An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.21(3); 2022 Oct

Psychiatric diagnosis and treatment in the 21st century: paradigm shifts versus incremental integration
Dan j. stein.
1 South African Medical Research Council Unit on Risk and Resilience in Mental Disorders, Department of Psychiatry and Neuroscience Institute, University of Cape Town, Cape Town South Africa
Steven J. Shoptaw
2 Division of Family Medicine, David Geffen School of Medicine, University of California Los Angeles, Los Angeles CA, USA
Daniel V. Vigo
3 Department of Psychiatry, University of British Columbia, Vancouver BC, Canada
4 Centre for Global Mental Health, Health Service and Population Research Department, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London UK
Pim Cuijpers
5 Department of Clinical, Neuro and Developmental Psychology, Amsterdam Public Health Research Institute, Vrije Universiteit Amsterdam, Amsterdam The Netherlands
Jason Bantjes
6 Alcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town South Africa
Norman Sartorius
7 Association for the Improvement of Mental Health Programmes, Geneva Switzerland
8 Department of Psychiatry, University of Campania “L. Vanvitelli”, Naples Italy
Psychiatry has always been characterized by a range of different models of and approaches to mental disorder, which have sometimes brought progress in clinical practice, but have often also been accompanied by critique from within and without the field. Psychiatric nosology has been a particular focus of debate in recent decades; successive editions of the DSM and ICD have strongly influenced both psychiatric practice and research, but have also led to assertions that psychiatry is in crisis, and to advocacy for entirely new paradigms for diagnosis and assessment. When thinking about etiology, many researchers currently refer to a biopsychosocial model, but this approach has received significant critique, being considered by some observers overly eclectic and vague. Despite the development of a range of evidence‐based pharmacotherapies and psychotherapies, current evidence points to both a treatment gap and a research‐practice gap in mental health. In this paper, after considering current clinical practice, we discuss some proposed novel perspectives that have recently achieved particular prominence and may significantly impact psychiatric practice and research in the future: clinical neuroscience and personalized pharmacotherapy; novel statistical approaches to psychiatric nosology, assessment and research; deinstitutionalization and community mental health care; the scale‐up of evidence‐based psychotherapy; digital phenotyping and digital therapies; and global mental health and task‐sharing approaches. We consider the extent to which proposed transitions from current practices to novel approaches reflect hype or hope. Our review indicates that each of the novel perspectives contributes important insights that allow hope for the future, but also that each provides only a partial view, and that any promise of a paradigm shift for the field is not well grounded. We conclude that there have been crucial advances in psychiatric diagnosis and treatment in recent decades; that, despite this important progress, there is considerable need for further improvements in assessment and intervention; and that such improvements will likely not be achieved by any specific paradigm shifts in psychiatric practice and research, but rather by incremental progress and iterative integration.
Psychiatry has over the course of its history been characterized by a range of different models of and approaches to mental disorder, each perhaps bringing forward some advances in science and in services, but at the same time also accompanied by considerable critique from within and without the field.
The shift away from psychoanalysis in the latter part of the 20th century was accompanied by key scientific and clinical advances, including the introduction of a wide range of evidence‐based pharmacotherapies and psychotherapies for the treatment of mental disorders. However, there has also been an extensive critique of pharmacological and cognitive‐behavioral interventions, whether focused on concerns about their “medical model” foundations, or emphasizing the need to build community psychiatry and to scale up these treatments globally 1 .
In the 21st century, global mental health has become an influential novel perspective on mental disorders and their treatment. This emergent discipline builds on advances in cross‐cultural psychiatry, psychiatric epidemiology, implementation science, and the human rights movement 2 . Global mental health has given impetus to a wide range of mental health research as well as to clinical strategies such as task‐shifting, with evidence that these are effective in diverse contexts and may be suitable for roll‐out at scale 3 . It is noteworthy, however, that global mental health has in turn been critiqued for inappropriate and imperial exportation of Western constructs to the global South 4 .
Psychiatric nosology has been a particular focus of both advances in and critique from the field. The 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐III) was paramount, providing an approach that attempted to eschew different models of etiology, focusing instead on reliable diagnostic constructs 5 . These constructs became widely used in epidemiological studies of mental illness, in psychiatric research on etiology and treatment, as well as in daily clinical practice throughout the world. The most recent editions of the DSM (DSM‐5) and of the International Classification of Diseases (ICD‐11) by the World Health Organization (WHO) have drawn on and given impetus to a considerable body of work in nosological science 6 , 7 .
Early on, psychoanalytic psychiatry criticized DSM diagnostic constructs for missing core psychic phenomena. With increasing concerns that these constructs have insufficient validity, neuroscientifically informed psychiatry has put forward approaches to assessing behavioral phenomena that emphasize laboratory models 8 . Despite the growing body of nosology science instantiated by the DSM‐5 and ICD‐11, many have argued for new paradigms of classification and assessment – e.g., the Research Domain Criteria (RDoC), the Hierarchical Taxonomy of Psychopathology (HiTOP) and other novel statistical approaches, and digital phenotyping.
Where do things stand currently with regard to psychiatry's models of and approaches to mental disorder? What are current clinical practices? What novel perspectives are being proposed, and what is the evidence base for them? To what extent will newly introduced models of clinical intervention, such as shared decision‐making or transdiagnostic psychotherapies, and novel approaches in psychiatric research, such as the use of “big data” in neurobiological research and treatment outcome prediction, have transformative impact for clinical practice in the foreseeable future?
In this paper we discuss proposed shifts to clinical neuroscience and personalized pharmacotherapy, innovative statistical approaches to psychiatric nosology and assessment, deinstitutionalization and community mental health care, the scale‐up of evidence‐based psychotherapy, digital phenotyping and digital therapies, and global mental health and task‐sharing approaches. We chose these novel perspectives because they have achieved particular prominence recently, and because many have argued that they will significantly impact psychiatric practice and research in the future.
We consider the extent to which proposed transitions from current practices to these novel perspectives reflect hype or hope, and whether they represent paradigm shifts or iterative progress in psychiatric research and practice. Although the contrast between hype and hope is itself likely oversimplistic, with many newly proposed models and approaches in psychiatry representing neither of these polar extremes, our point of departure is that false promises of paradigm shifts in health care may entail significant costs, while hope may justifiably be considered an important virtue for health professions 9 . We begin with a brief consideration of current models and approaches in psychiatric practice.
CURRENT MODELS AND APPROACHES IN PSYCHIATRY
Current practice in psychiatry varies in different parts of the world, but there are some important universalities. The duration and depth of training in psychiatry during the undergraduate and postgraduate years also differ across countries, but typically a general training in medicine and surgery is followed by specialized training in psychiatry, with exposure to both inpatient and outpatient settings. Globally, inpatient psychiatry focuses predominantly (but not exclusively) on severe mental disorders such as schizophrenia and bipolar disorder, while outpatient psychiatry focuses predominantly (but again not exclusively) on common mental disorders such as depression, anxiety disorders, and substance use disorders. In inpatient settings, psychiatrists are often leaders of a multidisciplinary team, with the extent and depth of this multidisciplinarity dependent on local resources. There are differences in sub‐specialization across the globe, but in many countries recognized sub‐specialties include child and adolescent psychiatry, geriatric psychiatry, and forensic psychiatry 10 .
A particularly important shift in the 20th century has been the process of deinstitutionalization, particularly in high‐income countries. Thus, there has been a decrease of bed numbers in specialized psychiatric hospitals, but an increase of these numbers in general medical hospitals, with variable strengthening of community services. It has been argued that, when it comes to mental health services, all countries are “developing”, since there is a relative underfunding of such services in relation to the burden of disease 1 .
Currently, the two major classification systems in psychiatry are the DSM‐5 and the ICD‐11. The DSM system is more commonly used by researchers, while the ICD is a legally mandated health data standard. The operational criteria and diagnostic guidelines included in the DSM‐III, the ICD‐10, and subsequent editions of the manuals have exerted considerable influence on modern psychiatry. They not only increase reliability of diagnosis, but also have clinical utility, since they provide clinicians with an approach to conceptualizing disorders and to communicating about them 11 , 12 . They have also played a key role in research, ranging from studies of the neurobiology of mental disorders, through to studies of interventions for particular conditions, and on to clinical and community epidemiological surveys.
However, there has also been considerable critique of the reliance of modern psychiatry on the DSM and the ICD. The notion that psychiatric diagnosis is itself “in crisis” has come both from within the field and from external critics. Two somewhat contradictory critiques have been that in daily practice the DSM and ICD criteria or guidelines are seldom applied formally by clinicians, and that over‐reliance on those criteria or guidelines leads to a checklist approach to assessment that ignores relevant symptoms and important contextual issues falling outside the focus of the nosologies. Additional key critiques have been that psychiatric diagnoses lack scientific validity, and that current nosologies are biased by influences such as that of the pharmaceutical industry 13 , 14 .
When thinking about etiology, many clinicians and researchers currently default to a biopsychosocial model acknowledging that a broad range of risk and protective factors are involved in the development and perpetuation of mental disorders. This model was introduced by G. Engel in an attempt to move from a reductionistic biomedical approach to include also psychological and social dimensions 15 . The model has important strengths insofar as it takes a systems‐based approach that considers a broad range of variables influencing disease onset and course, and attends to both the relevant biomedical disease and the patient's experience of illness 16 .
Nevertheless, the biopsychosocial approach has received significant critique. In particular, it has been argued that the biomedical model critiqued by Engel is a straw man, and that the biopsychosocial approach is overly eclectic and vague. By saying that all mental disorders have biological, psychological and social contributory factors, we are unable to be specific about any particular condition, and to target treatments accordingly 17 , 18 . While there are few data available on how rigorously psychiatrists consider the range of risk and protective factors in clinical work, a review of the research literature indicates ongoing work on multiple “difference‐makers”, distributed across a wide range of categories 19 .
Psychiatrists are trained to provide a range of both pharmacological and psychological interventions. However, data from psychiatric practice networks and from epidemiological surveys indicate that there has been a growing emphasis on pharmacotherapy interventions 20 , albeit with some exceptions 21 . Furthermore, the number of psychiatrists varies considerably from country to country, and from region to region within any particular country 22 . While primary care practitioners are also trained to deliver mental health treatments, and indeed provide the bulk of prescriptions for mental disorders in some regions, there is considerable evidence of underdiagnosis and undertreatment of such conditions in primary care settings.
Indeed, despite the development of a range of evidence‐based pharmacotherapies and psychotherapies in the last several decades, current data point to both a treatment gap and a research‐practice gap in mental health. The treatment gap refers to findings that, across the globe, many individuals with mental disorders do not have access to mental health care 23 . The research‐practice gap, also known as the “science‐practice” or “evidence‐practice gap”, refers to differences between treatments delivered in standard care and those supported by scientific evidence 24 . In particular, clinical practitioners have been criticized for employing an eclectic approach to choosing interventions, for not sufficiently adhering to evidence‐based clinical guidelines, and for not employing measurement‐based care.
The treatment gap and the research‐practice gap are of deep concern, given evidence of underdiagnosis and undertreatment, of misdiagnosis and inappropriate treatment, and of inadequate quality of treatment 25 , 26 . There are, however, some justifiable reasons for a gap between practice and research, including that the evidence base is relatively sparse for the management of treatment‐refractory and comorbid conditions, the relative lack of pragmatic “real‐world” research trials in psychiatry, and the possibly modest positive impact of guideline implementation on patient outcomes 27 , 28 . Indeed, several scholars have emphasized that including clinical experience and addressing patient values are key components of appropriate decision‐making 27 , 29 .
Considerably more research is needed to inform our knowledge of current psychiatric practice and its outcomes. Data from psychiatric practice networks have been useful in providing fine‐grained information in some settings, but much further work is warranted along these lines 30 . Data from randomized controlled trials indicate that psychiatric treatments are as effective as those in other areas of health care, but further evidence should be acquired using pragmatic designs in real‐world contexts 31 . Epidemiological data from across the globe suggest that individuals with mental disorders who received specialized, multi‐sector care are more likely than other patients to report being helped “a lot”, but there is an ongoing need for more accurate estimates of effective treatment coverage globally 32 .
In the interim, evidence of the treatment gap and the research‐practice gap in current mental health services has given impetus to the development of a number of novel diagnostic and treatment models and approaches, ranging from clinical neuroscience through to global mental health. Some of these models and approaches have achieved particular prominence in recent times, with proponents arguing that they will significantly impact psychiatric practice and research in the future. At times advocates for these perspectives and proposals have limited aims, while at other times they speak of paradigm shifts that will drastically alter or wholly reshape current clinical practices 33 , 34 , 35 , 36 . We next consider a number of these perspectives and proposals in turn.
CLINICAL NEUROSCIENCE AND PERSONALIZED PHARMACOTHERAPY
A key shift in 20th century psychiatry, at least in some parts of the world, was from psychoanalytic to biological psychiatry. The serendipitous discovery of a range of psychiatric medications in the mid‐20th century, and advances in molecular, genetic and neuroimaging methods, propelled this shift. More recently, terms such as clinical neuroscience, translational psychiatry, precision psychiatry, and personalized psychiatry have emerged, helping to articulate the conceptual foundations for a proposed psychiatric perspective aiming to replace or significantly augment current practice 37 , 38 , 39 .
The proposed paradigm of clinical neuroscience rests in part on a critique of current standard approaches. First, in terms of diagnosis, it has been argued that the DSM and ICD constructs are not sufficiently based on neuroscience 40 . Thus, for example, particular symptoms, which may involve quite specific neurobiological mechanisms, may be present across different diagnoses. Conversely, research findings demonstrate that there is considerable overlap of genetic architecture across different DSM and ICD mental disorders 41 . If current diagnostic constructs are not natural kinds, then arguably attempts to find specific biomarkers and develop targeted treatments for them are doomed to fail 42 , 43 .
The proposed new paradigm views psychiatry as a clinical neuroscience, which should rest on a firm foundation of neurobiological knowledge 44 . With advances in neurobiology, we will be better able to target relevant mechanisms and develop specific treatments for mental disorders. Neuroimaging and genomic research offer opportunities for personalizing psychiatric intervention: those with specific genetic variants may require tailoring of psychopharmacological intervention, while particular alterations in neural signatures may be used to choose a therapeutic modality or to alter parameters for neurostimulation.
The RDoC project, developed by the US National Institute of Mental Health (NIMH), has provided an influential conceptual framework for this proposed new paradigm 8 . Whereas the DSM‐III relied on the Research Diagnostic Criteria (RDC) in order to operationalize mental disorders, the RDoC project emphasizes domains of functioning that are underpinned by specific neurobiological mechanisms. Disruptions in these domains may lead to various symptoms and impairments. Domains of functioning are found across species, and their neurobiological substrates are sufficiently known to allow translational neuroscience, or productive movement from bench to bedside and back. Each domain of functioning can be assessed with specific laboratory paradigms.
The RDoC matrix initially included five domains of functioning and several “units of analysis” for assessing these domains (see Figure 1 ) 45 . Each domain in turn comprises a number of different “constructs” (or rows of the matrix): these were included on the basis of evidence that they entail a validated behavioral function, and that a neural circuit or system implements the function. Different “units of analysis” (or columns of the matrix) can be used to assess each construct: the center column refers to brain circuitry, with three columns to the left focusing on the genes, molecules and cells that comprise circuits, and three columns to the right focusing on circuit outputs (behavior, physiological responses, and verbal reports). A column to list paradigms is also included.

