- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Quality improvement...
Quality improvement into practice
Read the full collection.
- Related content
- Peer review
- Adam Backhouse , quality improvement programme lead 1 ,
- Fatai Ogunlayi , public health specialty registrar 2
- 1 North London Partners in Health and Care, Islington CCG, London N1 1TH, UK
- 2 Institute of Applied Health Research, Public Health, University of Birmingham, B15 2TT, UK
- Correspondence to: A Backhouse adam.backhouse{at}nhs.net
What you need to know
Thinking of quality improvement (QI) as a principle-based approach to change provides greater clarity about ( a ) the contribution QI offers to staff and patients, ( b ) how to differentiate it from other approaches, ( c ) the benefits of using QI together with other change approaches
QI is not a silver bullet for all changes required in healthcare: it has great potential to be used together with other change approaches, either concurrently (using audit to inform iterative tests of change) or consecutively (using QI to adapt published research to local context)
As QI becomes established, opportunities for these collaborations will grow, to the benefit of patients.
The benefits to front line clinicians of participating in quality improvement (QI) activity are promoted in many health systems. QI can represent a valuable opportunity for individuals to be involved in leading and delivering change, from improving individual patient care to transforming services across complex health and care systems. 1
However, it is not clear that this promotion of QI has created greater understanding of QI or widespread adoption. QI largely remains an activity undertaken by experts and early adopters, often in isolation from their peers. 2 There is a danger of a widening gap between this group and the majority of healthcare professionals.
This article will make it easier for those new to QI to understand what it is, where it fits with other approaches to improving care (such as audit or research), when best to use a QI approach, making it easier to understand the relevance and usefulness of QI in delivering better outcomes for patients.
How this article was made
AB and FO are both specialist quality improvement practitioners and have developed their expertise working in QI roles for a variety of UK healthcare organisations. The analysis presented here arose from AB and FO’s observations of the challenges faced when introducing QI, with healthcare providers often unable to distinguish between QI and other change approaches, making it difficult to understand what QI can do for them.
How is quality improvement defined?
There are many definitions of QI ( box 1 ). The BMJ ’s Quality Improvement series uses the Academy of Medical Royal Colleges definition. 6 Rather than viewing QI as a single method or set of tools, it can be more helpful to think of QI as based on a set of principles common to many of these definitions: a systematic continuous approach that aims to solve problems in healthcare, improve service provision, and ultimately provide better outcomes for patients.
Definitions of quality improvement
Improvement in patient outcomes, system performance, and professional development that results from a combined, multidisciplinary approach in how change is delivered. 3
The delivery of healthcare with improved outcomes and lower cost through continuous redesigning of work processes and systems. 4
Using a systematic change method and strategies to improve patient experience and outcome. 5
To make a difference to patients by improving safety, effectiveness, and experience of care by using understanding of our complex healthcare environment, applying a systematic approach, and designing, testing, and implementing changes using real time measurement for improvement. 6
In this article we discuss QI as an approach to improving healthcare that follows the principles outlined in box 2 ; this may be a useful reference to consider how particular methods or tools could be used as part of a QI approach.
Principles of QI
Primary intent— To bring about measurable improvement to a specific aspect of healthcare delivery, often with evidence or theory of what might work but requiring local iterative testing to find the best solution. 7
Employing an iterative process of testing change ideas— Adopting a theory of change which emphasises a continuous process of planning and testing changes, studying and learning from comparing the results to a predicted outcome, and adapting hypotheses in response to results of previous tests. 8 9
Consistent use of an agreed methodology— Many different QI methodologies are available; commonly cited methodologies include the Model for Improvement, Lean, Six Sigma, and Experience-based Co-design. 4 Systematic review shows that the choice of tools or methodologies has little impact on the success of QI provided that the chosen methodology is followed consistently. 10 Though there is no formal agreement on what constitutes a QI tool, it would include activities such as process mapping that can be used within a range of QI methodological approaches. NHS Scotland’s Quality Improvement Hub has a glossary of commonly used tools in QI. 11
Empowerment of front line staff and service users— QI work should engage staff and patients by providing them with the opportunity and skills to contribute to improvement work. Recognition of this need often manifests in drives from senior leadership or management to build QI capability in healthcare organisations, but it also requires that frontline staff and service users feel able to make use of these skills and take ownership of improvement work. 12
Using data to drive improvement— To drive decision making by measuring the impact of tests of change over time and understanding variation in processes and outcomes. Measurement for improvement typically prioritises this narrative approach over concerns around exactness and completeness of data. 13 14
Scale-up and spread, with adaptation to context— As interventions tested using a QI approach are scaled up and the degree of belief in their efficacy increases, it is desirable that they spread outward and be adopted by others. Key to successful diffusion of improvement is the adaption of interventions to new environments, patient and staff groups, available resources, and even personal preferences of healthcare providers in surrounding areas, again using an iterative testing approach. 15 16
What other approaches to improving healthcare are there?
Taking considered action to change healthcare for the better is not new, but QI as a distinct approach to improving healthcare is a relatively recent development. There are many well established approaches to evaluating and making changes to healthcare services in use, and QI will only be adopted more widely if it offers a new perspective or an advantage over other approaches in certain situations.
A non-systematic literature scan identified the following other approaches for making change in healthcare: research, clinical audit, service evaluation, and clinical transformation. We also identified innovation as an important catalyst for change, but we did not consider it an approach to evaluating and changing healthcare services so much as a catch-all term for describing the development and introduction of new ideas into the system. A summary of the different approaches and their definition is shown in box 3 . Many have elements in common with QI, but there are important difference in both intent and application. To be useful to clinicians and managers, QI must find a role within healthcare that complements research, audit, service evaluation, and clinical transformation while retaining the core principles that differentiate it from these approaches.
Alternatives to QI
Research— The attempt to derive generalisable new knowledge by addressing clearly defined questions with systematic and rigorous methods. 17
Clinical audit— A way to find out if healthcare is being provided in line with standards and to let care providers and patients know where their service is doing well, and where there could be improvements. 18
Service evaluation— A process of investigating the effectiveness or efficiency of a service with the purpose of generating information for local decision making about the service. 19
Clinical transformation— An umbrella term for more radical approaches to change; a deliberate, planned process to make dramatic and irreversible changes to how care is delivered. 20
Innovation— To develop and deliver new or improved health policies, systems, products and technologies, and services and delivery methods that improve people’s health. Health innovation responds to unmet needs by employing new ways of thinking and working. 21
Why do we need to make this distinction for QI to succeed?
Improvement in healthcare is 20% technical and 80% human. 22 Essential to that 80% is clear communication, clarity of approach, and a common language. Without this shared understanding of QI as a distinct approach to change, QI work risks straying from the core principles outlined above, making it less likely to succeed. If practitioners cannot communicate clearly with their colleagues about the key principles and differences of a QI approach, there will be mismatched expectations about what QI is and how it is used, lowering the chance that QI work will be effective in improving outcomes for patients. 23
There is also a risk that the language of QI is adopted to describe change efforts regardless of their fidelity to a QI approach, either due to a lack of understanding of QI or a lack of intention to carry it out consistently. 9 Poor fidelity to the core principles of QI reduces its effectiveness and makes its desired outcome less likely, leading to wasted effort by participants and decreasing its credibility. 2 8 24 This in turn further widens the gap between advocates of QI and those inclined to scepticism, and may lead to missed opportunities to use QI more widely, consequently leading to variation in the quality of patient care.
Without articulating the differences between QI and other approaches, there is a risk of not being able to identify where a QI approach can best add value. Conversely, we might be tempted to see QI as a “silver bullet” for every healthcare challenge when a different approach may be more effective. In reality it is not clear that QI will be fit for purpose in tackling all of the wicked problems of healthcare delivery and we must be able to identify the right tool for the job in each situation. 25 Finally, while different approaches will be better suited to different types of challenge, not having a clear understanding of how approaches differ and complement each other may mean missed opportunities for multi-pronged approaches to improving care.
What is the relationship between QI and other approaches such as audit?
Academic journals, healthcare providers, and “arms-length bodies” have made various attempts to distinguish between the different approaches to improving healthcare. 19 26 27 28 However, most comparisons do not include QI or compare QI to only one or two of the other approaches. 7 29 30 31 To make it easier for people to use QI approaches effectively and appropriately, we summarise the similarities, differences, and crossover between QI and other approaches to tackling healthcare challenges ( fig 1 ).

How quality improvement interacts with other approaches to improving healthcare
- Download figure
- Open in new tab
- Download powerpoint
QI and research
Research aims to generate new generalisable knowledge, while QI typically involves a combination of generating new knowledge or implementing existing knowledge within a specific setting. 32 Unlike research, including pragmatic research designed to test effectiveness of interventions in real life, QI does not aim to provide generalisable knowledge. In common with QI, research requires a consistent methodology. This method is typically used, however, to prove or disprove a fixed hypothesis rather than the adaptive hypotheses developed through the iterative testing of ideas typical of QI. Both research and QI are interested in the environment where work is conducted, though with different intentions: research aims to eliminate or at least reduce the impact of many variables to create generalisable knowledge, whereas QI seeks to understand what works best in a given context. The rigour of data collection and analysis required for research is much higher; in QI a criterion of “good enough” is often applied.
Relationship with QI
Though the goal of clinical research is to develop new knowledge that will lead to changes in practice, much has been written on the lag time between publication of research evidence and system-wide adoption, leading to delays in patients benefitting from new treatments or interventions. 33 QI offers a way to iteratively test the conditions required to adapt published research findings to the local context of individual healthcare providers, generating new knowledge in the process. Areas with little existing knowledge requiring further research may be identified during improvement activities, which in turn can form research questions for further study. QI and research also intersect in the field of improvement science, the academic study of QI methods which seeks to ensure QI is carried out as effectively as possible. 34
Scenario: QI for translational research
Newly published research shows that a particular physiotherapy intervention is more clinically effective when delivered in short, twice-daily bursts rather than longer, less frequent sessions. A team of hospital physiotherapists wish to implement the change but are unclear how they will manage the shift in workload and how they should introduce this potentially disruptive change to staff and to patients.
Before continuing reading think about your own practice— How would you approach this situation, and how would you use the QI principles described in this article?
Adopting a QI approach, the team realise that, although the change they want to make is already determined, the way in which it is introduced and adapted to their wards is for them to decide. They take time to explain the benefits of the change to colleagues and their current patients, and ask patients how they would best like to receive their extra physiotherapy sessions.
The change is planned and tested for two weeks with one physiotherapist working with a small number of patients. Data are collected each day, including reasons why sessions were missed or refused. The team review the data each day and make iterative changes to the physiotherapist’s schedule, and to the times of day the sessions are offered to patients. Once an improvement is seen, this new way of working is scaled up to all of the patients on the ward.
The findings of the work are fed into a service evaluation of physiotherapy provision across the hospital, which uses the findings of the QI work to make recommendations about how physiotherapy provision should be structured in the future. People feel more positive about the change because they know colleagues who have already made it work in practice.
QI and clinical audit
Clinical audit is closely related to QI: it is often used with the intention of iteratively improving the standard of healthcare, albeit in relation to a pre-determined standard of best practice. 35 When used iteratively, interspersed with improvement action, the clinical audit cycle adheres to many of the principles of QI. However, in practice clinical audit is often used by healthcare organisations as an assurance function, making it less likely to be carried out with a focus on empowering staff and service users to make changes to practice. 36 Furthermore, academic reviews of audit programmes have shown audit to be an ineffective approach to improving quality due to a focus on data collection and analysis without a well developed approach to the action section of the audit cycle. 37 Clinical audits, such as the National Clinical Audit Programme in the UK (NCAPOP), often focus on the management of specific clinical conditions. QI can focus on any part of service delivery and can take a more cross-cutting view which may identify issues and solutions that benefit multiple patient groups and pathways. 30
Audit is often the first step in a QI process and is used to identify improvement opportunities, particularly where compliance with known standards for high quality patient care needs to be improved. Audit can be used to establish a baseline and to analyse the impact of tests of change against the baseline. Also, once an improvement project is under way, audit may form part of rapid cycle evaluation, during the iterative testing phase, to understand the impact of the idea being tested. Regular clinical audit may be a useful assurance tool to help track whether improvements have been sustained over time.
Scenario: Audit and QI
A foundation year 2 (FY2) doctor is asked to complete an audit of a pre-surgical pathway by looking retrospectively through patient documentation. She concludes that adherence to best practice is mixed and recommends: “Remind the team of the importance of being thorough in this respect and re-audit in 6 months.” The results are presented at an audit meeting, but a re-audit a year later by a new FY2 doctor shows similar results.
Before continuing reading think about your own practice— How would you approach this situation, and how would you use the QI principles described in this paper?
Contrast the above with a team-led, rapid cycle audit in which everyone contributes to collecting and reviewing data from the previous week, discussed at a regular team meeting. Though surgical patients are often transient, their experience of care and ideas for improvement are captured during discharge conversations. The team identify and test several iterative changes to care processes. They document and test these changes between audits, leading to sustainable change. Some of the surgeons involved work across multiple hospitals, and spread some of the improvements, with the audit tool, as they go.
QI and service evaluation
In practice, service evaluation is not subject to the same rigorous definition or governance as research or clinical audit, meaning that there are inconsistencies in the methodology for carrying it out. While the primary intent for QI is to make change that will drive improvement, the primary intent for evaluation is to assess the performance of current patient care. 38 Service evaluation may be carried out proactively to assess a service against its stated aims or to review the quality of patient care, or may be commissioned in response to serious patient harm or red flags about service performance. The purpose of service evaluation is to help local decision makers determine whether a service is fit for purpose and, if necessary, identify areas for improvement.
Service evaluation may be used to initiate QI activity by identifying opportunities for change that would benefit from a QI approach. It may also evaluate the impact of changes made using QI, either during the work or after completion to assess sustainability of improvements made. Though likely planned as separate activities, service evaluation and QI may overlap and inform each other as they both develop. Service evaluation may also make a judgment about a service’s readiness for change and identify any barriers to, or prerequisites for, carrying out QI.
QI and clinical transformation
Clinical transformation involves radical, dramatic, and irreversible change—the sort of change that cannot be achieved through continuous improvement alone. As with service evaluation, there is no consensus on what clinical transformation entails, and it may be best thought of as an umbrella term for the large scale reform or redesign of clinical services and the non-clinical services that support them. 20 39 While it is possible to carry out transformation activity that uses elements of QI approach, such as effective engagement of the staff and patients involved, QI which rests on iterative test of change cannot have a transformational approach—that is, one-off, irreversible change.
There is opportunity to use QI to identify and test ideas before full scale clinical transformation is implemented. This has the benefit of engaging staff and patients in the clinical transformation process and increasing the degree of belief that clinical transformation will be effective or beneficial. Transformation activity, once completed, could be followed up with QI activity to drive continuous improvement of the new process or allow adaption of new ways of working. As interventions made using QI are scaled up and spread, the line between QI and transformation may seem to blur. The shift from QI to transformation occurs when the intention of the work shifts away from continuous testing and adaptation into the wholesale implementation of an agreed solution.
Scenario: QI and clinical transformation
An NHS trust’s human resources (HR) team is struggling to manage its junior doctor placements, rotas, and on-call duties, which is causing tension and has led to concern about medical cover and patient safety out of hours. A neighbouring trust has launched a smartphone app that supports clinicians and HR colleagues to manage these processes with the great success.
This problem feels ripe for a transformation approach—to launch the app across the trust, confident that it will solve the trust’s problems.
Before continuing reading think about your own organisation— What do you think will happen, and how would you use the QI principles described in this article for this situation?
Outcome without QI
Unfortunately, the HR team haven’t taken the time to understand the underlying problems with their current system, which revolve around poor communication and clarity from the HR team, based on not knowing who to contact and being unable to answer questions. HR assume that because the app has been a success elsewhere, it will work here as well.
People get excited about the new app and the benefits it will bring, but no consideration is given to the processes and relationships that need to be in place to make it work. The app is launched with a high profile campaign and adoption is high, but the same issues continue. The HR team are confused as to why things didn’t work.
Outcome with QI
Although the app has worked elsewhere, rolling it out without adapting it to local context is a risk – one which application of QI principles can mitigate.
HR pilot the app in a volunteer specialty after spending time speaking to clinicians to better understand their needs. They carry out several tests of change, ironing out issues with the process as they go, using issues logged and clinician feedback as a source of data. When they are confident the app works for them, they expand out to a directorate, a division, and finally the transformational step of an organisation-wide rollout can be taken.
Education into practice
Next time when faced with what looks like a quality improvement (QI) opportunity, consider asking:
How do you know that QI is the best approach to this situation? What else might be appropriate?
Have you considered how to ensure you implement QI according to the principles described above?
Is there opportunity to use other approaches in tandem with QI for a more effective result?
How patients were involved in the creation of this article
This article was conceived and developed in response to conversations with clinicians and patients working together on co-produced quality improvement and research projects in a large UK hospital. The first iteration of the article was reviewed by an expert patient, and, in response to their feedback, we have sought to make clearer the link between understanding the issues raised and better patient care.
Contributors: This work was initially conceived by AB. AB and FO were responsible for the research and drafting of the article. AB is the guarantor of the article.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: This article is part of a series commissioned by The BMJ based on ideas generated by a joint editorial group with members from the Health Foundation and The BMJ , including a patient/carer. The BMJ retained full editorial control over external peer review, editing, and publication. Open access fees and The BMJ ’s quality improvement editor post are funded by the Health Foundation.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Olsson-Brown A
- Dixon-Woods M ,
- Batalden PB ,
- Berwick D ,
- Øvretveit J
- Academy of Medical Royal Colleges
- Nelson WA ,
- McNicholas C ,
- Woodcock T ,
- Alderwick H ,
- ↵ NHS Scotland Quality Improvement Hub. Quality improvement glossary of terms. http://www.qihub.scot.nhs.uk/qi-basics/quality-improvement-glossary-of-terms.aspx .
- McNicol S ,
- Solberg LI ,
- Massoud MR ,
- Albrecht Y ,
- Illingworth J ,
- Department of Health
- ↵ NHS England. Clinical audit. https://www.england.nhs.uk/clinaudit/ .
- Healthcare Quality Improvement Partnership
- McKinsey Hospital Institute
- ↵ World Health Organization. WHO Health Innovation Group. 2019. https://www.who.int/life-course/about/who-health-innovation-group/en/ .
- Sheffield Microsystem Coaching Academy
- Davidoff F ,
- Leviton L ,
- Taylor MJ ,
- Nicolay C ,
- Tarrant C ,
- Twycross A ,
- ↵ University Hospitals Bristol NHS Foundation Trust. Is your study research, audit or service evaluation. http://www.uhbristol.nhs.uk/research-innovation/for-researchers/is-it-research,-audit-or-service-evaluation/ .
