

20 Thesis topics related to Healthcare Architecture

Healthcare Architecture is one of the most important, complex, and demanding fields as it requires precision, needs, and respect for privacy. As architects, we design these structures so that the public is able to walk through the health care system in a proper way. There are many students who work with the topic during their thesis project as it is not only challenging but also opens new doors into tackling pandemics such as Covid-19.
Here are 20 thesis topics related to healthcare architecture:

1. Children friendly healthcare design
Children’s hospitals have been one of the most challenging designs. As the hospital is the last place a child might want to go. So making hospitals less scary and motivating the children to accept the care is one of the biggest psychological challenges that the designer has to encounter. But when dealing with children it can help unleash the child inside the designer. So if you can design for those little ones; this one’s for you.
2. Multispecialty hospital design
A hospital design that deals with different types of multispeciality facilities available under one single roof. This design is in high demand in the urban context and is one of the biggest rising designs. As they’re able to adhere and cater to a large number of people with different ailments.
3. Drug rehabilitation center
Addiction has been and is going to be one of the biggest ailments that our generations have encountered. As there is a subsequent increase in the death rates that have been caused by an overdose of drugs. And somewhere there is a share of rehabilitation spaces too. As they need to feel less of a prison and more of a recovery center which can guarantee the addicted people that this is the road to recovery. Hence the role of architecture is highly important in this context. So if you would like to bring a change to this biggest problem of generation this one’s for you.
4. Redesigning intensive care units
One of the most unique and detailed topics of healthcare architecture which peek into the technicalities of the medical world. With a dominating services part. As including the technical part, there is a lot to design on this topic as it is one of the key elements of the hospitals.
5. Mental health hospital design
Still today mental health problems are always seen with a judgemental eye. And mental hospitals are still aren’t reached by the suffering people just out of the pressure and disgrace created around mental problems. This is why there is an immense need to break the imageability of the mental hospitals and redefine them in a new thought. A new image that can make it a lot less scary and way more approachable. So if you want to risk and break the mold; this is the best one.
6. Autistic healthcare redesign
Autistic care is one of the most creative and challenging ones. As they need for us to dwell into the life of autistic children and understand how their world works. And how can we make it better? Even though the percentage of their population might be small their needs are often ignored as most of the time they’re pushed into our normal worlds that don’t cater to their needs or care at all. So if you would like to step into their shoes and empathize. This one is a good option for you to choose from.
7. Advanced trauma recovery and care center
Trauma is a lot of complex phenomena that don’t just affect momentarily but can change a person’s life forever. Which makes these trauma recovery centers all the more important. They’re supposed to provide the care and refuge for them that can make them feel better and start their journey to recovery. It is a challenging phenomenon to give a solution to through architecture. But the built environment can do wonders that are beyond the comprehension of the human mind.
8. Cancer hospital and research center
Cancer hospitals are one of the most important elements of society and are always needed. With a large amount of infrastructure, technology, and care involved in making them. It undoubtedly makes it one of the most promising thesis topics.
9. Counseling Clinic: Rethinking mental healthcare
Counseling clinics are on a subsequent rise as they are easily approached and overall more preferred by the people who feel they need help. So this design doesn’t just need to step out from the big scary hospital vibe to a friendly place where one might feel like going to have some help. This thesis explores a lot of urban human psychology and the needs of today’s generations of healthcare. Indeed a topic for the promising future.
10. Juvenile trauma recovery center
With the considerable increase in juvenile crimes . Juvenile health and development have been the top priority of many countries worldwide. So out of the many efforts being done for their betterment, this one is one of the most crucial ones. This design needs to cater to the raging young minds while healing them of their trauma and help them walk the road of recovery without falling into the traps of crime. Children’s psychology will play a very important role in their recovery. Thus this project in a real sense is going to shape the future of tomorrow.
11. Pediatric hospital and care center
This one demands a good understanding of infant to toddler development and physiology. Their reactions in certain environments and how to make a peaceful place that can cater to these tender beings with care. It is a very creative and positive topic that prolifically deals with the news.
12. Lodging and care center for cancer patients
Peeking deeper into the journey of a cancer warrior. It gives us the chance to create a better environment for them when they’re battling and are feeling at their lowest. This calls for healing that is done through spaces that make them feel less pained and can provide hope. Something design is very much capable of.
13. Prison recovery and rehabilitation center
The time post-prison is as important as the time inside is. As the prisoners are often left in open with a shock of a new reality right ahead of them. Which at times is a lot to handle, especially in a positive mindset. Thus this rehab center won’t just make them prepared, but also will help them step into this new world as a better human.
14. Adaptive reuse of hospital buildings
The reuse of hospital spaces is challenging. But provides ample opportunities on the way depending on the context and background the design is going to set up in.
15. Cancer prevention, diagnosis, treatment, and survival unit
Covering the whole process of development and recovery this center is supposed to be the most important center in the life of the patients who are to be motivated and kept hopeful throughout. Which requires a conscious approach as a designer to make a space that can help them feel better and give them a will to survive.
16. Eldercare: Redefining healthcare for the elderly
Care for the elderly can be one of the needed topics in today’s world. As the care they need is much beyond a hospital. As they need a hospital that feels like hope. A place where they will be willing to stay rather than run away from. And the design can be the one that can create such an effect successfully.
17. Rural hospice center redesign
Hospice centers in rural areas serve as many other things rather than just healthcare architecture. They act as a refuge space for the general public and even an educational area. Considering its multidimensional use it can be used for many things. Thus providing it as an opportunity to work on a singular space that can serve as a multipurpose space .
18. Dementia: Care center redesign
The dementia care center is a healthcare architecture design that deals with the lives of dementia suffering patients. Which requires them to step into the shoes of the patients. As it can help us create a good environment for them.
19. Behavioral Healthcare facility
The behavioral health facility is the new healthcare facility that has been created. Which has been created to tackle the behavioral and other problems that are dealt with every day in the urban and rural contexts? Thus making it more approachable for the people suffering it. And thus it can become one of the futuristic architecture designs
20. Post-trauma recovery center
From the admission phase to the complete recovery. Different phases are involved and are needed to be catered carefully. Thus it makes the healthcare architecture of the space equally important in the healing of the trauma and the road towards recovery.

Renuka is an artist, architect, and writer. With a keen interest in psychology; she is passionate about 'User-centric and need-based designs'. As an empath herself she finds writing as a way to empower and voice people. While aiming to make this world a better place as a designer.
Eldridge London Architects + Designers-15 Iconic Projects

20 Thesis topics related to narrative architecture
Related posts.

Archi-Urbantecture
The Yas Viceroy Hotel: Iconic Design and Engineering

Assessing the Effectiveness of Experiential Learning in Design Education

Inclusivity and Diversity in Design Education: Fostering a More Representative Creative Industry

Digital Transformation in Design Education: Adapting to Technological Advancements

