Essay on AIDS for Students and Children
500+ words essay on aids.
Acquired Immune Deficiency Syndrome or better known as AIDS is a life-threatening disease. It is one of the most dreaded diseases of the 20 th century. AIDS is caused by HIV or Human Immunodeficiency Virus, which attacks the immune system of the human body. It has, so far, ended more than twenty-nine million lives all over the world. Since its discovery, AIDS has spread around the world like a wildfire. It is due to the continuous efforts of the Government and non-government organizations; AIDS awareness has been spread to the masses.


AIDS – Causes and Spread
The cause of AIDS is primarily HIV or the Human Immunodeficiency Virus. This virus replicates itself into the human body by inserting a copy of its DNA into the human host cells. Due to such property and capability of the virus, it is also known as a retrovirus. The host cells in which the HIV resides are the WBCs (White Blood Cells) that are the part of the Human Immune system.
HIV destroys the WBCs and weakens the human immune system. The weakening of the immune system affects an individual’s ability to fight diseases in time. For example, a cut or a wound takes much more time to heal or the blood to clot. In some cases, the wound never heals.
HIV majorly transmits in one of the three ways – Blood, Pre-natal and Sexual transmission. Transfusion of HIV through blood has been very common during the initial time of its spread. But nowadays all the developed and developing countries have stringent measures to check the blood for infection before transfusing. Usage of shared needles also transmits HIV from an infected person to a healthy individual.
As part of sexual transmission, HIV transfers through body fluids while performing sexual activity. HIV can easily be spread from an infected person to a healthy person if they perform unprotective sexual intercourse through oral, genital or rectal parts.
Pre-natal transmission implies that an HIV infected mother can easily pass the virus to her child during pregnancy, breastfeeding or even during delivery of the baby.
AIDS – Symptoms
Since HIV attacks and infects the WBCs of the human body, it lowers the overall immune system of the human body and resulting in the infected individual, vulnerable to any other disease or minor infection. The incubation period for AIDS is much longer as compared to other diseases. It takes around 0-12 years for the symptoms to appear promptly.
Few of the common symptoms of AIDS include fever , fatigue, loss of weight, dysentery, swollen nodes, yeast infection, and herpes zoster. Due to weakened immunity, the infectious person falls prey to some of the uncommon infections namely persistent fever, night sweating, skin rashes, lesions in mouth and more.
Get the huge list of more than 500 Essay Topics and Ideas
AIDS – Treatment, and Prevention
Till date, no treatment or cure is available for curing AIDS, and as a result, it is a life-threatening disease. As a practice by medical practitioners, the best way to curb its spread is antiretroviral therapy or ART. It is a drug therapy which prevents HIV from replicating and hence slows down its progress. It is always advisable to start the treatment at the earliest to minimize the damage to the immune system. But again, it is just a measure and doesn’t guarantee the cure of AIDS.
AIDS prevention lies in the process of curbing its spread. One should regularly and routinely get tested for HIV. It is important for an individual to know his/her own and partner’s HIV status, before performing any sexual intercourse activity. One should always practice safe sex. Use of condoms by males during sexual intercourse is a must and also one should restrict oneself on the number of partners he/she is having sex with.
One should not addict himself/herself to banned substances and drugs. One should keep away from the non-sterilized needles or razors. Multiple awareness drives by the UN, local government bodies and various nonprofit organizations have reduced the risk of spread by making the people aware of the AIDS – spread and prevention.
Life for an individual becomes hell after being tested positive for AIDS. It is not only the disease but also the social stigma and discrimination, felling of being not loved and being hated acts as a slow poison. We need to instill the belief among them, through our love and care, that the HIV positive patients can still lead a long and healthy life.
Though AIDS is a disease, which cannot be cured or eradicated from society, the only solution to AIDS lies in its prevention and awareness. We must have our regular and periodical health checkup so that we don’t fall prey to such deadly diseases. We must also encourage and educate others to do the same. With the widespread awareness about the disease, much fewer adults and children are dying of AIDS. The only way to fight the AIDS disease is through creating awareness.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

