- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
Critical Thinking in Medicine and Health
- First Online: 01 March 2020
Cite this chapter
- Louise Cummings 2
741 Accesses
1 Citations
This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations. Our cognitive resources are our only bulwark to the misinformation and faulty logic that exists in medicine and health. One resource in particular—reasoning—can counter the flawed thinking that pervades many medical and health issues. This chapter examines how concepts such as reasoning, logic and argument must be conceptualised somewhat differently (namely, in non-deductive terms) to accommodate the rationality of the informal fallacies. It also addresses the relevance of the informal fallacies to medicine and health and considers how these apparently defective arguments are a source of new analytical possibilities in both domains.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Albano, J. D., Ward, E., Jemal, A., Anderson, R., Cokkinides, V. E., Murray, T., et al. (2007). Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute, 99 (18), 1384–1394.
Article Google Scholar
Coxon, J., & Rees, J. (2015). Avoiding medical errors in general practice. Trends in Urology & Men’s Health, 6 (4), 13–17.
Google Scholar
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78 (8), 775–780.
Cummings, L. (2002). Reasoning under uncertainty: The role of two informal fallacies in an emerging scientific inquiry. Informal Logic, 22 (2), 113–136.
Cummings, L. (2004). Analogical reasoning as a tool of epidemiological investigation. Argumentation, 18 (4), 427–444.
Cummings, L. (2009). Emerging infectious diseases: Coping with uncertainty. Argumentation, 23 (2), 171–188.
Cummings, L. (2010). Rethinking the BSE crisis: A study of scientific reasoning under uncertainty . Dordrecht: Springer.
Book Google Scholar
Cummings, L. (2011). Considering risk assessment up close: The case of bovine spongiform encephalopathy. Health, Risk & Society, 13 (3), 255–275.
Cummings, L. (2012a). Scaring the public: Fear appeal arguments in public health reasoning. Informal Logic, 32 (1), 25–50.
Cummings, L. (2012b). The public health scientist as informal logician. International Journal of Public Health, 57 (3), 649–650.
Cummings, L. (2013a). Public health reasoning: Much more than deduction. Archives of Public Health, 71 (1), 25.
Cummings, L. (2013b). Circular reasoning in public health. Cogency, 5 (2), 35–76.
Cummings, L. (2014a). Informal fallacies as cognitive heuristics in public health reasoning. Informal Logic, 34 (1), 1–37.
Cummings, L. (2014b). The ‘trust’ heuristic: Arguments from authority in public health. Health Communication, 29 (10), 1043–1056.
Cummings, L. (2014c). Coping with uncertainty in public health: The use of heuristics. Public Health, 128 (4), 391–394.
Cummings, L. (2014d). Circles and analogies in public health reasoning. Inquiry, 29 (2), 35–59.
Cummings, L. (2014e). Analogical reasoning in public health. Journal of Argumentation in Context, 3 (2), 169–197.
Cummings, L. (2015). Reasoning and public health: New ways of coping with uncertainty . Cham, Switzerland: Springer.
Fowler, F. J., Jr., Levin, C. A., & Sepucha, K. R. (2011). Informing and involving patients to improve the quality of medical decisions. Health Affairs, 30 (4), 699–706.
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499.
Hamblin, C. L. (1970). Fallacies . London: Methuen.
Johnson, R. H. (2011). Informal logic and deductivism. Studies in Logic, 4 (1), 17–37.
Kahane, H. (1971). Logic and contemporary rhetoric: The use of reason in everyday life . Belmont, CA: Wadsworth Publishing Company.
Loucks, E. B., Buka, S. L., Rogers, M. L., Liu, T., Kawachi, I., Kubzansky, L. D., et al. (2012). Education and coronary heart disease risk associations may be affected by early life common prior causes: A propensity matching analysis. Annals of Epidemiology, 22 (4), 221–232.
Saposnik, G., Redelmeier, D., Ruff, C. C., & Tobler, P. N. (2016). Cognitive biases associated with medical decisions: A systematic review. BMC Medical Informatics and Decision Making, 16, 138. https://doi.org/10.1186/s12911-016-0377-1 .
Trowbridge, R. L. (2008). Twelve tips for teaching avoidance of diagnostic errors. Medical Teacher, 30, 496–500.
Walton, D. N. (1985a). Are circular arguments necessarily vicious? American Philosophical Quarterly, 22 (4), 263–274.
Walton, D. N. (1985b). Arguer’s Position . Westport, CT: Greenwood Press.
Walton, D. N. (1987). The ad hominem argument as an informal fallacy. Argumentation, 1 (3), 317–331.
Walton, D. N. (1991). Begging the question: Circular reasoning as a tactic of argumentation . New York: Greenwood Press.
Walton, D. N. (1992). Plausible argument in everyday conversation . Albany: SUNY Press.
Walton, D. N. (1996). Argumentation schemes for presumptive reasoning . Mahwah, NJ: Erlbaum.
Walton, D. N. (2010). Why fallacies appear to be better arguments than they are. Informal Logic, 30 (2), 159–184.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. Western Journal of Medicine, 172 (6), 390–393.
Woods, J. (1995). Appeal to force. In H. V. Hansen & R. C. Pinto (Eds.), Fallacies: Classical and contemporary readings (pp. 240–250). University Park: The Pennsylvania State University Press.
Woods, J. (2004). The death of argument: Fallacies in agent-based reasoning . Dordrecht: Kluwer Academic.
Woods, J. (2007). Lightening up on the ad hominem. Informal Logic, 27 (1), 109–134.
Woods, J. (2008). Begging the question is not a fallacy. In C. Dégremont, L. Keiff, & H. Rükert (Eds.), Dialogues, logics and other strange things: Essays in honour of Shahid Rahman (pp. 523–544). London: College Publications.
Download references
Author information
Authors and affiliations.
Department of English, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Louise Cummings
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Louise Cummings .
Chapter Summary
Medicine and health have tended to be overlooked in the critical thinking literature . And yet robust critical thinking skills are needed to evaluate the large number and range of health messages that we are exposed to on a daily basis.
An ability to think critically helps us to make better personal health choices and to uncover biases and errors in health messages and other information. An ability to think critically allows us to make informed decisions about medical treatments and is vital to efforts to reduce medical diagnostic errors.
A key element in critical thinking is the ability to distinguish strong or valid reasoning from weak or invalid reasoning. When an argument is weak or invalid, it is called a ‘fallacy’ or a ‘fallacious argument’.
The informal fallacies are so-called on account of the presence of epistemic and dialectical flaws that cannot be captured by formal logic . They have been discussed by many generations of philosophers and logicians , beginning with Aristotle .
Historically, philosophers and logicians have taken a pejorative view of the informal fallacies. Much of the criticism of these arguments is related to a latent deductivism in logic , the notion that arguments should be evaluated according to deductive standards of validity and soundness . Against deductive standards and norms, many reasonable arguments are judged to be fallacies.
Developments in logic , particularly the teaching of logic, forced a reconsideration of the prominence afforded to deductive logic in the evaluation of arguments. New criteria based on presumptive reasoning and plausible argument started to emerge. Against this backdrop, non-fallacious variants of most of the informal fallacies began to be described for the first time.
Today, some argument analysts characterize non-fallacious variants of the informal fallacies in terms of cognitive heuristics . During reasoning , these heuristics function as mental shortcuts, allowing us to bypass knowledge and come to judgement about complex health problems.
Suggestions for Further Reading
Sharples, J. M., Oxman, A. D., Mahtani, K. R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A., & Hoffmann, T. (2017). Critical thinking in healthcare and education. British Medical Journal, 357 : j2234. https://doi.org/10.1136/bmj.j2234 .
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. Its aim is to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health.
Hitchcock, D. (2017). On reasoning and argument: Essays in informal logic and on critical thinking . Cham: Switzerland: Springer.
This collection of essays provides more advanced reading on several of the topics addressed in this chapter, including the fallacies, informal logic , and the teaching of critical thinking . Chapter 25 considers if fallacies have a place in the teaching of critical thinking and reasoning skills.
Hansen, H. V., & Pinto, R. C. (Eds.). (1995). Fallacies: Classical and contemporary readings . University Park: The Pennsylvania State University Press.
This edited collection of 24 chapters contains historical selections on the fallacies, contemporary theory and criticism, and analyses of specific fallacies. It also examines fallacies and teaching. There are chapters on four of the fallacies that will be examined in this book: appeal to force; appeal to ignorance ; appeal to authority; and post hoc ergo propter hoc .
Diagnostic errors are a significant cause of death and serious injury in patients. Many of these errors are related to cognitive factors. Trowbridge ( 2008 ) has devised twelve tips to familiarize medical students and physician trainees with the cognitive underpinnings of diagnostic errors. One of these tips is to explicitly describe heuristics and how they affect clinical reasoning . These heuristics include the following:
Representativeness —a patient’s presentation is compared to a ‘typical’ case of specific diagnoses.
Availability —physicians arrive at a diagnosis based on what is easily accessible in their minds, rather than what is actually most probable.
Anchoring —physicians may settle on a diagnosis early in the diagnostic process and subsequently become ‘anchored’ in that diagnosis.
Confirmation bias —as a result of anchoring, physicians may discount information discordant with the original diagnosis and accept only that which supports the diagnosis.
Using the above information, identify any heuristics and biases that occur in the following scenarios:
Scenario 1: A 60-year-old man has epigastric pain and nausea. He is sitting forward clutching his abdomen. He has a history of several bouts of alcoholic pancreatitis. He states that he felt similar during these bouts to what he is currently feeling. The patient states that he has had no alcohol in many years. He has normal blood levels of pancreatic enzymes. He is given a diagnosis of acute pancreatitis. It is eventually discovered that he has had acute myocardial infarction.
Scenario 2: A 20-year-old, healthy man presents with sudden onset of severe, sharp chest pain and back pain. Based on these symptoms, he is suspected of having a dissecting thoracic aortic aneurysm. (In an aortic dissection, there is a separation of the layers within the wall of the aorta, the large blood vessel branching off the heart.) He is eventually diagnosed with pleuritis (inflammation of the pleura, the thin, transparent, two-layered membrane that covers the lungs).
Many of the logical terms that were introduced in this chapter also have non-logical uses in everyday language. Below are several examples of the use of these terms. For each example, indicate if the word in italics has a logical or a non - logical meaning or use:
University ‘safe spaces’ are a dangerous fallacy —they do not exist in the real world ( The Telegraph , 13 February 2017).
The MRI findings beg the question as to whether a careful ultrasound examination might have yielded some of the same information on haemorrhages ( British Medical Journal: Fetal & Neonatal , 2011).
The youth justice system is a slippery slope of failure ( The Sydney Morning Herald , 26 July 2016).
The EU countered with its own gastronomic analogy , saying that “cherry picking” the best bits of the EU would not be tolerated ( BBC News , 28 July 2017).
As Ebola spreads, so have several fallacies ( The New York Times , 23 October 2014).
Removing the statue of Confederacy Army General Robert E. Lee no more puts us on a slippery slope towards ousting far more nuanced figures from the public square than building the statue in the first place put us on a slippery slope toward, say, putting up statues of Hitler outside of Holocaust museums or of Ho Chi Minh at Vietnam War memorials ( Chicago Tribune , 16 August 2017).
We can expand the analogy a bit and think of a culture as something akin to a society’s immune system—it works best when it is exposed to as many foreign bodies as possible ( New Zealand Herald , 4 May 2010).
The Josh Norman Bowl begs the question : What’s an elite cornerback worth? ( The Washington Post , 17 December 2016).
The intuition behind these analogies is simple: As a homeowner, I generally have the right to exclude whoever I want from my property. I don’t even have to have a good justification for the exclusion. I can choose to bar you from my home for virtually any reason I want, or even just no reason at all. Similarly, a nation has the right to bar foreigners from its land for almost any reason it wants, or perhaps even no reason at all ( The Washington Post , 6 August 2017).
Legalising assisted suicide is a slippery slope toward widespread killing of the sick, Members of Parliament and peers were told yesterday ( Mail Online , 9 July 2014).
In the Special Topic ‘What’s in a name?’, an example of a question-begging argument from the author’s recent personal experience was used. How would you reconstruct the argument in this case to illustrate the presence of a fallacy?
On 9 July 2017, the effect of coconut oil on health was also discussed in an article in The Guardian entitled ‘Coconut oil: Are the health benefits a big fat lie?’ The following extract is taken from that article. (a) What type of reasoning is the author using in this extract? In your response, you should reconstruct the argument by presenting its premises and conclusion . Also, is this argument valid or fallacious in this particular context?
When it comes to superfoods, coconut oil presses all the buttons: it’s natural, it’s enticingly exotic, it’s surrounded by health claims and at up to £8 for a 500 ml pot at Tesco, it’s suitably pricey. But where this latest superfood differs from benign rivals such as blueberries, goji berries, kale and avocado is that a diet rich in coconut oil may actually be bad for us.
The article in The Guardian also makes extensive use of expert opinion. Two such opinions are shown below. (b) What three linguistic devices does the author use to confer expertise or authority on the individuals who advance these opinions?
Christine Williams, professor of human nutrition at the University of Reading, states: “There is very limited evidence of beneficial health effects of this oil”.
Tom Sanders, emeritus professor of nutrition and dietetics at King’s College London, says: “It is a poor source of vitamin E compared with other vegetable oils”.
The author of the article in The Guardian went on to summarize the findings of a study by two researchers that was published in the British Nutrition Foundation’s Nutrition Bulletin. The author’s summary included the following statement: There is no good evidence that coconut oil helps boost mental performance or prevent Alzheimer’s disease . (c) In what type of informal fallacy might this statement be a premise ?
Scenario 1: An anchoring error has occurred in which the patient is given a diagnosis of acute pancreatitis early in the diagnostic process. The clinician becomes anchored in this diagnosis, with the result that he overlooks two pieces of information that would have allowed this diagnosis to be disconfirmed—the fact that the patient has reported no alcohol use in many years and the presence of normal blood levels of pancreatic enzymes. By dismissing this information, the clinician is also showing a confirmation bias —he attends only to information that confirms his original diagnosis.
Scenario 2: A representativeness error has occurred. The patient’s presentation is typical of aortic dissection. However, this condition can be dismissed in favour of conditions like pleuritis or pneumothorax on account of the fact that aortic dissection is exceptionally rare in 20-year-olds.
(2) (a) non-logical; (b) non-logical; (c) non-logical; (d) non-logical; (e) non-logical; (f) logical; (g) logical; (h) non-logical; (i) logical; (j) logical
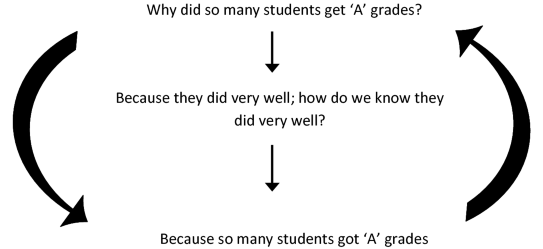
(3) The fallacy can be illustrated as follows. The head of department asks the question ‘Why did so many of these students get ‘A’ grades’? He receives the reply ‘Because they did very well’. But someone might reasonably ask ‘How do we know that they did very well?’ To which the reply is ‘Because so many students got ‘A’ grades’. The reasoning can be reconstructed in diagram form as follows:
The author is using an analogical argument , which has the following form:
P1: Blueberries, goji berries, kale, avocado and coconut oil are natural, exotic, pricey and surrounded by health claims.
P2: Blueberries, goji berries, kale and avocado have health benefits.
C: Coconut oil has health benefits.
This is a false analogy , or a fallacious analogical argument , because coconut oil does not share with these other superfoods the property or attribute < has health benefits >.
The author uses academic rank, field of specialization, and university affiliation to confer authority or expertise on individuals who advance expert opinions.
This statement could be a premise in an argument from ignorance .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cummings, L. (2020). Critical Thinking in Medicine and Health. In: Fallacies in Medicine and Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-28513-5_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-28513-5_1
Published : 01 March 2020
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-28512-8
Online ISBN : 978-3-030-28513-5
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Medical Student Guide For Critical Thinking

Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
To be more effective in their studies, students must think their way through abstract problems, work in teams and separate high quality from low quality information. These are the same qualities that today's medical students are supposed to possess regardless of whether they graduate in the UK or study medicine in Europe .
In both well-defined and ill-defined medical emergencies, doctors are expected to make competent decisions. Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more.
This article will explain why critical thinking is a must for people in the medical field.
Definition of Critical Thinking
You can find a variety of definitions of Critical Thinking (CT). It is a term that goes back to the Ancient Greek philosopher Socrates and his teaching practice and vision. Critical thinking and its meaning have changed over the years, but at its core always will be the pursuit of proper judgment.
We can agree on one thing. Critical thinkers question every idea, assumption, and possibility rather than accepting them at once.
The most basic definition of CT is provided by Beyer (1995):
"Critical thinking means making reasoned judgements."
In other words, it is the ability to think logically about what to do and/or believe. It also includes the ability to think critically and independently. CT is the process of identifying, analysing, and then making decisions about a particular topic, advice, opinion or challenge that we are facing.
Steps to critical thinking
There is no universal standard for becoming a critical thinker. It is more like a unique journey for each individual. But as a medical student, you have already so much going on in your academic and personal life. This is why we created a list with 6 steps that will help you develop the necessary skills for critical thinking.
1. Determine the issue or question
The first step is to answer the following questions:
- What is the problem?
- Why is it important?
- Why do we need to find a solution?
- Who is involved?
By answering them, you will define the situation and acquire a deeper understanding of the problem and of any factors that may impact it.
Only after you have a clear picture of the issue and people involved can you start to dive deeper into the problem and search for a solution.
2. Research
Nowadays, we are flooded with information. We have an unlimited source of knowledge – the Internet.
Before choosing which medical schools to apply to, most applicants researched their desired schools online. Some of the areas you might have researched include:
- If the degree is recognised worldwide
- Tuition fees
- Living costs
- Entry requirements
- Competition for entry
- Number of exams
- Programme style
Having done the research, you were able to make an informed decision about your medical future based on the gathered information. Our list may be a little different to yours but that's okay. You know what factors are most important and relevant to you as a person.
The process you followed when choosing which medical school to apply to also applies to step 2 of critical thinking. As a medical student and doctor, you will face situations when you have to compare different arguments and opinions about an issue. Independent research is the key to the right clinical decisions. Medical and dentistry students have to be especially careful when learning from online sources. You shouldn't believe everything you read and take it as the absolute truth. So, here is what you need to do when facing a medical/study argument:
- Gather relevant information from all available reputable sources
- Pay attention to the salient points
- Evaluate the quality of the information and the level of evidence (is it just an opinion, or is it based upon a clinical trial?)
Once you have all the information needed, you can start the process of analysing it. It’s helpful to write down the strong and weak points of the various recommendations and identify the most evidence-based approach.
Here is an example of a comparison between two online course platforms , which shows their respective strengths and weaknesses.
When recommendations or conclusions are contradictory, you will need to make a judgement call on which point of view has the strongest level of evidence to back it up. You should leave aside your feelings and analyse the problem from every angle possible. In the end, you should aim to make your decision based on the available evidence, not assumptions or bias.
4. Be careful about confirmation bias
It is in our nature to want to confirm our existing ideas rather than challenge them. You should try your best to strive for objectivity while evaluating information.
Often, you may find yourself reading articles that support your ideas, but why not broaden your horizons by learning about the other viewpoint?
By doing so, you will have the opportunity to get closer to the truth and may even find unexpected support and evidence for your conclusion.
Curiosity will keep you on the right path. However, if you find yourself searching for information or confirmation that aligns only with your opinion, then it’s important to take a step back. Take a short break, acknowledge your bias, clear your mind and start researching all over.
5. Synthesis
As we have already mentioned a couple of times, medical students are preoccupied with their studies. Therefore, you have to learn how to synthesise information. This is where you take information from multiple sources and bring the information together. Learning how to do this effectively will save you time and help you make better decisions faster.
You will have already located and evaluated your sources in the previous steps. You now have to organise the data into a logical argument that backs up your position on the problem under consideration.
6. Make a decision
Once you have gathered and evaluated all the available evidence, your last step is to make a logical and well-reasoned conclusion.
By following this process you will ensure that whatever decision you make can be backed up if challenged
Why is critical thinking so important for medical students?
The first and most important reason for mastering critical thinking is that it will help you to avoid medical and clinical errors during your studies and future medical career.
Another good reason is that you will be able to identify better alternative options for diagnoses and treatments. You will be able to find the best solution for the patient as a whole which may be different to generic advice specific to the disease.
Furthermore, thinking critically as a medical student will boost your confidence and improve your knowledge and understanding of subjects.
In conclusion, critical thinking is a skill that can be learned and improved. It will encourage you to be the best version of yourself and teach you to take responsibility for your actions.
Critical thinking has become an essential for future health care professionals and you will find it an invaluable skill throughout your career.
We’ll keep you updated

Science-Based Medicine
Exploring issues and controversies in the relationship between science and medicine