- ↵ University of Sheffield. Differentiating audit, service evaluation and research. 2006. https://www.sheffield.ac.uk/polopoly_fs/1.158539!/file/AuditorResearch.pdf .
- ↵ Royal College of Radiologists. Audit and quality improvement. https://www.rcr.ac.uk/clinical-radiology/audit-and-quality-improvement .
- Gundogan B ,
- Finkelstein JA ,
- Brickman AL ,
- Health Foundation
- Johnston G ,
- Crombie IK ,
- Davies HT ,
- Hillman T ,
- ↵ NHS Health Research Authority. Defining research. 2013. https://www.clahrc-eoe.nihr.ac.uk/wp-content/uploads/2014/04/defining-research.pdf .
- Log In / Register
- Education Platform
- Newsletter Sign Up
Case Studies

- How to Improve
- Improvement Stories
- Publications
- IHI White Papers
- Audio and Video
Case studies related to improving health care.
first < > last
- An Extended Stay A 64-year-old man with a number of health issues comes to the hospital because he is having trouble breathing. The care team helps resolve the issue, but forgets a standard treatment that causes unnecessary harm to the patient. A subsequent medication error makes the situation worse, leading a stay that is much longer than anticipated.
- Mutiny The behavior of a superior starts to put your patients at risk. What would you do? The University of Rochester’s Dr. Paul Griner presents the final installment in a series of case studies for the IHI Open School.
- On Being Transparent You are the CEO and a patient in your hospital dies from a medication error. What do you do next? The University of Rochester’s Dr. Paul Griner presents the fourth in a series of case studies.
- Locked In A cancer diagnosis leads to tears and heartache. But is it correct? Dr. Paul Griner, Professor Emeritus of Medicine at the University of Rochester, presents the third in a series of case studies for the IHI Open School.
- Confidentiality and Air Force One A difficult patient. A difficult decision. The University of Rochester’s Dr. Paul Griner presents the second in a series of case studies.
- The Protective Parent During a 50-year career in medicine, Dr. Paul Griner accumulated hundreds of patient stories. Most of his stories – including this case study "The Protective Parent" - are from the 1950s and 1960s, prior to what we now refer to as “modern medicine.”
- Advanced Case Study Between Sept. 30th and Oct. 14th, 2010, students and residents all over the world gathered in interprofessional teams and analyzed a complex incident that resulted in patient harm. Selected teams presented their work to IHI faculty during a series of live webinars in October.
- A Downward Spiral: A Case Study in Homelessness Thirty-six-year-old John may not fit the stereotype of a homeless person. Not long ago, he was living what many would consider a healthy life with his family. But when he lost his job, he found himself in a downward spiral, and his situation dramatically changed. John’s story is a fictional composite of real patients treated by Health Care for the Homeless. It illustrates the challenges homeless people face in accessing health care and the characteristics of high-quality care that can improve their lives.
- What Happened to Alex? Alex James was a runner, like his dad. One day, he collapsed during a run and was hospitalized for five days. He went through lots of tests, but was given a clean bill of health. Then, a month later, he collapsed again, fell into a deep coma, and died. His father wanted to know — what had gone wrong? Dr. John James, a retired toxicologist at NASA, tells the story of how he uncovered the cause of his son’s death and became a patient safety advocate.
- Improving Care in Rural Rwanda When Dr. Patrick Lee and his teammates began their quality improvement work in Kirehe, Rwanda, last year, the staff at the local hospital was taking vital signs properly less than half the time. Today, the staff does that task properly 95% of the time. Substantial resource and infrastructure inputs, combined with dedicated Rwandan partners and simple quality improvement tools, have dramatically improved staff morale and the quality of care in Kirehe.

A quality improvement evaluation case study: impact on public health outcomes and agency culture
Affiliation.
- 1 Center for Health Equity & Quality Research, University of Florida College of Medicine-Jacksonville, Jacksonville, FL 32209, USA. [email protected]
- PMID: 23597806
- DOI: 10.1016/j.amepre.2013.01.011
Background: Quality improvement (QI) is increasingly recognized as an important strategy to improve healthcare services and health outcomes, including reducing health disparities. However, there is a paucity of evidence documenting the value of QI to public health agencies and services.
Purpose: The purpose of this project was to support and assess the impact on the outcomes and organizational culture of a QI project to increase immunization rates among children aged 2 years (4:3:1:3:3:1 series) within a large public health agency with a major pediatric health mission.
Methods: The intervention consisted of the use of a model-for-improvement approach to QI for the delivery of immunization services in public health clinics, utilizing plan-do-study-act cycles and multiple QI techniques. A mixed-method (qualitative and quantitative) model of evaluation was used to collect and analyze data from June 2009 to July 2011 to support both summative and developmental evaluation. The Florida Immunization Registry (Florida SHOTS [State Health Online Tracking System]) was used to monitor and analyze changes in immunization rates from January 2009 to July 2012. An interrupted time-series application of covariance was used to assess significance of the change in immunization rates, and paired comparison using parametric and nonparametric statistics were used to assess significance of pre- and post-QI culture items.
Results: Up-to-date immunization rates increased from 75% to more than 90% for individual primary care clinics and the overall county health department. In addition, QI stakeholder scores on ten key items related to organizational culture increased from pre- to post-QI intervention. Statistical analysis confirmed significance of the changes.
Conclusions: The application of QI combined with a summative and developmental evaluation supported refinement of the QI approach and documented the potential for QI to improve population health outcomes and improve public health agency culture.
Copyright © 2013 American Journal of Preventive Medicine. Published by Elsevier Inc. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Child, Preschool
- Immunization / statistics & numerical data*
- Organizational Case Studies
- Organizational Culture
- Outcome Assessment, Health Care*
- Public Health
- Quality Improvement*

Patient Safety and Quality Improvement in Healthcare
A Case-Based Approach
- © 2021
- Rahul K. Shah 0 ,
- Sandip A. Godambe 1
Children’s National Health System, Washington, USA
You can also search for this editor in PubMed Google Scholar
Children's Hospital of The King's Daughters, Norfolk, USA
- Provides case-based approaches with tangible examples
- Includes diagrams and images to enhance learning
- Includes key learning points within each chapter
- Provides a question and answer section at the conclusion of each chapter
36k Accesses
6 Citations
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents (22 chapters)
Front matter, introduction: a case-based approach to quality improvement.
- Sandip A. Godambe, Rahul K. Shah
Organizational Safety Culture: The Foundation for Safety and Quality Improvement
- Michael F. Gutzeit, Holly O’Brien, Jackie E. Valentine
Creation of Quality Management Systems: Frameworks for Performance Excellence
- Adam M. Campbell, Donald E. Lighter, Brigitta U. Mueller
Reliability, Resilience, and Developing a Problem-Solving Culture
- David P. Johnson, Heather S. McLean
Building an Engaging Toyota Production System Culture to Drive Winning Performance for Our Patients, Caregivers, Hospitals, and Communities
- Jamie P. Bonini, Sandip A. Godambe, Christopher D. Mangum, John Heer, Susan Black, Denise Ranada et al.
What to Do When an Event Happens: Building Trust in Every Step
- Michaeleen Green, Lee E. Budin
Communication with Disclosure and Its Importance in Safety
- Kristin Cummins, Katherine A. Feley, Michele Saysana, Brian Wagers
Using Data to Drive Change
- Lisa L. Schroeder
Quality Methodology
- Michael T. Bigham, Michael W. Bird, Jodi L. Simon
Designing Improvement Teams for Success
- Nicole M. Leone, Anupama Subramony
Handoffs: Reducing Harm Through High Reliability and Inter-Professional Communication
- Kheyandra D. Lewis, Stacy McConkey, Shilpa J. Patel
Safety II: A Novel Approach to Reducing Harm
- Thomas Bartman, Jenna Merandi, Tensing Maa, Tara C. Cosgrove, Richard J. Brilli
Bundles and Checklists
- Gary Frank, Rustin B. Morse, Proshad Efune, Nikhil K. Chanani, Cindy Darnell Bowens, Joshua Wolovits
Pathways and Guidelines: An Approach to Operationalizing Patient Safety and Quality Improvement
- Andrew R. Buchert, Gabriella A. Butler
Accountable Justifications and Peer Comparisons as Behavioral Economic Nudges to Improve Clinical Practice
- Jack Stevens
Diagnostic Errors and Their Associated Cognitive Biases
- Jennifer E. Melvin, Michael F. Perry, Richard E. McClead Jr.
An Improvement Operating System: A Case for a Digital Infrastructure for Continuous Improvement
- Daniel Baily, Kapil Raj Nair
Patient Flow in Healthcare: A Key to Quality
- Karen Murrell
It Takes Teamwork: Consideration of Difficult Hospital-Acquired Conditions
- J. Wesley Diddle, Christine M. Riley, Darren Klugman
- Emergency Preparedness
- Workforce and Patient Experience
- Performance Excellence
- Incident Reporting
- Hand Hygiene and Stethoscope Hygiene
- Clinical Effectiveness
- STEEP Principles
About this book
Editors and affiliations.
Rahul K. Shah
Children's Hospital of The King's Daughters, Norfolk, USA
Sandip A. Godambe
About the editors
Bibliographic information.
Book Title : Patient Safety and Quality Improvement in Healthcare
Book Subtitle : A Case-Based Approach
Editors : Rahul K. Shah, Sandip A. Godambe
DOI : https://doi.org/10.1007/978-3-030-55829-1
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG 2021
Hardcover ISBN : 978-3-030-55828-4 Published: 16 December 2020
Softcover ISBN : 978-3-030-55831-4 Published: 17 December 2021
eBook ISBN : 978-3-030-55829-1 Published: 15 December 2020
Edition Number : 1
Number of Pages : XIX, 383
Number of Illustrations : 11 b/w illustrations, 118 illustrations in colour
Topics : Practice and Hospital Management , General Practice / Family Medicine , Primary Care Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Call for Papers
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 7, Issue 2
- Continuous quality improvement methodology: a case study on multidisciplinary collaboration to improve chlamydia screening
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Allison Ursu 1 ,
- Grant Greenberg 2 and
- Michael McKee 3
- 1 Department of Family Medicine , University of Michigan Medical School , Ann Arbor , Michigan , USA
- 2 Department of Family Medicine , Lehigh Valley Health Network , Allentown , Pennsylvania , USA
- 3 Family Medicine , University of Michigan Medical School , Ann Arbor , MI , United States
- Correspondence to Dr Allison Ursu; awessel{at}med.umich.edu
This article illustrates quality improvement (QI) methodology using an example intended to improve chlamydia screening in women. QI projects in healthcare provide great opportunities to improve patient quality and safety in a real-world healthcare setting, yet many academic centres lack training programmes on how to conduct QI projects. The choice of chlamydia screening was based on the significant health burden chlamydia poses despite simple ways to screen and treat. At the University of Michigan, we implemented a multidepartment process to improve the chlamydia screening rates using the plan-do-check-act model. Steps to guide QI projects include the following: (1) assemble a motivated team of stakeholders and leaders; (2) identify the problem that is considered a high priority; (3) prepare for the project including support and resources; (4) set a goal and ways to evaluate outcomes; (5) identify the root cause(s) of the problem and prioritise based on impact and effort to address; (6) develop a countermeasure that addresses the selected root cause effectively; (7) pilot a small-scale project to assess for possible modifications; (8) large-scale roll-out including education on how to implement the project; and (9) assess and modify the process with a feedback mechanism. Using this nine-step process, chlamydia screening rates increased from 29% to 60%. QI projects differ from most clinical research projects by allowing clinicians to directly improve patients’ health while contributing to the medical science body. This may interest clinicians wishing to conduct relevant research that can be disseminated through academic channels.
- chlamydia screening
- quality improvement
- healthcare delivery
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0
https://doi.org/10.1136/fmch-2018-000085
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Healthcare organisations continually strive to improve patient care services and quality through initiatives driven by their leadership and healthcare payers (eg, Centers for Medicare and Medicaid Services). 1 Quality improvement (QI) projects in healthcare provide opportunities to advance best practices and enhance the redesign of healthcare to improve patient quality and safety. 2 3
The modern study of QI has its origins in industry dating back to the first automotive assembly lines designed by Henry Ford in the early 1900s. Subsequently, work by Edwards Deming led to what is now commonly referred to as the ‘Plan/Do/Check/Adjust’ (PDCA) cycle. 4 Concurrent to the development of PDCA, Juran 5 developed what would become known as ‘total quality management’, which led to further developments in quality management methodology and philosophy such as Lean and Six Sigma. The same principles that apply to industry are now commonly applied to healthcare models of improvement. Unlike most research projects, QI tends to lack a true ‘control’ arm, but QI still lends itself to rigorous academic reporting. To facilitate this, the Standards for Quality Improvement Reporting Excellence guidelines were developed to provide a standard structure for reporting and publishing QI. 6
Despite the growth in knowledge around QI, and the development of QI as an academic discipline, many clinicians lack the training, skills and access to resources to conduct QI. QI projects require a blend of social science, engineering and research methodology skills. Academic healthcare institutions now recognise this need, and many offer training to their medical students, residents, faculty and staff. 7–9 Unlike many clinical research projects, QI projects are often smaller scale and occur on a compressed time frame.
While there are several tools to facilitate a QI project, here we focus on the standard PDCA methodology as defined by Deming. In our example, we engaged clinicians to participate by also coupling the project with the opportunity to obtain continuing medical educational credits. By aligning the QI need with the ability to meet board recertification requirements, active participation in the QI project is directly rewarded, and facilitates broader perspectives and more robust solutions.
The PDCA model follows a four-step cycle to achieve continuous improvement. 10 This method is also applicable to new projects or processes, products, or services. When followed, PDCA facilitates more robust project planning, root cause analysis, data collection and review, and ability to maintain focus. ‘Plan’ signifies developing an understanding of the possible countermeasure leading to an improvement. ‘Do’ is implementing the countermeasure. ‘Check’ is analysing the data that inform the effectiveness of the countermeasure on the topic of improvement. ‘Adjust’ is applying the learning from the data analysis and either developing refinements to the original countermeasure or developing a new countermeasure.
Incorporating a tool such as ‘The Model for Improvement’ can help QI teams focus on what they are seeking to achieve. The Model for Improvement has three key questions:
What are we trying to accomplish?
How will we know if a change is an improvement?
What changes can we make that will result in improvement?
Chlamydia screening QI project for illustrating the features of a QI project
There were 1.5 million chlamydia infections reported to the Centers for Disease Control and Prevention in 2015, with nearly 80% of these being reported from outside of sexually transmitted diseases clinics. 11 Adolescents and young adults between the ages of 16 and 24 account for half of these infections; they also have the highest burden of the disease in the USA, four times higher than the general public. Rates of infection have continued to increase since 2013. In 2017, the rate for women is approximately 687 per 100 000. 12 The estimated annual cost of chlamydia infection in the USA is estimated to be between $250 and $770 million. 13
Multiple national physician and public health groups recommend chlamydia screening for sexually active women younger than 25 years old in order to reduce the rates of infection and sequelae of the disease. These sequelae include pelvic inflammatory disease (PID), chronic pelvic pain, tubo-ovarian abscesses and infertility. There is also evidence that chlamydia infection facilitates the transmission of HIV. 14 Randomised control trials have shown that screening for chlamydia can reduce PID rates. 15 However, screening rates remain low.
The objective of this paper is to provide readers an overview on what resources and training programmes are recommended to support these QI endeavours. The following section provides a step-by-step process on how a specific QI project was designed and implemented to address poor chlamydia screening and treatment for young women at a large healthcare institution. Improvement in screening for chlamydia was chosen as a QI effort as this infection is the most commonly reported sexually transmitted disease in the USA, occurring at a rate of over 3265.7 cases per 100 000 in women aged 15–19, and 3985.8 cases per 100 000 in women aged 20–24. 16 Untreated chlamydia infection can lead to complications such as PID, infertility and tubal pregnancy.
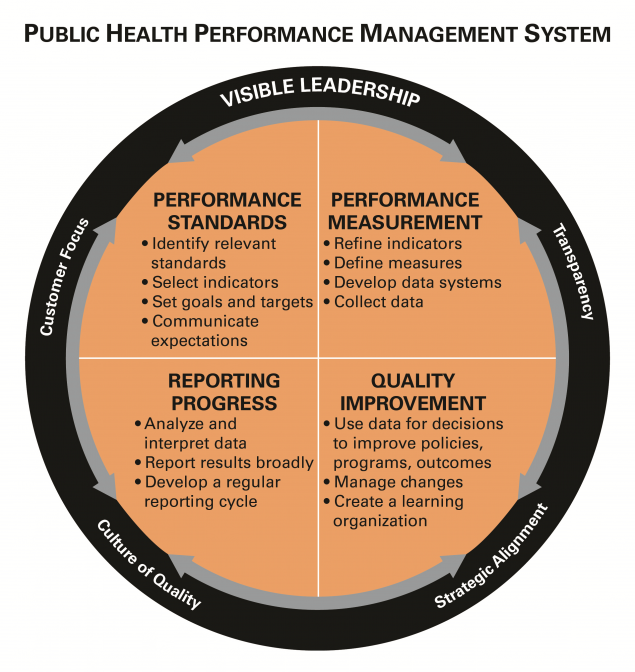
We used PDCA and the Model for Improvement steps to implement QI to improve chlamydia screening in women aged 16–24, and use this project as an exemplar to illustrate the steps of QI. We chose a focus on chlamydia screening due to the health burden that the infection poses, the availability of non-invasive screening tests, success of treatment and our institution’s low rates of screening which needed improvement. The chlamydia screening QI project was a multidepartment collaboration (ie, family medicine, internal medicine, paediatrics, obstetrics and gynaecology, and the University Health Service) of the University of Michigan Health System, an academic institution located in Midwestern USA. Representatives from each department worked together to produce a standard approach to develop the workflow, educational materials and a clinical decision support tool that was integrated into the electronic health record (EHR). To gain skills in QI, several members (GG and so on) of our team gained training in Lean healthcare, epidemiology and process change. For data collection we used outputs from our EHR, conducted interviews of clinicians and staff to understand the current state and challenges in chlamydia screening, and conducted clinical observations in the involved specialties. We assessed progress continually, with quarterly reporting to local clinical teams. The focus of this report is a 1-year period from 21 May 2014 to 31 May 2015.
Here we illustrate nine essential steps for conducting a QI project.
