion about them.
Positive results
If the genetic test result is positive, that means the genetic change that was being tested for was detected. The steps you take after you receive a positive result will depend on the reason you had genetic testing.
If the purpose is to:
- Diagnose a specific disease or condition, a positive result will help you and your doctor determine the right treatment and management plan.
- Find out if you are carrying a gene that could cause disease in your child, and the test is positive, your doctor, medical geneticist or a genetic counselor can help you determine your child's risk of actually developing the disease. The test results can also provide information to consider as you and your partner make family planning decisions.
- Determine if you might develop a certain disease, a positive test doesn't necessarily mean you'll get that disorder. For example, having a breast cancer gene ( BRCA1 or BRCA2 ) means you're at high risk of developing breast cancer at some point in your life, but it doesn't indicate with certainty that you'll get breast cancer. However, with some conditions, such as Huntington's disease, having the altered gene does indicate that the disease will eventually develop.
Talk to your doctor about what a positive result means for you. In some cases, you can make lifestyle changes that may reduce your risk of developing a disease, even if you have a gene that makes you more susceptible to a disorder. Results may also help you make choices related to treatment, family planning, careers and insurance coverage.
In addition, you may choose to participate in research or registries related to your genetic disorder or condition. These options may help you stay updated with new developments in prevention or treatment.
Negative results
A negative result means a mutated gene was not detected by the test, which can be reassuring, but it's not a 100 percent guarantee that you don't have the disorder. The accuracy of genetic tests to detect mutated genes varies, depending on the condition being tested for and whether or not the gene mutation was previously identified in a family member.
Even if you don't have the mutated gene, that doesn't necessarily mean you'll never get the disease. For example, the majority of people who develop breast cancer don't have a breast cancer gene ( BRCA1 or BRCA2 ). Also, genetic testing may not be able to detect all genetic defects.
Inconclusive results
In some cases, a genetic test may not provide helpful information about the gene in question. Everyone has variations in the way genes appear, and often these variations don't affect your health. But sometimes it can be difficult to distinguish between a disease-causing gene and a harmless gene variation. These changes are called variants of uncertain significance. In these situations, follow-up testing or periodic reviews of the gene over time may be necessary.
Genetic counseling
No matter what the results of your genetic testing, talk with your doctor, medical geneticist or genetic counselor about questions or concerns you may have. This will help you understand what the results mean for you and your family.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- National Library of Medicine. Help me understand genetics. Genetics Home Reference. https://ghr.nlm.nih.gov/primer. Accessed Feb. 13, 2017.
- Frequently asked questions about genetic testing. National Human Genome Research Institute. https://www.genome.gov/19516567/faq-about-genetic-testing/. Accessed Feb. 13, 2017.
- Genetic testing for hereditary cancer syndromes. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/genetics/genetic-testing-fact-sheet. Accessed Feb. 13, 2017.
- Raby BA, et al. Genetic testing. http://www.uptodate.com/home. Accessed Feb. 13, 2017.
- Grody WW, et al. ACMG position statement on prenatal/preconception expanded carrier screening. Genetics in Medicine. 2013;15:482.
- Genetic testing. American Medical Association. https://www.ama-assn.org/content/genetic-testing. Accessed Feb. 13, 2017.
- Frequently asked questions. Prenatal genetic diagnostic tests. FAQ164. Pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/-/media/For-Patients/faq164.pdf?dmc=1&ts=20161216T1208042192. Accessed Feb. 13, 2017.
- Breast cancer risk factors you cannot change. American Cancer Society. https://www.cancer.org/cancer/breast-cancer/risk-and-prevention/breast-cancer-risk-factors-you-cannot-change.html. Accessed Feb. 21, 2017.
- Atwal PS (expert opinion). Mayo Clinic, Jacksonville, Fla. Feb. 24, 2017.
- Genetic Testing for Breast Cancer
- Genetics and Cardiomyopathy
- Male hypogonadism
- Mapping the Genome
- Pregnancy after miscarriage
- Primary progressive aphasia
News from Mayo Clinic
- To combat heart disease and cancer, genomics researcher looks abroad Sept. 17, 2024, 02:00 p.m. CDT
- Mayo pioneers population science to advance personalized medicine Aug. 14, 2024, 02:30 p.m. CDT
- Tomorrow's Cure: How a lifetime of exposures impact health - exposome explained July 03, 2024, 12:21 p.m. CDT
- A Scientific Statement from the American Heart Association June 21, 2024, 02:40 p.m. CDT
- RegenBio Summit: Could a molecular scissors heal disease? June 17, 2024, 01:31 p.m. CDT
- New Mayo Clinic technology helps solve the unsolvable in rare disease diagnoses June 05, 2024, 11:00 a.m. CDT
- Mayo's new 'omics' strategy leaps into the future May 09, 2024, 12:40 p.m. CDT
- Genomics study enrolls 100,000 participants March 07, 2024, 03:30 p.m. CDT
- Comprehensive testing helps diagnose and manage rare genetic disorder Feb. 25, 2024, 12:00 p.m. CDT
- A silent tumor, precancerous polyps and the power of genetic screening Feb. 11, 2024, 12:00 p.m. CDT
- Understanding triple-negative breast cancer and its treatment Jan. 04, 2024, 04:00 p.m. CDT
- Mayo Clinic's DNA study reveals BRCA1 mutations in 3 sisters, prompts life-changing decisions Nov. 04, 2023, 11:00 a.m. CDT
- Beyond BRCA1/2: Pinpointing the risk of inherited breast cancer genes Oct. 28, 2023, 11:00 a.m. CDT
- Mayo Clinic and Oxford Nanopore announce collaboration to advance precision medicine for cancer and genetic disorders Oct. 19, 2023, 02:07 p.m. CDT
- Mayo Clinic Q and A: Understanding carrier screening for family planning Oct. 17, 2023, 02:40 p.m. CDT
- Mayo Clinic study sheds light on rare genetic disorder and blood cancers Oct. 11, 2023, 04:30 p.m. CDT
- New Mayo Clinic individualized medicine leader on a quest to bring cutting-edge medicine to all Sept. 23, 2023, 11:00 a.m. CDT
- Mayo Clinic cancer researchers targeting racial disparities in genomic data Sept. 02, 2023, 11:00 a.m. CDT
- Science Saturday: Mayo Clinic researchers use new innovative technology to diagnose teen brothers with ultra-rare genetic disorder Aug. 19, 2023, 11:00 a.m. CDT
- Science Saturday: A novel testing approach for newly identified VEXAS syndrome July 08, 2023, 11:00 a.m. CDT
- Mayo Clinic uses genomic testing broadly for rare diseases, improves patient care June 26, 2023, 09:02 p.m. CDT
- Science Saturday: Mayo Clinic doctor visits of the future could be powered by 'omics' research May 27, 2023, 11:00 a.m. CDT
- Researchers test DNA editing, recommend steps to improve accuracy May 02, 2023, 03:00 p.m. CDT
- Mayo Clinic in a new era of discoveries with rapid genome sequencing April 25, 2023, 03:00 p.m. CDT
- Science Saturday: A big step forward, bringing DNA sequencing data to routine patient care April 08, 2023, 11:00 a.m. CDT
- 9 common questions about genetic testing for cancer Feb. 06, 2023, 03:00 p.m. CDT
- Science Saturday: Mayo researchers streamline genetic testing in heart failure clinic, improve clinical care Jan. 28, 2023, 12:00 p.m. CDT
- Identifying inherited gene mutations in pancreatic cancer can lead to targeted therapies, better survival Nov. 24, 2022, 03:30 p.m. CDT
- Gather your family health history this Thanksgiving; it could save your life Nov. 22, 2022, 03:30 p.m. CDT
- Mayo Clinic Q and A: Genetic counseling after cancer diagnosis Nov. 14, 2022, 01:37 p.m. CDT
- A rare genetic cause for a common medical condition Nov. 09, 2022, 04:12 p.m. CDT
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
- Genetic Counseling and Hypertension Risks Words: 831
- Genetic Testing and Privacy & Discrimination Issues Words: 2476
- Advantages and Disadvantages of Genetic Testing Words: 617
- Genetic Testing, Its Background and Policy Issues Words: 1106
- The Importance of Heredity and Genetics Words: 547
- Link Between Obesity and Genetics Words: 2806
- Eugenics, Human Genetics and Their Societal Impact Words: 1668
- Genetic Technologies in the Healthcare Words: 592
- Genetic Diseases: Hemophilia Words: 1493
- The Potential Benefits of Genetic Engineering Words: 1091
Genetic Tests: Pros and Cons
Technological advancements enable people to access high-quality healthcare services and a larger bulk of data related to their health status. One of the recent innovations that are seen as revolutionary became the democratization of genetic testing. This kind of service was once associated with diverse restrictions but is now available to millions of people (Topol, 2016). Topol (2016) also notes that it was highly popularized in the 2000s when Angelina Jolie underwent the procedure that resulted in a media campaign. The celebrity spoke openly about her health status and the steps she underwent to ensure a high quality of life in the future. Clearly, genetic testing can help in identifying serious health issues or potential hazards, but it is critical to consider certain downsides of the procedure as well.
The major benefit of having a genetic test implemented is rather obvious and is related to accessing data regarding one’s health conditions. A patient can learn about some hereditary disorders that can pose a threat to their health (Topol, 2016). For instance, if there is a family history of cancer, the chances of having this chronic disease are rather high. Many people want to know for sure whether they are prone to developing cancer when their relatives are diagnosed with this health issue. Such was the case with Angelina Jolie, whose mother died after a long struggle. An obvious benefit of the procedure can be a clear and detailed description of a person’s health prospects that can be the ground for the development of an effective prevention plan (Grifantini, 2017). A person can access qualified care and receive a well-developed plan with the description of the necessary lifestyle changes to reduce the chances of developing the illness. As mentioned above, the procedure is now rather affordable, and people can have it even without any consultations with their physicians.
However, it is essential to consider the dark side of the matter before having a genetic test conducted. First, although the advancements in this kind of testing are remarkable, there is still a lack of qualified personnel who can properly interpret the results of genetic tests (Grifantini, 2017). Moreover, some errors are possible due to imperfections in equipment or procedures. Thus, a patient risks receiving erroneous results that can lead to wrong diagnoses and treatment plans. Mental health is another area to pay attention to when considering the relevance of genetic testing. People may develop depressive symptoms or other mental health issues when they learned about the health issues they have. A story about another Hollywood celebrity is well-known as well. After receiving screening results, Robin Williams committed suicide while the results turned out to be erroneous (Phillips, 2016). The celebrity was desperate and had to endure tremendous psychological load. Likewise, the person may feel devastated and develop numerous serious health issues after learning about the possibility of having some disorder.
It is also necessary to add that the possibility of having a disorder does not mean developing this disease (Grifantini, 2017). Moreover, comorbidity of illnesses is often considerable, and the prevention plan developed by a physician can contribute to the development of other health problems. Finally, Grifantini (2017) emphasizes that data confidentiality is one of the major vulnerabilities associated with genetic testing as laboratories often provide patient data to third parties.
In conclusion, it is necessary to note that genetic testing can be a good choice if a person understands related benefits and hazards. It is pivotal to address highly qualified medical staff and facilities with the corresponding reputation. The patient should receive all the details and have additional tests if necessary. People are willing to know more about their own bodies, but some are not ready for such knowledge. Finally, genetic testing is still undergoing transformations and further improvements, so it may be safer to avoid such procedures under certain circumstances.
Grifantini, K. (2017). What’s happening to your DNA data?: Genetic testing services abound, but consumers opting to use them should be aware of the pitfalls . IEEE Pulse, 8 (6), 10-14.
Phillips, K. (2016). ‘ The hardest role of his life’: Widow describes disease that drove Robin Williams to suicide . The Washington Post .
Topol, E. (2016). The patient will see you now: The future of medicine is in your hands . Basic Books.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, March 21). Genetic Tests: Pros and Cons. https://studycorgi.com/genetic-tests-pros-and-cons/
"Genetic Tests: Pros and Cons." StudyCorgi , 21 Mar. 2022, studycorgi.com/genetic-tests-pros-and-cons/.
StudyCorgi . (2022) 'Genetic Tests: Pros and Cons'. 21 March.
1. StudyCorgi . "Genetic Tests: Pros and Cons." March 21, 2022. https://studycorgi.com/genetic-tests-pros-and-cons/.
Bibliography
StudyCorgi . "Genetic Tests: Pros and Cons." March 21, 2022. https://studycorgi.com/genetic-tests-pros-and-cons/.
StudyCorgi . 2022. "Genetic Tests: Pros and Cons." March 21, 2022. https://studycorgi.com/genetic-tests-pros-and-cons/.
This paper, “Genetic Tests: Pros and Cons”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: November 9, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
Learn about DNA Tests
- Best for Accuracy
- Best For Health
- Best For Ancestry
- Best for Privacy
- Best DNA Test for Dogs
- Best DNA Test for Cats
- 23andMe Review
- Ancestry DNA Review
- Living DNA Review
Learn about Interpreting Results
- Download DNA
- 23andMe Results
- Data Deletion
- Chromosome Analysis
- DNA Painter
- DNA Statistics
What Are The Pros And Cons Of DNA Testing?

In This Article
DNA testing has many benefits. Primarily, it’s a convenient and trustworthy way to understand your genetics, personal relationships, and any diseases you may be at risk for, which can help you make any necessary lifestyle changes to live your best.
However, DNA tests can also potentially cause more anxiety because of the process and even return inconclusive or concerning results that may be costly to follow up on.
DNA testing has several pros and cons, but we’d say that, overall, it’s worth it if you have the budget and want to know more about yourself.
Your DNA gives you better insights into your genes. Inside these genes are instructions for your cells and the genetic variants that make you you.

Clinical genetic testing done by health care providers is different from direct-to-consumer (DTC) tests. Many at-home DNA tests provide information on ancestry and traits. Some offer insights into inherited health conditions.
5 Benefits of Genetic Testing
Genetic tests can analyze your genes to see which variants you have. They can reveal a lot about your appearance, behavior, and health.
Here are some benefits of DNA testing:
1. Make Informed Health Decisions
Sometimes, gene variants can undergo changes. These genetic mutations can increase your risk for certain diseases or cause health problems and genetic disorders.
Genes can also directly affect your health. They can influence your appetite and how you metabolize fats or absorb nutrients, among other things.
At-home genetic testing tends to focus on the prevention of diseases that you may have inherited or are at risk for. Clinical DNA tests are often used to diagnose illness.
Knowing your risks and medical history can help you take on a more proactive approach towards your health. For example, you can adjust your diet and lifestyle habits to curb any potential of developing diseases you may be genetically disposed to.
Some of the most common diseases DNA tests can detect or prepare you for are:
- Hereditary cancers or other types of cancer (like pancreatic cancer, colorectal cancer, or even ovarian cancer)
- Single gene disorders, like Fragile X syndrome or familial hypercholesterolemia
- Celiac disease
- Alzheimer’s
Making smarter health decisions can lower your risk for genetic disease and prevent an existing health problem from getting worse.
If you’re unsure about what to do with your DNA results, you can talk to your healthcare provider or a genetic counselor. Genetic counseling can help you understand which particular disease you’re most at risk for and which genetic disorder you may have. You can also proceed to medical care if necessary.
More importantly, they can tell you what to do about them. They can help you explore your options, get early treatment, and provide professional disease prevention advice.
2. Help With Family Planning
DNA tests can identify genetic mutations that you may have and could potentially pass on to your children. You can take your results to genetic counselors and make informed choices.
If you’re considering a sperm donor, an egg donor, or a surrogate, DNA testing can help you choose the best candidates for producing healthy offspring.
However, “bad genes” shouldn’t stop you from having children. Being at risk for these conditions does not mean that these conditions will truly develop.
Remember that DNA tests can only reveal potential diseases you may develop. There is currently no scientific way to verify with certainty if they will.