Critical Thinking in Medicine
Cognitive Errors and Diagnostic Mistakes is a superb new guide to critical thinking in medicine written by Jonathan Howard. It explains how our psychological foibles regularly bias and betray us, leading to diagnostic mistakes. Learning critical thinking skills is essential but difficult. Every known cognitive error is illustrated with memorable patient stories.
Rodin’s Thinker is doing his best to think but if he hasn’t learned critical thinking skills, he is likely to make mistakes. The human brain is prone to a multitude of cognitive errors.
Critical thinking in medicine is what the Science-Based Medicine ( SBM ) blog is all about. Jonathan Howard has written a superb book, Cognitive Errors and Diagnostic Mistakes: A Case-Based Guide to Critical Thinking in Medicine , that epitomizes the message of SBM . In fact, in the Acknowledgements, he credits the entire team at SBM for teaching him “an enormous amount about skepticism and critical thinking”, and he specifically thanks Steven Novella, Harriet Hall (moi!), and David Gorski.
Dr. Howard is a neurologist and psychiatrist at NYU and Bellevue Hospital. The book is a passionate defense of science and a devastating critique of Complementary and Alternative Medicine ( CAM ) and pseudoscience. Its case-based approach is a stroke of genius. We humans are story-tellers; we are far more impressed by stories than by studies or by textbook definitions of a disease. Dr. Howard points out that “Anecdotes are part of the very cognition that allows us to derive meaning from experience and turn noise into signal.” They are incredibly powerful from an emotional standpoint. That’s why he chose to begin every discussion of a cognitive error with a patient’s case, an anecdote.
CAM knows how effective this can be; that’s why it relies so heavily on anecdotes. When doctors think of a disease, they are likely to think of a memorable patient they treated with that disease, and that patient’s case is likely to bias their thinking about other patients with the same disease. If there is a bad outcome with a treatment, they will remember that and may reject that treatment for the next patient even if it is the most appropriate one. Dr. Howard uses patient stories to great advantage, first providing the bare facts of the case and then letting the patient’s doctors explain their thought processes so we can understand exactly where and why they went wrong. Then he goes on to explain the psychology behind the cognitive error, with study findings, other examples, and plentiful references. If readers remember these cases, they might avoid similar mishaps.
An encyclopedia of cognitive errors
The book is encyclopedic, running to 30 chapters and 588 pages. I can’t think of anything he failed to mention, and whenever an example or a quotation occurred to me, he had thought of it first and included it in the text. I couldn’t begin to list all the cognitive errors he covers, but they fall roughly into these six categories:
- Errors of overattachment to a particular diagnosis
- Errors due to failure to consider alternative diagnoses.
- Errors due to inheriting someone else’s thinking.
- Errors in prevalence perception or estimation.
- Errors involving patient characteristics or presentation context.
- Errors associated with physician affect, personality, or decision style.
A smattering of examples
There is so much information and wisdom in this book! I’ll try to whet your appetite with a few excerpts that particularly struck me.
- Discussing an issue with others who disagree can help us avoid confirmation bias and groupthink.
- Negative panic: when a group of people witness an emergency and fail to respond, thinking someone else will.
- Reactance bias: doctors who object to conventional practices and want to feel independent may reject science and embrace pseudoscience.
- Cyberchondria: using the Internet to interpret mundane symptoms as dire diagnoses.
- Motivated reasoning: People who “know” they have chronic Lyme disease will fail to believe 10 negative Lyme tests in a row and then believe the 11 th test if it is positive.
- The backfire effect: “encountering contradictory information can have the paradoxical effect of strengthening our initial belief rather than causing us to question it.”
- Biases are easy to see in others but nearly impossible to detect in oneself.
- Checklists for fake diseases take advantage of the Forer effect . As with horoscopes and cold readings, vague, nonspecific statements convince people that a specific truth about them is being revealed. Fake diseases are unfalsifiable: there is no way to rule them out.
- When presenting risk/benefit data to patients, don’t present risk data first; it will act as an “anchor” to make them fixate on risk.
- The doctor’s opinion of the patient will affect the quality of care.
- Randomness is difficult to grasp. The hot hand and the gambler’s fallacy can both fool doctors. If the last two patients had disease X and this patient has similar symptoms, the doctor will think he probably has disease X too. Or if the doctor has just seen two cases of a rare disease, it will seem unlikely that the next patient with similar symptoms will have it too.
- Apophenia : the tendency to perceive meaningful patterns with random information, like seeing the face on Mars.
- Information bias: doctors tend to think the more information, the better. But tests are indicated only if they will help establish a diagnosis or alter management. They should not be ordered out of curiosity or to make the clinician feel better. Sometimes doctors don’t know what to do with the information from a test. This should be a lesson for doctors who practice so-called functional medicine : they order all kinds of nonstandard tests whose questionable results give no evidence-based guidance for treating the patient. Doctors should ask “How will this test alter my management?” and if they can’t answer, they shouldn’t order the test.
- Once a treatment is started, it can be exceedingly difficult to stop. A study showed that 58% of medications could be stopped in elderly patients and only 2% had to be re-started.
- Doctors feel obligated to “do something” for the patient, but sometimes the best course is to do nothing. “Just don’t do something, stand there.” At the end of their own life, 90% of doctors would refuse the treatments they routinely give to patients with terminal illnesses.
- Incidentalomas: when a test reveals an unsuspected finding, it’s important to remember that abnormality doesn’t necessarily mean pathology or require treatment.
- Fear of possible unknown long-term consequences may lead doctors to reject a treatment, but that should be weighed carefully against the well-known consequences of the disease itself.
- It’s good for doctors to inform patients and let them participate in decisions, but too much information can overwhelm patients. He gives the example of a patient with multiple sclerosis whose doctor describes the effectiveness and risks of 8 injectables, 3 pills, and 4 infusions. The patient can’t choose; she misses the follow-up appointment and returns a year later with visual loss that might have been prevented.
- Most patients don’t benefit from drugs; the NNT tells us the Number of patients who will Need to be Treated for one person to benefit.
- Overconfidence bias: in the Dunning-Kruger effect, people think they know more than the experts about things like climate change, vaccines and evolution. Yet somehow these same people never question that experts know how to predict eclipses.
- Patient satisfaction does not measure effectiveness of treatment. A study showed that the most satisfied patients were 12% more likely to be admitted to the hospital, had 9% higher prescription costs, and were 26% more likely to die.
- The availability heuristic and the frequency illusion: “Clinicians should be aware that their experience is distorted by recent or memorable [cases], the experiences of their colleagues, and the news.” He repeats Mark Crislip’s aphorism that the three most dangerous words in medicine are “in my experience”.
- Illusory truth: people are likely to believe a statement simply because they have heard it many times.
- What makes an effective screening test? He covers concepts like lead time bias, length bias, and selection bias. Screening tests may do more harm than good. The PSA test is hardly better than a coin toss.
- Blind spot bias: Everyone has blind spots; we recognize them in others but can’t see our own. Most doctors believe they won’t be influenced by gifts from drug companies, but they believe others are unconsciously biased by such gifts. Books like this can make things worse: they give us false confidence. “Being inclined to think that you can avoid a bias because you [are] aware of it is a bias in itself.”
- He quotes from Contrived Platitudes: “Everything happens for a reason except when it doesn’t. But even then you can in hindsight fabricate a reason that will satisfy your belief system.” This is the essence of what CAM does, especially the versions that attribute all diseases to a single cause.
Some juicy quotes
Knowledge of bias should contribute to your humility, not your confidence.
Only by studying treatments in large, randomized, blinded, controlled trials can the efficacy of a treatment truly be measured.
When beliefs are based in emotion, facts alone stand little chance.
CAM , when not outright fraudulent, is nothing more than the triumph of cognitive biases over rationality and science.
Reason evolved primarily to win arguments, not to solve problems.
He includes a thorough discussion of the pros and cons of limiting doctors’ work hours, with factors most people have never considered, and a thorough discussion of financial motivations.
The book is profusely illustrated with pictures, diagrams, posters, and images from the Internet like “The Red Flags of Quackery” from sci-ence.org. Many famous quotations are presented with pictures of the person quoted, like Christopher Hitchens and his “What can be asserted without evidence can be dismissed without evidence”.
He never goes beyond the evidence. Rather than just giving study results, he tells the reader when other researchers have failed to replicate the findings.
We rely on scientific evidence, but researchers are not immune from bias. He describes the many ways research can go astray: 235 biases have been identified that can lead to erroneous results. As Ioannidis said, most published research findings are wrong. But all is not lost: people who understand statistics and the methodologies of science can usually distinguish a good study from a bad one.
He tells the infamous N-ray story. He covers the file drawer effect, publication bias, conflicts of interest, predatory journals, ghostwriting, citation plagiarism, retractions, measuring poor surrogates instead of meaningful clinical outcomes, and outright fraud. Andrew Wakefield features prominently. Dr. Howard’s discussions of p-hacking, multiple variables, random chance, and effect size are particularly valuable. HARKing is Hypothesizing After the Results are Known. It can be exploited to create erroneous results.
He tells a funny story that was new to me. Two scientists wrote a paper consisting entirely of the repeated sentence “Get me off your fucking mailing list” complete with diagrams of that sentence. It was rated as excellent and was accepted for publication!
Conclusion: Well worth reading for doctors and for everyone else
As the book explains, “The brain is a self-affirming spin-doctor with a bottomless bag of tricks…” Our brains are “pattern-seeking machines that fill in the gaps in our perception and knowledge consistent with our expectations, beliefs, and wishes”. This book is a textbook explaining our cognitive errors. Its theme is medicine but the same errors occur everywhere. We all need to understand our psychological foibles in order to think clearly about every aspect of our lives and to make the best decisions. Every doctor would benefit from reading this book, and I wish it could be required reading in medical schools. I wish everyone who considers trying CAM would read it first. I wish patients would ask doctors to explain why they ordered a test.
The book is not inexpensive. The price on Amazon is $56.99 for both softcover and Kindle versions. But it might be a good investment: you might save much more money that that by applying the principles it teaches, and critical thinking skills might even save your life. Well-written, important, timely, easy, and entertaining to read, lots of illustrations, packed with good stuff. Highly recommended.
View all posts
- Posted in: Book & movie reviews , Critical Thinking , Neuroscience/Mental Health , Science and Medicine
- Tagged in: bias , CAM , cognitive errors , diagnostic mistakes , Jonathan Howard
Posted by Harriet Hall
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
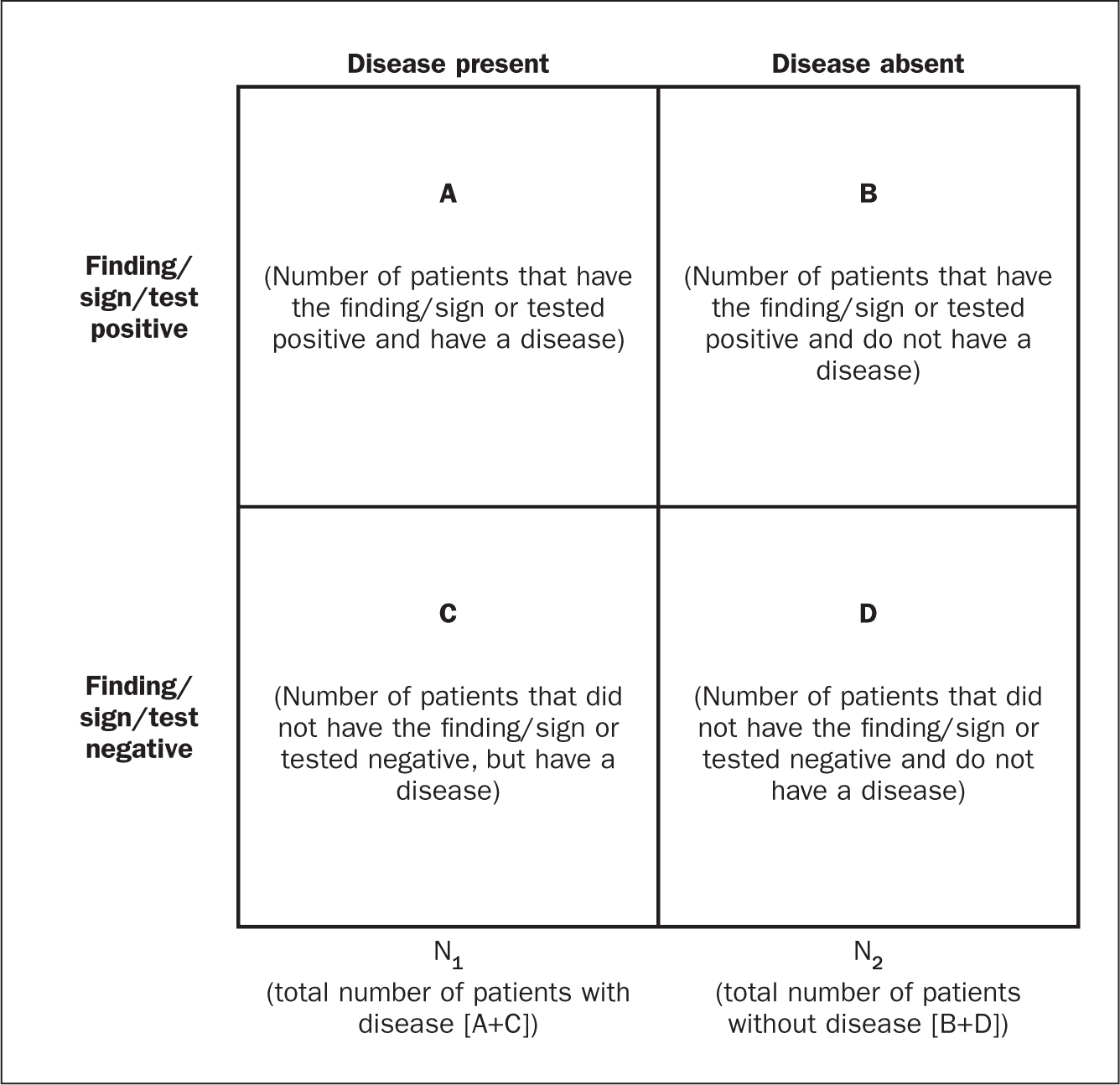
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?
- Educational advances in emergency medicine
- Open access
- Published: 16 April 2020
How to think like an emergency care provider: a conceptual mental model for decision making in emergency care
- Nasser Hammad Al-Azri 1
International Journal of Emergency Medicine volume 13 , Article number: 17 ( 2020 ) Cite this article
13k Accesses
14 Citations
11 Altmetric
Metrics details
General medicine commonly adopts a strategy based on the analytic approach utilizing the hypothetico-deductive method. Medical emergency care and education have been following similarly the same approach. However, the unique milieu and task complexity in emergency care settings pose a challenge to the analytic approach, particularly when confronted with a critically ill patient who requires immediate action. Despite having discussions in the literature addressing the unique characteristics of medical emergency care settings, there has been hardly any alternative structured mental model proposed to overcome those challenges.
This paper attempts to address a conceptual mental model for emergency care that combines both analytic as well as non-analytic methods in decision making.
The proposed model is organized in an alphabetical mnemonic, A–H. The proposed model includes eight steps for approaching emergency cases, viz., awareness, basic supportive measures, control of potential threats, diagnostics, emergency care, follow-up, groups of particular interest, and highlights. These steps might be utilized to organize and prioritize the management of emergency patients.
Metacognition is very important to develop practicable mental models in practice. The proposed model is flexible and takes into consideration the dynamicity of emergency cases. It also combines both analytic and non-analytic skills in medical education and practice.
Combining various clinical reasoning provides better opportunity, particularly for trainees and novices, to develop their experience and learn new skills. This mental model could be also of help for seasoned practitioners in their teaching, audits, and review of emergency cases.
“It is one thing to practice medicine in an emergency department; it is quite another to practice emergency medicine. The effective practice of emergency medicine requires an approach, a way of thinking that differs from other medical specialties” [ 1 ]. Yet, common teaching trains future emergency practitioners to “practice medicine in an emergency department.”
Emergency care is a complex activity. Emergency practitioners are like circus performers who have to “spin stacks of plates, one on top of another, of all different shapes and weights” [ 2 ]. This can be further complicated by simultaneous demands from various and multiple stakeholders such as administrators, patients, and colleagues. Add to that the time-bound interventions and parallel tasks required and it can be thought of no less than being chaotic.
There is a tendency to distinguish emergency care from other medical practices as being more action-driven than thought-oriented [ 3 ]. This probably stems from the presumption that emergency medicine follows the same strategy as other medical disciplines so it is judged within the same parameters. Another explanation for this is that emergency practitioners are seen to act immediately on their patients when other medical specialties might take longer time preparing for this action. However, the chaotic environment is different and it requires complex decision-making skills and strategies. Unlike general medical settings, in EM, often a history is unobtainable, and a physical examination and medical investigations are not readily available in a critically ill patient. Despite this, emergency medicine is still being taught using the conceptual model of general medicine that follows an information-gathering approach seeking optimal decision-making. In medical decision-making, the commonly adopted hypothetico-deductive method involving history taking, physical examination, and investigations corresponds to the general approach of medicine.
Importance of rethinking existing medical emergency care mental model
Education in medical emergency care adopts a strategy similar to that of general medicine despite the fact that it is not optimal in emergency departments. Emergency care providers cannot anticipate what condition their patients will be in and they cannot follow the steps of detailed history taking, complete physical examination, ordering required investigations, and, using the results, plan the management of their patient. Classical clinical decision theory may not fit dynamic environments like emergency care. Patients in the emergency department are usually critical, time is limited, and information is scarce or even absent, and decisions are still urgently required.
Croskerry (2002) has noted: “In few other workplace settings, and in no other area of medicine, is decision density as high” [ 4 ] as in emergency medicine. In an area where an information gap can be found in one third of emergency department visits, and more so in critical cases [ 5 ], an information-seeking strategy is unlikely to succeed. Moreover, diagnostic closure is usually the short-term target in the hypothetico-deductive method while this is less of a concern in emergency care. Instead, the short-term priorities in emergency care include assessment of acuity and life-saving [ 6 ]. Figure 1 presents a comparison of the conventional general medicine decision-making approach and how emergency care setting differs relatively with regard to those basic characteristics.
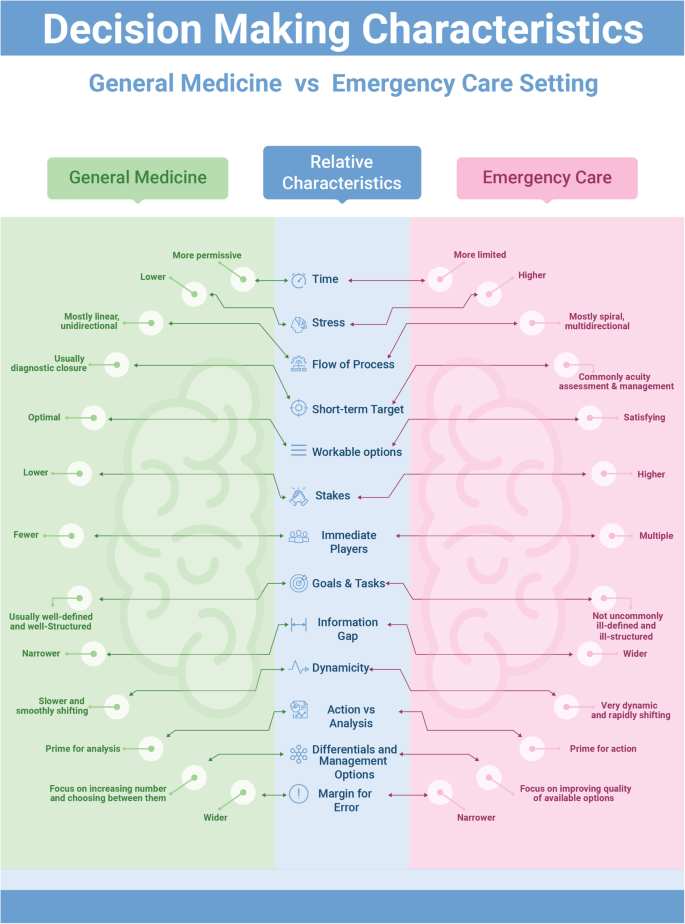
Comparing conventional decision-making in general medicine vs. emergency care setting
Hence, a different mental model with a distinctive approach for emergency care is required. Mental models are important to describe, explain, and predict situations [ 7 ]. This is the roadmap through the wilderness of emergency care rather than a guide on driving techniques. Experts are differentiated from novices in several aspects: sorting and categorizing problems, using different reasoning processes, developing mental models, and organizing content knowledge better [ 8 ]. In addition, experienced physicians form more rapid, higher quality working hypotheses and plans of management than novices do. Novices are especially challenged in this area, since teaching general problem solving was replaced with problem-based learning, as the emphasis shifted toward “helping students acquire a functional organization of content with clinically usable schemas” [ 9 ]. The proposed model is intended to better organize the knowledge and approach required in emergency care, which may eventually help improve the practice, particularly of novices.
Clinical decision-making in emergency care requires a unique approach that is sensitive to the distinctive milieu where emergency care takes place [ 10 ]. Xiao et al. (1996) have identified four components of task complexity in emergency medical care [ 11 ]. These include multiple and concurrent tasks, uncertainty, changing plans of management, and compressed work procedures with high workload. Such complex components require an approach that accommodates such factors and balances the various needs in a timely and priority-based, situationally adaptable methodology.
A different model for emergency care
This article addresses a general mental approach involving eight steps arranged with an initialism mnemonic, A–H. Figure 2 presents an infographic of the lifecycle of this A–H decision-making process. These steps represent the lifecycle of decision-making in emergency practice and form the core of the proposed conceptual model. Every emergency care encounter starts with the first step of situational awareness (A) where the provider starts to build up a workable mental template of the case presentation. This process is ongoing throughout the encounter to reflect the dynamic nature of emergency cases. The second to fourth steps (B–D) involve a triaging process in order to prioritize the most appropriate management at that point in time, through a series of risk-stratification stages. Then, additional emergency management (E) follows based on the flow of the case from earlier steps. Following emergency management, a planning step regarding further care (F) for the patient is required. The following step concerns emergency patients who may represent special high risk groups (G) with special precautions and particular diagnostic and management approaches to be considered. This step is, in fact, a mandate throughout the process but included here as a reminder. The final step is a reflection of the entire process that highlights (H) the learning aspects from the case management. Throughout the process, the first and last steps are ongoing as they reflect the dynamicity of the situation.
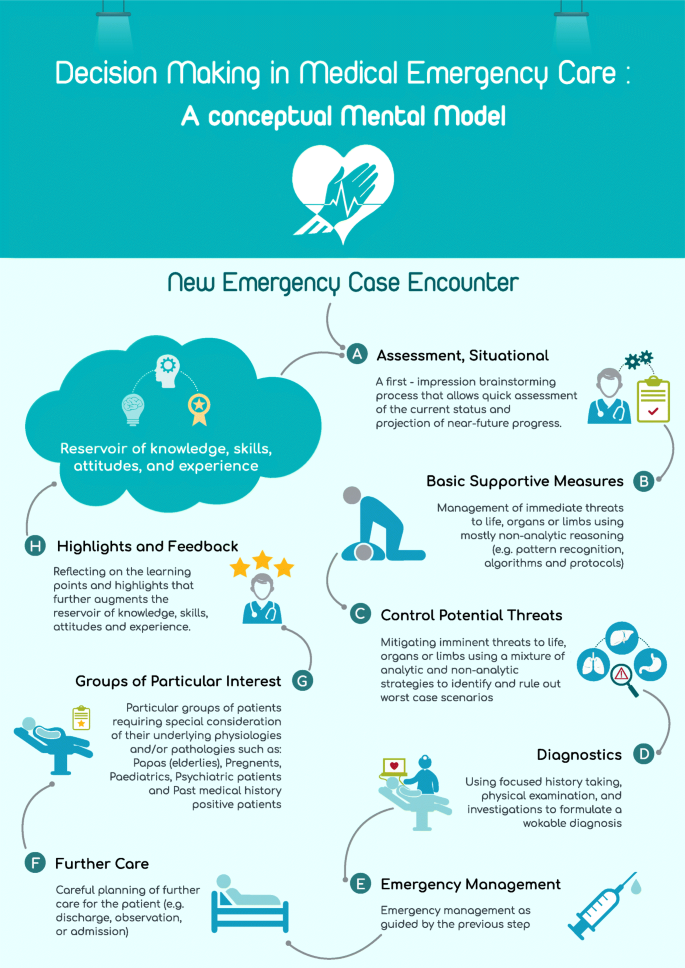
Situational decision-making model lifecycle
A: (awareness, situational)
It is likely that the first thought of an emergency care provider, when confronted with an acutely ill patient, is the issue of time: “how much time do I have to act and how much time do I have to think?” [ 12 ]. The mental brainstorming that takes place in a matter of seconds is a very valuable and indispensable part of every single emergency encounter. Providers’ prior beliefs, expectations, emotions, knowledge, skills, and experience all contribute to the initial approach adopted. Individuals vary in the importance they attach to different factors [ 13 ], and this variation is reflected in the decisions they make. The importance of this mental process is, unfortunately, not reflected in either general medicine or emergency medicine education and research. Traditionally, “medical education has focused on the content rather than the process of clinical decision making” [ 6 ].
The notion of “situational awareness” (SA) is a useful concept to borrow from aviation sciences. Situational awareness has been defined as the individual’s “perception of the elements of the environment within a volume of time and space, the comprehension of their meaning and the projection of their status in the near future” [ 14 ]. As noted from the definition, SA tries to amalgamate the experiences and background of the practitioner with the current situation in order to enable a more educated prediction of what will happen next. Although the concept originated outside of the medical field, it has already been utilized in several medical disciplines including surgery, anesthesiology, as well as quality care, and patient safety [ 15 , 16 , 17 ]. Moreover, SA has been discussed in several emergency care mandates and it is recommended for inclusion in the non-technical skills training of teams in acute medicine [ 15 ].
This emphasizes that an attentiveness to the dynamic nature of priorities in emergency management is as important as knowledge and skills. As such, SA provides a mental model that encourages emergency care practitioners to stay alert for changes in the surrounding environment and relate those changes to case management. The importance of this step in the model is that it prods us to go beyond our immediate perceptions and gut feelings and develop an overall view of the situation [ 18 ]. Practically, decision-making in emergency care has historically depended more on rapid situational assessment rather than optimal decision-making strategies as in the hypothetico-deductive method [ 19 ]. SA is probably one of the most neglected, yet distinguishing, skills in emergency medicine education.
B: (basic life, organ, and limb supportive measures)
The second step in emergency decision-making involves a clinical triaging process. The purpose of this triage is to prioritize time-bound interventions or treatment for the patient. Immediate risks to life, organs, or limbs take priority in case management. This precedes any analytical thinking provided by detailed history taking, physical examination, or investigations, even though a focused approach might be necessary. This step maintains the dynamicity of the process of decision-making and allows the practitioner a holistic view of available and appropriate options rather than ordinary linear thinking. It also provides flexibility of movement between treatment options in response to dynamic changes in the condition.
Life-threatening conditions always take precedence in emergency management. The next priority is to manage immediate risks to body organs or limbs; this is the essence of medical emergency management. Therefore, the aim of this step on basic supportive action (B) is to save the vitals of the patient. This is where advanced cardiac and trauma life support algorithms and emergency management protocols are important.
A useful approach at this step is pattern recognition. In real practice, when confronted with a critically ill or crashing patient, the emergency care provider usually abandons the time-consuming hypothetico-deductive method; pattern recognition offers a rapid assessment and clinical plan that permits immediate life-, organ-, or limb-saving measures to take place [ 20 ]. Pattern recognition, known also as non-analytic reasoning, is a central feature of the expert medical practitioner’s ability to rapidly diagnose and respond appropriately, compared to novices who struggle with linear thinking skills [ 21 , 22 , 23 ]. This approach could be further augmented by the availability of algorithms and protocols that allow immediacy of perception and initiation of management [ 4 ], as well as by including it in clinical teaching and education.
C: (control potential life, organ, and limb threats)
While emergency care providers must prioritize immediate threats to life, organs, and limbs, they must also anticipate and recognize imminent threats to the same and control them (C). This is one of the biggest challenges in emergency care compared to other medical settings; oftentimes, the grey cases are the hidden tigers. In fact, seasoned emergency care providers know that even the most unremarkable patients may have a catastrophic outcome within moments [ 24 ]. Emergency care providers usually adopt mental templates for the top diagnoses that they need to exclude for every particular presentation. This is a step of “ruling out” worst diagnoses before proceeding. Croskerry (2002) asserts that this “rule out the worst case” strategy is almost pathognomonic of decision-making in the emergency department [ 4 ]. Many emergency presentations (e.g., poisoning, head injury, and chest pain) are true time bombs that any emergency care provider should be alert to.
This step presents an intermediate stage between the previous step (B) where pattern recognition and non-analytic reasoning dominates decision-making, and the next step (D) where the hypothetico-deductive approach with its analytic reasoning starts to play a major role in decision-making. As such, this step utilizes a mixture of the analytic and non-analytic reasoning to aid emergency care practitioners the “rule out the worst case” scenario in their patients. Examples of presentation-wise “worst case” scenarios are illustrated in Table 1 .
Once a potential threat is discovered, the practitioner will be situationally more aware and this will help to initiate measures that could prevent further deterioration of the condition. Again, this step is another that is practiced commonly by expert practitioners but is presented informally or insufficiently in emergency medicine training or education. Emergency care practitioners should focus more on this step due to its centrality in emergency care practice as well as its importance for ensuring safety of patients.
D: (diagnostics)
Once immediate and/ or imminent threats have either been excluded or managed, the emergency care provider may move on to the next step of formulating a workable clinical diagnosis (D) through the commonly adopted hypothetico-deductive medical model via a focused history taking, physical examination, and investigations. This is basically what all medical students are trained for in their undergraduate and postgraduate medical education. This step involves the utilization of existing tools for optimal decision-making within the available resources in the emergency department. Nevertheless, a final diagnosis may not be reachable in the emergency department setting.
E: (emergency management)
This is the step that naturally follows the diagnostic step (D). After collecting appropriate information regarding patient presentation through a focused history, examination and investigations, the emergency care provider may start emergency management and treatment as indicated. This does not contradict utilizing appropriate interventions in earlier steps (B, C) that aim to save life, organs, or limbs.
F: (further care)
While decisions about intervention(s) in emergency care are very difficult, often decisions about the further management of the patient are just as difficult [ 25 ]. Grey cases present the dilemma of whether to admit, keep for observation, or discharge. This decision is problematic because it entails not only technical aspects of the clinical status of the patient but also social, political, economic, and administrative factors along with the availability of supportive resources.
The initial brainstorm regarding imminent threats to life, organs, and limbs (C) continues to play a major role in the emergency provider’s decision-making. Discharging patients to their home carries risks related to a lack of clinical care and formal monitoring compared to admitted patients [ 26 ]. Hence, this step is pivotal in the emergency care of patients with significant implications in terms of outcome. Incorporating this step in the model is essential for the emergency care provider to have an integrative and holistic view of the case.
G: (groups of particular interest)
Certain groups of patients warrant particular concern while being managed in emergency care settings [ 27 ]. There are different reasons to consider these groups as high risk. Often, it is because they have underlying pathologies and/or physiologies that make them more prone for complications, acute exacerbations, and/or they are less likely to withstand the stress of acute illness. These groups include the elderly, pregnant women, children, psychiatric patients, and patients with a significant past medical history. These patients should cause particular concern that may justify a different and/or altered path of management at any step during the emergency care process.
H: (highlights)
Lack of informative feedback is one of the major drawbacks in emergency medicine that hinders learning and maintaining of cognitive and practical emergency care skills [ 28 ]. Feedback and highlighting of learning points is a crucial step in medical education and can be done in a variety of methods [ 29 ]. This is an ongoing step that starts at the case encounter and never ends during a practitioner’s career. Here, the practitioner reflects on the care and management provided during the encounter and makes a case for learning and advancing his knowledge, skills, and attitudes in emergency care. This step is usually done unconsciously. However, exposing this process to scrutiny and making it a formal step in the process of emergency care is likely to enhance experiential learning of the provider and, more importantly, offer feedback for the first step in the model that further augments situational awareness (A). This will add to the reservoir of understanding and attentiveness for future cases.
Thinking about thinking, also called metacognition, in emergency care is likely to reveal the strengths and weaknesses in current approaches and open doors for further development and improvement of emergency care. It is also likely to aid in recognizing opportunities for interventional thinking strategies [ 18 ]. This could be a step forward in preparing a broad-based, critical thinking pattern for physicians, who may save lives, organs, and limbs based on undifferentiated cases without having to depend on a diagnosis to do so.
The presented conceptual model attempts to contribute to the exposition and development of the forgotten skill of clinical reasoning with a particular reference to emergency and acute care. Moreover, it dissects the usually overlooked process of decision-making in emergency care [ 28 ]. The arrangement of the model components in alphabetical mnemonics may act as a reminder of a decision process that will reduce omission errors in clinical settings. Furthermore, functional categorization of the steps involved in decision-making, as well as in actual practice, will provide and develop further insight and awareness of cognitive strengths and weaknesses at different stages.
A significant advantage of the proposed conceptual mental model for emergency care is that it combines both analytic as well as non-analytic (also called naturalistic decision-making, NDM) strategies to aid medical emergency management. This model does not eliminate the need for the hypothetico-deductive analytic method but rather incorporates it within a more comprehensive approach and utilizes it when it is situationally appropriate along with the non-analytic method (Fig. 3 ). Combining different clinical reasoning strategies helps novice practitioners have greater diagnostic accuracy, improve performance, and avoid giving misleading information [ 30 , 31 ].

