Premed Research That Impresses Medical Schools
Here are at least six research areas where you can leverage experiences to stand out on your medical school applications.
Research that Impresses Medical Schools

Getty Images
When writing about research on applications, describe not only what was done, but also write what was learned through research experiences.
One question premedical students frequently ask is, “Do I need to do research in order to be competitive for medical school ?”
My short answer: No.
It's not necessary for a medical school applicant to be involved in research , let alone publish a paper, in order to have a strong application. However, research only strengthens one’s application and never hurts it. Research doesn't guarantee acceptance to a medical school, and it's not necessary to gain acceptance.
However, I encourage premed students to conduct research at some point during their premed careers. Being involved in a research project trains premeds to think critically about an unresolved problem.
Research allows us to gain a better understanding of the unknown. Our current medical knowledge is built on clinical research . Drugs we prescribe patients underwent rigorous clinical trial studies, for example, and diagnostic work-up and treatment plans rely on evidence-based medicine based on research data.
Many premed students think that the research they conduct needs to be medical or scientific in nature. Another common misconception is that a strong premed must be involved with basic science research, often called bench research. While many premeds conduct medical-related research, these beliefs are not true. I have mentored amazing premed students with research ranging from Shakespearean play analysis to the creation of medical devices for individuals with disabilities.

6 Types of Medical Research
Here are six common health-related research directions I commonly see among premeds that reflect the breadth of research you can pursue:
- Basic science research
- Clinical research
- Public health research
- Health public policy research
- Narrative medicine research
- Artificial intelligence research
Basic Science Research
Basic science research, often called “bench research,” is the traditional research conducted in a laboratory setting. It tackles our fundamental understanding of biology .
Premeds involved with basic science research often study cells, viruses, bacteria and genetics. This research may also include animal and tissue specimens.
Examples: A premed student interested in cancer biology may study the cellular pathway of a specific tumor suppressor gene. Another premed student may probe how gut bacteria affect protein folding.
Clinical Research
Clinical research is the arm of medical research that tests the safety and effectiveness of diagnostic products, drugs and medical devices. It involves human subjects.
Examples: A premed interested in COVID-19 may conduct clinical trial research on new COVID-19 treatments. Another premed interested in dementia studies whether sleep improves depression among Alzheimer’s patients.
Public Health Research
Public health research studies the health of communities and populations in order to improve the health of the general public. Topics can range from vaccine access, disease prevention and disease transmission to substance abuse, social determinants of health and health education strategies.
Examples: A student interested in health equity may conduct public health research on how health insurance status and geography affect heart attack mortality. A premed excited about environmental science may look at the health impacts of wildfire smoke.
Health Public Policy Research
Premeds engaged in health policy research aim to understand how laws, regulations and policies can influence population health. Premeds may engage in both domestic and global policy research.
Examples: A premed interested in nutrition researches the effectiveness of nutrition programs in the Philippines. Another premed interested in economics studies health insurance markets in America.
Narrative Medicine Research
Narrative medicine research involves gathering stories from patients and their loved ones in order to understand the patient experience. As noted on the Association of American Colleges website , “Those stories can illuminate how a person became ill, the tipping point that compelled them to seek help, and, perhaps most importantly, the social challenges they face in getting better.”
Examples: A premed student interested in how Asians perceive disease can interview Asian patients about their attitudes toward herbal medications in cancer treatments. Another premed student interested in caregiver support can interviews caregivers of patients on prolonged mechanical ventilation to understand families’ decision-making processes.
Artificial Intelligence Research
Medical research utilizing artificial intelligence is increasingly popular, and premeds can analyze a large set of information to find medical discoveries. Premeds who conduct AI research typically have a skillset in computer science.
Examples: A premedical student interested in radiology may use AI to analyze hundreds of chest X-rays to create a program that better detects pneumonias. Another premed student may create and refine an algorithm using EKGs to better pick up abnormal heartbeats.
Remember that research not limited to these six categories. I've also met premeds engaged in journalistic research and business consulting research. As long as you have a research question and a scientific approach to analyze the question, then your pursuit can usually be considered research.
How Research Can Strengthen Medical School Applications
Research can strengthen your medical school application in several ways.
First, when a research project is related to a student’s interests, research involvement shows the application committee that the student is committed to advancing that field .
When writing about your research on applications, not only describe what you did, but also write what you learned through your research experiences. These lessons can include adaptability, analytical thinking and resilience.
Furthermore, you can discuss research through writing stories on secondary applications . For example, a common secondary essay prompt asks you to discuss a time when you failed or faced a challenge. You can write an essay about a challenging time you faced in your research and discuss how you overcame it. This will allow the admissions committee to gain insights into how you critically think through a problem.
Second, medical schools greatly favor independent research, in which students are leading the projects. In independent research, a premed forms a research question and a hypothesis. Then, the student gathers, analyzes and interprets data.
A student conducting independent research is in contrast to a student who helps another researcher with part of a project, or a student who follows protocols such as clinical trials recruitment, without thinking critically through the research design and analysis.
Third, becoming an author on a published paper can be a significant milestone and a valuable boost for a premed’s application. Of course, being a first author on a manuscript is an excellent feat, but it is not necessary for being seen as a strong student.
Other than publishing in academic journals, premedical students can showcase their research through poster presentations and talks. Presenting research conveys that you are excited about sharing your work and that you can explain your research to others, even those outside your field. These are all strong ways to indicate achievement and passion related to research.
The Value of Research for Premeds
Conducting premed research can provide firsthand insight into how much research you want to pursue throughout your career. After conducting research, some students may decide to get an M.D.-Ph.D. joint degree. Other students may come to the realization that their strengths lie elsewhere and conduct minimal research as doctors.
Through research, aspiring physicians will develop important skills that will help them in patient care. They will learn how to read and write research papers and evaluate treatment options by analyzing how robust the evidence is toward a specific treatment.
There are many advantages of engaging in research as a premed, only one of which is improving your medical school application. Since research is the cornerstone of medical advancement, research can help you become a more thoughtful doctor.
Medical School Application Mistakes

Tags: medical school , research , graduate schools , education , students
About Medical School Admissions Doctor
Need a guide through the murky medical school admissions process? Medical School Admissions Doctor offers a roundup of expert and student voices in the field to guide prospective students in their pursuit of a medical education. The blog is currently authored by Dr. Ali Loftizadeh, Dr. Azadeh Salek and Zach Grimmett at Admissions Helpers , a provider of medical school application services; Dr. Renee Marinelli at MedSchoolCoach , a premed and med school admissions consultancy; Dr. Rachel Rizal, co-founder and CEO of the Cracking Med School Admissions consultancy; Dr. Cassie Kosarec at Varsity Tutors , an advertiser with U.S. News & World Report; Dr. Kathleen Franco, a med school emeritus professor and psychiatrist; and Liana Meffert, a fourth-year medical student at the University of Iowa's Carver College of Medicine and a writer for Admissions Helpers. Got a question? Email [email protected] .
Popular Stories
Best Colleges

Morse Code: Inside the College Rankings

The Short List: Grad School

Law Admissions Lowdown

You May Also Like
Medical school rankings coming soon.
Robert Morse and Eric Brooks June 6, 2024
15 B-Schools With Low Acceptance Rates
Ilana Kowarski and Cole Claybourn June 5, 2024
Advice About Online J.D. Programs
Gabriel Kuris June 3, 2024
Questions to Ask Ahead of Law School
Cole Claybourn May 31, 2024

Tips for Secondary Med School Essays
Cole Claybourn May 30, 2024

Ways Women Can Thrive in B-School
Anayat Durrani May 29, 2024

Study Away or Abroad in Law School
Gabriel Kuris May 28, 2024

A Guide to Executive MBA Degrees
Ilana Kowarski and Cole Claybourn May 24, 2024

How to Choose a Civil Rights Law School
Anayat Durrani May 22, 2024

Avoid Procrastinating in Medical School
Kathleen Franco, M.D., M.S. May 21, 2024

Teaching Medical Research to Medical Students: a Systematic Review
Affiliations.
- 1 Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 2 Division of Hepatobiliary & Pancreatic Surgery, Department of Surgery, National University Hospital, Singapore, Singapore.
- 3 Liver Transplantation, National University Centre for Organ Transplantation, National University Hospital, Singapore, Singapore.
- 4 Centre for Medical Education, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 5 Division of Colorectal Surgery, Department of Surgery, National University Hospital, 1E Kent Ridge Road, Singapore, 119228 Singapore.
- PMID: 34457935
- PMCID: PMC8368360
- DOI: 10.1007/s40670-020-01183-w
Phenomenon: Research literacy remains important for equipping clinicians with the analytical skills to tackle an ever-evolving medical landscape and maintain an evidence-based approach when treating patients. While the role of research in medical education has been justified and established, the nuances involving modes of instruction and relevant outcomes for students have yet to be analyzed. Institutions acknowledge an increasing need to dedicate time and resources towards educating medical undergraduates on research but have individually implemented different pedagogies over differing lengths of time.
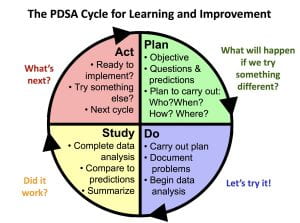
Approach: While individual studies have evaluated the efficacy of these curricula, the evaluations of educational methods and curriculum design have not been reviewed systematically. This study thereby aims to perform a systematic review of studies incorporating research into the undergraduate medical curriculum, to provide insights on various pedagogies utilized to educate medical students on research.
Findings: Studies predominantly described two major components of research curricula-(1) imparting basic research skills and the (2) longitudinal application of research skills. Studies were assessed according to the 4-level Kirkpatrick model for evaluation. Programs that spanned minimally an academic year had the greatest proportion of level 3 outcomes (50%). One study observed a level 4 outcome by assessing the post-intervention effects on participants. Studies primarily highlighted a shortage of time (53%), resulting in inadequate coverage of content.
Insights: This study highlighted the value in long-term programs that support students in acquiring research skills, by providing appropriate mentors, resources, and guidance to facilitate their learning. The Dreyfus model of skill acquisition underscored the importance of tailoring educational interventions to allow students with varying experience to develop their skills. There is still room for further investigation of multiple factors such as duration of intervention, student voluntariness, and participants' prior research experience. Nevertheless, it stands that mentoring is a crucial aspect of curricula that has allowed studies to achieve level 3 Kirkpatrick outcomes and engender enduring changes in students.
Supplementary information: The online version contains supplementary material available at 10.1007/s40670-020-01183-w.
Keywords: Curricula; Dreyfus model; Medical undergraduates; Research education; Skill acquisition.
© International Association of Medical Science Educators 2021.
Publication types
Why all medical students need to experience research
- Post author By Website Publications Officer
- Post date June 4, 2016

Medical students are very busy. The demands of studying medicine are extraordinary. Why then is it so important, on top of all there is to learn, to bother engaging in health and medical research? It is particularly important to consider this question at a time when, nationally and internationally, medical schools are including a research project as either a requirement of their program or a highly encouraged option. In fact, the Australian government is now supporting research by medical students with a specific category of scholarship funding from the National Health and Medical Research Council (NHMRC) available to students undertaking in a combined MBBS/PhD or MD/PhD program. [1]
As a Dean of Medicine, and passionate advocate of health and medical research (HMR) in Australia, I support the inclusion of research in medical programs. Research training and experience are not just ‘nice to have’ but a ‘must’ for our doctors of the future. Increased research training in medical programs is beneficial for a student’s professional pathway, their evolving practice and, most importantly, for the health of the patients and communities they serve. [2,3]
Demonstrated research experience at medical school is increasingly important in obtaining positions in training programs post-graduation. [4] Recognition of the importance of HMR in developing and applying the skills and knowledge acquired in their medical studies has seen many of the specialist colleges including research training and productivity (for example publications) in their approach to selection of trainees. Competition for vocational and advanced training places is fierce, and a professional resume that includes research productivity and qualifications is and will continue to be important. Some colleges may even move to requiring a PhD for entry into advanced training.
A research experience may be the first time a student has had to write and record what they do, think, and find coherently, concisely and precisely. This can contribute to developing lasting habits of critical thinking. In a landmark and classic essay, C. Wright Mills commented that there was never a time he was not thinking, reflecting, analysing, and writing – he was always working on an idea. [5] This is the mindset that research can build up, and this is surely the mindset we want in clinical medicine and population health, where continuing critical appraisal of new evidence and engagement with new ideas is vital. In addition to stimulating ongoing interest in learning, this intellectually curious mindset contributes to a sense of personal satisfaction and eagerness to engage in discovery and learning as part of a team. [3,6] Research achievements are rarely made by individuals in isolation. Developing a mindset of critical inquiry in individuals and teams clearly encourages research productivity in grants and publications in the longer term, [3] which can ‘future-proof’ careers at a time when research performance is important in professional esteem and progression. Even more importantly, involvement in research appears to improve clinical practice. Research-active healthcare providers appear to provide better care and achieve better patient outcomes, [7] making the investment of time in research training for medical students potentially very important to building a healthier society in the long term. Given the potential benefits to early career clinicians and to patients, it is important to expose recent medical graduates to research as well, and successful postgraduate training programs are also taking steps to include research training. [3,8]
So, what is the best way for medical schools and postgraduate training programs to provide research training that maximises these benefits? It is clear from the literature that the most important thing is to have protected time to pursue research. Whether the research is a programmed experience as part of a course (as is increasingly the case), or something pursued independently by the individual student or trainee, giving as much time as possible is key to getting the best quality outcomes. For recent graduates, hospitals need to allow time to do research. [8] For students, time should be set aside within the program. [4] Students and trainees also need to be mentored by experienced researchers to get the best results. [3] Research experiences for students and trainees that combine mentorship and protected time can deliver the biggest benefits to our future clinical leaders and society as they are most likely to result in high quality outputs that are published and improve knowledge and practice. Where possible, trainees without research degrees should try to enrol in these at the same time as pursuing their research experiences, through a university that offers flexible research training and options to submit theses by publication, as earning a research degree such as a PhD is increasingly becoming a prerequisite for obtaining research funding that can support a clinical research career.
In summary, more than ever before, being a doctor in the 21st century is a career of lifelong learning. The combination of continued, rapid growth in knowledge and advancing technology bringing that information to your fingertips, have brought both a richness to the practice of medicine as well as a challenge. There is a growing appreciation that researchers make better clinicians. Research exposure increases understanding of clinical medicine; facilitates critical thinking and critical appraisal; improves prospects of successful application for post graduate training, grants, and high impact publications; develops teamwork skills; and increases exposure to the best clinical minds. The government is lifting its investment in health and medical researchers like never before. The establishment of the Medical Research Future Fund by the Australian Government, for example, offers the promise of continued durable investment in HMR and innovation, and the NHMRC’s substantial investment in research training scholarships for current students and recent graduates signals the Government’s commitment to developing clinician researchers for the future.
I encourage all students to make the most of research opportunities in medical school and beyond, not only for the personal and professional benefits, but in contributing to the health of their patients and to the Australian community.
[1] NHMRC Funding Rules 2015: Postgraduate Scholarships – 6 Categories of Award – 6.2. Clinical Postgraduate Scholarship. 2015. https://www.nhmrc.gov.au/book/6-categories-award-3 (accessed Nov 2015).
[2] Laidlaw A, Aiton L, Struthers J, Guild S. Developing research skills in medical students: AMEE guide no. 69. Med Teach. 2012;34:754–71.
[3] Lawson PJ, Smith S, Mason MJ, Zyzanski SJ, Stange KC, Werner JJ, Flocke SA. Creating a culture of inquiry in family medicine. Fam Med. 2014;46(7):515–521.
[4] Collier AC. Medical school hotline: importance of research in medical education. Hawai’i Journal Med Public Health. 2012;71(2):53-6.
[5] Mills, CW. On intellectual craftsmanship. In: Seale, C. Editor. Social research methods: A reader. London: Routledge, 2004.
[6] von Strumm S, Hell B, Chamorro-Premuzic T. The hungry mind: intellectual curiosity is the third pillar of academic performance of university. Perspect Psychol Sci. 2011;6(6):574-88.
[7] Selby P, Autier P. The impact of the process of clinical research on health service outcomes. Ann Oncol 2011;22(Suppl 7):vii5-vii9.
[8] Chen JX, Kozin ED, Sethi RKV, Remenschneider AK, Emerick KS, Gray ST. Increased resident research over an 18-year period – a single institution’s experience. Otolaryngol Head Neck Surg. 2015;153(3):350-6.
Medical Research
How to conduct research as a medical student, this article will address how to conduct research as a medical student, including details on different types of research, how to go about constructing an idea and other practical advice., kevin seely, oms iv.
Student Doctor Seely attends the Rocky Vista University College of Osteopathic Medicine.
In addition to good grades, test performance, and notable characteristics, it is becoming increasingly important for medical students to participate in and publish research. Residency programs appreciate seeing that applicants are interested in improving the treatment landscape of medicine through the scientific method.
Many medical students also recognize that research is important. However, not all schools emphasize student participation in research or have associations with research labs. These factors, among others, often leave students wanting to do research but unsure of how to begin. This article will address how to conduct research as a medical student, including details on different types of research, how to go about constructing an idea, and other practical advice.
Types of research commonly conducted by medical students
This is not a comprehensive list, but rather, a starting point.
Case reports and case series
Case reports are detailed reports of the clinical course of an individual patient. They usually describe an unusual or novel occurrence or provide new evidence related to a specific pathological entity and its treatment. Advantages of case reports include a relatively fast timeline and little to no need for funding. A disadvantage, though, is that these contribute the most basic and least powerful scientific evidence and provide researchers with minimal exposure to the scientific process.
Case series, on the other hand, look at multiple patients retrospectively. In addition, statistical calculations can be performed to achieve significant conclusions, rendering these studies great for medical students to complete to get a full educational experience.
Clinical research
Clinical research is the peak of evidence-based medical research. Standard study designs include case-controlled trials, cohort studies or survey-based research. Clinical research requires IRB review, strict protocols and large sample sizes, thus requiring dedicated time and often funding. These can serve as barriers for medical students wanting to conduct this type of research. Be aware that the AOA offers students funding for certain research projects; you can learn more here . This year’s application window has closed, but you can always plan ahead and apply for the next grant cycle.
The advantages of clinical research include making a significant contribution to the body of medical knowledge and obtaining an understanding of what it takes to conduct clinical research. Some students take a dedicated research year to gain experience in this area.
Review articles
A literature review is a collection and summarization of literature on an unresolved, controversial or novel topic. There are different categories of reviews, including meta-analyses, systematic reviews and traditional literature reviews, offering very high, high and modest evidentiary value, respectively. Advantages of review articles include the possibility of remote collaboration and developing expertise on the subject matter. Disadvantages can include the time needed to complete the review and the difficulty of publishing this type of research.
Forming an idea
Research can be inspiring and intellectually stimulating or somewhat painful and dull. It’s helpful to first find an area of medicine in which you are interested and willing to invest time and energy. Then, search for research opportunities in this area. Doing so will make the research process more exciting and will motivate you to perform your best work. It will also demonstrate your commitment to your field of interest.
Think carefully before saying yes to studies that are too far outside your interests. Having completed research on a topic about which you are passionate will make it easier to recount your experience with enthusiasm and understanding in interviews. One way to refine your idea is by reading a recent literature review on your topic, which typically identifies gaps in current knowledge that need further investigation.
Finding a mentor
As medical students, we cannot be the primary investigator on certain types of research studies. So, you will need a mentor such as a DO, MD or PhD. If a professor approaches you about a research study, say yes if it’s something you can commit to and find interesting.
More commonly, however, students will need to approach a professor about starting a project. Asking a professor if they have research you can join is helpful, but approaching them with a well-thought-out idea is far better. Select a mentor whose area of interest aligns with that of your project. If they seem to think your idea has potential, ask them to mentor you. If they do not like your idea, it might open up an intellectual exchange that will refine your thinking. If you proceed with your idea, show initiative by completing the tasks they give you quickly, demonstrating that you are committed to the project.
Writing and publishing
Writing and publishing are essential components of the scientific process. Citation managers such as Zotero, Mendeley, and Connected Papers are free resources for keeping track of literature. Write using current scientific writing standards. If you are targeting a particular journal, you can look up their guidelines for writing and referencing. Writing is a team effort.
When it comes time to publish your work, consult with your mentor about publication. They may or may not be aware of an appropriate journal. If they’re not, Jane , the journal/author name estimator, is a free resource to start narrowing down your journal search. Beware of predatory publishing practices and aim to submit to verifiable publications indexed on vetted databases such as PubMed.
One great option for the osteopathic profession is the AOA’s Journal of Osteopathic Medicine (JOM). Learn more about submitting to JOM here .
My experience
As a second-year osteopathic medical student interested in surgery, my goal is to apply to residency with a solid research foundation. I genuinely enjoy research, and I am a member of my institution’s physician-scientist co-curricular track. With the help of amazing mentors and co-authors, I have been able to publish a literature review and a case-series study in medical school. I currently have some additional projects in the pipeline as well.
My board exams are fast approaching, so I will soon have to adjust the time I am currently committing to research. Once boards are done, though, you can bet I will be back on the research grind! I am so happy to be on this journey with all my peers and colleagues in medicine. Research is a great way to advance our profession and improve patient care.
Keys to success
Research is a team effort. Strive to be a team player who communicates often and goes above and beyond to make the project a success. Be a finisher. Avoid joining a project if you are not fully committed, and employ resiliency to overcome failure along the way. Treat research not as a passive process, but as an active use of your intellectual capability. Push yourself to problem-solve and discover. You never know how big of an impact you might make.
Disclaimers:
Human subject-based research always requires authorization and institutional review before beginning. Be sure to follow your institution’s rules before engaging in any type of research.
This column was written from the perspective from a current medical student with the review and input from my COM’s director of research and scholarly activity, Amanda Brooks, PhD.
Related reading:
H ow to find a mentor in medical school
Tips on surviving—and thriving—during your first year of medical school
Mile marker
20 reasons to love and hate retirement, road to residency, how to soften red flags on your eras application, ai and medicine, how dos can be at the forefront of the digital health revolution, emergency preparedness, high-altitude health care: navigating in-flight medical emergencies, creating change, do day 2024: advocating for student loan reform, health care worker safety and more, more in training.

AOA works to advance understanding of student parity issues
AOA leaders discuss student parity issues with ACGME, medical licensing board staff and GME program staff.

PCOM hosts annual Research Day showcasing scholarly activity across the college’s 3 campuses
Event highlighted research on important topics such as gun violence and COPD.
Previous article
Next article, one comment.
Thanks! Your write out is educative.
Leave a comment Cancel reply Please see our comment policy
- Premed Research
How Important is Research for Medical School
How important is research for medical school? Research is a critical part of your medical learning, and its important for both how to prepare for med school applications and of course your entire medical career. Research experience of any type is a valuable asset on medical school applications, and clinical research experience even more so. If you’ve completed a stint in a clinical research position, these can count towards how many clinical hours you need for medical school . Some of the most competitive or research-focused medical colleges even require students to have prior research experience to be accepted. Not every med school asks for research experience, but every medical student will need some research experience under their belts by the time they graduate. In this blog, we’ll look at how important research is for medical school, what research experience can do for you and where to look to find medical research opportunities.
>> Want us to help you get accepted? Schedule a free strategy call here . <<
Article Contents 6 min read
How important is research for medical school.
There are two sides to this question. The first is whether research experience is important for medical school applications. The second is whether gaining research experience is an important part of attending medical school. The answer to both of these is undoubtedly yes, research is very important for medical school.
Of course, there are some qualifications to this importance. Having research experience is not a hard requirement for the vast majority of medical school applications and students can still be accepted without pre-med research experience. For highly competitive medical schools, such as Stanford Medical School , or medical schools with a heavy focus on research, it may not only be a requirement but a huge asset and a way for you to ensure your medical school application stands out . For a majority of competitive, research-heavy medical colleges, up to 90% of matriculating students have prior research experience.
Check out our video for more advice on how to find premed research experience
It’s a good idea to check Medical School Admission Requirements ( MSAR ) to see if your choice of med school requires applicants to have any research experience, and if the admissions board has any preference for what type of research experience. A majority of schools will gladly accept students with research experience, but your priority should be on crafting an excellent med school app first and foremost. If you have a strong application and you have the time, you can consider looking for pre-med research opportunities to add to your application as a bonus.
But even if your choice of med school doesn’t require research experience, it is still extremely important to your journey as a med student and your future career as a doctor. If you are planning to apply to a very competitive medical school program, intend to pursue an MD/PhD program or are applying to a research-intensive medical college, research experience is an absolute must. And if none of these apply to you, eventually you will want to add research experience to your medical school resume, too.
First, let’s look at what research experience can do or your medical school applications.
Research experience for medical school applications
Research experience might be a necessary requirement for many med school applications, depending on the school and the program, but the type of research experience can vary significantly. For most med schools, they aren’t choosy about the type of research you have experience in, even if it’s not directly related to the medical field. Having any kind of research position in a scientific discipline will lend you invaluable experience and skills that will transfer to your time at med school.
But something that can help you stand out, and which medical schools value more heavily is clinical research experience. To gain clinical research as a premed might not always be possible for all students. Many try to find virtual research for premed students or look into virtual shadowing opportunities. But straight research experience and even shadowing experience is not considered actual clinical experience, and if you have any direct clinical experience on your med school application, it is considered an asset no matter where you apply.
Even if your choice of med school isn’t bothered by a lack of premed research experience or you don’t plan to pursue a career in medical research, this doesn’t mean you’re off the hook. Research is still an important aspect of medical school and being a practicing physician. Research experience provides you with pivotal skills you’ll employ as a doctor, but it can also broaden and deepen your medical knowledge and medical skills. Doctors rely on research to inform them and broaden their understanding of the medical field. And plenty of clinical physicians take the time to do their own research or publish research as a way to further their careers and open up new opportunities. Research experience also serves as a way to make your medical school resume stand out when you’re applying for jobs in residency and beyond. It might even be a requirement if you want to apply for research training positions or specialty medical research jobs.
For medical students in particular, they will be expected to undertake research projects and will be provided dedicated, protected research time to not only conduct their own individual or team research but to read the work of other researchers, too. Not all of your research experiences need to come directly through school, either. You can and are encouraged to pursue research opportunities outside med school as well. Any experiences you can add to your portfolio will be to your benefit. In short, research is a foundational part of the med school experience and in developing your skills as a medical professional.
So how can research experience help you in medical school? What advantages and benefits can it bring you? We’ll take a closer look at how important research is for medical school students and how it can be a long-term advantage in their careers.
In the vein of critically evaluating research work, conducting research will naturally develop your critical thinking and analysis skills. Throughout med school you will be asked to participate in, read about and conduct research, as doing so is part of the foundation of your medical knowledge. Research experience can also be influential in developing other important medical skills, too, such as better communication, teamwork and writing skills. It\u2019s also been shown through research that doctors who continue to learn about medicine and study medical research provide better care to patients overall. If nothing else, making a habit of regular research and study will keep you fresh and up to date on the medical field and its latest developments. "}]">
How to find medical research opportunities
Students who do want to attach some research experience to their applications or resumes often wonder where to start looking. Whether you’re a premed, current med school student or graduate student, gaining some research experience is important for your career. There are a number of places to look for opportunities, but the best ways are to use your network of contacts and ask them for recommendations. There are many programs, internships and study programs which offer research experience of any kind, and your school professors, mentors and advisors will have more insight into where to find them.
Research is a critical and eventual must-have skill and experience for medical school. Whether you add some research experience as a premed, med student or medical graduate depends on where you want to go to school and what your chosen career path as a medical professional will end up being. While you will almost certainly be given some research opportunities in medical school, it’s to your advantage to pursue some outside of your studies as well, to give yourself a competitive advantage in the job market, to continue your lifelong medical learning and to ensure you become the best doctor you can be for your future patients.
Research can a big advantage on both medical school applications and on medical school resumes for graduate medical students. Research experience is also very important to gain during your time at medical school, as it is a foundational skill you will need to become a physician.
Yes; research experience is not a definite requirement at most med schools and students without experience can still be accepted with a strong application. However, good research experience should not be considered a substitute for poor academic performance.
A majority of medical schools don’t require research experience for med school applications, with some exceptions. However, as a matriculating med school student you will be expected to gain research experience and participate in research projects during your school years.
Premed students can find valuable research positions through summer internship programs or by consulting with a college advisor. Professors and mentors are also a good option for finding research opportunities. Premeds can also look into study abroad programs that offer research experience.
No; most medical schools consider direct clinical experience more important than lab or field research for admissions. However, if you plan to apply for medical research positions, to a research-intensive med school program or want to pursue an MD/PhD, then research experience will be considered more important to have.
Research is part of the foundational skills med students will learn and will take with them into their future careers. Research experience can also provide a competitive advantage in the job market and prepare them for residency positions or work as a practicing physician.
Even if this is the case, research is a large part of being a physician and you will be required to gain at least a little experience with medical research throughout your med school career.
Generally speaking, no. Medical schools aren’t picky about the type of research experience you have, or even if the subject of the research undertaken was non-medical. Any research experience is valid.
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions, get started now.
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Premeds Research Webclass :
How to Get the Perfect Premed Research Experience
That Helped Me Get Accepted to SIX Med Schools
Time Sensitive. Limited Spots Available:
Would you like a Premed Research experience that admissions committees love?
Swipe up to see a great offer!

Comprehensive Guide to Research from the Perspective of a Medical Student
- By Dmitry Zavlin, M.D.
- February 9, 2017
- Medical Student , Pre-med
G uest post from Dmitry Zavlin, MD, a research fellow in Houston, Texas. He has been highly productive in his research endeavors and below describes a comprehensive guide to getting involved in research.
Without any doubt whatsoever, high USMLE scores, strong recommendation letters from faculty members, a multitude of away rotations, and an updated and accurate résumé make up the foundation of a strong application for a residency position. Nevertheless, from my personal experience, one topic remains crucial that many medical students either love or hate (or try not to think about it): research . It is an extracurricular activity that enables someone to stand out from the crowd and present oneself as a diverse and multitasking character. These traits are especially favorable when it comes to applying to competitive residency programs with high applicant to position ratios. I encourage every future graduate to look into this topic since – and as astonishing as this may seem – medical school is the ideal opportunity to get your name out there. You don’t need to take a year off from classes or be on an M.D., Ph.D. track. Even those students that do not seek academic careers have a benefit from engaging in scientific duties . It helps you understand the mechanisms of research, the bureaucratic obstacles, the medical challenges, and teaches you communication with peers and faculty. Furthermore, you learn how to read, analyze, and interpret scientific publications of others. And trust me, it’s not all gold that gets printed in journals . On first glance, getting involved in unpaid ventures while you are in class, on rotation, at home studying or just taking some time off for yourself might seem like a bad deal. Yet with a sincere approach towards this subject, you can strengthen your résumé, top off your application, and learn skills that will serve you well into your career as a doctor.
The following lines are intended to display my personal experience that I have made at my medical school and in my interactions with students, residents, fellows, and attendings at my current position.
Choosing your Project
First things first. Naturally, you would want to participate and conduct research in a field of medicine you might see yourself in after graduation. However, as mentioned before, this is not a K.O. criterion. Plenty of personal experiences tell me stories of students who were involved in one area and then switched and matched in a completely different specialty of medicine or completely left the patient-care sector. Therefore, consider your engagement in scientific tasks more of as a symbolization for your work ethic and your ability to perform in a team.
My first tip is to contact the department at your home medical school, introduce yourself, write 1-2 sentences describing your motivations and goals, and ask to sit down with some faculty members or scientific staff to discuss your involvement in any research activities.
Larger departments usually have secretaries or an academic office where your email is less likely to get lost compared to the inbox of a busy professor who receives hundreds of emails per day. Personally, I would aim for junior faculty and potentially senior residents who are experienced enough to conduct research on a high level but are not too far away from the life of a young medical student. Certain departments further have specific full-time research staff that is definitely a great resource for any scientific venture. While it may be helpful to work with the director and senior faculty directly, the sad reality is often that they typically have many academic and administrative duties and activities at their institutions that might not go along well with the schedule of an ambitious student and cause frustration in the long run.
When you meet, make sure to gain and write down as many details as possible:
- What is the topic, what is the goal of this project?
- What type of format is it? (See below)
- What is the current status?
- Who is involved in this research project, what is the team, what are the people to contact?
- What will be my duties?
- Any bureaucratic issues to be aware of (IRB approval, grants, finances)?
- What is the prognosis? Are there any deadlines?
Lastly, ask about the current literature on that topic so you know what your team’s role is going to be in this scientific field. Although one core concept of any research result is reproducibility, it often remains a challenge to publish a project that has already been performed and presented or printed before. Getting involved in an area that is in quick development with high turnaround is subsequently a strong recommendation.
Types of Evidence-Based Research
Now, I would like to talk about the most common options you will encounter when presented with an array of project offers. That way you know their perks and pitfalls before you commit to anything serious and long-lasting and potentially even waste any valuable and limited time of yours.
- Case Reports: These are the most basic and least powerful of scientific contributions to medicine. Give or take, a case report is the summarized hospital or clinic chart of a treated patient who presented with a problem A and was managed with therapy B. A case report that is typically 2-3 pages long with a short intro, a compact case discussion, and perhaps some photos is the closest thing you will get to a patient note you learned to write in early medical school. Their lack of medical value makes them hard to get published in journals and students should not solely rely on these projects as they may not ultimately be accepted by journals. Recommendation: 3/5
- Case Series, Retrospective Study: These layouts are my personal recommendation as they allow quality results within a short period and are not time-consuming or require large long-term commitment as others. Typical examples are an analysis of patients who presented with the same diagnosis or underwent an identical procedure. The difference between a case series and a retrospective study is that for the latter, the patients can be stratified into different subgroups (similar to “case control study”) and statistical calculations can be performed to achieve significant conclusions. Recommendation: 5/5
- Prospective Studies: In these studies, patients are gathered in one or multiple cohorts and are followed-up over long periods of time by lab results, imaging, physical exams etc. These require great time commitment and, from a student perspective, typically only allow a certain amount of participation. These are usually studies for physicians with long relationships with their patients. Recommendation: 3/5
- (Randomized) Clinical Trials : The peak of evidence-based medical research. Similar as prospective studies yet require more planning, IRB approval, and lots of work with industry, grants, protocols, etc. Student involvement is usually marginal. Recommendation: 2/5
- Basic Science, Animal Work: Although these projects require training, approval, and a large amount of preparation, student participation is common in many areas of basic science. The advantage of these laboratory activities is a certain amount of flexibility on when certain tasks and duties can be performed. Within certain limitations, a medical student can get involved in animal or basic science research and assist in specific jobs suitable to his or her personal schedule. Even partial involvement can be enough to get one’s name on a publication. However, lab work can be monotonous and frustrating at times when experiments do not deliver the anticipated results. Sitting in non-stimulation laboratories requires a certain type of character. Recommendation: 4/5
- Descriptions of Innovations: Purely descriptive publications of new surgical techniques, innovative technology, new pharmaceutical drugs, or simply personal statements on evolving subjects, etc. This type of work often demands a given level of expertise and is not typically suitable for graduate research. Recommendation: 2/5
- Reviews, Meta-Analyses: These types of written compositions are based on a literature review. The author’s job is to read through countless, often hundreds of previous publications and create a summary regarding a specific medical topic. Reviews and meta-analysis are particularly useful for issues that are prevalent and have delivered many reports in the past. Whereas a review merely lists the findings of previous research groups, a meta-analysis is able to pool data and conduct statistical analyses. These projects allow great flexibility and can be finished from any location but do not underestimate the time needed to achieve proper results. Recommendation: 4/5
Formats of Publication
What follows is a list of mediums that allow you to get your work to the public. Albeit the concept of most research activities is similar and progresses on akin paths, it is important to agree on a goal early in the research process. Journal articles, for example need to be of highest quality and impeccable when submitted. Presentations must be tailored accordingly depending on what audience you are planning to address. Book chapters need clear guidelines to ensure that your handiwork fits well to the other parts of the volume. Make sure to discuss this topic with your seniors to understand their expectations from you.
- Journal Articles: These are the highest quality format that you can use to submit your research work for the world to see. Upon arrival at the journal’s office, the editorial office first reviews your manuscript and determines its eligibility. Next, it is sent off to a number of anonymous reviewers who judge your documents and suggest if it is worth publication, if it needs changes, or if it should be rejected. Being an author on articles in peer-reviewed journal is the strongest support to improve your application. Recommendation: 5/5
- Podium Presentations: These are typically 5-15min PowerPoint conferences or similar in front of regional, national, and international audiences of students, residents, nurses, scientists, and board-certified physicians. While your work might be less accessible to the world than published articles, it is still recommended to submit your accomplishments to such conventions. Aim for national conferences rather than regional ones. Recommendation: 4/5 for (inter)national, 3/5 for regional conferences
- Poster Presentations: A classic poster session is where you travel to a conference, hang your poster with a summary of your research findings (similar to a short abstract) and are available for others to review your work and ask questions. In some cases, poster sessions are requested by conferences when you apply for podium presentations but your projects are not considered beneficial enough. Recommendation: 3/5
- Book Chapters: Senior physicians, faculty members, or experts on a certain field are sometimes asked to write segments of medical or scientific books that are soon to be brought on sale to the market. In certain cases, students or residents write segments of such book chapters for the senior author. From personal experience, these projects are a long-term process as they go into extreme medical detail. On the upside, publication with your name on it is almost guaranteed. Unfortunately, these types of publications are not of high evidence-based research and should only be considered as a secondary side project Recommendation: 3/5
Basic and Necessary Know-How
After choosing your project you need to learn and understand how the scientific process works once you have your results ready for publication. Conducting the studies, experiments, and the literature reviews is one part of the research job. Presenting your findings is the other side of the coin. Read many publications on the same subject and study what a paper is supposed to look like. Analyze the language the authors use. It has to be straight to the point, factual, objective, leave out unnecessary information yet avoid long soporific segments of repeating details. Your audience will want to hear a hypothesis, the methodology of your venture on how said hypothesis should be tested, your results, and an antiseptic interpretation thereof. Having a senior writer review your work is therefore crucial in the beginnings of a research career.
Next, and this may seem like a no-brainer, learn how to properly and efficiently use today’s available technology to your advantage. Learn the most important features of your word processing software. Get access to a tool that allows to sort and list literature references and full versions of articles, preferably in PDF format. If you share files with others or work simultaneously at different sites, use a cloud service to keep your files in synchronization across all your devices. Any photo, video, or graph-editing software with some artistic skills might come in handy as well. Lastly, learn some basic mathematical and statistical skills and obtain a statistical software. Research is nothing if you cannot back up your story by some hard numbers. Study what a t-test, a type I error, and a type II error are and how they work. Understand when you have to use chi-square and when the Fisher’s exact test . This list goes on and on. You do not need a Ph.D. degree in biometrics or stochastic calculus to be involved in medical research but even basic skills can set you far ahead of others and you will stand out from the crowd. Additionally, all these things I just mentioned facilitate your projects by incredible amounts and allow you to publish your results faster. Capitalize on the technology that is available today!
Finally, learn how to revise current literature and how to look for references to back up your ideas or contrast your data to those of other groups. In the end, research is a competition almost like any other business sector; except that money is not necessarily the number one objective but rather prestige and impact. Pubmed is a valuable search engine, for instance, that allows you to go through the MEDLINE database and find similar publications to your project. UpToDate is a practical tool that is constantly refreshed by countless experts and gives access to the latest guidelines on specific topics. One of my former attendings always said that publishing a paper is like selling a car: you have to know the market and emphasize the upsides of your work to gain interest of others. Have all these files clean and tide on your computer from day 1, so you can keep a good overview of things and track your progress.
Further Aspects to Consider
When you start a new research project, figure out who your team is that you will be working with as this will determine the authors and their order on a potential publication. Make sure your name appears on the final manuscript if you have brought significant effort and input towards the project. As the New England Journal of Medicine, one of the largest and most prestigious journals in the field, states:
“Credit for authorship requires (a) substantial contributions to the conception and design; or the acquisition, analysis, or interpretation of the data, (b) the drafting of the article or critical revision for important intellectual content, (c) final approval of the version to be published, and (d) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.”
The more work you put in, the further your name should appear up front. The final position of a scientific publication is usually reserved for the senior author (principal investigator) and the head of the team.
The last issue that needs to be mentioned here are finances. Even if you are working on a retrospective study and are just simply scrolling through patient charts to gather data, special software, travel to conferences, fees for journals (author processing charge for open access) can rapidly add up. Basic science ventures may require additional funding. Knowing your resources is crucial for any research. The discussion of money may seem like a sensitive subject and “above your pay grade” yet I recommend approaching this topic with open cards when the right moment comes.
Final Words
Despite the downsides of scientific work, I still believe the majority of students should experience the art of research that has made medicine what it is now. Yes, research is frequently frustrating and consumes many of your physical and mental resources. Yes, a majority of jobs after residency do not include research. Still, I will never forget the great feeling of my first accepted publication and when I immediately continued to strive towards the next challenge. Henceforward, research had something rewarding and appealing about it. In the long run, this highly dynamic profession is probably not suited for all future physicians, yet I can only repeat myself and encourage everyone to give it a try.
Dmitry Zavlin graduated with an M.D. from the Technical University of Munich in 2015.
He currently works as a research fellow in Houston.
To contact the author, please visit www.zavlin.com
Dmitry Zavlin, M.D.

First Day of Medical School – 4 Things to Know
Medical school is a completely different beast from your pre-med years in college. Here are four things you should know and prepare for in order to have the most productive, effective, and happy experience of medical school!
Premed and Medical Student Summer Research Guide
We break down the value of summer research, how to find research positions, and tips to make the most of summer research opportunities.

How to Find an Undergraduate Research Position
Research is a crucial component of any medical school application. Utilize the following tips to streamline the process of finding an ideal research position.
This Post Has One Comment
Awesome summary, really helpful for me as a med student!
Leave a Reply Cancel reply

Join the Insider Newsletter
Receive regular exclusive MSI content, news, and updates! No spam. One-click unsubscribe.
Customer Note Premed Preclinical Med Student Clinical Med Student
You have Successfully Subscribed!
A Realistic Guide to Medical School
Written by UCL students for students
Top 10 Tips: Getting into Research as a Medical Student
Introducing our new series: Top 10 Tips – a simple guide to help you achieve your goals!
In this blog post, Jessica Xie (final year UCL medical student) shares advice on getting into research as a medical student.

Disclaimers:
- Research is not a mandatory for career progression, nor is it required to demonstrate your interest in medicine.
- You can dip into and out of research throughout your medical career. Do not feel that you must continue to take on new projects once you have started; saying “no, thank you” to project opportunities will allow you to focus your energy and time on things in life that you are more passionate about for a more rewarding experience.
- Do not take on more work than you are capable of managing. Studying medicine is already a full-time job! It’s physically and mentally draining. Any research that you get involved with is an extracurricular interest.

I decided to write this post because, as a pre-clinical medical student, I thought that research only involved wet lab work (i.e pipetting substances into test tubes). However, upon undertaking an intercalated Bachelor of Science (iBSc) in Primary Health Care, I discovered that there are so many different types of research! And academic medicine became a whole lot more exciting…
Here are my Top 10 Tips on what to do if you’re a little unsure about what research is and how to get into it:
TIP 1: DO YOUR RESEARCH (before getting into research)
There are three questions that I think you should ask yourself:
- What are my research interests?
Examples include a clinical specialty, medical education, public health, global health, technology… the list is endless. Not sure? That’s okay too! The great thing about research is that it allows deeper exploration of an area of Medicine (or an entirely different field) to allow you to see if it interests you.
2. What type of research project do I want to do?
Research evaluates practice or compares alternative practices to contribute to, lend further support to or fill in a gap in the existing literature.
There are many different types of research – something that I didn’t fully grasp until my iBSc year. There is primary research, which involves data collection, and secondary research, which involves using existing data to conduct further research or draw comparisons between the data (e.g. a meta-analysis of randomised control trials). Studies are either observational (non-interventional) (e.g. case-control, cross-sectional) or interventional (e.g. randomised control trial).
An audit is a way of finding out if current practice is best practice and follows guidelines. It identifies areas of clinical practice could be improved.
Another important thing to consider is: how much time do I have? Developing the skills required to lead a project from writing the study protocol to submitting a manuscript for publication can take months or even years. Whereas, contributing to a pre-planned or existing project by collecting or analysing data is less time-consuming. I’ll explain how you can find such projects below.
3. What do I want to gain from this experience?
Do you want to gain a specific skill? Mentorship? An overview of academic publishing? Or perhaps to build a research network?
After conducting a qualitative interview study for my iBSc project, I applied for an internship because I wanted to gain quantitative research skills. I ended up leading a cross-sectional questionnaire study that combined my two research interests: medical education and nutrition. I sought mentorship from an experienced statistician, who taught me how to use SPSS statistics to analyse and present the data.
Aside from specific research skills, don’t forget that you will develop valuable transferable skills along the way, including time-management, organisation, communication and academic writing!
TIP 2: BE PROACTIVE
Clinicians and lecturers are often very happy for medical students to contribute to their research projects. After a particularly interesting lecture/ tutorial, ward round or clinic, ask the tutor or doctors if they have any projects that you could help them with!
TIP 3: NETWORKING = MAKING YOUR OWN LUCK
Sometimes the key to getting to places is not what you know, but who you know. We can learn a lot from talking to peers and senior colleagues. Attending hospital grand rounds and conferences are a great way to meet people who share common interests with you but different experiences. I once attended a conference in Manchester where I didn’t know anybody. I befriended a GP, who then gave me tips on how to improve my poster presentation. He shared with me his experience of the National institute of Health Research (NIHR) Integrated Academic Training Pathway and motivated me to continue contributing to medical education alongside my studies.
TIP 4: UTILISE SOCIAL MEDIA
Research opportunities, talks and workshops are advertised on social media in abundance. Here are some examples:
Search “medical student research” or “medsoc research” into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research Mentoring Scheme Mentee Scheme), NSAMR – National Student Association of Medical Research and International Opportunities for Medical Students .
Search #MedTwitter and #AcademicTwitter to keep up to date with ground-breaking research. The memes are pretty good too.
Opportunities are harder to come by on LinkedIn, since fewer medical professionals use this platform. However, you can look at peoples’ resumes as a source of inspiration. This is useful to understand the experiences that they have had in order to get to where they are today. You could always reach out to people and companies/ organisations for more information and advice.
TIP 5: JOIN A PRE-PLANNED RESEARCH PROJECT
Researchers advertise research opportunities on websites and via societies and organisations such as https://www.remarxs.com and http://acamedics.org/Default.aspx .
TIP 6: JOIN A RESEARCH COLLABORATIVE
Research collaboratives are multiprofessional groups that work towards a common research goal. These projects can result in publications and conference presentations. However, more importantly, this is a chance to establish excellent working relationships with like-minded individuals.
Watch out for opportunities posted on Student Training and Research Collaborative .
Interested in academic surgery? Consider joining StarSurg , BURST Urology , Project Cutting Edge or Academic Surgical Collaborative .
Got a thing for global health? Consider joining Polygeia .
TIP 7: THE iBSc YEAR: A STEPPING STONE INTO RESEARCH
At UCL you will complete an iBSc in third year. This is often students’ first taste of being involved in research and practicing academic writing – it was for me. The first-ever project that I was involved in was coding data for a systematic review. One of the Clinical Teaching Fellows ended the tutorial by asking if any students would be interested in helping with a research project. I didn’t really know much about research at that point and was curious to learn, so I offered to help. Although no outputs were generated from that project, I gained an understanding of how to conduct a systematic review, why the work that I was contributing to was important, and I learnt a thing or two about neonatal conditions.
TIP 8: VENTURE INTO ACADEMIC PUBLISHING
One of the best ways to get a flavour of research is to become involved in academic publishing. There are several ways in which you could do this:
Become a peer reviewer. This role involves reading manuscripts (papers) that have been submitted to journals and providing feedback and constructive criticism. Most journals will provide you with training or a guide to follow when you write your review. This will help you develop skills in critical appraisal and how to write an academic paper or poster. Here are a few journals which you can apply to:
- https://thebsdj.cardiffuniversitypress.org
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk
- https://cambridgemedicine.org/about
- https://www.bmj.com/about-bmj/resources-reviewers
Join a journal editorial board/ committee. This is a great opportunity to gain insight into how a medical journal is run and learn how to get published. The roles available depend on the journal, from Editor-in-Chief to finance and operations and marketing. I am currently undertaking a Social Media Fellowship at BJGP Open, and I came across the opportunity on Twitter! Here are a few examples of positions to apply for:
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk – various positions in journalism, education and website management
- https://nsamr.ac.uk – apply for a position on the executive committee or as a local ambassador
- Student BMJ Clegg Scholarship
- BJGP Open Fellowships
TIP 9: GAIN EXPERIENCE IN QUALITY IMPROVEMENT
UCL Be the Change is a student-led initiative that allows students to lead and contribute to bespoke QIPs. You will develop these skills further when you conduct QIPs as part of your year 6 GP placement and as a foundation year doctor.
TIP 10: CONSIDER BECOMING A STUDENT REPRESENTATIVE
You’ll gain insight into undergraduate medical education as your role will involve gathering students’ feedback on teaching, identifying areas of curriculum that could be improved and working with the faculty and other student representatives to come up with solutions.
It may not seem like there are any research opportunities up for grabs, but that’s where lateral thinking comes into play: the discussions that you have with your peers and staff could be a source of inspiration for a potential medical education research project. For example, I identified that, although we have lectures in nutrition science and public health nutrition, there was limited clinically-relevant nutrition teaching on the curriculum. I then conducted a learning needs assessment and contributed to developing the novel Nutrition in General Practice Day course in year 5.
Thanks for reaching the end of this post! I hope my Top 10 Tips are useful. Remember, research experience isn’t essential to become a great doctor, but rather an opportunity to explore a topic of interest further.
One thought on “Top 10 Tips: Getting into Research as a Medical Student”
This article was extremely helpful! Alothough, I’m only a junior in high school I have a few questions. First, is there anyway to prepare myself mentally for this challenging road to becoming a doctor? check our PACIFIC best medical college in Rajasthan
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Copyright © 2018 UCL
- Freedom of Information
- Accessibility
- Privacy and Cookies
- Slavery statement
- Reflect policy
Please check your email to activate your account.
« Go back Accept

Sign up to our Newsletter
Research for medical school admissions: what do you need to know.

