

Healthcare and Hospital Cafeteria Design Consultants
SERVING YOUR AREA
Ready to improve or build your food service operations? Contact us to talk to one of our experts right away!
or call 800-899-6604
Balancing Regulations, Labor, and Costs
Hospital kitchens and cafeterias represent some of the most demanding commercial cooking and dining spaces. Not only do they need to meet the needs of patients with restricted diets, but they must also be capable of efficiently providing a variety of menu items for staff and visitors. Hospital kitchens must also be capable of complying with strict hygienic standards.
Rapids Contract has addressed these demands and more in designing and installing hospital kitchens and cafeterias. While designing spaces, we balance regulations, labor and costs with the need for smooth workflow and service patterns. And, with our decades of experience and dedication to communication, we have forged relationships with contractors and fabricators to provide efficient installation and to elevate any kitchen or cafeteria into an attractive custom design.

Flexible, Labor-Saving Healthcare Kitchen Designs
Commercial healthcare dining has evolved to place an emphasis on labor-saving flexibility in the kitchen, ordering, and service areas. Rapids Contract’s designers know how to incorporate practical, functional time- and energy-savers into versatile spaces suited for room service orders, grab-and-go service, and dine-in visitors and staff.
Our CADD technology enables you to view your kitchen design in three dimensions well before the build begins. Our LEED-certified designer selects the best available on-demand technology that meets code and saves on costs. This includes eco scrappers, a green replacement for the commercial disposal, and other state-of-the-art appliances and lighting.
Get Ideas From Experts in The Industry
Experience with all types of facilites.

Streamlined Dine-In, Room Service, and Pick Up
For today’s hospital patients and cafeteria visitors, flexibility and flow are key to fast, convenient service. Let us show you how to streamline remote ordering for hospital room service and make it easy for visitors to find and purchase a variety of hot and cold foods. In addition, we can help you select energy-efficient equipment for display and contactless pickup save money over the long run and reduce the pressure on kitchen staff.
Project Management and Communication
One of the most important considerations in selecting a hospital kitchen design firm is how they will manage your project. At Rapids Contract, our project manager will be with you throughout the entire process. He or she will be on site during construction to coordinate with the trades, from fabricators to installers, and architects to general contractors. We take relationships with you and these key partners seriously, guiding the buildout for your hospital kitchen and cafeteria to align with your specifications, timeline, and budget.
FAQs for Healthcare Cafeterias
How long does it take to install a healthcare kitchen.
The time it takes to install a healthcare cafeteria can vary widely based on several factors, including the size of the kitchen, the complexity of the design, the type of equipment being installed, local regulations and permits, the availability of contractors and skilled labor, and the efficiency of the installation process.
In general, smaller and less complex kitchens in an existing foodservice space might take a few weeks to a couple of months to install, while larger and more intricate kitchens could take several months. Here are some key factors that can influence the installation timeline:
1. Design and Planning: The design phase can significantly impact the installation time. If the kitchen’s layout and design are well-prepared in advance, it can help streamline the installation process.
2. Equipment Selection and Availability: The type of equipment needed for the kitchen can affect the timeline. If specialized or custom equipment is required, it might take longer to source and install.
3. Permits and Regulations: Obtaining necessary permits and complying with local regulations can sometimes be a time-consuming process that impacts the installation timeline.
4. Construction and Infrastructure: If any modifications or construction work is required to accommodate the kitchen, such as plumbing, electrical, or ventilation systems, this can add to the installation time.
5. Skilled Labor and Contractors: Availability of skilled contractors, electricians, plumbers, and other professionals can influence how quickly the installation can be completed.
6. Project Management: Efficient project management can help keep the installation on track and avoid delays.
7. Unforeseen Issues: Unexpected challenges or issues that arise during installation, such as equipment malfunctions or structural problems, can extend the timeline.
8. Size and Complexity: Larger kitchens with more intricate setups, multiple workstations, and specialized equipment can naturally take longer to install.
9. Coordination and Scheduling: Coordinating the various tasks involved in the installation, such as equipment delivery, construction work, and inspections, requires careful scheduling.
It’s recommended to work closely with a firm like Rapids who has solutions engineers, designers, project managers, project coordinators, and support teams experienced in commercial kitchen installations. we can provide a more accurate estimate based on the specific details of your project and help manage the process to ensure it’s completed as efficiently as possible.
How much does a healthcare kitchen cost?
The cost of setting up a healthcare cafeteria can vary widely depending on several factors, including the size of the kitchen, the type of cuisine you’ll be preparing, the quality of equipment and materials you choose, location, and local regulations. Here are some of the major cost considerations:
1. Location: The cost of commercial real estate can vary greatly based on the region, city, and neighborhood where you plan to set up your kitchen.
2. Size and Layout: The overall square footage and layout of the kitchen will impact costs. A larger kitchen will require more equipment, materials, and space planning.
3. Equipment: The cost of commercial kitchen equipment varies based on the type and brand. High-quality, specialized equipment can be more expensive. Equipment includes ovens, stoves, refrigerators, freezers, fryers, grills, ventilation systems, dishwashers, and more.
4. Ventilation and Exhaust Systems: Proper ventilation and exhaust systems are crucial for a commercial kitchen to ensure air quality and safety. These systems can be a significant cost factor.
5. Utilities and Infrastructure: Costs associated with plumbing, electrical work, and gas lines installation or modifications need to be considered.
6. Construction and Renovation: If you’re building or renovating a space to accommodate the kitchen, construction costs can vary based on the extent of the work required.
7. Permits and Regulatory Compliance: Obtaining permits and complying with health and safety regulations may incur fees.
8. Interior Design and Finishes: The quality of finishes, such as flooring, countertops, and wall coverings, can impact costs.
9. Furniture and Fixtures: If you’re setting up a restaurant or eatery within the kitchen space, the cost of furniture and fixtures for the dining area should also be considered.
10. Labor Costs: Labor costs include not only the salaries of kitchen staff but also costs for installation, construction, and any specialized services needed.
11. Contingency: It’s wise to budget for unexpected costs that may arise during the setup process.
Due to the many variables involved, it’s challenging to provide an exact figure. However, to give you a rough idea, setting up a basic small-scale commercial kitchen could start around $50,000 to $100,000. Larger, more complex kitchens with high-end equipment and finishes could cost several hundred thousand dollars or even more.
To get a more accurate estimate for your specific situation, it’s recommended to consult with our commercial kitchen design and construction professionals. We can assess your needs, provide cost breakdowns, and help you plan a budget that aligns with your goals.
What layout options are available when designing a healthcare kitchen?
When designing a healthcare cafeteria, the layout should prioritize efficiency, speed, and safety. There are several layout options to consider, each with its own advantages depending on the size of the space, the menu, and the workflow. Here are some common layout options:
1. Assembly Line or Linear Layout: This layout resembles an assembly line, with different stations for each step of the food preparation process. It’s ideal for fast food chains with a limited menu of items that can be prepared quickly. The workflow progresses in a linear fashion, from order taking to food assembly.
2. U-Shaped Layout: A U-shaped layout places the cooking equipment and prep stations along the three sides of a U shape, with the middle left open for movement. This allows cooks to access equipment and ingredients without having to cross paths frequently.
3. L-Shaped Layout: In an L-shaped layout, the kitchen equipment and workstations are arranged along two adjacent walls in an L configuration. This can be effective for smaller spaces and helps streamline the workflow between cooking and preparation areas.
4. Island Layout: An island layout positions equipment and stations in the center of the kitchen, allowing cooks to access equipment from all sides. It’s suitable for larger kitchens with ample space and can provide a more flexible workflow.
5. Zoned Layout: This layout divides the kitchen into distinct zones, each dedicated to a specific task such as cooking, preparation, dishwashing, and storage. It’s efficient for larger kitchens and helps prevent congestion by keeping different tasks separate.
6. Open Kitchen Layout: An open kitchen layout allows customers to see the food preparation process, which can add transparency and a sense of freshness. This layout requires careful organization to maintain a clean and presentable appearance.
7. Parallel Layout: In a parallel layout, equipment and stations are placed along two parallel lines. This is useful for kitchens with a linear workflow, where tasks progress from one end to the other.
8. Zone and Flow Layout: This layout combines zoned areas with a logical flow of food preparation. It ensures that tasks progress smoothly and avoids unnecessary backtracking.
9. Hybrid Layout: Depending on the specific needs of your restaurant, a combination of different layouts can be used to optimize space and workflow. For example, a U-shaped layout for cooking and an assembly line for order preparation.
Remember that the layout should be tailored to your restaurant’s unique requirements, menu items, and anticipated customer flow. It’s important to consider factors like the placement of cooking equipment, prep stations, serving areas, and storage to create a seamless and efficient kitchen environment. Consulting with Rapids’ professional kitchen designers and solutions engineers can help you make informed decisions and create a layout that maximizes productivity and safety.
Where do you get your supplies from?
You can obtain foodservice equipment and supplies from various sources, both online and offline. Here are some common options:
Online Retailers: There are numerous online retailers that specialize in selling foodservice equipment and supplies but clearly Rapids Wholesale’s Webstore is the best in the business! In fact, over 75% of the K-12 school systems in our home state utilize our website for ordering equipment and smallwares. We work neighboring state school buying groups and independent schools as well! Our team can prepare a “market basket” of items your school uses most and provide negotiated discount pricing on those items! Reach out to find out more!
Restaurant Supply Stores: These are specialized stores that offer a wide range of commercial kitchen equipment and supplies. You can find everything from cooking appliances to utensils, furniture, and cleaning supplies. Rapids currently has Restaurant Supply Store locations in St. Paul, MN and Marion, IA.
Wholesale Distributors: Some distributors cater specifically to businesses in the food industry. They often offer bulk purchasing options and may have discounts for larger orders. Rapids Account Management Team is standing by to assist.
When sourcing foodservice equipment and supplies, consider factors like price, quality, warranty, and customer reviews. Compare options from different sources to make informed decisions that align with your budget and needs. Additionally, be aware of any local regulations or codes that might affect the type of equipment you can use in your commercial kitchen.

Previous Work – University of Iowa Stead Family Children’s Hospital
When the University of Iowa Stead Family Children’s Hospital envisioned their cafe, they saw a welcoming environment that was not only easily able to handle the flow of patients and their families, but could also offer a number of meal options.
Rapids helped bring the plan to fruition using our cafeteria and kitchen design services, as well as our equipment and smallwares fulfillment program. Our dedicated team worked on both the cafeteria and the Level 12 kitchenette, ensuring both had the same high-end look and quality materials – including equipment that is all run on electric power.
LET'S FIND YOUR SOLUTION
Rapids Contract serves the United States with locations in Iowa, Minnesota, and Missouri!
Get in touch with one of our experts and let us know how we can help with any of your foodservice needs.
Talk to one of our experts right away and get immediate assistance. We are open Mon - Fri, 8am - 5pm CST.

How Hospital Food Service Can Improve Patient Experiences And Outcomes
Food is fundamental to the human experience, and that’s doubly true for the patient experience
By Michael Tolliver / Special to Healthcare Facilities Today
Hospital meatloaf and pudding jokes never seem to go away, do they? If today’s patients still expect hospital food “isn’t going to be that great,” as Press Ganey has found [1] , maybe there’s something to the staying power of hospital food jokes. Maybe they’re proof of an ever-fresh opportunity to emotionally connect with patients.
On the other hand, hospitals have a lot to prioritize when it comes to the patient experience, so why should food take so much focus? HCAHPS may not ask directly about food, but studies show food service quality contributes to overall satisfaction of a hospital stay, not to mention patient recovery. [2]
That interdependence of food service and patient experience makes sense. Food doesn’t poke or prod a patient. It offers a comforting choice. A menu is much easier to understand than treatment options, and ordering food is the chance to make a positive decision for yourself.
Delivering on that promise of a positive outcome is the goal of great food service. Food is fundamental to the human experience, and that’s doubly true for the patient experience, since nutrition is key to patient health. Almost half of all deaths attributed to heart disease, stroke, and Type 2 diabetes are linked to poor diet. [3]
So how are hospitals helping patients learn about long-term nutritional health? How are they making the most of that opportunity to connect with patients through food? And how are they making sure it benefits the bottom line and sticks with patients, improving outcomes? Here’s a specially prepared selection of choice strategies, so let’s dig in.
Stealth health
The general trend toward health-conscious consumption does put pressure on menu creation, but for many patients (along with their stressed family and friends), healthy options can’t compete with the desire for comfort food. Giving people what they want is usually a hallmark of great service, but hospitals have a clear interest in reducing the risk of readmission, and that means meeting nutritional standards that contribute to recovery.
But as parents and nurses know, providing healthy food doesn’t guarantee it’ll be eaten. More than half of patients leave half or more of their meals uneaten, according to a 2019 study. The same study also noted that diminished nutritional intake delayed recovery and increased risk of complications. [4]
People want French fries. Instead of taking choices away and increasing the chance that patients order something they don’t really want (and don’t end up eating), the “stealth health” strategy make fries, burgers, and comfort food like mac and cheese healthier. A lot of hospitals no longer deep fry, for instance, but the most successful “stealth health” strategies focus on the positive. An enhanced flavor model makes palatable options healthier, and healthy options more palatable.
The key to a successfully implemented enhanced flavor profile is finding ways to efficiently produce on demand at scale. Prioritizing healthy food and patient choice means being smart about costs. With nutritional needs in hand and creative chefs on board, menu plans need to take sourcing and logistics into account. Great food service teams apply clear metrics and analytics to find the efficiency and cost savings needed to keep quality food affordable.
Choosy patients choose information
There’s also expectation management for dietary restrictions, and the importance of having information at hand for patients and guests who want to make more informed choices. Informative labels are just the first step. Information technology is the next one. Access to menus online helps everyone compare choices for themselves. The best systems prioritize user access to up-to-date menu information, and speed the user experience with tools that sort for vegetarian, diabetic, or other key factors and restrictions (such as salt and fat content, or allergens).
Many hospitals are finding the personal touch does wonders. When a dietitian sits with a patient and talks through their needs and wants, that’s both a service win and a healthcare win. Low salt and less grease may taste different, but with an enhanced flavor profile, change doesn’t have to be bad. Setting expectations helps patients focus on the positive, instead of what’s missing. Following up the in-person attention with in-room touch menus or online access enables choice and showcases the quality menu planners work so hard to provide.
Here’s where quality food really shines. What the dietitian helps patients learn, the food helps them accept, with tasty options and great service.
Room service Is the way
Anyone can order almost anything from a smartphone. Patients of every age bracket want to order what they want when they want it, and hospital food is no exception. Instead of sending up trays of unordered food that staff will have to throw away later, a room service model gives patients choice.
The benefits of the room service model are clear. Less than half as much wasted food (29% waste with a traditional model against 12% for the room service model) means patients are getting significantly better nutrition. Moving Press Ganey scores from 64 th to 95 th for “quality of food” is also a pretty powerful indicator of the impact on patient experience. [5]
If “hotel-style” room service sounds like it’s more expensive to run, think about this: the benefits in the study above also came with a 15% decrease in patient meal costs. The increased costs of room service turn out to be mainly start-up costs in equipment, software and training. [6]
Once those initial costs are dealt with (or, perhaps better for the hospital, avoided by bringing on a service partner with technical scope and labor expertise already in place), food costs can be reduced by room service models by reducing stock and inventory and eliminating overproduction. [7]
Retail, retail, retail
If the patients are getting room service, how does the retail cafeteria impact the patient experience? Family members eat there. Nurses and staff eat there. Improved employee engagement scores are a clear chance to increase your HCAHPS top box scores: 85% of engaged hospital employees demonstrate a genuinely caring attitude with patients as opposed to only 38% of disengaged employees. [8] But when the cafeteria is terrible, people will say so, out loud, a lot. That impression sticks in the mind of patients and can color lots of other judgements. And let’s be honest, family members often fill out surveys for patients. If they had a bad experience in the retail area, they might overlook how great the room service was for the patient.
Rising food costs and budget cuts may be squeezing the bottom line, but the retail portion of hospital food service is a chance to put all that meal planning, logistics, and service to work increasing retail revenues. On-demand dishes and healthier options, alongside amenities like coffee kiosks and food carts, keep everyone satisfied.
Retail is the chance to capitalize more on all the logistics work you’re doing to locally source ingredients, cook from fresh, and enhance flavors for patients. Now you can replace that tired cafeteria experience, and deliver that café, bistro, or restaurant feel that draws people in and delivers.
In some locations, a hospital can become a true dining destination for the greater community. Especially if the community lacks healthier, affordable options, hospital dining can be a boon to seniors and other community members looking to improve eating habits. Hospitals can increase their draw by promoting their tasty, healthy menu for community groups.
Hospitals with great retail programs can often offer nutritious food to at-risk groups at prices lower than local restaurants, without having to subsidize meals. Outreach programs like this both serve the community and create efficiency by generating revenue when staff may normally be underutilized.
The real trend is production management
There’s lots of trends to spot. Authentic foods from across the cultural spectrum, celebrity chef recipes, even setting up gardens on-site to grow their own produce – there are a lot of great ideas out there. They all come with their own stumbling blocks and start-up costs. Making sure that innovative, expanded menu options work for your hospital and your patients takes production expertise. Great ideas must be adapted for the healthcare environment and made efficient with flexible, intelligent production management.
For instance, farmer’s markets and local sourcing still have to meet regulations and strict processes, like chain of custody (recording who has what to help ensure quality control). And when a menu relies on a certain ingredient, great production teams know how to adapt or shift menu strategies when it’s not available. Keeping taste and quality high while working with the reality on the ground efficiently puts the patient experience first.
And for dessert…
Hating hospital food may be as American as apple pie, but savvy hospital directors know that lower expectation is an opportunity to exceed it. Where hospitals used to subsidize food, including huge discounts for employees to eat there, rising costs of food and food preparation have put that model to bed. When it comes to the bottom line, everything can look like a cost center, but food service done well can be a revenue generator.
Driving patient satisfaction and reducing readmissions are a tall order for any department. The right menu, the right food sourcing, the right service model, every element takes planning, resources, and commitment to implement efficiently. The right partner is ready to dump legacy caterer worries and woes and bring innovation and excitement to the table.
Michael V. Tolliver is Vice President Healthcare Operations at ABM .
October 5, 2020
Topic Area: Food Service
Recent Posts
Hais are worse than you thought.
No standards exist requiring a hospital room to be free of bacteria or viruses in sufficient numbers to cause an infection.
Ground Broken on New El Paso VA Health Care Center
The healthcare facility is anticipated to be completed in 2028.
Authorities Issue Joint Advisory on RansomHub Ransomware
RansomHub has impacted at least 210 organizations across critical infrastructure sectors, including healthcare.
9 Steps to a Successful Healthcare Capital Project
Navigating the future of the healthcare industry can be challenging, but prioritizing these key drivers for healthcare capital projects can help senior leaders make future-proof choices.
Steward Health Care to Sell Wadley Regional Medical Center in Texarkana
The facility is being sold to CHRISTUS Health.
News & Updates | Webcast Alerts Building Technologies | & More!
All fields are required. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

