
Subscribe or Renew

- Original Article
- Sep 26, 2024

Fractional Doses of Pneumococcal Conjugate Vaccine
Pneumococcal conjugate vaccines are an important but costly part of childhood vaccination. This trial assessed immunogenicity of fractional-dose regimens — a key consideration as countries transition out of Gavi support.
- Sep 25, 2024

Systematic vs. Targeted Biopsy for Prostate Cancer Screening
After 4 years of the GÖTEBORG-2 trial, MRI-targeted biopsy led to less detection of clinically insignificant prostate cancer than systematic biopsy without compromising the detection of cancer that may affect survival.
- Clinical Implications of Basic Research

Immunity and Early Colorectal Carcinogenesis
A recent study suggests that reexpression of a protein found during fetal development plays a role in the suppression of immunity in early colorectal adenomas and cancers.
- Interactive Medical Case

Avoiding Rash Decisions
This interactive feature describes a 40-year-old man who presented to the ED with a 5-day history of worsening sore throat, diffuse muscle aches, joint pains, and fevers with temperatures of up to 38.9°C. Test your diagnostic and therapeutic skills.
- Perspective
Celebrating Public Health
The winners of this year’s Lasker–Bloomberg Public Service Award, Quarraisha and Salim Abdool Karim, have dedicated their careers to translating scientific breakthroughs into improved human lives.
- Sep 21, 2024

Dobbs Revisited
After the Dobbs decision, an Ob/Gyn residency program in Wisconsin had to send its residents out of state to obtain abortion training. The process was complicated and costly.
Role of Physicians on Ethics Committees after Dobbs
Determining the legality of a necessary procedure such as abortion lies outside the domain of ethics committees, and committees that take on such a task contribute to the erosion of patient autonomy.
- Case Challenge

A 37-Year-Old Man with Fever, Myalgia, Jaundice, and Respiratory Failure
A 37-year-old man was transferred to the hospital because of fever, myalgia, and hypoxemia. Evaluation revealed leukocytosis, acute kidney failure, and conjugated hyperbilirubinemia.
What is the diagnosis? Cast your vote. Find the answers in the full text of the case, which publishes in the October 10, 2024, issue of the Journal .
Image Challenge
Original Research

Ziresovir in Hospitalized Infants with RSV
In a phase 3 trial involving infants in China, ziresovir, an orally administered RSV F protein inhibitor, led to an improvement in the Wang bronchiolitis score at day 3 and a decline in the RSV viral load by day 5.

Gene Therapy for Factor IX Deficiency
In participants with hemophilia B, fidanacogene elaparvovec was superior to factor IX prophylaxis, with a lower bleeding rate and stable factor IX expression.
- Sep 18, 2024

Blocking CSF1R in Chronic GVHD
A study in patients with chronic GVHD evaluated three doses of axatilimab, a colony-stimulating factor 1 receptor antibody. The lowest dose appeared to maximize response with the fewest adverse effects.
- Editorial Targeting CSF1R in Chronic GVHD — Lessons in Translation
- Editorial CSF1R Blockade for Refractory Chronic Graft-versus-Host Disease

Phase 2 Trial of Tulisokibart for Ulcerative Colitis
In this phase 2 trial, tulisokibart (a tumor necrosis factor–like cytokine 1A monoclonal antibody) was more effective than placebo in inducing clinical remission in patients with ulcerative colitis.
- Correspondence
- Sep 11, 2024

Influenza A(H5N1) in Wastewater in 10 U.S. Cities
Avian influenza A(H5N1) virus is spreading through dairy herds across the United States. In this report, wastewater surveillance shows the increase of H5N1 across 10 urban communities.
- Sep 16, 2024

Anti–Claudin 18.2 Antibody in Gastric Cancer
The addition of zolbetuximab, an anti–claudin 18.2 antibody, to chemotherapy in gastric and gastroesophageal junction adenocarcinoma led to longer progression-free and overall survival than chemotherapy alone.

Clinical Practice and Review
- Case Records of the Massachusetts General Hospital

A Woman with Kidney Lesions and Lytic Bone Disease
A 45-year-old woman was evaluated in the rheumatology clinic because of possible IgG4-related disease. She had polyclonal hypergammaglobulinemia, as well as kidney and bone lesions. What is the diagnosis?
- Images in Clinical Medicine

Button-Battery Ingestion
An 11-month-old girl presented with a 2-week history of progressive dysphagia and cough. A chest radiograph showed a foreign body with a “double-ring” sign. Torrential hematemesis subsequently developed.
Podcast: Intention to Treat

Brain Injury and Consciousness
New research using functional brain imaging reveals that many patients considered to be in a coma or vegetative state and who are unresponsive may actually be conscious and aware.

- Review Article
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome, characterized by fever, muscular rigidity, and dysautonomia, occurs with exposure to dopamine-blocking agents. Management, especially in critical care contexts, is described.

Central Nervous System Vasculitis
CNS vasculitis exists in medium- and large-vessel, small-vessel, and amyloid-deposition forms. Diagnosis is difficult, but the typical symptoms include acute focal deficits, cognitive impairment, and headache.
Accessible Weight Scales and Exam Tables
New U.S. rules issued in May 2024 will finally require all health care delivery organizations receiving federal funds to have medical diagnostic equipment that is accessible to patients with disability.

Featured Multimedia See all multimedia

Ziresovir in Hospitalized Infants with RSV Infection

PSA and MRI Prostate Cancer Screening

- Campus News /
WBCS Establishes Endowed Innovative Research Fund
September 27, 2024

Since 1998, WBCS, Inc. (formerly Wisconsin Breast Cancer Showhouse) – a grassroots, all-volunteer organization that draws support from businesses, nonprofits, and people from every walk of life – has partnered with the Medical College of Wisconsin Cancer Center’s efforts to eradicate breast cancer and prostate cancer in our community and across the country.
On September 3, executive leaders from MCW and the Medical College of Wisconsin Cancer Center hosted a ceremony to publicly announce WBCS’ newest gift: a $650,00 pledge to endow the WBCS Innovative Research Fund and support early-stage basic breast and prostate cancer research. At the ceremony, WBCS leaders presented an initial payment of $325,000.
MCW President and CEO John R. Raymond, Sr., MD , thanked WBCS leaders for their friendship and inspired leadership over the decades for bringing “the best and brightest here to do breast and prostate cancer research.” Joseph E. Kerschner, MD, Julia A. Uihlein, MA Dean of the School of Medicine, added, “It’s just so remarkable to think about how WCBS has contributed to the journey toward building a world-class cancer research and clinical education engine….”
Thus far, WBCS contributions to that journey have included funding endowed professorships in breast cancer research and prostate cancer research and providing critical seed grants for specific cancer-related research projects. For example, Todd Miller, PhD , the current holder of the WBCS Endowed Professorship of Breast Cancer Research, has used WBCS funding to launch two projects testing new research directions. The first aims to identify genes that control fatty acid saturation in breast cancer cells, with the goal of developing a drug target that can increase desaturation to sensitize cancer cells to a type of death called ferroptosis. The second hopes to explore opportunities for drug design by determining the structure of the FOXA1 protein, which is important in breast, prostate, and other cancers.

In total, MCW researchers have leveraged WBCS’s cumulative investments of $8.1 million to secure an extraordinary $137.6 million in competitive, external research funding from the National Institutes of Health and other funding agencies.
The endowed Innovative Research Fund reinforces WBCS’s position as MCW’s top philanthropic donor for adult cancer research. In notifying Gustavo Leone, PhD Director of the MCW Cancer Center , about the organization’s investment, Ellen Irion, WBCS Board Chair, wrote, “What an auspicious way to start our twenty-sixth year of mutual trust and partnership! The WBCS board is pleased to initiate this next phase in our relationship with the MCW Cancer Center.”
At the September 3 ceremony, Dr. Leone added that it “is the most exciting time in the history of research in relationship to cancer. All the pieces are coming together, and it’s especially true in Milwaukee.” The WBCS’s investment, he said, will help shift the focus “from short-term thinking to very long-term thinking.” The transparency of the WBCS’s involvement and the advances generated by WBCS funds will inspire and engage even more to invest in cancer research.
Ellen Irion noted that all the organization’s supporters, volunteers, and scientists felt “graced by the respect” MCW gives WBCS. “We don’t know that we would ever be treated the same way by any other institution.” WBCS, she concluded, is “deeply committed” to continue helping MCW accelerate promising research and launch groundbreaking clinical trials that will lead to lifesaving medical breakthroughs.

- Harvard Business School →
- Faculty & Research →
- September 2024
- HBS Case Collection
The Health Equity Accelerator at Boston Medical Center
- Format: Print
- | Language: English
- | Pages: 21
About The Author
Susanna Gallani
More from the authors.
- August 2024
- Faculty Research
Pioneering Pain Management: CWC Alliance Combats the Opioid Epidemic
- August 13, 2024
- Harvard Business School Working Knowledge
Can AI Save Physicians from Burnout?
- July 24, 2024
Providing Value and Equity in Medicare's Dementia Care Is a Must
- Pioneering Pain Management: CWC Alliance Combats the Opioid Epidemic By: Susanna Gallani, Karen L. Sedatole and Sarah Mehta
- Can AI Save Physicians from Burnout? By: Susanna Gallani, Lidia Moura and Katie Sonnefeldt
- Providing Value and Equity in Medicare's Dementia Care Is a Must By: Susanna Gallani and Lidia Moura
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Bone Miner Res
- PMC11425703