3. Discover Traits and How You Inherited Them
You may already know some of your traits. But genetic testing companies can dig deeper into your DNA and offer insights on traits you didn’t know you had.
Genetic tests can also help you understand where you inherited your traits. They can tell you which regions and groups of people you share DNA with.
If learning more about yourself is important to you, DNA tests can tell you more about where those traits came from and who you share them with.
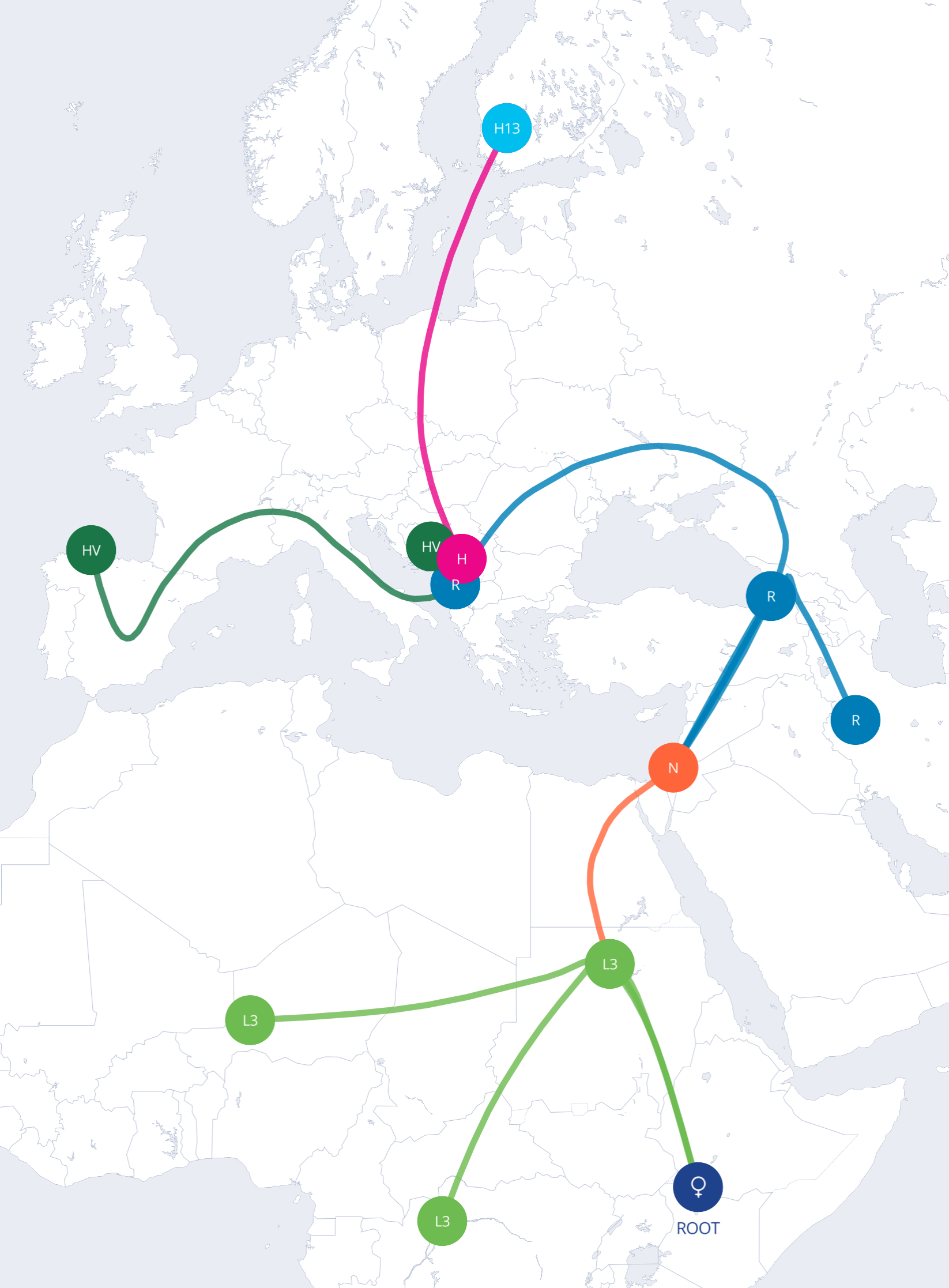
4. Learn Your Family History
DNA testing can help you find out where you’re from in terms of lineage. By comparing your genes with people from around the world, it can help you explore your ancestry and ethnic origins.
Your results will include regions and ethnicities which you share most of your DNA with. This suggests you have common ancestors.
If you’re interested in diving deeper into your family tree and how your ancestors contributed to who you are today, DNA tests could be a great help.

5. Connect With Possible Relatives
Some people use DNA tests to find lost family members and distant relatives. Some DNA testing companies also let you get in touch with them via their databases of users who have also taken the same test.
However, not all users will want to publicize their DNA information or results, so this isn’t always a guarantee.
Still, if you happen to find someone whose results overlap heavily with yours, it might be a cool new discovery and addition to your family tree.
Know Your DNA Reviews


Best DNA Kit
Don't miss out on the opportunity to learn more about yourself. Read our best DNA test page to find the best one for you.
5 Drawbacks of Genetic Testing
Of course, this isn’t to say that everyone should take a DNA test. Here are some cons of genetic testing:
1. Triggers Negative Emotions
Learning that you have a higher risk for health problems can be stressful.
Even if you know you have a family history when it comes to a certain disease, seeing it on your DNA results or waiting for confirmation can be a nerve-wracking experience.
If you have anxiety and other mental health issues or are currently under a lot of stress, you might want to avoid DNA testing. Wait until you have an adequate support system to help you deal with the results.
For example, finding out you have cancer risk can be distressing. Take a DNA test only if you feel emotionally ready for any negative reports.
Genetic testing results should be interpreted with the help of medical geneticists to avoid jumping to conclusions.
2. Involves Privacy Risks
DNA testing companies can keep your samples, information, and results after completing DNA analysis . This can put your data at risk in several ways:
- Your DNA data and personal information can be hacked
- DNA companies can share your information with third parties
- Changes in privacy policies can affect your DNA security
Always read a company’s privacy policies before buying a test. Make sure they won’t share your data with third parties like health insurance companies without consent.
Of course, you can trust some companies more than others. Here’s a complete guide on the most private DNA tests and what you can do to keep your data safe.

3. Affect Family and Personal Relationships
Keep in mind that your DNA test results won’t just affect you. What you can learn from it may also affect people in your family and other close relationships.
News of genetic disorders and health risks can cause distress to you and your family. If your family wasn’t aware of certain conditions in your lineage, they may not deal with the stress well.
You might also find lost relatives that your family doesn’t want to talk about or relatives that you didn’t know existed. Bringing this up can affect your relationship with them and may cause negative feelings to stew.
Ensure you’re careful with the information you share, are gentle with how you break sensitive news, and are mindful of what you divulge.
4. Not Everyone Wants to Be Found
DNA companies can connect you to genetic matches or people with similar DNA. However, they leave it up to members to decide if they want to be found or contacted.
This can limit your results to people who agreed to the DNA matching services. Even if you do find a match, they can stop contact before you can confirm a match.
Whichever the case, it’s important that you respect the privacy of your matches. Many people online know there are potential risks to having their information available online, so they may just want to be cautious.
5. It’s Not Always Accurate
The accuracy of genetic tests depends on several factors. These include the size of a company’s DNA database and the populations they compare your results with.
Accuracy can also vary for each person. For example, someone with European ancestry may get more accurate results from a company with reference groups from Europe.
But a person of Asian descent can’t expect the same accuracy from a company with very few members from Asia.
In fact, only a few DNA testing companies focus on minority ethnic groups. Most well-known DNA testing companies have more information on Western populations, like European and American populations. The small number of ethnic minorities in reference panels make it harder for people of color to get more precise results.
The accuracy of these tests will also depend on the type of DNA testing done. You can consult your medical practitioner for the best test that suits your purpose.
At-Home DNA Testing vs. Professional Testing
Genetic testing can be done at home or professionally in a medical setting. Here are the key differences between them:
At-Home Genetic Testing
At-home DNA tests, also known as direct-to-consumer or DTC kits, usually require a cheek swab. They’ll ask you to send a sample back for analysis.
Here are the pros of genetic testing when you do it at home:
- More accessible and affordable
- Convenient way to learn about your health, disease risks, and other traits
- Doesn’t need approval from a health insurance company
- They’ll send the results directly to you
- Sample collection is usually non-invasive
- Get your results within days of sending your sample

A DTC genetic test kit may have limitations when it comes to accuracy.
For example, if you’re concerned about developing cystic fibrosis, this test can only look into some (but not all) genetic markers that have been linked to it. A negative result doesn’t mean you’re not at risk.
Many DTC kits can provide you with a raw DNA file. This includes a comprehensive list of genetic variants that you tested positive for.
Unfortunately, they can be hard to interpret without a genetic counselor. They also need to be verified with clinical DNA tests before they can be trusted for medical decisions.
Because at-home genetic tests are customer-centered, they are mainly used to prevent diseases from progressing. A medical practitioner is the best person to help you achieve this goal.
Medical DNA Testing
This kind of test is performed by a healthcare professional. They will usually take your saliva sample or draw blood for DNA analysis.
A clinical DNA test looks for specific markers based on your medical background and family history. It’s expensive, but there’s no need to repeat the test for accuracy.

Processing and results will be subject to the doctor or lab conducting the test, but it’s usually preferred by people who trust a more controlled testing environment and professionals handling their samples.
Should You Take A Genetic Test?
You should consider genetic testing in these situations:
- Your family has a history of a genetic condition
- Certain health problems run in the family
- You want to know which illnesses a future child may inherit 1
- You want to see if your unborn child has a genetic illness 2
- You want to screen a newborn for genetic disorders 3
- You didn’t have the chance to know your family
- You want to learn more about your ancestors
- You want to find close relatives
DNA testing can be an effective planning tool, but it can also be a Pandora’s Box. It can open doors to things you may not be prepared to face yet.
Understanding the benefits and disadvantages of genetic testing is the best way to decide if it is right for you.
The results may not be what you want to learn, but there’s still power in knowing. Knowing may motivate you to better care for your health.
Before making a decision, you may talk to a certified genetic counselor. They’ll explain the process and the considerations you need to take.
Do DNA Testing Services Offer Consultations With Genetic Experts After You Get Your Results?
Some of them do. There are DNA testing services that come with a one-on-one consultation with a genetic counselor or geneticist. Many lab services also have doctors, counselors, and geneticists on call to discuss your results with you.
If not, they can often recommend someone you can talk to.
Do DNA Testing Services Offer Psychological Services After Testing or Getting Results?
Some of them do. It also depends on the company or testing service. However, you can also probably ask for a recommendation as many people often seek out psychological help after DNA test results.
How to Interpret My DNA Test Results?
Interpreting your DNA test results is best done by an expert. Talk to your healthcare provider, doctor, or genetic counselor for the best interpretations of your DNA test results.
Many DNA testing services also try to make their reports as digestible as possible for the average person. However, it can still be easy to take everything that’s reported at face value and jump to conclusions. It’s always best to consult a professional.
How Much Do DNA Tests Cost?
DNA tests can vary in price. There are some more affordable options at less than $100, but the most common range for comprehensive tests can be anywhere between $100 to more than $2000. It all depends on the kind of test you take, what it covers, and which company it’s from.
Is My Information Safe With DNA Tests?
Yes, for the most part. While there have been some cases where DNA testing companies have suffered security breaches, your private data should be safe.
Many companies offer the option to delete your DNA data from their databases altogether and even destroy your sample if you’re concerned about security breaches.
Again, not every database is fully secure, but big DNA companies are working constantly to tighten their security as much as possible.
The Best DNA Test
Looking for a DNA test that's accurate and can tell you about your health and heritage?
Related Pages

GPS Origins Review (2024)

Living DNA Review: See What 2024's Newest Family Test Can Tell You

How to Delete Your Data From Every DNA Testing Service

Best Native American DNA Test (2024)

Inherited Diseases and What Genetic Testing Can Uncover
- “ Carrier Screening .” The American College of Obstetricians and Gynecologists.
- “ Genetic Testing .” Nemours Children’s Health.
- “ Newborn Screening Tests .” Children’s Hospital of Philadelphia.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, Fullarton JE, Holtzman NA, et al., editors. Assessing Genetic Risks: Implications for Health and Social Policy. Washington (DC): National Academies Press (US); 1994.

