

Write an Error-free Research Protocol As Recommended by WHO: 21 Elements You Shouldn’t Miss!
Principal Investigator: Did you draft the research protocol?
Student: Not yet. I have too many questions about it. Why is it important to write a research protocol? Is it similar to research proposal? What should I include in it? How should I structure it? Is there a specific format?
Researchers at an early stage fall short in understanding the purpose and importance of some supplementary documents, let alone how to write them. Let’s better your understanding of writing an acceptance-worthy research protocol.
Table of Contents
What Is Research Protocol?
The research protocol is a document that describes the background, rationale, objective(s), design, methodology, statistical considerations and organization of a clinical trial. It is a document that outlines the clinical research study plan. Furthermore, the research protocol should be designed to provide a satisfactory answer to the research question. The protocol in effect is the cookbook for conducting your study
Why Is Research Protocol Important?
In clinical research, the research protocol is of paramount importance. It forms the basis of a clinical investigation. It ensures the safety of the clinical trial subjects and integrity of the data collected. Serving as a binding document, the research protocol states what you are—and you are not—allowed to study as part of the trial. Furthermore, it is also considered to be the most important document in your application with your Institution’s Review Board (IRB).
It is written with the contributions and inputs from a medical expert, a statistician, pharmacokinetics expert, the clinical research coordinator, and the project manager to ensure all aspects of the study are covered in the final document.
Is Research Protocol Same As Research Proposal?
Often misinterpreted, research protocol is not similar to research proposal. Here are some significant points of difference between a research protocol and a research proposal:
|
|
|
| A is written to persuade the grant committee, university department, instructors, etc. | A research protocol is written to detail a clinical study’s plan to meet specified ethical norms for participating subjects. |
| It is a plan to obtain funding or conduct research. | It is meant to clearly provide an overview of a proposed study to satisfy an organization’s guidelines for protecting the safety of subjects. |
| Research proposals are submitted to funding bodies | Research protocols are submitted to Institutional Review Boards (IRBs) within universities and research centers. |
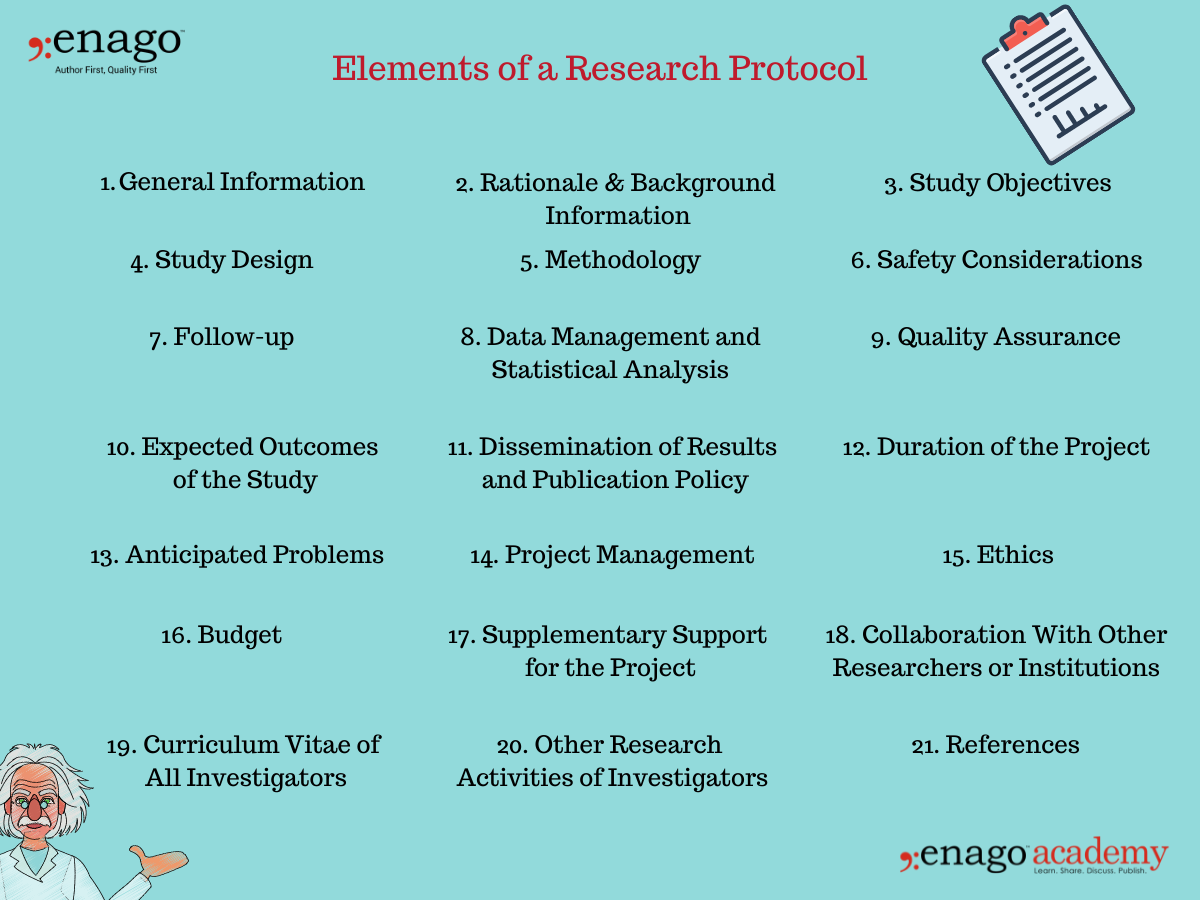
What Are the Elements/Sections of a Research Protocol?
According to Good Clinical Practice guidelines laid by WHO, a research protocol should include the following:
1. General Information
- Protocol title, protocol identifying number (if any), and date.
- Name and address of the funder.
- Name(s) and contact details of the investigator(s) responsible for conducting the research, the research site(s).
- Responsibilities of each investigator.
- Name(s) and address(es) of the clinical laboratory(ies), other medical and/or technical department(s) and/or institutions involved in the research.
2. Rationale & Background Information
- The rationale and background information provides specific reasons for conducting the research in light of pertinent knowledge about the research topic.
- It is a statement that includes the problem that is the basis of the project, the cause of the research problem, and its possible solutions.
- It should be supported with a brief description of the most relevant literatures published on the research topic.
3. Study Objectives
- The study objectives mentioned in the research proposal states what the investigators hope to accomplish. The research is planned based on this section.
- The research proposal objectives should be simple, clear, specific, and stated prior to conducting the research.
- It could be divided into primary and secondary objectives based on their relativity to the research problem and its solution.
4. Study Design
- The study design justifies the scientific integrity and credibility of the research study.
- The study design should include information on the type of study, the research population or the sampling frame, participation criteria (inclusion, exclusion, and withdrawal), and the expected duration of the study.
5. Methodology
- The methodology section is the most critical section of the research protocol.
- It should include detailed information on the interventions to be made, procedures to be used, measurements to be taken, observations to be made, laboratory investigations to be done, etc.
- The methodology should be standardized and clearly defined if multiple sites are engaged in a specified protocol.
6. Safety Considerations
- The safety of participants is a top-tier priority while conducting clinical research .
- Safety aspects of the research should be scrutinized and provided in the research protocol.
7. Follow-up
- The research protocol clearly indicate of what follow up will be provided to the participating subjects.
- It must also include the duration of the follow-up.
8. Data Management and Statistical Analysis
- The research protocol should include information on how the data will be managed, including data handling and coding for computer analysis, monitoring and verification.
- It should clearly outline the statistical methods proposed to be used for the analysis of data.
- For qualitative approaches, specify in detail how the data will be analysed.
9. Quality Assurance
- The research protocol should clearly describe the quality control and quality assurance system.
- These include GCP, follow up by clinical monitors, DSMB, data management, etc.
10. Expected Outcomes of the Study
- This section indicates how the study will contribute to the advancement of current knowledge, how the results will be utilized beyond publications.
- It must mention how the study will affect health care, health systems, or health policies.
11. Dissemination of Results and Publication Policy
- The research protocol should specify not only how the results will be disseminated in the scientific media, but also to the community and/or the participants, the policy makers, etc.
- The publication policy should be clearly discussed as to who will be mentioned as contributors, who will be acknowledged, etc.
12. Duration of the Project
- The protocol should clearly mention the time likely to be taken for completion of each phase of the project.
- Furthermore a detailed timeline for each activity to be undertaken should also be provided.
13. Anticipated Problems
- The investigators may face some difficulties while conducting the clinical research. This section must include all anticipated problems in successfully completing their projects.
- Furthermore, it should also provide possible solutions to deal with these difficulties.
14. Project Management
- This section includes detailed specifications of the role and responsibility of each investigator of the team.
- Everyone involved in the research project must be mentioned here along with the specific duties they have performed in completing the research.
- The research protocol should also describe the ethical considerations relating to the study.
- It should not only be limited to providing ethics approval, but also the issues that are likely to raise ethical concerns.
- Additionally, the ethics section must also describe how the investigator(s) plan to obtain informed consent from the research participants.
- This section should include a detailed commodity-wise and service-wise breakdown of the requested funds.
- It should also include justification of utilization of each listed item.
17. Supplementary Support for the Project
- This section should include information about the received funding and other anticipated funding for the specific project.
18. Collaboration With Other Researchers or Institutions
- Every researcher or institute that has been a part of the research project must be mentioned in detail in this section of the research protocol.
19. Curriculum Vitae of All Investigators
- The CVs of the principal investigator along with all the co-investigators should be attached with the research protocol.
- Ideally, each CV should be limited to one page only, unless a full-length CV is requested.
20. Other Research Activities of Investigators
- A list of all current research projects being conducted by all investigators must be listed here.
21. References
- All relevant references should be mentioned and cited accurately in this section to avoid plagiarism.
How Do You Write a Research Protocol? (Research Protocol Example)
Main Investigator
Number of Involved Centers (for multi-centric studies)
Indicate the reference center
Title of the Study
Protocol ID (acronym)
Keywords (up to 7 specific keywords)
Study Design
Mono-centric/multi-centric
Perspective/retrospective
Controlled/uncontrolled
Open-label/single-blinded or double-blinded
Randomized/non-randomized
n parallel branches/n overlapped branches
Experimental/observational
Endpoints (main primary and secondary endpoints to be listed)
Expected Results
Analyzed Criteria
Main variables/endpoints of the primary analysis
Main variables/endpoints of the secondary analysis
Safety variables
Health Economy (if applicable)
Visits and Examinations
Therapeutic plan and goals
Visits/controls schedule (also with graphics)
Comparison to treatment products (if applicable)
Dose and dosage for the study duration (if applicable)
Formulation and power of the studied drugs (if applicable)
Method of administration of the studied drugs (if applicable)
Informed Consent
Study Population
Short description of the main inclusion, exclusion, and withdrawal criteria
Sample Size
Estimated Duration of the Study
Safety Advisory
Classification Needed
Requested Funds
Additional Features (based on study objectives)
Click Here to Download the Research Protocol Example/Template
Be prepared to conduct your clinical research by writing a detailed research protocol. It is as easy as mentioned in this article. Follow the aforementioned path and write an impactful research protocol. All the best!
Clear as template! Please, I need your help to shape me an authentic PROTOCOL RESEARCH on this theme: Using the competency-based approach to foster EFL post beginner learners’ writing ability: the case of Benin context. I’m about to start studies for a master degree. Please help! Thanks for your collaboration. God bless.
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Promoting Research
Graphical Abstracts Vs. Infographics: Best practices for using visual illustrations for increased research impact
Dr. Sarah Chen stared at her computer screen, her eyes staring at her recently published…

- Publishing Research
10 Tips to Prevent Research Papers From Being Retracted
Research paper retractions represent a critical event in the scientific community. When a published article…

- Industry News
Google Releases 2024 Scholar Metrics, Evaluates Impact of Scholarly Articles
Google has released its 2024 Scholar Metrics, assessing scholarly articles from 2019 to 2023. This…
![outline of research protocol What is Academic Integrity and How to Uphold it [FREE CHECKLIST]](https://www.enago.com/academy/wp-content/uploads/2024/05/FeatureImages-59-210x136.png)
Ensuring Academic Integrity and Transparency in Academic Research: A comprehensive checklist for researchers
Academic integrity is the foundation upon which the credibility and value of scientific findings are…

