
- Critical Care Medicine
Explore the latest in critical care medicine, including management of respiratory failure, sepsis, HAI prevention, end-of-life care, and more.

Publication
Article type.
This trial protocol of Precision Resuscitation With Crystalloids in Sepsis (PRECISE) intends to test a machine learning algorithm to alert clinicians to the potential benefits of balanced crystalloids compared with normal saline in patients with a group D sepsis subphenotype.
- Noninvasive Ventilation in COPD—Pressure Matters JAMA Opinion September 16, 2024 Respiratory Failure and Ventilation Chronic Obstructive Pulmonary Disease Pulmonary Medicine Full Text | pdf link PDF
This randomized clinical trial compares the effect of high-intensity noninvasive positive pressure ventilation (NPPV) vs low-intensity NPPV on the need for endotracheal intubation in patients with an acute exacerbation of chronic obstructive pulmonary disease and hypercapnia.
This consensus study presents recommendations from a 51-member working group regarding kidney follow-up care for infants discharged from the neonatal intensive care unit.
This narrative review outlines diagnostic and treatment approaches to necrotizing soft tissue infections and suggests future directions while mentioning promising developments in their management.
This randomized clinical trial compares the effects of treatment with iloprost vs placebo on organ failure severity for adults in the intensive care unit with septic shock and endotheliopathy.
This cohort study of pediatric cardiac intensive care unit admissions explores whether an in-hospital cardiac arrest incidence reduction was maintained during a 2-year follow-up period among hospitals that engaged in a cardiac arrest prevention quality improvement project.
In this narrative medicine essay, a neonatologist through the complex forces of intensive care physician, son, and ethicist grapples with the impending loss of his father and ultimately understanding his father’s demand for autonomy in deciding his care.
This cohort study examines rates of vaccination for COVID-19 and for influenza among children receiving long-term home ventilation.
This cross-sectional study examines the longitudinal trends in endotracheal intubation and supraglottic airway utilization for airway management in a national emergency medical services cohort.
A man in his early 50s was admitted to the hospital after acute hypoxemic respiratory failure and cardiac arrest following aspiration, requiring 3 minutes of cardiopulmonary resuscitation. One day after extubation, he noticed blurry vision peripherally and difficulty focusing at near. What would you do next?
- A New Assay Might Speed Antimicrobial Susceptibility Testing in Sepsis JAMA News August 16, 2024 Infectious Diseases Antibiotic Use, Overuse, Resistance, Stewardship Resuscitation Sepsis Pathology and Laboratory Medicine Full Text | pdf link PDF
This cohort study assesses whether antithrombin III deficiency is associated with thrombohemorrhagic complications among patients with trauma.
In this narrative medicine essay, a pediatric critical care physician explores the right moment to speak with parents about their child’s life or death outcome, relying on the various elements involved in predicting an iffy endeavor.
This cohort study investigates the association between umbilical cord pH values and the risk of adverse neonatal outcomes among newborns in Denmark, which has universal umbilical cord pH measurement.
This systematic review and meta-analysis investigates the association between continuous positive airway pressure (CPAP) therapy and reduction of adverse hypertensive outcomes in pregnant women.
This systematic review and meta-analysis evaluates the clinical outcomes associated with daily sedation interruption vs continuous intravenous sedation in children receiving mechanical ventilation support.
This Medical News story discusses the rise in ransomware cyberattacks on health care, as well as new cybersecurity initiatives.
This cohort study evaluates patient and event characteristics associated with cardiopulmonary resuscitation (CPR) duration among pediatric patients with in-hospital cardiac arrest without return of circulation and whether hospitals with longer median durations of CPR have higher survival rates among all children requiring CPR.
This cohort study investigates the association of neonatal sepsis episodes with retinopathy of prematurity, including treatment-warranted cases, among very preterm infants in Germany and Norway.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy.
Hide this message
You are using an outdated browser. Please upgrade your browser to improve your experience and security.
The Directory of Open Access Journals
Quick search, critical care research and practice this journal has been awarded the doaj seal..
2090-1305 (Print) / 2090-1313 (Online)
- ISSN Portal
WeChat QR code

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Published: 17 June 2022
Redefining critical illness
- David M. Maslove ORCID: orcid.org/0000-0002-0765-7158 1 , 2 na1 ,
- Benjamin Tang ORCID: orcid.org/0000-0002-1469-9540 3 na1 ,
- Manu Shankar-Hari ORCID: orcid.org/0000-0002-5338-2538 4 , 5 ,
- Patrick R. Lawler 6 , 7 ,
- Derek C. Angus 8 , 9 ,
- J. Kenneth Baillie ORCID: orcid.org/0000-0001-5258-793X 5 , 10 , 11 ,
- Rebecca M. Baron 12 , 13 ,
- Michael Bauer ORCID: orcid.org/0000-0002-1521-3514 14 , 15 ,
- Timothy G. Buchman ORCID: orcid.org/0000-0001-7350-5921 16 , 17 ,
- Carolyn S. Calfee 18 ,
- Claudia C. dos Santos 7 , 19 ,
- Evangelos J. Giamarellos-Bourboulis ORCID: orcid.org/0000-0003-4713-3911 20 ,
- Anthony C. Gordon ORCID: orcid.org/0000-0002-0419-547X 21 ,
- John A. Kellum ORCID: orcid.org/0000-0003-1995-2653 8 ,
- Julian C. Knight 22 ,
- Aleksandra Leligdowicz ORCID: orcid.org/0000-0001-6055-4644 23 , 24 ,
- Daniel F. McAuley ORCID: orcid.org/0000-0002-3283-1947 25 , 26 ,
- Anthony S. McLean 3 ,
- David K. Menon ORCID: orcid.org/0000-0002-3228-9692 27 ,
- Nuala J. Meyer ORCID: orcid.org/0000-0003-4597-5584 28 ,
- Lyle L. Moldawer 29 ,
- Kiran Reddy ORCID: orcid.org/0000-0002-1621-1481 25 , 26 ,
- John P. Reilly ORCID: orcid.org/0000-0003-3937-5320 28 ,
- James A. Russell 30 ,
- Jonathan E. Sevransky 16 , 31 ,
- Christopher W. Seymour 8 ,
- Nathan I. Shapiro 13 , 32 ,
- Mervyn Singer ORCID: orcid.org/0000-0002-1042-6350 33 ,
- Charlotte Summers ORCID: orcid.org/0000-0002-7269-2873 34 ,
- Timothy E. Sweeney 35 ,
- B. Taylor Thompson 13 , 36 ,
- Tom van der Poll ORCID: orcid.org/0000-0002-9199-5079 37 ,
- Balasubramanian Venkatesh 38 , 39 ,
- Keith R. Walley 30 ,
- Timothy S. Walsh 40 ,
- Lorraine B. Ware 41 ,
- Hector R. Wong ORCID: orcid.org/0000-0001-7989-1173 42 na2 ,
- Zsolt E. Zador 43 &
- John C. Marshall 7 , 43 , 44
Nature Medicine volume 28 , pages 1141–1148 ( 2022 ) Cite this article
34k Accesses
155 Citations
168 Altmetric
Metrics details
- Laboratory techniques and procedures
- Therapeutics
- Translational research
Research and practice in critical care medicine have long been defined by syndromes, which, despite being clinically recognizable entities, are, in fact, loose amalgams of heterogeneous states that may respond differently to therapy. Mounting translational evidence—supported by research on respiratory failure due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection—suggests that the current syndrome-based framework of critical illness should be reconsidered. Here we discuss recent findings from basic science and clinical research in critical care and explore how these might inform a new conceptual model of critical illness. De-emphasizing syndromes, we focus on the underlying biological changes that underpin critical illness states and that may be amenable to treatment. We hypothesize that such an approach will accelerate critical care research, leading to a richer understanding of the pathobiology of critical illness and of the key determinants of patient outcomes. This, in turn, will support the design of more effective clinical trials and inform a more precise and more effective practice at the bedside.
Similar content being viewed by others

SepsEast Registry indicates high mortality associated with COVID-19 caused acute respiratory failure in Central-Eastern European intensive care units
A comparison of impact of comorbidities and demographics on 60-day mortality in ICU patients with COVID-19, sepsis and acute respiratory distress syndrome
Clinical relevance of timing of assessment of ICU mortality in patients with moderate-to-severe Acute Respiratory Distress Syndrome
A 66-year-old woman is admitted to the intensive care unit (ICU) with fever, cough and difficulty breathing. She is diagnosed with pneumonia, intubated and placed on mechanical ventilation. The following day, her chest X-ray reveals bilateral infiltrates, and arterial blood gas analysis shows severe hypoxemia. Her treating clinicians consider what to do next.
Were this patient admitted in 2019, her management might have been beset by more questions than answers. She has both sepsis, a syndrome of life-threatening organ dysfunction in the face of infection, and acute respiratory distress syndrome (ARDS), a syndrome of respiratory failure associated with lung injury and impaired gas exchange. Both of these syndromes have been the subject of many epidemiological and interventional studies, yet little of the resulting evidence is clinically actionable. There are no specific treatments for her sepsis beyond antmicrobials 1 , and the ventilation strategies used to treat ARDS might reasonably be applied to any patient in the ICU 2 .
Were she admitted today—and depending on geography and time of year—her condition might well be the result of critical Coronavirus Disease 2019 (COVID-19). She would still meet diagnostic criteria for both sepsis and ARDS and would ostensibly face a similar degree of therapeutic uncertainty. However, in the last few years, many large randomized trials have provided a wellspring of evidence suggesting that a patient in her condition is likely to benefit from corticosteroids 3 and interleukin-6 receptor antagonists 4 , 5 but that treatments for milder disease, including remdesivir 6 and systemic anticoagulation 7 , are unlikely to provide substantial benefit. To the great relief of many, the once arid landscape of clinical evidence in critical care has begun to germinate.
In what follows, we examine how advances in translational critical care brought us to this inflection point in our field and how these advances stand to fundamentally alter the way that we conceptualize and classify critical illness.
A new era in translational critical care research
The field of critical care medicine can be described by three stages of development (Fig. 1 ). In the first stage (‘Foundations’, c. 1955–1980s), mechanical ventilation and continuous monitoring of physiologic parameters were introduced to the care of the critically ill, along with higher nurse-to-patient ratios, standardized practices and an emerging recognition of critical care as a standalone medical specialty. These technological advances provided the basis for a physiology-based understanding of the host response to injury and saved the lives of patients who might otherwise have died. Critical illness was defined as organ-level pathophysiology (for example, shock and respiratory failure), and the delivery of intensive care services was centered on maintaining organ-level homeostasis (for example, assisted breathing and circulatory support).
