- Search Menu
- Sign in through your institution
- The Journals of Gerontology, Series A (1995-present)
- Journal of Gerontology (1946-1994)
- Advance Articles
- Editor's Choice
- Supplements
- Special Issues
- Translational articles
- Calls for Papers
- Author Guidelines
- Biological Sciences Submission Site
- Medical Sciences Submission Site
- Why Submit to the GSA Portfolio?
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About The Journals of Gerontology, Series A
- About The Gerontological Society of America
- Editorial Board - Biological Sciences
- Editorial Board - Medical Sciences
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- GSA Journals
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
C ognitive d ecline, d epression, t he h ormonal f ountain of y outh, f railty /s arcopenia, c ardiovascular d isease, i mmune s ystems and a ging, “t he m erchants of i mmortality ”, s ystems in g eriatrics, c onclusion.
- < Previous
The Top 10 Hot Topics in Aging
- Article contents
- Figures & tables
- Supplementary Data
John E. Morley, The Top 10 Hot Topics in Aging, The Journals of Gerontology: Series A , Volume 59, Issue 1, January 2004, Pages M24–M33, https://doi.org/10.1093/gerona/59.1.M24
- Permissions Icon Permissions
I enjoy talking with very old people. They have gone before us on a road by which we, too, may have to travel, and I think we do well to learn from them what it is like. —Socrates, in Plato's The Republic
EACH year in January, I have tried to review the cutting edge of geriatrics over the previous 2 years ( 1 , 2 ). This review is based to some extent on the high impact articles in the literature ( 3 , 4 ), but also on emerging areas. The Journals of Gerontology Series A also continue to welcome articles from some of our distinguished colleagues who have gone before us on the exploration of the wonders of aging and remain active contributors to the field of gerontology ( 5–8 ). This year, being my last year as editor of the Journal of Gerontology: Medical Sciences , I have decided to list what I believe are the top 10 hot areas in geriatrics.
There is no question that finding solutions to cognitive decline and the behavioral problems associated with it is a central area in geriatrics ( 9–11 ). Our knowledge of the pathophysiology of Alzheimer's disease is moving forward rapidly. While beta-amyloid has taken center stage, both as a neurotransmitter that produces learning and memory disturbances ( 12 , 13 ) as well as an initiator of tissue destruction, possibly through free radical activation ( 14 , 15 ), there is also increasing understanding of the tauopathies ( 16 ). A recent article showed that measuring tau protein in lip epithelial tissue could possibly be used to diagnose Alzheimer's disease ( 17 ).
There is an increasing awareness of the importance in early recognition of mild cognitive impairment ( 18 , 19 ). Acute illness causes not only short-term but also long-term functional decline in persons with preexisting cognitive impairment ( 20 ). In particular, it is now becoming clear that cognitive decline is associated with a decline in physical performance ( 19 , 21–27 ). This is in part due to the decrease in reaction time associated with central nervous system damage ( 22 ). Cognitive dysfunction, whatever the cause, is associated with a high rate of medical comorbidity ( 23 , 28 ) and earlier mortality ( 24 , 29 ). The effects on mortality are worsened when cognitive dysfunction coexists with depression ( 29 ).
Over the last decade, there has been much enthusiasm for the possibility that hormone replacement therapy may improve cognition and slow progression of Alzheimer's disease ( 30–33 ). However, the Women's Health Initiative (WHI) in older women showed that hormone replacement therapy resulted in both a greater degree of cognitive dysfunction and an increase in the incidence of Alzheimer's disease ( 34 , 35 ). At the same time, as these results have become known, there is an increasing belief that testosterone in males may improve cognitive function ( 36–38 ). A relationship between elevated homocysteine and vitamin B 12 and folate deficiency with Alzheimer's disease has been found ( 30 , 39 ). Other studies have suggested that hypercholesterolemia may play a key role in the development of Alzheimer's disease and worsening cognitive function ( 40 , 41 ). Centenarians with high HDL (high-density lipoprotein) levels have better cognitive function and exceptional longevity ( 42 ). It is possible that cholesterol-lowering, especially in mid-life, results in a decline in atherothrombotic brain infarction, which may, in itself, be a causative agent for Alzheimer's disease ( 43–46 ).
In the arena of treatment for Alzheimer's disease, data continue to emerge that cholinesterase inhibitors slow the progression of the disease ( 9 ). Memantine, a drug that modulates the glutamate/NMDA system, can now be added to our therapeutic armamentarium and may prove useful either alone or in combination with cholinesterase inhibitors ( 47 ). Studies continue to appear that gingko biloba is a useful therapeutic adjuvant for persons with Alzheimer's disease ( 48 ). The effects of gingko appear to be equivalent to some of the more mainstream therapeutic agents ( 49 ). There is an urgent need for high-quality, large (i.e., sufficiently well powered) studies utilizing this agent. An exciting recent study has shown that aerobic fitness reduces brain tissue loss in humans ( 50 ). Resistance exercise has recently been shown to improve function in people with dementia ( 51 ). These findings strongly reinforce the calls in the Journals to continue to exercise throughout life and maintain healthy lifestyle habits in order to compress morbidity ( 52–55 ).
While antibodies to beta-amyloid can reverse cognitive dysfunction in mice ( 48 , 49 ), the human immunization studies led to disastrous consequences, with some of the patients developing an inflammatory disease of the central nervous system ( 56 ). Thus, while we await the potential of antisense to beta-amyloid that can switch off its production or drugs that can inhibit the function of the amyloid precursor protein cleavage enzymes (secretases) ( 10 , 57 , 58 ), most of the care of patients with Alzheimer's disease still need to focus on end-of-life care ( 59 ). As has been demonstrated by Simmons and colleagues ( 60 ), feeding the older demented patient takes an inordinately long time. New methods need to be developed to accurately quantify the amount of food consumed by older patients ( 61 ). Protein energy malnutrition can cause a marked decline in quality of life in nursing homes ( 62 ). Small changes in the emotional status of institutionalized elders can markedly alter food intake ( 63 , 64 ). Innovative programs such as the “Eden” alternative or even mechanical pet therapy need to be put in place to improve quality of care in nursing homes ( 65–68 ). As so eloquently suggested by John Schnelle ( 69 ), we need to “capture the voice of cognitively impaired elders” to improve their quality of life. Kane and colleagues ( 70 ) have provided one approach to doing this. Kane ( 71 ) has also called for professionals who have the experience of having loved ones cared for in long-term care facilities to band together in an attempt to find new solutions that will improve the quality of care in institutions. Volicer ( 11 ) has provided great insight into the management of behavioral systems in the demented person. It is important to realize that behavioral management and appropriate attention to the caregiver's needs are far more powerful tools than the use of drugs to deal with behavioral problems. The recent explosion of the use of expensive antipsychotics, any of which have no proven efficacy, to treat behavioral problems in nursing homes is particularly to be deplored!
Finally, there is an increased awareness of the problems associated with driving in older cognitively impaired individuals and the need to more fully develop adequate transportation systems ( 72 , 73 ). Richardson and colleagues ( 74 ) have highlighted the importance of visual attention in maintaining driving skills. Global positioning devices are emerging as the best way to test true driving skills in older persons ( 75 ). Given the horrendous accident that occurred in California when an older person drove into a group of persons and couldn't stop, better testing tools are badly needed! Previously, a survey of geriatricians suggested that they have little comprehension when an older person is no longer a safe driver ( 76 ).
An excellent review by Dan Blazer has summarized that state of the art for the management of depression ( 77 ). Depression remains underrecognized and undertreated in older persons, highlighting the need for continued screening ( 51 , 53 , 63 , 78 ). Physicians need to be made more aware of the effectiveness of treatment for depression. This is particularly important, as depression is associated with worse outcomes following a myocardial infarction, in persons with diabetes or congestive heart failure, or in those undergoing rehabilitation ( 55 , 77 , 79 ). Persons with depression are more likely to fall ( 80 , 81 ). Depression is also associated with increased mortality ( 29 ). The good outcomes seen with electroconvulsive therapy, particularly when bipolar electrodes are used, needs to be more widely advertised among physicians and the elderly population. In addition, resistance exercise has been shown to be an excellent adjuvant therapy for depression ( 82 ).
The importance of mobility as an emerging area in geriatrics was highlighted by the fact that a single issue of the Journals was devoted to this topic ( 83–88 ). Lan and colleagues ( 89 ) have developed an objective index of mobility-related limitation. Walking speed is becoming recognized as an excellent measure of function. The ability to walk rapidly over a distance involves not only muscle strength ( 90–92 ), but also the integration of cardiovascular fitness ( 86 ), vision ( 93 ), postural stability ( 94 , 95 ), pain ( 91 ), and cognitive processing time ( 96 ). Habitual walking has been shown to decrease the onset of physical disability in older persons ( 97 ).
Undernutrition continues to be demonstrated to be a major factor associated with mortality in older persons ( 98 ). DeCastro ( 99 ) has painstakingly demonstrated the changes in eating behavior that occur with aging, including the decreased snacking between meals, that lead to the physiological anorexia of aging ( 100 , 101 ). Abnormal eating behaviors such as dietary restriction occur commonly in older women ( 102 ), but only in the minority of cases do they lead to disease processes such as recurrence of anorexia nervosa or anorexia tardive ( 103 ). The physiological factors involved in the pathophysiology of this aging-related anorexia have been recently reviewed in the Journals ( 95 , 104 ). Ghrelin, a hormone that stimulates eating and releases growth hormone, is emerging as a potentially important hormone in the regulation of feeding behavior. It is released from the stomach in response to fasting. Studies so far in older humans have shown no change or a small decrease with aging ( 105 , 106 ). PYY (3-36) , another gut hormone, has been shown to inhibit feeding in humans ( 107 ) and cause weight loss in mice ( 108 ). To date, however, the best evidence for the early satiation that occurs in older persons implicates cholecystokinin ( 109 ).
New approaches to the management of weight loss in older persons have included using taste enhancers ( 110 ) and giving caloric supplements between meals rather than with the meal ( 111 ). A clearly emerging area is the use of orexigenics to stimulate appetite ( 112 , 113 ). Yeh and colleagues ( 114 ) have shown in a controlled trial that megestrol acetate produces weight gain in malnourished older persons. Its effect appears to be mainly due to inhibition of cytokines. The orexigenic effect of megestrol has been confirmed in other studies ( 115 ). Megestrol, however, does decrease testosterone levels in males ( 116 ). Thus, in males, when it is used, consideration should be given to giving testosterone at the same time. Females have better weight gain than males when they are given megestrol. For centuries, cannabis has been known to create the desire to eat ( 117 ). Recently dronabinol, a pure tetrahydrocannabinol, has become available as an orexigenic. It has a smaller orexigenic effect than does megestrol. Its ideal use is most probably in the palliative care arena, where, not only does it increase food intake, but it also decreases pain and nausea and improves mood. There is a need for large studies to determine the utility of orexigenic agents in the treatment of undernutrition.
Unfortunately, little attention is being paid to the role of vitamin and trace element deficiency in the pathogenesis of functional impairment in older persons. Certainly, they can play an important role in delirium; now that the yellow intravenous multivitamin (“banana bag”) mix is widely available again, consideration should be given to its use in older hospitalized patients. Urinary incontinence is a major reason for institutionalization in older persons ( 118 , 119 ). Vitamin B 12 deficiency has been associated with the development of incontinence ( 120 ). Zinc deficiency is extremely common, especially in older diabetics ( 121 , 122 ). It is associated with anorexia, immune dysfunction, and poor wound-healing. More studies are needed on the role of zinc deficiency in chronically ill elderly individuals. Creatine supplementation enhances isometric strength when utilized together with resistance training in older adults ( 123 ).
While inadequate attention is paid to undernutrition and vitamin and mineral deficiency, a large amount of research is actively exploring the role of dietary restriction as a means to extend life span. Bodkin and colleagues ( 124 ) have suggested, from early studies in dietary-restricted rhesus monkeys, that this approach may decrease mortality and morbidity. Banks and colleagues ( 125 ), in studying Ethiopian baboons over the life span, suggested that dietary restriction really represents prevention of obesity, as baboons in the wild have minimal fat stores as measured by leptin. While dietary restriction does not appear to prevent central nervous system damage ( 126 ), it certainly decreases glycation in nonhuman primates ( 127 ) and improves beta-cell sensitivity ( 128 ). Banks and colleagues ( 129 ) found that some garbage-eating baboons in Kenya developed the metabolic (insulin resistance) syndrome. Their studies strongly suggested that the environment interacts with the genome to produce this syndrome, as not all the baboons were affected. In the human studies in Biosphere 2, caloric restriction appeared to have a number of potentially beneficial effects ( 130 ).
The WHI has created great disarray among the adherents to the concept that hormonal replacement will reverse the stigmata of aging. While the WHI did not show that estrogen/progestagen replacement increased mortality, it did show an increase in breast cancer, heart disease, and pulmonary embolism ( 131 , 132 ). This was offset by a decrease in colon cancer and hip fracture. This enormously expensive study was stopped prematurely based on a convoluted formula for early stoppage of the trial, thus leaving room for doubt about whether long-term hormone replacement therapy would increase or decrease mortality. In addition, as already alluded to, the study showed worsening cognitive function in the women receiving hormones ( 34 , 35 ). The estrogen-alone arm of this study continues and may help give further insight into these conundrums. Progesterone clearly increases the propensity to form thrombi and may also have played a major role in the pathogenesis of breast carcinogenesis. The women in this study were older, and thus the study provided little guidelines for the appropriate use of hormonal replacement therapy at the time of the menopause. However, it would seem clear that women in their sixties and beyond should not receive combination hormonal therapy.
In males, the enthusiasm for testosterone replacement continues unabated, but is based on a relatively small body of evidence-based medicine ( 36 , 133–135 ). A number of studies on testosterone replacement in older males have appeared in the Journals ( 136–139 ). Overall, testosterone in older men appears to be a quality-of-life drug improving libido ( 134 ) and the ability to obtain an erection when phosphodiesterase inhibitors are taken ( 140 ), as well as increasing muscle mass and possibly strength ( 141 ), and bone mineral density ( 142 , 143 ), while decreasing body fat ( 136 ). The effects of testosterone on cognition are controversial ( 36 , 138 , 141 , 142 , 144 , 145 ). Testosterone clearly increases hematocrit in older men. The effects of testosterone on prostate cancer carcinogenesis are controversial ( 36 , 133 ). The need for a large men's health study to determine the efficacy and safety of testosterone in older males should be a national imperative. The intriguing hypothesis of Bhasin and colleagues ( 146 ) that testosterone plays a role in determining the fate of mesenchymal pluripotent stem cells may hold a major key to understanding the aging process. The role of testosterone in the development of frailty in older women is also coming of age ( 147 ).
While data suggesting that growth hormone and insulin-growth factor-1 may play a role in maintaining muscle mass ( 144 , 148 , 149 ), the enthusiasm for the use of growth hormone in the aged appears to be ebbing ( 150 , 151 ). One publication did, however, suggest that, in a single large family, growth hormone dwarfs had a shorter life span than their normal-sized siblings ( 152 ). This would appear to be in contradiction to animals where growth hormone deficiency confers longevity ( 153 , 154 ).
The role of vitamin D beyond its importance in maintaining bone mineral density remains controversial. There is a suggestion that it may play a role in preventing disability in older persons ( 155 ). There is, however, evidence that physicians continue to fail to diagnose and treat osteoporosis in older persons ( 156 , 157 ).
As originally highlighted by Fried and colleagues ( 158 ) in the Journals , frailty is becoming a highly important geriatric syndrome. Frailty appears to be an important precursor of disability and functional decline (which in themselves are key predictors of mortality in older persons) ( 159 , 160–162 ). The causes of frailty are multiple and include not only alterations in muscle function, but also cognitive impairment and a decline in VO 2 max ( 163 , 164 ). Diseases such as diabetes and cardiovascular disease are clearly important in accelerating the onset of the frailty syndrome ( 165–169 ). Pain can increase the level of disability ( 170 ). As older adults are already performing their activities of daily living at close to maximum capacity, a small change can tip them over into the realm of disability ( 171 ). Exercise, particularly resistance exercise, appears to be the major weapon in the therapeutic armamentarium to reverse frailty and its consequences ( 172–181 ). Falls are a sentinel event that can cause a frail person to transition to disability and functional impairment ( 182 ). Fear of falling in frequent fallers can lead to further disability ( 183 ). The American Geriatrics Society guidelines represent an excellent approach to the management of falls ( 184 ).
Loss of muscle mass (sarcopenia) is a major proximate occurrence in the development of frailty in older persons ( 169 , 185 , 186 ). The importance of sarcopenia and its causes was highlighted by a series of review articles in the Journals towards the end of last year ( 187–194 ).
Cardiovascular disease is present in over half of the older population and an even greater number of nursing home residents ( 195 ). The Journals has continued to carry a number of review articles to keep its readers abreast of the rapid developments in this field ( 196–200 ). Many of these have been written by Bill Aronow, a true geriatric giant who ages extraordinarily successfully as one of the most productive geriatricians, at an age when most have retired, and as a highly competitive tennis player. As an iconoclast who hates to embrace new expensive therapy in the older person, your editor, nevertheless, feels it incumbent upon him to point out the growing evidence of the superiority of angiotensin receptor blockers for the treatment of hypertension and heart failure ( 201–203 ).
The management of hypertension in older persons, and particularly the old-old is one full of opinions and still short on evidence ( 197 , 204 ). To highlight this area, James Goodwin ( 205 ) wrote an excellent review article, which was subject to a careful dissection by a variety of commentators ( 206–214 ). It is this kind of discourse that forces us to carefully examine the true state of evidence-based medicine in the older person. It is very important that geriatricians do not fall into the trap of considering trials conducted in middle-aged persons or even the young old as being appropriate to guide aggressive therapy in our unique population.
Finally, when treating hypertension in older persons, it is important to remember that white coat hypertension, pseudohypertension, orthostasis, and postprandial hypotension occur commonly. Orthostatis and postprandial hypotension occur more commonly in the morning than later in the day ( 215 , 216 ). Postprandial hypotension appears to be due to the release of vasodilatory peptides, such as calcitonin gene-related peptide ( 217 ).
The deterioration of the immune system with aging is well recognized ( 218 , 219 ). The development of protein energy malnutrition can further cause deterioration in the immune system, resulting in a decrease in CD 4 + T cells ( 220 ). Both nutritional supplementation and exercise have been demonstrated to boost the immune system ( 154 , 221–223 ); older persons appear to be particularly susceptible to anthrax when used as a tool of bioterrorism ( 222 ). As might be expected, older persons have worse outcomes when exposed to some of the new infectious disease outbreaks such as West Nile Virus ( 224 ) and SARS ( 225 ). Transfusion-related West Nile virus is more common in older than in younger persons ( 224 ). This reminds us all of the importance of vaccination against influenza in our older population ( 226 , 227 ).
From the start of human history, alchemists have attempted to prolong the human life span ( 228 ). The extension of life remains an appropriate area of research for gerontologists, though we should continuously be on guard for science that extends longevity without compressing morality, as was the case for Tithonus, the morning lover of the goddess of dawn, Aurora. The appropriate approach to antiaging research has been the subject of a number of commentaries in the Journals ( 229–233 ). A particularly aggressive area of longevity research is to study the factors that distinguish the successful old-old, especially centenarians, from the rest of the population in the hope of unlocking the genetic keys of longevity ( 234–241 ). This area has been closely linked to similar research in animals ( 242 , 243 ).
The mechanisms of cellular senescence, as originally shown by Leonard Hayflick, remain an important arena of immortality research ( 244–246 ). It was these studies that led initially to the search for telomerase ( 247 ). Originally thought to hold the secrets to cellular mortality, this area is now more of one in which researchers are hoping to treat cancer by controlling the enzyme. Hayflick's original studies are also the basis for modern embryonic stem cell research an area that offers promise for tissue rejuvenation ( 248 ).
The ethics of longevity research, particularly in an era of capitalistic ownership of the “useful” human genes, is clearly a slippery slope. However, it should be recognized that, while the well-meaning argue how to move forward appropriately, those who are driven by fewer misgivings will likely not be deterred, allowing this area to be controlled by those who perhaps we would prefer did not hold the secrets to our future.
Kane ( 249 ) has argued that geriatrics is at the crossroads and that to some extent we have failed, and we should remove ourselves from the mainstream and become the physicians for chronic care hospitals. This viewpoint was hotly contested by a variety of gerontological experts ( 250–259 ).
While geriatrics has not always delivered at the level I think many of us who entered the field in the 1980s hoped for, it certainly has changed the face of modern medicine. My colleagues and I have previously argued that a major role of geriatricians and our health care colleagues is to develop and run systems that decrease errors and improve care for elderly patients ( 260–262 ). This argument was based on the pioneering work of Larry Rubenstein on the value of Geriatric Evaluation and Management Units ( 263 ), whose value has been clearly confirmed ( 264 , 265 ). The importance for the installation of effective Continuous Quality Improvement systems to prevent errors is no longer in doubt ( 266 , 267 ). The addition of a high-quality computerized medical record to such a system will further enhance care ( 268 ).
Since the introduction of the geriatric evaluation and management unit concept, geriatrics has provided a number of other innovative projects that improve patient outcomes, e.g., Acute Care For the Elderly Units (ACE) ( 269 ), Delirium Intensive Care Units ( 270 ), Subacute Care Units ( 271 ), a geriatric-friendly nurse in the emergency department ( 272 ), and Program of All-Inclusive Care for the Elderly (PACE) ( 273 ), we have recognized the importance of controlling the rampant polypharmacy created by our other subspecialty colleagues ( 274 ). We have shown the ability of early screening to detect treatable geriatric problems ( 275 , 276 ). The geriatric Glidepaths have been created to help primary care physicians provide appropriate care to the wide range of older persons they encounter in practice ( 277 ). While our colleagues and administrators have been slow to incorporate these systems, they are slowly penetrating the high-technological environment of modern medicine. None of these systems function without well-trained geriatricians at their helm.
The future of geriatrics would appear to be more exciting at this moment than any time in the past. To conclude this editorial, I would, however, like to look back into our past, because where we are today in geriatrics is reflective of the small steps of the giants who created modern American geriatrics. This year, David Solomon celebrated his 80th birthday and was appropriately honored by a special supplement of the Journal of the American Geriatrics Society ( 278–282 ). David, together with John Beck, created the “West Coast geriatrics culture.” While extraordinarily different men in both personality and interest, David and John are truly the giants of modern geriatrics following in the footsteps of Bob Butler's extraordinary achievement on the East Coast. I would like to add my happy birthday wishes to David and thank both David and John, not only for the inspiration they were to me, but also for their leadership in the gerontological world that I hold so close to my heart.
Morley JE. Hot topics in geriatrics. J Gerontol Med Sci. . 2003 ; 58A : 30 -36.
Morley JE. Drugs, aging, and the future. J Gerontol Med Sci. . 2002 ; 57A : M2 -M6.
Morley JE. Highly cited papers in the Journal . J Gerontol Med Sci. . 2003 ; 58A : 1098 -1102.
Morley JE. Citations, impact factor, and the Journal . J Gerontol Med Sci. . 2002 ; 57A : M765 -M769.
Bortz WM, II. A conceptual framework of frailty: a review. J Gerontol Med Sci. . 2002 ; 57A : M283 -M288.
Blumenthal HT. The aging-disease dichotomy: true or false? J Gerontol Med Sci. . 2003 ; 58A : 138 -145.
Butler RN. Report and commentary from Madrid: the United Nations World Assembly on Ageing. J Gerontol Med Sci. . 2002 ; 57A : M770 -M771.
Blumenthal HT. The autopsy in gerontological research: a retrospective. J Gerontol Med Sci. . 2002 ; 57A : M433 -M437.
Grossberg GT, Desai AK. Management of Alzheimer's Disease. J Gerontol Med Sci. 2003;331–353.
Banks WA, Morley JE. Memories are made of this: recent advances in understanding cognitive impairments and dementia. J Gerontol Med Sci. . 2003 ; 58A : 314 -321.
Volicer L, Hurley AC. Management of behavioral symptoms in progressive degenerative dementias. J Gerontol Med Sci. . 2003 ; 58A : 837 -845.
Flood JF, Roberts E, Sherman MA, Kaplan BE, Morley JE. Topography of a binding site for small amnestic peptides deduced from structure activity studies—relation to amnestic effect of amyloid beta-protein. Proc Natl Acad Sci U S A. . 1994 ; 91 : 380 -384.
Morley JE, Kumar VB, Bernardo AE, et al. Beta-amyloid precursor polypeptide in SAMP8 mice affects learning and memory. Peptides. . 2000 ; 21 : 1761 -1767.
Farr SA, Poon HF, Dogrukol-Ak D, et al. The antioxidants alpha-lipoic acid and N-acetylcysteine reverse memory impairment and brain oxidative stress in aged SAMP8 mice. J Neurochem. . 2003 ; 84 : 1173 -1183.
Khodr B, Howard J, Watson K, Khalil Z. Effect of short-term and long-term antioxidant therapy on primary and secondary ageing neurovascular processes. J Gerontol Biol Sci. . 2003 ; 58A : 698 -708.
Tonay M, Probst A. The neuropathological spectrum of neurodegenerative tauopathies. IUBMB Life. . 2003 ; 55 : 299 -305.
Hattori H, Matsumoto M, Iwai K, et al. The tau protein of oral epithelium increases in Alzheimer's disease. J Gerontol Med Sci. . 2002 ; 57A : M64 -M70.
Turner RS. Biomarkers of Alzheimer's disease and mild cognitive impairment: are we there yet? Exp Neurol. . 2003 ; 183 : 7 -10.
Nguyen HT, Black SA, Ray LA, Espino DV, Markides KS. Predictors of decline in MMSE scores among older Mexican Americans. J Gerontol Med Sci. . 2002 ; 57A : M181 -M185.
Sands LP, Yaffe K, Lui L-Y, Stewart A, Eng C, Covinsky K. The effects of acute illness on ADL decline over 1 year in frail older adults with and without cognitive impairment. J Gerontol Med Sci. . 2002 ; 57A : M449 -M454.
Blaum CS, Ofstedal MB, Liang J. Low cognitive performance, comorbid disease, and task-specific disability: findings from a nationally representative survey. J Gerontol Med Sci. . 2002 ; 57A : M523 -M531.
Tabbarah M, Crimmins EM, Seeman TE. The relationship between cognitive and physical performance: MacArthur Studies of Successful Aging. J Gerontol Med Sci. . 2002 ; 57A : M228 -M235.
Doraiswamy PM, Leon J, Cummings JL, Marin D, Neumann PJ. Prevalence and impact of medical comorbidity in Alzheimer's disease. J Gerontol Med Sci. . 2002 ; 57A : M173 -M177.
Bittles AH, Petterson BA, Sullivan SG, Hussain R, Glasson EJ, Montgomery PD. The influence of intellectual disability on life expectancy. J Gerontol Med Sci. . 2002 ; 57A : M470 -M472.
Binder EF, Kruse RL, Sherman AK, et al. Predictors of short-term functional decline in survivors of nursing home-acquired lower respiratory tract infection. J Gerontol Med Sci. . 2003 ; 58A : 60 -67.
McConnell ES, Pieper CF, Sloane RJ, Branch LG. Effects of cognitive performance on change in physical function in long-stay nursing home residents. J Gerontol Med Sci. . 2002 ; 57A : M778 -M784.
Sands LP, Yaffe K, Covensky K, et al. Cognitive screening predicts magnitude of functional recovery from admission to 3 months after discharge in hospitalized elders. J Gerontol Med Sci. . 2003 ; 58A : 37 -45.
Raji MA, Ostir GV, Markides KS, Goodwin JS. The interaction of cognitive and emotional status on subsequent physical functioning in older Mexican Americans: findings from the Hispanic established population for the epidemiologic study of the elderly. J Gerontol Med Sci. . 2002 ; 57A : M678 -M682.
Mehta KM, Yaffe K, Langa KM, Sands L, Whooley MA, Covinsky KE. Additive effects of cognitive function and depressive symptoms on mortality in elderly community-living adults. J Gerontol Med Sci. . 2003 ; 58A : 461 -467.
Whitmer RA, Haan MN, Miller JW, Yaffe K. Hormone replacement therapy and cognitive performance: the role of homocysteine. J Gerontol Med Sci. . 2003 ; 58A : 324 -330.
Asthana S. Estrogen and cognition: the story so far. J Gerontol Med Sci. . 2003 ; 58A : 322 -323.
Petitti DB, Buckwalter JG, Crooks VC, Chiu V. Prevalence of dementia in users of hormone replacement therapy as defined by prescription data. J Gerontol Med Sci. . 2002 ; 57A : M532 -M538.
Ott BR, Belazi D, Lapane KL. Cognitive decline among female estrogen users in nursing homes. J Gerontol Med Sci. . 2002 ; 57A : M594 -M598.
Schumaker SA, Legault C, Rapp SR, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women—the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA. . 2003 ; 289 : 2651 -2662.
Rapp SR, Espeland MA, Shumaker SA, et al. Effect of estrogen plus progestin on global cognitive function in postmenopausal women—the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA. . 2003 ; 289 : 2663 -2672.
Matsumoto AM. Andropause: clinical implications of the decline in serum testosterone levels with aging in men. J Gerontol Med Sci. . 2002 ; 57A : M76 -M99.
Kenny AM, Bellantonio S, Gruman CA, Acosta RD, Prestwood KM. Effects of transdermal testosterone on cognitive function and health perception in older men with low bioavailable testosterone levels. J Gerontol Med Sci. . 2002 ; 57A : M321 -M325.
Tariq SH. Knowledge about low testosterone in older men. J Gerontol Med Sci. . 2003 ; 58A : 382 -383.
Lokk J. News and views on folate and elderly persons. J Gerontol Med Sci. . 2003 ; 58A : 354 -361.
Adunsky A, Chesnin V, Davidson M, Gerber Y, Alexander K, Haratz D. A cross-sectional study of lipids and ApoC levels in Alzheimer's patients with and without cardiovascular disease. J Gerontol Med Sci. . 2002 ; 57A : M757 -M764.
Hajjar I, Schumpert J, Hirth V, Wieland D, Eleazer GP. The impact of the use of statins on the prevalence of dementia and the progression of cognitive impairment. J Gerontol Med Sci. . 2002 ; 57A : M414 -M418.
Atzmon G, Gabriely I, Greiner W, Davidson D, Schechter C, Barzilai N. Plasma HDL levels highly correlate with cognitive function in exceptional longevity. J Gerontol Med Sci. . 2002 ; 57A : M712 -M715.
Aronow WS, Ahn C, Gutstein H. Reduction of new coronary events and new atherothrombotic brain infarction in older persons with diabetes mellitus, prior myocardial infarction, and serum low-density lipoprotein cholesterol ≥125 mg/dl treated with statins. J Gerontol Med Sci. . 2002 ; 57A : M747 -M750.
Aronow WS, Ahn C. Risk factors for new atherothrombotic brain infarction in older Hispanic men and women. J Gerontol Med Sci. . 2002 ; 57A : M61 -M63.
Aronow WS, Ahn C, Gutstein H. Incidence of new atherothrombotic brain infarction in older persons with prior myocardial infarction and serum low-density lipoprotein cholesterol ≥125 mg/dl treated with statins versus no lipid-lowering drug. J Gerontol Med Sci. . 2002 ; 57A : M333 -M337.
Ostir GV, Raji MA, Ottenbacher KJ, Markides KS, Goodwin JS. Cognitive function and incidence of stroke in older Mexican Americans. J Gerontol Med Sci. . 2003 ; 58A : 531 -535.
Wilcock GK. Memantine for the treatment of dementia. Lancet Neurol. . 2003 ; 2 : 503 -505.
Andrieu S, Gillette S, Amouyal K, et al. Association of Alzheimer's disease onset with gingko biloba and other symptomatic cognitive treatments in a population of women aged 75 years and older from the PIDOS study. J Gerontol Med Sci. . 2003 ; 58A : 372 -377.
Fisher A, Morley JE. Antiaging medicine: the good, the bad, and the ugly. J Gerontol Med Sci. . 2002 ; 57A : M636 -M639.
Colcombe SJ, Erickson KI, Raz N, et al. Aerobic fitness reduces brain tissue loss in aging humans. J Gerontol Med Sci. . 2003 ; 58A : 176 -180.
Robison J, Gruman C, Gaztambide S, Blank K. Screening for depression in middle-aged and older Puerto Rican primary care patients. J Gerontol Med Sci. . 2002 ; 57A : M308 -M314.
Morley JE, Flaherty JH. It's never too late: health promotion and illness prevention in older persons. J Gerontol Med Sci. . 2002 ; 57A : M338 -M342.
Flaherty JH, McBride M, Marzouk S, et al. Decreasing hospitalization rates for older home care patients with symptoms of depression. J Am Geriatr Soc. . 1998 ; 46A : 31 -38.
Hubert HB, Bloch DA, Oehlert JW, Fries JF. Lifestyle habits and compression of morbidity. J Gerontol Med Sci. . 2002 ; 57A : M347 -M351.
Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults—a 3-year prospective study. Diabetes Care. . 1998 ; 21 : 231 -235.
Akiyama H, Barger S, Barnum S, et al. Inflammation and Alzheimer's disease. Neurobiol Aging. . 2000 ; 21 : 383 -421.
Banks WA, Farr SA, Butt W, Kumar VB, Franko MW, Morley JE. Delivery across the blood-brain barrier of antisense directed against amyloid beta: Reversal of learning and memory deficits in mice overexpressing amyloid precursor protein. J Pharmacol Exper Ther. . 2001 ; 297 : 1113 -1121.
Kumar VB, Vyas K, Franko M, et al. Molecular cloning, expression, and regulation of hippocampal amyloid precursor protein of senescence accelerated mouse (SAMP8). Biochem Cell Biol [Biochim Biol Cell]. . 2001 ; 79 : 57 -67.
Michel J-P, Pautex S, Zekry D, Zulian G, Gold G. End-of-life care of persons with dementia. J Gerontol Med Sci. . 2002 ; 57A : M640 -M644.
Simmons SF, Babineau S, Garcia E, Schnelle JF. Quality assessment in nursing homes by systematic direct observation: feeding assistance. J Gerontol Med Sci. . 2002 ; 57A : M665 -M671.
Berrut G, Favreau AM, Dizo E, et al. Estimation of calorie and protein intake in aged patients: validation of a method based on meal portions consumed. J Gerontol Med Sci. . 2002 ; 57A : M52 -M56.
Crogan NL, Pasvogel A. The influence of protein-calorie malnutrition on quality of life in nursing homes. J Gerontol Med Sci. . 2003 ; 58A : 159 -164.
Minicuci N, Maggi S, Pavan M, Enzi G, Crepaldi G. Prevalence rate and correlates of depressive symptoms in older individuals: the Veneto Study. J Gerontol Med Sci. . 2002 ; 57A : M155 -M161.
Paquet C, St-Arnaud-McKenzie D, Kergoat M-J, Ferland G, Dube L. Direct and indirect effects of everyday emotions on food intake of elderly patients in institutions. J Gerontol Med Sci. . 2003 ; 58A : 153 -158.
Morley JE, Flaherty JH. Putting the “home” back in nursing home. J Gerontol Med Sci. . 2002 ; 57A : M419 -M421.
Thoesen Coleman M, Looney S, O'Brien J, Ziegler C, Pastorino CA, Turner C. The Eden alternative: findings after 1 year of implementation. J Gerontol Med Sci. . 2002 ; 57A : M422 -M427.
Banks MR, Banks WA. The effects of animal-assisted therapy on loneliness in an elderly population in long-term care facilities. J Gerontol Med Sci. . 2002 ; 57A : M428 -M432.
Tamura T, Yonemitsu S, Itoh A, et al. Is an entertainment robot useful in the care of elderly people with severe dementia? J Gerontol Med Sci. . 2004 ; 59A : 83 -85.
Schnelle JF. Improving nursing home quality assessment: capturing the voice of cognitively impaired elders. J Gerontol Med Sci. . 2003 ; 58A : 238 -239.
Kane RA, Kling KC, Bershadsky B, et al. Quality of life measures for nursing home residents. J Gerontol Med Sci. . 2003 ; 58A : 240 -248.
Kane RL. Professionals with personal experience in chronic care (PPECC). J Gerontol Med Sci. . 2003 ; 58A : 867 .
Flaherty JH, Stalvey B, Rubenstein L. A consensus statement on nonemergent medical transportation services for older persons [Guest Editorial]. J Gerontol Med Sci. . 2003 ; 58A : 826 -831.
Margolis KL, Kerani PK, McGovern P, Songer T, Cauley JA. Ensrud KE for the Study of Osteoporotic Fractures Research Group. Risk factors for motor vehicle crashes in older women. J Gerontol Med Sci. . 2002 ; 57A : M186 -M191.
Richardson ED, Marottoli RA. Visual attention and driving behaviors among community-living older persons. J Gerontol Med Sci. . 2003 ; 58A : 832 -836.
Porter MM, Whitton MJ. Assessment of driving with the Global Positioning System and video technology in young, middle-aged, and older drivers. J Gerontol Med Sci. . 2002 ; 57A : M578 -M582.
Miller DJ, Morley JE. Attitudes of physicians toward elderly drivers and driving policy. J Am Geriatr Soc. . 1993 ; 41 : 722 -724.
Blazer DG. Depression in late life: review and commentary. J Gerontol Med Sci. . 2003 ; 58A : 249 -265.
Blazer DG. The prevalence of depressive symptoms. J Gerontol Med Sci. . 2002 ; 57A : M150 -M151.
Evans WJ. Exercise as the standard of care for elderly people. J Gerontol Med Sci. . 2002 ; 57A : M260 -M261.
Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R. Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol Med Sci. . 2002 ; 57A : M722 -M726.
Thomas VS, Hageman PA. Can neuromuscular strength and function in people with dementia be rehabilitated using resistance-exercise training? Results from a preliminary intervention study. J Gerontol Med Sci. . 2003 ; 58A : 746 -751.
Singh NA, Clements KM, Singh MAF. The efficacy of exercise as a long-term antidepressant in elderly subjects: a randomized, controlled trial. J Gerontol Med Sci. . 2001 ; 56A : M497 -M504.
Morley JE. Mobility performance: a high-tech test for geriatricians. J Gerontol Med Sci. . 2003 ; 58A : 712 -714.
Newman AB, Haggerty CL, Kritchevsky SB, Nevitt MC. Simonsick EM, for the Health ABC Collaborative Research Group. Walking performance and cardiovascular response: associations with age and morbidity—the Health, Aging and Body Composition Study. J Gerontol Med Sci. . 2003 ; 58A : 715 -720.
Lan T-Y, Deeg DJH, Guralnik JM, Melzer D. Responsiveness of the index of mobility limitation: comparison with gait speed alone in the longitudinal aging study Amsterdam. J Gerontol Med Sci. . 2003 ; 58A : 721 -727.
Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI Study: which influences mobility more? J Gerontol Med Sci. . 2003 ; 58A : 728 -733.
Alexander NB, Dengel DR, Olson RJ, Krajewski KM. Oxygen-Uptake (VO 2 ) kinetics and functional mobility performance in impaired older adults. J Gerontol Med Sci. . 2003 ; 58A : 734 -739.
Brandon LJ, Gaasch DA, Boyette LW, Lloyd AM. Effects of long-term resistive training on mobility and strength in older adults with diabetes. J Gerontol Med Sci. . 2003 ; 58A : 740 -745.
Lan T-Y, Melzer D, Tom BDM, Guralnik JM. Performance tests and disability: developing an objective index of mobility-related limitation in older populations. J Gerontol Med Sci. . 2002 ; 57A : M294 -M301.
Sicard-Rosenbaum L, Light KE, Behrman AL. Gait, lower extremity strength, and self-assessed mobility after hip arthroplasty. J Gerontol Med Sci. . 2002 ; 57A : M47 -M51.
Reid MC, Guo ZC, Towle VR, Kerns RD, Concato J. Pain-related disability among older male veterans receiving primary care. J Gerontol Med Sci. . 2002 ; 57A : M727 -M732.
Slade JM, Miszko TA, Laity JH, Agrawal SK, Cress ME. Anaerobic power and physical function in strength-trained and non-strength-trained older adults. J Gerontol Med Sci. . 2002 ; 57A : M168 -M172.
Cromwell RL, Newton RA, Forrest G. Influence of vision on head stabilization strategies in older adults during walking. J Gerontol Med Sci. . 2002 ; 57A : M442 -M448.
Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-Stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol Med Sci. . 2002 ; 57A : M539 -M543.
Hamerman D. Molecular-based therapeutic approaches in treatment of anorexia of aging and cancer cachexia. J Gerontol Med Sci. . 2002 ; 57A : M511 -M518.
Bean JF, Kiely DK, Leveille SG, et al. The 60 minute walk test in mobility-limited elders: What is being measured? J Gerontol Med Sci. . 2002 ; 57A : M751 -M756.
Wong CH, Wong SF, Pang WS, Azizah MY, Dass MJ. Habitual walking and its correlation to better physical function: implications for prevention of physical disability in older persons. J Gerontol Med Sci. . 2003 ; 58 : 555 -560.
Liu L, Bopp MM, Roberson PK, Sullivan DH. Undernutrition and risk of mortality in elderly patients within 1 year of hospital discharge. J Gerontol Med Sci. . 2002 ; 57A : M741 -M746.
de Castro JM. Age-related changes in the social, psychological, and temporal influences on food intake in free-living, healthy, adult humans. J Gerontol Med Sci. . 2002 ; 57A : M368 -M377.
Morley JE, Silver AJ. Anorexia in the elderly. Neurobiol Aging. . 1988 ; 9 : 9 -16.
Morley JE. Anorexia of aging—physiologic and pathologic. Am J Clin Nutr. . 1997 ; 66 : 760 -773.
Hays NP, Gathalon GP, Roubenoff R, Lipman R, Robert SB. The association of eating behavior with risk for morbidity in older women. J Gerontol Med Sci. . 2002 ; 57A : M128 -M133.
Miller DK, Morley JE, Rubenstein LZ, Pietruszka FM. Abnormal eating attitudes and body image in older undernourished individuals. J Am Geriatr Soc. . 1991 ; 39 : 462 -466.
Choy NL, Brauer S, Nitz J. Changes in postural stability in women aged 20 to 80 years. J Gerontol Med Sci. . 2003 ; 58A : 525 -530.
Strum K, MacIntosh CG, Parker BA, Wishart J, Horowitz M, Chapman IM. Appetite, food intake, and plasma concentrations of cholecystokinin, ghrelin, and other gastrointestinal hormones in undernourished older women and well-nourished young and older women. J Clin Endocrinol Metab. . 2003 ; 88 : 3747 -3755.
Rigamonti AE, Pincelli AI, Corra B, et al. Plasma ghrelin concentration in elderly subjects: comparison with anorexic and obese patients. J Endocrinol. . 2002 ; 175 : R1 -R5.
Batterham RL, Cohen MA, Ellis SM, et al. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. . 2003 ; 349 : 941 -948.
Morley JE, Flood JF. An investigation of tolerance to the actions of leptogenic and anorexigenic drugs in mice. Life Sci. . 1987 ; 41 : 2157 -2165.
MacIntosh CG, Morley JE, Wishart J, et al. Effect of exogenous cholecystokinin (CCK)-8 on food intake and plasma CCK, leptin, and insulin concentrations in older and young adults: evidence for increased CCK activity as a cause of the anorexia of aging. J Clin Endocrinol Metab. . 2001 ; 86 : 5830 -5837.
Mathey MFAM, Siebelink E, de Graaf C, Van Staveren WA. Flavor enhancement of food improves dietary intake and nutritional status of elderly nursing home residents. J Gerontol Med Sci. . 2001 ; 56A : M200 -M205.
Wilson MMG, Purushothaman R, Morley JE. Effect of liquid dietary supplements on energy intake in the elderly. Am J Clin Nutr. . 2002 ; 75 : 944 -947.
Morley JE. Anorexia and weight loss in older persons. J Gerontol Med Sci. . 2003 ; 58A : 131 -137.
Thomas DR. The relationship between functional status and inflammatory disease in older adults [Guest Editorial]. J Gerontol Med Sci. . 2003 ; 58A : 995 -998.
Yeh SS, Wu SY, Levine DM, et al. The correlation of cytokine levels with body weight after megestrol acetate treatment in geriatric patients. J Gerontol Med Sci. . 2001 ; 56A : M48 -M54.
Karcic E, Philpot C, Morley JE. Treating malnutrition with megestrol acetate: literature review and review of our experience. J Nutr Hlth Aging. . 2002 ; 6 : 191 -200.
Lambert CP, Sullivan DH, Evans WJ. Effects of testosterone replacement and/or resistance training on interleukin-6 tumor necrosis factor alpha, and leptin in elderly men ingesting megestrol acetate: a randomized controlled trial. J Gerontol Med Sci. . 2003 ; 58A : 165 -170.
Morley JE, Logi P, Bensusan AD. The subjective effects of dagga: including comparative studies with Britain and America. S Afr Med J. . 1973 ; 47 : 1145 -1149.
Wilson MMG. Urinary incontinence: bridging the gender gap. J Gerontol Med Sci. . 2003 ; 58A : 752 -754.
Nuotio M, Tammela TLJ, Luukkaala T, Jylha M. Predictors of institutionalization in an older population during a 13-year period: the effect of urge incontinence. J Gerontol Med Sci. . 2003 ; 58A : 756 -762.
Endo JO, Chen S, Potter JF, Ranno AE, Asadullah S, Lahiri P. Vitamin B 12 deficiency and incontinence: is there an association? J Gerontol Med Sci. . 2002 ; 57A : M583 -M587.
Kinlaw WB, Levine AS, Morley JE, Silvis SE, McClain CJ. Abnormal zinc metabolism in type II diabetes mellitus. Am J Med. . 1983 ; 75 : 273 -277.
Niewoehner CB, Allen JI, Boosalis M, Levine AS, Morley JE. Role of zinc supplementation in type II diabetes mellitus. Am J Med. . 1986 ; 81 : 63 -68.
Brose A, Parise G, Tarnopolsky MA. Creatine supplementation enhances isometric strength and body composition improvements following strength exercise training in older adults. J Gerontol Biol Sci. . 2003 ; 58A : 11 -19.
Bodkin NL, Alexander TM, Ortmeyer HK, Johnson E, Hansen BC. Mortality and morbidity in laboratory-maintained Rhesus monkeys and effects of long-term dietary restriction. J Gerontol Biol Sci. . 2003 ; 58A : 212 -219.
Banks WA, Phillips-Controy JE, Jolly CJ, Morley JE. Serum leptin levels in wild and captive populations of baboons (Papio): implications for the ancestral role of leptin. J Clin Endocrinol Metab. . 2001 ; 86 : 4315 -4320.
Morgan WW, Richardson AG, Nelson JF. Dietary restriction does not protect the nigrostriatal dopaminergic pathway of older animals from low-dose MPTP-induced neurotoxicity. J Gerontol Biol Sci. . 2003 ; 58A : 394 -399.
Sell DR, Lane MA, Obrenovich ME, et al. The effect of caloric restriction on glycation and glycoxidation in ski collagen of nonhuman primate. J Gerontol Biol Sci. . 2003 ; 58A : 508 -516.
Gresl TA, Colman RJ, Havighurst TC, Allison DB, Schoeller DA, Kemnitz JW. Dietary restriction and beta-cell sensitivity to glucose in adult male rhesus monkeys. J Gerontol Biol Sci. . 2003 ; 58A : 598 -610.
Banks WA, Altmann J, Sapolsky RM, Phillips-Conroy JE, Morley JE. Serum leptin levels as a marker for a syndrome X-like condition in wild baboons. J Clin Endocrinol Metab. . 2003 ; 88 : 1234 -1240.
Wolford RL, Mock D, Verdery R, MacCallum T. Calorie restriction in Biosphere 2: alterations in physiologic, hematologic, hormonal, and biochemical parameters in humans restricted for a 2-year period. J Gerontol Biol Sci. . 2002 ; 57A : B211 -B224.
Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. . 2003 ; 349 : 523 -534.
Roussouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women—principal results from the Women's Health Initiative randomized controlled trial. JAMA. . 2002 ; 288 : 321 -333.
Morley JE. The need for a men's health initiative. J Gerontol Med Sci. . 2003 ; 58A : 614 -617.
Anderson JK, Faulkner S, Cranor C, Briley J, Gevirtz F, Roberts S. Andropause: knowledge and perceptions among the general public and health care professionals. J Gerontol Med Sci. . 2002 ; 57A : M793 -M796.
Morley JE, Perry HM. Andropause: an old concept in new clothing. Clin Geriatr Med. . 2003 ; 19 : 507 -528.
Wittert GA, Chapman IM, Haren MT, Mackintosh S, Coates P, Morley JE. Oral testosterone supplementation increases muscle and decreases fat mass in healthy elderly males with low-normal gonadal status. J Gerontol Med Sci. . 2003 ; 58A : 618 -625.
Kenny AM, Prestwood KM, Gruman CA, Fabregas G, Biskup B, Mansoor G. Effects of transdermal testosterone on lipids and vascular reactivity in older men with low bioavailable testosterone levels. J Gerontol Med Sci. . 2002 ; 57A : M460 -M465.
Kenny AM, Prestwood KM, Gruman CA, Marcello KM, Raisz LG. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels. J Gerontol Med Sci. . 2001 ; 56A : M266 -M272.
Tariq SH, Haleem U, Omran ML, Kaiser FE, Perry HM, Morley JE. Erectile dysfunction: etiology and treatment in young and old patients. Clin Geriatr Med. . 2003 ; 19 : 539 -551.
Sih R, Morley JE, Kaiser FE, Perry HM, Patrick P, Ross C. Testosterone replacement in older hypogonadal men—a 12-month randomized controlled trial. J Clin Endocrinol Metab. . 1997 ; 82 : 1661 -1667.
Morley JE. Andropause: is it time for the geriatrician to treat it? J Gerontol Med Sci. . 2001 ; 56A : M263 -M265.
Christmas C, O'Connor KG, Harman SM, Tobin JD, et al. Growth hormone and sex steroid effects on bone metabolism and bone mineral density in healthy aged women and men. J Gerontol Med Sci. . 2002 ; 57A : M12 -M18.
Tan RS, Pu SJ. A pilot study on the effects of testosterone in hypogonadal aging male patients with Alzheimer's disease. Aging Male. . 2003 ; 6 : 13 -17.
Morley JE. Testosterone and behavior. Clin Geriatr Med. . 2003 ; 19 : 605 -616.
Bhasin S. The mechanisms of androgen effects on body composition: mesenchymal pluripotent cell as the target of androgen action. J Gerontol Med Sci. . 2003 ; 58A : 1103 -1110.
Morley JE, Perry HM, III. Androgens and women at the menopause and beyond. J Gerontol Med Sci. . 2003 ; 58A : 409 -416.
Waters DL, Yau CL, Montoya GD, Baumgartner RN. Serum sex hormones, IGF-1, and IGFBP3 exert a sexually dimorphic effect on lean body mass in aging. J Gerontol Med Sci. . 2003 ; 57A : 648 -652.
Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Develop. . 1999 ; 107 : 123 -136.
Bartke A, Coschigano K, Kopchick J, et al. Genes that prolong life: relationships of growth hormone and growth to aging and life span. J Gerontol Biol Sci. . 2001 ; 56A : B340 -B349.
Morley JE. Growth hormone: fountain of youth or death hormone? J Am Geriatr Soc. . 1999 ; 47 : 1475 -1476.
Benson A, Salemi S, Gallati S, et al. Reduced longevity in untreated patients with isolated growth hormone deficiency. J Clin Endocrinol Metab. . 2003 ; 88 : 3664 -3667.
Dozmorov I, Galecki A, Chang Y, Krzesicki, , Vergara M, Miller RA. Gene expression profile of long-lived Snell dwarf mice. J Gerontol Biol Sci. . 2002 ; 57A : B99 -B108.
Ikeno Y, Bronson RT, Hubbard GB, Lee S, Bartke A. Delayed occurrence of fatal neoplastic diseases in Ames Dwarf Mice: correlation to extended longevity. J Gerontol Biol Sci. . 2003 ; 58A : 291 -296.
Zamboni M, Zoico E, Tosoni P, et al. Relation between vitamin D, physical performance, and disability in elderly persons. J Gerontol Med Sci. . 2002 ; 57A : M7 -M11.
Kamel HK, Perry HM, Morley JE. Hormone replacement therapy and fractures in older adults. J Am Geriatr Soc. . 2001 ; 59 : 179 -187.
Kamel HK, Hussain MS, Tariq S, Perry HM, Morley JE. Failure to diagnose and treat osteoporosis in elderly patients hospitalized with hip fracture. Am J Med. . 2000 ; 109 : 326 -328.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotpye. J Gerontol Med Sci. . 2001 ; 56A : M146 -M156.
Thomas DR. Focus on functional decline in hospitalized older adults. J Gerontol Med Sci. . 2002 ; 57A : M567 -M568.
McCusker J, Kakuma R, Abrahamowicz M. Predictors of functional decline in hospitalized elderly patients: a systematic review. J Gerontol Med Sci. . 2002 ; 57A : M569 -M577.
Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community-living older persons. J Gerontol Med Sci. . 2003 ; 58A : 70 -75.
Valderrama-Gama E, Damian J, Ruigomez A, Martin-Moreno JM. Chronic disease, functional status, and self-ascribed causes of disabilities among noninstitutionalized older people in Spain. J Gerontol Med Sci. . 2002 ; 57A : M716 -M721.
Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol Biol Sci. . 2002 ; 57A : B115 -B125.
Morley JE, Perry HM, III, Miller DK. Something about frailty. J Gerontol Med Sci. . 2002 ; 57A : M698 -M704.
Ottenbacher KJ, Ostir GV, Peek MK, Goodwin JS, Markides KS. Diabetes mellitus as a risk factor for hip fracture in Mexican American older adults. J Gerontol Med Sci. . 2002 ; 57A : M648 -M653.
Newman AB, Gottdiener JS, McBurnie MA, et al. Associations of subclinical cardiovascular disease with frailty. J Gerontol Med Sci. . 2001 ; 56A : M158 -M166.
Rodriguez-Saldana J, Morley JE, Reynoso MT, et al. Diabetes mellitus in a subgroup of older Mexicans: prevalence, association with cardiovascular risk factors, functional and cognitive impairment, and mortality. J Am Geriatr Soc. . 2002 ; 50 : 111 -116.
Miller DK, Lui LYL, Perry HM, Kaiser FE, Morley JE. Reported and measured physical functioning in older inner-city diabetic African Americans. J Gerontol Med Sci. . 1999 ; 54 : M230 -M236.
Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol Med Sci. . 2002 ; 57A : M772 -M777.
Reid MC, Guo Z, Towle VR, Kersn RD. Concato. Pain-related disability among older male veterans receiving primary care. J Gerontol Med Sci. . 2002 ; 57A : M727 -M732.
Hortobagyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. J Gerontol Med Sci. . 2003 ; 58A : 453 -460.
Miszko TA, Cress ME, Slade JM, Covey CJ, Agrawal SK, Doerr CE. Effect of strength and power training on physical function in community-dwelling older adults. J Gerontol Med Sci. . 2003 ; 58A : 171 -175.
Nicklas BJ, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African American and Caucasian women. J Gerontol Med Sci. . 2003 ; 58A : 181 -189.
Figueroa A, Going SB, Milliken LA, et al. Effects of exercise training and hormone replacement therapy on lean and fat mass in postmenopausal women. J Gerontol Med Sci. . 2003 ; 58A : 266 -270.
Hortobagyi T. The positives of negatives: clinical implications of eccentric resistance exercise in older adults. J Gerontol Med Sci. . 2003 ; 58A : 417 -418.
LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol Med Sci. . 2003 ; 58A : 419 -424.
Carmeli E, Kessel S, Coleman R, Ayalon M. Effects of a treadmill walking program on muscle strength and balance in elderly people with down syndrome. J Gerontol Med Sci. . 2002 ; 57A : M106 -M110.
Trappe S, Williamson D, Godard M. Maintenance of whole muscle strength and size following resistance training in older men. J Gerontol Biol Sci. . 2002 ; 57A : B138 -B143.
Singh MAF. Exercise comes of age: rationale and recommendations for a geriatric exercise prescription. J Gerontol Med Sci. . 2002 ; 57A : M262 -M282.
Signorile JF, Carmel MP, Czaja SJ, et al. Differential increases in average isokinetic power by specific muscle groups of older women due to variations in training and testing. J Gerontol Med Sci. . 2002 ; 57A : M683 -M690.
Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, Bilbrew D. Effects of nurse counseling on walking for exercise in elderly primary care patients. J Gerontol Med Sci. . 2002 ; 57A : M733 -M740.
Morley JE. A fall is a major event in the life of an older person. J Gerontol Med Sci. . 2002 ; 57A : M492 -M495.
Murphy SL, Dubin JA, Gill TM. The development of fear of falling among community-living older women: predisposing factors and subsequent fall events. J Gerontol Med Sci. . 2003 ; 58A : 943 -947.
Lundebjerg N, Rubenstein LZ, Kenny RA, et al. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. . 2001 ; 59 : 664 -672.
Kenny AM, Dwason L, Kleppinger A, Iannuzzi-Sucich M, Judge JO. Prevalence of sarcopenia and predictors of skeletal muscle mass in nonobese women who are long-term users of estrogen-replacement therapy. J Gerontol Med Sci. . 2003 ; 58A : 436 -440.
Aronow WS, Ahn C. Elderly diabetics with peripheral arterial disease and no coronary artery disease have a higher incidence of new coronary events than elderly nondiabetics with peripheral arterial disease and prior myocardial infarction treated with statins and with no lipid-lowering drug. J Gerontol Med Sci. . 2003 ; 58A : 573 -575.
Morley JE. Sarcopenia revisited [Editorial]. J Gerontol Med Sci. . 2003 ; 58A : 909 -910.
Marcell TJ. Sarcopenia: causes, consequences, and preventions [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 911 -916.
Yarasheski KE. Exercise, aging, and muscle protein metabolism [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 918 -922.
Barton E, Morris C. Mechanisms and strategies to counter muscle atrophy [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 923 -926.
Leeuwenburgh C. Role of apoptosis in sarcopenia [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 999 -1001.
Bhasin S. Testosterone supplementation for aging-associated sarcopenia [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 1002 -1008.
Hawkins SA, Wiswell RA, Marcell TJ. Exercise and the master athlete—a model of successful aging? [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 1009 -1011.
Roubenoff R. Sarcopenia: effects on body composition and function [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 1012 -1017.
Aronow WS, Ahn C, Gutstein H. Prevalence and incidence of cardiovascular disease in 1160 older men and 2464 older women in a long-term health care facility. J Gerontol Med Sci. . 2002 ; 57A : M45 -M46.
Aronow WS. Management of the older person with atrial fibrillation. J Gerontol Med Sci. . 2002 ; 57A : M352 -M363.
Aronow WS. What is the appropriate treatment of hypertension in elders? J Gerontol Med Sci. . 2002 ; 57A : M483 -M486.
Vogel T, Verreault R, Turcotte J-F, Kiesmann M, Berthel M. Intracerebral aneurysms: a review with special attention to geriatric aspects. J Gerontol Med Sci. . 2003 ; 58A : 520 -524.
Aronow WS. Treatment of unstable angina pectoris/non-ST-segment elevation myocardial infraction in elderly patients [Review Article]. J Gerontol Med Sci. . 2003 ; 58A : 927 -933.
Aronow WS. Should hypercholesterolemia in older persons be treated to reduce cardiovascular events? J Gerontol Med Sci. . 2002 ; 57A : M411 -M413.
White HD. Should all patients with coronary disease receive angiotensin-converting-enzyme inhibitors? Lancet. . 2003 ; 362 : 755 -757.
Pfeffer MA, Swedberg K, Granger CB, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall Programme. Lancet. . 2003 ; 362 : 759 -766.
McMurray JJV, Ostergren J, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting enzyme inhibitors: the CHARM-Added trial. Lancet. . 2003 ; 362 : 767 -771.
Hajjar I, Miller K, Hirth V. Age-related bias in the management of hypertension: a national survey of physicians' opinions on hypertension in elderly adults. J Gerontol Med Sci. . 2002 ; 57A : M487 -M491.
Goodwin JS. Embracing complexity: a consideration of hypertension in the very old. J Gerontol Med Sci. . 2003 ; 58A : 653 -658.
Aronow WS. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 659 -660.
Denson S. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 660 -661.
Hajjar RR. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 661 -662.
Harris TB. Aging well and aging poorly: primary and secondary low blood pressure [Commentary]. J Gerontol Med Sci. . 2003 ; 58A : 662 -663.
Lowenthal DT. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 664 -665.
Michel J-P, Grab B, Perrenoud JJ. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 665 -666.
Newman AB. Commentary on “Embracing complexity: a consideration of hypertension in the very old.”. J Gerontol Med Sci. . 2003 ; 58A : 666 -667.
Thomas DR. The struggle to relate epidemiology to real people. J Gerontol Med Sci. . 2003 ; 58A : 667 -668.
Goodwin JS. Author's response to commentaries. J Gerontol Med Sci. . 2003 ; 58A : 669 -670.
Vloet LCM, Smits R, Jansen RWMM. Effect of meals at different mealtimes on blood pressure and symptoms in geriatric patients with postprandial hypotension. J Gerontol Med Sci. . 2003 ; 58A : 1031 -1035.
Morley JE. Postprandial hypotension—the ultimate Big Mac attack. J Gerontol Med Sci. . 2001 ; 56 : M741 -M743.
Edwards BJ, Perry HM III, Kaiser FE, et al. Relationship of age and calcitonin gene-related peptide to postprandial hypotension. Mech Ageing Develop. . 1996 ; 87 : 61 -73.
Breitbart E, Wang X, Leka LS, Dallal GE, Meydani SN, Stollar BD. Altered memory B-cell homeostasis in human aging. J Gerontol Biol Sci. . 2002 ; 57A : B304 -B311.
Li M, Torres C, Auna-Castillo C, et al. Defect in ERK2 and p54 JNK activation in aging mouse splenocytes. J Gerontol Biol Sci. . 2002 ; 57A : B41 -B47.
Kaiser FE, Morley JE. Idiopathic CD4+ T lymphopenia in older persons. J Am Geriatr Soc. . 1994 ; 42 : 1291 -1294.
McElhaney JE. Nutrition, exercise, and influenza vaccination. J Gerontol Med Sci. . 2002 ; 57A : M555 -M556.
Kohut ML, Cooper MM, Nickolaus MS, Russell DR, Cunnick JE. Exercise and psychosocial factors modulate immunity to influenza vaccine in elderly individuals. J Gerontol Med Sci. . 2002 ; 57A : M557 -M562.
Wouters-Wesseling W, Rozendaal M, Snijder M, et al. Effectof a complete nutritional supplement on antibody response to influenza vaccine in elderly people. J Gerontol Med Sci. . 2002 ; 57A : M563 -M566.
Pealer LN, Marfin AA, Petersen LR, et al. Transmission of West Nile virus through blood transfusion in the United States in 2002. N Engl J Med. . 2003 ; 349 : 1236 -1245.
Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med. . 2003 ; 348 : 1977 -1985.
McElhaney JE. Influenza: A preventable lethal disease. J Gerontol Med Sci. . 2002 ; 57A : M627 -M628.
Menec VH, MacWilliam L, Aoki FY. Hospitalizations and death due to respiratory illnesses during influenza seasons: a comparison of community residents, senior housing residents, and nursing home residents. J Gerontol Med Sci. . 2002 ; 57A : M629 -M635.
Chase P, Mitchell K, Morley JE. In the steps of giants: the early geriatrics texts. J Am Geriatr Soc. . 2000 ; 48 : 89 -94.
Smith JR, Olshansky SJ. Position statement on human aging. J Gerontol Biol Sci. . 2002 ; 57A : B291 .
Olshansky SJ, Hayflick L, Carnes BA. Position statement on human aging. J Gerontol Biol Sci. . 2002 ; 57A : B292 -B297.
Butler RN, Fossel M, Harman SM, et al. Is there an antiaging medicine? J Gerontol Biol Sci. . 2002 ; 57A : B333 -B338.
Bergamini E. In response to: “Is there an antiaging medicine?” [Letter]. J Gerontol Biol Sci. . 2003 ; 58A : 483 .
Fisher A, Morley JE. Antiaging medicine: the good, the bad, and the ugly. J Gerontol Med Sci. 57A:M636–M639.
Zuliani G, Cherubini A, Volpato S, et al. Genetic factors associated with the absence of atherosclerosis in octogenarians. J Gerontol Med Sci. . 2002 ; 57A : M611 -M615.
Barzilai N. Discovering the secrets of successful longevity. J Gerontol Med Sci. . 2003 ; 58A : 225 -226.
Choi Y-H, Kim J-H, Kim DK, et al. Distributions of ACE and APOE polymorphisms and their relations with dementia status in Korean centenarians. J Gerontol Med Sci. . 2003 ; 58A : 227 -231.
Evert J, Lawler E, Bogan H, Perls T. Morbidity profiles of centenarians: survivors, delayers, and escapers. J Gerontol Med Sci. . 2003 ; 58A : 232 -237.
Horiuchi S, Finch CE, Mesle F, Vallin J. Differential patterns of age-related mortality increase in middle age and old age. J Gerontol Biol Sci. . 2003 ; 58A : 495 -507.
Butler RN, Austad SN, Barzilai N, et al. Longevity genes: from primitive organisms to humans. J Gerontol Biol Sci. . 2003 ; 58A : 581 -584.
Da Cruz IBM, Oliveira G, Taufer M, et al. Angiotensin I-converting enzyme gene polymorphism in two ethnic groups living in Brazil's southern region: association with age. J Gerontol Med Sci. . 2003 ; 58A : 851 -856.
Tan Q, Yashin AI, Bladbjerg EM, et al. A case-only approach for assessing gene by sex interaction in human longevity. J Gerontol Biol Sci. . 2002 ; 57A : B129 -B133.
Jackson AU, Galecki AT, Burke DT, Miller RA. Mouse loci associated with life span exhibit sex-specific and epistatic effects. J Gerontol Biol Sci. . 2002 ; 57A : B9 -B15.
Hornsby PJ. Cellular senescence and tissue aging in vivo. J Gerontol Biol Sci. . 2002 ; 57A : B251 -B256.
Marcotte R, Wang E. Replicative senescence revisited. J Gerontol Biol Sci. . 2002 ; 57A : B257 -B269.
Smith JR, Venable S, Roberts TW, Metter EJ, Monticone R, Schneider EL. Relationship between in vivo age and in vitro aging: assessment of 669 cell cultures derived from members of the Baltimore Longitudinal Study of Aging. J Gerontol Biol Sci. . 2002 ; 57A : B239 -B246.
Nakamura E, Miyao K. Further evaluation of the basic nature of the human biological aging process based on a factor analysis of age-related physiological variables. J Gerontol Biol Sci. . 2003 ; 58A : 196 -204.
He Q, Li J, Bettiol E, Jaconi ME. Embryonic stem cells: new possible therapy for degenerative diseases that affect elderly people. J Gerontol Med Sci. . 2003 ; 58A : 279 -287.
Kane RL. The future history of geriatrics: Geriatrics at the crossroads. J Gerontol Med Sci. . 2002 ; 57A : M803 -M804.
Hazzard WR. Geriatrics at the crossroads—or simply early in the journey? [Commentary]. J Gerontol Med Sci. . 2002 ; 57A : M806 .
Warshaw G. Commentary on “The future history of geriatrics: geriatrics at the crossroads.”. J Gerontol Med Sci. . 2002 ; 57A : M806 -M807.
Rodin MB. Commentary on “The future history of geriatrics: geriatrics at the crossroads.”. J Gerontol Med Sci. . 2002 ; 57A : M807 -M808.
Flaherty JG. The adolescence of geriatrics [Commentary]. J Gerontol Med Sci. . 2002 ; 57A : M808 -M810.
Tangalos EG. Commentary on “The future history of geriatrics: geriatrics at the crossroads.”. J Gerontol Med Sci. . 2002 ; 57A : M811 .
Sinclair AJ. Commentary on “The future history of geriatrics: geriatrics at the crossroads.”. J Gerontol Med Sci. . 2002 ; 57A : M811 -M812.
Michel J-P, Pils K, Sieber C. Commentary on “The future history of geriatrics: geriatrics at the crossroads.”. J Gerontol Med Sci. . 2002 ; 57A : M812 -M813.
Kane RL. Authors' response to commentaries. J Gerontol Med Sci. . 2002 ; 57A : M813 -M814.
Thomas DR. The future history of geriatrics: consulting the experts [Letter]. J Gerontol Med Sci. . 2003 ; 58A : 92 .
Singh MAF. Commentary on “Dr. Kanes article. The future history of geriatrics: geriatrics at the crossroads” [Letter]. J Gerontol Med Sci. . 2003 ; 58A : 92 -93.
Morley JE, Miller DK. Total quality assurance: an important step in improving care for older individuals. J Am Geriatr Soc. . 1992 ; 50 : 974 -975.
Miller DK, Coe RM, Romeis JC, Morley JE. Improving quality of geriatric health care in four delivery sites—suggestions from practitioners and experts. J Am Geriatr Soc. . 1995 ; 43 : 60 -65.
Miller DK, Coe RM, Morley JE, Gettman J. Total quality management and geriatric care. Aust J Ageing. . 1998 ; 17 :(1 Suppl S): 60 -65.
Rubenstein LZ, Josephson KR, Wieland GD, English PA, Sayre JA, Kane RL. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med. . 1984 ; 311 : 1664 -1670.
Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. . 2002 ; 346 : 905 -912.
Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. . 1993 ; 342 : 1032 -1036.
Morley JE, Flaherty JH, Thomas DR. Geriatricians, continuous quality improvement, and improved care for older persons. J Gerontol Med Sci. . 2003 ; 58A : 809 -812.
Tsilimingras D, Rosen AK, Berlowitz DR. Patient safety in geriatrics: a call for action. J Gerontol Med Sci. . 2003 ; 58A : 813 -819.
Nebeker JR, Hurdle JF, Bair BD. Medical informatics in geriatrics. J Gerontol Med Sci. . 2003 ; 58A : 820 -825.
Palmer Rm, Landefeld CS, Kresevic D, Kowal J. A medical unit for the acute care of the elderly. J Am Geriatr Soc. . 1994 ; 42 : 545 -552.
Flaherty JH, Tariq SH, Raghavan S, Bakshi S, Moinuddin A, Morley JE. A model for managing delirious older inpatients. J Am Geriatr Soc. . 2003 ; 51 : 1031 -1035.
Makowski TR, Maggard W, Morley JE. The Life Care Center of St. Louis experience with subacute care. Clin Geriatr Med. . 2000 ; 16 : 701 -724.
Miller DK, Lewis LM, Nork MJ, Morley JE. Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc. . 1996 ; 44 : 513 -520.
Wieland D, Lamb VL, Sutton SR, et al. Hospitalization in the Program of All-Inclusive Care for the Elderly (PACE): rates, concomitants, and predictors. J Am Geriatr Soc. . 2000 ; 48 : 1373 -1380.
Flaherty JH. Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter medications—causes of confusion. Clin Geriatr Med. . 1998 ; 14 : 101–127 .
Miller DK, Brunworth D, Brunworth DS, Hagan R, Morley JE. Efficiency of geriatric case-finding in a private practitioners office. J Am Geriatr Soc. . 1995 ; 43 : 533 -537.
Miller DK, Morley JE, Rubenstein LZ, Pietruszka FM, Strome LS. Formal geriatric assessment instruments and the care of older general medical outpatients. J Am Geriatr Soc. . 1990 ; 38 : 645 -651.
Flaherty JH, Morley JE, Murphy DJ, Wasserman MR. The development of outpatient clinical Glidepaths. J Am Geriatr Soc. . 2002 ; 50 : 1886 -1901.
Yoshikawa TT, Reuben DB, Ouslander JG. Tribute to David H. Solomon, MD, for his contributions to geriatrics and gerontology, on his 80th birthday. J Am Geriatr Soc. . 2003 ; 51 :(7 Suppl S): S327 .
Yoshikawa TT, Reuben DB, Ouslander JG. Biographical sketch of David H. Solomon, MD. J Am Geriatr Soc. . 2003 ; 51 :(7 Suppl S): S330 -S332.
Warshaw WA, Gragg EJ. The training of geriatricians in the United States: three decades of progress. J Am Geriatr Soc. . 2003 ; 51 :(7 Suppl S): S338 -S345.
Reuben DB, Shekelle PG, Wenger NS. Quality of care for older persons at the dawn of the third millennium. J Am Geriatr Soc. . 2003 ; 51 :(7 Suppl S): S346 -S350.
Morley JE. Hormones and the aging process. J Am Geriatr Soc. . 2003 ; 51 :(7 Suppl S): S333 -S337.
| Month: | Total Views: |
|---|---|
| December 2016 | 2 |
| January 2017 | 205 |
| February 2017 | 706 |
| March 2017 | 464 |
| April 2017 | 43 |
| May 2017 | 26 |
| June 2017 | 69 |
| July 2017 | 43 |
| August 2017 | 243 |
| September 2017 | 522 |
| October 2017 | 400 |
| November 2017 | 737 |
| December 2017 | 2,602 |
| January 2018 | 4,618 |
| February 2018 | 4,700 |
| March 2018 | 4,999 |
| April 2018 | 4,276 |
| May 2018 | 3,689 |
| June 2018 | 3,453 |
| July 2018 | 3,473 |
| August 2018 | 4,227 |
| September 2018 | 5,572 |
| October 2018 | 4,805 |
| November 2018 | 5,726 |
| December 2018 | 4,153 |
| January 2019 | 4,255 |
| February 2019 | 4,126 |
| March 2019 | 4,394 |
| April 2019 | 4,658 |
| May 2019 | 4,865 |
| June 2019 | 4,180 |
| July 2019 | 4,133 |
| August 2019 | 4,697 |
| September 2019 | 5,501 |
| October 2019 | 3,785 |
| November 2019 | 2,915 |
| December 2019 | 2,082 |
| January 2020 | 3,273 |
| February 2020 | 3,085 |
| March 2020 | 2,087 |
| April 2020 | 2,095 |
| May 2020 | 1,206 |
| June 2020 | 1,579 |
| July 2020 | 1,237 |
| August 2020 | 1,373 |
| September 2020 | 2,140 |
| October 2020 | 2,189 |
| November 2020 | 1,847 |
| December 2020 | 1,360 |
| January 2021 | 1,806 |
| February 2021 | 2,061 |
| March 2021 | 1,955 |
| April 2021 | 1,768 |
| May 2021 | 1,510 |
| June 2021 | 1,347 |
| July 2021 | 1,170 |
| August 2021 | 1,467 |
| September 2021 | 2,213 |
| October 2021 | 1,939 |
| November 2021 | 1,407 |
| December 2021 | 1,093 |
| January 2022 | 1,237 |
| February 2022 | 1,417 |
| March 2022 | 1,408 |
| April 2022 | 1,323 |
| May 2022 | 1,105 |
| June 2022 | 901 |
| July 2022 | 762 |
| August 2022 | 1,020 |
| September 2022 | 1,472 |
| October 2022 | 1,352 |
| November 2022 | 1,071 |
| December 2022 | 697 |
| January 2023 | 1,058 |
| February 2023 | 1,034 |
| March 2023 | 888 |
| April 2023 | 714 |
| May 2023 | 791 |
| June 2023 | 536 |
| July 2023 | 604 |
| August 2023 | 723 |
| September 2023 | 807 |
| October 2023 | 841 |
| November 2023 | 726 |
| December 2023 | 593 |
| January 2024 | 857 |
| February 2024 | 911 |
| March 2024 | 892 |
| April 2024 | 792 |
| May 2024 | 790 |
| June 2024 | 619 |
| July 2024 | 446 |
| August 2024 | 621 |
| September 2024 | 327 |
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1758-535X
- Copyright © 2024 The Gerontological Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 02 November 2023
Driving the determinants of older people’s mental health in the context of urban resilience: a scoping review
- Sajad Vahabi 1 ,
- Azadeh Lak 2 &
- Niloofar Panahi 1
BMC Geriatrics volume 23 , Article number: 711 ( 2023 ) Cite this article
2009 Accesses
2 Citations
Metrics details
Population aging is a pervasive phenomenon occurring rapidly worldwide, while sustainable development goals are considered the mental health among older adults.
To investigate the factors affecting mental health, we conducted a scoping review of the 47 papers published between 2015 and 2022 to explore various dimensions affecting older adults’ mental health.
Our finding mirrors four dimensions of creating healthy and sustainable environments for older adults: person, place, processes, and resilience-related health in the living environment. The person dimension includes individual characteristics, attitudes and behaviors, and health status. The place dimension is divided into five categories: land use, access, physical form, public open spaces, and housing, while the process consists of the social, cultural, and economic environments. Resilience-related health dimension emphasizes the impact of natural and man-made disasters on older people’s mental health.
These findings can provide policymakers insights into developing community-based environmental intervention strategies to promote mental health among older adults and support healthy and active aging.
