Essay on Hospital
500 words essay on hospital.
Hospitals are institutions that deal with health care activities. They offer treatment to patients with specialized staff and equipment. In other words, hospitals serve humanity and play a vital role in the social welfare of any society. They have all the facilities to deal with varying diseases to make the patient healthy. The essay on hospital will take us through their types and importance.


Types of Hospitals
Generally, there are two types of hospitals, private hospitals and government hospitals. An individual or group of physicians or organization run private hospitals. On the other hand, the government runs the government hospital.
There are also semi-government hospitals that a private and organization and government-run together. Further, there are general hospitals that deal with different kinds of healthcare but with a limited capacity.
General hospitals treat patients from any type of disease belonging to any sex or age. Alternatively, there are specialized hospitals that limit their services to a particular health condition like oncology, maternity and more.
The main aim of hospitals is to offer maximum health services and ensure care and cure. Further, there are other hospitals also which serve as training centres for the upcoming physicians and offer training to professionals.
Many hospitals also conduct research works for people. The essential services which are available in a hospital include emergency and casualty services, OPD services, IPD services, and operation theatre.
Importance of Hospitals
Hospitals are very important for us as they offer extensive treatment to all. Moreover, they are equipped with medical equipment which helps in the diagnosis and treatment of many types of diseases.
Further, one of the most important functions of hospitals is that they offer multiple healthcare professionals. It is filled with a host of doctors, nurses and interns. When a patient goes to a hospital, many doctors do a routine check-up to ensure maximum care.
Similarly, when there are multiple doctors in one place, you can take as many opinions as you want. Further, you will never be left unattended with the availability of such professionals. It also offers everything under one roof.
For instance, in the absence of hospitals, we would have to go to different places to look for specialist doctors in their respective clinics. This would have just increased the hassle and waste energy and time.
But, hospitals narrow down this search to a great level. Hospitals are also a great source of employment for a large section of society. Apart from the hospital staff, there are maintenance crew, equipment handlers and more.
In addition, they also provide cheaper healthcare as they offer treatment options for patients from underprivileged communities. We also use them to raise awareness regarding different prevention and vaccination drives. Finally, they also offer specialized treatment for a particular illness.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Hospital
We have generally associated hospital with illness but the case is the opposite of wellness. In other words, we visit the hospital all sick and leave healthy or better than before. Moreover, hospitals play an essential role in offering consultation services to patients and making the population healthier.
FAQ of Essay on Hospital
Question 1: What is the importance of hospitals?
Answer 1: Hospitals are significant as they treat minor and serious diseases, illnesses and disorders of the body function of varying types and severity. Moreover, they also help in promoting health, giving information on the prevention of illnesses and providing curative services.
Question 2: What are the services of a hospital?
Answer 2: Hospitals provide many services which include short-term hospitalization. Further, it also offers emergency room services and general and speciality surgical services. Moreover, they also offer x-ray and radiology and laboratory services.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Medical Facilities Essays
Improving healthcare safety, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essays Examples >
- Essay Topics
Essays on Medical Facilities
21 samples on this topic
On this resource, we've put together a database of free paper samples regarding Medical Facilities. The intention is to provide you with a sample identical to your Medical Facilities essay topic so that you could have a closer look at it in order to get a clear idea of what a great academic work should look like. You are also advised to employ the best Medical Facilities writing practices displayed by competent authors and, eventually, create a top-notch paper of your own.
However, if putting together Medical Facilities papers entirely by yourself is not an option at this point, WowEssays.com essay writer service might still be able to help you out. For instance, our writers can develop an one-of-a-kind Medical Facilities essay sample solely for you. This example paper on Medical Facilities will be written from scratch and tailored to your original requirements, fairly priced, and delivered to you within the pre-set period. Choose your writer and buy custom essay now!
Managed Care Essay Sample
Introduction
Medical Informatics Case Study Example
Future trends in nursing practice essays examples.
The institutional affiliation
Good Literature Review About Managed Care And Quality Of Life
Healthcare marketing creative writing to use for practical writing help.
Letter to Chamber of Commerce
[Address: XYZ] [City, State, Zip]
Executive Vice President Local Chamber of Commerce
U.S. Chamber of Commerce 1615 H Street, NW Washington, DC 20062-2000 RE: Letter from owner of XYZ organization to the Executive Vice President of local chamber of commerce, introducing XYZ health care organization.
Dear Mr. Vice President,
Example Of We Can, But Dare We? Essay
Cultural privileges {type) to use as a writing model, fertility rate, death rate, and birth rate between 2000 and 2010 term papers example.
India’s Economy and Population
Perfect Model Essay On Cost Benefit Analysis
Attributes of the heics: a top-quality essay for your inspiration.
Implementation of the Hospital Emergency Incident Command System
Good Essay On Total Rewards- Makey Case
Demonstrating roles of the advanced practice registered nurse: free sample research paper to follow, good essay about health policy making, essay on awareness campaign grant.
List of Figures
Figure 1: Personal Hygiene advocacy Figure 2: Creating awareness on HIV Figure 3: EMS Ambulance in Action
Executive Summary/ Abstract
Inspiring Case Study About Defining Integrated Health System
Integrated Health System
Gender Segregation And Its Impact On The Employment Practices Of Doctors And Nurses: Literature Review You Might Want To Emulate
Economics essays examples.
Delivery date
Continuing Professional Development For Diagnostic Medical Sonography Research Papers Example
Telenursing {type) to use as a writing model.
275 words = 1 page double-spaced

Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
Don't have an Account?
Register Now!

