- Research article
- Open access
- Published: 22 July 2021

Health professionals and students’ experiences of reflective writing in learning: A qualitative meta-synthesis
- Giovanna Artioli ORCID: orcid.org/0000-0002-1810-0857 1 ,
- Laura Deiana 2 ,
- Francesco De Vincenzo 3 ,
- Margherita Raucci 1 ,
- Giovanna Amaducci 1 ,
- Maria Chiara Bassi 1 ,
- Silvia Di Leo 1 ,
- Mark Hayter 4 &
- Luca Ghirotto 1
BMC Medical Education volume 21 , Article number: 394 ( 2021 ) Cite this article
30k Accesses
30 Citations
11 Altmetric
Metrics details
Reflective writing provides an opportunity for health professionals and students to learn from their mistakes, successes, anxieties, and worries that otherwise would remain disjointed and worthless. This systematic review addresses the following question: “What are the experiences of health professionals and students in applying reflective writing during their education and training?”
We performed a systematic review and meta-synthesis of qualitative studies. Our search comprised six electronic databases: MedLine, Embase, Cinahl, PsycINFO, Eric, and Scopus. Our initial search produced 1237 titles, excluding duplicates that we removed. After title and abstract screening, 17 articles met the inclusion criteria. We identified descriptive themes and the conceptual elements explaining the health professionals’ and students’ experience using reflective writing during their academic and in-service training by performing a meta-synthesis.
We identified four main categories (and related sub-categories) through the meta-synthesis: reflection and reflexivity, accomplishing learning potential, building a philosophical and empathic approach, and identifying reflective writing feasibility. We placed the main categories into an interpretative model which explains the users’ experiences of reflective writing during their education and training. Reflective writing triggered reflection and reflexivity that allows, on the one hand, skills development, professional growth, and the ability to act on change; on the other hand, the acquisition of empathic attitudes and sensitivity towards one’s own and others’ emotions. Perceived barriers and impeding factors and facilitating ones, like timing and strategies for using reflective writing, were also identified.
Conclusions
The use of this learning methodology is crucial today because of the recognition of the increasing complexity of healthcare contexts requiring professionals to learn advanced skills beyond their clinical ones. Implementing reflective writing-based courses and training in university curricula and clinical contexts can benefit human and professional development.
Peer Review reports
Education of healthcare professionals supportstheir transformation into becoming competent professionals [ 1 ] and improves their reasoning skills in clinical situations. In this context, reflective writing (RW) is encouraged by both universities, and healthcare training providersencourage reflective writing (RW) since its utility in helping health students and professionals nurture reflection [ 2 ], which is considered a core element of professionalism. Furthermore, the ability to reflect on one’s performance is now seen to be a crucial skill for personal and professional development [ 3 ]. Writing about experiences to develop learning and growth through reflection is called ‘reflective writing’ (RW). RW involves the process of reconsidering an experience, which is then analyzed in its various components [ 4 , 5 ]. The act of transforming thoughts into words may create new ideas: the recollection of the experience to allow a deeper understanding of it, modifying its original perception, and creating new insights [ 6 ]. RWis the focused and recurrent inspection of thoughts, feelings, and events emerging from practice as applied to healthcare practice [ 7 ].
Reflection may be intended as a form of mental processing or thinking used by learners to fulfill a purpose or achieve some anticipated outcome [ 2 ]. This definition recalls Boud and colleagues’ view of reflection as a purposive activity directed towards goals [ 8 ]. For those authors, reflection involves a three-stage process, including recollection of the experience, attending to own feelings, and re-evaluating the experience. This process can be facilitated by reflective practices, among which RW is one of the main tools [ 9 ].
Between reflection-on-action (leading to adjustments to future learning and actions) and reflection-in-action (where adjustments are made at the moment) [ 10 ], RW can be situated in the former. It involves theprofessional’s reflections and analysis of experiences in clinical practice [ 11 , 12 ]. Mainly,RWinvolves the recurrent introspection ofone’s thoughts, feelings, and events within a particular context [ 13 ]. Several studies highlight how RWinfluencespromoting critical thinking [ 14 ], self-consciousness [ 15 ], and favors the development of personal skills [ 16 ], communication and empathy skills [ 4 , 17 ], and self-knowledge [ 3 ]. Thanks to the writing process, individuals may analyze all the components of their experience and learn something new, giving new meanings [ 5 ]. Indeed, putting down thoughts into words enables the individual to reprocess the experience, build and empower new insights, new learnings, and new ways to conceive reality [ 6 , 18 , 19 , 20 ].
Furthermore, RW provides an opportunity to give concrete meaning to one’s inner processes, mistakes, successes, anxieties, and worries that otherwise would remain disjointed and worthless [ 21 , 22 ]. The reflective approach of RW allows oneself to enter the story, becoming aware of our professional path, with both an educational and therapeutic effect [ 23 ].
Reflection as practically sustained by RW commonly overlaps with the process of reflexivity. As noted elsewhere [ 24 ], reflection and reflexivity originate from different philosophical traditionsbut have shared similarities and meanings. In the context of this article, we adopt two different working definitions of reflection and reflexivity. Firstly, we draw from the work of Alexander [ 25 ]: who explains reflection as the deliberation, pondering, or rumination over ideas, circumstances, or experiences yet to be enacted, as well as those presently unfolding or already passed [ 25 ]. Reflexivity at a meta-cognitive level relates to finding strategies to challenge and questionpersonal attitudes, thought processes, values, assumptions, prejudices, and habitual actions to understand the relationships’ underpinning structure with experiences and events [ 26 ]. In other words, reflexivity can be defined as “the self-conscious co-ordination of the observed with existing cognitive structures of meaning” [ 27 ].
Given those definitions,a philosophical framework for helping health trainees and professionals conduct an exercise that can be helpful to them, their practice, and – ultimately – their patients can be identified. There is a growing body of qualitative literature on this topic – which is valuable – but the nature of qualitative research is that it creates transferrable and more generalizableknowledge cumulatively. As such, bodies of qualitative knowledge must besummarized and amalgamated to provide a sound understanding of the issues – to inform practice and generate the future qualitative research agenda. To date, this has not been done for the qualitative work on reflective writing: a gap in the knowledge base our synthesis study intends to address by highlighting what connects students and professionals while using RW.
This systematic review addresses the following question: “What are the experiences of health professionals and students in applyingRWduring their education and training?”
This systematic review and meta-synthesis followed the 4-step procedure outlined by Sandelowski and Barroso [ 28 , 29 ], foreseeing a comprehensive search, appraising reports of qualitative studies, classification of studies, synthesis of the findings. Systematic review and meta-synthesis referto the process of scientific inquiry aimed at systematically reviewing and formally integrating the findings in reports of completed qualitative studies [ 29 ].
The article selection processwas summarized as a PRISMA flowchart [ 30 ]; the search strategy was based on PICo (Population, phenomenon of Interest, and Context),and the study results are reported in agreement with Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) guidelines [ 31 ].
Selection criteria
Inclusion criteria for the meta-synthesis were:
Primary qualitative studies published in peer-reviewed English journals.
With health professionals or health studentsas participants.
UsingRW in learning contexts (both pre-and in-service training).
Mixed methods where the qualitative part can be separated.
Articles should report the voice of participants (direct quotations).
Given the meta-synthesis indications, we excluded quantitative studies, non-primary research articles, meta-synthesis of qualitative studies, literature and systematic reviews, abstracts, unpublished reports, grey literature. In addition, we also excluded studies where participants were using RW in association with other learning tools and where the personal experience was not about using RW exclusively.
Data sources and searches
An experienced information specialist (MCB) performed the literature search on Medline, Embase, Cinahl, PsycInfo, Eric, and Scopus for research articles published from Jan 1st, 2008 to September 30th, 2019,to make sure we incorporated studies reflecting contemporary professional health care experience. Additional searchinginvolved reviewing the references or, and citations to, our included studies.
We filled an Excel file with all the titles and authors’ names. A filter for qualitative and mixed methods study was applied. Table 1 shows the general search strategy for all the databases based on PICo.
Four reviewers (GAr, MR, GAm, LD) independently screened titles and abstracts of all studies, then checked full-text articles based on the selection criteria. We also searched the reference lists of the full-text articles selected for additional potentially relevant studies. Any conflict was solved through discussion with three external reviewers (LG, MCB,SDL, and MH).
Quality appraisal
We used the Critical Appraisal Skills Programme (CASP): it provides ten simple guiding questions and examples to examine study validity, adequacy, and potential applicability of the results of qualitative studies. Guided by the work of Long and colleagues [ 32 ] and previously used in other meta-synthesis [ 33 ], we created 30 items from the 10 CASP questions on quality to ensure we could provide a detailed appraisal of the studies. FDV and LD independently assessed the quality of included studies with any conflicts solved by consulting a third reviewer (MCB and LG). Researchers scored primary studies weighingthe proposed items and ranking the quality of each included study [ 34 ] on high ( n > 20 items positively assessed), moderate (10 < n < 20), or low quality ( n < 10).
Analysis and synthesis
MCB created a data extraction table, GAr, GAm, and MRdescribed the included articles (Table 2 ). Quotations were extracted manually from the “results/findings” sections of the included studies by GAr, MCB, LDand inserted into adatabase. GAr, GAm, MR, and FDVperformed a thematic analysis of those sections, along with participants’ quotations. Then, they inductively derived sub-themes from the data, performing a first interpretative analysis of participants’ narratives (i.e., highlighting meanings participants interpreted about their experience). The sub-themes were compared and transferred across studies by adding the data into existing sub-themes or creating new sub-themes. Similar sub-themes were then grouped into themes, using taxonomic analysisto conceptually identify the sub-categories and the categories emerging from the participants’ narratives. This procedure allowed us to translate the themes identified from the original studies [ 28 ] into interpretative categories that could amalgamate and refine the experiences of health professionalsor health students on the use of RW [ 29 ]. The final categories are based on the consent of all the authors.
Literature search and studies’ characteristics
A total of 1488 articles were retrieved. Duplicates ( n = 251) were removed. Then, articles ( n = 1237) were identified and reviewed by title and abstract. We excluded n = 1152 articles because they did not match the specified inclusion criteria, based on the title and abstract. Consequently, we assessed 85 full-text articles. Sixty-eight records did not meet the inclusion criteria. At the end of the selection process, 17 reportsof qualitative research were selected. Figure 1 illustrates the search process.
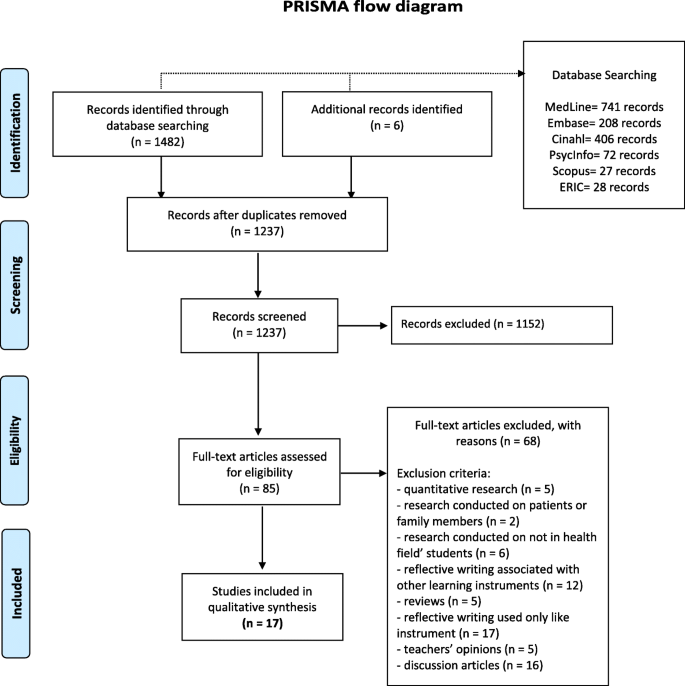
PRISMA flow diagram
Table 2 shows the characteristics of the included studies. Eleven studies involved healthcare students (58%, including nurses, midwives, physiotherapists, doctors, dentists, and oral health students), and six (32%, including doctors, occupational and radiation therapists) were referred to health professionals. In thirteen studies, participants were trained on RW before using it: this information could not be retrieved from the remaining articles.
Five articles reported studies conducted in the US, three in Australia, two in Canada, and two in Israel. The other studies were carried out in Italy, UK, Korea, Taiwan, and Sweden.
Critical appraisal results
We critically evaluatedall 17 studies to highlight the methodological strengthsand weaknesses of the selected studies. No article was removed on a quality assessment basis. Results of the quality appraisal are reported in Table 2 .