Situationally combined analytical and non-analytical decision-making methods
In addition, emergency care has been described as chaotic. Chaotic contexts are characterized by dominance of the unknowables, indeterminate relationships between the cause and effect, and a lack of existing manageable patterns [ 32 ]. In such contexts, the best approach to management is to act to establish order, then sense where stability is present and where it is not, and then respond to transform the situation from chaos to complexity [ 32 ]. The described model addresses those activities in order where the emergency care provider first acts (B), then senses (C), and finally responds (D, E) to establish a more stable context.
The suggested approach can be utilized by various groups of practitioners, such as physicians, nurses, and paramedics, hence the use of the term emergency care. Moreover, novices and trainees learn better by being exposed to the decision-making process involved, rather than just mimicking the actions of experts [ 3 ].
Medical education is required to produce a “broad-based physician, geared to solving undifferentiated clinical problems” [ 33 ]. Emergency medicine, as a generalist discipline, has probably high potential for that. The presented model could be used in several contexts. It could be used as a mental model that guides the practice of emergency care for novice practitioners or it could be used as a teaching tool for medical students and trainees, in not only emergency care, but also other specialties that may have exposure to emergency cases. In addition to novice providers, it has implications for physicians in emergency departments, paramedics in emergency medical services, general practitioners in rural clinics, nurse practitioners, or anyone else practicing emergency care. This may lead to the development of training and educational methods that suit each stage separately, as well as recognizing cognitive biases and avoiding them.
The model may also be used for audits and reviews of emergency case management, including self-audits, departmental or institutional audits, or peer reviews. Moreover, clinical decision-making aids could be further developed and tailored to the needs of the practice. For example, algorithms and pattern recognition are suitable for steps B and C teaching and decision-making, while event-driven and hypothetico-deductive approaches are more suitable for step D. This model is very broad-based. It is hoped that this conceptual model will help practitioners develop a more focused approach, a broader perspective, and a better ability to detect critical signals when managing undifferentiated emergency cases.
Availability of data and materials
Wears RL. Introduction: the approach to the emergency department patient. In: Wolfson AB, Hendey GW, Hendry PL, et. al. (eds). Harwood-Nuss’ Clinical Practice of Emergency Medicine. 4th edition. Lippincott Williams & Wilkins. 2005.
Groopman J. How doctors think. Boston: Houghton Mifflin Company; 2007.
Google Scholar
Geary U, Kennedy U. Clinical decision making in emergency medicine. Emergencias. 2010;22:56–60.
Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184–204.
Article Google Scholar
Stiell A, Forster AJ, Stiell IG, et al. Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ. 2003;169(10):1023–8.
PubMed PubMed Central Google Scholar
Kovacs G, Croskerry P. Clinical decision making: an emergency medicine perspective. Acad Emergency Med. 1999;6(9):947–52.
Article CAS Google Scholar
Burns K. Mental models and normal errors. In: Montgomery H, Lipshitz R, Brehmer B, editors. How Professionals Make Decisions. New Jersey: Lawrence Erlbaum Associates; 2005.
Gambrill E. Critical Thinking in clinical practice: improving the quality of judgments and decisions. 2nd ed. New Jersey: Wiley & Sons; 2005.
Elstein AS, Schwarz A. Clinical problem solving and diagnostic decision making: selective review of the cognitive literature. BMJ. 2002;324:729–32.
Croskerry P. Critical thinking and decisionmaking: avoiding the perils of thin-slicing. Ann Emergency Med. 2006;48(6):720–2.
Xiao Y, Hunter WA, Mackenzie CF, Jefferies NJ. Task complexity in emergency medical care and its implications for team coordination. Hum Factors. 1996;38(4):636–45.
Dailey RH. Approach to the patient in the emergency department. In: Rosen P, editor. Emergency medicine: concepts and clinical practice. St. Louis: Mosby; 2010. p. 137–50.
Lockey AS, Hardern RD. Decision making by emergency physicians when assessing cardiac arrest patients on arrival to hospital. Resuscitation. 2001;50(1):51–6.
Endsley MR. Design and evaluation for situation awareness enhancement. In: Proceedings of the Human Factors Society 32 nd Annual Meeting. Santa Monica, CA: Human factors Society; 1998. p. 97–101.
Flin R, Maran N. Identifying and training non-technical skills for teams in acute medicine. Qual Saf Health Care. 2004;13(Suppl 1):i80–4.
McIlvaine WB. Situational awareness in the operating room: a primer for the anesthesiologist. Seminars Anesthesia Perioperative Med Pain. 2007;26:167–72.
Wright MC, Taekman JM, Endsley MR. Objective measures of situation awareness in a simulated medical environment. Qual Saf Health Care. 2004;13(Suppl 1):i65–71.
Croskerry P. Cognitive forcing strategies in clinical decisionmaking. Annals of Emergency Medicine. 2003;41(1):110–20.
Bond S, Cooper S. Modelling emergency decisions: recognition-primed decision making. The literature in relation to an ophthalmic critical incident. J Clin Nurs. 2006;15:1023–32.
Sandhu H, Carpenter C. Clinical decisionmaking: opening the black box of cognitive reasoning. Ann Emerg Med. 2006;48(6):713–9.
Norman G, Young M, Brooks L. Non-analytical models of clinical reasoning: the role of experience. Med Edu. 2007;41(12):1140–5.
Sklar DP, Hauswald M, Johnson DR. Medical problem solving and uncertainty in the emergency department. Ann Emerg Med. 1991;20(9):987–91.
Szolovits P, Pauker S. Categorical and probabilistic reasoning in medical diagnosis. Artif Intell. 1978;11:115–44.
Mattu A, Goyal D. Emergency medicine: avoiding the pitfalls and improving the outcomes. Massachusetts: Blackwell Publishing; 2007.
Book Google Scholar
Frank LR, Jobe KA. Admission & discharge decisions in emergency medicine . Philadelphia: Hanley & Belfus; 2001.
Croskerry P, Campbell S, Forster AJ. Discharging safely from the emergency department. In Croskerry P. Patient safety in emergency medicine . Philadelphia: Wolters Kluwer; 2009.
Garmel GM. Approach to the emergency patient. In: Mahadevan SV, Garmel GM, editors. An introduction to clinical emergency medicine. Cambridge: Cambridge University Press; 2005.
Croskerry P, Sinclair D. Emergency medicine: a practice prone to error? CJEM. 2001;3(4):271–6.
Wald DA, Choo EK. Providing feedback in the emergency department. In: Rogers RL, Mattu A, Winters M, Martinez J, editors. Practical teaching in emergency medicine. West Sussex: Wiley-Blackwell; 2009. p. 60–71.
Chapter Google Scholar
Ark TK, Brooks LR, Eva KW. Giving learners the best of both worlds: do clinical teachers need to guard against teaching pattern recognition to novices? Acad Med. 2006;81(4):405–9.
Eva KW, Hatala RM, Leblanc VR, et al. Teaching from the clinical reasoning literature: combined reasoning strategies help novice diagnosticians overcome misleading information. Med Educ. 2007;41(12):1152–8.
Snowden DJ, Boone ME. A leader’s framework for decision making. Harv Bus Rev. 2007;85(1):68–76.
PubMed Google Scholar
Burdick WP. Emergency medicine’s role in the education of medical students: directions for change. Ann Emerg Med. 1991;20(6):688–91.
Download references
Acknowledgements
Nil declared
Author information
Authors and affiliations.
Emergency Department, Ibri Hospital, Ministry of Health, POB 134, 516 Akhdar, Ibri, Oman
Nasser Hammad Al-Azri
You can also search for this author in PubMed Google Scholar
Contributions
Solo author. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Nasser Hammad Al-Azri .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Solo author
Competing interests
The author declares that he has no competing interests.

Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Al-Azri, N.H. How to think like an emergency care provider: a conceptual mental model for decision making in emergency care. Int J Emerg Med 13 , 17 (2020). https://doi.org/10.1186/s12245-020-00274-0
Download citation
Received : 05 December 2019
Accepted : 25 March 2020
Published : 16 April 2020
DOI : https://doi.org/10.1186/s12245-020-00274-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Emergency care
- Emergency medicine
- Mental model
- Situational model
International Journal of Emergency Medicine
ISSN: 1865-1380
- General enquiries: [email protected]
Heterogeneity, Bayesian thinking, and phenotyping in critical care: A primer
Affiliations.
- 1 Department of Pharmacy, Piedmont Eastside Medical Center, Snellville, GA, and Department of Clinical and Administrative Pharmacy, University of Georgia College of Pharmacy, Athens, GA, USA.
- 2 Department of Pharmacy, University of North Carolina Medical Center, Chapel Hill, NC, USA.
- 3 Department of Clinical and Administrative Pharmacy, University of Georgia College of Pharmacy, Athens, GA, and Department of Pharmacy, Augusta University Medical Center, Augusta, GA, USA.
- PMID: 38742459
- DOI: 10.1093/ajhp/zxae139
Disclaimer: In an effort to expedite the publication of articles, AJHP is posting manuscripts online as soon as possible after acceptance. Accepted manuscripts have been peer-reviewed and copyedited, but are posted online before technical formatting and author proofing. These manuscripts are not the final version of record and will be replaced with the final article (formatted per AJHP style and proofed by the authors) at a later time.
Purpose: To familiarize clinicians with the emerging concepts in critical care research of Bayesian thinking and personalized medicine through phenotyping and explain their clinical relevance by highlighting how they address the issues of frequent negative trials and heterogeneity of treatment effect.
Summary: The past decades have seen many negative (effect-neutral) critical care trials of promising interventions, culminating in calls to improve the field's research through adopting Bayesian thinking and increasing personalization of critical care medicine through phenotyping. Bayesian analyses add interpretive power for clinicians as they summarize treatment effects based on probabilities of benefit or harm, contrasting with conventional frequentist statistics that either affirm or reject a null hypothesis. Critical care trials are beginning to include prospective Bayesian analyses, and many trials have undergone reanalysis with Bayesian methods. Phenotyping seeks to identify treatable traits to target interventions to patients expected to derive benefit. Phenotyping and subphenotyping have gained prominence in the most syndromic and heterogenous critical care disease states, acute respiratory distress syndrome and sepsis. Grouping of patients has been informative across a spectrum of clinically observable physiological parameters, biomarkers, and genomic data. Bayesian thinking and phenotyping are emerging as elements of adaptive clinical trials and predictive enrichment, paving the way for a new era of high-quality evidence. These concepts share a common goal, sifting through the noise of heterogeneity in critical care to increase the value of existing and future research.
Conclusion: The future of critical care medicine will inevitably involve modification of statistical methods through Bayesian analyses and targeted therapeutics via phenotyping. Clinicians must be familiar with these systems that support recommendations to improve decision-making in the gray areas of critical care practice.
Keywords: Bayesian analysis; acute respiratory distress syndrome; corticosteroids; mortality; phenotypes; sepsis.
© American Society of Health-System Pharmacists 2024. All rights reserved. For commercial re-use, please contact [email protected] for reprints and translation rights for reprints. All other permissions can be obtained through our RightsLink service via the Permissions link on the article page on our site—for further information please contact [email protected].
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Educators in academic surgery on managing expectations for surgery clerkship
Critical thinking, problem-solving, and emotional intelligence are a few of the skills medical students can learn during their surgical rotations. r. peter manes, md, saral mehra, md mba, kelly olino, md, and david stitelman, md, from the yale department of surgery discuss what makes a rewarding surgery clerkship experience..
In this series, Department of Surgery faculty, who were voted as top educators by the Yale School of Medicine's Class of 2024, share reflections on the role of academic surgeons in shaping medical education.
How do you engage and inspire students in the clerkshipexperience, while recognizing that the majority of students will not pursue surgery?
Tailor the educational experience.
R. Peter Manes: While many students are not interested in surgery, they all are curious, inquisitive individuals. It’s important to tailor the educational experience to the learner’s interests, while at the same time highlighting important concepts that every physician needs to know, no matter what career they pursue.
Use the Socratic method
Saral Mehra: I sometimes see students treated as invisible observers. If a student in my operating room or clinic made it this far in life; he/she is clearly a smart, educated, driven individual as clinical educators we need to see them as such. They are real people. Say good morning, ask questions, and make them feel a part of what is going on. Little acts and acknowledgements can go a long way to making students feel engaged and feel as though they belong.
In the operating room, and clinic, I like to use the Socratic method to teach. First, I warn them of my technique, and acknowledge I don’t expect them to know the answers to everything; it’s okay to not have an answer – but they must think. In this way, I can assess their current knowledge base, and adjust my questions to what will benefit them. I also have them write me diagrams and flow charts as they think through anatomy and differential diagnoses – the marking pens and sterile sheets make great writing apparatus.
In the clinic, or when not scrubbed in the operating room, I'll even tell them; it's okay to use your phone and resources to answer my questions- but take 5-10 minutes, figure out the answer, and then teach me. A little secret: if I ask a question for which I don't know the answer (or if a student asks me a question I can’t answer); I ask them to look it up and either tell me the next day or send me an email with the answer.
Success beyond a surgery rotation
Kelly Olino: Each student who comes in is trying to figure out how they belong and have to do this every single month. I think having a one-on-one meeting to begin each rotation and explaining the value of the opportunity they are being given and how valuable the time is to be dedicated to learning is key. We also discuss strategies for success beyond a surgery rotation- pursuing a love of knowledge, pushing for continuous improvement, and understanding that caring is the key to be a great doctor.
Create a shared vision
David Stitelman: Before cases, I like to discuss steps and anatomy with the resident and medical student. This helps us have a shared vision of what happens during cases. In terms of engagement, I also like to ask about undergraduate major, future plans and mentorship. In the Yale system, having a mentor is a big deal and making sure there is a faculty member watching out for the student is vital.
Featured in this article
- R Peter Manes, MD, FACS Associate Professor of Surgery (Otolaryngology); Residency Program Director, Otolaryngology Surgery; Clinical Site Director (YPB), Otolaryngology Surgery
- Saral Mehra, MD, MBA, FACS Associate Professor of Surgery (Otolaryngology); Section Chief, Head and Neck Surgery, Otolaryngology Surgery; Director, Head and Neck Oncologic and Reconstructive Surgery Fellowship, Surgery
- Kelly Olino, MD, FACS Assistant Professor of Surgery (Oncology); Leader, Skin Cancer Surgery, Melanoma Program; Clinical Director of the Smilow Melanoma Program, Yale Cancer Center; Co-Director Cutaneous Malignancy Tumor Board, Yale Cancer Center; Medical Student Clerkship Liaison for Division of Surgical Oncology, Surgery
- David Stitelman, MD Associate Professor of Surgery (Pediatrics)
Related Links
- Educators in academic surgery on giving and receiving feedback
- Educators in academic surgery on balancing education with other responsibilities
Main navigation
- Our Articles
- Dr. Joe's Books
- Media and Press
- Our History
- Public Lectures
- Past Newsletters
Subscribe to the OSS Weekly Newsletter!
Register for the oss 25th anniversary event, twisting facts about cancer.

- Add to calendar
- Tweet Widget
Let’s start with some facts. Antiperspirants, cell phones, root canals or wired bras do not cause cancer. Sugar or dairy products do not “feed” the disease. You cannot cure cancer with an alkaline diet, crystals, juices, shark cartilage, apricot pits, magnets, mistletoe, soursop, chlorella, black walnuts, coconut oil, cesium chloride, reiki, psychic surgery, baking soda, antineoplastons, bioresonance machines, orgone accumulators, Rife frequency generators or coffee enemas.
All of this comes to mind now because I was forwarded a link to a document entitled “Everyday Products Linked to Cancer” which also offers solutions to the problem. So, I clicked. I quickly learned that the discoverer of “the missing link” to “conquering cancer” is identified as a “natural health researcher and certified holistic cancer coach.” That immediately set my alarm bells ringing. This is not terminology that would ever be used to describe a legitimate scientist. And those bells really started to clamor when I encountered phrases like “groundbreaking,” “unveil cancer care known only to a few,” “challenge the one-sided, conventional understanding and offer more effective ways to conquer cancer,” “discover the proven protocols that have helped hundreds of thousands of people prevent and conquer cancer,” and “discover why many cancer treatments and prevention protocols fail.”
It seems Nathan Crane, also described as a “plant-based athlete,” has found the secret that has eluded thousands and thousands of researchers around the globe and is now equipped to “pave the way for future generations to live cancer free.” A search for this sage’s educational background reveals only that he went to Belgrade High School in Montana.
What is the key to living cancer-free? Staying away from “toxic household and personal care products” and “turning to nature” for replacements. Of course, we also need to fortify our body against toxins. How? By making use of “the power of nature’s detoxifiers.” Let me point out that the term “detoxify” is generally indicative of pseudoscience since the toxins being removed are never identified nor is the mechanism by which they are eliminated elucidated.
There is nothing novel in this “Conquering Cancer” manuscript. The Internet and bookstores brim with articles and books about purported carcinogens in everyday products and secret cures hidden by “Big Pharma” for fear of losing profits from the sale of ineffective, toxic chemotherapeutic agents. The idea of secret cures is nonsense, but when it comes to chemicals found in consumer products, there are some legitimate issues. However, fear-mongering documents, such as this one, generally smack of an ignorance of dose-response relationships and claim to have greater knowledge of the impact of these chemicals on health than what actually exists. Suppositions are presented as facts.
Some personal care products and cleaning agents contain chemicals that can be classified as endocrine disruptors or carcinogens. Furthermore, some of these can be detected in our bloodstream and urine. But it is critical to understand that the presence of a chemical cannot be equated to the presence of risk. Labeling a substance as an endocrine disruptor or carcinogen is in general based on cell culture or animal studies that use amounts far greater than what humans can possibly encounter. This does not mean that concerns about the likes of phthalates, bisphenol A, dioxane and nonylphenol ethoxylates should be swept under the carpet, but proclamations that “we’re poisoning ourselves” by using products that contain traces of these substances magnify whatever risk they may pose in an unrealistic fashion.
While reducing our use of products that contain chemicals that have the shadow of carcinogen or endocrine disruptor hanging over them has merit, the claim that turmeric, ginger, cayenne pepper, cinnamon, frankincense, Camu Camu or blueberries are “nature’s detoxifiers” and protect us from cancer is not evidence-based.
However, my biggest problem with this publication is the simplistic view it presents about preventing cancer. This is a very complex disease in which genetics, diet, infections, overweight, smoking, alcohol consumption, certain chemicals, exposure to ionizing radiation, changes in hormone levels, physical activity and age can all play roles. Suggestions that cancer risk can be significantly reduced by adding turmeric to the diet or replacing a commercial cleaning agent with vinegar, or switching from store-bought shampoo to a homemade concoction of aloe vera gel, coconut milk and castile soap, are naïve.
Something else is bothersome about this publication. The talk about “dangerous” everyday products and the use of herbs to “bolster our natural defenses” seems to be just bait to hook people to click on a link to a docuseries about “Conquering Cancer.” We are asked if we are “ready to explore the hidden cause of cancer that has eluded experts for years” and told that we will discover “how to starve your cancer cells without chemo, radiation or surgery.” The latter is a hallmark of quackery.
I did not take the bait because I follow cancer research closely and know that there are no hidden causes or magical cures. Certainly not any that have been discovered by a “certified holistic cancer coach.” I also suspect that if I were to click on the link for a “free ticket” to the series that promises to reveal “how natural, proven methods have helped over 591,753 people prevent and treat this life-threatening disease,” I might at some point be prompted to dig out my credit card for some over-hyped dietary supplement or a book with an assortment of twisted facts. But that’s just a guess.
@JoeSchwarcz
What to read next
Processed foods have many faces 17 may 2024.