Assessing Genetic Risks: Implications for Health and Social Policy.
- Hardcopy Version at National Academies Press
8 Social, Legal, and Ethical Implications of Genetic Testing
Each new genetic test that is developed raises serious issues for medicine, public health, and social policy regarding the circumstances under which the test should be used, how the test is implemented, and what uses are made of its results. Should people be allowed to choose or refuse the test, or should it be mandatory, as newborn screening is in some states? Should people be able to control access to the results of their tests? If test results are released to third parties such as employers or insurers, what protections should be in place to ensure that people are not treated unfairly because of their genotype?
The answers to these questions depend in part on the significance given to four important ethical and legal principles: autonomy, confidentiality, privacy, and equity. A review of the meaning of those concepts and how they are currently protected by the law provides a starting point for the development of recommendations on the degree of control people should have in deciding whether to undergo genetic testing and what uses should be made of the results. The task is a pressing one. In a 1992 national probability survey of the public, sponsored by the March of Dimes, 38 percent of respondents said that new types of genetic testing should be stopped altogether until the privacy issues are settled. 1
This chapter reviews some of the conflicts that will arise in the research and clinical settings, and suggests general principles that should be the starting point for policy analyses in this evolving field.
Since many of the references in this chapter are legal citations, its references appear in legal style as numbered end notes.
- KEY DEFINITIONS
Ethical Analysis
Autonomy can be defined as self-determination, self-rule, or self-governance. Autonomous agents or actions presuppose some capacity of reasoning, deciding, and willing. Moral, social, and legal norms establish obligations to respect autonomous agents and their choices. Respect for personal autonomy implies that agents have the right or power to be self-governing and self-directing, without outside control. In the context of genetic testing and screening, respect for autonomy refers to the right of persons to make an informed, independent judgment about whether they wish to be tested and then whether they wish to know the details of the outcome of the testing. Autonomy is also the right of the individual to control his or her destiny, with or without reliance on genetic information, and to avoid interference by others with important life decisions, whether these are based on genetic information or other factors. Respect for autonomy also implies the right of persons to control the future use of genetic material submitted for analysis for a specific purpose (including when the genetic material itself and the information derived from that material may be stored for future analysis, such as in a DNA bank or registry file).
Even though respect for autonomy is centrally important in our society, it is not absolute. It can be overridden in some circumstances, for example, to prevent serious harm to others, as is the case in mandatory newborn screening for phenylketonuria (PKU) and hypothyroidism.
Legal Issues
The legal concept of autonomy serves as the basis for numerous decisions protecting a person's bodily integrity. In particular, cases have held that competent adults have the right to choose whether or not to undergo medical interventions. 2 Before people make such a choice, they have a right to be informed of facts that might be material to their decision, 3 such as the nature of their condition and its prognosis, 4 the potential risks and benefits of a proposed test or treatment, 5 and the alternatives to the proposed intervention. 6 In the genetics context, health care providers have been held liable for not providing the information that a genetic test is available. 7
People also have a right to be informed about and to control the subsequent use of tissue that has been removed from their bodies. 8 There is some leeway under the federal regulations governing research involving human subjects for researchers to undertake subsequent research on blood samples provided for genetic tests (as in the newborn screening context) as long as the samples are anonymous and as long as the subsequent use was not anticipated at the time the sample was collected. 9 If the additional test was anticipated at the time the sample was collected, informed consent for that use should be obtained prior to the collection of the original sample.
Such an approach is thought appropriate to avert conflicts of interest, such as a physician/researcher suggesting that a patient undergo a particular test when the researcher actually wanted the tissue for the researcher's own additional use in a research or commercial project. In such a situation, the patient's autonomy is compromised even if the sample is used anonymously in the subsequent use. A report from the Office of Technology Assessment similarly stressed the importance of knowledge and consent:
The consent of the patient is required to remove blood or tissue from his or her body, and also to perform tests, but it is important that the patient be informed of all the tests which are done and that a concern for the privacy of the patient extends to the control of tissues removed from his or her body. 10
Among the various definitions of privacy, one broad definition captures its central element: privacy is "a state or condition of limited access to a person." 11 People have privacy if others lack or do not exercise access to them. They have privacy if they are left alone and do not suffer unauthorized intrusion by others. Once persons undergo genetic tests, privacy includes the right to make an informed, independent decision about whether—and which—others may know details of their genome (e.g., insurers, employers, educational institutions, spouses and other family members, researchers, and social agencies).
Various justifications have been offered for rules of privacy. First, some philosophers argue that privacy rights are merely shorthand expressions for a cluster of personal and property rights, each of which can be explicated without any reference to the concept of privacy. In making this argument, Judith Jarvis Thomson holds that privacy rights simply reflect personal and property rights, such as the rights not to be looked at, not to be overheard, and not to be caused distress. 12
A second justification holds that rights to privacy are important instruments or means to other goods, including intimate relations such as trust and friendship. Being able to control access to themselves enables people to have various kinds of relationships with different people, rather than being equally accessible to all others.
A third approach finds the basis for rights to privacy in respect for personal autonomy. Decisional privacy is often very close to personal autonomy. The language of personal autonomy reflects the idea of a domain or territory of self-rule, and thus overlaps with zones of decisional privacy.
Whatever their rationale or justification, rights of privacy are the subject of ongoing debate about their scope and weight. However, their scope is not unlimited, and they do not always override all other competing interests, such as the interests of others.
In the legal sphere, the principle of privacy is an umbrella concept encompassing issues of both autonomy and confidentiality. The right to make choices about one's health care is protected, in part, by the right to privacy guaranteed by the U.S. Constitution, as well as state constitutions. This includes a right to make certain reproductive choices, 13 such as whether to use genetic testing. 14 It also includes a right to refuse treatment.
An entirely different standard of privacy protects personal information. A few court decisions find protection for such information under the constitutional doctrine of privacy, 15 but more commonly, privacy protection against disclosure of personal information is found under common law tort principles. 16 In addition, there is a federal privacy act, 17 as well as state statutes protecting privacy.
Confidentiality
Confidentiality as a principle implies that some body of information is sensitive, and hence, access to it must be controlled and limited to parties authorized to have such access. The information provided within the relationship is given in confidence, with the expectation that it will not be disclosed to others or will be disclosed to others only within limits. The state or condition of nondisclosure or limited disclosure may be protected by moral, social, or legal principles and rules, which can be expressed in terms of rights or obligations.
In health care and various other relationships, we grant others access to our bodies. They may touch, observe, listen, palpate, and even physically invade. They may examine our bodies as a whole or in parts; and parts, such as tissue, may be removed for further study, as in some forms of testing. Privacy is necessarily diminished when others have such access to us; rules of confidentiality authorize us to control and thus to limit further access to the information generated in that relationship. For example, rules of confidentiality may prohibit a physician from disclosing some information to an insurance company or an employer without the patient's authorization.
Rules of confidentiality appear in virtually every code or set of regulations for health care relationships. Their presence is not surprising, because such rules are often justified on the basis of their instrumental value: if prospective patients cannot count on health care professionals to maintain confidentiality, they will be reluctant to allow professionals the full and complete access necessary for diagnosis and treatment. Hence, rules of confidentiality are indispensable for patient and social welfare; without those rules, people who need medical, psychiatric, or other treatment will refrain from seeking or fully participating in it. Another justification for rules of confidentiality is based on the principles of respect for autonomy and privacy, above. Respecting persons involves respecting their zone of privacy and accepting their decisions to control access to information about them. When people grant health care professionals access to them, they should retain the right to determine who else has access to the information generated in that relationship. Hence, the arguments for respect for autonomy and privacy support rules of confidentiality. Finally, duties of confidentiality often derive from explicit or implicit promises in the relationship. For instance, if the professional's public oath or the profession's code of ethics promises confidentiality of information, and the particular professional does not specifically disavow it, then the patient has a right to expect that information generated in the relationship will be treated as confidential. 18
There are at least two distinct types of infringements of rules of confidentiality. On the one hand, rules of confidentiality are sometimes infringed through deliberate breaches. On the other hand, rules of confidentiality are often infringed through carelessness, for example, when health care professionals do not take adequate precautions to protect the confidential information. Some commentators argue that both carelessness and modern practices of health care have rendered medical confidentiality a "decrepit concept," since it is compromised routinely in the provision of health care. 19
It is widely recognized that the rules of confidentiality are limited in at least two senses: (1) some information may not be protected, and (2) the rules may sometimes be overridden to protect other values. First, not all information is deemed confidential, and patients do not have a right to expect that such information will be protected from disclosure to others. For example, laws frequently require that health care professionals report gunshot wounds, venereal diseases, and other communicable diseases such as tuberculosis. Second, health care professionals may also have a moral or legal right (and sometimes even an obligation) to infringe rules of confidentiality, for example, to prevent a serious harm from occurring. In such cases, rules of confidentiality protect the information, but they can be overridden in order to protect some other value. Judgments about such cases depend on the probability of serious harm occurring unless confidentiality is breached. Any justified infringements of rules of confidentiality should satisfy the conditions identified earlier in the discussion of justified infringements of the principle of respect for autonomy.
The legal concept of confidentiality focuses on the information that people provide to their physicians. The protection of confidentiality is thought to serve an important public health goal in encouraging people to seek access to health care. It is thought that the patient's interest can be served only in an atmosphere of total frankness and candor. 20 Without the promise of confidentiality, people might avoid seeking medical treatment, thus potentially harming themselves as well as the community. In fact, the first doctor-patient confidentiality statute was passed in 1828 in New York during the smallpox epidemic to encourage people to seek health care. Various legal decisions have protected confidentiality of health care information, 21 as have certain state and federal statutes.
Confidentiality of health care information is also protected because disclosure of a person's medical condition can cause harm to him or her. An alternative set of legal principles-those penalizing discrimination (see below)-protects people against unfair uses of certain information.
Issues of justice, fairness, and equity crop up in several actions, practices, and policies relating to genetic testing. It is now commonplace to distinguish formal justice from substantive justice. Formal justice requires treating similar cases in a similar way. Standards of substantive or material justice establish the identity of the relevant similarities and differences and the appropriate responses to those similarities and differences. For instance, a society has to determine whether to distribute a scarce resource such as health care according to persons' differences in need, social worth, or ability to pay.
One crucial question is whether genetic disorders or predispositions provide a basis for blocking access to certain social goods, such as employment or health insurance. Most conceptions of justice dictate that employment be based on the ability to perform particular tasks effectively and safely. For these conceptions, it is unjust to deny employment to someone who meets the relevant qualifications but also has a genetic disease. Frequently these questions of employment overlap with questions of health insurance. Practices of medical underwriting in health insurance reflect what is often called "actuarial fairness"-that is, grouping those with similar risks together so insurers can accurately predict costs, and set fair and sufficient premium rates. Although actuarial fairness may be intuitively appealing, critics argue that it does not express moral or social fairness. According to Norman Daniels, there is "a clear mismatch between standard underwriting practices and the social function of health insurance" in providing individuals with resources for access to health care 22 (see Chapter 7 ).
The fundamental argument for excluding genetic discrimination in health insurance amounts to an argument for establishing a right to health care. One of the central issues in debates about the distribution of health care is one's view of the "natural lottery," in particular, a "genetic lottery." 23 The metaphor of a lottery suggests that health needs result largely from an impersonal natural lottery and are thus undeserved. But even if health needs are largely undeserved because of the role of chance, society's response to those needs may vary, as H. Tristram Engelhardt notes, depending on whether it views those needs as unfair or as unfortunate. 24 If health needs are unfortunate, but not unfair, they may be the object of individual or social compassion. Other individuals, voluntary associations, and even society may be motivated by compassion to try to meet those needs. If, however, the needs are viewed as unfair as well as unfortunate, society may have a duty of justice to try to meet those needs.
One prominent argument for the societal provision of a decent minimum of health care is that, generally, health needs are randomly distributed and unpredictable, as well as overwhelming when health crises occur. 25 Because of these features of health needs, many argue that it is inappropriate to distribute health care according to merit, societal contribution, or even ability to pay. Another version of the argument from fairness holds that health needs represent departures from normal species functioning and deprive people of fair equality of opportunity. Thus, fairness requires the provision of health care to "maintain, restore, or compensate for the loss of normal functioning" in order to ensure fair equality of opportunity. 26
Several committee members expressed concerns that these stated arguments are somewhat weakened by the fact that a number of diseases are not the result of random events, but are brought on or exacerbated by dispensable habits such as cigarette smoking and excessive alcohol ingestion. While our and other societies attempt to discourage such habits by education and taxation, there is general agreement that access to full health care must be ensured once illness develops. If a tendency to abuse alcohol, for example, were to have a genetic predisposition, an additional argument could be made for providing the same level of health care to everyone since a person does not choose his or her genetic propensities.
The argument that society should guarantee or provide a decent minimum of health care for all citizens and residents points toward a direction for health policy, but it does not determine exactly how much health care the society should provide relative to other goods it also seeks. And, within the health care budget, there will be difficult allocation questions, including how much should be used for particular illnesses and for particular treatments for those illnesses. Questions of allocation cannot be resolved in the abstract. In democratic societies, they should be resolved through political processes that express the public's will. In specifying and implementing a conception of a decent minimum, an adequate level, or a fair share of health care in the context of scarce resources, as the President's Commission noted in 1983, it is reasonable for a society to turn to fair, democratic political procedures to choose among alternative conceptions of adequate health care, and in view of "the great imprecision in the notion of adequate health care ... it is especially important that the procedures used to define that level be—and be perceived to be—fair." 27
The concept of equity serves as the underpinning for a variety of legal doctrines and statutes. Certain needy people are provided health care, including some genetics services, under government programs such as Medicaid (see Chapter 7 ). In addition, some legislative efforts have been made to prohibit discrimination based on genotype. For example, some states have statutes prohibiting discrimination in employment based on one's genotype. 28 And nearly all people over age 65 are deemed to have a right to care (under Medicare).
- CURRENT PRACTICE OF PROTECTION IN GENETICS
The development of genetic testing has raised numerous concerns about autonomy, confidentiality, privacy, and equity that are exacerbated by the range of contexts in which such tests are undertaken, the sheer volume of tests that could be offered, the many uses that can be made of test results, and the variety of institutions that store genetic information. To date, most genetic testing has been done in the reproductive context or with newborns, to identify serious disorders that currently or soon will affect the fetus or infant. However, the types of genetic conditions or predispositions that can potentially be tested for are much broader than those signaling serious, imminent diseases. These include characteristics (such as sex or height) that are not diseases, potential susceptibility to diseases if the person comes into contact with particular environmental stimuli, and indications that a currently asymptomatic person will suffer later in life from a debilitating disease such as Huntington disease. The genetic anomalies that can be tested for range widely in their manifestations, their severity, their treatability, and their social significance. People's ability to define themselves, to manage their destiny and self-concept, will depend in large measure on the control they have over whether they and others come to know their genetic characteristics.
Most medical testing is done within a physician-patient relationship. With genetic testing, however, the potential range of contexts in which it can be undertaken is large. Already, in the public health context, more than 4 million newborns are tested annually for metabolic disorders so that effective treatment can be started in a few hundred. Researchers are inviting people to participate in family studies and undergo genetic testing, including collection of DNA samples for present or future analyses. There are a growing number of nonmedical applications of genetic testing as well. In the law enforcement context, DNA testing is undertaken to attempt to identify criminal offenders. At least 17 states have DNA fingerprint programs for felons. 29 The armed services are collecting DNA samples from all members of the military, the primary purpose of which is to identify bodies of deceased soldiers. Employers and insurers may require people to undergo testing for genetic disorders for exclusionary purposes. One challenge for policy posed by this wide array of testing settings is that many of the existing legal precedents about autonomy, confidentiality, and privacy apply only to the traditional doctor-patient relationship. For example, some state statutes governing confidentiality deal only with information provided to physicians and might not cover information provided to Ph.D. researchers or employers.
There seems to be great variation among institutions and among providers in the amount of attention paid to autonomy, confidentiality, and privacy. For example, some obstetricians recognize the patient's autonomy by providing them the information about maternal serum alpha-fetoprotein (MSAFP) screening but acknowledging the patient's right to decide whether or not to undergo the test. Other obstetricians run the test on blood gathered from the woman for other purposes, so the woman does not even know she has been the subject of the test unless the obstetrician delivers the bad news that she has had an abnormal result.
Geneticists differ with respect to the emphasis they place on the confidentiality of the results of genetic testing. In a survey by Dorothy Wertz and John Fletcher, 30 numerous geneticists suggested that there were at least four situations in which they would breach confidentiality and disclose genetic information without the patient's permission, even over the patient's refusal: (1) 54 percent said they would disclose to a relative the risk of Huntington disease; (2) 53 percent said they would disclose the risk of hemophilia A; (3) 24 percent said they would disclose genetic information to a patient's employer; and (4) 12 percent said they would disclose such information to the patient's insurer. Primary care physicians may be even more likely to disclose such information. 31 Health care providers should explain their policies for disclosure in advance, including for disclosure to relatives.
Institutions that store DNA samples 32 or store the results of genetic tests also differ in the amount of respect they give to autonomy, confidentiality, and privacy. 33 Some institutions do additional tests on DNA samples without the permission of the person who provided the sample. Some share samples with other institutions. Some store samples or information with identifiers attached, rather than anonymously. Indeed, storage conditions themselves differ widely. Some newborn screening programs store filter papers in a temperature-controlled, secure setting; others merely pile them in a file cabinet or storage closet. Programs also differ in the length of time the sample or the test results are maintained.
Once DNA material has been submitted, there are few safeguards concerning other present or future uses that may be made of the material. DNA from the blood spots collected for newborn screening can now be extracted for further testing. 34 No standards or safeguards currently exist to govern the appropriate use of DNA analysis and storage from newborn screening tests. These possibilities raise questions about the need to obtain consent for additional and subsequent uses (particularly since consent is almost never obtained initially in newborn screening), as well as questions about the duty to warn if disorders are detected in the blood by using the new DNA extraction testing techniques.
The issue of confidentiality of genetic information will be underscored with the introduction of ''optical memory cards," a credit card-sized device that stores medical information. 35 These cards have already been introduced for use in Houston city health clinics. There is sufficient computer memory on the cards to include genetic information about the person and, in the future, to include a person's entire genome.
Congressional legislation has been introduced that would require all patients to use optical memory cards. This bill, the Medical and Health Insurance Information Reform Act of 1992, would mandate a totally electronic system of communication between health care providers and insurers. Such a system would be based either on the optical memory card (with a microchip capable of storing data) or on a card similar to an Automated Teller Card (which simply provides access to data stored elsewhere).
- APPLYING THE PRINCIPLES TO GENETIC TESTING
The principles of autonomy, privacy, confidentiality, and equity place great weight on individuals' rights to make personal decisions without interference. This is due, in part, to the importance placed on individuals in our culture and our legal system. However, individual rights are not without bound, and the area of genetics raises important questions of where individual rights end and where responsibilities to a group—such as one's family or the larger society—begin.
Medicine is generally practiced within this culture of individual rights (with provisions for patients' right to refuse treatment and right to control the dissemination of medical information about themselves), but there have been circumstances in which the medical model has been supplanted by the public health model, which encourages the prevention of disease—for example, by requiring that certain medical intervention (such as vaccinations) be undertaken and by warning individuals of health risks (e.g., through educational campaigns against smoking or through contact tracing with respect to venereal diseases). Some commentators have suggested that the public health model be applied to genetics, 36 with mandatory genetic screening and even mandatory abortion of seriously affected fetuses. A related measure might be warning people of their risk of genetic disorders.
There are several difficulties with applying the public health model to genetics, however. Certain infectious diseases potentially put society as a whole at immediate risk since the diseases can be transmitted to a large number of people in a short time. The potential victims are existing human beings who may be total strangers to the affected individual. In contrast to infectious disease, the transmission of genetic diseases does not present an immediate threat to society. Whereas infectious disease can cause rapid devastation to a community, the transmission of genetic disorders to offspring does not necessarily have an immediate detrimental effect, but rather creates a potential risk for a future generation in society. 37 U.S. Supreme Court cases dealing with fundamental rights have held that harm in the future is not as compelling a state interest as immediate harm. 38
Moreover, the very concept of "prevention" does not readily fit most genetic diseases. In the case of newborn screening for PKU, treatment can prevent mental retardation. However, with many genetic diseases today, the genetic disease itself is not being prevented, but rather the birth of a particular individual with the disease is prevented (e.g., when a couple, each of whom is heterozygous for a serious recessive disorder, chooses not to conceive or chooses to terminate the pregnancy of a fetus who is homozygous for the disorder). This sort of prevention cannot be viewed in the same way as preventing measles or syphilis, for example. There is a great variation among people in their view of disability and what constitutes a disorder to be "prevented." Many people will welcome a child with Down syndrome or cystic fibrosis into their family. In addition, some individuals have religious or other personal moral objections to abortion; even mandatory carrier status screening or prenatal screening without mandatory abortion may be objected to because people who object to abortion are concerned that the abortion rate will rise among those in the general population who learn of genetic risks to their fetus. Furthermore, some people with a particular disability or genetic risk may view mandatory genetic testing for that risk or disability as an attempt to eradicate their kind, as a disavowal of their worth.
Mandatory genetic testing might also have devastating effects on the individuals who are tested. Unlike infectious disease (which can be viewed as external to the person), genetic disease may be viewed by people as an intractable part of their nature. Persons who learn, against their will, that they carry a defective gene may view themselves as defective. This harm is compounded if they did not choose to learn the information voluntarily. This assault on personal identity is less likely with infectious diseases, although AIDS and genital herpes (for example) can also have a negative impact on self-image. Moreover, most genetic defects, unlike most infectious diseases, generally cannot now be corrected. 39 Thus, the unasked-for revelation that occurs through mandatory genetic testing can haunt the person throughout his or her life and can have widespread reverberations in the family, including others who may be at risk or related as partners. The information can serve as the basis for discrimination against the individual.
Additionally, policy concerns raised by attempts to stop the transmission of genetic diseases differ from those addressed to infectious diseases because genetic diseases may differentially affect people of different races or ethnic backgrounds. For that reason, some commentators contest the applicability of the infectious disease model to government actions regarding genetic disorders. Catherine Damme notes that "unlike infectious disease which [generally] knows no ethnic, racial, or gender boundaries, genetic disease is the result of heredity"—leaving open the possibility for discriminatory governmental actions. 40
The government has discretion with respect to which infectious diseases it tackles. For example, it can decide to require screening for syphilis but not chlamydia, or to require vaccinations for smallpox but not for diphtheria. Government action with respect to genetic diseases is likely to be regarded much differently, especially with respect to disorders for which an effective treatment does not exist and, consequently, the only medical procedure available is the abortion of an affected fetus. Minority groups who have been discriminated against in the past may view a screening program that targets only disorders that occur within their racial or ethnic group as an additional attack, and may view abstention from reproduction or the abortion of offspring based on genetic information as a form of genocide. 41
Those commentators who argue that the infectious disease precedents justify mandatory genetic screening fail to recognize that even in the case of infectious disease, very few medical procedures are mandated for adults. Adults are not forced to seek medical diagnosis and treatment even if they have a treatable infectious disease. Laws that required compulsory infectious disease screening prior to marriage (e.g., for venereal disease) are being repealed. For example, New York abolished its requirements for premarital gonorrhea and syphilis testing. One of the reasons for the abolition of the requirements was that they were not the most appropriate way to reach the population at risk. 42
Mandating diagnosis and treatment for genetic disorders is particularly problematic when the concept of disease is so flexible. Arno Motulsky has noted that "[t]he precise definition of 'disease' regardless of etiology, is difficult." 43 He notes that maladies such as high blood pressure and mental retardation are based on arbitrary cutoff levels. David Brock similarly noted that most disorders lie between the extremes of Tay-Sachs disease and alkaptonuria; what a physician advises "depends as much on the physician's ethical preconceptions as his medical experience." 44
