
- Baby & Toddler
- Breastfeeding

Top 10 Breastfeeding Problems Solved
Breastfeeding may be natural, but it’s not always easy. The truth is, there are several things that can pop up along your nursing journey, throwing up roadblocks on what might already be a pretty bumpy road. What is easy? Getting great advice from the experts that know breasts and babies best. We asked them for their best tips for how to handle the most common breastfeeding problems new moms face. Here’s what they said.
Problem #1: Latching Pain
Real talk: It’s 100 percent normal for your nipples to feel a little (or a lot) sore when you first start breastfeeding, especially if you’re a first-timer. But if the pain lasts longer than a few seconds into your feeding session, there may be an issue with baby’s latch . Remember, both you and baby are learning the ropes here, so an improper latch is one of the most common breastfeeding problems to surface.
Solution: First, gently rub your nipple under baby’s nose to encourage a wide-open mouth. “Most babies will ‘root’ at the breast and give you a good, open mouth when they’re ready to nurse,” says Stephanie Nguyen, RN, IBCLC, a lactation consultant and founder of Modern Milk , a breastfeeding clinic and prenatal-postnatal education center in Scottsdale, Arizona. “Next, place baby so their bottom lip is positioned well below your nipple, not at the base of the nipple,” she adds. “But be sure to bring baby onto your breast, rather than putting your breast in their mouth.” You’ll know baby is positioned correctly when their chin touches your breast, their lips are splayed out and you can’t see your nipple or part of the lower areola. (For more latching how-to, check out our latching guide .)
Problem #2: Cracked Nipples
This is one of those breastfeeding problems that can be the result of many different things: a shallow latch, pumping improperly, thrush and sometimes even dry skin. During your first week of breastfeeding, when baby is just learning to latch, you may even experience some bloody discharge, says Jane Morton, MD, a clinical professor of pediatrics emerita at Stanford Medical Center in Palo Alto, California, and founder of Droplet , an online resource for breastfeeding moms. Cracked nipples might be a little frightening (and uncomfortable), but this breastfeeding problem is nothing to worry about.
Solution: Your first step is to make sure baby is properly positioned. “When baby has a shallow latch, your nipple is positioned in the front of baby’s mouth, which means your nipple is rubbing along baby’s hard palate,” says Nguyen. Once you get a deeper latch, your nipple settles farther back in baby’s mouth where the soft palate lies, which is a much more comfortable (and effective) latch. It’s always best to have an OB or lactation consultant determine the cause of your cracked nipples before jumping into treatment, but for many moms, soothing gel pads, nursing ointments and/or taking a mild painkiller like acetaminophen (Tylenol) 30 minutes before nursing can help ease discomfort. Morton also suggests letting some milk stay on your nipples after a feeding and air dry to aid healing. And because cracked nipples can allow for bacteria to enter the breast, wash your sore nipples with soap and water at least twice a day. (For even more on how to heal your cracked nipples, see our primer .)
Problem #3: Engorgement
Engorged breasts (aka breasts bulging with a whole lot of milk) are very full, firm and taut, making it hard for baby to latch—and yes, like so many breastfeeding problems, engorged breasts can be pretty uncomfortable for mom. Your breasts may become engorged at the beginning of your breastfeeding journey when your milk first comes in and your body is still figuring out how to regulate milk production. Engorgement can also happen if you go too long between feedings or if baby isn’t properly draining your breasts of milk.
Solution: Try hand-expressing a little before feeding baby. This will get the milk flowing and soften the breast, making it easier for baby to latch and access milk, says Morton. Of course, the more you nurse, the less likely your breasts are to get engorged. (For more tips on relieving engorgement, read our guide on how to find relief .)
Check out The Bump’s Breastfeeding Solutions chart:

Problem #4: Clogged Ducts
When your breasts are overly full or you’ve gone longer than usual between feeds, milk can back up into your ducts, clogging them up . You’ll know you’ve got a plugged duct if there’s a hard lump on your breast, if your breast is sore to the touch, and/or there’s some redness. If you’ve got a fever too, that’s a sign of mastitis (see blow). Other causes of clogged ducts include: Compressing your breasts while sleeping; using wrong-sized pumping parts or an inefficient pump or having something hit your breast in the same spot, like the underwire of your bra. “But some women are simply more prone to plugged ducts and there may not actually be an underlying cause,” says Nguyen.
Solution: For clogged milk ducts, Morton encourages getting adequate rest (you should recruit your partner to pick up some slack when possible). You can also try feeding baby on the affected side first at each feeding until the duct is cleared. Applying warm compresses to your breasts and massaging them can also help break up the clog. “Vibration works too,” says Nguyen. “Try an electric massager or the end of an electric toothbrush.”
Problem #5: Mastitis
Mastitis is a bacterial infection in your breasts marked by flu-like symptoms such as fever and pain in your breasts, Morton says. It’s common within the first few weeks after birth (though it can also happen anytime during breastfeeding) and may be caused by other breastfeeding problems, such as clogged milk ducts, engorgement or even cracked nipples, which can allow bacteria to enter the breast, causing the infection.
Solution: The only way to treat mastitis is with antibiotics. “Your OB will make sure to prescribe one that’s safe and compatible with breastfeeding,” says Nguyen, who also recommends adding a probiotic to your daily routine whenever antibiotics are being used. At the same time, it’s still important to frequently empty your breasts. “If it’s too painful to nurse or baby refuses to nurse, pump to keep your breasts empty,” says Nguyen. “Milk backing up in your breasts can make mastitis worse.” Finally, warm compresses can help soothe discomfort.
Problem #6: Thrush
Thrush is a yeast infection in baby’s mouth, which can spread to your breasts. You’ll notice red, shiny and sometimes flaky nipples. You may also experience an itching sensation or deep, shooting breast pain.
Solution: Your doctor will need to prescribe an antifungal medication to put on your nipple and in baby’s mouth (OTC meds don’t cut it here). If you and baby are not both treated at the same time, you can easily pass the fungi back and forth, prolonging the healing, says Morton. To keep the yeast contained, make sure to sanitize all pump parts that come in contact with your breasts. “You’ll also want to wash all bras, clothing and nursing pads daily in hot water and vinegar to kill any yeast spores,” says Nguyen.
Problem #7: Low Milk Supply
In theory, breastfeeding is a supply-and-demand system. The more you nurse or pump, the more milk your body should make. That said, there can be many reasons for a low milk supply, so it’s always best to consult a lactation consultant to see what’s going on.
Solution: Frequent nursing and pumping during the day can help up your breast milk supply. While it’s important to stay hydrated and well nourished when nursing, surprisingly, downing an excess of fluids and consuming more calories hasn’t been shown to increase milk production, Morton notes. For more in-depth info on upping your supply, see more pro tips here .
Problem #8: Baby Sleeping at the Breast
Newborns can be especially sleepy in the first few weeks after birth, so nodding off while nursing is common—and even expected. However, snoozing at the breast can also occur if baby isn’t getting enough breast milk. “Milk flowing throughout the feeding will keep baby awake and engaged,” says Nguyen.
Solution: Milk flow is always fastest at the start at a feed, with the first let-down. So if you’re looking to increase efficiency, start with the fuller breast, then switch to the other sooner rather than later, Morton says. When baby’s sucking slows and their eyes are fluttering, massage your breast with your free hand. “Oftentimes, this will get milk flowing and perk baby up,” says Nguyen. “You can also try rubbing baby’s head, blowing gently in their face and gently shifting their position to wake her up.” Undressing your little one or even running a wet wipe down their cheek may also help.
Problem #9: Inverted Nipples
Unsure about the state of your nipples? Gently pinch your areola with your thumb and index finger. If your nipple retracts rather than protrudes, you may have inverted nipples . But take heart: Having flat or inverted nipples doesn’t mean you won’t be able to breastfeed. However, “it does mean that you’d likely benefit from some latching assistance with a lactation consultant,” says Nguyen.
Solution: In addition to getting some pro help, you can use a breast pump to get your milk flowing and pull your nipples out as much as possible before placing baby at your breast for a feed. You might also consider using nipple shields. “Nipple shields are thin, silicone shields that fit over the nipple that help the nipple protrude more, which makes latching easier,” says Nguyen. A lactation consultant can show you how to use them and make sure they’re fitting you properly so they don’t lead to other breastfeeding problems.
Problem #10: Painful Let-Down
The milk let-down sensation (aka “milk ejection reflex”) is often experienced as a tingling or a prickly pins-and-needles kind of feeling. But for some, the sensation is felt deep in the breasts and can hurt or be achy, especially when milk production is in overdrive.
Solution: When this pain develops due to an excessive amount of milk, try feeding baby longer on one particular breast and switching to the other only if you need to. However, if your prickly feeling morphs into more of a tiny-daggers-poking-your-breasts feeling, visit your healthcare provider. You may actually be experiencing a yeast or bacterial infection in your breasts. If you’ve got a fever, aches and chills, those are big red flags and call for treatment.
Expert bios:
Stephanie Nguyen, RN, MSN, WHNP-C, IBCLC, is a registered nurse, women’s health nurse practitioner and lactation consultant. She’s also the founder of Modern Milk , a breastfeeding clinic and prenatal-postnatal education center in Scottsdale, Arizona. She has a Master of Science degree in nursing from The University of Cincinnati and previously worked as a postpartum and labor/delivery nurse.
Jane Morton, MD, FABM, FAAP, is a pediatrician and international expert on breastfeeding. She is a clinical professor of pediatrics emerita at Stanford Medical Center in Palo Alto, California, and previously served as the director of the breastfeeding medicine program at Stanford University, as well as an executive board member of the American Academy of Pediatrics’ Section on Breastfeeding. She is also the founder of Droplet , an online resource for breastfeeding moms.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
31 Breastfeeding Tips Every Nursing Mom Should Know
12 Ways to Make Breastfeeding Easier
How to Eat a Healthy Breastfeeding Diet
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
BREASTFEEDING PROBLEMS OVERVIEW
Breast milk is the optimal source of nutrition for virtually all babies. It meets almost all of the nutritional needs of a full-term baby until approximately six months of age, when some pureed foods are usually added to the diet. Breastfeeding has many health benefits. (See "Patient education: Deciding to breastfeed (Beyond the Basics)", section on 'Why is breastfeeding important?' .)
Although experts recommend that babies be exclusively breastfed for at least six months, many people who start out breastfeeding stop before this time. Often, people stop because common problems interfere with their ability to breastfeed. Luckily, with guidance and support as well as appropriate medical treatment when needed, it is usually possible overcome these obstacles and continue breastfeeding for a longer time.
This topic discusses common problems associated with breastfeeding and how to handle them. Other aspects of breastfeeding are discussed elsewhere. (See "Patient education: Deciding to breastfeed (Beyond the Basics)" and "Patient education: Breastfeeding guide (Beyond the Basics)" and "Patient education: Health and nutrition during breastfeeding (Beyond the Basics)" and "Patient education: Pumping breast milk (Beyond the Basics)" .)
INADEQUATE MILK INTAKE
If your baby is not gaining weight well or has signs of dehydration, they may not be getting enough milk. This is not a reason to give up on breastfeeding, because, in most cases, this can be solved by figuring out the cause and some breastfeeding problem-solving.
Signs of inadequate intake — Ways of determining whether a baby is getting enough milk include:
● Baby's behaviors – You can get an idea of whether your baby is getting enough milk from how well they feed. During the first week of life, full-term babies (meaning that they were born within three weeks of their due date) generally breastfeed 8 to 12 times in 24 hours. During this first week, try to be sure that your baby feeds at least every four hours. After the first week, most babies will still wake frequently, but it's okay to let them sleep longer than four hours (unless they were born prematurely, in which case, they might need to feed more often). By four weeks after delivery, babies generally feed seven to nine times in 24 hours.
By the fifth day of life, most babies who are getting enough milk urinate six to eight times a day and have three or more bowel movements a day. Once your milk comes in, your baby's bowel movements should look pale yellow and seedy.
● Baby's weight – The most important sign of milk intake is the baby's weight. Full-term babies lose an average of 7 percent of their birth weight in the first three to five days of life. They typically get back to their birth weight within one to two weeks. Once your milk has come in (by day 3 to 5), your baby should not keep losing weight. If a baby has lost 10 percent of their weight or fails to return to their birth weight when expected, health care providers start to explore potential causes and solutions. If you weigh your baby at home, you need a digital infant scale to accurately weigh them. Remember to change the diaper first.
In some cases, the health care provider might ask you to weigh the baby before and after a feeding to see how much milk they drank. If you do this, leave the baby in the same diaper and clothes for the "before" and "after" weights (even if they wet the diaper or had a bowel movement during the feeding).
Your baby might go through periods when they seem hungrier than usual. As long as your baby is feeding well, having plenty of wet and dirty diapers and is gaining weight, they are most likely just having a growth spurt. If you keep breastfeeding frequently, your breasts will start making more milk to keep up with your baby's needs.
Causes of inadequate intake — Inadequate milk intake may be related to inadequate milk production, poor milk extraction by the baby, or a combination of these factors.
● Inadequate milk production – A common reason for inadequate milk production is not breastfeeding (or pumping) frequently enough. Frequent breastfeeding (or pumping) stimulates the breasts to make more milk. The baby might not breastfeed frequently enough because they are sleepy, separated from their mother too much, or being fed some formula (which makes them less hungry).
Less common reasons for inadequate milk production include insufficient development of the milk-producing tissue (called glandular tissue ( figure 1 )) during pregnancy, previous breast reduction surgery or radiation, hormonal imbalance, or certain medications that interfere with milk production. Breast augmentation surgery (breast implants) usually does not interfere with milk production.
● Poor milk extraction – Sometimes, a baby has difficulty getting the milk out of the breast even if the milk supply is adequate. This might be because they are not latching on to the breast effectively or not sucking well. This type of problem is more common in premature or slightly premature (also called "late preterm") babies. Occasionally, the baby does not feed well because of a medical problem, such as Down syndrome or tongue-tie (ankyloglossia). Many babies with ankyloglossia can breastfeed, particularly with guidance from a lactation specialist.
Management of inadequate intake
● Evaluation – If your baby has signs of inadequate milk intake, your health care provider will start with an evaluation which may include:
• Ask you about the changes in your breasts during pregnancy and after the birth and, specifically, whether you have engorgement
• Review any health problems that you or your baby have, as well as any medications you take and your relevant medical history (eg, whether you have had breast surgery or radiation in the past)
• Examine of your breasts (fullness, shape, and condition of the nipples)
• Examine the baby's mouth for signs of dehydration, any abnormalities, and/or an underlying medical problem
• Observe a breastfeeding session
● Management – In many cases, milk intake can be improved by using optimized breastfeeding techniques, including using comfortable positions ( figure 2 ) and helping the baby latch on properly ( figure 3 ). If you are having trouble with this, a health care provider can direct you to community resources (often a lactation consultant) for assistance. If you have a digital baby scale, your health care provider may have you check your baby's weight more frequently until you can be sure that they are feeding and growing well.
Stressful situations can interfere with milk let-down (when milk is released from the milk glands into the milk ducts ( figure 1 )); this makes it more difficult for the baby to extract milk. Staying calm and relaxed will help your milk flow.
Occasionally, a baby may need supplements of formula or expressed (pumped) breast milk to make sure that they are getting enough nutrition. However, in most cases, the supplements should be small and temporary while you work to increase your milk production and help the baby feed effectively. When possible, the supplemental formula should be given with a syringe, cup, spoon, or supplemental nursing system at the breast, rather than using a bottle and artificial nipple. This way, your baby won't be confused by the artificial nipple. Before starting a supplement, talk to your health care provider about whether it is necessary and how to give it to your baby safely.
Certain medications called galactagogues (or lactagogues) claim to increase milk production, but it's unclear whether these medications actually work and whether they are safe for a nursing baby, so most experts do not recommend using them. Herbal supplements to improve milk supply have also not been well studied for safety or efficacy.
NIPPLE AND BREAST PAIN
Several things can cause pain during breastfeeding. Most of these problems can be fixed, and you can continue breastfeeding.
To determine the cause of your pain, your health care provider will:
● Ask you about the pain (when it started, what makes it better or worse) and other aspects of your health including any skin conditions you have.
● Examine your nipples and breasts for signs of injury, infection, skin problems, or engorgement (which means that the breasts get overly full).
● Examine the baby for reasons that they might have difficulty breastfeeding, which include ankyloglossia (also called tongue-tie) and other mouth abnormalities.
● Observe you breastfeeding to see if the baby is latching on effectively. If the baby is not latching on properly, this can injure the nipple and also prevent the breast from emptying. This, in turn, can lead to engorgement, plugged ducts, and breast infections.
The main causes of nipple or breast pain are described below.
Nipple pain — Sore nipples are one of the most common complaints by people who are newly breastfeeding. Pain due to nipple injury needs to be distinguished from nipple sensitivity, which normally increases during pregnancy and peaks approximately four days after giving birth.
You can usually tell the difference between normal nipple sensitivity and pain caused by nipple injury based on when it happens and how it changes over time. Normal sensitivity typically subsides 30 seconds after the baby begins suckling. It also diminishes on the fourth day after giving birth and completely resolves when the baby is approximately one week old. Nipple pain caused by trauma, on the other hand, is more severe and persists or gets worse after suckling begins. Severe pain or pain that continues after the first week after birth is more likely to be due to nipple injury.
Normal nipple sensitivity — If you have some discomfort related to normal nipple sensitivity, keep in mind that this sensitivity usually goes away after the first few suckles of a feeding and stops happening after the first week or two of nursing. If you find the "pins and needles" sensation of milk let-down to be uncomfortable, rest assured that this discomfort also resolves in the first weeks of breastfeeding. If needed, you can take acetaminophen (sample brand name: Tylenol) or ibuprofen (sample brand names: Advil, Motrin) to ease your discomfort.
Nipple injury — Nipple injury usually is due to incorrect breastfeeding technique, particularly poor latch-on. Other factors that can make pain caused by injury worse include overuse of breast pads (pads inserted into the bra to absorb any leaking milk, which can keep the skin damp), use of potentially irritating products, and biting by an older baby.
Here are some things that you can do to prevent nipple injury:
● Learn how to position your baby so that the baby can latch on properly ( figure 2 ). If you feel pain while breastfeeding, try releasing the baby's mouth from the nipple, then helping them latch on properly ( figure 3 ). Videos that show how to latch a baby correctly are available here . If you are having trouble with this, get help from a health care provider or a lactation consultant.
● Try to keep your nipples dry and allow them to air-dry after feedings.
● Do not use harsh soaps or cleansers on your breasts.
● Avoid use or overuse of breast pads that have plastic backing.
● If your baby's mouth has any abnormalities, make sure to have them addressed as soon as possible. For example, if your baby has tongue-tie, surgery to correct it may make it easier for the baby to latch on properly.
● If your baby is biting your nipple, position the baby so that their mouth is wide open during feedings. That will make it harder to bite. Also, stick your finger between your nipple and the baby's mouth any time they bite you and firmly say "no." Then put the baby down in a safe place. The baby will learn not to bite you.
Here are some things you can do to promote healing if your nipples are already injured:
● Always start nursing with the breast that does not have the injury.
● If your nipples are cracked or raw, you can put expressed breast milk or an ointment on them, such as purified lanolin (if you are not allergic), and cover them with a nonstick pad. This will keep the injured part of your nipple from sticking to your bra. If you think that your nipple might be infected or you have a rash, see your health care provider.
● Use cool or warm compresses, if they seem to help. Avoid ice.
● Take a mild pain reliever, such as acetaminophen (sample brand name: Tylenol) or ibuprofen (sample brand names: Advil, Motrin), before feeding.
● If nipple pain prevents your baby from emptying your breasts, try using a pump or hand expression to empty your breasts. This will give your nipples a chance to heal and prevent engorgement. Use the milk you remove to feed your baby.
● Do not use vitamin E oil on your nipples. At high levels, it could be toxic to your baby.
Nipple eczema — Some people can get eczema (also called atopic dermatitis) in the nipple area. This usually causes itching or burning and a red, scaly rash ( picture 1 ). This is more common in people who have had eczema in other locations on their body. Other things that might cause nipple eczema or make it worse are use of irritating soaps or fragrances and overuse of breast pads. Occasionally, it can be caused by an allergic reaction to creams such as lanolin or foods that your baby has eaten before breastfeeding.
If you have a rash on your nipples, talk to your health care provider. They can help decide if it is caused by eczema or some other skin condition. If the problem is eczema, it might improve by avoiding hot showers and irritants (soaps or fragrances) and keeping your nipples dry, as discussed above. Or, your health care provider might recommend applying a cream that contains a steroid to your nipples. If you are using a prescription cream, you can continue breastfeeding but should gently wipe off visible cream that was not absorbed before each feeding.
Nipple vasoconstriction — Nipple vasoconstriction is when the blood vessels in the nipple tighten and do not let enough blood through. People with this problem can have pain, burning, or numbness in their nipples in response to cold, nursing, or injury. The nipples can also turn white or blue and then pink when the blood returns.
One way to tell nipple vasoconstriction apart from other causes of nipple pain is that it can be predictably triggered by cold, while other causes of pain cannot.
To manage nipple vasoconstriction, try to keep your whole body warm and dress warmly. Also, if possible, try to breastfeed in warm conditions. It might also help to avoid nicotine and caffeine since they can make the problem worse.
Engorgement — Engorgement is the medical term for when the breasts get too full of milk. It can make your breast feel full and firm and can cause pain and tenderness. Engorgement can sometimes impair the baby's ability to latch, which makes engorgement worse because the baby cannot then empty the breast.
Here are some things you can do to prevent and deal with engorgement:
● Learn how to position your baby so that the baby can latch on properly ( figure 3 and figure 2 ). If you are having trouble with this, get help from a health care provider or a lactation consultant.
● If the engorgement makes it hard for your baby to latch on, manually express a small amount of milk before each feeding to soften your areola and make it easier for the baby to latch on ( figure 4 ). To do this, place your thumb and forefingers well behind your areola (close to your chest) and then compress them together and toward your nipple in a rhythmic fashion. You can also use your hand to present your nipple in a way that is easier to latch on to and to help get milk out for the baby while the baby is suckling.
● You can use a breast pump to help soften your breast before a feeding, but be careful not to do it too much. Using a pump too much will stimulate your breast to make even more milk, which will make engorgement worse.
● Apply cool compresses between feedings. You can also try taking a warm shower; this can enhance let-down and may make it easier to get milk out.
● Take a mild pain reliever, such as acetaminophen (brand name: Tylenol) or ibuprofen (brand names: Advil and Motrin).
● Wear a bra that is supportive but not too tight.
Blocked ducts — A blocked or narrowed milk duct can cause a tender or painful lump to form on the breast. If the ducts near the surface of the nipple itself are blocked, a white dot or "bleb" can form at the end of the nipple ( picture 2 ).
Blocked ducts are caused by swelling or pressure in the affected area, which narrows the ducts so that the milk doesn't pass through easily. Things that can lead to a plugged milk duct include poor feeding technique (in particular, not varying your breastfeeding position), wearing tight clothing or an ill-fitting bra, abrupt decrease in feeding, engorgement, and infections.
Here are some things you can do to prevent and deal with a plugged duct:
● Learn how to position your baby so that the baby can latch on properly ( figure 3 and figure 2 ). If you are having trouble with this, get help from a health care provider or a lactation consultant. Make sure to vary your position during feedings so that every part of the breast can drain. You might even try to position the baby so that their chin is near the plugged area because this positioning can help drain that area best. Do not quit breastfeeding, as this could lead to engorgement and worsen the problem. Similarly, do not try to empty the breast with frequent or prolonged pumping, because this increases milk production and can lead to engorgement. However, you can try brief gentle pumping or manually expressing some milk after feedings to improve drainage.
● Try using cold or warm compresses or taking a warm shower and then very gently massaging your breast.
● Take a mild pain reliever, such as acetaminophen (sample brand name: Tylenol) or ibuprofen (sample brand names: Advil, Motrin).
● If your blockage does not get better within two days, see your health care provider since what appears to be a blocked duct may be something more concerning.
Galactoceles — Sometimes a blocked milk duct can cause a milk-filled cyst called a galactocele to form ( picture 3 ). Unless they are infected, galactoceles are usually painless, but they can get quite large. If necessary, a health care provider can drain a galactocele using a needle or suggest surgery if the problem is severe. If you have a persistent breast lump, be sure to see your health care provider because breast cancer can occur during lactation.
Mastitis — Mastitis is when part of the breast becomes inflamed and swollen. When this happens as a result of breastfeeding, it is called "lactational mastitis." It is most common during the first few months of breastfeeding. But it can happen at any time.
Mastitis starts out similar to engorgement, but usually affects one breast. The swelling in the breast puts pressure on the milk ducts. This causes the ducts to narrow, so milk cannot flow to the nipple as easily and the area becomes painful.
The goal of treatment is to ease discomfort and get the milk flowing again. To do this, you can try the steps listed above for relieving symptoms of engorgement (see 'Engorgement' above). In addition:
● Feed your baby when they show signs of being hungry ("feeding cues"). If milk is flowing from the breast with mastitis, you can feed your baby on that side. The milk is safe for the baby to drink.
● Hand expression is a gentle way to remove excess milk and help decrease inflammation ( figure 4 ).
Only use a breast pump if you need to. Do not try to empty your breast completely, as this can cause your body to produce more milk and make mastitis worse.
● Avoid using nipple shields.
● Drink plenty of fluids and rest when possible.
You do not need to stop breastfeeding if you have mastitis. Regular breastfeeding is actually the best way to help with swelling and keep milk from getting blocked again.
If milk flow is blocked for more than a day or two, this can lead to bacterial infection in the breast ("bacterial mastitis"). This can cause additional symptoms like fever, aches, or fatigue. Bacterial mastitis needs treatment with antibiotics. If you have an infection, continue to breastfeed. You will not pass the infection on to your baby.
MILK OVERSUPPLY
Some people make too much milk, which paradoxically can make breastfeeding difficult. Generally, the production of milk is determined by the baby's demand, but, in this case, the supply exceeds demand. The problem begins early in lactation and is most common for people breastfeeding their first child.
For people with an oversupply of milk, the rush of the milk can be so strong that it causes the baby to choke and cough and have trouble feeding or even to bite down to clamp the nipple. Babies whose mothers make too much milk can either gain weight quickly or gain too little weight because they cannot handle the flow of milk or because they do not get the hindmilk (last part of the milk) in the breast, which has the most calories.
If you have a problem with milk oversupply, don't worry. The problem usually goes away on its own. However, tell your health care provider about it so they can check whether you have any hormonal imbalances or take any medications that could make the problems worse.
Here are some things that you can do to deal with milk oversupply:
● Nurse in an upright position – Hold your baby upright to nurse and lean back or lie on your side ( figure 5 and figure 2 ). This will give the baby better control of the flow of milk.
● Use your fingers to reduce the flow of milk – Try putting a scissors-hold on your areola or pressing on your breast with the heel of your hand to restrict flow.
● Give the baby control – Let your baby interrupt feedings, and burp them often.
● Pump very little or not at all – Avoid pumping because it can stimulate even more milk production, but you can hand pump a little at the beginning of a feeding to relieve some of the pressure.
● Apply cold water or ice to your nipples to decrease leaking.
YEAST INFECTION
Yeast infections of the nipple or breast are poorly understood and researchers aren't sure what role they play in nipple pain.
Some health care providers diagnose yeast infections based on symptoms alone, especially:
● Breast pain out of proportion to any apparent cause
● History of vaginal yeast infections or a baby with a history of yeast infections such as thrush or diaper rash
● Shiny or flaky skin on the affected nipple
Other health care providers believe that the diagnosis should only be made if the yeast infection is proven. This can be done by seeing yeast under a microscope (looking at a skin scraping) or in a culture of breast milk.
Treatments include:
● Topical antifungals – Topical antifungals are creams or gels that contain medications called antifungal medicine, which kill yeast. If you are using any of these treatments, it's important to wipe any remaining medication that you can see off of your nipples before each feeding and reapply the medication after the feed. The antifungal medicine should be a cream or gel (the ointment form should not be used, because they contain paraffins that could be harmful to the baby).
Gentian violet was sometimes used as an antifungal, but there are some concerns about its safety and it has been removed from the market in some countries.
● Antifungal pills – If you do not get better with the options described above, your health care provider might prescribe antifungal pills for two weeks. You can continue to breastfeed while taking these pills since the typical amount of drug that makes it into breast milk is safe for breastfeeding babies. Prolonged treatment with antifungal pills is almost never necessary.
BLOODY NIPPLE DISCHARGE
Some people have bloody nipple discharge during the first days to weeks of lactation. This is more common with the first pregnancy and has been called "rusty pipe syndrome." It is thought to be caused by the increased blood flow to the breasts and ducts that happens when the body starts making milk. The color of the milk varies from pink to red or brown and generally goes away within a few days. This will not harm your baby, and you should continue breastfeeding. If you have bloody discharge for more than a week, you should see your health care provider.
WHEN TO SEEK HELP
If you are unable to breastfeed due to engorgement, pain, or difficulty latching your baby, help is available. Talk to your obstetrical or pediatric health care provider, nurse, lactation consultant, or a breastfeeding counselor.
FINDING A LACTATION CONSULTANT OR OTHER SUPPORT
Resources for finding a lactation consultant, peer support (online or in-person), and other types of support are listed in the table ( table 1 ).
WHERE TO GET MORE INFORMATION
Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website ( www.uptodate.com/patients ). Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below.
Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Common breastfeeding problems (The Basics) Patient education: Mastitis (The Basics) Patient education: Breastfeeding (The Basics) Patient education: Weaning from breastfeeding (The Basics) Patient education: Jaundice in babies (The Basics)
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Deciding to breastfeed (Beyond the Basics) Patient education: Breastfeeding guide (Beyond the Basics) Patient education: Health and nutrition during breastfeeding (Beyond the Basics) Patient education: Pumping breast milk (Beyond the Basics) Patient education: Raynaud phenomenon (Beyond the Basics) Patient education: Constipation in infants and children (Beyond the Basics)
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Ankyloglossia (tongue-tie) in infants and children Breastfeeding: Parental education and support Common problems of breastfeeding and weaning Lactational mastitis Maternal nutrition during lactation Nutrition in pregnancy: Dietary requirements and supplements Prevention of HIV transmission during breastfeeding in resource-limited settings The impact of breastfeeding on the development of allergic disease Safety of infant exposure to antidepressants and benzodiazepines through breastfeeding
Websites — The following organizations also provide reliable health information:
● United States National Library of Medicine
( www.medlineplus.gov/healthtopics.html )
● Centers for Disease Control and Prevention
( www.cdc.gov/breastfeeding )
● American Academy of Pediatrics
( www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/default.aspx )
● Academy of Breastfeeding Medicine
( www.bfmed.org/protocols )
● La Leche League International
( www.llli.org/resources )
● Office on Women's Health
( www.womenshealth.gov/patient-materials/health-topic/breastfeeding )
● LactMed database – For information about which medications are compatible with breastfeeding
( www.ncbi.nlm.nih.gov/books/NBK501922 )