Peer Review reports
There are more than 703 million older adults over age 65 worldwide. The increasing population of older people is caused by a decrease in the fertility rate and increasing life expectancy [ 1 ]. East and South-east Asia have the world’s largest aging adult population, with more than 260 million people, followed by Europe and North America, with more than 200 million people. By 2050, the older population will double to 1.5 billion [ 2 ]. Moreover, urban residents, that is, the people living in urban areas, comprise more than 55 percent of the world's population. Statistics predict that by 2050, more than 68% of the world's population will live in cities [ 3 ].
Moreover, the Organization for Economic Cooperation and Development (OECD) shows that the share of the population of people over 65 years old will increase to 25.1% in its member countries in 2050. Thus, cities particularly have many older residents, about 43.2% of the older adult population [ 4 ], indicating the coincidence of two significant phenomena of population aging and urbanization in the coming years. The Sustainable Development Goals (SDGs), developed by the United Nations, emphasize the health and well-being of all, especially older people [ 5 ]. The World Health Organization defines healthy aging as creating and sustaining functional capacity that leads to well-being in old age [ 6 ].
Recently, the mental health of older adults has been considered one of the significant issues that attracted the attention of researchers and policymakers. The World Health Organization (WHO) defines mental health as a state of well-being in which each person can realize their potential, cope with the stresses of life, work productively, and contribute to their community [ 7 ]. Hoisington et al. (2019) mentioned that Mental health includes emotional and social well-being components as well as social skills and cognitive functions affecting participation in basic tasks and social roles [ 8 ]. According to the Global Burden of Disease Survey (2015), depression and anxiety are the leading mental illnesses (ranked third and ninth, respectively) that cause the most problems worldwide, associated with various health problems, such as cardiovascular diseases and reduced quality of daily life, particularly among older people [ 9 ]. Older people’s mental health is becoming a growing public health concern [ 10 ].
Although national patterns of depression have been documented, research about older people has received less attention [ 11 ]. Specifically, neurological and psychiatric disorders account for 6.6% of all disabilities, the fifth leading cause of disease in the older population [ 12 ].
According to [ 13 ], with increased social participation among older adults, more time in physical activity, and more frequent contact with neighbors and children, their depression can be reduced [ 13 ]. Ko et al. 2019 believed that older men were significantly more likely to report feelings of loneliness, depression, and frequent suicidal thoughts than women. Older women were more likely to report higher stress levels and depressive symptoms. Older people who work suffer from more stress and, at the same time, experience fewer depressive symptoms [ 14 ].
Furthermore, the built environment is potentially involved in the mental disorders of older adults through its effects on social communication, access to green space, exposure to noise, traffic, or air pollution, and changes in individual behaviors, such as physical activity [ 15 ]. Evidence shows that the physical and social dimensions of the neighborhood environment play an essential role in older peoples’ health to predict health outcomes beyond individual deprivation and psychosocial characteristics [ 16 ]. For instance, according to research, older people living in pedestrian-friendly urban areas (with easier access to facilities, beautiful scenery, open spaces, and road safety) are generally more physically active and healthier [ 17 ]. Furthermore, older adults are more vulnerable to stressors or risks due to reduced physical performance against environmental barriers [ 18 ]. Compared to younger adults, older adults appear to be more vulnerable to changes in the built environment [ 19 ].
Today, urban resilience is considered a paradigm affecting all aspects of human life. Meerow (2016) proposed a new definition for urban resilience be defined as the following: “Urban resilience refers to the ability of an urban system and all its constituent socio-ecological and socio-technical networks across temporal and spatial scales to maintain or rapidly return to desired functions in the face of a disturbance, to adapt to change, and to quickly transform systems that limit current or future adaptive capacity [ 20 ]”. They added socio-economic dynamics such as public health, monetary capital, demographics, and Justice and equity to shape the other subsystems. The livelihoods and capacities of urban citizens have a significant role in enhancing urban resilience. Furthermore, after the COVID-19 outbreak, urban resilience is critical to urban and human health. Resilience is the capacity of a system or community at risk to withstand, adapt to, and recover from the effects of a hazard in a timely and effective manner [ 21 ].
The COVID-19 outbreak caused the disconnection of older adults from the outdoor environment, and older people with a history of depression reported higher levels of depression or sadness during the pandemic [ 22 ]. Fear of being infected with the virus, hospitalization of family members, disconnection of the senior from social support, and fear of losing a job can also affect older people’s mental health [ 22 , 23 , 24 ]. Although some studies show that younger people were more emotionally involved than seniors in disasters such as the COVID-19 pandemic, others show that older people suffer a more significant threat and death from catastrophes. Additionally, some authors have discovered a relationship between emotional well-being, resilience, and social support among caregivers exposed to social isolation [ 25 ].
In recent years, many studies have measured the impact of social, economic, health, individual, and demographic factors on the mental health of older adults; however, there is still no comprehensive model for measuring the factors affecting older adults' mental health in urban areas. This review study aims to find the factors affecting the mental health of older people living in urban environments by reviewing papers published in the last seven years by focusing on understanding the general determinants of older people’s mental health in the cities as a narrative systematic review. This study provides a deep understanding of the factors affecting the mental health of older adults for policymakers to make plans to increase the mental resilience of older adults and improve their quality of life.
A scoping review is a good tool for identifying domains or covering a body of literature on a particular topic, identifying knowledge gaps, existing literature, and concepts [ 26 ]. Arksey and O’Malley used a systematic scoping review for the first time in five main steps: identifying research questions, identifying related studies, selecting studies, charting and collecting data, and summarizing and reporting research results [ 27 ]. This method was then improved by Daudt et al. 2013, Levac et al. 2010, and Colquhoun et al. 2014 [ 28 , 29 , 30 ]. This study followed the PRISMA extension for scoping reviews (PRISMA-SCR) [ 31 ]. In recent years, some studies have been conducted on older people's mental health, each focusing on specific dimensions. Due to the complex nature of mental health, the scoping review is used in this study to identify knowledge gaps and reveal various factors affecting older people’s mental health.
Identifying research questions
The first step in the scoping review is to identify research questions to reveal and link them to the research objectives. This study aims to review the papers on the mental health of older adults to identify the factors that can affect the mental health of older adults living in the urban environment in the face of stressful aspects (conditions such as COVID-19) and lead to an increase in urban resilience among older people. For this purpose, the following questions have been used to refine the research.
What factors affect Older adults’ mental health living in urban environments?
What factors affect Older adults’ mental health living in the city In facing disasters and changes, ‘for instance, COVID-19’, to achieve urban resilience?
Identify related studies
We searched Scopus, PubMed, Web of Science, and Google Scholar for relevant papers from 2015 to 10 May 2022. Search strategies drafted by a professional person and refined through team discussion. The search terms were “mental health” and / OR “neighborhood” and / OR “urban area”, and “environment” and / OR “older people” and / OR “social environment” and / OR “built environment” and / OR “depression” and “anxiety” and “stress” and “Covid -19”. Article in Press in Scopus Database, Rural context-based, and non-English papers were excluded.
Selection of studies
One thousand nine hundred ninety-four papers were collected after searching the databases. First, 280 duplicate papers were removed, and then, based on the analysis of abstracts and titles, 1646 other papers were removed from the study. After a complete review of the papers, 21 were removed from the list due to their relevance to the rural environment, lack of suitable sample sizes, failure to calculate mental health or mental well-being, and relevance to nursing homes. To increase consistency among reviewers, All reviewers screened the first 60 publications and discussed the review’s screening and result.
Three authors did the initial review of the abstracts and titles, and after reviewing, all authors decided which paper would remain for further study. After this process, 47 papers complied with the criteria. It should be mentioned that 4 of the documents were review papers. The article selection process, the PRISMA process, is presented in Fig. 1 .
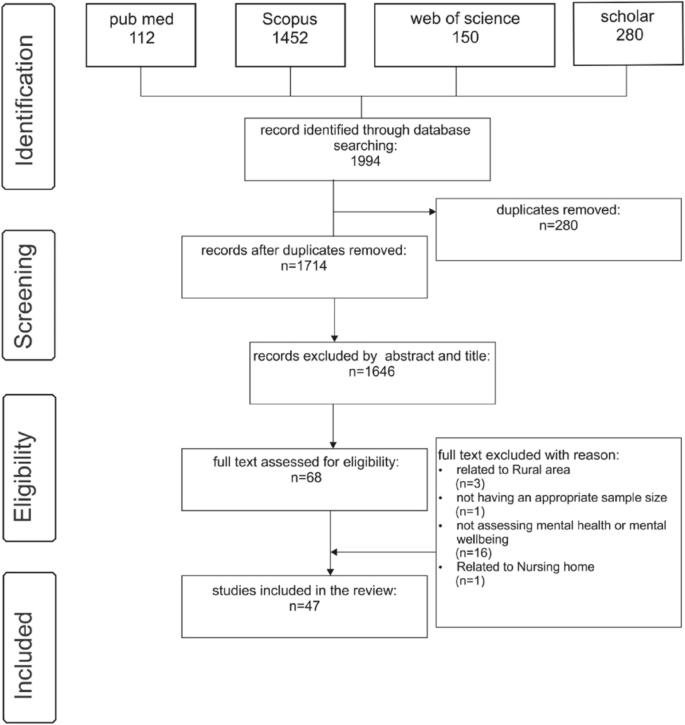
PRISMA flowchart for study selection
Charting and interpreting data
For data extraction and charting, this study follows [ 28 , 30 ] recommendations for scoping review data extraction and charting. In this regard, the authors chose the narrative review approach for data charting, as described in [ 30 ]. Based on this, Two reviewers developed an Excel file to examine which data needs to be extracted. Then, all related data were collected in an Excel file after selecting the papers. The Data included authors, year, geographical location, research scale, method, mental health measurement tool, personal factors, health factors, physical environment factors, social environment factors, economic factors, age of participants, and key findings.
Collecting, summarizing, and reporting the results
The last stage of the scoping review is collecting, summarizing, and reporting the results. Thematic analysis was used to combine, categorize, and codify the studies’ findings regarding the research questions and aims. Thematic analysis of the papers was done with an emphasis on the factors affecting older people’s mental health, such as the dimensions of the built environment, social environment, individual characteristics, and health status. Table 1 presents the categorizing process used in data analysis and coding.
Table 2 shows the characteristics of the reviewed papers. Twenty-seven studies (57.4%) are from Asia, ten studies (21.3%) are from Europe, and six studies (12.8%) are from America. In addition, the most significant number of studies is related to the Chinese mainland, with 11 (21.4%) studies, and Hong Kong, China, with eight studies (17%). Also, 41 (87.23 percent) studies were conducted with the quantitative method and 2 (4.25) with the qualitative approach. Four studies are review articles.
Analysis of assessment tools of mental health consisting of CES-D ( n = 11) and GDS-15 ( n = 9) was used in these studies to measure older adults' mental health. Tools such as HADS, UCLA, MSC, SF-12, SF-36, PSS, MMSE-2SV, SWLS, and GAI were also employed. Table 3 shows the mental health measurement tools used in the papers.
Older people studied in the papers were generally aged 60 and over (41.2 percent) and 65 and over (32.3 percent). Additionally, more than 74% of the studies mirror the environment dimension and its impact on mental health, as 46% examined the effects of the social environment on the mental health of older adults. In 14 papers, the impact of economic factors on older people’s mental health was studied; however, 46% of the papers considered personal health and its role in mental health. 46% of studies examined personal characteristics and their effect on mental health. Ten studies considered factors such as physical activity, social activity, the proportion of older people population, social relationships, household income, and social capital as mediating factors affecting older people’s mental health. Three papers examined the cultural aspects and their impact on mental health, and five studied the social health of older people against disasters, especially the COVID-19 virus. The main dimensions and codes are summarized in Fig. 2 .
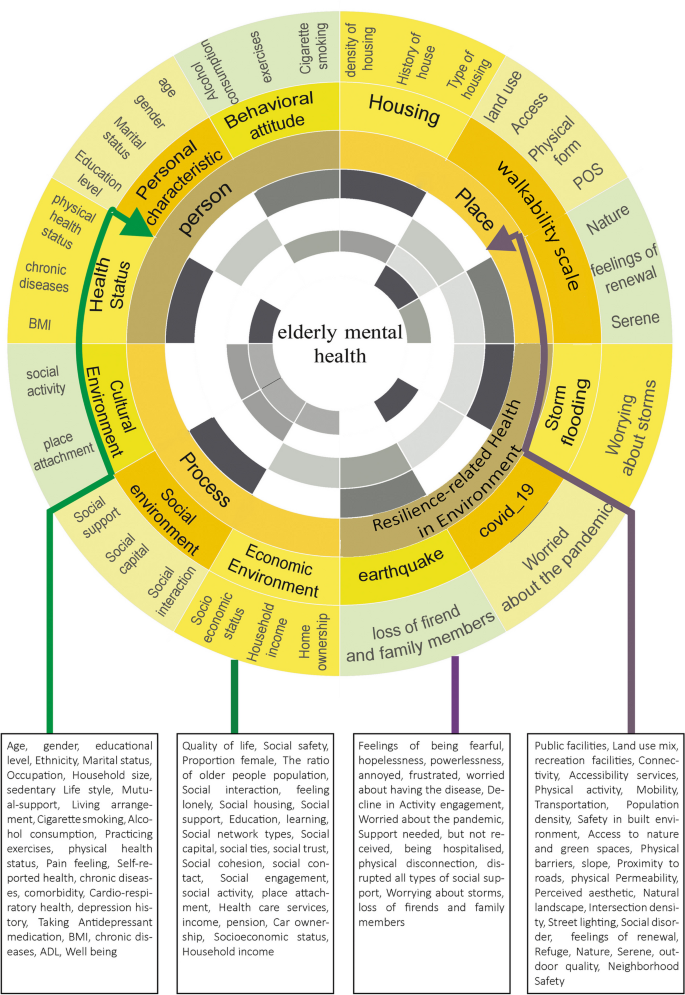
Determinant Model of older people’s mental health
According to the findings, intricate interactions between factors were investigated through the Co-occurrence of keywords with VOS Viewer for four mental health disorders reviewed in this study: mental health, well-being, anxiety, and depression. Each of these shows the different relationship between mental health and environmental determinants. Mental health factors include social support, social cohesion, social network, social capital, social status, land use, traffic, Healthcare, crime, income, health status, social environment, social behavior, residence characteristics, exercise, population density, green space and parks, residential environment, safety, neighborhood, perceived stress, demographic status, older adults population. Figure 3 shows the network visualization map.
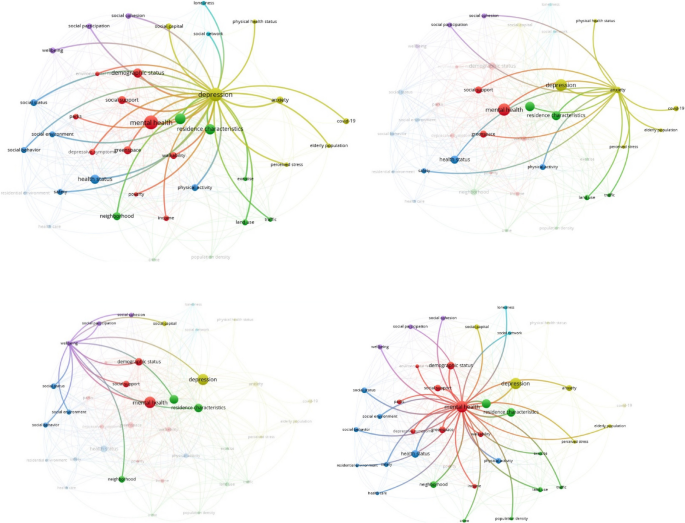
Term co-occurrence map for different mental health disorders from top-left: depression, anxiety, well-being, and overall mental health
Well-being is linked to social participation, cohesion, social support, social capital, demographic status, residence characteristics, social environment, and social behavior. Depression disorder is related to physical health status, walkability, health status, safety, income, neighborhood, physical activity, safety, land use, traffic, residence characteristics, green space and parks, social participation, social cohesion, social support, social capital, social network, demographic status, loneliness, poverty, neighborhood, social status. Anxiety disorder is connected to social support, social participation, social cohesion, residence characteristics, physical activity, older adult population, health status, land use, traffic, green space, COVID-19 outbreak, perceived stress, and safety. Additionally, as shown in the Co-occurrence term, depression highly impacts older people’s mental health.
The above findings explain that the various dimensions of mental health in older people are most influenced by environmental, individual, social, personal health, and economic factors. The paper’s review showed that older people’s mental health was associated with many factors, including the built and social environment. After thoroughly reviewing the papers, the factors affecting older people’s mental health were identified, and concepts related to various environmental dimensions were coded. The dimensions and criteria based on the Vos viewer are presented in Fig. 4 .
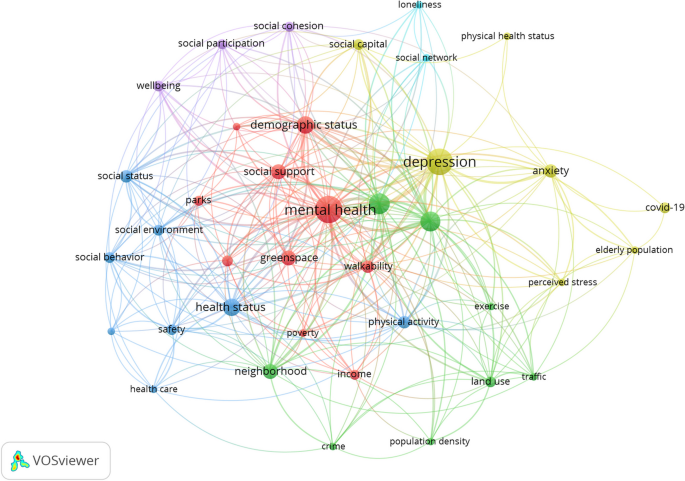
Term co-occurrence map of mental health disorders
Personal dimension
This dimension includes three sub-dimensions: personal characteristics, attitudes and behaviors, and health status. The following criteria and definitions of individual determinants have been extracted and coded from 32 papers. The papers have considered personal factors such as age, gender, education level, ethnicity, race, house ownership, employment, marriage, household size, sedentary lifestyle, mutual support, and living arrangement [ 32 , 33 , 34 , 35 ]. Three studies reported that living in areas with a high percentage of older people directly impacted older people’s health. Domènech-Abella et al. (2020) stated that a sedentary lifestyle and less physical activity reduce older people’s mental health. Attitudes and behaviors comprise three components: smoking, alcohol consumption, and physical exercise [ 13 , 14 , 36 ]. Byeon (2019) showed that older people who do flexibility exercises for an average of 1 to 4 days are 81 percent less likely to develop depression than those who do not. People who smoke are more likely to experience high-stress levels and depression [ 14 ].
Lam et al. (2020) showed a close relationship between personal characteristics such as physical and body weight and mental health. Moreover, individual health factors include physical health, well-being, pain sensation, functional ability, self-assessment of health, body mass index (BMI), restrictions on daily activities, chronic diseases, co-occurrence of multiple disorders, and lung diseases [ 31 , 35 , 39 , 47 ]. Therefore, people with a good BMI will be healthier and experience better mental health. Also, having two or more diseases simultaneously affects mental health [ 14 ].
Place-based dimension
The place dimension can affect older people’s mental health to a large extent, which is presented in 35 studies. The place-based features include land use, access, physical form, public open spaces, and housing. Eleven studies focused on land use, including proximity to services, public facilities, land use mix, and sports facilities [ 34 , 37 ]. Koohsari et al. (2019) report that women with better access to transportation stations have a higher level of mental health. Commercial and recreational facilities directly impact the mental health of older adults. The access factor is considered in 13 studies and includes connectivity, service access, mobility, pedestrian environment, and public transportation [ 38 , 39 , 40 ]. Low walkability of the built environment increases the chances of loneliness, which is associated with mental health [ 37 ].
Additionally, physical form, which was considered in 14 studies, includes population density, safety, access to green space, physical barriers, slope and topography, proximity to roads, physical permeability, familiarity with the environment, Environmental aesthetics, natural landscapes, and residential density [ 41 , 42 , 43 ]. Perception of safety is related to the physical and mental health of older people [ 44 ]. Furthermore, decreasing physical barriers and crime in the neighborhood increase older people’s mental health [ 18 ]. Public open space was considered in 13 papers, paying attention to issues such as street lighting, safety against crime, social disorders, availability of water spaces, recreational spaces, environmental cleanliness, noise pollution, congestion, Landscapes, outdoor quality, green and blue space coverage, restoration Serene, nature restoration, social restoration, landscape, restoration refuge and a sense of renewal [ 41 , 45 , 46 ].
More importantly, public open spaces significantly impact older people’s mental health, so green and blue infrastructures in the neighborhood and near beaches and lakes are associated with reduced use of antidepressants [ 10 ]. Green spaces are also associated with increased physical activity, improving mental health perception and well-being, and promoting older people’s mental health [ 34 , 47 ]. Ten papers consider housing quality, neighborhood safety, housing density, housing facilities, type of housing, length of stay, interior design, and house history [ 38 , 48 , 49 ]. The quality of housing and the neighborhood’s safety affect older adults' mental, physical, and mental health [ 50 ]. External building characteristics, interior design, home facilities, and interior home space profoundly impact the mental health of older people [ 49 ].
Procedural determinants
Procedural dimensions include social, cultural, and economic environments. The social environment affects the mental health of older adults in various ways. Chen et al. (2016) stated that older people, with the support of friends or family, have better mental health; additionally, social capital can play a supportive role in mental health [ 27 ]. The essential components of the social environment are presented in 21 papers, including quality of life and health, social safety, the ratio of women in the neighborhood, the ratio of older people population in the neighborhood, social interactions, feeling lonely, social housing, social support, education, learning, social network type, different types of social capital, Social nodes, trust, and social cohesion [ 34 , 38 , 51 , 55 ].
Besides, the cultural environment was repeated in three papers. Older people’s participation in social activities reduces stress and depression in older people [ 14 ]. This sub-theme profoundly affects the mental health of older adults and includes two criteria for social activities: the sense of place and identity [ 51 , 52 ].
According to our review, social and economic status is the most critical component of the economic factor. The economic environment is studied in 15 papers related to health: income/retirement, socio-economic status, car ownership, housing ownership, and household income [ 42 , 53 , 54 ].
Resilience-related health in environment dimension
Natural disasters and crises profoundly affect mental health. Five papers specifically address the issue of Covid-19 and its impact on older adults’ social health and resilience. With the Coronavirus outbreak, many older people were forced to stay home. Lockdowns and cocoons caused some problems profoundly affecting older people’s mental health. Dimensions introduced in these studies include cases of being affected by COVID-19, feeling lonely, fear, despair, helplessness and fatigue, fear of getting COVID-19, decreased participation in activities, need to receive support, frequent communication with others, hospitalization, disconnection, and loss of social support [ 23 , 24 , 55 ]. Older people’s physical activity has significantly decreased during the pandemic; thus, the severity of depression in women has increased [ 56 ]. Two studies have examined the impact of disasters on mental health, which refer to the fear of storms and the loss of families, respectively [ 57 , 58 ].
This study has used a scoping review to identify, select, and combine the findings of studies that have examined determinants affecting the mental health of older adults in urban areas in the context of urban resilience. We found that urban resilience refers to a city’s capacity to support its citizens and systems. Like humans, cities are resilient due to a variety of intricate variables. Surprisingly, however, there is a conceptual link between urban and psychological resilience because both ultimately benefit the person or citizen. As a result, the elements that contribute to urban resilience may also contribute to mental resilience and vice versa.
As a result, the conceptual similarity between urban and psychological resilience is rational, and the distinct characteristics that distinguish the two are likewise connected. Researching these elements and looking at resilience’s impact on mental health in urban settings would be fascinating. Based on reviewing the previous paper, we introduce the ideas of older adults’ mental health and urban resilience, describe urban resilience's functional link with older adults’ mental health, and pinpoint the characteristics of urban resilience in four dimensions of determinants associated with mental health in older people (anxiety, depression, mental health, and well-being), including personal and place-based factors, processes in the living environment (social, cultural, and economic), and environmental health (natural and man-made disasters).
Urban Resilience focuses on the system’s ability to maintain environmental harmony despite perturbations. Additionally, it aids in the recovery of individuals from disturbance. It deals with the capacity to adjust to and respond to structural change throughout time. Thus, most studies have pointed out the effect of older people’s characteristics on their mental health as the most influential factor. Regarding socio-economic processes, studies have emphasized the role of social capital, social interactions, perception of social security, and the economic status of older people in improving their mental health of the older people. This study scrutinizes the mental health of older adults by analyzing the geographical scope, tools for measuring older people's mental health, and key findings on the main reported determinants of older people’s mental health to provide comprehensive knowledge about the consequences of the results and gaps which can be helpful for physicians, researchers, and aging policymakers.
Based on the role of urban structure and place in building urban resilience, the place and land use range mix has been found in most studies. Still, some individual variables that refer to walkability in these studies (such as crosswalks, barrier-free sidewalks, and recreational environments) have a significant relationship with health. In particular, the presence of green space/park was the most studied variable in all areas related to mental health outcomes. A few studies paid attention to individual and place-based determinants. In contrast, the qualitative studies paid more attention to the perceptual characteristics of the quality of housing, the perception of environmental security, and the perception of the social environment.
In addition, perceptions of environmental health, fear of infectious diseases such as COVID-19, and injuries caused by natural and man-made disasters were considered in the papers. Most studies that looked at the impact of individual and environmental factors on older people’s mental health found significant relationships, with evidence supporting the moderating effects of demographic characteristics, health status, health behaviors, neighborhood walkability, and an area’s level of development intensity. The mediating results of both personal and place-based dimensions were not confirmed. Due to significant differences in research methodology, measurement methods, sample sizes, and neighborhood definition, direct comparisons between studies are impossible.
In addition, the results of the analysis of the keywords in VOS viewer showed that the study of factors such as Demographic Status, Health status, Social support, Green space, Walkability, Neighborhood Characteristics, Physical activity, Social Support, Social environment in research related to mental health is of great importance and has been studied more than the rest of the factors. Also, some factors such as traffic safety, safety, exercise, loneliness, social network, and physical health status have been less discussed.
Methodological limitations of review studies
A- Lack of standard tools in measuring the determinants of mental health: Contradictory findings on the role of the four dimensions on older people’s mental health may be partly due to the lack of clarity in the definition of standard mental health measurement tools for the four dimensions of individual, place, process, and environmental health. This problem is the most prevalent in place-based features, which mention various tools to study the effects of place-based features on older people’s mental health. Other studies have pointed to the lack of standard tools in investigating the factors affecting older people’s mental health [ 59 ]. Studies such as Ivey et al. (2015) point to using common mental health tools to link mental health and neighborhood measurement metrics using various data [ 44 ].
b- Lack of evaluation of specific Place-based features: Most Place-based features studied in the papers, such as public parks, access to public transportation, and land use composition, are among the common features necessary for healthy aging. Although an increasing number of studies have studied the separated criteria instead of integrated criteria to portray the role of individual and Place-based components, there is still a knowledge gap about place-based features that may affect the mental health of older adults. A small amount of literature outside the scope of this study, including unreviewed documents, suggests potential design solutions for adapting outdoor environments to mental health. They consider some design dimensions such as distinctive architectural features, ample street facilities (such as shaded chairs and lighting), a clear hierarchy of locations, comprehensive, simple, unobstructed sidewalks, and short and distinctive pedestrian crossings. These place-based features are attractive targets for interventions because they are generally more practical and sustainable than large-scale environmental or program-based interventions. Future studies need to identify valid and consistent ways to measure the role of specific design features and establish more robust paths between place-based characteristics and older people’s mental health. For example, green space is an essential Place-based feature playing a significant role in promoting the health of older people, particularly mental health [ 60 ]. However, our findings indicate that the total area/ratio of green space alone may not fully show a significant impact on health outcomes, and future research should consider the morphology and quality of green space for better assessment. There are no specific measuring tools for housing quality for older people, especially social housing. Studies conducted in this regard examined the needs and preferences of older adults and their effect on older people's mental health using qualitative methods.
Assessing the mental health of the older people
Mental health in older people has several definitions. Studies considered mental health in older adults as cognitive health; consequently, the loss of mental health is considered dementia in older people [ 59 ]. Another range of studies related to mental health emphasized some emotions such as stress, depression, and anxiety [ 15 , 34 , 43 , 56 , 61 , 62 ]. Despite different emotions in older people, there was no standard and comprehensive tool for mental health testing in older people. The most used tools were CES-D and GDS-15, which were used to study the rate of depression in older adults, and the others, the emotional disorders, in older adults received little attention. Especially when health is endangered in conditions such as pandemics or natural hazards, these instruments have little efficiency in measuring older people’s mental health, and most studies have turned to qualitative studies.
Study of mediating effects
Five studies looked at mediators focused on P.A. or walking outcomes using subjective self-reports, and three used objective measures (accelerometer measure of P.A.). In some papers, the mediating effects of subjectively estimated P.A. or walking were considerable. As respondents may not recall their previous physical activity accurately, this assessment approach frequently results in recall bias, limiting the capacity to find reliable relationships with cognitive function. Future studies should use objective techniques to capture P.A. levels more accurately and prove its mediation function in mental health conditions. Furthermore, more research is needed to understand the underlying mechanism of the long-term link between greenness and mental health. Depression was also discovered to mediate the relationship between urbanization and personal/crime-related safety [ 41 ].
In recent years, cities in North Africa and the Middle East have been experiencing special conditions under the influence of climatic phenomena. Every year, many people die due to dust. The vulnerable groups suffering from these changes are older people, who have to stay home because of the effects of these factors on health. Prolonged stay at home and disconnection from the external environment have affected older people’s mental health, so it is suggested that future research consider the effects of dust and climate change on older people’s mental health.
Strengths and limitations of the research
This research uses a scoping review method and a systematic search strategy based on research questions. In this study, a selection of scientific evidence and studies conducted on the mental health of older adults living in the city can be used to strengthen older people’s mental health in cities. This study also facilitates the formation of future research with a comprehensive view and by identifying different dimensions of mental health in older people. There are several limitations to the scoping review in this study. First, In this research, only four databases in English have been examined, which means that studies from other languages have not been included. Second, this study did not investigate factors such as dementia, schizophrenia, bipolar disorder, cognitive disorders, and suicide related to mental health disorders in older adults. Third, in this study, only research with the urban context is considered, and older people living in rural areas are out of the scope of this research. Fourth, different dimensions of the impact of the COVID-19 pandemic on the mental health of older people under environmental health are presented in this study. We suggest that in future research, the effect of the COVID-19 pandemic on the mental health of older adults living in cities be examined in more depth. Fifth, the significant studies included in this study are from developed countries in Asia, Europe, and America, so the findings of this study may be less applicable in developing countries. Sixth, Some natural disasters, such as floods and earthquakes, have not been investigated in this study. Still, since these factors affect the mental health of older people in resilient environments and there is a need to study in this field, some of the effects of these factors are shown in 5 4 to emphasize this issue. Only two factors were considered influential factors in mental health to highlight the importance of catastrophe on older people’s mental health. It is suggested that these factors’ role in older people’s mental health be examined in more detail in future research.
This study has presented a comprehensive and valid review of the papers about determinants of mental health of older adults in the context of the urban resilience approach that has been of interest in recent years. In this study, urban resilience is defined as the ability of the urban environment and its residents to maintain continuity in the face of shocks and stresses, especially for vulnerable older adults, so that they can adapt positively to achieve a sustainable environment. The results of this study have been presented in the form of a conceptual model that refers to the cognitive health component of older people, including personal and spatial dimensions, socio-economic and cultural processes, and health-oriented environments. The personal dimension refers to older adults’ demographic characteristics, health behaviors, and health status. The spatial dimension relates to land use, access, urban form, urban space, and the quality of older people’s neighborhoods.
Procedural components examine socio-cultural processes, economic conditions, and the policy-making and governance environment (including urban and health management). The difference between this study’s results and cognitive health components is the resilience-related health component, which tries to increase the adaptability of older adults in the face of shocks and disasters, including natural disasters and shocks caused by future infectious diseases that have affected the urban older people community during COVID-19. These components can make it possible to realize urban resilience with resilient residents.
Future related studies in designing a healthy and resilient environment for older people in a situation where climate changes, fine dust, and various phenomena resulting from global warming affect cities can effectively promote older people’s health and ultimately improve older adults’ health. The findings of this review can also provide insights for policymakers and those involved in planning and designing the development of environmental intervention strategies at the community level to promote mental health and resilience among older people and support healthy and active aging.
Availability of data and materials
After request, supporting data and data analysis materials are available from the corresponding author (AZ).
United Nations Department of Economic and Social Affairs PD. World Population Ageing 2020 Highlights: Living arrangements of older persons. In. United Nations Publication; 2020.
Nations U. World Population Ageing 2019 Highlights. United Nations; 2019.
Nations U. World Urbanization Prospects: The 2018 Revision. United Nations; 2018.
OECD. Ageing in Cities. In. Paris; 2015.
Pandey NM, Tripathi RK, Kar SK, Vidya K, Singh N. Mental health promotion for elderly populations in World Health Organization South-East Asia Region: Needs and resource gaps. World J Psychiatry. 2022;12(1):117.
Article CAS PubMed PubMed Central Google Scholar
Tavares RE, Jesus MC, Machado DR, Braga VAS, Tocantins FR, Merighi MAB. Healthy aging from the perspective of the elderly: an integrative review. Revista Brasileira de Geriatria e Gerontologia. 2017;20:878–89.
Article Google Scholar
WHO. Promoting mental health : concepts, emerging evidence, practice : summary report / a report from the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. Geneva: World Health Organization; 2004.
Hoisington AJ, Stearns-Yoder KA, Schuldt SJ, Beemer CJ, Maestre JP, Kinney KA, Postolache TT, Lowry CA, Brenner LA. Ten questions concerning the built environment and mental health. Build Environ. 2019;155:58–69.
Wang R, Liu Y, Lu Y, Zhang J, Liu P, Yao Y, Grekousis G. Perceptions of built environment and health outcomes for older Chinese in Beijing: A big data approach with street view images and deep learning technique. Comp Environ Urban Syst. 2019;78:101386.
McDougall CW, Hanley N, Quilliam RS, Bartie PJ, Robertson T, Griffiths M, Oliver DM. Neighbourhood blue space and mental health: A nationwide ecological study of antidepressant medication prescribed to older adults. Landsc Urban Plan. 2021;214:104132.
Yang KH, Han BH, Moore AA, Palamar JJ. Trends in major depressive episodes and mental health treatment among older adults in the United States, 2010–2019. J Affect Disord. 2022;318:299–303.
Article PubMed Google Scholar
Arias-Fernández L, Carcedo-Argüelles L, Martín-Payo R, López-García E, Rodríguez-Artalejo F, Lana A. Association between neighborhood physical characteristics and mental health among older adults in Spain. Geriatr Nurs. 2023;49:170–7.
Wang R, Feng Z, Liu Y, Lu Y. Relationship between neighbourhood social participation and depression among older adults: A longitudinal study in China. Health Soc Care Community. 2020;28(1):247–59.
Lee HJ, Lee DK. Do sociodemographic factors and urban green space affect mental health outcomes among the urban elderly population? Int J Environ Res Public Health. 2019;16(5):789.
Article PubMed PubMed Central Google Scholar
Pun VC, Manjourides J, Suh HH. Close proximity to roadway and urbanicity associated with mental ill-health in older adults. Sci Total Environ. 2019;658:854–60.
Article CAS PubMed Google Scholar
Toma A, Hamer M, Shankar A. Associations between neighborhood perceptions and mental well-being among older adults. Health Place. 2015;34:46–53.
Bhuyan MR, Yuen B. Older Adults’ Views of the Connections between Neighbourhood Built Environment and Health in Singapore. J Popul Ageing. 2022;15(1):279–99.
Zhao Y, Chung PK. Neighborhood environment walkability and health-related quality of life among older adults in Hong Kong. Arch Gerontol Geriatr. 2017;73:182–6.
Yue Y, Yang D, Owen N, Van Dyck D. The built environment and mental health among older adults in Dalian: The mediating role of perceived environmental attributes. Soc Sci Med. 2022;311:115333.
Meerow S, Newell JP, Stults M. Defining urban resilience: A review. Landsc Urban Plan. 2016;147:38–49.
Jha AK, Miner TW, Stanton-Geddes Z. Building urban resilience: principles, tools, and practice. World Bank Publications; 2013.
Paccagnella O, Pongiglione B. Depression deterioration of older adults during the first wave of the COVID-19 outbreak in Europe. Soc Sci Med. 2022;299:114828.
Khalaf OO, Abdalgeleel SA, Mostafa N. Fear of COVID-19 infection and its relation to depressive and anxiety symptoms among elderly population: online survey. MECP. 2022;29(1):7.
Google Scholar
Sit RWS, Lai HHK, Dong D, Wang B, Wong MCS, Chung RYN, Wong SYS. Explaining the psychosocial effects of COVID-19 among older Hong Kong Chinese people—a qualitative analysis. J Geriatr Psychiatry Neurol. 2022;35(2):206–14.
Perez-Rojo G, López J, Noriega C, Velasco C, Carretero I, López-Frutos P, Galarraga L. A multidimensional approach to the resilience in older adults despite COVID-19. BMC Geriatr. 2022;22(1):793.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):48.
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, Kastner M, Moher D. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Sohn SY, Joo WT, Kim WJ, Kim SJ, Youm Y, Kim HC, Park YR, Lee E. Social network types among older Korean adults: Associations with subjective health. Soc Sci Med. 2017;173:88–95.
Kabisch N, Püffel C, Masztalerz O, Hemmerling J, Kraemer R. Physiological and psychological effects of visits to different urban green and street environments in older people: A field experiment in a dense inner-city area. Landsc Urban Plan. 2021;207:103998.
Pun VC, Manjourides J, Suh HH. Association of neighborhood greenness with self-perceived stress, depression and anxiety symptoms in older U.S adults. Environ Health. 2018;17(1):39.
Guo Y, Liu Y, Lu S, Chan OF, Chui CHK, Lum TYS. Objective and perceived built environment, sense of community, and mental well-being in older adults in Hong Kong: A multilevel structural equation study. Landsc Urban Plan. 2021;209:104058.
Wang R, Liu Y, Xue D, Helbich M. Depressive symptoms among Chinese residents: how are the natural, built, and social environments correlated? BMC Public Health. 2019;19:1–8.
Domènech-Abella J, Mundó J, Leonardi M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, Ayuso-Mateos JL, Haro JM, Olaya B. Loneliness and depression among older European adults: The role of perceived neighborhood built environment. Health and Place. 2020;62:102280.
Khosravi H, Tehrani SO. Local Environment, Human Functions and the Elderly Depression and Anxiety. Ageing Int. 2019;44(2):170–88.
Lam WWY, Loo BPY, Mahendran R. Neighbourhood environment and depressive symptoms among the elderly in Hong Kong and Singapore. Int J Health Geogr. 2020;19(1):48.