Step 1. Assemble the team of stakeholders
The first step for implementing a QI project is to assemble a team of stakeholders and strong leaders ( figure 1 ). Effective teams are diverse, interdisciplinary and share a common goal. It is critically important to have buy-in from leadership to ensure that adequate resources and time are allocated towards the proposed QI project.
- Download figure
- Open in new tab
- Download powerpoint
Quality improvement step-by-step chart.
In our example we engaged all primary care-based departments caring for women aged 16–24 in an outpatient setting. This allowed us to standardise screening. A team was organised by a physician leader who had Lean training as well as a master’s degree in health system administration. The team included a project manager as well as other primary care stakeholders. Selection for local project leaders focused on recruiting individuals who were respected, visible and trusted within their own departments.
Step 2. Define the problem
Through a consensus decision-making process, prioritise the highest yield countermeasures which make the largest impact with the least effort ( figure 2 ). Methods for identifying a problem can come from chart review and clinical audit. In many places this can be facilitated through the use of EHR. Reports can be run that identify areas for improvement, for example patients needing cervical cancer screening, and these can be broken down by department, clinic and even provider. Epidemiological data can also identify problems. These could come from insurers or public health groups, for example, the Department of Public Health tracking chlamydia rates. Looking to the ‘Model for Improvement’, this step should partly answer the question of ‘What are we trying to achieve?’
Plan-do-check-adjust graph.
When we began the project, the study practices were screening 29% of eligible patients according to the Healthcare Effectiveness Data and Information Set (HEDIS). The eligible patients were women aged 16–24 who were deemed sexually active by a HEDIS algorithm. Our problem was defined as underperforming on chlamydia screening for women aged 16–24 years old.
Step 3. Identify stakeholders to build support for the project and assess level of interest
The next step is to prepare for the project ( figure 2 ). Research examples of similar projects and look for resources such as clinical guidelines to assist in developing your solution. The team needs to decide on a budget and timeline, determine if relevant data are already being collected, and establish what are the baseline data.
Our team began by identifying and recruiting clinician leaders from each of the stakeholder departments. From here we coordinated the work both with the operational leadership and clinical leadership of the local clinics as they would be responsible for insuring the process was in place and functioning. We also paired this QI project with the Part IV Maintenance of Certification (MOC) credit through the American Board of Medical Specialties Multi-Specialty Portfolio Program (MSPP). 17 An MOC project through MSPP provides physicians required credit towards maintaining board certification by conducting a QI project using the PDCA methodology. Additionally, we identified a toolkit for improving chlamydia screening. 18 The Agency for Healthcare Research and Quality has several examples on their website. 19
Step 4. Determine a goal and decide how to assess progress towards the goal and achievement of success
This involves deciding on a goal that is concrete, measurable, achievable and clinically important. This should be a discussion among the stakeholders, as what is important or achievable for one group may be different for another. Decide how to measure progress towards the goal, for example having monthly reports on screening rates that are reviewed by the stakeholders. This step fits into the ‘Model for Improvement’ under the first two questions noted in the Introduction section.
Our goal was to screen 57% (HEDIS 95th percentile) of eligible patients. Our measure of interest was the proportion of female patients aged 16–24 who had a chlamydia screen in the last 12 months. We planned to evaluate the project during an initial pilot period and once it was rolled out to all clinics, using the PDCA methodology. We agreed to meet monthly to review department-level data to allow for any further adjustments as needed. One example of an adjustment was changing the workflow to have a urine sample collected for any eligible patient prior to the visit. A model such as the above helped the team stay focused even in chaotic and demanding healthcare environments in which schedules and resources changed from day to day.
Step 5. Identify barriers
This can be done through brainstorming with stakeholders, surveying staff and through a root cause analysis ( figure 2 ). Physicians and non-physicians tend to jump to solutions instead of doing a root cause analysis. Root cause analysis is important to do so that the solution is sustainable. Root causes are underlying, can be controlled and managed. 20 They explain the what, why and how something occurs. The analysis involves data collection, recommendations and implementation very similar to the PDCA cycle. This process is slow and must be deliberate in order to create a new normal and ensure sustainability. This step addresses the ‘Model for Improvement’s’ last question.
In our case simply telling physicians to increase chlamydia screening will not work. The entire process must be changed. Some of the barriers we were able to identify were lack of knowledge of the screening recommendation, lack of knowledge of a non-invasive urine test for screening (no requirement for a pelvic exam), fear of breaking confidentiality for minors, not understanding the process of insurance coverage and insurances’ explanation of benefits to the parents of minors, discomfort discussing sexually transmitted infections during a clinic visit, lack of time in the visit to address sensitive issues, and a lack of a standardised approach to screening.
Step 6. Develop a countermeasure
As with defining the problem, a consensus among the team is crucial for success of the solution. This step is made easier when the problem and barriers have been clearly defined. The potential solution(s) must address the underlying causes of the problem. Solutions will also be more robust with input from the whole team. For example, if the front desk staff is responsible for giving patients information on screening, then input on how this is done best comes from them. There likely will be multiple solutions and they may vary by stakeholder.
We developed a standard approach for workflow, educational materials and a clinical decision support tool within the EHR to overcome our obstacles to screening. While not required for all QIs, a workflow was essential to our project. 21 The workflow streamlines discussion of screening, collection of screening sample, ordering test, follow-up of results and treatment. Because the workflow is standardised and easily visualised in the included flow sheet, it can be readily adapted to other clinical sites. The newly developed educational materials for staff, patients and parents explained the importance of screening, as well as the process for screening, and notification of results and treatment. These materials are also easily transferable to other sites. Lastly, the clinical decision support tool was an alert that is displayed in an area of the EHR called ‘best practice advisories’ (BPA). This notification is visible whenever the chart of an eligible patient is accessed. The automated alerts can easily be transferred to any healthcare system using an Epic EHR system ( figure 3 ).
Example of Chlamydia screening workflow. BPA, best practice advisories; MA, medical assistant; RN, registered nurseof M, University of Michigan.
Step 7. Test the process in a limited setting
Assessing the results and modifying the process on a small scale helps inform how the project is working ( figure 2 ). Typically, this involves conducting a pilot project. This is like a mini-PDCA cycle within the larger PDCA cycle of your QI project. This is where to test your initial problem, barriers, solutions and data collection, identify new barriers and solutions, and refine your process.
We carried out a pilot in three of our clinics: one family medicine, one paediatric and one internal medicine. These departments had representatives on the chlamydia QI team which facilitated the introduction and monitoring of the project. After 8 months the pilot clinics improved their chlamydia screening to 60% of eligible patients. During this time, feedback from the three clinics was used to adjust the process. For example, in paediatrics they felt that the discussion around chlamydia testing was too burdensome for all office visits given their high percentage of minor patients. They elected to use the workflow for chlamydia screening, and have the EHR alert, only during well-child exams rather than at all visits.
Step 8. Large scale project rollout
As illustrated in figure 1 , evaluating and modifying the project is a critical process more than a single step ( figure 2 ). This involves review of the data by the project team and by those who are doing the work, that is, medical assistants, office managers, physicians and nurses. All participants should be encouraged to provide feedback on the process, new barriers and new solutions. This can be done by surveying or interviewing the staff and by reviewing internal policies. 22–24
Following modifications informed by our pilot, we launched the project by activating the BPA and providing educational materials in all primary care clinics. This included presentations to educate the clinical providers and staff on the importance and need for process change to improve our low chlamydia screening rates. These occurred in the participating departments in large and small settings, for example at Grand Rounds as well as at medical assistant meetings for individual clinics.
Step 9. Evaluate and modify the QI project
As illustrated in figure 1, evaluating and modifying the project is a critical process more than a single step ( figure 2 ). This involves review of the data by the project team and by those who are doing the work, that is, medical assistants, office managers, physicians and nurses. All participants should be encouraged to provide feedback on the process, new barriers and new solutions. This can be done by surveying or interviewing the staff and by reviewing internal policies. 22–24
We met monthly to discuss the results from each of the participating departments. Shortly after a standard workflow and BPA had been implemented, the screening rate for women between 16 and 24 years old improved to 66% of eligible patients in family medicine clinics. We noticed an immediate improvement as soon as the process went live, and hypothesised the build-up and discussion of the project led to improvement before the process actually changed.
Additional barriers across departments identified were lack of adoption of the standard workflow among check-in staff, medical assistants and physicians. Our intervention to address this barrier was to standardise medical assistant workflow from intake to utilisation of the BPA particularly when the patient is 16–17 years old. A new standard workflow was agreed on and disseminated to each clinic. Two months after this intervention, our screening rates for 16–17 years old improved from 42% to 48%. Significantly, 4 years after our intervention, we have been able to maintain the rates of chlamydia screening well above our initial rate of 29%.
QI projects benefit from the step-by-step process outlined in the PDCA and Model for Improvement theories to effectively tackle potential challenges and improve the overall project’s relevance and success. The scale of the QI project can vary from a single clinical site to a large multispecialty group as the above example used. For example, Wakai et al 25 conducted a QI project in a single site but included an intervention. Focused on improvement of periodic assessments, they identified and addressed barriers and threats to the project’s success. QI projects can benefit from a mixed-methods approach, combining quantitative and qualitative analyses to better determine the next steps to the QI process. 22
Regardless of the model or the design used by the QI project, effective communication with all involved parties is key to successful QI projects. In hindsight, our project might have been more effective if we had communicated with our Department of Public Health about our change in approach to chlamydia screening. For example, in 2015, chlamydia incidence reached a record high prompting the Department of Public Health to declare an epidemic. The rate of positive screening tests was tracked by our microbiology lab and remained between 3.3% and 3.6%, although the number of tests increased by nearly 10 000 in 2015 compared with 2014, the year of our intervention. The increased positive tests were likely related to our increased screening efforts rather than a true outbreak.
Four years after intervening, the rates for chlamydia screening in our clinics ranged between 49% and 80% for 18–24 years old but 32%–63% for 16–17 years old. This is remarkable as achieving screening rates above 55% is difficult even in a research setting. 26 Despite the success in increasing screening rates for chlamydia, certain groups (ie, younger aged females) were still low. This highlights that QI projects may necessitate additional QI projects to address areas of concern that were discovered. For example, it was quickly noted that screening rates for 16–17 years old remained lower than for 18–24 years old. These data were not initially separated prior to our QI project or at the start of our intervention, limiting the ability to fully address this issue. We did however identify unique barriers mainly with the paediatric department that required modifications from the standard workflow that was working effectively for the chlamydia screening programme in other departments. The younger women, aged 16–17 years old, have special considerations for confidentiality, privacy and explanation of benefits forms designed to prevent accidental parent disclosures. In light of these findings, we plan to complete another MSPP MOC project for chlamydia screening to fully address these issues.
QI projects, including the one described above, have the ability to change healthcare delivery systems. Our QI project demonstrated the importance of chlamydia screening to the clinicians, and provided a feasible way to deliver care effectively to women aged 16–24 when coming for medical appointments. The use of a well-integrated BPA decreased clinicians’ mental demands by simply reminding and offering them of an evidence-based screening recommendation that could be selected with a single click.
There are several challenges and limitations to conducting QI projects. These projects require special skills that many clinicians lack. Furthermore, QI projects, similar to other research projects, need time, resources and commitment from multiple involved parties to successfully complete. The development and the design of QI projects should be carefully thought out, including how the project will be implemented, assessed, if needed, modified and communicated to others. QI projects, if not carefully designed, can be doomed by insufficient training or participation of all involved parties, poor fit with existing structural clinical flow or a perceived low priority of the project (eg, not a relevant or significant clinical issue). Also, if publication is a possibility, institutional review board approval should be requested.
Other resources
The Society of Teachers of Family Medicine (STFM) Conference of Practice Improvement is provided annually and features practical skills and resources for practice change. The STFM also has a rich online resource catalogue of courses, presentations and handouts on QI. Some academic institutions cover courses in business, public health and/or engineering schools. Furthermore, international organisations such as the World Organisation of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians 27 are committed to the improvement of patients’ quality of life and have offered QI workshops in the past. 28
Conclusions
Incorporating QI training programmes is a good investment for healthcare organisations and academic centres since they generate useful projects that will likely positively impact the overall healthcare system and improve dissemination of helpful and high-quality clinical strategies. The QI approach presented here can be applied to a myriad of clinical scenarios. Potential areas for improvement include any disease with a screening recommendation, for example lung cancer screening with low-dose CT scan. This project could also work for situations other than screening, such as triage of patient phone calls to clinic, or increasing uptake of the human papillomavirus vaccine. While QI projects require commitment and resources, as demonstrated here, these projects have the potential for primary care physicians to improve the health of the entire populations.
- Strategy CQ
- Hurtado MP SE ,
- Corrigan JM
- Juran JM GA
- Goodman D , et al
- Education QT
- Exchange AHCI
- Leaders APSfC
- Prevention CfDCa
- Incidence P and Cost of Sexually Transmitted Infections in the United States
- Fleming DT ,
- Wasserheit JN
- Gottlieb SL ,
- Chlamydia Statistics
- Program STatAM-SP
- Administration USDoHaHSHRaS
- Rooney JJ ,
- Bravata DM ,
- Sundaram V ,
- Lewis R , et al
- Creswell JC HM
- DeJonckheere M VL
- Engelman A ,
- Meeks LM MDF
- Simasek M ,
- Nakagawa U , et al
- Reid M , et al
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval This study was deemed not regulated by the University of Michigan Institutional Review Board.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:

Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
QOF quality improvement case studies
Three case studies developed by the Royal College of General Practitioners, National Institute for Health and Care Excellence and the Health Foundation which provide examples of how practices could approach their quality improvement activity.
QOF 2020/21 quality improvement cases studies
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- 10 Essential Public Health Services
- Cooperative Agreements, Grants & Partnerships
- Public Health Professional: Programs
- Health Assessment: Index
- Research Summary
- COVID-19 Health Disparities Grant Success Stories Resources
- Communication Resources
Performance Management and Quality Improvement: Definitions and Concepts
At a glance.
In the public health field, many initiatives and organizations focus on improving public health practice, using different terms. This page provides common definitions for public health performance management.
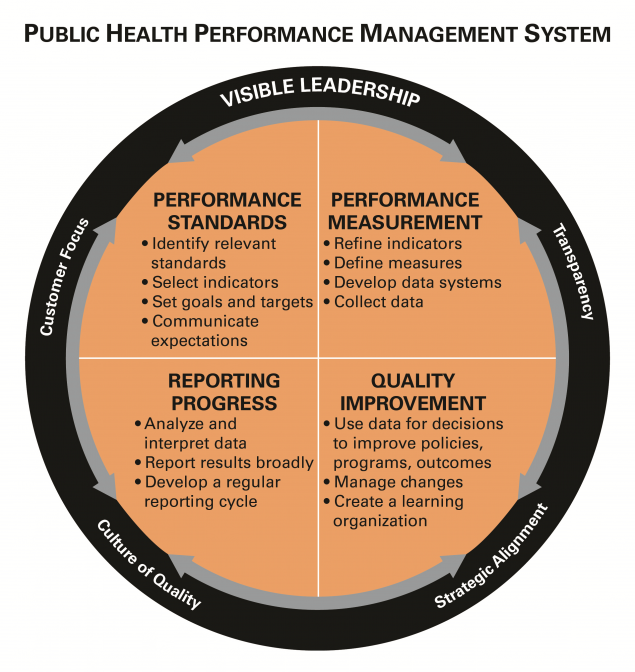
Definitions and concepts
There has been a rapidly growing interest in performance and quality improvement within the public health community, and different names and labels are often used to describe similar concepts or activities. Other sectors, such as industry and hospitals, have embraced a diverse and evolving set of terms but which generally have the same principles at heart (i.e., continuous quality improvement, quality improvement, performance improvement, six sigma, and total quality management).
In the public health field, an array of initiatives has set the stage for attention to improving public health practice, using assorted terms. The Turning Point Collaborative focused on performance management, the National Public Health Performance Standards Program created a framework to assess and improve public health systems, while the US Department of Health and Human Services has provided recommendations on how to achieve quality in healthcare . In 2011, the Public Health Accreditation Board launched a national voluntary accreditation program that catalyzes quality improvement but also acknowledges the importance of performance management within public health agencies. Regardless of the terminology, a common thread has emerged—one that focuses on continuous improvement and operational excellence within public health programs, agencies, and the public health system.
To anchor common thinking, below are links to some of the definitions that are frequently used throughout these pages.
Key definitions
- Riley et al, "Defining Quality Improvement in Public Health", JPHMP, 2010, 16(10), 5-7.
- Public Health Accreditation Board Acronyms and Glossary of Terms, Version 2022 [PDF]
Public Health Gateway
CDC's National Center for State, Tribal, Local, and Territorial Public Health Infrastructure and Workforce helps drive public health forward and helps HDs deliver services to communities.
- Research article
- Open access
- Published: 13 September 2017
Domains associated with successful quality improvement in healthcare – a nationwide case study
- Aleidis Skard Brandrud 1 ,
- Bjørnar Nyen 2 ,
- Per Hjortdahl 3 ,
- Leiv Sandvik 4 ,
- Gro Sævil Helljesen Haldorsen 5 ,
- Maria Bergli 1 ,
- Eugene C. Nelson 6 &
- Michael Bretthauer 7
BMC Health Services Research volume 17 , Article number: 648 ( 2017 ) Cite this article
11k Accesses
26 Citations
10 Altmetric
Metrics details
There is a distinct difference between what we know and what we do in healthcare: a gap that is impairing the quality of the care and increasing the costs. Quality improvement efforts have been made worldwide by learning collaboratives, based on recognized continual improvement theory with limited scientific evidence. The present study of 132 quality improvement projects in Norway explores the conditions for improvement from the perspectives of the frontline healthcare professionals, and evaluates the effectiveness of the continual improvement method.
An instrument with 25 questions was developed on prior focus group interviews with improvement project members who identified features that may promote or inhibit improvement. The questionnaire was sent to 189 improvement projects initiated by the Norwegian Medical Association, and responded by 70% (132) of the improvement teams. A sub study of their final reports by a validated instrument, made us able to identify the successful projects and compare their assessments with the assessments of the other projects. A factor analysis with Varimax rotation of the 25 questions identified five domains. A multivariate regression analysis was used to evaluate the association with successful quality improvements.
Two of the five domains were associated with success: Measurement and Guidance ( p = 0.011), and Professional environment ( p = 0.015). The organizational leadership domain was not associated with successful quality improvements ( p = 0.26).
