This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy.
Hide this message
You are using an outdated browser. Please upgrade your browser to improve your experience and security.

The Directory of Open Access Journals
Quick search, research reports in clinical cardiology.
1179-8475 (Online)
- ISSN Portal
Publishing with this journal
The journal charges up to:
as publication fees (article processing charges or APCs).
There is a waiver policy for these charges.
Look up the journal's:
- Aims & scope
- Instructions for authors
- Editorial Board
- Anonymous peer review
→ This journal checks for plagiarism .
Expect on average 16 weeks from submission to publication.
Best practice
This journal began publishing in open access in 2010 . What does DOAJ define as Open Accesss?
This journal uses a CC BY or a CC BY-NC license.
Attribution Attribution Non-Commercial
→ Look up their open access statement and their license terms .
The author does not retain unrestricted copyrights and publishing rights.
→ Learn more about their copyright policy .
Articles digitally archived in:
→ Find out about their archiving policy .
Deposit policy with:
- Sherpa/Romeo
Permanent article identifier:
Journal metadata
Publisher Dove Medical Press , United Kingdom Manuscripts accepted in English
LCC subjects Look up the Library of Congress Classification Outline Medicine: Internal medicine: Specialties of internal medicine: Diseases of the circulatory (Cardiovascular) system Keywords cardiovascular diseases heart disease cardiology
WeChat QR code

- Search Close search
- Find a journal
- Search calls for papers
- Journal Suggester
- Open access publishing
We’re here to help
Find guidance on Author Services
Citation search
Your download is now in progress and you may close this window.
- Choose new content alerts to be informed about new research of interest to you
- Easy remote access to your institution's subscriptions on any device, from any location
- Save your searches and schedule alerts to send you new results
- Export your search results into a .csv file to support your research
Login or register to access this feature
Register now or learn more

Research Reports in Clinical Cardiology
Publishes open access research on cardiovascular diseases and prevention, arrythmia, heart failure, adult congenital disease, methodologies and treatment.
Start a new submission or continue a submission in progress
- Instructions for authors
- Editorial policies
- Editing services site
- Journal metrics
- Aims & scope
- Journal information
- Editorial board
- News & calls for papers
Current issue
- All volumes & issues
- Most read articles
- Most cited articles
- New content alerts
Ready to submit? Start a new submission or continue a submission in progress
Journal overview
- Aims and scope
Research Reports in Clinical Cardiology publishes evidence-based original research, reports, editorials, perspectives, reviews and commentaries covering the following topics:
- metabolic disorders influencing cardiac risk
- coronary heart disease
- arrhythmias and pacing
- heart failure
- cardiomyopathies
- methodologies
- percutaneous and invasive techniques
- adult congenital heart disease
- cardiovascular genetics
Emphasis is placed upon translation of important basic research, updated information about classical topics, scholarly discussions of controversial topics, and incisive, salient manuscripts relevant either to conceptualization or practice of cardiology.
Research Reports in Clinical Cardiology will no longer consider meta-analyses for publication.
Explore articles
- Open access
Explore the most recently published articles
Latest issues
- Recent issues
Previous issue

Clinical Research in Cardiology
- Publishes articles from the field of clinical cardiology, angiology, heart and vascular surgery, and provides a current and competent overview on the diagnosis and therapy of heart and vascular diseases
- Forum for peer-reviewed original and review articles as well as critical perspective articles
- Official journal of the German Cardiac Society (DGK)
- Michael Böhm,
- Norbert Frey
Societies and partnerships
- Deutsche Gesellschaft für Pädiatrische Kardiologie (DGPK)
- Deutsche Gesellschaft für Prävention und Rehabilitation von Herz-Kreislauf-Erkrankungen (DGPR)

Latest issue
Volume 113, Issue 6
Spotlight: Special Issues in Medical Therapy
Latest articles
Inflammatory risk and clinical outcomes according to polyvascular atherosclerotic disease status in patients undergoing pci.
- Benjamin Bay
- Birgit Vogel
- Roxana Mehran

Long-term risk factor management and adverse events in patients with early-onset myocardial infarction—a “real-world” study
- Hatim Kerniss
- Luis Alberto Mata Marín
- Harm Wienbergen

German Cardiac Arrest Registry (G-CAR)—results of the pilot phase
- Janine Pöss
- Christoph Sinning
- the G-CAR Investigators

Use of coronary physiology to guide revascularization in clinical practice: results of the F(FR) 2 registry
- J. Michael Altstidl
- Stephan Achenbach
- Monique Tröbs

Clinical outcomes of single- versus two-stent PCI technique in severely calcified true bifurcation lesions after rotational atherectomy
- Mohamed Samy
- Ahmad Alali
- Nader Mankerious

Journal information
- Biological Abstracts
- Chemical Abstracts Service (CAS)
- Current Contents/Clinical Medicine
- Current Contents/Life Sciences
- Google Scholar
- INIS Atomindex
- Japanese Science and Technology Agency (JST)
- Norwegian Register for Scientific Journals and Series
- OCLC WorldCat Discovery Service
- Science Citation Index Expanded (SCIE)
- Semantic Scholar
- TD Net Discovery Service
- UGC-CARE List (India)
Rights and permissions
Editorial policies
© Springer-Verlag GmbH Germany, part of Springer Nature
- Find a journal
- Publish with us
- Track your research
Discover scientific knowledge and stay connected to the world of science
Discover research.
Access over 160 million publication pages and stay up to date with what's happening in your field.
Connect with your scientific community
Share your research, collaborate with your peers, and get the support you need to advance your career.
Visit Topic Pages
Measure your impact.
Get in-depth stats on who's been reading your work and keep track of your citations.
Advance your research and join a community of 25 million scientists
Researchgate business solutions.

Scientific Recruitment

Marketing Solutions

Clinical Cardiology Research and Reports

Quick Links
Journal highlights.
- Aerobic fitness
- Angina pectoris
- Angioplasty
- Aortic valve
- Cardiologist
- Chest drainage tubes
- Coronary arteries
- Coronary artery disease
- Echocardiogram (ECHO)
- Heart attack
- Heart monitor
- Heart-Lung Machine
- Median sternotomy
- Mitral valve
Pubmed Indexed Articles
Aims and scope.
Clinical Cardiology Research and Reports (CCRR) is a Peer-reviewed, Open Access journal that publishes original research articles, review articles, and clinical studies that focus on the diagnosis and treatment of cardiovascular disease. The journal welcomes submissions related to systemic hypertension, arrhythmia, congestive heart failure, valvular heart disease, vascular disease, congenital heart disease, and cardiomyopathy. Manuscript types include original article, review, case report, short communication, book review, letter to the editor, etc.
About Journal
Clinical Cardiology Research and Reports (CCRR) is a peer reviewed open access journal dedicated to publishing leading-edge research in cardiology. Studies pertaining to cardiac diseases such as: cong For more info
Journal particulars

Journal DOI
Current volume, google scholar.

Latest Articles
Review article aug 18, 2023, a review of cardiac resynchronization therapy: present and future.
Goldenberg H, Ishizu G, Yamamoto T, Fornwalt F, Metra T, Gardner J, A Review of Cardiac Resynchronization Therapy: Present and Future, V2(1).
DOI: Under Process
Short Communication Jul 08, 2023
Current perspectives of angina pectoris symptoms and treatment.
Silva M, Mancini B, Camici G*, Lennon N, Stone F, Current Perspectives of Angina Pectoris Symptoms and Treatment, V2(1).
Review Article Jun 29, 2023
Cardiac problems and outcomes of mitral valve regurgitation.
Bonow D, Harris H, Comin Y*, Badhwar D, Sampaio F. Cardiac Problems and Outcomes of Mitral Valve Regurgitation, J Clinical Cardiology Research and Reports. V2(I)
Review Article Mar 31, 2023
A clinical presentation of acute pulmonary embolism.
Boutitie F, Pasrija G, Goldhaber G, Pelletier T, Pruszczyk H, A Clinical Presentation of Acute Pulmonary Embolism, J Clinical Cardiology Research and Reports, V2(1).

Featured video: Clinical Cardiology Research and Reports
Javascript is currently disabled in your browser. Several features of this site will not function whilst javascript is disabled.
- Why Publish With Us?
- Editorial Policies
- Author Guidelines
- Peer Review Guidelines
- Open Outlook
- Submit New Manuscript
- Sustainability
- Press Center
- Testimonials
- Favored Author Program
- Permissions
- Pre-Submission

open access to scientific and medical research
- Expressions of interest for Editor-in-Chief - the International Medical Case Reports Journal Read more
Back to Journals » Research Reports in Clinical Cardiology » Aims and Scope

Research Reports in Clinical Cardiology
Issn: 1179-8475.
- About Journal
- Journal Metrics
- Peer Reviewers
- Article Publishing Charges
Aims and Scope
- Call For Papers
Editor-in-Chief: Dr Richard Kones
Research Reports in Clinical Cardiology publishes evidence-based original research, reports, editorials, perspectives, reviews and commentaries covering the following topics: • prevention • metabolic disorders influencing cardiac risk • coronary heart disease • arrhythmias and pacing • heart failure • cardiomyopathies • methodologies • treatment • percutaneous and invasive techniques • outcomes • adult congenital heart disease • cardiovascular genetics
Emphasis is placed upon translation of important basic research, updated information about classical topics, scholarly discussions of controversial topics, and incisive, salient manuscripts relevant either to conceptualization or practice of cardiology.
Research Reports in Clinical Cardiology will no longer consider meta-analyses for publication.
Related journals you may also be interested in:
- Diabetes, Metabolic Syndrome and Obesity
- Integrated Blood Pressure Control
- International Journal of Nephrology and Renovascular Disease
- Journal of Blood Medicine
- Vascular Health and Risk Management
Contact Us • Privacy Policy • Associations & Partners • Testimonials • Terms & Conditions • Recommend this site • Cookies • Top
Contact Us • Privacy Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Cardiol
- v.39(1); 2016 Jan

Objectives and Design of the Russian Acute Coronary Syndrome Registry (RusACSR)
Vladimir i. gridnev.
1 Department of New Cardiological Informational Technologies, Research Institute of Cardiology, Saratov State Medical University n.a. V.I. Razumovsky, Saratov, Russia
Anton R. Kiselev
Olga m. posnenkova, yulia v. popova, viktor a. dmitriev.
2 Department of Registries of Cardiovascular Diseases, Russian Cardiology Research and Production Complex, Moscow, Russia
Mikhail D. Prokhorov
3 Laboratory of Nonlinear Dynamics Modelling, Saratov Branch of the Institute of Radio Engineering and Electronics of the Russian Academy of Sciences, Saratov, Russia
Pavel Ya. Dovgalevsky
Elena v. oschepkova, associated data.
The Russian Acute Coronary Syndrome Registry ( RusACSR ) is a retrospective, continuous, nationwide, Web‐based registry of patients with acute coronary syndromes ( ACS ). The RusACSR is a database that uses a secure Web‐based interface for data entry by individual users. Participation in the RusACSR is voluntary. Any clinical center that provides health care to ACS patients can take part in the RusACSR . The RusACSR enrolls ACS patients who have undergone care in Russian hospitals from February 2008 to the present. Key data elements and methods of data analysis in the RusACSR are presented in this article. Up to 2015, 213 clinical centers from 36 regions of Russia had participated in the RusACSR . Currently, the database contains data on more than 250 000 ACS patients who underwent care from 2008 to 2015. Some current problems are highlighted in this article. The RusACSR is a perspective project for different epidemiologic studies in Russian ACS patients.
Introduction
There are a number of registries from various countries that include patients with acute coronary syndromes (ACS). 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 The main goal of these registries is to fill the gap between probative data of randomized controlled trials and real clinical practice. 12 , 13 The main functions of the ACS registries are (1) to report on clinical and demographic characteristics of patients with ACS in covered cohorts; and (2) to assess the treatment of ACS in accordance with the current guidelines.
The registries can also be used for epidemiologic studies, original studies, risk modeling, improving the quality of health care, and other objectives. The registry is an ideal tool for studying the real clinical practice, especially when it is necessary to improve the quality of health care.
It is known that the quality of health care in ACS patients, especially revascularization in ACS patients with ST‐segment elevation on electrocardiogram (STE‐ACS), requires improvement in many countries. 14 , 15 , 16 Within the framework of the Russian Federal Target Program Prevention and Control of Social Diseases (2007–2011) and the All‐Russian Vascular Program, in 2008 the Russian Acute Coronary Syndrome Registry (RusACSR; https://federalregistry.ru ) was established. This registry is still functioning.
The aim of this article is to describe the objectives and design of the RusACSR. The presented results may be interesting to a wide audience, as the RusACSR is currently the largest registry of ACS patients in Russia.
Description of the Russian Acute Coronary Syndrome Registry
The RusACSR has the following main objectives: (1) to create a national database with information on health care in ACS patients treated in Russia; (2) to obtain data on the demographic, clinical, and laboratory characteristics of ACS patients treated in Russia; (3) to identify the national features of associations between the characteristics of ACS and clinical outcomes, including mortality, complications, length of hospital stay, and quality of health care; and (4) to propose a practical guide for improving the quality and efficiency of ACS treatment in each clinical center participating in the RusACSR.
The Russian Cardiology Research and Production Complex (Moscow, Russia) was responsible for the development of the RusACSR and centralized data analysis at a federal level. The RusACSR was established in 2007 and 2008 by researchers, cardiologists, and information technology specialists from the Saratov Research Institute of Cardiology (Saratov, Russia). The current support of the RusACSR is carried out by the staff of both above‐mentioned organizations.
Participation
Participation in the RusACSR is voluntary and free of charge. Any clinical center that provides health care for ACS patients can participate in the RusACSR by sending a request to the technical support staff of the RusACSR. Starting in 2008, most of the main centers participating in the All‐Russian Vascular Program were invited to take part in the RusACSR by the Russian Cardiology Research and Production Complex. Up to 2015, 213 clinical centers from 36 regions of Russia had participated in the RusACSR (Figure (Figure1) 1 ) . 17