Design Education for Social Impact: Evaluating the Effectiveness of Community-Based Projects
- Architectural Community
- Architectural Facts
- RTF Architectural Reviews
- Architectural styles
- City and Architecture
- Fun & Architecture
- History of Architecture
- Design Studio Portfolios
- Designing for typologies
- RTF Design Inspiration
- Architecture News
- Career Advice
- Case Studies
- Construction & Materials
- Covid and Architecture
- Interior Design
- Know Your Architects
- Landscape Architecture
- Materials & Construction
- Product Design
- RTF Fresh Perspectives
- Sustainable Architecture
- Top Architects
- Travel and Architecture
- Rethinking The Future Awards 2022
- RTF Awards 2021 | Results
- GADA 2021 | Results
- RTF Awards 2020 | Results
- ACD Awards 2020 | Results
- GADA 2019 | Results
- ACD Awards 2018 | Results
- GADA 2018 | Results
- RTF Awards 2017 | Results
- RTF Sustainability Awards 2017 | Results
- RTF Sustainability Awards 2016 | Results
- RTF Sustainability Awards 2015 | Results
- RTF Awards 2014 | Results
- RTF Architectural Visualization Competition 2020 – Results
- Architectural Photography Competition 2020 – Results
- Designer’s Days of Quarantine Contest – Results
- Urban Sketching Competition May 2020 – Results
- RTF Essay Writing Competition April 2020 – Results
- Architectural Photography Competition 2019 – Finalists
- The Ultimate Thesis Guide
- Introduction to Landscape Architecture
- Perfect Guide to Architecting Your Career
- How to Design Architecture Portfolio
- How to Design Streets
- Introduction to Urban Design
- Introduction to Product Design
- Complete Guide to Dissertation Writing
- Introduction to Skyscraper Design
- Educational
- Hospitality
- Institutional
- Office Buildings
- Public Building
- Residential
- Sports & Recreation
- Temporary Structure
- Commercial Interior Design
- Corporate Interior Design
- Healthcare Interior Design
- Hospitality Interior Design
- Residential Interior Design
- Sustainability
- Transportation
- Urban Design
- Host your Course with RTF
- Architectural Writing Training Programme | WFH
- Editorial Internship | In-office
- Graphic Design Internship
- Research Internship | WFH
- Research Internship | New Delhi
- RTF | About RTF
- Submit Your Story
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Why hospital design matters: A narrative review of built environments research relevant to stroke care
Julie bernhardt, ruby lipson-smith, aaron davis, marcus white, heidi zeeman, natalie pitt, michelle shannon, maria crotty, leonid churilov.
- Author information
- Article notes
- Copyright and License information
Julie Bernhardt, 245 Burgundy Street, Heidelberg VIC 3084, Australia. Email: [email protected]
Received 2021 May 17; Accepted 2021 Aug 10; Issue date 2022 Apr.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License ( https://creativecommons.org/licenses/by-nc/4.0/ ) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages ( https://us.sagepub.com/en-us/nam/open-access-at-sage ).
Healthcare facilities are among the most expensive buildings to construct, maintain, and operate. How building design can best support healthcare services, staff, and patients is important to consider. In this narrative review, we outline why the healthcare environment matters and describe areas of research focus and current built environment evidence that supports healthcare in general and stroke care in particular. Ward configuration, corridor design, and staff station placements can all impact care provision, staff and patient behavior. Contrary to many new ward design approaches, single-bed rooms are neither uniformly favored, nor strongly evidence-based, for people with stroke. Green spaces are important both for staff (helping to reduce stress and errors), patients and relatives, although access to, and awareness of, these and other communal spaces is often poor. Built environment research specific to stroke is limited but increasing, and we highlight emerging collaborative multistakeholder partnerships (Living Labs) contributing to this evidence base. We believe that involving engaged and informed clinicians in design and research will help shape better hospitals of the future.
Keywords: Stroke, stroke rehabilitation, hospital design and construction, evidence-based design
Introduction
Imagine (re-)designing the very hospital you work in. What would you design differently? What would you change, to benefit you, your patients, and their families? What evidence might help guide those design decisions?
Healthcare facilities are among the most expensive buildings to construct, maintain, and operate. 1 Once built, hospitals remain in service for decades and are difficult to modify. With stakes this high, considering how building design best supports healthcare services is important. In this narrative review, we outline why the built environment matters, with particular focus on stroke care. We also discuss challenges inherent in designing healthcare environments, undertaking research and evaluating completed architecture.
The planning and design process for new healthcare environments is incredibly complex, but, in general, it occurs in three overlapping stages: (1) the planning stage in which the healthcare provider describes the users’ needs, model of care, and clinical program in a functional brief that summarizes the requirements for the new hospital; (2) the design stage in which these requirements are interpreted by architects to develop an initial concept which is then refined to a more detailed design; and (3) the delivery stage in which the building is constructed. The extent to which hospital staff and patients are included at each stage of this process can vary significantly between projects. 2
Healthcare professionals have long advocated for design features thought to benefit health and well-being, such as natural light, ventilation, and space between patients—for example, the circular hospital design proposed by the physician Antoine Petit 3 and long “Nightingale wards” proposed by Florence Nightingale. 4 Hospital design is now informed by a process termed “evidence-based design” (EBD), in which research evidence is used alongside other considerations such as the healthcare context, budget, and architects’ experience, to inform the design of the healthcare built environment. 5 , 6 In this context, the “healthcare built environment” encompasses: (1) the physical construction (layout, room dimensions, doors and window placement, outdoor and community access, etc.), (2) ambient features (noise, air quality, light, temperature, etc.), and (3) interior design (furniture, signage, equipment, artwork, etc.). 7 Analogous to evidence-based clinical practice, hospitals designed following best research evidence garnered from EBD processes have better safety, patient outcomes, staff retention, and operation costs. 8 , 9 The Center for Health Design, established in 1993 to advance EBD, now maintains a repository of over 5,000 articles on healthcare design ( https://www.healthdesign.org ).
The field is growing; however, many healthcare contexts, including stroke, have a limited built environment evidence base. 10 Establishing geographically organized stroke units has been an important focus 11 ; however, these studies rarely address specifics of the built environment, and we know little about optimal stroke unit design. Stroke clinical guidelines rarely mention the built environment nor provide guidance on how the environment might best support care. There are currently no stroke care-specific building standards, nor standardized checklists to evaluate the quality of these environments. 12
Why is the built environment neglected? Clinicians may identify as knowing less about how the environment might influence patient care or staff well-being. They may also feel uninformed about the design process and how to contribute their clinical expertise to influence decision-making. To begin to address these gaps, our objectives for this review were: (1) to introduce readers to healthcare built environment research and (2) to highlight evidence that underpins acute, subacute, or rehabilitation stroke care facility design. This review is in three parts:
Overview of healthcare built environment research;
Stroke care built environment evidence; and
Planning and design of new healthcare environments: Challenges and opportunities.
We include research from recent, relevant systematic reviews, other evidence summaries, and selected qualitative and mixed-methods research focusing on healthcare environments and design. Healthcare environments are complex and context-specific, with many interdependent variables that can rarely be isolated. This complex system does not readily lend itself to highly controlled experimental research designs in real-life settings. 13 Qualitative methods, such as case studies and pre- and post-occupancy evaluations (before and after a redesign or redevelopment), are common. With research still developing, heterogeneity exists in research designs, outcomes, environments, populations, and theoretical frameworks employed. 14 Hence, robust summary evidence derived from meta-analyses is lacking.
Healthcare built environment research
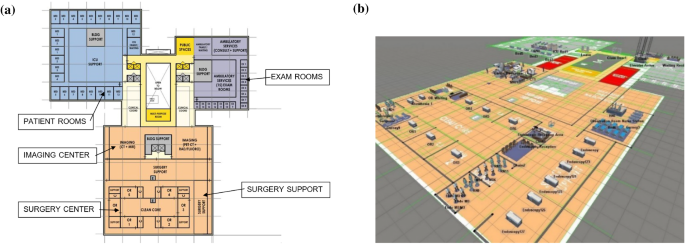
Research is dominated by studies conducted in acute environments such as emergency, surgery, and intensive care units (ICUs) ( Figure 1 ). 6 , 15 , 16 Older people, including those in dementia care, are frequently studied post-acute populations. 17
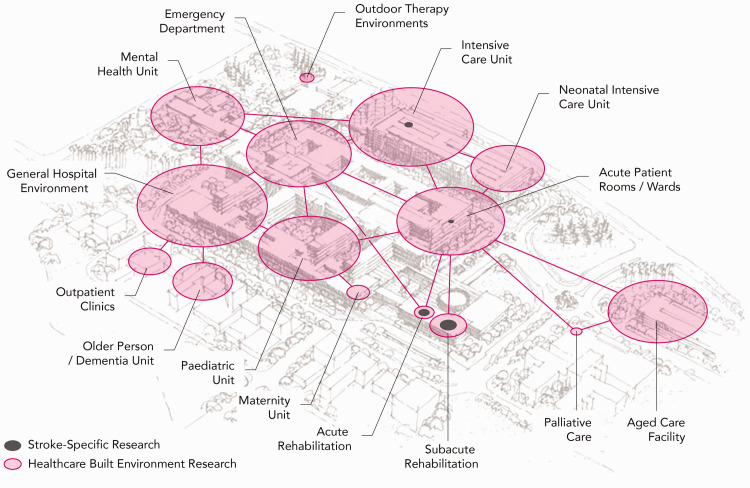
The volume of built environment research conducted in different healthcare settings. Circle size indicates the number of published research articles based on systematic literature review in preparation 18 and articles listed in the Centre for Healthcare Design research repository. Pink circles represent all built environment research, and the dark gray circles indicate stroke-specific research. (The aerial sketch in this image has been adapted with permission from Architectus + HDR.)
In this section, we introduce three topics relevant to most healthcare contexts: (1) design of internal spaces; (2) outdoor spaces; and (3) ambient features including light, noise, and air quality (with particular focus on infection control).
Internal spaces
The design of internal spaces, such as ward configuration, corridor design, and nurse station placements (centralized vs. decentralized), can influence patient visibility, safety, teamwork, distances staff walk in a shift, and time spent providing direct care to patients. 10 For example, open-plan, larger convex spaces can lead to greater patient visibility, and corridor width impacts staff circulation, informal communication, and teamwork. 19 In ICU, designs with centralized nurse stations and visibility of most patient rooms from that location are increasingly being replaced with decentralized nurses’ stations, arguably without strong evidence. 19 In emergency departments, with similar critical visibility requirements for teamwork and patient monitoring, some authors argue that physically separated zones or “pods” are neither efficient nor safe. 20 Decentralized nursing stations can lead to more patient room visits by staff. 21 , 22 This highlights current uncertainties.
The layout of hospital spaces and line of sight influences patient and visitor orientation and their ability to find their way around (“wayfinding”). 23 Signs, information boards, and “landmarks” (artwork, furniture, views, etc.) are typical wayfinding elements. 24 , 25 Inadequate wayfinding leads to delays in accessing services or finding people or places, associated stress, and higher staff burden as they provide directions for lost individuals. 25 While some standards exist, wayfinding is often not optimized in healthcare. 26
The proportion of single versus multiple(two or more)-bed rooms is a prominent ward design consideration. There is evidence that single rooms can support staff/patient communication, privacy, infection control, and noise reduction, but they are also associated with patient isolation and increased falls risk. 27 This evidence is, however, of mixed quality, limited to certain populations, with neutral and/or contrary results. 27 A higher proportion of single rooms generally results in longer corridors, longer staff walking distances, perceived decrease in patient visibility due to compromised sightlines, and higher construction and cleaning costs. 28 The inherent trade-offs will be different in every healthcare context. Less controversial is location of sinks and hand sanitizers; highly visible and standardized positioning promotes more consistent use. 29 , 30

