How Gender Reassignment Surgery Works (Infographic)
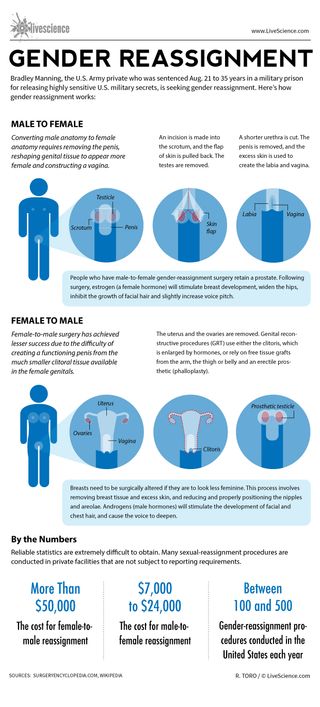
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.

Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Scientists made mice with Y chromosomes female by deleting just 6 tiny molecules
Man's years of premature ejaculation had a rare cause
Why are some people's mosquito bites itchier than others'? New study hints at answer
Most Popular
- 2 NASA's newly unfurled solar sail has started 'tumbling' end-over-end in orbit, surprising observations show
- 3 Over 40% of pet cats play fetch — but scientists aren't quite sure why
- 4 Massive helium reservoir in Minnesota could solve US shortage
- 5 Boat-ramming orcas may be using yachts as target practice toys, scientists suggest
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary , to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis )
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
- A to Z Guides
What Is Gender Affirmation Surgery?

Surgery to change the appearance of your body is a common choice for all kinds of people. There are many reasons that people might want to alter their appearance. For transgender or gender nonconforming people, making changes to their bodies is a way of affirming their identity.
A trans person can choose from multiple procedures to make their appearance match their self-identified gender identity. Doctors refer to this as gender "affirmation" surgery.
Trans people might decide to have surgery on their chest, genitals, or face. These surgeries are personal decisions, and each person makes their own choices about what is right for them.
Learn more about gender affirmation surgery and how it helps trans people.
What Does It Mean to Be Transgender or Nonbinary?
Transgender is a word to describe people whose gender identity or gender expression doesn't match the sex they were assigned at birth. Typically, parents and doctors assume a baby's gender based on the appearance of their genitals. But some people grow up and realize that their sense of who they are isn't aligned with how their bodies look. These people are considered transgender.
Trans people may identify as a different gender than what they were assigned at birth. For example, a child assigned male at birth may identify as female. Nonbinary people don't identify as either male or female. They may refer to themselves as "nonbinary" or "genderqueer."
There are many options for trans and nonbinary people to change their appearance so that how they look reflects who they are inside. Many trans people use clothing, hairstyles, or makeup to present a particular look. Some use hormone therapy to refine their secondary sex characteristics. Some people choose surgery that can change their bodies and faces permanently.
Facial Surgery
Facial plastic surgery is popular and accessible for all kinds of people in the U.S. It is not uncommon to have a nose job or a facelift . Cosmetic surgery is great for improving self-esteem and making people feel more like themselves. Trans people can use plastic surgery to adjust the shape of their faces to better reflect their gender identity.
Facial feminization. A person with a masculine face can have surgeries to make their face and neck look more feminine. These can be done in one procedure or through multiple operations. They might ask for:
- Forehead contouring
- Jaw reduction
- Chin surgery
- Hairline advancement
- Cheek augmentation
- Rhinoplasty
- Lip augmentation
- Adam's apple reduction
Facial masculinization. Someone with a feminine face can have surgery to make their face look more masculine. The doctor may do all the procedures at one time or plan multiple surgeries. Doctors usually offer:
- Forehead lengthening
- Jaw reshaping
- Chin contouring
- Adam's apple enhancement
Top Surgery
Breast surgeries are very common in America. The shorthand for breast surgeries is "top surgery." All kinds of people have operations on their breasts , and there are a lot of doctors who can do them. The surgeries that trans people have to change their chests are very similar to typical breast enhancement or breast removal operations.
Transfeminine. When a trans person wants a more feminine bustline, that's called transfeminine top surgery. It involves placing breast implants in a person's chest. It's the same operation that a doctor might do to enlarge someone's breasts or for breast reconstruction .
Transmasculine. Transmasculine top surgery is when a person wants a more masculine chest shape. It is similar to a mastectomy . The doctor removes the breast tissue to flatten the whole chest. The doctor can also contour the skin and reposition the nipples to look more like a typical man's chest.
Bottom Surgery
For people who want to change their genitals, some operations can do that. That is sometimes called bottom surgery. Those are complicated procedures that require doctors with a lot of experience with trans surgeries.
Transmasculine bottom surgery. Some transmasculine people want to remove their uterus and ovaries. They can choose to have a hysterectomy to do that. This reduces the level of female hormones in their bodies and stops their menstrual cycles.
If a person wants to change their external genitals, they can ask for surgery to alter the vaginal opening. A surgeon can also construct a penis for them. There are several techniques for doing this.
Metoidioplasty uses the clitoris and surrounding skin to create a phallus that can become erect and pass urine. A phalloplasty requires grafting skin from another part of the body into the genital region to create a phallus. People can also have surgery to make a scrotum with implants that mimic testicles.
Transfeminine bottom surgery. People who want to reduce the level of male hormones in their bodies may choose to have their testicles removed. This is called an orchiectomy and can be done as an outpatient operation.
Vaginoplasty is an operation to construct a vagina . Doctors use the tissue from the penis and invert it into a person's pelvic area. The follow-up after a vaginoplasty involves using dilators to prevent the new vaginal opening from closing back up.
How Much Does Gender Affirmation Surgery Cost?
Some medical insurance companies will cover some or most parts of your gender-affirming surgery. But many might have certain "exclusions" listed in the plan. They might use language like "services related to sex change" or "sex reassignment surgery." These limitations may vary by state. It's best to reach out to your insurance company by phone or email to confirm the coverage or exclusions.
If your company does cover some costs, they may need a few documents before they approve it.
This can include:
- A gender dysphoria diagnosis in your health records. It's a term used to describe the feeling you have when the sex you're assigned at birth does not match with your gender identity. A doctor can provide a note if it's necessary.
- A letter of support from a mental health professional such as a social worker, psychiatrist , or a therapist.
Gender affirmation surgery can be very expensive. It's best to check with your insurance company to see what type of coverage you have.
If you're planning to pay out-of-pocket, prices may vary depending on the various specialists involved in your case. This can include surgeons, primary care doctors, anesthesiologists, psychiatrists, social workers, and counselors. The procedure costs also vary, and the total bill will include a number of charges, including hospital stay, anesthesia, counseling sessions, medications, and the procedures you elect to have.
Whether you choose facial, top, or bottom or a combination of these procedures, the total bill after your hospital stay can cost anywhere from $5,400 for chin surgery to well over $100,000 for multiple procedures.
Recovery and Mental Health After Gender Affirmation Surgery
Your recovery time may vary. It will depend on the type of surgery you have. But swelling can last anywhere from 2 weeks for facial surgery to up to 4 months or more if you opted for bottom surgery.
Talk to your doctor about when you can get back to your normal day-to-day routine. But in the meantime, make sure to go to your regular follow-up appointments with your doctor. This will help them make sure you're healing well post-surgery.
Most trans and nonbinary people who get gender affirmation surgery report that it improves their overall quality of life. In fact, over 94% of people who opt for surgery say they are satisfied with the results.
Folks who have mental health support before surgery tend to do better, too. One study found that after gender affirmation surgery, a person's need for mental health treatment went down by 8%.
Not all trans and nonbinary people choose to have gender affirmation surgery, or they may only have some of the procedures available. If you are considering surgery, speak with your primary care doctor to discuss what operations might be best for you.
Top doctors in ,
Find more top doctors on, related links.
- Health A-Z News
- Health A-Z Reference
- Health A-Z Slideshows
- Health A-Z Quizzes
- Health A-Z Videos
- WebMDRx Savings Card
- Coronavirus (COVID-19)
- Hepatitis C
- Diabetes Warning Signs
- Rheumatoid Arthritis
- Morning-After Pill
- Breast Cancer Screening
- Psoriatic Arthritis Symptoms
- Heart Failure
- Multiple Myeloma
- Types of Crohn's Disease
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Preparing for Gender Affirmation Surgery: Ask the Experts
Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
What kind of care should I expect as a transgender individual?
What kind of care should I expect as a transgender individual? Before beginning the process, we recommend reading the World Professional Association for Transgender Health Standards Of Care (SOC). The standards were created by international agreement among health care clinicians and in collaboration with the transgender community. These SOC integrate the latest scientific research on transgender health, as well as the lived experience of the transgender community members. This collaboration is crucial so that doctors can best meet the unique health care needs of transgender and gender-diverse people. It is usually a favorable sign if the hospital you choose for your gender affirmation surgery follows or references these standards in their transgender care practices.
Can I still have children after gender affirmation surgery?
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals. Discuss all your options, such as sperm banking and egg freezing, with your doctor so that you can create the best plan for future family building. JHCTGEH has fertility specialists on staff to meet with you and develop a plan that meets your goals.
Are there other ways I need to prepare?
It is very important to prepare mentally for your surgery. If you haven’t already done so, talk to people who have undergone gender affirmation surgeries or read first-hand accounts. These conversations and articles may be helpful; however, keep in mind that not everything you read will apply to your situation. If you have questions about whether something applies to your individual care, it is always best to talk to your doctor.
You will also want to think about your recovery plan post-surgery. Do you have friends or family who can help care for you in the days after your surgery? Having a support system is vital to your continued health both right after surgery and long term. Most centers have specific discharge instructions that you will receive after surgery. Ask if you can receive a copy of these instructions in advance so you can familiarize yourself with the information.
An initial intake interview via phone with a clinical specialist.
This is your first point of contact with the clinical team, where you will review your medical history, discuss which procedures you’d like to learn more about, clarify what is required by your insurance company for surgery, and develop a plan for next steps. It will make your phone call more productive if you have these documents ready to discuss with the clinician:
- Medications. Information about which prescriptions and over-the-counter medications you are currently taking.
- Insurance. Call your insurance company and find out if your surgery is a “covered benefit" and what their requirements are for you to have surgery.
- Medical Documents. Have at hand the name, address, and contact information for any clinician you see on a regular basis. This includes your primary care clinician, therapists or psychiatrists, and other health specialist you interact with such as a cardiologist or neurologist.
After the intake interview you will need to submit the following documents:
- Pharmacy records and medical records documenting your hormone therapy, if applicable
- Medical records from your primary physician.
- Surgical readiness referral letters from mental health providers documenting their assessment and evaluation
An appointment with your surgeon.
After your intake, and once you have all of your required documentation submitted you will be scheduled for a surgical consultation. These are in-person visits where you will get to meet the surgeon. typically include: The specialty nurse and social worker will meet with you first to conduct an assessment of your medical health status and readiness for major surgical procedures. Discussion of your long-term gender affirmation goals and assessment of which procedures may be most appropriate to help you in your journey. Specific details about the procedures you and your surgeon identify, including the risks, benefits and what to expect after surgery.
A preoperative anesthesia and medical evaluation.
Two to four weeks before your surgery, you may be asked to complete these evaluations at the hospital, which ensure that you are healthy enough for surgery.
What can I expect after gender affirming surgery?
When you’ve finished the surgical aspects of your gender affirmation, we encourage you to follow up with your primary care physician to make sure that they have the latest information about your health. Your doctor can create a custom plan for long-term care that best fits your needs. Depending on your specific surgery and which organs you continue to have, you may need to follow up with a urologist or gynecologist for routine cancer screening. JHCTGEH has primary care clinicians as well as an OB/GYN and urologists on staff.
Among other changes, you may consider updating your name and identification. This list of resources for transgender and gender diverse individuals can help you in this process.
The Center for Transgender and Gender Expansive Health Team at Johns Hopkins
Embracing diversity and inclusion, the Center for Transgender and Gender Expansive Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital

Request an Appointment

Transgender Health: What You Need to Know

Gender Affirmation Surgeries

Facial Masculinization Surgery
Related Topics
- LGBTQ Health
- Gender Affirmation
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Semin Plast Surg
- v.25(3); 2011 Aug

Aesthetic and Functional Genital and Perineal Surgery: Male
Sex reassignment surgery in the female-to-male transsexual, stan j. monstrey.
1 Department of Plastic Surgery, Ghent University Hospital, Gent, Belgium
Peter Ceulemans
Piet hoebeke.
2 Department of Urology, Ghent University Hospital, Gent, Belgium
In female-to-male transsexuals, the operative procedures are usually performed in different stages: first the subcutaneous mastectomy which is often combined with a hysterectomy-ovarectomy (endoscopically assisted). The next operative procedure consists of the genital transformation and includes a vaginectomy, a reconstruction of the horizontal part of the urethra, a scrotoplasty and a penile reconstruction usually with a radial forearm flap (or an alternative). After about one year, penile (erection) prosthesis and testicular prostheses can be implanted when sensation has returned to the tip of the penis. The authors provide a state-of-the-art overview of the different gender reassignment surgery procedures that can be performed in a female-to-male transsexual.
Transsexual patients have the absolute conviction of being born in the wrong body and this severe identity problem results in a lot of suffering from early childhood on. Although the exact etiology of transsexualism is still not fully understood, it is most probably a result of a combination of various biological and psychological factors. As to the treatment, it is universally agreed that the only real therapeutic option consists of “adjusting the body to the mind” (or gender reassignment) because trying to “adjust the mind to the body” with psychotherapy has been shown to alleviate the severe suffering of these patients. Gender reassignment usually consists of a diagnostic phase (mostly supported by a mental health professional), followed by hormonal therapy (through an endocrinologist), a real-life experience, and at the end the gender reassignment surgery itself.
As to the criteria of readiness and eligibility for these surgical interventions, it is universally recommended to adhere to the Standards of Care (SOC) of the WPATH (World Professional association of Transgender Health) 1 . It is usually advised to stop all hormonal therapy 2 to 3 weeks preoperatively.
The two major sex reassignment surgery (SRS) interventions in the female-to-male transsexual patients that will be addressed here are (1) the subcutaneous mastectomy (SCM), often combined with a hysterectomy/ ovariectomy; and (2) the actual genital transformation consisting of vaginectomy, reconstruction of the fixed part of the urethra (if isolated, metoidioplasty), scrotoplasty and phalloplasty. At a later stage, a testicular prostheses and/or erection prosthesis can be inserted.
SUBCUTANEOUS MASTECTOMY
General principles.
Because hormonal treatment has little influence on breast size, the first (and, arguably, most important) surgery performed in the female-to-male (FTM) transsexual is the creation of a male chest by means of a SCM. This procedure allows the patient to live more easily in the male role 2 , 3 , 4 , 5 and thereby facilitates the “real-life experience,” a prerequisite for genital surgery.
The goal of the SCM in a FTM transsexual patient is to create an aesthetically pleasing male chest, which includes removal of breast tissue and excess skin, reduction and proper positioning of the nipple and areola, obliteration of the inframammary fold, and minimization of chest-wall scars. 4 , 5 Many different techniques have been described to achieve these goals and most authors agree that skin excess , not breast volume, is the factor that should determine the appropriate SCM technique. 2 , 3 , 4 , 5 Recently, the importance of the skin elasticity has also been demonstrated and it is important to realize that in this patient population, poor skin quality can be exacerbated when the patient has engaged in years of “breast binding” (Fig. 1 ). 6

(A,B) Result of long-term “breast binding.”
In the largest series to date, Monstrey et al 6 described an algorithm of five different techniques to perform an aesthetically satisfactory SCM (Fig. 2 ). Preoperative parameters to be evaluated include breast volume, degree of excess skin, nipple-areola complex (NAC) size and position, and skin elasticity.

Algorithm for choosing appropriate subcutaneous mastectomy technique.
Regardless of the technique, it is extremely important to preserve all subcutaneous fat when dissecting the glandular tissue from the flaps. This ensures thick flaps that produce a pleasing contour. Liposuction is only occasionally indicated laterally, or to attain complete symmetry at the end of the procedure. Postoperatively, a circumferential elastic bandage is placed around the chest wall and maintained for a total of 4 to 6 weeks.
The semicircular technique (Fig. 3 ) is essentially the same procedure as that described by Webster in 1946 7 for gynecomastia. It is useful for individuals with smaller breasts and elastic skin. A sufficient amount of glandular tissue should be left in situ beneath the NAC to avoid a depression. The particular advantage of this technique is the small and well-concealed scar which is confined to (the lower half of) the nipple-areola complex. The major drawback is the small window through which to work, making excision of breast tissue and hemostasis more challenging.

Semicircular technique. (A) Incisions and scar; (B) preoperative; (C) postoperative.
In cases of smaller breasts with large prominent nipples, the transareolar technique (Fig. 4 ) is used. This is similar to the procedure described by Pitanguy in 1966 8 and allows for subtotal resection and immediate reduction of the nipple. The resulting scar traverses the areola horizontally and passes around the upper aspect of the nipple.

Transareolar technique. (A,B) Incisions and scar; (C) preoperative; (D) postoperative.
The concentric circular technique (Fig. 5 ) is similar to that described by Davidson in 1979. 9 It is used for breasts with a medium-sized skin envelope (B cup), or in the case of smaller breasts with poor skin elasticity. The resulting scar will be confined to the circumference of the areola. The concentric incision can be drawn as a circle or ellipse, enabling deepithelialization of a calculated amount of skin in the vertical or horizontal direction. 4 , 5 Access is gained via an incision in the inferior aspect of the outer circle leaving a wide pedicle for the NAC. A purse-string suture is placed and set to the desired areolar diameter (usually 25–30 mm). The advantage of this technique is that it allows for reduction and/or repositioning of the areola, where required, and for the removal of excess skin.

Concentric circular technique. (A) incisions; (B) preoperative; (C) postoperative.
The extended concentric circular technique (Fig. 6 ) is similar to the concentric circular technique, but includes one or two additional triangular excisions of skin and subcutaneous tissue lateral and/ or medial. This technique is useful for correcting skin excess and wrinkling produced by large differences between the inner and outer circles. The resulting scars will be around the areola, with horizontal extensions onto the breast skin, depending on the degree of excess skin.

Extended concentric circular technique. (A) Incisions and scar; (B) preoperative preoperative; (C) postoperative.
The free nipple graft technique (Fig. 7 ) has been proposed by several authors for patients with large and ptotic breasts. 2 , 3 , 10 , 11 , 12 It consists of harvesting the NAC as a full-thickness skin graft; amputating the breast; and grafting the NAC onto its new location on the chest wall. Our preference is to place the incision horizontally 1 to 2 cm above the inframammary fold, and then to move upwards laterally below the lateral border of the pectoralis major muscle. The placement of the NAC usually corresponds to the 4th or 5th intercostal space. Clinical judgment is most important, however, and we always sit the patient up intraoperatively to check final nipple position. The advantages of the free nipple graft technique are easy chest contouring, excellent exposure and more rapid resection of tissue, as well as nipple reduction, areola resizing, and repositioning. The disadvantages are the long residual scars, NAC pigmentary and sensory changes, and the possibility of incomplete graft take.