- Awards + Events
- Architecture
- Interior Design
- Construction and Engineering
Operations and Facility Management
- Research and Theory
- Perspectives
- White Papers
- Ambulatory Care / Clinics
- Behavioral Health
- Cancer Care
- Emergency / Urgent Care
- Specialty Projects
- Landscaping / Exteriors
- FEATURED FIRMS
- Healthcare Design Showcase
- Breaking Through
- Remodel/Renovation Competition
- The HCD 10: Celebrating Healthcare Design Leaders
- HCD Product Innovation Awards
- HCD Conference + Expo
- Nightingale Awards
- Rising Star Competition
- HCD Webinar Schedule
- Furniture and Casegoods
- Building Products
- Ceiling and Wall Systems
- Infection Control
Good Taste: Designing Healthcare Dining Spaces
As competition surges among healthcare providers, delivering positive experiences for patients is inspiring projects that breathe new life into care spaces. But simultaneously, organizations are turning their attention to areas of the hospital that likewise improve staff and family satisfaction, and few spaces hold the potential to achieve this that the cafeteria does.
“The dining room in the hospital may not be a great source of revenue, but it does serve as an integral cog in the overall well-being and quality of the hospital services,” explains Yi Belanger, designer at Add Inc. , which is now with Stantec (Miami). “Patient and family member satisfaction ratings greatly rely on the overall experience of their hospital stay, and oftentimes, it means the hospital’s overall accommodations and service, including their dining space.”
On the flip side, hospitals with outdated dining facilities may suffer from perception coloring reality, leading patients and families to erroneously believe that the hospital itself is outdated.
A vast departure from the traditional single cafeteria line with limited food options and hours of operation, today’s hospital dining areas are designed as comfortable, hospitality-inspired spaces customized for the user experience. Embraced by staff and patient families, these spaces are viewed as a welcome amenity, particularly for those spending extended periods of time in the hospital.
Efficiency and flow To start, hospitals across the country are attempting to rectify the long-standing inefficiencies in cafeteria flow and service. Traditionally set up based on a lengthy serving line, entry and exit points were often unclear, and wandering patrons commonly threw a wrench in circulation.
To ensure a new space achieves optimal flow and space efficiencies, both in the serving/dining zones and back-of-house areas, Belanger says her team typically interviews the administrative, clinical, and kitchen staff to develop an understanding of workflow patterns in existing dining areas. Based on those conversations, the optimal amount of seating and square footage needed for circulation, serving, and egress emerges.
Another noted trend is breaking up the traditional food service line into multiple stations with varied food offerings: for example, a salad bar, prepackaged to-go meals, sandwich station, and condiment stands. “Signage can be used to effectively guide visitors, but the design team must create a flow that allows guests to visualize the menu offerings, traverse to the desired offering stations, and pay and exit from a controlled space in a minimal time frame. The design must also maximize the number of transactions within a specified time frame,” says David N. Moon, principal of Moon Mayoras Architects (San Diego).
Strategic seating When it comes to seating arrangements, the key is variety, incorporating options like a bar with stools, larger tables, smaller booths, and outdoor seating, if possible. “I like to create zones in these spaces for serving, dining, lounging, and personal space,” Belanger says. “These spaces can be equipped with movable furniture and modular systems that can be transformed for different functions during work hours and afterwards.”
Cindy Elkin, interior designer at RLF (Orlando), says that seating should support a variety of dining experiences and levels of social interaction. “To distinguish between these areas, we establish a flow of spaces and look at how we can manipulate the ceiling planes, wall boundaries, and seating heights to create spaces that are immediately identifiable as more intimate quiet areas or on-demand, energizing spaces,” she says.
For example, Kalloor recommends half-height walls to partition off small groupings of tables so that the numerous dining seats can be zoned into small compartments. These walls can also double as a barrier to shield these more private seating areas from traffic flow. “Patterned or colorful acrylic panels can also be used to serve as a vertical screen that helps to divide and organize space without the visual weight of a full wall,” she says.
To customize the space to specific user groups, Belanger recommends booth seating for the comfort and privacy of families, and unfixed tables and chairs in small and large clusters to support staff. Although preferences will vary from hospital to hospital, institutions generally require separate dining areas for doctors to support events like staff presentations, physician case studies, and educational programs often occurring during lunchtime. Some institutions may also require private areas for VIPs, such as hospital benefactors, foreign dignitaries, or celebrities.
Mastering materials As for how healthcare dining areas are being reimagined from an interiors perspective, the options for finishes are endless. “Dining spaces within a healthcare setting are the one place where designers can take more design risks,” says Margi Kaminski, senior associate vice president at RTKL (Chicago).
The materials palette can be much broader than that generally used in other healthcare spaces and may include accents such as high-gloss wall tiles in bold colors or patterned resin panels and textured glass. Kaminski also considers furnishings like sculptured chairs or decorative lighting for dining projects.
However, because dining spaces are housed within a high-use setting, designers must be “extra clever and creative in our material selections,” says Belanger, with furnishings and finishes specified that are durable and easily cleaned. “You want to create a space that performs like a high school cafeteria but looks more like a restaurant,” says Chris Youssef, an associate at Perkins Eastman (New York), “so mosaic tiles, glass, and wood laminates are the go-to materials that will give warmth, durability, and a higher-end look.”
Meanwhile, Belanger likes to introduce a lot of soft fabrics ingrained with stain-resistant properties and that fight wear and tear. Elkin adds visual interest to seating areas through texture, using rough and smooth surfaces to provide a backdrop while still maintaining cleanability and durability.
Kalloor turns to natural materials—in moderation—to finish a space. “While many natural materials may not be suitable for healthcare dining environments due to durability or sterility, when used selectively, they can add a lot of impact.” For instance, ceilings are a good place to incorporate the richness and beauty of wood, while natural stone tiles or glass mosaics can be integrated into the design in small doses and still deliver high design impact.
Another strategy, Kalloor says, is to use synthetic materials that mimic natural materials, colors, and patterns. “Examples include resilient flooring with a natural stone or wood look, engineered surface materials such as quartz or solid surface with visuals that imitate natural stone, and protective wall panels that are treated with a top layer that has an organic texture or wood panel appearance,” she says.
For flooring, Elkin recommends a balance of hard and soft flooring surfaces to create boundaries between different seating clusters and service areas. For example, hard-surface flooring, such as porcelain tiles, are typically installed in high-traffic circulation zones and at food service transition areas. Hard-surface flooring with minimal seams also minimizes crevices that may harbor dirt and germs. Poured composite floors like terrazzo o ffer can high-end visual appeal and come in a large variety of colors, visual textures, and custom patterns.
Up above An inherent piece of any dining space is all of the equipment required to operate, but one design trick is to shift attention elsewhere—specifically, up. “Designers use ceiling treatments as an opportunity to create interest and draw the eye up and away from the equipment in the serving areas and away from the cluster of chairs and tables in the dining room,” Kaminski says.
Kalloor adds that thoughtful ceiling design comes with even more benefits: “Ceiling treatments allow a large space to be visually compartmentalized into zones, they contribute the most to the acoustical quality within the space, and they tend be the only plane in the room that does not contain a lot of visual clutter.”
Belanger prefers gypsum ceilings in smaller dining and lounge spaces to create an upscale look, but in most applications specifies a smooth-finished acoustic ceiling tile. In place of standard 2-by-2-inch tiles, Kaminski recommends large-format, 48- by-48-inch options to create a more modern look. Barbara Bouza, managing director and principal at Gensler (Los Angeles), adds that high-performance mineral fiber and fiberglass materials will meet washability, noise level, anti-mold, and antibacterial requirements.
Let light in Lighting is another area where designers can boost the aesthetics of healthcare dining spaces. Whether it’s recessed down lights, decorative pendants, wall washers, rope lights, or indirect accent lights, there are plenty of options to help set the desired tone. For example, Kaminski says, “Mini-pendants over serving areas add a bit of fun, whereas clusters of drum fixtures in the dining area draw the eye upward to create a focal point above the sea of tables and chairs.”
Another trend Belanger sees is hospitals embracing LED lighting. “They understand that the initial cost is higher, but they save on the lifecycle cost almost immediately by reducing the frequency of maintenance calls to replace these fixtures,” she says. “I always like to give them direct/indirect LED fixtures with no more than 3500K for their general light over the food service and back-of-house areas,” she continues. Essentially, 3500K lighting provides a soft, warm light, whereas 4000K or higher takes on a more clinical/institutional look. With the softer light, a more restaurant-like environment is created.
“In the dining areas, I use recessed LED ‘high hats’ controlled by dimmers for different functions, ambience, and mood. LED decorative sconces and/or pendants make a world of difference in creating drama and appeal in a healthcare dining space. It also takes away the institutional look and makes the space feel like a restaurant,” she adds.
Of course, daylighting is also a desirable feature, driven by both newer energy code requirements and user preferences. “Allowing for daylight is key as this space is primarily used by hospital staff who are working in windowless spaces for much of the day,” Kalloor says. “If possible, the dining room should be designed along at least one exterior wall within the facility so that windows can stream light into the space.” Kalloor also recommends clerestory windows and skylights, in addition to conducting sunlight studies to optimize glazing placement and minimize glare.
Take out Moving forward, designers can anticipate that hospitals will continue prioritizing their dining areas, particularly given the elevated role that patient families are now playing in the healthcare process.
“With shortages in healthcare staff, specifically nursing, the family plays an important role in the caregiving experience and spends more time than ever in the hospital environment,” Bouza says. “These spaces offer visitors a welcome environment more conducive to working, having coffee, or even a small family meeting. A great dining space makes good business sense.”
Barbara Horwitz-Bennett is a contributing editor for Healthcare Design . She can be reached at [email protected] .
SIDEBAR : Back-of-house basics
Offering a take-away list of back-of-house best practices, food service consultant Richard Dieli of Dieli Murawka Howe (San Diego), suggests the following:
• Provide kitchen and ancillary spaces space for movement and storage of carts and mobile equipment in a safe and sanitary location.
• Provide more refrigeration than one thinks will be needed.
• Create a flow within the kitchen spaces that minimizes employee and mobile equipment cross traffic.
• Create a flow that allows easy access to refrigeration and storage for employees from all production areas.
• Install hand sinks in all production areas to promote food safety and reinforce a safe and sanitary work environment.
• Stay focused on utility costs. Utility and water usage are both deleterious to the environment and have a negative impact on the hospital’s bottom line.
• Optimize natural light. A pleasant work environment makes a healthier and happy employee, which in turn, will positively affect production.
Latest Operations and Facility Management

The HCD 10: UW Health, Outstanding Organization

The HCD 10: Tom Sorrell, Team MVP

The HCD 10: Stacey Johnson, Owner/Provider

The HCD 10: Deanne Avery, Facility Manager
Quality and standards of hospital food service; a critical analysis and suggestions for improvements
- September 2017
- Galle Medical Journal 22(2)

- Base Hospital Udugama

- University of Ruhuna
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Beraat Dener

- Hilal Betül Altintaş Başar

- Siti Hazimah Nor'hisham
- Nur Syazwani Mazlan
- Heng Chin Yee

- Mohd Shazali

- Amany M. Abdelhafez
- Lina Al Qurashi
- Reem Al Ziyadi
- Haneen Mograbi

- Vanessa A Theurer
- Andrew Fallon

- Mary Hannan-Jones

- J AM DIET ASSOC
- Patricia A. O'Hara
- Dan W. Harper
- Maris Kangas
- Nicole Lemire
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