Outdoor spaces
Hospital gardens were historically commonplace 31 ; however, less priority has been given to green space over time. Access to the outdoors and time in nature has been linked to stress reduction, improved physical symptoms, and emotional well-being in many healthcare settings. 32 Views of nature have been linked to reduced length of stay. 33 Good hospital garden design principles include creating opportunities for exercise, exploration, socialization, and to engage with and escape in nature. 32 Surprisingly, patients and visitors are often not aware of hospital gardens, and proactive approaches to increasing patient and family use of gardens have been recommended. 34 Usually conceptualized as spaces for patients and visitors, staff are often their primary users. 32 Outdoor spaces can be restorative for hospital staff, helping to reduce stress and improve attention, which may improve patient care and staff retention. 35
Ambient features
Ambient features, such as light and noise, can impact patient well-being and comfort, sleep, and communication with staff. 36 , 37 Light and noise also impact staff well-being and attention 38 and contribute to medication errors and other safety concerns. 39
Air quality is important for both comfort and infection control. Infection control is particularly prioritized in acute environments and is receiving deserved attention in the COVID-19 pandemic. A recent review of COVID-19 transmission showed that spatial configuration can affect patient density and thereby transmission. 40 Optimized systems for heating, ventilation, and air conditioning (HVAC) can filter microparticles such as viruses. Different HVAC systems also affect humidity, airflow velocities, air pressure—all important for exposure to active aerosols. Window ventilation, daylight, and electric UV light are recommended to aid disinfecting surfaces and use of surface materials that affect pathogen survival. 40
Stroke care built environment evidence
In this section, we outline how the built environment can influence important outcomes such as: (1) evidence-based stroke care, including rehabilitation; (2) efficiency of stroke care, staff processes, and communication; and (3) patient safety and well-being. The evidence-base specific to stroke care is small. 41 In Figure 2 , we summarize the design features and how they may influence a range of outcomes including patient and staff behavior. This should be considered illustrative rather than exhaustive. Where possible, we draw directly from stroke or brain injury-specific evidence, supplementing evidence from other populations where relevant.
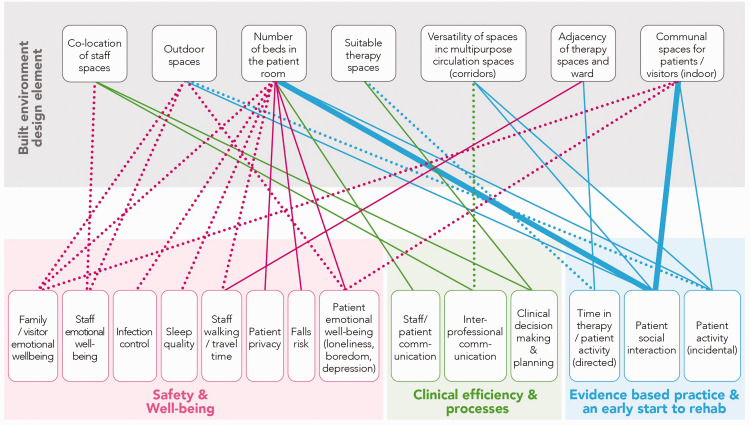
A summary of the evidence specific to stroke care environments. Dotted lines = a hypothesis, garnered from research in other populations; thin lines = limited evidence, < 3 studies; thick lines = moderate evidence, ≥ 3 studies, based on systematic literature review. 41
Evidence-based practice including rehabilitation
We found no stroke-specific research to underpin built environment recommendations for optimal delivery of either time-critical acute stroke treatments or evidence-based care, including rehabilitation. Guidelines recommend early commencement of both structured and incidental physical, cognitive, and social activity for all stroke patients, 42 , 43 although recommended levels vary. Patients in both acute and subacute environments spend most of their day alone and inactive in their bedroom. 44 , 45 While we can hypothesize that providing “draw-them-out” features on a ward may improve activity and engagement, evidence is limited. These features may include green spaces and indoor communal (social) spaces. Unfortunately, communal spaces, when present, often appear to be underutilized in both acute 46 and rehabilitation environments. 47 Many factors may influence whether patients use communal spaces, including not knowing they exist or where to find them, difficulty accessing them without help, or feeling they don’t have permission to use them. 48 In a Norwegian study across 11 stroke units with communal areas, patients were more active and spent less time in their bedroom in units where meals were served in the communal area. 49 Providing resources (games, music, books) in personalized activity packs and in communal spaces (“environmental enrichment”), with the aim to improve physical, social, and cognitive activity, has recently been tested in acute and subacute settings with mixed results. 50 – 52 Importantly, this approach relies on staff to encourage use and engagement, rather than embedding activity opportunities into the building itself. Hallways and circulation spaces are generally underrecognized as providing spaces for incidental activity and interaction. 53
There is limited stroke-specific research about the value or harm of single- versus multiple-bed rooms. A higher proportion of single rooms may be associated with lower levels of patient activity in acute stroke. 54 , 55 A systematic review of single- versus multiple-bed rooms in older people and those with neurological disorders found potential benefits (e.g. infection control, patient satisfaction) and harms (e.g. falls, isolation) with single rooms. 56 In rehabilitation facilities with a high proportion of single rooms, patients emphasize the importance of communal areas. 57 Further work is needed to identify and test how modifications to layout and communal and circulations spaces could enhance patient engagement, activity, and optimal care provision.
Efficiency of care, staff processes, and communication
Interprofessional communication and teamwork between physicians, nurses, and allied health professionals supports best practice stroke care. 11 Shared staff spaces support team communication and collaboration, enabling better understanding of patient needs, and greater knowledge about other team roles. 58 , 59
Therapy spaces are often discrete locations (e.g. gym, occupational therapy rooms), rather than being holistic, context-based environments that reflect the connectivity and continuity necessary for rehabilitation and transition beyond discharge. 60 , 61 Separation of clinical and therapy spaces can impact staff travel time, patient practice and activity, and even clinical decision-making. For example, Blennerhassett et al. 47 found that patients spent less time engaged in physical activity and more time in corridors when the ward was located further from the gym, on a separate floor. This also impacted wheelchair use and patient travel time. 47 Inaccessible therapy spaces can also change therapists’ intervention choices. 62
Safety and well-being
Falls are common after stroke, 63 yet the relationship between the built environment and falls is largely unexplored. The presence of a fellow patient (multiple-bed room) may help reduce falls, especially for older patients with neurological injury. 56 , 64 Roommates play an important role in monitoring the physical and mental health of others in stroke rehabilitation. 48 Stroke patients often experience loneliness when in hospital, 65 , 66 and some patients will choose a shared room over the privacy of a single room. 57 Sleep is important for recovery. Unsurprisingly, visual and aural privacy is less in multiple-bed rooms. However, noise traveling between corridors and bedrooms and lack of dedicated staff spaces for confidential conversations are also important. 48
Planning and design of new healthcare environments: Challenges and opportunities
Healthcare environments research and design is a multistakeholder endeavor involving government, healthcare providers, managers, clinical staff, patients, architects, quantity surveyors, construction companies, building managers, etc. This collaborative process can be challenging, 67 , 68 considering interdisciplinary differences in knowledge and approaches. 69 The complexity of hospital procurement and the fact that design and construction processes are foreign to many healthcare professionals adds further challenge. Clinicians often do not understand what the “user group” consultation process is supposed to achieve, and their involvement may be inconsistent throughout the design process, which limits their contribution to the process and ability to influence decisions. 67 While collaboration between architects and healthcare professionals is not new, 70 limited evidence informs current consultation processes. 67 , 71 High-quality healthcare environments are produced when shared decision-making and collaboration happens across healthcare, construction, and architecture to create designs based on evidence and end-users’ perspectives. 69
A number of research approaches are suggested to facilitate this collaboration, including participatory design, co-design, and Living Labs. 2 , 72 , 73 Over many years, our team has built partnerships between healthcare environment practitioners, clinicians, researchers, and people living with stroke, which have served to create a common understanding of the barriers and opportunities for redesigning and optimizing stroke care environments. With the creation of the Neuroscience Optimized Virtual Living Lab (NOVELL) for stroke rehabilitation redesign ( www.novellredesign.com ), we are working to develop new models for stakeholder engagement and research, and to contribute new evidence to stroke rehabilitation design.
In addition to collaboration challenges, research is infrequently embedded in the planning and design of new healthcare environments, and leaders in EBD have long called for appropriately funded, transparent, and freely available evaluations of completed buildings. 74 – 76 Given the cost of constructing and running healthcare buildings, the absence, or non-disclosure, of evaluations to determine whether desired outcomes were met is concerning. 77 , 78 Hospital design and construction is underpinned by technical and generic building guidelines and standards that differ within and between countries. The degree to which these standards are “evidence-informed” varies. In stakeholder consultations, understanding what is evidence-based and what is open to change can be difficult. Design innovation is essential if hospital buildings are to respond to new healthcare models or processes. For example, the recent COVID-19 induced surge in utilization of telehealth and other e-health technologies for rehabilitation, other treatment, and communication with people with stroke has implications for healthcare design, increasing demand for spaces for videoconferencing, equipment storage, and potential changes to waiting rooms and on-site consultation spaces. 79 , 80 Future design considerations for stroke recovery should also extend to the home environment. 81
The built environment matters. It can impact healthcare delivery and patient and staff outcomes. An evidence base is growing in some areas of healthcare design, while others require significant further research. The potential for both hospital and health services design innovation is strong. By continuing to build this evidence base, EBD can complement architectural processes to deliver high-performing healthcare assets. Involving engaged and informed clinicians in built environment design and research will help shape hospitals of the future.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: NOVELL is funded by the Felton Bequest and the University of Melbourne. Julie Bernhardt is funded by an NHMRC Research Fellowship (1154904). The Florey Institute of Neuroscience and Mental Health acknowledges support from the Victorian government and in particular funding from the Operational Infrastructure Support Grant.