The Research Domain Criteria matrix (from Cuthbert 45 )
The RDoC matrix is intended to include two further critical dimensions for integrating neuroscience and psychopathology, i.e. developmental trajectories and environmental effects 45 . Thus, from an RDoC perspective, many mental illnesses can be viewed as neurodevelopmental disorders, with maturation of the nervous system interacting with a range of external influences from the time of conception. Several key “pillars” of the RDoC framework, including its translational and dimensional focuses 8 , have been emphasized.
Anxiety, for example, can be studied in laboratory paradigms, and ranges from normal responses to threat through to pathological conditions. Indeed, a clinical neuroscience approach has contributed to the reconceptualization of several anxiety and related disorders 46 , 47 , 48 and to the introduction of novel therapeutic approaches for these conditions 49 . Further, work on stressors has usefully emphasized that environmental exposures become biologically embedded, with early adversity associated to alterations in both body and brain that occur irrespective of the DSM diagnostic category 50 , 51 .
The NIMH has linked the RDoC to funding applications, and this framework has given impetus to a range of clinical neuroscience research. Translational research will certainly advance our empirical knowledge of the neurobiology of behavior and of psychopathology. The RDoC has also prompted conceptual work related to the neurobiology of mental disorders, and the development of measures and methods. Indeed, to the extent that constructs in the RDoC matrix have validity as behavioral functions, and map onto specific biological systems such as brain circuits, the project summarizes key advances in the field, and provides useful guidance for ongoing research.
At the same time, it is relevant to note important limitations of the RDoC approach. First, the RDoC seems less an entirely new paradigm than a re‐articulation of existing ideas in biological psychiatry. Certainly, the importance of cross‐diagnostic neurobiological investigations of domains of functioning has long been emphasized 52 . Second, the neurobiology of any particular RDoC construct, such as social communication, may be enormously complex, so that alternative approaches to delineating the mechanisms involved in particular mental disorders may provide greater traction 53 . Third, methods used to measure domains in the RDoC framework may not be readily available to clinicians. The further one moves from academic centers to the practice of psychiatry in primary care settings around the globe, the less relevant an RDoC framework may be to daily clinical work.
Personalized and precision psychiatry are important aspirations of clinical neuroscience. The notion that psychiatric interventions need to be rigorously tailored to each individual patient makes good sense, given the substantial inter‐individual variability in the genome and exposome of those suffering from psychiatric disorders, as well as the considerable variation in response to current psychiatric interventions. With advances in genomic methods and findings, and the possibility that whole genome sequencing will become a standard clinical tool, with polygenic risk scores readily available, it is particularly relevant to consider the application of genomics to optimizing pharmacological and other treatments 54 .
The Clinical Pharmacogenetic Implementation Consortium (CPIC) has already provided a range of clinical guidelines for drugs used in psychiatry. For example, a CPIC guideline recommends that, given the association between the HLA‐B*15:02 variant and Stevens‐Johnson syndrome as well as toxic epidermal necrolysis after exposure to carbamazepine and oxcarbazepine, these drugs should be avoided in patients who are HLA‐B*15:02 positive and carbamazepine‐ or oxcarbazepine‐naïve 55 . The evidence base that pharmacogenomic testing improves outcomes is gradually beginning to accumulate, and recent guidelines have started to recommend a number of specific tests 56 .
From an RDoC perspective, particular domains of functioning involve specific neural circuits, which are in turn modulated by a range of molecular pathways. One notable recent development in these fields has been a focus on “big data”. Large collaborations in basic and clinical sciences have been established, which provide sufficient statistical power to advance the field in important ways.
Examples of such “big data” collaborations are the Enhancing Neuroimaging Meta‐analysis Consortium (ENIGMA) 57 , which includes tens of thousands of scans from across the world, and the Psychiatric Genetics Consortium (PGC) 58 , which includes hundreds of thousands of DNA samples from across the globe. The work of ENIGMA and PGC has been at the cutting edge of scientific research in psychiatry, and has provided crucial insights into mental disorders. Certain biological pathways, such as immune and metabolic systems, appear to play a role across different mental disorders, and genomic methods have contributed to delineating causal and modifiable mechanisms underlying these conditions 58 , 59 . At the same time, it must be acknowledged that to date few findings from this work have been successfully translated into daily clinical practice 36 , 54 , 60 .
In summary, clinical neuroscience provides an important conceptual framework that may generate some useful clinical insights, and that may be particularly helpful in guiding clinical research. This framework has contributed to the reconceptualization of a number of mental disorders, and has on occasion contributed to the introduction of new therapies 61 . As clinical neuroscience generates new evidence, this may be incorporated in nosological systems in the future. There are already good arguments for including advances in this area in the curriculum of psychiatric training, and for updating clinicians on progress in the field 62 .
At the same time, there are currently few biomarkers with clinical utility in psychiatry, and methods such as functional neuroimaging and genome sequencing, which are key for future advances in frameworks such as the RDoC, are not readily available to or useful for practicing clinicians 63 . The vast majority of clinical neuroscience publications appear to have little link to clinical practice. At best, therefore, we can expect that ongoing advances in clinical neuroscience will contribute to clinical practice via iterative advances in our conceptualization of mental disorders, and via the ongoing introduction of new insights and new molecules that emerge from laboratory studies.
Indeed, the claim that any particular laboratory, neuroimaging or genetic finding will dramatically change clinical practice should raise a red flag. The neurobiology of behaviors and psychopathology is complex, reproducibility of findings is an ongoing important issue, and clinical neuroscience investigations only occasionally impact clinical practice 64 . Indeed, we should be careful not to be over‐optimistic about clinical neuroscience constituting a paradigm shift. Neurobiological research has not to date provided a rich pipeline of accurate biomarkers for mental disorders, nor speedily found new molecular entities that are efficacious for these conditions, and we cannot, for example, expect that the DSM and ICD will be replaced by the RDoC anytime soon.
NOVEL STATISTICAL APPROACHES TO PSYCHIATRIC NOSOLOGY, ASSESSMENT AND RESEARCH
Disease taxonomies are particularly complex, and may not be able to follow historical models of scientific taxonomies, which have defined all elements of a given set. An often‐used example of the latter taxonomies is the periodic table of elements. Another venerable example is Linnaeus’ Systema Naturae and the resulting nomenclature of biological species. The periodic table of elements has the simplicity of small numbers plus the hard and fast rules of chemistry, while the Systema Naturae , despite having to deal with an ever‐expanding number of entities, is arguably based on direct observation of beings. In contrast, a disease taxonomy deals with thousands of unruly entities (versus 118 elements), which cannot be directly observed, apprehended or dissected (as animals or plants can).
Despite these challenges, disease taxonomies have sought to provide a shared, evidence‐based, clinically meaningful, comprehensive classification that is informed by etiology and therapeutics. The notion that underneath the observable syndrome lies a causal entity, that we should investigate and treat, lies at the heart of the practice of medicine 65 . Such “disease entities” have specific characteristics that make them clear and distinct from others (i.e., presentation, etiology, response to intervention), are transparent to the clinician, and are well‐grounded in evidence.
Psychiatry has long faced the challenges of producing a causal nosology that is able to direct treatment 66 . Pinel developed the first comprehensive nosology for people with severe mental disorders, along with moral treatment, the first therapeutic framework of the scientific era 67 . Soon afterward, Kahlbaum, Kraepelin and Bleuler laid a firm groundwork for clinical psychiatry through close observation and systematic documentation of the natural history of severe mental illness. Arguably, Freud further advanced nosology and therapeutics by focusing on a different set of disorders (usually milder but much more prevalent), which he termed neuroses (to highlight their difference from psychoses ), and by developing the concept and practice of psychotherapy. These frameworks gave impetus to subsequent advances in our understanding of and interventions for mental disorders.
Perceptions of insufficiently rapid and robust advances in treatments have led to criticism of current nosology 68 . In particular, the DSM and ICD have been criticized for overly focusing on reliability at the expense of validity. In this view, schizophrenia and bipolar disorder may be genuine disease entities, but our syndromic definition lacks specificity, and there are likely different causal pathways that lead to clinically meaningful subtypes of these disorders. Major depressive disorder, on the other hand, is likely to be a hodgepodge of mood syndromes, some non‐dysfunctional (i.e., non‐disorders) or non‐specific (i.e., combining depressive with anxiety symptoms), including only a few true but potentially diverse disease entities (e.g., melancholia, psychotic depression). And when it comes to, say, personality disorders, the disease‐entity concept is even more distant, and the search for new approaches is seen as particularly key.
One such novel paradigm is the HiTOP. This proposes a hierarchical framework that, based on the observed covariation of dimensional traits, is able to identify latent super‐spectra and spectra (supra‐syndromes), syndromes (our current disorders), and lower‐level components 69 , 70 , 71 , 72 . In this conceptual framework, a dimension consists of a continuous space in which an element occurs in differences of degree, but not of kind, between the normal and the pathological.
The HiTOP relies on factor analysis and related techniques, which tap into the covariation of observable traits to identify an unobserved, common factor that, once included in the model, explains the covariation 73 . Costa and McCrae's studies leading to the identification of five personality domains were a prime example of this approach. There is a common underlying reason that explains a person's tendency to worry about many things, think that the future looks bleak, be bothered by intrusive thoughts, and be grouchy 74 . That unobserved factor was conceptualized as “neuroticism”, and fully explains the covariation of these traits in any given individual. A similar approach to the study of childhood psychopathology led to the binary characterization of an “internalizing” and an “externalizing” dimension to childhood disorders 75 .
The HiTOP paradigm seeks to leverage these well‐established lines of research to develop a data‐driven nosology that is free from the theory‐driven dead weight built into current approaches. The key conceptual departure relies on the premise that, since evidence points towards psychopathological dimensions existing on a continuum, disorders should be similarly conceptualized, and nosology should move away from a focus on categorical entities. Instead of insisting on questionable boundaries, this approach proposes dimensional thresholds, which are empirically determined and do not involve any difference “in kind”. By grouping co‐occurring symptoms within the same syndrome, and non‐co‐occurring symptoms separately, within‐disorder heterogeneity is reduced. And by assigning overlapping syndromes to the same unobserved spectra, excess comorbidity found when using current categories is explained.
The resulting dimensional classification, the proponents of HiTOP argue, is consistent with evidence on risk factors, biomarkers, course of illness, and treatment response 69 . Figure 2 shows a schema of the proposed new nosology. An intriguing element of this approach is what has been termed “p”, or general psychopathology factor (at the top of Figure 2 ). In addition to super‐spectra and spectra, factor analysis ultimately points towards the existence of a single latent trait that would explain all psychopathology, comparable to the well‐established “g” factor for general intelligence 76 , 77 .

