- Member Login
- About The Project
- Case Studies

Case Study 3 – Palliative and End-of-Life Care
Click here to review the draft palliative and end-of-life care – interactive case study..
The following case vignette provides key concepts that could be considered when developing a plan of care for a patient who may require a controlled substance to manage their health concerns. As with any clinical situation, there are many patient variables that must be considered, including comorbid conditions, social determinants of health and their personal choices. You may choose to include different or additional health history and physical examination points, diagnostic tests, differential diagnoses and treatments depending on your patient’s context however this case vignette focuses on the aspects relevant to controlled substances.
Danny Kahan NP-Adult, specialty is palliative care Joshi Kamakani – 70 year old male with metastatic prostate cancer June Kamakani – patient’s wife Kelli Kamakani – patient’s 40 year old daughter
Danny is reviewing the patient history outside the house or in the car before visiting the patient.
Joshi Kamakani is a 70 year old retired engineer that the Palliative Care home care team and I have been looking after at home for the last two months. Joshi was diagnosed with inoperable prostate cancer three years ago and has been treated with ablative hormone therapy. Six months ago, Joshi started to have pain in his hips. His oncologist ordered a CT scan and found he had metastases in his ribs, pelvis and lumbar spine. Joshi and his wife June had a meeting with the team at the cancer centre and decided not to go ahead with any further cancer treatment. Our team has been involved since. June called me yesterday and asked me to make a home visit. Joshi has been having more pain this week and has been spending most of his time on the couch. He cannot get around without assistance and is very fatigued.
Joshi’s past medical history includes hypertension and reflux. He is taking Predisone 5 mg PO BID, Leuprorelin Depot 22.5mg IM every 3 months, hydrochlorothiazide 25 mg daily and pantoprazole 40 mg daily.
For pain, Joshi takes Morphine slow release 100 mg q12h and has not needed additional medication for breakthrough pain so far.
Takes place in the home. Patient is seen reclining on couch in first floor living room. Wife and daughter present.
Danny rings the doorbell and June lets him in.
June: Hi Danny. I’m so glad you’ve come.
Danny takes off his coat and shoes and walks into the living room. Kelli is sitting with her father who is covered up with a blanket on a couch in the main living area – he is awake but obviously drowsy. He smiles at Danny and holds out his hand. Danny shakes it a sits down in a chair opposite.
June: His pain killers just are not working any more – he’s uncomfortable when he is resting and it’s worse when he has to move around. It’s been happening for the last few weeks. He hasn’t had a fall but he is unsteady on his feet – especially soon after he get up. Joshi: I tried some acetaminophen from the drug store a few days ago but it really didn’t work. Kelli: Danny, you have to do something. He’s so uncomfortable. Danny: OK let’s talk about this a bit more. Joshi, were you sleepy after we increased the morphine 2 weeks ago? You were at 80 mg for each dose and now you are at 100 mg. Joshi: I was a bit sleepy for a few days and I had a bit of a weak stomach but that is gone now. I am a bit constipated though. Danny: when did you have your last bowel movement? Joshi: 4 days ago. Danny: OK we will have to address that today. I’d like to use the scale that I used at our last visit, it’s called the PPS, to assess your level of activity. ( Edmonton symptom assessment scale and Palliative Performance Score). Your PPS is 40% – last time I visited you were at 60%. June: yes, he is definitely having more trouble. I think the pain is preventing him from moving and that’s just making everything worse.
Danny: Joshi, your pain interference score tells me that the pain is severely interfering with your activity and I see that you are rating your current pain at rest at 6/10 and at 10/10 when you move. When I examined you, I did not note any changes from my last visit except for some new swelling over your left hip. June: Yes that’s where it is most sore – and before you ask, I am not going to the hospital for an xray. Kelli: Why can’t you just double his dose?
Danny [THINKS]: I will also add a bowel regime to address Joshi’s constipation and provide an order for a PRN anti-nauseant like metoclopramide or ondansetron. Joshi and his family will need to have education about the timeline of the peak benefit of the change in the regular dose, keeping track of PRN use, proper use of breakthrough medications (before care or any activity that causes pain), any other interventions we can include to help with his pain including adding other medications.
June: Danny, can I speak to you in private for a moment? June and Danny move to a private area of the house. Kelli and Joshi remain on the sofa. June: Danny, I have some concerns about having extra medication in the house and I need some advice on how to deal with this. My daughter had a real problem with drugs when she was in high school. She had to have treatment and as far as I know, she has been clean for the past 2 years. I have talked to her about having medication in the house and she tells me she’s not tempted but I really want to be sure we don’t have any incidents. I trust my daughter but I do worry that some things are beyond her control. Danny: Well June, it is always a good practice to have a plan for safe storage of medications. Here is some information about where you can purchase a locked box. I recommend you keep a key and have the hospice nurse take the other and have it numbered and controlled at the hospice office for the use of the nurses that care for Joshi. In the meantime, keep the medications in a place that you and Joshi can monitor and please keep a count of the medication in the containers and continue to write down when medication is given. June: Thanks Danny – I don’t want my daughter to think I don’t trust her. This should help.
Two weeks later – Danny is back in his office reviewing Joshi’s file with a Nurse Practitioner student…
Follow-up case question by Danny.
Student: Next up is Joshi Kamakani for review… Danny: Well, I’ve just been to see Joshi and his family. It has been two weeks since we increased his dose of morphine SR. We also added a neuropathic pain agent to help with his pain which has made him a bit more drowsy. He continues to take 20-30 mg breakthrough morphine/day and I noticed today that he has some myoclonus. Joshi’s pain is still in the moderate range with activity and now nausea is a problem.
Opioid rotation and opioid equianalgesia from NOUGG (McMaster Guidelines).
Danny: I think a rotation of opioid is the next step. Student: What medication should Danny consider and at what dose?
Danny: Joshi is using 270 mg oral morphine equivalents per day. To convert this dose to hydromorphone, the medication I have chosen to rotate to, we multiply by 0.2. Morphine 270 mg x 0.2 = 54 mg hydromorphone/day. We will want to convert 60% of the total daily dose so 54mg x .6 = 32mg. I want to give Joshi the new dose in a slow release form. It is most practical to provide Joshi with hydromorphone SR 15mg q12h and also provide him an additional 2-3 mg of hydromorphone immediate release for breakthrough pain. Providing him with the breakthrough dosing will be sure Joshi can have additional medication to help him until we are sure we have a stable, effective dose in 48-72 hours.
Learning Outcome
This interactive case study covered the following information:
- Opiate Titration
- Opiate Rotation
- Pain Assessment
- Assessment of adverse effects
- Safety Assessment
- Collaboration
- Family centred care
Masking is optional but encouraged in UPMC medical facilities and most patient care settings.
- Health Care Professionals
- Find a Doctor
- Services by Region

- Frequently Searched Services
- See All Services
- Locations by Region

- Locations by Type

- See All Locations
- Patient & Visitor Resources

- Patient Portals
- Find Covid-19 updates
- Schedule an appointment
- Request medical records
- Learn about financial assistance
- Find classes & events
- Send a patient an eCard
- Make a donation
- Read HealthBeat blog
- Explore UPMC Careers
- Medical Records
- Financial Assistance
- Classes & Events
- HealthBeat Blog
- Health Library
- Facts & Stats
- Supply Chain Management
- Community Commitment
- Support UPMC
- UPMC Enterprises
- UPMC International
- Physician Information
- Education & Training
- Departments
- Credentialing
Case Studies in Palliative and Supportive Care
One of the goals of the UPMC Palliative and Supportive Institute is to advance the practice of our specialty by sharing our knowledge with students and health care professionals around the world.
To this end, we share monthly synopses of notable or particularly interesting cases in which palliative care has played a role.
If you have any questions, opinions, or insight about any particular case, we encourage you to contact us .
Your health information, right at your fingertips. Select MyUPMC to access your UPMC health information. For patients of UPMC-affiliated doctors in Central Pa, select UPMC Central Pa Portal. Patients of UPMC Cole should select the UPMC Cole Connect Patient Portal.

The portal for all UPMC patients EXCEPT those in Central Pa.

The portal for UPMC patients in Central Pa.

The portal for UPMC Cole patients receiving inpatient care.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Health Serv Res

What is case management in palliative care? An expert panel study
Annicka g m van der plas.
1 Department of Public and Occupational Health, EMGO Institute for Health and Care Research, VU University Medical Center, Amsterdam, the Netherlands
2 Palliative Care Center of Expertise, VU University Medical Center, Amsterdam, the Netherlands
Bregje D Onwuteaka-Philipsen
Marlies van de watering.
3 Kennemer Gasthuis, Haarlem, the Netherlands
Wim J J Jansen
4 Department of Anaesthesiology, VU University Medical Center, Amsterdam, the Netherlands
5 Agora, National Support Center for Palliative Terminal Care, Bunnik, the Netherlands
Kris C Vissers
6 Department of Anaesthesiology, Pain, and Palliative Medicine, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands
Luc Deliens
7 End-of-Life Care Research Group, Ghent University and Vrije Universiteit Brussel, Brussels, Belgium
Associated Data
Case management is a heterogeneous concept of care that consists of assessment, planning, implementing, coordinating, monitoring, and evaluating the options and services required to meet the client's health and service needs. This paper describes the result of an expert panel procedure to gain insight into the aims and characteristics of case management in palliative care in the Netherlands.
A modified version of the RAND®/University of California at Los Angeles (UCLA) appropriateness method was used to formulate and rate a list of aims and characteristics of case management in palliative care. A total of 76 health care professionals, researchers and policy makers were invited to join the expert panel, of which 61% participated in at least one round.
Nine out of ten aims of case management were met with agreement. The most important areas of disagreement with regard to characteristics of case management were hands-on nursing care by the case manager, target group of case management, performance of other tasks besides case management and accessibility of the case manager.
Conclusions
Although aims are agreed upon, case management in palliative care shows a high level of variability in implementation choices. Case management should aim at maintaining continuity of care to ensure that patients and those close to them experience care as personalised, coherent and consistent.
Patients facing a life-threatening illness are likely to experience palliative care needs [ 1 , 2 ]. According to the World Health Organization (WHO), palliative care aims at improving the quality of life of patients and their families, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, emotional, and spiritual [ 3 ]. Palliative care is complex care. Firstly because it demands attention to and knowledge of not only disease, pain and symptom management, but also a range of other non-medical issues from reimbursement structures to availability of social services and spiritual care [ 3 ]. Gaps in the general and specialist knowledge required by the health care provider must be filled by access to reliable knowledge from others. Secondly, communication plays a pivotal role; several professionals and informal caregivers across settings can be involved and round-the-clock continuity of information is necessary to deliver consistent care sensitive to rapidly changing needs. In 98% of their palliative care patients, Dutch General Practitioners (GPs) cooperate with at least one other caregiver, with a mean number of four [ 4 ]. In the Netherlands, about half of patients experience one or more transfers in their last month of life [ 5 ], implying the need for communication across settings at least at the start of the transfer period. This will probably be even more true in future with increasing life expectancy and a growing number of patients with multiple chronic diseases [ 6 ] resulting in, among other things, more health care needs and more need for the coordination of care.
Case management has developed as a means of ensuring continuity of care for patients with complex care needs. It is a heterogeneous term for care that consists of assessment, planning, implementation, coordination, monitoring and evaluation of the options and services required to meet the client's health and service needs [ 7 ]. It has been used for many years in psychiatry [ 8 ], among frail elderly people [ 9 ] and many other populations. There have been varying research results on its effectiveness. There are numerous models of and variations in ways of delivering case management [ 10 ]. Adding to the confusion is the multitude of names given to case management; care management, care coordination, disease management, and managed care being some of the most common in the nursing field. Most studies compare one application of case management with care as usual, there is little research comparing different models or applications of case management. It is difficult to compare studies due to differing methodologies and outcome measures, and unclear definitions and descriptions of case management [ 11 - 13 ]. Therefore, we conclude that based on current research, for most medical conditions there is no way of identifying the best model for delivering case management.
The same can be said for case management in palliative care. No reviews on case management in palliative care were found and there is no definitive evidence of its effectiveness in palliative care. Some positive results are reported. In a randomised trial among patients with advanced chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF) or cancer, case management resulted in increased patient satisfaction with care and the earlier development of advance directives [ 14 ]. In patients with advanced illness (mostly cancer) receiving case management, compared with a matched historical control group, hospice use and number of hospice days increased [ 15 ]. There appear to be variations in the application of case management in palliative care. Differences can be seen in target populations (e.g. cancer only [ 16 ] or a range of diagnoses [ 17 ]), whether principles of disease management should be integrated [ 18 ] or focus should be solely on terminal care [ 19 ], whether case management should be delivered by a multidisciplinary team [ 20 ] or not [ 15 ] and a broad range of other variations. Again, these studies cannot be compared, therefore, no conclusions can be drawn as to which application of case management should be preferred.
The question of how case management should best be delivered in palliative care is unanswered. The purpose of this study was to formulate the aims of case management and describe essential characteristics of case management in palliative care in the Netherlands, as perceived by experts. The expert panel procedure also gave insight into which topics there is consensus between experts and what are the main differences in opinion between them.
The RAND® / University of California at Los Angeles (UCLA) appropriateness method is developed to combine scientific evidence with the collective judgment of experts to yield a statement regarding the appropriateness of performing a procedure at the level of patient-specific symptoms, medical history and test results [ 21 ]. The aim of this method is to reach consensus on which medical procedures are appropriate in certain medical conditions and circumstances. With a modified version of this method it is possible to investigate whether there is consensus or disagreement for a diverse range of topics. In three written rounds we consulted experts to formulate and rate aims and characteristics of case management in palliative care. Purpose of round 1 and 2 was to formulate a list of aims and characteristics, in the third round experts rated the aims and characteristics on importance for successful implementation of case management in palliative care.
Expert panel
We invited 73 experts with experience in palliative care to participate in the expert panel: general practitioners, coordinators of palliative care networks, case managers working in palliative care, researchers and policy makers in palliative care. The perspective of district nurses was included in the expert panel through case managers and scientists in the field of nursing. Two experts declined but proposed four others to take their places and the colleague of another was added leading to the questionnaire being sent to 76 experts. Of those, 46 (61%) participated in at least one round. Twenty-four experts gave their reasons for not participating: lack of time (n = 13), lack of knowledge about case management (n = 7), prolonged illness (n = 4). Four reactions in the first round and two in the second were not traceable because they were returned anonymously. This study is exempt from approval from an ethics committee.
Selection of aims and characteristics
We drafted a first list of aims and characteristics of case management in palliative care based on information from existing initiatives, literature and previous research. We used four headings to partition our list of aims and characteristics: aims of case management in palliative care, characteristics of content of case management in palliative care, characteristics of structure of case management in palliative care and general conditions. The 16 characteristics in the fourth section, general conditions, related so commonly to care in general (e.g. 'the caseload is in ratio with the terms of employment of the case manager and the necessary time investment for individual patients') that they were omitted for the purposes of this paper.
For the aims of case management in palliative care, we made use of the conceptual framework of continuity of care by Bachrach [ 22 ]. She identified seven dimensions in continuity of complex care. The dimensions put together describe an ideal model for care in situations where several health care providers, settings and/or needs are involved. Case management does not necessarily incorporate all elements in itself, but its task is to make sure the patient receives continuity of care. Bachrach listed these dimensions specifically for people with long-term mental disorders, and we hypothesised that they would be useful as a starting point in identifying the aims of case management in palliative care. We reformulated the characteristics to reflect palliative terminology and discourse. Additional to the seven characteristics derived from Bachrach, we added two more, one specifically on palliative care (care or coordination of care is aimed at quality of life and death) and the other because the literature suggests that continuity of care across settings is problematic in palliative care [ 23 , 24 ] and we hypothesised that case management should pay special attention to that aspect. In Table 1 the dimensions of Bachrach and the aims of case management are reported.
Transformation of dimensions of continuity of care to aims of case management in palliative care sent to the expert panel for feedback in round 1
In three written rounds the experts were asked to formulate and rate aims and characteristics of case management in palliative care. In the first round we presented the first draft of the list of aims and characteristics and the expert was asked to add and remove some, give textual feedback and feedback on the aims and characteristics included. For readability characteristics were clustered around themes within the sections; aims of case management in palliative care, characteristics of content of case management, characteristics of structure of case management, and general conditions. In the second round we sent a new draft based on the respondents' feedback, with the same question. No reaction was required if the participant agreed with the content and formulation. In order to be rated independently in the third round, the clusters were then divided into separate characteristics (see Table 2 for an example). Thus, a list of 41 clustered aims and characteristics was divided into 104 separate aims and characteristics. In the third round the expert panel rated all aims and characteristics on a nine-point scale, a score of one indicating that the aim or characteristic was 'not important for successful implementation' and of nine that it was 'very important for successful implementation' of case management in palliative care.
Example of a clustered characteristic in round 2 and division into separate characteristics for round 3
Data analysis
We calculated the mean, standard deviation, median and median absolute deviation (M.A.D.) for all aims and characteristics. Agreement was calculated according to the procedure described by the RAND Corporation specifically designed for expert panels with more than nine participants [ 21 ]. Thus, according to the RAND criteria, for an aim or characteristic to be considered important for successful implementation of case management two requirements for agreement had to be met:
1) the expert panel agreed with the aim or characteristic, meaning that an aim or characteristic was scored 7 to 9 by 80% of participants,
2) the expert panel agreed with each other, meaning that the Interpercentile Range Adjusted for Symmetry (IPRAS) is larger than the Interpercentile Range (IPR). We used .30 and .70 percentile scores to calculate the lower and upper limit of the IPR.
All other results are categorised as 'disagreement'. We used the M.A.D. as an estimator of dispersion to assess the level of disagreement within the expert panel. This measure is less susceptible to outliers than the standard deviation. To distinguish between a high and a moderate level of disagreement we used a cut off score of M.A.D. = 2.0.
Round 1 and 2
In the first round we received 35 reactions on the aims and characteristics. In Table 3 the response is shown differentiated by the discipline of the participants. Main topics addressed by the experts on the first draft were: inclusion of informal caregivers (family, partner) in case management, communication and role delineation between the case manager and other health care professionals and the necessity of tailoring care to individual needs and wishes. Also, wording of the aims and characteristics was altered accordingly to feedback from the expert panel. This resulted in an adapted draft sent around for round two. In the second round we received 12 reactions on the adapted draft. The feedback on this draft mainly concerned suggestions for improvements in detail. The complete list of aims and characteristics for case management in palliative care formulated after round two is reported in Additional file 1 .
Background characteristics of respondents per round
1 Some responses could not be traced, we are not certain whether the two unknown respondents from round two did or did not respond in round one. The total number may be between 4 and 6.
2 Some responses could not be traced, we are not certain whether the two unknown respondents from round two are unique, so the number of persons with one or more responses is between 46 and 48.
In the third round we received 34 reactions from the expert panel. Table 4 shows that agreement was reached on 35 aims and characteristics. Overall, about a third of the aims and characteristics met with agreement (34%), almost half with a moderate level of disagreement (49%), and less than a fifth (17%) with a high level of disagreement. Both aims and characteristics which are met with agreement and with a high level of disagreement are marked in the Additional file 1 . There were no notable differences between experts from different backgrounds on rating the aims and characteristics (see the Additional file 1 for mean and median scores).
Scoring of the aims and characteristics by the expert panel
Aims of case management in palliative care
In section one on aims almost all aims were met with agreement (90%) and none with a high level of disagreement. The one aim with a moderate level of disagreement (Additional file 1 , aim 1.2) used the term ‘care on demand’ ('vraaggestuurd'), which is used by Dutch policy makers to indicate that the patient is central to care as opposed to 'care as supplied' ('aanbod gestuurd') which prioritises the habits, rules and regulations of the institution delivering it. This characteristic was added at the request of some of the experts because they felt that aim 1.4 on individual care did not adequately cover the aspect of care on demand. However, we received questions on this term (e.g. 'does this mean that care should not be proactive?') that made clear that the denotation of the term is not well known among the expert panel. At the same time we received feedback indicating that the expert panel agrees that the patient should be at the centre of care and that it should be tailored to the individual needs of the patient and aim 1.4 was met with a high level of agreement.
Content of case management in palliative care
In section two on content of case management most characteristics were met with a moderate level of disagreement (44%), while another 40% were met with agreement and a small proportion with a high level of disagreement (17%). Within this section the highest level of disagreement (M.A.D. = 2.33) was on nursing care tasks (characteristic 2.1.a). This stems from the opinion of some experts that the number of health care providers surrounding the patient should be kept as low as possible. The district nurse can perform case management next to other duties. Others believe that district nurses, due to their busy schedules, do not have time to offer patients adequate comfort, reassurance and information and this will take second place to their nursing tasks. Comfort, reassurance and information may also be needed by patients who are not yet using care from a district nurse.
Structure of case management in palliative care
In section three on structure of case management most characteristics were met with a moderate level of disagreement (63%), while 22% encountered a high level of disagreement and only 15% were met with agreement. Within this section there were three characteristics with a joint highest level of disagreement (M.A.D. = 2.24): whether the case manager should combine case management with other tasks (e.g. consultation) (characteristic 3.5.b), whether she or he should be accessible 24 hours a day, seven days a week (characteristic 3.8.a), and if the target group she or he works for includes all patients with a life-threatening disease (characteristic 3.7.c).
This study shows that agreement was high on the aims of case management. However, how case management should be implemented, and exactly which elements of care it should include, is more open for debate. Disagreement was highest on topics regarding whether the case manager should perform hands-on nursing care themselves or not, on the target group, on accessibility of the case manager and on performance of other tasks besides case management.
Strengths and limitations
This is the first study using a structured procedure to report on the importance of the aims and characteristics of case management in palliative care. The expert panel reflects the opinions of case managers, coordinators of palliative care networks, general practitioners and other physicians, researchers and policy makers. There were no marked differences between experts from different backgrounds on rating the aims and characteristics. However, these opinions not necessarily reflect practice and we lack information on how often and how case management is implemented in the Netherlands. Also, our results may only be representative for mixed public-private health care systems with a strong primary care gatekeeper that resemble the Dutch system. The characteristics of case management may be different in other health care systems.
The aims that met agreement are in accordance with the general principles of palliative care and also reflect the patient advocacy model of case management [ 25 ]. This model offers comprehensive coordination of services aimed at quality of care and is distinguished from the interrogative model, which is more focused on clinical decision-making and emphasises cost-effectiveness. The aims also underline the importance of the seven dimensions of continuity of care formulated by Bachrach for psychiatric care [ 22 ]. This conceptual framework appears to be valid for complex continuous care in general, whether it is psychiatric care or palliative care.
Translation from aims to content of care is apparently relatively straightforward, with 40% agreement and only 17% strong disagreement on what care should be included. Offering information and support, identifying needs and adjusting care to match the patient's needs are the main tasks of the case manager. This can also be seen in descriptions of case management in palliative care [ 20 , 26 ], for cancer patients [ 27 ] and in a Delphi study on case management for patients with dementia [ 28 ]. Delivery of hands-on patient care is the most important area of disagreement within the expert panel. As mentioned in the results section, this stems from task alignment between the district nurse and case manager and whether these should be two different people or not. Besides, this also touches on the discussion whether palliative care should be part of primary (generalist) care, delivered by specialised palliative care providers, or in a cooperation between the two [ 29 ]. Case management could be delivered in a multidisciplinary team taking over all care, or case management can be guiding and assisting the primary health care providers (GP and district nurse) in their care for the patient. Another notable topic of disagreement is whether case management should stop before bereavement support is provided. The panel agrees that bereavement support is part of palliative care, reflected in agreement with characteristic 2.18.c. and aim 3. Whether there can be other endpoints for case management may be related to the target group, which is also a point of disagreement for the expert panel (reflected by characteristics 3.7 a, b and c). In a mixed-method study on case management for cancer patients, there are two distinct case management trajectories for patients receiving curative care and those receiving palliative care [ 27 ]. For curative patients case management can be short-term and stops when information needs are met. The discussion on bereavement support may also be a reflection of the Dutch reimbursement system, where it is not financed by public means and therefore any time the case manager spends on delivering it is not compensated.
Translation from aims to structure of case management is apparently less straightforward, with only 17% agreement and 22% strong disagreement. Characteristics such as the target group and the accessibility of the case manager may reflect the scope and depth of the case manager’s task: when can she or he work with the patient themselves and at what point does she or he refer to another professional? In the aforementioned Delphi study on case management for patients with dementia, no agreement could be reached on similar topics [ 28 ]. Apparently, in correspondence with applications of case management in cancer [ 11 ], CHF [ 12 ] and dementia [ 13 , 28 ], also in palliative care there is no unique best way to deliver case management according to experts.
Case management in palliative care should aim at maintaining continuity of care to ensure that patients and those close to them experience palliative care as personalised, coherent and consistent. There is a high level of agreement about the underlying dimensions of continuity of care [ 22 ]. The most important issues in implementation preferences are defining the target group of case management, the performance of other tasks besides case management, accessibility of the case manager and delivery of hands-on nursing care by the case manager. Research into the feasibility of different options and their effects on implementation could help health care planners make informed decisions on the best way to deliver case management.
Competing interests
The authors declare that they have no competing of interest.
Authors’ contributions
AvdP participated in the design of the study, carried out the measurements, analysed and interpreted the data, and drafted the manuscript. BO-P conceived of the study, participated in its design and coordination and made substantial contributions to the data interpretation and writing of the paper. MvdW, WJ, KV and LD participated in design of the study, interpretation of the data and critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6963/12/163/prepub
Supplementary Material
Aims and characteristics of case management in palliative care. This file contains a full list of all aims and characteristics of case management in palliative care, as formulated and rated by the expert panel. (PDF 129 kb)
Acknowledgements
The authors wish to thank ZONMw (grant number 80-82100-98-066) for their financial support. The funders had no role in data collection and analysis, selection of respondents, decision to publish, or preparation of the manuscript.
- Jaul E, Rosin A. Planning care for non-oncologic terminal illness in advanced age. IMAJ. 2005; 7 :5–8. [ PubMed ] [ Google Scholar ]
- McIlfatrick S. Assessing palliative care needs: views of patients, informal carers and healthcare professionals. JAN. 2007; 57 :77–86. doi: 10.1111/j.1365-2648.2006.04062.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sepulveda C, Marlin A, Yoshida T, Ullrich A. Palliative care: the World Health Organization's global perspective. J Pain Symptom Manag. 2002; 24 :91–96. doi: 10.1016/S0885-3924(02)00440-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Borgsteede SD, Deliens L, van der Wal G, Francke AL, Stalman WA, van Eijk JT. Interdisciplinary cooperation of GPs in palliative care at home: a nationwide survey in The Netherlands. Scand J Prim Health Care. 2007; 25 :226–231. doi: 10.1080/02813430701706501. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Abarshi E, Echteld M, Van den Block L, Donker G, Deliens L, Onwuteaka-Philipsen B. Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliat Med. 2010; 24 :166–174. doi: 10.1177/0269216309351381. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998; 51 :367–375. doi: 10.1016/S0895-4356(97)00306-5. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Commission for Case Manager Certification. Definition of Case management. Accessed 14-6-2010. http://www.cmsa.org/Home/CMSA/WhatisaCaseManager/tabid/224/Default.aspx .
- Dixon L, Goldberg R, Iannone V, Lucksted A, Brown C, Kreyenbuhl J. et al. Use of a critical time intervention to promote continuity of care after psychiatric inpatient hospitalization. Psychiatr Serv. 2009; 60 :451–458. doi: 10.1176/appi.ps.60.4.451. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, Mor V. et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ. 1998; 316 :1348–1351. doi: 10.1136/bmj.316.7141.1348. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huber DL. The diversity of case management models. Lippincotts Case Manag. 2002; 7 :212–220. doi: 10.1097/00129234-200211000-00002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wulff CN, Thygesen M, Sondergaard J, Vedsted P. Case management used to optimize cancer care pathways: a systematic review. BMC Health Serv Res. 2008; 8 :227–234. doi: 10.1186/1472-6963-8-227. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whellan DJ, Hasselblad V, Peterson E, O'Connor CM, Schulman KA. Metaanalysis and review of heart failure disease management randomized controlled clinical trials. Am Heart J. 2005; 149 :722–729. doi: 10.1016/j.ahj.2004.09.023. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pimouguet C, Lavaud T, Dartigues JF, Helmer C. Dementia case management effectiveness on health care costs and resource utilization: a systematic review of randomized controlled trials. J Nutr Health Aging. 2010; 8 :669–676. [ PubMed ] [ Google Scholar ]
- Engelhardt JB, Clive-Reed KP, Toseland RW, Smith TL, Larson DG, Tobin DR. Effects of a program for coordinated care of advanced illness on patients, surrogates, and healthcare costs: a randomized trial. Am J Manag Care. 2006; 12 :93–100. [ PubMed ] [ Google Scholar ]
- Spettell CM, Rawlins WS, Krakauer R, Fernandes J, Breton ME, Gowdy W. et al. A comprehensive case management program to improve palliative care. J Palliat Med. 2009; 12 :827–832. doi: 10.1089/jpm.2009.0089. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seow H, Piet L, Kenworthy CM, Jones S, Fagan PJ, Dy SM. Evaluating a palliative care case management program for cancer patients: the Omega Life Program. J Palliat Med. 2008; 11 :1314–1318. doi: 10.1089/jpm.2008.0140. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Head BA, Lajoie S, Augustine-Smith L, Cantrell M, Hofmann D, Keeney C. et al. Palliative care case management: increasing access to community-based palliative care for medicaid recipients. Prof Case Manag. 2010; 15 :206–217. [ PubMed ] [ Google Scholar ]
- Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. J Palliat Med. 2006; 9 :111–126. doi: 10.1089/jpm.2006.9.111. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Back AL, Li YF, Sales AE. Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med. 2005; 8 :26–35. doi: 10.1089/jpm.2005.8.26. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Holley APH, Gorawara-Bhat R, Dale W, Hemmerich J, Cox-Hayley D. Palliative access through care at home: experiences with an urban, geriatric home palliative care program. J Am Geriatr Soc. 2009; 57 :1925–1931. doi: 10.1111/j.1532-5415.2009.02452.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fitch K, Bernstein SJ, Aguilar MS, Burnand B, LaCalle JR, Lazaro P, The RAND/UCLA Appropriateness Method User's Manual. 2001.
- Bachrach LL. Continuity of care for chronic mental patients: a conceptual analysis. Am J Psychiatry. 1981; 138 :1449–1456. [ PubMed ] [ Google Scholar ]
- Hauser JM. Lost in transition: the ethics of the palliative care handoff. J Pain Symptom Manag. 2009; 37 :930–933. doi: 10.1016/j.jpainsymman.2009.02.231. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meier DE, Beresford L. Palliative care's challenge: facilitating transitions of care. J Palliat Med. 2008; 11 :416–421. doi: 10.1089/jpm.2008.9956. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Long MJ, Marshall BS. What price an additional day of life? A cost-effectiveness study of case management. Am J Manag Care. 2000; 6 :881–886. [ PubMed ] [ Google Scholar ]
- Head BA, Cantrell M, Pfeifer M. Mark's journey: a study in medicaid palliative care case management. Prof Case Manag. 2009; 14 :39–45. [ PubMed ] [ Google Scholar ]
- Howell D, Sussman J, Wiernikowski J, Pyette N, Bainbridge D, O'Brien M. et al. A mixed-method evaluation of nurse-led community-based supportive cancer care. Support Care Cancer. 2008; 16 :1343–1352. doi: 10.1007/s00520-008-0416-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Verkade PJ, van Meijel B, Brink C, van Os-Medendorp H, Koekkoek B, Francke AL. Delphi research exploring essential components and preconditions for case management in people with dementia. BMC Geriatr. 2010; 10 :54. doi: 10.1186/1471-2318-10-54. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gott M, Seymour J, Ingleton C, Gardiner C, Bellamy G. 'That's part of everybody's job': the perspectives of health care staff in England and New Zealand on the meaning and remit of palliative care. Palliat Med. 2012; 26 :232–241. doi: 10.1177/0269216311408993. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Case-based learning: palliative and end-of-life care in community pharmacy
Community pharmacists encounter patients at all stages in their life; however, patients who require palliative care require dedicated time and special consideration.