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Common breastfeeding challenges

Breastfeeding can be challenging, especially in the early days. But remember that you are not alone. Lactation consultants can help you find ways to make breastfeeding work for you and your baby. Some women face many different problems while breastfeeding, while others do not. Also, many women may have certain problems with one baby that they don't have with their second or third baby.
Challenge: Sore nipples
Many moms say that their nipples feel tender when they first start breastfeeding. Breastfeeding should feel comfortable once you and your baby have found a good latch and some positions that work.
What you can do
- Your baby should not be suckling from just the nipple. The baby should be nursing from most of the areola (the darker colored area around the nipple) and the nipple.
- A good latch is key, so visit the Getting a good latch section for detailed instructions. If your baby sucks only on the nipple, gently break your baby's suction to your breast by placing a clean finger in the corner of your baby's mouth. Then try again to get your baby to latch on. (Your nipple should not look flat or compressed when it comes out of your baby's mouth. It should look round and long or the same shape as it was before the feeding.)
- If you find yourself putting off feedings because breastfeeding is painful, get help from a lactation consultant. Delaying feedings can cause more pain and harm your milk supply.
- Try changing positions each time you breastfeed. The Breastfeeding holds section describes the various positions you can try.
- After breastfeeding, express a few drops of milk and gently rub the milk on your nipples with clean hands. Human milk has natural healing properties and contains oils that soothe.
- Use purified lanolin cream or ointment that is especially made for breastfeeding.
- Let your nipples air dry after feeding, or wear a soft cotton shirt.
- Get help from your doctor or lactation consultant before using creams, hydrogel pads (a moist covering for the nipple to help ease soreness), or a nipple shield (a plastic device that covers the nipple during breastfeeding). In some cases, you should not use these products. Your doctor or lactation consultant will help you make the choice that is best for you.
- Don't wear bras or clothes that are too tight and put pressure on your nipples.
- Change nursing pads (washable or disposable pads you can place in your bra to absorb leaks) often to avoid trapping in moisture that can cause cracked nipples.
- Avoid harsh soaps or ointments that contain astringents (like a toner) on your nipples. Washing with clean water is all that is needed to keep your nipples and breasts clean.
If you have very sore nipples, you can ask your doctor about using non-aspirin pain relievers.
Challenge: Low milk supply
Most mothers make plenty of milk for their babies. But many mothers worry about having enough milk. This video suggests that checking your baby's weight and growth is the best way to make sure he or she gets enough milk. Let your baby's doctor know if you are concerned.
For more ways to tell if your baby is getting enough milk, visit the How do I know if my baby is getting enough breastmilk? section.
There may be times when you think your supply is low, but it is actually just fine:
- When your baby is around 6 weeks to 2 months old, your breasts may no longer feel full. This is normal. At the same time, your baby may nurse for only five minutes at a time. This can mean that you and your baby are just getting used to breastfeeding — and getting good at it!
- Growth spurts can make your baby nurse longer and more often. These growth spurts often happen around 2 to 3 weeks, 6 weeks, and 3 months of age. Growth spurts can also happen at any time. Don't be worried that your supply is too low to satisfy your baby. Follow your baby's lead. Nursing more and more often will help increase your milk supply. Once your supply increases, you will probably be back to your usual routine.
- Make sure your baby is latched on and positioned well.
- Breastfeed often and let your baby decide when to end the feeding.
- Offer both breasts at each feeding. Have your baby stay at the first breast as long as he or she is still sucking and swallowing. Offer the second breast when the baby slows down or stops.
- Avoid giving your baby formula or cereal in addition to your breastmilk, especially in the first 6 months of life. Your baby may lose interest in your breastmilk, and your milk supply will decrease. If you need to supplement your baby's feedings with more milk, try using a spoon, cup, or a dropper filled with pumped breastmilk.
Check with your doctor for health issues, such as hormonal issues or primary breast insufficiency, if the above steps don't help.
Challenge: Oversupply of milk
An overfull breast can make breastfeeding stressful and uncomfortable for you and your baby.
- Breastfeed on one side for each feeding. Continue to offer that same breast for at least two hours until the next full feeding, gradually increasing the length of time per feeding.
- If the other breast feels unbearably full before you are ready to breastfeed on it, hand express for a few moments to relieve some of the pressure. You can also use a cold compress or washcloth to reduce discomfort and swelling.
- Feed your baby before he or she becomes overly hungry to prevent aggressive sucking. (Learn about hunger signs in the Tips for breastfeeding success section.)
- Burp your baby often if he or she is gassy so there is more room in baby's tummy for milk.
Challenge: Strong let-down reflex
Some women have a strong milk ejection reflex or let-down . This can happen along with an oversupply of milk.
- Hold your nipple between your first and middle fingers or with the side of your hand. Lightly press on milk ducts to reduce the force of the milk ejection.
- If your baby chokes or sputters when breastfeeding, unlatch him or her and let the extra milk spray into a towel or cloth.
- Allow your baby to latch and unlatch from the breast whenever he or she wants to.
- Try positions that reduce the force of gravity, which can make milk spray worse. These positions include the side-lying position and the football hold. (See the Breastfeeding holds section for illustrations of these positions.)
Challenge: Engorgement
It is normal for your breasts to become larger, heavier, and a little tender when they begin making milk. Sometimes, this fullness may turn into engorgement, when your breasts feel very hard and painful. Engorgement is the result of the milk building up. It usually happens during the third to fifth day after giving birth. But it can happen at any time, especially if you have an oversupply of milk or are not feeding your baby or expressing your milk often.
Engorgement can also cause:
- Breast swelling
- Breast tenderness
- Flattening of the nipple
- Low-grade fever
Engorgement can lead to plugged ducts or a breast infection, so it is important to try to prevent it before this happens.
- Breastfeed often after giving birth. As long as your baby is latched on and sucking well, allow your baby to feed for as long as he or she likes.
- Work with a lactation consultant to improve your baby's latch so that your baby can remove more milk from your breast.
- Breastfeed often on the engorged side to remove the milk, keep the milk moving freely, and prevent your breast from becoming too full.
- Do not use pacifiers or bottles to supplement feedings in the beginning. Try to wait to introduce pacifiers until your baby is 3 or 4 weeks old.
- Hand express or pump a little milk to soften the breast, areola, and nipple before breastfeeding.
- Massage the breast.
- Use cold compresses on your breast in between feedings to help ease the pain.
- If you are returning to work, try to pump your milk on the same schedule that your baby breastfed at home. Pump at least every four hours, or more often.
- Get enough rest, proper nutrition, and fluids.
- Wear a well-fitting, supportive bra that is not too tight.
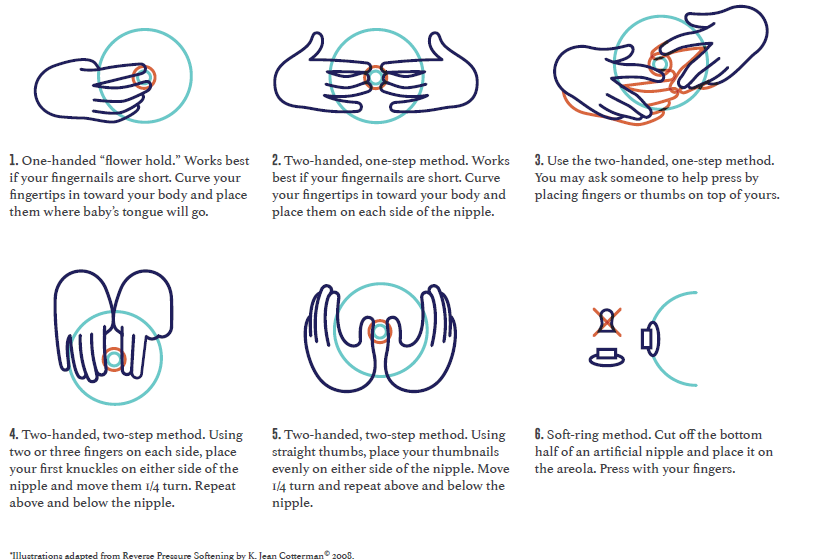
Try reverse pressure softening to make the areola soft around the base of the nipple and help your baby latch. Try one of the holds in the illustrations below. Press inward toward the chest wall and count slowly to 50. Use steady and firm pressure, but gentle enough to avoid pain. You may need to repeat each time you breastfeed for a few days.
- One-handed "flower hold." Works best if your fingernails are short. Curve your fingertips in toward your body and place them where baby's tongue will go.
- Two-handed, one-step method. Works best if your fingernails are short. Curve your fingertips in toward your body and place them on each side of the nipple.
- Two-handed, one-step method. You may ask someone to help press by placing fingers or thumbs on top of yours.
- Two-handed, two-step method. Using two or three fingers on each side, place your first knuckles on either side of the nipple and move them 1/4 turn. Repeat above and below the nipple.
- Two-handed, two-step method. Using straight thumbs, place your thumbnails evenly on either side of the nipple. Move 1/4 turn and repeat above and below the nipple.
- Soft-ring method. Cut off the bottom half of an artificial nipple and place it on the areola. Press with your fingers.
Challenge: Plugged ducts
Plugged ducts are common in breastfeeding mothers. A plugged milk duct feels like a tender and sore lump in the breast. If you have a fever or other symptoms then you probably have a breast infection rather than plugged ducts.
A plugged duct happens when a milk duct does not drain properly. Pressure then builds up behind the plug, and surrounding tissue gets inflamed. A plugged duct usually happens in only one breast at a time.
- Breastfeed on the side with a plugged duct as often as every two hours. This will help loosen the plug and keep your milk moving freely.
- Aim your baby's chin at the plug. This will focus his or her suck on the duct that is affected.
- Massage the area, starting behind the sore spot. Move your fingers in a circular motion and massage toward the nipple. Use a warm compress on the sore area.
- Rely on others to help you get extra sleep, or relax with your feet up to help speed healing. Often a plugged duct is a sign that you are doing too much.
- Wear a well-fitting, supportive bra that is not too tight, since a tight bra can constrict milk ducts. Consider trying a bra without an underwire.
- If you have plugged ducts that keep coming back, get help from a lactation consultant.
Challenge: Breast infection (mastitis)
Mastitis (mast-EYE-tiss) is soreness or a lump in the breast. It can cause symptoms such as:
- Fever and/or flu-like symptoms, such as feeling run down or very achy
- Yellowish discharge from the nipple that looks like colostrum
- Breasts that feel warm or hot to the touch and appear pink or red
A breast infection can happen when other family members have a cold or the flu. It usually happens in only one breast. It is not always easy to tell the difference between a breast infection and a plugged duct, because both have similar symptoms and can get better within 24 to 48 hours. Some breast infections that do not get better on their own need to be treated with prescription medicine from a doctor. (Learn more about medicines and breastfeeding in the Breastfeeding fact sheet .)
- Breastfeed on the infected side every two hours or more often. This will keep the milk moving freely and your breast from becoming too full.
- Massage the area, starting behind the sore spot. Move your fingers in a circular motion and massage toward the nipple.
- Apply heat to the sore area with a warm, wet cloth.
- Rely on others to help you get extra sleep, or relax with your feet up to help speed healing. Often a breast infection is a sign that you are doing too much and becoming overly tired.
- Wear a well-fitting, supportive bra that is not too tight, since a tight bra can constrict milk ducts.
Ask your doctor for help if you do not feel better within 24 hours of trying these tips, if you have a fever, or if your symptoms get worse. You might need medicine. See your doctor right away if:
- You have a breast infection in which both breasts look affected
- There is pus or blood in your breastmilk
- You have red streaks near the affected area of the breast
- Your symptoms came on severely and suddenly
Challenge: Fungal infections
A fungal infection, also called a yeast infection or thrush , can form on your nipples or in your breast. This type of infection thrives on milk and is an overgrowth of the Candida organism. Candida lives in our bodies and is kept healthy and at the correct levels by the natural bacteria in our bodies. When the natural balance of bacteria is upset, Candida can overgrow, causing an infection.
A key sign of a fungal infection is sore nipples that last more than a few days, even after your baby has a good latch. Or you may suddenly get sore nipples after several weeks of pain-free breastfeeding. Other signs are pink, flaky, shiny, itchy, or cracked nipples or deep pink and blistered nipples. You could also have achy breasts or shooting pains deep in the breast during or after feedings.
Causes of fungal infection include:
- Thrush in your baby's mouth, which can pass to you
- Nipples that are sore or cracked
- Receiving or taking antibiotics or steroids (often given to mothers during labor)
- A chronic illness like HIV , diabetes , or anemia
Fungal infections are treated with a medicine you rub on your breasts several times a day for about a week. It may take several weeks to clear up, so it is important to follow these tips to avoid spreading the infection:
- Change disposable nursing pads often.
- Wash any towels or clothing that comes in contact with the yeast in very hot water (above 122°F).
- Wear a clean bra every day.
- Wash your hands often.
- Wash your baby's hands often, especially if he or she sucks on his or her fingers.
- Boil every day all pacifiers, bottle nipples, or toys your baby puts in his or her mouth. (To boil them, place them in a pot of water and heat the water to a rolling boil. Boil the items for about 10 minutes.)
- After one week of treatment, throw away all pacifiers and nipples and buy new ones.
- Every day, boil all breast pump parts that touch your milk.
- Make sure other family members do not have thrush or other fungal infections. If they have symptoms, do not let them care for you or your baby until they get treated.
Challenge: Inverted, flat, or very large nipples
Some women have nipples that turn inward instead of pointing outward or are flat and do not protrude. Nipples can also sometimes flatten for a short time because of engorgement or swelling from breastfeeding. Inverted or flat nipples can sometimes make it harder to breastfeed. For breastfeeding to work your baby must latch on to both the nipple and the breast, so even inverted nipples can work just fine. Often, flat and inverted nipples will protrude more over time as the baby sucks more.
Very large nipples can make it hard for the baby to get enough of the areola into his or her mouth to compress the milk ducts and get enough milk.
- Talk to your doctor or a lactation consultant if you are concerned about your nipples.
- You can use your fingers to try to pull your nipples out. You can also talk to your doctor or nurse about using a device that gently suctions or pulls out inverted or temporarily flattened nipples.
- The latch for babies of mothers with very large nipples will improve with time as the baby grows. It might take several weeks to get the baby to latch well. But if you have a good milk supply, your baby will get enough milk even with a latch that isn't perfect.
Challenge: Nursing strike
A nursing "strike" is when your baby has been breastfeeding well for months and then suddenly begins to refuse the breast. A nursing strike can mean that your baby is trying to let you know that something is wrong. This usually does not mean that the baby is ready to wean (stop breastfeeding totally).
Not all babies will react the same way to the different things that can cause a nursing strike. Some babies will continue to breastfeed without a problem. Other babies may just become fussy at the breast. And other babies will refuse the breast entirely.
Some of the major causes of a nursing strike include:
- Having mouth pain from teething, a fungal infection like thrush, or a cold sore
- Having an ear infection, which causes pain while sucking or pressure while lying on one side
- Feeling pain from a certain breastfeeding position, perhaps from an injury on the baby's body or from soreness from an immunization
- Being upset about a long separation from the mother or a major change in routine
- Being distracted while breastfeeding, such as becoming interested in other things going on around the baby
- Having a cold or stuffy nose that makes breathing while breastfeeding difficult
- Getting less milk from the mother after supplementing breastmilk with bottles or overuse of a pacifier
- Responding to the mother's strong reaction if the baby has bitten her while breastfeeding
- Being upset by hearing arguing or people talking in a harsh voice while breastfeeding
- Reacting to stress, overstimulation, or having been repeatedly put off when wanting to breastfeed
If your baby is on a nursing strike, it is normal to feel frustrated and upset, especially if your baby is unhappy. Be patient with your baby and keep trying to offer your breasts. You may also want to pump your breastmilk to offer during the strike and to make sure you do not get engorged.
- Try to hand express or pump your milk as often as the baby used to breastfeed, to prevent engorgement and plugged ducts .
- Try another feeding method temporarily to give your baby your breastmilk, such as using a cup, dropper, or spoon.
- Keep track of your baby's wet and dirty diapers to make sure he or she is getting enough milk.
- Keep offering your breast to your baby. If your baby is frustrated, stop and try again later. You can also try offering your breast when your baby is very sleepy or is sleeping.
- Try breastfeeding positions where your bare skin is pressed next to your baby's bare skin.
- Focus on your baby, and comfort him or her with extra touching and cuddling.
- Try breastfeeding while rocking your baby in a quiet room without distractions.
Did we answer your question about breastfeeding challenges?
For more information about breastfeeding challenges, call the OWH Helpline at 1-800-994-9662 or check out the following resources from other organizations:
- Breastfeeding — Information from the Centers for Disease Control and Prevention.
- Breastfeeding — Information from the U.S. Library of Medicine.
- Breastfeeding Your Baby — Resource from the American College of Obstetricians and Gynecologists.
- Colic and Crying — Fact sheet from the National Library of Medicine.
- Breastfeeding with Sore Nipples — Information from La Leche League International.
- Is Thrush Causing My Sore Nipples? — Information from La Leche League International.
- Mastitis — Information from La Leche League International.
- Overcoming Breastfeeding Problems — Information from the U.S. Library of Medicine.
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