Tang S, Lee HF, Feng J. Social capital, built environment and mental health: A comparison between the local elderly people and the “laopiao” in urban China. Ageing Soc. 2022;42(1):179–203.
Barnett A, Zhang CJ, Johnston JM, Cerin E. Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int Psychogeriatr. 2018;30(8):1153–76.
Gan DRY. Neighborhood effects for aging in place: a transdisciplinary framework toward health-promoting settings. Hous Soc. 2017;44(1–2):79–113.
Koohsari MJ, McCormack GR, Nakaya T, Shibata A, Ishii K, Yasunaga A, Hanibuchi T, Oka K. Urban design and Japanese older adults’ depressive symptoms. Cities. 2019;87:166–73.
Ivey SL, Kealey M, Kurtovich E, Hunter RH, Prohaska TR, Bayles CM, Satariano WA. Neighborhood characteristics and depressive symptoms in an older population. Aging Ment Health. 2015;19(8):713–22.
Finlay J, Franke T, McKay H, Sims-Gould J. Therapeutic landscapes and well-being in later life: Impacts of blue and green spaces for older adults. Health Place. 2015;34:97–106.
Qiu L, Chen Q, Gao T. The effects of urban natural environments on preference and self-reported psychological restoration of the elderly. Int J Environ Res Public Health. 2021;18(2):1–14.
Abraham Cottagiri S, Villeneuve PJ, Raina P, Griffith LE, Rainham D, Dales R, Peters CE, Ross NA, Crouse DL. Increased urban greenness associated with improved mental health among middle-aged and older adults of the Canadian Longitudinal Study on Aging (CLSA). Environ Res. 2022;206:112587.
Domènech-Abella J, Switsers L, Mundó J, Dierckx E, Dury S, De Donder L. The association between perceived social and physical environment and mental health among older adults: mediating effects of loneliness. Aging Ment Health. 2021;25(5):962–8.
Li C, Zhou Y. Residential environment and depressive symptoms among Chinese middle- and old-aged adults: A longitudinal population-based study. Health Place. 2020;66:102463.
Liu Y, Dijst M, Faber J, Geertman S, Cui C. Healthy urban living: Residential environment and health of older adults in Shanghai. Health Place. 2017;47:80–9.
Hanslmaier M, Peter A, Kaiser B. Vulnerability and fear of crime among elderly citizens: what roles do neighborhood and health play? J Housing Built Environ. 2018;33(4):575–90.
Lu S, Liu Y, Guo Y, Ho HC, Song Y, Cheng W, Chui C, Chan OF, Webster C, Chiu RLH, et al. Neighborhood built environment and late-life depression: A multilevel path analysis in a Chinese society. J Gerontol B Psychol Sci Soc Sci. 2021;76(10):2143–54.
Curl A, Mason P. Neighbourhood perceptions and older adults’ well-being: Does walking explain the relationship in deprived urban communities? Transp Res Part A Policy Pract. 2019;123:119–29.
Mao S, Lu N, Xiao C. Perceived neighborhood environment and depressive symptoms among older adults living in Urban China: The mediator role of social capital. Health Soc Care Community. 2021.
Van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J Gerontol Series B. 2021;76(7):e249–55.
Li Y, Su S, Luo B, Wang J, Liao S. Physical activity and depressive symptoms among community-dwelling older adults in the COVID-19 pandemic era: A three-wave cross-lagged study. Int J Disaster Risk Reduct. 2022;70:102793.
Sirey JA, Berman J, Halkett A, Giunta N, Kerrigan J, Raeifar E, Artis A, Banerjee S, Raue PJ. Storm Impact and Depression Among Older Adults Living in Hurricane Sandy-Affected Areas. Disaster Med Public Health Prep. 2017;11(1):97–109.
Tsuboya T, Aida J, Hikichi H, Subramanian SV, Kondo K, Osaka K, Kawachi I. Predictors of depressive symptoms following the Great East Japan earthquake: A prospective study. Soc Sci Med. 2016;161:47–54.
Chen E, Wood D, Ysseldyk R. Online Social Networking and Mental Health among Older Adults: A Scoping Review. Can J Aging. 2022;41(1):26–39.
Lak A, Rashidghalam P, Myint PK, Baradaran HR. Comprehensive 5P framework for active aging using the ecological approach: an iterative systematic review. BMC Public Health. 2020;20(1):33.
Guo Y, Chang SS, Chan CH, Chang Q, Hsu CY, Yip PSF. Association of neighbourhood social and physical attributes with depression in older adults in Hong Kong: A multilevel analysis. J Epidemiol Community Health. 2020;74(2):120–9.
Ko H, Park YH, Cho B, Lim KC, Chang SJ, Yi YM, Noh EY, Ryu SI. Gender differences in health status, quality of life, and community service needs of older adults living alone. Arch Gerontol Geriatr. 2019;83:239–45.
Ruiz M, Scholes S, Bobak M. Perceived neighbourhood social cohesion and depressive symptom trajectories in older adults: a 12-year prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(10):1081–90.
Wang R, Lu Y, Zhang J, Liu P, Yao Y, Liu Y. The relationship between visual enclosure for neighbourhood street walkability and elders’ mental health in China: Using street view images. J Transp Health. 2019;13:90–102.
Liu Y, Lu S, Guo Y, Ho HC, Song Y, Cheng W, Chui CHK, Chan OF, Chiu RLH, Webster C, et al. Longitudinal associations between neighbourhood physical environments and depressive symptoms of older adults in Hong Kong: The moderating effects of terrain slope and declining functional abilities. Health Place. 2021;70:102585.
Cho S. Relationships between perceived neighborhood disorder and depressive symptomatology: the stress buffering effects of social support among older adults. Soc Work Public Health. 2022;37(1):45–56.
Tan TH. Perceived environmental attributes: their impact on older adults’ mental health in Malaysia. Int J Environ Res Public Health. 2022;19(6):3595.
Byeon H. Relationship between physical activity level and depression of elderly people living alone. Int J Environ Res Public Health. 2019;16(20):4051.
Chen YY, Wong GHY, Lum TY, Lou VWQ, Ho AHY, Luo H, Tong TLW. Neighborhood support network, perceived proximity to community facilities and depressive symptoms among low socio-economic status Chinese elders. Aging Ment Health. 2016;20(4):423–31.
Won J, Lee C, Forjuoh SN, Ory MG. Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Soc Sci Med. 2016;165:177–86.
Friesinger JG, Topor A, Bøe TD, Larsen IB. Studies regarding supported housing and the built environment for people with mental health problems: A mixed-methods literature review. Health Place. 2019;57:44–53.
Miao J, Wu X, Sun X. Neighborhood, social cohesion, and the Elderly’s depression in Shanghai. Soc Sci Med. 2019;229:134–43.
Download references
Acknowledgements
Not applicable.
This study hasn’t used any funding support.
Author information
Authors and affiliations.
Department of Urban Planning, Faculty of Arts, Tarbiat Modares University, Tehran, Iran
Sajad Vahabi & Niloofar Panahi
Department of Urban Planning, Faculty of Arts, Shahid Beheshti University, Tehran, Iran
You can also search for this author in PubMed Google Scholar
Contributions
The authors confirm contribution to the paper as follows: study conception and design: S.Vahabi and A.Lak.; data collection: S. Vahabi N. Panahi; analysis and interpretation of results: A.lak and S.Vahabi; draft manuscript preparation: S.Vahabi and A.Lak and N. Panahi. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Correspondence to Azadeh Lak .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table 1..
Reviewed article characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Vahabi, S., Lak, A. & Panahi, N. Driving the determinants of older people’s mental health in the context of urban resilience: a scoping review. BMC Geriatr 23 , 711 (2023). https://doi.org/10.1186/s12877-023-04387-y
Download citation
Received : 29 July 2022
Accepted : 05 October 2023
Published : 02 November 2023
DOI : https://doi.org/10.1186/s12877-023-04387-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older adults
- Mental health
- Scoping review
BMC Geriatrics
ISSN: 1471-2318
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Older adults’ suggestions of research topics on ageing well in urban environments – A participatory study
Roles Conceptualization, Investigation, Project administration, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute of General Practice and Family Medicine, Charité - Universitätsmedizin Berlin, Berlin, Germany
Roles Data curation, Formal analysis, Investigation, Project administration, Writing – original draft
Roles Supervision, Writing – review & editing
Affiliation Institute of Medical Sociology and Rehabilitation Science, Charité – Universitätsmedizin Berlin, Berlin, Germany
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing
- Philip Oeser,
- Nora Bruckmann,
- Paul Gellert,
- Wolfram J. Herrmann

- Published: October 4, 2023
- https://doi.org/10.1371/journal.pone.0292214
- Peer Review
- Reader Comments
Ageing societies and urbanization are global phenomena that pose new challenges for care delivery. It is important to create a scientific evidence base to prepare for these changes. Hence, the aim of our study was to assess which research agenda older adults living in an urban environment in Germany suggest.
A total of 1000 participants aged 65 years or older from five different neighborhoods of Berlin were randomly chosen and were sent a single item questionnaire allowing them to freely propose research topics regarding ageing well in the city. Codes were developed inductively and clustered into categories. In a second stage, these results were discussed with the participants and local stakeholders in a workshop and video calls.
102 persons suggested 18 research topics in 6 categories: health, living environment, social issues, mobility, and accessibility to information and communication. Proposed research topics ranged from accessibility of health care, green spaces and recreational means to social involvement and loneliness.
There is a substantial interest of older adults for research regarding their living situation. Research projects and local urban planning committees are encouraged to invite older adults to participate and integrate their perspectives suggested by older adults.
Citation: Oeser P, Bruckmann N, Gellert P, Herrmann WJ (2023) Older adults’ suggestions of research topics on ageing well in urban environments – A participatory study. PLoS ONE 18(10): e0292214. https://doi.org/10.1371/journal.pone.0292214
Editor: Grant Rich, Walden University, UNITED STATES
Received: August 7, 2023; Accepted: September 15, 2023; Published: October 4, 2023
Copyright: © 2023 Oeser et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data on Berlin neighborhood statistics is publicly available. Amt für Statistik Berlin-Brandenburg, Statistischer Bericht A | 16 – hj 2 / 20, available online at: [XLSX] https://download.statistik-berlin-brandenburg.de/ebfcd0da83f4fef4/474f2236e32a/SB_A01-16-00_2020h02_BE.xlsx [PDF] https://download.statistik-berlin-brandenburg.de/ffbcda9dc9cd780d/e7ab2379e8c3/SB_A01-16-00_2020h02_BE.pdf Senatsverwaltung für Stadtentwicklung, Bauen und Wohnen; Bericht Monitoring Soziale Stadtentwicklung Berlin 2019, available online at https://www.berlin.de/sen/sbw/stadtdaten/stadtwissen/monitoring-soziale-stadtentwicklung/bericht-2019/#Indikatoren The raw dataset consisting of the answers received from the participants of this study are available online under this identifier: https://zenodo.org/record/8318537 .
Funding: The project on which the article is based was supported by the Berlin Institute of Health (BIH) QUEST Center for Responsible Research. It was funded with 17,810 € in total over a duration of six months by the QUEST Grant for Patient and Stakeholder Engagement. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Ageing societies and urbanization are two global developments which pose challenges for healthy ageing in urban areas. The share of persons 70 years or older will double globally from 5.9% in 2020 to 11.3% in 2050, a shift that is also pronounced in Germany with an estimated increase from 15.9% in 2020 to 23.6% in 2050 [ 1 ]. An ageing population changes the demands for healthcare, with the focus shifting from acute care to long-term care, chronic conditions, and non-communicable diseases. Furthermore, the worldwide urban population is expected to increase from 4.22 billion in 2018 up to 6.68 billion in 2050, while the worldwide rural population is declining from 3.41 billion people in 2018 to 3.09 billion people in 2050 [ 2 ]. Germany already has a high degree of urbanization and ranks 14th in the decline of rural population until 2050. An urban living environment is associated with a high population density and more diverse population regarding gender, migration background and socio-economic status (SES) [ 3 ]. Healthcare and social care in urban areas are at the same time highly fragmented with several different providers available. Making cities age-friendly is becoming an important research area with a high public relevance [ 4 ].
What do older adults, the people who are directly affected, have to say about ageing well in urban environments? In a qualitative study from the United States based on interviews with community-dwelling adults older than 60 years, self-acceptance, self-growth and the pursuit of active engagement were defined as fundamental to ageing successfully [ 5 ]. A qualitative study with older adults on facilitators and barriers to growing old at home named physical and mental health, family environment and financial stability as key elements for quality of life while criticizing not being taken into account as a demographic by society, especially when living in an urban environment [ 6 ]. Reciprocal and trusting relationships with neighbors were the basis for satisfaction in another study on solitary older women’s perspectives on their residential living area and its impact on health and wellbeing [ 7 ]. Based on data from the Belgian Ageing Studies, it was shown how the physical environment can positively influence feelings of safety in older adults when the neighborhood is adapted to their physical needs [ 8 ]. A recent qualitative study in Germany on dementia risk reduction in urban environments, involving older adults and stakeholders, explored different perspectives on designing urban environments that support older adults’ needs to promote brain health, and encourages public policy to involve community members as co-creators for these spaces [ 9 ]. In an Australian study by the National Ageing Research Institute, the question of what older people want from healthcare was extensively assessed using a mixed-methods approach with focus group interviews and an online survey, emphasizing on topics surrounding health care [ 10 ].
Common to all these studies is that older adults merely participated in the research process and did not shape the research agenda themselves. Research on projects that allow older adults, as laypersons, to specifically define research topics is limited. Thus, the aim of our study was to assess which research agenda older adults living in an urban environment in Germany suggest.
This project had a participatory design following two stages: a survey stage and a workshop stage. First, we selected five different neighborhoods in Berlin to conduct the project. For the selection process, we used publicly available data from the Senate Department for Urban Development and Housing Berlin (Senatsverwaltung für Stadtentwicklung und Wohnen Berlin), and the Office of Statistics Berlin-Brandenburg (Amt für Statistik) [ 11 , 12 ] with an extensive insight in their demographics (number of inhabitants, share of inhabitants 65 years and older, SES, migration background). The selection was conducted jointly with local authorities, agreeing on neighborhoods with a heterogeneous population of older adults regarding socioeconomic status and migration background. Key figures of the five neighborhoods are presented in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0292214.t001
For the survey phase, we inquired at the Agency for Civil and Regulatory Affairs in Berlin (Landesamt für Bürger- und Ordnungsangelegenheiten, LABO) to randomly choose 200 citizens in each of these neighborhoods. Inclusion criteria were age of 65 years or older (the age of retirement in Germany), no active legal guardianship, and registration of main residency in the respective neighborhood. The study information and a single open-ended item was developed and pre-tested with other researchers and senior representatives from different neighborhoods in Berlin. The single open-ended item questionnaire was: “The following topics regarding ageing in the city should be researched in the future” [translation by the authors, original phrase in German: “Folgende Themen sollten zum Altwerden in der Stadt zukünftig erforscht werden”]. By giving no research question examples or topical suggestions, we aimed to achieve a variety of research themes. In the beginning of October 2021, we sent the study information to each citizen by mail, including one page with the single item questionnaire, and a stamped return envelope. We followed up with a reminder a week later, and another reminder two weeks after the initial letter was sent. The citizens had the possibility to anonymously submit their response by three different means: 1) respond via mail by using the stamped return envelope, 2) call us on a telephone hotline and leave a message on an answering machine, and 3) by using a website with the same open-ended questionnaire item allowing for direct text input in a text box. In case of phone calls, answers were transcribed into text by the second author.
Data analysis was conducted in six steps, of which the first four steps were conducted in a team (first, second, and last author). Those steps included 1) data familiarization through repeated reading and assurance to understand all answers, 2) splitting the answers into units of meaning, 3) constructing at least one code for each unit of meaning, 4) clustering of the codes into categories, 5) using the resulting coding scheme to code the whole text corpus, and 6) descriptive statistic of the coding results. For the data analyses, we used MAXQDA 2020 (VERBI Software, 2021). In many cases, one written response addressed several different topics, in these cases the responses were split into several single segments (462 segments in total, median = 4 segments per participant). Not all these segments were eventually classified into categories. For example, 14 of these segments described subjective conceptions on ageing in general, and 19 segments were complaints or opinions on (communal) political topics, so we decided to exclude them from further coding. The exemplary segments in the results section of this article were translated from German by the second author.
For the workshop phase, we sent a fourth letter to all citizens that were initially chosen to participate in the study and invited them to participate in a local workshop in each of the neighborhoods. Additionally, we invited local government representatives and stakeholders (i.e., NGOs) suggested by local government. The aim was to present the clusters with representative codes and relevant quotes and discuss them. The workshops were planned for November and December 2021. Due to increasing COVID-19 incidence in late 2021 in Berlin, only the workshop in Treptow-Köpenick could be conducted face-to-face. For the other neighborhoods, we offered the possibility to discuss the results via online meeting or through telephone calls to reduce risk of COVID-19 transmission.
Participants were informed about the content of the study, data protection and privacy rights. Participants were asked to answer without revealing any identifying information and were informed that by answering anonymously to the survey, implied consent was given to participation in the study and publication of its results. The study was approved by the ethics committee (Ethikkommission der Charité – Universitätsmedizin Berlin, Reference Number: EA1/254/21).
A total of 163 participants responded to the survey, of which 102 (10.2%) could be included in the evaluation. We received most of the valid responses (n = 78, 76.5%) via mail using the stamped return envelope. 91 (89.2%) of these answers could be assigned to a planning area: 30 (29.4%) came from Allende II (Treptow-Köpenick), 18 (17.6%) from Hohenschönhauser Straße (Lichtenberg), 15 (14.7) from Maulbeerallee (Spandau) and 14 (13.7%) from Treuenbrietzener Straße (Reinickendorf) and Böhlener Straße (Marzahn-Hellersdorf) respectively.
From the material, we constructed 18 codes which were clustered in six categories: Health, Living Environment, Social Issues, Mobility, Prevention, and Accessibility of Information and Communication. Fig 1 gives an overview of the categories, their respective codes and the number of individual participants whose answers contributed to these categories.
https://doi.org/10.1371/journal.pone.0292214.g001
Regarding health topics, responses from participants focused on health care delivery, but also on the adaptation of health care to the needs of older people and specific diseases. Participants mentioned the geographical distance to health services and the accessibility of health services as issues that should be investigated. The following quote demonstrates a specific research question on the distribution of allied health professions like physiotherapy:” I am 76 years old and had several surgeries last year , which is why I am very limited in my mobility . I would like to become fit again . However , there are not enough opportunities for physiotherapy to work on becoming fit again . Someone should think about this . How much and which kind of physiotherapy is actually needed per citizen depending on age . " (P14) Similarly, participants mentioned their desire that research on health services should have a stronger focus on older adults’ needs with regard to specific diseases and conditions:” Problems with pain are not taken seriously by doctors . (…) In the field of health care , we should research pain in old age . ” ( P 23)
Living environment
Respondents suggested further investigation into different topics in terms of lived environment, for example in the field of urban planning, green spaces and their impact on quality of life ( ”I would be interested to know about the influence of soil sealing of urban green spaces (…) on the quality of life and health of the older urban population . " P11). This also included comments on appropriate seating (i.e. benches, chairs), availability of public restrooms, and parks. Regarding their housing situation, participants expressed the importance of age-appropriate apartments, proposing to explore forms of assisted care living, the cause of rising rents, and the geographical distance and potentially difficult logistics of buying groceries and other supply of daily needs. Participants wished for further research on adjustments of the environment to their needs to be conducted.
Social issues
Loneliness was a topic that – despite being a well-established problem in literature – was still a prominent issue for older adults participating in our study, asking how to address the feeling of isolation in old age. Many participants wondered how social participation in the city can be strengthened while also highlighting the need for feeling safe and wondered how poverty in old age influences the possibility of interacting with others, social contacts and quality of life. Meeting places and leisure activities for older adults seem to be frequented regularly and rated as important social hubs. Some participants expressed that they would like to pursue their professional interests (” Looking for opportunities for successful older people to contribute their knowledge and experience “, P51) or get involved in cross-generational activities and networking (” Old people should be brought together with young people so that they’re not so lonely “, P97).
Research ideas for mobility included suggestions on individual traffic by car, bicycle or by foot. One participant mentioned the aspect of equality in traffic:” Research should look into a solution to increase traffic safety , where older adults have equal rights on the road . " (P90) Another respondent proposed the idea of bonus programs for older adults who relinquish their driver’s license. Few participants wrote about using the bicycle as means of transport, underlining the topic of safety on the road and the issues of sidewalks sometimes being shared by pedestrians and bikers at the same time. For some participants, the city in general did not seem very accessible. Use and accessibility of local public transport was also named a topic to be researched further:” I would like to use public transport again (e . g ., bus , train) . However , there is little attention to older adults with walking aids (e . g ., buses start too quickly after entering into) . " (P29)
Participants suggested that more research on prevention of diseases should be conducted. Specific research projects suggested were: age-appropriate physical and mental activities, at what age prevention should begin, how nutrition influences older adults’ health, but also proposing more research on early screening programs and dealing with substance abuse. A topic mentioned several times was preventing dementia:” Develop a screening program for early Alzheimer and dementia detection . If possible , include these in general preventive medical check-ups (like colon and breast cancer etc . ) for people in certain age groups . ” (P44)
Accessibility of information and communication
In this category, participants described their difficulties receiving relevant information in their area (i.e., on local age-centered activities, public transport schedules, for example through the internet or by other means). Participants also reported on problems with reading and understanding foreign languages, or medical jargon on their prescribed medication. They proposed to investigate ideas on how to reach older adults through different means (i.e., via doctors, media, and direct communication), underlining that digital information should not be seen as a mandatory information source for everyone.
When asked to suggest research topics from an older adults’ perspective, participants expressed their ideas on a wide range of topics that were clustered into six main categories: health, living environment, social issues, mobility, prevention and accessibility of information and communication. Most suggestions focused on topics of health care delivery and the living environment, but also tackled topics like social interaction and loneliness.
While differing in study design, the topics suggested in our research are in line with results of a qualitative study by Walker et al. [ 7 ], in which social networks, close relationships with other people in the neighborhood and proximity of services were defined as important by participants. The findings highlight that older adults suggest research topics from what they experience in their vicinity and what matters to them personally in their daily lives. In another study by Röhr et al., three main themes were defined regarding the design of urban environments to promote brain health: social participation, accessibility and proximity of health care, cultural events and public restrooms, as well as possibilities of local recreation and well-being [ 9 ]. All these topics were suggested by older adults in our study, who also mentioned the need for further investigation on disease prevention, specifically dementia prevention. Regarding health care topics, the National Ageing Research Institute of the Victorian Department of Health in Australia described older adults’ needs even more extensively than in the health segment of our study and defined important topics together with older adults, such as healthy and active ageing, independent living, sense of community, as well as care in medical crises and during end of life [ 10 ]. Self-acceptance and self-growth were found to be important for successful ageing in a study by Reichstadt et al. [ 5 ], but our participants did not specifically mention these themes as further research topics regarding urban ageing.
Research on participatory studies in which participants are actively engaged in designing a research agenda in an open format is limited, which makes it difficult to directly compare our results to similar projects. Also, the open format might have posed a potential intellectual challenge to the participants and may exclude older adults with a lower education from participation. Accordingly, only some of the responses were written in form of a definitive research topic. Responses were often phrased as issues and wishes or gave individual opinions on different topics ranging from national politics to general statements on growing old. We excluded the more general opinions that did not express any area for potential scientific research. Nevertheless, we were able to include many responses into our analysis to define categories, even when they were not specifically phrased as a hypothesis. Due to legal and ethical considerations, the letter sent out to the citizens contained five pages of descriptions on privacy and legal statements, which may have been discouraging especially for older adults who have a lower competency in reading. As the study information was only available in German, some citizens that received our mailings may have not understood their content. We received, however, one single answer in Russian which we had translated into German by a fellow researcher from our Institute. While the open format of the study might have been overwhelming for some, the overall response rate with more than 10% is still satisfactory for a postal survey with older adults who are not used to these kinds of projects. The age threshold that we chose as inclusion criteria (age 65 and older) was based on the earliest possible age of retirement in Germany, but it does not acknowledge possible differences in research ideas from the “young-old” adults (55–75 years) and the “old-old” adults (75+ and above) as described by Neugarten [ 13 ].
Unfortunately, the pandemic did not allow to conduct the second, workshop-based stage of the project as planned, so instead of five, only one workshop (in Treptow-Köpenick) could be conducted face-to-face. There, the panel consisted of older adults as well as local stakeholders (district officials, social workers) and allowed for a lively discussion on the presented topics, giving participants the chance to connect with each other. For the other four neighborhoods, we offered phone calls to present the results of the study individually and held video conferences with local stakeholders and interested participants. Online and via phone, the participation was not as strong as the local workshop, but it still gave us the possibility to present the results to stakeholders and interested citizens.
There is a substantial interest of older adults in urban environments on research regarding their living situation, especially focusing on health care delivery, living environment and psychosocial aspects, such as loneliness, interpersonal interaction, and concerns about living conditions. The focus on older adults’ daily lives should be more elaborated in the identified categories to promote aging well in cities. The suggested research topics can serve as a base for researchers on which to select themes that need further investigation, and involve different age groups of older adults to better reflect and integrate their perspectives.
Acknowledgments
We thank all participants and stakeholders for their contributions to this study. We also appreciate the assistance of our colleague Konrad Laker in language editing for the revised manuscript.
- 1. United Nations, Department of Economic and Social Affairs, World Population Prospects 2019, Online Edition. Rev. 1. Available: https://www.un.org/development/desa/pd/news/world-population-prospects-2019-0 .
- View Article
- Google Scholar
- PubMed/NCBI
- 11. Amt für Statistik Berlin-Brandenburg. Statistischer Bericht A I16–hj2/20. Available: https://www.statistik-berlin-brandenburg.de/publikationen/stat_berichte/2021/SB_A01-16-00_2020h02_BE.xlsx .
- 12. Senatsverwaltung für Stadtentwicklung und Wohnen Berlin. Monitoring Soziale Stadtentwicklung 2019. Available: https://www.berlin.de/sen/sbw/stadtdaten/stadtwissen/monitoring-soziale-stadtentwicklung/bericht-2019/ .
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Older Adults & Aging
Across asia, respect for elders is seen as necessary to be ‘truly’ buddhist.
Buddhists across the region also say that someone cannot be truly Buddhist if they do not respect deities or spirits.
As Biden and Trump seek reelection, who are the oldest – and youngest – current world leaders?
Though Biden is 81 years old, most global leaders are in their 50s and 60s, and the median age of current national leaders is 62.
U.S. centenarian population is projected to quadruple over the next 30 years
The number of Americans ages 100 and older is projected to more than quadruple over the next three decades.
Older Workers Are Growing in Number and Earning Higher Wages
Roughly one-in-five Americans ages 65 and older were employed in 2023 – nearly double the share of those who were working 35 years ago.
Dating at 50 and up: Older Americans’ experiences with online dating
One-in-six Americans ages 50 and older (17%) say they have ever used a dating site or app.
A record-high share of 40-year-olds in the U.S. have never been married
As of 2021, 25% of 40-year-olds in the United States had never been married, a significant increase from 20% in 2010.
Younger evangelicals in the U.S. are more concerned than their elders about climate change
Evangelical Protestant adults under 40 are more likely than older evangelicals to say climate change is an extremely or very serious problem.
Older Americans more wary than younger adults about prospect of driverless cars on the road
53% of those 50 and older say the widespread use of driverless vehicles would be a bad idea for society, as do 37% of adults ages 18 to 49.
Share of those 65 and older who are tech users has grown in the past decade
Adoption of key technologies by those in the oldest age group has grown markedly since about a decade ago.
Amid the pandemic, a rising share of older U.S. adults are now retired
As of the third quarter of 2021, 50.3% of U.S. adults 55 and older said they were out of the labor force due to retirement.
REFINE YOUR SELECTION
- Susannah Fox (19)
- Mary Madden (4)
- Renee Stepler (4)
- Richard Fry (4)
- D’Vera Cohn (3)
- Gretchen Livingston (3)
- Kathryn Zickuhr (3)
- Michelle Faverio (3)
- Amy Mitchell (2)
- Drew DeSilver (2)
- Jeffrey Gottfried (2)
- Katherine Schaeffer (2)
- Kim Parker (2)
- Lee Rainie (2)
- Michael Barthel (2)
- Pew Research Center Staff (2)
- Rakesh Kochhar (2)
- Tom Rosentiel (2)
- Aaron Smith (1)
- Adam Nekola (1)
- Andrew Perrin (1)
- Becka A. Alper (1)
- Christine Tamir (1)
- Dana Braga (1)
- Deborah Fallows (1)
- Eileen Patten (1)
- Elizabeth Grieco (1)
- Galen Stocking (1)
- Jeffrey S. Passel (1)
- John B. Horrigan (1)
- Justin Nortey (1)
- Katie Reilly (1)
- Laura Silver (1)
- Lauren Kent (1)
- Manolo Corichi (1)
- Mark Jurkowitz (1)
- Michael Lipka (1)
- Monica Anderson (1)
- Olivia Sidoti (1)
- Paul Taylor (1)
- Rich Morin (1)
- William Miner (1)
Research Teams
- Internet and Technology (39)
- Social Trends (30)
- Global (15)
- Religion (11)
- Politics (9)
- Journalism (8)
- Science (8)
- Global Migration and Demography (4)
- Data Labs (2)
- Methods (2)
- Pew Research Center (2)
- Race and Ethnicity (2)
901 E St. NW, Suite 300 Washington, DC 20004 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan, nonadvocacy fact tank that informs the public about the issues, attitudes and trends shaping the world. It does not take policy positions. The Center conducts public opinion polling, demographic research, computational social science research and other data-driven research. Pew Research Center is a subsidiary of The Pew Charitable Trusts , its primary funder.
© 2024 Pew Research Center
- Frontiers in Medicine
- Geriatric Medicine
- Research Topics
The Health of the Older Adults
Total Downloads
Total Views and Downloads
About this Research Topic
The global population is aging, and the growing awareness of the importance of promoting healthy aging is becoming increasingly relevant to physicians of many disciplines and fields of expertise. The complex issues affecting the health of older adults demand a multidisciplinary and coordinated personalized ...
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Research on the health of senior citizens from an interdisciplinary perspective: framework, core topics, and prospects
- Published: 07 December 2021
- Volume 5 , pages 345–362, ( 2021 )
Cite this article

- Xiaodan Wei ORCID: orcid.org/0000-0003-2899-3772 1
159 Accesses
2 Citations
1 Altmetric
Explore all metrics
The health of senior citizens is an important concern in the context of an aging population in China. Based on changes to and the characteristics of senior health in the new era, it is both important and necessary to promote research on senior health from an interdisciplinary perspective. An analytical framework that takes in society, behavior, psychology, environment, and genetic inheritance is the basis for interdisciplinary research on senior health. The core topics of this research focus on the factors that influence senior health, the allocation of resources for senior health, senior health equity, and the relationship of senior health to the labor market. At the same time, research on senior health is still subject to various constraints, such as the failure to develop a theoretical framework, insufficient depth and breadth of research practices, the need to better integrate the health data platforms, the relative weakness of human resources training efforts, and insufficient links and cooperation between government, enterprises, universities, and research institutes. In the future, comprehensively improving the research level of senior health in China must be a priority. A theoretical system for interdisciplinary research of senior health in China must be developed, and the focus of research should be in line with the national conditions. A unified sharing platform for data resources must be built, innovative training programs developed for human resources, and interconnections between government, enterprises, universities, and research institutes must be strengthened.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
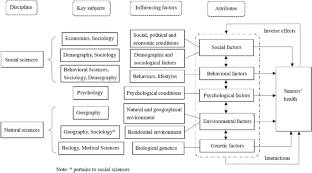
Similar content being viewed by others

Health Systems Research in Aging
Health of midlife and older adults in china: the role of regional economic development, inequality, and institutional setting.

Researching Quality of Life in Old Age: Some Conceptual and Methodological Principles
Explore related subjects.
- Medical Ethics
A feature of China’s population aging, which means that the aging level of rural areas is higher than that in urban areas.
A national development objective proposed by CPC, which requires more developed national economy and better systems by the centenary of CPC (2021) and the basic realization of modernization and the establishment of a prosperous, strong, democratic and civilized socialist country by the centenary of the founding of the PRC (2049).
The search expression “TI = senior * health OR TI = aging * health” was used to obtain sample articles from the CNKI database. Because the literature screening method proposed by Xiang and Wang ( 2019 ) was used here, the articles on senior health as selected for this paper diverge from those focused on medical or health care. That is, these articles are not focused on medical issues related to the various physical diseases that afflict the elderly. The specific search scope covered Social Sciences Series II, Economics and Management Sciences, Information Technology and some subcategories of Medical and Health Technology (i.e., Medical and Health Policies, Laws and Regulations; Medical Education and Marginal Medical Disciplines; and Preventive Medicine and Hygiene). A search for all articles published prior to December 31, 2020, found 1,319 articles. After excluding invalid articles such as review papers, news notices, general catalogues of journals, and editor’s messages, a total of 1,217 sample articles were obtained for analysis.
Based on the CSSCI journal catalog of Nanjing University (2019–2020), including the extended edition.
Bai, C. (2020). Study on the supply and effects of community health management service for urban–rural elderly under the background of pension combined with medical service: Evidence from CLHLS. Chinese Journal of Health Policy, 13 (3), 31–37. https://doi.org/10.3969/j.issn.1674-2982.2020.03.005
Article Google Scholar
Cai, F. (2020). How to reap the second demographic dividend? International Economic Review, 2 , 9–24.
Google Scholar
Cai, J. L., & Zhang, L. (2020). Socio-economic status and health inequality in the elderly: From the life course perspective. Expanding Horizons, 6 , 99–107. https://doi.org/10.3969/j.issn.1006-0138.2020.06.014
Christensen, K., Doblhammer, G., Rau, R., & Vaupel, J. (2009). Ageing populations: The challenges ahead. The Lancet, 374 (9696), 1196–1208. https://doi.org/10.1016/S0140-6736(09)61460-4
Dang, J. W. (2019). The science of ageing health: An important top-level thinking for coping with the ageing society. Scientific Research on Aging, 7 (7), 4–13. https://doi.org/10.3969/j.issn.2095-5898.2019.07.001
Du, P., & Dong, T. Y. (2015). Promoting healthy aging: Changing concept and policy innovations—The inspiration from the world report on ageing and health. Scientific Research on Aging, 3 (12), 3–10. https://doi.org/10.3969/j.issn.2095-5898.2015.12.001
Fang, T., & Yi, R. (2015). Influence of the retired young elderly’s health status on their labor participation. South China Population, 30 (2), 43–56. https://doi.org/10.3969/j.issn.1004-1613.2015.02.005
Gao, Y., & Yuan, X. (2020). Health transition and medical expenditure of the elderly in China. Population Research, 44 (2), 60–71.
Jiang, X. Q., & Liu, N. N. (2014). A study of the option of the elderly on long-term care, modes and influencing factors. Population Journal, 36 (1), 16–23. https://doi.org/10.3969/j.issn.1004-129X.2014.01.002
Jiang, X. Q., Wei, M., & Zhang, W. J. (2015). Study on the health status and influencing factors of China’s aging population. Population Journal, 37 (2), 46–56. https://doi.org/10.3969/j.issn.1004-129X.2015.02.006
Jiao, K. S. (2014). Influencing factors of health inequality. Sociological Studies, 29 (5), 24–46.
Jiao, K. S., & Bao, Z. M. (2020). Social change, life course and senior health. Sociological Studies, 35 (1), 149–169.
Jing, L. W., Hou, Q. H., Liu, Z., Sun, S. Y., & Huang, S. S. (2020). Analysis and countermeasures on social determinants of health equity among elderly in China. Chinese Journal of Health Policy, 13 (9), 1–7. https://doi.org/10.3969/j.issn.1674-2982.2020.09.001
Li, X. Y. (2020). Early roots of health inequality in the middle-aged and elderly people. Doctoral thesis, Shandong University, China. https://doi.org/10.27272/d.cnki.gshdu.2020.000048.
Li, Y., & Lu, J. H. (2020). Study of the effect of childhood adversity on depression among Chinese older adults. Population Journal, 42 (4), 56–69. https://doi.org/10.16405/j.cnki.1004-129X.2020.04.005
Li, Y., Lu, J. H., Cheng, Q., & Gu, D. N. (2020). Association between social participation and depression among older adults in China. Population and Development, 26 (3), 86–97.
Lu, J. H. (2018). Prospects of the interdisciplinary research on senior health in the new era. China Society Periodical, 23 , 30–31. https://doi.org/10.3969/j.issn.1674-3857.2018.23.016
Lu, J. H., & Guo, R. (2019). Compression or expansion of morbidity? A study on the long-term change trends of health among the elderly: 1998–2014. Population and Development, 25 (6), 76–86.
Lu, J. H., Li, Y., & Zheng, B. (2017). The relationship between self-reported health and social participation of Chinese elderly: Evidence from CLHLS Survey. Population Research, 41 (1), 15–26.
Lu, J. H., & Liu, Q. (2019). The research priorities and prospects of population studies in China under the background of population development shift. Population Journal, 41 (3), 5–15. https://doi.org/10.16405/j.cnki.1004-129X.2019.03.001
Lu, J. H., & Sha, D. (2018). Exploratory practices and policy reform strategy for the care for the disabled elderly against the backdrop of population aging. Studies on Socialism with Chinese Characteristics, 2 , 52–58.
Lu, J. H., & Wang, B. (2019). New trends of global public governance in the context of increasing life expectancy. Studies on Socialism with Chinese Characteristics, 6 , 69–75.
Lu, J. H., & Wang, B. (2020). The orientation, support, and mission of population studies under the era of China’s governance. Journal of the Party School of the Central Committee of the CPC, 24 (4), 122–129.
Lu, J. H., & Zhu, H. (2020). Discipline orientation, key issues and prospect of Chinese gerontology under the new form of aging society. Hebei Academic Journal, 40 (3), 11–18.
Qin, J., He, M., Zhang, Z. Y., Li, X. J., Zhang, N., Yu, J., & Rong, M. H. (2011). Interaction of ACE gene polymorphisms and environmental factors in longevity elderly in Bama of Guangxi. Chinese Journal of Gerontology, 31 (12), 2163–2166. https://doi.org/10.3969/j.issn.1005-9202.2011.12.001
Song, L. J., & Yang, L. (2020). The trajectory of health expectancy among elderly and its influencing factors: An empirical study based on CLHLS. Population and Economics, 3 , 58–73. https://doi.org/10.3969/j.issn.1000-4149.2020.00.009
Song, X. M. (2018). Life cycle health: Strategic thoughts for building a healthy China. Market and Demographic Analysis, 24 (1), 3–6.