Maps with clinical centers participated in the RusACSR. Abbreviations: RusACSR, Russian Acute Coronary Syndrome Registry.
The majority of centers participating in the RusACSR are located in the Central Federal Region of the Russian Federation, and several centers are located in the North‐West Federal Region, South Federal Region, Ural Federal Region, and Siberian Federal Region. Thus, registry centers represent federal districts where the majority of the Russian population lives. Of course, these regions are socioeconomically heterogeneous, but an annual public report contains the data on each region separately. 17
Design of the Russian Acute Coronary Syndrome Registry
The RusACSR is established as a retrospective, continuous, nationwide, Web‐based registry operating online ( https://federalregistry.ru ). The design of the RusACSR is based on the main points of the clinical guidelines on diagnosis and treatment of ACS. 18 , 19 , 20 , 21
Access to the Registry is given to registered members. Each user has a unique identification number and password to log in to the database. The Web forms are designed to be interactive. They limit or exclude certain options to avoid entry of conflicting or spurious data. Wherever possible, the data are entered by selection from drop‐down menus to minimize the number of keyboard errors. The purpose of all these measures is to maximize the accuracy of data.
The Web interface of the RusACSR contains 11 Web forms with the following titles: (1) personal data of ACS patients; (2) history of present event of ACS; (3) past history; (4) results of physical examination; (5) results of instrumental examinations; (6) results of laboratory tests; (7) invasive intervention; (8) prior therapy; (9) drug treatment of ACS; (10) recommendations at discharge; and (11) complications and outcomes.
The RusACSR enrolls patients who were admitted for ACS (ie, unstable angina or myocardial infarction [MI]) and underwent care in hospitals in Russia. Enrollment of patients started in February 2008 and has continued to the present day.
Inclusion criteria comprise any type of ACS (ie, unstable angina or MI) as a presumptive diagnosis, age ≥18 years, finished patient hospital chart, and absence of any exclusion criteria. 22
The RusACSR exclusion criteria are the following: (1) symptoms considered as consistent with acute cardiac ischemia are absent within the last 24 hours prior to admission; (2) patient was transferred into a registry hospital >24 hours after admission to the initial hospital; (3) patient was transferred out of a registry hospital <24 hours after admission; (4) symptoms considered as ACS at admission were not consistent with acute cardiac ischemia; and (5) ACS accompanied by a significant comorbidity, such as a motor vehicle accident, trauma, or severe gastrointestinal bleeding, and operation or procedure directly before admission. 22
A flow diagram of patient selection for inclusion in the RusACSR is presented in Figure Figure2 2 .

Flow diagram of patients' selection for inclusion to the RusACSR. Abbreviations: ACS, acute coronary syndrome; RusACSR, Russian Acute Coronary Syndrome Registry.
Data Elements
The key data elements and definitions of the RusACSR database were developed using the American College of Cardiology (ACC) 2001 Key Data Elements and Definitions for Measuring the Clinical Management and Outcomes of Patients with ACS 23 and the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 2011 Key Data Elements and Definitions of a Base Cardiovascular Vocabulary for Electronic Health Records. 24 After 2013, we adopted the RusACSR to the 2013 ACCF/AHA Key Data Elements and Definitions for Measuring the Clinical Management and Outcomes of Patients with ACS and Coronary Artery Disease. 25
Data on patient demographics, clinical characteristics, previous and hospital drug treatment, and reperfusion therapy are collected. Data on post‐hospital treatment of ACS patients are not included in the Registry. There is no capacity to follow patients after hospital discharge. (For details on the key data elements of the RusACSR database, see Supporting Information, Appendix A, in the online version of this article).
Data Collection
The centers participating in the RusACSR were asked to include all patients following inclusion/exclusion criteria treated for ACS during the year prior to the year of participation. The source of patient data is the hospital chart. To help the participants, a detailed user manual was developed. 22 This user manual is available on the RusACSR Web site.
The centers are interested in accurate data collection because these data are analyzed further by experts separately for each center and used on‐site for health care quality management. In each center, ≥1 physicians have been trained to log patient data into the Registry. The content of data‐entry Web forms is intuitive for 88% of untrained users. 26 Each year, experts from the RusACSR check the validity of entered data by reconciling randomly selected records with the data of patients' hospital charts. Currently, the RusACSR contains data on >250 000 ACS patients treated from 2008 to 2015. The main baseline characteristics of patients included in the RusACSR from February 1, 2008, to October 22, 2015, are presented in the Table Table1 1 .
Baseline Characteristics of ACS Patients Included in the RusACSR From February 1, 2008 to October 22, 2015
| Parameters | Values |
|---|---|
| Demographic and clinical characteristics (n = 254 584) | |
| Male sex | 49.8 |
| Age, y | 67 (58–77) |
| Prior MI | 28.6 |
| Prior chest pain | 55.5 |
| Prior PCI | 4.5 |
| Prior CABG | <0.1 |
| Prior CHF | 43.8 |
| Prior stroke and/or TIA | 7.6 |
| PVD | 6.3 |
| Family history of CAD | 19.9 |
| Hypertension | 79.3 |
| Smoking | 22.8 |
| DM | 15.3 |
| STE‐ACS patients | 33.6 |
| NSTE‐ACS patients | 49.2 |
| Heart rate at admission, bpm | 76 (68–86) |
| SBP at admission, mm Hg | 140 (120–160) |
| DBP at admission, mm Hg | 85 (80–90) |
| Killip class at admission (n = 169 007) | |
| I | 71.4 |
| II | 21.3 |
| III | 4.5 |
| IV | 2.8 |
| TC, mmol/L | 5.0 (4.2–6.0) |
| TG, mmol/L | 1.4 (1.0–2.0) |
| Cr, µmol/L | 92 (76–111) |
| Blood glucose, mmol/L | 5.6 (4.9–7.0) |
| ACS patients who underwent PCI | 16.6 |
| Prior medical therapy (n = 197 428) | |
| ASA | 45.6 |
| Clopidogrel | 9.5 |
| Nitrates | 34.6 |
| ACEIs | 47.8 |
| ARBs | 7.1 |
| β‐Blockers | 43.2 |
| Dihydropyridine CCBs | 9.1 |
| Non‐dihydropyridine CCBs | 2.0 |
| Warfarin | 1.9 |
| Reperfusion therapy in STE‐ACS patients (n = 85 496) | |
| Fibrinolitic therapy | 27.6 |
| Fibrinolitic therapy before hospital arrival | 8.0 |
| Time from chest pain (or its equivalent) to fibrinolitic therapy, min (n = 20 544) | 180 (120–300) |
| PCI (n = 85 496) | 29.4 |
| Primary PCI (n = 85 496) | 24.0 |
| Time from chest pain (or its equivalent) to PCI, min (n = 20 436) | 330 (200–750) |
| Drug therapy in ACS patients (STE‐ACS patients, n = 85 496; NSTE‐ACS patients, n = 125 228) | |
| Antiplatelet agents | |
| STE‐ACS patients | 97.8 |
| NSTE‐ACS patients | 97.3 |
| ASA | |
| STE‐ACS patients | 96.4 |
| NSTE‐ACS patients | 95.5 |
| Clopidogrel | |
| STE‐ACS patients | 84.4 |
| NSTE‐ACS patients | 76.4 |
| Anticoagulants | |
| STE‐ACS patients | 95.3 |
| NSTE‐ACS patients | 94.0 |
| β‐Blockers | |
| STE‐ACS patients | 89.0 |
| NSTE‐ACS patients | 89.8 |
| Statins | |
| STE‐ACS patients | 85.4 |
| NSTE‐ACS patients | 87.1 |
| ACEIs or ARBs | |
| STE‐ACS patients | 82.8 |
| NSTE‐ACS patients | 87.0 |
| Outcomes (STE‐ACS patients, n = 85 496; NSTE‐ACS patients, n = 125 228) | |
| In‐hospital cardiogenic shock | |
| STE‐ACS patients | 5.6 |
| NSTE‐ACS patients | 1.2 |
| Death during hospital stay | |
| STE‐ACS patients | 7.3 |
| NSTE‐ACS patients | 2.1 |
| Death during first day after admission | |
| STE‐ACS patients | 3.4 |
| NSTE‐ACS patients | 0.8 |
| GRACE risk score for in‐hospital death (STE‐ACS patients, n = 85 496; NSTE‐ACS patients, n = 125 228) | |
| STE‐ACS patients with data for calculating GRACE risk of in‐hospital death, n (%) | 40 214 (47.0) |
| NSTE‐ACS patients with data for calculating GRACE risk of in‐hospital death, n (%) | 27 896 (22.3) |
| STE‐ACS patients (n = 40 214) | |
| Low risk | 22.2 |
| Medium risk | 32.9 |
| High risk | 44.9 |
| NSTE‐ACS patients (n = 27 896) | |
| Low risk | 26.6 |
| Medium risk | 29.8 |
| High risk | 43.6 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitors; ACS, acute coronary syndrome; ARB, angiotensin II receptor blocker; ASA, aspirin; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CCB, calcium channel blocker; CHF, chronic heart failure; Cr, creatinine; DBP, diastolic blood pressure; DM, diabetes mellitus; GRACE, Global Registry of Acute Coronary Events; IQR, interquartile range; MI, myocardial infarction; NSTE‐ACS, non–ST‐segment elevation acute coronary syndrome; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; RusACSR, Russian Acute Coronary Syndrome Registry; SBP, systolic blood pressure; STE‐ACS, ST‐segment elevation acute coronary syndrome; TC, total cholesterol; TG, triglycerides; TIA, transient ischemic attack.
Data are presented as % or median (IQR), unless otherwise noted.
As for the proportion of ACS presentations included in the Registry since 2008, we have only an approximate estimation because the public statistics contain only the data on MI, and not on ACS morbidity across Russia. There are about 185 000 MIs per year in Russia. The RusACSR contains data on about 100 000 MI patients.
Data Security
Some of the main features of database and Web security issues should be mentioned briefly. As mentioned above, all users are assigned a unique username/password combination that is used to log on to the RusACSR. In this way, all transactions are recorded automatically in the Web server's log.
All the data are pseudonymously entered into a Web‐based database protected by a password on a safe server of the Russian Cardiology Research and Production Complex using secure sockets layer (SSL) connections. Subject identification is possible only at the local study site, and participating centers are exclusively able to review and modify the patient data. The data on ACS patients added to the RusACSR can be changed but cannot be removed. The transmitted data are stored in the central database on the central server at the Russian Cardiology Research and Production Complex.
The purpose of all the above‐mentioned measures is to ensure the confidentiality of the data.
Ethical Aspects
The study protocol including patient information and consent forms has been reviewed and approved by the Ethics Commission of the Russian Cardiology Research and Production Complex.
All patients must give informed consent before inclusion of their personal and clinical data in the RusACSR. The standard informed‐consent form is available on the RusACSR Web site. Patients gave their informed consent after transfer from an intensive care unit to a cardiac/coronary care unit. If patients died in the intensive care unit, consent was given by their relatives.
The appropriate measures are used to guarantee maximal data confidentiality. All patient‐related clinical data are anonymized locally.
Data Analysis
Within the RusACSR, an analytical module was created for the assessment of health care quality for ACS patients in Russia. The main aim of this analytical module is to implement the system analysis of clinical cases for the development of health care quality indicators for ACS patients to achieve the clinical result (for example, decrease of mortality).
We present the structure of a statistical report on health care in ACS patients that could be calculated in the RusACSR for each clinical center, region, or the whole of Russia (see Supporting Information, Appendix C, in the online version of this article). This report is calculated for any selected date range.
In the RusACSR, the completeness of execution of clinical guidelines in real clinical practice is evaluated using the developed clinical indicators, which are calculated automatically by using the database query for a required cohort of patients (in clinical units, in clinics, in regions of Russia, or in all participating clinics). These indicators were developed according to the ACCF/AHA methodology for the development of quality measures for cardiovascular technology. 27 (For details of clinical indicators, see Supporting Information, Appendix D, in the online version of this article.)
Based on the presented clinical indicators, the quality of care in ACS patients was compared among Russian hospitals. This approach allows us not only to evaluate the quality of care in a particular hospital based on clinical guidelines, but also to carry out a comparative evaluation with other hospitals in the city, region, or whole of Russia.
Disease registries allow data to be collected from large patient populations. Currently, the RusACSR is used for different goals by Russian researchers. A number of public reports on the quality of health care in ACS patients have been published recently. 17 , 28 Some authors already use the data from the RusACSR to assess the mortality 29 , 30 and appropriateness of percutaneous coronary intervention (PCI) in ACS patients in Russia, 31 to study the quality of health care in ACS patients, 32 , 33 , 34 , 35 , 36 , 37 and to analyze the clinical factors associated with PCI performance in Russia. 30 The results of the RusACSR have caused debate among Russian cardiologists. 38 Some authors reported their comments and suggestions with a view to improving this registry.
Because the RusACSR uses key data elements and definitions recommended by the ACCF/AHA, the results of our study have the potential to be used for cross‐country comparison with different registries in other European countries and the United States.
The ACC/AHA have proposed the performance measures for STEMI (ST‐segment elevation myocardial infarction) and NSTEMI (non–ST‐segment elevation myocardial infarction) patients. 39 The clinical indicators of the RusACSR have a similar goal. But our indicators were proposed in accordance with the national features of health care in ACS patients.
The evaluation of PCI in ACS patients has already become the target of some registries. 40 These registries have provided useful insights regarding the practice of interventional cardiology in various countries. The RusACSR plays a similar role in Russia.
According to some authors, the employment of ACS registries in small territories (small countries, separate regions, or cities) can improve the quality of health care in ACS patients. 41 The international experience shows that the most complete fulfillment of clinical guidelines in the care of STE‐ACS patients is achieved by using STEMI networks. 42 , 43 In Russia, several regions have already had a positive experience in implementing similar projects. Since 2008, the local STEMI networks based on the independent Samara STEMI Registry have been used successfully in the Samara region of Russia. 44 The RusACSR can become a basis for future development of similar networks in the whole of Russia.
The use of the RusACSR in practical health care is associated with the need to reorganize the workload of staff in centers providing care for ACS patients. Untrained users may have some difficulties with the use of the RusACSR. To solve this problem, we developed a user manual. 22 Another problem with the RusACSR is the formalization of medical information by users during the data transfer from a hospital chart to the Registry database. In our previous study, some problems were identified as the result of a test audit of 26 untrained users of the RusACSR. 26 This study showed that the main errors are the incompleteness of data entry and the semantic content of entered data. The errors relating to incompleteness of data entry were most frequent for heart rate and blood pressure data (33%), results of instrumental examinations (55%), results of laboratory tests (55%), invasive interventions (38%), and advice at discharge on smoking, nutrition, and weight management (28%). The semantic errors were most frequent in data on past history (68%), main symptom at admission (51%), date and time of arrival of ambulance with the patient (49%), electrocardiogram parameters (48%), creatine phosphokinases and troponins (38%), coronary angiography (55%), and advice at discharge on smoking, nutrition, and weight management (50%). It was found that the error rate does not depend on the medical experience of users. After the training, these users entered about 80% of the data correctly. That is why obligatory annual training was organized for all Registry users. However, the problem of human error has still not been completely solved.
Another problem with the RusACSR is covering the Russian population of ACS patients. At first, only clinical centers from the All‐Russian Vascular Program participated in the RusACSR. Currently, different centers participate in the Registry. Nevertheless, covering the Russian population of ACS patients is insufficiently representative. 38 The majority of centers that have participated in the RusACSR have quite good quality of health care, whereas most of the centers with low‐quality health care do not want to participate in the Registry. Widespread implementation of the RusACSR is the only solution to this problem.
The RusACSR is a perspective project for different epidemiologic studies in Russian ACS patients.
Supporting information
Appendix A. Key data elements of the database of the RusACSR
Appendix B. Addition data elements for coronary anatomy used in the RusACSR
Appendix C. Structure of statistical report on healthcare in ACS patients
Appendix D. Clinical indicators for assessment of quality of healthcare in ACS patients
Acknowledgments
The authors thank all participants of the RusACSR. This Registry is funded by the Russian Ministry of Health as a part of the Health National Project.
Drs. Gridnev, Kiselev, Posnenkova, and Prokhorov took part in the manuscript preparation. Drs. Gridnev, Kiselev, Posnenkova and Dmitriev designed the RusACSR. Drs. Dovgalevsky and Oschepkova contributed to the establishment of the federal RusACSR. Drs. Gridnev, Dovgalevsky, and Oschepkova contributed to the establishment of the local RusACSR. All authors reviewed and approved the final manuscript. The RusACSR is funded by the Russian Ministry of Health as a part of the Health National Project. The Russian Ministry of Health was not involved in the collection, analysis, and interpretation of data; in the manuscript preparation; or in making the decision to submit the article for publication. The authors have not received any financial support for the preparation of this article.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Clinical Research Article
- Open access
- Published: 22 June 2024
Cardiac evaluation of patients with juvenile dermatomyositis
- Gökmen Akgün 1 ,
- Betül Sözeri 2 ,
- Eviç Zeynep Başar 3 ,
- Nihal Şahin 4 ,
- Yunus Emre Bayrak 4 ,
- Kadir Ulu 2 ,
- Hüseyin Salih Güngör 3 ,
- Mustafa Doğan 3 ,
- Taliha Öner 5 ,
- Mehmet Karacan 5 ,
- Kadir Babaoğlu 3 ,
- Yonca Anık 6 &
- Hafize Emine Sönmez 4
Pediatric Research ( 2024 ) Cite this article
Metrics details
The present study aims to evaluate possible cardiac involvement in juvenile dermatomyositis (JDM) patients by conventional methods and cardiac magnetic resonance imaging (MRI) along with a systematic review of the literature on cardiac features in JDM.
The study group consisted of JDM patients who underwent cardiac MRI. We conducted a systematic review of the published literature involving JDM patients with cardiac involvement.
In the present study, although baseline cardiologic evaluations including electrocardiography and echocardiography were within normal limits, we showed late gadolinium enhancement on cardiac MRI in 3 of 11 JDM patients. In the literature review, we identified 25 articles related to cardiac involvement in JDM. However, none of them, except one case report, included cardiac MRI of JDM patients.
Cardiac abnormalities have been reported among the less frequent findings in patients with JDM. Cardiovascular complications during the long-term disease course are a leading cause of morbidity and mortality in these patients. Early detection of cardiac involvement by cardiac MRI in patients with JDM and aggressive treatment of them may improve the clinical course of these patients.
The myocardium in patients with JDM may be involved by inflammation.
Myocardial involvement may be evaluated by using contrast-enhanced cardiac MRI.
This is the first study evaluating cardiac involvement by cardiac MRI in JDM patients.
MRI may show early cardiac involvement in patients whose baseline cardiologic evaluations are within normal limits.
Early detection of cardiac involvement by cardiac MRI may improve the long-term prognosis of patients with JDM.
Similar content being viewed by others