Free nipple graft technique. (A) Incisions and scar; (B) preoperative; (C) postoperative.
Complications
Postoperative complications include hematoma (most frequent, despite drains and compression bandages), (partial) nipple necrosis, and abscess formation. This underscores the importance of achieving good hemostasis intraoperatively. Smaller hematomas and seromas can be evacuated through puncture, but for larger collections surgical evacuation is required.
Another not infrequent complication consists of skin slough of the NAC, which can be left to heal by conservative means. The exceptional cases of partial or total nipple necrosis may require a secondary nipple reconstruction. Even in the patients without complications, ~25% required an additional procedure to improve the aesthetic results. The likelihood of an additional aesthetic correction should be discussed with the patient in advance. 13 Tattoo of the areola may be performed for depigmentation.
The recommendations of the authors are summarized in their algorithm (Fig. 2 ), which clearly demonstrates that a larger skin envelope and a less elastic skin will require progressively a longer-incision technique. The FTM transsexual patients are rightfully becoming a patient population that is better informed and more demanding as to the aesthetic outcomes.
Finally, it is important to note that there have been reports of breast cancer after bilateral SCM in this population 14 , 15 , 16 because in most patients the preserved NAC and the always incomplete glandular resection leave behind tissue at risk of malignant transformation.
PHALLOPLASTY
In performing a phalloplasty for a FTM transsexual, the surgeon should reconstruct an aesthetically appealing neophallus, with erogenous and tactile sensation, which enables the patient to void while standing and have sexual intercourse like a natural male, in a one-stage procedure. 17 , 18 The reconstructive procedure should also provide a normal scrotum, be predictably reproducible without functional loss in the donor area, and leave the patient with minimal scarring or disfigurement.
Despite the multitude of flaps that have been employed and described (often as Case Reports), the radial forearm is universally considered the gold standard in penile reconstruction. 17 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28
In the largest series to date (almost 300 patients), Monstrey et al 29 recently described the technical aspects of radial forearm phalloplasty and the extent to which this technique, in their hands approximates the criteria for ideal penile reconstruction.
For the genitoperineal transformation (vaginectomy, urethral reconstruction, scrotoplasty, phalloplasty), two surgical teams operate at the same time with the patient first placed in a gynecological (lithotomy) position. In the perineal area, a urologist may perform a vaginectomy, and lengthen the urethra with mucosa between the minor labiae. The vaginectomy is a mucosal colpectomy in which the mucosal lining of the vaginal cavity is removed. After excision, a pelvic floor reconstruction is always performed to prevent possible diseases such as cystocele and rectocele. This reconstruction of the fixed part of the urethra is combined with a scrotal reconstruction by means of two transposition flaps of the greater labia resulting in a very natural looking bifid scrotum.
Simultaneously, the plastic surgeon dissects the free vascularized flap of the forearm. The creation of a phallus with a tube-in-a-tube technique is performed with the flap still attached to the forearm by its vascular pedicle (Fig. 8A ). This is commonly performed on the ulnar aspect of the skin island. A small skin flap and a skin graft are used to create a corona and simulate the glans of the penis (Fig. 8B ).

(A–D) Phallic reconstruction with the radial forearm flap: creation of a tube (urethra) within a tube (penis).
Once the urethra is lengthened and the acceptor (recipient) vessels are dissected in the groin area, the patient is put into a supine position. The free flap can be transferred to the pubic area after the urethral anastomosis: the radial artery is microsurgically connected to the common femoral artery in an end-to-side fashion and the venous anastomosis is performed between the cephalic vein and the greater saphenous vein (Fig. 8C ). One forearm nerve is connected to the ilioinguinal nerve for protective sensation and the other nerve of the arm is anastomosed to one of the dorsal clitoral nerves for erogenous sensation. The clitoris is usually denuded and buried underneath the penis, thus keeping the possibility to be stimulated during sexual intercourse with the neophallus.
In the first 50 patients of this series, the defect on the forearm was covered with full-thickness skin grafts taken from the groin area. In subsequent patients, the defect was covered with split-thickness skin grafts harvested from the medial and anterior thigh (Fig. 8D ).
All patients received a suprapubic urinary diversion postoperatively.
The patients remain in bed during a one-week postoperative period, after which the transurethral catheter is removed. At that time, the suprapubic catheter was clamped, and voiding was begun. Effective voiding might not be observed for several days. Before removal of the suprapubic catheter, a cystography with voiding urethrography was performed.
The average hospital stay for the phalloplasty procedure was 2½ weeks.
Tattooing of the glans should be performed after a 2- to 3-month period, before sensation returns to the penis.
Implantation of the testicular prostheses should be performed after 6 months, but it is typically done in combination with the implantation of a penile erection prosthesis. Before these procedures are undertaken, sensation must be returned to the tip of the penis. This usually does not occur for at least a year.
The Ideal Goals of Penile Reconstruction in FTM Surgery
What can be achieved with this radial forearm flap technique as to the ideal requisites for penile reconstruction?
A ONE-STAGE PROCEDURE
In 1993, Hage 20 stated that a complete penile reconstruction with erection prosthesis never can be performed in one single operation. Monstrey et al, 29 early in their series and to reduce the number of surgeries, performed a (sort of) all-in-one procedure that included a SCM and a complete genitoperineal transformation. However, later in their series they performed the SCM first most often in combination with a total hysterectomy and ovariectomy.
The reason for this change in protocol was that lengthy operations (>8 hours) resulted in considerable blood loss and increased operative risk. 30 Moreover, an aesthetic SCM is not to be considered as an easy operation and should not be performed “quickly” before the major phalloplasty operation.
AN AESTHETIC PHALLUS
Phallic construction has become predictable enough to refine its aesthetic goals, which includes the use of a technique that can be replicated with minimal complications. In this respect, the radial forearm flap has several advantages: the flap is thin and pliable allowing the construction of a normal sized, tube-within-a-tube penis; the flap is easy to dissect and is predictably well vascularized making it safe to perform an (aesthetic) glansplasty at the distal end of the flap. The final cosmetic outcome of a radial forearm phalloplasty is a subjective determination, but the ability of most patients to shower with other men or to go to the sauna is the usual cosmetic barometer (Fig. 9A-C ).

(A–C) Late postoperative results of radial forearm phalloplasties.
The potential aesthetic drawbacks of the radial forearm flap are the need for a rigidity prosthesis and possibly some volume loss over time.
TACTILE AND EROGENOUS SENSATION
Of the various flaps used for penile reconstruction, the radial forearm flap has the greatest sensitivity. 1 Selvaggi and Monstrey et al. always connect one antebrachial nerve to the ilioinguinal nerve for protective sensation and the other forearm nerve with one dorsal clitoral nerve. The denuded clitoris was always placed directly below the phallic shaft. Later manipulation of the neophallus allows for stimulation of the still-innervated clitoris. After one year, all patients had regained tactile sensitivity in their penis, which is an absolute requirement for safe insertion of an erection prosthesis. 31
In a long-term follow-up study on postoperative sexual and physical health, more than 80% of the patients reported improvement in sexual satisfaction and greater ease in reaching orgasm (100% in practicing postoperative FTM transsexuals). 32
VOIDING WHILE STANDING
For biological males as well as for FTM transsexuals undergoing a phalloplasty, the ability to void while standing is a high priority. 33 Unfortunately, the reported incidences of urological complications, such as urethrocutaneous fistulas, stenoses, strictures, and hairy urethras are extremely high in all series of phalloplasties, as high as 80%. 34 For this reason, certain (well-intentioned) surgeons have even stopped reconstructing a complete neo-urethra. 35 , 36
In their series of radial forearm phalloplasties, Hoebeke and Monstrey still reported a urological complication rate of 41% (119/287), but the majority of these early fistulas closed spontaneously and ultimately all patients were able to void through the newly reconstructed penis. 37 Because it is unknown how the new urethra—a 16-cm skin tube—will affect bladder function in the long term, lifelong urologic follow-up was strongly recommended for all these patients.
MINIMAL MORBIDITY
Complications following phalloplasty include the general complications attendant to any surgical intervention such as minor wound healing problems in the groin area or a few patients with a (minor) pulmonary embolism despite adequate prevention (interrupting hormonal therapy, fractioned heparin subcutaneously, elastic stockings). A vaginectomy is usually considered a particularly difficult operation with a high risk of postoperative bleeding, but in their series no major bleedings were seen. 30 Two early patients displayed symptoms of nerve compression in the lower leg, but after reducing the length of the gynecological positioning to under 2 hours, this complication never occurred again. Apart from the urinary fistulas and/or stenoses, most complications of the radial forearm phalloplasty are related to the free tissue transfer. The total flap failure in their series was very low (<1%, 2/287) despite a somewhat higher anastomotic revision rate (12% or 34/287). About 7 (3%) of the patients demonstrated some degree of skin slough or partial flap necrosis. This was more often the case in smokers, in those who insisted on a large-sized penis requiring a larger flap, and also in patients having undergone anastomotic revision.
With smoking being a significant risk factor, under our current policy, we no longer operate on patients who fail to quit smoking one year prior to their surgery.
NO FUNCTIONAL LOSS AND MINIMAL SCARRING IN THE DONOR AREA
The major drawback of the radial forearm flap has always been the unattractive donor site scar on the forearm (Fig. 10 ). Selvaggi et al conducted a long-term follow-up study 38 of 125 radial forearm phalloplasties to assess the degree of functional loss and aesthetic impairment after harvesting such a large forearm flap. An increased donor site morbidity was expected, but the early and late complications did not differ from the rates reported in the literature for the smaller flaps as used in head and neck reconstruction. 38 No major or long-term problems (such as functional limitation, nerve injury, chronic pain/edema, or cold intolerance) were identified. Finally, with regard to the aesthetic outcome of the donor site, they found that the patients were very accepting of the donor site scar, viewing it as a worthwhile trade-off for the creation of a phallus (Fig. 10 ). 38 Suprafascial flap dissection, full thickness skin grafts, and the use of dermal substitutes may contribute to a better forearm scar.

(A,B) Aspect of the donor site after a phalloplasty with a radial forearm flap.
NORMAL SCROTUM
For the FTM patient, the goal of creating natural-appearing genitals also applies to the scrotum. As the labia majora are the embryological counterpart of the scrotum, many previous scrotoplasty techniques left the hair-bearing labia majora in situ, with midline closure and prosthetic implant filling, or brought the scrotum in front of the legs using a V-Y plasty. These techniques were aesthetically unappealing and reminiscent of the female genitalia. Selvaggi in 2009 reported on a novel scrotoplasty technique, which combines a V-Y plasty with a 90-degree turning of the labial flaps resulting in an anterior transposition of labial skin (Fig. 11 ). The excellent aesthetic outcome of this male-looking (anteriorly located) scrotum, the functional advantage of fewer urological complications and the easier implantation of testicular prostheses make this the technique of choice. 39

Reconstruction of a lateral looking scrotum with two transposition flaps: (A) before and (B) after implantation of testicular prostheses.
SEXUAL INTERCOURSE
In a radial forearm phalloplasty, the insertion of erection prosthesis is required to engage in sexual intercourse. In the past, attempts have been made to use bone or cartilage, but no good long-term results are described. The rigid and semirigid prostheses seem to have a high perforation rate and therefore were never used in our patients. Hoebeke, in the largest series to date on erection prostheses after penile reconstruction, only used the hydraulic systems available for impotent men. A recent long-term follow-up study showed an explantation rate of 44% in 130 patients, mainly due to malpositioning, technical failure, or infection. Still, more than 80% of the patients were able to have normal sexual intercourse with penetration. 37 In another study, it was demonstrated that patients with an erection prosthesis were more able to attain their sexual expectations than those without prosthesis (Fig. 12 ). 32

(A,B) Phalloplasty after implantation of an erection prosthesis.
A major concern regarding erectile prostheses is long-term follow-up. These devices were developed for impotent (older) men who have a shorter life expectancy and who are sexually less active than the mostly younger FTM patients.
Alternative Phalloplasty Techniques
Metaidoioplasty.
A metoidioplasty uses the (hypertrophied) clitoris to reconstruct the microphallus in a way comparable to the correction of chordee and lengthening of a urethra in cases of severe hypospadias. Eichner 40 prefers to call this intervention “the clitoris penoid.” In metoidioplasty, the clitoral hood is lifted and the suspensory ligament of the clitoris is detached from the pubic bone, allowing the clitoris to extend out further. An embryonic urethral plate is divided from the underside of the clitoris to permit outward extension and a visible erection. Then the urethra is advanced to the tip of the new penis. The technique is very similar to the reconstruction of the horizontal part of the urethra in a normal phalloplasty procedure. During the same procedure, a scrotal reconstruction, with a transposition flap of the labia majora (as previously described) is performed combined with a vaginectomy.
FTM patients interested in this procedure should be informed preoperatively that voiding while standing cannot be guaranteed, and that sexual intercourse will not be possible (Fig. 13 ).

Results of a metoidioplasty procedure.
The major advantage of metoidioplasty is the complete lack of scarring outside the genital area. Another advantage is that its cost is substantially lower than that of phalloplasty. Complications of this procedure also include urethral obstruction and/or urethral fistula.
It is always possible to perform a regular phalloplasty (e.g., with a radial forearm flap) at a later stage, and with substantially less risk of complications and operation time.
FIBULA FLAP
There have been several reports on penile reconstruction with the fibular flap based on the peroneal artery and the peroneal vein. 27 , 41 , 42 It consists of a piece of fibula that is vascularized by its periosteal blood supply and connected through perforating (septal) vessels to an overlying skin island at the lateral site of the lower leg. The advantage of the fibular flap is that it makes sexual intercourse possible without a penile prosthesis. The disadvantages are a pointed deformity to the distal part of the penis when the extra skin can glide around the end of fibular bone, and that a permanently erected phallus is impractical.
Many authors seem to agree that the fibular osteocutaneous flap is an optimal solution for penile reconstruction in a natal male. 42
NEW SURGICAL DEVELOPMENTS: THE PERFORATOR FLAPS
Perforator flaps are considered the ultimate form of tissue transfer. Donor site morbidity is reduced to an absolute minimum, and the usually large vascular pedicles provide an additional range of motion or an easier vascular anastomosis. At present, the most promising perforator flap for penile reconstruction is the anterolateral thigh (ALT) flap. This flap is a skin flap based on a perforator from the descending branch of the lateral circumflex femoral artery, which is a branch from the femoral artery. It can be used both as a free flap 43 and as a pedicled flap 44 then avoiding the problems related to microsurgical free flap transfer. The problem related to this flap is the (usually) thick layer of subcutaneous fat making it difficult to reconstruct the urethra as a vascularized tube within a tube. This flap might be more indicated for phallic reconstruction in the so-called boys without a penis, like in cases of vesical exstrophy (Fig. 14 ). However, in the future, this flap may become an interesting alternative to the radial forearm flap, particularly as a pedicled flap. If a solution could be found for a well-vascularized urethra, use of the ALT flap could be an attractive alternative to the radial forearm phalloplasty. The donor site is less conspicuous, and secondary corrections at that site are easier to make. Other perforator flaps include the thoracodorsal perforator artery flap (TAP) and the deep inferior epigastric perforator artery flap (DIEP). The latter might be an especially good solution for FTM patients who have been pregnant in the past. Using the perforator flap as a pedicled flap can be very attractive, both financially and technically.