Meta-synthesis findings
Through the meta-synthesis, we identified four main categories (and related sub-categories): (i) reflection and reflexivity; (ii) accomplishing learning potential; (iii) building a philosophical and empathic approach; (iv) identifying reflective writing feasibility (for the complete dataset, please refer to supplemental material , where we have listed a selection of meaningful quotations of categories and sub-categories).
Given such categories, we developed an interpretative meta-synthesis model (Fig. 2 ) to illustrate the commonalities of the experience of using RW according to both students and professionals: RWas a vehicle for discovering reflection and allowing users to enter personal reflexivity to fulfillone’s learning potential, alongside the building of a philosophical and empathic approach. In their experience, reflection and reflexivity generate different skills and competencies: reflection matures skills such as professional skills and the ability to activate change and innovation. Reflexivity allows students and professionals to reach higher levels of competencyconcerning inner development and empathy reaching. Finally, from our analysis, participants, while recognizing the value of RW, also defined factors that could encourage or limit its use. Differences among participants’ groups are also outlined.
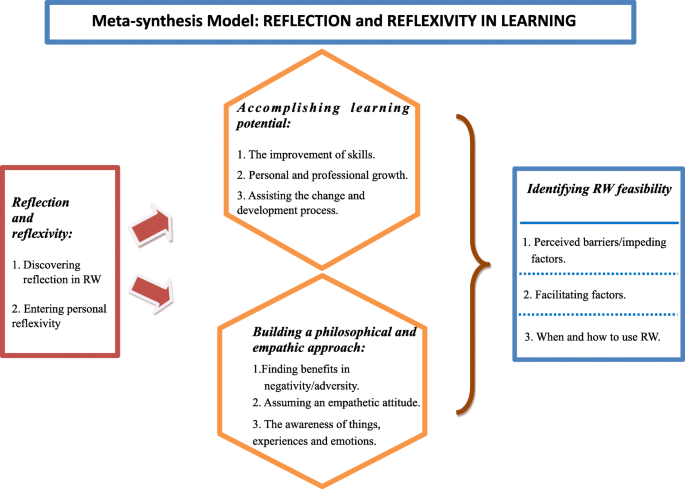
Meta-synthesis model: RW as experienced by health professionals and students
Reflection and reflexivity
Within this category, we collected the users’ narratives about the experience of applying RW and its disclosing capacity. By using RW, participants confronted themselves with both reflection and reflexivity. This category includes two sub-categories we named: discovering reflection and entering personal reflexivity.
Discovering reflection
The sub-category shows that experiencingRW deepened their reflection on experiences, practice, and profession. Thanks to RW, professionals, and students could explore previously unexplored topics and learn more about themselves.
“ Writing initiated me to think about my experiences … ” (professional) [ 46 ]. “ I think it’s good for physicians to reflect on what we’re doing ” (professional) [ 50 ]
The analysis showed that RW was considered reflective when it provided an opportunity for those who applied it to stop, reflect and conduct an inner discourse on topics never considered before [ 44 , 46 , 50 ]. Some students affirmed:
“ Helped (me) reflect on positive aspects ” (student) [ 40 ]. “ I don’t usually think too much about what happens to me, but through critical reflective journaling, I was able to think carefully about things happening around me. This activity helped me to look into my mind ” (student) [ 44 ]
This sub-category explains transversal meanings coming from uniformly professionals and students.
Entering personal reflexivity
This sub-category includes data about RW enabling users’reflexivity. In this context, RW was considered training for reflexivity as it enabled participants to question themselves more often [ 48 ], reflect on their experiences [ 35 ], attitudes, actions [ 38 , 45 ], and also reconsider their actions and identify their strengths and weaknesses [ 40 , 44 ].
“ The questions in this study do make me stop and think about things – how I feel about what I’m doing in residency ”(professional) [ 46 ]. “ Helped me ID (identify) my strengths and weaknesses ” (student) [ 40 ] RW also helped eradicate the background noise that my mind does not yet know how to filter out [ 51 ] .
Interesting to note that this sub-category is more present in students’ narratives. While professionals referred to self-reflection practices (probably already acquired in other contexts), students often reported how RW helped them discover reflexivity.
Accomplishing learning potential
Our analysis showed how users RW used the technique to “Accomplish learning potential.”
According to the studies’ participants, RWcan enable a learning performancethat would be difficult to reach otherwise. In this context, participants addressed RW as a tool for“accomplishing learning potential.”Within this category, three sub-categories were highlighted: the improvement of skills, personal and professional growth, and assisting the change and development process.
Improvement of skills
Participants agreed that the development of skills and abilities through RWwas aimed at their clinical skills and –in relevant areas such as question asking – encouraged reflection and research [ 35 , 46 ]. Communication skills were also enhanced, as were their relationship with patients, family,colleagues, and friends [ 35 , 38 , 46 ].
Participants said:
“ Through reflective journal writing, my attitude towards learning has changed. I have been encouraged to be a proactive learner. (...) I have been able to identify necessary places for improvement and through research, question asking, goal-setting (...). I have improved my skills in relevant areas” (student) [ 35 ]. “I feel that it [participation in the study] has been a positive experience by motivating me to improve on my clinical, communication skills, and also my relationships with colleagues, patients, family, and friends ” (professional) [ 46 ]
Participants also reported that,in their experience, RWprovided an opportunity to assess and improve themselves and to enhance their self-confidence [ 38 , 40 ]. Cognitive skills, includinggaining more profoundknowledge and problem-solving, along withtime-management [ 35 , 40 , 46 , 49 ], were also enhanced: RW,therefore,represented a learning mode [ 45 ].
“ Without reflection, I absolutely believe these skills would be more unattainable for me ”(student) [ 35 ]
This sub-category applies more to students’ narratives. Health students mentioned the tools helping them most to develop their skills. Professionals focused principally on what RWcould improve (communication skills or organizational skills).
Personal and professional growth
Participantsidentifiedthat RWhad promoted personal [ 51 ] and professional growth [ 35 , 46 ]. RW meant for participants:an ameliorated attitude towards work [ 46 ]; a development path for one’s job potential [ 38 ]; an enhancement of their introspective knowledge [ 51 ]; an enrichment of their expressive capability [ 38 ];an improvement of their interpersonal relationships with patients and colleagues [ 50 ] and developed their use of critical and reflective thinking [ 38 ].
“ Reflecting introduces a new aspect to clinic that focuses on the individual’s learning experience ” (student) [ 35 ]. “I think that it does change the way that you think about the practice of medicine and your own personal tendencies and your interactions with your patients and colleagues. And I think it can be a really powerful driver of culture change ” (professional) [ 50 ]
This sub-category is more represented among students than professionals. Students are ‘surprised’ at how important RW was to their learning. Professionals still recognized how RW was an essential driver of change for their clinic activities.
Assisting the change and development process
We labeledthe third sub-category“assisting the change and development process.”The changeinvolvedintroducing modifications tothe way of working [ 48 ], assessing what needed to be changed to achieve a work-life balance [ 51 ], understanding elements that did not allow change, and how to act on them in the future, and also considering new and important issues [ 46 ], further information [ 51 ] and new ways of thinking. This sub-category equally explained the meaning given to RW by students and professionals.
“ I think writing answer to some of these questions has allowed me to reflect back on the year and think about specific important topics that I might not have thought about again.” (professional) [ 46 ]. (Reflective journaling encouraged) “Assessing and focusing on the changes that need to be done to achieve the balance in my life and being able to integrate that with my family and in my work as a nurse.” (Student 16/RJ2) [ 51 ]
However, thischange process could not be possible without witnessing change and becoming aware of it [ 38 , 46 ]. This allowedparticipants to ‘see one’slearning history and path of growth,‘have a picture of the problem, handle things differently, and broadening their vision of the problem [ 48 ].
Building a philosophical and empathic approach
The “Reflection and reflexivity” category is closely aligned with the “Building a philosophical and empathic approach” category. Participants defined RW as a means for nurturing an intimate and profound level of learning, i.e., a philosophical and empathic approach towards real-life professional issues. The third category consists of three sub-categories: the ability to find benefits in negativity/adversity, assuming an empathetic attitude, and the awareness of things, experiences,emotions.
Finding benefits in negativity/adversity
According to participants, RWexerted a therapeutic effect by encouraging professionals and students to focus on the present (43)strictly. It seemed that RWeventually reduced their emotional stress [ 44 , 51 ]. Likewise,in the contextofnegative experiences [ 49 ], its practice acted as a catharsis [ 46 ] that could even allow them tolook back at those experiencesafresh – enabling a change in perspective [ 39 ].
“While writing the journal entry, I felt like I was unloading something from inside myself and being set free. This process made me feel better ” (student) [ 44 ]. “It is always good to pause to reflect on my experiences. The most cathartic question was a few months back when I got to describe my really bad experience.” (professional) [ 46 ] “Very therapeutic. I wrote on a bad experience, but at the end, we were laughing at it.” (professional) [ 49 ]
This specific approach allowed the practitioner/trainee to improve their self-care and focus on work objectives [ 51 ]:
“Self-reflection and reflective journaling promote self-understanding and is another part of self-care.” (Student 5/RJ3) [ 51 ]
Even if more emerging from students’ voices, professionals appeared genuinely amazed at how learning can be generated out of negativity.
Assuming an empathetic attitude
Study participants stressed the fact that RWhelped them develop empathetic attitudes. It seems that RWemphasized the importance of sensitivity and empathy by trying ‘to be in someone else’sshoes,’ especially that of patients or colleagues [ 36 , 37 , 44 ].
“How reflecting on patient encounters through field notes allowed her to “take a walk in someone else’s shoes ” (student) [ 36 ]. “It helps you see the humanity... ” (professional) [ 50 ]
This approach also applied in contexts outside of work and helped the practitioner take off his/her‘white coat’ and understand that before being a professional,he/shewas a person and a human being [ 36 , 37 , 46 , 50 ].
“ Which has made me more open to other’s ideas and thoughts ” (professional) [ 46 ]
As previously mentioned, according to the participants’ statements, awareness was the cornerstone to effective personal and professional growth [ 40 , 51 ].
This sub-category is equivalently present among the participants’ groups. Nonetheless, different meaningscould also be highlighted. Students appreciated RWby stressing its value of allowing them to enter deeply ‘into the other’ inner world (mainly patients). Professionals claimed they could recognize the profession’s human and relational aspects, whichcould also be helpful for their extra-professional relationships (family members, friends).
Awareness of things, experiences, emotions
Impartially balanced among professionals and students, awareness was cited in terms of ‘how things have affected me rather than simply continuing to work in a robotic manner’ [ 46 ], the awareness of who one was and who one has become thanks to the process of change [ 51 ]. This professional and relational awareness made it possible to think clearly about one’s practice and the health resources present in the context of belonging [ 50 ].
“Just being aware of what I know now and what I’ll know by the end of the semester … is a great way to learn who I am and what I can change about me for the better.” (Student 9/RJ1) [ 51 ]
The process of awareness that was facilitated by how their RW allowedthem to transform shapeless and straightforward ideasinto words and givethem a specific value and emotional charge [ 36 , 47 , 51 ]: it wasan authentic opportunity to turn emotions and feelings into something tangible –a journey of discovery and personal acceptance [ 43 ].
“ After two years or so, when you look back, it’s like, oh,that’s how I was feeling at the time, and right now, I feel differently. There is also this level of satisfaction. Like you have matured out of this thinking ” (professional) [ 47 ]
Identifying RW feasibility
The fourth category consists of three sub-categories: perceived barriers/impeding factors, facilitating factors, and when and how to use RW. Students and healthcare professionals who had the experience of practicing the RW in their work identified both limitations and facilitating factors and indications about when and how to use RW.
Perceived barriers/impeding factors
Some study participants (almost entirely students) identified several barriers to their activity. Some students could not see the benefits and thought RW was a waste of time [ 35 , 38 , 51 ]. However, others, who did see the potential benefits still felt that they lacked the time needed to devote to RW [ 42 ] or, sufficient mental space to report and describe a work situation, an excessive similarity of this activity to the regular working practice and, consequently, a lack ofmotivation to write [ 47 , 51 ]. In addition, some described the strainthey felt in writing down personal/professional experiences [ 47 ]. A lack of privacy was another problem, both for the concern about sharing the reflection and for the respect of confidentialityin writing itself [ 51 ]. Taken together,it appeared that some study participants did not recognizeRW as an effective means of help [ 39 , 50 ]. Althoughrealizing the potential of RW,others felt that their tutors did not provide noticeably clearexplanations of the aim of RW– which they would have found useful and motivating [ 45 ].