Tan, J. P., Liu, Y., Wang, X., & Wang, L. N. (2012). Trend of population aging in China and the status quo of the research into senior health. Chinese Journal of Gerontology, 32 (19), 4335–4337. https://doi.org/10.3969/j.issn.1005-9202.2012.19.125
Tong, Y. F., & Liao, Y. H. (2017). Impact of health status on the decision of labor force participation in the Chinese elderly. Chinese Journal of Population Science, 6 , 105–116.
Wang, F. B. H. (2017). Social cause or healthy option? An empirical study on the health inequality of elderly in China. China Sport Science and Technology, 53 (6), 13–20. https://doi.org/10.16470/j.csst.201706002
Wang, J. Y., & Li, T. R. (2020). The age mode of elderly disability in China and the disabled population projection. Population Journal, 42 (5), 57–72. https://doi.org/10.16405/j.cnki.1004-129X.2020.05.005
Wang, P., & Li, S. Z. (2012). The effect of intergenerational support on physical health of rural elderly under the background of out-migration of young adults. Population and Development, 18 (2), 61–71. https://doi.org/10.3969/j.issn.1674-1668.2012.02.012
Wang, W. Y., Li, Y. H., Li, H. R., Yu, J. P., & Xiao, Z. Y. (2015). Environmental mechanism of regional longevity in China. Scientific Decision-Making, 1 , 1–12. https://doi.org/10.3773/j.issn.1006-4885.2015.01.001 in Chinese.
Wang, W. Y., Yang, L. S., & Li, H. R. (2007). Environmental changes and health risks in China. Science and Society, 4 , 22–28. https://doi.org/10.3969/j.issn.2095-1949.2007.04.005
Wu, B. Y., Dong, H. L., Wang, Y. Y., & Zhang, X. Q. (2019). Discrimination of disability and its influence on health life expectancy in Chinese elderly population. Population Journal, 41 (1), 102–112. https://doi.org/10.16405/j.cnki.1004-129X.2019.01.009
Xiang, Y. H., & Wang, X. H. (2019). Current research situation and reflection on elderly health in China: A bibliometric analysis based on CNKI. Journal of Huazhong University of Science and Technology (social Science Edition), 33 (5), 20–27. https://doi.org/10.19648/j.cnki.jhustss1980.2019.05.03
Xu, M., & Liu, L. (2016). Could the new rural society endowment insurance affect the health improvement of the elderly: Evidence from Chinese longitudinal healthy longevity survey. Statistics and Information Forum, 31 (11), 87–94. https://doi.org/10.3969/j.issn.1007-3116.2016.11.015
Zeng, Y. (2011). A review on international trends in interdisciplinary research of factors affecting healthy aging. Chinese Science Bulletin, 56 (35), 2929–2940. https://doi.org/10.1360/972011-1891
Zeng, Y. (2012). Interdisciplinary research on healthy aging: Social, behavioral, environmental, genetic factors and their interactions. Chinese Journal of Health Policy, 5 (2), 5–11. https://doi.org/10.3969/j.issn.1674-2982.2012.02.002
Zeng, Y., Cheng, L. G., Chen, H. S., Cao, H. Q., Hauser, E., Liu, Y. Z., Vaupel, J., et al. (2010). Effects of FOXO genotypes on longevity: A bio-demographic analysis. The Journals of Gerontology Series a, Biological Sciences and Medical Sciences, 65 (12), 1285–1299. https://doi.org/10.1093/gerona/glq156
Zeng, Y., Nie, C., Min, J. X., Liu, X. M., Li, M. M., Chen, H. S., Vaupel, J., et al. (2016). Novel loci and pathways significantly associated with longevity. Scientific Reports . https://doi.org/10.1038/srep21243
Zeng, Y., & Shen, K. (2010). Main dimensions of health status among the Chinese elderly. Chinese Journal of Preventive Medicine, 2 , 108–114. https://doi.org/10.3760/cma.j.issn.0253-9624.2010.02.005
Zhang, Y. (2018). Impact of lifestyle on senior health and the associated inequalities. Doctoral thesis, Peking University, China.
Zhang, S. F., Tang, M., & Zhou, M. (2016). Exploring the system of disabled elderly care service: An analytical study on the living condition of the disabled elderly in China. Journal of xi’an Jiaotong University (social Sciences)., 36 (2), 83–90.
Zhang, W. J., & Du, P. (2009). Regional disparity in healthy life expectancy for the Chinese elderly: Expansion or compression. Population Research, 33 (5), 68–76.
Zhou, P. M., & Yuan, X. (2021). The impact of health on the economic participation of the elderly migrants. Lanzhou Academic Journal, 2 , 196–208. https://doi.org/10.3969/j.issn.1005-3492.2021.02.014
Zhu, Y. L., & Zhang, Z. X. (2019). The shift in senior health and the projected demand for elderly care workers. Chinese Journal of Population Science, 2 , 63–74.
Download references

Author information
Authors and affiliations.
Department of Sociology, Peking University, No. 5 Yiheyuan Road, Haidian District, Beijing, 100871, China
Xiaodan Wei
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Xiaodan Wei .
Ethics declarations
Conflict of interest.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Rights and permissions
Reprints and permissions
About this article
Wei, X. Research on the health of senior citizens from an interdisciplinary perspective: framework, core topics, and prospects. China popul. dev. stud. 5 , 345–362 (2021). https://doi.org/10.1007/s42379-021-00098-2
Download citation
Received : 27 August 2021
Accepted : 27 October 2021
Published : 07 December 2021
Issue Date : December 2021
DOI : https://doi.org/10.1007/s42379-021-00098-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Senior health
- Interdisciplinary
- Core topics
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.21(3); 2022 Oct
Mental health care for older adults: recent advances and new directions in clinical practice and research
Charles f. reynolds, 3rd.
1 University of Pittsburgh School of Medicine, Pittsburgh PA, USA
Dilip V. Jeste
2 Department of Psychiatry, University of California San Diego, La Jolla CA, USA
Perminder S. Sachdev
3 Centre for Healthy Brain Ageing, University of New South Wales, Sydney NSW, Australia
Dan G. Blazer
4 Department of Psychiatry and Behavioral Sciences, Duke University, Durham NC, USA
The world's population is aging, bringing about an ever‐greater burden of mental disorders in older adults. Given multimorbidities, the mental health care of these people and their family caregivers is labor‐intensive. At the same time, ageism is a big problem for older people, with and without mental disorders. Positive elements of aging, such as resilience, wisdom and prosocial behaviors, need to be highlighted and promoted, both to combat stigma and to help protect and improve mental health in older adults. The positive psychiatry of aging is not an oxymoron, but a scientific construct strongly informed by research evidence. We champion a broader concept of geriatric psychiatry – one that encompasses health as well as illness. In the present paper, we address these issues in the context of four disorders that are the greatest source of years lived with disability: neurocognitive disorders, major depression, schizophrenia, and substance use disorders. We emphasize the need for implementation of multidisciplinary team care, with comprehensive assessment, clinical management, intensive outreach, and coordination of mental, physical and social health services. We also underscore the need for further research into moderators and mediators of treatment response variability. Because optimal care of older adults with mental disorders is both patient‐focused and family‐centered, we call for further research into enhancing the well‐being of family caregivers. To optimize both the safety and efficacy of pharmacotherapy, further attention to metabolic, cardiovascular and neurological tolerability is much needed, together with further development and testing of medications that reduce the risk for suicide. At the same time, we also address positive aging and normal cognitive aging, both as an antidote to ageism and as a catalyst for change in the way we think about aging per se and late‐life mental disorders more specifically. It is in this context that we provide directions for future clinical care and research.
By the year 2050, according to the United Nations (UN), one in six persons will be 65+ years of age 1 . Given this increasing number of people entering the worldwide aging community, coupled with lower birth rates – especially in high‐income and some middle‐income countries – there is concern about the old‐age dependency ratio, that is, the number of people 65+ years of age per 100 persons in the working age group (ages 15‐64). That ratio is increasing significantly, especially in countries such as China 2 .
A common misconception is that elders are mostly a burden to society. The fact is, instead, that many of them keep on contributing in many ways, such as continued work, childcare, maintenance of the household, and meal preparation. Most live independently. Many contribute several hours a week to volunteer activities or serve in leadership roles in community organizations. Yet, as these elders continue to age, they often face increasing disabilities, perhaps minor initially but gradually leading to significant impairments.
Mental disorders are major contributors to these disabilities. They often coexist with each other, e.g. comorbid depression and cognitive impairment, or with physical diseases, e.g. hearing impairment and paranoid thoughts 3 . In many cases, comorbidity spans multiple mental and physical disorders.
Despite the “aging tsunami” we are currently witnessing, the rise of special care for older adults has been slow to develop. Psychiatry has lagged behind medicine, yet it is increasing its knowledge base as well as recruiting sub‐specialists, unfortunately not at a rate which can serve the unique needs of older adults with mental disorders, even in high‐income countries. The International Psychogeriatric Association, founded in 1982, has been instrumental in encouraging meetings and programs in many low‐ and middle‐income countries, as well as providing a forum for geriatric psychiatrists from throughout the world. In both clinical practice and research within geriatric psychiatry, interdisciplinary collaboration has been foundational and essential, given the complexity of the problems faced by older adults experiencing mental illness.
Both basic and applied research have appreciably increased the evidence base for the diagnosis, treatment and prevention of late‐life mental disorders. For example, although we have no pharmacological agent yet proven to prevent or retard the progression of Alzheimer's disease, evidence has accumulated to support the importance of preventive measures, such as education, physical activity and control of vascular risk factors 4 . In depression of older adults, treatment with a combination of pharmacotherapy and psychotherapy, especially learning‐based forms such as cognitive behavioral therapies (CBT), has been shown to be effective 5 , 6 . Alcohol use disorders among older adults are more common than often realized by clinicians, especially in men, so that careful screening for these disorders is now regarded as essential 7 .
While negative views of aging continue to permeate the beliefs of many, more positive views have emerged in recent years, as exemplified in the MacArthur Research Network on Successful Aging 8 . They have defined successful aging, in contrast to usual aging, as low probability of disease, high cognitive and physical function, and active engagement with life. Others have also included wisdom as a characteristic of positive aging 9 , 10 .
In this paper, we provide an overview of the burden of mental health problems in older adults, with a focus on neurocognitive disorders, major depressive disorder, schizophrenia, and substance use disorders. For each of these disorders – which can be better understood as groups of disorders – we cover the epidemiology, prevention, recent treatment advances, and emerging models of service delivery. Further, for each group of disorders, we touch briefly upon heterogeneity at several levels: etiology, clinical presentation, and variability in response to intervention. In so doing, we describe directions for the future of clinical practice and research.
We begin the overview by contextualizing considerations of neurocognitive disorders, major depression, schizophrenia, and substance use disorders within the sciences of positive aging and cognitive aging, including a summary of the social determinants of well‐being in older adults. Our view is that the positive elements of aging need to be highlighted, not only to reduce the triple jeopardies of ageism, mentalism and ableism (i.e., discrimination against people on the basis of their age, mental health problems, and disability), but also to provide hope to patients and family caregivers.
SOCIAL DETERMINANTS OF MENTAL HEALTH IN OLDER ADULTS
Social determinants of health are non‐medical factors that influence health outcomes and have a significant effect on health inequalities 11 . Prominent examples of these social determinants include nutrition, education, employment and living environment, and these apply to the entire population.
Older adults with mental disorders are impacted by several types of these determinants 12 : a) social determinants that affect overall health, b) unique social determinants of mental health, such as stigma against mental illnesses, mental health care disparity, flawed criminal justice system, and homelessness 13 , and c) aging‐related social determinants, such as ageism, workforce shortage, and social isolation/loneliness. There are, however, also some positive social determinants of health relevant to old age, such as wisdom, resilience, meaning in life, and community engagement. Evaluating and addressing these determinants at individual and community levels is critical for prevention of mental disorders and enhancement of well‐being in older adults in general 9 , 10 , 11 , 13 , 14 , 15 .
Ageism and stigma
Ageism is defined by stereotypes, prejudice and discrimination directed toward people on the basis of their age 16 . Called “an insidious scourge on society” 17 , it can be institutional, interpersonal and/or self‐directed. Aging and older adults are often discussed by the general public and the media using negative stereotypes, such as a decline in mental and cognitive function. Unfortunately, this type of pejorative view of later life may be internalized by older individuals themselves and enacted, creating a vicious circle resulting in poor mental health.
Ageism causes inequalities and has detrimental effects on the individual, community and society 17 . Combating ageism is one of the four action areas of the Decade of Healthy Ageing (2021‐2030) declared by the UN and the World Health Organization (WHO) 16 .
The stigma against mental disorders is even greater in later life. An example is the stigma against agitation in dementia patients, many of whom spend days or weeks in emergency rooms because long‐term care facilities would no longer admit them, and the society has not provided alternatives. Equally sadly, there are more people with severe mental disorders (excluding dementia) and substance use disorders who are aging in prisons and jails than in hospitals in the US 11 , 12 .
Workforce shortage
The geriatric mental health workforce is slim, even in the most developed countries 18 . Despite the increased number of older adults, the number of psychiatrists trained in geriatric psychiatry has not increased. We know what to do, but how to recruit professionals across multiple disciplines to improve geriatric care in various cultural contexts is an abiding question that needs to be addressed for the future of clinical care and research in this field.
Also as a consequence of this workforce shortage, with the increase of physical and functional challenges in older patients, the need for a caregiver usually arises. The primary caregiver is often a spouse or adult child of the older patient. The role of the caregiver is wrought with physical, psychological and emotional challenges when caring for someone with dementia and/or serious physical illness. The caregivers themselves often suffer from significant morbidity 19 .
Loneliness and social isolation
A recent report from the National Academies of Science, Engineering, and Medicine 20 highlighted the public health significance of loneliness (i.e., subjective distress arising from an imbalance between desired and perceived social relationships) and objectively measurable social isolation. Older adults are at a particularly high risk for both loneliness and social isolation 21 . Aging‐related risk factors include widowhood, physical disability, poor health, and caregiving responsibilities.
Loneliness and social isolation are associated with adverse mental and physical health outcomes – including alcohol and drug abuse, suicidality, poor nutrition, sedentary lifestyle, inadequate sleep, and worsening physical functioning 22 . Loneliness and social isolation are as dangerous to health as smoking and obesity 23 , and are an important risk factor for Alzheimer's disease, major depression, and generalized anxiety disorder, as well as for cardiovascular and metabolic diseases 24 , 25 , 26 . More Americans die from loneliness‐ and social isolation‐related conditions than from stroke or lung cancer 27 .
Loneliness is more common in people with severe mental disorders such as schizophrenia than in the general population 28 . The evidence base for social isolation regarding adverse outcomes is much greater than for loneliness, yet the evidence for adverse effects of loneliness is increasing 21 .
The National Academies report 20 urges further research to establish the strength of the predictive association of loneliness and social isolation with mortality, and to clarify how these two entities interact with other facets of social relationships, including social support.
Wisdom is a personality trait comprised of several components: prosocial attitudes and behaviors (empathy and compassion), self‐reflection, emotional regulation, acceptance of uncertainty and diversity of perspectives, social decision‐making and, possibly, spirituality 29 , 30 . Commonly used self‐report‐based scales for assessing wisdom with good psychometric properties include the San Diego Wisdom Scale or Jeste‐Thomas Wisdom Index 31 , the Three‐Dimensional Wisdom Scale 32 , and the Self‐Assessed Wisdom Scale 33 .
Across the lifespan, wisdom is associated with positive outcomes, including better overall physical and mental health, happiness, and lower levels of depression and loneliness 34 , 35 . Amongst older adults, numerous investigations have demonstrated that wisdom is associated with life satisfaction, subjective well‐being, and greater resilience 29 , 30 . These studies have reported that older adults score higher than younger adults on several components of wisdom, especially prosocial behaviors, self‐reflection, and emotional regulation 36 . Some empirical evidence indicates that wisdom has a curvilinear relationship with age, peaking in the 70s or early 80s 34 .
Neurobiological investigations show that prefrontal cortex (especially dorsolateral, ventromedial, and anterior cingulate), insula, and limbic striatum (especially amygdala) are involved in the various components of wisdom 29 . Intergenerational activities, such as grandparents' help in raising grandchildren, have been found to benefit both the generations biologically, cognitively and psychosocially 37 .
A number of recent clinical and biological studies have reported a strong inverse relationship between loneliness and wisdom, especially its compassion component 38 , 39 , 40 . This evidence suggests potential use of individual‐ and societal‐level interventions to enhance compassion and other components of wisdom in older adults, so as to reduce loneliness and improve well‐being 40 . There are indeed reports of psychosocial group interventions in older people producing a significant improvement in wisdom 41 .
Resilience is a trait or outcome that describes recovery or bounce‐back from adverse situations or a process of adapting well in the face of adversity, trauma, threats or other sources of major stress 21 . Commonly used measures of resilience include self‐report scales such as the Connor‐Davidson Resilience Scale 42 and the Grit Scale 43 . Resilience is highly relevant to healthy aging and well‐being, and should be viewed as a public health concept 44 . A framework for resilience to the challenges associated with aging is required to complement ongoing risk reduction policies, programs and interventions 45 .
Men experience greater feelings of loneliness and have increased difficulty in adjusting to widowhood compared to women, with the exception of veterans. Male veterans exposed to death while serving in the military show greater resilience and report less loneliness than civilian widowers 23 . Resilience has been shown to be associated with better health and functioning as well as greater longevity in all age groups, but especially in the very old adults 46 . Resilience interventions in older adults include mindfulness training, CBT, well‐being therapy, social support, lifestyle and mind‐body interventions, and phone coaching. Studies applying valid and reliable measures of resilience have reported positive outcomes with small to medium effect sizes using some of these interventions 47 .
The COVID‐19 pandemic has been particularly isolating to older adult populations, given their lower familiarity with technologies to facilitate social interactions or virtual visits by family, friends, or even health professionals. However, despite these obstacles, preliminary evidence indicates that older adults have been more resilient, experiencing fewer negative mental health outcomes compared to other age groups. In a recent study of over 5,000 American adults, adverse mental or behavioral health symptoms were much more prevalent among adults aged 18‐25 compared to those aged 65 years or older 48 .
Meaning in life
Meaning or purpose in life is the value and importance attributed to one's own life and activities, and the core significance of one's personal existence 49 . There are a number of validated instruments to assess meaning in life, such as the Meaning in Life Questionnaire 50 .
Multiple research studies have demonstrated a strong link between purpose in life and better physical, psychosocial and overall health outcomes, including social engagement, in older adult populations 51 , 52 . Meaning in life may also be a protective factor against suicide 53 . A recent study reported that the presence of meaning showed an inverted U‐shaped pattern across the life span, peaking around the age of 60 and decreasing subsequently as physical health declines 50 .
Life review therapy is an individual or group story‐telling intervention with a focus on integrating life stories through different phases in life. A randomized controlled trial found that life review therapy significantly improved the quality of life of older participants 54 . A meta‐analysis of randomized controlled trials showed that life review therapy has moderate effects on depressive symptoms in older adults 55 .
Community engagement
Community engagement is a key beneficial social determinant of mental health in older adults. There are many communities across the world, including those which are formally part of the WHO's Age‐Friendly Communities (AFC) Network, in which older adults are actively involved, valued and supported, with a focus on affordable housing, built environments conducive to active living, inexpensive and convenient transportation options, opportunities for social participation and leadership, intergenerational programs, and accessible health and wellness services 56 .
The Compassionate Communities and Cities (CCC) movement seeks to promote the motivation of communities and cities to take greater responsibility for the care of people near the end of life. A systematic review of the studies of CCC programs reported that the evidence for their implementation is still limited 57 . A global model for the development and evaluation of CCC in palliative care is warranted.
POSITIVE PSYCHIATRY AND SUCCESSFUL AGING
Positive psychiatry is the science and practice of psychiatry that seeks to understand and promote well‐being through assessment and interventions involving positive psychosocial factors in people with or without mental or physical illnesses 58 . A critical construct in positive psychiatry that relates to older adults is “successful aging”.
The definition of successful aging and its determinants remains variable. The original model by Rowe and Kahn 8 , derived from the MacArthur Research Network, included three domains: absence of disease and disability, high cognitive and physical functioning, and active engagement with life. This model has been criticized for its overemphasis on physical health, which fails to account for many older individuals with physical morbidity who subjectively rate themselves as aging successfully and report a high degree of satisfaction in later life stages 59 , and for ignoring a dynamic lifespan perspective 60 .
Qualitative studies of successful aging indicate that older adults consider the ability to adapt to circumstances and the positive attitude toward the future as being more important to their sense of well‐being than an absence of physical disease and disability 59 . Investigations have also revealed a paradox of aging: even as physical health declines, self‐rated successful aging and other indicators of psychosocial functioning improve in later life 61 . Largely similar findings have also been reported in Eastern cultures 62 .
A broad definition of successful aging should have the following components: a) subjective well‐being, with low level of perceived stress (the extent to which an individual perceives that current demands or challenges exceed his/her ability to cope with them); b) flourishing, which involves eudemonic well‐being, including meaning in life and close social relationships 63 ; c) post‐traumatic growth; d) sustained remission or recovery in people with severe mental disorders, that typically includes an absence or a marked reduction of symptoms along with functional independence.
Neuroscience research during the past three decades has demonstrated a neurobiological basis for successful aging, despite age‐associated degenerative changes. There is strong evidence for neuroplasticity in active older adults – i.e., if there is optimal physical, cognitive and social activity, the development of new synapses, dendrites, blood vessels, and even neurons in specific subcortical regions, such as the dentate gyrus of hippocampus, can and does take place 64 , 65 .
Clinical research supports a model in which positive psychological traits such as wisdom, resilience and social engagement interact with and feed into each individual's evaluation of the degree of well‐being and are stronger predictors of outcomes such as self‐rated successful aging than physical health. We must add that aging is characterized by notable heterogeneity and, therefore, the proposed model would not apply to all the older adults.
COGNITIVE AGING
Cognitive aging is a process that is ubiquitous with humans and occurs gradually throughout adult life 66 . Clinicians caring for older adults should be aware of this process because it does impact social functioning.
Episodic memory and executive function are crucial domains affected by the aging process, and exhibit on average a gradual decline over many years, accelerating in later life 67 . Even normal changes in cognition, however, are quite variable, within and between individuals 61 . Some functions may improve over time, such as wisdom, altruism, prosocial behaviors and reasoning ability in social conflicts 68 , 69 .
The evaluation of the person with potential cognitive aging cannot be limited to the use of typical screening tools such as the Mini‐Mental State Examination (MMSE) 70 or the Montreal Cognitive Assessment (MoCA) 71 . The family is perhaps the best source of information. Queries which can be informative include: “Is __ as sharp as he/she was before?”; “Does __ have greater difficulty managing finances and other business matters than in the past?”; “Has __ become lost for brief periods in familiar places?”; “Does ___ have more difficulty recalling the names of acquaintances of long standing but which he/she has not encountered recently?”; and “Does __ have more problems with cooking and have to refer to recipes more frequently than in the past?”. Individuals with cognitive aging may also be more reluctant to participate in social gatherings. Each of these changes in behavior may be barely noticeable, yet close friends and family typically do notice.
These age‐related problems do not derive simply from a milder form of neuronal loss or plaque formation which is less extensive than in Alzheimer's disease. Brain changes do occur, however, such as changes in astrocyte and microglial function and synaptic plasticity 72 . Genetic predisposition, traumatic brain injury, adverse environmental childhood exposures, and poor educational and cognitive enrichment experiences may also contribute 73 . In other words, many external experiences which potentially can be ameliorated render prevention of greater cognitive decline with aging important across the life cycle, though some causative factors are inherent to the aging brain.
Many comorbid conditions can cause or exacerbate cognitive aging, including diabetes mellitus, vascular conditions of the brain and heart, chronic lung and liver conditions, renal failure, sepsis, delirium, chronic obstructive pulmonary disease, multiple sclerosis, vision and hearing loss, and sleep disorders 74 . Successful treatment of these conditions can often mitigate the cognitive dysfunction 74 . Additionally, many mental disorders have been associated with cognitive decrements, such as major depression (especially treatment‐resistant forms), bipolar disorder, schizophrenia, various types of substance abuse, and anxiety disorders 75 .
A number of non‐pharmacological interventions may be effective on cognitive aging. These include exercise, which is perhaps the most important preventive tool. Physical activity has been found in several studies to assist individuals in maintaining both their physical and cognitive function throughout life, as well as preventing some important chronic conditions 76 . The evidence derives from both observational and intervention studies 77 , 78 .
In addition, reduction of cardiovascular and related metabolic risk factors, such as treating hypertension and diabetes as well as cessation of smoking and losing weight, have been demonstrated effective 79 . The mantra “What is good for the heart is good for the brain” appears to hold true 66 . For example, evidence is mounting that diets, such as the Dietary Approaches to Stop Hypertension (DASH) or the Mediterranean Diet, may be useful 80 , 81 .
Many medications, especially diphenhydramine and benzodiazepines, can produce cognitive decline, and clinicians must take care in their prescription to older adults. Long‐term effects, namely a persistence of cognitive dysfunction secondary to the drugs, are less substantiated by the literature. Sleep problems, such as chronic insomnia or sleep‐related breathing disorder such as obstructive sleep apnea, may also contribute 74 . Lack of education and little cognitive stimulation may also be involved, yet the evidence for these risk factors is not as strong as for those listed above 82 .
A number of somatic interventions have been suggested 66 . Yet, none of these has held up under strict empirical clinical trials. These include stimulant drugs, such as caffeinated beverages, brain stimulating computer‐based games, and electrical brain stimulation procedures, such as transcranial direct current stimulation 83 , 84 , 85 .
Given the lack of clearly effective interventions and the apparent minor impairment secondary to cognitive aging, clinicians may be hesitant to devote time to helping affected people and their families. Yet, cognitive aging can benefit from discussions by these clinicians with older adults and their relatives, as attention to risk and protective factors can have a significant positive impact.
One area where intervention can clearly be important is alerting the family of the potential for fraud perpetrated upon older adults 86 . The frequency of fraud has increased dramatically in high‐income countries, and perhaps in low‐ and middle‐income countries as well. When disturbing messages are delivered to these elders coupled with a demand for immediate response, the potential for fraud that can be very harmful is high. For example, in the US, elders may be telephoned with fraudulent alerts that they owe taxes and may be jailed if these are not paid immediately, coupled with a demand for their social security number. Warnings to older adults and their families can be most helpful in mitigating these threats 86 .
NEUROCOGNITIVE DISORDERS
The DSM‐5 87 has introduced the term “neurocognitive disorders” to describe the group of disorders with cognitive impairment as the salient feature, encompassing major (or dementia) and mild neurocognitive disorders, and delirium 88 . The term dementia, however, remains the most frequently used, and mild neurocognitive disorder is used interchangeably with the expression “mild cognitive impairment”.
The DSM‐5 has tried to bring coherence to the criteria for the various subtypes of these disorders under one framework, but its widespread adoption has been limited largely to psychiatry and psychology. The National Institute of Aging‐Alzheimer's Association (NIA‐AA) Criteria for dementia 89 and mild cognitive impairment 90 are widely used in the neurology literature. The DSM‐IV criteria for dementia 91 are still in use, with the major distinction from the DSM‐5 being that significant impairment in one cognitive domain is sufficient as long as the functional criteria are met.
The distinction between dementia and mild cognitive impairment is based on the severity of the cognitive deficits and, more importantly, on their functional consequences. For mild cognitive impairment, the International Working Group criteria are commonly applied 92 . With the increasing interest in preclinical syndromes, the concept of “subjective cognitive decline” (i.e., subjective report of decline in cognitive abilities from a previous level, unrelated to an acute event, with normal performance on standard cognitive tests, accounting for age, gender and education) has also received much attention in recent years 93 .
The DSM‐5 describes cognitive dysfunction by delineating six domains: complex attention, executive function, learning and memory, language, perceptual‐motor and social cognition. It recognizes that varying degrees of cognitive impairment are present in several mental disorders, but cognitive dysfunction must be the salient and defining feature for a diagnosis of neurocognitive disorder 88 . The formal acknowledgement of social cognition as a specific cognitive domain in the DSM‐5 has spurred much research and clinical interest 94 .
Dementia and mild neurocognitive disorder
Dementia and mild neurocognitive disorder are discussed together for several reasons. They are syndromes with shared etiology, with the main difference being the severity of cognitive impairment and its functional consequences 92 . Cognitive impairment should, in fact, be considered to be on a continuum, with mild cognitive impairment and dementia being categorical constructs imposed on that continuum. This is consistent with the understanding that the pathology underlying dementia, in particular that due to Alzheimer's disease 95 , can take several decades to build up in the brain, and cognitive impairment is similarly slow to develop and progress 95 .
Epidemiology
While there are many challenges in “counting” cases of dementia, partly related to the purpose for which this is being done 96 , several systematic efforts have been made. The latest global estimate from the Global Burden of Disease Study 2019 is 57.4 million (95% CI: 50.4‐65.1) cases worldwide in 2019, projected to increase to 152.8 million (95% CI: 130.8‐175.6) in 2050. This rise in prevalence is attributable to the increase in the elderly population, with the age‐standardized prevalence remaining stable 97 . There is much regional variation, with the smallest increases projected for Western Europe and high‐income Asia‐Pacific, and the largest increases for North Africa, Middle East, and Eastern sub‐Saharan Africa.
The incidence of dementia is showing a different trend, with several studies from high‐income countries, and one from Nigeria, showing a decline, especially in the last three decades 98 , 99 . No specific cause for this decline has been found, but changes in education, living conditions and health care are thought to have contributed.
The epidemiology of mild cognitive impairment has been less well studied. The published prevalence estimates vary by the diagnostic criteria being used 92 . Applying uniform criteria in the Cohort Studies of Memory in an International Consortium (COSMIC), the crude prevalence in those over 60 years was 5.9% (95% CI: 5.5‐6.3) overall, increasing from 4.5% at age 60‐69 to 5.8% at 70‐79, and to 7.1% at 80‐89 years. This was unaffected by gender and did not differ between White Caucasian and Chinese groups 100 .
Risk and protective factors
Twelve potentially modifiable risk/protective factors for dementia have been recently identified, as listed in Table Table1 1 101 . To the previously documented nine risk factors with good supporting evidence (less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact), three new ones have been added (excessive alcohol consumption, traumatic brain injury, and air pollution).
Modifiable risk factors of all‐cause dementia (adapted from Livingston et al 101 )
| Relative risk for dementia (95% CI) | Weighted population attributable fraction (%) | |
|---|---|---|
| Less education | 1.6 (1.3‐2.0) | 7.1 |
| Hearing impairment | 1.9 (1.4‐2.7) | 8.2 |
| Traumatic brain injury | 1.8 (1.5‐2.2) | 3.4 |
| Hypertension | 1.6 (1.2‐2.2) | 1.9 |
| Excessive alcohol consumption (>21 units/week) | 1.2 (1.1‐1.3) | 0.8 |
| Obesity (body mass index ≥30) | 1.6 (1.3‐1.9) | 0.7 |
| Smoking | 1.6 (1.2‐2.2) | 5.2 |
| Depression | 1.9 (1.6‐2.3) | 3.9 |
| Social isolation | 1.6 (1.3‐1.9) | 3.5 |
| Physical inactivity | 1.4 (1.2‐1.7) | 1.6 |
| Diabetes | 1.5 (1.3‐1.8) | 1.1 |
| Air pollution | 1.1 (1.1‐1.1) | 2.3 |
| Total | 39.7 |
Together, these factors account for about 40% of dementia risk worldwide, which can theoretically be prevented 102 . The potential is greater in low‐income countries, in which the prevalence of some of the risk factors is higher. An ambitious prevention program in terms of both policies and individual action has been therefore proposed, while recognizing that individual behavioral change, on which much of this depends, is difficult to achieve 102 . There has also been an international consensus on enlarging the vista of dementia to include cerebrovascular disease, with the Berlin manifesto of “preventing dementia by preventing stroke” 103 .
The evidence that the modification of lifestyle and other risk factors can slow cognitive decline and potentially delay the onset of dementia, or prevent it, is gradually accumulating 102 .
For most risk factors, the evidence comes largely from observational studies, although some controlled trials are also available 101 . While individual factors – such as education, physical activity, and control of vascular risk factors – are important to address, it is the lifelong cumulation of risk that appears to be most potent. Multimodal interventions over long periods have therefore been investigated.
The best‐known investigation is the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER Trial) 104 , a 2‐year multi‐domain randomized controlled trial in which the active arm included dietary counseling, physical exercise, cognitive training, and vascular and metabolic risk monitoring. Over 24 months, the improvement in global cognition was 25% higher in the intervention group compared to the general health advice control group. The improvement was observed regardless of demographic and socioeconomic factors, and was also seen in people with genetic susceptibility ( APOE*4 positive) to Alzheimer's disease 105 . Long‐term data from this trial, to explore whether the intervention did indeed prevent dementia, are not yet available.
While the FINGER trial generated much enthusiasm, two other large multi‐domain trials, the Multi‐domain Alzheimer Preventive Trial (MAPT) 106 from France and the Dementia by Intensive Vascular Care (PreDIVA) 107 from the Netherlands, were negative on their primary outcomes (respectively, cognitive decline and all‐cause dementia). Sub‐analyses of these trials, however, revealed that there was benefit in people with increased risk of dementia.
This highlighted the need for further research and resulted in the development of an international network of trials called the World‐Wide FINGERS (WW‐FINGERS) 108 , which encompasses 25 countries, including some low‐ and middle‐income countries. Some of the trials, such as the Maintain Your Brain Trial in Australia 109 , are completely online. This network, with the stated objective of data sharing and joint analyses, has the potential to provide the evidence base to develop prevention of dementia policies across communities and jurisdictions.
While policy change will need to await such evidence, it is reasonable, at an individual level, to advise older people at risk of cognitive decline to implement the measures of controlling vascular risk factors, optimizing their physical, mental and social activities, reducing stress, treating depression if present, and following a balanced Mediterranean‐like diet 110 . Indeed, it would be reasonable to argue that dementia prevention is a life‐long endeavor, the seeds of which are sown in childhood with good education and a nurturing environment.
Neuropsychiatric symptoms of dementia
Neuropsychiatric symptoms are a common reason for referral of a dementia patient to a psychiatric service. They also lead to much distress, both for the patient and his/her caregivers, and contribute to hospitalization and early admission to residential care 111 .
Several approaches have been used for the categorization of these symptoms, with none being completely satisfactory. They include agitation and aggression, psychotic symptoms (delusions, hallucinations), mood symptoms (depression, anxiety, elation, apathy), sleep and appetite disturbances, and ruminative, repetitive and somatoform behaviors 112 . Apathy has been reported to be the most common symptom, followed by depression and agitation/aggression 113 .
The Neuropsychiatric Inventory (NPI) 114 is the most commonly used instrument for the assessment of these symptoms in clinical trials, but it does not include all of them and is based on informant report. Other commonly used measures are the Behavioral Pathology in Alzheimer's Disease Rating Scale (BEHAVE‐AD) 115 and the Cohen‐Mansfield Agitation Inventory 116 .
Recent work has shown that neuropsychiatric symptoms may occur early in the course of dementia, at the stage of mild cognitive impairment or even before that. This has resulted in the concept of “mild behavioral impairment” 117 . There is some evidence that individuals with mild cognitive impairment who also have neuropsychiatric symptoms are at risk of faster progression to dementia 118 .
The treatment of neuropsychiatric symptoms remains a challenge. The current evidence suggests that the role of drug treatment is limited, and non‐pharmacological strategies are first line 119 , in particular some behavioral management techniques, especially those involving caregiver‐ and staff‐oriented interventions 120 . However, drug treatment is still common, with frequent adverse effects. Antipsychotics such as risperidone, aripiprazole and quetiapine have evidence supporting short‐term use for agitation or psychotic symptoms, but with increased risk of stroke and confusion or cognitive decline, along with extrapyramidal and metabolic adverse effects 121 . Other drugs used in some patients include antidepressants (e.g., citalopram, sertraline, mirtazapine), cholinesterase inhibitors, memantine, benzodiazepines and analgesics, all with limited evidence 112 .
A number of small drug trials have also been conducted to treat neuropsychiatric symptoms in frontotemporal dementia 122 and dementia with Lewy bodies 123 , but with limited evidence of success. A narrative review 124 and a Delphi consensus group 125 supported the use of donepezil and rivastigmine for neuropsychiatric symptoms of dementia with Lewy bodies, although a network meta‐analysis found that these drugs improved neuropsychiatric symptoms in Parkinson's disease dementia, but not in dementia with Lewy bodies 123 . Among antipsychotics, aripiprazole was reported in a small study to be effective and well tolerated for the treatment of psychotic symptoms in patients with dementia with Lewy bodies 126 .
There is an ongoing attempt to better understand the neurobiology of neuropsychiatric symptoms of dementia, so that rational therapeutics can be developed 112 .
Organization of services
The journey of a person with dementia is long and arduous, and often begins with a delay in diagnosis or its lack altogether. A pooled analysis reported that rates of undiagnosed dementia are as high as 70.7% in Canada, 43.1% in UK, 58.2% in Europe, and 61.7% worldwide 127 . The WHO Global Dementia Action Plan 128 aims to reduce this to 50% in 50% of countries by the year 2025.
The communication of the diagnosis to the patient and/or his/her family, once it is made, is often poor, with only 34% of primary care physicians and 48% of specialists routinely informing the individual about the diagnosis 129 . A negative reaction to the diagnosis is common, which is understandable considering the prevalent anti‐dementia stigma in society 130 , 131 .
The diagnosis of dementia should be followed by a management plan for the short and long term, to maintain optimal function and quality of life as long as possible. Too often, the diagnosis is followed instead by advice for disengagement from society 132 , which may set up the path to more rapid decline.
There are several worldwide challenges to providing high‐quality care to persons with dementia and their families. Both the direct and indirect costs of care are high, and public investment in this area has been inadequate, even in high‐income countries, although dementia was declared a public health priority by the WHO in 2015 133 .
The capacity to provide care at home is often insufficient, and systems to ensure the safety and quality of care are not commonly implemented. Institutional care is frequently of poor quality, because of lack of resources and adequately trained staff. People with young‐onset dementia and those from ethnic or other cultural minorities are often poorly catered for.
As the world faces a growing dementia population, the health services, and society in general, need a concerted and coordinated response underpinned by high quality. Several international examples of good practices are available for adoption in diverse settings 134 , 135 . The Global Dementia Observatory of the WHO monitors the public response to dementia in all countries on 35 key indicators, with the objective of achieving the global targets of the Global Dementia Action Plan by 2025 136 .