- International Student
- Essay Writing Center
- Sample Essays
Sample Medical School Essays
Applying to medical school is an exciting decision, but the application process is very competitive. This means when it comes to your application you need to ensure you’ve put your best foot forward and done everything you can to stand out from other applicants. One great way to provide additional information on why you have decided to pursue a career in medicine and why you’re qualified, is your medical school essay. Read these samples to get a good idea on how you can write your own top-notch essay.
This section contains five sample medical school essays
- Medical School Sample Essay One
- Medical School Sample Essay Two
- Medical School Sample Essay Three
- Medical School Sample Essay Four
- Medical School Sample Essay Five
Medical School Essay One
When I was twelve years old, a drunk driver hit the car my mother was driving while I was in the backseat. I have very few memories of the accident, but I do faintly recall a serious but calming face as I was gently lifted out of the car. The paramedic held my hand as we traveled to the hospital. I was in the hospital for several weeks and that same paramedic came to visit me almost every day. During my stay, I also got to know the various doctors and nurses in the hospital on a personal level. I remember feeling anxiety about my condition, but not sadness or even fear. It seemed to me that those around me, particularly my family, were more fearful of what might happen to me than I was. I don’t believe it was innocence or ignorance, but rather a trust in the abilities of my doctors. It was as if my doctors and I had a silent bond. Now that I’m older I fear death and sickness in a more intense way than I remember experiencing it as a child. My experience as a child sparked a keen interest in how we approach pediatric care, especially as it relates to our psychological and emotional support of children facing serious medical conditions. It was here that I experienced first-hand the power and compassion of medicine, not only in healing but also in bringing unlikely individuals together, such as adults and children, in uncommon yet profound ways. And it was here that I began to take seriously the possibility of becoming a pediatric surgeon.
My interest was sparked even more when, as an undergraduate, I was asked to assist in a study one of my professors was conducting on how children experience and process fear and the prospect of death. This professor was not in the medical field; rather, her background is in cultural anthropology. I was very honored to be part of this project at such an early stage of my career. During the study, we discovered that children face death in extremely different ways than adults do. We found that children facing fatal illnesses are very aware of their condition, even when it hasn’t been fully explained to them, and on the whole were willing to fight their illnesses, but were also more accepting of their potential fate than many adults facing similar diagnoses. We concluded our study by asking whether and to what extent this discovery should impact the type of care given to children in contrast to adults. I am eager to continue this sort of research as I pursue my medical career. The intersection of medicine, psychology, and socialization or culture (in this case, the social variables differentiating adults from children) is quite fascinating and is a field that is in need of better research.
Although much headway has been made in this area in the past twenty or so years, I feel there is a still a tendency in medicine to treat diseases the same way no matter who the patient is. We are slowly learning that procedures and drugs are not always universally effective. Not only must we alter our care of patients depending upon these cultural and social factors, we may also need to alter our entire emotional and psychological approach to them as well.
It is for this reason that I’m applying to the Johns Hopkins School of Medicine, as it has one of the top programs for pediatric surgery in the country, as well as several renowned researchers delving into the social, generational, and cultural questions in which I’m interested. My approach to medicine will be multidisciplinary, which is evidenced by the fact that I’m already double-majoring in early childhood psychology and pre-med, with a minor in cultural anthropology. This is the type of extraordinary care that I received as a child—care that seemed to approach my injuries with a much larger and deeper picture than that which pure medicine cannot offer—and it is this sort of care I want to provide my future patients. I turned what might have been a debilitating event in my life—a devastating car accident—into the inspiration that has shaped my life since. I am driven and passionate. And while I know that the pediatric surgery program at Johns Hopkins will likely be the second biggest challenge I will face in my life, I know that I am up for it. I am ready to be challenged and prove to myself what I’ve been telling myself since that fateful car accident: I will be a doctor.
Tips for a Successful Medical School Essay
- If you’re applying through AMCAS, remember to keep your essay more general rather than tailored to a specific medical school, because your essay will be seen by multiple schools.
- AMCAS essays are limited to 5300 characters—not words! This includes spaces.
- Make sure the information you include in your essay doesn't conflict with the information in your other application materials.
- In general, provide additional information that isn’t found in your other application materials. Look at the essay as an opportunity to tell your story rather than a burden.
- Keep the interview in mind as you write. You will most likely be asked questions regarding your essay during the interview, so think about the experiences you want to talk about.
- When you are copying and pasting from a word processor to the AMCAS application online, formatting and font will be lost. Don’t waste your time making it look nice. Be sure to look through the essay once you’ve copied it into AMCAS and edit appropriately for any odd characters that result from pasting.
- Avoid overly controversial topics. While it is fine to take a position and back up your position with evidence, you don’t want to sound narrow-minded.
- Revise, revise, revise. Have multiple readers look at your essay and make suggestions. Go over your essay yourself many times and rewrite it several times until you feel that it communicates your message effectively and creatively.
- Make the opening sentence memorable. Admissions officers will read dozens of personal statements in a day. You must say something at the very beginning to catch their attention, encourage them to read the essay in detail, and make yourself stand out from the crowd.
- Character traits to portray in your essay include: maturity, intellect, critical thinking skills, leadership, tolerance, perseverance, and sincerity.
Medical School Essay Two
If you had told me ten years ago that I would be writing this essay and planning for yet another ten years into the future, part of me would have been surprised. I am a planner and a maker of to-do lists, and it has always been my plan to follow in the steps of my father and become a physician. This plan was derailed when I was called to active duty to serve in Iraq as part of the War on Terror.
I joined the National Guard before graduating high school and continued my service when I began college. My goal was to receive training that would be valuable for my future medical career, as I was working in the field of emergency health care. It was also a way to help me pay for college. When I was called to active duty in Iraq for my first deployment, I was forced to withdraw from school, and my deployment was subsequently extended. I spent a total of 24 months deployed overseas, where I provided in-the-field medical support to our combat troops. While the experience was invaluable not only in terms of my future medical career but also in terms of developing leadership and creative thinking skills, it put my undergraduate studies on hold for over two years. Consequently, my carefully-planned journey towards medical school and a medical career was thrown off course. Thus, while ten-year plans are valuable, I have learned from experience how easily such plans can dissolve in situations that are beyond one’s control, as well as the value of perseverance and flexibility.
Eventually, I returned to school. Despite my best efforts to graduate within two years, it took me another three years, as I suffered greatly from post-traumatic stress disorder following my time in Iraq. I considered abandoning my dream of becoming a physician altogether, since I was several years behind my peers with whom I had taken biology and chemistry classes before my deployment. Thanks to the unceasing encouragement of my academic advisor, who even stayed in contact with me when I was overseas, I gathered my strength and courage and began studying for the MCAT. To my surprise, my score was beyond satisfactory and while I am several years behind my original ten-year plan, I am now applying to Brown University’s School of Medicine.
I can describe my new ten-year plan, but I will do so with both optimism and also caution, knowing that I will inevitably face unforeseen complications and will need to adapt appropriately. One of the many insights I gained as a member of the National Guard and by serving in war-time was the incredible creativity medical specialists in the Armed Forces employ to deliver health care services to our wounded soldiers on the ground. I was part of a team that was saving lives under incredibly difficult circumstances—sometimes while under heavy fire and with only the most basic of resources. I am now interested in how I can use these skills to deliver health care in similar circumstances where basic medical infrastructure is lacking. While there is seemingly little in common between the deserts of Fallujah and rural Wyoming, where I’m currently working as a volunteer first responder in a small town located more than 60 miles from the nearest hospital, I see a lot of potential uses for the skills that I gained as a National Guardsman. As I learned from my father, who worked with Doctors Without Borders for a number of years, there is quite a bit in common between my field of knowledge from the military and working in post-conflict zones. I feel I have a unique experience from which to draw as I embark on my medical school journey, experiences that can be applied both here and abroad.
In ten years’ time, I hope to be trained in the field of emergency medicine, which, surprisingly, is a specialization that is actually lacking here in the United States as compared to similarly developed countries. I hope to conduct research in the field of health care infrastructure and work with government agencies and legislators to find creative solutions to improving access to emergency facilities in currently underserved areas of the United States, with an aim towards providing comprehensive policy reports and recommendations on how the US can once again be the world leader in health outcomes. While the problems inherent in our health care system are not one-dimensional and require a dynamic approach, one of the solutions as I see it is to think less in terms of state-of-the-art facilities and more in terms of access to primary care. Much of the care that I provide as a first responder and volunteer is extremely effective and also relatively cheap. More money is always helpful when facing a complex social and political problem, but we must think of solutions above and beyond more money and more taxes. In ten years I want to be a key player in the health care debate in this country and offering innovative solutions to delivering high quality and cost-effective health care to all our nation’s citizens, especially to those in rural and otherwise underserved areas.
Of course, my policy interests do not replace my passion for helping others and delivering emergency medicine. As a doctor, I hope to continue serving in areas of the country that, for one reason or another, are lagging behind in basic health care infrastructure. Eventually, I would also like to take my knowledge and talents abroad and serve in the Peace Corps or Doctors Without Borders.
In short, I see the role of physicians in society as multifunctional: they are not only doctors who heal, they are also leaders, innovators, social scientists, and patriots. Although my path to medical school has not always been the most direct, my varied and circuitous journey has given me a set of skills and experiences that many otherwise qualified applicants lack. I have no doubt that the next ten years will be similarly unpredictable, but I can assure you that no matter what obstacles I face, my goal will remain the same. I sincerely hope to begin the next phase of my journey at Brown University. Thank you for your kind attention.
Additional Tips for a Successful Medical School Essay
- Regardless of the prompt, you should always address the question of why you want to go to medical school in your essay.
- Try to always give concrete examples rather than make general statements. If you say that you have perseverance, describe an event in your life that demonstrates perseverance.
- There should be an overall message or theme in your essay. In the example above, the theme is overcoming unexpected obstacles.
- Make sure you check and recheck for spelling and grammar!
- Unless you’re very sure you can pull it off, it is usually not a good idea to use humor or to employ the skills you learned in creative writing class in your personal statement. While you want to paint a picture, you don’t want to be too poetic or literary.
- Turn potential weaknesses into positives. As in the example above, address any potential weaknesses in your application and make them strengths, if possible. If you have low MCAT scores or something else that can’t be easily explained or turned into a positive, simply don’t mention it.
Medical School Essay Three
The roots of my desire to become a physician are, thankfully, not around the bedside of a sick family member or in a hospital, but rather on a 10-acre plot of land outside of a small town in Northwest Arkansas. I loved raising and exhibiting cattle, so every morning before the bus arrived at 7 a.m. I was in the barn feeding, checking cattle for any health issues and washing the show heifers. These early mornings and my experiences on a farm not only taught me the value of hard work, but ignited my interest in the body, albeit bovine at the time. It was by a working chute that I learned the functions of reproductive hormones as we utilized them for assisted reproduction and artificial insemination; it was by giving vaccinations to prevent infection that I learned about bacteria and the germ theory of disease; it was beside a stillborn calf before the sun had risen that I was exposed to the frailty of life.
Facing the realities of disease and death daily from an early age, I developed a strong sense of pragmatism out of necessity. There is no place for abstractions or euphemisms about life and death when treating a calf’s pneumonia in the pouring rain during winter. Witnessing the sometimes harsh realities of life on a farm did not instill within me an attitude of jaded inevitability of death. Instead, it germinated a responsibility to protect life to the best of my abilities, cure what ailments I can and alleviate as much suffering as possible while recognizing that sometimes nothing can be done.
I first approached human health at the age of nine through beef nutrition and food safety. Learning the roles of nutrients such as zinc, iron, protein and B-vitamins in the human body as well as the dangers of food-borne illness through the Beef Ambassador program shifted my interest in the body to a new species. Talking with consumers about every facet of the origins of food, I realized that the topics that most interested me were those that pertained to human health. In college, while I connected with people over samples of beef and answered their questions, I also realized that it is not enough simply to have adequate knowledge. Ultimately knowledge is of little use if it is not digestible to those who receive it. So my goal as a future clinical physician is not only to illuminate the source of an affliction and provide treatment for patients, but take care to ensure the need for understanding by both patient and family is met.
