Career mentorship, clinical and technology skills
- See us on facebook
- See us on youtube
- See us on instagram

APPLICATION GUIDE Clinical Science, Technology and Medicine Summer Internship
Applications Now Open
Applications open for the 2020 Clinical Science, Technology and Medicine Summer Internship program. Program application deadline is February 14, 2020.
How to write "the change you want to see in health care" essay

By SeventyFourImages via EnvatoElements
By Urvi Gupta
There are many ways of approaching an essay such as this one. Here are some methods that we find useful, and we hope they will be helpful to you as well.
The most powerful essays are those which could not be written by anyone other than yourself. Keep this in mind as you begin your brainstorm. Finding stories which are personal and teach the reader something about you is crucial.
Pull out some pen and paper. Set a 5-minute timer on your phone. Use this time to jot down every thought that comes into mind about the ways you wish our health care system was better. Try to keep your pen to the paper and keep writing throughout the 5 minutes.
Look over your list. Which ones stick out to you as the most compelling? Through your interactions with healthcare, have any of the challenges you brainstormed impacted you personally? Have you had any experiences where you worked towards any of these goals? Use these questions to pick 1-3 topics from your list.
Begin outlining your essay. For each of your topics, try to include answers to the following questions:
Briefly describe the topic/issue.
Why is this topic important to you specifically? How has it affected you/the people around you/the world? Give concrete examples.
How do you propose you can make it better? Again, be specific and try to draw inspiration from your own life.
Begin writing!
Read your draft out loud to yourself or a friend/family member to look for areas that are unclear or that could be improved.
Remember that it is less important as to what you pick for the change you want to see in health care and more important that you have something compelling and personal to say about it. We want to learn about you!
The views expressed here are the authors and they do not necessarily reflect the views and opinions of Stanford University School of Medicine. External websites are shared as a courtesy. They are not endorsed by the Stanford University School of Medicine.
The most powerful essays are those which could not be written by anyone other than yourself.
Urvi Gupta, BS SASI Teaching Assistant
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.

- Customer Reviews
- Extended Essays
- IB Internal Assessment
- Theory of Knowledge
- Literature Review
- Dissertations
- Essay Writing
- Research Writing
- Assignment Help
- Capstone Projects
- College Application
- Online Class
30+ Medical Argumentative Essay Topics for College Students
by Antony W
April 21, 2023