Our findings suggest that quality improvement projects with good guidance and focus on measurement for improvement have increased likelihood of success. The variables in these two domains are aligned with improvement theory and confirm the effectiveness of the continual improvement method provided by the learning collaborative. High performing professional environments successfully engaged in patient-centered quality improvement if they had access to: (a) knowledge of best practice provided by professional subject matter experts, (b) knowledge of current practice provided by simple measurement methods, assisted by (c) improvement knowledge experts who provided useful guidance on measurement, and made the team able to organize the improvement efforts well in spite of the difficult resource situation (time and personnel). Our findings may be used by healthcare organizations to develop effective infrastructure to support improvement and to create the conditions for making quality and safety improvement a part of everyone’s job.
Peer Review reports
Healthcare is suffering from serious unsolved problems that are threatening lives, increasing costs, and making the care unpredictable to the patient [ 1 , 2 , 3 , 4 , 5 , 6 , 7 ]. Improvement of quality in health care, is probably one of the greatest challenges of modern healthcare leadership. Quality improvement strategies sometimes fail to focus the changes on clinical, patient oriented improvements, and to involve the frontline healthcare professionals at an early stage of the change process [ 8 , 9 , 10 ].
The role of qualified improvement guidance has received little attention in the quality improvement literature [ 11 , 12 , 13 , 14 , 15 ]. A recent analysis of 35 systematic reviews explored the influence of context on the effectiveness of different quality improvement strategies. Improvement guidance was not found among a broad range of associated contextual factors that contribute to successful improvement. The analysis organized the findings based on the Model for Understanding Success in Quality (MUSIQ) model [ 16 , 17 ]. The MUSIQ model itself was based on a systematic review that included continual improvement interventions, but did not cover the role of improvement knowledge guidance [ 14 , 17 ]. A cluster-randomized trial aimed to compare clinic-level coaching with other learning collaborative components, found coaching to be equally effective with interest circle calls (group telephone conferences) in achieving clinical outcome improvements, but coaching was more cost-effective [ 18 ]. Godfrey did also find positive effects of systematic clinic-level coaching [ 19 , 20 ].
In a case study of 182 improvement teams Strating found that creating measurable targets is a crucial task in quality improvement [ 21 ]. In a systematic review of quality measurement . Thor et al. found statistical process control (SPC), to be a useful method for those who mastered the technique [ 22 ]. This underscores the importance of good measurement guidance.
Many healthcare organizations do not have a basic infrastructure to support improvement, and contextual factors generally receive scant attention in the current literature on quality improvement strategies [ 13 , 14 , 16 , 22 , 23 ]. Kringos et al. found that the availability and functionality of information technology and facilitated data collection improved the effectiveness of quality improvement intervention, as well as the involvement of multidisciplinary improvement teams [ 16 ].
Little evidence is found that leadership support is associated with successful quality improvement [ 24 , 25 , 26 ]. This may be typical for external initiated learning collaboratives, because we found a few studies where the frontline leaders have been directly included in the project planning and improvement guidance, with a positive leadership influence on the effectiveness of the improvement efforts [ 16 , 18 , 19 , 20 ].
Since 1994, and in spite of a limited underpinning of scientific evidence , the continual improvement method has been spread worldwide by thousands of improvement collaboratives [ 13 , 27 , 28 , 29 ]. Relatively little of that work is reported in the biomedical literature [ 30 ]. Systematic reviews and single studies of quality improvement efforts that are reported, indicate that a systematic and knowledge based approach is not enough to succeed without the presence of certain conditions for improvement, also described as context factors [ 13 , 14 , 16 , 31 ]. To meet these challenges, additional improvement approaches, including instruments for evaluating the underlying conditions for improvement, have been described [ 12 , 17 , 32 ]. In 2004 a systematic review recommended further research on factors that tend to produce adoptable changes in healthcare organizations [ 33 ]. A recent umbrella review of 35 systematic reviews of the influence of context factors on the effectiveness of (any) quality improvement intervention recommend further research to report the context factors in a systematic way to better appreciate their relative importance [ 16 ].
The present study explores the conditions for improvement in the context of 189 Norwegian clinical improvement projects initiated by the learning collaboratives of The Norwegian Medical Association. We asked participating clinicians to identify factors that may promote or inhibit quality improvement. Referring to the studies above, two of the unanswered questions are (1) “ What combination of what factors tend to produce “adoptable” improvement innovations ?” [ 33 ]. (2) How is the effectiveness of the continual improvement method? (The continual improvement method is described in Additional file 1 : Supplement 1). The purpose is to identify domains associated with success, as this knowledge may be used to develop an infrastructure and culture that promotes continual improvement in healthcare, without the help from a learning collaborative.
The method of the present study had four steps. First we developed a questionnaire for improvement teams. The instrument was based on a qualitative study of the conditions for change among 19 participants of the learning collaboratives of the Norwegian Medical Association (Sub study I, published in 2011) [ 23 ]. Second, we submitted the questionnaire to the 189 improvement teams of the same learning collaboratives. Third , we analyzed the data by comparing the reported conditions for improvement in the organizations of the successful projects versus the other (comparator) projects. We already knew the success level of the 189 projects from the validation of a Change Process and Outcome Scale instrument which was published in 2015 (Sub study II) [ 32 ].
The learning collaboratives
Between 1998 and 2011 The Norwegian Medical Association sponsored eight hospital related improvement collaboratives to support quality and safety improvement efforts in clinical environments (Table 1 ). The improvement collaboratives were based on the Breakthrough Series model of the Institute for Healthcare Improvement, aiming to accelerate improvement beyond what had been achieved by traditional educational approaches [ 34 ]. The model has two dimensions: the learning collaborative method (national level), and the systematic approach to continual improvement (organizational level) [ 11 , 22 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ] (described in Additional file 1 : Supplement 1). Each collaborative lasted from 6 to 9 months and engaged clinicians from 15 to 30 healthcare organizations who met to learn from each other and from recognized experts in specified topic areas (Table 1 ). The participating improvement teams sent 2–4 representatives from different disciplines involved in the topic (at least one physician) to three collaborative learning sessions, where the relevant subject matter experts of the collaborative (medicine, nursing, psychology, etc.) demonstrated the quality gaps within the topic to the participants. A team of 10–15 improvement knowledge experts (coaches) guided the improvement teams at, and in between the learning sessions.
Instrument development
The questionnaire was developed to identify the activities and conditions associated with successful quality improvement initiatives, and to study the effectiveness of the continual improvement method (Additional file 1 : Supplement 1). The instrument and its development is described in details in Additional file 1 : Supplement 2.
Sub study I
The first sub study was published in 2011 [ 23 ], and provided us with a large amount of relevant comments, and enabled us to develop a validated questionnaire reflecting the most interesting conditions for change reported by clinicians telling their improvement project stories from their own organizations, after participating in a learning collaborative of the Norwegian medical association.
Data collection
The questionnaire was submitted to former improvement team leaders between 2 and 4 years after the end of each improvement collaborative. We had access to their e-mail addresses from the improvement collaborative participant list. A link to an on-line questionnaire was e-mailed to the improvement team leaders. They were asked to think back on their improvement project and the promoting and inhibiting conditions for quality improvement that they encountered, and to show their level of agreement with the focus group comments that were included in the questionnaire.
If a Word-version of the questionnaire was preferred, the respondents returned their filled-in questionnaires by e-mail or “surface mail”. In cases of non-response from team leaders, we contacted other participants from the same team. In 36% of the teams, late responses lead to more than one response from the same team. Because the responses from team members mostly reflected different professions, and the inter-rater reliability of the same team ranged from poor to strong, we decided to let each team be represented by the average ratings of its responding members.
Project evaluation
This study is neither an experiment, nor a study of the experiments of others, aiming to bring evidence to the success of the projects in our material. This is a study of the conditions for making successful changes. The aim is to learn from healthcare professionals in the improvement teams of those projects who have been able to document improvements.
Sub study II
The second sub study was published in 2015 [ 32 ]. Seven improvement experts from different healthcare professions alternated in participating in a four-person review team. The reviewers were two physicians (BN and TSH), three nurses (GSH, ASB, and EA), one psychologist (LdG) and one bioengineer (AS). The improvement experts were not involved in the evaluation of projects they had participated in with coaching or other kinds of support. In this study we explored the final reports of the improvement teams. We developed a checklist to structure the study according to the recommended improvement method (Plan- Do-Study- Act-cycles) [ 38 ], to make it easier to discuss our observations an reflect on our different assessments of the project. The criterion to be classified as successful was to document significant improvements by recognized measurement methods, based on a clear linkage between vision, aims, change efforts and measurements.
We found that 72 projects (38%) were successful, ranging from 17 to 60% within each of the eight collaboratives. A majority (78%) presented their outcomes as a shift in the level in the desired direction on a control chart.
Data analysis
We analyzed the association between the assessments of the improvement teams (responses to 25 selected questions) and the success level of their projects. First, a logistic regression analysis was used to analyze the association between success and each of the 25 questions. Second, a factor analysis with Varimax rotation was used to identify the underlying structure of the 25 questionnaire items. Domains were extracted with an Eigen value greater than one. Kendall’s-tau-b correlation revealed that the conditions for a principal component analysis (PCA) were present. Third, when analyzing the multivariate associations between the five domains and success. Logistic regression analyses were performed, with success as the dependent variable, and the success domains as independent variables. Only domains which were significant in a bivariate analysis (defined as p < 0.05) were included in the multivariate regression analyses. The results from the regression analyses are presented as odds ratios with 95% confidence intervals and corresponding p -values. A significance level of 5% was used. All statistical analyses were performed using the software package IBM-SPSS version 21.
Our results are based on the answers to the 25 variables of the questionnaire from the successful versus the other projects. The questionnaires were returned by 53 physicians, 56 nurses, 38 psychologists, and 51 other healthcare professionals, representing 132 (70%) of the 189 improvement teams. Of the 132 responding projects, 54 (41%) had documented improvements in their final reports by recognized measure methods, and 78 (59%) had not been able to do so within the time frame of the learning collaborative (Table 2 ). The results of the 54 successful projects are presented in Additional file 1 : Supplement 3, not as a result of this study, but to illustrate the relationship between the changes they have made, and the conditions for change reflected in our findings.
Research question I: “What combination of what factors tend to produce “adoptable” improvement innovations?”
First, in a logistic regression analysis of the answers to the 25 questions of the questionnaire (Additional file 1 : Supplement 2) we identified the variables which were significant associated with success. Two variables were found in the final model: ( Q12) Good guidance & help with measurement, and (Q7) Someone in the improvement team enjoyed working with measurement (Table 3 ).
Second, to disentangle what combination of variables are underpinning successful improvement efforts, we performed a factor analysis of the 132 responses to the 25 questions. This analysis produced five domains: Domain I: “ Measurement and Guidance” (nine variables), Domain II: “ Leadership engagement ”(five variables), Domain III: “ Professional environment ” (seven variables), Domain IV: “ Group process” (two variables), and Domain V “ Leadership impact” (two variables) (Table 4 ).
Third, we studied the quartiles of the domains in the successful projects and compared the scores from the 54 successful projects with the 78 comparator projects within the five domains. Two domains were significantly associated with success: Domain I Measurement & Guidance ( p = 0.002) and Domain III Professional environment ( p = 0.002), (Table 5 ).
Finally, we made a logistic regression analysis of the five success domains. As shown in Table 6 , two domains were found in the final model: “ Measurement and Guidance” and “ Professional environment” , confirming the findings of the crude analyses displayed in Table 5 .
The complexity of our findings is displayed in Table 7 presenting the combination of variables that are underpinning the two success domains, illustrated by the proportion of successful and comparator projects scoring on the positive side of the scale (4 + 5) to each variable.
The first success domain “Measurement & Guidance” cover the two success variables from the first regression analysis: Good guidance & help with measurement, and Someone in the improvement team enjoyed working with measurement. In addition the findings suggest it was easier for the successful projects to get hold on their coach when needed (Q10), an availability they assessed as important to succeed (Q11). Further, did the control charts appear to be easy to communicate to their peers in the site (Q20), assessed as important when trying to make successful improvements (Q21).
The second success domain “Professional environment” indicate the importance of presenting patient focused aims when trying to engage of the professional environment in the improvement efforts (Q16), and the importance of presenting measurement to maintain motivation (Q23). Regardless of their success level, 83% reported they had been able to organize their improvement efforts well, in spite of a limited resource situation (Q5) (Table 7 ).
Research question 2: How is the effectiveness of the continual improvement method?
Our findings reflect the intellectual underpinnings of the continual improvement method presented in Additional file 1 : Supplement 1. High performing professional environments were successfully pursuing patient-centered quality improvement if they had access to a combination of: (a) knowledge of best practice , provided by professional subject matter experts, (b) knowledge of current practice provided by simple measurement methods, learned from (c) improvement knowledge experts who provided good guidance and help with measurement, and made the team able to organize the improvement efforts well in spite of the difficult resource situation (time and personnel).
Our findings support improvement knowledge guidance
Our study underscores the power of good guidance and help with measurement. In contrast to most learning collaboratives abroad, The Norwegian Medical Association invested in a team of 10–15 improvement knowledge experts (coaches) to guide their improvement teams [ 23 ]. The coaching team met regularly for education and training. A system of mentoring was developed to enable experienced coaches to support the novice coaches (Additional file 1 : Supplement 4).
Our findings support measurement for improvement as a cornerstone of the project
The present study highlights the importance of using measurement to understand and reflect on the variations in current practice, and to monitor the target process continually to maintain motivation for change. Learning from the final reports of the improvement projects, the sub study indicate that successful results are connected to a clear linkage between vision, aims and proper measurements, clear and understandable improvement efforts, and the ability to communicated this all to others in an understandable way [ 32 ]. Our findings support the findings of others indicating that by measuring and monitoring variation and change with control charts, it is easier to understand and manage performance from week-to-week, communicate progress, and motivate colleagues to sustain the improvements [ 43 , 44 , 45 , 46 , 47 , 48 ].
Our findings indicate common Interprofessional interest in the patients’ welfare
Our The glue for interprofessional collaboration is a common interest in the patient’s welfare, which has been emphasized as crucial by others [ 49 ]. We found that 92% of the 198 responding physicians, nurses, psychologists and other members of the improvement teams found patient-centered targets of “great” or “very great” importance for engaging their colleagues in quality improvement (Q16 Table 7 ).
Our findings call for an infrastructure for improvement in healthcare
We have found that successful quality improvement efforts depend on certain conditions for change in the participating organizations that to a certain degree have been facilitated by the national learning collaborative. However, if continual improvement efforts are to become part of everyone’s work in healthcare, an infrastructure for improvement that at least is providing similar conditions for change in the local context is essential. The infrastructure should include: (a) a system that promotes leadership’s engagement at every stage of the improvement work, (b) provides easy access to clinical data needed for improvement measurement and reflection, and (c) provides qualified improvement guidance to frontline clinical improvement teams [ 23 ].
Methodological considerations
A significant part of the overall spectrum of healthcare problems constitutes matters that are not principally biological. For this reason, it is essential to know how the philosophies of the social sciences and the biological sciences differ. One does not erroneously use the criteria for one area to judge another. The social sciences differ from the biological sciences in two aspects: They entail greater elements of overt interpretation that often enter into the collection of data. In many cases, a research result is an understanding, not an explanation. The difference between explanation and understanding however, is not as distinct as many believe [ 50 ], and in this study, we are including both.
The present study is exploring the conditions for making desired changes in healthcare. We are not reporting on a scientific experiment aiming to bring evidence to the success of the services and projects in our material. This study has been developed with the prerequisite of the known outcome of the learning collaborative projects of the Norwegian Medical Association.
Learning from high performers stems from a growing number of “positive deviance” approaches to quality improvement [ 50 , 51 , 52 , 53 ]. The aim of the present study is to learn from healthcare professionals in the improvement teams of those projects who have been able to document improvements based on a clear linkage between vision, aims, change efforts and measurements.
Process and outcome evaluation by improvement experts and improvement teams can illuminate the strategies and processes responsible for the improvement of the target process. In so doing, the process and outcome evaluation from sub study II [ 32 ], makes a relevant and important contribution to the development of potentially successful strategies to make positive changes in patient care [ 12 ].
It is a limitation that 75% of the projects covered by our research are from the psychiatric sector and one may conclude that the results are limited to this field. (Table 1 ) The general theoretical framework that we have used (see Additional file 1 : Supplement 1), the findings of others (see the Background section), and the matching conditions for improvement reported by the improvement teams from the non-psychiatric settings however, does not support this limitation [ 23 ].
It is a strength that the items used in the questionnaire was based on a data collection method that invites respondents to share their point of view, rather than respond to researcher-initiated questions [ 54 ]. We designed the questionnaire to be large enough to cover the most important comments, and short enough to get a decent response rate. As described in Additional file 1 : Supplement 2, this implied a step-wise reduction of the material from 233 (partly overlapping) comments to a final selection of 17. In spite of our systematic approach, we may unintentionally have excluded important comments in this process that should have been included in the study. The eight additional questions regarding the importance of the most critical incidents are meant to compensate for this limitation (Additional file 1 : Supplement 2).
Our findings suggest that quality improvement projects with good guidance and a sharp focus on measurement for improvement, have an increased likelihood of success.
The two success domains are well aligned with continual improvement theory. High performing professional environments were successfully pursuing patient-centered quality improvement if they had access to a combination of: (a) knowledge of best practice , provided by professional subject matter experts, (b) knowledge of current practice provided by simple measurement methods, learned from (c) improvement knowledge experts who provided good guidance and help with measurement, and made the team able to organize the improvement efforts well in spite of the difficult resource situation (time and personnel).
Our findings may be useful for healthcare organizations in the development of an effective infrastructure for improvement and thereby create necessary conditions for making quality and safety improvement a part of everyone’s job.
Havik OE. A general model for psychological reactions in somatic disease. How can we understand and care for the patients’ psychological needs? Nordisk Psykologi. 1989;41:161–76.
Article Google Scholar
Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US) 2000.
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press (US); 2001.
Google Scholar
Nelson EC, Batalden PB, Huber TP, Mohr JJ, Godfrey MM, Headrick LA, Wasson JH. Microsystems in health care: part 1. Learning from high-performing front-line clinical units. Jt Comm J Qual Improv. 2002;28:472–93.
PubMed Google Scholar
Deilkås ET. Report from a national medical record review using the global trigger tool. In: Report from the Norwegian knowledge Centre for the Health Services (editor); 2011.
Rotter T, Kinsman L, James E, Machotta A, Gothe H, Willis J, Snow P, Kugler J. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane systematic review and meta-analysis. Eval Health Prof. 2012;35:3–27.