I saw this combination of care and understanding while volunteering in an emergency room, where I was also exposed to other aspects and players in the medical field. While assisting a nurse perform a bladder scan and witnessing technicians carry out an echocardiogram or CT scan, I learned the important roles that other professionals who do not wear white coats have in today’s medical field. Medicine is a team sport, and coordinating the efforts of each of these players is crucial for the successful execution of patient care. It is my goal to serve as the leader of this healthcare unit and unify a team of professionals to provide the highest quality care for patients. Perhaps most importantly my time at the VA showed me the power a smile and an open ear can have with people. On the long walk to radiology, talking with patients about their military service and families always seemed to take their mind off the reason for their visit, if only for a few minutes. This served as a reminder that we are helping people with pasts and dreams, rather than simply remedying patients’ symptoms.
Growing up in a small town, I never held aspirations of world travel when I was young. But my time abroad revealed to me the state of healthcare in developing countries and fostered a previously unknown interest in global health. During my first trip abroad to Ghana, my roommate became ill with a severe case of traveler’s diarrhea. In the rural north of the country near the Sahara, the options for healthcare were limited; he told me how our professor was forced to bribe employees to bypass long lines and even recounted how doctors took a bag of saline off the line of another patient to give to him. During a service trip to a rural community in Nicaragua, I encountered patients with preventable and easily treatable diseases that, due to poverty and lack of access, were left untreated for months or years at a time. I was discouraged by the state of healthcare in these countries and wondered what could be done to help. I plan to continue to help provide access to healthcare in rural parts of developing countries, and hopefully as a physician with an agricultural background I can approach public health and food security issues in a multifaceted and holistic manner.
My time on a cattle farm taught me how to work hard to pursue my interests, but also fueled my appetite for knowledge about the body and instilled within me a firm sense of practicality. Whether in a clinic, operating room or pursuing public and global health projects, I plan to bring this work ethic and pragmatism to all of my endeavors. My agricultural upbringing has produced a foundation of skills and values that I am confident will readily transplant into my chosen career. Farming is my early passion, but medicine is my future.
Medical School Essay Four
I am a white, cisgender, and heterosexual female who has been afforded many privileges: I was raised by parents with significant financial resources, I have traveled the world, and I received top-quality high school and college educations. I do not wish to be addressed or recognized in any special way; all I ask is to be treated with respect.
As for my geographic origin, I was born and raised in the rural state of Maine. Since graduating from college, I have been living in my home state, working and giving back to the community that has given me so much. I could not be happier here; I love the down-to-earth people, the unhurried pace of life, and the easy access to the outdoors. While I am certainly excited to move elsewhere in the country for medical school and continue to explore new places, I will always self-identify as a Mainer as being from Maine is something I take great pride in. I am proud of my family ties to the state (which date back to the 1890’s), I am proud of the state’s commitment to preserving its natural beauty, and I am particularly proud of my slight Maine accent (we don’t pronounce our r’s). From the rocky coastline and rugged ski mountains to the locally-grown food and great restaurants, it is no wonder Maine is nicknamed, "Vacationland.” Yet, Maine is so much more than just a tourist destination. The state is dotted with wonderful communities in which to live, communities like the one where I grew up.
Perhaps not surprisingly, I plan to return to Maine after residency. I want to raise a family and establish my medical practice here. We certainly could use more doctors! Even though Maine is a terrific place to live, the state is facing a significant doctor shortage. Today, we are meeting less than half of our need for primary care providers. To make matters worse, many of our physicians are close to retirement age. Yet, according to the AAMC, only 53 Maine residents matriculated into medical school last year! Undoubtedly, Maine is in need of young doctors who are committed to working long term in underserved areas. As my primary career goal is to return to my much adored home state and do my part to help fill this need, I have a vested interest in learning more about rural medicine during medical school.
I was raised in Cumberland, Maine, a coastal town of 7,000 just north of Portland. With its single stoplight and general store (where it would be unusual to visit without running into someone you know), Cumberland is the epitome of a small New England town. It truly was the perfect place to grow up. According to the most recent census, nearly a third of the town’s population is under 18 and more than 75% of households contain children, two statistics which speak to the family-centric nature of Cumberland’s community. Recently rated Maine's safest town, Cumberland is the type of place where you allow your kindergartener to bike alone to school, leave your house unlocked while at work, and bring home-cooked food to your sick neighbors and their children. Growing up in such a safe, close-knit, and supportive community instilled in me the core values of compassion, trustworthiness, and citizenship. These three values guide me every day and will continue to guide me through medical school and my career in medicine.
As a medical student and eventual physician, my compassion will guide me to become a provider who cares for more than just the physical well-being of my patients. I will also commit myself to my patients’ emotional, spiritual, and social well-being and make it a priority to take into account the unique values and beliefs of each patient. By also demonstrating my trustworthiness during every encounter, I will develop strong interpersonal relationships with those whom I serve. As a doctor once wisely said, “A patient does not care how much you know until he knows how much you care.”
My citizenship will guide me to serve my community and to encourage my classmates and colleagues to do the same. We will be taught in medical school to be healers, scientists, and educators. I believe that, in addition, as students and as physicians, we have the responsibility to use our medical knowledge, research skills, and teaching abilities to benefit more than just our patients. We must also commit ourselves to improving the health and wellness of those living in our communities by participating in public events (i.e by donating our medical services), lobbying for better access to healthcare for the underprivileged, and promoting wellness campaigns. As a medical student and eventual physician, my compassion, trustworthiness, and citizenship will drive me to improve the lives of as many individuals as I can.
Cumberland instilled in me important core values and afforded me a wonderful childhood. However, I recognize that my hometown is not perfect. For one, the population is shockingly homogenous, at least as far as demographics go. As of the 2010 census, 97.2% of the residents of Cumberland were white. Only 4.1% of residents speak a language other than English at home and even fewer were born in another country. Essentially everybody who identified with a religion identified as some denomination of Christian. My family was one of maybe five Jewish families in the town. Additionally, nearly all the town’s residents graduated from high school (98.1%), are free of disability (93.8%), and live above the poverty line (95.8%). Efforts to attract diverse families to Cumberland is one improvement that I believe would make the community a better place in which to live. Diversity in background (and in thought) is desirable in any community as living, learning, and working alongside diverse individuals helps us develop new perspectives, enhances our social development, provides us with a larger frame of reference, and improves our understanding of our place in society.
Medical School Essay Five
“How many of you received the flu vaccine this year?” I asked my Bricks 4 Kidz class, where I volunteer to teach elementary students introductory science and math principles using Lego blocks. “What’s a flu vaccine?” they asked in confusion. Surprised, I briefly explained the influenza vaccine and its purpose for protection. My connection to children and their health extends to medical offices, clinics and communities where I have gained experience and insight into medicine, confirming my goal of becoming a physician.
My motivation to pursue a career in medicine developed when my mother, who was diagnosed with Lupus, underwent a kidney transplant surgery and suffered multiple complications. I recall the fear and anxiety I felt as a child because I misunderstood her chronic disease. This prompted me to learn more about the science of medicine. In high school, I observed patients plagued with acute and chronic kidney disease while briefly exploring various fields of medicine through a Mentorship in Medicine summer program at my local hospital. In addition to shadowing nephrologists in a hospital and clinical setting, I scrubbed into the operating room, viewed the radiology department, celebrated the miracle of birth in the delivery room, and quietly observed a partial autopsy in pathology. I saw many patients confused about their diagnoses. I was impressed by the compassion of the physicians and the time they took to reassure and educate their patients.
Further experiences in medicine throughout and after college shaped a desire to practice in underserved areas. While coloring and reading with children in the patient area at a Family Health Center, I witnessed family medicine physicians diligently serve patients from low-income communities. On a medical/dental mission trip to the Philippines, I partnered with local doctors to serve and distribute medical supplies to rural schools and communities. At one impoverished village, I held a malnourished two-year old boy suffering from cerebral palsy and cardiorespiratory disease. His family could not afford to take him to the nearest pediatrician, a few hours away by car, for treatment. Overwhelmed, I cried as we left the village. Many people were suffering through pain and disease due to limited access to medicine. But this is not rare; there are many people suffering due to inadequate access/accessibility around the world, even in my hometown. One physician may not be able to change the status of underserved communities, however, one can alleviate some of the suffering.
Dr. X, my mentor and supervisor, taught me that the practice of medicine is both a science and an art. As a medical assistant in a pediatric office, I am learning about the patient-physician relationship and the meaningful connection with people that medicine provides. I interact with patients and their families daily. Newborn twins were one of the first patients I helped, and I look forward to seeing their development at successive visits. A young boy who endured a major cardiac surgery was another patient I connected with, seeing his smiling face in the office often as he transitioned from the hospital to his home. I also helped many excited, college-bound teenagers with requests for medical records in order to matriculate. This is the art of medicine – the ability to build relationships with patients and have an important and influential role in their lives, from birth to adulthood and beyond.
In addition, medicine encompasses patient-centered care, such as considering and addressing concerns. While taking patient vitals, I grew discouraged when parents refused the influenza vaccine and could not understand their choices. With my experience in scientific research, I conducted an informal yet insightful study. Over one hundred families were surveyed about their specific reasons for refusing the flu vaccine. I sought feedback on patients’ level of understanding about vaccinations and its interactions with the human immune system. Through this project, I learned the importance of understanding patient’s concerns in order to reassure them through medicine. I also learned the value of communicating with patients, such as explaining the purpose of a recommended vaccine. I hope to further this by attending medical school to become a physician focused on patient-centered care, learning from and teaching my community.
Children have been a common thread in my pursuit of medicine, from perceiving medicine through child-like eyes to interacting daily with children in a medical office. My diverse experiences in patient interaction and the practice of medicine inspire me to become a physician, a path that requires perseverance and passion. Physicians are life-long learners and teachers, educating others whether it is on vaccinations or various diseases. This vocation also requires preparation, and I eagerly look forward to continually learning and growing in medical school and beyond.
To learn more about what to expect from the study of medicine, check out our Study Medicine in the US section.
Related Content:
Get the international student newsletter.
Healthcare Facility Essays (Examples)
Healthcare Provider Shortage
Us healthcare reimbursement and insurance issues.
Strata Decision Technology. (2020). Healthcare and hospital capital budget. Retrieved from https://www.stratadecision.com/healthcare-and-hospital-capital-budget/
The Karen Ann Quinlan Case Legal Aspects Of Healthcare
Quality and sustainability in health care, shortages of health care providers.
IOM. (2010). The future of nursing. Retrieved from http://nacns.org/wp-content/uploads/2016/11/5-IOM-Report.pdf " target="_blank" REL="NOFOLLOW">
Healthcare In The US Vs Healthcare In The UK France And India
Health care institutional organization and management.
Source Link: https://www.researchgate.net/figure/Organizational-Chart-of-Leadership-at-the-Mayo-Clinic-the-parent-organization-changed_fig2_234069825
Healthcare Marketing
Lane, T. (2019). Healthcare marketing laws. Retrieved from https://smallbusiness.chron.com/healthcare-marketing-laws-67307.html
Lifelong Learning Plan For A Healthcare Administrator
Gender and veterans differences in access to mental health care services.
Koo, K.H., Madden, E. & Maguen, S. (2015). Race, ethnicity, and gender differences in V.A. health care service utilization among U.S. veterans of recent conflicts. Psychiatric Services, 66(5), 507-513. https://doi.org/10.1176/appi.ps.201300498
Related Topics
- Healthcare Policy
- Healthcare Management
- Healthcare System
- Healthcare Services
- Healthcare Professional
- Healthcare Delivery
- Healthcare Sector
- Healthcare Environment
- Healthcare Fraud
Category Topics
- Female Circumcision
- Nursing Program
- Genetic Disease
- Sickle Cell
- Health Psychology
Improve your studying and writing skills
We have over 150,000+ study documents to help you.
Join thousands of other students and
"spark your studies"..
Study Guides
Writing Guides
Studying / Writing Tools
Customer Service
Your customer service team resolved my issue in minutes!