Penile reconstruction with a pedicled anterolateral thigh flap. (A) Preoperative and (B) postoperative results.
The Importance of a Multidisciplinary Approach
Gender reassignment, particularly reassignment surgery, requires close cooperation between the different surgical specialties. In phalloplasty, the collaboration between the plastic surgeon, the urologist, and the gynecologist is essential. 45 The actual penile reconstruction is typically performed by the plastic and reconstructive surgeon, and the contribution of the gynecologist, who performs a hysterectomy and a BSO (preferably through a minimal endoscopic access in combination with SCM), should not be underestimated.
However, in the long term, the urologist's role may be the most important for patients who have undergone penile reconstruction, especially because the complication rate is rather high, particularly with regard to the number of urinary fistulas and urinary stenoses. The urologist also reconstructs the fixed part of the urethra. He or she is likely the best choice for implantation and follow-up of the penile and/or testicular prostheses. They must also address later sequelae, including stone formation. Moreover, the surgical complexity of adding an elongated conduit (skin-tube urethra) to a biological female bladder, and the long-term effects of evacuating urine through this skin tube, demand lifelong urological follow-up.
Therefore, professionals who unite to create a gender reassignment program should be aware of the necessity of a strong alliance between the plastic surgeon, the urologist, mental health professional and the gynecologist. In turn, the surgeons must commit to the extended care of this unique population, which, by definition, will protract well into the future.
- Meyer W J, III, Bockting W O, Cohen-Kettenis P, et al. The Standards of Care for Gender Identity Disorders, 6th Version. J Psychol Human Sex. 2002; 13 :1–30. [ Google Scholar ]
- Lindsay W RN. Creation of a male chest in female transsexuals. Ann Plast Surg. 1979; 3 (1):39–46. [ PubMed ] [ Google Scholar ]
- Eicher W. Transsexualismus. Vol. 1992. Stuttgart: Fisher Verlag; pp. 120–123. [ Google Scholar ]
- Hage J J, Bloem J J. Chest wall contouring for female-to-male transsexuals: Amsterdam experience. Ann Plast Surg. 1995; 34 (1):59–66. [ PubMed ] [ Google Scholar ]
- Hage J J, Kesteren P J van. Chest-wall contouring in female-to-male transsexuals: basic considerations and review of the literature. Plast Reconstr Surg. 1995; 96 (2):386–391. [ PubMed ] [ Google Scholar ]
- Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008; 121 (3):849–859. [ PubMed ] [ Google Scholar ]
- Webster J P. Mastectomy for gynecomastia through a semicircular intra-areolar incision. Ann Surg. 1946; 124 :557–575. [ PubMed ] [ Google Scholar ]
- Pitanguy I. Transareolar incision for gynecomastia. Plast Reconstr Surg. 1966; 38 (5):414–419. [ PubMed ] [ Google Scholar ]
- Davidson B A. Concentric circle operation for massive gynecomastia to excise the redundant skin. Plast Reconstr Surg. 1979; 63 (3):350–354. [ PubMed ] [ Google Scholar ]
- Kluzák R. Sex conversion operation in female transsexualism. Acta Chir Plast. 1968; 10 (3):188–198. [ PubMed ] [ Google Scholar ]
- Hoopes J E. Surgical construction of the male external genitalia. Clin Plast Surg. 1974; 1 (2):325–334. [ PubMed ] [ Google Scholar ]
- Kenney J G, Edgerton M T. Reduction mammoplasty in gender dysphoria. Abstract presented at the 11th Symposium of the Harry Benjamin International Gender Dysphoria Association; septerber20–23, 1989; Cleveland, Ohio.
- Beer G M, Budi S, Seifert B, Morgenthaler W, Infanger M, Meyer V E. Configuration and localization of the nipple-areola complex in men. Plast Reconstr Surg. 2001; 108 (7):1947–1952. discussion 1953. [ PubMed ] [ Google Scholar ]
- Symmers W S. Carcinoma of breast in trans-sexual individuals after surgical and hormonal interference with the primary and secondary sex characteristics. BMJ. 1968; 2 (5597):83–85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Secreto G, Toniolo P, Berrino F, et al. Increased androgenic activity and breast cancer risk in premenopausal women. Cancer Res. 1984; 44 (12 Pt 1):5902–5905. [ PubMed ] [ Google Scholar ]
- Burcombe R J, Makris A, Pittam M, Finer N. Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual. Breast. 2003; 12 (4):290–293. [ PubMed ] [ Google Scholar ]
- Gilbert D A, Horton C E, Terzis J K, Devine C J, Jr, Winslow B H, Devine P C. New concepts in phallic reconstruction. Ann Plast Surg. 1987; 18 (2):128–136. [ PubMed ] [ Google Scholar ]
- Hage J J, Bouman F G, de Graaf F H, Bloem J J. Construction of the neophallus in female-to-lake transsexuals: the Amsterdam experience. J Urol. 1993; 6 :1463–1468. [ PubMed ] [ Google Scholar ]
- Chang T S, Hwang W Y. Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg. 1984; 74 (2):251–258. [ PubMed ] [ Google Scholar ]
- Hage J J, De Graaf F H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery. 1993; 14 (9):592–598. [ PubMed ] [ Google Scholar ]
- Fang R H, Kao Y S, Ma S, Lin J T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br J Plast Surg. 1999; 52 (3):217–222. [ PubMed ] [ Google Scholar ]
- Biemer E. Penile construction by the radial arm flap. Clin Plast Surg. 1988; 15 (3):425–430. [ PubMed ] [ Google Scholar ]
- Koshima I, Tai T, Yamasaki M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J Reconstr Microsurg. 1986; 3 (1):19–26. [ PubMed ] [ Google Scholar ]
- Meyer R, Daverio P J. One-stage phalloplasty without sensory deprivation in female transsexuals. World J Urol. 1987; 5 :9–13. [ Google Scholar ]
- Upton J, Mutimer K L, Loughlin K, Ritchie J. Penile reconstruction using the lateral arm flap. J R Coll Surg Edinb. 1987; 32 (2):97–101. [ PubMed ] [ Google Scholar ]
- Harashina T, Inoue T, Tanaka I, Imai K, Hatoko M. Reconstruction of penis with free deltoid flap. Br J Plast Surg. 1990; 43 (2):217–222. [ PubMed ] [ Google Scholar ]
- Sadove R C, Sengezer M, McRoberts J W, Wells M D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast Reconstr Surg. 1993; 92 (7):1314–1323. discussion 1324–1325. [ PubMed ] [ Google Scholar ]
- Santanelli F, Scuderi N. Neophalloplasty in female-to-male transsexuals with the island tensor fasciae latae flap. Plast Reconstr Surg. 2000; 105 (6):1990–1996. [ PubMed ] [ Google Scholar ]
- Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009; 124 (2):510–518. [ PubMed ] [ Google Scholar ]
- Weyers S, Selvaggi G, Monstrey S, et al. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol Surg. 2006; 3 :190–194. [ Google Scholar ]
- Selvaggi G, Monstrey S, Ceulemans P, T'Sjoen G, De Cuypere G, Hoebeke P. Genital sensitivity after sex reassignment surgery in transsexual patients. Ann Plast Surg. 2007; 58 (4):427–433. [ PubMed ] [ Google Scholar ]
- De Cuypere G, T'Sjoen G, Beerten R, et al. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005; 34 (6):679–690. [ PubMed ] [ Google Scholar ]
- Hage J J, Bout C A, Bloem J J, Megens J A. Phalloplasty in female-to-male transsexuals: what do our patients ask for? Ann Plast Surg. 1993; 30 (4):323–326. [ PubMed ] [ Google Scholar ]
- Vriens J P, Acosta R, Soutar D S, Webster M H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast Reconstr Surg. 1996; 98 (4):649–656. [ PubMed ] [ Google Scholar ]
- Felici N, Felici A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J Plast Reconstr Aesthet Surg. 2006; 59 (2):153–157. [ PubMed ] [ Google Scholar ]
- Matti B A, Matthews R N, Davies D M. Phalloplasty using the free radial forearm flap. Br J Plast Surg. 1988; 41 (2):160–164. [ PubMed ] [ Google Scholar ]
- Hoebeke P, Selvaggi G, Ceulemans P, et al. Impact of sex reassignment surgery on lower urinary tract function. Eur Urol. 2005; 47 (3):398–402. [ PubMed ] [ Google Scholar ]
- Selvaggi G, Monstrey S, Hoebeke P, et al. Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast Reconstr Surg. 2006; 118 (5):1171–1177. [ PubMed ] [ Google Scholar ]
- Hoebeke P, de Cuypere G, Ceulemans P, Monstrey S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J Urol. 2003; 169 (1):221–223. [ PubMed ] [ Google Scholar ]
- Eicher W. Surgical Treatment of Female-to-Male Transsexuals. In: Echer W, editor. Plastic Surgery in the Sexually Handicapped. Vol. 1989. Berlin: Springer; pp. 106–112. [ Google Scholar ]
- Hage J J, Winters H A, Lieshout J Van. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery. 1996; 17 (7):358–365. [ PubMed ] [ Google Scholar ]
- Sengezer M, Oztürk S, Deveci M, Odabaşi Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast Reconstr Surg. 2004; 114 (2):439–450. discussion 451–452. [ PubMed ] [ Google Scholar ]
- Felici N. Phalloplasty with Free Anterolateral Thigh Flap. Paper presented the XIX Biennial Symposium of the Harry Benjamin International Gender Dysphoria Association (HBIGDA); April 6–9, 2005; Bologna, Italy.
- Ceulemans P. The Pedicled Anterolateral Thigh Flap (ALT) Perforator Flap: A New Technique for Phallic Reconstruction. Paper presented at the XIV Biennial Symposium of the Harry Benjamin International Gender Dysphoria Association (HBIGDA); April 6–9, 2005; Bologna, Italy.
- Monstrey S, Hoebeke P, Dhont M, et al. Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir Belg. 2001; 101 (5):200–209. [ PubMed ] [ Google Scholar ]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.

A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Search Close Search submit
ISAPS Olympiad Word Congress 2025, Singapore: submit your abstract by October 18, 2024
Procedure: Male to Female Gender Reassignment Surgery (MTF GRS)
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of labia major/minor, clitoris and neovagina simultaneously.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Male gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as female smoothly such as breast aesthetic surgery, facial feminization surgery, body contouring, hair removal, voice change surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is quite complicated and only a handful of surgeons are able to perform this procedure. It can be completed in one stage or more stages depending on techniques and surgeons. The average surgical time ranges between 5-8 hours. There are several options of neovaginal construction depending on the type of tissue, single or in combination, such as penile skin, scrotal skin, large intestine, small intestine, or peritoneum.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-14 days depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What is the recovery process.
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patient can return to their normal lives but not have to do physical exercise during the first 2 months after surgery. The patient has to do vaginal dilation continuously for 6 months to maintain the neovagina canal until completely healed and is ready for sexual intimacy.
What are the results?
With the good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a female role completely and happily either on their own or with their male or female partners.
What are the risks?
The most frequent complication of MTF GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis, neovaginal contracture, unsightly scar or deformed genitalia, vaginal fistula, etc. The revision procedures to improve external appearance are composed of secondary labiaplasty/ urethroplasty/ perineoplasty/ and vulvaplasty. The other revision procedure is secondary vaginoplasty to help the patient able to have sexual intimacy with the partner.
- Patient Information
- Global Statistics
- Media Centre
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:
Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Gender reassignment surgery: an overview
Affiliation.
- 1 Gender Surgery Unit, Charing Cross Hospital, Imperial College NHS Trust, 179-183 Fulham Palace Road, London W6 8QZ, UK.
- PMID: 21487386
- DOI: 10.1038/nrurol.2011.46
Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics. Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available. The World Professional Association for Transgender Health currently publishes and reviews guidelines and standards of care for patients affected by gender dysphoria, such as eligibility criteria for surgery. This article presents an overview of the genital and nongenital procedures available for both male-to-female and female-to-male gender reassignment.
PubMed Disclaimer
Similar articles
- Gender identity disorder: general overview and surgical treatment for vaginoplasty in male-to-female transsexuals. Selvaggi G, Ceulemans P, De Cuypere G, VanLanduyt K, Blondeel P, Hamdi M, Bowman C, Monstrey S. Selvaggi G, et al. Plast Reconstr Surg. 2005 Nov;116(6):135e-145e. doi: 10.1097/01.prs.0000185999.71439.06. Plast Reconstr Surg. 2005. PMID: 16267416 Review.
- Current Concepts in Feminizing Gender Surgery. Safa B, Lin WC, Salim AM, Deschamps-Braly JC, Poh MM. Safa B, et al. Plast Reconstr Surg. 2019 May;143(5):1081e-1091e. doi: 10.1097/PRS.0000000000005595. Plast Reconstr Surg. 2019. PMID: 31033837 Review.
- [SEX REASSIGNMENT SURGERY WITH LAPAROSCOPIC SIGMOID COLON VAGINOPLASTY IN A MALE TO FEMALE TRANSSEXUAL: A CASE REPORT]. Ichihara K, Masumori N. Ichihara K, et al. Nihon Hinyokika Gakkai Zasshi. 2016;107(2):126-128. doi: 10.5980/jpnjurol.107.126. Nihon Hinyokika Gakkai Zasshi. 2016. PMID: 28442672 Japanese.
- Sexual Function in Post-surgical Transgender and Gender Diverse Individuals. Schoenbrunner A, Cripps C. Schoenbrunner A, et al. Obstet Gynecol Clin North Am. 2024 Jun;51(2):425-435. doi: 10.1016/j.ogc.2024.03.005. Epub 2024 Apr 9. Obstet Gynecol Clin North Am. 2024. PMID: 38777493 Review.
- Penile inversion vaginoplasty outcomes: Complications and satisfaction. Hontscharuk R, Alba B, Hamidian Jahromi A, Schechter L. Hontscharuk R, et al. Andrology. 2021 Nov;9(6):1732-1743. doi: 10.1111/andr.13030. Epub 2021 May 27. Andrology. 2021. PMID: 33955679 Review.
- Health Service Utilization and Its Associations with Depression and Sexual Risk Behaviors Among Transgender Women in Shanghai, China. Wang L, Harris R, Simoni JM, Yue Q, Fu J, Zheng H, Ning Z, Xavier Hall CD, Burns PA, Wong FY. Wang L, et al. Transgend Health. 2023 Dec 13;8(6):516-525. doi: 10.1089/trgh.2021.0009. eCollection 2023 Dec. Transgend Health. 2023. PMID: 38130986
- Chest Feminization in Transwomen with Subfascial Breast Augmentation-Our Technique and Results. Kanjoor JR, Khan TM. Kanjoor JR, et al. Aesthetic Plast Surg. 2024 Jul;48(13):2447-2458. doi: 10.1007/s00266-023-03726-z. Epub 2023 Nov 9. Aesthetic Plast Surg. 2024. PMID: 37945759
- Gender dysphoria: Quality of online information for gender reassignment surgery. Lo Torto F, Mori FR, Bruno E, Giacomini G, Turriziani G, Firmani G, Marcasciano M, Ribuffo D. Lo Torto F, et al. JPRAS Open. 2023 Sep 1;38:117-123. doi: 10.1016/j.jpra.2023.08.008. eCollection 2023 Dec. JPRAS Open. 2023. PMID: 37772032 Free PMC article.
- Principles and outcomes of gender-affirming vaginoplasty. Morrison SD, Claes K, Morris MP, Monstrey S, Hoebeke P, Buncamper M. Morrison SD, et al. Nat Rev Urol. 2023 May;20(5):308-322. doi: 10.1038/s41585-022-00705-y. Epub 2023 Feb 1. Nat Rev Urol. 2023. PMID: 36726039 Review.
- Considerations for secondary vaginoplasty. Shoham M, Pang JH, Satterwhite T. Shoham M, et al. Transl Androl Urol. 2022 Nov;11(11):1480-1483. doi: 10.21037/tau-22-660. Transl Androl Urol. 2022. PMID: 36507476 Free PMC article. No abstract available.
- Laryngoscope. 2005 Apr;115(4):611-8 - PubMed
- Eur Urol. 2005 Mar;47(3):398-402 - PubMed
- Nature. 1995 Nov 2;378(6552):68-70 - PubMed
- Plast Reconstr Surg. 2006 Oct;118(5):1171-1177 - PubMed
- Adv Exp Med Biol. 2002;511:75-100; discussion 100-5 - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Nature Publishing Group
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
EWTN News, Inc. is the world’s largest Catholic news organization, comprised of television, radio, print and digital media outlets, dedicated to reporting the truth in light of the Gospel and the Catholic Church.
- National Catholic Register
- News Agencies
- Catholic News Agency
- CNA Deutsch
- ACI Afrique
- ACI Digital
- Digital Media
- ChurchPOP Español
- ChurchPOP Italiano
- ChurchPOP Português
- EWTN News Indepth
- EWTN News Nightly
- EWTN Noticias
- EWTN Pro-life Weekly
- Register Radio
Get HALF OFF the Register!
National Catholic Register News https://www.ncregister.com/cna/biden-gender-reassignment-surgery-mandate-blocked

- Synod on Synodality
- Most Popular
- Publisher’s Note
- College Guide
- Commentaries
- Culture of Life
- Arts & Entertainment
- Publisher's Note
- Letters to the Editor
- Support the Register
- Print subscriptions
- E-Newsletter Sign-up
- EWTN Religious Catalogue
Biden ‘Gender-Reassignment’ Surgery Mandate Blocked
The ruling expands an earlier court decision that blocked the mandate for hospitals in Texas and Montana to all hospitals.

A U.S. district judge has placed a nationwide block on a Biden-Harris administration rule mandating that federally funded hospitals perform surgical interventions to alter the body’s appearance to mimic that of the opposite sex.
This comes after Texas and Montana sued the administration over changes it made in May to the Affordable Care Act’s section prohibiting discrimination based on sex.
The rule broadened the meaning of “sex” to include “gender identity.” This meant that federally funded hospitals were required to perform so-called “gender-reassignment” surgeries or face a range of penalties, including having their funding removed.
Texas and Montana argued that the change violated portions of state law that prohibit such surgical interventions performed on minors’ sexual and reproductive organs and ban Medicaid funding for these operations.
The two states argued that the Biden administration has given them “an impossible choice” to either “violate and abandon state law or risk devastating financial loss.”
The ruling, issued on Aug. 30 by Judge Jeremy Kernodle for the Eastern District of Texas, expanded an earlier court decision that blocked the mandate for hospitals in Texas and Montana. Kernodle said the Biden administration’s mandate is “unlawful” in all hospitals, not just those in Texas and Montana.
Texas Attorney General Ken Paxton called the ruling a “major victory for Americans across the country.”
“When Biden and Harris sidestep the Constitution to force their unlawful, extremist agenda on the American public, we are fighting back and stopping them,” said Paxton.
The Biden administration will likely appeal the ruling to the 5th Circuit Appellate Court.
- gender dysphoric youth
- transgender
- biden administration
- Related Stories
- Latest News

Federal Courts Rule in Favor of Transgender-Identifying Athletes in 2 States
Schools in New Hampshire and Virginia will allow boys who identify as girls to compete on girls’ teams.

Nebraska Supreme Court Upholds Abortion Restrictions, Ban on Sex Changes for Minors
Although the law remains in effect, Nebraskans will vote on a referendum on Nov. 5, which would establish a constitutional right to abortion in the state Constitution.

New Hampshire Becomes Latest State to Restrict Sex-Change Surgeries for Minors
Granite State also to restrict access to female athletic competitions in certain grades to only biological girls.

States, Doctors Sue Biden Administration Over Transgender Medical Mandate
Seven states and a group of pediatricians are suing President Joe Biden’s administration over a rule that would force doctors to provide sex-change procedures and require health insurers to cover them.

Trump-Vance Campaign Launches Catholics for Trump Coalition
The coalition emphasizes the defense of religious liberty, traditional values, and the sanctity of human life as priorities of the Republican nominee’s agenda.

Ortega Dictatorship in Nicaragua Deports Group of Foreign Priests and Nuns
Updated report cites 870 attacks by the Nicaraguan dictatorship against the Catholic Church since 2018, the year there were widespread demonstrations against the authoritarian regime and its unpopular proposed reforms.

Biden’s Claim That Harris Has ‘Moral Compass of a Saint’ Sparks Criticism From Theologians
“Someone who truly had the ‘moral compass of a saint’ would condemn abortion as murder instead of supporting it enthusiastically as Vice President Harris does,” Catholic philosopher Edward Feser said.

Pope Francis: Indonesia’s High Birth Rate Is an Example for Other Countries
'This might make one laugh, but there are some families that seem to prefer to have a cat or dog, but this, this doesn’t work,' Pope Francis added.

Mother Teresa Feared ‘Big Crowds’ — But She Loved Telling Them About the Eucharist
The mission and work of Mother Teresa can be seen in her profound Eucharistic life.

Medal of Honor Recipient Father Capodanno to Be Remembered in Annual Mass
As his cause for canonization proceeds, Servant of God Vincent Capodanno’s heroic and virtuous life is remembered every Sept. 4 with a memorial Mass at the Basilica of the National Shrine of the Immaculate Conception in Washington, D.C.

Should a Catholic Attend an Invalid Wedding?
DIFFICULT MORAL QUESTIONS: The moral legitimacy of attending such a ceremony is determined by several factors, including our duty to avoid scandal and the near occasion of sin.

‘The Crown’ Shows Us the Moral Power of Royal Virtue
A Look Back at Season 1 of the Netflix Miniseries on the Reign of Elizabeth II
French Priest Rescues Blessed Sacrament From Burning Catholic Church
Living ‘laudato si’ on an urban farm in tennessee, queering women’s boxing, bearing the wounds of christ: meet the stigmatists, catholic strategist promotes stewardship approach to foreign policy, american solidarity party fights for ballot access state-by-state, ‘witness to hope’ 25 years later, the mystery of consciousness: new study challenges ‘brain-death’ narrative, nebraska bishop calls for ‘developing authentically catholic schools’ in new pastoral letter, subscription options.