Step-by-Step Guide to Crafting a Business Plan for a Hospital

Get Full Bundle
| $169$99 | $59$39 | $39$29 | $15$9 | $25$15 | $15$9 | $15$9 | $15$9 | $19 |
Welcome to our blog post on how to write a business plan for a hospital! In today's rapidly growing healthcare industry, starting a hospital that focuses on providing quality, personalized medical services is a promising venture. According to recent statistics, the global healthcare market is projected to reach a value of $12.3 trillion by 2026, with a compound annual growth rate of 6.7%. This presents a great opportunity for entrepreneurs looking to make a difference in the lives of patients and contribute to the advancement of healthcare technology.
Before diving into the details of writing a business plan for your hospital, it's crucial to identify the market need and demand for this type of healthcare facility. Conducting a thorough market research will help you understand the current trends and assess the potential demand for specialized medical services. By analyzing competition and industry trends, you can gain insights into successful strategies and differentiate your hospital from others.
Developing a solid financial plan is essential for securing funding and partnerships. It involves outlining the hospital's projected revenue, expenses, and investment requirements. By preparing a comprehensive financial plan, you can demonstrate the viability and profitability of your venture to potential investors or lenders.
Defining the hospital's vision, mission, and values sets the foundation for its overall purpose. This helps in establishing a clear direction and guiding the decision-making process. Creating an organizational structure and identifying key roles ensures smooth operations and effective management of resources.
Formulating a comprehensive marketing strategy is crucial for attracting patients and building strong referral networks. It involves defining your target audience, identifying the best channels to reach them, and creating compelling messaging that highlights the unique benefits of your hospital.
Lastly, assessing the legal and regulatory requirements is vital to ensure compliance with healthcare laws and regulations. This includes obtaining the necessary licenses, permits, and certifications to operate your hospital.
By following these nine steps, you will be well-equipped to write a comprehensive business plan for your hospital. Stay tuned for our upcoming blog posts, where we will dive deeper into each step to provide you with practical insights and actionable tips.
Identify The Market Need And Demand
One of the first and most crucial steps in writing a business plan for a hospital is to identify the market need and demand for the services you intend to provide. Understanding the needs and preferences of potential patients is essential for developing a successful hospital that can effectively meet their healthcare requirements.
To gather this important information, conducting a thorough market research is key. This research should focus on the local healthcare landscape, demographics, and the specific services and medical treatments currently available in the area. By analyzing this data, you can identify any gaps or unmet needs in the market that your hospital can fulfill.
During the market research process, it is also important to evaluate the demographic trends and population dynamics in the area. Understanding factors such as age distribution, income levels, and prevalent medical conditions can help you tailor your services to the specific needs of the target population.
By thoroughly understanding the market need and demand for your hospital's services, you can develop a business plan that is aligned with the needs of the community you aim to serve. This will help ensure the success and sustainability of your hospital in the long run.
| Hospital Financial Model Get Template |
Conducting a Thorough Market Research
Conducting thorough market research is an essential step in developing a business plan for a hospital. This research will help you gain a clear understanding of the market need and demand, enabling you to make informed decisions about your hospital's offerings and target audience.
When conducting market research for a hospital, consider the following:
- Identify your target market: Determine the specific demographic and geographic characteristics of the population you intend to serve. This will help you tailor your services and marketing efforts accordingly.
- Analyze market trends: Stay updated with the latest trends in the healthcare industry. Identify emerging technologies, treatments, and practices that can distinguish your hospital from the competition.
- Assess competition: Study your competitors' offerings, pricing strategies, and marketing tactics. This will allow you to identify gaps in the market and position your hospital uniquely.
- Explore patient preferences: Understand what patients value when it comes to healthcare services. Conduct surveys or interviews to gather insights on their preferences, expectations, and experiences with existing healthcare providers.
- Evaluate regulatory factors: Familiarize yourself with the legal and regulatory requirements applicable to hospitals in your region. This includes licensing, documentation, and compliance with healthcare regulations.
Tips for Conducting Market Research for a Hospital
- Utilize online resources: Make use of online databases, industry reports, and market research tools to gather data on healthcare trends, market size, and consumer behavior.
- Engage with industry experts: Seek guidance from healthcare professionals, consultants, and experts who have in-depth knowledge of the industry. Their insights can provide valuable guidance during the research process.
- Consider qualitative and quantitative research: Combine qualitative methods like interviews and focus groups with quantitative techniques such as surveys and data analysis. This will provide a comprehensive understanding of your target market.
- Continuously update your research: Regularly review and update your market research to stay on top of industry developments and changing market dynamics. This will help you adapt your business plan accordingly.
By conducting thorough market research, you will be equipped with the necessary information to develop a business plan that aligns with the needs and expectations of your target market. This research will serve as a foundation for making informed decisions and ultimately contributing to the success of your hospital.
Analyze Competition And Industry Trends
One crucial step in developing a successful business plan for a hospital is to thoroughly analyze the competition and industry trends. This analysis provides valuable insights into the current market and helps identify opportunities and potential challenges that the hospital may face. Below are some important points to consider during this analysis:
Identify competitors: Begin by identifying existing hospitals and medical facilities that may be direct competitors. Research their offerings, facility size, capacity, and reputation within the community. Understanding their strengths and weaknesses will help you position your hospital effectively.
Study industry trends: Stay up-to-date with the latest trends in the healthcare industry. Identify key innovations, advancements in medical technology, and emerging treatments or services that could impact the hospital's success. This will help you adapt and stand out in a rapidly evolving industry.
Analyze market demand: Evaluate the current and projected demand for healthcare services in the target area. Consider factors such as population growth, demographic trends, and the prevalence of specific medical conditions. Understanding market demand will help in planning the hospital's service offerings and staffing requirements.
Evaluate competitive advantages: Identify what sets your hospital apart from the competition. This could include specialized services, unique treatment approaches, advanced technology, or a focus on personalized patient care. Highlighting these competitive advantages in your business plan will attract potential patients and investors.
- Use online resources, industry publications, and professional networks to gather information on competitors and industry trends.
- Engage with healthcare professionals, potential patients, and community members to gain insights into their expectations and preferences.
- Consider conducting surveys or focus groups to gather more specific feedback and opinions on the market and competition.
- Regularly revisit and update the analysis of competition and industry trends to stay ahead of the curve and maintain a competitive edge.
Develop A Solid Financial Plan
A solid financial plan is crucial for the success of any business, including a hospital. It provides a roadmap for achieving financial stability and sustainability. Here are some important steps to take when developing a solid financial plan for a hospital:
- Estimate costs and revenue: Start by estimating the costs involved in setting up and running the hospital. This includes expenses such as equipment, facility construction or lease, staff salaries, operational costs, and marketing expenses. Additionally, analyze the expected revenue sources, such as patient fees, insurance reimbursements, and potential partnerships or collaborations.
- Financial projections: Utilize the market research and competition analysis to make informed financial projections. This will include forecasting the number of patients, expected reimbursement rates, and expected revenue growth over a specific period of time. Be sure to consider factors such as seasonality, demand fluctuations, and potential economic changes.
- Budget allocation: Once you have estimated costs and revenue and made financial projections, prioritize how you will allocate your budget. Consider allocating resources for essential needs such as medical equipment, technology, employee training, marketing, and community outreach programs. Create a detailed budget plan that includes both recurrent and capital expenses.
Tips for developing a solid financial plan:
- Consult with financial advisors or experts in the healthcare industry to ensure accuracy and validity of financial projections.
- Consider different funding sources, such as private investors, loans, grants, or public funding programs specifically targeting healthcare projects.
- Account for contingency funds to handle unexpected expenses or emergencies.
- Regularly revisit and update your financial plan to reflect changing market conditions, trends, and regulatory requirements.
Developing a solid financial plan requires a thorough understanding of the healthcare industry, market dynamics, and financial management principles. It's essential to invest time and effort into this step to lay a strong foundation for the hospital's financial success.
Secure Funding and Partnerships
Once you have developed a solid financial plan, the next crucial step in starting a hospital is securing funding and building partnerships. This stage is vitally important as it determines the financial stability and sustainability of your hospital.
1. Identify potential funding sources: Start by exploring various funding options available to you. This may include approaching investors, applying for grants and loans, or seeking partnerships with other organizations. Assess the pros and cons of each option to determine the best fit for your hospital.
- Prepare a comprehensive business plan and financial projections to convince potential investors or lenders of your hospital's viability.
- Consider partnering with organizations that share a similar mission and vision to leverage their expertise, resources, and infrastructure.
2. Craft a compelling funding proposal: Develop a persuasive funding proposal that clearly outlines your hospital's mission, goals, financial needs, and potential benefits for investors or partners. Emphasize the unique value proposition and the impact your hospital can make in the healthcare industry.
3. Build strategic partnerships: Collaborate with other healthcare organizations, research institutions, or technology companies to access resources, expertise, and specialized services. Look for complementary strengths that align with your hospital's vision and objectives.
- Network within the healthcare industry to build connections and explore potential partnership opportunities.
- Consider joining professional associations or attending industry conferences to connect with potential partners.
4. Establish trust and credibility: Demonstrate your hospital's potential by showcasing the qualifications and expertise of your team, highlighting successful case studies, or sharing testimonials from satisfied patients or partners. Establishing credibility is crucial to attract investments and create fruitful partnerships.
5. Think beyond financial support: While securing funding is a primary concern, also consider the value that partners can bring beyond monetary contributions. Look for partners who can offer strategic guidance, business acumen, or access to a broader network of healthcare professionals and resources.
6. Seek legal and financial advice: Consult legal and financial experts to ensure that your funding and partnership agreements are robust and legally sound. They can assist in negotiating favorable terms and protecting your hospital's interests.
By carefully navigating the funding and partnership landscape, you can secure the necessary resources and allies to propel your hospital towards success. Remember, building strong partnerships is not just about financial support but also finding collaborative opportunities that align with your hospital's vision and values.
Define The Hospital's Vision, Mission, And Values
Defining the vision, mission, and values of your hospital is crucial for establishing its identity and guiding its direction. These elements serve as the foundation for your organization and shape its culture, goals, and strategies.
When crafting the vision statement , consider the long-term aspirations and purpose of your hospital. It should succinctly describe the desired future state and the impact you aim to make in the community. This statement should inspire and motivate both your staff and patients.
The mission statement clarifies the fundamental purpose and reason for the existence of your hospital. It outlines the primary services you will provide and the target population you aim to serve. This statement should be concise and clearly communicate the value you intend to deliver.
The values of your hospital outline the guiding principles and beliefs that underpin your organization's culture and conduct. These principles should align with the overall mission and vision. They provide a framework for decision-making, as well as help ensure consistency in providing patient care.
Tips for Defining Your Hospital's Vision, Mission, and Values:
- Involve key stakeholders, including staff, patients, and community members, in the process to gain diverse perspectives and foster a sense of ownership.
- Keep your statements concise and easily understandable to ensure clarity and coherence.
- Ensure that your vision, mission, and values are in line with the market need identified and the unique value proposition of your hospital.
- Regularly revisit and refine your vision, mission, and values to adapt to changes in the healthcare landscape and the evolving needs of your patients.
By clearly defining your hospital's vision, mission, and values, you establish a strong foundation that guides decision-making, fosters a sense of purpose among your staff, and communicates the unique value your hospital brings to the community.
Outline The Organizational Structure And Key Roles
In order to effectively run a hospital, it is crucial to clearly outline the organizational structure and identify the key roles within the healthcare facility. This will help ensure smooth operations, effective communication, and proper allocation of responsibilities. Here are some important steps to consider when outlining the organizational structure and key roles:
- Identify the leadership positions: Start by identifying the key leadership positions that will oversee the hospital's operations. This typically includes roles such as Chief Executive Officer (CEO), Chief Medical Officer (CMO), and Chief Nursing Officer (CNO).
- Define the departments: Next, outline the various departments within the hospital, such as administration, nursing, finance, human resources, and medical services. Each department should have a designated leader responsible for managing day-to-day operations and ensuring departmental goals are met.
- Establish reporting lines: Clearly define the reporting lines within the organizational structure to ensure efficient communication and decision-making processes. Indicate who reports to whom, and establish a hierarchical structure that promotes accountability and clarity.
- Identify key roles: Determine the key roles within each department and specify the responsibilities and qualifications for each position. This may include physicians, nurses, therapists, administrative staff, and other healthcare professionals required to deliver quality care.
- Promote teamwork and collaboration: Emphasize the importance of teamwork and collaboration among different departments and roles within the hospital. Encourage regular meetings, cross-functional projects, and open communication channels to foster a culture of cooperation and interdisciplinary care.
- Delegate authority: Delegate authority and empower individuals within their respective roles to make decisions and take ownership of their responsibilities. This encourages autonomy and accountability, and enables efficient problem-solving and decision-making processes.
- Consider developing an organizational chart to visually represent the hierarchical structure and reporting lines within the hospital.
- Regularly review and update the organizational structure to ensure it aligns with the evolving needs of the hospital and changing healthcare landscape.
- Communicate the organizational structure and key roles to all employees to ensure clarity and understanding of their responsibilities and reporting lines.
By carefully outlining the organizational structure and key roles, a hospital can establish a strong foundation for effective management, collaboration, and seamless delivery of quality healthcare services.
Formulate A Comprehensive Marketing Strategy
A comprehensive marketing strategy is essential for successfully promoting and positioning your hospital in the healthcare industry. It involves identifying your target audience, creating effective messaging, choosing the right marketing channels, and continuously evaluating and adapting your strategies to ensure maximum reach and impact.
When formulating your marketing strategy, keep the following key aspects in mind:
Tips for Formulating A Comprehensive Marketing Strategy:
- Identify your target audience: Determine the demographics and characteristics of the patients you want to attract. This enables you to tailor your marketing efforts towards their specific needs and preferences.
- Create compelling messaging: Develop a clear and persuasive message that highlights the unique value proposition of your hospital. Emphasize the personalized care, cutting-edge technology, and evidence-based treatment you offer.
- Choose the right marketing channels: Utilize a mix of traditional and digital marketing channels to reach your target audience effectively. Consider strategies such as search engine optimization (SEO), social media marketing, email campaigns, and referral programs.
- Build strong relationships: Cultivate relationships with referring physicians, healthcare professionals, and community organizations. Establish partnerships to increase referrals and enhance your reputation within the healthcare community.
- Monitor and evaluate: Regularly measure the effectiveness of your marketing efforts by tracking key performance indicators (KPIs). Analyze data, gather feedback, and adapt your strategies accordingly to ensure maximum impact and return on investment.
A comprehensive marketing strategy plays a vital role in attracting patients, establishing your hospital's brand, and maintaining a competitive edge in the healthcare industry. By understanding your target audience, crafting compelling messaging, choosing the right channels, and continuously evaluating your strategies, you can position your hospital as a trusted provider of high-quality and personalized medical services.
Assess Legal And Regulatory Requirements
Ensuring compliance with legal and regulatory requirements is crucial when setting up a hospital. This step involves researching, understanding, and meeting the various laws and regulations that govern the healthcare industry.
- Obtain necessary licenses and permits: Familiarize yourself with the licensing requirements specific to hospitals in your jurisdiction. Determine the necessary permits and certifications required to operate legally.
- Comply with healthcare regulations: Understand and comply with regulations related to patient privacy, data protection, health and safety standards, and medical waste management. Implement appropriate policies and protocols to ensure compliance.
- Stay updated with healthcare laws: Keep abreast of any changes or updates in healthcare laws and regulations that may have an impact on your hospital. This includes staying informed about reimbursement policies, billing regulations, and insurance requirements.
- Secure professional licenses and certifications: Ensure all healthcare professionals working at the hospital possess valid licenses and certifications. Perform necessary background checks and verification procedures to maintain quality and patient safety standards.
- Implement proper documentation and record-keeping practices: Establish systems for accurate and organized documentation to comply with medical record-keeping requirements. Adhere to guidelines for the storage, retention, and disposal of medical records.
- Seek legal counsel: Consult with healthcare attorneys or legal experts with experience in the healthcare industry to navigate the complex legal landscape.
- Stay updated with changes: Regularly review and update your knowledge on relevant laws and regulations to ensure ongoing compliance.
- Establish a compliance team: Assign responsibilities to a dedicated compliance team or officer to monitor and enforce adherence to legal and regulatory requirements.
In conclusion, developing a business plan for a hospital requires careful consideration and thorough research. By following the nine steps outlined in this checklist, you can ensure that your hospital is well-prepared to meet the market demand, provide high-quality care, and comply with legal and regulatory requirements. By focusing on personalized medical services, leveraging cutting-edge technology, and adopting a multidisciplinary approach to treatment, your hospital can strive towards providing the best possible outcomes for patients.
Related Blogs
- 7 Mistakes to Avoid When Starting a Hospital in the US?
- What Are The Top 9 Business Benefits Of Starting A Hospital Business?
- What Are Nine Methods To Effectively Brand A Hospital Business?
- Hospital Business Idea Description in 5 W’s and 1 H Format
- Own a Hospital Business: The Ultimate Acquisition Checklist!
- How To Name A Hospital Business?
- Hospital Owner Earnings: A Comprehensive Analysis
- How to Open a Hospital: Steps to Navigate Regulatory Requirements
- 7 Essential KPIs for Hospital Business Management
- How to Analyze Hospital Operating Expenses Efficiently
- What Are The Top Nine Pain Points Of Running A Hospital Business?
- Revolutionizing Healthcare: Unleash Success with Our Hospital Pitch Deck! Act Now.
- How to Improve Hospital Financial Performance: A Step-by-Step Guide
- What Are Nine Strategies To Effectively Promote And Advertise A Hospital Business?
- The Complete Guide To Hospital Business Financing And Raising Capital
- Strategies To Increase Your Hospital Sales & Profitability
- How To Sell Hospital Business in 9 Steps: Checklist
- Key Financial Aspects To Plan For When Starting A Hospital
- What Are The Key Factors For Success In A Hospital Business?
- Hospital Business: Evaluating its Worth
| Expert-built startup financial model templates |
Leave a comment
Your email address will not be published. Required fields are marked *
Please note, comments must be approved before they are published
Hospital Canteen SOP Template
- Great for beginners
- Ready-to-use, fully customizable Doc
- Get started in seconds
Hospital canteens play a vital role in providing nutritious meals to patients, staff, and visitors. But ensuring food safety and maintaining high standards can be a challenge. That's where ClickUp's Hospital Canteen SOP Template comes in!
With this template, you can streamline your Standard Operating Procedures (SOPs) for the hospital canteen, ensuring that your team:
- Follows strict hygiene and safety protocols to prevent foodborne illnesses
- Maintains proper food storage, handling, and preparation techniques
- Adheres to dietary restrictions and special meal requirements
- Monitors and maintains equipment and facilities for optimal performance
Whether you're managing a small hospital canteen or a large-scale operation, this template will help you maintain the highest standards of food safety and quality. Get started today and ensure a healthy dining experience for all!
Benefits of Hospital Canteen SOP Template
When it comes to running a hospital canteen smoothly and efficiently, having a standard operating procedure (SOP) template is a game-changer. Here are some of the benefits of using the Hospital Canteen SOP Template:
- Ensures consistent food quality and safety standards
- Streamlines daily operations and reduces errors
- Provides clear guidelines for staff on food preparation, handling, and storage
- Improves customer satisfaction by maintaining high service standards
- Helps with training new employees and maintaining a well-trained team
- Enhances overall efficiency and productivity in the canteen
Main Elements of Hospital Canteen SOP Template
ClickUp's Hospital Canteen SOP Template is designed to help you create and maintain standard operating procedures for your hospital canteen operations.
This Doc template contains all the necessary sections and content to guide you in creating a comprehensive SOP. It also includes ClickUp features such as:
- Custom Statuses: Create tasks with custom statuses to track the progress of each step in your SOP, such as "To Do," "In Progress," and "Completed."
- Custom Fields: Categorize and add attributes to your tasks to provide additional information and manage your canteen operations effectively.
- Custom Views: Utilize different views, such as List, Board, or Calendar, to visualize and manage your SOP tasks in a way that suits your workflow.
- Project Management: Enhance your SOP creation process with ClickUp's features like Tags, Dependencies, Priorities, and Integrations with other tools.
How to Use SOP for Hospital Canteen
Running a hospital canteen requires careful planning and adherence to standard operating procedures (SOPs). Here are four steps to effectively use the Hospital Canteen SOP Template in ClickUp:
1. Familiarize yourself with the template
Before diving into the SOP template, take some time to familiarize yourself with its structure and content. Understand the purpose and scope of the SOP, as well as the specific guidelines and procedures outlined within it. This will help you navigate the template more efficiently and ensure that you're following the correct protocols.
Use the Docs feature in ClickUp to access and read through the Hospital Canteen SOP Template.