- Reporting Research
How to Optimize Your Research Process: A step-by-step guide
For researchers across disciplines, the path to uncovering novel findings and insights is often filled…
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for…
Research Recommendations – Guiding policy-makers for evidence-based decision making
Demystifying the Role of Confounding Variables in Research

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
- AI in Academia
- Career Corner
- Diversity and Inclusion
- Infographics
- Expert Video Library
- Other Resources
- Enago Learn
- Upcoming & On-Demand Webinars
- Peer Review Week 2024
- Open Access Week 2023
- Conference Videos
- Enago Report
- Journal Finder
- Enago Plagiarism & AI Grammar Check
- Editing Services
- Publication Support Services
- Research Impact
- Translation Services
- Publication solutions
- AI-Based Solutions
- Thought Leadership
- Call for Articles
- Call for Speakers
- Author Training
- Edit Profile
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

In your opinion, what is the most effective way to improve integrity in the peer review process?
- Search Menu
- Sign in through your institution
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- Reasons to Submit
- About Journal of Surgical Protocols and Research Methodologies
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, contents of a research study protocol, conflict of interest statement, how to write a research study protocol.
- Article contents
- Figures & tables
- Supplementary Data
Julien Al Shakarchi, How to write a research study protocol, Journal of Surgical Protocols and Research Methodologies , Volume 2022, Issue 1, January 2022, snab008, https://doi.org/10.1093/jsprm/snab008
- Permissions Icon Permissions
A study protocol is an important document that specifies the research plan for a clinical study. Many funders such as the NHS Health Research Authority encourage researchers to publish their study protocols to create a record of the methodology and reduce duplication of research effort. In this paper, we will describe how to write a research study protocol.
A study protocol is an essential part of a research project. It describes the study in detail to allow all members of the team to know and adhere to the steps of the methodology. Most funders, such as the NHS Health Research Authority in the United Kingdom, encourage researchers to publish their study protocols to create a record of the methodology, help with publication of the study and reduce duplication of research effort. In this paper, we will explain how to write a research protocol by describing what should be included.
Introduction
The introduction is vital in setting the need for the planned research and the context of the current evidence. It should be supported by a background to the topic with appropriate references to the literature. A thorough review of the available evidence is expected to document the need for the planned research. This should be followed by a brief description of the study and the target population. A clear explanation for the rationale of the project is also expected to describe the research question and justify the need of the study.
Methods and analysis
A suitable study design and methodology should be chosen to reflect the aims of the research. This section should explain the study design: single centre or multicentre, retrospective or prospective, controlled or uncontrolled, randomised or not, and observational or experimental. Efforts should be made to explain why that particular design has been chosen. The studied population should be clearly defined with inclusion and exclusion criteria. These criteria will define the characteristics of the population the study is proposing to investigate and therefore outline the applicability to the reader. The size of the sample should be calculated with a power calculation if possible.
The protocol should describe the screening process about how, when and where patients will be recruited in the process. In the setting of a multicentre study, each participating unit should adhere to the same recruiting model or the differences should be described in the protocol. Informed consent must be obtained prior to any individual participating in the study. The protocol should fully describe the process of gaining informed consent that should include a patient information sheet and assessment of his or her capacity.
The intervention should be described in sufficient detail to allow an external individual or group to replicate the study. The differences in any changes of routine care should be explained. The primary and secondary outcomes should be clearly defined and an explanation of their clinical relevance is recommended. Data collection methods should be described in detail as well as where the data will be kept secured. Analysis of the data should be explained with clear statistical methods. There should also be plans on how any reported adverse events and other unintended effects of trial interventions or trial conduct will be reported, collected and managed.
Ethics and dissemination
A clear explanation of the risk and benefits to the participants should be included as well as addressing any specific ethical considerations. The protocol should clearly state the approvals the research has gained and the minimum expected would be ethical and local research approvals. For multicentre studies, the protocol should also include a statement of how the protocol is in line with requirements to gain approval to conduct the study at each proposed sites.
It is essential to comment on how personal information about potential and enrolled participants will be collected, shared and maintained in order to protect confidentiality. This part of the protocol should also state who owns the data arising from the study and for how long the data will be stored. It should explain that on completion of the study, the data will be analysed and a final study report will be written. We would advise to explain if there are any plans to notify the participants of the outcome of the study, either by provision of the publication or via another form of communication.
The authorship of any publication should have transparent and fair criteria, which should be described in this section of the protocol. By doing so, it will resolve any issues arising at the publication stage.
Funding statement
It is important to explain who are the sponsors and funders of the study. It should clarify the involvement and potential influence of any party. The sponsor is defined as the institution or organisation assuming overall responsibility for the study. Identification of the study sponsor provides transparency and accountability. The protocol should explicitly outline the roles and responsibilities of any funder(s) in study design, data analysis and interpretation, manuscript writing and dissemination of results. Any competing interests of the investigators should also be stated in this section.
A study protocol is an important document that specifies the research plan for a clinical study. It should be written in detail and researchers should aim to publish their study protocols as it is encouraged by many funders. The spirit 2013 statement provides a useful checklist on what should be included in a research protocol [ 1 ]. In this paper, we have explained a straightforward approach to writing a research study protocol.
None declared.
Chan A-W , Tetzlaff JM , Gøtzsche PC , Altman DG , Mann H , Berlin J , et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials . BMJ 2013 ; 346 : e7586 .
Google Scholar
- conflict of interest
- national health service (uk)
| Month: | Total Views: |
|---|---|
| January 2022 | 201 |
| February 2022 | 123 |
| March 2022 | 271 |
| April 2022 | 354 |
| May 2022 | 429 |
| June 2022 | 380 |
| July 2022 | 405 |
| August 2022 | 560 |
| September 2022 | 539 |
| October 2022 | 690 |
| November 2022 | 671 |
| December 2022 | 609 |
| January 2023 | 872 |
| February 2023 | 1,165 |
| March 2023 | 1,277 |
| April 2023 | 1,183 |
| May 2023 | 1,292 |
| June 2023 | 1,117 |
| July 2023 | 1,040 |
| August 2023 | 936 |
| September 2023 | 941 |
| October 2023 | 1,028 |
| November 2023 | 993 |
| December 2023 | 910 |
| January 2024 | 1,251 |
| February 2024 | 1,051 |
| March 2024 | 1,411 |
| April 2024 | 991 |
| May 2024 | 895 |
| June 2024 | 710 |
| July 2024 | 629 |
| August 2024 | 714 |
Email alerts
Citing articles via.
- Advertising and Corporate Services
- Journals Career Network
- JSPRM Twitter
Affiliations
- Online ISSN 2752-616X
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
The Research Protocol
- First Online: 17 December 2015
Cite this chapter

- Gilberto Lopes M.D., M.B.A. 2 ,
- Gustavo Werutsky 3 &
- Patricia Moretto M.D., M.Sc. 4
833 Accesses
2 Altmetric
The research protocol is defined as the most important document in clinical research which helps the researchers and the scientists to understand the necessity of the study and the way of execution and completion.
The protocol outlines the rationale for the study, its objective, the methodology used, and how the data will be managed and analyzed. It highlights how ethical issues have been considered, and where appropriate, how gender and minority issues are being addressed.
An additional step, after writing the protocol, particularly in large studies with teams of investigators, is to develop what may be called the operations manual for the study.
The full research protocol development takes usually 4 months, but is variable depending on the complexity of the research.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Research (See Clinical Research; Research Ethics)

Introduction to Clinical Research Concepts, Essential Characteristics of Clinical Research, Overview of Clinical Research Study Designs
The beginning – historical aspects of clinical research, clinical research: definitions, “anatomy and physiology,” and the quest for “universal truth”.
Conselho Nacional de Saúde (Brasil). Resolução n o 466, de 12 de dezembro de 2012. Brasília, 2012 [citado 2014 Mar 11]. http://www.conselho.saude.gov.br/web_comissoes/conep/index.html . Assessed November 2014.
IARC cancer statistics. http://globocan.iarc.fr/ . Assessed November 2014. OR http://www.iarc.fr/en/media-centre/pr/2014/pdfs/pr224_E.pdf . Assessed Nov 2014.
WHO. Cancer fact sheet. Geneva: WHO; 2014. Accessed Nov 2014.
Google Scholar
IAEA. A silent crisis: cancer treatment in developing countries. Vienna: Division of Public Information, IAEA; 2003.
Emanuel EJ, Wendler D, Killen J, Grady C. What makes clinical research in developing countries ethical? The benchmarks of ethical research. J Infect Dis. 2004;189(5):930–7. Epub 2004 Feb 17.
Download references
Author information
Authors and affiliations.
Oncoclinicas do Brasil, Rua Maranhão 569/4, São Paulo, SP, 01240-001, Brazil
Gilberto Lopes M.D., M.B.A.
Latin American Cooperative Oncology Group, 6681, 99A/806 Ipiranga Avenue, Porto Alegre, RS, 90619-900, Brazil
Gustavo Werutsky
Oncology, Caxias do Sul University Foundation, Caxias do Sul General Hospital, Rua Prof. Antônio Vignoli, 255 - Bairro Petrópolis, Caxias do Sul, RS, 95070-561, Brazil
Patricia Moretto M.D., M.Sc.
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gilberto Lopes M.D., M.B.A. .
Editor information
Editors and affiliations.
South African Medical Research Council, Francie van Zyl, Parrow, Cape Town, South Africa
Daniela Cristina Stefan
Barriers to Research in Developing Countries and Possible Steps to Overcome Them
The rise in the number of cancer cases, 14 million new cancer cases globally every year, with the majority of cases occurring in developing countries [ 1 ], has a great impact in those countries and must be addressed. Additionally, treatment options are both limited and expensive, and trial participation is an opportunity for better cancer care.
There are four key components to cancer control and, therefore, areas in need of research: prevention, early detection, diagnosis and treatment, and palliation, as stated by WHO [ 2 ]. In each of these areas, developing countries face major challenges, not only in dealing with the ongoing problems, but also with research opportunities.
The International Agency for Research on Cancer (IARC) uses the term “developing country” for less-developed regions such as: all regions of Africa, Asia (excluding Japan), Latin America and the Caribbean, Melanesia, Micronesia, and Polynesia [ 1 ].
In order to overcome barriers to doing research, and so that the results will have a chance to impact on local problems, some points have to be taken into consideration:
Choose a Relevant Topic to Your Community
Make sure that the many pressing problems in developing countries are being addressed, so local patients are able to see direct benefits. The research question has to be relevant for the population where it is tested. This is an ethics question, as well as a question that will improve accrual.
There is a broad consensus that efforts and scarce resources in developing countries should focus first and foremost on prevention and awareness rising, and secondly on early detection, treatment, and research. However, this should not prevent the progress and improvement of research capabilities in these countries.
Will the Protocol Be Feasible?
If the issue being looked at is technology, it should be noted that most health equipment used in developing nations is manufactured in the first world. Sometimes the equipment does not work on arrival, with lack of parts or trained technicians to fix it or do maintenance. Technical, social, cultural, and economic factors must be considered when looking at new technologies for these countries.
Researchers should also remember that in some countries there is limited access to radiotherapy, so research questions involving concurrent or sequential treatments may not be the best research option.
According to the International Atomic Energy Agency (IAEA) [ 3 ], although the developing world constitutes 85 % of the world’s population, it only has 2200 radiation therapy machines compared with the 4500 in the developed world. Those developing countries that have access to radiotherapy face considerable financial investment constrains and for up to 5 years are required to provide the necessary training, equipment set-up and maintenance, protocols, and quality control. Therefore, even if budget is not a concern for a specific study, creating a Radiotherapy Service for research purposes in a developing country would take a lot of planning, resources, and time.
In order to do the scans as planned in a protocol, radiologists with RECIST knowledge and time to do proper comparative reports are also needed and are not always available. Even with a central review, the delay in getting the images as planned could result in wrong clinical decisions and protocol violations.
The same applies to health workers, where it is sometimes necessary to train locals and adapt to the capabilities of the country. Obviously, if feasible, the improvement in capabilities would be welcome, as in addition to the research they could offer new treatments to patients and open the way for further research.
Funding and Economic Incentives
The challenges are many and substantial such as insufficient political priority and funding among donor agencies and governments of developing countries that have many competing priorities.
However, the local investigator must be familiarized with potential local and international sources: universities, government incentives, international for-profit initiatives, and creative not-for-profit partnerships.
Involvement in research with pharmaceutical companies, which can be lucrative to the institutions where it is done, is an obvious way to start, but usually some capabilities must already be in place to attract this kind of research. A pressing challenge is getting industry partners to invest in the clinical development of drugs that offer limited commercial opportunities. Despite the fact that the cost to approve drugs is lower in developing countries, it is still high and is a problem that universities and public institutions cannot overcome alone.
Intellectual Property
Partnership with industry may be necessary to develop early research in universities, and intellectual property licensing should be viewed as a requirement to attract industry partners. However, researchers must pay attention to patent systems before concluding agreements with pharmaceutical companies (who want a patent system that will protect their investments for as long as possible) and be careful, clearly stating on contracts who has ownership of the data collected, of publications or abstracts arising from study results, and of information obtained based on new data analyses.
Encouragement and Structure
In some developing countries, in addition to other research barriers, such as lack of diagnostic, treatment, and monitoring capacity, there is lack of academic staff (oncology and hematology expertise, specialized cancer nurses, pharmacists), qualified monitors, lack of encouragement to conduct and publish research, as well as lack of a research publishing infrastructure. Training personnel abroad, in other research centers, or in-house training before starting a project may be needed.
Planning and Accrual
Researchers may have problems with proper calculation for accrual, as most cancer registries in low- and middle-income countries have shortcomings and screening programs are largely absent. This can lead to erroneous assumptions regarding the relative frequencies of the varying levels of different cancers based on global trends, which can be misleading. These issues are major challenges for the future, but setting up an institutional cancer registry could be a good start in research planning.
In order to properly choose the study population, the researcher should take into consideration the contrasts in patient’s disease profiles: most cancer patients in developing countries have advanced or incurable cancers at the time their initial presentation, a different profile from that seen in developed countries. The prevalence and incidence can be also markedly different in comparison to developed countries for each disease site.
Developed countries often have relatively high rates of lung, colorectal, breast, and prostate cancer because of the earlier onset of the tobacco epidemic, the earlier exposure to occupational carcinogens, and the Western diet and lifestyle. In contrast, up to a fourth of cancers in developing countries are associated with chronic infections. Liver cancer is often causally associated with infection by the hepatitis B virus (HBV), cervical cancer is associated with infection by certain types of human papillomavirus (HPV), and stomach cancer is associated with Helicobacter pylori infection.
Weak referral systems can also make the accrual slow. This should be anticipated and should encourage creative solutions to strengthen it by the researchers. In some countries there are few cancer services. This can be helpful in the sense that it aggregates most of the cases in a few centers. However, if the health system is a mix of public and private, this dilutes the number of cases, increasing the numbers of institutions necessary for the accrual, and increasing the budget.
Issues During the Trial and for Follow-Up
There is sometimes a lack of awareness of the signs and symptoms of cancer and side effects from treatments, a lack of money to travel to a hospital, which could result in sub-notification of important events or delays in the notification and treatment of important side effects.
As health systems in developing countries are not set up for chronic disease management, chronic diseases such as cancer are often lost to follow-up. Therefore, organizing proper follow-up for patients enrolled in the trials could be a problem.