JL / Shutterstock.com
The World Health Organization (WHO) defines palliative care as an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness. This is achieved through the prevention and relief of suffering by means of early identification and impeccable assessment, and treatment of pain and other problems [1] .
Palliative care is often considered to be only for patients with cancer, but it also incl udes patients with conditions such as organ failure (e.g. heart failure , COPD, renal and hepatic failure), neurological conditions (e.g. multiple sclerosis , Parkinson’s disease and motor neurone disease), dementia, frailty , stroke and HIV/AIDS [2] , [3] , [4] .
The same can be said when considering symptoms (see Table) [5] . Being symptom-free is one of the most important factors for patients when considering end-of-life care [6] . Pharmacists have much to offer, not only in providing medicines required for symptom management, but also supporting patients and their carers to receive the right care at the right time [2] , [7] , [8] .
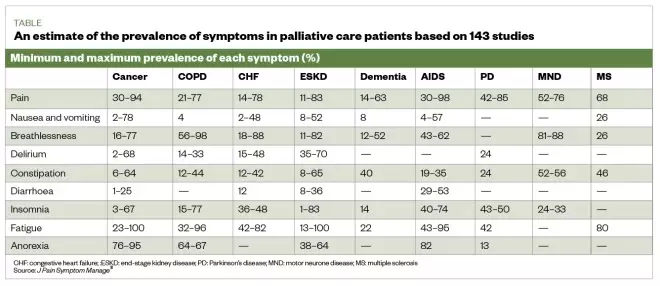
Table: an estimate of the prevalence of physical symptoms in palliative patients based on results from 143 studies
Source: J Pain Symptom Manage [5]
Symptom management
How symptoms are treated may change over time and may depend on many factors, including the symptom being treated, the patient’s ability to swallow (owing to disease process causing fatigue and weakness), and level of consciousness. Although most symptoms can be treated with oral preparations, it is likely that the oral route will become less available and a switch to parenteral preparations may be required.
The Gold Standards Framework recommends considering anticipatory prescribing of subcutaneous formulations for pain, nausea and vomiting, agitation/restlessness and excess respiratory secretions (also known as ‘death rattle’) [9] , [10] . The anticipatory prescribing of these medicines is part of advance care planning (i.e. the conversation between the patient’s families and carers about their future wishes and priorities for care) [11] , [12] .
The way symptoms are treated in patients receiving palliative care may change over time; however, several factors may influence this. For example, the Gold Standards Framework recommends considering subcutaneous formulations for:
- Nausea and vomiting;
- Agitation/restlessness;
- Excess respiratory secretions [12] .
Pharmacy schemes across the UK exist to act as stockists for locally selected anticipatory medicines, including alternative anti-emetics, opiates and steroids. See the Local Pharmaceutical Committee website for details (see Useful resources ). Be aware of the local pharmacies enrolled in these schemes, to ensure the pharmacy team can advise patients or carers if needed.
The Gold Standards Framework also suggests five steps for healthcare professionals to consider when advance care planning for patients, which are:
- Thinking about the future and what is important to the patient;
- Talking with family and friends about the patient’s choices so they are aware of them and can act as a spokesperson should the patient become unable to do this for themselves;
- Recording the patient’s wishes;
- Discussing plans with healthcare teams involved in the patient’s care (this may include conversations about resuscitation);
- Sharing information with the people who will need to be aware of it [12] .
An advance care plan can include many details, such as the desired extent of active treatment; the patient’s preferred place of care at the end of life; preferences for symptom management (e.g. the level of sedation a patient finds acceptable); people they would like to be present at end of life; spiritual and religious needs; and thoughts around funeral planning.
The Palliative Care Formulary provides excellent information and guidance on dosing and routes, which are often outside of the product license [10] . The National Institute for Health and Care Excellence (NICE) has also published several documents to support healthcare professionals in their approach to palliative care [13] (see Useful resources ).
Role of the pharmacist
Towards the end of a patient’s life, drug treatments should be as minimised when possible, with pharmacists reviewing and advising on deprescribing [7] , [14] . Pharmacists should also support patients in fulfilling their wishes to die in the place they choose with their symptoms well managed [8] .
The role of pharmacists in palliative care should be much greater than a supply function, although the importance of stocking anticipatory medicines should not be underestimated. Patients and their carers value more than the basic level of service from the pharmacy, and appreciate friendliness from staff who are familiar with them and can provide support with medicines and symptom management [15] .
The complex and often changing medicines regimens for palliative care patients can be challenging for medicines optimisation. Providing clear instructions on regimens and general communication can help (see Box 1 ) [10] . It is important to establish what medicines the patient is taking and when, and support and simplify their regimen if possible. For example, a patient is instructed to take paracetamol 1,000mg four times a day at 08:00, 12:00, 16:00 and 20:00, but wakes during the night with pain. Instead, the patient could be advised to take the paracetamol at equal intervals throughout the 24-hour period, (e.g. every six hours) [10] . However, this decision would need to take into consideration the patients waking hours and preferences.
The following case describes how pharmacists can assist patients nearing end of life with management of pain, nausea and constipation, and anticipatory prescribing.
Box: Considerations to take into account when communicating with palliative care patients and carers
Aims of communication :
- Information sharing;
- Reducing uncertainty;
- Facilitating choices and joint decision making;
- Creating, developing and maintaining relationships .
Getting started:
- Make time for the conversation, even if it is only for a few uninterrupted minutes;
- Ensure privacy;
- Introduce yourself;
- Indicate clearly that you have time to listen (e.g. offer to sit down with them);
- Use open questions to obtain information and allow the patient to talk (e.g. “what do you think this medicine is for?”);
- Engage using active listening (e.g. nodding and summarising to check information).
Be aware of non-verbal communication, such as:
- Facial expression;
- Eye contact;
- Posture (whether sitting or standing);
- Pitch and pace of voice;
- Use of appropriate touch.
Try to recognise barriers to good communication, for example:
- Language (patient’s own language or the use of jargon);
- Poor hearing, feeling generally unwell, fatigued, distracted by symptoms, fear and anxiety;
- Poor transfer of care information;
- Lack of time and privacy.
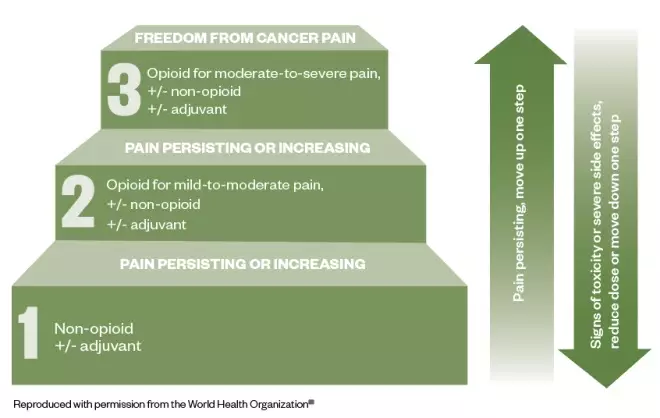
Figure: the three-step analgesic ladder
Source: World Health Organization [16]
This cancer pain management ladder provides a general guide to treatment based on the severity of pain
Palliative care part 1: pain management
Mary*, aged 54 years, comes into the pharmacy and asks to speak to the pharmacist about her prescribed medicines. She was recently diagnosed with metastatic pancreatic cancer, and her GP and palliative care team are working to manage her pain.
Two weeks ago, Mary was started on paracetamol 1,000mg four times per day and morphine sulphate liquid 5mg (2.5mL) every two to four hours as required. She was previously prescribed codeine 30–60mg four times per day, but this did not help to relieve her symptoms. On average, she has been taking six doses of morphine sulphate 5mg in each 24-hour period, and although this helps, it does not completely alleviate her pain.
Today, Mary has been prescribed morphine sulphate (MST; Napp Pharmaceuticals) 15mg twice daily and has been told to continue with her paracetamol and morphine sulphate liquid (for breakthrough pain). Mary explains that her GP said there may be a need to add a medicine for nerve pain. However, Mary goes on to say that she is worried that she is taking “too much” medicine and she is reluctant to take all of these medicines, especially if another may be added for nerve pain.
Actions and recommendations
The pharmacist should consider the following during the consultation:
- Communication — open questions should be used to determine how much has been explained to Mary about pain management. It may be that she has been given an explanation, but it is often worth covering these again;
- World Health Organization pain ladder — explain the use of the ladder (see Figure), including the need to use regular paracetamol;
- Analgesia — patients are often concerned by using more than one opiate. Patients may need to be encouraged to use their breakthrough analgesia when required, explaining how the dose is determined by the background analgesia may help [17] ;
- Keeping a diary — Mary should be encouraged to keep a pain diary. This can be a benefit as keeping a record of breakthrough doses may help when it comes to dose titration;
- Addressing patient concerns — explain to Mary that neuropathic agents may be used as an adjuvant if opiates fail to control the pain [18] ;
- Resources — recommend available online resources to Mary through the British Pain Society and the National Institute for Health and Care Excellence (see Useful resources) [17] , [19] .
Explain to Mary that as her opiate dose is increased, breakthrough doses will also increase. These should be one-sixth of the total daily opiate dose. For example, a dose of MST 30mg twice daily (60mg/24 hours), will require morphine sulphate (liquid or tablet) 10mg every 2–4 hours as required for breakthrough pain [10] , [14] .
When to refer
Mary should be referred back to her GP or the palliative care team if she requires frequent prescriptions for breakthrough medicines, which would indicate that her pain is not adequately managed, or she is experiencing unacceptable side effects (e.g. nausea or severe itch).
Palliative care part 2: nausea and constipation
Mary returns to the pharmacy ten days after starting on MST and her background dose is currently 30mg twice daily. She says that her pain is controlled, but she has been experienced nausea since the MST dose was increased two days ago. She also explains that she has not had “a proper bowel movement” for five days. Mary says she feels generally uncomfortable and has a feeling of fullness in her abdomen.
As a result, Mary is considering stopping the MST capsules. When questioned on her diet, Mary says she understands that dietary intake influences her bowels; however, she explains that her appetite is reduced owing to the abdominal discomfort. Mary would like to know if there is anything she can purchase that will help.
Constipation is the most commonly reported side effect of opiate treatment (up to 80% of patients) and can result in reduced quality of life and discontinuation of the offending medicine, which could result in a resurgence of pain [10] , [20] . When speaking with Mary about management, consider the following:
- Ascertain bowel pattern — the Bristol Stool chart can be used to support the consultation, but it is important to determine what is ‘normal’ for the patient and any other symptoms (e.g. colic) [21] . Mary confirms that her bowels feel sluggish and she is passing small, hard stools, which requires a lot of effort.;
- Maintaining a healthy diet — Mary’s dietary intake is reduced, but with resolution of constipation, this may improve. Encourage a healthy diet that includes whole grains, fruit and vegetables, and a good fluid intake [22] ;
- Laxatives — regular administration of laxatives to avoid constipation is advised [14] . The National Institute for Health and Care Excellence recommends the use of: stimulant laxatives (e.g. Senna [7.5–15mg at night, increasing to 30mg maximum in 24 hours] and sodium picosulphate [5–10mg at night]) and osmotic laxatives (e.g. lactulose [15–45mL daily in three divided doses] and macrogol compound [1–3 sachets daily in divided doses]) [22] . Docusate (up to 500mg daily in divided doses) is an alternative as both a softener and weak stimulant [10] . If tolerance to constipation does not occur, treatment with laxatives is advised for the duration of opiate use [20] . If titration of laxative is required then this occurs every 1–2 days according to response before switching to an alternative [10] ;
- Nausea — this common side effect occurs on initiation and dose increase, but is normally transient, lasting only a few days [15] , [23] , [24] . If patients are aware of this, they may feel more prepared and willing to accept it for a short period of time making the use of an antiemetic unnecessary [20] ;
- Non-pharmacological measures — pharmacy teams can recommend removal of certain stimuli (e.g. sight and smell of nausea-provoking foods) that lead to nausea and massage to help manage constipation [25] , [26] .
It is important to explain to Mary that opioid analgesics are a common cause of constipation, alongside other contributing factors, such as poor fluid, and dietary intake [27] .
Compliance with laxatives may be limited by patient factors, such as palatability, volume required and undesirable effects (e.g. flatulence and colic). Mary’s preference should be considered, especially as there is limited evidence for the use of laxatives, and management is generally dictated by best practice and expert opinion [14] .
The underlying aetiology of nausea and/or vomiting should be considered; gastric dysmotility and stimulation of the chemoreceptor trigger zone are most common with opiates, and can be managed with prokinetics (e.g. domperidone, metoclopramide) or a D2 receptor antagonist (e.g. haloperidol) [10] , [18] , [19] .
When the maximum licensed dose of laxatives is reached without adequate result, then there is a need to refer the patient.
If an antiemetic is considered necessary (e.g. owing to persistent or intolerable nausea ), the patient requires referral for thorough assessment [25] .
Palliative care part 3: Anticipatory prescribing
Mary’s husband, John*, brings a prescription for anticipatory medicines into the pharmacy. He is visibly upset and asks to speak to the pharmacist. He explains that the GP surgery called and asked for this prescription to be collected following a home visit from Mary’s community nurse.
During the visit, the nurse asked difficult questions about where Mary would like to be cared for when she becomes less well, and whether she would want to be resuscitated. The nurse had also suggested that Mary can stop her simvastatin, which she has been taking for the past 17 years.
John’s concerns
Although John is concerned because he knows Mary is unwell, he thinks these conversations suggest that Mary is nearing the end of her life.
When speaking with John, be empathetic while providing information. For example, explain:
- That anticipatory prescribing is part of advance care planning and does not signify that a patient is imminently dying. Medicines are prescribed in anticipation of symptoms, and should be put in place well in advance to enable rapid symptom relief [13] , [28] ;
- The possible use for each of the medicines (pain, nausea and vomiting, excess respiratory secretions, agitation and restlessness) [29] . It is unlikely that all would be needed, and possibly none at all. These medicines can be used for a more acute symptom, such as nausea or pain owing to infection, rather than only for use in the last few days of life;
- Stopping unnecessary medicines (i.e. those for long-term risk, such as statins for cardiovascular disease) should be considered to reduce tablet burden and potential side effects [7] ;
- These conversation can be distressing, but it provides an opportunity to consider serious issues during a time that is less critical and that some patients and carers may find comfort in the planning [30] .
After speaking with and explaining these points to John he appears to be more content and less worried. It is important to explain to him that the pharmacy team is available to speak to him or his wife if they have any further concerns.
*Case study is fictional
Useful resources
- Local Pharmaceutical Committee: lpc-online.org.uk/
[1] World Health Organization. WHO definition of palliative care. 2019. Available at: https://www.who.int/cancer/palliative/definition/en/ (accessed October 2019)
[2] World Health Organization. Palliative care. 2018. Available at: https://www.who.int/news-room/fact-sheets/detail/palliative-care (accessed October 2019)
[3] The Gold Standards Framework. PIG – Proactive identification guidance registration form. 2016. Available at: http://www.goldstandardsframework.org.uk/PIG (accessed October 2019)
[4] Marie Curie. Triggers for palliative care. 2015. Available at: https://www.mariecurie.org.uk/globalassets/media/documents/policy/policy-publications/june-2015/triggers-for-palliative-care-full-report.pdf (accessed October 2019)
[5] Moens K, Higginson IJ & Harding R. Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. J Pain Symptom Manag 2014;48(4):660–677. doi: 10.1016/j.jpainsymman.2013.11.009
[6] Kobewka D, Ronksley P, McIssac D et al. Prevalence of symptoms at the end of life in an acute care hospital: a retrospective cohort study. CMAJ Open 2017;5(1):E222–E228. doi: 10.9778/cmajo.20160123
[7] Walker KA, Scarpaci L & McPherson ML. Fifty reasons to love your palliative care pharmacist. American J Hosp Palliat Care 2010;27(8):511–513. doi: 10.1177/1049909110371096
[8] Macmillan Cancer Support. The Final Injustice: variation in end of life care in England. 2017. Available at: https://www.macmillan.org.uk/_images/MAC16904-end-of-life-policy-report_tcm9-321025.pdf (accessed October 2019)
[9] The Gold Standards Framework. Examples of Good Practice Resource Guide. Just in Case Boxes. 2006. Available at: https://www.goldstandardsframework.org.uk/cd-content/uploads/files/Library%2C%20Tools%20%26%20resources/ExamplesOfGoodPracticeResourceGuideJustInCaseBoxes.pdf (accessed October 2019)
[10] Twycross R, Wilcock A & Howard P. Palliative Care Formulary 6th Ed (PCF6). 2016. Available at: https://about.medicinescomplete.com/publication/palliative-care-formulary (accessed October 2019)
[11] National Palliative and End of Life Care Partnership. Ambitions for palliative and end of life care. 2015. Available at: http://endoflifecareambitions.org.uk/wp-content/uploads/2015/09/Ambitions-for-Palliative-and-End-of-Life-Care.pdf (accessed October 2019)
[12] Gold Standard Framework. Advance Care Planning. 2018. Available at: https://www.goldstandardsframework.org.uk/advance-care-planning (accessed October 2019)
[13] National Institute for Health and Care Excellence (NICE). Care of dying adults in the last days of life. NICE guideline [NG31]. 2015. Available at: https://www.nice.org.uk/guidance/ng31 (accessed October 2019)
[14] Royal Pharmaceutical Society. British National Formulary 76 . London: Pharmaceutical Press; 2001
[15] Edwards Z, Blenkinsopp A, Ziegler L & Bennett MI. How do patients with cancer pain view community pharmacy services? An interview study. Health Soc Care Community 2018;26(4):507–518. doi: 10.1111/hsc.12549
[16] World Health Organization. WHO’s cancer pain ladder for adults. 2019. Available at: https://www.who.int/cancer/palliative/painladder/en/ (accessed October 2019)
[17] National Institute for Health and Care Excellence (NICE). Palliative care for adults: strong opioids for pain relief. NICE guideline [CG140] 2016. Available at: https://www.nice.org.uk/guidance/cg140/ifp/chapter/Managing-side-effects (accessed October 2019)
[18] The British Pain Society. Cancer pain management. 2010. Available at: https://www.britishpainsociety.org/static/uploads/resources/files/book_cancer_pain.pdf (accessed October 2019)
[19] The British Pain Society. Patient publications. Available at: https://www.britishpainsociety.org/british-pain-society-publications/patient-publications/ (accessed October 2019)
[20] Rogers E, Mehta S, Shengelia R, & Carrington Reid M. Four strategies for managing opioid-induced side effects in older adults. Clin Geriatr 2013;21(4). PMID: 25949094
[21] National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Constipation in adults. 2019. Available at: https://cks.nice.org.uk/constipation#!scenarioRecommendation:1 (accessed October 2019)
[22] National Institute for Health and Care Excellence (NICE). Constipation in children and young people: diagnosis and management. Clinical guideline [CG99]. 2017. Available at: https://www.nice.org.uk/guidance/cg99/resources/cg99-constipation-in-children-and-young-people-bristol-stool-chart-2 (accessed October 2019)
[23] NHS. Morphine. 2018. Available at: https://www.nhs.uk/medicines/morphine/# (accessed October 2019)
[24] Cherny N, Ripamonti C, Pereira J et al. Strategies to manage the adverse effects of oral morphine: An evidence-based report. J Clin Oncol 2001;19(9):2542–2554. doi: 10.1200/JCO.2001.19.9.2542
[25] Chand S. Nausea and vomiting in palliative care. Pharm J 2014;292(7799)240. doi: 10.1211/PJ.2014.11135047
[26] National Institute for Health and Care Excellence (NICE). Clinical Knowledge Summary. Palliative care — nausea and vomiting. 2016. Available at: https://cks.nice.org.uk/palliative-care-nausea-and-vomiting (accessed October 2019)
[27] Watson M, Lucas C, Hoy A & Back I. Oxford Handbook of Palliative Care. Oxford University Press; 2005.
[28] National Institute for Health and Care Excellence (NICE). Care of dying adults in the last days of life. Quality standard [QS144]. 2017. Available at: https://www.nice.org.uk/guidance/qs144 (accessed October 2019)
[29] National Institute for Health and Care Excellence (NICE). Medicines guidance: prescribing in palliative care. Available at: https://bnf.nice.org.uk/guidance/prescribing-in-palliative-care.html (accessed October 2019)
[30] National Institute for Health and Care Excellence (NICE). End of life care for adults. 2017. Quality Standard [QS13]. Available at: https://www.nice.org.uk/guidance/qs13 (accessed October 2019)
You might also be interested in…

PJ view: Restore pharmacy opening hours to improve end-of-life care

Controlled drug stock licensing is working against high-quality palliative care for care home patients

How palliative care pharmacists in community practice are improving access to medicines

5 case studies: When is it time for palliative care versus hospice?
Never hesitate to say “I need help” if you’re struggling to cope with the pain and distress of a life-limiting illness. Hospice and palliative care providers are specially trained to hear your plea and will offer comfort, compassion and support.
“Just because you ask to speak with a palliative care or hospice care provider doesn’t mean you have to start service,” says Lisa Wasson, RN, clinical educator for HopeHealth.
Palliative care and hospice care are two different sets of services, although you might hear people use the terms interchangeably.
- Palliative care is for patients with a serious illness who are still receiving curative treatments, such as chemotherapy or dialysis. Palliative care providers offer medical relief from the symptoms or stress caused by either the illness itself or the treatment. They also help patients understand their options and establish goals of care.
- Hospice care is for patients with a life-limiting illness who have decided to stop curative treatments or have been given no further treatment options for cure or to prolong life. A full team of doctors, nurses, social workers, spiritual chaplains, hospice aides, grief support professionals and volunteers offer comfort and support to the patient and family.
To learn more about these differences, read The ABC’s of curative, palliative and hospice care .
5 case studies: Is palliative care or hospice care more appropriate?
Below are five fictional stories to give you a sense of when it could be helpful to ask for a palliative care or hospice care consultation. (Every medical case is unique, and only your health care provider can advise on your care.)
Case 1: An 86-year-old with Alzheimer’s disease is repeatedly hospitalized
Janet was diagnosed with Alzheimer’s disease nine years ago and lives at home in the care of her husband. She cannot make her needs known, is incontinent and depends on her husband to feed her. She has lost 20 pounds in six months and been hospitalized three times.
Palliative care or hospice? Janet would likely qualify for hospice care given how far along her disease has advanced.
Case 2: A man wishes to stop dialysis despite family’s wishes
Robert is 64 years old and has kidney failure, coronary artery disease and diabetes. He receives dialysis three times per week but wants to stop treatment. Today he was hospitalized after skipping two dialysis appointments. Robert’s family is concerned he is giving up, and they don’t know what to do.
Palliative care or hospice? Robert and his family need to get on the same page regarding his options and wishes. A good first step would be to ask a palliative care provider to guide that conversation with skill and sensitivity. Ultimately, Robert does have to the right to stop dialysis and choose hospice if he wishes.
“We deserve as much beauty, care and respect from the health care system at the end of life as we receive at the beginning when we are born” —Lisa Wasson, RN, CHPN
Case 3: A 30-year-old with breast cancer and her mother need support
Imani has undergone two rounds of chemotherapy and radiation for breast cancer. She has severe nausea and is losing weight due to poor appetite. Her mother, who works full time, is her primary caregiver.
Palliative care or hospice? Imani is actively fighting her disease with curative treatment and might qualify for palliative care. She would receive symptom management, support services to help her mother, and a conversation about her goals of care.
Case 4: A woman with autoimmune disorders battles depression
Cindy, age 52, has multiple autoimmune disorders, fibromyalgia pain and depression. She takes antidepressant medication, is self-isolating and cannot hold a job due to taking too many sick days.
Palliative care or hospice? Cindy is not a candidate for either palliative care or hospice care because she does not have a life-limiting disease. She still needs support, though, and would be referred to a case manager or social worker.
Case 5: A man with advanced ALS requests a do-not-resuscitate order
Carter has ALS, or amyotrophic lateral sclerosis, a progressive neurodegenerative disease. He has been hospitalized with infection five times and is on a ventilator. Carter is alert and told doctors he wants to return home and sign a do-not-resuscitate order (DNR). His family is upset about his decision.
Palliative care or hospice? While in the hospital, Carter can request to speak with a palliative care or hospice care provider to guide this sensitive conversation with his family. If he wishes to start hospice, a team will help him return home, tend to life-closure tasks and die in peace and comfort surrounded by his family.
Lisa Wasson hopes more patients and their families will seek to understand the benefits of hospice and palliative care. “We deserve as much beauty, care and respect from the health care system at the end of life as we receive at the beginning when we are born,” she says.
Questions about hospice care or palliative care? Contact us at (844) 671-HOPE or [email protected] .
Privacy overview.
May 14, 2024
Patients Fare Better When They Get Palliative Care Sooner, Not Later
Supportive care is often started late in an illness, but that may not be the best way
By Lydia Denworth