The Hierarchical Taxonomy of Psychopathology (HiTOP) model (from Krueger et al 69 )
If dimensional nosologies seek to overturn categorical ones, network analysis arguably aims to overturn both, insofar as it posits that the notion of an unobserved underlying construct is unwarranted, be it a categorical disease entity or a dimensional latent factor 78 . The network approach to psychopathology holds that mental disorders can be conceived as “problems in living”, and are best understood at the level of what is observable. Rather than by latent entities, disordered states are fully explained by the interaction between signs and symptoms (the “nodes” of the networks). These interactions are themselves the causal elements (i.e., a symptom causes another symptom, then another symptom, and so on), and a disorder is simply an alternative “stable state” of strongly connected symptom networks (as opposed to the “normal” steady state of health).
A conceptualization of disorders as “problems in living” does away with the medical notion of a disease as an underlying causal entity. In this view, deficiencies in our understanding of etiology are not necessarily due to diagnostic limitations or insufficiently accurate models for the unobserved but, on the contrary, may be due to our lack of attention to the surface, i.e. the symptoms themselves, which go about reinforcing each other while we are distracted by peeking behind imaginary curtains.
Unlike dimensional approaches, proponents of network analysis disavow any nosological hierarchy (super‐spectra, spectra, disorders, symptoms, etc.), and posit that there is only one level, that of symptoms, which can all cause and reinforce one another. Of note, network analysis posits that symptoms (or interacting nodes) can be activated by disturbances emerging from the “external field” (i.e., “external” to the symptom network, not necessarily to the body or person), such as the loss of a loved one (which may activate the symptom depressed mood, setting in motion the depressive network) or a brain abnormality (which may activate the symptom hallucination, setting in motion the psychotic network).
Whether an individual develops a new strongly connected network of symptoms in the face of a stressor depends on his/her “vulnerability”, which is based on the network's connectivity. Given a dataset with symptoms and/or signs for disorders, a network analysis can quantify all relevant nodes and interactions, including the frequency and co‐occurrence of symptoms, the strength and number of their associations, and the centrality of each symptom (i.e., the sum of the interactions with other nodes). Empirical work using network analysis potentially provides rigorous accounts of vulnerability to and evolution of mental disorders.
A number of other novel statistical approaches have also been put forward as potentially facilitating paradigm shifts in psychiatry. Psychiatry has long relied on linear models to explore associations and develop theories of risk and resilience for mental disorders. However, causal inference methods have now been developed in statistics, and provide new approaches to delineating causal relationships 79 . In genetics, Mendelian randomization provides an innovative method for addressing the causal relationships of different phenotypes, and has increasingly been employed in psychiatric research 80 . Neural networks and deep learning have played a key role in advancing artificial intelligence, and are increasingly being applied to the investigation of psychiatric disorders, including prediction of treatment outcomes 81 , 82 , 83 , 84 . While many view such techniques as allowing iterative advances, some are persuaded that they allow an entirely novel perspective and so constitute a paradigm shift in the field 85 .
Work on the HiTOP and network analysis has been important and useful in a number of respects. First, unbiased data‐driven approaches have an important role in strengthening the relevant science, whether of nosology, or of areas such as genetics. A focus on fear‐related anxiety disorders, for example, offers interesting avenues for research, both from a neuroscience and a therapeutic perspective, and network analysis has contributed insights into the presentation of some disorders 48 . Second, some dimensional constructs, including those of internalizing and externalizing disorders, have clinical utility. The “distress” subfactor reflects the notable overlap between depressive and anxious symptoms, and the association between symptoms from two different disorders (e.g., major depressive disorder and generalized anxiety disorder) may be stronger than associations “within” each disorder 86 . Third, the use of novel statistical methods to draw causal inferences has provided important insights into risk for and resilience to mental disorders 59 . For instance, network analysis offers a nuanced foundation for targeted treatment of the core symptoms of some mental disorders (e.g., reframing specific automatic thoughts through cognitive‐behavioral interventions).
At the same time, such approaches have important limitations. Notably, categorical and dimensional approaches are interchangeable: any dimension can be converted into a category, and any category can be converted into a dimension 87 . There is no reason to conceptualize mental disorders as exclusively dimensional. In physics, matter itself is sometimes better conceived in terms of waves (a dimensional concept) and other times in terms of particles (a categorical one). Similarly, in psychiatry, a pluralist approach that allows the employment of a range of different dichotomous and continuous constructs seems appropriate 88 , 89 .
Remarkably, the HiTOP employs DSM terminology at the disorder level. “Number‐driven” psychopathologies and their resulting nosologies may not necessarily lead to a shift in constructs grounded in long‐standing clinical practice and research. In the same vein, network analysis offers a useful model to understand the distribution of symptoms, identify therapeutic targets, and explain the effectiveness of symptomatic interventions. However, network analysis does not specify the particular levels of explanation that underlie a network structure; so, while it may be a useful organizing framework, it is unclear that it will provide novel insights into underlying etiological mechanisms.
Consider a set of patients presenting with the following symptoms, among others: headaches, vomiting and seizures. A factor analysis may point towards a latent factor explaining the covariation among them. Any clinician will know that, unless the cause is substance‐related, the first thing to rule out in these patients is a space‐occupying lesion in the brain, and that this unobserved element is only an intermediary that can itself be caused by multiple disease entities, most notably hemorrhage, infection and cancer. The fact that a latent factor may explain the covariation between anxious and depressive symptoms does not exclude that these symptoms are in fact caused by very different dysfunctions (upstream of the latent factor), and that other accompanying symptoms will hold the clue to the ultimate cause (just as high blood pressure, fever or weight loss would hold clues for a space‐occupying lesion syndrome).
Relatedly, consider the focus of the HiTOP on a general psychopathology factor “p”. This focus can be countered by a reductio ad absurdum argument suggesting that a latent factor “i” explains the covariation of any and all human illnesses. Given some datasets, we may find that the covariation of nausea, hemoptysis, jaundice and myocardial infarction is explained by a latent dimensional trait. We may choose to call this “sybaritism”, dimensionally distributed between one extreme (temperance) and another (debauchery). Readers who focus on values‐based medicine might well criticize the choice of words here, while those focused on evidence‐based medicine are unlikely to be persuaded that an approach that elides disease entities will advance studies of psychiatry, gastroenterology and cardiology 29 .
In a latent class analysis of depressive and anxious syndromes, Eaton et al 90 proposed an approach called “guided empiricism”, whereby they explicitly imposed a theory‐driven structure on various statistical models, compared them, and obtained the best empirical fit. Perhaps using such explicitly theory‐driven constraints is preferable to accepting hidden theoretical constructs. For example, rather than assuming that all the DSM depressive and some anxiety/stress related disorders are explained by a latent factor called “distress”, itself under a spectrum called “internalizing disorders”, a theory‐grounded structure can be imposed on the models to try to identify what is driving the overlap. Indeed, it should be emphasized that purportedly “number‐driven” nosologies all have built‐in qualitative components: from the questions in the scales used to measure traits, to the labels chosen for the latent factors, these classifications are theory‐laden.
In summary, the solution to nosologic challenges in psychiatry may not reside in the building of new nosologies or psychopathologies from scratch 91 , nor in the banishment of the “disease entity” concept, but rather in continuing the humble, laborious, iterative work of systematic clinical observation, painstaking research, and creative thinking, while purposefully comparing dimensional, categorical and hybrid models applied to the same datasets. The claim that a “quantitative” nosology is somehow “atheoretical” raises a red flag: where theory is seemingly absent, it is often hidden. Instead, we need thoughtful and explicit combinations of theories grounded on clinical practice and confirmatory quantitative evidence. Hypothesis formulation is a qualitative, creative, theory‐laden endeavour, while quantitative research helps us discard false theories and refine what we know (by proving hypotheses wrong or quantifying associations).
Similarly, etiological and treatment challenges in psychiatry are unlikely to be addressed merely by the employment of larger and larger datasets, using more and more sophisticated statistical methods. Certainly, big data consortia and sophisticated statistical analyses have yielded valuable insights into the nature of psychiatric disorders. However, it is important to recognize the limitations of any empirical dataset and any analytic method, as well as the value of a wide range of complementary research designs and statistical approaches – including the age‐old single‐case study, which may sometimes provide clinical insights that outweigh those from big data analyses 92 .
Indeed, the claim that a new statistical, bioinformatic or computational method will provide entirely novel insights that enable a paradigm shift in psychiatry should again raise a red flag. Furthermore, where solutions reside within a black box, there is ongoing uncertainty about the extent to which they will be able to provide clinically useful assistance 93 , 94 . Thoughtful and explicit combinations of existing and novel research designs and statistical methods should be employed, with the aim of achieving iterative and integrative progress in our diagnosis and treatment of psychiatric disorders.
DEINSTITUTIONALIZATION AND COMMUNITY MENTAL HEALTH CARE
The last 70 years have seen a seismic shift in models of mental health care delivery around the world. The first half of the 20th century was dominated by the growth of psychiatric hospitals, particularly in high‐income Western countries. By 1955, there were 558,239 severely mentally ill people living in psychiatric hospitals in the US, with a total population of 164 million at the time 95 . In the years that followed, there was a significant reduction in psychiatric hospital bed numbers in many high‐income countries, as part of a trend that came to be known as deinstitutionalization. In the UK, the US, Australia, New Zealand and countries in Western Europe, there was an 80‐90% reduction in psychiatric hospital beds between the mid‐1950s and the 1990s 96 .
Deinstitutionalization refers to the downscaling of large psychiatric institutions and the transition of patients into community‐based care. This is said to include three components: the discharge of people residing in psychiatric hospitals to care in the community, the diversion of new admissions to alternative facilities, and the development of new community‐based specialized services for those in need 97 . More recently, a focus in community‐based care has also been the development of models for integrating mental health into primary care, as well as of shared decision‐making and recovery approaches 98 . To the extent that these models propose new ways of addressing mental illness, as well as extensive scale‐up of community‐based services, many would argue that they constitute a crucial paradigm shift.
Deinstitutionalization was driven by three main forces. First, the introduction of new medications made it increasingly possible for people with severe and enduring mental disorders such as schizophrenia and bipolar disorder to live reasonably well in community settings. Second, the mushrooming of psychiatric hospitals had come with high costs, and deinstitutionalization was seen by many governments as a cost‐saving strategy. Third, the growth of the human rights movement in the 1950s and 1960s generated increasing public concern about practices in psychiatric institutions, including involuntary care. Films such as One Flew over the Cuckoo's Nest drew public attention to the conditions in those facilities and provided support to the idea that people living with mental disorders should have a choice over the nature and locus of their care. This trend was reinforced by research demonstrating that community‐based models of care, including for people with severe mental disorders, could be delivered effectively, in a manner that was more acceptable to service users, and in some cases less costly 97 .
However, in many regions of the world, these developments have not actually occurred. Particularly in many post‐colonial low‐income countries, for example in sub‐Saharan Africa and South Asia, large psychiatric hospitals have been left behind by departing administrations, and have remained the main locus of care. In these countries, there has been little substantial deinstitutionalization, and very limited scaling up of community‐based and primary care mental health services 22 . In low‐income countries, there were 0.02 psychiatric beds per 100,000 population in 2001, and this increased to 1.9 beds per 100,000 population in 2020.
The success of deinstitutionalization programmes in transitioning to community‐based care has been highly varied around the world. In some countries, such as Italy, legislation has mandated the establishment of community‐based services, and consequently these services have been widely implemented, although with substantial variation across the country 99 . In many other countries, funding did not follow people who were discharged from psychiatric hospitals into community settings. For example, in many parts of the US, deinstitutionalization has been associated with a burgeoning population of homeless mentally ill and mentally ill prisoners 95 .
In Central and Eastern Europe, even with recent reforms, studies have criticized the uneven pace of deinstitutionalization, the lack of investment in community‐based care, and the “reinstitutionalization” of many people with severe mental illness or intellectual disability 100 . In a tragic case in South Africa, deinstitutionalization of 2,000 people with severe mental illness or intellectual disability from the Life Esidimeni facility into unlicensed and unregulated community organizations led to the death of over 140 people, sparking a public outcry and a national enquiry by the Human Rights Commission 101 .
Importantly, deinstitutionalization has been associated with “revolving door” patterns of care, in which people are discharged from hospital after admission for an acute episode, but do not have adequate care and support in the community, and therefore relapse and need to be readmitted. Indeed, readmission rates have been an important indicator for service managers to monitor in the post‐deinstitutionalization era, and the focus of several intervention studies 102 .
The WHO has advocated for the development of community‐based services for mental disorders for many decades. In the early 2000s, it produced a set of guidelines for countries to develop national mental health policies, plans and services 103 . This included the now widely cited “optimal mix of services” to guide countries on how to balance hospital‐ and community‐based care. This model proposed a pyramid structure, in which specialist psychiatric inpatient care represents only a small proportion of services at the apex of the pyramid, and is supported by psychiatric services in general hospitals, specialist community outreach, primary care services, and self‐care at the base of the pyramid. Others have developed similar “balanced care” models 104 .
The 21st century has also seen the development of models for integrating mental health into primary care, such as collaborative care models 105 . These latter initially focused on managing people with comorbid depression and other chronic diseases. Subsequently this work has been expanded to include other mental disorders, through models in which a mental health specialist provides support to non‐specialist health care providers, who are the main point of contact for people needing care. The WHO has endorsed this approach, particularly through its flagship mhGAP programme, which provides clinical guidelines for the delivery of mental health care through non‐specialist health care platforms in primary care and general hospital settings 106 . The mhGAP Intervention Guide has now been implemented in over 100 countries.
In parallel, the latter part of the 20th century and early 21st century have seen the rapid development of shared decision‐making and recovery approaches to mental health care. Shared decision‐making involves clinicians and people with mental disorders working together to make decisions, particularly about care needs, in a collaborative, mutually respectful manner 98 . This approach is consistent with an emphasis on human rights, as well as on the importance of patients’ lived experience, explanatory models and specific values, and clearly deserves support 107 , 108 . Recovery models have challenged traditional roles of “patients” to reframe recovery as a way of living a satisfying, hopeful life that makes a contribution even within the limitations of illness 109 . The recovery movement has been highly influential, is now incorporated into mental health policies, and has shaped the design of mental health systems in several countries 109 .
Yet, despite the strong scientific and ethical principles supporting community‐based care, collaborative care and moves towards shared decision‐making and recovery approaches, there remain major challenges, and the proposed paradigm shift remains to a large extent aspirational. While community care models have been developed, tested and shown to be effective in landmark studies, there are few cases of countries systematically investing in these models at scale, in a manner that substantially influences the mental health of populations. In addition, although there are apparent advantages to approaches such as shared decision‐making, a wide range of barriers across individual, organizational and system levels have been reported 110 , and implementation remains limited in mental health care 98 .
Indeed, it has been noticed that the agreement about the concept of shared decision‐making among stakeholders is only superficial 98 . After all, clinicians may not support this approach if it leads to patients being more empowered, but less adherent to treatment recommendations. This example raises broader questions about community‐based care models: is the failure to systematically scale up these models just due to a lack of political will and related scarcity of resources, or are there fundamental concerns with the model? Our view is that both of these may be true.
There is certainly a lack of political will and investment. Despite the courageous campaigning by people with lived experience for their rights to make decisions about their care, together with the robust evidence of improved outcomes associated with community‐based collaborative care models, governments often remain indifferent 1 . In 2020, 70% of total government expenditure on mental health in middle‐income countries was allocated to mental hospitals, compared to 35% in high‐income countries 22 . These differences need to be viewed in the context of massive global inequities in governments’ commitments to mental health more broadly. While high‐income countries spend US$ 52.7 per capita on mental health, low‐income countries spend US$ 0.08 per capita 22 .
On the other hand, it may also be the case that community‐based care does not go far enough in addressing the social determinants of mental health. While many community‐based care models focus on individuals with a mental disorder and their immediate family, very few address the fundamental structural drivers of mental illness in populations, such as inequality, poverty, food insecurity, violence, and hazardous living conditions 111 , 112 . Successful community‐based mental health services arguably require the existence of viable communities.
The strategy of deinstitutionalization was founded on the premise that communities can provide a safe, supportive environment in which people with severe mental illness can thrive. In countries marked by high levels of poverty, inequality, civil conflict and domestic violence, this is certainly not the case. Advocating for community‐based care requires addressing the fundamental social injustices which precipitate and sustain mental illness in populations.
Furthermore, community‐based service planners may have not gone far enough in considering demand‐side drivers of mental health care. For example, in many low‐ and middle‐income countries, traditional and faith‐based healers continue to be major providers of care for people with severe mental disorders, due to the scarcity of mainstream mental health professionals, and shared beliefs about the causes and treatments of such conditions.
The effectiveness and cost‐effectiveness of collaborative shared care models with traditional and faith‐based healers has been documented in Ghana and Nigeria 113 . Similarly, the possibility of addressing demand‐side barriers by implementing a community informant detection tool, based on local idioms of distress and vignettes to identify people with various mental health conditions, has been demonstrated in Nepal 114 . These innovations from low‐ and middle‐income countries provide potential lessons for high‐income countries in developing collaborative care models that are aligned with the belief systems of mental health care users and address demand‐side barriers to care.
In summary, despite the development of community‐based services, collaborative care, shared decision‐making and recovery models, a paradigm shift towards the implementation of well‐functioning and effective community mental health care around the globe has not occurred. A red flag should be raised when plans for community‐based services are under‐resourced (for example, not providing sufficient human resources to do the work), or are over‐optimistic about implementation (for example, overlooking important barriers to shared decision‐making) 115 .
Nevertheless, community‐based models have many strengths, and should be incorporated into attempts to iteratively improve clinical practices and society responses to mental disorder. Indeed, it has been argued that the shift to community‐based services has not been a sudden change, but rather the culmination of a slow, gradual, evolutionary development, which has old historical roots and will hopefully continue over time 116 . Efforts to strengthen community‐based approaches around the world are needed to consolidate and extend the advances that have been achieved.
Taken together, the slow transition from institutional to community‐based mental health care is partly attributable to the failure of governments in low‐, middle‐ and high‐income countries to adequately invest in such care – to mandate the funding to follow people with mental disorders into their communities and provide them with the support and choices they need to live productive meaningful lives – and strategies are needed to persuade them to do so. But, perhaps to an equally important degree, there are shortcomings in models of community care, with unrealistic expectations of a dramatic paradigm shift.
CBT AND THE SCALE‐UP OF EVIDENCE‐BASED PSYCHOTHERAPY
Since its development in the 1970s, cognitive behavioral therapy (CBT) has been at the core of an important shift in clinical practice towards the use of evidence‐based psychotherapies. Hundreds of randomized controlled trials have examined the effects of CBT for a wide range of mental disorders, including depression, anxiety disorders, substance use disorders, bipolar disorder, psychotic disorders, somatoform disorders, eating disorders, personality disorders, and also other conditions, such as anger and aggression, chronic pain, and fatigue 117 . CBT has also been tested across age groups and specific target groups, such as women with perinatal conditions and people with general medical disorders 117 .
Several other types of psychotherapy have also been rigorously investigated, and even psychotherapies that had not traditionally been explored using randomized controlled trials, such as psychoanalytically oriented therapies and experiential therapies, have now also been tested using such methods 118 , 119 , 120 . Nevertheless, CBT is by far the best examined type of psychotherapy and therefore dominates the transition of the field towards the use of evidence‐based psychotherapies 121 .
CBT is highly consistent with a neurobiological model of mental disorders, insofar as it focuses on symptom reduction, improvement in functioning, and remission of the disorder. Furthermore, the literature on the neurobiological bases of behavioral and cognitive interventions has become increasingly sophisticated 122 , 123 , and a more recent literature on process‐based CBT aligns well with the focus of RDoC on transdiagnostic mechanisms 124 . CBT can therefore be readily combined with neurobiologically oriented approaches, especially pharmacotherapy.
However, despite the strength of the evidence and its compatibility with other evidence‐based interventions, CBT has not been integrated into mental health systems globally. In many countries, it is still often seen as a reductionist approach that does not tackle the real underlying problems. Psychoanalytic approaches remain dominant, for example, in France and in Latin America 125 .
In low‐ and middle‐income countries, psychotherapies in general are often not available for people suffering from mental disorders, due to lack of resources and trained clinicians. Even in high‐income countries such as the US, the uptake of psychotherapies has declined since the 1990s 20 , while the use of antidepressant medication has increased considerably 126 , despite the fact that most patients prefer psychotherapy over pharmacotherapy 127 .
In most treatment guidelines, CBT is recommended as a first‐line treatment for several mental disorders. However, the actual implementation of such guidelines in routine care has been consistently shown to be suboptimal 128 , 129 , 130 . In addition, when CBT is employed, it is unclear whether therapists actually use it as detailed in standardized treatment protocols, or whether they combine it with other approaches.
The Increasing Access to Psychological Therapies (IAPT) program in the UK represents the most ambitious attempt to address the barriers faced by evidence‐based psychotherapy, with scaling up of CBT across an entire country. The main goal of the program was to massively increase accessibility to evidence‐based psychotherapies for individuals suffering from common mental disorders, such as depression and anxiety disorders.
An important argument for massively scaling up evidence‐based therapies was economic. Depression and anxiety disorders often start during the working age, and therefore the economic costs associated with them are large, due to production losses and costs of welfare benefits. If these conditions are treated timeously, costs of treatment are balanced by increased productivity and reduced welfare costs 131 . A global return on investment analysis confirmed this assumption cross‐nationally, indicating that every invested US dollar would result in a benefit of 2.3 to 3 dollars when only economic costs are considered, and 3.3 to 5.7 dollars when the value of health returns is included 132 . Hence, the hope was that IAPT would pay for itself.
The IAPT model has a number of key features 133 . First, patients can be referred by a general practitioner or another health professional, but can also be self‐referred. People with depression, generalized anxiety disorder, mixed anxiety/depression, social anxiety disorder, post‐traumatic stress disorder (PTSD), panic disorder, agoraphobia, obsessive‐compulsive disorder, and health anxiety receive a person‐centered assessment that identifies the key problems, and an agreed‐upon course of treatment is defined 131 .
Second, IAPT works according to a stepped‐care model. Patients are first treated with an evidence‐based low‐intensity intervention, typically a self‐help intervention based on CBT. Only if this is not appropriate or patients do not recover, they receive a high‐intensity psychological treatment. Low‐intensity therapies are delivered by “psychological well‐being practitioners” who are trained to deliver guided self‐help interventions, either digitally, by telephone, or face to face. High‐intensity therapies are delivered by therapists who are fully trained in CBT or other evidence‐based interventions.
Third, the therapies offered by IAPT are those recommended by the UK National Institute for Health and Care Excellence (NICE). When the NICE recommends different therapies for a mental disorder, patients are offered a choice of which therapy they prefer. This means that IAPT does not only deliver CBT, although a recurring criticism has been that the program is overly focused on that type of psychotherapy.
Fourth, outcome data are routinely collected in IAPT. Patients are asked to fill in various validated questionnaires before each session, so that clinicians can review the outcomes and use them in treatment planning.
Between April 1, 2019 and March 31, 2020, 1.69 million patients were referred to IAPT, of whom 1.17 million started treatment, with 606 thousand completing treatment, and 51% of them reporting recovery. The proportion of those recovered, however, is substantially lower (26%) when it is calculated based on those who started treatment (assuming that dropouts did not recover), and it has been argued that IAPT outcomes have been reported in an overly positive way 134 , 135 .
An important issue is that the outcomes vary considerably across IAPT services. In 2015/2016, the lowest recovery rate was 21% and the highest was 63%. There is some evidence that recovery rates are higher with an increasing number of sessions and more patients stepping up to more intensive therapy 136 . Other variables that are associated with better outcomes include shorter waiting times, lower number of missed appointments, and a greater proportion of patients who go on with treatment after assessment 137 .
A recent systematic review and meta‐analysis of the IAPT program identified 60 open studies, of which 47 could be used to pool pre‐post outcome data 138 . Large pre‐post treatment effect sizes were found for depression (d=0.87, 95% CI: 0.78‐0.96) and anxiety (d=0.88, 95% CI: 0.79‐0.97), and a moderate effect for functional impairment (d=0.55, 95% CI: 0.48‐0.61).
The IAPT program arguably represents the state‐of‐the‐art for implementation of evidence‐based psychotherapy in routine clinical care. Indeed, it has served as a model for the development of similar programs in other countries 138 , including Australia 139 , Canada 140 , Norway 141 , and Japan 142 . More broadly, IAPT indicates recognition of the importance of mental health and of the allocation of sufficient resources to treatment of mental disorders, as well as acknowledgement of the importance of psychotherapies and their role in addressing mental disorders.
There are other large scale implementation programs of CBT, especially in digital mental health care. For example, MoodGYM 143 , an online CBT program for depression, had acquired over 850,000 users by 2015. Psychological task‐sharing interventions developed by the WHO, especially Problem Management Plus, have been tested in several randomized trials and are now being implemented in low‐ and middle‐income countries on a broad scale 144 , 145 . However, the IAPT program is still the largest systematic implementation program of psychotherapies across the world.
Given the ambitiousness of IAPT, with extensive and rigorous roll‐out across an entire country, it seems reasonable to raise the key question of whether this program has had real‐world impacts, including a reduction in the disease burden of mental disorders. A first issue, however, is that comparison of IAPT with other treatment services would require a community intervention trial in which people are randomized to either IAPT or “regular” mental health care. Such a trial has not been conducted and probably never will be. Thus, although it is possible to claim on the basis of outcome data from routine care that other services are as effective as IAPT 146 , or that IAPT services may not provide interventions that match the level of complexity of the problems of patients 147 , it is difficult to validate such claims.
A second issue is whether any mental health treatments, including IAPT, are truly capable of reducing the disease burden of mental disorders. A key modeling study has estimated that current treatments only reduce about 13% of the disease burden of mental disorders at a population level 148 . In optimal conditions, in which all those with a mental disorder receive an evidence‐based treatment, this percentage can be increased to 40%. So, even under optimal conditions of 100% uptake and 100% evidence‐based treatments, reduction of disease burden is not expected to be more than 40%. This is true for IAPT as well as other programs disseminated on a broad scale.
The limited ability of current treatments to reduce the disease burden of mental disorders raises the so‐called “treatment‐prevalence paradox” 149 . This refers to the fact that clinical treatment rates have increased in the past decades, while population prevalence rates of mental disorders have not decreased. Increased availability of treatments could shorten episodes, prevent relapses, and reduce recurrences, in turn leading to lower point prevalence estimates of depression, but this has not transpired. Most meta‐analyses indicate stable prevalence rates or even small increases in prevalence, despite increased uptake of services 150 and the demonstrated efficacy of psychiatric treatments 31 .
There are several possible explanations for this “treatment‐prevalence paradox” 149 . First, it is possible that prevalence rates of depression have dropped, but that at the same time incidence has increased due to societal changes. Second, it is possible that prevalence rates have dropped, but that emotional distress has been more often diagnosed as a depressive disorder over the past decades, thereby masking the drop. Third, it is possible that prevalence rates have not dropped, because treatments may not be as effective as the field would like 151 . Indeed, treatment effects may be overestimated in trials due to publication bias, selective outcome reporting, use of inappropriate control groups, or the allegiance effect. Moreover, treatments may not benefit chronic depressive patients, or treatments may have iatrogenic effects that block natural recovery and prolong depressive episodes 152 .
Taken together, the development of evidence‐based psychotherapies has been a remarkable step forward for psychiatry, and the scale‐up of such effective psychotherapies in IAPT and other large‐scale implementation programs has contributed to consolidating this advancement. That said, the several criticisms of IAPT suggest that it is by no means a panacea. Instead, the implementation of evidence‐based psychotherapies is arguably best conceptualized as representing incremental progress. The impact of evidence‐based treatments on the disease burden of mental disorders currently appears to be modest; and the time horizons for introduction of interventions that are notably more successful is unclear.
DIGITAL PHENOTYPING AND DIGITAL THERAPIES
Rapid technological advances and the expansion of the Internet have spurred the development and widespread use of a host of digital devices with the potential to transform psychiatric research and practice 153 . Indeed, the fourth industrial revolution and the nudge towards telepsychiatry by the COVID‐19 pandemic have already revealed that digital technologies provide novel opportunities to improve psychiatric diagnosis, expand the delivery of mental health care, and collect large quantities of data for psychiatric research 154 , 155 .
There are many examples of how these advances have enabled digital solutions in psychiatry 156 , 157 . To name a few, virtual reality can facilitate exposure therapy for phobias and PTSD 158 , chatbots can deliver remote CBT anonymously day‐and‐night 159 , computer analysis of closed circuit television (CCTV) images can identify suicide attempts in progress at suicide hot‐spots 160 , voice and facial recognition software may enhance psychiatric diagnosis 161 , 162 , wearable devices may enable real‐time monitoring and evaluation of patients 163 , analyses of human‐computer interaction may detect manic and depressive episodes in real‐time 164 , and suicide risk may be assessed by analysis of social media posts 165 .
Furthermore, the widespread use of digital medical records, the collection of vast quantities of data from individuals via smart devices, the ability to link multiple databases, and the use of machine learning algorithms have redefined the use of big data in psychiatry with the promise of overcoming the failures of conventional statistical methods and small samples to capture the underlying heterogeneity of psychiatric phenotypes 81 , 82 , 83 . The ability to access, store and manipulate data, together with the use of machine learning algorithms, promises to advance the practice of individualized medicine in psychiatry by allowing matching of patients with the most appropriate therapies 81 , 82 , 83 .
Smartphone use is now ubiquitous even in remote and resource‐constrained environments across the globe 166 , making these devices a powerful medium to improve access to psychiatric care 167 . Smartphones are already being used to deliver interventions for common mental disorders 168 , 169 , 170 , 171 , and more than 10,000 mental health apps are available in the commercial marketplace 172 . There is considerable potential to turn smartphones into cost‐effective and cost‐efficient treatment portals by literally placing mental health interventions in the hands of the 6,378 billion people who own these devices (i.e., 87% of the world's population), many of whom do not currently have access to mental health care.
As communication devices, smartphones can be used to facilitate peer support, deliver personalized messages, provide access to psychoeducational resources, and facilitate timely referrals to appropriate in‐person clinical care 153 . The communication capabilities of smartphones have enabled the expansion of telepsychiatry via high‐quality low‐cost voice and video calls 173 , with evidence indicating that the use of video conferencing is not inferior to in‐person psychiatric consultations 174 .
Because smartphones are equipped with a range of sensors and the ability to store and upload data, they can be easily used to collect real‐time active data (i.e., data which the user deliberately and actively provides in response to prompts). Active data collected via smartphones are already being used in psychiatry for ecological momentary assessments, cognitive assessments, diagnosis, symptom monitoring, and relapse prevention 175 , 176 . Beyond these clinical applications, smartphones are also powerful tools for data collection in psychiatric research 177 , 178 .
Digital devices, including smartphones and wearables, can also collect and store a host of passive data (that is, data generated as a by‐product of using the device for everyday tasks, without the active participation of the user) with near zero marginal costs. These passive data have been likened to fingerprints or digital footprints. They provide objective continuous longitudinal measures of individuals’ moment‐to‐moment behavior in their natural environments and could be used to develop precise and temporally dynamic markers of psychiatric illness, a practice known as digital phenotyping 155 , 179 .
If digital phenotyping delivers on its promises, it will enable continuous inexpensive surveillance of mental disorders in large populations, early identification of at‐risk individuals who can then be nudged to access psychiatric treatment, and early identification of treatment failure to prompt timely individualized treatment decisions 180 . These potential applications are important, given the dearth of accurate real‐time psychiatric surveillance systems in many parts of the world, individuals’ reluctance to seek treatment at the early stages of psychiatric illness, and the high rates of treatment failure which necessitate timely adjustments to management.
Identifying digital markers for mental disorders is, however, not without potential pitfalls, that will need to be mapped and navigated before digital phenotyping can realize its full potential. There are still unanswered questions about the sensitivity, reliability and validity of smartphone sensors for health monitoring and diagnosis 181 . Furthermore, there appears to be a bias in measurement of everyday activities from smartphone sensors, because of variations in how people use their devices 182 . It still remains to be seen if actuarial models developed from population level digital footprints are clinically useful at the level of individual patients, as well as how digital phenotyping can be meaningfully integrated into routine clinical practice, and how patients will respond to and accept passive monitoring of their day‐to‐day activities 180 , 183 .
Digital solutions are not without shortcomings, and a digital intervention is not necessarily better than no intervention 184 , 185 , 186 . Reviews of the quality and efficacy of mental health apps indicate that there is often little evidence to support the effectiveness of direct‐to‐consumer apps 184 , 185 , 186 . Even when mental health apps seem to be useful, data indicate that many of them suffer from high rates of attrition and are not used long enough or consistently enough to be effective 187 .
Concerns about data privacy and security are a significant obstacle to expanding the use of digital technologies in psychiatric practice and research 188 , 189 . Psychiatry is often concerned with deeply personal, sensitive, and potentially embarrassing information, that requires secure data storage and stringent privacy safeguards. The risks associated with collecting and storing digital mental health information need to be clearly articulated in terms that patients understand, so that they can provide informed consent. Privacy policies in digital solutions such as smartphone apps are unfortunately often written in inaccessible language and “legalese”, making them incomprehensible to many users 189 , and there is as yet insufficient regulation of mental health apps and no minimum safety standards 188 .
While digital technology use has increased across the globe, there are ongoing inequalities in the access to these technologies within and between countries 166 . The rapid digitalization of psychiatry may unintentionally exacerbate health inequalities if digital mental health solutions cannot be shared 190 . Psychiatry will need to grapple with thorny questions about how to share digital technologies with those most in need of access to mental health care, and how to develop digital solutions for culturally diverse resource‐constrained environments. High data costs, unstable Internet connections, and bandwidth limitations can create logistical constraints on the utilization of digital mental health solutions in low‐income countries 191 .
The development of digital mental health solutions has typically been driven by the information technology industry and commercial interests 172 . On the other hand, the demand for mental health apps has been largely driven by consumers through social media, personal searches, and word of mouth, rather than professional recommendations 192 . Commercialization of health care and the repositioning of patients as customers has certainly created some efficiencies in health care delivery 193 . However, the profit motive is not always aligned with good patient care, as illustrated by the recent opioid crisis 194 .
Ensuring that clinicians are part of the process of digitalization of psychiatry will entail training them to understand, use and develop digital technologies; establishing ethical guidelines for the use of these technologies; ensuring independent evaluation of the effectiveness of digital interventions by researchers who have no commercial interest in the products; and protecting patient safety by ensuring that the claims made about the benefits of digital solutions are supported by robust evidence.
Emerging evidence suggests that screen time may be associated with mental health problems, although most of the work in this area focuses on children and adolescents 195 , 196 , 197 . While research is mostly cross‐sectional, there are a small number of longitudinal studies showing that screen time has small to very small effects on subsequent depressive symptoms, and that these associations depend on device type and use 198 , 199 . If screen time is bad for mental health, would it be wise to promote the use of digital mental health interventions that entail more time online or in front of a screen? This is not an easy question to answer, and the answer is likely not a simple yes or no.
The challenge is to think about how digitizing psychiatry can be balanced with a careful understanding of the potential for digital devices to harm mental health. Few interventions in psychiatry are without potential side effects, and it would be naïve to think that digital ones are different. As with any psychiatric treatment, the prescription of digital interventions needs to be accompanied with consideration of the contraindications, advice about how to use the intervention to its maximum benefit, and warnings about potential side effects and how to manage them. To enable this we require data, which we do not yet have, about the contraindications and side effects of digital interventions 188 .
We already have evidence to show that digital technologies can be at least as effective as traditional practices in making a psychiatric diagnosis, identifying appropriate individualized interventions, and teaching psychological skills such as mindfulness and attentional training 180 , 200 , 201 . Yet, most clinicians would likely agree that psychiatric practice is fundamentally relational and that most mental illnesses have an interpersonal dimension. The increasing use of technology in psychiatry will change the relationship between physician and patient in ways that we probably do not yet understand and cannot anticipate.
How technology is utilized in psychiatry will be a function of how central we think relationships are in diagnosis and treatment, and whether or not we see digital technologies as primarily a tool to enhance the therapeutic relationship, or simply a conduit to deliver content or collect and process information 202 . Theories will need to be developed to conceptualize and understand the digital therapeutic relationship, while we hold in mind the potential to harness technology to deepen the relationship between clinicians and patients. Indeed, evidence suggests that digital interventions are most effective when they have at least some person‐to‐person interaction 179 , 200 .