- Patient Care & Health Information
- Diseases & Conditions
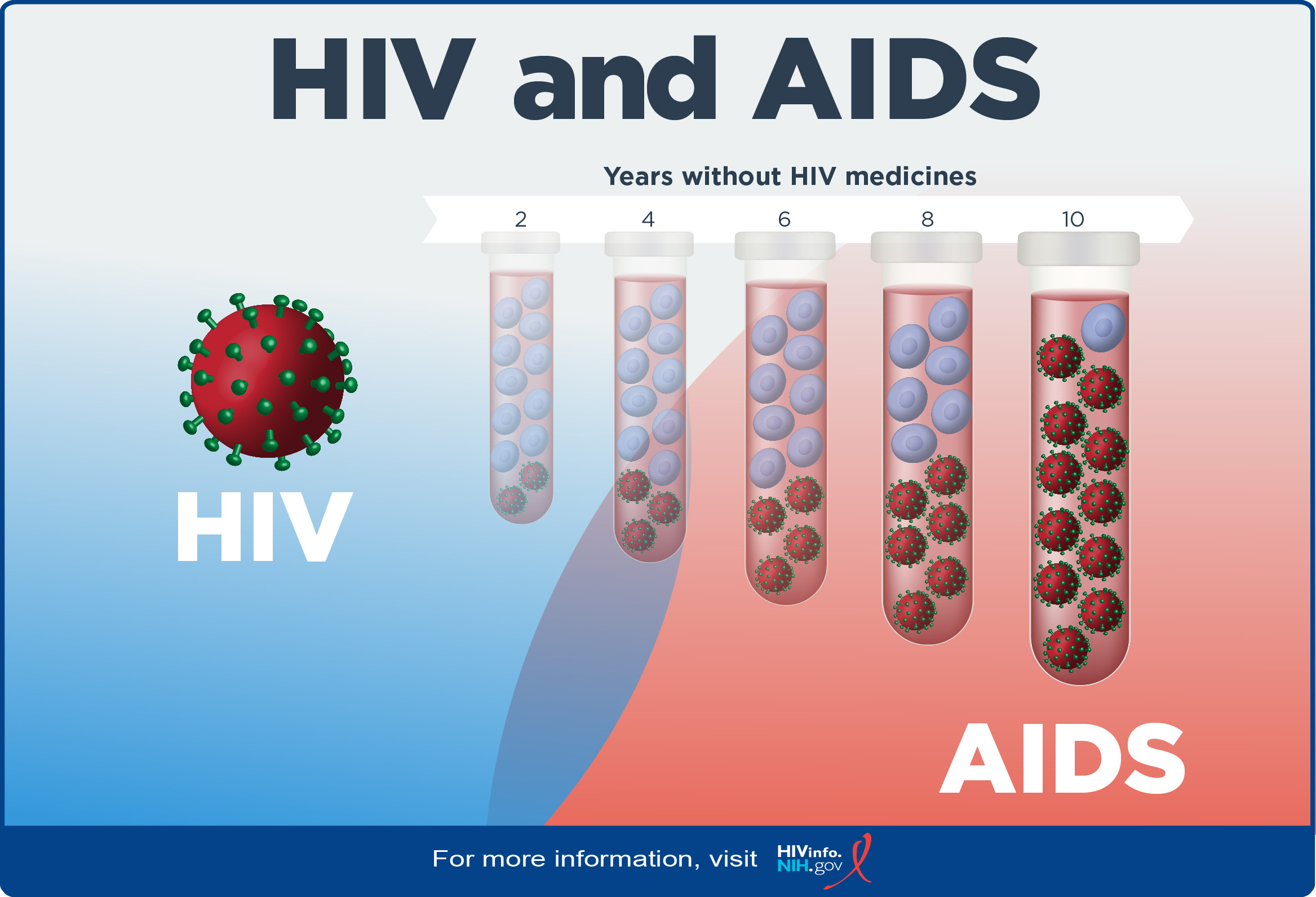
Acquired immunodeficiency syndrome (AIDS), is an ongoing, also called chronic, condition. It's caused by the human immunodeficiency virus, also called HIV. HIV damages the immune system so that the body is less able to fight infection and disease. If HIV isn't treated, it can take years before it weakens the immune system enough to become AIDS . Thanks to treatment, most people in the U.S. don't get AIDS .
HIV is spread through contact with genitals, such as during sex without a condom. This type of infection is called a sexually transmitted infection, also called an STI. HIV also is spread through contact with blood, such as when people share needles or syringes. It is also possible for a person with untreated HIV to spread the virus to a child during pregnancy, childbirth or breastfeeding.
There's no cure for HIV / AIDS . But medicines can control the infection and keep the disease from getting worse. Antiviral treatments for HIV have reduced AIDS deaths around the world. There's an ongoing effort to make ways to prevent and treat HIV / AIDS more available in resource-poor countries.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Assortment of Pill Aids from Mayo Clinic Store
The symptoms of HIV and AIDS vary depending on the person and the phase of infection.
Primary infection, also called acute HIV
Some people infected by HIV get a flu-like illness within 2 to 4 weeks after the virus enters the body. This stage may last a few days to several weeks. Some people have no symptoms during this stage.
Possible symptoms include:
- Muscle aches and joint pain.
- Sore throat and painful mouth sores.
- Swollen lymph glands, also called nodes, mainly on the neck.
- Weight loss.
- Night sweats.
These symptoms can be so mild that you might not notice them. However, the amount of virus in your bloodstream, called viral load, is high at this time. As a result, the infection spreads to others more easily during primary infection than during the next stage.
Clinical latent infection, also called chronic HIV
In this stage of infection, HIV is still in the body and cells of the immune system, called white blood cells. But during this time, many people don't have symptoms or the infections that HIV can cause.
This stage can last for many years for people who aren't getting antiretroviral therapy, also called ART. Some people get more-severe disease much sooner.
Symptomatic HIV infection
As the virus continues to multiply and destroy immune cells, you may get mild infections or long-term symptoms such as:
- Swollen lymph glands, which are often one of the first symptoms of HIV infection.
- Oral yeast infection, also called thrush.
- Shingles, also called herpes zoster.
Progression to AIDS
Better antiviral treatments have greatly decreased deaths from AIDS worldwide. Thanks to these lifesaving treatments, most people with HIV in the U.S. today don't get AIDS . Untreated, HIV most often turns into AIDS in about 8 to 10 years.
Having AIDS means your immune system is very damaged. People with AIDS are more likely to develop diseases they wouldn't get if they had healthy immune systems. These are called opportunistic infections or opportunistic cancers. Some people get opportunistic infections during the acute stage of the disease.
The symptoms of some of these infections may include:
- Fever that keeps coming back.
- Ongoing diarrhea.
- Swollen lymph glands.
- Constant white spots or lesions on the tongue or in the mouth.
- Constant fatigue.
- Rapid weight loss.
- Skin rashes or bumps.
When to see a doctor
If you think you may have been infected with HIV or are at risk of contracting the virus, see a healthcare professional as soon as you can.
More Information
- Early HIV symptoms: What are they?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
HIV is caused by a virus. It can spread through sexual contact, shooting of illicit drugs or use of shared needles, and contact with infected blood. It also can spread from parent to child during pregnancy, childbirth or breastfeeding.
HIV destroys white blood cells called CD4 T cells. These cells play a large role in helping the body fight disease. The fewer CD4 T cells you have, the weaker your immune system becomes.
How does HIV become AIDS?
You can have an HIV infection with few or no symptoms for years before it turns into AIDS . AIDS is diagnosed when the CD4 T cell count falls below 200 or you have a complication you get only if you have AIDS , such as a serious infection or cancer.
How HIV spreads
You can get infected with HIV if infected blood, semen or fluids from a vagina enter your body. This can happen when you:
- Have sex. You may become infected if you have vaginal or anal sex with an infected partner. Oral sex carries less risk. The virus can enter your body through mouth sores or small tears that can happen in the rectum or vagina during sex.
- Share needles to inject illicit drugs. Sharing needles and syringes that have been infected puts you at high risk of HIV and other infectious diseases, such as hepatitis.
- Have a blood transfusion. Sometimes the virus may be transmitted through blood from a donor. Hospitals and blood banks screen the blood supply for HIV . So this risk is small in places where these precautions are taken. The risk may be higher in resource-poor countries that are not able to screen all donated blood.
- Have a pregnancy, give birth or breastfeed. Pregnant people who have HIV can pass the virus to their babies. People who are HIV positive and get treatment for the infection during pregnancy can greatly lower the risk to their babies.
How HIV doesn't spread
You can't become infected with HIV through casual contact. That means you can't catch HIV or get AIDS by hugging, kissing, dancing or shaking hands with someone who has the infection.
HIV isn't spread through air, water or insect bites. You can't get HIV by donating blood.
Risk factors
Anyone of any age, race, sex or sexual orientation can have HIV / AIDS . However, you're at greatest risk of HIV / AIDS if you:
- Have unprotected sex. Use a new latex or polyurethane condom every time you have sex. Anal sex is riskier than is vaginal sex. Your risk of HIV increases if you have more than one sexual partner.
- Have an STI . Many STIs cause open sores on the genitals. These sores allow HIV to enter the body.
- Inject illicit drugs. If you share needles and syringes, you can be exposed to infected blood.
Complications
HIV infection weakens your immune system. The infection makes you much more likely to get many infections and certain types of cancers.
Infections common to HIV/AIDS
- Pneumocystis pneumonia, also called PCP. This fungal infection can cause severe illness. It doesn't happen as often in the U.S. because of treatments for HIV / AIDS . But PCP is still the most common cause of pneumonia in people infected with HIV .
- Candidiasis, also called thrush. Candidiasis is a common HIV -related infection. It causes a thick, white coating on the mouth, tongue, esophagus or vagina.
- Tuberculosis, also called TB. TB is a common opportunistic infection linked to HIV . Worldwide, TB is a leading cause of death among people with AIDS . It's less common in the U.S. thanks to the wide use of HIV medicines.
- Cytomegalovirus. This common herpes virus is passed in body fluids such as saliva, blood, urine, semen and breast milk. A healthy immune system makes the virus inactive, but it stays in the body. If the immune system weakens, the virus becomes active, causing damage to the eyes, digestive system, lungs or other organs.
- Cryptococcal meningitis. Meningitis is swelling and irritation, called inflammation, of the membranes and fluid around the brain and spinal cord, called meninges. Cryptococcal meningitis is a common central nervous system infection linked to HIV . A fungus found in soil causes it.
Toxoplasmosis. This infection is caused by Toxoplasma gondii, a parasite spread primarily by cats. Infected cats pass the parasites in their stools. The parasites then can spread to other animals and humans.
Toxoplasmosis can cause heart disease. Seizures happen when it spreads to the brain. And it can be fatal.
Cancers common to HIV/AIDS
- Lymphoma. This cancer starts in the white blood cells. The most common early sign is painless swelling of the lymph nodes most often in the neck, armpit or groin.
- Kaposi sarcoma. This is a tumor of the blood vessel walls. Kaposi sarcoma most often appears as pink, red or purple sores called lesions on the skin and in the mouth in people with white skin. In people with Black or brown skin, the lesions may look dark brown or black. Kaposi sarcoma also can affect the internal organs, including the lungs and organs in the digestive system.
- Human papillomavirus (HPV)-related cancers. These are cancers caused by HPV infection. They include anal, oral and cervical cancers.
Other complications
- Wasting syndrome. Untreated HIV / AIDS can cause a great deal of weight loss. Diarrhea, weakness and fever often happen with the weight loss.
- Brain and nervous system, called neurological, complications. HIV can cause neurological symptoms such as confusion, forgetfulness, depression, anxiety and difficulty walking. HIV -associated neurological conditions can range from mild symptoms of behavior changes and reduced mental functioning to severe dementia causing weakness and not being able to function.
- Kidney disease. HIV -associated nephropathy (HIVAN) is swelling and irritation, called inflammation, of the tiny filters in the kidneys. These filters remove excess fluid and waste from the blood and pass them to the urine. Kidney disease most often affects Black and Hispanic people.
- Liver disease. Liver disease also is a major complication, mainly in people who also have hepatitis B or hepatitis C.
There's no vaccine to prevent HIV infection and no cure for HIV / AIDS . But you can protect yourself and others from infection.
To help prevent the spread of HIV :
Consider preexposure prophylaxis, also called PrEP. There are two PrEP medicines taken by mouth, also called oral, and one PrEP medicine given in the form of a shot, called injectable. The oral medicines are emtricitabine-tenofovir disoproxil fumarate (Truvada) and emtricitabine-tenofovir alafenamide fumarate (Descovy). The injectable medicine is called cabotegravir (Apretude). PrEP can reduce the risk of sexually transmitted HIV infection in people at very high risk.
PrEP can reduce the risk of getting HIV from sex by about 99% and from injecting drugs by at least 74%, according to the Centers for Disease Control and Prevention. Descovy hasn't been studied in people who have sex by having a penis put into their vaginas, called receptive vaginal sex.
Cabotegravir (Apretude) is the first U.S. Food and Drug Administration-approved PrEP that can be given as a shot to reduce the risk of sexually transmitted HIV infection in people at very high risk. A healthcare professional gives the shot. After two once-monthly shots, Apretude is given every two months. The shot is an option in place of a daily PrEP pill.
Your healthcare professional prescribes these medicines to prevent HIV only to people who don't already have HIV infection. You need an HIV test before you start taking any PrEP . You need to take the test every three months for the pills or before each shot for as long as you take PrEP .
You need to take the pills every day or closely follow the shot schedule. You still need to practice safe sex to protect against other STIs . If you have hepatitis B, you should see an infectious disease or liver specialist before beginning PrEP therapy.
Use treatment as prevention, also called TasP. If you have HIV , taking HIV medicines can keep your partner from getting infected with the virus. If your blood tests show no virus, that means your viral load can't be detected. Then you won't transmit the virus to anyone else through sex.
If you use TasP , you must take your medicines exactly as prescribed and get regular checkups.
- Use post-exposure prophylaxis, also called PEP, if you've been exposed to HIV . If you think you've been exposed through sex, through needles or in the workplace, contact your healthcare professional or go to an emergency room. Taking PEP as soon as you can within the first 72 hours can greatly reduce your risk of getting HIV . You need to take the medicine for 28 days.
Use a new condom every time you have anal or vaginal sex. Both male and female condoms are available. If you use a lubricant, make sure it's water based. Oil-based lubricants can weaken condoms and cause them to break.
During oral sex, use a cut-open condom or a piece of medical-grade latex called a dental dam without a lubricant.
- Tell your sexual partners you have HIV . It's important to tell all your current and past sexual partners that you're HIV positive. They need to be tested.
- Use clean needles. If you use needles to inject illicit drugs, make sure the needles are sterile. Don't share them. Use needle-exchange programs in your community. Seek help for your drug use.
- If you're pregnant, get medical care right away. You can pass HIV to your baby. But if you get treatment during pregnancy, you can lessen your baby's risk greatly.
- Consider male circumcision. Studies show that removing the foreskin from the penis, called circumcision, can help reduce the risk of getting HIV infection.
- About HIV and AIDS . HIV.gov. https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/what-are-hiv-and-aids. Accessed Oct. 18, 2023.
- Sax PE. Acute and early HIV infection: Clinical manifestations and diagnosis. https://www.uptodate.com/contents/search. Accessed Oct. 18, 2023.
- Ferri FF. Human immunodeficiency virus. In: Ferri's Clinical Advisor 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Oct. 18, 2023.
- Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV . HIV.gov. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/immunizations. Accessed Oct. 18, 2023.
- AskMayoExpert. Human immunodeficiency virus (HIV) infection. Mayo Clinic; 2023.
- Elsevier Point of Care. Clinical Overview: HIV infection and AIDS in adults. https://www.clinicalkey.com. Accessed Oct. 18, 2023.
- Male circumcision for HIV prevention fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/nchhstp/newsroom/fact-sheets/hiv/male-circumcision-HIV-prevention-factsheet.html. Accessed Oct. 19, 2023.
- Acetyl-L-carnitine. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed. Oct. 19, 2023.
- Whey protein. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed. Oct. 19, 2023.
- Saccharomyces boulardii. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed Oct. 19, 2023.
- Vitamin A. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed Oct. 19, 2023.
- Red yeast rice. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed Oct. 19, 2023.
Associated Procedures
- Liver function tests
News from Mayo Clinic
- Mayo Clinic Minute: Know your status -- the importance of HIV testing June 25, 2024, 04:00 p.m. CDT
- Unlocking the mechanisms of HIV in preclinical research Jan. 10, 2024, 03:30 p.m. CDT
- Mayo Clinic expert on future of HIV on World AIDS Day Dec. 01, 2023, 05:15 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Introduction to HIV/AIDS
AIDS stands for Acquired Immune Deficiency Syndrome. AIDS is a serious condition that weakens the body's immune system, leaving it unable to fight off illness.
AIDS is the last stage in a progression of diseases resulting from a viral infection known as the Human Immunodeficiency Virus (HIV or AIDS virus). The diseases include a number of unusual and severe infections, cancers and debilitating illnesses, resulting in severe weight loss or wasting away, and diseases affecting the brain and central nervous system.
There is no cure for HIV infection or AIDS nor is there a vaccine to prevent HIV infection. However, new medications not only can slow the progression of the infection, but can also markedly suppress the virus, thereby restoring the body’s immune function and permitting many HIV-infected individuals to lead a normal, disease-free life.
How HIV/AIDS Affects The Body
The immune system is a network of cells, organs and proteins that work together to defend and protect the body from potentially harmful, infectious microorganisms (microscopic life-forms), such as bacteria, viruses, parasites and fungi. The immune system also plays a critical role in preventing the development and spread of many types of cancer .
When the immune system is missing one or more of its components, the result is an immunodeficiency disorder. AIDS is an immunodeficiency disorder.
Lymphocytes (white blood cells) are one of the main types of immune cells that make up the immune system. There are two types of lymphocytes: B cells and T cells. (T cells are also called CD4 cells, CD4 T cells, or CD4 cell lymphocytes). B cells secrete antibodies (proteins) into the body's fluids to ambush and attack antigens (foreign proteins such as bacteria, viruses or fungi). T cells directly attack and destroy infected or malignant cells in the body.
There are two types of T cells: helper T cells and killer T cells. Helper T cells recognize the antigen and activate the killer T cells. Killer T cells then destroy the antigen.
When HIV is introduced into the body, this virus is too strong for the helper T cells and killer T cells. The virus then invades these cells and starts to reproduce itself, thereby not only killing the CD4 T cells, but also spreading to infect otherwise healthy cells.
The HIV virus cannot be destroyed and lives in the body undetected for months or years before any sign of illness appears. Gradually, over many years or even decades, as the T cells become progressively destroyed or inactivated, other viruses, parasites or cancer cells (called "opportunistic diseases") which would not have been able to get past a healthy body's defense, can multiply within the body without fear of destruction. Commonly seen opportunistic diseases in persons with HIV infection include: pneumocystis carinii pneumonia , tuberculosis, candida (yeast) infection of the mouth, throat or vagina, shingles , cytomegalovirus retinitis and Kaposi's sarcoma.
AIDS is transmitted via three main routes:
The most common mode of transmission is the transfer of body secretions through sexual contact. This is accomplished through exposure of mucous membranes of the rectum, vagina or mouth to blood, semen or vaginal secretions containing the HIV virus.
Blood or blood products can transmit the virus, most often through the sharing of contaminated syringes and needles.
HIV can be spread during pregnancy from mother to fetus.
You cannot get AIDS/HIV from touching someone or sharing items, such as cups or pencils, or through coughing and sneezing. Additionally, HIV is not spread through routine contact in restaurants, the workplace or school. However, sharing a razor does pose a small risk in that blood from a minor nick can be transmitted from one person to another.
Immediately following infection with HIV, most individuals develop a brief, nonspecific “viral illness” consisting of low grade fever, rash, muscle aches, headache and/or fatigue. Like any other viral illness, these symptoms resolve over a period of five to 10 days. Then for a period of several years (sometimes as long as several decades), people infected with HIV are asymptomatic (no symptoms). However, their immune system is gradually being destroyed by the virus. When this destruction has progressed to a critical point, symptoms of AIDS appear. These symptoms are as follows:
extreme fatigue
rapid weight loss from an unknown cause (more than 10 lbs. in two months for no reason)
appearance of swollen or tender glands in the neck, armpits or groin, for no apparent reason, lasting for more than four weeks
unexplained shortness of breath, frequently accompanied by a dry cough, not due to allergies or smoking
persistent diarrhea
intermittent high fever or soaking night sweats of unknown origin
a marked change in an illness pattern, either in frequency, severity, or length of sickness
appearance of one or more purple spots on the surface of the skin, inside the mouth, anus or nasal passages
whitish coating on the tongue, throat or vagina
forgetfulness, confusion and other signs of mental deterioration
It can take as short as a year to as long as 10 to 15 years to go from being infected with HIV to "full-blown" AIDS.
According to the Center for Disease Control and Prevention, a person is considered to have AIDS when they have a T cell count (also called CD4 cell count) of 200 or less (healthy T cell levels range from 500 to 1500) or they have an AIDS-defining condition. The AIDS-defining conditions are:
· Candidiasis
· Cervical cancer (invasive)
· Coccidioidomycosis, Cryptococcosis, Cryptosporidiosis
· Cytomegalovirus disease
· Encephalopathy (HIV-related)
· Herpes simplex (severe infection)
· Histoplasmosis
· Isosporiasis
· Kaposi's sarcoma
· Lymphoma (certain types)
· Mycobacterium avium complex
· Pneumocystis carinii pneumonia
· Pneumonia (recurrent)
· Progressive multifocal leukoencephalopathy
· Salmonella septicemia (recurrent)
· Toxoplasmosis of the brain
· Tuberculosis
· Wasting syndrome
People who are not infected with HIV may also develop these diseases; the presence of any one of these conditions does not mean the person has AIDS. To be diagnosed with AIDS, a person must be infected with HIV.
Some people infected with HIV may develop a disease that is less serious than AIDS, referred to as AIDS Related Complex (ARC). ARC is a condition caused by the AIDS virus in which the patient tests positive for AIDS infection and has a specific set of clinical symptoms. However, ARC patients' symptoms are often less severe than those with classic AIDS because the degree of destruction of the immune system has not progressed as far as it has in patients with classic AIDS.
Symptoms of ARC may include loss of appetite, weight loss, fever, night sweats, skin rashes, diarrhea, tiredness, lack of resistance to infection or swollen lymph nodes .
Note: Not everyone who has been infected with HIV develops AIDS. Very rarely, some individuals can be infected with HIV yet maintain normal immune function and general good health even after 20 years of infection.
Screening for HIV infection is most commonly done by testing blood for HIV antibodies. A newer test, the Orasure test, involves collecting secretions between the cheek and gum and evaluating them for HIV antibodies. Orasure is essentially as accurate as a blood test, and, because it doesn't involve a needle stick, it is favored by many individuals. Orasure is available through physicians’ offices and many public health clinics. Finally, a new urine test available for screening, although if the test is positive, blood tests need to be performed for confirmation of the presence of HIV.
In 1996, a home HIV blood test (called Home Access) became available to the public. These home kits are available in pharmacies and by mail. The kit contains a few sharp tools called lancets, a piece of blotting paper marked with a unique identification number and a prepaid return envelope with a protective pouch. After pricking the finger with the lancet, a few drops of blood are blotted onto the paper, sealed into the envelope and sent to the address on the envelope. In about a week, the person calls a toll-free number to get the results of the test.
Anti-HIV (also called antiretroviral) medications are used to control the reproduction of the virus and to slow or halt the progression of HIV-related disease. When used in combinations, these medications are termed Highly Active Antiretroviral Therapy (HAART). HAART combines three or more anti-HIV medications in a daily regimen, sometimes referred to as a "cocktail". Anti-HIV medications do not cure HIV infection and individuals taking these medications can still transmit HIV to others. Anti-HIV medications approved by the U.S. Food and Drug Administration (FDA) fall into four classes:
1 . Nonnucleoside Reverse Transcriptase Inhibitors (NNRTIs), such as nevirappine (Viramune) and efavirenz (Sustiva), bind to and block the action of reverse transcriptase, a protein that HIV needs to reproduce.
2 . Nucleoside Reverse Transcriptase Inhibitors (NRTIs), such as zidovudine (Retrovir), tenofovir DF (Viread), and stavudine (Zerit), are faulty versions of building blocks that HIV needs to make more copies of itself. When HIV uses an NRTI instead of a normal building block, reproduction of the virus is stalled.
3 . Protease Inhibitors (PIs), such as lopinavir/ritonavir (Kaletra), disable protease, a protein that HIV needs reproduce itself.
4 . Fusion Inhibitors, such as enfuvirtide (Fuzeon ), are newer treatments that work by blocking HIV entry into cells.
(View more complete list of HIV drugs).
How many pills you will need to take and how often you will take them depends on what medications you and your doctor choose.
There is no one "best" regimen. You and your doctor will decide which medications are right for you. For people taking HAART for the first time, the recommended regimens are:
Sustiva + Truvada, Sustiva + Epzicom, or Atripla
Kaletra + Truvada, Kaletra + Epzicom, or Kaletra + Combivir
In general, taking only one or two drugs is not recommended because any decrease in viral load is almost always temporary without three or more drugs. The exception is the recommendation for pregnant women, who may take Combivir plus nevirapine to reduce the risk of passing HIV to their infants. If you are pregnant or considering becoming pregnant, there are additional treatment considerations. Recently, a number of drugs have been developed that combine two or even three separate medications in a single pill. Some of these, such as Truvada (emtricitabine + tenofovir) and Epzicom (abacavir + lamivudine) need be taken only once daily. Atripla (emtricitabine + tenofovir + efavirenz) combines three drugs in one pill and needs to be taken only once daily, thereby providing a complete HAART regimen with one pill once daily.
The treatment of HIV infection and AIDS is in a highly dynamic state. Individuals with this condition are advised to seek out experts in their local community who are current with the latest modes of therapy and ongoing clinical trials for evaluating newer therapies.
HIV/AIDS Medications
The following is a partial list of drugs approved for the treatment of HIV infection.
Nonnucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Delavirdine (Rescriptor, DLV) Pfizer
Efavirenz (Sustiva, EFV) Bristol-Myers Squibb
Nevirapine (Viramune, NVP) Boehringer Ingelheim
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Abacavir (Ziagen, ABC) GlaxoSmithKline
Abacavir,Lamivudine, Zidovudine (Trizivir) GlaxoSmithKline
Didanosine (Videx, ddI, Videx EC) Bristol-Myers Squibb
Emtricitabine (Emtriva, FTC, Coviracil) Gilead Sciences
Lamivudine (Epivir, 3TC) GlaxoSmithKline
Lamivudine, Zidovudine (Combivir) GlaxoSmithKline
Stavudine ( Zerit, d4T) Bristol-Myers Squibb
Tenofovir DF (Viread, TDF) Gilead Sciences
Zalcitabine (Hivid, ddC) Hoffmann-La Roche
Atripla (tenofovir, emtricitabine, efavirenz) Gilead Sciences
Zidovudine (Retrovir, AZT, ZDV) GlaxoSmithKline
Protease Inhibitors (PIs)
Amprenavir (Agenerase, APV) GlaxoSmithKline, Vertex Pharmaceuticals
Atazanavir (Reyataz, ATV) Bristol-Myers Squibb
Fosamprenavir (Lexiva, FPV) GlaxoSmithKline, Vertex Pharmaceuticals
Indinavir (Crixivan, IDV) Merck
Lopinavir, Ritonavir (Kaletra, LPV/r) Abbott Laboratories
Nelfinavir (Viracept, NFV) Agouron Pharmaceuticals
Ritonavir (Norvir, RTV) Abbott Laboratories
Saquinavir (Fortovase, SQV) Invirase Hoffmann-La Roche
Tipranavir (Aptivus) Boehringer-Ingelheim
Darunavir (Prezista) Tibotec Therapeutics
Fusion Inhibitors
Enfuvirtide (Fuzeon, T-20) Hoffmann-La Roche, Trimeris
Risk Prevention
The only way to protect from contracting AIDS sexually is to abstain from sex outside of a mutually faithful relationship with a partner whom the person knows is not infected with the AIDS virus. Otherwise, risks can be minimized if they:
Don't have sexual contact with anyone who has symptoms of AIDS or who is a member of a high risk group for AIDS.
Avoid sexual contact with anyone who has had sex with people at risk of getting AIDS.
Don't have sex with prostitutes.
Avoid having sex with anyone who has multiple and/or anonymous sexual partners.
Avoid oral, genital and anal contact with partner's blood, semen, vaginal secretions, feces or urine. Unless they know with absolute certainty that their partner is not infected, a latex condom should be used during each sexual act, from start to finish. The use of a spermicidal agent may provide additional protection.
Avoid anal intercourse altogether.
Don't share toothbrushes, razors or other implements that could become contaminated with the blood of anyone who is or might be infected with the AIDS virus.
Exercise caution regarding procedures, such as acupuncture, tattooing, ear piercing, etc., in which needles or other nonsterile instruments may be used repeatedly to pierce the skin and/or mucous membranes.
Such procedures are safe if proper sterilization methods are employed or disposable needles are used. Ask what precautions are taken before undergoing such procedures.
If an individual is scheduling surgery in the near future, and is able, they could consider donating blood for their own use. This will eliminate completely the already very small risk of contracting AIDS through a blood transfusion. It will also eliminate the risk of contracting other bloodborne diseases (such as hepatitis) from a transfusion.
If a person is an IV drug user, adhere to the prevention tips mentioned earlier, as well as:
Get professional help for terminating the drug habit.
Do not share needles or syringes. Be aware that some street sellers are resealing previously used needles and selling them as new.
Clean the needle before using.
Some people apparently remain well after infection of the AIDS virus. They may have no physically apparent symptoms of illness. However, if proper precautions are not used with sexual contacts and/or intravenous drug use, these infected individuals can spread the virus to others .
Anyone who thinks he or she is infected, or who is involved in high-risk behaviors, should not donate his/her blood, organs, tissues, or sperm as they may now contain the AIDS virus.
- Share via facebook
- Share via pinterest
- Share via twitter
- Share via mail
- Español (Spanish)
HIV Overview
Hiv and aids: the basics.
Note: Some individuals may prefer using the term “chestfeeding” rather than “breastfeeding.”
- The human immunodeficiency virus (HIV) is the virus that causes HIV infection. If untreated, HIV may cause acquired immunodeficiency syndrome (AIDS) , the most advanced stage of HIV infection.
- People with HIV who are not on medication and do not have consistent control of their HIV can transmit HIV through vaginal or anal sex, sharing of needles, pregnancy, and/or breastfeeding. If HIV is controlled, the risk of transmission is close to zero.
- Antiretroviral therapy (ART) is the use of HIV medicines that reduce the level of HIV in the blood (called viral load). ART is recommended for everyone who has HIV. ART cannot cure HIV infection, but HIV medicines help people with HIV have about the same life expectancy as people without HIV.
- HIV medicines (ART) can eliminate the risk of HIV transmission . For parents with HIV that want to breastfeed, the risk of transmitting HIV through breast milk is less than 1% with the consistent use of HIV medicine (ART) and an undetectable viral load.
- People on ART take a combination of HIV medicines (called an HIV treatment regimen ) every day (pills) or by schedule (injections). In many cases oral medicines may be combined into a single pill or capsule. There are newer long-acting medicines given by an injection every 2 months that may be used in some people.
What is HIV and AIDS?
HIV stands for human immunodeficiency virus , which is the virus that causes HIV infection. The abbreviation “HIV” can refer to the virus or to HIV infection.
AIDS stands for acquired immunodeficiency syndrome . AIDS is the most advanced stage of HIV infection.
HIV attacks and destroys the infection-fighting CD4 cells ( CD4 T lymphocyte ) of the immune system . The loss of CD4 cells makes it difficult for the body to fight off infections, illnesses, and certain cancers. Without treatment, HIV can gradually destroy the immune system, causing health decline and the onset of AIDS. With treatment, the immune system can recover.
How is HIV transmitted?
HIV can be transmitted from one person to another when certain bodily fluids are shared between people. Bodily fluids that can transmit HIV include blood, semen (“cum”), pre-seminal fluid (“pre-cum”), vaginal fluids, rectal fluids, and breastmilk. HIV can be transmitted during vaginal or anal sex, through sharing needles for injecting drugs or tattooing, by getting stuck with a needle that has the blood of someone with HIV on it, through pregnancy, and through breastfeeding.
The transmission of HIV from a birthing parent with HIV to their child during pregnancy, childbirth, or breastfeeding is called perinatal transmission of HIV. For more information on perinatal transmission, read the HIVinfo fact sheet on Preventing Perinatal Transmission of HIV .
You cannot get HIV by shaking hands or hugging a person who has HIV. You also cannot get HIV from contact with objects, such as dishes, toilet seats, or doorknobs, used by a person with HIV. HIV is not spread through the air or water or by mosquitoes, ticks, or other insects. Use the HIVinfo You Can Safely Share…With Someone With HIV infographic to spread this message.
What is the treatment for HIV?
Antiretroviral therapy (ART) is the use of HIV medicines to treat HIV infection. People on ART take a combination of HIV medicines (called an HIV treatment regimen ) every day (pills) or by schedule (injections). In many cases oral medicines may be combined into a single pill or capsule. There are newer long-acting medicines given by an injection every 2 months that may be used in some people.
ART is recommended for everyone who has HIV. ART prevents HIV from multiplying, which reduces the amount of HIV in the body (called the viral load ). Having less HIV in the body protects the immune system and prevents HIV infection from advancing to AIDS. ART cannot cure HIV, but HIV medicines can help people with HIV live long, healthy lives.
How can a person reduce the risk of transmitting HIV?
ART reduces the risk of HIV transmission. ART can reduce a person’s viral load to an undetectable level. An undetectable viral load means that the level of HIV in the blood is too low to be detected by a viral load test . People with HIV who maintain an undetectable viral load have no risk of transmitting HIV to their HIV-negative partner through sex.
HIV medicines taken during pregnancy, childbirth, and breastfeeding can also reduce the risk of perinatal (parent to infant) transmission of HIV. Previously, replacement feeding (properly prepared formula or pasteurized donor human milk from a milk bank) was recommended instead of breastfeeding since the risk of HIV transmission was considered high. Now, there is evidence that the risk of transmission through the breastmilk of someone consistently using ART and maintaining an undetectable viral load is low (less than 1%). Pregnant people with HIV can speak with their health care provider to determine what method of feeding their baby is right for them.
How can a person reduce the risk of getting HIV?
For people without HIV, there are several ways to reduce the risk of acquiring (getting) HIV infection. Using condoms correctly with every sexual encounter, particularly with partners that are HIV positive with a detectable viral load or with partners whose HIV status is unknown, can reduce the risk of acquiring HIV. Reducing HIV risk also involves limiting and reducing sexual partners, and avoiding sharing needles.
Persons who do not have HIV should talk to their health care provider about pre-exposure prophylaxis (PrEP) . PrEP is an HIV prevention option for people who do not have HIV but who are at risk of becoming infected with HIV. PrEP involves taking a specific HIV medicine every day or a long-acting injection. For more information, read the HIVinfo fact sheet on Pre-exposure Prophylaxis (PrEP) .
Persons who do not have HIV, but may have been exposed to HIV, should talk to their health care provider about post-exposure prophylaxis (PEP) within 72 hours after a possible exposure. For more information, read the HIVinfo fact sheet on Post-Exposure Prophylaxis (PEP) .
To learn more about reducing the risk of HIV transmission, read the HIVinfo fact sheet The Basics of HIV Prevention .
What are the symptoms of HIV and AIDS?
Within 2 to 4 weeks after infection with HIV, some people may have flu-like symptoms, such as fever, chills, or rash. The symptoms may last for a few days to several weeks. Other possible symptoms of HIV include night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, and mouth ulcers. Having these symptoms does not mean you have HIV. Other illnesses can cause the same symptoms. Some people may not feel sick during early HIV infection (called acute HIV ). During this earliest stage of HIV infection, the virus multiplies rapidly. After the initial stage of infection, HIV continues to multiply but at lower levels.
More severe symptoms of HIV infection for persons not on ART may not appear for many years until HIV has developed into AIDS. People with AIDS have weakened immune systems that make them prone to opportunistic infections. Opportunistic infections are infections and infection-related cancers that occur more frequently or are more severe in people with weakened immune systems than in people with healthy immune systems.
Without treatment, HIV transmission is possible at any stage of HIV infection—even if a person with HIV has no symptoms of HIV.
How is AIDS diagnosed?
Symptoms such as fever, weakness, and weight loss may be a sign that a person’s HIV has advanced to AIDS. However, a diagnosis of AIDS is based on the following criteria:
- A drop in CD4 count to less than 200 cells/mm 3 . A CD4 count measures the number of CD4 cells ( CD4 T lymphocyte ) in a sample of blood. OR
- The presence of certain opportunistic infections.
Although an AIDS diagnosis indicates severe damage to the immune system, HIV medicines can still help people at this stage of HIV infection.
This fact sheet is based on information from the following sources:
From Centers for Disease Control and Prevention:
- AIDS and Opportunistic Infections
- HIV and Pregnancy
From the Department of Health and Human Services (HHS):
- Introduction
- Infant Feeding for Individuals with HIV in the United States
From the National Institute of Allergy and Infectious Diseases (NIAID):
Also see the HIV Source collection of HIV links and resources.
You can Choose category
Cause and Effect Essay of AIDS/HIV
Hiv infection, causes of hiv/aids, effects of hiv/aids.
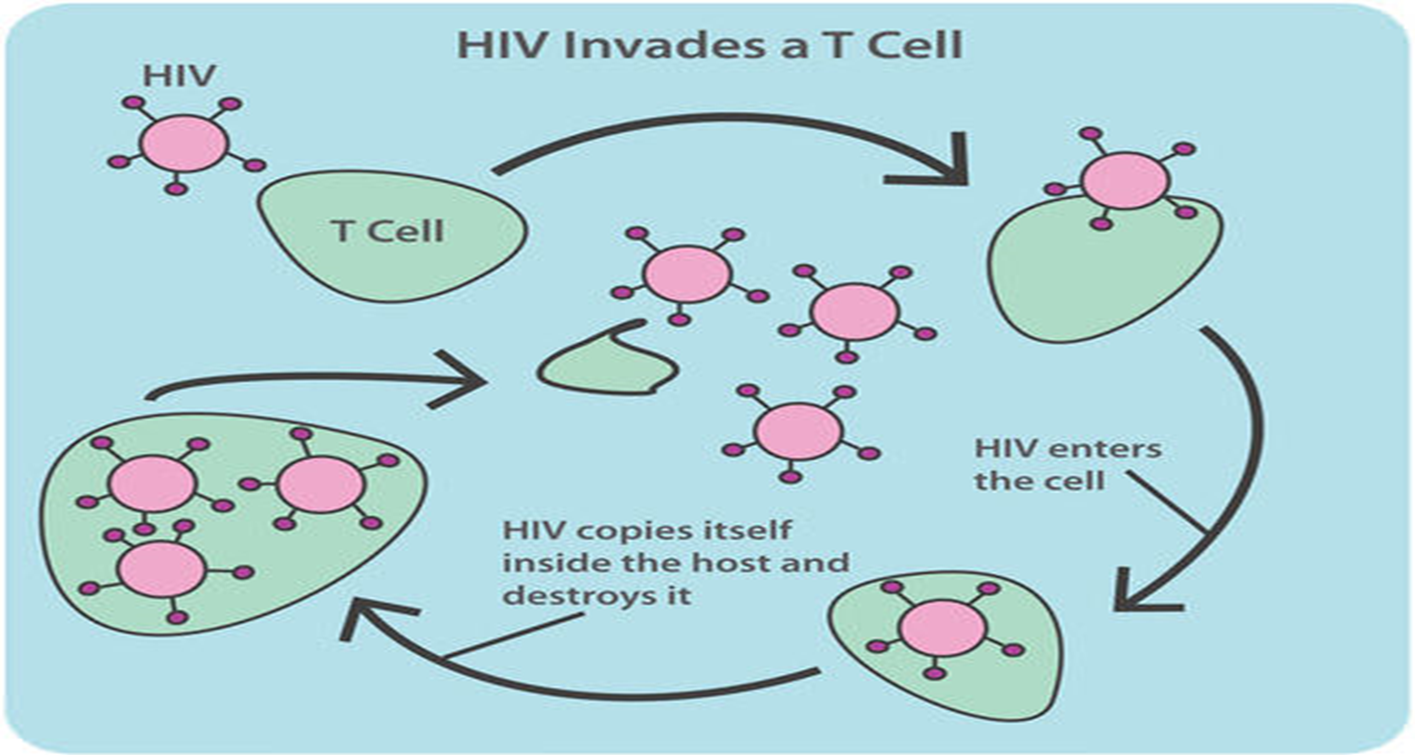
AIDS stands for “acquired immunodeficiency syndrome” which is an advanced stage of the human immunodeficiency virus (HIV) infection. AIDS is a chronic, life-threatening condition that results from HIV (Abraham, 2019). HIV interferes with the immune system by hindering the body’s ability to fight diseases and infections by destroying helper T cells which are responsible for keeping the human body immune from illnesses (K-12 Foundation 1). Medical practitioners say that AIDS is identified in a person when the CD4 count is below 200 cells per cubic millimeter (Abraham, 2019). After penetrating helper T cells, the virus copies itself in the host and destroys or infects the cell and other helper T cells throughout the body.
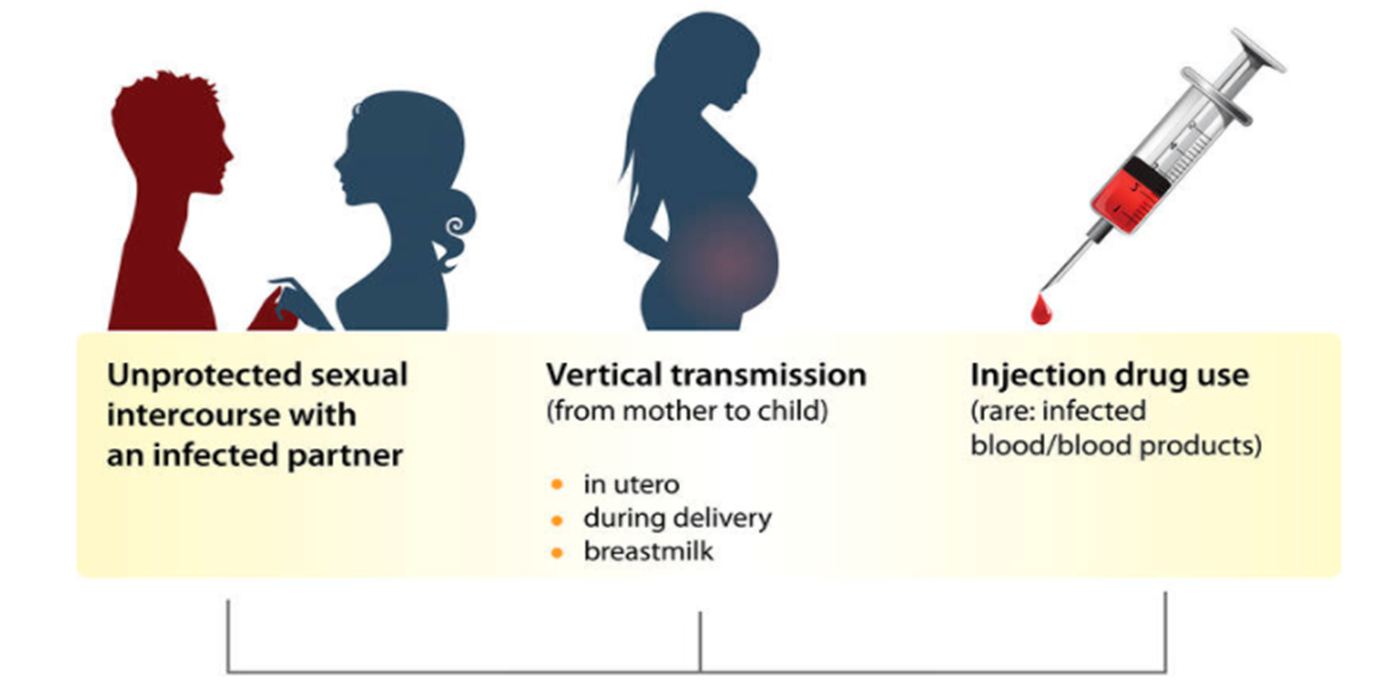
Figure 2 above illustrates the various ways that increase the chances of a person contracting the HIV virus. They comprise getting in contact with vaginal fluids, semen, and the blood of an infected person (Abraham, 2019). Moreover, the virus can be contracted by engaging in unprotected sexual activity with persons infected with the virus (Abraham 37). Another way a person can contract the virus is by sharing piercing instruments with infected persons. The virus also can pass from a mother to child while breastfeeding, during birth, or during pregnancy (Abraham, 2019). Without receiving suitable medication, it might take years before HIV makes the immune system weak to the point of developing AIDS (Abraham 25). These are some of the ways that the HIV virus can pass from an infected to a healthy person.
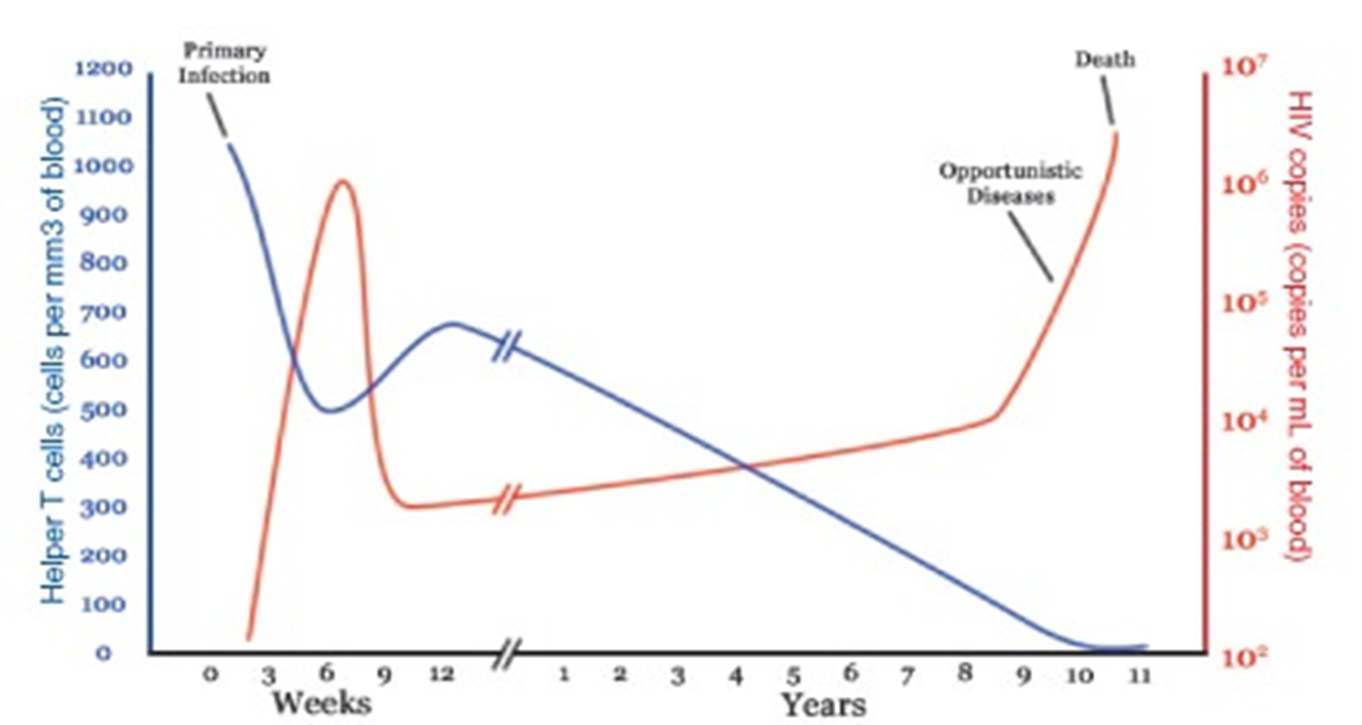
HIV/AIDS will have various effects on the body of a patient. For instance, HIV will destroy the CD4 cell count in the body of a patient which is vital for immunity from diseases and infections (Abraham, 2019). During the first several weeks, the body’s immune system tries to fight the virus. As evident in Figure 3 above, the human body’s response leads to a temporary reduction in the number of virus copies or the multiplication process. However, rapid reproduction makes it difficult for the immune system to completely destroy the pathological virus. Continued multiplication of the virus over the next several years results in further decline in helper T cells, consequently weakening the immune system further (K-12 Foundation 2. This compromise exposes the body to frequent infections.
Furthermore, a lack of appropriate medication will create a high risk of developing opportunistic diseases such as pneumonia, influenza, colds, breathing problems, fever, cough, pulmonary arterial hypertension (PAH), and cancer (Brady et al., 2019). Other consequences include loss of appetite, weight, and death.
Abraham, Thomas. “HIV and AIDS: The Causes and Effects.” HEKAMTHO (2019). Web.
Brady, Michael T., et al. “Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children.” Vaccine, 2019. Web.
Wilkin, Doughlas and Jean Brainard. “HIV and AIDS – Advanced.” K-12 Foundation, 2020. Web.
What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medicine as Prescribed
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Nutrition and People with HIV
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 25
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
What Is HIV?
HIV ( human immunodeficiency virus ) is a virus that attacks cells that help the body fight infection, making a person more vulnerable to other infections and diseases. It is spread by contact with certain bodily fluids of a person with HIV, most commonly during unprotected sex (sex without a condom or HIV medicine to prevent or treat HIV), or through sharing injection drug equipment.
If left untreated, HIV can lead to the disease AIDS ( acquired immunodeficiency syndrome ).
The human body can’t get rid of HIV and no effective HIV cure exists. So, once you have HIV, you have it for life. Luckily, however, effective treatment with HIV medicine (called antiretroviral therapy or ART) is available. If taken as prescribed, HIV medicine can reduce the amount of HIV in the blood (also called the viral load) to a very low level. This is called viral suppression. If a person’s viral load is so low that a standard lab can’t detect it, this is called having an undetectable viral load. People with HIV who take HIV medicine as prescribed and get and keep an undetectable viral load can live long and healthy lives and will not transmit HIV to their HIV-negative partners through sex .
In addition, there are effective methods to prevent getting HIV through sex or drug use, including pre-exposure prophylaxis (PrEP) , medicine people at risk for HIV take to prevent getting HIV from sex or injection drug use, and post-exposure prophylaxis (PEP) , HIV medicine taken within 72 hours after a possible exposure to prevent the virus from taking hold. Learn about other ways to prevent getting or transmitting HIV .
What Is AIDS?
AIDS is the late stage of HIV infection that occurs when the body’s immune system is badly damaged because of the virus.
In the U.S., most people with HIV do not develop AIDS because taking HIV medicine as prescribed stops the progression of the disease.
A person with HIV is considered to have progressed to AIDS when:
- the number of their CD4 cells falls below 200 cells per cubic millimeter of blood (200 cells/mm3). (In someone with a healthy immune system, CD4 counts are between 500 and 1,600 cells/mm3.) OR
- they develop one or more opportunistic infections regardless of their CD4 count.
Without HIV medicine, people with AIDS typically survive about 3 years. Once someone has a dangerous opportunistic illness, life expectancy without treatment falls to about 1 year. HIV medicine can still help people at this stage of HIV infection, and it can even be lifesaving. But people who start HIV medicine soon after they get HIV experience more benefits—that’s why HIV testing is so important.
How Do I Know If I Have HIV?
The only way to know for sure if you have HIV is to get tested . Testing is relatively simple. You can ask your health care provider for an HIV test. Many medical clinics, substance abuse programs, community health centers, and hospitals offer them too. If you test positive, you can be connected to HIV care to start treatment as soon as possible. If you test negative, you have the information you need to take steps to prevent getting HIV in the future.
To find an HIV testing location near you, use the HIV Services Locator .
HIV self-testing is also an option. Self-testing allows people to take an HIV test and find out their result in their own home or other private location. With an HIV self-test, you can get your test results within 20 minutes. You can buy an HIV self-test kit at a pharmacy or online. Some health departments or community-based organizations also provide HIV self-test kits for a reduced cost or for free. You can call your local health department or use the HIV Testing and Care Services Locator to find organizations that offer HIV self-test kits near you. (Contact the organization for eligibility requirements.)
Note: State laws regarding self-testing vary and may limit availability. Check with a health care provider or health department Exit Disclaimer for additional testing options.
Learn more about HIV self-testing and which test might be right for you .
Related HIV.gov Blogs
On national hiv testing day, level up your self-love by checking your status, june 27 is national hiv testing day, leaders’ reflections: the ongoing importance of national hiv testing day.
- HIV Testing Day National HIV Testing Day
- World AIDS Day
- HIVinfo.NIH.gov – HIV and AIDS: The Basics
- CDC – HIV Basics
- NIH – HIV/AIDS
- OWH – HIV and AIDS Basics
- VA – HIV/AIDS Basics
What Causes AIDS?
- Download PDF Copy