Medical argumentative essay topics give you some brilliant ideas that you can explore and defend depending on the research you’ve conducted.
As with any argumentative essay topic , a medical related essay also requires you to take a stance and use objective, verifiable, and reasonable evidence to defend your position.
However, the kinds of topics many students pick to explore in the medical field are often quite too common.
Think of type II diabetes, cardiovascular illness, breast cancer, and cirrhosis. These are topics you don’t want to cover for the simple reason that they are too common.
In this post, we give you a list of 30+ medical argumentative essay topics that aren’t too obvious.
These topic ideas should enable you to add a new spin to your work, so that you can write a medical essay that focuses on an issue that will capture the attention of your audience (reader) almost instantly.
30+ Medical Argumentative Essay Topics
Below is a list of 30+ essay topics that you may find interesting for your medical argumentative essay assignment :
Controversial Medical Argumentative Essay Topics
- The cost of healthcare in the United States of America is not justifiable
- Do homeless people deserve free healthcare simply because they don’t have money to pay medical bills?
- Unconventional medication should not be part of a state’s healthcare system
- There’s a strong link between poor health and poverty
- People should not turn to homeopathy because it isn’t more effective compared to seeking medical advice
- People with no health insurance cover deserve to get equal treatment at medical healthcare facilities
- Should the government take action against unexpected errors in medical settings?
- Doctors should not have the right to endorse medical products until verified for safety and effectiveness
- Healthcare institutions should provide opt-out and opt-in donor system
- There’s no true justification for the rising cost of healthcare in the United States of America
In theory, areas such as genetic engineering, diagnostics, and medical research can be interesting to explore within the medical field.
However, the assignment requires hours of intensive research, proper structuring, writing, and editing.
If you don’t have the time for all that, you can get argumentative assignment help from one of our team of writers.
Health Practices Argumentative Essay Topics
- The marijuana drug should be made legal worldwide
- TV shows on diet and weight loss don’t motivate people to improve their body image and self-esteem
- Is the state responsible for teaching people how to lead a healthy lifestyle?
- Communication authorities should impose an indefinite ban on TV shows that promote cosmetic surgery
- TV commercials that promote fast foods and alcohol should not be banned.
- It’s a waste of time to impose state regulation on fast food chains and alcohol sales as it undermines people’s freewill to food choices.
- Should we allow and encourage teenagers to use birth control pills?
- The state should not encourage the use of products manufactured at the cost of another person’s well-being.
- Exercise alone can’t improve your health
- Doctors should not ask for medical consent if they know they can save a patient from a particular illness
Medical Laws and Policies Argumentative Essay Topics
- Should the government declare euthanasia illegal?
- Doctors should not insist on providing medical treatment to minors if their parents are against such treatments.
- The vaccination of children against illnesses should be voluntary
- An organ transplantation committee should not consider an individual’s accomplishment to determine if they can receive an organ
- Patients should decide if they would like to use surrogate pregnancy for health reasons or on demand
- Is doctor-patient confidentially necessary anymore?
- There’s no concrete evidence that living a sedentary and lavish lifestyle is the number one cause of weight gain
- Should we support the legalization of abortion?
- Should patients with mental health conditions receive treatment in or outside of their community?
- People should not accept organ transplantation because of leading an unhealthy life
You may click here to place your order , and one of our writers who has experience in writing medical related essays will help you get the paper completed on time. Since we focus on custom writing, you don’t have to worry about plagiarism at all.
Argumentative Essay Topics on Medical Research
- Genetic engineering is humanly unethical and morally wrong and should therefore not be allowed
- Are there effective means to mitigate threats posed by medical research?
- There is no reasonable evidence that the Covid-19 global pandemic originated from a lab I Wuhan, China
- Medics should not use animals to test the effective of drugs on humans
- Computers used in medical research and diagnostic cannot replace doctors no matter how sophisticated they become.
- Should human beings be subject to mandatory medical testing without their consent?
- Should the federal government and health organizations, such as the UN and CDC, finance practical medical research?
- Do we need to have limits when subjecting human beings to absolutely necessary medical tests?
- The Corona virus is a biochemical weapon built in the lab to wipe out the human race
- There’s no sufficient evidence to prove that pills that delay aging can make the human race immortal
Medical Argumentative Essay Topics on Healthcare Management
- Is healthcare management doing enough to maintain the right standards in healthcare facilities?
- Are privately owned hospitals managed better than public hospitals?
- Registered nurses should not assume the role of a physician even in the event of a serious medical emergency
- Human Resource Management (HR) isn’t doing enough to improve and protect the quality of healthcare
- Do surgeons play an important role outside their medical capacities?
- Are healthcare institutions responsible for the protection of the environment?
- The relationship between and among medical staff can affect the quality of patients of different illnesses.
- There’s no relationship between a patient’s medical results and a hospital’s revenue.
- It’s easy to improve the relationship among staff members in a healthcare facility
- Should medical management allow and encourage intimate relationships among the staff members?
General Medical Argumentative Essay Topics
- Has the American government invested enough funds to improve healthcare service for its residents?
- There should be as many male nurses as there are female nurses
- Are data management systems in hospitals accurate and safe against breach?
- Do prisoners have the right to access quality healthcare?
- Electronic health record systems have more limitations than benefits.
related resources
- Argumentative Essay Topics on Racism
- Argumentative Essay Topics About Animals
- Music Argumentative Essay Topics
- Social Media Argumentative Essay Topics
- Technology Argumentative Essay Topics
About the author
Antony W is a professional writer and coach at Help for Assessment. He spends countless hours every day researching and writing great content filled with expert advice on how to write engaging essays, research papers, and assignments.
610 Healthcare Essay Topics & Research Questions to Write About
Are you looking for interesting healthcare essay topics? StudyCorgi has prepared an extensive list of health care topics to write about! Here, you’ll find title ideas for various healthcare fields, including healthcare management, ethics, administration, leadership, policy, finance, care quality, and issues faced by healthcare workers. Our topics are suitable for both high school students and college students. Check them out!
🏆 Best Health Care Topics to Write About
✍️ healthcare essay topics for college, 👍 good healthcare research topics & essay examples, 🌶️ hot medical essay topics to discuss, 🎓 most interesting health care essay examples, 💡 simple healthcare paper topics, 📌 easy healthcare essay topics, 👨⚕️ health titles for essays, 🏥 research topics about healthcare, 🚑 healthcare thesis topics, ❓ research questions about healthcare.
- Free Healthcare: Advantages and Disadvantages
- Application of Statistics in Healthcare
- Motivational Theories in Healthcare
- Artificial Intelligence in Healthcare
- Healthcare Information Systems: Components, Benefits
- The Importance of Healthcare Management
- Paired and Independent T-Test in Healthcare Scenario
- The Effects of the Lack of Teamwork in Healthcare This paper discusses the importance of interprofessional collaboration in healthcare and how a lack of teamwork negatively impacts patient outcomes.
- Hospital Revenue Sources and Models in Healthcare Industry Like any other business, healthcare organizations have to perform effective revenue management in order to maintain stable financial status and avoid critical losses.
- The US and New Zealand: Healthcare Profiles Comparison This essay compares the healthcare profiles of the United States and New Zealand and discusses how the latter may have paved the way for the former’s much-needed improvement.
- Statistics Application in Healthcare and Nursing Statistical analyses are efficient mechanisms for obtaining accurate data based on calculations and affecting not only the quality of care.
- Effects of Poor Communication in Healthcare Reviewing various categories of interactions within the healthcare system will enable an in-depth understanding of the effects of poor communication.
- Organization Theory Improving Healthcare Operations Organizational theories explain the relationships between the business and its environment and how it affects its operation mode.
- Supply and Demand of Healthcare and Automobiles This paper’s purpose is to examine the differences and peculiarities of the health care market, as well as analyze current trends in this field.
- Quality Management in Healthcare Quality management in healthcare is essential to ensure patient safety. It is helpful by providing the opportunity to evaluate quality in healthcare organizations.
- The Value of PowerPoint Presentations for Healthcare Management In the fast-evolving spheres like healthcare, technologies play a crucial role in the achievement of health-promotional, educational, strategic, and developmental goals.
- The Healthcare Manager’s Role in Information Technology Management This article focuses on the role that a healthcare manager plays in ensuring the efficient execution of medical operations through the use of new technologies.
- The U.S Healthcare System and the Roemer Model Roemer’s model of a healthcare system demonstrates how a socialist healthcare system operates. This paper explores the entire U.S healthcare system in relation to Roemer’s model.
- Pros and Cons of the Gatekeeper Healthcare System The article describes the levels of the healthcare system, its advantages and disadvantages, while the author believes that the advantages outweigh.
- Lack of Staffing and Training in Healthcare The essay discusses Lack of training affects the supply of trained nurses to health care organizations, thus, contributing to the nursing shortage in these organizations.
- Regression Analysis for Healthcare Organization The paper studies the regression analysis that enables managers to evaluate the patterns within the health care organization and make predictions for decision-making.
- Healthcare in Canada: Problems and Solutions The issue of the challenges that face Medicare in Canada is increasingly turning out to be a controversial subject; even as far as the politics of Canada are concerned.
- Risk Management in Healthcare Construction Projects A risk is any occurrence that has the potential to alter the progress of a project significantly. A risk may be positive or negative.
- Calgary Family Assessment Model in Healthcare Calgary Family Assessment Model is a tool utilized by health care specialists to evaluate the overall wellbeing of a family.
- Advantages of Computer Technology in Healthcare The emergence of computer technology within healthcare is the catalyst of changes that began to display the improvement of medical procedures and care quality.
- Role of Family in Healthcare and How Culture Affects Health Beliefs The paper will discuss how family shapes the role of care and attitudes towards health and how culture affects health beliefs and community health.
- Maternal Healthcare Overview Maternal health is a field that focuses on the well-being of women while pregnant, during childbirth, and throughout the postnatal period.
- Shared Decision-Making Principles in Healthcare The article argues that to provide effective care, healthcare workers need to understand the concepts of shared decision-making and follow the basic principles.
- Applying Ethical Principles in Healthcare Modern medical field requires new, high-quality ways of treating patients, considering the objective moral code.practice and help them in ethical decision-making process.
- Ethical Issues in Healthcare Essay: Ethical Dilemma This paper describes an ethical dilemma in healthcare, its specific characteristics, violated ethical principles, and existent barriers to ethical practice.
- Intercultural Communication in Business, Education, and Healthcare The rules of communication vary depending on different contexts; that’s why this paper aims to discuss intercultural communication in business, education, and healthcare.
- Expectancy Theory in the Healthcare Sector This paper explores the fundamentals of Expectancy Theory and applies it to the healthcare sector. Expectancy theory has found use in healthcare education contexts.
- Nursing Informatics Policy and Its Influence on Healthcare Delivery The development of nursing information structures is an essential factor in improving the delivery of health services. It includes the development of regulations.
- Healthcare Manager’s Conceptual, Technical, and Interpersonal Skills A healthcare manager is a person who facilitates, administrates, and influences the healthcare system as a manager is an indispensable part of the medical system.
- Creating App in Healthcare: Business Plan In order to create the most effective app in healthcare, it is necessary to monitor trends in this area and implement them.
- Healthcare Problems of Modern Society The public health system, as an organizational construct of a social institution, affects the formation and effective use of human capital.
- Artificial Intelligence in Healthcare: Pros & Cons Rapidly advancing artificial intelligence technologies are gradually changing health care practices and bring a paradigm shift to the medical system.
- Demand and Supply of Healthcare Workforce in Oman There has been continued indication of the shortages of physicians and nurses in hospitals across Oman and this is often seen in the media on regular basis.
- Healthcare Technological Trends and HRM Strategies Today our world is developing extremely quickly mainly due to the enormous technological development. This paper analyzes technological trends in the sphere of healthcare.
- Issues and Possible Solutions in the Healthcare Sector It is hard to disagree that healthcare is one of the most fundamental and intricate sectors playing a crucial role in people’s lives.
- Stages of Life and Influence of Age in Healthcare Age is a factor in the way patients interact with the healthcare system. This paper discusses the stages of life and the influence of age in healthcare from the patient’s perspective.
- Social Change: The Nurse’s Role in Global Healthcare To advocate for the global perspective on the issue of the opioid crisis and the need to change the current standards for opioid prescription.
- Healthcare Information System and Its Application In modern society, the healthcare information system plays a critical role in defining the quality of healthcare offered in healthcare centers.
- Healthcare Organizations’ Mission, Vision and Values This project identifies four health organizations coupled with reviewing their vision, mission, and values and proposes changes to the organizations’ missions, visions, and values.
- The Role of Cultural Relativism in Healthcare The Nacirema is a group of North Americans living in the territory between the “Canadian Cree, the Yaqui and Tarahumara of Mexico, and the Carib and Arawak of the Antilles”
- Virtual Reality in Healthcare and Education The beginnings of virtual reality can found throughout human history. This paper explores its emergence and development, and its influence in healthcare and education.
- Healthcare Problems in South Africa The state of health in South Africa differs from the most fundamental primary healthcare, provided for free by the government, to the highly professional and technologically advanced facilities.
- Patient-Centered Healthcare Coordination Plan The paper states that the goal of the eventual care coordination plan is to ensure that all the many aspects of healthcare are addressed.
- Comparing the American and Australian Healthcare Systems This paper will compare the American and Australian healthcare systems based on their costs, quality, and access and mention what the US can learn from the OCED member.
- Capstone Project Change Proposal in Healthcare Sector Nursing understaffing is caused primarily by the emotional exhaustion of medical workers due to the stressful workload in the sector.
- US and Canada Healthcare Systems Comparison Although Canada is similar to the U.S., its health care system cannot be copied as the two countries do not share the same social ethos and history.
- High Taxes’ Benefits for Education and Healthcare High taxes have more benefits than drawbacks for the citizens as the payments are allocated to develop essential systems, such as healthcare and education.
- Healthcare in the Russian Federation There are a number of key factors that lead to major Russian healthcare issues, such as chronic diseases, poor lifestyle habits, and lack of health promotion.
- Healthcare in the United Kingdom The purpose of this paper is to examine the healthcare in the United Kingdom, providing recent data and covering the main issues in this area.
- Change Management in Healthcare Changes in the healthcare field are always associated with difficulties since they affect the ways care is delivered, as well as medical professionals’ and clients’ experiences.
- HCA Healthcare Corporation’s Strategic Analysis HCA is a corporation that offers a broad scope of healthcare services in areas that encompass surgery, oncology, orthopedics, and cardiology to mention a few.
- Evaluation in Nursing Education and Healthcare Organization Evaluation and assessment are key components of nursing education and healthcare practice since they are concerned with quality appraisal and revealing the need for improvement.
- Ethics, Morals, and Values in Healthcare In healthcare, ethics, morals, and values play a rather crucial role. It is important to be able to differentiate between the concepts and understand their influence on the field.
- Performance Appraisals in Healthcare Settings The assessment of the achievements should be eliminated from the healthcare work setting because it focuses on the compensation rather than individual specifics.
- Russian and American Healthcare Systems Comparison The comparison of the health care system of Russia and the health care system in America shows that neither system meets the health care needs of its populations.
- Information Technology Applications in Healthcare Health IT applications as the most advanced tool that can potentially be used for enhancing patient education through patient-nurse communication.
- Irish Healthcare System: HR Management and Financing The management of the healthcare sector requires using not only adequate leadership practices and approaches to monitoring employee performance.
- Cultural Barriers in Healthcare Management There are numerous barriers including language, cultural competence, and structural access to health care which prevent participation from cultural or ethnic minorities.
- Leadership Theories in the Healthcare Industry There has been extensive research on the effectiveness of leadership style and of theories in different areas of work such as business, nursing, education, military, and politics.
- The US Healthcare Delivery System and Role of Nurses This paper aims to discuss changes implemented to reform the U.S. healthcare delivery system and the role of nurses in the altering environment.
- The Effectiveness of the Internet in Healthcare Healthcare organizations that are making use of the internet to manage their information have received significant attention.
- Financial Analysis in Healthcare Organizations There are four essential financial statements for a not-for-profit healthcare enterprise. They should be used for financial strategy formulation together.
- Evolution of Healthcare Information Systems Healthcare and hospital information systems have greatly changed in the past twenty years and this has been as a result of the improvement of information technology.
- Healthcare Management and Leadership The importance of healthcare management is being understood on the medicine front with various players and places.
- Ethical and Legal Issues in Healthcare Services The article is an analysis of a number of situations that a patient may face and contains a detailed analysis of each of them from a legal and ethical point of view.
- Healthcare Employee Recruitment and Selection Recruitment and selection are the starting points of staffing, which emphasizes their importance for providing the healthcare industry with employees.
- American and Spanish Healthcare Systems The paper is aimed to contrast and compare the information and statistics related to health care systems in the United States (US) and Spain.