Directions for future clinical practice and research in dementia are provided in Table 2 .
Directions for future clinical practice and research in dementia
| Neurocognitive disorders should remain categorized as mental disorders in the DSM and ICD, and psychiatry should play a major role in comprehensively assessing and treating these conditions. | |
| A global effort should be made to better understand the origins and disease mechanisms of the various dementia subtypes. | |
| An international effort should be promoted to improve epidemiology research on dementia in low‐ and middle‐income countries and to develop global platforms for data sharing. | |
| A global effort should be made to develop prevention strategies which are tailored to different populations based on differential risk factor profiles and behavioral repertoires. | |
| Clinical services and diagnostic pathways should be improved, so that patients with dementia and mild cognitive impairment can receive an early and accurate diagnosis. | |
| Better models of collaborative care for dementia should be developed that are accessible to all, both in the immediate period after a diagnosis and in the longer term. | |
| The neuropsychiatric symptoms of dementia should be better understood, so that neurobiologically informed treatments can be developed. | |
| The newly developed biomarkers of Alzheimer's disease should be made affordable and clinically available, and biomarkers should be developed for the other dementia subtypes. | |
| Drug development for dementia should become a global effort, with the objective that new treatments are tested in all populations, and when brought to the market are affordable and accessible to all. | |
| All societies should develop policies and procedures to address ageism and stigma against dementia. |
Specific dementias
There have been major advances in the last two decades in our understanding of the pathophysiology and biomarkers of specific dementias, in particular Alzheimer's disease. There have also been significant developments in the knowledge about pathology of dementia, including the description of a potentially new form, limbic‐predominant age‐related TDP‐43 encephalopathy (LATE).
Alzheimer's disease
While the hallmark features of plaques and tangles in Alzheimer's disease have been known for over a century, the understanding of the detailed pathologies involved is more recent. The pathogenesis of the protein abnormalities, the β‐amyloid (Aβ) peptides that aggregate to form the amyloid fibrils of the neuritic plaque, and the hyperphosphorylated tau that forms the neurofibrillary tangles, is now much better understood 137 .
This is associated with other processes such as neuroinflammation, oxidative stress, autophagy, dysfunction of the glymphatic system, alteration in blood vessels, leakage of the blood‐brain barrier, and abnormality in the gut microbiome, all contributing to the cellular pathology underlying Alzheimer's disease 138 .
There has long been a controversy on the relative importance of amyloid and tau in the pathogenesis of Alzheimer's disease. The most popular model is the “amyloid hypothesis”, which posits that Aβ, most likely in its soluble oligomeric form, initiates a pathophysiological cascade which leads to the hyperphosphorylation and misfolding of tau 139 . The misfolded tau is then propagated through the cortex in a prion‐like fashion, leading to cellular failure and the development of cognitive deficits 140 . The complex Aβ‐tau interactions are incompletely understood, and it seems likely that both pathologies are important and have a synergistic effect 139 .
Diagnosis and biomarkers
Alzheimer's disease accounts for 55‐60% of all cases of dementia. The clinical features are well described, with salience of disturbance of episodic memory in the early stages. The clinical criteria used most commonly are the NIA‐AA criteria for dementia 89 and mild cognitive impairment 90 due to Alzheimer's disease.
With the recent development of biomarkers for amyloid (A), tau (T) and neurodegeneration (N), Alzheimer's disease has also been described using the AT(N) framework, with a diagnosis requiring the presence of both A and T 141 . This approach distinguishes the pathological process of the disease from the clinical syndrome, recognizing that pathology precedes the development of neurodegeneration and clinical features by several years, if not decades.
A hypothetical model of dynamic biomarkers has been proposed to explain the pathophysiological process of Alzheimer's disease 142 , in which Aβ deposition occurs independently and accelerates tauopathy, which then leads to neurodegeneration detectable on magnetic resonance imaging (MRI) and positron emission tomography (PET) before cognitive symptoms become manifest.
There have been updates of the AT(N) classification to accommodate vascular pathology 143 and other pathologies such as neuroimmune dysregulation, synaptic disruption and blood‐brain barrier breakdown 144 .
One of the most significant recent advances in Alzheimer's disease has been the development of biomarkers, as listed in Table 3 . PET imaging was first established for amyloid 145 and later for tau 146 , and both are now in clinical use. It is now possible to assess amyloid and tau status with high specificity and sensitivity by the cerebrospinal fluid measurement of Aβ42 level, Aβ42/Aβ40 ratio and phospho‐tau (pTau) levels, for which standardized procedures have been developed 144 .
Biomarkers in the diagnosis of common dementing disorders
| Biomarker class | Imaging | Cerebrospinal fluid | Blood | |
|---|---|---|---|---|
| Alzheimer's disease | Amyloid (A) | PET (Pittsburgh compound‐B, F ligands) | Aβ42 level; Aβ42/Aβ40 ratio | Aβ42 level; Aβ42/Aβ40 ratio |
| Tau (T) | PET | pTau | pTau181; pTau217; pTau231 | |
| Neurodegeneration (N) | MRI, FDG PET | tTau; NfL | NfL | |
| Synaptic loss | FDG PET | Neurogranin | ||
| Neuroinflammation | TSPO PET | GFAP; TREM2 | GFAP | |
| Dementia with Lewy bodies | Neurodegeneration | MRI, FDG PET | ||
| Parkinsonism | DAT imaging, MIBG heart scintigraphy | |||
| Frontotemporal dementia | Neurodegeneration | MRI, FDG PET | NfL | NfL |
PET – positron emission tomography, FDG – fluorodeoxyglucose, MRI – magnetic resonance imaging, Aβ – amyloid beta, pTau – phosphorylated tau, tTau – total tau, NfL – neurofilament light chain, GFAP – glial fibrillary acidic protein, TREM2 – triggering receptor expressed on myeloid cells‐2, TSPO – translocator protein (18 kDa), DAT – dopamine transporter, MIBG – 123 I‐metaiodobenzylguanidine
More recently, the development of blood biomarkers for Alzheimer's disease has raised the prospect of affordable and readily accessible tests. While Aβ42/Aβ40 ratio shows promise, more work is needed to standardize its measurement before clinical use 147 . Some pTau fragments (pTau181, pTau217 and pTau231) in the blood have been shown to accurately reflect brain pathology and are rapidly emerging as biomarkers 148 . Blood levels of neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP) may accurately reflect neurodegeneration and neuroinflammation, respectively 148 .
The genetics of Alzheimer's disease has seen major advances in recent years. The fully penetrant mutations in three genes (amyloid precursor protein, presenilin 1 and presenilin 2), that cause disease of early onset, have been known for some time 149 . The main risk gene for sporadic disease is the ε4 allele of the apolipoprotein E gene ( APOE*4 ), which increases risk by 2‐3 fold in the heterozygous state and 10‐12 fold in the homozygous condition.
Genome‐wide association studies and next generation sequencing have led to the discovery of an additional >40 genes with small effect (odds ratios of 1.05 to 1.20). Collectively, the polygenic risk score for Alzheimer's disease can distinguish patients from controls with 75‐85% accuracy 150 .
The recent approval by the US Federal Drug Administration (FDA) of a disease‐modifying drug, aducanumab 151 , has been seen as a major milestone 152 . This is a human monoclonal antibody that targets the amyloid protein and is administered by monthly intravenous infusions.
However, its approval has generated considerable controversy. Phase 3 studies were initially terminated after a futility analysis, but a post‐hoc analysis led to “accelerated” approval by the FDA because it showed reduction of brain amyloid as a surrogate marker, even though the clinical benefit criterion was not met 153 , and the drug showed significant adverse effects in the form of cerebral edema and hemorrhage. This approval occurred despite the advice of the independent advisory committee of the FDA, and came with a price tag of US$ 56,000 per year for the drug.
The validity of reduced amyloid in the brain as a surrogate marker for clinical benefit has been questioned 154 . Nevertheless, many clinicians are preparing for the rollout of the drug in the US, and approval in other countries is being sought. The manufacturers of aducanumab have been given 6‐year approval by the FDA to provide evidence of clinical benefit. Guidelines for its appropriate use are beginning to be published 155 . Aducanumab may be the first of several disease‐modifying drugs coming to the clinic, and has generated renewed interest in drug treatment of Alzheimer's disease and other dementias.
Other dementias
Advances in other dementias – such as vascular dementia, dementia with Lewy bodies, and frontotemporal dementia – have been significant, but not as striking as those in Alzheimer's disease.
Vascular cognitive impairment and dementia
Vascular dementia has seen a broadening of the concept to vascular cognitive impairment and dementia 156 , and new diagnostic criteria 157 , 158 have been proposed.
Vascular dementia is the second most common form of dementia, accounting for about 15‐20% of all cases 159 . Vascular contributions to dementia are, however, much more common in autopsy studies, with up to 75% having some vascular pathology 160 and about one‐third having significant vascular pathology 161 .
Recently, international collaborations, such as the Stroke and Cognition Consortium (STROKOG) 162 and the METACOHORTS Consortium 163 , have been formed to expedite the development of new treatments and prevention efforts. A framework for research priorities in the cerebrovascular biology of cognitive decline has been proposed 164 . The priorities include the development and validation of imaging and biospecimen‐based biomarkers, better experimental models, and increased understanding of the underlying molecular and physiological mechanisms – white matter disease, infarction, microhemorrhage, vascular autoregulation, glymphatic flow, metabolic processes – and the interaction between vascular and Alzheimer pathologies 164 .
Dementia with Lewy bodies
Dementia with Lewy bodies has seen the publication of the fourth consensus report on its diagnosis and management 165 , which has clearly distinguished between clinical features and diagnostic biomarkers. The report gave more weighting to rapid eye movement (REM) sleep disorder, that involves recurrent dream enactment behavior, in the clinical criteria. The disproportionate deficits in the cognitive domains of attention, executive function and visual processing relative to memory and naming were highlighted.
While there are still no direct biomarkers to establish dementia with Lewy bodies, indicative biomarkers include reduced dopamine transporter (DAT) uptake in the basal ganglia on single photon emission computerized tomography (SPECT) or PET imaging 165 , 166 , reduced iodine‐metaiodobenzylguanidine (MIBG) myocardial scintigraphy uptake 165 , and polysomnographic confirmation of REM sleep without atonia 167 .
While the genetic architecture of this form of dementia is poorly understood, genome sequencing has identified new loci, and genetic risk scores suggest that it shares risk profiles with Alzheimer's and Parkinson's diseases 168 .
There is evidence for the beneficial effects of cholinesterase inhibitors, but not memantine, on cognition 169 , but parkinsonism is less likely to respond to dopaminergic drugs compared to Parkinson's disease, with an increased risk of psychosis 170 .
Frontotemporal dementia
Frontotemporal dementia is an umbrella term for a diverse group of neurodegenerative disorders characterized by atrophy in the frontal and temporal lobes, with a clinical picture dominated by a behavioral‐executive dysfunction (behavioral variant) or a language disturbance (semantic and progressive non‐fluent aphasia variants) 171 .
Because of the psychiatric features of the behavioral variant, psychiatrists are often the first professionals to see such patients 172 , and the condition may be misdiagnosed as obsessive‐compulsive disorder, schizophrenia, bipolar disorder or depression, because of some shared features 172 . Personality change is often an early feature of this behavioral variant; there may be features of borderline, antisocial, schizoid or schizotypal personality. Substance abuse may be present 172 . About 50% of patients with frontotemporal dementia initially receive one of the above‐mentioned psychiatric diagnoses, leading to a delay in the correct diagnosis of up to 5‐6 years 171 .
Frontotemporal dementia is usually a young‐onset disorder, being the second or third most common cause of dementia of young onset, accounting for 3‐26% of such cases in various studies 173 . About a third of cases are familial, with three autosomal dominant genes commonly implicated: progranulin (GRN), chromosome 9 open reading frame 72 (C9orf72), and microtubule‐associated protein tau (MAPT). However, several other genes have been involved. Rare mutations include TAR DNA‐binding protein 43 (TDP‐43), fused‐in sarcoma (FUS), valosin‐containing protein (VCP), and the CHMP2B genes. The C9orf72 mutations are the most common genetic form and may initially present as a late‐onset psychosis. These mutations have also been rarely reported in patients with schizophrenia and bipolar disorder 174 , 175 .
The inclusions in frontotemporal dementia contain tau, TDP‐43 or FUS proteins. There is increasing research in developing fluid biomarkers for this form of dementia, with NfL showing promise as marker of neurodegeneration 176 , but without specificity.
Differential diagnosis from psychiatric disorders and other neurodegenerative diseases is often aided by neuroimaging, using MRI and PET. There is predominant atrophy of frontal and temporal lobes, which is asymmetrical in the early stages, and this is associated with hypometabolism and hypoperfusion in these regions. Differential diagnosis from the frontal variant of Alzheimer's disease is assisted by amyloid imaging 177 .
There is currently no approved drug treatment for frontotemporal dementia. The focus of treatment is on the management of neuropsychiatric symptoms. The symptoms targeted have been apathy, disinhibition, obsessive‐compulsive and hoarding behaviors, loss of empathy and prosocial behavior, loss of insight, and psychosis, but results thus far have not been conclusive for the various interventions investigated 122 . Drugs to modulate the serotonergic and dopaminergic systems are used off‐label to treat these symptoms, but with modest success 122 .
Limbic‐predominant age‐related TDP ‐43 encephalopathy ( LATE )
LATE is a recently described entity which affects older people and presents with an amnestic picture resembling Alzheimer's disease 178 . Its pathology – which typically involves the amygdala, hippocampus and middle frontal gyrus – is common in older brains, seen in nearly 25% of brains at autopsy in a community cohort 179 .
The pathogenesis and clinical picture of this condition, and its status in relation to Alzheimer's disease and frontotemporal dementia, are only beginning to be understood.
The DSM‐5 recognizes delirium as a cognitive disorder with a disturbance of attention (i.e., reduced ability to direct, focus, sustain and shift attention) and awareness (i.e., reduced orientation to the environment). This often leads to what has been referred to as a confusional state or reduced level of consciousness 180 .
The presentation is multifaceted, with several cognitive domains being affected, along with altered sleep‐wake cycle, emotional lability, delusions, agitation, and other motor and behavioral disturbances. Two forms of delirium – hyperactive and hypoactive – have been described, with the hypoactive form being more common in older people and having a worse prognosis 181 .
Delirium remains a clinical diagnosis, with no validated biomarkers. Various inflammatory, metabolic and neurotransmitter‐based markers have been investigated, but their clinical application is limited 182 . The electroencephalogram (EEG) may be used as a supportive test, but it has low specificity and sensitivity, and its application is mainly to distinguish delirium from a primary mental disorder or a non‐convulsive status epilepticus 183 .
The lack of biomarkers and the diverse and sometimes subtle clinical features of delirium often result in its under‐recognition. In one study 184 , conducted in the context of palliative care, 60% of patients with delirium had not been diagnosed by the treating physician. A high index of suspicion, especially in older individuals in settings where delirium is most likely, is important, preferably complemented by a delirium screening tool 185 . One of the most widely used is the Confusion Assessment Method (CAM) 186 , which can alert the clinician to the likelihood of delirium in an individual case.
The pathophysiology of delirium is incompletely understood. Older age is an independent risk factor, and this has been attributed to several changes associated with brain aging, which include reduced blood flow and vascular density, neuronal loss, and changes in neurotransmitters and intracellular signal transduction systems 187 . Numerous predisposing and precipitating factors for delirium have been identified, resulting in its characterization as a state of acute brain failure through multiple pathways. Several hypotheses for its development have been proposed, such as the oxidative stress hypothesis 188 , the neuroinflammatory hypothesis 189 , the neuroendocrine hypothesis including the role of aberrant stress 190 , and the circadian rhythm dysregulation hypothesis 190 .
Since the various pathways do not occur in isolation, and do not lead to distinct consequences, delirium is best understood as a large‐scale neural network disruption 182 , with several processes (i.e., neuroinflammation, neurotransmitter dysregulation, oxidative stress, neuroendocrine disturbance, and circadian rhythm dysregulation) contributing to varying degrees in different situations.
Several clinical management guidelines for delirium have been published 191 , which include those from the UK National Institute for Health and Care Excellence (NICE) 192 and the American Geriatrics Society 193 . The emphasis is on prevention, with the use of multicomponent non‐pharmacological approaches. The various components are attention to the environment, encouraging ambulation and exercise, early mobilization following surgery, maintaining a fluid balance, attention to adequate nutrition, improving vision and hearing, sleep enhancement, infection prevention, pain management, hypoxia control, and optimization of medications 180 . A non‐pharmacological approach based on the above‐mentioned components is also the mainstay of treatment. Drug treatment is generally avoided, except for benzodiazepines in delirium from alcohol or benzodiazepine withdrawal.
While antipsychotics such as risperidone, haloperidol, ziprasidone and olanzapine are sometimes used to manage agitation or psychotic symptoms in delirium, there is a lack of strong evidence to support their use 194 .
LATE‐LIFE MAJOR DEPRESSION
The recognition of major depression is of great clinical importance across the life cycle, and no less so in older adults 195 . This condition presents increasing public health challenges to both high‐income and low‐ and middle‐income countries, reflecting demographic shifts to older populations and scarcity of treatment resources 195 , 196 . It is the second leading cause of disability worldwide, up from the third as of 1990 197 .
The hallmark of major depression in old age is its co‐occurrence with physical disorders and frailty, mild cognitive impairment, social determinants of health (e.g., major role transitions, bereavement, loneliness and social isolation), exposure to polypharmacy, and heightened risk for suicide. Late‐life major depression is also a significant source of caregiver burden for family members.
Approximately 6.7% to 7.5% of older adults report an episode of major depression within one year, among those attending primary care clinics 195 . Rates are still higher among medical inpatients and residents in long‐term care, rising with increasing disability and frailty. Women experience 1.7 times the risk as men. Prevalence rates are likely to be higher in marginalized groups, such as those of lower socioeconomic status. The lifetime suicide rate is 25 times greater in major depression than in the general population, with highest rates amongst older adults 196 , 197 , 198 .
Major depressive disorder and depressive symptoms not only bring suffering to those afflicted, but also produce amplification of disability from co‐occurring physical disorders, poor adherence to co‐prescribed treatments, failure to make healthy lifestyle choices, and increased risk for frailty, dementia, and early death. On the other hand, evidence‐based treatments work, if delivered appropriately, and may both prolong life and enhance its quality 199 .
In essence, the global public health and clinical burden of depression in old age has three dimensions: it is a mirror of brain aging, a mediator of bad outcomes, and a murderer that leads to dementia and to suicide. It is also an unwanted co‐traveler with the ills of aging: cancer, cardiovascular disease, and neurodegenerative disorders 195 , 196 , 197 .
Major depression in older adults is characterized by variability at multiple levels: etiopathogenesis, clinical presentation, and response to prevention and treatment. A staging‐model perspective, analogous to oncology, is useful 200 , 201 . Some older adults may present with mild or subsyndromal symptoms; some with new‐onset major depression; some with recurrent episodes which began earlier in life and show in later years shortening inter‐episode intervals and increasing treatment resistance; and still others are ravaged by chronic depression and its sequelae.
Staging has implications for differential diagnosis, intervention and prognosis 202 . Subsyndromal pictures represent opportunities for the indicated prevention of major depression. First episodes, while treatable, may also be prodromal expressions of dementia. Recurrent depressive episodes and chronic depression pose challenges of increasing treatment resistance and heightened risk for dementia. As in oncology, early intervention to prevent the transition to incident episodes and to recurrence may be life‐saving and life‐enhancing, by taking advantage of neuroprotective mechanisms early in the course of illness, while reversibility may still be attainable 200 , 201 .
In this context, the relationship of insomnia disorder to depression is clinically relevant, because insomnia is not only a symptomatic manifestation of major depression, but also a risk factor for incident and recurrent depressive episodes. Persistent insomnia (insomnia disorder) heightens the risk for a chronic relapsing course and thus warrants independent clinical attention to optimize outcomes 203 .
Insomnia may partially mediate depression risk for Alzheimer's and related dementias via beta‐amyloid accumulation, tau protein aggregation, inflammation and blood‐brain‐barrier disruption 204 , 205 , 206 . It is also a driver of suicidal ideation and behavior, and may be a modifiable risk factor for suicide 203 , 207 . .
A long‐term view of late‐life depression is necessary clinically: getting well is not enough, it is staying well that counts, given the propensity of depression to relapse, recurrence, chronicity, and treatment resistance, not to mention heightened risk for dementia and suicide.
Major depression can be prevented across the life cycle 196 , 208 . The case for its prevention in the later years of life is important from both public health and clinical perspectives. Major depression is prevalent, persistent and burdensome in respect to both morbidity and mortality. Treatment is only partially effective in reducing years lived with disability. There is, moreover, limited access to treatment, related to both mental health workforce issues and barriers confronting socially disadvantaged older adults and those from racial/ethnic minorities. The social inequalities of risk widen with age, generating disparities of access, utilization and response. This treatment gap reinforces the need for the development and implementation of pragmatic prevention programs 208 .
A meta‐analysis 209 estimated a reduction of about 20% in the incidence of major depressive episodes over 1‐2 years, compared with care as usual or waitlist, through the use of brief behavioral or learning‐based psychotherapies (such as CBT, interpersonal psychotherapy, problem‐solving therapy, and behavioral activation). The 38 randomized controlled trials included in the meta‐analysis enrolled mixed aged (adult and geriatric) participants, receiving care in high‐income countries. Studies investigated either indicated prevention (in persons already living with mild or subsyndromal symptoms) or selective prevention (in those with physical or psychosocial risk factors for depression, such as stroke or age‐dependent macular degeneration).
Only one randomized controlled trial of depression prevention specifically focused on older adults with mild symptoms (indicated prevention) has been conducted in a low‐ or middle‐income country 210 . The “DIL” intervention (meaning “Depression in Later Life” and also representing the local Konkani word for “heart”) was delivered by lay counselors to older adults at rural and urban primary care clinics in Goa, India. The intervention model was multi‐pronged, grounded in the strategies of behavioral activation 211 , but also including brief behavioral treatment for insomnia 212 , education in better self‐care for common physical disorders such as diabetes and osteoarthritis, and assistance in accessing medical and social services.
Over one year, DIL led to a reduction in the incidence of major depressive episodes compared to care as usual (4.4% versus 14.4%, log rank p=0.04) and in the burden of depressive and anxiety symptoms (group x time interaction: p<0.001). Participants randomly assigned to DIL reported to more frequently engage in pleasurable social and physical activities – a countermeasure to the “tension” and worry that plagued their daily lives. They took a more active hand in managing their health, coming to feel more in control and less helpless 210 . If these findings are replicated, the DIL intervention may be scalable to other low‐ or middle‐income countries.
More recently, the VITAL‐DEP randomized clinical trials examined the efficacy of two nutraceuticals, vitamin D and fish oils, in preventing incident and recurrent major depressive episodes in over 23,000 older adults, with an over‐sampling of African Americans 213 , 214 . The scope of the trials was wide, examining universal, selective and indicated prevention of depression. The trials did not, however, detect evidence for efficacy, relative to placebo, with either nutraceutical, despite a cogent neurobiological rationale for positing the prophylactic effect of each, singly and in combination. For example, vitamin D and/or fish oils could lower depression risk via reduction in inflammation and oxidative stress, and improvement in vascular/metabolic health and neuroprotection. These processes represent senescence‐associated secretory phenotypes (SASPs), i.e., molecular signatures of aging 215 .
Studies such as DIL and VITAL‐DEP highlight the importance of addressing the interplay between behavioral and biological factors involved in aging processes. Moreover, attention to workforce issues (via the use of task sharing or shifting to lay counsellors) and to the streamlining of evidence‐based behavioral interventions and psychotherapies, with sensitivity to differing cultural contexts, may help to optimize cost‐utility of prevention interventions. Identifying biomarkers of risk that may mediate or moderate response to preventive interventions remains a vital part of the research agenda in late‐life depression.
Treatment goals for major depressive disorder in older adults should include not only symptomatic remission, but also functional recovery; reduction of risk for relapse, recurrence and chronicity; and protection and maintenance of brain health and cognitive fitness 216 . Combined treatment (antidepressant medication plus depression‐specific psychotherapy) may be more effective than either alone in some populations, but side effect risks and patient demands/burdens may be greater 5 , 6 , 195 , 217 .
Psychotherapies may have a greater impact than antidepressant medication in the long run 216 , 217 . Moderators of outcome include individual patient‐level differences such as those concerning gender, ethnicity, disability status, neurocognitive performance, and physical comorbidity. Therapist competence (including ability to tailor treatment to the individual), therapeutic alliance, and patient preferences all influence the strength of response to treatment 6 .
The limitations of the available evidence include little comparative research, together with a need for greater attention to long‐term effects, comorbidity, and diverse populations. With respect to antidepressant pharmacotherapy, response rates in older adults are greater in trials lasting 10‐12 weeks than in those lasting 6‐8 weeks. Antidepressants are moderately effective in bringing about remission relative to pill placebo, with numbers needed to treat in the range of 8‐13 218 . Learning‐based psychotherapies (CBT, interpersonal psychotherapy, problem‐solving therapy, behavioral activation) are also moderately effective in bringing about remission 216 .
Continuing antidepressant medication in those who have initially done well appears to be effective in preventing relapse during 6‐12 months of continuation therapy, and in preventing recurrence for up to three years during longer‐term maintenance treatment, with reported numbers needed to treat of about 4 219 . Going forward, pharmacogenomics‐informed clinical decision making is likely to continue emerging as a useful strategy in probing treatment response variability (both efficacy and tolerability/safety) and contributing to better outcomes 220 , 221 .
Failure to achieve symptomatic remission after two or more trials of antidepressant pharmacotherapy is common in older adults with major depression. The largest published randomized controlled trial to date amongst older adults (“IRL GREY”) – a multi‐site, double‐blind, placebo‐controlled trial of aripiprazole augmentation of primary pharmacotherapy with venlafaxine – demonstrated efficacy for augmentation, yielding a 44% remission rate versus 29% with placebo (number needed to treat: 6.6) 222 . Aripiprazole was well tolerated in analyses of both cardiometabolic and neurological outcomes, and led to a reduction in the prevalence and severity of suicidal ideation.
A randomized pragmatic trial comparing augmentation versus switching class of antidepressant medications for treatment‐resistant late‐life major depression has recently been completed 223 . Preliminary analyses suggest that pharmacotherapy augmentation strategies (e.g., with bupropion or aripiprazole) are superior to switching strategies (to another monotherapy) in bringing about remission, and are no less safe with respect to such adverse events as falls.
A psychotherapy called “Engage”, rooted in a neurobiological framework addressing the reward system network, and streamlined for effective administration by community‐based psychotherapists, has been shown to be non‐inferior to problem‐solving therapy in late‐life depression 224 , and proposed for combination with pharmacotherapy in patients with persistent symptoms.
Prolonged grief disorder (PGD) is an important but often unrecognized factor in late‐life treatment‐resistant depression. The ICD‐11 and the DSM‐5‐TR have provided clinical guidelines and diagnostic criteria, respectively, for its diagnosis 225 . In PGD, acute grief becomes chronic, with intense yearning for the deceased, and accompanying symptoms of anguish, loneliness, suicidal ideation and pervasive functional impairment. PGD represents a failure to adapt to loss and to restore meaning in life without the lost loved one. This condition, which frequently coexists with major depression in older adults, responds well to grief‐specific psychotherapy, but not to antidepressant pharmacotherapy or to interpersonal psychotherapy for depression 226 .
We do not know if treating depression in older adults reduces the risk for dementia 101 . However, slowing cognitive decline in elderly with treatment‐resistant depression is now recognized as an important front in the fight against dementia, and a vital aspect in the staging of late‐life major depression 101 , 201 .
Progression of late‐life depression to Alzheimer's and related dementias is likely to be a multi‐mechanism process. Data‐driven proteomic analyses have revealed several biological pathways and molecular functions associated with cognitive impairment in late‐life major depression, related to neuro‐inflammatory control, neurotrophic support, cell survival/apoptosis, endothelial function, and lipid/protein metabolism 204 , 205 , 206 . Experimental studies of dementia prevention in late‐life major depression will need to monitor accumulation of tau and beta amyloid, and white matter disease, provide measures of cognitive and brain health, and document course of depressive illness.
The central question, as yet unanswered, is whether the modulation of biologic cascades related to the pathogenesis of cognitive impairment in late‐life major depression can also retard cognitive decline and reduce dementia incidence, particularly in more treatment‐resistant depression.
What do we know about the integration of primary care and behavioral health care for the treatment and prevention of major depression in older adults? How do we translate intervention science to real‐world care and management of suicide risk?
Collaborative care models integrate behavioral health care and primary care 227 , 228 . They are the best‐known real‐world enactments of measurement‐based care in older adults. Measurement‐based care includes standardized assessment of depressive symptoms, medication side effects, and patient adherence. It uses a multi‐step decision tree (algorithm) in treatment planning and patient follow‐up. While it provides feedback to assist in the management of patients, it is not a substitute for clinical judgment.
A Cochrane database systematic review has shown that collaborative care models (in mixed‐age samples) yield significant improvement in depression and anxiety outcomes compared with usual care. Improvement is evident over the short, medium and long term, with standardized mean differences of 0.25‐0.35 227 . Examples of successful models of collaborative care for midlife and older adults in high‐, middle‐ and low‐income countries include Improving Mood Promoting Access to Collaborative Care Treatment (IMPACT) 228 , Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) 229 , Friendship Bench in Zimbabwe 230 , and MANAS 231 and DIL 210 in India.
IMPACT and PROSPECT addressed population‐ and patient‐centered care in older adults with major depression. These studies, showcasing the principal characteristics of collaborative care, embodied evidence‐, team‐, measurement‐, and algorithmic‐based strategies to achieve and sustain remission in older adults attending rural and urban primary care clinics. These models facilitate a personalized approach to treating depression in older adults, starting with interventions requiring fewer specialized resources and moving to more elaborate interventions as needed.
In IMPACT 228 , over half of the participants in collaborative care reported at least a 50% reduction in depressive symptoms at 12 months, as compared with only 19% of participants in usual care. The benefits persisted for at least one year, when IMPACT resources were no longer available. IMPACT participants experienced more than 100 additional depression‐free days over a two‐year period.
In PROSPECT 229 , resolution of suicidal ideation was faster among intervention participants as compared with usual care; differences peaked at 8 months (70.7% vs. 43.9%). In addition, follow‐up after a median interval of 98 months found a 24% reduction in all‐cause mortality relative to care‐as‐usual participants 198 . Post‐hoc analysis showed that the decline in mortality reflected fewer deaths from cancer. The mechanism of this protective effect could involve an interplay between behavioral factors (e.g., better self‐care) and cellular or molecular processes of aging. Thus, a key question for research going forward is whether treating depression effectively modifies the risk architecture for cancer at either or both behavioral and molecular levels.
Further enhancements of collaborative care occur through the use of lay counsellors or community health workers, especially to reach under‐served racial/ethnic minorities. The MANAS 231 and the DIL 210 trials, deploying lay counsellors for the treatment and prevention of depression, respectively, in primary care patients (adults and older adults), provide compelling examples of task sharing/shifting to confront workforce issues that impede access to care in under‐resourced areas of the world.
Similarly, Chibanda et al 230 have shown that the use of lay health workers for delivering problem‐solving therapy (“Friendship Bench”) in a resource‐poor setting such as Zimbabwe may be effective in the primary care of common mental disorders. Community health workers and lay counselors perform a number of tasks, including screening for depression, relaying results to supervising clinicians, educating persons with depression and their caregivers about the illness and its treatment, facilitating identification of local resources for social and economic support, encouraging self‐care and cooperation with primary care for co‐occurring physical problems, and delivering depression‐specific psychotherapies, such as interpersonal therapy, behavioral activation, and problem‐solving therapy, in one‐on‐one or group formats.
Collaborative care models also facilitate re‐engineering care delivery to improve management of suicidal risk in depressed patients. In most countries, suicide rates are highest among older adults, and suicide attempts by older adults are frequently serious, with high lethality potential. Collaborative care promotes an explicit focus on factors that contribute to distress and to suicidal urges versus those that contribute to constraint and resistance 232 . It also integrates counseling with patients and family caregivers to reduce access to lethal means for suicide, together with safety planning and attention to family discord, victimization, and the need for social support. These and other elements of re‐engineering practice have been shown in the UK to yield suicide reductions of 22‐29% 233 .
Going forward, the use of machine learning to identify relevant data in electronic health records 234 and the use of adaptive screening tools 235 may improve our ability to match the intensity of services to level of suicide risk – thereby enacting a fundamental principle of collaborative, stepped‐based care. In addition, more research into both the short‐term and long‐term (maintenance) efficacy and safety of ketamine for the rapid reduction of suicidal ideation in older adults with major depression is warranted 236 . Finally, addressing depression‐related reductions in top‐down cognitive control should be a goal of psychotherapy in suicide attempters. Deficits in cognitive control result in disadvantageous decision‐making and limited problem‐solving, contributing to feelings of entrapment and hopelessness 237 .
Access to mental health services by older adults with major depression is driven by a shortage and skewed geographical distribution of providers. User‐facing apps coupled with assistance from coaches, and other telepsychiatry tools, can help address the treatment gap, but barriers related to culture, policy and funding issues remain 195 , 238 . Collaborative care models of service delivery should invest in supporting telepsychiatry.
In summary, the scalability of collaborative care is promising, not only because of its demonstrated effectiveness and, increasingly, the use of community health workers and lay counselors, but also because of its potential for cost‐offsetting impact. The evidence for cost‐effectiveness remains inconclusive, but certain policies do promote its implementation and uptake. For example, the Center for Medicare and Medicaid Services in the US now allows the use of current procedural terminology codes (so‐called CPT codes) to facilitate reimbursement of mental health specialists for work in primary care settings, including consultation on clinical management even when the psychiatrists may not have personally examined the patient.
Directions for future clinical practice and research in late‐life major depression are provided in Table 4 .
Directions for future clinical practice and research in late‐life depression
| Pragmatic intervention programs (e.g., collaborative, stepped‐care models) should be further developed and implemented, using both pharmacotherapy and depression‐specific psychotherapies (e.g., problem‐solving therapy, cognitive behavioral therapy, and interpersonal psychotherapy), amenable for use also in low‐ and middle‐income countries. | |
| Further comparative effectiveness/safety/tolerability research should be conducted to develop staged algorithms of care for use in both primary and specialty mental health settings, that will match needs of patients with intensity of intervention. | |
| Measurement‐based care should be promoted to optimize efficacy, tolerability, safety, and treatment adherence. | |
| The implications of staging models of depression for assessment, prevention and treatment should be further investigated. | |
| Indirect, less‐stigmatized approaches to depression prevention in older adults, such as treatment of insomnia disorder, should be further investigated. | |
| The use of lay counsellors, community health workers, and peer‐support specialists should be expanded through task sharing/shifting, to address the dearth of mental health specialists in low‐, middle‐ and high‐income countries. | |
| The use of telepsychiatry, especially to better reach under‐served and rural older adults, should be further integrated. | |
| There should be a focus on health‐span, not only on lifespan, in clinical care and in cost‐benefit analyses. | |
| A focus of research should be whether preventing and treating depression effectively modifies the risk for the major scourges of old age: cardiovascular disease, dementia and cancer. | |
| Further research should be conducted into suicide prevention in older adults, especially addressing high‐risk periods such as transitions from more to less intensive care settings. | |
| Research on ketamine should be expanded to include older adults, in order to further address the clinical care of those with treatment‐resistant depression, suicidal ideation, and cognitive impairment. | |
| Research in psychedelic‐assisted psychotherapy (e.g., psilocybin) for treatment‐resistant depression in older adults should be expanded. | |
| Pharmacogenomically‐informed clinical decision‐making for the care to older adults with major depression should be further explored. |
SCHIZOPHRENIA
The disorders that feature prominently in the differential diagnosis of an older adult with psychotic symptoms include schizophrenia, delusional disorder, substance/medication‐induced psychotic disorder, psychotic disorder due to another medical condition, and major or minor neurocognitive disorder with behavioral disturbance in the form of psychotic symptoms. Here we focus mainly on schizophrenia, as the prototypical psychotic disorder which has generated more research than most other mental disorders over the past 150 years.
A number of studies of schizophrenia in older adults have challenged the Kraepelinian concept of dementia praecox. While Eugen Bleuler also believed in worsening of this mental illness with age, his son Manfred disagreed, as he found that the course was highly heterogeneous. Half of the patients had an undulating course with remissions, and 12‐15% recovered fully 239 . Manfred Bleuler also reported that schizophrenia could have its onset in later life.
Although the Epidemiologic Catchment Area study found prevalence rates of schizophrenia of only 0.3% among persons aged 65 and over, it seemed to under‐sample in areas where persons with mental illness may be concentrated 240 . The actual prevalence rate is probably around 1%, and about 85% are living in the community 241 . A systematic review of literature published between 1960 and 2016 found that the pooled incidence of schizophrenia in those over 65 was 7.5 per 100,000 person‐years at risk, with an increased risk in women (OR=1.6, 95% CI: 1.0‐2.5) 242 .
Schizophrenia is associated with accelerated biological aging. Yet, it does not follow the course of known neurodegenerative disorders such as Alzheimer's disease, dementia with Lewy bodies, vascular dementia, and frontotemporal dementia, which are all accompanied by major atrophic changes in specific regions of the brain. There are no specific and observable degenerative changes that can be seen on an MRI or in neuropathological examinations of the brains of people with schizophrenia who die at older age 243 .
While there is aging‐associated cognitive decline, studies have found no significant difference in the rate of change in cognition in adults with versus without chronic schizophrenia 244 . However, cognitive trajectories differ significantly between institutionalized patients and outpatients with schizophrenia. The deterioration observed in the former patients seems to be related to greater illness severity, heavier medication load, vascular risk factors, and lack of stimulation 245 .
Several longitudinal investigations have shown that the clinical course of schizophrenia in late stages is often relatively stable and non‐deteriorating 246 , 247 , 248 . With aging, there is frequently an improvement in psychotic symptoms 246 . Most hospitalizations in older persons with schizophrenia are due to physical rather than psychological problems.
Studies have found that, relative to their younger counterparts, middle‐aged and older adults with schizophrenia tend to have better psychosocial functioning, including better adherence to medications and self‐rated mental health, and lower prevalence of substance use and psychotic relapse. A common explanation offered for this observation is the so‐called survivor bias – i.e., the sickest people died young from serious psychopathology, including suicide or drug use‐related events, so those who survive into older age are less sick. However, longitudinal studies show that, when people with schizophrenia are followed for many years, a sizable proportion do show progressive improvement in their functioning with age 248 . This improvement may reflect better ability to handle stress and engage in healthful behavior.
