Essay on Cancer for Students and Children
500+ words essay on cancer.
Cancer might just be one of the most feared and dreaded diseases. Globally, cancer is responsible for the death of nearly 9.5 million people in 2018. It is the second leading cause of death as per the world health organization. As per studies, in India, we see 1300 deaths due to cancer every day. These statistics are truly astonishing and scary. In the recent few decades, the number of cancer has been increasingly on the rise. So let us take a look at the meaning, causes, and types of cancer in this essay on cancer.
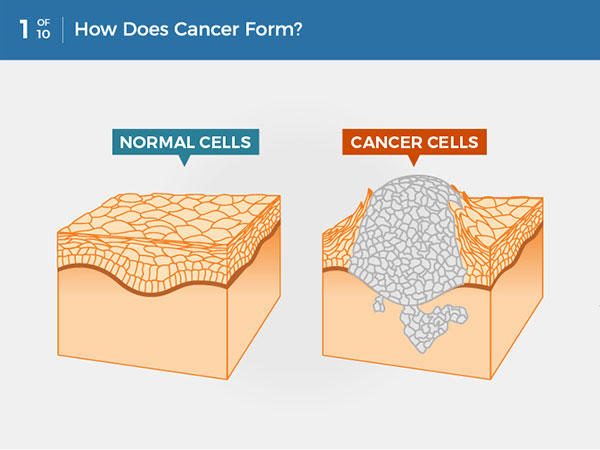
Cancer comes in many forms and types. Cancer is the collective name given to the disease where certain cells of the person’s body start dividing continuously, refusing to stop. These extra cells form when none are needed and they spread into the surrounding tissues and can even form malignant tumors. Cells may break away from such tumors and go and form tumors in other places of the patient’s body.


Types of Cancers
As we know, cancer can actually affect any part or organ of the human body. We all have come across various types of cancer – lung, blood, pancreas, stomach, skin, and so many others. Biologically, however, cancer can be divided into five types specifically – carcinoma, sarcoma, melanoma, lymphoma, leukemia.
Among these, carcinomas are the most diagnosed type. These cancers originate in organs or glands such as lungs, stomach, pancreas, breast, etc. Leukemia is the cancer of the blood, and this does not form any tumors. Sarcomas start in the muscles, bones, tissues or other connective tissues of the body. Lymphomas are the cancer of the white blood cells, i.e. the lymphocytes. And finally, melanoma is when cancer arises in the pigment of the skin.
Get the huge list of more than 500 Essay Topics and Ideas
Causes of Cancer
In most cases, we can never attribute the cause of any cancer to one single factor. The main thing that causes cancer is a substance we know as carcinogens. But how these develop or enters a person’s body will depend on many factors. We can divide the main factors into the following types – biological factors, physical factors, and lifestyle-related factors.
Biological factors involve internal factors such as age, gender, genes, hereditary factors, blood type, skin type, etc. Physical factors refer to environmental exposure of any king to say X-rays, gamma rays, etc. Ad finally lifestyle-related factors refer to substances that introduced carcinogens into our body. These include tobacco, UV radiation, alcohol. smoke, etc. Next, in this essay on cancer lets learn about how we can treat cancer.
Treatment of Cancer
Early diagnosis and immediate medical care in cancer are of utmost importance. When diagnosed in the early stages, then the treatment becomes easier and has more chances of success. The three most common treatment plans are either surgery, radiation therapy or chemotherapy.
If there is a benign tumor, then surgery is performed to remove the mass from the body, hence removing cancer from the body. In radiation therapy, we use radiation (rays) to specially target and kill the cancer cells. Chemotherapy is similar, where we inject the patient with drugs that target and kill the cancer cells. All treatment plans, however, have various side-effects. And aftercare is one of the most important aspects of cancer treatment.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