Study Spark - providing your mind the spark it needs to help improve your grades.
©2020 Study Spark LLC.
Studyspark.com uses cookies to offer our users the best experience. By continuing, you are agreeing to receive cookies. Privacy Policy

- Customer Reviews
- Extended Essays
- IB Internal Assessment
- Theory of Knowledge
- Literature Review
- Dissertations
- Essay Writing
- Research Writing
- Assignment Help
- Capstone Projects
- College Application
- Online Class
30+ Medical Argumentative Essay Topics for College Students
by Antony W
April 21, 2023

Medical argumentative essay topics give you some brilliant ideas that you can explore and defend depending on the research you’ve conducted.
As with any argumentative essay topic , a medical related essay also requires you to take a stance and use objective, verifiable, and reasonable evidence to defend your position.
However, the kinds of topics many students pick to explore in the medical field are often quite too common.
Think of type II diabetes, cardiovascular illness, breast cancer, and cirrhosis. These are topics you don’t want to cover for the simple reason that they are too common.
In this post, we give you a list of 30+ medical argumentative essay topics that aren’t too obvious.
These topic ideas should enable you to add a new spin to your work, so that you can write a medical essay that focuses on an issue that will capture the attention of your audience (reader) almost instantly.
30+ Medical Argumentative Essay Topics
Below is a list of 30+ essay topics that you may find interesting for your medical argumentative essay assignment :
Controversial Medical Argumentative Essay Topics
- The cost of healthcare in the United States of America is not justifiable
- Do homeless people deserve free healthcare simply because they don’t have money to pay medical bills?
- Unconventional medication should not be part of a state’s healthcare system
- There’s a strong link between poor health and poverty
- People should not turn to homeopathy because it isn’t more effective compared to seeking medical advice
- People with no health insurance cover deserve to get equal treatment at medical healthcare facilities
- Should the government take action against unexpected errors in medical settings?
- Doctors should not have the right to endorse medical products until verified for safety and effectiveness
- Healthcare institutions should provide opt-out and opt-in donor system
- There’s no true justification for the rising cost of healthcare in the United States of America
In theory, areas such as genetic engineering, diagnostics, and medical research can be interesting to explore within the medical field.
However, the assignment requires hours of intensive research, proper structuring, writing, and editing.
If you don’t have the time for all that, you can get argumentative assignment help from one of our team of writers.
Health Practices Argumentative Essay Topics
- The marijuana drug should be made legal worldwide
- TV shows on diet and weight loss don’t motivate people to improve their body image and self-esteem
- Is the state responsible for teaching people how to lead a healthy lifestyle?
- Communication authorities should impose an indefinite ban on TV shows that promote cosmetic surgery
- TV commercials that promote fast foods and alcohol should not be banned.
- It’s a waste of time to impose state regulation on fast food chains and alcohol sales as it undermines people’s freewill to food choices.
- Should we allow and encourage teenagers to use birth control pills?
- The state should not encourage the use of products manufactured at the cost of another person’s well-being.
- Exercise alone can’t improve your health
- Doctors should not ask for medical consent if they know they can save a patient from a particular illness
Medical Laws and Policies Argumentative Essay Topics
- Should the government declare euthanasia illegal?
- Doctors should not insist on providing medical treatment to minors if their parents are against such treatments.
- The vaccination of children against illnesses should be voluntary
- An organ transplantation committee should not consider an individual’s accomplishment to determine if they can receive an organ
- Patients should decide if they would like to use surrogate pregnancy for health reasons or on demand
- Is doctor-patient confidentially necessary anymore?
- There’s no concrete evidence that living a sedentary and lavish lifestyle is the number one cause of weight gain
- Should we support the legalization of abortion?
- Should patients with mental health conditions receive treatment in or outside of their community?
- People should not accept organ transplantation because of leading an unhealthy life
You may click here to place your order , and one of our writers who has experience in writing medical related essays will help you get the paper completed on time. Since we focus on custom writing, you don’t have to worry about plagiarism at all.
Argumentative Essay Topics on Medical Research
- Genetic engineering is humanly unethical and morally wrong and should therefore not be allowed
- Are there effective means to mitigate threats posed by medical research?
- There is no reasonable evidence that the Covid-19 global pandemic originated from a lab I Wuhan, China
- Medics should not use animals to test the effective of drugs on humans
- Computers used in medical research and diagnostic cannot replace doctors no matter how sophisticated they become.
- Should human beings be subject to mandatory medical testing without their consent?
- Should the federal government and health organizations, such as the UN and CDC, finance practical medical research?
- Do we need to have limits when subjecting human beings to absolutely necessary medical tests?
- The Corona virus is a biochemical weapon built in the lab to wipe out the human race
- There’s no sufficient evidence to prove that pills that delay aging can make the human race immortal
Medical Argumentative Essay Topics on Healthcare Management
- Is healthcare management doing enough to maintain the right standards in healthcare facilities?
- Are privately owned hospitals managed better than public hospitals?
- Registered nurses should not assume the role of a physician even in the event of a serious medical emergency
- Human Resource Management (HR) isn’t doing enough to improve and protect the quality of healthcare
- Do surgeons play an important role outside their medical capacities?
- Are healthcare institutions responsible for the protection of the environment?
- The relationship between and among medical staff can affect the quality of patients of different illnesses.
- There’s no relationship between a patient’s medical results and a hospital’s revenue.
- It’s easy to improve the relationship among staff members in a healthcare facility
- Should medical management allow and encourage intimate relationships among the staff members?

General Medical Argumentative Essay Topics
- Has the American government invested enough funds to improve healthcare service for its residents?
- There should be as many male nurses as there are female nurses
- Are data management systems in hospitals accurate and safe against breach?
- Do prisoners have the right to access quality healthcare?
- Electronic health record systems have more limitations than benefits.
related resources
- Argumentative Essay Topics on Racism
- Argumentative Essay Topics About Animals
- Music Argumentative Essay Topics
- Social Media Argumentative Essay Topics
- Technology Argumentative Essay Topics
About the author
Antony W is a professional writer and coach at Help for Assessment. He spends countless hours every day researching and writing great content filled with expert advice on how to write engaging essays, research papers, and assignments.