HIV or Human Immunodeficiency virus is a retrovirus that was first found in 1983. The virus is responsible for causing AIDS (acquired immunodeficiency syndrome).
Once within the body the HIV infects cells of the immune system that form the body’s defence system and makes them unable to fight off infections.
The virus enters the immune system’s CD4 cells, which protect the body against various bacteria, viruses and other germs. The CD4 cells are then used to make thousands of copies of the virus. These copies then leave the CD4 cells, killing them in the process.
As the virus starts to multiply the CD4 cell count thus decreases dramatically. HIV infection takes nearly 10 years or more to manifest into full blown AIDS case.
Beginning of the virus
HIV is thought to originate in Africa, where humans caught it from chimpanzees and other apes. The virus that affects the apes is very similar to HIV and is called SIVcpz (simian immunodeficiency virus). This virus spread to humans following contact with infected chimpanzee blood during the hunting of chimpanzees.
For many years the human type of HIV was limited to a remote part of Africa. With improved connections the virus began to spread worldwide.
Types of HIV virus
The virus changes very rapidly and is easily able to evade many of the body's defence systems.
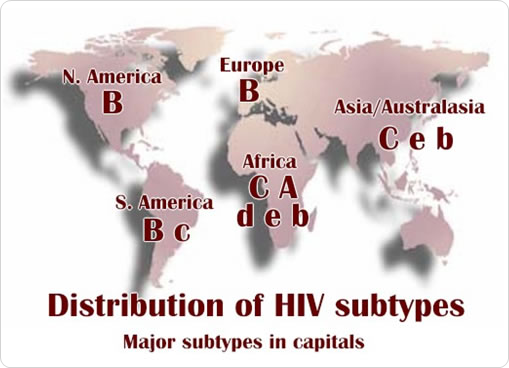
There are two types of HIV; they are HIV-1 and HIV-2 and they have many subtypes.
Related Stories
- Major UK study finds high demand and efficacy for HIV PrEP among sexual health service attendees
- Fear of stigma and rejection can lead to non-disclosure of STI status
- Nutrition's pivotal role in combating tuberculosis: addressing N-AIDS for better outcomes
HIV-1 is the cause of the current worldwide pandemic while HIV-2 is found in west Africa but rarely elsewhere.
HIV-2, which is transmitted in the same ways as HIV-1, causes AIDS much more slowly than HIV-1. HIV-1 resulted from human infection by SIVcpz that infects chimpanzees and HIV-2 resulted from infection by SIVsmm harbored by sooty mangabeys. HIV-2 is closely related to the SIV found in west Africa.
The strains of HIV-1 can be classified into four groups: the "major" group M, the "outlier" group O and two new groups, N and P. These four groups may represent four separate introductions of simian immunodeficiency virus into humans.
Of these, Group O appears to be restricted to west-central Africa and group N is rare.
More than 90 percent of HIV-1 infections belong to HIV-1 group M. Within group M there are known to be at least nine genetically distinct subtypes (or clades) of HIV-1. These are subtypes A, B, C, D, F, G, H, J and K.
Occasionally, two viruses of different subtypes can meet in the cell of an infected person and mix together their genetic material to create a new hybrid virus. Many of these new strains do not survive for long. These are called "circulating recombinant forms" or CRFs. For example, the CRF A/B is a mixture of subtypes A and B.
Distribution of HIV subtypes
- http://www.patient.co.uk/doctor/The-Human-Immunodeficiency-Virus-(HIV).htm
- http://www.nhs.uk/Conditions/HIV/Pages/Causes.aspx
- https://www.bbc.co.uk/
- https://cpha.ca
- https://www.trc-chennai.org/
- https://www.ncbi.nlm.nih.gov/
Further Reading
- All HIV/AIDS Content
- What is HIV/AIDS?
- HIV-1 versus HIV-2: What’s the Difference?
- AIDS Symptoms
- AIDS Pathophysiology
Last Updated: Jul 6, 2023