Andel C, Davidow SL, Hollander M, Moreno DA. The economics of health care quality and medical errors. J Health Care Finance. 2012;39:39–50.
Blumenthal D, Kilo CM. A report card on continuous quality improvement. Milbank Q. 1998;76:625–48.
Article CAS PubMed PubMed Central Google Scholar
Groene O, Klazinga N, Walshe K, Cucic C, Shaw CD, Sunol R. Learning from MARQuIS: future direction of quality and safety in hospital care in the European Union. Qual Saf Health Care. 2009;18(Suppl 1):i69–74.
Article PubMed PubMed Central Google Scholar
Rozenblum R, Lisby M, Hockey PM, Levtzion-Korach O, Salzberg CA, Efrati N, et al. The patient satisfaction chasm: the gap between hospital management and frontline clinicians. BMJ Qual Saf. 2013;22:242–50.
Article PubMed Google Scholar
Ovretveit J, Bate P, Cleary P, Cretin S, Gustafson D, McInnes K, McLeod H, Molfenter T, Plsek P, Robert G, et al. Quality collaboratives: lessons from research. Qual Saf Health Care. 2002;11:345–51.
Article CAS PubMed Google Scholar
Grol R, Wensing M, Eccles M, Davis D. Improving patient care: the implementation of change in healthcare. 2.ed. BMJ Books, Willey Blackwell; 2013.
Spencer E, Walshe K. National quality improvement policies and strategies in European healthcare systems. Qual Saf Health Care. 2009;18(Suppl 1):i22–7.
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, Margolis P. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88:500–59.
Glasgow JM, Davies ML, Kaboli PJ. Findings from a national improvement collaborative: are improvements sustained? BMJ Qual Saf. 2012;21:663–9.
Kringos DS, Sunol R, Wagner C, et al. The influence of context on the effectiveness ofhospital quality improvement strategies: a review of systematic reviews. BMC Health Serv Res. 2015;15:277.
Kaplan HC, Provost LP, Froehle CM, Margolis PA. The model for understanding success in quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21:13–20.
Gustafson DH, Quanbeck AR, Robinson JM, Ford JH, Pulvermacher A, French MT, et al. Which elements of improvement collaboratives are most effective? A cluster-randomized trial. Addiction. 2013;108:1145–57.
Godfrey MM, Andersson-Gare B, Nelson EC, Nilsson M, Ahlstrom G. Coaching interprofessional health care improvement teams: the coachee, the coach and the leader perspectives. J Nur Manag. 2014;22:452–64.
Godfrey MM. Improvement capability at the front lines of healthcare. Helping through leading and coaching. Jönköping University, School of Health Sciences; Dissertation Series No. 46, 2013.
Strating MMH, Nieboer AP, Zuiderent-Jerak T, Bal RA. Creating effective quality-improvement collaboratives: a multiple case study. BMJ Qual Saf. 2011;20:344–50.
Wilson T, Berwick DM, Cleary PD. What do collaborative improvement projects do? Experience from seven countries. Jt Comm J Qual Saf. 2003;29:85–93.
Brandrud AS, Schreiner A, Hjortdahl P, Helljesen GS, Nyen B, Nelson EC. Three success factors for continual improvement in healthcare: an analysis of the reports of improvement team members. BMJ Qual Saf. 2011;20:251–9.
Hulscher MEJL, Schouten LMT, Grol RPTM, Buchan H. Determinants of success of quality improvement collaboratives: what does the literature show? BMJ Qual Saf. 2013;22:19–31.
Øvretveit J. Leading improvement effectively: review of research (Editor). The Health Foundation; 2009.
Mills PD, Weeks WB. Characteristics of successful quality improvement teams: lessons from five collaborative projects in the VHA. Jt Comm J Qual Saf. 2004;30:152–62.
Leape LL, Rogers G, Hanna D, Griswold P, Federico F, Fenn CA, et al. Developing and implementing new safe practices: voluntary adoption through statewide collaboratives. Qual Saf Health Care. 2006;15:289–95.
Schouten LMT, Hulscher MEJL, van Everdingen JJE, Huijsman R, Grol RPTM. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ. 2008;336:1491–4.
Franco LM, Marquez L. Effectiveness of collaborative improvement: evidence from 27 applications in 12 less-developed and middle-income countries. BMJ Qual Saf. 2011;20:658–65.
Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney SE. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152.
Øvretveit J. Understanding the conditions for improvement: research to discover which context influences affect improvement success. BMJ Qual Saf. 2011;20(Suppl 1):i18–23.
Brandrud AS, Haldorsen GSH, Nyen B, Vardal M, Nelson E, Sandvik L, et al. Development and validation of the CPO scale: a new instrument for evaluation of health care improvement efforts. Q Manage Health Care. 2015;24:109–20.
Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629.
Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement; 2003. (Available on www.IHI.org . 8 Aug. 2017 at http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx ).
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290–8.
Minkman MMN, Schouten LMT, Huijsman R, van Splunteren PT. Integrated care for patients with a stroke in the Netherlands: results and experiences from a national breakthrough collaborative improvement project. Int J Integr Care. 2005;5:e14.
Batalden PB, Stoltz PK. A framework for the continual improvement of health care: building and applying professional and improvement knowledge to test changes in daily work. Jt Comm J Qual Improv. 1993;19:424–45.
CAS PubMed Google Scholar
Langley GJ, Moen RD, Nolan KM, Noland TW, Norman CL, Provost LP. The Improvement Guide. A Practical Approach på Enhancing Organizational Performance. 2.Ed. San Fransisco: Jossey-Bass; 2009.
Berwick DM. Continuous improvement as an ideal in health care. N Engl J Med. 1989;320:53–6.
Brennan S, McKenzie JE, Whitty P, Buchan H, Green S. Continuous quality improvement: effects on professional practice and healthcare outcomes (protocol). Cochrane Database Syst Rev. 2009:CD003319.
Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care. 2007;16:2–3.
Deming WE. Out of the crisis. MIT Press; 2000.
Thor J, Lundberg J, Ask J, Olsson J, Carli C, Harenstam KP, Brommels M. Application of statistical process control in healthcare improvement: systematic review. Qual Saf Health Care. 2007;16:387–99.
Nolan TW, Provost LP. Understanding variation. Qual Prog. 1990;23:70–8.
Wheeler DJ. Making sense of data: SPC for the service sector. Knoxville: SPC Press; 2003.
Henderson GR, Mead GE, van Dijke ML, Ramsay S, McDowall MA, Dennis M. Use of statistical process control charts in stroke medicine to determine if clinical evidence and changes in service delivery were associated with improvements in the quality of care. Qual Saf Health Care. 2008;17:301–6.
Neuhauser D, Provost L, Bergman B. The meaning of variation to healthcare managers, clinical and health-services researchers, and individual patients. BMJ Qual Saf. 2011;20:i36–40.
Solberg LI, Mosser G, McDonald S. The three faces of performance measurement: improvement, accountability, and research. Jt Comm J Qual Improv. 1997;23:135–47.
Berwick DM. What ‘patient-centered’ should mean: confessions of an extremist. Health Aff. 2009;28:w555–65.
Hofman B, Holm S. Philosophy of science. In: Laake P, Benestad HB, Olsen BR, editors. Research in medical and biological sciences. London: Academic Press Elsevier Ltd; 2015. p. 1–41.
Nelson EC, Batalden PB, Huber TP, et al. Microsystems in health care: part 1. Learning from high-performing front-line clinical units. Jt Comm J Qual Patient Saf. 2001;28:472–93.
Lawton R, Taylor N, Clay-Williams R, et al. Positive deviance: a different approach to achieving patient safety. BMJ Qual Saf. 2014;3:880–3.
Baxter R, Taylor N, Keller I, Lawton R. What methods are used to apply positive deviance within healthcare organizations? A systematic review. BMJ Qual Saf. 2016;25:190–201.
Gremler DD. The critical incident technique in service research. J Serv Res. 2004;7:65-89. doi: 10.1177/1094670504266138 .
Download references
Acknowledgements
The Norwegian Medical Association Quality Assurance Fund for Quality and Safety provided partial funding for the first part of the data collection of this study (2006-2008). The authors thank Lill de Grève (LdG), Ada Schreiner (AS), Tordis Sørensen Høifødt (TSH) and Ellen Andersen (EA) for their participation in the evaluation of the 189 projects. The authors thank H. Asbjørn Holm, Ole Tjomsland, and Lars Strauman for their help and support with this study.
Vestre Viken Health Trust (research team leader), South Eastern Norway Regional Health Authority funding our statistical support by the Oslo Center for Biostatistics and Epidemiology, Research support Services (co-supervisor). Norwegian Cancer Society and Research Council of Norway (main supervisor).
Availability of data and materials
Anonymised datasets are available from the corresponding author on request.
Author information
Authors and affiliations.
Quality Department, Vestre Viken Health Trust, Wergelandsgate 10, Postbox 800, 3004, Drammen, Norway
Aleidis Skard Brandrud & Maria Bergli
Municipality of Porsgrunn, Porstbox 128, N-3901, Porsgrunn, Norway
Bjørnar Nyen
Department of Family Medicine, Faculty of Medicine, University of Oslo, PO Box 1130, Blindern, NO-0318, Oslo, Norway
Per Hjortdahl
Oslo Center for Biostatistics and Epidemiology, Research support Services, Oslo University Hospital, Sogn Arena, Klaus Torgaards vei 3, 0372, Oslo, Norway
Leiv Sandvik
South Eastern Norway Regional Health Authority, PO Box 404, 2303, Hamar, Norway
Gro Sævil Helljesen Haldorsen
The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, 30 Lafayette Street, Lebanon, NH, USA
Eugene C. Nelson
Department of Health and Society, Faculty of Medicine, University of Oslo, PO Box 1130, Blindern, NO-0318, Oslo, Norway
Michael Bretthauer
You can also search for this author in PubMed Google Scholar
Contributions
ALL authors read and approved the final manuscript, agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. ASB was the research team leader and main responsible for planning and conducting the entire study. She has an intimate knowledge of the database and its content, and is main responsible for the data analysis and the manuscript. BNY collected data from one of the focus groups, participated in the development of the two instruments, participated in the evaluation of the improvement projects, has an intimate knowledge of the database and its content, assisted in the data analysis and participated in writing of the manuscript. PHJ supervised the planning and data collection part of the study, has an intimate knowledge of the database and its content, and participated in writing of the manuscript. LSA assisted in planning the research process, has an intimate knowledge of the database and its content, supervised the statistical analysis of the data, and participated in the writing of the manuscript. GSH collected data from one of the focus groups, participated in the development of the two instruments, participated in the evaluation of the improvement projects, and in the final preparation of the manuscript. MBE has an intimate knowledge of the database and its content, assisted in the analysis of the data and the literature review, and in the final preparation of the manuscript. ECN assisted in planning the research process, in outlining the contents of the article and in editing and reading the manuscript. MBR is the main supervisor of the study, has an intimate knowledge of the database and its content, assisted in the data analysis and participated in writing of the manuscript.
Corresponding author
Correspondence to Aleidis Skard Brandrud .
Ethics declarations
Ethics approval and consent to participate.
The dissertation proposal was evaluated by the regional ethics committee of South-East Norway 4 Oct 2012 and waived from formal approval according to Norwegian law due to the fact that it did not involve patient interventions. Later, the study was approved by the Data Protection Authority of Oslo University Hospital as required by Norwegian law. Informed consent was obtained from all informants of this study before enrolment. The thus, all necessary approval has been in place.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Supplement QI Success Domains. (DOCX 350 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Brandrud, A.S., Nyen, B., Hjortdahl, P. et al. Domains associated with successful quality improvement in healthcare – a nationwide case study. BMC Health Serv Res 17 , 648 (2017). https://doi.org/10.1186/s12913-017-2454-2
Download citation
Received : 16 October 2015
Accepted : 17 July 2017
Published : 13 September 2017
DOI : https://doi.org/10.1186/s12913-017-2454-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality improvement
- Learning collaboratives
- Continual improvement
- Conditions for change
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Continuous listening
- Crowdsourcing
- Digital feedback
- Digital rounding
- CAHPS & regulatory
- Healthcare big data
- Machine learning & AI
- Predictive analytics
- Natural language processing
- Key drivers analysis
- Transparency
- Effective reporting
- Data visualizations
- Interactive dashboards
- Industry benchmarks
- Review publishing
- Service recovery
- High reliability & PSO
- Core measures
Problems we solve
- Brand & growth
- Patient experience
- Health plan star ratings
- Employee experience
- Diversity, equity & inclusion
- Nursing excellence
- Patient & workforce safety
- Nurse leader
- Physician leader
- Technology & digital leader
- Marketing leader
- Experience leader
- Human resources
- Safety & quality leader
- Chief executive officer
- Culture & diversity leader
Your industry
- Health systems & providers
- Health plans
- Life sciences
- Strategic consulting
- Consulting overview
- Health plan
- Safety & high reliability
- Our team of experts
Insights & initiatives
- Centers of excellence
- Industry initiatives
- Safety 2025
- Equity partnership
- Workforce well-being
- Thought leaders
- Request a speaker
- Awards overview
- 2022 HX NDNQI Award winners
- 2022 HX Guardian of Excellence Award winners
- 2022 HX Pinnacle Excellence Award winners
- Case studies
- HX Insights 2024
- Pulse Podcast
- On-demand webinars
- Request a demo
Transforming health plan quality through improved experiences
Is your health plan’s quality ratings meeting your goals? Maybe you don't have access to current end-to-end experience data, which prevents you from improving quality in the way fully needed. Or you find it hard to prioritize quality efforts, because you don't have clear member insights to support needed changes. It's time for action. Today, taking a member-centric approach is essential for quality improvement. And that requires regularly listening to the member’s voice.
Traditional health plan quality improvement methods rely heavily on the Healthcare Effectiveness Data and Information Set (HEDIS) and Consumer Assessment of Healthcare Providers and Systems (CAHPS). While these are critical for many reasons, health plans can’t stop there. They must dig deeper to assess members’ needs, experiences, and expectations as they navigate their unique care journey.
Because healthcare is just that: a journey—and a nonlinear one at that. It’s not confined to a single experience, and it often has many overlapping or intersecting paths. People don’t think of their experiences in silos—the patient experience vs. consumer experience vs. member experience—and health plans can’t either. Every experience is unique in itself, and it takes a deeper understanding of each to learn how to effect real change.
Taking a member-centric approach to quality improvement is about connecting the dots throughout their healthcare journey, including but not confined to each episode of care, as well as over their lifetime.
To do this effectively, health plans must invest in:
- Understanding the member’s experience as an individual and patient
- Delivering patient support services that improve those in-care experiences
- Crafting a health plan experience that meets members wherever they are in their journey
But beyond the philosophical exercise of reframing how we think about healthcare through a Human Experience lens, health plans must be using their member data and applying it against everyday feedback across a member’s journey.
In a member-centric model, continuous feedback is essential for quality improvement. It's the tool that can contextualize situations and provide direct insights into member expectations and experiences. But exactly how do we go about collecting that feedback?
Collecting member feedback through a clinical quality lens
Continuously listening throughout the entire healthcare journey unlocks a deeper-level understanding of pain points and wins.
Capturing member feedback prior to a healthcare visit provides valuable insights into the member experience. This feedback can reveal potential barriers to care as well as any complexities in finding and accessing that care, which may lead to suboptimal quality outcomes or unmet member needs. Improving experiences leading up to a visit can have a tremendous impact on the long-term quality of care.
During the visit
Capturing member feedback about a specific healthcare visit, or across a care journey, identifies insights that requires immediate actions on the part of a health plan to improve their policies, network, or benefits—driving greater quality for members in the future. It may also help you address a specific member’s need where intervention in needed through a closed loop process.
Capturing member feedback days, weeks, and months after a visit helps a health plan quickly know when, where, and how to potentially support them in their care journey. It may help trigger health plan’s care and case management efforts to ensure the member is getting the needed post-visit care to improve quality outcomes.
While health plans invest a lot of their continuous listening programs focused on improving the experiences for net promoter scores (NPS), growth, and retention, these same measurement strategies can support improved outcomes while also supporting health plan affordability programs.
Final thoughts: The future of quality improvement
Continuous feedback powers a member-focused approach to quality improvement. It allows for health plans to see the entire healthcare experience through the lens of the member and patient—capturing a true Human Experience outlook. In the end, it’s a dynamic and responsive process, not a static one.
We need to move toward a future where every member feels supported and appreciated, and every health plan strives to help humans live healthier lives. After all, that's what quality improvement is all about.
To discuss capturing member feedback for quality improvement purposes, please reach out to Press Ganey’s team of health plan experts . They can discuss moving beyond traditional surveys to harness real-time member insights and proactively address the root causes negatively impacting experiences—and quality.
- Brand growth
- Health plan consulting
- Nursing consulting
- Copyright © 2023 Press Ganey
- Cookies settings
- Terms of service
- Legal and Privacy Policy
- Accessibility statement
- Cookie policy
- Copyright © 2024 Press Ganey
- Open access
- Published: 17 May 2024
Ensuring universal access to quality care for persons with presumed tuberculosis reaching the private sector: lessons from Kerala
- P. S. Rakesh 1 , 2 &
- Mohd Shannawaz 1
International Journal for Equity in Health volume 23 , Article number: 101 ( 2024 ) Cite this article
1 Altmetric
Metrics details
More than half of the people with Tuberculosis (TB) symptoms in India seek care from the private sector. People with TB getting treatment from private sector in India are considered to be at a higher risk for receiving suboptimal quality of care in terms of incorrect diagnosis and treatment, lack of treatment adherence support with a high loss to follow-up rate that could eventually increase their risk of drug resistance. The current study aims at documenting the approach and efforts taken by the Kerala state to partner with the private health care delivery providers for ensuring quality TB care to the people with presumed TB reaching them.
A case study approach was adopted with review of all available literature followed by five Key Informant Interviews to understand the case through a primary descriptive exploration. Grounded theory approach was used to generating the single theory of the case itself that explains it.
Kerala state has taken a variety of interventions to ensure universal access to TB care for citizens reaching the private sector with documented improvement in the quality of TB care. Key learnings from these initiatives were (i) patients need to be at the centre of partnerships, (ii) good governance is essential for ensuring Universal Health Coverage in a mixed health system, (iii) data intelligence is required to guide partnerships, (iv) identification of the correct ‘problems’ is crucial for effective design of partnerships and (v) a platform for meaningful dialogue of key stakeholders is needed.
Kerala experience demonstrated that if governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest.