“ To be honest, not a great deal ( … ) it wasn’t really some revelation ” (professional) [ 50 ]. “ I got a hard time referring it [my experience] to citations … I could have sat and cried yesterday when I did my essay … when I actually read it [my essay] I thought, oh I don’t know what it means, myself ” (Female 2 - student) [ 42 ]
Facilitating factors
This sub-category was exclusively interpreted from students’ narratives. They valued the perspectives to use RWin their practice seeing it as a valuable tool to be applied throughout their career [ 35 , 45 ],with many students reporting that they would continue with this technique [ 38 ]. Studentssaw RW as a valuable means of staying focused on their own goals and needs [ 40 , 51 ]. They remarked that it helped them reduce stress, gain clarity in one’s life and practice [ 41 ], and spiritually connect with themselves [ 45 , 51 ]. Furthermore, RW enabled studentsto discover more information about their health and well-being, ‘it also helped me tie in ideas and beliefs from different sources and relate it to my own’ [ 51 ]. RWhelped maintain awareness and recall the medical being/human being dichotomy [ 37 ]. It remindedstudentsof the difference between studying literature and refining manual skills and the ability to learn from experience and mistakes [ 35 ].
“ During the interview, I felt an element of being more like a ‘normal person’ having a ‘normal conversation’ with another human being. This was a strange realization because it reminded me of the dichotomy that physicians may experience, being doctor versus human ” (student) [ 37 ]
When and how to use RW
Health professionals (a few) and many students finally mentioned the time considered most appropriate to use RW, underlining its usefulness primarilywas during hardship rather than daily practice [ 47 ].Moreover,RWshould not be forced onto someone in any given moment but instead left to individual choice based on one’s spirit of the moment [ 40 , 46 ].
“. .. like if you had a patient die; that would be the only time you might write it down ” (professional) [ 47 ]
Otherparticipantsconsidered instructions on RW to be too forceful and notapplicable to their own experience of reflection [ 40 ]. ‘Reflection wasn’t just signing on the line.’ It allowed constructive feedback for the trainee or the professional. Constructive feedback could be positive or negative, but it was a powerful tool for thinking and examining things [ 45 ].
In this meta-synthesis of qualitative studies, we have interpreted the experiences of health professionals and students who used RWduring their education and training. Given the number of studies included, RW users’ experience was predominately investigated in students. This result, although not surprising, raises the question of whether RW in professional training is being used. RW is not used in professional training as often as it is in the academic training of healthcare students.
As to this review’s aim, we could highlight continuities and differences from study participants’ narratives. Our findings offer a conceptualization of usingRW in health care settings. According to the experience of both students (from different disciplines) and health professionals, RW allows its exponents to discover and practice reflectionas a form of cognitive processing [ 2 ] and enablethem to develop a better understanding of their lived situation. We also interpreted that RW allows users to make a ‘reflexive journey’ that involves them practicing meta-cognitive skills to challengetheir attitudes, pre-assumptions, prejudices, and habitual actions [ 24 , 26 ]. This was particularly true for students: “entering personal reflexivity” appears to be newer for them than for the professionals who are likely to acquire reflexivity during academic training. Students seemed more focused on tools than RW-related results. This consideration makes us affirm that reflective capacity is in progress for them.
Challenging pre-assumptions and entering reflexivityenabledRWusers to realize how RW may develop their learning potential to improve skills and personal/professional growth. Skills to be enhanced are quoted mainly by students. Conversely, professionals could comprehend the final purpose of learning, achievable through RW, in terms of communication or organizational abilities. Professionals interpreted skills from RW as abilities to apply in the clinical activities to find new solutions to problems.
The category “Accomplishing learning potential”confirms what many authors highlight: putting thoughts into words not only permits a deeper understanding of events [ 6 ], enhances professionalism [ 52 ] but also improves personal [ 16 ], communication, and empathy skills [ 4 , 17 ]. In this context, RW fulfills its mandate by letting human sciences [ 53 ] and evidence-based health disciplines affect clinical practice. As noted [ 54 ], students and health professionals’RW training allowed integrating scientific knowledge with behavioral and sociological sciences to supporttheir learning [ 55 ].
Users understood that RWcould be a powerful means of developing empathy and developing their philosophy of care: this consideration is in line with a recent study from Ng and colleagues [ 24 ]. Additionally, some authors [ 4 , 17 ] stressed these empathetic skills and “humanistic”competencies as essential to care for patients effectively [ 56 ]. Professionals were amazed how negativity could generate learning through RW. On the other hand, by recognizingand writing experienced negative situations, students could free themselves from feelings impeding empathy.
By employing RW, users reported factors that could encourage or limit its use. These findings further illustrate that RW is not always a tool that is easy to use without adequate training [ 57 ]. Almost exclusively, students reported hindering factors (limited time, difficulty in writing and understanding assignments, privacy issues, feeling bored or forced). As to professionals, few describedRW as a very stressful activity. Although students could identify impeding factors, they also recognized many positive ones. For professionals, RW was not to be used every day but in ‘extreme’ situations, requiring reflection and reflexivity to be applied. In general, enhancing motivation to write reflectively [ 58 ] should be the first goal of any training to make the process acceptable and profitable for trainees. If this first stage is not accomplished, it will reduce RW’sapparent professional and personal effectiveness among health professionals and students substantially.
Strengths, limitations, and research relaunches
This review may enrich our knowledge about providing RW as an educative tool for health students and professionals. However, the findings must be applied,taking into account some limitations. We focused our attention only on recent, primary, peer-reviewed studies within the time and publication limits. Qualitative studies often are available as grey literature: considering it may result in a different interpretation of students’ and professionals’ experience in using RW. Therefore, our conceptualization should be read bearing in mind a publication bias and the need to expand the literature search to other sources. Besides limiting the risk of missing published qualitative studies, we reviewed the reference listsof included studies for additional items. Our meta-synthesis is coherent to the interpretation of the included studies’ findings.
At least two reviewers have conducted each step of this systematic review. We purposely did not exclude studies based on a quality assessment to maintain a robust qualitative study sample size and valuable insights.
During analysis, all possible interpretations were screened by authors, and an agreement was reached. Nonetheless, we did not cover all the possible ways to interpret the voices of students and professionals.
Since RW is not used in professional training as often as it is in the academic training of healthcare students, a research relaunch could be investigatingwhether and to what extent RW is being used in in-service training programs. Moreover, the studies included in this review were conducted within Western countries. Students’ and professionals’ perspectives from Africa and Asia are underrepresented within the qualitative literature about experiences of using RW. Therefore, geographicalgeneralizations from the present meta-synthesis should be avoided, and our paper reveals the necessity for RW research in other cultures and settings. Nonetheless, authors of primary studies have paid little attention to cultural and regionaldiversity. Therefore, we recommend furtherinvestigations exploring the differences between cultural backgrounds and howRW is recognized within training programs in different countries. Finally, additional qualitative and quantitative research is required to deepen our understanding of RW’s clinical and psycho-social outcomes in high complexity health practice contexts.
Our analysis confirms the crucial role of RW in fostering reasoning skills [ 59 ] and awareness in clinical situations. While its utility in helping health students and professionals to nurture reflection [ 2 ] has been widely theorized, this meta-synthesis provide empirical evidence to support and illustrate this theoretical viewpoint. Finally, we argue that RWis even more critical given the increasing complexity of modern healthcare, requiringprofessionals to develop advanced skills beyond their clinical ones.
Practical implications
Two important implications can be highlighted:
students and professionals can recognize the potential of RW in learning advanced professional skills. ImplementingRW in academic training as well as continuing professional education is desirable.
Despite recognizing the effectiveness of RW in healthcare learning, students and professionals may face difficulties in writing reflectively. Trainers should acknowledge and address this.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Critical appraisal skills programme
Enhancing transparency in reporting the synthesis of qualitative research
Population, phenomena of interest and context
Preferred reporting items for systematic reviews and meta-analyses
Reflective writing
Mlinar Reljić N, Pajnkihar M, Fekonja Z. Self-reflection during first clinical practice: The experiences of nursing students. Nurse Educ Today. 2019;72:61–6. https://doi.org/10.1016/j.nedt.2018.10.019 .
Article Google Scholar
Moon JA. A handbook of Reflective and experiential learning: theory and practice. London: Routledge; 2004. p. 264.
Google Scholar
Borgstrom E, Morris R, Wood D, Cohn S, Barclay S. Learning to care: medical students’ reported value and evaluation of palliative careteaching involving meeting patients and reflective writing. BMC Med Educ. 2016;16:306.
Nelms Edwards C, Mintz-Binder R, Jones MM. When a clinical crisis strikes: lessons learned from the reflective writings ofnursing students. Nurs Forum. 2019;54(3):345–51. https://doi.org/10.1111/nuf.12335 .
Haugland BØ, Lassen RM, Giske T. Professional formation through personal involvement and value integration. Nurse Educ Pract. 2018;29:64–9. https://doi.org/10.1016/j.nepr.2017.11.013 .
Launer J. What’s the point of reflective writing? Postgrad Med J. 2015;91(1076):357 LP – 358. Available from: http://pmj.bmj.com/content/91/1076/357.abstract
Naber J, Markley L. A guide to nursing students’ written reflections for students and educators. Nurse Educ Pract. 2017;25:1–4. https://doi.org/10.1016/j.nepr.2017.04.004 .
Boud D, Keogh R, Walker D. Reflection, turning experience into learning [Internet]. 1985. Available from: http://www.123library.org/book_details/?id=110587
Ng SL, Kinsella EA, Friesen F, Hodges B. Reclaiming a theoretical orientation to reflection in medical education research: acritical narrative review. Med Educ. 2015;49(5):461–75. https://doi.org/10.1111/medu.12680 .
Mann K V. Reflection’s role in learning: increasing engagement and deepening participation. Perspect Med Educ. 2016;5(5):259–261. Available from: https://doi.org/ https://doi.org/10.1007/s40037-016-0296-y , 2016.
Jasper M, Rosser M, Mooney GP. Professional development, reflection and decision-making in nursing and health care. 2nd ed. London: Wiley-Blackwell; 2013. p. 254.
Burkhardt C, Crowl A, Ramirez M, Long B, Shrader S. A Reflective assignment assessing pharmacy students’ Interprofessional CollaborativePractice exposure during introductory pharmacy practice experiences. Am J Pharm Educ. 2019;83(6):6830. https://doi.org/10.5688/ajpe6830 .
Wilson H, Warmington S, Johansen M-L. Experience-based learning: junior medical students’ reflections on end-of-life care. Med Educ. 2019;53(7):687–697. Available from: https://doi.org/ https://doi.org/10.1111/medu.13907 .
Naber J, Wyatt TH. The effect of reflective writing interventions on the critical thinking skills anddispositions of baccalaureate nursing students. Nurse Educ Today. 2014;34(1):67–72. https://doi.org/10.1016/j.nedt.2013.04.002 .
Allan EG, Driscoll DL. The three-fold benefit of reflective writing: improving program assessment, student learning, and faculty professional development. Assess Writ [Internet]. 2014;21:37–55. Available from: https://www.sciencedirect.com/science/article/pii/S1075293514000087 . https://doi.org/10.1016/j.asw.2014.03.001 .
Peterson WJ, House JB, Sozener CB, Santen SA. Understanding the struggles to be a medical provider: view through medical StudentEssays. J Emerg Med. 2018;54(1):102–8. https://doi.org/10.1016/j.jemermed.2017.09.014 .
Liu GZ, Jawitz OK, Zheng D, Gusberg RJ, Kim AW. Reflective Writing for medical students on the surgical clerkship: oxymoron orAntidote? J Surg Educ. 2016;73(2):296–304. https://doi.org/10.1016/j.jsurg.2015.11.002 .
Craft M. Reflective writing and nursing education. J Nurs Educ. 2005;44(2):53–7. https://doi.org/10.3928/01484834-20050201-03 .
Tharenos CL, Hayden AM, Cook E. Resident self-portraiture: a reflective tool to explore the journey of becoming a doctor. J Med Humanit. 2019;40(4):529—551. Available from: https://doi.org/ https://doi.org/10.1007/s10912-018-9545-x .
Tsuruwaka M, Asahara K. Narrative writing as a strategy for nursing ethics education in Japan. Int J Med Educ. 2018 Jul;9:198–205. https://doi.org/10.5116/ijme.5b39.d5d2 .