Despite the fact that the public health model does not fit the situation of genetics, the individual rights model should not be seen as absolute. There are certain situations in which the values of autonomy, privacy, confidentiality, and equity should give way to prevent serious harm to others. Determining the exceptions to these general principles is no easy matter, however. There may be instances in which harm can be prevented by violating one of these principles, but in which the value of upholding the principles will nonetheless outweigh the chance of averting harm. In each instance, it will be necessary to assess several factors: How serious is the harm to be averted? Is violating one of the principles the best way to avert the harm? What will be the medical, psychological, and other risks of violating the principle? What will be the financial costs of violating the principle?
The following section addresses the issues raised by the application of these principles—autonomy, privacy, confidentiality, and equity—in the contexts of clinical genetics, other medical practices, genetics research, and so forth. It also provides guidance for determining the appropriate circumstances for exceptions to these principles. The chapter concludes with the committee's recommendations on these issues.
- ISSUES IN GENETIC TESTING
One important way to ensure autonomy with respect to genetic testing is to provide adequate information upon which a person can make a decision whether or not to undergo testing. A proper informed consent in medicine generally involves the presentation of information about the risks, benefits, efficacy, and alternatives to the procedure being undertaken. In addition, recent cases and statutes have recognized the importance of disclosures of any potential conflicts of interest that the health care professional recommending the test may have, such as a financial interest in the facility to which the patient is being referred. In the genetics context, this would include disclosure about equity holdings or ownership of the laboratory, dependence on test reimbursement to cover the costs of counseling, patents, and so forth. It would also include disclosure of any planned subsequent uses of the tissue samples, even if such uses are to be anonymous.
Various kinds of information are relevant to people who are attempting to exercise their autonomy by deciding whether or not to undergo genetic testing. This includes information about the severity, potential variability, and treatability of the disorder being tested for. If, for example, carrier status testing is being proposed for a pregnant woman or prenatal testing is being proposed for her fetus, she should be told whether the disorder at issue can be prevented or treated, or whether she will be faced with a decision about whether or not to abort (see Chapters 2 , 4 , and 5 ). The proposed informed consent guidelines for research involving genetic testing suggested by the Alliance of Genetic Support Groups provide an excellent starting point for the development of informed consent policies in the genetics area (see Chapter 4 ).
The potential development of multiplex testing adds another wrinkle to the issue of informed consent for genetic testing. If 100 disorders are tested from the same blood sample, it may be difficult to apply the current model of informed consent in which a health care provider gives information about each disorder and the efficacy of each test to the patient in advance of the testing. The difficulty in applying the traditional mechanisms for achieving informed consent does not provide an excuse for failing to respect a patient's autonomy and need for information, however. New mechanisms may have to be developed to protect these rights. It will be possible to have results reported back to the physician and patient only about those tests (or types of tests) the patient chooses. The choices can be made by the patient, based, for example, on the patient learning through a computer program about the various disorders and the various tests. Or the choices can be made according to general categories—for example, the patient might choose to have multiplex testing but choose not be informed of the results of testing for untreatable or unpreventable disorders 45 (see Chapters 1 , 3 , and 4 ).
In addition to the recognition that people are entitled to information before they make decisions, a second application of the autonomy principle comes with the recognition that the decision to participate in genetic testing and other genetics services must be voluntary. Voluntariness has been a recognized principle in past recommendations and practices involving genetics. This is in keeping with the recognized right of competent adults to refuse medical intervention, as well as the right to refuse even the presentation of medical information in the informed consent context. 46 If, for example, it becomes possible to accurately screen fetal cells isolated from a pregnant woman's blood in order to determine the genetic status of the fetus, state public health departments might be interested in requiring the test on the grounds that it is a minimally invasive procedure that can provide information to the woman (perhaps leading her to abort an affected fetus and saving the state money for care of that infant). Mandating such a test, however, would show insufficient respect for the woman's autonomy and would violate her right to make reproductive decisions.
Special Issues in the Screening and Testing of Children
The expansion of available tests fostered by the Human Genome Project will present complicated issues with respect to the testing of newborns and other children. Although there are clear legal precedents stating that adults are free to refuse even potentially beneficial testing and treatment, legal precedents provide that children can be treated without their consent (and over their parents' refusal) to prevent serious imminent harm. The U.S. Supreme Court has said that, while parents are free to make martyrs of themselves, they are not free to make martyrs of their children. 47 Medical intervention over parents' objection has been allowed in situations in which a child's life was in imminent danger and the treatment posed little risk of danger in itself. 48 Blood transfusions have been ordered for the children of Jehovah's Witnesses when the child's life was imminently endangered. 49
All states have programs to screen newborns for certain inborn errors of metabolism for which early intervention with treatment provides a clear medical benefit to the child, such as phenylketonuria. Currently, the statutes of at least two jurisdictions (the District of Columbia and Maryland) clearly provide that newborn screening is voluntary. 50 In at least two states (Montana and West Virginia), screening is mandatory and there is no legal provision for parental objection or refusal based on religious grounds. 51 In the rest of the states, there are grounds for parental refusal for religious or other reasons. However, although the majority of states allow objection to screening on some grounds, very few statutes require that the parents or guardians of an infant either be sufficiently informed that they can choose whether or not their infant should submit to the screening or be told they have the right to object. Two states (Missouri and South Carolina) have criminal penalties for parents who refuse newborn screening of their children. 52
The idea behind mandatory newborn screening is a benevolent one—to try to ensure that all children get the benefits of screening for PKU and hypothyroidism, for which early treatment can make a dramatic difference in the child's well-being by preventing mental retardation. Yet there is little evidence that it is necessary to make a newborn screening program mandatory to ensure that children are screened under the program. Recent studies show that the few states with voluntary newborn screening programs screen a higher percentage of newborns than some states with mandatory newborn screening programs; for 1990, voluntary programs reported reaching 100 percent of newborns in their states, while some states with mandatory programs report reaching 98 percent, and some even less than 96 percent. 53 Relevant research has suggested that even when a newborn screening program is completely voluntary and parents may refuse for any reason, the actual refusal rate is quite low, about 0.05 percent (27 of 50,000 mothers). In that study, most nurses reported that it required only one to five minutes to inform a mother about newborn screening. 54
Newborn screening for PKU—like a necessary blood transfusion for a child over the parents' refusal—has been justified on the basis of the legal doctrine of parens patriae, where the state steps in to order an intervention to protect a child from substantial, imminent harm. In the era of the Human Genome Project, when additional tests are being developed, some people are promoting newborn screening in part for less immediate and less clear benefits. Proposed guidelines have suggested that another benefit of newborn screening "might take the form of inscription in registries for later reproductive counseling (material PKU) or of surveillance of phenotypes (congenital adrenal hyperplasia)." 55 To achieve such an outcome, the resulting children would need to be followed until the age when reproductive counseling was appropriate—or when symptoms manifest—a daunting task in this age of mobility.
The first newborn screening programs were for disorders in which early treatment of the newborn was effective. Increasingly, however, testing is suggested for untreatable disorders. In such instances, the justification is not the benefit to the newborn but the benefit to the parents for future reproductive plans. For such reasons, several countries—and some states in the United States (e.g., Pennsylvania)—screen newborns for Duchenne muscular dystrophy. This medical intervention has no immediate medical benefit for the newborn, and carrier screening of the parents could be obtained through other methods, even when (as in the case of Duchenne muscular dystrophy and some other conditions) they may not realize they are at risk.
Moreover, screening newborns for genes for untreatable disorders or carrier status may have disadvantages. The children may be provided with information that, at the age of consent, they would rather not have. Parents might treat them differently if the results are positive. Parents may stigmatize or reject children with the abnormal genes, or may be less willing to devote financial resources to education or other benefits for such children. In addition, release of the test results might cause them to be uninsurable, unemployable, and unmarriageable.
There are additional benefits from voluntariness in newborn screening. Informing parents about newborn screening in advance of testing allows quality assurance: parents can check to see if the sample was actually drawn. As children are being released from the hospital increasingly early, due to insurance pressures, they might receive a false negative result because blood levels of phenylalanine have not yet risen sufficiently to be detected if elevated. Informed motivated parents may need to bring their babies to be screened after release from the hospital in order to ensure an accurate test result. The recommended informed consent process can provide the necessary education and motivation that will be required to make the return trip far better than mandatory programs.
In the postgenome era, people will be facing the possibility of undergoing many more genetic tests in their lifetimes, and will need to master a wealth of genetic information that is relevant to their health, their reproductive plans, and the choices they make about what to eat, where to live, and what jobs to take. The more settings in which they can be informed about genetics, the more able they will be to make these decisions. In addition, when newborn screening programs are voluntary, there is a greater chance that parents will be provided with material in advance about the disorder and have their questions answered, thus presenting the possibility that they will view it more seriously and will make a greater effort to ensure that the child receives proper treatment if a condition is detected. The disclosure of information to parents about newborn screening prior to newborn screening can be an important tool for public education about genetics.
Mandatory newborn screening should only be undertaken if there is strong evidence of benefit to the newborn from effective treatment at the earliest possible age (e.g., PKU and congenital hypothyroidism). Under this principle, screening for Duchenne muscular dystrophy would not be justified. In addition, mandatory newborn screening for cystic fibrosis would currently not be justified. 56 A prospective double-blind study in Wisconsin (the only controlled study on the subject) has not found benefits of early detection in newborn screening for CF; the treatment of children could be initiated with just as successful results based on the occurrence of symptoms. In addition to its lack of clear benefit, newborn screening for CF has a clear downside. Screening by its nature is overly broad; in newborn screening for cystic fibrosis, for example, "only 6.1 percent of infants with positive first tests [in the Colorado and Wyoming program] were ultimately found to have cystic fibrosis on sweat chloride testing." 57 Yet one-fifth of parents with false positives on newborn screening for cystic fibrosis "had lingering anxiety about their children's health." 58 Of the parents whose infants had initial, later disproven positive reports of CF in the Wisconsin study, 5 percent still believed a year later that their child might have CF. 59 Such a reaction may influence how parents relate to their child. A report on the Wisconsin newborn screening for CF stated that of the 104 families with false positives, 8 percent planned to change their reproductive plans and an additional 22 percent were not sure whether they would change their reproductive plans. 60 In fact, in France, the newborn screening program for cystic fibrosis was terminated at the request of parents who objected to the high number of false positives. 61 Denmark stopped screening for alpha-1-antitrypsin deficiency because of negative long-term effects on the mother-child interactions associated with identifying the infant's alpha-l-antitrypsin deficiency. 62
Even in cases where a treatment is available for a disorder detectable through newborn screening, it may not be of unequivocal benefit if started after symptoms appear. Treatment of children identified through screening for maple syrup urine disease may have only limited effectiveness at best, and parents may face a quandary about whether or not to treat. Even if hypothetical benefits exist, newborn screening programs need close scrutiny to determine if the necessary treatments are actually provided to the children. In states that support screening but not treatment, families may be unable to afford treatment and thus children may not benefit from screening. Many children with sickle cell anemia, for example, do not get their necessary penicillin prophylaxis. 63 Although most states provide education about diet and nutrition to parents of infants with PKU, not all states provide the expensive essential diet or other food assistance.
Beyond the issue of the testing of newborns in state-sponsored programs, there are more general issues regarding the genetic testing of children in clinical settings. Some technologies designed to identify affected individuals will also provide information about carrier status. If an infant is tested for sickle cell anemia, for example, the test will reveal whether the infant is a carrier. In that case, the carrier status information is a by-product of the test for sickle cell anemia since obtaining information on carrier status is not the primary purpose of the testing. Questions arise as to whether that information should be reported to the infant's parents.
One advantage to reporting the information is that it is relevant to the parents' future reproductive plans. If the infant is a carrier, at least one of the parents is a carrier. If both are carriers, then they are at 25 percent risk of having an affected child. On the other hand, there are disadvantages to the reporting of such information to parents. Unless education and counseling are available, they may erroneously worry that the child will be affected with a disease related to the carrier status. They may stigmatize the child or otherwise treat the child as different. In addition, the disclosure of the child's carrier status may result in disruption to the family if neither of the social parents is a carrier (which most often indicates that another man fathered the child).
Since numerous tests can be added in a newborn screening program using the initial filter paper spot, the pressure to add new tests may be difficult to resist. Under the American Society of Human Genetics (ASHG) guidelines, however, before tests are added, a rigorous analysis should be made about who will benefit, who will be harmed, and who consents. In state programs for newborn screening, subsequent anonymous uses of samples for research may be undertaken.
Voluntariness of Subsequent Uses
Many state newborn screening programs, as well as research and clinical facilities, store the filter paper spots or other DNA samples for long periods after their initial use in genetic testing. Some states use newborn screening spots to experiment with new tests, and this would seem permissible as long as the samples are not identified and the uses were not anticipated prior to the initial test. 64 If the samples are identified, the person's permission would be required. However, researchers constitute just one group that might want access to the newborn screening spots. Such spots are of interest to law enforcement officials; in one case, police contacted a newborn screening laboratory when they were trying to identify a young murder victim.
The American Society of Human Genetics issued a statement on DNA banking and DNA data banking in 1990. 65 ASHG recommended the purposes for which samples are acquired for DNA analysis be defined in advance:
Later access to DNA samples or to the profiles for other purposes should be permitted only when (a) a court orders the information to be released, (b) the data are to be anonymously studied, or (c) the individual from whom the sample was obtained provides written permission. In general, regardless of the purpose for which it was compiled, this information should be accorded at least the confidentiality that is accorded to medical records. 66
Confidentiality is meant to encourage the free flow of information between patient and physician so that the patient's sickness may be adequately treated. The protection of confidentiality is also justified as a public health matter, since ill people may not seek medical services in the first place if confidentiality is not protected. As a legal matter, confidentiality is generally protected in the doctor-patient relationship. However, genetic testing may not always occur within a doctor-patient relationship: a non-M.D. scientist may undertake the testing, or screening may occur in the employment setting. Moreover, it is not just the result of the test that raises concern about confidentiality. The sample itself may be stored (as in DNA banking or family linkage studies) for future use.
Genetic information is unlike other medical information. It reveals not only potential disease or other risks to the patient, but also information about potential risks to the person's children and blood relatives. The fact that geneticists may wish to protect third parties from harm by breaching confidentiality and disclosing risks to relatives is evidenced in the study by Wertz and Fletcher, cited earlier, in which half of the geneticists surveyed would disclose information to relatives over a patient's refusal. The geneticist's desire to disclose is based on the idea that the information will help the relative avoid harm. Yet this study indicated that about the same number of geneticists would disclose to the relative when the disorder was untreatable as when the disorder was treatable (53 percent would contact a relative about the risk of Huntington disease; 54 percent about the risk of hemophilia A). Since most people at risk for Huntington disease have not chosen testing to see if they have the genetic marker for the disorder, 67 geneticists may be overestimating the relative's desire for genetic information and infringing upon the relative's right not to know. They may be causing psychological harm if they provide surprising or unwanted information for which there is no beneficial action the relative can take.
In the legal realm, there is an exception to confidentiality: A physician may in certain instances breach confidentiality in order to protect third parties from harm, for example, when the patient might transmit a contagious disease 68 or commit violence against an identifiable individual. 69 In a landmark California case, for example, a psychiatrist was found to have a duty to warn the potential victim that his patient planned to kill her. 70
The principle of protecting third parties from serious harm might also be used to allow disclosure to an employer when an employee's medical condition could create a risk to the public. In one case, the results of an employee's blood test for alcohol were given to his employer. 71 The court held the disclosure was not actionable because the state did not have a statute protecting confidentiality, but the court also noted that public policy would favor disclosure in this instance since the plaintiff was an engineer who controlled a railroad passenger train.
An argument could be made that health care professionals working in the medical genetics field have disclosure obligations similar to those of the physician whose patient suffers from an infectious disease or a psychotherapist with a potentially violent patient. Because of the heritable nature of genetic diseases, a health professional who—through research, counseling, examination, testing, or treatment—gains knowledge about an individual's genetic status often has information that would be of value not only to the patient, but to his or her spouse or relatives, as well as to insurers, employers, and others. A counterargument could be made, however, that since the health professional is not in a professional relationship with the relative and the patient will not be harming the relative (unlike in the case of violence or infectious diseases), there should be no duty to warn.
The claims of the third parties to information, in breach of the fundamental principle of confidentiality, need to be analyzed, as indicated earlier, by assessing how serious the potential harm is, whether disclosure is the best way to avert the harm, and what the risk of disclosure might be.
Disclosing Genetic Information to Spouses
The genetic testing of a spouse can give rise to information that is of interest to the other spouse. In the vast majority of situations, the tested individual will share that information with the other spouse. In rare instances, the information will not be disclosed and the health care provider will be faced with the issue of whether to breach confidentiality. When a married individual is diagnosed as having the allele for a serious recessive disorder, the spouse might claim that the health care provider has a duty to share that information with him or her to facilitate reproductive decision making. 72 A few court cases have allowed physicians to disclose medical information about an individual in order to protect a spouse or potential spouse. 73 The foundation for this approach is laid by cases allowing disclosure of communicable diseases. 74 In situations such as disclosure of information about venereal disease or AIDS, the argument is made that sacrificing confidentiality, by notifying spouses and lovers, is necessary for public health and welfare, and is essential as a warning to seriously endangered third parties where the risk of transmission is high.
Since genetic disorders are not communicable to the spouse, a counter argument could be made that there is no legitimate reason for disclosing them. However, the spouse might have a great interest in the genetic information because he or she would like to protect any potential children from risk. Consider the case of a doctor who learns that a young man will later suffer from Huntington disease. The wife would appear to have at least some claim to that information since, if she and her husband have children, there will be a 50 percent chance that each child would inherit the disease. Similarly, each spouse would seem to have a claim to the information that the other was a carrier of a single gene for a recessive defect. Because of the importance of reproductive decisions, such information is crucial to the spouse.
Another instance in which genetic risk information arises in the marriage context is through prenatal screening. A fetus may be found to have an autosomal recessive disorder, which occurs only if both parents transmit the particular gene. If, in the course of prenatal diagnosis, it is learned that the mother is a carrier of the gene but her husband is not, the health care professional has knowledge that the husband is almost certainly not the father of the child. A claim could be made that the health care professional has a duty, or at least a right, to advise the husband of his misattributed paternity, so that he will know that any future children he has will not be at risk for that particular disorder.
On the other hand, an argument could be made that spouses should not be entitled to genetic risk information about a patient, even if it is arguably relevant to their future reproductive plans. 75 The right of reproductive decision making is viewed as the right of the individual. 76 The U.S. Supreme Court has held that a woman can abort without her husband's consent even if this will interfere with her husband's reproductive plans. 77 More recently, the U.S. Supreme Court held that a husband was not even entitled to notice that his wife intends to abort. 78 The court expressed concerns that the husband might react to the disclosure with violence, with threats to withhold economic support, or with psychological coercion. 79 Similar reactions could occur with information about misattributed paternity, particularly because the primary purpose of the testing was not to get paternity information.
Disclosing Genetic Information to Relatives
Blood relatives of the patient may have a more convincing claim than spouses for requiring that health care providers breach confidentiality. They could argue that the information about genetic risks or the availability of genetic testing may be relevant to their own future health care. 80 The strongest case for a warning would exist when there is a high likelihood that the relative has the genetic defect, the defect presents a serious risk to the relative, and there is reason to believe that the disclosure is necessary to prevent serious harm (e.g., by allowing for treatment or by warning the person to avoid harmful environmental stimuli). Malignant hyperthermia is an autosomal dominant genetic condition causing a fatal reaction to common anesthesia. Prompt warning of families can literally save lives, especially from death due to minor surgeries such as setting broken bones in children.
If the patient does not want to inform relatives, however, questions arise as to whether the health care provider or counselor should contact the relative over the patient's refusal. The President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research (1983) recommended that disclosure be made only if (1) reasonable attempts to elicit voluntary disclosure are unsuccessful; (2) there is a high probability of serious (e.g., irreversible or fatal) harm to an identifiable relative; (3) there is reason to believe that disclosure of the information will prevent harm to the relative; and (4) the disclosure is limited to the information necessary for diagnosis or treatment of the relative. 81
Even in the more compelling situation of disclosure to relatives, the health care provider is not in a professional relationship with the relative, and previous legal cases regarding a duty to provide genetic information have all involved a health care provider in a professional relationship with the person to be informed. Although infectious disease cases provide a precedent for warning strangers about potential risks, 82 genetic diseases are simply different from infectious diseases. The only potential argument that the health care professional could make for contacting the relative is that through diagnosis of the patient, the health care professional has reason to believe that the relative is at higher risk than the general population of being affected by a genetic disorder. If disorders are highly likely and are treatable or preventable, many medical geneticists would overrule a patient's refusal to disclose, and would inform a relative. Although there may be no legal obligation to single out relatives as creating a special duty for physicians, the knowledge that a defined, unknowing relative is at high risk for a serious or life-threatening, treatable disease may allow rare exceptions to the principle of confidentiality.
Confidentiality and Discrimination When Third Parties Seek Genetic Information
Many entities may have an interest in learning about people's genetic information. Insurers, employers, bankers, mortgage companies, educational loan officers, providers of medical services, and others have an interest in knowing about a person's future health status. Already, people have been denied insurance, employment, and loans based on their genotype. Such discrimination has occurred both when the information has been obtained through genetic testing and when the information has been obtained in other ways (e.g., inadvertent release of a relative's medical record or disclosure from payment for medical service for a child). 83
In the future, third parties may want access to genetic information or may wish to mandate genetic testing. In child custody cases, one spouse may claim that the other spouse should not get custody because of his or her genetic profile, for example, when the latter person has the gene for a serious, untreatable lateonset disorder. Professional schools (such as medical schools or law schools) may wish to deny admission to someone with such a disorder on the theory that such a person will have a shortened practice span.
Insurers underwriting individual health insurance currently use medical information to determine whether coverage should be granted and to determine how to price a particular policy. According to the Office of Technology Assessment, each year about 164,000 applicants are denied individual health insurance. 84 Far more Americans are covered by group plans—85 to 90 percent—with about 68 percent 85 covered by employment-based group plans rather than by individual plans. Although medical underwriting is not generally done as part of large employers' group policies, medical information is sometimes used against people in other ways in that context. People with medical problems or whose family members have medical problems have been refused jobs because employers do not want their insurance premiums increased due to payments for the care of the employee or the employee's family members.
In addition, employers that self-insure may choose to restrict coverage under their insurance plans so as not to pay for care for existing employees. One major airline already permanently excludes coverage for preexisting conditions for new employees. 86 Other employers have curtailed plan benefits once an employee has been diagnosed as having a particular disorder. In McGann v. H. & H. Music Co., for example, a man was covered by employer-provided commercial insurance that had a million dollar medical benefit maximum. 87 Once the employee was diagnosed as having AIDS, however, the employer switched to self-insurance and established a $5,000 limitation for AIDS, while keeping the million dollar cap for other disorders. The court held that an employer who is self-insured could modify its plan in this way—an ominous decision when one considers that at least 65 percent of all companies and 82 percent of companies with more than 5,000 employees are self-insured. 88 The U.S. Supreme Court decided not to hear the case and let stand the lower court's decision. Employees who are covered by their employers' self-insurance are thus in a precarious position, akin to having no insurance at all:
When one considers that many employees contribute substantial amounts of money to purchase this ''coverage," that many of them forego purchasing other insurance products in reliance on this coverage, and that few of them understand the precise nature of the self-insurance system, the entire system verges on fraud. 89