The cGAS–STING pathway as a therapeutic target in inflammatory diseases

Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update

Muscle abnormalities worsen after post-exertional malaise in long COVID
Introduction.
Juvenile dermatomyositis (JDM) is the most common idiopathic inflammatory myopathy presenting with the characteristic rash and proximal muscle weakness during childhood. 1 Although proximal muscle weakness and skin findings are the predominant features of the disease, cardiac findings may be accompanied at initiation or during the course of the disease. 2 Cardiac involvement in JDM is usually underestimated and studies regarding this issue are scarce. However, cardiac involvement may cause morbidity and mortality in the long-term period. Nonspecific sinus tachycardia is the most frequent cardiac abnormality in JDM. Left ventricular diastolic and systolic dysfunction, hypertension, atherosclerosis, coronary artery disease, and metabolic syndrome may also occur. 2 Increasingly, magnetic resonance imaging (MRI) studies begin to take an important place both in the diagnosis of the disease and detection of subclinical organ involvement. Adult studies showed that cardiac MRI may help to detect subclinical myocardial involvement. 3 , 4 However, there is no data about cardiac MRI findings in JDM patients. The present study aims to evaluate possible cardiac involvement in JDM patients by conventional methods and cardiac MRI along with a systematic review of the literature on cardiac features in JDM.
Material and methods
This cross-sectional study was conducted between June 2022 and December 2022. Patients who were followed up with a diagnosis of JDM were enrolled in the study. All patients fulfilled the Bohan and Peter 5 , 6 or EULAR/ACR 2017 classification criteria. 7 Demographic data, clinical manifestations, laboratory findings, treatments, and outcomes were obtained from patient charts. The disease activity was evaluated with the Childhood Myositis Assessment Scale (CMAS). 8
Initially, a standard 12-lead electrocardiogram (ECG) was performed in all patients. Subsequently, all of them were examined using transthoracic echocardiography (GE Vivid E9 ultrasound system, General Electric Healthcare, Horten, Norway). B-Mode and M-Mode echocardiographic images were obtained. Finally, all patients underwent cardiac MRI in a 1.5 T MR scanner (Philips Gyroscan Intera Master; Philips, Eindhoven, The Netherlands) equipped with a 30 mT/m maximum gradient strength and 150 mT/m/ms slew rate. Data were collected by utilizing a synergy body coin with the patient in the supine position. The vital signs of patients were monitored and recorded throughout the MR examination. The left ventricle (LV) was evaluated in the standard 17-segment model 9 (Supplementary Fig. 1 ). All images were analyzed by an experienced pediatric cardiologist (KB) and radiologist (YA).
The study respected the guidelines of the Helsinki Declaration concerning medical research in humans and received local Ethics Committee approval. Informed consent was obtained from each patient and/or parents.