The Standards for TB Care in India (STCI), which is a locally customized version of the International Standards of Tuberculosis Care , mentions 26 standards of care that every citizen of India should receive irrespective of the sector of treatment [ 1 ]. STCI deliberate on standard tools and strategies for early and complete detection of TB, standards of treatment in terms of drugs and regimens for best patient outcome, standards of public health actions and patient support such as adherence monitoring, clinical follow up, contact investigations and TB Preventive Therapy to the family. STCI lays down what is expected for quality TB care from the Indian healthcare system.
More than half of the people with TB symptoms in India seek care from the private sector [ 2 , 3 ]. Gaps in the TB care cascade such as people with TB not having access to correct and complete diagnosis, people diagnosed with TB not being started on correct treatment; and people started on treatment not completing treatment, were observed more among people with TB who were diagnosed in the private sector compared to the public sector [ 4 , 5 , 6 , 7 ]. There are also concerns about the suboptimal quality of care including incorrect diagnosis and non-standardized treatment regimens, lack of systems for treatment adherence support resulting in high loss to follow-up rate increasing the risk of drug resistance among the people who seek care from the private sector in India [ 4 , 5 , 6 , 7 ]. Many services assured in the public sector, such as free diagnostics including rapid molecular tests and drug susceptibility testing, free quality assured drugs, treatment adherence support and monitoring, contact investigation and TB preventive therapy, linkages to social welfare schemes rarely reach the patients who are treated in the private sector. Not having access to full range of quality TB care when and where the people need them, could be a hindrance to achieve Universal health coverage (UHC).
Realising the urgent need to engage private sector, the National Strategic Plan (NSP) for TB Elimination in India (2017–2025) enlisted various strategies to ensure that patients reaching the private sector receive care as per the STCI [ 8 ]. National TB Elimination Program (NTEP) has taken a variety of approaches including trainings, regulations, provisions of free services such as drugs and diagnostics, incentives and partnership schemes to engage with private sector [ 9 ]. Government of India has issued directives making TB notification mandatory as a first step to ensure STCI to all people affected with TB [ 10 ]. Provisions have been developed in Ni-kshay, the real time case-based web-based management information system of NTEP, where private providers can directly log in to the system using their user credentials and notify TB and report outcomes [ 11 ]. NTEP provides 500 INR (IUSD = 85 INR) as an incentive to the private provider to notify each TB patient and another 500 INR to report the treatment outcome [ 12 ]. Anti TB medicines have been included in schedule H1 which can only be sold on prescription of a Registered Medical Practitioner and details of the prescriber, the patient and the drug sold needs to be maintained by the chemists [ 13 ]. NTEP has also provisions for supplying free quality assured anti- TB drugs and free molecular tests and drug susceptibility tests to the patients reaching the private sector. Directly and through various agencies, NTEP intends to provide support for contact investigations and treatment adherence to all patients reaching private sector. NTEP guidance document on partnership (2019) details out about the purchase of various services from private sector [ 14 ]. Patient Provider Support Agencies (PPSA), predominantly Non-Governmental Agencies, are contracted in with the task of engaging with private sector for notifying cases to NTEP and coordinating with NTEP for free drugs and follow-up.
Despite all these initiatives in India, TB notifications and ensuring public health actions for people with TB have not been really converted into routine practice in private sector. NSP intended to achieve a target of two million TB notification from private sector in 2021; there is a gap of 1.3 million TB cases who are ‘missing’ in the surveillance system [ 2 , 9 ]. Studies, annual reports and evaluations revealed that Kerala state has successful ensured quality TB care to the people reaching the private sector [ 9 , 15 , 16 ]. The current study aims at documenting the approach and efforts taken by the Kerala TB Elimination program to partner with the ‘for profit’ formal private health care delivery providers for ensuring quality TB care with special emphasis on potential lessons to be learnt from the state. This is expected to help policy makers and programme managers in other parts of India and in other countries who face challenges in partnering with private sector for ensuring universal access to quality TB care.
Local setting
Kerala has experienced a 7.5% annual decline in the TB incidence since 2015 and has been certified for the same by Government of India under its sub-national TB free certification process [ 17 , 18 ]. The state TB program has been appreciated by the Joint Monitoring Mission (JMM) 2019, led by the World Health Organization and global developmental partners, for providing patient-centric TB care through systematic interventions [ 15 ]. Various efforts by the state for providing support to the people and family with TB were documented [ 19 ]. The private health care sector in Kerala accounts for more than 70% of all facilities and 60% of all inpatient beds. A significant proportion of people from low socio economic status also avail health care from private hospitals in the state for various reason such as long waiting time in public facilities, perceived low quality of care in public sector and proximity of health facilities [ 20 ]. National TB Prevalence survey (NTPS) revealed that among those with TB symptoms and sought health care in Kerala, 38% consulted the private sector first [ 2 ].
A case study approach was used to understand the case through a primary descriptive exploration. Review of all available literature followed by five Key Informant Interviews (KIIs) were conducted.
Desk review
Desk review of all available documents and studies were attempted first. All documents such as policy documents, operational plans, guidelines, annual reports and evaluation studies available in public domain in official websites of health department were referred to look for (1) policy and plan for engagement of private sector for TB care and (2) outcomes and data related to TB patients reaching the private sector. A high level of objectivity and sensitivity was maintained during the process; the authenticity of the documents were assessed, and the goals and biases were explored before examining the content. Literature search was done in MEDLINE, Embase and Web of Science using the key words (TB OR Tuberculosis) AND (Private hospital OR Private facility OR Private Partnership OR Private Practise OR Private Sector OR Public Private Partnership) AND Kerala. The search was carried out on 21st December 2022, and all studies including descriptive and analytical studies were included irrespective of the publication type. Studies published since 2000–2022 were included as our interest was in the recent situation, and earlier publications were difficult to access. Reference lists of papers identified in the searches, were scanned. Information was obtained about studies from state TB cell from where permissions for using TB-related data are sanctioned.
We used the operational definition provided by World Health Organisation which defined private health sector as ‘the individuals and organizations that are neither owned nor directly controlled by governments and are involved in provision of health services’ [ 21 ]. Reading abstracts, studies related to private sector and TB done in Kerala were included. We focussed on ‘for-profit’ healthcare providers, because they are more numerous and difficult to engage. We included only health service providers rather than manufacturers or distributors of medical equipment, technologies, consumables or drugs. All identified articles were screened for full-text review. Articles not focussing on ‘for-profit’ health sector and ‘quality of TB care’ were excluded.
Key informant interviews
Based on the literature review, additional five KIIs were conducted to fill in gaps in the information, to explore additional documents to be reviewed and to validate the observations from the literature. Key informants were persons with long experience in the field of TB control, who had broad knowledge of the TB scenario in the state, were aware of the TB programme activities over the years and who were involved in policy formulation and implementation related to TB and private sector. They were selected as they were the persons with the longest experience, each having more than 15 years of experience, in the field and had a broad overview of the TB and private sector engagement in the state. They were (i) a senior bureaucrat, involved in policy making (ii) a state-level programme manager responsible for TB programme activity implementation, (iii) a technical consultant for TB elimination from a global partner agency, responsible for guiding the state in TB policy formulation, implementation and supervision (iv) a senior leader of Indian Medical Association who was associated with TB projects implemented through IMA and (v) director of a 600 bedded private hospital. Participants were approached by phone, the purpose of the interviews were communicated and the prerequisites during the interview (stable internet connection, calm environment and with video switched on) were communicated. Two interviews were conducted in English and the rest in Malayalam, by PS (male, medical doctor with post-graduation in public health with 10 years of research experience), who was experienced in conducting qualitative studies and was fluent in the local language. All KIIs were conducted online using Zoom (Zoom Video Communications, San Jose, CA, USA) with video. One researcher recorded the proceedings, identifying key themes and monitored the verbal and non-verbal interactions. All participants who were contacted could participate. Major themes discussed were initiatives taken by the Government to engage private sector, major outcomes of such strategies and reasons for changing strategies. Each interview lasted for approximately 45 min (range: 25–75). No repeat interviews were attempted. KIIs were later transcribed verbatim and translated into English. Transcripts were returned to participants for comments.
Grounded theory approach was used to develop theory. We did not attempt to generate strong theories rather focussed on generating the single theory of the case itself that explains it. This was a deliberate attempt in order not to draw away our attention from features for understanding the case.
The transcripts were then manually coded by PS, emerging themes were identified. Citations with similar coding were grouped according to the predetermined themes. Themes were derived from the data. Recurrent themes were marked as important. All the flagged statements were put together and synthesised. The team went through the transcripts and notes and reached a consensus. Data triangulation was done comparing information from literature and qualitative interviews. Inductive thematic saturation was reached and no new codes emerged after the fourth interview. The study was approved by the Institutional Ethics Committee of Amity University, Noida, India.
PRISMA flow chart for the literature review were presented as Fig. 1 .
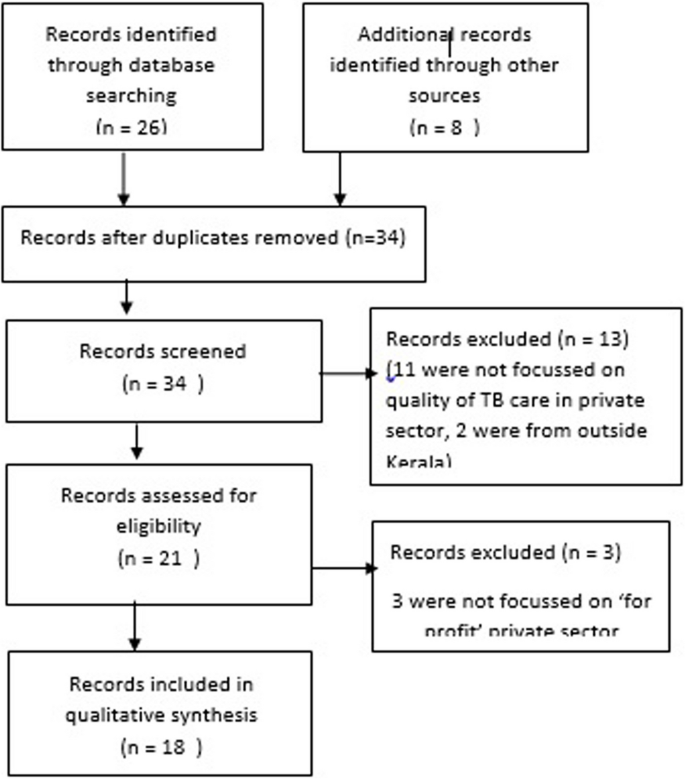
PRISMA flowchart indicating the results of literature search
The results of desk review and the KIIs are presented below.
Efforts for private sector engagement for TB care in Kerala
Many public-private mix strategies for TB care started in Kerala during the initial years of implementation of the National TB Elimination Program (NTEP), then called Revised National TB Control Program (RNTCP). Milestones of various initiatives by the state TB program to engage private sector for TB care ares described in Fig. 2 . Details of major initiatives by NTEP directly or in partnership with various stakeholders are compiled in Table 1 .
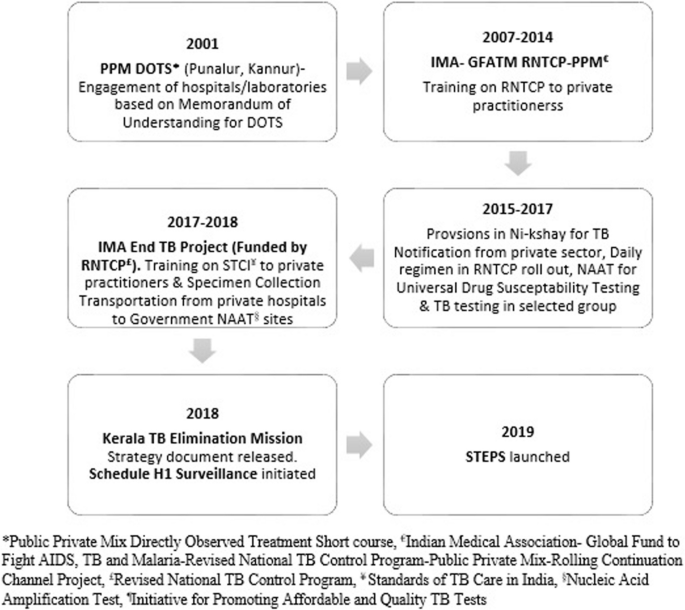
Milestone of Private Partnership for TB Care in Kerala
In 2016, even after the NTEP implemented a daily anti-TB regimen—the absence of which was cited as the major reason by the private sector for not participating—there was not much improvement in the private sector participation in terms of contributions towards TB notification or partnering with NTEP on signed partnership schemes. Operations researches conducted through the NTEP mechanisms, revealed many challenges for sub-optimal private sector participation [ 32 , 33 ]. Efforts were also put in place to understand the real problems of patients reaching the private sector [ 34 ]. A study that followed up a cohort of TB patients treated in private facilities in Kerala reported a loss to follow-up of 20–30% [ 34 ]. Limited ability to monitor and promote treatment adherence remained a major challenge in the private sector. Although NTEP documents the treatment outcome of every patient diagnosed/enrolled for treatment, such documentation is rare in the private sector. Lack of a network of field staff in the private sector limits the ability to monitor and support adherence to standards of care. STEPS (System for TB Elimination in Private Sector) evolved as a solution for ensuring standards of TB care in a patient-centric way for all patients accessing the private sector, addressing the concerns of the public and private sector [ 29 , 30 ]. A pilot STEPS centre in a private tertiary care centre in Kerala demonstrated that establishing STEPS centre within the hospital ensured 100% TB notification with a 4-fold increase in the number of patients notified over 6 months [ 35 ].Two interventions which emerged as prominent and replicable ones in our review are described below.
STEPS model
STEPS was envisioned as an equal partnership between the public and private sector for benefit of the society with improving standards of TB care as the outcome. Concept and evolution of STEPS are documented in detail elsewhere [ 30 ]. STEPS has three components: (i) a private hospitals TB consortium at district and state level consisting of hospital managements for policy support and review (ii) a coalition of medical professional associations at state and district levels for advocating with doctors and (iii) a STEPS centre in each private hospital. STEPS centre within a private hospital is a single window for diagnostic and treatment services, notification, patient linkage with social welfare, contact investigation, TB Preventive Therapy and treatment adherence support. A central person (STEPS lead) nominated by the hospital management, work together with contact persons (STEPS links) for each in-house department in a hub-and-spoke model. The STEPS lead and links are typically staff nurses. STEPS Links from various in-house clinical departments transfer the patients and related information to the STEPS Lead. Patients visit STEPS centre where education, counselling, support and linkages for molecular diagnostics, anti TB treatment initiation, contact investigations, TB Preventive Therapy, social welfare schemes and air borne infection control counselling are provided. STEPS Lead follows up the patient periodically over telephone and provides treatment adherence support, monitors adverse drug reactions, reminds clinical follow up and schedules reviews. Patient visits the concerned in house departments for clinical follow up. Through STEPS, private hospitals proactively supported patients to make decisions and participate in their own care. It also fosters customer loyalty. STEPS Lead enters information in NI-KSHAY. NTEP through its field staff and also through the five city officers of project JEET, a PPSA worked in the state for 2 years (2018–2019), provided customised and need based support to the patients reaching private hospitals, through the STEPS centres, including free diagnostics such as molecular tests and drug susceptibility testing, transportation of specimen from the hospitals for testing, free drugs, support for contact investigation, TB Preventive Therapy, Direct Benefit Transfer, linkages to social welfare services and retrieval if there is a lost to follow up. STEPS was implemented in all 14 districts of Kerala state, India since January 2019. Of the 446 hospitals mapped which manages more than 80% of the TB patients in the state, 318 established STEPS centres during 2019 and the remaining in 2020 [ 17 , 30 ].
Outcomes of STEPS
JMM (2019 November, India) visited Kerala and recommended supporting the establishment of STEPS Centres in all private health care facilities [ 15 ]. A formal evaluation of STEPS was conducted by a multi-disciplinary team in 2021 by (i) visiting 30 randomly selected STEPS centres for assessing infrastructure and process using a checklist, (ii) validating the patient data with Ni-kshay by telephonic interview of 57 TB patients (iii) analysing the quality of patient care indicators (iv) conducting in-depth interviews with 33 beneficiaries and stakeholders to understand their satisfaction and perceived benefits and (v) a cost analysis from the perspective of NTEP, private hospital and patients [ 31 ] .
Evaluation concluded that STEPS is a low cost, ‘patient centric’ model where the patient can approach any provider according to his/her choice and get uniform high quality TB care. Evaluation also revealed that STEPS was acceptable to all stakeholders and patient satisfaction was good. There was significant improvement in the quality of TB care indicators for patients diagnosed in private hospitals over the years in terms of notification, proportion with a microbiological confirmation of diagnosis, known HIV status, beneficiary receiving baseline rifampicin testing, Direct Benefit Transfer and the documented treatment success rate (Fig. 3 ).
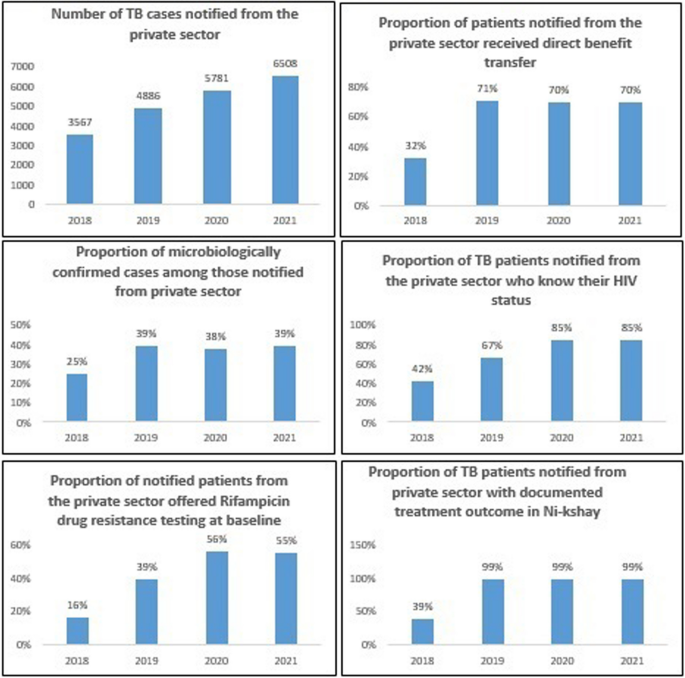
Trend in the indicator for ‘quality of care’ among the patients with TB who availed care from private sector in Kerala (2018–2021)
Number of specimens from private sector tested using molecular testing machines at public laboratories increased from 7606 in 2018 to 14,940 in 2021 [ 9 ]. STEPS led to a shift from using private anti-TB drugs to NTEP-supplied drugs and there was a drastic drop in the sale of anti-TB drugs in the state from 1.6 million rifampicin units in 2018 to 0.5 million rifampicin units in 2019 [ 16 , 17 , 31 ]. STEPS had also demonstrated good resilience in ensuring TB services during COVID-19 pandemic period [ 36 ].