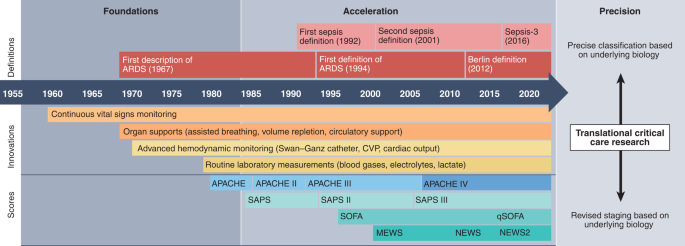
The first era, Foundations, spans from the founding of the discipline in the 1950s and 1960s to roughly the mid-1980s. In the second era, Acceleration, critical illness was better characterized through formal syndrome definitions and quantitative descriptions of illness severity. Outcomes improved, although few clinical studies yielded actionable results. A third era, Precision, is now emerging, based on a growing body of translational findings that reveal substantial biological heterogeneity within current critical care disease concepts. Parsing this heterogeneity to identify precise mechanisms of disease—along with ways to identify these clinically—will lead to more precise treatments and greater efficiency of care. Delineating these mechanisms and translating them to practice will be central tasks in critical care research in the coming decades. CVP, central venous pressure.
A second stage of development in the critical care field (‘Acceleration’, c. 1980s–2020) arose alongside advances in translational research that proffered an improved understanding of the pathophysiology of the host response. In this era, the field acquired structure, with the advent of quantitative scoring systems and standardized syndrome definitions. These included the APACHE score 8 as well as definitions for systemic inflammatory response syndrome (SIRS), sepsis 9 and ARDS 10 . Together, these laid the groundwork for rigorous clinical and translational studies, which, in combination with better organization and inter-disciplinary collaboration, led to tremendous improvements in outcomes for critically ill patients.
In recent years, emerging evidence has begun to suggest that, although initially useful in research and practice, current disease concepts do not sufficiently capture the full complexity of critical illness 11 , 12 . Advances in -omics science, data science and machine learning have generated evidence of heterogeneity in common ICU syndromes. Gene expression data from the blood of both pediatric and adult patients with sepsis have been used with hierarchical clustering algorithms to discover and validate distinct subsets of patients with shared transcriptomic responses to severe infection 13 , 14 , 15 , 16 , 17 , 18 , 19 . Similarly, latent class analysis (another statistical method to identify subgroups in populations) has been used with clinical and biomarker data from patients with ARDS to reveal hypo-inflammatory and hyper-inflammatory subtypes 20 , 21 , 22 . These findings clearly resonate with the day-to-day experience of clinicians caring for critically ill patients who, despite sharing common diagnoses, nonetheless exhibit substantial variability in clinical course and outcome 19 , 20 , 22 , 23 , 24 , 25 . There is an increasingly compelling need to reconsider the prevailing approach to the classification of critical illness 26 , 27 , 28 .
Critical care medicine is now on the cusp of a sea change—a third phase of development (‘Precision’; Fig. 1 ) defined by advances in translational science. This phase stands to be more disruptive than those preceding and will require a wholesale reconfiguration of existing classification frameworks.
Critical illness syndromes
Most of the illnesses treated in the ICU are clinical syndromes. Conditions like sepsis, ARDS, acute kidney injury, delirium and even chronic critical illness are characterized not by any particular biopsy feature, genetic mutation, microbial culture or serologic test but, rather, by collections of signs and symptoms that together paint the picture of a clinically recognizable entity. As a result, critical illness syndromes are heterogeneous by nature. For instance, sepsis can arise from a multitude of infections, caused by many different pathogens and resulting in different patterns of organ injury. ARDS may arise from either pulmonary triggers (such as pneumonia or aspiration) or non-pulmonary triggers (such as trauma or pancreatitis), and delirium may manifest as both agitation and somnolence. There is also temporal heterogeneity; a patient meeting diagnostic criteria for one syndrome at a given time may progress through different, often disparate, phases. Added to this is the tremendous heterogeneity in the host response to injury from one individual to the next.
Despite their limitations, syndromes enable the objective and reproducible assembly of patient cohorts and, as such, are useful in research and quality improvement. Syndromes can also be ‘prognostic’, meaning they can be used to estimate the likelihood of an outcome. For example, the current clinical criteria for septic shock are associated with a risk of death in excess of 40% 29 . These criteria do not, however, identify which patients are likely to respond to any specific treatment. Classifiers that exhibit this latter function are often called ‘predictive’. For example, coagulopathy due to thrombocytopenia is likely to improve with platelet transfusion, whereas that which is due to dysfibrinogenemia is not. This inherent limitation in the syndrome-based classification of critical illness arises because current criteria are based on clinical findings rather than on the underlying biological processes that give rise to them. An important question, therefore, is whether our current syndrome-based classification schema is fit for purpose and whether a new approach is needed.
A translational classification of critical illness
Illness classifications have been proposed and revised since antiquity, but, for the most part, the essential components have changed very little. An early taxonomy developed by Linnaeus in the 18th century bears striking resemblance to modern schemas such as the International Classification of Diseases (ICD) system, whereby individual diseases are specified on the basis of signs and symptoms, and the relationships between them are delineated, often as a nested hierarchy.
Important conceptual advances have, nonetheless, been made (Box 1 ). The TNM staging system in oncology has been useful in framing cancer not as a single disease but as a collection of related conditions whose optimal treatment depends on the extent of their progression. Adapting this concept to the ICU, the PIRO model (predisposition, insult, response, organ dysfunction) was proposed to underscore the notion that response to treatment is affected by more than whether certain syndromic criteria are met; a patient’s outcome is also strongly influenced by their baseline physiology, the nature of the precipitating insult and the way in which various organ systems respond 30 .
The PIRO model was an important early step toward acknowledging heterogeneity in critical illness. But translational and clinical evidence accrued in the last decade has deepened understanding of the complexity of critical illness and its biological determinants, compelling us to revisit the nosology of critical care. To best capitalize on these discoveries, a new framework must accommodate complexity and heterogeneity and must also establish a closer correspondence between diagnosis and treatment. In other words, critical illness classification should be not only prognostic, as syndromes are, but predictive as well, allowing researchers and practitioners to focus on measures that stand to improve outcomes.
Conceptually, a new classification system should encompass the inciting illness event, the physiologic disturbances produced and the treatments that could return the affected system(s) to a state of health. We advance a new concept here that begins with insults—events that instigate an acute departure from some baseline level of homeostasis, with the potential to elicit critical illness. Insults are myriad and diverse. Infection, trauma, stroke, hemorrhage, overdose and major surgery—all of these represent an abrupt change in baseline physiology, and all are common reasons for ICU admission. Insults give rise to perturbations in bodily systems that, in turn, lead to disease states, organ dysfunction and clinically overt morbidity.
The basis of this model is a more direct correspondence between insults and the pathophysiologic states they engender. This is achieved by placing the insult, along with its physiologic consequences and potential treatments, in a causal pathway. Causality is a key feature here and an important change from current syndromic classifications. For example, although we know that fluids will generally be helpful in septic shock, and low driving pressures during mechanical ventilation will be helpful in ARDS, the heterogeneity of these conditions limits the causal inferences that can be made, thereby hindering the clinical actionability of these principles in the treatment of any individual patient.
To enhance the precision of diagnosis in critical care, we invoke the concept of a treatable trait—a specific physiologic derangement characterized by biomarkers that portend a predictable response to a particular therapy 31 . Although biomarkers are often understood to refer to specialized laboratory tests, usually from blood or tissue, our use of the term here is more broadly construed. In the context of a treatable trait, we use the term ‘biomarker’ to mean any observable trait that corresponds with the biological abnormality of interest and that underpins a prediction around how a patient will respond to treatment. As such, biomarkers may include transcriptomic features derived from RNA sequencing, virulence factors identified by pathogen genomics, features seen on advanced imaging studies or even imbalances in the autonomic nervous system identified by millisecond-scale changes in heart rate variability. They may also include simple and routinely measured clinical variables, such as oxygen saturation, hemoglobin levels and glucose concentrations, which currently serve as usable biomarkers by enabling predictions about the effects of oxygen titration, transfusion and insulin therapy, respectively. The particular modality used is of secondary importance; what matters is that the trait can be measured, that it corresponds with the insult or physiological process causing harm and that it can be linked to treatment response.
Evidence suggests that disparate insults may give rise to shared molecular patterns of injury. Influential work by the Inflammation and the Host Response to Injury ( NCT00257231 ) program replicated clinical observations of pathophysiologic similarities across critical illness syndromes, by showing that molecular signatures in trauma and burn injuries include activation of similar infection-related and inflammation-related pathways 32 . This work has recently been extended, revealing molecular similarities between bacterial sepsis and COVID-19 viral sepsis 33 as well as between ARDS and pancreatitis 34 . These observations suggest that some signals might be generalizable across different forms of critical illness, precipitated by very different insults.
Such findings hint at a previously uncharacterized richness in the biological determinants of critical illness. Rather than a one-to-one correspondence between insult and disease state, a one-to-many relationship or even a many-to-many relationship is likely more appropriate. As traditional hierarchical models of classification cannot easily represent such a system, we offer the circular model shown in Fig. 2 to depict the precise biological processes that characterize a disease mechanism shared among different illness states, irrespective of the insult from which they arise. This configuration better accommodates the complexity of critical illness by acknowledging that certain states may be reached through different causal paths, and that, although the insult itself is important, it is the resultant physiologic state that may better characterize a patient’s current status.

Individual insults and biological abnormalities are combined in a circular model that accommodates connections between entities. In this example, four insults are portrayed (infection, trauma, surgery and pancreatitis). The same biological abnormality (represented by interconnecting bands) can arise from multiple different insults; for example, certain shared inflammation-mediated pathways may underpin each of the four insults shown.
To illustrate the potential utility of a model thus construed, consider the role of Toll-like receptor (TLR) signaling in critical illness. TLR pathways contribute to the inflammatory response and are known to be activated by various triggers, both exogenous (for example, bacterial endotoxin) and endogenous (for example, heme and hyaluronic acid) 35 . Indeed, upregulation of TLR pathways has been identified through gene expression profiling in the settings of both trauma 32 and sepsis 36 . However, given the heterogeneity of these clinical syndromes—as well as differences in the genetic determinants of the immune response to TLR activation 37 —the extent of TLR-mediated inflammation likely varies among patients. This biological heterogeneity may, in part, explain why inhibiting TLR-mediated inflammation does not appear to be an effective treatment for cohorts defined by diagnostic criteria for severe sepsis 38 . We might, however, hypothesize that this approach will be helpful in a subset of patients with sepsis with more pronounced dysregulation of TLR signaling. Moreover, we might also hypothesize that a subset of trauma patients who manifest maladaptive TLR pathway upregulation will also benefit from this approach, even though their illness state arose from a different insult. Answering this question would require a clinical trial in which patients are prospectively enrolled based on a treatable trait—in this case TLR upregulation—rather than on a clinical syndrome, such as sepsis or trauma.