Reports of the Death of Dental Cavities Are Greatly Exaggerated 17 May 2024

Methylene Chloride Can Strip Paint but Can Also Strip Years Off Your Life 15 May 2024

No, Eating French Fries is Not the Same as Smoking Cigarettes 10 May 2024

Navigating the Twisted World of Varicose Veins 10 May 2024
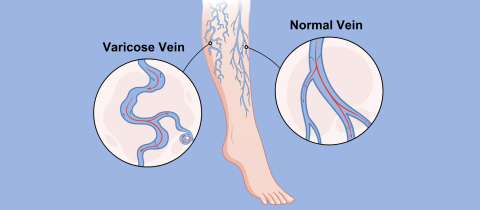
Pass on the Salt: Should We Ask for Potassium Chloride at the Dinner Table Instead? 17 May 2024

Department and University Information
Office for science and society.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Med Sci Monit
- v.17(1); 2011

Evidence and its uses in health care and research: The role of critical thinking
Milos jenicek.
1 Department of Clinical Epidemiology & Biostatistics, Michael G. de Groote School of Medicine, McMaster University, Hamilton, Ontario, Canada
Pat Croskerry
2 Department of Emergency Medicine, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada
David L. Hitchcock
3 David L. Hitchcock, Department of Philosophy, Faculty of Humanities, McMaster University, Hamilton, Ontario, Canada
Obtaining and critically appraising evidence is clearly not enough to make better decisions in clinical care. The evidence should be linked to the clinician’s expertise, the patient’s individual circumstances (including values and preferences), and clinical context and settings. We propose critical thinking and decision-making as the tools for making that link.
Critical thinking is also called for in medical research and medical writing, especially where pre-canned methodologies are not enough. It is also involved in our exchanges of ideas at floor rounds, grand rounds and case discussions; our communications with patients and lay stakeholders in health care; and our writing of research papers, grant applications and grant reviews.
Critical thinking is a learned process which benefits from teaching and guided practice like any discipline in health sciences. Training in critical thinking should be a part or a pre-requisite of the medical curriculum.
Sackett et al. originally defined evidence based medicine (EBM) as ‘… the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients’, and its integration with individual clinical expertise [ 1 ].’ In the nearly two decades that have intervened, there has been significant uptake of the idea that clinical care should be based upon sound, systematically researched evidence. There has been less emphasis on how clinical expertise itself might be improved, perhaps because the concept is more amorphous and difficult to define.
Clinical expertise is an amalgam of several things: there must be a solid knowledge base, some considerable clinical experience, and an ability to think, reason, and decide in a competent and well-calibrated fashion. Our focus here is on this last component: the faculties of thinking, reasoning and decision making. Clinicians must be able to integrate the best available critically appraised evidence with insights into their patients, the clinical context, and themselves [ 2 ]. To accomplish this integration, physicians need to develop their critical thinking skills. Yet historically this need has not received explicit attention in medical training. We believe that it should.
As an illustration of the use of critical thinking in clinical care, consider the following clinical scenario from emergency medicine : A 52-year-old male presents to the emergency department of a community centre with a complaint of constipation and is triaged with a low level acuity score to a ‘minors’ area. The department is extremely busy and several hours elapse before he is seen by the emergency physician. His principal complaint is constipation; he hasn’t had a bowel movement for 4 days. His abdomen is soft and non-tender. A large amount of firm stool is evident on rectal examination. He recalls a minor back strain a few days earlier. The physician orders a soapsuds enema and continues seeing other patients. After about 30 minutes he finds the nurse who administered the enema; she reports that it was ineffective. He orders a fleet enema which again proves ineffective. The nurse expresses her opinion that the patient is taking up too much time and suggests he be given an oral laxative and another fleet enema to take home with him. She is clearly unwilling to continue investing her effort in a patient with a trivial complaint. Nevertheless, the physician decides to administer a third enema himself. The third enema is only marginally effective and he then decides to disimpact the patient. The physician notes poor rectal tone and enquires further about the patient’s urination. He says he has been unable to urinate that day. On catheterisation he is found to have 1200cc. Neurological findings are equivocal: reflexes are present in both legs and there is some subjective diminished sensation.
A diagnosis of cauda equina syndrome is made and the emergency physician calls the neurosurgery service at a tertiary care hospital. It is now late in the evening. The neurosurgeon is reluctant to accept the working diagnosis. He suggests that the loss of sphincter tone might be due to the disimpaction, and argues that there was no significant history of back injury or convincing neurological findings. When the ED physician persists, the neurosurgeon suggests transferring the patient to the tertiary hospital ED for further evaluation and asks for a CT investigation of the patient’s lower spine before seeing him. The CT reveals only some minor abnormalities and the patient is kept overnight. An MRI is done in the morning. It shows extensive disc herniation with compression of nerve roots. The patient subsequently undergoes prolonged back surgery.
This case had a good outcome, although things might have been dramatically different. The patient might have suffered permanent neurological injury requiring lifelong catheterisation for urination.
Our scenario illustrates some key points about clinical decision making. At the outset, the patient presents with an apparently benign condition – constipation. The impression of a benign condition is incorporated at triage and results in a low-level acuity score and prolonged wait. The patient’s nurse also incorporates this diagnosis and exerts coercive pressure on the physician to discharge the patient. The neurosurgeon is dismissive of a physician’s assessment in a community centre ED, creating considerable inertia against referral. Thus the ED physician faces a variety of obstacles to ensure optimal patient care. These have little to do with EBM. He must resist and overcome a variety of cognitive, affective and systemic biases, his own as well as others’, and various contextual constraints. He must continue to think critically and persist in a course that has become increasingly challenging.
Our scenario also illustrates some key points about critical thinking. The initial impression of a benign condition of constipation is not the only diagnosis compatible with the patient’s symptoms. A health care professional reaching a preliminary diagnosis must be aware of the danger of fixing prematurely on this diagnosis and ignoring (or failing to look for) subsequent evidence that tells against it, as the nurse in our scenario was inclined to do. Observational and textual studies both indicate that the most common source of errors in reasoning is to close prematurely on a favoured conclusion and then ignore evidence that argues against that conclusion [ 3 ]. It is also important to keep in mind that a patient’s signs or symptoms may have more than one cause. Data that may confirm one of the causes does not necessarily rule out all the others. Attentive listening to the patient and careful looking in the data-gathering stage are essential to good medical practice, as Groopman has recently pointed out [ 4 ]. From a logical point of view, the physician’s diagnostic task is to gather data that will determine which one (or ones) of the possible causes is (or are) responsible for the patient’s problem. This goal will guide the selection of data and of additional tests. ‘Parallel’ or ‘lateral’ thinking [ 5 ] will help with the differential diagnosis.
Critical Thinking
Dewey’s original conceptualization [ 6 ] of what he called “reflective thinking” has spawned in the intervening century a variety of definitions of critical thinking, most notably that of Ennis as “ reasonable reflective thinking that is focused on deciding what to believe or what to do” [ 7 ] . Scriven and Paul have elaborated this definition as “… the intellectually disciplined process of actively and skilfully conceptualizing, applying, synthesizing or evaluating information gathered from, or generated by observation, experience, reflection, reasoning, or communication as a guide to belief or action ” [ 8 ].
The consensus of 48 specialists in critical thinking from the fields of education, philosophy and psychology was that it should be defined as ‘ purposeful self-regulatory judgment which results in interpretation, analysis, evaluation and inference, as well as explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations upon which that judgement is based ’ [ 9 ]. The list of additional definitions remains impressive [ 10 , 11 ].
Even more useful than these definitions are various lists of dispositions and skills characteristic of a “critical thinker” [ 7 , 9 , 12 ]. More useful still are criteria and standards for measuring possession of those skills and dispositions [ 13 ], criteria that have been used to develop standardized tests of critical thinking skills and dispositions [ 14 – 17 ] including some with specific reference to health sciences [ 18 ].
The elements of critical thinking subsume what has variously been described as clinical judgment [ 19 ] , logic of medicine [ 20 , 21 ] , logic in medicine [ 22 ] , philosophy of medicine [ 23 ] , causal inference [ 24 ] , medical decision making [ 25 ], clinical decision making [ 26 ], clinical decision analysis [ 27 ], and clinical reasoning [ 28 ]. An increasing number of monographs on logic and critical thinking in general have appeared [ 29 – 34 ] and their content is being adapted for medicine [ 35 – 37 ].
Everyday medical practice, whether in physicians’ offices or emergency departments or hospital wards, clearly involves “ reasonable reflective thinking that is focused on deciding what to believe (meaning the understanding of the problem) and/or what to do (i.e. deciding what to do to solve the problem)” [ 7 , 38 ]. Table 1 lists specific abilities underlying critical thinking in medical practice.
Specific abilities underlying critical thinking in medical practice.
Critical thinking is also called for in medical research and medical writing. Editors of leading medical journals have called for it. Edward Huth [ 39 , 40 ], former editor of Annals of Internal Medicine, has urged that medical articles reflect better and more organized ways of reasoning. Richard Horton [ 41 , 42 ], former editor of The Lancet , has proposed the use in medical writing of a contemporary approach to argument along the lines used by the philosopher Toulmin [ 40 , 41 ]. Subsequently, two of us have developed this approach in detail for medicine [ 43 , 44 ]. Dickinson [ 45 ] has called for an argumentative approach in medical problem solving and brought it to the attention to the world of medical informatics and beyond.
Dual Process Theory
An important component of critical thinking is being aware of one’s own thinking processes. In recent years, two general modes of thinking have been described under an approach described as dual process theory. The model is universal and has been directly applied to medicine [ 46 – 48 ] and nursing [ 49 ]. One mode is fast, reflexive, autonomous, and generally referred to as intuitive or System 1 thinking. The other is slow, deliberate, rule-based, and referred to as analytical or System 2 thinking. The mechanisms that underlie System 1 thinking are based on associative learning and innate dispositions: the latter are hard-wired, as a result of the evolutionary history of our species, to respond reflexively to certain cues in the environment. We have discrete, functionally-specialized mental programs that were selected when the brain was undergoing significant development especially spanning the last 6 million years of hominid evolution [ 50 ]. Although these programs may have served us well in our ancestral past, they may not be appropriate in some aspects of modern living. Some of this System 1 substrate also underlies various heuristics and biases in our thinking – the tendency to take mental short-cuts, or demonstrate reflexive responses in certain situations, often on the basis of past experience. Not surprisingly, most error occurs in System 1 thinking.
Contemplative , or fully reflective thinking, is System 2 thinking. It suits any practice of medicine or medical research activity where there is time to utilise the best critically appraised evidence in a step-by-step process of reasoning and argument. Contemplative, fully reflective thinking is appropriate, for example, in internal medicine, psychiatry, public health, and other specialties, in etiological research and clinical trials, and in writing up the results of such research [ 35 ].
In contrast, a shortcut or heuristic approach [ 51 ] with somehow truncated thinking is often dictated by the realities of emergency medicine, surgery, obstetrics or any situation where there is incomplete information, bounded rationality, and insufficient time to be fully reflective. The extant findings and the decision maker’s experience are all that is available. The quintessential challenge for well-calibrated decision making is to optimise performance in System 1. Hogarth [ 52 ] sees this challenge as educating our intuitive processes and has delineated a variety of strategies through which this might be accomplished.
No responsible physician would engage in reflective thinking on every occasion when a decision has to be made. Such acute emergencies as sudden complications of labour and delivery, ruptured aneurysms, multiple trauma victims and other immediately life-threatening situations generally leave no time for fully reflective thinking. A shortcut or heuristic approach is required [ 51 ], involving pattern recognition, steepest ascent reasoning, or algorithmic paths [ 21 , 53 ]. There is of course a place for reflective thinking before and after such time-constrained emergency decisions. More generally, reflective thinking is called for in any aspect of medical practice where there is time and reason for it.
The distinction should be made between the involuntary autonomous nature of System 1 thinking and a deliberate decision to use a shortcut for expediency, which is System 2 thinking. There is normally an override function of System 2 over System 1 but this may be deliberately lifted under extreme conditions.
Future Direction
Critical thinking is a learned process which benefits from teaching and guided practice like any other discipline in health sciences. It was already proposed as part of an early medical curriculum [ 54 ]. If we are to train future generations of health professionals as critical thinkers, we should do so in the spirit of critical thinking as it stands today. Clinical teachers should know how to run a Socratic discourse, and in which situations it is appropriate. They should be aware of contemporary models of argument. Clinical teachers should be trained and experienced in engaging with their interns and residents in meaningful discourse while presenting and discussing morning reports, at floor and other rounds, in morbidity and mortality conferences, or at less informal ‘hallway’, ‘elevator’ or ‘coffee-maker/drinking fountain’ teaching sites for busy clinicians. Such discourse is better than so-called “pimping”, i.e. quizzing of juniors with objectives ranging from knowledge acquisition to embarrassment and humiliation [ 37 , 55 ].
Also, somebody should point out to trainees the relevance to the health context of some basics of informal logic, critical thinking and argumentation, if those basics have been acquired as the result of studying for their first undergraduate degree.
Unquestionably, the appropriate critically appraised best evidence should be used as a foundation for reasoning and argument about how to care for patients. But, if we want to link the best available evidence to a patient’s biology, the patient’s values and preferences, the clinical or community setting, and other circumstances, we should take all these factors into account in using the best available evidence to get to the beliefs and decisions that have the best possible support.
Such a reflective integration cannot be mastered by mere exposure. A learning experience is required. Trainees in medicine need to learn how to think critically [ 56 ], just as they need to learn contemporary approaches to ‘rational’ medical decision making: how to use Bayes’ theorem in the diagnostic process, how to determine the sample size in a clinical trial, how to analyze survival curves in prognosis and outcomes studies, and how to calculate odds ratios in case control research. To understand each other, the teacher and the learner should both know the fundamentals of reasoning and argument in medicine. To achieve this understanding, we can either offer separate and distinct courses on critical thinking and decision making in medicine; or spread learning, practice and experience in critical thinking and decision making across various specialties; or do both. Only the future will show which of the alternatives is better. The integrated approach seems more promising, but harder to implement. Given the limitations on the current medical undergraduate curriculum, we might be hard-pressed to persuade a curriculum committee that precious space and time should be allocated to such concepts. The overriding rationale, however, should be that the knowledge of critical and reflective thinking is declarative knowledge (knowing how) and not simply an addition of procedural knowledge (know-how) or explicit knowledge. The old adage about it being preferable to teach someone how to fish rather than giving them fish applies. Any new additions will need to be streamlined and practical. A teaching module on critical thinking might for example include attention to how we reason and make decisions, factors that may impair decision making, the concept of critical thinking, situations where critical thinking is appropriate, some basic principles of logic and some logical fallacies. However the teaching, learning and practice of critical thinking is incorporated in the medical curriculum, it will need to include not only the contemplative, fully reflective thinking on hospital floors and in clinics but also the shortcut thinking [ 57 ] in such heuristic environments as operating theatres or emergency departments [ 46 , 48 , 58 – 60 ].
Similar education is required as a basis for framing grant applications and research reports as reasoned arguments, especially in the discussion section [ 61 , 62 ]. We may see a day when most medical journals are what Paton [ 63 ] terms “reflective journals”. If an application for a research grant, a research proposal, or a group of research findings (systematically reviewed or not) presented in a medical article are all exercises in argumentation and critical thinking, their authors, readers, and editors should find a common language for all these types of scientific and professional communication.
Almost four decades ago Feinstein [ 64 ] asked what kind of basic science clinical medicine needs. At that time, he had mostly clinical biostatistics and epidemiology in mind. Recently, Redelmeier et al. [ 65 ] proposed to add cognitive psychology as one more basic science. It is time, we think, to add critical thinking to that list.
Competing interests
None declared.
Source of support: None. Departmental support to produce the manuscript is acknowledged and appreciated
- Augsburg.edu
- Inside Augsburg
Search Strommen Center for Meaningful Work
- Faculty & Staff
- Graduate Students
- First Generation
- International
- Students With Disabilities
- Undocumented
- Business & Finance
- Culture and Language
- Environmental Sustainability
- Government, Law & Policy
- Health Professions
- Human & Social Services
- Information Technology & Data
- Marketing, Media & Communications
- Resumes and Cover Letters
- Expand Your Network / Mentor
- Explore Your Interests / Self Assessment
- Negotiate an Offer
- Prepare for an Interview
- Prepare for Graduate School
- Search for a Job / Internship
- Job Fair Preparation
- Start Your Internship
- Choosing a Major
- Career Collaborative
- Travelers EDGE
- Meet the Team
Critical Thinking: A Simple Guide and Why It’s Important
- Share This: Share Critical Thinking: A Simple Guide and Why It’s Important on Facebook Share Critical Thinking: A Simple Guide and Why It’s Important on LinkedIn Share Critical Thinking: A Simple Guide and Why It’s Important on X
Critical Thinking: A Simple Guide and Why It’s Important was originally published on Ivy Exec .
Strong critical thinking skills are crucial for career success, regardless of educational background. It embodies the ability to engage in astute and effective decision-making, lending invaluable dimensions to professional growth.
At its essence, critical thinking is the ability to analyze, evaluate, and synthesize information in a logical and reasoned manner. It’s not merely about accumulating knowledge but harnessing it effectively to make informed decisions and solve complex problems. In the dynamic landscape of modern careers, honing this skill is paramount.
The Impact of Critical Thinking on Your Career
☑ problem-solving mastery.
Visualize critical thinking as the Sherlock Holmes of your career journey. It facilitates swift problem resolution akin to a detective unraveling a mystery. By methodically analyzing situations and deconstructing complexities, critical thinkers emerge as adept problem solvers, rendering them invaluable assets in the workplace.
☑ Refined Decision-Making
Navigating dilemmas in your career path resembles traversing uncertain terrain. Critical thinking acts as a dependable GPS, steering you toward informed decisions. It involves weighing options, evaluating potential outcomes, and confidently choosing the most favorable path forward.
☑ Enhanced Teamwork Dynamics
Within collaborative settings, critical thinkers stand out as proactive contributors. They engage in scrutinizing ideas, proposing enhancements, and fostering meaningful contributions. Consequently, the team evolves into a dynamic hub of ideas, with the critical thinker recognized as the architect behind its success.
☑ Communication Prowess
Effective communication is the cornerstone of professional interactions. Critical thinking enriches communication skills, enabling the clear and logical articulation of ideas. Whether in emails, presentations, or casual conversations, individuals adept in critical thinking exude clarity, earning appreciation for their ability to convey thoughts seamlessly.
☑ Adaptability and Resilience
Perceptive individuals adept in critical thinking display resilience in the face of unforeseen challenges. Instead of succumbing to panic, they assess situations, recalibrate their approaches, and persist in moving forward despite adversity.
☑ Fostering Innovation
Innovation is the lifeblood of progressive organizations, and critical thinking serves as its catalyst. Proficient critical thinkers possess the ability to identify overlooked opportunities, propose inventive solutions, and streamline processes, thereby positioning their organizations at the forefront of innovation.
☑ Confidence Amplification
Critical thinkers exude confidence derived from honing their analytical skills. This self-assurance radiates during job interviews, presentations, and daily interactions, catching the attention of superiors and propelling career advancement.
So, how can one cultivate and harness this invaluable skill?
✅ developing curiosity and inquisitiveness:.
Embrace a curious mindset by questioning the status quo and exploring topics beyond your immediate scope. Cultivate an inquisitive approach to everyday situations. Encourage a habit of asking “why” and “how” to deepen understanding. Curiosity fuels the desire to seek information and alternative perspectives.
✅ Practice Reflection and Self-Awareness:
Engage in reflective thinking by assessing your thoughts, actions, and decisions. Regularly introspect to understand your biases, assumptions, and cognitive processes. Cultivate self-awareness to recognize personal prejudices or cognitive biases that might influence your thinking. This allows for a more objective analysis of situations.
✅ Strengthening Analytical Skills:
Practice breaking down complex problems into manageable components. Analyze each part systematically to understand the whole picture. Develop skills in data analysis, statistics, and logical reasoning. This includes understanding correlation versus causation, interpreting graphs, and evaluating statistical significance.
✅ Engaging in Active Listening and Observation:
Actively listen to diverse viewpoints without immediately forming judgments. Allow others to express their ideas fully before responding. Observe situations attentively, noticing details that others might overlook. This habit enhances your ability to analyze problems more comprehensively.
✅ Encouraging Intellectual Humility and Open-Mindedness:
Foster intellectual humility by acknowledging that you don’t know everything. Be open to learning from others, regardless of their position or expertise. Cultivate open-mindedness by actively seeking out perspectives different from your own. Engage in discussions with people holding diverse opinions to broaden your understanding.
✅ Practicing Problem-Solving and Decision-Making:
Engage in regular problem-solving exercises that challenge you to think creatively and analytically. This can include puzzles, riddles, or real-world scenarios. When making decisions, consciously evaluate available information, consider various alternatives, and anticipate potential outcomes before reaching a conclusion.
✅ Continuous Learning and Exposure to Varied Content:
Read extensively across diverse subjects and formats, exposing yourself to different viewpoints, cultures, and ways of thinking. Engage in courses, workshops, or seminars that stimulate critical thinking skills. Seek out opportunities for learning that challenge your existing beliefs.
✅ Engage in Constructive Disagreement and Debate:
Encourage healthy debates and discussions where differing opinions are respectfully debated.
This practice fosters the ability to defend your viewpoints logically while also being open to changing your perspective based on valid arguments. Embrace disagreement as an opportunity to learn rather than a conflict to win. Engaging in constructive debate sharpens your ability to evaluate and counter-arguments effectively.
✅ Utilize Problem-Based Learning and Real-World Applications:
Engage in problem-based learning activities that simulate real-world challenges. Work on projects or scenarios that require critical thinking skills to develop practical problem-solving approaches. Apply critical thinking in real-life situations whenever possible.
This could involve analyzing news articles, evaluating product reviews, or dissecting marketing strategies to understand their underlying rationale.
In conclusion, critical thinking is the linchpin of a successful career journey. It empowers individuals to navigate complexities, make informed decisions, and innovate in their respective domains. Embracing and honing this skill isn’t just an advantage; it’s a necessity in a world where adaptability and sound judgment reign supreme.
So, as you traverse your career path, remember that the ability to think critically is not just an asset but the differentiator that propels you toward excellence.