Subscriber Service Center Already a subscriber? Renew or manage your subscription here .
Subscribe and Save HALF OFF! Start your Register subscription today.
Give a Gift Subscription Bless friends, family or clergy with a gift of the Register.
Order Bulk Subscriptions Get a discount on 6 or more copies sent to your parish, organization or school.
Sign-up for E-Newsletter Get Register Updates sent daily or weeklyto your inbox.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 September 2024
Immune system adaptation during gender-affirming testosterone treatment
- Tadepally Lakshmikanth ORCID: orcid.org/0000-0001-7256-5770 1 na1 ,
- Camila Consiglio ORCID: orcid.org/0000-0002-8901-2328 1 , 2 na1 ,
- Fabian Sardh 3 , 4 ,
- Rikard Forlin 1 ,
- Jun Wang 1 ,
- Ziyang Tan 1 ,
- Hugo Barcenilla ORCID: orcid.org/0000-0002-7255-362X 1 ,
- Lucie Rodriguez ORCID: orcid.org/0000-0002-3692-9060 1 ,
- Jamie Sugrue 5 ,
- Peri Noori 3 ,
- Margarita Ivanchenko 1 ,
- Laura Piñero Páez 1 ,
- Laura Gonzalez 1 ,
- Constantin Habimana Mugabo 1 ,
- Anette Johnsson 1 ,
- Henrik Ryberg 6 , 7 ,
- Åsa Hallgren 3 ,
- Christian Pou 1 ,
- Yang Chen 1 ,
- Jaromír Mikeš ORCID: orcid.org/0000-0002-9941-7855 1 ,
- Anna James 1 ,
- Per Dahlqvist ORCID: orcid.org/0000-0002-6471-9503 8 ,
- Jeanette Wahlberg ORCID: orcid.org/0000-0003-4061-6830 9 ,
- Anders Hagelin 10 , 11 ,
- Mats Holmberg ORCID: orcid.org/0000-0003-2884-9981 10 , 11 ,
- Marie Degerblad 10 , 12 ,
- Magnus Isaksson 13 ,
- Darragh Duffy ORCID: orcid.org/0000-0002-8875-2308 5 ,
- Olle Kämpe ORCID: orcid.org/0000-0001-6091-9914 3 , 14 ,
- Nils Landegren 3 , 4 na1 &
- Petter Brodin ORCID: orcid.org/0000-0002-8103-0046 1 , 15 , 16 na1
Nature volume 633 , pages 155–164 ( 2024 ) Cite this article
Metrics details
- Epigenetics in immune cells
- Translational research
Infectious, inflammatory and autoimmune conditions present differently in males and females. SARS-CoV-2 infection in naive males is associated with increased risk of death, whereas females are at increased risk of long COVID 1 , similar to observations in other infections 2 . Females respond more strongly to vaccines, and adverse reactions are more frequent 3 , like most autoimmune diseases 4 . Immunological sex differences stem from genetic, hormonal and behavioural factors 5 but their relative importance is only partially understood 6 , 7 , 8 . In individuals assigned female sex at birth and undergoing gender-affirming testosterone therapy (trans men), hormone concentrations change markedly but the immunological consequences are poorly understood. Here we performed longitudinal systems-level analyses in 23 trans men and found that testosterone modulates a cross-regulated axis between type-I interferon and tumour necrosis factor. This is mediated by functional attenuation of type-I interferon responses in both plasmacytoid dendritic cells and monocytes. Conversely, testosterone potentiates monocyte responses leading to increased tumour necrosis factor, interleukin-6 and interleukin-15 production and downstream activation of nuclear factor kappa B-regulated genes and potentiation of interferon-γ responses, primarily in natural killer cells. These findings in trans men are corroborated by sex-divergent responses in public datasets and illustrate the dynamic regulation of human immunity by sex hormones, with implications for the health of individuals undergoing hormone therapy and our understanding of sex-divergent immune responses in cisgender individuals.
Gender-affirming hormone therapy (GAHT) enables the acquisition of secondary sex characteristics better aligned with gender identity in transgender individuals. It is important to understand how GAHT influences the immune response in these individuals, but this also provides a unique opportunity to investigate the immunomodulatory functions of gonadal steroids in vivo in humans of reproductive age. We performed longitudinal blood sampling of 23 trans men, who were assigned female sex at birth and undergoing masculinizing treatment with testosterone undecaonate starting at the age of 18–37 years. Blood samples were collected at baseline and following 3 and 12 months of testosterone treatment (Fig. 1a ). By analysing plasma proteins, immune cell phenotypes and functional immune cell responses in vitro, we searched for coordinated changes among cell populations and the protein mediators by which these communicate to understand global changes in response to testosterone treatment. Serum concentrations of bioavailable testosterone increased to male reference range values (Fig. 1b ), whereas oestradiol concentrations decreased from baseline to 3 months (Fig. 1c ), as did progesterone concentrations (Fig. 1d ). When integrating eight different hormones (Fig. 1b–d and Extended Data Fig. 1a ), a shared directionality was observed during testosterone therapy (Fig. 1e ). Five individuals received lower doses (Nebido, 750 mg) due to low body mass indices but their plasma hormone concentrations were comparable (Extended Data Fig. 1b ). Bulk mRNA sequencing (mRNA-seq) of longitudinal blood samples ( n = 60 from 20 out of 23 participants) showing decreasing transcripts enriched for Hallmark interferon (IFN)-α (IFNα) responses (Fig. 1f ), whereas upregulated transcripts were enriched for the Hallmark pathway of tumour necrosis factor (TNF) signalling through nuclear factor kappa B (NFκB) and Hallmark inflammatory responses (Fig. 1f ), indicating a previously unappreciated role for gonadal steroids in calibrating type-I interferon (IFN-I)/TNF cross-regulation.
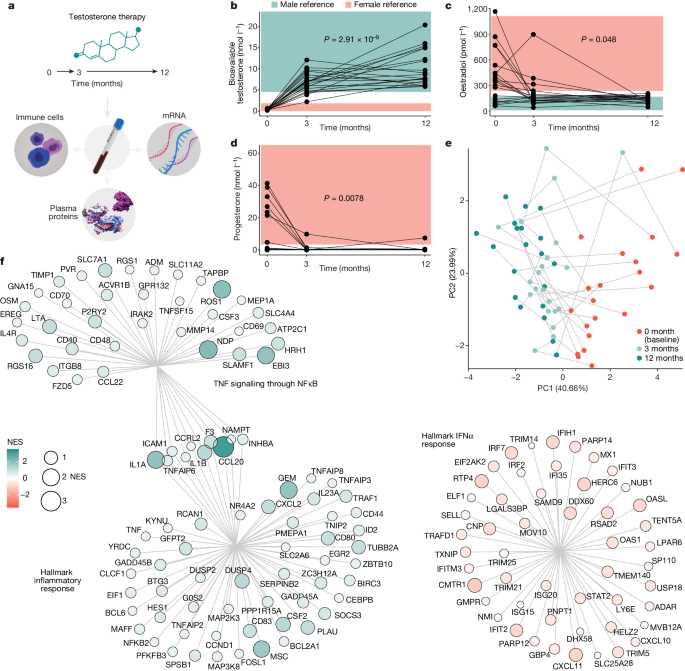
a , Systems-level assessment of blood immune system in individuals assigned female sex at birth (trans men) in blood samples collected at baseline, and after 3 and 12 months of oral testosterone therapy ( n = 23). b – d , Sex hormone concentrations measured in serum samples ( n = 66) using liquid chromatography with tandem mass spectrometry in a single experiment and shown in relation to female (pink) and male (blue) reference ranges before and during testosterone therapy. Kruskal–Wallis tests (5% false discovery rate (FDR) corrected) for bioavailable testosterone ( b ), oestradiol ( c ) and progesterone ( d ). e , PCA on the basis of nine sex hormones, first two principal components (PC1 and PC2; percentage variance explained) and sample points coloured by sample timepoint. f , Bulk RNA-seq from whole blood samples ( n = 60) and differently expressed mRNA transcripts analysed by normalized enrichment scores (NES) for Hallmark pathways. Hallmark IFNα responses decrease after 12 months of testosterone treatment, TNF signalling through NFκB and Hallmark inflammatory responses increased after 12 months of testosterone treatment as compared with baseline.
Testosterone-induced immune cell changes
We stabilized whole blood cells directly at blood collection, stained with a 50-parameter antibody panel and acquired 12,377,068 cells by mass cytometry. There was no significant change in total white blood cell (WBC) counts during testosterone treatment (Extended Data Fig. 2a ) and a total of 113 immune cell clusters were identified and embedded in a force-directed graph (Fig. 2a ) and annotated manually by median marker expression (Extended Data Fig. 2b ). Using mixed-effects models with age and study visit as fixed effects and participant as a random effect, we identified changes in several immune cell populations when comparing samples before and during testosterone treatment. We found an overall contraction of plasmacytoid dendritic cells (DCs) (pDCs), CD8 + mucosa-associated invariant T cells and CD24 + CD8 + central memory T cells (T CM ) during GAHT (Fig. 2b ).
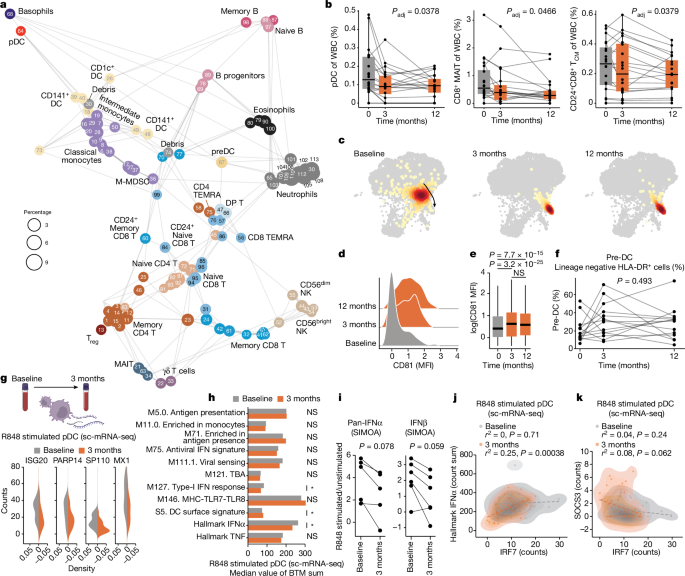
a , Immune cell clusters (FlowSOM) of 12,377,068 cells by 50-marker mass cytometry. N = 113 clusters annotated to lineages ( n = 35). Cluster-IDs match expression heatmap (Extended Data Fig. 2b ). b , Cell frequencies in n = 60 samples from 20 participants, four experiments, linear mixed-effects models with visit and age as fixed and participant as random effect. Boxplot centre, median; maximum, Q3 + 1.5 × IQR (IQR values ranging from Q1 to Q3); minimum whisker, Q1 − 1.5 × IQR; P values 5% FDR corrected. c , Two-dimensional embedding (ForceAtlas2) of pDCs ( n = 742) analysed by mass cytometry in a single donor and one representative experiment of four. d , CD81 expression in pDCs from samples in c . e , Summary of CD81 concentrations in pDCs from 18 donors across four experiments ( n = 15,197). Boxplot centre, median; maximum, Q3 + 1.5 × IQR (IQR values ranging from Q1 to Q3); minimum whisker, Q1 – 1.5 × IQR. Two-sided, uncorrected Wilcoxon rank sum test. f , Manually gated pre-DCs in lineage negative, HLA-DR + cells (Extended Data Fig. 2c ) in 42 samples, 14 participants from three experiments by one-way analysis of variance. g , Normalized counts of four IFN-I response genes in R848-stimulated pDCs by sc-mRNA-seq at baseline ( n = 41) and 3 months ( n = 47), of two experiments. Counts in stimulated cells, subtracting median counts in unstimulated pDCs. h , Median sums of genes assigned to indicated BTMs in R848-stimulated pDCs by sc-mRNA-seq at baseline and 3 months. * P < 0.05. Uncorrected, two-sided Student’s t -test. i , pan-IFNα and IFNb protein ratios (R848-stimulated versus unstimulated) in PBMC cultures; P values comparing ratios at baseline and 3 months by one-sided, paired Student’s t -tests. j , k , pDC sc-mRNA-seq of R848-stimulated pDCs at baseline ( n = 41) and 3 months ( n = 47) in two independent experiments by uncorrected, two-sided Student’s t -tests and R -values from Pearson correlation coefficients, IRF7 counts versus Hallmark IFNα count sum ( j ), and IRF7 versus SOCS3 counts ( k ). MAIT, mucosa-associated invariant T cells; MFI, mean fluorescence intensity; NS, non-significant.
Testosterone-mediated adaptation of pDCs
pDCs are efficient producers of IFN-I, and their contraction can contribute to the reduction in Hallmark IFNα transcripts by testosterone (Fig. 1f ). We also found pDC phenotypic changes upon testosterone treatment (Fig. 2c ), with surface expression of CD81 on pDCs increasing from 3 months (Fig. 2d,e ). CD5 + CD81 + pDCs were reported previously to differ from CD5 − CD81 − pDCs with attenuated type-I IFN responses and more potent regulatory T (T reg ) cell induction 9 . CD5 + DCs have since been shown to differ from classical pDCs and are termed AXL + SIGLEC6 + DCs (AS-DC) 10 , transitional DCs (tDCs) 11 or pre-DCs 12 . To study pre-DCs during GAHT, we gated these manually (Extended Data Fig. 2b ) 12 and found no change in abundance during testosterone therapy in vivo (Fig. 2f ).
Webb et al. previously reported lower frequencies of IFNα-producing pDCs upon TLR7/8 stimulation in transgender birth females as compared with postpubertal cisgender females 13 . To directly compare pDC functional responses before and after testosterone treatment in transgender birth female participants, we stimulated peripheral blood mononuclear cells (PBMCs) from baseline and after 3 months of testosterone by R848 (TLR7/8) and analysed individual pDCs by single-cell RNA sequencing (scRNA-seq). We verified pDC classification without pre-DC inclusion (Extended Data Fig. 3a ) 10 and found interferon-stimulated genes (ISGs), ISG20, PAPR14, SP110 and MX1 (counts) to be less induced after 3 months of testosterone as compared with baseline (Fig. 2g ). This corroborates a recent report of pDC responses in six trans men 14 . When investigating blood transcriptional modules (BTM) and hallmark gene pathways in these R848-stimulated pDC before and during testosterone, BTM S5 (DC surface signature) was induced, while the Hallmark IFNα gene set and the related M127 IFN-I response, were attenuated significantly (Fig. 2h ). We also investigated IFN-I protein secretion and found plasma pan-IFNα concentrations stable (Extended Data Fig. 3b ), while pan-IFNα and IFNb concentrations secreted upon R848 stimulation trended lower in PBMC cultures stimulated ex vivo with samples collected after 3 months of testosterone therapy as compared with baseline (Fig. 2i ). We conclude that pDCs contract in vivo and adapt phenotypically and functionally, leading to attenuated IFN-I responses during testosterone therapy.
Regulators of IFN-I responses in pDCs
IRF7 is a master regulator of IFN-I responses in pDCs 15 and individuals with loss of function mutations in IRF7 fail to control respiratory viruses such as influenza 16 and SARS-CoV-2 (ref. 17 ). We found IRF7 mRNA downregulated in pDCs following testosterone therapy, and IRF7 expression correlated with Hallmark IFNα transcripts in individual pDCs stimulated with R848 (Fig. 2j ). The suppressor of cytokine (SOCS) family of regulators are triggered by JAK-STAT signalling downstream of several cytokine receptors, providing negative feedback regulation. SOCS3 dampens IFN-I responses during flu infection 18 and we found SOCS3 (Fig. 2k ) and, to some extent, SOCS1 (Extended Data Fig. 3c,d ), upregulated in pDCs during in vivo testosterone therapy and inversely correlated with Hallmark IFNα and IRF7 following R848 stimulation (Extended Data Fig. 3e ). These results offer further insights to testosterone-mediated attenuation of IFN-I responses in pDCs.
Monocyte adaptation to testosterone therapy
Monocytes were also analysed by scRNA-seq following R848 stimulation, showing attenuated Hallmark IFNα responses after 3 months of testosterone therapy (Fig. 3a ). In contrast, Hallmark TNF responses upon R848 stimulation were potentiated in monocytes by testosterone therapy, indicating that the cross-regulation between IFN-I and TNF responses in blood mRNA-seq, is manifested in individual monocytes (Fig. 3a ). Stimulation with lipopolysaccharide (LPS) for 3 h showed further potentiated monocyte TNF responses by testosterone therapy (Fig. 3b ). Top genes involved in the Hallmark TNF response include IL-1, IL-6 and TNF but also NFκB pathway member NFKB1 were all induced more strongly by LPS stimulation after 3 months of testosterone in vivo (Fig. 3c ). TNF family proteins such as TNF, RANKL, TNFSFR9 and TRAIL were elevated in plasma during testosterone therapy (Fig. 3d and Extended Data Fig. 4a ). We treated blood from a healthy cisgender female participant with testosterone with or without the androgen receptor (AR) inhibitor enzalutamide and found RANKL was induced after 28 h in an AR-dependent manner (Extended Data Fig. 4b ). We conclude that, in contrast to attenuated IFN-I responses by pDCs and monocytes, Hallmark TNF responses are potentiated during testosterone treatment, further underscoring the cross-regulation of IFN-I and TNF regulated by sex hormones. These findings are important for understanding immunological consequences of masculinizing GAHT in trans men, but perturbations to this regulatory axis can also explain cytokine storms and excess mortality in cis male patients over female patients with COVID-19 and other severe infections.
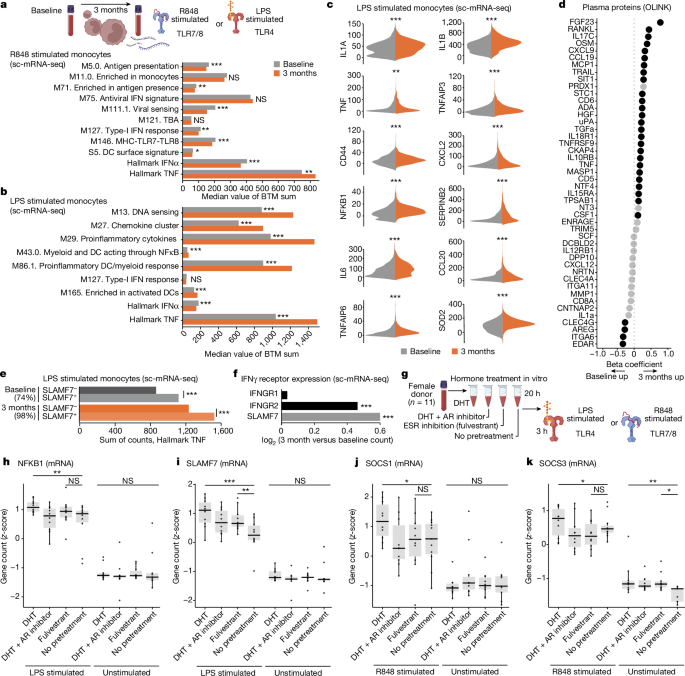
a , Median sum gene counts compared by two-sided, independent samples Student’s t -test, Bonferroni corrected P values for the indicated BTM in R848-stimulated (3 h) monocytes from baseline ( n = 466) and after 3 months of testosterone ( n = 851) treatment across two independent experiments. b , Median sum gene counts compared by two-sided, independent samples Student’s t -test with Bonferroni corrected P values for the indicated BTMs in LPS-stimulated (3 h) monocytes at baseline ( n = 1,297) and 3 months ( n = 1,050) from two independent experiments. c , log-transformed counts from sc-mRNA-seq of LPS-stimulated monocytes as in b after subtracting median expression of unstimulated cells at baseline ( n = 1,297; grey) and 3 months ( n = 1,050; orange) across two independent experiments. Twelve genes in the Hallmark TNF pathway are shown. d , Analysis of plasma proteins (Olink Target 96 inflammation and immune response panels) in samples from n = 20 participants at baseline and 3 months of testosterone in a single experiment. Black dots significantly different at 12 months over baseline ( P < 0.05) by Kruskal–Wallis tests. e , sc-mRNA-seq and Hallmark TNF responses upon LPS stimulation (3 h) in SLAMF7 high versus low monocytes as in b . Fraction of SLAMF7 + monocytes at baseline ( n = 1,297) and after 3 months of testosterone ( n = 1,050) shown on top. Two-sided, independent samples and uncorrected Student’s t -test; *** P < 0.001. f , The log 2 (fold change, 3 months versus baseline) gene counts for IFNGR1, IFNGR2 and SLAMF7 mRNA in monocytes (baseline, n = 1,297 and 3 months, n = 1,050). g , Blood from 11 healthy cis female participants incubated for 20 h with DHT with/without AR inhibitor (Enzalutamide) or ESR inhibitor/degrader (Fulvestrant) and then stimulated (3 h) by LPS or R848 and analysed for induced mRNA ( n = 560) by Nanostring nCounter. h – k , z -score transformed mRNA counts of LPS-induced NFKB1 ( h ), SLAMF7 ( i ), R848-induced SOCS1 ( j ) and SOCS3 ( k ). One-sided, paired measurements, uncorrected Student’s t -tests, * P < 0.05; ** P < 0.01; *** P < 0.001.
SLAMF7 is induced by testosterone
A recently described surface receptor, SLAMF7, potentiates TNF responses through an autocrine loop in myeloid cells 19 . We found SLAMF7 upregulation in T cells and monocytes during testosterone therapy. Pretreatment of blood cells from a cisgender female participant with dihydrotestosterone (DHT)—a form of testosterone not convertible to oestradiol by aromatase—followed by LPS stimulation for 3 h, induced TNF production in monocytes at amounts (mean fluorescence intensity) that correlated with SLAMF7 expression (Extended Data Fig. 4c ). scRNA-seq of monocytes from individuals undergoing GAHT and stimulated with LPS for 3 h ex vivo showed Hallmark TNF responses consistently more potent in SLAMF7 + than in SLAMF7 − monocytes, although both of these fractions were further enhanced by testosterone therapy (Fig. 3e ). SLAMF7 is induced by IFNγ 19 and we found one of its receptor genes, IFNGR2, upregulated in monocytes after testosterone treatment (Fig. 3f ). These findings indicate that SLAMF7 upregulation could contribute to testosterone-mediated potentiation of TNF responses in monocytes.
Relative effects of androgens and oestrogens
GAHT in individuals assigned female sex at birth decreases oestradiol concentrations rapidly and halts menstrual cycles. To investigate the relative contribution of increased testosterone and suppressed oestradiol on immune cell responses, we collected blood from 11 cisgender female participants of reproductive age and pretreated blood samples with testosterone, with and without the AR inhibitor enzalutamide as a control. Furthermore, as an alternative condition, we pretreated cells from the same donors with fulvestrant—a degrader of oestradiol-receptors (ESR) 1/2 (ESR1/2) to mimic the loss of ESR-mediated signals. We verified the expected hormone concentrations in each culture (Extended Data Fig. 4d ). After 20 h of pretreatment, we stimulated cultures with LPS or R848 (3 h) and induced n = 560 mRNA transcripts (Fig. 3g ). NFKB1 is a canonical LPS-induced gene, potentiated during GAHT, and also potentiated by 20 h pretreatment with DHT, but not Fulvestrant (Fig. 3h ). AR inhibition prevented the effect, indicating a direct role of androgen signalling in potentiating NFKB1 upon LPS stimulation (Fig. 3h ). Other Hallmark TNF pathway genes (IL-6, TNF and IL1B) were not induced significantly by either DHT or fulvestrant, indicating that further mechanisms or more time is required to mimic their induction in vivo (Extended Data Fig. 4e–g ). SLAMF7 upregulation after LPS was stronger in either DHT- or Fulvestrant-pretreated cells, indicating a balance between androgens and oestrogens regulating this factor (Fig. 3i ). Similarly STAT3 is an LPS response gene induced by either DHT or Fulvestrant, and this effect was visible even in unstimulated cultures without LPS (Extended Data Fig. 4h ).
Negative regulators of IFN-I responses—SOCS1 and SOCS3—were upregulated by DHT pretreatment in an AR-dependent manner, but not by ESR inhibition (Fulvestrant) (Fig. 3j,k ), verifying the direct effect of androgen signalling in suppressing IFN-I through these negative regulators in vivo during GAHT and in vitro.
T cell adaptation during GAHT
CD4/CD8 T cell ratios were higher in female in than male participants 20 , 21 but no decrease occurred during testosterone treatment (Extended Data Fig. 5a ), indicating that genetic factors rather than steroids are responsible for this. In 1889, Calzolari reported enlarged thymi in castrated male rabbits 22 and many subsequent studies confirmed this inhibitory effect on thymic output in mice 23 and humans 24 through AR-expressing thymic epithelial cells 25 . In our cohort, a slight reduction in naïve CD8 + T, but not CD4 + T cell proportions was seen after 12 months of testosterone treatment (Extended Data Fig. 5b,c ). T reg cells are more abundant in postpubertal male participants than in age-matched female participants 26 but, during GAHT, frequencies were stable over 12 months (Extended Data Fig. 5d ). Sex differences in CD4 + T cell polarization have been reported 27 , but in our sc-mRNA-seq data, no difference in T H 1, T H 2 or T H 17 marker genes occurred during testosterone therapy (Extended Data Fig. 5e–g ). T cell exhaustion in patients and mice with cancer has been linked to androgen signalling 28 , 29 , 30 . We found increased expression of a T cell exhaustion gene module in CD8 + T cells dominated by TIGIT mRNA upregulation (Extended Data Fig. 5h ). These findings illustrate how specific immune system components, reportedly divergent between male and female participants, are regulated by chromosomal differences, whereas others change dynamically in response to changing sex hormones.
Epigenetic induction of the NFκB pathway
As testosterone modulated monocyte function strongly during masculinizing GAHT, we performed NicheNet analyses to infer downstream consequences on other immune cell populations. We found monocyte-derived IL-6, TNF and IL-15 were upregulated by testosterone, and monocyte-released IL-12B as candidate genes to best explain several upregulated transcripts measured in NK and CD8 + T cells during GAHT (Fig. 4a ). The IFN-I regulator SOCS1 and the transcription factor (TF) RUNX3—important for maintaining cytotoxic function of CD8 + T cells 31 —can be explained by increased monocyte-derived IL-12B and IL-15. In NK cells, induced transcripts associated with cytotoxic function (GZMB, PRF1 and NKG7) were also explained by upregulated IL-15 and IL-12B (Fig. 4a ). Furthermore, upregulated IFNγ mRNA in NK cells was predicted as a downstream consequence of monocyte-derived IL-6, IL-15, IL-12B and TNF (Fig. 4a ).
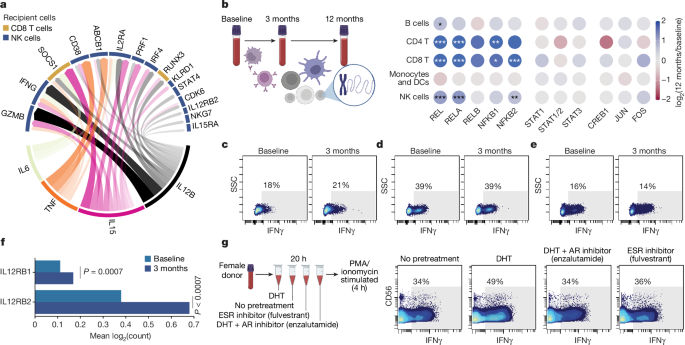
a , NicheNet analysis of monocytes from single-cell transcriptome data of LPS-stimulated PBMC comparing 3 months of in vivo testosterone treatment versus baseline. All target genes (top half of circle) are upregulated after testosterone treatment in vivo in NK cells and CD8 + T cells. Most explanatory genes in monocytes are shown in the lower half of the circle. Arrow width and density correspond to strength of inferred relationship. b , Blood T cells analysed for TF binding site chromatin accessibility as log-fold enrichment at 12 months versus baseline for a given TF with indicated cell populations using sc-ATAC-sequencing of PBMC ( n = 12,773) from three participants sampled before and during testosterone treatment. Cells were assigned to indicated cell populations on the basis of gene activity for canonical marker genes. Adjusted P values: * P < 0.05, ** P < 0.01, *** P < 0.001. c – e , PBMCs obtained at baseline or after 3 months of testosterone treatment were simulated with PMA/ionomycin for 4 h in vitro and intracellular IFNγ production in NK cells ( c ), CD8 + T cells ( d ) and CD4 + T cells ( e ) was analysed using flow cytometry. Numbers indicate percentage IFNγ + cells. f , Expression of IL12RB1 and IL12RB2 mRNA in NK cells at baseline and after 3 months of in vivo testosterone treatment by sc-mRNA-seq. Two-sided, independent samples and uncorrected Student’s t -test; *** P < 0.001. g , Blood from one healthy cisgender female participant was incubated for 20 h with DHT with/without Enzalutamide or Fulvestrant followed by stimulation with PMA/ionomycin for 4 h, staining for intracellular cytokines and analysis by mass cytometry. Manually gated NK cells are shown and the fraction of IFNγ + cells was determined on the basis of staining controls as indicated.
To investigate whether testosterone therapy would induce epigenetic adaptations in individual immune cells, we performed single-cell ATAC sequencing (sc-ATAC-seq) of ( n = 12,773) PBMCs from three participants sampled at baseline and after 3 and 12 months of testosterone treatment (Fig. 4b ). Given the altered IFN-I/TNF cross-regulation, we focussed on chromatin accessibility changes at JAK-STAT, AP-1, NFκB and MAPK TF binding sites. We found increased TF activity for all canonical NFκB binding sites, but not RELB (non-canonical NFκB) in T cells and NK cells, but not in B cells or myeloid/DCs following 12 months of testosterone treatment (Fig. 4b ). No significant changes were observed for STAT1, STAT2, STAT3, AP-1 (Fig. 4b ) or MAPK binding sites (data not shown), indicating that the canonical NFκB pathway is induced epigenetically in T/NK cells following testosterone treatment, possibly as a consequence of elevated TNF responses by myeloid cells, with broad functional implications for T/NK cell function and proliferation 32 .
Potentiation of IFNγ responses by NK
To further assess functional consequences of GAHT on lymphocytes, we stimulated PBMCs at baseline and following 3 months treatment with phorbol 12-myristate 13-acetate (PMA)/ionomycin and assessed intracellular IFNγ responses by flow cytometry. We found stronger IFNγ responses in NK cells following 3 months of testosterone treatment (Fig. 4c ), whereas CD8 + (Fig. 4d ) and CD4 + T cell responses were unchanged (Fig. 4e ). IL12RB1 and IL12RB2 mRNA in individual NK cells were induced during GAHT. Collectively, these findings support the view that NK cell function is potentiated during GAHT as a consequence of induced IL-12 responses by monocytes following testosterone treatment (Fig. 4f ).
We also aimed to distinguish relative effects of added testosterone through AR-signalling from the loss of oestradiol-mediated signals during GAHT. To this end, blood from five healthy cisgender female participants was preincubated with DHT, DHT + AR inhibitor (enzalutamide) or ESR inhibitor (fulvestrant) alone (20 h), before stimulation with PMA/ionomycin (4 h) (Fig. 4g ). Intracellular IFNγ was measured by mass cytometry and we found that pretreatment with DHT, but not loss of ESR signalling (fulvestrant), potentiated IFNγ responses by CD56 dim NK cells, but not T cells (Fig. 4g and Extended Data Fig. 5i ). These findings indicate a loop of potentiated IFNγ responses by NK cells and IFNγ-mediated upregulation of SLAMF7 on monocytes associated with potentiated TNF responses, triggering epigenetic activation of NFκB-regulated genes in T/NK cells and further enhancing IFNγ production by NK cells during testosterone therapy.
Corroborating findings in cisgender cohorts
To investigate whether observations made in individuals undergoing masculinizing GAHT could also explain divergent immune responses in cisgender individuals, we analysed several sc-mRNA-seq datasets of immune cells from male and female participants (Fig. 5a ). SARS-CoV-2 triggers sex-divergent immune responses and we found cross-regulated IFN-I and TNF responses in pDCs and monocytes, as shown by significantly higher Hallmark TNF responses in male monocytes and reduced IFN-I responses in two cohorts of adults less than 50 years of age (Fig. 5b,c ) 33 , 34 . In a separate sc-mRNA-seq dataset 35 of PBMCs from healthy volunteers stimulated in vitro with Candida albicans or Mycobacterium tuberculosis (mTB), greater IFN-I responses were seen in female pDCs and monocytes, while Hallmark TNF responses were higher in male monocytes (Fig. 5d ), further supporting sex hormone-mediated regulation of the IFN-I/TNF axis as an explanation for divergent responses by cis male and female participants across several cohorts.

a , Male and female patients infected with SARS-CoV-2. b , sc-mRNA-seq data from patients infected with SARS-CoV-2 selected for pDCs ( n = 144 (male, 103; female, 41)) and monocytes ( n = 33,887 (male, 18,262; female, 15,625)) and gene count sum for the indicated BTM. Two-sided, independent samples and uncorrected Student’s t -test: * P < 0.05; ** P < 0.01; *** P < 0.001. c , PBMC data from SARS-CoV-2 infected patients analysed by sc-mRNA-seq and divided into pDCs ( n = 21 (male, 10; female,11)) and monocytes ( n = 4,521 (male, 2,672; female, 1,849)). Two-sided, independent samples and uncorrected Student’s t -test: * P < 0.05; ** P < 0.01; *** P < 0.001. d , PBMCs from healthy male and female participants stimulated in vitro (3 h) and analysed by sc-mRNA-seq. pDCs ( n = 262 (male, 162; female, 100)) were selected from cells stimulated with C. albicans , and monocytes ( n = 12,961 (male, 6,652; female, 6,309)) were selected from cells stimulated with mTB. Two-sided, independent samples and uncorrected Student’s t -test: * P < 0.05; ** P < 0.01; *** P < 0.001. e , f , Monocytes in d subdivided according to SLAMF7 expression ( e ), and Hallmark TNF gene count following mTB stimulation in vitro for SLAMF7 + and SLAMF7 − monocytes ( f ). Two-sided, independent samples and uncorrected Student’s t -test: * P < 0.05; ** P < 0.01; *** P < 0.001. g , h , Single NK cell transcriptome analyses following in vitro exposure to mTB for 3 h ( g ) and 24 h ( h ) and mean mRNA count for IFNγ are shown. Two-sided, independent samples and uncorrected Student’s t -test: * P < 0.05; ** P < 0.01; *** P < 0.001.
Using the same dataset 35 , we found higher frequencies of SLAMF7 + monocytes in male participants (Fig. 5e ), and these SLAMF7 + monocytes produced stronger Hallmark TNF responses following mTB stimulation as compared with SLAMF7 − monocytes, indicating that this feature described during masculinizing GAHT also contributes to sex-divergent responses in cisgender individuals (Fig. 5f ). In PBMCs stimulated with mTB, sex-divergent NK cells responses were also found. After 3 h of mTB stimulation, the IFNγ mRNA response was stronger in female NK cells, probably reflecting differences in sensing mechanisms and initial IFN-I/II responses in female cells (Fig. 5g ). In contrast, after 24 h of mTB in vitro, secondary signals, such as monocyte-derived IL-6, TNF, IL-15 and IL-12B, are likely to influence, and in this case female NK cells have markedly reduced IFNγ mRNA, whereas male NK cells sustain a high IFNγ response transcriptionally (Fig. 5h ). This difference in response dynamics points towards cell–cell interactions and regulatory mechanisms divergent between sexes and corroborate our predictions from individuals undergoing GAHT. Testosterone-mediated potentiation of a monocyte–NK cell axis resulting in upregulated TNF and IFNγ can offer explanations for previously reported sex differences in mTB disease course 36 . Collectively, our results highlight previously unrecognized immunomodulatory effects of sex hormones in humans, calibrating an IFN-I/TNF axis across several immune cell populations with implications for understanding sex-divergent immune responses to infections, vaccines and autoantigens in immune-mediated diseases.
Sex hormones, in contrast to sex chromosomes, offer an opportunity for dynamic regulation of the human immune system in relation to changing needs over the course of life, and even during the course of the menstrual cycle in women of reproductive age. Sex chromosomes on the other hand, encode immunological differences between male and female individuals selected for throughout evolution 37 . The inactive X and active Y chromosomes can broadly modulate autosomal gene expression 8 , and gain-of-function mutations in the X-encoded gene TLR7 can trigger monogenic lupus-like disease with elevated IFN-I responses 38 .
GAHT enables the acquisition of secondary sex characteristics aligned with gender identity in transgender individuals but the immunological impacts and risks of immune-mediated and infectious diseases upon sex hormone therapy is unknown. Here we describe several layers of immunological adaptations in trans men, assigned female sex at birth and undergoing masculinizing testosterone treatment.
We find that testosterone increase and the resulting oestradiol suppression, alters a cross-regulation axis involving IFN-I and TNF. Similar cross-regulation has been described in vitro 39 and in vivo in healthy volunteers 40 , and in patients with female-dominated autoimmune lupus 41 , but its regulation by sex hormones is not previously known. Curiously, around 15% of patients treated with anti-TNF develop a lupus-like syndrome with autoantibodies against double-stranded RNA and elevated IFN-induced gene signatures 42 . Detailed studies of IFN-I and TNF cross-regulation have been performed in osteoclasts and show that TNF, RANKL and CSF1 induce NFκB-regulated genes, while inhibiting IFN-I (ref. 43 ). Conversely, IFN-I signalling through IFNAR1 limits this NFκB and AP-1 activation 43 . During GAHT, we find that plasma RANKL, CSF1 and TNF are all induced, NFκB TF binding sites exhibit more chromatin accessibility and Hallmark TNF responses are enhanced in an AR-dependent manner, indicating that IFN-I/TNF cross-regulation occurs at the system level and is calibrated by sex hormones in vivo.
The question arises as to whether observed changes are associated directly with testosterone treatment or occur indirectly due to reduced oestradiol signals. To test this question, we designed an in vitro system in which blood from 11 cis female donors was pretreated with either DHT (in the presence or absence of the AR inhibitor enzalutamide) or the ESR inhibitor fulvestrant only. Results showed that NFκB-mediated responses to LPS stimulation were potentiated by DHT alone through AR and not by loss of ESR-mediated signals. Inhibitors of IFN-I responses—SOCS1 and SOCS3—were also induced by DHT alone, indicating direct effects of androgens in suppressing IFN-I responses. It is conceivable that loss of oestradiol-mediated signals can also contribute to attenuated IFN-I responses through other mechanisms not investigated herein. In support of this, Seillet et al previously showed that oestradiol supplementation potentiates IFNα responses in postmenopausal women 44 and Griesbeck et al. reported that ESR signalling in mice potentiates IFNα responses in pDCs through IRF5 induction 45 . A case of a trans woman developing lupus during oestradiol therapy 46 points towards direct potentiating effects of oestradiol on IFN-I responses.
Male patients are at increased risk of severe disease following SARS-CoV-2 infection due to less efficient IFN-I responses and excessive inflammation mediated by IL-6, IFNγ, TNF and IL-1/18 (ref. 1 ). This could be explained in part by the testosterone-mediated potentiation of proinflammatory responses through IFNγ, SLAMF7 and TNF reported herein. Female patients with polycystic ovary syndrome have elevated testosterone concentrations, elevated plasma TNF 47 and are at greater risk of severe COVID-19 as compared with age-matched female control participants without polycystic ovary syndrome 48 . Not much is known about the severity of SARS-CoV-2 infections in individuals undergoing GAHT but one single-centre study found higher rates of symptomatic COVID-19 in trans men on testosterone therapy as compared with trans women on oestradiol 49 . Whether this reflects immune response differences and more symptomatic disease or differences in risks of contracting the virus through modulated ACE2 and or TMPRS2 expression remains to be determined.
Recent developments in immune-oncology have shown important roles for AR signalling in regulating T cell responses to tumours and limiting the efficacy of checkpoint blockade through T cell exhaustion 28 , 29 , 30 . We find upregulation of TIGIT—a marker of T cell exhaustion during masculinizing GAHT—in vivo, but we also find induction of TNF responses and IFNγ responses by NK cells, which seems at odds with reported impairments of T H 1 responses in male prostate cancer patients. However, analyses of chronic infection models (human immunodeficiency virus or lymphocytic choriomeningitis virus) have indicated TNF signalling in T cells as another important regulator of T cell exhaustion during chronic antigen stimulation 50 . It is tempting to speculate that the testosterone-driven induction of TNF described herein could be another driver of T cell exhaustion in cancer patients and a possible target for combination therapies in the future.
The main drawback of this study is the limited cohort size and the challenges in studying mechanisms of hormone-induced changes in human participants. Studies of model organisms are warranted to clarify mechanisms in vivo but, unlike higher order primates, laboratory mice do not menstruate 51 and also differ in their sex hormone regulation, affecting trade-off mechanisms in relation to changing needs. Performing in vitro experiments using human cells as described herein offers some mechanistic understanding but is limited in that such experiments are disconnected from physiological mechanisms of regulation in vivo through the nervous system or other endocrine pathways of importance.
Another challenge in human studies is separating the direct effects of gonadal steroids on a particular cell type from secondary effects mediated through cell–cell communication in vivo. Expression of the AR varies across cell populations, with maximal protein amounts found in pDCs followed by monocytes, while lymphocyte populations express lower amounts of AR protein (Extended Data Fig. 6a ). The two ESRs show variable expression across immune cell types but highest protein expression in pDCs (Extended Data Fig. 6b ). Analyses of mRNA from cell populations derived from fluorescence-activated cell sorting (FACS) show a similar pattern, with highest expression in pDCs in both male and female cells (Extended Data Fig. 6c ) and varied AR/ESR expression amounts across cell types, which offers another layer of complexity to the regulation of immunity by these hormones.
Life history theory provides a framework for understanding allocation of limited resources between critical traits such as reproduction, growth and maintenance, in which immunity is a key component 52 . Male investment into reproduction is much lower than that of females, and males allocate more resources into muscle growth and immune function and testosterone is a key regulator of such resource allocation in vertebrates 53 . Metcalf and Graham modelled trade-offs between sex-divergent recognition of pathogens (female superior) and pathogen-killing processes (male superior) and found that sexual maturation and changes in reproductive investments during the life course explains these observed divergent immune processes 54 . Our results corroborate this and adds mechanisms of hormone-mediated regulation of immunity in response to changing needs during the life course.
Evolutionary pressures from pathogens have shaped human immune systems and the risk of vertical transmission is a selective pressure unique to pregnant females 55 . It is thus tempting to speculate that potentiated IFN-I induced by elevated oestradiol amounts in pregnancy is selectively favoured to limit such vertical transmission of viruses. This also corroborates clinical observations of increased lupus flares mediated by IFN-I during pregnancy 56 . TNF is critical for the defence against Mycobacteria , Staphylococci and other common bacteria, but elevated TNF is also associated with failure of implantation 57 , pregnancy loss 58 and preeclampsia 59 . Evolutionary pressures to suppress TNF while potentiating IFN-I during the second half of the menstrual cycle and following implantation in pregnant people could increase the likelihood of reproductive success. Conversely, in male individuals, we speculate that increased investment into muscular growth could explain testosterone-mediated potentiation of TNF and suppression of IFN-I. Testosterone is induced following acute exercise and transient TNF responses by tissue macrophages is important for muscle regeneration and growth 56 . Chronically elevated TNF leads to muscle wasting. IFN-I directly inhibits myoblasts, leading to muscle weakening and wasting as seen in patients with autoimmune dermatomyositis 60 . To this end, it is conceivable that hormone control of the TNF/IFN-I axis reflects these different investments in reproduction and muscle growth, respectively, as predicted by life history theory.
Understanding the mechanisms by which gonadal steroids modulate immunity in individuals undergoing masculinizing GAHT are important to ensure the health and wellbeing of trans men and avoid long-term adverse outcomes such as severe infection and inflammatory disorders. These mechanisms can also help explain the divergent immune responses in cis men and women that are regulated dynamically by sex hormones in relation to ever changing needs during the human life course.
Inclusion and ethics
Twenty-three adult individuals who were assigned female sex at birth and who were undergoing masculinizing gender-affirming treatment were enroled at specialist centres for transgender medicine in Stockholm, Uppsala, Linköping and Umeå in Sweden between 2016 and 2023. The study was approved by the Swedish Ethical Review Authority (2016/1422-31/1). Informed consent was obtained from all individuals. Only individuals who had not previously received testosterone treatment and who had normal sex hormone concentrations were included. Additionally, individuals with autoimmune diseases, immunodeficiencies or signs of continuing infection/inflammation were excluded from the study.
Testosterone therapy
Venous blood samples were collected at three timepoints: baseline, 3 months and 12 months following testosterone injections (Testosterone Undecaonate, Nebido administered once every 12 weeks). All patients received 1,000 mg of Nebido except for four participants who received reduced doses of 750 mg due to low body mass indices or haematocrit values. The baseline sample was collected within the 2 weeks before the start of testosterone treatment.
Measurement of serum sex hormones
Serum concentrations of sex hormones were analysed using liquid chromatography with tandem mass spectrometry assays at Gothenburg University as described previously 61 . The same method was used to analyse sex hormones from resulting culture supernatants as shown in Extended Data Fig. 4d . Briefly, calibrator stock solutions were prepared for all sex hormones and each internal standard stock solution was made separately using 13 C 3 -labelled versions of each steroid, except for dehydroepiandrosterone, which was labelled with d6. Steroid hormones were analysed using a two-dimensional liquid chromatography system consisting of an Acquity ultra-performance liquid chromatography system and a TQ-XS triple quadrupole mass spectrometer from Waters. The lower limit of detection (LLOD) was defined as the lowest peak with a signal more than three times the noise level. The lower limit of quantification (LLOQ) was defined as the lowest peak that was reproducible with a coefficient of variation of less than 20% and an accuracy of 80% to 120%. To circumvent problems with endogenous steroid amounts, the determinations of LLOD and LLOQ were performed in human serum pools with isotope-labelled steroids spiked at four different concentrations.
The amounts of bioavailable testosterone were calculated according to the formulae below 62 :
in which rKb,ALB is the binding constant (0.601) for testosterone (TEST) to albumin (ALB), rKb,SHBG is the binding constant (1.0) for testosterone to sex hormone-binding globulin (SHBG) and P − ALB is a fixed value of 42.
Sample processing
A 4 ml sample of blood was drawn in EDTA-containing sterile vacutainer tubes from each participant in the sex reassignment therapy cohort and prepared as follows: 0.5 ml of blood was mixed with an equal amount of whole blood stabilizer 63 (Cytodelics AB), incubated for 10 min at ambient temperature and stored at −80 °C. A 1 ml aliquot of blood was mixed with PAXgene solution (BD Biosciences), incubated for 2 h at ambient temperature and stored at −80 °C. The remaining blood was centrifuged at 4 °C and 1,200 g for 10 min, after which plasma was collected and stored at −80 °C. The leftover blood after plasma removal was mixed equally with PBS and layered over Lymphoprep (STEMCELL Technologies) for PBMC isolation by density gradient centrifugation following the manufacturer’s protocol. Cells were washed, counted and cryopreserved in a solution of 90% FBS (Sigma-Aldrich) mixed with 10% dimethylsulfoxide (DMSO; Sigma-Aldrich), initially stored at −80 °C overnight and then transferred to −150 °C for future use.
Bulk RNA-seq of whole blood samples
To analyse changes in gene expression, we performed RNA-seq using RNA extracted from PAXgene blood samples. The RNA samples were prepared using a QIAcube with the PAXgene Blood RNA Kit (Qiagen). Before cDNA library preparation, the quality of the RNA was assessed by determining the RNA integrity number using the Agilent 2100 Bioanalyzer with the RNA 6000 Pico Kit. The RNA concentration was measured using the Qubit Fluorometer with the Qubit dsDNA HS Kit (ThermoFisher Scientific).
For final sequencing and cDNA library preparation, an Advanta RNA-Seq XT NGS Library Preparation Kit was used with the Juno system (Standard BioTools Inc.). We performed Bulk RNA-seq on a NovaSeq 6000 instrument using one flow cell SP-200 (Illumina) with paired-end reads and a read length 2 × 100.
Data analysis of bulk mRNA-seq data
Bulk RNA-seq results from 59 samples from 20 individuals undergoing testosterone treatment were preprocessed with Kallisto 64 . Quality control was provided by the National Genomics Infrastructure at Science for Life Laboratory, Stockholm, Sweden. To generate abundance estimates for all samples, the Kallisto program (v.0.46.2) was used to quantify abundances of transcript sequences in FASTA format using the Ensembl transcriptome Homo_sapiens.GRCh38.cdna.all.index ( https://ftp.ensembl.org/pub/release-109/fasta/homo_sapiens/cdna/ ) for the Kallisto index. The Kallisto outputs were then imported into R using the tximport package, and the effect of ‘visit’ on whole blood mRNA expression was assessed using DESeq2 (ref. 65 ) while accounting for interindividual variability and age effects. Before assessing differential gene expression, genes with fewer than 100 reads across samples were filtered out, as well as genes that did not have a normalized count of ten in at least one-fourth of the samples. The results from the differential gene expression analysis were used for gene set enrichment analysis of Hallmark pathways using clusterProfiler 66 .
scRNA-seq experiments
Cryopreserved PBMCs obtained at baseline and after 3 months of testosterone treatment were thawed in thawing medium (RPMI 1640 HyClone supplemented with 10% FBS, 1% penicillin-streptomycin and Benzonase-nuclease (Sigma-Aldrich)). Cells were counted using a Cellaca MX (Nexcelom), plated and incubated for 1 h at 37 °C and 5% CO 2 to rest. Samples were then either left untreated or stimulated ex vivo with LPS (100 ng ml −1 ) or R848 (1 μg ml −1 ) for 4 h. After stimulation, the cells were collected, and supernatants were stored for later analysis by SIMOA (Quanterix) 67 .
Viability and cell counts were assessed after resuspending collected cells in PBS with 0.04% BSA (ThermoFisher Scientific). The cells were then prepared for scRNA-seq using the 10x Genomics 3′ v.3.1 (dual index) kit according to the manufacturer’s instructions (catalogue no. CG000315 Rev B) on a Chromium Controller. Approximately 1 × 10 4 cells from each condition were loaded onto separate wells of a 10x Genomics chip and the Chromium Controller was used to create GEM emulsions. The target recovery was 6,000–7,000 cells per condition. The libraries were sequenced on an Illumina NovaSeq 6000 platform, using paired- end reads (configuration 28 × 10 × 10 × 90) with 20,000 reads per cell.
scRNA-seq data analyses
CellRanger with default parameters was used to process FASTQ-files and align sequencing reads from 10x Genomics 3′ HT v.3. and 3′ GE towards the human genome. Cells were further filtered using a bimodal distribution-based approach, excluding those with read counts below (considered low quality) or above (considered technical artifacts) cut-off thresholds. The cut-off thresholds for each sample were chosen on the basis of distribution shape of read counts to retain biologically relevant cells and to eliminate technical artifacts. Cells with mitochondrial gene expression above 10% were also filtered out. All scRNA-seq data were preprocessed in Python using Scanpy v.1.9.1. For each sample, normalization by counts per cell (target sum = 1 × 10 4 ) and feature scaling were applied to the CellRanger outputs for each sample, followed by linear dimensionality reduction using PCA and uniform manifold approximation and projection (on top 2000 variable genes), nearest neighbours ( n = 10) computation and identification of clusters (res = 1). Clusters were annotated on the basis of canonical marker genes. BTMs 68 were used to compare transcriptional patterns before and during testosterone treatment and in response to stimulation.
NicheNet analyses
The NicheNet analysis and circus plots were created following the standard workflow available from NicheNet 69 and circlize 70 . Specifically, differentially expressed genes between samples from baseline and after 3 months of testosterone treatment were identified using Seurat’s (v.4.3.0) built in function FindMarkers and filtered with an adjusted P value of less than 0.05 and an absolute value for the average fold change of at least 0.15. Ligand activities were calculated, and the top upstream ligands that could explain the observed target gene expression changes were selected. The ligand–target links were filtered on the basis of their weights (strength of the ligand–target relationship), with links belonging to the lowest 66% of scores being removed. The circos plot blocks were coloured according to a gene’s target cell, inferred as the cell type with the highest mean-value change between the two visits. The widths of the blocks indicate the potential of each receptor to be influenced by all shown ligands, with some interactions not visible due to the cut-off weight threshold. The transparency of the arrows indicates the regulatory potential of a ligand–target interaction (the more transparent, the weaker the regulatory potential).
sc-ATAC-seq and data analysis
sc-ATAC-seq experiments were conducted on the 10x Chromium platform, following a previously described protocol 71 . Briefly, cells were washed with PBS containing 0.04% BSA and nuclei subjected to isolation as per the manufacturer’s instructions. After counting, approximately 10,000 nuclei were used for tagmentation. The tagmented nuclei were then loaded for capture using the 10x Chromium controller. Following gel emulsion generation, we carried out linear amplification and DNA purification according to the manufacturer’s protocol. The resulting DNA was used for library construction, following the guidelines provided on the manufacturer’s website. The libraries were quantified using an Agilent Bioanalyzer and sequenced on an Illumina NovaSeq S4 sequencer, with the following setup: 50 bp read 1N, 8 bp i7 index, 16 bp i5 index and 50 bp read 2N. In this setup, 1N and 2N refer to the DNA insert sequencing, while i5 and i7 sequencing identify the individual barcodes of single cells.
The 10X Genomics cellranger pipeline (cellranger-atac mkfastq, count and aggr) was followed for 10x sc-ATAC-seq analysis. Cellranger aggr outputs were used for downstream analysis in R using the Signac package. We performed quality control using Signac’s default settings for transcriptional start site enrichment score, nucleosome banding pattern, sequencing depth and complexity, and fraction of fragments in peaks. The ratio of reads in genomic blacklist regions was calculated using the FractionCountsInRegion function with the blacklist for hg38. After quality control, a total of 143,624 peaks (features) across 12,773 cells remained for further analysis. The number of cells per sample varied between 636 and 4,632 for the eight total samples analysed. We applied frequency-inverse document frequency normalization, followed by feature selection and dimensionality reduction using singular value decomposition on the frequency-inverse document frequency matrix. We performed uniform manifold approximation and projection dimensionality reduction 72 on the first 30 latent semantic indexing components, with latent semantic indexing components capturing technical variation excluded from further analysis. K-nearest neighbour graph construction and clustering were done using the smart local moving algorithm, resulting in the identification of 21 unique clusters. Gene activities were used for cluster annotation, with gene activities determined using the GeneActivity function followed by log normalization. Five main immune clusters were identified and used for further analyses. TF motif analysis was conducted by identifying overrepresented motifs in a set of differentially accessible peaks between pre- and post-testosterone therapy (3 or 12 months) for all the five immune subsets using hypergeometric tests and P values corrected for several hypotheses (Benjamini–Hochberg).
Immune cell profiling by mass cytometry
Blood samples were mixed with a stabilizer 63 (Whole blood processing kit component; Cytodelics AB) within the first hour post blood-draw and cryopreserved according to the manufacturer’s recommendations. Samples were then thawed, fixed and lysed using Lysis and Wash buffers (Whole blood processing kit; Cytodelics AB). After fixation/lysis, 1–2 × 10 6 cells per sample were plated and cryopreserved using CRYO#20 (Cytodelics). For staining, cells were thawed at 37 °C, barcoded using an automated liquid handling robotic system (Agilent Technologies) 73 using the Cell-ID 20-plex Barcoding kit (Standard BioTools Inc.) as per the manufacturer’s recommendations and stained batch-wise after pooling. Cells were washed using cell staining buffer (CSB) (Standard BioTools Inc.), FcR blocked using an in-house-prepared blocking solution for 12 min at ambient temperature then stained using a cocktail of metal-conjugated antibodies targeting surface antigens (Broad extended panel) and incubated for 30 min at 4 °C. Cells were washed twice with CSB and fixed overnight using 2% formaldehyde in PBS (VWR international). The panel of antibodies used is listed in Supplementary Table 1 .
For cells from whole blood pretreated and stimulated in vitro, we performed intracellular staining. Cells were first stained with a cocktail of antibodies targeting surface antigens (Supplementary Table 2 ) and then washed twice with CSB, fixed and permeabilized using Foxp3/Transcription Factor Staining Buffer Set (ThermoFisher Scientific) according to the manufacturer’s instructions. Cells were then stained using a cocktail of metal-conjugated antibodies targeting intracellular antigens (Supplementary Table 3 ) and incubated for 1 h at ambient temperature. Cells were washed twice with CSB and fixed overnight using 2% formaldehyde in PBS.
For acquisition by CyTOF XT 73 , cells were stained with DNA intercalator (0.125 mM Iridium-191/-193 or MaxPar Intercalator-Ir (Standard BioTools Inc.) in 2% formaldehyde and incubated for 20 min at ambient temperature. Cells were washed twice with CSB followed by two washes with Maxpar Cell Acquisition Solution (CAS) Plus (Standard BioTools Inc.) before being filtered through a 35 mm nylon mesh, diluted to 500,000 cells ml −1 using CAS Plus and divided into polypropylene tubes. A total of 2 × 10 6 cells per tube in pelleted form were then placed in the chilled carousel of the CyTOF XT instrument (Standard BioTools Inc.). EQ Six (EQ6) element calibration beads (Standard BioTools Inc.) were added to a tube and placed in the carousel. The autosampler of the CyTOF XT dispensed CAS Plus to the pelleted sample tubes, mixed with EQ beads 0.1×, and then acquired on CyTOF XT mass cytometers at a rate of 300–500 cells s −1 using CyTOF software v.8.0 with noise reduction, event length limits of 10–150 pushes, and a flow rate of 0.030 ml min −1 .
Mass cytometry antibodies and reagents
Purified antibodies were obtained in carrier/protein-free buffer and coupled to lanthanide metals using the MaxPar X8 or MCP9 antibody conjugation kits (Standard BioTools Inc.) as per the manufacturer’s recommendations. Metal-conjugated antibodies were also purchased from Standard BioTools. The antibodies used for this study are listed in Supplementary Tables 1 – 3 .
Mass cytometry data analyses
Samples from participants undergoing sex reassignment therapy were processed through mass cytometry in four batches to investigate immune composition and phenotype. This involved analyzing.fcs files from 60 samples from 20 series of participants receiving testosterone treatment. Data analysis was conducted in R. The data were arcsin h transformed with a cofactor of five using the flowCore package. Beads and dead cells were filtered out. Batches were combined, and batch effects in marker expression were eliminated using the sva package. The resulting matrix was used for immune composition analysis with the FlowSOM package 74 .
Initially, 30 clusters were identified, neutrophil clusters were annotated, and the remaining non-neutrophil cells were clustered into a total of 100 clusters. A total of 113 unique clusters were annotated on the basis of median marker expression using the pheatmap package. A total of 12,377,068 cells from the 60 samples of participants undergoing testosterone treatment were further analysed. This analysis included investigating immune phenotypes using PAGA 75 (see below) and examining the effects of testosterone on immune cell composition using a mixed-effects model with the lme4 package. For linear mixed-effects models, the frequency of 35 immune subsets was modelled considering visit (baseline, 3 months and 12 months) and age as fixed effects, and participant ID as random effect. Significant visit effects were determined using a P value of 0.05 and a 5% FDR threshold, with beta coefficients indicating the directionality of the effect.
Spectral flow cytometry analysis of AR and ESR expression
For ESRa staining, PBMCs were extracted from heparinized whole blood, as described above. One million live cells were aliquoted per test, washed twice in ice-cold PBS, and incubated with LIVE/DEAD Fixable Blue dye (ThermoFisher Scientific) for 10 min at 4 °C. PBMCs were then washed in ice-cold FACS buffer (2% FBS, 0.5 mM EDTA in PBS) and FcR blocked using an in-house-prepared solution for 10 min at ambient temperature. The Horizon Brilliant Stain Buffer Plus (BD Biosciences) and extracellular antibodies (Supplementary Table 4 ) were added, and cells were incubated for 30 min at 4 °C followed by fixation and permeabilization with Fixative buffer (Cytodelics AB) or Foxp3/Transcription Factor Staining Buffer Set (ThermoFisher Scientific) according to the manufacturer’s instructions. Cells were mixed with FcR block buffer and, after 10 min at room temperature, intracellular antibodies (Supplementary Table 4 ) were added, and the samples were incubated for 30 min at 4 °C. For AR staining, WBCs from heparinized whole blood were prepared using a Cytodelics kit, and 1.5 million fixed-permeabilized cells was aliquoted per test and exposed to FcR block (BD Biosciences) for 30 min at 4 °C. Horizon Brilliant Stain Buffer Plus (BD Biosciences) and all-antibody cocktail (Supplementary Table 4 ) were added, and cells were incubated overnight at 4 °C. AR and ESRa antibody concentrations were established on the cell line MCF7 (ATCC); the specificity of AR antibody was also verified using a competitive displacement approach on MCF7 cells. Briefly, 60,000 cells were collected at passage two, fixed-permeabilized using Cytodelics kit, FcR blocked and stained as described for WBCs. Unconjugated antibodies and isotype controls information is present in Supplementary Table 4 . After a wash in cold FACS buffer, data were acquired using an Aurora spectral cytometer (Cytek Biosciences). Cytobank Community (Beckman Coulter) software was used for data analysis.
PBMC stimulation and intracellular staining by spectral flow cytometry
Cryopreserved PBMCs obtained from individuals undergoing gender-affirming testosterone treatment were collected at baseline and after 3 months of testosterone treatment. These cells were thawed in thawing medium (RPMI 1640 HyClone supplemented with 10% FBS, 1% penicillin-streptomycin and Benzonase-nuclease (Sigma-Aldrich).
The cells were then counted using a Cellaca MX (Nexcelom), plated and incubated for 1 h at 37 °C and 5% CO 2 to rest. After this, some samples were left untreated while others were stimulated ex vivo with PMA (50 ng ml −1 ) and Ionomycin (1 μg ml −1 ) for 4 h. Brefeldin A (5 μg ml −1 ) and Monensin (2 μg ml −1 ) were added during the last 3 h of stimulation.
Following stimulation, the cells were washed twice in ice-cold PBS and then incubated with LIVE/DEAD Fixable Blue dye for 10 min at 4 °C. The cells were then washed in ice-cold FACS buffer and FcR blocked using blocking solution prepared in-house for 10 min at ambient temperature.
Horizon Brilliant Stain Buffer Plus was added, and the cells were stained with a cocktail of fluorochrome conjugated antibodies targeting surface antigens for 30 min at 4 °C (Supplementary Table 4 ). The cells were then fixed using Fix, Lysis and Wash buffers (Whole blood processing kit; Cytodelics AB) and permeabilized using permeabilization buffer (ThermoFisher Scientific).
Next, the cells were stained with a cocktail of antibodies targeting intracellular antigens (Supplementary Table 4 ) for 30 min at 4 °C and then acquired using an Aurora spectral cytometer.
Plasma protein profiling by Olink
Plasma protein data was generated using the Olink assay, a proximity extension assay (Olink AB) 76 . Plasma (20 μl) from each sample was thawed and analysed using a Target Inflammation panel (Olink AB), at the Affinity Proteomics Stockholm, Science for Life Laboratory or Olink AB. In these assays, plasma proteins are dually recognized by pairs of antibodies coupled to a cDNA-strand that ligates when brought into proximity by its target, extended by a polymerase and detected using a Biomark HD 96.96 dynamic PCR array (Standard BioTools Inc.). Analyses of differentially abundant plasma proteins were performed using linear mixed-effects models considering age as fixed effects.
Whole blood pretreatment in vitro using testosterone and AR antagonist for Olink analysis
A blood sample obtained from a healthy female donor was mixed in equal ratio with WB-STIM buffer (Cytodelics AB) without phenol red. The sample was then split into three groups: untreated, treated with testosterone (Sigma-Aldrich) alone at 10 ng ml −1 , or treated with a combination of testosterone and the AR antagonist Enzalutamide (Sigma-Aldrich) at 2.3 μg ml −1 . All samples were incubated for 28 h at 37 °C and 5% CO 2 . After incubation, supernatants were collected, cryopreserved and later analysed using the Olink Target Inflammation panel (Olink AB) as described above.
Whole blood pretreatment and stimulation in vitro for Nanostring and mass cytometry analysis
For the in vitro pretreatment step, blood samples were mixed in equal ratio with WB-STIM buffer (Cytodelics AB) without phenol red and split as follows: untreated, treated with DHT (Sigma-Aldrich) alone at 10 ng ml −1 , treated with DHT combined with Enzalutamide (Sigma-Aldrich) at 2.3 μg ml −1 or treated with fulvestrant (Sigma-Aldrich) alone at 100 nM. Samples were incubated for 20 h at 37 °C and 5% CO 2 . DHT was chosen because this androgen cannot be converted to oestradiol by aromatase 77 . Fulvestrant is a degrader of the ESR and blocks oestradiol-mediated signalling 78 .
For Nanostring analyses, blood samples from healthy cisgender female donors ( n = 11) were pretreated and then immediately stimulated with either LPS (10 ng ml −1 ) or R848 (1 μM) for 3 h or left unstimulated as a control. Samples were then centrifuged at 4 °C and 1,200 g for 10 min and supernatants were collected, cryopreserved and analysed using SIMOA. The remaining 1 ml of blood was mixed with PAXgene solution (BD Biosciences), incubated for 2 h at ambient temperature and stored at −80 °C. RNA samples were prepared using a QIAcube with the PAXgene blood RNA kit (Qiagen) and analysed using the Nanostring nCounter Sprint Profiler system with a broad human immune response panel (Human Immunology v.2 Gene Expression CodeSet) as described previously 6 . For each sample, 100 ng of total RNA in a final volume of 5 μl was mixed with a capture probe and a reporter probe tagged with a fluorescent barcode from the gene expression code set. Probes and target transcripts were hybridized overnight at 65 °C for around 19 h according to the manufacturer’s recommendations. Hybridized samples were run on the Nanostring nCounter instrument using the corresponding protocol, in which excess capture and reporter probes were removed and transcript-specific ternary complexes were immobilized on the surface of the cartridge. The images from samples were scanned at high resolution by the nCounter instrument and gene expression data were collected after scanning and image processing.
For mass cytometry analyses of cytokine production, blood samples from healthy cisgender females ( n = 5) of reproductive age were collected before the ovulation phase of the menstrual cycle (day 1–10 from the first day of menstruation), pretreated and then immediately stimulated with either LPS (0.1 ng ml −1 ) or PMA (50 ng ml −1 ) combined with ionomycin (1 μg ml −1 ) for 4 h or left unstimulated as a control. Brefeldin A (5 μg ml −1 ) and Monensin (2 μg ml −1 ) were added in all conditions. Samples were then fixed and lysed using Lysis and Wash buffers (Whole blood processing kit; Cytodelics AB). After fixation/lysis, cells were cryopreserved using CRYO#20 (Cytodelics AB) and analysed using intracellular staining mass cytometry as described above.
Analyses of Nanostring gene expression data
Batch-normalized data were log-transformed and scaled to have unit variance and zero mean. This was followed by principal component analysis (PCA). The resulting PCAs were then plotted alongside the PCA loadings of hallmark TNF genes.
Quantification of IFNa and IFNb by Simoa
IFNa subtypes were quantified in plasma and in supernatants of ex vivo - stimulated PBMCs using Simoa digital ELISA (Quanterix) with HomeBrew assays as previously described 79 . Several IFNα subtypes were measured using a pan-IFNα subtype assay (Quanterix), with IFNa17 (PBL Assay Science) as a reference standard. Antibodies cloned from two patients with mutated APS1 were used for multi-IFNα subtype quantification. The 8H1 clone was coated on paramagnetic beads and used as the capture antibody (0.1 μg ml −1 ), and the 12H5 clone was biotinylated at a ratio of 30:1 and used as the detector. The limit of detection for IFNα was 0.03 fg ml −1 . IFNβ was also quantified in plasma from the cohort. For the IFNβ assay, the 710906-9 IFNβ antibody (PBL Assay Science) was coated on paramagnetic beads (0.3 μg ml −1 ) and used as a capture antibody. The 710323-9 antibody (PBL Assay Science) was biotinylated and used as the detector (30:1). Recombinant IFNβ (PBL Assay Science) served as a standard to determine unknown sample concentrations. The LOD for IFNβ was 0.3 pg ml −1 .
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Raw mass and flow cytometry data (FCS files) are available at FlowReposity.org ( https://flowrepository.org/id/FR-FCM-Z75Z ). Plasma protein (Olink), induced cytokines (SIMOA), blood mRNA-seq count tables, sc-mRNA-seq count tables as well as ATAC-seq data are available at Zenodo ( https://zenodo.org/doi/10.5281/zenodo.11517624 ) 80 .
Code availability
All scripts and data for reproduction of figures are available at GitHub ( https://github.com/Brodinlab/Gender-affirming-Testosterone-treatment ) and at Zenodo ( https://zenodo.org/doi/10.5281/zenodo.11517624 ) 80 .
Brodin, P. Immune determinants of COVID-19 disease presentation and severity. Nat. Med. 27 , 28–33 (2021).
Article CAS PubMed Google Scholar
Choutka, J., Jansari, V., Hornig, M. & Iwasaki, A. Unexplained post-acute infection syndromes. Nat. Med. 28 , 911–923 (2022).
Klein, S. L., Marriott, I. & Fish, E. N. Sex-based differences in immune function and responses to vaccination. Trans. R. Soc. Trop. Med. Hyg. 109 , 9–15 (2015).
Article CAS PubMed PubMed Central Google Scholar
Cooper, G. S. & Stroehla, B. C. The epidemiology of autoimmune diseases. Autoimmun. Rev. 2 , 119–125 (2003).
Article PubMed Google Scholar
Brodin, P. et al. Studying severe long COVID to understand post-infectious disorders beyond COVID-19. Nat. Med. 28 , 879–882 (2022).
Piasecka, B. et al. Distinctive roles of age, sex, and genetics in shaping transcriptional variation of human immune responses to microbial challenges. Proc. Natl Acad. Sci. USA 115 , E488–E497 (2018).
Brodin, P. et al. Variation in the human immune system is largely driven by non-heritable influences. Cell 160 , 37–47 (2015).
Blanton, LV. et al. Stable and robust Xi and Y transcriptomes drive cell-type-specific autosomal and Xa responses in vivo and in vitro in four human cell types. Cell. Genom. 4 , 100628 (2024).
Article Google Scholar
Zhang, H. et al. A distinct subset of plasmacytoid dendritic cells induces activation and differentiation of B and T lymphocytes. Proc. Natl Acad. Sci. USA 114 , 1988–1993 (2017).
Article ADS CAS PubMed PubMed Central Google Scholar
Villani, A.-C. et al. Single-cell RNA-seq reveals new types of human blood dendritic cells, monocytes, and progenitors. Science 356 , eaah4573 (2017).
Article PubMed PubMed Central Google Scholar
Sulczewski, F. B. et al. Transitional dendritic cells are distinct from conventional DC2 precursors and mediate proinflammatory antiviral responses. Nat. Immunol. 24 , 1265–1280 (2023).
See, P. et al. Mapping the human DC lineage through the integration of high-dimensional techniques. Science 356 , eaag3009 (2017).
Webb, K. et al. Sex and pubertal differences in the type 1 interferon pathway associate with both X chromosome number and serum sex hormone concentration. Front. Immunol. 9 , 3167 (2019).
Grünhagel, B. et al. Reduction of IFN-I responses by plasmacytoid dendritic cells in a longitudinal trans men cohort. iScience 26 , 108209 (2023).
Article ADS PubMed PubMed Central Google Scholar
Honda, K. et al. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature 434 , 772–777 (2005).
Article ADS CAS PubMed Google Scholar
Ciancanelli, M. J. et al. Life-threatening influenza and impaired interferon amplification in human IRF7 deficiency. Science 348 , 448–453 (2015).
Zhang, Q. et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 370 , eabd4570 (2020).
Pauli, E.-K. et al. Influenza A virus inhibits type I IFN signaling via NF-κB-dependent induction of SOCS-3 expression. PLoS Pathog. 4 , e1000196 (2008).
Simmons, D. P. et al. SLAMF7 engagement superactivates macrophages in acute and chronic inflammation. Sci. Immunol. 7 , eabf2846 (2022).
Uppal, S. S., Verma, S. & Dhot, P. S. Normal values of CD4 and CD8 lymphocyte subsets in healthy Indian adults and the effects of sex, age, ethnicity, and smoking. Cytometry B Clin. Cytom. 52B , 32–36 (2003).
Lee, B. et al. Age‐ and sex‐related changes in lymphocyte subpopulations of healthy Asian subjects: from birth to adulthood. Cytometry 26 , 8–15 (1996).
Halnan, E. T., Marshall, F. H. A. & Yule, G. U. On the relation between the thymus and the generative organs and the influence of these organs upon growth. Proc. R. Soc. B 88 , 68–86 (1914).
ADS Google Scholar
Dumont-Lagacé, M., St-Pierre, C. & Perreault, C. Sex hormones have pervasive effects on thymic epithelial cells. Sci. Rep. 5 , 12895 (2015).
Olsen, N. J. & Kovacs, W. J. Evidence that androgens modulate human thymic T cell output. J. Invest. Med. 59 , 32 (2011).
Olsen, N. J., Olson, G., Viselli, S. M., Gu, X. & Kovacs, W. J. Androgen receptors in thymic epithelium modulate thymus size and thymocyte development. Endocrinology 142 , 1278–1283 (2001).
Afshan, G., Afzal, N. & Qureshi, S. CD4 + CD25(hi) regulatory T cells in healthy males and females mediate gender difference in the prevalence of autoimmune diseases. Clin. Lab. 58 , 567–571 (2012).
PubMed Google Scholar
Kissick, H. T. et al. Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation. Proc. Natl Acad. Sci. USA 111 , 9887–9892 (2014).
Kwon, H. et al. Androgen conspires with the CD8 + T cell exhaustion program and contributes to sex bias in cancer. Sci. Immunol. 7 , eabq2630 (2022).
Guan, X. et al. Androgen receptor activity in T cells limits checkpoint blockade efficacy. Nature 606 , 791–796 (2022).
Yang, C. et al. Androgen receptor-mediated CD8 + T cell stemness programs drive sex differences in antitumor immunity. Immunity 55 , 1747 (2022).
Shan, Q. et al. The transcription factor Runx3 guards cytotoxic CD8 + effector T cells against deviation towards follicular helper T cell lineage. Nat. Immunol. 18 , 931–939 (2017).
Oh, H. & Ghosh, S. NF‐κB: roles and regulation in different CD4 + T‐cell subsets. Immunol. Rev. 252 , 41–51 (2013).
Consortium, et al. A blood atlas of COVID-19 defines hallmarks of disease severity and specificity. Cell 185 , 916–938.e58 (2022).
Zhao, X.-N. et al. Single-cell immune profiling reveals distinct immune response in asymptomatic COVID-19 patients. Signal Transduct. Target. Ther. 6 , 342 (2021).
Oelen, R. et al. Single-cell RNA-sequencing of peripheral blood mononuclear cells reveals widespread, context-specific gene expression regulation upon pathogenic exposure. Nat. Commun. 13 , 3267 (2022).
Hertz, D. & Schneider, B. Sex differences in tuberculosis. Semin. Immunopathol. 41 , 225–237 (2019).
Bellott, D. W. et al. Mammalian Y chromosomes retain widely expressed dosage-sensitive regulators. Nature 508 , 494–499 (2014).
Brown, G. J. et al. TLR7 gain-of-function genetic variation causes human lupus. Nature 605 , 349–356 (2022).
Palucka, A. K., Blanck, J.-P., Bennett, L., Pascual, V. & Banchereau, J. Cross-regulation of TNF and IFN-α in autoimmune diseases. Proc. Natl Acad. Sci. USA 102 , 3372–3377 (2005).
Rothuizen, L. E. et al. Influence of interferon β-1a dose frequency on PBMC cytokine secretion and biological effect markers. J. Neuroimmunol. 99 , 131–141 (1999).
Cantaert, T., Baeten, D., Tak, P. P. & van Baarsen, L. G. Type I IFN and TNFα cross-regulation in immune-mediated inflammatory disease: basic concepts and clinical relevance. Arthritis Res. Ther. 12 , 219 (2010).
Feldmann, M. & Maini, R. N. Anti-TNFα therapy of rheumatoid arthritis: what have we learned? Immunology 19 , 163–196 (2001).
Article CAS Google Scholar
Takayanagi, H. et al. RANKL maintains bone homeostasis through c-Fos-dependent induction of interferon-beta. Nature 416 , 744–749 (2002).
Seillet, C. et al. The TLR-mediated response of plasmacytoid dendritic cells is positively regulated by estradiol in vivo through cell-intrinsic estrogen receptor α signaling. Blood 119 , 454–464 (2012).
Griesbeck, M. et al. Sex differences in plasmacytoid dendritic cell levels of IRF5 drive higher IFN-α production in women. J. Immunol. 195 , 5327–5336 (2015).
Zandman-Goddard, G., Solomon, M., Barzilai, A. & Shoenfeld, Y. Lupus erythematosus tumidus induced by sex reassignment surgery. J. Rheumatol. 34 , 1938–1940 (2007).
Gao, L., Gu, Y. & Yin, X. High serum tumor necrosis factor-alpha levels in women with polycystic ovary syndrome: a meta-analysis. PLoS ONE 11 , e0164021 (2016).
de Medeiros, S. F., Yamamoto, M. M. W., de Medeiros, M. A. S., Yamamoto, A. K. L. W. & Barbosa, B. B. Polycystic ovary syndrome and risks for COVID-19 infection: a comprehensive review. Rev. Endocr. Metab. Disord. 23 , 251–264 (2022).
Durcan, E. et al. TransCOVID: does gender-affirming hormone therapy play a role in contracting COVID-19? J. Sex Marital Ther. 48 , 415–426 (2022).
Beyer, M. et al. Tumor-necrosis factor impairs CD4 + T cell–mediated immunological control in chronic viral infection. Nat. Immunol. 17 , 593–603 (2016).
Bellofiore, N., Rana, S., Dickinson, H., Temple-Smith, P. & Evans, J. Characterization of human-like menstruation in the spiny mouse: comparative studies with the human and induced mouse model. Hum. Reprod. 33 , 1715–1726 (2018).
Stearns, S. C. The Evolution of Life Histories (Oxford Univ. Press, 1992).
Muehlenbein, M. P. & Bribiescas, R. G. Testosterone-mediated immune functions and male life histories. Am. J. Hum. Biol. 17 , 527–558 (2005).
Metcalf, C. J. E. & Graham, A. L. Schedule and magnitude of reproductive investment under immune trade-offs explains sex differences in immunity. Nat. Commun. 9 , 4391 (2018).
Mitchell, E., Graham, A. L., Úbeda, F. & Wild, G. On maternity and the stronger immune response in women. Nat. Commun. 13 , 4858 (2022).
Warren, G. L. et al. Physiological role of tumor necrosis factor α in traumatic muscle injury. FASEB J. 16 , 1630–1632 (2002).
Romanowska-Próchnicka, K. et al. The role of TNF-α and anti-TNF-α agents during preconception, pregnancy, and breastfeeding. Int. J. Mol. Sci. 22 , 2922 (2021).
Babbage, S. J. et al. Cytokine promoter gene polymorphisms and idiopathic recurrent pregnancy loss. J. Reprod. Immunol. 51 , 21–27 (2001).
Anim-Nyame, N., Gamble, J., Sooranna, S. R., Johnson, M. R. & Steer, P. J. Microvascular permeability is related to circulating levels of tumour necrosis factor-α in pre-eclampsia. Cardiovasc. Res. 58 , 162–169 (2003).
Covert, L. T. et al. Effect of type I interferon on engineered pediatric skeletal muscle: a promising model for juvenile dermatomyositis. Rheumatology 63 , 209–217 (2023).
Article PubMed Central Google Scholar
Ohlsson, C. et al. Low progesterone and low estradiol levels associate with abdominal aortic aneurysms in men. J. Clin. Endocrinol. Metab. 107 , dgab867 (2021).
Google Scholar
Vermeulen, A. in The Endocrine Function of the Human Testis (eds James, V. H. T. et al.) 157–170 (Academic, 1973).
Brodin, P., Duffy, D. & Quintana-Murci, L. A call for blood—in human immunology. Immunity 50 , 1335–1336 (2019).
Bray, N. L., Pimentel, H., Melsted, P. & Pachter, L. Near-optimal probabilistic RNA-seq quantification. Nat. Biotechnol. 34 , 525–527 (2016).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15 , 550 (2014).
Yu, G., Wang, L.-G., Han, Y. & He, Q.-Y. clusterProfiler: an R package for comparing biological themes among gene clusters. Omics 16 , 284–287 (2012).
Wu, D., Milutinovic, M. D. & Walt, D. R. Single molecule array (Simoa) assay with optimal antibody pairs for cytokine detection in human serum samples. Analyst 140 , 6277–6282 (2015).
Li, S. et al. Molecular signatures of antibody responses derived from a systems biology study of five human vaccines. Nat. Immunol. 15 , 195–204 (2013).
Browaeys, R., Saelens, W. & Saeys, Y. NicheNet: modeling intercellular communication by linking ligands to target genes. Nat. Methods 17 , 159–162 (2020).
Gu, Z., Gu, L., Eils, R., Schlesner, M. & Brors, B. circlize implements and enhances circular visualization in R. Bioinformatics 30 , 2811–2812 (2014).
Satpathy, A. T. et al. Massively parallel single-cell chromatin landscapes of human immune cell development and intratumoral T cell exhaustion. Nat. Biotechnol. 37 , 925–936 (2019).
Becht, E. et al. Dimensionality reduction for visualizing single-cell data using UMAP. Nat. Biotechnol. 37 , 38–44 (2018).
Mikes, J., Olin, A., Lakshmikanth, T., Chen, Y. & Brodin, P. Mass cytometry, methods and protocols. Methods Mol Biol. 1989 , 111–123 (2019).
Gassen, S. V. et al. FlowSOM: using self‐organizing maps for visualization and interpretation of cytometry data. Cytometry A 87 , 636–645 (2015).
Wolf, F. A. et al. PAGA: graph abstraction reconciles clustering with trajectory inference through a topology preserving map of single cells. Genome Biol. 20 , 59 (2019).
Lundberg, M., Eriksson, A., Tran, B., Assarsson, E. & Fredriksson, S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res. 39 , e102–e102 (2011).
Swerdloff, R. S., Dudley, R. E., Page, S. T., Wang, C. & Salameh, W. A. Dihydrotestosterone: biochemistry, physiology, and clinical implications of elevated blood levels. Endocr. Rev. 38 , 220–254 (2017).
Nathan, M. R. & Schmid, P. A review of fulvestrant in breast cancer. Oncol. Ther. 5 , 17–29 (2017).
Rodero, M. P. et al. Detection of interferon alpha protein reveals differential levels and cellular sources in disease. J. Exp. Med. 214 , 1547–1555 (2017).
Folin, R., Tadepally, L. & Brodin, P. Gender-affirming-testosterone-treatment. https://doi.org/10.5281/zenodo.11517624 (2024).
Download references
Acknowledgements
We are grateful to the study participants and the patient organizations as well as clinical staff and colleagues for their involvement in study enrolment and sampling. We are grateful to B. Reinius, J. Rorbach and J. Zhang (Karolinska Institutet), D. Thomas (University of Cambridge) and G. Franzoso (Imperial College London) for helpful discussions and valuable input. We would like to thank the teams at the clinical centres for transgender medicine, especially S. Jarlvik Alm (Stockholm), I. Arnesjö and L.-G. Sjöström (Umeå), M. Svensson (Linköping) and K. Lindgren Freij (Uppsala). We are grateful for the support of European Research Council (StG 949609 to N.L.), the Marie Curie Actions (MSCA 101027744 to C.C. in P.B laboratory), Swedish Research Council (2019-01495, 2020-06190, 2020-02889, 2021-06529, 2021-05450, 2022-01567 to P.B., 2021-03118 to N.L. and 2020-02608 to O.K.), Karolinska Institutet (2018-02229 to P.B., 2019-00975 to N.L. and 2020-02139 to C.C.), Göran Gustafsson Foundation (GG2020-0040 to P.B., and 2141 and 2227 to N.L.), Knut & Alice Wallenberg Foundation (KAW2023-0344, 2019.0191 to P.B. 2018.0325 to O.K., and 2022.0146 to N.L. and O.K.), Supported by Academy of Medical Sciences and Department for Business, Energy and Industrial Strategy, UK (PA1032 to P.B.), Cornell Foundation (to N.L.), Tore Nilson Foundation (to N.L.), Magnus Bergvall Foundation (to N.L.), Selander Foundation (to N.L.), the Swedish Society of Medical Research (postdoctoral grant to N.L. and CG-22-0148-H-02 to P.B.), The Swedish Association for Endocrinologists (to N.L.) and the Swedish Society of Medicine (to N.L.) as well as The Human Immunome Project Michelson Prize (to C.C). We thank Affinity Proteomics for Olink data and National Genomics Infrastructure, SciLifeLab for sequencing data and V. Bondet (Institut Pasteur) for technical support with SIMOA assays. The computational analyses were enabled by resources at Uppsala Multidisciplinary Centre for Advanced Computational Science (UPPMAX).
Open access funding provided by Karolinska Institute.
Author information
These authors contributed equally: Tadepally Lakshmikanth, Camila Consiglio, Nils Landegren, Petter Brodin
Authors and Affiliations
Department of Women’s and Children’s Health, Karolinska Institutet, Solna, Sweden
Tadepally Lakshmikanth, Camila Consiglio, Rikard Forlin, Jun Wang, Ziyang Tan, Hugo Barcenilla, Lucie Rodriguez, Margarita Ivanchenko, Laura Piñero Páez, Laura Gonzalez, Constantin Habimana Mugabo, Anette Johnsson, Christian Pou, Yang Chen, Jaromír Mikeš, Anna James & Petter Brodin
Department of Laboratory Medicine, Lund University, Lund, Sweden
Camila Consiglio
Center for Molecular Medicine, Department of Medicine, Karolinska Institutet, Solna, Sweden
Fabian Sardh, Peri Noori, Åsa Hallgren, Olle Kämpe & Nils Landegren
Science for Life Laboratory, Department of Medical Biochemistry and Microbiology, Uppsala University, Uppsala, Sweden
Fabian Sardh & Nils Landegren
Translational Immunology Unit, Institut Pasteur, Paris, France
Jamie Sugrue & Darragh Duffy
Department of Clinical Chemistry, Sahlgrenska University Hospital, Gothenburg, Sweden
Henrik Ryberg
Department of Internal Medicine and Clinical Nutrition, University of Gothenburg, Gothenburg, Sweden
Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden
Per Dahlqvist
Department of Medicine, Örebro University, Örebro, Sweden
Jeanette Wahlberg
ANOVA, Karolinska University Hospital, Stockholm, Sweden
Anders Hagelin, Mats Holmberg & Marie Degerblad
Department of Medicine, Karolinska Institutet, Stockholm, Sweden
Anders Hagelin & Mats Holmberg
Department of Molecular Medicine and Surgery, Karolinska Institutet, Solna, Sweden
Marie Degerblad
Department of Medical Sciences, Uppsala University, Uppsala, Sweden
Magnus Isaksson
Department of Endocrinology, Metabolism and Diabetes, Karolinska University Hospital, Stockholm, Sweden
Medical Research Council, Laboratory of Medical Sciences, London, UK
Petter Brodin
Department of Immunology and Inflammation, Imperial College London, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
N.L., P.B. and O.K. designed the study. Experimental study coordination by T.L. Clinical enrolment and data collection was performed by P.D., J. Wahlberg, A. Hagelin, M.H., M.D. and M. Isaksson, coordinated by F.S. Sample preparation by T.L., F.S., P.N., L.P.P., L.G., C.H.M., A. Johnsson, Å. Hallgren. and C.P. Sex hormone analyses by H.R. Sex hormone receptor analyses by J.M. and M. Ivanchenko. SIMOA analyses by J.S. and D.D. In vitro stimulation experiments by T.L., H.B. and J. Wang and data analysis by P.B. Mass cytometry experiments by T.L. and data analysis by C.C., Z.T. and P.B. Olink, bulk mRNA and ATAC-seq data analysis by C.C. sc-mRNA-seq, Nanostring data and NicheNet analyses by R.F. Flow cytometry data analysis by T.L., H.B., J.M. and P.B. Manuscript written by P.B. with input from all co-authors.
Corresponding authors
Correspondence to Nils Landegren or Petter Brodin .
Ethics declarations
Competing interests.
P.B., T.L. and J.M. are cofounders of Cytodelics AB (Stockholm, Sweden), which produces and distributes the whole blood cell stabilizer solutions used in this study. P.B. is an executive board member of Kancera AB, scientific advisor for Pixelgen Technologies AB, Helaina Inc., Scailyte AG, Oxford Immune Algorithmics Ltd, Sention Health AB and the Swedish Olympic Committee. The other authors declare no competing interests.
Peer review
Peer review information.
Nature thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended data fig. 1 modeling of whole blood mrna transcriptome data..
Sex hormone measurements by LCMS over time during testosterone treatment in n = 22 subjects and 3 timepoints per subject. Shaded areas represent male (blue) and female (pink) reference ranges where available. P-values from Kruskal-Wallis tests (5% FDR corrected) b ) Testosterone and estradiol levels in patients receiving full dose (1000 mg, black) or reduced doses (750 mg, orange) of Nebido at one or more timepoints.
Extended Data Fig. 2 Immune cell changes during gender affirming testosterone therapy.
a ) White blood counts as measured by clinical chemistry analyses at baseline and following 3- and 12-months of testosterone therapy. Repeated measures ANOVA, unadjusted p-value. b ) Marker expression (Z-score transformed per marker) across all 113 immune cell clusters and n = 12,377,068 cells c ) Manual gating strategy to identify pDC, pre-DC and CD11c + DC populations among lineage negative HLA-DR + cells analyzed by Mass cytometry.
Extended Data Fig. 3 pDC functional responses.
a ) pDc and pre-DC marker genes as reported by Villani et al shown in n = 41 pDCs from baseline and n = 47 pDCs at 3-months from two independent experiments. Boxplot centre = median, max whisker = Q3 + 1.5*IQR (IQR = values ranging from Q1-Q3), min whisker = Q1 – 1.5*IQR. b ) Plasma pan-IFNα and IFNβ protein levels measured by SIMOA in 71 samples from 24 subjects across two experiments at baseline and following 3 and 12 months of testosterone therapy. Repeated measures ANOVA, unadjusted p-values. c ) pDC RNA counts for IRF7 vs SOCS1 following R848 stimulation in vitro comparing pDCs collected at baseline (n = 41) and following 3 months of testosterone (n = 47) across two independent experiments. Uncorrected, 2-sided t-tests and R-values from pearson correlation-coefficients, d ) pDC RNA counts for SOCS1 v.s. Hallmark IFNα following R848 stimulation and, e ) pDC RNA counts for SOCS3 v.s. Hallmark IFNα following R848 stimulation.
Extended Data Fig. 4 TNF family proteins and monocyte responses.
a ) Olink Target96 TM inflammation panel analyses of plasma samples from n = 20 subjects sampled 12 months after initiating Gender affirming testosterone therapy shown as mixed-effects modeling coefficients. b ) In vitro testosterone treatment (28 h) of blood from a healthy female with/without AR antagonist Enzalutamide and analyses by Olink Target 96 Inflammation. Linear mixed effects analysis with treatment as fixed effect and subject as random effect and 5% FDR corrected p-values, n.s: non-significant c ) Blood from a healthy female incubated (20 h) with dihydrotestosterone (DHT) with/without AR inhibitor (Enzalutamide) and stimulated by LPS (4 h) followed by Mass cytometry analysis of intracellular TNFα and SLAMF7 surface protein. Randomly down sampled (5%) of cells and visualized with dot size corresponding to SLAMF7 expression show TNFα hi cells predominantly expressing high SLAMF7 upon DHT pre-treatment. A single representative experiment of three. d ) Blood from eleven healthy cis females incubated (20 h) with dihydrotestosterone (DHT) with/without androgen receptor inhibitor (Enzalutamide) or oestradiol-receptor blocker and degrader (Fulvestrant). Resulting culture supernatants were analyzed for Androstenedione, DHEA, DHT, Estrone, Testosterone and 17a-Hydroxyprogesterone using GC-MS. e ) Cultures were stimulated by LPS for 3 h and analyzed for mRNA-abundances (n = 560) by Nanostring nCounter. Z-score transformed mRNA (counts) of LPS induced TNF, f ) IL6, g ) IL1B, and h ) STAT3. P-values: *p < 0.05, n.s: non-significant, by uncorrected pairwise t-tests. Boxplot centre = median, max whisker = Q3 + 1.5*IQR (IQR = values ranging from Q1-Q3), min whisker = Q1 – 1.5*IQR.
Extended Data Fig. 5 T cell adaptation to testosterone treatment.
a ) CD4/CD8 ratio, b ) Naive CD4 + T cells, and c ) Naive CD8 + T cell fractions before and during testosterone treatment. P-values from two-sided, paired and uncorrected t-tests. n.s = non-significant. d ) Mass cytometry analyses of Treg frequency. P-values from two-sided, paired and uncorrected t-tests. n.s = non-significant. e ) Single cell mRNA sequencing from PBMCs at baseline and after 3 months of testosterone in vivo selected on memory CD4 + T cells and transcripts related to Th1, f ) Th2 and g ) Th17 markers shown. h ) Expression of the indicated T cell exhaustion markers for CD8 + T cells at baseline and 3 months following testosterone analyzed by single cell mRNA sequencing. P-value from 2-sided, uncorrected t-test indicating global module expression at baseline vs. 3 months. i ) Five healthy female donors, pretreated with DHT, DHT + AR inhib. (Enzalutamide) or ESR inhibitor (Fulvestrant) followed by PMA/Ionomycin stimulation (4 h) and analyzed by intracellular IFNγ in CD4 + T, CD8 + T and NK cells analyzed by repeated measures ANOVA with Tukey’s Honest Significant Differences posthoc multiple hypothesis test.
Extended Data Fig. 6 Sex-hormone receptor expression.
a ) Flow cytometry analysis of intracellular staining of the androgen receptor, AR in the indicated cell populations. Staining control (fluorescence minus one, FMO) and mouse anti-human IgB 2B PE isotype control in grey. Mean Fluorescence Intensity, MFI is indicated. b ) Flow cytometry analysis of AR and pan-ESR in the indicated cell populations. Staining control (fluorescence minus one, FMO) in grey. c ) PBMCs from healthy men and women sorted based on canonical surface markers and subject to bulk mRNA-sequencing and expression nTPM (normalized Transcripts per million bases) for the indicated sex hormone receptor mRNA in three female and three male donors combined.
Supplementary information
Supplementary tables.
Table 1, Panel of antibodies for mass cytometry. Table 2, Antibodies for mass cytometry (extracellular antigens). Table 3, Antibodies for mass cytometry (intracellular antigens). Table 4, Antibodies for flow cytometry.
Reporting Summary
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Lakshmikanth, T., Consiglio, C., Sardh, F. et al. Immune system adaptation during gender-affirming testosterone treatment. Nature 633 , 155–164 (2024). https://doi.org/10.1038/s41586-024-07789-z
Download citation
Received : 06 April 2023
Accepted : 04 July 2024
Published : 04 September 2024
Issue Date : 05 September 2024
DOI : https://doi.org/10.1038/s41586-024-07789-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.