Schedule H1 surveillance
Since 2016, the Government of Kerala has enforced Schedule H1 implementation for anti-TB drugs as a joint venture by the drugs control department and state TB Elimination program, with monitoring from the top administrative level. From 2018 onwards, the state program managers of NTEP have modified it into a Schedule H1 surveillance system [ 28 ]. The process of schedule H1 surveillance and its benefits were documented through in-depth interviews of the drugs control department enforcement officers, chemist shop owners, private sector doctors, leaders of professional medical associations, and program managers and key staff of the TB Elimination Program in Kerala [ 28 ]. The TB Elimination Program of Kerala used the information from the Schedule H1 drug register to identify the missing TB cases from the surveillance system, identify providers who prescribed the anti TB drugs and extended support to them for ensuring STCI to their patients, and provide feedback to providers regarding prescription practices. The estimated number of un-notified TB cases per 100,000 people based on the total sales of rifampicin-containing products in Kerala showed an annual decline of 22% over the last few years, closing the gap in the surveillance system [ 17 ]. The major initiatives taken by the state for ensuring quality care to the patients reaching the private sector is represented schematically in Fig. 4 .
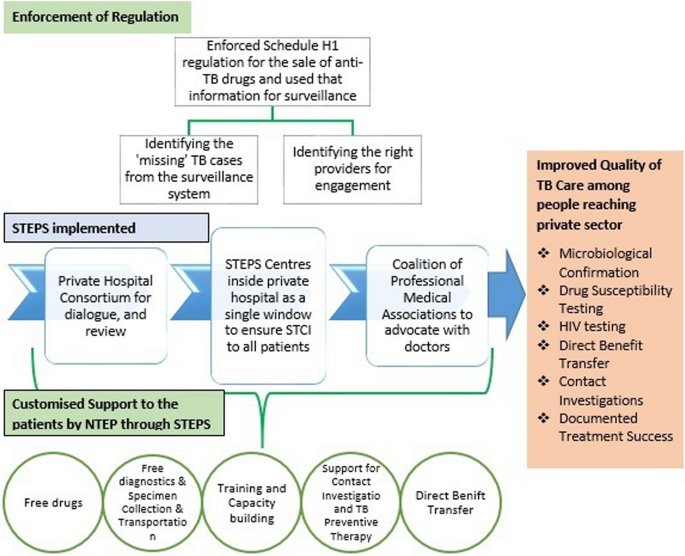
Schematic representation of major initiatives by Kerala to improve the quality of TB care among people reaching the private sector
Learnings from Kerala for engaging private sector for TB care
Vision of partnership: Most of the partnership models implemented in the country were mostly business-centred like incentive-based or service-purchase models that were similar to a client-vendor relationship rather than an equal partnership between the public and private sectors. Several models implemented in India that have successfully increased private case notifications were difficult to expand due to lesser emphasis on creating lasting partnerships and huge short-term financial implications [ 37 , 38 ]. As the intermediary agency who interacts with the private sector withdraws, the model collapses. Kerala state has literally redefined the ‘private sector engagement’ as a partnership for shared health outcomes. The vision of partnership that the state implemented through STEPS is in line with the recent vision shared by World Health Organization which described partnership as a means to “bring together a set of actors for the common goal of improving the health of populations based on mutually agreed roles and principles based on the principles of relative equality between the partners, mutual benefits to the stakeholders, autonomy, accountability and mutual commitment to agreed objectives” [ 39 ]. The state has proved that partnership with private sector is possible in the form of a relationship and not mere as contracts or purchase.
Strategic policy direction: Having a clear policy and strategy will help to avoid confusions among the stakeholders and will enable them to execute better. It should clearly define the goals and objectives of private sector engagement, clarify roles of all stakeholders, describe the institutional arrangements for engagement, outline the feasible strategies and arrangements to monitor performance. Health system decision makers need to know “where they are going” to be able to make efficient use of finite resources. The state has set a clear strategic policy direction with regard to engagement of private sector and trained all program managers regarding the same [ 29 ]
Strong governance mechanism: In Kerala, the state government focused on the governance of the whole health system – both private and public – to ensure access to quality TB care. The government efforts were successful in aligning the private sector with a common goal and making them commit to work to support the agenda. Both the sectors collectively delivered on the realization to ensure access and quality of TB care. Institutional mechanisms for periodic interaction between the public health system and the private sector were established. There was a clear understanding and delineation of the roles based on each stakeholder’s skills and expertise and there was mechanism to ensure accountability of both sectors. There was also a strong regulatory environment with regard to implementation of schedule H1 for anti-TB drugs, at the same time the information through the process has been used for generating data intelligence and ‘nudging’ positive behaviors among the private sector. The governance mechanisms ensured that the actors have the powers to do their jobs and to ensure that others do theirs. The government proactively promoted initiatives like IPAQT where TB tests are made available at affordable prices in the private sector [ 40 ]. Through ‘Coalition of Professional Medical Associations’ the government tried to bring in a social regulation too promoting STCI to every citizen.
Understanding the ‘problem’: Clear understanding of the ‘problem’ that is to be solved through partnership is critical in any successful partnership. The partnership needs to be tailor made to address the identified problems. Similarly understanding the behaviour of stakeholders and involving them from the planning phase are also important before developing any strategy. In Kerala, efforts were put in formally through operations research to identify the problem clearly and document the perceptions and concerns of different stakeholders [ 32 , 33 ]. STEPS evolved as a solution to address those concerns. Major challenges for ‘partnerships’ identified through various operations research done in the state and how that have been addressed through the STEPS is summarised in Table 2 . Kerala experience also reiterates that it is better to avoid over-reliance on pre-designed solutions when it comes to designing partnerships.
Generate data intelligence: There need to be systematic efforts for collection, compilation and analysis of data to guide the priorities for action. In Kerala, overall data regarding the sales of anti-TB drugs helped in (1) estimating the load of patients being treated in private sector and (2) monitor the trends. Granular information from schedule H1 data helped to (1) identify the potential providers for engagement and (2) identify the cases missed from the official surveillance system [ 28 ]. Experiences from the state iterate that pharmacy based surveillance of anti-TB drug sales has immense potential to improve the overall quality of TB care.
Enable stakeholders, foster relations and align structures: In Kerala, organizational structures were aligned towards the policy objectives that empowered the actors. ‘Private hospital consortium’ and ‘coalition of professional medical associations’ at state and district level enabled actors to work openly, sustainably, and effectively together, with trust. The consortium became the face of the private sector which facilitated dialogues between partners, catalyzed the implementation of policies and ensured that both the sectors are held accountable for their actions for the population. There were also district and sub-district wise WhatsApp groups with STEPS leads of all hospitals and the NTEP staff which facilitated smooth and easy communication. All such efforts to foster relations allowed stakeholders to move beyond simply understanding one another, to being able to work together.
Openness to change : Important strategic change that contributed to rapid scale-up and acceptance of STEPS were the attempts to gain the trust of hospital management, involvement of nurses for documentation and counselling, efforts for quality control through a coalition of professional medical associations, lack of formal memoranda of understanding, and lack of major financial transactions between partners [ 30 ]. Such flexibility and openness to change is crucial while governing mixed health systems.
Patient needs to be at the centre of every partnership: All public private partnership need to be ‘patient centric’ and their specific health needs and desired health outcomes should be the driving force. STEPS is a patient centric partnership where patient is the central figure in the continuum of care [ 30 , 31 ]. STEPS tells us that partnerships need to be designed after understanding the needs, preferences and circumstances of patients.
Equipping the public sector with the necessary skills and understanding to effectively engage with private sector: The state has undertaken a behavior change strategy for the NTEP staff to have a uniform outlook with regard to private sector engagement. Capacity of program managers and peripheral staff were built to deal with private sector in a more efficient way [ 31 ].
Incorporating UHC principles into a business model is possible: STEPS is a model based upon a self-initiated business promotion focusing on the concepts of ‘quality of care’ and ‘customer loyalty’ blended with the social responsibility of the private sector. STEPS centers used ‘after-sales support’ by following up every client, which could also be viewed as a business strategy which typically leads to higher customer satisfaction, brand loyalty, and even word-of-mouth marketing. Cost estimates revealed that implementing STEPS will be of benefit to private hospitals in terms of business returns [ 31 ].
The current study documents various approaches and efforts taken by the Kerala TB Elimination program to partner with the‘for profit’ formal private health care delivery providers for ensuring quality TB care. The current study attempts to synthesise the evidences generated from various studies conducted over different time periods and narrates a story which explains the changes in strategies, outcomes and the reasons for the same. Though the results are not meant to be generalized to other settings, it provides lot of insights to strengthen the private sector engagement in the country.
Though, Kerala state was proactive in engaging hospital and laboratories for DOTS (Directly Observed Treatment Short course) through formal memorandum of understanding through various partnership schemes and various efforts for capacity building, a significant chunk of private hospitals could not be engaged until 2018 resulting in sub-optimal quality of care to a significant proportion of people reaching the private sector in terms of not being offered treatment adherence support, baseline susceptibility testing for Rifampicin, contact investigations and linkages to social welfare schemes. After thorough understanding of the problem and the characteristics of the private sector and in consultation with the stakeholders, the state initiated STEPS which is an equal partnership model where both sectors have been made accountable to ensure uniform standards of TB care to the citizens reaching the private sector. Through enforcing schedule H1 regulations for the sales of anti-TB drugs, the state generated data and established an intelligence system for prioritising actions for partnerships and monitoring the outcomes. The implementation resulted in improvement in the quality of TB care among the people with TB reaching the private sector too.
Through the initiatives, Kerala has literality reframed ‘private sector engagement’ as ‘a partnership where both the sectors come together for the benefit of the society’. STEPS ensured that public resources are not diverted too much; and whatever is diverted through the STEPS is for the patient. In a country like India where most of the patients seek care from the private sector and the program managers are thriving to ensure quality of care in public sector with the limited resources, ‘purchasing’ of services and ‘incentivising’ of the private sector may not be the best way to create sustainable partnerships. Instead, the commitments to offer quality TB services need to be considered as the prime partnership option. Private sector will be more than willing to improve the quality of care to their clients as it improves patient satisfaction and provides good marketing advantage in the competitive healthcare. High out of pocket health expenditure will be the only concern then, which could be addressed to the needy through public provision of services through the private partner, promoting schemes such as IPAQT where TB tests are made available at affordable prices in the private sector or hospitals getting reimbursed for drugs and diagnostics through national health insurance schemes.
Kerala demonstrated that if Governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest. The case study reiterate that a good governance is essential for ensuring care in a mixed health system. The pursuit of UHC requires Governments to take ownership of healthcare, irrespective of where a person seeks care. WHO Advisory Group on the Governance of the Private Sector for Universal Health Coverage also emphasise a fundamental shift in the Governance behaviours to do business in a new way [ 39 ].
Data intelligence is crucial to successful governance. Good governance require data to identify whom to engage, monitor the progress and measure the impact. The state has used data coming out from the drug sales for the surveillance purpose. The state demonstrated that pharmacy based surveillance of anti-TB drug sales has immense potential to help the TB programs in improving the quality of care in private sector.
Success of STEPS also emphasises that successful private sector engagement initiatives need to have a platform for meaningful dialogue. Strengthening platforms, or structures for dialogue, and communication between sectors is important in building trust, and co-development of policies. Medical College Task Force is an example of a structured mechanism where NTEP interacts with all medical colleges [ 41 ]. It has state, zonal and national level structures. Similarly, a ‘Private Health Sector Task Force/consortium’ created at district, state, zonal and national level need to be established at the country level.
Kerala state has taken proactive role to partner with private sector after ensuring the quality of care in the public system. The model need to be customised and contextually adapted following the principles and approach and shall not be replicated as such, especially in settings where health systems are weak. It has also to be emphasised that the current experiences with the STEPS model in Kerala are with private hospitals and not with individual practitioners. It is also recommended that Kerala needs to systematically capture the patient’s cost and document the same for more meaningful insights.
Kerala state has taken a variety of interventions through STEPS to ensure universal access to TB care for citizens reaching the private sector with documented improvement in the quality of TB care. Kerala demonstrated that if Governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest. The case study reiterates that a good governance is essential for ensuring care in a mixed health system and such successful governance requires good data intelligence. Kerala reminds us that identifying the correct ‘problems’ are critical for effective design of partnerships and over reliance on pre designed solutions may not work.
Availability of data and materials
Data are available upon reasonable request. Data collected for the study, including individual de-identified participant data and a data dictionary defining each field in the set, study protocol, informed consent forms will be made available to others for a period of three years from the date of publication of the article, with a signed data access agreement and on due approval from the institutional ethics committee of Amity University, India, on submission of request to the principal investigator explaining the purpose for which the data will be used along with other relevant supporting documents.
World Health Organization (WHO) country Office for India. Standards for TB Care in India. WHO; 2014. [Accessed March 1, 2023]. Available from: https://apps.who.int/iris/bitstream/handle/10665/208894/stci_book.pdf
Indian Council of Medical Research. National TB prevalence survey 2019–2021. ICMR;2022[Accessed March 1 2023]. Available from: https://tbcindia.gov.in/showfile.php?lid=3659
Arinaminpathy N, Batra D, Khaparde S. The number of privately treated tuberculosis cases in India: an estimation from drug sales data. Lancet Infect Dis. 2016;16(11):1255–60.
Article PubMed PubMed Central Google Scholar
Stallworthy G, Dias HM, Pai M. Quality of tuberculosis care in the private health sector. J Clin Tuberc Other Mycobact Dis. 2020;20:100171.
Kwan A, Daniels B, Saria V. Variations in the quality of tuberculosis care in urban India: a cross-sectional, standardized patient study in two cities. PLoS Med. 2018;15(9):e1002653.
Rupani MP, Shah CJ, Dave JD, Trivedi AV, Mehta KG. ‘We are not aware of notification of tuberculosis’: A mixed-methods study among private practitioners from western India. Int J Health Plann Manag. 2021;36(4):1052–68.
Article Google Scholar
Satyanarayana S, Subbaraman R, Shete P, et al. Quality of tuberculosis care in India: a systematic review. Int J Tuberc Lung Dis. 2015;19(7):751–63.
Article CAS PubMed Google Scholar
Government of India. Ministry of health and family welfare (MOHFW). Central TB Division. National Strategic Plan for tuberculosis elimination 2017–2025. MOHFW; 2017. [Accessed March 1, 2023]. Available from: https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
Ministry of Health and Family Welfare. India TB Report 2022.CTD. [Accessed January 10,2023]. Available from: https://tbcindia.gov.in/WriteReadData/IndiaTBReport2022/TBAnnaulReport2022.pdf
Government of India. Ministry of Health and Family Welfare. Gazette of India notification G.S.R. 588(E). 2013. Drugs and cosmetics (fourth amendment) rules, 2013 [Accessed January 1, 2023].Available from: https://thehealthmaster.com/wp-content/uploads/2020/10/GSR-No.-588E-Dt-30-08-2013-Schedule-H1-Drugs-DC-fourth-Amendment-Rules-2013.pdf
Government of India. Ministry of Health and Family Welfare. National Tuberculosis Elimination Programme. NIKSHAY. [Accessed March 1, 2023]. Available from: https://www.nikshay.in/
Government of India. Ministry of Health and Family Welfare. Direct Benet Transfer Manual for National Tuberculosis Elimination Programme. [Accessed March 1, 2023]. Available from: https://tbcindia.gov.in/WriteReadData/l892s/23294204DBTManualForNTEP.pdf
Government of India. Ministry of health and family welfare. Gazette of India notification GSR 588(E). 2013. [Accessed March 1, 2023] https://thehealthmaster.com/wp-content/uploads/2020/10/GSR-No.-588E-Dt-30-08-2013-Schedule-H1-Drugs-DC-fourth-Amendment-Rules-2013.pdf
Government of India. Ministry of health & family welfare. Guidance document on partnerships 2019. [Accessed March 1, 2023] Available from: https://tbcindia.gov.in/WriteReadData/l892s/9531588006Guidance%20Doucument%20on%20Partnerships%20RNTCP%202019.pdf
Government of India, Ministry of Health & Family Welfare (MOHFW), Central TB Division. Report of the joint monitoring Mission. Revised National Tuberculosis Control Programme November 2019. MOHFW; 2019. [Accessed March 5, 2023]. Available from: https://tbcindia.gov.in/showfile.php?lid=3536
Government of Kerala Department of health and family welfare. Making the SDG a reality. Government of Kerala; 2021. [Accessed March 1, 2023]. https://www.keralahealthconference.in/e-Book.pdf
Government of Kerala. Kerala Health Conference-Making the SDG A reality—moving towards TB elimination—4 march 2021. [Video Recording]. Thiruvananthapuram: GOK. 2021. [Accessed March 4, 2023]. Available from: https://www.youtube.com/watch?v=C4Yr_FTMdgQ&t=3452s
Jeyashree K, Thangaraj J, Rade K, Modi B, Selvaraju S, Velusamy S, et al. Subnational TB claims verification group. Estimation of tuberculosis incidence at subnational level using three methods to monitor progress towards ending TB in India, 2015-2020. BMJ Open. 2022;12(7):e060197. https://doi.org/10.1136/bmjopen-2021-060197 .
Article PubMed Google Scholar
George LS, Rakesh PS, Sunilkumar M, Vijayakumar K, Kunoor A, Kumar VA. TB patient support systems in Kerala: A qualitative analysis. Indian J Tuberc. 2021;68(1):9–15. https://doi.org/10.1016/j.ijtb.2020.11.005 . Epub 2020 Nov 7
Manju R Nair, Ravi Prasad Varma. Availability, distribution and utilisation of health care services in Kerala. Thiruvananthapuram. 2021. [Accessed March 7, 2023] Available from: https://spb.kerala.gov.in/sites/default/files/inline-files/AvailDistribUtilisationHSKerala.pdf
World Health Organisation. The private health sector: an operational definition. Geneva. 2020. [Accessed on March 7, 2023]. Available from: https://www.who.int/docs/default-source/health-system-governance/private-health-sector-an-operational-definition.pdf
Kumar MK, Dewan PK, Nair PK, et al. Improved tuberculosis case detection through public-private partnership and laboratory-based surveillance, Kannur District, Kerala, India, 2001–2002. Int J Tuberc Lung Dis. 2005;9(8):870–6.