TLR signaling may also play an important role in the host response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Rapid whole-exome sequencing of probands with COVID-19 have identified deletions in the TLR7 gene that were associated with an extreme critical illness phenotype 39 . Although TLR signaling is implicated here as well, the nature of the derangement is different; loss-of-function variants lead to an impaired interferon-mediated response to the virus, and subsequent critical COVID-19. Rather than a TLR antagonist, we might reasonably hypothesize that a TLR agonist (such as imiquimod) would be effective in these cases. This would be a different treatable trait, one that might be shared by other conditions, including certain skin cancers 40 .
The conceptual critical care model we describe here has yet to be validated in prospective clinical trials; doing so will require studies that recruit patients based on treatable traits rather than syndrome criteria. However, early evidence for the feasibility and efficacy of this approach is mounting. For example, in oncology, the I-SPY platform uses molecular profiling of breast tumors to identify specific subtypes most likely to respond to certain treatments, such as the tyrosine kinase inhibitor neratinib 41 . This approach, often called predictive enrichment, is used to evaluate many breast cancer subtypes derived from tumor gene expression data, often coupled with adaptive randomization, a type of treatment allocation strategy that adjusts the randomization ratios according to interim results. The I-SPY consortium has recently expanded to launch I-SPY COVID, a phase 2 clinical trial platform designed to use adaptive randomization to rapidly evaluate the viability of new COVID-19 therapies, with those deemed potentially viable graduated to larger definitive trials 42 .
Within critical care, randomized trials are beginning to explore the use of predictive enrichment to reduce the heterogeneity of treatment effect seen when recruitment is based strictly on syndromic criteria. One example is the EUPHRATES study, which examined the use of polymyxin B hemoperfusion in patients with septic shock 43 . This therapy is designed to remove bacterial endotoxin from the circulation, and so, rather than enrolling all patients meeting syndrome criteria for septic shock, the investigators randomized only those patients with high baseline levels of circulating endotoxin. The EUPHRATES experience demonstrates the feasibility of using a biomarker to rapidly identify a specific subgroup of patients expected to be most responsive to treatment. It also illustrates the challenges in identifying treatable traits. With no difference in mortality seen between the treatment and placebo arms, this study highlights the importance of defining appropriate subgroups, developing predictive biomarkers and devising realistic measures of treatment response.
In many ways, recent COVID-19 clinical trials have also demonstrated the potential viability of using a treatable trait concept to disambiguate critical illness syndromes and increase the yield of actionable evidence. The role of corticosteroids in treating ARDS remains uncertain, but many patients with ARDS arising from COVID-19 appear to respond favorably to this treatment 3 . Here, a positive polymerase chain reaction (PCR) test for the SARS-CoV-2 virus might be seen as a biomarker for a subtype of ARDS with a greater than average likelihood of responding favorably to corticosteroid therapy. Adding further nuance is the predictive importance of dynamic patient factors, such as timing with respect to the initial insult and the severity of the resulting illness. Corticosteroids for COVID-19 appear to be most effective in those who are sickest and when given at a later phase of illness. With the success of the RECOVERY 3 and REMAP-CAP 4 studies, COVID-19 research also increased our familiarity with adaptive randomization.
In proposing this modernized conceptual model of critical illness, we hasten to add some potential limitations and nuances. First, although the model has direct implications for treatment, it leaves prognosis largely unchanged. Age, for example, may not be a treatable trait, but it is prognostic in most conditions. That said, critical care has no shortage of prognostic models, both general and disease-specific, that fulfil this function well.
Second, although we emphasize some of the key molecular findings that have shown promise in critical care, the critical illness concept proposed here by no means requires that a treatable trait be a molecular or genomic trait. Despite an increasing emphasis on molecular techniques in translational critical care research, there are no guarantees that increasing granularity will lead to tangible gains. Any feature that distinguishes a specific pathophysiologic process with causal links to treatment effects can serve this function.
Third, the discussion of a new conceptual model of critical illness raises some questions as to the fate of the critical illness syndromes that have, for decades, steered the field through a period of remarkable advancement. These are bedrock concepts in the modern ICU, and they are deeply ingrained in our systems of prognostication, record-keeping, disease surveillance, epidemiology, administration, quality improvement and research. It remains to be seen whether the field is ready for a wholesale shift away from syndromes or whether they will be retained in some capacity.
Lastly, the model proposed here is but one among many possible ways forward. Although we think that the principles outlined above address many of the challenges facing critical care, our overarching objective is to bring these challenges to light and suggest how progress might be made in addressing them.
Box 1 Precision diagnosis and treatment: lessons from other fields
When first diagnosed in the mid-19th century, Hodgkin lymphoma was identified as a painless enlargement of the lymph nodes. Around the turn of the 20th century, histologic examination revealed the presence of pathognomonic Reed–Sternberg cells within the affected nodes. Toward the end of that century, new techniques revealed that some cases were characterized by a specific translocation in the transcription factor BCL6 (ref. 59 ). At each stage in its evolution, the diagnosis of Hodgkin lymphoma has evolved further from the general to the specific and from its physical manifestations to its biological underpinnings. This march toward greater precision has changed diagnosis from an exercise driven by clinical signs and symptoms to one that is anchored in the underlying mechanisms of disease.
By contrast, diagnosis in critical care is still largely a clinical undertaking. Syndromes are identified and defined on the basis of derangements in vital signs, along with basic laboratory investigations. These abnormalities paint a picture of organ system dysfunction, with only inferences to link them to the underlying biology. The approach is inherently imprecise. For example, pulmonary embolism, viremia and gastrointestinal hemorrhage all culminate in tachycardia, but tachycardia on its own provides no insight into the underlying cause. These conditions have vastly different treatments, none of which is to treat the tachycardia itself. A contemporary model of critical illness must address this limitation and provide greater precision in diagnosis. This will allow clinicians to disambiguate clinical syndromes that, under current frameworks, encompass disparate disease states. More importantly, it will allow clinicians to target therapies to specific physiologic derangements.
The modern management of myelodysplastic syndromes (MDSs) is a useful example of precision in treatment. Long characterized as a group of related conditions characterized by low blood counts and a hypercellular, dysplastic bone marrow, advances in cytogenetics have allowed hematologists to better parse this syndrome, identifying a more precise subtype arising from a deletion of the long arm of chromosome 5 (del(5q)). All forms of MDS might be treated supportively with transfusion, but only del(5q) responds to lenalinomide. This molecular characterization of disease has been widely touted as the basis of precision medicine and provides an illustrative example of how the deconstructing of heterogeneous syndromes into biologically distinct subtypes can improve treatment.
Subtype discovery has recently become a major focus of critical care research as well. Different subtypes of sepsis have been identified using clinical data 60 but also on the basis of gene expression profiling 19 , 36 , 61 , 62 , 63 . Subtypes of ARDS have been identified in clinical profiling studies 20 , 61 and even found in patients deemed to be merely at risk for this syndrome 64 . Importantly, some of these subtypes have implications for treatment. Certain gene expression patterns in sepsis have been associated with a favorable response to glucocorticoids 65 , whereas others have been associated with harm from this same treatment 66 , 67 , 68 . Different ARDS subtypes may respond differently to fluids 22 . These subtypes begin to hint at ways we might connect diagnostics and therapeutics on a much deeper level.
The next phase of critical care
Upon arrival in the ICU, our patient is found to have a PCR-positive nasopharyngeal swab for the SARS-CoV-2 virus, worsening hypoxemia, decreased urine output and confusion. An echocardiogram reveals mild left ventricular dysfunction, and her D-dimer levels (a marker of blood clotting) are markedly elevated. By current standards, we might diagnose several syndromes—ARDS, sepsis, acute kidney injury, delirium and disseminated intravascular coagulation—each of which may be treated with different types of supportive care. These treatments may conflict with one another, and the lack of precision in our diagnoses makes it difficult to predict how she will respond to any of them.
A new conceptual model developed on the principles described above would support a more efficient approach in which syndrome labels are de-emphasized in favor of more precise biological descriptors. Genome sequencing may reveal that our patient has an allelic variant that puts her at much higher risk of severe lung inflammation than age-matched and sex-matched counterparts with the same presentation 44 , 45 . Transcriptome profiling could reveal her organ dysfunction to be largely the result of TNF/IL-1-mediated inflammation 46 , with little contribution from microvascular thrombosis. Heart rate variability analysis may reveal changes in autonomic function that portend delirium 47 . Moreover, these pathophysiologic features might not be confined to COVID-19 alone and may be seen in critical illness states arising from entirely different insults. These features will be understood as treatable traits, evoking a specific therapeutic course. The genetic polymorphism may be targeted with a known pharmacologic agent, she may be more likely to benefit from the inhibition of certain inflammatory pathways, and a sympatholytic medication may prove better than an anti-psychotic at preventing and treating agitation.
How do we get there?
The gulf between aspiration and achievement is wide. Many share the conviction that we need to move beyond syndromic characterization of the diseases of critical illness and to develop disease models based on shared biology 48 , 49 , 50 , 51 . Position papers and consensus conferences will be useful in cultivating and refining key concepts. But meaningful progress will also require concerted effort directed toward technical considerations as well. An overall approach to addressing the challenges is shown in Fig. 3 and must focus on theoretical and practical considerations across a range of key domains.