- 1. Chua G. New Royal Adelaide Hospital named third most expensive building in the world. Architecture & Design , 23 March 2015.
- 2. Donetto S, Pierri P, Tsianakas V, et al. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Des J 2015; 18: 227–248. [ Google Scholar ]
- 3. Petit A, Cellot Li, La Gardette P-Cdg. Mémoire sur la meilleure maniere de construire un hôpital de malades. A Paris: de l'imprimerie de Louis Cellot, 1774.
- 4. Nightingale F. Notes on hospitals . 3d ed., enlarged and for the most part rewritten. London: Longman, Green, Longman, Roberts, and Green, 1863.
- 5. Hamilton DK. The four levels of evidence-based practice. Healthc Des 2003; 3: 18–26. [ Google Scholar ]
- 6. Ulrich RS, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. HERD 2008; 1: 61–125. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Harris PB, McBride G, Ross C, et al. A place to heal: environmental sources of satisfaction among hospital patients 1. J Appl Soc Psychol 2002; 32: 1276–1299. [ Google Scholar ]
- 8. Berry LL, Parker D, Coile R, et al. The business case for better buildings. Front Health Serv Manag 2004; 21: 3–24. [ PubMed ] [ Google Scholar ]
- 9. Sadler BL, Berry LL, Guenther R, et al. Fable hospital 2.0: the business case for building better health care facilities. Hastings Cent Rep 2011; 41: 13–23. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Halawa F, Madathil SC, Gittler A, et al. Advancing evidence-based healthcare facility design: a systematic literature review. Health Care Manag Sci 2020; 23: 453–480. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Langhorne P, Ramachandra S and Collaboration SUT. Organised inpatient (stroke unit) care for stroke: network meta‐analysis. Cochrane Database Syst Rev 2020; 4: CD000197. [ DOI ] [ PMC free article ] [ PubMed ]
- 12. Elf M, Nordin S, Wijk H, et al. A systematic review of the psychometric properties of instruments for assessing the quality of the physical environment in healthcare. J Adv Nurs 2017; 73: 2796–2816. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Stichler JF, Hamilton DK. Rigor and replication. HERD 2008; 2: 3–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Shannon MM, Nordin S, Bernhardt J, et al. Application of theory in studies of healthcare built environment research. HERD 2020; 13: 154–170. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. O’Callaghan N, Dee A, Philip RK. Evidence-based design for neonatal units: a systematic review. Matern Health Neonatol Perinatol 2019; 5: 1–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Papoulias C, Csipke E, Rose D, et al. The psychiatric ward as a therapeutic space: systematic review. Br J Psychiatry 2014; 205: 171–176. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Joseph A, Choi Y-S, Quan X. Impact of the physical environment of residential health, care, and support facilities (RHCSF) on staff and residents: a systematic review of the literature. Environ Behav 2016; 48: 1203–1241. [ Google Scholar ]
- 18. Elf M, Anåker A, Marcheschi E, et al. The built environment and its impact on health outcomes and experiences of patients, significant others and staff—a protocol for a systematic review. Nurs Open 2020; 7: 895–899. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Hadi K, Zimring C. Design to improve visibility: impact of corridor width and unit shape. HERD 2016; 9: 35–49. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Pati D, Harvey TE, Jr, Pati S. Physical design correlates of efficiency and safety in emergency departments: a qualitative examination. Crit Care Nurs Q 2014; 37: 299–316. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Gurascio-Howard L, Malloch K. Centralized and decentralized nurse station design: an examination of caregiver communication, work activities, and technology. HERD 2007; 1: 44–57. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Fay L, Carll-White A, Schadler A, et al. Shifting landscapes: the impact of centralized and decentralized nursing station models on the efficiency of care. HERD 2017; 10: 80–94. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Rooke CN, Tzortzopoulos P, Koskela L, et al. Wayfinding: embedding knowledge in hospital environments. In: HaCIRIC International Conference 2009 Improving healthcare infrastructures through innovation , Hilton Metropole Hotel, Brighton, 23 April 2009.
- 24. Pati D, Harvey TE, Jr, Willis DA, et al. Identifying elements of the health care environment that contribute to wayfinding. HERD 2015; 8: 44–67. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Devlin AS. Wayfinding in healthcare facilities: contributions from environmental psychology. Behav Sci 2014; 4: 423–436. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Augur H. Poor healthcare wayfinding has hidden cost for hospital kontaktio, https://kontakt.io/blog/healthcare-wayfinding/ (2018, accessed 19 August 2021).
- 27. Taylor E, Card AJ, Piatkowski M. Single-occupancy patient rooms: a systematic review of the literature since 2006. HERD 2018; 11: 85–100. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Maben J, Griffiths P, Penfold C, et al. One size fits all? Mixed methods evaluation of the impact of 100% single-room accommodation on staff and patient experience, safety and costs. BMJ Qual Saf 2016; 25: 241–56. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Deyneko A, Cordeiro F, Berlin L, et al. Impact of sink location on hand hygiene compliance after care of patients with Clostridium difficile infection: a cross-sectional study. BMC Infect Dis 2016; 16: 1–7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Neo JRJ, Sagha-Zadeh R. The influence of spatial configuration on the frequency of use of hand sanitizing stations in health care environments. Am J Infect Control 2017; 45: 615–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Hickman C. Therapeutic landscapes: a history of English hospital gardens since 1800 : Manchester: Manchester University Press, 2013.
- 32. Marcus CC. Therapeutic landscapes. In: AS Devlin (ed) Environmental psychology and human well-being . London: Academic Press, 2018, pp.387–413.
- 33. Ulrich R. View through a window may influence recovery from surgery. Science 1984; 224: 420–421. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Whitehouse S, Varni JW, Seid M, et al. Evaluating a children's hospital garden environment: utilization and consumer satisfaction. J Environ Psychol 2001; 21: 301–314. [ Google Scholar ]
- 35. Nejati A, Rodiek S, Shepley M. The implications of high-quality staff break areas for nurses’ health, performance, job satisfaction and retention. J Nurs Manag 2016; 24: 512–523. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Aries MB, Aarts MP, van Hoof J. Daylight and health: a review of the evidence and consequences for the built environment. Light Res Technol 2015; 47: 6–27. [ Google Scholar ]
- 37. Johansson L, Bergbom I, Waye KP, et al. The sound environment in an ICU patient room—a content analysis of sound levels and patient experiences. Intensive Crit Care Nurs 2012; 28: 269–279. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Hadi K, DuBose JR, Ryherd E. Lighting and nurses at medical–surgical units: impact of lighting conditions on nurses’ performance and satisfaction. HERD 2016; 9: 17–30. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Chaudhury H, Mahmood A, Valente M. The effect of environmental design on reducing nursing errors and increasing efficiency in acute care settings: a review and analysis of the literature. Environ Behav 2009; 41: 755–786. [ Google Scholar ]
- 40. Dietz L, Horve PF, Coil DA, et al. 2019 novel coronavirus (COVID-19) pandemic: built environment considerations to reduce transmission. Msystems 2020; 5: e00245–20. [ DOI ] [ PMC free article ] [ PubMed ]
- 41. Lipson-Smith R, Pflaumer L, Elf M, et al. Built environments for inpatient stroke rehabilitation services and care: a systematic literature review. BMJ Open 2021; 11: e050247. [ DOI ] [ PMC free article ] [ PubMed ]
- 42. Stroke Foundation. Clinical guidelines for stroke management . Melbourne, Australia, 2021.
- 43. Rudd A, Bowen A, Young G, et al. National clinical guideline for stroke: 5th edition 2016. Clin Med 2017; 17: 154–155. [ DOI ] [ PMC free article ] [ PubMed ]
- 44. Janssen H, Ada L, Bernhardt J, et al. Physical, cognitive and social activity levels of stroke patients undergoing rehabilitation within a mixed rehabilitation unit. Clin Rehab 2014; 28: 91–101. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Fini NA, Holland AE, Keating J, et al. How physically active are people following stroke? Systematic review and quantitative synthesis. Phys Ther 2017; 97: 707–717. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Shannon MM, Elf M, Churilov L, et al. Can the physical environment itself influence neurological patient activity? Disabil Rehabil 2019; 41: 1177–1189. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Blennerhassett JM, Borschmann KN, Lipson-Smith RA, et al. Behavioral mapping of patient activity to explore the built environment during rehabilitation. HERD 2018; 11: 109–123. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Lipson-Smith RA. Space for recovery after stroke: exploring the role of the physical environment in inpatient rehabilitation facilities. PhD Thesis, The University of Melbourne, 2020.
- 49. Hokstad A, Indredavik B, Bernhardt J, et al. Hospital differences in motor activity early after stroke: a comparison of 11 Norwegian stroke units. J Stroke Cerebrovasc Dis 2015; 24: 1333–1340. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Rosbergen IC, Grimley RS, Hayward KS, et al. The impact of environmental enrichment in an acute stroke unit on how and when patients undertake activities. Clin Rehabil 2019; 33: 784–795. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Rosbergen IC, Grimley RS, Hayward KS, et al. Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: a controlled before–after pilot study. Clin Rehabil 2017; 31: 1516–1528. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Janssen H, Ada L, Middleton S, et al. Altering the rehabilitation environment to improve stroke survivor activity (AREISSA): a Phase II trial. Int J Stroke 2021: 17474930211006999. [ DOI ] [ PubMed ]
- 53. Colley J, Zeeman H, Kendall E. “Everything happens in the hallways”: exploring user activity in the corridors at two rehabilitation units. HERD 2018; 11: 163–176. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Anåker A, von Koch L, Sjöstrand C, et al. A comparative study of patients’ activities and interactions in a stroke unit before and after reconstruction—the significance of the built environment. PLoS One 2017; 12: e0177477. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Anåker A, von Koch L, Sjöstrand C, et al. The physical environment and patients’ activities and care: a comparative case study at three newly built stroke units. J Adv Nurs 2018; 74: 1919–1931. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Shannon M, Lipson-Smith R, Elf M, et al. Bringing the single versus multi-patient room debate to vulnerable patient populations: a systematic review of the impact of room types on hospitalized older people and people with neurological disorders. Intell Build Int 2020; 12: 180–198. [ Google Scholar ]
- 57. Killington M, Fyfe D, Patching A, et al. Rehabilitation environments: service users’ perspective. Health Expect 2019; 22: 396–404. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Paxino J, Denniston C, Woodward-Kron R, et al. Communication in interprofessional rehabilitation teams: a scoping review. Disabil Rehabil 2020: 1–17. [ DOI ] [ PubMed ]
- 59. Anåker A, von Koch L, Eriksson G, et al. The physical environment and multi-professional teamwork in three newly built stroke units. Disabil Rehabil 2020: 1–9. [ DOI ] [ PubMed ]
- 60. Thwaites K, Helleur E, Simkins I, et al. Restorative urban open space: exploring the spatial dimensions of human emotional fulfillment in urban open space. Landscape research 2005; 30: 525–547.
- 61. Wright CJ, Zeeman H, Biezaitis V. Holistic practice in traumatic brain injury rehabilitation: perspectives of health practitioners. PLoS One 2016; 11: e0156826. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Skubik-Peplaski C, Howell DM, Hunter EG, et al. Occupational therapists perceptions of environmental influences on practice at an inpatient stroke rehabilitation program: a pilot study. Phys Occup Ther Geriatr 2015; 33: 250–262. [ Google Scholar ]
- 63. Holloway RG, Tuttle D, Baird T, et al. The safety of hospital stroke care. Neurology 2007; 68: 550–555. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Singh I, Okeke J, Edwards C. Outcome of in-patient falls in hospitals with 100% single rooms and multi-bedded wards. Age Ageing 2015; 44: 1032–1035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. Anåker A, von Koch L, Heylighen A, et al. “It’s lonely”: patients’ experiences of the physical environment at a newly built stroke unit. HERD 2019; 12: 1937586718806696. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 66. Luker J, Lynch E, Bernhardsson S, et al. Stroke survivors’ experiences of physical rehabilitation: a systematic review of qualitative studies. Arch Phys Med Rehabil 2015; 96: 1698–708.e10. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Carthey J. Interdisciplinary user groups and the design of healthcare facilities. HERD 2020; 13: 114–128. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Miller TR, Baird TD, Littlefield CM, et al. Epistemological pluralism: reorganizing interdisciplinary research. Ecol Soc 2008; 13: 46.
- 69. Elf M, Fröst P, Lindahl G,et al. Shared decision making in designing new healthcare environments—time to begin improving quality. BMC Health Serv Res 2015; 15: 1–7. [ DOI ] [ PMC free article ] [ PubMed ]
- 70. Ehrström M, Jetsonen S, Lindh T, et al. Nomination of Paimio Hospital for inclusion in the world heritage list . Helsinki: National Board of Antiquities, 2005.
- 71. Hamilton DK. Incorporating credible evidence into the design process. HERD 2018; 11: 11–16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Hyysalo S, Hakkarainen L. What difference does a living lab make? Comparing two health technology innovation projects. CoDesign 2014; 10: 191–208. [ Google Scholar ]
- 73. Reay S, Collier G, Kennedy-Good J, et al. Designing the future of healthcare together: prototyping a hospital co-design space. CoDesign 2017; 13: 227–244. [ Google Scholar ]
- 74. Hamilton DK. Every facility project and every building is a research opportunity . Los Angeles, CA: SAGE Publications, 2009. [ DOI ] [ PubMed ]
- 75. Preiser WF. Continuous quality improvement through post-occupancy evaluation feedback. J Corp Real Estate 2003; 5: 42–56. [ Google Scholar ]
- 76. Shepley MM. Design evaluation. In: Marberry SO (ed) Healthcare design . New York: John Wiley, 1997, pp.73–104.
- 77. Hadjri K and Crozier C. Post‐occupancy evaluation: purpose, benefits and barriers. Facilities 2009; 27: 21–33.
- 78. Zimmerman A, Martin M. Post-occupancy evaluation: benefits and barriers. Build Res Inf 2001; 29: 168–174. [ Google Scholar ]
- 79. Hume R and Looney J. Designing for telemedicine spaces: planning for the next generation of health care delivery. Health Facilities Management , 3 February 2016, https://www.hfmmagazine.com/articles/1889-designing-for-telemedicine-spaces (accessed 18 August 2021).
- 80. Krupinski EA. Telemedicine workplace environments: designing for success. Healthcare 2014; 2: 115–122. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Kylén M, von Koch L, Pessah-Rasmussen H, et al. The importance of the built environment in person-centred rehabilitation at home: study protocol. Int J Environ Res Public Health 2019; 16: 2409. [ DOI ] [ PMC free article ] [ PubMed ]
- View on publisher site
- PDF (1.0 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Advertisement
The hospital of the future: rethinking architectural design to enable new patient-centered treatment concepts
- Original Article
- Published: 15 December 2021
- Volume 17 , pages 1177–1187, ( 2022 )
Cite this article

