Greater Good Science Center • Magazine • In Action • In Education

11 Questions to Ask About COVID-19 Research
Debates have raged on social media, around dinner tables, on TV, and in Congress about the science of COVID-19. Is it really worse than the flu? How necessary are lockdowns? Do masks work to prevent infection? What kinds of masks work best? Is the new vaccine safe?
You might see friends, relatives, and coworkers offer competing answers, often brandishing studies or citing individual doctors and scientists to support their positions. With so much disagreement—and with such high stakes—how can we use science to make the best decisions?
Here at Greater Good , we cover research into social and emotional well-being, and we try to help people apply findings to their personal and professional lives. We are well aware that our business is a tricky one.

Summarizing scientific studies and distilling the key insights that people can apply to their lives isn’t just difficult for the obvious reasons, like understanding and then explaining formal science terms or rigorous empirical and analytic methods to non-specialists. It’s also the case that context gets lost when we translate findings into stories, tips, and tools, especially when we push it all through the nuance-squashing machine of the Internet. Many people rarely read past the headlines, which intrinsically aim to be relatable and provoke interest in as many people as possible. Because our articles can never be as comprehensive as the original studies, they almost always omit some crucial caveats, such as limitations acknowledged by the researchers. To get those, you need access to the studies themselves.
And it’s very common for findings and scientists to seem to contradict each other. For example, there were many contradictory findings and recommendations about the use of masks, especially at the beginning of the pandemic—though as we’ll discuss, it’s important to understand that a scientific consensus did emerge.
Given the complexities and ambiguities of the scientific endeavor, is it possible for a non-scientist to strike a balance between wholesale dismissal and uncritical belief? Are there red flags to look for when you read about a study on a site like Greater Good or hear about one on a Fox News program? If you do read an original source study, how should you, as a non-scientist, gauge its credibility?
Here are 11 questions you might ask when you read about the latest scientific findings about the pandemic, based on our own work here at Greater Good.
1. Did the study appear in a peer-reviewed journal?
In peer review, submitted articles are sent to other experts for detailed critical input that often must be addressed in a revision prior to being accepted and published. This remains one of the best ways we have for ascertaining the rigor of the study and rationale for its conclusions. Many scientists describe peer review as a truly humbling crucible. If a study didn’t go through this process, for whatever reason, it should be taken with a much bigger grain of salt.
“When thinking about the coronavirus studies, it is important to note that things were happening so fast that in the beginning people were releasing non-peer reviewed, observational studies,” says Dr. Leif Hass, a family medicine doctor and hospitalist at Sutter Health’s Alta Bates Summit Medical Center in Oakland, California. “This is what we typically do as hypothesis-generating but given the crisis, we started acting on them.”
In a confusing, time-pressed, fluid situation like the one COVID-19 presented, people without medical training have often been forced to simply defer to expertise in making individual and collective decisions, turning to culturally vetted institutions like the Centers for Disease Control (CDC). Is that wise? Read on.
2. Who conducted the study, and where did it appear?
“I try to listen to the opinion of people who are deep in the field being addressed and assess their response to the study at hand,” says Hass. “With the MRNA coronavirus vaccines, I heard Paul Offit from UPenn at a UCSF Grand Rounds talk about it. He literally wrote the book on vaccines. He reviewed what we know and gave the vaccine a big thumbs up. I was sold.”
From a scientific perspective, individual expertise and accomplishment matters—but so does institutional affiliation.
Why? Because institutions provide a framework for individual accountability as well as safety guidelines. At UC Berkeley, for example , research involving human subjects during COVID-19 must submit a Human Subjects Proposal Supplement Form , and follow a standard protocol and rigorous guidelines . Is this process perfect? No. It’s run by humans and humans are imperfect. However, the conclusions are far more reliable than opinions offered by someone’s favorite YouTuber .
Recommendations coming from institutions like the CDC should not be accepted uncritically. At the same time, however, all of us—including individuals sporting a “Ph.D.” or “M.D.” after their names—must be humble in the face of them. The CDC represents a formidable concentration of scientific talent and knowledge that dwarfs the perspective of any one individual. In a crisis like COVID-19, we need to defer to that expertise, at least conditionally.
“If we look at social media, things could look frightening,” says Hass. When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell’s palsy. “We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.”
3. Who was studied, and where?
Animal experiments tell scientists a lot, but their applicability to our daily human lives will be limited. Similarly, if researchers only studied men, the conclusions might not be relevant to women, and vice versa.
Many psychology studies rely on WEIRD (Western, educated, industrialized, rich and democratic) participants, mainly college students, which creates an in-built bias in the discipline’s conclusions. Historically, biomedical studies also bias toward gathering measures from white male study participants, which again, limits generalizability of findings. Does that mean you should dismiss Western science? Of course not. It’s just the equivalent of a “Caution,” “Yield,” or “Roadwork Ahead” sign on the road to understanding.
This applies to the coronavirus vaccines now being distributed and administered around the world. The vaccines will have side effects; all medicines do. Those side effects will be worse for some people than others, depending on their genetic inheritance, medical status, age, upbringing, current living conditions, and other factors.
For Hass, it amounts to this question: Will those side effects be worse, on balance, than COVID-19, for most people?
“When I hear that four in 100,000 [of people in the vaccine trials] had Bell’s palsy, I know that it would have been a heck of a lot worse if 100,000 people had COVID. Three hundred people would have died and many others been stuck with chronic health problems.”
4. How big was the sample?
In general, the more participants in a study, the more valid its results. That said, a large sample is sometimes impossible or even undesirable for certain kinds of studies. During COVID-19, limited time has constrained the sample sizes.
However, that acknowledged, it’s still the case that some studies have been much larger than others—and the sample sizes of the vaccine trials can still provide us with enough information to make informed decisions. Doctors and nurses on the front lines of COVID-19—who are now the very first people being injected with the vaccine—think in terms of “biological plausibility,” as Hass says.
Did the admittedly rushed FDA approval of the Pfizer-BioNTech vaccine make sense, given what we already know? Tens of thousands of doctors who have been grappling with COVID-19 are voting with their arms, in effect volunteering to be a sample for their patients. If they didn’t think the vaccine was safe, you can bet they’d resist it. When the vaccine becomes available to ordinary people, we’ll know a lot more about its effects than we do today, thanks to health care providers paving the way.
5. Did the researchers control for key differences, and do those differences apply to you?
Diversity or gender balance aren’t necessarily virtues in experimental research, though ideally a study sample is as representative of the overall population as possible. However, many studies use intentionally homogenous groups, because this allows the researchers to limit the number of different factors that might affect the result.
While good researchers try to compare apples to apples, and control for as many differences as possible in their analyses, running a study always involves trade-offs between what can be accomplished as a function of study design, and how generalizable the findings can be.

The Science of Happiness
What does it take to live a happier life? Learn research-tested strategies that you can put into practice today. Hosted by award-winning psychologist Dacher Keltner. Co-produced by PRX and UC Berkeley’s Greater Good Science Center.
- Apple Podcasts
- Google Podcasts
You also need to ask if the specific population studied even applies to you. For example, when one study found that cloth masks didn’t work in “high-risk situations,” it was sometimes used as evidence against mask mandates.
However, a look beyond the headlines revealed that the study was of health care workers treating COVID-19 patients, which is a vastly more dangerous situation than, say, going to the grocery store. Doctors who must intubate patients can end up being splattered with saliva. In that circumstance, one cloth mask won’t cut it. They also need an N95, a face shield, two layers of gloves, and two layers of gown. For the rest of us in ordinary life, masks do greatly reduce community spread, if as many people as possible are wearing them.
6. Was there a control group?
One of the first things to look for in methodology is whether the population tested was randomly selected, whether there was a control group, and whether people were randomly assigned to either group without knowing which one they were in. This is especially important if a study aims to suggest that a certain experience or treatment might actually cause a specific outcome, rather than just reporting a correlation between two variables (see next point).
For example, were some people randomly assigned a specific meditation practice while others engaged in a comparable activity or exercise? If the sample is large enough, randomized trials can produce solid conclusions. But, sometimes, a study will not have a control group because it’s ethically impossible. We can’t, for example, let sick people go untreated just to see what would happen. Biomedical research often makes use of standard “treatment as usual” or placebos in control groups. They also follow careful ethical guidelines to protect patients from both maltreatment and being deprived necessary treatment. When you’re reading about studies of masks, social distancing, and treatments during the COVID-19, you can partially gauge the reliability and validity of the study by first checking if it had a control group. If it didn’t, the findings should be taken as preliminary.
7. Did the researchers establish causality, correlation, dependence, or some other kind of relationship?
We often hear “Correlation is not causation” shouted as a kind of battle cry, to try to discredit a study. But correlation—the degree to which two or more measurements seem connected—is important, and can be a step toward eventually finding causation—that is, establishing a change in one variable directly triggers a change in another. Until then, however, there is no way to ascertain the direction of a correlational relationship (does A change B, or does B change A), or to eliminate the possibility that a third, unmeasured factor is behind the pattern of both variables without further analysis.
In the end, the important thing is to accurately identify the relationship. This has been crucial in understanding steps to counter the spread of COVID-19 like shelter-in-place orders. Just showing that greater compliance with shelter-in-place mandates was associated with lower hospitalization rates is not as conclusive as showing that one community that enacted shelter-in-place mandates had lower hospitalization rates than a different community of similar size and population density that elected not to do so.
We are not the first people to face an infection without understanding the relationships between factors that would lead to more of it. During the bubonic plague, cities would order rodents killed to control infection. They were onto something: Fleas that lived on rodents were indeed responsible. But then human cases would skyrocket.
Why? Because the fleas would migrate off the rodent corpses onto humans, which would worsen infection. Rodent control only reduces bubonic plague if it’s done proactively; once the outbreak starts, killing rats can actually make it worse. Similarly, we can’t jump to conclusions during the COVID-19 pandemic when we see correlations.
8. Are journalists and politicians, or even scientists, overstating the result?
Language that suggests a fact is “proven” by one study or which promotes one solution for all people is most likely overstating the case. Sweeping generalizations of any kind often indicate a lack of humility that should be a red flag to readers. A study may very well “suggest” a certain conclusion but it rarely, if ever, “proves” it.
This is why we use a lot of cautious, hedging language in Greater Good , like “might” or “implies.” This applies to COVID-19 as well. In fact, this understanding could save your life.
When President Trump touted the advantages of hydroxychloroquine as a way to prevent and treat COVID-19, he was dramatically overstating the results of one observational study. Later studies with control groups showed that it did not work—and, in fact, it didn’t work as a preventative for President Trump and others in the White House who contracted COVID-19. Most survived that outbreak, but hydroxychloroquine was not one of the treatments that saved their lives. This example demonstrates how misleading and even harmful overstated results can be, in a global pandemic.
9. Is there any conflict of interest suggested by the funding or the researchers’ affiliations?
A 2015 study found that you could drink lots of sugary beverages without fear of getting fat, as long as you exercised. The funder? Coca Cola, which eagerly promoted the results. This doesn’t mean the results are wrong. But it does suggest you should seek a second opinion : Has anyone else studied the effects of sugary drinks on obesity? What did they find?
It’s possible to take this insight too far. Conspiracy theorists have suggested that “Big Pharma” invented COVID-19 for the purpose of selling vaccines. Thus, we should not trust their own trials showing that the vaccine is safe and effective.
But, in addition to the fact that there is no compelling investigative evidence that pharmaceutical companies created the virus, we need to bear in mind that their trials didn’t unfold in a vacuum. Clinical trials were rigorously monitored and independently reviewed by third-party entities like the World Health Organization and government organizations around the world, like the FDA in the United States.
Does that completely eliminate any risk? Absolutely not. It does mean, however, that conflicts of interest are being very closely monitored by many, many expert eyes. This greatly reduces the probability and potential corruptive influence of conflicts of interest.
10. Do the authors reference preceding findings and original sources?
The scientific method is based on iterative progress, and grounded in coordinating discoveries over time. Researchers study what others have done and use prior findings to guide their own study approaches; every study builds on generations of precedent, and every scientist expects their own discoveries to be usurped by more sophisticated future work. In the study you are reading, do the researchers adequately describe and acknowledge earlier findings, or other key contributions from other fields or disciplines that inform aspects of the research, or the way that they interpret their results?

Greater Good’s Guide to Well-Being During Coronavirus
Practices, resources, and articles for individuals, parents, and educators facing COVID-19
This was crucial for the debates that have raged around mask mandates and social distancing. We already knew quite a bit about the efficacy of both in preventing infections, informed by centuries of practical experience and research.
When COVID-19 hit American shores, researchers and doctors did not question the necessity of masks in clinical settings. Here’s what we didn’t know: What kinds of masks would work best for the general public, who should wear them, when should we wear them, were there enough masks to go around, and could we get enough people to adopt best mask practices to make a difference in the specific context of COVID-19 ?
Over time, after a period of confusion and contradictory evidence, those questions have been answered . The very few studies that have suggested masks don’t work in stopping COVID-19 have almost all failed to account for other work on preventing the disease, and had results that simply didn’t hold up. Some were even retracted .
So, when someone shares a coronavirus study with you, it’s important to check the date. The implications of studies published early in the pandemic might be more limited and less conclusive than those published later, because the later studies could lean on and learn from previously published work. Which leads us to the next question you should ask in hearing about coronavirus research…
11. Do researchers, journalists, and politicians acknowledge limitations and entertain alternative explanations?
Is the study focused on only one side of the story or one interpretation of the data? Has it failed to consider or refute alternative explanations? Do they demonstrate awareness of which questions are answered and which aren’t by their methods? Do the journalists and politicians communicating the study know and understand these limitations?
When the Annals of Internal Medicine published a Danish study last month on the efficacy of cloth masks, some suggested that it showed masks “make no difference” against COVID-19.
The study was a good one by the standards spelled out in this article. The researchers and the journal were both credible, the study was randomized and controlled, and the sample size (4,862 people) was fairly large. Even better, the scientists went out of their way to acknowledge the limits of their work: “Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.”
Unfortunately, their scientific integrity was not reflected in the ways the study was used by some journalists, politicians, and people on social media. The study did not show that masks were useless. What it did show—and what it was designed to find out—was how much protection masks offered to the wearer under the conditions at the time in Denmark. In fact, the amount of protection for the wearer was not large, but that’s not the whole picture: We don’t wear masks mainly to protect ourselves, but to protect others from infection. Public-health recommendations have stressed that everyone needs to wear a mask to slow the spread of infection.
“We get vaccinated for the greater good, not just to protect ourselves ”
As the authors write in the paper, we need to look to other research to understand the context for their narrow results. In an editorial accompanying the paper in Annals of Internal Medicine , the editors argue that the results, together with existing data in support of masks, “should motivate widespread mask wearing to protect our communities and thereby ourselves.”
Something similar can be said of the new vaccine. “We get vaccinated for the greater good, not just to protect ourselves,” says Hass. “Being vaccinated prevents other people from getting sick. We get vaccinated for the more vulnerable in our community in addition for ourselves.”
Ultimately, the approach we should take to all new studies is a curious but skeptical one. We should take it all seriously and we should take it all with a grain of salt. You can judge a study against your experience, but you need to remember that your experience creates bias. You should try to cultivate humility, doubt, and patience. You might not always succeed; when you fail, try to admit fault and forgive yourself.
Above all, we need to try to remember that science is a process, and that conclusions always raise more questions for us to answer. That doesn’t mean we never have answers; we do. As the pandemic rages and the scientific process unfolds, we as individuals need to make the best decisions we can, with the information we have.
This article was revised and updated from a piece published by Greater Good in 2015, “ 10 Questions to Ask About Scientific Studies .”
About the Authors
Jeremy Adam Smith
Uc berkeley.
Jeremy Adam Smith edits the GGSC’s online magazine, Greater Good . He is also the author or coeditor of five books, including The Daddy Shift , Are We Born Racist? , and (most recently) The Gratitude Project: How the Science of Thankfulness Can Rewire Our Brains for Resilience, Optimism, and the Greater Good . Before joining the GGSC, Jeremy was a John S. Knight Journalism Fellow at Stanford University.
Emiliana R. Simon-Thomas
Emiliana R. Simon-Thomas, Ph.D. , is the science director of the Greater Good Science Center, where she directs the GGSC’s research fellowship program and serves as a co-instructor of its Science of Happiness and Science of Happiness at Work online courses.
You May Also Enjoy

Why Is COVID-19 Killing So Many Black Americans?

How to Keep the Greater Good in Mind During the Coronavirus Outbreak

How to Form a Pandemic Pod

How Does COVID-19 Affect Trust in Government?