Dr. Ananya Mandal
Dr. Ananya Mandal is a doctor by profession, lecturer by vocation and a medical writer by passion. She specialized in Clinical Pharmacology after her bachelor's (MBBS). For her, health communication is not just writing complicated reviews for professionals but making medical knowledge understandable and available to the general public as well.
Please use one of the following formats to cite this article in your essay, paper or report:
Mandal, Ananya. (2023, July 06). What Causes AIDS?. News-Medical. Retrieved on September 15, 2024 from https://www.news-medical.net/health/What-Causes-AIDS.aspx.
Mandal, Ananya. "What Causes AIDS?". News-Medical . 15 September 2024. <https://www.news-medical.net/health/What-Causes-AIDS.aspx>.
Mandal, Ananya. "What Causes AIDS?". News-Medical. https://www.news-medical.net/health/What-Causes-AIDS.aspx. (accessed September 15, 2024).
Mandal, Ananya. 2023. What Causes AIDS? . News-Medical, viewed 15 September 2024, https://www.news-medical.net/health/What-Causes-AIDS.aspx.
Suggested Reading

If HIV/AIDS originated in Africa, how come the 1st cases of its sufferers, back in the early '70s were homosexuals in USA? I was a student nurse when I read about this scary disease in a magazine.
Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

How can microdialysis benefit drug development
Ilona Vuist
In this interview, discover how Charles River uses the power of microdialysis for drug development as well as CNS therapeutics.

Global and Local Efforts to Take Action Against Hepatitis
Lindsey Hiebert and James Amugsi
In this interview, we explore global and local efforts to combat viral hepatitis with Lindsey Hiebert, Deputy Director of the Coalition for Global Hepatitis Elimination (CGHE), and James Amugsi, a Mandela Washington Fellow and Physician Assistant at Sandema Hospital in Ghana. Together, they provide valuable insights into the challenges, successes, and the importance of partnerships in the fight against hepatitis.

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.


Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

Essay About HIV/AIDS
Introduction.
Human Immunodeficiency Virus, abbreviated as HIV, attacks the body’s immune system, and if left untreated, it can cause AIDS (Acquired Immune Deficiency Syndrome). HIV is a retroviral disease transmitted through unprotected sexual activity, from mother to child, blood transfusion, contact with infected body fluids, or hypodermic needles (Melhuish & Lewthwaite, 2018). The disease originated from a zoonotic animal, a chimpanzee in Central Africa. The virus version in chimpanzees, Simian Immunodeficiency Virus, is thought to have been passed to humans during their hunting activities way back in 1800. The disease has further been spread across Africa over the decades and eventually into other parts of the world. Its existence in the United States occurred between the mid to late 1970s.
Disease Manifestation
HIV weakens the immune system through infection and destruction of the CD4+ T cells, leading to immunodeficiency at the later stages of the disease. The virus adheres to the CD4+ protein on its surface and other cells to gain entry into the body ( Melhuish & Lewthwaite, 2018 ). Other coreceptors such as CCR5 and CXCR4 are essential in enabling the virus to gain complete access and cause infection to the body cells. HIV infection undergoes three stages: acute illness, chronic infection, and acquired immunodeficiency syndrome (AIDS) (Velloza et al., 2020). The first stage usually develops between 2 to 4 weeks after initial exposure. The stage often goes unrecognized because of the occasionally mild and nonspecific symptoms. Some of the clinical manifestations observed in the first stage include typical rushes distributed on the face and trunk, although they may also appear in the palms and soles. Oral and genital mucocutaneous ulceration is also another clinical manifestation that can be experienced during the first stage. In this stage, gastrointestinal manifestation, facial nerve palsy, acute encephalopathy, and many other clinical symptoms may participate.
In the second stage of infection, the virus continues to multiply but at low levels. Infected individuals who are in this stage may not have any alarming symptoms. The stage can last for up to 10 to 15 years, although it may move so fast in some individuals c. AIDs infection occurs in the third stage. The infection may be manifested by symptoms such as rapid loss of weight, recurring fever, extreme tiredness, prolonged swelling of the lymph glands in the groin, armpits, or neck, sores in the mouth, diarrhea that lasts for more than a week, or memory loss and other neurologic disorder (Nasuuna et al., 2018). When infected individuals are not treated, they may develop severe diseases such as serious bacterial infections, cryptococcal meningitis, tuberculosis, and cancers like Kaposi’s sarcoma and lymphomas.
Diagnosis and Treatment
HIV diagnosis can be made by a rapid diagnostic test that provides results on the same day. Individuals may also test themselves using an HIV self-test kit, although a confirmatory test has to be done later on by a qualified health professional (Mayo Clinic, 2020). The diagnostic test works by detecting antibodies produced by a person as part of their immune response to fight the virus. When the results turn out positive, immediate treatment should be done to manage the virus (Mayo Clinic, 2020). A combination of three or more antiretroviral drugs (ARVs) or antiretroviral therapy (ART) may suppress the symptoms and viral replication within an individual hence allowing recovery of the immune system and regain the ability to protect the body from opportunistic infections.
The public health measures of HIV prevention can be divided into three categories; primary, secondary, and tertiary prevention. Primary prevention measures protect an individual from acquiring HIV infection. It involves strategies such as abstaining from sex, not sharing needles and sharp objects and using condoms when engaging in sexual activities. Prevention medicines such as PrEP (pre-exposure prophylaxis) and PEP (post-exposure prophylaxis) may also be used to protect yourself from the infection (Mayo Clinic, 2020). Secondary HIV prevention involves measures that should be directed to infected individuals to prevent transmission to negative people (Mayo Clinic, 2020). Strategies used in secondary prevention entails giving health education to those who are infected, supporting ART adherence efforts, providing ongoing risk assessment regarding substance use and sexual behavior, encouraging infected individuals to disclose their HIV status to their sexual and drug use partners, prescribing condoms for positive individuals and providing counseling to them (Mayo Clinic, 2020). Tertiary prevention measures ensure the improved treatment to reduce the impact of HIV/AIDS disease and promote recovery. A tertiary prevention strategy aims at reducing complications that may be caused by HIV infection.
Surveillance measures
Local surveillance of HIV may be carried out using various reporting tools to fill HIV infection cases and later submitted to the local health departments for further analysis. The Centre for Disease Control and Prevention (CDC) plays a big role in collecting, analyzing, and disseminating data for national surveillance on HIV/AIDS. The CDC’s National surveillance system monitors HIV trends in the U.S (CDC, 2020). Moreover, the World Health organization can conduct international surveillance of HIV/AIDS, which surveys on HIV sentinel, STDs, and behavior.
Prevalence and Incidence
According to WHO (2020), the global prevalence of HIV is estimated to be over 37.7 million people, including 1.7 million children. The percentage prevalence in adults is 0.7%. Additionally, the incidence of HIV infection was 1.5 million (WHO, 2020). Most people living with HIV live in low and middle-income countries, with East and Southern Africa being the most affected region globally. In 2020, there were 670,000 new cases which amounted to 20.6 million infected individuals in East and Southern Africa.
Interesting facts
According to the WHO, some of the current interesting facts about HIV/AIDS is that it has claimed over 36.3 million people since its emergence; hence, it is still a major public health concern (WHO, 2021). Additionally, over 37.7 million were HIV positive in 2020, whereby 25.4 million were in the WHO African region. WHO also reports that over 680 thousand individuals succumbed to HIV-related infections, and over 1.5 million people acquired HIV/AIDS.
CDC. (2020, June 19). Tracking AIDS Trends . Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/statistics/surveillance/index.html
Eisinger, R. W., & Fauci, A. S. (2018). Ending the HIV/AIDS pandemic. Emerging infectious diseases , 24 (3), 413.
Mayo Clinic. (2020, February 13). HIV/AIDS – Symptoms and causes . https://www.mayoclinic.org/diseases-conditions/hiv-aids/symptoms-causes/syc-20373524
Melhuish, A., & Lewthwaite, P. (2018). Natural history of HIV and AIDS. Medicine , 46 (6), 356-361.
Nasuuna, E., Kigozi, J., Babirye, L., Muganzi, A., Sewankambo, N. K., & Nakanjako, D. (2018). Low HIV viral suppression rates following the intensive adherence counseling (IAC) program for children and adolescents with viral failure in public health facilities in Uganda. BMC Public Health , 18 (1), 1-9.
Velloza, J., Kemp, C. G., Aunon, F. M., Ramaiya, M. K., Creegan, E., & Simoni, J. M. (2020). Alcohol use and antiretroviral therapy non-adherence among adults living with HIV/AIDS in Sub-Saharan Africa: a systematic review and meta-analysis. AIDS and Behavior , 24 (6), 1727-1742.
WHO. (2021, June 9). HIV/AIDS . WHO | World Health Organization. https://www.who.int/news-room/fact-sheets/detail/hiv-aids
Cite This Work
To export a reference to this article please select a referencing style below:
Related Essays
Literature review of evidence-based research study regarding the fall prevention programs, strategies to mitigate web platform failure, end of life physician-assisted suicide, essay on genomic sequencing, iom future of nursing report and nursing, essay on health economics, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

HIV/AIDS epidemiology, pathogenesis, prevention, and treatment
The HIV-1 pandemic is a complex mix of diverse epidemics within and between countries and regions of the world, and is undoubtedly the defining public-health crisis of our time. Research has deepened our understanding of how the virus replicates, manipulates, and hides in an infected person. Although our understanding of pathogenesis and transmission dynamics has become more nuanced and prevention options have expanded, a cure or protective vaccine remains elusive. Antiretroviral treatment has transformed AIDS from an inevitably fatal condition to a chronic, manageable disease in some settings. This transformation has yet to be realised in those parts of the world that continue to bear a disproportionate burden of new HIV-1 infections and are most a% ected by increasing morbidity and mortality. This Seminar provides an update on epidemiology, pathogenesis, treatment, and prevention interventions pertinent to HIV-1.
HIV pandemic
An estimated 38·6 (33·4–46·0) million people live with HIV-1 worldwide, while about 25 million have died already. 1 In 2005 alone, there were 4·1 million new HIV-1 infections and 2·8 million AIDS deaths. 1 These estimates mask the dynamic nature of this evolving epidemic in relation to temporal changes, geographic distribution, magnitude, viral diversity, and mode of transmission. Today, there is no region of the world untouched by this pandemic ( figure 1 ). 2