In the last months of my mother’s life, before she went into hospice, she was seen at home by a nurse practitioner who specialized in palliative care. The focus is on improving patients’ quality of life and reducing pain rather than on treating disease. Mom had end-stage Alzheimer’s disease and could no longer communicate. It was a relief to have someone on hand who knew how to read her behavior (she ground her teeth, for instance, a possible sign of pain) for clues as to what she might be experiencing.
I was happy to have the help but wished it had been available earlier. I’m not alone in that. Evidence of the benefits of palliative care continues to grow. For people with advanced illnesses, it helps to control physical symptoms such as pain and shortness of breath. It addresses mental health issues, including depression and anxiety. And it can reduce unnecessary trips to the hospital. But barriers to access persist—especially a lack of providers. As a result, palliative care is too often offered late, when “the opportunity to benefit is limited,” says physician Kate Courtright of the Perelman School of Medicine at the University of Pennsylvania.
In 2021 only an estimated one in 10 people worldwide who needed palliative care received it, according to the World Health Organization. In the U.S., the numbers are better—the great majority of large hospitals include palliative care units—but it’s still hard for people who depend on small local hospitals or live in rural areas. Outpatient palliative care is especially hard to find.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Experts are also working to correct misconceptions. “When people hear the words ‘palliative care,’ they think ‘end-of-life care—I’m going to die,’ ” says physician Helen Senderovich, a palliative care expert at the University of Toronto. Although palliative medicine grew out of the hospice movement, it has evolved into a multidisciplinary specialty encompassing physical, psychological and spiritual needs of patients and their families throughout the trajectory of disease, Senderovich says. That path includes the time when treatments are still being tried.
So palliative care specialists have begun referring broadly to “supportive care”— “anything that is not directly modifying the disease,” says medical oncologist and palliative care specialist David Hui of the MD Anderson Cancer Center. For example, wound care and infusions to improve red blood cell counts in cancer patients are supportive; chemotherapy is not.
Generally, the earlier that supportive care is offered, the more satisfied patients report feeling. And ideally, people who need it now get referred to palliative medicine around the time they are diagnosed with a serious illness. An influential study in 2010 found that patients with lung cancer who received palliative care within eight weeks of diagnosis showed significant improvements in both quality of life and mood compared with patients who got only standard cancer care. Even though those receiving early palliative care had less aggressive care at the end of life, they lived an average of almost three months longer.
More recent studies have confirmed the life-quality advantages of earlier palliative care, although not all studies have shown longer survival. “Patients don’t just start having pain and anxiety and weight loss and tiredness only in the last days of life,” Hui says. Starting palliative care earlier allows patients and the care team to “think ahead and plan a little bit,” he adds.
Nor is palliative care effective only for cancer, although that’s where much of the research has been done. It benefits those with heart failure, chronic kidney disease, dementia, chronic obstructive pulmonary disease (COPD), Parkinson’s, and other serious illnesses.
In January 2024 the Journal of the American Medical Association published a pair of studies that broke “new ground” in developing sustainable, scalable palliative care programs, according to an accompanying editorial. One, the largest-ever randomized trial of palliative care, included more than 24,000 people with COPD, kidney failure and dementia across 11 hospitals in eight states. The researchers made palliative care an automated order, where doctors had to opt out of such care for their patients instead of going through an extra step of opting in. The rate of referrals to palliative care increased from 16.6 to 43.9 percent, says Courtright, lead author of the study. Length of hospital stay did not decline overall, but it did drop by 9.6 percent among those who received palliative care only because of the automated order.
The second study looked at 306 patients with advanced COPD, heart failure or interstitial lung disease. Half these people participated in palliative care via telehealth visits with a nurse to handle symptom management and a social worker to address psychosocial needs; the other people in the study did not get such care. Those who received the calls quickly showed improved quality of life, and the positive effects persisted for months after the calls concluded.
Because there are not enough palliative care providers, Hui advocates for a system that directs them to patients who would benefit most. Usually, and not surprisingly, those are people with the most severe symptoms. This system uses early screening of symptoms to identify these people. Hui calls the approach “timely” palliative care. “In reality, not every patient needs palliative care up front,” Hui says, so timely care uses scarce resources as effectively as possible.
I don’t know exactly when my mother needed to start palliative care, but I hope that going forward more caregivers and more families know to ask about it sooner.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.
- Open access
- Published: 18 May 2024
“Unless someone sees and hears you, how do you know you exist?” Meanings of confidential conversations – a hermeneutic study of the experiences of patients with palliative care needs
- Tove Stenman ORCID: orcid.org/0000-0002-1387-9152 1 ,
- Ylva Rönngren ORCID: orcid.org/0000-0002-0002-7866 1 ,
- Ulla Näppä ORCID: orcid.org/0000-0003-3075-0833 1 &
- Christina Melin-Johansson ORCID: orcid.org/0000-0001-9623-5813 1
BMC Nursing volume 23 , Article number: 336 ( 2024 ) Cite this article
Metrics details
Patients with palliative care needs live with the reality of limited time due to illness or age, eliciting emotional and existential responses. A failure to address their existential needs can lead to significant suffering. A person-centred approach is paramount to effectively address these needs, emphasising holistic care and effective communication. Although existing communication models focus on predefined frameworks, a need exists to explore more spontaneous and confidential conversations between patients and nurses. Confidential conversations have the potential to build therapeutic relationships and provide vital emotional support, highlighting the need for further research and integration into palliative care practice. This study aims to more deeply understand the meaning of confidential conversations for patients with palliative care needs.
In-depth interviews were conducted with 10 patients in the context of specialised palliative care. A hermeneutic analysis was used to gain a deeper understanding of the meanings of the conversations.
The patients had varying experiences and wishes concerning confidential conversations. They strived for self-determination in finding confidants, seeking trust and comfort in their interactions with nurses. Trust was crucial for creating a safe space where patients could express themselves authentically. In shared belonging, confidential conversations with a nurse provided validation and relief from life’s challenges. Experiences of feeling unheard or rejected by a nurse could intensify loneliness, prompting individuals to withdraw and remain silent. Regardless of the motives behind their choices, it was crucial that patients felt respect and validation in their decisions. Their autonomy could thus be recognised, and they felt empowered to make decisions based on their unique preferences.
Conclusions
Patients value trust and understanding, particularly in confidential conversations with nurses, which offer solace, validation and empowerment. However, indifference can increase patients’ suffering, fostering self-doubt and reluctance to engage further. To address this, health care can prioritise empathic communication skills, offer ongoing support to nurses, and promote continuity in care through investment in training and resources. Additionally, adopting a person-centred approach in confidential conversations is crucial, considering patients’ varying preferences.
Peer Review reports
Patients with palliative care needs live with the awareness that time is limited due to illness or advanced age [ 1 ]. Living with the uncertainty of life’s duration may evoke a range of reactions, emotions, and existential thoughts [ 2 ]. Death is difficult to come to terms with, and if a person cannot accept the reality of mortality, a risk of existential suffering arises [ 3 ]. Patients employ diverse strategies to handle their forthcoming death [ 2 ], one of which involves engaging in conversations with family, friends, and healthcare providers [ 1 , 2 ]. Conversations based on the individual patient’s specific needs, wishes, abilities, and conditions may be healing and even therapeutic [ 4 ]. Research indicates that engaging in conversations to express thoughts and emotions could benefit older people’s well-being [ 5 ]. Patients with palliative care needs strive to live a meaningful life. Focusing on living requires support from the healthcare system, including healthcare professionals, the environment, and the organisation of palliative care [ 6 ].
A person-centred approach is essential for addressing patients’ individual needs and goals. Essentially, person-centeredness embodies an ethical stance guiding both patients and professionals toward fostering healthful relationships within health care [ 7 ]. Palliative care philosophy is by nature person-centred and emphasises a holistic approach to the person and the goals of the hospice philosophy. This holistic approach addresses physical, psychological, social, and existential suffering and well-being [ 1 ]. A central approach involves communication and interaction between patients and nurses, grounded in patients’ beliefs, needs, stories, thoughts and feelings [ 8 , 9 ]. A person-centred approach may ensure holistic care by nurses to patients with palliative care needs [ 10 ]. Conversation between patients and nurses is anything but superficial; it is complex, effective, and confidential, offering important potential for interaction and emotional support [ 11 ]. Spontaneous and natural conversations are rarely described as they occur alongside other care activities, their apparent simplicity rendering them easily overlooked and invisible [ 12 , 13 ], however, they have potential and a unique opportunity to take advantage of support for patients with palliative care needs [ 12 ]. Patients with palliative care needs report receiving insufficient emotional and existential support [ 14 , 15 , 16 , 17 ]. This lack of support is associated with higher psychological stress and lower well-being [ 14 , 17 , 18 ].
In conversations, the nurse can support the individual patient’s specific needs of alleviation, and conversations are thus key within the fundamental framework of palliative care [ 1 ]. Conversations in palliative care that involve healthcare professionals are described as palliative care communication [ 19 ], advanced care planning [ 20 ], serious illness conversations [ 21 ] and existential conversations [ 22 ]. These different models of communication are not separate but can flow into each other, effectively meeting patients’ and relatives’ needs and preferences. Open and honest information, empathy and dedicated healthcare professionals contribute to effective communication. Open and honest communication may also arouse patients’ anxiety, stress and existential concerns [ 23 ].
Common to the conversations described is that either they are initiated by healthcare professionals and aim to exchange or obtain information or they have a predetermined purpose or content. Some communication models primarily focus on physicians and do not include the valuable communication skills that nurses possess. Therefore, further research is needed on spontaneous, naturally occurring communication by nurses in palliative care [ 23 ]. It is indicated that in a confidential conversation with a nurse, the atmosphere can be perceived as natural and spontaneous. Here, the patient can confide in the nurse about their wishes and thoughts. These interactions could facilitate the development of therapeutic relationships, allowing patients to express their thoughts, regardless of what they could be and gain support in their situation [ 24 ].
Confidential conversations and their content in the context of palliative care are under development as a research area and are further explored and developed in this study, grounded in patients’ perspectives and experiences. Complementary to other communication approaches, confidential conversations may be relevant to address patients’ emotional and existential concerns where support may be lacking. To enhance and expand communication as a fundamental aspect of palliative care, focusing on the significance of confidential conversations is crucial. Furthermore, this study intends to deepen the knowledge of the approaches that patients use in confidential conversations with nurses in the context of palliative care.
To more deeply understand the meanings of confidential conversations for patients with palliative care needs.
To develop a deeper understanding, a qualitative hermeneutic design inspired by Geanello’s [ 25 ] method was used. The analysis brings into the study Ricoeur’s theory of distanciation as part of the hermeneutic philosophy of understanding. Ricoeur’s hermeneutic theory aligns with the philosophical foundations of interpretive research and focuses on the relationship between ontology (the interpreter) and epistemology (interpretation). It allows researchers to use hermeneutic approaches to textual analysis, which is essential for understanding complex human experiences in the context of nursing [ 25 ].
Setting and participants
The setting for the study was palliative care units in a sparsely populated region in Northern Sweden, comprising four counties with a total of approximately 900,000 inhabitants [ 26 ]. The catchment area included two hospices, one hospital ward with round-the-clock care, and nine home health teams providing specialist palliative care [ 27 ].
Four specialist palliative care units providing care at home or in hospice participated One facility was excluded due to long travel distances and short treatment times, i.e. the enrolled patients were seriously affected by their illnesses. The patients received verbal information about the study from a unit manager, and the research group was notified of the patients´ contact details after their consent. Patients over 18 years old, who understood the meaning of participation and could participate in an interview of around 30 min could be included. A total of 19 patients were purposively sampled, and nine were excluded due to rapid deterioration, of whom three died. A total of 10 patients participated, six women and four men, aged 56–85 years (m 70) with advanced cancer. Nine were cared for in their homes by specialist palliative care teams, and one was cared for in a hospice. The performance status of the patients was 2.5 on the Eastern Cooperative Oncology Group Scale of Performance Status (ECOG PS). This indicates that the patients were confined to a bed or chair for more than 50% of their waking hours. The ECOG PS describes a patient’s level of functioning in daily life from 0 to 5, where 0 is fully functional and 5 is death [ 28 ].
Data collection
To enhance the research comprehension and generate novel insights, the research group conscientiously reflected on their positionalities and reflexivity both before and during the data collection and analysis. All researchers were registered nurses with extensive professional experience in fields where interpersonal conversations hold significant importance, including palliative care and psychiatric care. Recognising and acknowledging one’s pre-existing understandings is crucial, because it ensures that the subject is approached with appropriate depth and openness to novel perspectives. Awareness of one’s pre-understanding is important, giving the subject its proper dimensions and new perspectives [ 29 ].
Data were collected from November 2022 to February 2023 using qualitative interviews and demographic information questions (Supplementary File 1 ). The interviews were conducted by TS and YR with the support of an in-depth interview guide that contained open and follow-up questions to encourage the participants to reflect and deepen their thoughts [ 30 ]. Nine patients were interviewed face-to-face, and one was interviewed by telephone. The interviews began with a brief introduction of the interviewer and verbal information about the study, including that participation was voluntary. The interview prompts included: ‘Please, tell me about an occasion when you felt you had a confidential conversation with a nurse’. Follow-up questions and prompts were used, such as: ‘Can you elaborate?’ If they had not had a confidential conversation with a nurse, the follow-up question was whether they could speak more about that.
The interviews lasted between 22 and 77 min (m 36 min) and were digitally recorded. The visits at the patients’ residences lasted between one and three hours. To ensure reliability and dependability, the interviews were transcribed verbatim. The data were stored on a password-protected server at Mid Sweden University.
Data interpretation
The analysis was based on Ricouer’s method with distinction: explanation (content) and understanding (meaning). In the transition from speech to written text, the dialogue is made into writing, where meaning becomes more important than the words and allows for deeper interpretation. The text becomes autonomous and open to interpretation, overcoming the limitations of face-to-face dialogue [ 25 ].
In the first step, the interviews were transcribed and the text was organised. Repeated naïve reading initiated a preliminary interpretation, and new questions were raised and asked about the text. From part to whole, and from whole to part, an understanding crystallised. The hermeneutic circle characterizes this process. Returning to the data, the whole and the pre-understanding merged. Finally, a critical discussion of the themes was based on the pre-understanding of the research group. The analysis gave us a new understanding through the explanations of the text, and our horizons merged and expanded. Table 1 shows examples of the analysis process.
Ethical considerations
Ethical approval for the study was obtained from the Ethical Review Authority in Sweden (Dnr 2021–04066 and 2022-03769-02). Ethical considerations followed the research rules presented in the Declaration of Helsinki [ 31 ].
Even though patients with palliative care needs are in a vulnerable situation, they must be invited to participate in research. Ethical considerations are particularly important when collecting data because prognosis, energy and ability are considered, with flexibility for individual needs. A sensitive approach characterised by empathy was necessary for inclusion, but it also considered the patient’s self-determination [ 32 , 33 ].
Written consent was collected from operations managers, and written and oral consent was collected from the patients. They were informed that their participation was voluntary and that they could drop out of the study without explanation. The researchers performing the interviews had no professional relationship with the participants. The participants’ identities were coded, and transcribed material was stored in a locked cabinet. The unit manager would be contacted if the patients wanted support due to strong emotions during the interview.
The patients had varying experiences and requirements concerning confidential conversations. Some expressed a strong desire to talk and verbalise their thoughts, whereas others preferred to refrain from sharing their innermost thoughts with nurses. For some, remaining silent was their method of handling intense emotions, whereas others did not feel confident enough to disclose themselves in confidential conversations with a nurse. Regardless of the motives behind their choices, it was crucial that patients felt respect and validation in their decisions. Their autonomy could thus be recognised, and they felt empowered to make decisions based on their unique preferences.
In the analysis, three themes and seven subthemes emerged, All themes were interconnected and are presented in Table 2 .
Being self-determinant in finding appropriate confidants
In the confidential conversations, patients felt vulnerability and apprehension when expressing their deepest thoughts and emotions. Such revelations required a foundation of trust, leading patients to carefully select whom they confided in. They adeptly navigated various support structures and relationships to find the right confidant, whether seeking professional assistance or turning to trusted relatives or friends. This decision reflected a profound awareness of their need for trust and understanding.
To choose an appropriate dialogue partner
The patients highlighted the pivotal role of interpersonal skills by expressing an awareness of nurses’ communication abilities. They showed deep sensitivity to the nuances of verbal communication competence and demonstrated a genuine empathy for the challenges that nurses might face in engaging in confidential conversations. This had implications for the choice of confidant. One patient expressed this sentiment, saying: “…some nurses couldn’t talk… I noticed it right away… and I felt like this; I knew there were other nurses, so it didn’t matter.” (patient no. 207).
The patients perceived that some nurses were not feasible as dialogue partners due to their heavy workload. Their understanding extended beyond mere recognition of workload; they empathised with the nurses’ demanding work and the complexities of their roles. They accepted and respected the limitations that nurses faced. These encompassed factors beyond a heavy workload to include resources and time constraints, which could lead to emotional and psychological demands. The patients understood that these constraints did not indicate a lack of willingness to provide support. One patient said: “I find myself thinking, ‘Should I do this? Should I… maybe I shouldn’t… ask about this,’ especially when I sense the stress around me… I can save it for another time.” (patient no. 204).
The patients also did not expect the nurses to fulfil all their conversational needs. They recognised the broader context in which nurses operate. They acknowledged that nurses had multiple responsibilities, and they had a deep understanding of them being a part of a larger healthcare team with diverse responsibilities. This understanding reflected empathy towards the challenges that nurses faced and a realistic perspective of the healthcare system’s complexity.
In addition to formal care settings, patients sought support from personal networks outside the healthcare system. They leaned on family members, close friends and other professionals for alternative forms of support and confidential conversations. Within these networks, patients found the support they sought, underscoring their deliberate choice to seek assistance from sources they apprehended as capable of fostering meaningful and supportive interactions. This conscious decision underscored their commitment to prioritising relationships that could facilitate understanding and empathy.
To seek trust in interpersonal relations
The patients expressed that they sought special trust and trustworthiness in their confidant and that it required some form of relationship. They exhibited autonomy when considering issues that resonated with their unique experiences and needs. Trust played a central role, fostering a sense of security and comfort in sharing their innermost thoughts and emotions. One patient argued that:
Yes, maybe it could be that the more often you meet the same person, that that’s what’s important, that you get to meet the same person… yes, I could talk to them… then we talked about children and all sorts of things … But just that, I think that it’s important that you get to have … not have so many different people around you, then you get that feeling of trust. (patient no. 206)
Establishing trust within interpersonal relationships with nurses was pivotal for selecting a confidant, whether gradually developed or established in a single encounter. Furthermore, the initial interaction with a nurse significantly shaped the patient’s perception of trust, indicating that trust could be established in the immediacy of the encounter. Deepening trust within interpersonal relationships not only facilitated the selection of a confidant but also created an empowering atmosphere where patients felt comfortable having confidential conversations. This emphasised the profound impact of trust in interactions, as one patient confirmed:
I trust everyone who comes, but it’s difficult for me to open and talk freely… However, it is possible to talk… if I want to… I can talk to everyone who gets here. It’s reassuring when they’re [the nurses] attentive, but I don’t always feel the need to talk. However, I do feel comfortable talking with anyone in the staff. (patient no. 203)
Patients desired nurses to be attentive and available, ready to engage in confidential conversations when the patients felt comfortable. Creating a supportive environment and a solid relationship where patients felt empowered to express themselves authentically without fear of judgment or coercion was essential.
To preserve integrity
The intricate relationship between patients’ integrity and their willingness to share intimate thoughts and emotions was highlighted. Some reluctance was expressed to talk about personal feelings; exposing such vulnerable aspects of themselves felt unnecessary and even contrary to their sense of self. This sentiment was captured by one patient who had never before opened up to an outsider about deeply personal matters: “I think… I’ve never talked… with an outsider about personal things, that is, deeply personal things. I’ve never talked to anyone about it… Never. I don’t need it…” (patient no. 208).
Patients found vocalising personal issues overwhelming or unnecessary at times. Their reluctance to engage in conversation did not necessarily signify avoiding confrontation of their situation or rejecting support from nurses. Instead, it served as a protective barrier, allowing patients to maintain a sense of control and integrity amid vulnerability. It could also mean that they desired to be in solitude with their thoughts, which served as a means of preserving personal integrity. It provided a space for introspection and emotional processing.
Respecting the patients’ decisions regarding the initiation of confidential conversations was crucial. Choosing not to engage did not indicate a lack of need for support or understanding; rather, it reflected their preferences for navigating and processing their experiences while preserving their integrity.
Being in shared belonging
Patients found solace and validation in confidential conversations with nurses. The patients felt seen, understood and empowered by the nurses, which led them to express themselves authentically. These interactions offered relief from the challenges of illness and fostered emotional support, highlighting the importance of trust and genuine connection in relationships.
To find confirmation
The patients experienced a profound sense of confirmation in the confidential conversation and relationship with the nurse. The patients’ existence and experiences were not only acknowledged but also validated. In the confidential conversations, patients felt truly seen and understood as they articulated their innermost thoughts and emotions. This validation enhanced their sense of worth, reinforcing the belief that their voices mattered, as one patient stated: “So, it felt like… it felt like she [the nurse] thought it was important in some way, what I had to say” (patient no. 206).
Central to the success of these conversations was how nurses responded, and this success played a critical role in nurturing and maintaining patient–nurse relationships. The feeling of being confirmed and validated in the confidential conversation was strengthened by being met with genuine curiosity and openness from the nurse. One patient expressed it as:
They might have been running around, busy as could be, but still found a few minutes to spare for a chat… maybe just 2–3 min, but those brief moments meant the world to me. It was like, ‘Oh, how comforting, they made time for me.’ It was a tangible reminder of their presence. (patient no. 202)
This created an environment where patients felt comfortable and encouraged to authentically share their thoughts and feelings. By feeling validated and sensing genuine interest in their well-being, a sense of trust and connection was established, allowing meaningful and honest dialogue to develop naturally. Crucially, patients felt confirmation across the entire spectrum of emotions and subjects, unrestricted by judgment or devaluation. They found solace and affirmation in discussing even the most challenging topics, knowing that no subject was deemed too daunting or uncomfortable. As one patient expressed, “…when I share my innermost thoughts, however silly or ridiculous they may seem at times… to express them to someone, it holds significant meaning, allowing me to unburden myself…” (patient no. 208). This highlighted the transformative power of affirmation within the context of confidential conversations.
To find respite in the moment
Engaging in trusting conversations with a nurse went beyond simple dialogue; it provided patients with a break from the challenges of illness and forthcoming death. Within these conversations, patients found a space where they were seen as complete individuals with their hopes, fears and dreams, rather than just being defined by their medical conditions. This respite was not transient; it was a sanctuary where they felt understood and accepted, shielding them from the existential uncertainties such as fears related to death, loss of control and sorrow that often accompany serious illness. The patients felt empowered to share their innermost thoughts and feelings without fear of being judged or criticised, in the presence of trusted nurses. This allowed them to express themselves authentically, fostering a sense of empowerment. This was explained by one patient:
A nurse who stayed with me during a difficult conversation, even as I stood there, tears streaming down my face [cries] while discussing my illness. She simply stood there and stood and stood… listening attentively, unwavering. It was an incredible moment for me, a sense of relief washing over me, as if to say, ‘Now I can handle this [breathes out], I can manage.’ (patient no. 205).
Additionally, moments of shared laughter and joy provided patients with brief yet significant relief from their vulnerable situation. These confidential conversations became profound acts of validation and existential affirmation, offering a break and emotional support. The impact of such conversations is aptly captured in the following quote:
Yes, having someone who can listen and share a bit of the burden with you is truly comforting. It’s reminiscent of the care you received as a child when a mother figure would step in during tough times. It’s incredibly reassuring. (patient no. 209)
This sentiment underscores the profound comfort and reassurance that patients derive from these trusting interactions.
Being in-between
Being rejected when feelings and thoughts were expressed and the patient was vulnerable increased the feeling of loneliness. Opting not to start a confidential conversation following such experiences was not merely about avoiding discomfort but also a way to protect themselves. This meant trying to handle the complex feeling of wanting to have a confidential conversation but at the same time not being listened to or understood, a feeling of being in-between. This inner conflict discouraged patients from revealing themselves in confidential conversations with a nurse.
To feel rejected and lonely
Patients recounted situations where their attempts to communicate with nurses were met with indifference or dismissive remarks, which led to feelings of rejection and loneliness. These encounters left them with a sense of isolation and alienation as they struggled to find validation and understanding in their time of need. The feeling of being rejected was grounded in not feeling seen or listened to when they needed to talk, explained by one patient: “…I can’t expect every nurse to share my perspective on life or work, to come to me with enthusiasm. It’s just something you sense… It’s almost heart-breaking… if you need to talk to someone and then you’re… rejected.” (patient no. 202).
The patients felt neglected, which could lead to increased suffering when the nurse did not continue the conversation or they were met with uninterest. The absence of meaningful dialogue in these moments had significant existential implications, prompting patients to question their existence and purpose. They felt unheard and their needs unmet without acknowledgement and validation from the nurses.
These experiences of rejection and neglect could induce feelings of shame and guilt for burdening others with their difficulties. Despite their longing for connection and support, patients felt compelled to step back because they considered themselves burdensome rather than deserving of care and attention. One patient put it like this:
Yes… but I’ve encountered… well, they are nurses too, some who can be a bit snarky. Or who perhaps speaks a little too loudly. So, you notice these things, you notice them… and then I wonder… Is it because what I’m sharing is too heavy or not? (patient no. 204)
These encounters with indifference and dismissal not only left patients feeling rejected and lonely but also challenged their sense of self-worth. Beyond the absence of dialogue, it was a feeling of being unseen and unheard precisely when they needed acknowledgement the most. One patient said: “Unless someone sees you and hears you, how do you know you exist and why should you exist at all?” (patient no. 205).
To become silent if no one is listening
The experience of feeling rejected or neglected could deter the patient from attempting to initiate conversation again. Remaining silent after feeling silenced extended beyond a mere momentary response; it signalled a reluctance to seek help or a loss of confidence in the nurses’ ability to comprehend their needs. This loss of confidence also led patients to question the validity of their experiences and needs, fostering feelings of self-doubt and insecurity:
…Because it’s painful, you know, when you find yourself in situations like this, it’s like you start questioning yourself, feeling a bit unsure. How much can I ask for? Do I dare to speak up, or am I bothering? …But even then, you still can’t help to feel a bit hesitant, thinking, ‘Should I say this?’ (patient no. 204).
Maintaining silence was expressed as a form of self-preservation in vulnerable circumstances. Patients struggled with internal conflict, yearning to express themselves while simultaneously feeling unheard and unacknowledged. This conflict stemmed from a desire to address difficulties while safeguarding their vulnerability. This realisation highlighted a subtle yet profound disconnection as patients perceived the nurse’s lack of acknowledgement or recognition. Consequently, they hesitated to engage further in conversations, fearing continued neglect despite their escalating needs and suffering. This hesitation eroded the trust placed in the nurse, potentially deepening the detachment in the patient–nurse relationship. Such feelings could dissuade patients from seeking further dialogue. The following quote encapsulates the feeling of being dismissed:
Because… if I show… if I put my hand out and say, ‘I think it’s difficult today’… I feel so damn bad, and then [the nurse] says, ‘Well, what a shame,’ and then they leave… then I shut up. (patient no. 202)
Feeling rejected or neglected could discourage patients from initiating further conversation and cause them to remain silent. This reluctance reflected a loss of confidence in the nurse’s ability to understand their needs and led to feelings of self-doubt and insecurity.
This study aimed to more deeply understand the meanings of confidential conversation for patients with palliative care needs, an area of limited research. The findings underscore the importance of patient autonomy in selecting dialogue partners and shaping conversation dynamics. The patients strategically navigated support networks to find suitable confidants within and beyond healthcare settings.
It is indicated that confidential conversations, from a nursing perspective, occur at the patient’s initiative, often spontaneously, and with unforeseen content [ 24 ] and thus should be centred around the patient´s needs and preferences [ 34 ]. To adopt a person-centred approach, the patient must be acknowledged, invited and involved [ 34 , 35 ]. Patients are allowed to express their thoughts and concerns to a healthcare professional who actively listens and validates their experiences [ 34 ].
When some patients in our study wanted to talk, they actively chose who they would talk to, whether it was a family member, a friend, or someone on the healthcare staff. While some patients might not have considered nurses as their preferred conversational partners, for others, they were indispensable. This preference could evolve depending on the topic and situation [ 36 ]. Therefore, nurses and other health care professionals need to remain receptive and mindful of the ongoing, intricate and context-dependent nature of such interactions [ 23 , 36 ].
The process of choosing which nurse to talk to involves considering trust and confidence. Patients value trust in their relationships with nurses, regardless of the duration of their acquaintance. Studies by Ikander [ 37 ] emphasise the importance of establishing a relationship with nurses, and continuity of care, as highlighted by Engel [ 23 ], can facilitate conversations raised when living with the awareness that time is limited due to illness or advanced age.
In our study, patients viewed confidential conversations with nurses as valuable respites. When they engaged with attentive nurses, they felt validated and experienced relief. Participants emphasised the importance of mutual sharing during these interactions. Feeling valued and autonomous can be healing, fostering a return to one’s former self [ 38 ]. An authentic meeting reflects the patient’s human worth [ 39 ], aligning with a person-centred approach [ 7 ]. Patients noted various responses indicating interest and effort from nurses. Seemingly insignificant, small nursing actions can profoundly impact the patient’s well-being and sense of connection [ 40 ]. When nurses showed interest, patients felt validated and met with compassion. Establishing a compassionate relationship facilitates communication with patients facing life-threatening illnesses [ 41 , 42 ]. This caring relationship encompasses respect for patients’ autonomy, dignity and individual needs [ 38 ].
The nurse’s openness to the patient’s fragility and suffering may be a result of the ontological understanding of life. The encounter with suffering entails an ethical demand on the nurse, and this is an awareness and a call to relate to the basis of influence we have on each other [ 43 ]. By cultivating compassion as the cornerstone of care, nurses can create spaces of safety, trust and meaningful connection [ 40 ] for patients nearing the end of life. In the meeting, the nurse can recognise and honour the individual’s wholeness with dignity, to imagine them in a state of well-being and their wishes and desires [ 8 , 9 , 40 ]. The sense of being acknowledged and validated in confidential conversations serves as a vital form of support, offering respite and confirmation.
However, acknowledging the complexities of communication dynamics within these contexts is essential. Not all nurses may feel adequately equipped for or comfortable in such discussions [ 44 ]. Our study revealed that some patients experienced nurses who hesitated to engage in confidential conversations. The reluctance of some nurses to broach these sensitive topics may stem from various factors, including personal discomfort, lack of training or experience, or fear of causing emotional distress to the patient [ 34 ]. Rattner [ 45 ] investigated nurses’ feelings concerning intractable “nonphysical suffering” (emotional, psychological, spiritual and existential). The fact that they could not alleviate patients’ nonphysical suffering was difficult to deal with, and one solution was to ignore them instead. According to Rattner [ 46 ], despite the discomfort of being unable to help, healthcare professionals must dare to be present and validate the patient’s experiences. Otherwise, we close the door and suffering goes unspoken. In confidential conversations, nurses can affirm and support patients with courage, presence and time. However, factors such as understaffing and systemic barriers may hinder them from dedicating sufficient time, leading to feelings of inadequacy and moral distress [ 47 ]. Nevertheless, healthcare institutions must address these challenges.
In our study, patients who expected attentive listening and support from nurses but found these expectations unmet reported feeling disappointment and loneliness. Mirroring our findings, Tarbi et al. [ 38 ] highlighted how the absence of nurse connection can lead to feelings of rejection and isolation, contributing to existential loneliness. Moreover, limited healthcare support may hinder patients in addressing existential challenges, potentially leaving them feeling undervalued [ 39 ]. Arman et al. [ 48 ] suggested that a care relationship resulting in patient rejection and silence can increase existential suffering.
Neglect and indifference to patient needs, as described by Engel et al. [ 23 ], may increase feelings of guilt and shame among patients, rendering them vulnerable, as confirmed by previous studies [ 39 , 48 , 49 ]. Consequently, patients in our study may withdraw from interactions with nurses and remain silent. Regardless of its origin, unsatisfactory care prompts ethical consideration by healthcare personnel, touching on the right to autonomy [ 50 ].
Rattner [ 45 ] emphasised the importance of understanding that when patients do not talk, it does not mean that they do not want to talk. Since we do not know the reason why the patient does not want to talk, we can, with a person-centred approach, ensure that the opportunity for conversation is created. Tornöe et al. [ 51 ] suggested that nurses’ willingness to be present and cultivate silence can embolden them to remain engaged in conversations, encouraging patients to open up and find a moment of respite. By knowing this and through active listening, nurses can identify patient needs to minimise the risk of leaving them in existential loneliness. The patients in our study chose not to talk even if it could increase their suffering.
We discovered various reasons why a patient may choose not to engage in conversation. Apart from feeling unheard, this reluctance could stem from a lack of necessity to talk. Some patients chose not to talk as a means of introspection and self-preservation, finding solace in their thoughts and feelings. This choice may have stemmed from a reluctance to verbalise deeply personal matters or a desire to maintain control over their vulnerability [ 52 ]. Respecting patients’ decisions regarding communication was crucial in these instances, as part of a person-centred approach [ 10 ]. The realisation of limited time and the uncertainty of when death would occur led patients to attempt to navigate the situation through different strategies. Not talking could be a way of handling the difficulty [ 2 , 38 ]. Folkman et al. [ 53 ] noted that various forms of distraction and avoidance were ways of handling one’s situation. Distraction could be effective in dealing with particularly intense emotions and help reduce distress; however, avoiding thoughts and feelings associated with an event may risk increasing an individual’s anxiety over time [ 53 ]. With this understanding, nurses can recognise that patients handle their situations differently, with some preferring not to engage in conversation. By prioritising person-centred care, nurses can approach each patient individually, without imposing expectations, and embrace the diversity in their responses. By remaining emotionally and existentially attuned, nurses can acknowledge and validate the patient’s need for conversation and support.
The patients in our study spoke about their experiences of suffering when they were not treated as a whole person or their support needs were not met. Nurses can thus relieve suffering just by their presence and compassion, and confidential conversation can be one method. Nurses being open and responsive to patients’ ethical demands could be part of good care [ 40 ]. By actively listening, nurses can identify patients’ needs, preferences, fears and pains. Placing the patient at the forefront and ensuring they are treated with dignity and respect lays a foundation for person-centred care [ 34 ].
Limitations and methodological considerations
In our study’s methodology, we acknowledge the potential influence of the interview questions on patient responses. Despite efforts to design open-ended questions, certain prompts may inadvertently shape answers, potentially biasing the collected data.
During interviews, we maintained a reflective stance, continuously examining assumptions to minimise misinterpretations. Participants were encouraged to guide discussions and freely express their experiences in a supportive environment, facilitated by active listening techniques [ 54 ].
Including dying patients in research was crucial for evidence-based care and understanding their perspectives [ 32 , 33 ]. Challenges arose due to illness progression, leading to omission in some cases. Despite sample size limitations, the participants had profound experiences, enabling in-depth analysis.
In the analysis, we were vigilant about potential biases. The researchers independently coded transcripts and discussed interpretations to minimise individual interpretations. Seeking alternative perspectives enriched our understanding. Despite our inevitable perspectives, we prioritised methodological rigour. Through reflexivity, open-ended discussions and rigorous analysis, we aimed for valid and reliable findings.
We faced difficulties asking about existential support because participants found it hard to understand and relate to their experiences. After two interviews, we omitted the question from subsequent interviews. Instead, we focused conversations on exploring the diverse range of experiences that participants had. This approach allowed us to capture the richness and complexity of their interactions and perceptions.
The patients with palliative care needs in our study had different preferences and wishes regarding confidential conversations. Confidential conversations with nurses can offer patients solace, validation and empowerment and serve as an act of validation and existential affirmation, offering comfort amid vulnerability. Patients, discerning in their choice of confidants, prioritise trust and understanding in their relationships. Respecting their autonomy in initiating confidential conversations is essential, acknowledging their individual preferences and the need for personal integrity.
Nurses hold a crucial role in empowering patients to voice their concerns and preferences, especially during confidential conversations. Trustworthiness, familiarity and continuity are essential because patients rely on nurses to be attentive and accessible. Healthcare institutions and universities must invest in comprehensive training and resources to equip nurses with the necessary skills for confidential communication. Offering continuous support, including supervision and opportunities for reflection, enables nurses to evaluate their approach and avoid unintentionally contributing to patients’ feelings of rejection or isolation. Through a person-centred approach, patients’ unique preferences and the importance of maintaining personal integrity can be acknowledged and honoured – regardless of whether, how and when they want to have a confidential conversation.
Data availability
The datasets used and analysed during the current study are available from the corresponding author under the prerequisite that no sensitive, personal, or confidential data is revealed.
Abbreviations
World Health Organization (WHO). Palliative care – the essential facts. WHO: Geneva; 2020. https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/palliative-care/palliative-care-essential-facts.pdf?sfvrsn=c5fed6dc_1 .
Google Scholar
Werkander Harstäde C, Sandgren A. Confronting the forthcoming death: a classic grounded theory. J Palliat Care Med. 2016;6(6):1–7. https://doi.org/10.4172/2165-7386.1000289 .
Article Google Scholar
Yalom ID. Existential psychotherapy. London, England: Basic Books; 1980.
Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. https://doi.org/10.1016/j.pec.2008.11.015 .
Article PubMed Google Scholar
Tjernberg J, Bökberg C. Older persons’ thoughts about death and dying and their experiences of care in end-of-life: a qualitative study. BMC Nurs. 2020;19(1). https://doi.org/10.1186/s12912-020-00514-x .
Sandsdalen T, Hov R, Høye S, Rystedt I, Wilde-Larsson B. Patients’ preferences in palliative care: a systematic mixed studies review. Palliat Med. 2015;29(5):399–419. https://doi.org/10.1177/0269216314557882 .
Dewing J, McCormack B. Editorial: tell me, how do you define person-centredness? J Clin Nurs. 2017;26(17–18):2509–10. https://doi.org/10.1111/jocn.13681 .
Ternestedt B-M, Andershed B, Eriksson M, Johansson I. A good death: development of a nursing model of care. J Hosp Palliat Nurs. 2002;4(3):153–60. https://doi.org/10.1097/00129191-200207000-00015 .
Österlind J, Henoch I. The 6S-model for person‐centred palliative care: a theoretical framework. Nurs Philos. 2021;22(2). https://doi.org/10.1111/nup.12334 .
Abbaspour H, Heydari A. Concept analysis of end-of-life care. J Caring Sci. 2022. https://doi.org/10.34172/jcs.2022.037 .
Macdonald LM. Expertise in everyday nurse–patient conversations. Glob Qual Nurs Res. 2016;3(0). https://doi.org/10.1177/2333393616643201 .
Moran S, Bailey M, Doody O. An integrative review to identify how nurses practicing in inpatient specialist palliative care units uphold the values of nursing. BMC Palliat Care. 2021;20(1). https://doi.org/10.1186/s12904-021-00810-6 .
Sekse RJT, Hunskår I, Ellingsen S. The nurse’s role in palliative care: a qualitative meta-synthesis. J Clin Nurs. 2018;27(1–2):e21–38. https://doi.org/10.1111/jocn.13912 .
Wang T, Molassiotis A, Chung BPM, Tan J-Y. Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care. 2018;17(1). https://doi.org/10.1186/s12904-018-0346-9 .
Singer AE, Goebel JR, Kim YS, Dy SM, Ahluwalia SC, Clifford M, et al. Populations and interventions for palliative and end-of-life care: a systematic review. J Palliat Med. 2016;19(9):995–1008. https://doi.org/10.1089/jpm.2015.0367 .
Article PubMed PubMed Central Google Scholar
Van Lancker A, Van Hecke A, Verhaeghe S, Mattheeuws M, Beeckman D. A comparison of symptoms in older hospitalised cancer and non-cancer patients in need of palliative care: a secondary analysis of two cross-sectional studies. BMC Geriatr. 2018;18(1). https://doi.org/10.1186/s12877-018-0721-7 .
Hart NH, Crawford-Williams F, Crichton M, Yee J, Smith TJ, Koczwara B, et al. Unmet supportive care needs of people with advanced cancer and their caregivers: a systematic scoping review. Crit Rev Oncol Hematol. 2022;176:103728. https://doi.org/10.1016/j.critrevonc.2022.103728 .
Heus E, Zwan JM, Husson O, Frissen AR, Herpen CML, Merkx MAW, et al. Unmet supportive care needs of patients with rare cancer: a systematic review. Eur J Cancer Care. 2021;30(6). https://doi.org/10.1111/ecc.13502 .
Bigger SE, Zanville N, Wittenberg E, Towsley G, Glenn L. Palliative care communication among home health interprofessional staff: a randomized controlled trial of feasibility, acceptability, and preliminary effectiveness. Am J Hosp Palliat Care. 2024;41(2):203–10. https://doi.org/10.1177/10499091231165013 .
Fahner JC, Beunders AJM, Van Der Heide A, Rietjens JAC, Vanderschuren MM, Van Delden JJM, et al. Interventions guiding advance care planning conversations: a systematic review. J Am Med Dir Assoc. 2019;20(3):227–48. https://doi.org/10.1016/j.jamda.2018.09.014 .
Bernacki R, Hutchings M, Vick J, Smith G, Paladino J, Lipsitz S, et al. Development of the Serious Illness Care Program: a randomised controlled trial of a palliative care communication intervention. BMJ Open. 2015;5(10):e009032. https://doi.org/10.1136/bmjopen-2015-009032 .
Strang S, Henoch I, Danielson E, Browall M, Melin-Johansson C. Communication about existential issues with patients close to death – nurses’ reflections on content, process and meaning. Psychooncology. 2014;23(5):562–8. https://doi.org/10.1002/pon.3456 .
Engel M, Kars MC, Teunissen SCCM, Van Der Heide A. Effective communication in palliative care from the perspectives of patients and relatives: a systematic review. Palliat Support Care. 2023;21(5):890–913. https://doi.org/10.1017/S1478951523001165 .
Stenman T, Näppä U, Rönngren Y, Melin-Johansson C. Daring to deal with the difficult and unexpected: registered nurses’ confidential conversations with patients with palliative care needs: a qualitative interview study. BMC Palliat Care. 2023;22(1). https://doi.org/10.1186/s12904-023-01228-y .
Geanellos R. Exploring Ricoeur’s hermeneutic theory of interpretation as a method of analysing research texts. Nurs Inq. 2000;7(2):112–9. https://doi.org/10.1046/j.1440-1800.2000.00062.x .
Article CAS PubMed Google Scholar
Statistics Sweden. Folkmängd i riket, län och kommuner 31 December 2021. Accessed April 16. 2024. https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning/befolkningens-sammansattning/befolkningsstatistik/pong/tabell-och-diagram/helarsstatistik--kommun-lan-och-riket/folkmangd-i-riket-lan-och-kommuner-31-december-2021-och-befolkningsforandringar-2021/2021 .
Nationella rådet för palliativ vård (NRPV). Palliativguiden. 2022. Accessed April 16, 2024. https://www.nrpv.se/palliativguiden/ .
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–56.
Nystrom M, Dahlberg K. Pre-understanding and openness – a relationship without hope? Scand J Caring Sci. 2001;15(4):339–46. https://doi.org/10.1046/j.1471-6712.2001.00043.x .
Kvale S, Brinkmann S, Torhell S-E. Den Kvalitativa Forskningsintervjun. Lund: Studentlitteratur; 2014.
World Medical Association Declaration of Helsinki. JAMA. 2013;310(20):2191. https://doi.org/10.1001/jama.2013.281053 .
Article CAS Google Scholar
Bloomer MJ, Hutchinson AM, Brooks L, Botti M. Dying persons’ perspectives on, or experiences of, participating in research: an integrative review. Palliat Med. 2018;32(4):851–60. https://doi.org/10.1177/0269216317744503 .
Gysels M, Evans CJ, Lewis P, Speck P, Benalia H, Preston NJ, et al. MORECare research methods guidance development: recommendations for ethical issues in palliative and end-of-life care research. Palliat Med. 2013;27(10):908–17. https://doi.org/10.1177/0269216313488018 .
Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20(1):158. https://doi.org/10.1186/s12912-021-00684-2 .
Höglander J, Eklund JH, Spreeuwenberg P, Eide H, Sundler AJ, Roter D, et al. Exploring patient-centered aspects of home care communication: a cross-sectional study. BMC Nurs. 2020;19(1). https://doi.org/10.1186/s12912-020-00483-1 .
Fleischer S, Berg A, Zimmermann M, Wüste K, Behrens J. Nurse–patient interaction and communication: a systematic literature review. J Public Health. 2009;17(5):339–53. https://doi.org/10.1007/s10389-008-0238-1 .
Ikander T, Dieperink KB, Hansen O, Raunkiær M. Patient, family caregiver, and nurse involvement in end-of-life discussions during palliative chemotherapy: a phenomenological hermeneutic study. J Fam Nurs. 2022;28(1):31–42. https://doi.org/10.1177/10748407211046308 .
Tarbi EC, Gramling R, Bradway C, Meghani SH. If it’s the time, it’s the time: existential communication in naturally-occurring palliative care conversations with individuals with advanced cancer, their families, and clinicians. Pat Educ Couns. 2021. https://doi.org/10.1016/j.pec.2021.04.040 .
Haavisto E, Eriksson S, Cleland Silvia T, et al. Patients receiving palliative care and their experiences of encounters with healthcare professionals. OMEGA – J Death Dying. 2022;003022282210774. https://doi.org/10.1177/00302228221077486 .
Arman M, Rehnsfeldt A. The ‘little extra’ that alleviates suffering. Nurs Ethics. 2007;14(3):372–86. https://doi.org/10.1177/0969733007075877 .
Rochmawati E, Minanton M. Embedded spiritual conversation in cancer communication: lived experiences of nurses and patients/relatives. Int Nurs Rev. 2021;68(3):289–98. https://doi.org/10.1111/inr.12634 .
Sinclair S, Beamer K, Hack TF, McClement S, Raffin Bouchal S, Chochinov HM, et al. Sympathy, empathy, and compassion: a grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat Med. 2017;31(5):437–47. https://doi.org/10.1177/0269216316663499 .
Timmermann C, Uhrenfeldt L, Birkelund R. Ethics in the communicative encounter: seriously ill patients’ experiences of health professionals’ nonverbal communication. Scand J Caring Sci. 2017;31(1):63–71. https://doi.org/10.1111/scs.12316 .
Nyatanga B. Back to basics: communication in palliative care. Br J Community Nurs. 2022;27(1). https://doi.org/10.12968/bjcn.2022.27.1.46 .
Rattner M. Increasing our understanding of nonphysical suffering within palliative care: a scoping review. Palliat Support Care. 2022;20(3):417–32. https://doi.org/10.1017/S1478951521001127 .
Rattner M. Tellable and untellable stories in suffering and palliative care. Mortality. 2019;24(3):357–68. https://doi.org/10.1080/13576275.2018.1530206 .
Ulrich CM, Taylor C, Soeken K, O’Donnell P, Farrar A, Danis M, et al. Everyday ethics: ethical issues and stress in nursing practice. J Adv Nurs. 2010;66(11):2510–9. https://doi.org/10.1111/j.1365-2648.2010.05425.x .
Arman M, Rehnsfeldt A, Lindholm L, Hamrin E, Eriksson K. Suffering related to health care: a study of breast cancer patients’ experiences. Int J Nurs Pract. 2004;10(6):248–56. https://doi.org/10.1111/j.1440-172x.2004.00491.x .
Arman M. Empathy, sympathy, and altruism – an evident triad based on compassion. A theoretical model for caring. Scand J Caring Sci. 2023;00:1–10. https://doi.org/10.1111/scs.13163 .
Kalánková D, Stolt M, Scott PA, Papastavrou E, Suhonen R. Unmet care needs of older people: a scoping review. Nurs Ethics. 2021;28(2):149–78. https://doi.org/10.1177/0969733020948112 .
Tornøe K, Danbolt LJ, Kvigne K, Sørlie V. A mobile hospice nurse teaching team’s experience: training care workers in spiritual and existential care for the dying – a qualitative study. BMC Palliat Care. 2015;14(1). https://doi.org/10.1186/s12904-015-0042-y .
Tarbi EC, Meghani SH. A concept analysis of the existential experience of adults with advanced cancer. Nurs Outlook. 2019;67(5). https://doi.org/10.1016/j.outlook.2019.03.006 .
Folkman S, Greer S. Promoting psychological well-being in the face of serious illness: when theory, research, and practice inform each other. Psychooncology. 2000;9(1):11–9. https://doi.org/10.1002/(sici)1099-1611(200001/02)9:1%3C11::aid-pon424%3E3.0.co;2-z .
Louw S, Watson R, Jimarkon P. Active listening in qualitative research interviews. Proceedings of the International Conference: Doing Research in Applied Linguistics 2018 .
Download references
Acknowledgements
We especially want to thank the ten people who participated in the interviews and shared their experiences.
The authors received no financial support for the research, authorship, or publication of this article. The authors received financial support from Mid Sweden University for the research authorship, and open access.
Open access funding provided by Mid Sweden University.
Author information
Authors and affiliations.
Department of Health Sciences Nursing Science, Mid Sweden University, Östersund, S-831 25, Sweden
Tove Stenman, Ylva Rönngren, Ulla Näppä & Christina Melin-Johansson
You can also search for this author in PubMed Google Scholar
Contributions
TS, YR, UN, and CMJ considered the design, TS and YR collected the data, and TS and CMJ discussed the analysis and interpretation of data. TS, YR, UN, and CMJ contributed to the discussions of the result, and the writing and revision of the manuscript, and approved the final manuscript.
Corresponding author
Correspondence to Tove Stenman .
Ethics declarations
Ethics approval and consent to participate.
The Swedish Ethical Review Authority, Regional Ethics Committee in Stockholm, and Department of Other Research, (Dnr 2021–04066 and 2022-03769-02) approved the study. The ethical considerations followed the rules presented in the Declaration of Helsinki. TS and YR interviewed the participants after making personal contact; no further personal contact was made after the interviews. All the participants received written and verbal information about the study. All participants signed an informed consent and received information that participation was voluntary and that they could terminate participation without giving a reason. Once all the interviews were completed, they were transcribed verbatim and stored according to good research practice and ethical principles.
Consent for publication
Not applicable.
Competing interests
The authors TS, CMJ, UN, and YR declare no competing interests.
Author contributions
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Stenman, T., Rönngren, Y., Näppä, U. et al. “Unless someone sees and hears you, how do you know you exist?” Meanings of confidential conversations – a hermeneutic study of the experiences of patients with palliative care needs. BMC Nurs 23 , 336 (2024). https://doi.org/10.1186/s12912-024-01988-9
Download citation
Received : 12 September 2023
Accepted : 02 May 2024
Published : 18 May 2024
DOI : https://doi.org/10.1186/s12912-024-01988-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Confidential conversations
- Communication
- Palliative care
- Qualitative research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 10 May 2024
“So we brought these players together”: a qualitative study of educators’ experiences to analyze the challenges of creating an e-learning program for neuropalliative care
- Julia Bu 1 ,
- Susan DeSanto-Madeya 2 ,
- Mara Lugassy 3 ,
- Jessica Besbris 4 ,
- Sarah Bublitz ORCID: orcid.org/0000-0003-3258-543X 5 ,
- Neha M. Kramer 6 ,
- Roop Gursahani ORCID: orcid.org/0000-0002-6092-1595 7 ,
- Winnie Lau 8 ,
- Estella Kim 9 ,
- John Y. Rhee 10 &
- Piret Paal ORCID: orcid.org/0000-0002-1341-3248 11 , 12
BMC Medical Education volume 24 , Article number: 524 ( 2024 ) Cite this article
386 Accesses
5 Altmetric
Metrics details
In recent years, the subspecialty of neuropalliative care has emerged with the goal of improving the quality of life of patients suffering from neurological disease, though gaps remain in neuropalliative care education and training. E-learning has been described as a way to deliver interactive and facilitated lower-cost learning to address global gaps in medical care. We describe here the development of a novel, international, hybrid, and asynchronous curriculum with both self-paced modules and class-based lectures on neuropalliative care topics designed for the neurologist interested in palliative care, the palliative care physician interested in caring for neurological patients, and any other physician or advanced care providers interested in neuropalliative care.
The course consisted of 12 modules, one per every four weeks, beginning July 2022. Each module is based on a case and relevant topics. Course content was divided into three streams (Neurology Basics, Palliative Care Basics, and Neuropalliative Care Essentials) of which two were optional and one was mandatory, and consisted of classroom sessions, webinars, and an in-person skills session. Evaluation of learners consisted of multiple choice questions and written assignments for each module. Evaluation of the course was based on semi-structured qualitative interviews conducted with both educator and learner, the latter of which will be published separately. Audio files were transcribed and underwent thematic analysis. For the discussion of the results, Khan’s e-learning framework was used.
Ten of the 12 participating educators were interviewed. Of the educators, three identified as mid-career and seven as senior faculty, ranging from six to 33 years of experience. Nine of ten reported an academic affiliation and all reported association with a teaching hospital. Themes identified from the educators’ evaluations were: bridging the global gap, getting everybody on board, defining the educational scope, investing extensive hours of voluntary time and resources, benefiting within and beyond the curriculum, understanding the learner’s experience, creating a community of shared learning, adapting future teaching and learning strategies, and envisioning long term sustainability.
Conclusions
The first year of a novel, international, hybrid, and asynchronous neuropalliative care curriculum has been completed, and its educators have described both successes and avenues for improvement. Further research is planned to assess this curriculum from the learner perspective.
Peer Review reports
Though international humanitarian organizations consider palliative care an international public health priority [ 1 ], there is a large unmet global need for palliative care that is projected to grow wider in the coming years [ 2 ]. While models of palliative care originally focused on patients with cancer, the subspecialty of neuropalliative care developed to meet the unique needs of patients and caregivers suffering from neurological disease [ 3 ], as these patients uniquely face high symptom burden, functional decline, significant care giver needs, prognostic uncertainty, and complex decision making throughout the disease course [ 4 ]. Evidence has shown that implementation of palliative care improves patient and caregiver outcomes [ 3 ], as neuropalliative care strives to alleviate common sources of patient suffering by focusing on clear and compassionate communication, physical and spiritual symptoms support, caregiver support, and advance care planning [ 3 ].
There is, however, no uniformly agreed-upon optimal international model of palliative care for patients living with neurological disease [ 5 ]. A roadmap was published in 2018 as a framework for palliative care development in resource limited countries [ 6 ]. Possible proposed models include integrative (a neurologist with a specialist palliative care provider), disease specific interdisciplinary clinics, community-based palliative care services, and/or a specialized neuropalliative care provider [ 7 ], though as of 2020, there were only 63 neurologists who had active board certification in Hospice and Palliative Medicine (N. Kramer, personal communication, March 22, 2021).
Often cited barriers for integrating neuropalliative care into practice include education gaps of not only clinicians, including neurologists, palliative care providers, and primary care providers, but also patients and communities [ 3 ]. An ideal skillset for a neuropalliative clinician includes effective communication skills, navigating complex patient centered decision-making, managing end-of-life symptoms, and providing treatment options and anticipatory guidance [ 5 ]. Various curricula have been developed to disseminate core palliative skills, with online education being particularly helpful in providing lower-cost education, addressing global gaps in available resources that often primarily affect low-to-middle income countries.
E-Learning has been described as an innovative approach for delivering a learner-centered, interactive, and facilitated learning environment to anyone, anyplace, anytime, by utilizing the attributes and resources of various digital technologies along with other forms of learning materials suited for open and distributed learning environments. However, success in an e-learning system involves a systematic process of planning, designing, evaluating, and implementing online learning environments where learning is actively fostered and supported [ 8 ]. These initiatives range from smartphone application-based or online curricula [ 9 ] to Youtube videos [ 10 ]. In US-based online curricula in both primary palliative care [ 11 ] and neurological subspecialty [ 12 ], participants self-reported positive increase in knowledge and competence. Earlier studies on e-learning curriculum toolkit development in neuropalliative care focused on specific diseases [ 13 ]. Further creative approaches are needed to meet the need for palliative care expertise globally, and no prior online curricula has focused on neuropalliative education specifically.
We describe here the development of a novel, international, hybrid, and asynchronous curriculum with both self-paced modules and class-based lectures on neuropalliative topics. The course was targeted at physicians and advanced practice providers: neurologists interested in palliative care, palliative care physicians interested in learning unique aspects of care for patients with neurological disease, and any other clinician or advanced practice providers wishing to learn about the intersection of neurology and palliative care. We discuss the structure of this curriculum and explore the educators’ experiences. Since work on palliative care curricula is chronically underfunded, this paper provides some “lessons learned” to help with the general organization of e-learning.
The overall objectives of the E-learning program
The overarching objectives for this year-long course were to:
Bridge educational gaps by:
teaching palliative care basics to neurologists and other non-palliative providers.
teaching neurology basics to palliative care providers and other non-neurologists.
Provide a comprehensive neuropalliative skill set that will enhance all participants’ clinical approach to people living with serious neurological conditions.
Create a repository of multimodal resources (e.g. webinars, readings, interactive sessions) for use during and after the course.
Bring together interdisciplinary professionals in neurology, palliative care, and neuropalliative care in a shared environment to foster collaboration and networking across disciplines.
Methods and curriculum description
The course consisted of 12 modules, one per every four weeks over a twelve month period, beginning July 2022. Course participants from a variety of professional backgrounds were invited to participate, including neurologists, neurosurgeons, palliative care providers, geriatricians, physiatrists, internists, intensivists, pediatricians, and advanced practice providers. The course offering was listed in Indian neurology and palliative care websites and communication groups, as well as the International Neuropalliative Care Society website. Thirty-nine clinicians and one advanced practice provider registered for the course. Course content was divided into three streams: Neurology Basics, Palliative Care Basics, and Neuropalliative Care Essentials. Learners were encouraged to explore the first two streams to fill foundational gaps based on their training background and practice specialty, and all were expected to participate in the neuropalliative stream. Topics and objectives for each stream can be found in Table 1 and supplemental Table 1 respectively. Each module was built around an exemplary case. Traditional, bottom-up neurological education, from basic science through clinical skills and then on to diseases, is unworkable for non-neurologists [ 14 ] and likely contributes to “ neurophobia” [ 15 ]. This course used a phenomenological approach to enable learners to fill neuropalliative care knowledge and skill gaps using clinical context and relevance. These strategies included pre-recorded webinars and readings, group and individual assignments, monthly flipped classroom interactive sessions, and summative assessments including multiple choice questions and reflective exercises. The flipped classroom consisted of a case presentation and additional materials to supplement the webinar content, with open discussion from learners and educators. Learners were asked to complete a post-course evaluation, the results and analysis of which will be published separately. Learners were expected to spend an average of 2–3 h per week on course work. In order to pass the course, learners were required to attend 80% of flipped classroom sessions, complete 80% of Neuropalliative Care Essentials webinars, receive an 80% pass rate on multiple choice questions, and submit written assignments for each module. Learners were also expected to attend an 8-hour in-person session focused on developing neuropalliative communication skills, with additional opportunity for networking across disciplines.
Evaluation of the E-learning program from the educators’ perspective
To evaluate the e-learning program, a two-stage evaluation strategy based on semi-structured qualitative interviews was proposed to explore the experiences of educators and learners. In this paper, we report on educator experiences.
A semi-structured interview guide was developed by the research team. The interview guide consisted of four main questions: (1) How was your personal experience in developing this online course? What went well? What were the biggest challenges that had to be overcome? (2) Do you think this online course is a good model for the development of palliative care among healthcare professionals, and why? (3) What parts of the course did you find particularly useful? And where do you think the course could be improved? (4) And finally, what is your personal opinion of this online course? Any wishes for the future? The interviews were conducted in English with a recognition that this was not the native language of all educators.
Twelve experts involved in the curriculum’s development were identified and invited via email to participate in the study. The invitation included a statement, the interview questions, the purpose of data collection, and an informed consent statement. An appointment was then made for the interview. Interviews were conducted by two researchers using online videoconferencing. Introductory interviews were conducted prior to audio and video recording.
Ethical approval
Interviews were conducted as a component of program evaluation. Participation in the evaluation process was voluntary. Verbal and written consent to record and use the data for research purposes was obtained from all participants before the video recording began.
Data analysis
The audio files were transcribed verbatim and prepared for thematic analysis using Excel. First, the researchers familiarized themselves with the verbatim transcripts. Second, codes were identified by highlighting units of meaning in the text and labeling them to describe their content. Third, patterns between codes were identified, and codes were grouped together to identify themes. The themes were reviewed by splitting, combining, discarding, or recreating themes to make them more useful and accurate. Finally, the final list of themes was transferred to Miro Board to formulate the final list of themes. The formulation was done by a research group that discussed what was meant by each theme and how it contributed to the understanding of the data.
Data synthesis
For the discussion of the results, Khan’s e-learning framework with eight dimensions was applied to this work [ 8 ]: institutional, management, technological, pedagogical, ethical, interface design, resource support, and evaluation, described further in results section.
Of 12 educators, 10 agreed to participate in the evaluation. These included six from palliative care and four from neurology/neuropalliative care backgrounds. One was a nonclinical researcher. Four were from the USA, five were from India, and one was from Europe. Of the educators, three identified as mid-career and seven as senior faculty, ranging from 6 to 33 years of experience. Nine of ten reported an academic affiliation and all reported association with a teaching hospital.
The themes identified were as follows: (1) Bridging the global gap; (2) Getting everybody on board; (3) Defining the educational scope; (4) Investing extensive hours of voluntary time and resources; (5) Benefiting within and beyond the curriculum; (6) Understanding the learner’s experience; (7) Creating a community of shared learning; (8) Adapting future teaching and learning strategies; and (9) Envisioning long term sustainability.
Bridging the global gap
Educators agreed there is a need for education and training in neuropalliative care, though they noted worldwide there are few palliative care courses or the courses are limited to specific health systems or diseases. Educators noted online education and training help to disseminate information to a larger community, as there will be a greater demand for palliative care course, and felt this course needs to continue being offered internationally in the future.
Getting everybody on board
Educators noted currently there is little research about palliative care education online and found developing and implementing an online course is a navigation of a complex landscape of policies and requirements which may be specific to institutions, healthcare systems, or countries. Additionally, when tailoring a course to meet the goals of an international community, they emphasized local guidelines, cultural norms and systems of medical practice to consider, and a big challenge to get such varied communities on board. For example, one educator noted that in India, views on patient autonomy may be different than the West, which is pertinent for the clinician teaching palliative care to understand.
“India… is a collectivist society… we as a culture have willingly surrendered a good portion of… our personal autonomy to our families. The golden rule is you treat me like you would like to be treated… But the platinum rule is that you treat me the way I would like to be treated.” (009).
Defining the educational scope
Educators noted that neuropalliative care is an innovative specialty-based model of palliative care, and found that though the entire project was ambitious, it was helpful to consider and develop basic knowledge and skills needed to deliver neuropalliative care.
“I think the stream that brought it all together, these key neuropalliative issues, you know, are really incredibly important to the goal of this course to really focus on specific elements of palliative care for neurological patients.” (003). “So first we talked about who this course is for? Is it for neurologists? Is it for palliative care specialists? Is it appropriate for both? And is it aimed at non-physicians? So we thought about the audience and the medium: should it be in person or virtual? Should it be a combination? These were the first steps.” (005).
One theme noted by educators was the challenge to focus this course on the specific elements of palliative care for people with neurological problems. The course needed to provide relevant education for both palliative care providers and neurologists, and emphasis was placed on complex decision making. To meet the learners’ expectations and make the course engaging, they noted course content needed to be adapted to answer local questions. For example, changes in content were made to make it appropriate for India:
“I think if I did my best, I would miss the mark, and I would miss the mark in many ways, because there are nuances in the discussion of advance care planning in India and other countries, there are nuances in policy, there are nuances in the care that is provided and available. So I think having a course that’s really practical and real-world will be helpful for providers. You know, it’s helpful to have people who are on the ground and really know these systems.” (002).
Investing extensive hours of voluntary time and resource
“ This is the most extensive course I have ever tried to create! ” (005).
Educators acknowledged the discussion began during the [Covid-19] pandemic and the contemplation period took more time than expected. Coordination of a large planning group was complex and meticulous. It took numerous long phone calls to understand how online learning works and several months to discuss the curriculum content.
“ So we brought these players together for different groups of people and found a common time. I think that was one of the biggest challenges in working together and creating something where everyone could come together. It was difficult, but the result was very positive because everyone was willing to put in the time that was required. ” (007).
Despite being pro-bono work, educators admired how many people volunteered to create this program and its content, bringing various resources together to provide a rich and interactive curriculum.
Benefiting within and beyond the curriculum
Educators described benefiting beyond the curriculum itself as being a part of the curriculum designers and learning from international colleagues.
“It’s a journey for me… because this is a first for me. I wasn’t earlier part of any other course module or development techniques.” (001).
Educators reflected that putting the curricula itself together allowed them to learn not only about neuropalliative care, but about what topics may be important to local practice.
“I’m 63, that’s not an age at which I’m going to go do a fellowship now… the best way to learn is to teach”. (006)