In a Pandemic, Elbow Touches Might Keep Us Going

Why Your Sacrifices Matter During the Pandemic
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
18k Accesses
37 Citations
14 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
- Research Highlight
- Open access
- Published: 16 March 2020
SARS-CoV-2 and COVID-19: The most important research questions
- Kit-San Yuen 1 ,
- Zi -Wei Ye 2 ,
- Sin-Yee Fung 1 ,
- Chi-Ping Chan 1 &
- Dong-Yan Jin ORCID: orcid.org/0000-0002-2778-3530 1
Cell & Bioscience volume 10 , Article number: 40 ( 2020 ) Cite this article
86k Accesses
381 Citations
170 Altmetric
Metrics details
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and viral pathogenesis.
The 2019-nCoV causes an ongoing outbreak of lower respiratory tract disease called novel coronavirus pneumonia (NCP) by the Chinese government initially. The disease name was subsequently recommended as COVID-19 by the World Health Organization. Meanwhile, 2019-nCoV was renamed SARS-CoV-2 by the International Committee on Taxonomy of Viruses. As of February 24, 2020, more than 80,000 confirmed cases including more than 2,700 deaths have been reported worldwide, affecting at least 37 countries. The WHO has declared this a global health emergency at the end of January 2020. The epicenter of this ongoing outbreak is in the city of Wuhan in Hubei Province of central China and the Huanan seafood wholesale market was thought to be at least one of the places where SARS-CoV-2 from an unknown animal source might have crossed the species barrier to infect humans.
A pioneering study conducted in the city of Shenzhen near Hong Kong by a group of clinicians and scientists from the University of Hong Kong has provided the first concrete evidence for human-to-human transmission of SARS-CoV-2 [ 1 ]. This is an excellent example of how a high-quality clinical study can make a major difference in policy setting. Several important clinical features of COVID-19 have also been documented in this study. First, an attack rate of 83% within the family context is alarmingly high, indicating the high transmissibility of SARS-CoV-2. Second, the clinical manifestations of COVID-19 in this family range from mild to moderate, with more systematic symptoms and more severe radiological abnormalities seen in older patients. Generally, COVID-19 appears to be less severe than SARS. Third, an asymptomatic child was found to have ground-glass opacities in his lung and SARS-CoV-2 RNA in his sputum sample. This finding of asymptomatic virus shedding raises the possibility for transmission of SARS-CoV-2 from asymptomatic carriers to others, which is later confirmed by others [ 2 ]. Finally, the presentation of diarrhea in two young adults from the same family also suggests the possibility for gastrointestinal involvement in SARS-CoV-2 infection and fecal–oral transmission. The study has set the stage for the control and management of COVID-19 [ 1 ]. The work was completed timely and the investigators showed great courage and leadership in a very difficult time when the Chinese authority failed to recognize widespread person-to-person transmission of SARS-CoV-2 before January 20, 2020.
Several interesting papers on SARS-CoV-2 and COVID-19 have been published in the past few weeks to report on the evolutionary reservoir [ 3 ], possible intermediate host [ 4 ] and genomic sequence [ 5 ] of SARS-CoV-2 as well as clinical characteristics of COVID-19 [ 6 , 7 ]. In view of these findings and the urgent needs in the prevention and control of SARS-CoV-2 and COVID-19, in this commentary we highlight the most important research questions in the field from our personal perspectives.
The first question concerns how SARS-CoV-2 is transmitted currently in the epicenter of Wuhan. In order to minimize the spreading of SARS-CoV-2, China has locked down Wuhan and nearby cities since January 23, 2020. The unprecedented control measures including suspension of all urban transportation have apparently been successful in preventing further spreading of SARS-CoV-2 to other cities. However, the number of confirmed cases in Wuhan continued to rise. It is therefore crucial to determine whether the rise is due to a large number of infected individuals before the lock down and/or failure in the prevention of widespread intra-familial, nosocomial or community transmission. Based on the number of exported cases from Wuhan to cities outside of mainland China, it was predicted that there might be more than 70,000 individuals infected with SARS-CoV-2 on January 25, 2020 in Wuhan [ 8 ]. This should be determined experimentally in Wuhan as discussed below and it will reveal whether the real numbers of infected people and asymptomatic carriers are indeed underestimated severely. In addition to viral RNA detection, measurement of IgM and IgG antibodies as well as antigens would be very helpful. Several representative residential areas should be selected for detailed analysis so that a big picture can be deduced. The analysis should include all healthy and diseased individuals within the area with the aim of identifying people who have recovered from an infection or are having an active infection. The ratio of asymptomatic carriers should also be determined. The analysis should also be extended to detect RNA and antigen of influenza viruses. The activity of seasonal flu in Wuhan also reached a peak at the beginning of 2020. It will be of interest to see whether the flu season had ended and how many people having a fever now are actually infected with influenza virus. Precision control measures for SARS-CoV-2 should be tailor-designed for high-risk groups based on the results of this analysis. Differentiating people having a flu and preventing them from infecting with SARS-CoV-2 in a hospital setting might also be critical.
The second question is how transmissible and pathogenic is SARS-CoV-2 in tertiary and quaternary spreading within humans. Continued transmission of SARS-CoV-2 in Wuhan suggests that tertiary and quaternary spreading has occurred. Compared to the primary and secondary spreading during which SARS-CoV-2 was transmitted from animal to human and from human to human, has the transmission rate increased and has the pathogenicity decreased? Alternatively, is the virus less transmissible after several passages in humans? Retrospective analysis of all confirmed cases in Wuhan should be very informative. The answers to the above questions hold the key to the outcome of the outbreak. If the transmission is weakened, the outbreak may ultimately come to an end at which SARS-CoV-2 is eradicated from humans. On the contrary, if effective transmission can be sustained, the chance is increased that SARS-CoV-2 will become another community-acquired human coronavirus just like the other four human coronaviruses (229E, OC43, HKU1 and NL63) causing common cold only. The basic reproductive number (R 0 ) of SARS-CoV-2 has been estimated to be 2.68, resulting in an epidemic doubling time of about 6.4 days [ 8 ]. Other estimates of R 0 could go up to 4, higher than that of SARS-CoV, which is lower than 2. Determining the real R 0 will shed light on whether and to what extent infection control measures are effective.
The third question relates to the importance of asymptomatic and presymptomatic virus shedding in SARS-CoV-2 transmission. Asymptomatic and presymptomatic virus shedding posts a big challenge to infection control [ 1 , 2 ]. In addition, patients with mild and unspecific symptoms are also difficult to identify and quarantine. Notably, the absence of fever in SARS-CoV-2 infection (12.1%) is more frequent than in SARS-CoV (1%) and Middle East respiratory syndrome coronavirus (MERS-CoV; 2%) infection [ 6 ]. In light of this, the effectiveness of using fever detection as the surveillance method should be reviewed. However, based on previous studies of influenza viruses and community-acquired human coronaviruses, the viral loads in asymptomatic carriers are relatively low [ 9 ]. If this is also the case for SARS-CoV-2, the risk should remain low. Studies on the natural history of SARS-CoV-2 infection in humans are urgently needed. Identifying a cohort of asymptomatic carriers in Wuhan and following their viral loads, clinical presentations and antibody titers over a time course will provide clues as to how many of the subjects have symptoms in a later phase, whether virus shedding from the subjects is indeed less robust, and how often they might transmit SARS-CoV-2 to others.
The fourth question relates to the importance of fecal–oral route in SARS-CoV-2 transmission. In addition to transmission via droplets and close contact, fecal–oral transmission of SARS-CoV has been shown to be important in certain circumstances. Gastrointestinal involvement of SARS-CoV-2 infection and isolation of SARS-CoV-2 from fecal samples of patients are in support of the importance of fecal–oral route in SARS-CoV-2 transmission. Although diarrhea was rarely seen in studies with large cohorts [ 6 , 7 ], the possibility of SARS-CoV-2 transmission via sewage, waste, contaminated water, air condition system and aerosols cannot be underestimated, particularly in cases such as the Diamond Princess cruise ship with 3,700 people, among whom at least 742 have been confirmed to be infected with SARS-CoV-2 plausibly as the result of a superspreading event. Further investigations are required to determine the role of fecal–oral transmission in these cases and within the representative residential areas selected for detailed epidemiological studies in Wuhan as discussed earlier.
The fifth question concerns how COVID-19 should be diagnosed and what diagnostic reagents should be made available. RT-PCR-based SARS-CoV-2 RNA detection in respiratory samples provides the only specific diagnostic test at the initial phase of the outbreak. It has played a very critical role in early detection of patients infected with SARS-CoV-2 outside of Wuhan, implicating that widespread infection of the virus had occurred in Wuhan at least as early as the beginning of 2020. This has also pushed the Chinese authority to acknowledge the severity of the situation. Due to difficulties in sampling and other technical issues in this test, at one point in early February clinically diagnosed patients with typical ground glass lung opacities in chest CT were also counted as confirmed cases in order to have the patients identified and quarantined as early as possible. ELISA kits for detection of IgM and IgG antibodies against N and other SARS-CoV-2 proteins have also been available more recently. This has made specific diagnosis of ongoing and past infection possible. Particularly, seroconversion for IgM antibodies normally occurs a few days earlier than that of IgG. ELISA reagents for detection of SARS-CoV-2 antigens such as S and N are still in urgent need, and would provide another test highly complementary to viral RNA detection.
The sixth question concerns how COVID-19 should be treated and what treatment options should be made available. COVID-19 is a self-limiting disease in more than 80% of patients. Severe pneumonia occurred in about 15% of cases as revealed in studies with large cohorts of patients. The gross case fatality is 3.4% worldwide as of February 25, 2020. This rate is 4.4% for patients in Wuhan, 4.0% for patients in Hubei and 0.92% for patients outside of Hubei. The exceedingly high fatality in Wuhan might be explained by the collapse of hospitals, a large number of undiagnosed patients, suboptimal treatment or a combination of these. Up to date, we still do not have any specific anti-SARS-CoV-2 agents but an anti-Ebola drug, remdesivir, may hold the promise. As a nucleotide analog, remdesivir was shown to be effective in preventing MERS-CoV replication in monkeys. Severity of disease, viral replication, and lung damage were reduced when the drug was administered either before or after infection with MERS-CoV [ 10 ]. These results provide the basis for a rapid test of the beneficial effects of remdesivir in COVID-19. Other antiviral agents worthy of further clinical investigations include ribavirin, protease inhibitors lopinavir and ritonavir, interferon α2b, interferon β, chloroquine phosphate, and Arbidol. However, we should also bear in mind the side effects of these antiviral agents. For example, type I interferons including interferon α2b and interferon β are well known for their antiviral activity. Their beneficial effects at an early phase of infection are well expected. However, administration at a later stage carries the risk that they might worsen the cytokine storm and exacerbate inflammation. Notably, steroids have been experimentally used widely in the treatment of SARS and are still preferred by some Chinese physicians in the treatment of COVID-19. It is said to be capable of stopping the cytokine storm and preventing lung fibrosis. However, the window in which steroids might be beneficial to patients with COVID-19 is very narrow. In other words, steroids can only be used when SARS-CoV-2 has already been eliminated by human immune response. Otherwise, SARS-CoV-2 replication will be boosted leading to exacerbation of symptoms, substantial virus shedding, as well as increased risk for nosocomial transmission and secondary infection. In this regard, it will be of interest to determine whether the report of fungal infection in the lungs of some patients in Wuhan might be linked to misuse of steroids. Nevertheless, the screening of new pharmaceuticals, small-molecule compounds and other agents that have potent anti-SARS-CoV-2 effects will successfully derive new and better lead compounds and agents that might prove useful in the treatment of COVID-19.
The seventh question is whether inactivated vaccines are a viable option for SARS-CoV-2. The chance that SARS-CoV-2 will become endemic in some areas or even pandemic has increased in view of its high transmissibility, asymptomatic and presymptomatic virus shedding, high number of patients with mild symptoms, as well as the evidence for superspreading events. Thus, vaccine development becomes necessary for prevention and ultimate eradication of SARS-CoV-2. Inactivated vaccines are one major type of conventional vaccines that could be easily produced and quickly developed. In this approach, SARS-CoV-2 virions can be chemically and/or physically inactivated to elicit neutralizing antibodies. In the case of SARS-CoV and MERS-CoV, neutralizing antibodies were successfully and robustly induced by an inactivated vaccine in all types of animal experiments, but there are concerns about antibody-dependent enhancement of viral infection and other safety issues. While inactivated vaccines should still be tested, alternative approaches include live attenuated vaccines, subunit vaccines and vectored vaccines. All of these merit further investigations and tests in animals.
The eighth question relates to the origins of SARS-CoV-2 and COVID-19. To make a long story short, two parental viruses of SARS-CoV-2 have now been identified. The first one is bat coronavirus RaTG13 found in Rhinolophus affinis from Yunnan Province and it shares 96.2% overall genome sequence identity with SARS-CoV-2 [ 3 ]. However, RaTG13 might not be the immediate ancestor of SARS-CoV-2 because it is not predicted to use the same ACE2 receptor used by SARS-CoV-2 due to sequence divergence in the receptor-binding domain sharing 89% identity in amino acid sequence with that of SARS-CoV-2. The second one is a group of betacoronaviruses found in the endangered species of small mammals known as pangolins [ 4 ], which are often consumed as a source of meat in southern China. They share about 90% overall nucleotide sequence identity with SARS-CoV-2 but carries a receptor-binding domain predicted to interact with ACE2 and sharing 97.4% identity in amino acid sequence with that of SARS-CoV-2. They are closely related to both SARS-CoV-2 and RaTG13, but apparently they are unlikely the immediate ancestor of SARS-CoV-2 in view of the sequence divergence over the whole genome. Many hypotheses involving recombination, convergence and adaptation have been put forward to suggest a probable evolutionary pathway for SARS-CoV-2, but none is supported by direct evidence. The jury is still out as to what animals might serve as reservoir and intermediate hosts of SARS-CoV-2. Although Huanan seafood wholesale market was suggested as the original source of SARS-CoV-2 and COVID-19, there is evidence for the involvement of other wild animal markets in Wuhan. In addition, the possibility for a human superspreader in the Huanan market has not been excluded. Further investigations are required to shed light on the origins of SARS-CoV-2 and COVID-19.
The ninth question concerns why SARS-CoV-2 is less pathogenic. If the reduced pathogenicity of SARS-CoV-2 is the result of adaptation to humans, it will be of great importance to identify the molecular basis of this adaptation. The induction of a cytokine storm is the root cause of pathogenic inflammation both in SARS and COVID-19. SARS-CoV is known to be exceedingly potent in the suppression of antiviral immunity and the activation of proinflammatory response. It is therefore intriguing to see how SARS-CoV-2 might be different from SARS-CoV in interferon-antagonizing and inflammasome-activating properties. It is noteworthy that some interferon antagonists and inflammasome activators encoded by SARS-CoV are not conserved in SARS-CoV-2. Particularly, ORF3 and ORF8 in SARS-CoV-2 are highly divergent from ORF3a and ORF8b in SARS-CoV that are known to induce NLRP3 inflammasome activation. ORF3 of SARS-CoV-2 is also significantly different from the interferon antagonist ORF3b of SARS-CoV. Thus, these viral proteins of SARS-CoV and SARS-CoV-2 should be compared for their abilities to modulate antiviral and proinflammatory responses. The hypothesis that SARS-CoV-2 might be less efficient in the suppression of antiviral response and the activation of NLRP3 inflammasome should be tested experimentally.
Much progress has been made in the surveillance and control of infectious diseases in China after the outbreak of SARS-CoV in 2003. Meanwhile, virological research in the country has also been strengthened. The new disease report and surveillance system did function relatively well during the 2009 pandemic of swine flu. New viral pathogens such as avian influenza virus H7N9 and severe-fever-with-thrombocytopenia syndrome bunyavirus have also been discovered in recent years [ 11 , 12 ], indicating the strength and vigor of Chinese infectious disease surveillance and virological research. However, the ongoing outbreak of SARS-CoV-2 has not only caused significant morbidity and mortality in China, but also revealed major systematic problems in control and prevention of infectious diseases there. Unfortunately, many of the lessons from the 2003 outbreak have not been learned. Importantly, disease control professionals, practicing physicians and scientists are disconnected in the fight against SARS-CoV-2 and COVID-19. In addition, important decisions were not made by experts in the field. Hopefully, these issues will be dealt with swiftly and decisively during and after the outbreak.
Above we have discussed the two possibilities that this outbreak will unfold. If SARS-CoV-2 is not eliminated from humans through quarantine and other measures, it can still be eradicated by vaccination. If it attenuates to become another community-acquired human coronavirus causing mild respiratory tract disease resembling the other four human coronaviruses associated with common cold, it will not be a disaster either. Before SARS-CoV-2 attenuates further to a much less virulent form, early diagnosis and improved treatment of severe cases hold the key to reduce mortality. We should remain vigilant, but there are grounds for guarded optimism. Redoubling our research efforts on SARS-CoV-2 and COVID-19 will solidify the scientific basis on which important decisions are made.
Availability of data and materials
Not applicable.
Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Xing F, Liu J, Yip CCY, Poon RWS, Tsoi HW, Lo SKF, Chan KH, Poon VKM, Chan WM, Ip JD, Cai JP, Cheng VCC, Chen H, Hui CKM, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–23.
Article CAS Google Scholar
Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, Wang M. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585 .
Article PubMed Google Scholar
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020. https://doi.org/10.1038/s41586-020-2012-7 .
Lam TTY, Shum MHH, Zhu HC, Tong YG, Ni XB, Liao YS, Wei W, Cheung WYM, Li WJ, Li LF, Leung GM, Holmes EC, Hu YL, Guan Y. Identification of 2019-nCoV related coronaviruses in Malayan pangolins in southern China. BioRxiv. 2020. https://doi.org/10.1101/2020.02.13.945485 .
Article Google Scholar
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. https://doi.org/10.1016/S0140-6736(20)30251-8 .
The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China. China CDC Weekly. 2020;2(8):113–22.
Google Scholar
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019, novel coronavirus–infected pneumonia in Wuhan China. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585 .
Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689-97. https://doi.org/10.1016/S0140-6736(20)30260-9 .
Heimdal I, Moe N, Krokstad S, Christensen A, Skanke LH, Nordbø SA, Døllner H. Human coronavirus in hospitalized children with respiratory tract infections: a 9-year population-based study from Norway. J infect Dis. 2019;219(8):1198–206.
de Wit E, Feldmann F, Cronin J, Jordan R, Okumura A, Thomas T, Scott D, Cihlar T, Feldmann H. Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. PNAS. 2020. https://doi.org/10.1073/pnas.1922083117 .
Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Chen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Li X, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Zhang Y, Han J, Yu H, Li D, Gao GF, Wu G, Wang YU, Yuen Z, Shu Y. Human infection with a novel avian-origin influenza virus. N Engl J Med. 2013;368:1888–977.
Yu XJ, Liang MF, Zhang SY, Liu Y, Li JD, Sun YL, Zhang L, Zhang QF, Popov VL, Li C, Qu J, Li Q, Zhang YP, Hai R, Wu W, Wang Q, Zhan FX, Wang XJ, Kan B, Wang SW, Wan KL, Jing HQ, Lu JX, Yin WW, Zhou H, Guan XH, Liu JF, Bi ZQ, Liu GH, Ren J, Wang H, Zhao Z, Song JD, He JR, Wan T, Zhang JS, Fu XP, Sun LN, Dong XP, Feng ZJ, Yang WZ, Hong T, Zhang Y, Walker DH, Wang Y, Li DX. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med. 2011;364(16):1523–32.
Download references
Acknowledgements
We thank Pearl Chan, Hinson Cheung, Terence Lee and Kam-Leung Siu for critical reading of the manuscript.
Coronavirus research in our laboratory was funded by the Hong Kong Health and Medical Research Fund (HKM-15-M01) and Hong Kong Research Grants Council (T11-707/15-R).
Author information
Authors and affiliations.
School of Biomedical Sciences, The University of Hong Kong, 3/F Laboratory Block, 21 Sassoon Road, Pokfulam, Hong Kong
Kit-San Yuen, Sin-Yee Fung, Chi-Ping Chan & Dong-Yan Jin
Department of Microbiology, The University of Hong Kong, Pokfulam, Hong Kong
You can also search for this author in PubMed Google Scholar
Contributions
KSY and DYJ wrote the manuscript with inputs from ZWY, SYF and CPC. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Dong-Yan Jin .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
No potential conflict of interest was reported by the authors.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yuen, KS., Ye, Z.W., Fung, SY. et al. SARS-CoV-2 and COVID-19: The most important research questions. Cell Biosci 10 , 40 (2020). https://doi.org/10.1186/s13578-020-00404-4
Download citation
Received : 26 February 2020
Accepted : 07 March 2020
Published : 16 March 2020
DOI : https://doi.org/10.1186/s13578-020-00404-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- 2019 novel coronavirus (2019-nCoV)
- Novel coronavirus pneumonia (NCP)
Cell & Bioscience
ISSN: 2045-3701
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
More Questions and Answers About COVID-19 Vaccines
Interview by Stephanie Desmond
How is it possible that COVID-19 vaccines prevent serious illness and death but may not prevent mild infection? How effective are vaccines at preventing long-haul COVID? How soon might we see flu mRNA vaccines and would those have to go through clinical trials?
Josh Sharfstein answers a list of important questions about COVID-19 vaccines.
Most COVID vaccine information is focused on how effective they are at preventing serious disease, hospitalization, and death. How is it possible that the vaccine is more effective at preventing serious illness and death than it is preventing a mild infection?
It’s actually very common for vaccines to be much better at preventing serious illness and death than preventing infection or mild infection. For example, with the flu vaccine, people can still often get the flu, but they are much less likely to get seriously ill or die if they get the flu vaccine.
The question is why. It partly depends on how the immune system responds to vaccines. Any infection whatsoever is a certain type of immune response, and very few vaccines give what people call a “sterilizing immune response.”
What vaccines do cause is an immune response that is strong and multifaceted inside your body. So, even if you knew that the virus can replicate a bit for a mild infection, it can’t cause that huge overwhelming infection that really puts people at risk.
Early on in the pandemic, before we even had vaccines, some vaccine experts were saying the most important thing is going to be [preventing] serious illness and death, and [vaccines will] probably will be much better for that than for mild illness, just like almost every other vaccine out there. Sure enough, that proved to be the case.
How effective are vaccines at preventing long-haul COVID?
We don’t know. It’s a good question, because people can get these long-term symptoms from relatively mild infection.
There are some studies being set up to assess this, but we don’t know for sure. The safe bet would be that the chance of getting a long-haul infection is going to be much lower [for] someone who’s vaccinated compared to someone who’s not, just because that person is much less likely to get infected at all.
There’s also this related question of whether people with long-term symptoms from COVID actually might benefit from getting vaccinated. Somebody who had an infection and has been suffering some of those symptoms like fatigue and brain fog—does it get better if you get vaccinated? There’s no answer to that; however, at multiple clinical sites, some of the doctors are hearing from their patients that they’re feeling somewhat better. I think that the real answer to that, though, is going to depend on studies that will be completed, to see whether it makes a difference.
If I have no symptoms at all after receiving the Pfizer or Moderna vaccines, does this indicate that if I had gotten COVID, I would have been asymptomatic or had mild symptoms?
I do not think it means that.
What determines how sick you are from COVID-19 is a complex set of things that include how much virus your body actually took in. That’s one reason why people who get exposed to lower levels of virus are more likely to have an infection without symptoms, for example.
It also relates to different aspects of people’s immune system and probably some other factors we haven’t figured out, so I would not assume that the response to the vaccine is the same as the response to the actual virus.
Is this the first time mRNA technology has been used in a vaccine?
It is not, actually. There are several vaccines that are in development with mRNA technology. They’ve completed safety studies for them, and that includes influenza—so there could be an mRNA flu vaccine in the future—cytomegalovirus, Zika virus, and the rabies virus.
[These vaccine trials] haven’t made it all the way to the end [because] those were going through the regular vaccine process where you go one step at a time. Those companies aren’t going to invest in a big, next trial until they’ve really analyzed the data from the previous study.
In the case of [COVID-19 vaccines], we had a lot of urgency and all the money was put up, up front. The companies didn’t have to find the money for each stage—they were just able to just proceed from the safety study to the effectiveness study very quickly. This let the coronavirus vaccines go to the front of the line because of the urgency.
This is a technology that’s been well studied, not just for vaccines, but also for therapeutics.
Do you think that having successful mRNA COVID vaccines will pave the way for these other vaccines?
It’s going to be great for people’s comfort level with the vaccine, both at a level of understanding—like, “Wow, that’s going to be like the coronavirus vaccine, and it was so successful!”—and also scientifically, I think there’ll be a greater understanding of mRNA vaccines, and that will help with the development and the review of other mRNA vaccines for different different viruses.
Having said that, just because an mRNA vaccine works for coronavirus doesn’t mean it’s necessarily going to work for a rabies or influenza virus. They’re going to have to do studies to find out.
Do we know yet how soon flu vaccines may be made as mRNA vaccines, and will they have to go through clinical trials as a new vaccine?
I would expect that they would go to clinical trials … but I do know that some studies have already been done, and hopefully this will proceed and we’ll get another great vaccine.
One of the long-held goals for flu vaccination is a vaccine that lasts more than one year, and maybe a vaccine that doesn’t require a strain change every year. The mRNA vaccines may be a way to get to that goal, but there obviously has to be a lot more research.
Why are mRNA vaccines so encouraging for the future?
This is a platform that has certain advantages, among them, that you can stand it up so quickly. It doesn’t require a lot of different ingredients—it’s a very, very small number of things that go into the vaccine—and it can be updated, very quickly, so if you need to change the strain, it’s very possible to do that.
I think we’ll look back and think that mRNA kind of had its coming out party with coronavirus, but [was] around beforehand, and it will hopefully lead to some other important advances in medicine.
How are side effects from COVID-19 vaccines being monitored?
They’re being monitored in multiple ways. One thing that people who have gotten vaccinated know is that you have an opportunity to get texted about the potential side effects you’re experiencing. The Centers for Disease Control is looking at that from millions of people who are getting vaccinated to understand the profile of side effects. People also submit reports to the manufacturers and to the FDA about potential side effects, and there are studies that are done in large insurance databases or clinical databases where you can look at the people who got the vaccine compared to people who didn’t get the vaccine to see whether there’s any difference in case there’s a question about whether or not a particular side effect might be caused by the vaccine.
On a regular basis, there is a big group that comes together and looks at data from all these different sources to see what the safety profile is and, so far, it’s been very, very strong.
I was just looking at a 60-page document that’s posted on the CDC website where they went through all these different sources and they have a huge analysis of allergic reactions. I think the Pfizer vaccine had five serious allergic reactions per million doses given, and per 2.8 million for the Moderna vaccine. Almost always, those allergic reactions are in the first dose. Not always, but almost always.
It also talks about the evidence of the mild side effects people get. Seventy percent of the people get a sore arm; I think about a third got a headache, a third got fatigue, but then of course they feel better in just a couple of days.
They’ve been even doing studies in these insurance databases to compare people who are vaccinated and people who aren’t vaccinated just for things that people think “Well, maybe, could it possibly relate to this [vaccine]?” and they have not found any serious red flags coming up.
So, there’s a lot of analysis of safety data and there will continue to be. It’s a very important part of vaccination and the vaccination program to look at safety and not just in one way, but in multiple ways.
Does someone who recovered from COVID and then gets vaccinated have a higher immunity than someone who hasn’t had COVID and also gets vaccinated?
In general, people who have had COVID have some immune reaction to COVID when they recover. But it’s variable—some people may have a pretty mild immune reaction, and some people may have a very protective immune reaction—and right now, we don’t have an easy way to tell the difference between them.
That’s why vaccination is recommended for everyone, even if you’ve had COVID before. There will be studies of different types of people, their vaccination status and when they got vaccinated, and hopefully we’ll get a picture and some markers like a blood test that you could take to find out how protected you are. We have that for certain infectious diseases. You can, for example, for hepatitis B, see whether you have antibodies.
One of the things we’ll learn from some of these studies is, is there a way to test people for their ability to withstand a coronavirus infection? When we have that, I think that might be more important than these general questions because probably it will depend on the individual and having some way to test to figure that out over time is what will be helpful to people.
If I’ve had COVID, how long should I wait to get vaccinated? Is it okay to get my first dose if I no longer have symptoms?
The basic standard requirements are that if you are in that period where you’re sick and could be spreading COVID to stay home until you get better, which I think is around 10 days and no symptoms—then it’s fine to get vaccinated.
[Some] people have said you’re probably relatively protected from another infection for a couple months after that infection and, if you want to wait a couple of months to get vaccinated, you can do that. But there’s no requirement to do that. It’s perfectly fine to get vaccinated.
There are people who may get COVID right after their first shot, before there’s any protection, and they could get vaccinated for their second shot on time if they want, with one exception: If they’ve been treated for that COVID infection with antibody treatment, then there’s a recommendation to wait 90 days so that that antibody treatment doesn’t interfere with the vaccination.
What will happen if everyone gets vaccinated? Won’t the variants get tougher as their source of food gets eliminated?
The virus is constantly mutating and every time that it replicates, there’s a chance that you could develop a variant. If the virus can’t replicate, the virus can’t develop a variant. If the virus is replicating a lot, then you’re more likely to get variants.
The goal of a vaccination campaign now is to reduce the spread of the virus, which reduces the replication of the virus, which will reduce the chance that there will be more variants.
With less virus, fewer people are dying. And with less virus, fewer variants.
The CDC recently released guidance for what vaccinated people can do safely. What do you think of this?
One important principle is that vaccination is important to people both directly and indirectly.
Directly, it’s important if you’re protected, and there may be some things that are different, like you can meet up in small groups with people who are vaccinated.
There’s also the indirect benefit, which is the more people get vaccinated, the less coronavirus is spreading out there. The less coronavirus spreading out there, the easier it is to open things up again. That’s the indirect benefit, and that may not happen the day you get vaccinated or the day you’re protected from your vaccine. But, the more people in your community get vaccinated, the more likely the benefit is going to come help you.
This is exciting because we can see what the end of the pandemic might look like, but we just have to get there. We can’t trip on our way running too fast to the end of the pandemic.
Meanwhile, states like Texas and Mississippi have both rescinded their mask mandates. Is this getting a little too far ahead?
We have to push COVID as far into the end zone as it can go through good mask wearing, social distancing, and vaccination until we really are able to open things with competence. The risk of doing it too soon is that the virus keeps spreading, you get mutations, you get potential variants spreading, and we wind up taking a step back. That takes longer, in the end, to get to the place that we all want to go.
I’m also concerned about the mixed messaging. Mask wearing really does reduce infection, and we still have a lot of infections in the United States, even though it has come down. Just to hear from one level of government “Do this,” and another level of government “Do that,” it just stirs the pot again and makes it harder for people just to stick with the program long enough to put coronavirus back in a box, which I think is within reach.
Now, will what the governors do really upend that? We don’t know. But will it increase the risk of a problem? It might, and I think that’s why you hear so many people saying, “We’re headed toward the end zone, don’t blow it.”
Joshua Sharfstein, MD , is the vice dean for Public Health Practice and Community Engagement and a professor in Health Policy and Management . He is also the director of the Bloomberg American Health Initiative and a host of the Public Health On Call podcast.
Stephanie Desmon is the co-host of the Public Health On Call podcast. She is the director of public relations and marketing for the Johns Hopkins Center for Communication Programs , the largest center at the Bloomberg School of Public Health.
RELATED CONTENT
- Monica Gandhi and Vaccine Optimism (Podcast)
- Vaccine Week Finale: Q&A with Dr. Josh Sharfstein (podcast)
- For mRNA Vaccines, COVID-19 Is Just the Beginning
Facebook Live Q&A
This conversation is excerpted from a March 5 Facebook Live.
See More Like This
Related Content
Pandemic agreement may happen eventually ... but will the world be ready, what to know about the updated covid vaccine for fall, winter 2024–25, why we’re still waiting for a pandemic treaty, why covid surges in the summer, the problem with pulse oximeters: a long history of racial bias.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
SARS-CoV-2 and COVID-19: The most important research questions
Affiliations.
- 1 1School of Biomedical Sciences, The University of Hong Kong, 3/F Laboratory Block, 21 Sassoon Road, Pokfulam, Hong Kong.
- 2 2Department of Microbiology, The University of Hong Kong, Pokfulam, Hong Kong.
- PMID: 32190290
- PMCID: PMC7074995
- DOI: 10.1186/s13578-020-00404-4
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and viral pathogenesis.
Keywords: 2019 novel coronavirus (2019-nCoV); COVID-19; Novel coronavirus pneumonia (NCP); SARS-CoV-2.
© The Author(s) 2020.
PubMed Disclaimer
Conflict of interest statement
Competing interestsNo potential conflict of interest was reported by the authors.
Similar articles
- A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: lessons from other pathogenic viruses. Fung SY, Yuen KS, Ye ZW, Chan CP, Jin DY. Fung SY, et al. Emerg Microbes Infect. 2020 Mar 14;9(1):558-570. doi: 10.1080/22221751.2020.1736644. eCollection 2020. Emerg Microbes Infect. 2020. PMID: 32172672 Free PMC article. Review.
- Human and novel coronavirus infections in children: a review. Rajapakse N, Dixit D. Rajapakse N, et al. Paediatr Int Child Health. 2021 Feb;41(1):36-55. doi: 10.1080/20469047.2020.1781356. Epub 2020 Jun 25. Paediatr Int Child Health. 2021. PMID: 32584199 Review.
- [Diagnosis, treatment, control and prevention of SARS-CoV-2 and coronavirus disease 2019: back to the future]. Ye ZW, Jin DY. Ye ZW, et al. Sheng Wu Gong Cheng Xue Bao. 2020 Apr 25;36(4):571-592. doi: 10.13345/j.cjb.200115. Sheng Wu Gong Cheng Xue Bao. 2020. PMID: 32347053 Review. Chinese.
- Epidemiological feature, viral shedding, and antibody seroconversion among asymptomatic SARS-CoV-2 carriers and symptomatic/presymptomatic COVID-19 patients. Chen Y, Li P, Ding Y, Liu M, Liu L, Yi B, Wu T, Dong H, Lao X, Ding K, Wang H, Zhang D, Tan X, Wang Z, Xu G, Cao G. Chen Y, et al. J Infect Public Health. 2021 Jul;14(7):845-851. doi: 10.1016/j.jiph.2021.05.003. Epub 2021 May 27. J Infect Public Health. 2021. PMID: 34118734 Free PMC article.
- Virus shedding dynamics in asymptomatic and mildly symptomatic patients infected with SARS-CoV-2. Li W, Su YY, Zhi SS, Huang J, Zhuang CL, Bai WZ, Wan Y, Meng XR, Zhang L, Zhou YB, Luo YY, Ge SX, Chen YK, Ma Y. Li W, et al. Clin Microbiol Infect. 2020 Nov;26(11):1556.e1-1556.e6. doi: 10.1016/j.cmi.2020.07.008. Epub 2020 Jul 9. Clin Microbiol Infect. 2020. PMID: 32653662 Free PMC article.
- Interleukin-6 in COVID-19 Severity Stratification. da Silva FP, Luís MF, Jesus F, Ribeiro J, Almeida É, Braga S, Ferreira L. da Silva FP, et al. Tanaffos. 2023 Apr;22(4):382-388. Tanaffos. 2023. PMID: 39176139 Free PMC article.
- Impact of COVID-19 on child tuberculosis hospitalization. Zaidi S, Errami A, Belkhou I, Elkhaldi M, Ailal F, Benhsaien I, Adnane F, Amenzoui N, Abkari A, Bousfiha AA. Zaidi S, et al. Tunis Med. 2024 Jul 5;102(7):410-414. doi: 10.62438/tunismed.v102i7.4923. Tunis Med. 2024. PMID: 38982965 Free PMC article. English.
- The Development of Aptamer-Based Gold Nanoparticle Lateral Flow Test Strips for the Detection of SARS-CoV-2 S Proteins on the Surface of Cold-Chain Food Packaging. Li X, Wang J, Yang G, Fang X, Zhao L, Luo Z, Dong Y. Li X, et al. Molecules. 2024 Apr 13;29(8):1776. doi: 10.3390/molecules29081776. Molecules. 2024. PMID: 38675595 Free PMC article.
- Water-sanitation-health nexus in the Indus-Ganga-Brahmaputra River Basin: need for wastewater surveillance of SARS-CoV-2 for preparedness during the future waves of pandemic. Chakraborty P, Vinod PG, Syed JH, Pokhrel B, K Bharat G, Basu AR, Fouzder T, Pasupuleti M, Urbaniak M, Beskoski VP. Chakraborty P, et al. Int J Ecohydrol Hydrobiol. 2022 Apr;22(2):283-294. doi: 10.1016/j.ecohyd.2021.11.001. Epub 2021 Nov 15. Int J Ecohydrol Hydrobiol. 2022. PMID: 38620864 Free PMC article.
- The COVID-19 pandemic: Considerations for the waste and wastewater services sector. Nghiem LD, Morgan B, Donner E, Short MD. Nghiem LD, et al. Case Stud Chem Environ Eng. 2020 May;1:100006. doi: 10.1016/j.cscee.2020.100006. Epub 2020 Apr 30. Case Stud Chem Environ Eng. 2020. PMID: 38620229 Free PMC article.
- Chan JFW, Yuan S, Kok KH, To KKW, Chu H, Yang J, Xing F, Liu J, Yip CCY, Poon RWS, Tsoi HW, Lo SKF, Chan KH, Poon VKM, Chan WM, Ip JD, Cai JP, Cheng VCC, Chen H, Hui CKM, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. - DOI - PMC - PubMed
- Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, Wang M. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.1585. - DOI - PMC - PubMed
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 doi: 10.1038/s41586-020-2012-7. - DOI - PMC - PubMed
- Lam TTY, Shum MHH, Zhu HC, Tong YG, Ni XB, Liao YS, Wei W, Cheung WYM, Li WJ, Li LF, Leung GM, Holmes EC, Hu YL, Guan Y. Identification of 2019-nCoV related coronaviruses in Malayan pangolins in southern China. BioRxiv. 2020 doi: 10.1101/2020.02.13.945485. - DOI
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020 doi: 10.1016/S0140-6736(20)30251-8. - DOI - PMC - PubMed
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- The Lens - Patent Citations
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Questions and Answers about COVID-19 Vaccines
On this page, you will find answers to some of the most common questions people are asking about COVID-19 disease and vaccines. Just click on the question of interest and the answer will appear below it.
Can't find what you're looking for?
- Check the “Archived COVID-19 Questions” page.
- Ask your COVID-19 vaccine questions here.
You can also find information related to COVID-19 in these additional resources:
- Printable Q&A, "COVID-19 vaccines: What you should know" English | Spanish | Japanese
- “Look at Each Vaccine: COVID-19 Vaccine” webpage
- Animations: “How COVID-19 Viral Vector Vaccines Work” and “How mRNA Vaccines Work.”
What are the COVID-19 vaccine recommendations for the summer?
Although cases of COVID-19 have decreased, they continue to occur and will likely continue at low levels throughout the summer. For this reason, if someone is considered high risk and they have not been vaccinated in the last six months, they could consider getting a dose, particularly if they will be traveling or around a lot of people.
With this said, the COVID-19 vaccine will be updated this fall so that it protects against a common and currently circulating strain of SARS-CoV-2, the virus that causes COVID-19. The Food and Drug Administration (FDA) advisory committee is meeting in early June to review the data and make recommendations regarding which strain should be used. The updated vaccine will likely be available sometime in September, so people can get a booster dose before cases start to increase again in the fall or winter.
Those who get vaccinated against COVID-19 this summer (as described in the first paragraph) should wait at least four months before getting the updated version, putting them closer to winter for their next dose.
Watch this video in which Dr. Offit describes the considerations related to COVID-19 vaccination during the summer.
Last updated: June 4, 2024
Do DNA fragments in COVID-19 mRNA vaccines cause harm?
The short answer to this question is no, but let’s look a bit more closely.
The quantity
It is important to realize that mRNA vaccines undergo several steps during production, including multiple purification steps. This means that the amount of DNA fragments remaining in a dose of vaccine is extremely small. In fact, the leftover amount is so small that it can only be measured in nanograms, which are 1 billionth (with a “b”) of a gram or 1/1,000,000,000 of a gram. Think of it like one snowflake among 1,000,000,000 — an inconsequential quantity that would escape our notice unless we were looking for it.
The biology
With this said, some people might still be concerned that any DNA fragments are in the vaccine at all. First, it is important to realize that we are exposed to DNA fragments all the time. Anytime we eat plants or animals, we consume DNA, so our bodies need to protect against damage from foreign DNA. And while it is true that when we consume these fragments, they do not necessarily enter our bloodstream, like those in an injection will, we can still be reassured that our cells are designed to protect our DNA. Here are three relevant examples of how cells protect our DNA:
- Cytoplasm – As the vaccine is processed, DNA fragments may find their way to the cytoplasm of a cell, but our cells contain enzymes and immune system mechanisms for detecting and destroying anything foreign, so even if the fragments end up in our cell, they are destroyed.
- Nucleus – In our cells, our own DNA is housed inside the nucleus. The nuclear membrane acts like a moat around a castle, such that only with the appropriate “clearances” can something enter the nucleus. In our cells, these clearances are controlled by “nuclear access signals,” which are not part of (or accessible to) the DNA fragments.
- DNA – Further, for DNA to be changed, certain enzymes must be present. One example is integrase. Without integrase, our own DNA will not “open” to allow another piece of DNA to be added to it. In the example of the DNA fragments in vaccines, integrase is not present, so change cannot occur.
Some have also suggested that because the mRNA vaccine is delivered in lipid particles, the aforementioned description is not accurate. However, this is also a misconception. While the lipid particles help deliver the mRNA into a cell, the vaccine components are taken into compartments called endosomes. Endosomes contain acids and enzymes that break down the lipids and most of the DNA fragments, so they are quickly destroyed.
Watch this video as Dr. Offit describes these safety mechanisms.
To find out more about DNA and other vaccine ingredients, check the “Vaccine Ingredients” section of our website .
Read more about the misinformation surrounding DNA fragments in Dr. Offit’s Substack, “Beyond the Noise.”
Last updated: April 24, 2024
Are the mRNA vaccines a type of gene therapy?
The short answer to this question is no. Check out the article in our April 2024 Parents PACK newsletter to find out why.
If young children do not get severely ill from COVID-19, why should I consider giving this vaccine to my child who is younger than 5 years of age?
As parents weigh the relative risk and benefits of getting their youngest children vaccinated against COVID-19, some wonder about the need for their child to get a relatively new vaccine when the disease doesn’t seem too bad in most children. Most healthcare providers agree that the benefits of vaccination outweigh the risks for our youngest family members:
- As of April 2024, about 2,000 children 17 years of age or younger have died from COVID-19. While this is a small number compared with the more than 1.1 million deaths in the U.S., for those families, their world will never be the same.
- Millions of children have been infected with the virus that causes COVID-19. Some of those children were hospitalized with severe disease or developed a condition called multi-inflammatory syndrome in children (MIS-C), which can damage organs and on rare occasions be deadly. Importantly, it appears that newer variants are less likely to cause MIS-C. Watch this video in which Dr. Offit discusses this trend.
- Like adults, some children who have had COVID-19, even mild cases, have experienced lingering symptoms, commonly referred to as “long COVID.” In younger children it may be difficult for them to express what they are feeling or experiencing, which can make this condition even more difficult to identify and address.
- Millions of vaccines have been administered safely to children at this point.
For a more detailed look at the considerations related to COVID-19 vaccination of children and a series of resources, check out the March 2023 issue of Parents PACK and this April 2023 article penned by Dr. Offit, the VEC’s director .
Watch this short video of Dr. Offit discussing why children should get the COVID-19 vaccine.
What COVID-19 vaccines are currently available in the U.S.?
The U.S. has three approved COVID-19 vaccines; however, the two that are most often used based on the current vaccine recommendations are those described as “mRNA vaccines.” Find out more about each vaccine:
- Pfizer mRNA bivalent vaccine – This vaccine contains mRNA to protect against the spike protein from the XBB.1.5 variant of SARS-CoV-2, the virus that causes COVID-19. The bivalent Pfizer vaccine that contained two spike proteins is no longer authorized for use in the U.S. Available in three different doses based on the age of the individual (3 micrograms per dose for 6 months to 4 years, 10 micrograms per dose for 5 to 11 years, and 30 micrograms per dose for 12 years and older).
- Moderna mRNA bivalent vaccine – This vaccine also contains mRNA to protect against the spike protein from the XBB.1.5 variant of SARS-CoV-2. Likewise, the bivalent Moderna vaccine is no longer authorized for use in the U.S. Two doses are available and are based on the age of the individual (25 micrograms for 6 months to 11 years and 50 micrograms for 12 years and older).
- Novavax protein-based vaccine – This vaccine only contains the spike protein from the XBB.1.5 variant. This vaccine is approved for those 12 years and older who did not previously get a COVID-19 vaccine. In this situation it should be administered as a two-dose series separated by three to eight weeks. As a booster dose, it can be given as a single dose to those 18 years and older.
A fourth vaccine, J&J/Janssen adenovirus-based vaccine , is no longer available in the U.S., but it is still used in other countries. This vaccine contains a replication-defective adenovirus that has been altered to include the gene (DNA) of the spike protein for the original SARS-CoV-2 virus. Because of the availability of other vaccines and due to the rare but serious side effects associated with this vaccine (i.e., Guillain-Barre syndrome (GBS) and thrombosis with thrombocytopenia syndrome (TTS)), and its monovalent formula, this vaccine was removed from the U.S. vaccine supply in the spring of 2023.
What is the Novavax vaccine and who can get it?
The Novavax COVID-19 vaccine uses a “tried and true” approach to inducing immunity. Specifically, the vaccine delivers the spike protein and an adjuvant, which is something that increases immune responses to the protein. It is given as two doses, separated by 3-8 weeks, to those 12 years of age and older. This technology is exactly the same as that used to make one of the influenza vaccines (FluBlok) and very similar to that used to make the hepatitis B and human papillomavirus vaccines.
To find out more about the Novavax vaccine, watch this video of VEC Director, Paul Offit, MD, who is on the FDA’s advisory committee and, therefore, reviewed the data presented during the advisory committee meeting.
Who should get a booster dose of COVID-19 vaccine?
The general rule of thumb related to CDC guidance is that individuals in the U.S. receive a single booster at least eight weeks after their last dose of COVID-19 vaccine. However, some nuance exists for different age groups and vaccines, as shown on this CDC reference table . As such, if you are not sure whether you need an additional dose, we recommend speaking to your healthcare provider.
Adults 65 years of age and older can get up to two doses of the 2023-2024 vaccine separated by at least four months.
Moderately or severely immune compromised individuals may require more doses than their age-matched, immune competent counterparts; however, the recommendations vary based on vaccination history and age, so it is important to talk to your healthcare provider about your or a family member’s specific needs. The recommendations for this group are summarized on these CDC reference tables .
Watch this video to hear Dr. Paul Offit talk about who should get a COVID-19 booster dose.
My teen is a student-athlete and already had COVID-19, so does he need the COVID-19 vaccine? We are worried about myocarditis.
While myocarditis is rare, it is also real; so, we can understand why some parents may be hesitant to get their teens vaccinated. But it is important when making these decisions to realize that the choice not to vaccinate is also a choice to risk COVID-19, so let’s take a look.
Vaccination and myocarditis
By June 2022, almost 55 million doses of Pfizer’s mRNA vaccine were given to children and teens from 5 to 17 years of age. Of those, 635 cases of myocarditis were diagnosed. Most cases occurred in males, and the side effect was most likely to occur in the first seven days after the second dose, albeit a small number of cases occurred after receipt of the first dose or a booster dose.
When a group of 5- to 17-year-olds who experienced myocarditis after COVID-19 vaccination were followed to see how they did, about half were hospitalized and none died. Most of those who were hospitalized went home within three days. In addition, according to their cardiologists, three months after the event, more than 6 in 10 were fully recovered and an additional 2 in 10 had likely fully recovered, but tests were still outstanding.
COVID-19 disease and myocarditis
A review of the literature, published in August 2022, found that an individual is at least 7 times more likely to experience myocarditis resulting from a COVID-19 infection than from a COVID-19 vaccine.
These other considerations are important when deciding about COVID-19 vaccination of teens (or teen athletes):
- Studies have shown that children younger than 5 years of age do not experience myocarditis following receipt of the COVID-19 mRNA vaccines, so vaccinating young children before the risk of myocarditis increases is one way to avoid this potential side effect. Importantly, immunization of our youngest population against COVID-19 has been extremely limited, so it is possible that over time, as more youngsters are vaccinated, we would identify a low risk for myocarditis in young children as well. However, it is also possible that we would see a greater risk from infection compared with vaccination. These are the types of information we need to continue working toward understanding when it comes to this disease.
- For those at greater risk of this side effect, increasing the time between doses to at least eight weeks, appears to lessen the risk of this side effect.
- While older individuals can experience myocarditis in the first week after vaccination, the risk is greatest for males between 12 and 39 years of age. The risk for females is lower than for males, but still can occur and is more prevalent between 12 and 29 years of age.
- It is also important to realize that myocarditis following vaccination is short-lived and tends to resolve on its own, whereas myocarditis following an infection tends to be more severe.
- We are still learning about “long COVID,” the condition that causes people to experience symptoms well after their infection goes away. While we don’t yet know how often this occurs in younger people, it is clear that some young people suffer similar long-term consequences.
Watch this video to hear Dr. Paul Offit talk about COVID-19 vaccine and myocarditis in teens.
Last updated: September 20, 2023; reviewed April 24, 2024
Can someone with COVID-19 get the COVID-19 vaccine or booster?
In the U.S., the CDC recommends that anytime someone has a respiratory illness, they try to stay away from others until their symptoms start improving and they have not had a fever for at least 24 hours.
Likewise, while the CDC previously recommended delaying vaccination for patients who were treated with antibody-based therapies, data now demonstrate that the modest reduction in antibody responses seen in these patients does not warrant the delay. With this said, most recently infected individuals are still recommended to wait for about three months before getting vaccinated, so the antibodies introduced by treatment are unlikely to be problematic anyway.
Why are booster doses recommended?
The goal of vaccination is to prevent serious illness. This is achieved by generating immune memory cells, such as B cells and T cells. These cells are typically long-lived and reside in the bone marrow, bloodstream, and lymph glands to monitor for exposure to a pathogen. If the pathogen is detected, these memory cells quickly become activated and stimulate the immune response to efficiently fight the infection before the infection can get out of control and cause serious illness. In the case of COVID-19 mRNA vaccines, studies demonstrated that high levels of memory cells are generated, and as variants emerged, we saw that the levels of memory cells generated by both the mRNA (Pfizer and Moderna) and adenovirus-based (J&J/Janssen) vaccines were sufficient to prevent serious illness in most cases. As such, these findings would not warrant a booster dose.
However, a second goal of vaccination could be to prevent any level of illness, meaning that vaccinated people would not even experience mild or asymptomatic infection. To accomplish this, people need to have high levels of neutralizing antibodies circulating in their bloodstream. Neutralizing antibodies prevent the virus from attaching to and entering cells. Typically, neutralizing antibody levels fade over time. When this happens, a booster dose can stimulate the memory B and T cells to cause production of neutralizing antibodies, thereby increasing the level of detectable antibodies in the bloodstream and decreasing the chance for any level of illness for another brief period of time (a couple of months).
While prevention of any level of illness is a noble goal, historically, prevention of serious illness has been the goal of vaccination, particularly for respiratory infections, like COVID-19. These two goals have been at the heart of the scientific “debate” over the need for booster doses. In truth, prevention of serious illness is the only reasonable and attainable goal for a virus like SARS-CoV-2, which has a short incubation period.
Watch this video to hear Dr. Offit talk about the Fall 2023 COVID-19 recommendations.
Who is considered immune compromised when it comes to deciding about COVID-19 vaccines?
People should talk with their healthcare providers to determine whether they are considered moderately or severely immune compromised since each individual is unique. However, the CDC has provided some guidance that may help.
People typically considered moderately or severely immune compromised include the following:
- People currently being treated for cancers of the blood or organs (so-called “solid tumor” cancers)
- People with blood-related cancers, regardless of current treatment status, including those with chronic lymphocytic leukemia, non-Hodgkin lymphoma, multiple myeloma and acute leukemia
- People who received an organ transplant and take immunosuppressive medications to prevent rejection of the organ
- People who had a stem cell transplant or received CAR T-cell therapy less than 2 years ago or who are taking immunosuppressive medications
- People with conditions that are considered to cause permanent immune deficiency because the condition affects cells of their immune system, such as DiGeorge syndrome or Wiskott-Aldrich syndrome
- People infected with HIV whose infection is untreated or considered to be at an advanced stage
- High-dose corticosteroids (more than 20 mg prednisone or similar medications per day)
- Alkylating agents
- Antimetabolites
- Transplant-related immunosuppressive medications
- Cancer chemotherapeutic medications that are considered severely immunosuppressive (e.g., tumor-necrosis, or TNF, blockers)
- Biologic agents that suppress or modulate the immune response (e.g., B-cell depleting agents)
Some people 12 years of age and older in these groups may be eligible for ongoing protection through intravenous receipt of a monoclonal antibody product called Pemgarda. Treatments are required every three months. This product cannot be used for treating COVID-19. If you want to find out if you are eligible and could benefit from this product, speak to your healthcare provider who treats you for your immune-compromising condition.
People who should work with their healthcare provider to determine their need for additional doses include:
- People taking medications that make them uncertain whether they would be included in the list of individuals mentioned above
- People with immune-system-related conditions not specifically mentioned above
- People preparing to start one of the above-mentioned medications
People not considered to be in this category include:
- People who do not have compromised immunity.
- People without a spleen.
- People who had cancer but are no longer being treated.
- People with chronic conditions that do not involve the immune system or require treatment with high doses of corticosteroids, such as diabetes, asthma, COPD, kidney disease, heart conditions, sickle cell disease, among others. If you are not sure, check with your healthcare provider.
Can people get other vaccines at the same time as their COVID-19 vaccine?
Yes. The CDC has indicated that COVID-19 vaccine can be administered at the same visit as any other vaccines (including influenza and RSV vaccines as well as nirsevimab, the RSV monoclonal antibody prevention for infants).
One exception, however, is for people, particularly young males, who need both a COVID-19 and an orthopoxvirus (mpox or smallpox) vaccine. These people should consider waiting at least four weeks between receipt of the vaccines due to increased risk of myocarditis.
Vaccines given at the same visit should be given in different locations separated by at least one inch.
Watch this video to hear Dr. Hank Bernstein talk about getting the COVID-19 vaccine at the same time as other vaccines.
What is the difference between emergency use authorization and the normal process of vaccine approval?
The main difference between emergency use authorization, or EUA, and the normal process, which is via a biologic licensure application, or BLA, is how long data were collected prior to the vaccines being reviewed for use. So, when considered quite literally, the vaccines being used under EUA are no different than those that are used after the vaccines get full approval (BLA). The reason for the shortened timeline for COVID-19 vaccines was, of course, because of the pandemic. But, importantly, steps were not skipped to shorten the timeline, and at this point, these vaccines have been given safely to millions of people.
Were the COVID-19 vaccines approved by the FDA?
Even though the COVID-19 vaccines were initially released under Emergency Use Authorization (EUA), they were still approved by the Food and Drug Administration (FDA). The review process was the same, but because of the pandemic, the data could be submitted after a shorter period of participant follow-up than usual. However, even after submitting data (and getting an EUA), those studies continued.
Last updated: July 21, 2022; reviewed April 24, 2024
Is it safe for my teen to get the COVID-19 vaccine given the stories about myocarditis?
Cases of myocarditis, or inflammation of the heart, have been reported in a small number of people after receipt of the COVID-19 mRNA vaccine:
- The cases of myocarditis occur more often in boys and young men and more often after the second dose. Symptoms typically occur within 4 days after receipt of the dose. Recently immunized teens and young adults who experience chest pain or shortness of breath should be seen by a healthcare provider and report recent their vaccination.
- Myocarditis is somewhat common, particularly following viral infections. In fact, cases tend to occur more often in the spring due to viruses that circulate at this time of year (specifically, coxsackie B viruses). Typically, about 100-200 cases occur per million people per year.
- Available data suggest that the incidence of myocarditis following mRNA vaccines is about 1 to 10 per 100,000 vaccine recipients; however, this risk increases in males between 16 and 39 years of age to about 1 per 10,000 vaccine recipients. These numbers are lower in females. They are also lower than if people are infected with the virus that causes COVID-19, which increases the risk of myocarditis at least sevenfold.
- Parents and teens should watch for symptoms that may include chest pain, pressure, heart palpitations, difficulty breathing after exercise or lying down, or excessive sweating. One or more of these symptoms may also be accompanied by tiredness, stomach pain, dizziness, fainting, unexplained swelling, or coughing. If a recently vaccinated teen develops these symptoms or you are unsure, contact the child’s doctor or seek more immediate medical assistance if needed.
Find out more in this article from our Vaccine Update newsletter for healthcare providers.
Watch a video featuring one of our pediatric cardiologists, Dr. Matt Elias, discussing treating patients with myocarditis.
Last updated: April 26, 2023; reviewed April 24, 2024
Is it safe for my child to get the COVID-19 vaccine?
The mRNA vaccines are approved for those 6 months of age and older.
At this point, millions of children and teens have been safely vaccinated against COVID-19. The clinical trials in those 5 years of age and younger showed the vaccines to be safe and effective against severe disease. Moderna’s vaccine for the youngest children (6 months to 11 years of age) is one-half the dose (25 micrograms) of their vaccine for those 12 years and older (50 micrograms for 12 years and older). Pfizer’s vaccine for the youngest children (6 months to 4 years of age) is one-tenth the dose (3 micrograms) of their adult vaccine (30 micrograms for 12 and older). The Pfizer bivalent vaccine dose for 5- to 11-year-olds is one-third the adult dose (10 micrograms).
See more about the importance of vaccinating children against COVID-19:
- March 2023 issue of Parents PACK
- April 2023 article penned by Dr. Offit, the VEC’s director
- “Why Should Children Get the COVID-19 Vaccine?” (video featuring Dr. Offit)
If my child is near one of the cutoff ages for different doses (5 or 12 years of age), is it better to get them vaccinated or wait?
Since COVID-19 is still circulating and it takes several weeks for a person to be considered fully immunized, it is generally recommended to start the vaccination process with the vaccine the child is currently eligible to receive even if it is a lower dose.
If your child’s birthday occurs during the period between doses, the child will be offered the higher dose for their subsequent doses. Two exceptions are worth noting. First, if your child started with the Pfizer vaccine at age 4 and then turns 5, they will still be given the third dose of the vaccine for younger children (3 micrograms). Second, if your child is moderately or severely immune compromised and they transition from 11 to 12 years of age during their dosing, they may finish with the original doses or the doses for their age. Talk with your child’s healthcare provider if you feel your child might be in this situation.
What side effects will my child experience from the COVID-19 vaccine?
Side effects in children were similar to what has been found in other age groups, including pain at the injection site, fatigue, headache, fever, chills, muscle pain, or joint pain.
Even though a small number of cases of myocarditis, or heart inflammation, have been identified in teens and young adults, particularly in the 4 days after receipt of the second dose of the vaccine, this side effect has not been found in younger age groups, who receive lower doses. However, it is still important to monitor younger children for this potential side effect. Chest pain, shortness of breath, or related symptoms should be reported to a healthcare provider.
Other serious side effects have not been identified, nor have long-term effects. Find additional information:
- Long-term Side Effects of COVID-19 Vaccine? What We Know.
- Reproductive Health and COVID-19 Vaccines
Last updated: June 21, 2022; reviewed April 24, 2024
Can the COVID-19 vaccine affect puberty or fertility in my child?
No. The rumors related to COVID-19 vaccines affecting puberty or fertility are unfounded. The mRNA vaccines are processed near the injection site and activated immune system cells travel through the lymph system to nearby lymph nodes. In this manner, they are not traveling to other parts of the body. As such, there would not be a biological reason to expect that maturation or reproductive functionality of either males or females would be negatively affected by COVID-19 vaccination now or in years to follow. Importantly, due to reports of menstrual cycle changes following vaccination, studies have been, and continue to be, conducted. Studies to date have suggested about a one-day difference in menstrual cycles; however, further data are needed to understand this finding and these reports, particularly because many factors can affect the timing of an individual’s cycle. As such, analyzing the data carefully will be important. In addition, five large, national monitoring systems have not revealed any concerning findings related to miscarriage, stillbirth, preterm birth, birth defects, pregnancy or post-delivery complications or outcomes, infant or neonatal outcomes, menstrual irregularities or post-menopausal bleeding.
Watch this short video in which Dr. Paul Offit discusses COVID-19, the vaccines and infertility.
You can read more about fertility and COVID-19 vaccines in this Vaccine Update article.
If I got a COVID-19 vaccine in another country, can I get one in the U.S.?
Individuals vaccinated in another country are recommended to receive one dose of the 2023-2024 vaccine if they have not received an updated version approved by the FDA or WHO. The dose should be administered at least eight weeks after the most previous COVID-19 vaccine.
Young children (6 months to 4 years of age and people who are considered immune compromised should check with a healthcare provider, as the recommendations may vary somewhat for them based on U.S. recommendations for these groups.
To see which vaccines are approved by the WHO, check this webpage .
Last updated: September 20, 2023; reviewed April 24, 2024
Can I get the COVID-19 vaccine during my menstrual cycle?
Yes. Although minor changes (about one day in length) to the cycle have been observed, women do not need to schedule their COVID-19 vaccine around their menstrual cycle. The reasons for the changes are possibly the result of effects on specific types of immune system cells that are also present in the uterus or hormonal changes associated with the immune response.
Of note, the COVID-19 vaccine is not shed after vaccination, so being around recently vaccinated individuals would not be expected to affect someone’s cycle.
You can read more about menstruation and COVID-19 vaccines in this Vaccine Update article.
Last updated: December 23, 2022; reviewed April 24, 2024
Do the COVID-19 vaccines contain live virus?
The mRNA (Moderna and Pfizer) vaccines do not contain live virus. Each of these contain a single gene from the virus that causes COVID-19. The gene instructs our cells to make the protein, but no other proteins from the virus are made, so whole virus particles are never present. In this manner, people who were vaccinated cannot shed, or spread, the virus to other people as a result of vaccination. If, however, the individual subsequently becomes infected, they can spread the virus during the days before and early during their infection. Of note, the amount of virus shed by vaccinated people quickly decreases, so they generally shed less virus overall compared to unvaccinated, infected individuals. This is also the case for the J&J/Janssen vaccine; however, that version is no longer available in the U.S.
The Novavax vaccine does not contain live virus, either. It delivers the spike protein directly, rather than having our cells make the protein. As such, viral shedding does not occur following receipt of this version.
In this video, Dr. Paul Offit talks about the ingredients used in the COVID-19 mRNA vaccines.
Do the COVID-19 vaccines cause viral shedding?
Viral shedding occurs when a person is infected with a virus and whole viral particles produced during the infection are transmitted in the individual’s secretions. For viruses that infect the respiratory tract, like COVID-19, these particles are often found in secretions from the nose and mouth, such as saliva or mucus.
Some people wonder whether they can shed the virus as a result of vaccination. In the case of COVID-19 mRNA vaccines approved for use in the U.S., the short answer is no. The same is true of adenovirus-based vaccines (like J&J/Janssen) although this type of COVID-19 vaccine is no longer approved for use in the U.S. In both cases (mRNA- and adenovirus-based vaccines), only the gene for a single protein from the virus that causes COVID-19 – the spike protein – is introduced. As such, whole viral particles are never produced during vaccine processing. Indeed, people are not considered to be infected when they are vaccinated because the virus does not replicate in them. Further, the vaccines are processed near the site of injection, so the spike protein produced during processing would not be found in nasal or oral secretions. As such, they cannot “shed” the single protein either. Likewise, the Novavax vaccine, which delivers the spike protein directly, cannot result in viral shedding.
However, if vaccinated people are infected, the virus will replicate at low levels in their nasal or oral cavity before the immune system stops it. In this scenario, the individual can shed the virus beginning about two days before the start of symptoms and through the first three to four days after symptoms begin.
Read more about viral shedding in this Parents PACK article, “Viral Shedding and COVID-19 — What Can and Can’t Happen."
Watch this short video of Dr. Offit answering the question, “Can I spread coronavirus to others when I get the COVID-19 vaccine?”.
How do mRNA vaccines work?
People make mRNA all the time. In our cells, DNA in the nucleus is used to make mRNA, which is sent to the cytoplasm where it serves as a blueprint to make proteins. Most of the time, the proteins that are produced are needed to help our bodies function.
mRNA vaccines take advantage of this process by introducing the mRNA for an important protein from the virus that the vaccine is trying to protect against. In the case of COVID-19, the important protein is the spike protein of the SARS-CoV-2 virus. The mRNA that codes for the SARS-CoV-2 spike protein is delivered to our muscle cells, which make the protein. The protein is then processed by immune system cells, called dendritic cells, which express the spike protein on the cell surface, travel to a local lymph node, and stimulate other cells of the immune system (B cells) to make antibodies. These antibodies protect us, so that if we are exposed to SARS-CoV-2 in the future, our immune system is ready and we don’t get sick.
The vaccine is processed over a 1- to 2-week period after vaccination during which time the immune response develops. However, the mRNA only directs protein production in the cell for 1 to 3 days before it breaks down. Once it breaks down, the cell stops making the spike protein.
- Watch an animation of how COVID-19 mRNA vaccines work.
- See more about dendritic cells and the adaptive immune system in this animation.
- Watch this short video of Dr. Offit describing how mRNA vaccines work.
Last updated July 29, 2021; reviewed April 24, 2024
How do adenovirus vector vaccines work?
Although COVID-19 adenovirus-based vaccines are no longer used in the U.S., they remain in use in some other countries. These vaccines take advantage of a class of relatively harmless viruses, called adenoviruses. Some adenoviruses cause the common cold, but others can infect people without causing illness. To use these viruses for vaccine delivery, scientists choose types of adenovirus that do not cause illness and to which most people have not been exposed. They alter the virus by removing two of the genes that enable adenovirus to replicate in people, and they replace one of those genes with the one for the SARS-CoV-2 spike protein.
Like human cells, adenoviruses contain DNA as their genetic material. So, when an adenovirus vaccine is administered, it enters muscle cells where it releases the DNA that includes the gene for the spike protein, and the genetic material enters the nucleus of the cell. In the nucleus, the DNA is used to make messenger RNA (mRNA), which is released into the cytoplasm to serve as a blueprint for making proteins. The DNA from the viral vector, however, cannot insert into the cell’s DNA. The mRNA causes the SARS-CoV-2 protein to be produced. Specialized cells of the immune system, called dendritic cells, put pieces of the newly produced SARS-CoV-2 spike protein on their surface and travel to a draining lymph node where they stimulate other cells of the immune system; specifically, B cells that make antibodies, T cells that help B cells make antibodies, and other T cells that can kill virus-infected cells. Antibodies against the spike protein will now prevent the virus from causing an infection in the future.
Watch an animation of how COVID-19 viral vector vaccines work.
Find out more about adenovirus vaccines in this Vaccine Update article, “Getting Familiar with COVID-19 Adenovirus-replication-deficient Vaccines.”
How does the protein-based vaccine (Novavax) work?
The Novavax COVID-19 vaccine delivers the SARS-CoV-2 spike protein into our muscle. Once in our muscle, immune system cells that circulate throughout our body recognize the protein as foreign and attack it. Specialized immune system cells, called dendritic cells, put pieces of the protein on their surface and travel to nearby lymph nodes to activate other parts of the immune system. It takes about 1 to 2 weeks for the vaccine to be processed. The result is immunologic memory cells that are specialized to recognize the viral spike protein in the event of a future encounter with the virus.
This process takes advantage of our adaptive immune system, which responds to foreign proteins every day. To find out more about this part of our immune system, watch this animation .
Watch this short video of Dr. Offit describing the Novavax COVID-19 vaccine.
How did the vaccine companies (e.g., Pfizer and Moderna) decide which mRNA to use?
In order for a virus to reproduce and cause infection, it must get into cells and take over the cellular machinery . Because viruses attach to cells using a particular protein on their surface , in this case the SARS-CoV-2 spike protein, scientists understood that blocking that attachment would be a direct way to prevent infection. One way to block this attachment is with antibodies that bind to the surface protein. As such, when the genome was published, scientists developing the nucleic acid or protein subunit vaccines (i.e., those that only used part of the virus) chose the gene for the spike protein, anticipating that this would be the most direct route to developing an effective vaccine. The 2023-2024 COVID-19 mRNA vaccines use mRNA for the spike protein from a newer variant of the virus (XBB.1.5), so that the antibodies our immune system produces more closely match the surface protein of the SARS-CoV-2 viruses currently circulating.
Last updated: September 21, 2023; reviewed April 24, 2024
Who should NOT get the COVID-19 vaccine?
Most people are able to get COVID-19 vaccine. But a few groups of people either should not get the vaccine or should get a particular version. Likewise, some individuals should consult with their doctor or follow special procedures.
People who should NOT get any COVID-19 vaccine:
- Those younger than 6 months of age.
- People currently or recently experiencing a COVID-19 infection; these people can get vaccinated once they have been without a fever for 24 hours and their primary symptoms have resolved although it is recommended that these individuals wait at least three months to be vaccinated so they develop a more robust immune response to the vaccine dose.
People who cannot get the mRNA vaccine (Pfizer or Moderna), but may be able to get the Novavax vaccine:
- Anyone with a previous severe allergic reaction (i.e., one that causes anaphylaxis, any reaction that causes swelling that affects the airway (i.e., tongue, uvula, or larynx), or diffuse rash that also involves respiratory surfaces, such as Stevens-Johnson Syndrome) to a COVID-19 mRNA vaccine dose or an mRNA vaccine component.
- Anyone with a known polyethylene glycol (PEG) allergy.
People who cannot get the protein-based vaccine (Novavax), but may be able to get the mRNA (Pfizer or Moderna) vaccine:
- Anyone with a previous severe allergic reaction (i.e., one that causes anaphylaxis), any reaction that causes swelling that affects the airway (i.e., tongue, uvula, or larynx), or diffuse rash that also involves respiratory surfaces, such as Stevens-Johnson Syndrome, to a COVID-19 protein-based vaccine (Novavax) dose or one of its components.
- Anyone with a known polysorbate allergy.
People who may get the vaccine after considering risks and benefits and/or consulting with their healthcare provider:
- Individuals with a history of a non-severe, immediate (within 4 hours) allergic reaction to a previous dose of COVID-19 vaccine. (These individuals should be observed for 30 minutes after receipt of the vaccine.)
- People who have a severe or immediate allergic reaction to one of the types of vaccines and for whom the cause of the reaction is unknown (i.e., which component caused the reaction) should consult an allergist or immunologist to determine whether the individual can get the other version. If they proceed, they should be vaccinated at a location with medical facilities and staff prepared to respond to medical emergencies.
- People who cannot get one type of COVID-19 vaccine may be able to get the other type.
- People who are moderately or severely ill (regardless of whether they have a fever) may delay vaccination until they feel better.
- People with a history of MIS-C or MIS-A should delay vaccination until at least 90 days after diagnosis and they experience a return of normal cardiac function and are considered clinically recovered.
- People who experienced myocarditis or pericarditis within 3 weeks of receipt of COVID-19 vaccine are typically advised not to get additional doses of any COVID-19 vaccine. In some instances, individuals and their healthcare providers may decide to proceed with an additional dose based on the risk-benefit assessment. In this situation, symptoms should have resolved and at least 8 weeks should have passed before any additional doses are administered. Note: This does not apply to people with history of myocarditis or pericarditis unrelated to COVID-19 vaccination (including from COVID-19 infection, prior to COVID-19 vaccination, or more than 3 weeks after COVID-19 vaccination), nor does it apply to people with a history of heart disease.
People who should follow special procedures
- Pregnant people who develop a fever after vaccination should take acetaminophen. (See more in the pregnancy-related questions lower on this page.)
- People treated with convalescent plasma should not receive measles- or varicella-containing vaccines until at least 7 months after receipt of the plasma.
- People with a known COVID-19 exposure can get vaccinated if they don’t have symptoms.
- People with a current infection should wait at least until symptoms resolve but may have a better immune response to the vaccine if they wait at least 3 months after start of symptoms.
Watch this video of Dr. Offit answering the question, “Who Should Not Get the COVID-19 mRNA Vaccines?”.
Where can I get the vaccine?
COVID-19 vaccines are generally widely available. As such, we recommend checking for vaccine at your provider’s office, local pharmacies, healthcare facilities, or mobile clinics. For children younger than 5 years of age, we recommend contacting your child’s healthcare provider or checking with clinics or pharmacies before going for vaccination as some may have certain age requirements for administering vaccines.
Last updated: Nov. 10, 2021; reviewed April 24, 2024
What are the side effects of the COVID-19 vaccine?
Common side effects are caused as part of the immune response to each vaccine.
mRNA vaccines: Older children and adults
- Muscle aches
Side effects occurred during the first week after vaccination but were most likely one or two days after receipt of the vaccine. During clinical trials, side effects were more frequent following the second dose and more likely to be experienced by younger, rather than older, adults. Although most people will not have significant side effects, some people may wish to schedule their vaccination, so that they will not need to call out of work the next day if they don’t feel well.
A small number of people who get the mRNA vaccine experience mild, short-lived inflammation of the heart, called myocarditis. About 1 to 10 of every 100,000 mRNA vaccine recipients experience this condition, but it is most likely in adults 39 years and younger and more often occurs in males. This condition tends to occur within 4 days of receipt of the second dose, but it can occur after any dose and up to several days after vaccination. Recently vaccinated individuals who experience chest pain or shortness of breath should seek medical care. This condition tends to resolve within 2-3 weeks and does not cause long-term heart damage. Importantly, COVID-19 infections can also cause myocarditis, and this tends to occur more frequently after infection compared with vaccination. (See “My teen is a student-athlete and already had COVID-19, so does he need the COVID-19 vaccine? We are worried about myocarditis.” on this page for more detailed information.)
mRNA vaccines: Children younger than 5 years of age
Young children who received either the Pfizer or Moderna mRNA vaccine commonly experienced:
- Pain, tenderness, and swelling near the injection site
- Irritability
- Decreased appetite
Older children in this age group, who are better able to communicate what they are feeling, sometimes also experienced headaches, chills, achiness or joint pain, and nausea or vomiting. These effects were somewhat more likely after receipt of the Moderna vaccine, which is a higher dose, but occurred infrequently overall.
Myocarditis was not detected in this age group, either in clinical trials or since the vaccines have been in use; however, because COVID-19 mRNA vaccines are a rare cause of myocarditis in older adolescents and young adults, it is possible that it could be observed in younger children. Experience with these vaccines in older children and adults suggest that the likelihood of myocarditis is significantly lower following vaccination compared with infection. Also, the doses given to this age group are even lower than those given to older children and adults. However, parents and care providers should still monitor their children in the days following vaccination and contact healthcare providers or seek emergency care should concerns arise.
Protein-based vaccine: Adults
The most common side effects from the protein-based vaccine (Novavax) are:
- Injection site pain and less often redness or swelling
A small number of cases of myocarditis have occurred in individuals who received this vaccine; however, additional data are necessary to determine the level of risk. Recently vaccinated individuals who have heart-related symptoms should seek medical care.
Adenovirus-based vaccine: Adults
Adenovirus-based vaccines are no longer available in the U.S., but they are still used in some other countries.
The most common side effects from the adenovirus vaccine (Johnson & Johnson/Janssen) are:
Side effects occurred during the first seven to eight days after vaccination but were most likely to occur one or two days after receipt of the vaccine. Side effects were more often experienced by younger, rather than older vaccine recipients.
Two rare, but potentially dangerous conditions, have been identified following receipt of the adenovirus-based vaccines, such as the J&J/Janssen version:
- Thrombosis with thrombocytopenia syndrome, or TTS, occurs in about 1-2 of every 1 million vaccine recipients and develops up to 3 weeks after getting vaccinated. Individuals between 18 and 64 years of age, both female and male, who got the J&J/Janssen vaccine have experienced this condition; however, women between the ages of 30 and 49 years of age are at the greatest risk. Anyone who got the J&J/Janssen vaccine less than 3 weeks ago should seek medical care if they develop severe headache, shortness of breath, severe abdominal pain, unexplained leg pain, easy bruising, or small red spots on the skin. Anyone seeking medical care with one or more of these symptoms should mention their recent receipt of the vaccine, so healthcare providers can order the appropriate diagnostic tests and treatments.
- Guillain-Barré syndrome, or GBS, occurs in about 1 of every 100,000 vaccine recipients, most often during the first 3 weeks after getting vaccinated. The condition has most often been identified in males between 50 and 64 years of age, but it can occur in females and those 65 years and older on occasion. While rare, most cases have required hospitalization and at least one person has died. Anyone who recently received an adenovirus-based COVID-19 vaccine and experiences muscle weakness or paralysis should seek medical treatment and inform the healthcare provider of the recent vaccination. It should also be noted that COVID-19 infection has been associated with GBS; so, natural infection with SARS-CoV-2 also appears to be a rare cause of GBS. Find out more about GBS in this Parents PACK article, “Guillain-Barré Syndrome (GBS) & Vaccines: The Risks and Recommendations.”
Can I take medicine for the side effects after I get the vaccine?
The CDC has indicated that you can take anti-fever or anti-inflammatory medications if necessary following COVID-19 vaccination, but it is important to know that doing so could diminish the level of immunity that develops. This is true anytime you take these types of medications, whether following vaccination or to treat illness. Generally speaking, the “symptoms” people experience following vaccination or during illness, such as fever, redness at the injection site, or fatigue, are caused by your immune system response. For example, fever is your body turning up its “thermostat” to make the immune system more efficient and the pathogen less efficient. For these reasons, if you are not very uncomfortable, it is better not to take these medications.
Some wonder how long they should wait after vaccination before taking these types of medicines, so their immune response is not affected. As a rule of thumb, the immune response following receipt of the mRNA vaccine develops over a week or two after vaccination and for the adenovirus vaccine, over the course of about four weeks, but the greatest chance of affecting your immune response would be in the first few days after receipt of the vaccine. Indeed, in the adenovirus vaccine studies, about 1 in 4 vaccine recipients took fever-reducing medication (antipyretics), and most people were still protected from severe disease and all were protected against hospitalization. Responses to the protein-based vaccine (Novavax) develop over a period of a couple of weeks, but side effects, like fever, are most likely in the first couple of days after receipt of the vaccine.
Find out more in this Parents PACK article, "Medications and COVID-19 Vaccines: What You Should Know."
If I don’t have side effects, does that mean the vaccine did not work?
Many people will get the vaccine and not experience side effects. This does not mean that the vaccine did not work for them. In the clinical trials side effects occurred at varying rates, for example only about 1 to 20 of every 100 people who received the mRNA vaccine had a fever, but we know that the mRNA vaccine worked for more than 90 of every 100 people.
Last updated: March 1, 2021; reviewed April 24, 2024
What are the expected long-term side effects of the vaccination for COVID-19?
- Most negative effects occur within 6 weeks of receiving a vaccine, which is why the FDA asked the companies to provide 8 weeks of safety data after the last dose.
- mRNA vaccines: The mRNA in the vaccine breaks down quickly because our cells need a way to stop mRNA from making too many proteins or too much of a single protein. But, even if for some reason our cells did not breakdown the vaccine mRNA, the mRNA stops making the protein within about a week, regardless of the body’s immune response to the protein. Read more about COVID-19 mRNA vaccines in this Parents PACK article, “Long-term Side Effects of COVID-19 Vaccine? What We Know.” Watch a short video of Dr. Paul Offit explaining why COVID-19 vaccines would not be expected to cause long-term side effects.
- Protein-based vaccines: The protein is processed within a few days.
Although no longer available in the U.S., it is worth mentioning that the DNA from adenovirus-based vaccines does not break down as quickly as mRNA. The DNA in the vaccine cannot alter our DNA because a gene for the enzyme integrase is not present. These vaccines are processed within about 4 weeks, so they would not be expected to cause any long-term effects either.
Should I stop taking my daily dose of aspirin before getting the COVID-19 vaccine?
If your daily dose of aspirin was prescribed by your physician following a stroke or heart attack, we recommend speaking to that doctor about whether to stop taking your medication for a day or two prior to vaccination. If, however, your daily dose of aspirin is because you have risk factors for a stroke or heart attack (such as high blood pressure or high levels of “bad” cholesterol) but have never had a stroke or heart attack, you should talk to your doctor about discontinuing the aspirin not only prior to your COVID-19 vaccine, but all together. The data show that while daily aspirin helps prevent second strokes or heart attacks, it does not help prevent first occurrences, even in people who are at increased risk. Our director, Dr. Paul Offit, carefully reviewed the data related to this topic for his book, Overkill: When Modern Medicine Goes Too Far .
Last updated: Jan. 24, 2022; reviewed April 24, 2024
What should I do if I took pain medicine before getting the COVID-19 vaccine?
While your initial immune response may have been lower, you will likely still have developed some immunity. Even if your immune response is somewhat lower overall, you are likely to develop sufficient levels of immunity to reduce your chance for infection. In addition, even if you were infected, you would be likely to experience disease that is less severe and of shorter duration.
Can additional doses of the COVID-19 vaccine be from a different company?
Previously unvaccinated children 6 months to 4 years of age and those 5 years and older who are unvaccinated or partially vaccinated AND moderately or severely immune compromised should get all doses of the same brand, except in certain situations. If you are in this group, talk to your healthcare provider to determine the recommendations for your situation.
Those 5 years and older who have completed their initial vaccine series according to the recommendations for their age and immune status can get any brand. For people who are not immune compromised, they are generally considered to have completed their initial series after at least one previous dose. For those who are severely or moderately immune compromised, they are generally considered to have completed their initial series after at least 3 doses of mRNA vaccine or 1 dose of adenovirus- or protein-based vaccine PLUS 1 or more doses of mRNA vaccine. If you are unsure of whether you can switch brands based on your vaccination history, talk to your healthcare provider to help determine the recommendation for your situation.
How long do I need to wait if I had or need to get a non-COVID-19 vaccine?
In most cases, individuals do not need to delay receipt of COVID-19 vaccine and other vaccines; however, if given during the same appointment, the vaccines should be administered in different locations (different arms or separated by at least one inch on the same arm).
The one exception is that people who need to get both an orthopoxvirus vaccine (mpox/smallpox) and a COVID-19 vaccine, particularly teen and young adult males, should consider waiting for 4 weeks between receipt of the two vaccines due to known or potential risks of myocarditis related to individual orthopox and COVID-19 mRNA and protein-based vaccines. However, if the individual is at risk for mpox due to an outbreak or exposure or at risk for severe COVID-19, they should not delay their vaccination given that they would be trading a real risk for a theoretical risk by delaying.
Watch this short video in which Dr. Hank Bernstein explains the benefits of receiving routine vaccines at the same time as the COVID-19 vaccine.
What is multisystem inflammatory syndrome (MIS-C or MIS-A)?
Multisystem inflammatory syndrome can occur in children (MIS-C) or adults (MIS-A). Development of symptoms typically occurs about 4 to 6 weeks after SARS-CoV-2 infection and can occur even in those who did not experience symptoms of COVID-19. Often multiple organs and body systems are involved, including effects on the gastrointestinal tract, heart, kidneys, skin, lungs, and eyes. Individuals with unexplained rash, vomiting or diarrhea, shortness of breath or chest pain or palpitations should seek medical care. Some people with MIS-C or MIS-A will require admission to intensive care and a small number may require mechanical ventilation.
Find out more about MIS-C and long COVID-19 in this video with one of CHOP’s infectious diseases pediatricians.
Watch this short video in which Dr. Offit discusses whether MIS-C after COVID-19 infection is going away.
Watch this short video in which Dr. Caroline Diorio explains the importance of getting kids vaccinated against COVID-19.
Last updated: December 30, 2022; reviewed April 24, 2024
What is long COVID?
Long COVID, also known as post-COVID conditions or long-term COVID, is characterized by long-lasting symptoms related to previous SARS-CoV-2 infection. Symptoms can last for weeks or months after viral clearance and resolution of the initial infection. Examples of the types of symptoms that affected individuals report include fatigue, difficulty thinking or concentrating (“brain fog”), headache, change in or loss of taste or smell, dizziness, heart palpitations, chest pain, shortness of breath, cough, joint or muscle pain, anxiety, depression, sleep problems, feelings like “pins and needles,” diarrhea or stomach pain, rash, changes in menstrual cycle, or fever. Symptoms sometimes appear or worsen after physical or mental activity. People, particularly those who experienced severe COVID-19 infections, may also develop new chronic conditions, such as diabetes, heart conditions or neurological conditions.
Scientists continue to research long COVID. Current theories about the causes include:
- Long-term SARS-CoV-2 replication or reactivation of other viruses that remain in the body from previous infections
- Changes to the immune system’s ability to self-regulate after infection with the virus
- Blood clots (specifically microclots) caused by infection in an array of body organs
- Damage to mitochondria, which are the energy factories in our cells
Watch this short video in which Dr. Offit discusses what we are learning about long COVID and how some of these possibilities would be resolved by different approaches to treatment.
Does a vaccinated person present a risk to an unvaccinated person?
Vaccinated people do not shed virus following vaccination. COVID-19 vaccines do not contain live viruses, nor do they cause production of whole viral particles. As such, there is no infectious virus to spread from a vaccinated person to someone else.
But a vaccinated person can still be infected and potentially spread the virus to others. If they do not have symptoms, they may spread the virus without even knowing they are infected. While vaccinated individuals who become infected can be a source of viral spread, they do not appear to spread as much virus as unvaccinated individuals who become infected because their immune response is able to respond to the infection more quickly – shortening the length of infection and, therefore, the amount of virus produced.
Read more, “Vaccinated or Unvaccinated: What You Should Know.”
What ingredients are in the COVID-19 mRNA vaccine?
The mRNA vaccines include:
- mRNA – The mRNA is for the spike protein of the XBB.1.5 strain of SARS-CoV-2, the virus that causes COVID-19.
- Lipids - These are molecules that are not able to dissolve in water. They protect the mRNA, so that it does not break down before it gets into our cells. These can be thought of as little “bubbles of fat,” which surround the mRNA like a protective wall. There are four different lipids in the Pfizer vaccine and three in the Moderna vaccine. One of the lipids in both vaccines is cholesterol. The lipids are the most likely components of the vaccine to cause allergic reactions.
- Salts and amines - The Pfizer vaccine contains four salts. One is table salt. The salts are used to keep the pH of the vaccine similar to that found in the body, so that the vaccine does not damage cells when it is administered. The Moderna vaccine also contains four chemicals to balance the pH, but two are in a class of organic compounds known as “amines” and two are acetic acid and its salt form, sodium acetate. Acetic acid is the main component of vinegar (other than water).
- Sugar – This ingredient is literally the same as that which you put in your coffee or on your cereal. It is used in both of the vaccines to help keep the “bubbles of fat” from sticking to each other or to the sides of the vaccine vial.
These are the only ingredients in the mRNA vaccines.
NOT in the COVID-19 mRNA vaccines:
- Animal Products
- Antibiotics
- Blood products
- Egg Proteins
- Fetal material
- Pork products
- Preservatives, like thimerosal
Note: The trace quantities of small DNA fragments, which are contained in several biologics, including other vaccines, are well within the levels established as safe by the FDA. To find out more about DNA fragments, see “Do DNA fragments in COVID-19 mRNA vaccines cause harm?” at the beginning of this page.
Watch this short video in which Dr. Paul Offit talks about the ingredients of COVID-19 mRNA vaccines.
What ingredients are in the COVID-19 adenovirus-based vaccine?
Adenovirus-based vaccines are no longer available in the U.S.; however, they are used in other countries.
The adenovirus vaccine includes:
- Adenovirus type 26 (Ad26) containing SARS-CoV-2 spike protein gene and altered so that it cannot replicate
- Stabilizers – Salts, alcohols, polysorbate 80, and hydrochloric acid
- Manufacturing by-products – amino acids
Because the adenovirus-based COVID-19 vaccine is grown in fetal cells and although the product is highly purified, remnants of the fetal cells may remain in the final product.
NOT in the COVID-19 adenovirus vaccines:
- Preservatives, like thimerosal
What ingredients are in the COVID-19 protein-based vaccine (Novavax)?
The protein-based vaccine includes:
- SARS-CoV-2 spike protein from the XBB.1.5 version of the virus
- An adjuvant derived from the soap bark tree (Quillaja saponaria), called Matrix-M
- Stabilizers – Salts (including table salt), polysorbate 80, and hydrochloric acid
NOT in the COVID-19 protein-based vaccine:
Do COVID-19 vaccines contain antibiotics?
No. COVID-19 vaccines do not contain antibiotics.
Watch this short video in which Dr. Hank Bernstein discusses which ingredients are and are not in the COVID-19 mRNA vaccines.
Can mRNA vaccines change the DNA of a person?
Since mRNA is active only in a cell’s cytoplasm and DNA is located in the nucleus, mRNA vaccines do not operate in the same cellular compartment that DNA is located.
Further, mRNA is quite unstable and remains in the cell cytoplasm for only a limited time (See “What stops the body from continuing to produce the COVID-19 spike protein after getting an mRNA vaccine?” below.) mRNA never enters the nucleus where the DNA is located, so it can’t alter DNA. For more details, see “Do DNA fragments in COVID-19 mRNA vaccines cause harm?” at the beginning of this page.
Watch this short video in which Dr. Paul Offit explains why it’s not possible for mRNA vaccines to alter a person’s DNA.
Can adenovirus-based vaccines change the DNA of a person?
Although adenovirus-based vaccines are no longer available in the U.S., they are still used in some other countries and some people in the U.S. received them previously, so it is useful to know that they cannot change a person’s DNA. Adenovirus-based vaccines contain DNA, which enters the nucleus of cells after vaccination, but the virus cannot replicate and the vaccine does not include a necessary enzyme, called integrase. Therefore, the vaccine cannot change a person’s DNA.
What stops the body from continuing to produce the COVID-19 spike protein after getting a COVID-19 mRNA or adenovirus-based vaccine?
Both the mRNA and adenovirus vaccines result in production of spike protein that results from mRNA blueprints. Because our cells are continuously producing proteins, they need a way to ensure that too many proteins do not accumulate in the cell. So, generally speaking, mRNA is always broken down fairly quickly. Even if for some reason our cells did not breakdown the vaccine mRNA, the mRNA stops making the protein within about a week, regardless of the body’s immune response to the protein. Once the mRNA is broken down, the blueprint is gone, so the cell can no longer continue to make spike proteins.
Likewise, while the adenovirus-based vaccine delivers DNA and the DNA lasts longer than mRNA, studies have shown that adenovirus-based DNA does not last longer than a few weeks.
Watch this short video in which Dr. Hank Bernstein explains how the mRNA from the COVID-19 vaccine is broken down and removed from the body.
For more details on the process by which spike protein production is limited, see the “mRNA vaccine” section of this article .
Last updated March 28, 2023; reviewed April 24, 2024
Will the spike protein from current vaccines cause an issue if there are future variants?
The spike protein does not remain in the body for an extended time, nor does it travel around the body. The only thing that remains after the vaccine is processed are antibodies and memory immune cells. To date, previous vaccination against COVID-19 has produced immunologic memory that remains effective against newer variants. However, 2023-2024 COVID-19 vaccines were updated for a newer variant, XBB.1.5.
Is it okay to donate blood after getting the COVID-19 vaccine?
Giving blood after getting the COVID-19 vaccine will not diminish the resulting immune response, which mostly builds in the lymph nodes near the injection site. Likewise, the American Red Cross (ARC) does not require a delay following vaccination with the vaccines currently approved for use in the U.S.; however, individuals must know which brand of vaccine they received and show the immunization card if possible. More details about blood donation are available on the ARC website.
Last updated: March 18, 2021; reviewed April 24, 2024
Are COVID-19 vaccines made in fetal cells?
The mRNA vaccines (those by Pfizer and Moderna) and the protein-based vaccine (Novavax) do not contain fetal cells.
But the adenovirus-based vaccines (no longer used in the U.S.), like Johnson & Johnson/Janssen’s, use cells originally isolated from fetal tissue (often referred to as fetal cells). These fetal cells are used to grow the vaccine virus.
To replicate, a virus needs to take over a cell’s machinery (See this animation ); however, the adenoviruses used in these vaccines have been altered, making them unable to complete the replication process. So, to make the vaccine, these altered viruses need to infect cells that have been changed in a way that allows the defective virus to reproduce. The special cells for this process were isolated decades ago from one of two terminated fetuses and later adapted for the adenovirus reproduction process. Neither of these are used to produce any existing vaccines grown in fetal cells :
- HEK-293 — This is a kidney cell line that was isolated from a terminated fetus in 1972.
- PER.C6 — This is a retinal cell line that was isolated from a terminated fetus in 1985.
These two cell lines have been maintained in the laboratory, and no additional fetuses are needed to produce adenovirus-vector vaccines.
In this short video, Dr. Paul Offit addresses fetal cells and COVID-19 vaccines.
You can find out more about the adenovirus-based vaccines and fetal cells in this Vaccine Update article .
Last updated September 21, 2023; reviewed April 24, 2024
How long will vaccine immunity last?
Discussions related to immunity following COVID-19 vaccination have been fraught with confusion and misinformation. To understand what we have learned from scientific studies, it is important to understand some basics related to immunity in general.
A quick look at immunity
When we are infected with a pathogen, our immune system responds by making B cells and T cells. Some of the B cells are short-lived and have the job of being antibody-producing factories that work to stop the infection. A small number of B cells are long-lived to form one part of our immunologic memory. Likewise, some T cells work to kill virus-infected cells to stop the infection and others serve as army generals, producing chemical signals to control the immune response (ramp it up or down as needed). And, as with B cells, a small number of T cells remain long after the infection to form another part of our immunologic memory.
The long-lasting B and T cells protect us against future infections. If the pathogen is detected, these cells reproduce, so that our immune system overcomes the infection more quickly than it did during the first infection. Whereas first infections can take about a week to control, our immune system is usually at full speed within 3 to 5 days during subsequent infections.