Launer J. Managing the threat to reflective writing. Postgrad Med J. 2018 ;94(1111):314 LP – 315. Available from: http://pmj.bmj.com/content/94/1111/314.abstract
Rojí R, Noguera-Tejedor A, Pikabea-Díaz F, Carrasco JM, Centeno C. Palliative care bedside teaching: A qualitative analysis of medical Students’Reflective writings after clinical practices. J Palliat Med. 2017;20(2):147–54. https://doi.org/10.1089/jpm.2016.0192 .
Artioli G, Artioli F. Autobiografia e apprendimento in tirocinio [autobiography and learning in traineeship]. In: Alastra V, editor. Ambienti narrativi, territori di cura e formazione [Narrative settings, care and education territories]. Milano: FrancoAngeli; 2016. p. 114–25.
Ng SL, Wright SR, Kuper A. The divergence and convergence of critical reflection and critical reflexivity:implications for health professions education. Acad Med. 2019;94(8):1122–8. https://doi.org/10.1097/ACM.0000000000002724 .
Alexander PA. Reflection and reflexivity in practice versus in theory: challenges of conceptualization, complexity, and competence. Educ Psychol. 2017;52(4):307–314. Available from: https://doi.org/ https://doi.org/10.1080/00461520.2017.1350181 .
Verdonk P. When I say … reflexivity. Med Educ. 2015;49(2):147–8. https://doi.org/10.1111/medu.12534 .
Siraj-Blatchford I, Siraj-Blatchford J. Reflexivity, social justice and educational research. Cambridge J Educ. 1997;27(2):235–248. Available from: https://doi.org/ https://doi.org/10.1080/0305764970270207 , Reflexivity, Social Justice and Educational Research.
Sandelowski M, Barroso J, Voils CI. Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Res Nurs Health. 2007;30(1):99–111. Available from: https://pubmed.ncbi.nlm.nih.gov/17243111 . https://doi.org/10.1002/nur.20176 .
Sandelowski M, Barroso J. Handbook for synthesizing qualitative Research. New York, NY, US: Springer Publishing Company; 2006. p. 312.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Med. 2009;6(7):e1000097. Available from: https://doi.org/ https://doi.org/10.1371/journal.pmed.1000097 .
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181. https://doi.org/10.1186/1471-2288-12-181 .
Long HA, French DP, Brooks JM. Optimizing the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Heal Sci. 2020;1(1):31–42. Available from: https://doi.org/ https://doi.org/10.1177/2632084320947559 .
Barisone M, Bagnasco A, Hayter M, Rossi S, Aleo G, Zanini M, et al. Dermatological diseases, sexuality and intimate relationships: A qualitativemeta-synthesis. J Clin Nurs. 2020;29(17–18):3136–53. https://doi.org/10.1111/jocn.15375 .
Boeije HR, van Wesel F, Alisic E. Making a difference: towards a method for weighing the evidence in a qualitativesynthesis. J Eval Clin Pract. 2011;17(4):657–63. https://doi.org/10.1111/j.1365-2753.2011.01674.x .
Tsang AKL, Walsh LJ. Oral health students’ perceptions of clinical reflective learning--relevance totheir development as evolving professionals. Eur J Dent EducOff J AssocDent Educ Eur. 2010;14(2):99–105. https://doi.org/10.1111/j.1600-0579.2009.00598.x .
Wald HS, Reis SP, Monroe AD, Borkan JM. “The loss of my elderly patient:” interactive reflective writing to support medicalstudents’ rites of passage. Med Teach. 2010;32(4):e178–84. https://doi.org/10.3109/01421591003657477 .
Garrison D, Lyness JM, Frank JB, Epstein RM. Qualitative analysis of medical student impressions of a narrative exercise in thethird-year psychiatry clerkship. Acad Med. 2011;86(1):85–9. https://doi.org/10.1097/ACM.0b013e3181ff7a63 .
Kuo C-L, Turton M, Cheng S-F, Lee-Hsieh J. Using clinical caring journaling: nursing student and instructor experiences. J Nurs Res. 2011;19(2):141–9. https://doi.org/10.1097/JNR.0b013e31821aa1a7 .
Bagnato S, Dimonte V, Garrino L. The reflective journal: A tool for enhancing experience- based learning in nursing students in clinical practice. J Nurs Educ Pract. 2013;3(3):102–11.
Constantinou M, Kuys SS. Physiotherapy students find guided journals useful to develop reflective thinkingand practice during their first clinical placement: a qualitative study. Physiotherapy. 2013;99(1):49–55. https://doi.org/10.1016/j.physio.2011.12.002 .
Jonas-Dwyer DRD, Abbott P V, Boyd N. First reflections: third-year dentistry students’ introduction to reflective practice. Eur J Dent Educ [Internet]. 2013 Feb 1;17(1):e64–9. Available from: https://doi.org/10.1111/j.1600-0579.2012.00763.x.
Bowman M, Addyman B. Academic reflective writing: a study to examine its usefulness. Br J Nurs. 2014 Mar;23(6):304–9. https://doi.org/10.12968/bjon.2014.23.6.304 .
Binyamin G. Growing from dilemmas: developing a professional identity through collaborativereflections on relational dilemmas. Adv Health Sci Educ Theory Pract. 2018 Mar;23(1):43–60. https://doi.org/10.1007/s10459-017-9773-2 .
Hwang B, Choi H, Kim S, Kim S, Ko H, Kim J. Facilitating student learning with critical reflective journaling in psychiatricmental health nursing clinical education: A qualitative study. Nurse Educ Today. 2018;69:159–64. https://doi.org/10.1016/j.nedt.2018.07.015 .
Persson EK, Kvist LJ, Ekelin M. Midwifery students’ experiences of learning through the use of written reflections -an interview study. Nurse Educ Pract. 2018 May;30:73–8. https://doi.org/10.1016/j.nepr.2018.01.005 .
Levine RB, Kern DE, Wright SM. The impact of prompted narrative writing during internship on reflective practice: aqualitative study. Adv Health Sci Educ Theory Pract. 2008;13(5):723–33. https://doi.org/10.1007/s10459-007-9079-x .
Cashell A. Radiation therapists’ perspectives of the role of reflection in clinical practice. J Radiother Pract. 2010/09/15. 2010;9(]):131–141. Available from: https://www.cambridge.org/core/article/radiation-therapists-perspectives-of-the-role-of-reflection-in-clinical-practice/7E45C6571ACD2FDEDA1556A18C82782D
Vachon B, Durand M-J, LeBlanc J. Using reflective learning to improve the impact of continuing education in thecontext of work rehabilitation. Adv Health Sci Educ Theory Pract. 2010;15(3):329–48. https://doi.org/10.1007/s10459-009-9200-4 .
Karkabi K, Wald HS, Cohen Castel O. The use of abstract paintings and narratives to foster reflective capacity in medical educators: a multinational faculty development workshop. Med Humanit. 2013/11/22. 2014;40(1):44–48. Available from: https://pubmed.ncbi.nlm.nih.gov/24273319
Caverly T, Matlock D, Thompson J, Combs B. Qualitative evaluation of a narrative reflection program to help medical trainees recognize and avoid overuse: “Am I doing what’s right for the patient?” Patient Educ Couns. 2018;101(3):475—480. Available from: https://doi.org/ https://doi.org/10.1016/j.pec.2017.09.001 .
Padykula BM. RN-BS students’ reports of their self-care and health-promotion practices in aHolistic nursing course. J Holist NursOff J Am Holist Nurses’Assoc. 2017;35(3):221–46. https://doi.org/10.1177/0898010116657226 .
Bjerkvik LK, Hilli Y. Reflective writing in undergraduate clinical nursing education: A literature review. Nurse Educ Pract. 2019;35:32–41. https://doi.org/10.1016/j.nepr.2018.11.013 .
Ng SL, Mylopoulos M, Kangasjarvi E, Boyd VA, Teles S, Orsino A, et al. Critically reflective practice and its sources: A qualitative exploration. Med Educ. 2020;54(4):312–319. Available from: https://doi.org/ https://doi.org/10.1111/medu.14032 .
Chaudhary ZK, Mylopoulos M, Barnett R, Sockalingam S, Hawkins M, O’Brien JD, et al. Reconsidering Basic: Integrating Social and Behavioral Sciences to Support Learning. Acad Med. 2019 Nov;94(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the58th Annual Research in Medical Education Sessions):S73–8.
Wald HS, White J, Reis SP, Esquibel AY, Anthony D. Grappling with complexity: medical students’ reflective writings about challengingpatient encounters as a window into professional identity formation. Med Teach. 2019;41(2):152–60. https://doi.org/10.1080/0142159X.2018.1475727 .
Smith T. Guided reflective writing as a teaching strategy to develop nursing student clinical judgment. Nurs Forum. 2020;n/a(n/a). Available from: https://doi.org/ https://doi.org/10.1111/nuf.12528 , 56, 2, 241, 248.
Whitmore CA, Sakai J, Mikulich-Gilbertson SK, Davies RD. A four-week Reflective Writing program in the psychiatry clerkship: testing Effectson Reflective capacity. Acad psychiatryj Am Assoc DirPsychiatr Resid Train Assoc Acad Psychiatry. 2019;43(2):171–4.
Rajhans V, Eichler R, Sztrigler Cohen O, Gordon-Shaag A. A Novel method of enhancing students’ involvement in reflective writing. Clin Teach. 2020;n/a(n/a). Available from: https://doi.org/ https://doi.org/10.1111/tct.13303 , 18, 2, 174, 179.
Uygur J, Stuart E, De Paor M, Wallace E, Duffy S, O’Shea M, et al. A Best Evidence in Medical Education systematic review to determine the most effective teaching methods that develop reflection in medical students: BEME Guide No. 51. Med Teach. 2019;41(1):3–16. Available from: https://doi.org/ https://doi.org/10.1080/0142159X.2018.1505037 .
Download references
Acknowledgments
We thank Dr. Silvia Tanzi for her insightful feedback about this work and Manuella Walker for assisting in the final editing of the paper.
Not applicable.
Author information
Authors and affiliations.