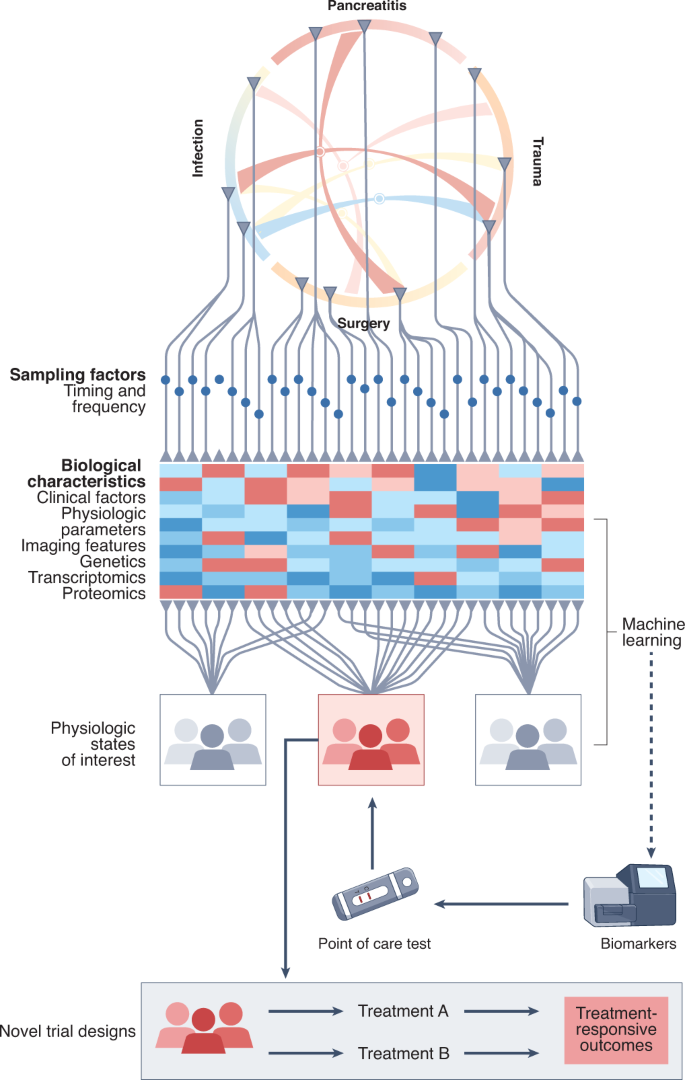
At the top of the figure, the circular model shows how different insults can give rise to shared biological abnormalities, with each gray triangle representing a patient with a specific insult. To characterize the patient response to injury, samples are collected at various times (blue dots) and used to generate biological characteristics. Tests may include blood tests, physiologic waveforms and imaging studies, as well as genomic, transcriptomic and proteomic profiling, and may be added to existing data such as age, comorbidities, environmental factors and functional status. The heat map depicts the clustering of these data to identify physiologic states of interest, which may be used to place patients into cohorts or to describe any single patient along a temporal trajectory of injury response. Note that each patient, when assessed at multiple points, may remain in an unchanged physiologic state or move to another. Unsupervised machine learning and other statistical techniques are used for subtype discovery, with supervised machine learning deployed to identify potential biomarkers. These are developed into tests that can be used at the point of care, including as an enrichment strategy for recruitment into prospective trials. Endpoints that directly reflect the response to treatment are defined and may include proximal outcomes that can be located in a causal pathway with the treatment. A physiologic state of interest and its corresponding predictive biomarker constitute a ‘treatable trait’, which, upon demonstration of efficacy in clinical trials, can be integrated into clinical care pathways.
Basic science
The concept of a ‘treatable trait’ generally implies that the underlying mechanism is understood and that the treatment relates to the mechanism. Thus, detailed preclinical work aimed at mechanistic understanding of putative treatable traits must be undertaken in earnest .
Biomarker development
On a practical level, operationalizing the treatable trait concept will, in some cases, necessitate the development of novel biomarkers that can be used in the ICU environment. This will require close collaboration with clinical chemists and laboratory experts to create validated assays that can be run in a clinical lab, respecting both the multifocal nature of critical care and the rapid turnaround times needed to inform decision-making. Assays run on readily available samples such as blood, urine, exhaled gases or even physiologic signals are more likely to be adopted than more invasive assays, such as tissue biopsies. Similarly, tests based on faster modalities, such as PCR or molecular barcoding platforms, will see greater uptake than more cumbersome sequencing technologies. Developing viable biomarker assays will involve addressing many hurdles, including identifying physiologically important disease states, describing the appropriate clinical interpretation of test results and satisfying regulatory requirements. Entirely new technologies will undoubtedly be explored to meet the exigencies of finding biomarkers of treatable traits in the ICU.
Outcome measures
Outcomes must be devised that can readily determine whether biomarker-informed treatment has been effective. Current outcomes such as mortality, organ support-free days and coarse measures of neurologic function may lack the necessary specificity to adjudicate the success of a given treatment. For instance, a patient with COVID-19 may respond favorably to corticosteroids, only to succumb later to a pulmonary embolism or bacterial coinfection. We must consider the relative importance of intermediate outcomes as well as outcomes that may not be considered patient-centered by current standards 52 .
Data integration
The noise resulting from large numbers of variables, the confounding effects of differing approaches to treatment and healthcare delivery and the diminishing realistic size of individual effects all argue for the integration of data on a grand scale and over a sustained period of time. Data from electronic health records, next-generation sequencing and multi-omics biology provide the substrate, and data science and enhanced statistical and machine learning approaches provide the methods. The precedents set by the Framingham Heart Study 53 , the Human Genome Project 54 or the insights in particle physics generated by the large Hadron collider all speak to the power of the creation, curation and sharing of large amounts of data.
Novel trial designs
Causal inference is challenged by confounding. Randomization provides the most reliable means of reducing confounding, thereby establishing causality. Large randomized clinical trials, therefore, provide powerful but under-used opportunities for causal inference, whereas emerging methods, such as Mendelian randomization 55 , enable more robust inferences of causality from random biologic variability. The use of platform trials, which incorporate adaptive designs that evaluate multiple treatments, has shown promise in efficiently weighing the effectiveness of multiple different treatments and can accommodate heterogeneity in the study population 56 , as evidenced by the success of the RECOVERY and REMAP-CAP studies 3 , 7 .
National and international collaboration of investigator-led research consortia
Large-scale, multi-national and multi-institutional collaborations such as CERN, LIGO and the Human Genome Project are becoming more common. The move toward open science and the creation of shared data repositories emphasize the will and provide the platforms for collaboration. Collaboration among national clinical research groups is increasing in areas such as emerging infectious diseases, cancer, stroke and thrombosis. In critical care, the International Forum for Acute Care Trialists (InFACT) has provided a forum for early discussions on the staging and stratification of critical illness. Collaboration at the scale needed to address the challenge is becoming possible.
The management of patients with cancer was transformed in 1933 by the creation of the Union for International Cancer Control and by the development of the TNM staging system, first proposed by Pierre Denoix in the 1940s 57 , 58 . The treatment of cardiovascular disease has been shaped by the Framingham Heart Study, with its comprehensive characterization of the natural history of a disease over time 53 . A similar approach will be needed to reframe critical illness. Owing to the rapid changes and multi-organ manifestations seen in critical illness, it is likely to be more complicated and to take a correspondingly greater effort than the precedents of oncology and cardiology. It is achievable, but it will require collaboration at a global scale—in reaching agreement on terminology and approaches to taxonomy, in creating shared data repositories to test and validate models and in incorporating models into randomized trials to evaluate causal inference. For all the upheaval it has created, COVID-19 has shown that such an aspiration in global research collaboration is not only desirable but also possible.
Marshall, J. C. Why have clinical trials in sepsis failed? Trends Mol. Med. 20 , 195–203 (2014).
Article PubMed Google Scholar
Writing Group for the PReVENT Investigators. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial. JAMA 320 , 1872–1880 (2018).
The Recovery Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med. 384 , 693–704 (2021).
Article Google Scholar
REMAP-CAP Investigators et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N. Engl. J. Med. 384 , 1491–1502 (2021).
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA 326 , 499–518 (2021).
Beigel, J. H. et al. Remdesivir for the treatment of Covid-19—final report. N. Engl. J. Med. 383 , 1813–1826 (2020).
Article CAS PubMed Google Scholar
REMAP-CAP Investigators et al. Therapeutic anticoagulation with heparin in critically ill patients with Covid-19. N. Engl. J. Med. 385 , 777–789 (2021).
Knaus, W. A., Draper, E. A., Wagner, D. P. & Zimmerman, J. E. APACHE II: a severity of disease classification system. Crit. Care Med. 13 , 818–829 (1985).
Bone, R. C. et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101 , 1644–1655 (1992).
Bernard, G. R. et al. Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med. 20 , 225–232 (1994).
Leligdowicz, A. & Matthay, M. A. Heterogeneity in sepsis: new biological evidence with clinical applications. Crit. Care 23 , 80 (2019).
Article PubMed PubMed Central Google Scholar
Prescott, H. C., Calfee, C. S., Thompson, B. T., Angus, D. C. & Liu, V. X. Toward smarter lumping and smarter splitting: rethinking strategies for sepsis and acute respiratory distress syndrome clinical trial design. Am. J. Respir. Crit. Care Med. 194 , 147–155 (2016).
Wong, H. R. et al. Identification of pediatric septic shock subclasses based on genome-wide expression profiling. BMC Med. 7 , 34 (2009).
Article PubMed PubMed Central CAS Google Scholar
Wong, H. R. et al. Genomic expression profiling across the pediatric systemic inflammatory response syndrome, sepsis, and septic shock spectrum. Crit. Care Med. 37 , 1558–1566 (2009).
Article CAS PubMed PubMed Central Google Scholar
Wong, H. R., Freishtat, R. J., Monaco, M., Odoms, K. & Shanley, T. P. Leukocyte subset-derived genomewide expression profiles in pediatric septic shock. Pediatr. Crit. Care Med. 11 , 349–355 (2010).
PubMed PubMed Central Google Scholar
Wong, H. R. et al. Toward a clinically feasible gene expression-based subclassification strategy for septic shock: proof of concept. Crit. Care Med. 38 , 1955–1961 (2010).
Wong, H. R. et al. Validation of a gene expression-based subclassification strategy for pediatric septic shock. Crit. Care Med. 39 , 2511–2517 (2011).
Maslove, D. M., Tang, B. M. & McLean, A. S. Identification of sepsis subtypes in critically ill adults using gene expression profiling. Crit. Care 16 , R183 (2012).
Sweeney, T. E. et al. Unsupervised analysis of transcriptomics in bacterial sepsis across multiple datasets reveals three robust clusters. Crit. Care Med. 46 , 915–925 (2018).
Calfee, C. S. et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir. Med. 2 , 611–620 (2014).
Calfee, C. S. et al. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest 147 , 1539–1548 (2015).
Famous, K. R. et al. Acute respiratory distress syndrome subphenotypes respond differently to randomized fluid management strategy. Am. J. Respir. Crit. Care Med. 195 , 331–338 (2017).
Cohen, M. J. et al. Identification of complex metabolic states in critically injured patients using bioinformatic cluster analysis. Crit. Care 14 , R10 (2010).
Davenport, E. E. et al. Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Respir. Med. 4 , 259–271 (2016).
Scicluna, B. P. et al. Classification of patients with sepsis according to blood genomic endotype: a prospective cohort study. Lancet Respir. Med. 5 , 816–826 (2017).