Systematic review of the literature
A systematic review of the literature on cardiac involvement in JDM was conducted. Relevant documents were searched according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) principles by using Medline and PubMed databases (Supplementary Fig. 2 ). 10 The following keywords were used: (“Juvenile dermatomyositis” OR “JDM” OR “Dermatomyositis, Juvenile” OR “Juvenile Myositis” OR “Myositis, Juvenile”) AND (“cardiac involvement” OR “cardiac manifestation” OR “heart involvement” OR “heart manifestation”). Articles only in English were included in the search. All related articles, including randomized and nonrandomized controlled trials, observational studies (case-control, cohort studies, and case series), and single case reports, were included. Two authors (GA and HES) independently reviewed all possibly eligible studies. Finally, discrepancies were resolved by discussion with the two experienced authors (KB and BS).
Baseline characteristics of our patients
A total of 11 patients were included in the study. Four (36.4%) were male and 7 (63.6%) were female. The median age at evaluation was 11 (7–17) years. The median duration of the disease was 24 (1–102) months. All the patients had heliotrope rash and proximal muscle weakness. Gottron papules were present in 10 patients, calcinosis in 2, and lipodystrophy in 2, concomitantly. The median CMAS score was 35 (22–48) at the time of diagnosis and 52 (41–52) at the time of cardiac evaluation. None of the patients had pulmonary or gastrointestinal involvement. Anti-nuclear antibody (ANA) was positive in 10 patients, anti-transcription intermediary factor 1γ (Anti-TIF1γ) in 2, anti-NXP2 in 1, and anti-Mi2 alfa and beta in 1 patient. Nailfold capillaroscopy findings revealed scleroderma pattern in 5 patients and non-scleroderma pattern in 5 patients (Table 1 ). None of them had additional cardiac risk factors including smoking, obesity, hypertension, dyslipidemia, and metabolic syndrome.
Cardiac features of our patients
Electrocardiographic examination showed normal sinus rhythm with normal QRS voltage and axis in all patients. None of them had arrhythmia at the time of evaluation. Conventional echocardiographic parameters were within the normal range (Table 1 ). Three of 11 patients (27.2%) had myocardial late gadolinium enhancement (LGE) on cardiac MRI similar to the appearance in myocarditis. Segment 17 (apex) was involved in 2 patients, and segments 1,2 5,6,9,10,11,14 (basal anterior, basal anteroseptal, basal inferolateral, basal anterolateral, mid inferoseptal, mid inferior, mid inferolateral, and apical septal) were involved in 1 patient (Fig. 1 ). Furthermore, one patient showed impaired right ventricular ejection fraction (EF) which was not shown in conventional echocardiography. Patients with myocardial late gadolinium enhancement were younger than others, but there were no differences between these two groups in terms of clinical and laboratory findings.
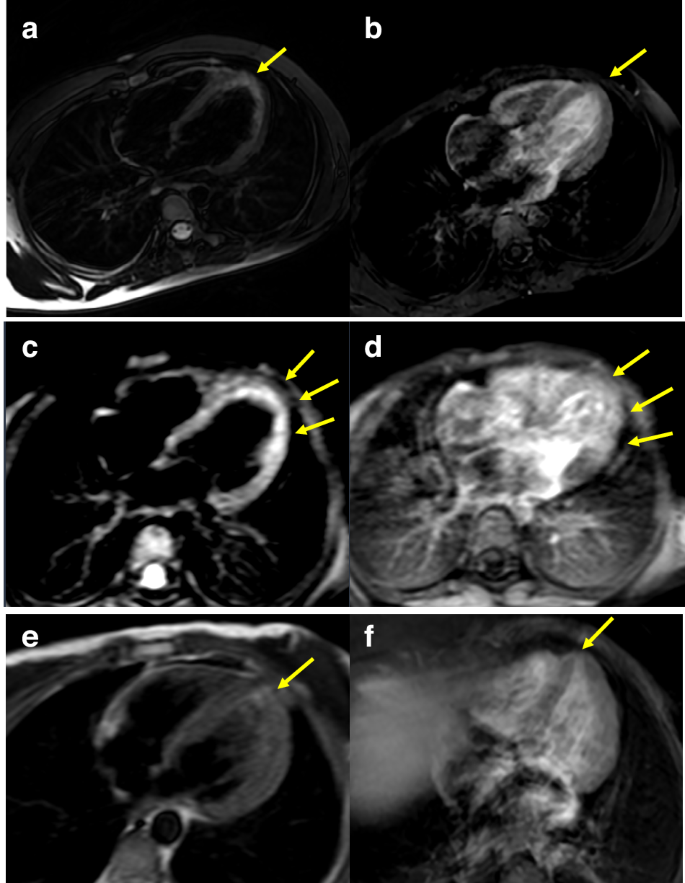
Myocardial images of T2 scans ( a , c , e ) and late gadolinium enhancement T1 scans ( b , d , f ) on cardiac MRI. Cardiac MRI axial plane: ( a , c , e ) are T2 weighted fat saturated images and ( b , d , f ) are postcontrast late enhancement T1 weighted images. Myocardial edema is seen on segment 17 (apex) on images ( a ) and ( e ) and on segments 1, 2, 5, 6, 9, 10, 11, and 14 (basal anterior, basal anteroseptal, basal inferolateral, basal anterolateral, mid inferoseptal, mid inferior, mid inferolateral and apical septal) on the image ( c ). On postcontrast images ( b ) ( d ) and ( f ) contrast enhancement is seen on the segments parallel with myocardial edema areas on T2W-fat-saturated images.
Cardiac features of patients with JDM in the literature
Supplementary Fig. 2 lists the schematic analyzes of the systematic literature review. At first, 84 related articles were identified. After the title and abstract review, 25 articles were included. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 Of these 25 articles, 7 were case report and 18 were observational studies (Table 2 ). However, none of them, except one, included cardiac MR findings of JDM patients. Stewart et al. 32 reported a 14-year-old girl diagnosed with JDM who had first-degree heart block and low voltages on ECG. Her disease evolved into multisystem involvement during hospitalization and treatment. Conduction disturbance progressed to atrial fibrillation. Her echocardiographic examination and cardiac MRI were normal. The disease course of the patient was complicated by macrophage activation syndrome. She was treated successfully with immunosuppressive therapy. Karaca et al. 16 reported another case report of conduction disturbance in an 11-year-old boy with JDM. The patient had sinus bradycardia with a heart rate of 40–44 per minute. After treatment with intravenous immunoglobulin (IVIG) and steroids, bradycardia was resolved spontaneously. A case-control study by ref. 13 including 25 patients with JDM reported one patient whose initial presentation was cardiac failure due to myocarditis and another two patients with asymptomatic ECG abnormalities. Ghosh et al. 30 reported a 10-year-old girl with a complete heart block secondary to JDM. She had normal systolic and diastolic functions. After treatment with methylprednisolone, ECG returned to sinus rhythm. Another case-control study by ref. 19 reported that diastolic dysfunction detected by tissue Doppler imaging was present in 22% of patients with JDM, pericarditis in 11%, and ECG abnormalities in 17% during 16 years of clinical follow-up. In their ensuing study, ref. 21 reported that patients with JDM had systolic dysfunction represented by decreased long-axis strain on color tissue Doppler echocardiography. Barth et al. 23 investigated 55 JDM patients aged 6–48 years using 24-h ambulatory Holter ECG and stated that patients with JDM had decreased heart rate variability (HRV). HRV is related to the heart rate. Insufficient response of inflamed myocardium and conduction tissue to vagal and sympathetic stimulus may be the reason for decreased HRV. Cantez et al. 27 reviewed retrospectively 105 patients with JDM. They found that ECG abnormalities (prolonged QTc and PR interval, bundle branch block) were present in 6% of the patients and echocardiographic abnormalities (atrioventricular-semilunar valve regurgitations) in 25%. However, their ECG and echocardiographic findings were mild or trivial and unlikely to be linked to the underlying disease. Diniz et al. 31 investigated 35 patients with JDM using conventional 2D and speckle-tracking echocardiography. They found that patients with JDM had lower LV global peak longitudinal systolic strain as well as lower peak circumferential systolic strain values than controls, although all the patients had normal LV ejection fraction (EF) on 2D conventional echocardiography. These results indicate that speckle-tracking echocardiography may be more sensitive than conventional 2D echocardiography in detecting early subclinical myocardial impairment in JDM patients. Diastolic dysfunction represented by low early diastolic tissue velocity (e’) and systolic dysfunction represented by decreased longitudinal strain were reported by ref. 34 including 57 patients with JDM. Patients with JDM generally have subclinical silent cardiac involvement during childhood, although there are few case reports of pericardial tamponade resulting in congestive heart failure which was treated by open drainage 11 and ventricular arrhythmias treated by amiodarone. 36 Overt cardiovascular disease and death resulting from cardiovascular involvement in JDM are more common in adult populations during long-term follow-up.
The myocardium in patients with JDM can be involved by inflammation just as the skeletal muscle. In the present study, we showed myocardial involvement by using contrast-enhanced cardiac MRI in 3 of 11 JDM patients whose baseline cardiologic evaluations including ECG and echocardiography were within normal limits. To our best knowledge, this is the first study evaluating cardiac involvement by cardiac MRI in JDM patients. Adults, with dermatomyositis and polymyositis frequently have cardiac involvement such as conduction abnormalities, atrial and ventricular arrhythmias, pericarditis, and myocarditis. 16 Cardiac involvement in JDM may either develop acutely or manifest during the disease course. Systemic vasculopathy and elevated interferon signature play a central role in the pathogenesis of idiopathic inflammatory myopathies. Both factors result in endothelial dysfunction which leads to cardiovascular manifestation during the disease. 2 Rhythm and conduction problems and myocarditis are the most observed cardiac abnormalities in the acute phase of the disease. Rider et al. 20 evaluated 374 patients with juvenile idiopathic inflammatory myopathy. Abnormal ECG findings were present in 56 (15%) of the patients. However, the study did not specify the abnormal ECG findings. Cantez et al. 27 showed prolonged QTc or prolonged PR in 6 of 69 JDM patients. Barth et al. 29 demonstrated pathologic ECG findings in 10 (17%) of 58 JDM patients. Furthermore, patients presenting with varying degrees of heart block have been reported. 30 , 32 Besides these acute complications, reduced aerobic capacity, systolic and diastolic dysfunction, and impaired cardiometabolic measures have been demonstrated in long-term follow-up. 14 , 15 , 19 , 21 , 26 , 28 , 33 , 35
Current recommendation guidelines do not provide a recommendation on how often and by which method patients with JDM should be screened for cardiac aspects. Cardiac MRI may be a valuable prospective technique to detect subclinical myocardial involvement. However, it is recommended that cardiac MRI should only be performed in patients with abnormalities on ECG or echocardiography. 37 Cardiac MRI studies conducted in recent years have revealed that myocardial involvement is higher than previously thought. For instance, Rosenbohm et al. 38 demonstrated signs of myocardial inflammation in 62.3% of 53 polymyositis (PM)/dermatomyositis (DM) patients by cardiac MRI. In the aforementioned study, they reported that the lateral segments of the left ventricle were significantly more often affected than the anterior or septal segments. Another study by ref. 4 showed late gadolinium enhancement (LGE) involving around 5% of the mass of the myocardium in 9 of 16 adult patients with PM/DM. The most affected part of the heart was interventricular septum ( n = 8) followed by lateral wall ( n = 5), inferior wall ( n = 3), apex ( n = 2), and anterior wall of the left ventricle ( n = 1). They also found that LGE was more common in patients with PM compared to those with DM. 4 Diederichsen et al. 39 evaluated cardiac abnormalities by cardiac MRI in newly diagnosed, untreated patients with idiopathic inflammatory myopathies. They detected systolic dysfunction by cardiac MRI in 2 of 14 patients with idiopathic inflammatory myopathies. Most recently, ref. 40 suggested that characteristics of cardiac dysfunction may be different between subgroups of idiopathic inflammatory myopathies, and they confirmed their hypothesis by mapping cardiac MRI parameters. They found higher global extracellular volume values in the PM group compared to the DM group. The number of affected ventricular segments in PM patients was higher than in DM patients. In our study, 3 of 11 patients had intramyocardial late gadolinium enhancement. Of them, 2 were diagnosed 3 months ago and the other patient was following for 12 months after the diagnosis. All three patients were in clinically inactive stage.
Due to the rare nature of the disease, there is no randomized controlled study on this subject. Accurate and timely treatment may prevent permanent cardiac damage in patients with JDM. Long-term follow-up of patients with JDM have shown frequent cardiovascular complications such as coronary artery disease, hypertension, atherosclerosis in adolescence and adulthood. Despite the fact that JDM can often cause significant cardiovascular morbidity and mortality during the long-term course of the disease, cardiac involvement is often overlooked at the onset of the disease. A cardiac MRI study by ref. 41 showed that myocardial LGE on contrast-enhanced magnetic resonance imaging of 4 adult patients with idiopathic inflammatory myopathies had markedly regressed after 6 months of corticosteroid and immunosuppressive therapy. They suggested that patients with cardiac involvement may require more aggressive treatments. IVIG is an anti-inflammatory and immunomodulatory drug commonly used in myocarditis to reduce the damage of inflammatory cytokines in cardiac myositis. 42 In our study, IVIG was given to 2 patients after cardiac MRI while one could not be treated with IVIG due to financial problems.
Late gadolinium enhancement on cardiac MRI may be seen in various cardiac diseases. Cardiomyopathies, autoimmune and inflammatory diseases, and metabolic and storage diseases cause LGE on cardiac MRI. Accumulation of amyloid fibrils in amyloidosis and glycosphingolipids in Anderson-Fabry disease deteriorate myocardial structure and cause intramyocardial fibrosis. Viral myocarditis, sarcoidosis, and systemic sclerosis are other causes of intramyocardial fibrosis due to inflammation with ischemic damage. Intramyocardial fibrosis and LGE can be found in arrhythmogenic right ventricular cardiomyopathy and dilated or hypertrophic cardiomyopathies. 43 Myocardial segments involved by contrast media and the pattern of gadolinium distribution may vary from patient to patient even if they have the same disease. Therefore, the clinical value of LGE distribution patterns in providing precise diagnosis remains to be clarified. In our 2 patients, intramyocardial LGE was present in the left ventricular apex. The remaining patient had more diffuse myocardial contrast enhancement (basal anterior, basal anteroseptal, basal anterolateral, basal inferolateral, mid inferior, mid inferoseptal, mid inferolateral, and apical septal segments).
Although conventional echocardiography and ECG findings were completely normal, myocardial involvement was detected in 3 patients in our study. All patients underwent repeat cardiac MRIs. Intramyocardial LGE was resolved in both patients after 6 months of treatment. A similar result was present in Allanore et al.’s study. 41
The small sample size is one of the important limitations of the study. Furthermore, all patients were at different periods of the disease. Another limitation is that our findings are not enough to make a contribution to predictive factors for cardiac involvement. Cardiac MRIs are difficult to implement in childhood patients. Unfortunately, it was inevitable that motion artifacts would occur. Changes seen may be the result of slow flow within the trabeculae and could be artifacts. However, in the present study, complete myocardial involvement suggests actual myocardial involvement rather than an artifact. Furthermore, there was an absence of involvement in the basal segment of the left ventricular free wall. Thus, the present involvement should not be construed as an artifact. Additionally, myocardial suppression was performed via a look-locker program that provides different TI values, and the best one was chosen. However, due to motion artifacts and high cardiac rate, the images included were a little inferior quality. Therefore, we believe that further studies are needed to decide on which JDM patients should be evaluated by cardiac MRI, and further studies in a larger cohort are needed to confirm our results.