Enter the URL below into your favorite RSS reader.
Challenges in public health facilities and services: evidence from a geographically isolated and disadvantaged area in the Philippines
- Citation (BibTeX)
View more stats
The study describes the conditions of public health sector in the Island Municipality of Jomalig, Quezon Province in Luzon, Philippines. Located at the far north-eastern side of the Quezon Province, Jomalig Island can be reached through a motor boat at around 4-5 hours (or more depending on the sea condition). Given the geographical disadvantage, challenges in economic and social services in the island are apparent. That includes deficiencies in basic public utility services such as water and electricity. The paper showcases a needs assessment on public health facilities and services in a far-flung municipality in the Philippines. This study examines the challenges in public health aspirations in a location considered to be a geographically isolated and disadvantaged area (GIDA).
The study made use of key informant interviews (KIIs) among health professionals and village health workers in the island. Aside from the KIIs, the study included the World Health Organization’s (WHO) tracer checklist on general readiness. The checklist was administered but in interview style. The participants were the public health staff in the island. The researcher was able to interview the health professionals (nurses and a midwife) manning the main public health facility in the island municipality while in the case of the other villages, health volunteers or the Barangay Health Worker (BHWs) were interviewed.
There are deficiencies in facilities, offered services and health staff. Deficiencies are seen too based on the domains under the WHO Tracer Checklist. Mortality and morbidity rates were not at alarming rate though reports of hypertension and diarrhea are common. The relatively “complete” health services are only available at the island’s main health center yet unfortunately, some people who seek treatment and health care could not visit due to distance and the accompanying expenditures. Other factors affecting health status of the population include the reliance to “faith healers” (quack doctors or Albularyos) and the delay of parental reports of their health condition and the condition of their children, both of which result to the “escalation” of illness. Among others, challenges and aspirations of the island’s public health sector include electric supply, better budgetary allocation for their facilities, and equipment and additional training for the barangay (village) health workers.
Conclusions
Enduring the underfinanced and undermanned health facilities, the island’s population also suffers the consequences on overall health owing to limited movements and communication due to the geographical characteristics of the municipality. Emergency boats per village, health education campaign that focuses on eliminating open defecation and reliance on quack doctors, stand-by generators for the health centers, and radio communication system are strongly recommended to mitigate the negative impacts of living within GIDA communities.
High incidence of poverty is recorded in far-flung areas, which also comes with households having greater chances of living in poor conditions for a long time. In addition, geographically isolated areas are also associated with poor basic services and facilities such as schools, sanitation, electricity and clinics or health centers. 1 Some of these conditions have led to the deaths of poor children 2 or have put them in poor health conditions. 3 Moreover, positive health-seeking behaviour are not observed among the poor in contrast to population of higher economic classes. 4 This is not surprising since the less fortunate succumb to the consequences of poverty as they suffer the incapability to cope with health expenditures. 5 That is why community economic development is a crucial component in forming health-seeking behaviour 6 in these very areas. Governments have pursued nonetheless strategies to encourage the poor to utilize health facilities and services like giving incentives 7 , 8 and enrolling them in social insurance schemes. 9
However, aside from poverty, the conditions of public health facilities including the quality of health professionals and workers determine also the trajectories of health outcomes. 10 While, for example, improved access to better public health facilities and their services can reduce the mortality and morbidity rates associated with unhygienic medical procedures 11 , some health workers were found out to be prescribing drugs despite being untrained to do so 12 , which could lead to serious health complications among the public. Indeed, public health facilities and services are marred with concerns. Aside from the infrastructural and training aspects, problems in human resources and leadership contribute negatively to health-related services. 13 Such findings echoed what was underscored in the earlier study 14 where poor management in the provincial and local level were found out to be contributory to low-quality service in these health facilities.
Obviously, geographically isolated and disadvantaged areas (GIDA) reveal not only deficiencies in health facilities and services but also to the number of people accessing them compare to urban, city spaces. Policy makers should concern themselves to health outcomes especially in the midst of this gross inequalities. 15 Unfortunately, policy makers have rarely focus on including the poor in the implementation and formulation of strategies. 16
GIDA areas in the Philippines are particularly suffering under these conditions. Aside from the lack of health facilities (or the deficiencies therein), health professionals are either concentrated in the urban areas or leaving the country. 17 Despite the shortage of health professionals, the Philippines continue to be a major exporter of such human resources. 18 Inadequate pay is identified as one of the reasons health personnel are considering leaving public health facilities. 19
With all these on the background, the study examines the health needs of a far eastern island municipality in the Philippines. This aims to explore the deficiencies in health facilities and services in the island and how its location contributes significantly in the overall health-seeking behavior and health status of the population. The study provides insights as to how these geographically isolated and disadvantaged areas are challenged in terms of the desires to health care services and to recommend potential “small” solutions while recognizing budgetary constraints on the part of the government.
Study location
The research locale was the Island Municipality of Jomalig, part of the Quezon Province in Luzon, Philippines. Located at the far north-eastern side of the Quezon Province, Jomalig Island can be reached through a motor boat at around 4-5 hours (or more depending on the sea condition). Given the geographical disadvantage, challenges in economic and social services in the island are apparent. That includes deficiencies in basic public utility services such as water and electricity. In addition, most roads are not yet cemented which can turn easily into mud during rainy seasons. Health centers are visited by a doctor once or twice a month. The Philippine Statistics Authority indicates that Jomalig is a 5th class municipality which means that the locality has an annual income of 1 to 3 million pesos only.
Participants
The participants of the study were basically the public health staff in the island. The researcher was able to interview the health professionals (nurses and a midwife) manning the main public health facility in the island municipality while in the case of the other villages, only health volunteers or the Barangay Health Worker (BHWs) were interviewed. Some village officials were also able to give information about the status of their health facilities and services through informal conversations.
Data collection
The data were gathered through Key Informant Interviews (KIIs) with the assigned health professional (nurse or midwife) and the Barangay Health Worker (BHWs) for each particular barangay or community. The KIIs also made use of the World Health Organization’s Service Availability and Readiness Assessment (SARA) on general service readiness indicators. 20 The researcher made used of this WHO Tracer (Appendix S1 in the Online Supplementary Document ) to survey the level of general readiness of this island’s facilities to cater the health needs of its population. Each KII took place inside the health center “facilities”. The KII had two parts, the first was on the open-ended questions that inquired about the conditions of public health facilities in the area and the consequences of which in the general health of the population. The second part was on answering the WHO Tracer.
The data obtained from the KII were transcribed and then thematically analyzed. The result of WHO tracer checklist is presented in prose form under the given domains of the checklist.
Ethical approval
The researcher secured prior approval before the actual gathering of data among the participants. The researcher asked the permission of the head of the main health center of the island before the actual conduct of KII with their health staff in the center and in other villages. Aside from securing permission to conduct KIIs with the BHWs, the researcher also asked and informed each respective village official (village captain) about the undertaking. The researcher also sought the permissions of the participants about the use of a voice-recording device.
Key findings of this research are divided into several categories: (a) Mortality and Morbidity Rates (b) Health Services (c) Other factors affecting health status of the population (d) Challenges and Aspirations, and (e) WHO Tracer Items for assessing general readiness. These results are presented according to the themes that emerged from the interviews.
Mortality and morbidity rates
All barangays reported no alarming rates of mortality. Rare are cases of mortality due to illnesses but some minimal cases of death are reportedly due to natural death and hypertension. Consistently, all Barangays recorded cases of ordinary colds and cough and especially diarrhea. In two Barangays, Casuguran and Gango, health professionals noticed increased complaints of children’s wounds. The changing weather in the island is seen as a strong factor that causes colds and cough among children. The striking consistency of diarrhea in these communities is attributed to the open defecation practices of some residents in far-flung communities (in sitios or sub-villages]. Health professionals believe that such a practice contaminates the water source below and even in the seas where they just throw their faeces:
“They will just go somewhere private and defecate there. Some others would put their human waste in the plastic bag and then throw it in the waters. It made their water supply contaminated and especially diarrhea is more common to children who play and swim in the contaminated waters.”
Health services
Common to all Barangays are the general consultation services (with BP Monitoring], in which, health professionals sometimes are “forced” to issue prescription due to the absence of doctor in the island. Some minor surgeries can also be done in these health centers but are protocoled to be done in the main health center in Barangay Talisoy. Family planning, including its free counselling and contraceptives, is also offered in all Barangays. Deworming and immunization are also consistently offered and done in the health centers. However, in a sitio (sub-village) in Barangay Casuguran, immunization was not consistently held due to the lack of proper refrigeration for the vaccines. People in that Sitio could not just go in the Health center of their Barangay because of the travel cost and distance. Pre-natal check-ups are also offered in the centers with the lying-in services except in Barangay Bukal. Feeding programs are also held in Barangays Gango and Casuguran to counter malnutrition. TB dots program as well as the Grantisadong Pambata Program (Immunization) are offered in the centers. Anti-rabies shots are not offered even in Barangay Talisoy, so people have to go to Polilio or Lucena (Other Towns in the Province) for such injections.
Other factors affecting health status of the population
a. Albularyo-based treatment and other old beliefs and practices – Some part of the population still prioritise going to quack doctors over health professional and the BHWs for proper medical treatment. The implication is that those who came to Albularyos (faith healers) first then go to the health centers afterwards had their health conditions deteriorate or worsen. The idea of going first to Albularyos is reinforced by the belief that when people go to health centers, something bad will happen. A health professional also reported about people pouring amoxicillin to their open wounds instead of taking it in. Thus, wounds are not treated properly. Pregnant women also choose hilot (a birthing method characterized primarily by “massage”) over health center’s lying-in for proper birth delivery, which sometimes results to maternal and child death.
b. Poverty/Lack of income – the economic status of the general population spells a lot about the health status of people. It resulted to malnourishment of children, in fact in 2012, DSWD lists Jomalig as one of the top municipalities which have severe case of malnourishment among children. Money becomes also a terrible problem with the locals because they just cannot travel to their health center (in case they are from sitios going to the center) or from the island going to hospitals in other municipalities and cities of the Quezon province. Habal-habal (motorcycle - local mode of transportation) is also costly at the rate of hundreds, as well as the boat from the island going to other towns (especially if it’s a special trip) just to seek medical attention.
c. Geographical location and sea conditions – the distance to better health facilities also has great impact to the overall health status of the population. Intensive medical attention and comprehensive check-up are just few of the things that cannot be accessed easily due to proximity of the people from these facilities, its cost and travel hours make health needs more challenging to access for the poor population. Taking also into account the sea conditions, people just cannot sail even in emergency situations due to safety concerns, leaving patients in a very difficult position. Weather also is believed to be of a significant factor. Health workers attributed cases of cough and colds to the changing weather in the island.
d. Environment – unclean water sources are also factors in some communities due primarily to open defecation practices of some locals. Aside from irresponsible garbage dumping, the interviewees revealed that there are communities that almost half of the total number of households has no toilets of their own, affecting ground water below and even the immediate sea water close to those communities.
e. People’s stubbornness – parents play cards during the day that their children are left outside playing, in which they usually left these children unmonitored on their recreational activities in dirty areas and in the sea. Health workers believe that such is one of the causes why commonly complaint illnesses including wounds among children persist. This stubbornness also led to some parents consulting or bringing their children during evening or night when the official time of health workers has already passed but which ultimately results to the illnesses not being assessed earlier, and therefore not treated in its supposedly earlier stage.
Challenges and aspirations
a. Electricity - Supply of electricity has always been the challenge. In five Barangays, limited electricity negatively impacts health care services in the centers. Barangay Talisoy enjoys at least a consistent electric supply during 8AM to 5PM services due to the generator. Lying-ins in those barangays, thus, become not ideal place for those who are about to give birth.
b. Equipment and facilities – three out of the two barangays do not have a health center on their own. Those three barangays were offered to only use a vacant room inside their Barangay hall (Village Local Office). Except for the main health center, the other four centers have no adequate facilities and own source of water for sanitation purposes. Most of the lying-ins are only in their structural form, however, beds and other equipment related to lying-in services are lacking. Medicines and equipment, especially for emergency situations are also lacking and insufficient such as nebulizers for some Barangays. Even adult scale to be used for mothers is also lacking in some Barangays.
c. Transportation – vital emergency transportation both in land and sea is also not available for the general population. Thus, health services are severely affected in terms of bringing patients to the main health center and even to some hospitals in the Quezon province. A nurse proposed that at least one emergency fast craft boat be deployed in the Island in case of emergency.
d. Barangay health workers – some health workers (health professionals and BHWs) believe that the training for BHWs is insufficient and thus more training is needed. One thing that sometimes discourage BHWs from attending training is the transportation cost when going to the main health center. A health professional from Barangay Bukal proposed that the honorarium should be raised from its value, in 2015, of Php. 500.00 or US$9.61.
e. Health professionals (nurses and midwives) – part of the struggle in the island for these health professionals is their extended working hours. Supposedly from 8AM to 5PM only, their doors are knocked even in the evening for consultations.
The WHO Tracer Items for assessing general readiness, presented in five domains (basic amenities, basic equipment, standard precaution for prevention of infections, laboratory and medicine and commodities).
a) Basic amenities
Health centers in the island during supposedly working hours do not have electric supply. Only Barangay Talisoy out of five Barangays, being the main health center in the island, enjoys a generator at times. It also lacks improved water source;
“Our health center cannot be said to have improved water source since we only rely on underground source of water”
Only three out of five health centers have rooms for a private patient consultation. Only one among all the barangay health centers has no access to adequate sanitation facility. All health centers in the island have no communication equipment. Instead they use their own personal phones to contact health authorities outside the island and within. However, only Barangay Talisoy has a good network signal, other areas in the island either has no or fluctuating signal, making reporting of health cases for the health workers difficult. One health professional even narrated that one time he really struggled to report and ask for a medical advice from the doctor when a resident was accidently hit in the face with a fallen coconut;#:
“It was really difficult. We need instructions from a doctor but we could not communicate.”
Additionally, health centers have no computers. Email and internet are only accessible (with considerable degree of difficulty) through the health workers’ personal phones and laptops. The Island has no emergency vehicle.
b) Basic equipment
Generally, all health centers except one, Barangay Gango, have adult scales while child/Infant scale, thermometer, stethoscope and sphygmomanometer are available to all villages. Only the main health center has a refrigeration equipment. This is the reason why some vaccines are only accessible to the main health center:
“People from other villages have no choice but to go here in the town center for vaccination. All vaccines are here because other health centers have no refrigerators.”
Two of the Barangay health centers, Barangay Bukal and Apad, mentioned that they only use natural light source, all others are with available generators.
c) Standard precaution for prevention of infections
Sterilization equipment is available only at the main health center while all health centers (including the main] have adequate storage and disposal of sharps, sharps box/container, disinfectant, single use – standard disposable syringes, latex gloves and masks. Unfortunately, soap or hand disinfectant storage and safe disposal of infectious wastes are not adequate even in the main health center. The guidelines for standard precaution is available only at Barangay Talisoy.
d) Laboratory
Almost all health centers in the island have no basic laboratory test equipments and paraphernalia. Except for the main health center which can cater whole blood glucose by glucometer, urine dipstick and urine pregnancy test, all others have none. The tracer checklist provided 9 basic laboratory items for general readiness, thus only 3 among those 9 are said to be readily available in the island, specifically in the main health center in Barangay Talisoy.
e) Medicine and commodities
Of these standard 14 essential medicines, only three are not available in the main health centers such as the Atenolol, Amitriptyline and Ceftriaxone. The available medicines in the main health center are generally available also in the health centers in other Barangays. The availability of the most number of these medicines from the checklist means that, in so far as the item for medicines and commodities are concerned, there is relatively general readiness.
The island municipality is far from being an ideal place to have a medical treatment, even to be sick. Aside from health centers being underequipped and undermanned, infrastructures such as roads and health facilities in the Island cannot be said to have a supporting environment to cater quality health services. Health centers in the area could only respond and treat to basic illnesses that require no complex medical procedures and medication. At the end of the day, patients with deeper health issues as well as those with emergency cases that require major surgery and immediate medical attention still have to seek help outside Jomalig. Dental services are not also available.
Travel costs, distance, transportation and poor network signal in some areas all play roles leading to mortality and morbidity among the population. Among the very poor people, who are also the most vulnerable to sickness in Jomalig, is the struggle to report their illnesses at times due to expensive travel cost from the sitios to health centers. Even if they are able to consult health professionals in their respective health centers, cases which have to be treated somewhere else like in Lucena, Polilio, and Panganiban or in Manila are left in the same status since travelling is costly, how much more the cost of having to be treated. They even have term called “pasahirap” to refer to free ride boat passengers. This is why transportation system is a crucial strategy in serving socially excluded population. 21 Not only the distance affects negatively the population to access health services but also the services being done and offered by health workers. Some BHWs are reportedly not so consistent in attending training sessions and reporting cases in their respective areas due to the travel cost. In emergency cases also, availability of transportation and the distance are all crucial factors for attending to the patients’ needs. Added to this is the status of network signal in the island. Communication between health authorities in the island is hampered by poor or even absent signals in some areas. Immediate medical advice and other related medical instructions are not followed immediately because of poor signal in some areas, thus putting peoples’ health and life at risk.
Other factors that negatively affect the health status of population are beliefs which are counter-scientific in nature and those that exhibit people’s stubbornness. Albularyos are flourishing and people are buying their services that sometimes led to the “escalation” of illness. People’s attitude also in terms of sanitation, of practicing open defecation despite local authorities’ intervention, grows problematic as cases of diarrhea increase also. Thus, peoples’ unwillingness to health measures in the island has compounded the already fragile health services provided by the health centers.
The health services in the island are therefore far from being perfectly dependable. In the World Health Organization (WHO) tracer for general readiness, the island’s health centers can be said to have limited capacity. The absence of electricity, strong communication signal, emergency transport, proper facilities and basic lab tests have all been part of the struggles of health workers to deliver efficient and quality health services. However, to mitigate the impact of having not so effective health services in the island, the population must start to work on better environment and eradicate old popular beliefs that are not helpful in sustaining positive health outcomes. By transforming those sets of beliefs and practices into behaviors consistent with attempts to achieve good health and preservation of life, health centers in the island can monitor more effectively the real health status of people within their jurisdiction, save government resources and help more patients in the process.
Methodological limitations
Readers are asked to take caution in the appreciation of the findings. The data used on this article lifted up from a fieldwork done in 2015. Three years have passed since the last time the researcher visited the particular communities under consideration. Since then, public health facilities and services may have been improved and do not now reflect the current conditions. Nonetheless, these reports are still relevant in public health discussions with special attention on rural health.
CONCLUSIONS
Given these results, the island municipality has apparent deficiencies in public health facilities and services which obviously led to poor health outcomes and health-related practices among the population. The government has to quickly act on financing facilities including the additional and training of health staff in GIDA areas in order to effectively provide just even the most minimum of quality health service. Emergency boats per village, health education campaign that focuses on eliminating open defecation and reliance on quack doctors, stand-by generators for the health centers, and radio communication system are strongly recommended.
Acknowledgements
The researcher is forever grateful to Tatay Erning (+) who died this year (2019) in one of the health centers in the Island. He was the habal-habal (single motorcycle) driver who accompanied and serviced the researcher going and traversing difficult, muddy roads to every village of the island.
Competing interests
The author completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author), and declare no conflicts of interest.
Correspondence to:
Zaldy C Collado Social Development Research Center De la Salle University 2401 Taft Ave Malate Manila, 1004 Philippines [email protected]
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.