HSex=heterosexual. MSM=Men who have sex with men. IDU=injection drug users. Based on Joint UNAIDS and WHO AIDS epidemic update December, 2005.
Heterosexual transmission remains the dominant mode of transmission and accounts for about 85% of all HIV-1 infections. Southern Africa remains the epicentre of the pandemic and continues to have high rates of new HIV-1 infections. 3 Although overall HIV-1 prevalence remains low in the emerging epidemics in China and India, the absolute numbers, which are fast approaching those seen in southern Africa, are of concern. 1 Outside of sub-Saharan Africa, a third of all HIV-1 infections are acquired through injecting drug use, most (an estimated 8·8 million) of which are in eastern Europe and central and southeast Asia. 1 The rapid spread of HIV-1 in these regions through injecting drug use is of importance, since it is a bridge for rapid establishment of more generalised epidemics.
A defining feature of the pandemic in the current decade is the increasing burden of HIV-1 infections in women, 4 which has additional implications for mother-to-child transmission. Women now make up about 42% of those infected worldwide; over 70% of whom live in sub-Saharan Africa. 1 Overall, a quarter of all new HIV-1 infections are in adults aged younger than 25 years. 1 HIV-1 infection rates are three to six times higher in female adolescents than in their male counterparts, 1 , 5 – 7 and this difference is attributed to sexual coupling patterns of young women with older men. Population prevalence of HIV-1 infection, concurrent sexual relationships, partner change, sexual practices, the presence of other sexually transmitted diseases, 8 – 11 and population mobility patterns 12 – 14 for economic and other reasons (eg, natural disasters and wars) further increase the probability of HIV-1 acquisition. 3 , 15 Emerging data accord with strong links between risk of sexual HIV-1 acquisition and episodic recreational drug or alcohol use. 16
Although sub-Saharan Africa continues to bear a disproportionate burden of HIV-1 infections, there is now an increasing number of countries reporting stabilisation or declines in prevalence (eg, Zambia, Tanzania, Kenya, Ghana, Rwanda, Burkina Faso, and Zimbabwe). 1 There is some evidence to attribute these reductions to effective changes in sexual behaviour, such as postponement of sexual debut, reduction in casual relationships, and more consistent condom use in casual relationships. 17 , 18 However, increasing morbidity and mortality rates associated with a maturing HIV-1 epidemic need to be considered when interpreting these data. 19 For example, the death of a few high-risk individuals who are key to transmission chains could exert a major effect on sexual networks and result in major reductions in infection rates. 20 Additionally, since most HIV-1 estimates are based on surveys in antenatal populations, increasing morbidity and mortality could cause the numbers of women in this group to decrease, and thus lead to underestimates of the true prevalence in these countries. 19
Although the relative contribution of cell-free virus compared with cell-associated virus in HIV-1 transmission remains unclear, there is growing evidence that viral load is predictive of transmission risk. 21 , 22 The highest levels of viraemia are seen during acute infection and advanced HIV-1 disease. 22 Further, co-infections with other sexually transmitted diseases in asymptomatic HIV-1 infected people can increase viral shedding to levels similar to those seen during acute infection. 23 Thus, sexually transmitted diseases could enhance HIV-1 transmission to rates similar to those seen during primary infection. 24 This observation could help to explain why the efficiency of HIV-1 transmission exceeds, in some settings, the earlier mathematical projections. 25 Thus, identification and treatment of recently infected people is an important means to reduce transmission. However, most people are unaware of their HIV-1 status during these crucial first months of infection. Several screening strategies based on laboratory testing and clinical algorithms are being developed and tested 26 for efficient identification of early infection before antibody development. 27 Additionally, a more aggressive management of sexually transmitted infections in settings with generalised epidemics has the potential to affect current epidemic trajectories. 24
Based on their genetic make-up, HIV-1 viruses are divided into three groups (eg, M [main], N, and O group, figure 2 ). These HIV-1 groups and HIV-2 probably result from distinct cross-species transmission events. 28 Pandemic HIV-1 has diversified into at least nine subtypes ( figures 1 and and2) 2 ) and many circulating recombinant forms, 29 , 30 which encode genetic structures from two or more subtypes (eg, A/E=CRF01; A/G=CRF02). The continuously evolving HIV-1 viral diversity poses an immense challenge to the development of any preventive or therapeutic intervention. 29

The HIV-1 pandemic is largely due to viral isolates belonging to the HIV-1 M-group, with HIV-1 subtype C being the most prevalent (red). Recombinant circulating forms cluster with the M-group but have been omitted for clarity. HIV-1 M group and the contemporary SIV strains identified in wild chimpanzees in Cameroon (SIVcpzLB7/EK5 28 ) are highlighted. HIV-1 sequences cluster closely with SIV from chimpanzees (SIVcpz), whereas HIV-2 resembles SIV from macaques and sooty mangabeys (SIVmac/SIVsm).
In terms of viral diversity, subtype C viruses continue to dominate and account for 55–60% of all HIV-1 infections worldwide ( figure 1 ). 30 Non-subtype B isolates might differ in their virological characteristics from the subtype B isolates (eg, viral load, chemokine co-receptor usage, transcriptional activation in specific biological compartments). 31 – 33 However, the clinical consequences of subtype variations remain unclear.
Infection with two or more genetically distinct viruses could lead to new recombinant viruses. Recombination takes place at a higher rate than initially predicted, 30 and circulating recombinant forms account for as much as 20% of infections in some regions (eg, southeast Asia). 31 These findings are in agreement with the occurrence of co-infections with multiple distinct isolates in a close temporal context. 34 – 36 Further, superinfections in which time points of virus acquisition are months to years apart have been described, although at a much lower frequency than co-infections. 34 , 37 – 39 Collectively, these observations challenge the assumption that HIV-1 acquisition happens only once with a singular viral strain and that, thereafter, the infected individual is protected from subsequent infections. 40 This lack of immunisation has substantial implications for vaccine development. Emerging evidence suggests that clinical progression to AIDS might be more rapid in individuals with dual infections, 35 and encouraging safer sex practices in viraemic HIV-1-infected people might be appropriate to keep recurrent exposure to new viral strains to a minimum.
Pathogenesis of HIV-1
The worldwide spread of HIV-1 indicates that the virus effectively counteracts innate, adapted, and intrinsic immunity. 41 , 42 Despite its modest genome size (less than 10 kb) and its few genes ( figure 3 ), HIV-1 excels in taking advantage of cellular pathways while neutralising and hiding from the different components of the immune system. 43 – 45 Notably, our understanding of pathogenesis is often derived from studies of subtype B viruses and non-human primate studies.

(A) Envelope glycoproteins gp120/41 form the spikes on the virion’s surface. During maturation the gag protein is cleaved and Gag p24 forms the core. The viral genome, viral reverse transcriptase (RT), integrase as well as a number of host proteins are encapsidated. (B) Dir erent steps of the viral life cycle on a cellular level and the potential targets for treatment interventions. (C) HIV-1 has evolved strategies to counteract the restriction factors TRIM5α and APOBEC3G/3F. If left unchecked by HIV-1 Vif, APOBEC3G/3F is encapsidated into the egressing virion, and on infection of a target cell leads to G-to-A hypermutations in the viral genome. Rhesus TRIM5α inhibits HIV-1 replication early after infection of the target cell before the step of reverse transcription.
The HIV-1 life cycle is complex ( figure 3 ) and its duration and outcome is dependent on target cell type and cell activation. 46 In the early steps, HIV-1 gains access to cells without causing immediate lethal damages but the entry process can stimulate intracellular signal cascades, which in turn might facilitate viral replication. 47 , 48 The two molecules on the HIV-1 envelope, the external glycoprotein (gp120) and the transmembrane protein (gp41), form the spikes on the virion’s surface. 49 During the entry process, gp120 attaches to the cell membrane by first binding to the CD4+ receptor. Subsequent interactions between virus and chemokine co-receptors (eg, CCR5, CXCR4) trigger irreversible conformational changes. 49 , 50 The actual fusion event takes place within minutes by pore formation, 50 , 51 and releases the viral core into the cell cytoplasm. After the core disassembles, the viral genome is reverse transcribed into DNA by the virus’ own reverse transcriptase enzyme. 46 Related yet distinct viral variants can be generated during this process since reverse transcriptase is error prone and has no proofreading activity. 46 At the midpoint of infection, the viral protein integrase in conjunction with host DNA repair enzymes inserts the viral genome into gene-rich, transcriptionally active domains of the host’s chromosomal DNA. 52 – 54 An integrase binding host factor, LEDGF/p75 (lens epithelium-derived growth factor), facilitates integration, 55 , 56 which marks the turning point by irreversibly transforming the cell into a potential virus producer. In the late steps, production of viral particles needs host driven as well as virus driven transcription. 46 Viral proteins are transported to and assemble in proximity to the cell membrane. Virus egress from the cell is not lytic and takes advantage of the vesicular sorting pathway (ESCRT-I, II, III), which normally mediates the budding of endosomes into multivesicular bodies. 57 , 58 HIV-1 accesses this protein-sorting pathway by binding TSG101 via its late domain, a short sequence motif in p6 of Gag. 59 , 60 Cleavage of the Gag-Pol poly-protein by the viral protease produces mature infectious virions. 46 , 61
Since cytoplasmic molecules of the producer cell and components from its cell surface lipid bilayer are incorporated into the new viral particle, virions bear characteristics of the cells in which they were produced. 62 Incorporated host molecules can determine the virus’ phenotype in diverse ways (eg, shape the replicative features in the next cycle of infection or mediate immune activation of bystander cells 62 ).
Studies of the early events that happen after HIV-1 breaches the mucosal barrier suggest the existence of a window period in which viral propagation is not yet established and host defences could potentially control viral expansion. 63 The important co-receptors for HIV-1 infection are two chemokine receptors—CCR5 and CXCR4. Independently of the transmission route, most new infections are established by viral variants that rely on CCR5 usage. 64 CXCR4-tropic viruses generally appear in late stages of infection and have been associated with increased pathogenicity and disease progression. 65
Compelling evidence from non-human primate models (eg, simian immunodeficiency virus [SIV] infection of rhesus macaques) suggest that vaginal transmission results in infection of a small number of CD4+ T lymphocytes, macrophages, and dendritic cells located in the lamina propria. 63 Potential pathways for virus transmission involve endocytosis, transcytosis, and virus attachment to mannose C-type lectin receptors (eg, DC-SIGN) located on dendritic cells and macrophages. 66 The initial replication takes place in the regional lymph organs (eg, draining lymph nodes) and is composed of few viral variants, and leads to modest primary amplification. With migration of infected T lymphocytes or virions into the bloodstream, secondary amplification in the gastrointestinal tract, spleen, and bone marrow results in massive infection of susceptible cells. In close temporal relation with the resulting peak of viraemia (eg, 10 6 to 10 7 copies per mL plasma), clinical symptoms can be manifest during primary HIV-1 infection ( figure 4 ). The level of viraemia characteristic for the chronic phase of infection in an individual (viral set point) differs from the peak viraemia by one or two orders of magnitude. This reduction is largely attributed to HIV-1 specific CD8+ responses but target cell limitation could also play a part. The viral population is most homogeneous early after transmission, but as viral quasi-species diversify in distinct biological compartments, mutant viruses that are resistant to antibody neutralisation, cytotoxic T cells, or antiretroviral drugs are generated and archived in long-lived cells (ie, viral reservoirs).