Goal-directed osteoporosis treatment: ASBMR/BHOF task force position statement 2024
Felicia cosman.
Department of Medicine, Columbia University College of Physicians and Surgeons, New York , NY 10032, United States
E Michael Lewiecki
New Mexico Clinical Research & Osteoporosis Center, Division of Metabolic Bone Diseases, Albuquerque, NM 87106, United States
Richard Eastell
Division of Clinical Medicine, University of Sheffield, Sheffield S10 2RX, United Kingdom
Peter R Ebeling
Department of Medicine, School of Clinical Sciences, Monash University, Clayton, VIC 3168, Australia
Suzanne Jan De Beur
Division of Endocrinology and Metabolism, University of Virginia, Charlottesville, VA 22908, United States
Bente Langdahl
Department of Endocrinology, Aarhus University Hospital, Aarhus N 8200, Denmark
Department of Clinical Medicine, Aarhus University, Aarhus N 8200, Denmark
Department of Internal Medicine, Severance Hospital, Endocrine Research Institute, Yonsei University College of Medicine, Seoul 03722, South Korea
Ghada El-Hajj Fuleihan
Calcium Metabolism and Osteoporosis Program, WHO Collaborating Center for Metabolic Bone Disorders, American University of Beirut, Beirut 1107, Lebanon
Douglas P Kiel
Marcus Institute for Aging Research, Hebrew Senior Life, Boston, MA 02131, United States
Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02215, United States
John T Schousboe
Division of Research and Evaluation, HealthPartners Institute, Bloomington MN 55425, United States
Division of Health Policy and Management, University of Minnesota, Minneapolis, MN 55425, United States
Joao Lindolfo Borges
Brazil Clinical Research Center, Brasilia 71625-175, Brazil
Angela M Cheung
Department of Medicine and Joint Department of Medical Imaging, University Health Network, Toronto, ON M5G 2C4, Canada
Centre of Excellence in Skeletal Health Assessment, University of Toronto, Toronto, ON M5G 2C4, Canada
Adolfo Diez-Perez
Department of Medicine, Institute Hospital del Mar of Medical Investigation, Barcelona 08003, Spain
Peyman Hadji
Department of Obstetrics and Gynecology, Frankfurt Center of Bone Health and Phillipps-University of Marburg, Frankfurt 60313, Germany
Sakae Tanaka
Department of Orthopaedic Surgery, Faculty of Medicine, The University of Tokyo, Hongo, Bunkyo-ku, Tokyo 113-0033, Japan
Friederike Thomasius
Department of Clinical Osteology, Frankfurt Center of Bone Health and Endocrinology, Frankfurt 60313, Germany
Department of Endocrinology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
Steven R Cummings
San Francisco Coordinating Center, CPMC Research Institute, Department of Epidemiology and Biostatistics, University of California, San Francisco, CA 94158, United States
The overarching goal of osteoporosis management is to prevent fractures. A goal-directed approach to long-term management of fracture risk helps ensure that the most appropriate initial treatment and treatment sequence is selected for individual patients. Goal-directed treatment decisions require assessment of clinical fracture history, vertebral fracture identification (using vertebral imaging as appropriate), measurement of bone mineral density (BMD), and consideration of other major clinical risk factors. Treatment targets should be tailored to each patient’s individual risk profile and based on the specific indication for beginning treatment, including recency, site, number and severity of prior fractures, and BMD levels at the total hip, femoral neck, and lumbar spine. Instead of first-line bisphosphonate treatment for all patients, selection of initial treatment should focus on reducing fracture risk rapidly for patients at very high and imminent risk, such as in those with recent fractures. Initial treatment selection should also consider the probability that a BMD treatment target can be attained within a reasonable period of time and the differential magnitude of fracture risk reduction and BMD impact with osteoanabolic versus antiresorptive therapy. This position statement of the ASBMR/BHOF Task Force on Goal-Directed Osteoporosis Treatment provides an overall summary of the major clinical recommendations about treatment targets and strategies to achieve those targets based on the best evidence available, derived primarily from studies in older postmenopausal women of European ancestry.
Introduction
Since our last report in 2017, 1 the emergence of new medical evidence and development of new therapeutic agents have prompted a need to revisit the concept of goal-directed treatment (treat-to-target) for osteoporosis. For these reasons, the American Society for Bone and Mineral Research (ASBMR) and Bone Health & Osteoporosis Foundation (BHOF, formerly National Osteoporosis Foundation) re-assembled an international task force of clinical scientists and expert physicians to update the previous report and develop a pragmatic approach to aid clinicians in managing patients with osteoporosis. Multiple drafts of this document were extensively vetted by all authors. Comments, suggestions and edits were carefully considered and text was accepted or modified until all authors were in agreement. Pharmaceutical companies provided no funding for the development of this manuscript and had no role in its concept, writing, or revisions. There was no external funding from any source. All coauthors approved the final version of the position statement.
The most recent guidelines from the American Association of Clinical Endocrinology, Endocrine Society, North American Menopause Society (now The Menopause Society), BHOF, European Society for Clinical, and Economic Aspects of Osteoporosis and Osteoarthritis/International Osteoporosis Foundation and National Osteoporosis Guideline Group 2–7 have included a new very high fracture risk category. A subset of very high-risk patients is also at imminent risk of fracture for 2 yr following an incident fracture 2 , 4 , 5 , 8–16 or after multiple prior fractures. 2 , 17–20
Since the last report, two new osteoanabolic agents, abaloparatide and romosozumab, have been approved for treatment of patients with osteoporosis in the USA and in many other countries. Head-to-head studies in high or very high-risk patients demonstrate that osteoanabolic agents are more effective in preventing osteoporotic fractures than bisphosphonates 21–25 and denosumab. 26 Additionally, the Foundation for the National Institutes of Health/Study to Advance bone mineral density (BMD) as a Regulatory Endpoint collaboration (FNIH/SABRE) showed a strong relationship between BMD increases with treatment compared with placebo, and the magnitude of anti-fracture efficacy in a meta-regression of over 50 clinical trials. 27–29 In clinical trials, the increase in total hip (TH) and femoral neck (FN) BMD in treated patients compared with placebo explained a somewhat greater proportion of the anti-fracture effect than change in lumbar spine (LS) BMD. 28
Data from trials with antiresorptive and osteoanabolic agents show an inverse relationship between the BMD level achieved in patients on treatment and the subsequent risk of fracture. 30–33 New evidence shows that TH BMD appears to be the most useful treatment target because it consistently predicts the risk of both vertebral and nonvertebral fractures, whereas the LS BMD level after treatment predicts the risk of vertebral fracture but does not predict the risk of nonvertebral fractures as consistently. 33 In addition, new evidence provides guidance for identifying a BMD target. 32 , 33 Other studies have confirmed the benefit of treating with an osteoanabolic medication before an antiresorptive drug, compared with the reverse order, to maximize gains in BMD, particularly in the hip 34–38 and the probability of achieving different BMD treatment targets beginning with osteoanabolic rather than antiresorptive agents at varying starting BMD levels. 39–41
It is common clinical practice and a requirement of many health insurers to prescribe an oral bisphosphonate as initial treatment for all patients with osteoporosis, unless a contraindication is present. However, this “step therapy” approach does not provide the most effective treatment for all high and very high-risk patients. In contrast, goal-directed treatment individualizes treatment decisions based on an individual’s fracture risk, taking into account fracture history, BMD, and other risk factors, aiming at prespecified individualized treatment targets. Based on these considerations, some patients will benefit most from osteoanabolic therapy as initial treatment.
Goal-directed therapy is a strategy for the long-term management of patients receiving treatment for osteoporosis. Achieving treatment targets might require intensification of therapy if a fracture occurs or the patient remains far from a BMD target despite osteoporosis treatment. This intensification could include replacing a bisphosphonate with denosumab, replacing a bisphosphonate or perhaps denosumab with an osteoanabolic agent, or adding an osteoanabolic agent to ongoing treatment with a bisphosphonate or denosumab. It might also include a repeat course of osteoanabolic medication. It must be acknowledged, however, that the BMD effects of switching from antiresorptive to osteoanabolic agents are not as robust as those seen when initiating treatment with an osteoanabolic agent (especially when switching from denosumab). 38 In addition, the evidence supporting the safety and efficacy of repeat courses of osteoanabolic agents is extremely limited. Extended use beyond 24 mo and repeated use of branded teriparatide is approved in the USA when a patient remains at or has returned to having a high risk for fracture.
This report represents the consensus of the ASBMR/BHOF Task Force on Goal-Directed Osteoporosis Treatment, based on interpretation of the best evidence available. This position statement is not a clinical guideline. It begins with a summary overview of the main principles, followed by a description of the evidence underlying these principles. It is focused on postmenopausal White women for whom the vast majority of evidence is available. For physicians who are not confident prescribing goal-directed therapy or managing very-high risk patients, referral to an osteoporosis specialist should be considered.
Summary of major principles
Treatment targets.
Treatment targets should be individualized, based in large part on the specific indication for beginning treatment, including recency of fracture, number and site of prior fractures, severity of vertebral fracture(s), BMD at the TH, FN, and/or LS, age, and other strong risk factors for fracture.
- Patients at imminent risk of fracture: Patients with a recent fracture are at very high risk of more fractures over the next 2 yr; this risk is largely independent of baseline T-score. The treatment goal for these patients is to rapidly and maximally reduce fracture risk. Greater BMD increases are associated with greater reduction in fracture risk. Some patients who have had multiple prior fractures (even if not within the last 2 yr) are also at imminent risk. Many of these patients also have sustained very-high risk. For these patients, the treatment goal is rapid and maximal reduction in fracture risk, but more sustained treatment is likely required than for a single recent fracture.
- For patients who are not at imminent risk of fracture, baseline T-scores, fracture history, and other major risk factors guide the selection of treatment targets.
- In patients on osteoporosis treatment, TH T-score best reflects subsequent fracture risk at both vertebral and nonvertebral sites. In patients on osteoporosis treatment, T-score at the FN also reflects subsequent risk of fracture at both vertebral and nonvertebral sites. Since reproducibility is better for the TH than the FN, it is the preferred region of interest for a treatment target. For patients with an isolated T-score < −2.5 at the FN, the FN T-score can be the treatment target. Improving T-score to levels > −2.5 is associated with lower risk for nonvertebral and vertebral fractures. A T-score > −2.5 should be the minimum treatment target. In some patients, achieving a higher T-score target might be warranted, based on other risk factors.
- In patients on osteoporosis treatment, LS T-score reflects subsequent risk of vertebral fracture, but the association with nonvertebral fracture is less consistent. Improving LS T-score to levels > −2.5 is associated with lower vertebral fracture risk; a T-score > −2.5 should be the minimum treatment target. In some patients, achieving a higher target T-score might be warranted based on other risk factors.
- For countries with different T-score intervention thresholds, T-score targets should be adjusted accordingly.
- Patients with baseline T-score > − 2.5: For patients with baseline T-scores > −2.5 who are recommended for treatment because of high fracture risk (such as prior fracture or high-risk medical conditions), increasing BMD remains associated with reduced fracture risk. Greater BMD increases with larger T-score improvements are associated with greater fracture-risk reduction, but a T-score target is not easily defined in these patients.
Selecting treatment to achieve treatment targets
- Initial treatment: Selection of initial treatment should consider the probability that a treatment target can be attained over a reasonable period of time, with greater urgency for patients at imminent fracture risk (recent fracture or some multiple prior fractures). Data to guide these decisions include the likelihood that a treatment can provide at least a 50% probability of attaining the T-score target over 3 yr, depending on the initial BMD. For some patients, it might be appropriate to select treatment to achieve a higher T-score target, reach the treatment target faster, or provide a higher probability of achieving the treatment target.
- Sequence of treatment: Treatment sequence is important for attaining T-score targets particularly in patients with baseline T-scores far below the treatment target. Selection of initial therapy should acknowledge the differential impact on BMD for osteoanabolic-first versus antiresorptive-first treatment sequences. Greater and faster BMD increases at the hip and spine are seen with osteoanabolic-first followed by antiresorptive treatment strategies, compared with the reverse order.
Determining if treatment targets have been achieved
To determine whether a treatment target has been achieved requires repeat BMD testing and assessment for new fractures, including vertebral imaging. Having a baseline vertebral image before starting treatment allows confirmation that an incident vertebral fracture has occurred on follow-up vertebral imaging. If a patient experiences one or more new fractures, it indicates that the most important treatment target has not been met, regardless of the T-scores achieved. Monitoring for achievement of a treatment target is distinct from monitoring for treatment responses. To achieve a treatment target, a treatment response is necessary. Treatment response, which can be assessed by measurement of biochemical turnover markers, depends on patient adherence and type and duration of prior osteoporosis medication.
- When a treatment target has not been achieved or is unlikely to be achieved, consider changing to more potent therapy (or continuing the highest potency treatment sequence).
- When a treatment target has been reached, maintenance of BMD is the focus. This may involve continuing treatment, changing treatment, pausing treatment, or administering intermittent bisphosphonates.
Review of the evidence to support major principles and actionable steps in patient management
To establish a treatment target and select initial therapy requires assessment of fracture risk, including vertebral imaging when appropriate, and BMD measurement when available. Indications for BMD testing and vertebral imaging are available in the BHOF Clinician’s Guide 6 and the International Society for Clinical Densitometry Position Statements. 42 Treatment targets should reflect the underlying clinical scenarios; specific BMD treatment targets and choice of therapeutic agents should be individualized.
Treatment targets and selection of treatment for patients at imminent risk
Recent fracture and imminent risk of subsequent fracture.
Multiple recent studies in different regions of the world confirm the importance of recent fracture as a predictor of subsequent fracture. 8–16 Overall, these large database studies show that the risk of fracture is increased dramatically for up to 2 yr after the occurrence of the first fracture, with the annual risk remaining high but declining after that time. Risk increases very rapidly after an initial fracture, with the highest risk seen within the first few months after the fracture. 10 One of the most comprehensive studies utilized a Medicare database to evaluate 377,500 women age 65 yr and older who had a first clinical fracture. 8 Women with fractures of the digits, skull, patella, sternum, scapula, and ribs were excluded. Fracture risk was assessed for up to 5 subsequent yr. Average risk of subsequent fracture was 10% in the very next year and 18% in the 2 yr following the first fracture. The site of the first fracture was associated with varying risks of subsequent fracture ( Figure 1 ). 8 The magnified short-term risk was particularly high after vertebral and pelvic fractures and lowest for ankle fractures, though even ankle fractures were still associated with a subsequent 1-yr risk of just below 5% and 2-yr risk of almost 10% (which is still considered imminent risk). 43 Therefore, in patients at imminent risk, especially those with recent fractures of the spine, hip, and pelvis, rapid and maximum fracture risk reduction is the first and most important treatment target.

One-year risk of recurrent fracture in women > 65 years of age, based on site of initial fracture, from Medicare database of 377,561 women with first fracture. Adapted from reference 8 .
Multiple prior fractures and imminent risk of subsequent fracture
Patients with multiple prior fractures may also be at imminent risk for more fractures. 2 , 17–20 Fracture site, severity, and time from last fracture occurrence remain important determinants of subsequent risk. In many patients with two or more fractures, rapid and maximum fracture risk reduction is the most important treatment goal. This is particularly pertinent for women with fracture sites that include spine, hip, or pelvis and for patients whose fractures were not remote (more than 10 yr earlier). Additionally, in many patients with multiple fractures, very-high risk persists, especially if there are no modifiable risk factors. Treatment targets might include attaining higher T-score targets than specified below. Furthermore, these patients might require a more prolonged and intensive course of therapy even after achieving T-score targets.
Selecting initial treatment for patients at imminent risk
Since osteoanabolic agents reduce fracture risk faster and to a greater extent than antiresorptive agents, 21–26 osteoanabolic therapy may be better for patients at imminent fracture risk, especially after recent major fractures such as spine, hip, and pelvis ( Figure 1 ). 8 Initiating treatment with osteoanabolic agents followed by antiresorptive agents also increases BMD more than the reverse treatment sequence. Therefore, BMD treatment targets are more likely to be achieved rapidly with an osteoanabolic-first treatment sequence. For patients with other recent fractures, osteoanabolic agents, bisphosphonates, or denosumab may be appropriate, depending site of fracture and BMD. A consensus regarding which recent non-hip, non-spine, non-pelvis fractures should prompt use of osteoanabolic therapy versus bisphosphonates or denosumab is needed.
Treatment targets and selection of treatment for patients with T-scores ≤ −2.5
Why is bmd a good target for osteoporosis treatment and what is the best skeletal site.
In a large meta-regression of pharmaceutical clinical trials, 2-yr mean BMD differences between active and placebo-treated patients in the TH, FN, and LS were associated with fracture risk reduction; 27–29 larger mean BMD increases predicted greater reductions in fracture risk. Mean TH and FN BMD increments explained a somewhat larger proportion of fracture risk reduction than mean LS BMD increments ( Table 1 ). 28 LS BMD is more likely affected by degenerative artifact and aortic calcification. Of the two hip regions of interest, the TH has better reproducibility than the FN. 28
Proportion of treatment-related fracture reduction effect explained by BMD increment at the TH, FN, and LS (95% CI).
| Total Hip | Femoral Neck | Lumbar Spine | |
|---|---|---|---|
| 59% (50-69) | 61% (51-72) | 31% (19-44) | |
| 63% (38-88) | 67% (40-95) | 52% (23-82) | |
| 48% (21-76) | 44% (12-77) | 42% (9-75) |
Adapted from reference 28 .
Mean TH BMD level after treatment is predictive of subsequent risk of both nonvertebral and vertebral fractures. 30–33 The relationship between mean LS BMD level after treatment has not been tested in as many clinical trials, since several studies did not assess LS BMD in all individuals at all time points. 30 , 31 In trials where LS BMD has been measured in the full population, mean LS T-score reflects subsequent risk of vertebral fracture consistently; however, the association with nonvertebral fracture is not universal. For example, in a post hoc analysis from the ARCH study (Active-controlled fracture study in postmenopausal women with osteoporosis at high risk), mean LS BMD attained after 1 yr of treatment with alendronate or romosozumab was associated with subsequent risk of vertebral fracture but not nonvertebral fracture ( Figure 2 ). 33