This is particularly true, given that many people choose jobs because of the health benefits. 90 The Equal Employment Opportunity Commission is reportedly endeavoring to use the Americans with Disabilities Act to challenge companies' practices of setting caps on health insurance payouts for employees with AIDS. 91
The advent of genetic testing, as well as the increasing identification of genetic diseases, makes genetic information, like other medical information, available for use as a basis for medical underwriting in health insurance. The danger, according to one study, is that "genetic testing made possible as we continue to map the human genome may result in many more individuals being denied private insurance coverage than ever before." 92 Genetic tests are not necessary to find out genetic information on applicants. Insurers already obtain genetic information from medically underwritten applicants through family histories and laboratory tests (e.g., cholesterol levels). This was of as much concern to the committee as the use of genetic information from other sources. Although insurers generally do not perform or require genetic tests when doing medical underwriting, they may seek to learn the results of any genetic tests from which an applicant may have information. This could deter people from seeking these tests.
The existence of medical underwriting can lead people to avoid needed medical services:
If people worry that their use of health services may disqualify them from future insurance coverage, they may limit their use of needed services, fail to submit claims for covered expenses, or pressure physicians to record diagnoses that are less likely to attract an underwriter's attention. The last two actions add error to data bases used for health care research and monitoring. 93
A survey of insurers undertaken by the Office of Technology Assessment (OTA) of the U.S. Congress found that insurers see a role for genetic information in medical underwriting. OTA surveyed commercial insurers, Blue Cross and Blue Shield companies, and large health maintenance organizations, which offered individual and medically underwritten small-group health insurance coverage. Data were gathered on underwriting practices, including requirements for diagnostic tests or physical examinations before an insurance policy can be issued. Data on reimbursement practices, as well as general attitudes toward genetic testing, were also obtained.
Insurers generally believed that it was fair for them to use genetic tests to identify those at increased risk of disease; slightly more than one-fourth of medical directors indicated that they disagreed somewhat that such use was fair.
Three-quarters of the responding companies said they thought "an insurer should have the option of determining how to use genetic information in determining risk." 94
OTA's survey of insurers found that genetic information is not viewed as a special type of information. 95 What seems important to insurers when making insurability and rating decisions is the particular condition, not that the condition is genetically based. OTA found that the majority of insurers did not anticipate using specific genetic tests in the future. However, a majority of medical directors from commercial insurers agreed with the statement that "it's fair for insurers to use genetic tests to identify individuals with increased risk of disease." In a comparison survey, OTA found that 14 percent of responding genetic counselors reported that they had clients who had experienced difficulties obtaining or retaining health care coverage as a result of genetic testing.
Surveys by Paul Billings and colleagues, 96 as well as by the Office of Technology Assessment, 97 uncovered specific examples of people being denied health insurance coverage based on their genotype. These incidents include cases in which a person with a positive test for a genetic disorder had his or her insurance canceled or "rated up" as a result; 98 where genetic disorders such as alpha-antitrypsin were defined as preexisting conditions, thus excluding payment for therapy; where a particular genetic condition resulted in exclusion from maternity coverage; 99 and where the birth of a child affected with a serious recessive disorder led to the inability of the parents and unaffected siblings to obtain insurance. 100
Genetic information provides serious challenges to the traditional operation of insurance. Health insurance in this country is premised on the notion that risks can be predicted on a population-wide basis, but not well on an individual basis; thus insurance becomes a mechanism for spreading risks. If, through genetic testing or the use of genetic information acquired by other means, insurers can learn of people's actual future health risks (e.g., the risk of a serious late-onset disorder), the benefit of risk spreading will be lost; the individual will be changed an amount equal to future medical costs, which may in some cases make insurance prohibitively expensive.
Currently it is permissible in most states to do medical underwriting based on genetic information. However, the expansion of genetic testing presents a serious challenge to medical underwriting and could lead to an alternative policy approach in which medical underwriting is eliminated altogether. Originally, health insurance was based on health risks for entire communities, known as community rating, rather than on individual rating of health risks or conditions. Insurers gradually began to offer lower rates to employers based on the generally better health and lower risks of employed persons, and competition ensued among insurers to insure the "best" (i.e., lowest) risks. This has led to many of the problems in our current health insurance system in which some people have become permanently uninsurable. 101 In a system of community rating,
. . there would be no place for [the use of the results of] genetic testing, since applicants would not be rated according to their individual health risks and conditions. 102
Rochester, New York has had a successful system of community rating; a key factor in its success has been the belief of large employers who would normally self-insure that their participation in a system that emphasizes risk sharing and collective strategies to contain costs, results in a system that will keep costs lower over the long term than they would be in a segmented, risk-rated competitive health insurance market. 103 The states of Maine and New York have recently passed legislation requiring health insurers offering policies in their states to return to community rating by 1993. 104 Several other states have introduced legislation to protect people from discrimination based on their genotype. In addition, more general antidiscrimination laws may provide some remedy for people who are discriminated against because of their genotype.
Much of this legislation has been a direct response to the debacle in the early 1970s with respect to sickle cell screening. When mandatory sickle cell screening laws were adopted, some insurers and employers began making decisions about insurance coverage and employment opportunities based on the results of the testing. In particular, carriers of sickle cell trait were denied jobs and charged higher insurance rates without evidence that possession of the trait placed a person at a higher risk of illness or death. 105 As a result, some states have adopted laws protecting people with sickle cell trait. At least two states prohibit denying an individual life insurance 106 or disability insurance, 107 or charging a higher premium, 108 solely because the individual has sickle cell trait. A few states have similarly adopted statutes to prohibit mandatory sickle cell screening as a condition of employment, 109 to prohibit discrimination in employment against people with sickle cell trait, 110 and to prohibit discrimination by unions against people with sickle trait. 111
More recently, some states have adopted laws with a broader scope. A California statute prohibits discrimination by insurance companies against people who carry a gene that has no adverse effects on the carrier, but may affect his or her offspring. 112 Under a Wisconsin law, 113 insurers are prohibited from requiring that applicants undergo DNA testing to determine the presence of a genetic disease or disorder, or the individual's predisposition for a particular disease or disorder. Nor may insurers ask whether the individual has had a DNA test or what the results of the test were. Insurers are also prohibited from using DNA test results to determine rates or other aspects of coverage. However, insurance discrimination based on genetic information not obtained through DNA testing is not forbidden by the law.
There is also much concern about the use of genetic information in the employment context. The Council of Ethical and Judicial Affairs of the American Medical Association has taken the position that it is inappropriate for employers to perform genetic tests to exclude workers from jobs. 114 The opinion acknowledges that the protection of public safety is an important rationale for medical tests of employees. However, the opinion states:
Genetic tests are not only generally inaccurate when used for public safety purposes, but also unnecessary. A more effective approach to protecting the public's safety would be routine testing of a worker's actual capacity to function in a job that is safety-sensitive. 115
The opinion points out that capacity testing is more appropriate because it would not cause discrimination against someone who has the gene for a disorder but who is totally asymptomatic, yet it would "detect those whose incapacity would not be detected by genetic tests, either because of a false-negative test result or because the incapacity is caused by something other than the disease being tested for." 116
In the employment context, a New Jersey law prohibits employment discrimination based on an "atypical hereditary cellular or blood trait." 117 In New York, a statute prohibits genetic discrimination based on sickle cell trait, Tay-Sachs trait, or Cooley anemia (beta-thalassemia) trait. 118 In Oregon, Wisconsin, and Iowa, even more comprehensive laws prohibit genetic screening as a condition of employment. 119
At the federal level, it is still an open question whether the Americans with Disabilities Act (ADA) 120 will provide adequate protection against genetic discrimination. There are three definitions of persons considered to have a disability and, therefore, protected under the statute. Individuals currently with a disability comprise the first group, persons with a history of a disability comprise the second group, and persons who have the appearance of being disabled constitute the third. This later category should protect carriers of genetic disease who are themselves healthy but could be refused employment because they have a high risk of giving birth to a child with a genetic disorder that might be expensive in insurance or health care costs to the employer. This third category for those with the appearance of disability should also protect persons with an increased risk of disease due to genetic susceptibility to breast cancer, or who have a gene for a late-onset disorder such as Huntington disease.
The NIH-DOE Joint Working Group on Ethical, Legal, and Social Implications (ELSI) of the Human Genome Project petitioned the Equal Employment Opportunity Commission (EEOC), which is responsible for implementing the law. ELSI requested that the EEOC broaden its proposed rulemaking to include these protections related to genetic testing and genetic disorders, or susceptibility to a genetic disorder.
However, according to an interpretation by the EEOC, the act does not protect carriers of genetic diseases who are themselves healthy but could be refused employment because they have a 25 percent risk of giving birth to a child with a genetic disorder. Also, the EEOC does not view a person with an increased risk of disease due to genetic factors, or who has the gene for a late-onset disorder such as Huntington disease, as having a disability and thus being protected by the law.
Legislation has been introduced to extend the definition of disability to a "genetic or medically identified potential of, or predisposition toward, a physical or mental impairment that substantially limits a major life activity." 121
Another limitation of the ADA is that it allows employers to request any type of medical testing on an employee after a conditional offer of employment is made. In contrast, statutes in 11 states limit such testing to that which is job related. 122
There may in fact be a narrow set of circumstances in which genetic testing may be appropriate to determine a person's ability to undertake a particular job. For example, a person with an active seizure disorder might be excluded from a job in which he or she could cause serious harm. Such a possibility would seem to be appropriate only if the potential harm were serious and screening were the most appropriate way to avert the harm. The committee was concerned, however, that employers might confuse having the gene for, or a genetic predisposition to, a particular disorder with currently being symptomatic. The possibility that someone, later in life, might become incapable of doing a job does not provide a sufficient rationale for not letting him or her undertake the job at the current time. Consequently, in most situations, periodic medical screening for symptoms rather than genetic screening will be a more appropriate means of determining whether an employee presents a serious risk of harm to third parties. 123
- FINDINGS AND RECOMMENDATIONS
Overall Principles
The committee recommends that vigorous protection be given to autonomy, privacy, confidentiality, and equity. These principles should be breached only in rare instances and only when the following conditions are met: (1) the action must be aimed at an important goal—such as the protection of others from serious harm—that outweighs the value of autonomy, privacy, confidentiality, or equity in the particular instance; (2) it must have a high probability of realizing that goal; (3) there must be no acceptable alternatives that can also realize the goal without breach of these principles; and (4) the degree of infringement of the principle must be the minimum necessary to realize the goal.
The committee recommends that regardless of the institutional structure of the entity offering genetic testing or other genetics services, there be a mechanism for advance review of the new genetic testing or other genetics services not only to assess scientific merit and efficacy, but also to ensure that adequate protections are in place for autonomy, privacy, confidentiality, and equity . The usual standards for review of research should be applied no matter what the setting. In particular, an institutional review board (IRB) should review the scientific and ethical issues related to new tests and services in academic research centers, state public health departments, and commercial enterprises.
These reviews should include any proposed investigational use of genetic tests, as well as more extensive pilot studies. In all instances the review body should include people from inside and outside the institution, including community representatives, preferably consumers of genetic services. In the clinical practice setting, professional societies should be encouraged to review studies and issue guidelines, thereby supplementing the guidance provided by IRBs (see Chapter 3 ).
The committee also recommends that the National Institutes of Health (NIH) Office of Protection from Research Risks provide guidance and training on how review bodies should scrutinize the risks to human subjects of genetic testing . IRBs may also need technical advice from a local advisory group on genetics (see Chapter 1 ). To the extent that a National Advisory Committee on Genetic Testing and its Working Group on Genetic Testing are established (see Chapter 9 ), these bodies should be consulted by IRBs and the NIH Office of Protection from Research Risks.
All laboratories offering genetic testing are included under the Clinical Laboratory Improvement Amendments of 1988 (CLIA88), and the committee recommends that the Health Care Financing Administration expand its existing lists of covered laboratory tests to include the full range of genetic tests now in use (see Chapter 3 ).
New tests, not validated elsewhere, that are added to the battery of tests should be considered investigational if they are used to make a clinical decision . The committee recommends that IRB approval be obtained in universities, commercial concerns, and other settings where new tests for additional disorders are being undertaken, even if the tests rely on existing technologies. IRB approval should be obtained before new tests are added to newborn screening.
Informed Consent
The committee recommends that for a proper informed consent to be obtained from a person who is considering whether to undergo genetic testing, the person should be given information about the risks, benefits, efficacy, and alternatives to the testing; information about the severity, potential variability, and treatability of the disorder being tested for; and information about the subsequent decisions that will be likely if the test is positive (e.g., whether the person will have to make a decision about abortion). Information should also be disclosed about any potential conflicts of interest of the person or institution offering the test (e.g., equity holdings or ownership of the laboratory performing the test, dependence on test reimbursement to cover the costs of counseling, patents). The difficulty in applying the traditional mechanisms for achieving informed consent should not be considered an excuse for failing to respect a patient's autonomy and need for information.
The committee recommends that research be undertaken to determine what patients want to know in order to make a decision about whether or not to undergo a genetic test . People may have less interest in information about the label for the disorder and its mechanisms of action than they have in information about how certainly the test predicts the disorder, what effects the disorder has on physical and mental functioning, and how intrusive, difficult, or effective any existing treatment protocol would be. Research is also necessary to determine the advantages and disadvantages of various means of conveying that information (e.g., through specialized genetic counselors, primary care providers, single-disorder counselors, brochures, videos, audiotapes, and computer programs). People also need to know about potential losses of insurability or employability or social consequences that may result from knowledge about the disorder for which testing is being discussed.
Multiplex Testing
Performing multiple genetic tests on a single sample of genetic material—often using techniques of automation—has been called multiplex testing. The committee recommends that informed consent be gained in advance of such multiplex testing. New means (such as interactive or other types of computer programs, videotapes, and brochures) should be developed to provide people—in advance of testing—with the information described in the previous recommendations, such as descriptions of the nature of tests that are included in multiplex testing and the nature of the disorders being tested for (discussed in Chapter 4 ). A health care provider or counselor should also provide information about each of the tests, or if that is not possible because of the number of tests being grouped together, the provider or counselor should supply information about the categories of disorders so that the person will be able to make an informed decision about whether to undergo the testing.
The committee identified the area of multiplex testing as one in which more research is needed to develop ways to ensure that patient autonomy is recognized . The more general research the committee has advocated on determining what information should be conveyed and how it should be conveyed should be supplemented with additional research dealing with the unique case of multiplex testing where many disorders could be tested for at once, and those disorders may have differing characteristics. In multiplexing, tests should be grouped so that tests requiring similar demands for informed consent and education and counseling may be offered together. Only certain types of tests should be multiplexed; some tests should only be offered individually, especially tests for untreatable fatal disorders (e.g., Huntington disease).
The committee also recommends that research be undertaken to make decisions about which tests to group together in multiplex testing, based on the type of information the tests provide. The committee believes strongly that tests for untreatable disorders should not be multiplexed with tests for disorders that can be cured or prevented by treatment or by avoidance of particular environmental stimuli.
Voluntariness
The committee reaffirms that voluntariness should be the cornerstone of any genetic testing program. The committee found no justification for a state sponsored mandatory public health program involving genetic testing of adults, or for unconsented-to genetic testing of patients in the clinical setting.
Screening and Testing of Children
The committee recommends that newborn screening programs be voluntary. The decision to make screening mandatory should require evidence that—without mandatory screening—newborns will not be screened for treatable illnesses in time to institute effective treatment (e.g., in PKU or congenital hypothyroidism) . The committee bases its recommendation and preference for voluntariness on evidence from studies of existing mandated and voluntary programs that demonstrate that the best interests of the child can be served without abrogating the principle of voluntariness. Voluntary programs have delivered services as well or better than mandated programs. There is no evidence that a serious harm will result if autonomy is recognized, just as there is no evidence that mandating newborn screening is necessary to ensure that the vast majority of newborns are screened.
The committee recommends that newborn screening should not be undertaken in state programs unless there is a clear, immediate benefit to the particular infant being screened . In particular, screening should not be undertaken if presymptomatic identification of the infant and early intervention make no difference, if necessary and effective treatment is not available, or if the disorder is untreatable and screening is being done to provide information merely to aid the parents' (or the infant's) future reproductive plans. The committee recommends that states that screen newborns have an obligation to ensure treatment of those detected with the disorder under state programs, without regard to ability to pay for treatment.
The committee recommends that in the clinical setting, children generally be tested only for disorders for which a curative or preventive treatment exists and should be instituted at that early stage . Childhood screening is not appropriate for carrier status, untreatable childhood diseases, and late-onset diseases that cannot be prevented or forestalled by early treatment. Because only certain types of genetic testing are appropriate for children, tests specifically directed to obtaining information about carrier status, untreatable childhood diseases, or late-onset diseases, should not be included in the multiplex tests offered to children. Research should be undertaken to determine the appropriate age for testing and screening for genetic disorders in order to maximize the benefits of therapeutic intervention and to avoid the possibility that genetic information will be generated about a child when there is no likely benefit to the child in the immediate future.
The majority of the committee recommends that carrier status of newborns and other children be reported to parents only after the parents have been informed of the potential benefits and harms of knowing the carrier status of their children . Because of the risk of stigma for the newborn, such pretest information should be provided to parents when they are informed about newborn screening. Provision should be made for answering any questions the parents may have; these questions are best answered in the context of genetic counseling. The decisions of the parents about whether to receive such information should always be respected (see Chapter 4 ). Where such information is not disclosed after parents are given the option to get such information and then knowingly refuse the information, the courts should take this policy analysis and the recommendation of this committee into consideration and not find liability if parents sue because the carrier status of their child was not disclosed and they subsequently give birth to an affected child. Research is needed on the consequences of revealing carrier status in newborns to identify both harms and benefits from disclosing such information in the future.
Subsequent Uses
The committee recommends that before genetic information is obtained from individuals (or before a sample is obtained for genetic testing), they (or, in the case of minors, their parents) be told what specific uses will be made of the information or sample; how—and for how long—the information or sample will be stored; whether personal identifiers will be stored; and who will have access to the information or sample, and under what conditions . They should also be informed of future anticipated uses for the sample, asked permission for those uses, and told what procedures will be followed if the possibility for currently unanticipated uses develops. The individuals should have a right to consent or to object to particular uses of the sample or information.
Subsequent anonymous use of samples for research is permissible, including in state newborn screening programs. Except for such anonymous use, the newborn specimen should not be used for additional tests without informed consent of the parents or guardian.
If genetic test samples are collected for family linkage studies or clinical purposes, they should not be used for law enforcement purposes (except for body identification). If samples are collected for law enforcement purposes, they should not be accessible for other nonclinical uses such as testing for health insurance purposes.
Disclosure to Spouses and Relatives
As a matter of general principle, the committee believes that patients should be encouraged and aided in sharing appropriate genetic information with spouses . Mechanisms should be developed to aid a tested individual in informing his or her spouse and relatives about the individual's genetic status and informing relatives about genetic risks. These mechanisms would include the use of written materials, referrals for counseling, and so forth.
On balance, the committee recommends that health care providers not reveal genetic information about a patient's carrier status to the patient's spouse without the patient's permission. Furthermore, information about misattributed paternity should be revealed to the mother but should not be volunteered to the woman's partner.
Although confidentiality may be breached to prevent harm to third parties, the harm envisioned by the cases generally has been substantial and imminent. 124 The spouse's claim of future harm due to the possibility of later conceiving a child with a genetic disorder would not be a sufficient reason to breach confidentiality. The committee found no evidence of a trend on the part of people to mislead their spouses about their carrier status. Moreover, since most people do tell their spouses about genetic risks, breaching of confidentiality would be needed only rarely.
The committee believes that patients should share genetic information with their relatives so that the relatives may avert risks or seek treatment . Health care providers should discuss with patients the benefits of sharing information with relatives about genetic conditions that are treatable or preventable or that involve important reproductive decision making. The committee believes that the disadvantages of informing relatives over the patient's refusal generally outweigh the advantages, except in the rare instances described above.
The committee recommends that confidentiality be breached and relatives informed about genetic risks only when attempts to elicit voluntary disclosure fail, there is a high probability of irreversible or fatal harm to the relative, the disclosure of the information will prevent harm, the disclosure is limited to the information necessary for diagnosis or treatment of the relative, and there is no other reasonable way to avert the harm . When disclosure is to be attempted over the patient's refusal, the burden should be on the person who wishes to disclose to justify to the patient, to an ethics committee, and perhaps in court that the disclosure was necessary and met the committee's test.
If there are any circumstances in which the geneticist or other health care professional could breach confidentiality and disclose information to a spouse, relative, or other third party—for example, to an employer—those circumstances should be explained in advance of testing; and, if the patient wishes, the patient should be given the opportunity to be referred to a health care provider who will protect confidentiality.
On a broader scale, the committee recommends that:
- all forms of genetic information be considered confidential and not be disclosed without the individual's consent (except as required by law), including genetic information that is obtained through specific genetic testing of a person as well as genetic information about a person that is obtained in other ways (e.g., physical examination, knowledge of past treatment, or knowledge of a relative's genetic status);
- confidentiality of genetic information should be protected no matter who obtains or maintains that information, including genetic information collected or maintained by health care professionals, health care institutions, researchers, employers, insurance companies, laboratory personnel, and law enforcement officials; and
- to the extent that current statutes do not ensure such confidentiality, they should be amended so that disclosure of genetic information is not required.
The committee recommends that codes of ethics of those professionals providing genetics services (such as those of the National Society of Genetic Counselors (NSGC), or of geneticists, physicians, and nurses) contain specific provisions to protect autonomy, privacy, and confidentiality . The committee endorses the NSGC statement of a guiding principle on confidentiality of test results:
The NSGC support individual confidentiality regarding results of genetic testing. It is the right and responsibility of the individual to determine who shall have access to medical information, particularly results of testing for genetic conditions. 125
The committee also endorses the principles on DNA banking and DNA data banking contained in the 1990 ASHG statement.
To further protect confidentiality, the committee recommends that
- patients' consent be obtained before the patient's name is provided to a genetic disease registry and that consent be obtained before information is redisclosed;
- each entity that receives or maintains genetic information or samples have procedures in place to protect confidentiality, including procedures limiting access on a need-to-know basis, identifying an individual who has responsibility for overseeing security procedures and safeguards, providing written information to each employee or agent regarding the need to maintain confidentiality, and taking no punitive action against employees for bringing evidence of confidentiality breaches to light;
- any entity that releases genetic information about an individual to someone other than that individual ensure that the recipient of the genetic information has procedures in place to protect the confidentiality of the information;
- any entity that collects or maintains genetic information or samples separate them from personal identifiers and instead link the information or sample to the individual's name through some form of anonymous surrogate identifiers;
- the person have control over what parts of his or her medical record are available to which people; if an optical memory card is used, this could be accomplished through a partitioning-off of data on the card; and
- any individual be allowed access to his or her genetic information in the context of appropriate education and counseling, except in the early research phases during the development of genetic testing when an overall decision has been made that results based on the experimental procedure will not be released and the subjects of the research have been informed of that restriction prior to participation.
Discrimination in Insurance and Employment
In general, the committee recommends that principles of autonomy, privacy, confidentiality, and equity be maintained, and the disclosure of genetic information and the taking of genetic tests should not be mandated . Such a position, however, is in conflict with some current practices in insurance and employment.