Juvenile dermatomyositis is a multisystemic disease characterized by diffuse inflammation of skin and muscles. Cardiac involvement may occur in the course of the disease, however, remains unrecognized due to the lack of overt clinical manifestations in childhood. When considering that long-term cardiovascular complications seen in patients with JDM have significant effects on morbidity and mortality, early detection of cardiac involvement by cardiac MRI and aggressive treatment of these patients may improve the long-term prognosis of patients with JDM.
Data availability
All data generated or analyzed during this study are included in this published article. For additional information concerning these data, the corresponding author can be contacted.
McCann, L. J., Livermore, P., Wilkinson, M. G. L. & Wedderburn, L. R. Juvenile dermatomyositis. Where are we now? Clin. Exp. Rheumatol. 40 , 394–403 (2022).
Article PubMed Google Scholar
Mondal, S., Barman, P. & Vignesh, P. Cardiovascular abnormalities in juvenile dermatomyositis: a scoping review for the clinical rheumatologists. Front. Med. 9 , 827539 (2022).
Article Google Scholar
Mavrogeni, S. et al. Myocarditis during acute inflammatory myopathies: evaluation using clinical criteria and cardiac magnetic resonance imaging. Int. J. Cardiol. 164 , e3–e4 (2013).
Mavrogeni, S., Douskou, M. & Manoussakis, M. N. Contrast-enhanced CMR imaging reveals myocardial involvement in idiopathic inflammatory myopathy without cardiac manifestations. JACC Cardiovasc. Imaging 4 , 1324–1325 (2011).
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (first of two parts). N. Engl. J. Med. 292 , 344–347 (1975).
Article CAS PubMed Google Scholar
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (second of two parts). N. Engl. J. Med. 292 , 403–407 (1975).
Lundberg, I. E. et al. 2017 European League Against Rheumatism/American College of rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Arthritis Rheumatol. 69 , 2271–2282 (2017).
Article PubMed PubMed Central Google Scholar
Huber, A. M. et al. Validation and clinical significance of the childhood myositis assessment scale for assessment of muscle function in the juvenile idiopathic inflammatory myopathies. Arthritis Rheum. 50 , 1595–1603 (2004).
Cerqueira, M. D. et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105 , 539–542 (2002).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372 , 71 (2021).
Pereira, R. M., Lerner, S., Maeda, W. T., Goldenstein-Schainberg, C. & Cossermelli, W. Pericardial tamponade in juvenile dermatomyositis. Clin. Cardiol. 15 , 301–303 (1992).
Jimenez, C., Rowe, P. C. & Keene, D. Cardiac and central nervous system vasculitis in a child with dermatomyositis. J. Child Neurol. 9 , 297–300 (1994).
Shehata, R. et al. Juvenile dermatomyositis: clinical profile and disease course in 25 patients. Clin. Exp. Rheumatol. 17 , 115–118 (1999).
CAS PubMed Google Scholar
Hicks, J. E., Drinkard, B., Summers, R. M. & Rider, L. G. Decreased aerobic capacity in children with juvenile dermatomyositis. Arthritis Rheum. 47 , 118–123 (2002).
Takken, T., Spermon, N., Helders, P. J., Prakken, A. B. & Van Der Net, J. Aerobic exercise capacity in patients with juvenile dermatomyositis. J. Rheumatol. 30 , 1075–1080 (2003).
PubMed Google Scholar
Karaca, N. E., Aksu, G., Yeniay, B. S. & Kutukculer, N. Juvenile dermatomyositis with a rare and remarkable complication: sinus bradycardia. Rheumatol. Int. 27 , 179–182 (2006).
Sallum, A. M. et al. Risk factors associated with calcinosis of juvenile dermatomyositis. J. Pediatr. 84 , 68–74 (2008).
Sakurai, N., Nagai, K., Tsutsumi, H. & Ichimiya, S. Anti-CADM-140 antibody-positive juvenile dermatomyositis with rapidly progressive interstitial lung disease and cardiac involvement. J. Rheumatol. 38 , 963–964 (2011).
Schwartz, T., Sanner, H., Husebye, T., Flato, B. & Sjaastad, I. Cardiac dysfunction in juvenile dermatomyositis: a case-control study. Ann. Rheum. Dis. 70 , 766–771 (2011).
Rider, L. G. et al. The myositis autoantibody phenotypes of the juvenile idiopathic inflammatory myopathies. Medicine 92 , 223–243 (2013).
Article CAS PubMed PubMed Central Google Scholar
Schwartz, T., Sanner, H., Gjesdal, O., Flato, B. & Sjaastad, I. In juvenile dermatomyositis, cardiac systolic dysfunction is present after long-term follow-up and is predicted by sustained early skin activity. Ann. Rheum. Dis. 73 , 1805–1810 (2014).
Schwartz, T. et al. In active juvenile dermatomyositis, elevated eotaxin and MCP-1 and cholesterol levels in the upper normal range are associated with cardiac dysfunction. Rheumatology 53 , 2214–2222 (2014).
Barth, Z. et al. In juvenile dermatomyositis, heart rate variability is reduced, and associated with both cardiac dysfunction and markers of inflammation: a cross-sectional study median 13.5 years after symptom onset. Rheumatology 55 , 535–543 (2016).
Khera, R., Khare, S. & Singh, S. K. Acute presentation of juvenile dermatomyositis with subclinical cardiac involvement: a rare case. J. Clin. Diagn. Res. 10 , SD01–SD03 (2016).
PubMed PubMed Central Google Scholar
Saini, I., Kalaivani, M. & Kabra, S. K. Calcinosis in juvenile dermatomyositis: frequency, risk factors and outcome. Rheumatol. Int. 36 , 961–965 (2016).
Berntsen, K. S. et al. Submaximal exercise capacity in juvenile dermatomyositis after longterm disease: the contribution of muscle, lung, and heart involvement. J. Rheumatol. 44 , 827–834 (2017).
Cantez, S., Gross, G. J., MacLusky, I. & Feldman, B. M. Cardiac findings in children with juvenile Dermatomyositis at disease presentation. Pediatr. Rheumatol. Online J. 15 , 54 (2017).
Silverberg, J. I., Kwa, L., Kwa, M. C., Laumann, A. E. & Ardalan, K. Cardiovascular and cerebrovascular comorbidities of juvenile dermatomyositis in US children: an analysis of the National Inpatient Sample. Rheumatology 57 , 694–702 (2018).
Barth, Z. et al. Association between nailfold capillary density and pulmonary and cardiac involvement in medium to longstanding juvenile dermatomyositis. Arthritis Care Res. 71 , 492–497 (2019).
Article CAS Google Scholar
Ghosh, R. et al. Juvenile dermatomyositis presenting as complete heart block in a 10-year-old girl. Paediatr. Int. Child Health 40 , 251–254 (2020).
Diniz, M. F. R. et al. Echocardiographic study of juvenile dermatomyositis patients: new in sights from speckle-tracking-derived strain. Clin. Rheumatol. 40 , 1497–1505 (2021).
Stewart, J. A., Price, T., Moser, S., Mullikin, D. & Bryan, A. Progressive, refractory macrophage activation syndrome as the initial presentation of anti-MDA5 antibody positive juvenile dermatomyositis: a case report and literature review. Pediatr. Rheumatol. Online J. 20 , 16 (2022).
Witczak, B. N. et al. Body composition in long-standing juvenile dermatomyositis: associations with disease activity, muscle strength and cardiometabolic measures. Rheumatology 61 , 2959–2968 (2022).
Witczak, B. N. et al. Associations between cardiac and pulmonary involvement in patients with juvenile dermatomyositis-a cross-sectional study. Rheumatol. Int. 42 , 1213–1220 (2022).
Marstein, H. S. et al. Adipose tissue distribution is associated with cardio-metabolic alterations in adult patients with juvenile-onset dermatomyositis. Rheumatology 62 , SI196–SI204 (2023).
Singh, S. & Bansal, A. Twelve years experience of juvenile dermatomyositis in North India. Rheumatol. Int. 26 , 510–515 (2006).
Zhang, L., Wang, G. C., Ma, L. & Zu, N. Cardiac involvement in adult polymyositis or dermatomyositis: a systematic review. Clin. Cardiol. 35 , 686–691 (2012).
Rosenbohm, A. et al. Early diagnosis of cardiac involvement in idiopathic inflammatory myopathy by cardiac magnetic resonance tomography. J. Neurol. 262 , 949–956 (2015).
Diederichsen, L. P. et al. Cardiac abnormalities assessed by non-invasive techniques in patients with newly diagnosed idiopathic inflammatory myopathies. Clin. Exp. Rheumatol. 33 , 706–714 (2015).
Feng, C. et al. Myocardial involvement characteristics by cardiac MR imaging in patients with polymyositis and dermatomyositis. Rheumatology 61 , 572–580 (2022).
Allanore, Y. et al. Effects of corticosteroids and immunosuppressors on idiopathic inflammatory myopathy related myocarditis evaluated by magnetic resonance imaging. Ann. Rheum. Dis. 65 , 249–252 (2006).
Canter, C. E. & Simpson, K. E. Diagnosis and treatment of myocarditis in children in the current era. Circulation 129 , 115–128 (2014).
Satoh, H. et al. Distribution of late gadolinium enhancement in various types of cardiomyopathies: significance in differential diagnosis, clinical features and prognosis. World J. Cardiol. 6 , 585–601 (2014).
Download references
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and affiliations.
Department of Pediatric Cardiology, City Hospital, Kocaeli, Turkey
Gökmen Akgün
Department of Pediatric Rheumatology, University of Health Sciences, Ümraniye Research and Training Hospital, Istanbul, Turkey
Betül Sözeri & Kadir Ulu
Department of Pediatric Cardiology, Kocaeli University, Faculty of Medicine, Kocaeli, Turkey
Eviç Zeynep Başar, Hüseyin Salih Güngör, Mustafa Doğan & Kadir Babaoğlu
Department of Pediatric Rheumatology, Kocaeli University, Faculty of Medicine, Kocaeli, Turkey
Nihal Şahin, Yunus Emre Bayrak & Hafize Emine Sönmez
Department of Pediatric Cardiology, University of Health Sciences, Ümraniye Research and Training Hospital, Istanbul, Turkey
Taliha Öner & Mehmet Karacan
Department of Radiology, Kocaeli University, Faculty of Medicine, Kocaeli, Turkey
You can also search for this author in PubMed Google Scholar
Contributions
G.A., B.S., E.Z.B., and Y.A. were involved in gathering data, formal analysis, and writing the original draft. N.Ş., Y.E.B., K.U., H.S.G., M.D., T.Ö., M.K., K.B., supported gathering data and contributed to analyzing and interpreting data. H.E.S. conceived the study and revised the manuscript. All authors reviewed and revised the manuscript and approved the final version of the manuscript.
Corresponding author
Correspondence to Hafize Emine Sönmez .
Ethics declarations
Competing interests.
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclosures
No financial disclosures.
Informed Consent Written informed consent was obtained from patients and their parents.
Supplementary information
Supplementary figures, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Akgün, G., Sözeri, B., Başar, E.Z. et al. Cardiac evaluation of patients with juvenile dermatomyositis. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03336-8
Download citation
Received : 01 November 2023
Revised : 14 May 2024
Accepted : 31 May 2024
Published : 22 June 2024
DOI : https://doi.org/10.1038/s41390-024-03336-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
June 18, 2024 , Vol 331, No. 23, Pages 1977 - 2058
Audio highlights.
- Audio: Krill Oil for Knee Osteoarthritis, EHR Prompts to Improve Antibiotic Selection, FTC Action on Prescription Drugs, and more
Krill Oil for Knee Osteoarthritis : A Randomized Clinical Trial
This randomized clinical trial assesses the effect of krill oil supplementation vs placebo on knee pain improvement in patients with knee osteoarthritis, significant knee pain, and effusion-synovitis.
Stewardship Prompts to Improve Antibiotic Selection for Pneumonia : The INSPIRE Randomized Clinical Trial
This clinical trial examines the effect of an antibiotic stewardship bundle (education, feedback, and real-time multidrug-resistant organism risk-based CPOE prompts) vs routine stewardship on antibiotic selection during the first 3 hospital days in adults with pneumonia.
- Audio: Stewardship Prompts to Improve Antibiotic Selection for Pneumonia and Urinary Tract Infection
Stewardship Prompts to Improve Antibiotic Selection for Urinary Tract Infection : The INSPIRE Randomized Clinical Trial
This clinical trial evaluates whether computerized provider order entry prompts providing patient- and pathogen-specific multidrug-resistant organism risk estimates could reduce use of empiric extended-spectrum antibiotics for treatment of urinary tract infections.
Dispensing of Glucagon-Like Peptide-1 Receptor Agonists to Adolescents and Young Adults, 2020-2023
This study uses data from US retail pharmacies to assess national GLP-1RA dispensing to adolescents and young adults from 2020-2023.
Health and the 2024 US Election
Shingles vaccination in medicare part d after inflation reduction act elimination of cost sharing.
This cross-sectional study uses data from retail pharmacies to examine shingles vaccine uptake among Medicare Part D beneficiaries following an IRA policy to eliminate cost sharing.
US Public Health Preparedness and Response to Highly Pathogenic Avian Influenza A(H5N1) Viruses
US public health preparedness and response to highly pathogenic avian influenza A(H5N1) viruses are assessed in this survey study conducted by the CDC.
Federal Trade Commission Actions on Prescription Drugs, 2000-2022
This Special Communication examines the Federal Trade Commission’s policy and legal actions related to alleged misconduct, consolidation, and anticompetitive behavior in the pharmaceutical market between 2000 and 2022.
- Audio: The Federal Trade Commission’s Role in the Oversight of Drug Companies
- Editorial Federal Trade Commission Oversight of the Pharmaceutical Industry Amy Kapczynski, JD JAMA
Conveying Risks of Harm in Alzheimer Disease by Amyloid Lowering
This Viewpoint discusses how data gaps in published research impede clinicians’ ability to clearly discuss the risks and benefits of amyloid-lowering drugs for treating Alzheimer disease.
Heard but Excluded: A Language Manifesto
This Viewpoint discusses dismantling language barriers via multipronged approaches grounded in innovation, human-centered design, and systems thinking in 3 key areas.
Advancing Access to Cell and Gene Therapies in Medicaid
This Viewpoint presents the components of the payment model and the implementation challenges among the Center for Medicare and Medicaid Innovation, state Medicaid agencies, patients, and manufacturers.
The Other Side of the Curtain
In this narrative medicine essay, a newly minted pediatric critical care physician learns firsthand what holistic medical care is from the love and attention she received during a hospitalization for mediastinal lymphoma.
Harnessing the Electronic Health Record to Improve Empiric Antibiotic Prescribing
Federal trade commission oversight of the pharmaceutical industry, chronic chagas disease in the us.
This JAMA Insights provides recommendations for Chagas disease screening, diagnosis, and management in the US
Blood Testing for Phosphatidylethanol
A 36-year-old man with obesity and dyslipidemia presented with elevated liver enzymes following a liver transplant to treat acute-on-chronic liver failure due to alcohol-associated hepatitis. What would you do next?
AI in Medicine
How artificial intelligence will enhance imaging access and analysis.
This Medical News article is an interview with Saurabh Jha, a cardiothoracic radiologist and an associate professor of radiology at the University of Pennsylvania, and JAMA Editor in Chief Kirsten Bibbins-Domingo.
- Audio: AI in Radiology: Enhancing Analysis, Education, and Access
Monoclonal Antibody Authorized to Protect At-Risk People From COVID-19
Microneedle vaccine patches generated immune response in children, federal trade commission bans noncompete clauses, blood pressure drugs linked to more fractures, falls in va nursing homes, new drug for utis gets the greenlight, progress in heart failure deaths reversed over past decade, hhs commits millions to improving maternal, infant health, lower dose of mpox vaccine was safe, effective, monoclonal antibody protected majority of children from malaria, a good prognosis, congress, the doctor, social isolation and loneliness in older adults.