Essay on Healthcare in India
Students are often asked to write an essay on Healthcare in India in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Healthcare in India
Introduction.
Healthcare in India is a critical sector. It includes public and private hospitals, clinics, and other medical facilities.
Public Healthcare
The government provides public healthcare. It’s often free or low-cost, making it accessible to many people.
Private Healthcare
Private healthcare, on the other hand, is usually more expensive. However, it tends to have better facilities and shorter wait times.
India faces challenges in healthcare, like inadequate facilities in rural areas and a shortage of trained medical professionals.
Despite these challenges, India is striving to improve its healthcare system for everyone.
250 Words Essay on Healthcare in India
Healthcare in India is a multifaceted system, encompassing public and private sectors, traditional and modern medicine, and urban and rural disparities. This essay explores the current state of healthcare in India, its challenges, and potential solutions.
Current State of Healthcare
India’s healthcare sector has made significant strides, with increased life expectancy and decreased infant mortality. However, it is riddled with disparities. While urban areas enjoy better healthcare facilities, rural regions grapple with inadequate infrastructure and lack of trained medical personnel.
The challenges are manifold. Accessibility and affordability remain major concerns. A large portion of the population lacks access to quality healthcare, while high out-of-pocket expenses push many into poverty. Furthermore, there is a significant shortage of healthcare professionals, particularly in rural areas.
Public-Private Partnership
A public-private partnership (PPP) is seen as a viable solution. The private sector’s resources and efficiency can supplement the public sector’s reach and affordability. However, the implementation of PPPs requires stringent regulations to prevent exploitation.
Role of Technology
Technology can bridge the urban-rural divide. Telemedicine, AI, and mobile health technologies can facilitate remote consultations, predictive diagnostics, and health monitoring, making healthcare more accessible and affordable.
While India’s healthcare system faces significant challenges, the combination of public-private partnerships and technology can pave the way for an efficient, inclusive, and affordable healthcare system. It is crucial for policymakers, healthcare providers, and technology companies to work together towards this common goal.
500 Words Essay on Healthcare in India
India’s healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation’s development agenda.
The Landscape of Indian Healthcare
India’s healthcare infrastructure is a mix of public and private providers. The public system, under the aegis of the Ministry of Health and Family Welfare, provides primary, secondary, and tertiary care. However, it suffers from inadequate funding, lack of infrastructure, and a dearth of healthcare professionals. The private sector, on the other hand, is burgeoning. It is technologically advanced, offers high-quality services, but is often criticized for being expensive and inaccessible to the poor.
Healthcare Accessibility and Affordability
Access to quality healthcare is a significant issue in India. Rural areas, in particular, face a shortage of healthcare facilities and professionals. The urban-rural divide is stark, with the majority of quality healthcare services concentrated in cities. Affordability is another concern. High out-of-pocket expenses push many into poverty every year. The situation calls for a robust health insurance framework to protect citizens from catastrophic health expenditures.
Government Initiatives
Recognizing these challenges, the Indian government has launched various initiatives. The National Health Mission aims to improve health outcomes, particularly for the rural population. The Ayushman Bharat scheme, launched in 2018, provides health insurance coverage to the underprivileged, aiming to make healthcare more affordable. These initiatives, while commendable, need effective implementation and monitoring to ensure their success.
Technological Innovations
Technological innovations have the potential to revolutionize India’s healthcare landscape. Telemedicine, artificial intelligence, and digital health records can address the issues of accessibility and affordability. Telemedicine can bridge the urban-rural divide by providing remote consultations. AI can assist in disease prediction and management, while digital health records can streamline patient data, improving efficiency and patient care.
Challenges and Future Prospects
Despite these advancements, India’s healthcare system faces significant challenges. The COVID-19 pandemic has exposed the fragility of the healthcare infrastructure, with hospitals overwhelmed and resources stretched thin. India also grapples with a dual disease burden – communicable diseases like tuberculosis and non-communicable diseases like diabetes and heart disease.
The future of healthcare in India lies in adopting a holistic approach. This includes increasing public health expenditure, strengthening primary healthcare, improving health literacy, and leveraging technology.
India’s healthcare sector, while fraught with challenges, is teeming with potential. With the right mix of policy interventions, technology adoption, and a focus on equitable access, India can transform its healthcare landscape, ensuring a healthier future for its citizens. The journey is long and arduous, but with concerted efforts, a robust and inclusive healthcare system is achievable.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Handloom and Indian Legacy
- Essay on Growth of Banking Sector in India
- Essay on Greatness of India
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

- Share full article
Advertisement
Supported by
Guest Essay
Doctors Need a Better Way to Treat Patients Without Their Consent

