- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Clinical problem...
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature
- Related content
- Peer review
This article has a correction. Please see:
- Clinical problem solving and diagnostic decision making: selective review of the cognitive literature - November 02, 2006
- Arthur S Elstein , professor ( aelstein{at}uic.edu ) ,
- Alan Schwarz , assistant professor of clinical decision making.
- Department of Medical Education, University of Illinois College of Medicine, Chicago, IL 60612-7309, USA
- Correspondence to: A S Elstein
This is the fourth in a series of five articles
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 , 2 , 3 and decision making. 4 , 5 , 6 , 7 , 8 Problem solving research was initially aimed at describing reasoning by expert physicians, to improve instruction of medical students and house officers. Psychological decision research has been influenced from the start by statistical models of reasoning under uncertainty, and has concentrated on identifying departures from these standards.
Summary points
Problem solving and decision making are two paradigms for psychological research on clinical reasoning, each with its own assumptions and methods
The choice of strategy for diagnostic problem solving depends on the perceived difficulty of the case and on knowledge of content as well as strategy
Final conclusions should depend both on prior belief and strength of the evidence
Conclusions reached by Bayes's theorem and clinical intuition may conflict
Because of cognitive limitations, systematic biases and errors result from employing simpler rather than more complex cognitive strategies
Evidence based medicine applies decision theory to clinical diagnosis
Problem solving
Diagnosis as selecting a hypothesis.
The earliest psychological formulation viewed diagnostic reasoning as a process of testing hypotheses. Solutions to difficult diagnostic problems were found by generating a limited number of hypotheses early in the diagnostic process and using them to guide subsequent collection of data. 1 Each hypothesis can be used to predict what additional findings ought to be present if it were true, and the diagnostic process is a guided search for these findings. Experienced physicians form hypotheses and their diagnostic plan rapidly, and the quality of their hypotheses is higher than that of novices. Novices struggle to develop a plan and some have difficulty moving beyond collection of data to considering possibilities.
It is possible to collect data thoroughly but nevertheless to ignore, to misunderstand, or to misinterpret some findings, but also possible for a clinician to be too economical in collecting data and yet to interpret accurately what is available. Accuracy and thoroughness are analytically separable.
Pattern recognition or categorisation
Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not depend as much on strategy as on mastery of content. Further, the clinical reasoning of experts in familiar situations frequently does not involve explicit testing of hypotheses. 3 10 , 11 , 12 Their speed, efficiency, and accuracy suggest that they may not even use the same reasoning processes as novices. 11 It is likely that experienced physicians use a hypothetico-deductive strategy only with difficult cases and that clinical reasoning is more a matter of pattern recognition or direct automatic retrieval. What are the patterns? What is retrieved? These questions signal a shift from the study of judgment to the study of the organisation and retrieval of memories.
Problem solving strategies
Hypothesis testing
Pattern recognition (categorisation)
By specific instances
By general prototypes
Viewing the process of diagnosis assigning a case to a category brings some other issues into clearer view. How is a new case categorised? Two competing answers to this question have been put forward and research evidence supports both. Category assignment can be based on matching the case to a specific instance (“instance based” or “exemplar based” recognition) or to a more abstract prototype. In the former, a new case is categorised by its resemblance to memories of instances previously seen. 3 11 This model is supported by the fact that clinical diagnosis is strongly affected by context—for example, the location of a skin rash on the body—even when the context ought to be irrelevant. 12
The prototype model holds that clinical experience facilitates the construction of mental models, abstractions, or prototypes. 2 13 Several characteristics of experts support this view—for instance, they can better identify the additional findings needed to complete a clinical picture and relate the findings to an overall concept of the case. These features suggest that better diagnosticians have constructed more diversified and abstract sets of semantic relations, a network of links between clinical features and diagnostic categories. 14
The controversy about the methods used in diagnostic reasoning can be resolved by recognising that clinicians approach problems flexibly; the method they select depends upon the perceived characteristics of the problem. Easy cases can be solved by pattern recognition: difficult cases need systematic generation and testing of hypotheses. Whether a diagnostic problem is easy or difficult is a function of the knowledge and experience of the clinician.
The strategies reviewed are neither proof against error nor always consistent with statistical rules of inference. Errors that can occur in difficult cases in internal medicine include failure to generate the correct hypothesis; misperception or misreading the evidence, especially visual cues; and misinterpretations of the evidence. 15 16 Many diagnostic problems are so complex that the correct solution is not contained in the initial set of hypotheses. Restructuring and reformulating should occur as data are obtained and the clinical picture evolves. However, a clinician may quickly become psychologically committed to a particular hypothesis, making it more difficult to restructure the problem.
Decision making
Diagnosis as opinion revision.
From the point of view of decision theory, reaching a diagnosis means updating opinion with imperfect information (the clinical evidence). 8 17 The standard rule for this task is Bayes's theorem. The pretest probability is either the known prevalence of the disease or the clinician's subjective impression of the probability of disease before new information is acquired. The post-test probability, the probability of disease given new information, is a function of two variables, pretest probability and the strength of the evidence, measured by a “likelihood ratio.”
Bayes's theorem tells us how we should reason, but it does not claim to describe how opinions are revised. In our experience, clinicians trained in methods of evidence based medicine are more likely than untrained clinicians to use a Bayesian approach to interpreting findings. 18 Nevertheless, probably only a minority of clinicians use it in daily practice and informal methods of opinion revision still predominate. Bayes's theorem directs attention to two major classes of errors in clinical reasoning: in the assessment of either pretest probability or the strength of the evidence. The psychological study of diagnostic reasoning from this viewpoint has focused on errors in both components, and on the simplifying rules or heuristics that replace more complex procedures. Consequently, this approach has become widely known as “heuristics and biases.” 4 19
Errors in estimation of probability
Availability —People are apt to overestimate the frequency of vivid or easily recalled events and to underestimate the frequency of events that are either very ordinary or difficult to recall. Diseases or injuries that receive considerable media attention are often thought of as occurring more commonly than they actually do. This psychological principle is exemplified clinically in the overemphasis of rare conditions, because unusual cases are more memorable than routine problems.
Representativeness —Representativeness refers to estimating the probability of disease by judging how similar a case is to a diagnostic category or prototype. It can lead to overestimation of probability either by causing confusion of post-test probability with test sensitivity or by leading to neglect of base rates and implicitly considering all hypotheses equally likely. This is an error, because if a case resembles disease A and disease B equally, and A is much more common than B, then the case is more likely to be an instance of A. Representativeness is associated with the “conjunction fallacy”—incorrectly concluding that the probability of a joint event (such as the combination of findings to form a typical clinical picture) is greater than the probability of any one of these events alone.
Heuristics and biases
Availability
Representativeness
Probability transformations
Effect of description detail
Conservatism
Anchoring and adjustment
Order effects
Decision theory assumes that in psychological processing of probabilities, they are not transformed from the ordinary probability scale. Prospect theory was formulated as a descriptive account of choices involving gambling on two outcomes, 20 and cumulative prospect theory extends the theory to cases with multiple outcomes. 21 Both prospect theory and cumulative prospect theory propose that, in decision making, small probabilities are overweighted and large probabilities underweighted, contrary to the assumption of standard decision theory. This “compression” of the probability scale explains why the difference between 99% and 100% is psychologically much greater than the difference between, say, 60% and 61%. 22
Support theory
Support theory proposes that the subjective probability of an event is inappropriately influenced by how detailed the description is. More explicit descriptions yield higher probability estimates than compact, condensed descriptions, even when the two refer to exactly the same events. Clinically, support theory predicts that a longer, more detailed case description will be assigned a higher subjective probability of the index disease than a brief abstract of the same case, even if they contain the same information about that disease. Thus, subjective assessments of events, while often necessary in clinical practice, can be affected by factors unrelated to true prevalence. 23
Errors in revision of probability
In clinical case discussions, data are presented sequentially, and diagnostic probabilities are not revised as much as is implied by Bayes's theorem 8 ; this phenomenon is called conservatism. One explanation is that diagnostic opinions are revised up or down from an initial anchor, which is either given in the problem or subjectively formed. Final opinions are sensitive to the starting point (the “anchor”), and the shift (“adjustment”) from it is typically insufficient. 4 Both biases will lead to collecting more information than is necessary to reach a desired level of diagnostic certainty.
It is difficult for everyday judgment to keep separate accounts of the probability of a disease and the benefits that accrue from detecting it. Probability revision errors that are systematically linked to the perceived cost of mistakes show the difficulties experienced in separating assessments of probability from values, as required by standard decision theory. There is a tendency to overestimate the probability of more serious but treatable diseases, because a clinician would hate to miss one. 24
Bayes's theorem implies that clinicians given identical information should reach the same diagnostic opinion, regardless of the order in which information is presented. However, final opinions are also affected by the order of presentation of information. Information presented later in a case is given more weight than information presented earlier. 25
Other errors identified in data interpretation include simplifying a diagnostic problem by interpreting findings as consistent with a single hypothesis, forgetting facts inconsistent with a favoured hypothesis, overemphasising positive findings, and discounting negative findings. From a Bayesian standpoint, these are all errors in assessing the diagnostic value of clinical evidence—that is, errors in implicit likelihood ratios.
Educational implications
Two recent innovations in medical education, problem based learning and evidence based medicine, are consistent with the educational implications of this research. Problem based learning can be understood as an effort to introduce the formulation and testing of clinical hypotheses into the preclinical curriculum. 26 The theory of cognition and instruction underlying this reform is that since experienced physicians use this strategy with difficult problems, and since practically any clinical situation selected for instructional purposes will be difficult for students, it makes sense to provide opportunities for students to practise problem solving with cases graded in difficulty. The finding of case specificity showed the limits of teaching a general problem solving strategy. Expertise in problem solving can be separated from content analytically, but not in practice. This realisation shifted the emphasis towards helping students acquire a functional organisation of content with clinically usable schemas. This goal became the new rationale for problem based learning. 27
Evidence based medicine is the most recent, and by most standards the most successful, effort to date to apply statistical decision theory in clinical medicine. 18 It teaches Bayes's theorem, and residents and medical students quickly learn how to interpret diagnostic studies and how to use a computer based nomogram to compute post-test probabilities and to understand the output. 28
We have selectively reviewed 30 years of psychological research on clinical diagnostic reasoning. The problem solving approach has focused on diagnosis as hypothesis testing, pattern matching, or categorisation. The errors in reasoning identified from this perspective include failure to generate the correct hypothesis; misperceiving or misreading the evidence, especially visual cues; and misinterpreting the evidence. The decision making approach views diagnosis as opinion revision with imperfect information. Heuristics and biases in estimation and revision of probability have been the subject of intense scrutiny within this research tradition. Both research paradigms understand judgment errors as a natural consequence of limitations in our cognitive capacities and of the human tendency to adopt short cuts in reasoning.