This JAMA Patient Page discusses social isolation and loneliness as important public health concerns, especially among older adults.
- Editor's Note Illness, Isolation, and the Poetry of Illumination Rafael Campo, MD, MA JAMA
Maintenance of Certification’s Value to Patients and Physicians
Maintenance of certification’s value to patients and physicians—reply, time to ivt treatment and functional outcomes in acute ischemic stroke, time to ivt treatment and functional outcomes in acute ischemic stroke—reply, phoenix criteria for pediatric sepsis and septic shock, phoenix criteria for pediatric sepsis and septic shock—reply, latest from the uspstf.
- USPSTF Recommendation: Interventions for High Body Mass Index in Children and Adolescents
- USPSTF Recommendation: Screening for Breast Cancer
- USPSTF Recommendation: Interventions to Prevent Falls in Community-Dwelling Older Adults
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Frontiers in Cardiovascular Medicine
- Cardio-Oncology
- Research Topics
Case Reports in Cardio-Oncology: 2024
Total Downloads
Total Views and Downloads
About this Research Topic
This Research Topic is the third volume of 'Case Reports in Cardio-Oncology'. Please see the previous volume here. This Research Topic aims to collect all the Case Reports submitted to the Cardio-Oncology section. If submitted directly to this collection the paper will be personally assessed by a Senior Associate Editor before the beginning of the peer-review process. Please make sure your article adheres to the following guidelines before submitting it. Case Reports highlight unique cases of patients that present with an unexpected diagnosis, treatment outcome, or clinical course: 1) Rare cases with Typical features 2) Frequent cases with Atypical features 3) Cases with a convincing response to new treatments, i.e. single case of off-label use Case Report format: - Maximum word count: 3000 words - Title: Case Report: “area of focus” - Abstract. - Introduction: including what is unique about the case and medical literature references. - Case description: including de-identified patient information, relevant physical examination and other clinical findings, relevant past interventions, and their outcomes. - A figure or table showcasing a timeline with relevant data from the episode of care. - Diagnostic assessment, details on the therapeutic intervention, follow-up, and outcomes, as specified in the CARE guidelines. - Discussion: strengths and limitations of the approach to the case, discussion of the relevant medical literature (similar and contrasting cases), take-away lessons from the case. - Patient perspective. Please, note that authors are required to obtain written informed consent from the patients (or their legal representatives) for the publication. IMPORTANT: Only Case Reports that are original and significantly advance the field will be considered.
Keywords : case reports
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines.
| Manuscript Summary | |
| Manuscript |
Participating Journals
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Value of comparative studies of "real clinical practice" in modern cardiology. Position paper based on the expert council discussion dated 12/18/2020
Affiliations.
- 1 I. M. Sechenov First Moscow State Medical University (Sechenov University). Moscow, Russia.
- 2 Russian National Research Medical University named after Pirogov, Moscow, Russia.
- 3 Research Institute for Complex Issues of Cardiovascular Diseases, Kemerovo, Russia.
- 4 Russian State University of Peoples' Friendship, Moscow, Russia.
- 5 Almazov National Medical Research Center, St. Petersburg, Russia.
- 6 Kazan State Medical University, Kazan, Russia.
- 7 Russian Medical Academy of Postgraduate Education, Moscow, Russia.
- 8 Samara Regional Clinical Cardiological Dispensary, Russia Samara State Medical University, Samara, Russia.
- 9 Perm State Medical University named after Academician Wagner E.A., Perm, Russia.
- 10 Volgograd State Medical University, Volgograd, Russia.
- 11 National Medical Research Centre for Therapy and Preventive Medicine, Moscow, Russia Robertson Centre for Biostatistics, Glasgow, Great Britain.
- 12 National Medical Research Centre for Therapy and Preventive Medicine, Moscow, Russia.
- 13 Scientific Medical Research Center of Cardiology, Moscow, Russia.
- 14 Privolzhsky Research Medical University of the Ministry of Health of the Russia, Nizhny Novgorod, Russia.
- 15 Novosibirsk State Medical University, Novosibirsk, Russia.
- PMID: 34112079
- DOI: 10.18087/cardio.2021.5.n1646
On December 18, 2020, an expert council was held with the participation of members of the Russian Society of Cardiology, the Eurasian Association of Ther-apists, the National Society for Atherothrombosis, the National Society for Evi-dence-Based Pharmacotherapy, and the Russian Heart Failure Society. The event was devoted to the discussion of the correct use of research data of "real clinical practice" in decision making.
PubMed Disclaimer
Similar articles
- [Focus ultrasound for cardiology practice. Russian consensus document]. Mareev YV, Dzhioeva ON, Zorya OT, Pisaryuk AS, Verbilo SL, Skaletsky KV, Ionin VA, Drapkina OM, Alekhin MN, Saidova MA, Safarova AF, Garganeeva AA, Boshchenko AA, Ovchinnikov AG, Chernov MY, Ageev FT, Vasyuk YA, Kobalava ZD, Nosikov AV, Safonov DV, Khudorozhkova ED, Belenkov YN, Mitkov VV, Mitkova MD, Matskeplishvili ST, Mareev VY. Mareev YV, et al. Kardiologiia. 2021 Nov 30;61(11):4-23. doi: 10.18087/cardio.2021.11.n1812. Kardiologiia. 2021. PMID: 34882074 Russian.
- The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Mullens W, Damman K, Harjola VP, Mebazaa A, Brunner-La Rocca HP, Martens P, Testani JM, Tang WHW, Orso F, Rossignol P, Metra M, Filippatos G, Seferovic PM, Ruschitzka F, Coats AJ. Mullens W, et al. Eur J Heart Fail. 2019 Feb;21(2):137-155. doi: 10.1002/ejhf.1369. Epub 2019 Jan 1. Eur J Heart Fail. 2019. PMID: 30600580 Review.
- [Russian Heart Failure Society, Russian Society of Cardiology. Russian Scientific Medical Society of Internal Medicine Guidelines for Heart failure: chronic (CHF) and acute decompensated (ADHF). Diagnosis, prevention and treatment]. Mareev VY, Fomin IV, Ageev FT, Begrambekova YL, Vasyuk YA, Garganeeva AA, Gendlin GE, Glezer MG, Gote SV, Dovzhenko TV, Kobalava ZD, Koziolova NA, Koroteev AV, Mareev YV, Ovchinnikov AG, Perepech NB, Tarlovskaya EI, CHesnikova AI, Shevchenko AO, Arutyunov GP, Belenkov YN, Galyavich AS, Gilyarevskiy SR, Drapkina OM, Duplyakov DV, Lopatin YM, Sitnikova MY, Skibitskiy VV, SHlyakhto EV. Mareev VY, et al. Kardiologiia. 2018 SJun;58 Suppl 6:1-164. Kardiologiia. 2018. PMID: 30081796 Russian. No abstract available.
- Review of the International Society for Heart and Lung Transplantation Practice guidelines for management of heart failure in children. Colan SD. Colan SD. Cardiol Young. 2015 Aug;25 Suppl 2:154-9. doi: 10.1017/S1047951115000955. Cardiol Young. 2015. PMID: 26377722 Review.
- Organization of heart failure management in European Society of Cardiology member countries: survey of the Heart Failure Association of the European Society of Cardiology in collaboration with the Heart Failure National Societies/Working Groups. Seferovic PM, Stoerk S, Filippatos G, Mareev V, Kavoliuniene A, Ristic AD, Ponikowski P, McMurray J, Maggioni A, Ruschitzka F, van Veldhuisen DJ, Coats A, Piepoli M, McDonagh T, Riley J, Hoes A, Pieske B, Dobric M, Papp Z, Mebazaa A, Parissis J, Ben Gal T, Vinereanu D, Brito D, Altenberger J, Gatzov P, Milinkovic I, Hradec J, Trochu JN, Amir O, Moura B, Lainscak M, Comin J, Wikström G, Anker S; Committee of National Heart Failure Societies or Working Groups of the Heart Failure Association of the European Society of Cardiology. Seferovic PM, et al. Eur J Heart Fail. 2013 Sep;15(9):947-59. doi: 10.1093/eurjhf/hft092. Epub 2013 Jun 19. Eur J Heart Fail. 2013. PMID: 23787723
- Search in MeSH
LinkOut - more resources
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Acute Coronary Syndromes
- Cardiac Surgery
- Heart Failure
- Heart Health
- Heart Rhythm
- Hypertension
- Interventional Cardiology
- Mitral Valve
- Pharmaceutics
- Structural Heart Disease
- Tricuspid Valve
- Vascular & Endovascular
- Chest Pain Guidelines
- Compensation
- Education & Training
- Patient Care
- Policy & Regulations
- Professional Associations
- Cardiac Imaging
- Informatics
- Nuclear Cardiology
- Remote Monitoring
- Experience Stories
- Webinars & Videos
Search form
1.6 million excess black deaths owed to inequities in cardiac care, jacc report card reveals.
![research reports in clinical cardiology The American College of Cardiology (ACC) this week published a report card on highlighting the excess cardiovascular mortality among Black Americans between 2000-2022.[1] The ACC said it highlights the "persistent and tragic inequities" in cardiovascular care and outlines the years of life lost to the Black community because of their higher cardiovascular disease death rates. #healthdisparities](https://cardiovascularbusiness.com/sites/default/files/styles/top_stories/public/2018-08/blackpatientpills.jpg.webp?itok=6GMknDiV)
The Journal of the American College of Cardiology (JACC) this week published a report card on the excess cardiovascular mortality among Black Americans between 2000-2022.[1] The ACC said it highlights the "persistent and tragic inequities" in cardiovascular care and outlines the years of life lost to the Black community because of higher cardiovascular disease death rates.
The report showed the Black population experienced 1.6 million excess deaths overall and millions of potential life-years lost. Heart disease was the leading cause of age-adjusted excess mortality among Black Americans. This includes deaths due to ischemic heart disease, hypertension, cerebrovascular disease and heart failure.
“Our study reveals that Black Americans, because of their higher cardiovascular mortality rates compared with white Americans, have suffered almost 800,000 excess deaths, which translates to about 24 million additional years of life lost between 2000 and 2022,” JACC incoming editor-in-chief Harlan M. Krumholz, MD , SM, FACC, who is also senior author of the study, said in a statement. “This staggering figure highlights the critical need for systemic changes in addressing cardiovascular inequities.”
Krumholz said the goal of the report card is to promote accountability and serve as a catalyst for action that addresses the ongoing problem.
“We are reminded of the stark reality that Black Americans continue to face significant disparities in cardiovascular outcomes,” explained Jennifer H. Mieres, MD , FACC, in an accompanying editorial.[2] She is the chair of the ACC Diversity and Inclusion Committee and senior vice president of the Center for Equity of Care at Northwell Health in New Hyde Park, New York. She said the report card serves as a reminder that all Americans have not benefited equally from significant advances made in the treatment and prevention of cardiovascular diseases.
“Bringing an equity lens to the redesign of CV health by addressing the social determinants of health and the systemic barriers that contribute to structural racism are critical for solving for cardiovascular health disparities and ensuring equity of care,” Mieres said.
Despite advancements in medicine, access to care has impacted the higher numbers of Black cardiovascular deaths
This report highlights persistent and significant racial disparities in cardiovascular disease outcomes between Black and white Americans. The key finding is that between 2000 and 2022, Black Americans had almost 800,000 excess age-adjusted deaths and 24 million excess years of potential life lost due to cardiovascular disease.
"Despite the triumphant reduction in cardiovascular morbidity and mortality over the last 50 years, those declines evolved at racially disproportionate rates resulting in not just health inequities, but life inequities. The disparities are evident across different subcategories, including ischemic heart disease, hypertension, cerebrovascular disease, and heart failure. Moreover, the sharp increases during the pandemic indicate the specific vulnerability of this group during a public health crisis and the need to mitigate this risk in future pandemics," the authors of the report wrote.
The ACC said in a statement the social determinants of health have a detrimental impact in creating barriers that prevent the most vulnerable Americans from receiving the cardiovascular care they need. The ACC has established multiple programs to address these inequities, including the Diversity and Inclusion Program . Its Internal Medicine Program introduces groups who have been historically underrepresented in cardiology to a career in cardiology by connecting them with the mentors, peer network and resources they need to understand career opportunities in the field.
The ACC Clinical Trials Research (CTR) program is also designed to increase the number of historically underrepresented minorities in cardiology to serve as leaders in cardiovascular clinical trials research to ensure diversity of thought, experience and perspective. The ACC also wants to ensure that the evidence base in studies includes data more closely reflecting the demographics of the actual cardiovascular patient population.
How the study was conducted
Krumholz and fellow researchers used the U.S. Centers for Disease Control and Prevention’s Wide-ranging ONline Data for Epidemiologic Research (WONDER) national death certificate data to collect primary cause of death stats in 5-year age groups from Black and white populations.
They calculated age-adjusted mortality rates (AAMR) for each disease condition by weighting the crude death rate by the fraction of individuals in that age group according to the 2000 population distribution. The excess AAMR was computed by subtracting the estimated AAMR of white people from the AAMR of Black people. Years of life lost (YPLL), defined as the number of years a person would have lived had they not died when they did, was estimated by multiplying the 5-year age group crude mortality rate by the life expectancy of white people for that age group, gender, and year. The excess YPLL was computed by subtracting the estimated YPLL of white people from the estimated YPLL of Black people.
Related Cardiac Health Disparities Content:
Cdc-funded program improved cardiovascular health of low-income nebraska women, rising amputation rates spark new pad initiative in miami, health disparities are causing serious harm, leading to 400 amputations per day, cardiologist details the many health disparities he encounters in rural mississippi, why health equity is important in cardiology, how cardiologists can address health disparities in their communities, aha president michelle albert on addressing health equity issues in cardiology, video: health equity and diversity is a business model.
References:
1. Adith S. Arun, Mitsuaki Sawano, Yuan Lu, Frederick Warner, César Caraballo, Rohan Khera, Melvin R. Echols, Clyde W. Yancy, and Harlan M. Krumholz. Excess Cardiovascular Mortality Among Black Americans 2000-2022: A JACC Report Card. J Am Coll Cardiol. Jun 18, 2024. Epublished DOI: 10.1016/j.jacc.2024.06.004.
2. Jennifer H. Mieres, Jeffrey T. Kuvin, and Robert O. Roswell. Cardiovascular Health, Juneteenth 2024: Are We Thriving Together or Not? J Am Coll Cardiol. Jun 18, 2024. Epublished DOI: 10.1016/j.jacc.2024.06.005.