Reilly, J. P., Christie, J. D. & Meyer, N. J. Fifty years of research in ARDS. Genomic contributions and opportunities. Am. J. Respir. Crit. Care Med. 196 , 1113–1121 (2017).
Seymour, C. W. et al. Precision medicine for all? Challenges and opportunities for a precision medicine approach to critical illness. Crit. Care 21 , 257 (2017).
Calfee, C. S. Opening the debate on the new sepsis definition. Precision medicine: an opportunity to improve outcomes of patients with sepsis. Am. J. Respir. Crit. Care Med. 194 , 137–139 (2016).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315 , 801–810 (2016).
Marshall, J. C. The PIRO (predisposition, insult, response, organ dysfunction) model: toward a staging system for acute illness. Virulence 5 , 27–35 (2014).
Russell, C. D. & Baillie, J. K. Treatable traits and therapeutic targets: goals for systems biology in infectious disease. Curr. Opin. Syst. Biol. 2 , 140–146 (2017).
Xiao, W. et al. A genomic storm in critically injured humans. J. Exp. Med. 208 , 2581–2590 (2011).
Sweeney, T. E. et al. Validation of inflammopathic, adaptive, and coagulopathic sepsis endotypes in Coronavirus Disease 2019. Crit. Care Med. 49 , e170–e178 (2021).
Neyton, L. P. A. et al. Molecular patterns in acute pancreatitis reflect generalizable endotypes of the host response to systemic injury in humans. Ann. Surg. 275 , e453–e462 (2022).
Lorne, E., Dupont, H. & Abraham, E. Toll-like receptors 2 and 4: initiators of non-septic inflammation in critical care medicine? Intensive Care Med. 36 , 1826–1835 (2010).
Maslove, D. M. & Wong, H. R. Gene expression profiling in sepsis: timing, tissue, and translational considerations. Trends Mol. Med. 20 , 204–213 (2014).
Kim, S. et al. Characterizing the genetic basis of innate immune response in TLR4-activated human monocytes. Nat. Commun. 5 , 5236 (2014).
Opal, S. M. et al. Effect of eritoran, an antagonist of MD2-TLR4, on mortality in patients with severe sepsis: the ACCESS randomized trial. JAMA 309 , 1154–1162 (2013).
van der Made, C. I. et al. Presence of genetic variants among young men with severe COVID-19. JAMA 324 , 663–673 (2020).
Article PubMed CAS Google Scholar
Migden, M. R., Chang, A. L. S., Dirix, L., Stratigos, A. J. & Lear, J. T. Emerging trends in the treatment of advanced basal cell carcinoma. Cancer Treat. Rev. 64 , 1–10 (2018).
Park, J. W. et al. Adaptive randomization of neratinib in early breast cancer. N. Engl. J. Med. 375 , 11–22 (2016).
I-SPY Covid Consortium. Clinical trial design during and beyond the pandemic: the I-SPY COVID trial. Nat. Med. 28 , 9–11 (2022).
Article CAS Google Scholar
Dellinger, R. P. et al. Effect of targeted polymyxin B hemoperfusion on 28-day mortality in patients with septic shock and elevated endotoxin level: the EUPHRATES randomized clinical trial. JAMA 320 , 1455–1463 (2018).
Pairo-Castineira, E. et al. Genetic mechanisms of critical illness in COVID-19. Nature 591 , 92–98 (2021).
Kousathanas, A. et al. Whole genome sequencing reveals host factors underlying critical Covid-19. Nature https://doi.org/10.1038/s41586-022-04576-6 (2022).
Lee, J. S. et al. Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19. Sci. Immunol. 5 , eabd1554 (2020).
Oh, J. et al. Prediction and early detection of delirium in the intensive care unit by using heart rate variability and machine learning. Physiol. Meas. 39 , 035004 (2018).
Marshall, J. C. et al. Measures, markers, and mediators: towards a staging system for clinical sepsis. Crit. Care Med. 31 , 1560–1567 (2003).
Wu, A. C. et al. Current status and future opportunities in lung precision medicine research with a focus on biomarkers. An American Thoracic Society/National Heart, Lung, and Blood Institute research statement. Am. J. Respir. Crit. Care Med. 198 , e116–e136 (2018).
Maslove, D. M., Lamontagne, F., Marshall, J. C. & Heyland, D. K. A path to precision in the ICU. Crit. Care 21 , 79 (2017).
Matthay, M. A. et al. Acute respiratory distress syndrome. Nat. Rev. Dis. Prim. 5 , 18 (2019).
Gajic, O., Ahmad, S. R., Wilson, M. E. & Kaufman, D. A. Outcomes of critical illness: what is meaningful? Curr. Opin. Crit. Care 24 , 394–400 (2018).
Mahmood, S. S., Levy, D., Vasan, R. S. & Wang, T. J. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet 383 , 999–1008 (2014).
Green, E. D., Watson, J. D. & Collins, F. S. Human Genome Project: twenty-five years of big biology. Nature 526 , 29–31 (2015).
Emdin, C. A., Khera, A. V. & Kathiresan, S. Mendelian randomization. JAMA 318 , 1925–1926 (2017).
Berry, S. M., Connor, J. T. & Lewis, R. J. The platform trial: an efficient strategy for evaluating multiple treatments. JAMA 313 , 1619–1620 (2015).
Gospodarowicz, M. et al. History and international developments in cancer staging. Cancer Prev. Cont. 2 , 262–268 (1998).
CAS Google Scholar
Mackillop, W. J., O’Sullivan, B. & Gospodarowicz, M. The role of cancer staging in evidence-based medicine. Cancer Prev. Cont. 2 , 269–277 (1998).
Bakhirev, A. G., Vasef, M. A., Zhang, Q. Y., Reichard, K. K. & Czuchlewski, D. R. Fluorescence immunophenotyping and interphase cytogenetics (FICTION) detects BCL6 abnormalities, including gene amplification, in most cases of nodular lymphocyte-predominant Hodgkin lymphoma. Arch. Pathol. Lab. Med. 138 , 538–542 (2014).
Seymour, C. W. et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 321 , 2003–2017 (2019).
Shankar-Hari, M. & Rubenfeld, G. D. Population enrichment for critical care trials: phenotypes and differential outcomes. Curr. Opin. Crit. Care 25 , 489–497 (2019).
Wong, H. R. & Marshall, J. C. Leveraging transcriptomics to disentangle sepsis heterogeneity. Am. J. Respir. Crit. Care Med. 196 , 258–260 (2017).
Sweeney, T. E. & Khatri, P. Generalizable biomarkers in critical care: toward precision medicine. Crit. Care Med. 45 , 934–939 (2017).
Kitsios, G. D. et al. Host–response subphenotypes offer prognostic enrichment in patients with or at risk for acute respiratory distress syndrome. Crit. Care Med. 47 , 1724–1734 (2019).
Wong, H. R. et al. Combining prognostic and predictive enrichment strategies to identify children with septic shock responsive to corticosteroids. Crit. Care Med. 44 , e1000–e1003 (2016).
Wong, H. R. et al. Developing a clinically feasible personalized medicine approach to pediatric septic shock. Am. J. Respir. Crit. Care Med. 191 , 309–315 (2015).
Wong, H. R., Hart, K. W., Lindsell, C. J. & Sweeney, T. E. External corroboration that corticosteroids may be harmful to septic shock endotype a patients. Crit. Care Med. 49 , e98–e101 (2021).
Antcliffe, D. B. et al. Transcriptomic signatures in sepsis and a differential response to steroids. From the VANISH randomized trial. Am. J. Respir. Crit. Care Med. 199 , 980–986 (2019).
Download references
Acknowledgements
The authors would like to acknowledge the pioneering work of Hector Wong, whose leadership was instrumental in establishing the use of genome-wide analysis to more richly describe the heterogeneity of host responses to infection. His mentorship, generosity, collegiality, vision and tireless dedication will be deeply missed. Development of the concepts shaping this Perspective was facilitated through meetings of the Staging and Stratification Working Group of the International Forum for Acute Care Trialists.
Author information
These authors contributed equally: David M. Maslove, Benjamin Tang.
Deceased: Hector R. Wong.