What Is Cancer?
Get email updates from NCI on cancer health information, news, and other topics
Get email updates from NCI
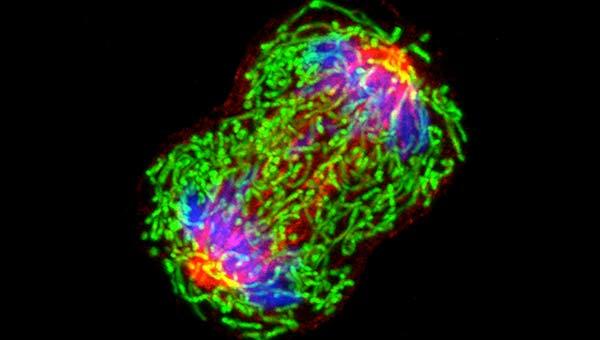
A dividing breast cancer cell.
The Definition of Cancer
Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body.
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
Sometimes this orderly process breaks down, and abnormal or damaged cells grow and multiply when they shouldn’t. These cells may form tumors, which are lumps of tissue. Tumors can be cancerous or not cancerous ( benign ).
Cancerous tumors spread into, or invade, nearby tissues and can travel to distant places in the body to form new tumors (a process called metastasis ). Cancerous tumors may also be called malignant tumors. Many cancers form solid tumors, but cancers of the blood, such as leukemias , generally do not.
Benign tumors do not spread into, or invade, nearby tissues. When removed, benign tumors usually don’t grow back, whereas cancerous tumors sometimes do. Benign tumors can sometimes be quite large, however. Some can cause serious symptoms or be life threatening, such as benign tumors in the brain.
Differences between Cancer Cells and Normal Cells
Cancer cells differ from normal cells in many ways. For instance, cancer cells:
- grow in the absence of signals telling them to grow. Normal cells only grow when they receive such signals.
- ignore signals that normally tell cells to stop dividing or to die (a process known as programmed cell death , or apoptosis ).
- invade into nearby areas and spread to other areas of the body. Normal cells stop growing when they encounter other cells, and most normal cells do not move around the body.
- tell blood vessels to grow toward tumors. These blood vessels supply tumors with oxygen and nutrients and remove waste products from tumors.
- hide from the immune system . The immune system normally eliminates damaged or abnormal cells.
- trick the immune system into helping cancer cells stay alive and grow. For instance, some cancer cells convince immune cells to protect the tumor instead of attacking it.
- accumulate multiple changes in their chromosomes , such as duplications and deletions of chromosome parts. Some cancer cells have double the normal number of chromosomes.
- rely on different kinds of nutrients than normal cells. In addition, some cancer cells make energy from nutrients in a different way than most normal cells. This lets cancer cells grow more quickly.
Many times, cancer cells rely so heavily on these abnormal behaviors that they can’t survive without them. Researchers have taken advantage of this fact, developing therapies that target the abnormal features of cancer cells. For example, some cancer therapies prevent blood vessels from growing toward tumors , essentially starving the tumor of needed nutrients.
How Does Cancer Develop?
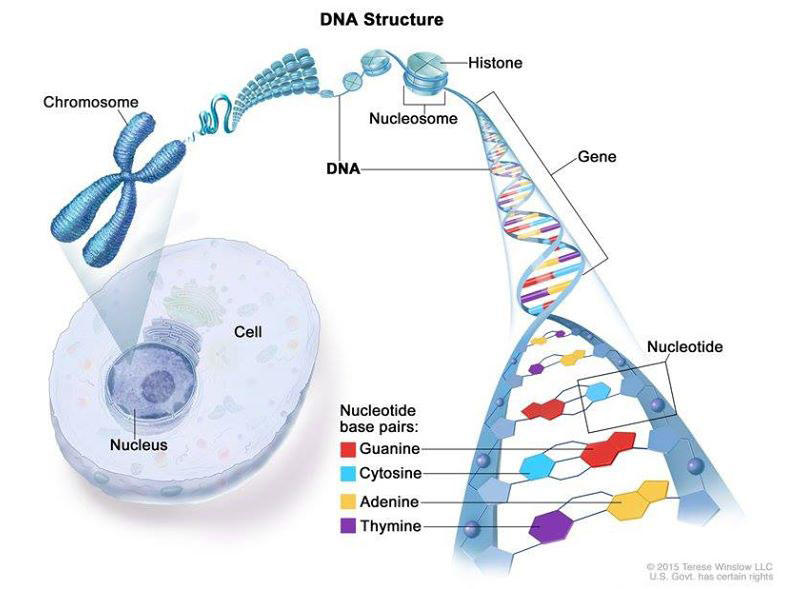
Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes.
Cancer is a genetic disease—that is, it is caused by changes to genes that control the way our cells function, especially how they grow and divide.
Genetic changes that cause cancer can happen because:
- of errors that occur as cells divide.
- of damage to DNA caused by harmful substances in the environment, such as the chemicals in tobacco smoke and ultraviolet rays from the sun. (Our Cancer Causes and Prevention section has more information.)
- they were inherited from our parents.
The body normally eliminates cells with damaged DNA before they turn cancerous. But the body’s ability to do so goes down as we age. This is part of the reason why there is a higher risk of cancer later in life.
Each person’s cancer has a unique combination of genetic changes. As the cancer continues to grow, additional changes will occur. Even within the same tumor, different cells may have different genetic changes.
Fundamentals of Cancer
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues.
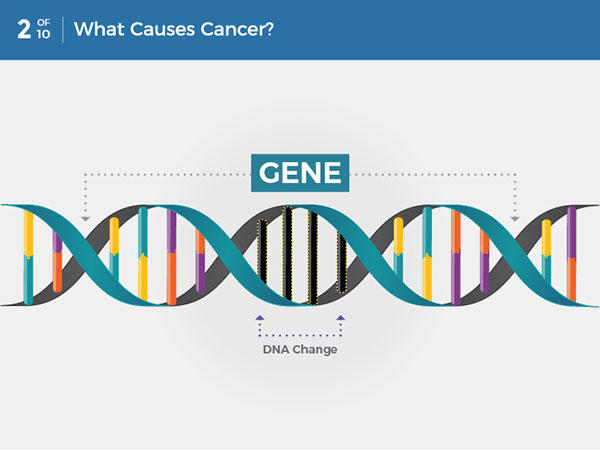
Cancer is caused by changes to DNA. Most cancer-causing DNA changes occur in sections of DNA called genes. These changes are also called genetic changes.
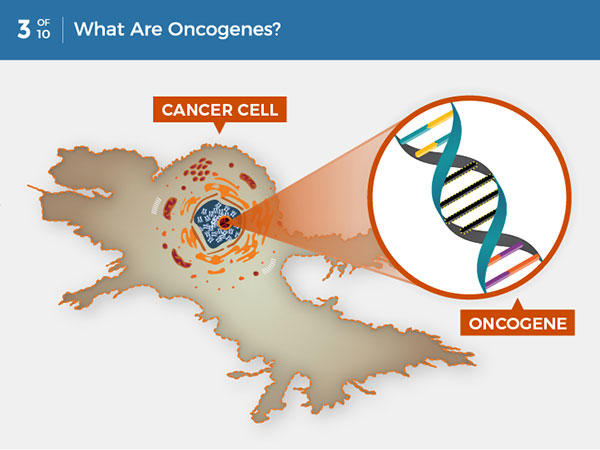
A DNA change can cause genes involved in normal cell growth to become oncogenes. Unlike normal genes, oncogenes cannot be turned off, so they cause uncontrolled cell growth.
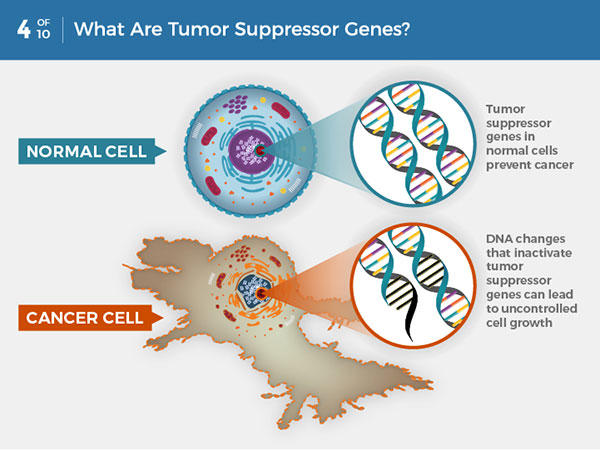
In normal cells, tumor suppressor genes prevent cancer by slowing or stopping cell growth. DNA changes that inactivate tumor suppressor genes can lead to uncontrolled cell growth and cancer.
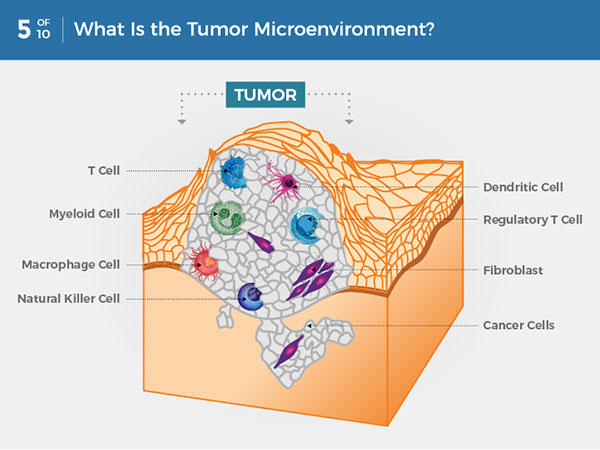
Within a tumor, cancer cells are surrounded by a variety of immune cells, fibroblasts, molecules, and blood vessels—what’s known as the tumor microenvironment. Cancer cells can change the microenvironment, which in turn can affect how cancer grows and spreads.
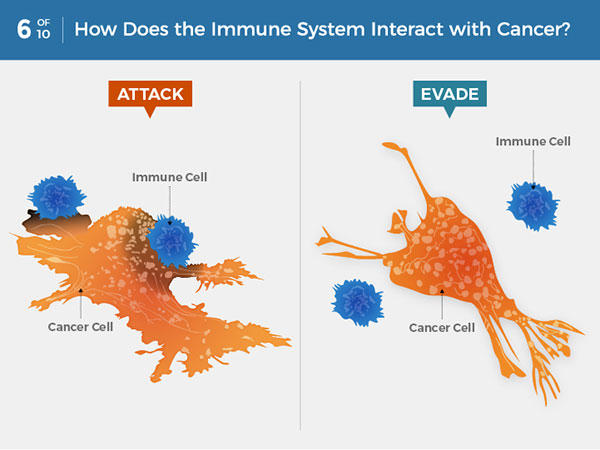
Immune system cells can detect and attack cancer cells. But some cancer cells can avoid detection or thwart an attack. Some cancer treatments can help the immune system better detect and kill cancer cells.
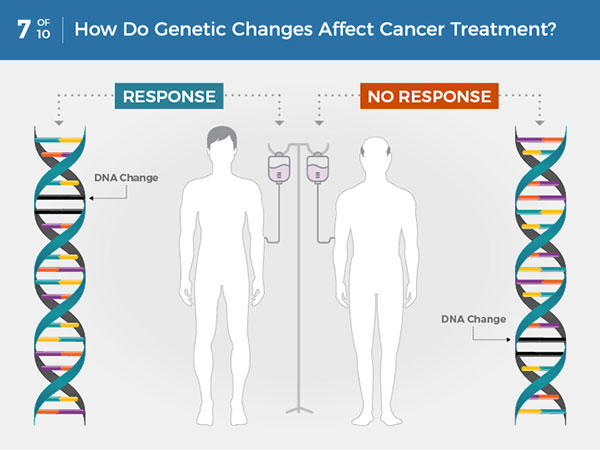
Each person’s cancer has a unique combination of genetic changes. Specific genetic changes may make a person’s cancer more or less likely to respond to certain treatments.
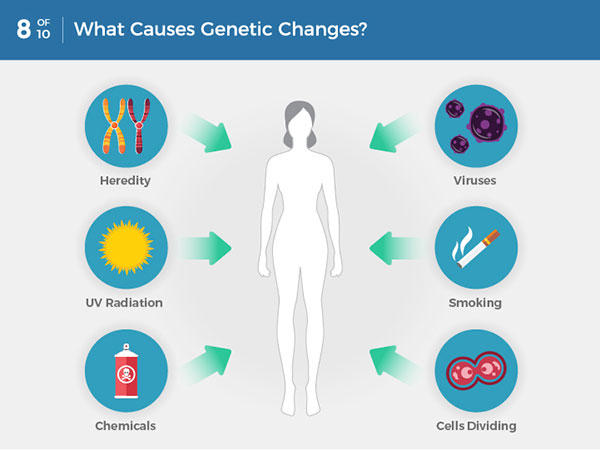
Genetic changes that cause cancer can be inherited or arise from certain environmental exposures. Genetic changes can also happen because of errors that occur as cells divide.
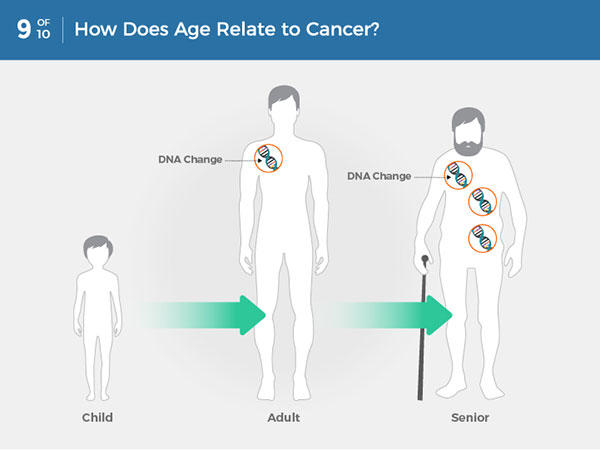
Most often, cancer-causing genetic changes accumulate slowly as a person ages, leading to a higher risk of cancer later in life.
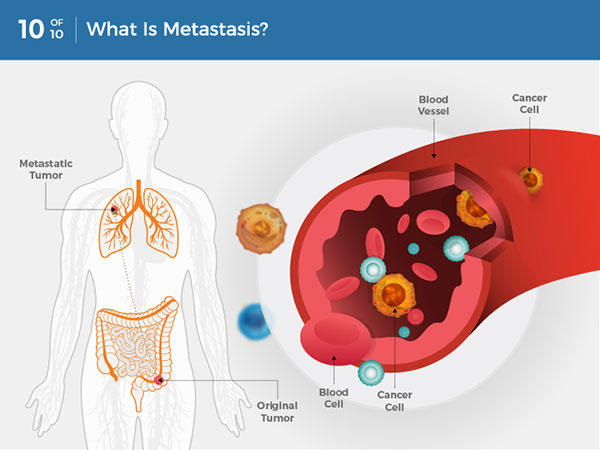
Cancer cells can break away from the original tumor and travel through the blood or lymph system to distant locations in the body, where they exit the vessels to form additional tumors. This is called metastasis.
Types of Genes that Cause Cancer
The genetic changes that contribute to cancer tend to affect three main types of genes— proto-oncogenes , tumor suppressor genes , and DNA repair genes. These changes are sometimes called “drivers” of cancer.
Proto-oncogenes are involved in normal cell growth and division. However, when these genes are altered in certain ways or are more active than normal, they may become cancer-causing genes (or oncogenes), allowing cells to grow and survive when they should not.
Tumor suppressor genes are also involved in controlling cell growth and division. Cells with certain alterations in tumor suppressor genes may divide in an uncontrolled manner.
DNA repair genes are involved in fixing damaged DNA. Cells with mutations in these genes tend to develop additional mutations in other genes and changes in their chromosomes, such as duplications and deletions of chromosome parts. Together, these mutations may cause the cells to become cancerous.
As scientists have learned more about the molecular changes that lead to cancer, they have found that certain mutations commonly occur in many types of cancer. Now there are many cancer treatments available that target gene mutations found in cancer . A few of these treatments can be used by anyone with a cancer that has the targeted mutation, no matter where the cancer started growing .
When Cancer Spreads
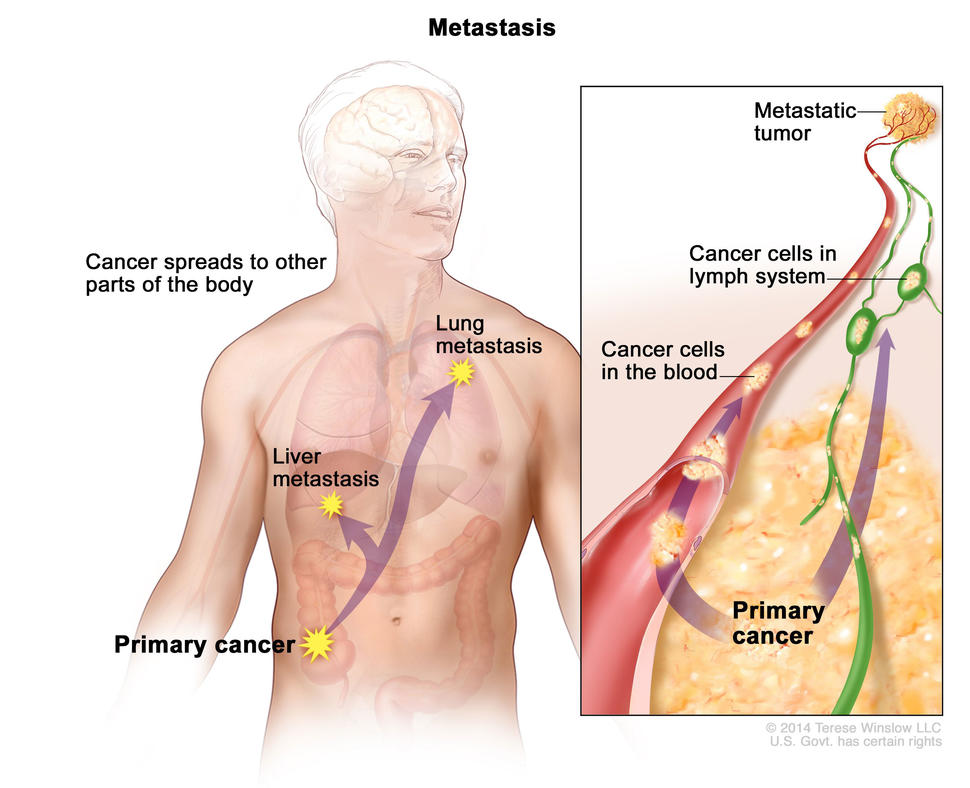
In metastasis, cancer cells break away from where they first formed and form new tumors in other parts of the body.
A cancer that has spread from the place where it first formed to another place in the body is called metastatic cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
Metastatic cancer has the same name and the same type of cancer cells as the original, or primary, cancer. For example, breast cancer that forms a metastatic tumor in the lung is metastatic breast cancer, not lung cancer.
Under a microscope, metastatic cancer cells generally look the same as cells of the original cancer. Moreover, metastatic cancer cells and cells of the original cancer usually have some molecular features in common, such as the presence of specific chromosome changes.
In some cases, treatment may help prolong the lives of people with metastatic cancer. In other cases, the primary goal of treatment for metastatic cancer is to control the growth of the cancer or to relieve symptoms it is causing. Metastatic tumors can cause severe damage to how the body functions, and most people who die of cancer die of metastatic disease.
Tissue Changes that Are Not Cancer
Not every change in the body’s tissues is cancer. Some tissue changes may develop into cancer if they are not treated, however. Here are some examples of tissue changes that are not cancer but, in some cases, are monitored because they could become cancer:
- Hyperplasia occurs when cells within a tissue multiply faster than normal and extra cells build up. However, the cells and the way the tissue is organized still look normal under a microscope. Hyperplasia can be caused by several factors or conditions, including chronic irritation.
- Dysplasia is a more advanced condition than hyperplasia. In dysplasia, there is also a buildup of extra cells. But the cells look abnormal and there are changes in how the tissue is organized. In general, the more abnormal the cells and tissue look, the greater the chance that cancer will form. Some types of dysplasia may need to be monitored or treated, but others do not. An example of dysplasia is an abnormal mole (called a dysplastic nevus ) that forms on the skin. A dysplastic nevus can turn into melanoma, although most do not.
- Carcinoma in situ is an even more advanced condition. Although it is sometimes called stage 0 cancer, it is not cancer because the abnormal cells do not invade nearby tissue the way that cancer cells do. But because some carcinomas in situ may become cancer, they are usually treated.
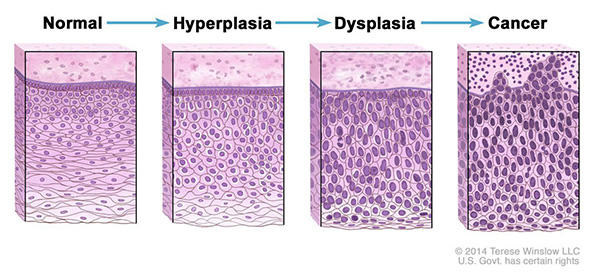
Normal cells may become cancer cells. Before cancer cells form in tissues of the body, the cells go through abnormal changes called hyperplasia and dysplasia. In hyperplasia, there is an increase in the number of cells in an organ or tissue that appear normal under a microscope. In dysplasia, the cells look abnormal under a microscope but are not cancer. Hyperplasia and dysplasia may or may not become cancer.
Types of Cancer
There are more than 100 types of cancer. Types of cancer are usually named for the organs or tissues where the cancers form. For example, lung cancer starts in the lung, and brain cancer starts in the brain. Cancers also may be described by the type of cell that formed them, such as an epithelial cell or a squamous cell .
You can search NCI’s website for information on specific types of cancer based on the cancer’s location in the body or by using our A to Z List of Cancers . We also have information on childhood cancers and cancers in adolescents and young adults .
Here are some categories of cancers that begin in specific types of cells:
Carcinomas are the most common type of cancer. They are formed by epithelial cells, which are the cells that cover the inside and outside surfaces of the body. There are many types of epithelial cells, which often have a column-like shape when viewed under a microscope.
Carcinomas that begin in different epithelial cell types have specific names:
Adenocarcinoma is a cancer that forms in epithelial cells that produce fluids or mucus. Tissues with this type of epithelial cell are sometimes called glandular tissues. Most cancers of the breast, colon, and prostate are adenocarcinomas.
Basal cell carcinoma is a cancer that begins in the lower or basal (base) layer of the epidermis, which is a person’s outer layer of skin.
Squamous cell carcinoma is a cancer that forms in squamous cells, which are epithelial cells that lie just beneath the outer surface of the skin. Squamous cells also line many other organs, including the stomach, intestines, lungs, bladder, and kidneys. Squamous cells look flat, like fish scales, when viewed under a microscope. Squamous cell carcinomas are sometimes called epidermoid carcinomas.
Transitional cell carcinoma is a cancer that forms in a type of epithelial tissue called transitional epithelium, or urothelium. This tissue, which is made up of many layers of epithelial cells that can get bigger and smaller, is found in the linings of the bladder, ureters, and part of the kidneys (renal pelvis), and a few other organs. Some cancers of the bladder, ureters, and kidneys are transitional cell carcinomas.
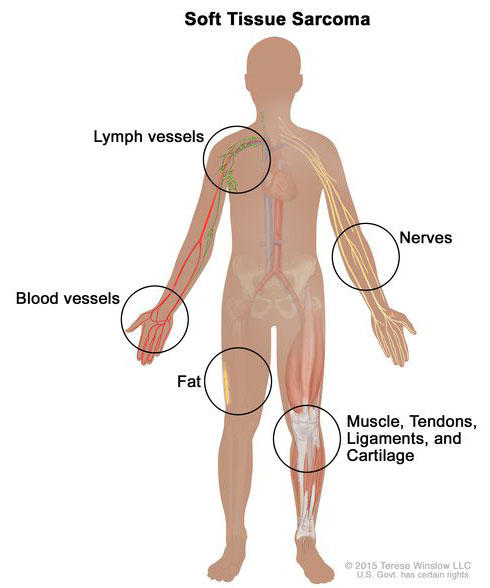
Soft tissue sarcoma forms in soft tissues of the body, including muscle, tendons, fat, blood vessels, lymph vessels, nerves, and tissue around joints.
Sarcomas are cancers that form in bone and soft tissues, including muscle, fat, blood vessels, lymph vessels , and fibrous tissue (such as tendons and ligaments).
Osteosarcoma is the most common cancer of bone. The most common types of soft tissue sarcoma are leiomyosarcoma , Kaposi sarcoma , malignant fibrous histiocytoma , liposarcoma , and dermatofibrosarcoma protuberans .
Our page on soft tissue sarcoma has more information.
Cancers that begin in the blood-forming tissue of the bone marrow are called leukemias. These cancers do not form solid tumors. Instead, large numbers of abnormal white blood cells (leukemia cells and leukemic blast cells) build up in the blood and bone marrow, crowding out normal blood cells. The low level of normal blood cells can make it harder for the body to get oxygen to its tissues, control bleeding, or fight infections.
There are four common types of leukemia, which are grouped based on how quickly the disease gets worse (acute or chronic) and on the type of blood cell the cancer starts in (lymphoblastic or myeloid). Acute forms of leukemia grow quickly and chronic forms grow more slowly.
Our page on leukemia has more information.
Lymphoma is cancer that begins in lymphocytes (T cells or B cells). These are disease-fighting white blood cells that are part of the immune system. In lymphoma, abnormal lymphocytes build up in lymph nodes and lymph vessels, as well as in other organs of the body.
There are two main types of lymphoma:
Hodgkin lymphoma – People with this disease have abnormal lymphocytes that are called Reed-Sternberg cells. These cells usually form from B cells.
Non-Hodgkin lymphoma – This is a large group of cancers that start in lymphocytes. The cancers can grow quickly or slowly and can form from B cells or T cells.
Our page on lymphoma has more information.
Multiple Myeloma
Multiple myeloma is cancer that begins in plasma cells , another type of immune cell. The abnormal plasma cells, called myeloma cells, build up in the bone marrow and form tumors in bones all through the body. Multiple myeloma is also called plasma cell myeloma and Kahler disease.
Our page on multiple myeloma and other plasma cell neoplasms has more information.
Melanoma is cancer that begins in cells that become melanocytes, which are specialized cells that make melanin (the pigment that gives skin its color). Most melanomas form on the skin, but melanomas can also form in other pigmented tissues, such as the eye.
Our pages on skin cancer and intraocular melanoma have more information.
Brain and Spinal Cord Tumors
There are different types of brain and spinal cord tumors. These tumors are named based on the type of cell in which they formed and where the tumor first formed in the central nervous system. For example, an astrocytic tumor begins in star-shaped brain cells called astrocytes , which help keep nerve cells healthy. Brain tumors can be benign (not cancer) or malignant (cancer).
Our page on brain and spinal cord tumors has more information.
Other Types of Tumors
Germ cell tumors.
Germ cell tumors are a type of tumor that begins in the cells that give rise to sperm or eggs. These tumors can occur almost anywhere in the body and can be either benign or malignant.
Our page of cancers by body location/system includes a list of germ cell tumors with links to more information.
Neuroendocrine Tumors
Neuroendocrine tumors form from cells that release hormones into the blood in response to a signal from the nervous system. These tumors, which may make higher-than-normal amounts of hormones, can cause many different symptoms. Neuroendocrine tumors may be benign or malignant.
Our definition of neuroendocrine tumors has more information.
Carcinoid Tumors
Carcinoid tumors are a type of neuroendocrine tumor. They are slow-growing tumors that are usually found in the gastrointestinal system (most often in the rectum and small intestine). Carcinoid tumors may spread to the liver or other sites in the body, and they may secrete substances such as serotonin or prostaglandins, causing carcinoid syndrome .
Our page on gastrointestinal neuroendocrine tumors has more information.
The Unique Hell of Getting Cancer as a Young Adult