What we have learned about COVID-19 immunity
During a COVID-19 infection, our immune systems produce B cells, antibodies, T cells, chemical signals and immunologic memory — just as in other infections. Antibodies have been found to be important for stopping COVID-19 infections, so in the period of weeks to a few months after an infection or vaccination, lingering antibodies afford protection. But, antibodies are not long lived, so after a few months, we need to rely on immunologic memory. Memory B and T cells have been shown to be important for protection against future infections, particularly certain subsets of T cells. However, as described in the previous paragraph, immunologic memory takes a few days (3 to 5 days) to ramp up. So, during this period, the virus will reproduce in the upper respiratory tract, causing cold-like symptoms (e.g., nasal and sinus congestion, runny nose and coughing) for some and positioning the individual to spread the virus to others (even if they don’t have symptoms). Because of this gap period during which symptoms and transmission can occur, some feel the vaccine doesn’t work. However, the same situation is possible following infection or vaccination, and it will always be the case because of the biology of immunologic memory.
With this said, we have also learned that certain groups of people are at increased risk for severe disease if they are infected. This happens for two reasons — their immune system is not strong enough to overcome the infection by the time their immunologic memory ramps up or one or more components of their immunologic memory is lacking. For these people, help in the form of recently developed antibodies (e.g., vaccination during the part of the year when COVID-19 is circulating) or early treatment with antiviral medications (e.g., Paxlovid™) is most important. The people in these groups include those who are:
- Elderly (65 years and older)
- Moderately or severely immune compromised
- Diagnosed with a chronic disease, particularly heart, kidney, liver or lung disease, diabetes, and obesity, among others.
A new monoclonal antibody product, called Pemgarda, is available for some eligible individuals who are at least 12 years of age and are considered moderately or severely immune compromised. Pemgarda is given intravenously every three months. To find out more about the product and who is eligible, talk to your healthcare provider.
In this short video, Dr. Hank Bernstein talks about how long COVID-19 vaccine immunity lasts.
If you had COVID-19, do you still need to get the vaccine?
People who had COVID-19 are recommended to get the vaccine about 3 to 4 months after they have recovered. Some studies have indicated two benefits:
- Vaccination more consistently produces protective immune responses than infection.
- Vaccination provides a wider breadth of protection based on the types of memory responses produced.
In addition, studies have suggested that “hybrid immunity,” that is immunity developed as a result of both infection and vaccination, provides better protection than either vaccination or infection alone.
Watch this video of Dr. Offit explaining why people previously infected with COVID-19 can benefit from receiving the vaccine.
Is a coronavirus vaccine necessary?
SARS-CoV-2 infections can be a minor hindrance or lead to severe disease or even death. Likewise, some people, including children, experience lingering symptoms, called “long COVID,” which is yet to be understood. This virus will continue to circulate in the United States and the world for decades if not longer. While hygiene measures, such as social distancing, handwashing, and wearing masks, offer some help, the best way to stop this virus is to generate SARS-CoV-2-specific immunity. At this point, most people have some immunity either from vaccination or from infection. However, two points are worth considering:
- Most of the individuals being hospitalized for COVID-19 at this point are either individuals who are in a high-risk group or individuals who are unvaccinated.
- Studies have shown that “hybrid immunity,” which is immunity generated when someone has had both vaccination and an infection, is likely superior to immunity generated from infection alone. As such, even people who were previously infected, can benefit from vaccination.
For more information, watch this short video of Dr. Paul Offit addressing “Why does it matter if I don’t get the COVID-19 vaccine?”
How long before a coronavirus vaccine takes effect?
The Pfizer mRNA vaccine requires one to three doses for those greater than 6 months old, depending on age. Protection against severe disease is greatest about two weeks after the last recommended dose. For those getting a single dose (ages 5 years and older), the working assumption is that these individuals were likely exposed to the virus in the community, so the dose of vaccine will enhance their immunologic memory. Unfortunately, we cannot be sure that these individuals were equally immune to begin with, so time will tell whether their immunity is as robust as it is for those who had multiple doses.
The Moderna mRNA vaccine requires one or two recommended doses depending on age. The same working assumption as described in the Pfizer vaccine paragraph above relates to single dose recipients here as well (those 5 years of age and older).
Currently, the broadest, longest-lasting immunity is induced by either three doses of an mRNA-containing vaccine or at least two doses plus a natural infection.
The protein-based vaccine (Novavax) requires two doses. Immunity will be most robust about two weeks after the second dose.
Do the variants affect vaccine effectiveness?
Current vaccines will protect most against severe disease and death independent of what variants are circulating; however, neutralizing antibodies that develop shortly after receipt of a dose will fade in a few months, so people can still develop mild illness. For some with immune conditions that affect their response to the vaccine or infection and for those of older age, immune protection is less robust, so they are more likely to benefit from an additional dose. See more details in the answer to “How long will vaccine immunity last?”
Can pregnant people get the COVID-19 vaccine?
With data from tens of thousands of pregnant people now in hand, no concerns have been identified and the vaccine works. Further, we now know that:
- Pregnant people are at higher risk for severe COVID-19 compared with those of the same age who are not pregnant.
- Vaccination during pregnancy also affords some protection to the baby in the months after delivery and before they are old enough to be vaccinated.
Pregnant people who get the COVID-19 vaccine should take acetaminophen if they develop a fever after vaccination, as fever during pregnancy can negatively affect a developing baby. Taking acetaminophen during pregnancy has been found to be safe.
In this short video, Dr. Hank Bernstein discusses COVID-19 vaccination during pregnancy.
You can read more about pregnancy and COVID-19 vaccines in this Vaccine Update article.
Drs. Paul Offit and Ripudaman Minhas discuss vaccines, pregnancy, development and autism in this video.
Last updated: April 27, 2023; reviewed April 24, 2024
Can I get the COVID-19 vaccine if I am breastfeeding?
Yes. COVID-19 is not transmitted through breast milk and vaccination has not caused a concern either.
In addition, breastfeeding does not need to be delayed for any period of time before or after vaccination.
Babies may benefit from antibodies or immune cells introduced through breast milk after the mother is vaccinated. This is called passive immunity.
Both the Academy of Breastfeeding Medicine and the American College of Obstetricians and Gynecologists support this approach.
Hear from Dr. Caroline Diorio, a pediatric oncologist, about the importance of getting the COVID-19 vaccine during pregnancy.
In this short video, Dr. Hank Bernstein discusses COVID-19 vaccination when breastfeeding.
You can read more about breastfeeding and COVID-19 vaccines in this Vaccine Update article.
Drs. Paul Offit and Amna Husain discuss vaccines and breastfeeding in this video.
Can I get the COVID-19 vaccine if I am trying to get pregnant?
Yes, people who are trying to get pregnant can get the COVID-19 vaccine. Likewise, vaccination can be finished during pregnancy, and it is important to do so since pregnancy increases one’s risk of being hospitalized and having preterm births if infected with COVID-19 before delivery.
Last updated: June 23, 2022; reviewed April 24, 2024
Should I delay getting pregnant if I got the COVID-19 vaccine?
No, you do not need to delay pregnancy. The COVID-19 vaccines do not present a cause for concern related to pregnancy.
Last updated: Jan. 25, 2022; reviewed April 24, 2024
Why was I told to wait a month after getting the COVID-19 vaccine before getting a mammogram?
Some people experience swelling of the lymph nodes under their vaccinated arm after getting the COVID-19 mRNA vaccine. Because this could be mistakenly identified as spread of breast cancer to lymph nodes, delaying the mammogram can prevent the chance of this happening.
Why was I asked if I recently received the COVID-19 vaccine on the questionnaire for my MRI?
People occasionally experience swelling of the lymph nodes near the vaccine injection site, which could interfere with interpreting the results of the MRI depending on what location is being imaged.
Last updated: Jan. 25, 2022; reviewed April 24, 2024
Is it necessary to wait to get blood work done after getting the COVID-19 vaccine?
Generally speaking, it would be recommended to wait about a week after getting the mRNA vaccine and a few weeks after getting the adenovirus-based vaccine before getting bloodwork. Delays are not likely to be needed after receipt of the protein-based vaccine. However, it would be better to inquire with the healthcare provider who ordered the bloodwork as they have the benefit of knowing the reason for the bloodwork, the type of tests ordered, and the patient’s medical history. As such, they will be in the best position to offer this guidance for each individual situation.
If I have an autoimmune or immune-compromising condition, can I be vaccinated?
Most people with immune-compromising conditions may get the COVID-19 vaccine as long as they do not have a severe allergy to a vaccine component (i.e., one that causes anaphylaxis or requires medical intervention).
However, it is recommended that individuals with compromised immune systems discuss their personal risks and benefits with a healthcare provider to determine whether to receive the vaccine or if they may need additional doses.
Knowing the potential for a lower immune response, if someone with an immune-compromising condition decides to get vaccinated, it will be important to get all recommended doses, depending on their condition. Some people may be eligible for ongoing treatment with a monoclonal antibody product called Pemgarda, and some may choose to continue practicing other public health measures during periods of high virus circulation.
Last updated: June 23, 2022; reviewed April 24, 2024
Can I get the COVID-19 vaccine if I had Guillain-Barré syndrome (GBS)?
People with a history of Guillain-Barré syndrome (GBS) can get the COVID-19 vaccine, as long as they do not have another condition that puts them among the people recommended against vaccination. A small number of cases of GBS (about 1 of 100,000 people) have been identified following receipt of the adenovirus-based COVID-19 vaccine (J&J/Janssen); however, this vaccine is no longer used in the U.S.
A note about GBS and influenza vaccines
Some people wonder if they can get the COVID-19 vaccine if they developed GBS following receipt of an influenza vaccine. Since COVID-19 and influenza (flu) vaccines are made differently, people with this history would not be expected to have an issue with COVID-19 vaccine. As such, they are still recommended to get COVID-19 vaccine.
Finally, many people are incorrectly told that if they had GBS, they cannot get a flu vaccine. However, most people with a history of GBS can get the flu vaccine. Only people who were diagnosed with GBS less than 6 weeks after receipt of influenza vaccine are considered to have a “precaution” for receipt of influenza vaccine, meaning that the patient and the healthcare provider should discuss the relative risks and benefits associated with getting the influenza vaccine. In fact, studies have shown that influenza disease presents a greater risk of GBS than influenza vaccination. Find out more:
- ”Vaccines and Guillain-Barré Syndrome” webpage
- Guillain-Barré Syndrome (GBS) & Vaccines: The Risks and Recommendations , September 14, 2021, Parents PACK newsletter
Can I still get vaccinated if I have a cold?
People with mild cold-like symptoms are not prevented from getting the COVID-19 vaccine. However, if they are not feeling well, their symptoms just started, or their symptoms are getting worse, they may want to delay vaccination until they feel better; otherwise, they might not be able to tell effects of illness from those of the vaccine. If they are uncertain, they should speak to their doctor, who has the benefit of their medical history and will be in the best position to help them weigh the potential pros and cons. This advice is similar for other vaccines as well.
If I am taking anticoagulants (blood thinners), can I get the COVID-19 vaccine?
Patients on blood thinners can get the COVID-19 vaccine. However, because the vaccine is given intramuscularly, the risk for bleeding is slightly greater for these individuals. As such, they should tell the healthcare provider administering the vaccine about their use of an anticoagulant. The vaccine itself does not increase the risk for this group of patients. The same advice is true for other vaccines that are injected as well.
Last updated: April 28, 2023; reviewed April 24, 2024
If I am currently taking antibiotics, can I get the COVID-19 vaccine?
As long as you are not still sick from your recent infection, you can get the COVID-19 vaccine even if you are taking an antibiotic. But, if you are still having symptoms, you should wait until you are feeling better, so that it is easier to tell if any new symptoms are from your infection or the vaccination.
Last updated: Sept. 28, 2021; reviewed April 24, 2024
If I am taking antivirals, can I get the COVID-19 vaccine?
You do not need to stop taking antiviral medication before vaccination. Because the COVID-19 vaccines being used in the U.S. do not rely on viral replication, antivirals should not affect development of the immune response. However, if you are still experiencing symptoms of the infection for which the antivirals were prescribed, you should wait until you are feeling better before getting the vaccine. This will allow you to distinguish symptoms from your infection with side effects from the vaccine.
If I am taking biologics, can I get the COVID-19 vaccine?
Taking biologics, like Humira, is not a reason to forgo COVID-19 vaccination as per CDC guidelines. However, patients taking these types of medication may wish to consult with their doctor to discuss the potential risks and benefits of getting the COVID-19 vaccine, given that these types of medications are often prescribed for individuals with immune-compromising conditions. As a result, there may be other considerations related to the potential risks and benefits of vaccination.
For general information about vaccines and biologics, check out this printable Q&A sheet.
Last updated: Jan. 25, 2021; reviewed April 24, 2024
How long should I wait to get the COVID-19 vaccine after getting a steroid injection or vice versa?
You should speak with your doctor to determine whether the quantity of steroids that you are receiving is suppressing your immune system. If so, you should hold off on receiving vaccines until the effect of the steroids has worn off.
Does the COVID-19 vaccine cross the blood-brain barrier?
It would not be expected that the COVID-19 vaccines would cross the blood-brain barrier (BBB) for a few reasons.
mRNA vaccines:
- Most of the protein that is made is bound to cells - The vaccine is injected into muscle, where mRNA from the vaccine causes production of COVID-19 spike protein. The protein (not the mRNA) is then processed by dendritic cells where pieces of the protein are put on the cell surface before the dendritic cell travels to the nearest lymph node and stimulates other cells of the immune system to make an immune response against the protein. This process is typical of our adaptive immune system, which you can find out more about in this animation , or you can watch this animation that describes how the mRNA vaccine is processed .
- Even if the protein left the cell whole (which it doesn’t), it is too large to cross the BBB.
Adenovirus vaccine (no longer used in the U.S.):
- As with the mRNA vaccine, pieces of the protein that result from vaccine processing are put on dendritic cells that travel to the nearest lymph node. See how the adenovirus-based vaccine is processed in this animation .
- The virus used to deliver the vaccine is also too large to cross the BBB.
Protein-based vaccines (e.g., Novavax) would not be expected to cross the BBB either as the proteins are too large.
Does the COVID-19 vaccine cause antibody-dependent enhancement (ADE)?
Antibody-dependent enhancement (ADE) occurs when the antibodies from a previous infection (or vaccination) help the virus gain access to cells rather than blocking access to cells. Getting an infection after vaccination does NOT provide evidence of ADE. These are two distinct immunologic phenomena.
ADE has not been identified as a concern related to SARS-CoV-2 infection or following COVID-19 vaccination. In fact, a body of evidence has suggested that ADE is not a concern:
- First, most people have been infected with other coronaviruses in their lifetime, and ADE has not been identified as a result of these infections.
- Second, in human studies, people previously infected with coronavirus were infected with different types of coronavirus, and they did not experience enhanced disease.
- Third, experimental animals vaccinated against SARS-CoV-2 did not develop enhanced disease when challenged, or infected, with the virus.
- Fourth, when people with COVID-19 received plasma containing SARS-CoV-2 antibodies, they did not experience enhanced disease.
- Finally, millions of people have been vaccinated against COVID-19. Some of them have subsequently been infected with SARS-CoV-2, and none of them have shown evidence of ADE.
Watch a short video in which Dr. Paul Offit explains why COVID-19 vaccines are unlikely to cause ADE.
Does the COVID-19 vaccine cause fertility issues?
Infertility has not been found to be an issue in women or men infected with or vaccinated against COVID-19.
Unfortunately, misinformation about fertility-related issues continues to circulate. These concerns take a few forms:
- Compromised fertility in the vaccine recipient – Some concerns related to a placental protein, called syncytin-1. This protein is associated with the placenta during pregnancy. Online claims early during the pandemic promoted a paper suggesting that a small number of similar amino acids in the spike protein and the placental protein would cause vaccine-induced antibodies to react against syncytin-1. Since human proteins are made using the same 20 amino acid building blocks, many proteins have short sections that are similar to one another. However, most of our antibodies do not cross-react with other proteins because a variety of other factors come into play. The most important of which is antibody specificity to the three-dimensional version of its target. As such, while a theoretical paper like the one previously mentioned can generate an interesting hypothesis, the idea requires clinical confirmation, which never materialized for this idea that unfortunately spread quickly and, quite frankly, unnecessarily scared people.
- Some concerns related to males, and whether the vaccines could decrease sperm count. While fever can cause a temporary decrease in sperm count, there is no biologically plausible reason to expect that the vaccines would cause any long-term effect on sperm count.
- Compromised fertility in individuals near someone who recently received COVID-19 vaccine – This misperception conflates two concepts: effects on fertility and viral shedding. As mentioned above, the vaccines do not affect fertility in the vaccinated person, so there would not be a reason to expect that they would affect someone else’s fertility. Second, it assumes that recently vaccinated individuals shed virus or spike protein. Neither of these occur. While these vaccines cause the body to generate spike protein, they do not cause production of whole virus particles, nor do parts of the vaccine migrate to the nasal cavity. As such, a recently vaccinated person does not shed any part of the virus and cannot, therefore, spread vaccine-related components to another person.
This Parents PACK article about vaccination of children 5 to 11 years of age also addresses fertility-related concerns.
Is there any hope that a vaccine will help people with lingering aftereffects from coronavirus?
Clinical studies are underway to determine whether antiviral medications might help ease the lingering effects of COVID-19 infection, and studies of vaccination have suggested that by decreasing the severity of infection, fewer people experience long-term symptoms. However, vaccination does not appear to help ease symptoms in people who are already suffering the lingering effects of an infection.
Does the COVID-19 vaccine contain blood products?
The COVID-19 vaccines available in the U.S. do not contain any blood products, including red blood cells, white blood cells or platelets.
Watch this short video in which Dr. Offit talks about the ingredients used in the COVID-19 mRNA vaccines.
Do COVID-19 vaccines contain a microchip?
COVID-19 vaccines do not contain microchips. This idea is based on a false narrative and misinformation campaign waged online. You can find out more about where this idea came from on snopes.com .
Last updated: Dec. 15, 2020; reviewed April 24, 2024
If my baby has had some of her vaccines, is she protected from COVID-19?
A baby’s other vaccines will not protect them from COVID-19.
If the baby is at least 6 months of age, she can receive the COVID-19 vaccine; however, she should not be considered immune until at least 2 weeks after receipt of her last dose.
COVID-19 video resources
This section of the page will house video resources and interviews related to COVID-19.
Vaccine Makers Project videos and animations The Vaccine Makers Project (VMP) is the classroom program of the Vaccine Education Center (VEC). VMP resources include a variety of science-based animations that show not only how COVID-19 vaccines work, but also how viruses take over our cells and how our immune systems work.
Talking about Vaccines with Dr. Paul Offit: COVID-19 This VEC playlist features several short videos in which Dr. Offit addresses common questions about COVID-19.
Talking about Vaccines with Dr. Hank Bernstein: COVID-19 This playlist features a series of short videos in which Dr. Hank Bernstein answers common questions about COVID-19 vaccines.
Reviewed by Paul A. Offit, MD, on April 24, 2024
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- COVID-19 is a disease caused by a virus. The most common symptoms are fever, chills, and sore throat, but there are a range of others.
- Most people make a full recovery without needing hospital treatment. People with severe symptoms should seek medical care as soon as possible.
- Over 760 million cases and 6.9 million deaths have been recorded worldwide since December 2019, but the actual number is thought to be higher.
- Over 13 billion vaccine doses have been administered as of June 2023.
COVID-19 is the disease caused by the SARS-CoV-2 coronavirus. It usually spreads between people in close contact.
COVID-19 vaccines provide strong protection against severe illness and death. Although a person can still get COVID-19 after vaccination, they are more likely to have mild or no symptoms.
Anyone can get sick with COVID-19 and become seriously ill or die, but most people will recover without treatment.
People over age 60 and those with existing medical conditions have a higher risk of getting seriously ill. These conditions include high blood pressure, diabetes, obesity, immunosuppression including HIV, cancer and pregnancy. Unvaccinated people also have a higher risk of severe symptoms.
People may experience different symptoms from COVID-19. Symptoms usually begin 5–6 days after exposure and last 1–14 days.
The most common symptoms are:
- fever
- sore throat.
Less common symptoms are:
- muscle aches and heavy arms or legs
- severe fatigue or tiredness
- runny or blocked nose, or sneezing
- new and persistent cough
- tight chest or chest pain
- shortness of breath
- hoarse voice
- numbness or tingling
- appetite loss, nausea, vomiting, abdominal pain or diarrhoea
- loss or change of sense of taste or smell
- difficulty sleeping.
People with the following symptoms should seek immediate medical attention:
- difficulty breathing, especially at rest, or unable to speak in sentences
- drowsiness or loss of consciousness
- persistent pain or pressure in the chest
- skin being cold or clammy, or turning pale or a bluish colour
- loss of speech or movement.
People who have pre-existing health problems are at higher risk when they have COVID-19; they should seek medical help early if worried about their condition. These include people taking immunosuppressive medication; those with chronic heart, lung, liver or rheumatological problems; those with HIV, diabetes, cancer. obesity or dementia.
People with severe disease and those needing hospital treatment should receive treatment as soon as possible. The consequences of severe COVID-19 include death, respiratory failure, sepsis, thromboembolism (blood clots), and multiorgan failure, including injury of the heart, liver or kidneys.
In rare situations, children can develop a severe inflammatory syndrome a few weeks after infection.
Some people who have had COVID-19, whether they have needed hospitalization or not, continue to experience symptoms. These long-term effects are called long COVID (or post COVID-19 condition). The most common symptoms associated with long COVID include fatigue, breathlessness and cognitive dysfunction (for example, confusion, forgetfulness, or a lack of mental focus or clarity). Long COVID can affect a person’s ability to perform daily activities such as work or household chores.
Most people will recover without needing treatment in a hospital.
For those who need it, doctors will suggest treatments for COVID-19 based on the severity of the disease and the risk of it getting worse. They will consider the person’s age and if they have other health problems.
More on treatment
People should get vaccinated as soon as it’s their turn. They should follow local guidance on vaccination and ways to protect themselves against COVID-19.
COVID-19 vaccines provide strong protection against serious illness, hospitalization and death.
To prevent the spread of COVID-19:
- avoid crowds and keep a safe distance from others, even if they don’t appear to be sick;
- wear a properly fitted mask if you feel sick, have been close to people who are sick, if you are at high-risk, or in crowded or poorly ventilated areas;
- clean your hands frequently with alcohol-based hand rub or soap and water;
- cover your mouth and nose with a bent elbow or tissue when you cough or sneeze;
- dispose of used tissues right away and clean your hands; and
- if you develop symptoms or test positive for COVID-19, self-isolate until you recover.
Vaccination against COVID-19 is based on priority groups such as people aged 60 years and over, and those with underlying medical problems such as high blood pressure, diabetes, chronic health problems, immunosuppression (including HIV), obesity, cancer, pregnant persons, and unvaccinated people. In March 2023, WHO updated its recommendations on primary series vaccination (two doses of any vaccine) as well as the need for booster doses. These recommendations are time-limited and can change at any time depending on how the SARS-CoV-2 virus is circulating in your area or country. It is important to stay up to date with local guidelines and recommendations provided by your local health authority.
Since its introduction, COVID-19 vaccines have saved millions of lives across the world by providing protection against severe disease, hospitalization, and death. Even though vaccines protect against severe disease and death, it is still possible to spread SARS-CoV-2 to others after being vaccinated.
WHO response
The World Health Organization is the global coordinating agency for the response to the COVID-19 pandemic. The Organization works with Member States and partners on all aspects of the pandemic response, including facilitating research, developing guidance, coordinating vaccine development and distribution, and monitoring daily case numbers and trends around the world.
Since April 2020, the Access to COVID-19 Tools (ACT) Accelerator, launched by WHO and partners, has supported the fastest, most coordinated, and successful global effort in history to develop tools to fight a disease. COVAX, the vaccines pillar of the ACT-Accelerator is a ground-breaking global collaboration to accelerate the development, production, and equitable access to COVID-19 tests, treatments, and vaccines.
WHO provides global coordination and member state support on vaccine safety monitoring. It developed the target product profiles for COVID-19 vaccines and provides R&D technical coordination.
WHO also leads work to improve global capacity and access to oxygen production, distribution and supply to patients.
Although WHO announced the end of the emergency phase of COVID-19 in May 2023, the Organization continues to coordinate the global response.
All information on COVID-19
WHO's work on coronavirus disease
MINI REVIEW article
Covid-19: emergence, spread, possible treatments, and global burden.

- 1 Department of Pharmacology, Manipal College of Pharmaceutical Sciences, Manipal Academy of Higher Education, Manipal, India
- 2 Department of Health Sciences, School of Education and Health, Cape Breton University, Sydney, NS, Canada
The Coronavirus (CoV) is a large family of viruses known to cause illnesses ranging from the common cold to acute respiratory tract infection. The severity of the infection may be visible as pneumonia, acute respiratory syndrome, and even death. Until the outbreak of SARS, this group of viruses was greatly overlooked. However, since the SARS and MERS outbreaks, these viruses have been studied in greater detail, propelling the vaccine research. On December 31, 2019, mysterious cases of pneumonia were detected in the city of Wuhan in China's Hubei Province. On January 7, 2020, the causative agent was identified as a new coronavirus (2019-nCoV), and the disease was later named as COVID-19 by the WHO. The virus spread extensively in the Wuhan region of China and has gained entry to over 210 countries and territories. Though experts suspected that the virus is transmitted from animals to humans, there are mixed reports on the origin of the virus. There are no treatment options available for the virus as such, limited to the use of anti-HIV drugs and/or other antivirals such as Remdesivir and Galidesivir. For the containment of the virus, it is recommended to quarantine the infected and to follow good hygiene practices. The virus has had a significant socio-economic impact globally. Economically, China is likely to experience a greater setback than other countries from the pandemic due to added trade war pressure, which have been discussed in this paper.
Introduction
Coronaviridae is a family of viruses with a positive-sense RNA that possess an outer viral coat. When looked at with the help of an electron microscope, there appears to be a unique corona around it. This family of viruses mainly cause respiratory diseases in humans, in the forms of common cold or pneumonia as well as respiratory infections. These viruses can infect animals as well ( 1 , 2 ). Up until the year 2003, coronavirus (CoV) had attracted limited interest from researchers. However, after the SARS (severe acute respiratory syndrome) outbreak caused by the SARS-CoV, the coronavirus was looked at with renewed interest ( 3 , 4 ). This also happened to be the first epidemic of the 21st century originating in the Guangdong province of China. Almost 10 years later, there was a MERS (Middle East respiratory syndrome) outbreak in 2012, which was caused by the MERS-CoV ( 5 , 6 ). Both SARS and MERS have a zoonotic origin and originated from bats. A unique feature of these viruses is the ability to mutate rapidly and adapt to a new host. The zoonotic origin of these viruses allows them to jump from host to host. Coronaviruses are known to use the angiotensin-converting enzyme-2 (ACE-2) receptor or the dipeptidyl peptidase IV (DPP-4) protein to gain entry into cells for replication ( 7 – 10 ).
In December 2019, almost seven years after the MERS 2012 outbreak, a novel Coronavirus (2019-nCoV) surfaced in Wuhan in the Hubei region of China. The outbreak rapidly grew and spread to neighboring countries. However, rapid communication of information and the increasing scale of events led to quick quarantine and screening of travelers, thus containing the spread of the infection. The major part of the infection was restricted to China, and a second cluster was found on a cruise ship called the Diamond Princess docked in Japan ( 11 , 12 ).
The new virus was identified to be a novel Coronavirus and was thus initially named 2019-nCoV; later, it was renamed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) ( 13 ), and the disease it causes is now referred to as Coronavirus Disease-2019 (COVID-19) by the WHO. The virus was suspected to have begun its spread in the Huanan seafood wholesale market in the Wuhan region. It is possible that an animal that was carrying the virus was brought into or sold in the market, causing the spread of the virus in the crowded marketplace. One of the first claims made was in an article published in the Journal of Medical Virology ( 14 ), which identified snakes as the possible host. A second possibility was that pangolins could be the wild host of SARS-CoV-2 ( 15 ), though the most likely possibility is that the virus originated from bats ( 13 , 16 – 19 ). Increasing evidence and experts are now collectively concluding the virus had a natural origin in bats, as with previous such respiratory viruses ( 2 , 20 – 24 ).
Similarly, SARS and MERS were also suspected to originate from bats. In the case of MERS, the dromedary camel is an intermediate host ( 5 , 10 ). Bats have been known to harbor coronaviruses for quite some time now. Just as in the case of avian flu, SARS, MERS, and possibly even HIV, with increasing selection and ecological pressure due to human activities, the virus made the jump from animal to man. Humans have been encroaching increasingly into forests, and this is true over much of China, as in Africa. Combined with additional ecological pressure due to climate change, such zoonotic spillovers are now more common than ever. It is likely that the next disease X will also have such an origin ( 25 ). We have learned the importance of identification of the source organism due to the Ebola virus pandemic. Viruses are unstable organisms genetically, constantly mutating by genetic shift or drift. It is not possible to predict when a cross-species jump may occur and when a seemingly harmless variant form of the virus may turn into a deadly strain. Such an incident occurred in Reston, USA, with the Reston virus ( 26 ), an alarming reminder of this possibility. The identification of the original host helps us to contain future spreads as well as to learn about the mechanism of transmission of viruses. Until the virus is isolated from a wild animal host, in this case, mostly bats, the zoonotic origin will remain hypothetical, though likely. It should further be noted that the virus has acquired several mutations, as noted by a group in China, indicating that there are more than two strains of the virus, which may have had an impact on its pathogenicity. However, this claim remains unproven, and many experts have argued otherwise; data proving this are not yet available ( 27 ). A similar finding was reported from Italy and India independently, where they found two strains ( 28 , 29 ). These findings need to be further cross-verified by similar analyses globally. If true, this finding could effectively explain why some nations are more affected than others.
Transmission
When the spread of COVID-19 began ( Figure 1 ), the virus appeared to be contained within China and the cruise ship “Diamond Princess,” which formed the major clusters of the virus. However, as of April 2020, over 210 countries and territories are affected by the virus, with Europe, the USA, and Iran forming the new cluster of the virus. The USA ( Figure 2 ) has the highest number of confirmed COVID-19 cases, whereas India and China, despite being among the most population-dense countries in the world, have managed to constrain the infection rate by the implementation of a complete lockdown with arrangements in place to manage the confirmed cases. Similarly, the UK has also managed to maintain a low curve of the graph by implementing similar measures, though it was not strictly enforced. Reports have indicated that the presence of different strains or strands of the virus may have had an effect on the management of the infection rate of the virus ( 27 – 29 ). The disease is spread by droplet transmission. As of April 2020, the total number of infected individuals stands at around 3 million, with ~200,000 deaths and more than 1 million recoveries globally ( 30 , 34 ). The virus thus has a fatality rate of around 2% and an R 0 of 3 based on current data. However, a more recent report from the CDC, Atlanta, USA, claims that the R 0 could be as high as 5.7 ( 35 ). It has also been observed from data available from China and India that individuals likely to be infected by the virus from both these countries belong to the age groups of 20–50 years ( 36 , 37 ). In both of these countries, the working class mostly belongs to this age group, making exposure more likely. Germany and Singapore are great examples of countries with a high number of cases but low fatalities as compared to their immediate neighbors. Singapore is one of the few countries that had developed a detailed plan of action after the previous SARS outbreak to deal with a similar situation in the future, and this worked in their favor during this outbreak. Both countries took swift action after the outbreak began, with Singapore banning Chinese travelers and implementing screening and quarantine measures at a time when the WHO recommended none. They ordered the elderly and the vulnerable to strictly stay at home, and they ensured that lifesaving equipment and large-scale testing facilities were available immediately ( 38 , 39 ). Germany took similar measures by ramping up testing capacity quite early and by ensuring that all individuals had equal opportunity to get tested. This meant that young, old, and at-risk people all got tested, thus ensuring positive results early during disease progression and that most cases were mild like in Singapore, thus maintaining a lower death percentage ( 40 ). It allowed infected individuals to be identified and quarantined before they even had symptoms. Testing was carried out at multiple labs, reducing the load and providing massive scale, something which countries such as the USA did quite late and India restricted to select government and private labs. The German government also banned large gatherings and advocated social distancing to further reduce the spread, though unlike India and the USA, this was done quite late. South Korea is another example of how a nation has managed to contain the spread and transmission of the infection. South Korea and the USA both reported their first COVID-19 cases on the same day; however, the US administration downplayed the risks of the disease, unlike South Korean officials, who constantly informed their citizens about the developments of the disease using the media and a centralized messaging system. They also employed the Trace, Test, and Treat protocol to identify and isolate patients fast, whereas the USA restricted this to patients with severe infection and only later broadened this criterion, like many European countries as well as India. Unlike the USA, South Korea also has universal healthcare, ensuring free diagnostic testing.
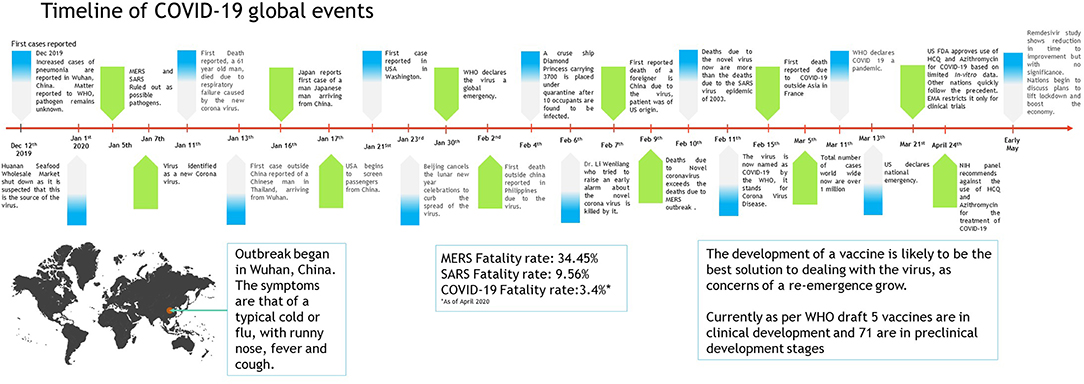
Figure 1 . Timeline of COVID-19 progression ( 30 – 32 ).
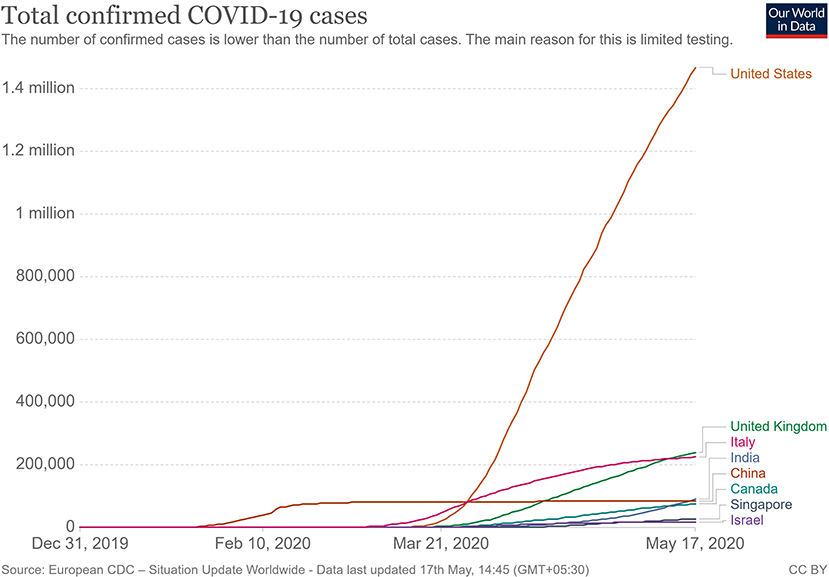
Figure 2 . Total confirmed COVID 19 cases as of May 2020 ( 33 ).
The main mode of transmission of 2019-nCoV is human to human. As of now, animal-to-human transfer has not yet been confirmed. Asymptomatic carriers of the virus are at major risk of being superinfectors with this disease, as all those infected may not develop the disease ( 41 ). This is a concern that has been raised by nations globally, with the Indian government raising concerns on how to identify and contain asymptomatic carriers, who could account for 80% of those infected ( 42 ). Since current resources are directed towards understanding the hospitalized individuals showing symptoms, there is still a vast amount of information about asymptomatic individuals that has yet to be studied. For example, some questions that need to be answered include: Do asymptomatic individuals develop the disease at any point in time at all? Do they eventually develop antibodies? How long do they shed the virus for? Can any tissue of these individuals store the virus in a dormant state? Asymptomatic transmission is a gray area that encompasses major unknowns in COVID-19.
The main route of human-to-human transmission is by droplets, which are generated during coughing, talking, or sneezing and are then inhaled by a healthy individual. They can also be indirectly transmitted to a person when they land on surfaces that are touched by a healthy individual who may then touch their nose, mouth, or eyes, allowing the virus entry into the body. Fomites are also a common issue in such diseases ( 43 ).
Aerosol-based transmission of the virus has not yet been confirmed ( 43 ). Stool-based transmission via the fecal-oral route may also be possible since the SARS-CoV-2 has been found in patient feces ( 44 , 45 ). Some patients with COVID-19 tend to develop diarrhea, which can become a major route of transmission if proper sanitation and personal hygiene needs are not met. There is no evidence currently available to suggest intrauterine vertical transmission of the disease in pregnant women ( 46 ).
More investigation is necessary of whether climate has played any role in the containment of the infection in countries such as India, Singapore, China, and Israel, as these are significantly warmer countries as compared with the UK, the USA, and Canada ( Figure 2 ). Ideally, a warm climate should prevent the virus from surviving for longer periods of time on surfaces, reducing transmissibility.
Pathophysiology
On gaining entry via any of the mucus membranes, the single-stranded RNA-based virus enters the host cell using type 2 transmembrane serine protease (TMPRSS2) and ACE2 receptor protein, leading to fusion and endocytosis with the host cell ( 47 – 49 ). The uncoated RNA is then translated, and viral proteins are synthesized. With the help of RNA-dependant RNA polymerase, new RNA is produced for the new virions. The cell then undergoes lysis, releasing a load of new virions into the patients' body. The resultant infection causes a massive release of pro-inflammatory cytokines that causes a cytokine storm.
Clinical Presentation
The clinical presentation of the disease resembles beta coronavirus infections. The virus has an incubation time of 2–14 days, which is the reason why most patients suspected to have the illness or contact with an individual having the illness remain in quarantine for the said amount of time. Infection with SARS-CoV-2 causes severe pneumonia, intermittent fever, and cough ( 50 , 51 ). Symptoms of rhinorrhoea, pharyngitis, and sneezing have been less commonly seen. Patients often develop acute respiratory distress syndrome within 2 days of hospital admission, requiring ventilatory support. It has been observed that during this phase, the mortality tends to be high. Chest CT will show indicators of pneumonia and ground-glass opacity, a feature that has helped to improve the preliminary diagnosis ( 51 ). The primary method of diagnosis for SARS-CoV-2 is with the help of PCR. For the PCR testing, the US CDC recommends testing for the N gene, whereas the Chinese CDC recommends the use of ORF lab and N gene of the viral genome for testing. Some also rely on the radiological findings for preliminary screening ( 52 ). Additionally, immunodiagnostic tests based on the presence of antibodies can also play a role in testing. While the WHO recommends the use of these tests for research use, many countries have pre-emptively deployed the use of these tests in the hope of ramping up the rate and speed of testing ( 52 – 54 ). Later, they noticed variations among the results, causing them to stop the use of such kits; there was also debate among the experts about the sensitivity and specificity of the tests. For immunological tests, it is beneficial to test for antibodies against the virus produced by the body rather than to test for the presence of the viral proteins, since the antibodies can be present in larger titers for a longer span of time. However, the cross-reactivity of these tests with other coronavirus antibodies is something that needs verification. Biochemical parameters such as D-dimer, C-reactive protein, and variations in neutrophil and lymphocyte counts are some other parameters that can be used to make a preliminary diagnosis; however, these parameters vary in a number of diseases and thus cannot be relied upon conclusively ( 51 ). Patients with pre-existing diseases such as asthma or similar lung disorder are at higher risk, requiring life support, as are those with other diseases such as diabetes, hypertension, or obesity. Those above the age of 60 have displayed the highest mortality rate in China, a finding that is mirrored in other nations as well ( Figure 3 ) ( 55 ). If we cross-verify these findings with the population share that is above the age of 70, we find that Italy, the United Kingdom, Canada, and the USA have one of the highest elderly populations as compared to countries such as India and China ( Figure 4 ), and this also reflects the case fatality rates accordingly ( Figure 5 ) ( 33 ). This is a clear indicator that aside from comorbidities, age is also an independent risk factor for death in those infected by COVID-19. Also, in the US, it was seen that the rates of African American deaths were higher. This is probably due to the fact that the prevalence of hypertension and obesity in this community is higher than in Caucasians ( 56 , 57 ). In late April 2020, there are also claims in the US media that young patients in the US with COVID-19 may be at increased risk of stroke; however, this is yet to be proven. We know that coagulopathy is a feature of COVID-19, and thus stroke is likely in this condition ( 58 , 59 ). The main cause of death in COVID-19 patients was acute respiratory distress due to the inflammation in the linings of the lungs caused by the cytokine storm, which is seen in all non-survival cases and in respiratory failure. The resultant inflammation in the lungs, served as an entry point of further infection, associated with coagulopathy end-organ failure, septic shock, and secondary infections leading to death ( 60 – 63 ).
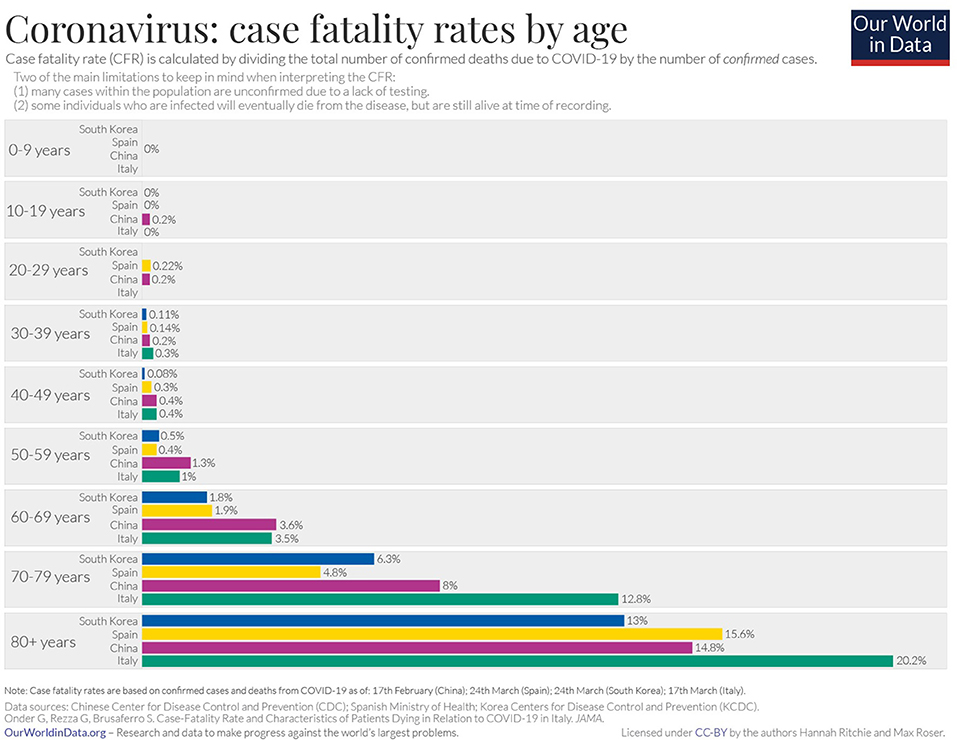
Figure 3 . Case fatality rate by age in selected countries as of April 2020 ( 33 ).
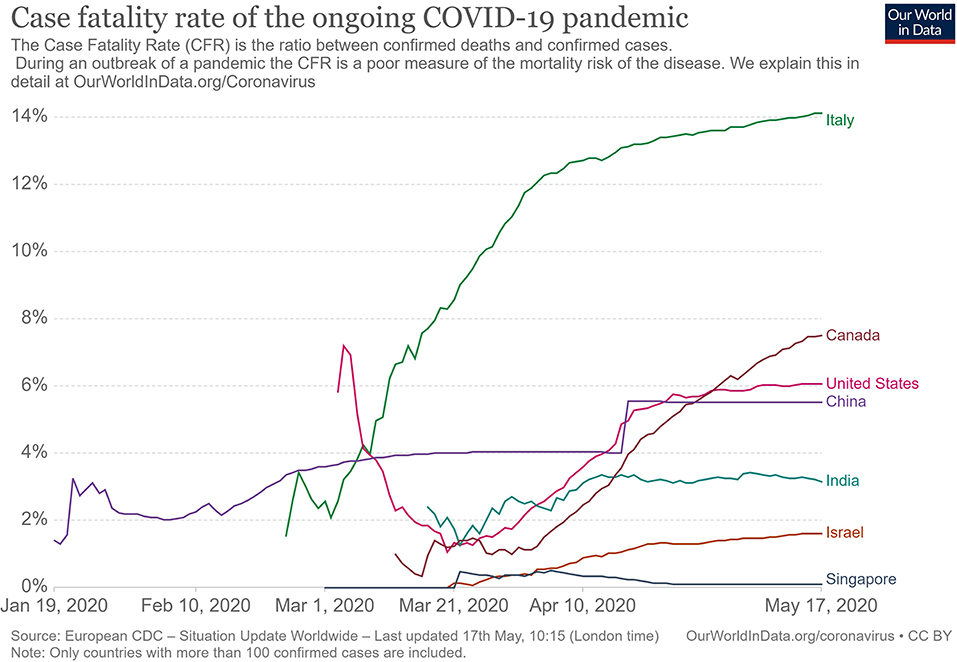
Figure 4 . Case fatality rate in selected countries ( 33 ).
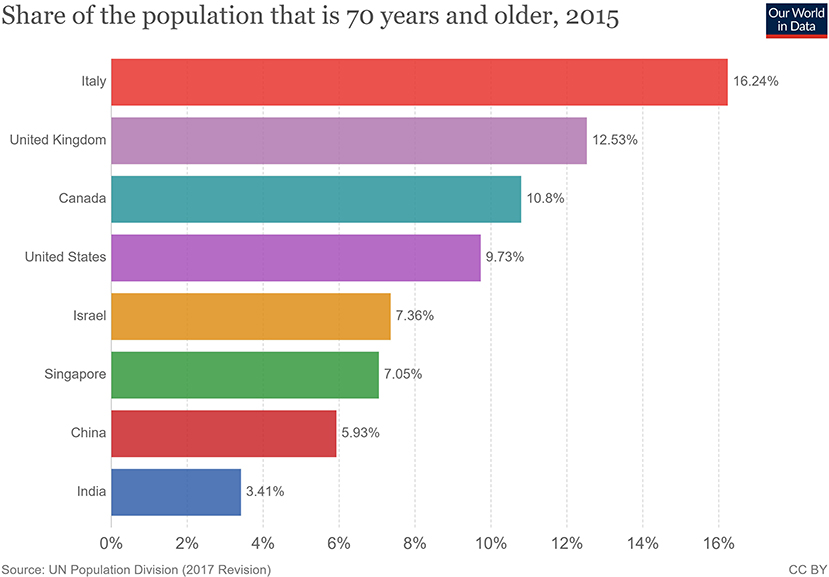
Figure 5 . Population share above 70 years of age ( 33 ).
For COVID-19, there is no specific treatment available. The WHO announced the organization of a trial dubbed the “Solidarity” clinical trial for COVID-19 treatments ( 64 ). This is an international collaborative study that investigates the use of a few prime candidate drugs for use against COVID-19, which are discussed below. The study is designed to reduce the time taken for an RCT by over 80%. There are over 1087 studies ( Supplementary Data 1 ) for COVID-19 registered at clinicaltrials.gov , of which 657 are interventional studies ( Supplementary Data 2 ) ( 65 ). The primary focus of the interventional studies for COVID-19 has been on antimalarial drugs and antiviral agents ( Table 1 ), while over 200 studies deal with the use of different forms of oxygen therapy. Most trials focus on improvement of clinical status, reduction of viral load, time to improvement, and reduction of mortality rates. These studies cover both severe and mild cases.
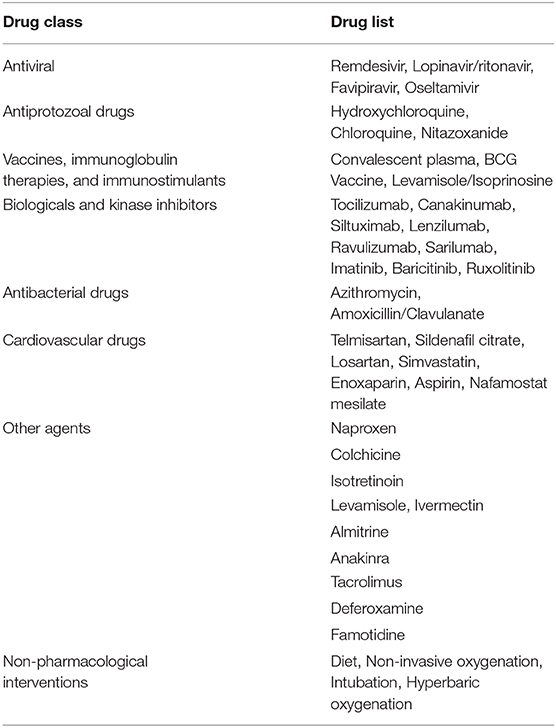
Table 1 . List of therapeutic drugs under study for COVID-19 as per clinical trials registered under clinicaltrials.gov .
Use of Antimalarial Drugs Against SARS-CoV-2
The use of chloroquine for the treatment of corona virus-based infection has shown some benefit in the prevention of viral replication in the cases of SARS and MERS. However, it was not validated on a large scale in the form of a randomized control trial ( 50 , 66 – 68 ). The drugs of choice among antimalarials are Chloroquine (CQ) and Hydroxychloroquine (HCQ). The use of CQ for COVID-19 was brought to light by the Chinese, especially by the publication of a letter to the editor of Bioscience Trends by Gao et al. ( 69 ). The letter claimed that several studies found CQ to be effective against COVID-19; however, the letter did not provide many details. Immediately, over a short span of time, interest in these two agents grew globally. Early in vitro data have revealed that chloroquine can inhibit the viral replication ( 70 , 71 ).
HCQ and CQ work by raising the pH of the lysosome, the cellular organelle that is responsible for phagocytic degradation. Its function is to combine with cell contents that have been phagocytosed and break them down eventually, in some immune cells, as a downstream process to display some of the broken proteins as antigens, thus further enhancing the immune recruitment against an antigen/pathogen. The drug was to be administered alone or with azithromycin. The use of azithromycin may be advocated by the fact that it has been seen previously to have some immunomodulatory role in airway-related disease. It appears to reduce the release of pro-inflammatory cytokines in respiratory illnesses ( 72 ). However, HCQ and azithromycin are known to have a major drug interaction when co-administered, which increases the risk of QT interval prolongation ( 73 ). Quinine-based drugs are known to have adverse effects such as QT prolongation, retinal damage, hypoglycemia, and hemolysis of blood in patients with G-6-PD deficiency ( 66 ). Several preprints, including, a metanalysis now indicate that HCQ may have no benefit for severe or critically ill patients who have COVID-19 where the outcome is need for ventilation or death ( 74 , 75 ). As of April 21, 2020, after having pre-emptively recommended their use for SARS-CoV-2 infection, the US now advocates against the use of these two drugs based on the new data that has become available.
Use of Antiviral Drugs Against SARS-CoV-2
The antiviral agents are mainly those used in the case of HIV/AIDS, these being Lopinavir and Ritonavir. Other agents such as nucleoside analogs like Favipiravir, Ribavirin, Remdesivir, and Galidesivir have been tested for possible activity in the prevention of viral RNA synthesis ( 76 ). Among these drugs, Lopinavir, Ritonavir, and Remdesivir are listed in the Solidarity trial by the WHO.
Remdesivir is a nucleotide analog for adenosine that gets incorporated into the viral RNA, hindering its replication and causing chain termination. This agent was originally developed for Ebola Virus Disease ( 77 ). A study was conducted with rhesus macaques infected with SARS-CoV-2 ( 78 ). In that study, after 12 h of infection, the monkeys were treated with either Remdesivir or vehicle. The drug showed good distribution in the lungs, and the animals treated with the drug showed a better clinical score than the vehicle group. The radiological findings of the study also indicated that the animals treated with Remdesivir have less lung damage. There was a reduction in viral replication but not in virus shedding. Furthermore, there were no mutations found in the RNA polymerase sequences. A randomized clinical control study that became available in late April 2020 ( 79 ), having 158 on the Remdesivir arm and 79 on the placebo arm, found that Remdesivir reduced the time to recovery in the Remdesivir-treated arm to 11 days, while the placebo-arm recovery time was 15 days. Though this was not found to be statistically significant, the agent provided a basis for further studies. The 28-days mortality was found to be similar for both groups. This has now provided us with a basis on which to develop future molecules. The study has been supported by the National Institute of Health, USA. The authors of the study advocated for more clinical trials with Remdesivir with a larger population. Such larger studies are already in progress, and their results are awaited. Remdesivir is currently one of the drugs that hold most promise against COVID-19.
An early trial in China with Lopinavir and Ritonavir showed no benefit compared with standard clinical care ( 80 ). More studies with this drug are currently underway, including one in India ( 81 , 82 ).
Use of Convalescent Patient Plasma
Another possible option would be the use of serum from convalescent individuals, as this is known to contain antibodies that can neutralize the virus and aid in its elimination. This has been tried previously for other coronavirus infections ( 83 ). Early emerging case reports in this aspect look promising compared to other therapies that have been tried ( 84 – 87 ). A report from China indicates that five patients treated with plasma recovered and were eventually weaned off ventilators ( 84 ). They exhibited reductions in fever and viral load and improved oxygenation. The virus was not detected in the patients after 12 days of plasma transfusion. The US FDA has provided detailed recommendations for investigational COVID-19 Convalescent Plasma use ( 88 ). One of the benefits of this approach is that it can also be used for post-exposure prophylaxis. This approach is now beginning to be increasingly adopted in other countries, with over 95 trials registered on clinicaltrials.gov alone, of which at least 75 are interventional ( 89 ). The use of convalescent patient plasma, though mostly for research purposes, appears to be the best and, so far, the only successful option for treatment available.
From a future perspective, the use of monoclonal antibodies for the inhibition of the attachment of the virus to the ACE-2 receptor may be the best bet. Aside from this, ACE-2-like molecules could also be utilized to attach and inactivate the viral proteins, since inhibition of the ACE-2 receptor would not be advisable due to its negative repercussions physiologically. In the absence of drug regimens and a vaccine, the treatment is symptomatic and involves the use of non-invasive ventilation or intubation where necessary for respiratory failure patients. Patients that may go into septic shock should be managed as per existing guidelines with hemodynamic support as well as antibiotics where necessary.
The WHO has recommended that simple personal hygiene practices can be sufficient for the prevention of spread and containment of the disease ( 90 ). Practices such as frequent washing of soiled hands or the use of sanitizer for unsoiled hands help reduce transmission. Covering of mouth while sneezing and coughing, and disinfection of surfaces that are frequently touched, such as tabletops, doorknobs, and switches with 70% isopropyl alcohol or other disinfectants are broadly recommended. It is recommended that all individuals afflicted by the disease, as well as those caring for the infected, wear a mask to avoid transmission. Healthcare works are advised to wear a complete set of personal protective equipment as per WHO-provided guidelines. Fumigation of dormitories, quarantine rooms, and washing of clothes and other fomites with detergent and warm water can help get rid of the virus. Parcels and goods are not known to transmit the virus, as per information provided by the WHO, since the virus is not able to survive sufficiently in an open, exposed environment. Quarantine of infected individuals and those who have come into contact with an infected individual is necessary to further prevent transmission of the virus ( 91 ). Quarantine is an age-old archaic practice that continues to hold relevance even today for disease containment. With the quarantine being implemented on such a large scale in some countries, taking the form of a national lockdown, the question arises of its impact on the mental health of all individuals. This topic needs to be addressed, especially in countries such as India and China, where it is still a matter of partial taboo to talk about it openly within the society.
In India, the Ministry of Ayurveda, Yoga, and Naturopathy, Unani, Siddha and Homeopathy (AYUSH), which deals with the alternative forms of medicine, issued a press release that the homeopathic, drug Arsenicum album 30, can be taken on an empty stomach for 3 days to provide protection against the infection ( 92 ). It also provided a list of herbal drugs in the same press release as per Ayurvedic and Unani systems of medicine that can boost the immune system to deal with the virus. However, there is currently no evidence to support the use of these systems of medicine against COVID-19, and they need to be tested.
The prevention of the disease with the use of a vaccine would provide a more viable solution. There are no vaccines available for any of the coronaviruses, which includes SARS and MERS. The development of a vaccine, however, is in progress at a rapid pace, though it could take about a year or two. As of April 2020, no vaccine has completed the development and testing process. A popular approach has been with the use of mRNA-based vaccine ( 93 – 96 ). mRNA vaccines have the advantage over conventional vaccines in terms of production, since they can be manufactured easily and do not have to be cultured, as a virus would need to be. Alternative conventional approaches to making a vaccine against SARS-CoV-2 would include the use of live attenuated virus as well as using the isolated spike proteins of the virus. Both of these approaches are in progress for vaccine development ( 97 ). Governments across the world have poured in resources and made changes in their legislation to ensure rapid development, testing, and deployment of a vaccine.
Barriers to Treatment
Lack of transparency and poor media relations.
The lack of government transparency and poor reporting by the media have hampered the measures that could have been taken by healthcare systems globally to deal with the COVID-19 threat. The CDC, as well as the US administration, downplayed the threat and thus failed to stock up on essential supplies, ventilators, and test kits. An early warning system, if implemented, would have caused borders to be shut and early lockdowns. The WHO also delayed its response in sounding the alarm regarding the severity of the outbreak to allow nations globally to prepare for a pandemic. Singapore is a prime example where, despite the WHO not raising concerns and banning travel to and from China, a country banned travelers and took early measures, thus managing the outbreak quite well. South Korea is another example of how things may have played out had those measures by agencies been taken with transparency. Increased transparency would have allowed the healthcare sector to better prepare and reduced the load of patients they had to deal with, helping flatten the curve. The increased patient load and confusion among citizens arising from not following these practices has proved to be a barrier to providing effective treatments to patients with the disease elsewhere in the world.
Lack of Preparedness and Protocols
Despite the previous SARS outbreak teaching us important lessons and providing us with data on a potential outbreak, many nations did not take the important measures needed for a future outbreak. There was no allocation of sufficient funds for such an event. Many countries experienced severe lack of PPE, and the lockdown precautions hampered the logistics of supply and manufacturing of such essential equipment. Singapore and South Korea had protocols in place and were able to implement them at a moment's notice. The spurt of cases that Korea experienced was managed well, providing evidence to this effect. The lack of preparedness and lack of protocol in other nations has resulted in confusion as to how the treatment may be administered safely to the large volume of patients while dealing with diagnostics. Both of these factors have limited the accessibility to healthcare services due to sheer volume.
Socio-Economic Impact
During the SARS epidemic, China faced an economic setback, and experts were unsure if any recovery would be made. However, the global and domestic situation was then in China's favor, as it had a lower debt, allowing it to make a speedy recovery. This is not the case now. Global experts have a pessimistic outlook on the outcome of this outbreak ( 98 ). The fear of COVID-19 disease, lack of proper understanding of the dangers of the virus, and the misinformation spread on the social media ( 99 ) have caused a breakdown of the economic flow globally ( 100 ). An example of this is Indonesia, where a great amount of fear was expressed in responses to a survey when the nation was still free of COVID-19 ( 101 ). The pandemic has resulted in over 2.6 billion people being put under lockdown. This lockdown and the cancellation of the lunar year celebration has affected business at the local level. Hundreds of flights have been canceled, and tourism globally has been affected. Japan and Indonesia are estimated to lose over 2.44 billion dollars due to this ( 102 , 103 ). Workers are not able to work in factories, transportation in all forms is restricted, and goods are not produced or moved. The transport of finished products and raw materials out of China is low. The Economist has published US stock market details indicating that companies in the US that have Chinese roots fell, on average, 5 points on the stock market as compared to the S&P 500 index ( 104 ). Companies such as Starbucks have had to close over 4,000 outlets due to the outbreak as a precaution. Tech and pharma companies are at higher risk since they rely on China for the supply of raw materials and active pharmaceutical ingredients. Paracetamol, for one, has reported a price increase of over 40% in India ( 104 – 106 ). Mass hysteria in the market has caused selling of shares of these companies, causing a tumble in the Indian stock market. Though long-term investors will not be significantly affected, short-term traders will find themselves in soup. Politically, however, this has further bolstered support for world leaders in countries such as India, Germany, and the UK, who are achieving good approval ratings, with citizens being satisfied with the government's approach. In contrast, the ratings of US President Donald Trump have dropped due to the manner in which the COVID-19 pandemic was handled. These minor impacts may be of temporary significance, and the worst and direct impact will be on China itself ( 107 – 109 ), as the looming trade war with the USA had a negative impact on the Chinese and Asian markets. The longer production of goods continues to remain suspended, the more adversely it will affect the Chinese economy and the global markets dependent on it ( 110 ). If this disease is not contained, more and more lockdowns by multiple nations will severely affect the economy and lead to many social complications.
The appearance of the 2019 Novel Coronavirus has added and will continue to add to our understanding of viruses. The pandemic has once again tested the world's preparedness for dealing with such outbreaks. It has provided an outlook on how a massive-scale biological event can cause a socio-economic disturbance through misinformation and social media. In the coming months and years, we can expect to gain further insights into SARS-CoV-2 and COVID-19.
Author Contributions
KN: conceptualization. RK, AA, JM, and KN: investigation. RK and AA: writing—original draft preparation. KN, PN, and JM: writing—review and editing. KN: supervision.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge the contributions made by Dr. Piya Paul Mudgal, Assistant Professor, Manipal Institute of Virology, Manipal Academy of Higher Education towards inputs provided by her during the drafting of the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00216/full#supplementary-material
Supplementary Data 1, 2. List of all studies registered for COVID-19 on clinicaltrials.gov .
1. McIntosh K, Dees JH, Becker WB, Kapikian AZ, Chanock RM. Recovery in tracheal organ cultures of novel viruses from patients with respiratory disease. Proc Natl Acad Sci USA. (1967) 57:933–40. doi: 10.1073/pnas.57.4.933
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Esper F, Weibel C, Ferguson D, Landry ML, Kahn JS. Evidence of a novel human coronavirus that is associated with respiratory tract disease in infants and young children. J Infect Dis. (2005) 191:492–8. doi: 10.1086/428138
3. Stöhr K. A multicentre collaboration to investigate the cause of severe acute respiratory syndrome. Lancet. (2003) 361:1730–3. doi: 10.1016/S0140-6736(03)13376-4
4. Peiris JSM, Lai ST, Poon LLM, Guan Y, Yam LYC, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. (2003) 361:1319–25. doi: 10.1016/S0140-6736(03)13077-2
5. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. (2015) 386:995–1007. doi: 10.1016/S0140-6736(15)60454-8
6. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. (2012) 367:1814–20. doi: 10.1056/NEJMoa1211721
7. Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. (2009) 7:439–50. doi: 10.1038/nrmicro2147
8. Li W, Moore MJ, Vasllieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. (2003) 426:450–4. doi: 10.1038/nature02145
9. Ge X-Y, Li J-L, Yang X-L, Chmura AA, Zhu G, Epstein JH, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. (2013) 503:535–8. doi: 10.1038/nature12711
10. Wang M, Hu Z. Bats as animal reservoirs for the SARS coronavirus: Hypothesis proved after 10 years of virus hunting. Virol Sin. (2013) 28:315–7. doi: 10.1007/s12250-013-3402-x
11. Diamond Princess Cruise Ship in Japan Confirms 99 New Coronavirus Cases | World news | The Guardian. Available online at: https://www.theguardian.com/world/2020/feb/17/coronavirus-japan-braces-for-hundreds-more-cases-as-another-china-city-locked-down (accessed February 17, 2020).
Google Scholar
12. Diamond Princess Coronavirus & Quarantine Updates - Notices & Advisories - Princess Cruises. Available online at: https://www.princess.com/news/notices_and_advisories/notices/diamond-princess-update.html (accessed February 17, 2020).
13. Gorbalenya AE, Baker SC, Baric RS, Groot RJ, de Drosten C, Gulyaeva AA, et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. (2020) 5:536–44. doi: 10.1038/s41564-020-0695-z
14. Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol . (2020) 7:jmv.25682. doi: 10.1002/jmv.25682
15. Cyranoski D. Did pangolins spread the China coronavirus to people? Nature . (2020) doi: 10.1038/d41586-020-00364-2
CrossRef Full Text | Google Scholar
16. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. (2020) 395:565–74. doi: 10.1016/S0140-6736(20)30251-8
17. Wassenaar TM, Zou Y. 2019_nCoV: Rapid classification of betacoronaviruses and identification of traditional Chinese medicine as potential origin of zoonotic coronaviruses. Lett Appl Microbiol. (2020) 70:324–48. doi: 10.1111/lam.13285
18. Velavan TP, Meyer CG. The Covid-19 epidemic. Trop Med Int Heal . (2020) 25:278–80. doi: 10.1111/tmi.13383
19. Guarner J. Three Emerging Coronaviruses in Two Decades. Am J Clin Pathol . (2020) 153:420–21. doi: 10.1093/ajcp/aqaa029
20. Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. (2005) 310:676–9. doi: 10.1126/science.1118391
21. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
22. Menachery VD, Yount BL, Debbink K, Agnihothram S, Gralinski LE, Plante JA, et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nat Med. (2015) 21:1508–13. doi: 10.1038/nm.3985
23. COVID-19 Coronavirus Epidemic has a Natural Origin—ScienceDaily. Available online at: https://www.sciencedaily.com/releases/2020/03/200317175442.htm (accessed April 22, 2020).
24. Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med . (2020) 26:450–2. doi: 10.1038/s41591-020-0820-9
25. Prioritizing Diseases for Research and Development in Emergency Contexts. Available online at: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts (accessed April 22, 2020).
26. Albariño CG, Guerrero LW, Jenks HM, Chakrabarti AK, Ksiazek TG, Rollin PE, et al. Insights into Reston virus spillovers and adaption from virus whole genome sequences. PLoS ONE. (2017) 12:e0178224. doi: 10.1371/journal.pone.0178224
27. Yao H, Lu X, Chen Q, Xu K, Chen Y, Cheng L, et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. medRxiv. (2020). doi: 10.2139/ssrn.3578153
28. Stefanelli P, Faggioni G, Lo Presti A, Fiore S, Marchi A, Benedetti E, et al. Whole genome and phylogenetic analysis of two SARS-CoV-2 strains isolated in Italy in January and February 2020: additional clues on multiple introductions and further circulation in Europe. Eurosurveillance. (2020) 25:2000305. doi: 10.2807/1560-7917.ES.2020.25.13.2000305
29. Yadav P, Potdar V, Choudhary M, Nyayanit D, Agrawal M, Jadhav S, et al. Full-genome sequences of the first two SARS-CoV-2 viruses from India. Indian J Med Res. (2020) 151:200–9. doi: 10.4103/ijmr.IJMR_663_20
30. WHO | Coronavirus disease 2019 (COVID-19) Situation Report – 26. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
31. WHO | Middle East Respiratory Syndrome Coronavirus (MERS-CoV). World Health Organization (2020).
32. WHO | Summary of Probable SARS Cases With Onset of Illness From 1 November 2002 to 31 July 2003. World Health Organization (2015).
33. Worldometer. Coronavirus cases. Worldometer. (2020) 1−22.
34. Update on the Outbreak of New Coronavirus Pneumonia as of 24 hours on 15 February. Beijing (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml (accessed February 16, 2020).
35. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. (2020) 26. doi: 10.3201/eid2607.200282
36. 83% of India's Coronavirus Patients Are Below the Age of 50: Health ministry data - India News. Available online at: https://www.indiatoday.in/india/story/83-of-india-s-coronavirus-patients-are-below-the-age-of-50-health-ministry-data-1663314-2020-04-04 (accessed April 23, 2020).
37. 42% of Coronavirus Patients in 21-40 age bracket: Govt. Available online at: https://economictimes.indiatimes.com/news/politics-and-nation/42-of-coronavirus-patients-in-21-40-age-bracket-govt/articleshow/74987254.cms (accessed April 23, 2020).
38. Why COVID-19 Case Counts Are so Low in Singapore Hong Kong and Taiwan | Advisory Board Daily Briefing. Available online at: https://www.advisory.com/daily-briefing/2020/03/19/asian-countries (accessed April 29, 2020).
39. Coronavirus: Why so Few Deaths Among Singapore's 14000 Covid-19 Infections? | South China Morning Post. Available online at: https://www.scmp.com/weekasia/health-environment/article/3081772/coronavirus-why-so-few-deaths-among-singapores-14000 (accessed April 29, 2020).
40. Stafford N. Covid-19: Why Germany's case fatality rate seems so low. BMJ. (2020) 7:369. doi: 10.1136/bmj.m1395
41. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med . (2020) 382:970–1. doi: 10.1056/NEJMc2001468
42. Coronavirus pandemic | 80% of COVID-19 Cases Either Asymptomatic or Show Mild Symptoms. Health ministry - Moneycontrol.com. Available online at: https://www.moneycontrol.com/news/india/coronavirus-pandemic-80-of-covid-19-cases-either-asymptomatic-or-show-mild-symptoms-health-ministry-5170631.html (accessed April 24, 2020).
43. WHO | Q&A on Coronaviruses. Available online at: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed February 16, 2020).
44. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med . (2020) 382:929–36. doi: 10.1056/NEJMoa2001191
45. Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. (2020) 5:335–37. doi: 10.1016/S2468-1253(20)30048-0
46. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. (2020) 395:809–15. doi: 10.1016/S0140-6736(20)30360-3
47. Fehr AR, Perlman S. Coronaviruses: An overview of their replication and pathogenesis. In: Coronaviruses: Methods and Protocols (New York: Springer), 1–23. doi: 10.1007/978-1-4939-2438-7_1
48. Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. (2020) 92:418–23. doi: 10.1002/jmv.25681
49. Hoffmann M, Kleine-Weber H, Schroeder S, Mü MA, Drosten C, Pö S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80. doi: 10.1016/j.cell.2020.02.052
50. Cheng VCC, Chan JFW, To KKW, Yuen KY. Clinical management and infection control of SARS: Lessons learned. Antiviral Res. (2013) 100:407–19. doi: 10.1016/j.antiviral.2013.08.016
51. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
52. Udugama B, Kadhiresan P, Kozlowski HN, Malekjahani A, Osborne M, Li VYC, et al. Diagnosing COVID-19: the disease and tools for detection. ACS Nano . (2020) 14:3822–35. doi: 10.1021/acsnano.0c02624
53. Testing, | CDC,. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/testing/index.html (accessed April 29, 2020).
54. Advice on the Use of Point-of-Care Immunodiagnostic Tests for COVID-19. Available online at: https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19 (accessed April 29, 2020).
55. Zhang Yanping. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. (2020) Available online at: http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9bfea8db1a8f51 (accessed February 18, 2020).
56. Petersen R, Pan L, Blanck HM. Racial and ethnic disparities in adult obesity in the United States: CDC's tracking to inform state and local action. Prev Chronic Dis. (2019) 16:180579. doi: 10.5888/pcd16.180579
57. Wang L, Southerland J, Wang K, Bailey BA, Alamian A, Stevens MA, et al. Ethnic differences in risk factors for obesity among adults in California, the United States. (2017) 2017:2427483. doi: 10.1155/2017/2427483
58. Covid-19 Causes Sudden Strokes in Young Adults Doctors Say - CNN. Available online at: https://edition.cnn.com/2020/04/22/health/strokes-coronavirus-young-adults/index.html (accessed April 24, 2020).
59. Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost . (2020) 1–4. doi: 10.1111/jth.14828
60. Lancet T, Medicine R. Comment Understanding pathways to death in patients with. Lancet Respir Med. (2020) 2019:2019–21. doi: 10.1016/S2213-2600(20)30165-X
61. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA . (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
62. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
63. Doctors Warn COVID-19 Might Cause Strokes in Young Adults. Available online at: https://nypost.com/2020/04/23/doctors-warn-covid-19-might-cause-strokes-in-young-adults/ (accessed April 24, 2020).
64. “Solidarity” Clinical Trial for COVID-19 Treatments. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments (accessed April 23, 2020).
65. Search, of: COVID-19 - List Results - ClinicalTrials.gov . Available online at: https://www.clinicaltrials.gov/ct2/results?cond=COVID-19&term=&cntry=&state=&city=&dist= (accessed May 1, 2020).
66. De Wilde AH, Jochmans D, Posthuma CC, Zevenhoven-Dobbe JC, Van Nieuwkoop S, Bestebroer TM, et al. Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob Agents Chemother. (2014) 58:4875–84. doi: 10.1128/AAC.03011-14
67. Tai DYH. Pharmacologic treatment of SARS: current knowledge and recommendations. Ann Acad Med Singapore. (2007) 36:438–43.
PubMed Abstract | Google Scholar
68. Sheahan TP, Sims AC, Leist SR, Schäfer A, Won J, Brown AJ, et al. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. (2020) 11:222. doi: 10.1038/s41467-019-13940-6
69. Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. (2020) 14:72–73. doi: 10.5582/bst.2020.01047
70. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. (2020) 30:269–71. doi: 10.1038/s41422-020-0282-0
71. Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. (2005) 2:1–0. doi: 10.1186/1743-422X-2-69
72. Cramer CL, Patterson A, Alchakaki A, Soubani AO. Immunomodulatory indications of azithromycin in respiratory disease: a concise review for the clinician. Postgrad Med. (2017) 129:493–9. doi: 10.1080/00325481.2017.1285677
73. Plaquenil™ Hydroxychloroquine Sulfate Tablets USP Description. Available online at: http://www.cdc.gov/malaria (accessed April 21, 2020).
74. Magagnoli J, Narendran S, Pereira F, Cummings T, Hardin JW, Sutton SS, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. medRxiv. (2020) doi: 10.1101/2020.04.16.20065920
75. Shamshirian A, Hessami A, Heydari K, Alizadeh-Navaei R, Ebrahimzadeh MA, Ghasemian R, et al. Hydroxychloroquine Versus COVID-19: A Rapid Systematic Review and Meta-Analysis. medRxiv. (2020) doi: 10.1101/2020.04.14.20065276
76. Li G, De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV). Nat Rev Drug Discov . (2020) 19:149–50. doi: 10.1038/d41573-020-00016-0
77. Warren TK, Jordan R, Lo MK, Ray AS, Mackman RL, Soloveva V, et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. (2016) 531:381–5. doi: 10.1038/nature17180
78. Williamson BN, Feldmann F, Schwarz B, Meade-White K, Porter DP, Schulz J, et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. bioRxiv. (2020) doi: 10.1101/2020.04.15.043166
79. Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. (2020) 395:1569–78. doi: 10.1016/S0140-6736(20)31022-9
80. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe covid-19. N Engl J Med . (2020) 382:1787–99. doi: 10.1056/NEJMoa2001282
81. Search, of: Lopinavir, Ritonavir, | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=Lopinavir%2CRitonavir&cond=COVID&draw=4&rank=22#rowId21 (accessed April 23, 2020).
82. Bhatnagar T, Murhekar M, Soneja M, Gupta N, Giri S, Wig N, et al. Lopinavir/ritonavir combination therapy amongst symptomatic coronavirus disease 2019 patients in India: protocol for restricted public health emergency use. Indian J Med Res. (2020) 151:184–9. doi: 10.4103/ijmr.IJMR_502_20
83. Yeh K-M, Chiueh T-S, Siu LK, Lin J-C, Chan PKS, Peng M-Y, et al. Experience of using convalescent plasma for severe acute respiratory syndrome among healthcare workers in a Taiwan hospital. J Antimicrob Chemother. (2005) 56:919–22. doi: 10.1093/jac/dki346
84. Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically Ill patients with COVID-19 with convalescent plasma. JAMA . (2020) 323:1582–9. doi: 10.1001/jama.2020.4783
85. Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infect Dis . (2020) 7:1–6. doi: 10.1093/ofid/ofaa102
86. Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest . (2020) 138745:1–22. doi: 10.1172/JCI138745
87. Ye M, Fu D, Ren Y, Wang F, Wang D, Zhang F, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. J Med Virol. (2 020) doi: 10.1002/jmv.25882
88. Recommendations for Investigational COVID-19 Convalescent Plasma | FDA. Available online at: https://www.fda.gov/vaccines-blood-biologics/investigational-new-drug-ind-or-device-exemption-ide-process-cber/recommendations-investigational-covid-19-convalescent-plasma (accessed April 23, 2020).
89. Search, of: plasma | Interventional Studies | COVID - List Results - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/results?term=plasma&cond=COVID&Search=Apply&age_v=&gndr=&type=Intr&rslt= (accessed April 23, 2020).
90. Infection Prevention and Control. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (accessed February 17, 2020).
91. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med . (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
92. Press Information Bureau AYUSH Advisory for Corona virus. Press Inf Bereau. Available online at: https://pib.gov.in/PressReleasePage.aspx?PRID=1600895 (accessed February 17, 2020).
93. CanSino, Biologics : China Announces First Human Trials of Covid-19 Vaccine | MarketScreener,. Available online at: https://www.marketscreener.com/CANSINO-BIOLOGICS-INC-59318312/news/CanSino-Biologics-China-announces-first-human-trials-of-Covid-19-vaccine-30183232/ (accessed April 7, 2020).
94. Safety, and Immunogenicity Study of 2019-nCoV Vaccine (mRNA-1273) for Prophylaxis SARS CoV-2 Infection - Full Text View - ClinicalTrials.gov . Available online at: https://clinicaltrials.gov/ct2/show/NCT04283461 (accessed April 7, 2020).
95. NIH, Clinical Trial of Investigational Vaccine for COVID-19 Begins | National Institutes of Health (NIH),. Available at: https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins (accessed April 7, 2020).
96. Novel, Coronavirus vaccine manufacturing contract signed — The Jenner Institute,. Available online at: https://www.jenner.ac.uk/about/news/novel-coronavirus-vaccine-manufacturing-contract-signed (accessed April 7, 2020).
97. Xie L, Sun C, Luo C, Zhang Y, Zhang J, Yang J, et al. SARS-CoV-2 and SARS-CoV Spike-RBD structure and receptor binding comparison and potential implications on neutralizing antibody and vaccine development. bioRxiv [Preprint]. (2020). doi: 10.1101/2020.02.16.951723
98. The Global Economic Impact of the Coronavirus Outbreak – Harvard Gazette. Available online at: https://news.harvard.edu/gazette/story/2020/02/the-global-economic-impact-of-the-coronavirus-outbreak/ (accessed February 17, 2020).
99. Shimizu K. 2019-nCoV, fake news, and racism. Lancet . (2020) 395:685–6. doi: 10.1016/S0140-6736(20)30357-3
100. ROHDE RODNEY. 2019 Novel Coronavirus (2019-nCoV) Update: Uncoating the Virus. Am Soc Microbiol. (2020). Available online at: https://asm.org/Articles/2020/January/2019-Novel-Coronavirus-2019-nCoV-Update-Uncoating
101. Virus-free Indonesia more threatened by COVID-19 than Singapore Malaysia: Survey - World - The Jakarta Post. Available online at: https://www.thejakartapost.com/news/2020/02/18/virus-free-indonesia-more-threatened-by-covid-19-than-singapore-malaysia-survey.html (accessed February 18, 2020).
102. Japan, May Lose $1,.29 Billion in Tourism Revenue Due to COVID-19 Outbreak | The Japan Times. Available online at: https://www.japantimes.co.jp/news/2020/02/16/business/economy-business/japan-lose-billion-tourism-revenue-covid19-outbreak/#.XkvxX0fitPY (accessed February 18, 2020).
103. Coronavirus's Effect on Tourism Will Carry Into 2021 Experts Say - Bloomberg. Available online at: https://www.bloomberg.com/news/articles/2020-02-13/coronavirus-s-effect-on-tourism-will-carry-into-2021-experts-say (accessed February 18, 2020).
104. The, week in charts - The cost of covid-19 | Graphic detail | The Economist,. Available online at: https://www.economist.com/graphic-detail/2020/02/14/the-cost-of-covid-19 (accessed February 17, 2020).
105. coronavirus: Covid-19 Impact: Pharma Companies Feel the Pain as Prices of Key Inputs Shoot Up - The Economic Times. Available online at: https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/covid-19-impact-pharma-companies-feel-the-pain-as-prices-of-key-inputs-shoot-up/articleshow/74144044.cms?from=mdr (accessed February 17, 2020).
106. Coronavirus Outbreak: Paracetamol Prices Jump 40% In India As Coronavirus Shuts Down China. Available online at: https://www.ndtv.com/india-news/coronavirus-outbreak-paracetamol-prices-jump-40-in-india-as-coronavirus-shuts-down-china-2181480 (accessed February 18, 2020).
107. The coronavirus could cripple China's economy for longer than Wall Street wants to believe | Business Insider India. Available online at: https://www.businessinsider.in/international/news/the-coronavirus-could-cripple-chinas-economy-for-longer-than-wall-street-wants-to-believe/articleshow/74162183.cms (accessed February 17, 2020).
108. Viral Slowdown - How China's Coronavirus Epidemic Could Hurt the World Economy | Leaders | The Economist. Available online at: https://www.economist.com/leaders/2020/02/13/how-chinas-coronavirus-epidemic-could-hurt-the-world-economy (accessed February 17, 2020).
109. China's Economic Battle With COVID-19 | The ASEAN Post. Available online at: https://theaseanpost.com/article/chinas-economic-battle-covid-19 (accessed February 17, 2020).
110. The Coronavirus Could Cost China's Economy $60 Billion this Quarter. - CNN. Available online at: https://edition.cnn.com/2020/01/31/economy/china-economy-coronavirus/index.html (accessed February 18, 2020).
Keywords: 2019-nCoV, COVID-19, SARS-CoV-2, coronavirus, pandemic, SARS
Citation: Keni R, Alexander A, Nayak PG, Mudgal J and Nandakumar K (2020) COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. Front. Public Health 8:216. doi: 10.3389/fpubh.2020.00216
Received: 21 February 2020; Accepted: 11 May 2020; Published: 28 May 2020.
Reviewed by:
Copyright © 2020 Keni, Alexander, Nayak, Mudgal and Nandakumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krishnadas Nandakumar, mailnandakumar77@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Research article
- Open access
- Published: 02 June 2021
How do you feel during the COVID-19 pandemic? A survey using psychological and linguistic self-report measures, and machine learning to investigate mental health, subjective experience, personality, and behaviour during the COVID-19 pandemic among university students
- Cornelia Herbert ORCID: orcid.org/0000-0002-9652-5586 1 ,
- Alia El Bolock 1 , 2 &
- Slim Abdennadher 2
BMC Psychology volume 9 , Article number: 90 ( 2021 ) Cite this article
117k Accesses
37 Citations
Metrics details
The WHO has raised concerns about the psychological consequences of the current COVID-19 pandemic, negatively affecting health across societies, cultures and age-groups.
This online survey study investigated mental health, subjective experience, and behaviour (health, learning/teaching) among university students studying in Egypt or Germany shortly after the first pandemic lockdown in May 2020. Psychological assessment included stable personality traits, self-concept and state-like psychological variables related to (a) mental health (depression, anxiety), (b) pandemic threat perception (feelings during the pandemic, perceived difficulties in describing, identifying, expressing emotions), (c) health (e.g., worries about health, bodily symptoms) and behaviour including perceived difficulties in learning. Assessment methods comprised self-report questions, standardized psychological scales, psychological questionnaires, and linguistic self-report measures. Data analysis comprised descriptive analysis of mental health, linguistic analysis of self-concept, personality and feelings, as well as correlational analysis and machine learning. N = 220 (107 women, 112 men, 1 = other) studying in Egypt or Germany provided answers to all psychological questionnaires and survey items.
Mean state and trait anxiety scores were significantly above the cut off scores that distinguish between high versus low anxious subjects. Depressive symptoms were reported by 51.82% of the student sample, the mean score was significantly above the screening cut off score for risk of depression. Worries about health (mental and physical health) and perceived difficulties in identifying feelings, and difficulties in learning behaviour relative to before the pandemic were also significant. No negative self-concept was found in the linguistic descriptions of the participants, whereas linguistic descriptions of feelings during the pandemic revealed a negativity bias in emotion perception. Machine learning (exploratory) predicted personality from the self-report data suggesting relations between personality and subjective experience that were not captured by descriptive or correlative data analytics alone.
Despite small sample sizes, this multimethod survey provides important insight into mental health of university students studying in Egypt or Germany and how they perceived the first COVID-19 pandemic lockdown in May 2020. The results should be continued with larger samples to help develop psychological interventions that support university students across countries and cultures to stay psychologically resilient during the pandemic.
Peer Review reports
Only in a few month, the COVID-19 epidemic developed into a serious pandemic affecting all countries around the globe. Physical and social distancing and global lockdown of public, social, and work life was and still is a necessity in many countries to fight the pandemic without vaccine. Scientific progress in understanding the behaviour of the virus has grown rapidly since the outbreak of the pandemic, while scientific understanding of the psychological consequences of the pandemic is still at a developing stage. Empirical studies investigating mental health, well-being, subjective experience and behaviour during the COVID-19 pandemic are currently underway and several survey studies from several countries have meanwhile been published. First published surveys investigated the mental health of Covid-19 survivors or of health care professionals enrolled in the treatment of COVID-19 patients [ 1 , 2 ]. Moreover, first observations from surveys investigating psychological reactions of the general population in the hot spot countries immediately after the outbreak of the COVID-19 pandemic in 2020 have meanwhile been published e.g., [ 3 , 4 , 5 ]. The results suggest a significant increase in mental ill health among populations during the first few months of the COVID-19 pandemic, supporting earlier observations from previous epi- and pandemics [ 6 ]. The World Health Organization (WHO) expects mental health burdens in the general population to be particularly pronounced in people who have already been at risk of or suffering from affective disorders before the pandemic (see for an overview [ 7 , 8 ]). Similarly, patients in general as well as patients with a chronic mental disorder in particular, are expected to suffer from impairments in mental health and well-being due to their medical and psychotherapeutic treatment being reduced or cancelled as a consequence of the pandemic lockdown [ 8 ]. In addition, health care professionals involved in the treatment of COVID-19 patients as well as workers with system-relevant jobs are supposed to be at special risk of developing stress-related symptoms and diseases such as post-traumatic stress disorder, chronic fatigue, anxiety, and depressive disorder [ 1 , 2 , 8 ].
However, the current COVID-19 pandemic is not just threatening specific parts of the population. On the contrary. The spread of the virus around the world, its exponential increase in infection probability, and its high lethality bear constant threats for whole societies and for each individual as the pandemic is still evident now, one year after the pandemic outbreak.
Therefore, according to the WHO, primary mental health prevention targeting either the general public or specific population groups should be an indispensable goal of crisis management of the current COVID-19 pandemic [ 8 ] comprising all age-groups from youth, adolescence to adulthood.
Notably, fighting the COVID-19 pandemic currently still requires behaviour change in everybody including daily behaviour (work, business, family, and leisure) as well as changes in health behaviour and social behaviour. In each country so far, the COVID-19 pandemic lockdowns affected daily behaviour routines including work, business, family, and leisure time activities. The COVID-19 pandemic lockdowns started in China in January 2020 and only a few months later, lockdowns followed in many countries around the globe including Germany and Egypt in March 2020. Crucially, in all countries, the first lockdowns came by far and large unexpected to the population. The restrictions in daily life and behaviour may therefore not be tolerated equally well by everybody. Accordingly, health care professionals and the WHO have suggested that counseling programs supporting and assisting people in behaviour change need to become part of the COVID-19 pandemic prevention initiatives [ 8 , 9 ] to avoid unnecessary mental health burdens in the general public.
However, in order to successfully support mental health, well-being, and behaviour in those social domains of life most seriously affected by the current COVID-19 pandemic, a better scientific understanding is required of how individual people experience and psychologically react to the current COVID-19 pandemic, how they think, feel, suffer and cope with the situation, and how they are handling threat perception, how they perceive and regulate emotions and behaviour [ 10 ].
Academia and education are two social and public domains that have been seriously affected by the pandemic lockdown in every country. Concerning Germany, in March 2020 the different states of Germany decided to postpone all academic teaching at higher education institutions to an indefinite period. The universities’ infrastructure including libraries were closed and students were not allowed to come to the university. Similarly, concerning Egypt, public and private universities responded in a similar manner as mandated by the government by closing the campus for students and switching all teaching activities to e-learning. Teaching courses including classes, laboratory courses, seminars, preparatory and induction courses were suspended for the summer term 2020. Teaching during the summer term was announced to be offered as online e-learning format. The lockdown situation in the two countries was thus almost identical for university students concerning the aspects of their social and academic life.
Working at home without any possibility of coming to the university campus and not being able of attending to lectures and courses face-to-face together with peers, tutors, and teachers require from students to learn and adapt to new behaviour rules. Psychologically, pandemics increase uncertainty [ 11 ]. Uncertainty causes stress and increases the risk for mental ill health if it conflicts with behaviour routines and habits [ 11 ]. Despite most of the students being digital natives, the abrupt switch from face-to-face communication to digital, computer-assisted forms of teaching and sole reliance on digital interaction as the only means of social interaction might not be tolerated mentally and physically equally well by all students. Whether the current pandemic situation and its consequences are experienced as a threat may depend on the students’ individual character, i.e., the student’s personality and self-concept as well as his/her current cognitive, affective, and motivational state.
Recent observations from published survey studies among Chinese students after the lockdown reported an increase in general anxiety within about 25% of the student participants. Anxiety symptoms ranged from mild to moderate to severe anxiety [ 3 ]. Moreover, pandemic self-isolation was found to be associated with complex patterns of psychopathology amongst students including an increase in symptoms of obsessive–compulsive disorder, hypochondria, depression, and neurasthenia [ 4 ]. Meanwhile published survey studies from several countries in Europe and across the world support negative changes in mental health among university students immediately after the first lockdowns in 2020, specifically in relation with quarantine and self-isolation [ 12 , 13 , 14 , 15 , 16 ].
Nationwide surveys conducted before the COVID-19 pandemic already reported elevated mental health problems and stress-related symptoms including anxiety and depression among university students [ 17 , 18 , 19 , 20 , 21 ], and this, although university students across countries might belong to the young educated low-risk population. In a recent online study including N = 185 university students studying in Germany, 36.6% of the students (women and men) reported to experience depressive symptoms, 41.83% (women and men) reported high levels of state anxiety, and mental stress due to excessive demands and uncertainty in finances, job, or social relationships [ 21 ]. This prevalence of academic stress and mental health burdens have been found among university students all over the globe [ 17 , 18 , 19 , 20 ], including Egypt [ 22 , 23 ].
Thus, as a population group, university students may be particularly vulnerable to stress-related lifestyle changes affecting mental health that are associated with the current COVID-19 pandemic. Individual differences in mental health may also exist and influence how the students perceive and how well they adapt and cope with the current COVID-19 pandemic situation and to what degree they are motivated to change their behaviour in response to the pandemic consequences in social and academic life and teaching. Psychological theories and models of behaviour change, e.g., Health Belief Model, Transtheoretical Model, or Social Cognitive Theory [ 24 , 25 , 26 ], all agree in that individual factors, specifically those related to emotion- and self-regulation can explain how people perceive themselves, whether and why they change their behaviour and why others do not. Threat perception has been suggested to play an outstanding role [ 27 ], because pandemics threaten the whole person, i.e. our self and the self-concept. Personality traits although considered stable may play a critical role in threat perception, in mental health and behaviour because they influence and modulate the person’s feelings, beliefs, and the person’s trust in one’s own self-regulatory abilities required to change one’s own behaviour [ 27 ]. Moreover, stable personality traits and a positive self-concept are considered general important stress buffers and protectors of mental health, whereas neuroticisms, trait anxiety, difficulties in describing and identifying feelings as well as an overall negative self-concept are considered significant risk factors of mental ill-health, specifically of anxiety disorder and depressive disorder [ 28 , 29 , 30 ].
These examples underscore the complexity and dynamics of how individual traits and state-like individual psychological factors as well as characteristics of the situation interact and influence subjective experience and behaviour. Methodologically, this raises questions of how interactions between situation, person and behaviour can best be assessed, investigated, modeled and predicted in relation to the COVID-19 pandemic in which little empirical evidence is available so far and different aggregated data measures of qualitative and quantitative origin might be used to best capture the internal personal variables of interest (e.g., feelings, worries, self-concept, or personality traits) that provide insight into the subjective experience and the perceived changes in health and behaviour of individual persons behaving in the context of the COVID-19 pandemic.
Computational modeling and machine learning have been already successfully applied in the field of pandemic research to predict transmission rates of the virus based on global behavioural changes of the general population [ 31 ]. These approaches require huge data sets (big data). In health behaviour research, first attempts have been made to apply computational models to data sets comprising smaller sample sizes to model behaviour of individuals, for instance, in response to behavioural interventions supporting health prevention [ 32 ]. These computational models build on psychological theories of human behaviour. Character Computing is one of these psychologically-driven approaches, whose computational models include stable character traits (e.g., personality, self-concept) and cognitive, affective, and motivational state variables and behavioural indicators as input to take into consideration the dynamic interactions between situation (S), person (P) and behaviour (B) (for an overview, see [ 33 , 34 , 35 ] and Fig. 1 ). The computational models are not fixed but can be improved and extended, e.g., by ontologies [ 36 ] or automated data processing, the more empirical evidence and data is available [ 32 , 33 , 34 , 35 ].
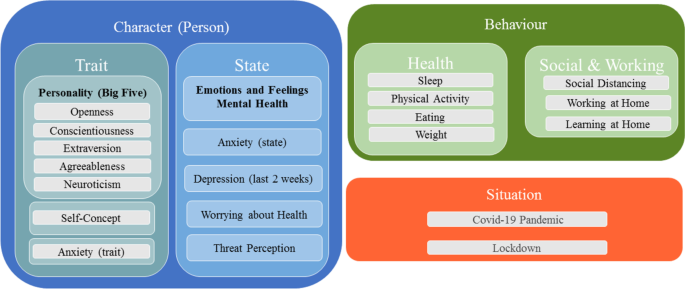
Illustration of the dynamic relationships between situation, a person’s character (traits and states), and behaviour change
Aim of this online survey study
Based on the challenges of the COVID-19 pandemic outlined above, this online survey study is aimed at contributing to the scientific understanding of the psychological consequences of the pandemic by investigating mental health, subjective experience, and behaviour among university students studying in Egypt or Germany after the first pandemic lockdown in May 2020. As outlined above, university students may be particularly sensitive to lifestyle changes related to the COVID-19 pandemic, negatively affecting the students’ mental health, their subjective experience and behaviour. Moreover, as also explained above, the students’ personality traits and self-concept might constitute important stable psychological variables that could influence mental health as well as subjective experience and behaviour related to the COVID-19 pandemic. Therefore, to fully capture these psychological aspects, psychological assessment included a number of psychological variables ranging from stable personality traits and self-concept to state-like psychological variables sensitive to situational change and related to (a) mental health (current depressive symptoms and state anxiety), (b) pandemic threat and emotion perception including current feelings, (c) worries about health including perceived changes in paying attention to bodily symptoms, and (d) self-reported perceived changes in health behaviour (weight, eating, sleeping, physical activity), social and learning behaviour (difficulties in self-regulated learning). To capture all aspects summarized under (a)–(d), the assessment methods comprised a mix of self-report tools (survey items, standardized psychometric scales, psychological questionnaires, and linguistic self-report measures).
Data analysis included (a) descriptive analysis for prevalence estimation of mental health variables, (b) linguistic analysis of self-concept, personality and feelings during the pandemic and (c) correlational analysis and machine learning tools. Machine learning tools were used for exploratory purpose only to further explore the idea of whether machine learning algorithms could despite small sample sizes be trained to predict stable personality traits from the self-report data of the students. Knowing whether stable personality traits (that due to their stability cannot easily be changed by health care interventions) can be predicted from the students’ self-report data could help develop individualized health care interventions that take the students’ personality development into account. The online survey was distributed among university students studying at universities in Egypt and also in Germany. Both countries were equally affected by the lockdowns in May 2020. With respect to the already published survey studies (see above), all attesting an increase in mental ill health among university students during the COVID-19 pandemic the following main research questions were addressed:
RQ1 Mental health: Can the present online survey study confirm high state anxiety and depressive symptoms reported in previous studies in the current sample of university students during the time period of the first COVID-19 pandemic lockdown in May 2020? Crucially, are the self-reported symptoms of anxiety and depression when assessed on standardized psychological screening and assessments tools beyond the cut off scores of clinical samples, and comparable or even higher than the prevalence rates reported in pre-pandemic surveys?
RQ2 Threat perception and worries about health: Do university students report to experience threat, negative feelings and worries about health during the COVID-19 pandemic?
RQ3 Emotion perception: Do university students report to perceive difficulties in emotion perception in the time period of the first pandemic lockdown relative to before the pandemic?
RQ4 Health behaviour, social behaviour and learning: Do university students report to perceive changes in health behaviour (e.g., weight, eating, sleeping, physical activity, paying attention to bodily symptoms), and do they report to experience difficulties in self-regulation during learning (teaching), and in social behaviour in the time period of the first pandemic lockdown?
RQ5 Self-concept and personality: Do university students report a positive or a negative self-concept? Are mental health variables correlated with the students’ personality?
RQ6 Exploratory analysis: Can machine learning despite small data sample sizes predict stable personality traits from the self-report data of the students?
Participants
The survey study was designed and conducted by the Department of Applied Emotion and Motivation Psychology of Ulm University and administered via Ulm University and LimeSurvey software ( https://www.limesurvey.org/de/ ). The survey was advertised among others via the university’s international office to reach specifically students studying in Egypt. The survey was provided in English language (i.e., the academic language), and proficiency in English language was a prerequisite for taking part in the study. Participants were fully debriefed about the purpose of the survey, participation was voluntary and anonymous (see ethics statement). After registration, participants answered questions about their language proficiency, age, gender, their university, study year, and their living situation (alone, with friends or family). Only university students who were aged 18 years and older, and who provided informed consent were able to participate in the study. The survey items were structured in blocks of items and questionnaires: sociodemographic (1), personality (Big-Five) and anxiety (state and trait) (2), survey items about teaching, survey items about health including the linguistic task (self-concept) (3–4), and finally, emotion perception and depression screening (5). The blocking of the serial order of these topics lead to partial drop-outs across the survey, particularly across blocks (see below).
An overview of the complete study-design is provided in the flow-diagram in Fig. 2 . An overview of the online survey items and questionnaires can be found in the Additional file 1 .
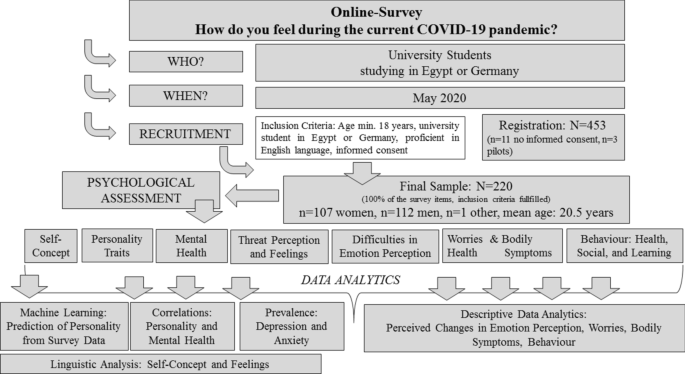
Design of the survey including data collection and recruitment of participants and data analytics. Please see sections ““ Aim of this online survey study ” and “ Methods ” for detailed explanation
Study sample, survey drop-out and missing data
In total, N = 453 university students registered for the study and answered the inclusion and exclusion criteria. Of these, n = 3 were pilots and n = 11 participants did not give informed consent or did not explicitly state that they want to get their data published in scientific research, and were therefore excluded from the study sample. N = 439 volunteers (n = 215 men, n = 219 women, n = 5 did prefer not to name their gender; mean age : 20.69 years, SD = 2.87 years) completed the sociodemographic questions. Of these, n = 19 (4.3%) did not report to study in Germany or Egypt and were excluded. Of the 420 university students who reported to study in Egypt or Germany, n = 325 participants (n = 167 men, n = 156 women, n = 2 did prefer not to name their gender; mean age : 20.38 years, SD = 1.76 years, range: 18–33 years) filled in the personality and anxiety questionnaires only, while n = 220 participants (n = 112 men, n = 107 women, n = 1 did prefer not to name the gender; mean age : 20.45 years, SD = 1.88 years, range: 18–33 years) completed the entire survey. This corresponds to a survey completion rate of 0.49 (division of the number of participants who complete the entire survey (n = 220) by the total number of participants who register for the survey (n = 453)). This rate falls within the rate expected for online surveys (20–50%).
Analysis of the drop-outs (including e.g., univariate measures of variance (ANOVA)), showed no difference in age between the groups (i.e., the sample who filled in the sociodemographic items only (n = 95) versus the sample who filled in the personality and anxiety questionnaires only (n = 105) versus the final sample (n = 220), F (417,2) = 1.72, p = .18. In addition, the student samples did not differ with respect to gender, i.e., the % of the number of women and men. Analysis of anxiety and personality scores likewise suggests that the final sample and the sample who dropped-out after filling in the personality or anxiety questionnaires (n = 220 versus n = 105) did not differ in state anxiety or in the scores on any of the Big-Five personality dimension. (state anxiety: F (323,1) = 1.77, p > .18; Openness: F (323,1) = 0.16, p > .69; Conscientiousness: F (323,1) = 2.82, p > .13; Extraversion: F (332,1) = 0.94, p > .33; Agreeableness: F (323,1) = .062, p > .43; Neuroticism: F (323,1) = 1.22, p > .27). Mean scores of trait anxiety differed between the final sample and the sample who dropped out (n = 220: mean : 46.02, SD = 11.2, range : 26–79 vs. n = 105: mean : 49.02, SD = 10.98, range : 26–77, F (323,1) = 5.78, p = .017). However, using median tests (which are less susceptible to outliers) showed no significant difference in the distribution of trait anxiety scores between the samples (median-test = 1.59, p = .21), see Fig. 3 for an overview.
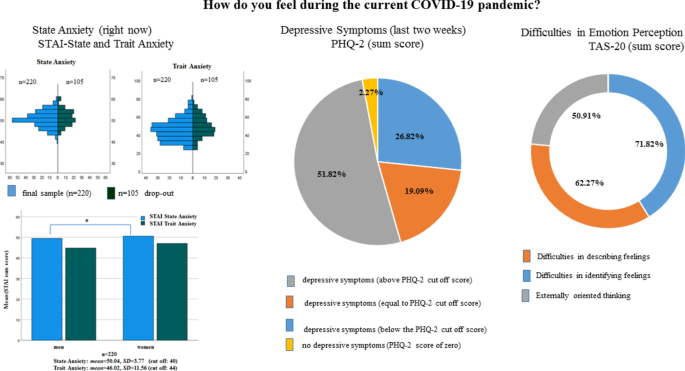
State and Trait Anxiety distributions across the final sample and drop outs (left upper column). Mean state and trait anxiety scores in women and man in the final sample (left lower column), significant results ( p < .05) are illustrated by lines and cross. Percentage of students reporting depressive symptoms (middle column). Right column: Percentage of students reporting changes in emotion perception on the TAS-20 questionnaire and subscales after the COVID-19 pandemic outbreak
The survey was programmed such that it produced as little missing data as possible. Therefore, missing data of single items in a questionnaire or in a block of open items could be excluded and missing scores were therefore not imputed. Regarding the self-generated prompts, participants were free to answer the prompts (self-concept and feeling descriptions). Inspection of the data shows that in the full sample, 5 participants did not fill in all of self-descriptive prompts, leaving open 1, 2 or 3 of the descriptions, respectively.
Measures: survey items and questionnaires
The online survey included several self-report measures comprising a mix of single items with open and closed questions, standardized psychometric scales, and standardized psychological questionnaires. The section below and Table 1 provide an overview of the survey items, questionnaire measures and hypotheses grouped according to the psychological domains and research questions of interest (for an overview, see also RQ1–RQ6 in the section “ Aim of this online survey study ”).
Mental health: anxiety (trait/state), current depressive symptoms (last 2 weeks)
As illustrated in Table 1 , the participants anxiety proneness including trait and state anxiety as well as their current self-reported depressive symptoms (last 2 weeks) were assessed with psychological questionnaires including the Spielberger Trait and State Inventory (STAI, [ 37 ]), and the Patient Health Questionnaire (PHQ-2, [ 38 ]). The STAI is available in many different languages and has shown similar values of internal consistencies among university students from European and Arabic countries [ 39 ]. Whereas the trait scale of the STAI asks for how one generally feels, the instruction of the state scale of the STAI asks for how one feels right now. The PHQ-2 has proven to be a robust screening for depressive symptoms across different cultures including European and Arabic countries [ 40 ]. It asks for the presence of depressive symptoms over a time period of the last two weeks.
Threat perception, feelings, and perceived difficulties in emotion perception during the COVID-19 pandemic
Threat perception as well as discrete emotions and feelings in response to the COVID-19 pandemic situation were assessed by single survey items. Specifically, these items asked the participants about how the current COVID-19 pandemic situation makes them feel in terms of valence (positive/pleasant-negative/unpleasant), arousal (low/calm-high/aroused), and dominance (feeling in or out of control of the situation). The 9-point Self-Assessment Manikin scales (SAM, [ 41 ]) were used for valence, arousal and dominance assessment. The SAM scales are one of the most robust and frequently used scales for the unbiased, non-verbal assessment of emotions and feelings on the three dimensions of emotions including valence, arousal and dominance [ 41 ]. In accordance with the literature [ 41 ], the SAM scales ranged from 1 (negative/unpleasant, low arousal/calm, out of control) to 9 (positive/pleasant, high arousal/aroused, in control). In addition, we asked the participants to indicate which kind of discrete emotions they experienced in response to the COVID-19 pandemic. Participants could choose among six discrete emotions (sad, anxious, angry, disgusted, happy, surprised, or neutral). In addition, participants were given five prompts to describe their current feelings in response to the COVID-19 pandemic situation (“I feel ….”). In order to assess potential difficulties in emotion perception, participants filled in the Toronto Alexithymia Scale (TAS-20; [ 42 ]), which comprises the three subscales “Difficulty Describing Feelings”, “Difficulty Identifying Feelings”, and “Externally-Oriented Thinking”. Since we were interested in perceived changes since the pandemic outbreak, participants were instructed to answer each item of the TAS-20 questionnaire relative to before the pandemic.
Worries about health and perceived changes in behaviour during the COVID-19 pandemic
Worries about health, perceived changes in paying attention to bodily symptoms (e.g., taste, smell, cardiovascular, respiration/breathing, appetite/eating/drinking), as well as perceived changes in health behaviour (weight, eating behaviour, sleep and physical activity behaviour) as well as perceived difficulties in social behaviour (social distancing) and self-regulatory learning (i.e., difficulties in paying attention to the content provided by e-learning, difficulties in studying with the same effort as before the pandemic situation) were assessed via single survey items. The single item questions that asked for worries and perceived changes in behaviour could be answered with “yes” or “no”; “yes” meaning an increase and “no” meaning no change in relation to before the pandemic. The items on health behaviour included items asking in both directions, e.g., whether one eats more or less, sleeps more or less, exercises more or less than before the pandemic. The single item questions of paying attention to bodily symptoms could be answered on 10-point Likert scales such that change scores could be calculated based on the participants’ answers allowing evaluation of the degree of change as increase, decrease or no change during the pandemic situation in relation to before the pandemic (see Table 1 for an overview).
Personality and self-concept
As illustrated in Table 1 , the participants’ personality traits were assessed with the Big Five Personality Inventory (BFI-40, [ 43 ]). The BFI-40 is a standardized self-report measure that has been validated in different cultural populations and age groups [ 44 ]. The self-concept was assessed using a modified short version of the twenty statements tests (TST, [ 45 ]). The TST is a cross-cultural tool for the assessment of different facets of the self-concept including actual, ideal, and ought selves. In the present study, participants had to generate self-descriptions for the actual self only. In line with the instruction of the TST [ 45 ], participants were asked to provide five words to the prompts “I am ….” in order to describe themselves.
Mental health: anxiety (trait and state) and current depressive symptoms
In line with previous pre-pandemic surveys among university students (see Background for an overview), we expected a high prevalence of anxiety and depressive symptoms in the present sample of university students irrespective of their culture or country in which they study. Prevalence rates for self-reported current depressive symptoms assessed with the screening tool of the PHQ-2 asking for depressive symptoms in the last 2 weeks (PHQ-2 items: item1: “little interest or pleasure in doing things”; item 2: “feeling down, depressed or hopeless”) and state anxiety (asking for how one feels right now) might be expected to be even higher than prevalence rates reported in previous surveys before the pandemic situation.
Threat perception, feelings, and difficulties in emotion perception
We expected threat perception to the COVID-19 pandemic to be associated with self-reported unpleasantness, feelings of moderate to high levels of arousal, self-reported perceived lack of dominance (feeling less in control of the situation) on the Self-Assessment Manikin (SAM) scales. In addition, we expected self-reports of feelings of anger, sadness, and anxiety towards the pandemic as assessed by the survey items assessing discrete emotions. We also explored whether students report to perceive changes in emotion perception since the pandemic outbreak relative to before the pandemic outbreak. Specifically, we explored whether participants report difficulties in describing and identifying feelings and report externally oriented thinking on the TAS-20 as potential maladaptive adaptions in coping with the pandemic lockdown. As mentioned above, the instruction of the TAS-20 items asked the participants to answer the items in relation to before the pandemic.
Worries about health, perceived changes in behaviour during the COVID-19 pandemic
We expected that the majority of students will report to be more worried about their mental and physical health than before the pandemic. Moreover, we expected a higher awareness of bodily symptoms (i.e., paying more attention to perceived changes in smell, taste, cardiovascular functions, breathing/respiration, and appetite/eating/drinking) relative to before the pandemic. Given that the lockdown in every country had effects on the students’ work and leisure time activities, we also expected that participants will report changes in health behaviour including a decrease in regular physical activity compared to before the pandemic lockdown including self-reported changes in eating- and sleeping behaviour and weight. We also expected difficulties in learning and social behaviour (see Table 1 ).
Moreover, we examined how university students see themselves (self-concept). In particular, we explored whether the students would report a positive or negative self-concept and compared their linguistic descriptions of the self to their descriptions of their current feelings pandemic-related feelings (“I feel …) and their personality. Regarding personality, we explored whether stable psychological personality traits (Big Five and trait anxiety) would be correlated with state anxiety and depressive symptoms and the students’ perceived changes in emotion perception. Finally, we examined for exploratory purpose, whether machine learning could predict the students’ personality traits from their reports (for details see “Data Analysis” section).
Descriptive analyses and statistics
To answer the hypotheses outlined above, the participants’ answers (questionnaires, single items) were analysed descriptively to provide insight into how many students on average reported anxiety and depressive symptoms as well as how many students reported to perceive changes in subjective experience (threat perception, difficulties in emotion perception, worries about health, bodily symptoms) and behaviour (health, social, learning). Analysis of the questionnaires (PHQ-2, STAI, TAS-20, BFI-40) followed the guidelines and manuals and were calculated as sum scores or mean scores (non-normalized). For the PHQ-2, STAI and TAS-20, cut off scores are available from the literature (see “ Results ” section). These cut off scores were also used in the present study to discriminate between high versus low trait anxiety, high versus low state anxiety, depressive symptoms, and difficulties in emotion perception. Means and standard deviations were calculated for all questionnaire data and for the closed survey items using Likert scales or the SAM scales. The questionnaire data and answers to the survey items were tested statistically for significance by means of non-parametric or parametric statistical tests as appropriate. The respective test statistics are presented in brackets in the “ Results ” sections. Given the drop-out across blocks of the survey (see section about Sample size, survey drop-out and missing data), the results for each scale, item or questionnaire were calculated for the available sample who filled in the questions and the final sample (n = 220) who filled in the complete survey and who reported to study in Egypt or Germany. P values are reported uncorrected and two tailed if not otherwise specified. The SPSS software (IBM SPSS Statistics Software, Version 27) was used for all statistical testing including correlation analysis (see below).
Correlational analysis
Correlation analyses (Pearson) were used to assess the relationships between the Big Five personality traits (BFI-40), mental health variables (STAI: trait and state anxiety, PHQ2: screening for depressive symptoms), and difficulties in emotion perception (TAS-20). P values are reported uncorrected and two tailed if not otherwise specified.
Linguistic analysis of self-concept and feelings
The open-ended linguistic answers assessing the self-concept (“I am …”) and feelings in response to the pandemic (“I feel …”) were analysed with computer-assisted text analysis tools including Linguistic Inquiry of Word Count (LIWC; [ 46 ]). The dictionary of the LIWC software contains words and word stems, grouped into semantic categories related to psychological constructs. The categories provided by the LIWC allow the assessment of the polarity of words (positive or negative). The LIWC analysis produces reliably results with about 500 words and more. Therefore, in the present study, words generated by each participant were accumulated across participants and entered as a whole text corpus for words generated for the prompts “I am …” (self-concept) or for the prompt “I feel …” (feelings in response to the pandemic), respectively. This allows the evaluation of the self-concept and current pandemic feelings of the university sample as a whole. For the linguistic analysis no statistic testing was performed.
Machine learning (exploratory analysis)
Machine learning (ML) was used for exploratory purpose only and the ML algorithms were chosen to combine the different psychological variables that were descriptively analysed in order to explore whether individual personality traits including the Big Five and trait anxiety can be predicted and classified by automated machine learning tools. To this end, the questionnaire scores and answers to the different survey items were preprocessed according to the following procedure: the participants’ Big Five personality traits from the BFI-40, the state and trait anxiety scores (from the STAI including for each individual, a difference score for self-reported trait and state anxiety), depression (PHQ-2), perceived changes regarding difficulties in emotion perception (TAS-20) as well as the participants’ answers on the SAM scales for threat perception (e.g., valence, arousal, dominance) were normalized (z-scores). The participants’ answers to the discrete emotions elicited during the pandemic, difference scores assessing increase in current anxiety (difference score comparing STAI state vs. STAI trait) as well as the participants’ answers to the survey items asking for worries and perceived changes in health and behaviour were labeled as positive or negative or set to zero if the students reported no change. The answers to the survey items asking for perceived changes in paying attention to bodily sensations/symptoms were combined to a total score denoting the total perceived changes in attention towards bodily sensations/symptoms and the total change was labeled as positive or negative depending on whether attention increased or decreased relative to before the pandemic or set to zero if there was no change. Sociodemographic variables such as country or university were no contribution factors in prediction and classification. After data preprocessing and data labeling, the dataset for machine learning comprised continuous features and discrete categorical features. The whole dataset was denoted “X” and the continuous or discrete features were denoted “y” in the feature matrix. The machine learning libraries of the Python software package ( https://www.python.org/ ) were used for automated data analysis. Data analysis was based on regression models. Gradient Boosting Regression (GBR) and Support Vector Regression (SVR) were chosen for the regression models. The principle of Gradient Boosting Regression is to build multiple regression models based on decision trees. Decision tree models are supervised machine learning algorithms that have tree structures that recursively break down the dataset into smaller datasets through branching operations while comparing the final node results with the target values. Decision tree models provide the best fit for small sample sizes to avoid overfitting the data. The same holds true for support vector machine algorithms. Support Vector Regressions (SVR) aim at finding the best fitting line in continuous data within a predefined threshold error. The evaluation of the accuracy of the prediction is evaluated based on the root mean squared error (RMSE). Depending on the type of data to be predicted, RMSE within 10–20% of the range is considered a good result. Especially with human self-report, data accuracies are usually much lower than in other more deterministic domains of machine learning e.g., natural language processing or bioinformatics. One reason for the lower accuracies in human behaviour data is the higher variance in the data itself [ 47 ]. To account for this, we accepted a RMSE of up to 16.6% as sufficient for the decision that the data can be predicted by the model accurately.
We used the classical train/test split approach with a ratio of 8:2. Train/test split is a common validation approach frequently used in ML studies including those with smaller sample sizes [for a critical review see [ 48 ]). No k-fold cross validation (CV) approach was chosen as it has been shown that k-fold CV can lead to overestimation especially with small sample sizes, whereas train/test split and nested CV approaches have been shown to be equally reliable even with small sample sizes [ 48 ]. We also performed hyperparameter tuning, an algorithm frequently used and recommended in machine learning to choose and select during training the best model while avoiding biasing the data, and the number of features and the feature-to-sample ratio) was kept in an optimal range (less features than samples) for avoiding overfitting [ 48 ].
Descriptive data analytics
Mental health: anxiety (trait and state) and depressive symptoms.
The mean state and trait anxiety scores of the university students who completed the entire survey and who studied in Egypt or in Germany (n = 220) were above the cut off scores that according to the literature distinguishes between high versus low anxious subjects [ 49 ]. The mean state anxiety score as measured with the STAI inventory was significantly above the cut of score of 40 (n = 220, mean : 50.04, SD = 3.77; T = 39.47, df = 219, cut off: 40, p < 0.001). A cut off score below or above a score of 44 in the trait STAI scale differentiates between low trait anxious and high anxiety prone individuals [ 49 ]. The mean score for trait anxiety was significantly higher than this cut off score (n = 220, mean: 46.02, SD = 11.56; T = 2.60, df = 219, cut off: 44, p < 0.01). Given the drop-out of n = 105 students, the analysis of the mean state and trait anxiety scores were recalculated for the final sample including those students who dropped out. The analysis showed that also in this larger sample of n = 325 students the cut off scores were significantly above the cut off scores (state anxiety: n = 325; mean : 50.23, SD = 3.75; T = 49.13, df = 324, cut off: 40, p < 0.001; trait anxiety: n = 325; mean : 47.08, SD = 11.52; T = 4.72, df = 324, cut off: 44, p < 0.001) and in addition, trait anxiety scores (trait) did not differ significantly between women and men in this sample (trait anxiety: n = 325; mean-woman : 47.94, SD = 11.82; men: 45.96, SD = 10.91; F (321,1) = 2.45, p > 0.12). However, women reported higher state anxiety scores than men. This difference in state anxiety scores between women and men was significant (state anxiety: n = 325; mean-woman : 50.81, SD = 3.62; men: 49.63, SD = 3.79; F (321,1) = 8.08, p < 0.005) and was also significant in the n = 220 sample. There was no significant difference in state anxiety scores between students studying in Egypt or Germany, neither in the n = 220 sample nor in the sample comprising n = 325 students (n = 220, state anxiety: Egypt- mean : 50.16, SD = 3.75, Germany- mean : 49.08, SD = 3.86, Mann – Whitney-U = -1.39, p = 0.16; n = 325, state anxiety: Egypt- mean = 50.32, SD = 3.70, Germany- mean : 49.45, SD = 4.22, Mann – Whitney-U = -1.24, p = 0.22). However, students studying in Egypt reported higher trait anxiety compared to the students studying in Germany (n = 325, trait anxiety: Egypt- mean : 47.62, SD = 11.60, Germany- mean : 42.24, SD = 9.75, n = 220, trait anxiety: Egypt- mean : 46.49, SD = 11.57, Germany- mean : 42.40, SD = 10.93), but this difference was not significant in the final sample (n = 220, Mann – Whitney-U = − 1.39, p = 0.16). The results are illustrated and summarized in Fig. 3 .
For the PHQ-2 screening for depressive symptoms a sum score greater than 3 on both items is associated with depression proneness [ 38 ]. In the sample of university students who completed the entire survey and therefore had filled in the PHQ-2 depression screening, the mean sum score was mean: 3.48, SD = 1.58, and significantly above the cut off score ( T = 4.51, df = 219, cut off = 3, p < 0.0001). 51.82% (n = 114) of the students had sum scores greater than the cut off (> 3), and 19.09% (n = 42) had a sum score of 3 (cut off). Only 26.82% (n = 59) of the sample scored below the PHQ-2 cut off score (< 3), and only 2.27% (n = 5) did report to not suffer from loss of interest or pleasure in doing things (PHQ-2 item 1) or from feeling down, depressed or hopeless during the last two weeks (PHQ-2 item 1) (see Fig. 3 for an overview on state anxiety and depressive symptoms). The PHQ-2 scores did not differ between students studying in Egypt or Germany (n = 220, Egypt- mean : 3.51, SD = 1.56, Germany- mean : 3.24, SD = 1.79, Mann – Whitney-U = − 0.643, p = 0.52) nor did they differ between women and men (n = 220, woman- mean : 3.48, SD = 1.54, men- mean : 3.47, SD = 1.63, F (217,1) = 0.00, p = 0.98).
Descriptive analysis of the items assessing threat perception (SAM; Self-Assessment Manikin scales ranging from 1 (unpleasant, not aroused, or no control) to 9 (pleasant, very highly aroused, in control)) showed that, the students (n = 220) felt slightly unpleasant ( mean : 4.19, SD = 1.97). In addition, 55% (n = 120) of the final study sample (n = 220) reported a score from 1 to 4, i.e., from high unpleasantness to moderate unpleasantness on the 9-point SAM valence scale. On average, the students did not feel much in or out of control of the situation ( mean : 5.07, SD = 2.41) on the 9-point SAM scale for dominance. Nevertheless, 37.55% of the study sample reported a score from 1 (no control) to 4 (loss of control) on the SAM scale for dominance. Mean physiological arousal was rated as moderate ( mean : 5.40, SD = 2.22). However, 50% of the university students (n = 110) reported an arousal score of 6 (aroused) to 9 (very high arousal) on the SAM arousal scale. Given the drop-out of students, comparisons of the ratings (valence, arousal, or control) were performed between samples (n = 220 and n = 59 who completed the ratings but did not fill in the entire survey). This showed that the ratings did not differ between the samples ( Mann – Whitney-U -tests, all p > 0.70). From the set of discrete emotions (including sadness, anger, fear, disgust, happiness, surprise, or neutral emotions), 66.8% reported to feel not neutral, 93.2% reported to feel not happy, 56.4% reported to feel sad, 75.9% reported to feel angry, 92.3% reported to feel surprised, 87.7% reported to feel disgusted, and 52.7% reported to feel afraid by the current pandemic situation. The distribution of “yes” versus “no” answers differed significantly for the categories feel neutral, happy, surprised, disgusted, or angry, respectively, (non-parametric test for binomial distribution: all p < 0.001). From all students who completed these items (n = 277) the same significant results were obtained for the answers concerning discrete emotions.
16.88% of the students of the final sample (n = 220) had a total TAS-20 score greater than the critical TAS-20 cut off score (TAS-20 cut off > 60, [ 30 ]). From the three subscales of the TAS-20 questionnaire, changes in self-reported difficulties in emotion perception in relation to the pandemic as compared to before the pandemic were reported by 62.27% (n = 137) for items belonging to the subscale “Difficulty describing feelings”, and by 71.82% (n = 158) for the items belonging to the subscale “Difficulty identifying feelings” and by 50.91% (n = 112) for the items belonging to the subscale “Externally Orienting Thinking”. The distributions of the TAS-20 scores of the three subscales did not differ between students studying in Egypt or Germany ( Mann – Whitney-U , all p > 0.50). However, woman (n = 107) reported higher scores on the subscales “Difficulties identifying feeling” compared to men (n = 112), F (217,1) = 217.1, p = 0.035.
Worries about health
In the final sample who completed the survey (n = 220), 65.5% (n = 144 students) of the study sample reported to worry about their mental health more due to the COVID-19 pandemic than before the pandemic, whereas 34.5% (n = 76) answered to worry not more than before the pandemic. 71.4% (n = 157) of the students reported to worry more about their physical health than before the pandemic, whereas 28.6% (n = 63) answered to worry not more about their physical health than before the pandemic. The distributions of “yes” versus “no” differed significantly for both, worries about mental and physical health, respectively (non-parametric test for binomial distribution: all p < 0.001) and this also held true when considering all students who filled in these items (n = 227). Self-reported worries about mental health and physical health were significantly related (χ2 = 100.43, df = 2, p < 0.001). 65% (n = 143 of n = 220) reported to worry in both domains (mental health and physical health) more than before the pandemic and this also held true when considering all students who filled in these items (n = 227), see Fig. 4 a.
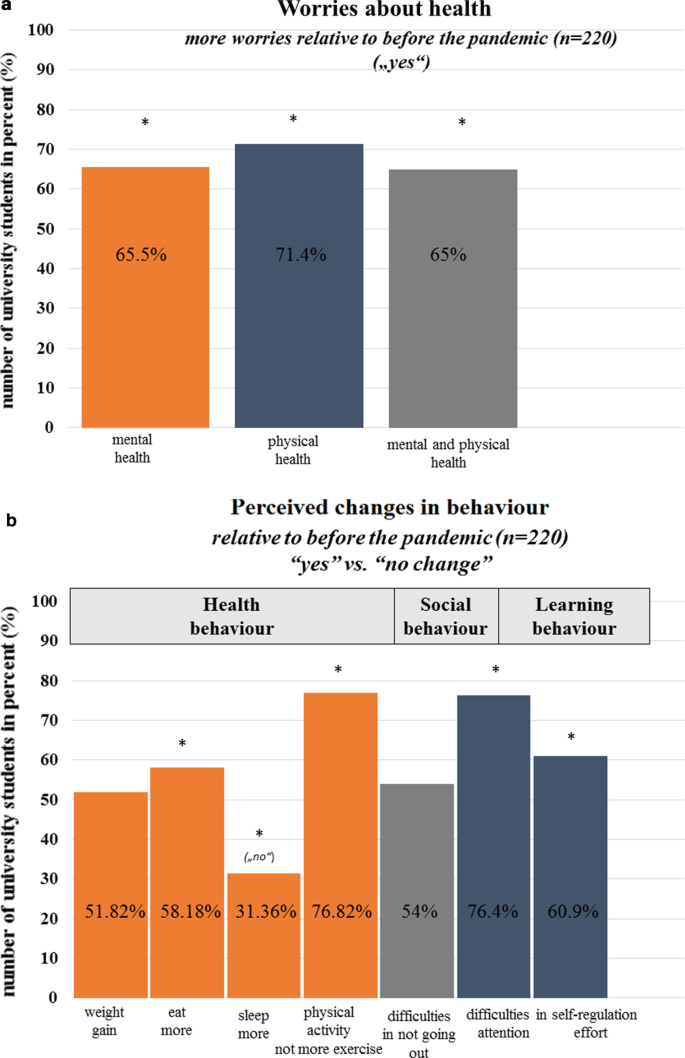
a Worries about mental health or physical health or both (mental and physical health). The cross represents significant results, p < .05. b Perceived changes in health behaviour including weight, eating, sleeping, and physical activity. The cross represents significant results, p < .05
Behaviour: health
Across health behaviour domains (weight, eating, sleep, physical activity), 52.3%, 58.2%, 31.8%, and 76.4% of the study sample (n = 220) reported to have gained weight, to eat more than before the pandemic and to not sleep more or exercise more than before the pandemic situation. The distributions of “yes” versus “no” answers were significantly different for the domains of eating, sleep and exercise/physical activity (non-parametric test for binomial distribution: eat, sleep, exercise/physical activity all p < 0.001) and this again held true when considering all students who filled in the items (n = 227). Paying attention to bodily sensations and symptoms (i.e., changes in taste, smell, appetite/eating/drinking, cardiovascular functions, breathing/respiration) did however not change significantly relative to before the pandemic outbreak. On average, on Likert scales ranging from 1 (“decrease”) to 5 (“no change”) to 10 (“increase”), participants reported not to pay more attention to or to be more aware of bodily sensations and symptoms than before the pandemic (smell: mean : 5.18, SD = 1.21, taste: mean : 5.15, SD = 1.27, bodily symptoms: mean : 5.84, SD = 1.74, cardiac symptoms: mean : 5.78, SD = 1.66, breathing: mean : 5.77, SD = 1.64, eating and drinking/appetite: mean : 5.52, SD = 2.09). The answers on these rating scales did not differ between students studying in Egypt or Germany (all p > 0.16), but comparisons between women and men showed that women scored significantly higher on the scale asking for attention to bodily symptoms than men (woman- mean : 6.18, SD = 1.90, men- mean : 5.50, SD = 1.53, F (217,1) = 8.50, p > 0.002). This again held true when considering all students who filled in the items (n = 227).
Behaviour: social distancing and learning
Being asked about their social situation of self-isolation, teaching and learning behaviour, 54% of the student sample (n = 220) replied to have difficulties in not going out during the pandemic. 76.4% replied to have difficulties in self-regulated learning, being unable of focusing their attention on the teaching content. Of these students, 60.9% replied to have difficulties in studying with the same self-regulatory effort because of being anxiously preoccupied with the current pandemic situation (see Fig. 4 b). The distributions of “yes” versus “no” answers were significantly different for the domains of learning (non-parametric test for binomial distribution: eat, sleep, exercise/physical activity all p < 0.002) and this again held true when considering all students who filled in these items (n = 305, all p < 0.001).
Linguistic self-concept and self-descriptions of current feelings
Linguistic self-descriptions (“I am …”) showed a positivity bias. Overall, more positive words than negative words were used by the students to describe themselves (see Fig. 5 ). As mentioned above, linguistic analysis of the university students’ self-descriptions about how the current COVID-19 pandemic situation makes them feel (“I feel …”) showed the reverse pattern with more negative words than positive words being used by the study sample to complete the prompt “I feel ….” (see Fig. 5 ). In addition, Fig. 6 shows the most prominent examples, i.e., the words most often used by the students to describe their feelings during the pandemic.in the prompt “I feel …”.
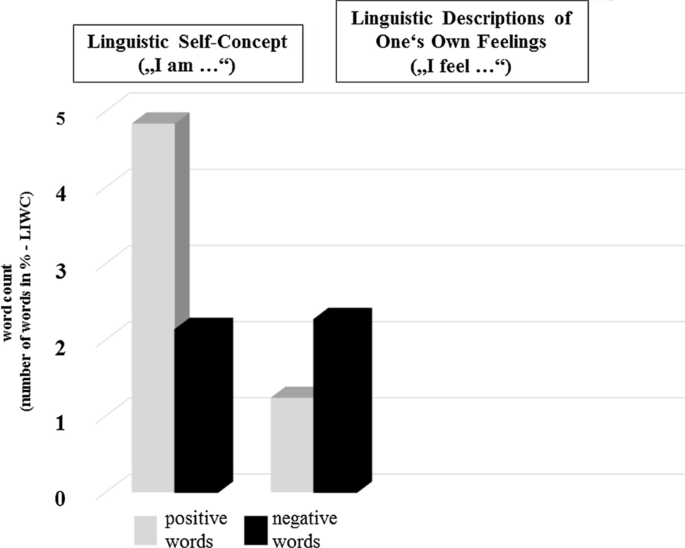
Percentage of negative and positive words. Left column: Self-concept: “I am …”. Right column: Current feelings during the pandemic “I feel …”
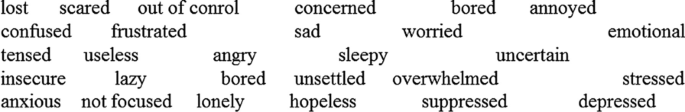
Summary of the words most often used by the university students to describe their feelings in response to the pandemic
Personality: Big Five
The final student sample (n = 220) scored low on the BFI-40 subscales for extraversion ( mean : 24.5, SD = 5.65), neuroticism ( mean : 25.37, SD = 6.51), and reported moderate scores on the conscientiousness scale ( mean : 30.69, SD = 6.07), the openness scale ( mean : 36.85, SD = 5.07), and the agreeableness scale ( mean : 33.42, SD = 4.50) and as described earlier (see section “ Study sample, survey drop-out and missing data ”), the BFI-40 scores of the samples (n = 220 vs. n = 105 who dropped-out) did not differ in the five personality dimensions. The Big Five personality traits were significantly correlated with self-reported depressive and anxiety symptoms as well as with the self-reported difficulties in emotion perception. Table 2 shows a summary of the correlations between measures of personality traits (BFI-40), trait anxiety (STAI-trait scale), state anxiety (STAI-state scale), self-reported depressive symptoms (PHQ-2), and perceived difficulties in emotion perception (TAS-20) as obtained from the final sample (n = 220).
Automated data analytics, machine learning (exploratory)
The university students’ personality traits (Big Five) and trait anxiety could be predicted from the psychological variables (trait and state) summarized in Table 3 through feature importance extraction by Support Vector Regression. The table and the numbers in percent show the major contributing factors to the prediction of the respective trait listed in the left column (under “Measure”). Table 4 shows the prediction accuracy suggesting that prediction of all trait attributes have similar error rates.
The COVID-19 pandemic is taking its toll. Concerns have been raised by the WHO (2020) [ 8 ], that the COVID-19 pandemic will cause “a considerable degree of fear, worry and concern in the population” (cited from WHO, 2020 [ 8 ]) and that stress and anxiety as well as depression will increase considerably during the COVID-19 pandemic, rendering affective disorders a public mental health concern of the COVID-19 pandemic [ 8 ]. In the present survey, mental health (depressive symptoms, state and trait anxiety), subjective experience (threat perception, current feelings, perceived difficulties in emotion perception, worries about health during the pandemic) as well as perceived changes in behaviour (related to health, social behaviour and learning/teaching) was assessed among university students studying in Egypt or Germany, respectively. The survey was administered in May 2020, shortly after the lockdown in these countries. Going beyond previous surveys, the students’ self-concept and the Big Five of human personality were additionally assessed to explore psychological patterns between personality traits, mental health, and perceived changes in subjective experience by means of correlation analysis and machine learning.
Mental health among university students
Regarding pandemic risk groups, previous cross-cultural pre-pandemic surveys have shown high prevalence rates of anxiety and depression among university students across countries [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]. Therefore, the WHO’s concerns about the psychological consequences of the COVID-19 pandemic on mental health and well-being might affect university students as a population group as well. The results obtained from this sample of university students who study in Egypt or Germany during the first lockdown period confirm these concerns. In particular, the results confirm previous pre-pandemic results about mental health of university students and they seem to confirm the concerns of the WHO regarding mental health and threat perception during the current pandemic. The mean state anxiety score (assessed with standardized questionnaires including the Spielberger Trait-State Anxiety Inventory, STAI) was significantly above the cut off score that, according to the literature [ 34 ], discriminate high from low anxious subjects. In addition, state anxiety scores were significantly higher in woman than man. Moreover, 51.82% (n = 114) of the students had sum scores greater than the cut off (> 3), and 19.09% (n = 42) had a sum score of 3 (cut off). Only 26.82% (n = 59) of the sample scored below the PHQ-2 cut off score (< 3), and only 2.27% (n = 5) did report to not suffer from loss of interest or pleasure in doing things (PHQ-2 item 1) or from feeling down, depressed or hopeless during the last two weeks (PHQ-2 item 1), and self-reported depressive symptom did not differ among students studying in Egypt or Germany or in woman or men (see Fig. 3 for an overview on state anxiety and depressive symptoms). Thus, in total, 51.82% and 19.09% of the final student sample (n = 220) reported depressive symptoms at and above the cut off score for depressive symptoms [ 38 ], thus feeling depressed or hopeless and reporting a loss of interest and pleasure in the items of the PHQ-2 questionnaire during most of the days of the last 2 weeks of the COVID-19 pandemic. Prevalence rates from previous surveys among university students reported a prevalence of anxiety symptoms or depressive symptoms above 35% among university students before the pandemic (e.g., for depression or anxiety [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]). A recent online study [ 21 ], including N = 185 university students studying in Germany found that 36.6% of the university students (women and men) report experiencing depressive symptoms, 41.83% (women and men) reported experiencing high levels of state anxiety, and all students reported experiencing stress due to excessive demands and uncertainty in finances, job, or social relationships. These prevalence rates have actually been found in cohort studies including university students all over the globe, irrespective of culture before the outbreak of the pandemic [ 17 , 18 , 19 , 20 , 21 , 22 , 50 , 51 , 52 , 53 ]. In relation to these pre-pandemic prevalence rates, the prevalence of state anxiety and of depressive symptoms in the current sample seem to have more than doubled during the pandemic time period.
The scores for state anxiety need to be seen in relation to the results obtained for trait anxiety. As mentioned above, trait anxiety scores were even higher in those students who dropped-out, however state anxiety scores did not differ across students who completed the survey and those who did not. Students with high state anxiety during the pandemic may be at special risk of suffering from anxiety proneness in the long run. Therefore, surveys among university students should be continued to further explore the development of anxiety and particularly also of depressive symptoms during the current pandemic as well as the comorbidity of anxiety with depressive symptoms as a consequence of the COVID-19 pandemic. Very recent surveys among university students from Greece (Europe) and the United States conducted in a similar time period (during the first lockdowns in these countries) report similar high percentage numbers of anxiety, depression and mental health burdens [ 12 , 13 ]). Given that the STAI asks for feelings of stress, worry, discomfort, experienced on a day to day basis one could expect changes in other psychological domains as well (see below).
Threat perception and perceived difficulties in emotion perception
Being asked about their feelings during the pandemic, 55% of the students reported unpleasantness and 37.55% of the students rated to be in loss of control of the situation, and about 50% reported moderate to high physiological arousal. Moreover, university students reported a mix of discrete emotions in response to the pandemic. In particular, there was a significant loss of happiness, and a change in feelings of surprise, disgust and anger. In line with this, as illustrated in Fig. 5 , linguistic analysis of the participants’ answers to the questions “I feel …” also suggest a negativity bias in the linguistic descriptions of the students’ feelings: In summary, there was more intense use of negative than positive words to describe one’s feelings in response to the pandemic. Thus, feelings of threat and negative emotions were also reflected in the self-generated linguistic answers of the students, supporting a general increase in anxiety during the first period of the COVID-19 pandemic among university students. Similarly, and in line with the scores obtained from the depression screening instrument (PHQ-2), linguistic analysis of the questions “I feel …” revealed a high percentage of words such as feeling depressed, down or hopeless (see Fig. 6 ). Thus, anxiety and depression related words were amongst the most frequently used words when participants were asked to describe in their own words, how the current COVID-19 pandemic situation makes them feel. The study sample also reported to have perceived difficulties in emotion perception during the pandemic. Using the three subscales of the Toronto Alexithymia Scale (TAS-20), the participants were instructed to rate whether they experience difficulties in emotion perception relative to before the pandemic situation. Especially difficulties in identifying and describing feelings were reported. Moreover, the sum scores of the TAS-20 were significantly correlated with the students’ anxiety scores and the intensity of self-reported depressive symptoms (see Table 2 ). Taken together, these results are of particular interest in light of discussions which mental health interventions might help university students to cope with the threat provoked by the pandemic situation. Given that previous research has shown that high scores on the TAS-20 promote psychopathology [ 28 , 29 ], the reports of the students about them perceiving difficulties in identifying one’s feelings in response to the pandemic situation relative to before the pandemic outbreak should be taken seriously and investigated in further studies in larger student cohorts.
Worries about health and health behaviour during the COVID-19 pandemic
Moreover, the university students’ worries about health should be taken seriously. Chronic worrying is a sign of chronic distress and constitutes a risk factor of later development of general anxiety disorder [ 54 ]. In the current study, 65.5% of the final student sample (n = 220) reported being worried about their mental health and 71.4% reported to worry about their physical health more often than before the pandemic. The majority of the student sample did, however, not report to pay more attention to bodily sensations or symptoms (taste, smell, cardiovascular, respiration/breathing) than before the pandemic. However, worries about mental and physical health were accompanied by perceived changes in health behaviour. The percentage of “yes” and “no”-answers differed significantly for changes in health behaviour related to eating and physical activity behaviour since the outbreak of the pandemic. We did not ask the students for their eating behaviour or their physical activity level before the pandemic. Thus, the questions asking for perceived changes during relative to before the pandemic might have the potential of a memory bias. Nevertheless, pre-pandemic surveys report that up to 30% of university students do not exercise at a regular basis and do not meet the WHO’s weekly or daily physical activity recommendations (for an overview see [ 55 ]). The present results suggest a reduction in physical activity during the pandemic and physical inactivity and sedentarism are among the major risk factors promoting negative lifestyle-related diseases in the long run [ 55 ].
Learning behaviour during the COVID-19 pandemic
The pandemic might have negative effects on student’s teaching and learning behaviour. In the present sample of university students, difficulties in teaching and learning were reported by the majority of students. One interpretation of these results is, that pandemic situations such as the current COVID-19 pandemic are characterized by uncertainty, fear, and threat, i.e., factors that are known to impact self-regulation. Previous research has shown that self-regulation is negatively related with threat perception [ 27 ] because responding to fear, anxiety and to threatening events depletes top-down control and self-regulatory resources [ 56 , 57 ] that are also required for academic performance. In line with this, students reported having difficulties in focusing and concentrating on the teaching content during the current COVID-19 pandemic situation (see Fig. 4 b). Self-learning formats such as e-learning may accentuate these effects.
Self-concept and personality of university students, and machine learning
When asked to describe themselves with a modified version of the TST asking for descriptions of the students’ “actual self”, positive word use outweighed negative word use. When the student sample was considered as a whole, linguistic analysis of word use (see Fig. 5 ) supported a clear bias towards positivity that also accords with previous results that seeing yourself in a positive light correlates with positive self-descriptions and preferential processing of positive words [ 58 , 59 , 60 , 61 ]. Although this result must be seen in relation to a general positivity bias in written and spoken language (most languages having more positive than negative words [ 62 ], the analysis of word use suggests that the pandemic situation at the time of the survey did not provoke a threat to the self-concept of this university student sample and this, although linguistic analysis of the answers to the prompt that asked for feelings during the pandemic (see also Fig. 5 ) revealed a negativity bias as immediate negative responses to the pandemic situation in line with the results observed for the survey items asking for threat perception. Symptoms of state anxiety and current depressive symptoms may therefore reflect temporary changes of the university students to the pandemic situation that however occur immediately in response to the pandemic lockdown.
Psychological theories agree that individual factors such as one’s personality are correlated with subjective experience, well-being, mental health, and behaviour, e.g., [ 63 , 64 ]. In line with this, analyses showed correlations between the Big Five (BFI-40) personality traits and the university students’ self-reported symptoms of anxiety, depression and their perceived difficulties in emotion perception. Statistically, correlation analysis, linear regression analysis, multivariate structural equation models, mediator analysis, or moderator analysis may all be feasible statistical methods to describe the relationship between psychological variables. However, in the present study we attempted to apply supervised machine learning algorithms that are built on regression models to further explore whether personality traits were not only correlated with mental health variables but could be predicted from the self-reported subjective experience of the participants obtained from this survey’s multimethod assessment. The observed results are promising despite the relatively small datasets used for training and prediction. The algorithms provided relatively accurate models for the prediction of personality traits from self-report data. As illustrated in Table 3 , neuroticism as one of the big five personality traits (shown to be related to mental ill health [ 63 , 64 ]) and in the present study sample significantly correlated with both, self-reported anxiety and depressive symptoms (see Table 2 ) could best be predicted by changes in current anxiety (threat perception, difference scores state vs trait anxiety), by the students’ self-reported trait and state anxiety, by their self-reported perceived difficulties in emotion perception (describing one’s feelings reported on the TAS-20), by self-reported changes in physical health behaviour (eating) and by self-reported difficulties in social distancing. Very recent results from surveys investigating the role of personality factors during the current COVID-19 pandemic also found that people’s self-reported psychological perceptions of and reactions towards the pandemic also depend on stable personality traits including the Big Five (for an overview [ 65 ]). Interestingly, there is also evidence that expression on personality traits such as the Big Five can change in conjunction with mental ill health [ 66 ]. Our results and these recent results suggest that future studies exploring the psychological consequences of the COVID-19 pandemic should include the assessment of personality traits in their anamnestic exploration of mental health and self-reported experience.
Limitations
The present study adds to the evidence reported in the literature about the negative consequences of the current COVID-19 pandemic on mental health and well-being of university students. By using a mix of self-report measures it allows detailed insight into the subjective experiences associated with the pandemic in this population group in the psychological domains of mental health, health behaviour change and learning. However, some limitations already discussed in the sections above should be stressed. First, there was a high drop-out whose percentage was within the upper range of the expected drop-out rates for online surveys (20–50%). Although drop-outs were statistically assessed and compared to the final sample as far as appropriate, suggesting no bias by age or gender or the student’s personality, the drop-out reduced the final sample size reducing the power of the study. Thus, further data is required to demonstrate the generalizability of the present observations and to further explore possible cultural differences. In the present study sample, the reported significant differences between gender and students studying in Egypt or Germany might be tentative due to the small study samples. Power calculations suggest an ideal sample size of about N = 271 (90% confidence) or N = 385 (95% confidence) participants (margin of error of 5%). Although this sample size was reached in the beginning, it was reduced by the successive drop-out across the blocks of survey items. Second, statistics revealed significant results for the quantitative measures, however, the results of the linguistic tasks (self-concept and feeling prompts) could be reported only descriptively. The LIWC software was used for linguistic analysis. This allowed word categorization with high accuracy and validity [ 46 ] providing interesting insight that otherwise might have gone unnoticed and confirmed the results obtained from quantitative measures. Third, due to the small sample size the machine learning approach is exploratory and challenged by limitations. While machine learning tools have already been applied in many domains of psychology (e.g., in the domain of Affective Computing and Health Psychology), their use is still relatively under investigated in studies using psychology data obtained from multimethod approaches as the current one [ 67 ]. Existing studies using machine learning for analyzing personality- and behaviour-related data, mainly target personality prediction from larger datasets (e.g., [ 68 ]). In the present study, we followed guidelines and recommendations from existing machine learning studies discussing possible solutions for application of machine learning tools with small sample sizes (see for an overview [ 69 , 70 , 71 ]), using sample size of about 200 and support vector machines (SVM similar to SVR used in our study) for estimation of depressive symptoms, for personality trait and perceived stress prediction based on sample sizes ranging from 150 to 250 participants [ 69 , 70 , 71 ], as in the present study. In line with these previous studies applying machine learning tools to smaller sample sizes, we applied machine learning to a mix of measures that captured subjective experience in relation to the current COVID-19 pandemic situation in line with the recommendations from psychologically-driven computational approaches that suggest to include trait and state measures for prediction [ 25 , 26 ]. Nevertheless, the present approach is exploratory and application of machine learning to small sample sizes need to be critically discussed, e.g., for a detailed discussion see [ 48 ], as it can lead to overfitting or overestimation. One recommendation to avoid such problems with small sample sizes is to use nested cross validation and control feature-to-sample ratio [ 48 ]. It will be interesting to follow-up the present ML results in future COVID-19 survey studies and use additional data collected during the course of the pandemic for validation and training in order to confirm the results from ML in hopefully larger samples, supporting the combination of machine learning and classical data analytics in the domain of psychology.
This survey investigated the subjective experience of university students studying in Egypt or Germany during the COVID-19 pandemic in May 2020, i.e., in the time period after the first pandemic lockdown in the countries. Perceived changes in all psychological domains including state anxiety, depressive symptoms, threat perception, emotion perception, worries about health and behaviour (health, social distancing, and learning) were reported in the majority of students taking part in the survey. Recent COVID-10 surveys report similar high prevalence rates among university students across the globe [ 3 , 4 , 12 , 13 ]. Although the results of this survey are tentative, the multimethod approach of this survey, using multiple scales, descriptive, correlational, and linguistic analysis, provides a valuable contribution to previously published COVID-19 studies. Moreover, the approach of combining descriptive analysis with machine learning should and could be followed-up in larger samples during the second period of the current pandemic. Crucially, despite the small sample size, the present results of self-reported anxiety and depressive symptoms among university students, that also seem to be supported by recent surveys including university students from other countries [ 3 , 4 , 12 , 13 ] should be taken serious as they suggest that there is an urgent need to develop interventions that help prevent mental health among university students in order to avoid negative consequences in health and learning behaviour in response to the pandemic and provide health care to those students who might be at special risk of mental ill health.
Questionnaire/survey
The questionnaires and self-assessment scales used in this study are standardized questionnaires and standardized scales whose references are cited in the manuscript in brackets. The single survey questions e.g., health and teaching have been developed for the purpose of this survey and are summarized in Table 1 in the manuscript. An overview of the online survey can be found in the supplement of this manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Due to the informed consent form in which the possibility of raw data being published online was not explicitly stated, the raw data cannot be made accessible in online repositories.
Abbreviations
BFI five inventory [ 43 ]
Decision tree regression
Gradient Boosting Regression
Linguistic inquiry of word count [ 46 ]
Personal Health Questionnaire 2 [ 38 ]
Root mean squared error
Self-Assessment Manikin scales [ 41 ]
Spielberger Trait State Anxiety Inventory [ 37 ]
Support Vector Regression
Toronto Alexithymia Scale [ 42 ]
World Health Organization
Bohlken J, Schömig F, Lemke MR, Pumberger M, Riedel-Heller SG. COVID-19-Pandemie: Belastungen des medizinischen Personals [COVID-19 pandemic: stress experience of healthcare workers—a short current review]. Psychiatr Prax. 2020;47:190–7. https://doi.org/10.1055/a-1159-5551 .
Article PubMed PubMed Central Google Scholar
Petzold MB, Plag J, Ströhle A. Umgang mit psychischer Belastung bei Gesundheitsfachkräften im Rahmen der Covid-19-Pandemie [Dealing with psychological distress by healthcare professionals during the COVID-19 pandemia]. Nervenarzt. 2020;91:417–21. https://doi.org/10.1007/s00115-020-00905-0 .
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. https://doi.org/10.1016/j.psychres.2020.112934 .
Chen B, Sun J, Feng Y. How have COVID-19 isolation policies affected young people’s mental health? – Evidence from Chinese College Students. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.01529 .
Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.01540 .
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, Di Bernardo A, Capelli F, Pacitti F. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr. 2020;55:137–44. https://doi.org/10.1708/3382.33569 .
Article PubMed Google Scholar
World Health Organization (2020). Mental health and COVID-19. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/mental-health-and-covid-19 . Accessed 29 June 2020.
Betsch C. How behavioural science data helps mitigate the COVID-19 crisis. Nat Hum Behav. 2020. https://doi.org/10.1038/s41562-020-0866-1 .
van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ et al. Using social and behavioural science to support COVID-19 pandemic response; 2020. https://www.nature.com/articles/s41562-020-0884-z . Accessed 28 June 2020.
Greco V, Roger D. Uncertainty, stress, and health. Personal Individ Differ. 2003;34:1057–68. https://doi.org/10.1016/s0191-8869(02)00091-0 .
Article Google Scholar
Patsali ME, Mousa DPV, Papadopoulou EV, Papadopoulou KK, Kaparounaki CK, Diakogiannis I, Fountoulakis KN. University students’ changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. 2020;292:113298.
Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020;22(9):e21279.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, Debien C, Molenda S, Horn M, Grandgenèvre P, Notredame CE. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3(10):e2025591.
Kaparounaki CK, Patsali ME, Mousa DPV, Papadopoulou EV, Papadopoulou KK, Fountoulakis KN. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020;290:113111.
Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4):e7541.
PubMed PubMed Central Google Scholar
Duffy A, Saunders KE, Malhi GS, Patten S, Cipriani A, McNevin SH, MacDonald E, Geddes J. Mental health care for university students: a way forward? Lancet Psychiatry. 2019;6(11):885–7.
Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract. 2010;16(1):1–6.
Brown JSL. Student mental health: some answers and more questions. J Ment Health. 2018;27:193–6. https://doi.org/10.1080/09638237.2018.1470319 .
Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47:391–400. https://doi.org/10.1016/j.jpsychires.2012.11.015 .
Herbert C, Meixner F, Wiebking C, Gilg V. Regular physical activity, short-term exercise, mental health, and well-being among university students: the results of an online and a laboratory study. Front Psychol. 2020;11:509. https://doi.org/10.3389/fpsyg.2020.00509 .
El-Gilany AH, Amro M, Eladawi N, Khalil M. Mental health status of medical students: a single faculty study in Egypt. J Nerv Ment Dis. 2019;207(5):348–54.
Abdallah AR, Gabr HM. Depression, anxiety and stress among first year medical students in an Egyptian public university. Int Res J Med Med Sci. 2014;2(1):11–9.
Google Scholar
Champion VL, Skinner CS. The health belief model. Health Behav Health Educ Theory Res Pract. 2008;4:45–65.
Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50(2):248–87.
Prochaska JO, Johnson S, Lee P. The trans theoretical model of behavior change. In: Shumaker SA, Ockene JK, Riekert KA, editors. The handbook of health behavior change. Berlin: Springer; 2009. p. 59–83.
Fernandes O, Portugal LCL, Alves RCS, Campagnoli RR, Mocaiber I, David IPA, Erthal FCS, Volchan E, de Oliveira L, Pereira MG. How you perceive threat determines your behaviour. Front Hum Neurosci. 2013;7:632.
Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. 2000;48:99–104. https://doi.org/10.1016/S0022-3999(99)00083-5 .
Marchesi C, Brusamonti E, Maggini C. Are alexithymia, depression, and anxiety distinct constructs in affective disorders? J Psychosom Res. 2000;49:43–9. https://doi.org/10.1016/S0022-3999(00)00084-2 .
Beck AT. Cognitive therapy and the emotional disorders. London: Penguin; 1979.
Verelst F, Willem L, Beutels P. Behavioural change models for infectious disease transmission: a systematic review (2010–2015). J R Soc Interface. 2016. https://doi.org/10.1098/rsif.2016.0820 .
Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, Rivera DE, et al. Building new computational models to support health behaviour change and maintenance: new opportunities in behavioural research. Transl Behav Med. 2015;5:335–46. https://doi.org/10.1007/s13142-015-0324-1 .
Herbert, C. An experimental-psychological approach for the development of character computing. In: Character computing (pp. 17–38). Springer, Cham; 2020.
El Bolock A, Abdennadher S, Herbert C. Applications of character computing from psychology to computer science. In: Character computing. Springer, Cham; 2020. p. 53–71.
Herbert C, El Bolock A, Abdennadher S. A psychologically driven, user-centered approach to character modeling. In: Character computing. Springer, Cham; 2020. p. 39–51.
El Bolock A, Herbert C, Abdennadher S. CCOnto: towards an ontology-based model for character computing. In: International conference on research challenges in information science. Springer, Cham; 2020. p. 529–535.
Spielberger CD. State-trait anxiety inventory for adults. 1983.
Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–71.
Bahammam MA. Validity and reliability of an Arabic version of the state-trait anxiety inventory in a Saudi dental setting. Saudi Med J. 2016;37(6):668.
AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, Shuqdar RM, AlOwaybil R. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16(1):32.
Bradley MM, Lang PJ. Measuring emotion: the self-assessment manikin and the semantic differential. J Behav Therapy Exp Psychiatry. 1994;25(1):49–59.
Bagby RM, Ayearst LE, Morariu RA, Watters C, Taylor GJ. The Internet administration version of the 20-item Toronto Alexithymia Scale. Psychol Assess. 2014;26(1):16.
John OP, Donahue EM, Kentle RL. Big five inventory. J Personal Soc Psychol. 1991. https://doi.org/10.1037/t07550-000 .
Schmitt DP, Allik J, McCrae RR, Benet-Martínez V. The geographic distribution of Big Five personality traits: patterns and profiles of human self-description across 56 nations. J Cross Cult Psychol. 2007;38(2):173–212.
Rees A, Nicholson N. The twenty statements test. Essential guide to qualitative methods in organizational research. 2004. p. 86–97.
Pennebaker JW, Francis ME, Booth RJ. Linguistic inquiry and word count: LIWC 2001. Mahway Lawrence Erlbaum Assoc. 2001;71(2001):2001.
Guo Y, Graber A, McBurney RN, Balasubramanian R. Sample size and statistical power considerations in high-dimensionality data settings: a comparative study of classification algorithms. BMC Bioinform. 2010;11(1):447.
Vabalas A, Gowen E, Poliakoff E, Casson AJ. Machine learning algorithm validation with a limited sample size. PLoS ONE. 2019;14(11):e0224365.
Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res. 2011;63(Suppl. 11):467–72.
Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the world health organization world mental health surveys. Psychol Med. 2016;46:2955–70. https://doi.org/10.1017/S0033291716001665 .
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127:623–38. https://doi.org/10.1037/abn0000362 .
January J, Madhombiro M, Chipamaunga S, Ray S, Chingono A, Melanie A. Prevalence of depression and anxiety among undergraduate university students in low- and middle-income countries: a systematic review protocol; 2018. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0723-8 . Accessed 29 June 2020.
Stock C, Kücük N, Miseviciene I, Guillén-Grima F, Petkeviciene J, Aguinaga-Ontoso I, Krämer A. Differences in health complaints among university students from three European countries. Prev Med. 2003;37:535–43.
Andrews G, Hobbs MJ, Borkovec TD, Beesdo K, Craske MG, Heimberg RG, Rapee RM, Ruscio AM, Stanley MA. Generalized worry disorder: a review of DSM-IV generalized anxiety disorder and options for DSM-V. Depress Anxiety. 2010;27:134–47. https://doi.org/10.1002/da.20658 .
World Health Organization. Physical activity; 2020. https://www.who.int/dietphysicalactivity/pa/en/ . Accessed 29 June 2020.
Wagner DD, Heatherton TF. Self-regulatory depletion increases emotional reactivity in the amygdala. Social Cogn Affect Neurosci. 2013;8:410–7. https://doi.org/10.1093/scan/nss082 .
Hoyle RH. Personality and self-regulation: trait and information-processing perspectives. J Pers. 2006;74(6):1507–26.
Diener E, Diener C. Most people are happy. Psychol Sci. 1996;7(3):181–5.
Herbert C, Junghofer M, Kissler J. Event related potentials to emotional adjectives during reading. Psychophysiology. 2008;45:487–98. https://doi.org/10.1111/j.1469-8986.2007.00638.x .
Herbert C, Kissler J, Junghöfer M, Peyk P, Rockstroh B. Processing of emotional adjectives: evidence from startle EMG and ERPs. Psychophysiology. 2006;43:197–206. https://doi.org/10.1111/j.1469-8986.2006.00385.x .
Watson LA, Dritschel B, Obonsawin MC, Jentzsch I. Seeing yourself in a positive light: brain correlates of the self-positivity bias. Brain Res. 2007;1152:106–10.
Dodds PS, Clark EM, Desu S, Frank MR, Reagan AJ, Williams JR, Mitchell L, et al. Human language reveals a universal positivity bias. Proc Natl Acad Sci USA. 2015;112:2389–94. https://doi.org/10.1073/pnas.1411678112 .
Hayes N, Joseph S. Big 5 correlates of three measures of subjective well-being. Personal Individ Differ. 2003;34(4):723–7.
Jylhä P, Isometsä E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depress Anxiety. 2006;23(5):281–9.
Jorm AF, Christensen H, Henderson AS, Jacomb PA, Korten AE, Rodgers B. Predicting anxiety and depression from personality: is there a synergistic effect of neuroticism and extraversion? J Abnorm Psychol. 2000;109(1):145.
Karsten J, Penninx BW, Riese H, Ormel J, Nolen WA, Hartman CA. The state effect of depressive and anxiety disorders on big five personality traits. J Psychiatr Res. 2012;46(5):644–50.
Stachl C, Pargent F, Hilbert S, Harari GM, Schoedel R, Vaid S, Bühner M. Personality research and assessment in the era of machine learning. Eur J Personal. 2019;34(5):613–31.
Azucar D, Marengo D, Settanni M. Predicting the Big 5 personality traits from digital footprints on social media: a meta-analysis. Personal Individ Differ. 2018;124:150–9.
Singh C. Using data analysis and machine learning for studying and predicting depression in users on social media. Doctoral dissertation, Carleton University; 2020.
Marouf AA, Ashrafi AF, Ahmed T, Emon T. A machine learning based approach for mapping personality traits and perceived stress scale of undergraduate students. Int J Mod Educ Comput Sci. 2019;11(8):42.
Tandera T, Suhartono D, Wongso R, Prasetio YL. Personality prediction system from facebook users. Procedia Comput Sci. 2017;116:604–11.
Download references
Acknowledgements
Not applicable.
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the DAAD/BMBF (principal investigators: CH, SA) and by the budgetary resources of the Department of Applied Emotion and Motivation Psychology, and the open access publication fund of Ulm University. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Applied Emotion and Motivation Psychology, Institute of Psychology and Education, Faculty of Engineering, Computer Science and Psychology, Ulm University, Albert Einstein Allee 47, 89081, Ulm, Germany
Cornelia Herbert & Alia El Bolock
Computer Science Department, Faculty of Media Engineering and Technology, German University in Cairo - GUC, New Cairo City, Egypt
Alia El Bolock & Slim Abdennadher
You can also search for this author in PubMed Google Scholar
Contributions
CH conceptualized and designed the study and the survey. CH was involved in data recruitment, in data preprocessing and CH performed data analytics for descriptive and correlational data and results (descriptive data analytics, statistical analysis), and CH interpreted the result, CH supervised the machine learning part, created figures and tables and drafted and wrote the manuscript and revised it for scientific content. AB helped in the survey, performed the machine learning part, the machine learning part was also supervised by SA. All authors read and approved the manuscript.
Corresponding author
Correspondence to Cornelia Herbert .
Ethics declarations
Ethics approval and consent to participate.
The present survey follows ethical guidelines: all students took part voluntarily in the survey. They gave written informed consent prior to filling out the survey. The participants were fully debriefed about the purpose of the study. They were informed that they will be questioned about their health, teaching and learning behaviour, and their subjective experience with the current COVID-19 pandemic situation. They were informed that they can withdraw from the study at any time during the survey without giving reasons or without negative consequences on confidentiality. They were debriefed in detail about data privacy. No individual ethics approval was submitted before the start of the survey. The survey contains questionnaires that are part of online studies that had received approval in previous studies of the corresponding author by the local ethics committee of Ulm University.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. An overview of the online survey items and questionnaires.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Herbert, C., El Bolock, A. & Abdennadher, S. How do you feel during the COVID-19 pandemic? A survey using psychological and linguistic self-report measures, and machine learning to investigate mental health, subjective experience, personality, and behaviour during the COVID-19 pandemic among university students. BMC Psychol 9 , 90 (2021). https://doi.org/10.1186/s40359-021-00574-x
Download citation
Received : 12 August 2020
Accepted : 26 April 2021
Published : 02 June 2021
DOI : https://doi.org/10.1186/s40359-021-00574-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Corona virus
- Personality
- Mental health
- Emotion perception
- Self-concept
- Linguistic analysis
- Machine learning
- Character computing
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Raise research question about covid-19