Both approaches have focused more on the mistakes made by both experts and novices than on what they get right, possibly leading to overestimation of the frequency of the mistakes catalogued in this article. The reason for this focus seems clear enough: from the standpoint of basic research, errors tell us a great deal about fundamental cognitive processes, just as optical illusions teach us about the functioning of the visual system. From the educational standpoint, clinical instruction and training should focus more on what needs improvement than on what learners do correctly; to improve performance requires identifying errors. But, in conclusion, we emphasise, firstly, that the prevalence of these errors has not been established; secondly, we believe that expert clinical reasoning is very likely to be right in the majority of cases; and, thirdly, despite the expansion of statistically grounded decision supports, expert judgment will still be needed to apply general principles to specific cases.
Series editor J A Knottnerus
Preparation of this review was supported in part by grant RO1 LM5630 from the National Library of Medicine.
Competing interests None declared.
“The Evidence Base of Clinical Diagnosis,” edited by J A Knottnerus, can be purchased through the BMJ Bookshop ( http://www.bmjbookshop.com/ )
- Elstein AS ,
- Shulman LS ,
- Bordage G ,
- Schmidt HG ,
- Norman GR ,
- Boshuizen HPA
- Kahneman D ,
- Sox HC Jr . ,
- Higgins MC ,
- Mellers BA ,
- Schwartz A ,
- Chapman GB ,
- Sonnenberg F
- Glasziou P ,
- Pliskin J ,
- Brooks LR ,
- Coblentz CL ,
- Lemieux M ,
- Kassirer JP ,
- Kopelman RI
- Sackett DL ,
- Haynes RB ,
- Guyatt GH ,
- Richardson WS ,
- Rosenberg W ,
- Tversky A ,
- Fischhoff B ,
- Bostrom A ,
- Quadrell M J
- Redelmeier DA ,
- Koehler DJ ,
- Liberman V ,
- Wallsten TS
- Bergus GR ,
10 Evidence-Based Practice Examples

Evidence-based practice is, as the name suggests, the idea that occupational practices should be based on scientific evidence.
Evidence-based practices were first introduced in medicine. Since then, they have become common in nursing (Ellis, 2016), education (Pring & Thomas, 2004), management, psychology (Hersen & Sturmey, 2012), architecture, urban planning, public policy (Loversidge & Zurmehly, 2019), law, philanthropy, and other fields.
A simple example of evidence-based practice is when a therapist chooses to pivot to a new therapy strategy with a patient after receiving compelling new evidence in the academic literature that demonstrates its effectiveness.
Definition of Evidence-Based Practice
Evidence-based practice requires a systematic approach to the translation of research findings into practice.
Supporters of evidence-based practice claim that it can to bridge the gap between research and practical application (Reynolds, 2000, p. 19).
Evidence-based practices distinguish between research that has immediate practical significance and research that doesn’t.
In the case of medicine, this:
“….helps doctors to ignore the vast quantities of clinical research which are not of direct relevance to practice” (Reynolds, 2000, p. 19).
Evidence-based medicine, which is where evidence-based practice originated, consists of five explicit steps (Reynolds, 2000, pp. 22-23):
- A Specific Question: First, the clinician, faced with a patient or group of patients, constructs a specific question concerning their care. This could relate to the diagnosis of the problem, the most effective treatments and their possible side-effects, or the best method of delivering services to meet patients’ needs.
- Finding the Best Evidence: The second stage consists of finding, as efficiently as possible, the best evidence to answer the clinical question.
- Evaluating the Validirty and Usefulness: Third, the clinician evaluates the evidence for its validity and usefulness.
- Applying the Practice: Fourth, the results are applied to the specific patient or group of patients.
- Evaluating the Practice: Finally, the outcome of the intervention is evaluated.
Evidence-based practices in other fields tend to follow a similar process that is modified to fit the context.
Evidence-Based Practice Examples
1. hand hygeine (healthcare).
Hand washing in hospitals emerged rather late in human history – around the 1840s according to the History Channel . This was based on some rather gruesome evidence.
Doctors began to notice that mothers’ deaths during childbirth were far higher in the doctors’ wards (about 98.4 deaths per 1000 births) compared to midwives’ wards (36.2 per 1000 births).
One Hungarian doctor, Ignaz Semmelweis, started conducting some tests to see why women were dying at such high rates in doctors’ wards. At first, he thought the priests’ bells were scaring women as priests would walk through doctors’ wards only. But rerouting the priests did nothing.
Then, he noticed that the doctors did a range of tasks during their day the midwives didn’t – including handling cadavers. He hypothesized that the doctors might be bringing matter from the cadavers into the wards on their hands. So, he made them wash their hands.
The result was fantastic – deaths during childbirth plummeted in the doctors’ wards.
Interestingly, it took Semmelweis a long time to convince other European doctors to follow his evidence-based practice, but eventually, his arguments won everyone over.
2. Cognitive Behavioral Therapy (Psychotherapy)
Cognitive Behavioral Therapy (CBT) is a psychological treatment grounded in empirical research.
It aims to help people re-frame their thoughts by identifying when a thought might be leading them astray. Amd teaches them to reframe their thoughts into ones that are more productive.
This therapy has been demonstrated to be effective for a range of disorders, including depression, anxiety disorders, and eating disorders.
Therapists and councillors have been compelled to bring CBT into their practice, and often replace medicinal treatments with CBT, due to substantial evidence that it is as effective as, or more effective than, psychiatric medications.
This intervention, then, is an example of how a therapeutic treatment is used because evidence suggests it’s highly effective.
3. Play-Based Learning (Education)
There was a period of time where play in the classroom was considered unacceptable – children should learn through repetition and rote learning!
But learning theorists in the early- to mid-20th Century, including Maria Montessori, Rudolph Steiner, and Mildred Parten, presented new evidence that play-based learning supports children’s cognitive development .
Following this evidence, a range of school curricula around the world have proactively encouraged play as a means for stimulating learning and development in the classroom.
4. Hot Spots Policing (Criminal Justice)
Hot spots policing focuses on small geographic areas or places, usually in urban settings, where crime is concentrated.
The majority of criminal events occur in these relatively few places, often termed ‘hot spots.’
Criminologists have found ample evidence that focussing resources on these hot spots can help to reduce crime rates, improve public safety, and more efficiently distribute police resources.
As a meta-analysis by Braga, Papachristos and Hureau (2014) concludes:
“The results of our research suggests that hot spots policing generates small but noteworthy crime reductions, and these crime control benefits diffuse into areas immediately surrounding targeted crime hot spots.”
Strategies used during hot spot policing include increasing police patrols, and problem-oriented policing strategies. Nevertheless, strategies need to be carefully catered in order to ensure prejudice, profiling, and discrimination do not occur.
5. Motivational Interviewing (Social Work)
Motivational Interviewing (MI) is a counseling approach designed to create safe spaces for clients to share their thoughts, have them heard with empathy, and lastly, to motivate clients to achieve change in their lives.
The eventual goal is to instil intrinsic motivation within the client, which can lead to long-term changes in behavior.
The concept has gained prominence in social work practice because a substantial corpus of evidence has emerged underpinning its effectiveness.
For example, two meta-analyses have found MI to effect change for clients:
“MI produced statistically significant, durable results” (Lundahl et al., 2010)
“Psychologists and physicians obtained an effect in approximately 80% of the studies, while other healthcare providers obtained an effect in 46% of the studies. When using motivational interviewing in brief encounters of 15 minutes, 64% of the studies showed an effect.” (Rubak et al., 2005)
6. Dialectical Behavioral Therapy (Psychology)
DBT is a cognitive-behavioral treatment developed by Marsha Linehan for individuals with borderline personality disorder who engage in self-harming behaviors.
DBT combines principles of behavioral psychology, which are used to promote change, with mindfulness and acceptance strategies from eastern meditation traditions.
The efficacy of DBT has been shown in numerous randomized controlled trials for a variety of behavioral, emotional, and cognitive outcomes.
7. Formative Assessment (Education)
Formative assessment is an educational approach that involves testing students’ learning and development part-way through a unit of work.
It generally involves giving students pop quizzes or in-class assessments, followed by feedback on their work that they can use to identify weaknesses to work on prior to a final test.
It’s also extensively used to adjust teaching strategies mid-stream to better suit students’ needs.
Meta-analyses consistently find that it can help support student learning and outcomes:
“…meta-analysis research found consistent positive effects of formative assessment on student learning” (Lee et al., 2020, p. 125)
This ongoing, interactive assessment allows teachers to identify and address gaps in students’ understanding, helping students to learn more effectively. Evidence indicates that formative assessment can significantly enhance student learning.
8. Action Research (Various Fields)
Action research embraces the principles of evidence-based practice by empowering practitioners to gather their own evidence in their own contexts.
It is a method of research that involves practitioners conducting studies of their own practice, often in collaboration with their clients, patients, and students.
The action researcher conducts analysis of their own practice then uses the feedback gathered during their research process to make adjustments to their practice. Following this, more action research studies will take place, with scholars continuing to update and improve their work over time with the support of evidence collected during their research.
One big benefit of an action research approach is that the data is collected in their own settings, making the findings of the case studies extremely relevant to their practice.
9. Effective Altruism (Philanthropy)
Effective Altruism is a philosophy and social movement that advocates for making the world a better place in the most effective way possible.
It is unique in the fact that it researches the most effective companies to donate to, based on factors like bang-for-your-buck, how much money is wasted on administration and marketing, and so on. The idea is to ensure your philanthropic donations do the most good in the world.
Often, it finds that people should donate to highly efficient charities who work on causes such as global poverty in the developing world, where one dollar can go a long way in saving and improving lives.
10. Use of Checklists in Surgery (Healthcare)
Checklists are used in medicine, particularly in surgical procedures, to reduce errors and improve patient safety.
The WHO’s Surgical Safety Checklist is a prominent example. It includes a series of checks to be done before induction of anesthesia, before the incision of the skin, and before the patient leaves the operating room.
The introduction of this checklist in healthcare has resulted in significant reductions in both morbidity and mortality (Kramer & Drews, 2016), leading to its widespread adoption.
Evidence-based practice has underpinned significant improvements in outcomes across multiple professions, from healthcare to social work, to education. By basing your work on evidence rather than anecdote or assumptions, we can have higher standards in our professions and better serve our communities. However, this comes with burdens, such as the need for ongoing professional development and consistent action research to assess whether outcomes of interventions match our expectations.
Braga, A. A., Papachristos, A. V., & Hureau, D. M. (2014). The effects of hot spots policing on crime: An updated systematic review and meta-analysis. Justice quarterly , 31 (4), 633-663.
Ellis, P. (2016). Evidence-based Practice in Nursing . SAGE Publications.