W hen I got diagnosed with Stage 3b Hodgkin Lymphoma at age 32, it was almost impossible to process. Without a family history or lifestyle risk factors that put cancer on my radar, I stared at the emergency room doctor in utter disbelief when he said the CT scan of my swollen lymph node showed what appeared to be cancer—and lots of it. A few days away from a bucket list trip to Japan, I’d only gone to the emergency room because the antibiotics CityMD prescribed to me when I was sick weren’t working.I didn’t want to be sick in a foreign country. So when the doctor told me of my diagnosis, the only question I could conjure was: “So Tokyo is a no-go?”
Around the world, cancer rates in people under 50 are surging, with a recent study in BMJ Oncology showing that new cases for young adults have risen 79% overall over the past three decades. In the U.S. alone, new cancer diagnoses in people under 50 hit 3.26 million, with the most common types being breast, windpipe, lung, bowel, and stomach. A new feature in the Wall Street Journal highlights the mad dash among doctors and researchers to determine what’s causing this troubling rise. Strangely, overall cancer rates in the U.S. have dropped over the past three decades, while young people—particularly with colorectal cancers—are increasingly diagnosed at late stages. “We need to make it easier for adolescents and young adults to participate in clinical trials to improve outcomes and study the factors contributing to earlier onset cancers so we can develop new cures,” says Julia Glade Bender, MD, co-lead of the Stuart Center for Adolescent and Young Adult (AYA) Cancers at Memorial Sloan Kettering in New York City (where I am currently a patient.)
Doctors suspect that lifestyle factors and environmental elements, from microplastics to ultra-processed foods, could be to blame. But many adults in their 20s and 30s, such as myself, were otherwise healthy before their diagnoses. It felt like all those years of forcing myself to run, eat high-fiber foods, and choke down kombucha were for nothing.
Cancer is hell at any age, but the challenges facing young adults are especially steep, as the disease disrupts a formative period for building a career, family, and even healthy self-esteem, from body image to gender identity. It’s critical that our approach to treating and supporting these patients reflects the severity of this disruption. In recent years, a growing number of cancer hospitals have developed young adult-specific programming like support groups, information sessions on dating and sexual health, and even mobile apps to help counter social alienation. But there is still a long way to go.
Read more: Why I Stopped Being A “Good” Cancer Patient
Shockingly enough, canceling my trip to Japan was the least of my worries. Beyond the excruciating physical side effects of high-dose chemotherapy and a number of life-threatening complications, cancer pulverized my self-esteem into nothingness, as I watched peers get married and promoted from my bed. Thankfully, after switching to a new hospital, I found support groups that connected me with a community of peers who got it, as well as social workers who work exclusively with young adults and thus recognized many of my biggest challenges, like social isolation, financial strain, the dating nightmare, and hating my bald head.
Perhaps the biggest reason I resented cancer was for disrupting a milestone I’d worked for my whole life: a book launch. (My diagnosis came two months before my first book was published.) Young adulthood is meant to be littered with these kinds of professional and personal benchmarks, many of which are hard enough to accomplish without tumors; dating, for instance, is impossible for me even as a healthy person. Now I have to re-enter the pool older, weaker, and more traumatized?
“Young adult patients may be trying to assert independence from parents, establish a career or intimate relationship, or even be parents themselves,” says Bender. “Most will be naïve to the medical system or a serious health condition.” And so they require flexible, creative clinicians who can help navigate them “to and through the best available therapy and back to their lives, inevitably ‘changed’ but intact.” Not only do these patients need specialized psychosocial support, but research initiatives should prioritize developing treatments that minimize long-term toxicities.
Given that many young patients haven’t yet built financial stability and are often in some form of debt, organizations like Young Adults Survivors United (YASU) have emerged to support young adult survivors and patients through the financial overwhelm. Stephanie Samolovitch, MSW and founder of YASU, says that there’s still an enormous need for resources supporting young adult cancer patients and survivors.
“Cancer causes a young adult to be dependent again, whether it’s moving back in with parents, getting rides to appointments, or asking for financial help,” says Samolovitch, who was diagnosed with leukemia in 2005, two weeks before her 20th birthday. “Young adults never expect to apply for Medicaid or Social Security Disability during our twenties or thirties, yet cancer doesn't give us a choice sometimes. That causes stress, shame, depression, and anxiety when trying to navigate the healthcare system.”
Read more: How to Create an Action Plan After a Cancer Diagnosis
When Ana Calderone, a 33-year-old magazine editor, was diagnosed with stage 2 breast cancer at 30, the most challenging part of getting diagnosed so young was “everything.”
“I felt like it set my whole life back, which sounds stupid because I was literally fighting for my life,” she says. “Who cares if I had to delay my wedding a year because I was still getting radiation treatment? But it was really hard at the time. Everything was delayed, and still is.”
During chemo, Calderone’s doctors gave her a shot that she still receives to try and preserve her ovaries, and she’s been able to try IVF twice. She says she had to proactively advocate for those things with her care team. While Calderone is currently cancer free, she still must take medication that has further delayed her plans to build a family. “I’m fairly confident I’d have a child by now if I didn’t get cancer. That’s been the most devastating part,” she says. “My oncologist would consider letting me get pregnant in two more years, which would be 4.5 years post-diagnosis, and even that is still a risk.”
For 32-year-old Megan Koehler, whose son was one and a half when she was diagnosed with Hodgkin Lymphoma, the hardest part “was knowing the world continued on while I spent days in bed,” she says. “My coworkers still worked on projects I was supposed to be part of, and the worst was knowing my son was growing up, learning to speak sentences, and just becoming a toddler without me – or so it felt that way.”
She remembers crying for most of his second birthday because she was in bed post chemo, feeling devastated that she didn’t have the energy to spend the day with him. During a 50-plus day hospital stay caused by an adverse reaction to a chemotherapy drug, she would Facetime him and cry when he spoke in sentences, because he wasn’t doing that before she was admitted. While she’s grateful for the support she had from her husband and mother, she felt alienated. “I spoke to a few people my age via social media, but no one in person. My center mostly catered to the older generations, so it was somewhat isolating. I did have a great relationship with a few of the infusion nurses who were around my age.”
While oncologists may be rightly focused on saving patients’ lives, there must be more consideration for quality of life during and after treatment – both physical and mental. “More questions need to be asked about their relationships, fertility options, and any mental health concerns or symptoms,” says Samolovitch. From a research perspective, initiatives must expand to pinpoint not only the reason for the rise of cancer in young adults, but find ways to screen and diagnose earlier.
Towards the beginning of my treatment, before I switched hospitals, my oncologist seemed to treat my concerns about self-esteem and hair loss as trivial compared to the real work of saving my life. At my weakest, I had to advocate repeatedly to get accurate information on cold capping, a process of scalp cooling that can preserve most of your hair during chemotherapy, and I had to beg again and again for a social worker to reach out to me, which took weeks.
It’s a beautiful thing that more young adults with cancer are surviving their illnesses. But that means they’ll have decades of life ahead of them. Providers must do a better job supporting young adult patients through all the collateral damage that comes with cancer and its treatment.
More Must-Reads from TIME
- How Donald Trump Won
- The Best Inventions of 2024
- Why Sleep Is the Key to Living Longer
- Robert Zemeckis Just Wants to Move You
- How to Break 8 Toxic Communication Habits
- Nicola Coughlan Bet on Herself—And Won
- Why Vinegar Is So Good for You
- Meet TIME's Newest Class of Next Generation Leaders
Contact us at [email protected]