SPH Convocation Season 2024

Grads Take the Stage as ‘Architects of a Brighter, Healthier Future’
Coe in maternal and child health podcast–c2: critical conversations that lie at the heart of health justice ., coe in maternal and child health podcast–c2: critical conversations that lie at the heart of health justice, with dr. lisa erlanger., in the latest episodes of c2: critical conversations that lie at the heart of health justice , listen a two-part conversation on weight stigma with dr. lisa erlanger, professor of family medicine at the university of washington..
This podcast is hosted by the Center of Excellence in Maternal and Child Health Education, Science and Practice at the School of Public Health. These episodes serve to generate conversations in classrooms and living rooms about issues and strategic solutions critical to the health of communities and families, focusing on how we can achieve health justice as a collective. The Center has launched two seasons of C2: Critical Conversations that Lie at the Heart of Health Justice.
In the second episode of this two-part series, the CoE continues their conversation with Dr. Lisa Erlanger, a board-certified family physician and clinical professor of family medicine at the University of Washington. She is a leader in the growing movement for weight-inclusive primary care and speaks nationally about anti-fat bias, weight-inclusive primary care, and eating disorders.

Join this CoE conversation which explores the foundations of weight-inclusive primary care and “peel back the onion” that is diet culture. The discussion also addresses research and everyday discourse about weight can be misleading and what we can do to fix these misconceptions.
For Part 1 of this conversation, click below:
For more information about Dr. Erlanger and her work, click the link below: https://sites.google.com/view/drlisaerlanger
Explore Related Topics:
- Share this story
- 0 Comments Add
CoE in Maternal and Child Health Podcast–C2: Critical Conversations that Lie at the Heart of Health Justice.
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
- Military & Veterans
- Transfer Students
- Education Partnerships
- COVID-19 Info
- 844-PURDUE-G
- Student Login
- Request Info
- Bachelor of Science
- Master of Science
- Associate of Applied Science
- Graduate Certificate
- Master of Business Administration
- ExcelTrack Master of Business Administration
- ExcelTrack Bachelor of Science
- Postbaccalaureate Certificate
- Certificate
- Associate of Applied Science (For Military Students)
- Programs and Courses
- Master of Public Administration
- Doctor of Education
- Postgraduate Certificate
- Bachelor of Science in Psychology
- Master of Health Care Administration
- Master of Health Informatics
- Doctor of Health Science
- Associate of Applied of Science (For Military Students)
- Associate of Science (For Military Students)
- Master of Public Health
- Executive Juris Doctor
- Juris Doctor
- Dual Master's Degrees
- ExcelTrack Master of Science
- Master of Science (DNP Path)
- Bachelor of Science (RN-to-BSN)
- ExcelTrack Bachelor of Science (RN-to-BSN)
- Associate of Science
- Doctor of Nursing Practice
- Master of Professional Studies
The average Purdue Global military student is awarded 54% of the credits needed for an associate's and 45% of the credits needed for a bachelor's.
- General Education Mobile (GEM) Program
- AAS in Health Science
- AS in Health Science
- BS in Organizational Management
- BS in Professional Studies
- AAS in Criminal Justice
- AAS in Small Group Management
- AAS Small Group Management
- Master's Degrees
- Bachelor's Degrees
- Associate's Degrees
- Certificate Programs
- Noncredit Courses
- Tuition and Financial Aid Overview
- Financial Aid Process
- Financial Aid Awards
- Financial Aid Resources
- Financial Aid Frequently Asked Questions
- Financial Aid Information Guide
- Tuition and Savings
- Aviation Degree Tuition and Fees
- Professional Studies Tuition and Fees
- Single Courses and Micro-Credentials
- Time and Tuition Calculator
- Net Price Calculator
- Military Benefits and Tuition Assistance
- Military Educational Resources
- Military Tuition Reductions
- Military Spouses
- Student Loans
- Student Grants
- Outside Scholarships
- Loan Management
- Financial Literacy Tools
- Academic Calendar
- General Requirements
- Technology Requirements
- Work and Life Experience Credit
- DREAMers Education Initiative
- Student Identity
- Student Experience
- Online Experience
- Student Life
- Alumni Engagement
- International Students
- Academic Support
- All Purdue Online Degrees
- Career Services
- COVID-19 FAQs
- Student Accessibility Services
- Student Resources
- Transcript Request
- About Purdue Global
- Accreditation
- Approach to Learning
- Career Opportunities
- Diversity Initiatives
- Purdue Global Commitment
- Cybersecurity Center
- Chancellor's Corner
- Purdue Global Moves
- Leadership and Board
- Facts and Statistics
- Researcher Request Intake Form
Most Commonly Searched:
- All Degree Programs
- Communication
- Criminal Justice
- Fire Science
- Health Sciences
- Human Services
- Information Technology
- Legal Studies
- Professional Studies
- Psychology and ABA
- Public Policy
- Military and Veterans
- Tuition and Fee Finder
- Financial Aid FAQs
- Military Benefits and Aid
- Admissions Overview
- Student Experience Overview
- Academic Support Overview
How to Improve Critical Thinking in the Workplace