Plasma viraemia (top), and dynamic changes of the CD4+ T-lymphocyte compartments (bottom). Primary infection characterised by high plasma viraemia (red line, top), low CD4 cells (green line, bottom), and absence of HIV-1 specific antibodies (orange line, bottom). Viraemia drops as cytotoxic CD8+ T-lymphocytes (CTL) develop (blue line, bottom) and an individual viral-load set point is reached during chronic infection. Viral set points dir er greatly among individuals (eg, red dotted line, top) and predict disease progression. Viral diversity increases through out the disease (closed circles, top). The risk of transmission is highest in the first weeks when viraemia peaks (closed circles, top). GALT=gut-associated lymphoid tissues.
A pronounced depletion of activated as well as memory CD4+ T cells located in the gut-associated lymphoid tissues has been seen in individuals identified early after infection. 67 The preferential depletion of the CD4+ cells in the mucosal lymphoid tissues remains despite years of antiretroviral treatment, a striking observation that contrasts with the fact that the number of CD4+ T lymphocytes in the peripheral blood can return to normal under antiretroviral treatment.
A gradual destruction of the naive and memory CD4+ T-lymphocyte populations is the hallmark of HIV-1 infection, with AIDS being the last disease stage ( figure 4 ). 68 Despite the frequent absence of symptoms during early and chronic phase, HIV-1 replication is dynamic throughout the disease. The half-life of a single virion is so short that half the entire plasma virus population is replaced in less than 30 minutes, 69 and the total number of virions produced in a chronically infected person can reach more than 10¹P particles per day. 69 , 70 The turnover rates of lymphocyte populations are upregulated many fold during HIV-1 infection, whereas cell proliferation decreases once viral replication is reduced by antiretroviral treatment. 71 , 72 Different depletion mechanisms have been proposed, with an emerging consensus favouring generalised immune activation as cause for constant depletion of the CD4+ cell reservoir. 73
Immune activation predicts disease progression 74 and, thus, seems to be a central feature of pathogenic HIV-1 infections. Recently, Nef proteins from SIV lineages that are non-pathogenic in their natural hosts (eg, African green monkeys) have proved to down-regulate CD3-T-cell receptors, resulting in reduced cell activation and apoptosis. 75 HIV-1 Nef fails to quench T-cell activation, possibly leading to the high degree of immune activation seen in infected people.
Understanding the mechanisms that lead to protection or long-lasting control of infection will guide vaccine development by providing correlates of protection. Natural resistance to HIV-1 infection is rare and varies greatly between individuals. Two groups—long-term non-progressors and highly exposed persistently seronegative individuals—have been studied widely to identify innate and acquired protective determinants ( table 1 ). 76 Host resistance factors consist of human leucocyte antigen (HLA) haplotypes, autoantibodies, mutations in the promoter regions, and coding regions of the co-receptors CCR5 and CCR2, as well as the up-regulation of chemokine production ( table 1 ). 76 , 77 Indeed, individuals encoding a truncated CCR5 version (CCR5Δ32) have slower disease progression (heterozygote) or are resistant to CCR5-using viruses (homozygote). 78 The CCL3L1 gene encodes MIP1α, a CCR5 co-receptor ligand and chemokine with antiviral activity. Recent findings show that CCL3L1 gene copies vary individually and higher numbers of gene duplications result in reduced susceptibility to infection, 77 , 79 possibly by competitive saturation of CCR5 co-receptor. Cytotoxic T-lymphocyte responses, helper T-cell functions, and humoral responses are some of the acquired factors that modulate the risk of transmission in highly exposed persistently seronegative individuals, 76 and could also contribute to spontaneous control of replication in long-term non-progressors. The putative protective role of cytotoxic T-lymphocyte activity has been suggested in seronegative sex workers and in some long-term non-progressors. 76 , 80
Some of the host factors affecting susceptibility to HIV-1 infection
| Innate | Genetic | Acquired | Intrinsic |
|---|---|---|---|
| Autoantibodies | HLA haplotype | Cytotoxic T-cell activity | APOBEC3G/3F |
| Chemokines | CCR5 gene/promoter | Helper T-cell function | TRIM5α |
| Cytokines | CCR2 gene/promoter | Neutralising antibodies | |
| CCL3L1 gene copy number |
HLA=human leucocyte antigen. CCR5=chemokine receptor 5. CCR2=chemokine receptor 2. CCL3L1=CC chemokine ligand like-1, APOBEC3G/3F=apolipoprotein B mRNA editing complex 3.
Mammalian cells are not welcoming micro-environments, but rather deploy a defensive web to curb endogenous and exogenous viruses. HIV-1’s ability to circumvent these defences is as impressive as its efficiency to exploit the cellular machinery. APOBEC3G/3F and TRIM5α are recently described intrinsic restriction factors that are constitutively expressed in many cells. 81 , 82 Both gene loci have been under strong selective pressure throughout primate evolution, 83 indicating an ancient need to neutralise foreign DNA and maintain genome stability that precedes the current HIV-1 pandemic.
APOBEC3 enzymes (A3) belong to the superfamily of cytidine deaminases, 84 a group of intracellular proteins with DNA/RNA editing activity. 84 , 85 Most representatives of the APOBEC3 group have some mutagenic potential and restrict endogenous retroviruses and mobile genetic elements. The deaminases A3G, A3F, and A3B have potent antiviral activity, with the first two being expressed in cells that are susceptible to HIV-1 infection (T-lymphocytes, macrophages). HIV-1 evades APOBEC3 mutagenesis by expressing Vif, which leads to APOBEC3G/3F but not A3B degradation. 42 , 86 – 90
We still need to establish how the mechanisms of DNA editing and antiviral activity are interwoven, since some antiviral activity can be maintained despite defective DNA editing. 91 The early replication block in non-stimulated CD4+ T cells has been attributed to low molecular mass complexes of APOBEC3G. 92 Hypermutated genomes in HIV-1 infected patients 93 and mutations in Vif resulting in abrogated or differential APOBEC3 neutralisation capacity have been described. 94 , 95 The degree to which APOBEC3G/3F mRNA expression predicts clinical progression remains an area of intensive investigation. 96 , 97
Several representatives of the heterogeneous family of tripartite motif proteins (TRIM) inhibit retroviruses in a species-specific manner. 81 , 98 TRIM5α from rhesus macaques and African green monkeys inhibit HIV-1 replication, whereas the human homologue is inactive against SIV and HIV-1, leading to the recorded susceptibility of human cells to both viruses. 81 Rhesus TRIM5α recognises the capsid domain of HIV-1 Gag and manipulates the kinetics of HIV-1 core disassembly within minutes after cell entry. 99 , 100 Thus, experimental approaches to render HIV-1 resistant to rhesus TRIM5α could lead to immunodeficiency viruses capable of replicating in rhesus macaques. Such a non-primate model would allow testing of antiviral treatment and vaccine interventions with HIV-1 viruses instead of SIV or SIV/HIV chimeric viruses.
Clinical management
The diagnosis of HIV-1 infection is based on the detection of specific antibodies, antigens, or both, and many commercial kits are available. Serological tests are generally used for screening. A major advance has been the availability of rapid HIV-1 antibody tests. These assays are easy to do and provide results in as little as 20 minutes, 101 enabling specimen collection and proper diagnosis at the same visit. Rapid tests are important tools for surveillance, screening, and diagnosis, and can be reliably done on plasma, serum, whole blood, or saliva by health-care providers with little laboratory expertise. The two limitations of these serological tests are detection of infection during primary infection when antibodies are absent, and in infants younger than 18 months who might bear maternal HIV-1 antibodies. In these instances direct virus detection is the only option (eg, quantification of viral RNA [standard] or p24 antigen in heat denatured serum [less expensive]).
For staging purposes, measurement of CD4+ cells and viraemia is required. Plasma viral load is widely used to monitor therapeutic success on antiretroviral treatment. Several commercially available tests provide sensitive quantification of plasma HIV-1 RNA copies. The newer versions of the Amplicor and Quantiplex (Roche, Indianapolis, IN, USA, and Bayer Diagnostics, Walpole, MA, USA, respectively) assays have overcome initial suboptimum performance for non-B subtypes. 102 While the viral load determines the rate of destruction of the immune system, the number of CD4+ cells reveals the degree of immunodeficiency and is, therefore, used to assess the stage of infection. CD4+ cell counts together with clinical manifestations (eg, occurrence of opportunistic infections) are key criteria for HIV-1 disease classification. Flow cytometry analysis is the standard method for CD4+ cells quantification.
Standard methods for quantifying viral load and CD4+ cell counts need advanced laboratory infrastructures, and assays require a specimen to be tested within a short time of collection. These requirements pose challenges for resource-constrained settings. The use of dried blood spot specimen has resolved some of the difficulties associated with transportation of samples needed for virological assessments. 103 Measurement of reverse transcriptase activity in plasma samples, simplification of gene amplification methods (eg, Taqman technology), and paper-strip quantification (dipstick assays) might provide cost-effective alternatives for the future. 104 – 106 Similarly microcapilliary flow-based systems, CD4+ chips, or total white counts (panleucocyte gating) provide alternatives for establishment of the level of immunodeficiency in resource-limited settings. 107 – 110
Drug treatment
Antiretroviral compounds.
Antiretroviral treatment is the best option for longlasting viral suppression and, subsequently, for reduction of morbidity and mortality. However, current drugs do not eradicate HIV-1 infection and lifelong treatment might be needed.
20 of the 21 antiretroviral drugs currently approved by the US Food and Drug Administration target the viral reverse transcriptase or protease ( table 2 ). Eight nucleoside/nucleotide analogues and three non-nucleoside reverse transcriptase inhibitors inhibit viral replication after cell entry but before integration. Fixed-dose combination tablets simplify treatment regimens by reducing the daily pill burden, and drugs with long half-lives allow once or twice daily dosing. Eight protease inhibitors prevent the maturation of virions resulting in production of non-infectious particles. The recently approved darunavir (June, 2006) is the first of its class that retains activity against viruses with reduced susceptibility to protease inhibitors. Enfuvirtide targets a gp41 region of the viral envelope and stops the fusion process before the cell is infected. This drug needs to be injected twice daily and its use is reserved for treatment of heavily drug-experienced patients since it can help overcome existing drug resistance. 111 , 112 Development of new antiretrovirals focuses on molecules that target entry, reverse transcription, integration, or maturation. Compounds that have been designed to inhibit resistant viruses are urgently needed since many patients treated during the past decades harbour viral strains with reduced susceptibilities to many if not all available drugs ( table 3 ).
Antiretroviral drugs currently approved by US Food and Drug Administration
| Entry | Reverse transcriptase | Protease | |||
|---|---|---|---|---|---|
| Nucleoside | Nucleotide | Non-nucleoside | |||
| Single compound tablets | Enfuvirtide | Abacavir | Tenofovir | Delaviridine | (Fos)-Amprenavir |
| Didanosine | Efavirenz | Atazanavir | |||
| Emtricitabine | Nevirapine | Darunavir | |||
| Lamivudine | Indinavir | ||||
| Stavudine | Nelfinavir | ||||
| Zalcitabine | Ritonavir | ||||
| Zidovudine | Saquinavir | ||||
| Tripanavir | |||||
| Fixed-dose combination tablets | Abacavir/lamivudine (Epzicom) | Lopinavir/ritonavir | |||
| Zidovudine/lamivudine (Combivir) | |||||
| Tenofovir/emtricitabine (Truvada) | |||||
| Abacavir/lamivudine/zidovudine (Trizavir) | |||||
| Tenofovir/emtricitabine/efavirenz (Atripla) | |||||
Drugs belong to five drug classes and target three dir erent viral steps (entry, reverse transcription, or protease). Availability of these drugs in resource-limited countries is subject to country specific licensing agreements.
Antiretrovirals currently in phase II/III of clinical development
| Drug | Mechanism | Activity against PI and RT resistant strains | |
|---|---|---|---|
| Maraviroc | MVC | CCR5 inhibitor | Yes, but not X4 variants |
| Vicriviroc | SCH D | Yes, but not X4 variants | |
| Etravirine | TMC-125 | Non-nucleoside reverse transcriptase inhibitor | Yes, also NNRTI-resistant strains |
| TMC-278 | Yes, also NNRTI-resistant strains | ||
| n/a | MK-0518 | Integrase strand transfer inhibitor | Yes |
| n/a | GS-9137 | Yes |
The goal of antiretroviral treatment is to decrease the morbidity and mortality that is generally associated with HIV-1 infection. A combination of three or more active drugs is needed to achieve this aim in most patients. Effective treatment returns to near normal the turnover rates of both CD4+ and CD8+ T-cell populations. 72 Potent but well tolerated drugs with long half-lives and simplified regimens improve the options for first-line and second-line chemotherapeutic interventions.
Combination antiretroviral treatment
High rate of viral replication, low fidelity of reverse transcription, and the ability to recombine are the viral characteristics that lead to the diversity of HIV-1 species (quasi-species) in chronically infected individuals. This high genetic variability provided the rationale for highly active antiretroviral treatments (HAART). By combination of several potent antiretroviral agents, viral replication is suppressed to such low levels that emergence of drug resistant HIV-1 variants was, if not prevented, at least delayed. By doing so, CD4+ T-lymphocyte numbers increase, leading to a degree of immune reconstitution that is sufficient to reverse clinically apparent immunodeficiency. Widespread introduction of HAART in industrialised countries resulted in a striking decrease in morbidity and mortality, putting forward the hope that HIV-1 infection can be transformed into a treatable chronic disease. 113 – 115
A set of criteria composed of plasma viraemia concentration, absolute or relative CD4+ cell counts, and clinical manifestations, is used to recommend initiation of HAART. The benefits of treatment clearly outweigh the potential side-effects in patients with clinical signs of immunodeficiency (eg, AIDS defining illnesses) or with CD4+ numbers less than 200 per μL (recommendation of US Department of Health and Human Services, October, 2005). However, the best time point to begin treatment remains controversial in asymptomatic patients with modest depletion of CD4+ T cells (eg, more than 350 per μL) and modest levels of viraemia (eg, less than 100 000 copies per mL). 116 Studies with clinical endpoints supporting the validity of early versus late interventions in asymptomatic patients are difficult to do and insufficient clinical data are currently available. Early depletion of gut CD4+ T lymphocytes, 117 increasing viral diversity, and the poor regenerative abilities of key populations of the immune system provide arguments for beginning treatment as early as possible. The wide application of this principle is restricted by long-term drug toxicities that lead to reduction of quality of life, and by treatment costs. Toxicities (eg, renal, hepato, mitochondrial), metabolic changes (eg, lipodystrophy, diabetes mellitus), and immune reconstitution disease are some of the long-term problems that complicate decade-long HAART. 118 – 121
One strategy addressing life-long daily compliance to HAART has been structured treatment interruptions. The rationale for this approach was based on the premise that the body’s own immune system could keep the virus in check if exposed to a very modest level of viral replication. If successful, this strategy could limit drug toxicity and reduce treatment costs. 122 Although preliminary findings for this strategy were mixed in terms of benefits, 123 – 125 the recent early closure of the SMART trial was based on increased morbidity and mortality in the treatment interruption arm. 126 Thus, in the absence of clinical benefits, most investigators strongly discourage treatment interruptions except as needed to address treatment intolerance.
HAART in resource-constrained settings
The transformation of AIDS into a chronic disease in industrialised countries has yet to be realised in resource-constrained settings. Access to HAART is an absolute humanitarian necessity to avert mortality in people who are central to the future survival of their countries. 127 Despite restricted health infrastructures and diverse co-morbidities in these regions, remarkable therapeutic success rates have been shown, with adherence rates at least comparable with those reported in industrialised countries. 128 – 131 WHO and UNAIDS treatment guidelines focusing on resource-limited settings suggest use of standard first-line regimen followed by a set of more expensive second-line options 132 and proposes the use of standardised decision-making steps (eg, when to start, to substitute for side-effects, to switch for virological failure). 132 , 133 In many countries, treatment options are limited not only by the costs of HAART but also by restrictive licensing policies, and current estimates suggest that 80% of people infected with HIV-1 with a clinical need for treatment do not yet have access to antiretroviral drugs. 1 Thus, efforts and strategies to further scale up treatment access are crucial, 134 – 137 since antiretroviral treatment is also an effective intervention for prevention. 138
Drug resistance
Emergence of drug resistance is the most common reason for treatment failure. Insufficient compliance, drug side-effects, or drug-drug interactions can lead to suboptimum drug concentrations, resulting in viral rebound. Viral resistance has been described to every antiretroviral drug and therefore poses a serious clinical as well as public-health problem. 139 HIV-1 subtypes differ in the sequence of mutations leading to drug resistance, and some naturally occurring polymorphisms might actually modulate resistance. 140 , 141 Drug-resistant HIV-1 is transmissible and can be detected in up to 20% of newly infected individuals in countries with broad access to antiretrovirals. 34 The prevalence of drug resistance in the untreated population remains low in regions with poor access to treatment. 142
Short-term antiretroviral-based interventions are effective in prevention of mother-to-child transmission. However, these interventions could result in drug resistant viral variants in the mother, baby, or both. 143 Around half the women who received one dose of nevirapine to prevent mother-to-child transmission harbour viruses resistant to non-nucleoside reverse transcriptase inhibitors (NNRTI). 144 , 145 These resistant viruses replicate efficiently and can be transmitted by breast milk, 146 and minor resistant populations present long after the intervention can possibly decrease the effectiveness of subsequent NNRTI-based treatment regimens. 147 The combination of short-course zidovudine, lamivudine, and nevirapine prevents peripartum transmission while reducing the risk of nevirapine resistant viruses. 148
Viral reservoirs
Viral reservoirs consist of anatomical sanctuaries and a small pool of infected long-lived memory T lymphocytes. HIV-1 latency in long-lived cell populations (eg, memory T lymphocytes, macrophages) poses an obstacle to eradication because current antiviral combination treatments fail to eliminate integrated proviruses from resting cells. Different strategies, including immune-modulatory molecules (interleukin 2, anti-CD3 mAb, interleukin 7), have been used to reactivate resting cells in the setting of HAART. Histone deacetylase-1 inhibitors, like valproic acid, release an inherent transcriptional block and by doing so facilitate viral long terminal repeat-driven expression. 149 Augmenting standard antiretroviral treatment with enfuviridine and valproic acid reduced the number of latently infected CD4+ T cells (29–84%), but to establish the relative contribution of each drug with respect to the final outcome is difficult. 150
Mother-to-child transmission
Prevention of mother-to-child transmission has seen advances in both industrialised and resource-constrained settings. 151 – 153 Intrapartum transmission has been reduced by increasing access to interventions such as one dose of nevirapine to mother and newborn baby. 154 Concerns about drug-resistant viral strains have led to several trials with combination treatments to reduce transmission during the intrapartum period. 148 , 152 , 155 In some settings, elective delivery by caesarean section can further reduce HIV-1 transmission during the intrapartum period, but the benefits of the intervention could be countered by post-partum sepsis and increasing maternal mortality. 156
Because HIV-1 can be transmitted by breastfeeding, replacement feeding is recommended in many settings. Poor access to clean running water precludes, however, the use of formula feeding under these circumstances, 157 and exclusive breastfeeding with abrupt weaning is one option for reducing transmission. 158 A potential novel intervention still being tested is the daily use of antiretrovirals during breastfeeding. More attention is starting to focus on the pregnant mother, especially initiation of antiretroviral therapy in mothers with low CD4+ counts during pregnancy and thereafter. 159 , 160 Only limited data are available regarding the health of uninfected children born to HIV-1-positive mothers. 161 In a European cohort of exposed-uninfected children, no serious clinical manifestations were apparent, at least in the short term to medium term (median follow-up 2 years). 162
Sexual transmission
Reduction of heterosexual transmission is crucial for control of the epidemic in many parts of the world. 1 , 163 Prevention is achieved through reduction in the number of discordant sexual acts or reduction of the probability of HIV-1 transmission in discordant sexual acts. The first can be achieved through abstinence and sex between concordantly seronegative individuals. Abstinence and lifelong monogamous relationships might not be adequate solutions for many people and therefore several interventions aimed at lowering the risk of transmission per discordant sexual act are in the process of clinical testing. Male and female condoms provide a proven and affordable prevention option. 164 , 165 In combination, these options are also more commonly referred to as the ABC (abstinence, be faithful, condom use) approach.
Other biomedical prevention interventions include male circumcision, antiretrovirals for prevention (eg, pre-exposure or post-exposure), chemoprophylactic treatment of herpes simplex virus-2 (HSV-2), microbicides, and vaccines. Results from one of three independent phase III male circumcision trials underway in South Africa, Kenya, and Uganda has helped to allay some of the ambivalence around the protective effect of male circumcision. 8 , 166 The findings from the South African trial show a 60% protective effect of male circumcision. 167 The possible mechanism relates to the fact that the foreskin has apocrine glands that secrete lysozymes but also Langerhans cells expressing CD4 and other receptors. 168 , 169 These skin-specific dendritic cells can uptake virus and are believed to play a part in transport of the virus to susceptible T cells. Immunofluorescence studies of foreskin mucosa suggest that these tissues might be more susceptible to HIV-1 infection than cervical mucosa. 170 Findings from this proof-of-concept trial need to be compared with evidence from the two trials still underway in Kenya and Uganda, and to acceptability data, behaviour change after circumcision, surgical complication rates, and logistics of undertaking the procedures before policy formulation and wide-scale access as a prevention strategy. 171 – 173
Since high plasma viraemia increases the risk of transmission by as much as an order of magnitude, 21 does reducing viral load in the infected partner through, for example, antiretroviral treatment reduce the risk of HIV-1 transmission in the uninfected sexual partner? A trial to explore this question is currently being run jointly by the HIV Prevention Trials Network ( www.hptn.org ) and the Adult Clinical Trials Group. Mathematical projections estimate up to 80% HIV-1 reduction, 174 , 175 but scarce observational data currently exist. 176 Post-exposure prophylaxis is recommended after occupational (eg, needle stick) 177 and non-occupational (eg, rape, sexual abuse) 178 exposure, although data for efficacy and optimum drug combinations are few. 179 Some clinical trials assessing the benefits of once daily pre-exposure chemoprophylaxis with antiretroviral compounds with long biological half-life (eg, tenofovir) have been put on hold or stopped. 175 , 180 Neither the overall idea of pre-exposure prophylaxis nor the drug itself, which is well tolerated, was at the root of the protests. Concerns were centred on clinical trials in resource-poor settings and the perceived scarcity of adequate interventions protecting these vulnerable populations.
HSV-2 might increase both the risk of transmitting and acquiring HIV-1. 181 , 182 Antivirals (eg, aciclovir, valaciclovir) are effective in reducing viral shedding 183 – 185 and HSV-2 transmission in discordant heterosexual couples. 182 The future of HSV-2 prevention might reside in the vaccine that is currently under development. 186 Whether prophylactic use of aciclovir in populations with high HSV-2 prevalence and incidence rates results in reduced HIV-1 incidence rates remains unresolved but several trials addressing this issue are underway, including HPTN039.
Gender disparities lie at the centre of women’s vulnerability. Prevention options need to be provided that can be used by women independently of their male sexual partner’s knowledge or consent. 187 Notwithstanding that redressing these disparities is a long-term challenge, several preventive interventions can be implemented in the interim on the basis of our incomplete understanding at a biological level of HIV-1 risk for women. For example, there seems to be a correlation between levels of sexual hormones (eg, progesterone) and transmission risk. 188 Observational studies also highlight the relation between abnormal vaginal flora and increased risk of HIV-1 infection. 189 , 190 The high prevalence of vaginal infections such as bacterial vaginosis (30–50%), vulvovaginal candidosis (10–13%), and trichomonas vaginalis (7–23%) in African women is associated with a substantial risk of HIV-1 acquisition. 189 In addition to increasing access to female condoms and treatment of other sexually transmitted infections, trials are underway to assess the use of other barrier methods such as cervical caps, invisible condoms, diaphragms, and diaphragms combined with micro bicides. 190 The control of vaginal infections is a potentially important method for decreasing HIV-1 acquisition that has yet to be tested. Periodic presumptive treatment for vaginal infections is being explored as an HIV-1 prevention strategy. 191
Microbicides
Microbicides are an additional important biomedical intervention technology that is covert and under women’s control. 192 These topical products potentially could be used to prevent rectal and vaginal transmission of HIV-1, but proof of concept has been elusive. Although the three phase III trial results of the first microbicidal product (nonoxynol-9) done in the mid-1980s and 1990s did not show protective effects, 193 , 194 they have informed the medical knowledge in terms of product selection, clinical testing, and safety assessments. The past 5 years have seen major advances in investment and product development. 66 , 195 , 197 Early clinical testing of multiple products including the launch of advanced clinical trials for five different products is continuing ( table 4 ). The development of antiretroviral gels increased the specificity of these third generation microbicides in relation to surfactants, vaginal enhancers, or entry inhibitors that have dominated the product pipeline so far ( figure 5 ). The first antiretroviral gel to undergo early testing is tenofovir gel, and the findings in terms of safety profile, tolerance, low systemic absorption, and slight adverse events are promising. 192 As with vaccines, a major obstacle is the absence of a surrogate marker of protection. Additional challenges are adherence to product use and the high rates of pregnancy in trial participants.