Reviewed by:
Jonathan Preminger
Former Admissions Committee Member, Hofstra-Northwell School of Medicine
Reviewed: 4/25/24
There are several ways in which you can make your application for medical school more attractive to the eyes of admissions committees.
While research experience is not a requirement for most schools, having a research background that is sound, aligns with your major and interests, is fundamentally strong, and overall complements your application’s theme is a perfect way to be a competitive candidate and enhance your possibilities of getting into medical school.
This guide will teach you all that you need to know about research for medical school, ensuring you’ll gain successful and meaningful experiences.
Get The Ultimate Guide on Writing an Unforgettable Personal Statement

Importance of Research for Medical School

Your MCAT , GPA, extracurriculars, and clinical experience all play a role in your admissions chances. But research is also key! Most but not all students accepted to medical school have research experience.
According to a survey of incoming medical students conducted by the AAMC , 60% of students participated in some kind of laboratory research for college students. Experts in the field have made their ideas about it very clear; Dr. Petrella, a Stanford University Ph.D. and mentor, states:
“Our belief is that an exercise science curriculum provides students the opportunity to become responsible professionals of competence and integrity in the area of health and human performance.”
Today, we’ll talk about how to prepare for and strategically use research to enhance your application and make it more interesting and rich in the eyes of the admissions committee. But first, take a quick look at why you should gain research experience in your undergraduate career.

What Counts as Research for Medical School?
While most research is good research, some things should be taken into consideration before jumping into the next opportunity available:
- Clinical research is great but research in the humanities or social sciences also counts
- Good research experience develops your writing skills, critical thinking skills, professionalism, integrity, and ability to analyze data
- It’s important to contribute to the research for a long period of time—several months rather than a couple weeks
- You can participate in research part-time or full-time; both count
- You should get involved in research related to your major, desired career, and interests
- Be committed and deeply involved in the research—you’ll be asked about it in interviews!
- Being published as a top contributor of any related research papers looks the best
Overall, there isn’t really “bad” research experience, so long as you’re committed, make clear contributions, and are genuinely passionate about the subject!
How to Gain Research Experience as a Pre Med
There are several ways to become involved in research and find research opportunities during your undergraduate years. Research opportunities will be available through the university you’re attending, so make sure to maintain a good relationship and communication with your professors.
One of the best ways to secure a research position is to have a conversation with your professors. They may be looking for a student to help them with an upcoming project, and even if they don’t have any opportunities to offer you, they can easily refer to other staff members who might.
Try navigating through your university’s website as well; many schools will have a student job board that may host research opportunities. For example, if you were a premed student at the University of Washington , you’d be able to check the Undergraduate Research Program (URP) database in order to filter and find research opportunities.
How Many Hours of Research Do You Need For Medical School?
Since research is not a requirement at most medical schools, there’s no minimum number of hours you should be spending at the lab. Some students report entering medical school with over 2,000 hours of research experience, while others had no more than 400.
This may seem like a lot but bear in mind that a semester or summer of research involvement sums up to around 500-800 hours. This can be more than enough to show your abilities, commitment, and critical thinking skills.
The hours you should dedicate to research widely depend on your personal circumstances and other aspects of your application. If you have the bandwidth to dedicate more hours to research, you should, but never compromise your grades for it.

6 Types of Medical Research
There are six main types of research that pre-med students commonly participate in:
Basic Science Research
Basic science research involves delving into the intricacies of biology in laboratory settings. It's one of the most common pre-med research opportunities and typically entails studying genes, cellular communication, or molecular processes.
Clinical Research
Clinical research is all about working with real patients to learn about health and illness. It's hands-on and great for getting a feel for healthcare.
Public Health Research
Public health research focuses on analyzing population health trends and developing strategies for disease prevention and health promotion. It's a great area for pre-med students interested in community health, although it is a little harder to get involved in.
Health Public Policy Research
Health public policy research examines the impact of healthcare regulations and policies on access to care and health outcomes. Although less common among pre-med students, it offers insights into the broader healthcare system, involving analyses of policy effectiveness and healthcare disparities.
Narrative Medicine Research
Narrative medicine research explores the role of storytelling and patient experiences in healthcare delivery. It's a more human side of medicine, focusing on empathy and connection.
Artificial Intelligence Research
Artificial intelligence research can be difficult for pre-meds to get involved in, but it offers innovative solutions to complex medical problems, such as developing AI algorithms for disease diagnosis and treatment planning.
Tips to Make the Best out of Research Hours
Now that we've covered the importance of research experience for med school application, we'll go over some tips to help you make the most of your research experience!
Have Noteworthy Research Experience
Having noteworthy research experience is a plus in your application, but it doesn’t end here. The ultimate goal of research is to actually become involved in the most recent projects, discoveries, and questions in your field of study, and prepare you for potential research later in your graduate career.
Use Research as an Opportunity to Gain Skills
Make your best effort to see research experience not only as a way to make your resume and application look better, but also as an opportunity to gain skills and face challenges that will help you become a dedicated professional, and will help you succeed in any your future endeavors.
Be Clear With Your Goals
Before getting started with your research hours, make sure the research question is perfectly clear to you, and that you’re familiar and interested in what the research is aiming to find or prove. By doing this, you’ll be off to a great start, and your research experience will be valuable from the beginning.
Understand the Project and Be Engaged
Once you’re involved in research, make sure you try your best to perfectly understand every part of it. Shallow and meaningless research experiences won’t get you very far.
During your interview you'll be asked about the research project – regardless of your level of contribution, it’s important for you to be clear, confident, and perfectly articulate to make yourself a competitive candidate.
Take Your Experience Seriously
Also, take your time at the lab very seriously. Try approaching your research contribution as a job; show up in time just like you would show up in time for work, put your best effort in it, and above all, be professional.
Build Relationships With Your Supervisors
Another tip for maximizing your research experience is to make a connection and form a relationship with the mentor or the professor that will, or is already working with you. By forming strong bonds and relationships, you’ll have the opportunity to ask your mentor for a letter of recommendation.
So, do take every hour spent seriously and work hard to make a good impression. This way, you’ll kill two birds with one stone: you’ll gain research experience while obtaining strong recommendations.
What Kind of Research do Medical Schools Prefer? (Science vs Non-Science)
That is a somewhat tricky question. The simple answer is that any research that can show your involvement and commitment and aligns with the theme of your application is beneficial. However, there are a lot of layers to it.
Probably the most common type of research among applicants –which is also highly valued by medical schools – is science and lab research. If you’re a science major in college, this is probably the way you’d want to go; laboratory-based research.
With that said, if your major is in the social sciences or humanities, getting involved in research related to your major and your interests is something that medical schools will find attractive.
After all, the majority of schools use a holistic approach to admissions and want their potential candidates to be widely and well-educated individuals.
1. Is Research Experience More Important Than Clinical Experience For Medical School?
The short answer to this is no. Even though the majority of applicants have research experience, for many deans of admissions, clinical experience is equally and sometimes even more valuable. The clinical experience involves patient interaction, which is undoubtedly crucial preparation for a life-long career as a physician.
However, getting your first research experience as early as possible in your undergraduate years will help you determine if research is something you’d like to pursue in the future. Plus, it will make it easier for you to secure more research positions in your graduate years, so you should definitely go for it if it's of your interest.
2. Is Research Experience More Important Than Physician Shadowing?
While both experiences are relevant, research has the added benefit of allowing you to gain hands-on experience. However, don’t forget that doctor shadowing also adds a lot of value to your application, since it serves the purpose of actually seeing what being a physician is, and such experience could determine your interest in moving forward.
You should also take into account what your medical school of choice expects. For example, for research-focused schools like the Mayo Clinic , research experience will definitely be more important and you should plan on putting most of your energy there.
3. Should I Take A Gap Year Before Medical School To Gain Research Hours?
Taking a gap year gives you the opportunity to refine your application and fully focus on what you want to improve. Whether it’s worth it or not depends on your personal and academic circumstances. Remember, it’s not necessarily about how many hours you complete, but the level of contribution you make and your interest in it!
4. Should I Participate In Many, Short-Lived Research Experiences Or In A Few Long Ones?
Always choose quality over quantity when it comes to research experience. One long research experience will impress the admissions committee far more than several short ones! More time spent on a project often means greater contributions made, and it demonstrates interest, persistence, and resilience.
5. Should I Look For Research Opportunities Even If My GPA Is A Bit Low?
If you’ve gone through a hard time and your GPA is suffering a little bit, definitely focus your energy on that before committing to long hours in the lab. Your GPA and MCAT scores are the non-arguable parts of your application; make sure these are as impeccable as possible, and as soon as there’s an improvement, move on to research.
That doesn’t mean that you should completely forget about the “extras” of your application; as long as you keep a balance between a good GPA, scores, work, and extracurriculars, you’ll be on the right path to creating a competitive application.
6. What Does It Mean To Be Published In Research? Is It Important To Medical Schools?
Being published means that your name appears on written documents about research, and it is, indeed, important, but not necessary. We’re not talking about being the first author in a publication, since this is almost impossible for an undergraduate student.
However, appearing as a co-author on any presentation, publication, or poster will help you build a reputation.
7. What Should I Do If I Don’t Have Research Experience?
Ultimately, if you don’t have any research experience and do not have time or do not plan on being part of any research, focus and invest time in your clinical experience as well as volunteering and community service. Also, work on maintaining a good GPA and improving your MCAT score.
Keep in mind, though, that MD-PhD candidates do need to get involved in research before applying, and a big emphasis should be placed on research in these cases.
8. Does Clinical Research Count Also As Clinical Experience?
Clinical research can count as both clinical experience and research experience in your AMCAS application.
9. Is Research Required For Medical School?
Research experience is not required for most medical schools. However, having research experience will help you stand out and present yourself as a more competitive candidate during the application process.
Final Thoughts
Participating in research for medical school can play an important role in the quality of your application. For this reason, knowing how to make your experiences as valuable and rich as possible will play a key role in ensuring the research complements your application and overall profile.
Research is the perfect way to build a strong skill set that will aid you as a medical student and make you a better physician!
Schedule A Free Consultation
You may also like.

How to Become a Gastroenterologist

Medical Schools in Nebraska: List + How to Get In

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 23 March 2022
Student wellness trends and interventions in medical education: a narrative review
- Harrison J. Klein 1 &
- Sarah M. McCarthy 1
Humanities and Social Sciences Communications volume 9 , Article number: 92 ( 2022 ) Cite this article
13k Accesses
25 Citations
2 Altmetric
Metrics details
- Science, technology and society
Medical education is a time wrought with personal and professional stressors, posing serious challenges to maintaining student wellness. Extensive research has thus been conducted to identify these stressors and develop practical solutions to alleviate their harmful effects. This narrative review of quantitative and qualitative literature summarizes trends in student wellness and examines interventions deployed by medical schools to ameliorate student distress. Current trends indicate that mental illness, substance use, and burnout are more prevalent in medical students compared to the general population due to excessive academic, personal, and societal stressors. Pass/fail grading systems and longitudinal, collaborative learning approaches with peer support appear to be protective for student wellness. Additionally, maintaining enjoyable hobbies, cultivating social support networks, and developing resiliency decrease distress in medical students on an individual level. Faculty and administrator development is also a necessary component to ensuring student wellness. The COVID-19 pandemic has posed unique challenges to the medical education system and has stimulated unprecedented innovation in educational technology and adaptability. Particularly, the discontinuation of the clinical skill evaluation components for both osteopathic and allopathic students should be a focus of medical student wellness research in the future.
Similar content being viewed by others
Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value

Academic burnout among master and doctoral students during the COVID-19 pandemic

Online education and the mental health of faculty during the COVID-19 pandemic in Japan
Defining student wellness.
Defining student wellness has challenged stakeholders throughout the medical education system. The term “wellness” first appeared in literature following World War II, though the concept extends back to Christian ethics of the 19th century that linked physical well-being to moral character (Kirkland, 2014 ). Implicit within these origins of wellness is a responsibility of the individual to contribute to their own well-being. This is reflected in Kirkland’s premise that “each individual can and should strive to achieve a state of optimal functioning” ( 2014 ). Contemporary researchers characterize wellness similarly to the World Health Organization’s (WHO) definition of human health. In the preamble to the WHO’s constitution, health is defined as a “state of complete physical, mental, and social well-being and not merely the absence of disease” (Grad, 2002 ). Wellness can therefore be succinctly defined as self-aware, intentional prevention of distress and promotion of well-being (Kirkland, 2014 ).
Human wellness’s inherent multidimensionality often poses a challenge to quantitative research methods. Most studies thus ultimately measure some combination of indicators for distress and well-being. Addiction, mental disorders, suicidal ideation, and burnout are common indicators of distress assessed through various screening methods (Jackson et al., 2016 ; Moir et al., 2018 ; Dyrbye and Shanafelt, 2016 ). On the contrary, Gallup-Healthways Well-Being Index Composite Score examines well-being across several domains of life, including: life evaluation, emotional health, physical health, healthy behavior, work environment, and basic access. The Well-Being Composite Score thus emphasizes the presence of health rather than absence of disease (Kirkland, 2014 ). Though methodologies and definitions vary across studies and reviews, the fundamental characteristics of wellness appear constant: absence of disease and presence of health. Investigations using this paradigm have identified professional education, particularly medical education, as a time of increased distress and diminished wellness (Dyrbye et al., 2014 ). We have thus undertaken a review of contemporary literature to identify trends in student wellness, as well as the interventions deployed to address such trends. This narrative review outlines the prevalence and contributing factors to mental illness, addiction, and burnout in the medical student population. We then describe several intervention strategies used by medical schools to address student wellness deficits, including: wellness committees, pass-fail (P/F) grading, mindfulness training, curricular alterations, and developing more wellness-aware faculty/administration. In compiling this review, we hope to provide a snapshot of contemporary student wellness that may be used to guide medical schools seeking to improve the student experience during the COVID-19 pandemic and its aftermath.
Mental well-being
As previously mentioned, directly measuring wellness is a challenge in educational research. Therefore, most studies assess wellness of student populations by examining rates of mental illness or distress (Kirkland, 2014 ). Numerous studies have revealed that mental health issues are virtually ubiquitous in the medical education system. Dyrbye and colleagues report that medical school appears to be a peak time for distress in a physician’s training ( 2014 ). Localization of distress to the training process is evidenced by higher rates of depression, fatigue, and suicidal ideation in medical students as compared to age-matched controls from the general population, with these symptoms declining to the same levels as control populations within 5 years after completing post-graduate education (Dyrbye et al., 2014 ). Further, Jackson et al determined that a majority of medical students exhibited either burnout, depressive symptoms, suicidal ideation, alcohol abuse/dependence, or a combination of these factors at the time of survey ( 2016 ). A meta-analysis conducted by Rosenstein and colleagues revealed that 27% of medical students met criteria specifically for depression or depressive symptoms ( 2016 ). This increased prevalence of mental illness is not restricted to medical education. A survey of law students revealed that 17% screened positively for depression, 37% screened positively for anxiety, and 27% screened positively for an eating disorder. These statistics indicate increasing trends of mental illness across graduate education as a whole, rather than medical education alone (Organ et al., 2016 ).
This prolific mental distress can substantially impact medical students’ ability to meet academic demands (Dyrbye et al., 2014 ). As such, substantial research has been conducted investigating factors that contribute to mental illness in an academic setting. Surprisingly, students begin medical school with mental health better than similarly aged peers. However, these roles quickly reverse, with medical student mental health ultimately becoming worse than control populations (Dyrbye and Shanafelt, 2016 ). It seems that medical education may actually select for individuals prone to developing psychological distress (Bergmann et al., 2019 ). Moir et al. report that the majority of medical students are considered Type A individuals, displaying high levels of ambition and competition. Though these qualities facilitate academic success, they also lead to hostility and frustration with challenging situations (Moir et al., 2018 ). Medical students were also found to have high levels of conscientiousness (Moir et al., 2018 ). Conscientiousness is a component of the Big 5 Personality model, which uses the qualities of neuroticism, extraversion, openness, agreeableness, and conscientiousness as the most basic descriptors of an individual’s personality (Shi et al., 2018 ). Conscientiousness is characterized by diligence and careful attention to detail, thus predicting high levels of academic success. However, increased conscientiousness may also exacerbate the likelihood of mental and physical distress due to inordinate demands placed on one’s self (Bergmann et al., 2019 ). Student age was also found to correlate with mental well-being. Younger students were found to approach their studies with dualistic orientations, seeking an explicit, incontrovertible knowledge of medicine. Diagnostic challenges and knowledge gaps ubiquitous in clinical medicine can thus be frustrating to younger students (Lonka et al., 2008 ). It is worth noting that, despite the importance of addressing mental health issues, some authors feel categorizing symptoms of depression and burnout leads to over-medicalization of human suffering and is not useful (Moir et al., 2018 ).
The aforementioned qualities of medical students facilitate development of both maladaptive perfectionism and imposter syndrome, heightening mental wellness concerns in this population (Bubenius and Harendza, 2019 ; Hu et al., 2019 ; Henning et al., 1998 ; Seeliger and Harendza, 2017 ; Thomas and Bigatti, 2020 ). The prevalence of imposter syndrome has been estimated between 22.5–46.6% in medical students, however, the prevalence of perfectionism has proven much more difficult to measure (Thomas and Bigatti, 2020 ). Maladaptive perfectionism is a multifactorial entity encompassing inordinate self-expectations, negative reactions to failure, and a persistent lack of satisfaction in performance (Bubenius and Harendza, 2019 ; Thomas and Bigatti, 2020 ). This emphasis on perfection prevents students from appreciating their vulnerability and thus delays self-recognition of mental distress (Seeliger and Harendza, 2017 ). Not surprisingly, maladaptive perfectionism has thus demonstrated an association with anxiety, depression, bulimia nervosa, anorexia nervosa, and chronic fatigue syndrome (Thomas and Bigatti, 2020 ). The strength of these associations was further demonstrated by Bubenius and Harendza’s use of maladaptive perfectionism as a predictor of depressive symptoms in German medical school applicants ( 2019 ). Imposter syndrome is a phenomenon often associated with maladaptive perfectionism and is characterized by anxiety, lack of self-confidence, depression, and frustration with one’s performance (Clance and Imes, 1978 ). While imposter syndrome bears an uncanny resemblance to perfectionism, the difference lies in imposter syndrome’s characteristic fear of being discovered as undeserving of a place in medical school, regardless of actual accomplishments (Clance and Imes, 1978 ). Imposter syndrome has been associated with a lack of resilience and this, similar to perfectionism, can increase psychological distress (Levant et al., 2020 ). The combined effects of imposter syndrome and maladaptive perfectionism predispose students to mental health issues and thus deserve special attention in studies geared toward well-being interventions. Of note, preliminary work by Chand and colleagues has demonstrated that cognitive behavioral therapy may be especially effective in ameliorating the deleterious effects of maladaptive perfectionism (Chand et al., 2018 ). Treatment for imposter syndrome, however, appears to be a significant gap in wellness literature (Bravata et al., 2020 ).
Deeply intertwined with imposterism and perfectionism is the medical student’s experience of shame. Shame is characterized as a negative emotional response to life events. These life events can take many forms, though personal mistakes within a hostile environment are a common instigator of shame (Bynum et al., 2019 ). Perfectionism and imposter syndrome thus provide a fertile soil of negative self-evaluation in which shame can flourish (Bynum et al., 2020 ). Feelings of shame are further exacerbated by factors within the medical school environment. Mistreatment by colleagues or preceptors, receiving low test scores, underrepresentation within classes, institutional expectations, and social comparison were reported as contributors to shame by medical students in a hermeneutic analysis (Bynum et al., 2021 ). Regardless of origin, shame has been recognized as a “destabilizing emotion,” leading to student isolation, psychological distress, and difficulty with identity formation (Bynum et al., 2021 ). Explorations of shame as a contributor to medical student distress are limited in the current literature. Thus, wellness researchers must dedicate studies to characterizing and preventing this significant, but potentially modifiable, contributor to student distress (Bynum et al., 2019 ).
Medical students’ educational environment can also have a profound impact on mental health, particularly during the early days of training. The transition between college and professional school is marked by anxiety, stress, and financial upheaval. Thus, students may feel more vulnerable than ever as they begin their professional education in a new environment in which they are unaware of available mental health resources, leading to isolation and unnecessary suffering (Organ et al., 2016 ). Even for those aware of these resources, significant stigma still surrounds mental illness in professional education. This is emphasized in Organ et al’s finding that only 50% of law students with mental health issues actually receive professional counseling. Their findings suggest that this reluctance largely stems from fear of professional repercussions if administrators discover a student’s mental health diagnosis (Organ et al., 2016 ). While this study was conducted in law students, Hankir et al found similar trends in both medical students and physicians by examining autobiographical narratives published to combat the stigma against help-seeking behavior (Hankir et al., 2014 ). Hankir and colleagues have elucidated several phenomena that contribute to medical students delaying or even avoiding treatment for mental distress. Self-stigma operates as a powerful deterrent to help-seeking and seems to stem from internalization of society’s expectation that medical students are mentally and physically invincible. This leads to feelings of decreased self-esteem and self-efficacy, as well as fear of stigmatization from the general public (Hankir et al., 2014 ; Fischbein and Bonfine, 2019 ). Rahael Gupta, now a psychiatry resident, brought this stigma to public light as she shared her personal experience with depression during medical school in her short film project entitled “Physicians Connected.” The film, conveyed line-by-line through Gupta’s colleagues at the University of Michigan, highlights the unspoken rule that mental distress is a black mark on a future physician’s career (Gupta, 2018 ). Gupta’s efforts, and those similar, underscore a growing call for public discourse, rather than concealment, of mental well-being within the medical profession. This call is echoed with Robyn Symon’s film “Do No Harm: Exposing the Hippocratic Hoax,” which further explores the toxic culture of medical education that drives physicians and medical students to commit suicide. Both Gupta and Symon highlight the taboo of mental distress within the medical field, which instead prioritizes efficiency and academic success over student and physician well-being. Both films characterize this lack of help-seeking behavior as products of the healthcare system’s toxic structure, rather than individual student distress interacting with a demanding work life (Gupta, 2018 ; Symon 2020 ).
Substance use
In addition to impaired academic performance, mental illness also increases risk for development of substance use disorder in medical students (McLellan, 2017 ). Thus, the pervasiveness of mental illness during medical education warrants careful analysis of substance use patterns in the student population. Alcohol abuse or dependence has already been well documented in the professional education system (Dyrbye and Shanafelt, 2016 ; Organ et al., 2016 ; Jackson et al., 2016 ). Alarmingly, despite 43% of law students reporting a recent occurrence of binge drinking, only 4% had sought professional assistance for alcohol or drug misuse. This trend again highlights significant mental health and addiction stigma throughout the graduate education system (Organ et al., 2016 ). Medical students, and all those in the medical field, may be uniquely affected by this prevalence of substance use. For example, the American Foundation for Suicide Prevention produced a documentary entitled “Struggling in Silence: Physician Depression and Suicide,” which highlights the powerful role that substance use plays in medical student and physician suicide specifically. With a greater knowledge of and access to potentially lethal substances, those in the medical field are at heightened risk for suicide completion, especially with the inhibition-lowering effects of some drugs (AFSP, 2002 ).
Alcohol dependence is of particular concern in medical education due to implications in hindering student career progression and compromised patient safety. Despite this concern, alcohol use is prevalent among medical students. A survey of 855 medical students across 49 schools in the United States revealed that 33.8% of students reported consuming 5 or more drinks in one sitting within the past two weeks, meeting the criteria for binge drinking (Ayala et al., 2017 ). Further, survey responses from 4402 medical students in the U.S. demonstrated that 32.4% met criteria for alcohol abuse/dependence, compared to 15.6% in a control sample of similarly aged but non-medical student counterparts (Jackson et al., 2016 ). The substantial academic stress of a professional education is a clear driving force behind this trend, though several compounding risk factors have been identified. Young males were identified as at an increased risk for alcohol dependence compared to their female colleagues (Jackson et al., 2016 ; Organ et al., 2016 ). Jackson and colleagues further identified that students who were unmarried, diagnosed with a mood disorder, low-income, or burdened with educational debt from professional and undergraduate studies were at increased risk for alcohol dependence ( 2016 ). While ethnicity’s relationship to alcohol use was not explored in medical students, a survey of over 11,000 law students from 15 law schools in 2016 determined that ethnic minorities were more likely to report an increase in drinking whereas Caucasian students were more likely to demonstrate a positive CAGE screening (Organ et al., 2016 ). The CAGE screen is a 4-item questionnaire developed by John Ewing in 1984 to identify drinking problems. The CAGE screen has a 93% sensitivity and 76% specificity for identifying problem drinking whereas alcoholism identification has a sensitivity of 91% and specificity of 77% (Williams, 2014 ). This increased alcohol use in both Caucasian and ethnic minority students demonstrates a need for culturally tailored and inclusive prevention programs.
Though alcohol is the most commonly abused drug amongst medical students, illicit drug use has also been reported at concerning levels. A survey of 36 United States medical schools revealed that approximately one-third of students had used illicit drugs within the past 12 months (Shah et al., 2009 ). Papazisis and colleagues similarly examined illicit drug use in undergraduate medical students in Greece, finding a lifetime substance use rate of ~25% ( 2017 ). Marijuana was the most common illicit drug used in both studies (Shah et al., 2009 ; Papazisis et al., 2017 ). Use of prescription medications without a prescription was also found amongst law students, particularly stimulants such as Ritalin, Adderall, and Concerta (Organ et al., 2016 ). These findings suggest that the competitive culture of graduate education may drive students to engage in recreational drug use, particularly those struggling to meet academic demands or suffering from mental distress.
Student burnout
Burnout was canonically defined by Freudenberger in 1974 as a state of physical and mental exhaustion caused by or related to work activities, often manifesting when heightened professional stress conflicts with personal ideals or expectations (Freudenberger, 1974 ; Rodrigues et al., 2018 ; Baro Vila et al., 2022 ). Though originally a descriptive disorder, burnout is now recognized in the International Classification of Diseases, 10th revision, under code Z73.0 (Lacy and Chan, 2018 ). Burnout is traditionally diagnosed with the Maslach Burnout Inventory, a 22-item questionnaire that characterizes each of the three burnout domains: emotional exhaustion, depersonalization, and personal accomplishment (Dyrbye and Shanafelt, 2016 ). Emotional exhaustion is associated with feelings of being overworked and a subsequent loss of compassion. Depersonalization is characterized by a sense of detachment from colleagues/patients and, when combined with emotional exhaustion, can result in unprofessional behavior. The personal accomplishment domain mainly describes an individual’s feelings of competence and professional satisfaction (Lacy and Chan, 2018 ). In addition to each domain’s unique consequences, burnout domains interact to cause an extinction of motivation when efforts no longer produce desired results (Vidhukumar and Hamza, 2020 ). Approximately 50% of fourth year medical students were found to have burnout when surveyed with the Maslach Burnout Inventory (Dyrbye and Shanafelt, 2016 ). This value holds true internationally according to a survey of medical students conducted in India (Vidhukumar and Hamza, 2020 ). Additionally, burnout increases as training progresses, particularly the depersonalization component (Dyrbye and Shanafelt, 2016 ). Burnout thus increases feelings of callousness towards patients, leading to unprofessional and potentially dangerous conduct. Burnout in medical school also appears to affect specialty choice; burned out individuals were more likely to choose specialties with more controllable lifestyles and higher pay (Dyrbye and Shanafelt, 2016 ). Investigating causes of burnout is thus of utmost importance to understand potential influences on medical student career trajectory and ensuring patient safety.
Identified causes of burnout appear to differ between the years of medical training. Preclinical years are characterized by dissatisfaction with the learning environment and lack of faculty support. Clinical years are characterized by dissatisfaction with the learning environment, clerkship disorganization, and working with cynical or abusive residents and/or attending physicians (Dyrbye and Shanafelt, 2016 ). Reed and colleagues found a positive correlation between the time spent in exams and burnout whereas a negative correlation was observed with increased patient interaction ( 2011 ). Several correlates of burnout outside of medical schools’ learning environments and curricula have also been described, including: female gender, dissatisfaction with career options, non-ethnic minority status, high educational debt, residency competition, expanding knowledge-base, workforce shortage, and stressful events in one’s personal life (Dyrbyre and Shanafelt, 2016 ; Vidhukumar and Hamza, 2020 ). Erosion of social ties during medical education also contributes to the burnout spiral, as socialization is protective against burnout symptoms (Bergmann et al., 2019 ; Busireddy et al., 2017 ). No associations between contact days, time in didactic learning or clinical experiences, and any measure of student well-being and burnout prevalence were found (Reed et al., 2011 ).
Interventions to improve well-being
Medical schools have implemented several interventions to reduce student distress and enhance wellness. Though interventional approaches are varied, researchers have identified salient features common to most successful wellness interventions. For example, Dyrbye and colleagues underline the importance of well-being committees that can liaise between administration, faculty, and students, lessening fear of admonishment for seeking help or acknowledging distress ( 2019 ). Additionally, Moir et al reports that student buy-in is absolutely essential, as disengaged wellness lectures offer little, if any, benefit ( 2016 ). Interventions appear most effective when they are designed to reduce student burdens, rather than adding to the already overwhelming schedule and content of medical school (Busireddy et al., 2017 ). Finally, administrations often pose an obstacle to wellness initiatives, especially those who believe that well-being is of minor importance. This obstacle is reflected by the low prevalence of medical schools with official wellness competencies built into the curriculum (Dyrbye et al., 2019 ). We will now explore some of the specific interventions medical schools have employed to improve student wellness.
Transitioning to a Pass/Fail (P/F) grading scheme is a wellness initiative that has received substantial attention in the United States, especially in light of findings that grade evaluation systems are a larger determinant of student well-being compared to content of educational contact hours (Reed et al., 2011 ; Spring et al., 2011 ). The Mayo Medical School examined the feasibility and effects of P/F grading by introducing the system to first-year medical students in 2006. Rohe and colleagues found that these first-year medical students reported less stress, better overall mood, and greater group cohesion compared to their graded peers. These characteristics persisted into the second year of medical school, even when grading reverted to a traditional 5-level schema (Rohe et al., 2006 ). While critics of P/F grading argue that students will be less motivated to excel academically, evidence suggests that first-year residents from P/F schools performed similarly to residents from graded schools (Rohe et al., 2006 ). Additionally, a P/F system reduces extrinsic motivation and intense competition while increasing cohesion and peer cooperation (Moir et al., 2018 ; Rohe et al., 2006 ). These qualities are essential in the increasingly team-based healthcare landscape. Though transitioning to a P/F system reduced medical student distress during the preclinical years, it is important to note that the transition did not decrease test anxiety for the United States Medical Licensing Exam (USMLE) Step 1 (Williams et al., 2015 ; Rohe et al., 2006 ). Determining test anxiety for USMLE Step 1 will be an active area of research in the face of a new P/F grading for the licensure exam.
Allopathic and osteopathic medical programs are infamous for their academic rigors and intense curricular designs. These curricula are often described as competitive, leisure and socialization-deficient, and requiring exclusive dedication. These characteristics predispose medical students to decreased quality of life (Bergmann et al., 2019 ). As such, altering the curricula of these programs has been investigated as a means to prevent, rather than react to, student distress through a person-in-context perspective (Dyrbye et al., 2005 ; Slavin et al., 2012 ; Slavin et al., 2014 ). It has long been documented that the undergraduate medical curriculum is overflowing with information (D’Eon and Crawford, 2005 ). Rather than identifying salient features for inclusion in courses, medical school faculty often address this surplus of information by cramming unrealistic amounts of information into lectures (D’Eon and Crawford, 2005 ; Dyrbye et al., 2005 ). As mentioned earlier, wellness initiatives are often more effective when they reduce student burdens, rather than adding additional requirements (Busireddy et al., 2017 ). Though this may lead one to believe that shortening curricular hours is an intuitive wellness initiative, this measure only led to workload compression and feelings of being unprepared for clinical practice when used as a unifocal intervention (Dyrbye and Shanafelt 2016 ; Busireddy et al., 2017 ; Dyrbye et al., 2019 ). This continually expanding mass of information thus poses two challenges to wellness initiatives. First, medical students’ schedules are often too consumed by curricular hours to engage in additional wellness programming, especially without an external motivator. Second, the amount of information itself imposes feelings of distress on students, exacerbating the already-stressful nature of medical school and predisposition to mental health issues. Beyond the quantity of curricular hours, delivery and content of those hours is also important to student wellness. Lonka and colleagues found that a collaborative approach to learning increased satisfaction and decreased the perceived workload ( 2008 ). The collaborative environment of problem-based learning may thus offer some improvement to curriculum-induced stress, though current evidence is weak (Camp et al., 1994 ). Incorporating self-care workshops into the curriculum also appears to ameliorate the depersonalization component of burnout (Busireddy et al., 2017 ). In light of these promising results, it follows that the most powerful approach to improving student wellness through curricular restructuring is a multifactorial one. This multifactorial approach is best appreciated in the wellness initiatives within the Vanderbilt University School of Medicine and the Saint Louis University School of Medicine (Drolet and Rodgers, 2010 ; Slavin et al., 2014 ).
The Vanderbilt wellness initiative is composed of three arms: the Advisory College System, the Student Wellness Committee, and Vanderbilt Medical Student LIVE. The Advisory College is composed of both students and faculty that offer personalized advising and mentorship to students within the school. The Student Wellness Committee emphasizes student-led wellness initiatives and serves as an interface with faculty. Lastly, Vanderbilt Medical Student LIVE is an adjunct curriculum that fosters self-care and personal growth amongst the physicians in training (Drolet and Rodgers, 2010 ). The wellness program at the Saint Louis University School of Medicine is structured differently, though shares similar goals. The program entitled Mental Health 3.0 radically, but feasibly and efficiently, altered the structure of the School’s curriculum. Grading was converted to a P/F basis, with only the median exam score and 75 th percentile reported to students. Student contact hours were reduced by 10% during the preclinical curriculum and faculty were advised on how to appropriately identify topics for inclusion in their lectures. Longitudinal electives were instituted following contact hour reduction to encourage student growth and interest identification while forming relationships with fellow students and faculty. These electives were complemented by the formation of five learning communities to further enhance student immersion in areas of interest. Lastly, resilience and mindfulness training was incorporated into the mandatory curriculum while offering an increased number of social events (Slavin et al., 2014 ; Slavin, 2019 ). This wellness initiative was continually expanded and improved to include an early entry and exit to third-year clinical rotations, which minimized stress entering fourth year, and a confidential depression/anxiety tracking system to screen students for worrisome mental health issues (Slavin and Chibnall, 2016 ; Slavin, 2019 ). Comparison between these wellness initiatives reveals that whereas Slavin and colleagues have produced significant declines in student depression, anxiety, and stress with increased group cohesion (Slavin et al., 2014 ; Slavin, 2019 ), the impacts of curricular changes at the Vanderbilt University School of Medicine have not yet been quantified (Drolet and Rodgers, 2010 ). In addition to minimizing student distress, the Mental Health 3.0 program also increased student flourishing (Slavin and Chibnall, 2016 ). The success of Mental Health 3.0 provides strong evidence that diminished medical student well-being is likely a product of multiple factors within the medical learning environment rather than intrinsic student qualities alone (Slavin, 2019 ).
Mindfulness practices have also become increasingly popular as a wellness intervention. Mindfulness is defined as the non-judgmental awareness of one’s own experience with the goal of increasing concentration, insight, and relaxation. Employing mindfulness techniques has been demonstrated to decrease stress and anxiety, though its effects are not as apparent in reducing burnout symptoms (Williams et al., 2015 ). This lack of effect on burnout symptoms may be due to the focus of mindfulness practices, which is on the individual experience rather than improving the structural entities that cause burnout in the first place (Moir et al., 2018 ). Mindfulness practices implemented through peer-support groups in a United States medical school failed to demonstrate improvement in student anxiety, depression, quality of life, or resiliency. Though this may have been due to insufficient peer training, a non-blinded study design, or limited participation, these results lend further support to the need for structural corrections to the medical education system rather than improvement in students’ attitudes or outlooks (Moir et al., 2018 ). This is in contrast to the results obtained when primary care doctors underwent a 52-hour mindfulness training course. Post-course surveys revealed reduced burnout and improved empathy sustained for 3 months post-intervention (Dyrbye and Shanafelt, 2016 ). Comparison of factors contributing to burnout between medical students and practicing clinicians, as well as determining prerequisites for successful implementation of mindfulness programs, may thus be potential areas for research.
Administration and faculty personnel serve as educators and role models for students. Interventions centered on these individuals can thus facilitate a top-down approach to increasing student wellness. A primary concern for German medical students was a lack of coherent information management by faculty with regard to academic expectations, exacerbating the stress of exams and assignments. Solutions offered by students included recording lectures for later viewing and professors providing explicit learning objectives. These students also reported that attendance policies are often too strict and may impede self-care practices, such as utilizing the school counseling system. Proposed solutions were to loosen attendance requirements via a self-reporting absence system (Dederichs et al., 2020 ). Beyond their academic roles, faculty also often serve as mentors to students. The Liaison Committee on Medical Education requires that schools implement a mentoring system for their students, and these mentors are typically medical school faculty. However, Andre et al proposed a vertical mentoring system that complements faculty involvement with senior students in a program entitled “Mentors in Medicine.” This peer-mentoring system was found to be better suited for day-to-day navigation of medical school, while faculty were better suited to offer more long-term career support (Andre et al., 2017 ). Further integration of mentoring to include financial advisors may reduce distress in students with large amounts of educational debt (Dyrbye et al., 2019 ). Faculty commitment to wellness initiatives facilitates the development of communal concern for student wellness, extending beyond the Office of Student Affairs (Slavin et al., 2014 ). Moving forward, faculty and administration will continue to play pivotal roles in student wellness as the medical education system adapts to the technology and challenges of a post-pandemic landscape.
Though a majority of reviewed literature focused on the preclinical years of medical school, important developments have been made in clinical education as well. Dyrbye and Shanafelt found that a longitudinal rotation curriculum, in which students spend several contiguous months at one training site rather than smaller stints at several training sites, facilitates development of meaningful relationships with preceptors, increasing satisfaction and reducing burnout (Dyrbye and Shanafelt, 2016 ). This is congruent with Slavin and Chibnall’s finding that deploying effective wellness initiatives is made difficult by the changing environment of clinical rotations and lack of control over clinician interactions with students (Slavin and Chibnall, 2016 ). Further work by Slavin and Chibnall indicates that negative experiences (e.g., mistreatment) during clinical years are a product of resident burnout, which itself results from toxic healthcare structures and environments (Slavin and Chibnall, 2016 ). For example, residents often experience sleep deprivation, adjustment difficulties, interpersonal conflict, demanding workloads, and a lack of control over their schedule. Interplay between these factors and resident burnout increases likelihood for development of depression and suicidal ideation (Nene and Tadi, 2021 ). These deleterious resident symptoms may then translate to negative interactions with medical students. Improving the medical student experience can thus be facilitated by ameliorating resident burnout. A potential target for resident burnout interventions is resiliency, which has demonstrated a protective effect against burnout (Sheer et al., 2021 ; Nituica et al., 2021 ; Rodrigues et al., 2018 ). For example, implementation of the Gabbe Health and Wellness program, which was structured around an interprofessional Mindfulness in Motion training, significantly increased resiliency in residents at the Ohio State University Wexner Medical Center (Moffatt-Bruce et al., 2019 ). The Mindfulness in Motion training consists of a weekly group meeting with five sequential segments: prompted reflective writing, video presentation on mind/body connectivity, voluntary sharing of reflective responses, video instruction on yoga and mindfulness practices, and a closing meditation (Klatt et al., 2020 ). Though yielding promising results, these methods remain reactive, similar to most medical student wellness initiatives, and do not address the underlying structural causes of burnout within the healthcare system. While current literature lacks specific explorations of the healthcare system’s tendency toward reactive change, as opposed to proactive, this may be an extension of the field’s prioritization of efficiency and academic success over well-being, as mentioned previously (Gupta, 2018 ; Symon, 2020 ). Addressing the correction of such structures is beyond the scope of this review, but deserves serious attention in wellness research. In addition, further explorations of student and resident wellness may involve elucidating the specific motivations within medical culture that keep wellness a low priority within program structuring.
Based on reviewed literature, the following interventions were demonstrated to improve student well-being: transitioning to a P/F grading system, collaborative learning approaches, longitudinal clinical rotation sites, and peer-mentoring programs. General measures for reducing distress include: maintaining hobbies, socialization, positive outlook, avoiding delayed gratification mindsets, learned resiliency, and choosing medicine based off of one’s own interests. Mental Health 3.0 offers an evidence-based approach for successfully implementing these interventions. Measures that did not demonstrate significant improvement include: peer-led mindfulness groups and shortening curricular hours (Vidhukumar and Hamza, 2020 ; Dyrbye and Shanafelt, 2016 ).
The COVID-19 pandemic caused both immediate and long-term changes to the delivery of medical education. At the onset of the pandemic, medical students were removed from clinical rotations to protect against infection. While this ensured their safety, these students were also deprived of peer-engagement due to asynchronous virtual learning. This shift undoubtedly contributed to increased feelings of isolation and risk for burnout (Klasen et al., 2021 ). Despite numerous challenges, the pandemic has also provided opportunities for medical educators to innovate with new technology. For example, senior students on emergency medicine rotations have served as a source of virtual follow-up for emergency department (ED) visits after reviewing medical records. This has allowed students to continue clinical skill development while ensuring safety from infection and proper supervision. Virtual ED follow-ups reflect a growing trend for web-side encounters to serve as a temporary substitute or supplement for clinical rotations (Klasen et al., 2021 ). These digital learning structures were well-received by students, which predicts the persistence of virtual learning in medical school curricula after the COVID-19 pandemic resolves (Dederichs et al., 2020 ). Despite this apparent positive reception, online learning poses challenges to students’ psychological well-being. The asynchronous nature of virtual education modalities lends to feelings of isolation and a lack of motivation during the preclinical years of medical school (Klasen et al., 2021 ). Combined with the already taxing nature of medical education, the stressors of online learning may ultimately exacerbate existing student wellness concerns. Students featured in “Four Years in Blue: The University of Michigan Medical School Documentary” expressed concern for their future clinical training, specifically with regard to availability of personal protective equipment and physician safety. The students also reported feelings of sadness due to a loss of participation in important class milestones, such as a residency match day celebration (Michigan Medicine, 2020 ). Future alterations to the global medical education system in light of the pandemic will thus be an active area of research for years to come. Most notably, the pandemic appears to have served as an impetus for the National Board of Medical Examiners and National Board of Osteopathic Medical Examiners to indefinitely suspend the Step 2-Clinical Skills and Level 2-Performance Evaluation requirement for both allopathic and osteopathic students, respectively (AACOM, 2021 ; USMLE, 2021 ). Student response to this change and its potential effect on student performance should be thoroughly evaluated in future research.
Conclusions and future work
Further reports of wellness programs and interventions aimed at reducing student stress, developing coping strategies, and preventing burnout are needed. As demand for physicians increases and medical school curricula continue to expand, the potential for worsening student wellness increases. COVID-19, stress of licensure exam preparation, and the increasing cost of medical school all add to the brewing pot of pervasive mental illness, substance use, and burnout in the medical student population. Our review of contemporary literature suggests that transitioning to a P/F grading system and implementing longitudinal, collaborative learning approaches with peer support offer solutions to deteriorating medical student wellness. Electives should also be incorporated within the curriculum to further enhance student engagement and excitement for learning (Slavin, 2014 ). Academic faculty should be specifically targeted with instruction on how to reduce extraneous information within courses (Slavin et al., 2014 ; Slavin, 2019 ). Students should also be encouraged to maintain enjoyable hobbies, cultivate social support networks, and maintain a positive outlook to develop resiliency and protect their mental health (Vidhukumar and Hamza, 2020 ; Dyrbyre and Shanafelt, 2016 ). Cognitive behavioral therapy and training in cognitive restructuring techniques should be made available to students in order to address feelings of shame, maladaptive perfectionism, and imposter syndrome (Bynum et al., 2020 ; Chand et al., 2018 ; Slavin et al., 2014 ; Slavin, 2019 ). Confidential depression/anxiety tracking systems to screen students for worrisome mental health issues may also aid in identifying at risk students before mental distress becomes fulminant (Slavin, 2019 ). Faculty and administrators must also strive to improve student wellness from a top-down approach, ensuring that students feel safe to express wellness concerns and seek support when necessary. This may be accomplished through faculty training sessions or development of student liaison committees (Dyrbye et al., 2019 ; Andre et al., 2017 ). Programs at the Saint Louis University School of Medicine and Vanderbilt University School of Medicine offer successful templates for implementation of such programming. With the implementation of any intervention, of course, stringent evaluation guidelines must be employed to ensure optimal improvement to student wellness while avoiding unnecessary burdens to students’ overwhelming schedule.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
American Association of Colleges of Osteopathic Medicine (2021) AACOM, AOA, NBOME support suspension of COMLEX-USA Level 2-PE and continued osteopathic assessment. AACOM. https://www.aacom.org/news-and-events/news-detail/2021/02/17/aacom-aoa-nbome-support-suspension-of-comlex-usa-level-2-pe-and-continued-osteopathic-assessment . Accessed 16 Apr 2021
American Foundation for Suicide Prevention (2002) Struggling in silence: physician depression and suicide. State of the Art, Inc
Andre C, Deerin J, Leykum L (2017) Students helping students: vertical peer mentoring to enhance the medical school experience. BMC Res Note 10(1):176. https://doi.org/10.1186/s13104-017-2498-8
Article Google Scholar
Ayala EE, Roseman D, Winseman JS, Mason HRC (2017) Prevalence, perceptions, and consequences of substance use in medical students. Med Educ Online 22(1):1392824. https://doi.org/10.1080/10872981.2017.1392824
Article PubMed PubMed Central Google Scholar
Baro Vila RC, Burgos LM, Sigal A, Costabel JP, Alves de Lima A (2022) Burnout syndrome in cardiology residents. Impact of the COVID-19 pandemic on burnout syndrome in cardiology residents. Curr Probl Cardiol 47(1):100873. https://doi.org/10.1016/j.cpcardiol.2021.100873
Article PubMed Google Scholar
Bergmann C, Muth T, Loerbroks A (2019) Medical students’ perceptions of stress due to academic studies and its interrelationships with other domains of life: a qualitative study. Med Educ Online 24(1):1603526. https://doi.org/10.1080/10872981.2019.1603526
Bravata DM, Watts SA, Keefer AL, Madhusudhan DK, Taylor KT, Clark DM, Nelson RS, Cokley KO, Hagg HK (2020) Prevalence, predictors, and treatment of impostor syndrome: a systematic review. J Gen Intern Med 35(4):1252–1275. https://doi.org/10.1007/s11606-019-05364-
Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M (2017) Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ 9(3):294–301. https://doi.org/10.4300/JGME-D-16-00372.1
Bußenius L, Harendza S (2019) The relationship between perfectionism and symptoms of depression in medical school applicants. BMC Med Educ 19(1):370. https://doi.org/10.1186/s12909-019-1823-4
Bynum IV WE, Artino AR, Uijtdehaage S, Webb A, Varpio L (2019) Sentinel emotional events: the nature, triggers, and effects of shame experiences in medical residents. Acad Med 94(1):85–93. https://doi.org/10.1097/ACM.0000000000002479
Bynum IV WE, Teunissen WP, Varpio L (2021) In the “Shadow of Shame”: a phenomenological exploration of the nature of shame experiences in medical students. Acad Med 96(11S):S23–S30. https://doi.org/10.1097/ACM.0000000000004261
Bynum IV WE, Uijtdehaage S, Artino Jr AR, Fox JW (2020) The Psychology of shame: a resilience seminar for medical students. MedEdPORTAL 16:11052. https://doi.org/10.15766/mep_2374-8265.11052
Bynum IV WE, Varpio L, Lagoo J, Teunissen PW (2021) ‘I’m unworthy of being in this space’: The origins of shame in medical students. Med Educ 55(2):185–197. https://doi.org/10.1111/medu.14354
Camp DL, Hollingsworth MA, Zaccaro DJ, Cariaga-Lo LD, Richards BF (1994) Does a problem-based learning curriculum affect depression in medical students? Acad Med 69(10 Suppl):S25–7. https://doi.org/10.1097/00001888-199410000-00031 . PMID: 7916817
Article CAS PubMed Google Scholar
Chand SP, Chibnall JT, Slavin SJ (2018) Cognitive behavioral therapy for maladaptive perfectionism in medical students: a preliminary investigation. Acad Psychiatry 42(1):58–61. https://doi.org/10.1007/s40596-017-0708-2
Clance PR, Imes SA (1978) The imposter phenomenon in high achieving women: dynamics and therapeutic intervention. Psychothe. Theory Res Pract 15:241–247. https://doi.org/10.1037/h0086006
Dederichs M, Weber J, Muth T, Angerer P, Loerbroks A (2020) Students’ perspectives on interventions to reduce stress in medical school: a qualitative study. PLoS ONE 15(10):e0240587. https://doi.org/10.1371/journal.pone.0240587
Article CAS PubMed PubMed Central Google Scholar
D’Eon M, Crawford R (2005) The elusive content of the medical-school curriculum: a method to the madness. Med Teach 27(8):699–703. https://doi.org/10.1080/01421590500237598
Drolet BC, Rodgers S (2010) A comprehensive medical student wellness program—design and implementation at Vanderbilt School of Medicine. Acad Med 85:103–110. https://doi.org/10.1097/00001888-199410000-00031
Dyrbye LN, Sciolla AF, Dekhtyar M, Rajasekaran S, Allgood JA, Rea M, Knight AP, Haywood A, Smith S, Stephens MB (2019) Medical school strategies to address student well-being: a national survey. Acad Med 94(6):861–868. https://doi.org/10.1097/ACM.0000000000002611
Dyrbye LN, Shanafelt T (2016) A narrative review on burnout experienced by medical students and residents. Med Educ 50(1):132–149. https://doi.org/10.1111/medu.12927
Dyrbye LN, Thomas MR, Shanafelt TD (2005) Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc 80(12):1613–22. https://doi.org/10.4065/80.12.1613
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89(3):443–451. https://doi.org/10.1097/ACM.0000000000000134
Fischbein R, Bonfine N (2019) Pharmacy and medical students’ mental health symptoms, experiences, attitudes and help-seeking behaviors. Am J Pharm Educ 83(10):7558. https://doi.org/10.5688/ajpe7558
Freudenberger H (1974) Staff burn-out. J Soc Issues 30(1):159–165. https://doi.org/10.1111/j.1540-4560.1974.tb00706.x
Grad FP (2002) The preamble of the constitution of the World Health Organization. Bull WHO 80(12):981–984
PubMed Google Scholar
Gupta R (2018) Physicians connected. https://www.youtube.com/watch?v=Xtfsrqp9XH4&t=191s . Accessed 9 Jan 2022
Hankir AK, Northall A, Zaman R (2014) Stigma and mental health challenges in medical students. BMJ Case Rep. https://doi.org/10.1136/bcr-2014-205226 . PMID: 25183806; PMCID: PMC4158203
Henning K, Ey S, Shaw D (1998) Perfectionism, the imposter phenomenon and psychological adjustment in medical, dental, nursing and pharmacy students. Med Educ 32(5):456–64. https://doi.org/10.1046/j.1365-2923.1998.00234.x
Hu KS, Chibnall JT, Slavin SJ (2019) Maladaptive perfectionism, imposterism, and cognitive distortions: threats to the mental health of pre-clinical medical students. Acad Psychiatry 43:381–385. https://doi.org/10.1007/s40596-019-01031-z
Jackson ER, Shanafelt TD, Hasan O, Satele DV, Dyrbye LN (2016) Burnout and alcohol abuse/dependence among U.S. medical students. Acad Med 91(9):1251–1256. https://doi.org/10.1097/ACM.0000000000001138
Kirkland A (2014) What is wellness now? J Health Polit Policy Law 39(5):957–70. https://doi.org/10.1215/03616878-2813647
Klasen JM, Meienberg A, Bogie BJM (2021) Medical student engagement during COVID‐19: lessons learned and areas for improvement. Med Educ 55(1):115–118. https://doi.org/10.1111/medu.14405
Klatt MD, Bawa R, Gabram O, Blake A, Steinberg B, Westrick A, Holliday S (2020) Embracing change: a mindful medical center meets COVID-19. Glob Adv Health Med 9(Dec):2164956120975369. https://doi.org/10.1177/2164956120975369
Lacy BE, Chan JL (2018) Physician burnout: the hidden health care crisis. Clin Gastroenterol Hepatol 16(3):311–317. https://doi.org/10.1016/j.cgh.2017.06.043
Levant B, Villwock JA, Manzardo AM (2020) Imposterism in third-year medical students: an item analysis using the Clance imposter phenomenon scale. Perspect Med Educ 9(2):83–91. https://doi.org/10.1007/s40037-020-00562-8
Lonka K, Sharafi P, Karlgren K, Masiello I, Nieminen J, Birgegard G, Josephson A (2008) MED NORD–A tool for measuring medical students’ well-being and study orientations. Med Teach 30(1):72–79. https://doi.org/10.1080/01421590701769555
McLellan AT (2017) Substance misuse and substance use disorders: why do they matter in healthcare? Trans Am Clin Climatol Assoc 128:112–130
PubMed PubMed Central Google Scholar
Moffatt-Bruce SD, Nguyen MC, Steinberg B, Holliday S, Klatt M (2019) Interventions to Reduce Burnout and Improve Resilience: Impact on a Health System’s Outcomes. Clin Obstet Gynecol 63(3):432–443
Moir F, Henning M, Hassed C, Moyes SA, Elley CR (2016) A peer-support and mindfulness program to improve the mental health of medical students. Teach Learn Med 28(3):293–302. https://doi.org/10.1080/10401334.2016.1153475
Moir F, Yielder J, Sanson J, Chen Y (2018) Depression in medical students: current insights. Adv Med Educ Pract 9:323–333. https://doi.org/10.2147/AMEP.S137384
Nene Y, Tadi P (2021) Resident Burnout In: StatPearls. StatPearls Publishing. Available via: https://www.ncbi.nlm.nih.gov/books/NBK553176/?report=classic . Accessed 19 Feb 2022
Nituica C, Bota OA, Blebea J, Cheng CI, Slotman GJ (2021) Factors influencing resilience and burnout among resident physicians-a National Survey. BMC Med Educ 21(1):514. https://doi.org/10.1186/s12909-021-02950-y
Organ JM, Jaffe DB, Bender KM (2016) Suffering in silence: the survey of law student well-being and the reluctance of law students to seek help for substance use and mental health concerns. J Legal Educ 66(1):116–156
Google Scholar
Papazisis G, Tsakiridis I, Koulas I, Dagklis T, Kouvelas D (2017) Prevalence of illicit drug use among medical students in Northern Greece and association with smoking and alcohol use. Hippokratia 21(1):13–18
CAS PubMed PubMed Central Google Scholar
Reed DA, Shanafelt TD, Satele DW, Power DV, Eacker A, Harper W, Moutier C, Durning S, Massie FS, Thomas MR, Sloan JA, Dyrbye LN (2011) Relationship of pass/fail grading and curriculum structure with well-being among preclinical medical students: a multi-institutional study. Acad Med 86(11):1367–1373. https://doi.org/10.1097/ACM.0b013e3182305d81
Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Gonçalves AK (2018) Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS ONE 13(11):e0206840. https://doi.org/10.1371/journal.pone.0206840
Rohe DE, Barrier PA, Clark MM, Cook DA, Vickers KS, Decker PA (2006) The benefits of pass-fail grading on stress, mood, and group cohesion in medical students. Mayo Clin Proc 81(11):1443–1148. https://doi.org/10.4065/81.11.1443
Rosenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen C, Mata DA (2016) Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA 31(21):2214
Seeliger H, Harendza S (2017) Is perfect good?-dimensions of perfectionism in newly admitted medical students. BMC Med Educ 17(1):206. https://doi.org/10.1186/s12909-017-1034-9
Shah AA, Bazargan-Hejazi S, Lindstrom RW, Wolf KE (2009) Prevalence of at-risk drinking among a national sample of medical students. Subst Abus 30(2):141–149. https://doi.org/10.1080/08897070902802067
Sheer AJ, Estores IM, Nickels R, Radhakrishnan N, Goede DL, Mramba LK, Lo MC (2021) Improving burnout and well-being among medicine residents: impact of a grassroots intervention compared to a formal program curriculum. J Educ Health Promot 10:250. https://doi.org/10.4103/jehp.jehp_1378_20
Shi J, Yao Y, Zhan C, Mao Z, Yin F, Zhao X (2018) The relationship between big five personality traits and psychotic experience in a large non-clinical youth sample: the mediating role of emotion regulation. Front Psychiatry 9:648. https://doi.org/10.3389/fpsyt.2018.00648
Slavin S (2019) Reflections on a decade leading a medical student well-being initiative. Acad Med 94(6):771–774. https://doi.org/10.1097/ACM.0000000000002540
Slavin SJ, Chibnall JT (2016) Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med 91(9):1194–1196. https://doi.org/10.1097/ACM.0000000000001226
Slavin SJ, Schindler D, Chibnall JT (2014) Mental health 3.0: improving student wellness through curricular changes. Acad Med 89(4):573–577. https://doi.org/10.1097/ACM.0000000000000166 . Medical Student
Slavin SJ, Schindler D, Chibnall JT, Fendell G, Shoss M (2012) PERMA: A model for institutional leadership and culture change. Acad Med 87:1481
Spring L, Robillard D, Gehlbach L, Simas TA (2011) Impact of pass/fail grading on medical students’ well-being and academic outcomes. Med Educ 45(9):867–77. https://doi.org/10.1111/j.1365-2923.2011.03989.x . PMID: 21848714
Symon R (2020) Do no harm: exposing the hippocratic hoax. Symon Productions
Thomas M, Bigatti S (2020) Perfectionism, imposter phenomenon, and mental health in medicine: a literature review. Int J Med Educ 11:201–213. https://doi.org/10.5116/ijme.5f54.c8f8
United States Medical Licensing Examination (2021) Work to relaunch USMLE Step 2 CS discontinued. USMLE. https://www.usmle.org/announcements/?ContentId=309 . Accessed 16 Apr 2021
University of Michigan Medical School (2020) Four Years in Blue: The University of Michigan Medical School Documentary. Michigan Medicine
Vidhukumar K, Hamza M (2020) Prevalence and correlates of burnout among undergraduate medical students-a cross-sectional survey. Indian J Psychol Med 42(2):122–127
Article CAS Google Scholar
Williams D, Tricomi G, Gupta J, Janise A (2015) Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry 39(1):47–54. https://doi.org/10.1007/s40596-014-0197-5
Williams N (2014) The CAGE questionnaire. Occup Med 64(6):473–474. https://doi.org/10.1093/occmed/kqu058
Download references
Acknowledgements
We thank Ericka Allen, of the Lake Erie College of Osteopathic Medicine, for assistance in proofreading and revisions of this manuscript.
Author information
Authors and affiliations.
Lake Erie College of Osteopathic Medicine, Erie, PA, USA
Harrison J. Klein & Sarah M. McCarthy
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sarah M. McCarthy .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
Not applicable.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Klein, H.J., McCarthy, S.M. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun 9 , 92 (2022). https://doi.org/10.1057/s41599-022-01105-8
Download citation
Received : 30 August 2021
Accepted : 24 February 2022
Published : 23 March 2022
DOI : https://doi.org/10.1057/s41599-022-01105-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Addressing medical student burnout through informal peer-assisted learning: a correlational analysis.
- Paola Campillo
- Frances Ramírez de Arellano
- Legier V. Rojas
BMC Medical Education (2024)
Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support
- Helen M West
- Oscar T Edginton
BMC Psychology (2024)
The influence of medical students’ life values on their perception of future professional activity during the Covid-19 pandemic
- Inna Diachenko
- Svitlana Kalishchuk
- Taras Bulanov
Current Psychology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Focusing on positive thinking
You can learn to turn negative thinking into positive thinking. The process is simple, but it does take time and practice — you're creating a new habit, after all. Following are some ways to think and behave in a more positive and optimistic way:
- Identify areas to change. If you want to become more optimistic and engage in more positive thinking, first identify areas of your life that you usually think negatively about, whether it's work, your daily commute, life changes or a relationship. You can start small by focusing on one area to approach in a more positive way. Think of a positive thought to manage your stress instead of a negative one.
- Check yourself. Periodically during the day, stop and evaluate what you're thinking. If you find that your thoughts are mainly negative, try to find a way to put a positive spin on them.
- Be open to humor. Give yourself permission to smile or laugh, especially during difficult times. Seek humor in everyday happenings. When you can laugh at life, you feel less stressed.
- Follow a healthy lifestyle. Aim to exercise for about 30 minutes on most days of the week. You can also break it up into 5- or 10-minute chunks of time during the day. Exercise can positively affect mood and reduce stress. Follow a healthy diet to fuel your mind and body. Get enough sleep. And learn techniques to manage stress.
- Surround yourself with positive people. Make sure those in your life are positive, supportive people you can depend on to give helpful advice and feedback. Negative people may increase your stress level and make you doubt your ability to manage stress in healthy ways.
- Practice positive self-talk. Start by following one simple rule: Don't say anything to yourself that you wouldn't say to anyone else. Be gentle and encouraging with yourself. If a negative thought enters your mind, evaluate it rationally and respond with affirmations of what is good about you. Think about things you're thankful for in your life.
Here are some examples of negative self-talk and how you can apply a positive thinking twist to them:
Practicing positive thinking every day
If you tend to have a negative outlook, don't expect to become an optimist overnight. But with practice, eventually your self-talk will contain less self-criticism and more self-acceptance. You may also become less critical of the world around you.
When your state of mind is generally optimistic, you're better able to handle everyday stress in a more constructive way. That ability may contribute to the widely observed health benefits of positive thinking.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Forte AJ, et al. The impact of optimism on cancer-related and postsurgical cancer pain: A systematic review. Journal of Pain and Symptom Management. 2021; doi:10.1016/j.jpainsymman.2021.09.008.
- Rosenfeld AJ. The neuroscience of happiness and well-being. Child and Adolescent Psychiatric Clinics of North America. 2019;28:137.
- Kim ES, et al. Optimism and cause-specific mortality: A prospective cohort study. American Journal of Epidemiology. 2016; doi:10.1093/aje/kww182.
- Amonoo HL, et al. Is optimism a protective factor for cardiovascular disease? Current Cardiology Reports. 2021; doi:10.1007/s11886-021-01590-4.
- Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/paguidelines/second-edition. Accessed Oct. 20, 2021.
- Seaward BL. Essentials of Managing Stress. 4th ed. Burlington, Mass.: Jones & Bartlett Learning; 2021.
- Seaward BL. Cognitive restructuring: Reframing. Managing Stress: Principles and Strategies for Health and Well-Being. 8th ed. Burlington, Mass.: Jones & Bartlett Learning; 2018.
- Olpin M, et al. Stress Management for Life. 5th ed. Cengage Learning; 2020.
- A very happy brain
- Being assertive
- Bridge pose
- Caregiver stress
- Cat/cow pose
- Child's pose
- COVID-19 and your mental health
- Does stress make rheumatoid arthritis worse?
- Downward-facing dog
- Ease stress to reduce eczema symptoms
- Ease stress to reduce your psoriasis flares
- Forgiveness
- Job burnout
- Learn to reduce stress through mindful living
- Manage stress to improve psoriatic arthritis symptoms
- Mayo Clinic Minute: Meditation is good medicine
- Mountain pose
- New School Anxiety
- Seated spinal twist
- Standing forward bend
- Stress and high blood pressure
- Stress relief from laughter
- Stress relievers
- Support groups
- Tips for easing stress when you have Crohn's disease
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Positive thinking Stop negative self-talk to reduce stress
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
What admission officers wish premeds knew before applying
New section.
What exactly do medical schools look for in applications? We asked three admission officers what they want applicants to know before applying to medical school.
It’s common to wonder what medical schools are looking for in an application and how you can make sure you’re prepared when you apply and interview. To help answer these questions, we asked three admission officers what they want applicants to know before applying so they can be successful. Their answers include being able to tell your story, having clinical experience, and making sure your goals are aligned with the school’s mission statement. Here’s what they shared.
“At the core of any patient encounter, there is a story. As physicians, we are primed to listen to stories, so a good story is key when a physician reads a medical school application or evaluates answers during the interview. Most medical school applicants have enough volunteer, work, shadowing, and research experiences to fill every space in their AMCAS application and prompt in their secondary applications. However, while many are very good at accumulating experiences, they are sometimes not so good at putting these experiences in context or effectively communicating them to interviewers and application reviewers. The applicant should be able to put all his or her experiences in the context of why they want to be a physician and describe their journey. Novelists, English professors, and screen writers call this this the ‘arc of the story.’ For example, the arc could be that a topic in class led to a research opportunity that led to a showing experience that then led to working with a group that is involved in that issue. This is different than the applicant that has a dozen unrelated experiences and is unable to connect them. In short, the applicant should be able to tell a good story that makes sense and engages the interviewer or reviewer rather than give a checklist of research, shadowing, and volunteering. Most applicants will not have a perfect story where everything falls into place, but that is OK. The most interesting stories have lots of twist and turns.”
-David D. Grier, MD , Associate Dean for Student Admissions, Wake Forest School of Medicine
“The professional opportunities for physicians are quite wide, and include options in research, administration, and industry. However, if you are considering applying to medical school, you should know that the curriculum prepares you to be a competent clinician. With that in mind, schools want you to bring some experience in the world of patient care. Your ability to speak first-hand of the impact of clinical volunteer work on your future career plans is a compelling aspect of the selection and admissions process. I feel that it makes sense to postpone applications until you have accumulated at least one year of clinical experiences.”
- Jorge A. Girotti, PhD, MHA, Associate Dean for Admissions and Special Curricular Programs, University of Illinois College of Medicine
“It is very important for medical school applicants to do their research before applying. Exploring a medical school’s mission statement is a great way to determine if your goals are in alignment. If a medical school’s mission is to serve disadvantaged populations, your application should show similar evidence of your interests. Your application should highlight the goals of the school and how your experiences will contribute to the overall mission.
By reviewing your application, an admissions committee should be able to identify your motivation for medicine as well as your motivation for applying to their medical school. One of the best ways an applicant can demonstrate fit is how you respond to secondary application questions. These critical mini-essays typically ask applicants how they identify with a school’s mission and how much an applicant understands the field of medicine. For example, a secondary question may ask what about your experience with caring for others. You can demonstrate caring in multiple ways: caring for a loved one, shadowing, working in hospice, or other experiences that allowed you to observe patient care whether it is formal or informal.
Another way to understand fit is to understand a medical school’s admissions criteria. If a medical school suggests applicants should have research experience, then applicants should show substantial evidence of working in a lab or research publications. Each medical school has their own unique admissions requirements that are tailored to their specific missions. Applicants should be diligent about examining this information before submitting an application.”
-Tanisha Price-Johnson, Executive Director, Admissions, University of Arizona College of Medicine – Tucson
Back to The Library