Employers want critical thinkers — those with sound judgment who can evaluate and analyze issues, make decisions, and overcome obstacles. Hiring managers are looking for people who can think critically and resolve issues quickly and effectively.
The National Association of Colleges and Employers ( NACE ) lists critical thinking as one of the eight career readiness competencies that demonstrate a recent college graduate has been educated for success in the workplace. Career readiness is “key to ensuring successful entrance into the workforce,” NACE reports.
Employers have not been shy about the lack of critical thinking skills in the workforce.
According to a 2023 ZipRecruiter skills hiring report , for which more than 2,000 U.S. employers were surveyed, the top three skills employers say candidates are “most lacking in” are:
- Time management
- Professionalism
- Critical thinking
In addition, the global management consulting firm McKinsey and Company projects that the demand for skills such as critical thinking and decision-making will grow by 19% in the U.S. and by 14% in Europe through 2030.
Critical thinkers, where are you? Hone your critical thinking skills, and become an indispensable member of your team with these five steps.
1. Formulate Your Questions
First thing to do: Identify the problem and the questions you need to ask. When you ask smart questions from the beginning, you can get a clearer picture of the issues involved. Questions to ask during this stage include:
- What’s happening?
- Why is this happening?
- What is most concerning about X?
- What is holding people back from solving X?
- What is the desired outcome?
2. Gather Information
Now it’s time to perform research. Depending on the nature of your problem, you may need to interview people, gather data and statistics, get historical project information, etc.
Make sure to get diverse input, too. It’s natural to want to talk with like-minded people, but this does nothing to help you get diverse perspectives and potential solutions.
In the research phase, consider asking stakeholders:
- How would you solve the problem?
- What other ways have you tried so far?
- What do you need to happen for this problem to be solved?
- Is there anything we haven’t discussed that you need me to know?
Don’t be afraid to ask for clarity. If someone you’re interviewing says something you’re not familiar with, ask them to tell you more about it. How does it fit into the problem or solution?
Aim to ask open-ended yet short questions. “How can I better understand this issue?” and “What if we tried a new approach?” can help others frame and communicate their own hypotheses.
3. Question Your Assumptions
Critical thinking depends on objectivity. You just collected a slew of facts in step two; now it’s time to vet your information.
If it’s from an online source, make sure the site is reputable and trustworthy. What’s their motive in sharing this information? Is the information complete and current? Are they trying to get you to take action (for example, send money or vote for them)?
Look for evidence that the source itself received diverse input. Ask if someone’s voice is missing in the presentation of the facts.
Finally, as you move to step four to apply the information, keep this question in mind: “Am I making any assumptions about this information?” Decisions need facts, not assumptions, to support them.
4. Apply the Information to Identify the Best Solution
Ask yourself this at the start of this step: “Are there any viewpoints I missed?” If all stakeholders have had an equal voice, you’re good to proceed. At this stage, you will use reason and logic to synthesize your information and arrive at the best solution. Questions to consider include:
- Are there other factors I haven’t considered?
- Have I evaluated the information from every perspective?
- Are my conclusions supported by sufficient evidence?
After completing the due diligence outlined above, you are ready to form your own opinion about the problem and devise a solution — or, solutions. There may be more than one, so plan to present them all.
5. Communicate and Evaluate Your Solution
Now you will share your findings with the stakeholders, such as your manager, executives, coworkers, and anybody else who should be involved.
After you’ve implemented your solution, evaluate whether it was effective. Did it solve the initial problem? What lessons can you take from this experience? How will you improve your critical thinking for next time?
Earn a College Degree Online With Purdue Global
As you navigate the working world, consider Purdue Global if a certificate or college degree could help you achieve your goals. With more than 175 online programs , you can earn a certificate or degree while still working and taking care of your family. Reach out for more information .
See Notes and Conditions below for important information.
About the Author
Purdue Global
Earn a degree you're proud of and employers respect at Purdue Global, Purdue's online university for working adults. Accredited and online, Purdue Global gives you the flexibility and support you need to come back and move your career forward. Choose from 175+ programs, all backed by the power of Purdue.
- General Education
- Legal Studies & Public Policy
- Online Learning
Your Path to Success Begins Here
Learn more about online programs at Purdue Global and download our program guide.
Connect with an Advisor to explore program requirements, curriculum, credit for prior learning process, and financial aid options.
Employment and Career Advancement: Purdue Global does not guarantee employment placement or career advancement. Actual outcomes vary by geographic area, previous work experience and opportunities for employment.
- Share full article
Advertisement
Supported by
Guest Essay
Doctors Need a Better Way to Treat Patients Without Their Consent

By Sandeep Jauhar
Dr. Jauhar is a cardiologist in New York who writes frequently about medical care and public health.
Not long ago, I took care of a middle-aged man at my hospital who had severe heart failure requiring life support. When he was disconnected from machines after a few days of treatment, he began to display psychotic symptoms, including delusional thinking, tangential speech and paranoia. He had a long history of untreated schizophrenia, I learned, which had estranged him from family members and friends, with whom he had virtually no contact.
My patient demanded to leave the hospital. However, sending him home was going to be a problem. He could not take care of himself. There was little chance he would take his medications, including a blood thinner to dissolve a clot in his heart before it caused a stroke. He was even less likely to take psychiatric drugs that he did not believe he needed.
My colleagues and I didn’t know what to do, so we called the treating psychiatrist. The psychiatrist immediately declared that our patient lacked the capacity to discharge himself from the hospital. The patient could not grasp the implications of this choice, for instance, or properly weigh its risks and benefits. The psychiatrist said the patient should remain in the hospital to receive psychiatric treatment, even against his will.
The psychiatrist’s opinion made sense to me. Patients with untreated schizophrenia have a higher rate of death than those who undergo treatment. Hopefully treatment would restore my patient’s judgment to the point where he would take his medications when he went home — or even decide not to take them, but to make that risky decision in the full appreciation of the likely consequences. (If autonomy means anything, it means that patients have the right to make bad decisions, too.) Treating him, even over his objections, seemed to be in his best interests.
However, according to New York law — and the law of other states — such involuntary treatment would require a court order. As doctors, we would have to plead our case before a judge. But was a judge without medical or psychiatric expertise the best person to decide this man’s fate?
In this case and also more generally, I think the answer is no. The law ought to be changed to keep such decisions in hospitals — in the hands of doctors, medical ethicists and other relevant experts.
Doctors don’t always have to resort to the courts to treat patients without their consent. There are some notable exceptions, such as during a life-threatening emergency (if a competent patient has not previously refused such treatment) or when there is a pressing societal interest (such as requiring patients with communicable tuberculosis to take antibiotics).
But judicial review has been the cornerstone of “treatment over objection,” as it’s known, for the past four decades or so. Appellate courts in the 1980s ruled that judicial hearings in such cases are needed to safeguard patients’ rights. For example, in 1983, in Rogers v. Commissioner of Department of Mental Health, the Massachusetts Supreme Judicial Court declared that a judge could override medical judgments favoring involuntary psychiatric treatment.
The underlying motivation behind judicial review was and remains laudable: to avoid the sort of paternalistic abuses that have characterized too much of medical history. Doctors often used to withhold bad news from patients, to cite just a small example. Involuntary treatment, even with benevolent intentions, reeks of such paternalism.
But though medical practice is by no means perfect, times have changed. The sort of abuse dramatized in the 1975 movie “One Flew Over the Cuckoo’s Nest,” with its harrowing depiction of forced electroconvulsive therapy, is far less common. Doctors today are trained in shared decision-making. Safeguards are now in place to prevent such maltreatment, including multidisciplinary teams in which nurses, social workers and bioethicists have a voice.
In addition to being less necessary to prevent abuse than they once were, courts are by nature poorly suited for making decisions about treatment over objection. For one thing, they are slow: Having to go to court often results in delays, sometimes up to a week or more, which can harm patients who need care urgently.
Moreover, judges have neither the experience nor the expertise to properly evaluate psychological states, assess decision-making capacity or determine whether a proposed treatment’s benefits outweigh its risks. It is no surprise that by some estimates 95 percent or more of requests for treatment over objection are approved by judges, who invariably haven’t met the patient and must rely on information provided by the treating medical team.
A better system for determining whether a patient should be treated over his or her objection would be a hospital hearing in which a committee of doctors, ethicists and other relevant experts — all of whom would be independent of the hospital and not involved in the care of the patient — engaged in conversation with the medical team and the patient and patient’s family. Having hearings on site would expedite decisions and minimize treatment delays. The committee would make the final decision.
Of course, such a committee would have to be granted immunity from legal liability (as with judges in our current system), so that experts would be willing to serve and speak candidly. Patients’ interests could be safeguarded by requiring the committee to publish its reasoning. Periodic audits by a regulatory body could ensure that the committee’s deliberations were meeting medical and ethical standards.
In the event that the committee could not reach a consensus on the best course of action (or if there were allegations of wrongdoing), then the parties involved could appeal to a judge. But that would be the exception rather than the rule.
In the case of my patient with heart failure, the decision ultimately didn’t have to go before a judge. Multiple discussions involving the patient, the hospital ethics and palliative care teams, social workers, nurses, psychiatrists and other doctors — discussions that in many respects served the function of a formal committee of the sort I’m proposing — yielded an agreement with the patient that his interests would be best served by sending him home with hospice care.
Capacity must be judged relative to the decision being made, and it became clear over the course of hospitalization that our patient understood the terminal nature of his condition and had the capacity to choose hospice care. Forced treatment was unlikely to significantly improve his psychiatric symptoms before the natural progression of heart failure caused his death.
So he was discharged home. It was the best decision under the circumstances, one reached by expert deliberation, not legal procedure. He passed away a few weeks later without, fortunately, ever setting foot in court.
Sandeep Jauhar ( @sjauhar ) is a doctor at Northwell Health in New York and the author, most recently, of “ My Father’s Brain : Life in the Shadow of Alzheimer’s.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .

IMAGES
VIDEO
COMMENTS
Critical thinking, the ability to think clearly and rationally about what to do or what to believe, is essential for the practice of medicine. Few doctors are likely to argue with this. Yet, until recently, the UK regulator the General Medical Council and similar bodies in North America did not mention "critical thinking" anywhere in their ...
Other constraints such as authoritarianism, intimidation and financial pressures may act against the expression of being critical or even the cultivation of critical thinking. The issue of the constraints on critical thinking and the potential hazards it entails will require further consideration by those who encourage being critical in medicine.
Critical thinking/problem-solving skills should emphasize self-examination. It should teach an individual to accomplish this using a series of steps that progress in a logical fashion, stressing that critical thinking is a progression of logical thought, not an unguided process. Pedagogy.
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. ... Delva D, Fischer M, Konopasek L, Schwartzstein RM, Gusic M. Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med ...
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
The Internal Medicine Journal (IMJ) is a ... Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking. It is important to define these skills explicitly, explain their rationales, describe methods of instruction and provide examples of optimal application. ...
Abstract. Critical thinking is essential to a health professional's competence to assess, diagnose, and care for patients. Defined as the ability to apply higher-order cognitive skills (conceptualization, analysis, evaluation) and the disposition to be deliberate about thinking (being open-minded or intellectually honest) that lead to action ...
There are several reasons why it is important to have a set of critical thinking skills that can be applied to medicine and health. As the scenario in Sect. 1.1 illustrates, we cannot evade the relentless exposure to medical and health messages that is part of our daily lives. We would be naïve to think that all, or even most, of these messages are conveying claims that represent some ideal ...
Evaluation of research behind evidence-based medicine requires critical thinking and good clinical judgment. Sometimes the research findings are mixed or even conflicting. As such, the validity, reliability, and generalizability of available research are fundamental to evaluating whether evidence can be applied in practice. To do so, clinicians ...
Current best practices in teaching critical thinking in medicine In the context of the 2011 Millennium Conference, the consensus among experts in critical thinking was that in order to teach critical thinking, learners must learn about both . 4 metacognition* and cognitive skills. The field of metacognition includes neurobiology, cognitive
The issue of the constraints on critical thinking and the potential hazards it entails will require further consideration by those who encourage being critical in medicine. Citing Literature. Volume 18, Issue 5. October 2012. Pages 938-944. Related; Information; Close Figure Viewer. Return to Figure.
Building on the conceptual framework first established by the Foundation for Critical Thinking, 19 the milestones for critical thinking articulated here were also heavily influenced by the Dreyfus model of the stages of expertise, 20 which has been applied extensively in nursing 21 and in medicine. 16 The language used in specialty board ...
Understanding Critical Thinking to Create Better Doctors Abstract Medical students master an enormous body of knowledge, but lack systematic problem solving ability ... 1Dept. of Psychiatry and 2 Dept. of Preventive and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry-605006, India
Medistudents team. August 18, 2021. Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
Critical Thinking in Medicine. Cognitive Errors and Diagnostic Mistakes is a superb new guide to critical thinking in medicine written by Jonathan Howard. It explains how our psychological foibles regularly bias and betray us, leading to diagnostic mistakes. Learning critical thinking skills is essential but difficult.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England (Health Education England (HEE), 2017).This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles (Faculty of Intensive Care Medicine ...
Current research related to critical thinking has focused on medicine, nursing, physical therapy, pharmacy, and dental programs, but there has been no description of assessing sonography students. The Dreyfus model has been used as a framework to describe acquired skills that reflects students' progress from novice to expert clinicians. This ...
General medicine commonly adopts a strategy based on the analytic approach utilizing the hypothetico-deductive method. Medical emergency care and education have been following similarly the same approach. ... This could be a step forward in preparing a broad-based, critical thinking pattern for physicians, who may save lives, organs, and limbs ...
Teaching and Assessing Critical Thinking and Clinical Reasoning Skills in Medical Education. of teaching which dates back to 470-399 BC dur ing Socrates era (Paul, Elder, & Bartell, 1997). This ...
Purpose: To familiarize clinicians with the emerging concepts in critical care research of Bayesian thinking and personalized medicine through phenotyping and explain their clinical relevance by highlighting how they address the issues of frequent negative trials and heterogeneity of treatment effect. Summary: The past decades have seen many ...
Critical thinking, problem-solving, and emotional intelligence are a few of the skills medical students can learn during their surgical rotations. R. Peter. ... In this series, Department of Surgery faculty, who were voted as top educators by the Yale School of Medicine's Class of 2024, share reflections on the role of academic surgeons in ...
But twisting science snarls my mind. Particularly when it comes to mangling facts about the causes and treatment of cancer. Let's start with some facts. Antiperspirants, cell phones, root canals or wired bras do not cause cancer. Sugar or dairy products do not "feed" the disease. You cannot cure cancer with an alkaline diet, crystals ...
Critical thinking is also called for in medical research and medical writing. Editors of leading medical journals have called for it. Edward Huth [39,40], former editor of Annals of Internal Medicine, has urged that medical articles reflect better and more organized ways of reasoning.Richard Horton [41,42], former editor of The Lancet, has proposed the use in medical writing of a contemporary ...
7 Program in Ethics and Decision Making in Critical Illness, Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA. 8 Center for Bioethics and Medical Humanities, Northwestern University Feinberg School of Medicine, Chicago, IL. Supplemental digital content is available for this article.
Critical thinking acts as a dependable GPS, steering you toward informed decisions. It involves weighing options, evaluating potential outcomes, and confidently choosing the most favorable path forward. ☑ Enhanced Teamwork Dynamics. Within collaborative settings, critical thinkers stand out as proactive contributors. They engage in ...
stigma CoE in Maternal and Child Health Podcast-C2: Critical Conversations that Lie at the Heart of Health Justice, with Dr. Lisa Erlanger. In the latest episodes of C2: Critical Conversations that Lie at the Heart of Health Justice, listen a two-part conversation on weight stigma with Dr. Lisa Erlanger, professor of family medicine at the University of Washington.
This paper examines the predictors of belief in the efficacy of complementary and alternative medicine (CAM) and its use, including cognitive factors (scientific reasoning, health literacy, locus of control), beliefs (holistic and magical health beliefs pseudoscientific beliefs, and trust in doctors), sociodemographic factors, and cancer diagnosis. The sample consisted of 177 women (41.8% with ...
Hone your critical thinking skills, and become an indispensable member of your team with these five steps. 1. Formulate Your Questions. First thing to do: Identify the problem and the questions you need to ask. When you ask smart questions from the beginning, you can get a clearer picture of the issues involved.
Dr. Jauhar is a cardiologist in New York who writes frequently about medical care and public health. Not long ago, I took care of a middle-aged man at my hospital who had severe heart failure ...
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. ... 3 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, Massachusetts; Corresponding Author: Margaret M. Hayes.