Understanding the learner’s experience
Educators noted understanding the audience is vital; the learners were all busy clinicians, and self-paced learning meant that not everyone came prepared. Educators reflected on this lack of engagement and suggested a more rigorous selection process for learners is needed for future offerings of the course. They believed as the goal of a curriculum is for learners to learn, learner engagement and retention of information is imperative. Educators reflected that learner feedback of the course is vital to course evaluation.
“Something that the group noticed was that the palliative care folks were much more engaged than the neurologists. So we really wanted to understand why that was and what we could improve for the neurologists to make it more interesting for them and make them feel like they could really benefit from this course.” (005).
Educators reflected that currently how this course impacted learner clinical practice is unknown. Though available feedback can be used to modify the course, reasons for learner attrition is also difficult to ascertain. Educators felt that for future iterations of the course, soliciting feedback from learners at the beginning and middle of the course may aid in these evaluation gaps.
Creating a community of shared learning
One theme that was reported by educators was that online learning is about building a community, so conversations between course participants are essential. One aim was to make this course a place for networking.
“You might want to divide the participants into small groups to do small projects together. That way they get to know a few others and have a chance to share ideas and set a goal. I also think that the monthly sessions at via zoom should be much more interactive so that the course participants have a lot more say. I think that would be a space for growth.” (004).
Educators reflected that content needs to become more concise to allow for synchronous online activities, regular check-ins about personal practice, and discussions about what was learned. Educators felt that small group assignments improve cross-country collaboration, and allowing time for discussion can foster teaching among learners, as practitioners may know more about the community and its needs than some educators.
Adapting future teaching and learning strategies
Educators identified that there is room for growth; questions abound for what teaching strategies need to be changed next course offering. Currently, the focus is on webinars. Educators felt the content could be consolidated by having some essential knowledge acquisition through self-directed learning and currently the course is very theoretical. They thought it may benefit from more practical cases specific to the clinician’s area of expertise, such as with inclusion of patient and family voices or with more skill development sessions. The bulk of the curriculum focused on current knowledge.
“Put them in break-out rooms, you know, and discuss face to face. That will enhance our learning. And then give them cases, break them up into groups of five, and show them how they could do it. Those kinds of discussions would show what they have learned over the last month. So we need to incorporate more of these skill-based sessions.” (007).
In terms of performance assessment, educators felt the MCQs should be replaced at least in part by practical tasks.
Envisioning long term sustainability
Educators noted in the first year, the goal was to create all the content and get the pilot course started. For subsequent iterations, educators posed questions to consider including: What happens next time? How can awareness be spread about the course? How can more participants attend the live sessions? A course is only helpful if learners complete the course. Would conferring a degree instead of a certificate improve participation? From the educator side, more comfort with the online curriculum is needed:
“I have some people who are known as educators, but they had a very hard time transitioning to online content and asynchronous content and building a community. If you’re not used to watching YouTube, you may have a hard time engaging with it.” (008).
The demand for palliative care for people with neurological disease and their caregivers is rising globally. Palliative care education and curricular development is central to improving access to high quality palliative care. Targeted initiatives to improve healthcare workers competencies in symptom control, communication, advance care planning are needed. Integrating palliative care into public health systems is important for the sustainability of palliative care around the world. The resources for planning and creating educational activities ‘ rest on the shoulders of champions ’ [ 16 ]; however the lack of explicit funding for creation and maintenance of such educational activities, such as e-learning programs, is a well-known barrier.
For the e-learning program described here, the educators’ evaluations indicate that the program is consistent with the mission of the International Neuropalliative Care Society (INPCS) to build an international neuropalliative care community. This course not only addresses common topics relevant to caring for patients with serious neurological conditions and their caregivers, but it also highlights the importance of multidisciplinary practice and integrative care and provides enhanced opportunities for interprofessional collaboration and education. All these components have been highlighted as priorities in the field of neuropalliative care [ 5 ].
There are some lessons to be learned from the educators’ evaluation of the e-learning program relevant to individuals designing a curriculum in a newly defined field, such as neuropalliative care. Khan’s E-Learning Framework with eight dimensions has been applied to this work: institutional, management, technological, pedagogical, ethical, interface design, resource support, and evaluation. All dimensions work to foster analysis and evaluation of every aspect of the e-learning design process [ 8 ]. This evaluation identified four main learning points, which are discussed below.
Allow spaces to learn from learners. Khan’s E-Learning Framework supports educators’ experiences that managing people, content, and the e-learning environment is time-consuming and largely a voluntary task that requires getting everyone on board. While curriculum developers may feel compelled to provide as much information as possible, socioeconomically and culturally familiar content may be more relevant to learners. Planning events in which learners can learn from each other through discussion and networking can also increase the amount of actionable information shared. Mindfulness of nurturing learning cultures whilst building global learning platforms cannot be overlooked [ 17 ]. A recent study proposed four dimensions that can be factors of convergence or divergence for learners: management of time and learning activities, management of the learning space, management of interpersonal relations, and style of communication [ 18 ]. Most importantly, online learning networks foster community growth [ 19 , 20 ] which benefits any new field. Neuropalliative care is a newly defined field with limited availability of evidence-based information. Available evidence is collected from certain populations, socioeconomic and cultural contexts, and therefore, entails little social and cultural diversity. Getting everyone on board means also adding learners’ voices to the curriculum via enabling spaces for exchange, reflection and obtaining new insights from learners [ 21 ].
Plan your e-learning as if there will not be a second time . The evaluation for e-learning and assessment of learners’ experiences was of concern, which is closely related to the pedagogical and ethical dimensions of e-learning programs. Educators clearly pointed out the monotony in teaching and assessment strategies, as well as the need for changes related to improving the collective learning experience, incorporating patient and caregiver voices, and providing workshops to improve practical skills. Although educators are well aware of the importance of such improvements, the enormous amount of volunteer work involved raises the question of whether educators would be motivated enough to work a second time, adding to concerns of long-term sustainability of such e-learning programs. At this time, similar to the seeds that grew this current project, the field of neuropalliative care relies on practitioners dedicated to the field to continue providing volunteer time to advance the field’s missions, including engaging new communities nationally and internationally [ 3 ]. As communities and professional organizations further realize the importance of neuropalliative care in holistically supporting patients with serious neurological disease, it is our hope that educational initiatives like this one continue to flourish.
Focus on learner progress, support, and professional gains throughout the process. The institutional dimension addresses administrative, academic affairs, and learner services issues related to e-learning. Different organizations may have different requirements, which can cause delays and interruptions in the process. In the current project, the different requirements were successfully brought together. The dimension of resource support of e-learning to promote meaningful learning was discussed by educators. As learners invest many hours in participating in e-learning programs, the return on investment must be clear. Successful self-directed learning requires commitment and guidance, and therefore, in order to provide the best care for people with neurological conditions, healthcare providers motivated to improve their knowledge and skills must be provided with sufficient learning time, financial support, and professional development. The E-learning module structure was chosen for this current endeavor to balance the motivation of learners with practical availability of time in a clinician’s work schedule for optional learning, though educators felt that certain key clinical skills of the palliative care toolkit such as communication skills are better practiced by live faculty-led sessions. Further work evaluating the learner’s perspectives is needed to elucidate the ideal balance of asynchronous modules vs. live sessions for neuropalliative skills, though the asynchronous module option, touted by this project’s educators as well as in prior literature [ 11 ], appears to remain the most practical way to deliver education to a busy and geographically diverse audience.
In terms of e-learning programs, the first step is to help learners determine their motivation for taking the course through screening. Recently novel approaches to predict learners’ success have been proposed [ 22 , 23 ]. Secondly, regular hands-on assignments and assessments can help motivate and focus learners. Finally, there is the question of whether a certificate is sufficient motivation or whether the course should lead to a degree that can be used to achieve subspecialization in neuropalliative care. An exploration of learners’ feedback from this educational endeavor will be published separately.
Be aware of your blind spots. The interface design, online support, and technology infrastructure were not discussed by educators involved, which suggests a knowledge gap in this area, and confirms the perception that online teaching needs new kinds of educators [ 24 ]. User friendliness and questions regarding learning infrastructure are important factors that enhance learners’ experience. Professional companies with better understanding of how e-learning functions should be involved from the beginning. In terms of evaluation, it has been indicated that the capability of monitoring and storing user traffic is useful to understand a learner’s behavior, proficiency, accumulated knowledge and learning curve [ 25 ], which can be considered for future iterations of this course.
Success factors in e-learning implementation effectiveness have been related to technology, learner, instructor, content, and institution support [ 26 ]. We describe here the educators’ reflections of designing and implementing an international e-learning program in neuropalliative care, highlighting their perceived successes such as bridging gaps in education, building international communities, themselves learning from experts outside the curriculum, as well as avenues for improvement such as in integrating technology [ 22 ] and questioning sustainability. Furthermore, analysis of learner evaluations will provide further insights to help understand how this e-learning program is perceived and its educational benefits from the learners’ perspective.
Data availability
Data sharing is not applicable as no datasets were generated or analyzed during the current study. Copies of interview transcripts are available upon request from the first author.
Gómez-Batiste X, Murray SA, Thomas K, et al. Comprehensive and Integrated Palliative Care for people with Advanced Chronic conditions: an Update from several European initiatives and recommendations for policy. J Pain Symptom Manage. 2017;53:509–17. https://doi.org/10.1016/j.jpainsymman.2016.10.361 .
Article Google Scholar
Connor SR, Centeno C, Garralda E, Clelland D, Clark D. Estimating the number of patients receiving Specialized Palliative Care globally in 2017. J Pain Symptom Manage. 2021;61(4):812–6. https://doi.org/10.1016/j.jpainsymman.2020.09.036 .
Kluger BM, Hudson P, Hanson LC, et al. Palliative care to support the needs of adults with neurological disease. Lancet Neuro. 2023;22:619–31. https://doi.org/10.1016/S1474-4422(23)00129-1 .
Taylor LP, Besbris JM, Graf WD, Rubin MA, Cruz-Flores S, Epstein LG, Ethics. Law, and Humanities Committee, a joint committee of the American Academy of Neurology, American Neurological Association, and Child Neurology Society. Clinical Guidance in Neuropalliative Care: An AAN Position Statement. Neurology. 2022;98(10):409–416. https://doi.org/10.1212/WNL.0000000000200063 . PMID: 35256519.
Grossman CH, Hearn R, McPhee M, Fisher F, Wools C, Mathers S. Neuropalliative care for progressive neurological diseases: a scoping review on models of care and priorities for future research. Palliat Med. 2023;37(7):959–97. https://doi.org/10.1177/02692163231175696 .
Callaway MV, Connor SR, Foley KM, World Health Organization Public Health Model. A Roadmap for Palliative Care Development. J Pain Symptom Manage. 2018;55:S6–13. https://doi.org/10.1016/j.jpainsymman.2017.03.030 .
Gursahani R, Lorenzl S. International models of neuropalliative care. In: Miyasaki JM and Kluger BM eds. Handbook of Clinical Neurology Elsevier B.V. 2022:74–84. https://doi.org/10.1016/B978-0-323-85029-2.00012-9 .
Khan BH. (2010) The Global E-Learning Framework. In R.A. Wisher and. B.H. Khan, editors, Learning on demand: ADL and the future of e- learning. Washington, DC.
Wittenberg-Lyles E, Goldsmith J, Platt CS. Palliative Care Communication. Semin Oncol Nurs. 2014;30(4):280–6. https://doi.org/10.1016/j.soncn.2014.08.010 .
Liu M, Cardenas V, Zhu Y, Enguidanos S. YouTube Videos as a Source of Palliative Care Education: a review. J Pall Med. 2019;22:1568–73. https://doi.org/10.1089/jpm.2019.0047 .
Berke C, Mollman S, Skoglund A, Pravecek B, Perrenoud M, Stewart C. New ways to impact primary palliative care practices using online continuing education. 2023;17:1–20. https://doi.org/10.1177/26323524231179977 .
Loebel EM, Stein LK, Fara M, Farouk S, Chadha N. Curriculum Innovations: Eye-ing Enhanced Educational Methods for Neurology Trainees: Pilot of an Online, Case-based Neuro-ophthalmology Interactive Workshop. Neurol Edu 2023, 2 (1) e200052; DOI: 10.1212/NE9.0000000000200052.
Gatsios D, Antonini A, Gentile G, et al. Education on palliative care for Parkinson patients: development of the best care for people with late-stage Parkinson’s disease curriculum toolkit. BMC Med Educ. 2021;21:538. https://doi.org/10.1186/s12909-021-02964-6 .
Menken M. Demystifying neurology. BMJ. 2002;324(7352):1469–70.
Chhetri SK. E-learning in neurology education: principles, opportunities and challenges in combating neurophobia. J Clin Neurosci. 2017;44:80–3.
Paal P, Brandstötter C, Elsner F, Lorenzl S, Osterbrink J, Stähli A. European interprofessional postgraduate curriculum in palliative care: a narrative synthesis of field interviews in the region of Middle, Eastern, and Southeastern Europe and Central and West Asia. Palliative & Supportive Care. Cambridge University Press; 2022. p. 1–10.
Goodfellow R, Lamy M. (2010). Learning Cultures in Online Education. Design and technology education: an international journal, 14.; Hameed, N., Shaikh, M.U., Hameed, F., & Shamim, A. (2016). Cultural Differences in E-Learning: Exploring New Dimensions. ArXiv, abs/1607.01359 .
Latrous WO, Khadraoui M. Cultural challenges of E-Learning experiences: an exploratory research. Int J E Serv Mob Appl. 2020;12:18–37.
Yang L, Ouyang F. Building Online Learning Community for Higher Education. ICCIA. 2012. https://doi.org/10.2991/iccia.2012.267 .
McArdle G, Monahan T, Bertolotto M. (2007). WEB-BASED COMMUNITIES IN E-LEARNING. In Proceedings of the Third International Conference on Web Information Systems and Technologies - Volume 3: WEBIST; ISBN 978-972-8865-79-5; ISSN 2184–3252, SciTePress, pages 265–272. https://doi.org/10.5220/0001264802650272 .
Colosimo AL. Guides: e-Learning kit: Building community. https://libraryguides.mcgill.ca/elkit/community (2016). Accessed 3, Nov 2023.
Divyabharathi D, Sheshasaayee DA. (2018). A Study on improvised models for E-Learning Systems Success. International Journal of Emerging Technologies and Innovative Research 2018.
Benabbes K, Housni K, Hmedna B, Zellou A, Mezouary AE. A New Hybrid Approach to Detect and Track Learner’s Engagement in e-Learning. IEEE Access. 2023;11:70912–29. https://doi.org/10.1109/ACCESS.2023.3293827 .
Jokinen H, Pramila-Savukoski SP, Kuivila HM et al. Development and psychometric testing of hybrid education competence instrument for social and health care, and health sciences educators. Nurse Educ Today. 2023;105999.
Burdescu DD, Mihăescu MC. How Learner’s proficiency may be increased using knowledge about users within an E-Learning platform. Informatica (Slovenia). 2006;30:433–8.
Google Scholar
Yodihartomo F, Wijaya C, Aurelia H. R.D. (2022). Analyzing Success Factors of E-Learning Effectiveness at Higher Education in Indonesia: A Review. 2022 6th International Conference on Information Technology, Information Systems and Electrical Engineering (ICITISEE) , 519–524.
Download references
Acknowledgements
To the faculty members of this project, who are key stakeholders, participants, and visionaries of this project.
The authors have no funding sources to declare.
Author information
Authors and affiliations.
University of California San Diego, San Diego, CA, USA
College of nursing, University of Rhode Island, Rhode Island, USA
Susan DeSanto-Madeya
Westchester Medical Center, Valhalla, NY, USA
Mara Lugassy
Cedars-Sinai Medical Center, Los Angeles, CA, USA
Jessica Besbris
Institute of Palliative Care, Paracelsus Medical University, Salzburg, Austria
Sarah Bublitz
Rush University Medical Center, Chicago, IL, USA
Neha M. Kramer
P. D. Hinduja National Hospital, Mumbai, India
Roop Gursahani
University of North Carolina, Chapel Hill, NC, USA
University of California, Berkeley, Berkeley, CA, USA
Estella Kim
Dana Farber Cancer Institute, Harvard Medical School, Boston, MA, USA
John Y. Rhee
Department of Ethnology, Institute of Cultural Studies, University of Tartu, Tartu, Estonia
You can also search for this author in PubMed Google Scholar
Contributions
JBu, EK conducted participant interviews. JBu, SDSM, ML, PP analyzed and interpreted the interview transcripts JBu, SDSM, ML, JBe, NK, WL, PP as a major contributor in writing the manuscript All authors read and approved the final manuscript.
Corresponding author
Correspondence to Julia Bu .
Ethics declarations
Ethics approval and consent to participate.
Ethics waiver provided by Salzburg Ethics Committee (Ethikkommission für das Bundesland Salzburg) reference number pf_415. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bu, J., DeSanto-Madeya, S., Lugassy, M. et al. “So we brought these players together”: a qualitative study of educators’ experiences to analyze the challenges of creating an e-learning program for neuropalliative care. BMC Med Educ 24 , 524 (2024). https://doi.org/10.1186/s12909-024-05437-8
Download citation
Received : 03 December 2023
Accepted : 17 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12909-024-05437-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Neuropalliative education e-learning
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Standardizing Integrated Oncology and Palliative Care Across Service Levels: Challenges in Demonstrating Effects in a Prospective Controlled Intervention Trial
- Original Research
- Open access
- Published: 14 May 2024
Cite this article
You have full access to this open access article