Geddes, J. (2000). Evidence-Based Practice in Mental Health. In Trinder, L., & Reynolds, S. (2000). Evidence-Based Practice: A Critical Appraisal . Blackwell.
Guyatt, G., Cairns, J., Churchill, D., Cook, D., Haynes, B., Hirsh, J., Irvine, J., Levine, M., Levine, M., Nishikawa, J., Sackett, D., Brill-Edwards, P., Gerstein, H., Gibson, J., Jaeschke, R., Kerigan, A., Neville, A., Panju, A., Detsky, A., … Tugwell, P. (1992). Evidence-Based Medicine: A New Approach to Teaching the Practice of Medicine. JAMA , 268 (17), 2420–2425. https://doi.org/10.1001/jama.1992.03490170092032
Lee, H., Chung, H. Q., Zhang, Y., Abedi, J., & Warschauer, M. (2020). The effectiveness and features of formative assessment in US K-12 education: A systematic review. Applied Measurement in Education , 33 (2), 124-140.
Hersen, M., & Sturmey, P. (2012). Handbook of Evidence-Based Practice in Clinical Psychology, Adult Disorders . John Wiley & Sons.
Hjørland, B. (2011). Evidence-based practice: An analysis based on the philosophy of science. Journal of the American Society for Information Science and Technology , 62 (7), 1301–1310. https://doi.org/10.1002/asi.21523
Ioannidis, J. P. A., Fanelli, D., Dunne, D. D., & Goodman, S. N. (2015). Meta-research: Evaluation and Improvement of Research Methods and Practices. PLoS Biology , 13 (10), e1002264. https://doi.org/10.1371/journal.pbio.1002264
Kramer, H. S., & Drews, F. A. (2017). Checking the lists: A systematic review of electronic checklist use in health care. Journal of biomedical informatics , 71 , S6-S12.
Loversidge, J. M., & Zurmehly, J. (2019). Evidence-Informed Health Policy . Sigma Theta Tau.
Lundahl, B. W., Kunz, C., Brownell, C., Tollefson, D., & Burke, B. L. (2010). A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on social work practice , 20 (2), 137-160.
MacAskill, W. (2017). Effective Altruism: Introduction. Essays in Philosophy , 18 (1), 1–5. https://doi.org/10.7710/1526-0569.1580
MacAskill, W., & Pummer, T. (2020). Effective Altruism. In International Encyclopedia of Ethics (pp. 1–9). John Wiley & Sons, Ltd. https://doi.org/10.1002/9781444367072.wbiee883
Parry, G. (1992). Improving psychotherapy services: Applications of research, audit and evaluation. British Journal of Clinical Psychology , 31 , 3–19. https://doi.org/10.1111/j.2044-8260.1992.tb00964.x
Pring, R., & Thomas, G. (2004). Evidence-based Practice in Education . McGraw-Hill Education (UK).
Reynolds, S. (2000). The Anatomy of Evidence-Based Practice: Principles and Methods. In Trinder, L., & Reynolds, S. (2000). Evidence-Based Practice: A Critical Appraisal . Blackwell.
Rosenberg, W., & Donald, A. (1995). Evidence based medicine: An approach to clinical problem-solving. BMJ (Clinical Research Ed.) , 310 (6987), 1122–1126. https://doi.org/10.1136/bmj.310.6987.1122
Rubak, S., Sandbæk, A., Lauritzen, T., & Christensen, B. (2005). Motivational interviewing: a systematic review and meta-analysis. British journal of general practice , 55 (513), 305-312.
Sackett, D. L., Rosenberg, W. M. C., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. BMJ , 312 (7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71
Smolen, P., Zhang, Y., & Byrne, J. H. (2016). The right time to learn: Mechanisms and optimization of spaced learning. Nature Reviews. Neuroscience , 17 (2), 77–88. https://doi.org/10.1038/nrn.2015.18
Sutherland, W. (2003). Evidence-based Conservation. Conservation in Practice , 4 (3), 39–42. https://doi.org/10.1111/j.1526-4629.2003.tb00068.x
Tabibian, B., Upadhyay, U., De, A., Zarezade, A., Schölkopf, B., & Gomez-Rodriguez, M. (2019). Enhancing human learning via spaced repetition optimization. Proceedings of the National Academy of Sciences , 116 (10), 3988–3993. https://doi.org/10.1073/pnas.1815156116
Tolin, D. F. (2010). Is cognitive–behavioral therapy more effective than other therapies?: A meta-analytic review. Clinical psychology review , 30 (6), 710-720.

Tio Gabunia (B.Arch, M.Arch)
Tio Gabunia is an academic writer and architect based in Tbilisi. He has studied architecture, design, and urban planning at the Georgian Technical University and the University of Lisbon. He has worked in these fields in Georgia, Portugal, and France. Most of Tio’s writings concern philosophy. Other writings include architecture, sociology, urban planning, and economics.
- Tio Gabunia (B.Arch, M.Arch) #molongui-disabled-link 6 Types of Societies (With 21 Examples)
- Tio Gabunia (B.Arch, M.Arch) #molongui-disabled-link 25 Public Health Policy Examples
- Tio Gabunia (B.Arch, M.Arch) #molongui-disabled-link 15 Cultural Differences Examples
- Tio Gabunia (B.Arch, M.Arch) #molongui-disabled-link Social Interaction Types & Examples (Sociology)

Chris Drew (PhD)
This article was peer-reviewed and edited by Chris Drew (PhD). The review process on Helpful Professor involves having a PhD level expert fact check, edit, and contribute to articles. Reviewers ensure all content reflects expert academic consensus and is backed up with reference to academic studies. Dr. Drew has published over 20 academic articles in scholarly journals. He is the former editor of the Journal of Learning Development in Higher Education and holds a PhD in Education from ACU.
- Chris Drew (PhD) #molongui-disabled-link 25 Positive Punishment Examples
- Chris Drew (PhD) #molongui-disabled-link 25 Dissociation Examples (Psychology)
- Chris Drew (PhD) #molongui-disabled-link 15 Zone of Proximal Development Examples
- Chris Drew (PhD) #molongui-disabled-link Perception Checking: 15 Examples and Definition
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Exercises in Clinical Reasoning
Diagnostic Schema
- DS Introduction
- Case 1: 31M with pleuritic chest pain
- Teaching Slides
- Instructor Guide
- Case 2: 27M with DOE
Introduction
A diagnostic schema is a cognitive tool that allows clinicians to systematically approach a clinical problem by providing an organizing scaffold.
For example, a commonly used schema for acute kidney injury (AKI) separates this problem into pre-renal, intrinsic, and post-renal causes. By approaching AKI using these categories, clinicians can systematically access and explore individual illness scripts as potential diagnoses.
- Because they can be retrieved and manipulated as a single item within the working memory, schema also help clinicians to manage their cognitive load and maintain the bandwidth for effective problem-solving.
Examples of Basic Diagnostic Schema
Bilateral lower extremity edema.
1. Cardiac 2. Liver 3. Renal 4. Vascular 5. Lymphatic
1. Blood Loss 2. Decreased Production 3. Increased Destruction
Intrinsic Renal Injury in AKI
1. Glomerular 2. Tubular 3. Interstitial 4. Vascular
Benefits of Diagnostic Schema
Tether diagnostic thinking to a logical framework.
A logical framework (e.g. structural/anatomic, physiologic, systems-based) is more easily remembered.
Avoid missing diagnoses
A diagnostic schema helps clinicians avoid leaving off categories of illnesses, or anchoring on the most familiar diagnoses.
Trigger search for differentiating features
Diagnostic schema can help trigger clinicians to perform differentiating historical or physical exam maneuvers to refine the differential diagnosis. (e.g. the schema for volume overload triggers the clinician to check the jugular venous pressure as that will help to differentiate among the potential diagnostic categories for this problem)
Teach others how to reason
A schema is easily an efficient way to teach others how to approach a clinical problem ("think aloud").
Creating Diagnostic Schema
Through deliberate practice, learners adapt and individualize their schema — tying these frameworks to prior clinical knowledge and experience, which keeps them robust and accessible. Over time individuals may find that collapsing certain categories, or creating new ones, allows a schema to “work” best for them.
Finding Schemas
- Symptom to Diagnosis: An Evidence Based Guide by Adam S. Cifu and Scott Stern
- The Clinical Problem Solvers (podcast)
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Cases : Clinical Problem-Solving Cases
Harriet S.MeyerMD, Contributing EditorJonathan D.EldredgeMLS, PhD, Journal Review EditorRobertHoganMD, adviser for new media
Not Available
Developing practical clinical problem-solving skills is an important professional endeavor for health care providers. Patient management problems and clinical problem-solving cases have been incorporated into certifying examinations and continuing education programs. Such simulations, in print or electronic form, allow users to select diagnostic or treatment options for hypothetical patients with immediate feedback on management decisions. The course of such simulated patient cases depends on user choices. Patient simulations have been popular and effective but difficult to develop.
Cases : Clinical Problem-Solving Cases . JAMA. 2000;283(13):1755–1756. doi:10.1001/jama.283.13.1755-JBK0405-4-1
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
How to Write a Clinical Problem Solving Manuscript
- First Online: 04 November 2016
Cite this chapter

- Gurpreet Dhaliwal 4 &
- Gabrielle N. Berger 5
1599 Accesses
A clinical problem solving (CPS) exercise highlights the process by which an experienced clinician approaches a diagnostic puzzle. Compared to a traditional case report, a CPS article places greater emphasis on conveying and analyzing clinical reasoning. CPS manuscripts are more likely to be published if they adhere to a standard framework. Identifying a suitable case and constructing a CPS manuscript requires thoughtful planning and commitment. Writing and editing the case discussion, selecting coauthors, and formatting the manuscript may take up to a year from start to finish. This chapter is a step-by-step guide to writing a successful CPS manuscript.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Tarter L, Yazdany J, Moyers B, Barnett C, Dhaliwal G. The Heart of the Matter. N Engl J Med. 2013;368(10):944–50. doi: 10.1056/NEJMcps1114207 .
Article CAS PubMed Google Scholar
Keenan CR, Dhaliwal G, Henderson MC, Bowen JL. A 43-year-old woman with abdominal pain and fever. J Gen Intern Med. 2010;25(8):874–7. doi: 10.1007/s11606-010-1372-3 .
Article PubMed PubMed Central Google Scholar
Download references

Author information
Authors and affiliations.
Department of Medicine, University of California San Francisco, San Francisco, CA, USA
Gurpreet Dhaliwal
Division of General Internal Medicine, Department of Medicine, University of Washington School of Medicine, Seattle, WA, USA
Gabrielle N. Berger
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gurpreet Dhaliwal .
Rights and permissions
Reprints and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Dhaliwal, G., Berger, G.N. (2017). How to Write a Clinical Problem Solving Manuscript. In: Writing Case Reports. Springer, Cham. https://doi.org/10.1007/978-3-319-41899-5_10
Download citation
DOI : https://doi.org/10.1007/978-3-319-41899-5_10
Published : 04 November 2016
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-41898-8
Online ISBN : 978-3-319-41899-5
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Lesson 3: Clinical Problem Solving
- 1 UNIT 3: CLINICAL PROBLEM SOLVING
- 2.1 3.1: TAKING THE PATIENT’S HISTORY
- 2.2 3.2: PHYSICAL EXAMINATION
- 2.3 3.3: FURTHER INVESTIGATIONS
- 3.1 3.4 FEVERS
- 4 Assignment
UNIT 3: CLINICAL PROBLEM SOLVING
Introduction:.
Welcome to the first unit of the Child Health Course. In this unit, you will be acquainted with the basics of clinical problem solving. Clinical problem solving is the process of making a correct diagnosis. That is starting from a problem and working it out until you establish what is wrong with your patient and then solving it. It involves taking your patient’s history, carrying out a physical examination and making relevant investigations to establish what the problem is. Once this is identified then you need plan how to manage the problem (ie. the solutions).
Please read each section thoroughly and do the activities as you go. Take as much time as you need to do each activity. If you have any difficulty completing any activity, study the section again and if you still cannot do.the activity write to your tutor for assistance.
3.1: TAKING THE PATIENT’S HISTORY
In clinical problem solving, it is important that you begin with history taking.
Check your answers as you read on.
History taking can be defined as a systematic inquiry into the patient or client’s life. It is the process of obtaining relevant information from the patient or patient’s caretaker (such as the mother or father) for the purpose of making a diagnosis.
History taking in children is different and more detailed than in adults. Often you must take the history from the mother, the father or guardian. Ordinarily, it is the mother that brings her child to the clinic, so we will refer only to the mother in our discussion. If the father or another guardian brings the child, the procedure remains the same.
You should sit next to the mother and child as you take the history. Do not have any barrier, such as a desk, between you and them. In this position, you can then easily begin examining the child while he or she is sitting on the mother’s lap. Watch what the child is doing while you take the history, as you can learn a lot from observation. If the child is breastfed, encourage the mother to feed the child while you take the history.
What are the components of a child's history?
The following is a list of the components of a child's history:
- Identification data
- Presenting complaint
- History of presenting complaints
- Systemic review
- Past medical history
- Treatment history
- Developmental milestones
- Nutritional history
- Immunisation history
- Family social history
We shall now look at each of these components in more detail:
a) Identification data: This is the child's personal information. It includes the child’s names, age, sex, tribe, religion, next of kin (parents) and address (residential), and the date of seeing the child in the health unit. After all these have been recorded the child should then be weighed and the weight recorded also.
b) Presenting complaint: The presenting complaint is the problem(s) that has caused the caretaker to bring the child for medical help. For instance, it may be:
- fever (the child feels hot)
It is important to establish the duration of each complaint. For example, if the child has a cough, ask "How long has the child been coughing?" If there is more than one complaint, ask which complaint came first, which was next and finally, which came last. You should then present these complaints in order beginning with the one that came first.
When writing down the patient’s history, always use the caretaker’s words. For instance, if the mother says that the child feels hot, then write: “the child feels hot.” Avoid describing it as a high temperature.
c) History of the presenting complaint: The history of the presenting complaint is additional information about the presenting complaint. You must ask more questions about the symptoms that the mother has mentioned. This means asking questions like:
- “When did the illness begin?”
- “How did it start?”
- “Was it sudden or was the onset slow?”
Find out when each symptom began and whether it seems to be getting better or worse. Ask about associated symptoms. For example, a cough may present with difficulty in breathing, diarrhoea may present with blood in stool or with vomiting. Fever may be constant or on and off. Ask and then listen until the mother has finished talking . Avoid interrupting her as much as possible to be sure you have all the information she can offer. You can then ask leading questions to help her remember what she might have forgotten. She may answer in the positive or negative.
d) Systemic review
In a systemic review we try to find out how the presenting complaint has affected the child's other systems like feeding/drinking habits, respiration, playing, and sleeping as well as gastrointestinal and urinary habits. This is also important in excluding symptoms from other systems or symptoms shared by many systems. This may also remind a mother of important symptoms she had earlier left out.
For ALL sick children aged 2 months up to 5 years, check for these general danger signs:
Ask the caretaker:
- Is the child able to drink or breastfeed?
- Does the child vomit everything?
- Has the child had convulsions?
Look and determine:
- Is the child lethargic or unconscious?
- Is the child breathing fast?
- Is the child dehydrated?
If the answer is “yes” to any of the above questions, the child has one or more of the general danger signs and needs URGENT attention. Refer appropriately. See Appendix 1 for a chart on how to assess and classify the sick child age 2 months up to 5 years.
e) Past medical history: A past medical history is important. Ask:
- Has the child had the same illness before? This information is important because some illnesses can be recurrent, such as convulsions;
- What other illnesses has the child had in the past? This question is important because the present illness may be a complication of a previous illness. For instance, a child may be malnourished as a complication of measles.
- Ask if the child has had hospital admission and if so for what.
- Ask to see the child’s old medical forms or medical card. This is a good way to get an accurate past medical history.
f) Treatment history: Before mothers seek professional attention, they will often try other remedies at home or from other sources. Always ask about any other treatment received by the child during the present illness before prescribing more. Determine if there has been any response to this treatment
g) Immunisation history: Because of the importance of disease prevention, particularly the six killer diseases, it is absolutely necessary to ascertain the immunisation status of every child. Ask every mother about vaccines already received by the child. Look at the immunization card to ascertain which immunization the child has received and has not received.
h) Nutritional history: Malnutrition is a risk factor for all types of illness, especially in children. Well-nourished children rarely fall sick. Therefore it is important to find out:
- If the child is still breastfed
- If the child is breastfed exclusively
- How often it is breastfed
- What other foods the child receives, how much and how often
- Whether there are any feeding problems
- Find out whether the child is bottle fed, especially those with diarrhoeal illness
Whatever interferes with a child’s nutrition has a direct bearing on the child’s health and should be dealt with.
i) Developmental history: In normal childhood growth and development there are certain milestones to be passed at certain ages. The following is a brief summary of developmental assessment needed:
Ask about the antenatal care and the delivery of the child:
- Did the mother attend antenatal care?
- Did the mother suffer any illnesses during pregnancy?
- Was the delivery spontaneous or assisted?
- Was it a home or hospital delivery?
- Was the child born at term?
- Were there any complications during or after delivery?
- What was the birth weight?
- Did the child cry at birth?
- Did the child breathe spontaneously at birth?
All of this information is needed for assessing the health of the child.
Table 1.1: Developmental Milestones
j) Family and social history: It is important to obtain information about the health of the rest of the family. Ask:
- Is anyone else in the family ill?
- What is the general health of other siblings? Find out if any have died.
- Where and with whom does the family live?
- Are both parents alive and staying together?
- Any other family diseases, such as sickle cell disease, asthma, etc.
- Is family income adequate and what is the source of their income?
- Does the family have an adequate source of food, water and other resources?
- What is the source of water
Family and social status can influence a child’s health and should not be left out in history taking.
POINTS TO NOTE WHEN TAKING CHILDRENS HISTORY: In taking the history of a child, it is important to treat the caretaker with respect and courtesy. When a child is sick, the caretaker feels worried and may be impatient about getting treatment. The following points are important to keep in mind when taking a child’s medical history.
- Always greet the mother appropriately and ask her to sit with her child.
- Establish good communication with the mother from the beginning of the visit and let her feel at ease with no embarrassment.
- Listen carefully to what the mother tells you. This will show that you are taking her concerns seriously.
- Use words the mother understands. When necessary, paraphrase your questions.
- Give the mother time to answer the questions. For example, she may need time to decide if the symptom or sign you asked about is present or not.
- Ask additional questions when the mother is not sure about an answer.
- Use good questioning techniques. Ask open-ended questions, encouraging the mother to give you the information you need. Avoid questions that call for just a “Yes” or “No” response.
- With babies and young children you have to take the history from the parent or guardian who brings the child. Older children can speak for themselves, but you need to hear the parent’s story as well. When speaking to a child, address him or her by name.
An accurate history is the first and most important step in making a correct diagnosis and will direct further investigations as well as the management of an illness. History taking accounts for over 70% of the diagnosis. It should precede both physical examination and treatment of all except extremely ill patients like those with convulsions or coma.
Now that you have finished reading the material on taking the medical history of a child, you are ready for the next activity.
3.2: PHYSICAL EXAMINATION
Conducting a physical examination is the next step after history taking. It is guided by the history that has been taken. Complete the following activity before proceeding with the reading material.
Did your answer include any of the followings? Proceed with the reading.
A health worker conducts a physical examination in order to assess the bodily state of a patient or client by doing the followings:
a) Inspection: Look and see. This is the first step.
b) Palpation: Touch and feel.
c) Percussion: Use the middle fingers of both hands to elicit resonance in cavities like the thoracic and abdominal cavities.
d) Auscultation: Use a stethoscope to detect sounds in the thoracic and abdominal cavities. The same is used for detecting pulsation, such as the brachial pulse when taking blood pressure.
Physical examinations are classified, or divided, into two main types:
- General examination
- Systemic examination
While this classification applies to adults there are some modifications when it comes to children. In carrying out a physical examination of a child, ensure that:
- The child is comfortable
- There is adequate light
- It is carried out gently
- The child is calm
- You talk to him as you proceed with the examination
- The child has all the clothes removed
EXAMINING A CHILD:
Examining a child begins as soon as the child arrives in your clinic. Notice what the child is doing while you talk to the mother. Is he/she lively, playing, interested in its surroundings? Or is the child obviously ill or sick looking? Observe how well a baby feeds when put to the breast.
Do as much as you can without taking the child away from the mother. Examine small children while they are sitting on the mother’s lap.
Leave until last that part of the examination that is likely to make the child cry. For example, babies and small children must be completely undressed for a thorough physical examination, but this sometimes makes them cry. Therefore, observe carefully, count respiratory rate and listen with stethoscope before undressing the baby.
ALWAYS take the temperature. In babies and infants below one year of age the most reliable way of taking the temperature is rectally. If you are the one to take the temperature and you decide to use this method, do it at the end of the examination. The normal range of temperature is 36.5 - 37.5oC.
You may not need to do a complete examination for every child but the following FIVE points should always be checked.
- Assess the general condition of the child
- Look and listen to the way the child is breathing
- Count the respiratory rate
- Look for signs of dehydration, anaemia, wasting, oedema and cyanosis;.
- Check for neck stiffness
ASK YOURSELF: How does the child look?
- Is she or he well? A bit unwell? Or severely ill?