Relationship between T-score attained after one year of treatment with either alendronate or romosozumab and subsequent risk of nonvertebral (left) or vertebral fracture (right) for the total hip (A and B), femoral neck (C and D) and lumbar spine (E and F). 33
For all of these reasons, the single best skeletal site for a T-score target is the TH. This might be important in some clinical situations, for example where the TH T-score is already > −2.5, but LS T-score is below. Medication choice might differ in this type of patient, rather than the reverse situation where LS T-score is > −2.5, but TH T-score is lower (see below). In patients who have only a FN T-score < −2.5 or a LS T-score < −2.5, a T-score > −2.5 at the respective skeletal site should be the treatment target.
What is the rationale for choosing the minimum target of > −2.5?
In some countries, a T-score < −2.5 represents an indication for pharmacologic treatment regardless of other risk factors. 6 However, since fracture risk is dependent on other factors, notably age and prevalent fracture, 44 , 45 a T-score > −2.5 should be considered the minimal target . For countries with different or no T-score intervention thresholds, T-score targets should be adjusted accordingly. 46
Patients with other important risk factors might warrant higher T-score targets. This is demonstrated very clearly in analyses from the denosumab FREEDOM trial (Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Mo) and its extension. 32 The relationship between attained T-score on denosumab treatment and subsequent fracture risk is maintained in individuals with and without prior fracture, but the risk at all BMD levels is much higher in those with a fracture history ( Figure 3 ). 32 These data support setting higher T-score targets in patients with a history of fracture. Higher T-score targets might also be suggested for patients with advanced age, recent falls history, and poor physical function. 47–49 In these patients, T-score targets of −2.0 or even −1.5 might be appropriate. In the ARCH trial, where all patients had fractures at entry, progressive lowering of subsequent fracture risk was observed as 1 yr TH T-scores approached −1.5. 33

Relationship between T-score attained on denosumab and subsequent risk of nonvertebral fracture in full population (A), by age < 75 vs. > 75 yr (B), and by prior history of fracture (C). 32
A higher T-score target might also be considered in patients for whom a pause in medication is being considered. Anyone who stops osteoporosis medication will lose bone eventually, though the rate of loss is dependent on what medication is being discontinued. Bone loss rates after stopping bisphosphonates are much slower than bone loss rates after stopping all other agents. Therefore, medication pauses should only be considered in patients whose last treatment is a bisphosphonate. Aiming for a higher T-score in those patients being considered for a medication pause might permit maintenance of T-score above −2.5 even after the expected bone loss occurs (see section below on BMD maintenance for further discussion).
Selecting initial treatment to achieve target BMD
The choice of therapeutic agent is dependent on which skeletal site has the lowest T-score and exactly what the starting BMD is at that site. When selecting initial treatment, the clinician should consider the probability that BMD targets can be attained with a specific treatment over a reasonable period of time (see “Probability of Attaining BMD Treatment Targets” below). Selection of initial therapy should also acknowledge the differential impact on BMD for osteoanabolic-first versus antiresorptive-first treatment sequences and the differential effects of medications on hip and spine BMD.
Goal-directed therapy choices should also consider other important clinical factors:
- In patients with TH T-score −2.5 to −2.8 (inclusive) and LS T-score −2.5 to −3.0 (inclusive) : bisphosphonates, denosumab, and osteoanabolic agents are all likely to enable the achievement of T-scores > −2.5 at both TH and LS within 3 yr. Treatment choices should consider a patient’s fracture history, including the skeletal site and timing of prior fracture. For patients with no prior fracture or a fracture other than spine, hip, or pelvis, bisphosphonates and denosumab are both highly likely to enable achievement of treatment targets within 3 yr and are the most appropriate choice. In contrast, in patients who have had a major fracture such as the spine, hip, or pelvis, osteoanabolic agents should be considered. This is most important if those fractures occurred somewhat recently (eg, more than 2 yr before, but within the last decade). In those patients, choosing osteoanabolic agents as initial therapy might enable patients to achieve treatment targets faster, to achieve higher T-score targets, or to have a higher probability of achieving the treatment target when beginning treatment. 39–41 Individual patient factors and local/regional guidance should be considered when deciding treatment based on site of prior fracture or T-score intervention threshold. 46
- In patients with very low BMD (TH T-scores < −2.8 or LS T-scores < −3.0): osteoanabolic agents might be required to achieve BMD treatment targets (see next section on probability of attaining BMD targets). Osteoanabolic agents and osteoanabolic-first treatment sequences produce larger BMD gains in both TH and LS compared with antiresorptive agents alone. Therefore, osteoanabolic agents should be considered as initial therapy for these patients when possible. In patients who start with a TH T-score < −3.5, it might be impossible to achieve a treatment target with any current medication in 3 yr; however, treatment decisions should aim to improve TH T-score to levels as close to the target as possible. Bisphosphonates or denosumab might be the first choice in some patients with no other risk factors, especially in countries where T-score intervention thresholds are lower.
Probability of attaining BMD treatment targets
Table 2 provides estimates of the lowest starting TH or LS T-score that would allow at least a 50% probability of attaining a T-score > −2.5 at that site, based on data available for different therapeutic agents over ~3 yr of treatment. These data can be helpful in making initial treatment decisions.
Lowest baseline T-score that permits > 50% of women to achieve a T-score > −2.5 in approximately 3 yr.
| Total Hip | Lumbar Spine | |
|---|---|---|
| −2.7 | −3.0 | |
| −2.8 | −3.1 | |
| −2.9 | −3.5 | |
| −2.9 | −3.5 | |
| −3.1 | −3.7 |
Adapted from references 39–41 .
Probabilities with romosozumab followed by alendronate or denosumab versus alendronate only
In a post hoc analysis of the ARCH and FRAME (Fracture study in postmenopausal women with osteoporosis) studies, the probability of attaining BMD targets over a total of 3 yr of therapy with alendronate alone, 1 yr of romosozumab followed by alendronate, or 1 yr of romosozumab followed by denosumab was determined ( Figure 4 ; Table 2 ). 39 In patients with TH T-score of −2.7, the probability of achieving a TH T-score > −2.5 with alendronate alone over 3 yr was > 50%, whereas this probability was only 9% for those who started with TH T-score of −3.0. For romosozumab followed by alendronate, the corresponding probabilities were 73% and 38%, respectively. For romosozumab followed by denosumab, these probabilities were 90% and 61%, respectively. 39

Probability of attaining T-score above −2.5 for TH (A) and LS (B) over 3 yr during treatment with alendronate, romosozumab followed by alendronate, or romosozumab followed by denosumab, based on starting T-score. 39
For women who began with LS T-scores of −3.0, the probability of achieving a LS T-score above −2.5 with alendronate alone was 55%, while it was only 11% with a starting LS T-score of −3.5. With romosozumab followed by alendronate, these probabilities were 81% and 46% respectively for starting T-scores of −3.0 and −3.5, respectively. With romosozumab followed by denosumab, the probabilities were 93% and 67%, respectively.
Probabilities with abaloparatide for 18 mo followed by alendronate for 2 yr
In a post hoc analysis of the ACTIVE study (Abaloparatide Comparator Trial in Vertebral Endpoints) and its extension, the probability of attaining BMD targets with abaloparatide for 18 mo followed by alendronate for 2 yr was determined. 40 Women with baseline TH T-scores as low as −2.9 and baseline LS T-scores as low as −3.5 had a > 50% probability of attaining a T-score above −2.5 at each respective site with abaloparatide followed by alendronate ( Table 2 ).
Probabilities with denosumab over 3 yr
In a post hoc analysis of the FREEDOM study, the probability of attaining BMD targets with 3 yr of denosumab treatment was determined. 41 There was a > 50% probability that women with starting TH T-scores > −2.8 and LS T-scores > −3.1 could achieve target T-scores above −2.5 with 3 yr of denosumab treatment ( Table 2 ).
Importance of treatment sequence
BMD increases with osteoanabolic agents are lower, particularly in the TH, when patients transition from a bisphosphonate or denosumab. Upon transition from a bisphosphonate to teriparatide, TH BMD declines consistently for at least 12 mo and hip strength is not improved for at least 1 yr. 34 , 35 Data are not currently available to assess the BMD effects of a treatment sequence beginning with an antiresorptive and switching to abaloparatide. When patients on denosumab are switched to teriparatide, TH BMD declines rapidly and remains below the on-denosumab baseline for a full 2 yr. 36 Upon transition from a bisphosphonate to romosozumab, TH BMD and hip strength improve 35 although not as markedly as seen with romosozumab in treatment naïve individuals. After 1 yr of denosumab treatment, upon transition to romosozumab, TH BMD remains stable; 50 however, the BMD effect with romosozumab might differ after a longer preceding denosumab treatment duration. LS BMD increments are also lower with osteoanabolic agents upon transition from antiresorptive agents; however, the difference is not as marked as it is in the TH. 34–38 , 50
Choice of treatment after osteoanabolic
In patients initially treated with osteoanabolic therapy for 1-2 yr (as appropriate for the agent used), the subsequent choice of antiresorptive agent should take into account the repeat BMD level and other clinical risk factors. Patients who are still far from BMD targets might benefit from denosumab to attain BMD targets, since denosumab increases BMD more than bisphosphonates after osteoanabolic treatment. 38 In patients who are close to BMD targets after osteoanabolic treatment, intravenous or oral bisphosphonates can be considered as follow-up therapy. In some countries, it might be possible to consider another course of osteoanabolic therapy some years later for those who still have T-scores below −2.5. If another course of osteoanabolic therapy is foreseen, bisphosphonates may be the better intermediate treatment choice. This would avoid the overshoot bone remodeling seen after denosumab discontinuation, which might mitigate the effect of the second course of osteoanabolic treatment. 38
Treatment targets and selection of treatment for patients with T-scores > −2.5
More than half of all patients who have adulthood fractures have BMD levels above osteoporosis range. 51–53 For patients with baseline T-scores > −2.5 who have had a single prior fracture that occurred more than 2 yr earlier, subsequent risk might differ substantially by skeletal site and time since fracture. Prior vertebral, hip, and pelvic fractures are associated with higher and more persistent risk than other fractures. For higher-risk patients who require treatment, increasing BMD is associated with reduced fracture risk. 54 There is a paucity of evidence to guide the actual BMD level to target in these patients. Percentage increase in BMD is a function of baseline BMD, with lower percentage increases expected in those with higher baseline BMD. 54 Another level of uncertainty is how percentage changes in BMD relate to T-score unit changes. These relationships are specific for different populations at different starting BMD levels. For example, in the ARCH study, where all women began with T-scores < −2.0, mean BMD percentage increments with 1 yr of alendronate or romosozumab treatment were compared with mean T-score changes ( Table 3 ). 33 With 1 yr of alendronate, BMD increments of 2.9% in TH and 5.1% in LS corresponded to T-score unit changes of 0.2 and 0.3, respectively. With romosozumab, BMD increases of 6% in TH and 14% in LS BMD were associated with T-score unit increases of 0.3 and 0.9. BMD gain and T-scores continue to increase over at least 1-2 subsequent yr. TH T-score increments of at least 0.2 units and LS increments of at least 0.5 units are achievable over 3 yr with most therapies (bisphosphonates, denosumab, and osteoanabolic agents) and would be expected to reduce risk of both vertebral and nonvertebral fracture. 55–62 Therefore, these T-score changes can be considered treatment targets in these patients.
Relationship between % BMD increase and T-score change in the TH and LS at 1 yr after treatment with romosozumab or alendronate.
| Romosozumab ( = 1739) | Alendronate ( = 1726) | |||
|---|---|---|---|---|
| Mean % change BMD | Mean change T-score | Mean % change BMD | Mean change T-score | |
| 6.3% | 0.31 | 2.9% | 0.15 | |
| 13.9% | 0.90 | 5.1% | 0.34 | |
Adapted from reference 33 .
For patients with no prior fracture, T-score above −2.5, but high fracture probability according to a fracture risk algorithm, initiation of treatment with an antiresorptive agent may be appropriate, with a goal of increasing TH T-score by 0.2 (3%) and LS T-score by 0.5 (6%).
An algorithm, which presents treatment targets and principles guiding selection of initial treatments for individual patients, is provided in Figure 5 .

Goal directed therapy algorithm. Treatment targets and initial treatment selection, guided by fracture history (site, number and recency) and BMD. 1 Risk likely differs based on fractures that occurred a few years earlier vs. very remote events (eg 15 yr earlier). 2 Many, but not all, patients with multiple fractures are at imminent risk, based on fracture sites and time from fracture occurrence. 3 In some countries, T-score intervention thresholds are lower; T-score targets should be adjusted accordingly. 4 There is no consensus about which recent fracture sites should be recommended for osteoanabolic treatment vs. BP or DMAB or what T-score should prompt use of osteoanabolic treatment in patients with recent “other fractures.” 5 BP or DMAB might be first choice in some patients with no other risk factors, especially in countries where T-score intervention thresholds are lower. 6 Choosing osteoanabolic agents provides a higher probability of achieving treatment targets, achieving treatment targets faster, and achieving higher T-score targets. Abbreviations: TH, total hip; FN, femoral neck; LS, lumbar spine; BP, bisphosphonates; DMAB, denosumab.
Determining whether patients have achieved treatment targets is distinct from monitoring for treatment responses; patients might have had a good treatment response yet still be at high risk of fracture if treatment targets have not been achieved.
When treatment targets have not been met
Patients with clinical fractures or confirmed vertebral fractures while on medication have not achieved treatment targets and are at imminent risk of more fractures. While a fracture on treatment does not necessarily represent treatment failure, it does suggest that fracture risk is higher than previously recognized. After an evaluation for secondary causes of osteoporosis, interventions to reduce falls risk and improve treatment adherence should be implemented and patients should be started or continued on the most potent medication (or medication sequence) for at least the next 2 yr. This strategy could also consider switching to or adding an osteoanabolic agent to ongoing antiresorptive medication. In women who have already been treated with osteoanabolic medication and remain at very high risk, another course of osteoanabolic medication (either using the same or different medication) could be considered. The optimal timing of a second course of treatment and how to maximize BMD gain after antiresorptive therapy is unknown, although repeated use of branded teriparatide is approved in some countries, if a patient remains at or has returned to a high risk for fracture. This approach might also be appropriate for women whose BMD levels remain below the target or those who lose BMD despite therapy. Continuing an antiresorptive medication, such as denosumab, is also a potential strategy, especially when osteoanabolic options are limited. 63
When treatment targets have been achieved
For patients who have achieved treatment targets, benefits are expected to wane if medication is discontinued. BMD declines rapidly after discontinuation of most agents and important clinical consequences might occur, such as multiple vertebral fractures after denosumab discontinuation. 64 , 65 Upon cessation of denosumab, after short-term use (< 3 yr), transition to bisphosphonates appears to be effective at mitigating bone loss and risk of multiple vertebral fractures, but the most effective regimen after long-term use remains uncertain. 38 , 64 , 65 In contrast to denosumab discontinuation, with cessation of bisphosphonate treatment, residual effects can persist for several years after discontinuation, 66 , 67 particularly for zoledronic acid. 67 Therefore, when treatment targets have been met with a nonbisphosphonate, transitioning to a bisphosphonate may serve to maintain BMD gains. In one study of women with low bone mass, a single infusion of zoledronic acid was able to maintain BMD for up to 5 yr. 68 Administration of periodic zoledronic acid, with a dose interval beyond 1 yr, might therefore be useful for long-term maintenance of treatment targets achieved. Periodic administration of oral bisphosphonates might also permit maintenance of BMD targets. For patients who have achieved treatment targets with bisphosphonate therapy, a pause in treatment (“bisphosphonate holiday”) may be considered. More information is needed to clarify the optimal dosing regimen to avoid rare but important side effects associated with bisphosphonate duration, such as atypical femur fractures and osteonecrosis of the jaw, while maximizing the likelihood of maintaining BMD.
Limitations
The evidence used here is based almost solely on women self-reporting as White, primarily 60 yr of age and older. It needs to be clarified how recommendations should differ in lower risk populations (younger patients; men; women of other ethnicities, race, or geographical location). Furthermore, specific BMD levels are associated with a wide variation in absolute fracture risk, depending on ethnicity and geography. Indications for treatment vary in different regions of the world and the treatment targets suggested here should be modified according to local considerations. The treatment targets might also differ in patients with secondary osteoporosis conditions such as glucocorticoid-induced osteoporosis or in patients with diabetes mellitus.
A consensus is needed to confirm which fractures constitute a risk high enough to warrant initial use of osteoanabolic therapy. This is true for both patients with recent fractures and fractures that occurred more than 2 yr earlier. Consensus is also needed on defining an acceptable level of fracture risk after treatment. Reducing fracture risk is the treatment goal; currently, BMD targets are the best way to determine if this goal has been achieved. Determining whether BMD treatment targets have been met requires good quality, reliable BMD data, and interpretation. With a very low starting T-score, especially in the TH, treatment targets might not be attainable even with the most potent currently available therapy; however, the concept of choosing treatment sequences likely to attain BMD levels close to the target is still appropriate. The data to derive probabilities of attaining treatment targets are from post-hoc analyses, with two of the studies published only as abstracts at the current time. There is a paucity of evidence about treatment targets for patients who have fractures with starting T-scores above −2.5. Making treatment decisions based on at least a 50% probability of achieving the BMD target is intended as a general guide, not a rule.
The approach presented in this position statement does not take into account limitations imposed by health systems and insurers, cost, cost-effectiveness, or patient preferences. Osteoanabolic agents are relatively expensive (vs. antiresorptive agents) and often require a pre-approval process. Medication authorization, insurance coverage, medication cost, and out of pocket costs to consumers vary considerably around the world. These factors must be considered when treatment decisions are discussed with individual patients. There are few data addressing the optimal timing and effectiveness of repeat courses of osteoanabolic treatment after antiresorptive medication. Furthermore, this is not feasible in many countries.
Evidence about what to do once treatment targets are reached is also limited. While intravenous zoledronic acid may be the best option for many patients, the minimal effective dose and dosing interval to maintain BMD and fracture risk reduction, while avoiding rare complications, such as atypical femur fracture, is likely to vary among individuals and by prior osteoporosis treatment administered. In addition, some patients might not be candidates for bisphosphonates; these patients have very limited BMD maintenance options. Here, bisphosphonates are considered as a class with few distinctions among the agents, although most of the data available utilize alendronate or zoledronic acid.
Finally, including patients in decision-making regarding treatment targets, initial treatment selection and maintenance of treatment targets will likely add to the success of the goal directed therapy approach. 69 , 70
The ASBMR/BHOF Task Force on Goal-Directed Osteoporosis Treatment suggests that rapid fracture risk reduction should be the predominant treatment goal for patients at very high and imminent risk of fracture. The Task Force also recommends considering using BMD goals to guide clinical decisions for initiating and continuing treatment. Specific BMD targets and treatment decisions should be tailored to each patient’s clinical risk profile and BMD. Considerations presented here may be modified in the future as more evidence becomes available.
Contributor Information
Felicia Cosman, Department of Medicine, Columbia University College of Physicians and Surgeons, New York , NY 10032, United States.
E Michael Lewiecki, New Mexico Clinical Research & Osteoporosis Center, Division of Metabolic Bone Diseases, Albuquerque, NM 87106, United States.
Richard Eastell, Division of Clinical Medicine, University of Sheffield, Sheffield S10 2RX, United Kingdom.
Peter R Ebeling, Department of Medicine, School of Clinical Sciences, Monash University, Clayton, VIC 3168, Australia.
Suzanne Jan De Beur, Division of Endocrinology and Metabolism, University of Virginia, Charlottesville, VA 22908, United States.
Bente Langdahl, Department of Endocrinology, Aarhus University Hospital, Aarhus N 8200, Denmark. Department of Clinical Medicine, Aarhus University, Aarhus N 8200, Denmark.
Yumie Rhee, Department of Internal Medicine, Severance Hospital, Endocrine Research Institute, Yonsei University College of Medicine, Seoul 03722, South Korea.
Ghada El-Hajj Fuleihan, Calcium Metabolism and Osteoporosis Program, WHO Collaborating Center for Metabolic Bone Disorders, American University of Beirut, Beirut 1107, Lebanon.
Douglas P Kiel, Marcus Institute for Aging Research, Hebrew Senior Life, Boston, MA 02131, United States. Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02215, United States.
John T Schousboe, Division of Research and Evaluation, HealthPartners Institute, Bloomington MN 55425, United States. Division of Health Policy and Management, University of Minnesota, Minneapolis, MN 55425, United States.
Joao Lindolfo Borges, Brazil Clinical Research Center, Brasilia 71625-175, Brazil.
Angela M Cheung, Department of Medicine and Joint Department of Medical Imaging, University Health Network, Toronto, ON M5G 2C4, Canada. Centre of Excellence in Skeletal Health Assessment, University of Toronto, Toronto, ON M5G 2C4, Canada.
Adolfo Diez-Perez, Department of Medicine, Institute Hospital del Mar of Medical Investigation, Barcelona 08003, Spain.
Peyman Hadji, Department of Obstetrics and Gynecology, Frankfurt Center of Bone Health and Phillipps-University of Marburg, Frankfurt 60313, Germany.
Sakae Tanaka, Department of Orthopaedic Surgery, Faculty of Medicine, The University of Tokyo, Hongo, Bunkyo-ku, Tokyo 113-0033, Japan.
Friederike Thomasius, Department of Clinical Osteology, Frankfurt Center of Bone Health and Endocrinology, Frankfurt 60313, Germany.
Weibo Xia, Department of Endocrinology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China.
Steven R Cummings, San Francisco Coordinating Center, CPMC Research Institute, Department of Epidemiology and Biostatistics, University of California, San Francisco, CA 94158, United States.
Author contributions
Felicia Cosman (Conceptualization, Data curation, Project administration, Writing—original draft, Writing—review & editing), E. Michael Lewiecki (Conceptualization, Supervision, Writing—original draft, Writing—review & editing), Richard Eastell (Conceptualization, Writing—original draft, Writing—review & editing), Peter Ebeling (Conceptualization, Writing—original draft, Writing—review & editing), Suzanne Jan de Beur (Conceptualization, Writing—original draft, Writing—review & editing), Bente Langdahl (Conceptualization, Writing—original draft, Writing—review & editing), Yumie Rhee (Conceptualization, Writing—original draft, Writing—review & editing), Ghada El-Hajj Fuleihan (Writing—review & editing), Douglas Kiel (Writing—review & editing), John Schousboe, (Writing—review & editing), Joao Borges (Writing—review & editing), Angela Cheung (Writing—review & editing), Adolfo Diez-Perez (Writing—review & editing), Peyman Hadji (Writing—review & editing), Sakae Tanaka (Writing—review & editing), Friederike Thomasius (Writing—review & editing), Weibo Xia (Writing—review & editing), and Steven R. Cummings (Conceptualization, Supervision, Writing—original draft, Writing—review & editing).
The authors received no funding for this project.
Conflicts of interest
F.C.: Amgen: investigator, consultant, advisor, speaker; Radius Health: investigator, consultant, speaker; Enterabio, Biocon, CuraTeQ, Pfizer/Myovant/Sumitomo, Theramex, UCB: consultant.
E.M.L.: Amgen: investigator, consultant, speaker; Radius: investigator, consultant; Ultragenyx: investigator; Kyowa Kirin: consultant, speaker; Angitia and Ascendis: consultant.
R.E. : AstraZeneca, Immunodiagnostic Systems, Sandoz, Samsung, CL Bio, CuraTeQ, Biocon, Takeda, UCB: consultant; Pharmacosmos, Alexion, UCB and Amgen: speaker; Alexion and Osteolabs: grants.
P.R.E. : Amgen: grant funds, speaker; Alexion: grant funds, speaker, consultant; Sanofi: investigator; Kyowa Kirin: speaker.
S.J.d.B. : Ultragenyx: investigator, consultant; Kyowa Kirin: investigator, consultant; Ascendis: consultant; Inozyme: consultant; BridgeBio: investigator; Mereo: Investigator.
B.L. : Amgen: investigator, advisor, speaker; UCB: investigator, advisor, speaker; Gedeon-Richter: advisor, speaker; Astellas; speaker; Astra-Zeneca: speaker.
Y.R. : Amgen: investigator, speaker; Alexion: grant funds; Sanofi: investigator; Kyowa Kirin: investigator, speaker; Daewoong: investigator; Dongkook: investigator; Donga ST: investigator.
D.P.K.: Amgen: grant funds, Radius Health: consultant and grant funds, Agnovos: Data and Safety Monitoring Board.
G.E.H.F.: None.
J.T.S. : None.
J.L.C.B. : None.
A.C. : Amge n: investigator, consultant, speaker; Incyte: investigator; Ipsen: investigator, consultant, speaker; Sanofi: investigator.
A.D.P.: Theramex: speaker and advisor.
P.H.: Amgen, Besins, Exeltis, Gedeon Richter, Hexal, Sandoz, Stada, Theramex and UCB: speaker and consultant.
S.T. : Amgen, Asahi Kasei Pharma and Daiichi-Sankyo Co: speaker.
F.T. : Amgen, Fresenius, Gedeon-Richter, Stada, Theramex, UCB: Advisor and speaker; Abbvie, Alexion: speaker.
W.X. : None.
S.R.C. : Amgen: speaker.
The Common App is Open. Class of 2029, Apply Today!
10 Clinical Research Jobs in the Greater Boston Area
- Careers for Veterans
- College Advice
- Completing Your Degree
- Dental Hygiene
Seven Behind the Scenes Medical Jobs With No Patient Contact
30 Clinical Research and Regulatory Affairs Skills You Need to Advance Your Career
- Seven Regulatory Affairs Jobs in Boston and How Regis Prepares You
- Is a Master's in Regulatory Affairs and Clinical Research Worth It?
- Should I Get a Master's Degree or Certificate in Regulatory Affairs and Clinical Research?
- How To Get a Regulatory Affairs and Clinical Research Certificate and What You Can Do With It?
- Their Choice was Consistent: Physician Assistant
- The Nuclear Option
- Compassion, Ethics, and Values. All in a Day’s Work for a Social Worker
- Master's in Counseling vs Master's in Social Work
- Master's in Counseling Salary and Career Outlook
- MA in Counseling vs MS in Counseling: What's the Difference?
- What Can You Do With a Master's Degree in Counseling?
- How to Become a Licensed Counselor in Massachusetts
- What Can You Do With a Master's Degree in ABA?
- ABA vs Counseling: Which Master's Degree is Right for You?
- How to Become a Board Certified Behavior Analyst (BCBA): Five Steps
- Applied Behavior Analysis: What It is and How It Works
- How to Become a Counselor: Six Key Steps
- What Can You Do With a Bachelor's Degree in Psychology?
- Seven Top Public Health Careers in the Merrimack Valley
- Five Health Sciences Careers (and What They Pay) in the Merrimack Valley
- What Can You Do With a Health Sciences Degree?
- Marketing and Communications
- Medical Imaging
- Occupational Therapy
- Online Learning
- Public Health
- Speech-Language Pathology
Today, the field of clinical research is bridging the gap between the developmental aspects of healthcare and the public health impact of medical innovation. Working in this field can be incredibly rewarding, allowing you to make a difference in the lives of others with little to no patient contact .
Those interested in clinical research careers have numerous options available to them throughout the United States, but the Greater Boston area offers a wealth of opportunities as a major hub for both healthcare and the life sciences.
If you’re curious about the professional landscape in Boston, Massachusetts, here’s an overview of the clinical research landscape in the region, the top 10 high-paying careers you can expect, and the best places to work in clinical research in the Greater Boston area.
Want to learn more about working in Regulatory and Clinical Research Management? Download Our Free Guide!


Why Work in the Greater Boston Area?
While understanding the various career paths available to you in clinical research is essential to your long-term success in the field, it is equally important to determine the best location for you to work in.
For example, the Greater Boston area holds one of the largest concentrations of biotech startups and biopharma companies in the world . As a result, it attracts a great deal of incubator organizations and venture capital firms interested in supporting research and development projects across a variety of life science and healthcare businesses.
At the center of all this activity, there are also thriving research organizations, healthcare facilities, and educational institutions with renowned life science programs. As you would expect, this creates a direct pipeline of young talent for the biotech and biopharma companies in the area.
While there are plenty of job opportunities in Boston, the level of talent in the region has also led to more desirable salaries post-graduation. According to our analysis of job postings data, clinical research professionals in the Greater Boston area make an average salary of $90,000—increasing at an annual rate of 34.4 percent. This can attract even more aspiring clinical research professionals to the New England area.
Whether you're just starting out or trying to advance your career, Boston is a prime destination for anyone seeking a dynamic career in clinical research. According to our analysis of job postings data, here are the top clinical research jobs Boston has to offer:
- Laboratory managers: Oversee the day-to-day operations of clinical labs, including safety compliance, supply management, security protocols, and staffing
- Research laboratory managers: Lead research teams, coordinate projects, and ensure lab operations run smoothly
- Laboratory supervisors: Responsible for managing teams of lab technicians, directing daily activities, and implementing proper lab safety protocols
- Web operations managers: Oversee an organization’s online presence, including website management, data collection systems, and patient outreach
- Quality control laboratory supervisors: Ensure all aspects of lab operations, such as staff, processes, and equipment, are set up to maintain accuracy and compliance
- Laboratory operations managers: Handle the administrative and logistical aspects of research laboratories, from budgeting to safety compliance to resource allocation
- Clinical laboratory managers: Specialize in overseeing medical laboratories in healthcare institutions, ensuring timely and accurate test results
- Clinical laboratory supervisors: Oversee the work of lab technicians and technologists to ensure high standards of patient care
- Managers: Work at different levels of clinical research organizations, which often involves project management, team leadership, and strategic planning
- Field service supervisors: Manage clinical operations that involve researching, gathering resources, and communicating with patients in off-site locations

While the top jobs in this field are for experienced clinical researchers, skilled professionals are in high demand at all levels. Therefore, landing an entry-level job is a crucial step toward a rewarding clinical research career.
For those just starting out in clinical research, here are the top entry-level positions you should consider applying to:
- Clinical trial assistant: Aid in conducting trials, helping to perform interviews, collecting data and records, and performing routine lab duties
- Clinical research coordinator: Supervise research trials and conduct screenings to find patients who are the right fit
- Data coordinator: Manage the data collection processes for clinical research projects, ensuring accuracy and safe handling of patient information
- Clinical research associate: Monitor the success of research trials, ensuring the right protocols are being implemented
If you’re serious about exploring clinical research careers, these entry-level positions can be incredibly beneficial in your pursuit of a higher level research role. To ensure you get the most out of these roles, remember to network with other professionals to better understand the types of industries and roles available to you.
With this knowledge and foundational industry experience you could even transition into the following roles after a few years, including:
- Senior clinical research specialist: Part of the leadership team on research trials that monitor the clinical team, research participants, and quality assurance protocols
- Senior data coordinator: Manage a team of data coordinators and work with other team leaders to develop data management policies that support the research studies
- Research program leader: Responsible for developing and managing the goals and procedures of research studies, coordinating with team leads to carry out these goals
- Clinical research lab/pharmacy director: Oversee the operation of clinical research laboratories or pharmacies within healthcare institutions
Where Can You Work in Clinical Research in the Greater Boston Area?
One of the greatest advantages of working in a clinical research industry hub like Boston is the variety of employers and projects available to you. If you want to build a diverse work history that demonstrates expertise and leadership skills, working in the Greater Boston area provides ample opportunity to collaborate with a wide range of teams and eventually progress to high-level roles.
Top Industries
Choosing the right industry is very important to your long-term success as a clinical research professional. While there is plenty of skills overlap between industries, making an industry shift mid-career can be stressful and overwhelming. Therefore it’s important to know all your options before choosing which industry to work in.
According to our analysis of job postings data, there are six industries that are hiring a large number of clinical research professionals in the Greater Boston Area, including:
- Colleges, Universities, and Professional Schools: Academic institutions often conduct cutting-edge research, such as observational studies and clinical trials.
- General Medical and Surgical Hospitals: Healthcare institutions require clinical research expertise to drive advancements in patient care and treatment.
- Employment Placement Agencies: Recruitment agencies connect clinical research professionals with job opportunities in various sectors.
- Research and Development in the Physical, Engineering, and Life Sciences: R&D departments in life science industries, such as pharmaceutics, actively seek clinical research talent to lead product development teams.
- Offices of All Other Miscellaneous Health Practitioners: Specialized healthcare practices often engage in clinical research activities to better understand public health trends and needs.
- Research and Development in Biotechnology: R&D teams in biotech are often responsible for groundbreaking studies in medical technology.
Top Companies Hiring
Once you know what industry you hope to work in, conducting some research on companies in that sector can ensure you feel fulfilled at work. According to our analysis of job postings data, the top companies hiring clinical research professionals in Boston include:
- Mass General Brigham
- Harvard University
- Boston University
- Massachusetts Institute of Technology
- Massachusetts General Hospital
- Dana-Farber Cancer Institute
Take the Next Step Toward a Clinical Research Career
Although the robust ecosystem of biotech companies, healthcare institutions, and research organizations makes the Greater Boston area an ideal place to grow your clinical research career, the competitive landscape also means it’s important to distinguish yourself in the job market.
An undergraduate degree in a relevant field is the minimum requirement for most entry-level jobs. However, aspiring professionals also have the option to pursue certificate programs or even a master’s degree to build specific skill sets in clinical research.
While this additional education might seem like an unnecessary additive, according to our analysis of job postings data, most employers expect entry-level researchers to have a developed skill set . In fact, approximately 29 percent require a master’s degree, rather than a bachelors, along with past industry experience.
To ensure you don’t get left behind in this thriving field, consider earning an MS in Regulatory and Clinical Research Management (RCRM) at Regis College. Through the specialized curriculum, exciting internship opportunities, and job placement resources for post-graduation, Regis can fully prepare you to take on any leadership role in clinical research.
To learn more about Regis’s graduate degree, contact an admission counselor to discover how the program can jumpstart your career.

Related Blogs

Hoping to advance your career in regulatory affairs and clinical research? Here are 30 clinical research and regulatory affairs skills you should develop.

What Is Regulatory Affairs?
Wondering what regulatory affairs is, and the role it plays in healthcare? Here’s an overview of regulatory affairs, and its importance in consumer safety.
Want to work in healthcare, but don’t have a clinical background? Here’s a list of seven behind the scenes medical jobs that don’t involve patient contact.
January 03, 2024
- 235 Wellesley Street, Weston MA 02493
- 781.768.7000
- © 2024
- Privacy Policy
Center for regenerative medicine

Discover CReM
Research at CReM
Cores & Protocols
Mentorship & Outreach
CReM in the News!
Financial support.
Human health and development depend on dynamic networks of physical, and functional, interactions between proteins. However, the details of these networks – how they are formed and how they function – are largely unknown.
Upcoming Seminars
Klaus kaestner, phd, ms.
Thomas and Evelyn Suor Butterworth Professor in Genetics Associate Director, Penn Diabetes Research Center
Smilow Center for Translational Research
University of Pennsylvania Perelman School of Medicine
Philadelphia, PA
Special Guests
Pulin li, phd.
Eugene Bell Career Development Professor of Tissue Engineering; Core Member, Whitehead Institute
Jeremy Reiter, MD, PhD
Professor and Chair of Biochemistry and Biophysics Smith Cardiovascular Research Building University of California, San Francisco San Francisco, CA
We Are Hiring
Make a donation, research programs.
- Publications

New publication from the Murphy Lab: A specialized population of monocyte-derived tracheal macrophages promote airway epithelial regeneration through a CCR2-dependent mechanism
Click here to read the article.
Alveolar epithelial type I cells (AT1s) line the gas exchange barrier of the distal lung and have been historically challenging to isolate or maintain in cell culture. Here, we engineer a human in vitro AT1 model system via directed differentiation of induced pluripotent stem cells (iPSCs). We use primary adult AT1 global transcriptomes to suggest benchmarks and pathways, such as Hippo-LATS-YAP/TAZ signaling, enriched in these cells. Next, we generate iPSC-derived alveolar epithelial type II cells (AT2s) and find that nuclear YAP signaling is sufficient to promote a broad transcriptomic shift from AT2 to AT1 gene programs. The resulting cells express a molecular, morphologic, and functional phenotype reminiscent of human AT1 cells, including the capacity to form a flat epithelial barrier producing characteristic extracellular matrix molecules and secreted ligands. Our results provide an in vitro model of human alveolar epithelial differentiation and a potential source of human AT1s.

New Publication from the Kotton Lab on the generation of human alveolar epithelial type I cells from pluripotent stem cells
Kotton and colleagues generate human alveolar epithelial type I cells (AT1s) from induced pluripotent stem cells (iPSCs). The resulting cells can be grown as 3D organoids or in 2D air-liquid interface cultures, displaying many of the molecular, morphologic, and functional phenotypes of primary AT1s.
Click here to see the article

CReM Researchers Awarded $14 Million to Understand and Treat Genetic Lung Diseases
A team of researchers led by Darrell N. Kotton, MD, the David C. Seldin Professor of Medicine, has been awarded a five-year, $14 million grant from the NIH’s National Heart, Lung, and Blood Institute (NHLBI) for their research, “Developing Pluripotent Stem Cells to Model and Treat Lung Disease.” The new award will fund an integrated, multi-investigator program project grant where four interacting labs headed by four physician-scientists, all located in the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center, will develop next generation stem cell-based therapies for currently incurable genetic lung diseases affecting children and adults, including childhood and adult interstitial lung diseases, an inherited form of emphysema, cystic fibrosis and primary ciliary dyskinesia.

The Kotton Lab publishes new paper on iPSC modeling of childhood interstitial lung disease caused by ABCA3 mutations
Mutations in ATP-binding cassette A3 (ABCA3), a phospholipid transporter critical for surfactant homeostasis in pulmonary alveolar type II epithelial cells (AEC2s), are the most common genetic causes of childhood interstitial lung disease (chILD). Treatments for patients with pathological variants of ABCA3 mutations are limited, in part due to a lack of understanding of disease pathogenesis resulting from an inability to access primary AEC2s from affected children. Here, we report the generation of AEC2s from affected patient induced pluripotent stem cells (iPSCs) carrying homozygous versions of multiple ABCA3 mutations. We generated syngeneic CRISPR/Cas9 gene-corrected and uncorrected iPSCs and ABCA3-mutant knockin ABCA3:GFP fusion reporter lines for in vitro disease modeling. We observed an expected decreased capacity for surfactant secretion in ABCA3-mutant iPSC-derived AEC2s (iAEC2s), but we also found an unexpected epithelial-intrinsic aberrant phenotype in mutant iAEC2s, presenting as diminished progenitor potential, increased NFκB signaling, and the production of pro-inflammatory cytokines. The ABCA3:GFP fusion reporter permitted mutant-specific, quantifiable characterization of lamellar body size and ABCA3 protein trafficking, functional features that are perturbed depending on ABCA3 mutation type. Our disease model provides a platform for understanding ABCA3 mutation–mediated mechanisms of alveolar epithelial cell dysfunction that may trigger chILD pathogenesis.
Click here to read the article

Latest publication from the Murphy Lab featured on the cover of Blood Advances: De Novo Hematopoiesis from the Fetal Lung!
Hemogenic endothelial cells (HECs) are specialized cells that undergo endothelial-to-hematopoietic transition (EHT) to give rise to the earliest precursors of hematopoietic progenitors that will eventually sustain hematopoiesis throughout the lifetime of an organism. Although HECs are thought to be primarily limited to the aorta-gonad-mesonephros (AGM) during early development, EHT has been described in various other hematopoietic organs and embryonic vessels. Though not defined as a hematopoietic organ, the lung houses many resident hematopoietic cells, aids in platelet biogenesis, and is a reservoir for hematopoietic stem and progenitor cells (HSPCs). However, lung HECs have never been described. Here, we demonstrate that the fetal lung is a potential source of HECs that have the functional capacity to undergo EHT to produce de novo HSPCs and their resultant progeny. Explant cultures of murine and human fetal lungs display adherent endothelial cells transitioning into floating hematopoietic cells, accompanied by the gradual loss of an endothelial signature. Flow cytometric and functional assessment of fetal-lung explants showed the production of multipotent HSPCs that expressed the EHT and pre-HSPC markers EPCR, CD41, CD43, and CD44. scRNA-seq and small molecule modulation demonstrated that fetal lung HECs rely on canonical signaling pathways to undergo EHT, including TGFβ/BMP, Notch, and YAP. Collectively, these data support the possibility that post-AGM development, functional HECs are present in the fetal lung, establishing this location as a potential extramedullary site of de novo hematopoiesis.

New publication from the Murphy Lab in Science Advances! They led a Team demonstrating that immune cells drive NET tumor progression and susceptibility to therapies
Neuroendocrine tumors (NETs) are rare cancers that most often arise in the gastrointestinal tract and pancreas. The fundamental mechanisms driving gastroenteropancreatic (GEP)–NET growth remain incompletely elucidated; however, the heterogeneous clinical behavior of GEP-NETs suggests that both cellular lineage dynamics and tumor microenvironment influence tumor pathophysiology. Here, we investigated the single-cell transcriptomes of tumor and immune cells from patients with gastroenteropancreatic NETs. Malignant GEP-NET cells expressed genes and regulons associated with normal, gastrointestinal endocrine cell differentiation, and fate determination stages. Tumor and lymphoid compartments sparsely expressed immunosuppressive targets commonly investigated in clinical trials, such as the programmed cell death protein–1/programmed death ligand–1 axis. However, infiltrating myeloid cell types within both primary and metastatic GEP-NETs were enriched for genes encoding other immune checkpoints, including VSIR (VISTA), HAVCR2 (TIM3), LGALS9 (Gal-9), and SIGLEC10. Our findings highlight the transcriptomic heterogeneity that distinguishes the cellular landscapes of GEP-NET anatomic subtypes and reveal potential avenues for future precision medicine therapeutics.

Kotton Lab featured in Boston University Article on Lung Disease Research
For more than 20 years, a team of Boston University scientists have been on a quest to not just figure out how to treat incurable lung diseases, but also how to regenerate damaged lungs so they’re as good as new.
That is the goal of pulmonologist Darrell Kotton and his lab at the Center for Regenerative Medicine (CReM), a joint effort between the University and Boston Medical Center, BU’s primary teaching hospital. By refining their work using sophisticated stem cell technology, Kotton and his team are closer to realizing that vision than ever before.
In two new studies published in Cell Stem Cell, BU researchers detail how they engineered lung stem cells and successfully transplanted them into injured lungs of mice. Two lines of cells targeted two different parts of the lung: the airways, including the trachea and bronchial tubes, and the alveoli, the delicate air sacs that deliver oxygen to the bloodstream. Their findings could eventually lead to new ways for treating lung diseases, including severe cases of COVID-19, emphysema, pulmonary fibrosis, and cystic fibrosis, a disease caused by a genetic mutation.

The Mostoslavsky Lab Publishes New Platform to Make T Cells from iPSCs
A robust method of producing mature T cells from iPSCs is needed to realize their therapeutic potential. NOTCH1 is known to be required for the production of hematopoietic progenitor cells with T cell potential in vivo. Here we identify a critical window during mesodermal differentiation when Notch activation robustly improves access to definitive hematopoietic progenitors with T/NK cell lineage potential. Low-density progenitors on either OP9-hDLL4 feeder cells or hDLL4-coated plates favored T cell maturation into TCRab+CD3+CD8+ cells that express expected T cell markers, upregulate activation markers, and proliferate in response to T cell stimulus. Single-cell RNAseq shows Notch activation yields a 6-fold increase in multi-potent hematopoietic progenitors that follow a developmental trajectory toward T cells with clear similarity to post-natal human thymocytes. We conclude that early mesodermal Notch activation during hematopoietic differentiation is a missing stimulus with broad implications for producing hematopoietic progenitors with definitive characteristics.
Click here to access the full article

New Publication for the Murphy Lab, A ‘Blueprint’ for Longevity feature in USA Today, the New York Post and 75 other Media Outlets
Age-related changes in immune cell composition and functionality are associated with multimorbidity and mortality. However, many centenarians delay the onset of aging-related disease suggesting the presence of elite immunity that remains highly functional at extreme old age.
To identify immune-specific patterns of aging and extreme human longevity, we analyzed novel single cell profiles from the peripheral blood mononuclear cells (PBMCs) of a random sample of 7 centenarians (mean age 106) and publicly available single cell RNA-sequencing (scRNA-seq) datasets that included an additional 7 centenarians as well as 52 people at younger ages (20–89 years).
The analysis confirmed known shifts in the ratio of lymphocytes to myeloid cells, and noncytotoxic to cytotoxic cell distributions with aging, but also identified significant shifts from CD4+ T cell to B cell populations in centenarians suggesting a history of exposure to natural and environmental immunogens. We validated several of these findings using flow cytometry analysis of the same samples. Our transcriptional analysis identified cell type signatures specific to exceptional longevity that included genes with age-related changes (e.g., increased expression of STK17A, a gene known to be involved in DNA damage response) as well as genes expressed uniquely in centenarians’ PBMCs (e.g., S100A4, part of the S100 protein family studied in age-related disease and connected to longevity and metabolic regulation).
Collectively, these data suggest that centenarians harbor unique, highly functional immune systems that have successfully adapted to a history of insults allowing for the achievement of exceptional longevity.
Click here to see the article Click here to see the USA Today Article

The latest publication from the Kotton lab detailing the transcriptomic programs of iPSC-derived alveolar cells
Dysfunction of alveolar epithelial type 2 cells (AEC2s), the facultative progenitors of lung alveoli, is implicated in pulmonary disease pathogenesis, highlighting the importance of human in vitro models. However, AEC2-like cells in culture have yet to be directly compared to their in vivo counterparts at single-cell resolution. Here, we performed head-to-head comparisons among the transcriptomes of primary (1°) adult human AEC2s, their cultured progeny, and human induced pluripotent stem cell–derived AEC2s (iAEC2s). We found each population occupied a distinct transcriptomic space with cultured AEC2s (1° and iAEC2s) exhibiting similarities to and differences from freshly purified 1° cells. Across each cell type, we found an inverse relationship between proliferative and maturation states, with preculture 1° AEC2s being most quiescent/mature and iAEC2s being most proliferative/least mature. Cultures of either type of human AEC2s did not generate detectable alveolar type 1 cells in these defined conditions; however, a subset of iAEC2s cocultured with fibroblasts acquired a transitional cell state described in mice and humans to arise during fibrosis or following injury. Hence, we provide direct comparisons of the transcriptomic programs of 1° and engineered AEC2s, 2 in vitro models that can be harnessed to study human lung health and disease.

| The Center for Regenerative Medicine 670 Albany St 2nd Floor Boston MA 02118 Boston University & Boston Medical Center |
Quick links
Research at the crem, cores & protocols.
© 2021 CReM. All Rights Reserved.
Privacy policy Terms of use

Welcome to CReM
My name is Gabrielle. I'm the Administrative Assistant at CReM. Leave us a short message down below. We will get back to you ASAP!
The Wilson lab is focused on two major aspects of regenerative medicine:
1) Developing gene therapy approaches for the study and treatment of lung diseases: The ability to manipulate gene expression in specified lung cell populations has both experimental and therapeutic potential for lung disease. By developing viral vectors that transduce specific lung cell types in vivo, we hope to minimize potential off-target effects while maximizing our ability to target diseased cell populations. We work with lentiviral and AAV vectors to overexpress or knockdown expression of genes important to disease pathogenesis in the lung.
2) Utilizing induced pluripotent stem cells (iPSC) to study human lung and liver diseases: The Wilson lab is interested in the application of patient-derived iPS cells for the study of lung and liver diseases, such as alpha-1 antitrypsin deficiency (AATD).
The Hawkins Lab is interested in how the human lung develops and responds to injury to better understand human lung disease. Induced pluripotent stem cells (iPSCs) offer a unique opportunity to model human lung disease and bridge the gap between research in animal models and humans.
Using this iPSC platform, we are focused on understanding the molecular mechanisms that control human lung development. We hope to apply this knowledge to advance our understanding of and develop precision medicine approaches for lung disease.
The Murphy laboratory is composed of dynamic and passionate researchers who utilize multiple stem cell-based platforms to answer basic biological questions and combat disease. Central directions of the laboratory include: developmental hematopoiesis, the modeling of blood-borne disease, and discovery and therapeutic intervention in sickle cell disease, amyloidosis, and aging.
The Murphy Lab has pioneered: The world’s largest sickle cell disease-specific iPSC library and platforms and protocols that can used to recapitulate hematopoietic ontogeny and to develop and validate novel therapeutic strategies for the disease; The successful modeling of a protein folding disorder called familial amyloidosis demonstrating the ability to model a long-term, complex, multisystem disease in a relatively short time, using lineage-specified cells (hepatic, cardiac and neuronal) derived from patient-specific stem cells; The first iPSC library created from subjects with exceptional longevity (centenarians) that serves as an unlimited resource of biomaterials to fuel the study of aging and the development of novel therapeutics for aging-related disease.
www.murphylaboratory.com
@DRGJMurphy
The Serrano Lab studies neurodevelopment and cardiovascular development in the context of rare multi-systemic disorders originated by pathogenic variants in epigenetic modifiers like KMT2D.
We aim to identify shared molecular and cellular mechanisms driving cardiovascular and brain development with particular interest in cell differentiation, migration, and cell cycle progression.
Our lab combines rare disease modeling in zebrafish together with cardiovascular and neurobiology techniques and human iPSC-derived brain organoids and endothelial cells.
We believe that a patient-forward focus to our projects will help us to get better understanding of disease mechanisms through basic science research. To this end, we are active in the collaborative community among field experts and rare disease patient-advocacy groups who drive our research program to identify therapeutic targets in patient-specific iPS cells.
The Mostoslavsky Lab is a basic science laboratory in the Section of Gastroenterology in the Department of Medicine at Boston University.
Our goal is to advance our understanding of stem cell biology with a focus on their genetic manipulation via gene transfer and their potential use for stem cell-based therapy.
The Mostoslavsky’s Lab designed and constructed the STEMCCA vector for the generation of iPS cells, a tool that has become the industry standard for nuclear reprogramming. Project areas in the lab focuses on the use of different stem cell populations, including embryonic stem cells, induced Pluripotent Stem (iPS) cells, hematopoietic stem cells and intestinal stem cells and their genetic manipulation by lentiviral vectors.
Our laboratory have already established a large library of disease-specific iPS cells with a particular interest in utilizing iPS cells to model diseases of the liver, the gastrointestinal tract, prion-mediated neurodegenerative diseases and immune-based inflammatory conditions, using iPSC-derived microglia, macrophages and T/NK cells.
The Gouon-Evans lab investigates cellular and molecular mechanisms driving liver development, regeneration and cancer. We specifically interrogate the role of progenitor/stem cells and how they share similar molecular signature and functions during these 3 processes.
Our innovative tools include: 1) directed differentiation of human pluripotent stem cells (PSC) to generate in vitro liver progenitors and their derivative hepatocytes, the main functional cell type of the liver, 2) mouse models with lineage tracing strategy to track in vivo the fate of progenitor cells, 3) PSC derivative cell transplantation into mouse models with damaged livers as cell therapy for liver diseases, 3) dissection of liver cancer specimens from patients to identify and define the impact of specific cancer stem cells in liver oncogenesis.
Projects in the Gouon-Evans lab will lead to a better understanding of the liver development, to the establishment of multi-modular approaches for improving liver regeneration with PSC derivatives, and will reveal the impact of specific cancer stem cells as a target for diagnosis and therapy in liver oncogenesis.

