- Search Menu
- Sign in through your institution
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Answer to part 1, answer to part 2, answer to part 3, answer to part 4, answer to part 5.
- < Previous
Educational Case: A 57-year-old man with chest pain
Contributed equally.
- Article contents
- Figures & tables
- Supplementary Data
Nikhil Aggarwal, Subothini Selvendran, Vassilios Vassiliou, Educational Case: A 57-year-old man with chest pain, Oxford Medical Case Reports , Volume 2016, Issue 4, April 2016, Pages 62–65, https://doi.org/10.1093/omcr/omw008
- Permissions Icon Permissions
This is an educational case report including multiple choice questions and their answers. For the best educational experience we recommend the interactive web version of the exercise which is available via the following link: http://www.oxfordjournals.org/our_journals/omcr/ec01p1.html
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by paramedics in the community. He smoked 20 cigarettes daily (38 pack years) but was not aware of any other cardiovascular risk factors. On examination he appeared comfortable and was able to complete sentences fully. There were no heart murmurs present on cardiac auscultation. Blood pressure was 180/105 mmHg, heart rate was 83 bpm and regular, oxygen saturation was 97%.
What is the most likely diagnosis?
An ECG was requested and is shown in figure 1.
How would you manage the patient? (The patient has already received 300 mg aspirin).
30 minutes later the patient's chest pain returned with greater intensity whilst waiting in the emergency department. Now, he described the pain as though “an elephant is sitting on his chest”. The nurse has already done an ECG by the time you were called to see him. This is shown in figure 2.

ECG on admission.

ECG 30 minutes after admission.
What would be the optimal management for this patient?
He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home. The patient is keen to return to work and asks when he could do so.
When would you advise him that he could return to work?
One week later, he receives a letter informing him that he is required to attend cardiac rehabilitation. The patient is confused as to what cardiac rehabilitation entails, although he does remember a nurse discussing this with him briefly before he was discharged. He phones the hospital in order to get some more information.
Which of the following can be addressed during cardiac rehabilitation?
A - Acute coronary syndrome
Although the presentation could be attributable to any of the above differential diagnoses, the most likely etiology given the clinical picture and risk factors is one of cardiac ischemia. Risk factors include gender, smoking status and age making the diagnosis of acute coronary syndrome the most likely one. The broad differential diagnosis in patients presenting with chest pain has been discussed extensively in the medical literature. An old but relevant review can be found freely available 1 as well as more recent reviews. 2 , 3
C - Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg,
In patients with ACS, medications can be tailored to the individual patient. Some medications have symptomatic benefit but some also have prognostic benefit. Aspirin 4 , Clopidogrel 5 , Atenolol 6 and Atorvastatin 7 have been found to improve prognosis significantly. ACE inhibitors have also been found to improve left ventricular modeling and function after an MI. 8 , 9 Furthermore, GTN 10 and morphine 11 have been found to be of only significant symptomatic benefit.
Oxygen should only to be used when saturations <95% and at the lowest concentration required to keep saturations >95%. 12
There is no evidence that diltiazem, a calcium channel blocker, is of benefit. 13
His ECG in figure 1 does not fulfil ST elevation myocardial infarction (STEMI) criteria and he should therefore be managed as a Non-STEMI. He would benefit prognostically from beta-blockade however his heart rate is only 42 bpm and therefore this is contraindicated. He should receive a loading dose of clopidogrel (300 mg) followed by daily maintenance dose (75 mg). 14 , 15 He might not require GTN if he is pain-free but out of the available answers 3 is the most correct.
D - Proceed to coronary angiography
The ECG shows ST elevation in leads V2-V6 and confirms an anterolateral STEMI, which suggests a completely occluded LAD. This ECG fulfils the criteria to initiate reperfusion therapy which traditionally require one of the three to be present: According to guidance, if the patient can undergo coronary angiography within 120 minutes from the onset of chest pain, then this represents the optimal management. If it is not possible to undergo coronary angiography and potentially percutaneous intervention within 2 hours, then thrombolysis is considered an acceptable alternative. 12 , 16
≥ 1 mm of ST change in at least two contiguous limb leads (II, III, AVF, I, AVL).
≥ 2 mm of ST change in at least two contiguous chest leads (V1-V6).
New left bundle branch block.
GTN and morphine administration can be considered in parallel but they do not have a prognostic benefit.
E - Not before an exercise test
This patient is a lorry driver and therefore has a professional heavy vehicle driving license. The regulation for driving initiation in a lorry driver following a NSTEMI/ STEMI may be different in various countries and therefore the local regulations should be followed.
In the UK, a lorry driver holds a category 2 driving license. He should therefore refrain from driving a lorry for at least 6 weeks and can only return to driving if he completes successfully an exercise evaluation. An exercise evaluation is performed on a bicycle or treadmill. Drivers should be able to complete 3 stages of the standard Bruce protocol 17 or equivalent (e.g. Myocardial perfusion scan) safely, having refrained from taking anti-anginal medication for 48 hours and should remain free from signs of cardiovascular dysfunction during the test, notably: angina pectoris, syncope, hypotension, sustained ventricular tachycardia, and/or electrocardiographic ST segment shift which is considered as being indicative of myocardial ischemia (usually >2 mm horizontal or down-sloping) during exercise or the recovery period. 18
For a standard car driving license (category 1), driving can resume one week after successful intervention providing that no other revascularization is planned within 4 weeks; left ventricular ejection fraction (LVEF) is at least 40% prior to hospital discharge and there is no other disqualifying condition.
Therefore if this patent was in the UK, he could restart driving a normal car one week later assuming an echocardiogram confirmed an EF > 40%. However, he could only continue lorry driving once he has passed the required tests. 18
E - All of the above
Cardiac rehabilitation bridges the gap between hospitals and patients' homes. The cardiac rehabilitation team consists of various healthcare professions and the programme is started during hospital admission or after diagnosis. Its aim is to educate patients about their cardiac condition in order to help them adopt a healthier lifestyle. This includes educating patients' about their diet, exercise, risk factors associated with their condition such as smoking and alcohol intake and finally, about the medication recommended. There is good evidence that adherence to cardiac rehabilitation programmes improves survival and leads to a reduction in future cardiovascular events. 19 , 20
Oille JA . Differential diagnosis of pain in the chest . Can Med Assoc J . 1937 ; 37 (3) : 209 – 216 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC536075/ .
Google Scholar
Lee TH , Goldman L . Evaluation of the patient with acute chest pain . N Engl J Med . 2000 ; 342 (16) : 1187 – 1195 . http://www.nejm.org/doi/full/10.1056/NEJM200004203421607 .
Douglas PS , Ginsburg GS . The evaluation of chest pain in women . N Engl J Med . 1996 ; 334 (20) : 1311 – 1315 . http://www.nejm.org/doi/full/10.1056/NEJM199605163342007 .
Baigent C , Collins R , Appleby P , Parish S , Sleight P , Peto R . ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group . BMJ . 1998 ; 316 (7141) : 1337 – 1343 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28530/ .
Yusuf S , Zhao F , Mehta S , Chrolavicius S , Tognoni G , Fox K . Clopidogrel in unstable angina to prevent recurrent events trail investigators . effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation . N Engl J Med . 2001 ; 345 (7) : 494 – 502 . http://www.nejm.org/doi/full/10.1056/NEJMoa010746#t=articleTop .
Yusuf S , Peto R , Lewis J , Collins R , Sleight P . Beta blockade during and after myocardial infarction: An overview of the randomized trials . Prog Cardiovasc Dis . 1985 ; 27 (5) : 335 – 371 . http://www.sciencedirect.com/science/article/pii/S0033062085800037 .