Azienda USL-IRCCS di Reggio Emilia, Viale Umberto I, 50, 42123, Reggio Emilia, Italy
Giovanna Artioli, Margherita Raucci, Giovanna Amaducci, Maria Chiara Bassi, Silvia Di Leo & Luca Ghirotto
Medical and Surgical Department, University of Parma, Parma, Italy
Laura Deiana
European University of Rome, Rome, Italy
Francesco De Vincenzo
Faculty of Health Sciences, University of Hull, Hull, UK
Mark Hayter
You can also search for this author in PubMed Google Scholar
Contributions
GArwas responsible for the original concept. MCB performed the literature search on databases. MCB, GAr, GAm, LD, MR were responsible of data curation. GAr, MR, GAm, and LD screened titles and abstracts of all studies. LG, MCB, SDL, and MH served as external auditors. FDV and LD assessed the quality of included studies. MCB and LG gave a third opinion in case of disagreement. GAr, GAm, MR, and FDV derived sub-categories from the data. GAr, LG, MH drafted the first version of the manuscript. FDV, LD composed tables, and figures. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Giovanna Artioli .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
Meta-synthesis framework with participants’ narratives.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Artioli, G., Deiana, L., De Vincenzo, F. et al. Health professionals and students’ experiences of reflective writing in learning: A qualitative meta-synthesis. BMC Med Educ 21 , 394 (2021). https://doi.org/10.1186/s12909-021-02831-4
Download citation
Received : 27 October 2020
Accepted : 14 July 2021
Published : 22 July 2021
DOI : https://doi.org/10.1186/s12909-021-02831-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care education
- reflective writing
- Health professionals
- Health students
- qualitative meta-synthesis
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Ali M. Communication skills 1: benefits of effective communication for patients. Nursing Times. 2017; 113:(12)18-19
Barber C. Communication, ethics and healthcare assistants. British Journal of Healthcare Assistants. 2016; 10:(7)332-335 https://doi.org/10.12968/bjha.2016.10.7.332
Berlo DK. The process of communication; an introduction to theory and practice.New York (NY): Holt, Rinehart and Winston; 1960
Bramhall E. Effective communication skills in nursing practice. Nurs Stand. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Bumb M, Keefe J, Miller L, Overcash J. Breaking bad news: an evidence-based review of communication models for oncology nurses. Clin J Oncol Nurs. 2017; 21:(5)573-580 https://doi.org/10.1188/17.CJON.573-580
Caldwell L, Grobbel CC. The importance of reflective practice in nursing. International Journal of Caring Sciences. 2013; 6:(3)319-326
Communication skills for workplace success employers look for these communication skills. The Balance (online). 2019. http://tinyurl.com/yyx3eeoy (accessed 27 June 2019)
Evans N. Knowledge is power when it comes to coping with a devastating diagnosis. Cancer Nursing Practice. 2017; 16:(10)8-9 https://doi.org/10.7748/cnp.16.10.8.s7
Gibbs G. Learning by doing: a guide to teaching and learning methods.Oxford: Further Education Unit, Oxford Polytechnic; 1988
Gillett A, Hammond A, Martala M. Successful academic writing.Harlow: Pearson Education Limited; 2009
Hanratty B, Lowson E, Holmes L Breaking bad news sensitively: what is important to patients in their last year of life?. BMJ Supportive & Palliative Care. 2012; 2:(1)24-28 https://doi.org/10.1136/bmjspcare-2011-000084
Hemming L. Breaking bad news: a case study on communication in health care. Gastrointestinal Nursing. 2017; 15:(1)43-50 https://doi.org/10.12968/gasn.2017.15.1.43
Macmillan Cancer Support. Cancer clinical nurse specialists (Impact Briefs series). 2014. http://tinyurl.com/yb96z88j (accessed 27 June 2019)
Healthcare professionals: acknowledging emotional reactions in newly-diagnosed patients. 2012. http://www.justgotdiagnosed.com (accessed 27 June 2019)
Oelofsen N. Using reflective practice in frontline nursing. Nurs Times. 2012; 108:(24)22-24
Paterson C, Chapman J. Enhancing skills of critical reflection to evidence learning in professional practice. Phys Ther Sport. 2013; 14:(3)133-138 https://doi.org/10.1016/j.ptsp.2013.03.004
Pincock S. Poor communication lies at heart of NHS complaints, says ombudsman. BMJ. 2004; 328 https://doi.org/10.1136/bmj.328.7430.10-d
Royal College of Nursing. Revalidation requirements: reflection and reflective discussion. 2019. http://tinyurl.com/yy8l68cy (accessed 27 June 2019)
Schildmann J, Cushing A, Doyal L, Vollmann J. Breaking bad news: experiences, views and difficulties of pre-registration house officers. Palliat Med. 2005; 19:(2)93-98 https://doi.org/10.1191/0269216305pm996oa
Shipley SD. Listening: a concept analysis. Nurs Forum. 2010; 45:(2)125-134 https://doi.org/10.1111/j.1744-6198.2010.00174.x

Reflecting on the communication process in health care. Part 1: clinical practice—breaking bad news
Beverley Anderson
Macmillan Uro-oncology Clinical Nurse Specialist, Epsom and St Helier NHS Trust
View articles · Email Beverley
This is the first of a two-part article on the communication process in health care. The interactive process of effective communication is crucial to enabling healthcare organisations to deliver compassionate, high-quality nursing care to patients, in facilitating interactions between the organisation and its employees and between team members. Poor communication can generate negativity; for instance, misperception and misinterpretation of the messages relayed can result in poor understanding, patient dissatisfaction and lead to complaints. Reflection is a highly beneficial tool. In nursing, it enables nurses to examine their practice, identify problems or concerns, and take appropriate action to initiate improvements. This two-part article examines the role of a uro-oncology clinical nurse specialist (UCNS). Ongoing observations and reflections on the UCNS's practice had identified some pertinent issues in the communication process, specifically those relating to clinical practice and the management of practice-related issues and complaints. Part 1 examines the inherent problems in the communication process, with explanation of their pertinence to delivering optimal health care to patients, as demonstrated in four case studies related to breaking bad news to patients and one scenario related to communicating in teams. Part 2 will focus on the management of complaints.
In health care, effective communication is crucial to enabling the delivery of compassionate, high-quality nursing care to patients ( Bramhall, 2014 ) and in facilitating effective interactions between an organisation and its employees ( Barber, 2016 ; Ali, 2017 ). Poor communication can have serious consequences for patients ( Pincock, 2004 ; Barber, 2016 ; Ali, 2017 ). Misperception or misinterpretation of the messages relayed can result in misunderstanding, increased anxiety, patient dissatisfaction and lead to complaints ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ; Evans, 2017 ; Doyle, 2019 ), which, as evidence has shown, necessitates efficient management to ensure positive outcomes for all stakeholders—patients, health professionals and the healthcare organisation ( Barber, 2016 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). Complaints and their management will be discussed in Part 2.
Reflection is a highly beneficial tool ( Oelofsen, 2012 ), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes ( Bramhall, 2014 ). The author, a uro-oncology clinical nurse specialist (UCNS), is required to ensure that appropriate reassurance and support is given to patients following the receipt of a urological cancer diagnosis ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ). Support consists of effective communication, which is vital to ensuring patients are fully informed and understand their condition, prognosis and treatment and, accordingly, can make the appropriate choices and decisions for their relevant needs ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ; Doyle, 2019 ).
Reflection is a process of exploring and examining ourselves, our perspectives, attributes, experiences, and actions and interactions, which helps us gain insight and see how to move forward ( Gillett et al, 2009:164 ). Reflection is a cycle ( Figure 1 ; Gibbs, 1988 ), which, in nursing, enables the individual to consciously think about an activity or incident, and consider what was positive or challenging and, if appropriate, plan how a similar activity might be enhanced, improved or done differently in the future ( Royal College of Nursing (RCN), 2019 ).
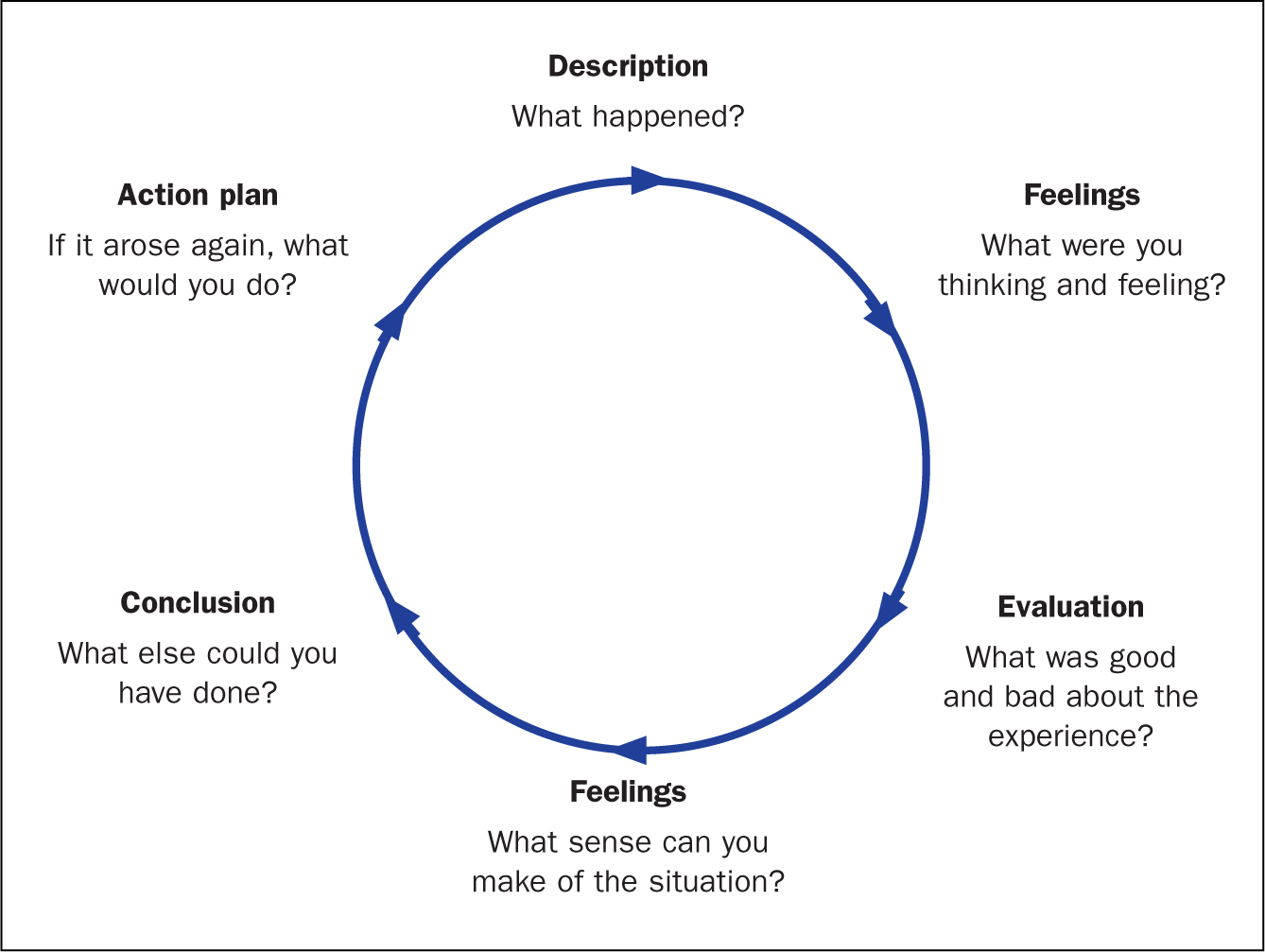
Reflective practice
Reflective practice is the ability to reflect on one's actions and experiences so as to engage in a process of continuous learning ( Oelofsen, 2012 ), while enhancing clinical knowledge and expertise ( Caldwell and Grobbel, 2013 ). A key rationale for reflective practice is that experience alone does not necessarily lead to learning—as depicted by Gibbs' reflective cycle (1988) . Deliberate reflection on experience, emotions, actions and responses is essential to informing the individual's existing knowledge base and in ensuring a higher level of understanding ( Paterson and Chapman, 2013 ). Reflection on practice is a key skill for nurses—it enables them to identify problems and concerns in work situations and in so doing, to make sense of them and to make contextually appropriate changes if they are required ( Oelofsen, 2012 ).
Throughout her nursing career, reflection has been an integral part of the author's ongoing examinations of her practice. The process has enabled numerous opportunities to identify the positive and negative aspects of practice and, accordingly, devise strategies to improve both patient and practice outcomes. Reflection has also been a significant part author's professional development, increasing her nursing knowledge, insight and awareness and, as a result, the author is an intuitive practitioner, who is able to deliver optimal care to her patients.
Communication
Figure 2 provides a visual image of communication—it is both an expressive, message-sending, and a receptive, message-receiving, process ( Berlo, 1960 ; McClain, 2012 ; Evans, 2017 ). This model was originally designed to improve technical communication, but has been widely applied in different fields ( Berlo, 1960 ). Communication is the sharing of information, thoughts and feelings between people through speaking, writing or body language, via phone, email and social media ( Bramhall, 2014 ; Barber, 2016 ; Doyle, 2019 ). Effective communication extends the concept to require that transmitted content is received and understood by someone in the way it was intended.
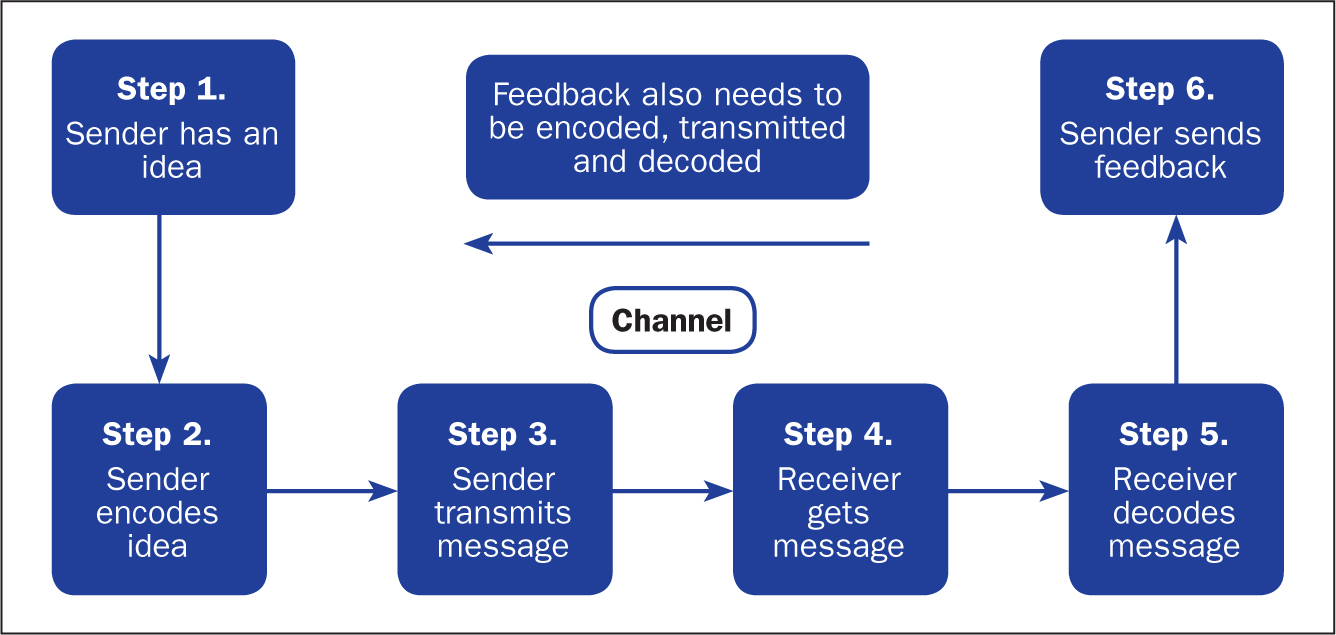
The process is more than just exchanging information. It is about the components/elements of the communication process, ie understanding the emotion and intentions behind the information—the tone of voice, as well as the actual words spoken, hearing, listening, perception, honesty, and ensuring that the messages relayed are correctly interpreted and understood ( Bramhall, 2014 ; Barber, 2016 ; Evans, 2017 ; Doyle, 2019 ). It is about considering emotions, such as shock, anger, fear, anxiety and distress ( Bumb et al, 2017 ; Evans, 2017 ). Language and conceptual barriers may also negatively impact on the efficacy of the communication being relayed.