By Sandeep Jauhar
Dr. Jauhar is a cardiologist in New York who writes frequently about medical care and public health.
Not long ago, I took care of a middle-aged man at my hospital who had severe heart failure requiring life support. When he was disconnected from machines after a few days of treatment, he began to display psychotic symptoms, including delusional thinking, tangential speech and paranoia. He had a long history of untreated schizophrenia, I learned, which had estranged him from family members and friends, with whom he had virtually no contact.
My patient demanded to leave the hospital. However, sending him home was going to be a problem. He could not take care of himself. There was little chance he would take his medications, including a blood thinner to dissolve a clot in his heart before it caused a stroke. He was even less likely to take psychiatric drugs that he did not believe he needed.
My colleagues and I didn’t know what to do, so we called the treating psychiatrist. The psychiatrist immediately declared that our patient lacked the capacity to discharge himself from the hospital. The patient could not grasp the implications of this choice, for instance, or properly weigh its risks and benefits. The psychiatrist said the patient should remain in the hospital to receive psychiatric treatment, even against his will.
The psychiatrist’s opinion made sense to me. Patients with untreated schizophrenia have a higher rate of death than those who undergo treatment. Hopefully treatment would restore my patient’s judgment to the point where he would take his medications when he went home — or even decide not to take them, but to make that risky decision in the full appreciation of the likely consequences. (If autonomy means anything, it means that patients have the right to make bad decisions, too.) Treating him, even over his objections, seemed to be in his best interests.
However, according to New York law — and the law of other states — such involuntary treatment would require a court order. As doctors, we would have to plead our case before a judge. But was a judge without medical or psychiatric expertise the best person to decide this man’s fate?
In this case and also more generally, I think the answer is no. The law ought to be changed to keep such decisions in hospitals — in the hands of doctors, medical ethicists and other relevant experts.
Doctors don’t always have to resort to the courts to treat patients without their consent. There are some notable exceptions, such as during a life-threatening emergency (if a competent patient has not previously refused such treatment) or when there is a pressing societal interest (such as requiring patients with communicable tuberculosis to take antibiotics).
But judicial review has been the cornerstone of “treatment over objection,” as it’s known, for the past four decades or so. Appellate courts in the 1980s ruled that judicial hearings in such cases are needed to safeguard patients’ rights. For example, in 1983, in Rogers v. Commissioner of Department of Mental Health, the Massachusetts Supreme Judicial Court declared that a judge could override medical judgments favoring involuntary psychiatric treatment.
The underlying motivation behind judicial review was and remains laudable: to avoid the sort of paternalistic abuses that have characterized too much of medical history. Doctors often used to withhold bad news from patients, to cite just a small example. Involuntary treatment, even with benevolent intentions, reeks of such paternalism.
But though medical practice is by no means perfect, times have changed. The sort of abuse dramatized in the 1975 movie “One Flew Over the Cuckoo’s Nest,” with its harrowing depiction of forced electroconvulsive therapy, is far less common. Doctors today are trained in shared decision-making. Safeguards are now in place to prevent such maltreatment, including multidisciplinary teams in which nurses, social workers and bioethicists have a voice.
In addition to being less necessary to prevent abuse than they once were, courts are by nature poorly suited for making decisions about treatment over objection. For one thing, they are slow: Having to go to court often results in delays, sometimes up to a week or more, which can harm patients who need care urgently.
Moreover, judges have neither the experience nor the expertise to properly evaluate psychological states, assess decision-making capacity or determine whether a proposed treatment’s benefits outweigh its risks. It is no surprise that by some estimates 95 percent or more of requests for treatment over objection are approved by judges, who invariably haven’t met the patient and must rely on information provided by the treating medical team.
A better system for determining whether a patient should be treated over his or her objection would be a hospital hearing in which a committee of doctors, ethicists and other relevant experts — all of whom would be independent of the hospital and not involved in the care of the patient — engaged in conversation with the medical team and the patient and patient’s family. Having hearings on site would expedite decisions and minimize treatment delays. The committee would make the final decision.
Of course, such a committee would have to be granted immunity from legal liability (as with judges in our current system), so that experts would be willing to serve and speak candidly. Patients’ interests could be safeguarded by requiring the committee to publish its reasoning. Periodic audits by a regulatory body could ensure that the committee’s deliberations were meeting medical and ethical standards.
In the event that the committee could not reach a consensus on the best course of action (or if there were allegations of wrongdoing), then the parties involved could appeal to a judge. But that would be the exception rather than the rule.
In the case of my patient with heart failure, the decision ultimately didn’t have to go before a judge. Multiple discussions involving the patient, the hospital ethics and palliative care teams, social workers, nurses, psychiatrists and other doctors — discussions that in many respects served the function of a formal committee of the sort I’m proposing — yielded an agreement with the patient that his interests would be best served by sending him home with hospice care.
Capacity must be judged relative to the decision being made, and it became clear over the course of hospitalization that our patient understood the terminal nature of his condition and had the capacity to choose hospice care. Forced treatment was unlikely to significantly improve his psychiatric symptoms before the natural progression of heart failure caused his death.
So he was discharged home. It was the best decision under the circumstances, one reached by expert deliberation, not legal procedure. He passed away a few weeks later without, fortunately, ever setting foot in court.
Sandeep Jauhar ( @sjauhar ) is a doctor at Northwell Health in New York and the author, most recently, of “ My Father’s Brain : Life in the Shadow of Alzheimer’s.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Planning of Medical Facilities and Amenities Research Paper
Introduction, regulatory requirements, color and noise issues, equipment needed, electronic items needed, budget planning and cost estimates, the role of stakeholders, gantt chart.
Planning of medical facilities and amenities calls for extra care and caution to ensure adherence to all the laid down procedures, regulations, and certification. This in turn ensures conduct of work within the budget limits and the stakeholders achieve their targeted goals.
The research paper examines an in-depth analysis of the creation of a medical care amenity, while examining the laid down regulations, all important parameters, and time required for finishing the project, the total cost of the project and the equipment needed in the project.
Concerning this, the equipments used in the medical field are highly regulated. They are under a high level of maintenance and safety than most of the machines and equipments found in the market. This is because there are those patients who respond very slowly or are unable to respond to hazardous conditions.
Some of the medical equipment in use today act as life support and their failure lead to loss of life. Before designing the phase of any equipment, it is important to understand its regulatory requirements and the certification required of it. This is advantageous in that it not only reduces the costs, but it also increases the safety of the product and the turn around time required for certification.
The licensing regulations of each State lay down the specific design on the use of medical facility within its premises. These are the FGI guidelines used in the construction of and design of medical facilities Kunders (2004). The different states call for the use of codes in International Building.
In addition, the states get accreditation from the Joint Commission on the Accreditation of Healthcare organizations Kunders (2004). The National Fire Protection Association (NFPA) provides guidelines ensuring compliance with fire codes within the health facility.
This is to protect patients from fire outbreaks within the health centers. The guidance of fire safety within the facilities requires adherence to the standards contained in the NFPA 101 and NFPA 99.
Health facility must also follow the American Disability Act in order to protect the physically challenged patients. The facilities must also follow the OSHA regulations especially in the design of their laboratories. Medical facilities should be accessible to those seeking medical care. Therefore, they should have designs that enhance care to patients. This is especially in tall buildings, which should have lifts, and they should be accessible to people with disability.
The design of the medical facility should ensure that there are fire assembly points in case of fire outbreak within the premises. The design of the facility is environmental friendly to avoid polluting the environment. Patients’ experiences within a health facility are many and varied. To take good care and ensure wellbeing of patients, health facilities apply aesthetics that ensure comfort of the patient while in the facility.
Additionally, the medical facilities need to be sustainable and environmental friendly because they make use of a lot of human power, raw materials, water, and energy. Therefore, the designs must follow the laid down regulations.
It is important to choose the best color for the medical facility. The colors used in the medical facility aims at capturing, coordinating and calming the best mood and mental state of the patients and providing a serene environment for the patient so that they recover fast Kunders (2004). The ambiance provided by colors makes it fast for patients to recover.
When the colors are not calm, they interfere with the health and the recovery process of the patient. Therefore, they threaten the recovery process of the patient. There should be enough signboards in and around hospitals to ensure maximum silence Kunders (2004). There should be no hooting by cars in and around hospitals.
This ensures that noise is at minimum to enable patients have ample time for rest and sleep and this makes them feel secure. The privacy of the patient is very important, medical facilities should guarantee the patient’s privacy, and there should be no disclosure of private and confidential information of the patient without the consent of the patient Kunders (2004).
Medical facilities across the board have similar health care equipment. The equipments in use in our medical facility are; trolleys, sinks, room dividers, heating and ventilation systems, lavatories, X-ray machines, wheel chairs and tables, laboratory kits, waste containers, examination beds, desks and chairs. The National Clearing House for Educational Facilities (NCHEF) provides for these lists of equipment (clark, 2009).
Medical facilities require electronic items to fasten the process of service delivery and to ensure that patients have the best care and diagnoses, and administration of best treatment. Electrically modified devices are the best to conform to the hospital safety standards.
The devices also assist patients in the recovery process. They include fans, electronic beds, computers, DVD players, play station, blood pressure monitors, ultrasound systems, emergency oxygen systems, and dental instruments among others (clark, 2009).
Buildings in use require conversion to medical facility, which marks the start of budget planning. The budget should take care of materials, wages, transport, and architectural costs. Installation of medical equipments is after completion of the conversion process.
The stakeholders of a medical facility are the community and inside stakeholders Tregunno (2004). People working in the facility such as doctors, nurses and cooks forms part of the inside stakeholder. Physicians ensure design of medical facilities in a way that not only promotes the wellbeing of the patient but also their own wellbeing.
Nurses require a facility that will enable them provide the best care to patients Kunders (2004). Doctors provide medical care and they prescribe medicine to patients. The community stakeholders ensure that there is enough supply of medicine, food, security and there is adherence to government policies.
The care personnel make sure the facility ensures maximum interaction between nurses and physicians. The facility should ensure outside stakeholders like emergency personnel have easy access to the facility to enhance patient care.
The outside stakeholders look forward to a facility that is responsive to their needs and a facility that does not harm them. The facility should meet the needs of the surrounding stakeholders Kunders (2004)
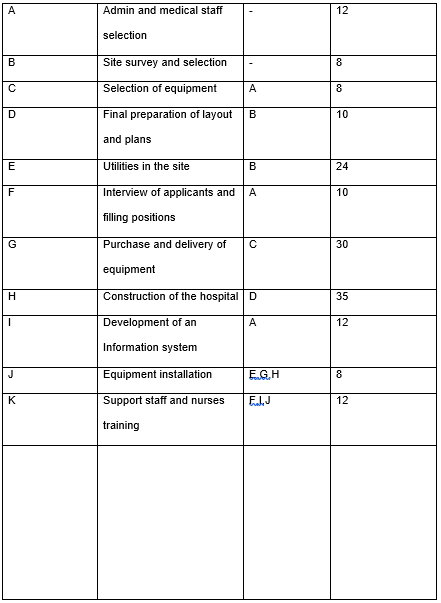
Clark, W. (2009). The Gantt chart:a working tool of management . London: Pitman. Web.
Kunders, G. (2004). Hospitals: Facilities Planning and Management . New York: Tata McGraw-Hill Education. Web.
Tregunno, D. (2004). Health, Nursing & Environmental Studies. New York: Palgrave Macmillan. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, April 19). Planning of Medical Facilities and Amenities. https://ivypanda.com/essays/facility-planning-research-paper/
"Planning of Medical Facilities and Amenities." IvyPanda , 19 Apr. 2019, ivypanda.com/essays/facility-planning-research-paper/.
IvyPanda . (2019) 'Planning of Medical Facilities and Amenities'. 19 April.
IvyPanda . 2019. "Planning of Medical Facilities and Amenities." April 19, 2019. https://ivypanda.com/essays/facility-planning-research-paper/.
1. IvyPanda . "Planning of Medical Facilities and Amenities." April 19, 2019. https://ivypanda.com/essays/facility-planning-research-paper/.
Bibliography
IvyPanda . "Planning of Medical Facilities and Amenities." April 19, 2019. https://ivypanda.com/essays/facility-planning-research-paper/.
- Etihad Airlines: Operational Decision Making
- Boutique Hotels: Starting and Running
- The SWOT Analysis: Cityville
- Scientific Management in the Modern Organizations
- The Manager of the Century: Following the Track of a Born Leader
- The Notion of the Work-Life Balance
- Management vs. Leadership
- Emotional Intelligence in the Organizational Behavior Context
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Perspective
When pto stands for 'pretend time off': doctors struggle to take real breaks.
Mara Gordon

A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off. Wolfgang Kaehler/LightRocket via Getty Images hide caption
A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off.
A few weeks ago, I took a vacation with my family. We went hiking in the national parks of southern Utah, and I was blissfully disconnected from work.
I'm a family physician, so taking a break from my job meant not seeing patients. It also meant not responding to patients' messages or checking my work email. For a full week, I was free.
Taking a real break — with no sneaky computer time to bang out a few prescription refill requests — left me feeling reenergized and ready to take care of my patients when I returned.
But apparently, being a doctor who doesn't work on vacation puts me squarely in the minority of U.S. physicians.
Research published in JAMA Network Open this year set out to quantify exactly how doctors use their vacation time — and what the implications might be for a health care workforce plagued by burnout, dissatisfaction and doctors who are thinking about leaving medicine.
"There is a strong business case for supporting taking real vacation," says Dr. Christine Sinsky , the lead author of the paper. "Burnout is incredibly expensive for organizations."