Schwartz GG , Olsson AG , Ezekowitz MD et al. . Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial . JAMA . 2001 ; 285 (13) : 1711 – 1718 . http://jama.jamanetwork.com/article.aspx?articleid=193709 .
Pfeffer MA , Lamas GA , Vaughan DE , Parisi AF , Braunwald E . Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction . N Engl J Med . 1988 ; 319 (2) : 80 – 86 . http://content.onlinejacc.org/article.aspx?articleid=1118054 .
Sharpe N , Smith H , Murphy J , Hannan S . Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction . The Lancet . 1988 ; 331 (8580) : 255 – 259 . http://www.sciencedirect.com/science/article/pii/S0140673688903479 .
Ferreira JC , Mochly-Rosen D . Nitroglycerin use in myocardial infarction patients . Circ J . 2012 ; 76 (1) : 15 – 21 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527093/ .
Herlitz J , Hjalmarson A , Waagstein F . Treatment of pain in acute myocardial infarction . Br Heart J . 1989 ; 61 (1) : 9 – 13 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1216614/ .
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation . Eur Heart J . 2012 ; 33 (20) : 2569 – 2619 . http://eurheartj.oxfordjournals.org/content/33/20/2569 .
The effect of diltiazem on mortality and reinfarction after myocardial infarction . the multicenter diltiazem postinfarction trial research group . N Engl J Med . 1988 ; 319 (7) : 385 – 392 . http://www.nejm.org/doi/full/10.1056/NEJM198808183190701 .
Jneid H , Anderson JL , Wright RS et al. . 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update) A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2012 ; 60 (7) : 645 – 681 . http://circ.ahajournals.org/content/123/18/2022.full .
Hamm CW , Bassand JP , Agewall S et al. . ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the european society of cardiology (ESC) . Eur Heart J . 2011 ; 32 (23) : 2999 – 3054 . http://eurheartj.oxfordjournals.org/content/32/23/2999.long .
O'Gara PT , Kushner FG , Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2013 ; 61 (4) : 485 – 510 . http://content.onlinejacc.org/article.aspx?articleid=1486115 .
BRUCE RA , LOVEJOY FW Jr . Normal respiratory and circulatory pathways of adaptation in exercise . J Clin Invest . 1949 ; 28 (6 Pt 2) : 1423 – 1430 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC439698/ .
DVLA . Https://Www.gov.uk/current-medical-guidelines-dvla-guidance-for-professionals-cardiovascular-chapter-appendix .
British Heart Foundation . Http://Www.bhf.org.uk/heart-health/living-with-heart-disease/cardiac-rehabilitation.aspx .
Kwan G , Balady GJ . Cardiac rehabilitation 2012: Advancing the field through emerging science . Circulation . 2012 ; 125 (7) : e369–73. http://circ.ahajournals.org/content/125/7/e369.full .
Author notes
- knowledge acquisition
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Case study 1: acute myocardial infarction
Sep 12, 2014
350 likes | 1.4k Views
Case study 1: acute myocardial infarction. Megan Fuchs Good Sam Dietetic Intern January 5, 2012. Patient Profile Personal Information. 46 year old white male Lives in Cincinnati, OH with wife, daughter, and grandson Leads a physically active lifestyle
Share Presentation
- kcal intake
- current admission
- high blood pressure
- diet education low sodium

Presentation Transcript
Case study 1: acute myocardial infarction Megan Fuchs Good Sam Dietetic Intern January 5, 2012
Patient ProfilePersonal Information • 46 year old white male • Lives in Cincinnati, OH with wife, daughter, and grandson • Leads a physically active lifestyle • Works in maintenance – constant movement • Lifts weights and swims regularly • No ethnic or religious considerations
Patient ProfileAdmission • JD presented to the Western Ridge ER with complaints of chest pain, N/V, and diaphoresis • Found to be having an acute inferior myocardial infarction (MI) • Immediately transferred to GSH ER • At GSH, doctors confirmed the diagnosis of an acute inferior MI based on • EKG results consistent with MI • Noted sinus arrhythmia • Rate of 89 • Marked segment elevation in inferior leads
Patient profilePast medical History • Splenectomy(as a child, unknown reason for removal) • Surgical removal of the spleen due to rupture, enlargement, certain blood disorders, cancer, infections, or non-cancerous tumors • Spleen is an important part of fighting infection – filters damaged red blood cells • Complications may include hemorrhage, blood clots, infection, or injury to other organs • Hypertension(HTN) • High blood pressure • Diagnosed when ones blood pressure is 140/80 mmHg • Factors affecting BP include amount of water and salt in the body; function of the kidneys, nervous system, and blood vessels • Increased risk of developing HTN if one is obese, stressed/anxious, high salt diet, family history, diabetes, smoker, or African American
Patient ProfileFamily History Very strong history of heart failure
Patient profileHealth History • Generally sleeps well, 6-8 hours a night • Physically Active Lifestyle • Maintenance worker – uses stairs, walks to and from buildings • Lifts weights and swims 3-4 times/week • Non-smoker • Occasionally drinks alcohol • No substance abuse
Patient ProfileHealth History • Height: 5’9” • Weight: 267.7 lb • Weight history: 5 lb weight gain/loss throughout the year • No large amount of weight loss or gain • Appetite • Prior to admission – very good appetite, enjoys all foods but eats very little vegetables • JD and his wife enjoy shopping and cooking together • During hospital stay – appetite improved but was initially very poor
Patient profilehealth history • No dental problems • No chewing or swallowing problems • Normal digestion • Elimination – regular bowel movements
Disease BackgroundAcute Inferior Myocardial infarction • Myocardial Infarction or Heart Attack • Occurs when blood flow to part of the heart is blocked resulting in damage or death to the muscle • Usually caused by a blood clot or plaque formation blocking the coronary artery, which supplies the heart with oxygen and blood
Disease BackgroundPathophysiology/etiology • Most common etiologic factor: presence of atherosclerotic plaque blocking the coronary arteries • Plaque leads to the disruption of blood flow through the coronary arteries to the heart • Size of the thrombus determines the percent of blockage, ultimately determining the extent of damage • Decreased blood flow for an amount of time can trigger a process known as ischemic cascade • Causing the heart muscle to die and potentially resulting in cardiac arrhythmia
Disease BackgroundSymptoms • Most often characterized by • Chest pain • Tightness in chest • Feeling of heaviness in the chest area • Nausea • Vomiting • SOB • Sweating • Often mistaken for heart burn or indigestion during initial onset • Usually chest pain or tightness will last longer than 20 minutes and increase in intensity
Medical DiagnosisTreatment • Initial Treatment • Nitroglycerin or morphine to numb chest pain • Angioplasty for stent placement to unclog artery – most common emergency treatment • Drug therapy to break apart clots – thrombolytic therapy • Open heart surgery – most severe cases • After initial treatment • Medication to help protect the heart from future cardiovascular events – blood thinner, beta-blocker, or ACE inhibitor • Lifestyle changes • Slowly incorporating exercise • Changing dietary habits • Maintaining control of BP, blood sugar, and cholesterol levels
Disease BackgroundNutritional Intervention Low sodium, low fat, low cholesterol ≤ 30% total kcal from fat – less than 1/3 of those kcal should be saturated 200 mg/day cholesterol Sodium Weigh loss if overweight should be stressed
Disease BackgroundEvidenced Based Research • The New England Journal of Medicine • Goal: to determine if salt reduction in diet would decrease cardiovascular disease • The effects of salt reduction in association with CVD was compared • Decrease in cost of HTN medication was determined • Results • Reducing dietary salt to 3gm a day would reduce new cases of • CHD by 60,000-120,000 • MI by 54,000-99,000 • Stroke by 32,000-66,000 • Medical costs related to CVD would decrease by 10 billion to 24 billion dollars annually
Disease BackgroundPrognosis • Usually, patients without complications can return to normal activity – slowly! • The prognosis is dependent on how much of the heart muscle was damaged • Amount of damage will determine how fast one returns to normal activities • Level of damage may cause arrhythmia, valve problems, or heart rupture • If the heart is no longer able to pump blood as well as it used to, heart failure may be a concern
Application to patient • Initial Diagnosis: Acute Inferior Myocardial Infarction • November 20, 2011 • Symptoms: Chest pain (7 out of 10), nausea, vomiting, and diaphoresis • Sinus arrhythmia, marked segment elevation of inferior leads • Symptoms lasting 2 hr total • JD had a very good understanding of his diagnosis • Although discouraged because he lead an active lifestyle • Unaware of unhealthy eating habits in relation to diagnosis • Connection to strong family history of heart disease
Current Admission • Diagnosis • Acute Inferior Myocardial Infarction • Diagnostic procedures • Metabolic panel, chest panel, and complete blood count • Echocardiogram showed mild decrease in the left atrium, left ventricular function decreased, ejection factor of 45-50%, and trace mitral regurgitation • Chest x-ray found the trachea, heart, and mediastinal structures to be normal, along with clear lungs and pleural spaces
Current admission • Diagnostic procedures cont. • Coronary angiography summary noted • dominant right system single vessel disease • left ventriculography demonstrated severe inferior hypokinesis • The right coronary artery was proximally occluded and enlarged with no collateralization • Initially JD’s cardiac enzymes were • CK: 252 • MB: 4.4 • Troponin: 0.01
Current AdmissionTreatment Stent placement to the right coronary artery occlusion JD was started on the beta-blocker Carvedilol to control his hypertension and treat his valve dysfunction in combination with a statin JD was also prescribed plavix and advised to take an aspirin to help avoid future cardiovascular events
Current AdmissionMedications • Chewable Aspirin • Colace • Coreg • Heparin • Lipitor • Maalox • Morphine • Nitroglycerin • Plavix • Prinivil • Tylenol • Xanax • Zofran
Nutrition Care ProcessNutrition Assessment • Current Diet Order • Cardiac: low fat/cholesterol, 3 gram Na, 0 caffeine • Diet History • Prior to admission JD did not follow any specific diet restrictions; 3 meals a day with an evening snack • Fast food (White Castle, Skyline), Sit down restaurants (Applebee’s 1-2 times/week), and home cooked meals (~4 times/week) • Ate very little vegetables; liked apples, oranges, and grapes; drank 2% milk • Both JD and his wife cook and grocery shop together • JD expressed interest in learning new recipes and substituting items to make each meal more heart healthy
Nutrition Care ProcessNutrition Assessment • 24 hour recall • 25% po intake at breakfast – couple bites of low sodium scrambled eggs and whole wheat english muffin with a small amount of jelly, few sips of orange juice • 100% po intake at lunch – meatloaf, red skin mashed potatoes, vegetable medley (corn, red peppers, green beans), dinner roll, and 4 oz apple juice • 100% po intake at dinner – oven baked chicken, sliced potatoes, vegetables (yellow squash, carrots, and peppers), and 8 oz skim milk • JD avoided his deserts because he is not big on sweets
Nutrition Care ProcessNutrition Assessment • JD had no prior MNT • Prior to admission JD clearly stated he ate few, if any vegetables and likes some fruits. Also, most of his meals during the week consist of fast food. JD’s diet is mainly high fat, high sodium foods • While in the hospital, JD received well balanced meals, and surprisingly he ate the vegetables! • Level of nutritional risk: moderate risk due to high-risk diagnosis and obesity (167% IBW)
Nutrition Care ProcessNutritionAssessment Anthropometrics Biochemical Labs • Height: 5’9” • Weight: 267.7 lb (122 kg) • IBW: 160 lb ± 10% • %IBW: 167% • ABW: 187 lb (85 kg) • Usual wt: 250 lb (114 kg) • % weight change: +7% • BMI: 39.45 kg/m2
Nutrition care processnutrition assessment Macronutrient Needs Calories: 2125 kcal (25 kcal/kg ABW) Protein: 68-85 gm (0.8-1.0 gm/kg ABW) Carbohydrates: 292 gm/day (55% total kcal) Fat: 71 gm/day (30% total kcal) *16.5 gm saturated fat/day (7% total fat)
Nutrition Care ProcessNutrition Diagnosis • Nutrition Diagnosis • NC-3.3 Overweight/obesity • PES Statement • Overweight/obesity related to excessive kcal intake as evidenced by 167% IBW and a BMI of 39.45 kg/m2 • Goals included appropriate weight loss, appropriate oral intake, and appropriate kcal intake • Recommendation • A critical aspect of JD’s recovery is a decrease in weight and a more restrictive diet than he was used to – diet education is key in preventing future cardiac events
Nutrition Care ProcessNutrition Intervention • Plan • Limit foods high in fat, cholesterol, and sodium • Cholesterol intake should be < 200 mg/day • Total percent of fat from kcal should be ≤ 30% • Increase MUFA and decrease saturated fats (7% of kcal/day) • Decreasing total kcal intake to obtain appropriate weight loss • Implement • Provided JD with a list of heart healthy foods • Explained what foods were high in fat, cholesterol, and sodium • Reviewed sources of saturated fat and MUFA • Explained how to read a nutrition fact label • Provided tips eating out • Diet education – low sodium, low fat, low cholesterol – and weight loss are the most important nutrition interventions for JD.
Nutrition Care ProcessMonitoring and Evaluation • While in the hospital JD was receiving a cardiac diet per MD order • Extensive diet education was provided • JD expressed great intentions to follow a low fat, low cholesterol, low sodium diet at home • Monitoring JD’s progress • Keeping track of his daily sodium, cholesterol, and fat intake – comparing day to day • Writing down times a week he eats out and what he ate
Summary • 46 year old male living a moderately active lifestyle • PMH: hypertension and splenectomy • Current medical diagnosis: acute inferior myocardial infarction • Stent placement, EF 45-50% • Medications: carvedilol, aspirin, plavix, statin • Cardiac diet per MD • Educated on importance of low sodium, low fat, low cholesterol diet, along with weight loss • Encouraged to keep records of fat, cholesterol, and sodium for self monitoring
References • Mayo Foundation for Medical Education and Research. Splenectomy. Available at http://www.mayoclinic.com/health/splenectomy/MY01271. Accessed 11/30/2011. • Dugdale, DC. PubMed Health. Hypertension. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001502/. Accessed 11/30/2011. • Chen, MA. PubMed Health. Heart Attack. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001246/. Accessed 11/30/2011. • Khera, AV. Cuchel, M. de la Llera-Moya, M. Rodrigues, A. Burke, MF. Jafri, K. French, BC. Phillips, JA. Muchsavage, ML. Wilensky, RL. Mohler, ER. Rothblat, GH. Rader, DJ. Cholesterol Efflux Capacity, High-Density Lipoprotein Function, and Atherosclerosis. N Engl J Med 2011; 364:127-35. • Siri-Tarino, PW. Sun, Q. Hu, FB. Krauss, RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J ClinNutr 2010; 91:535-46.
References • Bibbins-Domingo, K. Chertow, GM. Coxson, PG. Moran, A. Lightwood, JM. Pletcher, MJ. Goldman, L. Projected Effect of Dietary Salt Reductions on Future Cardiovascular Disease. N Engl J Med 2010; 362:590-9. • TriHealth, Inc. Eating with your Hearts Consent. The Heart and Vascular Center. • Lee, CD. Jacobs, DR. Schreiner, PJ. Iribarren, C. Hankinson, A. Abdominal Obesity and Coronary Artery Calcification in Young Adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J ClinNutr 2007; 86:48-54. • Martin, T. The Normal Range for Creatine Kinase Blood Test. Available at http://www.brighthub.com/science/medical/articles/75706.aspx. Accessed 11/30/2011. • The American Association for Clinical Chemistry. CK-MD, The Test. Available at http://labtestsonline.org/understanding/analytes/ckmb/tab/test. Accessed 11/30/2011. • Pronsky, ZM. Crowe, SR JP. Food Medication Interactions, 16th edition. 2010; p. 3-339. • Khan, S. Myocardial Infarction Pathophysiology. Available at http://www.buzzle.com/articles/myocardial-infarction-pathophysiology.html. Accessed 12/30/11.
- More by User
Evidence Based Strategies for Acute Myocardial Infarction Care: STEMI
Evidence Based Strategies for Acute Myocardial Infarction Care: STEMI. Scott A. Sample DO, FACC Cardiovascular Interventionist April 2010. Why a Systems Approach to Acute Coronary Syndrome Care?.
809 views • 23 slides
Coronary Artery Disease and Acute Myocardial Infarction
Coronary Artery Disease and Acute Myocardial Infarction. NPN 200 Fall 2006. Coronary Artery Disease. Atherosclerosis Define: thickness and hardening of the arteries caused by deposits of fat and fibrin which harden.
746 views • 23 slides
Management of Acute Myocardial Infarction
Management of Acute Myocardial Infarction. Minimal Acceptable vs Optimal Care. Hussien H. Rizk, MD Cairo University. Background. Suspicious chest pain: extremely common cause of ER visits Acute MI: the most costly cardiac cause of ER visits
1.36k views • 14 slides
Universal Definition of Myocardial Infarction, hsTroponin and Clinical Coding of Myocardial Infarction
Contents. Universal definition of MIHigh sensitivity troponin T assayICD 10 coding of acute IHDSummary of suggestions/proposals. Classification of Acute Myocardial Infarction. Type 1: Spontaneous MI related to ischaemia due to a primary coronary event, such as plaque erosion and/or rupture, fissu
844 views • 19 slides
Valsartan in Acute Myocardial Infarction Trial Investigators
VALIANT Trial. Valsartan in Acute Myocardial Infarction Trial Investigators . Presented at American Heart Association Scientific Sessions 2003 Marc A. Pfeffer, et al. N Engl J Med 2003;349:1893-906. VALIANT Trial.
633 views • 5 slides
Evidence Based Strategies for Acute Myocardial Infarction Care: Unstable Angina/Non-STEMI
Evidence Based Strategies for Acute Myocardial Infarction Care: Unstable Angina/Non-STEMI . Scott A. Sample DO, FACC Cardiovascular Interventionist April 2010. Why a Systems Approach to Acute Coronary Syndrome Care?.
1.39k views • 26 slides
Population Trends in the Incidence and Outcomes of Acute Myocardial Infarction
Population Trends in the Incidence and Outcomes of Acute Myocardial Infarction. Robert W. Yeh, MD MSc Massachusetts General Hospital Alan S. Go, MD Kaiser Division of Research University of California, San Francisco. BACKGROUND. The “Ecosystem” of Acute Myocardial Infarction.
638 views • 17 slides
The Tilarginine Acetate Injection in a Randomized International Study in Unstable Acute Myocardial Infarction Patients
The Tilarginine Acetate Injection in a Randomized International Study in Unstable Acute Myocardial Infarction Patients with Cardiogenic Shock (TRIUMPH). Judith S. Hochman on behalf of TRIUMPH Investigators. TRIUMPH was supported by ArgiNOx Pharmaceuticals, Inc.
500 views • 34 slides
Ambulance Victoria and MonashHEART Acute Myocardial Infarction (Mon-AMI) 12 lead ECG project. An update
Ambulance Victoria and MonashHEART Acute Myocardial Infarction (Mon-AMI) 12 lead ECG project. An update. On behalf of the MonAMI Team A Hutchison, Y Malaiapan , B Barger, I Jarvie , E Watkins, G Braitberg , T Kambourakis , JD Cameron, IT Meredith.
469 views • 18 slides
Myocardial Infarction Chapter 18
Myocardial Infarction Chapter 18. Acute Myocardial Infarction (AMI). AKA ST segment elevation myocardial infarction (STEMI) Occlusion of coronary artery causes myocardium to be ischemic and tissue death occurs. AMI continued. Until the ‘80’s, AMI was treated symptomatically
484 views • 17 slides
Chapter 53. Management of ST-Elevation Myocardial Infarction. ST-Elevation Myocardial Infarction (STEMI). Myocardial infarction (MI): necrosis of the myocardium resulting from ischemia STEMI: acute MI caused by complete interruption of regional myocardial blood flow
489 views • 16 slides
Acute Myocardial Infarction
Acute Myocardial Infarction. Dr. Meg- angela Christi Amores. one of the most common diagnoses in hospitalized patients mortality rate from AMI is ~30 % more than half of these deaths occurring before the stricken individual reaches the hospital. Acute MI.
827 views • 14 slides
Myocardial Infarction
Myocardial Infarction. What is Myocardial Infarction? Myocardial Infarction is a result of critical imbalance between coronary blood supply and myocardial demand ( myocytes die due to myocardial ischemia ) . . Incidence of Myocardial Infarction in young Saudi population.
4.29k views • 53 slides
Cardiovascular Care of Older Adults: Acute Myocardial Infarction
Cardiovascular Care of Older Adults: Acute Myocardial Infarction. Karen P. Alexander MD Associate Professor Medicine Duke Clinical Research Institute Duke University Medical Center Durham, NC. Outline. Understand the presentation of ACS in older adults
880 views • 47 slides
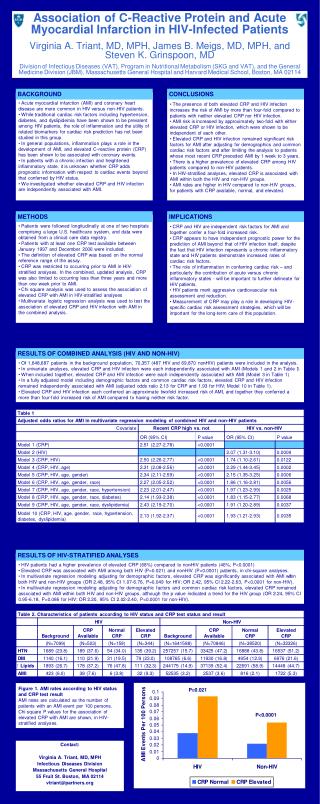
Association of C-Reactive Protein and Acute Myocardial Infarction in HIV-Infected Patients
Association of C-Reactive Protein and Acute Myocardial Infarction in HIV-Infected Patients Virginia A. Triant, MD, MPH, James B. Meigs, MD, MPH, and Steven K. Grinspoon, MD
166 views • 1 slides
ACUTE MYOCARDIAL INFARCTION
ACUTE MYOCARDIAL INFARCTION. AMI. Myocardial Infarction. Occurs when there is a sudden and total occlusion or near-occlusion of blood flowing through an affected coronary artery to an area of heart muscle
2.95k views • 73 slides
Acute Coronary Syndromes
Acute Coronary Syndromes. At the end of this self-study the participant will: Describe the pathophysiology of Acute Coronary Syndromes List signs and symptoms of: Stable angina Unstable angina Acute myocardial infarction. What is ACS?.
2.76k views • 17 slides
Acute coronary disorders Drugs in cardiopulmonary resuscitation
Acute coronary disorders Drugs in cardiopulmonary resuscitation. Advanced Life Support (ALS) algorithm. Acute coronary syndromes. Definitions. The acute coronary syndromes comprise: Unstable angina Non-Q wave myocardial infarction Q wave myocardial infarction
1.02k views • 70 slides
Myocardial Infarction. By Dr. Hanan Said Ali. Learning Objectives. Define of myocardial infarction. Explain Pathophysiology of MI. Enumerate Clinical Manifestation of MI. Identify the diagnostic measures of MI. Discus complication of myocardial infarction.
1.54k views • 33 slides
Myocardial ischemia and infarction
Myocardial ischemia and infarction. Physiology Factors determining myocardial oxygen supply and demand Myocardial oxygen demand 2. Mechanisms of myocardial ischemia 3. Acute adaptations to ischemia 4. Ischemic myocardial disease 5. Myocardial infarction.
1.48k views • 47 slides
Acute Myocardial Infarctions
Acute Myocardial Infarctions. Howard L. Sacher, D.O. Chief, Division of Cardiology Adjunct Clinical Associate Professor of Medicine New York College of Osteopathic Medicine. To understand current concepts of the pathophysiology of acute myocardial infarction (AMI).
1.32k views • 104 slides

Table S2. Sequences of primers used for RT-PCR
Supplementary Materials. Table S1. Features of patients with acute myocardial infarction or unstable angina and control subjects. AMI: acute myocardial infarction. * ANOVA test after the values were logarithm-transformed, # Chi-square test. ACEI: angiotensin convert enzyme inhibitors.
203 views • 8 slides
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Patient presentation.
Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency department because this episode was unrelenting and more severe. Mr. Smith describes his current pain as severe and sharp, and also complains of nausea and shortness of breath. Vital signs are HR: 110 BP: 150/90 RR: 30 Temp 97.6 O2 Sat: 92% on 2L nasal cannula, EKG shows ST segment elevation in leads II, III and AVf. Labs were drawn, including an elevated troponin (4.23 ng/ml), and slightly elevated white blood cell count (13.6 × 10 9 /L) .
Past Medical History
Type II diabetes (age 47), dyslipidemia (age 33), atherosclerosis (age 52), hypertension (age 49), obesity (age 33), viral pneumonia (age 29), hiatal hernia (age 28), peptic ulcer disease (age 41)
Family Medical History
Mother (deceased) – atrial fibrillation (diagnosed at age 45), died of MI (age 65)
Father (83) – obesity, type II diabetes (diagnosed at 50), COPD (diagnosed at 55)
Social History
Smoker (20 pack years), worked in an office sitting at a desk his whole career (35 years), recently began working out at his local gym since retiring this year.
Myocardial Infarction (MI) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Definition of Myocardial Infarction (MI)
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. It is a leading cause of death worldwide and a significant public health concern.
Introduction to Myocardial Infarction (MI)
This nursing case study aims to provide a comprehensive understanding of myocardial infarction by delving into its various aspects, including its pathophysiology, risk factors, clinical presentation, diagnostic methods, and management strategies. Through the exploration of a fictional patient’s journey, we will shed light on the intricate nature of this life-threatening condition and highlight the importance of early recognition and intervention.
Background and Significance of Myocardial Infarction
Myocardial infarction is a sudden and often catastrophic event that can have profound consequences on an individual’s health and well-being. Understanding its underlying mechanisms and risk factors is essential for healthcare professionals, as timely intervention can be life-saving. This case study not only serves as a learning tool but also emphasizes the critical role of medical practitioners in identifying and managing myocardial infarctions promptly.
Pathophysiology of Myocardial Infarction
A crucial aspect of comprehending myocardial infarction is exploring its pathophysiology. We will delve into the intricate details of how atherosclerosis, the buildup of plaque in coronary arteries, leads to the formation of blood clots and the subsequent interruption of blood flow to the heart muscle. This disruption in blood supply triggers a cascade of events, ultimately resulting in the death of cardiac cells.
Risk Factors of Myocardial Infarction
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction.
Clinical Presentation Myocardial Infarction
Recognizing the signs and symptoms of myocardial infarction is crucial for timely intervention. We will present a fictional patient’s experience, illustrating the typical clinical presentation, which often includes chest pain or discomfort, shortness of breath, nausea, lightheadedness, and diaphoresis. Through this patient’s journey, we will highlight the importance of accurate symptom assessment and prompt medical attention.
Diagnostic Methods for Myocardial Infarction
Modern medicine offers various diagnostic tools to confirm a myocardial infarction swiftly and accurately. This case study will explore these diagnostic methods, such as electrocardiography (ECG), cardiac biomarkers, and imaging techniques like coronary angiography. By understanding these diagnostic modalities, healthcare professionals can make informed decisions and initiate appropriate treatments promptly.
Management Strategies for Myocardial Infarction
The management of myocardial infarction involves a multidisciplinary approach, including medication, revascularization procedures, and lifestyle modifications. We will discuss the fictional patient’s treatment plan, emphasizing the importance of reestablishing blood flow to the affected heart muscle and preventing further complications.
Nursing Case Study for Myocardial Infarction (MI)
Having established a foundational understanding of myocardial infarction, we will now delve deeper into Mr. Salazar’s case, tracing his journey through diagnosis, treatment, and recovery. This in-depth examination will shed light on the real-world application of the principles discussed in the introduction, providing valuable insights into the clinical management of myocardial infarction and its impact on patient outcomes.
Mr. Salazar, a 57-year-old male, arrives at the Emergency Department (ED) with complaints of chest pain that began approximately one hour after dinner while he was working. He characterizes the discomfort as an intense “crushing pressure” located centrally in his chest, extending down his left arm and towards his back. He rates the pain’s severity as 4/10. Upon examination, Mr. Salazar exhibits diaphoresis and pallor, accompanied by shortness of breath (SOB).
What further nursing assessments need to be performed for Mr. Salazar?
- Heart Rate (HR): The number of heartbeats per minute.
- Blood Pressure (BP): The force of blood against the walls of the arteries, typically measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
- Respiratory Rate (RR): The number of breaths a patient takes per minute.
- Body Temperature (Temp): The measurement of a patient’s internal body heat.
- Oxygen Saturation (SpO2): The percentage of oxygen in the blood.
- S1: The first heart sound, often described as “lub,” is caused by the closure of the mitral and tricuspid valves.
- S2: The second heart sound, known as “dub,” results from the closure of the aortic and pulmonic valves.
- These sounds provide important diagnostic information about the condition of the heart.
- Clear: Normal, healthy lung sounds with no added sounds.
- Crackles (Rales): Discontinuous, often high-pitched sounds are heard with conditions like pneumonia or heart failure.
- Wheezes: Whistling, musical sounds often associated with conditions like asthma or chronic obstructive pulmonary disease (COPD).
- Pulses refer to the rhythmic expansion and contraction of arteries with each heartbeat. Common pulse points for assessment include the radial artery (wrist), carotid artery (neck), and femoral artery (groin). Evaluating pulses helps assess the strength, regularity, and rate of blood flow.
- Edema is the abnormal accumulation of fluid in body tissues, leading to swelling. It can occur in various body parts and may indicate underlying conditions such as heart failure, kidney disease, or localized injury. Edema assessment involves evaluating the degree of swelling and its location.
- Skin condition (temperature, color, etc.)
What interventions do you anticipate being ordered by the provider?
- Oxygen therapy involves administering oxygen to a patient to increase the level of oxygen in their blood. It is used to treat conditions such as respiratory distress, and hypoxia (low oxygen levels), and to support patients with breathing difficulties.
- Nitroglycerin is a medication used to treat angina (chest pain) and to relieve symptoms of heart-related conditions. It works by relaxing and widening blood vessels, which improves blood flow to the heart, reducing chest pain.
- Aspirin is a common over-the-counter medication and antiplatelet drug. In the context of myocardial infarction (heart attack), it is often administered to reduce blood clot formation, potentially preventing further blockage in coronary arteries.
- A 12-lead EKG is a diagnostic test that records the electrical activity of the heart from 12 different angles. It provides information about the heart’s rhythm, rate, and any abnormalities, helping diagnose conditions like arrhythmias, heart attacks, and ischemia.
- Cardiac enzymes are proteins released into the bloodstream when heart muscle cells are damaged or die, typically during a heart attack. Measuring these enzymes, such as troponin and creatine kinase-MB (CK-MB), helps confirm a heart attack diagnosis and assess its severity.
- A chest X-ray is a diagnostic imaging procedure that creates images of the chest and its internal structures, including the heart and lungs. It is used to identify issues like lung infections, heart enlargement, fluid accumulation, or fractures in the chest area.
- Possibly an Echocardiogram
Upon conducting a comprehensive assessment, it was observed that the patient exhibited no signs of jugular vein distention (JVD) or edema. Auscultation revealed normal heart sounds with both S1 and S2 present, while the lungs remained clear, albeit with scattered wheezes. The patient’s vital signs were recorded as follows:
- BP 140/90 mmHg SpO 2 90% on Room Air
- HR 92 bpm and regular Ht 173 cm
- RR 32 bpm Wt 104 kg
- Temp 36.9°C
The 12-lead EKG repor t indicated the presence of “Normal sinus rhythm (NSR) with frequent premature ventricular contractions (PVCs) and three- to four-beat runs of ventricular tachycardia (VT).” Additionally, there was ST-segment elevation in leads I, aVL, and V2 through V6 (3-4mm), accompanied by ST-segment depression in leads III and aVF.
Cardiac enzyme levels were collected but were awaiting results at the time of assessment. A chest x-ray was also ordered to provide further diagnostic insights.
In response to the patient’s condition, the healthcare provider prescribed the following interventions:
- Aspirin: 324 mg administered orally once.
- Nitroglycerin: 0.4 mg administered sublingually (SL), with the option of repeating the dose every five minutes for a maximum of three doses.
- Morphine: 4 mg to be administered intravenously (IVP) as needed for unrelieved chest pain.
- Oxygen: To maintain oxygen saturation (SpO2) levels above 92%.
These interventions were implemented to address the patient’s myocardial infarction (heart attack) and alleviate associated symptoms, with a focus on relieving chest pain, improving oxygenation, and closely monitoring vital signs pending further diagnostic results.
What intervention should you, as the nurse, perform right away? Why?
- Apply oxygen – this can be done quickly and easily and can help to prevent further complications from low oxygenation.
- Oxygen helps to improve oxygenation as well as to decrease myocardial oxygen demands.
- Often it takes a few minutes or more for medications to be available from the pharmacy, so it makes sense to take care of this intervention first.
- ABC’s – breathing/O 2 .
What medication should be the first one administered to this patient? Why? How often?
- Nitroglycerin 0.4mg SL – it is a vasodilator and works on the coronary arteries. The goal is to increase blood flow to the myocardium. If this is effective, the patient merely has angina. However, if it is not effective, the patient may have a myocardial infarction.
- Aspirin should also be given, but it is to decrease platelet aggregation and reduce mortality. While it can somewhat help prevent the worsening of the blockage, it does little for the current pain experienced by the patient.
- Morphine should only be given if the nitroglycerin and aspirin do not relieve the patient’s chest pain.
What is the significance of the ST-segment changes on Mr. Salazar's 12-lead EKG?
- ST-segment changes on a 12-lead EKG indicate ischemia (lack of oxygen/blood flow) or infarction (death of the muscle tissue) of the myocardium (heart muscle).
- This indicates an emergent situation. The patient’s coronary arteries are blocked and need to be reopened by pharmacological (thrombolytic) or surgical (PCI) intervention.
- Time is tissue – the longer the coronary arteries stay blocked, the more of the patient’s myocardium that will die. Dead heart tissue doesn’t beat.
Mr. Salazar’s chest pain was unrelieved after three (3) doses of sublingual nitroglycerin (NTG). Morphine 5 mg intravenous push (IVP) was administered, as well as 324 mg chewable baby aspirin. His pain was still unrelieved at this point
Mr. Salazar’s cardiac enzyme results were as follows:
Troponin I 3.5 ng/mL
Based on the results of Mr. Salazar's labs and his response to medications, what is the next intervention you anticipate? Why?
- Mr. Salazar needs intervention. He will either receive thrombolytics or a heart catheterization (PCI).
- Based on the EKG changes, elevated Troponin level, and the fact that his symptoms are not subsiding, it’s possible the patient has a significant blockage in one or more of his coronary arteries.
- It seems as though it may be an Anterior-Lateral MI because ST elevation is occurring in I, aVL, and V 2 -V 6 .
Mr. Salazar was taken immediately to the cath lab for a Percutaneous Coronary Intervention (PCI). The cardiologist found a 90% blockage in his left anterior descending (LAD) artery. A stent was inserted to keep the vessel open.
What is the purpose of Percutaneous Coronary Intervention (PCI), also known as a heart catheterization?
- A PCI serves to open up any coronary arteries that are blocked. First, they use contrast dye to determine where the blockage is, then they use a special balloon catheter to open the blocked vessels.
- If that doesn’t work, they will place a cardiac stent in the vessel to keep it open.[ /faq]
[faq lesson="true" blooms="Application" question="What is the expected outcome of a PCI? What do you expect to see in your patient after they receive a heart catheterization?"]
- Blood flow will be restored to the myocardium with minimal residual damage.
- The patient should have baseline vital signs, relief of chest pain, normal oxygenation status, and absence of heart failure symptoms (above baseline).
- The patient should be able to ambulate without significant chest pain or SOB.
- The patient should be free from bleeding or hematoma at the site of catheterization (often femoral, but can also be radial or (rarely) carotid.
Mr. Salazar tolerated the PCI well and was admitted to the cardiac telemetry unit for observation overnight. Four (4) hours after the procedure, Mr. Salazar reports no chest pain. His vital signs are now as follows:
- BP 128/82 mmHg SpO 2 96% on 2L NC
- HR 76 bpm and regular RR 18 bpm
- Temp 37.1°C
Mr. Salazar will be discharged home 24 hours after his arrival to the ED and will follow up with his cardiologist next week.
What patient education topics would need to be covered with Mr. Salazar?
- He should be taught any dietary and lifestyle changes that should be made.
- Diet – low sodium, low cholesterol, avoid sugar/soda, avoid fried/processed foods.