Challenges of effective communication
The following sections explain the challenges involved in communication—namely, conveying a cancer diagnosis or related bad news.
Tone of voice and words spoken
According to Barber (2016) , when interacting with patients, especially communicating ‘bad news’ to them, both the tone of voice and the actual words spoken are important. The evidence has shown that an empathetic and sensitive tone is conducive to providing appropriate reassurance and in aiding understanding ( McClain, 2012 ; Evans, 2017 ; Hemming, 2017 ). However, an apathetic and insensitive tone will likely evoke fear, anxiety and distress ( Pincock, 2004 ; Ali, 2017 ; Doyle, 2019 ). In terms of the words used, the use of jargon, or highly technical language and words that imply sarcasm and disrespect, can negatively impact on feelings and self-confidence ( Doyle, 2019 ).
Hearing what is being conveyed is an important aspect of effective communication. When interacting with patients it is vital to consider potential barriers such as language (ie, is the subject highly technical or is English not the patient's first language) and emotions (ie shock, anger, fear, anxiety, distress) ( Bumb et al, 2017 ; Evans, 2017 ). A patient may fail to hear crucial information because he or she is distressed during an interaction, or may be unable to fully understand the information being relayed ( Bumb et al, 2017 ). Good communication involves ascertaining what has been heard and understood by the patient, allowing them to express their feelings and concerns, and ensuring these are validated ( Evans, 2017 ).
Listening to the patient
Listening is a deliberate act that requires a conscious commitment from the listener ( Shipley, 2010 ). The key attributes of listening include empathy, silence, attention to both verbal and non-verbal communication, and the ability to be non-judgemental and accepting ( Shipley, 2010 ). Listening is an essential component of effective communication and a crucial element of nursing care ( Shipley, 2010 ; Evans, 2017 ; Doyle, 2019 ). In health care, an inability to fully listen to and appreciate what the patient is saying could result in them feeling that their concerns are not being taken seriously. As observed by the author in practice, effective listening is essential to understanding the patient's concerns.
Perception, interpretation, understanding
Relevant and well-prepared information is key to the patient's perception and interpretation of the messages relayed ( McClain, 2012 ). It is vital to aiding their understanding and to informing their personal choices and decisions. If a patient were to misinterpret the information received, this could likely result in a misunderstanding of the messages being relayed and, consequently, lead to an inability to make clear, informed decisions about their life choices ( McClain, 2012 ; Bramhall, 2014 ).
Fully informing the patient and treating them with honesty, respect and dignity
In making decisions about their life/care, a patient is entitled to all information relevant to their individual situation and needs (including those about the actual and potential risks of treatment and their likely disease trajectory) ( McClain, 2012 ). Information equals empowerment—making a decision based on full information about a prognosis, for example, gives people choices and enables them to put their affairs in order ( Evans, 2017 ). Being honest with a patient not only shows respect for them, their feelings and concerns, it also contributes to preserving the individual's dignity ( Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). However, as observed in practice, a reluctance on the health professional's part to be totally open and honest with a patient can result in confusion and unnecessary emotional distress.
When reflecting on the efficacy of the communication being relayed, it is important for health professionals to acknowledge the challenges and consider how they may actually or potentially impact on the messages being relayed ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Communication and the uro-oncology clinical nurse specialist
It is devastating for a patient to receive the news that they have cancer ( Bumb et al, 2017 ). Providing a patient with a cancer diagnosis—the ‘breaking of bad news’, defined as any information that adversely and seriously affects an individual's view of his or her future ( Schildmann et al 2005 )—is equally devastating for the professional ( Bumb et al, 2017 ; Hemming, 2017 ). It is thus imperative to ensure the appropriate support is forthcoming following receipt of bad news ( Evans, 2017 ).
Integral to the delivery of bad news is the cancer CNS, in this context, the UCNS, who is acknowledged to be in the ideal position to observe the delivery of bad news (usually by a senior doctor in the urology clinic), and its receipt by patients ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ), and to offer appropriate support afterwards ( Evans, 2017 ). Support includes allocating appropriate time with the patient, and their family, after the clinic appointment to ensure they have understood the discussion regarding the diagnosis, prognosis and treatment options ( Evans, 2017 ; Hemming, 2017 ). In this instance, effective communication, as well as the time required, is usually tailored to each individual patient, allowing trust to be built ( Bumb et al, 2017 ; Evans, 2017 ; Hemming, 2017 ).
In the performance of her role, the UCNS is fully aware of the importance placed on delivering bad news well. She has seen first hand how bad news given in a less than optimal manner can impact on the patient's emotions and their subsequent ability to deal with the results. Hence, her role in ensuring that the appropriate support is forthcoming following the delivery of bad news is imperative. It is important to understand that the delivery of bad news is a delicate task—one that necessitates sensitivity and an appreciation of the subsequent impact of the news on the individual concerned. It should also be acknowledged that while the receipt of bad news is, understandably, difficult for the patient, its delivery is also extremely challenging for the health professional ( Bumb et al, 2017 ).
Communicating bad news
The primary functions of effective communication in this instance are to enhance the patient's experience and to motivate them to take control of their situation ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Telling a patient that they have a life-threatening illness such as cancer, or that their prognosis is poor and no further treatment is available to them, is a difficult and uncomfortable task for the health professional ( Bumb et al, 2017 ). It is a task that must be done well nonetheless ( Schildmann, 2005 ). Doing it well is reliant on a number of factors:
- Ensuring communicated information is sensitively delivered ( Hanratty et al 2012 ) to counter the ensuing shock following the patient's receipt of the bad news ( McClain, 2012 )
- Providing information that is clear, concise and tailored to meeting the individual's needs ( Hemming, 2017 )
- Acknowledging and respecting the patient's feelings, concerns and wishes ( Evans 2017 ).
This approach to care is important to empower patients to make the right choices and decisions regarding their life/care, and gives them the chance to ‘put their affairs in order’ ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ).
Choices and decision-making
Case studies 1 and 2 show the importance of honesty, respect, listening and affording dignity to patients by health professionals, in this case senior doctors and the UCNS. The issue of choice and decision-making is highlighted. It is important to note that, while emphasis is placed on patients receiving all the pertinent information regarding their individual diagnosis and needs ( McClain 2012 ), despite receipt of this information, a patient may still be unable to make a definite decision regarding their care. A patient may even elect not to have any proposed treatment, a decision that some health professionals find difficult to accept, but one that must be respected nevertheless ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ).
Case study 1. Giving a poor prognosis and accepting the patient's decision
Jane Green, aged 48, received a devastating cancer diagnosis, with an extremely poor prognosis. It was evident that the news was not what she expected. She had been convinced that she had irritable bowel syndrome and, hence, a cancer diagnosis was quite a shock. Nevertheless, she had, surprisingly, raised a smile with the witty retort: ‘Cancer, you bastard—how dare you get me.’ Mrs Green had been married to her second husband for 3 years. Sadly, her first husband, with whom she had two daughters, aged 17 and 21, had died from a heart attack at the age of 52. His sudden death was hugely upsetting for his daughters; consequently, Mrs Green's relationship with her girls (as she lovingly referred to them) was extremely close. The legacy of having two parents who had died young was not one Mrs Green wished to pass on to her daughters. Her main concern, therefore, was to minimise the inevitable distress that would ensue, following her own imminent death.
In the relatively short time that Mrs Green had to digest the enormity and implications of her diagnosis, she had been adamant that she did not wish to have any life-prolonging interventions, particularly if they could not guarantee a reasonable extension of her life, and whose effects would impact on the time she had left. This decision was driven by previously having observed her mother-in-law's experience of cancer: its management with chemotherapy and the resultant effect on her body and her eventual, painful demise. Mrs Green's memory of this experience was still vivid, and had heightened her fears and anxieties, and reinforced her wish not to undergo similar treatment.
Mrs Green requested a full and honest discussion and explanation from the consultant urologist and the UCNS regarding the diagnosis and its implications. This included the estimated prognosis, treatment interventions and the relevant risks and benefits—specifically, their likely impact on her quality of life. In providing Mrs Green with this information, the consultant and the UCNS had ensured information was clear and concise, empathetic and sensitive to her needs ( Shipley, 2010 ; Hanratty, et al, 2012 ; Evans, 2017 ; Hemming, 2017 ) and, importantly, that her request for honesty was respected. Not disclosing the entire truth can ‘inadvertently create a false sense of hope for a cure and perceptions of a longer life expectancy’ ( Bumb et al, 2017:574 ). Being honest had empowered Mrs Green to come to terms with both the diagnosis and prognosis, to consider the options as well as the risks and benefits. She had a choice between quantity of life and quality of life. Mrs Green elected for quality of life and, accordingly, made decisions that she felt were in her own, and her family's, best interests.
Despite receiving pertinent information and sound advice on why a patient should agree to treatment intervention, they may still elect not to have any treatment ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ). This decision, as observed by the UCNS in practice, is difficult for some health professionals to accept. In Mrs Green's case, accepting her decision not to have any treatment was extremely difficult for both the consultant and the UCNS. In an attempt to try to change Mrs Green's mind, the consultant asked the UCNS to speak to her. The UCNS was aware that the consultant's difficulty to accept the decision was compounded by Mrs Green's age (48) and a desire to give her more time. However, the UCNS had listened closely to Mrs Green's wishes and, in view of her disclosure regarding the experience of her mother-in-law's death, her first husband's untimely death, her fear of upsetting her daughters and her evident determination to keep control of her situation, the UCNS felt compelled to respect her decision.
Following the consultant's request, the UCNS spoke to Mrs Green but, on hearing what she had to say regarding her decision not to have more treatment, concluded that she had to respect Mrs Green's decision. She also clarified whether Mrs Green were willing to continue communication with her GP and ensured that the GP was fully updated regarding current events. Mrs Green had thanked the staff for all their support, but did not wish to continue follow-up with the service. The GP assured the UCNS that she would keep a close eye on Mrs Green and her family.
Case study 2. Giving an honest account of disease progression
The following case study explains how a reluctance by health professionals to be totally honest with a patient had inadvertently hampered the individual's ability to make informed decisions regarding his life choices.
Mr Brown, aged 87, had been previously diagnosed and treated for cancer. On his referral to the urology clinic, his disease had progressed to the metastatic stage, which had limited his management options to palliative care.
Since we have established that delivering bad news to a patient is a difficult task ( Bumb et al, 2017 ), it is not surprising that some health professionals fail to be totally honest with the patient for fear of upsetting them. During the consultation, it transpired that Mr Brown had other serious illnesses and was being managed by other clinicians. Seemingly, previous communications with these clinicians had left Mr Brown and his family unenlightened about his prognosis and his future prospects. In hindsight, the family would have appreciated total honesty sooner, since this would have allowed them to make realistic decisions.