Boston University’s Chronic Traumatic Encephalopathy (CTE) Center conducts high-impact, innovative research on chronic traumatic encephalopathy and other long-term consequences of repetitive brain trauma in athletes, military personnel, first responders, victims of physical violence, and others affected by head trauma. The mission of the CTE Center is to conduct state-of-the-art research on CTE, including its neuropathology and pathogenesis, clinical presentation, genetics and other risk factors, biomarkers, methods of detection during life, and methods of prevention and treatment.
Latest Stories
Younger exposure to football linked to worse cognitive outcomes in later life.
Healio | Among men who played American football, researchers found that exposure to the sport at a younger age was Read more
Publication Database
Characterizing Neurobehavioral Dysregulation Among Former American Football Players: Findings From the DIAGNOSE CTE Research Project
The Journal of Neuropsychiatry and Clinical Neurosciences | Pulukuri SV, Fagle TR, Trujillo-Rodriguez D, van Amerongen S, Bernick C, Geda Read more
Cognition Mediates the Association Between Cerebrospinal Fluid Biomarkers of Amyloid and P-Tau and Neuropsychiatric Symptoms
Journal of Alzheimer's disease | Frank B, Walsh M, Hurley L, Groh J, Blennow K, Zetterberg H, Tripodis Y, Budson Read more

Best Medical Schools in Boston (Ultimate Guide)
If you’re thinking about studying medicine in Boston (or any other allied health/medical studies program), you’ll want to know where the best medical schools in the city are.
Luckily, you have a ton of great options – 3 of the major ones are even located within a 5-mile radius of each other!
This article picks the best of them and provides you with all the necessary information (tuition fees, programs, locations, admissions data, etc.) you’ll likely want to know.
As a med student myself, I know how valuable quick overviews like this can be!
Ready to get started? Let’s go.
Best Medical Schools in Boston
There are 3 allopathic (MD) schools in the Boston area. These offer 4-year medical degrees, giving board licensure as a practicing physician.
All admissions data is taken from the American Association of Medical Colleges ( Source ). Ranking data is taken from U.S. News.
1. Harvard Medical School
| 25 Shattuck Street, Boston, MA 02115-6092 | |
| 1 in Research/8 in Primary Care | |
| 519.46 | |
| 3.7% | |
| $64,984 | |
| 3.92 | |
| 700 | |
| 14:1 |
Harvard Medical School is one of the top med schools in the world and is hugely selective.
The school offers medical degrees in Medicine, Dentistry, Public Health, Medical Information Management, and more.
Situated off Shattuck Street, close to Boston’s Central Village, the main campus buildings make up the Longwood Medical and Academic Area.
The school itself is affiliated with Massachusetts General Hospital.
See the website for admissions information, medical school requirements, and more.
DETAILS
- Name : Harvard Medical School
- Phone : 617-432-1000
- Website : hms.harvard.edu
Related : How Hard Is It To Get Into Harvard Medical School? (Explained!)
2. Boston University School of Medicine
| 72 E. Concord Street, L-103, Boston, MA 02118 | |
| 33 in Research/44 in Primary Care | |
| 517 | |
| 5.75% | |
| $64,884 | |
| 3.81 | |
| 663 | |
| 1.7:1 |
Founded in 1848, Boston University School of Medicine is famous for being one of the first institutions in the world to formally educate female physicians.
The school offers medical degrees in Medicine, Dentistry, Occupational Therapy, Physical Therapy, General Health Services, Health Management and Administration, and more.
Situated off Concord Street, in Boston’s South End, the main campus buildings are close to Frederick Douglass Square Historic District.
The school itself is affiliated with Boston Medical Center.
- Name : Boston University School of Medicine
- Phone : 617-358-9600
- Website : bumc.bu.edu
3. Tufts University School of Medicine
| 136 Harrison Avenue, Boston, MA 02111 | |
| 55 in Research/51 in Primary Care | |
| 508 | |
| 4.92% | |
| $65,052 | |
| 3.3 | |
| 809 | |
| 1.4:1 |
Tufts University School of Medicine consistently ranks among the world’s best medical research institutions for clinical medicine.
The school offers medical degrees in Medicine, Dentistry, Veterinarian, Nutrition, Occupational Health, Health Care Administration, and more.
Situated on Harrison Avenue, close to Boston Common, the main campus buildings are located in Chinatown.
The school itself is affiliated with Tufts Medical Center.
- Name : Tufts University School of Medicine
- Phone : 617-636-7000
- Website : medicine.tufts.edu
Four-Year Medical Studies Schools in Boston
There are several other great options for broader medical studies in Boston. These offer health and medical degrees in fields like nursing, physical therapy, pharmacy, physician assistant, and more.
4. Northeastern University
| 360 Huntington Avenue, Boston, MA 02115 | |
| 49 | |
| 1410-1540 (ACT 33-35) | |
| 18.1% | |
| $57,592 | |
| Private | |
| 15,156 | |
| 14:1 |
Northeastern University is a private research university with its main campus in Boston.
The school offers medical studies degrees in Pharmacy, Pharmacy Administration, Nursing, Physical Therapy, Health Care Administration, Physician Assistant, Medical Information Management, and more.
Situated on Huntington Avenue, close to the Museum of Fine Arts Boston, the main campus buildings are between West Fens and South End.
See the website for admissions information, course requirements, and more.
- Name : Northeastern University
- Phone : 617-373-2000
- Website : northeastern.edu
5. Boston College
| 140 Commonwealth Avenue, Chestnut Hill, MA 02467 | |
| 36 | |
| 1330-1500 (ACT 31-34) | |
| 27.2% | |
| $61,706 | |
| Private | |
| 9,445 | |
| 11:1 |
Boston College is a private, Jesuit research university in Chestnut Hill, Massachusetts.
The school offers medical studies degrees in Physician Assistant, Genetic Counseling, Public Health, Nursing, Physical and Occupational Therapy, Optometry, Pharmacy, and more.
It is just over 10 miles from downtown Boston.
- Name : Boston College
- Phone : 617-552-3100
- Website : bc.edu
6. Brandeis University
| 415 South Street, Waltham, MA 02454 | |
| 42 | |
| 1320-1510 (ACT 31-33) | |
| 34% | |
| $60,391 | |
| Private | |
| 3,493 | |
| 10:1 |
Brandeis University is a private research university in Waltham, Massachusetts.
The school offers medical studies degrees in Global Health Policy, Health Informatics, International Public Health, Genetic Counseling, Medical Information Management, and more.
- Name : Brandeis University
- Phone : 781-736-3237
- Website : brandeis.ed u
Two-Year Medical Studies Schools in Boston
There are also some great two-year schools for medical studies in Boston. These institutions offer courses like phlebotomy, surgical technician, pharmacy technician, radiation therapist, and more.
7. Bay State College
| 31 St. James Ave, Boston, MA 02116 | |
| 38-49 in Regional Colleges North | |
| 67% | |
| $29,200 | |
| 609 | |
| 9:1 |
Bay State College is a private, for-profit college in the Back Bay neighborhood of Boston, Massachusetts
The school offers medical studies courses in Health Sciences, Nursing, Physical and Occupational Therapy Assistant, Medical Assistant, and more.
- Name : Bay State College
- Phone : 617-217-9080
- Website : baystate.edu
8. Bunker Hill Community College
| 250 New Rutherford Ave, Boston, MA 02129-2925 | |
| N/A | |
| 100% | |
| $4,464 (in-state)/$9,408 (out-of-state) | |
| 12,522 | |
| 25:1 |
Bunker Hill Community College is a public multi-campus community college serving the Greater Boston area.
The school offers medical studies courses in Health Sciences, Phlebotomy, Patient Care Technician, Medical Assistant and Medical Interpreting.
- Name : Bunker Hill Community College
- Phone : 617-228-2000
- Website : bhcc.edu
9. Massachusetts Bay Community College
| 50 Oakland St, Wellesley Hills, MA 02481-5399 | |
| N/A | |
| 100% | |
| $5,088 (in-state)/$10,032 (out-of-state) | |
| 4,368 | |
| 15:1 |
Massachusetts Bay Community College is a public community college in Norfolk and Middlesex Counties.
The school offers medical studies courses in Health Sciences, Surgical Technician, Radiologist, EMT, Medical Administration, Nursing, and more.
- Name : Massachusetts Bay Community College
- Phone : 781-239-3000
- Website : massbay.edu
Boston is home to some of the best medical schools and medical study colleges in the entire state of Massachusetts.
If you’re interested in medical or allied health careers in the city, it’s a great idea to go deeper into your research. This website is home is hundreds of articles discussing medical school life and healthcare careers. Feel free to browse around or search for more information.
To get the best out of your time, I recommend checking the admissions guidelines and eligibility of the courses that most interest you, directly on each Boston-based college’s website.
That’s where you’ll get the most up-to-date and accurate information!
Related Questions
What is the best medical school in massachusetts.
The best medical school in the state is Boston’s Harvard Medical School. It has the highest ranking, as per U.S. News, in Research and Primary Care, out of all medical schools in Massachusetts.
You can see the exact stats of each school above.
What are the best pre-med schools in Boston?
Because you can study any undergrad major as a pre-med, the best schools are usually those with the highest ranking, smallest class sizes, best opportunities for research and clinical experience, and other extracurricular involvements.
Boston schools that best fit that criteria include:
- Boston University
- Boston College
- Harvard University
- Tufts University
- Brandeis University
You can check out their pre-med offerings via the websites listed above.
Are there any osteopathic (DO) medical schools in Boston?
There is no osteopathic (DO) medical school in Boston.
The closest osteopathic medical school to Boston city and metro is Wheaton College Massachusetts , based out of Norton, MA.
Wheaton College Massachusetts is located approximately 27 miles southwest of the city.
Does Boston College have a medical school?
Boston College does not have a medical school.
As mentioned before, its Pre-Health Program is one of the best in the state, however.
What about medical billing and coding schools in Boston?
The following schools are good choices for medical billing and coding in or close to the city:
- Massachussetts Bay Community College (Wellesley Hills, MA )
- Fisher College (Boston, MA)
- Roxbury Community College (Roxbury Crossing, MA)
What are the best medical assistant schools in Boston?
The following schools offer medical assistant courses in or close to the city:
- Bay State College (Boston, MA)
- Bunker Hill Community College (Boston, MA)
- North Shore Community College (Danvers, MA)
- Northern Essex Community College (Haverhill, MA)
Born and raised in the UK, Will went into medicine late (31) after a career in journalism. He’s into football (soccer), learned Spanish after 5 years in Spain, and has had his work published all over the web. Read more .
16 Best Medical schools in Boston, MA
Updated: February 29, 2024
- Art & Design
- Computer Science
- Engineering
- Environmental Science
- Liberal Arts & Social Sciences
- Mathematics
Below is a list of best universities in Boston ranked based on their research performance in Medicine. A graph of 6.19M citations received by 162K academic papers made by 16 universities in Boston was used to calculate publications' ratings, which then were adjusted for release dates and added to final scores.
We don't distinguish between undergraduate and graduate programs nor do we adjust for current majors offered. You can find information about granted degrees on a university page but always double-check with the university website.
1. Boston University
For Medicine
2. Northeastern University