- Anne-Tove Brenne ORCID: orcid.org/0000-0003-2730-6299 1 , 2 ,
- Erik Torbjørn Løhre 1 , 2 ,
- Anne Kari Knudsen 3 , 4 ,
- Jo-Åsmund Lund 5 , 6 ,
- Morten Thronæs 1 , 2 ,
- Bardo Driller 1 , 5 , 7 ,
- Cinzia Brunelli 8 &
- Stein Kaasa 3 , 4 , 9
183 Accesses
1 Altmetric
Explore all metrics
Introduction
Patients with cancer often want to spend their final days at home. In Norway, most patients with cancer die in institutions. We hypothesized that full integration of oncology and palliative care services would result in more time spent at home during end-of-life.
A prospective non-randomized intervention trial was conducted in two rural regions of Mid-Norway. The hospitals’ oncology and palliative care outpatient clinics and surrounding communities participated. An intervention including information, education, and a standardized care pathway was developed and implemented. Adult non-curative patients with cancer were eligible. Proportion of last 90 days of life spent at home was the primary outcome.
We included 129 patients in the intervention group (I) and 76 patients in the comparison group (C), of whom 82% of patients in I and 78% of patients in C died during follow-up. The mean proportion of last 90 days of life spent at home was 0.62 in I and 0.72 in C ( p = 0.044), with 23% and 36% ( p = 0.073), respectively, dying at home. A higher proportion died at home in both groups compared to pre-study level (12%). During the observation period the comparison region developed and implemented an alternative intervention to the study intervention, with the former more focused on end-of-life care.
A higher proportion of patients with cancer died at home in both groups compared to pre-study level. Patients with cancer in I did not spend more time at home during end-of-life compared to those in C. The study intervention focused on the whole disease trajectory, while the alternative intervention was more directed towards end-of-life care. “Simpler” and more focused interventions on end-of-life care may be relevant for future studies on integration of palliative care into oncology.
Trial Registration
ClinicalTrials.gov Identifier: NCT02170168.
Plain Language Summary
Palliative care is an important part of cancer care to improve patients’ quality of life. To be cared for and die in the preferred place are quality markers in palliative care. Patients with cancer often want to spend their final days at home. In Norway, most patients with cancer die in institutions. We hypothesized that full integration of cancer and palliative care would result in more time spent at home during end-of-life. An intervention that included information, education, and a standardized care pathway was developed and implemented in a region of Mid-Norway (the intervention region, I). A similar region served as comparison region (C). Adult patients with cancer treated with non-curative intent were eligible. Altogether, 129 patients in I and 76 patients in C were included in the study, of whom 82% in I and 78% in C died during follow-up. The mean proportion of time spent at home last 90 days of life was 0.62 in I and 0.72 in C ( p = 0.044), and 22.6% and 35.6% ( p = 0.073) died at home, respectively. A higher proportion died at home in both groups compared to pre-study national levels (12%). During the study period, C developed and implemented an alternative intervention to the study intervention, with the former placing more focus on end-of-life care compared to the she study intervention that focused on the whole disease trajectory. This may explain why the intervention did not result in more time spent at home during end-of-life as compared to C. “Simpler” interventions directed towards the study’s primary outcome may be relevant for future studies on integration of palliative care into oncology.
Similar content being viewed by others

PALLiON – PALLiative care Integrated in ONcology: study protocol for a Norwegian national cluster-randomized control trial with a complex intervention of early integration of palliative care

Care plus study: a multi-site implementation of early palliative care in routine practice to improve health outcomes and reduce hospital admissions for people with advanced cancer: a study protocol