- Exercise – 30-45 minutes of moderate activity 5-7 days a week, u nless instructed otherwise by a cardiologist. This will be determined by the patient’s activity tolerance – how much can they do and still be able to breathe and be pain-free?
- Stop smoking and avoid caffeine and alcohol.
- Medication Instructions
- Nitroglycerin – take one SL tab at the onset of chest pain. If the pain does not subside after 5 minutes, call 911 and take a second dose. You can take a 3rd dose 5 minutes after the second if the pain does not subside. Do NOT take if you have taken Viagra in the last 24 hours.
- Aspirin – take 81 mg of baby aspirin daily
- Anticoagulant – the patient may be prescribed an anticoagulant if they had a stent placed. They should be taught about bleeding risks.
- When to call the provider – CP unrelieved by nitroglycerin after 5 minutes. Syncope. Evidence of bleeding in stool or urine (if on anticoagulant). Palpitations, shortness of breath, or difficulty tolerating activities of daily living.
Linchpins for Myocardial Infarction Nursing Case Study
In summary, Mr. Salazar’s case highlights the urgency of recognizing and responding to myocardial infarction promptly. The application of vital signs, EKG, cardiac enzymes, and medications like aspirin, nitroglycerin, and morphine played a pivotal role in his care. Diagnostic tools like echocardiography and chest X-rays contributed to a comprehensive evaluation.
Nurses must remain vigilant and compassionate in such emergencies. This case study emphasizes the importance of adhering to best practices in the assessment, diagnosis, and management of myocardial infarction, with the ultimate goal of achieving favorable patient outcomes.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
Acute coronary syndrome, associated data.

The paramedics brought a 60-year-old man to the emergency department after a sudden onset of shortness of breath with a subsequent drop in the Glasgow Coma Scale (GCS). On arrival the patient looked peri-arrest. His O 2 saturations were 84% on 15 L of oxygen. He had gasping breathing with a completely silent chest and the GCS was 6/15 (E=1, V=1, M=4). The blood gas revealed type-2 respiratory failure. The chest X-ray was unremarkable and ECG was not indicative for cardiac catheterisation lab activation. Bedside shock scan was done which showed global hypokinesia of the left ventricle. In spite of unconvincing ECG and chest X-ray, an acute cardiac event was diagnosed in view of an abnormal bedside echo. The patient was transferred to the cardiac catheterisation lab for urgent percutaneous coronary intervention which revealed critical stenosis of the left main stem coronary artery, which was successfully stented. The patient had a good recovery from the life-threatening event.
Patients with undifferentiated shock can be a real challenge for the Emergency Physician. To diagnose the underlying cause in a shocked patient in a timely manner is vital as the treatment options may be completely different and are also time critical. It is imperative for emergency physicians to equip themselves with ultrasound skills as it can play a key role in the patient's management.
This case is an excellent example of the importance of bedside ultrasound scan utilisation. The patient's presentation was very atypical for an acute coronary event. His bedside ECG ( figure 1 ) and chest X-ray (CXR; figure 2 ) were not helpful in the diagnosis until an ultrasound scan ( video 1 ) revealed a significant left ventricle wall motion abnormality and explained the patient's condition.

ECG showing sinus tachycardia with QRS at upper normal limit of 120 ms. The voltage criteria for left ventricular hypertrophy is met. No features to suggest acute ST-elevation myocardial infarction are obvious.

Chest anteroposterial supine X-ray not showing any major areas of airspace opacification or pneumothorax.
Video 1
A sub-xiphoid view of heart during bedside ultrasound shock scan shows almost globally akinetic left ventricle .Right ventricle seems to be contracting normally. No pericardial fluid was seen.
Case presentation
Our patient was a 60-year-old man who was brought to the emergency department (ED) by paramedics after a sudden onset of shortness of breath.
On scene when attended by the paramedics the patient was in significant respiratory distress and was diaphoretic. There was no history of chest pain. On arrival to the ED, he was unresponsive but the airway was patent. The patient's breathing effort was very poor and he was gasping. His trachea was central and chest was completely silent. His breathing was supported initially with a bag valve mask and then subsequently the patient was intubated in view of his low Glasgow Coma Scale (GCS). He was easy to ventilate and the chest movements were bilateral and equal. His first blood pressure reading was 170/110 mm Hg and pulse rate was about 120/min. His neck veins were not engorged and he had equal blood pressure in both arms. His GCS was 6/15 (E=1, V=1, M=4). The rest of the examination was unremarkable. We could not figure out the cause of the patient's acute deterioration after completing the primary survey.
The patient was continuously monitored and serial ECGs were carried out. The ECGs were discussed with the Cardiology Registrar who was not convinced of any acute cardiac event.
The patient had no significant medical or surgical history and was not on any medications.
Investigations
Routine bloods in the ED were:
- Haemoglobin 158 g/L
- White cell count 17.1×10 9 /L
- Sodium 136 mmol/L
- Potassium 4 mmol/L
- Urea 6.1 mmol/L
- Creatinine 97 μmol/L
- Estimated glomerular filtration rate 73 mL/min/L.73 m 2
- C reactive protein <5 mg/L
- Troponin I 115 μg/L
- International normalised ratio 1.0
- D-dimer 0.95 μg/L
- Arterial blood gas: pH 6.98, pCO 2 16.02 kPa, pO 2 21.7 kPa, HCO 3 27.8 mmol/L, base excess −7.5, lactate 2.7.
CXR showed no significant pathology.
ECG showed sinus tachycardia with left ventricular hypertrophy.
Focused bedside cardiac ultrasound scan 1 and shock scan 2 conducted by the ED Registrar showed global hypokinesia of the left ventricle.
Official echo performed later by the cardiologist showed severe systolic dysfunction and apical thrombus.
The coronary angiogram revealed severe ostial stenosis of the left main coronary artery.
Differential diagnosis
A patient with low GCS, shortness of breath and type-2 respiratory failure may have wide differentials like life-threatening asthma, tension pneumothorax, acute cardiac events or massive pulmonary embolism. Treatment of each is quite different and time critical. An early shock scan using ultrasound helped us narrow our differential towards a cardiac pathology.
On the way to hospital, paramedics had given the patient salbutamol and ipratropium nebulisation, intravenous hydrocortisone (100 mg) and intravenous furosemide (40 mg).
In the ED, initially the patient's breathing was supported with bag-valve-mask ventilation with 15 L of O 2 . The patient was also given intravenous salbutamol 0.5 mg bolus, magnesium sulfate 2 g and 500 mL of 0.9% normal saline.
ITU were consulted to secure the airway. The patient was intubated and transferred to the cardiac catheterisation laboratory for immediate percutaneous coronary intervention (PCI).
Outcome and follow-up
A 4.5×13 mm stent was placed in the left main artery during emergency PCI. Postprocedure, the patient was admitted to the intensive care unit for 1 day and then transferred to the ward for monitoring. After a few days of observation the patient was discharged home with medicines and for follow-up in the cardiology clinic.
We found the patient's presentation very challenging. The patient had no chest pain and had low GCS. His CXR and ECG were non-diagnostic. Atypical presentations in acute coronary syndrome are known phenomenon where there is absence of chest pain. Although some high-risk factors have been identified, 3 for example older age (72.9 years), female gender, non-white race and comorbidities (diabetes, stroke and heart failure); our patient had none of them. The National Registry of Myocardial Infarction 2 database showed that 33% patients did not present with chest pain. 4 Patients with myocardial infarction without chest pain are less quickly diagnosed and treated and have higher adjusted odds of hospital mortality, regardless of whether they have an ST-segment elevation. 5 6 The presence of silent chest is a possible presentation in early stages of cardiogenic shock and has mortality of about 70% due to the difficulty in diagnosis. 7 Although our patient was presented atypically with very little history available as a result of low GCS and non-specific ECG, a quick bedside (see video 1 ) echo which showed a globally hypokinetic left ventricle proved to be a life saver as the right diagnosis was made and critical minutes were saved by not making other unnecessary investigations such as CT of the head.