Authors and Affiliations
Department of Critical Care Medicine, Queen’s University, Kingston, Ontario, Canada
David M. Maslove
Kingston Health Sciences Center, Kingston, Ontario, Canada
Department of Intensive Care Medicine, Nepean Hospital, Sydney, New South Wales, Australia
Benjamin Tang & Anthony S. McLean
The Queen’s Medical Research Institute, Centre for Inflammation Research, Institute for Regeneration and Repair, Edinburgh, UK
Manu Shankar-Hari
Intensive Care Medicine, Royal Infirmary of Edinburgh, NHS Lothian, Edinburgh, UK
Manu Shankar-Hari & J. Kenneth Baillie
Cardiac Intensive Care Unit, Peter Munk Cardiac Centre, University Health Network, Toronto, Ontario, Canada
Patrick R. Lawler
Interdepartmental Division of Critical Care Medicine, University of Toronto, Toronto, Ontario, Canada
Patrick R. Lawler, Claudia C. dos Santos & John C. Marshall
Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, PA, USA
Derek C. Angus, John A. Kellum & Christopher W. Seymour
University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Derek C. Angus
Roslin Institute, University of Edinburgh, Edinburgh, UK
J. Kenneth Baillie
Pandemic Science Hub, Centre for Inflammation Research, University of Edinburgh, Edinburgh, UK
Division of Pulmonary and Critical Care Medicine, Brigham and Women’s Hospital, Boston, MA, USA
Rebecca M. Baron
Harvard Medical School, Boston, MA, USA
Rebecca M. Baron, Nathan I. Shapiro & B. Taylor Thompson
Department of Anesthesiology and Intensive Care Medicine, Jena University Hospital, Jena, Germany
Michael Bauer
Center for Sepsis Care & Control, Jena University Hospital, Jena, Germany
Emory Critical Care Center, Emory University, Atlanta, GA, USA
Timothy G. Buchman & Jonathan E. Sevransky
Santa Fe Institute, Santa Fe, NM, USA
Timothy G. Buchman
Division of Pulmonary, Critical Care, Allergy, and Sleep Medicine; Department of Medicine, University of California, San Francisco, San Francisco, CA, USA
Carolyn S. Calfee
Keenan Centre for Biomedical Research of Saint Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada
Claudia C. dos Santos
4th Department of Internal Medicine, National and Kapodistrian University of Athens, Medical School, Athens, Greece
Evangelos J. Giamarellos-Bourboulis
Division of Anaesthetics, Pain Medicine and Intensive Care, Imperial College London, London, UK
Anthony C. Gordon
Wellcome Centre for Human Genetics, University of Oxford, Oxford, UK
Julian C. Knight
Department of Medicine, Division of Critical Care, University of Western Ontario, London, Ontario, Canada
Aleksandra Leligdowicz
Department of Microbiology and Immunology, University of Western Ontario, London, ON, Canada
Regional Intensive Care Unit, Royal Victoria Hospital, Belfast, UK
Daniel F. McAuley & Kiran Reddy
Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University Belfast, Belfast, UK
Division of Anaesthesia, Department of Medicine, University of Cambridge, Cambridge, UK
David K. Menon
Department of Medicine, Pulmonary, Allergy, and Critical Care Division, University of Pennsylvania, Philadelphia, PA, USA
Nuala J. Meyer & John P. Reilly
Sepsis and Critical Illness Research Center, Department of Surgery, University of Florida College of Medicine, Gainesville, FL, USA
Lyle L. Moldawer
Centre for Heart Lung Innovation and Critical Care Medicine, University of British Columbia, Vancouver, British Columbia, Canada
James A. Russell & Keith R. Walley
Division of Pulmonary, Allergy, Critical Care and Sleep, School of Medicine, Emory University, Atlanta, GA, USA
Jonathan E. Sevransky
Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA
Nathan I. Shapiro
Bloomsbury Institute of Intensive Care Medicine, Division of Medicine, University College London, London, UK
Mervyn Singer
Department of Medicine, University of Cambridge School of Medicine, Cambridge, UK
Charlotte Summers
Inflammatix, Inc, Burlingame, CA, USA
Timothy E. Sweeney
Divisions of Biostatistics and Pulmonary/Critical Care Medicine, Massachusetts General Hospital, Boston, MA, USA
B. Taylor Thompson
Amsterdam UMC, University of Amsterdam, Amsterdam, Netherlands
- Tom van der Poll
Department of Intensive Care, Wesley and Princess Alexandra Hospitals, Brisbane, Queensland, Australia
Balasubramanian Venkatesh
The George Institute for Global Health, University of New South Wales, Sydney, New South Wales, Australia
Usher Institute for Population Health Sciences, Deanery of Molecular, Genetics, and Population Health Sciences, University of Edinburgh, Edinburgh, UK
Timothy S. Walsh
Departments of Medicine and Pathology, Microbiology and Immunology, Vanderbilt University School of Medicine, Nashville, TN, USA
Lorraine B. Ware
Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Hector R. Wong
Department of Surgery, University of Toronto, Toronto, Ontario, Canada
Zsolt E. Zador & John C. Marshall
Departments of Surgery and Critical Care Medicine, Unity Health Toronto, Toronto, Ontario, Canada
John C. Marshall
You can also search for this author in PubMed Google Scholar
Contributions
B.T. and J.C.M. conceived of the idea, with all authors making important conceptual contributions and refining the writing of the manuscript. D.M.M., B.T., M.S.-H., P.R.L. and J.C.M. formed the primary writing group.
Corresponding author
Correspondence to David M. Maslove .
Ethics declarations
Competing interests.
R.M.B. reports having served on advisory boards for Merck and Genentech. M.B. is a stockholder of SmartDyeLivery, a company developing nanodrugs for sepsis. T.G.B. has no direct conflicts of interest. His employer, Emory University, collects a stipend for his service as Editor-in-Chief of Critical Care Medicine from the Society of Critical Care Medicine. Emory University also collects a stipend from the US Government for his service as senior advisor to the Biomedical Advanced Research and Development Authority. C.S.C. receives grant funding from the NIH, US Food and Drug Administration, US Department of Defense, Quantum Leap Healthcare Collaborative and Roche-Genentech and has provided consulting services for Quark, Vasomune, Gen1e Life Sciences, Cellenkos, and Janssen. A.C.G. is supported by an NIHR Research Professorship (RP-2015-06-018) and the NIHR Imperial Biomedical Research Centre. Outside of this work he has received personal fees from 30 Respiratory paid to his institution. Outside the submitted work, D.F.M. reports personal fees from consultancy for GlaxoSmithKline, Boehringer Ingelheim, Bayer, Novartis, Sobi and Eli Lilly and from sitting on a Data Monitoring and Ethics Committee for trials undertaken by Vir Biotechnology and Faron Pharmaceuticals. In addition, his institution has received funds from grants from the National Institute for Health and Care Research (NIHR), the Wellcome Trust, Innovate-UK, the Medical Research Council (MRC) and the Northern Ireland HSC R&D Division. D.F.M. also holds a patent for an anti-inflammatory treatment issued to Queen’s University Belfast. D.F.M. was Director of Research for the UK Intensive Care Society (term ended in June 2021) and is NIHR/MRC Efficacy and Mechanism Evaluation Programme Director. D.K.M. reports grants from the European Union, the NIHR and the Canadian Institute for Advanced Research supporting the submitted work; grants from GlaxoSmithKline and Lantmannen; and consulting fees from Calico, GlaxoSmithKline, Lantmannen, NeuroTrauma Sciences and Integra Neurosciences outside the submitted work. L.L.M. reports grants and contracts from the NIGMS, NICHD, and NIAID (NIH), as well as subcontracts from Inflammatix and Beckman-Coulter through awards from BARDA (HHS). In addition, L.L.M. participates in clinical studies supported by RevImmune, Immunex, Faraday and Beckman-Coulter. J.A.R. reports patents owned by the University of British Columbia that are related to (1) the use of PCSK9 inhibitor(s) in sepsis and (2) the use of vasopressin in septic shock, as well as (3) a patent owned by Ferring Pharmaceuticals for the use of selepressin in septic shock. J.A.R. is an inventor on these patents. J.A.R. was a founder, director and shareholder in Cyon Therapeutics and is a shareholder in Molecular You Corp. J.A.R. is no longer actively consulting for any industry. J.A.R. reports receiving consulting fees in the last 3 years from SIB Therapeutics (developing a sepsis drug), Ferring Pharmaceuticals (manufactures vasopressin and is developing selepressin) and PAR Pharma (sells prepared bags of vasopressin). J.A.R. was a funded member of the Data and Safety Monitoring Board of a National Institutes of Health-sponsored trial of plasma in COVID-19 (PASS-IT-ON) (2020–2021). J.A.R. reports having received an investigator-initiated grant from Grifols (titled ‘Is HBP a mechanism of albuminʼs efficacy in human septic shock?’) that was provided to and administered by the University of British Columbia. J.A.R. has received four grants for COVID-19 research from the Canadian Institutes of Health Research and two grants from the St. Paul’s Foundation. J.A.R. was also a non-funded science advisor and member of the Government of Canada COVID-19 Therapeutics Task Force (2020–2021). N.I.S. reports research funding from the National Institutes of Health, Luminos, Inflammatix and Google and is a consultant for Diagnostic Robotics. M.S. has served on advisory boards for infection and sepsis-related projects from Abbott, AM Pharma, Aptarion, Biotest, Biomerieux, deePull, Pfizer, Roche, Safeguard Biosystems and Spiden, and from Deltex Medical, Fresenius and Nestle outside the submitted work. M.S. holds a patent owned by University College London related to a sulphide-releasing molecule for ischaemia-reperfusion injury and a pending patent for phytosterol use in sepsis. UCL also holds shares in Deltex Medical and receives research funding from the Medical Research Council, Wellcome Trust, NIHR, Innovate UK, the European Commission and the UCL Technology Fund. T.E.S. is stockholder in, and employee of, Inflammatix, which is developing a rapid test for sepsis endotypes. Outside the submitted work, B.T.T. reports personal fees from consultancy for Bayer and Genentech. B.V. reports being an NHMRC Investigator Fellow.
Peer review
Peer review information.
Nature Medicine thanks Robert Stevens and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Maslove, D.M., Tang, B., Shankar-Hari, M. et al. Redefining critical illness. Nat Med 28 , 1141–1148 (2022). https://doi.org/10.1038/s41591-022-01843-x
Download citation
Received : 12 January 2022
Accepted : 28 April 2022
Published : 17 June 2022
Issue Date : June 2022
DOI : https://doi.org/10.1038/s41591-022-01843-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Early physical rehabilitation dosage in the intensive care unit associates with hospital outcomes after critical covid-19.
- Kirby P. Mayer
- Evan Haezebrouck
- Joshua K. Johnson
Critical Care (2024)
Analysis of influencing factors and construction of risk prediction model for postoperative thrombocytopenia in critically ill patients with heart disease
- Changjun Song
Journal of Cardiothoracic Surgery (2024)
Monocyte state 1 (MS1) cells in critically ill patients with sepsis or non-infectious conditions: association with disease course and host response
- Giuseppe G. F. Leite
- Justin de Brabander
The role of lipid emulsions containing omega-3 fatty acids for medical and surgical critical care patients
- Christian Stoppe
- Robert G. Martindale
- Jayshil J. Patel
Biological basis of critical illness subclasses: from the bedside to the bench and back again
- Joseph Stevens
- Oğuzhan Tezel
- Mihir R. Atreya
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- SCCM Connect
- Log In Log In Forgot Password? Forgot Username? New User? Sign Up Free
Forgot username? Forgot password? New User? Sign Up Free
- Membership and Community
- Critical Care Congress
- Clinical Resources
- Overview Membership and Community
- Become a Member
- Get Involved
- Career and Leadership
- Connect with SCCM Members
- SCCM Apparel and Merchandise
- Overview Education
- Educational Programming
- Airway and Mechanical Ventilation Management
- Adult Critical Care Review and Assessment
- Pediatric Critical Care Review and Assessment
- Latest Updates
- Hosted Training
- Accredited Education and Subject Matter Expert Resources
- Learning Categories
- Overview Critical Care Congress
- 2025 Critical Care Congress
- 2024 Critical Care Congress
- How to Claim ACE/MOC
- Past Congress Resources
- Abstracts and Case Reports
- Session Proposals
- Congress FAQs
- Future Congress Dates
- Congress Highlights
- Congress Digital
- Congress Literature Releases
- Exhibitor, Support, and Advertising Opportunities
- Overview Research
Discovery, the Critical Care Research Network
- Critical Care Innovation Incubator
- Research Grants
- Research Surveys
- SCCM-Weil Research Trust
- Overview Clinical Resources
- Quality Improvement
- ICU Liberation Campaign
- Sepsis Resources
- Diagnostic Excellence
- Choosing Wisely
- Well-Being Resources
- Patient Management During Outbreaks and Disasters
- Patient-Centered Outcomes Research Institute Projects
- Global Health
- Crisis Response
- Humanitarian Activities
- Collaboratives
- Browse the LearnICU Catalog
- SCCM Resource Library
- Critical Care Quick Study
- Overview Become a Member
- Associate Member Benefits
- Professional Member Benefits
- Select Member Benefits
- Renew or Upgrade
- Overview Get Involved
- Specialty Sections
- Knowledge Education Groups
- Committees and Volunteer Opportunities
- SCCM Social Media
- Overview Career and Leadership
- Career Central
- American College of Critical Care Medicine
- Early Career Professionals
- Leadership, Empowerment, and Development
- Overview Connect with SCCM Members
- Overview SCCM Apparel and Merchandise
- Overview Educational Programming
- Critical Care Ultrasound
- Critical Care Pharmacotherapy
- Critical Care Echocardiography
- Neurocritical Care
- Critical Care Knowledge Assessment
- Virtual Critical Care Rounds
- Fundamentals
- Current Concepts
- Overview Latest Updates
- Overview Hosted Training
- Opportunities
- Hosted Training Calendar
- Instructors, Directors, and Consultants
- Free Critical Care Training
- Overview Accredited Education and Subject Matter Expert Resources
- Overview Learning Categories
- Overview 2025 Critical Care Congress
- Overview 2024 Critical Care Congress
- Overview Abstracts and Case Reports
- Overview Congress Highlights
- Overview Congress Digital
- Overview Congress Literature Releases
- Overview Exhibitor, Support, and Advertising Opportunities
- Overview Discovery, the Critical Care Research Network
- Discovery Town Hall
- Data Science Campaign
- Submit a Clinical Investigator Proposal
- Discovery Research Collaboratives
- Discovery Resources
- Clinical Investigators Meetings
- Overview Critical Care Innovation Incubator
- Overview Journals
- Critical Care Medicine Journal
- Pediatric Critical Care Medicine Journal
- Critical Care Explorations Journal
- SCCM COVID-19 Journal Articles
- Journal Audio Summaries
- Overview Research Grants
- Overview Research Surveys
- Overview SCCM-Weil Research Trust
- Overview Quality Improvement
- ICU Centers of Excellence Program
- Overview Global Health
- Overview Collaboratives
- Overview LearnICU
SCCM is performing maintenance on its websites. For the best browsing experience, please use Microsoft Edge or Safari. Those using Chrome or Firefox may experience access issues at this time.