Dave Fornell has covered healthcare for more than 17 years, with a focus in cardiology and radiology. Fornell is a 5-time winner of a Jesse H. Neal Award, the most prestigious editorial honors in the field of specialized journalism. The wins included best technical content, best use of social media and best COVID-19 coverage. Fornell was also a three-time Neal finalist for best range of work by a single author. He produces more than 100 editorial videos each year, most of them interviews with key opinion leaders in medicine. He also writes technical articles, covers key trends, conducts video hospital site visits, and is very involved with social media. E-mail: [email protected]
Related Content
Around the web.
Eleven medical societies have signed on to a consensus statement aimed at standardizing imaging for suspected cardiovascular infections.
Kate Hanneman, MD, explains why many vendors and hospitals want to lower radiology's impact on the environment. "Taking steps to reduce the carbon footprint in healthcare isn’t just an opportunity," she said. "It’s also a responsibility."
Philips introduced a new CT system at ECR aimed at the rapidly growing cardiac CT market, incorporating numerous AI features to optimize workflow and image quality.
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- Wunderkinds Nomination
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Millions fewer people may need statins, a new study suggests. But guidelines have yet to agree
By Elizabeth Cooney June 10, 2024

I t’s a familiar scene for patients during a routine primary care visit. The doctor scans blood test results, notes high cholesterol flagged by a standard calculator to assess risk of heart attack or stroke, then decides — and ideally discusses — whether to recommend taking a statin to cut the risk over time.
That conversation may happen less often if changes in the risk model presented by the American Heart Association in November translate into new guidelines for prescribing statins. Those guidelines haven’t been recalibrated yet, but a new analysis suggests that the new risk model could mean far fewer Americans — as many as 40% less than current calculators say — would be candidates for cholesterol-lowering drugs to prevent cardiovascular disease.
advertisement
To reach this conclusion, published Monday in a JAMA Internal Medicine study , researchers analyzed data from 3,785 adults who were 40 to 75 years old and took part in the National Health and Nutrition Examination Survey from January 2017 to March 2020. Their 10-year risk of artery-narrowing cardiovascular disease was computed using the AHA’s Predicting Risk of cardiovascular disease EVENTs (PREVENT) equations from 2023 and then compared to risk estimates using the previous tool from 2013, the Pooled Cohort Equations (PCE) on which current guidelines are based.
Those 2013 equations were widely criticized as overestimating risk . The 2023 version, drawing on billing and electronic health record data from a more diverse real-world population, incorporated current statin use as well as metabolic and kidney diseases.
Sign up for Morning Rounds
Understand how science, health policy, and medicine shape the world every day
Chiadi Ndumele, chair of the American Heart Association’s CKM Scientific Advisory Group, emphasized that the actual PREVENT risk thresholds for statin use in cardiovascular prevention will need to be decided in clinical guidelines, and that has not yet occurred. He also acknowledged criticism of the earlier risk model.
“We updated the AHA risk prediction model to PREVENT reflecting the growing influence of inter-related metabolic risk factors (obesity, diabetes, metabolic syndrome) and chronic kidney disease on cardiovascular disease risk,” Ndumele, director of obesity and cardiometabolic research at Johns Hopkins University, told STAT in an email. “It is therefore not surprising that the investigators found about twice the predicted event rate for the PCEs vs. PREVENT, reflecting this difference.”
Under the current guidelines, most people with a 10-year risk of 7.5% or more for developing cardiovascular disease are advised to take a statin, while at a 5% risk, they’re told only that they and their doctors should consider doing so.
“Analyses are underway,” Ndumele said. “Guidelines will have to consider whether and how to update recommendations to include PREVENT risk thresholds to guide clinical decision making.”
Related: Reversing progress, stroke rates are rising, especially in working-age adults
What’s changed in the JAMA Internal Medicine analysis is how many people might be at risk, based on the new components put into the calculator. Overall, 4% of people had a 10-year risk of developing cardiovascular disease, compared to the 8% previously predicted by the PCE. The number of adults recommended for statins could drop from 45.4 million to 28.3 million.
Race, now recognized as a social not biological construct, was excluded in the newer equations. That meant 5.1% of Black adults were computed to be at risk, compared to 10.9% from the previous calculator. For older adults ages 70 to 75, the proportion at risk was 10.2%, down from 22.8%.
In a paradox, the study found that while fewer people might be eligible for statins, which now can cost as little as $40 a year, the estimates also say most people who would be advised to take them aren’t doing so.
“The prior risk equations and the PREVENT equations that we focus on in this study really seek to give doctors and patients sort of a starting percentage to say, is it worth having a conversation about statins?” lead study author Timothy Anderson, a primary care physician and an assistant professor of medicine at University of Pittsburgh Medical Center, told STAT. “When we’re seeing risk rates cut in half, I think that really is something that’s likely to impact how doctors and patients talk about these meds.”
The biggest predictor of risk remains age, Anderson said. “If you’re a borderline risk now, you’re likely to be higher risk in five years. And that’s a complicated set of conversations for primary care doctors and patients to have.”
That concerns Steven Nissen, a cardiologist at the Cleveland Clinic, who was not part of the study. “Age is the most powerful factor in the calculators, so if you wait until somebody is 60 or 65, you’re playing catch-up,” he said. “I tend to lean toward treating rather than not treating when it’s a borderline case, but only when the patient and I have a conversation.”
Nissen has been leading an effort in collaboration with AstraZeneca to make the 5-milligram dose of its drug, rosuvastatin, available without a prescription. He urged shared decision-making between doctor and patient, aware that busy primary care physicians may be pressed for time.
“Good medicine involves judgment. And the calculator is not a replacement for good medical judgment, which may come to a different conclusion,” he said. “I’m not very supportive of either calculator because I think that in general, it’s good to have a lower LDL,” or “bad” cholesterol.
There are a multitude of factors affecting cardiovascular health, and statins are just one piece, said Gregg Fonarow, chief of cardiology at UCLA, citing the AHA’s recent projection that 61% of the U.S. population will likely have cardiovascular disease. He did not take part in the current study.
Related: Decline in heart failure deaths has been undone, led by people under 45
“So many cardiovascular events are preventable, not just through medication but through lifestyle modification. We need to do such a better job with prevention,” Fonarow said. “This really represents an opportunity to use the new enhanced PREVENT risk score and better inform individuals of risk, but importantly, not just for 10-year risk, but their lifelong risk for disease.”
Ndumele said PREVENT will help guide use of preventive therapies beyond statins, relevant for people with cardiovascular-kidney-metabolic syndrome, a disorder in which metabolic risk factors, chronic kidney disease, and the cardiovascular system interact to cause multi-organ dysfunction and poor cardiovascular outcomes.
“I think the challenge with this paper is the assumption that the same threshold will be used for the recommendation of statin use,” Ndumele said. “Risk estimates from PREVENT are much closer to what is observed in reality than they were for PCEs, but there is need for discussion about the optimal risk threshold for preventive statin use in guidelines.”
Nissen said any changes should be thought through carefully, with this caveat: “The take-home message is that any of these calculators are the best guess about risk,” he said, “but the decision to treat is different from simply calculating a risk.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies . Our financial supporters are not involved in any decisions about our journalism.
About the Author Reprints
Elizabeth cooney.
Cardiovascular Disease Reporter
Elizabeth Cooney is a cardiovascular disease reporter at STAT, covering heart, stroke, and metabolic conditions.
cardiovascular disease
public health
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