Need for Palliative Care Research
In some developing countries, there is lack of trained personnel to administer palliative care or pain killers such as morphine. This is particularly startling given that approximately 70 % of the patients seen at these hospitals are at such an advanced stage of cancer upon arrival that they are beyond cure and palliative care and pain management is the only benefit they can still receive. Studies in the palliative setting, which should be relatively easy to accrue, could have a major impact in the quality of life of patients and in the training of local health workers.
Ethics Barriers
The ethics principles in clinical research were established in order to avoid previous abuses/misconducts, such as the Tuskegee Study of Untreated Syphilis (TSUS).
Based on the influential codes of ethics and regulations that guide ethical clinical research (Nuremberg Code Footnote 1 ; Declaration of Helsinki 1 , Belmont Report 1 , CIOMS 1 , U.S. Common Rule 1 ), seven main principles have been described as guiding the conduct of ethical research 1 : social and clinical value; scientific validity; fair subject selection; favorable risk-benefit ratio; independent review; informed consent; and respect for potential and enrolled subjects.
The trial should follow the ethics rules from the country where it was originally written and in the other countries where the research will be developed. Some areas of ethics controversy in developing countries are: the standard of care to be used (as the local standard of care could mean no treatment or less than the “worldwide best”) and the quality of informed consent (due to lack of knowledge, language/cultural barriers, high workload, and time constraints). The discussion about valid science, social benefits, and favorable risk:benefit ratio to justify less than the worldwide best care has to take place early on in the protocol design to avoid an unethical and/or unfeasible trial. Efforts should be taken to improve the quality of informed consent, such as researchers training and observance to the GCP.
Not all the population in developing countries is vulnerable, but a great deal of them is at increased risk of exploitation due to poverty, limited healthcare services, illiteracy, cultural and linguistic differences, and limited understanding of the nature of scientific research. To make things worse, regulatory infrastructures, which could minimize this risk, may lack effectiveness or be nonexistent. As suggested by Emanuael et al. [ 4 ], “collaborative partnerships between researchers and sponsors in developed countries and researchers, policy makers, and communities in developing countries help to minimize the possibility of exploitation by ensuring that a developing country determines for itself whether the research is acceptable and responsive to the community’s health problems.”
Lastly, the many differences between developed and developing countries, in addition to the various sociocultural groups existing in a country, must be taken into consideration during the research protocol conception and execution. Specifically, issues to keep private information confidential, to find the person responsible for giving consent, and how best to explain the clinical trial purpose, benefits, risks, and involved procedures could arise due to local peculiarities.
Rights and permissions
Reprints and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Lopes, G., Werutsky, G., Moretto, P. (2016). The Research Protocol. In: Stefan, D. (eds) Cancer Research and Clinical Trials in Developing Countries. Springer, Cham. https://doi.org/10.1007/978-3-319-18443-2_5
Download citation
DOI : https://doi.org/10.1007/978-3-319-18443-2_5
Published : 17 December 2015
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-18442-5
Online ISBN : 978-3-319-18443-2
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Human Subjects Office
Protocol template.
Researchers use study protocols to provide specific details about the study, including background, purpose, study design, safety assessments and analysis plan. If a formal protocol does not exist, the IRB may require the UI investigator to supply one (e.g., an investigator initiated study or a complex study) The UI IRB recommends using an NIH Protocol Outline Template for Phase I, Phase II-III, or Behavioral and Social Science Research (BSSR) Involving Humans. The NIH and FDA provide a Protocol Template tool for creating a Protocol. Information described in the HawkIRB application must be consistent with the corresponding protocol.
Please refer to the UI Operations Manual, UI IRB Standard Operating Procedures & Researcher Guide (Section II Part 1.A, Part 18.A., and Part 19.A.), and The Point for assistance in aligning the protocol with the institutional guidelines.
Phase 1 or non-Clinical Trial : For studies that involves a Phase 1 clinical or therapeutic intervention, see Protocol Outline template .
Phase II-III Clinical Trials : For the FDA/NIH draft protocol template for Phase II through III trials, use the Phase 2 and 3 Clinical Trials that Require FDA-IND or IDE Application .
Behavioral and Social Science Research (BSSR) Involving Humans Protocol Template : Template for behavioral and social science researchers prepare research protocols for human studies measuring a social or behavioral outcome or testing a behavioral or social science-based intervention, use the Behavioral and Social Science Research (BSSR) Involving Humans protocol recommended by NIH.

- Planning a Research Project
- Getting Started
- Study Designs
- Data Management
- Budgets & Funding This link opens in a new window
- Writing Proposals This link opens in a new window
- Ethics Approval

Clinical Resource Guides
Databases and Apps A-Z
Education and Training
Equipment Booking
Keeping up to date
Research Repository
Research Toolkit
What does the library have?
What the library can do for you
- Evidence-Based Practice Guide
- Systematic Review Guide
- Quality Improvement Projects
- Ethics and Law Resource Guide
- Research and Grant Proposals
- Literature Searching Guide
- Grey Literature Guide
- Data Collection & Storage
- Statistics for Research
- Writing, Referencing & Publishing
- Communicating Research Findings
- Research Promotion & Impact
- Templates & examples
- Registration & publication
- Monash Health requirements
What is a study protocol?
A protocol is a detailed plan for a research study, outlining the specifics of how the research will be conducted. It is an essential document that helps to ensure research is conducted in a safe and ethical manner, and that the integrity of the research is preserved throughout the life of the study.
Common elements of a protocol
Melbourne Children's Trials Centre. (2017). Developing, amending and complying with research protocols. https://www.mcri.edu.au/images/research/training-resources/research-process-resources/guideline_developing_research_protocols.pdf
See the Data Management page in this guide for information on creating a data management plan (DMP), plus online tools and templates.
Literature review
Protocols draw on relevant literature at multiple points, e.g. in background information, when providing a rationale for the study, and when discussing known risks and benefits. If you haven't yet completed a literature search, now is the time to do one!
The Library offers training and guidance on conducting literature reviews, including a webinar on literature searching and a Literature Searching Guide .
Library research support
The Library offers various forms of research support depending on the purpose of your research. Our research support includes:
- Research consultations
- Literature search service
- Literature review report service
- Feedback on your literature search strategy
- Co-authorship for systematic reviews and other evidence synthesis projects
Complete this online form to request research support and learn more about each service offered.
Request research support
For an overview of Library research support, click the link below.
Library Research Support Services
Additional resources
- Protocol writing in clinical research (2016) by A. Al-Jundi & S. Sakka
- Write an error-free research protocol as recommended by WHO: 21 elements you shouldn't miss! (2022) by U. Bhosale
- How to Write a Research Protocol: Tips and Tricks (2018) by M. Cameli
- Guidance: Developing a protocol for a clinical research project (n.d.) by the Clinical Research Development Office, RCH
Protocol templates
The Murdoch Children's Research Institute (MCRI) provides annotated protocol templates for the following study designs:
- Clinical trial - drug/device intervention
- Clinical trial - intervention is not drug/device
- Observational studies
- Clinical audits / Quality assurance
To access the templates, click the blue button below and scroll down to the section on Clinical Research Development Office (CRDO) resources.
MCRI protocol templates
Qualitative studies
The NHS Health Research Authority offers a protocol template for qualitative research at the bottom of the page linked below.
NHS Qualitative protocol template
Example protocols
- RCT - A clinical investigation evaluating efficacy of a full-thickness placental allograft (Revita) in lumbar microdiscectomy outcomes
- Observational study - Prospective observational long-term safety registry of Multiple Sclerosis patients who have participated in cladribine clinical trials (PREMIERE)
- Systematic review and meta-analysis - Protocol for a systematic review and meta-analysis on the associations between shift work and sickness absence
Tip: The results of your literature search may include published protocols relevant to your research question.
Journal requirements
Journals that publish study protocols provide guidelines for the content required in protocol manuscripts. It can be helpful to review these guidelines even if you do not intend to publish your protocol in a peer-reviewed journal.
Search for the manuscript guidelines for your preferred journal(s) or review the examples below.
- BMC Nursing
Registering or publishing your protocol
Researchers are encouraged to submit their protocol for publication in a scholarly journal, and/or register their protocol in a relevant database. Many funding agencies also require grant recipients to register or publish their study protocol.
Where to register your protocol
Your study design generally determines where you register your protocol. See the table below for options on where to register your protocol.
| Systematic reviews, rapid reviews, | (Open Science Framework) |
| Clinical trials
| One or more trials registries (ANZTCR) (International Clinical Trials Registry Platform) (Open Science Framework) |
| Observational Studies
| (ANZTCR) (Open Science Framework) |
| Qualitative studies | (ANZTCR) (Open Science Framework) |
Where to publish your protocol
There are two main options:
- E.g. Journal of Clinical Epidemiology , Journal of Allied Health , Journal of Clinical Nursing
- E.g. BMC Trials , JMIR Research Protocols , Contemporary Clinical Trials
Be aware of predatory publishers - Check our our Writing, Referencing & Publishing Guide or our Predatory Publishing A-Z for more information.