A central component of the Society's mission is the support of quality-based improvement initiatives and the support of multiprofessional research at all levels.
The critical care professionals dedicated to research are vitally important to the present and future of the specialty. Researchers -- be their focus on basic, applied or translational research -- are at the forefront of advancing knowledge that can be leveraged to treat disease, to improve quality of care, and to enhance patient experiences and outcomes. Integration of research topics and techniques into the educational programs, publications and communications of the Society remains a priority.
The Research Section supports research development among Society members and promotes communication about opportunities and networks.
The Society of Critical Care Medicine's (SCCM) peer-reviewed journals help readers stay ahead of the latest advances in critical care technology and research. They offer innovative findings that continually improve the practice of critical care. Learn More
SCCM offers several grant opportunities for critical care professionals seeking funding for activities that aim to improve care. Learn More
The Society of Critical Care Medicine (SCCM) offers a service to disseminate research surveys for individuals or institutions. Learn More
- Discovery VIRUS COVID-19 Registry
- STOP-Trauma ICU Learning Collaborative
- Discovery Data Coordinating Center
Critical Care Research and Practice
Subject Area and Category
- Critical Care and Intensive Care Medicine
Hindawi Limited
Publication type
20901305, 20901313
Information
How to publish in this journal
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
| Category | Year | Quartile |
|---|---|---|
| Critical Care and Intensive Care Medicine | 2013 | Q2 |
| Critical Care and Intensive Care Medicine | 2014 | Q2 |
| Critical Care and Intensive Care Medicine | 2015 | Q1 |
| Critical Care and Intensive Care Medicine | 2016 | Q2 |
| Critical Care and Intensive Care Medicine | 2017 | Q2 |
| Critical Care and Intensive Care Medicine | 2018 | Q2 |
| Critical Care and Intensive Care Medicine | 2019 | Q2 |
| Critical Care and Intensive Care Medicine | 2020 | Q2 |
| Critical Care and Intensive Care Medicine | 2021 | Q2 |
| Critical Care and Intensive Care Medicine | 2022 | Q2 |
| Critical Care and Intensive Care Medicine | 2023 | Q2 |
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
| Year | SJR |
|---|---|
| 2013 | 0.665 |
| 2014 | 0.643 |
| 2015 | 0.971 |
| 2016 | 0.690 |
| 2017 | 0.499 |
| 2018 | 0.668 |
| 2019 | 0.519 |
| 2020 | 0.532 |
| 2021 | 0.452 |
| 2022 | 0.508 |
| 2023 | 0.558 |
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
| Year | Documents |
|---|---|
| 2012 | 85 |
| 2013 | 30 |
| 2014 | 28 |
| 2015 | 19 |
| 2016 | 28 |
| 2017 | 15 |
| 2018 | 32 |
| 2019 | 23 |
| 2020 | 40 |
| 2021 | 61 |
| 2022 | 38 |
| 2023 | 26 |
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
| Cites per document | Year | Value |
|---|---|---|
| Cites / Doc. (4 years) | 2012 | 0.000 |
| Cites / Doc. (4 years) | 2013 | 2.024 |
| Cites / Doc. (4 years) | 2014 | 2.539 |
| Cites / Doc. (4 years) | 2015 | 2.636 |
| Cites / Doc. (4 years) | 2016 | 2.617 |
| Cites / Doc. (4 years) | 2017 | 2.086 |
| Cites / Doc. (4 years) | 2018 | 1.856 |
| Cites / Doc. (4 years) | 2019 | 1.830 |
| Cites / Doc. (4 years) | 2020 | 1.908 |
| Cites / Doc. (4 years) | 2021 | 2.282 |
| Cites / Doc. (4 years) | 2022 | 2.160 |
| Cites / Doc. (4 years) | 2023 | 2.062 |
| Cites / Doc. (3 years) | 2012 | 0.000 |
| Cites / Doc. (3 years) | 2013 | 2.024 |
| Cites / Doc. (3 years) | 2014 | 2.539 |
| Cites / Doc. (3 years) | 2015 | 2.636 |
| Cites / Doc. (3 years) | 2016 | 2.545 |
| Cites / Doc. (3 years) | 2017 | 1.467 |
| Cites / Doc. (3 years) | 2018 | 1.806 |
| Cites / Doc. (3 years) | 2019 | 1.640 |
| Cites / Doc. (3 years) | 2020 | 2.057 |
| Cites / Doc. (3 years) | 2021 | 2.158 |
| Cites / Doc. (3 years) | 2022 | 1.976 |
| Cites / Doc. (3 years) | 2023 | 2.043 |
| Cites / Doc. (2 years) | 2012 | 0.000 |
| Cites / Doc. (2 years) | 2013 | 2.024 |
| Cites / Doc. (2 years) | 2014 | 2.539 |
| Cites / Doc. (2 years) | 2015 | 2.379 |
| Cites / Doc. (2 years) | 2016 | 2.213 |
| Cites / Doc. (2 years) | 2017 | 1.277 |
| Cites / Doc. (2 years) | 2018 | 1.372 |
| Cites / Doc. (2 years) | 2019 | 1.745 |
| Cites / Doc. (2 years) | 2020 | 1.800 |
| Cites / Doc. (2 years) | 2021 | 1.825 |
| Cites / Doc. (2 years) | 2022 | 1.861 |
| Cites / Doc. (2 years) | 2023 | 1.909 |
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
| Cites | Year | Value |
|---|---|---|
| Self Cites | 2012 | 0 |
| Self Cites | 2013 | 3 |
| Self Cites | 2014 | 2 |
| Self Cites | 2015 | 4 |
| Self Cites | 2016 | 3 |
| Self Cites | 2017 | 0 |
| Self Cites | 2018 | 1 |
| Self Cites | 2019 | 0 |
| Self Cites | 2020 | 0 |
| Self Cites | 2021 | 7 |
| Self Cites | 2022 | 3 |
| Self Cites | 2023 | 6 |
| Total Cites | 2012 | 0 |
| Total Cites | 2013 | 172 |
| Total Cites | 2014 | 292 |
| Total Cites | 2015 | 377 |
| Total Cites | 2016 | 196 |
| Total Cites | 2017 | 110 |
| Total Cites | 2018 | 112 |
| Total Cites | 2019 | 123 |
| Total Cites | 2020 | 144 |
| Total Cites | 2021 | 205 |
| Total Cites | 2022 | 245 |
| Total Cites | 2023 | 284 |
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
| Cites | Year | Value |
|---|---|---|
| External Cites per document | 2012 | 0 |
| External Cites per document | 2013 | 1.988 |
| External Cites per document | 2014 | 2.522 |
| External Cites per document | 2015 | 2.608 |
| External Cites per document | 2016 | 2.506 |
| External Cites per document | 2017 | 1.467 |
| External Cites per document | 2018 | 1.790 |
| External Cites per document | 2019 | 1.640 |
| External Cites per document | 2020 | 2.057 |
| External Cites per document | 2021 | 2.084 |
| External Cites per document | 2022 | 1.952 |
| External Cites per document | 2023 | 2.000 |
| Cites per document | 2012 | 0.000 |
| Cites per document | 2013 | 2.024 |
| Cites per document | 2014 | 2.539 |
| Cites per document | 2015 | 2.636 |
| Cites per document | 2016 | 2.545 |
| Cites per document | 2017 | 1.467 |
| Cites per document | 2018 | 1.806 |
| Cites per document | 2019 | 1.640 |
| Cites per document | 2020 | 2.057 |
| Cites per document | 2021 | 2.158 |
| Cites per document | 2022 | 1.976 |
| Cites per document | 2023 | 2.043 |
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
| Year | International Collaboration |
|---|---|
| 2012 | 31.76 |
| 2013 | 26.67 |
| 2014 | 17.86 |
| 2015 | 10.53 |
| 2016 | 10.71 |
| 2017 | 0.00 |
| 2018 | 18.75 |
| 2019 | 17.39 |
| 2020 | 22.50 |
| 2021 | 22.95 |
| 2022 | 10.53 |
| 2023 | 19.23 |
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
| Documents | Year | Value |
|---|---|---|
| Non-citable documents | 2012 | 0 |
| Non-citable documents | 2013 | 4 |
| Non-citable documents | 2014 | 6 |
| Non-citable documents | 2015 | 6 |
| Non-citable documents | 2016 | 3 |
| Non-citable documents | 2017 | 4 |
| Non-citable documents | 2018 | 4 |
| Non-citable documents | 2019 | 3 |
| Non-citable documents | 2020 | 0 |
| Non-citable documents | 2021 | 0 |
| Non-citable documents | 2022 | 0 |
| Non-citable documents | 2023 | 0 |
| Citable documents | 2012 | 0 |
| Citable documents | 2013 | 81 |
| Citable documents | 2014 | 109 |
| Citable documents | 2015 | 137 |
| Citable documents | 2016 | 74 |
| Citable documents | 2017 | 71 |
| Citable documents | 2018 | 58 |
| Citable documents | 2019 | 72 |
| Citable documents | 2020 | 70 |
| Citable documents | 2021 | 95 |
| Citable documents | 2022 | 124 |
| Citable documents | 2023 | 139 |
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
| Documents | Year | Value |
|---|---|---|
| Uncited documents | 2012 | 0 |
| Uncited documents | 2013 | 21 |
| Uncited documents | 2014 | 27 |
| Uncited documents | 2015 | 41 |
| Uncited documents | 2016 | 21 |
| Uncited documents | 2017 | 34 |
| Uncited documents | 2018 | 24 |
| Uncited documents | 2019 | 32 |
| Uncited documents | 2020 | 24 |
| Uncited documents | 2021 | 21 |
| Uncited documents | 2022 | 35 |
| Uncited documents | 2023 | 36 |
| Cited documents | 2012 | 0 |
| Cited documents | 2013 | 64 |
| Cited documents | 2014 | 88 |
| Cited documents | 2015 | 102 |
| Cited documents | 2016 | 56 |
| Cited documents | 2017 | 41 |
| Cited documents | 2018 | 38 |
| Cited documents | 2019 | 43 |
| Cited documents | 2020 | 46 |
| Cited documents | 2021 | 74 |
| Cited documents | 2022 | 89 |
| Cited documents | 2023 | 103 |
Evolution of the percentage of female authors.