STAT Plus: The CEO of Kaiser’s new health network shares why he’s making a bet on a tiny North Carolina hospital system

STAT Plus: Jury orders Stanford to pay millions to employee in racial harassment case

STAT Plus: A primer on HELIOS-B, an enormous stock-moving event for Alnylam Pharmaceuticals

STAT Plus: Top FDA official Peter Marks overruled staff, review team to approve Sarepta gene therapy

STAT Plus: Why a big California employer ditched Elevance for some of its health plans
- UTHealth Houston

Kiran K. Mallula, MD, MS
- Associate Professor, Pediatric Cardiology
- Director, Cardiac Catheterization Laboratories
- Education & Training
Areas of Interest
Publications, memberships.
Languages Spoken: English, Hindi, Telugu, Sanskrit
Clinical Interests
Hybrid/fusion imaging
Transcatheter valve therapies
Interventional MRI
Research Interests
Principal Investigator, Utility of ECHOPIXEL 3D viewer in procedural planning
Principal investigator, Transcatheter Fontan fenestration in children: A multicenter experience.
McPeters R, Chicarelli E, Manning D, Mallula KK , Krulisky J. Case of bronchopulmonary sequestration in a newborn
Krulisky J, Siwik E, Mallula KK . Comparative outcomes of transcatheter closure of secundum ASDs with the ASO and GSO devices: A single center experience.
Mallula KK , Patel S, Avula S, Sernich S, Pettitt T, Siwik ES. Utility of a hybrid approach for Post-Fontan reinterventions: Case series and current review of literature.
Participation in A Prospective Data Registry for the Congenital Cardiovascular Interventional Study Consortium: Risk Stratification for Cardiac Catheterization Procedures
Uppu SC, Chandrasekaran S, Mallula KK. Constrictive pericarditis in a patient with sinus venosus atrial septal defect and anomalous right upper pulmonary venous return. Ann Pediatr Cardiol 2009;2(1):87-8.
Mallula K , Amin Z. Recent changes in instructions for use for the Amplatzer atrial septal defect occluder: How to incorporate these changes while using transesophageal echocardiography or intracardiac echocardiography? Pediatr Cardiol 2012;33(7):995-1000.
Mallula KK . et. al. Sinus venosus atrial septal defect: Postoperative outcomes after repair http://search.proquest.com/docview/1026799439
Ghawi H, Gendi S, Mallula K , Zghouzi M, Faza N, Awad S. Fetal left and right ventricle myocardial performance index: Defining normal values for the second and third trimesters – single tertiary center experience. Pediatr Cardiol 2013;34(8):1808-15.
Mallula K , Patel N, Amin Z. New design of the amplatzer membranous VSD occluder: A step forward? Pediatr Cardiol 2013;34(8):2068-72.
Mallula KK , Patel ND, Hijazi ZM, Joshi S, Naheed Z. Double-outlet right ventricle with an intact ventricular septum: A unique stage 1 palliation. Pediatr Cardiol 2013;34(8):2086-8
Mallula KK , Sosnowski C, Awad S. Spectrum of Cantrell’s pentalogy: Case series from a single tertiary care center and review of the literature. Pediatr Cardiol 2013;34(7):1703-10
Severin PN, Awad S, Shields B, Hoffman J, Bonney W, Cortez E, Ganesan R, Patel A, Barnes S, Al-Anani S, Mallula K , et. al. The pediatric cardiology pharmacopeia: 2013 update. Pediatr Cardiol 2013;34(1):1-29.
Mallula KK , Gupta U, Hasbani K. A rare case of Cardiac Aspergilloma diagnosed by cardiac MRI. Case of the week Number 14-02. Society of Cardiovascular Magnetic Resonance http://scmr.org/caseoftheweek/2014/6994.html#.Uw0kiLTiZRk (2/2014)
Patel ND, Mallulla KK , Abdulla RI. Atrial flutter demonstrated by M-mode echocardiography. Pediatr Cardiol 2014;35(5):893-5.
Mallula K , Vaughn G, El-Said H, Lamberti JJ, Moore JW. Comparison of ductal stenting versus surgical shunts for palliation of patients with pulmonary atresia and intact ventricular septum. Catheter Cardiovasc Interv 2015;85(7):1196-202
Mallula KK , Kenny D, Hijazi ZM. Transjugular melody valve placement in a small child with protein losing enteropathy. Catheter Cardiovasc Interv 2015;85(2):267-7
Mallula KK , Patel ND, Abdulla RI, Bokowski JW. Tetralogy of fallot with left superior vena cava and coronary sinus atrial septal defect: a rare association. Pediatr Cardiol 2015;36(5):1100-1
Vaughn GR, Moore JW, Mallula KK, Lamberti JJ, El-Said HG. Transcatheter stenting of the systemic-to-pulmonary artery shunt: A 7-year experience from a single tertiary center. Catheter Cardiovasc Interv 2015
Guillot M, Ascuitto R, Ross-Ascuitto N, Mallula KK, Siwik E. Computational fluid dynamics as a complementary study for transcatheter endovascular stent implantation for recoarctation of the aorta associated with minimal pressure drop: An aneurysmal ductal ampulla with aortic isthmus narrowing, Cardiol Young. 2019 Jun; 29(6):768-776.
Krulisky J, Mallula KK. Transcatheter exclusion of a large RVOT aneurysm in a systemic right ventricle. Journal of American College of Cardiology: Case Reports (In press, March 2020)
Guruchandrasekar S, Mallula KK , Siwik ES. Endovascular repair of thoracic aortic pseudoaneurysms in children. Journal of American College of Cardiology: Case Reports (In Press, April 2020)
Non-refereed
Lilje C, Mallula KK , Ward K, Congeni J. A teenager with shortness of breath and headaches. Consultant360:volume 15(7), July 2016. https://www.consultant360.com/articles/teenager-history-shortness-breath-and-headaches
Book Chapters:
Mallula KK , Kenny D, Hijazi Z. Tricuspid valve insufficiency: SAPIEN valve in the tricuspid position. Structural, Valvular and Congenital Heart Disease Interventions, 2nd Edition (Horst Sievert, Shakeel A. Qureshi, Neil Wilson, Ziyad M. Hijazi, eds), October 2012
Mallula KK , Amin Z. Pulmonary atresia with intact ventricular septum. Atlas of Neonatal Cardiology, 1st edition, July 2013
Mallula KK , Amin Z. Hybrid closure of Muscular Ventricular Septal Defects. Chapter in Fetal and Hybrid Procedures in Congenital Heart diseases, 1st edition, November 2015
Book Reviews:
Mallula KK , Hijazi, Z. iBook Review, The Illustrated Field Guide to Congenital Heart Disease and Repair, 3rd Edition. Congenital Cardiology Today, August 2013.
2014 Medium to longer term outcomes of percutaneous transcatheter closure of congenital ventricular septal defects. Oral presentation at PICS-AICS 2013, Miami, FL. https://youtu.be/_hWFK2zGDpc?t=4412
2015 Ductal stenting: Is it time to redefine the palliative strategy in patients with pulmonary atresia with intact ventricular septum and critical pulmonary stenosis? Oral presentation at PICS-AICS 2014, Chicago, IL. https://youtu.be/awfuFwmNdls?t=4681
2015 Update on 2014 live cases, PICS-AICS 2015, Las Vegas, NV. https://youtu.be/Y4ZKGIKSeBM
2017 Live Cases Update, PICS-AICS 2017, Miami, FL. https://youtu.be/pV8faM-FIWQ?t=81
Electronic and Multi-Media:
01/16 https://www.medtronic.com/physicianlocator/googleMaps/showResults?therapy=47&locationRadio=allUS&searchByFilterName=zipCode&zipOrCityRadius=50&searchByFilterValue=77584
08/18 https://www.chnola.org/blog/2018/august/understanding-heart-failure-in-children/ Blog from Children’s Hospital for parents with kids with heart failure.
10/18 https://childrensconnection.blog/2018/10/11/fixing-broken-hearts-with-cardiac-catheterization/ Blog from Children’s Hospital related to anticipatory guidance for parents with kids who need a catheterization procedure.
02/19 https://www.wdsu.com/article/heart-surgery-saves-8-month-old-babys-life/26112715 Local news report about the care provided by the Heart team at Children’s Hospital to treat a Honduran child.
Fellow, SCAI
Fellow, PICS
Fellow, AAP
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies

IMAGES
VIDEO
COMMENTS
Journal overview. Research Reports in Clinical Cardiology publishes evidence-based original research, reports, editorials, perspectives, reviews and commentaries covering the following topics: Emphasis is placed upon translation of important basic research, updated information about classical topics, scholarly discussions of controversial ...
Clinical Application of PINK1 and ACSL4 Protein Levels in the Acute Myocardial Infarction Patients and Prognosis Evaluation After PCI. Ao W, Duan P, Luo P, Xiang D, Wang Q, Ren Y, He Q. Research Reports in Clinical Cardiology 2024, 15:45-53. Published Date: 4 June 2024.
Research Reports in Clinical Cardiology, Volume 15, Issue (2024) See all volumes and issues. Volume 15, 2024 Vol 14, 2023 Vol 13, 2022 Vol 12, 2021 Vol 11, 2020 Vol 10, 2019 Vol 9, 2018 Vol 8, 2017 Vol 7, 2016 Vol 6, 2015 Vol 5, 2014 Vol 4, 2013 Vol 3, 2012 Vol 2, 2011 Vol 1, 2010. Select to download all citations or PDFs.
Research Reports in Clinical Cardiology, Volume 12, Issue (2021) See all volumes and issues. Vol 15, 2024 Vol 14, 2023 Vol 13, 2022 Volume 12, 2021 Vol 11, 2020 Vol 10, 2019 Vol 9, 2018 Vol 8, 2017 Vol 7, 2016 Vol 6, 2015 Vol 5, 2014 Vol 4, 2013 Vol 3, 2012 Vol 2, 2011 Vol 1, 2010. Download citations Download PDFs Download issue.
Dr Richard Kones. Editor in Chief. Dr Kones. Department of Cardiology, Cardiometabolic Research Institute, Houston, TX, USA. Richard Kones MD began as a mathematically inclined chemical engineer, and then attended NYU School of Medicine in a special pilot program. Inspired by a mentor in the Physiology department, he conducted independent ...
A peer-reviewed, open access journal in cardiovascular diseases, heart disease & cardiology. This website uses cookies to ensure you get the best experience. ... Research Reports in Clinical Cardiology 1179-8475 (Online) Website ISSN Portal About ...
Publishes open access research on cardiovascular diseases and prevention, arrythmia, heart failure, adult congenital disease, methodologies and treatment. ... Research Reports in Clinical Cardiology Research Reports in Clinical Cardiology Search in: Advanced search Citation search.
Research Reports in Clinical Cardiology 2022, 13:1-7. Published Date: 13 January 2022. An international, peer-reviewed, open access, online journal publishing original research, reports, editorials, reviews and commentaries on all aspects of cardiology in the clinic and laboratory.
Overview. Clinical Research in Cardiology is an international journal dedicated to clinical cardiovascular research. Publishes articles from the field of clinical cardiology, angiology, heart and vascular surgery, and provides a current and competent overview on the diagnosis and therapy of heart and vascular diseases.
JAMA Cardiology Clinical Challenge. has active quiz. Matthew G. Peters, MD; et al. ... and Policy Promoting EDI in Genetics Research PTSD and Cardiovascular Disease Red Blood Cell Transfusion: 2023 AABB International Guidelines Reimagining Children's Rights in the US Spirituality in Serious Illness and Health The US Medicaid Program: Coverage ...
Introduction: The findings of many new cardiology clinical trials over the last year have been published or presented at major international meetings. This paper aims to describe and place in context a summary of the key clinical trials in cardiology presented between January and December 2016. Methods: The authors reviewed clinical trials ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on CLINICAL CARDIOLOGY. Find methods information, sources, references or conduct a literature review on ...
Research Reports in Clinical Cardiology | Read 153 articles with impact on ResearchGate, the professional network for scientists. Published by Dove Medical Press Online ISSN: 1179-8475
1 Clinical Research Center, Laval University, Quebec Heart and Lung Institute, 2725, chemin Ste-Foy, Quebec City, Qc, GIV 4G5, Canada. [email protected]. ... This analysis reports on the total cardiovascular or fatal events in the REWIND participants METHODS: We compared the total incidence of MACE or non-cardiovascular deaths ...
Phase II clinical research design in cardiology: learning the right lessons too well: observations and recommendations from the Cardiovascular Cell Therapy Research Network (CCTRN) Circulation . 2013 Apr 16;127(15):1630-5. doi: 10.1161/CIRCULATIONAHA.112.000779.
Aims and scope. Clinical Cardiology Research and Reports (CCRR) is a Peer-reviewed, Open Access journal that publishes original research articles, review articles, and clinical studies that focus on the diagnosis and treatment of cardiovascular disease. The journal welcomes submissions related to systemic hypertension, arrhythmia, congestive ...
Research Reports in Clinical Cardiology, Volume 13, Issue (2022) Browse this journal. Current issue; List of issues; Most read articles; Research Reports in Clinical Cardiology, Volume 13, Issue (2022) See all volumes and issues. Volume 13, 2022. Select to download all citations or PDFs.
7 Cardiovascular Research, Departments of Genetics, Pharmacology and Physiopathology of Heart, Blood Vessels and ... controls. If these findings are confirmed in larger studies, this easy to perform maneuver may serve as an effective clinical diagnostic test for CRDS and become an important part of the evaluation of cardiac arrest. Editor's ...
Research Reports in Clinical Cardiology publishes evidence-based original research, reports, editorials, perspectives, reviews and commentaries covering the following topics: • prevention • metabolic disorders influencing cardiac risk • coronary heart disease • arrhythmias and pacing • heart failure • cardiomyopathies • methodologies • treatment • percutaneous and invasive ...
The Russian Acute Coronary Syndrome Registry (RusACSR) is a retrospective, continuous, nationwide, Web‐based registry of patients with acute coronary syndromes (ACS).The RusACSR is a database that uses a secure Web‐based interface for data entry by individual users. Participation in the RusACSR is voluntary. Any clinical center that provides health care to ACS patients can take part in the ...
A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105 , 539-542 (2002).
Keep up to date with the latest research, clinical reviews, and opinions. [Skip to Navigation] Our website uses cookies to enhance your experience. ... and Policy Promoting EDI in Genetics Research PTSD and Cardiovascular Disease Red Blood Cell Transfusion: 2023 AABB International Guidelines Reimagining Children's Rights in the US ...
DALLAS - June 22, 2024 - A weekly dose of semaglutide 2.4 mg significantly reduced the risk of major adverse cardiovascular events (MACEs) in people with overweight or obesity and cardiovascular disease but not diabetes, regardless of blood sugar level, according to a clinical trial including researchers from UT Southwestern Medical Center. The findings, published in Diabetes Care, also ...
This Research Topic is the third volume of 'Case Reports in Cardio-Oncology'. Please see the previous volume here.This Research Topic aims to collect all the Case Reports submitted to the Cardio-Oncology section. If submitted directly to this collection the paper will be personally assessed by a Senior Associate Editor before the beginning of the peer-review process.
13 Scientific Medical Research Center of Cardiology, Moscow, Russia. 14 Privolzhsky Research Medical University of the Ministry of Health of the Russia, Nizhny Novgorod, ... and the Russian Heart Failure Society. The event was devoted to the discussion of the correct use of research data of "real clinical practice" in decision making. MeSH terms
The Journal of the American College of Cardiology (JACC) this week published a report card on the excess cardiovascular mortality among Black Americans between 2000-2022.[1] The ACC said it highlights the "persistent and tragic inequities" in cardiovascular care and outlines the years of life lost to the Black community because of higher cardiovascular disease death rates.
Browse the list of issues and latest articles from Research Reports in Clinical Cardiology. Volume 13 2022.
One report looks at the projected increase in cardiovascular disease rates in the decades ahead, while the other projects their total related costs. "The landscape of cardiovascular disease in the U.S. is seeing the arrival of a near-perfect storm," Dr. Dhruv S. Kazi, vice chair of the advisory writing group, said in a news release. Kazi is ...
There are a multitude of factors affecting cardiovascular health, and statins are just one piece, said Gregg Fonarow, chief of cardiology at UCLA, citing the AHA's recent projection that 61% of ...
Master of Science (Clinical Research) RUSH University, Chicago, Illinois Fellowship in Pediatric Cardiology ... Journal of American College of Cardiology: Case Reports (In Press, April 2020) Non-refereed. Lilje C, Mallula KK, Ward K, Congeni J. A teenager with shortness of breath and headaches. Consultant360:volume 15(7), July 2016. https://www ...