Relevant Prompt documents include:
- Research Agreements Procedure
- Publication and dissemination of research findings
- Intellectual Property
- Research Ethics and Governance – Protocol and Investigational Brochure Content, Design, Amendments and Compliance
- Privacy and Confidentiality in Research
- Research Ethics and Governance – Authorship for Research
Visit the Forms Library from Research Support Services for links and more information.
Research - Forms Library
Research agreements
The Research Agreements Procedure provides guidance on which agreement to use in which circumstance and the pathway to follow for seeking review and approval. There are preferred templates for various types of studies, such as collaborative or investigator-initiated studies.
For more information, visit the Research Agreements page from Research Support Services.
Research Agreements page
Protocol amendments
Once your protocol is finalised and ethics approval has been granted, you must notify the Monash Health Research Support Services team regarding protocol amendments .
Monash Health acknowledges the Traditional Custodians of the land, the Wurundjeri and Boonwurrung peoples, and we pay our respects to them, their culture and their Elders past, present and future.
We are committed to creating a safe and welcoming environment that embraces all backgrounds, cultures, sexualities, genders and abilities.
- << Previous: Study Designs
- Next: Data Management >>
- Last Updated: Aug 22, 2024 1:16 PM
- URL: https://monashhealth.libguides.com/planning_research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Bras Pneumol
- v.49(6); 2023
- PMC10760430
Crafting a research protocol: a stepwise comprehensive approach
Elaboração de um protocolo de pesquisa: abordagem abrangente passo a passo, ricardo gassmann figueiredo.
1 . Programa de Pós-Graduação em Saúde Coletiva, Universidade Estadual de Feira de Santana - PPGSC-UEFS - Feira de Santana (BA) Brasil.
2 Methods in Epidemiologic, Clinical, and Operations Research-MECOR-program, American Thoracic Society/Asociación Latinoamericana del Tórax, Montevideo, Uruguay.
Cecilia María Patino
3 Department of Preventive Medicine, Keck School of Medicine, University of Southern California, Los Angeles (CA) USA.
Juliana Carvalho Ferreira
4 . Divisão de Pneumologia, Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, São Paulo (SP) Brasil.
PRACTICAL SCENARIO
A group of researchers plan to conduct a cross-sectional study to estimate the prevalence of frailty in elderly patients with moderate to severe asthma and to report a measure of association between asthma control and frailty. 1 The research protocol outlines the complex interactions of asthma control in frail patients and motivation to address this research question. Study design, objectives, methods, ethical issues, risks, and impact were also detailed in the protocol.
WHAT IS A RESEARCH PROTOCOL?
A well-structured research protocol guides researchers through the intricate process of conducting rigorous research. A research protocol is designed to be concise and self-contained, and to summarize the core aspects of the study. Self-discipline is vital in this process, as it requires the investigator to structure the central concepts of the study and reveal particular issues that demand attention. 2 The research protocol often serves as the foundation for the development of manual of operating procedures, which includes comprehensive information on the organization and policies of the study, as well as an operational approach to the procedures outlined in the study protocol; therefore, both documents complement each other.
ELEMENTS OF A RESEARCH PROTOCOL
The research protocol framework (outlined in Chart 1 ) usually includes a title, rationale, background information, objectives, methodology, data management, statistical plan, quality control, ethics, budget, developing plan, timeline, references, and appendices, although the sections included vary depending on institutional templates.
| Step | Description |
|---|---|
| Title | Concise, reflecting study main ideas, and attracting reader’s attention |
| Background and rationale | What is the problem? Why is it important? What is known about it? |
| Objectives | Specific, measurable, and established prior to carrying out the study |
| Relevance and study design | Contributions of the study to the field, aligned with rationale and objectives |
| Methods | Participants, exposures/intervention, outcomes, study setting, eligibility criteria, participant timeline, sample size, recruitment, and blinding Detailed script: How will the study be conducted? Why was the described design chosen? |
| Data collection, access, and management | Methods for data storage, security, privacy, and treatment of missing data |
| Statistical plan | Descriptive statistics, hypothesis testing, sample size, and power calculation |
| Quality control | Credibility of the research: instruments, data collection, data acquisition |
| Ethics | Ethical dilemmas, application to ethics research committees, Informed consent form |
| Roles and responsibilities | Affiliations, roles, and responsibilities of protocol contributors |
| Budget | Detailed expenses: personnel, equipment, consumables, logistics |
| Funding | Sources of financial support |
| Dissemination plan | Effective communication of research findings |
| Timeline | Be realistic about project management throughout the research |
| References | Check publishers’ guidelines, consider using reference manager software |
| Appendices | Extensive descriptions of procedures, questionnaires, and informed consent forms |
| Protocol version | Indicator of version and date of the protocol |
The title should be concise, descriptive, and engage readers, effectively reflecting the core of the research. 3 The background section outlines the driving factors and motivation for conducting the research. It should provide a broad context, elucidate the problem, address specific knowledge gaps, and establish the rationale for the study. In our practical example, the authors provided background information about how the multidimensional aspects of frailty are imbricated into proper asthma management in patients with advanced age. This section should align with the objectives, highlighting the potential impact of the study. Research objectives should be clear, measurable, precise, and set before conducting the study. 2 After the statement of the primary objective, secondary aims might be appropriate. The objectives will guide the study design and methodology, directing attention toward the intended research outcomes.
The methods section is a detailed blueprint of the research project and the basis for the manual of operating procedures. It should detail the study design, participant selection (eligibility, sampling, and recruitment), variables, data acquisition, data management (storage, security, privacy, and treatment of missing data), statistical plan, and sample size calculation. The scientific robustness of the study relies on its methodology, ensuring validity and replicability. The statistical plan should clearly outline the analysis methods, software used, and criteria for determining statistical significance. Quality control mechanisms uphold the internal validity of the study. This segment should describe measures to minimize bias and ensure data quality. 2 Steps might include regular data verification, calibration and certification of instruments, as well as research personnel training.
Ethical considerations are paramount in research. This section should document the issues that are likely to raise ethical concerns, including informed consent forms, confidentiality, data protection, and potential ethical dilemmas. 3 Moreover, it should also mention approvals obtained from institutional review boards. The budget section details the financial requirements of the research. It includes costs with personnel, equipment, materials, logistics, consumables, and contingencies. A realistic and well-planned timeline is crucial for successful project management.
Deficiencies in effectively disseminating and transferring research-based knowledge into clinical practice can impair the potential benefits of the research project. Therefore, most health research funding agencies expect commitment from investigators to disseminate the study findings actively. Integrating a dissemination plan in the research protocol will facilitate effective communication of research outcomes to the scientific community and those who can apply the knowledge in real-world situations.
KEY MESSAGES
- A comprehensive research protocol not only provides a roadmap for the implementation of the study but also ensures that the research question is addressed according to high-quality research standards.
- Quality control is essential to improve internal validity of the study.
- A structured approach to conducting research reduces the likelihood of misleading conclusions and biases, ensuring validity and reproducibility of the study.

Protocol Outline
| A. B. C. Appendix A
The IHRIRB’s assessment of your research proposal involves a series of steps: (1) identifying the risks associated with the research, as distinguished from the risks the participants would experience even if not participating in the research; (2) determining that risks will be minimized; (3) identifying the probable benefits to be derived from the research; (4) determining that risks are reasonable in relation to the benefits to the participants, if any, and the importance of the knowledge to be gained; (5) ensuring that potential participants will be provided with an accurate and fair description of the risks or discomforts of the anticipated benefits; and (6) determining the intervals of periodic review. To ensure that the IHRIRB completes their review in a timely manner, your proposal must include the following information, as applicable: ¨ Cover letter with a list of all investigators and a contact person and telephone number ¨ Detailed protocol of study design, sampling, analyses, timelines, evaluation, and community involvement ¨ Informed consent and assent forms ¨ Other attachments, such as a copy of scripts or survey that will be used, materials that will be distributed, etc. If your proposal is missing any required items, review of your proposal will be delayed. SAMPLE PROTOCOL OUTLINE POSTED BELOW.
Your research Protocol should discuss in detail how you plan to carry out the research, how you will analyze the data that you collect, and what you plan to do with the results. The following are points that you should address in your protocol.
¨ Provide relevant research background and explain why this activity is necessary or important. ¨ Describe the potential impact of the proposed research.
¨ Provide a complete description of the study design, sequence, and timing of all study procedures that will be performed. Provide this information for pilot, screening, intervention, and follow-up phases. Include all materials that will be used in the procedure, such as surveys, scripts, questionnaires, etc. Attach flow sheets if they will help the reader understand the procedures. ¨ Describe how study procedures differ from standard care or procedures (e.g., medical, psychological, educational, etc.). ¨ If any deception or withholding of complete information is required, explain why this is necessary and attach a debriefing statement. ¨ Describe where the study will take place ¨ A letter of approval and cooperation from each participating site is needed. For example, if the study will be conducted in the local school system, an approval letter from the School Board and Superintendent are necessary.
¨ Explain how the nature of the research requires or justifies using the participant population. ¨ Provide the approximate number and ages for the control and experimental groups. ¨ Describe the gender and minority representation of the participant population. ¨ Describe the criteria for selection for each participant group. ¨ Describe the exclusion criteria exclusion for each participant group. ¨ Describe the source for participants and attach letters of cooperation from agencies, institutions, or others involved in the recruitment. ¨ Explain who will approach the participants and how the participants will be approached. Explain what steps you will take to avoid coercion and protect privacy. Submit advertisements, flyers, contact letters, and phone contact protocols. ¨ Explain if participants will receive payments, services without charge, or extra course credit. ¨ Explain if participants will be charged for any study procedures.
¨ Describe the nature and amount of risk of injury, stress, discomfort, invasion of privacy, and other side effects from all study procedures, drugs, and devices. Describe the amount of risk the community may be subjected to. ¨ Describe how due care will be used to minimize risks and maximize benefits. ¨ Describe the provisions for a continuing reassessment of the balance between risks and benefits. ¨ Describe the data and safety monitoring committee, if any. ¨ Describe the expected benefits for individual participants, the community, and society.
¨ Describe how adverse effects will be handled. ¨ Discuss if facilities and equipment are adequate to handle possible adverse effects. ¨ Explain who will be financially responsible for treatment of physical injuries resulting from study procedures (e.g., study sponsor, subject, organization compensation plan, etc.).
¨ Explain if data will be anonymous (no possible link to identifiers). ¨ Explain if identifiable data will be coded and if the key to the code will be kept separate from the data. ¨ Explain if any other agency or individual will have access to identifiable data. ¨ Explain how data will be protected (e.g., computer with restricted access, locked file, etc.).
¨ If the consent form is written, submit copies of all consent and assent forms for each participant group. If an oral consent or assent script will be used, submit written scripts for each group. ¨ If you will not use a consent form or script, submit written justification of waiver of consent.
¨ List all non-investigational drugs or other substances that will be used during the research. Include the name, source, dose, and method of administration. ¨ List all investigational drugs or substances to be used in the study. Include the name, source, dose, method of administration, IND number, and phase of testing. (INDs must be registered with the appropriate institutional pharmacy.) Provide a concise summary of drug information prepared by the investigator, including available toxicity data, reports of animal studies, description of studies done in humans, and drug protocol. ¨ List all investigational devices to be used. Provide the name, source, description of purpose, method, and Food and Drug Administration IDE number. If no IDE is available, explain why the device qualifies as a non-significant risk. Attach a copy of the protocol, descriptions of studies in humans and animals, and drawings or photographs of the device.
¨ Describe how materials with potential radiation risk will be used (e.g., X-rays and radioisotopes). ¨ If you will use materials with potential radiation risk, describe the status of annual review by the Radiation Safety Committee. If the annual review has been approved, attach a copy of the approval. ¨ Describe the medical, academic, or other personal records that will be used. ¨ Describe the type of audio-visual recordings, tape recordings, or photographs that will be made. ¨ Explain if the Scientific Instrument Division will test all instruments. If not, describe the safety testing procedures. ¨ Do the PI or sponsor have relevant insurance coverage? If so, state company name and policy number. This excerpt should be read in conjunction with the Guidelines. Appendix C
© 2018 |