Why Does Student Mental Health Suffer During Summer? Here’s What the Data Says
May 23, 2024
Data that highlights how summer affects student mental health and how to access mental healthcare during the summertime (and year-round).
By: Charlie Health Editorial Team
Clinically Reviewed By: Dr. Don Gasparini
Learn more about Clinical Review Process
Table of Contents
After the demands of the school year, many students eagerly await summer vacation. However, while summertime may bring warm weather, rest, and summer camp for some students, experts agree that it can be a trying time for young people’s mental health. During summer, many children and adolescents experience a shift from the structured support of school to a more unstructured environment, which can take a toll on their mental health.
These effects, though, are not felt equally. Research shows that students from marginalized backgrounds who disproportionately depend on schools for essential resources like food, medical and mental healthcare, and supervision are at a higher risk for negative emotional outcomes during the summer. For example, a multi-campus study of about 28,200 undergraduate students found that first-generation college students were more likely than continuing-generation college students to experience financial hardships, food and housing insecurity, and adverse mental health outcomes during the summer of 2020.
This is not to say that summertime is inherently harmful to students’ mental health. For many, summer vacation brings mental health benefits, like a break from school work and time with loved ones. A study of students across four years of college, for instance, showed a consistent “anticipatory stress spike” of 17% in the last two weeks of summer break as students faced the school year to come.