2. Customize the template to your hospital's needs
Every hospital has unique requirements and regulations when it comes to running a canteen. Take the time to tailor the SOP template to fit your hospital's specific needs. This may involve adding or removing certain sections, updating procedures to align with your hospital's policies, or incorporating any additional guidelines or regulations that are relevant to your canteen operations.
Utilize the custom fields feature in ClickUp to make necessary modifications and personalize the Hospital Canteen SOP Template.
3. Train your canteen staff
Once you have finalized the customized SOP template, it's crucial to train your canteen staff on its contents and expectations. Schedule a training session to go over each section of the SOP, explaining the procedures, guidelines, and best practices outlined in the document. Ensure that your staff understands their roles and responsibilities, as well as the importance of adhering to the SOP for maintaining a safe and efficient canteen environment.
Create tasks in ClickUp to assign training sessions and track the progress of each staff member.
4. Regularly review and update the SOP
SOPs are not set in stone and should be reviewed and updated periodically to reflect any changes in regulations, hospital policies, or best practices. Schedule regular reviews of the Hospital Canteen SOP to ensure it remains up-to-date and relevant. Encourage feedback from your canteen staff and consider their suggestions for improvement. By continuously evaluating and updating the SOP, you can ensure that your canteen operations stay in compliance and consistently meet the highest standards.
Set recurring tasks in ClickUp to remind yourself to review and update the Hospital Canteen SOP on a regular basis.
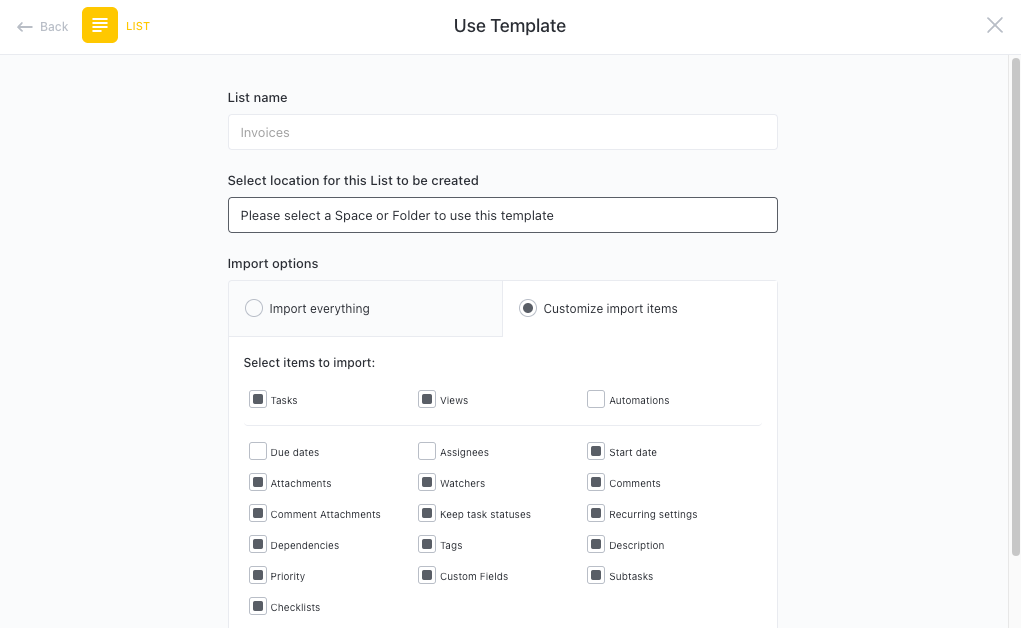
Get Started with ClickUp's Hospital Canteen SOP Template
Hospital canteen managers can use this Hospital Canteen SOP Template to streamline operations and ensure a smooth running canteen for staff and patients.
First, hit “Add Template” to sign up for ClickUp and add the template to your Workspace. Make sure you designate which Space or location in your Workspace you’d like this template applied.
Next, invite relevant members or guests to your Workspace to start collaborating.
Now you can take advantage of the full potential of this template to manage your canteen:
- Create Docs to outline the Standard Operating Procedures (SOPs) for each area of the canteen, such as food preparation, cleaning, and cashier duties
- Assign tasks to team members to ensure everyone is aware of their responsibilities
- Utilize Checklists for daily opening and closing procedures to maintain cleanliness and hygiene
- Attach relevant documents such as menus, ingredient lists, and special dietary requirements for easy reference
- Set up recurring tasks to schedule regular equipment maintenance and cleaning
- Use the Gantt chart view to create a timeline for menu planning and ordering supplies
- Collaborate using Comments for seamless communication and feedback on menu ideas and customer preferences
Related Templates
- Applied Energy Management SOP Template
- Safety in Pharmaceutical Industry SOP Template
- Petroleum Engineering SOP Template
- Safety in Factory SOP Template
- Employee Onboarding SOP Template
Template details
Free forever with 100mb storage.
Free training & 24-hours support
Serious about security & privacy
Highest levels of uptime the last 12 months
- Product Roadmap
- Affiliate & Referrals
- On-Demand Demo
- Integrations
- Consultants
- Gantt Chart
- Native Time Tracking
- Automations
- Kanban Board
- vs Airtable
- vs Basecamp
- vs MS Project
- vs Smartsheet
- Software Team Hub
- PM Software Guide

Serving our Healthcare Providers
We service America’s hospital systems, doctor offices, and healthcare facilities. For these teams and visitors, taking care of the patient is their top priority. Often, they keep going and forget to grab a bite to eat. By partnering with us, we’ll help make it easy for these caregivers to take a break and refuel, so they can get back to what they need to do.
From open retail markets for the break room to markets with access-controlled doors for the lobby, our technology provides flexibility for a variety of spaces.
Our snack, drink, fresh food, and coffee vending machines offer the options you need for your break room or lobby.
It's Easy to Get Started

Let us know you're ready to provide the best break possible by completing our online form .

We’ll meet with you to review your service needs, space requirements, and develop a plan for you.

We’ll agree on what happens next and when.
Guangdong Grace Kitchen Equipment Co., Ltd

What are the main points of the design plan of the hospital canteen kitchen?

Quick Links
- Applications
- Western Cooking Range
- Bakery Equipment
- Refrigeration Equipment
- Snacks Food Equipment

Better Touch Better Business
For more products related question ,Welcome to inquiry us .
Follow us at

版权所有 © 2019 格雷斯厨房设备有限公司 | 版权所有

Hello, please leave your name and email here before chat online so that we won't miss your message and contact you smoothly.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Availability of Healthy Food and Beverages in Hospital Outlets and Interventions in the UK and USA to Improve the Hospital Food Environment: A Systematic Narrative Literature Review
Associated data.
Not applicable.
The aims of this systematic review are to determine the availability of healthy food and beverages in hospitals and identify interventions that positively influence the hospital food environment, thereby improving the dietary intake of employees and visitors. Embase, Medline, APA PsycInfo, Scopus, Google Scholar and Google were used to identify publications. Publications relating to the wider hospital food environment in the UK and USA were considered eligible, while those regarding food available to in-patients were excluded. Eligible publications ( n = 40) were explored using a narrative synthesis. Risk of bias and research quality were assessed using the Quality Criteria Checklist for Primary Research. Although limited by the heterogeneity of study designs, this review concludes that the overall quality of hospital food environments varies. Educational, labelling, financial and choice architecture interventions were shown to improve the hospital food environment and/or dietary intake of consumers. Implementing pre-existing initiatives improved food environments, but multi-component interventions had some undesirable effects, such as reduced fruit and vegetable intake.
1. Introduction
Overweight and obesity are extremely prevalent across the UK and USA. In 2018, it was estimated that 67% of men and 60% of women in the UK had overweight or obesity [ 1 ], along with 71.6% of American adults in 2015/2016 [ 2 ]. A high body mass index (BMI) is linked to a range of non-communicable diseases, such as hypertension, type 2 diabetes and coronary heart disease [ 3 ], which has led to a significant number of hospital admissions associated with weight-related disorders. Between 2014 and 2015, it was estimated that the economic cost of overweight and obesity-related health complications to the National Health Service (NHS) was GBP 6.1 billion [ 4 ], while the healthcare cost of obesity in America was approximately USD 149.4 billion [ 5 ].
In addition to the high prevalence of obesity and overweight in the general population, healthcare employees demonstrate similar weight-management issues. One study carried out by Kyle et al. (2017) used data from the 2008–2012 Health Survey for England and found that 25.1% of the nurses surveyed had a BMI of 30 kg/m 2 or higher, classifying them as ‘obese’. Furthermore, 32% of unregistered care workers, 26% of non-health-related NHS employees and 12% of other healthcare professionals also had a BMI of 30 kg/m 2 or higher. These values are similar among American hospital staff members, with 27% of American nurses estimated to be obese [ 6 ].
A key cause of obesity is eating an excess of unhealthy foods. In the UK, the Office for Health Improvement and Disparities advises infrequent consumption of foods high in fat, salt and sugar [ 7 ]. American guidelines reflect the same general recommendations; according to the 2015–2020 Dietary Guidelines for Americans, a healthy diet should involve the restriction of saturated and trans fats, added sugars and salt [ 8 ]. Therefore, unhealthy foods can be defined as products that are high in these substances.
The range of healthy or unhealthy food and beverages available, food marketing techniques and the cost of food items in a specified setting can be referred to as the food environment [ 9 ]; this has a significant impact on the nutritional quality of food consumed by the general public. Studies have shown that there is an association between easier access to fast food and greater BMI and odds of obesity [ 10 ], suggesting that the food environment has a strong influence on weight status.
The general public has an expectation of hospitals and other healthcare environments to promote healthy behaviours, with 97% of participants in one survey indicating that hospitals should act as positive role models for healthy lifestyle behaviours [ 11 ]. Despite this, unhealthy foods are often found in hospital food outlets.
The aim of this review is to explore the extent to which healthy food and drink options are available to employees and visitors in hospital food environments and to determine which interventions are effective in reducing the purchase and consumption of unhealthy foods and beverages. This research may identify interventions that can improve the health and wellbeing of hospital employees and visitors, potentially leading to policy change to ensure healthy food is predominant in the wider hospital food environment.
2. Materials and Methods
The protocol associated with this systematic review was registered with PROSPERO, an international database of prospectively registered systematic reviews (reference number CRD42021223249). An amendment was made on 12 August 2021, detailing the repetition of database searching and a revised quality assessment method.
To find literature relevant to the current hospital food environment and interventions to improve the nutritional quality of food available to employees and visitors, a systematic search was carried out using five electronic databases: Embase, Medline, APA PsycInfo (all accessed via Ovid), Scopus and Google Scholar. Google was also utilised to ascertain suitable grey literature. Initial searches were carried out on 23 October 2020 and repeated on 21 July 2021 to detect new publications.
Suitable keyword search terms were identified; controlled search terms included “hospital”, “convenience food”, “healthy diet”, “automatic food dispensers” and “nutritional value”. Key words were amended slightly for each database; full search terms are listed in Appendix A .
Eligibility criteria were established to aid the selection of relevant publications. Some criteria were used to narrow the scope of the research to facilitate a detailed review of source material within the timeframe available. Two researchers carried out independent eligibility screening using Rayyan [ 12 ], and disputes were resolved via discussion with a third researcher.
Publications were included in the present review if they related to the wider hospital food environment (i.e., food outlets accessible to hospital employees and/or visitors) in the UK or the USA. No restrictions were placed on publication dates. Publications were excluded if they focused on food available only to patients in hospital wards. Additional exclusion criteria included studies with no full-text sources available, studies written in a language other than English and studies which involved systematic reviews or meta-analyses.
Search results were imported to Endnote [ 13 ]; duplicates were removed before the sample was exported to Rayyan [ 12 ]. Studies were initially screened based on the adherence of their titles and abstracts to the eligibility criteria. Included studies were further refined by screening full texts and removing ineligible records.
Several key pieces of data were extracted from each study in a standardised template by one researcher. Extracted information included author names, year of publication, country, study design, aim, duration, intervention/observation methods, outcome measures and results. A quality assessment and risk of bias analysis was also carried out on each source by one researcher using the Quality Criteria Checklist for Primary Research from the Academy of Nutrition and Dietetics [ 14 ]. See Appendix B , Table A1 for the full data extraction table.
The key outcomes of interest were the nutritional quality of food and beverages currently available to employees and visitors in hospitals as well as interventions aiming to improve the nutritional quality of products, awareness of nutritional values, dietary intake or overall health of hospital employees and visitors. Summary measures for these outcomes varied greatly between eligible publications. Due to the heterogeneity of summary measures and study designs, a quantitative synthesis or meta-analysis was not possible; consequently, a narrative synthesis was undertaken.
Studies were initially grouped into categories based on study type (i.e., observations and interventions). Interventions were allocated to sub-categories to allow for a well-structured narrative synthesis. Sub-categories included educational, labelling, financial, choice architecture, pre-existing guideline implementation and multi-component interventions.
Of the 806 search results initially identified from databases and search engines, 40 studies met the eligibility criteria. The most common reason for exclusion was the irrelevance of study outcomes to the research question. This was often due to a focus on patient meals rather than the food available to hospital employees and visitors. A PRISMA flow diagram [ 15 ] displays the inclusion and exclusion process ( Figure 1 ).

PRISMA 2009 flow diagram [ 15 ], detailing the number of studies included and excluded at each stage of the screening process.
3.1. Participant Characteristics
Fifteen publications reported the number of hospital employees, students or visitors involved in observations or interventions [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ], while twelve reported the number of food outlets [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ] and ten reported the number of healthcare facilities involved [ 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 ]. Three studies recorded the number of food outlets and survey respondents [ 53 , 54 , 55 ]. In total, the eligible publications reported the involvement of 18,171 participants, 139 food outlets and 529 hospitals and healthcare facilities.
3.2. Countries
In the UK, 5 interventions [ 31 , 34 , 38 , 39 , 40 ], 7 observations [ 17 , 23 , 35 , 37 , 44 , 45 , 51 ] and 1 mixed methods design [ 41 ] were reported; in the USA, 14 interventions [ 16 , 20 , 24 , 25 , 28 , 29 , 30 , 33 , 36 , 42 , 43 , 48 , 53 , 54 , 55 ], 10 observations [ 18 , 19 , 21 , 27 , 32 , 46 , 47 , 49 , 50 , 52 ] and 2 mixed methods studies [ 22 , 26 ] were reported.
3.3. Study Design
Observational studies ( n = 17) employed a range of techniques, such as interviews, focus groups and cohort studies. Of the intervention studies ( n = 20), 8 utilised a randomised controlled trial design [ 16 , 28 , 29 , 31 , 33 , 34 , 38 , 53 ], and 12 utilised quasi-experimental methods [ 20 , 24 , 25 , 30 , 36 , 39 , 40 , 42 , 43 , 48 , 54 , 55 ]; additionally, 3 studies employed mixed methods [ 22 , 26 , 41 ], incorporating a range of techniques, such as conducting interviews and collecting sales figures. The full data extraction can be seen in Table A1 . According to the Quality Criteria Checklist for Primary Research, 11 of the eligible publications met high quality and risk of bias standards [ 16 , 18 , 26 , 27 , 28 , 29 , 31 , 38 , 48 , 49 , 53 ], while 29 were considered neither particularly strong nor particularly weak ( Table A1 ) [ 17 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 30 , 32 , 33 , 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 50 , 51 , 52 , 54 , 55 ].
3.4. Observations
Five observational studies explored hospital food outlet adherence to pre-existing standards and guidelines [ 32 , 35 , 37 , 46 , 51 ]. Sustain (2017) found variation in the hospital food environments between 30 hospitals, with around 50% complying with standards listed in the NHS contract. Healthy options were also found to be more prevalent than unhealthy options in vending machines [ 51 ]. Similarly, James et al. (2017) investigated 30 food outlets across two NHS hospitals and their adherence to The National Institute for Health and Care Excellence (NICE) Quality Standard 94. Quality Standard 94 includes three quality statements relating to the availability of healthy options in vending machines (statement 1), nutritional information on menus (statement 2) and prominent display of healthy options (statement 3). Adherence to statements 1 and 2 was poor; only 10% of food products and 53% of drinks available in vending machines were classified as healthy and nutritional information was not available on menus at either hospital. Adherence to statement 3 was mixed, as both healthy and unhealthy options were displayed prominently in food outlets [ 35 ].
In 19 facilities across California, Lawrence et al. (2009) found that 81% of food in vending machines did not adhere to the California state nutrition standards for schools. Carbonated drinks were the most common beverages in vending machines, with advertisements for these beverages being prevalent. At the time of the study, 60% of facilities had already adopted or were beginning to implement nutritional standards for vending machines [ 46 ].
Mohinra et al. (2021) investigated the food environment in a dental hospital and found that beverages met Commissioning for Quality and Innovation (CQUIN) targets for sugar content; however, foods high in fat, salt and sugar were displayed in prominent locations, and unhealthy options were more affordable than healthy options [ 37 ].
Derrick et al. (2015) assessed the nutritional quality of cafeteria meals in relation to LiVe Well Plate guideline adherence. On average, food outlets that adhered to the LiVe Well Plate guideline had significantly higher nutrition composite scores than those which did not, particularly for point-of-purchase options, suggesting healthier food environments [ 32 ].
The diverse nutritional quality of cafeteria meals was also reported by Jaworowska et al. (2018). Variation was identified between different meals in the same outlet and between the same meals at different facilities; the majority of meals were high in saturated fat, while 69% of meat-based dishes and 43% of vegetarian dishes were high in salt content [ 44 ].
Findings were similar within paediatric hospitals or clinics. Across 14 facilities, Lesser et al. (2012) reported that most food outlets offered healthy options and half displayed nutritional information at the point of purchase. However, the majority had high-calorie options positioned close to point-of-purchase and promoting unhealthy options on signs was more common than promoting healthy options. Furthermore, half of the cafeterias had no healthy hot meals [ 47 ]. In vending machines accessible to children, Kibblewhite et al. (2010) found that none of the food-based or mixed food and drink vending machines contained 50% or more healthy food options. Meanwhile, 13% of drinks machines in paediatric clinics and 9% of drinks machines in other areas of the hospital contained 50% or more healthy options. Advertisements for brands associated with unhealthy products were also commonly found on vending machines [ 45 ].
Parental visitors to a paediatric hospital were broadly dissatisfied with the food environment. Food options were considered restrictive, and concerns were raised regarding the quality, freshness and positioning of products. Participants also felt that food available in the hospital food environment contradicted healthy eating messaging on signage [ 23 ].
Interviews, focus groups and surveys were also carried out with hospital employees and non-parental visitors. Bak et al. (2020) reported that nursing students believed that few healthy food options were available in hospitals. The students indicated that subsidising healthy foods could improve the hospital food environment and positively influence eating behaviours among nurses [ 17 ]. Barriers and facilitators to healthy eating were identified via interviews with 17 food service managers, carried out by Lederer et al. (2014). Only four of the respondents reported that their cafeteria followed nutrition standards set by the hospital ( n = 3) or by the American Heart Association and the Academy of Nutrition and Dietetics ( n = 1). The majority of respondents said that consumer-related factors, such as customer satisfaction and demand, were barriers to healthy food implementation [ 21 ]. Consumer satisfaction was also cited as a potential barrier by food service managers in a study by Jilcott Pitts et al. (2016). Other challenges included profit implications and training costs, while potential facilitators of healthy eating included altered positioning of healthy and unhealthy options and signage promoting healthy options [ 19 ]. Furthermore, Liebert et al. (2013) also highlighted profits and resources as potential barriers to implementing nutrition interventions. Despite this, over 80% of respondents were concerned about eating well and stated that they would be more likely to do so if healthy options were cheaper than unhealthy options. Additionally, 73% were in favour of the taxation and subsidisation of products based on nutritional content [ 22 ].
The impact of hospital location or average visitor socioeconomic status on the hospital food environment was also explored. Winston et al. (2013) found no significant relationship between the socioeconomic status of the local area and the nutrition composite score of the hospital [ 52 ]. In contrast, a study by Goldstein et al. (2014) found that physicians seeing mostly patients of higher socioeconomic status were more likely to report high levels of nutritional support compared to those seeing patients of lower socioeconomic status [ 18 ].
3.5. Interventions
Hospital food environment interventions can be grouped into several categories. Studies incorporating interventions from three or more categories are classified as “multi-component”; these studies are grouped and explored separately under the “Multi-Component Interventions” subheading.
3.5.1. Educational
Educational interventions aim to increase consumer knowledge of the nutritional guidelines or the nutritional content of foods. Of the seven educational interventions, four utilised signage or flyers to increase awareness of the nutritional content of products.
Allan and Powel (2020) assessed the impact of point-of-purchase signage on the nutritional quality of purchases and found that signage reduced the calorie content of purchases, reduced sugar content in some circumstances and had no impact on fat content [ 31 ]. Webb et al. (2011) also introduced nutritional labelling on posters or nutritional labelling on posters and a point-of-purchase menu board. More consumers noticed the nutritional information when posters and menu boards were used, compared to only posters. Nutritional labelling on posters and menu boards was also associated with the increased purchase of lower-calorie snacks and side dishes but made no significant difference in the nutritional content of entrée purchases [ 55 ].
When combining signage with traffic light labelling, Sonnenberg et al. (2013) found that nutritional content, taste and price became more important to consumers, while convenience became less important. Participants who were influenced by nutritional information bought more healthy products than those who were not [ 25 ]. Block et al. (2010) introduced signage and flyers about the health implications of regular soft-drink consumption, along with taxation. Education alone had no significant effect on sugar-sweetened soft drink sales. However, education enhanced the effects of taxation, reducing soft drink sales by 10% compared to price increases alone [ 53 ].
Two studies used digital methods to deliver nutritional information [ 16 , 28 ]. Abel et al. (2015) sent texts or emails to participants regarding calorie reference values. Participants who received the information were twice as likely to know reference values compared to a control group, but this did not appear to alter calorie consumption or portion sizes [ 16 ]. Thorndike et al. (2021) used emails (and letters) to provide feedback on food choices. The number of healthy purchases increased while the number of unhealthy purchases decreased. These effects remained significant at a 24-month follow-up, but there was no significant change in weight status [ 28 ].
Another study by Thorndike et al. (2016) used social norm feedback in combination with financial incentives. Social norm feedback alone led to a 1.8% increase in healthy purchases, but this was not statistically significant. Combining social norm feedback with a financial incentive resulted in a 2.2% increase in healthy purchases, and employees rated healthiest at baseline were influenced most greatly by the interventions [ 29 ].
3.5.2. Labelling
Six studies explored the effects of labelling [ 25 , 27 , 30 , 33 , 42 , 54 ]. Elbel et al. (2013) added ‘less healthy’ labels to some items, and this increased purchase of healthier options by 7% [ 33 ]. Sato et al. (2013) added calorie, fat and sodium content information to packaging. A non-significant increase in healthier options sold was observed, along with a significant decrease in the total number of meals sold per day. Despite this, 71% of customers who noticed the intervention reacted positively to it, and 50% claimed that the labels influenced them to purchase a healthier option [ 54 ].
The most common form of labelling was traffic light labelling. Sonnenberg et al. (2013) investigated the impacts of traffic light labelling and nutritional signage on customer food-related attitudes. The intervention increased the importance of health and nutrition to participants, and more participants claimed to use nutritional information when making food choices during the intervention compared to pre-intervention. More healthy options were purchased by those who were influenced by the labels than those who were not [ 25 ].
Traffic light labelling reduced the number of unhealthy purchases in three studies. Whitt et al. (2018) assessed the impact of traffic light labelling on food choices compared to cartoon labelling. Traffic light labelling decreased unhealthy food purchases by 7% from baseline, while cartoon labelling increased the number of unhealthy purchases by 1% from baseline and by 5% from the washout period [ 42 ]. In two studies, Thorndike et al. (2014, 2019) found that traffic light labelling decreased the proportion of red-labelled products purchased [ 30 ], which resulted in fewer calories purchased and potential employee weight loss [ 27 ].
3.5.3. Financial
The effects of financial interventions were primarily investigated via taxation and subsidisation of products. Elbel et al. (2013) found that taxing unhealthy products increased the proportion of healthy purchases by 11.5% from baseline and that this was associated with fewer unhealthy purchases and an increased proportion of healthy beverage purchases [ 33 ]. Similarly, Block et al. (2010) found that increasing the prices of sugar-sweetened soft drinks decreased sales by 26% [ 53 ]. Patsch et al. (2016) utilised taxation and subsidisation and found significant increases in the proportion of healthy alternatives sold along with decreases in the number of traditional, less healthy products sold [ 24 ].
In addition to feedback-based interventions, Thorndike et al. (2016) offered financial incentives for healthy purchases. Feedback plus a financial incentive led to a 2.2% increase in healthy purchases, compared to a 1.8% increase for feedback alone and a 0.1% increase for the control group [ 29 ]. In a second study by Thorndike et al. (2021), the intervention increased the purchase of healthy products by 7.3% and decreased the purchase of unhealthy options by 3.9%. This effect did not lead to significant weight loss in the intervention group [ 28 ].
3.5.4. Choice Architecture
Choice architecture was implemented in several ways; the most prevalent method was altering the proportion of healthy and unhealthy products available to purchase. Three studies focused on products available in vending machines. Griffiths et al. (2020), Grivois-Shah et al. (2018) and Pechey et al. (2019) found an increase in the number of healthy products purchased [ 43 ], a decrease in the amount of calories purchased [ 34 , 38 ] and mixed results regarding the financial impact of the intervention [ 34 , 43 ]. Simpson et al. (2018) conducted a similar study in a hospital shop but found no significant difference in the relative proportion of healthy options sold between pre- and post-intervention sales data [ 40 ].
Thorndike et al. (2014) took a different approach and utilised choice architecture by making healthy options more visible. The impact of choice architecture itself is unknown, as it was only assessed in combination with traffic light labelling. Nevertheless, the overall intervention decreased the proportion of unhealthy product sales by 3% and increased the proportion of healthy product sales by 5% after two years [ 30 ].
Public Health England, as previously known (2018), investigated the impact of altering product positioning in vending machines; this is explored in more depth in the ‘Implementing Standards and Guidelines’ section [ 39 ].
3.5.5. Implementing Standards and Guidelines
Three studies assessed the impacts of supporting the implementation of pre-existing standards for hospital food outlets [ 39 , 41 , 48 ]. Moran et al. (2016) encouraged the implementation of the Healthy Hospitals Food Initiative and improved adherence to the programme. The nutritional quality of the hospital food environment also improved [ 48 ].
Stead et al. (2020) focused on the implementation of Healthcare Retail Standards in hospital shops. Compliance with these standards had no effect on the number of fruit products available but decreased the number of chocolate-based options and the number of promotions for these products. The standards also reduced meal-deal sales [ 41 ].
Public Health England (2018) altered the content of vending machines in line with Government Buying Standards for Food and Catering. In drinks machines, these changes decreased calorie and sugar content of purchases and increased proportion of ‘diet’ beverages sold. In food machines, sales of crisps decreased while sales of confectionary and dried fruit and nut products increased [ 39 ].
3.5.6. Multi-Component Interventions
Stites et al. (2015) carried out a study involving choice architecture, financial incentives and educational components. Hospital employees were taught mindfulness techniques, encouraged to pre-order meals and, for part of the intervention, provided with vouchers for the cafeteria. This intervention resulted in lower calorie and fat purchases compared to a control group, with and without the vouchers. Despite the dietary changes, weight loss was not significant among the intervention group [ 26 ].
LaCaille et al. (2016) incorporated signage, traffic light labelling and choice architecture into a nutrition intervention, alongside encouraging physical activity participation. The control group experienced a greater average reduction in waist circumference than the intervention group after six months (but not after 12 months). As well as this, the intervention group experienced a significant decrease in fruit, vegetable and fibre intake over the course of the study. Consumption of foods high in sugar and fat also decreased [ 20 ].
Mazza et al. (2017) also reported mixed results. Financial interventions and traffic light labelling were combined with health and social norm messaging and choice architecture. Financial interventions and traffic light labelling increased healthy beverage purchases by 2.9%. The addition of health and social norm messaging and grouping items into nutritional categories further increased healthy beverage purchases. Healthy crisp sales increased by 5.4% when traffic light labelling was introduced and by 6% when health messaging was implemented. However, healthy crisp sales decreased by 5.9% when the price of water was reduced, suggesting that this financial intervention nullified the beneficial effects of traffic light labelling [ 36 ].
4. Discussion
The observational studies carried out across the UK and USA suggest that the quality of the wider food environment is diverse. Compliance with pre-existing standards and guidelines is varied [ 32 , 35 , 37 , 46 , 51 ] and the nutritional quality of cafeteria meals differs between meals and facilities [ 44 , 47 ]. A lack of healthy food options was reported in vending machines, while the availability of healthy beverage options was slightly greater [ 45 ]. Hospital visitors and employees reported concerns regarding the quality, freshness and positioning of healthy and unhealthy options [ 23 ] and believed there was a lack of healthy options available [ 17 ]. Barriers to the implementation of healthy eating initiatives were also identified, including customer satisfaction [ 19 , 21 ] and profit implications [ 19 , 22 ], although participants were in favour of a financial intervention to encourage healthy food and beverage choices [ 22 ]. Findings relating to the impact of socioeconomic status on the hospital food environment are inconsistent [ 18 , 52 ].
Utilising signage and flyers is associated with the reduced calorie content of purchases [ 31 ], and displaying nutritional information on menu boards and posters increases the purchase of low-calorie options compared with using posters alone [ 55 ]. Digital methods of communicating nutritional information can increase knowledge of reference values [ 16 ] and increase purchase frequency of healthy options whilst decreasing purchase frequency of unhealthy options [ 28 ], but effects on calorie consumption are contested [ 16 , 28 ] and these interventions have no significant impact on weight-related outcomes [ 28 ]. Moreover, educational interventions can be successfully incorporated with traffic light labelling [ 25 ] and financial interventions [ 29 , 53 ].
Adding simple labels to products, marking them as ‘less healthy’ or giving some nutritional information, is associated with an increase in the number of healthy purchases [ 33 ] but also with decreased total purchases per day [ 54 ]. Nevertheless, labelling interventions are viewed positively by consumers [ 54 ]. Traffic light labelling has been shown to increase the importance of nutrition to participants [ 25 ], increase the number of healthy purchases [ 25 ], reduce the number of unhealthy purchases [ 30 , 42 ] and reduce the calorie content of purchases [ 27 ]. It was predicted that this could lead to consumer weight loss, provided that no other lifestyle alterations occurred [ 27 ].
Taxation on unhealthy products or subsidisation of healthy products was found to be associated with an increased proportion of healthy purchases [ 24 , 33 ] and a decreased number of sugar-sweetened soft drink purchases [ 53 ]. Financial incentives were also found to effectively increase healthy purchases and decrease unhealthy purchases [ 28 , 29 ], but no impact on weight-related outcomes was identified [ 28 ].
Altering the proportion of healthy options available to purchase from vending machines was found to increase healthy purchases [ 43 ] and decrease the calorific content of purchases [ 34 , 38 ]. This type of intervention may have undesirable financial outcomes for food outlets, but this remains unclear [ 34 , 43 ].
One study found no change in the proportion of healthy options sold before and after a choice architecture intervention in a hospital shop [ 40 ]. However, another study reported that displaying healthy options more prominently reduced unhealthy purchases and increased healthy purchases when combined with traffic light labelling [ 30 ]. Choice architecture interventions also increased ‘diet’ beverage sales and reduced the total sugar content of purchases [ 39 ].
Encouraging implementation of pre-existing standards and guidelines is associated with an overall improvement in the hospital food environment [ 48 ] and decreased availability of unhealthy products [ 41 ]. In beverage vending machines, implementing governmental standards increased the proportion of ‘diet’ beverage sales and reduced the sugar and calorie content of purchases [ 39 ]. However, adherence to these standards has also been shown to reduce sales of meal deals [ 41 ] and increase sales of confectionary [ 39 ].
Multi-component interventions have been carried out with a range of study designs. These interventions have been shown to reduce calorie and fat content of purchases [ 26 ], reduce consumption of foods high in sugar and fat [ 20 ], increase healthy beverage purchases [ 36 ] and increase the purchase of healthy snack options [ 36 ]. However, certain multi-component interventions have also resulted in decreased fruit, vegetable and fibre intake [ 20 ] and decreased sales of healthy snack options [ 36 ]. These interventions were not associated with significant weight loss [ 20 , 26 ].
This review has several strengths. Study screening was independently conducted by two researchers, and the process was blinded to reduce the impact of researcher bias. Additionally, conducting a narrative synthesis allowed the integration of material that would have been incomparable using quantitative synthesis. Therefore, the heterogeneous data have been compiled into a useful summary to inform further research. However, the heterogeneity of study designs and outcome measures restricts the use of quantitative synthesis and meta-analysis to summarise findings. Additionally, many studies involve multiple interventions, making it difficult to determine the impact of each intervention on outcomes. This limits the strength of recommendations.