Although more than half the U.S. population (approximately 156 million people) is covered by some kind of life insurance, 126 the use of genetic information in medical underwriting 127 decisions about life insurance appears to raise different and somewhat lesser concerns than the use of genetic information in health insurance underwriting. More of life insurance has historically been medically underwritten. Complaints of genetic discrimination in life insurance have been made. 128 Apparently, fewer Americans believe that life insurance is a basic right. In contrast, the Canadian Privacy Commission believes that life insurance is a basic right, and recommends that Canadians be permitted to purchase up to $100,000 in basic life insurance without genetic or other restrictions; underwriting for larger amounts of life insurance could be subject to a variety of life-style and health restrictions, including the use of genetic information. 129 Most of the committee agrees with the spirit of the Canadian Commission's recommendation that a limited amount of life insurance be available to everyone without regard to health or genetic status. However, health insurance was considered a much more pressing ethical, legal, and social issue.
The committee recommends that legislation be adopted so that medical risks, including genetic risks, not be taken into account in decisions on whether to issue or how to price health care insurance . Because health insurance differs significantly from other types of insurance in that it regulates access to health care, an important social good, risk-based health insurance should be eliminated. A means of access to health care should be available to every American without regard to the individual's present health status or condition, including genetic makeup. Any health insurance reform proposals need to be evaluated to determine their effect on genetic testing and the use of genetic information in health insurance (see Chapter 7 ).
The committee recommends that the unfair practices highlighted by the McGann case be prevented. Such situations could be eliminated by Congress in three ways. First, the antidiscrimination provision of the Employee Retirement Income Security Act (ERISA, see Chapter 7 ), section 510, could be amended to prohibit various types of employer conduct. For example, the legislation could prohibit: (1) the alteration of benefits or the alteration of benefits without a certain notice period; (2) the reduction of coverage for only a single medical condition; (3) the reduction of benefits after a claim for benefits already had been submitted, and so forth. At the very least, the committee recommends that an amendment be adopted making those practices illegal.
A second way of legislatively preventing McGann-type situations would be to amend the ERISA preemption provision, section 514. By amending this section to limit the preemptive effect of ERISA (e.g., that permits ERISA provisions to override state insurance regulations) or to eliminate ERISA preemption entirely, the result would be to allow the states to regulate self-insured employer benefits in the same way that state insurance commissions regulate commercial health insurance benefits. Although state regulation may be preferable to no regulation, it could lead to the burdensome multiplicity of state regulations that ERISA was intended to eliminate. For this reason, the committee believes that federal prohibition of the type of conduct in the McGann case would be preferable.
A third way to eliminate discrimination in employee health benefits by selfinsured employers would be to amend section 501 of the ADA. The ADA is essentially neutral on the issue of health benefits; clauses on preexisting conditions, medical underwriting, and other actuarially based practices, to the extent permitted by state law, do not violate the ADA. Thus, the ADA could be amended to prohibit differences in health benefits that result in discrimination against individuals with disabilities. Amending the ADA in this manner would, in effect, mandate uniform coverage (although it is not clear what conditions would be covered) at community rates for employees. If Congress wanted to mandate that all employers offer a package of health benefits, a good argument could be made that it ought to do so separately and not via amendments to the ADA.
The committee recommends that legislation be adopted so that genetic information cannot be collected on prospective or current employees unless it is clearly job related. Sometimes employers will have employees submit to medical exams to see if they are capable of performing particular job tasks. The committee recommends that if an individual consents to the release of genetic information to an employer or potential employer, the releasing entity should not release specific information, but instead answer only yes or no regarding whether the individual was fit to perform the job at issue.
The committee recommends that the EEOC recognize that the language of the Americans with Disabilities Act provides protection for presymptomatic people with a genetic profile for late-onset disorders, unaffected carriers of disorders that might affect their children, and people with genetic profiles indicating the possibility of increased risk of a multifactorial disorder. The committee also recommends that state legislatures adopt laws to protect people from genetic discrimination in employment. In addition, the committee recommends an amendment to the ADA (and adoption of similar state statutes) limiting the type of medical testing employers can request or the medical information they can collect to that which is job related.
Ultimately, new laws on a variety of other topics may also be necessary to protect autonomy, privacy, and confidentiality in the genetics field, and to protect people from inappropriate decisions based on their genotypes . 130 The ability of genetics to predict health risks for asymptomatic individuals and their potential offspring presents challenges in the ethical and social spheres. The committee recommends that careful consideration be given to the development of policies for the implementation of genetic testing and the handling of genetic test results .
March of Dimes Birth Defects Foundation, Genetic Testing and Gene Therapy: National Survey Findings 18 (September 1992). New York.
See, e.g., Satz v. Perlmutter, 362 So.2d 160 (Fla. App. 1978) aff'd 379 So.2d 359 (Fla. 1980).
See, e.g., Salgo v. Leland Stanford Jr. Univ. Bd. of Trustees, 154 Cal. App. 2d 560, 317 P.2d 170 (1957); Canterbury v. Spence, 464 F.2d 772 (D.C. Cir.), cert. denied, 409 U.S. 1064 (1972).
Gates v. Jensen, 92 Wash.2d 246, 595 P.2d 919 (1979).
Salgo v. Leland Stanford Jr. Univ. Bd. of Trustees, 154 Cal. App. 2d 560, 317 P.2d 170 (1957).
Kogan v. Holy Family Hospital, 95 Wash.2d 306, 622 P.2d 1246 (1980).
See, e.g., Becker v. Schwartz, 46 N.Y.2d 401, 386 N.E.2d 807, 413 N.Y.S.2d 895 (1978). For a review of relevant cases, see Lori B. Andrews, ''Torts and the Double Helix: Liability for Failure to Disclose Genetic Risks," 29 U. Houston L. Rev. 143 (1992).
L. Andrews, "My Body, My Property," 16(5) Hastings Center Report 28 (1986). See also Moore v. Regents of the University of California.
The federal regulations governing informed consent in the context of human experimentation provide that informed consent is not necessary for research on pathological or diagnostic specimens "if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects." 45 C.F.R. § 46.101(b)(5) (1991).
Similarly, some state human experimentation laws do not seem to extend their coverage to research on removed parts. In Virginia, for example, the law does not cover "the conduct of biological studies exclusively utilizing tissue or fluids after their removal or withdrawal from a human subject in the course of standard medical practice." Va. Code Ann. § 37.1-234(1) (1984). Under the New York law, human research is defined to exclude "studies exclusively utilizing tissue or fluids after their removal or withdrawal from a human subject in the course of standard medical practice." N.Y. Public Health Law § 2441(2) (McKinney 1977).
Office of Technology Assessment (OTA), U.S. Congress, Human Gene Therapy 72 (Washington, D.C.: U.S. Government Printing Office, 1984).
Ferdinand D. Schoeman, "Privacy: Philosophical Dimensions of the Literature," in Philosophical Dimensions of Privacy: An Anthology, ed., Ferdinand D. Schoeman (New York: Cambridge University Press, 1984).
See Judith Jarvis Thomson, "The Right to Privacy," Philosophy and Public Affairs 4(summer):315-333, (1975).
See, e.g., Griswold v. Connecticut, 381 U.S. 479 (1965); Roe v. Wade, 410 U.S. 113 (1973); Planned Parenthood v. Casey,__ U.S._ _, , 112 S.Ct. 2791 (1992).
Lifchez v. Hartigan, 735 F. Supp. 1361 (N.D. III. 1991), affd without opinion sub. nom.; Scholber v. Lifchez, 914 F.2d 260 (7th Cir. 1990), cert. denied, 111 S.Ct. 787 (1991).
Carter v. Broadlawn Medical Center, 667 F. Supp. 1269, 1282 (S.D. Iowa 1987). In that case, the court held that the privacy of patient records in a county hospital is protected by the Fourteenth Amendment's concept of personal liberty. See also Whalen v. Roe, 429 U.S. 589, 599 n. 23 (1977).
Horne v. Patton, 291 Ala. 701, 287 So.2d 824 (1973); MacDonald v. Clinger, 84 A.D.2d 482, 444 N.Y.S.2d 801 (1982).
Privacy Act of 1974, 5 U.S.C. § 552a (1991).
For further discussion of these arguments (and others in this section), see Tom L. Beauchamp and James F. Childress, Principles of Biomedical Ethics, 3rd ed. (New York: Oxford University Press, 1989, chap. 7).
Mark Siegler, "Confidentiality in Medicine—A Decrepit Concept," N. Engl. J. Med. 307: 1518-1521 (1982).
Research has found that people who are told that their answers would not be confidential provide less intimate information. Woods and McNamara, "Confidentiality: Its Effect on Interviewee Behavior," 11 Prof. Psychology 714, 719 (1980).
See, e.g., Horne v. Patton, 291 Ala. 701, 287 So.2d 824 (1973); MacDonald v. Clinger, 84 A.D.2d 482,444 N.Y.S.2d 801 (1982). See W. Prosser and W.P. Keeton, Prosser and Keeton on Torts 856-863 (1984). See also S. Newman, "Privacy in Personal Medical Information: A Diagnosis," 33 U. Fla. L. Rev. 394-424 (1981). According to the latter article, the tort of invasion of privacy has been rejected only in Rhode Island, Nebraska and Wisconsin. Id. at 403. However, two of these states now recognize it by statute. R.I. Gen. Laws § 9-1-28 (1984); Wisc. Stat. § 895.50 (1985-86).
Norman Daniels, "Insurability and the HIV Epidemic: Ethical Issues in Underwriting," 68 The Milbank Quarterly 497-515 (1990). See also Mark A. Rothstein, "The Use of Genetic Information in Health and Life Insurance." In Friedman, T. (ed.) Molecular Genetic Medicine (New York: Academic Press, 1993).
On the natural lottery, see H. Tristram Engelhardt, Jr., Foundations of Bioethics (New York: Oxford University Press, 1986).
See Gene Outka, "Social Justice and Equal Access to Health Care," Journal of Religious Ethics 2 (1974). See also President's Commission for the Study of Ethical Problems in Biomedical and Behavioral Research, Securing Access to Health Care, Vol. 1 : Report (Washington, D.C.: U.S. Government Printing Office, 1983).
Normal Daniels, "Equity of Access to Health Care: Some Conceptual and Ethical Issues," Milbank Memorial Fund Quarterly/Health and Society 60 (1982). See also Norman Daniels, Just Health Care (New York: Cambridge University Press, 1985).
President's Commission for the Study of Ethical Problems in Biomedical and Behavioral Research, Securing Access to Health Care, Vol. 1: Report (Washington, D.C.: U.S. Government Printing Office, 1983), p. 42.
Rothstein, "Genetic Discrimination in Employment and the American with Disabilities Act," 29 Houston L Rev. 23, 31 (1992). See also the discussion infra in this chapter, "Discrimination."
Office of Technology Assessment (OTA), U.S. Congress, Genetic Witness: Forensic Uses of DNA Tests (Washington, D.C.: U.S. Government Printing Office, 1990).
D. C. Wertz and J.C. Fletcher, Ethics and Human Genetics: A Cross-Cultural Perspective (New York: Springer-Verlag, 1989); and D.C. Wertz and J.C. Fletcher, "An International Survey of Attitudes of Medical Geneticists Toward Mass Screening and Access to Results," 104 Public Health Reports 35-44 (1989).
G. Geller, E. Tambor, G. Chase, K. Hofman, R. Faden, N. Holtzman. "How Will Primary Care Physicians Incorporate Genetic Testing: Directiveness in Communication," 31 Medical Care 625-631 (1993).
There are several reasons why institutions store DNA samples, rather than just information from samples. The first is for future potential clinical benefit, such as when a new test may be developed that could provide a more accurate diagnosis. The second is for litigation purposes, so that the sample can be retested if the results are challenged. The third is for research purposes, to use the DNA for the development of additional tests.
Philip Reilly, Presentation to Ethical, Legal, and Social Implications Program Committee, January 1991.
Yoichi Matsubara, Kuniaki Narisawa, Keiya Tada, Hiroyuki Ikeda, Yao Ye-Qi, David M. Danks, Anne Green, Edward R.B. McCabe, "Prevalence of K329E Mutation in Medium-Chain AcylCoA Dehydrogenase Gene Determined from Guthrie Cards," 338 Lancet 552-553 (1991).
Joe Abernathy, "City Health Clinics Unveil Controversial 'Smart Card'," Houston Chronicle, October 11, 1992, sec. A, p. 1.
See, e.g., M. Shaw, "Conditional Prospective Rights of the Fetus," 5 J. Legal Med. 63 (1989).
Moreover, it should be noted that this risk (transmission of genetic disease to offspring) is one that society has always lived with, and seems to have flourished despite that risk.
For example, in The New York Times v. United States, 403 U.S. 713 (1971), the U.S. Supreme Court, in a per curiam opinion held that the government had not met its "heavy burden" of proving that national security required that the Pentagon Papers be suppressed. The logic of the case was explained further in the concurrences; the right of free speech is to be infringed by a prior restraint only when disclosure "will surely result in direct, immediate, and irreparable damage to our Nation or its people." Id. at 730 (Stewart, J., concurring). Or when there is "governmental allegation and proof that publication must inevitably, directly, and immediately cause the occurrence of an event kindred to imperiling the safety of a transport already at sea ..." during wartime. Id. at 726-727 (Brennan, J., concurring).
The standard of irreparability for granting an injunction against protected speech is an absolute, not a comparative standard. Even if the speech could cause great harm, that would not be sufficient. As Justice White pointed out in his concurrence in New York Times, it is not sufficient that there may be "substantial damage to public interests." Id. at 731 (White, J., concurring). Similarly, Justice Stewart said "I am convinced that the Executive is correct with respect to some of the documents involved [i.e., they should not, in the national interest, be published]. But I cannot say that disclosure of any of them will surely result in direct, immediate, and irreparable harm to our Nation or its people. That being so, there can under the First Amendment be but one judicial resolution of the issue before us." Id. at 730 (White, J., concurring).
Even if irreparable harm were a possibility, New York Times indicates that an injunction should not be issued against the press unless such harm would come about directly and immediately. The term "immediately" is easy enough to understand; it requires a present, not future, harm. The term "directly" relates to the lack of intervening influences during that time period. The irreparable harm would not occur directly if another important influence would or could intervene. Another way of expressing the immediacy and directness that is necessary is by saying the harm is "inevitable"—it will occur within a short period of time during which nothing will or could change it or stop it.
Even when a prior restraint is not at issue, high standards are required for showing a compelling state interest when a fundamental right is at issue. Also in the First Amendment area, speech that is not false should not be the basis for subsequent punishment unless it provided an immediate threat of serious harm. (See, e.g., Bridges v. California, 314 U.S. 252, 263 (1941) ("the substantial evil must, be extremely serious and the degree of imminence extremely high before utterances can be punished").)
AIDS, of course, is an infectious disease that cannot be cured and that is strongly identified with certain minority groups (e.g., homosexuals). It is interesting to note that for many of the same reasons that are applicable to mandatory genetic screening, mandatory AIDS screening has not been adopted. Instead, anonymous voluntary screening has been the model.
C. Damme, "Controlling Genetic Disease Through Law," 15 U. Cal. Davis L. Rev. 801, 807 (1982).
Such charges were leveled by blacks when mandatory sickle cell carrier screening was put into place.
L. Andrews, Medical Genetics: A Legal Frontier 233 (1987).
A. G. Motulsky, "The Significance of Genetic Disease," 59, 61 in B. Hilton, D. Callahan, M. Harris, P. Condliffe, B. Berkley, eds., Ethical Issues in Human Genetics: Genetic Counseling and the Use of Genetic Knowledge (Fogarty International Proceedings No. 13, 1973).
Statement of D. Brock in B. Hilton et al., eds., id. at 90.
The idea of choosing by category was discussed by Alta Charo, J.D., at the committee's June 1992 workshop.
e.g., Cobbs v. Grant, 8 Cal.3d 829, 104 Cal. Rptr. 505, 502 P.2d 1, 12 (1972). Some states' informed consent statutes explicitly recognize a right to refuse information. Alaska Stat. § 09.55.556(b)(2) (1983); Del. Code Ann. tit. 18, § 6852(b)(2) (Supp. 1984); N.H. Rev. Stat. Ann. § 507-C:2(II)(b)(3) (1983); N.Y. Public Health Law § 2805-d(4)(b) (McKinney 1985); Or. Rev. Stat. § 677.097(2) (1985); Utah Code Ann. § 78-14-5(2)(c) (1977); Vt. Stat. Ann. tit. 12, § 1909(c)(2) (Supp. 1991); Wash. Rev. Code Ann. § 7.70.060(2) (Supp. 1991).
Prince v. Massachusetts, 321 U.S. 158, 170 (1944).
In re Green, 448 Pa. 338, 292 A.2d 387, 392 (1972). See also Brown and Truit, "The Right of Minors to Medical Treatment," 28 DePaul L. Rev. 289, 299 (1979).
Jehovah's Witnesses v. King County Hospital 278 F. Supp. 488 (W.D. Wash. 1967), 390 U.S. 598 (1968), denied, 391 U.S. 961 (1968).
D.C. Code Ann. § 6-314(3) (1989); Md. Health-Gen. Code Ann. § 13-102(10) and 109(e)(f) (1982).
Iowa Admin. Code § 641-4.1 (136A) (1992); Mich. Comp. Laws Ann. § 333.5431(1) (West 1992); Mont. Code Ann. § 50-19-203(1) (1991); W. Va. Code Ann. § 16-22-3 (Supp. 1992).
Mo. Ann. Stat. § 191.331(5) (Vernon 1990); S.C. Code § 44-37-30(B) (1991).
Council of Regional Networks for Genetic Services (CORN), Newborn Screening: 1990, Final Report (February 1992). New York.
R. R. Faden, A. J. Chwalow, N. A. Holtzman, and S. Horn, "A Survey to Evaluate Parental Consent As Public Policy for Neonatal Screening," 72 Am. J. Pub. Health 1347 (1982).
"Consensus Statement Proposed for Routine Newborn Genetic Screening." Based on October 1989 conference in Quebec, Canada. Reported in Bartha Maria Knoppers and Claude M. LaBerge (eds.), "Genetic Screening: From Newborns to Data Typing," Excerpta Medica 382 (1990).
Currently, Colorado and Wyoming include cystic fibrosis testing as a part of their mandatory newborn screening program; Wisconsin includes cystic fibrosis in newborn screening as part of an experimental research protocol.
Neil A. Holtzman, "What Drives Neonatal Screening Programs," 325 New Engl. J. Med. 802809 (Sept. 12, 1991), referring to K.B. Hammond, S.H. Abman, R.J. Sokol, F.J. Accurso, "Efficacy of Statewide Newborn Screening for Cystic Fibrosis by Assay of Trypsinogen Concentration, 325 New Engl. J. Med. 769-74 (1991).
Id., citing P. Farrell, personal communication.
Norm Fost presentation, June 1992 committee workshop.
Statement of Claude LaBerge at June 1992 committee meeting.
See T. McNeil, B. Harty, T. Thelin, E. Aspergren-Jansson, T. Sveger, "Identifying Children at High Somatic Risk: Long-Term Effects on Mother-Child Interactions," Acta-Psychiatrica Scandinavica 74(6):555-562 (December 1986).
Ellen Wright Clayton, "Screening and Treatment of Newborns," 29 Houston L. Rev. 85 (1992).
The federal regulations governing informed consent in the context of human experimentation provide that informed consent is not necessary for research on pathological or diagnostic specimens "if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects." 45 C.F.R. § 46.101(b)(4)(1991).
Similarly, some state human experimentation laws do not seem to extend their coverage to research on removed parts. In Virginia, for example, the law does not cover "the conduct of biological studies exclusively utilizing tissue or fluids after their removal or withdrawal from a human subject in the course of standard medical practice." Va. Code Ann. § 37.1-234(1) (1990). Under the New York law, human research is defined to exclude "studies exclusively utilizing tissue or fluids after removal or withdrawal from a human subject in the course of medical practice."
Some researchers argue that blood and urine left over after a patient's tests are done should be available without requiring the patient's informed consent. However, the issue is not as straightforward as it might seem. Research surreptitiously done on a patient's blood might generate information that could be damaging to the patient. If a cystic fibrosis test were being developed with excess blood from a PKU test, and the blood tested positive for cystic fibrosis, it could be argued that, depending on how reliable the test seemed, the infant's parents should be informed. But if the result ultimately turned out to be a false positive, the family may have been harmed by unnecessary worry. With respect to research on leftover blood from adults, if testing is being developed for a potentially stigmatizing disorder (such as AIDS) or a disorder that might influence employment or other opportunities for the person (such as Huntington disease) the risks to the patient if confidentiality were compromised might be so high that it would seem unethical not to solicit the individual's consent before the research is undertaken.
ASHG Ad Hoc Committee on Individual Identification by DNA Analysis, "Individual Identification by DNA Analysis: Points to Consider," Am. J. Hum. Genet. 46:631-634 (1990).
Id. at 632.
Nancy Wexler, "The Tiresias Complex: Huntington's Disease as a Paradigm of Testing for Late-Onset Disorders," FASEB Journal 6:2820-2825 (1990).
See, e.g., Skillings v. Allen, 143 Minn. 323, 173 N.W. 663 (1919); Davis v. Rodman, 147 Ark. 385, 227 S.W. 612 (192 1). For a more recent case, regarding a duty to warn third parties of communicable diseases, see Gammill v. U.S., 727 F.2d 950 (10th Cir. 1984).
Tarasoffv. Regents of the University of California, 131 Cal. Rptr. 14, 17 Cal. App. 3d 425, 551 P.2d 334 (1976).
Collins v. Howard, 156 F. Supp. 322, 325 (S.D. Ga. 1957) (dicta).
The individual generally asks that his or her spouse be informed as well. Statement of J. Lejeune in B. Hilton, D. Callahan, M. Harris, P. Condliffe, B. Berkeley, eds., Ethical Issues in Human Genetics: Genetic Counseling and the Use of Genetic Knowledge, 70 (Fogarty International Proceedings No. 13, 1973).
In a March of Dimes-sponsored national public opinion survey, 71 percent of respondents said that if a doctor of a woman who plans to have children finds through testing that her children might inherit a serious or fatal genetic disease, the doctor has an obligation to tell her husband. March of Dimes Birth Defects Foundation, Genetic Testing and Gene Therapy: National Survey Findings 7 (New York, September 1992). However, in some instances, an individual may or may not want personal genetic information disclosed to his or her spouse.
Berry v. Moensch, 8 Utah 2d 191, 331 P.2d 814 (1958); Curry v. Corn, 52 Misc.2d 1035, 277 N.Y.S.2d 470 (1966) (during marriage, each has the right to know the existence of any disease that may have bearing on the marital relation).
See, e.g., Simonsen v. Swenson 104 Neb. 224, 177 N.W. 831 (1920).
The man whose nonpaternity is shown through prenatal screening might argue that, in addition to its relevance to his future childbearing plans, the information that he is not the father of his wife's child has an immediate financial implication since he might not wish to support the child. However, state paternity statutes preserve that a child born during a marriage is the husband's child and require him to support the child, even if it could conceivably be shown through genetic testing that he was not the biological father of the child. The logic behind such cases is that there is a societal interest in the integrity of the family.
Eisenstadt v. Baird, 405 U.S. 438 (1972).
Planned Parenthood v. Danforth, 428 U.S. 52 (1976).
Planned Parenthood v. Casey,__ U.S. , 112 S.Ct. 2791 (1992).
If a patient is the carrier of the gene for a serious autosomal recessive disorder, his or her relatives might also argue that they would be harmed by not knowing that they, too, are at risk of having children with that disorder. However, the risk to future offspring may be too remote to warrant breaching confidentiality, as it is in the case of a spouse.
The President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research, Screening and Counseling for Genetic Conditions 6 (1983).
See, e.g. Simonsen v. Swenson, 104 Neb. 224, 177 N.W. 831 (1920).
In one instance, for example, a woman was denied disability insurance when her father's medical records were released to the insurer.
Office of Technology Assessment, U.S. Congress, Medical Testing and Health Insurance 73 (1988).
S. Rep. 100-360, 100th Cong., 1st Sess. 20 (1988).
Report of Committee on Employer-Based Health Benefits, citing Seeman (1993).
McGann v. H. & H. Music Co., 946 F.2d 401 (5th Cir. 1991 ), cert. denied sub nom.; Greenberg v. H. & H. Music Company,__U.S.__ 112 S.Ct. 1556 (1992).
Eric Zicklin, "More Employers Self-Insure Their Medical Plans, Survey Finds," Business and Health 74 (April 1992).
Mark Rothstein, "The Use of Genetic Information in Health and Life Insurance," in Molecular Genetic Medicine, ed., Ted Friedman (New York: Academic Press, 1993).
According to American Healthline, Briefing on Health Insurance, November 17, 1992, more than half of Americans would not accept a job that did not provide health insurance.
"EEOC Said Ready to 'Fast Track' Complaints of Insurance Caps under Title I of the ADA," 7 No. 18 AIDS Policy & Law 1-2 (October 2, 1992).
N. Kass, "Insurance for the Insurers," Hastings Center Report, 6-11 (November-December 1992).
Institute of Medicine (IOM), National Academy of Sciences, M. Field and D. H. Shapiro (eds.) Employment and Health Benefits: A Connection at Risk. Committee on Employer-Based Health Insurance (Washington, D.C.: National Academy Press, 1993).
OTA, 1992a, p. 180.
OTA, 1992b.
See, e.g., P.R. Billings, M.A. Kohn, M. de Cuevas, J. Beckwith, J.S. Alper, M.R. Natowicz, "Discrimination as a Consequence of Genetic Testing," 50 Am. J. Hum. Genet. 476-482 (1992).
U.S. Congress, Office of Technology Assessment, Cystic Fibrosis and DNA Tests: Implications of Carrier Screening (Washington, D.C.: U.S. Government Printing Office, 1992a).
The disorders included adult polycystic kidney disease, Huntington disease, neurofibromatosis, Marfan syndrome, Down syndrome, Fabray disease.
The conditions included a balanced translocation.
The disorder was cystic fibrosis.
Kass, 1992.
Report of Institute of Medicine Committee on Employer-Based Health Benefits.
See Kass, 1992 for descriptions of these plans.
P. Reilly, Genetics, Law and Social Policy 62-86 (Cambridge, Mass.: Harvard University Press, 1977).
Fla. Stat. Ann. § 626.9706(1) (West 1984); La. Rev. Stat. Ann. § 22:652.1(D) (West Supp. 1992).
22 Fla. Stat. Ann. § 626.9707(1) (West 1984); La. Rev. Stat. Ann. § 22:652. 1(D) (West Supp. 1992).
Fla. Stat. Ann. § 626.9706(2) (West 1984) (life insurance), § 626.9707(2) (West 1984) (disability insurance); La. Rev. Stat. Ann. § 22:652.1(D) (West Supp. 1992).
This same law appears in three places in the Florida statutes: Fla. Stat. Ann. § 448.076 (West 1981); § 228.201 (West Supp. 1989); and § 63.043 (West 1985).
Fla. Stat. Ann. § 448.075 (West 1981); N.C. Gen. Stat. § 95-28. 1(1989); La. Rev. Stat. Ann. § 23: 1002(A) (West 1985).
La. Rev. Stat. Ann. § 23:1002(C)(I) (West 1985).
Cal. Ins. Code § 10143 (West Supp. 1992).
1991 Wisc. Act 269, codified as Wisc. Stat. Ann. § 631.89.
Council on Ethical and Judicial Affairs, "Use of Genetic Testing by Employers," 266 JAMA 1827 (1991).
Id. at 1828.
N.J. Stat. Ann. § 10:5-12(a) (West Supp. 1992).
N.Y. Civ. Rights Law § 48 (McKinney 1992).
1992 Iowa Legis. Serv. 93 (West); Or. Rev. Stat. § 659.227 (1991); 1991 Wis. Laws 117.
104 Stat. 327 (1991). For sections of the Americans With Disabilities Act relating to employment, see 42 U.S.C.A. § 12101-12117 (Supp. 1992).
L. Gostin and W. Roper. "Update: The Americans with Disabilities Act," Health Affairs 11(3):248-258.
Alaska Stat. § 18.80.220(a)(1) (1991); Cal. Gov't Code § 12940(d) (West Supp. 1991); Colo. Rev. Stat. § 24-34-402(1)(d) (1988); Kan. Stat. Ann. § 44-1009(a)(3) (Supp. 1991); Mich. Comp. Laws Ann. § 37.1206(2) (West 1985); Minn. Stat. Ann. § 363.02(1)(8)(i) (West Supp. 1991); Mo. Ann. Stat. § 213.055.1(1)(3) (Vernon Supp. 1992); Ohio Rev. Code Ann. § 4112.02(E)( 1) (Anderson 1991); 43 Pa. Cons. Stat. Ann. § 955(b)(1) (1991); R.I. Gen. Laws § 28-5-7(4)(A) (Supp. 1991); Utah Code Ann. § 34-35-6(1)(d) (Supp. 1991).
Office of Technology Assessment (OTA), U.S. Congress, Genetic Screening in the Workplace, OTA-BA-456 (Washington, D.C.: U.S. Government Printing Office, 1990).
See, e.g., Simonsen v. Swenson, 104 Neb. 224, 177 N.W. 831 (1920); Tarasoff v. Regents of the University of California, 131 Cal. Rptr. 14, 17 Cal. App. 3d 425, 551 P.2d 334 (1976).
National Society of Genetic Counselors (NSGC), "Guiding Principles," Perspectives on Genetic Counseling (October 1991).
American Council on Life Insurance, 1992 Life Insurance Fact Book 19 (1992).
Medical underwriting is the evaluation of a person's insurability, usually assessed through a combination of answers to a written questionnaire and physical examination to identify certain conditions determined by medical underwriters (and underwriting manuals) to reduce life expectancy below actuarial norms. Standards for medical underwriting vary substantially by insurance company, and underwriting decisions are considered crucial business decisions by insurers and are thus considered "trade secrets."
Paul Billings, "Testimony Before Human Resources and Intergovernmental Relations Subcommittee of the Committee on Government Operations," U.S. House of Representatives, 102nd Congress, July 23, 1992.
Canadian Privacy Commission, Genetic Testing and Privacy (Ottawa, 1992).
Neil A. Holtzman and Mark A. Rothstein, "Invited Editorial: Eugenics and Genetic Discrimination," 50 Am. J. Hum. Genet. 457-459 (1992).
- Cite this Page Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, Fullarton JE, Holtzman NA, et al., editors. Assessing Genetic Risks: Implications for Health and Social Policy. Washington (DC): National Academies Press (US); 1994. 8, Social, Legal, and Ethical Implications of Genetic Testing.
- PDF version of this title (3.1M)
In this Page
Other titles in this collection.
- The National Academies Collection: Reports funded by National Institutes of Health
Recent Activity
- Social, Legal, and Ethical Implications of Genetic Testing - Assessing Genetic R... Social, Legal, and Ethical Implications of Genetic Testing - Assessing Genetic Risks
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Genetic Testing Overview
- Genetic Testing FAQs
- Who Should Get Genetic Testing?
- Hereditary Cancer Syndromes
Pros & Cons of Genetic Testing
Genetic testing for cancer looks for specific inherited changes (mutations) in a person’s genes that are associated with a high-to-moderate increased risk of cancer. And while there are certainly benefits to being tested for these mutations, it is important to understand that there are also limitations. For example, a positive result from cancer genetic testing doesn’t necessarily mean that you will develop cancer but can weigh heavily on the minds of you or your loved ones. On the other hand, a negative result doesn’t guarantee that you won’t develop cancer.
At Rocky Mountain Cancer Centers, we feel that in order to make the best decision you must first weigh the pros and cons. In this section, we want to help you understand both the advantages and disadvantages of genetic testing for cancer.
Some advantages, or pros, of genetic testing, include:
- A sense of relief from uncertainty
- A greater understanding of your health and your cancer risk
- Information to help make informed medical and lifestyle decisions
- Opportunity to help educate other family members about the potential risk
Some disadvantages, or risks, that come from genetic testing can include:
- Testing may increase your stress and anxiety
- Results in some cases may return inconclusive or uncertain
- Negative impact on family and personal relationships
- You might not be eligible if you do not fit certain criteria required for testing
If genetic testing is something that interests you and you would like to learn more about it, please visit our Genetic Testing FAQs page .
- For Individuals & Families
- For Employers & Employees
- For Physicians
- Patient Portal
- For Prospective Physicians
- Cost of PartnerMD
- Find a Doctor
- Find a Location
- Learning Center
- Health Insurance
« View All Posts
The Pros and Cons of Genetic Testing
December 21st, 2022 | 3 min. read
By Jim Mumper, M.D.