Problem Solving For Breastfeeding Parents
Woman’s lactacation resources .
Breastfeeding can be challenging at times, but you are not alone. Our lactation consultants are trained to help you find ways to breastfeeding success. Our lactation consultants are trained to help you find ways to breastfeeding success and are a phone call away.
Call Woman’s Warmline at 225-924-8239.
We provide free lactation phone consultation and troubleshooting advice from a registered nurse. This service is available to the entire community.
Schedule a Woman’s BreastTime virtual consultation.
Woman’s offers virtual breastfeeding appointments with our lactation nurses in the convenience of your own home via iPhone™, iPad™ or Android phone.
Common Challenges and How to Tackle Them
Sore nipples are common for many moms during the first few days of breastfeeding. The best treatment for sore nipples is prevention.
Here are some tips:
Check the position of the baby when he latches on.
Smooth lanolin over your nipples after each nursing session.
Let your nipples air dry after each nursing session.
Alternate the breast you begin with for each session.
Put a safety pin on the side of your bra to help you remember which breast you started on.
You should also not hear any clicking or sucking sound. If you do, your baby isn't positioned right. Bring your baby closer to you and have his mouth cover as much of the areola as possible. Correct positioning/latch is most important prevention of sore nipples.
Thrush is a yeast infection that may form on the breast and be passed to your baby's mouth. It causes nipple or breast pain that lasts throughout the feeding and doesn't improve even after your baby has a better latch or changes position.
Symptoms are very sore nipples, achy or painful breasts or pink, flaky, shiny, itchy or cracked nipples. Overly moist breasts, sore or cracked nipples, a diet high in sugar or yeasty foods or taking antibiotics, birth control pills or steroids can all lead to thrush.
If your baby has thrush, creamy white patches may appear inside of his mouth or on his tongue. He might also get a red, bumpy diaper rash that won't heal.
If you suspect thrush, contact your doctor and your baby's doctor. You'll need to treat both your breasts and your baby's mouth with a prescription antifungal or with the over-the-counter antifungal gentian violet. To prevent thrush, air-dry your nipples, use nipple pads in your bra and wear a clean bra every day.
A couple of days after giving birth, your breasts increase in size and feel full and heavy. This engorgement is normal. It's caused by an increase in the volume of milk in your breasts and by increased blood flow and tissue swelling. Your breasts may feel slightly warm to the touch and be slightly reddened. This signals the beginning of milk production.
Here are some tips for relieving engorgement:
Use warm compresses
Let warm water run over your breasts in the shower
Lay cabbage leaves on your breasts to relieve pressure
Try pumping some milk between feedings
Allow your baby to finish the first breast first
Apply cold compresses in between feedings
A plugged duct is a sore, tender lump in the breast that occurs when a milk duct is not draining well. Most plugged ducts go away within a couple of days without developing into mastitis (breast infection).
To manage plugged ducts:
Change your baby's breastfeeding positions
Nurse frequently on the affected side
Apply a heating pad or warm compresses
Gently massage the area
If you feel like you have the flu and one breast is red, hot and sore, you may have mastitis. Usually an antibiotic clears up this infection. In the meantime, keep nursing and/or pumping on that side as much as possible, even though it may be uncomfortable.
To prevent mastitis, make sure you empty your breasts regularly. If you do take antibiotics, add a probiotic (good bacteria such as lactobacillus) supplement or eat a container of live culture yogurt every day.
Breastfeeding is a supply-and-demand activity. The more you nurse, the more milk your body makes. So when your baby goes through a growth spurt and seems to be nursing all the time, keep in mind he is signaling your body to up the milk production to meet his new nutritional needs.
For the baby who refused the breast, cup feeding can be an alternative. In cup feeding the baby laps the milk with his tongue; never pour the milk down a baby’s throat.
- Jose Ruiz III MD
- Viviana Ellis MD
- Ilanna Loeffel MD
- Camilo Gonima MD
- Paula Bilica DO
- John Adams MD
- Patient Testimonials
- Gynecologic Surgery
- Annual Wellness
- Patient Resources
- Patient Portal
- Appointment
Solving Common Breastfeeding Problems

Common breastfeeding problems and solutions
Many common breastfeeding problems can be resolved with simple positional corrections, a good routine, and at-home comfort measures.
Sore nipples
- Ensure the baby latches onto the entire areola, not just the nipple.
- Change the baby’s feeding position to get a better latch.
- Treat cracked nipples with breast milk or breastfeeding cream.
Overfull breasts
- Feed as often as your baby is interested, on one side per feeding.
- Use warm showers and massage to relieve discomfort.
- Hand-express milk to decrease pressure.
Not enough milk
- Breastfeed often, offering both breasts.
- Pump after and between feedings to increase milk supply.
- Get rest and stay hydrated.
Plugged milk duct
- Breastfeed frequently on the side with the plugged duct.
- Massage the sore area, moving toward the nipple.
- Apply a warm compress to the area.
Get help for serious breastfeeding challenges
Some breastfeeding problems are more serious, so don’t hesitate to reach out to our team for help if you experience severe pain, swelling or redness in your breasts. If you see signs of infection, be sure to contact our San Antonio OBGYNs for treatment options.
Breast infection
- Continue to breastfeed on the side with the infection.
- Apply a warm, wet compress to the area.
- Discuss an antibiotic with your doctor.
Fungal infection
- Contact your doctor for antifungal medication for anyone affected.
- Clean your hands and the baby’s hands often.
- Wear a clean bra every day.
Give yourself a break
Breastfeeding is not always easy and can cause stress for a new mom, so it’s important to have tools and resources to improve the experience. Our San Antonio OBGYNs encourage women to take these steps to make it easier.
- Be patient with yourself and be confident. Even experienced moms can have difficulty. Know that breastfeeding challenges are common, and you will find solutions.
- Don’t be afraid to ask the people around you for help. Being a new mom is an exhausting, emotional time. Rely on family and friends for additional support, whether it’s cooking, cleaning or caring for the baby while you rest.
- Find support in a community. Talk with others who are also new moms, or look for a breastfeeding organization. Breastfeeding support communities are available in many areas and online.
- Look to professionals for guidance. Your OBGYN, the baby’s pediatrician, and lactation consultants are all great resources for help overcoming breastfeeding challenges.
If you have breastfeeding problems or need additional support, our San Antonio OBGYNs are available to help. Contact Legacy Women’s Health for an appointment.
- Tips for Hot Flashes
- You Shouldn’t Have to Squeeze When You Sneeze
You are using a very outdated browser and will have a difficult time navigating and viewing this site. Please upgrade your browser and experience the web as it is intended!

- Cardiology - Provided by UCHealth
- Contact Lens Ordering
- Dermatology
- Endocrinology & Diabetes
- ENT | Otolaryngology – Ear, Nose & Throat
- Family Medicine
- Gastroenterology
- General Surgery
- Internal Medicine
- Laboratory - Provided by LabCorp
- Obstetrics and Gynecology
- Ophthalmology
- Optical Services
- Orthopedics
- Pediatric Orthopedics
- Podiatry - Foot & Ankle
- Radiology - Provided by Health Images
- Rheumatology
- Urgent Care
- After Hours Medical Care in Boulder
- Billing and Business Office
- Contracted Insurance List
- Healthcare Pricing
- Inclement Weather FAQs for Patients
- Minor Consent Form
- Request Medical Records
- Surprise Billing Disclosure

Chesney Kennedy, MD: Breastfeeding – Embrace Imperfection and Find Support
By Dr. Chesney Kennedy with assistance from Rebecca Harris, RN, IBCLC (International Board of Lactation Consultant)
Embracing Imperfection in Breastfeeding