Developing a Protocol for Systematic and Scoping Reviews
- Protocol Templates
- Making Your Protocol Available
- Additional Resources
- Related Guides
- Getting Help
What is a Protocol?
In the evidence synthesis process, the first step is determining a research question (Uman, 2011). The next step is deciding which type of review to conduct based on your research question. Before conducting the actual literature review and research, the team must develop a protocol.
The protocol of an evidence synthesis outlines the rationale, hypothesis, and methods researchers are planning to use in conducting their review (Page et. al, 2021). Protocols must be completed before the actual review is conducted, and is then used as a guide for the research team. Outlining the team's steps in the research process is not only essential for collaboration, but in establishing authorship and credibility. In order for your review to be legitimate, you must outline and justify the measures taken to search and review the relevant literature.
Once a protocol is developed, it is uploaded and shared for other researchers to review. This is done to allow for potential replication in research measures.
- Systematic Review
- Scoping Review
What is a Systematic Review?
A systematic review is a form of evidence synthesis where a comprehensive literature review relating to one specific research question is conducted (Newman & Gough, 2020). Literature reviewed includes studies, papers, essays, research, and unpublished studies. The goal is to be as comprehensive as possible and to prevent bias in literature selected. Once all of the literature is reviewed, poorly done studies are filtered and the researcher is able to make recommendations regarding future directions of research applying to the area of focus.
For more information on conducting a systematic review at Duquesne, see our Systematic Review library guide .
What is a Scoping Review?
A scoping review is a form of evidence synthesis where the author's goal is determining the scope of literature surrounding a particular area of interest (Munn et. al, 2018). This is contrary to a systematic review, which aims to gather all of the literature relating to a focused research question (Pham et. al, 2014). Also referred to as mapping, the scoping review's purpose is to amass literature in one area - what is consistent/inconsistent in the literature? What are trends in research being done in this area? What are the gaps? This is useful information to have as it informs future research.
For more information on conducting a scoping review at Duquesne, see our Scoping Review library guide .
What to Include in Your Protocol
Depending on the type of evidence synthesis you aspire to conduct, a protocol may need to follow a template. Potential requirements for these protocols include description of the following elements (Uman, 2011):
- Inclusion and exclusion criteria
- Eligibility
- Keywords used in searches, synonyms
- Types of studies reviewed
- Examples of search terms
- Justification of how studies are being assessed
- Ways of preventing bias
- Next: Protocol Templates >>
- Last Updated: Feb 5, 2024 3:28 PM
- URL: https://guides.library.duq.edu/protocols
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 14, Issue 5
- Use of social network analysis in health research: a scoping review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Eshleen Grewal 1 ,
- Jenny Godley 2 , 3 , 4 ,
- Justine Wheeler 5 ,
- http://orcid.org/0000-0001-9008-2289 Karen L Tang 1 , 3 , 4
- 1 Department of Medicine , University of Calgary , Calgary , Alberta , Canada
- 2 Department of Sociology , University of Calgary , Calgary , Alberta , Canada
- 3 Department of Community Health Sciences , University of Calgary , Calgary , Alberta , Canada
- 4 O’Brien Institute for Public Health , University of Calgary , Calgary , Alberta , Canada
- 5 Libraries and Cultural Resources , University of Calgary , Calgary , Alberta , Canada
- Correspondence to Dr Karen L Tang; klktang{at}ucalgary.ca
Introduction Social networks can affect health beliefs, behaviours and outcomes through various mechanisms, including social support, social influence and information diffusion. Social network analysis (SNA), an approach which emerged from the relational perspective in social theory, has been increasingly used in health research. This paper outlines the protocol for a scoping review of literature that uses social network analytical tools to examine the effects of social connections on individual non-communicable disease and health outcomes.
Methods and analysis This scoping review will be guided by Arksey and O’Malley’s framework for conducting scoping reviews. A search of the electronic databases, Ovid Medline, PsycINFO, EMBASE and CINAHL, will be conducted in April 2024 using terms related to SNA. Two reviewers will independently assess the titles and abstracts, then the full text, of identified studies to determine whether they meet inclusion criteria. Studies that use SNA as a tool to examine the effects of social networks on individual physical health, mental health, well-being, health behaviours, healthcare utilisation, or health-related engagement, knowledge, or trust will be included. Studies examining communicable disease prevention, transmission or outcomes will be excluded. Two reviewers will extract data from the included studies. Data will be presented in tables and figures, along with a narrative synthesis.
Ethics and dissemination This scoping review will synthesise data from articles published in peer-reviewed journals. The results of this review will map the ways in which SNA has been used in non-communicable disease health research. It will identify areas of health research where SNA has been heavily used and where future systematic reviews may be needed, as well as areas of opportunity where SNA remains a lesser-used method in exploring the relationship between social connections and health outcomes.
- Protocols & guidelines
- Social Interaction
- Social Support
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-078872
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This is a novel scoping review that fills an important gap—how and where social network analysis (SNA) (as a data collection and analytical tool) has been used in health research has not been systematically documented despite its increasing use in the discipline.
The breadth of the scoping review allows for a comprehensive mapping of the use of SNA to examine social connections and non-communicable disease and health outcomes, without limiting to any one population group or setting.
The use of the Arksey and O’Malley framework as well as the Levac et al recommendations to guide our scoping review will ensure that a rigorous and transparent process is undertaken.
Due to the scope of the review and the large volume of anticipated studies, only published articles in the English language will be included.
Introduction
Social connections are known to influence health. 1 People with many supportive social connections tend to be healthier and live longer than people who have fewer supportive social connections, while social isolation, or the absence of supportive social connections, is associated with the deterioration of physical and psychological health, and even death. 2–5 These associations hold even when accounting for socioeconomic status and health practices. 6 Additionally, having a low quantity of supportive social connections is associated with the development or worsening of medical conditions, such as atherosclerosis, hypertension, cardiovascular disease and cancer, potentially through chronic inflammation and changes to autonomic regulation and immune responses. 7–13 Unsupportive social connections can also have adverse effects on health due to emotional stress, which can then lead to poor health habits, psychological distress and negative physiological responses (eg, increased heart rate and blood pressure), all of which are detrimental to health over time. 14 The health of individuals is therefore connected to the people around them. 15
Social networks can influence health via five pathways. 15 16 First, networks can provide social support, to meet the needs of the individual. Dyadic relationships can provide informational, instrumental (ie, aid and assistance with tangible needs), appraisal (ie, help with decision-making) and/or emotional support; this support can be enhanced or hindered by the overall network structure. 17 In addition to the tangible aid and resources that are provided, social support—either perceived or actual—also has direct effects on mental health, well-being and feelings of self-efficacy. 18–20 Social support may also act as a buffer to stress. 16 19 The second pathway by which social networks influence health, and in particular health behaviours such as alcohol and cigarette use, physical activity, food intake patterns and healthcare utilisation, is through social influence. 16 21 That is, the attitudes and behaviour of individuals are guided and altered in response to other network members. 22 23 Social influence is difficult to disentangle from social selection from an empirical standpoint. That is, similarities in behaviour may be due to influences within a network, or alternatively, they may reflect the known phenomenon where individuals tend to form close connections with others who are like them. 22 24 The third pathway is through the promotion of social engagement and participation. Individuals derive a sense of identity, value and meaning through the roles they play (eg, parental roles, community roles, professional roles, etc) in their networks, and the opportunities for participation in social contexts. 16 The fourth pathway by which networks affect health is through transmission of communicable diseases through person-to-person contact. Finally, social networks overlap, resulting in differential access to resources and opportunities (eg, finances, information and jobs). 15 16 An individual’s structural position can result in differential health outcomes, similar to the inequities that stem from differences in social status. 16
There has been an explosion of literature in the area of social networks and health. In their bibliometric analysis, Chapman et al found that the number of studies that examine social networks and health has sextupled since 2000. 25 Similarly, the value of grants and contracts in this topic area, as awarded by the National Science Foundation and the National Institutes of Health, has increased 10-fold. 25 A turning point in the field was the HIV epidemic, where there was an urgent need to better understand its spread. 25 The exponential rise in the number of studies since then that examine social networks and health appears to reflect a widespread understanding that an individual’s health cannot be isolated from his or her social networks and context. There is, however, significant heterogeneity in what aspect of, and how, social networks are being studied. For example, many health research studies use proxies for social connectedness such as marital status or living alone status (as these variables tend to be commonly included in health surveys), without considering the quality of those social connections, and without further exploring the broader social network and their characteristics. 16 26 These proxy measures do little to describe the structure, quantity, quality or characteristics of social connections within which individuals are embedded. Another common approach in health research is to focus on social support measures and their effects on health. Individuals are asked about perceived, or received, social support (for example, through questions that ask about the availability of people who provide emotional support, informational support and/or assistance with daily tasks, with either binary or a Likert scale of responses). 27 28 While important, social support measures do not assess the structure of social networks and represent only one of many different mechanisms by which social networks influence health. 17 23
Social network analysis
Social network analysis (SNA) is a methodological tool, developed in the 1930s by social psychologists, used to study the structure and characteristics of the social networks within which individuals are embedded. 16 29 It has evolved over the past 100 years and has been used by researchers in many social science disciplines to analyse how structures of relationships impact social life. 29 30 SNA has the following key properties 3 30 31 : (1) it relies on empirical relational data (ie, data on actors (nodes) and the connections (ties) between them); (2) it uses mathematical models and graph theory to examine the structure of relationships within which individual actors are embedded; and (3) it models social action at both the group and the individual level arising from the opportunities and constraints determined by the system of relationships. The premise of SNA is that social ties are both drivers and consequences of human behaviour, and are therefore the object of study. 15 16 23 32 Social networks are comprised of nodes, representing the members within a network, connected by ties, representing relations among those individuals. 33 There are two types of SNA: egocentric network analysis and whole network analysis. Egocentric network analysis describes the characteristics of an individual’s (ie, the ‘egos’) personal network, while whole network analysis examines the structure of relationships among all the individuals in a bounded group, such as a school or classroom. 3
In egocentric network analysis, a list of ‘alters’ (ie, nodes) to whom the ego is connected, is obtained through a name generator. Name generator questions ask for a list of alters based on role relations (eg, friends or family), affect (eg, people to whom the ego feels close), interaction (eg, people with whom the ego has been in contact) or exchange (eg, people who provide social and/or financial support). 34 These are followed by name interpreters, where the ego is asked questions about the characteristics of each named alter. 35 Analyses of these data involve constructing measures that describe these egocentric networks. Such measures include network size, network density (ie, how tightly knit the network is), the strength of relationships (ie, the intensity and duration of relationships between ego and alter), network function (ie, the resources and/or support provided through the network) and the diversity of relations within the network (‘heterogeneity’). 23 36 In whole network analysis, the network boundary is determined a priori and network members are known, for example, through membership lists or rosters. 37 Each network member is surveyed, to identify the other network members with whom they are connected and/or affiliated; attributes of each member are obtained through surveying the network members themselves. Variables are constructed at the individual and network levels. Individual-level measures include the number of ties to other network members (‘degree’), types of relationships, and the strength and diversity of relationships. Network-level measures include but are not limited to: density (representing how tightly knit or ‘glued’ together the network is), reciprocity (ie, the proportion of network ties that are reciprocated), isolates (ie, nodes with no ties to other network members), centralisation (or the extent to which the network ties are focused on one node or a set of nodes), cliques and equivalence (ie, sets of nodes that have the same pattern of ties and therefore occupy the same position in the network). 33 38 The constructed measures can then be included in statistical models to explore associations between individual and/or network-level measures, and outcomes. 33 39
Study rationale
In medicine and health research, there has traditionally been a dichotomy between the individual and the context in which the individual is situated—such as in their relationships with others. 40 As such, epidemiology of diseases has historically focused on individual-level traditional risk and protective factors—such as biological markers, genetics, lifestyle and health behaviours, and psychological conditions. 41 While criticisms of this individualistic focus abound, attempts to develop and use different approaches in medicine and research have lagged behind. 42 The use and adoption of methods, like SNA, that frame issues of health and wellness differently, has the potential to offer new insights and solutions to clinical and healthcare delivery problems, 42 by more holistically considering ‘different levels of change’ beyond the individual. 41 We seek to examine the extent to which SNA has transcended the boundaries of its disciplines of origin in the social sciences, into health research. For example, while Chapman et al have clearly shown an explosion of publications at this intersection, 25 it remains unclear whether these studies use SNA tools (which were developed specifically to interrogate the nature and characteristics of social networks), or whether they suffer from the known problem of conflation of constructs like social support, social capital and social integration. 15 43 Many studies that report the impact of ‘social networks’ on health outcomes do not use SNA methods but rather use self-reported network size (without probing the network and its structure), 44 45 social support, 46 marital status 47 48 and/or household members 47 as proxies.