Digital technologies may change the way psychiatry is practiced, but to date much of the research in this area has been experimental, with proof‐of‐concept and clinical trials in highly controlled settings using very small samples 172 . The translational potential of these technologies has not yet been realized, and we still have some way to go to bring digital advances in mental health “from code to clinic” 172 . There are relatively few examples of digital technologies other than teleconferencing being used routinely in everyday real‐world psychiatric practice, and there is an urgent need for pragmatic trials and translational research to understand the barriers to adoption and implementation of new technologies 203 . The attitudes of clinicians and patients towards digital solutions in psychiatry and their perceptions of the effectiveness and safety of these devices are important determinants of how widely new technologies will be adopted.
Taken together, the science is still too young to let us know the extent to which the introduction of digital technologies will truly constitute a paradigm shift in psychiatric diagnosis and treatment, and whether these technologies will deliver on their promise to reduce the burden of disease caused by mental disorders. The available evidence gives cause for optimism and suggests that these technologies could assist in iteratively progressing the science and practice of psychiatry. However, there are many red flags when it comes to digital psychiatry, including overpromising with regards to efficacy and overlooking the human relationship. In order for iterative progress to happen, we will need continuous critical reflection, with an ongoing emphasis on equitable access, appropriate regulation, and quality assurance 204 .
GLOBAL MENTAL HEALTH AND TASK‐SHARING
The concept of global health emerged in the aftermath of World War II, when cross‐national organizations were needed to coordinate health efforts, particularly against infectious diseases 205 . The WHO was established in 1948, and became a key advocate for global health, exemplifying the key pillars of this approach, including the recognition that health is a public good requiring support from all sectors of the governments, that health involves a continuum ranging from wellness to illness, and that the determinants of health are biological, sociocultural and environmental 206 . Global health saw the protection of human rights as a central concern of all action concerning health, and expected that action to improve health includes the formulation of working policies addressing upstream social determinants of health, and a strengthening of health services 207 .
With growing recognition of the burden of non‐communicable diseases, including mental, neurological and substance use disorders, global mental health became an important focus. B. Chisholm, a psychiatrist who was the first WHO Director General, introduced the mantra “No health without mental health” 208 . An early 4x4 model of non‐communicable diseases emphasized the comorbidity of cardiovascular diseases, diabetes, cancer and respiratory diseases with tobacco use, unhealthy diet, physical inactivity and harmful alcohol use as risk factors for these conditions. A later 5x5 approach has emphasized that these non‐communicable diseases are commonly comorbid with mental disorders, and that childhood adversity is an important common risk factor 209 .
Over the past several decades, global mental health has become a significant discipline, with specific departments established at several leading universities, textbooks and journals devoted to the subject, and significant support for research obtained from funders 210 . In addition to a focus on mental health as a public good and human right, on mental health as entailing a continuum and a life course approach, on the importance of social determinants of mental health, and on the need of strengthening mental health services, work in global mental health has emphasized the efficacy of task‐shifting interventions, the importance of addressing stigma, and the value of including service users’ perspectives in research and planning 1 , 2 .
Early work by the WHO, and subsequent work by others in global mental health, has led to important contributions. A first key contribution has been the recognition of the burden of mental disorders, and advocacy that this burden needs to be urgently and appropriately addressed. There are far too few mental health clinicians in low‐ and middle‐income countries, where the vast majority of the world's population resides 22 .
A second key contribution has been a focus on addressing mental health in primary care. In the 1970s, the WHO conducted a multinational collaborative study demonstrating the feasibility and effectiveness of offering community‐based mental health care, delivered by primary health care workers, in developing countries 211 . A few years later, in 1978, the Primary Health Care Conference in Alma Ata, composed of representatives of almost all countries in the world, included the promotion of mental health into the list of essential components of primary health care.
Nevertheless, global health in general and global mental health in particular have faced many challenges. Early hopes were that globalization would entail a border‐free world with easy communication, trade, and mutual support. However, globalization has also arguably allowed unidirectional unloading of products of the North to the less industrially developed South, and a simultaneous migration of many individuals, including health professionals, from the global South to the North. Colonial practices, including large psychiatric hospitals, have remained in existence in many low‐income countries. Rapid urbanization and breakdown of traditional communities, which provided some support to vulnerable individuals, have further complicated the provision of health care. The introduction of digital technologies – which has been considered as a potential equalizer – also runs the risk of creating a new divide, the digital divide.
In terms of the clinical practice of psychiatry, while the numbers of psychiatrists and other mental health care workers has significantly increased across the globe, their inequitable distribution has not significantly improved 22 . There are still many countries with only a few psychiatrists, and the brain drain – the movement of fully trained psychiatrists from the global South to the North – continues 212 . Training programs which can be used for primary health care providers in mental health have been produced by the WHO and other agencies, and the situation has improved in some countries, but the numbers of those left with no adequate care remain high. Primary care practitioners are not always willing to accept responsibility for the treatment of mental disorders, and many well‐trained psychiatrists have continued to work in private health care services that reach only a minority of those who need help.
Earlier sections of this paper considered some of the concerns about current psychiatry nosology raised by neurobiologically‐focused and “number‐driven” researchers. But even from a public health perspective, application of key aspects of the chapter on mental disorders of the ICD rises problems 213 . First, most practicing clinicians feel that in daily work the number of diagnostic categories proposed for use should follow the number of options for therapeutic interventions, and so ICD approaches may be too complex. Second, reporting about inpatient mental health services to national authorities in most instances follows the guidelines provided by hospitals, which do not allow for the collection of sufficiently detailed or validated data. The interpretation of findings may be made even more difficult by the fact that in federal countries the rules of reporting to the central authority differ from area to area.
Global mental health has been crucially important in putting forward a number of innovative models and approaches. At the same time, critics might suggest that the strategies of global mental health are not so much an entirely new paradigm but instead a re‐packaging of long‐standing ideas in the field, and that each of these strategies has important limitations which deserve emphasis.
First, global mental health has focused on the notion of “task‐shifting”. This involves the use of non‐specialized health care workers, who are trained and supervised by mental health specialists. Systematic reviews have concluded that there is now considerable evidence for the efficacy of this approach 3 , 214 . Nevertheless, this strategy is not a panacea. There are limits to what can be done by untrained personnel. The treatment of more complex conditions, such as treatment‐refractory mental disorders, requires well‐trained clinicians. Moreover, significant supervision and monitoring may be required, and this entails human and financial resources. There is now interest in how to assess therapist competence in task‐shifting trials 215 , 216 . Finally, there is a difference between demonstration projects conducted by academic researchers and real‐life scale‐up projects undertaken by governments. Pharmacotherapy outcomes are worse in real‐world pragmatic trials than in academic‐centre explanatory trials, and we might expect that the same will hold true in the case of task‐shifting research.
A second important strategy of global mental health has been to build the investment case for mental health, demonstrating the return on investment for countries scaling up community‐based care. As noted earlier, this gave key impetus to the implementation of psychotherapies in the UK. However, a number of challenges remain. Many economic returns accrue to sectors outside ministries of health, which traditionally hold mental health budgets. Economic returns on scaled‐up mental health care are likely to accrue through improved labour market participation, reduced homelessness, and savings to correctional services and police services, and not necessarily to the health sector. Moreover, such savings might only be realized at some time in the future, creating what has been termed pernicious “diagonal accounting” 217 . Finally, it must be conceded that not all investment in mental health – for example, care for those with severe neurodevelopmental disorders – will yield significant economic returns.
A third key strategy of global mental health has been to focus on building stronger, better coordinated advocacy, with partnerships between people with lived experience and clinicians to campaign for better and more resources for mental health care. It has been argued that ongoing dialogue between the various stakeholders involved in community‐based care is essential to reach common ground on service development priorities. This should also include maximizing opportunities for leadership from people with lived experience, to address demand‐side barriers to community‐based mental health care. Nevertheless, there are key barriers to advocacy work, including low mental health literacy of policy‐makers, and a gap in frameworks linking research to policy 218 .
A fourth key strategy of global mental health has been to focus on stigma reduction strategies. Certainly, reducing stigma and discrimination against people living with mental illness is vital if we are to promote care in the community. Furthermore, there is a growing evidence base for the positive impact of stigma reduction campaigns for mental health, such as the World Psychiatric Association's “Open the Doors” program. At the same time, there are important challenges to acknowledge. Much more needs to be done to both improve the effectiveness of these interventions and extend stigma reduction programmes to a range of different countries 219 . Stigma reduction strategies should not deny the dysfunction that accompanies severe mental disorders (services for such conditions remain sorely needed), and they need to also highlight that individuals suffering from psychiatric disorders have “responsibility without blame” 220 . Finally, it is notable that, in some contexts, providing neurobiologically focused information increases rather than decreases stigma 221 .
A fifth key strategy of global mental health is to address social determinants of mental disorders. Governments need to address fundamental social injustice such as rampant inequality, high unemployment, civil conflict and violence, particularly gender‐based violence, that drive mental disorders in populations 222 . That said, the evidence base for population‐level interventions to address the social determinants of mental health is rather sparse and of low quality 223 . Ironically, global mental health has been accused of ignoring key contextual data 224 , and of perpetuating some of the sociopolitical inequities it critiques 225 . Less contentiously, while some clinicians may well contribute to efforts focused on social determinants, the majority will focus on providing direct clinical care. Public mental health skills are needed to supplement, rather than replace, standard clinical training.
Taken together, it is clear that the concepts and methods of global mental health have many strengths, have contributed to important advances, and should be incorporated into further attempts to incrementally improve health policies as well as clinical practice. As always, discourse about a paradigm shift and over‐optimism about the extent of envisaged change raise red flags. Indeed, the key strategies of global mental health that may facilitate ongoing incremental progress may themselves require iterative attention: we need to continue to be innovative about task‐sharing, to gradually strengthen the investment case, to steadily develop better advocacy strategies, to further reduce stigma about mental disorders and increase mental health literacy, and to better address social determinants of these conditions.
Kuhn's notion of scientific paradigms has been extraordinarily influential 226 . He argued that most of science is “normal”: scientists have a particular conceptual framework, with various exemplars that are key for the field, which allows them to address a range of relatively minor “puzzles” 227 . However, from time to time, there is a paradigm shift, with an entirely new conceptual framework and new exemplars coming to fore and causing a “crisis”, and so entailing a major revolution in the field. Thus, for example, at one point phlogiston was thought to explain combustion, but this paradigm was replaced by one that emphasized the importance of oxygen, providing an entirely new perspective. Notably, from a “critical” perspective, scientific paradigms are incommensurable; those who adopt different paradigms are really talking past one another, and the shift from one paradigm to another happens not because of scientific advancement, but rather due to a sociopolitical shift in the field 228 , 229 .
From this perspective, psychiatry has been characterized by a history of continual paradigm shifts, with the field lurching over time from one set of models to another, with no substantive scientific advances in our knowledge, but rather merely a responsiveness to the prevailing sociopolitical winds of the day 229 . Thus, as noted earlier, psychiatry has seen movements from psychodynamic approaches to neuroscientific ones, and from institutional care to community‐based care. While a good deal of the critique of psychiatry has come from external fields, there is a significant contribution from within the discipline, with proponents of new paradigms at times being very critical of current practices. The idea that psychiatry is in crisis seems to be prevalent and persistent in both the professional literature and in social media 230 , 231 , 232 , 233 , 234 .
We would argue strongly against this view of psychiatry. This is not to disagree that there have been important shifts in the field over its history: there certainly have been. Nor is it to disagree with the valid points that sociopolitical and sociocultural factors are key to such issues as determining budgets for mental health services, and in influencing the experience and expression of mental disorders 235 . Nor is to deny or downplay the many crucial challenges that continue to face psychiatry as a profession, and psychiatrists as practitioners 236 , 237 . And perhaps most importantly, it is not to ignore or to minimize the enormity of the treatment and the research‐practice gaps discussed in detail earlier in this paper. Clearly, considerably more needs to be done to improve mental health care services, and to effectively address the burden of disease due to mental disorder.
However, we wish to emphasize that there has been a gradual accretion of knowledge about mental disorders, and that our understanding of their causes and our ability to manage them has significantly increased over time. We also wish to argue that the different proposals for the field discussed in this paper are not necessarily incommensurable paradigms, but rather are important perspectives that can productively be drawn on and integrated into contemporary practice 238 . The integration of clinical neuroscience and global mental health, for example, may facilitate advances in precision public mental health 239 . Space precludes a detailed consideration of a range of other innovative perspectives that may also contribute to the incremental and integrative advance of psychiatric practice, including collaborative care 240 , preventive psychiatry 241 , evolutionary psychiatry 242 , positive psychiatry 243 , intergenerational psychiatry 244 , and welfarist psychiatry 245 .
Perhaps most importantly, we would wish to problematize the notion that psychiatry is in perennial and perpetual crisis. Tools provided by “critical” authors, who emphasize the sociopolitical aspects of science and medicine, may be in fact be useful in investigating why psychiatry is so often viewed in this way, and why a view of psychiatry as steadily accreting knowledge and improving clinical practices is less often put forward than seems reasonable, even from within the field. Are there specific interests that stand to gain from negative views of the psychiatric profession? What are the benefits to particular authors of being overly critical of existing practices and of promising entirely novel or disruptive solutions? What can be done to encourage those without and within the field to emphasize that scientific progress is often iterative and incremental, with gradual consolidation of knowledge, with inclusion and integration of a range of different models and approaches?
We have noted in this paper a number of red flags, which seem indicative of overly optimistic promises of a paradigm shift in psychiatry practice and research, and that may inadvertently even support an antipsychiatry position that discourages patients from seeking sorely needed professional care, or policy‐makers from funding desperately needed mental health care services. A few of these red flags deserve particular emphasis here.
First, given the complexity of mental disorders, and the need to avoid both a brainless and a mindless psychiatry 246 , various forms of reductionism serve as red flags, whether these involve neuro‐reductionism (e.g., mental disorders are merely brain disorders) or culturalism (e.g., mental disorders merely reflect social inequalities). As a field, we should promote the breadth and depth of psychiatric concepts and findings, emphasizing that psychiatry builds bridges across biological, psychological and social domains, and that – despite the complexity of mental disorders – this has allowed important insights into their phenomenology and etiology, and has facilitated the development of a broad range of different evidence‐based treatment modalities and types of intervention. The complexity of mental disorders may, however, mean that there are few “silver bullets” in psychiatry: any individual mental health intervention may have only modest effect sizes, and reduction of disease burden due to mental disorders is a massive goal, likely requiring a broad range of interventions 247 .
Second, economic over‐optimism may be a red flag: bringing new drugs to market requires significant financial investment, deinstitutionalization is not an inexpensive option, and it is a challenge to demonstrate that large‐scale implementation programs such as IAPT save money. While a range of different metaphors may be useful in describing psychiatric work, and in encouraging policy‐makers to fund mental health services, we need perhaps to be particularly careful of seeing patients as merely consumers, and psychiatry as simply providing a return on investment. Similarly, while a collaborative relationship between professional clinicians and patient partners may be useful in encouraging shared decision‐making, this metaphor of psychiatric work and mental health services may miss some aspects of the clinical encounter. The metaphor of clinicians providing care is a crucial one, and we need to call for more such care, even if at times it is somewhat expensive 115 .
Third, calls for a radical transformation of psychiatry's research agenda are a red flag. Hubris may result in downplaying what has already been achieved over decades, or in overly focusing on one or other favoured perspective. A more humble position that emphasizes how difficult is to know what approaches and models will lead to the largest advances, that encourages a broad range of promising work, that insists on principles of reproducible science including the common metrics agenda, and that acknowledges the key role of serendipity, is appropriate 64 , 248 , 249 . Analogously, calls for a radical transformation or narrowing of the training curriculum also constitute a red flag: psychiatry trainees need exposure to a broad range of concepts and methods, including neuroscience, statistics, evidence‐based psychotherapy, digital psychiatry, and public mental health. The field needs well‐rounded graduates who are able to access and employ the full range of concepts and findings from our rich discipline.
How can we facilitate an ongoing focus on incremental advances in clinical practice, with integration of a range of different perspectives and findings? It may be useful to approach the issues discussed in this paper with a particular knowledge of how science works, and with a particular attitude towards progress.
From the perspective of knowledge, it seems useful to emphasize that concepts of scientific crisis and paradigm shifts often serve as rhetorical devices, that in sciences ranging from physics to psychiatry multiple approaches and models are potentially useful, and that in psychiatry there is a particular need for pluralistic and pragmatic approaches that integrate a range of different concepts, methods and findings 229 , 250 . From the perspective of attitude, we would emphasize the value of staying hopeful, avoiding hype, and committing to the important work of closing the treatment gap as well as the research‐practice gap.
Thus, in terms used earlier in this paper, the solution to challenges in psychiatric diagnosis and treatment is unlikely to lie in entirely novel paradigms, but rather in the humble, laborious, iterative work of systematic clinical observation, painstaking research, and creative thinking. In the case of psychiatric assessment, for example, we have elsewhere argued for the need for more work on post‐diagnostic assessments and measures that are consistent with measurement‐based care and that promote personalized psychiatry 251 , 252 , 253 . In the case of psychiatric treatment, addressing the treatment and the research‐practice gaps will require more attention to expanding innovative delivery models that will reach more people in need 254 , systematic adoption and roll‐out of integrated evidence‐based interventions 255 , and an iterative discovery‐confirmation process to assess and improve efficacy 256 .
In conclusion, this review of a range of proposed approaches to and models of diagnosis and treatment of mental disorders suggests caution in concluding that we are facing a crisis in psychiatry which necessitates a disruptive transitioning from traditional to new practices. We argue instead that an approach which emphasizes paradigm shifts should be replaced by one that focuses on the importance and value of incremental and integrative advances. In particular, we caution against an advocacy for paradigm shifts that inadvertently represents a disguised manifestation of antipsychiatry, and we instead suggest the need for a position that emphasizes both the accomplishments and limitations of psychiatric diagnosis and treatment, and that is cautiously optimistic about their future.
FORUM – PSYCHIATRIC PRACTICE AND RESEARCH: THE VALUE OF INCREMENTAL AND INTEGRATIVE ADVANCES