Outpatient and Inpatient Structures: What Does It Need to Integrate Palliative Care Services?
Avoid common mistakes on your manuscript.
Modern palliative care (PC) is an important part of oncology, and early introduction is recommended in conjunction with anticancer therapy [ 1 , 2 , 3 ]. PC can be delivered in a variety of settings, including inpatient units, outpatient clinics, nursing homes, and the home (home-based care) [ 4 , 5 ]. The increasing incidence and prevalence of cancer warrant rethinking the care delivery models [ 3 ]. In scattered populated areas, decentralized PC services are useful [ 6 ].
PC interventions are often complex [ 7 , 8 ]. The use of scientifically recommended methods, such as randomized controlled trials (RCTs) to study their effects may be difficult due to poor recruitment, high attrition rates, bias, confounding, and small sample sizes [ 7 ]. However, well-founded study objectives evaluated by sound and time-responsive outcome measures are recommended [ 7 ]. Time spent at home is recognized as a valid outcome to assess the quality of end-of-life (EOL) care and is in line with patients’ preferences [ 9 , 10 , 11 ]. In Norway, the majority of patients with cancer die in institutions, and this represents a pattern strengthened over the past decades [ 12 ]. Compared to other European countries, Norway is at bottom of the list of patients with cancer dying at home [ 13 ]. Prior to the Covid-19 pandemic, only 10–12% of patients with cancer died at home in Norway [ 14 ]; this had increased to 16% in 2021. Being able to spend the last phase of life at home and die at home if preferred depends on several factors, such as family support and easy access to healthcare services [ 15 , 16 ].
Implementing PC interventions into existing healthcare structures is challenging [ 17 , 18 ]. Albeit the benefits of early integration of PC in oncology having been known for more than a decade, precise knowledge on which ‘active components’ in PC improve outcomes is still lacking [ 8 ]. Published research mainly addresses physical, psychological, social, and EOL care aspects [ 1 , 2 , 19 , 20 , 21 , 22 ], but few studies have addressed the coordination of care.
In previously publications, we described the development and implementation of a regional oncology and PC program [ 17 , 23 ]. The program consisted of a complex intervention and represented full integration of oncology and PC throughout the entire disease trajectory, including improved care coordination within and between services at different levels of healthcare [ 23 ]. The development of the program was based on results from earlier studies in the areas of oncology and PC care and focused on increasing time spent at home at the EOL for patients with cancer [ 2 , 17 , 23 , 24 , 25 ]. From this studies, we concluded that development of the program was feasible, and healthcare providers reported that it improved cancer care. However, the program was only used to a limited extent in clinical practice. To evaluate its effectiveness on clinical outcomes, we conducted a prospective controlled non-randomized intervention trial in two health regions in Mid-Norway. This paper presents the clinical outcomes of this intervention trial. We hypothesized that the measurable effects of the complex intervention would increase during the project period, and that a major part of this change would be caused by the complex intervention and not only by general work to improve healthcare services. Time spent at home during the last 90 days of life was chosen as primary clinical outcome.
Design and Participants
This prospective controlled non-randomized intervention trial was conducted in two regions of Mid-Norway, the Orkdal Region [ 23 ] and the Romsdal Region. Two hospitals in these regions, Orkdal Hospital and Molde Hospital, respectively, coordinated the trial. Characteristics of the two regions are given in Table 1 .
Patients in the intervention group (I) resided in 13 municipalities neighboring Orkdal Hospital. Patients in the comparison group (C) were recruited from Molde Hospital and nine adjacent municipalities.
Inclusion and Exclusion
Eligibility criteria were: advanced loco-regional and/or metastatic cancer; adult residents (> 18 years of age) of the participating municipalities; and capability to comply with study procedures and read and write Norwegian. Patients receiving anticancer therapy with a curative intent were excluded.
The Intervention Group
A complex intervention focusing on introducing PC along the entire disease trajectory was introduced in the intervention group. The intervention was based on previous studies and complied with national standards for palliative cancer care [ 24 , 25 , 26 , 27 , 28 , 29 ]. The activities and strategies included in the intervention are summarized in Table 2 , and details on implementation have been described elsewhere [ 17 , 23 ]. The main components were:
A standardized care pathway (SCP) with integrated and coordinated oncology and PC services throughout the disease trajectory and across healthcare levels.
An educational program intended to improve healthcare professionals’ (HCPs’) knowledge and skills in oncology and PC.
An information program on oncology and PC aimed at the public, patients, and carers.
The intervention hospital had an outpatient clinic providing integrated oncology and PC services at all stages of the disease, delivered by one team of HCPs consisting of an oncologist and oncology nurse, a physiotherapist, an occupational therapist, a chaplain, a dietitian, and a social worker [ 23 ]. The patients were thus not referred to PC when needed. Due to the lack of oncologists with formal training in palliative medicine in Norway, medical residents in oncology trained in palliative medicine in cancer during their oncology fellowship provided care and advice [ 23 ]. Home care nurses, nurses at nursing homes, and general practitioners (GPs) in the communities could contact the intervention hospital around the clock, where they had access to nurses and physicians trained in oncology and PC at the outpatient clinic Monday to Friday between 08 a.m. and 16 p.m [ 23 ]. Out of hours, the internal medicine department at Orkdal Hospital or Cancer Clinic at Trondheim University Hospital could be contacted.
The Comparison Group
The comparison hospital had a cancer outpatient clinic and a PC team of whom 50% were physicians with formal training in palliative medicine (Table 1 ). Patients were referred to the PC team based on needs and symptom burden. The primary focus of the team was providing PC and included home visits upon request and providing support for the patients and their families. Nurses from the communities and the local hospital collaborated on education in a PC network at least once a year. PC physicians collaborated with GPs through visits to the GP offices, visits with the GP to patients at home or in nursing homes, and through bi-annual PC training courses. In addition, home care nurses, nursing home nurses, and GPs could contact a hospital PC physician around the clock. A project focusing on structured advance care planning (ACP) and a palliative plan in primary healthcare to all individuals with life-limiting illnesses, such as incurable cancer, was launched in the comparison region in 2015, and systematically implemented from January to June 2018 (Table 3 ) [ 30 ].
Data Collection and Assessments
Data were managed by 29 community nurses and The Trial Office, Trondheim University Hospital. Paper-based forms were used. At inclusion, information on patient demographics, cancer diagnosis, disease stage and location of metastases, present anticancer treatment, medications, place of care, and performance status were registered. Updates on the patients’ general condition, use of hospital services and admissions, and use of community healthcare services (days in rehabilitation and nursing homes included) were collected every 4 weeks. Date and place of death were recorded.
Patients received questionnaires at inclusion every 4 weeks for 2 years or until death. Patients included in the study for > 2 years received questionnaires every 6 months after 2 years to avoid loss of motivation to participate. Data on symptom intensity and quality of life (QoL) were collected using the European Association for Palliative Care (EAPC) basic dataset [ 31 ] and European Organization for Research and Treatment of Cancer “Quality of Life Questionnaire Core 15 palliative” (EORTC QLQ C15-PAL) [ 32 ]. Furthermore, every 12 weeks the patients stated preferred places of terminal care and death. These questions formulated were introduced by: “We know from experience that you might change your mind over time. We would like to get your opinion about the next questions again, independently of what you have answered earlier.” (1) “Many persons, sick and healthy, think of where they, once in time, prefer to die. When time comes, and you yourself could chose, where would you prefer to die?” (2) “If you could choose where to be cared for at the end of life, where would you prefer to receive treatment and care?” Response categories were “Home”, “Nursing home”, “Hospital,” or “Others.” The last recorded response was used for analysis.
Pre-study data on cancer deaths and place of death were obtained from the Norwegian Cause of Death Registry. The Norwegian Cancer Registry provided data on cancer incidence and prevalence (Table 1 ).
The primary outcome was the proportion of the final 90 days of life spent at home. The secondary outcome was the number of home deaths. Death at preferred place and patients’ health-related QoL as measured by EORTC QLQ C15-PAL served as exploratory outcomes [ 32 ].
Data Analyses and Statistics
We calculated that 250 deaths would allow a power of 90% for the detection of at least a 20% difference in the mean proportions of time spent at home during the final 90 days of life between I and C, provided a C proportion of 45% and with a two-sided significance level of 5%.
The proportion of the final 90 days of life spent at home was calculated by subtracting the number of days spent in hospital, nursing homes, or rehabilitation institutions from the number of days at home. Residency in sheltered municipal housing was defined as “home,” while residency in a nursing home was not. Day of discharge was counted as inpatient-day and day of admission was not. For patients who died prior to 90 days after inclusion, the proportion of remaining lifespan spent at home was used. Home death was analyzed as dying at home compared to dying elsewhere. The global QoL item of the EORTC QLQ-C15-PAL was used for analysis of QoL at inclusion and before death.
Descriptive statistics were used to analyze population characteristics and calculate death at preferred place. Pearson’s Chi-square test was used for group comparisons, and the Welch t -test was used in case of unequal variances. The proportion of the final 90 days of life spent at home was approximately normally distributed. A two-sided independent t -test was used to compare means of proportions. Logistic regression was used to estimate odds ratio (OR) for dying at home in the compared groups. To compare deaths at preferred place between the two groups, Pearson’s Chi-square test was used. The global QoL item of EORTC QLQ-C15-PAL was scored from 1 (“very poor”) to 7 (“excellent”), and the result was calculated following the procedures of the EORTC QLQ-C15-PAL Scoring Manual: Score = ([Raw score − 1]/6) × 100 [ 33 ].
Kaplan–Meier estimates were used to calculate time from inclusion to end of follow-up or death, and to calculate time from last reported preferred place of terminal care and preferred place of death to death. Linear and logistic regression models were used to explore possible influences by demographic and clinical differences on the proportion of the final 90 days spent at home and home deaths, respectively. For both models, a univariate analysis with “region” as the independent variable was performed as the first step; this was followed by multivariate analyses that were performed to adjust for variables differing between the two compared groups.
P values ≤ 0.05 were considered to be statistically significant.
For all analyses, Stata Statistical Software Release 16.0 and 17.0 (StataCorp LP, College Station, TX, USA) were applied.
Ethics and Consent
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Committee for Medical Research Ethics Central Norway, REK Central (2014/212). Written informed consent was obtained from all participants included in the study. In cases where the participant was competent to give oral informed consent but not able to write, an adult family member or HCP signed a proxy consent.
Protocol Deviations
Patients were entered in the study from November 2014 to December 2017; the follow-up period ended December 2019 (Table 3 ). Due to the inclusion rates and survival rates being different from assumed, the preplanned inclusion and follow-up periods were prolonged by 1 and 2 years, respectively. The study was closed before reaching the planned 250 analyzable deaths and, in addition, the C proportion was smaller (36%) than assumed in the study power calculations.
Patient Characteristics
Eligible patients were recruited from the outpatient clinics, with 130 patients included in I and 78 patients included in C (Fig. 1 ). One patient in each group withdrew consent and one patient in the comparison group did not fulfill inclusion criteria.
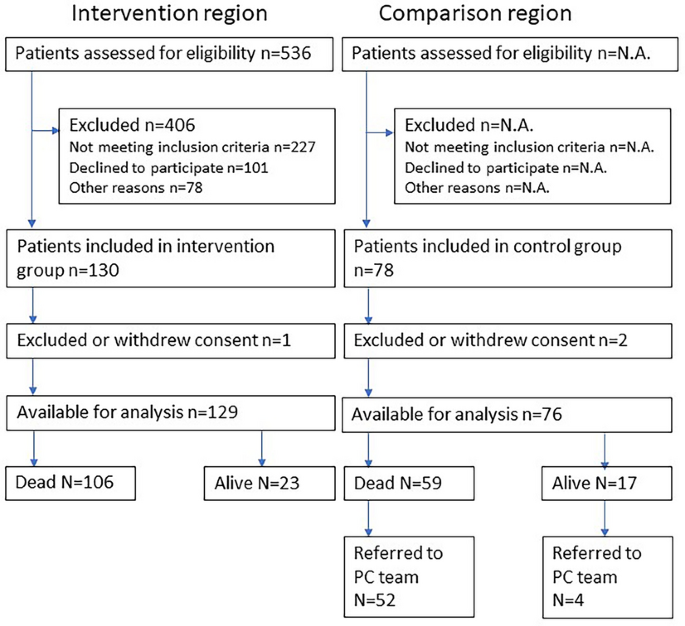
Study flow diagram. N.A. not assessed, PC palliative care
Patient characteristics at inclusion are given in Table 4 . Mean age was 70.7 (range 38–92) years in I and 68.1 (range 47–84) years in C. In I and C, 57% and 82% of patients, respectively, had a Karnofsky Performance Status (KPS) of at least 90% [ 34 ]. Compared to patients in C, fewer patients in I received medical anticancer therapy at inclusion, and they also lived farther away from the hospital.
Median time from inclusion to end of follow-up or death was 425 (95% CI 272–557) days in I and 403 (95% CI 268–635) days in C. In C, 56 patients (74%) were referred to the PC team. By the end of the study period, 106 (82%) patients in I and 59 (78%) patients in C died (Fig. 1 ); of these, 16 in I and nine in C died before reaching 90 days of observation.
Primary Outcome
Patients who died before study closure were analyzed for the primary outcome. The mean number of days of inclusion was 81 (range 1–90) in I and 85 (range 20–90) in C. The mean proportion of time spent at home during the last 90 days of life was 0.62 (95% CI 0.56–0.68) in I and 0.72 (95% CI 0.64–0.80) in C (Fig. 2 a; Electronic Supplementary Material [ESM] Table S1 ), with a statistical difference of 0.10 (95% CI 0.00–0.20, p = 0.044) in favor of C. When adjusting for education level, performance score, symptom score (< 4 or ≥ 4), anticancer therapy (yes/no), and distance from home to hospital, the difference was 0.15 (95% CI 0.03–0.27, p = 0.018) in favor of C.
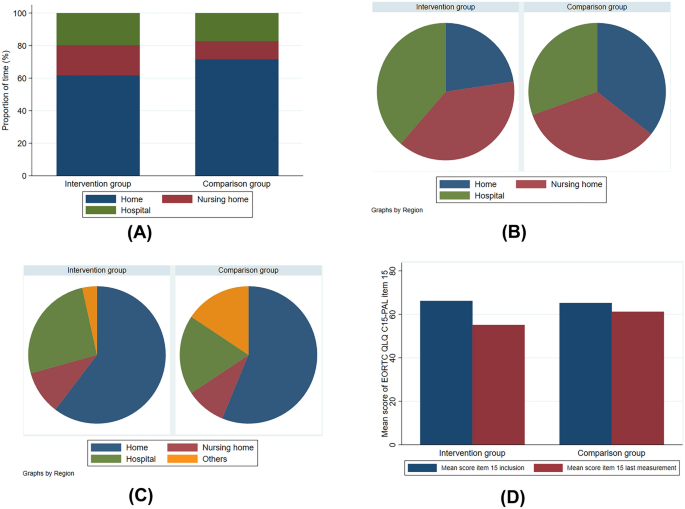
Primary, secondary, and exploratory outcomes. a Mean proportion of time spent in different care settings during the last 90 days of life. b Actual place of death. c Preferred place of death. d Mean score of EORTC QLQ C15-PAL item 15 at inclusion and last measurement before death. EORTC QLQ C15-PAL European Organization for Research and Treatment of Cancer “Quality of Life Questionnaire Core 15 palliative”
Secondary and Exploratory Outcomes
Twenty-four (22.6%) and 21 (35.6%) patients died at home in I and C, respectively (Fig. 2 b; ESM Table S2; p = 0.73). Univariate logistic regression analysis showed an OR of 1.9 (95% CI 0.94–3.8; p = 0.075) in favor of dying at home in C. When adjusting for education level, performance score, symptom score (< 4 or ≥ 4), anticancer therapy (yes/no), and distance from home to hospital, the OR was 2.6 (95% CI 0.97–6.7, p = 0.059) in favor of C. Forty-one (38.7%) patients in I and 18 (30.5%) patients in C died in hospital; the corresponding numbers for deaths in nursing homes were 41 (38.7%) and 20 (34.0%), respectively (Fig. 2 b; ESM Table S2).
Of the patients who had died, 90 patients (response rate = 85%) in I and 45 patients (response rate = 76%) in C had stated a preferred place of death. In both groups, approximately one third of the responses were collected fewer than 90 days prior to death. In their response to the question on preferred place of death, 57 (63.3%) patients in I and 25 (55.6%) patients in C preferred home death (Fig. 2 c; ESM Table S3), while 55 (64.7%) and 32 (69.6%) patients in I and C, respectively, preferred terminal home care. Thirty-four (37.8%) patients in I and 14 (31.1%) patients in C died at the preferred place (Pearson χ 2 p = 0.45).
QoL, as scored by EORTC QLQ C15-PAL item 15, revealed no mean group differences at inclusion: 66.2 ( n = 99, 95% CI 61.3–71.0) in I versus 65.2 ( n = 46, 95% CI 58.0–72.4) in C ( p = 0.82) (Fig. 2 d). Comparison of the mean decline in scores from inclusion to last measurement revealed a significant difference in favor of C: − 18.3 ( n = 73, 95% CI − 24.5 to − 12.1) in I versus − 7.2 ( n = 44, 95% CI − 16.3 to 1.9) in C ( p = 0.04) (Fig. 2 d).
Statement of Principal Findings
In both groups, the proportion of home deaths among patients with cancer increased from the pre-study period of 12% to 22.6% (I) and 35.6% (C). It also increased more than in the general population of Norway during the same period (12% in 2019) [ 14 ].
We assumed that C represented the general situation for PC in Norway. However, during the study period, an intervention directed towards EOL care was initiated in C [ 30 ]. Consequently, the study consisted of two different interventions, both of which were having a positive effect on the proportion of home deaths in both groups, as compared to pre-study levels. Patients in C spent more time at home compared to patients receiving the intervention measures in I during the final 90 days of life. Hence, measurable effects of the complex intervention did not increase during the project period as we hypothesized. The difference between the groups in proportion of home deaths did not reach statistical significance. There were no group differences in deaths at preferred place. The decline in QoL during the study period for the patients who died was larger in I.
Appraisal of Methods
We chose a study design consisting of an intervention group and a control group. The rationale for a control group was to better be able to measure a potential intervention effect. An RCT or a cluster-randomized trial was not feasible due to small-scale conditions and the system-level nature of the intervention. Given the complex nature of the intervention, a study design with baseline observations before implementation of the complex intervention may also be an appropriate design.
Since the effect of the intervention in C was larger than anticipated, we compared the content of the interventions related specifically towards EOL care. The interventions in both groups included those that focused on EOL care and, in particular, home care. The actual study intervention had a broader aim and included the entire disease trajectory. Patients were exposed to the intervention for a mean of 14 months prior to death. In C, the applied intervention was more directed towards EOL, with ACP introduced in primary care to the patients at a mean of 114 days prior to death [ 30 ]. The comparison region (C) had a PC specialist who worked 50%, and the nurses and GPs had special training in PC. Consequently, an unintended intervention with focus on EOL was implemented in the comparison region during the study period. The intervention region lacked a physician with formal competence in PC, which may also had a negative influence on the results.
Patients with advanced cancer were recruited regardless of life expectancy and PC needs. A median follow-up of > 1 year is unusual in PC trials [ 35 ]. The long follow-up in the present study was in line with our aim to provide the patients with the intervention over a substantial period before they reached the final phase of their life. One may argue whether study endpoints focusing on the entire disease trajectory, such as regular measurement of symptom burden, quality of life, and satisfaction with care, would have been more appropriate in this case than study endpoints directed towards EOL, and whether the study design at all allowed for assumptions on causality [ 36 , 37 ].
Previously published results revealed that the SCP was used to a limited extent [ 17 ]. Hence, insufficient implementation of the intervention and lack of adherence may also have affected the results. Potential effects of the intervention were measured as early as at the initiation of the implementation process, possibly before effects were evident. Furthermore, no pilot study on intervention acceptance and uptake in clinical practice was conducted.
The study was conducted with protocol deviations. The preplanned inclusion and follow-up periods were prolonged, and the study was closed before reaching the number of patients and group proportions used for power calculations [ 38 ]. Temporal trends are likely to occur and be evident in a long study period [ 39 ]. In our case, implementation of the intervention in the comparison region started before the end of the follow-up period of our study [ 30 ].
Comparison with Previous Work and Possible Reasons Why the Intervention Failed
Implementing complex interventions with the intentions to alter HCPs’ behavior is difficult [ 18 , 39 , 40 ]. A cluster-randomized trial in Mid-Norway evaluating a care pathway for home-dwelling elderly after hospital discharge was inconclusive due to incomplete use of the intervention [ 41 ]. The authors of that study suggested that intervention adherence should be ensured before study start. Another Norwegian cluster-randomized trial investigating the effect of PC on the use of anticancer treatment at the EOL found no differences between the groups [ 42 ]. As in our study, the intervention did not have the desired effect, probably due to the HCPs having a too low fidelity to the intervention to change clinical practice [ 42 ]. The reasons for insufficient implementation in our study are heterogenous and may include factors such as differences in hospital and primary care cultures, lack of management anchoring, different information and communications technology systems, and preconceptions about PC referrals [ 17 , 18 , 43 , 44 ]. Implementation of the intervention stretched over a 5-year period, and change in key staff during this period may have contributed negatively to the follow-up of adherence to the SCP [ 17 ]. Data from the comparison region showed that 50% of patients with advanced cancer got an ACP in primary care between 2018 and 2020 [ 30 ]. The intervention in the Romsdal Region was simpler, had a stronger focus on EOL care, and involved HCPs who had devoted their time and focus on EOL care.
A study comparing hospital expenditures for dying patients with cancer demonstrated that Norway is at the top of the list in terms of per capita hospital days during the last 180 days of life [ 45 ]. Currently there is a national political effort to better facilitate EOL home care and home death [ 46 ]. In 2010, 44% of all cancer deaths in Norway occurred in hospitals; by 2019 this proportion had decreased to 33% [ 14 ]. During the same period, the proportion of cancer deaths at home was stable (11% vs. 12%) [ 14 ]. In our study, we found that more than half of the patients preferred home death, which is not in line with what happens in “real life.”
Implications for Further Work
Our intervention was complex and insufficiently implemented [ 17 ]. In the comparison group (C), the ACP project in primary healthcare probably had a higher uptake than the more comprehensive SCP in I [ 30 ]. The ACP intervention was highly anchored and represented a ‘simpler’ intervention than the SCP, with the former more focused on the clinical endpoints chosen for this study. One may reflect whether an SCP containing fewer ‘active PC components’ would be less challenging to implement, and whether it represents possible strategy for the future efforts to study integration of PC into “main stream” oncology. Still, the dilemma remains: Which are the most important components of early integrated PC, and how do we develop interventions simple enough for practicality and complex enough for effect [ 47 ]?
In the current study, most of the patients in both groups were cared for close to their homes and died in their municipalities [ 15 ]. Care and death where preferred are regarded as important healthcare quality measures [ 46 ]. Most of the included patients preferred to be cared for and die at home. However, a substantial fraction preferred to be cared for and die in nursing homes or hospitals. Identifying these patients is important both from research and healthcare planning perspectives.
Patients in the intervention group (I) did not spend more of their final 90 days of life at home than patients in the comparison group (C). The situation in C differs from the general situation in Norway in general. The study intervention focused on the whole disease trajectory, while an alternative intervention in C was more directed towards EOL care. “Simpler” interventions may be relevant for future studies of integration of PC into oncology.
Data Availability
The data analysed during the current study are available from the corresponding author on reasonable request.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Article CAS PubMed Google Scholar
Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–30.
Article PubMed Google Scholar
Kaasa S, Loge JH, Aapro M, et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol. 2018;19(11):e588–653.
Rocque GB, Cleary JF. Palliative care reduces morbidity and mortality in cancer. Nat Rev Clin Oncol. 2013;10(2):80–9.
World Health Organization. Palliative care. Key facts 2018. https://www.who.int/news-room/fact-sheets/detail/palliative-care . Accessed 24 Oct 2019.
Official Norwegian Report. NOU 2017:16 På liv og død-Palliasjon til alvorlig syke og døende (In Norwegian). Oslo: Departementenes sikkerhets-og serviceorganisasjon; 2017.
Google Scholar
Higginson IJ, Evans CJ, Grande G, et al. Evaluating complex interventions in end of life care: the MORECare statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med. 2013;11:111.
Article PubMed PubMed Central Google Scholar
Fulton JJ, LeBlanc TW, Cutson TM, et al. Integrated outpatient palliative care for patients with advanced cancer: A systematic review and meta-analysis. Palliat Med. 2019;33(2):123–34.
Groff AC, Colla CH, Lee TH. Days spent at home—a patient-centered goal and outcome. N Engl J Med. 2016;375(17):1610–2.
Andersen SK, Croxford R, Earle CC, Singh S, Cheung MC. Days at home in the last 6 months of life: a patient-determined quality indicator for cancer care. J Oncol Pract. 2019;15(4):e308–15.
Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3(3):287–300.
Kalseth J, Theisen OM. Trends in place of death: The role of demographic and epidemiological shifts in end-of-life care policy. Palliat Med. 2017;31(10):964–74.
Cohen J, Houttekier D, Onwuteaka-Philipsen B, et al. Which patients with cancer die at home? A study of six European countries using death certificate data. J Clin Oncol. 2010;28(13):2267–73.
Norwegian Institute of Public Health. Norwegian Cause of Death Registry [Web page]. Oslo: Norwegian Institute of Public Health; 2022 [updated 09 June 2022 June 09]. https://statistikkbank.fhi.no/dar/index.jsp?headers=DODSSTED&stubs=EU_SHORT_CODE&measure=common&virtualslice=Freq_value&layers=DAAR&layers=virtual&study=http%3A%2F%2F10.0.3.47%3A80%2Fobj%2FfStudy%2Fd3b.eu-shortlist.dodssted&DAARsubset=2020&DAARslice=2020&mode=cube&DODSSTEDslice=Total&virtualsubset=Freq_value&v=2&EU_SHORT_CODEslice=Total&DODSSTEDsubset=Total%2C1+-+9&measuretype=4&cube=http%3A%2F%2F10.0.3.47%3A80%2Fobj%2FfCube%2Fd3b.eu-shortlist.dodssted_C1&EU_SHORT_CODEsubset=Total%2C02_1&top=yes . Accessed 06 Feb 2023.
Barlund AS, Andre B, Sand K, Brenne AT. A qualitative study of bereaved family caregivers: feeling of security, facilitators and barriers for rural home care and death for persons with advanced cancer. BMC Palliat Care. 2021;20(1):7.
Nysaeter TM, Olsson C, Sandsdalen T, Wilde-Larsson B, Hov R, Larsson M. Preferences for home care to enable home death among adult patients with cancer in late palliative phase—a grounded theory study. BMC Palliat Care. 2022;21(1):49.
Brenne AT, Lohre ET, Knudsen AK, et al. Implementing a standardized care pathway integrating oncology, palliative care and community care in a rural region of mid-Norway. Oncol Ther. 2021;9(2):671–93.
Hjermstad MJ, Hamfjord J, Aass N, et al. Using process indicators to monitor documentation of patient-centred variables in an integrated oncology and palliative care pathway-results from a cluster randomized trial. Cancers (Basel). 2021;13(9):2194.
Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol. 2017;35(8):834–41.
Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302(7):741–9.
Article CAS PubMed PubMed Central Google Scholar
Groenvold M, Petersen MA, Damkier A, et al. Randomised clinical trial of early specialist palliative care plus standard care versus standard care alone in patients with advanced cancer: the Danish Palliative Care Trial. Palliat Med. 2017;31(9):814–24.
Vanbutsele G, Pardon K, Van Belle S, et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19(3):394–404.
Brenne AT, Knudsen AK, Raj SX, et al. Fully integrated oncology and palliative care services at a local hospital in mid-Norway: development and operation of an innovative care delivery model. Pain Ther. 2020;9(1):297–318.
Jordhoy MS, Fayers P, Saltnes T, Ahlner-Elmqvist M, Jannert M, Kaasa S. A palliative-care intervention and death at home: a cluster randomised trial. Lancet. 2000;356(9233):888–93.
Morita T, Miyashita M, Yamagishi A, et al. Effects of a programme of interventions on regional comprehensive palliative care for patients with cancer: a mixed-methods study. Lancet Oncol. 2013;14(7):638–46.
Morita T, Miyashita M, Yamagishi A, et al. A region-based palliative care intervention trial using the mixed-method approach: Japan OPTIM study. BMC Palliat Care. 2012;11:2.
St. Olavs Hospital HF. Forbedringsprogram 2013. https://ekstranett.helse-midt.no/1010/Sakspapirer/41-12%20Vedlegg%202%20Forbedringsprogram%20for%202013.pdf . (In Norwegian only]. Accessed 12 Dec 2017.
Norwegian Ministry of Health and Care Services. The Coordination Reform Proper Treatment—at the right place and right time (white paper). Norwegian Ministry of Health and Care Services; 2009. Report No. 47 (2008–2009) to the Storting. https://www.regjeringen.no/contentassets/d4f0e16ad32e4bbd8d8ab5c21445a5dc/en-gb/pdfs/stm200820090047000en_pdfs.pdf . Accessed 11 Dec 2017.
The Norwegian Directorate of Health. Nasjonalt handlingsprogram for palliasjon i kreftomsorgen [Norwegian National Giudelines]. Oslo: The Norwegian Directorate of Health; 2019. https://www.helsedirektoratet.no/tema/palliasjon . (In Norwegian). Accessed 18 Oct 2019
Driller B, Talseth-Palmer B, Hole T, Stromskag KE, Brenne AT. Cancer patients spend more time at home and more often die at home with advance care planning conversations in primary health care: a retrospective observational cohort study. BMC Palliat Care. 2022;21(1):61.
Sigurdardottir KR, Kaasa S, Rosland JH, et al. The European Association for Palliative Care basic dataset to describe a palliative care cancer population: results from an international Delphi process. Palliat Med. 2014;28(6):463–73.
Groenvold M, Petersen MA, Aaronson NK, et al. The development of the EORTC QLQ-C15-PAL: a shortened questionnaire for cancer patients in palliative care. Eur J Cancer. 2006;42(1):55–64.
Groenvold M, Petersen MA, on behalf of the EORTC Quality of Life Group EQoL. Addendum to the EORTC QLQ-C30 Scoring Manual: scoring of the EORTC QLQ-C15-PAL. 2006. http://www.dmcgpal.dk/files/addendum%20to%20the%20eortc%20qlq%20final%20july%202006.pdf . Accessed 09 Sept 2021.
Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer. 1980;45(8):2220–4.
Bouca-Machado R, Rosario M, Alarcao J, Correia-Guedes L, Abreu D, Ferreira JJ. Clinical trials in palliative care: a systematic review of their methodological characteristics and of the quality of their reporting. BMC Palliat Care. 2017;16(1):10.
Sourial N, Longo C, Vedel I, Schuster T. Daring to draw causal claims from non-randomized studies of primary care interventions. Fam Pract. 2018;35(5):639–43.
Kacha AK, Nizamuddin SL, Nizamuddin J, Ramakrishna H, Shahul SS. Clinical study designs and sources of error in medical research. J Cardiothorac Vasc Anesth. 2018;32(6):2789–801.
Haun MW, Estel S, Rucker G, et al. Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev. 2017; 6:CD011129.
Shanbhag D, Graham ID, Harlos K, et al. Effectiveness of implementation interventions in improving physician adherence to guideline recommendations in heart failure: a systematic review. BMJ Open. 2018;8(3): e017765.
Evans-Lacko S, Jarrett M, McCrone P, Thornicroft G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv Res. 2010;10:182.
Rosstad T, Salvesen O, Steinsbekk A, Grimsmo A, Sletvold O, Garasen H. Generic care pathway for elderly patients in need of home care services after discharge from hospital: a cluster randomised controlled trial. BMC Health Serv Res. 2017;17(1):275.
Hjermstad MJ, Pirnat A, Aass N, et al. PALLiative care in ONcology (PALLiON): a cluster-randomised trial investigating the effect of palliative care on the use of anticancer treatment at the end of life. Palliat Med. 2024;38(2):229–39.
Rosstad T, Garasen H, Steinsbekk A, Sletvold O, Grimsmo A. Development of a patient-centred care pathway across healthcare providers: a qualitative study. BMC Health Serv Res. 2013;13:121.
Sommerbakk R, Haugen DF, Tjora A, Kaasa S, Hjermstad MJ. Barriers to and facilitators for implementing quality improvements in palliative care—results from a qualitative interview study in Norway. BMC Palliat Care. 2016;15:61.
Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272–83.
Norwegian Ministry of Health and Care Services. Lindrende behandling og omsorg—Vi skal alle dø en dag. Men alle andre dager skal vi leve (white paper). Norwegian Ministry of Health and Care Services; 2020. Report No. 24 (2019–2020) to the Storting. https://www.regjeringen.no/no/dokumenter/meld.-st.-24-20192020/id2700942/ . Accessed 1 Oct 2020.
Lohre ET, Thronaes M, Brunelli C, Kaasa S, Klepstad P. An in-hospital clinical care pathway with integrated decision support for cancer pain management reduced pain intensity and needs for hospital stay. Support Care Cancer. 2019;28(2):671–82.
Download references
Acknowledgements
The authors thank the Norwegian Cause of Death Registry and Cancer Registry of Norway for providing data. We also thank the study nurses Kjellrun Gravdal and Randi Sunde for their work in the inclusion of participants and data collection, the Study Office at the Cancer Clinic, St. Olav’s Hospital Trondheim University Hospital, and all healthcare professionals at Orkdal Hospital, Molde Hospital, and in the 22 participating municipalities, for their contribution. Finally, we express our gratitude to all patients who participated.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
This work was supported by Norwegian Foundation Dam for Health and Rehabilitation [grant number 148113], the Norwegian Cancer Society, the Norwegian Directorate of Health [grant number 11/2341-26], Norwegian Women’s Public Health Association Orkdal, European Palliative Care Research Centre (PRC), St. Olavs’ Hospital Trondheim University Hospital, and Norwegian University of Science and Technology. The Rapid Service Fee was funded by Norwegian University of Science and Technology. The funding sources were not involved in preparation of the article.
Author information
Authors and affiliations.
Department of Clinical and Molecular Medicine, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway
Anne-Tove Brenne, Erik Torbjørn Løhre, Morten Thronæs & Bardo Driller
Cancer Clinic, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
Anne-Tove Brenne, Erik Torbjørn Løhre & Morten Thronæs
Department of Oncology, Oslo University Hospital, Oslo, Norway
Anne Kari Knudsen & Stein Kaasa
European Palliative Care Research Centre (PRC), Oslo University Hospital and University of Oslo, Oslo, Norway