We will therefore undertake a scoping review to map the use of SNA as a data collection and analytical method in health research. More specifically, the scoping review will examine how SNA has been used to study associations across social networks and individual health and well-being (including both physical and psychological health), health knowledge, health engagement, health service use and health behaviours. Scoping reviews are a knowledge synthesis approach that aims to uncover the volume, range, reach and coverage of a body of literature on a specific topic. 49 They differ from systematic reviews, another type of knowledge synthesis, in their objectives. Systematic reviews seek to answer clinical or epidemiological questions and are conducted to fill gaps in knowledge. 50 Systematic reviews are used to establish the effectiveness of an intervention or associations between specific exposures and outcomes. On the other hand, scoping reviews do not seek to provide an answer to a question, but rather, aim to create a map of the existing literature. 49 They are used to provide clarity to the concepts and definitions used in literature, examine the way in which research is conducted in a specific field or on a specific topic, and uncover knowledge gaps. 49 A scoping review, therefore, is well suited as a research method to address our research question, of mapping the ways in which SNA has been used in health research. This scoping review can identify areas (eg, specific populations and specific health outcomes) where there has been a plethora of SNA research warranting future systematic reviews. It can also identify areas within health research where the use of SNA is scarce, highlighting topics, populations or outcomes for future study.
This scoping review will be limited to studies that use SNA in exploring network components and their associations with non-communicable diseases and health and well-being outcomes, for three reasons. The first is feasibility, given the large volume of studies anticipated, based on Chapman et al ’s bibliometric study on this topic. 25 Second, the use of SNA in understanding disease transmission of communicable diseases (such as sexually transmitted infections) is well established; its application to HIV was in fact one of the catalysts, as previously mentioned, to its broader uptake in health research. 25 Third, SNA in health research has shifted from focusing on communicable diseases to focusing on non-communicable diseases and their risk factors; SNA is now being applied much more frequently to the latter conditions than the former ones. 51
Methods and analysis
The scoping review will be informed by the framework developed by Arksey and O’Malley 52 for conducting scoping reviews, as well as the additional recommendations made by Levac et al . 53 Arksey and O’Malley’s framework recommends that the review process be organised into the following five steps: identifying the research question; identifying relevant studies; study selection; charting the data; and collating, summarising and reporting the results. 52 The reporting of this review will adhere to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews. 54
Patient and public involvement
No patients will be involved.
Step 1: identifying the research question
A preliminary search of the literature identified a gap related to SNA and how it has been used to study the relationship between social networks and individual well-being and health outcomes. This led to the development of the research question that will guide this scoping review: how have social network analytical tools been used to study the associations between social networks and individual patient health? In this case, SNA is defined as a data analysis technique that uses either an egocentric or whole network analysis approach. For egocentric network analysis, we will include studies that involve peer nomination (ie, use of a name generator) and the collection of one or more characteristics of alters (ie, use of name interpreter(s)).
Step 2: identifying relevant studies
A search strategy will be constructed through consultation with an academic librarian (JW). The main concepts from the research question will be used for a preliminary search in Google Scholar. Additionally, the lead authors will provide the librarian with key studies that will be text-mined for relevant terms. These key studies will include a variety of populations (across different countries and age groups) and health outcomes. 55–58 Key studies will be searched in Ovid MEDLINE for appropriate subject headings. In consultation with team members, the librarian (JW) will construct a pilot search strategy. A title/abstract/keyword search will be conducted in Ovid MEDLINE against the known seed/key studies. Table 1 lists example keywords and terms relating to social networks that will be used, with the full search strategy detailed in online supplemental appendix A .
Supplemental material
- View inline
Search terms relating to social network analysis
Due to a significant number of irrelevant articles surrounding communicable diseases using this search strategy, we will exclude records with these terms in either the title or keyword fields. Table 2 lists the terms related to communicable diseases.
Search terms relating to communicable diseases
Of note, the search strategy will not include terms that relate to health-related outcomes of interest (outside of excluding communicable diseases). Prior literature has shown that the inclusion of outcome concepts in a search strategy reduces the recall and sensitivity of a search strategy. 59 60 This problem is further exacerbated when only generic health terms (for example, ‘morbidity’ or ‘health status’) or specific health terms (eg, specific diseases or conditions such as ‘diabetes mellitus’) are used. 61 Because the objective of this scoping review is to examine and map the use of SNA in health research, the outcomes of interest are very broad, including: physical health and well-being, psychological health and well-being, healthcare engagement, health knowledge, health behaviours, healthcare access and use, disease prevalence and outcomes (spanning every organ system), and mortality. It will be impossible for a search strategy to be sufficiently comprehensive, to capture all possible generic and specific terms relating to this broad range of outcomes. In keeping with recommendations to minimise the number of elements in a search strategy 62 —and in particular outcome elements 63 —our search strategy will entail searching for SNA terms in health databases without specifying health outcomes.
The search strategy will first be created in Medline (Ovid), then translated and adapted for the databases: (1) EMBASE (Ovid), (2) APA PsycInfo (Ovid) and (3) CINAHL (EBSCO). A search will be completed in April 2024. No date filters will be applied to the search. However, animal-only studies will be excluded. The current version of the search strategy including limits and filters, for all databases, is included in online supplemental appendix A .
Step 3: study selection
The criteria that will be used to determine which studies to include are as follows:
Studies that employ SNA as a data collection and/or analysis technique, as defined above. Of note, studies that elicit only the number of friends or other social contacts, without collection of any information about these social contacts, are not considered to be SNA and are therefore not included in the scoping review.
Studies that explore the social networks of individuals in whom the health outcome is measured.
Studies must include the exploration of non-communicable health outcomes. Examples include self-rated health or other global measures of health (including measures of physical health, mental health and well-being), health practices (eg, physical activity, dietary patterns, smoking, alcohol use, substance use), sexual and reproductive health, healthcare-seeking behaviours (eg, medication adherence, acute care use, attachment to a primary care provider), health knowledge, health beliefs, healthcare engagement, non-communicable disease prevalence and mortality.
The criteria that will be used to exclude studies are as follows:
Studies that explore the social networks of organisations or healthcare providers, rather than the social networks of the individual about whom the health outcome is measured or reported.
Studies that describe or use data analysis techniques other than SNA (eg, using proxies for social networks/social support that do not include peer nomination (such as marital status or living alone status), or studies where study participants report the number of social contacts but where no other information about each social contact is collected).
Studies that focus exclusively on online social networks (eg, social media, online forums, online support groups).
Studies related to prevention, transmission or outcomes of communicable diseases.
Non-English studies, for feasibility purposes.
We will not limit studies based on the study population or country in which the SNA is conducted. Studies in paediatric and adult populations will be included. The reasons for excluding SNA studies that focus solely on social media and online networks are twofold. First, we anticipate a very large number of articles, given the broad populations and outcomes of interest, and for feasibility purposes, we have needed to narrow the research objective to in-person and/or offline social networks only. Second, there are likely inherent differences in online and offline social networks. Individuals use health-related social networking sites and online networks primarily for information seeking, connection with others who share a similar lived experience while being able to maintain some emotional distance and interacting with health professionals 64 ; this differs from in-person networks, which individuals go to more for emotional and tangible or instrumental support. Friends met on online networks vary from friends met in person in other important ways. They tend to have less similarity in terms of age, gender and place of residence, 65 and the network ties more commonly arise spontaneously—that is, without common acquaintances or affiliations. 66 The social patterns and interactions among individuals and their online network contacts are also different—with entire relationships built on text-based interactions. 66 Therefore, while online social networks are an important area of study, they appear to be inherently different from the study of offline social networks, and are therefore excluded from this scoping review.
For the first step of the screening process, after removing duplicate articles, two reviewers will independently assess the titles and abstracts of the studies to determine whether they meet the inclusion criteria. Any studies that do not meet the inclusion criteria will be excluded from the review. Studies that either one of the two reviewers feels are potentially relevant will be included in the full-text review, to ensure that no article is prematurely excluded at this stage. During the second step of the screening process, two reviewers will independently review the full texts of the studies to ensure they meet the inclusion criteria. Conflicts will be resolved by third and fourth reviewers with expertise in SNA (JG) and health outcomes (KLT). The number of studies included in each step of the screening process will be reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses diagram. 67
Step 4: charting the data
A data charting document ( online supplemental appendix B ) will be created to extract data from the studies in the review. This document will include information about the authors, year of publication, study location, study population characteristics, outcomes of interest to this scoping review, and the scales and measures used for each outcome. Data about the social network analytical method will also be extracted, including whether studies used egocentric versus whole networks, the name generator used (in egocentric network studies) or the relationship being explored, the maximum number of peer nominations allowed, the lookback period used, whether (and which) alter attributes were collected, and whether alter-to-alter tie data were collected. Data extraction will be performed by at least one reviewer, with a second reviewer separately checking and confirming the inputted data. Disagreements in data extraction will be resolved through a consensus, and through the input of reviewers with content and methods expertise (KLT, JG).
Step 5: collating, summarising and reporting results
The results of the review will be presented in the form of figures and tables and will include descriptive numerical summaries. The numerical summary will include information about the number of studies included in the review, where the studies were conducted, when they were published and characteristics of the populations, such as the sample sizes and mean age. It will also include characteristics of the SNA conducted in these studies, including the number that are whole network studies versus egocentric network studies, the data sources used and the attributes of the social connections that are collected and analysed. Results will be synthesised in text, as well as through tables and figures.
Ethics and dissemination
This review does not require ethics approval. Data will be extracted from published material. Once the scoping review is complete, an article will be written to convey the findings of this review, and it will be submitted for publication in a peer-reviewed journal. We anticipate the results of this review will map out the ways in which SNA has been used in health research. Specifically, this scoping review will identify areas of potential saturation where SNA has been heavily used, opportunities for future systematic reviews (where there is a large body of primary research studies requiring synthesis) and health research gaps (eg, the health outcomes where SNA has been minimally used). The scoping review will also shed light on characteristics of SNA that have been used (eg, whether egocentric networks vs whole networks are used and in what settings, and whether a broad range of social network characteristics are captured and analysed), which will serve to inform the conduct of future SNA studies in health research.
Ethics statements
Patient consent for publication.
Not applicable.
- Schaefer DR
- Christiansen J ,
- Qualter P ,
- Friis K , et al
- Leong D , et al
- Umberson D ,
- Glymour MM ,
- Everson-Rose SA ,
- Robles TF ,
- Kiecolt-Glaser JK
- Kiecolt-Glaser JK ,
- McGuire L ,
- Robles TF , et al
- O’Brien E , et al
- Shattuck EC
- Christakis NA
- Berkman LF ,
- Brissette I , et al
- McFarlane AH ,
- Bellissimo A ,
- Rueger SY ,
- Malecki CK ,
- Pyun Y , et al
- Siciliano MD
- de la Haye K ,
- Barnett LM , et al
- Murray JM ,
- Sánchez-Franco SC ,
- Sarmiento OL , et al
- Pescosolido BA ,
- Borgatti SP
- Chapman A ,
- Verdery AM ,
- Holt-Lunstad J ,
- Gjesfjeld CD ,
- Greeno CG ,
- Poston WS , et al
- Fredericks KA ,
- Carrington P
- Crossley N ,
- Bellotti E ,
- Edwards G , et al
- Wasserman S ,
- Burgette JM ,
- Rankine J ,
- Culyba AJ , et al
- Kirkengen AL ,
- Ekeland T-J ,
- Getz L , et al
- Pescosolido BA
- Lucivero F , et al
- Vettore MV ,
- Ahmad SFH ,
- Machuca C , et al
- De Gagne JC
- Palmer Kelly E ,
- García EL ,
- Banegas JR ,
- Pérez-Regadera AG , et al
- Hempler NF ,
- Joensen LE ,
- Peters MDJ ,
- Stern C , et al
- Higgins JPT ,
- Chandler J , et al.
- Valente TW ,
- Colquhoun H ,
- Tricco AC ,
- Zarin W , et al
- Christakis NA ,
- Mohr P , et al
- O’Malley AJ ,
- Arbesman S ,
- Steiger DM , et al
- Watkins SC ,
- Jato MN , et al
- Frandsen TF ,
- Nielsen MFB ,
- Bruun Nielsen MF ,
- Lindhardt CL , et al
- Maclean A ,
- Sweeting H , et al
- Bramer WM ,
- de Jonge GB ,
- Rethlefsen ML , et al
- Lefebvre C ,
- Glanville J ,
- Briscoe S , et al
- Colineau N ,
- Doerfel ML ,
- Shamseer L ,
- Clarke M , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
Contributors KLT and JG conceived of the study protocol. KLT, JG, EG and JW developed and revised the study protocol, the search strategy and the inclusion/exclusion criteria. EG and KLT drafted the protocol manuscript, and all authors provided critical revisions.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Study Protocol
The landscape of spiritual health and spirituality in Canada: A scoping review protocol
Roles Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Health, Society and Aging, McMaster University, Hamilton, Ontario, Canada, ICES, Toronto, Ontario, Canada, Faculty of Liberal Arts, Wilfrid Laurier University, Waterloo, Ontario, Canada
Roles Writing – review & editing
Affiliation Department of Health Sciences, Wilfrid Laurier University, Waterloo, Ontario, Canada
Affiliation Department for the Study of Religions, Wake Forest University, Winston-Salem, North Carolina, United States of America
Affiliation Faculty of Liberal Arts, Wilfrid Laurier University, Waterloo, Ontario, Canada
- Helana Marie Boutros,
- Merna Mina,
- Nelly Van Doorn-Harder,
- Maurita T. Harris