- Healthcare Disparities in the LGBT Community Apart from the disparities representatives of the LGBT community face in everyday life, they also deal with some major challenges as to their access to appropriate health care services.
- Quality Improvement Team in Healthcare Institution The essay considers creation of an interdisciplinary quality improvement team, risks associated with working with such teams and the ways to address these issues.
- The Challenges Faced by Healthcare Workers The challenges faced by healthcare workers include transitioning from volume-based healthcare to value-based healthcare, increasing costs and expenses, and provider shortages.
- Modern Healthcare Management: The Role of Information Technologies The introduction of IT in medicine made it possible to bring its advancement to a new level and had a beneficial effect on improving the provision of medical care to the patients.
- Categorical Variables in a Healthcare Research Such categories as age, gender, height, weight can be applied in healthcare research. This paper describes categorical variables and analyzes categorical variables’ application.
- US and Singapore Healthcare Systems Comparison The Healthcare system is a major concern for many countries. Comparing and contrasting the quality of healthcare in the U.S. and Singapore might provide valuable insights.
- Healthcare Regulatory Agencies in the US The purpose of this paper is to identify 5 major healthcare regulatory agencies in the US, describe the agency, level of regulatory authority, and role within the US healthcare system.
- Conflict Resolution in a Healthcare Setting The senior management of a healthcare setting must find a way to resolve a conflict in order not to undermine employees’ productivity and the quality of the provided care.
- Customer Focus in Healthcare Project Management There are certain changes in project management that take place when the organization decides to focus more on customer preferences.
- Project Management in Healthcare Project management in healthcare involves several skills and techniques that improve the efficiency of operations in medical facilities.
- Importance of Education for Healthcare Professionals Education are important in promoting quality healthcare services by providing healthcare practitioners with knowledge and skills in handling different healthcare conditions.
- Effects of Poor Workplace Culture on Healthcare Organizations The current paper provides a unique outlook on the fundamental value held by workplace culture in healthcare organizations.
- Management and Leadership in Healthcare The effectiveness of management of a medical organization can only be guaranteed by the figure of the chief physician as the main head of the clinic.
- How Digital Literacy Skills Will Help Me in the Healthcare Setting This article serves as an overview of the literature on nurses’ use of and access to health-related information on the Internet (HRI).
- Spain’s Current Healthcare System Governments across the globe implement powerful measures and allocate adequate resources to support their respective healthcare systems.
- Healthcare Delivery Models in Germany, the UK, and the US The goal of the research paper is to compare and contrast healthcare delivery models in three countries: Germany, the United Kingdom, and the U.S.
- Healthcare Services: Right or Privilege? It is believed that all people should have free access to healthcare. But today it is a privilege that only particular people can access even though it should be a human right.
- Quality Improvement in Healthcare Improving quality in health care is one of the essential tasks. The quality of hospital services depends on external factors, such as industrial manufacturing processes.
- Cost Allocation in Healthcare Analysis This essay aims to discuss the cost allocation process in the context of healthcare, including its goals, key steps, and methods.
- The Issue of Ethics in Healthcare The most frequently found ethical problems are those that require a simple distinction of what is right and wrong.
- Implementation of Healthcare Organizational Design In the case of a healthcare organization, the organization and management structure should support the design.
- Administrative and Financial System in Healthcare Administrative and financial system applications have advantages and disadvantages for healthcare; however, their benefits prevail over the challenges.
- Healthcare Robotics Impact Today, robotics enters many spheres of life, including education, social life, and healthcare. The use of robots in healthcare allows advancing patient care and achieving better health outcomes.
- Steps in the Process of Risk Management in Healthcare Risk management is essential for any enterprise, but for healthcare organizations, it has even greater significance because, frequently, people’s lives are at stake.
- Time Management in the Healthcare Sector Effective time management is a core component of the healthcare sector. The integration of time management strategies requires specific resources.
- Agile-Scrum in Healthcare Project Management The paper illustrates agile’s integration in the healthcare industry and showcases how more project management schemes are needed to boost its application in the sector.
- Analysis of Limited Access to Healthcare The analysis will primarily focus on geographic and related factors in regards to the issue of healthcare access.
- Healthcare Environment: Challenges to Teamwork and Collaboration Collaboration among staff members is one of the vital requirements for effective management of key tasks and responsibilities in the healthcare environment.
- Healthcare Professions: EMT and Occupational Therapist This paper discusses such healthcare professions in the U.S. healthcare system as emergency medical technician (EMT) and occupational therapist.
- GBMC HealthCare System’s Competitive Advantage Strategic planning helps GBMC maintain steady value growth, decrease financial risks, and plan development for the services and employees.
- Racial and Ethnic Disparities in Healthcare The government can improve health outcomes by ensuring equitable access to diagnosis, treatment, and management of chronic illnesses for marginalized populations.
- Staffing Process in Healthcare The paper analyzes the essential functions, values, and components of effective health care organizational leadership and the challenges of leading modern healthcare organizations.
- Mintzberg’s Configuration in a Healthcare Organization The paper compares Mintzberg’s five basic organizational configurations, identifies the predominant design that works best for a health care organization.
- Leadership and Change in Healthcare Management The paper outlines the essence of leadership and change in healthcare management focusing on the Patient safety, Understanding organizations, Health care management.
- Practice in the Field of Healthcare: Literature Review The purpose of this study has been to determine how the evidence supports practice in the health care industry as well as the various problems health care.
- Cash Versus Accrual Accounting Methods in Healthcare Organizations This paper will focus on analyzing the advantages and disadvantages of integrating accrual versus cash accounting methods in private physician practices and public hospitals.
- GE Energy and GE Healthcare: Strategic Customer Relationships This article seeks to discuss the benefits of building strategic customer relationships for GE Energy and GE healthcare and their customers.
- Conflict Stages and Its Resolution in Healthcare The purpose of this paper is to describe the case related to the development of a conflict in a healthcare setting, identify its type and discuss four stages of a conflict.
- Comparison of Healthcare Systems: The United States and Switzerland According to AHRQ, there are cases when health disparities in the quality of care and access may be observed. It particularly relates to ethnic minorities and immigrants with low income.
- Healthcare Human Resources Management and Changes Human resource management is a vital emphasis of management in organizations. This essay explores the significance of HRM in the context of the health care industry.
- Research Designs in Healthcare Research The paper introduces various research methods and types of designs, explaining how they can be applied within the healthcare industry.
- The Right to Healthcare as a Basic Human Right This paper argues for the implementation of a universal healthcare system in the United States and emphasizes that healthcare is a basic human right.
- Hospital Ownership Types and Impacts on Healthcare Finance The paper states that there is a significant difference in the level of the financial well-being of private, non-profit, and public hospitals.
- Benefits of Health Information Technology Information technology can assist patients in getting their medications, which can be prescribed on video and audio devices.
- Healthcare: The Importance of Accessibility Healthcare plays a significant role in treating life-threatening illnesses, and the accessibility for everyone would save countless lives.
- Performance Appraisal Process in a Healthcare Organization The immediate goals of a nursing performance appraisal have to involve the improvement of care performance, which should lead to a positive healthcare organization outcome.
- The Healthcare Information: Security and Privacy All employees should participate in a mandatory training program that is aimed at raising awareness of the importance of handling patient health records securely.
- IT in Healthcare: Barcode Medication Administration System The integration of the information systems into the medical has improved a lot of issues, including reduction of errors relating to administration transcription.
- Ethical Professional Codes of Healthcare The current case study describes the basic principles of healthcare ethics. They include autonomy, beneficence, justice, and non-maleficence.
- Healthcare System in Republic of Panama The paper discusses the organization of the Panama health care system, patients’ bill of rights, medical ethical issues and complexities of advanced directives.
- Financial Management Role in Healthcare With the introduction of the Affordable Care Act, electronic health records, and the Medicare billing system, the financial aspect of healthcare requires extra attention.
- Medical Technologies Developing Healthcare In this case, the primary goal of this paper is to highlight a substantial role of technology in the advancement of medicine.
- The Consent Role and Aspects in Healthcare Consent represents a kind of agreement that is defined between two or more parties and highlights certain capacities and freedoms that are preserved by that agreement.
- Patient Identity Management Policy in Healthcare The prime reason to implement Patient Identity Management strategies considers the linkage and quantity of electronic healthcare data.
- Cybersecurity and Protection in Healthcare Studying the topic of cybersecurity in healthcare is a valuable source for creating the best ways to protect against hacker attacks.
- Healthcare Social Issue for Indigenous People in Canada It is worth pointing out that the social issue associated with the indigenous population of Canada and the health care system is relevant and open.
- Healthcare Reimbursement Models The paper discusses healthcare reimbursement models. They are payment systems that allow healthcare organizations to be reimbursed for their patients’ services.
- Importance of Radiology and Imaging Service in Healthcare Health sectors have been improved since the introduction of radiology. Diseases such as cancer can be treated through this process.
- The Ontological Basis for Participant Action Research in Healthcare The paper is interested in describing the ontological and epistemological basis for participant action research in healthcare with particular emphasis on non-medical prescribing.
- Partnering to Heal: Healthcare-Associated Infections Prevention The essay explains how healthcare providers and family members could have prevented the occurrence of healthcare-associated infections.
- Leadership in Motivating Healthcare Staff to Increase Performance Transformation leadership is an approach that efficiently works to motivate healthcare staff to increase performance and teamwork and to improve patients’ outcomes.
- Healthcare Accreditation and Licensing Accreditation and licensure are essential processes that potentially render healthcare provision more systematized and standardized.
- Quality Healthcare and Its Aims Organizations and healthcare providers develop analytic frameworks for assessing quality to improve outcomes. Patient-centered care is an aim proposed by the Institute of Medicine.
- Absenteeism and Lateness in the Healthcare Field Absenteeism and lateness are widespread and significant issues in any professional sphere. However, such problems acquire more importance when they occur in the healthcare field.
- Policies and Protocols in Healthcare Policies and protocols in a healthcare environment are essential, as they guide medical professionals in providing high-quality, evidence-based care to all patients.
- Healthcare Database Design and Development The healthcare databases for patient data and human resources are likely to be different. Similarly, the database scope can define the specific needs and issues.
- The Internet of Things (IoT) and Healthcare The Internet of Things (IoT) is a term that defines the way objects (things) can be connected to the Internet, which provides them with the capability to transmit information.
- Malnutrition and Patient Safety Healthcare Policy The paper considers patient safety as the health care policy issue of high priority. Especially, it focuses on poor nutrition as the neglected aspect of patient safety.
- Efficacy of Telemedicine and Its Application in Healthcare The technology of telehealth or Telemedicine is being applied actively in healthcare. There are various studies that examine the influence of Telemedicine on participants.
- Graphs, Statistical and Clinical Significance in Healthcare In healthcare and medicine, there can be two different types of significance: clinical and statistical, and it is important to understand the difference between the types.
- Role of Ethics in Healthcare Leadership Healthcare administrators use the principle of nonmaleficence to resolve challenges associated with service delivery.
- Restraint and Seclusion in Healthcare Restraint and seclusion have been used as measures of addressing patients’ behaviors that could cause harm to them and other people around.
- Non-traditional Healthcare Practices: Can It Replace the Actual Medicine? The three cultures that will be examined in this study will consist of the Filipino, Chinese and Finnish cultures. Their non traditional health practices significantly diverged from one another.
- Factors of Decision-Making by Healthcare Managers Healthcare managers occasionally encounter situations that require them to make critical decisions in healthcare facilities.
- Professional Relationships in Healthcare Successful professional relationships are essential to working effectively in healthcare settings and maintaining a positive climate within the organization.
- The Action Research in Healthcare Action research is a methodology used to identify clinical practice problems and develop potential solutions to improve the quality of care.
- The Healthcare System: Effects of Social Media Healthcare professionals are grasping social media as an instrument in careers advancement. Registered nurses and health practitioners must be registered for vocational reasons.
- Leadership in Healthcare Management & Administration Healthcare management needs administrators with a deep understanding of the medical practice and requires them to be influential leaders.
- United Healthcare Firm’s Readiness to Meeting Healthcare Needs The paper analyzes United Healthcare is an incorporated public firm in the US known for offering healthcare products and insurance services.
- Quality Improvement and Measurement Tools in Healthcare Quality tools are widely used to define and assess healthcare problems, especially in healthcare facilities that prioritize quality and safety problems.
- Quality Improvement and Transformation of Healthcare This paper proposes one solution for improving persistent quality issues by including health care providers in the quality improvement process.
- The German Healthcare System: Key Aspects The German Healthcare System is among the most advanced healthcare systems that provide quality healthcare services, which are not only accessible but also affordable.
- Teamwork and Collaboration in Healthcare Successful health outcomes are best attained when there are teamwork and collaboration among the individuals involved.
- Major Third-party Payers to Healthcare Providers This paper includes a brief discussion of major reimbursement methods that are currently used in the country of the USA.
- Ethical and Religious Directives for Catholic Healthcare Services The sixth edition of ethical and religious directives for Catholic healthcare services was created under the patronage of the US Conference of Catholic Bishops.
- Healthcare Professional Training and Development The articles that will be discovered in this paper mainly cover the topic of training and development of staff in healthcare establishments.
- Interpersonal Communication Skills in Healthcare The problem of miscommunication in healthcare persists and tends to have negative impacts on patient outcomes, including those related to safety.
- Healthcare Disparities and Potential Solutions The purpose of the paper is to expand on healthcare disparities, contributing factors, potential solutions, and the details of their implementation.
- NMC Healthcare Organization and Its Culture NMC Healthcare has several strengths that contribute towards its success. Having been operating for more than four decades, the firm has gained vast experience.
- Blockchain Revolution in the Healthcare Industry How Blockchain Could Revolutionize the Healthcare Industry by Krupa Bathia examines how modern technologies can be considered to maximize or streamline healthcare delivery.
- The Implication of Information Technology on Marketing Strategy of Healthcare Industry The growth of information technology has transformed marketing strategies of most industries. In the healthcare industry, IT has changed the way marketers relate with customers.
- Mental Healthcare Provision & Barriers to Innovation Mental health providers require innovative ways of improving care delivery, but they are experiencing significant challenges in adopting innovations.
- Organizational Change in Healthcare The change in the management aspect of the healthcare sector administration poses an excellent example to the impact upon all stakeholders.
- Culture of the Nacirema in Modern Healthcare Constant development and improvement in healthcare are crucial for quality care and positive patient outcomes, including an examination of the Nacirema culture’s practices.
- Marijuana and Its Use in Healthcare The research suggests considering the use of marijuana as a medication for treatment because it can help to stop certain diseases and help reduce the risk of mental illness.
- Strategic and Program Evaluation in Healthcare
- Healthcare Facility Expansion Funding
- Aspects of Palliative Care in Healthcare
- The Basic Level of Healthcare: H. Engelhardt’s and N. Daniels’ Perspectives
- Strategic Planning in Healthcare
- Using of Virtual Reality in Healthcare
- Healthcare Professional Burnout and Its Effects
- Artificial Intelligence: Integrated in Healthcare
- Perfect Competition and the Cost of Healthcare
- Cuban Cultural Communication in Relation to Healthcare
- Roles of a Financial Manager in Healthcare
- Informatics Technologies in Healthcare
- Compensation Structure in Healthcare
- Organizational Performance and Structure in Healthcare
- Theory, Risk, and Quality Management in Healthcare Facilities
- Indian Healthcare Information System
- Implementing Effective Management in Healthcare
- Using of Statistics in Healthcare
- Behavioral Cues in Healthcare Behaviors
- Healthcare Management: Past, Present, and Future
- Building Trust Within the Healthcare Setting
- Implementation Strategy in the Healthcare Sector: Implementation Stages Analysis
- Afro-Latin Culture and Approach to Healthcare
- Patient Safety in the Healthcare Workplace Culture
- Unionization and Magnet Accreditation in Healthcare
- Healthcare for Hindus: Purnell Model for Cultural Competence
- Effective Professional Teamwork in Healthcare
- South African and Namibian Healthcare
- United Healthcare Group and Its Strategic Plan
- Team-Based Healthcare in Nursing Practice
- Diagnosis-Related Groups in Healthcare Research
- Future Trends in Healthcare
- Application of Blockchain in Healthcare
- Interprofessional Collaboration Examples in Nursing Case Study
- Risk and Quality Management in Healthcare
- The Gibbs Reflection Cycle Method in Healthcare
- Corruption in South Africa’s Healthcare Sector
- Organizational Theory in Healthcare
- Ethical Dilemmas in Healthcare
- Scheduling Management in Healthcare
- Strategic Planning and Leadership in Healthcare
- Career in Healthcare Administration
- The Importance of Interdisciplinary Collaboration in Healthcare
- Clinical Career Ladders in Healthcare
- Interprofessional Communication in the Healthcare Team
- Women’s Healthcare: Eugenics and Sterilization
- Communication Skills in Healthcare Workers
- Servant Leadership in Healthcare
- Incivility Within a Healthcare Setting
- Healthcare Documentation: Standards and Regulations
- The Analysis of Healthcare Organization
- Healthcare: Interprofessional Collaboration
- Tuberculosis Infections and Healthcare in Brunei