Current Psychiatry Research and Reviews

About the journal
Latest published, current state of application of formal thought disorder screening methods in first-degree relatives of patients with schizophrenia: a narrative review, omega-3 fatty acid supplementation improves attention deficit-hyperactivity disorder symptoms in children.
Copyright © 2024 The Author(s). Published by Bentham Science Publishers
- Psychiatry and Behavioral Health
Explore the latest in psychiatry, including recent guidelines and advances in management of anxiety, depression, bipolar disease, and more.
Publication
Article type.
This randomized clinical trial evaluates the use of a digital version of generalized cognitive behavioral therapy strategies in the treatment of individuals with alcohol use disorder.
- Digital Cognitive Behavioral Therapy Intervention for Alcohol Use Disorder JAMA Network Open Opinion September 26, 2024 Mobile Health and Telemedicine Alcohol Psychotherapy Substance Use and Addiction Medicine Full Text | pdf link PDF open access
This prognostic study develops a model based on administrative data for regular US Army soldiers that can predict suicides 1 to 120 months after leaving active service.
- Actualizing Military Suicide Prevention Through Digital Health Modernization JAMA Psychiatry Opinion September 25, 2024 Suicide Violence War Full Text | pdf link PDF
This systematic review and meta-analysis evaluates the association of direct and indirect psychotherapy with suicidal ideation and attempts.
This Viewpoint examines the US Supreme Court’s opinion on Harrington v Purdue Pharma and the implications it could have on public health, individuals affected by opioid misuse, and bankruptcy law.
This cohort study uses current US hospital discharge data to examine readmission rates of infants with and without neonatal opioid withdrawal syndrome.
This randomized clinical trial investigates whether in-home delivery of a daily voice-activated cognitive behavioral therapy program improves insomnia symptoms among survivors of breast cancer.
- Perceived CTE and Suicidality—Is Perception Reality? JAMA Neurology Opinion September 23, 2024 Neurology Traumatic Brain Injury Suicide Full Text | pdf link PDF
- Suicide and the Epidemiology of a Toxin That Kills Quickly—Data Sharing Between Public Health Agencies JAMA Network Open Opinion September 23, 2024 Public Health Toxicology Suicide Full Text | pdf link PDF open access
This cohort study evaluates associations between prenatal exposure to maternal SARS-CoV-2 infection with rates of positive Modified Checklist for Autism in Toddlers, Revised screenings.
This case series study defines a new approach for identifying sodium nitrite deaths based on forensic confirmation and compares its findings with those of current poison center surveillance.
This cross-sectional study among American Indian/Alaska Native adolescents living on or near the Cherokee Nation Reservation examines the potential of Tribal identity to attenuate the association between pain interference and substance use.
This systematic review and meta-analysis evaluates the efficacy of gamified digital mental health interventions in treating anxiety, depression, and attention-deficit/hyperactivity disorder among children and adolescents.
This cross-sectional study gathered data using surveys from former professional players of American-style football to gauge how many perceive that they have chronic traumatic encephalopathy and determine clinically relevant correlates, including suicidality.
This cross-sectional study assessed which community asset categories may be associated with youth mental health symptoms.
- Action Needed to Ease Parental Stress, US Surgeon General Warns JAMA News September 20, 2024 Media and Youth Pediatrics Child and Adolescent Psychiatry Surgery Adolescent Medicine Full Text | pdf link PDF free
- Detection and Referral of Depression in Patients With Visual Impairment: A Call for Practical Training and Methods JAMA Ophthalmology Opinion September 19, 2024 Ophthalmology Depressive Disorders Full Text | pdf link PDF has multimedia
This Korean population-based cohort study evaluated the incidence rates and risks of depressive disorder in patients with retinitis pigmentosa.
This Viewpoint discusses the limitations of clinical prediction models in psychiatric research.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Psychiatric disorders articles from across Nature Portfolio
Psychiatric disorders are a heterogeneous group of mental disorders, manifesting as unusual mental or behavioural patterns that cause distress or disability to the individual.
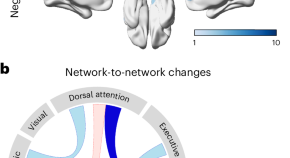
Mapping connectivity and network alterations in youth depression by functional brain imaging
Analyses of functional MRI brain images of young people with depression revealed that altered brain connectivity associated with this disorder is circumscribed to specific networks and hub regions, including the default mode and attentional networks. The magnitude of these connectivity changes is a reliable predictor of depression symptom severity.
Related Subjects
- Autism spectrum disorders
- Bipolar disorder
- Obsessive compulsive disorder
- Post-traumatic stress disorder
- Schizophrenia
Latest Research and Reviews