- Published: August 29, 2024
- https://doi.org/10.1371/journal.pone.0309294
- Reader Comments
Introduction
Currently, literature on spiritual health remains limited. Even more so, literature on spiritual health remains limited in Canada. This is exacerbated by the fact that spiritual health is a term that remains widely contested with no concrete definition. Meanwhile, the semantic connection between “religion” and “spirituality” remains ambiguous in the West and scholars hold different positions. In this paper, we outline our scoping review protocol to describe the current landscape of spiritual health and spirituality (in relation to health) research in Canada, including the meaning and understanding behind these two concepts.
Methods and analysis
This protocol for our scoping review is documented in accordance with the PRISMA-P reporting guidelines and adheres to Arksey and O’Malley’s scoping review methodology. We will conduct a search strategy across select electronic databases and review the reference lists of chosen papers. Two reviewers, HMB and MM, will independently and blindly screen all title/abstracts and full-text studies for eligibility. Any Canadian-situated studies that centrally mention and focus on “spirituality” or “spiritual health” will be included. Relevant variables will be extracted through an iterative process, with the data charting being continuously reviewed and refined. Findings from this scoping review will support the future of health research and conceptual expansion of health beyond the mental, physical and social. Approval from a research ethics board is not required, nor has it been obtained, as the data is derived from journal articles and academic publications.
Citation: Boutros HM, Mina M, Van Doorn-Harder N, Harris MT (2024) The landscape of spiritual health and spirituality in Canada: A scoping review protocol. PLoS ONE 19(8): e0309294. https://doi.org/10.1371/journal.pone.0309294
Editor: Magdalena Szaflarski, University of Alabama at Birmingham, UNITED STATES OF AMERICA
Received: July 7, 2024; Accepted: August 7, 2024; Published: August 29, 2024
Copyright: © 2024 Boutros et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: No datasets were generated or analysed during the current study. All relevant data from this study will be made available upon study completion.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Spiritual health is conceptualized, theorized, and studied substantially against two disciplines in the literature: health promotion and nursing practice. This is not to say that theology and philosophy do not play a role in contributing to the current understanding of spiritual health. There is an inevitable distinctive flavour of these disciplines in nursing practice and health promotion, but it is a flavour more so subconsciously underpinned instead of explicitly expressed [ 1 – 3 ].
Today, the term “spiritual health” is a growing linguistic term that is being used across different countries and different continents, having had linguistic use since the 1980s [ 4 – 17 ]. Furthermore, there have been multiple studies whose research objectives define spiritual health [ 6 , 11 , 12 , 14 ], only one of which is based in Canada [ 18 ]. However, despite this growing emphasis on wholeness and holism, there remains a noticeable absence of discussion surrounding spirituality and spiritual health [ 19 ].
It can be argued that the re-introduction in the 1980s of spiritual health in disciplines, such as health promotion and nursing practice, is precipitated by a convicting desire to counter Descartes-infused biomedical practices within healthcare and health promotion practice. In the 17 th century, Descartes argued that the human body is mechanistically understood and conceptualized, independent of the mind [ 14 , 20 , 21 ]. This philosophy led to mind-body dualism and its mutational offshoots contributed to 21st-century biomedicine today, where biomedicine particularly focuses on relieving physical symptoms of disease and illness instead of focusing on etiology and prevention [ 14 , 20 ].
While the negative implications of the current biomedical approach arguably placed a new enthusiasm for spiritual health on the map, health was not always biomedically conceptualized [ 22 ]. Historically, a holistic understanding of health was spawned in Ancient Greek medicine [ 20 ]. Unlike its modern biomedical counterpart, Ancient Greek medicine argued that it was insufficient to define health as the absence of disease and unpleasant symptoms [ 20 ]. Instead, Ancient Greeks asserted that health is more wholly characterized by an individual’s sound spiritual base and a satisfying, full life [ 11 , 20 , 22 ]. Therefore, the physician’s role in Ancient Greek medicine was centralized around restoring order instead of simply removing unpleasant symptoms [ 20 ]. For example, Hippocrates asserted that a person’s worldview or way of life is a normative feature for one’s health. This implies that a person’s beliefs and value systems are decisive factors for their health. Therefore, it is reasonable to assume that in-depth awareness of the multi-dimensional role that beliefs and value systems play leads to the integration of these beliefs in one’s daily life, which impacts one’s well-being [ 11 , 23 ]. It is also reasonable to assume that if a person’s beliefs and value systems are dichotomous and logically inconsistent with their life patterns and behaviour, wholeness cannot be achieved, and their well-being may be negatively impacted [ 11 ].
As part of a slow-growing paradigm shift, the World Health Organization (WHO) expanded its definition of health “from the absence of disease and illness” to include an element of wholeness where health is defined as “a state of complete physical, mental and social well-being” [ 15 ]. However, WHO has yet to include a spiritual dimension of health [ 15 , 19 ]. In this sense, the dimension of spiritual health today remains Hippocratic in an expansionist way but not necessarily a normative feature in health, even if there is a competing shift away from the biomedical approach to health. While biomedical approaches remain strong, there is a growing re-permeation of “wholeness” in health circles: it is the helping disciplines of nursing practice and health promotion that illuminate the resurgence and need for spiritual health today [ 7 , 13 , 14 , 24 ].
Literature on spiritual health remains limited across many countries, including Canada. The most recent reviews on spiritual health were published in 2007 and 2022 and identified several gaps in spiritual health research [ 1 , 9 ]. This is exacerbated by the fact that spiritual health is a term that remains widely contested with no concrete definition. Meanwhile, the semantic connection between “religion” and “spirituality” remains ambiguous in the West and scholars hold different positions [ 24 – 26 ]. Critical to the wellness and health discussion is the discourse on “spiritual, but not religious” or “spiritual and religious.” The definition of spirituality arguably has become more elastic especially now since people no longer wish to conform to established religious structures such as churches, mosques and the like. This has important implications since Canada is considered a multicultural country whose citizens practice a variety of different religions and spiritualties and uphold diverse worldviews. Thus, a knowledge synthesis of spiritual health and spirituality (in relation to health) is invaluable.
This scoping review protocol aims to build on the previous knowledge synthesis work of Litalien et al., 2022, who conducted a systematic literature review exploring the influence of religiosity and spirituality on health across Canada [ 27 ]. While Litalien et al. focus on the influence of religiosity and spirituality on health, our scoping review specifically focuses on the relationship between spirituality and health (its influence, its conceptualization and so forth), and the implicit relationship between spirituality and religion in the context of Canada today. Furthermore, we build on Litalien et al.’s search strategy by expanding it to enhance its robustness. This scoping review protocol also aligns with previous calls to action–in health promotion and curricula–to emphasize and promote spiritual health in the Canadian context [ 18 , 19 , 28 ]. Since spiritual health is a growing term, it is intellectually reasonable to assume that research on spiritual health may not necessarily be linguistically framed in those exact words. Instead, many researchers may do work related to spiritual health, but may reciprocally relate spirituality to health [ 24 , 25 , 29 , 30 ]. Thus, this scoping review is exploratory beyond the term, “spiritual health” and explores spirituality in relation to other dimensions of health as well. Finally, this scoping review protocol heeds the call that spirituality is salient to health [ 19 , 24 ].
Scoping review objectives
The main aim of this scoping review will be to outline and describe the current landscape of spiritual health and spirituality (in relation to health) research in Canada, including the meaning and understanding behind these two concepts. Secondary aims will include determining the proportion of studies that demonstrate a link between (a) spirituality and health to religion and (b) spiritual health to religion. Based on these objectives, this scoping review will be exploratory.
A scoping review will be conducted to examine the current landscape of spirituality and spiritual health and wellness research [ 31 ]. This approach was selected because it enables a broader examination of spirituality and spiritual health, rather than concentrating on specific outcomes [ 32 ]. As a form of knowledge synthesis, conducting a scoping review will capture developments in spiritual health and spirituality research across disciplines. All in all, our aim is to gather recent research on spirituality and spiritual health, which can guide future projects in this field [ 33 ].
This scoping review is an initial preliminary step to understanding spiritual health in Canada. The results from this scoping review will inform the study design of future research projects and future work on spirituality and spiritual health across Canada. Research ethics board approval is not required since data are from publications or publicly shared reports.
Protocol design
This scoping review will adhere to Arksey and O’Malley’s methodology for scoping review [ 31 ]. Based on this methodology, there are six different stages in developing a scoping review: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) charting the data; (5) collating, summarizing, and reporting the results and (6) consulting with relevant stakeholders (which is optional according to Arksey and O’Malley). Thus, we will adhere to Arksey and O’Malley’s methodology while incorporating Levac et al.’s approach, namely, to consult with stakeholders as a knowledge translation requirement [ 34 ]. In our case, we will consult Dr. Nelly Van Doorn-Harder throughout the scoping review process. Nelly van Doorn-Harder is a scholar of religion. Presently, she is a professor at Wake Forest University (North Carolina, USA) and the Vrije Universiteit (Amsterdam, Netherlands). Her expertise in religious studies, interfaith engagement and anthropology background will inform this work and ensure that this scoping review is relevant for multiple communities [ 35 ]. To present the search findings, the Preferred Reporting Items for Systematic Reviews and Meta-Analysis will be utilized [ 36 ].
Stage 1: Identifying the research question
The research questions are:
- RQ1: What research currently exists on spirituality (in relation to health) and spiritual health in Canada?
- RQ2: How are spirituality (in relation to health) and spiritual health conceptualized and understood?
- RQ3: Does the mention of spirituality converge with the mention of religion in the context of health?
Stage 2: Identifying relevant studies— Search strategy and information sources
This stage will be characterized by an iterative process. This will comprise of reviewing the literature, refining the search strategy, and incorporating additional sources found in the reference lists of selected papers. Initial screening of titles and abstracts will precede the full-text review of chosen studies. The research team has collaboratively developed and finalized the search strategy, as well as the eligibility criteria. The study is scheduled to take place from April 2024 to August 2024.
Relevant studies for this review will be identified through a comprehensive search conducted in the following electronic databases: ProQuest Databases (including MEDLINE and APA PsychINFO), EBSCO Host Databases, Scopus, Embase, Web of Science, Anthropology Plus, and PubMed. The search strategy will involve systematically combining keywords and Boolean operators (AND/OR) across each database.
Search String 1: (spirituality or spiritual needs or spiritual care or spiritu*)
Search String 2: (Canada or Canadian or Canadians or in Canada)
Search String 3: (health or wellbeing or well being or well-being or quality of life or wellness or physical health or social health or spiritual health or intellectual health or emotional health or financial health or environmental health or occupational health or intellectual health)
Particularly for Search String 3, we ensured that it encapsulates at least eight dimensions of well-being, as per Colorado State University’s “Health Education and Prevention” information [ 37 ]. The full search strategy across all databases is provided in this protocol’s supplementary material (see S1 Table ). Search results will be saved as.ris files and imported into Covidence for study screening and data management [ 38 ].
To ensure a comprehensive literature coverage of spirituality and spiritual health in Canada is attained, a Google search will also be conducted (for the first 100 hits) to identify relevant journal articles and academic publications in line with this scoping review. To identify additional studies that are in line with this scoping review’s inclusion and exclusion criteria, forward and backward citation searches of all included publications will be conducted.
Stage 3: Study selection
The review process will involve two stages of screening: first, a review of titles and abstracts, and second, a full-text review. Two researchers (HMB and MM) will independently screen all imported citations for titles and abstracts in a double-blind manner, applying the predefined inclusion and exclusion criteria. Covidence will handle duplicate removal prior to title and abstract screening, and any remaining duplicates will be manually removed by HMB and MM. In cases of disagreement/ conflict on title and abstract inclusion, the third reviewer (MTH) will review the studies and make a final decision to exclude ineligible studies and resolve conflicts on Covidence. Studies included by both HMB and MM will proceed to full-text review. During the full-text review stage, the same two reviewers (HMB and MM) will independently screen studies against the same predefined inclusion and exclusion criteria. Any discrepancies in full-text inclusion will be reviewed by the third reviewer (MTH), who will make final decisions to exclude ineligible studies and resolve conflicts on Covidence, prior to proceeding to the data extraction phase.
Inclusion criteria
Published in the English language
Peer-reviewed journal articles
Research is focused within the Canadian context
Available electronically in full text
Current studies that mention and focus on any type of “spirituality” or “spiritual health”
Must mention some aspect of health, well-being or wellness (it could also mention an aspect antithetical to health, such as illness, distress, etc.)
All articles until the present day
Exclusion criteria
Grey literature
Printed in languages other than English
Papers without evaluation and reporting of results/ or knowledge contributions
Exclude any studies loosely tied to spirituality/health and spiritual health. For example, a study focusing on the correlates of smoking, mentioning briefly that “spiritual and social health are important.”
Stage 4: Data collection
Data extraction for study details will be organized in a charting table on an Excel spreadsheet for full-text studies, relevant forward and backward citations of full-text studies and hand searched studies. The team will employ an iterative approach through team meetings and email exchanges to review, refine and consistently update the data extraction table. Relevant variables will be extracted, including, but not limited to author(s), year of publication, journal of publication, open/ closed access, year of data collected (if applicable), methodology, findings, and knowledge contributions.
Stage 5: Data summary and synthesis of results
The search results will be reported using the Preferred Reporting Items for Systematic reviews and Meta-Analysis extension Protocols (PRISMA-P) as per PLOS ONE knowledge synthesis journal requirements (See S2 Table ) [ 39 ]. As a scoping review aims to outline key concepts and define the boundaries of a topic or field, this review will not conduct critical appraisal of the included studies [ 31 , 32 ]. Instead, this scoping review will offer a comprehensive overview of all studies that are included [ 31 , 32 ]. Data will be synthesized and summarized from our data extraction table to create a narrative report detailing available data on the following themes: (1) the extent to the relationship between spirituality and religion in Canada is intertwined/ interchangeable or disparate (i.e. may present themselves in micro discourse analysis of research and personal narratives regarding the relationship between spirituality and religion), (2) whether religion and/or spirituality contains negative connotations (i.e. public discourse, literature, historical contexts where religion or spirituality reflected social conflict, oppression or discrimination) (3) theoretical versus empirical paper, (4) the extent that spirituality been conceptualized in relation to health (i.e. theoretical models, empirical research, interventions or therapeutic approaches that integrate spirituality into healthcare settings) and (5) the context in which religion is mentioned (i.e. immigration, colonialism, religious rituals or practices observed in public spaces etc.), (6) cultural influences (i.e. indigenous perspectives, immigrant communities, geographical differences etc.) and (7) interfaith dialogue (between different religious and spiritual groups in Canada).
Stage 6: Consultation
This scoping review will be fundamentally informed and supported by faculty members and academics within religious studies, health anthropology and/or interdisciplinary health academic backgrounds. At Stage 3 of the research, researchers who actively research within these particular fields will be contacted to gain a deeper understanding of spirituality and spiritual health within the context of Canada. This will be based on authorship frequency relative to other authors in the research and Religious Studies and Health Promotion stakeholders within HMB’s network. These two critical pathways to consultation will lead to the co-interpretation and enrichment of extracted knowledge alongside HMB and MM.
Supporting information
S1 table. detailed search strategy across all selected databases for this scoping review protocol..
Detailed search strategy across all selected databases for this scoping review protocol.
https://doi.org/10.1371/journal.pone.0309294.s001
S2 Table. Completed PRISMA-P checklist for scoping review protocol.
Completed PRISMA-P checklist for scoping review protocol.
https://doi.org/10.1371/journal.pone.0309294.s002
- View Article
- PubMed/NCBI
- Google Scholar
- 12. Fisher J. W. (2009). Understanding and assessing spiritual health. In De Souza M., Francis L. J., O’Higgins-Norman J., & Scott D. (Eds.), International Handbook of Education for Spirituality , Care and Wellbeing (Vol. 3, pp. 69–88). Springer Netherlands. https://doi.org/10.1007/978-1-4020-9018-9_5 .
- 21. Williams B. (1967). René Descartes. In Edwards P. (Ed.), The encyclopedia of philosophy (Vols. 1 and 2, pp. 344–354). Macmillan.
- 37. 8 Dimensions of Well-Being | Health Education & Prevention | CSU Pueblo . (n.d.). Retrieved March 14, 2024, from https://www.csupueblo.edu/health-education-and-prevention/8-dimension-of-well-being.html .
- 38. Covidence systematic review software, Veritas Health Innovation, Melbourne Australia. www.covidence.org .