- Carlos Amato 1 ,
- Leslie McCanne 1 ,
- Chengyuan Yang 1 ,
- Daniel Ostler 2 ,
- Osman Ratib 3 ,
- Dirk Wilhelm 2 , 4 &
- Lukas Bernhard ORCID: orcid.org/0000-0002-9729-8928 2
12k Accesses
5 Citations
19 Altmetric
Explore all metrics
Today’s hospitals are designed as collections of individual departments, with limited communication and collaboration between medical sub-specialties. Patients are constantly being moved between different places, which is detrimental for patient experience, overall efficiency and capacity. Instead, we argue that care should be brought to the patient, not vice versa, and thus propose a novel hospital architecture concept that we refer to as Patient Hub . It envisions a truly patient-centered, department-less facility, in which all critical functions occur in the same building and on the same floor.
To demonstrate the feasibility and benefits of our concept, we selected an exemplary patient scenario and used 3D software to simulate resulting workflows for both the Patient Hub and a traditional hospital based on a generic hospital template by Kaiser-Permanente.
According to our workflow simulations, the Patient Hub model effectively eliminates waiting and transfer times, drastically simplifies wayfinding, reduces overall traveling distances by 54%, reduces elevator runs by 78% and improves access to quality views from 67 to 100% for patient rooms, from 0 to 100% for exam rooms and from 0 to 38% for corridors. In addition, the interaction of related medical fields is improved while maintaining the quality of care and the relationship between patients and caregivers.
With the Patient Hub concept, we aim at rethinking traditional hospital layouts. We were able to demonstrate, alas on a proof-of-concept basis, that it is indeed feasible to place the patient at the very center of operations, while increasing overall efficiency and capacity at the same time and maintaining the quality of care.
Similar content being viewed by others

The Architecture of New Hospitals: Complex yet Simple and Beautiful

Improving the Patient Room: Lessons from Acuity Adaptable Room
A hierarchical facility layout planning approach for large and complex hospitals.
Avoid common mistakes on your manuscript.
Current healthcare systems around the world are characterized by the organizational principles of segmentation and separation of medical specialties. They are structured into departments and facilities which offer the best service in their respective field but are not properly coordinated or tightly linked to the rest of the healthcare ecosystem. Consequently, today’s hospitals seem more a collection of different “departments” and medical fields than a fully integrated cooperative and service-oriented facility. Each department uses its own workflow schemes or standard operative procedures (SOP), employs specially trained personnel, and runs its medical service in well-circumscribed and precisely defined structures and areas. Communication between disciplines is often limited to the absolute minimum necessary for coordination tasks, e.g., regarding forwarding of relevant patient information and time scheduling of examinations or interventions.
The current system requires patients to step from doctor to doctor and from department to department to collect the jigsaw puzzle pieces of their disease. It is a serious drawback of current hospital structures that patients often need to tell their medical history and symptoms over and over again to the medical staff of different disciplines and subspecialties. The request and scheduling of different diagnostic examinations across departments are often confined to a very succinct standard requisition, neglecting the exchange of any additional patient-specific information (e.g., the anatomical reconstruction after gastric surgery in case of a postoperative CT scan to rule out complications). This data that are essential for appropriate programming and interpretation of diagnostic procedures is often non-accessible to the physician performing the exams. We call this “incremental care” and in this traditional model, the patient is constantly moved around to receive care (Fig. 1 depicts an exemplary traditional patient’s pathway). While some of these issues could be addressed by optimizing the clinical communication and data storage infrastructure, we believe that by means of architectural choices it becomes possible to further benefit and simplify the necessary workflows and to reduce the amount of required technology.
Traditional Incremental “Patient to Care” flow: the patient is constantly being moved between departments, typically starting from clinical reception, followed by examinations, diagnostics, treatments, ward stays and other way stations. Due to the highly fragmented structure, a direct access of external parties, especially academia and industry, is aggravated
Current hospitals are organized around well-separated specialized clinics and expert units, which all by themselves are perfectly tuned for economically optimized and efficient use of their dedicated infrastructure (e.g., the operating room in surgery or the MRI in radiology) and make efforts to reduce the cost of personnel wherever possible. Profit has become the main driver of healthcare and everything else including patient satisfaction and even quality of care often comes as a second priority. However, financial profit is generally not assessed on a global scale of patient management services but rather on the level of subsystems and specialized services, with a focus on separated profit centers which results in higher global costs rather than reducing them due to inefficient coordination and consolidation of clinical pathways. “Service-oriented” care units refer more to medical services (or equipment) and teams providing dedicated care, rather than to patient-centered care facilities. This often results in inefficient workflows such as excessive and unnecessary time spent in waiting rooms, which is becoming prevalent in large facilities.
Although system optimization works well for a specialized and restricted field, e.g., a department or a single facility, the entire healthcare system has grown enormously toward becoming rigid, not-adaptive, and slow. It is not designed for the active prevention of disease, but for mere reaction in case an adverse health event or development arises. This approach entails that the patient suffers more overall, since diseases are allowed to develop and manifest themselves before they are finally diagnosed and treatment can be started. At the same time, the burden for clinical care facilities increases as well, since treatments become more complex and result in longer durations of stay. The preventive approach has been advocated for quite some time now [ 1 ] and its benefits have become very obvious during the recent Covid-19 pandemic [ 2 ].
Although “interdisciplinary care” and “overarching approach” represent typical buzzwords of modern treatment concepts, the integration of involved clinical disciplines remains on a low level. One notable exception is acute trauma or emergency management where any active action is focused on the patient and collaboration is crucial to handling critically vital situations. The growing field of emergency medicine could serve as a model for a more global paradigm shift, as an example of healthcare delivery that is, above all, patient-centered. In such a context, interdisciplinary communication is highly standardized involving all persons and services required for well-protocoled patient management scenarios. Services are brought to the patient, and not vice versa, and anything and everybody involved is geared to facilitate a fast and comprehensive treatment. It has been shown that the patient-centered multidisciplinary approach, at least for acute trauma, can save lives and is superior to traditional concepts [ 3 ]. So, one might ask whether such an approach could also be beneficial for other indications or even for general care? And if so, will this new concept maintain the current standard of care and the relationship between caregivers and patients?
As a central building block for addressing the issues described in the previous we present our new hospital concept that we refer to as Patient Hub . It envisions a truly patient-centered, department-less facility, where all the critical functions occur on one floor. While our idea is not intended to solve all of today’s hospital design flaws (and we are fully aware that one solution will never fit all models), we aim at providing concepts and tools to help re-think traditional designs.
We developed a novel, one-of-a-kind design concept for the hospital of the future. The envisioned facility is fully patient-centered and strives for a workflow-oriented design by clustering related functionalities and processes in defined hubs, all located on the same floor and in close proximity to each other. In order to demonstrate the effectiveness and added value of our proposed hospital architecture, we benchmarked this new concept against a traditional design. For that, we reconstructed both the Patient Hub and an exemplary traditional hospital layout using 3D simulation software and compared them with regard to workflow efficiency and patient satisfaction. For the initial analysis presented here, we chose a typical patient scenario based on a common real-world case.
The patient hub concept
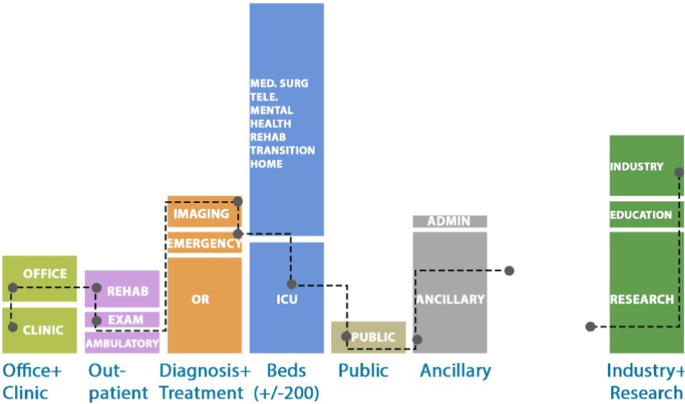
Today’s hospital buildings are often fancier versions of the 1960s bed-tower-on-diagnostic-and-treatment podium model, with a lot of newer technology crammed inside. In accordance with the principle of decentralization, which is prevalent in many healthcare systems around the world [ 4 ], such environments are characterized by being divided into departments and individual silos, each possessing its own organizational structure (including permanent staff, assigned space and beds), optimized for operational and financial efficiency. The patient is moved around from place to place to receive care, instead of bringing the care and technology to the patient (e.g., infrastructure like CT or MRI is often inconveniently and remotely located in a different building, as illustrated by Fig. 2 ).
Functional stacking of (traditional) Template Hospital used for simulation comparison
In contrast, our Patient Hub concept is a radical departure from the way traditional hospitals are designed. It envisions a transformative “one of a kind” and truly patient-centered, department-less facility. We propose a highly centralized clinical layout, where all relevant medical fields of expertise are available within the same space surrounding the patient (see Figs. 3 and 4 ). They form clusters which contain functionalities of equal classes, as for example examination , out-patient care or administration . For the patient, the whole system has a single-entry point to simplify wayfinding and is designed to minimize patient movement. The centralized clinical layout brings together staff from all specialties to encourage clinical collaboration and care coordination, thereby stimulating health care performance [ 5 ]. Instead of facilities being distributed along the hospital, and most often on different levels or even buildings, the new design concept aims at achieving a logical and self-explaining layout by bringing together what belongs together. However, the vision of the Patient Hub encompasses much more than a traditional hospital: This new environment (or ecosystem) co-locates outpatient, inpatient, rehabilitation, wellness and prevention, ancillary support spaces, and industry (research and development) all under one roof. It is envisioned to be no longer just a site for the treatment of the sick but a health-oriented all-encompassing facility, which is achieved by implementing patient-centered structures and workflows as well as by an expansion of services to also incorporate prevention and wellness.
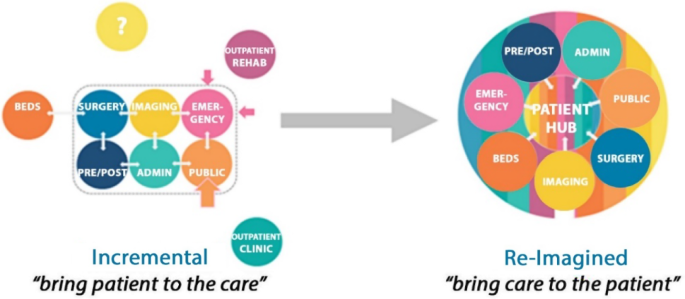
Re-imagined healthcare paradigm: changing from incremental “patient to care” approach toward a re-imagined “care to patient” approach
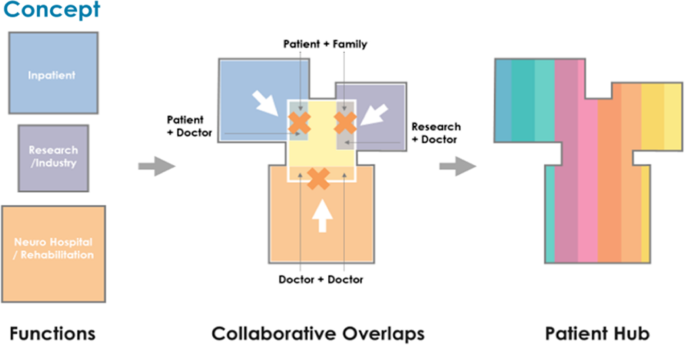
Concept diagram illustrating “all under one roof” collaborative Patient Hub concept
Instead of being department-oriented, the Patient Hub design follows a more functional approach. To avoid getting lost in the sub-channels of the system (different departments with specific ecosystems), the architecture is logically constructed and patient-centered. It features a single point of entry, and a central meet and commute “core” to which the relevant facilities (housing, examination, out-patient care, administration) are linked, just as the arms of a tree are joined to the trunk. For the reduction or even full avoidance of patient moves, the respective areas cluster the required functionalities on one site. This will be done irrespective of the affiliated department or responsibility. Instead of passing from the radiologic department in level A to cardiology in level D to complete the pre-operative check-up, the patent will now move from one to the other door, as depicted in Fig. 5 .