Another limitation of this review is our pragmatic decision to restrict the search to studies carried out in the UK and USA. This decision was taken because the number of studies carried out in the UK and USA allowed for an in-depth analysis of all relevant literature within the available time frame. It should be noted that the exclusion of studies from other countries limits the wider generalisability of findings.
Furthermore, some studies took place several years ago, meaning that information about the ‘current hospital food environment’ may no longer be valid. One observation found that 60% of facilities were beginning to adopt vending machine nutrition standards in 2009 [ 46 ], so vending machine nutritional quality could have since changed. Nevertheless, poor nutritional quality in vending machines was reported in 2017 [ 35 ], indicating that concerns about healthy vending machine options may remain relevant.
The majority of interventions discussed in this review can be used to improve nutrition awareness, eating behaviour or the overall hospital food environment. Studies that surveyed hospital employees or visitors on their acceptance of these interventions reported that over 70% of responses were positive [ 22 , 54 ].
Some studies show that combining multiple interventions can improve the nutritional quality of food purchases. However, multi-component interventions may have the potential to lead to detrimental impacts, such as reduced fruit and vegetable consumption and reduced sales of healthy snacks [ 20 , 36 ]. Consequently, more robust study designs are required to identify the most effective intervention combinations in multi-component studies.
Further interventions are needed in the UK to investigate the most effective methods of improving the nutritional quality of employee and visitor diets. Research into the associations between food environment and food intake in a variety of settings, other than hospitals, would also be valuable. Moreover, some interventions included in this review would benefit from being replicated to generate an evidence base with consistent outcome measures. This would produce more homogenous data, facilitating quantitative synthesis and meta-analysis. A more precise estimated effect size would be generated, thereby strengthening practice and policy recommendations.
Timely implementation of public health interventions, such as altering food environments and encouraging healthier diets, is especially pertinent in the wake of the COVID-19 pandemic. Dietary patterns high in fat, salt and sugar contribute to the prevalence of obesity and type II diabetes, which increase the risk of severe COVID-19 outcomes [ 56 ]. By altering the hospital food environment, healthy food and beverages could be made the easiest option to purchase, thereby improving dietary quality and potentially reducing the risk of ill-health among hospital employees and visitors. Food environment interventions could also reduce the discrepancy between health messaging and poor hospital food environments, ensuring that hospitals act as positive role models for healthy lifestyle behaviours.
5. Conclusions
In conclusion, the quality of the hospital food environment varies within and between facilities. Hospital visitors and employees are generally receptive to food environment interventions and a variety of designs can be used to improve the hospital food environment and increase the proportion of healthy purchases. However, multi-component interventions can have neutral or detrimental effects on participant eating behaviours depending on the design. Therefore, further research that also encompasses studies beyond the UK and USA is required to determine the most effective combinations within multi-component interventions.
Acknowledgments
Guidance on database searching was provided by Aimee Cook, a Medical Sciences Librarian at Newcastle University Library.
Appendix A.1. Scopus Search Criteria
Hospital AND (food OR nutrition*) AND (“convenience food” OR “fast food” OR “healthy food” OR snack OR fat OR salt OR sugar OR calorie OR beverage) AND (catering OR outlet OR vending AND machine OR cafe* OR restaurant OR canteen OR “hospital shop” OR “hospital store” OR “gift shop”) AND (policy OR “food preference” OR “consumer attitudes” OR choice OR decision OR “health promotion” OR diet OR healthy OR options) AND (LIMIT-TO (AFFILCOUNTRY, “United States”) OR LIMIT-TO (AFFILCOUNTRY, “United Kingdom”)) AND (LIMIT-TO (LANGUAGE, “English”)).
Appendix A.2. Embase, Medline and APA PsycInfo Controlled Vocabulary Search
Hospital AND (Food OR Food product OR Convenience food OR Packaged food OR Fat OR Dietary fat OR Fat intake OR Dietary fat OR Sodium chloride OR Salt intake OR Dietary salt OR Sugar OR Dietary sugar OR Sugar intake OR Beverage OR Sugar-sweetened beverage OR Calorie) AND (Catering service OR Food outlet OR Food service OR Vending machine OR Automatic food dispensers OR Commercial food OR Cafeteria OR Cafeteria diet OR Restaurant OR Canteen OR Shop OR Store OR Retail OR Commerce) AND (Nutrition policy OR Healthcare policy OR Government policy making OR Public health OR Healthcare planning OR Health policy OR Nutrition OR Nutritional value OR Nutritive value OR Food preference OR Feeding behaviour OR Consumer attitudes OR Consumer satisfaction OR Eating behaviour OR Choice OR Decision making OR Health promotion OR Food availability OR Diet OR Healthy diet OR Food options).
Full data extraction for n = 40 studies, including quality assessment and risk of bias analysis, carried out using the Quality Criteria Checklist for Primary Research [ 14 ].
| Citation, Country | Study Design, Duration | Aim of Study | Participants/ Hospitals | Intervention | Outcome Measures | Results | Risk of Bias Analysis |
|---|---|---|---|---|---|---|---|
| Abel et al. (2015) [ ], USA | RCT, 4 weeks | Assess knowledge of government reference values among the public and assess the impact of email/text interventions on calorie reference value knowledge. | = 246 hospital employees and students | Assess knowledge of reference values, deliver weekly text or email prompts regarding calorie intake, then administer a follow-up test to assess impact of intervention. | Knowledge of government reference values and impact of intervention on self-reported calorie consumption. | At baseline, 42.2% of participants knew the 2000 calorie reference value. Following text intervention, participants 2x as likely to know the reference value as the control group ( = 0.047, odds ratio = 2.2, 95% confidence interval [1.01, 4.73]). No significant difference between text and email conditions. 52% of participants would use the information when making future food decisions. 32% stated that the intervention led to lower calorie intake than if the information was available on menus and posters—no statistically significant change in self-reported calorie consumption or portion size. | + |
| Allan and Powell (2020) [ ], UK | RCT, 6 months | Reduce purchase of unhealthy single-serve snacks. | 30 hospital food outlets | Implement tailored point-of-purchase signs displaying calorific values of the items for sale. | Average energy, fat and sugar content of purchases per day, average cost of each purchase and total number of purchases per day. | Purchases significantly lower in calories (95% CI: −0.83, −2.85, < 0.001), sugar content and cost (95% CI: −0.46, −1.32, < 0.001) post-intervention compared to pre-intervention. This was also true for calories ( = 0.049) and cost ( = 0.03) comparing intervention to the control site. No significant differences in fat content ( = 0.07), sugar content ( = 0.48) or number of purchases ( = 0.64) between intervention and control sites. | + |
| Bak et al. (2020) [ ], UK | Observational, 2 h (per focus group) | Investigate beliefs of student nurses about causes of nurses’ health-related behaviours, plus strategies to improve these behaviours. | 20 undergraduate nursing students | Ask student nurses about underlying factors for health-related behaviours, reasoning behind these behaviours and identifying stakeholders responsible for implementing solutions. | Student views regarding the underlying causes of health-related behaviours among nurses and how these could be improved. | Four key causes of negative health-related behaviours identified: Knowledge, shift-work, culture and stress. Several students reported snacking was common during night-shifts and few healthy food options were available within hospitals. They also suggested that high stress triggers a desire to eat “comfort foods”, which are often high in fat. The idea of subsidising healthy food options for staff was raised as a possible strategy to improve food-related behaviours. | ∅ |
| Block et al. (2010) [ ], USA | RCT, 6 weeks | Assess the impact of increasing the prices of sugar-sweetened soft drinks and educational interventions on beverage sales. | = 1 hospital food outlet and 154 survey respondents | 5 phase intervention involving 35% price increase on soft drinks, an educational campaign (posters and flyers) and combined price increase and educational campaign. | Number and category of drinks purchased per day and total number of beverage sales. | Sales of regular, sugar-sweetened soft drinks significantly decreased during intervention, while sales of diet soft drinks increased. Regular soft drink sales decreased by 26% during price increase (95% CI = 39.0, 14.0) and 36% (95% CI = 49.0, 23.0)in the combination phase (education and price increase). Education alone did not significantly impact sales of regular soft drinks, despite a 9% sales increase (95% CI = −4.0, 22.0). 44% of survey participants noticed an intervention, with 82% being aware of the educational phase and 18% being aware of the price increase. | + |
| Derrick et al. (2015) [ ], USA | Observational, short duration | Describe nutrition environments in hospitals that participate in the One Health Care System and investigate the impact of the LiVe Well Plate initiative. | 21 hospital food outlets | Assess food environment using the Hospital Nutrition Environment Scan, including signage, menu information and pricing strategies. Implement the LiVe Well Plate in low-scoring hospitals based on menu factors. | Nutrition composite scores of cafeterias and nutrition scores based on barriers and facilitators, grab-and-go items, menu offering and point-of-purchase options. | Mean nutrition composite score was 49.2 ± 8.1 in hospitals which adhered to the LiVe Well Plate and 29.7 ± 11.3 in hospitals which did not. Those adhering to the initiative had significantly higher scores for facilitators and barriers ( < 0.001) and point-of-purchase options ( = 0.013) than the other group and two locations promoted healthy food choices via pricing. No significant differences between groups for grab-and-go ( = 0.178) or menu options ( = 0.172). | ∅ |
| Elbel et al. (2013) [ ], USA | RCT, 6 months | Investigate the impact of taxation and food labelling interventions on healthy produce purchases. | 1 hospital food outlet | 5 phase intervention involving product labelling, a 30% taxation on less healthy items, a combined intervention and a combined intervention with taxation rationale stated on products. | Number and nutritional quality of purchases. | At baseline, 47.2% of purchases were healthy (95% CI = 43%, 52%). This rose to 54% in the labelling condition (95% CI = 49%, 58%) and 59% under the taxation conditions (95% CI = 56%, 61%; not shown). Taxation conditions did not significantly differ ( on Wald test = 0.82); all increased probability of healthy purchase by 10–12% ( < 0.001). Taxation associated with fewer unhealthy food choices (AME = −9.41%, 95% CI = −13.80%, −5.03%, < 0.001) and more healthy beverage purchases (AME = 5.87%, 95% CI = 2.36%, 9.38%, = 0.001). Unclear if taxation had a greater impact than labelling. | ∅ |
| Goldstein et al. (2014) [ ], USA | Observational, short duration | Investigate physician perspectives on hospital support available to promote healthy hospital environments. | 1485 physicians | Physicians were asked to rate their place of work based on support offered for achievement and maintenance of a healthy food environment and physical activity. | Physician rating of hospital support | Health-promoting environments were mostly rated ‘good’, with 70% of respondents suggesting that nutrition environments were supportive. Responses varied according to socioeconomic status of the average patient (higher ratings were given by physicians seeing lower middle class [OR: 1.74 (1.27–2.39)], upper middle class [2.23 (1.61–3.09)] to affluent patients [2.91 (95% CI: 1.49–5.66)] compared to physicians seeing very poor to lower/middle-class patients). 40% of respondents stated that their facilities supported healthy nutrition. | + |
| Griffiths et al. (2020) [ ], UK | RCT, 24 weeks | Assess health benefits and cost-effectiveness of replacing regular snacks with healthy options. | = 2 hospital food outlets | Vending machines in 2 locations were exposed to alternating “healthy” or “unhealthy” conditions, with all products costing the same amount. | Sales volume, profit and calories sold. Compensatory behaviours (sales data from nearby shop), number of items purchased by each customer and time taken to complete each purchase | The healthy condition was associated with a 61% decrease in calories purchased, which was significant (SE = 579.23; t = −3.868; < 0.0001) and a GBP 1116 decrease in profits. There was no significant impact on number of sales and no significant association between calorie content and sales volume. No significant difference in sales from a local shop (SE = 0.848; t = 0.249; = 0.81), suggesting no compensatory behaviours. No significant difference in the likelihood of single versus multiple item purchases between conditions (χ (1) = 2.20, = 0.14). | ∅ |
| Grivois-Shah et al. (2018) [ ], USA | Quasi-Experimental, 6 months | Assess the impact of increasing the proportion of healthy options in vending machines on calorie, fat, sugar and salt purchase, plus sales revenue. | 23 hospitals | Proportion of healthy “Right Choice” items in vending machines was increased from 20% to 80%. | Percentage of healthy options vended and total number of items vended. Mean revenue, calorific value, fat content and sodium content per site, per month. | The intervention increased average number of “Right Choice” items purchased from vending machines from 9.9% to 35%. Percentage change in average monthly revenue was not significantly different between baseline and post-intervention (95% CI = −12.6 to 7.8, = 0.5766). On average, the intervention reduced average fat content by 27.4% per month (95% CI = −37.4 to −15.9, < 0.0001), sugar content by 11.8% per month (95% CI = −22.0 to −0.3, = 0.0447), sodium content by 25.9% per month (95% CI = −33.9 to 17.0, < 0.0001) and calorie content by 16.7% per month (95% CI = −25.5 to −6.8, = 0.0016). Beverage profit declined by 11.1% (95% CI = −19.9 to −1.3, = 0.0274) while number sold increased by 16.2% (95% CI = 3.7 to 30.2, = 0.0100). | ∅ |
| James et al. (2017) [ ], UK | Observational, 2 weeks | Assess adherence to NICE quality statements 1–3 of quality standard 94 at two NHS hospitals. | 30 hospital food outlets | Food environments were assessed using the Consumer Nutrition Environment Tool. Adherence to quality statements was measured. Statement 1 regarding healthy options in vending machines, statement 2 about nutritional information on menus and statement 3 regarding prominent display of healthy options. | Proportion of healthy and less healthy options in vending machines, clarity of nutrition information on menus and prominence of healthy food and beverages displayed. | 10% of food products and 53% of drinks in vending machines were considered healthy, making adherence to quality statement 1 poor. Food items were given a C-NET score of 18.3. Nutritional information was not available on menus at either facility, so adherence to quality statement 2 was also poor. Adherence to quality statement 3 was inconsistent, as both healthy and less healthy products were prominently displayed in cafeterias. 25% of cafeteria options were healthy. | ∅ |
| Jaworowska et al. (2018) [ ], UK | Observational, 2 months | Describe nutritional quality of hot lunches in NHS hospital staff canteens. | 8 hospitals | Nutritional composition of canteen meals was assessed using meal samples from each canteen. | Energy, protein, total fat, saturated fat, carbohydrates, fibre and sodium content of meals. | Meals containing meat had a higher energy density than vegetarian meals and were also higher in salt content (0.61 vs. 0.49 g; < 0.05) and protein per 100g (9.8 vs. 4.8 g; < 0.05). Significant variation in nutritional composition between different meals. According to standard cafeteria portion sizes, 67% of meat-based and 80% of vegetarian meals were high in saturated fat, while 69% of meat-based and 43% of vegetarian dishes were high in salt (red light according to the traffic light labelling system). Meals varied significantly between hospitals, especially per portion. | ∅ |
| Jilcott Pitts et al. (2016) [ ], USA | Observational, short duration | Describe barriers and facilitators to the implementation of healthy service guidelines and strategies for health promotion. | 9 food service managers and operators | Information about hospital size, types of food available and current nutrition initiatives was gathered via a quantitative survey and more in-depth information was obtained from qualitative interviews. | Difficulty or ease of guideline implementation, price outcomes, barriers and facilitators to implementation and potential behavioural design strategies to promote healthy eating. | Challenges raised regarding implementation of guidelines including profit implications, customer dissatisfaction and difficulties with changing obligations to food strategies. Suggested strategies to encourage healthier choices included signage and icons on healthier items, positioning of healthy options and marketing techniques. Additional training costs were anticipated to arise from altering the food environment. | ∅ |
| Kibblewhite et al. (2010) [ ], UK | Observational, short duration | Describe products available in vending machines close to paediatric wards and outpatient clinics. | 13 hospitals | Percentages of healthy and unhealthy vending machine items accessible to children were calculated. | Number of healthy and unhealthy items in vending machines and advertising for unhealthy brands. | In paediatric clinics, 13% of the drinks-only machines contained over 50% healthy options, while none of the food-only machines reached this target. The mixed food and drink machine met the target for drinks, but not food. In other areas of the hospital which were accessible to children, 9% of drinks machines contained over 50% healthy options compared to 27% for food machines. Mixed machines contained 50% healthy drinks but not food. 55% of machines in paediatric clinics and 72% in other areas displayed commercial logos, mostly associated with unhealthy products. | ∅ |
| LaCaille et al. (2016) [ ], USA | Quasi-Experimental, 12 months | Assess the efficacy of , an obesity-prevention programme. | 900 hospital and primary care clinic employees | A multi-component intervention was implemented, including traffic light labelling, choice architecture, pedometer usage and signage was launched. | Weight, BMI, waist circumference, physical activity levels and dietary behaviour after 6 months and 1 year | No significant change in weight (95% CI = −1.13, 1.56, = 0.76) or BMI between groups (95% CI = −0.17, 2.39, = 0.09) or in weight (95% CI = −0.36, 0.89, 0.40) or BMI (95% CI = −0.27, 0.95, = 0.27) over time. The control group had a significantly greater decrease in waist circumference than the intervention group at 6 months (95% CI = 1.28 to 4.72, = 0.001) but not at 12 months (95% CI = −1.06, 2.16, 0.51). There was a significant decrease in fruit and vegetable intake over 12 months in the intervention group (95% CI = −13.13, −2.23, = 0.007), but consumption of foods high sugar and fat, like cookies, cakes and brownies, also significantly decreased (95% CI = −0.12, −0.01, = 0.02). The intervention caused employees to view their employer as more committed to improving health and wellbeing (95% CI = 0.06, 0.23, = 0.002) and 86% wanted the intervention to continue. | ∅ |
| Lawrence et al. (2009) [ ], USA | Observational, short duration | Describe the range of healthy and unhealthy vending machine options and healthcare settings. | 19 healthcare facilities | Numbers of healthy and unhealthy products in vending machines were recorded and the quality and quantity of food products were compared between 3 types of environment. | Percentage of healthy options in vending machines, advertising and implementation of standards. | In hospitals and clinics, carbonated beverages were the most prevalent drink, accounting for 30% of drinks in hospitals and 38% in clinics). 81% of food across all sites did not adhere to standards, 75% of vending machines displayed advertisements for carbonated beverages and 60% of facilities with vending machines were in the process of adopting nutritional standards for the machines. | ∅ |
| Lederer et al. (2014) [ ], USA | Observational, short duration | Describe the nutritional knowledge, practices and attitudes of hospital cafeteria managers in hospitals following the Healthy Hospitals Food Initiative (HHFI). | 17 cafeteria managers | A 22 question survey was delivered to participants who approved menus, had influence over food purchases and monitored food preparation. | Nutritional practices, standards and policies. | 4 of 17 participants said that their cafeteria followed hospital nutrition standards. 13 claimed to think about nutrition when planning menus, but most respondents ranked consumer preferences and cost as the 2 main considerations. 14 participants reported reducing sodium content of meals by cooking from scratch, buying products with lower sodium content and decreasing the salt content of recipes. 16 respondents cited consumer-related factors as limitations to healthy food implementation, such as lack of demand, customer satisfaction and lack of consumer education around healthy eating. Environmental factors were also a concern for 6 participants, such as an inability to move cafeteria fixtures to make healthy options more prominent. | ∅ |
| Lesser et al. (2012) [ ], USA | Observational, short duration | Describe the quality of the food environments in outlets at a children’s hospital | 14 hospitals | The Nutrition Environment Measures Study in Restaurants was adapted for use in cafeterias. Items in hospital cafeterias were scored according to healthy or unhealthy status. | Nutritional quality of food in hospital cafeterias and healthy eating prompts. | Majority of venues offered healthy options, like low-fat milk, fresh fruit and a salad bar. Around 50% of cafeterias displayed point-of-purchase nutritional information, while less than 33% displayed signage promoting healthy menu choices. High-calorie options were available near point-of-purchase in 81% of venues, 50% offered discounts for multiple purchases, 38% displayed signage promoting unhealthy eating and 50% had no healthy hot meals. NEMS-C scores ranged from 13 to 30, with a mean of 19.1. | ∅ |
| Liebert et al. (2013) [ ], USA | Mixed Methods, 2 years | Research and plan the Better Bites intervention programme to improve food choices of hospital employees. | 100 hospital employees | Employees were interviewed using the Nutrition Environment Measures Study in Restaurants and other surveys. Best practices were identified for planning and developing the Better Bites intervention. | Barriers and facilitators to healthy eating, perceptions of healthy food availability and likelihood of behaviour modification following interventions. | Majority of respondents supported the intervention but concerns were raised about profits, resources and ability to change eating behaviours. 82% of respondents were concerned about eating well and 83% reported being more likely to buy healthy items if cheaper than unhealthy items. 73% in favour of reducing healthy option prices and increasing unhealthy option prices. | ∅ |