Shots - Health News
Health workers know what good care is. pandemic burnout is getting in the way.
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days of vacation or less per year. That's a little more than the average American: Most workers who have been at a job for a year or more get between 10 and 14 days of paid vacation time , according to the U.S. Bureau of Labor Statistics.
However, most doctors don't take real vacation. Over 70% of doctors surveyed said they worked on a typical vacation day.
"I have heard physicians refer to PTO as 'pretend time off,'" Sinsky says, referring to the acronym for "paid time off."
Sinsky and co-authors found that physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less, since vacation time is linked to well-being and job satisfaction .
And all those doctors toiling away on vacation, sitting poolside with their laptops? Sinsky argues it has serious consequences for health care.
Physician burnout is linked to high job turnover and excess health care costs , among other problems.
Still, it can be hard to change the culture of workaholism in medicine. Even the study authors confessed that they, too, worked on vacation.
"I remember when one of our first well-being papers was published," says Dr. Colin West , a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the revisions up at the family cabin in northern Minnesota on vacation."
Sinsky agreed. "I do not take all my vacation, which I recognize as a delicious irony of the whole thing," she says.
She's the American Medical Association's vice president of professional satisfaction. If she can't take a real vacation, is there any hope for the rest of us?
I interviewed a half dozen fellow physicians and chatted off the record with many friends and colleagues to get a sense of why it feels so hard to give ourselves a break. Here, I offer a few theories about why doctors are so terrible at taking time off.
We don't want to make more work for our colleagues
The authors of the study in JAMA Network Open didn't explore exactly what type of work doctors did on vacation, but the physicians I spoke to had some ideas.
"If I am not doing anything, I will triage my email a little bit," says Jocelyn Fitzgerald , a urogynecologist at the University of Pittsburgh who was not involved in the study. "I also find that certain high-priority virtual meetings sometimes find their way into my vacations."
Even if doctors aren't scheduled to see patients, there's almost always plenty of work to be done: dealing with emergencies, medication refills, paperwork. For many of us, the electronic medical record (EMR) is an unrelenting taskmaster , delivering a near-constant flow of bureaucratic to-dos.
When I go on vacation, my fellow primary care doctors handle that work for me, and I do the same for them.
But it can sometimes feel like a lot to ask, especially when colleagues are doing that work on top of their normal workload.
"You end up putting people in kind of a sticky situation, asking for favors, and they [feel they] need to pay it back," says Jay-Sheree Allen , a family physician and fellow in preventive medicine at the Mayo Clinic.
She says her practice has a "doctor of the day" who covers all urgent calls and messages, which helps reduce some of the guilt she feels about taking time off.
Still, non-urgent tasks are left for her to complete when she gets back. She says she usually logs in to the EMR when she's on vacation so the tasks don't pile up upon her return. If she doesn't, Allen estimates there will be about eight hours of paperwork awaiting her after a week or so of vacation.
"My strategy, I absolutely do not recommend," Allen says. But "I would prefer that than coming back to the total storm."
We have too little flexibility about when we take vacation
Lawren Wooten , a resident physician in pediatrics at the University of California San Francisco, says she takes 100% of her vacation time. But there are a lot of stipulations about exactly how she uses it.
She has to take it in two-week blocks — "that's a long time at once," she says — and it's hard to change the schedule once her chief residents assign her dates.
"Sometimes I wish I had vacation in the middle of two really emotionally challenging rotations like an ICU rotation and an oncology rotation," she says, referring to the intensive care unit. "We don't really get to control our schedules at this point in our careers."
Once Wooten finishes residency and becomes an attending physician, it's likely she'll have more autonomy over her vacation time — but not necessarily all that much more.
"We generally have to know when our vacations are far in advance because patients schedule with us far in advance," says Fitzgerald, the gynecologist.
Taking vacation means giving up potential pay
Many physicians are paid based on the number of patients they see or procedures they complete. If they take time off work, they make less money.
"Vacation is money off your table," says West, the physician well-being researcher. "People have a hard time stepping off of the treadmill."
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount regardless of patient volume. That means the more patients doctors cram into their schedules, the more money they make. Going on vacation could decrease their take-home pay.
But West says it's important to weigh the financial benefits of skipping vacation against the risk of burnout from working too much.
Physician burnout is linked not only to excess health care costs but also to higher rates of medical errors. In one large survey of American surgeons , for example, surgeons experiencing burnout were more likely to report being involved in a major medical error. (It's unclear to what extent the burnout caused the errors or the errors caused the burnout, however.)
Doctors think they're the only one who can do their jobs
When I go on vacation, my colleagues see my patients for me. I work in a small office, so I know the other doctors well and I trust that my patients are in good hands when I'm away.

Doctors have their own diagnosis: 'Moral distress' from an inhumane health system
But ceding that control to colleagues might be difficult for some doctors, especially when it comes to challenging patients or big research projects.
"I think we need to learn to be better at trusting our colleagues," says Adi Shah , an infectious disease doctor at the Mayo Clinic. "You don't have to micromanage every slide on the PowerPoint — it's OK."
West, the well-being researcher, says health care is moving toward a team-based model and away from a culture where an individual doctor is responsible for everything. Still, he adds, it can be hard for some doctors to accept help.
"You can be a neurosurgeon, you're supposed to go on vacation tomorrow and you operate on a patient. And there are complications or risk of complications, and you're the one who has the relationship with that family," West says. "It is really, really hard for us to say ... 'You're in great hands with the rest of my team.'"
What doctors need, says West, is "a little bit less of the God complex."
We don't have any interests other than medicine
Shah, the infectious disease doctor, frequently posts tongue-in-cheek memes on X (formerly known as Twitter) about the culture of medicine. Unplugging during vacation is one of his favorite topics, despite his struggles to follow his own advice.
His recommendation to doctors is to get a hobby, so we can find something better to do than work all the time.
"Stop taking yourself too seriously," he says. Shah argues that medical training is so busy that many physicians neglect to develop any interests other than medicine. When fully trained doctors are finally finished with their education, he says, they're at a loss for what to do with their newfound freedom.
Since completing his training a few years ago, Shah has committed himself to new hobbies, such as salsa dancing. He has plans to go to a kite festival next year.
Shah has also prioritized making the long trip from Minnesota to see his family in India at least twice a year — a journey that requires significant time off work. He has a trip there planned this month.
"This is the first time in 11 years I'm making it to India in summer so that I can have a mango in May," the peak season for the fruit, Shah says.
Wooten, the pediatrician, agrees. She works hard to develop a full life outside her career.
"Throughout our secondary and medical education, I believe we've really been indoctrinated into putting institutions above ourselves," Wooten adds. "It takes work to overcome that."
Mara Gordon is a family physician in Camden, N.J., and a contributor to NPR. She's on X as @MaraGordonMD .
- American Medical Association

IMAGES
VIDEO
COMMENTS
500 Words Essay On Hospital. Hospitals are institutions that deal with health care activities. They offer treatment to patients with specialized staff and equipment. In other words, hospitals serve humanity and play a vital role in the social welfare of any society. They have all the facilities to deal with varying diseases to make the patient ...
Introduction. Health is a critical aspect and should be handled with importance. This is because human bodies are susceptible to various health related issues that would require medical attention failure to which death would occur. Health care facilities are, therefore, a key component and should be maintained at the best condition possible to ...
Medical Facilities Essays. Improving Healthcare Safety. Safety in healthcare is an important issue needing sustained concentration and refining. Research estimates that 1 in 10 healthcare users have suffered from some form of harm, resulting in more than 3 million casualties each year (WHO, 2023). In poor to middle-income countries, the ...
Hartford Hospital in Hartford, Connecticut.A hospital is one common type of health facility. An eye, ear, nose, and throat clinic in Durham, North Carolina, illustrating a common smaller facility.. A health facility is, in general, any location where healthcare is provided. Health facilities range from small clinics and doctor's offices to urgent care centers and large hospitals with elaborate ...
An expensive health care system translates to an increasing proportion of the population being unable to access the much needed medical care. The New York Times reports that according to census survey carried out in the year 2007, an estimated 45.6 million people in the USA were uninsured and hence unlikely to receive comprehensive medical care from hospitals (1).
They also assess the future evolution of payment systems leading toward sustainable health, changes in provider roles, and the entrance of new nontraditional players. For more on this topic, watch Health Systems in 2030, a free NEJM Catalyst virtual event held on March 4, 2021.
The intention is to provide you with a sample identical to your Medical Facilities essay topic so that you could have a closer look at it in order to get a clear idea of what a great academic work should look like. You are also advised to employ the best Medical Facilities writing practices displayed by competent authors and, eventually, create ...
Schneck Medical Center: The Baldrige Award Schneck Medical Center: Overview The Schneck Medical Center according to the National Institute of Standards and Technology -- NIST (2011) "is a 93-bed nonprofit hospital providing primary and specialized services to the residents of Jackson County, Ind., and surrounding communities." The facility as NIST (2011) further points out, offers a variety of ...
This essay discusses health policies, the determinants of health, and the connections between the two. The determinants of health are individual and environmental factors that affect people's physical and mental well-being and the ability to […] Healthcare Services: Internal and External Factors.
Healthcare Facilities Essay. Satisfactory Essays. 706 Words. 3 Pages. Open Document. Research the websites of two competitors and assess the effectiveness of their online presence. Identify specific areas where those websites are superior to yours whether in form or function. Also identify areas where your own website is superior.
Analysis. 1. There has been widespread debate in recent years concerning whether healthcare should be private or public. 2. In my opinion, despite the importance of government regulation in the healthcare industry, a freer system will naturally encourage greater innovation. Paraphrase the overall essay topic. Write a clear opinion.
Essay: Evidence-based health-care architecture. This is a time of enormous investment in new health-care buildings. The UK plans to create upwards of a hundred hospitals and thousands of primary-care clinics and surgery centres. In the USA, more than $200 billion will be spent on new hospitals over the next decade.
Medical School Essay Four. Prompt: Tell us more about who you are. I am a white, cisgender, and heterosexual female who has been afforded many privileges: I was raised by parents with significant financial resources, I have traveled the world, and I received top-quality high school and college educations.
View all our healthcare facility essays. These healthcare facility essays include examples, outlines, titles, topics, introductions, conclusions, and resources to assist you. ... Quinlan were unsuccessful and after it became apparent that her comma was irreversible, she was transferred to another medical facility, i.e. St. Clare's in Danville.
This is precisely why we included the numerous sample medical school personal statement essays at the end of this guide. ... at an assisted living facility. One of his patients was an injured former athlete who was having trouble standing. His wife held back tears as he grimaced and repeatedly referred to "passing on." Dr. Sekhon studied ...
The role of nurses is changing in the healthcare facilities. According to Stangeland (2010), nurses were traditionally regarded as assistants to medical doctors who were expected to follow instructions on how to handle patients in different settings. However, this role is changing as nurses find themselves in situations where they have to make ...
Think of type II diabetes, cardiovascular illness, breast cancer, and cirrhosis. These are topics you don't want to cover for the simple reason that they are too common. In this post, we give you a list of 30+ medical argumentative essay topics that aren't too obvious. These topic ideas should enable you to add a new spin to your work, so ...
This essay is about learning medical facilities medical facilities medical facilities play pivotal role in the healthcare ecosystem, serving as the cornerstone. Skip to document. ... This essay is about learning medical facilities. Course. Healthcare Settings, Claim Cycle, and Claims Processing (ME2550) 58 Documents. Students shared 58 ...
Aside from health centers being underequipped and undermanned, infrastructures such as roads and health facilities in the Island cannot be said to have a supporting environment to cater quality health services. Health centers in the area could only respond and treat to basic illnesses that require no complex medical procedures and medication.
In one of my earliest pieces, I wrote about a local boy's suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon ...
250 Words Essay on Healthcare in India Introduction. Healthcare in India is a multifaceted system, encompassing public and private sectors, traditional and modern medicine, and urban and rural disparities. This essay explores the current state of healthcare in India, its challenges, and potential solutions. Current State of Healthcare
The law ought to be changed to keep such decisions in hospitals — in the hands of doctors, medical ethicists and other relevant experts. Doctors don't always have to resort to the courts to ...
Planning of medical facilities and amenities calls for extra care and caution to ensure adherence to all the laid down procedures, regulations, and certification. This in turn ensures conduct of work within the budget limits and the stakeholders achieve their targeted goals. We will write a custom essay on your topic.
Write a letter to the editor of a newspaper demanding better medical facilities in govt. hospitals.2 April 2020The EditorThe Bangladesh ObserverDhakaDear Sir,I would be delighted if you could publish the following letter in your esteemed daily.Yours faithfully,Mustafizur Rahman314 Elephant Road, DhakaDemanding Better Medical Facilities in Government HospitalsThe healthcare facilities provided ...
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount ...