TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works
Home > SD > DENTISTRY > ETD-PROSTHODONTICS

Theses, Dissertations and Projects - Prosthodontics
Theses/dissertations from 2022 2022.
Effect of Splinting Implant Scan Bodies Intraorally on The Trueness of Complete Arch Digital Impressions: A Clinical Study , Kawther Mahmoud Ali
Theses/Dissertations from 2019 2019
In-vitro Comparison of Retention Among Contemporary and Conventional Post-and- Cores , Hatem Alqarni
Three Dimensional Analysis of Intraoral Scanners Accuracy: An In-Vitro Study , Rami Ammoun
Complications associated with mandibular fixed complete arch prostheses based on implant distribution , Shivani Karre
Theses/Dissertations from 2018 2018
The Wear of Acrylic Resin and Composite Resin Teeth against Polished and Glazed Zirconia , Abdulkareem Alshehri
In-vitro Evaluation of Accuracy of Conventional and CAD/CAM Removable Partial Denture Frameworks , Pooya Soltanzadeh
Theses/Dissertations from 2017 2017
Effect of Image Sharpening on Radiographic Image Quality , Jefferson Lee Clark
Theses/Dissertations from 2016 2016
Comparison of Retention between Milled and Conventional Denture Bases: A Clinical Study , Abdulaziz Abdullah AlHelal
Effects of Microwave Irradiation on the Dimensional Stability of Complete Denture Bases , Miguel Pappaterra
Theses/Dissertations from 2015 2015
Effect of Diamond Bur and Root Canal Irrigants on Retention of Fiber Posts , Rami Jekki
Comparison of Maxillary Anterior Teeth Width to Facial Dimensions among Three Races , Ewa Parciak
Are Bone Turnover Markers and Vitamin D levels associated with Frequency of Complete Denture Relines? , Shweta Puri
Theses/Dissertations from 2014 2014
Comparison of Occlusal Plane Orientation Obtained Using Five Facebow Systems , Thomas C. Maveli
Theses/Dissertations from 2013 2013
Evaluation of Accuracy of Impression Materials with Different Mixing Techniques , James Ywom
Theses/Dissertations from 2012 2012
In‐Vitro Comparison of Tensile Bond Strength of Denture Adhesives on Denture Bases , Doris Rachel Kore
Effect of Time on Gypsum-Impression Material Compatibility , John Boram Won
Theses/Dissertations from 2009 2009
Effect of Auxiliary Preparation Elements on Resistance Form of Complete Crowns , Manuel H. Guevara
The Effect of Auxiliary Preparation Elements on the Resistance Form of Complete Metal Crowns , Mostafa Nazari
Immediate Loading of Unsplinted Implants in the Anterior Mandible for Overdentures , Phillip Roe
Theses/Dissertations from 2008 2008
Effect of Gutta Percha on the Retention of a Post Using Different Cements , Saeda H. Basta
An In-Vitro Investigation of the Physical Properties of Alginate Alternatives , Rishi Dinesh Patel
Theses/Dissertations from 2006 2006
A Comparison of Cadiax Axiography & NewTom 3G Tomography Condylar Measurements , David Phillip Brock
Theses/Dissertations from 2003 2003
Dental Treatment Options for Snoring - A Pilot Study , Kainaz Khushrooh Byramjee
Theses/Dissertations from 1999 1999
Marginal Discrepancy of Components Utilized for Implant Framework Construction , Mathew Thomas Kattadiyil
Theses/Dissertations from 1973 1973
Effect of Post-Operative Use of Chlorhexidine on Regeneration of Bifurcation Defects in Dogs , Gary Bogle
- Collections
- Disciplines
Advanced Search
- Notify me via email or RSS
Author Corner
- Faculty Research (Pure)
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Prosthodontics Thesis Topics
It is important to choose the thesis topics carefully while pursuing MDS course. The thesis topic should be easy as well as interesting. Many a times the residents mistake a complex thesis topic to be a good thesis topic while an easy topic can also be a good topic. So there is no point in taking complex thesis topics. Prosthodontics is a specialized branch of dentistry that focuses on the restoration and replacement of missing or damaged teeth. Prosthodontists, experts in this field, employ a combination of artistry and advanced dental technology to enhance the oral health and quality of life for their patients. From crafting dental prostheses to addressing complex cases involving multiple missing teeth or congenital anomalies, prosthodontics stands at the forefront of dental innovation.
Embarking on a journey in prosthodontics is a profound exploration into the realm of dental science, and for those pursuing a Master of Dental Surgery (MDS), the selection of an appropriate thesis topic holds paramount significance. Prosthodontics, often referred to as the art and science of dental prosthetics, plays a pivotal role in restoring oral function, aesthetics, and overall well-being. In the pursuit of academic excellence, the choice of an orthodontics thesis topic becomes a critical juncture, shaping the trajectory of one’s research and contributing to the collective knowledge in the field.
Prosthodontics, an essential branch of dentistry, focuses on the design, manufacture, and fitting of artificial replacements for teeth and other parts of the mouth. This field provides fertile ground for research, and delving into prosthodontics thesis topics can significantly impact patient care outcomes. For students and professionals exploring advanced research, prosthodontics thesis topics may include innovations in dental materials or the effectiveness of new digital impression techniques.
Additionally, prosthodontics thesis topics that investigate the biomechanics of dentures or the integration of implantology with aesthetic considerations are crucial for advancing the field and enhancing the functional aesthetics in dental restorations.
The scope of prosthodontics extends beyond mere tooth replacement; it encompasses the intricate art of smile design, facial aesthetics, and the restoration of oral function. Patients who seek prosthodontic care often present with diverse challenges, and prosthodontists are equipped with a comprehensive skill set to address these issues, ensuring optimal outcomes in terms of both form and function.
As MDS candidates delve into the world of prosthodontics, the selection of a thesis topic becomes a defining aspect of their academic journey. The process of identifying a suitable research topic requires careful consideration and an understanding of the current trends, challenges, and advancements within the field. This is where the strategic choice of keywords, such as “orthodontics thesis topics,” comes into play, guiding prospective researchers towards relevant and impactful areas of study.
A well-chosen prosthodontics thesis topic serves as the foundation for a rigorous and insightful exploration into a specific aspect of prosthodontics. It not only reflects the researcher’s interests and expertise but also contributes to the evolving body of knowledge in the discipline. The impact of research in prosthodontics is far-reaching, influencing clinical practices, treatment modalities, and even the development of new technologies.
In the multifaceted world of prosthodontics, the journey towards an MDS thesis is an odyssey of discovery, innovation, and scholarly pursuit. The choice of an orthodontics thesis topic is a pivotal decision that shapes the trajectory of a researcher’s academic and professional endeavors.
Through strategic use of keywords and a thoughtful exploration of the significance of the chosen topic, MDS candidates can not only enhance the visibility of their work but also contribute meaningfully to the ever-evolving tapestry of prosthodontic knowledge. As the field continues to advance, the commitment to choosing impactful orthodontics thesis topics remains an enduring testament to the dedication of researchers in propelling prosthodontics into the futur
PROSTHODONTICS THESIS TOPICS (2024 Update)

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 May 2019
Advances in materials and concepts in fixed prosthodontics: a selection of possible treatment modalities
- Daniel Edelhoff 1 ,
- Michael Stimmelmayr 2 ,
- Josef Schweiger 3 ,
- M. Oliver Ahlers 4 &
- Jan-Frederik Güth 2
British Dental Journal volume 226 , pages 739–748 ( 2019 ) Cite this article
7495 Accesses
16 Citations
Metrics details
The introduction of adhesive techniques in combination with translucent restorative materials has greatly influenced treatment concepts in fixed prosthodontics. Modern production technologies offer access to new polymer materials that provide innovative pre-treatment options for complex prosthetic rehabilitations. Additionally, computer-aided design and manufacturing (CAD/CAM) provides access to new ceramic types and thus extends the range of indications for metal-free restorative options. With these developments, important changes of treatment concepts in fixed prosthodontics have occurred which affect the professional life of dental practitioners with a focus on prosthetic dentistry. This article gives an overview of the advances in selected fields of fixed prosthodontics and provides support in material selection for different kinds of indications, from single-tooth restorations to fixed dental prostheses.
You have full access to this article via your institution.
Similar content being viewed by others

Modern partial dentures - part 2: a review of novel metal-free materials and innovations in polymers

Modern partial dentures - part 1: novel manufacturing techniques
Ceramics overview
Presents innovative pre-treatment options with CAD/CAM polymers in complex rehabilitations.
Demonstrates less invasive preparation options for bonded all-ceramic veneers and occlusal onlays.
Identifies the potential and limitations of all-ceramic restorations for the abraded dentition.
Provides material selection criteria to ensure durable anterior cantilever resin-bonded FDPs and conventional FDPs.
Introduction
Treatment options in fixed prosthodontics have changed significantly in recent decades. Three main developments have strongly influenced these changes. First, minimally invasive treatments have increasingly become feasible in restorative dentistry, thanks to the introduction of the adhesive technique in combination with restorative materials with translucent properties comparable to those of natural teeth. Mechanical anchorage of restorations via conventional cementation, a predominantly subtractive method, is gradually being superseded by a primarily defect-orientated additive approach. Second, modifications of conventional treatment procedures have led to the development of an economical approach to the removal of healthy tooth structure, as the planned outcome is defined in a wax-up before the treatment itself is commenced. This wax-up is then used for reference during tooth preparation. Third, digital technology delivers important additional information including 3D data, for analysis, diagnostics, communication, restorative designs and treatment planning, improving reproducibility. Also, the computer-aided design/manufacturing (CAD/CAM) process facilitates more standardised fabrication processes and quality improvements in materials, and provides access to new materials offering favourable options during the pre-treatment period as well as for subsequent definitive restorations. Similarly, the introduction of cantilever resin-bonded fixed dental prostheses and implants permits the preservation of tooth structure for teeth that would otherwise have had to be prepared as abutment teeth.
This article demonstrates the advances in materials and strategies in fixed prosthodontics by discussing a selection of possible treatment modalities and supports these concepts by citing the available scientific literature.
At present, conventional treatment with metal-based crowns and fixed dental prostheses (FDPs) are considered the gold standard for clinical success and survival. 1 However, the extensive removal of tooth structure associated with full coverage crowns and FDPs on prepared abutment teeth remains a major drawback. A retrospective clinical study has demonstrated that the 15-year survival probability of vital pulps was 81.2% in metal-ceramic single crowns and only 66.2% in FDP abutments. 2 Foster found an endodontic complication rate of 21% for FDP abutments after six years. 3 . An initial quantification of hard tissue removal with different preparation configurations revealed that up to 72% of the clinical crown will be removed in full crown preparations in the anterior and posterior regions. 4 , 5 In contrast, all-ceramic anterior veneer preparations are associated with removing tooth structure in the amount of between 7% (partial veneers) and 30% (extended veneers). 4 For occlusal onlays with proximal extensions, 32% of the tooth structure was removed. 5 These findings were confirmed in a study that used state-of-the-art measuring techniques and are increasingly affecting treatment decisions in prosthodontics. 6
Several in vitro studies on endodontically-treated teeth have found that preserving greater amounts of natural tooth structure has a significant positive effect on fracture resistance in all tooth types. 7 , 8 Up to 45% more tooth structure can be preserved by opting for partial rather than complete coverage when restoring endodontically-treated molars. 9 Similar results were found for retainer preparations for resin-bonded FDPs and attachments. 10 , 11
It is noteworthy that clinical studies on all-ceramic partial coverage crowns have shown no or very low endodontic complication rates, at observation periods between seven and 12.6 years, compared to studies on metal-ceramic full coverage crowns. 12 For veneer restorations, the rate of endodontic complications was as low as 2.51% after an observation period of 20 years. 13 Hence, less invasive preparation and restoration designs appear to have a favourable effect on the vitality of restored teeth. Against this background, fixed prosthodontics has been undergoing a paradigm shift towards less invasive methods in recent years. Prosthetic concepts have also become increasingly well-differentiated in recent decades. 10 , 14 , 15
Predominantly subtractive concepts, to provide mechanical retention for traditionally cemented restorations, are being replaced by less invasive, primarily defect-orientated procedures wherever feasible. 16 In the case of pronounced dental hard tissue loss, additive approaches offer innovative reversible pre-treatment options and functional restorations. 17 , 18 In addition, modifications are being made to traditional procedures, such as defining the treatment goal in the lead-up to the treatment itself with the aid of a diagnostic wax-up. 19 The wax-up provides orientation for tooth preparation and a more economical approach when it comes to removing healthy dental hard tissue. 20
This article intends to describe innovative pre-treatment options and methods that allow the removal of hard tissues to be substantially reduced. Metal-free CAD/CAM materials will be presented and discussed, focusing on selected polymers and all-ceramic materials.
Innovative pre-treatment with CAD/CAM polymers
Pre-treatment with occlusal splints is an important step in a structured concept for complex prosthetic rehabilitations and serves to determine and stabilise a physiological condylar position. Furthermore, it permits evaluating acceptance of the intended vertical dimension. Conventional positional splints are a proven, established and relatively low cost pre-treatment. Their chemical composition allows the splints to be modified to follow adaptive changes in condylar position. However, the willingness of patients to wear conventional splints during daytime is limited, mostly due to aesthetic and phonetic restrictions, limiting their efficiency. 21 In addition, conventional positioning splints are generally provided for only one jaw. In bimaxillary restorative treatments, therefore, they attempt to represent the entire change in vertical dimension in a single appliance and cannot simulate the position of the occlusal plane of the subsequent restoration. Despite these limitations, conventional relaxation and positioning splints continue to be the method of choice for initial pain relief and functional rehabilitation.
With the introduction of CAD/CAM-milled polymers, novel alternatives to splints have become available. Designed according to a diagnostic wax-up and milled and finished to full contour from tooth-coloured polycarbonate, these splints approximate the definitive restoration in terms of function and aesthetics ( Fig. 1 ). Removable monomaxillary or bimaxillary full contour splints provide the option of conservative, surgical, periodontal and restorative interventions beneath them without adverse effects on the newly defined aesthetic and functional situation ( Figs 2 and 3 ). At the end of the 'test drive' period, a segmented transfer to the final restoration can be performed, facilitating the treatment of complex rehabilitations ( Figs 4 and 5 ). 17

Industrial prefabricated CAD/CAM disc made of tooth-coloured polycarbonate (Temp Premium Flexible; Zirkonzahn, Gais, Italy) after milling two fully-contoured removable splints

Fully-contoured CAD/CAM occlusal splints for bimaxillary application (maxilla and mandible) after separation from the polycarbonate disc. The material exhibits an extremely high degree of flexibility and, even when extremely thin (0.3 mm), has a high fracture resistance

Preoperative frontal view of a female patient with a right cleft lip and palate. Tooth 12 is missing and the dentition exhibits severe tooth wear that has led to a change in intercuspal position and a decrease in the vertical dimension of occlusion

After a successful clinical evaluation of aesthetics and function over at least three months, the transition to the definitive restoration can proceed segment by segment, using the reciprocal transfer method for the evaluated jaw relation. The right quadrant was prepared and the maxillary splint separated in half with a separating disk

With the left half of the splint inserted in the still unprepared left quadrant, the jaw relation was registered using a high precision bisacrylate registration material (LuxaBite; DMG, Hamburg, Germany), which can be corrected with Aluwax (American Dental Systems, Vaterstetten, Germany). Limitations of this technique exist in patients who suffer from instable temporomandibular joints or who are occlusion-sensitive. In these cases, the techniques featured in the subsequent illustrations should be used
An additional pre-treatment option is the application of polymethyl methacrylate (PMMA) repositioning onlays and veneers, bonded to the compromised tooth or existing restorations ( Figs 6 , 7 and 8 ). They can be made conventionally or by CAD/CAM. 22 , 23 Given the higher edge stability compared to ceramics, polymer-based materials can be milled to very thin layers of up to 0.3 mm and can thus serve as pure additive restorations without any tooth preparation. 23 However, this pre-treatment option is more complicated because the bonded PMMA restorations are difficult to modify intraorally, their reversibility is limited, and they are relatively expensive. Nevertheless, because the contours of these temporary restorations are identical to the intended restored situation and because they are inserted permanently, patients can even eat with them, which makes the evaluation period as realistic and effective as possible.

CAD/CAM repositioning onlays made of PMMA (TelioCAD; Ivoclar Vivadent, Schaan, Liechtenstein). These extra thin additive PMMA restorations can be bonded to existing restorations for occlusal correction as a fixed pre-treatment and simultaneously for a 'test drive' of the new occlusion

Preoperative situation of a patient seeking treatment for bite correction because of severe pain in function as a consequence of a generalised malocclusion

Occlusal PMMA veneers bonded to existing restorations. Before adhesive placement with a low viscosity resin cement, the existing metal ceramic restoration with gold margins were tribochemically air-abraded (CoJet; 3M, Seefeld, Germany), then cleaned and coated with a primer
According to the authors' experience, both monomaxillary and bimaxillary full contour simulation splints, as well as repositioning onlays and repositioning veneers, enjoy substantially better patient acceptance than conventional positional splints and provide new 'test drive' options to explore the aesthetics, phonetics and function of complex prosthetic rehabilitations. They can serve to identify the most adequate occlusion concept, especially in patients sensitive to occlusal changes. In complex prosthetic rehabilitations, they permit a conversion to the definitive restoration, a segment at a time ( Fig. 9 ). However, relevant clinical studies are still absent.
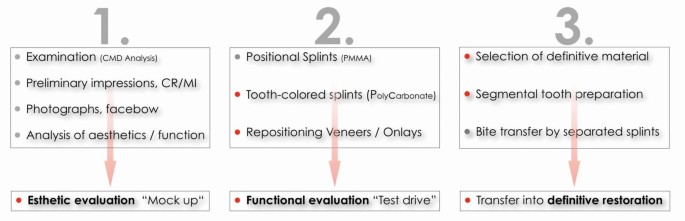
Overview of the pre-treatment options for complex prosthetic rehabilitations with major changes in aesthetics and function, and the transition to definitive restorations
Conversion to definitive all-ceramic restorations
All-ceramic anterior veneers.
Encouraged by positive long-term clinical results, there has been a steady expansion of the range of indications for all-ceramic veneers, even going so far as to re-evaluate previous contraindications to open up possible new fields of application. 24 , 25 , 26 , 27 , 28 , 29 Against this background, ceramic veneers have shed their reputation of being purely aesthetic adjuncts, turning into a serious treatment alternative, in addition to conventional, far more invasive types of restorations. 30 , 31 , 32 Today, veneers are also used to restore the biomechanics of the dentition, establish adequate function, mask highly discoloured endodontically-treated teeth, and for other purposes. 33 Silicate ceramic materials are the material of choice to replace lost natural enamel thanks to their enamel-like optical and mechanical properties. 34 , 35 However, veneer preparation, provisionalisation and adhesive bonding place greater demands on the operator's skills than complete-coverage crown preparation and conventional cementation. Enamel preservation represents a determining factor for the success of a veneer restoration. 36 , 37 Therefore, veneers should be designed using a mainly additive approach.
Veneer preparations are subject to stringent principles, but they still offer a high degree of flexibility in terms of the restorative design, depending on the clinical situation (tooth position, degree of destruction, occlusal conditions, periodontal surroundings etc). 38 , 39 This is true for both the incisal design and for its interproximal extension. 38 , 24 Preparing a palatal chamfer offers the highest degree of freedom in positioning the incisal edge, which is particularly important if a large amount of hard tissue has been lost. 38 , 39 , 40
Similar considerations apply to the interproximal extension of the preparation ( Fig. 10 ). 35 , 24 If the popular medium wrap design is used, the contact area, and thus the width of the existing tooth, are maintained and, consequently, the height is determined by the defined width to height ratio ( Fig. 11 ). By contrast, a long wrap design eliminates the contact areas due to their deep interproximal extension, offering considerably more scope for variation regarding the shape and position of the restoration ( Fig. 12 ). The long wrap design is therefore advantageous in severe discolouration, diastemas, extensive shape modifications, slide midline corrections, black triangles and large fillings. Furthermore, the long wrap design is recommended for veneers in the immediate vicinity of crowns, as it allows the contact area between the two restorations to be executed in ceramics. Interproximal preparation can be conveniently accomplished with oscillating preparation instruments (for example, Sonic Line; Komet Dental, Lemgo, Germany) and Soflex discs (2382 M; 3M, Seefeld, Germany). 41 In periodontally compromised situations, the long wrap design may be combined with a horizontal insertion axis, 42 eliminating the need for an extensive reduction of the coronal tooth structure. The width can be smaller cervically than incisally. Substantial amounts of hard tissue can be preserved with this configuration. On the downside, however, the clinical and technical implementation of this technique is difficult.
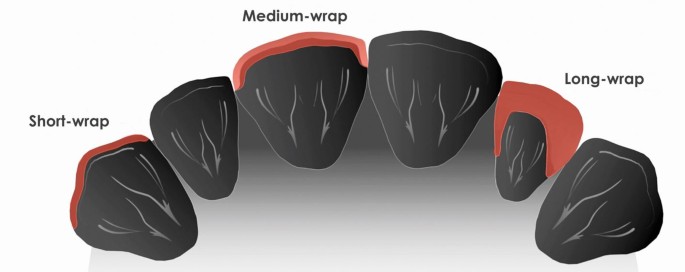
Design options for the interproximal extension. Left to right, with increasing levels of invasiveness. Short wrap design: easy to implement, but with a visible adhesive joint. Medium wrap design: retains the contact point, with the adhesive joint not visible. Long wrap design: removes the contact point and requires a deeper (approximately two thirds) interproximal preparation

Veneer preparation in medium wrap design, preserving the contact points, and try-in of definitive feldspathic veneers, sintered on refractory dies (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)

Veneer preparation in long wrap design, opening the contact points, and try-in of the definitive veneers made of feldspathic ceramics using the sintering technique on refractory dies (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)
Circular preparation designs (360° veneers), also known as 'full wrap' veneer designs, are particularly recommended for complex cases that require increasing the vertical dimension of occlusion to close the resultant free space on the palatal aspect of the maxillary anterior teeth ( Fig. 13 ). Essentially, a diagnostic template or silicone mould should be manufactured from the wax-up and used as a guide during tooth preparation, reducing the amount of tissue removed, by taking into account the previously defined external contour of the future veneer ( Fig. 14 ). 35 , 37 , 43 If severe discolouration is present, the preparation may be slightly deeper to provide sufficient scope for masking the tooth. 33 Luting composites can also be used to slightly modify the final colour of ceramic veneers. 44 In a retrospective ten-year cohort study, these veneers have been shown to offer a 93.5% survival probability. 13 First interim results of a prospective clinical study on veneers with a long wrap design have been promising; however, no sufficient data are as yet available on either long wrap or full wrap veneers. 45 The survival rates of ceramic veneers are also influenced by other parameters, including the amount of available enamel, the optical and mechanical properties of the material used, the preparation design, tooth function and occlusion, the degree of destruction and the vitality of the tooth to be treated (vital or endodontically-treated), as well as the level of experience of the restorative team. 13 , 31 , 36 , 37

Veneer preparation in full wrap design (360° veneers) and try-in of the definitive monolithic bichromatic veneers made of lithium disilicate ceramic (IPS e.max Press Multi; Ivoclar Vivadent; Otto Prandtner, MDT, Munich, Germany)
Template-guided veneer preparation. The silicon index was made on the wax-up and then seated on the prepared teeth to control the removal of hard tissue against to the planned contour of the definitive restoration using a special probe featuring a millimetre scale (CP-15UNC, University of North Carolina; Hu-Friedy, Tuttlingen, Germany)
All-ceramic occlusal onlays
Adhesively connected all-ceramic occlusal onlays are a reliable treatment option for the posterior region. 46 , 47 In this context, it should be borne in mind that most clinical long-term studies are based on leucite-reinforced glass ceramics, whereas considerably stronger ceramic materials based on lithium disilicate are available today. 12 , 48 With the decreasing incidence of caries, accompanied by an increasing incidence of biocorrosive defects, including in generalised form, changed defect morphologies of the dental hard tissue are gaining in importance. 49 , 50 Thus, the requirement profile for minimally invasive, defect-orientated, adhesively-cemented single-tooth restorations has changed. Restorative treatment in the posterior region now focuses increasingly on occlusal defects, seeking to restore adequate function, aesthetics and biomechanics, and to help prevent further pathological wear.
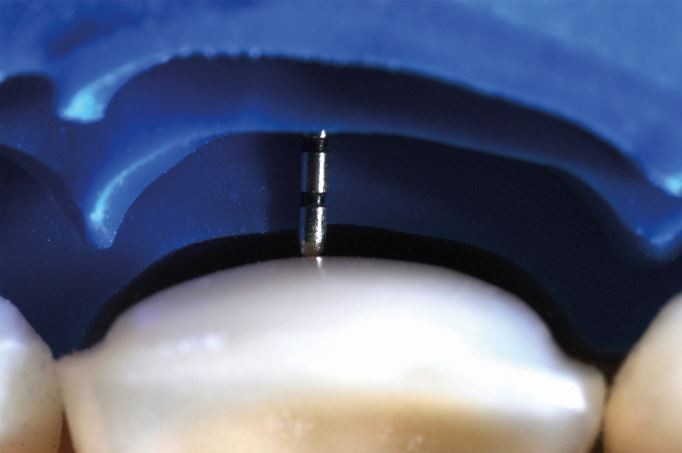
In view of the sometimes extreme changes in occlusal contour due to tooth wear, adhesively-cemented occlusal onlays made of high-strength glass ceramics are a more desirable type of restoration than conventional full crowns, which are twice as invasive. 5 As they permit a defect-orientated preparation and eliminate the need for a retentive preparation design, all-ceramic onlays are a sensible treatment option and avoid conventional invasive methods. 14 , 51 The supragingival preparation margins of occlusal onlays offer numerous advantages in terms of better control during preparation, reduced loss of dental hard tissue, less or no traumatic interference with the marginal gingiva, easier conventional and digital impression-taking, more available enamel for bonding and well-controlled adhesive cementation, possibly under rubber dam ( Figs 15 and 16 ).
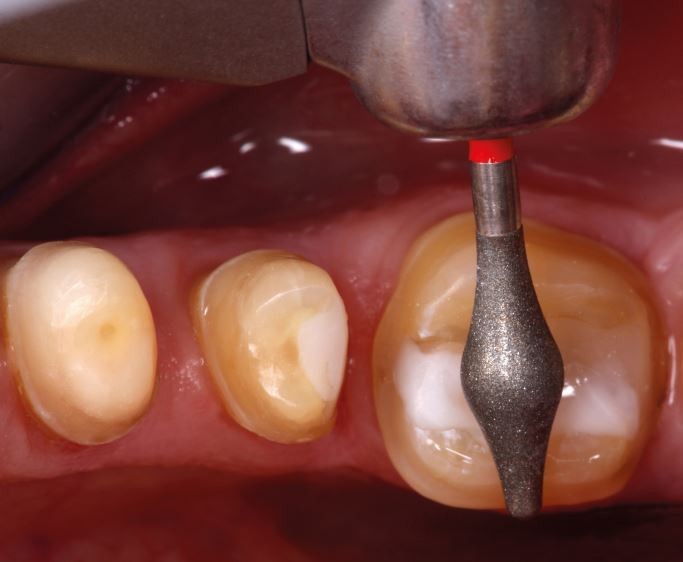
Preparation of an occlusal plateau for a lithium disilicate ceramic occlusal onlay. The specific geometry of the abrasive body (here: OccluShaper as finisher, Komet Dental, Lemgo, Germany) creates anatomically-shaped convex cusp support for the future occlusal onlay while leaving enough space in the central fissure to implement an immediate side shift (ISS) during dynamic occlusion
Occlusal onlay preparations are associated with a gentle removal of tooth structure, especially if the preparation does not extend beyond the equator into the infrabulge (red marked area)
Since the introduction of lithium disilicate, the recommended preparation depths for glass ceramic onlays have been reduced significantly. Today, a minimum occlusal thickness of 1 mm is recommended for monolithic restorations (staining technique) ( Figs 17 and 18 ). Discussions are currently underway about further reductions in layer thickness if appropriate enamel support is present. 14 , 48

Monolithic occlusal onlays made of IPS e.max Press (degree of turbidity: HT) with an occlusal thickness of 1 mm and a 0.5 mm circular border (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)

Try-in of the lithium disilicate ceramic occlusal onlays (IPS e.max Press, degree of turbidity: HT) with a colour-keyed dyed try-in paste (Variolink Esthetic, Try-in, colour: warm; Ivoclar Vivadent)
Glass ceramic onlays appear to be ideally suited for rebuilding abraded and eroded posterior teeth because they offer enamel-like properties and a favourable interface behaviour. 51 They allow particularly gentle preparation of the tooth structure, as long as the preparation does not extend beyond the equator into the infrabulge (Fig. 16). Consequently, these onlays can help avoid conventional, much more invasive prosthetic procedures. It is essential for the preparation margins to be located predominantly in enamel. Extensive silicate ceramic onlays have displayed a favourable stress response pattern and with almost exclusively compressive forces at the interface in in vitro studies. 51 However, all transitions should be rounded and soft to prevent stress peaks within the restoration (Fig. 15). 52
It is generally useful to distinguish between pure onlays, involving only occlusal surfaces, and onlay veneers, involving the vestibular surface. The latter are indicated if a major shade modification in the aesthetic region (premolar) is required (Fig. 15). 23 In a controlled prospective clinical study, silicate ceramic onlays showed satisfactory long-term results after 12 years. They are also suited for use in extensive tooth structure defects. 53 Another clinical study with an observation period of 12.6 years revealed failure rates of 20.9% in vital teeth and 39% in endodontically-treated teeth. 47
Resin-bonded anterior all-ceramic FDPs
Resin-bonded fixed dental prostheses (RBFDPs) in the anterior region were first described in the 1970s. 54 In a literature review, RBFDPs comprising two retainers showed a significantly lower probability of survival than full crown abutments over a period of ten years. 1 However, it should be borne in mind that anterior maxillary teeth are considered to be particularly vulnerable to vitality loss when used as full crown abutments in conventional FDPs. 2 The tooth structure removal on anterior maxillary central incisors was measured to be up to 72.1% for full crown abutments and only 12.4% after preparation of wing retainers for an RBFDP. 4 With the introduction of metal-based cantilever RBFDPs (cRBFDPs) in the 1980s, invasiveness levels were further reduced and the need for unphysiological splinting of abutment teeth was eliminated. 55 , 56 In the anterior region, cRBFDPs were identified to have a lower clinical failure rate than two retainer RBFDPs. 57 , 58 The principles of minimally invasive treatment also favour cRBFPDs. 58 In the 1990s, glass-infiltrated aluminium oxide ceramics were used for the first time in a clinical study to manufacture all ceramic RBFDPs with two retainers. 59 With greater popularity and better access to CAD/CAM technology, zirconia-based cRBFDPs became the therapy of choice where metal-free cRBFDPs are indicated. 60 , 61
Today, most cRBFDPs are made with frameworks made of materials with a high modulus of elasticity, such as base-metal alloys or zirconia ceramics ( Fig. 19 ). They are used in the anterior region as an alternative to implant-supported restorations for single teeth if implant treatment is contraindicated, extensive surgical interventions should be avoided, the space available is insufficient for implant treatment, the patient is too young or too old, or if an implant is simply not wanted. 55 , 61 In a clinical trial investigating the impact of complications of anterior single-tooth restorations, the oral health-related quality of life was similar irrespective of whether implant-supported single crowns or cRBFDPs were used. 62

CAD/CAM zirconia-based cantilever resin-bonded fixed dental prosthesis (cRBFDPs) for the replacement of two missing maxillary lateral incisors (left and right) in a young female patient (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)
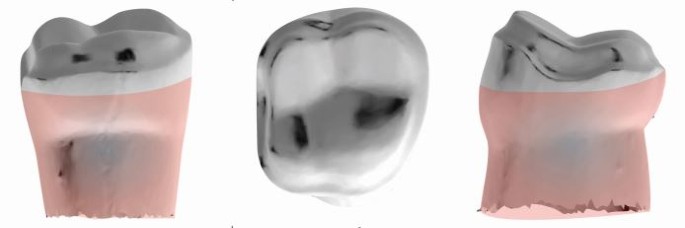
One of the most important indications is in the anterior region of the maxilla, as the highest incidence of dental agenesis is reported to affect maxillary lateral incisors, with a higher prevalence in female than male patients. 63 In the same meta-analysis, bilateral agenesis of maxillary lateral incisors was found more frequently than unilateral agenesis ( Fig. 20 ). If a maxillary lateral incisor is missing, central incisors will be the abutments of choice for cRBFDPs due to their larger proximal contact area (PCA) (Figs 20 and 21 ). 64 Removing between 0.5 mm and 0.7 mm of tooth structure is recommended in preparation for the wing-shaped retainer, with either a slight chamfer or slight rounded shoulder as a finishing line. Instead of retentive grooves associated with metal-based RBFDPs, a flat proximal box 0.5 mm in depth and 2 × 2 mm in width is recommended at the connector side for pontics of all-ceramic cRBFDPs (Fig. 21). 60 , 65 Additional requirements include healthy abutment teeth that are primarily free of both caries and fillings, enough interocclusal space (approximately 0.8 mm) and sufficient amounts of enamel. 61 Where central incisors show major carious lesions, extended fillings, endodontic treatment or similar, the canine can be selected as the abutment tooth for cRBFDPs.

Post-orthodontic palatal view of the anterior tooth display of a young female patient with bilateral agenesis of the maxillary lateral incisors. The recipient site of the pontic had been pre-treated for an improved emergence profile
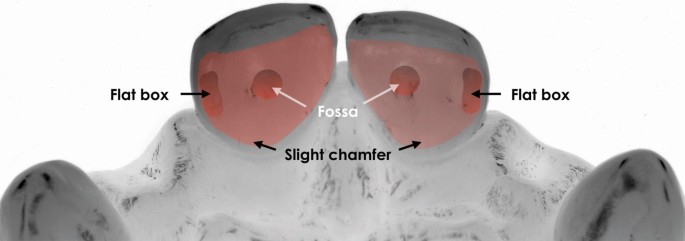
For zirconia-based cantilevered RBFDPs, a flat proximal box 0.5 mm in depth and 2×2 mm in width is recommended at the connector side for the pontic
One of the most frequent minor complications is debonding. A reliable procedure for binding to either tooth hard tissue or zirconia is considered the most important prerequisite for the long-term clinical success of zirconia-based cRBFDPs. 66 Where bonding to enamel represents a predictable and well-established procedure, different methods to generate a reliable adhesion to zirconia surfaces are described. 67 Based on the results of a systematic review, the physico-chemical conditioning of zirconia, including moderate airborne particle abrasion and the use of MDP-based resin cements, were found to produce reliable adhesion ( Figs 22 and 23 ). 68 Following these protocols, this type of minimally invasive restoration can satisfy high aesthetic demands while requiring relatively little treatment time ( Figs 24 and 25 ). Since the preparation takes place almost exclusively within the enamel, local anaesthetics are usually not required.

For a reliable bond to the zirconia wing, the internal surface was air-abraded with carborundum (50 μ m grain) at 1 bar of pressure. For better control of the air abrasion process, a black marker was applied to the internal surface of the wing. In a second step, the air-abraded zirconia was cleaned and a MDP primer was applied ahead of the luting composite

Postoperative palatal view after the adhesive placement of two zirconia cRBFDPs with an ovate pontic design. Since the distal contact area of the pontics can be accessed by dental floss, hygiene procedures are simplified compared to two retainer RBFDPs

Post-orthodontic frontal view of a young female patient with congenitally missing maxillary lateral incisors (orthodontic procedures: Professor A. Wichelhaus, LMU Munich, Germany)

Postoperative frontal view after adhesive insertion of the zirconia cRBFDPs restorations. Both canines and centrals received bonded no-prep feldspathic veneer restorations made using the refractory-die technique (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)
Data from clinical studies on zirconia cRBFDPs show excellent clinical results. In a four-year clinical study, with 15 zirconia cRBFDPs, a survival rate of 100% was reported. 69 Two early debondings could be successfully reattached. In a clinical long-term study of a total of 108 anterior zirconia cRBFDPs, 75 in the maxilla and 33 in the mandible, a ten-year survival rate of 98.2% and a corresponding success rate of 92.0% were reported. Six debondings and one restoration loss were recorded; all debonded zirconia cRBFDPs could be rebonded. 10 In carefully selected cases, lithium disilicate ceramics might be suitable as a framework material for cRBFDPs. 70
Conventional FDPs made of zirconia
Lithium disilicate ceramics was introduced in 1998 as a reliable metal-free material for different types of single-tooth restorations. For single crowns, long-term clinical survival rates comparable to metal ceramic crowns have been reported. 71 , 72 , 73 In contrast, conventional three-unit FDPs made of lithium disilicate ceramics are recommended for only limited indications (anterior dentition with second premolar as distalmost abutment), and survival rates were strongly correlated with the framework design, veneered or monolithic. 74 , 75 , 76 The introduction of CAD/CAM technology gave rise to the first generation of yttrium-stabilised polycrystalline tetragonal zirconia (3Y-TZP), with significant higher flexural strengths than all dental glass or oxide ceramics available at this time. 77 Because of their high opacity, the first generation of zirconia was used predominantly as a framework material that was manually veneered by a sintering ceramic for aesthetic reasons. Specific material properties of zirconia in contrast to metal alloys, such as a different coefficient of thermal expansion and extreme low thermal conductivity, required new veneering materials and new firing parameters. 78 The combination of the optical properties of both the dentin-like zirconia framework and the enamel-like ceramic veneer greatly raised the aesthetic standards for metal-free FDPs in the anterior and posterior jaw ( Figs 26 , 27 , 28 , 29 and 30 ). 79 In clinical studies, the first generation of zirconia ceramics rarely exhibited framework fractures, but many cases of minor and major chipping of the veneer as the most frequent complication. 80 , 81 , 82 In a randomised clinical trial (RCT), zirconia FDPs with up to five units demonstrated satisfying long-term results comparable to those of the metal ceramic control group. 83 Nevertheless, a higher rate of framework fractures, debonding, chipping and inferior marginal adaption was reported.

Palatal view of a four-unit FDP with a CAD/CAM zirconia framework and a manually sintered ceramic veneer (IPS e.max ZirCAD LT [3Y-TZP]/IPS e.max Ceram; Ivoclar Vivadent). The ceramic gingiva replica was also sintered onto the zirconia framework (laboratory procedures: Oliver Brix, CDT, Bad Homburg, Germany)

Try-in of the four-unit zirconia-based FDP on two implants (Screw-line, 3.8/13 mm; Camlog, Wimsheim, Germany) in the lateral incisor positions 12 and 22, with zirconia hybrid abutments

Basal view of a posterior three-unit FDP with a CAD/CAM zirconia framework (3Y-TZP, Lava Plus; 3M) and manually-sintered ceramic veneer (IPS e.max Ceram; Ivoclar Vivadent) to replace tooth 36 (laboratory procedures: Otto Prandtner, MDT, Munich, Germany)

Abutment teeth 35 and 37 prepared for a three-unit zirconia FDP with ceramic veneer

Postoperative situation after adhesive placement of the three-unit zirconia FDP with sintered ceramic veneer
The use of monolithic zirconia would reduce the risk of chipping and improve the stability of the restoration while simplifying the CAD/CAM procedure. 84 One important prerequisite for using zirconia in monolithic restorations was improved aesthetics through reduced opacity and the option of individual staining. New formulas resulted in new types of zirconia ceramics with greater translucency. 85 Four generations of zirconia ceramics are now available that can be differentiated by their admixture of aluminium and yttrium oxides. Not only their optical characteristics but also the mechanical properties are influenced as a result of a matter of changes in refractive index, grain size, and crystalline composition ( Figs 31 , 32 and 33 ). 86 , 87 Recently innovative CAD/CAM-materials were introduced, which combine two different zirconia compositions in one disc (gradient technology). New generations of zirconia ceramics promise new indications. All relevant long-term clinical trials refer to restorations made of 3Y-TZP zirconia. Many open questions remain, related especially to the third and fourth zirconia generations. Long-term clinical stability, wear behaviour and bonding options have not yet been fully verified. 88 Initial in vitro studies have demonstrated a significant increase of translucency in novel zirconia materials, but associated with a significant reduction in flexural strength. 89

Occlusal view of a CAD/CAM posterior three-unit FDP made of monolithic multilayer zirconia (3Y-TZP zirconia; Katana HT/ML, Kuraray Noritake, Tokyo, Japan). Surface staining was applied, without sintered ceramic veneer

Intraoral view of the prepared abutment teeth 14 and 16

Try-in of the three-unit FDP made of monolithic multilayer zirconia (3Y-TZP zirconia, Katana HT/ML; Kuraray Noritake)
For 5Y-TZP zirconia, flexural strength and translucency parameters between those of 3Y-TZP and lithium disilicate ceramic are reported. Both the short-term and long-term bond strengths of 5Y-TZP and 3Y-TZP were shown to be similar to lithium disilicate. 5Y-TZP demonstrated no measurable material wear, and antagonist enamel wear was comparable to other materials tested. 88
With the introduction of digital technologies and access to new restorative materials, clinicians are facing a continuously increasing range of treatment options in fixed prosthodontics. These options allow strategies and materials to be selected specifically for the individual patient's needs. However, clinicians and technicians need well-developed skills, experiences and knowledge to select the right therapy based on scientific data.
A paradigm shift towards less invasive treatment options is obvious; the overall aim is to reach the treatment goal while removing the least possible amount of natural tissue. Reliable bonding to natural enamel and tooth-coloured materials have ushered in a shift towards much more conservative preparation designs than was previously thought possible. 4 , 5
Minimally invasive restorations are considered beneficial because of the low risk of damaging the pulp, better hard tissue protection, easier impression-taking, a better view of the site during preparation and adhesive fixation, and less interference with the marginal gingiva. While these possibilities inspire a great deal of excitement, we should bear in mind that the methods described above involve a high degree of technique sensitivity regarding preparations (mainly enamel), adhesive bonding and fine-tuning of the static and dynamic occlusion. 24 , 52 , 61 , 90 , 91
While clinical long-term studies 10 , 13 , 46 , 47 , 91 exist on minimally invasive restorative methods using ceramic materials, valid clinical data on the long-term behaviour of minimally invasive definitive restorations made of CAD/CAM composite resins are still lacking. 92 , 93 The intermediate three-year results of a five-year prospective clinical study with 45 inlays and 58 partial-coverage restorations made of CAD/CAM polymer-infiltrated ceramics have demonstrated good performance. 94 However, a significant decrease in marginal adaption and an increase in marginal discolouration and surface roughness were observed over time. 94 A randomised clinical trial with indirect composite resin and glass ceramic veneers showed similar survival rates of 87% and 93.5%, respectively. However, changes in surface characteristics were more frequent in the composite material. 95
The clinical results with direct composites as a definitive restorative material were initially good, especially in the anterior region. 96 , 97 However, clinical follow-ups showed that in more complex cases, direct posterior composite restorations discernibly deteriorated after five and a half years and more, in terms of surface texture, anatomical shape and marginal fit. 98 The survival rates of composite resin as a restorative material in complex direct rehabilitations depend on the tooth position, being most unfavourable in the case of molars. 99
Numerous in vitro studies on CAD/CAM composite resins and polymer-infiltrated ceramics have examined their optical and mechanical properties, surface and wear behaviour, as well as bonding options. In one of these in vitro studies, CAD/CAM composite resins showed higher flexural strengths than leucite ceramics and polymer-infiltrated ceramics, but lower strengths than lithium disilicate ceramics. 100 Glass ceramics showed lower discolouration rates than CAD/CAM composites and less two-body wear. 100 In multiple in vitro studies, ceramics showed superior gloss retention compared to hybrid ceramics, composites and acrylic polymers. 101 , 102 , 103
Since ceramics are expected to exhibit lower wear than resin composites under clinical conditions, the long-term stability after an increase in the vertical dimension of occlusion in complex rehabilitations, where ceramics are used in the antagonist jaw, might be superior to that of resin composite materials. 104 , 105 Finally, because CAD/CAM composite resins show a high degree of conversion, a reliable bond to the internal surface of the restoration is difficult to achieve. A reliable bond to luting composites seems to be achieved only by air abrasion and special pre-treatment strategies. 106
Despite the numerous in vitro studies on CAD/CAM composite resins and polymer-infiltrated ceramics, controlled, randomised clinical trials still remain the gold standard against which to compare the clinical performance of new materials. As a consequence, the authors still consider all-ceramic restorations the treatment of choice for definitive restorations, especially in complex rehabilitations where the masticatory forces are borne solely by the restorations. However, the preparations should be as minimally invasive as possible and developed individually in accordance with the chosen material and type of restoration.
According to the authors, clinical evidence for CAD/CAM composite resins is limited to single-tooth restorations with enamel margins within a functional masticatory system, where bite forces are additionally distributed to adjacent natural teeth. Here the use of a composite restoration can help preserve the natural tooth structure on the antagonistic dentition. 100
Dentists providing fixed prosthetic restorations have a vast array of treatment alternatives to conventional and, essentially, more invasive procedures. The introduction of digital technologies has paved the way for innovative treatment strategies and restorative concepts in terms of new diagnostic tools, benefits in communication and treatment planning, and access to new materials with extended indications. The introduction of new polymer materials supports innovative reversible pre-treatment concepts, such as: CAD/CAM tooth-coloured fully-contoured removable splints; and new CAD/CAM ceramics which provide new indications for definitive restorations. Many metal-free treatment modalities introduced in the last decades are now backed up by valid long-term data. Regarding the material class of ceramics, the relevant treatment options are considered to be scientifically validated for numerous indications. On the other hand, sufficient long-term results on the use of CAD/CAM composite resins and polymer-infiltrated ceramics for definitive restorations and novel classes of zirconia are not available yet. Generally, the methods described in this article are technique-sensitive and therefore require the clinician and technician to have well-developed skills and experience. And with all that, the present report has only been able to touch upon a small section of the spectrum of present-day fixed prosthodontics.
Pjetursson B E, Lang N P. Prosthetic treatment planning on the basis of scientific evidence. J Oral Rehabil 2008; 35 (Spec Iss): 72-79.
Cheung G S, Lai S C, Ng R P. Fate of vital pulps beneath a metal-ceramic crown or a bridge retainer. Int Endod J 2005; 38: 521-530.
Foster L V. Failed conventional bridge work from general dental practice: clinical aspects and treatment needs of 142 cases. Br Dent J 1990; 168: 199-201.
Edelhoff D, Sorensen J A. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent 2002; 87: 503-509.
Edelhoff D, Sorensen J A. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent 2002; 22: 241-249.
Al-Fouzan A F, Tashkandi E A. Volumetric measurements of removed tooth structure associated with various preparation designs. Int J Prosthodont 2013; 26: 545-548.
Chun Y H, Raffelt C, Pfeiffer H et al. Restoring strength of incisors with veneers and full ceramic crowns. J Adhes Dent 2010; 12: 45-54.
Soares P V, Santos-Filho P C, Martins L R, Soares C J. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: fracture resistance and fracture mode. J Prosthet Dent 2008; 99: 30-37.
Murphy F, McDonald A, Petrie A, Palmer G, Setchell D. Coronal tooth structure in root-treated teeth prepared for complete and partial coverage restorations. J Oral Rehabil 2009; 36: 451-461.
Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent 2017; 65: 51-55.
Jagodin S, Sasse M, Freitag-Wolf S, Kern M. Influence of attachment design and material on the retention of resin-bonded attachments. Clin Oral Investig 2019; 23: 1217-1223.
Guess P C, Selz C F, Steinhart Y N, Stampf S, Strub J R. Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7year results. Int J Prosthodont 2013; 26: 21-25.
Beier U S, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont 2012; 25: 79-85.
Fradeani M, Barducci G, Bacherini L, Brennan M. Esthetic rehabilitation of a severely worn dentition with minimally invasive prosthetic procedures (MIPP). Int J Periodontics Restorative Dent 2012; 32: 135-147.
Walls A W. The use of adhesively retained all-porcelain veneers during the management of fractured and worn anterior teeth: Part 2. Clinical results after 5 years of follow-up. Br Dent J 1995; 178: 337-340.
Loomans B, Opdam N, Attin T et al . Severe tooth wear: European consensus statement on management guidelines. J Adhes Dent 2017; 19: 111-119.
Edelhoff D, Schweiger J, Prandtner O, Trimpl J, Stimmelmayr M, Güth J F. CAD/CAM splints for the functional & esthetic evaluation of new defined occlusal dimensions. Quintessence Int 2017; 48: 181-191.
Opdam N, Frankenberger R, Magne P. From 'direct versus indirect' toward an integrated restorative concept in the posterior dentition. Oper Dent 2016; 41 (Spec Iss): S27-S34.
Edelhoff D, Ahlers M O. Occlusal onlays as a modern treatment concept for the reconstruction of severely worn occlusal surfaces. Quintessence Int 2018; 49: 521-533.
Edelhoff D, Prandtner O, Saeidi Pour R, Liebermann A, Stimmelmayr M, Güth J F. Anterior restorations: The performance of ceramic veneers. Quintessence Int 2018; 49: 89-101.
Leib A M. Patient preference for light-cured composite bite splint compared to heat-cured acrylic bite splint. J Periodontol 2001; 72: 1108-1112.
Ahlers M O. Determination of vertical dimension when using repositioning onlays for second stage restorative treatment after functional therapy. J Craniomandibular Function 2014; 6: 131-148.
Edelhoff D, Beuer F, Schweiger J, Brix O, Stimmelmayr M, Güth J F. CAD/CAM-generated high-density polymer restorations for the pre-treatment of complex cases. Quintessence Int 2012; 43: 457-467.
Rouse J S. Full veneer versus traditional veneer preparation: A discussion of interproximal extension. J Prosthet Dent 1997; 78: 545-549.
Simonsen R J. From prevention to therapy: minimal intervention with sealants and resin restorative materials. J Dent 2011; 39 (Spec Iss): S27-S33.
Stappert C F, Stathopoulou N, Gerds T, Strub J R. Survival rate and fracture strength of maxillary incisors, restored with different kinds of full veneers. J Oral Rehabil 2005; 32: 266-272.
Vailati F, Belser U C. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 1. Eur J Esthet Dent 2008; 3: 30-44.
Vailati F, Belser U C. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 2. Eur J Esthet Dent 2008; 3: 128-146.
Vailati F, Belser U C. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 3. Eur J Esthet Dent 2008; 3: 236-257.
Belser U C, Magne P, Magne M. Ceramic laminate veneers: continuous evolution of indications. J Esthet Dent 1997; 9: 197-207.
Peumans M, van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent 2000; 28: 163-177.
Chu S J, Mieleszko A J. Color-matching strategies for non-vital discolored teeth: part 1. Laboratory ceramic veneer fabrication solutions. J Esthet Restor Dent 2014; 26: 240-246.
Magne P, Douglas W H. Porcelain veneers: dentin bonding optimization and biomimetic recovery of the crown. Int J Prosthodont 1999; 12: 111-121.
Magne P, Douglas W H. Interdental design of porcelain veneers in the presence of composite fillings: finite element analysis of composite shrinkage and thermal stresses. Int J Prosthodont 2000; 13: 117-124.
Burke F J. Survival rates for porcelain laminate veneers with special reference to the effect of preparation in dentin: a literature review. J Esthet Restor Dent 2012; 24: 257-265.
Gurel G, Sesma N, Calamita M A, Coachman C, Morimoto S. Influence of enamel preservation on failure rates of porcelain laminate veneers. Int J Periodontics Restorative Dent 2013; 33: 31-39.
Schmidt K K, Chiayabutr Y, Phillips K M, Kois J C. Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. J Prosthet Dent 2011; 105: 374-382.
Magne P, Douglas W H. Design optimization and evolution of bonded ceramics for the anterior dentition: a finite-element analysis. Quintessence Int 1999; 30: 661-672.
Albanesi R B, Pigozzo M N, Sesma N, Laganá D C, Morimoto S. Incisal coverage or not in ceramic laminate veneers: A systematic review and meta-analysis. J Dent 2016; 52: 1-7.
Faus-Matoses I, Solá-Ruiz F. Dental preparation with Sonic vs. high-speed Finishing: analysis of microleakage in bonded veneer restorations. J Adhes Dent 2014; 16: 29-34.
Magne P, Belser U. Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach . New Malden: Quintessence, 2002.
Rieder C E. The use of provisional restorations to develop and achieve esthetic expectations. Int J Periodontics Restorative Dent 1989; 9: 122-139.
Xu B, Chen X, Li R, Wang Y, Li Q. Agreement of try-in pastes and the corresponding luting composites on the final color of ceramic veneers. J Prosthodont 2014; 23: 308-312.
Guess P C, Stappert C F. Midterm results of a 5year prospective clinical investigation of extended ceramic veneers. Dent Mater 2008; 24: 804-813.
Frankenberger R, Taschner M, Garcia-Godoy F, Petschfelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent 2008; 10: 393-398.
van Dijken J W, Hasselrot L. A prospective 15-year evaluation of extensive dentinenamelbonded pressed ceramic coverages. Dent Mater 2010; 26: 929-939.
Ma L, Guess P C, Zhang Y. Load-bearing properties of minimal-invasive monolithic lithium disilicate and zirconia occlusal onlays: finite element and theoretical analyses. Dent Mater 2013; 29: 742-751.
Kreulen C M, van 't Spijker A, Rodriguez J M, Bronkhorst E M, Creugers N H J, Bartlett D W. Systematic review of the prevalence of tooth wear in children and adolescents. Caries Res 2010; 44: 151-159.
Jaeggi T, Grüninger A, Lussi A. Restorative therapy of erosion. Monogr Oral Sci 2006; 20: 200-214.
Magne P, Belser U. Porcelain versus compositeinlays/onlays: effect of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodontics Restorative Dent 2003; 23: 543-555.
Ahlers M O, Mörig G, Blunck U, Hajtó J, Pröbster L, Frankenberger R. Guidelines for the preparation of CAD/CAM ceramic inlays and partial crowns. Int J Comput Dent 2009; 12: 309-325.
Rochette A L. Attachment of a splint to enamel of lower anterior teeth. J Prosthet Dent 1973; 30: 418-423.
Briggs P, Dunne S, Bishop K. The single unit, single retainer, cantilever resin-bonded bridge. Br Dent J 1996; 181: 373-379.
Hopkins C. An immediate cantilevered Rochette bridge. Br Dent J 1981; 151: 292-295.
Botelho M G, Chan A W, Leung N C, Lam W Y. Long-term evaluation of cantilevered versus fixed-fixed resin-bonded fixed partial dentures for missing maxillary incisors. J Dent 2016; 45: 59-66.
Wei Y R, Wang X D, Zhang Q et al . Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J Dent 2016; 47: 1-7.
Kern M, Sasse M. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J Adhes Dent 2011; 13: 407-410.
Kern M. RBFDPs: Resin-Bonded Fixed Dental Prostheses . 1st ed. New Malden: Quintessence, 2018.
Sasse M, Kern M. All-ceramic resin-bonded fixed dental prostheses: treatment planning, clinical procedures, and outcome. Quintessence Int 2014; 45: 291-297.
Lam W Y, McGrath C P, Botelho M G. Impact of complications of single tooth restorations on oral health-related quality of life. Clin Oral Implants Res 2014; 25: 67-73.
Polder B J, Van't Hof M A, Van der Linden F P, Kuijpers-Jagtman A M. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol 2004; 32: 217-226.
Stappert C F, Tarnow D P, Tan J H, Chu S J. Proximal contact areas of the maxillary anterior dentition. Int J Periodontics Restorative Dent 2010; 30: 471-477.
Kern M, Schwarzbach W, Strub J R. Stability of all-porcelain, resin-bonded fixed restorations with different designs: an in vitro study. Int J Prosthodont 1992; 5: 108-113.
Blatz M B, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res 2018; 97: 132-139.
Inokoshi M, Van Meerbeck B. Adhesively luted zirconia restorations: why and how? J Adhes Dent 2014; 16: 294.
Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent 2015; 17: 7-26.
Sailer I, Hämmerle C H. Zirconia ceramic single-retainer resin-bonded fixed dental prostheses (RBFDPs) after 4 years of clinical service: a retrospective clinical and volumetric study. Int J Periodontics Restorative Dent 2014; 34: 333-343.
Sailer I, Bonani T, Brodbeck U, Hämmerle C H. Retrospective clinical study of single-retainer cantilever anterior and posterior glass-ceramic resin-bonded fixed dental prostheses at a mean follow-up of 6 years. Int J Prosthodont 2013; 26: 443-450.
Simeone P, Gracis S. Eleven-Year Retrospective Survival Study of 275 Veneered Lithium Disilicate Single Crowns. Int J Periodontics Restorative Dent 2015; 35: 685-694.
Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig 2013; 17: 275-284.
van den Breemer C R, Vinkenborg C, van Pelt H, Edelhoff D, Cune M S. The clinical performance of monolithic lithium disilicate posterior restorations after 5: 10, and 15 years: A retrospective case series. Int J Prosthodont 2017; 30: 62-65.
Teichmann M, Göckler F, Wübbels A, Weber V, Yildirim M, Wolfart S, Edelhoff D. Ten-year survival and complication rates of lithium-disilicate (Empress 2) tooth-supported crowns, implant-supported crowns, and fixed dental prostheses. J Dent 2017; 56: 65-77.
Sola-Ruiz M F, Lagos-Flores E, Roman-Rodriguez J L, Highsmith Jdel R, Fons-Font A, Granell-Ruiz M. Survival rates of a lithium disilicate-based core ceramic for three-unit esthetic fixed partial dentures: a 10-year prospective study. Int J Prosthodont 2013; 26: 175-180.
Kern M, Sasse M, Wolfart S. Ten-year outcome of three-unit fixed dental prostheses made from monolithic lithium disilicate ceramic. J Am Dent Assoc 2012; 143: 234-240.
Manicone P F, Rossi Iommetti P, Raffaelli L. An overview of zirconia ceramics: basic properties and clinical applications. J Dent 2007; 35: 819-826.
Tholey M J, Swain M V, Thiel N. Thermal gradients and residual stresses in veneered Y-TZP frameworks. Dent Mater 2011; 27: 1102-1110.
Pecho O E, Ghinea R, Ionescu A M, Cardona Jde L, Paravina R D, Pérez Mdel M. Color and translucency of zirconia ceramics, human dentine and bovine dentine. J Dent 2012; 40 (Spec Iss): e34-e40.
Heintze S D, Rousson V. Survival of zirconiaand metal-supported fixed dental prostheses: a systematic review. Int J Prosthodont 2010; 23: 493-502.
Ioannidis A, Bindl A. Clinical prospective evaluation of zirconia-based three-unit posterior fixed dental prostheses: Up-to ten-year results. J Dent 2016; 47: 80-85.
Teichmann A, Wienert A L, Rückbeil M, Weber V, Wolfart S, Edelhoff D. Ten-year survival and chipping rates and clinical quality grading of zirconia-based fixed dental prostheses. Clin Oral Investig 2018; 22: 2905-2915.
Sailer I, Balmer M, Hüsler J, Hämmerle C H F, Känel S, Thoma D S. 10-year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J Dent 2018; 76: 32-39.
Guess P C, Zavanelli R A, Silva N R, Bonfante E A, Coelho P G, Thompson V P. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont 2010; 23: 434-442.
Zhang Y, Lawn B R. Novel zirconia materials in dentistry. J Dent Res 2018; 97: 140-147.
Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int 2017; 48: 369-380.
Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int 2017; 48: 441-450.
Sailer I, Strasding M, Valente N A, Zwahlen M, Liu S, Pjetursson B E. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin Oral Implants Res 2018; 29 (Spec Iss): 184-198.
Kwon S J, Lawson N C, McLaren E E, Nejat A H, Burgess J O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent 2018; 120: 132-137.
Frankenberger R, Reinelt C, Petschelt A, Krämer N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent Mat 2009; 25: 960-968.
Beier U S, Kapferer I, Dumfahrt H. Clinical long-term evaluation and failure characteristics of 1: 335 all-ceramic restorations. Int J Prosthodont 2012; 25: 70-78.
Fasbinder D J, Dennison J B, Heys D R, Lampe K. The clinical performance of CAD/CAM-generated composite inlays. J Am Dent Assoc 2005; 136: 1714-1723.
Vanoorbeek S, Vandamme K, Lijnen I, Naert I. Computer-aided designed/computer-assisted manufactured composite resin versus ceramic single-tooth restorations: a 3-year clinical study. Int J Prosthodont 2010; 23: 223-230.
Spitznagel F A, Scholz K J, Strub J R, Vach K, Gierthmuehlen P C. Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin Oral Investig 2018; 22: 1973-1983.
Gresnigt M M, Kalk W, Ozcan M. Randomized clinical trial of indirect resin composite and ceramic veneers: up to 3year follow-up. J Adhes Dent 2013; 15: 181-190.
Schmidlin P R, Filli T, Imfeld C, Tepper S, Attin T. Three-year evaluation of posterior vertical bite reconstruction using direct resin compositea case series. Oper Dent 2009; 34: 102-108.
Wolff D, Kraus T, Schach C et al . Recontouring teeth & closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent 2010; 38: 1001-1009.
Attin T, Filli T, Imfeld C, Schmidlin P R. Composite vertical bite reconstructions in eroded dentitions after 5.5 years: a case series. J Oral Rehabil 2012; 39: 73-79.
Loomans B A C, Kreulen C M, Huijs-Visser H E C E et al . Clinical performance of full rehabilitations with direct composite in severe tooth wear patients: 3.5 Years results. J Dent 2018; 70: 97-103.
Stawarczyk B, Liebermann A, Eichberger M, Güth J F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J Mech Behav Biomed Mater 2015; 55: 1-11.
Partin-Agarwal K, Terwilliger R J, Lien W, Jessup J P, Motyka N C, Vandewalle K S. Polish retention of ceramic-polymer CAD/CAM materials. Gen Dent 2018; 66: 65-70.
Koizumi H, Saiki O, Nogawa H, Hiraba H, Okazaki T, Matsumura H. Surface roughness & gloss of current CAD/CAM resin composites before & after toothbrush abrasion. Dent Mater J 2015; 34: 881-887.
Mörmann W H, Stawarczyk B, Ender A, Sener B, Attin T, Mehl A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and Martens hardness. J Mech Behav Biomed Mater 2013; 20: 113-125.
Matzinger M, Hahnel S, Preis V, Rosentritt M. Polishing effects and wear performance of chairside CAD/CAM materials. Clin Oral Investig 2019; 23: 725-737.
D'Arcangelo C, Vanini L, Rondoni G D, Vadini M, De Angelis F. Wear Evaluation of Prosthetic Materials Opposing Themselves. Oper Dent 2018; 43: 38-50.
Reymus M, Roos M, Eichberger M, Edelhoff D, Hickel R, Stawarczyk B. Bonding to new CAD/CAM resin composites: influence of air abrasion and conditioning agents as pretreatment strategy. Clin Oral Investig 2019; 23: 529-538.
Download references
Author information
Authors and affiliations.
Director and Chair, Department of Prosthetic Dentistry, University Hospital, LMU, Munich, Germany
Daniel Edelhoff
Associate Professor, Department of Prosthetic Dentistry, University Hospital, LMU, Munich, Germany
Michael Stimmelmayr & Jan-Frederik Güth
Dental Technician, Head of Dental Laboratory, Department of Prosthetic Dentistry, University Hospital, LMU, Munich, Germany
Josef Schweiger
Department of Prosthetic Dentistry, Centre for Dental and Oral Medicine, University Medical Centre Hamburg-Eppendorf, University of Hamburg, Hamburg, Germany; Director, CMD-Centre Hamburg-Eppendorf, Hamburg, Germany
M. Oliver Ahlers
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Daniel Edelhoff .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Edelhoff, D., Stimmelmayr, M., Schweiger, J. et al. Advances in materials and concepts in fixed prosthodontics: a selection of possible treatment modalities. Br Dent J 226 , 739–748 (2019). https://doi.org/10.1038/s41415-019-0265-z
Download citation
Published : 24 May 2019
Issue Date : May 2019
DOI : https://doi.org/10.1038/s41415-019-0265-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Time-dependent degree of conversion, martens parameters, and flexural strength of different dual-polymerizing resin composite luting materials.
- Matthias Kelch
- Bogna Stawarczyk
- Felicitas Mayinger
Clinical Oral Investigations (2022)
Material selection for tooth-supported single crowns—a survey among dentists in Germany
- Angelika Rauch
- Annett Schrock
- Sebastian Hahnel
Clinical Oral Investigations (2021)
Biomechanical planning for minimally invasive indirect restorations
- Deborah I. Bomfim
- Noushad M. Rahim
- Rupert S. Austin
British Dental Journal (2020)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

The Use and Performance of Artificial Intelligence in Prosthodontics: A Systematic Review
Selina a bernauer, nicola u zitzmann.
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected]
Received 2021 Sep 7; Accepted 2021 Oct 1; Collection date 2021 Oct.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( https://creativecommons.org/licenses/by/4.0/ ).
(1) Background: The rapid pace of digital development in everyday life is also reflected in dentistry, including the emergence of the first systems based on artificial intelligence (AI). This systematic review focused on the recent scientific literature and provides an overview of the application of AI in the dental discipline of prosthodontics. (2) Method: According to a modified PICO-strategy, an electronic (MEDLINE, EMBASE, CENTRAL) and manual search up to 30 June 2021 was carried out for the literature published in the last five years reporting the use of AI in the field of prosthodontics. (3) Results: 560 titles were screened, of which 30 abstracts and 16 full texts were selected for further review. Seven studies met the inclusion criteria and were analyzed. Most of the identified studies reported the training and application of an AI system ( n = 6) or explored the function of an intrinsic AI system in a CAD software ( n = 1). (4) Conclusions: While the number of included studies reporting the use of AI was relatively low, the summary of the obtained findings by the included studies represents the latest AI developments in prosthodontics demonstrating its application for automated diagnostics, as a predictive measure, and as a classification or identification tool. In the future, AI technologies will likely be used for collecting, processing, and organizing patient-related datasets to provide patient-centered, individualized dental treatment.
Keywords: artificial intelligence, machine learning, deep learning, neural networks, reconstructive dentistry, prosthetic treatment
1. Introduction
“Digital transformations”, “digitized workflows”, “technical developments”: these terms describe some of the game changers of the 21st century, both in social life as well as dental medicine [ 1 ]. The use of mobile devices, tablets, and smartphones, and the easy access to technology and the World Wide Web, have changed the cultural habits of our society in general [ 1 ]. It is not surprising that more advanced technologies, such as artificial intelligence (AI), are also finding increasing application in daily life. Generally speaking, AI imitates the cognitive processes of human intelligence by using machines and software-type algorithms to manage complex tasks [ 2 , 3 ].
AI applications are commonplace in digital everyday life, for example in the form of virtual assistants such as “Siri” or “Alexa” [ 1 , 4 ], and AI applications are implemented in various engineering fields [ 5 , 6 , 7 ]. In medicine, AI algorithms are ubiquitously used for image processing via feature extraction of specific images and target conducting [ 8 ]. For example, AI algorithms can be used for analyzation of chest X-ray and lung CT image samples images of COVID-19 patients and thus decrease the picture diagnostic time of the radiologist and accelerate clinical decisions [ 9 ]. Furthermore, technological advances are increasingly noticeable in dentistry, but are still restrained compared to medicine. Digital dental processes are continuously being standardized and are becoming part of routine treatment protocols [ 10 , 11 , 12 ]. In particular, computer-aided design/computer-aided manufacturing (CAD/CAM) procedures have found their way into everyday clinical and laboratory practice [ 10 , 13 ]. Digitization in dentistry continues to develop and new trends are emerging, including the application of AI.
AI is a widely used term that warrants a precise definition ( Figure 1 ); in general, algorithms that simulate the processes of human intelligence to resolve problems are summarized under the term AI [ 4 , 14 ]. Intelligence is defined as: “the ability of a system to act appropriately in an uncertain environment, where appropriate action is that which increases the probability of success, and success is the achievement of behavioral subgoals that support the system’s ultimate goal” [ 15 ]. Strong and weak AI can be differentiated. Strong AI describes a system “that was operated in the same way as human intelligence through non-natural, artificial hardware, and software construction” [ 4 ]. Weak AI, on the other hand, does not aim to mimic human intelligence in its entirety, but rather is a system, in which the advantages of medical and logical algorithms can be used by humans. Weak AI recognizes that computer-integrated technology is different from human intellectual performances [ 4 ].
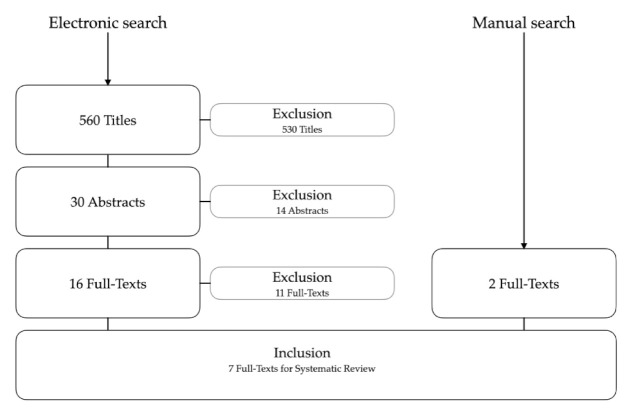
Flowchart of the electronic and manual search strategy.
Inspiration for the formation of artificial networks can be found in the biology of the human brain. “An artificial neuron is a mathematical function conceived as a coarse model of a biological neuron. The principle is to simulate the transfer of information through a neuron: weighted nodes receive the inputs (representing the synapses), sum them to produce an activation (representing the axon), and pass this activation to a nonlinear function called activation or transfer function, in order to generate the output signal. Each neuron acts as an elementary processing unit. The output signal of one unit will feed the other units, organized in layers, and so on, forming an artificial neural network (ANN)” [ 16 ]. There are typically three phases in the development and application of an ANN: (a) the training phase, where the ANN learns; (b) the validation phase, where the ANN’s results and reference values are reconciled; and (c) the inference or application phase, where the ANN is used in real cases [ 14 ].
Machine learning (ML) is part of weak AI; by recognizing patterns, the computer system is able to learn and make predictions [ 4 , 17 ]. After being trained on existing datasets, the ML system is able to provide accurate predictions on new data. Often the training datasets need to be simplified, so that the algorithm can recognize the desired pattern. Depending on how carefully these interventions are made, the performance of ML systems varies [ 16 ]. Current examples of ML systems include translators such as DeepL, diagnosis tools, and speech recognition frameworks [ 18 ]. Deep learning (DL) is part of ML that describes “a set of computational models composed of multiple layers of data processing, which make it possible to learn by representing these data through several levels of abstraction” [ 16 ]. Compared to ML, deep neural networks (DNNs) are able to independently learn and hierarchize the training dataset but require, therefore, larger amounts of data. It comes with the advantage that new feature extractors are not needed for every problem [ 16 ]. DL works via a backpropagation algorithm to train neural networks [ 16 ]. Convolutional neural networks (CNN) are a special part of DL, used especially for image processing and analyses of radiological datasets [ 16 ].
AI technologies are well suited for repetitive work using large datasets. The greater the workload, the more precise the performance of AI becomes [ 1 ]. Since dentistry provides many areas for assisting work and automation of simple routine tasks, AI could find applications here and support dentists to improve quality of work and accuracy [ 18 ].
The domain of AI in (dental) medicine is image data processing in radiological workflows, especially for detection of caries and periapical endodontic lesions [ 16 ], as well as automatic identification and classification of oral implant systems [ 19 ]. In prosthodontics, however, AI technology is still scarce due to complex diagnostics and treatment requiring individual protocols.
Therefore, the aim of this systematic review was to analyze the recent scientific literature on the diagnostic performance and the clinical applications of AI in applied prosthodontics. The remainder of this systematic review was structured as follows: (a) introduction of the search strategy and related inclusion criteria for data extraction; (b) summary of the obtained findings of the identified and included studies; (c) critical discussion of the results; (d) conclusions.
2. Materials and Methods
This systematic review was conducted in accordance with the guidelines of PRISMA (Preferred Reporting Items of Systematic Reviews and Meta-Analyses) [ 20 ].
2.1. Search Strategy
Based on the PICO criteria, a search strategy was developed and an electronic search was conducted. The PICO question was formulated as follows: What are the current clinical applications and diagnostic performance of AI in the field of prosthodontics?
A systematic electronic search of PubMed MEDLINE, EMBASE, and CENTRAL was performed for English-language publications; in addition, Google Scholar was reviewed. Search syntax was categorized into population, intervention, comparison, and outcome (PICO). Each category was assembled from a combination of Medical Subject Headings (MeSH Terms) as well as free-text words in simple or multiple conjunctions: ((Prosthodontics [Mesh]) OR (prosthetic treatment) OR (reconstructive therapy)) AND ((Artificial Intelligence [Mesh]) OR (Machine Learning OR Deep Learning OR Neural Networks [Mesh])) ( Table 1 ).
Search strategy according to the PICO criteria.
Additional manual searches of the bibliographies of all full-text articles and related reviews selected from the electronic search were also performed. Furthermore, manual searching was conducted in the following journals: Journal of Prosthodontic Research, Journal of Prosthetic Dentistry, Clinical Oral Implants Research, International Journal of Oral Maxillofacial Implants, Clinical Implant Dentistry and Related Research, Implant Dentistry, and Journal of Implantology.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria for the studies were defined as follows:
Studies at all levels of evidence, except expert opinion;
Articles published in English;
Articles published in the last 5 years (up to 30 June 2021).
Exclusion criteria for the studies were defined as follows:
Review articles, letter to editors and case reports involving less than 5 cases;
Animal studies;
Full-text not available/accessible.
2.3. Data Extraction
Two reviewers (S.B. and T.J.) independently screened the titles and abstracts that were identified in the searches according to the defined inclusion and exclusion criteria. If sufficient information could not be extracted from titles and abstracts, the full text was consulted. The full texts of potentially relevant articles were obtained and reviewed in detail by both reviewers, from which the final list of articles was selected for further analysis. Disagreements were resolved by discussion.
The following information was collected from selected articles:
Author(s), year of publication, country, study design;
Total number of patients/datasets;
Training/validation datasets;
Test datasets;
Aim of the study;
AI application; and
The information extracted from the articles was tabulated. Assessment of risk of bias was carried out for each included study, using the Newcastle–Ottawa Assessment Scale ( http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed on 7 September 2021)) to assess the quality of the studies ( Table 2 ).
Presentation of risk of bias evaluation for included studies.
3.1. Included Studies
The systematic search was finished on 30 June 2021. A total of 560 article titles were screened and 30 abstracts were considered for further analysis. Subsequently, the full texts of 16 articles were analyzed to determine if they met the inclusion criteria. After further examination, 11 articles were excluded due to the following reasons:
Not a study in the field of AI application in prosthodontics ( n = 6);
Not a clinical study ( n = 3);
Full text not available ( n = 1);
Missing information on AI technology ( n = 1).
Moreover, two other articles meeting the inclusion criteria were added from manual searching; subsequently, a total of seven full-text articles were included for data extraction ( Figure 1 ).
3.2. Descriptive Analysis
The seven included full-text articles came from diverse areas of the field of prosthodontics and demonstrated a wide range of the use of AI. Six studies investigated the training and application of different AI systems [ 19 , 22 , 23 , 24 , 25 , 26 ] and one study explored the function of an intrinsic AI system of a specific CAD software for designing prosthetic reconstructions [ 21 ]. Direct comparisons of the identified and included studies were not feasible because of the heterogeneity of the specific aims, defined outcomes, and topics within the field of reconstructive dentistry. Therefore, the analysis of the information reported by the included studies follows a descriptive approach. The detailed data extraction is summarized in Table 3 .
Characteristics and outcomes of the studies included.
AI: artificial intelligence; ANN: artificial neural network; CNN: convolutional neural networks; n: number; n.r.: not reported.
All included studies were designed as non-randomized, retrospective cohort studies. Three of the publications were from one research group with a special focus on radiographic image analysis [ 19 , 23 , 24 ]. The number of datasets used for AI training in the studies varied considerably (from 43 to 10770). Five of the studies included investigated CNN models, one study applied an ANN model, and another study used an intrinsic AI and algorithms of a commercially available laboratory CAD software.
4. Discussion
This systematic review focused on applied AI technologies in prosthodontics, and it was demonstrated that AI was used for automated diagnostics, as a predictive measure, and as a classification or identification tool. The findings indicated that, in the wider field of prosthodontics, AI has been applied to CAD/CAM systems, implant prosthetics, tooth preservation, and orofacial anatomy. Since digital technologies are developing rapidly and the observed turnover rate of obsolete software is about 1.5–2 years, the current search was limited to the last 5 years. The aim of this systematic review was not to provide a historical overview of AI technology in dentistry in general. Rather, the manuscript focused on prosthetic AI applications. Furthermore, the systematic search focused on clinical trials and case series with at least 5 patients to increase the scientific level (and to avoid including technical reports).
The overall number of eligible studies investigating AI applications in prosthodontics was relatively low ( n = 7). Although automated detection of caries has been investigated in AI dental imaging diagnostics a few years ago, the use of AI technology in prosthodontics is (still) rare. Prosthodontics itself is a diverse and complex area of dental medicine and one that may benefit from the routine application of AI technologies. Long-term success relies on good prognosis of abutment teeth (and/or implants) in all facets of periodontal, endodontic, operative and reconstructive principles, and include patient-specific factors, such as load situation, personal and medical issues, and supportive care [ 27 ]. Successful prosthetic reconstructions require the use of a synoptic treatment concept with sufficient backward planning and a clean practical implementation, including dental laboratory workflows. Furthermore, the various different patient-related factors must be taken into account; many intraoral situations are not directly comparable, with the exception of edentulous patients. One factor is that the number of teeth to be replaced varies extremely from 1 to 28. Mathematically, the number of possible situations, starting from 28 teeth, would be the factorial of 27, i.e., 27×, 26×, 25×, 24×, etc. The number of options, combined with the factors mentioned above, makes prosthetic therapy a demanding and complex specialty, which requires a certain knowledge in adjacent disciplines. AI technologies are particularly suited to dealing with complex situations with multiple possible factors; therefore, the application of AI to prosthetic workflows is of high interest.
This systematic review revealed that AI systems are currently mainly limited to test versions of automated diagnostics, especially in dental imaging and radiology [ 3 ], and classification tools such as for periodontally compromised teeth, dental cusps, or caries. Encouragingly, the identified studies all reported high performance of the different AI systems investigated ( Table 3 ), i.e., including high diagnostic accuracy for dental caries [ 23 ], and very good prediction accuracy for debonding of CAD/CAM crowns [ 22 ].
AI is increasingly being applied to dentistry including in diverse areas of prosthetic research for efficient data processing. The first application of AI within dentistry was in the classification of diagnostic images and processing of data from surface scanning techniques, because the digitally coded images could easily be transferred into AI systems [ 3 , 17 ]. The application of AI in diagnostics continues to be developed. AI technologies in dentistry have the power to become central in the triad of patient data management, health care application, and services, and can facilitate future developments in patient-centered individualized treatment [ 3 ].
Beyond prosthodontics, AI was previously linked to other dental disciplines [ 2 ]. In tooth preservation, radiologically driven AI analyses can help detect root fractures and identify periapical pathologies [ 28 ] or classify root morphologies [ 29 ]. In periodontology, disease progression can be evaluated while clinical and radiological periodontal parameters are automatically determined following AI technology. In oral surgery, AI can be used to screen radiological images for pathological changes, such as cysts and bony tumors [ 2 ]. Furthermore, there are possible applications in implantology. AI-based treatment planning in CAD/CAM implant dentistry could be of great interest in order to simplify virtual 3D treatment planning, and, consecutively, robotic insertion of dental implants using AI applications [ 30 ].
AI will certainly play a significant role in dentistry in the future and the development of these technologies is awaited with excitement. AI has a disruptive potential to renew processes in all fields of dentistry; but, due to the complexity of prosthetic treatment concepts, the adoption of AI technology in prosthodontics is still rather hesitant. AI systems are particularly beneficial for processing and analyzing large amounts of data to classify outcomes, and for processing repetitive workflows. AI algorithms will likely provide support in evidence-based dental decision making, particularly for less experienced practitioners, and facilitate the analysis of individual patient cases. More homogeneous treatment protocols could be ensured that still allow for individualized and personalized treatment. Chen et al. developed a prototype decision model to assist (unexperienced) dentists in choosing appropriate removable prosthetic options [ 31 ]. Such supportive tools in therapy planning of (complex) patient cases in prosthodontics enable the further development of tele-dentistry.
The combination of AI technologies in the field of prosthodontics could lead to a wide variety of novel options, such as AI systems for generating occlusal surface design for crowns accounting for existing intraoral wear facets, as automatic set-up designers for complete dentures, for determining the emergence profile in implantology, or in automatic framework designs for removable partial dentures [ 32 ]. Finally, as an educational tool, AI already provides the opportunity to support less experienced undergraduate students in their professional development [ 33 ].
In principle, there are no limitations to using the power of AI in prosthodontics. In many cases, however, it is (unfortunately) financial factors that trigger the development and standard implementation of new AI technologies in the most economically profitable areas—and tend to prevent interesting dental applications because a market appears too small for the dental industry. Nevertheless, future developments and research on AI can be eagerly awaited.
Although this seems to be very promising, the obstacles of AI systems should not be ignored. Based on this systematic literature search, the identified trials must be seen as pilot studies and experimental, and the technologies used in these studies are not yet suitable for everyday clinical routine in the focus of prosthodontics. At the moment, AI is mainly used in undergraduate dental education and for academic research. Improvements in the technology and user interfaces is needed before the techniques can be implemented into routine dental practice. Some intermediate steps still need to be developed to make AI attractive and helpful for its routine implementation. Beyond the technical possibilities, the cost–benefit ratio and ethical aspects of the use of patient-specific data also need to be critically examined in future research on AI technology in (reconstructive) dentistry [ 3 ].
5. Conclusions
While the number of studies reporting the use of AI in prosthodontics identified in this systematic review was relatively low (inclusion of seven out of sixteen full-texts), these studies reflect an honest overview of the latest developments in AI focusing on diagnostics, predictive measures, classification, and identification tools. Prosthodontics is the dental discipline with the greatest variance in terms of diagnostics and, in particular, treatment options. Therefore, it does not seem surprising that the results of this systematic review are comparably diverse and heterogeneous.
In addition, dentistry is (still) lagging behind medicine in terms of routine use of AI technology. Nevertheless, AI applications in prosthodontics have the potential to open up a wide range of opportunities for clinicians and patients, and could be used as a supplementary future basic tool for collecting, processing, and organizing patient-related datasets to provide patient-centered, individualized, and personalized treatment. Possible applications of AI algorithms are very diverse in prosthodontics and one can eagerly await further research foci and developments.
The step-by-step implementation of digital applications (in dentistry) is linked to the necessary technical development and is dependent on the flexibility of the users in everyday life. The willingness to learn new treatment protocols and to trust computerized applications has been proven as a strong negative driver for dentists [ 34 ]. In addition, new technologies require continuous investment of the dental community. As long as the research results are not demonstrating superiority, the routine implementation of AI applications in prosthodontics will be delayed. Here, the university and dental schools need to foster AI technology in research and education.
A critical topic and crucial factor for the successful rehabilitation of complex prosthetic cases is the correct clinical definition of vertical and horizontal maxillo-mandibular relationships. AI technology could be used for automatic registering of jaw relationships based on radiological landmarks in cone-beam computed tomography. In this context, the configuration of virtual dental articulators could be synchronized with the radiological situation to simulate individual patient movements for treatment simulation and final fabrication of prosthetic reconstructions.
The use of AI technologies in prosthodontics is conceivable in many ways (and absolutely desirable) from the clinicians’ point of view, but not least the demand and the economic efficiency will decide whether the MedTech industry will push AI in prosthodontics as fast and to what extent.
Author Contributions
Conceptualization, S.A.B. and T.J.; methodology, S.A.B. and T.J.; formal analysis, S.A.B. and T.J.; investigation, S.A.B. and T.J.; data curation, S.A.B. and T.J.; writing—original draft preparation, S.A.B.; writing—review and editing, T.J. and N.U.Z.; visualization, S.A.B.; supervision, T.J. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement.
The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Joda T., Bornstein M.M., Jung R.E., Ferrari M., Waltimo T., Zitzmann N.U. Recent trends and future direction of dental research in the digital era. Int. J. Environ. Res. Public Health. 2020;17:1987. doi: 10.3390/ijerph17061987. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Shan T., Tay F., Gu L. Application of artificial intelligence in dentistry. J. Dent. Res. 2021;100:232–244. doi: 10.1177/0022034520969115. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Joda T., Yeung A., Hung K., Zitzmann N., Bornstein M. Disruptive Innovation in Dentistry: What It Is and What Could Be Next. J. Dent. Res. 2020:0022034520978774. doi: 10.1177/0022034520978774. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Park W.J., Park J.-B. History and application of artificial neural networks in dentistry. Eur. J. Dent. 2018;12:594. doi: 10.4103/ejd.ejd_325_18. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Ganguly B., Chaudhuri S., Biswas S., Dey D., Munshi S., Chatterjee B., Dalai S., Chakravorti S. Wavelet kernel-based convolutional neural network for localization of partial discharge sources within a power apparatus. IEEE Trans. Ind. Inform. 2020;17:1831–1841. doi: 10.1109/TII.2020.2991686. [ DOI ] [ Google Scholar ]
- 6. Moradi M.J., Hariri-Ardebili M.A. Developing a Library of Shear Walls Database and the Neural Network Based Predictive Meta-Model. Appl. Sci. 2019;9:2562. doi: 10.3390/app9122562. [ DOI ] [ Google Scholar ]
- 7. Roshani M., Phan G.T., Ali P.J.M., Roshani G.H., Hanus R., Duong T., Corniani E., Nazemi E., Kalmoun E.M. Evaluation of flow pattern recognition and void fraction measurement in two phase flow independent of oil pipeline’s scale layer thickness. Alex. Eng. J. 2021;60:1955–1966. doi: 10.1016/j.aej.2020.11.043. [ DOI ] [ Google Scholar ]
- 8. Ren R., Luo H., Su C., Yao Y., Liao W. Machine learning in dental, oral and craniofacial imaging: A review of recent progress. PeerJ. 2021;9:e11451. doi: 10.7717/peerj.11451. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Alafif T., Tehame A.M., Bajaba S., Barnawi A., Zia S. Machine and Deep Learning towards COVID-19 Diagnosis and Treatment: Survey, Challenges, and Future Directions. Int. J. Environ. Res. Public Health. 2021;18:1117. doi: 10.3390/ijerph18031117. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Miyazaki T., Hotta Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011;56:97–106. doi: 10.1111/j.1834-7819.2010.01300.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Bernauer S.A., Müller J., Zitzmann N.U., Joda T. Influence of Preparation Design, Marginal Gingiva Location, and Tooth Morphology on the Accuracy of Digital Impressions for Full-Crown Restorations: An In Vitro Investigation. J. Clin. Med. 2020;9:3984. doi: 10.3390/jcm9123984. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Gintaute A., Straface A., Zitzmann N.U., Joda T. Die Modellgussprothese 2.0: Digital von A bis Z. Swiss. Dent. J. 2020;130:229–235. doi: 10.61872/sdj-2020-03-02. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Saravi B., Vollmer A., Hartmann M., Lang G., Kohal R.-J., Boeker M., Patzelt S. Clinical performance of CAD/CAM All-ceramic tooth-supported fixed dental prostheses: A systematic review and meta-analysis. Materials. 2021;14:2672. doi: 10.3390/ma14102672. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Currie G. Intelligent imaging: Anatomy of machine learning and deep learning. J. Nucl. Med. Technol. 2019;47:273–281. doi: 10.2967/jnmt.119.232470. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Albus J.S. Outline for a theory of intelligence. IEEE Trans. Syst. Man Cybern. 1991;21:473–509. doi: 10.1109/21.97471. [ DOI ] [ Google Scholar ]
- 16. Meyer P., Noblet V., Mazzara C., Lallement A. Survey on deep learning for radiotherapy. Comput. Biol. Med. 2018;98:126–146. doi: 10.1016/j.compbiomed.2018.05.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Hung K., Montalvao C., Tanaka R., Kawai T., Bornstein M.M. The use and performance of artificial intelligence applications in dental and maxillofacial radiology: A systematic review. Dentomaxillofacial Radiol. 2020;49:20190107. doi: 10.1259/dmfr.20190107. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Grischke J., Johannsmeier L., Eich L., Griga L., Haddadin S. Dentronics: Towards robotics and artificial intelligence in dentistry. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2020;36:765–778. doi: 10.1016/j.dental.2020.03.021. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Lee J.-H., Jeong S.-N. Efficacy of deep convolutional neural network algorithm for the identification and classification of dental implant systems, using panoramic and periapical radiographs: A pilot study. Medicine. 2020;99 doi: 10.1097/MD.0000000000020787. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Lerner H., Mouhyi J., Admakin O., Mangano F. Artificial intelligence in fixed implant prosthodontics: A retrospective study of 106 implant-supported monolithic zirconia crowns inserted in the posterior jaws of 90 patients. BMC Oral Health. 2020;20:1–16. doi: 10.1186/s12903-020-1062-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Yamaguchi S., Lee C., Karaer O., Ban S., Mine A., Imazato S. Predicting the debonding of CAD/CAM composite resin crowns with AI. J. Dent. Res. 2019;98:1234–1238. doi: 10.1177/0022034519867641. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Lee J.-H., Kim D.-H., Jeong S.-N., Choi S.-H. Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J. Dent. 2018a;77:106–111. doi: 10.1016/j.jdent.2018.07.015. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Lee J.-H., Kim D.-h., Jeong S.-N., Choi S.-H. Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm. J. Periodontal Implant. Sci. 2018;48:114. doi: 10.5051/jpis.2018.48.2.114. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Raith S., Vogel E.P., Anees N., Keul C., Güth J.-F., Edelhoff D., Fischer H. Artificial Neural Networks as a powerful numerical tool to classify specific features of a tooth based on 3D scan data. Comput. Biol. Med. 2017;80:65–76. doi: 10.1016/j.compbiomed.2016.11.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Wei J., Peng M., Li Q., Wang Y. Evaluation of a Novel Computer Color Matching System Based on the Improved Back-Propagation Neural Network Model. J. Prosthodont. 2018;27:775–783. doi: 10.1111/jopr.12561. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Zitzmann N.U., Krastl G., Hecker H., Walter C., Waltimo T., Weiger R. Strategic considerations in treatment planning: Deciding when to treat, extract, or replace a questionable tooth. J. Prosthet. Dent. 2010;104:80–91. doi: 10.1016/S0022-3913(10)60096-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Lee J.-H., Kim D.-H., Jeong S.-N. Diagnosis of cystic lesions using panoramic and cone beam computed tomographic images based on deep learning neural network. Oral Dis. 2020;26:152–158. doi: 10.1111/odi.13223. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Hiraiwa T., Ariji Y., Fukuda M., Kise Y., Nakata K., Katsumata A., Fujita H., Ariji E. A deep-learning artificial intelligence system for assessment of root morphology of the mandibular first molar on panoramic radiography. Dentomaxillofacial Radiol. 2019;48:20180218. doi: 10.1259/dmfr.20180218. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Kurt Bayrakdar S., Orhan K., Bayrakdar I.S., Bilgir E., Ezhov M., Gusarev M., Shumilov E. A deep learning approach for dental implant planning in cone-beam computed tomography images. BMC Med. Imaging. 2021;21:86. doi: 10.1186/s12880-021-00618-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Chen Q., Wu J., Li S., Lyu P., Wang Y., Li M. An ontology-driven, case-based clinical decision support model for removable partial denture design. Sci. Rep. 2016;6:1–8. doi: 10.1038/srep27855. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Joda T., Gallucci G., Wismeijer D., Zitzmann N. Augmented and virtual reality in dental medicine: A systematic review. Comput. Biol. Med. 2019;108:93–100. doi: 10.1016/j.compbiomed.2019.03.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Zitzmann N.U., Matthisson L., Ohla H., Joda T. Digital undergraduate education in dentistry: A systematic review. Int. J. Environ. Res. Public Health. 2020;17:3269. doi: 10.3390/ijerph17093269. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Van der Meer W.J., Andriessen F.S., Wismeijer D., Ren Y. Application of intra-oral dental scanners in the digital workflow of implantology. PLoS ONE. 2012;7:e43312. doi: 10.1371/journal.pone.0043312. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
- View on publisher site
- PDF (504.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Glimpse into the future of prosthodontics: The synergy of artificial intelligence
Artak heboyan, nazia yazdanie, naseer ahmed.
- Author information
- Article notes
- Copyright and License information
Author contributions: Heboyan A, Yazdanie N, and Ahmed N contributed to this paper; Yazdanie N and Ahmed N designed the overall concept and outline of the manuscript; Heboyan A contributed to the discussion and design of the manuscript; Heboyan A, Yazdanie N, and Ahmed N contributed to the writing, and editing the manuscript and review of literature.
Corresponding author: Artak Heboyan, DDS, MD, MSc, PhD, Associate Professor, Department of Prosthodontics, Yerevan State Medical University after Mkhitar Heratsi, No. 2 Koryun Street, Yerevan 0025, Armenia. [email protected]
Received 2023 Sep 21; Revised 2023 Oct 26; Accepted 2023 Nov 17; Issue date 2023 Nov 26.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.
Prosthodontics, deals in the restoration and replacement of missing and structurally compromised teeth, this field has been remarkably transformed in the last two decades. Through the integration of digital imaging and three-dimensional printing, prosthodontics has evolved to provide more durable, precise, and patient-centric outcome. However, as we stand at the convergence of technology and healthcare, a new era is emerging, one that holds immense promise for the field and that is artificial intelligence (AI). In this paper, we explored the fascinating challenges and prospects associated with the future of prosthodontics in the era of AI.
Keywords: Artificial intelligence, Prosthodontics, Treatment planning, Patient-centric care, Three-dimensional printing
Core Tip: Prosthodontics and artificial intelligence working together will raise the standard of dental care in the twenty-first century and improve the quality of life for many people who require dental replacements.
INTRODUCTION
Artificial intelligence (AI) has transformed diagnoses in healthcare, including the prosthodontics field[ 1 - 3 ]. Machine learning (ML) algorithms can evaluate exponential patient data, such as patient interviews, radiographs, and intraoral scans to detect oral diseases early with a high accuracy[ 4 ]. AI can help prosthodontists discover oral conditions earlier, allowing them to intervene rapidly and deliver highly effective treatments[ 5 ]. Furthermore, AI-powered treatment planning can improve decision-making in prosthodontic procedures. AI can offer customized treatment plans by analyzing patient-specific data, ensuring that prosthetic solutions are matched to the individual needs. This improves not just patient satisfaction but also treatment efficacy[ 3 , 6 ].
While AI generally involves the application of advanced algorithms and ML technologies to complete tasks that would typically require human intelligence. ML in medicine particularly refers to the use of algorithms that can acquire information from data to improve performance on a certain task. This maybe acquired from huge datasets involve teaching models, patient histories or medical photographs to recognize configurations and associations that would be challenging for individuals to distinguish. ML can be applied for a variety of healthcare applications including treatment outcomes prediction, patients’ possible medical conditions identification, or treatment plans optimization[ 7 , 8 ].
The future of prosthodontics will be characterized by a shift towards greater customization[ 2 ]. AI algorithms can analyze a patient's unique oral anatomy and recommend the most suitable materials, designs, and manufacturing techniques for prosthetic devices. This level of personalization ensures that patients receive prostheses that fit seamlessly, enhancing comfort and functionality[ 9 ]. Furthermore, the integration of AI with three-dimensional printing technology allows for the rapid fabrication of complex dental prosthesis. This combination enables the fabrication of precise crowns, bridges and dentures. As a result, prosthodontists would provide rapid, cost-effective, and aesthetically acceptable solutions to their patients[ 10 ].
The chatbots and virtual assistants driven by AI are already revolutionizing patient interaction in healthcare. These technologies in prosthodontics can give patients with information, support, and appointment reminders. AI-powered tele-prosthodontics services can offer remote consultations and follow-ups, increasing access to dental treatment for people living in distant or underserved areas[ 11 , 12 ]. Furthermore, AI can improve the patient experience by anticipating and resolving potential issues before they arise. Prosthodontists can offer pro-active interventions and recommendations by continuously monitoring and analyzing patient data, assuring the long-term success of prosthetic treatment[ 13 ].
While the future of prosthodontics with AI holds immense promise, it also presents several challenges and ethical considerations. Ensuring data privacy, security, and informed consent are crucial aspects of integrating AI into healthcare[ 14 ]. Taking into consideration that patient records are mostly confidential, there is an expected disagreement among organizations to exchange patients` medical data and personal information. AI systems raise some significant concerns regarding data safety and privacy. Since health-related data are significant and vulnerable, hackers sometimes can target them, thus, preserving the privacy of medical data is crucial. Patient informed consent is another key factor for data confidentiality since healthcare specialists may permit widespread usage of patient medical data for AI research without demanding patient consent[ 15 , 16 ]. Moreover, there is a need for rigorous training and education to equip prosthodontists with the skills required to harness the power of AI effectively.
Finally, there are possible threats to healthcare providers and humans connected to potential misuse of AI-systems. Limitations in the use of AI in dentistry may be related to lack of transparency and accountability as well as bias and discrimination. AI-based systems may be inadequate in their understanding of the context of human oral health and disease. Nowadays, job displacement is not a significant shortcoming of AI application in dentistry, especially for prosthodontics, but it is likely that some procedures could be replaced by AI devices. However, AI systems may not be available or affordable to all human beings and communities, which may lead to discriminations in access to healthcare[ 16 , 17 ].
AI will open up new possibilities for prosthodontics and take it into unexplored landscape. Dental prosthetic solutions will soon be more precise and available than ever due to AI-powered diagnostics, treatment planning, customization and patient-centered care. It is crucial to keep an eye out for emerging ethical and regulatory issues as we proceed along this transformational route. Prosthodontics and AI working together will raise the standard of dental care in the twenty-first century and improve the quality of life for many people who require dental replacement and rehabilitation.
Conflict-of-interest statement: The authors declare no conflict of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: September 21, 2023
First decision: October 24, 2023
Article in press: November 17, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: Armenia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corte-Real A, Portugal S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
Contributor Information
Artak Heboyan, Department of Prosthodontics, Yerevan State Medical University after Mkhitar Heratsi, Yerevan 0025, Armenia. [email protected].
Nazia Yazdanie, Department of Prosthodontics, FMH College of Medicine and Dentistry, Lahore 54000, Pakistan.
Naseer Ahmed, Department of Prosthodontics, Altammash Institute of Dental Medicine, Karachi 75500, Pakistan.
- 1. Fatima A, Shafi I, Afzal H, Díez IT, Lourdes DRM, Breñosa J, Espinosa JCM, Ashraf I. Advancements in Dentistry with Artificial Intelligence: Current Clinical Applications and Future Perspectives. Healthcare (Basel) 2022;10 doi: 10.3390/healthcare10112188. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Chadha U, Abrol A, Vora NP, Tiwari A, Shanker SK, Selvaraj SK. Performance evaluation of 3D printing technologies: a review, recent advances, current challenges, and future directions. Progress in Additive Manufacturing. 2022 [ Google Scholar ]
- 3. Ritushree T, Dhaded S, Konin P. Future of prosthodontics together with artificial intelligence and robotics. Guident. 2022:16. [ Google Scholar ]
- 4. Zhang X, Liang Y, Li W, Liu C, Gu D, Sun W, Miao L. Development and evaluation of deep learning for screening dental caries from oral photographs. Oral Dis. 2022;28:173–181. doi: 10.1111/odi.13735. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Singi SR, Sathe S, Reche AR, Sibal A, Mantri N. Extended Arm of Precision in Prosthodontics: Artificial Intelligence. Cureus. 2022;14:e30962. doi: 10.7759/cureus.30962. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Chau RCW, Chong M, Thu KM, Chu NSP, Koohi-Moghadam M, Hsung RT, McGrath C, Lam WYH. Artificial intelligence-designed single molar dental prostheses: A protocol of prospective experimental study. PLoS One. 2022;17:e0268535. doi: 10.1371/journal.pone.0268535. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Marino R, Uribe S, Chen R, Schwendicke F, Giraudeau N, Scheerman J. Terminology of e-Oral Health: Consensus Report of the IADR's e-Oral Health Network Terminology Task Force. 2023 Preprint. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Mohammad-Rahimi H, Rokhshad R, Bencharit S, Krois J, Schwendicke F. Deep learning: A primer for dentists and dental researchers. J Dent. 2023;130:104430. doi: 10.1016/j.jdent.2023.104430. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Alammar A, Kois JC, Revilla-León M, Att W. Additive Manufacturing Technologies: Current Status and Future Perspectives. J Prosthodont. 2022;31:4–12. doi: 10.1111/jopr.13477. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Rokaya D, Kongkiatkamon S, Heboyan A, Dam VV, Amornvit P, Khurshid Z, Srimaneepong V, Zafar MS. 3D-Printed Biomaterials in Biomedical Application. Functional biomaterials: Drug delivery and biomedical applications. 2022:319–339. [ Google Scholar ]
- 11. Mariño R, Ghanim A. Definition of Teledentistry, e-Health Care in Dentistry and Oral Medicine: A Clinician’s Guide. 2018; 3-14. [ Google Scholar ]
- 12. Chen YW, Stanley K, Att W. Artificial intelligence in dentistry: current applications and future perspectives. Quintessence Int. 2020;51:248–257. doi: 10.3290/j.qi.a43952. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Khan B, Fatima H, Qureshi A, Kumar S, Hanan A, Hussain J, Abdullah S. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed Mater Devices. 2023:1–8. doi: 10.1007/s44174-023-00063-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Kim CS, Samaniego CS, Sousa Melo SL, Brachvogel WA, Baskaran K, Rulli D. Artificial intelligence (A.I.) in dental curricula: Ethics and responsible integration. J Dent Educ. 2023 doi: 10.1002/jdd.13337. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Schwendicke F, Büttner M. Artificial intelligence: advances and pitfalls. Br Dent J. 2023;234:749–750. doi: 10.1038/s41415-023-5855-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Ayad N, Schwendicke F, Krois J, van den Bosch S, Bergé S, Bohner L, Hanisch M, Vinayahalingam S. Patients' perspectives on the use of artificial intelligence in dentistry: a regional survey. Head Face Med. 2023;19:23. doi: 10.1186/s13005-023-00368-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Kelly CJ, Karthikesalingam A, Suleyman M, Corrado G, King D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019 doi: 10.1186/s12916-019-1426-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (341.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
Theses, Dissertations and Projects - Prosthodontics . Follow. Theses/Dissertations from 2022 PDF. Effect of Splinting Implant Scan Bodies Intraorally on The Trueness of Complete Arch Digital Impressions: A Clinical Study, Kawther Mahmoud Ali. Theses/Dissertations from 2019 PDF. In-vitro ...
Research - Removable Prosthodontics Optimization of the dimension of computer numerical control-milled polyetheretherketone clasps: An in vitro evaluation of accuracy Na Zhang,
List of more than 2000 premium prosthodontics thesis topics for MDS to choose from. The topics include thesis done in various universities as well as recent paper published in Prosthodontics Journals. ... treatment modalities, and even the development of new technologies. In the multifaceted world of prosthodontics, the journey towards an MDS ...
The Journal of Prosthodontics is the official journal of the American College of Prosthodontists (ACP), the organization that represents the specialty of prosthodontics and ensures national recognition of the specialty. We promote the advanced study and practice of prosthodontics, implant, esthetic and reconstructive dentistry. We support researchers and practicing clinicians with publication ...
Removable prosthodontics; Latest Research and Reviews. An in vitro evaluation of tensile strength of molar endocrown milled from various computer aided design and manufacturing materials.
This article gives an overview of the advances in selected fields of fixed prosthodontics and provides support in material selection for different kinds of indications, from single-tooth ...
Read the latest articles of Journal of Prosthodontic Research at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature. ... Removable Prosthodontics. 11 November 2019. Fixed Prosthodontics. 11 November 2019. Clinical Epidermiology. 11 November 2019. View all special issues and article collections.
In addition, new technologies require continuous investment of the dental community. As long as the research results are not demonstrating superiority, the routine implementation of AI applications in prosthodontics will be delayed. Here, the university and dental schools need to foster AI technology in research and education.
Read the latest articles of The Journal of Prosthetic Dentistry at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature. ... Report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. Georgios Maroulakos, Geoffrey A. Thompson, Elias D. Kontogiorgos. May 2019 ...
Prosthetic dentistry or prosthodontics is one of the branches of dentistry, mainly deals with replacement and rehabilitation of missing teeth with the help of fixed and removable prosthesis or ...
Latest Advances in Prosthodontics: Improving Patient-Centered Outcomes. ... Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently. Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more ...
The goals of applying an evidence-based approach to prosthodontics involve finding and compiling the latest scientific information available pertaining to prosthodontics and its techniques, critically analyzing the scientific evidence behind the existing treatment protocol, and seeking improvement in the research, and reporting studies that are ...
AI will open up new possibilities for prosthodontics and take it into unexplored landscape. Dental prosthetic solutions will soon be more precise and available than ever due to AI-powered diagnostics, treatment planning, customization and patient-centered care. It is crucial to keep an eye out for emerging ethical and regulatory issues as we ...
The Journal of Prosthetic Dentistry is the leading professional journal devoted exclusively to prosthetic and restorative dentistry.The Journal is the official publication for 24 leading U.S. international prosthodontic organizations. The monthly publication features timely, original peer-reviewed articles on the newest techniques, dental materials, and research findings.
The field of prosthodontics and restorative dentistry commonly deal with complex restorative reconstructions. Alongside an increasing demand for complete mouth rehabilitations because of multifactorial causative elements, 1-3 a systematic approach is necessary to ensure appropriate diagnosis, planning, and treatment. 4 Historically, conventional methods have achieved successful treatment ...
The present topic aims to collect and disseminate original research papers, reviews, and technical reports on the state of the art in the field of fixed prosthodontics and implant therapy. Potential fields include but are not limited to the following: Fixed prosthodontics on natural teeth; Implant prosthodontics; CAD/CAM materials; 3D-printed ...
Prosthodontics is the dental specialty pertaining to the diagnosis, treatment planning, rehabilitation and maintenance of the oral function,... | Explore the latest full-text research PDFs ...
PDF | On Jan 1, 2020, Kokila Vellingiri and others published Current Trends in Fixed Prosthodontics | Find, read and cite all the research you need on ResearchGate
The editors of the Journal of Prosthodontics are pleased to present this virtual issue compiling twelve clinical reports published in the Journal of Prosthodontics over the last two years.. Clinical reports, which typically detail the presentation, treatment, and follow-up of an individual patient, highlight some of the most important work prosthodontists do for patients.
New Content Alerts; Pricing; Reprints; Sponsoring Organizations; Academy of Prosthodontics, The; The Italian Academy of Prosthetic Dentistry; American Academy of Fixed Prosthodontics, The; American Academy of Maxillofacial Prosthetics, The; Academy of Advanced Prosthodontics in Taiwan (no website) American Academy of Restorative Dentistry, The