| Mazza et al. (2017) [ ], USA | Quasi-Experimental, short duration (around 15 days per intervention) | Comparing the impacts of a range of interventions, combined with traffic light labelling, on beverage and crisp (potato chip) sales. | = 1 hospital food outlet | Interventions, such as price increases, health messaging, social norm messaging and grouping items into nutritional categories, were assessed for efficacy alongside a traffic light labelling intervention. | Daily number of healthy (green-labelled) purchases. | Traffic light labelling increased healthy beverage purchases by 2.9% compared to a price increase alone ( < 0.0001). When labelling and price changes were combined with subsequent interventions, colour grouping, social norm feedback and oppositional pairing reduced healthy beverage purchases by 2% ( < 0.0001), 1.7% ( < 0.01) and 6.9% ( = 0.01), respectively. For crisps, traffic light labelling increased percentage of healthy crisps sold by 5.4% ( = 0.001), compared to a sugar sweetened beverage price increase. When water price decreased, healthy crisp sales decreased by 5.9% ( = 0.003). Health messaging increased healthy crisp sales by 6% compared to control conditions ( = 0.004). | ∅ |
| McSweeney et al. (2018) [ ], UK | Observational, short duration | Assess parental perspectives of food available in a children’s hospital and the barriers and facilitators to healthy eating. | 18 parents | Parents were interviewed regarding ease of healthy eating in the hospitals until no new themes were raised. | Themes centred around food accessibility and nutritional quality of food in hospitals. | Purchases were influenced by cost and speed. Parents described the food choice as restrictive, especially for children, vegetarians and those trying to eat healthier. Quality of food was said to vary between outlets and concerns about freshness, presentation and location of unhealthy options were raised. Maintenance of a healthy diet was considered difficult, as food available contradicted healthy eating messages shown on signs. A discount or loyalty card was proposed to make healthy food cheaper to repeat visitors. | ∅ |
| Mohindra et al. (2021) [ ], UK | Observational, 2 weeks | Describe nutritional quality of products available in a dental hospital, along with the price and positioning of high fat, salt and sugar products. | 1 hospital food outlet | An audit of coffee shop food and beverage options was carried out using Commissioning for Quality and Innovation (CQUIN) indicator 1b targets for 2018/19 | Nutritional content of packaged food and drinks and fresh food, total sugar content in products and the price, quantity and variety of each product category. | A variety of pre-packaged sandwiches, wraps and salads was available, compared to just 1 packaged vegetable product, 3 packaged fruit products and 3 fresh fruit products. 42% of packaged sandwiches, wraps and salads contained less than 400 kcal and below 5 g saturated fat per 100 g. 50% of cakes and 66% of biscuits adhered to the CQUIN guideline of containing less than 250 kcal per portion and 12% of cakes contained more sugar per portion than the daily recommended sugar intake from SACN. All crisps and popcorn met targets for saturated fat, while 73% contained less than the PHE salt target. All cold drinks met the CQUIN targets per 100 mL, but portion sizes varied widely and, as such, so did sugar content per portion. All hot drinks met the CQUIN targets. Unhealthy foods were displayed prominently compared to fresh fruit and packaged fruit was more expensive than packaged biscuits. Low-fat sandwiches were also more expensive than high-fat sandwiches. | ∅ |
| Moran et al. (2016) [ ], USA | Quasi-Experimental, 3 years | Implement the Healthy Hospitals Food Initiative (HHFI) in public and private hospitals to establish nutrition standards and assess outcomes. | 40 hospitals | HHFI implementation was supported by dieticians, promotional materials and monthly progress reports to identify achievements and next steps. | Degree of HHFI implementation and nutritional quality of food options. | At baseline, all public hospitals ( 16) had implemented standards for patient meals and vending machines, but none had implemented cafeteria standards. No hospital met the criteria for sodium or whole grains, and none offered an affordable healthy meal. Following intervention, 12 public hospitals met cafeteria standards, while 71% of private hospitals had implemented standards for patient meals, 58% for beverage vending machines, 50% for food vending machines and 67% for cafeterias. 21% of hospitals achieved sodium standards, 61% achieved standards for whole grains and 68% offered a healthy, affordable meal. | + |
| Mulder et al. (2020) [ ], USA | Observational, 11 months | Describe national prevalence of workplace policies, practices and interventions to support employee health. | 338 hospitals | Senior hospital employees responded to the Workplace Health in America survey. | Hospital size and worksite health-promotion factors. | 81.7% of hospitals provided health promotion or wellness programmes in the previous year and likelihood of implementation varied based on hospital size ( < 0.01) and type ( < 0.05). Of those which offered programmes, 53.7% provided healthy diet advice (95% CI, 47.6–59.8%) and 59.9% had programmes to tackle obesity (95% CI, 53.9–65.9%). Of the hospitals which had wellness programmes and contained food outlets, 48.6% displayed nutritional information about calories, sodium or fat (95% CI, 42.3–54.8%), 54.7% used symbols to identify healthy choices (95% CI, 48.4–61.0%) and 19.2% subsidised healthy foods and beverages (95% CI, 14.2–24.1%). | + |
| Patsch et al. (2016) [ ], USA | Quasi-Experimental, 1 year | Assess the impact of subsidisation of healthy food and taxation of unhealthy food on sales and financial outcomes. | 2800 hospital visitors and employees | Three food items were paired with healthier ‘Better Bites’ alternatives at two hospitals (PH and SFMC). Products were labelled as such and signage was added to canteens. Healthy product cost decreased by 35%, while unhealthy product cost increased by 35%. | Average weekly healthy (Better Bites) and less healthy sales, change in the proportion of healthy and less healthy products sold at each facility and financial outcomes. | At PH, relative traditional burger sale decreased by 47.9% (z = ± 35.85, < 0.001) while the Better Bites option experienced a relative increase of 600% (z = ± 35.85, < 0.001). Better Bites salad sales demonstrated a relative increase of 2.6% (z = ± 1.18, = 0.238). At SFMC, proportion of traditional burger sales experienced a relative decrease of 20.4% (z = ± 14.87, < 0.001) and the Better Bites burger demonstrated a relative increase of 371.2% (z = ± 14.87, < 0.001), but sales remained lower than those of traditional burgers. At this site, Better Bites salad sales showed a relative increase of 71.1% (z = ± 5.32, < 0.001). | ∅ |
| Pechey et al. (2019) [ ], UK | RCT, 28 weeks | Assess the impact of altering the absolute and relative availability of healthier and less healthy vending machine products. | 10 hospital food outlets | Vending machines were subjected to five conditions and 20% of items were changed in each condition. Proportion of healthier and less healthy items available was altered each time. | Energy purchased from each vending machine under every condition and number of products vended each week. | Altering the proportion of healthy and unhealthy options did not significantly alter energy purchased from food (decrease less healthy: = 0.407, increase healthier: = 0.103, decrease healthier: = 0.350, increase less healthy: = 0.180). When the number of unhealthy beverages decreased, energy purchased from beverages decreased by 53% ( = 0.001). Total sales did not decrease. | + |
| Public Health England (2018) [ ], UK | Quasi-Experimental, 9 months | Assess the impact of nutrition standard implementation and choice architecture on the nutritional quality of vending machine products. | 17 food outlets | In phase 1, vending machine content was altered to adhere to best practice Government Buying Standards for Food and Catering but healthy items were displayed less prominently. In phase 2, standards were upheld and healthier items were displayed more prominently. | Number of items sold, mean energy content per product and mean sugar content per product. | In drinks machines, total sales increased by 2.5% as fewer sugar-sweetened beverages and more ‘diet’ beverages were sold. Energy per item sold decreased (−36.2%), along with total sugar content (−36.4%). In food machines, overall sales decreased throughout the intervention (−3.2% in phase 1, −11.8% between phase 1 and 2), mainly due to reduced purchase of crisps (−29.1% in phase 1, −23.1% between phase 1 and 2). Confectionary and dried fruit and nuts sales increased in phase 1 (+14.2% and +23.2%) and decreased slightly (but remained above baseline) in phase 2 (−8.2% and −0.8%) and total energy from food decreased in phase 1 (−10.5%) and phase 2 (−9.5%). | ∅ |
| Sato et al. (2013) [ ], USA | Quasi-Experimental, 12 weeks | Assess the impact of food labelling on the purchase of healthier entrees in cafeterias and on financial outcomes. | 1 hospital food outlet and = 131 participants surveyed | Following baseline data collection from receipts, labels were added to entrees, displaying information on calorie, fat and sodium content. Customers were surveyed on their usage of these labels. | Change in the nutritional content of purchases pre- and post-intervention and customer preferences on labelling and views regarding the influence of labelling. | Mean percentage of healthier options sold increased by 0.7% while regular menu sales decreased by 0.7% ( = 0.837). Overall, total entrée sales decreased by around 8% ( < 0.0001) and average price increased by 50 cents. 77% of customers who purchased entrees claimed to have noticed the labels and at least 71% of these respondents expressed positive feelings towards the labels. 50% of those who noticed labels and purchased an entrée claimed that labels influenced their purchase, persuading them to select healthier options. | ∅ |
| Sharma et al. (2016) [ ], USA | Observational, 2 months | Describe current policies and practices associated with nutrition and physical activity environments in hospitals and compare them between facilities. | 5 hospitals | The Environmental Assessment Tool was used to assess healthy food availability in six cafeterias and six vending machines. Mean score was calculated at each healthcare facility. | Environmental Assessment Tool factors, such as physical activity and nutrition support. | All hospitals offered nutrition education classes and provided healthy vending machines and cafeteria options. Healthy food availability scores ranged from 62–75% and varied within hospitals. Healthy food availability in vending machines scored 13–36%, while healthy drink availability scored between 0–40%. | ∅ |
| Simpson et al. (2018) [ ], UK | Quasi-Experimental, 6 months | Assess the feasibility of increasing proportion of healthy options in a hospital shop and the impact on financial outcomes and consumer acceptability. | 1 hospital food outlet | Portion sizes, promotions, prices, positioning and healthy option availability were adjusted to diminish barriers and implement facilitators to healthy eating. Intervention results were assessed soon after implementation and at a later date. | Relative sales of healthy food products, change in sales within food categories and change in profits. | Adding fruit to the meal deal increased units of fruit sold from 40 to over 900 per week. Total sales increased by 11% but no significant change in relative proportion of healthy food sales. In follow-up, sales increased by 27% but change in relative proportion of healthy food sales remained unchanged. Sales of sweets and chocolate decreased, but sales of other unhealthy products did not. 35% of respondents said the shop sold a good range of healthy options pre-intervention, compared to 60% post-intervention. | ∅ |
| Sonnenberg et al. (2013) [ ], USA | Quasi-Experimental, 3 months | Assess the impact of product labelling on consumer awareness of healthy purchases. | 204 (baseline) 253 (following intervention) hospital employees and visitors | Traffic light labelling and signage were introduced. A dietician was present in the first two weeks of intervention and nutritional information flyers were made available. Consumers were surveyed following purchase of items. | Public perspectives on important factors when purchasing food and beverages, nutritional value of products and the influence of traffic light labelling on purchases. | At baseline, 46% of respondents stated health and nutrition were important factors when making food choices, increasing to 61% following intervention ( = 0.004). Taste ( = 0.04) and price ( = 0.02) also became more important, while convenience became slightly less important ( = 0.06). Increased participants reporting usage of nutritional information when making choices (15% to 33%, < 0.001). Those who noticed and were influenced by labels bought more green-labelled items and fewer red-labelled items compared to those who did not ( < 0.001). | ∅ |
| Stead et al. (2020) [ ], UK | Mixed Methods, 18 months (short reassessment 1 year later) | Describe the process of Healthcare Retail Standard implementation and how the standards impact healthy product promotion. | 17 hospital food outlets | Data on chocolate and fresh fruit was gathered following implementation of the Healthcare Retail Standards (HRS) and interviews were conducted with managers to understand awareness and attitudes regarding the standards. | Number of relevant products on display and number of promotions for relevant products. | 12 of 13 shops achieved compliance with the HRS. Mean number of fruit products available did not change, while mean number of chocolate products decreased from an average of 60 to 29. Chocolate promotions in shops decreased from 166 to 38. Managers raised concerns about reduced uptake of meal deals. Allowing introduction of baked crisps into the meal deal slightly increased sales, but not to pre-intervention levels. | ∅ |
| Stites et al. (2015) [ ], USA | Mixed Methods, 12–16 weeks | Assess the impact of mindfulness and pre-ordering meals on nutritional quality of purchases by hospital employees. | 26 hospital employees | In the full-intervention, mindful eating educational sessions were combined with encouragement to pre-order canteen meals. Vouchers were also issued. In the partial intervention, vouchers were not issued. Mindful Eating Questionnaires were administered at the beginning and end of the study. | Amount of energy and fat in lunches purchased by employees. | Average calorie content of lunches was 601 kcal and fat content was 4.9 g for the intervention group compared to 745.7 kcal (95% CI = −254.0 to −35.1, = 0.01) and 13.8 g (95% CI = −15.2 to −2.6, = 0.005) for the delayed treatment group. Calorie (95% CI −81.3 to −52.6, < 0.001) and fat content (95% CI = −4.1 to −2.8, < 0.001) also decreased when the financial incentive was removed. Mindful eating behaviours increased from pre- to post-intervention ( < 0.001), but weight loss was not statistically significant e ( = 0.099). 92% of participants expressed interest in using a pre-ordering system in the future. | + |
| Sustain (2017) [ ], UK | Observational, short duration | Describe current availability of healthy food and drinks in hospitals and determine hospital adherence to nutritional standards. | 30 hospitals | Surveys were sent to hospitals and assessed fresh food availability, healthy options and access to facilities during breaks. | Information on hospital food standards and types of food available to staff and visitors. | 50% of hospitals adhered to all five standards stated in the NHS contract, while 67% reported meeting or working towards health and wellbeing CQUIN targets. 40% of facilities had 24-h access to healthy foods, 25% met the criteria for having a food and drink strategy and 77% offered fresh food to staff. Two hospitals met all of the criteria for healthy food available to staff and visitors and 23 met the goal of having two portions of vegetables per main meal. Six hospitals had 70% or more products in hospital shops with green or orange traffic light labels. Vending machines selling mostly healthy options ( 138) were more prevalent than those selling less healthy options ( 90); 21 hospitals offered meal deals, including healthy options. | ∅ |
| Thorndike et al. (2014) [ ], USA | Quasi-Experimental, 2 years | Assess the impact of traffic light labelling and choice architecture on hospital cafeteria sales. | 2285 hospital employees | Traffic light labelling was introduced and, after three months, a choice architecture intervention was also introduced. | Proportion of healthy and unhealthy sales every 3 months. | After one year, proportion of red-labelled items sold decreased from 24% to 21% ( 0.001) and proportion of green-labelled items increased from 41% to 45% ( < 0.001). After two years, proportion of red-labelled items sold remained the same, while proportion of green-labelled items increased to 46% ( < 0.001). Results were statistically similar among all populations and sales were stable for two years. | ∅ |
| Thorndike et al. (2016) [ ], USA | RCT, 6 months | Investigate the impact of social norm feedback and financial incentives on nutritional quality of purchases. | 2672 hospital employees | Participants were randomised to three groups, feedback (monthly comparison to other employee purchases), feedback and incentive (financial reward for healthy purchases) or control | Proportion of healthy items bought at baseline and at end of intervention. | The feedback incentive condition led to a 2.2% in green-labelled purchases ( = 0.03) compared to 0.1% for the control. The feedback only condition led to a non-signifcant1.8% increase ( = 0.03). There was a significant relationship between health classification at baseline and the impact of interventions on food choices ( < 0.001). | + |
| Thorndike et al. (2019) [ ], USA | Observational, 2 years | Investigate the relationship between workplace cafeteria healthy eating programmes and reduced calorie purchases among employees throughout a two year intervention. | 5695 hospital employees | Sales data was gathered before and after implementation of traffic light labelling. | Calories sold at baseline and end of intervention, plus weight change of employees. | After one year, mean calorie content per transaction decreased by 19 kcal from baseline (95% CI, −23 to −15 kcal, < 0.001). After two years, there had been a mean decrease of 35 kcal, with red-labelled item purchases decreasing by 42 kcal per transaction from baseline (95% CI, −45 to −39 kcal, < 0.001). The dynamic model suggested that frequent users of the hospital cafeteria would lose 1.1 kg in one year and 2 kg in three years as a result of cafeteria interventions, assuming no other changes to eating or exercising behaviour. | + |
| Thorndike et al. (2021) [ ], USA | RCT, 2 years | Assess the impact of an automated behavioural intervention on weight status and nutritional intake of hospital employees. | 602 hospital employees | Two emails were sent per week, providing feedback on purchasing behaviour and offering personalised advice. 1 letter was also sent per month, comparing participants to peers and offering financial incentives for healthy choices. | Change in weight from baseline to 12 months and 24 months, cafeteria purchases and calories purchased per day. | After 1 year (95% CI, −0.6 to 1.0, = 0.70) and 2 years (95% CI, −0.3 to 1.4, = 0.20), there was no significant difference in weight change between the intervention and control groups. Following the first year, purchases of green-labelled items had increased by 7.3% (95% CI, 5.4 to 9.3) and purchases of red-labelled items had decreased by 3.9% compared to baseline (95% CI, −5.0 to −2.7). Number of calories purchased per day decreased by 49.5 kcal compared to the control group (95% CI, −5.0 to −2.7). Differences remained significant after 2 years. After 1 year, 92% of survey respondents in the intervention group stated that at least one of the intervention methods had supported healthy decision-making. | + |
| Webb et al. (2011) [ ], USA | Quasi-Experimental, 3 months | Gather views of hospital food outlet users and assess the impact of calorie-labelling on purchasing behaviour. | 6 hospital food outlets and 554 survey respondents | Cafeterias were subjected to one of three conditions: No labelling, calorie and nutrient labelling on posters and labelling on posters in addition to point-of-purchase menu board labelling. | Attitudes, awareness and usage of calorie information by consumers and the daily number and type of purchases made. | 69% of survey respondents using food outlets with menu boards and posters noticed calorie information compared to 58% using outlets with just posters. 32% of respondents noticed calorie information and a third of these participants indicated that it influenced their purchases. Average number of daily purchases remained the same. Proportion of lower-calorie side dishes purchased increased by 4.8% at the menu-board site and decreased by 4.8% at the no labelling site ( = 0.0007). Proportion of low-calorie snacks purchased increased by 1.3% at the menu board site and decreased by 8.1% at the no labelling site ( < 0.006). Changes to entrée purchases were modest. | ∅ |
| Whitt et al. (2018) [ ], USA | Quasi-Experimental, 4 months | Compare the impacts of traffic light labelling and cartoon labelling on food choices in a children’s hospital cafeteria. | 1 hospital food outlet | Products were given a traffic light colour sticker for unhealthy, neutral and healthy, or a Spongebob Squarepants sticker for healthy items. | Proportion of daily healthy, neutral and unhealthy purchases. | Traffic light labelling led to the lowest number of unhealthy food purchases, at 30%, which was significantly lower than the 37% value at baseline ( < 0.001). Cartoon labelling increased the number of unhealthy purchases, with a 5% increase from washout (χ = 5.73 ( = 0.057)). | ∅ |
| Winston et al. (2013) [ ], USA | Observational, 4 months | Assess the impact of socioeconomic status of an area on hospital nutrition composite scores. | 39 hospitals | The Hospital Nutrition Environment Scan for Cafeterias, Vending Machines and Gift Shops was used to score the hospital food environment. | Barriers and facilitators for a healthy diet. | Average score was less than 25% of possible points and were higher for vending machines (33%) than for cafeterias or gift shops. There was no significant association between socioeconomic status of the area and the nutrition composite score. Less than half of the shelf space in cafeterias was used for healthier items and 85% of cafeterias displayed unhealthy options near the point-of-purchase. Use of a contracted food service was linked to provision of a healthy combination meal and the availability of nutritional information. | ∅ |
+: The report has met targets for quality (such as generalisability, inclusion and exclusion and data collection and analysis) and risk of bias. ∅: Report quality is neither particularly strong nor particularly weak. --: Targets for quality and bias have not been met.
Author Contributions
Author contributions to this review are as follows: Conceptualisation, L.M., S.S. and S.R.; methodology, L.M., S.S. and S.R.; validation, L.M., S.S. and S.R.; investigation, S.R.; resources, S.R.; data curation, S.R. and L.M.; writing—original draft preparation, S.R.; writing—review and editing, S.R., L.M. and S.S; visualisation, S.R.; supervision, L.M. and S.S.; project administration, L.M. and S.S.; funding acquisition, L.M. and S.S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding. We are grateful to Newcastle University for supporting this work.
Institutional Review Board Statement
Informed consent statement, data availability statement, conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dolgoprudny
| Overview | Map | Directions | Satellite | Photo Map |
| Overview | Map | Directions |
| Satellite | Photo Map |
| Tap on the map to travel |
- Type: City with 118,000 residents
- Description: human settlement in Dolgoprudny Urban Okrug, Moscow Oblast, Russia
- Postal code: 141707
Notable Places in the Area
Church of saint vladimir in vinogradovo.