Most parents I serve in my Boulder and Longmont pediatrics practice do not live in an extended family situation, surrounded by grandparents and aunties who are always around to help a baby latch onto the breast. Most families live in single-family homes and are lucky if they have helpers nearby, so there can be a sense of isolation. On top of that, many of the breastfeeding parents I work with have been perfectionists their whole lives—excelling in school, careers, and hobbies. They expect breastfeeding to go just as smoothly.
However, my observations over the years have taught me that birthing and breastfeeding can be areas of life over which we do not have much control. It can feel humbling and aggravating when our assumptions of how it should be do not pan out. Most breastfeeding parents have a deep, innate sense that breastfeeding should always feel beautiful, natural, and accessible. However, if that were the case, we would not have lactation consultants at every hospital and birth center.
Building Your Support Team
I encourage breastfeeding parents to gather their team of lactation consultant(s), medical provider(s), and trusted friends and family for help and support.
I also encourage every breastfeeding parent to trust themselves. I have seen breastfeeding parents who breastfeed easily from day one (rare). I have seen breastfeeding parents who have hired three different lactation consultants in the first month until they figured it out and thought they might lose their minds… but they didn’t. I have seen breastfeeding parents who decide that the process of breastfeeding is not good for their own mental health, and so they opt for formula instead (or a combination of breastfeeding and formula). I could go on…there are so many different scenarios. All of these paths are fine.
Most importantly, your baby is growing, and the breastfeeding parent’s emotional and physical health are optimized. Whatever path you choose will be right for you — even if it is not what you imagined. So again, allow yourself lots and lots of room for imperfection as you slowly learn how to breastfeed.
Practical Tips and Resources
In this article, I describe breastfeeding tips and resources in Boulder County that can support you in whatever path you choose. I have collaborated with my friend Rebecca Harris, Lactation Consultant, Nurse, and mother of three who resides and practices in the Bay Area in California. She became a lactation consultant years ago when I became a pediatrician, and we worked together at the same pediatric clinic. Rebecca brings 20 years of breastfeeding experience and has comprehensive breastfeeding knowledge at her fingertips. We used to joke that most mammals wake their sleepy newborns for feeding by licking their cheeks, and maybe humans could try it, too. While everything in this article is based on evidence-based medicine, this is our recommended personal approach based on years of observation and experience with moms and babies. Let me know if you try it!
Overview of Breastfeeding Tips and Resources
Let this article be a launching point. Rebecca and I believe it contains excellent practical advice. Ultimately, your breastfeeding plan will be unique to your situation. Your breastfeeding journey will come together with intuition and support.
We cover the following topics:
Benefits of Breastfeeding
- What to Expect in the First Few Days After Your Baby is Born
- A Breastmilk-Making Plan
- A Triple Feeding Plan
- Nipple Pain and Mild Engorgement Tips
- What to Avoid While Breastfeeding
- How to Clean Pump Parts\Helpful Pumping Accessories
- Breastmilk Storage
- How to Warm up Breastmilk
Reputable Website Resources
- Great Books for Parents on Baby’s First Year
- Boulder County (and surrounding area) Offerings for Breastfeeding Support, Lactation Consultants, Parent Support Groups
Breastfeeding your baby has so many health benefits for both the breastfeeding baby and the parent. Studies show that breastfed babies have lower risks of asthma, type I diabetes, and sudden infant death syndrome. Breastfed babies are also less likely to have ear infections and stomach bugs. The antibodies passed to your baby from the breastmilk help babies develop a robust immune system. Breastfeeding parents have a lower risk of developing breast cancer, ovarian cancer, Type II diabetes, and high blood pressure.
Some parents are unable or choose not to breastfeed (or exclusively breastfeed) for various reasons. There is absolutely nothing wrong with that, either. We are fortunate to live in a time when we have excellent formulas and donor breast milk.
Whatever your feeding plan is (or evolves into) for your baby, we can support you in the direction you wish to go.
What to Expect in the First Week
When your baby is born – whether it is in a hospital, birth center, or your home, a lactation consultant will visit at some point to help you get started with breastfeeding. If you are not offered this service automatically, request it. Most hospitals and birth centers have lactation nurses you can continue seeing after you leave. I recommend setting up an appointment with a lactation nurse before you leave the hospital and continuing to see them at least weekly until you feel completely comfortable with breastfeeding. The Lactation Network is a national organization that contracts with insurance providers to allow breastfeeding parents six free lactation support appointments. Visit their website at https://lactationnetwork.com/
After your baby’s birth, breastmilk takes around 3-5 days to come in fully. At times, it can take longer. We sometimes see this when moms experience stress, cesarean section, diabetes, or thyroid conditions. We can support you through this.
Your baby does not need much milk in the first couple of days. Babies are born with large glycogen supplies in their liver, keeping their blood sugar levels up. The milk volume will almost double daily in the baby’s first week. Here are typical volumes of what full-term babies need each day after birth. This is helpful if you need to supplement with pumped breast milk, donor breast milk, or formula during the first week of life. Often, no supplementation is necessary, but sometimes it is… and that is okay! You can decide whether or not to supplement with help from your pediatrician or lactation consultant.
Count your baby’s diapers as evidence of adequate intake. In general, the average amount for each feeding is (8-12+ feedings within 24 hours):
- Notes for intake: 30ml = 1 ounce
- Notes for output: Between days 2 and 3, baby’s stool changes from black to green, then to yellow, with a yellow “seedy” look by day 5.
You may need to supplement less as your milk supply increases and the infant’s latch and sucking improves. Please follow up with your pediatrician or lactation consultant to ensure your infant gains weight appropriately and that your milk supply can be assessed.
A Breast Milk Making Plan
Keep in mind that a breastfeeding plan is dynamic. A lactation consultant and your pediatrician will assist you with making adjustments as your milk supply develops and your baby grows into breastfeeding.
Spend time skin-to-skin, cuddling with your baby as often as possible. Skin-to-skin contact helps raise your prolactin level and naturally increases your milk production. It also helps boost your oxytocin level, a hormone that helps your milk to let down.
More breast stimulation and removal = more milk
Attempt breastfeeding at least 8-12+ times within 24 hours or every 0-3 hours. This will continue for about the first two weeks. All babies lose some weight right after birth. This is normal! Your baby will have a check-up at 2-3 days of age, and your pediatrician will ensure that the baby has not lost too much weight. At your two-week check-up, your pediatrician will check to see if your baby has regained their birth weight. Many parents are surprised to learn that babies are mostly nocturnal for the first six weeks after birth, so they may want to feed often at night. This is normal and to be expected. On days 2-4, you may experience “cluster feeding” when babies want to feed about every 30 minutes throughout the night, and this may continue when your baby is going through growth spurts within the first year of life.
A breastfeeding plan generally looks like this:
- Breastfeed on demand at least 8-12+ times per 24 hours (This may be every 0-3 hours).
- Alternate which breast the breastfeeding parent starts with. The breastfeeding parent can use a rubber band on their wrist to keep track.
- Breastfeed on one side for as long as the baby is actively feeding (usually about 10-20 min). Offer both breasts at each feeding.
- Hand-express for comfort, if needed. Watch this video on how to express your first milk .
A “Triple Feed” Plan
This plan be necessary in the following situations, which are pretty common:
- If a baby loses more than 10% of their birth weight within the first few days of life.
- If a baby isn’t removing breast milk well from the breast.
- If the breastfeeding parent is working on building their milk supply.
The Triple Feed Plan looks like this:
- Nurse on demand, at least every 3 hours.
- Pump right afterward for 10-15 minutes. Gently massage breasts while pumping. Suction should be comfortable at the highest level.
- Offer back your expressed milk via a syringe, cup, or bottle.
Record times, lengths of feeds, and amount of expressed milk fed to baby for at least the first two weeks.
Note: To shorten this cycle, have a helper feed your baby the pumped breastmilk (from your previous pump session) while you are pumping new fresh milk. Pumped breast milk is safe to stay at room temperature for 4-6 hours, so it is fine to sit on the counter and be used for the next feeding.
Tips for Nipple Pain or Mild Engorgement:
- Visit this website overview of mastitis and engorgement
- If you can, continue to breastfeed on demand at least every three hours. Try using reverse pressure softening or a little hand expression to help soften the areola, which relieves discomfort and makes it easier for the baby to latch.
- Watch this video showing reverse pressure softening
- If needed for missed feedings or in place of a breastfeeding session, pump your breasts for up to 10 minutes
- Offer all your expressed breastmilk back to your baby via bottle, finger feeder, or cup.

Avoid These Things That are Known to Reduce Breastmilk Supply
- Birth control pills and injections
- Decongestants, antihistamines
- Severe weight loss diets
- Mints, parsley, sage (excessive amounts)
Cleaning Pump Parts
- After using your pump parts, give them a good hot rinse and let them dry in a clean place away from bathroom or kitchen use and splatters
- Once a day, do a good scrubby wash on all parts
- Never wash the tubes, as they are for suction only
- You can also put milky pump parts in the refrigerator and use them un-rinsed at the next pumping session
Helpful Pumping Accessories
- Photo of baby, item of baby’s clothing, or the recorded sound of baby crying (these stimulate milk letdown reflex)
- Hands-free pumping bra
- High-quality breast pump or hospital-grade pump with breast milk storage bags
- Insulated tote with cooler packs to cool, store, and transport breast milk
Breast Milk Storage: Rule of Fives
A general rule of thumb is breast milk lasts:
- Five hours at room temperature.
- Five days in the refrigerator.
- Five months in the freezer.
Warming up Breast Milk
- To warm refrigerated breast milk, place it in a bowl of warm tap water surrounding the bottle, adding warm water if needed. The milk needs to be heated enough to remove the chill. Never microwave breastmilk
- Frozen milk can be thawed in a bowl of warm water, adding warm water as the water cools
- Frozen milk can be thawed in the refrigerator, but once the last ice crystals have melted, it must be used within 24 hours. Do not refreeze breast milk
- It is desirable to store some milk in feeding-size portions and have some in 1-2 oz increments to defrost as needed
- Kellymom.com — Latching, positioning, plugged ducts, mastitis, dairy, and other food sensitivities
- La Leche League International
- La Leche League – Safe Sleep
- Babycenter.com — Breastfeeding tips are under the “Baby” tab. They also have a great section on starting solid foods.
- Jane Morton, MD, IBCLC: Maximizing Milk production with a hospital-grade pump
- Working Moms – “Work and Pump”
- Global Health Media – A good latch video
- SimpliFed.com — Virtual breastfeeding support
Books for Parents in Baby’s First Year
- Happiest Baby on the Block by Harvey Karp, MD (sleep and soothing)
- Baby411 by Ari Brown and Denise Fields
- What to Expect the First Year by Heidi Murkoff
Local Breast Feeding Support, Lactation Services, and Parent Support Groups:
- Avista Hospital Lactation Department
- Birth Center of Boulder
- Boulder Community Health Lactation Support
- Boulder Medical Center lactation appointments: Erin Harper-Sanchez, CNM
- CommonSpirit Longmont United Hospital Lactation Consultant
- UCHealth Birth Center at Longs Peak Hospital
After all this advice, and I know these can be challenging times…I wish you happy moments with this sweet new person in your life. Cheers!
- Diana West, IBCLC, Diane Wiessinger, and Teresa Pitman from La Leche League International. The Womanly Art of Breastfeeding . July 13, 2010
- Diana West, IBCLC and Lisa Marasco, M.A., IBCLC. Making More Milk, The Breastfeeding Guide to Increasing Your Milk Production . November 18, 2019
- World Health Organization. Breastfeeding. Available at: https://www.who.int/health-topics/breastfeeding (Accessed on December 18, 2020)

Dr. Chesney Kennedy, MD – Pediatrician
About Chesney Kennedy Pediatrician in Longmont and Boulder
Dr. Chesney Kennedy is your dedicated partner in pediatric healthcare, serving families in Longmont and Boulder, Colorado. With a solid commitment to the well-being of children and teenagers, she goes above and beyond to create an inclusive and welcoming environment for all, including the LGBTQIA+ community, ensuring that everyone feels comfortable and respected in her practice. Specializing in:
General Pediatrics
- Newborn Care
- Well-Child and Preventive Care
- Personalized Primary Care: Tailored healthcare solutions to address the unique needs of each child
- Sick Visits
- Mental Health: Support for depression, anxiety, and ADHD
- Sports Physicals
- Vaccinations
Dr. Chesney’s services for teens include:
- Birth Control: Providing a range of options, including IUDs, Nexplanon®, birth control pills, Depo shots, and counseling
- Emergency Contraception: Offering Plan B
- Heavy Periods: Dr. Kennedy is here to address and manage heavy and irregular menstrual cycles
- Pregnancy Options & Counseling
- Sexually Transmitted Infections: Offering testing, diagnosis, and treatment
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills. Geneva: World Health Organization; 2013.

Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills.
13 breastfeeding.

- What is in this session?
Breastfeeding plays a crucial role in the health, growth and development of babies and has benefits for the mother too. Women may need some help to successfully feed their babies. They need support and reassurance as they learn this skill. This session focuses on the initiation of breastfeeding following birth and when and how to refer women who are experiencing difficulties.
If necessary and where possible, you should refer women to see a trained breastfeeding counsellor and/or use support materials, such as “the WHO and UNICEF training materials”.
Breastfeeding counselling, a training course (1993) http://www.who.int/child_adolescent_health/documents/who_cdr_93_3/en/index.html

Infant and young child feeding counselling, an integrated course (2006) http://www.who.int/nutrition/publications/infantfeeding/9789241594745/en/

- What skills will I develop?
- Providing information and demonstrating breastfeeding techniques
- Encouragement and support
- Shared problem-solving

- What am I going to learn?
By the end of this session you should be able to:
- Communicate the advantages and benefits of breastfeeding for both mother and baby
- Demonstrate how to breastfeed a baby, including positioning and attachment
- Assess actual and potential difficulties and how to work with women on ways to overcome them
- Explain the opportunities for HIV-infected mothers to breast feed and improve HIV-free survival of their baby
- Breastfeeding
During pregnancy and after the birth it is important to discuss with women the importance of exclusive breastfeeding for six months. Try to include the partner or other family members and communicate to them all about the benefits of breastfeeding for the mother and baby, the process of breastfeeding and when and how long to feed for. You should also discuss continued breastfeeding after six months and introduction of other foods in addition to breast milk. You might find it useful to refer to more specialized breastfeeding tools and materials to support your discussion.
What is so good about breastfeeding?
- Breast milk provides all the nutrients that a baby needs for the first six months of life to grow and develop.
- Breast milk continues to provide high-quality nutrients and helps protect against infection up to two years of age or more.
- Breast milk protects babies from infections and illnesses.
- Babies find breast milk easy to digest.
- The baby's body uses breast milk efficiently.
- Breastfeeding can contribute to birth spacing.
- Breastfeeding helps the mother's uterus to contract reducing the risk of bleeding after birth.
- Breastfeeding lowers the rate of breast and ovarian cancer in the mother.
- Breastfeeding promotes a faster return to mother's pre-pregnancy weight.
- Breastfeeding promotes the emotional relationship, or bonding, between mother and infant.
As well as benefits for the baby in terms of survival, breastfeeding has other advantages. It is easier to carry out than feeding formula; it takes no preparation; is always at the correct temperature, it is always clean and is always available. It is the perfect nutrition for babies.
Communicate information on the advantages of breastfeeding (including health benefits, economic benefits, etc.), to help women decide which method of feeding they will choose. Be sure to also discuss the risks of not breastfeeding. Answer any questions or concerns the woman may have. For example, some women do not realize that it is normal for the baby to lose weight in the first three or four days after birth and that this is not a reflection of how she is breastfeeding or the quality of her breast milk. Women can still breastfeed while taking most medications, such as antibiotics, antiretroviral or TB medication.
Some women may choose not to breastfeed. You should respect this decision, even if you disagree with it and support her to replacement feed safely.

Women need support to help them decide and carry out their infant feeding choice
Risks of not breastfeeding.
- Babies may get sick more often with diarrhoea, malnutrition and pneumonia and are at increased risk of dying.
- Babies do not get natural protection to illnesses.
Initiating skin-to-skin contact and breastfeeding
After birth, dry the baby. Place him/her on the mother's chest, preferably with skin-to-skin contact. Use a blanket to cover both baby and the mother, to keep the baby warm. When the baby seems ready, encourage the mother to help the baby to her breast. Babies show they are ready to take the breast when they start “rooting”, or looking for the breast. Some babies need encouragement to latch-on at this stage.
It is important for all mothers to start skin-to-skin contact from birth as soon as possible following birth – preferably in the first hour. They should let their baby suckle when they appear to be ready. Some babies may take longer to start breastfeeding. As a health worker you have an important role in helping the mother to do this. Early contact will help a mother to bond with her baby - that is, to develop a close, loving relationship. It also makes it more likely that she will start to breastfeed.
SKIN-TO-SKIN CONTACT HELPS
- to keep the baby warm
- to establish breastfeeding
- to encourage mother-child bonding.
Positioning and attachment
To help a mother learn how to breastfeed first encourage her to get herself into a comfortable position. Show her how to hold the baby straight, with both the baby's head and body turned to face her breast and with the baby's nose opposite her nipple. She should hold the baby close supporting the whole body, not just the neck and shoulders. Refer to breastfeeding aids and materials to help you become more familiar with correct positioning and attachment.

Encourage and support women as they learn to breastfeed
Observe the mother breastfeeding her baby and offer help and assistance if needed. Look for signs of good attachment and effective suckling (slow deep sucks with pauses). If the attachment is not good, encourage the mother to reposition the baby. Show the mother how to take the baby off the breast, by inserting her little finger into the corner of the baby's mouth. Keep encouraging and reassuring the mother the whole time. Encourage her to reposition the baby until she feels comfortable and the baby is sucking well. Reassure her that there is no need to rush, even if the baby is crying.
Correct breastfeeding positioning occurs when the baby's:
- head and whole body are well supported and held close to mother
- face and stomach face the mother
- ear and shoulder are in one straight line, neck is not twisted.
Good attachment occurs when the baby's:
- mouth covers most of areola (dark part of the nipple) with some of the areola visible above the mouth
- mouth is wide open
- chin touches the breast
- lower lip is turned outwards.
Effective suckling occurs when:
- slow, deep firm sucks alternate with bursts of suckling
- no other sounds except swallowing sounds are heard.
Exclusive breastfeeding
All mothers should be encouraged to exclusively breastfeed their babies until they are six months old. Exclusive breastfeeding means that the baby is not given any other food or drink, not even water. They are only given breast milk. Make sure that you or others in the facility do not give the baby anything that will interfere with exclusive breastfeeding.
To encourage and support exclusive breastfeeding there are key things you can do:
- Encourage breastfeeding frequently, day and night, and advise the mother to allow the baby to feed for as long as he/she wants. Tell her it is quite normal for a baby to feed up to eight times a day. Explain to her the signs a baby will show when he/she needs to be fed (such as “rooting”, looking for the nipple, sucking on the hand).
- Reassure the parents that there is no need to give the baby any other drink or food, not even water – breast milk has all a baby needs.
- Help the mother whenever she needs assistance and especially if she is a first time or adolescent mother or a mother with other special needs.
- Explain to the mother she should let the baby finish the first breast and come off on its own before offering the second breast.
- Encourage the mother to start each feed with a different breast. For example, if the left breast is used to start one feed, at the next feeding start with the right breast.
- If it is necessary to express breast milk, show the mother how to do this and show her how to feed expressed breast milk by cup. You may need to refer her to a trained infant feeding counsellor for this.
- Reassure the mother that her body will make enough breast milk to satisfy her baby's needs. Just because a baby is crying, it does not mean that she does not have enough breast milk. A baby who is demanding more breast feeds may be growing. By allowing the baby to suckle more often, her body will produce more breast milk to meet her baby's needs.
- Explain that the mother can provide all the breast milk her baby needs for the first 6 months and beyond.
- Explain that the mother can continue breastfeeding if she has to return to work or school, either by expressing breast milk or feeding more often when she is at home.
- Advise her to seek help (or come back to see you) if the baby is not feeding well or if she has any difficulties or concerns with breastfeeding, sore nipples or painful breasts. If needed, refer her to a trained infant feeding counsellor.

In many health facilities breastfeeding is supported in a number of different ways. This activity is designed to get you and your colleagues to assess how you provide breastfeeding counselling and support, and what could be improved or strengthened.
- At what point in pregnancy did the health worker discuss breastfeeding with them?
- Do they think these discussions should have started earlier in pregnancy or later, or was this the right time?
- Do they remember what was discussed with them? (Make a list of the different points discussed.)
- Did they feel the information was clear and easy for them to understand?
- After birth, what advice and support was given to them to breastfeed their babies? When was this given?
- Was skin-to-skin contact promoted after birth (the baby placed on the mother's upper abdomen)? How soon after birth was it started?
- Was ongoing support, advice and reassurance given to them? How was this given?
- Who gave them support and advice once they were home? Did they feel they had enough support and advice or did they need more? What additional support and advice did they think would be helpful?
- What are some of the barriers women face to exclusive breastfeeding and how can the health staff help them to solve these?
- Ask women for suggestions on how staff could better respond to their needs.
- Discuss the responses with the rest of the group working through this handbook if applicable. Do you need to do anything differently? How can you as a team better respond to the support women need to successfully breastfeed? With the manager, make a plan for any changes that should be introduced, including reviews to check on how you are progressing. For example, you could carry out this activity again, six months after making changes to evaluate whether you have made any improvements.

Discussion of breastfeeding should start during pregnancy by asking women how they plan to feed the baby. At this time you do not need to overload women with too much information. Stick to the basic facts about the benefits of breastfeeding for the baby and for the mother. Talk to women about the benefits of initiating skin-to-skin contact as soon as possible following the birth (preferably within one hour) to facilitate early initiation of breastfeeding. You should help the mother with the first breastfeed to show her how to position and attach the baby. Demonstrations are important as breasfeeding is a skill that mothers learn. Have dolls available to demonstrate position. Remember to provide as much support and reassurance as each woman needs - it will vary according to the woman.
Consider how you might be able to provide support and reassurance to women once they have left the health facility and are at home. Once home many women experience feeding problems such as engorged breasts or cracked nipples. Others may be pressured by family members to offer supplementary foods or drinks. How can you work with women to overcome some of these problems? One way is to talk with all family members on the importance of exclusive breastfeeding. You can also make sure you assess breastfeeding at any visit or meeting during the postnatal period. Also consider holding a special session for breastfeeding problems.
Often in the community, groups exist to support women who are breastfeeding. Find out what support exists, or contact women who have successfully breastfed and see if they would be available to support women after birth.
Before discharge and if the mother returns to the health facility during the postnatal period you need to assess how breastfeeding is going. You should also assess breastfeeding and provide relevant information during routine visits and at any time if there is feeding difficulty or the mother is concerned about feeding.
- Supporting breastfeeding
Women need extra support, encouragement and reassurance while breastfeeding. Although we view breastfeeding as a natural process, it is still a skill that has to be learned. Initially breastfeeding can seem demanding, as the baby may have a desire to feed/suck frequently. Babies however, begin to establish their own pattern over time, and the mother will begin to feel more comfortable and at ease.
Some women also find that the initial ‘let down’ reflex is very strong which causes them pain or they get strong after-pains as their wombs contract. Reassure them that this will pass. The ‘let down’ reflex may also cause them to leak milk when they have sexual intercourse. Reassure them that this is normal and that they may need to tell their husband or partner that this is normal.
Sometimes husbands or partners may feel excluded from the breastfeeding process. Encourage them to be involved in other ways. This may ease the situation and help men to provide more support for breastfeeding; for example, by asking him to fetch the baby for the feed, helping make the woman comfortable, or looking after the other children while she is feeding. Massaging the baby, and humming to calm a crying baby are other very useful ways of involving men.
Many women find breastfeeding difficult due to problems such as engorgement or sore nipples. Engorgement may happen a few days after birth or at any time when the baby's feeding pattern changes. The breasts become overfull with milk and tissue fluid; milk does not flow well and the skin is tight (especially the nipple). This makes it difficult for the baby to latch on. Sometimes the skin looks red and the woman has a fever which usually disappears in 24 hours. To prevent engorgement, help women to start breastfeeding soon after birth, ensure good attachment and encourage unrestricted breastfeeding. To treat engorgement, recommend that the mother puts warm compresses on her breasts or takes a warm shower and expresses enough milk to reduce discomfort which helps make attachment easier. After expressing milk she can use cold compresses to reduce the inflammation. Cracked or sore nipples occur mainly because the baby is not attaching properly. Help the mother to make sure the baby is attaching properly.
Support for feeding preterm and/or low birth weight babies
Low birth-weight or preterm babies should be fed their mother's own breast milk. The mother may need extra support to initiate breastfeeding or expressing breastmilk as soon as possible after birth. Because low birth-weight babies can sometimes get easily tired when feeding, it is particularly important that the mother feeds her baby as often as possible, responding to demand and at least 8 feeds during 24 hours, during the day and night
If a mother cannot feed her own baby, it is still best for a low birth-weight baby to be fed human breast milk. Another woman could feed the baby, so long as she is not HIV-infected. Some facilities have established breast milk banks, where breast milk from healthy donor women is collected, pasteurised and kept frozen. If your facility does not have a breast milk bank, maybe the local referral hospital can put you in contact with a breast milk bank. Try to find out about breast milk banks in your area and keep this information available for mothers who cannot breastfeed for a while due to health problems. If the low birth-weight or preterm baby cannot be fed breast milk, either by the mother, a wet nurse or from a breast milk bank, then the baby can be given standard infant formula by cup. Look at Session 26 of the WHO Breastfeeding Counselling: A training course ( http://www.who.int/maternal_child_adolescent/documents/who_cdr_93_3/en/ ), for further information on how to help a mother breastfeed a low birth-weight baby.

Encouraging continuous skin-to-skin contact can help low birth weight babies keep warm and support breastfeeding on demand. Make sure parents are aware of all the newborn danger signs and that they understand it is especially important to bring a low birth-weight newborn to a health facility if they have any worries, as these small babies are at particular risk from infections and feeding difficulties.
Support for the mother who is not yet breastfeeding
If the mother or baby is ill or the baby is too small to suckle you need to give extra support and help. First teach the mother how to express milk and feed the baby by cup. If you have not been trained to do this, you should refer to an infant feeding counsellor where possible. If the mother and baby are separated for any reason then reassure the mother about the baby's progress whenever she asks. Encourage the mother to start breastfeeding the baby as soon as she or the baby is able.
Support for breastfeeding twins
Many mothers who give birth to two or more babies are worried they will not have enough milk. Reassure her that she will have enough milk for both babies. Encourage the mother to feed one baby at a time until breastfeeding is established. You can then show her different ways she can feed the babies and work with her to find out which method she is most comfortable with. If one twin is weaker or smaller than the other, make sure that the weaker twin also gets enough milk.
Advice to women who are not breastfeeding
Some women may not be able to breastfeed and others may choose not to. A woman's right to take an informed decision should be supported and respected. If after discussing the benefits of breastfeeding and the risks of not breastfeeding the mother decides not to breastfeed, she should be shown alternative methods.
These mothers need to learn how to safely prepare and feed formula to their babies. You may also have other women whose babies have died or who have had a stillbirth. These women may experience discomfort in their breasts for a period of time. Advise them not to stimulate the breasts or nipples. Show them how to support the breasts with a firm well fitting bra or a cloth. Teach the mother how to express just a little milk to relieve discomfort but not enough to stimulate more milk production.
Advise all women to seek care if their breasts become painful, swollen, and red or if they feel ill.
- Mothers who are HIV-positive
Babies of HIV-positive mothers can benefit from breastfeeding for all the same reasons outlined above. HIV may pass from an HIV-infected mother to her baby during pregnancy, childbirth and breastfeeding. Antiretroviral treatments can dramatically reduce the risk of mother-to-child transmission during breastfeeding and increase the chance of HIV-free survival of the baby (that is, staying free of HIV infection and also staying alive). Although there is still a small chance that the baby could become HIV positive even when the mother is being treated with antiretroviral drugs, babies who are not breastfed, but given replacement feeds, are more likely to die from infections.
National health authorities should have a policy to indicate whether health services should promote and support breastfeeding or replacement feeding among HIV-infected mothers. You need to be aware of this recommendation and you should develop the skills to support women to achieve this. However, it is a mother's right to choose how to feed her baby and you will need to support her choice. Mothers who are aware they are HIV infected should be counselled on safe infant feeding by a trained infant feeding counsellor. Where specialist help is not available, you should support women as best you can.
Ask her to repeat back to you in her own words to make sure she has understood the information correctly. Work together to make a plan that she can implement in order to carry out safe infant feeding.
Women who are HIV-positive and plan to breastfeed need support, particularly in the early stages when breastfeeding is being initiated. Try to help the women to avoid getting mastitis or nipple damage, as these difficulties increase the risk of transmission to the baby. Advise the woman to return if she has any problems with her breasts.
Women who have chosen replacement feeding for their babies must have regular follow-up to ensure that the baby is growing and to support replacement feeding. These women need extra support and reassurance, especially if they are from a community where breastfeeding is the norm. Many communities may stigmatize or shun a woman who chooses replacement feeding. Work with families and communities to support women in their choice of infant feeding.
WHO RECOMMENDATIONS FOR INFANT FEEDING FOR HIV-POSITIVE WOMEN
Mothers known to be HIV positive should be provided with lifelong antiretroviral therapy or antiretroviral prophylaxis (preventative treatment) to reduce HIV transmission to the baby during pregnancy, childbirth and breastfeeding.
National health authorities should decide whether health services in that country should principally promote and support breastfeeding or promote and support replacement feeding among HIV-infected mothers.
In settings where national authorities recommend breastfeeding, HIV infected mothers and/ or their babies should be given antiretroviral treatment or prophylaxis to reduce the risk of transmission throughout the breastfeeding period.
These mothers should exclusively breastfeed their babies for the first 6 months of life, then introduce appropriate complementary foods with continued breastfeeding for the first 12 months of life. Mothers should stop breastfeeding only when they can provide a safe and adequate diet.
If a mother decides to stop breastfeeding, she should do so gradually within one month.
HIV infected mothers should only give commercial infant formula milk as a replacement feed to their baby when specific conditions of safety and hygiene, affordability and supply of formula, access to health care and family support for replacement feeding are met.
Guidelines on HIV and infant feeding 2010. Principles and recommendations for infant feeding in the context of HIV and a summary of evidence
http://www.who.int/maternal_child_adolescent/documents/9789241599535/en/

What did I learn?

Breastfeeding should be encouraged and supported for all women. In this session you examined how to explain the importance of exclusive breastfeeding for six months and continued breastfeeding up to two years or beyond. You learned how to support women and how to demonstrate ways to effectively breastfeed soon after the birth. You also learned that mother who are HIV-infected can also breastfeed and give their baby all the benefits of breast milk with very little risk of transmitting HIV.
Take some time to reflect on how you can improve your own skills in communicating breastfeeding and demonstrating how to position and attach the baby. You could use your notebook to write down tips or advice you can give to women who are experiencing problems.
Encourage women to learn from one another; often women have helpful home remedies or suggestions for alleviating some of the discomforts associated with breastfeeding in the early stages. Determine what support exists in the community. Make contacts with these groups.
Finally, remember that it is important for successful breastfeeding that the woman has the support of her partner and her family.
All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob ). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep ).
- Cite this Page Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills. Geneva: World Health Organization; 2013. 13, BREASTFEEDING.
- PDF version of this title (5.7M)
In this Page
Other titles in this collection.
- WHO Guidelines Approved by the Guidelines Review Committee
PUBLICATIONS
Attitudes towards breastfeeding, breastfeeding, kangaroo care with premies, milk banking.
- Skin to Skin
Sore Nipples
Powdered Baby Formula Sold in North America: Assessing the Environmental Impact K Cadwell, A Blair, C Turner-Maffei, M Gabel, and K Brimdyr – Breastfeeding Medicine (ahead of print) DOI: 10.1089/bfm.2020.0090
Childhood Obesity and Breastfeeding Rates in Pennsylvania Counties—Spatial Analysis of the Lactation Support Landscape A Blair, E MacGregor, N Lee – Frontiers in Public Health, April 2020 DOI: 10.3389/fpubh.2020.00123
A Survey of Knowledge, Attitudes, and Practices of Providers and Staff at Al-Zahraa University Hospital Regarding the Baby-Friendly Hospital Initiative and the International Code of Marketing Breast Milk Substitutes SM Abd El-Ghany, AAW Korraa, EA Ahmed, IMW Salem, SA Eslam, AA El-Taweel, K Cadwell – The Journal of Perinatal Education , October 2019. DOI: 10.1891/1058-1243.28.4.210
Case Studies in Breastfeeding: Problem-solving Skills & Strategies (2nd ed.) K Cadwell, C Turner-Maffei – Sandwich, Mass.: Healthy Children Project, Inc., 2019
Call for Improved Military Policy to Support Breastfeeding Among U.S. Armed Forces E Drake, K Cadwell, JE Dodgson – Nursing Outlook, May-June 2017; 65(3):343-345. Epub 2017 Apr 18. DOI: 10.1016/j.outlook.2017.04.007
Intrapartum Administration of Synthetic Oxytocin and Downstream Effects on Breastfeeding: Elucidating Physiologic Pathways K Cadwell, K Brimdyr – Intrapartum Administration of Synthetic Oxytocin and Downstream Effects on Breastfeeding: Elucidating Physiologic Pathways. Ann Nurs Res Pract. 2017; 2(3): 1024.
Pocket Guide for Lactation Management K Cadwell, C Turner-Maffei – Sudbury, Mass.: Jones and Bartlett Publishers, 2021
Breastfeeding AZ: Terminology and Telephone Triage K Cadwell, C Turner-Maffei – Sudbury Mass.: Jones and Bartlett Publishers, 2012
Evaluation of mothers’ knowledge, attitudes, and practice towards the ten steps to successful breastfeeding in Egypt AMAM Abul-Fadl, M Shawky, A El-Taweel, K Cadwell, C Turner-Maffei – Breastfeeding Medicine, 2012
The Curriculum in Support of the Ten Steps to Successful Breastfeeding: A 20-Hour Interdisciplinary Breastfeeding Management Course for the United States. (3rd ed.). K Cadwell & C Turner-Maffei, Sandwich, Mass: Health Education Associates, Inc., 2011
Continuity of care in breastfeeding: Best practices in the maternity setting K Cadwell, C Turner-Maffei – Sudbury, Mass.: Jones and Bartlett Publishers, 2009
Improved breastfeeding success through the baby-friendly hospital initiative. D Meyers, C Turner-Maffei, American Family Physician, 78(2), 180, 182, 2008.
100 questions & answers about breastfeeding. K Cadwell, C Turner-Maffei, AC Blair, Sudbury, Mass.: Jones & Bartlett Publishers, 2008
Lactation resources for clinicians C Turner‐Maffei – Journal of Midwifery & Women’s Health, 2007
Maternal and infant assessment for breastfeeding and human lactation: a guide for the practitioner (2nd ed.) K Cadwell, C Turner-Maffei, B O’Connor, A Blair, L Arnold, & E Blair, Sudbury, Mass.: Jones and Bartlett Publishers, 2006
Maternal and Infant Assessment for Breastfeeding and Human Lactation: A Guide for the Practitioner K Cadwell, C Turner‐Maffei, B O’Connor, A Blair – Journal of Midwifery & Women’s Health, 2004
Overcoming barriers to implementing the Ten Steps to Successful Breastfeeding—Final report C Turner-Maffei, K Cadwell – Sandwich, MA: Baby-Friendly USA, 2004
Reclaiming breastfeeding for the United States: Protection, promotion and support K Cadwell, C Turner-Maffei, A Blair, L Arnold, Z Maja McInerney, C Cadwell, K Brimdyr – Jones and Bartlett Publishers, Inc., 2002
Fielding questions about breastfeeding BL Philipp, K Cadwell – Contemporary Pediatrics – Montvale, 1999
Global participatory action research (GLOPAR) K Cadwell, E White – Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 11(4), 262, 1995
Skin-to-Skin
Skin-to-skin contact after birth: Developing a research and practice guideline K Brimdyr, J Stevens, K Svensson, A Blair, C Turner-Maffei, J Grady, L Bastarache, A al Alfy, J Crenshaw, E Giugliani, U Ewald, R Haider, W Jonas, M Kagawa, S Lilliesköld, R Maastrup, R Sinclair, E Swift, Y Takahashi, K Cadwell – Acta Paediatrica, May 2023 DOI: 10.1111/apa.16842
Connecting the dots between fetal, premature and full-term behaviour while in skin-to-skin contact: The nine stages of instinctive behaviour K Brimdyr, K Cadwell – Breastfeeding Review, November 2021
The nine stages of skin‐to‐skin: practical guidelines and insights from four countries K Brimdyr, K Cadwell, K Svensson, Y Takahashi, E Nissen, AM Widström – Maternal & Child Nutrition, June 2020 DOI: 10.1111/mcn.13042
A plausible pathway of imprinted behaviors: Skin-to-skin actions of the newborn immediately after birth follow the order of fetal development and intrauterine training of movements AM Widström, K Brimdyr, K Svensson, K Cadwell, E Nissen – Medical Hypotheses, January 2020 DOI: 10.1016/j.mehy.2019.109432
A low-cost intervention to promote immediate skin-to-skin contact and improve temperature regulation in Northern Uganda E Nissen, K Svensson, S Mbalinda, K Brimdyr, P Waiswa, B Mpora Odongkara, A Hjelmstedt, June 2019 DOI: 10.12968/ajmw.2018.0037
The effect of labor medications on normal newborn behavior in the first hour after birth: A prospective cohort study K Brimdyr, K Cadwell, AM Widström, K Svensson, R Phillips – Early Human Development, May 2019 DOI: 10.1016/j.earlhumdev.2019.03.019
Skin-to-skin contact the first hour after birth, underlying implications and clinical practice AM Widström, K Brimdyr, K Svensson, K Cadwell, E Nissen – Acta Pædiatrica, February 2019 DOI: 10.1111/apa.14754
Mapping, Measuring, and Analyzing the Process of Skin-to-Skin Contact and Early Breastfeeding in the First Hour After Birth K Cadwell, K Brimdyr, R Phillips – Breastfeeding Medicine, September 2018 DOI: 10.1089/bfm.2018.0048
An implementation algorithm to improve skin-to-skin practice in the first hour after birth K Brimdyr, K Cadwell, J Stevens, Y Takahashi – Maternal and Child Nutrition, April 2018 DOI: 10.1111/mcn.12571
The Association Between Common Labor Drugs and Suckling When Skin-to-Skin During the First Hour After Birth K Brimdyr, K Cadwell, AM Widström, K Svensson, M Neumann, E Hart, S Harrington, R Phillips – Birth: Issues in Perinatal Care, October 2017 PMID:26463582
A realistic evaluation of two training programs on implementing skin-to-skin as a standard of care K Brimdyr, AM Widström, K Cadwell, K Svensson, C Turner-Maffei – The Journal of perinatal education, 2012 DOI: 10.1891/1058-1243.21.3.149
Effect of early skin to skin contact on preterm neonates’ vital parameters NM Samra, K Brimdyr – Journal of Arab Child, 2011
An overview of PRECESS
A Realistic Evaluation of Two Training Programs on Implementing Skin-to-Skin as a Standard of Care. K Brimdyr, AM Widström, K Cadwell, K Svensson, C Turner-Maffei. J Perinat Educ. 2012 Summer;21(3):149-57. doi: 10.1891/1058-1243.21.3.149. PMID: 23730126 Free PMC Article
Use of a video-ethnographic intervention (PRECESS Immersion Method) to improve skin-to-skin care and breastfeeding rates. JT Crenshaw, K Cadwell, K Brimdyr, AM Widström, K Svensson, JD Champion, RE Gilder, EH Winslow. Breastfeed Med. 2012 Apr;7(2):69-78. doi: 10.1089/bfm.2011.0040. Epub 2012 Feb 7. PMID: 22313390
Effect of intermittent kangaroo mother care on weight gain of low birth weight neonates with delayed weight gain. NM Samra, AE Taweel, K Cadwell. J Perinat Educ. 2013 Fall;22(4):194-200. doi: 10.1891/1058-1243.22.4.194. PMID: 24868132 Free PMC Article
The effect of kangaroo mother care on the duration of phototherapy of infants re-admitted for neonatal jaundice. NM Samra, A El Taweel, K Cadwell. J Matern Fetal Neonatal Med. 2012 Aug;25(8):1354-7. doi: 10.3109/14767058.2011.634459. Epub 2011 Nov 28. PMID: 22122062
Evaluation of mothers’ knowledge, attitudes, and practice towards the ten steps to successful breastfeeding in Egypt. AM Abul-Fadl, M Shawky, A El-Taweel, K Cadwell, C Turner-Maffei. Breastfeed Med. 2012 Jun;7(3):173-8. doi: 10.1089/bfm.2011.0028. PMID: 22803928
Evaluation of mothers’ knowledge, attitudes, and practice towards the ten steps to successful breastfeeding in Egypt. AM Abul-Fadl, M Shawky, A El-Taweel, K Cadwell, C Turner-Maffei, Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 7, 173–178. 2012
Effect of components of a workplace lactation program on breastfeeding duration among employees of a public-sector employer. JA Balkam, K Cadwell, SB Fein. Matern Child Health J. 2011 Jul;15(5):677-83. doi: 10.1007/s10995-010-0620-9. PMID: 20552261
Latching-on and suckling of the healthy term neonate: breastfeeding assessment. K Cadwell. J Midwifery Womens Health. 2007 Nov-Dec;52(6):638-42. Review. PMID: 17984002
Pain reduction and treatment of sore nipples in nursing mothers. K Cadwell, C Turner-Maffei, A Blair, K Brimdyr, Z Maja McInerney. J Perinat Educ. 2004 Winter;13(1):29-35. PMID: 17273373 Free PMC Article
The relationship between positioning, the breastfeeding dynamic, the latching process and pain in breastfeeding mothers with sore nipples. A Blair, K Cadwell, C Turner-Maffei, K Brimdyr. Breastfeed Rev. 2003 Jul;11(2):5-10. PMID: 14768311
Human milk in the NICU: policy into practice L Arnold, Sudbury, MA: Jones and Bartlett, 2010
U.S. health policy and access to banked donor human milk LDW Arnold, Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 3(4), 221–229, 2008
Global health policies that support the use of banked donor human milk: a human rights issue LDW Arnold, International Breastfeeding Journal, 1, 26, 2006
The ethics of donor human milk banking LDW Arnold, Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 1(1), 3–13, 2006
The cost-effectiveness of using banked donor milk in the neonatal intensive care unit: prevention of necrotizing enterocolitis. LDW Arnold, Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 18(2), 172–177, 2002
Trends in donor milk banking in the United States. LD Arnold, Advances in Experimental Medicine and Biology, 501, 509–517, 2001
Recommendations for collection, storage, and handling of a mother’s milk for her own infant in the hospital setting (3rd ed.) . LD Arnold, Human Milk Banking Association of North America, 1999
How to order banked donor milk in the United States: what the health care provider needs to know. LD Arnold, Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 14(1), 65–67, 1998
Donor milk banking in China: the ultimate step in becoming baby friendly. LD Arnold, Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 12(4), 319–321, 1996
Storage containers for human milk: an issue revisited. LD Arnold, Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 11(4), 325–328, 1995
A plausible causal relationship between the increased use of fentanyl as an obstetric analgesic and the current opioid epidemic in the US. K Brimdyr, K Cadwell – Medical Hypotheses, October 2018, Volume 119, Pages 54-57.
- Latest Updates
- Global Impact
- Cape and Islands
- Meet the Team
- Lactation Counselor Training Course
- CLC Certification
- Online Learning
- Lactation Courses
- International Conference
- Upcoming Courses
- College Credit Recommendations
- Books & Videos
- Publications
Healthy Children Project, Inc. | 159 Long Pond Drive, Harwich, MA 02645
Copyright Healthy Children Project, Inc.
- Online Maternal & Infant Assessment Course
- Online Advanced Issues in Lactation Practice Course
- 2024 Breastfeeding Symposium at Sea
- Research Team

- Kindle Store
- Kindle eBooks
- Parenting & Relationships
Promotions apply when you purchase
These promotions will be applied to this item:
Some promotions may be combined; others are not eligible to be combined with other offers. For details, please see the Terms & Conditions associated with these promotions.
Buy for others
Buying and sending ebooks to others.
- Select quantity
- Buy and send eBooks
- Recipients can read on any device
These ebooks can only be redeemed by recipients in the US. Redemption links and eBooks cannot be resold.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Follow the author

Case Studies in Breastfeeding: Problem-Solving Skills & Strategies Kindle Edition
- Print length 251 pages
- Language English
- Sticky notes On Kindle Scribe
- Publication date September 2, 2020
- File size 12801 KB
- Page Flip Enabled
- Word Wise Enabled
- Enhanced typesetting Enabled
- See all details
Customers who read this book also read

Editorial Reviews
About the author, product details.
- ASIN : B08HDLVQ2B
- Publication date : September 2, 2020
- Language : English
- File size : 12801 KB
- Text-to-Speech : Enabled
- Screen Reader : Supported
- Enhanced typesetting : Enabled
- X-Ray : Not Enabled
- Word Wise : Enabled
- Sticky notes : On Kindle Scribe
- Print length : 251 pages
- #78 in Breastfeeding
- #174 in Education Problem Solving
- #2,272 in Baby & Toddler Parenting
About the author
Karin cadwell.
Discover more of the author’s books, see similar authors, read author blogs and more
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Top reviews from other countries
Report an issue
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Welcome to parenthood — it's quite a ride! Have questions about baby sleep habits , baby care and feeding, health, development , and safety? We can help you solve breastfeeding and baby sleep problems, start solid foods, handle crying, know what your baby's ready for, track your baby's development , find great childcare and baby activities, and more.
Baby topics