After fully assessing Mr Brown's case (and in light of this disclosure) the doctor decided to be totally honest with Mr Brown and his family regarding his current situation and the choices available to him. Explanations were empathetic and sensitive to Mr Brown's and his family's feelings ( Hanratty et al, 2012 ; Evans, 2017 ). While the news was not entirely unexpected, Mr Brown and his family appreciated the consultant's candour. In this instance, the consultant had respected Mr Brown's entitlement to total honesty. By receiving all the facts, and the appropriate reassurance and support from the UCNS, Mr Brown could now consider his options and, with his family's support, proceed to put his affairs in order.
Management and treatment of cancer
The management and treatment of cancer is determined by several factors. These include: the grade and stage of the individual's disease—whether the disease is low-grade/low-risk, intermediate-grade/intermediate-risk, or high-grade/high-risk. For some low-grade/low-risk disease, the recommended treatment of choice is surgery alone. However, in certain cases, further review of the staging and histology might reveal features of cancer within the sample that are at a high-risk of local recurrence, necessitating additional treatment intervention, ie chemotherapy or radiotherapy, to minimise this threat.
Following the primary treatment intervention (ie surgery), for low-risk/low-grade disease, the risk of local recurrence is usually low, as is the need for additional treatment intervention (chemotherapy or radiotherapy). Nonetheless, local recurrence is still a possibility. A failure to make the patient aware of this possibility creates a lack of trust and a false sense of hope ( Bumb et al, 2017 ), and evokes unnecessary emotional distress for the patient, their families and carers ( McClain, 2012 ).
As previously explained, the term ‘fully informed’ relates to a patient's entitlement to all information relevant to their situation and needs (including those about the actual and potential risks) ( McClain 2012 ). Informed knowledge is power, thus honesty is imperative ( Evans, 2017 ). The following case studies highlight the consequence of failing to fully inform patients about risks and diagnosis.
Case study 3. Consequences of not being fully informed
Mr White, aged 36, had been diagnosed with a low-grade/low-risk cancer. After the initial diagnosis was explained, Mr White was explicitly told by the doctor that after surgery he would not require any additional treatment. However, a subsequent review of his staging and histology revealed features of cancer within the sample that were at a high risk of local recurrence. Therefore the decision was made to offer Mr White additional treatment with radiotherapy to reduce the risk of recurrence down the line. Understandably, this news and the ensuing emotional impact—fear, anxiety and distress—was significant for Mr White. The author contends that, to avoid inciting these emotions, Mr White should have been fully informed, at the initial diagnosis, of the potential risks that further treatment might be necessary, no matter how unlikely these risks were perceived to be. Having observed the emotional impact on Mr White, and other similar cases in local practice, the author proposed that, when delivering a cancer diagnosis, consideration must be given not only to the physical, but also the emotional/psychological impact of the diagnosis on the individuals concerned and all risks, even those deemed small, discussed.
The following case study illustrates how a lack of honesty can lead to misinterpretation and misunderstanding of the messages relayed ( McClain, 2012 ; Bramhall, 2014 ) and, accordingly, raises questions regarding the patient's care.
Case study 4. Consequences of ‘sugar-coating’ a diagnosis
Mrs Black, aged 78, had been diagnosed with a low-grade/low-risk bladder cancer, for which the recommended treatment is a course of six doses of intravesical chemotherapy (mitomycin). In providing Mrs Black with the diagnosis, the doctor had failed to clarify that the term ‘bladder polyp/wort’ in fact meant cancer. It is evident to the UCNS that the doctor's intention was to reduce the impact of the news for Mrs Black. However, if a cancer diagnosis is not clearly explained at the outset ( Evans, 2017 ), then, as the UCNS's personal observations in practice have shown, the offer of subsequent cancer treatments will raise questions. In a follow-up meeting with the UCNS, Mrs Black queried why she was having a cancer treatment, when a cancer diagnosis had not been clearly given ( Bumb et al, 2017 ). In this instance, Mrs Black's query placed the UCNS in an uncomfortable position, but one in which she ultimately had to be honest in her response.
Despite the physician's good intentions, a lack of honesty or in this case ‘sugar-coating’ the truth was an infringement of Mrs Black's right to receive full and honest information regarding her diagnosis and treatments and impacted her ability to make clear decisions regarding her care ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ).
Scenario: communicating in teams
In the UCNS's experience, effective communication is crucial when communicating in teams. The UCNS's observations in practice evoked reflection on past experiences of poor communication and its ensuing impact on her feelings, including hurt and, to some extent, a degree of anger.
Seemingly, poor communication is ingrained in all areas of practice and is highly evident in teams ( Doyle, 2019 ). The ability to communicate effectively is essential to team cohesiveness. One of the chief requirement is to facilitate an environment in which individuals can grow and excel, thus good/effective communication is vital. As previously stated, the tone of voice and actual words spoken are important ( Bramhall, 2014 ; Evans, 2017 ; Doyle, 2019 ). A tone that is respectful and conducive to elevating the individual's self-esteem and morale, ultimately increases self-worth and confidence. Conversely, a patronising attitude—a tone of voice and words spoken that imply sarcasm and disrespect—can, and often does, result in hurt feelings and a significant loss of confidence ( Doyle, 2019 ). Some senior professionals clearly believe in a hierarchy of entitlement to respect in the way that individuals communicate with other team members. A patronising tone of voice and words that imply sarcasm and disrespect impact significantly on individual team members' morale, self-esteem, self-worth, confidence and professional standing. This can lead to disharmony within the clinical environment. This could be communication between a consultant and a junior doctor, or a junior doctor and senior nurse, for example.
As health professionals, admittedly, we could all attest to poor communication at some point in our careers. Nevertheless, we have a responsibility to work and communicate effectively with other team members ( Ali, 2017 ; Doyle, 2019 ). The objective here is in facilitating a happy and functional team, one that demonstrates professionalism and competency in providing the care necessary to improving patients' experiences and outcomes ( Ali, 2017 ; Doyle, 2019 ). Securing improvements necessitates the health professional reflecting on their communication skills, acknowledging their limitations and initiating steps to address these ( Barber, 2016 ).
These case studies and scenario provide an insight into the UCNS's observations and reflections on her area of clinical practice and highlight the importance of effective communication. Acknowledgement of the inherent challenges within the communication process are clearly explained, with consideration given to the actual and potential impact in terms of patient, health professionals and clinical practice outcomes ( Oelofsen, 2012 ; RCN, 2019 ).
Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life, but seemingly few people, including health professionals, have mastered the skill of truly effective communication. There are evident pitfalls that could lead to patient care being compromised as a result of poor communication between health professionals. The UCNS's role in delivering bad news and supporting patients involves ensuring that patients are adequately informed to enable them to take control of their individual situation and, accordingly, that they are able to make the appropriate choices and decisions for their respective needs. Poor communication within teams can affect patient care and staff morale, and learning how to communicate more effectively is beneficial in terms of improving staff interactions with each other. Essentially, communicating effectively is everyone's responsibility; hence, all health professionals should look at the way they interact and communicate with each other and take the necessary steps to improve this extremely important activity.
- The cancer clinical nurse specialist (CNS) role is pivotal when patients receive bad news. It is crucial not only to the individual's understanding of the diagnosis, prognosis and treatment options, but also to the provision of appropriate support following the bad news and countering the ensuing impact of the news on the patient
- Reflection is a powerful tool, one that enables nurses to examine their practice, identifying salient issues and initiate change/improvements
- Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life—few people (in this context health professionals) have mastered the skill of truly effective communication
- Poor communication has implications for the patient, health professional and the health organisation
CPD reflective questions
- Reflection on practice is a key skill for nurses that enables them to identify salient issues and initiate actions to address these. How well do you think you reflect in practice, and does this provide the insight you seek?
- Effective communication is an important interpersonal skill. How well do you communicate with patients and colleagues in your area of practice? Reflect on any situations that you find difficult
- The issue of poor communication within teams and its impact on team members has been highlighted in this article. Have you observed poor communication within your team or within your area of practice? If so, how could this be improved?
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About The British Journal of Social Work
- About the British Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
- < Previous
Reflective Practice (Key Themes in Health and Social Care)
- Article contents
- Figures & tables
- Supplementary Data
David Wilkins, Reflective Practice (Key Themes in Health and Social Care), The British Journal of Social Work , Volume 44, Issue 3, April 2014, Pages 787–788, https://doi.org/10.1093/bjsw/bcu026
- Permissions Icon Permissions
Reflective practice, as noted by the authors of this book, is generally accepted as being a ‘good thing’, certainly in social work, but also in other areas of health and social care more generally as well. However, somewhat refreshingly for a book on the topic, the authors also make a case for the relative paucity of evidence we have as to why reflective practice is a good thing and how reflective practice might make a difference, either in terms of the professional engaging in reflective practice or, more importantly, in terms of outcome for the ‘service user’. One potential problem with this contention is that, via Google Scholar, it is relatively easy to find over half a million results for the search phrase ‘reflective practice social work’, which suggests that it is hardly a topic that has gone unnoticed.
Nevertheless, it does appear to be the case that much of this work, if not all, is written with the starting premise that reflective practice is a good thing rather than examining whether it is, why and how. Understandably, the authors of this book do tentatively conclude that, despite the absence of a strong evidence base either way, reflective practice is a skill-set worth developing for social workers and they also highlight the necessity of reflective practice being demonstrated ‘through doing’ rather than perhaps being seen as a mindset or ‘only’ as a way of thinking to be used in particular settings or contexts, such as supervision.
Email alerts
Citing articles via.
- X (formerly Twitter)
- Recommend to your Library
Affiliations
- Online ISSN 1468-263X
- Print ISSN 0045-3102
- Copyright © 2024 British Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Reflective Practice in Social Care and Social Work
Reflective practice is when you critically explore and evaluate your experiences, so that you may make positive changes to your approach. During reflection, you will record your behaviour and thought process as well as any related emotions; doing so will allow you to consider and alter your approach where necessary for future situations.
Exploring your experiences in an objective and comprehensive manner, and identifying both your strengths and areas for change is vital to improving your performance.
Reflective practice is applied successfully across many areas of care, including the following:
- Social care
- Social work
- Counselling
- Support Work
- Child support services
Table of Contents
Why Reflective Practice is so Important in Social Care and Social Work
Ever since its development in the 1980s, reflective practice has increasingly been considered critical for the development of health workers. The rise of professional health and social care standards has required those working with the vulnerable to show advanced understanding and continued self-development to justify their credentials: this involves ongoing displays of reflective practice.
In this way, reflective practice becomes the backbone of your CPD (Continuing Professional Development). CPD is employed in many industries, including social work, as the determined commitment of an individual to self-improvement across their careers. In fields such as social care and social work, nothing less is expected.
How to Perform Reflective Practice in Social Care and Social Work
Gibbs reflective cycle provides a popular framework for effective reflective practice:
Description
Detail the event you are reflecting on as much as possible: Where you were, who you were with, what you were doing and why, what others were doing; context of the event as a whole, and what transpired.
Recall your thoughts throughout the event; namely why the event sticks in your mind. How were you feeling at the offset, and how did your feelings progress? How did you feel about what you were thinking? How did other people and the outcome of the event make you feel? Now you’ve had time to reflect, how do you feel about it now?
Decide which things about the experience were good or bad; what was an improvement and what didn’t go so well.
Go into more detail by breaking the event down into component areas and focussing on these. This is more in-depth than the Evaluation stage; Include not just what went well, but consider what you did well and didn’t, along with how others did
Using your analysis, you will develop insight into the behaviour of yourself and the others involved, and how this contributed to the outcome of the event, remembering that this all for your growth and betterment. Ask yourself bluntly what you could have done differently.
Action Plan
Consider the circumstances of the event happening again: what would you do this time? What would do differently, and what would stay the same? What actions or preparations can be made to improve for when this situation comes again? This is the end of the cycle; and the basis of the next cycle also begins here.
Example of Reflective Practice in Social Care and Social Work
In a social care role, reflective practice could be applied to any of your interactions with your patients. For example, if you are offering encouragement or hopeful optimism to a client in a very difficult situation, but are then met unexpectedly with a negative or even aggressive response; there is much to learn from the situation, your actions and the actions of the client.
In this example, you may come to the conclusion that your positive remarks had been superficial and appeared patronising. You may have not completely understood the amount of pressure placed upon the client. Your instant reaction may have been to attribute your client’s behaviour to their personality. You should realise that distress in the client’s situation is normal, and to acknowledge that with the client. Showing that you are capable of coping with the clients distress will provide a better result for the clients and the case.
In a social work role, reflective practice could be applied to any interaction with another person you encounter in your role, such as dealing with a colleague. A difficult situation that required careful behaviour and responses from yourself may not have had the best outcome; due in part to the actions of a co-worker.