Re-imagined “Care to Patient” flow diagram indicating functional adjacency needed to deliver patient-centered care
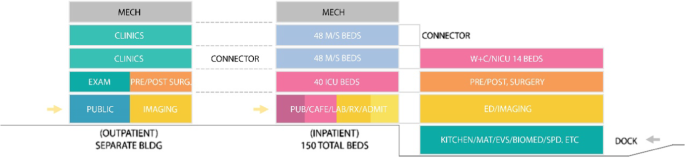
By avoiding duplicating functionalities which today are replicated in every department (e.g., waiting rooms, registration area, observation area) the Patient-hub concept aims at saving space, simplifying patient pathways, and facilitating implementation and adaptation of new treatment concepts. While keeping this functional patient-hub design with all required functionalities being logically distributed on one floor, we envision different levels of the building to be adaptable to different patient needs and specialties, like surgery, medical treatment, rehabilitation, etc. (see Fig. 6 ).
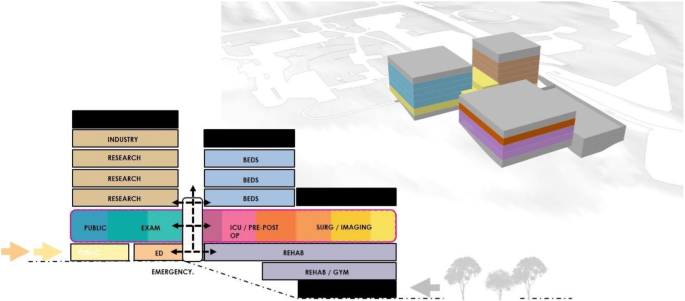
Patient Hub functional stacking and 3D massing
Due to its horizontal layout and resulting space demands, the Patient Hub layout in its most essential form is best suited for freestanding greenfield hospitals. The hub floor of our current design requires an 8,000–9,000 square meter floor plate but can be scaled up and down depending on the number of beds and procedure space needed. Since a further increase of the horizontal expansion would start to contradict the goal of having a compact centralized hub with streamlined workflows and short routes, we instead propose to stack multiple independent Patient Hub units vertically. Thereby, it becomes possible to retain the compact size of each hub and keep all movements of a given patient on the same floor, while making more efficient use of the available building ground and increasing the overall capacity.
Patient scenario
Our exemplary scenario revolves around a patient being diagnosed for rectal cancer. First, the patient receives general examination and diagnostics according to current guidelines [ 6 ], which include endoscopy, pelvic MRI and CT. After physical examination, which, due to his age and existing comorbidities includes cardiologic assessment, the case is discussed in multidisciplinary consultations such as tumor conferences and the patient is scheduled for surgery. Preparation measures for surgery include obtaining the patient’s informed consent by the surgeon and anesthesia, as well as preoperative preparation such as bowel cleansing and blood tests. After the intervention, observation in the ICU is carried out for one day, before the patient is returned to the regular ward. In our scenario, an eventless postoperative course is observed, which is why only a chest x-ray is performed to examine the postoperative lung status. No other tests or assessment of anastomotic healing are undertaken. During the hospitalization, the patient has an interview with the surgeon, to discuss upon the results of surgery and eventually additional treatments, and another interview with the social worker to decide upon auxiliary measures. Finally, the patient is discharged from the clinic.
The case above describes a common situation that clinicians are dealing with regularly and is based on the organizational structure and standard operating procedures of a university hospital. We analyzed the necessary steps along this clinical pathway for a traditionally designed hospital. Even though we chose a complication-free course for our scenario, the resulting list of necessary steps contains 95 entries, many of which are describing a change of the patient’s location or time spent within various waiting rooms. Refer to Table 1 for an excerpt of this list.
Workflow simulation
Using the 3D simulation software FlexSim Healthcare™ (FlexSim Software Products, Inc., Orem, Utah, USA), we developed dynamic models for comparing various quality measures between our two different hospital layouts. FlexSim Healthcare is a standalone healthcare simulation product aiming to model patient flows and other healthcare processes. It is designed to help healthcare organizations to evaluate different scenarios and validate them before they are implemented. For that, one or several architectural models can be created, followed by the definition of patient journeys. During execution of the simulation, FlexSim can monitor data contributing to patient satisfaction, including the total time spent, time spent for each treatment, time proportion of receiving care, travel distances, etc. It can also be used to analyze staff and equipment utilization rates and help to balance staff workload and amount of equipment.
Modelling of architectural layout
We selected Kaiser Anaheim hospital, a traditional hospital with a similar size, to be compared to the Patient Hub. The construction of this hospital was based on a generic “template” hospital plan developed and used by Kaiser-Permanente, the US largest non-profit Health Management Organization (HMO) (Fig. 7 ). This plan was developed when the organization was required to replace half of its hospital beds in California due to new seismic regulations and resulted in a prototypical hospital “template” that can be built on virtually any site, with few modifications [ 7 ], with a minimum of effort, lead time, and government review [ 8 ]. The design aimed at incorporating the best known clinical practices and design success stories and was optimized for a fast and efficient construction process [ 7 ]. Due to these characteristics, and a broad and successful implementation, we have selected this layout as the best comparison available today.
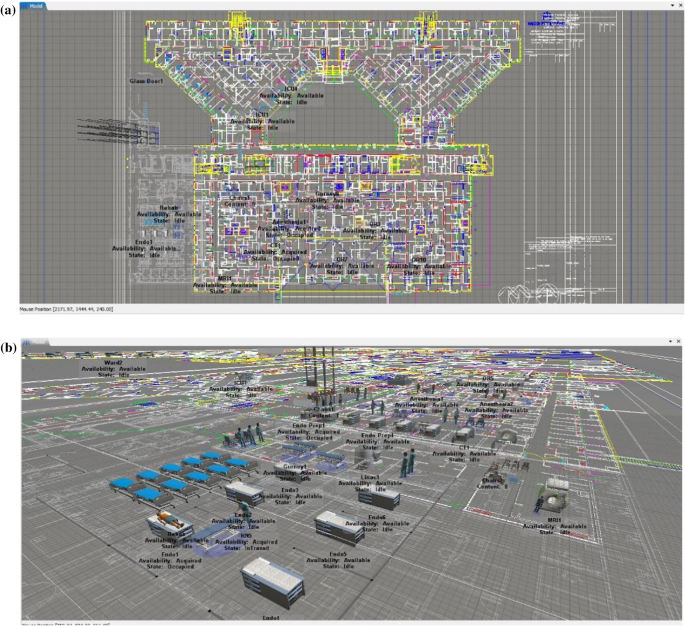
Simulations within FlexSim Healthcare for a traditional hospital (Kaiser-Permanente); a 2D overview floor plan; b 3D rendering of 2nd floor; the right parts of the images show the linear workflow used for the simulation
The second model (see Fig. 8 ) represents our Patient Hub, i.e., a hypothetical department-less hospital layout based on patient-centered care activities and concentrated on a single floor. Both buildings were modeled in FlexSim based on the floor plans. The model elements essential to this process were those affecting patient travel distance and waiting time, including vertical transportation, wall arrangement and the available medical equipment.
a 2D view of main Patient Hub floor showing diagnostic and treatment, outpatient, universal inpatient patient ward and patient experience / public / interdisciplinary coordination core blocks; b 3D rendering of Patient Hub floor within FlexSim environment; showing simulation workflow study to determine and test ideal functional adjacencies
Definition of patient treatment journey
After implementing the models, we defined the patient scenario (see previous section) and created a list of healthcare services that this patient needs to receive. We programed the full process based on this list, from patient first entering the hospital, walking to each exam rooms, receiving direct care (endoscopy, CT, MRI, surgery), receiving indirect care (observation rooms, patient ward), consultation and rehabilitation, and finally leaving the hospital.
Definition of staff and equipment
We assigned medical staff (doctors, nurses, technicians, etc.), medical equipment (CT, MRI etc.) and transit equipment (wheelchairs, gurneys, etc.) to the simulation models. For each model, 2 CT machines, 1 MRI machine, 1 ergometer, 4 gurneys and 4 wheelchairs were available. The patients were supervised by 4 Doctors of Medicine (MD) and 4 Registered Nurses (RN) per medical specialty. Numbers were based on the size of the functioning area (according to industry standards) and are the same for both models in order to not affect the simulation results. We programed the full process of staff providing direct and indirect care including escorting and monitoring patients.
Using FlexSim we simulated the whole process from entering the hospital to exiting, and monitored key statistics including travel distance, major milestones, treatment times, waiting times, time proportion, utilization rate for both patient and staff. For both scenarios, we simulated the arrival of three patients every half hour between 8am and 9:30am, which amounts to a total of nine patients.
Comparative parameters
For measuring the performance of the two models, we selected multiple parameters, with a high focus on improving the patient experience:
Waiting and Transfer Time
Travel Distance
Number of Elevator Runs
Access to Respite Spaces, Nature and Quality Views
The first parameter Waiting and Transfer Time is arguably the most relevant for patient experience, staff workload and overall efficiency alike. By decreasing this parameter, the overall duration of the hospital stay can be shortened and resting/recovery time for the patient (i.e., time spent in the ward) can be maximized. Furthermore, staff members are less overburdened and can potentially use the gain in time for other tasks or patients, thus improving staff satisfaction and economic interests of the hospital. Admittedly, reducing transfer times likewise can serve to increase the throughput of patients, however, we did not intend to improve on this measure.
The parameter Travel Distance refers to the length of the path that each single patient needs to travel during the hospital stay. We split this into the following three parts reflecting the different stages of the patient’s pathway: Endoscopy , CT + MRI + Cardiology and Anesthesia + OR + ICU . Decreasing travel distance is desirable since long transfers between distant departments are a burden for patient and personnel alike and extend the duration of hospital stays.
Wayfinding refers to the complexity of the patient’s traveling route within the hospital. A high number of turns, stop-and-go’s, transfers paired with rather chaotic paths and destinations scattered across different buildings indicate a poor performance with respect to this parameter. Short and infrequent transfers paired with simple and uncomplicated routes within the same building and on the same floor indicate a good performance. For our initial assessment, we interpreted the patient’s path as a graph and used the number of nodes and edges as an abstract measure of complexity. In addition, we considered the number of locations requiring signage as a more user-oriented parameter.
The Number of Elevator Runs is another measure for the complexity of patient transfers. Elevators often are bottlenecks within hospital buildings and contribute to elongated transfer times, which is disadvantageous from patient, staff and economic perspectives. Therefore, a low number of elevator runs indicates better performance. Furthermore, elevator operation typically accounts for 3 to 8% of the total energy consumption of a building [ 9 ]. Thus, a decrease can have a positive impact on the hospital’s CO 2 footprint.
Hospital stays can be associated with high mental stress or anxiety for many reasons, such as individual ailments and separation from the outside world and everyday life. The bleak, functional and sterile look that hospital interiors tend to have, may further amplify this effect. However, there is overwhelming evidence and research indicating that having frequent Access to Respite Spaces, Nature and Quality Views influence our health outcomes and help mitigate this problem [ 10 , 11 , 12 ]. To evaluate the performance of our models with regard to this parameter, we analyzed the number of patient rooms, examination rooms and corridors providing quality views to gardens surrounding or located in between hospital buildings.
Numeric results of the workflow simulations for the parameters and models explained in the Methods section are given in Table 2 .
Our results presented in the previous section are promising, since a considerable improvement for every selected parameter can be observed. We see this as a proof-of-concept of our ideas. However, we want to stress that the investigated scenario is only a first step toward proving the feasibility of the Patient Hub concept. Other patient scenarios and combinations of them will lead to even more complicated situations and workflows, where we believe the benefits of the new patient-centered layout will become even more obvious—due to the reduction of bottlenecks and resulting improvements of target parameters relevant for patient experience. Generally, we interpret the simulation results as evidence for the postulation that, as healthcare strategies are expected to evolve toward more ambulatory and short-term hospitalization, facilities should focus more on optimizing their workflows rather than maintaining the priority of traditional inpatient procedures of hospitalized patients. Our study also concludes that a patient experience measurement or scoring system should be formally included in all hospital design simulations, although the construction of such an integrated index is still pending and requires the involvement of experts from different fields.
Clearly, the proposed layout has not yet been fully implemented in the real world and thus may be prone to problems that cannot be identified using the proof-of-concept approach presented in the manuscript. As of now, a test pilot project with limited scale is under construction in Philadelphia, which will accommodate 150 beds. This test project will be a valuable source of insights regarding problems and limitations of the Patient Hub concept.
Still, there are limitations that we are already aware of, especially regarding the size of the Patient Hub. It is neither reasonable nor feasible to scale up a single floor facility indefinitely to accommodate for more and more patients. The strengths of the centralized layout would be mitigated by the huge size and the whole system would presumably become sluggish and less efficient. Also, the available building ground would not be used very efficiently, as compared to a multi-level building. A possible solution to this is the stacking of multiple patient hubs (e.g., with different specializations) on top of each other. However, this would mean that diagnosis and treatment services need to be duplicated, which has been done in the past, but is not preferred by most hospital operators due to financial concerns.
A further limitation is that an integration of the Patient Hub concept into existing facilities is not possible. Thus, it is exclusively applicable to new building projects.
As of now, the proposed concepts mainly focus on architectural design and a translation to the real world will certainly require many more building blocks, such as AI (notably workflow scheduling/optimization), big data (collection and processing of health data) and robotics (e.g., self-driving assistance systems). In particular, we envision the entire infrastructure, including technical devices, spaces and functional units to become adaptive and mobile. For example, a medical / surgical patient room could be utilized as an ICU site (Universal Room). Intervention rooms could be suitable for surgery, interventional radiology or cardiologic manipulations. CT scanners and other assistance systems could be designed as self-navigating systems, to move independently to desired locations.
While we plan to incorporate such considerations into future work, we advocate a very deliberate use of technology, governed by the paradigm of bringing care to the patient and not solely by economic interests. As argued before, the new patient-centered approach is expected to increase patient satisfaction, to reduce overall procedure times (if combined with an intelligent real-time scheduling and organization system) and to even be superior regarding infection prevention. Moreover, such an adaptive environment will most likely contribute to the physicians’ satisfaction as well as foster collaborative and interdisciplinary work. At the same time, it will allow for fast and easy adjustment of the entire system according to the current number of patients and the prevailing diseases they are suffering from (e.g., in case of a pandemic). As shown in Fig. 9 , we envision the Patient-Hub to behave according to an expanding core model, where all activities can be centralized during times of low demand (e.g., at night) and expanded by reactivating auxiliary areas from hibernation to deal with higher workloads. A centralized layout would facilitate such an expansion and retraction as opposed to a traditional layout where all core functionalities are distributed throughout the hospital.
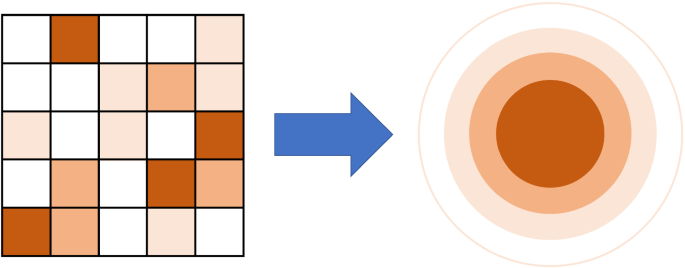
Functional design changes from a distributed pattern to an expanding core concept
The Patient Hub Design maintains the patient–caregiver relationship and the principle of patient-centered care delivery by preserving core aspects of current hospitals such as wards and operating theaters, which, however, are functionally rearranged and smartly repositioned within the Patient Hub. This rearrangement not only improves patient experience but also the patient-related communication and collaboration of physicians, further improving workflow and information exchange.
We believe “departments” will no longer define the basic structure of a hospital. Instead, patient requirements and functionalities, such as “operative care,” “infectious disease recovery”, “conservative oncology” or “preventive care” will be brought into focus. By using this revised interpretation of interdisciplinary patient-centered care for our Patient Hub concept, we are able to improve patient and healthcare workers experience and satisfaction while maintaining the current standard of care.
Lastly, we do not believe that economic parameters are deteriorated by the patient-centered approach. On the contrary, our simulation results show significant increases in efficiency throughout the facility, with less required staff members and less time required per patient. Therefore, we expect our approach to not only be beneficial for patients and employees, but to be cost effective and economically reasonable at the same time.
We have presented our vision of a novel patient-centered department-less hospital design referred to as the Patient Hub. While the realization of this vision clearly requires disruptive change regarding many aspects (such as clinical workflows, application of technology, functioning of the healthcare system in general), our main aim herein was to focus on re-inventing the architectural layout. For benchmarking the performance of our concept with regard to patient experience, we have defined a patient scenario and created simulation models for both the Patient Hub layout and a standard hospital template by Kaiser-Permanente. The simulation results were highly promising, showing clear advantages of the Patient Hub layout throughout all benchmark parameters. We see this as a proof-of-concept of our ideas and as an important validation before implementing the Patient Hub in the real-world.
Hood L, Balling R, Auffray C (2012) Revolutionizing medicine in the 21st century through systems approaches. Biotechnol J 7(8):992–1001. https://doi.org/10.1002/biot.201100306
Article CAS PubMed PubMed Central Google Scholar
Evans S, Agnew E, Vynnycky E, Stimson J, Bhattacharya A, Rooney C, Warne B, Robotham J (2021) The impact of testing and infection prevention and control strategies on within-hospital transmission dynamics of COVID-19 in English hospitals. Philosophical transactions of the Royal Society of London. Series B Biol Sci 376(1829):20200268. https://doi.org/10.1098/rstb.2020.0268
Article CAS Google Scholar
Hußmann B, Waydhas C, Lendemans S (2013) Schockraummanagement beim Schwer- und Schwerstverletzten: Eine interdisziplinäre Aufgabe [Emergency trauma room management in severely and most severely injured patients: a multidisciplinary task]. In: Janssens U, Joannidis M, Mayer A (eds) Weiterbildung Intensivmedizin und Notfallmedizin. Springer, Berlin Heidelberg, Berlin, Heidelberg, pp 21–31
Chapter Google Scholar
Saltman RB (ed) (2007) Decentralization in health care. Strategies and outcomes. European Observatory on Health Systems and Policies Series. Open University Press, Maidenhead
Google Scholar
Ridgely MS, Ahluwalia SC, Tom A, Vaiana ME, Motala A, Silverman M, Kim A, Damberg CL, Shekelle PG (2020) What are the determinants of health system performance? findings from the literature and a technical expert panel. Jt Comm J Qual Patient Saf 46(2):87–98. https://doi.org/10.1016/j.jcjq.2019.11.003
Article PubMed Google Scholar
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen Y-J, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wuthrick E, Gregory KM, Gurski L, Freedman-Cass DA (2018) Rectal cancer, version 2.2018, NCCN clinical practice guidelines in oncology. J National Compr Cancer Network JNCCN 16(7):874–901. https://doi.org/10.6004/jnccn.2018.0061
Article Google Scholar
Building Design & Construction (2008) Kaiser Permanente’s Template for Success. https://www.bdcnetwork.com/kaiser-permanente%E2%80%99s-template-success . Accessed September 6th, 2021
Kaiser Permanente (2011) Creating the ultimate patient experience. https://about.kaiserpermanente.org/our-story/our-history/creating-the-ultimate-patient-experience . Accessed September 6th, 2021
de Almeida A, Hirzel S, Patrão C, Fong J, Dütschke E (2012) Energy-efficient elevators and escalators in Europe: an analysis of energy efficiency potentials and policy measures. Energy Build 47:151–158. https://doi.org/10.1016/j.enbuild.2011.11.053
Facility Guidelines Institute (2014) Guidelines for design and construction of hospitals and outpatient facilities. American hospital association. American society for healthcare engineering
Kaplan S (1995) The restorative benefits of nature: Toward an integrative framework. J Environ Psychol 15(3):169–182. https://doi.org/10.1016/0272-4944(95)90001-2
Ulrich RS (1984) View through a window may influence recovery from surgery. Science 224(4647):420–421. https://doi.org/10.1126/science.6143402
Article CAS PubMed Google Scholar
Download references
Not applicable.
Author information
Authors and affiliations.
CannonDesign, Los Angeles, CA, USA
Carlos Amato, Leslie McCanne & Chengyuan Yang
Research Group MITI, Klinikum rechts der Isar, Technical University Munich, Munich, Germany
Daniel Ostler, Dirk Wilhelm & Lukas Bernhard
Department of Radiology and Medical Informatics, University of Geneva, Geneva, Switzerland
Osman Ratib
Department of Surgery, Klinikum rechts der Isar, Technical University Munich, Munich, Germany
Dirk Wilhelm
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Carlos Amato .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or living animals performed by any of the authors.
Informed consent
This article does not contain patient data.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Amato, C., McCanne, L., Yang, C. et al. The hospital of the future: rethinking architectural design to enable new patient-centered treatment concepts. Int J CARS 17 , 1177–1187 (2022). https://doi.org/10.1007/s11548-021-02540-9
Download citation
Received : 06 July 2021
Accepted : 29 November 2021
Published : 15 December 2021
Issue Date : June 2022
DOI : https://doi.org/10.1007/s11548-021-02540-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered healthcare
- Hospital of the future
- Clinical workflow
- Find a journal
- Publish with us
- Track your research
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Download Free PDF
Sustainable Healthcare Architecture - Designing a Healing Environment