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Why is cancer so hard to cure?
Share this:.
By Jessica Saenz
Today, we know more about cancer than ever before. More treatments are available to patients than at any other time in history, and researchers make discoveries about how to prevent and treat the disease every day. Yet, some types of cancer are increasing and, in some cases, affecting younger age groups.
Why does cancer continue to outsmart us?
Mark McNiven, Ph.D. , a researcher, director of the Mayo Clinic Center for Biomedical Discovery and co-leader of Mayo Clinic Comprehensive Cancer Center ’s Cancer Cell Genomics, Signaling and Metastasis Research Program , says the answer isn’t a single silver bullet. He and Tanios Bekaii-Saab, M.D. , a medical oncologist and chair of the Division of Hematology and Oncology at Mayo Clinic in Arizona and chair of Mayo Clinic Comprehensive Cancer Center’s Gastrointestinal Cancer Disease Group , explain how cancer works and why it's so hard to cure:
What is cancer?
Cells in the body follow instructions that determine every function in their life cycle, from division to purpose to death. "Normally, when cells reproduce to a certain number or density, they signal to each other to stop growing," says Dr. McNiven. When a change or mutation occurs in a cell, it may begin to disregard instructions and multiply erratically. This process is known as cancer.
So, how does this disregard for instructions become deadly? The repercussions of uncontrolled cell growth differ for each cancer type, but Dr. McNiven says the result is often organ failure. "Each cell in our body has a particular function. When cells become cancerous, they no longer function as if they were from that tissue or organ of origin. They turn into nondescript cells that accumulate, grow and take nutrition from your body," he says.
Cancer isn’t one disease: it's many diseases.
Cancer is a broad term encompassing many diseases that stem from the unchecked growth of cells. But even within one type of cancer, there can be many variations that respond to different treatments. These variations are called cancer subtypes.
"If you take a tumor and slice it into multiple pieces and look at the genetic composition — even within that same tumor — we are likely to find different subpopulations of cells with different genetic compositions. And that likelihood increases as the tumor grows," says Dr. Bekaii-Saab.
Dr. Bekaii-Saab says cancer specialists used to think they could treat each cancer type the same way. "But it turns out that each type of cancer has to be broken down into multiple groups. And with each of those small subgroups, we have a specific target that appears to be most relevant for the originating cancer type," he says.
Not all cancer subtypes have a treatment. That's because cancer scientists are still discovering gene alterations linked to cancer and researching drugs that could affect their function. Still, Dr. Bekaii-Saab says researchers have made significant progress in recent years, and the pace of research is accelerating. "The world of targeting cancer at the genetic and molecular level is moving fast. Finding targets and translating research into the clinical setting — it's moving at an astronomical rate and will likely accelerate further with the integration of artificial intelligence and machine learning."