It is important when finding yourself feeling frustrated, angry or anxious at work to recognise the emotion, and to understand by objectively analysing why it is that you feel like this. If a difficult situation or experience has caused you to become defensive or argumentative, consider an application of Reflective Practice to improve your responses in the future.

DSDWEB: FREE STUDY GUIDES FOR CARE QUALIFICATIONS
Answers for the Care Certificate and Levels 2, 3, 4 & 5 Diploma/NVQ
Learn, Do Not Copy! ALL DSDWEB RESOURCES ARE FREE. Please do pay for anything purporting to be from DSDWEB.
Write a reflective account detailing an example of how you have, or could have, used a person centred approach in a sensitive or complex situation.
The account must contain a description of how person centred values were or could be put into practice in the situation.
I was supporting a young adult with a learning disability in his home. His girlfriend was visiting and they were watching a movie in his lounge and had been asked to be left alone together, so I respected their wishes and went to bring the laundry in from outside. The client’s lounge is joined to the conservatory via a pair of french doors and many windows and when I came back inside, I saw that he and his girlfriend were both topless and kissing in his lounge.
This was a sensitive situation because although I respected my client and his girlfriend had the right to intimacy, there was a problem with privacy because the conservatory was a thoroughfare for both staff and my client’s housemate as well as his housemate’s friends. The windows also meant that they could potentially be viewed by neighbours. This could lead to future embarrassment, complaints by neighbours or even a complaint to the police, which would all heighten the anxiety of both individuals. It was also the first time that they had displayed sexual intimacy towards each other so it came as a surprise.
I went around to the other door (that didn’t have windows), knocked and apologised for disturbing them but explained that I needed to come in and talk to them before they went any further and to put their tops back on. When they were dressed I entered the room and explained my concerns. My client was upset at first because he thought he’d done something wrong but I told him that it was not my place to stop consenting adults from being intimate (and then I checked that they were both consensual) but it was my job to ensure that they were protected from the potential implications of them having sex where others could see them. I then suggested that they go up to his bedroom and reminded them that he had condoms in his bedside drawer and that he should use one. They went upstairs to continue in private.
In this situation, I took into account my client’s right to privacy, despite me having to disturb him to ensure he had privacy from others. I respected my client and his girlfriend’s right to choose to have sexual intercourse (knowing that they both had capacity to make the decision) and tried to behave with dignity and respect in a sensitive situation.
Leave a comment Cancel reply
You must be logged in to post a comment.
- Food & Water
- Education & Work
- Where We Work
- Women's Economic Justice
- Case Studies
- Reports & Resources
- Reports & Resources Archive
- How to Help
- Organize Locally
- Attend an Event
- Ways to Give
News & Stories
- Latest Stories
- Crisis Response
- Education & Work
- Food & Nutrition
- Thought Leadership
- Media & Press
- Press Releases
- Media Coverage
- Press Resources
- Mission & Vision
- Global Advisory Council
- Strategic Partners
- Our History
- Equity and Inclusion
- News & Stories
The most essential back to school supply in Mozambique? Water.

Since the local school only offers up to seventh grade, some children must repeat grades to continue their education. All photos: Sarah Easter/CARE
By Sarah Easter October 29, 2024
Classrooms are full in northern Mozambique. In Cabo Delgado, there are 100 students in one small room, four children to a bench. Half of the school’s 1,072 students attend in the morning, the other half in the afternoon.
“It is not easy, but at least they have a school to go to,” one of the teachers reflected.
There are classes up to the seventh grade here, and the student ages range. Some children repeat grades because there is no higher-level school, while other students have been out of school for several years. The ongoing conflict in Cabo Delgado has forced hundreds of thousands of people from their homes, leaving many families in a desperate search for food, shelter, and safety.
Yet, regardless of their background or age, these students come together to sing, learn, and study.

High hopes in a land of scarcity
Farsana is 15 and in the seventh grade. She is not sure if she will be able to continue her education after finishing this grade, as the nearest school offering higher levels is too far away, and her family cannot afford to send her. But Farsana has high hopes.
“I want to be a doctor to help other people,” she says. Her 18-year-old brother is in the same class, because he can’t attend a higher-level school. Farsana and her brother’s school time is in the afternoon, from 12:30 to 5:30. In the morning, they help their parents in the fields.
“I cut grass, so my parents can plant the seeds, and I help with harvesting,” she says.

“We do not have any running water. We collect rainwater during the rainy season, but it is not enough for all the children for the whole year. On a hot day, we would need at least 250 gallons of water each day for drinking, hand washing, and the latrines,” says the school’s director.
For Farsana, the lack of water is a big problem.
“It is not easy. Some weeks we have no water at all. We cannot wash our hands. We have no water to drink. We then have to go and find water somewhere in the village. It is so difficult to concentrate when I don’t have any water to drink,” she says.

Water as school supply
“If the water tank is empty, we have to ask the children to bring water to school. We have a system in place, where the classes are on weekly water duty in shifts so that everyone contributes,” says the director.
When Farsana’s class is on water duty, she uses her mother’s bucket to carry five gallons of water to the school’s water tank.
“Sometimes I find a waterhole that has enough water. Sometimes I go to the river and sometimes we have to buy it,” she says.

Addressing menstrual and other hygiene needs in schools
The school’s latrines also lack access to water, which makes hygiene a big challenge for the school and the students.
“Especially for the girls on their period, not having access to water is a problem,” says the director. There is not enough water in the school to wash the cloths they use for menstrual hygiene.
“I use a plastic bag and take it home to wash it there,” explains Farsana. Buying soap to wash the cloth is another challenge for her.
Farsana is part of a girls group at school that learns about menstrual hygiene from a CARE volunteer. She has also received a menstrual hygiene kit, which includes underwear, three washable cloths pads, and a cycle tracker.

“Before I used the traditional way, where we tie parts of our capulanas around our legs. But that was not clean or safe and you could not sit comfortably like that. Now it is a lot easier for me,” Farsana says.
Capulanas are the traditional cloth Mozambiquan woman and girls use as skirts. It is a length of material about 2 metres by 1 metre. It can either be used as a wrap-around skirt, dress or can become a baby carrier on the back. It is considered a complete piece of clothing.

What CARE is doing
Together with Farsana’s school and financial support from the Austrian Development Agency, CARE is evaluating the area to find ideal spots to build a waterhole for the school. Additionally, CARE plans to rehabilitate the water tank to increase its capacity from 1,300 gallons to 3,000 gallons and improve the rainwater collection system.
CARE plans to rebuild the latrines, making them bigger with water access and a waste management system.
“I am looking forward to when CARE finishes the waterhole,” Farsana says, “because that will make our lives a lot easier. Water is important, not just for drinking but also for hygiene and to stay healthy.
- Girls' Education
- Menstrual Hygiene
Related Stories
By CARE Staff · October 30, 2024
Northern Syria is grappling with rising malnutrition and inadequate healthcare. The humanitarian response is critically underfunded, yet CARE and its partners remain committed to assisting those in need. Read More
Syria: “When we get sick, we just suffer through it”
Media & press.
October 18, 2024
The hunger we are seeing across Gaza is shocking and unconscionable and in every respect it’s getting worse. Whether or not the existence of famine can be determined doesn’t matter – widespread death, child wasting, malnutrition, illness, and severe trauma – all immense and preventable forms of suffering that have been happening for the past year. Read More
CARE statement on IPC report on hunger in Gaza
October 17, 2024
Thirteen days since the Israeli military issued mass forced displacement orders to various parts of northern Gaza, CARE’s partner Palestinian NGO Juzoor for Health and Social Development, has sadly lost two of their staff members just the past week, Dr. Ahmad Al-Najar, while he was performing his duties at a medical point in Al-Falouja, Jabalia on October 15, and midwife Ms. Laila Jneid, who was killed along with her parents on October 12. Read More
Israeli siege of northern Gaza: Hundreds of thousands endure catastrophic conditions

COMMENTS
What is reflective practice? Reflective practice is a strategy or approach with a rich history across several disciplines. Predominantly starting in education and philosophy, the approach evolved and gained attention in healthcare in the late 20 th century to improve patient care and promote continuous professional development.. Over time it slowly began to be adopted in social care to help ...
Background Reflective writing provides an opportunity for health professionals and students to learn from their mistakes, successes, anxieties, and worries that otherwise would remain disjointed and worthless. This systematic review addresses the following question: "What are the experiences of health professionals and students in applying reflective writing during their education and ...
Learn what a reflective account is, why it is important for health and social care professionals, and how to write one. Explore different types of reflective accounts, models, and examples based on real scenarios.
This reflective essay was co-written by two social workers at very different points in their career paths. At the time of writing, [Rebecca] was newly qualified and embarking on her first role in palliative care. ... of palliative care social work that should be embraced and communicated to level the playing field with other health care ...
Learn how to use Gibbs' Reflective Cycle, a model for reflective learning, to improve your skills and patient care in health and social care. The cycle has six stages: Description, Feelings, Evaluation, Analysis, Conclusion, and Action Plan.
degree in social care and at least three years work experience in social care. These criteria were used to ensure that participants had the opportunity to learn about self- awareness and reflection and to practise it in the workplace. The participants were selected from students studying a Masters in Advanced Social Care Practice.
A student nurse shares an incident where she observed a doctor not washing her hands before examining a patient. She reflects on her feelings, evaluation, analysis and action plan to improve her practice and patient safety.
Critically reflect on an encounter with a service user in a health care setting. This essay aims to critically reflect on an encounter with a service user in a health care setting. The Gibbs' Reflective Cycle will be used as this is a popular model of reflection. Reflection is associated with learning from experience.
Faculty Of Public Health Tips On Writing Effective Reflective Notes Faculty of Public Health - September 2012. Email: [email protected] Page 4 Figure 1 shows that the reflective thinking process starts with you. Before you can begin to assess the words and ideas of others, you need to pause and identify and examine your own 'baseline' position.
Including an up-to-date overview of the framework written by Jan Fook, this helpful text makes a significant contribution in terms of the practical theorizing of critical reflection. It will be of use to health and social care professionals keen to practice creatively and effectively, especially those undertaking short courses or further ...
Introduction Primary care is said to be the "first point of contact" for people when accessing the health care system in Ireland (Department of health and children 2001). The World health organisation(1978) outline that one of the main roles of primary health care is to provide access to care for the most vulnerable but also to identify and ...
Reflection is a process of thinking analytically about your professional practice and learning from it. It can help you maintain good practice, improve your service and your wellbeing. Learn more about reflection, what it is not, and how to do it effectively.
Reflective practice, by its nature, is a process of sense making leading to action. Elsewhere, I have proposed a model of effective reflection and how this could be implemented on an individual or small group basis for professionals at all levels of seniority across the health and social care field.
Learn how to use reflective practice to improve your health and care work and meet your standards. Find out about different types of reflection, examples of case studies and a template to guide your own activities.
These case studies will help you to reflect on your practice, and provide a summary of reflective models that can help aid your reflections and make them more effective. Templates are also provided to guide your own activities. Remember, there is no set way to reflect and you can adapt these activities to suit your learning style and your role.
Reflection is a highly beneficial tool (Oelofsen, 2012), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes (Bramhall, 2014).
Reflective Practice (Key Themes in Health and Social Care), Janet Hargreaves and Louise Page, Cambridge, Polity Press, 2013, pp. xi + 192, ISBN-10: 074565424X, £14.23 (pb), £12.81 ... Reflective Practice (Key Themes in Health and Social Care), The British Journal of Social Work, Volume 44, Issue 3, April 2014, Pages 787-788, ...
The social care sector is an area that has been recently professionalised and its origins were primarily focused on residential care for young people and those with disabilities. The Health and Social Care Professionals Act 2005 established a registration board for social care work and other healthcare professions (Share and Lalor, 2009).
In a social care role, reflective practice could be applied to any of your interactions with your patients. For example, if you are offering encouragement or hopeful optimism to a client in a very difficult situation, but are then met unexpectedly with a negative or even aggressive response; there is much to learn from the situation, your ...
A care worker shares how they used a person centred approach in a sensitive situation with a client and his girlfriend. They respected their privacy, intimacy and dignity, but also ensured their safety and well-being.
Thirteen days since the Israeli military issued mass forced displacement orders to various parts of northern Gaza, CARE's partner Palestinian NGO Juzoor for Health and Social Development, has sadly lost two of their staff members just the past week, Dr. Ahmad Al-Najar, while he was performing his duties at a medical point in Al-Falouja ...