what is covid 19?
where did it come from?
why does it keeps spreading?
when did it start spreading?
Explanation:
in making research question be guided by the 5 w's

- Can you briefly explain what this novel coronavirus is?
- What do we know about how SARS-CoV-2 is spread and why it's spreading so quickly?
- What are the incubation period and symptoms of COVID-19?
- How can I protect myself from the coronavirus?
- How effective are masks and when should I wear one?
- How often and after what activities should you cleanse your hands?
- What is “social distancing” and will it help?
- Are some people at risk for getting very sick with COVID-19?
- How does COVID-19 affect children?
- Are asymptomatic patients less contagious? Are presymptomatic people less contagious?
New questions in English
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study
Contributed equally to this work with: Dominika Maison, Diana Jaworska, Dominika Adamczyk, Daria Affeltowicz
Roles Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Faculty of Psychology, University of Warsaw, Warsaw, Poland
Roles Formal analysis, Investigation, Writing – original draft, Writing – review & editing
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Roles Conceptualization, Formal analysis, Investigation, Methodology
- Dominika Maison,
- Diana Jaworska,
- Dominika Adamczyk,
- Daria Affeltowicz

- Published: October 11, 2021
- https://doi.org/10.1371/journal.pone.0258133
- Peer Review
- Reader Comments
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6 th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed that for all respondents the greatest challenges and the source of the greatest suffering were: a) limitation of direct contact with people; b) restrictions on movement and travel; c) necessary changes in active lifestyle; d) boredom and monotony; and e) uncertainty about the future.
Citation: Maison D, Jaworska D, Adamczyk D, Affeltowicz D (2021) The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study. PLoS ONE 16(10): e0258133. https://doi.org/10.1371/journal.pone.0258133
Editor: Shah Md Atiqul Haq, Shahjalal University of Science and Technology, BANGLADESH
Received: April 6, 2021; Accepted: September 18, 2021; Published: October 11, 2021
Copyright: © 2021 Maison et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files ( S1 Dataset ).
Funding: This work was supported by the Faculty of Psychology, University of Warsaw, Poland from the funds awarded by the Ministry of Science and Higher Education in the form of a subsidy for the maintenance and development of research potential in 2020 (501-D125-01-1250000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The coronavirus disease (COVID-19), discovered in December 2019 in China, has reached the level of a pandemic and, till June 2021, it has affected more than 171 million people worldwide and caused more than 3.5 million deaths all over the world [ 1 ]. The COVID-19 pandemic as a major health crisis has caught the attention of many researchers, which has led to the creation of a broad quantitative picture of human behavior during the coronavirus outbreak [ 2 – 4 ]. What has been established so far is, among others, the psychological symptoms that can occur as a result of lockdown [ 2 ], and the most common coping strategies [ 5 ]. However, what we still miss is an in-depth understanding of the changes in the ways of coping with challenges over different stages of the pandemic. In the following study, we used a longitudinal qualitative method to investigate the challenges during the different waves of the coronavirus pandemic as well as the coping mechanisms accompanying them.
In Poland, the first patient was diagnosed with COVID-19 on the 4 th March 2020. Since then, the number of confirmed cases has grown to more than 2.8 million and the number of deaths to more than 73,000 (June 2021) [ 1 ]. From mid-March 2020, the Polish government, similarly to many other countries, began to introduce a number of restrictions to limit the spread of the virus. These restrictions had been changing from week to week, causing diverse reactions in people [ 6 ]. It needs to be noted that the reactions to such a dynamic situation cannot be covered by a single study. Therefore, in our study we used qualitative longitudinal research in order to monitor changes in people’s emotions, attitudes, and behavior. So far, few longitudinal studies have been carried out that investigated the various issues related to the COVID-19 pandemic; however, all of them were quantitative [ 7 – 10 ]. The qualitative approach (and especially the use of enabling and projective techniques) allows for an in-depth exploration of respondents’ reactions that goes beyond respondents’ declarations and captures what they are less aware of or even unconscious of. This study consisted of six stages of interviews that were conducted at key moments for the development of the pandemic situation in Poland. The first stage of the study was carried out at the moment of the most severe lockdown and the biggest restrictions (March 2020) and was focused on exploration how did people react to the new uncertain situation. The second stage of the study was conducted at the time when restrictions were extended and the obligation to cover the mouth and nose everywhere outside the household were introduced (middle of April 2020) and was focused at the way how did people deal with the lack of family gatherings over Easter. The third stage of the study was conducted at the moment of announcing the four stages of lifting the restrictions (April 2020) and was focused on people’s reaction to an emerging vision of getting back to normalcy. The fourth stage of the study was carried out, after the introduction of the second stage of lifting the restrictions: shopping malls, hotels, and cultural institutions were gradually being opened (May 2020). The fifth stage of the study was conducted after all four stages of restriction lifting were in place (June 2020). Only the obligation to cover the mouth and nose in public spaces, an order to maintain social distance, as well as the functioning of public places under a sanitary regime were still in effect. During those 5 stages coping strategies with the changes in restrictions were explored. The sixth and last stage of the study was a return to the respondents after a longer break, at the turn of October and November 2020, when the number of coronavirus cases in Poland began to increase rapidly and the media declared “the second wave of the pandemic”. It was the moment when the restrictions were gradually being reintroduced. A full description of the changes occurring in Poland at the time of the study can be found in S1 Table .
The following study is the first qualitative longitudinal study investigating how people cope with the challenges arising from the COVID-19 pandemic at its different stages. The study, although conducted in Poland, shows the universal psychological relations between the challenges posed by the pandemic (and, even more, the restrictions resulting from the pandemic, which were very similar across different countries, not only European) and the ways of dealing with them.
Literature review
The COVID-19 pandemic has led to a global health crisis with severe economic [ 11 ], social [ 3 ], and psychological consequences [ 4 ]. Despite the fact that there were multiple crises in recent years, such as natural disasters, economic crises, and even epidemics, the coronavirus pandemic is the first in 100 years to severely affect the entire world. The economic effects of the COVID-19 pandemic concern an impending global recession caused by the lockdown of non-essential industries and the disruption of production and supply chains [ 11 ]. Social consequences may be visible in many areas, such as the rise in family violence [ 3 ], the ineffectiveness of remote education, and increased food insecurity among impoverished families due to school closures [ 12 ]. According to some experts, the psychological consequences of COVID-19 are the ones that may persist for the longest and lead to a global mental health crisis [ 13 ]. The coronavirus outbreak is generating increased depressive symptoms, stress, anxiety, insomnia, denial, fear, and anger all over the world [ 2 , 14 ]. The economic, social, and psychological problems that people are currently facing are the consequences of novel challenges that have been posed by the pandemic.
The coronavirus outbreak is a novel, uncharted situation that has shaken the world and completely changed the everyday lives of many individuals. Due to the social distancing policy, many people have switched to remote work—in Poland, almost 75% of white-collar workers were fully or partially working from home from mid-March until the end of May 2020 [ 15 ]. School closures and remote learning imposed a new obligation on parents of supervising education, especially with younger children [ 16 ]. What is more, the government order of self-isolation forced people to spend almost all their time at home and limit or completely abandon human encounters. In addition, the deteriorating economic situation was the cause of financial hardship for many people. All these difficulties and challenges arose in the aura of a new, contagious disease with unexplored, long-lasting health effects and not fully known infectivity and lethality [ 17 ]. Dealing with the situation was not facilitated by the phenomenon of global misinformation, called by some experts as the “infodemic”, which may be defined as an overabundance of information that makes it difficult for people to find trustworthy sources and reliable guidance [ 18 ]. Studies have shown that people have multiple ways of reacting to a crisis: from radical and even violent practices, towards individual solutions and depression [ 19 ]. Not only the challenges arising from the COVID-19 pandemic but also the ways of reacting to it and coping with it are issues of paramount importance that are worth investigating.
The reactions to unusual crisis situations may be dependent on dispositional factors, such as trait anxiety or perceived control [ 20 , 21 ]. A study on reactions to Hurricane Hugo has shown that people with higher trait anxiety are more likely to develop posttraumatic symptoms following a natural disaster [ 20 ]. Moreover, lack of perceived control was shown to be positively related to the level of distress during an earthquake in Turkey [ 21 ]. According to some researchers, the COVID-19 crisis and natural disasters have much in common, as the emotions and behavior they cause are based on the same primal human emotion—fear [ 22 ]. Both pandemics and natural disasters disrupt people’s everyday lives and may have severe economic, social and psychological consequences [ 23 ]. However, despite many similarities to natural disasters, COVID-19 is a unique situation—only in 2020, the current pandemic has taken more lives than the world’s combined natural disasters in any of the past twenty years [ 24 ]. It needs to be noted that natural disasters may pose different challenges than health crises and for this reason, they may provoke disparate reactions [ 25 ]. Research on the reactions to former epidemics has shown that avoidance and safety behaviors, such as avoiding going out, visiting crowded places, and visiting hospitals, are widespread at such times [ 26 ]. When it comes to the ways of dealing with the current COVID-19 pandemic, a substantial part of the quantitative research on this issue focuses on coping mechanisms. Studies have shown that the most prevalent coping strategies are highly problem-focused [ 5 ]. Most people tend to listen to expert advice and behave calmly and appropriately in the face of the coronavirus outbreak [ 5 ]. Problem-focused coping is particularly characteristic of healthcare professionals. A study on Chinese nurses has shown that the closer the problem is to the person and the more fear it evokes, the more problem-focused coping strategy is used to deal with it [ 27 ]. On the other hand, a negative coping style that entails risky or aggressive behaviors, such as drug or alcohol use, is also used to deal with the challenges arising from the COVID-19 pandemic [ 28 ]. The factors that are correlated with negative coping include coronavirus anxiety, impairment, and suicidal ideation [ 28 ]. It is worth emphasizing that social support is a very important component of dealing with crises [ 29 ].
Scientists have attempted to systematize the reactions to difficult and unusual situations. One such concept is the “3 Cs” model created by Reich [ 30 ]. It accounts for the general rules of resilience in situations of stress caused by crises, such as natural disasters. The 3 Cs stand for: control (a belief that personal resources can be accessed to achieve valued goals), coherence (the human desire to make meaning of the world), and connectedness (the need for human contact and support) [ 30 ]. Polizzi and colleagues [ 22 ] reviewed this model from the perspective of the current COVID-19 pandemic. The authors claim that natural disasters and COVID-19 pandemic have much in common and therefore, the principles of resilience in natural disaster situations can also be used in the situation of the current pandemic [ 22 ]. They propose a set of coping behaviors that could be useful in times of the coronavirus outbreak, which include control (e.g., planning activities for each day, getting adequate sleep, limiting exposure to the news, and helping others), coherence (e.g., mindfulness and developing a coherent narrative on the event), and connectedness (e.g., establishing new relationships and caring for existing social bonds) [ 22 ].
Current study
The issue of the challenges arising from the current COVID-19 pandemic and the ways of coping with them is complex and many feelings accompanying these experiences may be unconscious and difficult to verbalize. Therefore, in order to explore and understand it deeply, qualitative methodology was applied. Although there were few qualitative studies on the reaction to the pandemic [e.g., 31 – 33 ], they did not capture the perception of the challenges and their changes that arise as the pandemic develops. Since the situation with the COVID-19 pandemic is very dynamic, the reactions to the various restrictions, orders or bans are evolving. Therefore, it was decided to conduct a qualitative longitudinal study with multiple interviews with the same respondents [ 34 ].
The study investigates the challenges arising from the current pandemic and the way people deal with them. The main aim of the project was to capture people’s reactions to the unusual and unexpected situation of the COVID-19 pandemic. Therefore, the project was largely exploratory in nature. Interviews with the participants at different stages of the epidemic allowed us to see a wide spectrum of problems and ways of dealing with them. The conducted study had three main research questions:
- What are the biggest challenges connected to the COVID-19 pandemic and the resulting restrictions?
- How are people dealing with the pandemic challenges?
- What are the ways of coping with the restrictions resulting from a pandemic change as it continues and develops (perspective of first 6 months)?
The study was approved by the institutional review board of the Faculty of Psychology University of Warsaw, Poland. All participants were provided written and oral information about the study, which included that participation was voluntary, that it was possible to withdraw without any consequences at any time, and the precautions that would be taken to protect data confidentiality. Informed consent was obtained from all participants. To ensure confidentiality, quotes are presented only with gender, age, and family status.
The study was based on qualitative methodology: individual in-depth interviews, s which are the appropriate to approach a new and unknown and multithreaded topic which, at the beginning of 2020, was the COVID-19 pandemic. Due to the need to observe respondents’ reactions to the dynamically changing situation of the COVID-19 pandemic, longitudinal study was used where the moderator met on-line with the same respondent several times, at specific time intervals. A longitudinal study was used to capture the changes in opinions, emotions, and behaviors of the respondents resulting from the changes in the external circumstances (qualitative in-depth interview tracking–[ 34 ]).
The study took place from the end of March to October 2020. Due to the epidemiological situation in the country interviews took place online, using the Google Meets online video platform. The audio was recorded and then transcribed. Before taking part in the project, the respondents were informed about the purpose of the study, its course, and the fact that participation in the project is voluntary, and that they will be able to withdraw from participation at any time. The respondents were not paid for taking part in the project.
Participants.
In total, 115 interviews were conducted with 20 participants (6 interviews with the majority of respondents). Two participants (number 11 and 19, S2 Table ) dropped out of the last two interviews, and one (number 6) dropped out of the last interview. The study was based on a purposive sample and the respondents differed in gender, age, education, family status, and work situation (see S2 Table ). In addition to demographic criteria intended to ensure that the sample was as diverse as possible, an additional criterion was to have a permanent Internet connection and a computer capable of online video interviewing. Study participants were recruited using the snowball method. They were distant acquaintances of acquaintances of individuals involved in the study. None of the moderators knew their interviewees personally.
A total of 10 men and 10 women participated in the study; their age range was: 25–55; the majority had higher education (17 respondents), they were people with different professions and work status, and different family status (singles, couples without children, and families with children). Such diversity of respondents allowed us to obtain information from different life perspectives. A full description of characteristics of study participants can be found in S2 Table .
Each interview took 2 hours on average, which gives around 240 hours of interviews. Subsequent interviews with the same respondents conducted at different intervals resulted from the dynamics of the development of the pandemic and the restrictions introduced in Poland by the government.
The interviews scenario took a semi-structured form. This allowed interviewers freely modify the questions and topics depending on the dynamics of the conversation and adapt the subject matter of the interviews not only to the research purposes but also to the needs of a given respondent. The interview guides were modified from week to week, taking into account the development of the epidemiological situation, while at the same time maintaining certain constant parts that were repeated in each interview. The main parts of the interview topic guide consisted of: (a) experiences from the time of previous interviews: thoughts, feeling, fears, and hopes; (b) everyday life—organization of the day, work, free time, shopping, and eating, etc.; (c) changes—what had changed in the life of the respondent from the time of the last interview; (d) ways of coping with the situation; and (e) media—reception of information appearing in the media. Additionally, in each interview there were specific parts, such as the reactions to the beginning of the pandemic in the first interview or the reaction to the specific restrictions that were introduced.
The interviews were conducted by 5 female interviewers with experience in moderating qualitative interviews, all with a psychological background. After each series of interviews, all the members of the research teams took part in debriefing sessions, which consisted of discussing the information obtained from each respondent, exchanging general conclusions, deciding about the topics for the following interview stage, and adjusting them to the pandemic situation in the country.
Data analysis.
All the interviews were transcribed in Polish by the moderators and then double-checked (each moderator transcribed the interviews of another moderator, and then the interviewer checked the accuracy of the transcription). The whole process of analysis was conducted on the material in Polish (the native language of the authors of the study and respondents). The final page count of the transcript is approximately 1800 pages of text. The results presented below are only a portion of the total data collected during the interviews. While there are about 250 pages of the transcription directly related to the topic of the article, due to the fact that the interview was partly free-form, some themes merge with others and it is not possible to determine the exact number of pages devoted exclusively to analysis related to the topic of the article. Full dataset can be found in S1 Dataset .
Data was then processed into thematic analysis, which is defined as a method of developing qualitative data consisting of the identification, analysis, and description of the thematic areas [ 35 ]. In this type of analysis, a thematic unit is treated as an element related to the research problem that includes an important aspect of data. An important advantage of thematic analysis is its flexibility, which allows for the adoption of the most appropriate research strategy to the phenomenon under analysis. An inductive approach was used to avoid conceptual tunnel vision. Extracting themes from the raw data using an inductive approach precludes the researcher from imposing a predetermined outcome.
As a first step, each moderator reviewed the transcripts of the interviews they had conducted. Each transcript was thematically coded individually from this point during the second and the third reading. In the next step, one of the researchers reviewed the codes extracted by the other members of the research team. Then she made initial interpretations by generating themes that captured the essence of the previously identified codes. The researcher created a list of common themes present in all of the interviews. In the next step, the extracted themes were discussed again with all the moderators conducting the coding in order to achieve consistency. This collaborative process was repeated several times during the analysis. Here, further superordinate (challenges of COVID-19 pandemic) and subordinate (ways of dealing with challenges) themes were created, often by collapsing others together, and each theme listed under a superordinate and subordinate category was checked to ensure they were accurately represented. Through this process of repeated analysis and discussion of emerging themes, it was possible to agree on the final themes that are described below.
Main challenges of the COVID-19 pandemic.
Challenge 1 –limitation of direct contact with people . The first major challenge of the pandemic was that direct contact with other people was significantly reduced. The lockdown forced many people to work from home and limit contact not only with friends but also with close family (parents, children, and siblings). Limiting contact with other people was a big challenge for most of our respondents, especially those who were living alone and for those who previously led an active social life. Depending on their earlier lifestyle profile, for some, the bigger problem was the limitation of contact with the family, for others with friends, and for still others with co-workers.
I think that because I can’t meet up with anyone and that I’m not in a relationship , I miss having sex , and I think it will become even more difficult because it will be increasingly hard to meet anyone . (5 . 3_ M_39_single) . The number In the brackets at the end of the quotes marks the respondent’s number (according to Table 1 ) and the stage of the interview (after the dash), further is information about gender (F/M), age of the respondent and family status. Linguistic errors in the quotes reflect the spoken language of the respondents.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0258133.t001
Changes over time . Over the course of the 6 months of the study, an evolution in the attitudes to the restriction of face-to-face contact could be seen: from full acceptance, to later questioning its rationale. Initially (March and April), almost all the respondents understood the reasons for the isolation and were compliant. At the beginning, people were afraid of the unknown COVID-19. They were concerned that the tragic situation from Italy, which was intensively covered in the media, could repeat itself in Poland (stage 1–2 of the study). However, with time, the isolation started to bother them more and more, and they started to look for solutions to bypass the isolation guidelines (stage 3–4), both real (simply meeting each other) and mental (treating isolation only as a guideline and not as an order, perceiving the family as being less threatening than acquaintances or strangers in a store). The turning point was the long May weekend that, due to two public holidays (1 st and 3 rd May), has for many years been used as an opportunity to go away with family or friends. Many people broke their voluntary isolation during that time encouraged by information about the coming loosening of restrictions.
During the summer (stage 5 of the survey), practically no one was fully compliant with the isolation recommendations anymore. At that time, a growing familiarity could be observed with COVID-19 and an increasing tendency to talk about it as “one of many diseases”, and to convince oneself that one is not at risk and that COVID-19 is no more threatening than other viruses. Only a small group of people consciously failed to comply with the restrictions of contact with others from the very beginning of the pandemic. This behavior was mostly observed among people who were generally less anxious and less afraid of COVID-19.
I’ve had enough. I’ve had it with sitting at home. Okay, there’s some kind of virus, it’s as though it’s out there somewhere; it’s like I know 2 people who were infected but they’re still alive, nothing bad has happened to anyone. It’s just a tiny portion of people who are dying. And is it really such a tragedy that we have to be locked up at home? Surely there’s an alternative agenda there? (17.4_F_35_Adult and child)
Ways of dealing . In the initial phase, when almost everyone accepted this restriction and submitted to it, the use of communication platforms for social meetings increased (see Ways of dealing with challenges in Table 1 ) . Meetings on communication platforms were seen as an equivalent of the previous face-to-face contact and were often even accompanied by eating or drinking alcohol together. However, over time (at around stage 4–5 of the study) people began to feel that such contact was an insufficient substitute for face-to-face meetings and interest in online meetings began to wane. During this time, however, an interesting phenomenon could be seen, namely, that for many people the family was seen as a safer environment than friends, and definitely safer than strangers. The belief was that family members would be honest about being sick, while strangers not necessarily, and—on an unconscious level—the feeling was that the “family is safe”, and the “family can’t hurt them”.
When it became clear that online communication is an insufficient substitute for face-to-face contacts, people started to meet up in real life. However, a change in many behaviors associated with meeting people is clearly visible, e.g.: refraining from shaking hands, refraining from cheek kissing to greet one another, and keeping a distance during a conversation.
I can’t really say that I could ‘feel’ Good Friday or Holy Saturday. On Sunday, we had breakfast together with my husband’s family and his sister. We were in three different places but we connected over Skype. Later, at noon, we had some coffee with my parents, also over Skype. It’s obvious though that this doesn’t replace face-to-face contact but it’s always some form of conversation. (9.3_F_25_Couple, no children)
Challenge 2 –restrictions on movement and travel . In contrast to the restrictions on contact with other people, the restrictions on movement and the closing of borders were perceived more negatively and posed bigger challenges for some people (especially those who used to do a lot of travelling). In this case, it was less clear why these regulations were introduced (especially travel restrictions within the country). Moreover, travel restrictions, particularly in the case of international travels, were associated with a limitation of civil liberties. The limitation (or complete ban) on travelling abroad in the Polish situation evoked additional connotations with the communist times, that is, with the fact that there was no freedom of movement for Polish citizens (associations with totalitarianism and dictatorship). Interestingly, the lack of acceptance of this restriction was also manifested by people who did not travel much. Thus, it was not just a question of restricting travelling abroad but more of restricting the potential opportunity (“even if I’m not planning on going anywhere, I know I still can”).
Limitations on travelling around the country were particularly negatively felt by families with children, where parents believe that regular exercise and outings are necessary for the proper development of their children. For parents, it was problematic to accept the prohibition of leaving the house and going to the playground (which remained closed until mid-May). Being outdoors was perceived as important for maintaining immunity (exercise as part of a healthy lifestyle), therefore, people could not understand the reason underlying this restriction and, as a consequence, often did not accept it.
I was really bothered by the very awareness that I can’t just jump in my car or get on a plane whenever I want and go wherever I want. It’s not something that I have to do on a daily basis but freedom of movement and travelling are very important for me. (14.2_M_55_Two adults and children)
Changes over time . The travel and movement limitations, although objectively less severe for most people, aroused much greater anger than the restrictions on social contact. This was probably due to a greater sense of misunderstanding as to why these rules were being introduced in the first place. Moreover, they were often communicated inconsistently and chaotically (e.g., a ban on entering forests was introduced while, at the same time, shopping malls remained open and masses were allowed to attend church services). This anger grew over time—from interview to interview, the respondents’ irritation and lack of acceptance of this was evident (culminating in the 3 rd -4 th stage of the study). The limitation of mobility was also often associated with negative consequences for both health and the economy. Many people are convinced that being in the open air (especially accompanied by physical activity) strengthens immunity, therefore, limiting such activity may have negative health consequences. Some respondents pointed out that restricting travelling, the use of hotels and restaurants, especially during the holiday season, will have serious consequences for the existence of the tourism industry.
I can’t say I completely agree with these limitations because it’s treating everything selectively. It’s like the shopping mall is closed, I can’t buy any shoes but I can go to a home improvement store and buy some wallpaper for myself. So I don’t see the difference between encountering people in a home improvement store and a shopping mall. (18.2_F_48_Two adults and children)
Ways of dealing . Since the restriction of movement and travel was more often associated with pleasure-related behaviors than with activities necessary for living, the compensations for these restrictions were usually also from the area of hedonistic behaviors. In the statements of our respondents, terms such as “indulging” or “rewarding oneself” appeared, and behaviors such as throwing small parties at home, buying better alcohol, sweets, and new clothes were observed. There were also increased shopping behaviors related to hobbies (sometimes hobbies that could not be pursued at the given time)–a kind of “post-pandemic” shopping spree (e.g., a new bike or new skis).
Again, the reaction to this restriction also depended on the level of fear of the COVID-19 disease. People who were more afraid of being infected accepted these restrictions more easily as it gave them the feeling that they were doing something constructive to protect themselves from the infection. Conversely, people with less fears and concerns were more likely to rebel and break these bans and guidelines.
Another way of dealing with this challenge was making plans for interesting travel destinations for the post-pandemic period. This was especially salient in respondents with an active lifestyle in the past and especially visible during the 5 th stage of the study.
Today was the first day when I went to the store (due to being in quarantine after returning from abroad). I spent loads of money but I normally would have never spent so much on myself. I bought sweets and confectionery for Easter time, some Easter chocolates, too. I thought I’d do some more baking so I also bought some ingredients to do this. (1.2_ F_25_single)
Challenge 3 –necessary change in active lifestyle . Many of the limitations related to COVID-19 were a challenge for people with an active lifestyle who would regularly go to the cinema, theater, and gym, use restaurants, and do a lot of travelling. For those people, the time of the COVID constraints has brought about huge changes in their lifestyle. Most of their activities were drastically restricted overnight and they suddenly became domesticated by force, especially when it was additionally accompanied by a transition to remote work.
Compulsory spending time at home also had serious consequences for people with school-aged children who had to confront themselves with the distance learning situation of their children. The second challenge for families with children was also finding (or helping find) activities for their children to do in their free time without leaving the house.
I would love to go to a restaurant somewhere. We order food from the restaurant at least once a week, but I’d love to go to the restaurant. Spending time there is a different way of functioning. It is enjoyable and that is what I miss. I would also go to the cinema, to the theater. (13.3_M_46_Two adults and child.)
Changes over time . The nuisance of restrictions connected to an active lifestyle depended on the level of restrictions in place at a given time and the extent to which a given activity could be replaced by an alternative. Moreover, the response to these restrictions depended more on the individual differences in lifestyle rather than on the stage of the interview (except for the very beginning, when the changes in lifestyle and everyday activities were very sudden).
I miss that these restaurants are not open . And it’s not even that I would like to eat something specific . It is in all of this that I miss such freedom the most . It bothers me that I have no freedom . And I am able to get used to it , I can cook at home , I can order from home . But I just wish I had a choice . (2 . 6_F_27_single ).
Ways of dealing . In the initial phase of the pandemic (March-April—stage 1–3 of the study), when most people were afraid of the coronavirus, the acceptance of the restrictions was high. At the same time, efforts were made to find activities that could replace existing ones. Going to the gym was replaced by online exercise, and going to the cinema or theater by intensive use of streaming platforms. In the subsequent stages of the study, however, the respondents’ fatigue with these “substitutes” was noticeable. It was then that more irritation and greater non-acceptance of certain restrictions began to appear. On the other hand, the changes or restrictions introduced during the later stages of the pandemic were less sudden than the initial ones, so they were often easier to get used to.
I bought a small bike and even before that we ordered some resistance bands to work out at home, which replace certain gym equipment and devices. […] I’m considering learning a language. From the other online things, my girlfriend is having yoga classes, for instance. (7.2_M_28_Couple, no children)
Challenge 4 –boredom , monotony . As has already been shown, for many people, the beginning of the pandemic was a huge change in lifestyle, an absence of activities, and a resulting slowdown. It was sometimes associated with a feeling of weariness, monotony, and even of boredom, especially for people who worked remotely, whose days began to be similar to each other and whose working time merged with free time, weekdays with the weekends, and free time could not be filled with previous activities.
In some way, boredom. I can’t concentrate on what I’m reading. I’m trying to motivate myself to do such things as learning a language because I have so much time on my hands, or to do exercises. I don’t have this balance that I’m actually doing something for myself, like reading, working out, but also that I’m meeting up with friends. This balance has gone, so I’ve started to get bored with many things. Yesterday I felt that I was bored and something should start happening. (…) After some time, this lack of events and meetings leads to such immense boredom. (1.5_F_25_single)
Changes over time . The feeling of monotony and boredom was especially visible in stage 1 and 2 of the study when the lockdown was most restrictive and people were knocked out of their daily routines. As the pandemic continued, boredom was often replaced by irritation in some, and by stagnation in others (visible in stages 3 and 4 of the study) while, at the same time, enthusiasm for taking up new activities was waning. As most people were realizing that the pandemic was not going to end any time soon, a gradual adaptation to the new lifestyle (slower and less active) and the special pandemic demands (especially seen in stage 5 and 6 of the study) could be observed.
But I see that people around me , in fact , both family and friends , are slowly beginning to prepare themselves for more frequent stays at home . So actually more remote work , maybe everything will not be closed and we will not be locked in four walls , but this tendency towards isolation or self-isolation , such a deliberate one , appears . I guess we are used to the fact that it has to be this way . (15 . 6_M_43_Two adults and child) .
Ways of dealing . The answer to the monotony of everyday life and to finding different ways of separating work from free time was to stick to certain rituals, such as “getting dressed for work”, even when work was only by a computer at home or, if possible, setting a fixed meal time when the whole family would gather together. For some, the time of the beginning of the pandemic was treated as an extra vacation. This was especially true of people who could not carry out their work during the time of the most severe restrictions (e.g., hairdressers and doctors). For them, provided that they believed that everything would return to normal and that they would soon go back to work, a “vacation mode” was activated wherein they would sleep longer, watch a lot of movies, read books, and generally do pleasant things for which they previously had no time and which they could now enjoy without feeling guilty. Another way of dealing with the monotony and transition to a slower lifestyle was taking up various activities for which there was no time before, such as baking bread at home and cooking fancy dishes.
I generally do have a set schedule. I begin work at eight. Well, and what’s changed is that I can get up last minute, switch the computer on and be practically making my breakfast and coffee during this time. I do some work and then print out some materials for my younger daughter. You know, I have work till four, I keep on going up to the computer and checking my emails. (19.1_F_39_Two adults and children)
Challenge 5 –uncertainty about the future . Despite the difficulties arising from the circumstances and limitations described above, it seems that psychologically, the greatest challenge during a pandemic is the uncertainty of what will happen next. There was a lot of contradictory information in the media that caused a sense of confusion and heightened the feeling of anxiety.
I’m less bothered about the changes that were put in place and more about this concern about what will happen in the future. Right now, it’s like there’s these mood swings. […] Based on what’s going on, this will somehow affect every one of us. And that’s what I’m afraid of. The fact that someone will not survive and I have no way of knowing who this could be—whether it will be me or anyone else, or my dad, if somehow the coronavirus will sneak its way into our home. I simply don’t know. I’m simply afraid of this. (10.1_F_55_Couple, no children)
Changes over time . In the first phase of the pandemic (interviews 1–3), most people felt a strong sense of not being in control of the situation and of their own lives. Not only did the consequences of the pandemic include a change in lifestyle but also, very often, the suspension of plans altogether. In addition, many people felt a strong fear of the future, about what would happen, and even a sense of threat to their own or their loved ones’ lives. Gradually (interview 4), alongside anxiety, anger began to emerge about not knowing what would happen next. At the beginning of the summer (stage 5 of the study), most people had a hope of the pandemic soon ending. It was a period of easing restrictions and of opening up the economy. Life was starting to look more and more like it did before the pandemic, fleetingly giving an illusion that the end of the pandemic was “in sight” and the vision of a return to normal life. Unfortunately, autumn showed that more waves of the pandemic were approaching. In the interviews of the 6 th stage of the study, we could see more and more confusion and uncertainty, a loss of hope, and often a manifestation of disagreement with the restrictions that were introduced.
This is making me sad and angry. More angry, in fact. […] I don’t know what I should do. Up until now, there was nothing like this. Up until now, I was pretty certain of what I was doing in all the decisions I was making. (14.4_M_55_Two adults and children)
Ways of dealing . People reacted differently to the described feeling of insecurity. In order to reduce the emerging fears, some people searched (sometimes even compulsively) for any information that could help them “take control” of the situation. These people searched various sources, for example, information on the number of infected persons and the number of deaths. This knowledge gave them the illusion of control and helped them to somewhat reduce the anxiety evoked by the pandemic. The behavior of this group was often accompanied by very strict adherence to all guidelines and restrictions (e.g., frequent hand sanitization, wearing a face mask, and avoiding contact with others). This behavior increased the sense of control over the situation in these people.
A completely opposite strategy to reducing the feeling of uncertainty which we also observed in some respondents was cutting off information in the media about the scale of the disease and the resulting restrictions. These people, unable to keep up with the changing information and often inconsistent messages, in order to maintain cognitive coherence tried to cut off the media as much as possible, assuming that even if something really significant had happened, they would still find out.
I want to keep up to date with the current affairs. Even if it is an hour a day. How is the pandemic situation developing—is it increasing or decreasing. There’s a bit of propaganda there because I know that when they’re saying that they have the situation under control, they can’t control it anyway. Anyhow, it still has a somewhat calming effect that it’s dying down over here and that things aren’t that bad. And, apart from this, I listen to the news concerning restrictions, what we can and can’t do. (3.1_F_54_single)
Discussion and conclusions
The results of our study showed that the five greatest challenges resulting from the COVID-19 pandemic are: limitations of direct contact with people, restrictions on movement and travel, change in active lifestyle, boredom and monotony, and finally uncertainty about the future. As we can see the spectrum of problems resulting from the pandemic is very wide and some of them have an impact on everyday functioning and lifestyle, some other influence psychological functioning and well-being. Moreover, different people deal with these problems differently and different changes in everyday life are challenging for them. The first challenge of the pandemic COVID-19 problem is the consequence of the limitation of direct contact with others. This regulation has very strong psychological consequences in the sense of loneliness and lack of closeness. Initially, people tried to deal with this limitation through the use of internet communicators. It turned out, however, that this form of contact for the majority of people was definitely insufficient and feelings of deprivation quickly increased. As much data from psychological literature shows, contact with others can have great psychological healing properties [e.g., 29 ]. The need for closeness is a natural need in times of crisis and catastrophes [ 30 ]. Unfortunately, during the COVID-19 pandemic, the ability to meet this need was severely limited by regulations. This led to many people having serious problems with maintaining a good psychological condition.
Another troubling limitation found in our study were the restrictions on movement and travel, and the associated restrictions of most activities, which caused a huge change in lifestyle for many people. As shown in previous studies, travel and diverse leisure activities are important predictors of greater well-being [ 36 ]. Moreover, COVID-19 pandemic movement restrictions may be perceived by some people as a threat to human rights [ 37 ], which can contribute to people’s reluctance to accept lockdown rules.
The problem with accepting these restrictions was also related to the lack of understanding of the reasons behind them. Just as the limitation in contact with other people seemed understandable, the limitations related to physical activity and mobility were less so. Because of these limitations many people lost a sense of understanding of the rules and restrictions being imposed. Inconsistent communication in the media—called by some researchers the ‘infodemic’ [ 18 ], as well as discordant recommendations in different countries, causing an increasing sense of confusion in people.
Another huge challenge posed by the current pandemic is the feeling of uncertainty about the future. This feeling is caused by constant changes in the rules concerning daily functioning during the pandemic and what is prohibited and what is allowed. People lose their sense of being in control of the situation. From the psychological point of view, a long-lasting experience of lack of control can cause so-called learned helplessness, a permanent feeling of having no influence over the situation and no possibility of changing it [ 38 ], which can even result in depression and lower mental and physical wellbeing [ 39 ]. Control over live and the feeling that people have an influence on what happens in their lives is one of the basic rules of crisis situation resilience [ 30 ]. Unfortunately, also in this area, people have huge deficits caused by the pandemic. The obtained results are coherent with previous studies regarding the strategies harnessed to cope with the pandemic [e.g., 5 , 10 , 28 , 33 ]. For example, some studies showed that seeking social support is one of the most common strategies used to deal with the coronavirus pandemic [ 33 , 40 ]. Other ways to deal with this situation include distraction, active coping, and a positive appraisal of the situation [ 41 ]. Furthermore, research has shown that simple coping behaviors such as a healthy diet, not reading too much COVID-19 news, following a daily routine, and spending time outdoors may be protective factors against anxiety and depressive symptoms in times of the coronavirus pandemic [ 41 ].
This study showed that the acceptance of various limitations, and especially the feeling of discomfort associated with them, depended on the person’s earlier lifestyle. The more active and socializing a person was, the more restrictions were burdensome for him/her. The second factor, more of a psychological nature, was the fear of developing COVID-19. In this case, people who were more afraid of getting sick were more likely to submit to the imposed restrictions that, paradoxically, did not reduce their anxiety, and sometimes even heightened it.
Limitations of the study.
While the study shows interesting results, it also has some limitations. The purpose of the study was primarily to capture the first response to problems resulting from a pandemic, and as such its design is not ideal. First, the study participants are not diverse as much as would be desirable. They are mostly college-educated and relatively well off, which may influence how they perceive the pandemic situation. Furthermore, the recruitment was done by searching among the further acquaintances of the people involved in the study, so there is a risk that all the people interviewed come from a similar background. It would be necessary to conduct a study that also describes the reaction of people who are already in a more difficult life situation before the pandemic starts.
Moreover, it would also be worthwhile to pay attention to the interviewers themselves. All of the moderators were female, and although gender effects on the quality of the interviews and differences between the establishment of relationships between women and men were not observed during the debriefing process, the topic of gender effects on the results of qualitative research is frequently addressed in the literature [ 42 , 43 ]. Although the researchers approached the process with reflexivity and self-criticism at all stages, it would have seemed important to involve male moderators in the study to capture any differences in relationship dynamics.
Practical implications.
The study presented has many practical implications. Decision-makers in the state can analyze the COVID-19 pandemic crisis in a way that avoids a critical situation involving other infectious diseases in the future. The results of our study showing the most disruptive effects of the pandemic on people can serve as a basis for developing strategies to deal with the effects of the crisis so that it does not translate into a deterioration of the public’s mental health in the future.
The results of our study can also provide guidance on how to communicate information about restrictions in the future so that they are accepted and respected (for example by giving rational explanations of the reasons for introducing particular restrictions). In addition, the results of our study can also be a source of guidance on how to deal with the limitations that may arise in a recurrent COVID-19 pandemic, as well as other emergencies that could come.
The analysis of the results showed that the COVID-19 pandemic, and especially the lockdown periods, are a particular challenge for many people due to reduced social contact. On the other hand, it is social contacts that are at the same time a way of a smoother transition of crises. This knowledge should prompt decision-makers to devise ways to ensure pandemic safety without drastically limiting social contacts and to create solutions that give people a sense of control (instead of depriving it of). Providing such solutions can reduce the psychological problems associated with a pandemic and help people to cope better with it.
Conclusions
As more and more is said about the fact that the COVID-19 pandemic may not end soon and that we are likely to face more waves of this disease and related lockdowns, it is very important to understand how the different restrictions are perceived, what difficulties they cause and what are the biggest challenges resulting from them. For example, an important element of accepting the restrictions is understanding their sources, i.e., what they result from, what they are supposed to prevent, and what consequences they have for the fight against the pandemic. Moreover, we observed that the more incomprehensible the order was, the more it provoked to break it. This means that not only medical treatment is extremely important in an effective fight against a pandemic, but also appropriate communication.
The results of our study showed also that certain restrictions cause emotional deficits (e.g., loneliness, loss of sense of control) and, consequently, may cause serious problems with psychological functioning. From this perspective, it seems extremely important to understand which restrictions are causing emotional problems and how they can be dealt with in order to reduce the psychological discomfort associated with them.
Supporting information
S1 table. a full description of the changes occurring in poland at the time of the study..
https://doi.org/10.1371/journal.pone.0258133.s001
S2 Table. Characteristics of study participants.
https://doi.org/10.1371/journal.pone.0258133.s002
S1 Dataset. Transcriptions from the interviews.
https://doi.org/10.1371/journal.pone.0258133.s003
- 1. JHU CSEE. COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020 [cited 2021 Jun 1]. https://github.com/CSSEGISandData/COVID-19#covid-19-data-repository-by-the-center-for-systems-science-and-engineering-csse-at-johns-hopkins-university .
- View Article
- PubMed/NCBI
- Google Scholar
- 5. Gerhold L. COVID-19: Risk perception and coping strategies. Results from a survey in Germany. PsyArXiv [Preprint]. 2020 Mar 25.
- 6. Nowakowska K. Rok z koronawirusem: Od paniki, przez luz, do fatalizmu. [A year with coronavirus—from panic through chill to fatalism]. Dziennik Gazeta Prawna [Internet]. 2021 Mar 4 [cited 2021 Jun 1]. https://www.gazetaprawna.pl/wiadomosci/kraj/artykuly/8111858,szczepienia-maseczki-rok-z-koronawirusem-zycie-codzienne.html
- 11. Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. IESE Business School Working Paper No. WP-1240-E. 2020 Mar 23.
- 15. ARC. Praca z domu w polskim wydaniu—badanie na zlecenie Gumtree.pl we współpracy z Randstat Polska [The Polish way of working from home—a study commissioned by Gumtree.pl in collaboration with Randstat Polska]. 2020 [cited 2021 Jun 1]. https://www.randstad.pl/strefa-pracownika/centrum-prasowe/badanie-gumtreepl-we-wspolpracy-z-randstad-potrafimy-sie-zorganizowac-choc-czasem-lubimy-sobie-poprzeszkadzac-praca-z-domu-w-polskim-wydaniu/
- 16. Sierpowska, I. O edukacji w czasie pandemii [On Education during pandemic]. Centrum Prasowe SWPS [Internet]. 2020 Sep 8. [cited 2021 Jun 1]. https://www.swps.pl/centrum-prasowe/informacje-prasowe/22390-o-edukacji-w-czasie-pandemii-2?dt=1622540060078
- 17. Polish Academy of Sciences. Understanding COVID-19. Report by the COVID-19 team at the President of the Polish Academy of Sciences. 2020 Sep 14. [Cited 2021 Jun 1]. https://informacje.pan.pl/images/2020/opracowanie-covid19-14-09-2020/ZrozumiecCovid19_opracowanie_PAN.pdf
- 25. Brown, K. The pandemic is not a natural disaster. The New Yorker [Internet]. 2020 Apr 13 [cited 2021 Jun 1]. https://www.newyorker.com/culture/annals-of-inquiry/the-pandemic-is-not-a-natural-disaster .
- 34. Maison D. Qualitative marketing research. Understanding consumer behaviour. London: Routledge; 2019.
- 36. Argyle M. Causes and correlates of happiness. In: Kahneman D, Diener E, Schwarz N, editors. Well-Being: The Foundations of Hedonic Psychology. New York: Russell Sage Foundation; 1999. p. 353–373.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study
Dominika maison.
Faculty of Psychology, University of Warsaw, Warsaw, Poland
Diana Jaworska
Dominika adamczyk, daria affeltowicz, associated data.
All relevant data are within the manuscript and its Supporting Information files ( S1 Dataset ).
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6 th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed that for all respondents the greatest challenges and the source of the greatest suffering were: a) limitation of direct contact with people; b) restrictions on movement and travel; c) necessary changes in active lifestyle; d) boredom and monotony; and e) uncertainty about the future.
Introduction
The coronavirus disease (COVID-19), discovered in December 2019 in China, has reached the level of a pandemic and, till June 2021, it has affected more than 171 million people worldwide and caused more than 3.5 million deaths all over the world [ 1 ]. The COVID-19 pandemic as a major health crisis has caught the attention of many researchers, which has led to the creation of a broad quantitative picture of human behavior during the coronavirus outbreak [ 2 – 4 ]. What has been established so far is, among others, the psychological symptoms that can occur as a result of lockdown [ 2 ], and the most common coping strategies [ 5 ]. However, what we still miss is an in-depth understanding of the changes in the ways of coping with challenges over different stages of the pandemic. In the following study, we used a longitudinal qualitative method to investigate the challenges during the different waves of the coronavirus pandemic as well as the coping mechanisms accompanying them.
In Poland, the first patient was diagnosed with COVID-19 on the 4 th March 2020. Since then, the number of confirmed cases has grown to more than 2.8 million and the number of deaths to more than 73,000 (June 2021) [ 1 ]. From mid-March 2020, the Polish government, similarly to many other countries, began to introduce a number of restrictions to limit the spread of the virus. These restrictions had been changing from week to week, causing diverse reactions in people [ 6 ]. It needs to be noted that the reactions to such a dynamic situation cannot be covered by a single study. Therefore, in our study we used qualitative longitudinal research in order to monitor changes in people’s emotions, attitudes, and behavior. So far, few longitudinal studies have been carried out that investigated the various issues related to the COVID-19 pandemic; however, all of them were quantitative [ 7 – 10 ]. The qualitative approach (and especially the use of enabling and projective techniques) allows for an in-depth exploration of respondents’ reactions that goes beyond respondents’ declarations and captures what they are less aware of or even unconscious of. This study consisted of six stages of interviews that were conducted at key moments for the development of the pandemic situation in Poland. The first stage of the study was carried out at the moment of the most severe lockdown and the biggest restrictions (March 2020) and was focused on exploration how did people react to the new uncertain situation. The second stage of the study was conducted at the time when restrictions were extended and the obligation to cover the mouth and nose everywhere outside the household were introduced (middle of April 2020) and was focused at the way how did people deal with the lack of family gatherings over Easter. The third stage of the study was conducted at the moment of announcing the four stages of lifting the restrictions (April 2020) and was focused on people’s reaction to an emerging vision of getting back to normalcy. The fourth stage of the study was carried out, after the introduction of the second stage of lifting the restrictions: shopping malls, hotels, and cultural institutions were gradually being opened (May 2020). The fifth stage of the study was conducted after all four stages of restriction lifting were in place (June 2020). Only the obligation to cover the mouth and nose in public spaces, an order to maintain social distance, as well as the functioning of public places under a sanitary regime were still in effect. During those 5 stages coping strategies with the changes in restrictions were explored. The sixth and last stage of the study was a return to the respondents after a longer break, at the turn of October and November 2020, when the number of coronavirus cases in Poland began to increase rapidly and the media declared “the second wave of the pandemic”. It was the moment when the restrictions were gradually being reintroduced. A full description of the changes occurring in Poland at the time of the study can be found in S1 Table .
The following study is the first qualitative longitudinal study investigating how people cope with the challenges arising from the COVID-19 pandemic at its different stages. The study, although conducted in Poland, shows the universal psychological relations between the challenges posed by the pandemic (and, even more, the restrictions resulting from the pandemic, which were very similar across different countries, not only European) and the ways of dealing with them.
Literature review
The COVID-19 pandemic has led to a global health crisis with severe economic [ 11 ], social [ 3 ], and psychological consequences [ 4 ]. Despite the fact that there were multiple crises in recent years, such as natural disasters, economic crises, and even epidemics, the coronavirus pandemic is the first in 100 years to severely affect the entire world. The economic effects of the COVID-19 pandemic concern an impending global recession caused by the lockdown of non-essential industries and the disruption of production and supply chains [ 11 ]. Social consequences may be visible in many areas, such as the rise in family violence [ 3 ], the ineffectiveness of remote education, and increased food insecurity among impoverished families due to school closures [ 12 ]. According to some experts, the psychological consequences of COVID-19 are the ones that may persist for the longest and lead to a global mental health crisis [ 13 ]. The coronavirus outbreak is generating increased depressive symptoms, stress, anxiety, insomnia, denial, fear, and anger all over the world [ 2 , 14 ]. The economic, social, and psychological problems that people are currently facing are the consequences of novel challenges that have been posed by the pandemic.
The coronavirus outbreak is a novel, uncharted situation that has shaken the world and completely changed the everyday lives of many individuals. Due to the social distancing policy, many people have switched to remote work—in Poland, almost 75% of white-collar workers were fully or partially working from home from mid-March until the end of May 2020 [ 15 ]. School closures and remote learning imposed a new obligation on parents of supervising education, especially with younger children [ 16 ]. What is more, the government order of self-isolation forced people to spend almost all their time at home and limit or completely abandon human encounters. In addition, the deteriorating economic situation was the cause of financial hardship for many people. All these difficulties and challenges arose in the aura of a new, contagious disease with unexplored, long-lasting health effects and not fully known infectivity and lethality [ 17 ]. Dealing with the situation was not facilitated by the phenomenon of global misinformation, called by some experts as the “infodemic”, which may be defined as an overabundance of information that makes it difficult for people to find trustworthy sources and reliable guidance [ 18 ]. Studies have shown that people have multiple ways of reacting to a crisis: from radical and even violent practices, towards individual solutions and depression [ 19 ]. Not only the challenges arising from the COVID-19 pandemic but also the ways of reacting to it and coping with it are issues of paramount importance that are worth investigating.
The reactions to unusual crisis situations may be dependent on dispositional factors, such as trait anxiety or perceived control [ 20 , 21 ]. A study on reactions to Hurricane Hugo has shown that people with higher trait anxiety are more likely to develop posttraumatic symptoms following a natural disaster [ 20 ]. Moreover, lack of perceived control was shown to be positively related to the level of distress during an earthquake in Turkey [ 21 ]. According to some researchers, the COVID-19 crisis and natural disasters have much in common, as the emotions and behavior they cause are based on the same primal human emotion—fear [ 22 ]. Both pandemics and natural disasters disrupt people’s everyday lives and may have severe economic, social and psychological consequences [ 23 ]. However, despite many similarities to natural disasters, COVID-19 is a unique situation—only in 2020, the current pandemic has taken more lives than the world’s combined natural disasters in any of the past twenty years [ 24 ]. It needs to be noted that natural disasters may pose different challenges than health crises and for this reason, they may provoke disparate reactions [ 25 ]. Research on the reactions to former epidemics has shown that avoidance and safety behaviors, such as avoiding going out, visiting crowded places, and visiting hospitals, are widespread at such times [ 26 ]. When it comes to the ways of dealing with the current COVID-19 pandemic, a substantial part of the quantitative research on this issue focuses on coping mechanisms. Studies have shown that the most prevalent coping strategies are highly problem-focused [ 5 ]. Most people tend to listen to expert advice and behave calmly and appropriately in the face of the coronavirus outbreak [ 5 ]. Problem-focused coping is particularly characteristic of healthcare professionals. A study on Chinese nurses has shown that the closer the problem is to the person and the more fear it evokes, the more problem-focused coping strategy is used to deal with it [ 27 ]. On the other hand, a negative coping style that entails risky or aggressive behaviors, such as drug or alcohol use, is also used to deal with the challenges arising from the COVID-19 pandemic [ 28 ]. The factors that are correlated with negative coping include coronavirus anxiety, impairment, and suicidal ideation [ 28 ]. It is worth emphasizing that social support is a very important component of dealing with crises [ 29 ].