Dolgoprudnenskoye Cemetery

Locales in the Area

Lianozovo District

- Categories: city or town , big city and locality
- Location: Moscow Oblast , Central Russia , Russia , Eastern Europe , Europe
- View on OpenStreetMap
Dolgoprudny Satellite Map
Popular Destinations in Moscow Oblast
Curious places to discover.

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Information
Find all the information of Dolgoprudny or click on the section of your choice in the left menu.
- Update data
| Country | |
|---|---|
| Oblast |
Dolgoprudny Demography
Information on the people and the population of Dolgoprudny.
| Dolgoprudny Population | 112,007 inhabitants |
|---|---|
| Dolgoprudny Population Density | 5,411.0 /km² (14,014.3 /sq mi) |
Dolgoprudny Geography
Geographic Information regarding City of Dolgoprudny .
| Dolgoprudny Geographical coordinates | Latitude: , Longitude: 55° 55′ 60″ North, 37° 30′ 0″ East |
|---|---|
| Dolgoprudny Area | 2,070 hectares 20.70 km² (7.99 sq mi) |
| Dolgoprudny Altitude | 183 m (600 ft) |
| Dolgoprudny Climate | Humid continental climate (Köppen climate classification: Dfb) |
Dolgoprudny Distance
Distance (in kilometers) between Dolgoprudny and the biggest cities of Russia.
Dolgoprudny Map
Locate simply the city of Dolgoprudny through the card, map and satellite image of the city.
Dolgoprudny Nearby cities and villages
Dolgoprudny Weather
Weather forecast for the next coming days and current time of Dolgoprudny.
Dolgoprudny Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Dolgoprudny.
| Day | Sunrise and sunset | Twilight | Nautical twilight | Astronomical twilight |
|---|---|---|---|---|
| 27 August | 04:25 - 11:31 - 18:37 | 03:45 - 19:17 | 02:54 - 20:08 | 01:52 - 21:10 |
| 28 August | 04:27 - 11:31 - 18:34 | 03:47 - 19:14 | 02:57 - 20:05 | 01:56 - 21:05 |
| 29 August | 04:29 - 11:30 - 18:32 | 03:49 - 19:11 | 02:59 - 20:02 | 01:59 - 21:01 |
| 30 August | 04:31 - 11:30 - 18:29 | 03:52 - 19:08 | 03:02 - 19:58 | 02:03 - 20:57 |
| 31 August | 04:33 - 11:30 - 18:26 | 03:54 - 19:06 | 03:04 - 19:55 | 02:06 - 20:53 |
| 1 September | 04:35 - 11:29 - 18:24 | 03:56 - 19:03 | 03:07 - 19:52 | 02:10 - 20:49 |
| 2 September | 04:37 - 11:29 - 18:21 | 03:58 - 19:00 | 03:09 - 19:49 | 02:13 - 20:45 |
Dolgoprudny Hotel
Our team has selected for you a list of hotel in Dolgoprudny classified by value for money. Book your hotel room at the best price.
| Just 6 km from Sheremetyevo Airport, this hotel in Khimki offers an international restaurant with karaoke facilities, soundproofed rooms, and free Wi-Fi. The Moscow Ring Road is 7 km away... | from | |
| The lakeside Holiday Inn Vinogradovo offers contemporary accommodation within 10 km from Sheremetyevo Airport. It features an indoor pool and a fitness center with mini-gym and 2 saunas... | from | |
| Free Wi-Fi is offered at this 3-star hotel, located 200 metres from the Klyazma River in Khimki. Features include an indoor pool and tennis court. A balcony and a TV are standard in all Park Hotel Olympiets rooms... | from | |
| This 4-star hotel is located just a 20-minute drive from the Crocus Expo Centre, guests can use a free transfer to get there. The hotel offers free Wi-Fi, a restaurant serving European and Russian cuisine, and a 24-hour reception and taxi service... | from | |
| Offering excellent motorway links and just a 10-minute walk from Moscow Lianozovo Park, these apartments are fitted with flat-screen TVs, a microwave and a refrigerator... | from | |
Dolgoprudny Nearby
Below is a list of activities and point of interest in Dolgoprudny and its surroundings.
Dolgoprudny Page
| Direct link | |
|---|---|
| DB-City.com | Dolgoprudny /5 (2021-10-07 13:22:49) |

- Information /Russian-Federation--Moscow-Oblast--Dolgoprudny#info
- Demography /Russian-Federation--Moscow-Oblast--Dolgoprudny#demo
- Geography /Russian-Federation--Moscow-Oblast--Dolgoprudny#geo
- Distance /Russian-Federation--Moscow-Oblast--Dolgoprudny#dist1
- Map /Russian-Federation--Moscow-Oblast--Dolgoprudny#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Dolgoprudny#dist2
- Weather /Russian-Federation--Moscow-Oblast--Dolgoprudny#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Dolgoprudny#sun
- Hotel /Russian-Federation--Moscow-Oblast--Dolgoprudny#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Dolgoprudny#around
- Page /Russian-Federation--Moscow-Oblast--Dolgoprudny#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data
COMMENTS
3. The Delivery Network: At initial stages, small delivery network with around 4 backup. Rather than increasing the men, we would like to invest more on proper food temperature control mechanism. using the latest version of vehicles gives good fuel economy, thus saving. 4. Sterilized packaging: The packaging.
Hospitals take a fresh look on cafeteria design
8 Ways to Improve Hospital Foodservice for Patients
LET'S FIND YOUR SOLUTION. Rapids Contract serves the United States with locations in Iowa, Minnesota, and Missouri! SUBMIT INQUIRY. TALK TO AN EXPERT | 866-875-4241. Rapids Contract offers comprehensive design for healthcare and hospital cafeterias, kitchens, serving lines, and other food service areas.
It offers a comforting choice. A menu is much easier to understand than treatment options, and ordering food is the chance to make a positive decision for yourself. Delivering on that promise of a positive outcome is the goal of great food service. Food is fundamental to the human experience, and that's doubly true for the patient experience ...
Canteen-proposal - Datta Tiffins - Free download as Word Doc (.doc), PDF File (.pdf), Text File (.txt) or read online for free. The document is a proposal from Datta Tiffins to provide canteen services at M.M. Joshi Eye Hospital. It outlines Datta Tiffins' commitment to providing hygienic and healthy food options. It details the services offered such as meals, snacks and beverages.
7 Ways to Increase Sales in Your Hospital Cafeteria
Good Taste: Designing Healthcare Dining Spaces
Modern hospital kitchen design chooses to emphasize wellness, hope, and fresh, local ingredients. Steam trays and cafeteria-style dining are things of the past. Appliances like microgreen growers allow kitchens to have access to fresh greens year-round, regardless of the climate or season. Since hospital kitchens serve the local community as ...
Context and Policy Issues. Hospital food services play a critical role in the management of all hospitalized patients. Optimal nutritional intake is considered crucial for both patient health and patient satisfaction with their hospital experience. 1, 2 Inadequate food intake throughout the course of admission may result in nutritional status deterioration, 3 which is associated with prolonged ...
Investigation of the Hospital Food and Nutrition Service (HFNS) of 37 hospitals by means of structured interviews assessing two quality control corpora, namely nutritional care quality (NCQ) and ...
2. Craft a compelling funding proposal: Develop a persuasive funding proposal that clearly outlines your hospital's mission, goals, financial needs, and potential benefits for investors or partners. Emphasize the unique value proposition and the impact your hospital can make in the healthcare industry. 3.
That's where ClickUp's Hospital Canteen SOP Template comes in! With this template, you can streamline your Standard Operating Procedures (SOPs) for the hospital canteen, ensuring that your team: Follows strict hygiene and safety protocols to prevent foodborne illnesses. Maintains proper food storage, handling, and preparation techniques.
How to Write an Effective Business Plan in Medicine
Serving our Healthcare Providers. We service America's hospital systems, doctor offices, and healthcare facilities. For these teams and visitors, taking care of the patient is their top priority. Often, they keep going and forget to grab a bite to eat. By partnering with us, we'll help make it easy for these caregivers to take a break and ...
3. Standards for kitchen design of hospital canteens Hospital canteens have very strict requirements on the place, because the hospital is a very clean place with higher sanitation standards than other places. 1. Do not choose areas prone to pollution in dry terrain, water supply and drainage conditions and power supply areas.
1. Introduction. Overweight and obesity are extremely prevalent across the UK and USA. In 2018, it was estimated that 67% of men and 60% of women in the UK had overweight or obesity [], along with 71.6% of American adults in 2015/2016 [].A high body mass index (BMI) is linked to a range of non-communicable diseases, such as hypertension, type 2 diabetes and coronary heart disease [], which has ...
Canteen Proposal | PDF | Cafeteria | Tableware
Business-Plan-For Canteen Inside Campus - Free download as Word Doc (.doc), PDF File (.pdf), Text File (.txt) or read online for free. This document outlines a business plan for a startup called Food Arcade, which will be an arcade-themed food establishment. The summary includes: 1) Food Arcade aims to be a unique dining experience that combines video games and classic arcade games with ...
Dolgoprudny is a town in Moscow Oblast, Russia, located about 20 kilometers north of Moscow city center. The town's name is derived from Russian "Долгий пруд" —a long and narrow pond situated in the northeastern part of the town. Photo: Георгий Долгопский, CC BY-SA 4.0. Ukraine is facing shortages in its brave fight ...
Dolgoprudny Geographical coordinates: Latitude: 55.9333, Longitude: 37.5 55° 55′ 60″ North, 37° 30′ 0″ East Dolgoprudny Area: 2,070 hectares 20.70 km² (7.99 sq mi): Dolgoprudny Altitude: 183 m (600 ft) Dolgoprudny Climate: Humid continental climate (Köppen climate classification: Dfb)
Contacts Warehouse and Оffice. Industrial Park Sheremetyevo. 141400, Moscow Oblast, Khimki city, Klyazma area, 1g. Phone: +7 (495) 6519231 Fax: +7 (495) 6519232
Sheremetyevo International Airport (SVO/UUEE) is an international airport located in Khimki, Moscow Oblast.Sheremetyevo serves as the main hub for Russian flag carrier Aeroflot and its branch Rossiya Airlines, Nordwind Airlines or Ural Airlines. The product is equipped with an automatic installer, which means that the scenery will be ...