Early detection is critical to curing cancer but isn’t always possible.
The possibility of a cure is highest when cancer is caught at its earliest stage when it can be removed surgically or targeted with treatment. Regular screening can lead to early detection or even prevention of certain cancers such as colon and breast cancer . "More than half of patients diagnosed with cancer will survive longer than 10 years. That's increased from a much smaller percentage two decades ago, partly because we're detecting cancer earlier, but also due to significant advances in treatment options," says Dr. Bekaii-Saab.
But not every cancer causes symptoms — or symptoms that are easily distinguishable from other health conditions. And screening tests aren’t yet available for every cancer.
Uterine cancer , for example, is the most common gynecologic cancer , but no standard screening test exists. People are encouraged to report unusual symptoms to their healthcare professional and keep up with annual pelvic exams. If uterine cancer symptoms are subtle, mistaken for symptoms of other health conditions, or nonexistent, then the cancer has time to progress into later stages.
While most cancers may not be curable in later stages, Dr. Bekaii-Saab says treatment advances mean people with cancer can often live a meaningful life span. "Patients' lives are being prolonged, and their quality of life improves significantly if we find the right treatment match. Although we're not curing them at this stage, and cancer will likely take their life at some point, we're extending their survival and preserving their quality of life for many years."
Treatments must fit each person — and their cancer.
Each cancer is unique, and so is each person diagnosed with cancer. When developing cancer treatment plans, care teams consider cancer type, subtype and stage, the general health of the patient, and the patient’s preferences. Treatments must be effective in killing the cancer while also being well tolerated by the patient.
Most treatments carry risks, but as your cancer team designs your care plan, they can help you weigh the risks and benefits of cancer treatment to help you determine what you are comfortable with and what's most important to your quality of life.
Weighing risks and benefits includes considering other health conditions (comorbidities) to determine if treatment could complicate them. "We must consider different genetic drivers, previous exposures, comorbidities and other factors so we can treat everyone with the right level of care," says Dr. Bekaii-Saab.
Lack of representation in clinical trials and access to cancer care has hindered progress.
Clinical trials help medical researchers understand how to diagnose, treat and prevent cancer and other diseases and conditions. Historically, people from minority populations have had limited access to clinical trials.
"For the last 100 years, we have focused most of our studies and treatments around white men of Northern European descent, but that is only part of the population," says Dr. McNiven. "It turns out that people respond differently to treatments based on their heritage and genetic makeup, where they live, and what they eat."
Increasing participation of people from diverse populations in clinical trials can help researchers learn more about cancer cures for everyone.
Dr. Bekaii-Saab says matters that might seem small to some — like transportation, time off work or even parking fees — can be barriers that prohibit people from accessing cancer care and clinical trials. "If we want to achieve true health equity and representation in clinical trials and cure more cancers, we have to think about how to make clinical care and research trials more accessible."
Learn more about cancer treatment and find cancer clinical trials at Mayo Clinic.
Join the Cancer Support Group on Mayo Clinic Connect , an online patient community moderated by Mayo Clinic for patients and caregivers.
Also, read these articles:
- Clinical trials: A significant part of cancer care
- Dear Mayo Clinic: 5 advances in cancer treatment
- Reduce your risk for the 4 most common cancers
- Dear Mayo Clinic: Genetic counseling after cancer diagnosis
Related Posts

Findings show extended progression-free survival for people with meningiomas who received a radiopharmaceutical approved for neuroendocrine tumors.

Mayo Clinic study findings reveal a protein that increases glioblastoma malignancy, a new understanding of the tumor's biology, and a potential new treatment strategy.

Dr. Elizabeth Cathcart-Rake explains the value of specialized cancer care for LGBTQ+ people and how she hopes to pave the way for improved outcomes with the Rainbows Breast Cancer Clinic.
Ernest and Isadora Rosenbaum Library