Both schizophrenia and aging are characterized by heterogeneity. It is not surprising, therefore, that the course of schizophrenia in later life is highly variable, ranging from complete remission to a dementia‐like state 241 . Reported predictors of sustained remission include greater social support, being (or having been) married, higher level of cognitive/personality reserve, and early initiation of treatment. Patients with very chronic illness, severe symptoms including disorganized thinking and behavior, resistance to treatment, and brain abnormalities are at higher risk of poor prognosis 247 , 248 .
It is important to recognize that some people with schizophrenia can and do have positive traits and states such as resilience and happiness. One study using a validated scale of happiness found that, although the mean level was lower in patients with schizophrenia than in healthy comparison subjects, 38% of the patients had happiness ratings in the highest range, despite worse physical health and objectively more stressors 249 . Associations of greater happiness include higher levels of resilience, optimism, and personal mastery, and healthier levels of biomarkers of stress 250 .
There are possible neurobiological explanations for improvement in mental function with aging in general, including in patients with schizophrenia. These include aging‐associated reductions in dopaminergic, noradrenergic and serotonergic activity leading to decreased severity of positive symptoms and decreased impulsivity; reduced stimulation of reward circuitry resulting in decreased illicit substance use; and reduced amygdala activation with negative emotional stimuli contributing to decreased emotional negativity. Several studies have reported posterior‐to‐anterior shift with aging (PASA), resulting in better executive functioning 251 . Obviously, these are largely speculative hypotheses in terms of inferring causality.
Compared to the general population, persons with schizophrenia have an 8.5‐fold greater risk of suicide. However, much less is known regarding suicidal behavior in older patients with schizophrenia 252 . The literature mostly consists of mixed samples of middle‐aged and older individuals. It suggests that depressive symptoms, hopelessness, previous attempts, low quality of life, and history of trauma are likely risk factors 252 , 253 , 254 . While depression is a well‐known risk factor for suicide in schizophrenia, a qualitative study found that delusions and hallucinations were central to suicidal behavior in some patients 255 .
Patients with schizophrenia require thorough assessment for the presence and nature of suicidal ideation or behavior, suicide risk, and factors contributing to suicidality. An integrated approach incorporating different psychosocial modalities relevant to the individual is recommended. CBT helps persons with schizophrenia having suicidal ideation or behavior 256 . Second‐generation antipsychotics may be more effective than first‐generation ones in reducing suicide risk, although few studies have examined their impact on suicidality in older patients with schizophrenia 257 . While clozapine has been reported to be particularly effective in reducing suicidal behavior, its use in older patients is restricted due to its strong anticholinergic side effects as well as granulocytopenia. While there is some evidence for a possible antisuicidal role of selective serotonin reuptake inhibitors in patients with schizophrenia, there is a dearth of such studies in older patients 258 .
Late‐onset schizophrenia and very late‐onset schizophrenia‐like psychosis
The term “late‐onset schizophrenia” was coined by Manfred Bleuler in 1943 to describe a form of schizophrenia with an onset between the ages of 40 and 60 259 . He found that 15% of his patients with schizophrenia met this definition, with only a small number of cases presenting later. These patients' symptoms were fundamentally similar to those in persons with earlier onset, and there were no cognitive or physical signs suggesting a degenerative brain disease.
Roth and Kay 260 described “late paraphrenia”, characterized by a well‐organized system of paranoid delusions with onset after age 45, with or without hallucinations, in the setting of a well‐preserved personality and affective response. They did not consider this to be a subtype of schizophrenia.
The DSM has changed its stance on distinguishing late‐onset from earlier‐onset schizophrenia over the past four editions. The DSM‐III did not allow a diagnosis of schizophrenia if symptoms emerged after the age of 45 261 . The DSM‐III‐R removed this restriction and introduced a “late‐onset” specifier for onset after age 44 years 262 . That specifier was removed in the DSM‐IV 91 .
In 2000, the International Late‐Onset Schizophrenia Group proposed the term “late‐onset schizophrenia” for cases with onset between 40 and 60 years, and “very late‐onset schizophrenia‐like psychosis” for those presenting first after age 60 263 . This distinction was supported by empirical evidence, although the threshold of 40 years for the diagnosis of the former condition was somewhat arbitrary. The group felt that both conditions had clinical usefulness and that their identification could promote research in the field. Late‐onset schizophrenia appeared to be as stable a diagnosis as early‐onset schizophrenia; both diagnoses remained unchanged in up to 93% of cases in a follow‐up, and only rarely were they reclassified as mood disorders 263 , 264 . However, few studies have focused on the diagnosis of very late‐onset schizophrenia‐like psychosis. The DSM‐5 88 does not use an age cutoff in the diagnostic criteria for schizophrenia, nor does the ICD‐11 265 .
Studies have shown similarity between late‐onset and early‐onset schizophrenia in terms of family history of the illness, presence of minor physical anomalies, brain abnormalities such as slightly enlarged ventricles on MRI, nature of psychopathology, and type of cognitive impairment 266 . However, there are also differences between the two conditions. A noteworthy difference is related to gender. Early‐onset schizophrenia is more common in men, whereas late‐onset schizophrenia is much more common in post‐menopausal women than in age‐comparable men, suggesting a possible protective effect of estrogen in pre‐menopausal women. The finding does not seem to arise from gender differences in care‐seeking and societal role expectations or in delay between symptom emergence and service contact 263 .
The higher frequency of late‐onset schizophrenia in women has led to trials of estrogen therapy. In a recent 8‐week, double‐blind, randomized, placebo‐controlled parallel‐group study of 200 women with schizophrenia randomized to a 200 μg estradiol patch or placebo added to antipsychotics, participants receiving estradiol had significant improvement in positive and negative symptoms as well as general psychopathology 267 . Obviously, further clinical trials of this type are needed to establish the value of estrogen in women with late‐onset schizophrenia.
The severity of psychopathology as well as that of cognitive impairment tends to be lower in late‐onset than early‐onset schizophrenia 263 , and patients with the former condition may require lower dosages of antipsychotics than age‐comparable persons with the latter 259 . Thus, late‐onset schizophrenia may be a distinct subtype of the illness.
Aging‐associated psychosocial factors such as retirement, financial difficulties, bereavement, deaths of peers, or physical disability may contribute to the precipitation of the symptoms of schizophrenia in later life 263 . However, the role of these factors has not been studied systematically. Sensory deficits, especially long‐standing conductive deafness, are common in the late‐onset form 264 , but may primarily reflect the patients' reluctance to seek corrective measures or their inability to get correction of these deficits because of poor access to quality health care. Premorbid educational, occupational and psychosocial functioning is less impaired in the late‐onset than in the early‐onset form 268 . The relatives of patients with very late‐onset schizophrenic‐like psychosis have a lower morbid risk for schizophrenia than the relatives of those with the early‐onset form 266 .
Late‐onset schizophrenia does not appear to be a prodrome of Alzheimer's disease, as patients do not demonstrate faster decline in memory beyond age‐associated loss 244 , 266 . Individuals with schizophrenia are known to have reduced cognitive reserve that puts them at increased risk of a dementia diagnosis as they age. However, there is no evidence of higher rates of Alzheimer's disease in patients with schizophrenia 268 . A post‐mortem study found that Alzheimer's disease pathology was rare among cognitively impaired persons with very chronic psychosis 243 .
Treatment: pharmacotherapy
Antipsychotics constitute the backbone of treatment of schizophrenia at all ages, including older patients. During the last three decades, first‐generation antipsychotics have been largely replaced in older persons by second‐generation ones, because of the side effects of the former, such as tardive dyskinesia. However, the newer drugs have proven to be far from optimal in terms of both efficacy and safety. While they control the positive symptoms and prevent relapses similarly to first‐generation medications, they are no more efficacious than the older drugs.
One study compared the longer‐term safety and effectiveness of the four most commonly used second‐generation antipsychotics (aripiprazole, olanzapine, quetiapine and risperidone) in 332 patients, aged >40 years, having psychosis associated with schizophrenia, mood disorders, post‐traumatic stress disorder, or dementia 269 . The overall results suggested a high discontinuation rate (median duration 26 weeks prior to discontinuation), lack of significant improvement in psychopathology, and high cumulative incidence of metabolic syndrome (37% in one year) and of serious (24%) and non‐serious (51%) adverse events with all the four antipsychotics 269 .
Pharmacokinetic and pharmacodynamic changes that occur with age lead to an increased sensitivity to antipsychotics in older individuals, and increase the risk of side effects, especially parkinsonism, tardive dyskinesia, sedation, hypotension and falls 270 . Given the improvement in psychotic symptoms with age in a number of patients with schizophrenia, a progressive reduction in daily dose over a period of weeks or months may be attempted. A watchful eye should be kept on signs of early relapse, so that the dose can be increased as and when needed. In a minority of aging patients with schizophrenia, eventual discontinuation of antipsychotics is feasible, but the patients should be followed carefully 271 .
Modifiable risk factors for tardive dyskinesia should be identified, to minimize its incidence and severity. These include diabetes mellitus, smoking, substance abuse including alcohol and cocaine, and anticholinergic co‐treatment 272 . Two novel vesicular monoamine transporter type 2 (VMAT2) function inhibitors, valbenazine and deutetrabenazine, have been approved in the US as add‐on therapy for persons with tardive dyskinesia 273 . VMAT2 inhibitors may be used to address tardive dyskinesia‐associated impairments and impact on psychosocial functioning 274 .
Treatment: psychosocial interventions
Clinicians should combine pharmacotherapy with appropriate psychosocial interventions in older patients with schizophrenia. There are three skills training programs specifically designed for older adults with severe mental illness and shown to be effective in randomized clinical trials: cognitive‐behavioral social skills training (CBSST), functional adaptation skills training (FAST), and Helping Older People Experience Success (HOPES). They are all group‐based; provide accommodations for persons with physical or cognitive disabilities; help develop skills in incremental steps; and use age‐appropriate psychosocial training techniques to meet the needs of older persons 275 .
The CBSST 276 , 277 is a manualized group intervention, within the framework of the biopsychosocial stress‐vulnerability model of schizophrenia, consisting of three modules, each with four‐weekly sessions, to be repeated, for a total of 24 sessions. The modules focus on thought challenging, seeking social support, and solving problems, with homework assignment after each session. Skills include promoting cognitive behavioral strategies, recognition of early warning signs of relapse, improved communication with health care professionals and social interactions in everyday activities, treatment adherence, and behavioral strategies for coping with psychiatric symptoms.
Randomized controlled trials of CBSST in older adults with schizophrenia have shown a high rate of adherence and low dropout rates 276 . While there was no significant change in psychopathology in pharmacologically stabilized patients, there was significant improvement in social activities, cognitive insight and mastery of problem‐solving skills, as well as a reduction in defeatist attitudes, at the end of the intervention. Some improvement was sustained 6 months post‐treatment 277 .
The FAST 278 focuses on communication, transportation, medication management, social skills, organization and planning, and financial management in 24 semi‐weekly two‐hour group sessions. Active learning approaches include in‐session skills practice, behavioral modeling, role‐playing and reinforcement, and homework practice assignments.
A randomized controlled trial including 240 older adults with schizophrenia showed that FAST participants, compared to a time‐equivalent attention‐control group, had significant improvement in everyday functional skills as well as social and communication skills at the end of treatment and three months later 278 . A pilot study of an adapted version of the FAST program showed improved functioning and well‐being in middle‐aged and older Latinos with severe mental illness 279 .
The HOPES 280 integrates psychosocial skills training and preventive health care management. The skills training component includes classes, role‐play exercises, and community‐based homework assignments in social skills, community living skills, and healthy living. The weekly skills class curriculum provided over 12 months consists of seven modules: communicating effectively, making and keeping friends, making the most of leisure time, healthy living, using medications effectively, and making the most of a health care visit.
A randomized controlled trial of HOPES including 183 older adults with severe mental illness showed significantly greater improvement in skills performance, psychosocial functioning, self‐efficacy, and psychopathology at one‐year and three‐year follow‐up compared to usual care 281 . A greater proportion of HOPES participants received flu shots, hearing tests, eye exams, mammograms, PAP smears, and completed advanced directives than the usual care recipients.
Randomized controlled trials have also shown significant improvement with other manualized psychosocial interventions in older patients with schizophrenia, such as supported employment without and with compensatory cognitive training to help them obtain and retain paid jobs 282 , 283 .
Recent advances in technology along with the COVID‐19‐associated social distancing have hastened a rapid growth of psychosocial interventions administered remotely. For example, computer‐initiated text messaging three times per day for 12 weeks, or live telephone interaction two times per week, can be used to promote self‐management in people with severe mental illness. Following initial training in the use of the necessary technology, people with schizophrenia have minimal dropout rates, few broken devices, and high patient satisfaction 284 . There is a need for more research in this area among older adults with schizophrenia.
In the past few decades, there has been a dramatic decline in the number of persons with schizophrenia living in mental institutions, and an increase in the number of older outpatients 241 . Thus, there is an increasing pressure for community programs to provide services to older persons. As mentioned above, older persons with schizophrenia have higher frequency and severity of physical diseases than people without severe mental illness, and yet receive much less than adequate health care. Also, for schizophrenia patients of all ages, the Epidemiologic Catchment Area Study reported a lifetime prevalence of 33% and 28% for alcoholism and drug abuse disorders, respectively 285 .
Structural barriers in the health care system as well as physician attitudes create impediments to care. A Scottish study reported that primary care doctors were less willing to have persons with schizophrenia on their practice list, and more likely to believe that such persons were apt to be violent 286 . In the US, there are considerable racial inequalities in health status due to diminished access to health care, poorer health practices, and lower socioeconomic status among marginalized ethnic groups compared to non‐Latino Whites 287 .
The excess risk of early mortality, physical comorbidity, early institutionalization, and high costs among older adults with schizophrenia require the development and dissemination of effective and sustainable integrated care models that simultaneously address both mental and physical health care needs. Current evidence‐based integrated care models primarily adopt three approaches: psychosocial skills training, integrated illness self‐management, and collaborative care and behavioral health homes. The next step should be the development of innovative models that build on these approaches by incorporating novel uses of telehealth, mobile health technology, and peer support, and strategies implemented successfully in developing economies 275 .
An optimal mental health care system for older persons with schizophrenia should have a full multidisciplinary range of clinical, rehabilitative, preventive and supportive services 288 . These include comprehensive assessment; case management; intensive outreach; smooth coordination of mental health, physical health, and social services; appropriate community and inpatient mix; and provisions for maintenance of family caregivers' mental and physical health. Unfortunately, such a system does not exist, and services remain fragmented and under‐utilized by this highly disenfranchised population 289 .
Successful aging with schizophrenia
Despite the above‐mentioned biological and societal issues, successful aging is not an oxymoron even among aging adults with schizophrenia. The clinical practice of positive psychiatry discussed above applies to these people too. The strategies necessary for seeking this goal include appropriate pharmacotherapy and psychosocial interventions, along with healthful diet, physical exercise, non‐toxic environment (e.g., cessation of smoking), and positive attitude on everyone's part. It is never too early nor too late to start on this path.
Positive psychiatric care of people with schizophrenia should include assessment not just of psychopathology but also of well‐being, strengths, perceived stressors, and lifestyle. This can be done by completing validated brief questionnaires in waiting room or online at home. Using these data, the clinician can identify treatment targets such as lifestyle (e.g., sedentary behavior) or social network, and implement appropriate interventions 290 .
A prescription given to a person with schizophrenia must go beyond an antipsychotic drug. It must include enhancement of personal psychosocial strengths, appropriately individualized behavioral interventions, and healthy lifestyle strategies such as physical, cognitive and social activities, adequate sleep, and nutritious diet. In the coming years, there will be an increasing use of digital technologies to disseminate evidence‐based interventions to large numbers of patients. Directions for future clinical practice and research in older adults with schizophrenia are provided in Table 5 .
Directions for future clinical practice and research in older people with schizophrenia
| A full multidisciplinary range of clinical, rehabilitative, preventive and supportive services – including comprehensive assessment, case management, intensive outreach, and smooth coordination of mental health, physical health, social services and peer support – should be implemented. | |
| Efficacious antipsychotics without metabolic side effects should be investigated. | |
| Well‐designed randomized controlled trials of psychotherapeutic interventions incorporating principles of cognitive behavioral therapy and socialization training should be conducted. | |
| Individual or group interventions, such as cognitive training, to promote brain fitness in older patients should be used. | |
| Treatment targets such as lifestyle (e.g., sedentary behavior) should be identified, and appropriate interventions (e.g., regular physical activities) should be implemented. | |
| “Wellness within illness” should be assessed and promoted: well‐being, resilience, optimism, personal mastery, wisdom, social engagement, and social support. | |
| Social determinants of mental health in aging, such as loneliness and social isolation, should be evaluated, and interventions targeting these features in individual patients – e.g., psychosocial skills training – should be used. | |
| Mobile interventions, including use of smartphones to deliver psychosocial interventions, should be implemented to promote self‐management of illness, using user‐friendly technologies. | |
| Collaborative care and behavioral health homes should be further established and evaluated. | |
| Medications and non‐pharmacological treatments for cognitive impairment in older patients with schizophrenia should be investigated. | |
| Pragmatic trials of hormone therapies such as estrogen derivatives in post‐menopausal women with schizophrenia should be conducted. | |
| Anti‐suicidal medications useful for older patients with schizophrenia should be investigated. | |
| Effectiveness and safety of anti‐inflammatory and other medications to slow down accelerated aging in schizophrenia should be explored. | |
| Digital phenotyping at the level of sensors, data science and health care should be investigated, to help in relapse prediction and prevention in old age schizophrenia, possibly using machine learning and other relevant technologies. | |
| Further research on caregivers of older people with schizophrenia should be conducted, and further appropriate interventions should be developed. |
All this must be accompanied by community support. Just as it takes a village to raise a child, it takes a community, which does not carry stigma against mental illnesses and their treatments, to provide optimal care to older people with schizophrenia.
SUBSTANCE USE DISORDERS
Substance use disorders are often overlooked worldwide as causes of problems for older adults, overshadowed by emergencies such as the opioid crisis among young and middle‐aged adults in high‐income countries. The extant literature reflects this deficit. Empirical studies of substance use among older adults are sparse to non‐existent from virtually all low‐ and middle‐income countries, and infrequent even in high‐income countries. Yet, these disorders are more frequent than many mental health workers believe, and their adverse consequences can be highly impairing.
In addition, interventions directed to these disorders in the elderly have been sparsely studied. Usually, however, diagnoses and interventions for younger adults can be applied to these elders, with judicious implementation which considers the biological, psychological and social factors unique to the elderly 291 , 292 .
Among the older adults, there are many challenges which may be exacerbated by alcohol and drug misuse, including functional and cognitive decline, compromised immune function, falls, other household injuries and depression. This reinforces the need for psychiatrists and all physicians to be more alert to and screen for substance use disorders, despite the many competing health concerns with which older adults present to them 293 .
Epidemiological studies from the US and many parts of Europe have found that the number of older persons in treatment for drug use problems has increased in recent years, most likely due to the aging of the baby‐boom generation who were born between 1946 and 1964. As birth rates in high‐income countries have now declined, the baby boomers have contributed to the “squaring of the age pyramid” leading to major increases in persons 65+ years who bring with them higher levels of illicit drug use and prescription drug misuse than previous age cohorts 294 , 295 .
In the US, nearly 1 million adults aged 65 and older live with a substance use disorder, as reported in 2018 data 296 . While the total number of admissions due to substance use disorders between 2000 and 2012 differed slightly, the proportion of admissions of older adults increased from 3.4% to 7.0% during this time 297 . In a study from Germany among subjects aged 60‐79 years, 69% consumed alcohol regularly and 17% consumed it at some risk 295 . From 2007 to 2016, prevalence rates of drug use among those in the 50‐59 and 60 and older age groups in Australia increased by 60‐70% 295 .
Yet another factor requires physicians, especially those who treat many older adults, to be more vigilant. Older adults in high‐income countries take a plethora of prescribed and over‐the‐counter medications 298 . Over a seven‐year period, non‐medical use or misuse of pain relievers doubled (from 0.8% in 2012 to 1.7% in 2019) among people aged 65 or older in the US, while among the total population there was a slight decrease (from 4.8% in 2012 to 3.5% in 2019) 296 . Combinations of acetaminophen and hydrocodone or propoxyphene were the most commonly used drugs 299 .
Social factors are the most important risks for substance use in older adults. For example, being divorced, separated or single is associated with increased or unhealthy drinking in late life in the US, though this may differ across genders 300 , 301 . Another factor is having drugs available in the house or from friends. Risk factors for drug use in late life further include physical problems, especially uncontrolled pain following surgery. Pain from back or shoulder strain may also be involved.
Mental health problems also contribute to increased drug use, especially depression and anxiety. Men are more like to have a long history of alcohol intake which extends into late life, and they tend to drink greater quantities. Overall decline in physical health may contribute as well 292 .
Screening and diagnosis
The first step by the clinician in addressing potential drug use is screening. Many tools have been demonstrated effective in eliciting the problem among older adults. These include the Alcohol Use Disorders Identification Test‐Concise (AUDIT‐C) 302 and the CAGE Questionnaire Adapted to Include Drugs (CAGE‐AID) 303 . The AUDIT‐C questions specific amounts of alcohol a person consumes 302 . The CAGE‐AID focuses upon the symptoms that derive from substance use disorder. Both the AUDIT and CAGE screening scales are used internationally.
The CAGE‐AID tool contains the following four questions, which can be used for both alcohol and other substance use 303 : 1. Have you ever felt that you should Cut down on your drinking or drug use?; 2. Have people Annoyed you by criticizing your drinking or drug use?; 3. Have you ever felt bad or Guilty about your drinking or drug use?; 4. Have you ever had a drink or used drugs first thing in the morning to steady your nerves or to get rid of a hangover ( Eye‐opener )?
This screening should be part of the usual evaluation of the older adult, for all too often the clinician may wrongly assume that the elder has no problem with substances. Substance use may be overlooked by family members or not considered important. Clinicians may also believe that problems from substance use are not critical or that little can be done to decrease use 292 .
The DSM‐5 criteria capture a wider proportion of older adults with substance use disorders compared to DSM‐IV ones. Even so, many elders will likely remain unidentified 304 . Age‐associated physiological changes that increase the effects of alcohol and other substances cause older adults to experience a reduction of tolerance to these substances, thus interfering with one of the hallmarks of substance use disorder, namely increased tolerance 291 . Furthermore, interruption in social and vocational activities or other social consequences of drinking or drug use may be less likely to occur or less noticeable in old age.
Using item response theory with the 2009 National Survey on Drug Use and Health data, one study explored whether there were age‐related biases among the DSM‐5 criteria for alcohol use disorder 304 . The findings revealed that there were differential responses among older versus middle‐aged adults, such that older adults were half as likely to endorse the criteria related to tolerance, activities to obtain alcohol, social/interpersonal problems, and physically hazardous situations. The criteria that were most effective in identifying alcohol use disorder among older adults were unsuccessful efforts to cut back, withdrawal, and social and interpersonal problems.
Treatment and organization of services
Some assume that older adults who abuse substances experience such a chronic condition that they will not respond to treatment. On the contrary, they have demonstrated treatment outcomes that are as good, or even better, than those seen in younger groups 291 .
Nevertheless, access to specialized services tailored for older adults is limited 305 . Brief interventions by health care professionals are the first and one of the most important steps in a treatment plan. The older adult who is gently alerted about the problems with substances may take heed when the health care professional warns of the danger, yet otherwise ignoring warnings coming from friends and family.
A common thread of most brief interventions is the use of elements of motivational interviewing 306 . Such interventions provide education about the substance and how it might be harmful, thereby enhancing motivation for change. One approach is “normative feedback”, in which a patient's drinking is compared with his/her peers. This feedback is then combined with brief advice about how to cut down or eliminate substance use 306 .
This approach on the surface is appealing to clinicians working with older adults and the elders themselves 306 . Unfortunately, little high‐quality evidence of the effectiveness of standardized brief interventions, such as motivational interviewing, is available, although naturalistic studies are promising 292 . Older persons are more likely to complete treatment than younger persons.
Medication use is essential for withdrawal from alcohol and other substances. Symptoms associated with alcohol withdrawal include increased pulse rate, blood pressure and temperature, as well as restlessness, disturbed sleep, anxiety and, when severe, delirium, seizures and hallucinations 292 . Medications used to alleviate alcohol withdrawal syndromes are usually benzodiazepines, which are tapered over a few days, primarily to prevent delirium and seizures. They should only be used on a short‐term basis.
Only two medications have been used extensively for the treatment of alcohol use disorder in older adults. Disulfiram was the first, yet the data on its use in preventing alcohol abuse among older adults are unclear. Furthermore, clinicians have been reluctant to use the medication, given its side effects if alcohol is ingested. Nevertheless, at a usual dose of 250 mg daily, the drug is considered safe for older adults who are otherwise in good health 307 . Of interest, limited data indicate some efficacy for naltrexone in the treatment of alcohol use disorder among older adults 308 .
Buprenorphine is the preferred treatment for opioid dependence, and appears to be safer than methadone. Nevertheless, to prescribe buprenorphine in the US requires special training. Drugs approved by the US FDA for the treatment of opioid dependence include sublingual buprenorphine and buprenorphine/naloxone tablets or strips. Because of safety issues, buprenorphine/naloxone is the preferred formulation 309 , 310 . Treatment with buprenorphine is safe and effective. Many patients can manage the induction period on their own at home.
Naltrexone is the most well‐studied medication used for substance use disorder treatment among older adults, and it has demonstrated effectiveness with this population. Naltrexone is an opioid receptor antagonist and is thought to reduce craving for opioids as well as alcohol by blocking dopamine release in the brain. Its major limitation in older adult people, many of whom have chronic pain, is that it blocks the effect of opiate‐based pain medications, often used following surgery. It can also potentiate the symptoms of a preexisting major depression. Patients with histories of comorbid depression should therefore be closely monitored 311 . Naltrexone is usually accepted by older adults, and its effectiveness is about equivalent of what is found in younger adults 308 .
Overall, group support for abuse and addiction is the most valuable long‐term intervention. Groups such as Alcoholics or Narcotics Anonymous (AA) can help older adults with a substance use disorder by reducing isolation, shame and stigma, though there have been no systematic studies on their effects. Elders use AA frequently worldwide in over 180 countries 312 . Yet they may face the same barriers to participation in self‐help groups as they do with formal treatment: stigma and shame of needing to attend to these issues in late life. If their primary substance use problem is alcohol, they often experience discomfort in attending meetings that include younger poly‐substance users. Such discomfort may not be as acute for baby boomers.
Traditional self‐help groups can be modified for older adults. For example, slowing the pace of the meeting to reflect cognitive changes in aging, and devoting attention to handling losses and extending social support, could be critical for recovery 291 , 313 .
Despite decades of research and clinical trials, the treatment and prevention of substance use disorders in older adults has been of marginal success. This is frustrating to patients as well as clinicians. The need for improved treatments tailored for older adults is critical (see Table 6 ).
Directions for future clinical practice and research in late‐life substance use disorders
| Clinicians and lay persons should be educated about the importance of substance use disorders in older adults, including their medical sequelae such as falls, cognitive decline, and worsening of co‐occurring physical and mental disorders. | |
| Screening for substance use disorders should be integrated in both primary care and specialty mental health services for older adults. | |
| The most important risk factors for substance use disorders in older adults – particularly social isolation, loneliness, bereavement, and felt loss of purpose and meaning in life – should be better known, evaluated and addressed. | |
| Self‐help groups should be adapted for older adults, e.g., by slowing the pace to accommodate cognitive impairment, and/or by addressing issues related to social support. | |
| The silos of mental health and substance abuse services should be broken down. | |
| Possible adaptations of diagnostic criteria/guidelines for substance use disorders should be considered to improve their performance in older adults. | |
| Further research should be conducted into the effectiveness of standardized brief interventions, such as motivational interviewing, in older adults. | |
| Further research should be carried out into the effectiveness and safety of using medications such as buprenorphine and naltrexone in older adults with substance use disorders. | |
| Factors in midlife which predispose to the development of substance use disorders in late life should be explored. | |
| Differences in substance use disorders by ethnicity, gender and geography should be investigated, and risks associated with disruptions in the lives of older adults that might lead to these disorders should be explored. |
CONCLUSIONS
Mental disorders in older adults are a leading cause of suffering and disability in the world, much of it avoidable. These disorders are common, impairing social functioning and economic productivity, undermining adherence to co‐prescribed medical treatments, and increasing the risk for loss of independence and early mortality from suicide and physical illness. Prevention, timely recognition and treatment are global public health and moral priorities.
Within the broader context of a positive psychiatry of aging, and as a countermeasure to ageism and stigma, it is essential to champion the assessment and promotion of wellness within illness, in order to enhance well‐being, resilience, optimism, and self‐efficacy/personal mastery. Moreover, it is important to evaluate the social determinants of mental illness in older adults, particularly loneliness and social isolation, and to use interventions that target these issues in individual patients and the family caregivers.
Because older adults with mental illness often engage in unhealthy lifestyles, particularly lack of physical activity, it is important to identify and implement appropriate interventions that will repay both mental and physical health benefits. Interventions to promote brain and cognitive fitness may be offered in individual and in group formats that provide rewards and reinforcement for adopting healthier behaviors in physical activity, diet and sleep.
Recent technological developments now allow the use of mobile interventions, including “just‐in‐time” interventions such as the use of smartphones for computer‐initiated text‐messaging or live telephone interactions to promote and enhance self‐management of illness. In addition, further use and investigation of digital phenotyping at the levels of sensors, data science and health care may prove useful in relapse prevention – given the frequently relapsing and chronic course of mental disorders in old age.
Future practice and research need to combat the fragmentation of clinical care through the establishment and evaluation of collaborative care and behavioral health homes. Such models should build on comprehensive approaches incorporating novel use of telehealth, mobile health technology, and peer support, capitalizing on strategies implemented successfully in low‐ and middle‐income countries. Team‐based care needs to become increasingly measurement‐based and interdisciplinary, incorporating and enacting a range of clinical, rehabilitative, preventive and supportive services. These services should include comprehensive assessment, clinical management, intensive outreach, and coordination of mental health, physical health and social services.
We also underscore the importance of care that is not only patient‐focused but also family‐centered. The caregivers of older persons with mental disorders are themselves burdened and in need of information and support. Including them as informal members of the caregiving team repays benefits to the identified patient and to caregivers alike and facilitates accurate clinical assessment and targeted interventions to promote wellness and to prevent serious adverse events (including suicide).
Cutting across all of the diagnostic entities considered in this paper is the need for further investigations of medications that can ameliorate cognitive impairment and slow down its progression. Medications that may reduce risk for suicide are also sorely needed, together with research on how best to use them within clinical care and systems of care. Further development and evaluation of medications without metabolic, cardiovascular and neurological side effects is needed to optimize safety and tolerability as well as efficacy and effectiveness.
Mental disorders of old age are heterogeneous at multiple levels: etiopathogenesis, clinical presentation, and response to intervention. They reflect genetic, environmental, social and developmental vulnerabilities as well as resilience. Taking these dimensions into account is critical to implementing personalized and effective treatment approaches and to doing meaningful research.
Because response variability to medications and other psychosocial and psychotherapeutic interventions is great among older adults, further investigation of moderators and mediators of response variability during acute, continuation and maintenance treatment is needed. This may allow clinicians to better personalize treatment, by understanding what works for whom, when and how. Finally, in the translational and clinical neuroscience space, further investigation of anti‐inflammatory medications to slow down accelerated aging is highly relevant to advances in clinical care.
Fortunately, science in the service of promoting healthy brain aging and cognitive fitness in the later years of life has become increasingly compelling. We believe that strategies for health promotion and care for older adults living with mental disorders are deeply linked.
Drawing upon the lessons learned in cardiovascular medicine and oncology, we suggest that detecting and diagnosing later‐life mental disorders early in their course is crucial to preventing their complications (such as treatment resistance, cognitive impairment, and mortality). Early detection and diagnosis facilitate care that is both evidence‐based and proportionate to the needs of the individual patient and family caregivers. Staging approaches that take into account where a patient is in the trajectory of his/her illness have clear clinical relevance, power and utility across the life cycle into old age.
Given the complexity of mental disorders in older adults, team‐based collaborative care models provide an evidence‐based and scalable way for health systems to implement prevention and personalized care. Furthermore, the use of telemedicine and the integration of peer‐support specialists, lay counselors and community health workers are helping to bridge the gap created by the worldwide paucity of geriatric mental health clinicians. They are also powerful antidotes to the barriers posed by fear and stigma.
In essence, addressing the rights and needs of older people and their families living with mental disorders remains a global public health and – no less – a moral imperative born of progress in discovery and applied sciences.
ACKNOWLEDGEMENT
The authors would like to thank C. Buchweitz, D. Korzon and S. Dean for their assistance with finalizing the manuscript.
178 Interesting Topics in Aging
🏆 best psychology of aging research topics, 👍 good essay topics on aging, ⭐ simple & easy gerontology topics, 📌 most interesting aging topics to write about, ❓ aging research topics and questions.
- The Concept of Aging Process The science dealing with the process of aging is termed ‘gerontology’ and this science tries to elucidate the factors and details of the process of aging.
- The Aging Population Impacts on labour Impacts on healthcare Impacts on government spending The increase in the proportion of the people who are old leads to a decrease of the number of people who are within the working […]
- Aging as a Social Problem The social challenges of the old people are further worsened by the economic constrains, and labeling. Ageism is another social challenge and it refers to a situation where people look down upon the elderly people […]
- Anti-Aging Products: Pros and Cons While the subject on anti-aging products is politicized over time, the manufacturers of the products defend themselves by saying that the customers are informed, they understand the risks associated with anti-aging products, and they choose […]
- Physical Exercise Program Importance in Old Age As such, regular physical and mental exercise is integral in helping the aged people to boost their strength, confidence and intrinsic health.
- Generation Gap: Childhood, Adulthood, Old Age At the same period, the younger generation says about the impact of the modern tendencies, changes of the way of life that give an opportunity to claim that the younger generation is more advanced.
- Mental Health and Wellness in Aging Population This research proposal will examine the aspects of wellness with regards to the dimensions of mental health and among the aged.
- Aging Theories and Interview With the Elderly For a better understanding of both the process of aging and the theories we have studied in class, I have conducted an interview with an elderly person, and the results of it are presented in […]
- Elderly and Aging in American and Viking Societies In the end, the conclusions are drawn to understand the significance of elderly and attitudes towards the aging process in each society.
- Physical Appearance in Old Age and Social Degradation People consider old age as a social problem and, in fact, many people do not want to age. There is the need to expand research and training to eliminate the problem of ageism within the […]
- Old Age Dependency Overview and Analysis This paper seeks to describe how the use of this metric can become an evidence-based approach for formulating new policies and frameworks to maximize the economic output of the elderly, engage them in productive activities, […]
- Adulthood and Aging – Widower’s and Widow’s Syndrome According to the information on the site, studies have been carried out to compare the death rate for a group of widows/widowers to that of a control group.
- The Ideas for Skin Care and Anti-Aging Products In this essay, we are going to use the ideas for skin care and anti-aging products in a bid to explore further the topic of ideation and to put it into practice.
- The Myth of Mental and Physical Deterioration in Old Age The findings of these studies suggest that mental deterioration is not inevitable, as the participants were found to preserve high cognitive function and mental health.
- The Aging Population’s Retirement Security There is a continuous increase in the aging population number, without any retirement security hence a need for a collective effort to ensure stability and dignity for the elderly population in the future.
- Global Issues: Addressing an Aging Population An important issue that is currently facing the world community is aging due to the increasing number of older people. Migration leaves the countries in which people are moving with a significant number of older […]
- Vital Signs: A Window Into Aging and Health However, it is always the nurse’s duty to assess vital signs and set up the proper follow-up in the event that irregularities are discovered.
- Aging in the United States and Japan Further, the physical health of aging in Japan is highly regarded, whereas, in the US, the aging is most are separated and left indoors. The US and Japan encourage the aging to spend most of […]
- Aging, Chronic Conditions, and End of Life Essentially, the quality of life of the dying person and those who are important to them is attempted to be improved by effective end-of-life care.
- Free Radical Theory Among Aging Theories According to the theory of mutation accumulation, genes useful in early human life are maintained by natural selection, in contrast to genes useful in old age.
- The Policies and Deficits Affecting Aging in the United States This paper discusses the policies and deficits affecting aging in the United States and the role of government in ensuring that they are protected.
- Visible and Invisible Aging Article by Clarke & Griffin The authors initially identified two possible approaches to the problem from different angles: the popularity of youth in society and the lack of respect for older people, and they outlined the inverse proportion of the […]
- Scientific Theories on Phenomenon of Old Age The social component of this issue becomes no less important, and the author, moving from social integration and issues of suicide among the elderly, begins to reveal in more detail the section on the dynamism […]
- Financial Stability in Old Age The financial and economic factors are among those aspects that put the aging population at risk of physical and mental complications and expose them to health inequalities.
- Aging: Subcategories, Longevity, and Human Services The middle-old subgroup often experiences chronic pain, deals with stressors correlating with the deaths of friends and spouses, and encounters balance problems.
- Aging Process in Relation to Abuse One category of the characteristics of the aging process are specific physiological changes, such as various neurological disorders, impaired cognition, memory loss, the loss of learning ability, and a decline in special senses.
- Small-Group Communication: Innovation in Aging A small group is essentially an assemblage of two or more individuals that communicate while engaging in certain events or an interconnected aim and can exercise correlation amongst each other. Every team member can acquire […]
- Aging Changes and Dealing With Them For example, immediate tasks such as the state of a cooked meal usually remain in the short-term memory and then vanish; deliberately learned math course sticks in the memory for a while, being an example […]
- Taste: Entry and Profits in an Aging Economy Now, I understand that taste is a more complicated category in the economy that features the concepts of utility and consumer inertia.
- Personality, Cognition, and Physical State of Old Age This work is aimed at revealing my personal views on the aspects of personality, cognition, and physical state of old age and assessing the theoretical background that describes the relevant states and their prerequisites.
- Health Care Within Aging White Veterans With Dementia Since this condition is heavily linked with damage to the brain, these people should be addressed in a friendly manner to avoid misunderstanding.
- Applying Neural Stem Cells to Counteract Brain Aging Pluripotent stem cells, or PSCs, are the best candidates for in vitro generation and cultivation of neural stem cells. Neural stem cells: Origin, heterogeneity and regulation in the adult mammalian brain.
- Effects of Aging on the Integumentary and Musculoskeletal Systems The second part is a summary of the information available on the changes that occur in the integumentary system with age.