- Medicines and Healthcare Regulatory Agency (MHRA)
- Electronic Resources in Healthcare
- System Failures in Healthcare Facilities
- Incivility Within the Healthcare Metaparadigm
- Healthcare Delivery System in the US and Its Components
- Cash vs. Accrual Accounting for Healthcare Organization
- Marketing Change in Healthcare
- Developing a Feedback-Rich Environment in the Healthcare
- Incomplete or Missing Documentation: Patient Safety in Healthcare
- Patient Safety Culture in the Healthcare Workplace
- Organizational Culture in Healthcare
- Big Data and Data Mining in Healthcare Education
- Information Systems in Healthcare
- Workplace Interpersonal Conflicts Among the Healthcare Workers
- Continuous Quality Improvement Strategies in Healthcare
- High-Reliability Healthcare Organization’s Traits
- Access of Healthcare: Factors Affecting the Access of Care and Barriers
- Healthcare Organization: Finance and Accounting
- Technologies and Expenditures in Healthcare
- Patients Safety and Needs in Healthcare Environment
- Conflict Management in Healthcare Facilities
- Healthcare Quality, Safety, and High-Reliability
- Healthcare Quality Initiatives and Their Importance
- Data Breaches and Cyber Attacks on Healthcare Organizations
- Information Security Policies in Healthcare Organizations
- Fraud and Abuse in Healthcare: Analysis
- Information Technology Projects in the Healthcare Sector
- Jehovah’s Witnesses’ Views on Healthcare
- Healthcare Administrator: Profession Overview
- The Concept of Accountability in Healthcare
- Mental Healthcare Aspects of Latinos
- Telehealth and Its Impact on the Healthcare System
- Overworked Healthcare Systems: The Case of the US and Canada
- Fraud Schemes in the Healthcare Industry
- Healthcare Industry Challenges: Information and Service Integration
- Healthcare Delivery Systems in Different Countries
- The Pain Rating Scales in Healthcare
- Sexual Issues Confronting Healthcare Providers in the 21st Century
- The Implementation of a Safety Improvement Initiative in Healthcare Institutions
- Medication Error Impact on Healthcare Quality
- Healthcare Marketing and Its Evolution
- Performance Management System in Healthcare
- The Forced-Air Prewarming Strategy in Healthcare
- Poverty and Poor Health: Access to Healthcare Services
- Organizational Mission, Vision, and Values in Healthcare
- Ethics in the Healthcare Industry: Armando Dimas’ Case
- Nurse’s Role in Healthcare Sentinel Events
- Quality and Risk Management in Healthcare
- Leadership in Healthcare Institutions
- Healthcare Innovations and Improvements
- Theory of Planned Behavior and Educational Intervention in Prevention of Healthcare-Associated Infections
- Healthcare System in the Republic of Panama
- Vanguard Healthcare Services, LLC: Health Organization Case Study
- Cost, Access, and Quality in Healthcare
- The Importance of Effective Healthcare Communication
- Nursing Informatics in Healthcare
- Technology and Future Trends in Healthcare
- Mobile Apps Utilization in Modern Health Care
- Stage-Of-Life and Healthcare Experiences
- Healthcare Root-Cause Analysis and Safety Improvement Plan
- Cloudlet Architecture in Healthcare Computing
- Autism and Associated Healthcare Issues
- Impact of Technology on the Healthcare System
- United Healthcare Organization and Citizens’ Needs
- AIDET Communication Process in the Healthcare
- Robotic Technologies in the Healthcare Sector
- New Sustainable Development Goals in Healthcare
- Chinese Cultural Beliefs: Healthcare Assessment
- Pressure Ulcers as a Healthcare Project Topic
- Personality Type and Leadership in Healthcare
- Teamworking Skills in Healthcare
- Healthcare Project Management Office’s Responsibilities
- Cross-Cultural Healthcare and Its Implications
- Healthcare Financing: Equipment Replace Proposal
- Trends in the Healthcare Sector
- Emotional Intelligence and Feelings in Healthcare
- LGBT Healthcare Disparity: Theoretical Framework
- Levine’s Conservation Theory in Healthcare Research
- Healthcare Change Management and Workforce Retention
- Tenet Healthcare Corporation: Training and Development
- Ways to Improve the US Healthcare System
- Code of Conduct in Healthcare Organizations
- Three-Step Change Theory and Its Phases in Healthcare
- Healthcare Quality Improvement Team Meeting Plan
- Emotional Intelligence in Healthcare Leaders and Nurses
- How Big Data Is Used in Health Care
- Healthcare Conflict Resolution Case
- Healthcare Technological Advancements: Pros & Cons
- Religion and Ethics in Healthcare Provision
- Healthcare Quality Improvement and Stakeholders
- Nursing Quality Models in Healthcare Institutions
- Healthcare Governance and Its Common Features
- Healthcare Information Technology: Information Needs and Implementation of the Health Information System
- Big Data in the Healthcare Sector: Pros and Cons
- Using Smartphones in Healthcare: Ethical Issues
- Constructing Team Values in Healthcare
- Epidemiological Data and Its Role in Healthcare
- Beliefs, Perceptions, and Behaviors Impacting Healthcare Utilization
- Advocacy and Communication in Healthcare
- Strategic Planning Processes in Healthcare
- Risk Management in Healthcare Settings
- Effective Communication and Quality in Healthcare
- Analysis of Innovation in Healthcare
- Trinity Healthcare’s Internal and External Barriers
- Healthcare Informatics: Introduction to Theory
- Stakeholders’ Conflict of Interests in Healthcare Provision
- Elder Abuse in the US Healthcare System
- Voluntary Accreditation in Healthcare: Requirements, Compliance, and Standards
- Data Analytics and System Performance in Healthcare
- Integration of Health Information Management System (HIMS) into Healthcare
- Safety Culture in the Healthcare Workplace
- Aspects of Healthcare Costs
- The Smartphone Technology in the Healthcare Sector
- Operation Management and Value Chain in Healthcare
- “The HR Challenges Shaping the Healthcare Industry” Article Summary
- Racial Disparities in Healthcare Through the Lens of Systemic Racism
- Abbreviated Quantitative Healthcare Research Plan
- Healthcare Issues: The Cultural Assessment Framework
- Strategic Management Techniques and Tools in Healthcare
- Transformational Leadership in Healthcare
- Intentional Exaggeration: Healthcare Plans and Products
- Six Sigma’ Management Strategy in Healthcare
- Patient Rights When Interacting With Healthcare Providers
- Informatics in the Clinic Area Healthcare
- Leadership in Healthcare Overview
- The Practice Reality of Quality Improvement in Healthcare
- Reducing the Number of Healthcare-Associated Infections
- Accountability in the Healthcare Industry
- Statistical Process Control in the Healthcare
- Replication and Its Importance in Healthcare Research
- The Launch of Healthcare Projects
- The Importance of Moral Courage in the Healthcare
- Healthcare Marketing and Strategy in Prenatal Care Practice
- Theory of Control in the Healthcare
- Healthcare: New Treatment Methods
- Hospital-Acquired Pressure Ulcers in US Healthcare Organizations
- Evidence-Based Conflict Resolution Strategies in Healthcare
- Leadership Styles and Theories in Healthcare
- Cultural Pluralism and Sexism in Healthcare
- Improving Healthcare Quality With Bar-Coded Medication Administration
- Science of Human Flourishing in Healthcare
- Medical Devices Trade Agreements for Healthcare
- Transgender People and Healthcare Barriers
- Healthcare Delivery Models and Nursing Trends
- Healthy Relationships in the Healthcare Workplace
- Tenet Healthcare Corporation’s Training and Development Plan
- ABC Healthcare Cyber and Computer Network Security
- Muslim Faith and Healthcare Relationship
- Healthcare Marketing Communication and Strategies
- Healthcare Policy, Leadership and Performance
- Healthcare Workforce and Human Resource Management
- Healthcare Informatics: Infrastructure Evaluation
- Healthcare Regulatory Agencies
- Using Technology in Healthcare Setting
- Austrian vs. American Healthcare Systems
- Sickle Cell Disease and Healthcare Decisions
- The PICOT Framework in Healthcare
- Financial Viability in Healthcare
- The Christian and Buddhist Perspectives in Healthcare
- Healthcare Mission and Philosophy: Mercy Hospital Inc.
- Healthcare in the United States: Timeline and Reforms
- Healthcare Access: Financial Barriers
- Simulation in Healthcare Operational Decision-Making
- The United States Healthcare System Analysis
- The National Healthcare Quality and Disparities Report
- Factors Facilitating Quality Improvement in Healthcare
- Leadership Models in Healthcare
- Policies Addressing LGBT (Queer) Healthcare Disparities
- Quality Healthcare Improvement for Pregnant Women in New York City
- Negligence and Battery in Healthcare Units
- Risk Management, Quality and Safety in Healthcare
- Healthcare Affordability in the United States
- Healthcare Quality and Outcomes: Measurement and Management
- The Policy Standard in China’s Healthcare System
- Healthcare Financial Elements
- Patient-Centered Medical Home: Marketing in Healthcare
- How Analytics Can Help Improve Healthcare Decision-Making
- Evidence-Based Practice in Healthcare Organizations
- The Impact of Genomics on Policy and Practice in Healthcare
- Healthcare Costs Affected by the COVID-19 Pandemic
- Monitoring Compliance of IV Pump Integration in a Healthcare Setting
- Geography and Healthcare Equity in the U.S.
- Navigating Organizational Theories in Healthcare
- Challenges and Complexities in the U.S. Healthcare System
- The US vs. New Zealand Healthcare Systems
- Dental Healthcare Persons’ Infection Control
- Monitoring and Controlling Functions in Healthcare Organizations
- Abuses in a Healthcare Context
- The Canadian Healthcare System’s Key Challenges
- Healthcare as a Basic Human Right
- Data Analytics and Its Role in Healthcare
- Business Analytics in Healthcare
- Impacts of Organizational Culture and Structure on Healthcare Outcomes
- Healthcare Service Management Course
- Healthcare Organization Assessment
- Advanced Practice Nurse: Healthcare Policy
- Business Needs in the Healthcare Sector
- Information Technologies in Healthcare
- Management Tasks in Healthcare Organizations
- Healthcare Risk Management – Balancing Safety and Efficiency
- Informed Decision-Making in Healthcare
- Diversity in Healthcare Organizations
- Managing Incremental Healthcare Costs in a Post Pandemic World
- Healthcare Change Implementation and Management Plan
- Healthcare Data Quality Elements
- Standardization as a Procedural Issue in Healthcare
- Cultural Diversity and Sensitivity in Healthcare
- Leading Interprofessional Collaboration in Healthcare
- Barriers to Healthcare in Refugee Communities
- Policy Analysis in Healthcare Industry
- Healthcare Research: Systematic Search Strategy
- Refugees’ Adjustment and Accessibility of Healthcare
- Professional Services Automation System in Healthcare
- VITAS Healthcare: Program Evaluation Proposal
- Healthcare Research Designs and Sampling Methods
- Healthcare Policy Evaluation in the US vs. Mexico
- Prevention in Healthcare and Social Science
- Interprofessional Team Management in Healthcare
- Implications of Healthcare Fraud and Abuse
- Impacts of Technology on the Healthcare System
- Healthcare Advocacy Plan for Nassau County
- Incorporating Telehealth Into the Healthcare System
- Healthcare Program: Informational Campaign on Dementia
- Initial Beliefs: Evidence-Based Management in Healthcare
- Q.I. Program for Vaccination Among Healthcare Workers
- How Healthcare Organizations Deal With COVID-19 Financial Issues
- Billing and Coding Regulations in Healthcare
- Vocal Biomarkers in Healthcare
- Communication Problems in Healthcare Attendants
- Climate Change as a Healthcare Priority
- Rising Healthcare Costs as a Policy Issue
- Electronic Vulnerability in Healthcare
- Statistical Analysis in Healthcare
- Access to Healthcare Services and Language Interpretation
- The Healthcare Labour Shortage: Practice, Theory, Evidence
- Healthcare Financing: USA vs. Switzerland
- Discussion: The Use of RFID in Healthcare
- Healthcare Insurance Organizations’ Risk of Fraud
- The Healthcare Center for the Homeless
- Project Evaluation in Healthcare
- Healthcare Language Barrier for Afghani Refugees
- The Socio-Ecological Model of Access to Healthcare
- Advantages of Accreditation of Healthcare Organizations
- Technologies in Healthcare Delivery
- Antibiotics: The Use in Healthcare
- Challenges of Virtual Assistance Technology Implementation for Healthcare
- Universal Healthcare as a Basic Right of Humanity
- Evaluation of Virtual Reality in Healthcare
- Healthcare Interprofessional Team Members’ Perspectives on Caring
- Leadership Versus Management: Healthcare Leadership
- Third-Party Payers in Healthcare Reimbursement
- Organizational Change Regarding Language Barriers in Healthcare
- The Triple Aim Framework and Financial Issues in Healthcare
- How 911 Dispatcher Technology Has Reduced Healthcare Costs
- Applying Lean Principles in Healthcare
- Reducing Healthcare Expenses: Structural and Individual Measures
- Hansen vs. Baxter Healthcare Corporation
- The Role of Differential Diagnosis in Healthcare
- Issues in Healthcare and Effective Communication with Organization Stakeholders
- Healthcare Collection Policies and Procedures
- Issues of Healthcare in the US
- Healthcare Services for Vulnerable Populations in Georgia
- Report Specifications in Healthcare
- Importance of Healthcare Advocacy Plan
- The Healthcare Costs Regulation Strategies
- Malpractice, Abuse, and Neglect in Healthcare
- Healthcare Cost and Utilization Project
- The Healthcare Administrator: Leadership Abilities
- Queer People (LGBTQIA) in Healthcare System Context
- Informatics Systems in Healthcare
- Auburn Hospital’s Comprehensive Healthcare Strategies
- Healthcare during Tornados: Business Continuity
- Qualitative Research in Healthcare
- Interoperability in Healthcare
- Theories and Approaches in Healthcare
- The Significance of Healthcare Policy
- Legal and Ethical Issues in Healthcare System
- Consumer Involvement in the Healthcare System
- Significance of Accreditation in Healthcare
- Healthcare Trends and Innovations
- Pediatric and Adult Anatomy for Healthcare Providers
- Licensed Professional Counseling in Mental Healthcare
- Healthcare Errors, Risks, and Project Management
- A Strategic Plan for a Healthcare Organization
- Technology in the Healthcare System
- Healthcare Insurance in the USA
- Population Aging and Healthcare Concerns
- Implementing and Evaluating a Healthcare Organization’s Strategic Plan
- Galen’s Experiential Philosophic Approach to Healthcare
- Economic Issues Confronting Healthcare System
- Doctor Michael R. Walker as Leader in Healthcare
- Role of Advance Directives in Healthcare
- Nursing Informatics: Healthcare Blockchain System
- “Top Challenges Facing the Healthcare Industry Today”: Three Challenges
- Healthcare Information Systems
- Technology in Healthcare and Care Coordination
- Universal Healthcare in the United States
- Simulation Training for Healthcare Staff
- Mandatory COVID-19 Vaccination for Healthcare Employees
- Regulation of Patient Healthcare Records Release
- Telemedicine as a Healthcare Provision Technique
- Healthcare for Queer (LGBTQIA+) Patients
- The American College of Healthcare Executives: Leadership Reflection
- Strategic Planning Process in Healthcare
- The Assessment Process in Healthcare
- Competitive Forces in the Healthcare Market
- Impact of Obesity on Healthcare System
- Care Coordination Process in the Healthcare
- Social Welfare Policy and Healthcare Insurance
- Interprofessional Teamwork in Healthcare
- Quality Performance Is a Goal in Healthcare
- Revenue Cycle Processes and Pricing in Healthcare
- Billing Specialists in Healthcare
- Healthcare: Auditing Practices
- Community Healthcare Agency at Fairfax
- The Adoption of the EHR Framework in Healthcare Facilities
- Should Free Healthcare be a Right in America?
- Unlisted Procedures and Services in Healthcare
- Creating Value in Healthcare Settings
- Healthcare Disparity in the African American Community
- The Introduction of a Vaccine Against COVID-19 Among Healthcare Staff in Moldova
- The Healthcare Availability in the USA
- Improving a Healthcare Compliance Program
- The Healthcare Situation in the USA
- Human Resource Management: Healthcare
- Artificial Intelligence: Human Trust in Healthcare
- Researching of Fraud and Abuse in Healthcare
- Ethics of Care (EOC) and Healthcare
- Genetic Technologies in the Healthcare
- Racial Inequality, Immigration, and Healthcare in the US
- Occupational Stress Management in Healthcare
- Cybersecurity in Healthcare Organizations
- Impact of IT on Healthcare During COVID-19
- Nurses’ Knowledge to Be Successful Healthcare Professionals
- The Risk of Using Abbreviations in Modern Healthcare
- The Use of Unmanned Aircraft Systems (UAS) in the Healthcare
- Women’s Healthcare and Social Darwinism
- Telepsychiatry as Innovative Healthcare Practice
- Language and Culture: Impact on Healthcare
- Health Costs and Insurance in Healthcare
- Fraud in the Healthcare Industry
- Providing Quality Care in Healthcare Setting
- Occupational Therapy in Modern Healthcare Market
- Responsible Citizenship in Healthcare Administration
- Handwashing Compliance of Healthcare Workers
- Healthcare and Governmental Efforts
- Followership and Leadership in Healthcare
- Reducing Risks Facing a Healthcare Organization
- Public Education Initiatives in the Area of Healthcare
- Followership-Leadership Interaction in Healthcare
- The Importance of In-Team Communication in Primary and Emergency Healthcare
- Healthcare Leadership and Management Functions
- Mental Healthcare Services for Transgender Individuals
- Social Justice and Barriers in Healthcare
- Analysis of Implicit Bias in Healthcare
- Accreditation, Regulation, and Certification in the Healthcare Field
- Healthcare Settings: Financial Challenges
- Patient Consent in Healthcare Diagnostics
- Cultural Diversity in Healthcare
- Standard of Care in Healthcare System
- Joe Biden’s New Reform on Healthcare
- The Culture of an Open Attitude in Healthcare
- Global Issues in Healthcare: Cultural Competence and Patient Safety
- Language, Culture, and Healthcare
- International Classification of Functioning in Healthcare
- What Are the Cross Cultural Healthcare Perspectives?
- How to Estimate the Optimal Size of Secondary Healthcare Providers in Slovenia?
- How Health Policy Shapes Healthcare Sector Productivity?
- How HRM Provides a Mandatory Organized Structure in the Healthcare System?
- How Medical Robotics Affect Healthcare Costs and Patient Care?
- How Medicare Has Impacted Healthcare Within the United States of America?
- How Reliable Are Surveys of Client Satisfaction With Healthcare Services?
- How Retractable Syringe Development Impacted Society and Healthcare?
- What Are the Applications of Simulation Within the Healthcare Context?
- What Are the Factors Influencing Healthcare Service Quality?
- What Is “Quality Improvement” and How Can It Transform Healthcare?
- What Is Interprofessional and Multiprofessional Collaboration in Healthcare?
- What Is Jamaica’s Ethnomedicine Potential in the Healthcare System?
- What Are the Characteristics of Healthcare Wastes?
- What Is a Canadian Model of Integrated Healthcare?
- What Are the Trends and Approaches in Lean Healthcare?
- Whar Are the Emerging Information Technologies for Enhanced Healthcare?
- What Are the Challenges for Design Researchers in Healthcare?
- How Well-organized Logistics Can Service Healthcare?
- What Are the Theories on Implementation of Change in Healthcare?
- How the Blockchain Technology Was Implemented in Healthcare?
- How To Improve Healthcare With Interactive Visualization?
- What Are the Essentials of Economic Evaluation in Healthcare?
- How Mobile Devices Are Transforming Healthcare?
- How to Develop Machine Learning Models for Healthcare?
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, December 21). 610 Healthcare Essay Topics & Research Questions to Write About. https://studycorgi.com/ideas/healthcare-essay-topics/
"610 Healthcare Essay Topics & Research Questions to Write About." StudyCorgi , 21 Dec. 2021, studycorgi.com/ideas/healthcare-essay-topics/.
StudyCorgi . (2021) '610 Healthcare Essay Topics & Research Questions to Write About'. 21 December.
1. StudyCorgi . "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
Bibliography
StudyCorgi . "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
StudyCorgi . 2021. "610 Healthcare Essay Topics & Research Questions to Write About." December 21, 2021. https://studycorgi.com/ideas/healthcare-essay-topics/.
These essay examples and topics on Healthcare were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 8, 2024 .
Home — Essay Samples — Nursing & Health — Health Care
Essays on Health Care
Five nursing pillars, optometrist: advantages and disadvantages, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Occupational Therapy Application
Aspects of nursing shortage, the importance of nursing philosophy, examples of icare values in healthcare, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Fresh Fruit, Broken Bodies: a Summary and Analysis
Analysis of "a walk to beautiful", universal health care: persuasive speech outline, the importance of hand washing in nursing, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Sick Around America Documentary Analysis
Middle range theory of acute pain, patch adams reflection paper, nursing personal statement, self-assessment in nursing, vimax extender analysis, delegation in nursing case study, cleveland clinic mission statement, challenges of istj in nursing, topics in this category.
- Affordable Care Act
- Universal Health Care
- Nursing Care Plan
- Health Care Policy
- Healthcare Crisis
- Opioid Epidemic
- Nursing Theory
Popular Categories
- Public Health Issues
- Maintaining Health
- Anatomy & Physiology
- Infectious Diseases
- Nutrition & Dieting