Department of Oncology, Møre Og Romsdal Hospital Trust, Ålesund, Norway
Jo-Åsmund Lund & Bardo Driller
Department of Health Sciences in Ålesund, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Ålesund, Norway
Jo-Åsmund Lund
Department for Research and Innovation, Møre Og Romsdal Hospital Trust, Ålesund, Norway
Bardo Driller
Palliative Care, Pain Therapy and Rehabilitation Unit, Fondazione IRCCS Instituto Nazionale dei Tumori, Milan, Italy
Cinzia Brunelli
Institute of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, Norway
Stein Kaasa
You can also search for this author in PubMed Google Scholar
Contributions
Anne Kari Knudsen, Jo-Åsmund Lund, Morten Thronæs, and Stein Kaasa designed the study. Anne-Tove Brenne, Erik Torbjørn Løhre, Anne Kari Knudsen, and Bardo Driller recruited participants and collected data. Anne-Tove Brenne, Anne Kari Knudsen, and Cinzia Brunelli analyzed the data. Anne-Tove Brenne, Erik Torbjørn Løhre, and Stein Kaasa wrote the manuscript. Anne-Tove Brenne had the primary responsibility for the final content. All authors commented on previous versions of the manuscript, read, and approved the final version and consented to submission.
Corresponding author
Correspondence to Anne-Tove Brenne .
Ethics declarations
Conflict of interest.
Anne-Tove Benne, Erik Torbjørn Løhre, Anne Kari Knudsen, Jo-Åsmund Lund, Morten Thronæs, Bardo Driller, and Cinzia Brunelli declare that they have no competing interests. Stein Kaasa led the committee constituted by the Government from May 2016 to December 2017 that published the Official Norwegian Report on palliative care [ 6 ]. Anne Kari Knudsen’s affiliation has changed since the time of the study, and is now affiliated with County Governor Oslo and Viken, Oslo, Norway.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Committee for Medical Research Ethics Central Norway, REK Central (2014/212). Written informed consent was obtained from all individual participants included in the study. In cases where the participant was competent to give oral informed consent but not able to write, an adult family member or HCP signed a proxy consent.
Additional information
Anne Kari Knudsen’s affiliations have changed since the time of this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 177 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/ .
Reprints and permissions
About this article
Brenne, AT., Løhre, E.T., Knudsen, A.K. et al. Standardizing Integrated Oncology and Palliative Care Across Service Levels: Challenges in Demonstrating Effects in a Prospective Controlled Intervention Trial. Oncol Ther (2024). https://doi.org/10.1007/s40487-024-00278-3
Download citation
Received : 26 February 2024
Accepted : 16 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1007/s40487-024-00278-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- End-of-life
- Integration
- Palliative care
- Regional model
- Time at home
- Find a journal
- Publish with us
- Track your research
In People with Young-Onset Dementia, A Closer Look at Palliative Care
—a study from the netherlands examined palliative care practices in patients with young-onset dementia, concluding that a palliative approach is appropriate even in this population..
By Brett Moskowitz, MA Reviewed by Sejal Makvana Bhavsar, MD
For those with young-onset dementia (YOD)—defined as individuals developing symptoms before age 65—palliative care strategies have not been well studied, according to the investigators of a newly published study on palliative care in nursing home residents with YOD. 1
Baseline palliative care for people with dementia should address treatment, behavioral and psychological symptoms, comorbidities, and other health problems. 2 Another component of palliative care is advance care planning (ACP), which can include communication between the healthcare team, the patient, caregivers responsible for the patient’s care, as well as healthcare proxies. 3 The authors cite recent evidence that ACP actually improves end-of-life outcomes. 4
.jpg)
Special care units specifically for patients with YOD are available across the Netherlands and are supported by a national care program. 5,6 “Therefore,” write the authors, “the Dutch setting offers the opportunity to study palliative care practices in the unique context of infrastructure established for specialized nursing home care for young people living with dementia.” By using data from this population, the authors’ aim was to provide additional context and information about this under-studied population. 1
The study examined palliative care organizations and ACP using data collected between 2016 and 2022 from a baseline questionnaire completed by physicians, family caregivers, and nursing staff—the observational Care4Youngdem-study. The population was derived from a cohort that included 185 Dutch nursing home residents (from 16 long-term care institutions) with YOD (mean age = 63.9 years; 50.3% female; 42.2% diagnosed with Alzheimer’s disease dementia, the most common dementia subtype) for whom data was collected and available from all three respondents: physicians, family caregivers, and nursing staff. Included on the questionnaires were items on sociodemographics, quality of life measured with the quality of life in late-stage dementia (QUALID) scale, dementia-related somatic health problems, symptoms, pain medication, psychotropic drugs, and ACP. 1
As determined by family caregivers and nursing staff, respectively, the mean QUALID score among this patient cohort was 24.0 (SD 7.9), and 25.3 (SD 8.6). The most common dementia-related health issue was swallowing problems, occurring in 11.4% of patients. 1
Physicians and nursing staff, respectively, reported observed agitation at 42.0% and 40.5%. They also reported pain, respectively, at 18.6% and 30.2%. Family caregivers observed agitation and pain, respectively, at 34.6% and 25.2%, at least once a week over the previous month. 1
In this population, 29.5% were administered pain medication, and treatment with psychotropics was prescribed in 72.3% of cases—primarily antipsychotics (41.6%) and antidepressants (39.9%). Only 5.4% had written advance directives, and 27.2% had provided written treatment preferences from the former general practitioner. Comfort was the most common global care goal, noted by 73.9%. All interventions other than hospitalizations and antibiotics were more likely to include do-not-treat orders compared to do-treat orders. 1
Higher QOL scores—as indicated by lower QUALID scores—were given by family caregivers compared to nursing staff on average: 24.0 (SD 7.9) versus 25.3 (SD 8.6). The difference was even greater when assessing patients with advanced dementia, where mean QUALID scores were 24.8 (SD 8.7) among family caregivers and 28.6 (SD 9.2) among nursing staff. 1
“We discovered that neuropsychiatric symptoms caused larger symptom burden than physical symptoms,” says the study’s lead investigator, Jasper Maters, MD, of Radboud University Medical Center, Nijmegen, in the Netherlands. “Most residents have comfort care goals despite a relatively young age. Our findings should encourage healthcare professionals to start the conversation about treatment preferences in a timely manner, even before nursing home admission.”
The authors noted that this was the first study of palliative care-related characteristics of a YOD population in the Netherlands living in YOD-specific care units, with data given from three perspectives. They wrote that one of the strengths of this study was the use of validated instruments (eg, QUALID scores) that allow these data to be compared with other populations. However, one limitation could be that the findings are characteristic of this type of facility, which may not translate to different types of practices. Also, detailed data on diagnostic work-up of dementia type were not required in this questionnaire. Therefore, the accuracy of diagnoses could not be confirmed. 1
The authors concluded that palliative care should be considered appropriate for most people with YOD, and that ACP should be considered earlier in the disease process. 1 Maters and his colleagues are conducting additional research to further elucidate the impact of palliative care. “We have collected data on end-of-life care and hope to find out the effects of palliative care and advance care planning on end-of-life outcomes including comfort and family satisfaction,” he says.
Published: May 15, 2024
- 1. Maters J, van der Steen JT, de Vugt ME, Bakker C, Koopmans RTCM. Palliative care in nursing home residents with young-onset dementia: professional and family caregiver perspectives. J Alzheimers Dis . 2024;97:573-586. doi:10.3233/JAD-230486
- 2. van der Steen JT, Radbruch L, Hertogh CM, et al; European Association for Palliative Care. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med . 2014;28:197-209. doi:10.1177/0269216313493685
- 3. Rietjens JAC, Sudore RL, Connolly M, et al; European Association for Palliative Care. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol . 2017;18:e543-e551. doi:10.1016/S1470-2045(17)30582-X
- 4. Wendrich-van Dael A, Bunn F, Lynch J, et al. Advance care planning for people living with dementia: an umbrella review of effectiveness and experiences. Int J Nurs Stud . 2020;107: 103576. doi:10.1016/j.ijnurstu.2020.103576
- 5. Mulders AJ, Zuidema SU, Verhey FR, Koopmans RT. Characteristics of institutionalized young onset dementia patients–the BEYOnD study. Int Psychogeriatr . 2014;26:1973-1981. doi:10.1017/S1041610214001859
- 6. Bakker C, Verboom M, Koopmans R. Reimagining postdiagnostic care and support in young-onset dementia. J Am Med Dir Assoc . 2022;23:261-265. doi:10.1016/j.jamda.2021.12.008
In dementia, some symptoms vary by social and cultural factors, heart rate variability: a possible marker for agitation in alzheimer’s disease, is dementia risk altered by triglyceride levels in a higher “normal” range, singing away dementia-related verbal agitation—is that possible, depression and incident dementia: untangling this knot, for alzheimer’s disease, nordic walking may have possible cognitive benefits, acute agitation in long-term care residents: more injectables used during covid, alzheimer’s disease symptoms and their effects on caregivers.
.jpg)
- Study Protocol
- Open access
- Published: 18 May 2024
Co-designing strategies to improve advance care planning among people from culturally and linguistically diverse backgrounds with cancer: iCanCarePlan study protocol
- Ashfaq Chauhan 1 ,
- Upma Chitkara 1 ,
- Ramya Walsan 1 ,
- Ursula M. Sansom-Daly 2 , 3 , 4 ,
- Elizabeth Manias 5 ,
- Davinia Seah 6 ,
- Angie Dalli 7 ,
- Nadine El-Kabbout 8 ,
- Thit Tieu 9 , 10 ,
- Mashreka Sarwar 10 ,
- Misbah Faiz 11 ,
- Nancy Huang 12 ,
- Vitor Moraes Rocha 13 ,
- Abhijit Pal 14 &
- Reema Harrison 1
BMC Palliative Care volume 23 , Article number: 123 ( 2024 ) Cite this article
2 Altmetric
Metrics details
Advance care planning (ACP) describes the process of supporting individuals at any age or stage of health to consider and share their personal values, life goals, and preferences regarding future health care. Engaging in ACP is associated with better-quality of care in which people receive care in lines with their wishes, values and preferences. Direct translations of ACP guides and resources do not attend to the considerable inter- and intra-ethnic variations in cultural and religious or spiritual beliefs that shape preferences among people from culturally and linguistically diverse (CALD) backgrounds. ICanCarePlan is a three-year project that aims to determine the prevalence of ACP documentation among people from CALD backgrounds with cancer, identify resources available and their use to support ACP among CALD communities, identify barriers and facilitators of person-centred ACP, and to develop, through co-design with consumers and clinicians, approaches that enhance the process ACP for people from CALD backgrounds.
A mixed-method sequential approach will be used comprising of four studies. Study one is retrospective medical record review of approximately 1500 medical records to establish the prevalence of ACP documentation among CALD patient records in cancer services. Study two is a document analysis synthesising the resources available in the Australian health system to support ACP. Study three is a qualitative study with healthcare staff and consumers to explore barriers and enablers of person-centred ACP. Evidence generated from studies one to three will inform the conduct of co-design with stakeholders to develop approaches to improve ACP processes among CALD communities. Language, technical and financial support for meaningful involvement with consumers from CALD backgrounds throughout this project is outlined. A plan for distress management is also made due to sensitive nature of the topic. The research project has also established a project steering group consisting of three consumer members who are from CALD backgrounds.
The project will address a national priority issue for a growing population of CALD communities in Australia. The project will provide novel evidence of ACP among CALD communities and novel strategies developed with stakeholders to enhance uptake and experiences of ACP.
Peer Review reports
Introduction
Advance care planning (ACP) describes the process of supporting individuals at any age or stage of health to consider and share their personal values, life goals, and preferences regarding future health care [ 1 , 2 , 3 ]. ACP is a part of person-centred care; ACP should occur across the continuum of care, integrating specific values, goals and preferences with shared decision-making as care evolves [ 1 , 2 ]. For people with life-limiting disease, ACP provides individuals with opportunities to extend their autonomy in decision making to stages of life in which they are unable to make decisions for themselves [ 4 ]. ACP aids families and health care providers to make informed choices and to develop care plans aligning with patients’ values, goals and personal preferences [ 5 ]. In enhancing person-centred care and decision-making, ACP is associated with reduced hospitalisation, intensive care unit admission, invasive medical procedures at the end of life, and reduced stress, anxiety and depression amongst patients and support persons [ 5 , 6 , 7 , 8 , 9 , 10 ]. As a result, ACP is ultimately associated with improved quality of life for patients and carers [ 4 ].
Culturally and linguistically diverse (CALD) is a term used in Australian context to describe people who are born overseas or have a parent born overseas, or who speak a language other than English at home or engage in a cultural or religious practices that are different to the mainstream practices [ 11 , 12 ]. A narrative review of 43 studies published between 2017 and 2022 identified that culture, ethnicity and language proficiency influence opportunities for ACP, exposing CALD communities to potentially burdensome health care at the end of their life [ 13 ]. The review also identified that rate of uptake of ACP and the patient’s desire to talk and plan about death was related to length of stay in the destination country, acculturation and cultural and religious beliefs of ACP akin to defeat and competing with God [ 13 ]. Effective communication between healthcare staff and consumers (patients and their family or care support person) is an essential element of the ACP process [ 14 , 15 ]. Limited proficiency in English language was identified as a key factor contributing to poor quality ACP; a systematic review of 10 studies examining the use of interpreters among people with cancer with low-English proficiency identified inadequate goals of care discussions when professional interpreters were not used [ 16 ].
ACP can take many forms; when formally documented, an Advance Care Directive (ACD) is a formal plan of a person’s wishes and preferences about their future care. ACP often occurs informally and includes any instance of information sharing between healthcare staff, patients and/or their support person about their wishes, values and preferences for care [ 5 , 6 , 17 ]. There is limited evidence of the uptake of any form of ACP among people from CALD backgrounds experiencing cancer; limited administrative socio-cultural data available in patient records is a key challenge for generating this evidence. One large prospective audit study of 4,187 records of adults aged 65 years and over showed that there was a lower prevalence of completed advance care directives among those born outside of Australia (21.9%) compared to those born in Australia (28.9%) [ 17 ]. Further, the extent to which socio-cultural variables such as language spoken at home, preferred language, interpreter use, country of birth or parent’s country of birth, religion and time spent in the country of residence collectively influence the uptake of ACP is unclear.
Intra- and inter-group differences in the preferences, customs, values and expectations of care towards the end of life are notable among diverse CALD populations, reinforcing the importance of ACP for CALD communities. Documented differences include sharing the burden of worry and/or caregiving, attitudes towards explicit talk about death and dying within clinical encounters, traditional approaches as part of supportive care, and desire to be cared for/to die at home [ 7 , 8 ]. Yet healthcare staff and consumers have limited access to support them in engaging in ACP. Direct translations of ACP guides and resources do not attend to the range of cultural, religious or spiritual beliefs that shape preferences for end-of-life care (care delivered to the patient at the end of their life) for people from CALD backgrounds [ 18 , 19 , 20 ]. . Such guides may require cultural adaptation in their content and/or implementation – beyond direct language translation – to address the cultural and ethnic factors that shape preferences regarding end-of-life care and to support healthcare staff to engage in such communications. Without culturally and linguistically appropriate resources, people from CALD backgrounds may be left without the required support to engage in ACP and may be exposed to poor quality of care at the end of their life that is not aligned with their preferences, values or needs [ 21 , 22 ].
The iCanCarePlan project aims to address this gap by supporting ACP among people with cancer from CALD backgrounds. The project aims to provide novel evidence of the uptake and experience of ACP among CALD communities, resources available to support staff and consumers, and to co-design evidence-based approaches to improve the process of ACP between healthcare staff and CALD populations .
To determine the uptake and nature of ACP amongst people from CALD backgrounds experiencing cancer and examine socio-cultural factors predicting the uptake.
To characterise the resources available to support ACP in the Australian health system context and determine the extent of their relevance for people from CALD backgrounds.
To explore barriers and facilitators to ACP amongst people from CALD backgrounds with cancer and their clinicians.
To co-design a new or adapted culturally appropriate strategy to support person-centred, high-quality ACP for people from CALD backgrounds experiencing cancer.
Methods and analysis
Study design.
A mixed method sequential approach will be used comprising four studies (Fig. 1 ). A mixed-method approach [ 23 , 24 ] was selected to integrate information about the evidence of the extent of ACP (uptake and nature of ACP) among CALD populations, then identify resources available to support healthcare staff and consumers and the factors (barriers and facilitators) that have impact on ACP with CALD communities. This knowledge will inform a co-design process as the final study of the project. Co-design workshops will be conducted with consumer, policy and clinician stakeholders to collectively identify the target issue(s), design a solution(s) and develop a plan that will be used by the project team to implement the proposed solution(s).
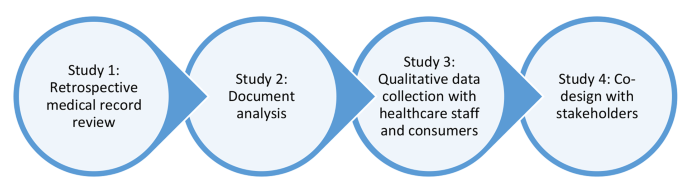
Pictorial representation of iCanCarePlan project comprising of four studies
Study 1: retrospective medical record review
Retrospective medical record review will be used to address objective one as an established approach to data collection pertaining to ACP. This approach has been used in past studies to determine the prevalence of ACP documentation [ 5 , 17 ]. This study methods will be guided by our prior medical record review research in Australian cancer services [ 25 ].
Study 1 will be conducted across three health services providing comprehensive cancer and/or palliative care to patients from CALD backgrounds with cancer. These services provide care in inpatient, outpatient and in the community setting. The services are located in three distinct government administrative areas in the state of New South Wales that have large population of people from diverse CALD backgrounds [ 26 ]. These three health services have been purposefully selected as they attend to a diverse demographic of CALD communities [ 26 ].
A total of 1500 medical records will be reviewed (500 at each site). This sample size is sufficient to address the study objectives. To determine the prevalence of ACP documentation based on estimated rate of 25% of ACP completion and 5% margin of error, a minimum sample size required is 300 records [ 27 ]. We will also explore association between prevalence of any ACP documentation with the seven socio-cultural variables that are recommended by the Australian Bureau of Statistics in their Standards for Statistics on Cultural and Language Diversity [ 28 ]. These seven variables are country of birth, language spoken at home, preferred language, interpreter required, year of arrival in Australia, religious affiliation and if one/both parents born overseas. Based on the formula n = 100 + 50(i) where (i) is the number of independent variables, minimal sample size required to examine the association is 450 medical records [ 29 ]. The sample size of 1500 is sufficient to explore the association between the presence of any ACP documentation and the seven socio-cultural variables outlined [ 29 ].
Eligibility and recruitment
A medical record will be eligible for inclusion if: (a) it belonged to a person from CALD background (born outside of Australia or had any/both parents born outside of Australia, speaks a language other than English at home or requires an interpreter) AND (b) there is a diagnosis of cancer that has poor prognosis, AND (c) it belongs to a person with cancer who had their first episode of care between January 2017 – December 2020 (an ‘episode of care’ defined as being seen by a health professional at the participating health service for a cancer-related illness and/or management for the first time). No age restrictions will be in place. Inclusion of cancers with poor prognosis for adults (> 18 years of age) and children and young adults (< 18 years of age) is based on identification by Cancer Australia National Cancer Control Indicators (Supplementary File A ) [ 30 , 31 ]. Records that do not meet the eligibility criteria will be excluded.
Data extraction
Each service will generate a list of patient records and the research team will apply the inclusion criteria to select eligible records using a random number generator. Once the eligible patient records are identified, a data extraction template (Supplementary File B ) will be used to collect data. Each medical record will be retrospectively reviewed from the time of their first episode of care to the current date or until the date for when the data is available.
Data analysis
Data analysis will be carried out using the R statistical software package. The primary outcome of interest will be the prevalence and type of ACP documentation (such as presence of an Advance Care Directive, resuscitation plan, conversation about goals of care or place of death) in the paper and/or electronic based medical records of patients with cancer from CALD backgrounds. Descriptive statistics (e.g., frequency, percent, sum, mean, median, standard deviation) will be used to describe the sample characteristics and frequency and nature of ACP documentation. Chi-square tests of independence will be used to compare key variables (such as age, sex, country of birth, language spoken at home, interpreter required, preferred language etc.) and logistic regression will be used to identify the association between the presence of ACP documentation to socio-cultural variables of the diverse CALD populations.
Study 2: document analysis
Altheide’s document analysis approach will be used to address objective two, to characterise and explore the relevance of current resources available to healthcare staff and consumers from CALD backgrounds that support them during the process of ACP [ 15 , 32 , 33 ].
The study will examine resources available at all levels of the Australian healthcare system. The websites of Australian government departments and health agencies at national, state and local health administrative levels will be searched. Relevant non-government organisations that have key focus on ACP, palliative and end-of-life care will be searched to identify and include eligible resources for analysis.
Eligibility and inclusion
Eligible data sources will comprise of contemporary resources (available in print, audio or video format) published from January 2013 to June 2023. Resources that provide guidance for the communication process for ACP (for example: question guides, how to guides, fact sheets, toolkits, techniques for communication other similar documents) will be eligible for inclusion. Strategic plans, policy documents, frameworks and implementation plans will be excluded as they do not provide the information relevant to the study objective. Resources relating to education modules and professional development courses will also be excluded.
The data extraction will be completed in accordance with the iterative process of search, selection and extraction outlined in prior research using the Altheide’s approach [ 15 ]. Two researchers will complete an initial search of the eligible organisations (Supplementary File C ) websites using key words (palliative care, end-of-life care, life support care, advance care directive, advance care planning, advanced personal plan, life wishes, substitute decision-maker, carer decision maker) to identify initial set of resources. These key words have been developed using collective knowledge and experience of the research team and relevant literature [ 34 , 35 ]. These resources will then be subjected to inclusion criteria by the two same researchers who completed the initial search and eligible resources will be identified. Any discrepancies during this stage will be resolved through discussion with the project lead. Data extraction tool will be developed and used to collect consistent information from the eligible documents relevant to study objective. The two researchers will complete the data extraction using the data extraction tool for the subset of the resources. The findings will be compared and discussed in a meeting with the project lead. Following this, one researcher will complete the data extraction of the remaining eligible resources with findings discussed in regular meetings with the project lead.
Narrative synthesis will be employed for evidence synthesis [ 15 ]. Contents of the eligible resources that provide guidance or support to consumers from CALD backgrounds or healthcare staff for the ACP will form the unit of analysis. The data extracted will be analysed to present the characteristics of the resources. Frequency, count and proportion of the resources will be presented under the categories of total number of resources, form (print, audio, video), source (government or non-government), target group (healthcare staff and/or consumers) and type of settings (such as primary, secondary, community, specialist or other). This will be followed by presenting a narrative description of operationalisation of ACP process with consumers from CALD backgrounds. We will examine the extent of cultural, religious or spiritual, language and other specific considerations for ACP with diverse CALD communities outlined or discussed in the included resources. We will also examine consumer involvement in development of the resources.
Study 3: qualitative data collection with healthcare staff and consumers
Qualitative data in the form of focus groups or interviews with healthcare staff and consumers will be used to address the objective three. Focus groups and semi-structured interviews provide a flexible approach to data collection to obtain in- depth data on experiences and expectations of ACP [ 36 , 37 ]. Given the nature of the discussion, some participants (especially consumers from CALD backgrounds) may not wish to participate in the focus groups. These participants will be provided the opportunity to participate via one-on-one semi-structured interviews with the researcher.
Evidence of the current barriers and enablers to ACP and use of current resources with CALD communities experiencing cancer will be captured nationally through focus groups with healthcare staff and consumers from CALD backgrounds accessing cancer care.
Number of the focus groups will be determined by emerging findings and point of saturation [ 36 , 38 ]. Approximately four to six focus groups (two-three focus groups with healthcare staff and two-three with CALD consumers and consumer representatives), with a total of up to 48 participants will be conducted. Each focus group will consist of six to eight participants. This sample size is sufficient to allow in-depth discussion on the topic while managing the amount of information collected to analyse the data [ 36 ].
Recruitment and eligibility
Healthcare staff working in cancer or palliative care for a minimum of six months, consumer representatives from consumer organisations that cater to cancer and palliative care, and consumers from CALD backgrounds who have used cancer or palliative care services will be eligible to participate in this study. All eligible participants will be 18 years of age or older and willing to provide consent for participation.
Participant recruitment and data collection will be an iterative process with focus groups and/or interviews conducted concurrently. Purposive sampling will be used to recruit participants through multiple channels (social media, networks and consumer organisations). Recruitment will be based on participant opt-in; contact details of the research team will be distributed through study advertisements (poster, social media posts) and potential participants will be provided with opportunity to contact research team first. Eligibility screen will be conducted, and eligible participants will be provided with study information sheet and consent form (PICF) prior to data collection. For participants who require language support during screening and recruitment, bilingual fieldworkers or interpreters will be used to convey the information and obtain consent as required. PICFs will be made available to participants in their preferred non-English language as needed.
Based on our previous work [ 39 ], we have established a project steering group that consists of three consumer members from CALD backgrounds with lived experience of cancer. Feedback from these three consumer members was sought for developing consumer facing research material such as the participation information sheet and recruitment advertisement to facilitate participation of consumers from CALD backgrounds in interviews or focus-groups and subsequent co-design workshops. These consumer members will also support the research team in developing a recruitment strategy for recruiting people from CALD backgrounds in this research.
Data collection
Data collection will commence after the consent is obtained and recorded. An interview guide informed by thematic domains framework (TDF) will be used to guide the qualitative data collection [ 40 , 41 ]. The TDF is selected to elicit responses from the participants to identify factors (barriers and facilitators) responsible for delivery of quality ACP with people from CALD backgrounds with cancer [ 42 ]. The focus groups/interviews will be conducted either online, face-to-face or using a hybrid model (combination of face-to-face and online participation) as suitable to the participants.
Data will be analysed using the Framework method [ 43 ]. TDF will be used as the framework for this analysis. Study data will be managed using NVivo [ 41 ]. The audio recording of the focus groups/interviews will be transcribed verbatim. Data will be transferred to NVivo, and analysis will be conducted in it. Data analysis will draw out common experiences and perceptions regarding the barriers and facilitators to ACP amongst people from CALD backgrounds experiencing cancer against the TDF framework. Data will be both inductively and deductively analysed. The data will be analysed and coded under the categories of TDF. A working analytical framework will be developed in the initial stage through an iterative process of re-reading and coding the transcripts between two researchers and the project lead. A Framework Matrix charting the final categories and codes will be developed. Following this, themes will be developed with preliminary themes refined in consultation with contribution from the wider research team.
Study 4 – co-design approaches to improve quality ACP
Adapted experienced-based co-design (EBCD) approach will be used to conduct this study. This approach has been used in our prior work to co-design health service interventions with relevant stakeholders including consumers from CALD backgrounds [ 39 , 44 ]. Adapted EBCD consist of two adaptations made to the co-design approach. These two adaptations are (a) inclusion of a preparatory stage to identify and meet various support needs of the co-design members and (b) inclusion of a consumer co-facilitator to mitigate power imbalance during co-design workshops [ 39 , 44 ]. These two adaptations aim to improve the meaningful participation of co-design members and improve their experiences of co-design process [ 39 ]. Following the preparatory phase, a series of three co-design workshops will be conducted accompanied by an introductory meeting between all co-design members and a set of preparatory meetings in between co-facilitators prior to each workshop (Fig. 2 .).
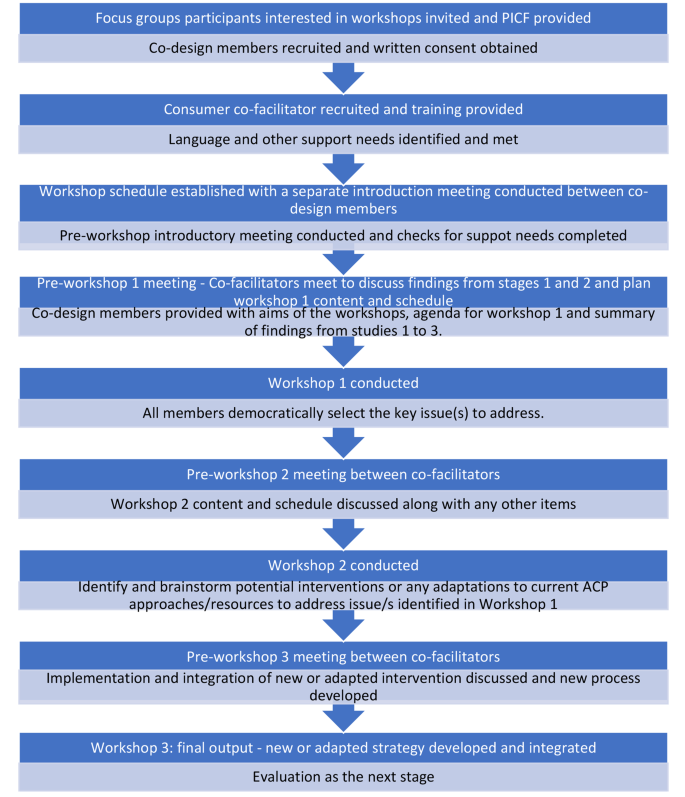
Co-design process
Preparatory work prior to co-design
Preparatory work will be undertaken to support meaningful participation of consumers from CALD backgrounds in co-design workshops [ 39 , 45 ]. This involves identifying and meeting the support needs of the co-design members and ensuring equal power distribution between all members during co-design.
Identifying support requirements
Based on our prior work [ 39 , 44 , 45 ], language, technological and financial support needs of the co-design members will be identified and addressed to enhance equal participation of all co-design members in the co-design workshops [ 45 ]. Professional interpreters or bilingual research fieldworkers will be used to provide language support as required by potential participants. Through our existing consumer co-facilitator network [ 46 ], we have access to bilingual research fieldworkers who can speak 11 languages. The members of this network are trained in conducting research and have knowledge of the research project. In a case where the language support is not provided with bilingual research fieldworker, an interpreter will be used. The mode of meeting (online, face to face or hybrid) will be determined based on the preferences of co-design members. Technical support will be provided via one-to-one communication with participants to facilitate online participation in the co-design workshops where necessary. Consumers and their representatives will be remunerated for their time to take part in the project appropriate to the nature of their roles based on the rates proposed by Health Consumers New South Wales [ 47 , 48 ].
Strategies to mitigate power imbalance during co-design
To enhance meaningful participation of consumers from CALD backgrounds and to minimise the power imbalance between researchers and consumers in co-design workshops, consumer co-facilitators will assist the research co-facilitator to conduct the co-design workshops [ 49 ]. Employing consumer and research co-facilitators in co-design encourages a more inclusive culture to encourage engagement and provide co-facilitators to adequately identify and address any issues and shifts in power dynamics [ 49 ]. Consumer co-facilitators will be provided a role description and receive training in the research topic and co-facilitation prior to the co-design workshops.
Co-design procedure
Approximately 4–6 members (2–3 consumers/consumer representatives and two-three healthcare staff) will be involved as members of the co-design group [ 39 , 50 ]. Based on our prior work with diverse consumers, this size of group membership provides an opportunity for all members to contribute fully and effectively including with use of interpreters and support persons [ 44 ]. The co-design group will also consist of research co-facilitators, a consumer co-facilitator and a bilingual fieldworker as needed relevant to the study population [ 39 ]. Those who have taken part in the focus groups/interviews will be requested to indicate their interest if they wish to be contacted about co-design workshops. Those who indicate willingness to be contacted will provide their email and telephone contact details for this purpose and be invited to take part as co-design members until 4–6 members have been recruited. The consumer co-facilitator will be recruited to co-facilitate each group via the existing consumer co-facilitator network. If any member withdraws from the co-design group, a new member will be invited to join the process. Recordings of the initial session(s) will be shared with the new members if they are joining late in the process. The change in co-design group members in between workshops would not impact the validity of the process but may introduce broader range of perspective enhancing the process. Written consent will be obtained prior to the conduct of co-design workshops.
Co-design workshops
The codesign groups will be convened to adapt, design and implement solutions to the priority issues identified through studies one to three. Written informed consent will be obtained prior to the conduct of co-design workshops. A suitable place to conduct the workshops will be identified in consultation with the co-design members. The co-design group will meet for no more than 10 h in total; approximately for 2.5 h for three times over a period of six weeks. The duration and timing of the groups will be determined by the members to ensure suitability. A separate introductory meeting will be conducted between the group members for 30-minute prior to first co-design workshop. In this meeting, the group will develop terms of reference that will determine their ways of working and the preferred mode of meeting (online, face to face or hybrid) and meeting duration and frequency. Co-facilitators will meet prior to each co-design workshop to determine the scope and content of each workshop based on the progress to that point. The co-facilitators will also contact co-design members in between workshops to address any queries or concerns or to receive any feedback that members were not able to provide in the workshop. Preparatory meetings in between the workshops will allow co-facilitators to integrate theory into the content of the subsequent workshops [ 51 ].
Ensuring study quality
The programme of work has been through independent peer review process as part of the Cancer Institute New South Wales Career Development Fellowship grant awarded to project lead (RH). This programme of work is funded based on the scientific quality of the proposal. The funding also requires an annual progress report to the funder. To further ensure the study quality, a project reference group has been established that meets twice in a year. The reference group consist of three consumer members with lived experience of cancer along with members from relevant policy, research, consumer interest and cancer and palliative care relevant organisations. Terms of reference have been co-developed with member of the project reference group. The main function of the reference group is to provide oversight on the project processes and progress against the research objectives.
The research project has received ethics approval from two National Health and Medical Research Council (NHMRC) accredited Human Research Ethics Committees (Reference number: 2023/ETH00216 and 520,231,235,452,528) by South-Western Sydney Local Health District Human Research Ethics Committee and Macquarie University Human Research Ethics Committee. Through the ethics applications and approvals, various ethical considerations have been explored and a risk mitigation plan created for each matter employing three main strategies.
Firstly, recognising the complexity of the programme of work involved, a research team consisting of project lead, project manager and associate investigators has been established. The research team will provide accountability for the conduct of the research activities. Secondly, recognising involvement of consumers from diverse language and cultural backgrounds and risk associated with potential for ineffective communication, budget has been allocated for translating consumer facing material and employing bilingual fieldworkers or interpreters in the research activities.
Thirdly, recognising the sensitivity of the topic area, the discussion about ACP may bring about distress to potential participants during qualitative data collection and in co-design workshops. This issue may arise in group discussions or during one-on-one interviews [ 52 ]. A process will be implemented whereby a list of supportive organisations will be provided to the participants prior, during and after each focus group/interview and co-design workshops. At the start of each focus group or interview and co-design workshop, research team will inform participant to let the research team know if they experience any distress. Participants will also be informed that they do not have to answer every question, that they can take a break from discussion at any time if they wish and if online, they can close their camera or video application if they need to [ 53 ]. During the discussion, if the researcher think that the participant is experiencing distress, the researcher will pause the discussion and ask if the participant requires a break. The researcher will also offer the list of support organisations if the participant wishes to speak with a relevant organisation. Participant will be asked if they require a referral for further support or if they require the researcher or the research team to contact their local general practitioner [ 53 ]. After each discussion, the researcher will follow-up with participants and co-design members to check on them. The project team also includes a practising clinical psychologist who could provide referrals for further support as needed.
Anticipated operational difficulties
The main anticipated difficulty relating to this program of work is recruitment of consumers from CALD backgrounds in qualitative data collection. Discussion about experiences and expectations of ACP may bring distress among consumers from any backgrounds, but particularly for people from CALD backgrounds where cultural meaning of disease such as cancer and death and dying is different to that of the non-CALD population [ 54 , 55 ]. Further varied cultural practices may dictate consumers readiness to talk about their experiences of ACP. Perception of a cancer as a ‘shameful’, stigmatised disease may further complicate the recruitment process [ 56 ]. To mitigate this issue, an iterative collaborative approach will be used. The researchers will identify and partner with community representatives, leaders and organisations working closely with various CALD communities to identify a recruitment strategy that would work for recruiting consumers from a particular community. This approach will be undertaken with help of the project steering group members, especially consumer members, who will assist with identification of these networks and introduce the research team where necessary. Through these connections, avenues for distributing recruitment material to recruit participants from CALD background and suitable approach for data collection (e.g. via focus group or on-one interview and most appropriate modality) will be determined. The iterative collaborative approach of working with consumer members of the project steering group and community representatives, leaders and organisations may also assist in identifying priority CALD communities to conduct language, culture or religion specific focus-groups or interviews. This approach will allow us to generate knowledge of the issues that may pertain to range of CALD populations but also be specific for some CALD communities.
Potential research, policy and practice implications
The Australian National Consensus Statement on essential elements for safe and high quality end-of-life care highlights ACP as an essential element of person-centred high quality end-of-life care [ 57 ]. Provision of culturally appropriate resources and communication have been highlighted in the Consensus Statement for achieving safe and high quality end-of-life care for people from CALD backgrounds [ 57 ]. Need for meaningful ACP conversations with priority population groups such as those from CALD backgrounds have also been identified as a national information priority by Australian Institute of Health and Welfare considering increasing population of people from diverse CALD backgrounds [ 58 ].
This program of work will contribute to advancing research, policy and practice for meaningful ACP with CALD communities in the following four ways. The medical record review study will provide a real-world data on ‘what is happening’. This study will identify gaps for communities for ACP processes and documentation. The document analysis study will help understand the current state of ‘what is available’. This study will identify gaps in the resources and where the adaptation or new strategy are required to support healthcare staff or consumers to facilitate meaningful ACP. Qualitative data collected through focus groups or interviews will inform ‘how the conversations are happening’. This study will help understand needs, desires, barriers and facilitators for meaningful ACP and will directly inform how the strategy need to be tailored to suit the needs of CALD populations. Co-design will then help partner with end service users to directly shape the strategy to improve ACP that they receive. The co-designed strategy developed will be reported in the context of quality ACP issue addressed, the adaptation made to the process, the population who co-designed the strategy and the target population for whom the co-designed strategy is relevant for. The co-design strategy will also report on potential process and outcome success measures. Application of the strategy to address diverse cultural needs will be discussed along with the need for future adaptations to suit diverse CALD populations. The plan for implementation and evaluation of the strategy will follow as next steps separate to this programme of work.
The project will address a national priority issue for a growing population of CALD communities in Australia. The project will provide novel evidence of ACP among CALD communities and novel strategies developed with stakeholders to enhance uptake and experiences of ACP. communities in Australia. The project will also provide important process related knowledge for enhancing participation of consumers from CALD communities in research concerning sensitive topics. Implementation and evaluation of the co-designed approach will be the next step.
Data availability
No datasets were generated or analysed during the current study.
Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, et al. Defining Advance Care planning for adults: a Consensus Definition from a Multidisciplinary Delphi Panel. J Pain Symptom Manag. 2017;53(5):821–e321.
Article Google Scholar
Rosa WE, Izumi S, Sullivan DR, Lakin J, Rosenberg AR, Creutzfeldt CJ, et al. Advance Care Planning in Serious Illness: a narrative review. J Pain Symptom Manag. 2023;65(1):e63–78.
Rietjens JAC, Sudore RL, Connolly M, van Delden JJ, Drickamer MA, Droger M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–51.
Article PubMed Google Scholar
Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000–25.
Detering KM, Buck K, Ruseckaite R, Kelly H, Sellars M, Sinclair C, et al. Prevalence and correlates of advance care directives among older australians accessing health and residential aged care services: multicentre audit study. BMJ Open. 2019;9(1):e025255.
Article PubMed PubMed Central Google Scholar
Ruseckaite R, Detering KM, Evans SM, Perera V, Walker L, Sinclair C, et al. Protocol for a national prevalence study of advance care planning documentation and self-reported uptake in Australia. BMJ Open. 2017;7(11):e018024.
Johnson S, Butow P, Kerridge I, Tattersall M. Advance care planning for cancer patients: a systematic review of perceptions and experiences of patients, families, and healthcare providers. Psychooncology. 2016;25(4):362–86.
Licqurish S, Phillipson L, Chiang P, Walker J, Walter F, Emery J. Cancer beliefs in ethnic minority populations: a review and meta-synthesis of qualitative studies. Eur J Cancer Care. 2017;26(1):e12556.
Spelten ER, Geerse O, van Vuuren J, Timmis J, Blanch B, Duijts S, et al. Factors influencing the engagement of cancer patients with advance care planning: a scoping review. Eur J Cancer Care (Engl). 2019;28(3):e13091.
Roeland EJ, Lindley LC, Gilbertson-White S, Saeidzadeh S, Currie ER, Friedman S, et al. End-of-life care among adolescent and young adult patients with cancer living in poverty. Cancer. 2020;126(4):886–93.
Australian Instiotut of Health and Welfare. Cultural and linguistic diversity measures in aged care: working paper. Canberra: AIHW; 2014.
Australian Institute of Health and Welfare. Australia’s Health 2018 Canberra AIHW; 2018.
Glyn-Blanco MB, Lucchetti G, Badanta B. How do cultural factors influence the provision of end-of-life care? A narrative review. Appl Nurs Res. 2023;73:151720.
Green A, Jerzmanowska N, Green M, Lobb EA. Death is difficult in any language’: a qualitative study of palliative care professionals’ experiences when providing end-of-life care to patients from culturally and linguistically diverse backgrounds. Palliat Med. 2018;32(8):1419–27.
Chauhan A, Walpola RL, Manias E, Seale H, Walton M, Wilson C, et al. How do health services engage culturally and linguistically diverse consumers? An analysis of consumer engagement frameworks in Australia. Health Expect. 2021;24(5):1747–62.
Silva MD, Genoff M, Zaballa A, Jewell S, Stabler S, Gany FM, et al. Interpreting at the end of life: a systematic review of the impact of interpreters on the delivery of Palliative Care services to Cancer patients with Limited English proficiency. J Pain Symptom Manage. 2016;51(3):569–80.
Sinclair C, Sellars M, Buck K, Detering KM, White BP, Nolte L. Association between Region of Birth and Advance Care Planning Documentation among older Australian migrant communities: a Multicenter Audit Study. Journals Gerontology: Ser B. 2021;76(1):109–20.
Harrison R, Walton M, Chitkara U, Manias E, Chauhan A, Latanik M, et al. Beyond translation: engaging with culturally and linguistically diverse consumers. Health Expect. 2020;23(1):159–68.
de Arruda-Colli MNF, Sansom-Daly U, Dos Santos MA, Wiener L. Considerations for the cross-cultural adaptation of an advance care planning guide for youth with cancer. Clin Pract Pediatr Psychol. 2018;6(4):341–54.
PubMed PubMed Central Google Scholar
Evans HE, Jessop S, Bedoya SZ, Lyon ME, Wiener L, Sansom-Daly UM. Examining the Cultural appropriateness of Advance Care Planning Tools for adolescents and Young adults with Cancer: an example of cross-cultural adaptation of the voicing my CHOiCES Tool. Curr Probl Cancer. 2023;47(5):101010.
Harley HYK, Joesph L, Delan D, Bridget C. Experience and perspectives on palliative or end-of-life care of Chinese people and their families as immigrants to high-income countries: a systematic review and thematic synthesis. BMJ Global Health. 2020;5(12):e003232.
Francois K, Lobb E, Barclay S, Forbat L. The nature of conflict in palliative care: a qualitative exploration of the experiences of staff and family members. Patient Educ Couns. 2017;100(8):1459–65.
Shorten A, Smith J. Mixed methods research: expanding the evidence base. Evid Based Nurs. 2017;20(3):74.
Tashakkori A, Creswell JW. Editorial: the New era of mixed methods. J Mixed Methods Res. 2007;1(1):3–7.
Chauhan A. Consumer engagement for patient safety: strategies for consumer engagement for culturally and linguistically diverse consumers in cancer services. Macquarie University; 2023.
Australian Bureau of Statistics. Data by region ABS; 2023.
Johnston KM, Lakzadeh P, Donato BMK, Szabo SM. Methods of sample size calculation in descriptive retrospective burden of illness studies. BMC Med Res Methodol. 2019;19(1):9.
Australian Bureau of Statistics. Latest release: standards for statistics on Cultural and Language Diversity. Canberra, ACT: ABS; 2022.
Google Scholar
Bujang MA, Sa’at N, Sidik T, Joo LC. Sample size guidelines for logistic regression from Observational studies with large Population: emphasis on the Accuracy between statistics and parameters based on Real Life Clinical Data. Malays J Med Sci. 2018;25(4):122–30.
Cancer Australia. National Cancer Control indicators - five-year relative survival by stage at diagnosis for childhood cancers. Sydney, Australia: Cancer Australia; 2021.
Cancer Australia. National Cancer Control indicators – 5-year relative survival from diagnosis. 2022. Sydney, Australia: Cancer Australia; 2022.
Altheide DL, Qualitative Media A. 1996 2020/09/01. Thousand Oaks, California: SAGE Publications, Inc. https://methods.sagepub.com/book/qualitative-media-analysis .
Esbati A, Barnes M, Henderson A, Taylor J. Legislation, policies and guidelines related to breastfeeding and the Baby Friendly Health Initiative in Australia: a document analysis. Aust Health Rev. 2018;42(1):72–81.
Tran J, Sellars M, Nolte L, White BP, Sinclair C, Fetherstonhaugh D, et al. Systematic review and content analysis of Australian health care substitute decision making online resources. Aust Health Rev. 2021;45(3):317–27.
Pereira-Salgado A, Mader P, Boyd LM. Advance care planning, culture and religion: an environmental scan of Australian-based online resources. Aust Health Rev. 2018;42(2):152–63.
Morgan D. Focus Groups as Qualitative Research. Thousand Oaks, California1997. https://methods.sagepub.com/book/focus-groups-as-qualitative-research .
Jamshed S. Qualitative research method-interviewing and observation. J Basic Clin Pharm. 2014;5(4):87–8.
Krueger RA. Focus groups: a practical guide for applied research. California: Sage; 2014.
Harrison R, Walton M, Manias E, Wilson C, Girgis A, Chin M, et al. Codesigning consumer engagement strategies with ethnic minority consumers in Australian cancer services: the CanEngage Project protocol. BMJ Open. 2021;11(8):e048389.
McGowan LJ, Powell R, French DP. How can use of the theoretical domains Framework be optimized in qualitative research? A rapid systematic review. Br J Health Psychol. 2020;25(3):677–94.
Francis JJ, O’Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci. 2012;7(1):35.
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117.
Chauhan A, Newman B, Roberto E, Walpola RL, Seale H, Chin M, et al. Making it meaningful’: co-designing an intervention to improve medication safety for people from culturally and linguistically diverse backgrounds accessing cancer services. Patient Experience J. 2023;10(2):34–48.
Chauhan A, Leefe J, She EN, Harrison R. Optimising co-design with ethnic minority consumers. Int J Equity Health. 2021;20(1):240.
Easpaig BRNG, Shé ÉN, Chauhan A, Newman B, Joseph K, Tieu NT et al. Enabling the space and conditions for co-leadership in co-design: an evaluation of co-facilitator training for CALD consumers. Public Health Res Pract. 2022.
Health Consumers NSW. Remuneration and reimbursement guidelines for consumer involvement in health and medical research. Sydney: Health Consumers NSW; 2022.
Health Consumers NSW. Remuneration and reimbursement of health consumers. Sydney: Health Consumers NSW; 2022.
Harrison R, Newman B, Chauhan A, Sarwar M. Employing cofacilitation to balance power and priorities during health service codesign. Health Expectations. 2023;n/a(n/a).
Dimopoulos-Bick T, Dawda P, Maher L, Verma R, Palmer V. Experience-based Co-design: tackling common challenges. J Health Des. 2018;3:86–93.
Reema H, Éidín NS, Deborah D, Ashfaq C, Bronwyn N. Creating space for theory when co-designing healthcare interventions. J Eval Clin Pract 2022.
Sansom-daly UM, Wakefield CE, McGill BC, Patterson P. Ethical and Clinical Challenges Delivering Group‐based cognitive‐behavioural therapy to adolescents and young adults with Cancer using Videoconferencing Technology. Australian Psychol. 2015;50(4):271–8.
Sansom-Daly UM, Wakefield CE, Bryant RA, Butow P, Sawyer S, Patterson P, et al. Online group-based cognitive-behavioural therapy for adolescents and young adults after cancer treatment: a multicenter randomised controlled trial of recapture Life-AYA. BMC Cancer. 2012;12:339.
Wiener L, McConnell DG, Latella L, Ludi E. Cultural and religious considerations in pediatric palliative care. Palliat Support Care. 2013;11(1):47–67.
Chauhan A, Walton M, Manias E, Walpola RL, Seale H, Latanik M, et al. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health. 2020;19(1):118.
Hughson J-a, Woodward-Kron R, Parker A, Hajek J, Bresin A, Knoch U, et al. A review of approaches to improve participation of culturally and linguistically diverse populations in clinical trials. Trials. 2016;17(1):263.
Australian Commission on Safety and Quality in Health Care. National Consensus Statement: essential elements for safe and high–quality end–of–life care. Sydney: ACSQHC; 2023.
Australian Institute of Health and Welfare in collaboration with the Palliative Care and End-of-Life Care Data Development Working Group. National Palliative Care and End-of-Life Care Information priorities. Canberra: AIHW; 2022.
Download references
Acknowledgements
We would like to thank Sheetal Challam, Philippa Sambevski, Lisa Woodland, Lukas Hofstatter, Nadine El-Kabbout, Mashreka Sarwar, Thit Tieu, Elizabeth Manias, Angie Dalli, Ursula Sansom-Daly, Misbah Faiz and Vitor Moraes Rocha for their continuing support as members of the iCanCarePlan project steering group.
This research project is funded by Cancer Institute NSW via a Career Development Fellowship awarded to project lead Professor Reema Harrison. The Fellowship application underwent scientific peer review by the funding body as part of the funding process.
Author information
Authors and affiliations.
Centre for Health Systems and Safety Research, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, North Ryde, NSW, Australia
Ashfaq Chauhan, Upma Chitkara, Ramya Walsan & Reema Harrison
Behavioural Sciences Unit, School of Clinical Medicine, Discipline of Paediatrics & Child Health, UNSW Medicine and Health, Randwick Clinical Campus, UNSW Sydney, Sydney, NSW, Australia
Ursula M. Sansom-Daly
Kids Cancer Centre, Sydney Children’s Hospital, Sydney, NSW, Australia
Sydney Youth Cancer Service, Nelune Comprehensive Cancer Centre, Prince of Wales Hospital, Sydney, NSW, Australia
School of Nursing and Midwifery, Monash University, Melbourne, Victoria, Australia
Elizabeth Manias
Sacred Heart Supportive and Palliative Care, St Vincent’s Hospital Sydney, Sydney, NSW, Australia
Davinia Seah
Australian Commission on Safety and Quality in Health Care, Sydney, NSW, Australia
Angie Dalli
Nafs Counselling, Sydney, NSW, Australia
Nadine El-Kabbout
Sisters’ Cancer Support Group Inc., Sydney, NSW, Australia
Centre for Health Systems and Safety Research, Australian Institute of Health Innovation, Macquarie University, North Ryde, NSW, Australia
Thit Tieu & Mashreka Sarwar
District Clinical Governance, South Western Sydney Local Health District, Sydney, NSW, Australia
Misbah Faiz
Macarthur Cancer Therapy Centre, South Western Sydney Local Health District, Sydney, NSW, Australia
Nancy Huang
Murray Primary Health Network, Bendigo, Victoria, Australia
Vitor Moraes Rocha
Liverpool Hospital, South Western Sydney Local Health District, Sydney, NSW, Australia
Abhijit Pal
You can also search for this author in PubMed Google Scholar
Contributions
RH conceived the project and is the project lead. AC, UC, RW and UMSD contributed to design of individual studies through regular meeting. AC and UC will be largely responsible for collecting data for the studies outlined in the project. EM, DS, AD, NEK, TT, MS, MF, NH, VR and AP provided guidance on the conduct of the studies. AC drafted the initial and subsequent draft of the manuscript with RH. UC, RW, UMSD, EM, DS, AD, NEK, TT, MS, MF, NH, VR, AP and RH provided intellectual content to the manuscript, edited and reviewed the final draft. RH acquired the funding for the project.
Corresponding author
Correspondence to Ashfaq Chauhan .
Ethics declarations
Ethics approval and consent to participate.
The research project has received ethics approval from two National Health and Medical Research Council (NHMRC) accredited Human Research Ethics Committees (Reference number: 2023/ETH00216 and 520231235452528) by South-Western Sydney Local Health District Human Research Ethics Committee and Macquarie University Human Research Ethics Committee. While no direct patient data is collected for the protocol manuscript, informed written consent will be obtained from participants prior to data collection where applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chauhan, A., Chitkara, U., Walsan, R. et al. Co-designing strategies to improve advance care planning among people from culturally and linguistically diverse backgrounds with cancer: iCanCarePlan study protocol. BMC Palliat Care 23 , 123 (2024). https://doi.org/10.1186/s12904-024-01453-z
Download citation
Received : 11 January 2024
Accepted : 08 May 2024
Published : 18 May 2024
DOI : https://doi.org/10.1186/s12904-024-01453-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Advance care planning
- End-of-life care
- Culturally and linguistically diverse
- Person-centred care
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Click here to review the draft Palliative and End-of-Life Care - Interactive Case Study. The following case vignette provides key concepts that could be considered when developing a plan of care for a patient who may require a controlled substance to manage their health concerns. As with any clinical situation, there are many patient ...
own decisions about their health care. The five case studies presented in this issue of Healing Hands will highlight issues and challenges that clinicians may confront while providing palliative care to patients experiencing homelessness. Case #1: Mr. J Case study Mr. J was a man in his mid-50s who was admitted to a recuperative care program in ...
Case 2.18 Fungating Wounds and the Palliative Care Patient 220 Laura C. Harmon Case 2.19 Pressure Ulcer Care in Palliative Care 229 Laura C. Harmon Case 2.20 Treating Ascites 239 ... Case Studies In Palliative and End-of-Life Care is written for clinicians caring for patients and their families across diagnoses, illness trajectories, settings ...
The following is a case study of a patient who resided in the CCU for over 8 months. ... Most people approaching end of life die in the hospital and 20% of those die in a CCU. 2 Palliative and end-of-life care are realistic and ethical options that should be considered much sooner for many patients in the CCU. 3 Clinical team members need to ...
The UPMC Palliative and Supportive Institute shares monthly cases on areas such as managing pain, dealing with grief, and other palliative care topics. View current cases here. View archived cases below. If you have questions or insights about a case, feel free to contact the institute. Browse the extensive archive of palliative and supportive ...
One of the goals of the UPMC Palliative and Supportive Institute is to advance the practice of our specialty by sharing our knowledge with students and health care professionals around the world. To this end, we share monthly synopses of notable or particularly interesting cases in which palliative care has played a role. If you have any ...
Case Studies in Palliative and End-of-Life Care uses a case-based approach to provide students and practitioners with an important learning tool to improve critical thinking skills and encourage discussion toward improving experiences for patients and their families. The book is organized into three sections covering subjects related to communication, symptom management, and family care.
Many randomized, controlled trials and case-control studies of palliative care interventions to date have shown reductions in patients' symptoms and health care utilization and improvements in ...
Patient-centered family meetings "Patient-centered" palliative care is critical as it focuses on the patient's quality of life 18 and the imperative to address patient's end-of-life clinical, psychosocial, and spiritual concerns and needs in a timely manner. Patient-centered care may be defined as health care that is respectful and responsive to patients' preferences and needs while also ...
Medicare's new focus on end-of-life care has driven nurses and other clinicians to re-examine when advanced care planning should begin, and serious illness discussions should be conducted. This article will address barriers to, cultural influences on, framing of, and documentation of serious illness discussions using a case study approach.
A case study: highlighting the importance of multidisciplinary working in palliative care for a patient with psychological trauma. Hos Pal Med Int Jnl. 2020;4(2):46‒49. DOI: 10.15406/hpmij.2020.04.00185 The value and power of the MDT approach is illustrated in this case report, whereby a lady who has suffered for a large part of her
Maintaining patients' autonomy at the end of life is a challenging subject that needs to be addressed using a contextualized approach. One alternative demarche in setting care goals and shared decision-making may be "relational autonomy". To this end, the case of an end-stage patient in the need of palliative care and the related ethical ...
Palliative Care. The Case for Hospital Palliative Care—Improving Quality. Reducing Cost. 3 Hallmarks of a Vital Trend Based on need, not prognosis, palliative care responds to the episodic, complex, and long-term nature of serious illness. The pillars of palliative care are: → Improved quality leading to lower costs—of hospital care.
2. Explain the importance of honoring Advance Directives. 3. Demonstrate influence of multicultural background of health care providers and the care perspective. 4. Explain how an interdisciplinary Palliative Care Team utilizing a transdisciplinary approach impacts patient outcomes.
Organisational case study methodology will be used to guide the study design. In total, 50 cases will be conducted in five European countries (10 per country). A case involves a semi-structured interview with a relative and an HCP closely involved in the care of a deceased patient who received some type of palliative sedation at the end-of-life.
The Journal of Palliative Care is a quarterly, peer-reviewed, international and interdisciplinary forum for practical, critical thought on palliative care and palliative medicine.JPC publishes high-quality original research, opinion papers/commentaries, narrative and humanities works, case reports/case series, and reports on international activities and comparative palliative care.
Effective integration between hospices, palliative care services and other local health care services to support patients with palliative care needs is an important international priority. A previous model suggests that integration involves a cumulative stepped process of engagement with other organisations labelled as 'support, supplant or supplement', but the extent to which this model ...
Study design. The qualitative case study model proffered by Robert Stake [30,31,32] was adopted in examining the emergence of EoLC in Macao, and developing a theoretical understanding of the EoLC establishment from a social movement perspective.The 'EoLC within the context of Macao' was determined as 'the case', in order to reinforce the focus of enquiry for the present study.
Hospice Case Studies Case 1 . Ms. Wamser is an 87-year-old woman with a hx of hypertension, hypothyroidism and advanced dementia consistent with Alzheimer's type dementia. She experienced a gradual functional decline and ... The correct answer is "C" complex wound care. Patient with open wounds requiring "frequent skilled
In the aforementioned Delphi study on case management for patients with dementia, no agreement could be reached on similar topics . ... Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med. 2005; 8:26-35. doi: 10.1089/jpm.2005.8.26.
The complex and often changing medicines regimens for palliative care patients can be challenging for medicines optimisation. ... Case study. Palliative care part 1: pain management. Mary*, aged 54 years, comes into the pharmacy and asks to speak to the pharmacist about her prescribed medicines. She was recently diagnosed with metastatic ...
Indeed, it has been conjectured that the level of suffering described by MS patients is comparable with that experienced by amyotropic lateral sclerosis and cancer patients—common recipients of palliative care. 5,28 Thus, a case study is presented to demonstrate the need for conjunctive palliative care (see Table 2).
Case 5: A man with advanced ALS requests a do-not-resuscitate order. Carter has ALS, or amyotrophic lateral sclerosis, a progressive neurodegenerative disease. He has been hospitalized with infection five times and is on a ventilator. Carter is alert and told doctors he wants to return home and sign a do-not-resuscitate order (DNR).
The rate of referrals to palliative care increased from 16.6 to 43.9 percent, says Courtright, lead author of the study. Length of hospital stay did not decline overall, but it did drop by 9.6 ...
Background Patients with palliative care needs live with the reality of limited time due to illness or age, eliciting emotional and existential responses. A failure to address their existential needs can lead to significant suffering. A person-centred approach is paramount to effectively address these needs, emphasising holistic care and effective communication. Although existing communication ...
Background: Few studies have explored the outcomes of patients placed on comfort care with respect to hospice disposition. The objective of this study was to perform a retrospective analysis of patients who transitioned to comfort care. Methods: We conducted a retrospective study of patients placed on the comfort care order set between July 1st, 2021, until June 30th, 2022.
Though international humanitarian organizations consider palliative care an international public health priority [], there is a large unmet global need for palliative care that is projected to grow wider in the coming years [].While models of palliative care originally focused on patients with cancer, the subspecialty of neuropalliative care developed to meet the unique needs of patients and ...
Introduction Patients with cancer often want to spend their final days at home. In Norway, most patients with cancer die in institutions. We hypothesized that full integration of oncology and palliative care services would result in more time spent at home during end-of-life. Methods A prospective non-randomized intervention trial was conducted in two rural regions of Mid-Norway. The hospitals ...
Family caregivers observed agitation and pain, respectively, at 34.6% and 25.2%, at least once a week over the previous month. 1. In this population, 29.5% were administered pain medication, and ...
Green A, Jerzmanowska N, Green M, Lobb EA. Death is difficult in any language': a qualitative study of palliative care professionals' experiences when providing end-of-life care to patients from culturally and linguistically diverse backgrounds. Palliat Med. 2018;32(8):1419-27. Article PubMed Google Scholar