N9=nonoxonol-9. CS=cellulose sulphate.
Summary of microbicides currently undergoing advanced clinical testing
| Phase | Mode of action | Effective against | |
|---|---|---|---|
| Carraguard | III | Seaweed polymer, entry inhibitor | HIV-1/HIV-2, human papilloma virus, herpes simplex virus |
| Cellulose sulphate | III | Entry inhibitor | Broad range of sexually transmitted diseases; also active as contraceptive |
| PRO2000 | III | Entry inhibitor | HIV-1/HIV-2, human papillomavirus, chlamydia |
| Savvy (C31G) | III | Surfactant | Broad range of sexually transmitted diseases; also active as contraceptive |
| Tenofovir gel | IIb | Nucleotide reverse transcriptase inhibitor | HIV-1/HIV-2 |
| Buffer gel+PRO2000 | IIb/III | Natural vaginal defence/entry inhibitor | HIV-1/HIV-2, chlamydia, gonorrhoea, human papillomavirus, bacterial vaginosis |
| Tenofovir gel+oral | II | Nucleotide reverse transcriptase inhibitor | HIV-1/HIV-2 |
A safe, protective, and inexpensive vaccine would be the most efficient and possibly the only way to curb the HIV pandemic. 198 Despite intensive research, development of such a candidate vaccine remains elusive. Safety concerns prohibit the use of live-attenuated virus as immunogen. 199 Many different approaches with recombinant technologies have been pursued over the past two decades. Initially, efforts were focused on generating neutralising antibodies with recombinant monomeric envelope gp120 (AIDSVAX) as immunogen. 200 , 201 This vaccine did not induce neutralising antibodies and, not unexpectedly, the phase III trials failed to show protection. 202 , 203 Antibody mediated HIV-1 neutralisation is complicated by the high genetic diversity of the variable Env regions, epitopes masked by a carbohydrate shield (glycosylation), and conformational or energetic constraints. 204 Since CD8 T-cell responses control to some extent viral replication in vivo, recent vaccine development has focused on eliciting cellular immune responses. Overcoming pre-existing immunity against replication incompetent immunogenic vectors (eg, recombinant adenovirus type 5) is one of the challenges. 205 Safety and immunogenicity studies using replication defective vaccine vectors are continuing after preliminary studies in non-human primates showed some protection. 204 The immune system generally fails to spontaneously clear HIV-1 and the true correlates of protection continue to be ill defined. 198 , 206 However, the general belief is that approaches aimed at eliciting both humoral and cell mediated immunity are most promising to prevent or at least control retroviral infection. 198
Conclusions
An important gateway to both prevention and care is knowledge of HIV-1 status. 207 Fear of knowledge of status, including stigma and discrimination, has discouraged many from seeking voluntary counselling and testing services. 208 As access to antiretroviral interventions (prevention of mother-to-child transmission, antiretroviral treatment) increases, the opportunities for HIV-1 testing will grow and create opportunities for a prevention-care continuum, with the voluntary counselling and testing services as a point of entry. These changes will result in a shift in prevention efforts from a focus on individuals not infected with HIV-1 to a more effective continuum of prevention that includes uninfected, recently infected, infected, and asymptomatic people, as well as those with advancing HIV disease and on antiretroviral therapy.
HIV/AIDS is an exceptional epidemic that demands an exceptional response. Much progress has been made in a short space of time, despite many scientific and programmatic challenges ( figure 6 ). In the absence of a protective vaccine or a cure, prevention and access to antiretroviral treatments are the best options to slow down the HIV-1 pandemic. Broad implementation of these principles needs improved infrastructures in resource-constrained regions, which have been and will continue to be most affected. The fact that HIV-1 is predominantly sexually transmitted and disproportionately affects populations that are already socially or economically marginalised, or both, poses many ethical, social, economic, and political challenges.

Estimates place the cross species transmission events leading to the worldwide spread of HIV-1 to the early decades of the 20th century. Numbers circled by a hexagon identify the specific year of an event. PEPFAR=President’s Emergency Plan for AIDS Relief.
In view of the immediacy of the problem, and the fact that both research and programmes are mainly funded by the public sector, there is a greater demand from civil society for co-ownership of research and accountability for use of public funds. On the one hand, this co-ownership defines a changing role and responsibility of science in society, and on the other hand, shows a necessary synergy between activism and science. This partnership has been invaluable for antiretroviral drug development, treatment access in resource-constrained settings, and the scale-up of interventions to reduce mother-to-child transmission.
The increasing number of infected women and the disproportionate burden of infection in resource-constrained settings creates a scientific imperative to ensure research is done for people and in settings who stand to benefit most. The most affected countries face many other economic, political, and development challenges, which have raised issues in undertaking multicentre and multicountry research. Research addressing women-specific topics (such as effect of sexual hormones on transmission and disease progression, viral diversity, and antiretroviral potency) and women-specific prevention interventions including microbicides is crucial. We are probably at one of the most hopeful and optimistic points in our response to the pandemic. There is definitely more attention being directed to HIV-1, more resources ( panel ), more civil society mobilisation, more governments speaking up, more possibilities for treatment, and more evidence about what prevention and treatment strategies will work than in previous years. The unrelenting growth of the pandemic tells us that current strategies are not enough. Clearly, we need to do some things differently, while also increasing the scale and magnitude of current strategies in keeping with the pandemic.
PanelOnline resources
Epidemiology.
http://www.unaids.org/en/HIV_data/default.asp
Treatment recommendations
Centers for Disease Control and Prevention
http://www.cdc.gov/hiv/topics/treatment/index.htm
HIV-1 drug resistance
Stanford University HIV Drug Resistance Database
http://hivdb.stanford.edu/index.html
International AIDS Society–USA
http://www.iasusa.org/resistance_mutations/index.html
Microbicide
Alliance for Microbicide Development
http://www.microbicide.org
HIV Prevention Trials Network
http://www.hptn.org/index.htm
International AIDS Vaccine Initiative
http://www.iavi.org
Search strategy and selection criteria
A comprehensive literature review was undertaken by searching the PubMed database online, for English language publications between January, 2000, and June, 2006. The database search terms included keywords such as “HIV/AIDS”, “epidemiology”, “prevention”, “pathogenesis”, “HSV-2”, “male circumcision”, “PMTCT”, “scaling up treatment”, “resource constrained settings”, “antiretroviral pre-exposure prophylaxis”, “HAART”, “restriction”, “host factor”, “HIV pathogenesis”, “resistance”, “latency”. Various combinations of these words were entered. All duplicate articles were removed. A subset of relevant articles was chosen and full-text manuscripts were summarised.
Acknowledgments
We thank P D Bieniasz, W Cates, L Chakrabarti, C Cheng-Mayer, J Coovadia, H Gayle, P A Fryd, R Gray, S Abdool Karim, L Kuhn, K Mayer, P Mane, L C F Mulder, L Myer, and M Wawer for helpful discussions. M Boettiger and C Baxter assisted with literature searches. This work was supported by NIH grant RO1AI064001 (VS), by grant 1 U19AI51794 (QAK) from CAPRISA that forms part of the Comprehensive International Program of Research on AIDS (CIPRA) funded by the National Institute of Allergy and infectious Disease (NIAID), National Institutes of Health (NIH) and the US Department of Health and Human Services (DHHS) and grant D43 TW00231 (QAK) from the Columbia University-Southern African Fogarty AIDS International Training and Research Program.
Conflict of interest statement
D D Ho sits on the scientific advisory boards for Monogram, Osel, Achillion, Valiant, Oyagen, Lavipharm, and XTL. Products or work from these companies are not discussed in the review. He holds patents on vaccine candidates. The other authors declare no conflict of interest.
Talk to our experts
1800-120-456-456
- Essay on AIDS

HIV (human immunodeficiency virus) is an infection that causes cells in the body that help it fight infections, making a person more susceptible to other infections and diseases. Interaction with certain bodily secretions of an HIV-positive individual, most commonly during unprotected intercourse (sex without the use of a condom or HIV treatment to prevent or treat HIV), or sharing injection drug equipment spreads the virus.
If HIV is not treated, it can progress to AIDS (acquired immunodeficiency syndrome). HIV cannot be eradicated by the human body, and there is no effective HIV cure. As a result, whether you have HIV, you will have it for the rest of your life.
Long and Short AIDS Essay in English
There are many diseases causing microorganisms, like bacteria, viruses, fungi etc. The symptoms of the diseases depend on the type of microorganism that is spreading it. It can vary from mild to severe. AIDS which stands for Acquired Immunodeficiency Syndrome is a viral disease that is rampant in growth. It was only in the last century that this viral disease has proved to be lethal and fatal, taking away about twenty million lives globally. The awareness about the disease and the virus causing it which is HIV or Human Immunodeficiency Virus is more now compared to earlier. In this HIV AIDS essay, we can go through the important information about it and burst some myths.
Below are different ways to write an AIDS essay in English. The essay on HIV AIDS can be of 2 formats, a long essay on HIV AIDS or a short AIDS essay.
Short Essay on Aids
This AIDS essay is a brief one and will cover the important notes about the disease and the ways one can prevent it.
The way of occurrence of this disease is in the name itself, AIDS stands for Acquired Immunodeficiency Syndrome. The disease is acquired via the virus which is called Human Immunodeficiency Virus. It is not an auto-immune disease in the early stages of infection where the immune system in the body fights off infection to protect the body from diseases that go against itself. The virus enters from an outside source and destroys the efficiency of our immune system.
AIDS is transmitted through contact. The contact with infected blood of the HIV OR AIDS patient in any form can easily transfer this viral disease. It can also be transmitted through contact with semen or vaginal fluids of the infected person. This occurs in the case when one is sexually exposed to a person with HIV.
HIV once enters the body, invades and conquers the immune system making the body susceptible to other diseases. It is then very easy for the simple flu or cold infection to be severe as the immune system is no longer fit to fight it.
When detected in the early period can be battled with, but more often than not people assume the symptoms to not be AIDS so it spreads and kills the individual. To be protected when having sex and not sharing any form of toiletries with others is the way to prevent and keep this deadly virus at bay.
Long Essay on AIDS
This is the long format of an essay on HIV AIDS where its workings, causes and effects and remedies are discussed.
There are some diseases that have been borne by the living in this world which has created a ruckus in human history and the struggle to find a permanent cure still exists. AIDS is one such disease. Acquired Immunodeficiency Syndrome is the name of the disease which is also shortened as AIDS.
It has since only the 20 th century affected the human race and many people lost their lives, more than 20 million of them. The virus that aids in the transmission of this disease is Human Immunodeficiency Virus or also called HIV. Due to the same property of immunodeficiency, it is referred to as HIV/AIDS.
Since it affects the immune system severely, the cells and the workings of it in our body must be clearly understood. The immune system’s role in the body is that of a soldier wherein it identifies any sort of anomalies that enters or infiltrates the body and prepares antibodies against it. And kills them in order to prevent infection that has the probability of causing a harmful disease.
Since the cells of the immune system have already created the antibodies, the cell memory is activated when the entry occurs again and the immune system fights and destroys such foreign and harmful matter.
What Happens when HIV Enters the Body?
When a person is infected with the Human immunodeficiency virus, it directly attacks the immune system making the cells weak and incapable of creating antibodies for this particular virus. As they become weak their function to perform the task of defending against other microorganism entrants is also weakened.
When the fighter in our bodies becomes weak, we are more likely to fall ill. The illness can be a simple flu or an allergy and our body cannot fight any further. The symptoms once infected will start to appear within the first two weeks. The symptoms are very flu-like for instance, one will be more tired than usual and fatigue will be more frequent and regular. Other symptoms include sore throat and fever. The risk of opportunistic infections like tuberculosis and herpes also increases. Some people however remain asymptomatic even for longer periods after being infected with the virus.
Cause of HIV/AIDS
The main and only cause of this dreadful disease is the contact through blood, semen, pre-seminal fluid, vaginal fluids, rectal fluids and breast milk. The semen and vaginal fluids are transferred through sex and rectal fluids through anal sex. When people have multiple partners, and they have unprotected sex the transmission is highly likely. The contact through blood can also be via the unhygienic practice of sharing an infected person’s razors, blades. Even unsterilized syringes while taking drugs or even a tattoo parlor where they use unsterilized machines on the body can transmit the virus easily. The transmission means are endless so one must proceed with utmost caution to keep themselves safe either way.
What is the Life Expectancy for the Patients Carrying HIV or AIDs with Them?
Many factors can affect the life expectancy of people living with HIV. Depending on these factors there are many differences in the outcomes between people, and other factors. The factors on which life expectancy depend are:
Access to effective HIV treatment and quality health care.
Start HIV treatment as soon as possible after HIV infection, before your CD4 cell count drops to a low level. The sooner you are diagnosed and start HIV treatment, the better your long-term chances are.
Having serious HIV-related illnesses in the past. This may occur before HIV is diagnosed and/or before HIV treatment is started. These diseases have a detrimental effect on life expectancy.
Results one year after starting HIV treatment. Studies show that life expectancy is better for people who respond well within a year of starting treatment than people who do not respond. In particular, people with a CD4 count of at least 350 and an undetectable viral load during the year have a much better chance long-term.
Year of Diagnosis - HIV treatment and medical care have improved over the years. People who have been diagnosed in recent years are expected to live longer than people who were diagnosed long ago.
Heart diseases, liver diseases, cancer and other health conditions are more likely to be the cause of death than HIV or AIDs.
Injecting drug use - Life expectancy is short for people with HIV who inject drugs, due to drug overdose and viral infections.
Social and Economic Conditions - there are significant differences in life expectancy depending on where you grew up, your income, education, social status and more.
Gender – Men are supposed to live for a shorter period of time than women.
Genetics - you may have certain conditions if close relatives have.
Mental and Emotional Well-being - high levels of stress are associated with reduced life expectancy.
Lifestyle - longevity for people who eat a balanced diet, are physically active, maintain a healthy weight, avoid alcohol abuse or use drugs, and stay in touch with the community. Avoiding smoking is very important in life.
There are a few myths surrounding this disease. It is believed earlier that AIDS can spread even through contact or touch without any exchange of fluids. Like through a hug or just by being near the infected person. That myth has been debunked and it is absolutely untrue. One can freely hug an AIDS patient without worry.
The other one was when kissing, there is an exchange of saliva which is also a fluid and AIDS can spread through kissing, which also proved to be untrue. And HIV always means AIDS that is fatal was another rumor or myth, and this myth is proven wrong where many people have lived longer with HIV by medication and taking care of their health.
There is no permanent cure yet for treating HIV/AIDS, so it is our responsibility to look out for ourselves. The way one can first prevent themselves from being infected is by getting vaccinated. It is important to get tested in your adult life if you have multiple sexual partners and also get your partner tested for the same. The other way is being monogamous. The most used form of prevention is having protected and safe sex and using condoms that creates a barrier for transmission. Do check for sterilized needles in case you decide to get a tattoo or injected. Lessen the use of alcohol and drugs as that is anyway weakening and altering the immune system.
According to the estimates of the Indian government 2.40 million Indians are living with HIV wherein, the infected ones fall in the age group of 15-49, and 39 %of them that is 9,30,00 of them are women. The numbers are alarming and the rate of increase is not slowing down anytime soon. We as a country must break the traditions and conversations about sex should be open and safe. It is high time we lose our lives to this disease which can be prevented.