Scientists have attempted to systematize the reactions to difficult and unusual situations. One such concept is the “3 Cs” model created by Reich [ 30 ]. It accounts for the general rules of resilience in situations of stress caused by crises, such as natural disasters. The 3 Cs stand for: control (a belief that personal resources can be accessed to achieve valued goals), coherence (the human desire to make meaning of the world), and connectedness (the need for human contact and support) [ 30 ]. Polizzi and colleagues [ 22 ] reviewed this model from the perspective of the current COVID-19 pandemic. The authors claim that natural disasters and COVID-19 pandemic have much in common and therefore, the principles of resilience in natural disaster situations can also be used in the situation of the current pandemic [ 22 ]. They propose a set of coping behaviors that could be useful in times of the coronavirus outbreak, which include control (e.g., planning activities for each day, getting adequate sleep, limiting exposure to the news, and helping others), coherence (e.g., mindfulness and developing a coherent narrative on the event), and connectedness (e.g., establishing new relationships and caring for existing social bonds) [ 22 ].
Current study
The issue of the challenges arising from the current COVID-19 pandemic and the ways of coping with them is complex and many feelings accompanying these experiences may be unconscious and difficult to verbalize. Therefore, in order to explore and understand it deeply, qualitative methodology was applied. Although there were few qualitative studies on the reaction to the pandemic [e.g., 31 – 33 ], they did not capture the perception of the challenges and their changes that arise as the pandemic develops. Since the situation with the COVID-19 pandemic is very dynamic, the reactions to the various restrictions, orders or bans are evolving. Therefore, it was decided to conduct a qualitative longitudinal study with multiple interviews with the same respondents [ 34 ].
The study investigates the challenges arising from the current pandemic and the way people deal with them. The main aim of the project was to capture people’s reactions to the unusual and unexpected situation of the COVID-19 pandemic. Therefore, the project was largely exploratory in nature. Interviews with the participants at different stages of the epidemic allowed us to see a wide spectrum of problems and ways of dealing with them. The conducted study had three main research questions:
- What are the biggest challenges connected to the COVID-19 pandemic and the resulting restrictions?
- How are people dealing with the pandemic challenges?
- What are the ways of coping with the restrictions resulting from a pandemic change as it continues and develops (perspective of first 6 months)?
The study was approved by the institutional review board of the Faculty of Psychology University of Warsaw, Poland. All participants were provided written and oral information about the study, which included that participation was voluntary, that it was possible to withdraw without any consequences at any time, and the precautions that would be taken to protect data confidentiality. Informed consent was obtained from all participants. To ensure confidentiality, quotes are presented only with gender, age, and family status.
The study was based on qualitative methodology: individual in-depth interviews, s which are the appropriate to approach a new and unknown and multithreaded topic which, at the beginning of 2020, was the COVID-19 pandemic. Due to the need to observe respondents’ reactions to the dynamically changing situation of the COVID-19 pandemic, longitudinal study was used where the moderator met on-line with the same respondent several times, at specific time intervals. A longitudinal study was used to capture the changes in opinions, emotions, and behaviors of the respondents resulting from the changes in the external circumstances (qualitative in-depth interview tracking–[ 34 ]).
The study took place from the end of March to October 2020. Due to the epidemiological situation in the country interviews took place online, using the Google Meets online video platform. The audio was recorded and then transcribed. Before taking part in the project, the respondents were informed about the purpose of the study, its course, and the fact that participation in the project is voluntary, and that they will be able to withdraw from participation at any time. The respondents were not paid for taking part in the project.
Participants
In total, 115 interviews were conducted with 20 participants (6 interviews with the majority of respondents). Two participants (number 11 and 19, S2 Table ) dropped out of the last two interviews, and one (number 6) dropped out of the last interview. The study was based on a purposive sample and the respondents differed in gender, age, education, family status, and work situation (see S2 Table ). In addition to demographic criteria intended to ensure that the sample was as diverse as possible, an additional criterion was to have a permanent Internet connection and a computer capable of online video interviewing. Study participants were recruited using the snowball method. They were distant acquaintances of acquaintances of individuals involved in the study. None of the moderators knew their interviewees personally.
A total of 10 men and 10 women participated in the study; their age range was: 25–55; the majority had higher education (17 respondents), they were people with different professions and work status, and different family status (singles, couples without children, and families with children). Such diversity of respondents allowed us to obtain information from different life perspectives. A full description of characteristics of study participants can be found in S2 Table .
Each interview took 2 hours on average, which gives around 240 hours of interviews. Subsequent interviews with the same respondents conducted at different intervals resulted from the dynamics of the development of the pandemic and the restrictions introduced in Poland by the government.
The interviews scenario took a semi-structured form. This allowed interviewers freely modify the questions and topics depending on the dynamics of the conversation and adapt the subject matter of the interviews not only to the research purposes but also to the needs of a given respondent. The interview guides were modified from week to week, taking into account the development of the epidemiological situation, while at the same time maintaining certain constant parts that were repeated in each interview. The main parts of the interview topic guide consisted of: (a) experiences from the time of previous interviews: thoughts, feeling, fears, and hopes; (b) everyday life—organization of the day, work, free time, shopping, and eating, etc.; (c) changes—what had changed in the life of the respondent from the time of the last interview; (d) ways of coping with the situation; and (e) media—reception of information appearing in the media. Additionally, in each interview there were specific parts, such as the reactions to the beginning of the pandemic in the first interview or the reaction to the specific restrictions that were introduced.
The interviews were conducted by 5 female interviewers with experience in moderating qualitative interviews, all with a psychological background. After each series of interviews, all the members of the research teams took part in debriefing sessions, which consisted of discussing the information obtained from each respondent, exchanging general conclusions, deciding about the topics for the following interview stage, and adjusting them to the pandemic situation in the country.
Data analysis
All the interviews were transcribed in Polish by the moderators and then double-checked (each moderator transcribed the interviews of another moderator, and then the interviewer checked the accuracy of the transcription). The whole process of analysis was conducted on the material in Polish (the native language of the authors of the study and respondents). The final page count of the transcript is approximately 1800 pages of text. The results presented below are only a portion of the total data collected during the interviews. While there are about 250 pages of the transcription directly related to the topic of the article, due to the fact that the interview was partly free-form, some themes merge with others and it is not possible to determine the exact number of pages devoted exclusively to analysis related to the topic of the article. Full dataset can be found in S1 Dataset .
Data was then processed into thematic analysis, which is defined as a method of developing qualitative data consisting of the identification, analysis, and description of the thematic areas [ 35 ]. In this type of analysis, a thematic unit is treated as an element related to the research problem that includes an important aspect of data. An important advantage of thematic analysis is its flexibility, which allows for the adoption of the most appropriate research strategy to the phenomenon under analysis. An inductive approach was used to avoid conceptual tunnel vision. Extracting themes from the raw data using an inductive approach precludes the researcher from imposing a predetermined outcome.
As a first step, each moderator reviewed the transcripts of the interviews they had conducted. Each transcript was thematically coded individually from this point during the second and the third reading. In the next step, one of the researchers reviewed the codes extracted by the other members of the research team. Then she made initial interpretations by generating themes that captured the essence of the previously identified codes. The researcher created a list of common themes present in all of the interviews. In the next step, the extracted themes were discussed again with all the moderators conducting the coding in order to achieve consistency. This collaborative process was repeated several times during the analysis. Here, further superordinate (challenges of COVID-19 pandemic) and subordinate (ways of dealing with challenges) themes were created, often by collapsing others together, and each theme listed under a superordinate and subordinate category was checked to ensure they were accurately represented. Through this process of repeated analysis and discussion of emerging themes, it was possible to agree on the final themes that are described below.
Main challenges of the COVID-19 pandemic
Challenge 1 –limitation of direct contact with people . The first major challenge of the pandemic was that direct contact with other people was significantly reduced. The lockdown forced many people to work from home and limit contact not only with friends but also with close family (parents, children, and siblings). Limiting contact with other people was a big challenge for most of our respondents, especially those who were living alone and for those who previously led an active social life. Depending on their earlier lifestyle profile, for some, the bigger problem was the limitation of contact with the family, for others with friends, and for still others with co-workers.
I think that because I can’t meet up with anyone and that I’m not in a relationship , I miss having sex , and I think it will become even more difficult because it will be increasingly hard to meet anyone . (5 . 3_ M_39_single) . The number In the brackets at the end of the quotes marks the respondent’s number (according to Table 1 ) and the stage of the interview (after the dash), further is information about gender (F/M), age of the respondent and family status. Linguistic errors in the quotes reflect the spoken language of the respondents. Table 1 Challenges and ways to cope with them. Challenge Ways to cope Social isolation Meetings on online platforms Circumventing the rules (e.g., exceptions for the family in the restriction of face-to-face meetings) Restriction on movement and travel “Rewarding oneself”, “indulging”–hedonic behaviors Making future travel plans Necessary change in active lifestyle Looking for “substitutes”, e.g., online exercises, using movie streaming platforms Dreaming about the future after the pandemic (e.g., travelling abroad) Boredom, monotony Rituals Looking for new challenges and experiences (e.g., baking bread) Uncertainty about the future Looking for information about the number of COVID-19 infections and deaths Cutting off from information Open in a separate window
Changes over time . Over the course of the 6 months of the study, an evolution in the attitudes to the restriction of face-to-face contact could be seen: from full acceptance, to later questioning its rationale. Initially (March and April), almost all the respondents understood the reasons for the isolation and were compliant. At the beginning, people were afraid of the unknown COVID-19. They were concerned that the tragic situation from Italy, which was intensively covered in the media, could repeat itself in Poland (stage 1–2 of the study). However, with time, the isolation started to bother them more and more, and they started to look for solutions to bypass the isolation guidelines (stage 3–4), both real (simply meeting each other) and mental (treating isolation only as a guideline and not as an order, perceiving the family as being less threatening than acquaintances or strangers in a store). The turning point was the long May weekend that, due to two public holidays (1 st and 3 rd May), has for many years been used as an opportunity to go away with family or friends. Many people broke their voluntary isolation during that time encouraged by information about the coming loosening of restrictions.
During the summer (stage 5 of the survey), practically no one was fully compliant with the isolation recommendations anymore. At that time, a growing familiarity could be observed with COVID-19 and an increasing tendency to talk about it as “one of many diseases”, and to convince oneself that one is not at risk and that COVID-19 is no more threatening than other viruses. Only a small group of people consciously failed to comply with the restrictions of contact with others from the very beginning of the pandemic. This behavior was mostly observed among people who were generally less anxious and less afraid of COVID-19.
I’ve had enough. I’ve had it with sitting at home. Okay, there’s some kind of virus, it’s as though it’s out there somewhere; it’s like I know 2 people who were infected but they’re still alive, nothing bad has happened to anyone. It’s just a tiny portion of people who are dying. And is it really such a tragedy that we have to be locked up at home? Surely there’s an alternative agenda there? (17.4_F_35_Adult and child)
Ways of dealing . In the initial phase, when almost everyone accepted this restriction and submitted to it, the use of communication platforms for social meetings increased (see Ways of dealing with challenges in Table 1 ) . Meetings on communication platforms were seen as an equivalent of the previous face-to-face contact and were often even accompanied by eating or drinking alcohol together. However, over time (at around stage 4–5 of the study) people began to feel that such contact was an insufficient substitute for face-to-face meetings and interest in online meetings began to wane. During this time, however, an interesting phenomenon could be seen, namely, that for many people the family was seen as a safer environment than friends, and definitely safer than strangers. The belief was that family members would be honest about being sick, while strangers not necessarily, and—on an unconscious level—the feeling was that the “family is safe”, and the “family can’t hurt them”.
When it became clear that online communication is an insufficient substitute for face-to-face contacts, people started to meet up in real life. However, a change in many behaviors associated with meeting people is clearly visible, e.g.: refraining from shaking hands, refraining from cheek kissing to greet one another, and keeping a distance during a conversation.
I can’t really say that I could ‘feel’ Good Friday or Holy Saturday. On Sunday, we had breakfast together with my husband’s family and his sister. We were in three different places but we connected over Skype. Later, at noon, we had some coffee with my parents, also over Skype. It’s obvious though that this doesn’t replace face-to-face contact but it’s always some form of conversation. (9.3_F_25_Couple, no children)
Challenge 2 –restrictions on movement and travel . In contrast to the restrictions on contact with other people, the restrictions on movement and the closing of borders were perceived more negatively and posed bigger challenges for some people (especially those who used to do a lot of travelling). In this case, it was less clear why these regulations were introduced (especially travel restrictions within the country). Moreover, travel restrictions, particularly in the case of international travels, were associated with a limitation of civil liberties. The limitation (or complete ban) on travelling abroad in the Polish situation evoked additional connotations with the communist times, that is, with the fact that there was no freedom of movement for Polish citizens (associations with totalitarianism and dictatorship). Interestingly, the lack of acceptance of this restriction was also manifested by people who did not travel much. Thus, it was not just a question of restricting travelling abroad but more of restricting the potential opportunity (“even if I’m not planning on going anywhere, I know I still can”).
Limitations on travelling around the country were particularly negatively felt by families with children, where parents believe that regular exercise and outings are necessary for the proper development of their children. For parents, it was problematic to accept the prohibition of leaving the house and going to the playground (which remained closed until mid-May). Being outdoors was perceived as important for maintaining immunity (exercise as part of a healthy lifestyle), therefore, people could not understand the reason underlying this restriction and, as a consequence, often did not accept it.
I was really bothered by the very awareness that I can’t just jump in my car or get on a plane whenever I want and go wherever I want. It’s not something that I have to do on a daily basis but freedom of movement and travelling are very important for me. (14.2_M_55_Two adults and children)
Changes over time . The travel and movement limitations, although objectively less severe for most people, aroused much greater anger than the restrictions on social contact. This was probably due to a greater sense of misunderstanding as to why these rules were being introduced in the first place. Moreover, they were often communicated inconsistently and chaotically (e.g., a ban on entering forests was introduced while, at the same time, shopping malls remained open and masses were allowed to attend church services). This anger grew over time—from interview to interview, the respondents’ irritation and lack of acceptance of this was evident (culminating in the 3 rd -4 th stage of the study). The limitation of mobility was also often associated with negative consequences for both health and the economy. Many people are convinced that being in the open air (especially accompanied by physical activity) strengthens immunity, therefore, limiting such activity may have negative health consequences. Some respondents pointed out that restricting travelling, the use of hotels and restaurants, especially during the holiday season, will have serious consequences for the existence of the tourism industry.
I can’t say I completely agree with these limitations because it’s treating everything selectively. It’s like the shopping mall is closed, I can’t buy any shoes but I can go to a home improvement store and buy some wallpaper for myself. So I don’t see the difference between encountering people in a home improvement store and a shopping mall. (18.2_F_48_Two adults and children)
Ways of dealing . Since the restriction of movement and travel was more often associated with pleasure-related behaviors than with activities necessary for living, the compensations for these restrictions were usually also from the area of hedonistic behaviors. In the statements of our respondents, terms such as “indulging” or “rewarding oneself” appeared, and behaviors such as throwing small parties at home, buying better alcohol, sweets, and new clothes were observed. There were also increased shopping behaviors related to hobbies (sometimes hobbies that could not be pursued at the given time)–a kind of “post-pandemic” shopping spree (e.g., a new bike or new skis).
Again, the reaction to this restriction also depended on the level of fear of the COVID-19 disease. People who were more afraid of being infected accepted these restrictions more easily as it gave them the feeling that they were doing something constructive to protect themselves from the infection. Conversely, people with less fears and concerns were more likely to rebel and break these bans and guidelines.
Another way of dealing with this challenge was making plans for interesting travel destinations for the post-pandemic period. This was especially salient in respondents with an active lifestyle in the past and especially visible during the 5 th stage of the study.
Today was the first day when I went to the store (due to being in quarantine after returning from abroad). I spent loads of money but I normally would have never spent so much on myself. I bought sweets and confectionery for Easter time, some Easter chocolates, too. I thought I’d do some more baking so I also bought some ingredients to do this. (1.2_ F_25_single)
Challenge 3 –necessary change in active lifestyle . Many of the limitations related to COVID-19 were a challenge for people with an active lifestyle who would regularly go to the cinema, theater, and gym, use restaurants, and do a lot of travelling. For those people, the time of the COVID constraints has brought about huge changes in their lifestyle. Most of their activities were drastically restricted overnight and they suddenly became domesticated by force, especially when it was additionally accompanied by a transition to remote work.
Compulsory spending time at home also had serious consequences for people with school-aged children who had to confront themselves with the distance learning situation of their children. The second challenge for families with children was also finding (or helping find) activities for their children to do in their free time without leaving the house.
I would love to go to a restaurant somewhere. We order food from the restaurant at least once a week, but I’d love to go to the restaurant. Spending time there is a different way of functioning. It is enjoyable and that is what I miss. I would also go to the cinema, to the theater. (13.3_M_46_Two adults and child.)
Changes over time . The nuisance of restrictions connected to an active lifestyle depended on the level of restrictions in place at a given time and the extent to which a given activity could be replaced by an alternative. Moreover, the response to these restrictions depended more on the individual differences in lifestyle rather than on the stage of the interview (except for the very beginning, when the changes in lifestyle and everyday activities were very sudden).
I miss that these restaurants are not open . And it’s not even that I would like to eat something specific . It is in all of this that I miss such freedom the most . It bothers me that I have no freedom . And I am able to get used to it , I can cook at home , I can order from home . But I just wish I had a choice . (2 . 6_F_27_single ).
Ways of dealing . In the initial phase of the pandemic (March-April—stage 1–3 of the study), when most people were afraid of the coronavirus, the acceptance of the restrictions was high. At the same time, efforts were made to find activities that could replace existing ones. Going to the gym was replaced by online exercise, and going to the cinema or theater by intensive use of streaming platforms. In the subsequent stages of the study, however, the respondents’ fatigue with these “substitutes” was noticeable. It was then that more irritation and greater non-acceptance of certain restrictions began to appear. On the other hand, the changes or restrictions introduced during the later stages of the pandemic were less sudden than the initial ones, so they were often easier to get used to.
I bought a small bike and even before that we ordered some resistance bands to work out at home, which replace certain gym equipment and devices. […] I’m considering learning a language. From the other online things, my girlfriend is having yoga classes, for instance. (7.2_M_28_Couple, no children)
Challenge 4 –boredom , monotony . As has already been shown, for many people, the beginning of the pandemic was a huge change in lifestyle, an absence of activities, and a resulting slowdown. It was sometimes associated with a feeling of weariness, monotony, and even of boredom, especially for people who worked remotely, whose days began to be similar to each other and whose working time merged with free time, weekdays with the weekends, and free time could not be filled with previous activities.
In some way, boredom. I can’t concentrate on what I’m reading. I’m trying to motivate myself to do such things as learning a language because I have so much time on my hands, or to do exercises. I don’t have this balance that I’m actually doing something for myself, like reading, working out, but also that I’m meeting up with friends. This balance has gone, so I’ve started to get bored with many things. Yesterday I felt that I was bored and something should start happening. (…) After some time, this lack of events and meetings leads to such immense boredom. (1.5_F_25_single)
Changes over time . The feeling of monotony and boredom was especially visible in stage 1 and 2 of the study when the lockdown was most restrictive and people were knocked out of their daily routines. As the pandemic continued, boredom was often replaced by irritation in some, and by stagnation in others (visible in stages 3 and 4 of the study) while, at the same time, enthusiasm for taking up new activities was waning. As most people were realizing that the pandemic was not going to end any time soon, a gradual adaptation to the new lifestyle (slower and less active) and the special pandemic demands (especially seen in stage 5 and 6 of the study) could be observed.
But I see that people around me , in fact , both family and friends , are slowly beginning to prepare themselves for more frequent stays at home . So actually more remote work , maybe everything will not be closed and we will not be locked in four walls , but this tendency towards isolation or self-isolation , such a deliberate one , appears . I guess we are used to the fact that it has to be this way . (15 . 6_M_43_Two adults and child) .
Ways of dealing . The answer to the monotony of everyday life and to finding different ways of separating work from free time was to stick to certain rituals, such as “getting dressed for work”, even when work was only by a computer at home or, if possible, setting a fixed meal time when the whole family would gather together. For some, the time of the beginning of the pandemic was treated as an extra vacation. This was especially true of people who could not carry out their work during the time of the most severe restrictions (e.g., hairdressers and doctors). For them, provided that they believed that everything would return to normal and that they would soon go back to work, a “vacation mode” was activated wherein they would sleep longer, watch a lot of movies, read books, and generally do pleasant things for which they previously had no time and which they could now enjoy without feeling guilty. Another way of dealing with the monotony and transition to a slower lifestyle was taking up various activities for which there was no time before, such as baking bread at home and cooking fancy dishes.
I generally do have a set schedule. I begin work at eight. Well, and what’s changed is that I can get up last minute, switch the computer on and be practically making my breakfast and coffee during this time. I do some work and then print out some materials for my younger daughter. You know, I have work till four, I keep on going up to the computer and checking my emails. (19.1_F_39_Two adults and children)
Challenge 5 –uncertainty about the future . Despite the difficulties arising from the circumstances and limitations described above, it seems that psychologically, the greatest challenge during a pandemic is the uncertainty of what will happen next. There was a lot of contradictory information in the media that caused a sense of confusion and heightened the feeling of anxiety.
I’m less bothered about the changes that were put in place and more about this concern about what will happen in the future. Right now, it’s like there’s these mood swings. […] Based on what’s going on, this will somehow affect every one of us. And that’s what I’m afraid of. The fact that someone will not survive and I have no way of knowing who this could be—whether it will be me or anyone else, or my dad, if somehow the coronavirus will sneak its way into our home. I simply don’t know. I’m simply afraid of this. (10.1_F_55_Couple, no children)
Changes over time . In the first phase of the pandemic (interviews 1–3), most people felt a strong sense of not being in control of the situation and of their own lives. Not only did the consequences of the pandemic include a change in lifestyle but also, very often, the suspension of plans altogether. In addition, many people felt a strong fear of the future, about what would happen, and even a sense of threat to their own or their loved ones’ lives. Gradually (interview 4), alongside anxiety, anger began to emerge about not knowing what would happen next. At the beginning of the summer (stage 5 of the study), most people had a hope of the pandemic soon ending. It was a period of easing restrictions and of opening up the economy. Life was starting to look more and more like it did before the pandemic, fleetingly giving an illusion that the end of the pandemic was “in sight” and the vision of a return to normal life. Unfortunately, autumn showed that more waves of the pandemic were approaching. In the interviews of the 6 th stage of the study, we could see more and more confusion and uncertainty, a loss of hope, and often a manifestation of disagreement with the restrictions that were introduced.
This is making me sad and angry. More angry, in fact. […] I don’t know what I should do. Up until now, there was nothing like this. Up until now, I was pretty certain of what I was doing in all the decisions I was making. (14.4_M_55_Two adults and children)
Ways of dealing . People reacted differently to the described feeling of insecurity. In order to reduce the emerging fears, some people searched (sometimes even compulsively) for any information that could help them “take control” of the situation. These people searched various sources, for example, information on the number of infected persons and the number of deaths. This knowledge gave them the illusion of control and helped them to somewhat reduce the anxiety evoked by the pandemic. The behavior of this group was often accompanied by very strict adherence to all guidelines and restrictions (e.g., frequent hand sanitization, wearing a face mask, and avoiding contact with others). This behavior increased the sense of control over the situation in these people.
A completely opposite strategy to reducing the feeling of uncertainty which we also observed in some respondents was cutting off information in the media about the scale of the disease and the resulting restrictions. These people, unable to keep up with the changing information and often inconsistent messages, in order to maintain cognitive coherence tried to cut off the media as much as possible, assuming that even if something really significant had happened, they would still find out.
I want to keep up to date with the current affairs. Even if it is an hour a day. How is the pandemic situation developing—is it increasing or decreasing. There’s a bit of propaganda there because I know that when they’re saying that they have the situation under control, they can’t control it anyway. Anyhow, it still has a somewhat calming effect that it’s dying down over here and that things aren’t that bad. And, apart from this, I listen to the news concerning restrictions, what we can and can’t do. (3.1_F_54_single)
Discussion and conclusions
The results of our study showed that the five greatest challenges resulting from the COVID-19 pandemic are: limitations of direct contact with people, restrictions on movement and travel, change in active lifestyle, boredom and monotony, and finally uncertainty about the future. As we can see the spectrum of problems resulting from the pandemic is very wide and some of them have an impact on everyday functioning and lifestyle, some other influence psychological functioning and well-being. Moreover, different people deal with these problems differently and different changes in everyday life are challenging for them. The first challenge of the pandemic COVID-19 problem is the consequence of the limitation of direct contact with others. This regulation has very strong psychological consequences in the sense of loneliness and lack of closeness. Initially, people tried to deal with this limitation through the use of internet communicators. It turned out, however, that this form of contact for the majority of people was definitely insufficient and feelings of deprivation quickly increased. As much data from psychological literature shows, contact with others can have great psychological healing properties [e.g., 29 ]. The need for closeness is a natural need in times of crisis and catastrophes [ 30 ]. Unfortunately, during the COVID-19 pandemic, the ability to meet this need was severely limited by regulations. This led to many people having serious problems with maintaining a good psychological condition.
Another troubling limitation found in our study were the restrictions on movement and travel, and the associated restrictions of most activities, which caused a huge change in lifestyle for many people. As shown in previous studies, travel and diverse leisure activities are important predictors of greater well-being [ 36 ]. Moreover, COVID-19 pandemic movement restrictions may be perceived by some people as a threat to human rights [ 37 ], which can contribute to people’s reluctance to accept lockdown rules.
The problem with accepting these restrictions was also related to the lack of understanding of the reasons behind them. Just as the limitation in contact with other people seemed understandable, the limitations related to physical activity and mobility were less so. Because of these limitations many people lost a sense of understanding of the rules and restrictions being imposed. Inconsistent communication in the media—called by some researchers the ‘infodemic’ [ 18 ], as well as discordant recommendations in different countries, causing an increasing sense of confusion in people.
Another huge challenge posed by the current pandemic is the feeling of uncertainty about the future. This feeling is caused by constant changes in the rules concerning daily functioning during the pandemic and what is prohibited and what is allowed. People lose their sense of being in control of the situation. From the psychological point of view, a long-lasting experience of lack of control can cause so-called learned helplessness, a permanent feeling of having no influence over the situation and no possibility of changing it [ 38 ], which can even result in depression and lower mental and physical wellbeing [ 39 ]. Control over live and the feeling that people have an influence on what happens in their lives is one of the basic rules of crisis situation resilience [ 30 ]. Unfortunately, also in this area, people have huge deficits caused by the pandemic. The obtained results are coherent with previous studies regarding the strategies harnessed to cope with the pandemic [e.g., 5 , 10 , 28 , 33 ]. For example, some studies showed that seeking social support is one of the most common strategies used to deal with the coronavirus pandemic [ 33 , 40 ]. Other ways to deal with this situation include distraction, active coping, and a positive appraisal of the situation [ 41 ]. Furthermore, research has shown that simple coping behaviors such as a healthy diet, not reading too much COVID-19 news, following a daily routine, and spending time outdoors may be protective factors against anxiety and depressive symptoms in times of the coronavirus pandemic [ 41 ].
This study showed that the acceptance of various limitations, and especially the feeling of discomfort associated with them, depended on the person’s earlier lifestyle. The more active and socializing a person was, the more restrictions were burdensome for him/her. The second factor, more of a psychological nature, was the fear of developing COVID-19. In this case, people who were more afraid of getting sick were more likely to submit to the imposed restrictions that, paradoxically, did not reduce their anxiety, and sometimes even heightened it.
Limitations of the study
While the study shows interesting results, it also has some limitations. The purpose of the study was primarily to capture the first response to problems resulting from a pandemic, and as such its design is not ideal. First, the study participants are not diverse as much as would be desirable. They are mostly college-educated and relatively well off, which may influence how they perceive the pandemic situation. Furthermore, the recruitment was done by searching among the further acquaintances of the people involved in the study, so there is a risk that all the people interviewed come from a similar background. It would be necessary to conduct a study that also describes the reaction of people who are already in a more difficult life situation before the pandemic starts.
Moreover, it would also be worthwhile to pay attention to the interviewers themselves. All of the moderators were female, and although gender effects on the quality of the interviews and differences between the establishment of relationships between women and men were not observed during the debriefing process, the topic of gender effects on the results of qualitative research is frequently addressed in the literature [ 42 , 43 ]. Although the researchers approached the process with reflexivity and self-criticism at all stages, it would have seemed important to involve male moderators in the study to capture any differences in relationship dynamics.
Practical implications
The study presented has many practical implications. Decision-makers in the state can analyze the COVID-19 pandemic crisis in a way that avoids a critical situation involving other infectious diseases in the future. The results of our study showing the most disruptive effects of the pandemic on people can serve as a basis for developing strategies to deal with the effects of the crisis so that it does not translate into a deterioration of the public’s mental health in the future.
The results of our study can also provide guidance on how to communicate information about restrictions in the future so that they are accepted and respected (for example by giving rational explanations of the reasons for introducing particular restrictions). In addition, the results of our study can also be a source of guidance on how to deal with the limitations that may arise in a recurrent COVID-19 pandemic, as well as other emergencies that could come.
The analysis of the results showed that the COVID-19 pandemic, and especially the lockdown periods, are a particular challenge for many people due to reduced social contact. On the other hand, it is social contacts that are at the same time a way of a smoother transition of crises. This knowledge should prompt decision-makers to devise ways to ensure pandemic safety without drastically limiting social contacts and to create solutions that give people a sense of control (instead of depriving it of). Providing such solutions can reduce the psychological problems associated with a pandemic and help people to cope better with it.
Conclusions
As more and more is said about the fact that the COVID-19 pandemic may not end soon and that we are likely to face more waves of this disease and related lockdowns, it is very important to understand how the different restrictions are perceived, what difficulties they cause and what are the biggest challenges resulting from them. For example, an important element of accepting the restrictions is understanding their sources, i.e., what they result from, what they are supposed to prevent, and what consequences they have for the fight against the pandemic. Moreover, we observed that the more incomprehensible the order was, the more it provoked to break it. This means that not only medical treatment is extremely important in an effective fight against a pandemic, but also appropriate communication.
The results of our study showed also that certain restrictions cause emotional deficits (e.g., loneliness, loss of sense of control) and, consequently, may cause serious problems with psychological functioning. From this perspective, it seems extremely important to understand which restrictions are causing emotional problems and how they can be dealt with in order to reduce the psychological discomfort associated with them.
Supporting information
Funding statement.
This work was supported by the Faculty of Psychology, University of Warsaw, Poland from the funds awarded by the Ministry of Science and Higher Education in the form of a subsidy for the maintenance and development of research potential in 2020 (501-D125-01-1250000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2021; 16(10): e0258133.
Decision Letter 0
17 May 2021
PONE-D-21-11248
The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study.
Dear Dr. Dominika,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Please submit your revised manuscript by six weeks. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Shah Md Atiqul Haq
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. In order to improve reporting, in your methods section, please provide additional information about the participant recruitment method, including a description of any inclusion/exclusion criteria that were applied to participant recruitment and a description of how participants were recruited.
3.We note that you have indicated that data from this study are available upon request. PLOS only allows data to be available upon request if there are legal or ethical restrictions on sharing data publicly. For information on unacceptable data access restrictions, please see http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions .
In your revised cover letter, please address the following prompts:
a) If there are ethical or legal restrictions on sharing a de-identified data set, please explain them in detail (e.g., data contain potentially identifying or sensitive patient information) and who has imposed them (e.g., an ethics committee). Please also provide contact information for a data access committee, ethics committee, or other institutional body to which data requests may be sent.
b) If there are no restrictions, please upload the minimal anonymized data set necessary to replicate your study findings as either Supporting Information files or to a stable, public repository and provide us with the relevant URLs, DOIs, or accession numbers. Please see http://www.bmj.com/content/340/bmj.c181.long for guidelines on how to de-identify and prepare clinical data for publication. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories .
We will update your Data Availability statement on your behalf to reflect the information you provide.
4. Please include a copy of Table 3 which you refer to in your text on page 32.
Additional Editor Comments:
Dear authors/writers.
I would like to ask you to revise the article as suggested by the commenters.
You also need to focus on the discussion section. This section should be logical, concise, and have a strong conclusion.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: No
Reviewer #3: Partly
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #3: No
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: No
Reviewer #3: Yes
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: GENERAL COMMENTS
This manuscript analyses in depth the reactions of a Polish sample during the COVID pandemic. Its main strength is the longitudinal perspective qualitative study. However, the present manuscript fails at research structure and it is recommended to relay into its main contribution.
I have suggested some changes or recommendation which I hope the authors find them in a constructive manner.
My recommendation for this article is a major revision.
SPECIFIC COMMENTS
INTRODUCTION
Please add a reference for making those statements (L. 34, 51,54, 131, 136)
L 43 This study is not the first with a qualitative methodology, please revise the whole manuscript.
L 54 which reactions are going to be reported? reactions in people, policies, government ¿?
L 66-88 Authors describe the 6 stages and the research questions could fit better at the procedure subsection in the methods section. I would suggest describing the evolution of the COVID19 different stages in Poland should be detailed as the reader could understand better the study.
L 99 include the name of the main author of the 3C model
Still in this part, I would suggest authors linking the natural disaster situation and this health pandemic situation.
L 186 please provide the first author of this model
L 199-201 This sentence is no needed:
"However, it needs to be noted that Polizzi and colleagues (12) did not validate the
model in an empirical study but based their recommendations on theoretical considerations and conclusions from previous research."
L 209-211- It seems that some other qualitative studies have been done on COVID 19. Then please review the writing of the whole manuscript as it may not be the first qualitative study. Although, authors could point out their main contribution comparing their study with the previous study: it is a longitudinal study.
L 224-226 The aims or research questions should be in the same line as the results structure:
A) COVID 19 Challenges and how to cope with them over time.
B) How the psychological principles for natural disasters (3c's) could be a reference model to analyse the COVID 19 reactions?
The authors do not mention here in these research questions the 3C's models which should be taken into consideration.
L 219 an "s" is missing previous to reactions.
L 228 Please omit the word research and insert Methods
The divide the content into these subsections:
L 245 google meets is an online video platform not for chat (writing). The authors should clarify this point.
L 246 it is strange to say "use a video camera" when the computers have it already and in google meet you only have to "open" it.
L 254 Please take into account this matter in the limitations sections as those with less than higher education may be in a worse financial situation so this study may be biased in that way.
The sample is 20 participants which were interviewed 6 times.
Table 1- Please explain at the bottom the meaning of
Table 1- Please make a support sentence of why dividing the sample into more or less than 40 years old. One participant with 40 is young or old?
L 276 up to here there were in-depth- interviews…now you write here semi-structured interviews. Please define which was taken into consideration.
L 300-305- after the procedure the data analysis subsection should be mentioned. Could please give us some information about:
It is an inductive, deductive or mixed approach.
• How many pages were analyzed from the transcription?
• How many units of content did you find?
• Did you divide them into dimensions after or previously? To facilitate the analysis. Which criteria were taken?
• Did you find supra or subordinate factors in the analysis?
How did you find an agreement about the units of contents between the 5 researchers?
L 580 please check the spelling as "wanin" is not a word.
Table 2. Could this table be organized with the units of content found in each challenge and ways to cope?
L 821 Should state Table 3 now is Table 2 written.
L 693 This model has been explained before in the introduction please do not repeat the information in the results section.
The question is why this model could be adequate for analyzing the reactions during health pandemic situation?
L 824 Please separate Discussion and conclusions
Within the discussion authors should:
First paragraph: relate the main results with the aims-research questions of the study.
Second: detail and compare each result with previous results
Third: add the limitations of the study
Fourth: add some practical implications of the study
Fith: the final paragraph should be the conclusions.
Right now the discussion is too long in terms of length and the authors within 3 pages only have 8 references.
It could be shortened and more focused on the contribution of the paper.
Reviewer #2: (1) Is the manuscript technically sound, and do the data support the conclusions? [NO]
Three main problems:
First, the authors do not describe how the subjects were recruited, aside from saying it was a purposive sample. This is inadequate. Were there prior relationships between the subjects and the investigators?
Second, more needs to be said about the development of the data themes. The five challenges surely do not capture all the richness of 120 interviews. It would be helpful to hear about variability within the major themes as well as about what minor themes were identified.
Third, the conclusions go beyond the data presented in the results. Statements such as (line 719) “The analysis of the results showed that the first solution (full submission to orders) occurred more often in people with higher COVID-19 anxiety.” are unsupported by data presented in the results. Worse, we are not even told how anxiety was measured. The conclusion is peppered with unsupported statements of this sort, which are testable, but no results have been shown.
I recommend a table or tables showing the emergence of the major themes (concerns) across time and across subject characteristics. This would provide a framework for presenting and testing statements such as the one identified above.
(2) Has the statistical analysis been performed appropriately and rigorously? [NO]
There are appropriate qualitative statistics for testing most, if not all, of the conclusions the authors wish to highlight.
(3) Have the authors made all data underlying the findings in their manuscript fully available? [NO]
Generally, interview data can be anonymized by appropriate redaction of names and other sensitive material. If this is not possible, the code sheets showing the extraction of themes from the interviews would be the next best thing.
(4) Is the manuscript presented in an intelligible fashion and written in standard English? [NO]
There are some problems of English grammar, although these are not any worse than many late drafts by authors whose first language is English.
• E.g.: lines 101, 104-107, 219, 634.
• Table 1. Use of undefined acronym (DINKS).
Reviewer #3: This is a longitudinal, qualitative study on the challenges arising from the COVID-19 pandemic and the way people deal with them. As the pandemic is still ongoing, the impact may yet to be concluded in the background. This is a long article and many parts can be condensed and tightened up. For instance, the description about interviews on page 14 is redundant. Some other themes also seem redundant in some ways. Ways of dealing and change of lifestyle may be considered to be combined.
The authors claimed that none of the studies have employed qualitative methods, but is there any literature of quantitative study on similar topics, as this may serve as a baseline for this study.
There are also some concerns about methodology and results as follows:
1. The authors interviewed 20 participants, six times each, and totaling 120 interviews. The interviewees range from 25-55. Why were participants divided into two age cohorts on the basis of age 40? There were 6 out of 20 interviewers who are over 40. The dividing of the age groups needs clearer reasoning. Particularly, most of citations used as evidence are based on groups under 40 years old.
2. The Interviews were conducted online by 5 female interviewers with experience in Psychology. Does the gender of the interviewers make any difference? The educational background and occupations of the interviewees were included in the demographics, but how this factor may affects the results is not explained.
3. All the interviews were transcribed, but there is no description about the ways for ensuring data accuracy and translation. (I suppose the interview was conducted in Polish?)
1. The authors used quotations of the interviewees to support the thematic points. Some point has 2 or 3 citations, some used only one. As this is already a fairly long article, one more representative citation for each point might be enough? Or, the responses can be integrated into the description of the findings using quotation.
2. Most of citations used as evidence are under aged 40 groups. This requires some further discussion and explanation.
3. The authors may consider restructure the results section and tighten up some findings.
4. Do different age, occupation, lifestyle, even occupation have any impact on how the interviewees experience different restriction.
5. The limitation of this study needs to be described, such as the representativeness of the respondents
Compared with the long presentation of results, the discussion is quite brief. Some parts require further explanation. For instance, p.40 “the study allowed deep understanding to be gained of the difficulties….” is not clear.
The paper ends abruptly. It requires a conclusion section to summarize the findings and its contribution/ or significance.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Cristina López de Subijana
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
12 Jul 2021
Dear Reviewers,
Thank you for your valuable time and useful contribution to our article titled “The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study”. We appreciate the inputs you have given, and we are sure that it will definitely help improve our manuscript.
Please see the "Response to Reviewers" file for detailed information on the changes made and responses to all comments. In general, we have made significant changes to the paper presented. First, we significantly restructured the method description section. We provided additional information about the participant recruitment method, including a description of inclusion criteria that were applied to participant recruitment and a description of how participants were recruited. As suggested, we have described the study procedure and the data analysis process itself in more detail. We have also shortened the description of the results, not limiting the description of the conclusions themselves, but reducing the number of quotations illustrating the obtained data. The discussions and conclusions section has been rewritten - according to your suggestions it includes the main results of the study, their comparison with previous results, limitations of the study, some practical implications of the study. Moreover, the whole article was corrected in terms of language and formatting (correcting errors in table names).
We would like to thank you once again for all your comments and suggestions for changes to our article. We hope that after the changes we have made, the manuscript meets PLOS ONE standards, requirements, and publication criteria, and will appeal to the journal’s readers.
Submitted filename: Response to Reviewers.docx
Decision Letter 1
26 Jul 2021
PONE-D-21-11248R1
Dear Dominika Adamczyk,
Please submit your revised manuscript by four weeks. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
Dear author,
Please address the comments and suggestions asked by the reviewers.
Best of luck
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
Reviewer #2: Partly
3. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #2: N/A
4. Have the authors made all data underlying the findings in their manuscript fully available?
Reviewer #2: Yes
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: Dear Authors,
The manuscript has improved in the way now it is better supported and structured. Still I would suggest authors to shorten the length of the article. Almost fifty pages is too much for a research article. I would suggest to review each part and try to shorten some pages in each section. For example introduction is 5 pages and literature review another 5 pages. Research articles are normally around 3 pages for the whole introduction.
Reviewer #2: From a snowball sample of 20 respondents, the authors collected 115 interviews in six waves between March and October 2020 regarding perceptions of and responses to the COVID-19 pandemic. Themes were extracted from the interviews and organized into five major challenges that the respondents faced during this period. These challenges were found to be consistent with John Reich’s “3-Cs” and theory of resilience in natural disasters.
Generally, this is an interesting, opportunistic use of the pandemic. The topic is not insignificant. The snowball technique of sample development, while it has flaws, is an accepted method for small scale, investigative studies. The interview and data collection methodology, as described, appears to be generally rigorous. The issue of the uniform gender of the interviewers seems to me, given the small sample size, to be less of an issue than the relatively large number of interviewers for the sample. Fortunately, the study includes no sub-group analysis, so these issues become largely irrelevant. There is, inevitably, some danger that the analytic framework espoused by the authors influenced the data collection process, but, given the exploratory nature of the study, this is not a large concern.
The introduction, literature review, motivation for the study, methods, description of the participants, and description of the analytic process are all well done. Table 1 would be more informative if it showed the distribution of subjects over demographic characteristics, rather than listing each subject.
The reporting of the results I find less satisfactory. The methodology describes extracting themes from the interview data. The results report on challenges. Are the five challenges the only themes that were extracted? Are the challenges composed of clusters of themes? Do the challenges capture all the themes identified? By focusing on challenges, are the authors not talking about successful coping behaviors? For example, the subjects’ reactions to the limitations on travel are uniformly portrayed as negative (limitations on freedom, etc.) did none of the subjects perceive this as an appropriate public health measure that gave the subjects some control over the situation? A table showing the count of themes occurrences by study period would be greatly appreciated.
The interpretation of the results in the context of Reich’s framework is totally baffling in that it does not appear to refer to the results at all. There is one mention of one of the challenges in this section. Table 3 refers to some things that might be themes, but without a proper reporting of the themes, we don’t really know and are unable to judge its completeness. Without a better tie to the data, this section should be deleted.
The discussion and conclusion are generally adequate, given my concerns above. The limitations are accurately stated. My greatest concern here is that the process of focusing on concerns has caused the authors to lose sight of successful coping behaviors.
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Author response to Decision Letter 1
31 Aug 2021
Dear Editor and Reviewers,
Thank you once again for your valuable time and useful contribution to our article titled “The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study”. The two most important changes we have made are the removal of the part of the description of the results presenting them in the light of the 3C theory and the significant shortening of the whole article. Please find our answers to the reviewers’ comments below.
Reviewer #1:
• Still I would suggest authors to shorten the length of the article. Almost fifty pages is too much for a research article. I would suggest to review each part and try to shorten some pages in each section. For example introduction is 5 pages and literature review another 5 pages. Research articles are normally around 3 pages for the whole introduction.
- This is the main change we have made in the revised article. We have significantly shortened the text, as suggested by both reviewers.
Reviewer #2:
• Table 1 would be more informative if it showed the distribution of subjects over demographic characteristics, rather than listing each subject.
- In our view, presenting the demographic characteristics of each respondent adds value to the text and shows the diversity of the respondents. However, in line with previous suggestions regarding the length of the text, we have decided to move the table to an appendix.
• The reporting of the results I find less satisfactory. The methodology describes extracting themes from the interview data. The results report on challenges. Are the five challenges the only themes that were extracted? Are the challenges composed of clusters of themes? Do the challenges capture all the themes identified?
- As presented in the text, the manuscript contains only part of the results, as it would be impossible to present all the findings from such a large number of interviews. For example, we do not describe specific changes in emotions here, and some residual information on this topic was removed from the text after the previous round of reviews because it would have been misleading throughout the text.
• By focusing on challenges, are the authors not talking about successful coping behaviors?
• For example, the subjects’ reactions to the limitations on travel are uniformly portrayed as negative (limitations on freedom, etc.) did none of the subjects perceive this as an appropriate public health measure that gave the subjects some control over the situation?
• My greatest concern here is that the process of focusing on concerns has caused the authors to lose sight of successful coping behaviors.
- We understand where these doubts come from, but we cannot write about the positive aspects of the changes described, as they did not appear in our study. The participants perceived these limitations in an unambiguously negative way - perhaps a study conducted over a different period or one in which the participants retrospectively evaluate certain changes would have provided different results. However, in this paper, we describe the experience at the time of the study.
• The interpretation of the results in the context of Reich’s framework is totally baffling in that it does not appear to refer to the results at all. There is one mention of one of the challenges in this section. Table 3 refers to some things that might be themes, but without a proper reporting of the themes, we don’t really know and are unable to judge its completeness. Without a better tie to the data, this section should be deleted.
- After careful consideration, we decided to comply with the above comment and remove the section presenting the results in the light of Reich's theory.
Decision Letter 2
20 Sep 2021
PONE-D-21-11248R2
Dear Dr. Dominika Adamczyk,
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Dear authors,
The article is now accepted.
Best wishes,
Reviewer #1: Dear authors and editor,
The authors have shortenen the article as suggested.
It is present form the article is well structured, written and could be published.
Reviewer #2: I want to thank the authors for their hard work on this article. I would also like to suggest to them that "qualitative methods" refers to certain data collection modalities. There are appropriate statistics to use with qualitative data. Also, their adoption of an entirely narrative form of reporting does little to sharpen or clarify their findings. The article would have more punch if it were less discursive and more focused on the findings. However, I now feel I'm stepping into the role of advisor, which is not necessarily the job of a reviewer.
Acceptance letter
28 Sep 2021
Dear Dr. Adamczyk:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Shah Md Atiqul Haq
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 03 July 2020
Six months of coronavirus: the mysteries scientists are still racing to solve
- Ewen Callaway ,
- Heidi Ledford &
- Smriti Mallapaty
You can also search for this author in PubMed Google Scholar
In late December 2019, reports emerged of a mysterious pneumonia in Wuhan, China, a city of 11 million people in the southeastern province of Hubei. The cause, Chinese scientists quickly determined, was a new coronavirus distantly related to the SARS virus that had emerged in China in 2003, before spreading globally and killing nearly 800 people.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 583 , 178-179 (2020)
doi: https://doi.org/10.1038/d41586-020-01989-z
Ellinghaus, D. et al. Preprint at medRxiv https://doi.org/10.1101/2020.05.31.20114991 (2020).
Long, Q.-X. et al. Nature Med . https://doi.org/10.1038/s41591-020-0965-6 (2020).
Article Google Scholar
Grifoni, A. et al. Cell 181 , 1489–1501 (2020).
Article PubMed Google Scholar
Ni, L. et al. Immunity 52 , 971–977 (2020).
Callow, K. A., Parry, H. F., Sergeant, M. & Tyrrell, D. A. Epidemiol. Infect. 105 , 435–446 (1990).
MacLean, O. A. et al. Preprint at bioRxiv https://doi.org/10.1101/2020.05.28.122366 (2020).
van Doremalen, N. et al. Preprint at bioRxiv https://doi.org/10.1101/2020.05.13.093195 (2020).
Zhou, P. et al. Nature 579 , 270–273 (2020).
Zhou, H. et al. Curr. Biol. 30 , 2196–2203 (2020).
Latinne, A. et al. Preprint at bioRxiv https://doi.org/10.1101/2020.05.31.116061 (2020).
Lam, T. T.-Y. et al. Nature https://doi . org/10.1038/s41586-020-2169-0 (2020).
Zhang, T., Wu, Q. & Zhang, Z. Curr. Biol. 30 , 1346–1351 (2020).
Download references
Reprints and permissions
Related Articles