Genetic testing continues to increase in popularity. However, it is not for everyone . Results of genetic testing can often be uninformative and ultimately can cause more stress and anxiety over the possibility of a disease you may never get.
Genetic testing should be encouraged only when there is effective therapy available to prevent or treat the condition tested for. There is little value in genetic tests that do not allow you to take action to reduce or change your risk for a particular disease.
In other words, genetic testing is a good idea only when the pros of genetic testing outweigh the cons of your situation. It’s shouldn’t be a one-size-fits-all approach.
It’s important to talk to your doctor about your motivations and concerns so you can make the best decision for your health.
So what are the pros of genetic testing? What are the cons? Let’s dive in.
What are the pros of genetic testing?
1. treatment of disease.
If you already have a disease, understanding whether you have a genetic variant could inform treatment protocols.
For example, women with breast cancer often struggle with whether they should undergo chemotherapy.
A 2018 study published in the New England Journal of Medicine found “that many women with early-stage invasive breast cancer could safely forgo chemotherapy, if they score in the mid-range or lower for risk that their cancer will recur, as measured by a commonly used genomic test .”
The right genetic test for the right individual might provide information that would allow a doctor to recommend a different type of treatment. This is where genetic tests can be highly valuable.
2. Lifestyle changes for disease prevention.
If you don’t already have a disease, knowing you have a genetic variant for a particular disease could lead you to make positive lifestyle/behavioral changes to help lower the risk of getting that disease.
This can be useful for a disease such as Alzheimer’s. If you know you are more at risk for developing Alzheimer’s due to a genetic variant, you can change your lifestyle to try to lower your risk ahead of time.
3. Stress relief from lack of genetic variants.
Learning whether you do or don’t have a genetic variant can often provide relief from the “fear of the unknown.”
Think about the stress that comes from an online search of a simple symptom and the litany of diseases that appear as a result. It’s worrisome for everyone.
For some types of cancer and other diseases, genetic testing can reveal that you are not predisposed to develop that disease, which could reduce your stress.
What are the cons of genetic testing?
1. a negative test could mask additional causes..
The result of any genetic test does not mean you definitely will not get a certain disease. It simply means you don’t have the genetic variant for that particular disease.
Diseases have other causes, such as environmental factors (like toxins in the air or water) and lifestyle habits (like an unhealthy diet or smoking). Just because a genetic test turns up negative doesn’t make it a lock that you won’t develop that disease.
2. A positive test could unnecessarily increase stress.
Just like knowledge could decrease stress if it comes back negative, a positive test can also unnecessarily increase stress.
If a genetic test comes back positive for a certain disease, it doesn’t mean you will automatically get that disease.
You could get a positive test in your 40s and spend the rest of your life worried about whether that disease is going to come. And it may not. A positive genetic test just means you’re at a greater risk to develop it down the line, but doesn't guarantee anything.
There’s also the risk of “genetic purgatory.” You could have a gene that’s tested as a “variant of unknown significance,” or VUS, resulting in the mind game of “maybe it’s bad, maybe it isn’t.”
This can lead to mental anguish or worse — unnecessary medical interventions.
3. The cost of genetic testing can be high.
While the cost of genetic sequencing has dropped steadily since its inception in the late 1980s, the National Human Genome Research Institute estimates the cost at around $1,000. As for health insurance coverage, that can vary as well, including partial coverage or complete coverage, depending on the test.
4. Genetic testing can come with privacy concerns.
Privacy concerns plague all of us in this digital world, and the same is true for genetic testing. Who controls the info? Who has access?
According to the National Center for Biotechnology Information , the Health Insurance Portability and Accountability Act (HIPAA) “does not extend to DTC genetic testing companies" because they are not defined as "covered entities" under HIPAA.
5. You could get an inadequate interpretation of your results.
Qualified interpretation of results is essential. Not everyone is qualified to interpret results. Direct-to-consumer kits can prove especially problematic for this reason. This is why genetic counseling exists.
The National Society of Genetic Counselors says, “Genetic counselors are healthcare professionals with unique specialized graduate degrees and experience in the areas of both medical genetics and counseling. Genetic counselors work as members of a healthcare team, providing risk assessment, education, and support to individuals and families at risk for, or diagnosed with, a variety of inherited conditions. Genetic counselors also interpret genetic testing, provide supportive counseling, and serve as patient advocates.”
Genetic Testing at PartnerMD
PartnerMD believes that the highest level of care is individualized, personal, and based on our knowledge of you as a person.
We follow the directive of the American Medical Association’s Code of Medical Ethics, which states, “Physicians should not encourage testing unless there is effective therapy available to prevent or ameliorate the condition tested for.”
If you are ready to take the next step, we recommend having a conversation with your doctor to figure out if it is the right fit for you. In addition, check out these resources for more information:
What is Genetic Testing?
5 genetic testing questions you need to ask.
- Is Genetic Testing Right for Everyone?
- What is Genetic Counseling and Why is it Important?
Jim Mumper, M.D.
As a family medicine physician and Chief Medical Officer of PartnerMD, Dr. Jim Mumper brings over 30 years of experience in primary care. Every time he sees you, his goal is to show kindness and meet your needs. He co-founded PartnerMD to focus on personalized, preventive care. Dr. Mumper's leadership has been vital in establishing PartnerMD as a leading concierge medical practice dedicated to patient-centered care.
Don't forget to share this post:
Related Articles
What is opendna what can it tell you about your heart health.
July 11th, 2024 | 2 min. read
What is Genetic Counseling? Why is it Important?
January 2nd, 2023 | 3 min. read
December 27th, 2022 | 3 min. read
December 16th, 2022 | 3 min. read
Your Family Health History Offers Clues to Your Genetic Profile
October 24th, 2018 | 3 min. read
Do Your Genes Affect How Long You'll Live?
September 26th, 2018 | 3 min. read
DNA Testing: Curiosity vs. Medical Necessity
September 6th, 2018 | 3 min. read
How Knowing Your Family Medical History Can Change Your Life
July 20th, 2016 | 2 min. read