Most Popular
13 days ago
From Karl Marx to Toga Shortages: Reddit’s Funniest Essay Mistakes
Health care essay topics.

In today’s rapidly developing world, the importance of healthcare professionals cannot be overstated. As the demand for quality medical services continues to grow, the significance of individuals pursuing careers in this field becomes increasingly evident. The healthcare sector plays a pivotal role in society, addressing a wide range of medical needs and improving overall well-being. It is no wonder that many students are drawn to this career path, driven by a genuine passion for helping others and positively impacting people’s lives. With numerous sub-disciplines and specializations available, the healthcare field offers diverse opportunities for students to explore their interests and contribute to improving global health. We’ve assembled a list of the most relevant healthcare essay topics to shed some light on the issues students often struggle with. In case you feel that you need professional help, turn to the best online essay writing service for guidance.
Most Popular Health Care Topics 2023

Health Care essay topics
What are some interesting healthcare essay topics.
When it comes to healthcare essay topics, there are numerous intriguing options to explore. One interesting topic could be the impact of technology on patient care. This could involve examining the benefits and challenges associated with advancements such as electronic health records, telemedicine, or artificial intelligence in diagnosing diseases. Another fascinating subject could be the ethics of organ transplantation, delving into the complex considerations surrounding organ allocation and the implications for patients and society. Furthermore, topics like the future of personalized medicine, healthcare disparities, or the role of nurses in primary care could provide rich areas for exploration and analysis.
How do I choose a topic for my healthcare essay?
Choosing a topic for your healthcare essay requires careful consideration of various factors. First and foremost, reflect on your interests within the field of health care. Consider the areas that resonate with you the most, whether medical advancements, patient advocacy, health policy, or ethical dilemmas. Additionally, it’s crucial to assess the availability of research and credible sources on the chosen topic. Ensure that there is sufficient literature and evidence to support your arguments. Furthermore, align your subject with the assignment requirements and guidelines provided by your instructor. Finally, strive to select a topic that allows you to contribute a unique perspective, offer potential solutions to existing problems, or provoke critical thinking.
What are the current trends in health care that can be explored in an essay?
Several current trends in health care offer opportunities for exploration in an essay. One prominent trend is the adoption of electronic health records (EHRs) and their impact on patient privacy and data security. You could delve into the benefits and challenges of EHR implementation, analyzing how they affect patient care and confidentiality. Another trend worth exploring is the rise of telehealth services, particularly in light of the COVID-19 pandemic. Investigate the benefits, limitations, and long-term implications of telemedicine regarding access to care, quality of care, and patient satisfaction. Additionally, you could examine the utilization of big data and analytics in healthcare decision-making, the development of precision medicine and gene therapy, the integration of mental health care into primary care settings, or the exploration of social determinants of health.
Are there any ethical issues related to health care that can be discussed in an essay?
Health care encompasses a myriad of ethical issues that provide fertile ground for discussion in an essay. One such issue is end-of-life care and euthanasia, where you can explore the moral, legal, and personal considerations surrounding the right to die with dignity and the role of physicians in this process. Another relevant topic involves the allocation of scarce resources, particularly in organ transplantation. This subject raises ethical dilemmas regarding fairness, equity, and the criteria used to determine who receives organs. Other potential ethical issues include the use of placebos in clinical practice, conflicts of interest in pharmaceutical research, genetic engineering, and cloning, patient autonomy and informed consent, the role of artificial intelligence in decision-making, privacy concerns in health data sharing, and the ethical implications of healthcare disparities.
How can I find credible sources for my healthcare essay topic?
Finding credible sources is essential for a well-researched healthcare essay. To locate reliable information, start by exploring reputable academic databases such as PubMed, JSTOR, or Google Scholar. These platforms provide access to peer-reviewed articles and research papers authored by experts in the field. Additionally, visit respected health organizations’ websites like the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), National Institutes of Health (NIH), or professional associations related to your topic of interest. These sources often publish reliable reports, guidelines, and studies. When evaluating sources, ensure they come from reputable authors, institutions, and respected peer-reviewed journals. Pay attention to the publication date to ensure you’re accessing the most current information.
What are some controversial issues in health care that can be debated in an essay?
Health care is rife with controversial issues that spark lively debates. One such issue is abortion rights and reproductive health, exploring topics like access to abortion services, ethical considerations, and the role of legislation in reproductive healthcare decisions. Another contentious subject involves mandatory vaccination policies, where you can examine the balance between public health and individual autonomy, considering issues of personal belief exemptions and community immunity. Additional controversial issues include the legalization of medical marijuana, the use of animals in medical research, healthcare access for undocumented immigrants, the impact of private healthcare insurance on accessibility and equity, regulation of alternative medicine practices, and debates surrounding physician-assisted suicide.
How does the Affordable Care Act impact the healthcare system?
The Affordable Care Act (ACA), also known as Obamacare, has a significant impact on the U.S. healthcare system. The ACA aimed to increase access to healthcare and improve affordability. One of its key provisions is the requirement for individuals to have health insurance, which expands coverage and reduces the number of uninsured Americans. The ACA provides subsidies to help individuals and families afford insurance, particularly those with lower incomes. It also expanded Medicaid eligibility, enabling more low-income individuals to access healthcare. The law prohibits insurance companies from denying coverage or charging higher premiums based on pre-existing conditions. Additionally, the ACA emphasizes preventive care by requiring insurance plans to cover preventive services without cost-sharing. However, the ACA has been a subject of ongoing debates and legal challenges, with criticisms including concerns about affordability, individual mandates, the effects on insurance premiums and choice, and the balance between federal and state control over healthcare policies.
Can I write an essay on the importance of preventive care in health care?
Certainly, you can write an essay on the importance of preventive care in health care. Preventive care focuses on proactive measures to maintain and promote health, aiming to prevent the onset of diseases or detect them early when they are more manageable. In your essay, you can emphasize the benefits of preventive care, such as reduced healthcare costs by preventing expensive treatments and hospitalizations. You can discuss the various components of preventative care, including vaccinations, routine screenings, healthy lifestyle interventions, and early detection of diseases. Additionally, explore the impact of preventive care on population health outcomes, emphasizing the significance of education and public health campaigns in promoting preventive measures. Highlight the importance of healthcare policies and initiatives prioritizing and facilitating access to preventive care services for individuals and communities.
What are the challenges faced by the healthcare industry today?
The healthcare industry faces several challenges in today’s complex landscape. One of the significant challenges is rising healthcare costs. Factors such as technological advancements, increased demand for services, and an aging population contribute to escalating expenses. This poses challenges in terms of affordability, equitable access, and financial sustainability of healthcare systems. Additionally, healthcare disparities are a pressing issue, with certain populations facing barriers to accessing quality care due to factors like socioeconomic status, race, ethnicity, or geographic location. Other challenges include healthcare workforce shortages, particularly in rural areas, as well as the rapid pace of medical advancements, which necessitates continuous training and education for healthcare professionals. Ethical dilemmas, such as balancing patient autonomy and best practices, also present challenges in decision-making. Lastly, issues related to data privacy and cybersecurity have emerged with the increased adoption of electronic health records and the need to protect sensitive patient information.
Are there any specific healthcare policies or regulations that can be analyzed in an essay?
Yes, numerous specific healthcare policies or regulations can be analyzed in an essay. One example is the Health Insurance Portability and Accountability Act (HIPAA), which protects patient privacy and regulates the use and disclosure of health information. You can explore the impact of HIPAA on healthcare practices, patient rights, and data security. Another policy is the Medicare Access and CHIP Reauthorization Act (MACRA), which introduced the Quality Payment Program (QPP) to shift healthcare reimbursement from fee-for-service to value-based care. Analyzing the effects of MACRA and QPP on healthcare delivery and quality improvement efforts could make for an informative essay. Other policies and regulations that can be analyzed include the Health Information Technology for Economic and Clinical Health (HITECH) Act, the 21st Century Cures Act, the Stark Law, the Anti-Kickback Statute, or state-specific healthcare regulations. By examining these policies, you can assess their goals, impact on healthcare stakeholders, and potential benefits and challenges associated with their implementation.
Follow us on Reddit for more insights and updates.
Comments (0)
Welcome to A*Help comments!
We’re all about debate and discussion at A*Help.
We value the diverse opinions of users, so you may find points of view that you don’t agree with. And that’s cool. However, there are certain things we’re not OK with: attempts to manipulate our data in any way, for example, or the posting of discriminative, offensive, hateful, or disparaging material.
Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
More from Academic Writing Tips