CAS PubMed Google Scholar
World Health Organization (WHO). Public–Private Mix for DOTS Global Progress. Report of the Second Meeting of the PPM Subgroup for DOTS Expansion . WHO; 2004. [Accessed April 17, 2023].Available from: https://apps.who.int/iris/handle/10665/68619
Ferroussier O, Kumar MK, Dewan PK, Nair PK, Sahu S, Wares DF, et al. Cost and cost-effectiveness of a public-private mix project in Kannur District, Kerala, India, 2001-2002. Int J Tuberc Lung Dis. 2007 Jul;11(7):755–61.
Greaves F, Ouyang H, Pefole M, MacCarthy S, Cash RA. Compliance with DOTS diagnosis and treatment recommendations by private practitioners in Kerala, India. Int J Tuberc Lung Dis. 2007;11(1):110–2.
Chugh S. IMA GFATM RNTCP PPM project: milestones in sight one year after. J Indian Med Assoc. 2008;106(7):454–8.
PubMed Google Scholar
Rakesh PS, Balakrishnan S, Jayasankar S, Asokan RV. TB management by private practitioners – is it bad everywhere? Indian J Tuberc. 2016;63(4):251–4. https://doi.org/10.1016/j.ijtb.2016.09.009 .
Ps R, Balakrishnan S, Ramachandran R, Nandhan S, Samuel NI, Pp P, et al. Using a pharmacy-based surveillance system to improve standards for TB Care in Kerala. India Glob Health Sci Pract. 2021;9(4):846–54. https://doi.org/10.9745/GHSP-D-21-00346 .
Government of Kerala. Kerala TB Elimination Mission. August 2017. [Accessed on March 2, 2023] Available online: https://dhs.kerala.gov.in/wp-content/uploads/2021/01/KeralaTB-Elimination-Mission_Strategy-activity-plan-and-budget..pdf .
Balakrishnan S, Rakesh PS, Sunilkumar M, Sankar B, Ramachandran R, Ameer KA, et al. STEPS: A solution for ensuring standards of TB Care for Patients Reaching Private Hospitals in India. Glob Health Sci Pract. 2021;9(2):286–95. https://doi.org/10.9745/GHSP-D-20-00449 .
Rakesh PS, Balakrishnan S, Sunilkumar M, Alexander KG, Vijayan S, Roddawar V, et al. STEPS - a patient centric and low-cost solution to ensure standards of TB care to patients reaching private sector in India. BMC Health Serv Res. 2022;2(1):2. https://doi.org/10.1186/s12913-021-07342-y .
Rakesh PS, Nair S, Philip S, Varma RP. Barriers for involvement of private doctors in RNTCP – qualitative study from Kerala, India. J Family Med Prim Care. 2019;8(1):160–5. https://doi.org/10.4103/jfmpc.jfmpc_208_18 .
Philip S, Isaakidis P, Sagili KD, Meharunnisa A, Mrithyunjayan S, Kumar AM. "They know, they agree, but they don't do"--the paradox of tuberculosis case notification by private practitioners in Alappuzha district, Kerala, India. PLoS One. 2015;10(4):e0123286. https://doi.org/10.1371/journal.pone.0123286 .
Article CAS PubMed PubMed Central Google Scholar
Kunoor A, James PT, Raj M, Rajesh CT, Nair P, Rakesh PS. Outcomes of patients treated with individualised anti-tuberculosis regimens in a tertiary care center in India. Public Health Action. 2017;7(4):308. https://doi.org/10.5588/pha.17.0062 .
Nair P, James PT, Kunoor A, Rakesh PS. How we ensured 100% TB notification: experiences from a private tertiary care hospital in India. Public Health Action. 2017;7(2):179–80. https://doi.org/10.5588/pha.16.0128 .
Khobragade RN, Kelkar RU, Sunilkumar M, Cency B, Murthy N, Surendran D, et al. Health system resilience: ensuring TB services during COVID-19 pandemic in Kerala. India Indian J Tuberc. 2022;69(4):427–31. https://doi.org/10.1016/j.ijtb.2021.10.004 . Epub 2021 Oct 13y
Government of India, Ministry of Health & family welfare, National Tuberculosis Elimination Programme (NTEP). Universal access to TB care (UATBC): concurrent assessment report. NTEP; 2016. [Accessed March 9, 2021]. Available from: https://tbcindia.gov.in/index1.php?sublinkid=4711&level=3&lid=3265&lang=1.
Shibu V, Daksha S, Rishabh C, Sunil K, Devesh G, Lal S, et al. Tapping private health sector for public health program? Findings of a novel intervention to tackle TB in Mumbai. India Indian J Tuberc. 2020;67(2):189–201.
World Health Organisation. Engaging the private health service delivery sector through governance in mixed health systems: strategy report of the WHO advisory group on the governance of the private sector for universal health coverage. Geneva: WHO; 2020. [Accessed on Feb 3,2023]. Available from: https://www.who.int/activities/strengthening-private-sector-engagement-for-uhc
Initiative for Promoting Affordable and Quality TB Tests (IPAQT). [Online] Available at: https://healthmarketinnovations.org/program/initiative-promoting-affordable-and-quality-tb-tests-ipaqt
Central TB Division. Training modules (5-9) for programme managers & medical officers. New Delhi July 2020. [Accessed on March 3, 2023] Available from: https://tbcindia.gov.in/WriteReadData/NTEPTrainingModules5to9.pdf
Download references
Acknowledgements
This research received no external funding.
Author information
Authors and affiliations.
Amity Institute of Public Health & Hospital Administration, Amity University, Noida, India
P. S. Rakesh & Mohd Shannawaz
The Union South East Asia Office, New Delhi, India
P. S. Rakesh
You can also search for this author in PubMed Google Scholar
Contributions
PSR & MS have substantial participation in the conception, design, collection of data, analysis and interpretation of the data. PSR wrote the manuscript, MS reviewed and edited it. Both approved the final version of the paper.
Corresponding author
Correspondence to P. S. Rakesh .
Ethics declarations
Ethics approval and consent to participate.
This study involves human participants. The study was approved by institutional review board and ethics committee of Amity University, Noida, India. Participants gave written informed consent to participate in the study before taking part.
Consent for publication
Not Applicable as no personal information regarding participants are revealed.
Competing interests
PS Rakesh was closely associated with the state TB Elimination program, Kerala in multiple roles such as WHO consultant & State Technical consultant for IMA-GFATM-RNTCP-PPM Project and was part of all major recent initiatives for private sector engagement. He also contributed to most of the studies and evaluations regarding private sector engagement for TB care in the state, which were mentioned in the current study. This could be a potential personal conflict of interest as his views and ideologies can influence this research.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1..
Abstract in Malayalam.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rakesh, P.S., Shannawaz, M. Ensuring universal access to quality care for persons with presumed tuberculosis reaching the private sector: lessons from Kerala. Int J Equity Health 23 , 101 (2024). https://doi.org/10.1186/s12939-024-02151-1
Download citation
Received : 11 March 2023
Accepted : 15 March 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12939-024-02151-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Public private partnership
- Private sector engagement
- Schedule H1
- Standards of TB care
- Universal access to TB care
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Adv Pract Oncol
- v.12(4); 2021 May

Quality Improvement Projects and Clinical Research Studies

Every day, I witness firsthand the amazing things that advanced practitioners and nurse scientists accomplish. Through the conduct of quality improvement (QI) projects and clinical research studies, advanced practitioners and nurse scientists have the opportunity to contribute exponentially not only to their organizations, but also towards personal and professional growth.
Recently, the associate editors and staff at JADPRO convened to discuss the types of articles our readership may be interested in. Since we at JADPRO believe that QI projects and clinical research studies are highly valuable methods to improve clinical processes or seek answers to questions, you will see that we have highlighted various QI and research projects within the Research and Scholarship column of this and future issues. There have also been articles published in JADPRO about QI and research ( Gillespie, 2018 ; Kurtin & Taher, 2020 ). As a refresher, let’s explore the differences between a QI project and clinical research.
Quality Improvement
As leaders in health care, advanced practitioners often conduct QI projects to improve their internal processes or streamline clinical workflow. These QI projects use a multidisciplinary team comprising a team leader as well as nurses, PAs, pharmacists, physicians, social workers, and program administrators to address important questions that impact patients. Since QI projects use strategic processes and methods to analyze existing data and all patients participate, institutional review board (IRB) approval is usually not needed. Common frameworks, such as Lean, Six Sigma, and the Model for Improvement can be used. An attractive aspect of QI projects is that these are generally quicker to conduct and report on than clinical research, and often with quantifiable benefits to a large group within a system ( Table 1 ).
Clinical Research
Conducting clinical research through an IRB-approved study is another area in which advanced practitioners and nurse scientists gain new knowledge and contribute to scientific evidence-based practice. Research is intended for specific groups of patients who are protected from harm through the IRB and ethical principles. Research can potentially benefit a larger group, but benefits to participants are often unknown during the study period.
Clinical research poses many challenges at various stages of what can be a lengthy process. First, the researcher conducts a review of the literature to identify gaps in existing knowledge. Then, the researcher must be diligent in their self-reflection (is this phenomenon worth studying?) and in developing the sampling and statistical methods to ensure validity and reliability of the research ( Higgins & Straub, 2006 ). A team of additional researchers and support staff is integral to completing the research and disseminating findings. A well-designed clinical trial is worth the time and effort it takes to answer important clinical questions.
So, as an advanced practitioner, would a QI project be better to conduct than a clinical research study? That depends. A QI project uses a specific process, measures, and existing data to improve outcomes in a specific group. A research study uses an IRB-approved study protocol, strategic methods, and generates new data to hopefully benefit a larger group.
In This Issue
Both QI projects and clinical research can provide evidence to base one’s interventions on and enhance the lives of patients in one way or another. I hope you will agree that this issue is filled with valuable information on a wide range of topics. In the following pages, you will learn about findings of a QI project to integrate palliative care into ambulatory oncology. In a phenomenological study, Carrasco explores patient communication preferences around cancer symptom reporting during cancer treatment.
We have two excellent review articles for you as well. Rogers and colleagues review the management of hematologic adverse events of immune checkpoint inhibitors, and Lemke reviews the evidence for use of ginseng in the management of cancer-related fatigue. In Grand Rounds, Flagg and Pierce share an interesting case of essential thrombocythemia in a 15-year-old, with valuable considerations in the pediatric population. May and colleagues review practical considerations for integrating biosimilars into clinical practice, and Moore and Thompson review BTK inhibitors in B-cell malignancies.
- Higgins P. A., & Straub A. J. (2006). Understanding the error of our ways: Mapping the concepts of validity and reliability . Nursing Outlook , 54 ( 1 ), 23–29. 10.1016/j.outlook.2004.12.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillespie T. W. (2018). Do the right study: Quality improvement projects and human subject research—both valuable, simply different . Journal of the Advanced Practitioner in Oncology , 9 ( 5 ), 471–473. 10.6004/jadpro.2018.9.5.1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kurtin S. E., & Taher R. (2020). Clinical trial design and drug approval in oncology: A primer for the advanced practitioner in oncology . Journal of the Advanced Practitioner in Oncology , 11 ( 7 ), 736–751. 10.6004/jadpro.2020.11.7.7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
1. Introduction. The Patient Safety and Quality Improvement (QI) movements in healthcare have been slow to achieve momentum in improving outcomes [].Braithwaite et al. (2018) estimate that in healthcare organisations, nearly two-thirds of initiatives experience implementation failure [].Changes in healthcare tend to be project-based with whole system change, which acknowledges the ...
Definitions of quality improvement. Improvement in patient outcomes, system performance, and professional development that results from a combined, multidisciplinary approach in how change is delivered. 3. The delivery of healthcare with improved outcomes and lower cost through continuous redesigning of work processes and systems. 4.
Implementation science and quality improvement both use tests of change to adapt interventions in a particular context. The context in which the changes are made affects the effectiveness of tests of change, irrespective of the methods that are used. Fidelity in tests of change refers to both the faithful use of data to drive the iterations of ...
In accordance with Key Driver 3: Optimize health information systems to extract data and support use of evidence in practice, the case study discusses how the practice used its electronic health record to develop a registry and identify and engage patients, as called for by Key Driver 5: Engage with patients and families in evidence-based care ...
What constitutes 'quality' in the context of healthcare provision is likely very different depending on who you ask. For patients it might relate to how quickly an appointment can be secured, the ease of communication or the outcome of a procedure; for clinicians perhaps it has more to do with access to state of the art equipment, dependable resources and decreasing risk; for the manager ...
Prepared for the Agency for Healthcare Research and Quality . working paper series. RAND working This product is part of the RAND Health ... The Six Steps to Quality Improvement THE CASE STUDY IN MORE DETAIL Background Step 1: Use Patient Experience Data to Flag Problems and Confirm Findings Step 2: Select Measures, Decide What Should be ...
We would like to show you a description here but the site won't allow us.
Studies of QIC consistently note that health care professionals' engagement is a critical contributor to QIC implementation and outcomes, 5,6,8,9 although the nature of professionals' engagement and how to facilitate it has only recently been explored in further depth. 5,8,10,11 This literature has shown that professionals are less likely to engage in QICs when they perceive them as a ...
Background: Quality improvement (QI) is increasingly recognized as an important strategy to improve healthcare services and health outcomes, including reducing health disparities. However, there is a paucity of evidence documenting the value of QI to public health agencies and services. Purpose: The purpose of this project was to support and assess the impact on the outcomes and organizational ...
Impact Case Studies. AHRQ's evidence-based tools and resources are used by organizations nationwide to improve the quality, safety, effectiveness, and efficiency of health care. The Agency's Impact Case Studies highlight these successes, describing the use and impact of AHRQ-funded tools by State and Federal policy makers, health systems ...
End of chapter commentary by the editors highlight important concepts and connections between various chapters in the text. Patient Safety and Quality Improvement in Healthcare: A Case-Based Approach presents a novel approach towards hospital safety and quality with the goal to help healthcare providers reach zero harm within their organizations.
The 2019/20 changes to the Quality and Outcomes Framework included the introduction of a quality improvement (QI) domain. This booklet contains three case studies developed by the Royal College of General Practitioners, National Institute for Health and Care Excellence and the Health
impairing the quality of the care and increasing the costs. Quality improvement efforts have been made worldwide by learning collaboratives, based on recognized continual improvement theory with limited scientific evidence. The present study of 132 quality improvement projects in Norway explores the conditions for improvement from the perspectives
Definitions of quality improvement. Improvement in patient outcomes, system performance, and professional development that results from a combined, multidisciplinary approach in how change is delivered. 3. The delivery of healthcare with improved outcomes and lower cost through continuous redesigning of work processes and systems. 4.
This article illustrates quality improvement (QI) methodology using an example intended to improve chlamydia screening in women. QI projects in healthcare provide great opportunities to improve patient quality and safety in a real-world healthcare setting, yet many academic centres lack training programmes on how to conduct QI projects. The choice of chlamydia screening was based on the ...
This article represents one substudy that is part of a broader qualitative, multilevel design single embedded case study, investigating regulatory quality improvement implementation and work across three levels of the specialised Norwegian healthcare system. 37 53 The case was defined as the design, implementation and enactment of the Quality ...
Quality improvement and coaching. The field of QI in healthcare is characterised as a change management approach towards achieving an evidence-based, effective, high-quality, patient-centred, safe, accessible and equitable healthcare service (IOM [Institute of Medicine], Citation 2001; National Board of Health and Welfare, Citation 2006).QI in healthcare is especially influenced by Edward ...
6 February 2020. Topic: General practice, Primary care. Publication type: Case study. Three case studies developed by the Royal College of General Practitioners, National Institute for Health and Care Excellence and the Health Foundation which provide examples of how practices could approach their quality improvement activity.
In 2011, the Public Health Accreditation Board launched a national voluntary accreditation program that catalyzes quality improvement but also acknowledges the importance of performance management within public health agencies. Regardless of the terminology, a common thread has emerged—one that focuses on continuous improvement and ...
Implementation Case Studies Prepared for: Agency for Healthcare Research and Quality 540 Gaither Road Rockville, MD 20850 Contract No. HHSA290200600019 ... innovation, and change and related work in health care, such as quality improvement. At the most basic level, hospitals, medical groups, and other health care organizations that attempt to ...
Quality improvement (QI) is a process of approaching systemic problems in healthcare. The healthcare system comprises many people with different scopes of training and expertise functioning in social hierarchies [3] that use many pieces of technology, such as the electronic medical record.
There is a distinct difference between what we know and what we do in healthcare: a gap that is impairing the quality of the care and increasing the costs. Quality improvement efforts have been made worldwide by learning collaboratives, based on recognized continual improvement theory with limited scientific evidence. The present study of 132 quality improvement projects in Norway explores the ...
Continuous feedback powers a member-focused approach to quality improvement. It allows for health plans to see the entire healthcare experience through the lens of the member and patient—capturing a true Human Experience outlook. In the end, it's a dynamic and responsive process, not a static one. We need to move toward a future where every ...
They also assess the future evolution of payment systems leading toward sustainable health, changes in provider roles, and the entrance of new nontraditional players. For more on this topic, watch Health Systems in 2030, a free NEJM Catalyst virtual event held on March 4, 2021.
Kerala demonstrated that if Governments take a proactive role in engaging the private sector, in an informed and evidence-based way, they can leverage the advantages of the private sector while protecting the public health interest. The case study reiterates that a good governance is essential for ensuring care in a mixed health system and such ...
What is Quality Improvement (QI)? Paul Batalden and Frank Davidoff, in 2008, described QI as "the combined and unceasing efforts of everyone—healthcare professionals, patients and their families, researchers, payers, planners and educators—to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development" .
Since 2004, the agency has developed more than 400 Impact Case Studies that illustrate AHRQ's contributions to healthcare improvement. Available online and searchable via an interactive map , the Impact Case Studies help to tell the story of how AHRQ-funded research findings, data and tools have made an impact on the lives of millions of ...
Figure 1: The benefits of the National Digital Health Strategy. Important aspects of the patient-centric strategy are the level of benchmarking performed to determine best-in-class approaches to digital health, especially in Africa, enhanced patient experiences, alignment with human rights principles and the UN's SDGs, operational excellence ...
Quality Improvement. As leaders in health care, advanced practitioners often conduct QI projects to improve their internal processes or streamline clinical workflow. These QI projects use a multidisciplinary team comprising a team leader as well as nurses, PAs, pharmacists, physicians, social workers, and program administrators to address ...