IMAGES
VIDEO
COMMENTS
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Double incision. With this procedure, incisions are typically made at the top and bottom of the pectoral muscle and the chest tissue is removed. The skin is pulled down and reconnected at the ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria. Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX ...
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly refer to many procedures an individual may have ...
A trans person can choose from multiple procedures to make their appearance match their self-identified gender identity. Doctors refer to this as gender "affirmation" surgery. Trans people might ...
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia ...
During this period, 214 patients underwent penile inversion vaginoplasty. Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18-61 years); the average of operative time was 3.3 h (range 2-5 h); the average duration of hormone therapy before surgery was 12 years (range 1-39).
410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
The two major sex reassignment surgery (SRS) interventions in the female-to-male transsexual patients that will be addressed here are (1) the subcutaneous mastectomy (SCM), often combined with a hysterectomy/ ovariectomy; and (2) the actual genital transformation consisting of vaginectomy, reconstruction of the fixed part of the urethra (if ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria ...
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of ...
Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female ...
The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The number worldwide is estimated ...
For surgery, have completed at least six months of hormone treatment (or longer if needed for the surgery). Have a health care professional: Confirm that there are no other possible causes for gender dysphoria. Assess their mental and physical health and whether treatment would harm them. Discuss the risks and benefits of treatment.
This meant that federally funded hospitals were required to perform so-called "gender-reassignment" surgeries or face a range of penalties, including having their funding removed.
303 See Other. openresty