- Is the child fully alert? Drowsy/lethargic? Unconscious?
If a sick child seems to be sleeping, awaken the child to make sure he or she is not unconscious at the end of your examination. Remember to count the respiratory rate first.
EXAMINATION PROCEDURE
The following procedure can be used in examining a child:
- Inspect (look at) how the child is breathing.
- Count the respiratory rate.
- 60/min and above is fast breathing in children up to the age of 2 months.
- 50/min and above is fast breathing in children aged 2 months up to one year.
- 40/mm and above is fast breathing in children aged 1-5 years.
Fast breathing is a sign of serious illness and may be caused by any of the following:
a) Pneumonia: Fast, shallow breathing, grunting, flaring of the nostrils and fever. Chest indrawing may be present in severe pneumonia.
b) Asthma: Recession between and below the ribs plus wheezing, in children above 2 years of age.
c) Bronchiolitis: Recession and wheezes or crackles (in an infant under 15 months).
d) Severe dehydration/Acidosis: Rapid, deep breathing in a clear chest.
4. Palpate the abdomen for:
- Any areas of tenderness or masses
- Enlargement of the liver or spleen
5. Check the genitalia. Look for hernia. Palpate both testes in males.
6. Check for anaemia in the conjunctive, on the tongue, nailbed, palm, etc.
7. Check for jaundice in the white part of the eye and the palms and soles.
8. Check for cyanosis in the eye, palms and soles even if it is difficult in dark skinned children;
9. Check for dehydration.
- Sunken eyes
- Very slow skin pinch (a slow pinch that goes back very slowly)
- Failure to drink or drinking poorly
- Slow skin pinch
- Drinking eagerly
10. Palpate for enlarged lymph nodes in the neck, armpits and groin.
11. Palpate for tenderness or swelling of bones or joints. Make sure the child is moving all four limbs normally.
12. Inspect the ears using an auriscope. In otitis media you will see a bright red ear drum with or without pus. In case of a foreign body in the ears, refer appropriately.
13. Inspect the throat using a torch and spatula. Are the tonsils inflamed? Is there oral thrush, koplik spots or any other abnormality?
14. Finally, if the child is unable to sit, stand, walk or if the child’s movements do not seem normal, first rule out neck stiffness. If the child cannot perform these movements because of illness, the child may be very seriously ill. Refer appropriately.
At the end of the physical examination, you must decide what is wrong with the patient. You must also decide on management and follow up. It is important to explain your decision to the mother. This is also a good time to give health education. Time spent talking after you have made your diagnosis is time well spent. Mothers frequently imagine that their children are much worse than they are, and this is because they have not been reassured. Parents have a right to know about the condition of their child as well as the required treatment. They will have confidence in you if you give them this information.
Now that you have read the section on physical examination, you are ready to complete the next activity.
3.3: FURTHER INVESTIGATIONS
When you have taken the patient’s history and conducted a physical examination, you may find it necessary to confirm your suspicion with some sort of investigations. An investigation can range from a simple laboratory procedure to radiological scanning or other complex procedure.
There are a number of investigations that are commonly carried out at health facilities. These are listed below, along with the reasons for each investigation:
1. Blood slide for malaria parasites could be used for the following reasons:
- Diagnosis of malaria
- Rule out malaria in a child with fever
- As a follow up of treatment for malaria
- For screening donated blood
- To investigate anaemia
A malaria blood slide may be a thick blood film used for screening for parasites, especially when they may be scanty, or for counting malaria parasites. A thin film may also be used for identification of the various species of malaria parasites, or for typing of the parasites.
2. White blood cell (WBC) total count and differential. This may be ordered for
- Pyrexia of unknown origin (P.U.O.)
- Lymphocyte count
3. VDRL/RPR. This can be used to:
- Diagnose syphilis
- Screening in antenatal clinics
- Screening of contact
- Screening for blood transfusion.
4. Haemoglobin (Hb) estimation. Haemoglobin is the red pigment inside red blood cells that transports oxygen from the lungs to body tissues, and carries carbon dioxide from the tissues to the lungs for excretion. Reduction in the circulating Hb below normal levels is referred to as anaemia . Reasons for Hb estimation are:
- To diagnose anaemia
- To screen for anaemia during pregnancy, assess blood donors and in medical examination
- To monitor and follow up during treatment for anaemia
Normal ranges of Hb are:
- Males: 13.0 - 18.0g/dl
- Females: 12.0 - 16.0g/dl
- Infants: 13.5 - 19.5g/dl
- Children 1-7 yrs: 11.0 - 14.0g/dl
5. Urinalysis. Reasons for carrying out urinalysis are
- Nephrotic syndrome
- Glomerulonephritis
- To diagnose Schistosoma Haematobium
- To check bleeding in the urinary tract
- To rule out TB of the urinary tract.
- To rule out urinary tract infections (UTI)
6. Stool for microscopic examination. Stool may be examined in cases of:
- Abdominal pains/distension/worm infection
- Diarrhoea/dysentery
- Skin itching
7. Blood grouping and counting. This may be ordered:
- Before blood transfusion
- In screening of antenatal mothers
- In paternity disputes
- In population surveys
- In forensic medicine (criminology)
8. Sputum microscopy for acid-alcohol fast bacilli (AAFBs). It is carried out by the Zeihl Neelsen staining method. This is often ordered:
- To rule out TB
- To diagnose TB
- For follow up in treatment of TB
9. Laboratory screening for HIV. This test may be required for:
- Screening donated blood
- For surveillance purposes
- Conforming a clinical diagnosis of HIV/AIDS
- Satisfying some authorities such as churches, governments, etc.
For proper patient management, the three procedures of history taking, physical examination and investigation should be carried out.
We hope you now understand the process of clinical problem solving and that you are now able to reach the correct diagnosis. Next, we shall discuss a common complaint that children present with in our health facilities, that is Fever.
Fever is one of the most common complaints at out patient clinics. It is the most common symptom of various childhood illneses. Sometimes parents think fever is synonymous with malaria and therefore treat their children unnecessarily with antimalarial tablets. It is therefore important that as a health worker you understand what fever is, its causes, and how to management. This will also help you to counsel and educate the mothers appropriately.
Types of Fevers:
There are at least four different types of fevers.
- Intermittent fever, in which the body temperature falls to normal every day before rising again.
- Persistent/continuous fever, in which there is persistent elevation of body temperature without significant variation
- Remittent fever, in which the fever falls each day but does not reach normal Levels.
- Relapsing fever, in which short febrile periods occur between one or more days of normal temperature.
Causes of Fevers in Children:
There are various causes of fever in children. These include the following.
- Malaria: This is the commonest cause of fever in the malaria endemic areas. Malaria is confirmed by the finding of malaria parasites in a blood slide. However, one negative blood slide does not always rule out malaria. Carry out at least two slides and if both are negative, malaria is unlikely.
- Pneumonia: Count the rate of breathing and look for chest indrawing. See Unit 8 on Upper Respiratory Infections for more information.
- Meningitis: Check for neck stiffness and irritability. If in doubt, do a lumbar puncture.
- Otitis media: Check ear drums for signs of infection. See Unit 9 for more information
- Tonsillitis: Inspect the throat, examine the tonsils and feel the cervical lymph glands.
- Early measles: Look for Koplik’s spots.
- Urinary tract infections: Check urine for protein and pus cells.
- Typhoid: Look for a history of fever rising slowly over a week, with loss of appetite, headache and increasing toxaemia. Abdominal distension and cough develop in the second week. Diarrhoea comes late and stools may be haemorrhagic. Isolated cases are rare: typhoid tends to occur in epidemics.
- Hepatitis: Look for dark urine, tender liver with jaundice.
- Osteitis/osteomyelitis: Tender bone, very localised at first.
- Rheumatic fever: Fleeting joint pain and swelling, tachycardia, rashes, fever.
- Rheumatoid arthritis: Peripheral joint pains and swelling not fleeting, lymph node enlargement, splenonegaly, rash.
- Septicaemias: Toxaemia, rashes, and jaundice. Think of coliform septicaemia in neonates, staphylococcal septicaemia in infancy, salmonella or meningococcal septicaemia in older children, and salmonella septicaemia in children with sickle cell anaemia. Do a blood culture.
- Tuberculosis: Low grade fever, weight loss, failure to thrive. Do chest X-ray.
- In some areas: Relapsing fever or trypanosomiasis. Do clinical examination, blood slide and CSF examination.
- Immunization: BCG, DPT, measles, and other vaccinations can cause fever.
Sometimes a fever is due to an unknown reason. This is called fever of unknown origin (FUO) or pyrexia of unknown origin (PUO). In this case the fever is most likely as a result of a virus. If you come across many cases of fever of unknown origin in a household or in the community, you should report this to the health authorities for more sophisticated tests.
Management of Fever
The general condition of the child is important for the management. Ask yourself when doing the examination: Does he behave normally? What other symptoms are present beside the fever? Dehydration? Malnutrition?
a. If the fever is high (38.5 oC), give paracetamol either as tablets (500mg) or as a suspension (125 mg in 5 mls). Give in dosage of:
- 5 – 10 mg/kg body weight, 3/12 of age
- 125 mg from 3/12 to 1 year of age
- 125 - 250 mg from 1 year to 5 years
- 250 – 500 mg from 6 years to 12 years.
Administer paracetamol every 6 hours. However, note that paracetamol overdose may cause liver damage. Paracetamol can also hide diagnostic fever patterns without curing the disease.
b. Feverish children should be undressed allow them to get rid of the heat. Wearing warm clothes can worsen the fever. High body temperature can precipitate convulsions.
c. Children who have fever need to take extra fluids, so make sure that they have plenty to drink. If they are unable to drink, give fluids by nasogastric tube. If they are obviously dehydrated, they need rehydration urgently and if they have collapsed give intravenous fluids.
Complications of Fever
Complications of fever include:
- Dehydration
Convulsions are controlled using an anticonvulsant like Diazepam, paraldehyde, etc. It is important that you manage them as an emergency because convulsions can cause brain damage. They are prevented by proper fever management.
Dehydration is managed by rehydration as already discussed above.
Prevention of Fever in Children
From what we have covered in this section, you should now know that the causes of fever are many and varied. It is, therefore, difficult to suggest a single preventive measure for fever. To prevent fever, you have to prevent its cause. Therefore you must find the cause.
You have now come to the end of this unit. It is hoped that you have achieved all the objectives. Have a look at the learning objectives again. If you feel confident that you have covered them well, then complete the Tutor Marked Assignment before you proceed to the next unit.
PRACTICAL ACTIVITY
Visit the laboratory facility nearest to your health facility and find out the following from the laboratory technologist:
What are the common types of investigations they carry out in that laboratory
What percentage of their clients are children?
What are the common tests carried out among children
How does a positive malaria blood slide look like?
Write a report of your findings and send it to the tutor together with your assignment.
Enjoy the rest of the course!!
Navigation menu
Personal tools.
- Request account
- View source
- View history
- Recent changes
- Practice editing
- Community portal
- Mailing list
Print/export
- Create a book
- Download as PDF
- Printable version
- What links here
- Related changes
- Upload file
- Special pages
- Permanent link
- Page information
- This page was last modified on 10 September 2007, at 15:47.
- This page has been accessed 15,131 times.
- Content is available under the Creative Commons Attribution Share Alike License unless otherwise noted.
- Privacy policy
- About WikiEducator
- Disclaimers
Clinical problem-solving in nursing: insights from the literature
Affiliation.
- 1 [email protected]
- PMID: 10759980
- DOI: 10.1046/j.1365-2648.2000.01342.x
This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on how clinicians problem-solve. The nursing process, which is heavily used and frequently described as a problem-solving approach to nursing care, requires a deductive reasoning process which is not the problem-solving process in use during care-giving activities. More knowledge is required on what process is in place as we develop as a profession. The literature highlights the complexities involved in attempting to uncover thinking processes. The main research approaches to discovering problem-solving strategies in the past three decades have been from a cognitive perspective, with two main theories, decision-theory and information processing-theory, underpinning the majority of studies conducted. None of the research approaches used to date has resulted in the identification of a general model of problem-solving that is consistent across tasks or disciplines. However, early hypothesis activation with subsequent testing of the hypothesis seems to be consistent in clinicians across disciplines.
Publication types
- Clinical Competence*
- Education, Nursing*
- Nursing Process*
- Problem Solving*
- MRCP Part 1
- MRCP Part 2
- MRCS Part A
- MRCS Part B
- Internal Medicine Training
- Core Surgical Training
- Anaesthetics CT1 / ACCS
- Cardiothoracic Surgery ST1
- Emergency Medicine ACCS
- GP Selection Centre
- Histopathology ST1
- Neurosurgery ST1
- Obs and Gynae ST1
- Ophthalmology ST1
- Paediatrics ST1
- Public Health Medicine ST1
- Radiology ST1
- Clinical Oncology ST3
- Combined Infection Training ST3
- Dermatology ST3
- Emergency Medicine ST3
- General Surgery ST3
- Haematology ST3
- Intensive Care Medicine ST3
- Medical Oncology ST3
- Obs and Gynae ST3
- Paediatrics ST3
- Plastic Surgery ST3
- Trauma & Orthopaedic Surgery ST3
- Urology ST3
- Vascular Surgery ST3
- Acute Internal Medicine ST4
- Anaesthetics ST4
- Cardiology ST4
- Emergency Medicine ST4
- Endocrinology and Diabetes Mellitus ST4
- Gastroenterology ST4
- Neurology ST4
- Psychiatry ST4
- Renal Medicine ST4
- Respiratory Medicine ST4
- Rheumatology ST4
- NHS Consultant Interview
- Leadership and Management
- Teach the Teacher
- Foundation Ranker
- Find Locum Work

MSRA Practice Questions
The Multi-Specialty Recruitment Assessment (MSRA) is used as part of the Specialty Training (ST) recruitment process by a wide range of specialities. To support your MSRA preparation, this guide provides information on the structure of the exam and how to prepare, as well as example MSRA practice questions.
For more details relating to the specialties which currently require completion of the MSRA, as well as information about exam dates, how the MSRA is scored and tips on how to do well, visit our MSRA: Complete Guide 2024.
Structure of MSRA
Based on the Foundation Programme curriculum, the MSRA is designed to assess essential competencies and your ability to apply your knowledge to clinical decisions.
The MSRA is separated into the following two parts:
Professional Dilemmas Paper
- Duration: 95 minutes
- Number of questions: 50 scenarios
- Part 1: Ranking – For these scenarios, you need to judge the appropriateness of actions in response to the situation and rank them in order, from most to least appropriate.
- Part 2: Multiple Choice – For each scenario you will be given eight plausible actions and be required to select the three most appropriate, when used in unison, to fully resolve the situation.
- Assessment area: This is a Situational Judgement Test (SJT). The paper assesses your professional attributes, behaviours and judgements in relation to clinical scenarios. It focuses on the following core areas: professional integrity, coping with pressure, and empathy and sensitivity.
Clinical Problem Solving Paper
- Duration: 75 minutes
- Number of questions: 86 questions
- Extended Matching Questions – You’ll be given a set of responses and need to identify the most appropriate option in relation to multiple, independent scenarios.
- Single Best Answers – You’ll be given a set of responses and need to identify the most appropriate option for a single scenario.
- Assessment area: The paper assesses your ability to apply your clinical knowledge, judgement and problem solving skills to make appropriate clinical decisions. It focuses on the following core competencies: investigation, diagnosis, emergency care, prescribing and management (non-prescribing).
Check out our MSRA: Complete Guide 2024 for more information on each of the MSRA papers and what’s assessed. The practice question section below also provides further details on the clinical topics covered in the Clinical Problem Solving Paper scenarios.
How to prepare for the MSRA
It’s essential that you identify what’s required for both the Professional Dilemmas and Clinical Problem Solving papers and allocate enough time to adequately prepare for them. As mentioned previously, our MSRA guide provides a comprehensive overview of what’s expected in each section of the MSRA, and is a useful reference point for all your MSRA queries.
As the Professional Dilemmas paper focuses on assessing your professional attributes and behaviours, revisiting the General Medical Council’s (GMC’s) good medical practice guidance and generic professional capabilities framework may be helpful in your MSRA preparations. Likewise, the Clinical Problem Solving paper assesses your ability to apply your clinical knowledge and problem solving skills to clinical scenarios, and therefore some direct revision of clinical theory may be required. However, for each the focus is on applying this knowledge and skills, and making sound judgements in relation to clinical scenarios; as such, dedicating time to practice questions and mock exams will be invaluable, as these provide the opportunity to explore the types of scenarios and questions you’ll encounter during the MSRA exam.
While many may advise dedicating as much time as possible to your preparations to do well in an exam, in fact, making the most effective use of your revision time will have a more significant impact than simply allocating more time to it. With the added challenge of preparing for the MSRA while working a full-time job, it’s essential that you focus on the effective use of practice questions, rather than aimlessly completing as many questions as you can in the time you have available.
Our adaptive MSRA question bank uses state-of-the-art algorithms to automatically identify your strengths and weaknesses, personalising your learning to ensure you focus on the topics which will have the biggest impact on your MSRA preparations, and ultimately your exam score. By ensuring that you’re asked the right questions at the right time, and spending more time mastering the topics that you need to focus on, you’ll make the most effective use of your valuable revision time. To access thousands of professionally written MSRA questions and take your exam preparations to the next level, visit our MSRA question bank and start preparing for the MSRA more efficiently.
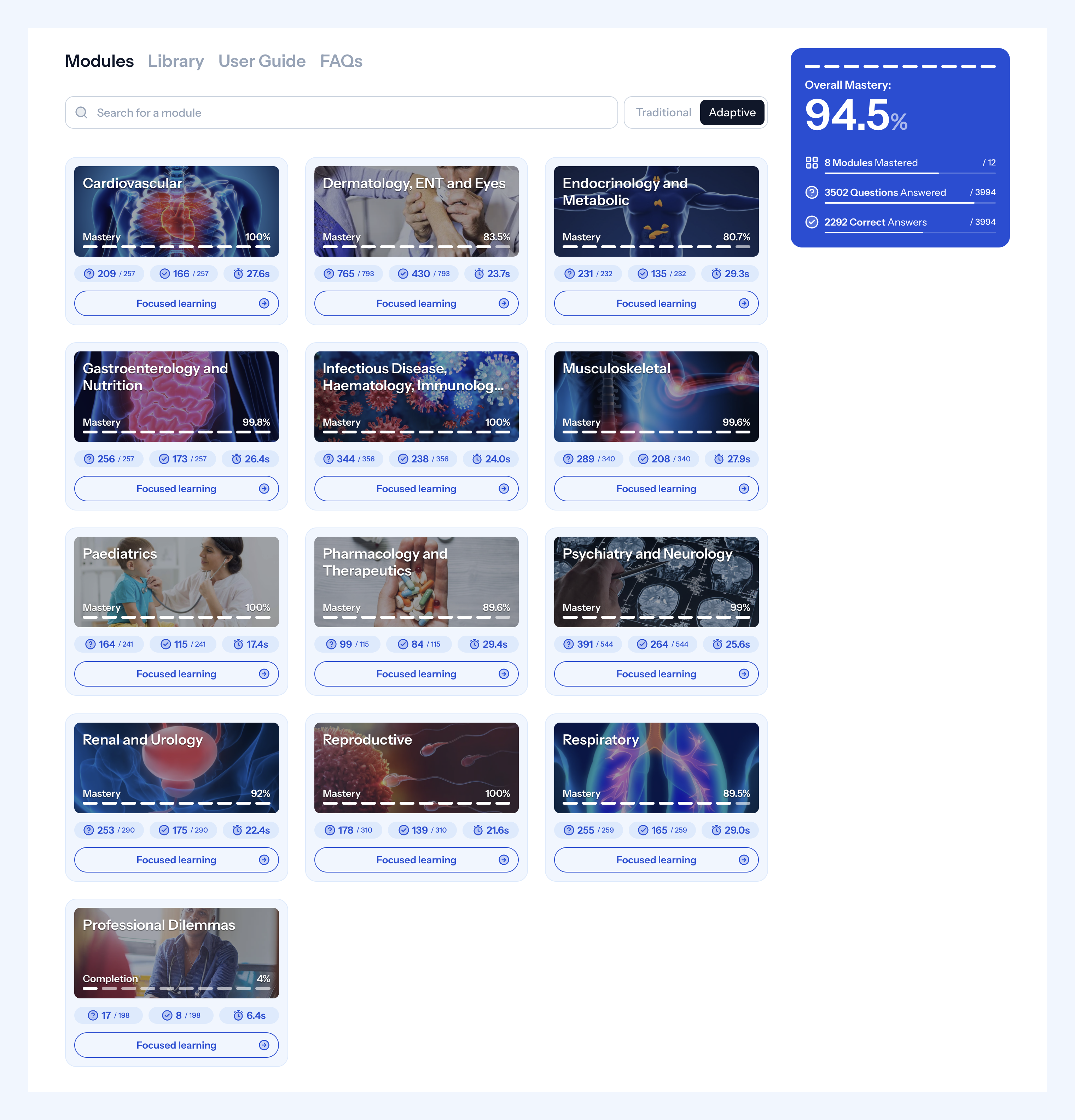
This is an image of the question bank dashboard, so you know what to expect when you purchase. You will be able to clearly see what areas of the syllabus you have “mastered” and which areas require further study.
Practice questions
This section provides examples of the type of questions you’ll experience in each section of the MSRA. You can also find more information about MSRA preparation and practice questions in our ‘ MSRA Question Bank’ and ‘MSRA Exam Revision’ blogs.
Professional Dilemmas Practice Questions
As highlighted in the structure section, the Professional Dilemmas paper contains two types of questions: ranking and multiple choice.
Ranking questions
With ranking questions, you’ll be presented with a scenario and possible actions, from which you need to judge the appropriateness of these responses. You’ll be required to rank each action in order from the most appropriate (1) to the least appropriate (5) in relation to the scenario given.
Multiple choice questions
For the multiple choice questions, you’ll be presented with a scenario and eight plausible actions, from which you need to judge the most appropriate responses to the situation given. You’ll be required to select three options that, when combined, give the most appropriate response to the scenario.
👉 MSRA Professional Dilemmas Example Questions from the Medibuddy MSRA question bank
Clinical Problem Solving Practice Questions
As mentioned previously, the Clinical Problem Solving paper contains two types of questions: extended matching questions and single best answer questions. For both, you’ll be presented with a set of responses and asked to judge which is the most appropriate in relation to a given scenario. The difference being, for the extended matching questions, these same responses must be judged against multiple, independent scenarios; whereas, for the single best answer questions, the given responses are only judged against a single scenario.
Scenarios in the Clinical Problem Solving paper cover the following topics:
- Cardiovascular
- Dermatology / ENT / Eyes
- Endocrinology / Metabolic
- Gastroenterology / Nutrition
- Infectious Disease / Haematology / Immunology / Allergies / Genetics
- Musculoskeletal
- Paediatrics
- Pharmacology and Therapeutics
- Psychiatry / Neurology
- Renal / Urology
- Reproductive
- Respiratory
In the examples below, you’ll see a mixture of extended matching questions and single best answer questions, across the various topic areas.
👉 MSRA Clinical Problem Solving Example Questions from the Medibuddy MSRA question bank
For more questions written for the MSRA exam, check out our MSRA question bank . We offer three subscriptions, so you can choose the best subscription for you based on when you are taking your exam.
Further reading
MSRA Complete Guide 2024
MSRA Exam Revision
Msra question bank, msra ai powered, adaptive question bank.
With over 4000 questions specifically written for the MSRA, our adaptive MSRA question bank has all you need to score highly.
Find out more
MSRA: Complete Guide 2024
Over half of all junior doctors applying for Specialty Training posts each year

If you’re applying for a Specialty Training (ST) post in 2024, you may need to

If you’re required to undertake the Multi-Specialty Recruitment Assessment (MS

Take your subscriptions with you
Our mobile app allows you to access your interview and exam question banks wherever you are.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.324(7339); 2002 Mar 23
Evidence base of clinical diagnosis
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature.
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 – 3 and decision making. 4 – 8 Problem solving research was initially aimed at describing reasoning by expert physicians, to improve instruction of medical students and house officers. Psychological decision research has been influenced from the start by statistical models of reasoning under uncertainty, and has concentrated on identifying departures from these standards.
Summary points
- Problem solving and decision making are two paradigms for psychological research on clinical reasoning, each with its own assumptions and methods
- The choice of strategy for diagnostic problem solving depends on the perceived difficulty of the case and on knowledge of content as well as strategy
- Final conclusions should depend both on prior belief and strength of the evidence
- Conclusions reached by Bayes's theorem and clinical intuition may conflict
- Because of cognitive limitations, systematic biases and errors result from employing simpler rather than more complex cognitive strategies
- Evidence based medicine applies decision theory to clinical diagnosis
Problem solving
Diagnosis as selecting a hypothesis.
The earliest psychological formulation viewed diagnostic reasoning as a process of testing hypotheses. Solutions to difficult diagnostic problems were found by generating a limited number of hypotheses early in the diagnostic process and using them to guide subsequent collection of data. 1 Each hypothesis can be used to predict what additional findings ought to be present if it were true, and the diagnostic process is a guided search for these findings. Experienced physicians form hypotheses and their diagnostic plan rapidly, and the quality of their hypotheses is higher than that of novices. Novices struggle to develop a plan and some have difficulty moving beyond collection of data to considering possibilities.
It is possible to collect data thoroughly but nevertheless to ignore, to misunderstand, or to misinterpret some findings, but also possible for a clinician to be too economical in collecting data and yet to interpret accurately what is available. Accuracy and thoroughness are analytically separable.
Pattern recognition or categorisation
Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not depend as much on strategy as on mastery of content. Further, the clinical reasoning of experts in familiar situations frequently does not involve explicit testing of hypotheses. 3 , 10 – 12 Their speed, efficiency, and accuracy suggest that they may not even use the same reasoning processes as novices. 11 It is likely that experienced physicians use a hypothetico-deductive strategy only with difficult cases and that clinical reasoning is more a matter of pattern recognition or direct automatic retrieval. What are the patterns? What is retrieved? These questions signal a shift from the study of judgment to the study of the organisation and retrieval of memories.
Problem solving strategies
- Hypothesis testing
- Pattern recognition (categorisation)
- By specific instances
- By general prototypes
Viewing the process of diagnosis assigning a case to a category brings some other issues into clearer view. How is a new case categorised? Two competing answers to this question have been put forward and research evidence supports both. Category assignment can be based on matching the case to a specific instance (“instance based” or “exemplar based” recognition) or to a more abstract prototype. In the former, a new case is categorised by its resemblance to memories of instances previously seen. 3 , 11 This model is supported by the fact that clinical diagnosis is strongly affected by context—for example, the location of a skin rash on the body—even when the context ought to be irrelevant. 12
The prototype model holds that clinical experience facilitates the construction of mental models, abstractions, or prototypes. 2 , 13 Several characteristics of experts support this view—for instance, they can better identify the additional findings needed to complete a clinical picture and relate the findings to an overall concept of the case. These features suggest that better diagnosticians have constructed more diversified and abstract sets of semantic relations, a network of links between clinical features and diagnostic categories. 14
The controversy about the methods used in diagnostic reasoning can be resolved by recognising that clinicians approach problems flexibly; the method they select depends upon the perceived characteristics of the problem. Easy cases can be solved by pattern recognition: difficult cases need systematic generation and testing of hypotheses. Whether a diagnostic problem is easy or difficult is a function of the knowledge and experience of the clinician.
The strategies reviewed are neither proof against error nor always consistent with statistical rules of inference. Errors that can occur in difficult cases in internal medicine include failure to generate the correct hypothesis; misperception or misreading the evidence, especially visual cues; and misinterpretations of the evidence. 15 , 16 Many diagnostic problems are so complex that the correct solution is not contained in the initial set of hypotheses. Restructuring and reformulating should occur as data are obtained and the clinical picture evolves. However, a clinician may quickly become psychologically committed to a particular hypothesis, making it more difficult to restructure the problem.
Decision making
Diagnosis as opinion revision.
From the point of view of decision theory, reaching a diagnosis means updating opinion with imperfect information (the clinical evidence). 8 , 17 The standard rule for this task is Bayes's theorem. The pretest probability is either the known prevalence of the disease or the clinician's subjective impression of the probability of disease before new information is acquired. The post-test probability, the probability of disease given new information, is a function of two variables, pretest probability and the strength of the evidence, measured by a “likelihood ratio.”
Bayes's theorem tells us how we should reason, but it does not claim to describe how opinions are revised. In our experience, clinicians trained in methods of evidence based medicine are more likely than untrained clinicians to use a Bayesian approach to interpreting findings. 18 Nevertheless, probably only a minority of clinicians use it in daily practice and informal methods of opinion revision still predominate. Bayes's theorem directs attention to two major classes of errors in clinical reasoning: in the assessment of either pretest probability or the strength of the evidence. The psychological study of diagnostic reasoning from this viewpoint has focused on errors in both components, and on the simplifying rules or heuristics that replace more complex procedures. Consequently, this approach has become widely known as “heuristics and biases.” 4 , 19
Errors in estimation of probability
Availability —People are apt to overestimate the frequency of vivid or easily recalled events and to underestimate the frequency of events that are either very ordinary or difficult to recall. Diseases or injuries that receive considerable media attention are often thought of as occurring more commonly than they actually do. This psychological principle is exemplified clinically in the overemphasis of rare conditions, because unusual cases are more memorable than routine problems.
Representativeness —Representativeness refers to estimating the probability of disease by judging how similar a case is to a diagnostic category or prototype. It can lead to overestimation of probability either by causing confusion of post-test probability with test sensitivity or by leading to neglect of base rates and implicitly considering all hypotheses equally likely. This is an error, because if a case resembles disease A and disease B equally, and A is much more common than B, then the case is more likely to be an instance of A. Representativeness is associated with the “conjunction fallacy”—incorrectly concluding that the probability of a joint event (such as the combination of findings to form a typical clinical picture) is greater than the probability of any one of these events alone.
Heuristics and biases
- Availability
- Representativeness
Probability transformations
- Effect of description detail
- Conservatism
- Anchoring and adjustment
- Order effects
Decision theory assumes that in psychological processing of probabilities, they are not transformed from the ordinary probability scale. Prospect theory was formulated as a descriptive account of choices involving gambling on two outcomes, 20 and cumulative prospect theory extends the theory to cases with multiple outcomes. 21 Both prospect theory and cumulative prospect theory propose that, in decision making, small probabilities are overweighted and large probabilities underweighted, contrary to the assumption of standard decision theory. This “compression” of the probability scale explains why the difference between 99% and 100% is psychologically much greater than the difference between, say, 60% and 61%. 22
Support theory
Support theory proposes that the subjective probability of an event is inappropriately influenced by how detailed the description is. More explicit descriptions yield higher probability estimates than compact, condensed descriptions, even when the two refer to exactly the same events. Clinically, support theory predicts that a longer, more detailed case description will be assigned a higher subjective probability of the index disease than a brief abstract of the same case, even if they contain the same information about that disease. Thus, subjective assessments of events, while often necessary in clinical practice, can be affected by factors unrelated to true prevalence. 23
Errors in revision of probability
In clinical case discussions, data are presented sequentially, and diagnostic probabilities are not revised as much as is implied by Bayes's theorem 8 ; this phenomenon is called conservatism. One explanation is that diagnostic opinions are revised up or down from an initial anchor, which is either given in the problem or subjectively formed. Final opinions are sensitive to the starting point (the “anchor”), and the shift (“adjustment”) from it is typically insufficient. 4 Both biases will lead to collecting more information than is necessary to reach a desired level of diagnostic certainty.