- Successful Aging and Its Key Constituents Therefore, aging is a stage of life, which can be as happy and prosperous as other phases of life. Thus, this research is pretty informative and contributes to people’s understanding of the peculiarities of successful […]
- Aging Population and Its Effect on the US Healthcare However, on the flip side, growth in the number of older adults in relation to the young population would also signify a reduction in the labor force and, consequently, a decline in national income.
- Researching of Theories of Aging Social isolation among the elderly in the US can be reduced through the application of the activity theory. This theory suggests that individuals enjoy old age by finding new activities to do to substitute the […]
- Colorado Springs: Aging Services Network The Colorado Department of Human Services is the highest department over CDAAS and provides the same services. The Long-Term Care Ombudsman Program focuses on a broader range of services, including recreational, and economic counseling, to […]
- Aging Services Network Map Evaluation Summit View Assisted Living is a home care service located in the Garwyn Oaks neighborhood of Baltimore. The area has a good selection of assisted living facilities for senior citizens who want to get more […]
- Aging: Concepts and Controversies An analysis of the college admission process reveals one challenge facing counselors: that there is a necessity of providing the certain measures to avoid the discrimination of the disabled.
- Perceptions of Aging Adults This paper sets out to explore the difference between grandparents and baby boomers; whether baby boomers are younger, energetic, or are similar; the differences in our perceptions of aging today versus 30 years ago, the […]
- Effects of Age and Aging on the Immune Response to Diseases Such as COVID-19 The purpose of this paper is to address the effects of age and aging on the immune response to diseases such as COVID-19.
- Aging Population Study by Christensen Kaare et al. The descriptive approach in the Aging Population: The Challenges Ahead, the article written by Christensen Kaare et al, systematically and accurately elaborates on life expectancy trends in developed nations.
- Aging and Beauty Standards: Overcoming Social Prejudice The ethical issue is that in an attempt to change one’s body and make it similar to those that are presented in the media and by stars, people lose their identities and opinions.
- Reflection Essay: Aging and Sugar I want to go on trips around the world with my family and engage in new challenges. In order to do that, now I should care about my health and economic welfare.
- Healthy Aging in the United Arab Emirates Report: This part highlights the current plan for aged care in the UAE, presupposing increasing investment in the sphere and attraction of private companies, communities’ preferences for aged care, resources provided by the UAE to […]
- Caring for the Elderly and Biological Process of Aging Robnett and Chop believe strongly that ‘a wider knowledge of the mechanisms that tend to affect the aging process can play a significant role towards identifying new interventions that have the potential to alter the […]
- Benefits of Exercises in the Aging Population Balance issues and falls are very frequent in the elderly, and they significantly contribute to the increased rates of institutionalization. This makes Tai Chi an important intervention in enhancing balance and reducing the risk of […]
- Aging as Social Problem in North American Society In the North American society, individuals attaining the age of sixty-five are expected to retire to pave way for the new generation to manage the economy. In other words, the project would have a number […]
- Person’s Aging Process and Media Impact As a result, the old are naturally the leaders of the society and are even expected to make the most consequential decisions that affect the entire society.
- Myth: The Aging Population Is to Blame for Uncontrollable The issue of aging of the population is very critical, especially because it becomes worrisome when the health expenses increase and policymakers left with a dilemma on what to focus on in addressing the situation.
- Aging and Oral Health Implications in Australia Consequently, parallel to the observation of AHMAC Steering Committee for National Planning for Oral Health, that those preserved teeth are predisposed to developing diseases of the mouth, and because of various influences of population aging, […]
- Aging Body and Sensory Changes and Adaptation From a critical perspective, it is evident that Joseph is proud of his life and the fact that he has left behind a legacy.
- The Aspect of Aging Ageism The old people, on the other hand, are so susceptible to ageism because old age is the last stage of life and that makes the elderly vulnerable to death.
- The Science Behind Bacterial Aging A bacterium is one of the organisms that undergo asymmetric division of cells hence does not undergo aging. In this bacterium, it is evident that the DNA process stopped because the stalk cell turned out […]
- Aging Theory and Medication Adherence for Geriatric Patients The following will be the goals and objectives of the Practicum Experience in this course. Define the phrase ‘theory of aging’ Explain how the aging process can be altered.
- Aging Changes Explained Effects of aging on the nervous system lead to a reduction in the velocity of signal transmission due to varied effects on the nerve cells or on the neurotransmitter secretion.
- Aging Population in the Western United States The older population in the western US is disproportionately compromised because the climate has a great impact on the health of older people, yet these older people’s adaptability is compromised.
- Impact of Aging on the Human Body The free radical theory has it that the radicals produced by body cells can also destroy them, and as a result, the aging of cells occurs.
- Human Growth Hormone: Finding a Remedy Against Aging The methods he used in this research and conclusions were documented in the New England journal of medicine on the 5th of July 1990.
- Aging: The Terms This authority is attributed to the authoritative role of the father and the grandfather in the presidency of the emotional and economical demands of their generation group.
- Experience of Aging in Indiana: Interviews Study The questions with the President of CICOA were more structures and had a formal nature, including questions such as the state of health service for the elderly, challenges in providing services, the plans for overcoming […]
- Aging Issues in Canada In denial, people deny the fact that they are in the situation they are in and mostly they say, “This cannot be happening, not to me”.
- The Impact of Culture on Aging: Psychological and Sociological Analysis Analyzing the impact of American culture on the process of aging, disease management and pain control, we should first identify the main features of American mentality.
- Neurogenetics Effects on Cognition in Aging Brains According to Wong et al, Alzheimer’s disease is usually associated with a mutation in three genes: the amyloid precursor protein gene and two presenilin genes.
- The Causes and Effects of Social Cognition and Aging The brain, as the most complex organ in a human’s body, is especially susceptible to drastic changes from a plethora of factors.
- Changes in the Aging Brain: Overview The changes the brain undergoes while aging weakens its functions and can result in the development of cognitive disorders, such as Alzheimer’s disease. According to Vandenbroucke, these deviations indicate the importance of the choroid plexus […]
- The Link Between Cognition and Aging Brain The problems of changes in the cognitive functions of the brain over time are one of the leading causes of depression, delirium, and dementia in older adults.
- Senior Centers and Places of Worship as Primary Active Aging Settings There is a variety of places that can accommodate the elderly or help to fulfill their needs for community interactions, and among these places are community settings and places of worship.
- Interviews About the Realities of Aging However, inasmuch as he does not want to get to the point of needing specialized care, which is his greatest fear, he is aware of the reality and possibility of that time coming at some […]
- The Problem of Aging, and the Needs of Aging Employees The aim of this research is to investigate the significance of workplace design changes and altering concepts of project management careers as a result of aging.
- Old Age Phobia: Problems and Solutions Most of the countries of the world share the same view regarding the issue of the fear of aging. Thus, the perception of age is never well-received by the community and there is such a […]
- Demand for Health Care in the USA: Old Age The question therefore arises is that what determines the demand for health in the US. Therefore, he concludes that age is not a determining factor in the increase of health care expenses.
- The Great Down-Aging Syndrome: Why 40 Is the New 20 It has also been observed that the middle-aged people are fervent consumers of those products that are mainly used by the young. Not all middle-aged consumers are attracted to products that are meant for the […]
- Perspectives on Aging in the US The analysis of US trends influencing the growth of the population is to be performed through national, economical and regional trends development.
- Development Psychology: Aging Attitudes in Mass Media Considering the problem of attitudes towards aging in mass media, one can observe that the elderly population is having been viewed in a different manner if compared to the people of young age.
- Psychology of Aging Analysis The regulation of social life can be a promising quality of life in later adulthood. Lifestyle factors have a tremendous effect on the quality of life and well-being in later years.
- Maccianti on Fiduciary Responsibility of an Aging Owner The framework used in the critique is to evaluate the options available regarding Michael and to attempt to trace the cause of the present problem for the purpose of possibly preventing a similar situation in […]
- Healthy Musculoskeletal System and Aging Once we reach the age of 30, our bones stop growing and making new cells, and we are left to live the rest of our lives with the current condition of our bones.
- Adult Development and Aging But nowadays, the issue of adulthood is gradually becoming one of the most important because the borders between adolescence and adulthood are not fixed which leads to the mixture of generations, and to the process […]
- Aging and Death Relations The growth of damages in the organ elements that are required for the creation of new cells of the body leads to death.
- Aging Services in Modern Society This project there is ensuring that the staffs are committed to caring for elderly people. There is a team that is responsible for research in this project.
- Health and Wellness of Aging: Abuse and Illness In the case of abuse, the situation deteriorates, and the senior individual cannot recuperate quickly, which affects the way they function.
- Health & Wellness of Aging. Gerontological Society of America The Gerontological Society of America is an organization, which aims to research and ensure the health and wellness of aging among American older adults.
- Online Dating for Aging Adults Considering the benefactors of the relationships that aging people develop through dating sites and applications also helps to determine the actual value of the tools in question.
- Aging Services Access Barriers and Counterstrategies However, by improving the reciprocity between a patient and a nurse with the help of different types of media, one can address the issues temporarily, at the same time working on long-term goals such as […]
- Aging in Rural Places: Retirement and Leisure Therefore, strategies for assisting older adults to transfer to a new stage of their development and retain the extent of their activity are important goals. Moreover, it is critical to ensure that the healthcare needs […]
- Aging Population of the World as a Healthcare Issue The area of healthcare is the domain that has been affected by the rise in the number of aging people to the greatest extent.
- Gerontology: The Aging and Disability Programs The practitioner is in charge of taking care of older adults, and the administrator is involved in greeting and guiding the clients.
- Normal Aging of Brain Structures and Cognition Evidence of brain changes can be seen as early as the middle age in that there is a decrease in the number of neurotransmitter binding sites, as well as a decrease in the level of […]
- Care Coordination for Aging Population in the Clinical Setting However, the described solution to the health problems of aging patients may entail difficulties in coordinating the work of the health experts involved in a team.
- Aging and Barriers to Healthcare in Rural Areas For this purpose, the integration of innovative technology and the reconsideration of the current infrastructure will have to be seen as possible solutions.
- Strategies to Slow the Brain Aging Aging may result in severe effects on the brain and lead to cumulative damage and the impairment of cognitive functions. However, it is possible to prevent and slow the effects of brain aging.
- Primary Prevention for the Aging Population Among the examples of primary prevention, the best strategies for caring for the aging population include vaccination, health education, and the promotion of a healthy lifestyle.
- Aging Word and Meaning Behind Its Use While this is a natural process, this paper explains why people use the word “aging” in a derogatory manner. The use of the word in a respectful manner will empower more senior citizens to pursue […]
- The Concept of Successful Aging Medical specialists and theorists of psychology create a variety of concepts and definitions that in their opinion most fully reflect the idea of successful aging.
- Aging and Policy Issues in Rural Places As someone who has quite extensive experience of working with older adults and elderly patients in the oncology, medical-surgical nursing, and telemetry units, I have to confirm that meeting the needs of patients in a […]
- Successful and Unsuccessful Aging: My Grandfather’ Story In this paper, special attention will be paid to the story of my grandfather and his style of life that turns out to be a strong example for me.
- Women’s Aging Fears in Personal Fashion Blogs I would like to stress that it should be age-appropriate and modern at the same time. Moreover, I learned that there is a need for the development and implementation of relevant programs aimed to improve […]
- Cataract Development and Aging Factor The problem of cataract blindness is essential to discuss because the occurrence of the condition in aging adults increases at an extremely high rate.
- Aging Population Impact on the Labor Market These employees are also special in the fact that they have the capacity to stay with one firm for a very long time.
- Aging Ethical Issues and Cultural Differences In other words, the biggest misconception that seems to have been accepted in society is the fact that the embryo is the standard to the right to life.
- Canada’s Aging and Demographic Dynamics That is, the issue of ‘Canada’s aging’ is closely interconnected with other qualitative aspects of contemporary Canadian living, concerned with the government’s continual endorsement of the policy of multiculturalism and affected by the overall socio-economic […]
- Getting Old: Healthy or Unhealthy Aging It is wise to choose a healthy lifestyle to enjoy the goodness that life has to offer. One is able to concentrate on their career and be able to plan for retirement.
- How Can We Delay the Aging Process in Skin? Hsu, Li, and Fuchs note that the intrinsic and extrinsic biological factors such as the changes in the stratum corneum structure and corneum along with the occurrence of lipids justify the use chemical peels as […]
- Aging and Its Cultural and Ethnic Factors The main idea that I am going to promote throughout the paper’s entirety is that the aging-related issues cannot be referred to as such that represent the value of a ‘thing in itself’ in the […]
- Suadi vs. Australian Aging and Occupational Therapy Therefore, the objective of the given paper is to investigate the current system of occupational therapy operations in Saudi Arabia and identify the gaps to fill. The focus of the study is occupational therapy for […]
- Dementia, Aging, Gerontology: Theories and Care Proponents of the theory, Elaine Cumming and William Henry take the psychosocial perspective in explaining the unhealthy collective relationships the aging person’s experience in the latest phases of their lives.
- Aging Population Issues in American Prison System A case of an increase in the number of elderly people in prison was reported in 2000 when the number of elderly prisoners was only 3% of total America’s prison population, but in 10 years […]
- Physical Changes and Aging in Psychology It is important to understand various provisions of physical changes in the context of human development. It is crucial to understand various provisions of growth and physical development with respect to aging.
- Holistic Approach to Successful Aging Based on the above statistics, it is apparent that the USA will experience an absolute aging society in the future. One of the great accomplishments of healthcare in the 21st century is an improvement in […]
- Aging and Parkinson’s Disease Parkinson’s disease refers to a condition, where a portion of the brain is damaged progressively over a period of many years.
- Geriatrics: Aging Effects on Individuals and Society Individuals at the age of 60 and above are referred to as the elderly. The term chronological age refers “to the age of a human being from the day of his or her birth”.
- Canadian Healthcare Spending on Aging Population The increase in the aging population corresponds with the increase in life expectancy in the country. In this paper, the impact of the aging population on the healthcare expenditure in Canada will be discussed.
- The Exercise and Diet’ Implications on Aging Studies have also shown that regular exercise and healthy eating habits among the aging population helps to improve the rate of glucose metabolism in the body.
- Aging Offenders in Prison The increased number of elderly inmates is partly due to the introduction of longer sentences in the 1970s and 1980s as US took a tough approach to crime.
- Impact of Aging Population on the US Economy Due to the advanced age of the patients in this case and the complexity of the care they require, the available caregivers will be forced to compromise the health of their patients in an attempt […]
- Sociological Theories and the Process of Aging Functionalists agree with proponents of conflict theory that the society experiences some breakdowns and that mistreatment of the poor in the society is a reality.
- Aging Issues: Elderly, Cultural Values and Support The provision of long term care for the elderly is one of the issues in aging. These factors include the sources of long term care finances, the processes used in the determination of a person’s […]
- Physical Aging: Ectocranial Suture Closure One essential aspect of forensic science is the ability to determine the age of the skeletal remains at the time of death.
- Aging as a Social Process Society is able to grow and progress because of the values and conventions that the elderly pass on to the upcoming generations.
- Aging Population in Singapore In light of the abovementioned demographic trends, it is imperative that the government put in place strategies and programmes to address isolation and depression facing the ageing populations.
- Function Plasticity in Cognitive Aging The extensive available literature covering plasticity of the brain and the perceptual psychophysics of aging strongly emphasize that the negative consequences of brain plasticity is a significant contributor to cognitive decline related to advancements in […]
- Third Age Living and Computer Technologies in Old Age Learning This essay gives an analysis of factors which have contributed to the successful achievement of the Third Age by certain countries as a life phase for their populations.
- Public Policy: Obesity and Aging Society In the realm of the United States’ health care, the aging society is drawing much attention based on the evident increase of obesity prevalence among older citizens that has resulted to an increase in many […]
- Is Aging Infrastructure Slowing the U.S.? The deteriorating state of infrastructure has been linked to the current economic crisis that is being experienced in the United States of America.
- Aging, Culture, Ethnicity and Family Care The research by the author shows the limitations of the informal structures in dealing with the elderly. She is the organizer of the family reunions and the custodian of the family history.
- Aging in Society and Community The superb comedy movie also looks at the major life changes, such as retirement and life of widowhood, transformations in living arrangements, and economic and political issues that define the habits of the old people […]
- The Problem of Population Aging in the US Given that the retirement age is the determinant of labour force participation, increased retirement age would significantly reverse economic crisis due to population aging.
- What Are the Negative Stereotypes About Aging?
- What Are the Reproductive Problems in Aging Men?
- What Are Your Attitudes About Aging?
- Why Is Researching Aging Important?
- What Is the Main Danger for Aging People?
- What Are the Stages of Aging?
- Why Is Aging Important in Society?
- What Are the Pillars of Aging?
- What Are the Factors That Influence Aging?
- What Are the Two Theories of Successful Aging?
- What Are the Hallmarks of Aging?
- What Are the Keys to Successful Aging?
- Does Language Comprehension Decline With Age?
- What Is Current Research on Aging?
- What Are the Six Principles Important in Treat Aging People?
- What Is Wisdom in Aging?
- What Vitamin Increases Longevity of Aging People?
- What Are the Types of Aging?
- What Are the Things That Will Increase the Life Expectancy of Aging People?
- What Are the Factors of Aging?
- What Is Body Type Best for the Longevity of Aging People?
- What Is a Healthy Aging Concept?
- What Is the Real Cause of Aging?
- What Is the Most Important Intervention for Aging People?
- Is Healthy Aging Possible?
- What Is the Main External Cause of Aging?
- What Are the Two Main Reasons for the Aging Population?
- What Are the Theories of Aging?
- How Can We Solve the Problem of Aging Population?
- What Are the Problems of Ageing?
- Dementia Research Ideas
- Gerontology Titles
- Demography Paper Topics
- Genetics Research Ideas
- Dermatology Topics
- Memory Research Ideas
- Parkinson’s Disease Questions
- Nursing Home Questions
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 21). 178 Interesting Topics in Aging. https://ivypanda.com/essays/topic/aging-essay-topics/
"178 Interesting Topics in Aging." IvyPanda , 21 Feb. 2024, ivypanda.com/essays/topic/aging-essay-topics/.
IvyPanda . (2024) '178 Interesting Topics in Aging'. 21 February.
IvyPanda . 2024. "178 Interesting Topics in Aging." February 21, 2024. https://ivypanda.com/essays/topic/aging-essay-topics/.
1. IvyPanda . "178 Interesting Topics in Aging." February 21, 2024. https://ivypanda.com/essays/topic/aging-essay-topics/.
Bibliography
IvyPanda . "178 Interesting Topics in Aging." February 21, 2024. https://ivypanda.com/essays/topic/aging-essay-topics/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Health Topics A-Z
Languages offered: English | Español
NIA provides health information informed by research and reviewed by experts to help you learn about healthy aging and common health conditions in older adults. Browse our health topics below.
You can also explore:
- Free print and PDF publications
- Information for health professionals
- Infographics, videos, and more
Browse A-Z Health Topics
A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z
Advance care planning Aging in place Alcohol misuse or alcohol use disorder Alzheimer’s and dementia Alzheimer’s and relationships Alzheimer’s caregiving Alzheimer’s causes and risk factors Alzheimer's changes in behavior and communication Alzheimer’s symptoms and diagnosis Alzheimer’s treatment Assisted living and nursing homes
Bladder health and incontinence Brain donation Brain health
Caregiving Clinical trials and studies Constipation COVID-19
Elder abuse End of life Exercise and physical activity
Falls and falls prevention Fatigue Flu Frontotemporal disorders
Grief and mourning
Health care professionals information Healthy aging Healthy eating, nutrition, and diet Hearing and hearing loss Heart health High blood pressure HIV/AIDS Hospice and palliative care
Immunizations and vaccines
Legal and financial planning Lewy body dementia Loneliness and social isolation Long-distance caregiving Long-term care
Medical care and appointments Medicines and medication management Memory loss and forgetfulness Menopause Mental and emotional health
Organ donation Osteoarthritis Osteoporosis
Pain Parkinson’s disease Prostate health
Safety Sexuality Shingles Skin care Sleep Stroke
Teeth and mouth
Vascular dementia Vision and vision loss Vitamins and supplements
nia.nih.gov
An official website of the National Institutes of Health
Best Senior Thesis Topics
Table of contents
- 0.1 Key Points:
- 1 The Importance Of A Good Senior Thesis Topics
- 2.1 1. Identify your interests and passions
- 2.2 2. Consider the scope and feasibility of the topic
- 2.3 3. Seek guidance from your professors and advisors
- 3 Good Senior Thesis Topics
- 4 Senior Thesis Topics For High School And College Students
- 5 Psychology Senior Thesis Ideas
- 6 English Literature Senior Thesis Topics
- 7 Graphic Design Senior Thesis Ideas
- 8 Political Science Senior Thesis Topics
- 9 History Senior Thesis Ideas
- 10 Criminal Justice Senior Thesis Ideas
- 11 Conclusion
Senior thesis topics are research projects students undertake in their final year of undergraduate studies or graduate programs. These senior thesis topics allow students to demonstrate their expertise in academic writing.
School senior thesis topics can cover a wide range of disciplines. This spans science and humanities to social sciences and engineering. All of these allow students to explore their academic interests in depth and make valuable contributions to their respective fields against any grade stereotypes or even gender stereotypes.
With a thousand ideas, it may be hard to nail a good topic. This article covers a series of college and high school senior thesis topics for different subjects.
Key Points:
- School senior thesis topics allow students to dig deep into a specific study area within their chosen field.
- A strong senior thesis topic can potentially make a valuable impact on the academic community and shape future research in the field.
The Importance Of A Good Senior Thesis Topics
Well-selected senior thesis topics capture the interest of the student and hold significance in their field of study. This is important for the following reasons.
Firstly, well-chosen school senior thesis topics provide students with an opportunity to explore a specific area of study. This fosters a sense of ownership and engagement with the research process. These personal investment projects enhance motivation and dedication, resulting in a higher quality of work. However, not every student had the luxury of time. In case you have a question like, who can write my thesis , there are professional platforms that can render such a service. With 24/7 customer support and experienced writers, for you to write a thesis becomes so easy.
Secondly, good high school senior thesis topics enable students to make original contributions to their field by conducting research, analyzing data, and generating new insights. This can lead to advancements in knowledge and potential solutions to existing problems.
Lastly, a strong senior thesis topic demonstrates students’ ability to think critically and develop analytical skills. It requires formulating search questions, designing methods, and interpreting complex data. These processes cultivate intellectual maturity, problem-solving abilities, and effective communication skills.
Tips On How To Select The Best Senior Thesis Topic?
Selecting the best high school senior thesis topic requires a thoughtful and systematic approach. With numerous options available, it is important to consider the topic selection process carefully. Nonetheless, you can buy thesis paper pieces online if you cannot spare that much time for the steps involved, with professors available to help. Listed below are some tips to help you choose the best senior thesis topics.
1. Identify your interests and passions
Choose topics in the subjects that excite you and the areas of study that keep you on your toes. This will keep you energetic throughout the search process and increase the worth of your work.
2. Consider the scope and feasibility of the topic
Ensure that the topic is manageable within the given timeframe and aligns with the resources and expertise available to you. It is essential to strike a balance between a topic that is challenging enough to showcase your abilities and one that is realistic and achievable.
3. Seek guidance from your professors and advisors
They possess valuable expertise and can provide insights into potential research areas or suggest topics based on your academic strengths. They can also provide ideas on how to write a thesis for research paper pieces – a crucial aspect of research writing. Engage in discussions with them to receive feedback and better understand the viability and relevance of your topic ideas.
Good Senior Thesis Topics
The right thesis topic showcases a student’s expertise and passion and sets the stage for a quality research experience.
However, the steps of choosing a senior thesis topic can be overwhelming. Below is a curated list of topic ideas for your next project.
- The Impact of Artificial Intelligence on Job Automation: Analyzing the Effect on Employment Trends.
- Accessing the Effects of Plastics in the Evolution of Marine Ecology
- A Closer Look at the Relationship Between Social Media Usage and Mental Health Outcomes.
- Exploring the Thin Line Between Genetic Engineering and Moral Ethics
- A Case Study on the Impact of Climate Change on Ecological Biodiversity
- Analyzing the Impact of Corporate Social Responsibility Initiatives on Consumer Behavior and Brand Perception.
- Exploring the Intersection of Gender and Leadership: A Comparative Study of Leadership Styles and Organizational Performance.
- Investigating the Psychological Effects of Virtual Reality: Examining its Potential in Therapy and Mental Health Treatment.
- Assessing the Impacts of Global Warming Policies on Energy Transition: Case Studies from Different Countries.
- Exploring the Representation of Race and Identity in Contemporary Literature: Comparative Analysis of Works by Diverse Authors.
Senior Thesis Topics For High School And College Students
When it comes to selecting senior thesis topics, both high school and college students are faced with a challenge. This challenge is finding a subject that aligns with academic interests and demonstrates their research abilities.
An important point to remember is to seek help from your professors. They provide valuable advice on questions like – how to finish my thesis and strategic planning to craft a good one if you feel unsure. Listed are some popular topics for both college and high school senior thesis.
- The Impact of Social Media on Mental Health: An Analysis of the Relationship between Social Media Usage and Psychological Well-being in Society.
- Renewable Energy Solutions: Assessing the Feasibility and Environmental Benefits of Implementing Solar Energy Systems in a Local Community.
- Cultural Differences in Perception of Beauty: Examining how cultural norms shape the perception of beauty and body image ideals.
- The Effects of Climate Change on Biodiversity: Investigating the Relationship between Global Warming and Species Extinction Rates.
- Gender Equality in the Workplace: Analyzing the Factors Affecting the Gender Pay Gap
- Cybersecurity and Data Privacy: Assessing the Best Practices for Protecting Personal and Organizational Data in the Digital Age.
- The Influence of Music on Emotion and Memory: Investigating the Cognitive and Psychological Effects of Music and Its Potential Therapeutic Applications.
- Evaluating the Effectiveness of Sports Injuries Prevention Programs among Professional Athletes
- Sustainable Agriculture Practices: Analyzing the Environmental, Economic, and Social Benefits of Organic Farming
- Urbanization and Urban Planning: Evaluating the Impacts of Rapid Urban Growth on Infrastructure, Transportation, and Quality of Life in Urban Society.
Psychology Senior Thesis Ideas
When selecting psychology senior thesis topics and how to write them, the choices can be vast and exciting. This list explores some topics to help most students generate compelling senior thesis best topics.
- The Impact of Childhood Trauma on Adult Mental Health: Physiological Responses Study
- Examining the Effects of Mindfulness-Based Interventions on Social Anxiety Disorder and Stress in College Students
- The Relationship Between Social Media Use and Romantic Relationships in Adolescents
- Investigating the Role of Parenting Styles in the Development of Emotional Intelligence in Children
- Exploring the Effects of Sleep Deprivation on Cognitive Functioning and Executive Functioning
- The Influence of Personality Traits on Career Choice and Self Esteem
- Understanding the Psychology of Eating Disorders and Self-Esteem in Young Adults
- Investigating the Impact of Social Support Therapy on Depression Treatment and Anxiety Reduction
- The Relationship Between Sleep Quality and Cardiovascular Dysfunction in Children
- Examining the Effects of Exercise on Eating Disorders and Anxiety Symptoms in Individuals with Major Depression
English Literature Senior Thesis Topics
With a vast landscape of works in literature and critical theories to explore, finding the perfect English literature senior thesis topics can be exciting and challenging. Students can draw inspiration for writing from the following listed English literature senior thesis topics:
- Exploring gender roles in Shakespeare’s Tragedies: The Differences of Women like Ophelia, Lady Macbeth, and Desdemona.
- The Influence of Colonialism in Postcolonial Literature: A Study of Chinua Achebe’s Things Fall Apart and Joseph Conrad’s Heart of Darkness.
- Shakespearean Tragedy in Modern Context: A Comparative Study of Hamlet and Arthur Miller’s Death of a Salesman
- An Analysis of Gothic Elements in the Books of Mary Shelley and Edgar Allan Poe.
- The Illustration of Mother Nature in Samuel Taylor Coleridge and William Wordsworth’s Poetry.
- Politics and Religion in Literature Periods
- The Portrayal of Social Class, Civil Rights and Inequality in Women from Jane Austen’s Novels.
- Social Critique and Satire in the Novels of Charles Dickens
- A Comparative Study of Gender and Sexuality in the Works of Virginia Woolf
- The Influence of Colonialism and Imperialism on Heart of Darkness and Wide Sargasso Sea.
Graphic Design Senior Thesis Ideas
Writing a senior thesis in graphic design can be interesting as it offers students an opportunity to showcase their creative prowess. Some topics to refine for creative folks in this field are:
- Designing Dynamic Interactions in the Digital World for the Human Mind.
- Visual Storytelling: Examining the Role of Graphic Design in Narrative Communication
- The Intersection of Graphic Design and Social Justice: Using Design as a Catalyst for Promoting Positive Social Impact.
- Sustainable Design Practices in Graphic Design: Exploring Eco-Friendly Approaches and Materials.
- The Evolution of Branding in the Digital Age: Analyzing the Shift from Traditional to Digital Branding Strategies.
- Graphic Design for User Experience: Investigating the Creation and Impact of Visual Design on User Engagement and Satisfaction.
- Visualizing Data: Exploring Innovative Techniques for Information Design and Data Visualization.
- Exploring Cultural Identity through Graphic Design: Examining the Representation of Identity and Diversity in Visual Communication.
- The Power of Color in Graphic Design: Investigating the Psychological and Emotional Effects of Color in Visual Communication.
- Designing for Accessibility: Examining Inclusive Design Principles and Practices in Graphic Design.
Political Science Senior Thesis Topics
Science senior thesis topics offer a chance to demonstrate your research writing skills and critical thinking abilities. The thesis topics you choose will shape your writing and research journey and ultimately determine the success of your thesis.
Therefore, getting all the help you need can help you generate interesting political science senior thesis topics. So, some interesting political science senior thesis topics to look into include:
- Analysis of European Union Protests and the Use of Social Media in Political Mobilization.
- Investigating how Gender Quotas Affect the Political Representation of Women in Parliamentary Systems.
- The Influence of Political Campaigns on Voter Behavior: A Case Study of a Recent National Election.
- Assessing the connection between governance stability and disparities in wealth in modern society.
- Analysis of Right- and Left-Wing Populist Leaders’ Political Rhetoric Use in Populist Movements.
- Evaluating how well international human rights treaties work to encourage adherence to human rights.
- An analysis of non-governmental organizations’ (NGOs) influence on environmental policy in modern society.
- Public Trust in Politics and National Scandals: A Comparative Analysis of Previous Cases.
- Exploring the Rise of Authoritarianism in Democracies: Factors and Challenges.
- Investigating the Influence of Media Ownership and Control on Media Bias in Political Reporting.
History Senior Thesis Ideas
History is a vast field with countless potential topics to explore for writing. This makes the selection process both exciting and daunting.
However, with careful consideration and planning process, researchers can write and find the perfect history senior thesis topics. Some history senior thesis topics that showcase history students’ analytical skills and intellectual prowess are:
- The Impact of the Industrial Revolution on Modern Society and Culture in the Renaissance Era
- Breaking Gender Limitations: The Contribution of Women to the Equal Rights Campaign
- The Causes and Consequences of the Cold War: A Comparison of the USA and the USSR
- Evaluating the Causes and Effects of the French Revolution
- The African-American Experience during the Reconstruction Era: Progress and Challenges
- The Role of Propaganda in World War II Development: Analysis of Nazi and Allied Strategies
- The Rise and Fall of Colonialism: Examining the Impact of European Powers on Africa
- The Origins and Development of Ancient Greece Culture
- The Great Depression: A Case Study on its Effects on the Society.
- The Impact of Rational Concepts on the American Revolution and the Rise of the US.
Criminal Justice Senior Thesis Ideas
Criminal justice senior thesis topics should address significant issues within the field. This gives students the chance to contribute to understanding the challenges and improvement of the criminal justice system. Listed are some senior thesis topics to consider:
- The Impact of Body-Worn Cameras on Police Accountability and Public Trust
- The Effectiveness of Restorative Justice Practices in Reducing Recidivism Rates
- A Look at the Correlation between Mental Health and Criminal Behavior
- Exploring the Impact of Race and Ethnicity in the Law Enforcement System’s Sentencing Inequalities
- Analyzing the Effectiveness of Drug Courts in Keeping Substance Abuse Offenders Out of the Regular Law Enforcement System
- The Use of Risk Assessment Tools in Sentencing and Parole Decision-Making
- Investigating the Factors Influencing False Confessions and Their Implications for the Criminal Justice System
- Evaluation of the Impact of Capital Punishment on Criminal Activity Suppression and Community Response.
- Investigating the Links Between Halt and Search and Racism in Policing
- Rates of Juvenile Delinquency and Relapse and the Effectiveness of Rehab Initiatives
Senior thesis topics chosen with careful deliberation allow students to demonstrate their prowess in academic research. It is an opportunity for students to make original contributions to their fields, advance knowledge, and potentially impact the broader academic community.
The selection of good senior thesis topics for writing should be based on personal interest, feasibility, and relevance. This ensures a meaningful and successful research project. Good luck!
Readers also enjoyed
WHY WAIT? PLACE AN ORDER RIGHT NOW!
Just fill out the form, press the button, and have no worries!
We use cookies to give you the best experience possible. By continuing we’ll assume you board with our cookie policy.

IMAGES
VIDEO
COMMENTS
The role of testosterone in the development of frailty in older women is also coming of age (147). While data suggesting that growth hormone and insulin-growth factor-1 may play a role in maintaining muscle mass (144, 148, 149), the enthusiasm for the use of growth hormone in the aged appears to be ebbing (150, 151).
The state of well-being is a multifaceted phenomenon that refers to an individual's subjective feelings, and exploring perspectives of older adults on aging well is developing to be an important area of research. Therefore, the aim of this study was to explore perceptions on aging well among older adult Palestinians ≥60 years.
The suggested research topics can serve as a base for researchers on which to select themes that need further investigation, and involve different age groups of older adults to better reflect and integrate their perspectives. ... If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text ...
Digital technology may be beneficial in improving people's cognitive ability as suggested by Wu et al. (2019).In the first paper of the special issue, Wu et al. (2019) explore the use of technology in memory clinics suggesting how the use of technology can be beneficial for people's mental and physical health, through stimulating cognitive abilities including executive functioning, memory ...
Materials and procedure. We developed focus groups materials based on previous research (Venkatesh et al., 2003; Zhou et al., 2014; Chan et al., 2016).A number of different devices were made available to the participants during the second half of the focus groups to gain feedback from older adults on any likely preferences for size, style, etc., to better direct the selection of the tablet ...
Specifically, senior citizens broadly face major problems such as. loneliness, abuse, health care, income, housing and transport, security etc. These problems are. interlinked or inter- dependent ...
A scoping review is a good tool for identifying domains or covering a body of literature on a particular topic, identifying knowledge gaps, existing literature, and concepts [].Arksey and O'Malley used a systematic scoping review for the first time in five main steps: identifying research questions, identifying related studies, selecting studies, charting and collecting data, and summarizing ...
Inflammatory Bowel Disease in the Elderly: Epidemiology, Pathophysiology, Clinical Aspects and Treatment Strategies. John Triantafillidis. 529 views. Advances our understanding of human aging and the fundamental link with age-related diseases, ultimately leading to improved healthspans.
Social determinants of health. Quality of care. In 2018 the US population ages sixty-five and older numbered 52.4 million, with older adults representing 15.6 percent of the population. 1 By 2030 ...
T. Cederholm and I. BosaeusN Engl J Med 2024;391:155-165. Malnutrition occurs in up to 10% of community-dwelling older people and contributes to morbidity and mortality. The two main pathologic ...
on Pervasive Health and Technology Research Article. 1. An Empirical Study on Ch allenges Face d by the Elderly. in Care Centres. J ieLi1,*, Wei WeiGoh1, NZ Jhanjhi1, Filzah Binti Md Isa2, Sumathi ...
Background Ageing societies and urbanization are global phenomena that pose new challenges for care delivery. It is important to create a scientific evidence base to prepare for these changes. Hence, the aim of our study was to assess which research agenda older adults living in an urban environment in Germany suggest. Methods A total of 1000 participants aged 65 years or older from five ...
Older Americans more wary than younger adults about prospect of driverless cars on the road. 53% of those 50 and older say the widespread use of driverless vehicles would be a bad idea for society, as do 37% of adults ages 18 to 49. short readsJan 13, 2022.
The research problem of this thesis was elderly people's coping at home. The research questions were how elderly people cope with their lives at home and what kind of physical, social and ... It is necessary to research about this topic to improve the situation. The method of this research is narrative literature review. Data was collected ...
The global population is aging, and the growing awareness of the importance of promoting healthy aging is becoming increasingly relevant to physicians of many disciplines and fields of expertise. The complex issues affecting the health of older adults demand a multidisciplinary and coordinated personalized approach. The acquisition of an array of medical conditions and comorbidities with ...
The health of senior citizens is an important concern in the context of an aging population in China. Based on changes to and the characteristics of senior health in the new era, it is both important and necessary to promote research on senior health from an interdisciplinary perspective. An analytical framework that takes in society, behavior, psychology, environment, and genetic inheritance ...
By the year 2050, according to the United Nations (UN), one in six persons will be 65+ years of age 1.Given this increasing number of people entering the worldwide aging community, coupled with lower birth rates - especially in high‐income and some middle‐income countries - there is concern about the old‐age dependency ratio, that is, the number of people 65+ years of age per 100 ...
In this essay, we are going to use the ideas for skin care and anti-aging products in a bid to explore further the topic of ideation and to put it into practice. Reflection Essay: Aging and Sugar. I want to go on trips around the world with my family and engage in new challenges.
The data gathered revealed that Senior Citizens were "Moderately Aware" of most of the parameters presented such as the 20% discount, government assistance, and priority in express lanes.
Highlighted Topics. Alzheimer's and Dementia. Brain Health. Caregiving. Clinical Trials and Studies. Exercise and Physical Activity. Healthy Eating. Menopause. NIA provides health information informed by research and reviewed by experts to help you learn about healthy aging and common health conditions in older adults.
The state of well-being is a multifaceted phenomenon that refers to an individual's subjective feelings, and exploring perspectives of older adults on aging well is developing to be an important area of research. Therefore, the aim of this study was to explore perceptions on aging well among older adult Palestinians ≥60 years. Methods. A ...
In contemporary Pakistani society the senior citizens are facing problems in the form of low social status, poverty/lack of pension and deprivation from the authority of property control, ageism ...
Senior thesis topics are research projects students undertake in their final year of undergraduate studies or graduate programs. These senior thesis topics allow students to demonstrate their expertise in academic writing. School senior thesis topics can cover a wide range of disciplines. This spans science and humanities to social sciences and ...