Healthcare facility design is a complex endeavor that forces function to follow both form and quality. Healthcare facilities serve a wide range of functions from medical applications (i.e. diagnostic, treatment, emergency rooms, clinics, etc.) to functional programs (i.e. food services, housekeeping, waiting rooms, meeting areas, office space, etc.). Designers of a healthcare facility are required to look at every aspect of human life. These facilities are spaces people live (temporally for treatment) and work in, where they are born and die. With modern medicine’s reliance on technology and demanding building programs, designers of modern hospitals may view healthcare architecture as incompatible with the principles of sustainable design. However, sustainability is not only a moral obligation for the healthcare field, it is beneficial to the patient and fosters a healing environment. Sustainable practices should be adopted for future constructions and renovations of healthcare facilities. These practices will not only save money during the lifespan of most healthcare facilities, they will also make spaces more effective for healing.
Related papers
International Journal of Sustainable Development and Planning
Technological progress has had negative effects as well as positive effects if it affects the life industry and the entire ecosystem significantly through the great consumption of natural resources, and here the construction sector in general and the health sector, in particular, have a role in this. From the perspective of keeping pace with technological development, responding to environmental changes, and paying attention to hospital environments (especially since the emergence of modern epidemics), and because the construction sector is the largest consumer of energy in the world, which made international organizations move towards creating a sustainable environment in the construction of hospital buildings by reducing energy consumption. This research focused on studying the components and principles of sustainable design for hospital buildings and the environmental, economic, health, and social benefits of sustainable development in the healthcare industry. In addition to the ...
Architectoni.ca, 2012
Sustainability is the important concepts in 20th century. Several definitions of sustainable development have been put forth, including the following common one: development that meets the needs of the present without compromising the ability of future generations to meet their own needs. Sustainability relies on high efficiency and the uninterrupted function of a continuing social, economic and ecological system in such a way that does not degrade and consume the resources used. Sustainable architecture is explained as a long term thought and action philosophy including the processes of building programming, usage, management throughout its economic life, destruction of the building or reuse. “The characteristics of sustainable design are its ability to integrate the life cycles of building systems with ecological systems in biosphere. The aim of this study is to reveal what design inputs can be driven in hospital buildings that differ in terms of design, application process and human environment relationships in use. When the continuously dense usage situations of hospitals are considered, the concept of “green hospital” is used to define the hospitals fulfilling at least one of the alternatives such as choosing environmental settlement design, buying nature friendly building materials and products, being environmentally sensitive during the construction of the hospital building and keeping this sensitivity going in service production process. Green hospital defines a facility which recycles, reuses the materials, reducing wastes and giving more clean air to the environment. This approach based on an environmentalist management understanding is seen under the headlines like management of waste and hazardous materials, water management, energy management and air emission regulating system and innovator environmental designs.
E3S Web of Conferences
The problems of necessity of sustainable and ecological approaches in architectural design of hospitals are raised in the research. The best international experience of designing and operating hospitals designed on the principles of sustainable development is considered. Examples and implementation examples of healthcare institutions integrating energy efficient technologies are analyzed and illustrated: natural ventilation, solar panels, rainwater collection, filtration and reuse of wastewater, greening of the roof and walls, sun protection, aerodynamic volumetric and spatial form. Studying and using the proven experience of the best examples of ecological hospital buildings, recognized and certified at the highest levels of the world institutions for the development of a sustainable future, will allow Ukraine to create the conditions for solving the crisis both in the sphere of health care and in the ecologically preserved environment of the country.
IAI INTERNATIONAL ACADEMIC INSTITUTE, 2019
Increasing environmental problems due to overpopulation, and the negative impacts of these problems on living creatures have brought sustainability forward. Nowadays, when energy consumption is intensified, the exhaustion of fossil fuels which are used as resources has encouraged developing countries to use renewable energy sources. Especially in buildings such as hospitals, energy consumption, and waste management have been given significance. Hospitals are not only those that heal patients with disease, but also those used by staff, attendants and medical students, and are intended to protect their current health. As hospital buildings are associated with hygiene and health, these structures must meet those expectations. Hospitals are institutions that reinforce their energy consumption by having high amounts of energy and continuous waste production. Because of the fact that hospital buildings provide service for 7 days and 24 hours, they consume a large amount of energy and produce both chemical and domestic waste. It is known that this situation harms the environment much more than expected. In addition to energy consumption, there are chemicals that adversely affect human health in unsustainable structures. These chemicals are found in interior materials and furnitures as well as in construction materials. The presence of such harmful chemicals in hospitals contrasts with the aims of such structures which aim to provide health services. Those problems had created the need for "green hospitals" which are taking advantage of renewable energy sources, using environmentally friendly construction materials, planning waste management and providing green environments. Green hospital design includes the use of daylight, proper artificial lighting, vernacular architecture forms and materials, natural and non-toxic materials, good indoor air quality and ergonomics. These structures made with an environmentalist approach contribute to the good management of energy consumption, while reducing the stress on the patients with the elements such as air conditioning and lighting-which has an effect on healing patients. At the same time, depending on the innovative design concept by the green hospital design, hospital staff and visitors feels more comfortable inside the structure. The aim of this study is to describe the green hospital concepts and investigate the effects of green hospital elements into interior space. Acquired information is going to be used in case studies such as; USA/Colorado's first Leed certified hospital called Boulder Community Foothills Hospital and VKV American Hospital which had gained importance with the leadership of green hospital building structure in Turkey. Examples are going to be compared due to green building systems and their reflection to interior space.
In hospital buildings wherever most, patients look for medical treatment and employees provides continuous support, making a healing atmosphere is primarily necessary and relevant. Healing suggests redressing ills and establishing a method that leads towards health. The term ‘Healing Architecture’ that has been coined recently, is employed to invoke a way of a nonstop process; It has been known for a protracted time that the natural atmosphere is closely connected with health and its close environmental conditions have an effect on human health. However, there's little proof to counsel that the physical aspects of designed atmosphere will have an effect on human health. These physical aspects of healing atmosphere serve for all users of the care facility: employees, clinicians, directors, patients and families. Existing studies have shown that in a very newer hospital atmosphere higher health outcome will be achieved once the physical aspects like access to outside read, patient...
The complexity of designing healthcare facilities functionally and psychologically is apparent. Apart from building services, various requirements of the Ministry of Health (MoH) are expected to be followed by healthcare designers. This paper outlines the role and importance of physical built environment in the design of hospitals as a means to create a healing environment. Lighting (day and artificial lighting) will be one of the focus areas to be examined in the study of healing architecture. At the outset, the existing conditions in 100 to 150 bedded hospital buildings in Malaysia will be reviewed and further investigation will be carried out with particular attention to the design and implementation of lighting and its relationship to other environmental factors. The paper concludes with the discussion on the influence of lighting in hospital design as one of the physical aspects in creating a healing environment. Conference theme: Daylighting and lighting
The article deals with important issues of the ecological approach to the health care facilities design within the general world's attention to the problem of sustainable development of the urban environment. Taking as the example the innovative foreign experience of implemented projects of medical institutions, as well as design, competitive and conceptual proposals revealed the latest idea of coexistence and harmonization of natural and man-made worlds within the medical environment that meets the challenges and needs of the XXI century. It is the concept of the hospital-park, that synthetically combines the architectural environment, natural environment, as well as man-made oasis and creates the basis for emergent results both in the medical field and in the need for a neat attitude to our planet. The article reveals the possibilities of designing a hospital-park of different stories and in different initial conditions: in a dense urban environment with a minimum size of the ...
Journal of environmental and natural studies :, 2024
Aşk ile Çalışan Yorulmaz, Ali Akyıldız Armağanı-II, 2024
Pontificia Universidad Católica del Perú, 2008
The Palgrave Encyclopedia of Imperialism and Anti-Imperialism, 2021
Bulletin archéologique des Écoles françaises à l'étranger, 2023
Anales del Seminario de Historia de la Filosofía, 2021
International Journal of Health Services, 2008
Anatolian Journal of Psychiatry, 2021
International Conference on Electrical and Electronics Engineering, 2009
Rishabh Sharma, 2024
Surface and Coatings Technology, 2009
Ambient Science, 2018
EAS journal of dentistry and oral medicine, 2024
Related topics
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