The Will to Live
Ernest H. Rosenbaum, M.D. Isadora R. Rosenbaum, M.A.
As medical professionals, we have always been fascinated by the power of the will to live. Like all creatures in the animal world, human beings have a fierce instinct for survival. The will to live is a force within all of us to fight for survival when our lives are threatened by a disease such as cancer. Yet this force is stronger in some people than in others.
Many physicians have seen how two patients of similar ages and with the same diagnosis, degree of illness, and treatment program experience vastly different results.
Sometimes the biology of a cancer will dictate the course of events regardless of the patient’s attitude and fighting spirit. These events are often beyond our control. But patients with positive attitudes are better able to cope with disease-related problems and may respond better to therapy. Many physicians have seen how two patients of similar ages and with the same diagnosis, degree of illness, and treatment program experience vastly different results. One of the few apparent differences is that one patient is pessimistic and the other optimistic.
We have known for over 2,000 years— from the writings of Plato and Galen— that there is a direct correlation between the mind, the body, and one’s health. “The cure of many diseases is unknown to physicians,” Plato concluded, “because they are ignorant of the whole. For the part can never be well unless the whole is well.”
Recently there has been a shift in health care toward recognizing this wisdom, namely that the psychological and the physical elements of a body are not separate, isolated, and unrelated, but are vitally linked elements of a total system. Health is increasingly being recognized as a balance of many inputs, including physical and environmental factors, emotional and psychological states, and nutritional habits and exercise patterns.
Researchers are now experimenting with methods of actively enlisting the mind in the body’s combat with cancer, using techniques such as meditation, biofeedback, and visualization (creating in the mind positive images about what is occurring in the body). Some doctors and psychologists now believe that the proper attitude may even have a direct effect on cell function and consequently may be used to arrest, if not cure, cancer. This new field of scientific study, called psychoneuroimmunology, focuses on the effect that mental and emotional activity have on physical well-being, indicating that patients can play a much larger role in their recovery.
It will be many years before we know whether it is possible for the mind to control the immune defense system. Experiments with biofeedback and visualization are helpful in that they encourage positive thinking and provide relaxation, thereby increasing the will to live. But they can also be damaging if a patient puts all of his or her faith in them and ignores conventional therapy.
The Power of the Mind
The mind’s role in causing and curing disease has been debated endlessly. Speculation abounds, particularly in the case of cancer. But no studies have proven in a scientifically valid way that a person can control the course of his or her cancer with the mind, although patients often believe otherwise. There are many individual cases that attest to the power of positive attitudes and emotions. One patient with high-risk cancer had a mastectomy at age twentynine. At thirty-one, she had advanced Stage IV cancer with widespread massive liver and bone involvement and, subsequently, extensive lung metastases. She also had an amazingly strong will to live.
“I would get out of bed every morning as if nothing was wrong,” she once said. “I may have known I was going to have to face things and could feel sick during the day, but I never got out of bed that way. There was a lot I was fighting for. I had a three-year-old child, a wonderful life, and a magical love affair with my husband.” Thirty years later, she is still alive, still on chemotherapy, and still living an active life.
We often ask our patients to explain how they are able to transcend their problems. We have found that however diverse they are in ethnic or cultural background, age, educational level, or type of illness, they have all gone through a similar process of psychological recovery.
We often ask our patients to explain how they are able to transcend their problems. We have found that however diverse they are in ethnic or cultural background, age, educational level, or type of illness, they have all gone through a similar process of psychological recovery. They all consciously made a “decision to live.” After an initial period of feeling devastated, they simply decided to assess their new reality and make the most of each day.
Their “will to live” means that they really want to live, whether or not they’re afraid to die. They want to enjoy life, they want to get more out of life, they believe that their life is not over, and they’re willing to do whatever they can to squeeze more out of it.
The threat of death often renews our appreciation of the importance of life, love, friendship, and all there is to enjoy. We open up to new possibilities and begin taking risks we didn’t have the courage to take before. Many patients say that facing the uncertainties of living with an illness makes life more meaningful. The smallest pleasures are intensified and much of the hypocrisy in life is eliminated. When bitterness and anger begin to dissipate, there is still a capacity for joy.
One patient wrote, “I love living, I love nature. Being outdoors, feeling the sun on my skin or the wind blowing against my body, hearing birds sing, breathing in the spray of the ocean. I never lose hope that I may somehow stumble upon or be graced with a victory against this disease.”
Strengthening Your Will to Live
Unfortunately, and quite understandably, many patients react to the diagnosis of cancer in the same way that people in primitive cultures react to the imposition of a curse or spell: as a sentence to a ghastly death. This phenomenon, known as “bone pointing,” results in a paralytic fear that causes the victim to simply withdraw from the world and await the inevitable end. In modern medical practice, a similar phenomenon may occur when, out of ignorance or superstition, a patient believes the diagnosis of cancer to be a death sentence. However, the phenomenon of self-willed death is only effective if the person believes in the power of the curse.
In the treatment of cancer, we’ve seen patients fail on their first course of chemotherapy, fail again on the second and third treatments, then—with more advanced disease—a fourth treatment is highly successful.
In all things, you have to take a risk if you want to win, to get a remission or recover with the best quality of life. Just the willingness to take a risk seems to generate hope and a positive atmosphere in which the components of the will to live are enhanced. There are many other ways of strengthening the will to live.
Getting Involved The best thing a patient can do to strengthen the will to live is to get involved as an active participant in combating his or her disease. When patients approach their disease in an aggressive fighting posture, they are no longer helpless victims. Instead, they become active partners with their medical support team in the fight for improvement, remission, or cure. This partnership must be based on honesty, open communication, shared responsibility, and education about the nature of the disease, therapy options, and rehabilitation. The result of this partnership is an increased ability to cope that, in turn, nurtures the will to live.
Helping and Sharing with Others – A way to strengthen this partnership is to extend the relationship to others. The emotional experience of sharing and enjoying your family and partnerships supports your love for life and your will to survive.
As you make the transition from helpless victim to activist, one of the most important realizations is that you have everything to do with how others perceive you and treat you. If you can accept your condition and hold self-pity at bay, others won’t feel sorry for you. If you can discuss your disease and medical therapy in a matter-of-fact manner, they’ll respond in kind without fear or awkwardness. You are in charge. You can subtly and gently put your family, friends, and coworkers at ease by being frank about what you want to talk about or not talk about and by being explicit about whether and when you want their help.
Sharing your life with others and receiving aid or support from friends and family will improve your ability to cope and help you fight for your life. A person who is lonely or alone often feels like a helpless victim. There is a need to share your own problems, but helping others find solutions to or cope better with the problems of daily living gives strength to both the giver and the receiver. There are few more satisfying experiences in life than helping a person in need.
Patients can also take part in psychological support programs, either through private counseling or through group therapy. Sharing frustrations with others in similar circumstances often relieves the sense of isolation, terror, and despair cancer patients often feel.
Those who must live with cancer can live to the maximum of their capacity by
- living in the present, not the past,
- setting realistic goals and being willing to compromise,
- regaining control of their lives and maintaining a sense of independence and self-esteem,
- trying to resolve negative emotions and depression by actively doing things to help themselves and others, and
- following an improved diet and exercising regularly.
Nurturing Hope
Of all the ingredients in the will to live, hope is the most vital. Hope is the emotional and mental state that motivates you to keep on living, to accomplish things, and to succeed. A person who lacks hope can give up on life and lose the will to live. Without hope, there is little to live for. But with hope, a positive attitude can be maintained, determination strengthened, coping skills sharpened, and love and support more freely given and received.
Even if a diagnosis is such that the future seems limited, hope must be maintained. Hope is what people have to live on. Take away hope, and you take away a chance for the future, which leads to depression. When people fall to that low emotional state, their bodies simply turn off.
Hope can be maintained as long as there is even a remote chance for survival. It can be kindled and nurtured by minor improvements or a remission and maintained when crises or reversals occur. There may be times when you will feel exhausted and drained by never-ending problems and feel ready to give up the struggle to survive. All too often it seems easier to give up than to keep on fighting. Frustrations and despair can sometimes feel overwhelming. Determination or dogged persistence is needed to accomplish the difficult task of fighting for your health.
The experience of cancer not only is destructive in a physical way, but can be a major deterrent to your fighting attitude and will to live. But even during the roughest times, there are often untapped reserves of physical and emotional strength to call upon to help you survive one more day. These reserves can add meaning to your life as well as serve as a lighthouse that leads you to a safe haven during a turbulent storm.
Hope has different meanings for each person. It is a component of a positive attitude and acceptance of our fate in life. We use our strengths to gain success to live life to the fullest. Circumstances often limit our hopes of happiness, cure, remission, or increased longevity. We also live with fears of poverty, pain, a bad death, or other unhappy experiences.
You may worry so much that you lose sight of the possibility of recovery and lose your sense of optimism. On the other hand, you may become so hopeful and confident that you lose sight of reality. Your main challenge is balancing your worry and your hope.
Hope is nourished by the way we live our lives. Achieving the best quality of life requires settling old problems, quarrels, and family strife as well as completing current tasks. Problems that have not been resolved need to have completion. New tasks should be undertaken. If the future seems limited, you can achieve the satisfaction of knowing that you have taken care of your affairs and not left the burden to your family or others. By doing so, you can achieve peace of mind, which will also help strengthen your will to live. With each passing day, try to complete what you can and have that satisfaction that you have done your best.
Be bold, be venturesome, and be willing to experience each day to the fullest to enhance your enjoyment of life. As long as fear, suffering, and pain can be controlled, life can be lived fully until the last breath. Each of us has the capacity to live each day a little better, but we need to focus on both purpose and goals and set into action a realistic daily plan—often altered many times—to help us achieve them. These resources are the foundation of the will to live. Only by using the power of the will to live—nourished by hope—can we achieve the sublime feelings of knowing and experiencing the wonders of life and appreciate its meanings through vital living.
Related Articles