IMAGES
VIDEO
COMMENTS
Get a custom essay on Genetic Testing: Advantages and Disadvantages. At the same time, I acknowledge all the benefits that genetic testing can bring in terms of diagnosing a wide range of diseases and conditions. Fearing that they might discover hereditary predispositions to some untreatable diseases, many people choose not to get tested.
Pros and Cons of Genetic Testing: What to Know Before You Go. Genetic testing, when appropriate, is a powerful tool to gauge a patient's risk for disease. A Michigan Medicine genetic counselor explains the process. On the surface, the concept seems like a no-brainer: A sample of blood or saliva can offer clues to your body's genetic defects ...
Genetic testing is a type of health program that involves the identification of any changes in genes, chromosomes, and proteins. Here are 12 Pros and Cons of Genetic Testing. Find out what is, why it is needed, how the genetic testing is done, advantages & disadvantages of it and how accurate it can be before taking.
What Are the Advantages and Disadvantages of DTC Genetic Testing? The advantages of DTC genetic testing can be described as follows [1,2]. First, DTC genetic testing may provide an opportunity for consumers to recognize the importance of genetics in diverse phenotypes, including diseases. If the test results indicate that a consumer has a ...
Genetic testing has potential benefits whether the results are positive or negative for a gene mutation. Test results can provide a sense of relief from uncertainty and help people make informed decisions about managing their health care. For example, a negative result can eliminate the need for unnecessary checkups and screening tests in some ...
Overview. Genetic testing involves examining your DNA, the chemical database that carries instructions for your body's functions. Genetic testing can reveal changes (mutations) in your genes that may cause illness or disease. Although genetic testing can provide important information for diagnosing, treating and preventing illness, there are ...
Testing can only reveal what scientists know so far about the link between genes and disease. It can tell you if you have the rare genetic mutation that appears to raise one's lifetime risk of ...
In general, the advantages and disadvantages of genetic testing are numerous, and people have to understand that it is impossible to predict the results, as well as to be ready for the information. Serious decisions should be made, and significant steps should be taken by people who use genetic testing. Geneticists have to be ready to cooperate ...
Genetic Tests: Pros and Cons. Topic: Genetics Words: 640 Pages: 2. Technological advancements enable people to access high-quality healthcare services and a larger bulk of data related to their health status. One of the recent innovations that are seen as revolutionary became the democratization of genetic testing.
Here are some cons of genetic testing: 1. Triggers Negative Emotions. Learning that you have a higher risk for health problems can be stressful. Even if you know you have a family history when it comes to a certain disease, seeing it on your DNA results or waiting for confirmation can be a nerve-wracking experience.
Applied Clinical Genomics is the application of genetic information to the clinical setting, including improved diagnosis of disease and tailored treatment efficacy and safety. By discovering and defining the genes that underlie susceptibility to disorders, genetic information can be used to identify and better define those genes that play ...
Each new genetic test that is developed raises serious issues for medicine, public health, and social policy regarding the circumstances under which the test should be used, how the test is implemented, and what uses are made of its results. ... Research is also necessary to determine the advantages and disadvantages of various means of ...
Some advantages, or pros, of genetic testing, include: A sense of relief from uncertainty. A greater understanding of your health and your cancer risk. Information to help make informed medical and lifestyle decisions. Opportunity to help educate other family members about the potential risk.
My current opinion is that despite the many advantages of genetic testing, the disadvantages still outweigh them. I feel this way for a variety of reasons: 1) Preimplantation Genetic Diagnosis is eerily similar eugenics; 2) Discrimination may occur as a result of the information provided by genetic testing; 3) Abnormal results may cause ...
Genetic tests may be used to identify increased risks of health problems, to choose treatments, or to assess responses to treatments." In this essay I will be writing about what genetic testing is, the different types of testing done, the advantages of getting tested, and some of the disadvantages of getting tested. …show more content…
Genetic testing may have limited useful and reliable applications especially in the case of diseases whose genes are few and have been correctly identified. Huntington gene is one example. People with Huntington disease have 36 to more than 120 CAG (Huntington disease is also known as CAG trinucleotide repeat expansion). People with 36 to 40 ...
Introduction to Genetic Testing: Currently, genetic testing is a voluntary test. It is taken to identify the presence of a gene that causes disease or to identify mutations that can lead to a disease. Chromosomes, proteins, and genes are tested through several different methods, including molecular, chromosomal, and biochemical methods.
2. A positive test could unnecessarily increase stress. Just like knowledge could decrease stress if it comes back negative, a positive test can also unnecessarily increase stress. If a genetic test comes back positive for a certain disease, it doesn't mean you will automatically get that disease. You could get a positive test in your 40s and ...
Genetic predictive testing is a good option for at-risk individuals to know if they will develop the disease. Therefore in this paper, I will discuss HD genetic testing advancements, as well as the advantages and disadvantages of the test. HD is an inherited neurological disorder that results in involuntary movements as well as cognitive and ...