IMAGES
VIDEO
COMMENTS
Open in a separate window. First section: Description of the core center, contacts of the investigator/s, quantification of the involved centers. A research protocol must start from the definition of the coordinator of the whole study: all the details of the main investigator must be reported in the first paragraph.
The research protocol is a document that describes the background, rationale, objective (s), design, methodology, statistical considerations and organization of a clinical trial. It is a document that outlines the clinical research study plan. Furthermore, the research protocol should be designed to provide a satisfactory answer to the research ...
The protocol is the detailed plan of the study. Every research study should have a protocol, and the protocol should be written. The written protocol: • forces the investigators to clarify their thoughts and to think about all aspects of the study; • is a necessary guide if a team (not a single investigator) is working on the research;
The protocol should explicitly outline the roles and responsibilities of any funder(s) in study design, data analysis and interpretation, manuscript writing and dissemination of results. ... The spirit 2013 statement provides a useful checklist on what should be included in a research protocol . In this paper, we have explained a ...
The Research Protocol A research protocol outlines the plan for how a study is run. The study plan is developed to answer research questions. It provides evidence for feasibility of a study, detailed objectives, design, methodology, analytical/statistical considerations and how the study will be conducted and evaluated. A well-written and
Research Protocol A research protocol also known as a research proposal, study plan and/or project plan is a document which describes in detail the plan for conducting a research study. The terms study and project are often used interchangeably. A well written and comprehensive research protocol is essential for a high-quality research project. A
Protocol writing allows the researcher to review and critically evaluate the published literature on the interested topic, plan and review the project steps and serves as a guide throughout the investigation. The proposal is an inevitable document that enables the researcher to monitor the progress of the project [ 5 ].
Writing of the research protocol should precede application for ethical and regulatory approval; and the final protocol will be required upfront by ethical committees and research and development departments. The length of the research protocol will be governed by the size and nature of the study - a multicenter drug trial will clearly have a ...
A research protocol is the road map you will follow in writing a grant proposal and carrying out your research. This chapter provides a long list of elements that may be included, such as study design, safety considerations, quality assurance, and ethical outcomes. Also included in the chapter are sections on what makes a good research protocol ...
The research protocol is defined as the most important document in clinical research which helps the researchers and the scientists to understand the necessity of the study and the way of execution and completion. The protocol outlines the rationale for the study, its objective, the methodology used, and how the data will be managed and analyzed.
The aim of this guide is to help researchers write a research study protocol for an observational study. The guide will take you through each section of the protocol giving advice and examples of the information required in that section. This is a guide only and for those requiring more information on particular topics; some useful references ...
If a formal protocol does not exist, the IRB may require the UI investigator to supply one (e.g., an investigator initiated study or a complex study) The UI IRB recommends using an NIH Protocol Outline Template for Phase I, Phase II-III, or Behavioral and Social Science Research (BSSR) Involving Humans.
Adapted from World Health Organization, Recommended Format for a Research Protocol G-XXX, 2014 08 15 Page 1 of 3. Key Elements of a Research Protocol . All protocols must include the following: ... Clearly outline the statistical methods to be used, including: i. Rationale for choice of sample size (power calculation and justification).
Abstract. A research protocol is best viewed as a key to open the gates between the researcher and his/her research objectives. Each gate is defended by a gatekeeper whose role is to protect the resources and principles of a domain: the ethics committee protects participants and the underlying tenets of good practice, the postgraduate office ...
A badly written protocol can contribute substantially to approval times especially for investigator-initiated studies. The protocol provides the scientific basis for the proposed research; it defines the study objectives, the population to be studied, the procedures to be followed, the evaluations to be performed and the plan for analysis; and lastly, it discusses the administrative aspects of ...
The statement of purpose then outlines exactly what is to be studied. in the proposed study, how it is to be studied, in whom, ... A research protocol is a detailed plan of a study.
It must convey exactly what you are going to do, in whom, where, when, and how. Methods must relate directly to and only to the specific objectives of the study. In the above example, recording the birthweight of all participants and a history of TB between the ages of 6 and 9 years would address objective 1.
The Research Protocol. A research protocol outlines the plan for how a study is run. The study plan is developed to answer research questions. It provides evidence for feasibility of a study, detailed objectives, design, methodology, statistical considerations and how the study will be conducted and evaluated. A well-written and complete ...
A protocol is a detailed plan for a research study, outlining the specifics of how the research will be conducted. It is an essential document that helps to ensure research is conducted in a safe and ethical manner, and that the integrity of the research is preserved throughout the life of the study. A protocol -- or Project Description -- is a ...
A research protocol is designed to be concise and self-contained, and to summarize the core aspects of the study. Self-discipline is vital in this process, as it requires the investigator to structure the central concepts of the study and reveal particular issues that demand attention. 2 The research protocol often serves as the foundation for ...
Research Protocol Outline. Your research Protocol should discuss in detail how you plan to carry out the research, how you will analyze the data that you collect, and what you plan to do with the results. The following are points that you should address in your protocol. Introduction and Background. ¨ Provide relevant research background and ...
Protocol Templates Download Version; Descriptive Study Template: This template should only be used for for studies limited to (1) the use of existing data or specimens, (2) where the only study procedure is a retrospective chart review or use of existing biological samples and (3) where the analysis plan is limited to purely descriptive summary statistics.
The protocol of an evidence synthesis outlines the rationale, hypothesis, and methods researchers are planning to use in conducting their review (Page et. al, 2021). Protocols must be completed before the actual review is conducted, and is then used as a guide for the research team. Outlining the team's steps in the research process is not only ...
Introduction Social networks can affect health beliefs, behaviours and outcomes through various mechanisms, including social support, social influence and information diffusion. Social network analysis (SNA), an approach which emerged from the relational perspective in social theory, has been increasingly used in health research. This paper outlines the protocol for a scoping review of ...
Approval from a research ethics board is not required, nor has it been obtained, as the data is derived from journal articles and academic publications. ... In this paper, we outline our scoping review protocol to describe the current landscape of spiritual health and spirituality (in relation to health) research in Canada, including the ...