The Role of the Clergy
Religion and Spirituality

The Art of Forgiveness

Coping with Cancer


Coping with Depression

When Your Spouse Has Cancer

The Waiting Process

Patient Stories

One Patients Way of Coping

Feeling Right When Things Go Wrong

I Live a Disease-Threatening Life

The Scent of an Orange

In Touch with My Dream

I Don't Have Time Not to Live

A Cup of Breath

One in a Million

Expedition Inspiration

To Call Forth That Spark
Ernest h. rosenbaum, m.d..
Clinical Professor of Medicine, University of California, San Francisco, Comprehensive Cancer Center; Adjunct Clinical Professor, Department of Medicine, Stanford University Medical Center; Director, Stanford Cancer Supportive Care Programs National/International, Stanford Complementary Medicine Clinic, Stanford University Medical Center, Stanford, California. More
Ernest H. Rosenbaum’s career has included a fellowship at the Blood Research Laboratory of Tufts University School of Medicine (New England Center Hospital) and MIT. He teaches at the University of California, San Francisco, Comprehensive Cancer Center, was the cofounder of the Northern California Academy of Clinical Oncology, and founded the Better Health Foundation and the Cancer Supportive Care Program at the Stanford Complementary Medicine Clinic, Stanford University Medical Center.
His passionate interest in clinical research and developing ways to improve patient care and communication with patients and colleagues has resulted in over fifty articles on cancer and hematology in various medical journals. He has also participated in many radio and television programs and frequently lectures to medical and public groups.
He has written numerous books, including Living with Cancer: A Home Care Training Program for Cancer Patients; Decisions for Life: You Can Live Ten Years Longer with Better Health; Cancer Supportive Care: A Comprehensive Guide for Cancer Patients and Their Families; Nutrition for the Cancer Patient; Everyone’s Guide to Cancer Therapy; and Everyone’s Guide to Cancer Survivorship. For Everyone’s Guide to Cancer Therapy, Ernest Rosenbaum, M.D., Malin Dollinger, M.D., and Greg Cable received and Honorable Mention in 1991 from the American Medical Writers Association for Excellence in Medical Publications. Ernest and Isadora Rosenbaum received the same award in 1982 for their book, A Comprehensive Guide for Cancer Patients and Their Families.
Isadora Rosenbaum, M.A.
Isadora Rosenbaum is a medical assistant who worked in immunology research and is currently at an oncology practice at the UCSF Comprehensive Cancer Center offering advice and psychosocial support. She coauthored Nutrition for the Cancer Patient and The Comprehensive Guide for Cancer Patients and Their Families. She has written chapters in Everyone’s Guide to Cancer Therapy, Living with Cancer, and You Can Live 10 Years Longer with Better Health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 13 January 2020
The global challenge of cancer
Nature Cancer volume 1 , pages 1–2 ( 2020 ) Cite this article
28k Accesses
56 Citations
32 Altmetric
Metrics details
Cancer is a multifaceted global health issue that continues to demand action. We are launching Nature Cancer to inform, inspire and convene scientists across the multidisciplinary arena of cancer research, aiming to advance biomedical knowledge and treatment strategies within the greater framework of society.
Cancer is a disease that spans the breadth of human experience. Observed in hominid fossils and human mummies, first described in ancient times by Egyptian and later by Greek physicians, it has manifested itself throughout human history. Affecting people of all ages, cancer cuts through society, causing suffering on a global scale. According to the World Health Organization, cancer is responsible for one in six deaths, which makes it the second most common cause of death globally.
Through the ages, physicians who observed and described this disease were faced with its seeming intractability. The emergence of modern medicine changed that view through an initially slow accumulation of biological and therapeutic knowledge that accelerated with the advent of molecular cell biology and genetics in the latter part of the 20th century. This progress, together with more recent technological advances, have permitted an unprecedented understanding of the disease. Today the word ‘cancer’ refers to hundreds of distinct disease types that share similar fundamental properties. The importance of the tissue and cell type from which the disease originates is clear. It is known that the function of cancer cells at the molecular and metabolic level is crucial but is also highly context dependent. Cancer is also appreciated as a disease of change—a condition characterized by plasticity and heterogeneity, that evolves at genetic, phenotypic and pathological levels, and progresses through different stages clinically. Beyond decoding of the genetic fingerprint and molecular makeup of a specific cancer type, we understand the importance of the systemic and local tumor environment in how the disease develops and manifests. The interplay with the immune system and immune tumor microenvironment has become especially apparent in recent years. Indeed, today we recognize that cancer heterogeneity, evolution and the local and systemic environment all have key roles not only in disease development but also in the response or resistance to therapy and disease recurrence.
Technological advances such as next-generation sequencing, integrated ‘-omics’, imaging and single-cell methodologies have allowed profiling of different tumor types at a resolution and scale that were not possible previously. The ability to generate and share big data is fundamentally altering the way this disease is understood and treated—for example, by allowing the identification of biomarkers to select patients for clinical trials and evaluate therapy responses. Data science has become a core part of a field that is increasingly embracing computation, as in the form of artificial intelligence for extracting information from complex datasets. Nevertheless, the potential of such approaches to revolutionize data analysis for cancer screening, diagnosis and therapy decisions comes with challenges.
Viewing cancer as a systemic disease characterized by evolution, heterogeneity and environmental inputs may seem commonplace now, but in reality, revealing one layer of complexity only underscores other complex features that need to be appreciated. The size, quality and complexity of large datasets, such as those of The Cancer Genome Atlas, the International Cancer Genome Consortium and the Human Cell Atlas (among others), mean that considerable work is needed to decode, interpret and contextualize findings. Identifying tumor cell–intrinsic genomic and epigenomic attributes provides only a snapshot of tumor development and progression. A more complete picture may emerge with longitudinal information, as well as profiling of different cellular constituents of tumors, such as stromal and immune cells. Integrative ‘-omics’ and single-cell approaches provide the ability to do so; however, additional factors need to be considered. Among them are the peculiarities of the particular tissue and tumor type, the size and characteristics of human-participant cohorts or the choice of preclinical animal model systems, the resolution and strength of the chosen methodology and the quality of analytical tools. How data from individual patients versus larger cohorts are handled and analyzed, the information that can be obtained from each type of analysis and the extent to which tumor profiling studies may be more broadly generalizable, given the degree of inter-patient heterogeneity, are questions with which this field continues to grapple.
The developments noted above have also revolutionized the approach to treatment. The more granular understanding of cancer’s molecular drivers and tumor-cell-intrinsic or extrinsic vulnerabilities, and the addition of next-generation sequencing testing to clinical practice, have given rise to targeted therapies and the concept of precision oncology—treatment tailored to the individual patient, aiming to hit cancer-specific vulnerabilities, thereby hopefully reducing toxicities and improving quality of life for patients receiving treatment. High-throughput approaches, computational science, bioengineering and nanomedicine are changing the landscape of drug and diagnostics development. The hard-won advances in tumor immunology have led to an explosion of cancer immunotherapies. These therapeutic breakthroughs in precision medicine and immuno-oncology have successfully introduced several therapeutic modalities into the clinic. However, as with historical cancer treatments, these new modalities still encounter the setbacks of therapy resistance and lack of response, as well as their own serious adverse events. To that end, studying the fundamental mechanisms underlying these processes to devise new therapeutic strategies, and exploring innovative treatment combinations, represent major areas of focus.
An additional key consideration in the effort against cancer is the influence of the environment, daily habits and culture. We are gaining a better understanding of these facets of the disease, but such factors are often difficult to quantify and control in a real-world setting, or to model in the laboratory. The often late-stage presentation, and therefore late diagnosis, of the disease continues to hamper therapy options, and metastasis remains a major cause of cancer deaths and a main focus of foundational cancer research. Socioeconomic factors lend an additional, devastating dimension: according to the World Health Organization, 70% of cancer deaths occur in low- or middle-income countries, but even in high-income societies, certain parts of the population bear a disproportionate burden of suffering. A large fraction of cancer cases and deaths may be preventable with greater epidemiological and mechanistic understanding of environmental and behavioral risk factors. The development and wider adoption of the Pap test and HPV vaccines against cervical cancer are singular successes that exemplify the importance of early detection and prevention in neutralizing the threat of cancer in a broad population. However, this remains a disease of disparities. Therefore, it is essential to deepen our appreciation of the underlying causes of these inequalities and to work toward reversing them, always keeping the patient at the forefront of the cross-disciplinary scientific endeavor in this field. Developing more-effective screening and diagnostic means and working toward providing accessible and affordable high-quality cancer care for the wider population will be essential for addressing cancer-health disparities.
It has been thousands of years since the ancient Greek physician Hippocrates strove to understand this disease and named it ‘cancer’ from the Greek word karkinos , meaning ‘crab’, possibly as an allusion to the blood vessels emanating from tumors. We are now in the enviable position of having a much more refined understanding of the disease and we know that cancer has no panacea. Instead, it requires synthesis of knowledge, collaboration between fields and a deeper appreciation of the challenges facing patients, clinicians and scientists from different disciplines. Fortunately, this is an era of thriving biomedical research that has seen the field of cancer research expand into a vibrant, multidisciplinary community that seeks new and innovative ways to engage collectively and to tackle this disease.
As we launch Nature Cancer , we seek to provide a unique forum that embraces the breadth of this community, from foundational preclinical science to translational and clinical work. Through our pages, we aim to increase the knowledge of cancer formation, development and progression, to explore innovative approaches to cancer diagnosis, treatment and prevention, and to understand the societal impact of this disease. Ultimately, our goal is to become a point of convergence for scientists from diverse fields and to lend a new voice to discussing and contextualizing the most exciting findings and pressing issues in cancer research today. Our inaugural issue encapsulates the diversity of science we aim to bring to you and the conversations we seek to start. As we realize our first steps into this field, we thank our authors and referees and welcome our readers.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
The global challenge of cancer. Nat Cancer 1 , 1–2 (2020). https://doi.org/10.1038/s43018-019-0023-9
Download citation
Published : 13 January 2020
Issue Date : January 2020
DOI : https://doi.org/10.1038/s43018-019-0023-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Data-driven energy landscape reveals critical genes in cancer progression.
npj Systems Biology and Applications (2024)
Health Economic Evidence and Modeling Challenges for Liquid Biopsy Assays in Cancer Management: A Systematic Literature Review
- Mussab Fagery
- Hadi A. Khorshidi
- Maarten IJzerman
PharmacoEconomics (2023)
Fundamental concepts of protein therapeutics and spacing in oncology: an updated comprehensive review
- Bahareh Farasati Far
- Maryam Safaei
- Mohammad Reza Naimi-Jamal
Medical Oncology (2023)
Prediction of biomarkers and therapeutic combinations for anti-PD-1 immunotherapy using the global gene network association
- Chia-Chin Wu
- Y. Alan Wang
- P. Andrew Futreal
Nature Communications (2022)
Subcellular proteomics
- Josie A. Christopher
- Charlotte Stadler
- Kathryn S. Lilley
Nature Reviews Methods Primers (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Talk to our experts
1800-120-456-456
- Essay on Cancer: Empowering Hope and Health