| Year | Female Percent |
|---|---|
| 2012 | 27.81 |
| 2013 | 40.18 |
| 2014 | 34.03 |
| 2015 | 30.43 |
| 2016 | 40.63 |
| 2017 | 44.71 |
| 2018 | 38.82 |
| 2019 | 39.01 |
| 2020 | 36.76 |
| 2021 | 38.10 |
| 2022 | 37.80 |
| 2023 | 44.44 |
Evolution of the number of documents cited by public policy documents according to Overton database.
| Documents | Year | Value |
|---|---|---|
| Overton | 2012 | 12 |
| Overton | 2013 | 4 |
| Overton | 2014 | 3 |
| Overton | 2015 | 2 |
| Overton | 2016 | 1 |
| Overton | 2017 | 0 |
| Overton | 2018 | 3 |
| Overton | 2019 | 2 |
| Overton | 2020 | 0 |
| Overton | 2021 | 0 |
| Overton | 2022 | 0 |
| Overton | 2023 | 0 |
Evoution of the number of documents related to Sustainable Development Goals defined by United Nations. Available from 2018 onwards.
| Documents | Year | Value |
|---|---|---|
| SDG | 2018 | 5 |
| SDG | 2019 | 3 |
| SDG | 2020 | 9 |
| SDG | 2021 | 27 |
| SDG | 2022 | 10 |
| SDG | 2023 | 11 |
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2024. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy

- Featured Feed
- Collections
- Become A Contributor
- Account Settings
- My Public Profile
- Feed Subscriptions
- Change My Institution
Use the journals feature with a free QxMD account.
Use Read by QxMD to access full text via your institution or open access sources.
Read also provides personalized recommendations to keep you up to date in your field.
Existing User
New to Read
Sign up for a free QxMD account to keep track of pertinent research with access to hundreds of Journal Publications.
Critical Care Research and Practice
All material on this website is protected by copyright, Copyright © 1994-2024 1994-{new Date().getFullYear()} by WebMD LLC. By using this service, you agree to our terms of use and privacy policy .
Save your favorite articles in one place with a free QxMD account.
Search tips.
Use Boolean operators: AND/OR
diabetic AND foot diabetes OR diabetic
Exclude a word using the 'minus' sign
Virchow -triad
Use Parentheses
water AND (cup OR glass)
Add an asterisk (*) at end of a word to include word stems
Neuro* will search for Neurology, Neuroscientist, Neurological, and so on
Use quotes to search for an exact phrase
"primary prevention of cancer" (heart or cardiac or cardio*) AND arrest -"American Heart Association"
We want to hear from doctors like you!
Take a second to answer a survey question.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Crit Care Res Pract
| 2020 to 2024 |  | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
IMAGES
VIDEO
COMMENTS
Critical Care Research and Practice is an open access journal publishing articles related to anesthesiology, perioperative and critical care medicine, and the integration of intraoperative management in preparation for postoperative critical care management. As part of Wiley's Forward Series, this journal offers a streamlined, faster ...
The Association of the Pulmonary Artery Pulsatility Index and Right Ventricular Function after Cardiac Surgery. Johnny Wei, Abigail Kee, Rachel Dukes, Jack Franke, Vincent Leonardo, Brigid C. Flynn. , 5408008. First Published: 13 February 2024.
Explore the latest in critical care medicine, including management of respiratory failure, sepsis, HAI prevention, end-of-life care, and more. This narrative review outlines diagnostic and treatment approaches to necrotizing soft tissue infections and suggests future directions while mentioning promising developments in their management.
Critical Care Research and Practice is a peer-reviewed, open access journal that offers a forum for physicians and health professionals who work in the area of health services research in critical care. The journal publishes original research articles and review articles related to anesthesiology, perioperative and critical care medicine, as well as the integration of intraoperative management ...
Aims and scope. Critical Care Research and Practice is an open access journal publishing articles related to anesthesiology, perioperative and critical care medicine, and the integration of ...
Potentiate critical care research both through research funding portfolios and by enhancing knowledge dissemination: Develop real-time updates to clinical practice guidelines: Advocate for equitable and inclusive critical care, particularly in underresourced care settings: Expand and support a global network of critical care professionals
A peer-reviewed, open access journal in & critical care. ... Critical Care Research and Practice This journal has been awarded the DOAJ Seal. 2090-1305 (Print) / 2090-1313 (Online) ... Best practice. This journal began publishing in open access in 2010.
A peer-reviewed, open access journal in & critical care. A peer-reviewed, open access journal in & critical care. This website uses cookies to ensure you get the best experience. ... Critical Care Research and Practice This journal has been awarded the DOAJ Seal. 2090-1305 (Print) / 2090-1313 (Online) Website ...
Research and practice in critical care medicine have long been defined by syndromes, which, despite being clinically recognizable entities, are, in fact, loose amalgams of heterogeneous states ...
TRANSLATING RESEARCH INTO CRITICAL CARE PRACTICE. Table 2 summarizes the major critical care practice recommendations developed over the past 25 years that are relatively low-cost and supported by high-quality evidence demonstrating improved patient outcomes. Despite their benefits, most of these best practices have not been fully integrated ...
Research. A central component of the Society's mission is the support of quality-based improvement initiatives and the support of multiprofessional research at all levels. The critical care professionals dedicated to research are vitally important to the present and future of the specialty. Researchers -- be their focus on basic, applied or ...
Awareness and Perception of Healthcare Providers about Proxy Consent in Critical Care Research. Rania Mahafzah, Karem H. Alzoubi, Omar F. Khabour, Rana Abu-Farha, 7614517; First Published: 30 September ... Evaluation of Paediatric Critical Care Needs and Practice in Nigeria: Paediatric Residents' Perspective. Moses Temidayo Abiodun, Fidelis E ...
Between January 2022 (Volume 31, Issue 1) and the current May 2023 journal issue (Volume 32, Issue 3), AJCC published 71 reports of original research. These recent papers addressed a wide range of research topics, including bedside patient care, palliative and end-of-life care, intensive care unit (ICU) survivorship, measurement and prediction of patient problems, family concerns ...
Sample of convenience was done. Intensivists were contacted using social media platforms and personal networking and via critical care societies. The survey was designed using Google™ forms online and sent out from February 17 th, 2020 to 23 rd September, 2020, to critical care professionals in 34 countries worldwide (Figure (Figure1). 1 ...
A peer-reviewed, Open Access journal that publishes research articles, review articles, and clinical studies related to critical care medicine. See the journal's SJR, citation impact, publication type, ISSN, scope, and quartile ranking in Egypt and other countries.
BACKGROUND: Previous research suggests that patients from rural areas who are critically ill with complex medical needs or require time-sensitive subspecialty interventions face worse healthcare outcomes and delays in care when compared to those from urban areas. The critical care resuscitation unit (CCRU) at our quaternary care center was established to expedite the transfer of critically ill ...
The Development of Critical Care Medicine in China: From SARS to COVID-19 Pandemic Haiyan Yin , Shan Wang , Youfeng Zhu , Rui Zhang , Xiaoling Ye , Jianrui Wei , Peter C. Hou , 3956732
Neonatal resuscitation is a critical procedure aimed at ensuring the successful transition of newborns from intrauterine to extrauterine life. Traditionally, this involves immediate clamping and cutting of the umbilical cord, but recent advances have introduced intact cord resuscitation (ICR) as an alternative approach. This review aims to comprehensively analyze ICR, exploring its evolution ...
Advertising Policy. Critical Care Research and Practice accepts advertisements that are relevant to the journal's subject community, promote high quality products and services, and are provided by reputable organizations who display a true commitment to science and medicine. This journal can earn revenue from advertising sales income. Wiley's advertising policy safeguards editorial ...
Crit Care Res Pract; Critical Care Research and Practice Vols. 2010 to 2024; 2010 to 2024; 2020 to 2024 ... v.2016 2016: v.2017 2017: v.2018 2018: v.2019 2019: 2010 to 2014: v.2010 2010: v.2011 2011: v.2012 2012: v.2013 2013: v.2014 2014: Articles from Critical Care Research and Practice are provided here courtesy of Hindawi Limited. Follow ...
2 Both The Faculty of Architecture of the KU Leuven is developing the concept of Academic Design Offices (ADO) in order to clarify, intensify and render more explicit the connection between education, design practice and research, avoiding the threat of parallel circuits of practice and academia in Architecture. ADOs consist of multidisciplinary teams where researchers, artists, practitioners ...
Research published in the journal must be: Scientifically valid - adhering to accepted community standards of research. Technically accurate in its methods and results. Representative of a specific advance, or replication, or null/negative result, which is worthy of publication.
Background Ventilator-associated pneumonia (VAP) is the most common nosocomial infection in intensive care units (ICUs) and is a common cause of morbidity and mortality in intensive care patients. ... Nursing in Critical Care. Early View. RESEARCH ARTICLE. ... Relevance to Clinical Practice.