It is difficult for everyday judgment to keep separate accounts of the probability of a disease and the benefits that accrue from detecting it. Probability revision errors that are systematically linked to the perceived cost of mistakes show the difficulties experienced in separating assessments of probability from values, as required by standard decision theory. There is a tendency to overestimate the probability of more serious but treatable diseases, because a clinician would hate to miss one. 24
Bayes's theorem implies that clinicians given identical information should reach the same diagnostic opinion, regardless of the order in which information is presented. However, final opinions are also affected by the order of presentation of information. Information presented later in a case is given more weight than information presented earlier. 25
Other errors identified in data interpretation include simplifying a diagnostic problem by interpreting findings as consistent with a single hypothesis, forgetting facts inconsistent with a favoured hypothesis, overemphasising positive findings, and discounting negative findings. From a Bayesian standpoint, these are all errors in assessing the diagnostic value of clinical evidence—that is, errors in implicit likelihood ratios.
Educational implications
Two recent innovations in medical education, problem based learning and evidence based medicine, are consistent with the educational implications of this research. Problem based learning can be understood as an effort to introduce the formulation and testing of clinical hypotheses into the preclinical curriculum. 26 The theory of cognition and instruction underlying this reform is that since experienced physicians use this strategy with difficult problems, and since practically any clinical situation selected for instructional purposes will be difficult for students, it makes sense to provide opportunities for students to practise problem solving with cases graded in difficulty. The finding of case specificity showed the limits of teaching a general problem solving strategy. Expertise in problem solving can be separated from content analytically, but not in practice. This realisation shifted the emphasis towards helping students acquire a functional organisation of content with clinically usable schemas. This goal became the new rationale for problem based learning. 27
Evidence based medicine is the most recent, and by most standards the most successful, effort to date to apply statistical decision theory in clinical medicine. 18 It teaches Bayes's theorem, and residents and medical students quickly learn how to interpret diagnostic studies and how to use a computer based nomogram to compute post-test probabilities and to understand the output. 28
We have selectively reviewed 30 years of psychological research on clinical diagnostic reasoning. The problem solving approach has focused on diagnosis as hypothesis testing, pattern matching, or categorisation. The errors in reasoning identified from this perspective include failure to generate the correct hypothesis; misperceiving or misreading the evidence, especially visual cues; and misinterpreting the evidence. The decision making approach views diagnosis as opinion revision with imperfect information. Heuristics and biases in estimation and revision of probability have been the subject of intense scrutiny within this research tradition. Both research paradigms understand judgment errors as a natural consequence of limitations in our cognitive capacities and of the human tendency to adopt short cuts in reasoning.
Both approaches have focused more on the mistakes made by both experts and novices than on what they get right, possibly leading to overestimation of the frequency of the mistakes catalogued in this article. The reason for this focus seems clear enough: from the standpoint of basic research, errors tell us a great deal about fundamental cognitive processes, just as optical illusions teach us about the functioning of the visual system. From the educational standpoint, clinical instruction and training should focus more on what needs improvement than on what learners do correctly; to improve performance requires identifying errors. But, in conclusion, we emphasise, firstly, that the prevalence of these errors has not been established; secondly, we believe that expert clinical reasoning is very likely to be right in the majority of cases; and, thirdly, despite the expansion of statistically grounded decision supports, expert judgment will still be needed to apply general principles to specific cases.
This is the fourth in a series of five articles
Series editor: J A Knottnerus
Preparation of this review was supported in part by grant RO1 LM5630 from the National Library of Medicine.
Competing interests: None declared.

“The Evidence Base of Clinical Diagnosis,” edited by J A Knottnerus, can be purchased through the BMJ Bookshop ( www.bmjbookshop.com )
- CPSolvers Academy
- Morning Report
- Diagnostic frameworks
Illness scripts
- Residency Match
- Spaced Learning
Acute Hypertension
Acute Respiratory Distress Syndrome
Adrenal Insufficiency
Alpha-1 Antitrypsin Deficiency
Anaplasmosis
Antibody-Mediated Encephalitis
Behcet’s Disease
Bowel Obstruction
Brain Abscess
Celiac Disease
Community Acquired Pneumonia
Congenital Long QT Syndrome
COVID-19 – Part 1
COVID-19 – Part 2
COVID vs Influenza
COVID-19- Patient Infographics
Crohn’s Disease
Cushing’s – The Journey
Endocarditis (overview)
Endocarditis (native-valve)
Endometriosis
Entamoeba Histolytica
Eosinophilic granulomatosis with polyangitis
Extra-articular features of RA
Generalized Tonic Clonic Seizure
Gilbert Syndrome
Granulomatosis with polyangiitis
Granulomatous Infection – by exposure
Hemochromatosis
Hepatitis A
Hepatitis B
Hepatitis C
Hereditary Spherocytosis
Histoplasmosis
Hypersensitivity Pneumonitis
IgA Nephropathy
IgG4-Related Disease
Invasive Aspergillus
Lyme Disease
Methamphetamine Intoxication
Multiple Myeloma
Multiple Sclerosis
Mycoplasma Pneumoniae
Native Valve Endocarditis 1.0
Nephrogenic Diabetes Insipidus
Neurosyphillis
Parapneumonic Effusion
Paraproteinemia
Parkinson’s
Paroxysmal Nocturnal Hemoglobinuria
Pelvic Inflammatory Disease (PID)
Pheochromocytoma
Plummer Vinson Syndrome
Primary Sclerosing Cholangitis
Protein Losing Enteropathy
Pyoderma Gangrenosum
Pyogenic Liver Abscess
Relapsing Polychondritis
Rheumatoid Arthritis
Sarcoidosis
Sjogren’s
Spinal Epidural Abscess
Spontaneous Bacterial Peritonitis
Subclavian Steal Syndrome
Systemic Sclerosis
Thrombotic Thrombocytopenic Purpura (TTP)
Tumor Lysis Syndrome
Typhoid Fever
Visceral Leishmaniasis
Waldenström’s Macroglobulinemia
Yellow Nail Syndrome

COMMENTS
This is the fourth in a series of five articles This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential ...
What Is Clinical Reasoning? Clinical reasoning is usually defined in a very general sense as "The thinking and decision -making processes associated with clinical practice" (Higgs and Jones 2000) or simply "diagnostic problem solving" (Elstein 1995).. For the purpose of this book, we define clinical reasoning as the mental process that happens when a doctor encounters a patient and is ...
The ECR series utilizes a clinical problem-solving format that allows you to receive and digest information the way it would be received in a real clinical scenario. Parallel expert commentary. The series includes meta-cognitive commentary from an expert diagnostician. This parallel process allows the reader to understand the framework by which ...
Solving a clinical problem in one discipline holds little predictive value for how one will do with a problem in another area. Even in problems with the same diagnosis, there is little consistency in performance. ... or some part of it. A few examples are provided in the table. Each method addresses a component of the larger clinical reasoning ...
Here, the problem space is almost infinite and largely undifferentiated, and the prevalence of serious and specific diseases is low. 9 For example, even among patients presenting with chest pain, only 1.5% to 3.5% have an acute coronary syndrome. 10 Similarly, merely 1% of cases of abdominal pain are caused by neoplastic disease. 11 Pulmonary ...
The problem representation during the clinical reasoning process. The PR is linked to hypothesis-generation and can act as a guide during the diagnostic journey. It allows clinicians to distill the case into its most relevant features, which facilitates efficient diagnostic schema and illness script selection.
The clinical problem solving/diagnostic reasoning session is designed to provide a window into the master clinician's thought process and reasoning strategies. The session serves as a valuable tool to learn and teach the process of hypothesis generation (eliciting the right question), problem representation (problem list), prioritized ...
An illness script is a clinical reasoning tool used by clinicians to collect and retrieve clinically relevant information about a particular condition. In the reasoning process, we use illness scripts to compare and contrast a patient's clinical presentation (i.e., the patient's "script") against our own mental models of a disease (i.e ...
For example, research on medical problem solving typically employs cases that can best be called "medical whodunnits,"—clear-cut cases in which a single diagnosis can account for all the findings. ... Clinical problem analysis is an explicitly analytic and systematic approach to clinical problem solving in the sense that it makes optimal ...
The Clinical Problem Solvers Democratizing clinical reasoning education Podcast Morning Report RLR CPSolvers Frameworks - Scripts Get Involved!
A simple example of evidence-based practice is when a therapist chooses to pivot to a new therapy strategy with a patient after receiving compelling new evidence in the academic literature that demonstrates its effectiveness. ... Evidence based medicine: An approach to clinical problem-solving. BMJ (Clinical Research Ed.), 310(6987), 1122 ...
A diagnostic schema is a cognitive tool that allows clinicians to systematically approach a clinical problem by providing an organizing scaffold. For example, a commonly used schema for acute kidney injury (AKI) separates this problem into pre-renal, intrinsic, and post-renal causes. By approaching AKI using these categories, clinicians can ...
Developing practical clinical problem-solving skills is an important professional endeavor for health care providers. Patient management problems and clinical problem-solving cases have been incorporated into certifying examinations and continuing education programs. Such simulations, in print or electronic form, allow users to select ...
IN this issue of the Journal we begin a new series, "Clinical Problem-Solving," which focuses on the difficult diagnostic, therapeutic, and ethical challenges that physicians face every day. Each i...
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
A clinical problem solving (CPS) exercise highlights the process by which an experienced clinician approaches a diagnostic puzzle. It is constructed in a manner that emphasizes thought process and reasoning as the case unfolds. A CPS manuscript is a variation on the traditional case report which allows the authors to explore a clinical dilemma ...
Vasculopathy - CNS. Visceral Air. Visual Field Defects. Weakness Thought Train. Weight loss. Wide complex tachycardia. Frameworks alphabetically Cardiac Neuro Lung GI Renal Infectious Liver Rheum Blood Electrolytes Endocrine Miscellaneous Icons made by Kara Lau All Frameworks Abdominal DistensionAbdominal Pain OverviewAbdominal Pain - Image ...
In this unit, you will be acquainted with the basics of clinical problem solving. Clinical problem solving is the process of making a correct diagnosis. That is starting from a problem and working it out until you establish what is wrong with your patient and then solving it. It involves taking your patient's history, carrying out a physical ...
Abstract. This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on how clinicians problem-solve.
For example, in a patient with moderate abdominal pain, ... Elstein noted that solving one clinical problem is not a strong predictor of solving the second problem; he called this as "content specificity" which was in contrast with the general long-held belief that problem solving was an independent ability associated with expertise.
In the examples below, you'll see a mixture of extended matching questions and single best answer questions, across the various topic areas. 👉 MSRA Clinical Problem Solving Example Questions from the Medibuddy MSRA question bank. For more questions written for the MSRA exam, check out our MSRA question bank. We offer three subscriptions ...
Pattern recognition or categorisation. Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not ...
AcromegalyAcute HypertensionAcute Respiratory Distress SyndromeAdrenal InsufficiencyAlpha-1 Antitrypsin DeficiencyAnaplasmosisAntibody-Mediated ...