Raising Cancer Awareness: Promoting Early Detection and Healthy Living
Cancer is often regarded as one of the most feared diseases globally, being a major cause of death. Its life-threatening nature in any form makes it a difficult topic for many to discuss openly. However, spreading awareness about cancer can provide significant benefits to the public, encouraging early detection and prevention.
Also Check for National Cancer Awareness Day: Empowering Hope and Health
Long Essay on Cancer
In a recent study conducted in 2018, it was found that around 9.5 million people died that year owing to cancer. The World Health Organisation has revealed that cancer is the second leading cause of death across the world. The statistics in India are also no better and as per recent figures about 1300 people die every day owing to cancer of different types. Cancer types and causes have seen a steady increase in the past decade which does not bode well for the world population.
Cancer is one of the most serious health challenges facing humanity today, affecting millions of people around the world. It is a condition where the cells in the body grow uncontrollably, sometimes forming tumours, and spread to other parts of the body.
If left untreated, cancer can lead to life-threatening complications. However, with advancements in medical science, many cancers can be treated, especially when detected early.
What is Cancer?
Cancer is one of the most serious health challenges facing humanity today, affecting millions of people around the world. It is a condition where the cells in the body grow uncontrollably, sometimes forming tumours, and spread to other parts of the body. If left untreated, cancer can lead to life-threatening complications. However, with advancements in medical science, many cancers can be treated, especially when detected early.
Types of Cancer
Some of the most common types of cancer include breast cancer, lung cancer, colorectal cancer, prostate cancer, skin cancer, and blood cancer (leukaemia). Breast cancer mainly affects women but can also occur in men, while lung cancer is often linked to smoking. Colorectal cancer typically affects older adults, and prostate cancer occurs in men. Skin cancer is largely caused by overexposure to ultraviolet radiation, while leukaemia affects the blood and bone marrow.
Cancer Causes
In the present-day living environment, several factors are liable to cause cancer. However, in many cases, one single factor cannot be attributed or held responsible for causing cancer in an individual. The substances that are known to be cancer-causing or increasing the risks of cancer are known as carcinogens. Carcinogens can range from anything from pollutants to tobacco to something as simple as processed meats.
The effect of carcinogens, however, on different individuals is different and it is also dependent on several factors, be it physical, lifestyle choice, or biological. The causes of cancer vary depending on the type, but there are several common risk factors. Genetics can play a role, meaning individuals with a family history of cancer may be more likely to develop the disease. Lifestyle choices such as smoking, excessive alcohol consumption, poor diet, and lack of exercise can also increase the risk. Environmental factors, including pollution, radiation, and exposure to harmful chemicals, are known to trigger cancer. Some infections, like human papillomavirus (HPV), can lead to cancers such as cervical cancer.
Cancer Treatment
Once diagnosed, the treatment of cancer depends on its type and stage. The main treatment options include surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. Surgery is used to remove tumours, while chemotherapy and radiation therapy work by destroying cancer cells. Immunotherapy helps the body’s immune system fight cancer, and targeted therapies are designed to attack specific cancer cells without harming normal cells.
Cancer Awareness
Prevention plays a crucial role in reducing the risk of developing cancer. Avoiding tobacco is one of the most effective ways to prevent cancer, as smoking is a leading cause of lung and other cancers. A healthy diet rich in fruits, vegetables, and whole grains can also lower cancer risk. Regular physical activity and maintaining a healthy weight are important for overall health and cancer prevention. Additionally, certain vaccines, such as the HPV vaccine, can prevent infections that lead to cancer. Regular screenings, such as mammograms or colonoscopies, are vital for detecting cancer in its early stages when it is most treatable.
Short Essay on Cancer
To provide you with a grasp on the subject matter, we have provided a short essay on cancer here. Cancer is a disease in which the cells in specified or different parts of the body start dividing continuously. Cancer is usually caused by specific substances that affect several factors in our body. These specific substances are called carcinogens.
Cancer can be caused owing to exposure to pollution, radiation, harmful substances, poor lifestyle choices, etc. Cancer is best treated when detected early. Usually, surgery as well as other treatments such as chemotherapy, radiation therapy, etc. are used to treat cancer.
Cancer awareness is one of the best means that help prevent and fight the disease.
Tips to Write An Essay on Cancer
Do the Research : Gather valid information on cancer to write a comprehensive and accurate essay.
Analyse the Question : Understand the essay prompt and the key terms needed to focus on the most relevant points about cancer.
Focus on Essential Information : Instead of covering all types of cancer, prioritize the most important facts to keep the essay concise.
Define Terms Clearly : Explain the terms and types of cancer, along with how they affect the body and possible treatments.
Organise the Structure : Start with an introduction, followed by the body discussing types and treatments, and end with a clear conclusion.
Cancer is, undoubtedly, one of the most life-shattering diseases. Together, let us make an effort to take on this disease with more care and hope.
FAQs on Essay on Cancer: Empowering Hope and Health
1. What is an essay on Cancer?
An essay on cancer discusses its causes, types, prevention, and treatment, raising awareness about the disease.
2. How do I write a short essay on Cancer?
A short essay on cancer should cover its definition, common types, symptoms, and the importance of early detection.
3. What should be included in a Cancer introduction?
A cancer introduction explains what cancer is, how it develops, and its impact on individuals and society.
4. What are some social awareness of Cancer slogans?
Social awareness cancer slogans include "Fight Cancer, Spread Hope" and "Early Detection Saves Lives."
5. What are common breast Cancer symptoms?
Common breast cancer symptoms include lumps, changes in breast shape, and unusual discharge from the nipple.
6. What is Breast Cancer?
Breast cancer is a type of cancer that forms in the cells of the breasts, often detected through mammograms.
7. What is Prostate Cancer?
Prostate cancer is a type of cancer that occurs in the prostate gland, commonly affecting men over 50.
8. What are general Cancer symptoms?
General cancer symptoms include unexplained weight loss, persistent fatigue, and abnormal lumps or swelling.
9. What are common blood Cancer symptoms?
Common blood cancer symptoms include frequent infections, fatigue, bruising, and bleeding easily.
10. What are the symptoms of lung Cancer?
Lung cancer symptoms include persistent cough, chest pain, and shortness of breath, often worsening over time.
11. What is skin Cancer?
Skin cancer is a type of cancer that begins in the skin cells, often caused by excessive exposure to ultraviolet (UV) rays.

Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Cancer Research Catalyst The Official Blog of the American Association for Cancer Research

Home > Cancer Research Catalyst > Cancer Survivors: In Their Words
Cancer Survivors: In Their Words
This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we’ve published from cancer survivors at different stages of their treatment.

In this essay , psychiatrist Adam P. Stern’s cerebral processing of his metastatic kidney cancer diagnosis gives rise to piercing questions. When he drops off his 3-year-old son to daycare, he ponders a simple exchange: his son’s request for a routine morning hug before he turns to leave. “Will he remember me, only a little, just enough to mythologize me as a giant who used to carry him up the stairs? As my health declines, will he have to learn to adjust to a dad who used to be like all the other dads but then wasn’t?” he questions.

In another essay from a parent with a young child, Amanda Rose Ferraro describes the abrupt change from healthy to not healthy after being diagnosed with acute myeloid leukemia in May 2017. After a 33-day hospital stay, followed by weeklong chemotherapy treatments, Ferraro’s cancer went into remission, but a recurrence required more chemotherapy and a stem cell transplant. Ferraro describes harrowing guilt over being separated from her 3-year-old son, who at one point wanted nothing to do with her. “Giving up control is hard, but not living up to what I thought a mother should be was harder. I had to put myself first, and it was the hardest thing I had ever done,” she writes.
In January 1995, 37-year-old Melvin Mann was diagnosed with chronic myelogenous leukemia, which would eventually mean he would need to take a chance on a phase I clinical trial that tested an experimental drug called imatinib—a treatment that would go on to receive U.S. Food and Drug Administration approval under the brand name Gleevec. It would also mean trusting a system with a documented history of negligence and abuse of Black people like him: “Many patients, especially some African Americans, are afraid they will be taken advantage of because of past unethical experiments like the infamous Tuskegee syphilis study,” Mann writes, before describing changes that make current trials safer. Mann’s been on imatinib ever since and has enjoyed watching his daughter become a physician and celebrating 35 years of marriage.

In another essay , Carly Flumer addresses the absurdity of hearing doctors reassure her that she had a good cancer after she was diagnosed with stage I papillary thyroid cancer in 2017. “What I did hear repeatedly from various physicians was that I had the ‘good cancer,’ and that ‘if you were to have a cancer, thyroid would be the one to get,’” she writes.
In another piece for Cancer Today , Flumer shares how being diagnosed with cancer just four months after starting a graduate program shaped her education and future career path.
For Liza Bernstein, her breast cancer diagnosis created a paradox as she both acknowledged and denied the disease the opportunity to define who she was. “In the privacy of my own mind, I refused to accept that cancer was part of my identity, even though it was affecting it as surely as erosion transforms the landscape,” she writes . “Out in the world, I’d blurt out, ‘I have cancer,’ because I took questions from acquaintances like ‘How are you, what’s new?’ literally. Answering casual questions with the unvarnished truth wasn’t claiming cancer as my identity. It was an attempt to dismiss the magnitude of it, like saying ‘I have a cold.’” By her third primary breast cancer diagnosis, Bernstein reassesses and moves closer to acceptance as she discovers her role as advocate.

As part of the staff of Cancer Today , a magazine and online resource for cancer patients, survivors and caregivers, we often refer to a succinct tagline to sum up our mission: “Practical knowledge. Real hope.” Part of providing information is also listening closely to cancer survivors’ experiences. As we celebrate National Cancer Survivor Month, we elevate these voices, and all patients and survivors in their journeys.
Cancer Today is a magazine and online resource for cancer patients, survivors, and caregivers published by the American Association for Cancer Research. Subscriptions to the magazine are free to cancer patients, survivors and caregivers who live in the U.S.
- About This Blog
- Blog Policies
- Tips for Contributors

Clinical Trials Highlighted at the AACR Annual Meeting 2015

Pausing Breast Cancer Treatment to Get Pregnant, and Other News from SABCS 2022

Two New Therapeutics Approved For Treating Multiple Myeloma
Cancel reply
Your email address will not be published. Required fields are marked *
Join the Discussion (max: 750 characters)...
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Share Your Story
- National Cancer Research Month
- Patient Advocate Events

IMAGES
VIDEO
COMMENTS
Cancer might just be one of the most feared and dreaded diseases. In this Essay on Cancer will discuss its Type, Causes, and Treatment.
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues. Cancer is caused by changes to DNA. Most cancer-causing DNA changes occur in sections of DNA called genes. These changes are also called genetic changes.
In this article, we examine types of cancer, how the disease develops, and how doctors may treat it. We also explore different types of cancer and disease outlook.
Cancer is hell at any age, but the challenges facing young adults are especially steep, as the disease disrupts a formative period for building a career, family, and even healthy self-esteem,...
Early detection is critical to curing cancer but isn’t always possible. The possibility of a cure is highest when cancer is caught at its earliest stage when it can be removed surgically or targeted with treatment. Regular screening can lead to early detection or even prevention of certain cancers such as colon and breast cancer.
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020 (1). The most common in 2020 (in terms of new cases of cancer) were: breast (2.26 million cases); lung (2.21 million cases); colon and rectum (1.93 million cases);
The experience of cancer not only is destructive in a physical way, but can be a major deterrent to your fighting attitude and will to live. But even during the roughest times, there are often untapped reserves of physical and emotional strength to call upon to help you survive one more day.
Cancer is a disease that spans the breadth of human experience. Observed in hominid fossils and human mummies, first described in ancient times by Egyptian and later by Greek physicians, it has...
Discover how spreading awareness about cancer can bring hope and improve health. Learn about prevention, early detection, and the importance of education in fighting cancer.
The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we’ve published from cancer survivors at different stages of their treatment.