Using Grammarly Placed A Student On Academic Probation
Is Summarizing Books a Good Way to Retain Knowledge? Redditors Weigh In
Remember Me
What is your profession ? Student Teacher Writer Other
Forgotten Password?
Username or Email
Should Healthcare Be Free? Essay on Medical System in America
Introduction, problem statement, why healthcare should be free, why healthcare should be paid, works cited.
The US government has historically taken a keen interest in the health of its citizens. As far back as the beginning of the 1900s, President Theodore Roosevelt declared that “nothing can be more important to a state than its public health: the state’s paramount concern should be the health of its people” (Gallup and Newport 135). Despite these, the United States is classified as the nation with the most expensive, and yet inefficient, health care system among developed nations.
An expensive health care system translates to an increasing proportion of the population being unable to access the much needed medical care. The New York Times reports that according to census survey carried out in the year 2007, an estimated 45.6 million people in the USA were uninsured and hence unlikely to receive comprehensive medical care from hospitals (1). Due to the perceived inefficiencies, there has been agreement that the current health care system is faulty and therefore in need of radical changes to make it better.
Majority of American’s are greatly dissatisfied with the current health care system which is extremely expensive and highly inefficient. While an effective system can be deemed to be one which is efficient, acceptable and at the same time equitable, the current system is lacking in this attributes.
The aim of this paper will be to analyze the effects that free health care system in America would have. This paper will argue that a health care system which guarantees free health care for all Americans is the most effective system and the government should therefore adopt such a system.
Free health care would result in a healthier nation since people would visit the doctors when necessary and follow prescriptions. Research by Wisk et al. indicated that both middle and lower class families were suffering from the high cost of health care (1). Some families opted to avoid going to the doctor when a member of the family is sick due to the high cost of visiting the doctor and the insurance premiums associated with health care.
In the event that they go to the doctor, they do not follow prescriptions strictly so as to reduce cost. Brown reveals that “60 percent of uninsured people skipped taking dosages of their medication or went without it because it cost too much” (6). Such practices are detrimental to a person’s health and they cost more in the long run.
The last few years have been characterized by financial crises and recessions which have negatively affected the financial well being of many Americans. In these economic realities, the cost of health care has continued to rise to levels that are unaffordable to many Americans. This loss of access to health care has led to people being troubled and generally frustrated. A report by Brown indicates that the price for prescription drugs in the US has escalated therefore becoming a financial burden for the citizens (6).
The productivity of this people is thereby greatly decreased as they live in uncertainty as to the assurance of their health and thereby spend more time worrying instead of being engaged in meaningful activities that can lead the country into even greater heights of prosperity. Free health care would lead to a peace of mind and therefore enable people to be more productive.
Since medical care is not free, many people have to make do with curative care since they cannot afford to visit medical facilities for checkups or any other form of preventive medical care. This assertion is corroborated by Colliver who reveals that many people are opting to go without preventative care or screening tests that might prevent more serious health problems due to the expenses (1).
Research shows that approximately 18,000 adults die annually due to lack of timely medical intervention (The New York Times 1). This is mostly as a result of lack of a comprehensive insurance cover which means that the people cannot receive medical attention until the disease has progressed into advanced stages. This is what has made medical care so expensive since “sick patients need more care than relatively healthy ones” (Sutherland, Fisher, and Skinner 1227).
This is an opinion shared by Sebelius who reveals that 85% of medical costs incurred in the country arise from people ailing from chronic conditions (1). She further notes that if screened early, these diseases such as diabetes and obesity can be prevented thus saving the medical cost to be incurred in their treatment. It therefore makes sense to have a health care system that makes it possible for everyone to access preventive care thus curbing these conditions before they are fully blown.
While most people assume that free health care will result in better services as more people will be able to access health care, this is not the case. The increase in people who are eligible for health care will lead to an increase in the patients’ level meaning that one may have to wait for long before receiving care due to shortage of medical personnel or the rationing of care.
A European doctor, Crespo Alphonse, reveals that when health care is free, people start overusing it with negative implications for the entire system (AP). In addition to this, free health care would invariably lead to cost cutting strategies by hospitals.
This would lead to scenario where finding specialized care is hard and the rate of medical mistakes would increase significantly. As a matter of fact, a survey on Switzerland hospitals found that medical errors had jumped by 40% owing to the introduction of mandatory health insurance (AP). While it is true that free health care will increase the number of people visiting the doctor, this may be a positive thing since it will encourage preventive care as opposed to the current emphasis on curative care.
Free health care is a move towards a socialistic system. As it is, the US is a nation that is built on strong capitalistic grounds. This is against the strong capitalistic grounds on which the United States society is build on. While detractors of the private insurance firms are always quick to point out that the firms make billions of dollars from the public, they fail to consider the tax that these firms give back to the federal government (Singer 1).
Free health care would render players in the health industry such as private insurance companies unprofitable. Free health care will bring about a shift from a profit oriented system to a more people oriented system. Without money as a motivation, research efforts will plummet thereby leading to a decrease in the medical advancement as investment in research will not be as extensive (Singer 1).
The Associate Press reveals that doctors may also lack to be as motivated if they are no incentives and thereby the quality of their work may weaken (1). As such, a free health care system would have far reaching consequences for the economy of the nation since the health care industry is a profitable industry for many.
The Healthcare system is one of the most important components of the U.S. social system since full productivity cannot be achieved without good health. This paper has argued that a free health care system would be the most effective system for America. To reinforce this assertion, the paper has articulated the benefits that the country would accrue from free health care.
With free health care, all Americans would be able to access health services when they need it leading to increased quality of life. In addition, many people would make use of preventive healthcare services, therefore reducing the financial burden that the expensive curative services result in.
The paper has taken care to point out that free health care has some demerits, most notably of which is overloading the health services with a high number of patients. Even so, the observably advantages to be reaped from the system far outweigh the perceived risks. As it is, decades of reform on the US health care system have failed to provide any lasting solution to the problem.
Making health care free for all may be the strategy that will provide a solution for the ideal health care system that has thus far remained elusive. From the arguments presented in this paper, it can irrefutably be stated that free health care will result in a better health care system for the country.
Associate Press. (AP). Europe’s free health care has a hefty price tag . 2009. Web.
Brown, Paul. Paying the Price: The High Cost of Prescription Drugs for Uninsured Americans. U.S. PIRG Education Fund, 2006.
Colliver, Victoria. “Jump in middle-income Americans who go without health insurance,” San Francisco Chronicle (SFGate), 2006.
Gallup, Andrew, and Newport Francis. The Gallup Poll: Public Opinion . Gallup Press, 2005. Print.
Sebelius, Kathleen. Health Insurance Reform Will Benefit All Americans . 2009. Web.
Singer, Peter. Why We Must Ration Health Care . 2009. Web.
Sutherland, Jason., Fisher Elliott, and Skinner Jonathan. “Getting Past Denial – The High Cost of Health Care in the United States” . New England Journal of Medicine 361;13, 2009).
The New York Times. The Uninsured . 2009. Web.
Wisk, Lauren. High Cost a Key Factor in Deciding to Forgo Health Care . 2011. Web.
- The US Healthcare Financing Concerns
- Hospice – Dying with Comfort and Dignity
- Assessing the Role of Conflict in the Health Care Environment
- Africa Regional Conference: Should Democracy Be Promoted in Africa?
- Why did Tunisia and Egypt’s governments fall? Will they become democracies?
- The Spread of Democracy
- Trustee vs. Delegate Models of Representation
- The United States Constitution
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, October 12). Should Healthcare Be Free? Essay on Medical System in America. https://ivypanda.com/essays/free-health-care-in-america/
"Should Healthcare Be Free? Essay on Medical System in America." IvyPanda , 12 Oct. 2018, ivypanda.com/essays/free-health-care-in-america/.
IvyPanda . (2018) 'Should Healthcare Be Free? Essay on Medical System in America'. 12 October.
IvyPanda . 2018. "Should Healthcare Be Free? Essay on Medical System in America." October 12, 2018. https://ivypanda.com/essays/free-health-care-in-america/.
1. IvyPanda . "Should Healthcare Be Free? Essay on Medical System in America." October 12, 2018. https://ivypanda.com/essays/free-health-care-in-america/.
Bibliography
IvyPanda . "Should Healthcare Be Free? Essay on Medical System in America." October 12, 2018. https://ivypanda.com/essays/free-health-care-in-america/.