Dysfunction in sensorimotor and default mode networks in major depressive disorder with insights from global brain connectivity
Using a large multisite dataset of people with major depressive disorder and healthy controls, the authors show global brain connectivity alterations in the sensorimotor, visual, and default mode networks.
- Yajuan Zhang
- Chu-Chung Huang
- Chun-Yi Zac Lo
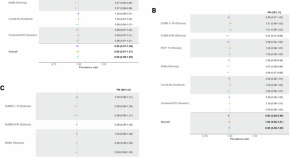
Mental illness and COVID-19 vaccination: a multinational investigation of observational & register-based data
Monitoring COVID-19 vaccine uptake in those at risk of severe disease, such as people with mental illness, is important. Here, the authors use cohort and/or health registry data from five countries in northern Europe and investigate vaccine uptake by mental illness and treatment status.
- Mary M. Barker
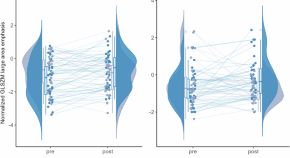
MRI textural plasticity in limbic gray matter associated with clinical response to electroconvulsive therapy for psychosis
- Eugenie Choe
- Jun Soo Kwon
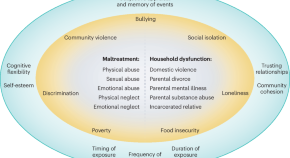
Revisiting the use of adverse childhood experience screening in healthcare settings
Screening for adverse childhood experiences can improve mental health outcomes through personalized treatments in at-risk individuals or preventative strategies at the population level. In this Review, Danese et al. synthesize the challenges and opportunities of these screening measures and related analytical methods.
- Andrea Danese
- Kirsten Asmussen
- Angela Sweeney
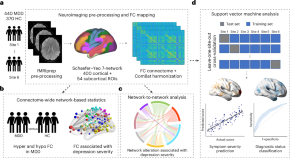
A mega-analysis of functional connectivity and network abnormalities in youth depression
This mega-analysis of brain resting-state functional connectivity in young individuals with major depressive disorder scanned at six sites across four countries identified hub regions of the attentional and default mode networks as predictors of depression severity.
- Nga Yan Tse
- Aswin Ratheesh
- Andrew Zalesky
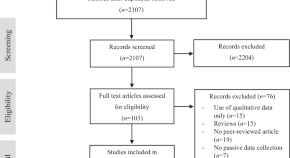
A systematic review on passive sensing for the prediction of suicidal thoughts and behaviors
- Rebekka Büscher
- Tanita Winkler
- Lasse B. Sander
News and Comment
Revolutionary drug for schizophrenia wins US approval
The medication is the first in decades to have a different mode of action than do current drugs, achieving better symptom relief with fewer side effects.
- Elie Dolgin
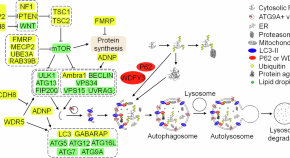
Impaired macroautophagy confers substantial risk for intellectual disability in children with autism spectrum disorders
- Audrey Yuen Chang
- Guomei Tang
Found: a brain-wiring pattern linked to depression
The disease has a consistent mark in the brain even when symptoms are absent.
- Sara Reardon

Reorienting social communication research via double empathy
- Oluwatobi Abubakare

Could video games be good for your health?
A large causal analysis based on a natural experiment suggests that gaming improves psychological well-being, but these benefits tapered off after more than 3 hours of gaming per day.
- Karen O’Leary
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Specialties
- Drugs misuse (including addiction)
- Drugs: psychiatry
- Somatoform disorders
- Suicide (psychiatry)
- Sleep disorders
- Sexual and gender disorders
- Psychotic disorders (incl schizophrenia)
- Psychotherapy
- Psychiatry of old age
- Child and adolescent psychiatry
- Anxiety disorders (including OCD and PTSD)
- Alcohol-related disorders
- Adjustment disorders
- Mood disorders (including depression)
- Personality disorders
- Memory disorders (psychiatry)
- Impulse control disorders
- Eating disorders
Psychiatry from BMJ
Psychiatry from BMJ aims to provide you with a mixture of the most important psychiatry resources that we publish with the latest, continually updated research articles from the BMJ and all of our specialist journals, plus online education from BMJ Learning.
Latest from The BMJ
Subscribe to The BMJ
Submit your paper
Psychiatry key external links
Nice guidance: mental health and behavioural conditions, international psychiatry, the psychiatrist, american journal of psychiatry, rss feed for british journal of psychiatry most frequently read articles, nice guidelines on psychiatry topics, royal college of psychiatrists, evidence-based mental health, key psychiatry resources from bmj, doctors accessing mental-health services: an exploratory study, obsessive-compulsive disorder: a guide to recognition and management, suicide risk management.

- Allergy & Immunology
- Anesthesiology
- Critical Care
- Dermatology
- Diabetes & Endocrinology
- Emergency Medicine
- Family Medicine
- Gastroenterology
- General Surgery
- Hematology - Oncology
- Hospital Medicine
- Infectious Diseases
- Internal Medicine
- Multispecialty
- Ob/Gyn & Women's Health
- Ophthalmology
- Orthopedics
- Pathology & Lab Medicine
- Plastic Surgery
- Public Health
- Pulmonary Medicine
- Rheumatology
- Transplantation
- Today on Medscape
- Business of Medicine
- Medical Lifestyle
- Science & Technology
- Medical Students
- Pharmacists
Expert Calls for Research into GLP-1s for Mental Illness
Kate Johnson
September 24, 2024
MILAN — Recent research allaying concerns about suicidality linked to glucagon-like peptide 1 (GLP-1) receptor agonists, along with evidence of these agents' potential psychiatric and cognitive benefits, has prompted the lead investigator of a major analysis to urge researchers to explore the potential of these drugs for mental illness.
"So far, we've been talking about the safety from a neuropsychiatric perspective in diabetes, but there is also the safety and benefit in people with mental disorders," Riccardo De Giorgi, MD, PhD, from the Department of Psychiatry, University of Oxford, Oxford, England, told Medscape Medical News .
The results of the meta-analysis were previously reported by Medscape Medical News and reviewed by De Giorgi at the 37th European College of Neuropsychopharmacology (ECNP) Congress . De Giorgi broached whether GLP-1 inhibitors such as semaglutide might also offer the same benefits in patients without diabetes as they do in those with diabetes, in terms of cognitive deficits and substance use or mood disorders.
Noting that GLP-1s are not approved for psychiatric disorders, De Giorgi said it can't be assumed that the "metabolic or maybe even more general mechanisms that are being modified with these medications in diabetes or even in obesity are the same for people with psychiatric disorders. We're talking about very different things. From a clinical perspective, you could do real harm," he told Medscape Medical News .
Yet De Giorgi emphasized the importance of exploring the potential benefits of these medications in psychiatry.
"From a research perspective…I am very worried about missing an opportunity here. This happened with rimonabant, a cannabis medication that was used for weight loss back in 2012 and was withdrawn quite dramatically in Europe immediately after licensing because it increased suicide risk. Since then, nobody has been touching the cannabinoid system, and that's a shame because in psychiatry, we don't have that much we can work on. So we don't want to miss an opportunity with the GLP-1 system — that's why we need to be cautious and look at safety first," he said.
Signal of Efficacy?
De Giorgi's research suggested several potential neurobiological effects of GLP-1 inhibition in diabetes research.
"There was a bit of a signal specifically for the big three dementias — vascular, Lewy Body, and frontotemporal — although there was not enough power," he reported. "We also saw a reduced risk in nicotine misuse, especially amongst other substance use disorders…and finally a more tentative association for reduced depression," he added.
He noted that GLP-1s for psychiatric illness likely have limitations and may not cure mental disorders but could help specific subsets of patients. He pointed out that rather than aiming for large-scale studies, the focus should be on small, incremental studies to advance the research.
Asked by the session chair, John Cryan, PhD, from University College Cork, Cork, Ireland, and chair of the ECNP Scientific Committee whether improvement in patients' mood could be attributed to weight loss, De Giorgi replied no.
"We now have quite a lot of studies that show that if there is an effect or association it is seen quite a bit earlier than any weight loss. Remember, weight loss takes quite a lot of time, and at quite high doses, but more provocatively, even if that's the case, does it matter? We as psychiatrists do worry that we need to disentangle these things, but they don't do that in cardiology, for example. If they see a benefit in mortality they don't really care if it's specifically an effect on heart failure or ischemic disease," said De Giorgi.
Regardless of their neuropsychiatric potential, the cardiometabolic benefits of GLP-1 inhibitors are sorely needed in the psychiatric population, noted two experts in a recent JAMA Psychiatry viewpoint article .
Sri Mahavir Agarwal, MD, PhD, and Margaret Hahn, MD, PhD, from the University of Toronto and the Schizophrenia Division at the Centre for Addiction and Mental Health, in Toronto, Ontario, Canada, pointed out in a recent editorial published in JAMA Psychiatry that "individuals with severe mental illness (SMI) have exceedingly high rates of metabolic comorbidity; three of four are overweight or obese, whereas the prevalence of type 2 diabetes (T2D) is several-fold higher than in the general population. Consequently, individuals with SMI die 15-20 years earlier from cardiovascular disease (CVD) than do those in the general population with CVD," they noted.
"The arrival of semaglutide has infused significant enthusiasm in the field of mental health research. The proximal effects of weight and related CV comorbidities are significant in themselves. It is plausible that semaglutide could act through neurogenesis or secondary benefits of improving metabolic health on other important outcomes, such as cognitive health and quality of life, thereby filling an unmet need in the treatment of SMI," Agarwal and Hahn added.
An Exciting Opportunity
Current research investigating GLP-1s in psychiatry and neurology is increasingly focused on neuroinflammation, said De Giorgi.
Research shows significant evidence that certain medications may help reduce dysfunctional inflammatory processes linked to various cognitive and psychiatric disorders, he added.
Many patients with established psychiatric conditions also have physical health issues, which contribute to increased mortality risk, said De Giorgi. It's crucial to understand that if these treatments improve mortality outcomes for psychiatric patients, the specific mechanisms involved are secondary to the results. Psychiatrists must be equipped to prescribe, manage, and initiate these therapies, he added.
"While trials involving psychosis patients are ongoing, we are making progress and should seize this opportunity" said De Giorgi.
Cryan agreed: "I think we'll get there. What these drugs have shown is that you can, through a single mechanism, have multitude effects related to brain-body interactions, and why not focus that on mood and anxiety and cognitive performance? It's exciting no matter what. We now need to do longitudinal, cross-sectional, placebo-controlled trials in specific patient populations," Cryan said.
This study received funding from the National Institute for Health and Care Research Oxford Health Biomedical Research Centre and Medical Research Council. De Giorgi's co-authors reported receiving funding for other work from Novo Nordisk, Five Lives SAS, Cognetivity Ltd., Cognex Ltd., P1vital, Lundbeck, Servier, UCB, Zogenix, J&J, and Syndesi. Cryan reported no relevant disclosures.
Send comments and news tips to [email protected] .
TOP PICKS FOR YOU
- Perspective
- Drugs & Diseases
- Global Coverage
- Additional Resources
- Biosimilars May Finally Stop the Rocketing Cost of Insulin
- Reducing Albumin Improves Kidney and Heart Function in People With Type 2 Diabetes
- Low Co-Pays Drive Better Adherence to New Diabetes Drugs
- Diseases & Conditions Type 2 Diabetes Mellitus
- Diseases & Conditions Pediatric Type 2 Diabetes Mellitus
- Diseases & Conditions Type 2 Diabetes Mellitus and TCF7L2
- Drugs exenatide injectable suspension
- Type 2 Diabetes Mellitus
- Pediatric Type 2 Diabetes Mellitus
- Type 2 Diabetes Mellitus and TCF7L2
- Pediatric Type 1 Diabetes Mellitus
- Fast Five Quiz: Atrial Fibrillation and Diabetes
- Perioperative Management of the Diabetic Patient
- Bedridden Breakdown: Classifying Pressure Injuries
- Diabetes Mellitus Type 2 News & Perspectives
- What's the Goal in Treating Type 2 Diabetes?
- Denosumab for Osteoporosis May Prevent Type 2 Diabetes
Advertisement
- Register for Free
- My account Orders Downloads Address Payment methods Account details
- About About Psychiatrist.com About JCP About PCC About CME Institute
Error: Search field were incomplete.