3. Boston College
4. University of Massachusetts - Boston
5. MGH Institute of Health Professions

6. Simmons University

7. MCPHS University

8. Suffolk University

9. New England College of Optometry

10. Fisher College

11. Emerson College
12. Bay State College

13. Emmanuel College
14. Wentworth Institute of Technology
15. Berklee College of Music
16. New England Law - Boston

Universities for Medicine near Boston
| University | City | ||
|---|---|---|---|
| 3 | 44 | Cambridge, Massachusetts | |
| 5 | 1 | Cambridge, Massachusetts | |
| 7 | 50 | Medford, Massachusetts | |
| 7 | 429 | Brookline, Massachusetts | |
| 14 | 528 | Newton, Massachusetts | |
| 14 | 560 | Waltham, Massachusetts | |
| 16 | 168 | Waltham, Massachusetts | |
| 18 | 675 | Wellesley, Massachusetts | |
| 21 | 282 | Wellesley, Massachusetts | |
| 32 | 561 | Framingham, Massachusetts |
Medicine subfields in Boston
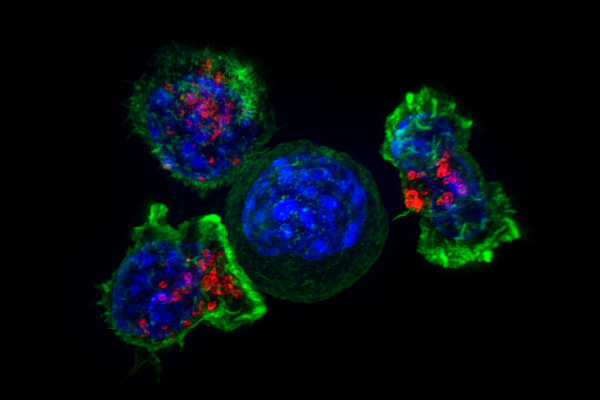
BU-BMC Cancer Center
Bridging the clinical oncology and biomedical research communities at the boston university medical and the charles river campuses and boston medical center., translating scientific findings into clinical results.
The BU-BMC Cancer Center provides high-quality patient care in combination with innovative research programs that directly transform cancer management through the discovery of personalized approaches for cancer detection and treatment.
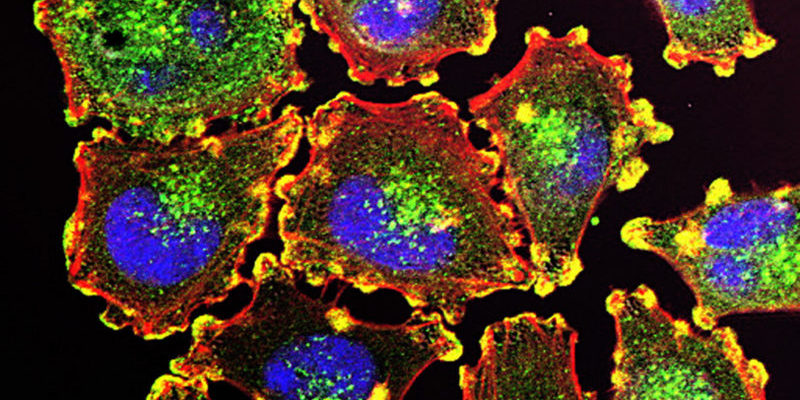
Join the Cancer Center
About Health Informatics Lab
The Health Informatics Lab (HILab) is part of the Master of Science in Health Informatics and the Health Informatics certificate at the Department of Computer Science , Metropolitan College, Boston University. The HILab is committed to excellence in research and education in health informatics and biomedicine. We are located at the Charles River campus.
Health informatics is an interdisciplinary field at the intersection of computer science, informatics, and biomedicine. The HILab brings together computer scientists, biologists, and clinical scientists to work together on human health through advanced uses of information technologies. The HILab simultaneously supports education and research in Health Informatics by engaging the faculty and students in research projects and by the provision of educational and research resources.
The HILab contributes to the improvement of healthcare by pursuing research and development in health informatics, bioinformatics, and clinical research. Our work involves the standardization and cataloging of medical algorithms, the development of classification algorithms for bioinformatics, and the implementation of knowledge-based systems for biomedicine.
For our latest research activities, click here .
Boston University Metropolitan College
MET Health Informatics Research Lab
Useful Links
Subscribe now.
Don’t miss our future updates! Get Subscribed Today!
© 2023 Trustees of Boston University
- Admitted Graduate Students
- Current Graduate Students
- Current Undergraduate Students
BC.EDU LINKS

- Boston College
- Campus Life
- Jesuit, Catholic
- Academic Calendar
- BC Magazine
- Directories
- Offices, Services, Resources
- Agora Portal
- Maps & Directions
- Undergraduate
Summer Research Experiences
- Science Education
- Health Professions
- Professional Development Events and Activities

Lists and Directories of Summer Research Experiences
- National Science Foundation (NSF) - Research Experiences for Undergraduates (REUs) NOTE: Please also see Resources for Students Applying for REUs.
- National Institutes of Health (NIH) Summer Internships
- American Association of Medical Colleges (AAMC)
- Faculty for Undergraduate Neuroscience (FUN) - Neuroscience Internships Listing
- American Physiological Society (APS)
- Biomedical Science Careers Program
- SACNAS (Society for the Advancement of Chicanos and Native Americans in Science)
- Boston College EagleLink Service (sign in required)
Specific Programs
- Amgen Scholars Program Note: Amgen has multiple sites available at research universities. Application deadline depends on specific site.
- Baylor College of Medicine - SMART program
- Summer Medical and Research Training - Houston, TX
- Brigham and Women's Hospital STARS Program
- Summer Training in Academic Research and Scholarship
- Centers for Disease Control and Prevention (CDC)
- Cold Spring Harbor (NY)
- Columbia University IGERT on Optical Techniques for Actuation, Sensing & Imaging of Biological Systems
- Cincinnati Children's Hospital - Summer Undergraduate Research
- Harvard-MIT Health Sciences and Technology Summer Institute
- Harvard Summer Research Program in Kidney Medicine
- Harvard Stem Cell Institute
- Joslin Diabetes Center Summer Research
- Johns Hopkins University Summer Research
- The Jackson Lab - Summer Biomedical Research (Bar Harbor, ME)
- Sackler Institute of Graduate Biomedical Sciences, NYU School of Medicine
- Marine Biological Laboratory
- Mayo Clinic Summer Research Program (Rochester, MN)
- MIT Lincoln Laboratory Summer Research Program
- NASA Undergraduate Research Program
- Nemours / Alfred I. duPont Hospital for Children (Wilmington, DE)
- Mass General Hospital - Summer Research Trainee Program
- Mass General Hospital - Wellman Center for Photomedicine
- Roswell Park Cancer Institution Summer Research Program (Buffalo, NY)
- Thomas Jefferson University Research Program (Philadelphia, PA)
- University of Massachusetts Medical School (Worcester, MA)
- University of Connecticut Health Center
- University of Texas Southwestern Graduate School of Biomedical Sciences - SURF program
- University of California, San Francisco Summer Research Training Program
- University of Wisconsin, Madison Summer Research Program in Biology
- Wadsworth Laboratories (New York State Department of Health)
Biotech Opportunities
- Massachusetts Biotechnology Council
- Stryker Orthopaedics
- Biogen Idec
Environmental Sciences
- Environmental Protection Agency (EPA)
- United States Department of Agriculture (USDA)
- NSF REU sites focusing on Ocean Sciences
- RISE (Research Internships in Science & Engineering) (Germany)
- John Innes Centre and Sainsbury Laboratory (United Kingdom)
- Institut Pasteur (Paris)
- The Atlantis Fellowship (Europe and Latin America)
Biology Department 355 Higgins Hall
617-552-3540

IMAGES
VIDEO
COMMENTS
Research in Action. In an immersive seminar to Latin America, an interdisciplinary group of Boston College faculty focuses on human rights and reconciliation, international partnerships. Two book projects, Hope: Promise, Possibility, and Fulfillment and The Holy Spirit: Setting the World on Fire are notable examples of how STM faculty members ...
Boston College is committed to providing an array of research opportunities for undergraduates. In the humanities, the sciences, business, and education, students have a chance to gain exposure to new methods and lead their own research projects. No matter your interests, fellowships across disciplines provide funding to gain practical ...
Targeting cancer. An international research team led by a Boston College professor has uncovered a drug and diet pairing that could fight a deadly brain cancer. Researchers have paired a specialized diet and a tumor-fighting drug and found the non-toxic combination helps to destroy the two major cells found in an aggressive form of brain cancer ...
Review Article. Sep 18, 2024. CME. Perspective. Sep 21, 2024. The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles ...
BU showcase includes Han, Grinstaff, Khalil, Chen, and Paschalidis. By Andrew Thurston. As part of the weeklong celebration marking this Friday's formal installation of Melissa L. Gilliam as Boston University's 11th president, BU researchers shared a glimpse into their work and how they are changing the world for the better, at Wednesday's Inauguration 2024 Research on Tap event at the ...
Currently ranked #39 nationally by US News and World Report, Boston College's reputation for research output stretches far and wide. ... Part 4: Getting into medical school as a Boston College premed. Successfully gaining acceptance into medical school is a true exercise in patience and persistence. It may seem at some times to be a drawn out ...
Through research, health care education, workforce development, and community health initiatives, AHW drives change. ... On September 3, executive leaders from MCW and the Medical College of Wisconsin Cancer Center hosted a ceremony to publicly announce WBCS' newest gift: a $650,00 pledge to endow the WBCS Innovative Research Fund and support ...
Lydia Bischoff, B.S., Research Associate Lillie Mitchell (BC'25) Sophie Jalkut (BC'24), continuing as Research Assistant Jack Weidenbach, Research Assistant ... Boston College (applying to medical school) Ben Lamarre (BC'23) Boston College (researcher @ MGH) Elizabeth Mortati (BC'23) Boston College (medical student at SUNY Downstate) Lydia Boer ...
Boston University Medical Campus Boston University's programs in Clinical Research aim to meet the needs of health professionals engaged in the full-spectrum of patient-oriented research. We offer both master's degree and certificate programs to individuals seeking careers in clinical research in industry or academic settings.
Program at a Glance. Graduate Certificate. 16 Credits Required. $925 Current Cost per Credit. 8-12 months Completion Time. Clinical research is the fastest-growing discipline in the burgeoning medical device and pharmaceutical industries. Keeping pace with the ever-increasing body of knowledge and new regulatory procedures generated by ...
BOSTON - Boston Medical Center (BMC) researchers have established Boston Health Equity & community-Aligned Learning Health System (Boston HEALHS), a new program that will support comparative effectiveness research to accelerate enhanced health equity, patient care, and community engagement. Boston HEALHS will be supported by a $5 million grant from the federal Agency for Healthcare Research ...
Gallani, Susanna, Mary Witkowski, and Katie Sonnefeldt. "The Health Equity Accelerator at Boston Medical Center." Harvard Business School Case 125-039, September 2024.
Douglas P Kiel, Marcus Institute for Aging Research, Hebrew Senior Life, Boston, MA 02131, United States. Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02215, United States. ... Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China. Steven R Cummings, ...
That topic is one of the key areas of interest for Rebecca Carrier, a Northeastern University professor of chemical engineering and the head of the university's Advanced Drug Delivery Research Lab. "So mucus, why is it so interesting?" Carrier asked recently in front of an audience at the Curry Student Center on the Boston campus.
If you would like to show your support for the research Dr. Seyfried and his lab undertake, you can easily contribute a donation through the Boston College Development page. Please select the "Area of Support*" section, scroll down and choose the "Other" category, and type in "Biology Cancer Research - Dr. Seyfried" in the text field.
According to our analysis of job postings data, clinical research professionals in the Greater Boston area make an average salary of $90,000—increasing at an annual rate of 34.4 percent. This can attract even more aspiring clinical research professionals to the New England area.
Center for Regenerative Medicine of Boston University and Boston Medical Center DISCOVER CReM contact us Positions available Financial Support CReM response to COVID-19 Discover CReM About CReM Human health and development depend on dynamic networks of physical, and functional, interactions between proteins. However, the details of these networks - how they are formed and how
Today, the school is home to more than 640 funded research programs. Students at the Boston University School of Medicine have several distinct ways to earn an M.D., including the Early Medical ...
Boston University's Chronic Traumatic Encephalopathy (CTE) Center conducts high-impact, innovative research on chronic traumatic encephalopathy and other long-term consequences of repetitive brain trauma in athletes, military personnel, first responders, victims of physical violence, and others affected by head trauma. The mission of the CTE ...
All admissions data is taken from the American Association of Medical Colleges (Source). Ranking data is taken from U.S. News. 1. Harvard Medical School. Location: 25 Shattuck Street, Boston, MA 02115-6092. National University Rank: 1 in Research/8 in Primary Care. Average MCAT:
The Health Center provides students access to board-certified physicians, nurse practitioners, registered nurses, and on-site specialty consultants affiliated with some of Boston's finest hospitals. The center provides both inpatient and outpatient services. The Health Center is located on the ...
Experience what sets our students, faculty, and researchers apart. We do more than teach medicine and conduct research, we live it - in Boston and all over the world. Every day we learn, teach and discover in places not everyone goes - the front lines of medicine and science. Learn More.
Washington 8. Milwaukee 8. Claremont 7. New Orleans 7. Albany 7. Ranking methodology. Below is the list of 16 best universities for Medicine in Boston, MA ranked based on their research performance: a graph of 6.19M citations received by 162K academic papers made by these universities was used to calculate ratings and create the top.
Translating Scientific Findings into Clinical Results. The BU-BMC Cancer Center provides high-quality patient care in combination with innovative research programs that directly transform cancer management through the discovery of personalized approaches for cancer detection and treatment.
Research; Campus Life; Jesuit, Catholic; Resources. Academic Calendar; BC Magazine; BC News; Directories; ... For medical and psychological emergencies on campus, contact Boston College Police at 617-552-4444. Phone: 617-552-3225 Fax: 617-552-3603. [email protected]. Hours of Operation.
For more information about the PROVEn registry, please email research coordinator Nellie Shippen or call (617) 414-1987. Providing research, support, guidance and resources to all department faculty engaged in psychiatric and interdisciplinary research, the Psychiatry Research Centers' research initiatives encompass a variety of specialties ...
The Health Informatics Lab (HILab) is part of the Master of Science in Health Informatics and the Health Informatics certificate at the Department of Computer Science, Metropolitan College, Boston University. The HILab is committed to excellence in research and education in health informatics and biomedicine. We are located at the Charles River ...
CSTM Clough School of Theology and Ministry. LAW Boston College Law School. LSEHD Lynch School of Education and Human Development. MCAS Morrissey College of Arts and Sciences. MCBC Messina College. SSW School of Social Work. WCAS Woods College of Advancing Studies. " A key reason that Jesuit education has emphasized the liberal arts for the ...
Joslin Diabetes Center Summer Research. Johns Hopkins University Summer Research. The Jackson Lab - Summer Biomedical Research (Bar Harbor, ME) Sackler Institute of Graduate Biomedical Sciences, NYU School of Medicine. Marine Biological Laboratory. Mayo Clinic Summer Research Program (Rochester, MN) MIT Lincoln Laboratory Summer Research Program.