FAQs on Essay on AIDS
1. Is AIDS an Autoimmune Disease?
In the early stages of HIV infection that leads to AIDS, the immune system only weakens so it is not an auto-immune disease. But during the later and final stages, the workings of the immune system are similar to that of an auto-immune system where it works against itself. And in such cases, the body of the individual is susceptible to many more diseases. AIDS, a disease found in immune deficiency disorder, is caused by HIV and weakens the human immune system. Autoimmune diseases, on the other hand, are where the immune system turns, attacking healthy cells.
2. Does one die from HIV Infection?
The HIV infection results in many symptoms that make the body weaker day by day. But some do not even suffer those symptoms and they may live longer than the ones showing severe symptoms. In any case, it is important to take medications that are prescribed to reduce the severity of symptoms and live a little longer. The best way is to keep healthy and lead an active lifestyle as much as possible. Although the death toll from AIDS has dropped dramatically around the world, this situation increases the risk of contracting a fatal disease — potentially leading to death. No treatment or cure is present for HIV.
3. What method was adopted by the hospitals to report HIV or AIDs cases?
The doctors took the active initiative for the reporting and diagnosis of HIV or AIDs cases all over the world. The methods that all the French hospital wards were known for, for their role in controlling HIV infection, were asked to report the 2000 deaths among HIV-positive adults. The causes of death were recorded using a standard questionnaire. The Mortality 2000 study was launched to explain the distribution of the leading causes of death of HIV-positive people at the national level in France in the year 2000.
4. What is the way of determining the root cause of death in AIDs patients?
Following the International Classification of Diseases, 10th Revision (ICD-10) to death, the information contained in the questionnaire was used to determine the single cause of death. The causes of AIDS were categorized as one cause of death, followed by definitions of AIDS-related diseases. If a standard questionnaire was lost, summarized quarter notices were used to determine the underlying cause of death, if possible. Determination of the AIDs cases was set to the most important things in the list, which was done from the abstracted quarterly notifications from the questionnaires.
5. Is Vedantu a reliable website for knowing about AIDs disease?
Vedantu is the most reliable website for referring to information about AIDs disease. Being one of the most dangerous diseases in the world with no proper treatment or cure, the world's physicians are still under pressure to decipher the way to save a person from this disease. The Vedantu website contains authentic or updated information about this disease and thus the readers and viewers can rely on this source of information for perfect knowledge about the disease and its prevention also.
- Fact sheets
Facts in pictures
Publications.
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Health topics /
Human immunodeficiency virus (HIV) is an infection that attacks the body’s immune system, specifically the white blood cells called CD4 cells. HIV destroys these CD4 cells, weakening a person’s immunity against opportunistic infections, such as tuberculosis and fungal infections, severe bacterial infections and some cancers.
WHO recommends that every person who may be at risk of HIV should access testing. People at increased risk of acquiring HIV should seek comprehensive and effective HIV prevention, testing and treatment services. HIV infection can be diagnosed using simple and affordable rapid diagnostic tests, as well as self-tests. It is important that HIV testing services follow the 5Cs: consent, confidentiality, counselling, correct results and connection with treatment and other services.
People diagnosed with HIV should be offered and linked to antiretroviral treatment (ART) as soon as possible following diagnosis and periodically monitored using clinical and laboratory parameters, including the test to measure virus in the blood (viral load). If ART is taken consistently, this treatment also prevents HIV transmission to others.
At diagnosis or soon after starting ART, a CD4 cell count should be checked to assess a person’s immune status. The CD4 cell count is a blood test used to assess progression of HIV disease, including risk for developing opportunistic infections and guides the use of preventive treatment. The normal range of CD4 count is from 500 to 1500 cells/mm3 of blood, and it progressively decreases over time in persons who are not receiving or not responding well to ART. If the person’s CD4 cell count falls below 200, their immunity is severely compromised, leaving them susceptible to infections and death. Someone with a CD4 count below 200 is described as having an advanced HIV disease (AHD) .
HIV viral load measures the amount of virus in the blood. This test is used to monitor the level of viral replication and effectiveness of ART. The treatment goal is to reduce the viral load in the blood to undetectable levels (less than 50 copies/ml), and the persistent presence of detectable viral load (greater than 1000 copies/ml) in people living with HIV on ART is an indicator of inadequate treatment response and the need to change or adjust the treatment regimen.
WHO’s 2022–2030 global health sector strategy on HIV aims to reduce HIV infections from 1.5 million in 2020 to 335 000 by 2030, and deaths from 680 000 in 2020 to under 240 000 in 2030.
Many people do not feel symptoms of HIV in the first few months after infection and may not know that they are infected. Others may experience influenza-like symptoms, including fever, headache, rash and sore throat. However, these first few months are when the virus is most infectious.
As the disease progresses, symptoms will be expanded and more pronounced. These can include swollen lymph nodes, weight loss, fever, diarrhoea and cough. HIV weakens the body’s ability to fight other infections, and without treatment people will become more susceptible to other severe illnesses such as tuberculosis , cryptococcal meningitis, bacterial infections and some cancers including lymphomas and Kaposi’s sarcoma.
Diagnosis of HIV uses rapid tests that provide same-day results and can be done at home, although a laboratory test is required to confirm the infection. This early identification greatly improves treatment options and reduces the risk of transmission to other people including sexual or drug-sharing partners.
HIV is fully preventable. Effective antiretroviral treatment (ART) prevents HIV transmission from mother to child during pregnancy, delivery and breastfeeding. Someone who is on antiretroviral therapy and virally suppressed will not pass HIV to their sexual partners.
Condoms prevent HIV and other sexually transmitted infections, and prophylaxis use antiretroviral medicines to prevent HIV. Male circumcision is recommended in high-burden countries in eastern and southern Africa. Harm reduction (needle syringe programmes and opioid substitution therapy) prevents HIV and other blood-borne infections for people who inject drugs .
HIV is treated with antiretroviral therapy consisting of one or more medicines. ART does not cure HIV but reduces its replication in the blood, thereby reducing the viral load to an undetectable level.
ART enables people living with HIV to lead healthy, productive lives. It also works as an effective prevention, reducing the risk of onward transmission by 96% .
ART should be taken every day throughout the person’s life. People can continue with safe and effective ART if they adhere to their treatment. In cases when ART becomes ineffective - HIV drug resistance - due to reasons such as lost contact with health care providers and drug stockouts, people will need to switch to other medicines to protect their health.
- HIV and AIDS
- HIV drug resistance
- Coronavirus disease (COVID-19) and people living with HIV
- Guidelines on HIV
- Country profiles
- HIV testing services dashboard
- HIV data and statistics
- Global Health Observatory HIV data repository:
- The epidemic
- The response
- Global health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections, for the period 2022–2030 (WHA75.20)
- Global health sector strategies on HIV, viral hepatitis and sexually transmitted infections, for the period 2016–2021 (WHA69.22)
- Global health sector strategy on HIV/AIDS, 2011–2015 (WHA64.14)
- Global health-sector strategy for HIV/AIDS (WHA56.30)
- HIV/AIDS: confronting the epidemic (WHA53.14)
- Global HIV, Hepatitis and STIs Programmes
- Vaccine development
Long-acting injectable lenacapavir proves effective in HIV prevention for women
A seventh case of HIV cure reported at AIDS 2024
Unfinished business: only the urgent and accelerated delivery of HIV services will keep the promise of ending AIDS in children by 2030
WHO releases technical brief on reducing HIV-related stigma and discrimination in healthcare settings

World AIDS Day 2023: Let Communities Lead
Tackling health facility intersectional stigma faced by key populations in Ghana
Countries take up new WHO recommendations on self-testing for PrEP and PEP
Using art to increase condom awareness
Donors making a difference: WHO, communities and partners collaborate to end infectious diseases

Men lag behind women in the response to the HIV epidemic

Monoclonal antibodies for HIV prevention

HIV and cervical cancer

World AIDS Day 2021 – Community-based health workers can deliver safe and effective HIV services

Don’t let the opportunity pass: Integrating STIs into HIV and key population services

Have you heard about Zero Risk and HIV?
Celebrating Condoms
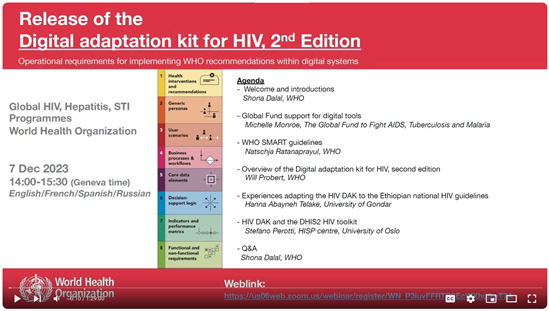
Webinar: release of the 2nd edition of the Digital adaptation kit for HIV

HTS Info app
WHO's current HIV testing services guidelines and information Download IOS | Download play store

WHO's consolidated guidelines for HIV treatment and care app. Download IOS | Download play store
Oral PrEP Tool app
The WHO PrEP Implementation Tool app for health workers Download IOS | Download play store

Implementing the global health sector strategies on HIV, viral hepatitis and sexually...

Guidelines for HIV post-exposure prophylaxis
Despite advancements in testing and treatment, over one million people became infected with HIV in 2022. This warrants a need for a revitalized focus on...

Consolidated guidelines on differentiated HIV testing services
These guidelines outline a public health approach to strengthening and expanding HIV testing services (HTS). They present and discuss key updates...
WHO Youtube Channel

HIV/AIDS - WHO videos playlist
Related health topics.
Sexually transmitted infections (STIs)
Tuberculosis

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
HIV and AIDS and Mental Health
What is hiv.
HIV, or human immunodeficiency virus , is the virus that causes AIDS (acquired immunodeficiency syndrome). HIV can be transmitted during sexual intercourse, by sharing syringes, or during pregnancy, childbirth, or breastfeeding.
HIV weakens the immune system by destroying CD4+ T cells, a type of white blood cell that is important for fighting off infections. The loss of these cells means that people living with HIV are more vulnerable to other infections and diseases.
Today, effective anti-HIV medications allow people with HIV to lead long, healthy lives. When taken as prescribed, these daily medications, called antiretroviral therapy (ART), can suppress the amount of virus in the blood to a level so low that it is undetectable by standard tests.
Why are people with HIV and AIDS at a higher risk for mental disorders?
The stress associated with living with a serious illness or condition, such as HIV, can affect a person’s mental health. People with HIV have a higher chance of developing mood, anxiety, and cognitive disorders. For example, depression is one of the most common mental health conditions faced by people with HIV.
It is important to remember that mental disorders are treatable. People who have a mental disorder can recover.
HIV and related infections can also affect the brain and the rest of the nervous system. This may change how a person thinks and behaves. Also, some medications used to treat HIV may have side effects that affect a person's mental health.
Situations that can contribute to mental health problems for anyone:
- Having trouble getting mental health services
- Experiencing a loss of social support, resulting in isolation
- Experiencing a loss of employment or worries about being able to perform at work
- Dealing with loss, including the loss of relationships or the death of loved ones
In addition, people with HIV include may also experience situations that negatively impact their mental health, such as:
- Having to tell others about an HIV diagnosis
- Managing HIV medicines and medical treatment
- Facing stigma and discrimination associated with HIV/AIDS
Understanding how living with HIV can affect mental health and knowing what resources are available can make it easier for people to manage their overall health and well-being.
What other complications can be caused by HIV?
HIV causes significant inflammation in the body. This inflammation can cause neurological complications by damaging the spinal cord and brain, which form the central nervous system.
Despite effective ART, people with HIV are still at risk for central nervous system diseases associated with HIV. These diseases can be neurological (affecting the nervous system) or neurocognitive (affecting cognition or mental processing).
Severe neurological impairments such as dementia, brain atrophy, and encephalitis (inflammation of the brain) are less common in people who use ART, compared to people with HIV who are not on ART. However, there are still less severe forms of central nervous system diseases associated with HIV.
Researchers are working to better understand how HIV affects the central nervous system. This information will be helpful to develop new treatments to improve the lives of people with HIV. Understanding which types of cells in the central nervous system are targeted by the HIV infection and how those cells are damaged may help shape efforts to prevent, treat, and cure HIV.
Research efforts also focus on understanding why HIV is harder to eliminate in some tissues in the body and what strategies might be more effective on those cells.
How can people with HIV improve their mental health?
Research shows that HIV treatment should begin as soon as possible after diagnosis to achieve the best health outcomes. Following a treatment plan, such as taking the medications prescribed by a health care provider, is critical for controlling and suppressing the virus.
Following the treatment plan can be difficult, but there are strategies that can help such as following a treatment plan, creating a routine, setting an alarm, and downloading a reminder app on a smartphone.
Starting ART can affect mental health in different ways. Sometimes ART can relieve anxiety because knowing that you are taking care of yourself can provide a sense of security. However, coping with the reality of living with a chronic illness like HIV can be challenging. In addition, some antiretroviral medicines may cause symptoms of depression, anxiety, and sleeplessness and may make some mental health issues worse.
For these reasons, it is important for people with HIV to talk to a health care provider about their mental health before starting ART. These conversations should continue throughout treatment.
People with HIV should talk with their provider about any changes in their mental health , such as thinking or how they feel about themselves and life in general. People with HIV should also discuss any alcohol or substance use with their provider.
People with HIV should also tell their health care provider about any over-the-counter or prescribed medications they may be taking, including any mental health medications , because some of these drugs may interact with antiretroviral medications. Learn tips for talking with a health care provider about your mental health .
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions, including mental illnesses. The goal of clinical trials is to determine if a new test or treatment works and is safe.
Although individual participants may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago.
Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and if one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- ClinicalTrials.gov: HIV/AIDS and Depression : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Adults - HIV/AIDS Issues : List of studies being conducted on the NIH Campus in Bethesda, MD
Federal Resources
- Centers for Disease Control and Prevention (CDC): HIV Basics
- HIV.gov: Mental Health and HIV
- HIV.gov: HIV Basics
- HIVinfo.NIH.gov: HIV and Mental Health
- National Institute of Allergy and Infectious Diseases: HIV/AIDS
- National Institute of Neurological Diseases and Stroke: Neurological Complications of AIDS
Free Brochures
- Depression : This brochure provides information about depression including the different types of depression, signs and symptoms, how it is diagnosed, treatment options, and how to find help for yourself or a loved one.
- Chronic Illness & Mental Health: Recognizing and Treating Depression : This brochure provides information about depression and mental health for people living with chronic illnesses, including children and adolescents. It discusses symptoms, risk factors and treatment options.
- Tips for Talking with A Health Care Provider About Your Mental Health : This fact sheet provides five tips to help prepare and guide you on how to talk to a health care provider about your mental health and get the most out of your visit.
Research and Statistics
- NIMH Division of AIDS Research
- CDC: HIV Statistics Center
Last Reviewed: November 2023
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.

IMAGES
VIDEO
COMMENTS
500+ Words Essay on AIDS. Acquired Immune Deficiency Syndrome or better known as AIDS is a life-threatening disease. It is one of the most dreaded diseases of the 20 th century. AIDS is caused by HIV or Human Immunodeficiency Virus, which attacks the immune system of the human body. It has, so far, ended more than twenty-nine million lives all ...
With the use of antiretroviral therapy, a person can maintain a chronic HIV diagnosis without developing AIDS for decades. Symptoms of AIDS can include: recurrent fever. chronic swollen lymph ...
Scanning electron micrograph of HIV-1, colored green, budding from a cultured lymphocyte. HIV is the cause of the spectrum of disease known as HIV/AIDS. HIV is a retrovirus that primarily infects components of the human immune system such as CD4 + T cells, macrophages and dendritic cells. It directly and indirectly destroys CD4 + T cells.
Untreated HIV / AIDS can cause a great deal of weight loss. Diarrhea, weakness and fever often happen with the weight loss. Brain and nervous system, called neurological, complications. HIV can cause neurological symptoms such as confusion, forgetfulness, depression, anxiety and difficulty walking.
HIV causes other infections to get worse, such as hepatitis C, hepatitis B and mpox. Transmission. HIV can be transmitted via the exchange of body fluids from people living with HIV, including blood, breast milk, semen, and vaginal secretions. HIV can also be transmitted to a child during pregnancy and delivery.
Causes. AIDS is transmitted via three main routes: The most common mode of transmission is the transfer of body secretions through sexual contact. This is accomplished through exposure of mucous ...
The human immunodeficiency virus (HIV) is the virus that causes HIV infection. If untreated, HIV may cause acquired immunodeficiency syndrome (AIDS), the most advanced stage of HIV infection.; People with HIV who are not on medication and do not have consistent control of their HIV can transmit HIV through vaginal or anal sex, sharing of needles, pregnancy, and/or breastfeeding.
Introduction. Human immunodeficiency virus or HIV is the cause of HIV infection that leads to the autoimmune disorder acquired immune deficiency syndrome (AIDS) [] (Fig. 1).The major cause of spreading of HIV is through unprotected sex, during pregnancy from mother to foetus, through contaminated hypodermic needles and infected blood transfusions [].
The time between HIV transmission and an AIDS diagnosis is usually 10-15 years, but sometimes longer. There is a very small number of people who have managed to control the HIV infection without ART and are called 'elite-controllers'. This situation is very rare and most people will need ART to avoid becoming ill.
HIV/AIDS will have various effects on the body of a patient. For instance, HIV will destroy the CD4 cell count in the body of a patient which is vital for immunity from diseases and infections (Abraham, 2019). During the first several weeks, the body's immune system tries to fight the virus. As evident in Figure 3 above, the human body's ...
AIDS is the late stage of HIV infection that occurs when the body's immune system is badly damaged because of the virus. In the U.S., most people with HIV do not develop AIDS because taking HIV medicine as prescribed stops the progression of the disease. A person with HIV is considered to have progressed to AIDS when: the number of their CD4 ...
What Causes AIDS? HIV or Human Immunodeficiency virus is a retrovirus that was first found in 1983. The virus is responsible for causing AIDS (acquired immunodeficiency syndrome). Once within the ...
HIV/AIDS catastrophe has been one of the defining features of the past quarter of a century. Although it is short-lived in the scheme of public-health crises, the pandemic ranks among the most ...
Introduction. Human Immunodeficiency Virus, abbreviated as HIV, attacks the body's immune system, and if left untreated, it can cause AIDS (Acquired Immune Deficiency Syndrome). HIV is a retroviral disease transmitted through unprotected sexual activity, from mother to child, blood transfusion, contact with infected body fluids, or hypodermic ...
Abstract. Acquired immunodeficiency syndrome (AIDS) of humans is caused by two lentiviruses, human immunodeficiency viruses types 1 and 2 (HIV-1 and HIV-2). Here, we describe the origins and evolution of these viruses, and the circumstances that led to the AIDS pandemic. Both HIVs are the result of multiple cross-species transmissions of simian ...
HIV/AIDS (UNAIDS) global plan10 decreased by 38% between 2009 and 2012, because of increased access to antiretrovirals to prevent mother-to-child transmission. However, access to antiretroviral therapy is much lower in children than adults.3 HIV is a major contributor to the global burden of disease. In 2010, HIV was the leading cause of ...
HIV/AIDS is an exceptional epidemic that demands an exceptional response. Much progress has been made in a short space of time, despite many scientific and programmatic challenges ( figure 6 ). In the absence of a protective vaccine or a cure, prevention and access to antiretroviral treatments are the best options to slow down the HIV-1 pandemic.
AIDS Essay. HIV (human immunodeficiency virus) is an infection that causes cells in the body that help it fight infections, making a person more susceptible to other infections and diseases. Interaction with certain bodily secretions of an HIV-positive individual, most commonly during unprotected intercourse (sex without the use of a condom or ...
World AIDS Day 2021 - Community-based health workers can deliver safe and effective HIV services. 28 March 2024. Don't let the opportunity pass: Integrating STIs into HIV and key population services. 1 March 2024. Have you heard about Zero Risk and HIV? 13 February 2024. Celebrating Condoms.
AIDS (acquired immunodeficiency syndrome) is caused by the progression of the HIV virus. HIV stands for human immunodeficiency virus. Unlike some other viruses, the human body can't get rid of HIV completely. According to AIDS.gov, once you have HIV, you have it for life. HIV attacks the body's immune system, specifically the CD4 cells (T ...
HIV, or human immunodeficiency virus , is the virus that causes AIDS (acquired immunodeficiency syndrome). HIV can be transmitted during sexual intercourse, by sharing syringes, or during pregnancy, childbirth, or breastfeeding. HIV weakens the immune system by destroying CD4+ T cells, a type of white blood cell that is important for fighting ...
The HIV-1 pandemic is a complex mix of diverse epidemics within and between countries and regions of the world, and is undoubtedly the defining public-health crisis of our time. Research has deepened our understanding of how the virus replicates, manipulates, and hides in an infected person. Although our understanding of pathogenesis and transmission dynamics has become more nuanced and ...