Postdoctoral Fellow in Biomedical Optics and Medical Physics
We seek skilled and enthusiastic candidates for Postdoctoral Fellow positions in the Biomedical Optical Imaging for cancer research.
Dallas, Texas (US)
UT Southwestern Medical Center, BIRTLab
Associate Professor
J. Craig Venter Institute is conducting a faculty search for Associate Professors position in Rockville, MD and San Diego, CA campuses.
Rockville, Maryland or San Diego, California
J. Craig Venter Institute
Associate Professor position (Tenure Track), Dept. of Computational & Systems Biology, U. Pittsburgh School of Medicine. Please apply by Dec. 2, 2024.
University of Pittsburgh, Pittsburgh
University of Pittsburgh | DCSB
Assistant Professor
Assistant Professor position (Tenure Track), Dept. of Computational & Systems Biology, U. Pittsburgh School of Medicine. Please apply by Dec. 2, 2024.
Independent Group Leader Positions in Computational and/or Experimental Medical Systems Biology
NIMSB is recruiting up to 4 Independent Group Leaders in Computational and/or Experimental Medical Systems Biology
Greater Lisbon - Portugal
NOVA - NIMSB
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine (2021)
Chapter: 8 major findings and research questions, 8 major findings and research questions, introduction.
The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. The significant effect on vulnerable populations, such as essential workers and the elderly, is well documented, as is the devastating effect the COVID-19 pandemic had on the economy, particularly brick-and-mortar retail and hospitality and food services. Concurrently, the deaths of unarmed Black people at the hands of law enforcement officers created a heightened awareness of the persistence of structural injustices in U.S. society.
Against the backdrop of this public health crisis, economic upheaval, and amplified social consciousness, an ad hoc committee was appointed to review the potential effects of the COVID-19 pandemic on women in academic science, technology, engineering, mathematics, and medicine (STEMM) during 2020. The committee’s work built on the National Academies of Sciences, Engineering, and Medicine report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine: Opening Doors (the Promising Practices report), which presents evidence-based recommendations to address the well-established structural barriers that impede the advancement of women in STEMM. However, the committee recognized that none of the actions identified in the Promising Practices report were conceived within the context of a pandemic, an economic downturn, or the emergence of national protests against structural racism. The representation and vitality of academic women in STEMM had already warranted national attention prior to these events, and the COVID-19
pandemic appeared to represent an additional risk to the fragile progress that women had made in some STEMM disciplines. Furthermore, the future will almost certainly hold additional, unforeseen disruptions, which underscores the importance of the committee’s work.
In times of stress, there is a risk that the divide will deepen between those who already have advantages and those who do not. In academia, senior and tenured academics are more likely to have an established reputation, a stable salary commitment, and power within the academic system. They are more likely, before the COVID-19 pandemic began, to have established professional networks, generated data that can be used to write papers, and achieved financial and job security. While those who have these advantages may benefit from a level of stability relative to others during stressful times, those who were previously systemically disadvantaged are more likely to experience additional strain and instability.
As this report has documented, during 2020 the COVID-19 pandemic had overall negative effects on women in academic STEMM in areas such productivity, boundary setting and boundary control, networking and community building, burnout rates, and mental well-being. The excessive expectations of caregiving that often fall on the shoulders of women cut across career timeline and rank (e.g., graduate student, postdoctoral scholar, non-tenure-track and other contingent faculty, tenure-track faculty), institution type, and scientific discipline. Although there have been opportunities for innovation and some potential shifts in expectations, increased caregiving demands associated with the COVID-19 pandemic in 2020, such as remote working, school closures, and childcare and eldercare, had disproportionately negative outcomes for women.
The effects of the COVID-19 pandemic on women in STEMM during 2020 are understood better through an intentionally intersectional lens. Productivity, career, boundary setting, mental well-being, and health are all influenced by the ways in which social identities are defined and cultivated within social and power structures. Race and ethnicity, sexual orientation, gender identity, academic career stage, appointment type, institution type, age, and disability status, among many other factors, can amplify or diminish the effects of the COVID-19 pandemic for a given person. For example, non-cisgender women may be forced to return to home environments where their gender identity is not accepted, increasing their stress and isolation, and decreasing their well-being. Women of Color had a higher likelihood of facing a COVID-19–related death in their family compared with their white, non-Hispanic colleagues. The full extent of the effects of the COVID-19 pandemic for women of various social identities was not fully understood at the end of 2020.
Considering the relative paucity of women in many STEMM fields prior to the COVID-19 pandemic, women are more likely to experience academic isolation, including limited access to mentors, sponsors, and role models that share gender, racial, or ethnic identities. Combining this reality with the physical isolation stipulated by public health responses to the COVID-19 pandemic,
women in STEMM were subject to increasing isolation within their fields, networks, and communities. Explicit attention to the early indicators of how the COVID-19 pandemic affected women in academic STEMM careers during 2020, as well as attention to crisis responses throughout history, may provide opportunities to mitigate some of the long-term effects and potentially develop a more resilient and equitable academic STEMM system.
MAJOR FINDINGS
Given the ongoing nature of the COVID-19 pandemic, it was not possible to fully understand the entirety of the short- or long-term implications of this global disruption on the careers of women in academic STEMM. Having gathered preliminary data and evidence available in 2020, the committee found that significant changes to women’s work-life boundaries and divisions of labor, careers, productivity, advancement, mentoring and networking relationships, and mental health and well-being have been observed. The following findings represent those aspects that the committee agreed have been substantiated by the preliminary data, evidence, and information gathered by the end of 2020. They are presented either as Established Research and Experiences from Previous Events or Impacts of the COVID-19 Pandemic during 2020 that parallel the topics as presented in the report.
Established Research and Experiences from Previous Events
| Leading up to the COVID-19 pandemic, the representation of women has slowly increased in STEMM fields, from acquiring Ph.D.s to holding leadership positions, but with caveats to these limited steps of progress; for example, women representation in leadership positions tends to be at institutions with less prestige and fewer resources. While promising and encouraging, such progress is fragile and prone to setbacks especially in times of crisis (see ). | |
| Social crises (e.g., terrorist attacks, natural disasters, racialized violence, and infectious diseases) and COVID-19 pandemic-related disruptions to workload and schedules, added to formerly routine job functions and health risks, have the potential to exacerbate mental health conditions such as insomnia, depression, anxiety, and posttraumatic stress. All of these conditions occur more frequently among women than men. As multiple crises coincided during 2020, there is a greater chance that women will be affected mentally and physically (see and ). |
___________________
1 This finding is primarily based on research on cisgender women and men.
| Structural racism is an omnipresent stressor for Women of Color, who already feel particularly isolated in many fields and disciplines. Attempts to ensure equity for all women may not necessarily create equity for women across various identities if targeted interventions designed to promote gender equity do not account for the racial and ethnic heterogeneity of women in STEMM (see , , and ). |
Impacts of the COVID-19 Pandemic during 2020
| While some research indicates consistency in publications authored by women in specific STEMM disciplines, like Earth and space sciences, during 2020, several other preliminary measures of productivity suggest that COVID-19 disruptions have disproportionately affected women compared with men. Reduced productivity may be compounded by differences in the ways research is conducted, such as whether field research or face-to-face engagement with human subjects is required (see ). | |
| Many administrative decisions regarding institutional supports made during 2020, such as work-from-home provisions and extensions on evaluations or deliverables, are likely to exacerbate underlying gender-based inequalities in academic advancement rather than being gender neutral as assumed. For example, while colleges and universities have offered extensions for those on the tenure track and federal and private funders have offered extensions on funding and grants, these changes do not necessarily align with the needs expressed by women, such as the need for flexibility to contend with limited availability of caregiving and requests for a reduced workload, nor do they generally benefit women faculty who are not on the tenure track. Furthermore, provision of institutional support may be insufficient if it does not account for the challenges faced by those with multiple marginalized identities (see and ). | |
| Organizational-level approaches may be needed to address challenges that have emerged as a result of the COVID-19 pandemic in 2020, as well as those challenges that may have existed before the pandemic but are now more visible and amplified. Reliance on individual coping strategies may be insufficient (see and ). | |
| The COVID-19 pandemic has intensified complications related to worklife boundaries that largely affect women. Preliminary evidence |
| from 2020 suggests women in academic STEMM are experiencing increased workload, decreased productivity, changes in interactions, and difficulties from remote work caused by the COVID-19 pandemic and associated disruptions. Combined with the gendered division of nonemployment labor that affected women before the pandemic, these challenges have been amplified, as demonstrated by a lack of access to childcare, children’s heightened behavioral and academic needs, increased eldercare demands, and personal physical and mental health concerns. These are particularly salient for women who are parents or caregivers (see ). | |
| During the COVID-19 pandemic, technology has allowed for the continuation of information exchange and many collaborations. In some cases technology has facilitated the increased participation of women and underrepresented groups. However, preliminary indicators also show gendered impacts on science and scientific collaborations during 2020. These arise because some collaborations cannot be facilitated online and some collaborations face challenges including finding time in the day to engage synchronously, which presents a larger burden for women who manage the larger share of caregiving and other household duties, especially during the first several months of the COVID-19 pandemic (see ). | |
| During the COVID-19 pandemic in 2020, some professional societies adapted to the needs of members as well as to broader interests of individuals engaged in the disciplines they serve. Transitioning conferences to virtual platforms has produced both positive outcomes, such as lower attendance costs and more open access to content, and negative outcomes, including over-flexibility (e.g., scheduling meetings at non-traditional work hours; last-minute changes) and opportunities for bias in virtual environments (see ). | |
| During the COVID-19 pandemic in 2020, many of the decision-making processes, including financial decisions like lay-offs and furloughs, that were quickly implemented contributed to unilateral decisions that frequently deviated from effective practices in academic governance, such as those in crisis and equity-minded leadership. Fast decisions greatly affected contingent and nontenured faculty members—positions that are more often occupied by women and People of Color. In 2020, these financial decisions already had negative, short-term effects and may portend long-term consequences (see ). | |
| Social support, which is particularly important during stressful situations, is jeopardized by the physical isolation and restricted social interactions that have |
| been imposed during the COVID-19 pandemic. For women who are already isolated within their specific fields or disciplines, additional social isolation may be an important contributor to added stress (see ). | |
| For women in the health professions, major risk factors during the COVID-19 pandemic in 2020 included unpredictability in clinical work, evolving clinical and leadership roles, the psychological demands of unremitting and stressful work, and heightened health risks to family and self (see ). |
RESEARCH QUESTIONS
While this report compiled much of the research, data, and evidence available in 2020 on the effects of the COVID-19 pandemic, future research is still needed to understand all the potential effects, especially any long-term implications. The research questions represent areas the committee identified for future research, rather than specific recommendations. They are presented in six categories that parallel the chapters of the report: Cross-Cutting Themes; Academic Productivity and Institutional Responses; Work-Life Boundaries and Gendered Divisions of Labor; Collaboration, Networking, and Professional Societies; Academic Leadership and Decision-Making; and Mental Health and Well-being. The committee hopes the report will be used as a basis for continued understanding of the impact of the COVID-19 pandemic in its entirety and as a reference for mitigating impacts of future disruptions that affect women in academic STEMM. The committee also hopes that these research questions may enable academic STEMM to emerge from the pandemic era a stronger, more equitable place for women. Therefore, the committee identifies two types of research questions in each category; listed first are those questions aimed at understanding the impacts of the disruptions from the COVID-19 pandemic, followed by those questions exploring the opportunities to help support the full participation of women in the future.
Cross-Cutting Themes
- What are the short- and long-term effects of the COVID-19 pandemic on the career trajectories, job stability, and leadership roles of women, particularly of Black women and other Women of Color? How do these effects vary across institutional characteristics, 2 discipline, and career stage?
2 Institutional characteristics include different institutional types (e.g., research university, liberal arts college, community college), locales (e.g., urban, rural), missions (e.g., Historically Black Colleges and Universities, Hispanic-Serving Institutions, Asian American/Native American/Pacific Islander-Serving Institutions, Tribal Colleges and Universities), and levels of resources.
- How did the confluence of structural racism, economic hardships, and environmental disruptions affect Women of Color during the COVID-19 pandemic? Specifically, how did the murder of George Floyd, Breonna Taylor, and other Black citizens impact Black women academics’ safety, ability to be productive, and mental health?
- How has the inclusion of women in leadership and other roles in the academy influenced the ability of institutions to respond to the confluence of major social crises during the COVID-19 pandemic?
- How can institutions build on the involvement women had across STEMM disciplines during the COVID-19 pandemic to increase the participation of women in STEMM and/or elevate and support women in their current STEMM-related positions?
- How can institutions adapt, leverage, and learn from approaches developed during 2020 to attend to challenges experienced by Women of Color in STEMM in the future?
Academic Productivity and Institutional Responses
- How did the institutional responses (e.g., policies, practices) that were outlined in the Major Findings impact women faculty across institutional characteristics and disciplines?
- What are the short- and long-term effects of faculty evaluation practices and extension policies implemented during the COVID-19 pandemic on the productivity and career trajectories of members of the academic STEMM workforce by gender?
- What adaptations did women use during the transition to online and hybrid teaching modes? How did these techniques and adaptations vary as a function of career stage and institutional characteristics?
- What are examples of institutional changes implemented in response to the COVID-19 pandemic that have the potential to reduce systemic barriers to participation and advancement that have historically been faced by academic women in STEMM, specifically Women of Color and other marginalized women in STEMM? How might positive institutional responses be leveraged to create a more resilient and responsive higher education ecosystem?
- How can or should funding arrangements be altered (e.g., changes in funding for research and/or mentorship programs) to support new ways of interaction for women in STEMM during times of disruption, such as the COVID-19 pandemic?
Work-Life Boundaries and Gendered Divisions of Labor
- How do different social identities (e.g., racial; socioeconomic status; culturally, ethnically, sexually, or gender diverse; immigration status; parents of young children and other caregivers; women without partners) influence the management of work-nonwork boundaries? How did this change during the COVID-19 pandemic?
- How have COVID-19 pandemic-related disruptions affected progress toward reducing the gender gap in academic STEMM labor-force participation? How does this differ for Women of Color or women with caregiving responsibilities?
- How can institutions account for the unique challenges of women faculty with parenthood and caregiving responsibilities when developing effective and equitable policies, practices, or programs?
- How might insights gained about work-life boundaries during the COVID-19 pandemic inform how institutions develop and implement supportive resources (e.g., reductions in workload, on-site childcare, flexible working options)?
Collaboration, Networking, and Professional Societies
- What were the short- and long-term effects of the COVID-19 pandemic-prompted switch from in-person conferences to virtual conferences on conference culture and climate, especially for women in STEMM?
- How will the increase in virtual conferences specifically affect women’s advancement and career trajectories? How will it affect women’s collaborations?
- How has the shift away from attending conferences and in-person networking changed longer-term mentoring and sponsoring relationships, particularly in terms of gender dynamics?
- How can institutions maximize the benefits of digitization and the increased use of technology observed during the COVID-19 pandemic to continue supporting women, especially marginalized women, by increasing accessibility, collaborations, mentorship, and learning?
- How can organizations that support, host, or facilitate online and virtual conferences and networking events (1) ensure open and fair access to participants who face different funding and time constraints; (2) foster virtual connections among peers, mentors, and sponsors; and (3) maintain an inclusive environment to scientists of all backgrounds?
- What policies, practices, or programs can be developed to help women in STEMM maintain a sense of support, structure, and stability during and after periods of disruption?
Academic Leadership and Decision-Making
- What specific interventions did colleges and universities initiate or prioritize to ensure that women were included in decision-making processes during responses to the COVID-19 pandemic?
- How effective were colleges and universities that prioritized equity-minded leadership, shared leadership, and crisis leadership styles at mitigating emerging and potential negative effects of the COVID-19 pandemic on women in their communities?
- What specific aspects of different leadership models translated to more effective strategies to advance women in STEMM, particularly during the COVID-19 pandemic?
- How can examples of intentional inclusion of women in decision-making processes during the COVID-19 pandemic be leveraged to develop the engagement of women as leaders at all levels of academic institutions?
- What are potential “top-down” structural changes in academia that can be implemented to mitigate the adverse effects of the COVID-19 pandemic or other disruptions?
- How can academic leadership, at all levels, more effectively support the mental health needs of women in STEMM?
Mental Health and Well-being
- What is the impact of the COVID-19 pandemic and institutional responses on the mental health and well-being of members of the academic STEMM workforce as a function of gender, race, and career stage?
- How are tools and diagnostic tests to measure aspects of wellbeing, including burnout and insomnia, used in academic settings? How does this change during times of increased stress, such as the COVID-19 pandemic?
- How might insights gained about mental health during the COVID-19 pandemic be used to inform preparedness for future disruptions?
- How can programs that focus on changes in biomarkers of stress and mood dysregulation, such as levels of sleep, activity, and texting patterns, be developed and implemented to better engage women in addressing their mental health?
- What are effective interventions to address the health of women academics in STEMM that specifically account for the effects of stress on women? What are effective interventions to mitigate the excessive levels of stress for Women of Color?
This page intentionally left blank.
The spring of 2020 marked a change in how almost everyone conducted their personal and professional lives, both within science, technology, engineering, mathematics, and medicine (STEMM) and beyond. The COVID-19 pandemic disrupted global scientific conferences and individual laboratories and required people to find space in their homes from which to work. It blurred the boundaries between work and non-work, infusing ambiguity into everyday activities. While adaptations that allowed people to connect became more common, the evidence available at the end of 2020 suggests that the disruptions caused by the COVID-19 pandemic endangered the engagement, experience, and retention of women in academic STEMM, and may roll back some of the achievement gains made by women in the academy to date.
The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine identifies, names, and documents how the COVID-19 pandemic disrupted the careers of women in academic STEMM during the initial 9-month period since March 2020 and considers how these disruptions - both positive and negative - might shape future progress for women. This publication builds on the 2020 report Promising Practices for Addressing the Underrepresentation of Women in Science, Engineering, and Medicine to develop a comprehensive understanding of the nuanced ways these disruptions have manifested. The Impact of COVID-19 on the Careers of Women in Academic Sciences, Engineering, and Medicine will inform the academic community as it emerges from the pandemic to mitigate any long-term negative consequences for the continued advancement of women in the academic STEMM workforce and build on the adaptations and opportunities that have emerged.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.

IMAGES
COMMENTS
When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell's palsy. "We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.". 3.
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
The sixth question concerns how COVID-19 should be treated and what treatment options should be made available. COVID-19 is a self-limiting disease in more than 80% of patients. Severe pneumonia occurred in about 15% of cases as revealed in studies with large cohorts of patients. The gross case fatality is 3.4% worldwide as of February 25, 2020.
These and related questions are revisited at the end of 2021 to shed light on the roadmap of bringing an end to the pandemic. Keywords: SARS-CoV-2, COVID-19, Pandemic, Endemic, Vaccines, Antivirals. When only slightly more than 80,000 confirmed cases of SARS-CoV-2 infection were reported worldwide and right before COVID-19 was declared a ...
As reported by the CDC, from February 12 to April 2, 2020, of 149,760 cases of confirmed COVID-19 in the United States, 2572 (1.7%) were children aged <18 years, similar to published rates in ...
COVID-19 CLINICAL TRIAL RECOMMENDATIONS-As multiple federal research agencies have demonstrated, it is most ethical and prudent to enroll patients with COVID-19 in clinical trials rather than use clinically unproven therapies. There are multiple ongoing trials, some with adaptive designs, which potentially can quickly answer pressing questions on
Our findings on academic outcomes indicate that COVID-19 has led to a large number of students delaying graduation (13%), withdrawing from classes (11%), and intending to change majors (12%). Moreover, approximately 50% of our sample separately reported a decrease in study hours and in their academic performance.
variation in the e ects of COVID-19 across students. In terms of labor market expectations, on average, students foresee a 13 percentage points decrease in. the probability of. on, a reduction of 2 percent in their reservation wages, a. d a2.3 percent decrease in their expected earn. ID-19 demonstrate that stude.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and viral pathogenesis.
In the case of [COVID-19 vaccines], we had a lot of urgency and all the money was put up, up front. The companies didn't have to find the money for each stage—they were just able to just proceed from the safety study to the effectiveness study very quickly.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and ...
The WHO Covid-19 Research Database was maintained by the WHO Library & Digital Information Networks and was funded by COVID-19 emergency funds. The database was built by BIREME, the Specialized Center of PAHO/AMRO. Its content spanned the time period March 2020 to June 2023. It has now been archived, and no longer searchable since January 2024.
Ask your COVID-19 vaccine questions here. You can also find information related to COVID-19 in these additional resources: Printable Q&A, "COVID-19 vaccines: What you should know" English | Spanish | Japanese. "Look at Each Vaccine: COVID-19 Vaccine" webpage. Animations: "How COVID-19 Viral Vector Vaccines Work" and "How mRNA Vaccines ...
WHO and its partners are committed to accelerating the development of COVID-19 vaccines while maintaining the highest standards on safety. Vaccines go through various phases of development and testing - there are usually three phases to clinical trials, with the last one designed to assess the ability of the product to protect against disease, which is called efficacy.
COVID-19 is the disease caused by the SARS-CoV-2 coronavirus. It usually spreads between people in close contact. COVID-19 vaccines provide strong protection against severe illness and death. Although a person can still get COVID-19 after vaccination, they are more likely to have mild or no symptoms. Anyone can get sick with COVID-19 and become ...
Although, there is a variety of modeling approaches that have been proposed so far for prediction and evaluation of the COVID-19 disease, there are more questions that can still be answered. There are some related works that sensitivity analysis used in their studies [13,17]. They used this technique only for special variables and parameters.
The new virus was identified to be a novel Coronavirus and was thus initially named 2019-nCoV; later, it was renamed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) , and the disease it causes is now referred to as Coronavirus Disease-2019 (COVID-19) by the WHO. The virus was suspected to have begun its spread in the Huanan seafood ...
Background The WHO has raised concerns about the psychological consequences of the current COVID-19 pandemic, negatively affecting health across societies, cultures and age-groups. Methods This online survey study investigated mental health, subjective experience, and behaviour (health, learning/teaching) among university students studying in Egypt or Germany shortly after the first pandemic ...
Raise research question about covid-19 - 14388557. answered Raise research question about covid-19 See answers Advertisement Advertisement erickamozo07 erickamozo07 Answer: what is covid 19? where did it come from? ... Brainly.ph. PL: Brainly.pl ...
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed ...
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6 th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages.
Six months of coronavirus: the mysteries scientists are still racing to solve. From immunity to the role of genetics, Nature looks at five pressing questions about COVID-19 that researchers are ...
Major Findings and Research Questions INTRODUCTION. The COVID-19 pandemic, which began in late 2019, created unprecedented global disruption and infused a significant level of uncertainty into the lives of individuals, both personally and professionally, around the world throughout 2020. The significant effect on vulnerable populations, such as ...