Study Finds High COVID Vaccination Rates Among Mentally Ill, But Gaps Persist
by Denis Storey September 26, 2024 at 11:03 AM UTC
Clinical relevance: New research confirms high COVID vaccination rates, but those with untreated mental health conditions are less likely to get vaccinated.
- Data from more than 325,000 people in five countries showed that 85 percent of them received the first vaccine dose.
- Individuals with untreated mental health conditions are less likely to be vaccinated.
- The study highlights the need for targeted interventions to boost vaccination rates in vulnerable groups.
In a classic case of “good news, bad news,” a vast multinational study confirms that work toward COVID vaccination rates has worked. But that work is still unfinished.
The paper , appearing in Nature Communications, explains that the good news is that COVID vaccination rates remain high – regardless of one’s mental health condition. But the bad news is that those with untreated mental health conditions might be less likely to get vaccinated.
This research, based on data from seven cohort studies within the COVIDMENT consortium and compared against the Swedish national registers, offers new insight into vaccination trends among this already vulnerable demographic
Methodology and Results
The study’s authors look at data pulled from seven studies that spanned five countries – Sweden, Norway, Iceland, Estonia, and Scotland – as part of the COVIDMENT consortium. The data covered more than 325,000 individuals. The Swedish National Registry provided data points for more than 8 million people.
The researchers found that 85 percent of individuals received the first dose of the COVID vaccine (until Sept. 30, 2021).
“The high vaccination coverage among most individuals with mental illness shows that the COVID-19 vaccination campaign has been successful,” lead author Mary Barker , a postdoctoral researcher at the Institute of Environmental Medicine , Karolinska Institutet, said in a press release.
The team determined mental illness using self-reported measures, clinical diagnoses, and prescription data. By pooling results through meta-analyses, the research revealed that most individuals with mental illness showed no significant difference in vaccination rates compared to the general population.
But, the Swedish registry data revealed a small dropoff – 9 percent – in the uptake of both the first and second vaccine doses among those with mental illness. This reduction appeared to be more noticeable among those not using psychiatric medications. For example, those struggling with substance use disorder were 16 percent less likely to be vaccinated.
All of this, the authors concluded, suggests that those managing mental health conditions without medical help could be at higher risk of lower vaccination rates.
Pushing For Further COVID Research
The researchers wanted to clear up earlier conflicting reports about the relationship between mental illness and COVID-19 vaccine rates. Some studies linked schizophrenia and substance use disorders with lower vaccine uptake. Others found higher vaccination rates among individuals with anxiety or depression.
This new analysis suggests that medication status may play a key role in these trends, as individuals using psychiatric medications such as antidepressants tend to have similar vaccination rates as the general population.
But the team also insisted that more research should follow.
“More research is needed to explore the reasons behind these associations in order to improve current and future vaccination strategies and ultimately ensure equitable protection against infectious diseases,” Barker added. “As individuals with mental illness are at higher risk of severe COVID-19 outcomes, high vaccination coverage is especially important in this group.”
In short, these findings highlight the need for more targeted public health interventions to address lower vaccination rates among specific subgroups, particularly those managing mental health conditions without medication – or help of any kind.
Further Reading
Lockdowns May Have Accelerated Brain Aging, Especially in Girls
Rethinking Mental Health in a Post-COVID World
New Research Validates Long COVID’s Existence
Stanford Accelerated Intelligent Neuromodulation Therapy
Dr. Nolan Williams delves into the innovative Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT) for treating resistant depression. Explore groundbreaking research, clinical trials, and the transformative potential of personalized brain stimulation techniques in imp...
Nolan Williams
Systematic Review

Breast Cancer and Depression: A Scoping Review of Indian Literature
This scoping review explores depression prevalence, correlates, impact, and interventions in breast cancer patients, with a focus on the Indian context.
M. Vaseel and others
Search Articles
Related articles, table of contents.
Risk of Incident Psychosis and Mania With Prescription Amphetamines
Information & authors, metrics & citations, conclusions:, get full access to this article.
View all available purchase options and get full access to this article.
Information
Published in.
- Schizophrenia Spectrum and Other Psychotic Disorders
- Bipolar and Related Disorders
- Substance-Related and Addictive Disorders
Competing Interests
Funding information, export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
View Options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - American Journal of Psychiatry
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
View options
Share article link.
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Microsoft Research Lab – Asia
Nnscaler: exploring a new paradigm for parallel execution in deep learning, share this page.
Author: Youshan Miao
Today, deep learning has permeated our daily lives. As the size of models continues to grow, training these models on massive GPU accelerators has become increasingly time-consuming and costly. To effectively harness the power of massive GPUs and enhance efficiency, researchers have been developing various parallel strategies to improve performance across multiple devices. However, many potentially efficient parallel strategies remain unexplored. Fully exploring these possibilities to further unlock performance remains a major challenge in both research and application.
Recently, researchers from Microsoft Research Asia proposed nnScaler, a framework that supports freely expressing parallel strategies through a set of parallel primitives while minimizing search costs by utilizing a strategy-constrained search space.
Parallel primitives: A unified framework to describe parallel strategies
Mainstream training systems, such as Megatron-LM, DeepSpeed, and Alpa, typically incorporate built-in parallel strategies like data-parallelism, tensor-parallelism, and pipeline-parallelism, which can be combined through configuration. While this approach is efficient for most cases and convenient for users, it may overlook more efficient strategies. Including new efficient parallel strategies often require substantial modifications to the underlying system code, which is impractical.
Therefore, researchers revisited the fundamental components of parallel strategies. The execution of deep learning models can usually be represented as a data-flow graph, where tensors (representing data) are the edges, and tensor operators are the vertices. The process of parallelization involves transforming the computation data-flow graph, originally designed for single-device execution, into a distributed data-flow graph for multi-device execution. Thus, researchers propose a set of basic operations as parallel primitives, including:
- op-trans : Describes how operators and tensors are partitioned.
- op-assign : Assigns the partitioned operators to specific devices.
- op-order : Specifies the execution order of operators on the same device.
By utilizing these primitives, we can precisely describe how each operator and tensor in the data-flow graph is partitioned and scheduled across devices (spatially) and over time (temporal order on the same device).

These parallel primitives can naturally express various widely used parallel strategies. For instance, data-parallelism can be expressed as partitioning all forward pass and backward pass operators along the data sample dimension and distributing them evenly across all devices, while copying the optimizer operators to each device. All operators on each device maintain the same execution order as in the original graph. The introduction of parallel primitives allows for the flexible description and integration of various parallel strategies within a unified framework, significantly expanding the representational scope of parallel strategy spaces.
This universality not only systematically expresses existing parallel strategies but also provides the potential to explore new ones. For example, for operators that produce intermediate results too large for a single device, the original strategy might be tensor-parallelism with communication coordination. However, using parallel primitives, we can partition the tensor for that specific operator and schedule all partitions on the same device for sequential execution, successfully executing the operation while avoiding communication overhead, as shown in the figure below.

Enhancing efficiency through expert-guided strategy search
While parallel primitives expand the strategy space, this expansion also introduces a new challenge—the vast strategy space makes it difficult to complete searches within a limited time. With a multitude of possible combinations, efficiently finding the optimal strategy becomes a pressing issue.
nnScalerleverages domain expert wisdom to guide effective strategy searches. This guidance can be described through parallel primitives, seamlessly integrating into the system. For example, as shown in the figure below, researchers can constrain the operator’s partitioning scheme to the options specified in the algo set and limit the partitioning to the number of pieces specified by num.

By setting specific constraints, experts can significantly narrow the search space, making the search process more efficient and targeted. Experiments have shown up to 10x increase in search efficiency without compromising the effectiveness of the strategies.
This approach can uncover high-performance strategies that existing methods overlook and complete searches in a shorter time, thereby improving the efficiency of deep learning training. nnScaler has been validated in the training of multiple deep learning models, demonstrating significant performance improvements.
For more details, please refer to the nnScaler paper: https://www.usenix.org/conference/osdi24/presentation/lin-zhiqi (opens in new tab)
By introducing parallel primitives and expert-guided strategy searches, nnScaler has effectively addressed many issues in the design of parallel strategies for deep learning. This method not only significantly expands the space of parallel strategies, but also provides new directions and tools for future research in parallel strategies. Researchers are eager to see this method demonstrate its potential in broader applications, bringing more possibilities to the development of deep learning.
- Follow on X
- Like on Facebook
- Follow on LinkedIn
- Subscribe on Youtube
- Follow on Instagram
- Subscribe to our RSS feed
Share this page:
- Share on Facebook
- Share on LinkedIn
- Share on Reddit

IMAGES
VIDEO
COMMENTS
Formerly Archives of General Psychiatry. Explore the latest science of anxiety, autism, depression, OCD, psychosis, psychotherapy, schizophrenia, and more. ... Economics, and Policy Promoting EDI in Genetics Research PTSD and Cardiovascular Disease Red Blood Cell Transfusion: 2023 AABB International Guidelines Reimagining Children's Rights in ...
C.J. RosenN Engl J Med 2024;391:561-562. New infections with SARS-CoV-2 continue 4 years after the pandemic began, despite advances in vaccines, antiviral medications, and preventive measures. 1 ...
The devastation wreaked by psychiatric illnesses strongly underlies the need for novel, rapid, and more effective treatments. The latest treatments—including psychotropic medications ...
A survey of US twelfth graders in 2023 found that 11 percent reported using delta-8 THC within the past 12 months, compared with 30 percent reporting marijuana use [15]. Delta-8 THC use was lower in states with cannabis legalization (8 versus 14 percent) or delta-8 THC regulation (6 versus 14 percent).
Don't miss the newest articles. Keep up to date with the latest research, clinical reviews, and opinions. [Skip to Navigation] ... This Viewpoint discusses the limitations of clinical prediction models in psychiatric research. Original Investigation. Patient Self-Guided Interventions to Reduce Sedative Use and Improve Sleep: ...
Arulpragasam, A. R. et al. Low intensity focused ultrasound for non-invasive and reversible deep brain neuromodulation—a paradigm shift in psychiatric research. Front. Psychiatry 13, 825802 ...
Abstract. In contrast to most fields of medicine, progress to discover and develop new and improved psychiatric drugs has been slow and disappointing. The vast majority of currently prescribed ...
Major depressive disorder (MDD) affects a substantial portion of the population; however, much is still unknown about the pathophysiology of this disorder. Treatment resistance highlights the heterogeneous nature of MDD and the need for treatments to target more than monoamine neurotransmission. This review summarizes research into the new and emerging targets of MDD. These include drugs such ...
Depression is a common psychiatric disorder and a major contributor to the global burden of diseases. According to the World Health Organization, depression is the second-leading cause of disability in the world and is projected to rank first by 2030 [1]. Depression is also associated with high rates of suicidal behavior and mortality [2].
When I give presentations about JAMA Psychiatry and in my Year in Review articles, I highlight our journal's ambition to be the outlet for the best psychiatric research articles. Original Investigations are the lifeblood of our journal and will remain that way. We have always prioritized meaningful advances coming from rigorous and definitive research over flashy topics that may be popular ...
Discover clinical research, reviews, and provacative comment and opinion from The Lancet Psychiatry, providing a clear, ... as preferred first-choice medications for the short-term treatment of ADHD. New research should be funded urgently to assess long-term effects of these drugs. The Lancet Psychiatry ISSN 2215-0366. Lancet Journals. The Lancet;
Objective: Current information on treatment and clinical characteristics of U.S. adults with schizophrenia spectrum disorders (i.e., schizophrenia, schizoaffective, and schizophreniform disorders) may help inform public health policy and service development for this population. Methods: Data were from the U.S. Mental and Substance Use Disorders Prevalence Study, conducted from October 2020 to ...
In this 6-week, double-blind study, patients with major depression remained on their antidepressant treatment and also received either placebo, cariprazine 1.5 mg/day, or cariprazine 1.5 mg for 2 weeks and then increased to 3 mg/day. A total of 751 patients were included in the modified intention-to-treat analysis.
Jonathan E Alpert, Linda L Carpenter, Adrienne Grzenda, John H Krystal, William M McDonald, Charles B Nemeroff. Full-Text HTML. PDF. Peruse the current issue of The Lancet Psychiatry, a monthly journal focussed on all aspects of psychiatry.
Psychiatric nosology has been a particular focus of debate in recent decades; successive editions of the DSM and ICD have strongly influenced both psychiatric practice and research, but have also led to assertions that psychiatry is in crisis, and to advocacy for entirely new paradigms for diagnosis and assessment.
The new research in this issue includes data from the Kaiser Permanente registry that characterizes racial and ethnic disparities in the diagnosis of affective and nonaffective psychotic disorders. Another study uses GWAS data from the Psychiatric Genetics Consortium to explore the genetic underpinnings of the increased incidence of ...
Psychiatric research news. Read current research on psychiatric disorders such as depression, OCD, schizophrenia, panic disorder, bipolar disorder and more.
This journal provides rapid publication of complete research reports and reviews in the field of psychiatry. The scope of the journal encompasses: Biochemical, physiological, neuroanatomic, genetic, neurocognitive, and psychosocial determinants of psychiatric disorders. Diagnostic assessments of …. View full aims & scope.
Read the latest articles of Current Psychiatry Research and Reviews at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature
Psychiatry and Behavioral Health. Explore the latest in psychiatry, including recent guidelines and advances in management of anxiety, depression, bipolar disease, and more. This cross-sectional study assessed which community asset categories may be associated with youth mental health symptoms. This Korean population-based cohort study ...
Psychiatric disorders articles from across Nature Portfolio. Psychiatric disorders are a heterogeneous group of mental disorders, manifesting as unusual mental or behavioural patterns that cause ...
Psychiatry from BMJ aims to provide you with a mixture of the most important psychiatry resources that we publish with the latest, continually updated research articles from the BMJ and all of our specialist journals, plus online education from BMJ Learning. Latest from The BMJ . Endgames An adolescent with disabling abdominal pain. Published ...
MILAN — Recent research allaying concerns about suicidality linked to glucagon-like peptide 1 (GLP-1) receptor agonists, along with evidence of these agents' potential psychiatric and cognitive ...
PsychiatryOnline.org is the platform for all American Psychiatric Association Publishing journals, DSM, and bestselling textbooks, as well as APA Practice Guidelines, and continuing medical education. ... LATEST ARTICLES MOST CITED. 12 Sep 2024. ... 1 Dec 2011 New Research Full Access.
In a classic case of "good news, bad news," a vast multinational study confirms that work toward COVID vaccination rates has worked. But that work is still unfinished. The paper, appearing in Nature Communications, explains that the good news is that COVID vaccination rates remain high - regardless of one's mental health condition.But the bad news is that those with untreated mental ...
Objective: Amphetamine prescribing has increased in the United States in recent years. Previous research identified an increased risk of incident psychosis with prescription amphetamines. The purpose of this study was to examine the impact of dose levels of prescription amphetamines on the risk of this rare but serious adverse outcome. Methods: A case-control study using electronic health ...
Author: Youshan Miao Today, deep learning has permeated our daily lives. As the size of models continues to grow, training these models on massive GPU accelerators has become increasingly time-consuming and costly. To effectively harness the power of massive GPUs and enhance efficiency, researchers have been developing various parallel strategies to improve performance across multiple […]