Bedside ultrasound is widely used by most physicians during the management of trauma patients but its use in the assessment of sick medical patients is still not considered an important diagnostic tool. There is enough evidence 8 to suggest that the use of ultrasound during the initial assessment of sick medical patients can increase the diagnostic accuracy significantly as shown in this case.
Learning points
- Ultrasound is an important tool for emergency and acute care physicians.
- Bedside ultrasound should be performed early during the initial assessment of sick medical patients to diagnose life-threatening emergencies.
- Acute coronary syndrome (ACS) with flash pulmonary oedema can mimic life-threatening asthma and respiratory failure.
- Atypical presentations of ACS should always be kept in mind.
Contributors: Both the authors have dealt with the patient and contributed to the case report.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.

IMAGES
VIDEO
COMMENTS
Case presentation on Myocardial Infarction. Ram Bahadur Basyal, a 59-year-old male, was admitted to the hospital with complaints of chest pain, shoulder pain, shortness of breath, and vomiting. He was diagnosed with anteroseptal myocardial infarction. His condition gradually improved over his hospital stay through medication, oxygen ...
Case Presented by Final Year MBBS sudents of Frontier Medical College at the 1st Clinico-Pathological Conference for the year 2015.The Presentation is divided into two parts. First part is about a case of an Acute ST Segment elevated Myocardial Infarction with. Its management at the Hospital and the findings.
Jan 2, 2019 • Download as PPTX, PDF •. 11 likes • 2,352 views. N. Netal Patel. this is a case study on a patient with myocardial infarction. Health & Medicine. 1 of 32. Download now. Case on myocardial infarction - Download as a PDF or view online for free.
Case presentation on MYOCARDIAL INFARCTION. Aug 18, 2019 • Download as PPTX, PDF •. 8 likes • 4,981 views. Vigneswari Paladugu. A blockage of blood flow to the heart muscle. A heart attack is a medical emergency.A heart attack usually occurs when a blood clot blocks blood flow to the heart.Without blood,tissues loses oxygen and dies.
Case presentation myocardial infarction. Jan 15, 2016 • Download as PPTX, PDF •. 15 likes • 8,417 views. Crystal Capistrano. case study. Health & Medicine. 1 of 56. Download now. Case presentation myocardial infarction - Download as a PDF or view online for free.
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
MYOCARDIAL INFARCTION MI is defined as a diseased condition which is caused by reduced blood flow in a coronary artery due to atherosclerosis & occlusion of an artery by an embolus or thrombus. MI or heart attack is the irreversible damage of myocardial tissue caused by prolonged ischaemia & hypoxia. ... studies revealed a prediction that India ...
Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Read more. Education. 1 of 31.
STEMI comprises 25-40% of myocardial infarction presentations. In-hospital mortality 5-6%. One year mortality 7-18% has significantly decreased with appropriate care including primary PCI and GDMT. Benjamin EJ, et al. Heart Disease and Stroke Statistics 2017 Update, Report From The AHA.
Presentation Transcript. Case study 1: acute myocardial infarction Megan Fuchs Good Sam Dietetic Intern January 5, 2012. Patient ProfilePersonal Information • 46 year old white male • Lives in Cincinnati, OH with wife, daughter, and grandson • Leads a physically active lifestyle • Works in maintenance - constant movement • Lifts ...
Smith describes his current pain as severe and sharp, and also complains of nausea and shortness of breath. Vital signs are HR: 110 BP: 150/90 RR: 30 Temp 97.6 O2 Sat: 92% on 2L nasal cannula, EKG shows ST segment elevation in leads II, III and AVf. Labs were drawn, including an elevated troponin (4.23 ng/ml), and slightly elevated white blood ...
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental ...
Case Presentation on MI - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. The document describes a case study of a 60-year-old female patient admitted to the hospital with symptoms of myocardial infarction including chest pain and shortness of breath. It provides details on her medical ...
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be "silent" and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death.[1] Most myocardial infarctions are due to underlying coronary artery disease, the ...
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
A Case Report: Acute Myocardial Infarction in a 29-year-old Male. 2/5/2019 Aaron Tiffee, MD, FACEP , Zariad Saran, DO , Tyler Ingersoll, MS. The HEART score is a go-to tool in assessing the risk of an acute coronary syndrome. But in this case, a score of 3 did not mean the 29-year-old patient was safe. Cardiovascular disease (CVD) is currently ...
Most deaths from myocardial infarction occur in the first hours of disease onset, with 40-65% occurring within the first hour and approximately 80% in the first 24 hours 5,6. The recently implemented therapies for MI treatment have been proven to modify patient evolution and prognosis.
2. Epidemiology and risk factors. Multiple studies have explored the epidemiology of MINOCA within their population with prevalence found to be between 5-25% of all MI events [6, 7, 8].The VIRGO study reported that among young adults aged 18-55, women had 5 times greater odds of having MINOCA than men and they had comparable clinical outcomes as those who had myocardial infarction due to ...
PK !¤F$¶Û ! ppt/presentation.xmlìšßn£F Æï+õ ,n+Çó fˆâ¬œd]UJ¥h"}‚Ç Z p6Ùjß½3˜˜sr ››¦ µVÊ Î™áÌï› ù gŸž7ùäÉÖMV 󀟰`b‹´\eÅÃøz·œš`Ò´I±Jò²°óàÅ6Á§ó_ 9«N«Ú6¶h"Ö5 ¸nŠæ4™ m[ ÎfMúh7IsRV¶p±uYo'ÖýZ?ÌVuòÝu¿Ég‚±h¶I²"èÛ×ïi_®×Yj¯Êt»q—ßuRÛ¼«£y̪海ê=½ÁQà'šäÉÞnï Û.Ë¢m àÜ ...
1. Introduction. Cardiovascular disease, including myocardial infarction (MI), continues to be one of the leading causes of all deaths. The risk of death is at least 30% higher than in the overall reference population at both 1-3 and 3-5 years after MI [].In Poland, about 1.2-1.5 million people suffer from coronary heart disease, and about 100,000 people experience MI.
The National Registry of Myocardial Infarction 2 database showed that 33% patients did not present with chest pain. 4 Patients with myocardial infarction without chest pain are less quickly diagnosed and treated and have higher adjusted odds of hospital mortality, regardless of whether they have an ST-segment elevation. 5 6 The presence of ...
ED treatment. Internal STEMI Code paged at 22:55 Patient arrived at 22:57 Interventions Chest X‐Ray Assessment Repeat 12 Lead EKG. 5,000 Units IV Heparin. ED treatment. 22:05 (8 minutes after arrival) Compressions started Defibrillated at 150 J. ED treatment. 18 minutes in ED. Interventions Continued 180 mg ticagrelor Patient undressed ...
This case study describes a 54-year-old male patient who presented to the emergency department with complaints of chest pain, breathlessness, and giddiness. He was diagnosed with a ST-segment elevated myocardial infarction. His medical history included diabetes and smoking. A physical exam found mild chest pain and normal vital signs. Investigations revealed elevated liver enzymes, cholesterol ...