Writing a Medicine Essay: Guide, Types, Tips, and Topics

A medical essay is a written paper that is focused on a medical topic. It is mostly an essay written by medical students. Your instructor may assign this type of paper to gauge your understanding of a particular health issue. While it might seem simple, writing these essays is challenging, especially for first-timers. This is because they require scientific accuracy, clear undressing of the given topic, and clinical insights. In the essay, you are required to demonstrate your knowledge and skills of the various medical concepts and their application in the real world. This means that every claim and argument you make must be supported with scientific evidence.
If you are wondering how to write a medical essay, we will provide you with all the tips and steps you need to write a high-quality essay.
Different Types of Medical Essays
There are many types of medical essays you will come across in school that vary based on the purpose, subject matter, and formatting style. These are:
Argumentative Essays
These types of medical essays take a stance on medical issues and require the support of well-researched, accurate, and current information. An argumentative essay is usually assigned as a capstone project in your final years and requires lengthy and detailed research to establish your position on a topic.
When writing an argumentative medical essay, your goal should be to convince the readers to agree with your point of view by presenting a strong argument. Some of the topics you may cover include the impact of technology, the effectiveness of particular medical treatments, etc.
Compare and Contrast Essays
These types of essays deal with two or more subjects in a particular category of the medical field and compare their similarities and contrast their differences. Your instructor will assign a compare and contrast essay to challenge your analytical and comparative skills and see whether you can make meaningful arguments about a given topic.
Compare and contrast essays rely on factual analysis, so you must support all your arguments with sufficient scientific evidence. Additionally, it would be best if you used special transition words and phrases such as in comparison, by contrast, likewise, similarly, the same as, both, also, etc.
Expository Essays
Expository means intended to explain. This type of medical essay aims to explain a particular medical topic clearly and consciously. Expository essays require you to investigate a particular topic, evaluate the available evidence, expound on the claims, and explain a focused idea clearly.
Use accurate and current information from reliable sources when writing expository essays to ensure you provide well-structured, logical, and clear arguments.
Descriptive Medical Essays
This type of literature helps in communicating a particular information, for instance, a specific medical condition, treatment, theory or procedure, in a descriptive manner. Descriptive essays provide a comprehensive and effective description in a way that readers will feel like they are experiencing the subject firsthand.
To write descriptive essays, you must use words and phrases that pique curiosity to bring your narrative to life. Ensure you also integrate thoughts, feelings, smells, tastes and sounds into your essay.
Overall, descriptive medical essays help to provide an objective portrayal of a medical subject to help readers better and understand the complex topics in the medical world.
Overall, no matter which type of essay you are writing, there should be a clear and logical flow of information from one part of an essay to another.
Outline of a Medical Essay
Are you asking what are the parts of a medical essay?—the answer is simple. An essay on medicine must include the following parts: introduction, body paragraphs and conclusion.
Introduction
An introduction of a medical essay introduces your topic and provides some background information about the subject being discussed.
It also includes the reason for writing the essay and provides brief points of what you will cover in the body of the paper. An introduction should also include your thesis statement which offers a concise summary of your essay and state the claim you will be making in your paper.
Your introduction should be concise and quickly hook the readers to ensure they read the rest of the essay.
Body Paragraphs
The body section of your medical essay is where you delve into the main claim of your paper. It could have two supporting paragraphs or five. There is no limit to how many numbers of paragraphs you can write unless your professor provides a specific number.
When supporting your thesis statement with multiple sources, the best thing to do is to have only one paragraph per idea and source cited. For instance, if you are writing an argumentative medical essay, one paragraph should provide a single aspect of your arguments supported by credible evidence.
The conclusion of your medical essay should provide a summary of what you have discussed in the body of your paper. It contains three sections:
- A restatement of your thesis statement without using the exact wording.
- General conclusions and state why your essay is essential.
- The final part brings everything together clearly and concisely to show readers you have understood the topic under discussion.
Avoid bringing in any new information in the conclusion section of your paper. The goal here is to provide readers with a closure.
Use the following format to organize your essay:
1. Introduction
- Background information
- Thesis statement
2. Body Paragraphs
1. First point
- Introduction statement.
- Supporting evidence (facts, statistics, etc).
- Conclusion statement transitioning to the next paragraph.
2. Second point
- Supporting evidence (facts, statistics, etc.).
3. Third point
3. Conclusion
- Restatement of the thesis statement.
- General conclusion.
- Closing statement.
This is just a basic outline you can follow when writing your medical essay. Depending on the type of essay you are writing, you may need to include some information.
Steps for Writing a Great Medical Essay
Follow these steps when writing your medical essay. Remember, there are no right or wrong ways to write an essay. It can be a messy process as long as you ensure that there is a good flow of information.
Read the Assignment Prompt
Writing a high-quality health and medicine essay requires that you first understand your instructors' expectations. Therefore, begin by reading the prompt given, which will have all the information about the rules, guidelines and instructions that you must follow.
How well you write an essay can differentiate a high-quality medical essay from a low-quality paper. Your instructor will expect you incorporate relevant scientific evidence in your essay and demonstrate an understanding of it to show that you possess the right knowledge about the medical field.
Your instructor will also want to see whether you can accurately dissect the chosen topic into different components and explain it well to the readers.
So, by reading and understanding what is expected, you can clearly articulate your facts and express your ideas.
Chose a Great Medical Essay Topic
To write a great medical essay topic, you must choose an interesting topic that will be easy to write about. There are various interesting topics for medical essays that you can choose from, which range from various subjects in medicine.
Choose a topic that you are familiar with or one you will be able to write about. There are various interesting topics for a medical essay which you can choose from for your paper.
In addition to choosing an interesting topic, ensure you keep the following in mind:
- The topic of your choice should be relevant to the assignments.
- Think about the scope of the paper. Will you be writing about a specific medical topic or discussing medicine in general?
Once you have chosen a topic, research to locate information about it, begin by writing down what you already know about the topic, and then use that to develop probing questions such as why, what if, etc.
Identify keywords that are related to your topic, as they will help in locating specific information. At this point, it’s important to do background research about the topic to ensure that there is enough to write about it. Doing this will help you achieve a basic understanding of the chosen topic before delving deeper, which means you can formulate the topic and broaden or narrow it.
Conduct Research
Doing thorough research lays the foundation for a high-quality essay, as you will have sufficient information to take a critical approach to the chosen topic. So, go through the different types of scientific literature, such as PubMed, EMBASE, and Cochrane Library, to find scientific articles. These resources are credible and will give you the information needed to write a high-quality essay.
Remember, a medical essay seeks to understand your understanding of scientific knowledge and evidence acquired both in theory and practice. So, to be able to demonstrate this knowledge, you must have relevant, accurate information from a variety of credible sources.
Please note that there are two types of research you can conduct depending on the topic. Primary and secondary research. Primary research is where you collect information firsthand through methods such as interviews, questionaries etc. Secondary research, on the other hand, is where you obtain information from information collected by other researchers, such as books, journals, etc. This is the most common form of research because it saves you time, money, and energy, unlike primary research.
Create an Outline
Like other types of essays, your medical essay should have an outline that organizes your thoughts and ideas before writing. Your outline should tell readers what your essay will cover and ensure you prevent a clear and well-structured argument. In other words, your outline is a roadmap. When you get stuck during the writing process, it will help you get right back on track.
As mentioned, your medical essay outline has three main parts: Introduction, body paragraphs, and conclusion.
Some of the tips that can help you create a good outline for your essay on medicine.
- Begin by first writing several ideas that you intend to include in your essay on medicine. Think of these ideas as the skeleton of your paper.
Begin Drafting
Now that you have prepared adequately for the topic at hand, you can start writing. Start by writing your introduction, which begins with a hook to capture the reader's attention, followed by some background information about the topic, and then a thesis presentation.
However, if you want to capture all ideas and ensure you write an engaging introduction, write it after. There is no right or wrong way to do this, as long as your introduction achieves its intended purpose.
When writing the body paragraphs, ensure you support your ideas with accurate information from reliable sources. Include both in-text citations and a reference list or bibliographic section at the end of the paper.
For every piece of evidence you provide, ensure you expound on it and connect it to your ideas under the paragraph and to the overall argument. Do this by explaining, interpreting and expanding on your evidence. If you are providing a counterargument, debunk the evidence provided.
Ensure you have included as much information as possible to ensure the readers get a comprehensive understanding of the topic.
Revise and Edit Your Draft
Revising refers to looking at the essay from a fresh perspective. It is an ongoing process involving reviewing the arguments, evidence and presentations. Learning how to revise an essay will ensure that your essay meets all the criteria for medical paper writing and that it has addressed all the necessary points. Based on the revisions, you could alter or rewrite the ideas or arguments of your essay.
Editing, on the other hand, refers to improving the appearance of your essay by correcting grammar, spelling and function errors. The goal is to make your essay as clear and effective as possible.
When revising and editing, pretend to be one of your readers. Ask yourself whether you are satisfied with what you are reading.
Read your medical essay out loud to pick out any problems with unity and coherence. As you read, check for clarity and a good flow of your ideas. Check for areas that are confusing and redundant and ensure you correct them.
Medical Essay Topics
Here is a list of medical essay topics you can borrow to write your essay.
Argumentative Medical Essay Topics
- Is universal healthcare a fundamental right or a financial burden?
- The Gender Bias in Medical Research and Treatment: How It Affects Women’s Health
- Should people be compelled to donate their organs after death?
- Are Vaccines necessary for public health or an infringement on personal freedoms?
- Is medical marijuana a viable treatment option or a gateway drug?
- How can society break the barriers to seeking mental health treatment?
- Is obesity a result of personal choices or environmental factors?
- What can be done to combat this growing threat of antibiotic resistance
- Genetically modified organisms (GMOs) foods: Are they safe?
- Euthanasia: Is it compassionate or a violation of human dignity?
- Alternative medicine vs. conventional medicine: Which is more effective in overall health?
- Is low-fat better than low-carb?
- Negative Effects of Total Isolation on Physical and Mental Health.
- Mental Health Benefits Associated with Physical Activity.
Expository Medical Essay Topics
- Risk of postoperative atrial fibrillation in patients receiving red blood cell transfusion.
- What causes HIV/AIDS stereotypes?
- Challenges of precision medicine
- What are the ethics of genetics testing?
- The need for government intervention in negotiating drug prices
- Addressing health disparities among the African community.
- Mental health stigma is the barrier to seeking treatment.
- Implications of fast food joints.
- Role of education in promoting healthy eating habits among teenagers.
- Use of stem cells for cancer treatment.
- Incorporating alternative medicine into modern medicine.
- Controversy in the American healthcare system.
Descriptive Medical Essay Topics
- The importance of preventative medicine in maintaining good health.
- Importance of genetics in influencing the development of diseases.
- The impact of lifestyle choices on overall health and well-being.
- What's the link between mental health and physical health?
- The benefits of integrative medicine in treating chronic health conditions.
- The role of proper nutrition in preventing and treating illnesses.
- The effects of stress on the body and strategies for managing stress.
- The use of technology in healthcare delivery and an improving patient outcome.
- What are the challenges of healthcare access for low-income populations?
- Ethical considerations in end-of-life care and decision making.
- Benefits and drawbacks of health technology.
Compare and Contrast Medical Essays
- Western medicine vs traditional Chinese medicine.
- Conventional medicine vs. Alternative medicine.
- A holistic approach to health and wellness compared to allopathic medicine.
- Examine the benefits and drawbacks of prescription medications versus natural remedies for chronic health conditions.
- Preventive medicine vs. Reactive medicine.
- Health insurance: public vs. private.
- Generic drugs vs. brand name drugs.
- Assisted living vs. nursing homes.
- Telemedicine vs. in-person appointments.
- Change in lifestyle vs mental health medication.
- UK vs Us: Mental health treatment.
- Hospital patient care vs at-home patient care.
Tips for Writing a Good Medical Essay
Vary the length of the sentences.
Long sentences can be monotonous and lull readers to sleep. It is important to mix your essay with short sentences to make the readers feel like they are reading natural speech. This will persuade readers to stay invested in your essay's message.
Use Active Voice
The active voice is more direct and makes your health and medical essay easier to read, especially if you are writing about a complex topic. It creates a stronger and more direct tone that captures and maintains the reader's interest, which is important, especially when trying to convince readers about a particular topic.
Use Vivid Verbs
Use vivid verbs instead of weak verbs, which will just clutter your essay and make it difficult for readers to understand the messages. Vivid verbs help paint a clear picture of the topic, thus making your arguments more persuasive.
Final Word on Writing Medical Essays
It could be an essay about healthcare policy, the pathophysiology of a certain disorder (autism, genetic disorders, or chronic disorders), medical processes, or healthcare issues. Once you are assigned to write an essay on medicine topics, you need to take the steps we have outlined above. Go through the pre-writing, writing, and post-writing steps above and see for yourself your capabilities.
Remember, a great medical essay involves following a clear structure and incorporating clear arguments supported by information from reliable sources. By following the above steps and tips, you can write a great medical essay that communicates your ideas and provides insights into complex subjects in medicine.
If you are stuck and need a professional writer to handle your paper, you can trust our medicine writers. These astute writers are experienced in research writing and have a background in medicine. Sign up, place an order, and get everything done within the shortest turnaround time.
Struggling with
Related Articles

Epidemiology Research Essay: A Guide with Steps, Insights, & Tips
Best Nursing Topics and Ideas for Presentations