Mental Health Tips for High School Students, According to Therapists
Ashley Laderer
For those students whose mental health does suffer during summer vacation, experts believe there are steps that can be taken to improve well-being, like making structured summer programs more accessible. However, while there’s extensive research on summer’s impact on students (particularly marginalized students), it’s often underutilized in policy and practice.
To assess how summer affects student’s mental health, Charlie Health looked at the numbers, including data on summer crime rates and food insecurity, which play a role in well-being. We also offer some tips on how to access mental healthcare during the summer (and year-round).
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
Thank you for signing up!
You can unsubscribe anytime., many students lose necessary school-based mental health services during the summer.
Students are six times more likely to access mental healthcare when services are offered in school, according to U.S. Secretary of Education Miguel Cardona. For those many students who access mental healthcare at school , this support abates over the summer, possibly exacerbating or leading to increased mental health issues. As research has consistently shown, mental health conditions often worsen when left unaddressed.
Increased summer crime rates can take a toll on student mental health
Crime rates and the risk of crime victimization generally increase during the summer, according to The Department of Justice, and exposure to violence can take a toll on mental health. For example, a 2018 study found that depression symptoms are 61% higher in crime hot spots than cold spots (3.68 versus 2.28, where higher ratings mean greater symptoms), and PTSD symptoms are 85% higher in those places with more crime (0.72 versus 0.39). Children and youth from low-income families and neighborhoods and those who are minorities are at greatest risk since they disproportionately live in areas with higher levels of crime — over three-quarters (77.71%) of those studied in crime hot spots were African American, and over half (54.55%) had a household income of $25,000 or less, the study found.
Many students face food insecurity over the summer, resulting in mental health issues
Access to school-based food and nutrition programs is curtailed during the summer, resulting in an increased risk of food insecurity among children and youth. Research has consistently found that food insecurity is positively correlated with mental health conditions and symptoms, like rates of depression and stress. A study based on national data of U.S. adolescents found that food insecurity was linked to higher chances of mood, anxiety, behavior, and substance use disorders. A rise in food insecurity resulted in a 14% increase in the likelihood of experiencing a mental health disorder in the past year, the 2012 study found.
How to address student mental health during summer vacation
Addressing student mental health during summer vacation is, first and foremost, a systemic issue. Above all, lawmakers need to allocate enough resources and funding to services that improve mental healthcare for students — year-round and during the summer, and particularly within marginalized communities. Below are some other steps that can be taken to address student mental health during the summer.
Find accessible summer programs
Maintain a consistent routine
Seek mental healthcare, find accessible summer programs .
As mentioned, experts have found summer programs to be effective in promoting mental health outcomes among students. However, summertime learning and enrichment opportunities often draw on the resources available through a child’s parents and their local communities. As a result, children from more economically advantaged families and neighborhoods have greater access to resources from their families and communities. However, families can explore various local resources that may offer accessible summer programming — such as community centers and libraries — and get in touch with schools, local government agencies, or nonprofit organizations that may have information about program scholarships.
Establishing a consistent daily schedule can help students maintain a sense of structure and predictability during the oft-unstructured summer time of vacation. Try encouraging regular sleep patterns, mealtimes, and unstructured leisure time. Also, it’s a bonus if some of the time is set aside for self-care practices like relaxation techniques, exercise, or hobbies, which can promote stress management and overall well-being.
If a student’s mental health is suffering during summer vacation, it’s important to seek professional support. One way to do this is to specifically look for providers who work with students over the summer or organizations focused on mental healthcare for students. If you’re looking for more than once-weekly mental health support for students, consider Charlie Health’s student-specific Reset & Recharge summer program. This 9-12 week program helps students (11-23) reset their mental health and recharge their coping skills in virtual peer groups, preparing them for the school year ahead.
https://www.pearsonassessments.com/professional-assessments/blog-webinars/blog/2023/07/why-does-summer-break-impact-student-mental-health.html
https://pubmed.ncbi.nlm.nih.gov/31940162/
https://escholarship.org/uc/item/19d5c0ht#main
https://home.dartmouth.edu/news/2024/03/study-tracks-shifts-student-mental-health-during-college
https://www.ed.gov/news/press-releases/biden-harris-administration-takes-action-help-schools-deliver-critical-health-care-services-millions-students
https://bjs.ojp.gov/content/pub/pdf/ics.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6394830/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9014344/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3632292/
https://www.ncbi.nlm.nih.gov/books/NBK552656/
Comprehensive mental health treatment from home
90% of Charlie Health clients and their families would recommend Charlie Health
More like this

How to Build Resilience in Students
Charlie Health Editorial Team

How to Talk About Tragedy & School Shootings

How Family Therapy Can Help Your Teen

We're building treatment plans as unique as you.
Need additional mental health support? Charlie Health can help
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J R Soc Med
- v.101(3); 2008 Mar 1
Involving medical students in research
Undergraduate research is not a new phenomenon in medicine. Charles Best was a medical student at the time that he and his supervisor, Frederick Banting, discovered insulin. Insulin arises from the pancreatic islets of Längerhans, themselves discovered in 1869 by medical student Paul Längerhans. In biomedical research, Alan Hodgkin, formerly professor of biophysics at the University of Cambridge, won the Nobel Prize in 1972 for work on nerve transmission that he began as an undergraduate.
Medical student research can be mandatory, elective or extracurricular. In Germany, medical school graduates practice medicine but cannot assume the title ‘Doctor’ until they have submitted a thesis. As a result, around 90% of practicing German physicians have undertaken a period of research. 1 Although research is usually voluntary for UK medical students, there is increasing undergraduate interest in research and publication. The 2007 MTAS form, for example, awards credit to medical graduates for a first author paper in a peer-reviewed journal.
The GMC document Tomorrow's Doctors states that medical school graduates must be able to ‘critically evaluate evidence’ and ‘use research skills to develop greater understanding and to influence their practice’. 2 It has been suggested that a period of research might help fulfill this requirement of new doctors. 3 , 4 Despite this possibility, medical students have only limited opportunities to pursue original research. However, a number of institutions offer intercalated degree courses in which students suspend their medical training to undertake a second degree, often with a strong research component. These attract around a third of UK medical students each year. 5 , 6
Reasons for medical students choosing to intercalate are varied and include improving their long-term career prospects as well as establishing a broad knowledge base. 6 The opportunity to conduct original research is, however, less frequently given as a reason for pursuing an intercalated degree. 5 , 6 In addition, two thirds of new doctors in the UK have not undertaken an intercalated degree 5 , 6 and may graduate without experiencing research. A number of barriers explain the reluctance of medical students to intercalate. One survey found the most common reasons were financial constraints, lack of interest, and reluctance to prolong medical training. 6
Nevertheless, there are many benefits of undergraduate participation in research. For example, student researchers can greatly increase the publication output of their medical school. Academic supervisors at one German institution have reported that students appear as co-authors on approximately 28% of papers published in Medline-indexed journals. 8
Research experience may also boost the career profile of graduating medical students. When a cohort of students at the Stanford University School of Medicine was encouraged to participate in research, 75% gained authorship of a paper and 52% presented data to a national conference. 3 In Germany, around 66% of medical students obtain a Medline-indexed publication before qualifying. This does not include data presented to meetings or published in peer-reviewed journals not indexed by Medline. 8
In addition to boosting graduate employability, publication as an undergraduate can have long-term career implications for doctors. For example, one survey of academic physicians found that career success is independently associated with having conducted research as a student. 9 In addition, physicians who undertook extracurricular research at medical school produced four times as many publications as their peers. 10
Undergraduate research may also provide a solution for countries in which academic medicine is experiencing a crisis in recruiting postgraduate clinical researchers. 11 For example, a survey of medical student researchers found that 75% were motivated to pursue further research and 60% aspired to a full-time academic career. 3
Those students not considering research careers may nevertheless develop skills transferable to clinical practice. In particular, medical student research may help instil a culture of evidence-based medicine (EBM) in clinical medicine. According to one author, ‘the practice of EBM is not a “behaviour”… it is an internalized spirit of enquiry born of a deep understanding… of the value and the limitations of biomedical research’. 5 Indeed, there is evidence to suggest that research experience as an undergraduate may foster this ‘deeper understanding’. 3–5 According to one survey, American medical students participating in research found that the experience ‘taught them to ask questions, review the literature critically, and analyse data’. 3 Students undertaking a mandatory literature review further developed ‘critical appraisal, information literacy, and critical thinking skills’ and the opportunity to make ‘contacts for postgraduate training’. 4
Despite these apparent benefits, there are objections to involving undergraduates in research. Intensive projects may, for example, disrupt the progress of students through the core medical curriculum. Similarly, supervision requirements may distract faculty members from their own clinical and research commitments. However, students do not have to run a clinical trial to learn about the research process. If there are not pre-existing clinical projects suitable for student participation, undergraduates might be involved in critically appraising literature for a review article, or preparing patient case reports for publication. Projects such as these require little supervision while still immersing students in the research culture of their profession.
In summary, research opportunities for medical students are often confined to intercalated degree courses; potentially increasing financial burden, prolonging the curriculum and delaying clinical experience. As a result, around two thirds of medical students eschew the opportunity to intercalate 5 , 6 and miss out on conducting original research. Nevertheless, the benefits of student participation in research are well-documented for graduates, institutions and the academic community as a whole. 3–5 , 7–10 As a result, senior doctors should strongly consider involving motivated students in elective or extracurricular research projects. Furthermore, medical educators should recognize the value of student research and incorporate opportunities into the curriculum wherever practicable. Only in these ways can we secure a future for academic medicine and foster a genuine respect for EBM in tomorrow's doctors.
DECLARATIONS —
Competing interests DM is an undergraduate medical student and Editor of Reinvention: A Journal of Undergraduate Research . He has received research funding from the Reinvention Centre for Undergraduate Research at the University of Warwick and Oxford Brookes University
Funding None
Ethical approval Not applicable
Guarantor DM
Contributorship DM is the sole contributor
Acknowledgements
The author would like to thank Mina Aletrari for reviewing earlier drafts of this paper

IMAGES
VIDEO
COMMENTS
Deadline: July 16, 2024. One method to sharpen your critical analysis skills and prepare for medical school is to participate in research opportunities for premed students as either an undergraduate or during the time between college and medical school. "Any and all research—including non-medical research—is beneficial," said Haidn ...
In particular, medical research equips clinicians with skills to critically analyze the clinical relevance of papers to provide invaluable insights into novel treatments. The integration of research into medical education has been documented to have translated into skills valuable to future clinical practice.
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started ### This article contains: Students often go into medicine because of a desire to help others and improve patients' physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care ...
Here are six common health-related research directions I commonly see among premeds that reflect the breadth of research you can pursue: Basic science research. Clinical research. Public health ...
Introduction. Research is essential to advance medical knowledge. It is crucial to understand problems that affect the health of individuals, communities, and health systems. 1 Unfortunately, in the previous two decades, the number of physician-scientists on staff in medical school faculties has declined by approximately 25%. The learning environment in how research methodologies are ...
Research in Medical Education: A Primer for Medical Students II. Why should I do a MedEd research project? Why are medical students especially qualified to do MedEd research? As medical students, you are front and center of the medical education process! Oftentimes, great ideas about "what works" in education are dashed on the shoals of ...
1.1. Research in the medical career: when and why? The main reason for researching and publishing high quality scientific articles lies in learning to use and critique evidence for responsible decision making based on it, trying to avoid as much as possible medical failures during clinical practice [11,12].On the other hand, this tool helps to optimize overall critical thinking, personal ...
A research project might require you to first take coursework in basic lab sciences, statistics, or another advanced topic specific to the project. Other PIs may prefer to train you "on-the-job" through their graduate or post-doc students. This will impact when you are ready to join a project. Finding the right research project.
Phenomenon: Research literacy remains important for equipping clinicians with the analytical skills to tackle an ever-evolving medical landscape and maintain an evidence-based approach when treating patients. While the role of research in medical education has been justified and established, the nuances involving modes of instruction and relevant outcomes for students have yet to be analyzed.
A research experience may be the first time a student has had to write and record what they do, think, and find coherently, concisely and precisely. This can contribute to developing lasting habits of critical thinking. In a landmark and classic essay, C. Wright Mills commented that there was never a time he was not thinking, reflecting ...
Avoid joining a project if you are not fully committed, and employ resiliency to overcome failure along the way. Treat research not as a passive process, but as an active use of your intellectual capability. Push yourself to problem-solve and discover. You never know how big of an impact you might make.
Extra-curricular, research-related activities are a key method by which students develop interest in their field of choice, and a competitive edge in medical students. The lack of research education and opportunities within medical school teaching tends to force medical students to look beyond their degree to obtain this experience, and is ...
Summer programs at the National Institutes of Health (NIH) provide an opportunity to spend a summer working at the NIH side-by-side with some of the leading scientists in the world, in an environment devoted exclusively to biomedical research. Find opportunities available for current medical students.
The first is whether research experience is important for medical school applications. The second is whether gaining research experience is an important part of attending medical school. The answer to both of these is undoubtedly yes, research is very important for medical school. Of course, there are some qualifications to this importance.
It helps you understand the mechanisms of research, the bureaucratic obstacles, the medical challenges, and teaches you communication with peers and faculty. Furthermore, you learn how to read, analyze, and interpret scientific publications of others. And trust me, it's not all gold that gets printed in journals.
TIP 4: UTILISE SOCIAL MEDIA. Research opportunities, talks and workshops are advertised on social media in abundance. Here are some examples: Facebook. Search "medical student research" or "medsoc research" into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research ...
Importance of Research for Medical School. Your MCAT, GPA, extracurriculars, and clinical experience all play a role in your admissions chances. But research is also key! Most but not all students accepted to medical school have research experience. According to a survey of incoming medical students conducted by the AAMC, 60% of students ...
Medical education is a time wrought with personal and professional stressors, posing serious challenges to maintaining student wellness. Extensive research has thus been conducted to identify ...
Guaranteed income programs have been successful in low-income countries. Now, researchers hope to test their effectiveness in the U.S. May 30, 2024. AAMCNews. Women are changing the face of medicine in America. Data from the past 18 years show how women have driven growth in the supply of physicians and expanded their presence in some of the ...
Introduction and background. Memory can be trained to seemingly impossible levels [], indicating that there may be potential for improvement of how knowledge is acquired in medical school.Accordingly, there have been recommendations for improving medical education based on the available evidence in cognitive science regarding learning [2, 3].As technology continues to expand, more web-based ...
This program is designed for students from historically marginalized groups including low-income and first-generation students. The goal of RISE is to equip students to take on larger, more intensive academic-year and summer experiences for later in their college career. Each student receives $2,500 in scholarships and funds to cover on-campus ...
When newer studies adjusted for such factors, they found a possible association between coffee and decreased mortality. Coffee may offer some protection against: Parkinson's disease. Type 2 diabetes. Liver disease, including liver cancer. Heart attack and stroke. Coffee still has potential risks, mostly due to its high caffeine content.
Positive thinking often starts with self-talk. Self-talk is the endless stream of unspoken thoughts that run through your head. These automatic thoughts can be positive or negative. Some of your self-talk comes from logic and reason. Other self-talk may arise from misconceptions that you create because of lack of information or expectations due ...
Get full tuition covered for up to 4 years. If you're in the Army or haven't joined yet but want to serve, the U.S. Army's Health Professions Scholarship Program (HPSP) will help pay for medical school. So, you can: Graduate from medical school without debt. Earn a $2,700+ monthly allowance. Receive a $20,000 signing bonus.
In short, the applicant should be able to tell a good story that makes sense and engages the interviewer or reviewer rather than give a checklist of research, shadowing, and volunteering. Most applicants will not have a perfect story where everything falls into place, but that is OK. The most interesting stories have lots of twist and turns.".
For example, "exercise enhances synaptic plasticity and blood flow while reducing inflammation and increasing the expression of neurotrophic factors like BDNF ," Glatt explained. "These ...
After the demands of the school year, many students eagerly await summer vacation. However, while summertime may bring warm weather, rest, and summer camp for some students, experts agree that it can be a trying time for young people's mental health. During summer, many children and adolescents experience a shift from the structured support of school to a more unstructured environment, which ...
Involving medical students in research. Undergraduate research is not a new phenomenon in medicine. Charles Best was a medical student at the time that he and his supervisor, Frederick Banting, discovered insulin. Insulin arises from the pancreatic islets of Längerhans, themselves discovered in 1869 by medical student Paul Längerhans.