COMMENTS
The architectural design of healthcare institutions impacts patient experience and health outcomes. Facing challenges like demographic aging and evolving treatments, this study...
Here are 20 thesis topics related to healthcare architecture: ©Pinterest. 1. Children friendly healthcare design. Children’s hospitals have been one of the most challenging designs. As the hospital is the last place a child might want to go.
The extensive literature review conducted in this study illuminates the intrinsic relationship between architecture and healthcare, particularly underscoring architecture’s pivotal role in enhancing the quality of care and overall patient experience within healthcare institutions.
In this narrative review, we outline why the healthcare environment matters and describe areas of research focus and current built environment evidence that supports healthcare in general and stroke care in particular.
This thesis will largely serve to create a discursive space examining architecture and health, by privileging a nursing perspective, which is all too often absent from built environment narratives.
As a new paradigm in healthcare design in the 21st century, evidence-based design (EBD) has played a critical role in the changing hospital architectural design process and shaping new images of hospital architecture.
Objective: This study assesses how architectural design strategies impact the flexibility of hospitals to change over time. Background: Most hospitals are designed for highly specialized medical functions, which is often in conflict with the need to design the hospital facility to accommodate evolvement and change of functions over time.
By using this revised interpretation of interdisciplinary patient-centered care for our Patient Hub concept, we are able to improve patient and healthcare workers experience and satisfaction while maintaining the current standard of care.
Sustainable Healthcare Architecture - Designing a Healing Environment. Sara Bensalem. Healthcare facility design is a complex endeavor that forces function to follow both form and quality.
Architecture Research for Care and Health. This edition of HERD features a selection of six papers presented at ARCH19. Together with the keynotes, these papers give complementary per-spectives on how to activate and apply research-based knowledge into architectural practice.