- Newborn Baby Care & Feeding
- Newborn Baby Sleep
- The Early Weeks

- Postpartum Complications
- Postpartum Weight & Body Image
- Contraception
- Postpartum Depression & Emotional Health
- Postpartum Nutrition
- Postpartum Relationships & Sex
- Recovering From Birth
- Postpartum Fitness

- Baby Development Delays
- Physical Development
- Social & Emotional Development
- Encouraging Baby Development
- Your Baby's Brain Development
- Your Baby's Developing Senses
- Your Baby's Developmental Milestones
- Your Baby's Firsts

- Behavior Basics
- Bonding & Attachment

- Games & Activities

- Your Newborn
- Your Baby From 2 to 6 Months
- Your Baby From 7 to 11 Months

- Bedtime Routines
- Sleep Problems & Solutions
- Sleep Basics
- Your Baby's Naps

- Breast Pumping & Bottle Feeding
- Breastfeeding Basics
- Nursing Problems & Solutions
- Special Nursing Situations
- Is It Safe: Breastfeeding

- Soothing Your Baby
- Why Babies Cry

- Baby Poop 101
- Diaper Rash (birth to 12 mo.)
- Diapering Basics

- Bottles & Nipples
- Choosing & Using Baby Formula

- Baby Sleep & Feeding Schedules
- Creating Your Baby's Routine

- Baby Food Ideas & Recipes
- Feeding Problems & Solutions
- Solid Feeding Basics
- Food Safety

- Baby Bath Basics

- Parenting in the NICU
- Preemie Care & Feeding
- Preemie Development
- Life as a Preemie Parent

- Childcare Basics
Latest in Baby


Breastfeeding challenges and product fixes for common problems
Breastfeeding can be difficult, but thankfully there are products available to help.
Breastfeeding is a natural process, but it doesn’t always come easily. Many new mothers encounter challenges such as latch issues, low milk supply, engorgement, and sore nipples.
These challenges can often leave new mums feeling overwhelmed and frustrated so it’s important to remember that every breastfeeding journey is unique and seeking support from lactation consultants or support groups can be helpful.
There are also several products now available to help new mums overcome their breastfeeding issues.
By understanding the cause of the issue and learning to deal with it effectively, the sooner you can get back to enjoying the experience of breastfeeding your baby.
We take a closer look at some common breastfeeding issues and the products that offer relief and support.
Products to help with breastfeeding
Help to soothe and heal sore nipples.
One of the most common complaints from breastfeeding mothers is sore and cracked nipples . The initial days of nursing can be uncomfortable as both mother and baby adapt to the process.
Most nipple pain can be attributed to the latch or attachment of your baby. It may take a little time to get this right.
Using a nipple balm or nipple shields can provide relief by soothing and protecting the delicate skin.
GAIA Skin Naturals Nipple Balm, RRP $12.95
GAIA Skin Naturals Nipple Balm , a nourishing balm to moisturise, soothe and protect your sensitive areas. The balm is made from natural ingredients meaning there is no need to rinse before feeding.
Silverette Nursing Cups, The Original Nursing Cups, RRP $85 – $96
Silverette Nursing Cups, The Original Nursing Cups are made from 925 silver that has antimicrobial, anti-inflammatory, anti-fungal AND antibacterial benefits. The can be worn between feeds to naturally prevent, protect and soothe soreness, irritation or cracked nipples from breastfeeding or expressing milk.
Try this to relieve engorgement
When milk production exceeds the baby’s demand, breasts can become overly full, hard and painful. In addition to the pain associated with being full, engorgement may also cause your nipples to flatten, making it difficult for your baby to latch on properly, which can lead to the pain described above.
Massaging the breasts, applying warm compresses, and using breast pumps to express milk can help to alleviate this discomfort.
Multi-Mam Compresses Sore Nipples 12 Pack, RRP $19.99
Multi-Mam Compresses help alleviate breastfeeding discomforts such as nipple pain, swelling and sensitivity. The compress supports the natural healing process and has a direct cooling and soothing effect on sore nipples.
Get rid of blocked ducts
Blocked ducts or ‘clogged’ milk ducts occur when the flow of breast milk is obstructed within one or more milk ducts, causing milk to back up and accumulate in the affected area.
You may feel this as a sharp pain, and may notice a lump or a red patch on your breast.
Clogged milk ducts are painful and make feeding and pumping unpleasant, but it’s essential to address a blocked duct as it can lead to mastitis if it’s not cleared quickly.
To alleviate a blocked duct keep feeding from the affected breast, and gently massage towards your nipple as you feed. Applying some heat to the area can help as well.
Adding a breast pump to your new routine is an excellent way to assist you to continue to collect and express milk gently and effectively.
Welcare Nuture Wearable Breast Pump, RRP $99.95
Compact, portable & lightweight, the Wearable Electric Breast Pump fits discreetly in any well-fitting nursing bra for hands-free, wireless pumping.
The pump has three modes to choose from including massage, suction and expression and nine adjustable suction levels.
Ways to allieve the pain of mastitis
Sometimes a blocked duct may become infected – this is called mastitis.
The most common cause of mastitis is hyperlactation or an oversupply of milk. This oversupply of milk causes your milk ducts to narrow because the surrounding tissue puts pressure on the ducts.
You may have a swollen, red area on your breast, a high temperature, and feel really unwell. See your GP as you may antibiotics, but don’t stop feeding from the affected side.
It is really important to keep the milk moving in that breast, either by the baby feeding and/or expressing or pumping.
Lansinoh® TheraPearl 3-in-1 Breast Therapy, RRP $30.95
Lansinoh® TheraPearl 3-in-1 Breast Therapy offers two re-usable hot or cold breast therapy packs. Use it cold to help relieve pain and swelling caused by engorgement and mastitis. Use it warm to encourage let down and to stimulate milk flow and reduce time spent expressing with a breast pump.
For more information or help seven days a week, call the National Breastfeeding Helpline on 1800 686 268 FREE or visit the Australian Breastfeeding Association website .
The post Breastfeeding challenges and product fixes for common problems appeared first on Bounty Parents .
This article may contain affiliate links that Microsoft and/or the publisher may receive a commission from if you buy a product or service through those links.


COMMENTS
It could be a plugged duct, Neal says. There are a number of possible causes for this, but the cure is the same: get the milk flowing again in this area. Try to position the baby so that her chin points towards the tender area and massage the breast in that spot while the baby nurses. Apply heat between feedings.
Problem #10: Painful Let-Down. The milk let-down sensation (aka "milk ejection reflex") is often experienced as a tingling or a prickly pins-and-needles kind of feeling. But for some, the sensation is felt deep in the breasts and can hurt or be achy, especially when milk production is in overdrive.
Regular breastfeeding is actually the best way to help with swelling and keep milk from getting blocked again. If milk flow is blocked for more than a day or two, this can lead to bacterial infection in the breast ("bacterial mastitis"). This can cause additional symptoms like fever, aches, or fatigue.
Common breastfeeding challenges include: Sore nipples. Many moms say that their nipples feel tender when they first start breastfeeding. Low milk supply. Moms sometimes worry about whether they are making enough milk for baby. Cluster feeding and growth spurts. In cluster feedings, your baby feeds very frequently.
6) Supply. 7) White, Painful Nipples. 8) Engorgement. 9) Breasts feel soft. 10) Itching, Stinging, and Burning Nipples. 10) Baby Choking, Refusing to Nurse, has lots of gas, spitting up extra, etc. 11) Inverted or Flat Nipples. 12) White Dot on Nipple.
Breastfeeding Problem-Solving Guide. The following recommendations are general guidelines. If you are still having problems after trying some of these suggestions, contact a lactation consultant or your healthcare provider. Remember: If your baby is gaining weight, then your milk supply is fine.
Here are seven breastfeeding problem-solving tips from a lactation consultant. ... Thrush, a fungal infection, is another common problem among breastfeeding mothers and babies. This is an infection caused by the overgrowth of yeast. It can cause sore nipples, achy breasts and white spots on the inside of your baby's cheeks, tongue or gums. ...
Breastfeeding can be challenging, especially in the early days. But remember that you are not alone. Lactation consultants can help you find ways to make breastfeeding work for you and your baby. Some women face many different problems while breastfeeding, while others do not. Also, many women may have certain problems with one baby that they ...
Case Studies in Breastfeeding: Problem-Solving Skills & Strategies combines logic, wisdom, critical thinking, and theory to convey a deeper understanding of how to act in accordance with the highest needs of the breastfeeding dyad. In this book, authors Karin Cadwell and Cindy Turner-Maffei develop a consultative framework and utilize their ...
By hcproject July 25, 2019. Originally published in 2003, HCP faculty members Karin Cadwell and Cynthia Turner-Maffei recently published an updated 2019 edition of Case Studies in Breastfeeding: Problem-Solving Skills and Strategies. The new book, which is 220 pages long, shares a step-by-step, consultative framework for addressing both common ...
Case Studies in Breastfeeding: Problem Solving Skills and Strategies combines logic, wisdom, and theory in order to convey a deeper understanding of how to act in accordance with the highest needs of the breastfeeding mother and baby. In this book, authors Karin Cadwell, PhD, RN, IBCLC and Cindy Turner-Maffei, MA, IBCLC develop a consultative framework and present illustrative case studies ...
Find out which breastfeeding problems are the most common and how to solve them! Breastfeeding creates a unique bond between a mother and her baby and at the...
A new learn-at-home module, "Case Studies in Breastfeeding: Problem Solving Skills and Strategies," is now available from Health Education Associates. The module is based on the popular book by the same name authored by HCP faculty members Karin Cadwell and Cindy Turner-Maffei.
This is very common about 2-6 days after the baby's birth, especially if the baby is not able to feed frequently or for long enough, if he is not positioned well, or if supplements are given. Engorgement is caused by a build-up of milk. Your baby may not be able to get a good mouthful of breast tissue in his mouth if the breast is too swollen ...
The Ultimate Breastfeeding Book of Answers: The Most Comprehensive Problem-Solving Guide to Breastfeeding from the Foremost Expert in North America, Revised & Updated Edition [Newman M.D., Jack, Pitman, Teresa] on Amazon.com. *FREE* shipping on qualifying offers. The Ultimate Breastfeeding Book of Answers: The Most Comprehensive Problem-Solving Guide to Breastfeeding from the Foremost Expert ...
Problem Solving For Breastfeeding Parents . Woman's Lactacation Resources . Breastfeeding can be challenging at times, but you are not alone. Our lactation consultants are trained to help you find ways to breastfeeding success. Our lactation consultants are trained to help you find ways to breastfeeding success and are a phone call away.
Solving Common Breastfeeding Problems. It's widely known that breastfeeding is a healthy choice for both mom and baby. But, many women encounter breastfeeding challenges. Sometimes, despite our best efforts, it just doesn't work as well as we'd like. The good news is that through education and preparation, most breastfeeding problems can ...
This book is Print On Demand. Orders can take 4-6 weeks to fulfill. Case Studies in Breastfeeding: Problem Solving Skills and Strategies combines logic, wisdom, and theory in order to convey a deeper understanding of how to act in accordance with the highest needs of the breastfeeding mother and baby.In this book, authors Karin Cadwell, PhD, RN, IBCLC and Cindy Turner-Maffei, MA, IBCLC develop ...
Breastfed babies are also less likely to have ear infections and stomach bugs. The antibodies passed to your baby from the breastmilk help babies develop a robust immune system. Breastfeeding parents have a lower risk of developing breast cancer, ovarian cancer, Type II diabetes, and high blood pressure.
Breastfeeding plays a crucial role in the health, growth and development of babies and has benefits for the mother too. Women may need some help to successfully feed their babies. They need support and reassurance as they learn this skill. This session focuses on the initiation of breastfeeding following birth and when and how to refer women who are experiencing difficulties.
Case Studies in Breastfeeding: Problem-Solving Skills & Strategies. Karin Cadwell, Karin Cadwell. Jones & Bartlett, 2004 195 pp, $34.95, pb. Search for more papers by this author. Cynthia Turner-Maffei, Cynthia Turner-Maffei. Jones & Bartlett, 2004 195 pp, $34.95, pb. Search for more papers by this author.
Case Studies in Breastfeeding: Problem Solving Skills and Strategies combines logic, wisdom, and theory in order to convey a deeper understanding of how to act in accordance with the highest needs of the breastfeeding mother and baby. In this book, authors Karin Cadwell, PhD, RN, IBCLC and Cindy Turner-Maffei, MA, IBCLC develop a consultative framework and present illustrative case studies ...
Breastfeeding: A Problem-Solving Manual, Third Edition. Kathleen G. Auerbach, PhD, IBCLC. Journal of Human Lactation 1991 7: 1, 35-35 Download Citation. If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click ...
Book Review: Case Studies in Breastfeeding: Problem-Solving Skills and Strategies. Nicole J. Bernshaw, MSc, IBCLC. Journal of Human Lactation 2004 20: 2, 243-243 Download Citation. If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software ...
Case Studies in Breastfeeding: Problem-solving Skills & Strategies (2nd ed.) K Cadwell, C Turner-Maffei - Sandwich, Mass.: Healthy Children Project, Inc., 2019. Call for Improved Military Policy to Support Breastfeeding Among U.S. Armed Forces E Drake, K Cadwell, JE Dodgson - Nursing Outlook, May-June 2017; 65(3):343-345. Epub 2017 Apr 18.
Case Studies in Breastfeeding: Problem-Solving Skills & Strategies combines logic, wisdom, critical thinking, and theory to convey a deeper understanding of how to act in accordance with the highest needs of the breastfeeding dyad. In this book, authors Karin Cadwell and Cindy Turner-Maffei develop a consultative framework and utilize their ...
Case Studies in Breastfeeding: Problem Solving Skills and Strategies 2nd Edition. 2019, by Karin Cadwell & Cindy Turner-Maffei. This text combines logic, wisdom, and theory in order to convey a deeper understanding of how to respond in accordance with the highest needs of the breastfeeding dyad. The authors develop a consultative framework and ...
Welcome to parenthood — it's quite a ride! Have questions about baby sleep habits, baby care and feeding, health, development, and safety?We can help you solve breastfeeding and baby sleep problems, start solid foods, handle crying, know what your baby's ready for, track your baby's development, find great childcare and baby activities, and more.
Massaging the breasts, applying warm compresses, and using breast pumps to express milk can help to alleviate this discomfort. Multi-Mam Compresses Sore Nipples 12 Pack, RRP $19.99. Multi-Mam ...