The Latest pediatric nursing research topics
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Healthcare Writing

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Subsections
How to build a better health system: 8 expert essays

We need to focus on keeping people healthy, not just treating them when they're sick Image: REUTERS/Rupak De Chowdhuri
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Global Future Council on Health and Healthcare
Introduction
By Francesca Colombo , Head, Health Division, Organisation for Economic Co-operation and Development (OECD) and Helen E. Clark , Prime Minister of New Zealand (1999-2008), The Helen Clark Foundation
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis . COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention . Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage , that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide , mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
OECD Economic Outlook 2020 , Volume 2020 Issue 1, No. 107, OECD Publishing, Paris
OECD Employment Outlook 2020 : Worker Security and the COVID-19 Crisis, OECD Publishing, Paris
OECD Health at a Glance 2019, OECD Publishing, Paris
https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf
OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris
Working for Health and Growth: investing in the health workforce . Report of the High-Level Commission on Health Employment and Economic Growth, Geneva.
Colombo F., Oderkirk J., Slawomirski L. (2020) Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries . In: Haring R., Kickbusch I., Ganten D., Moeti M. (eds) Handbook of Global Health. Springer, Cham.
2. Improving population health and building healthy societies in times of COVID-19
By Helena Legido-Quigley , Associate Professor, London School of Hygiene and Tropical Medicine
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale .
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.¹ Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.¹
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganés to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David's father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city's central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN's Agenda 2030 , Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
The stories of Maria, David and Ruben are real stories featured in the Documentary: The impact of COVID19 in urban outskirts, Directed by Jose A Guardiola. Available here. Permission has been granted to narrate these stories.
Buck, D., Baylis, A., Dougall, D. and Robertson, R. (2018). A vision for population health: Towards a healthier future . [online] London: The King's Fund. [Accessed 20 Sept. 2020]
Wilton Park. (2020). Healthy societies, healthy populations (WP1734). Wiston House, Steyning. Retrieved from https://www.wiltonpark.org.uk/event/wp1734/ Cohen B. E. (2006). Population health as a framework for public health practice: a Canadian perspective. American journal of public health , 96 (9), 1574–1576.
3. Imagine a 'well-care' system that invests in keeping people healthy
By Maliha Hashmi , Executive Director, Health and Well-Being and Biotech, NEOM, and Jan Kimpen , Global Chief Medical Officer, Philips
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).⁴,⁵ Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.

The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
Anderson, G. (2011). Responding to the growing cost and prevalence of people with multiple chronic conditions . Retrieved from OECD.
Institute for Health Metrics and Evaluation. GBD Data Visualizations. Retrieved here.
OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD. (2017). Obesity Update . Retrieved here.
Malik, V. S., Willett, W. C., & Hu, F. B. (2013). Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology , 9 (1), 13-27.
Lang, J., Cluff, L., Payne, J., Matson-Koffman, D., & Hampton, J. (2017). The centers for disease control and prevention: findings from the national healthy worksite program. Journal of occupational and environmental medicine , 59 (7), 631.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How much do OECD countries spend on prevention? Retrieved from OECD.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.
Richardson, A. K. (2012). Investing in public health: barriers and possible solutions. Journal of Public Health , 34 (3), 322-327.
Yong, P. L., Saunders, R. S., & Olsen, L. (2010). Missed Prevention Opportunities The healthcare imperative: lowering costs and improving outcomes: workshop series summary (Vol. 852): National Academies Press Washington, DC.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved here .
McDaid, D., F. Sassi and S. Merkur (Eds.) (2015a), “Promoting Health, Preventing Disease: The Economic Case ”, Open University Press, New York.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved from OECD.
4. Why e arly detection and diagnosis is critical
By Paul Murray , Head of Life and Health Products, Swiss Re, and André Goy , Chairman and Executive Director & Chief of Lymphoma, John Theurer Cancer Center, Hackensack University Medical Center
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund , typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.¹ During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.

Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes. Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology New early detection technologies can improve the ability to identify symptoms and diseases early: i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease. ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.⁴
4. Regulation and Intervention Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients' inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care. Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
OECD Health Working Papers No. 101 "How much do OECD countries spend on prevention" , 2017
World Health Organization; Global Health Observatory (GHO) data; https://www.who.int/gho/health_workforce/physicians_density/en/
Saving lives, averting costs; A report for Cancer Research UK, by Incisive Health, September 2014
Liquid Biopsy: Market Drivers And Obstacles; by Divyaa Ravishankar, Frost & Sullivan, January 21, 2019
Liquid Biopsies Become Cheap and Easy with New Microfluidic Device; February 26, 2019
How America’s 5 Top Hospitals are Using Machine Learning Today; by Kumba Sennaar, February 19, 2019
5. The business case for private investment in healthcare for all
Pascal Fröhlicher, Primary Care Innovation Scholar, Harvard Medical School, and Ian Wijaya, Managing Director in Lazard’s Global Healthcare Group
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap , increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets . Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.

Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
- Small market size . Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
- Talent . Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
- Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
- Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
- Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
- Economic growth rates . A growing middle class is expanding the potential market for healthcare products and services.
- Alignment of incentives . A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
- Emergence of National Health Insurance Schemes . South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products .
- Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
- Aggregation of existing players.
- Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
- Telemedicine . Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
- Cost effective diagnostics . Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly , and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
John E. Ataguba, Associate Professor and Director, University of Cape Town and Matthew Guilford, Co-Founder and Chief Executive Officer, Common Health
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs ,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India , forfeited Eid bonuses for nurses in Indonesia , and hospital bankruptcies in the United States . In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020 , and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries , and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically , incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. L essons in integrated care from the COVID-19 pandemic
Sarah Ziegler, Postdoctoral Researcher, Department of Epidemiology and Biostatistics, University of Zurich, and Ninie Wang, Founder & CEO, Pinetree Care Group.
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service . These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed . These strategies call for countries to:
- Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
- Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
- Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
- Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
- Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12: 6049–57.
- WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization, 2016.
- WHO. COVID-19 significantly impacts health services for noncommunicable diseases. June 2020.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicalbe diseases in the COVID-19 response. The Lancet. 2020. 395:1678-1680
- WHO. Framework on integrated people-centred health services. Geneva: World Health Organization, 2016.
8 . Why access to healthcare alone will not save lives
Donald Berwick, President Emeritus and Senior Fellow, Institute for Healthcare Improvement; Nicola Bedlington, Special Adviser, European Patient Forum; and David Duong, Director, Program in Global Primary Care and Social Change, Harvard Medical School.
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
1. United Nations General Assembly. Political declaration of the high-level meeting on universal health coverage. New York, NY2019.
2. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on. Institute of Health Equity;2020.
3. National Academies of Sciences, Engineering, and Medicine: Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: Improving health care worldwide. Washington, DC: National Academies Press;2018.
4. World Health Organization, Organization for Economic Co-operation and Development, World Bank Group. Delivering quality health services: a global imperative for universal health coverage. World Health Organization; 2018.
5. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196-e1252.
6. Ricci-Cabello I, Violán C, Foguet-Boreu Q, Mounce LT, Valderas JM. Impact of multi-morbidity on quality of healthcare and its implications for health policy, research and clinical practice. A scoping review. European Journal of General Practice. 2015;21(3):192-202.
7. Valtis YK, Rosenberg J, Bhandari S, et al. Evidence-based medicine for all: what we can learn from a programme providing free access to an online clinical resource to health workers in resource-limited settings. BMJ global health. 2016;1(1).
8. Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America . Washington, DC: National Academies Press 2012.
Medical School Examples

Craft a Winning Medical School Essay with Examples and Proven Tips
Published on: May 8, 2023
Last updated on: Jan 31, 2024

Share this article
Are you dreaming of becoming a doctor or a health care professional?
The first step towards achieving that goal is to get accepted into a top-tier medical school.
But with so many other qualified medical students competing for the same spot, how do you stand out from the crowd?
It all starts with your medical school essay.
Your essay is your opportunity to your unique qualities, experiences, and aspirations.
In this blog, we'll provide you with examples that will help you catch the attention of admissions committees.
From purpose to common mistakes to avoid, we'll cover everything you need to get accepted into the medical school of your dreams.
So, let's dive in!
On This Page On This Page -->
Types of Medical School Examples
Medical school essays come in many different forms, each with its own unique requirements and purpose.
In this section, we'll discuss some of the most common types of medical school essays and what you need to know to write them successfully.
Personal Statements
Personal statements are the most common type of medical school essay. They are usually a one-page essay that introduces you to the admissions officers.
It explains why you want to pursue medicine as a career. Personal statements should be engaging, and memorable, and show off your unique qualities.
An outline offers a framework to help you craft a compelling narrative that showcases your strengths and experiences.
Check out this personal statement example that can help future physicians getting into the schools of their dreams.
Medical School Personal Statement Examples pdf
Secondary Essays
Secondary essays are additional essays that some medical schools require in addition to the personal statement.
They often ask specific questions about your background, experiences, or interests. They give you an opportunity to show off your future patient care and problem-solving skills.
Here is a brief example of a secondary application medical school essay:

Paper Due? Why Suffer? That's our Job!
Diversity Essays
Diversity essays ask you to write about your experiences with diversity and how they have influenced you to pursue a career and your interest in medicine.
These essays are becoming increasingly common in medical school applications as schools strive to build a more diverse and inclusive student body.
Good Medical School Essay Examples
Are you struggling to write a standout medical school essay? They say that the best way to learn is by example. That's especially true when it comes to public health school essays.
We'll provide you with some of the best examples to help you craft an essay that will help your career in medicine.
Medical College Essay Examples
Personal Statement Medical School Examples Pdf
Medical School Covid Essay Examples
Challenging Medical School Essay Examples
Writing a medical school essay is more than just telling a story about yourself. It's an opportunity to demonstrate your critical thinking and analytical skills.
In this section, we'll highlight some of the challenging medical school essay examples. This will give you a sense of what admissions committees are looking for. You can learn how to exceed those expectations by writing a successful medical school essay.
Greatest Challenge Medical School Essay Examples
Successful Medicine Personal Statement Examples
Medical School Scholarship Essay Examples
Medical School Essay Examples for Different Schools
Each medical school has its own unique mission, values, and admissions criteria, and your essay should reflect that.
In this section, we'll explore how to tailor your medical school essay for different schools and showcase some examples of successful essays.
Letâs explore these Stanford and Harvard medical school essay examples:
Medical School Personal Statement Examples Harvard
Medical School Personal Statement Examples Stanford
Tips on Crafting an Excellent Medical School Personal Statement
The medical school personal statement is your opportunity to showcase your unique qualities and experiences.
Here are some tips to help you craft an excellent personal statement:

Start Early
Don't wait until the last minute to start writing your personal statement. Give yourself plenty of time to brainstorm, write, and revise your essay. Starting early also allows you to get feedback from mentors, professors, or peers.
Focus on Your Story
Your personal statement should tell a story that showcases your journey to medicine. Highlight the experiences and qualities that have led you to pursue a career in medicine. Tell them how you plan to use your skills to make a difference.
Be Specific
Use specific examples to illustrate your experiences and achievements. Don't just list your accomplishments, but show how they have prepared you for a career in medicine. Use concrete details to make your essay more engaging and memorable.
Show, Don't Tell
Instead of simply stating your qualities, show them through your experiences and actions. For example, donât say you're a team player. Describe a time when you worked effectively in a team to achieve a goal.
Tailor Your Essay to the School
As mentioned earlier, each medical school has its own unique mission and values. Tailor your personal statement to each school to demonstrate your fit with their program and values.
Mistakes to Avoid in a Medical School Personal Statement
When it comes to your medical school personal statement, there are some common mistakes you should avoid:
Avoid using cliched phrases and ideas that are overused in personal statements. Admissions committees want to see your unique perspective and experiences. They do not want generic statements that could apply to anyone.
Negativity
Don't focus on negative experiences or aspects of your life in your personal statement. Instead, focus on your strengths and how you have grown from challenges.
Lack of Focus
Make sure your personal statement has a clear focus and theme. Don't try to cover too many topics or experiences in one essay. Instead, focus on one or two experiences that are meaningful to you and illustrate your journey to medicine.
Too Formal or Informal Tone
Make sure your personal statement strikes the right tone. Avoid being too formal or using overly complex language. Also, avoid being too informal or using slang.
Plagiarism
Never copy someone else's personal statement or use a template to write your own. Admissions committees can easily spot plagiarism, and it will result in an immediate rejection.
Grammatical and Spelling Errors
Proofread your personal statement thoroughly for grammatical and spelling errors. Even a few small errors can detract from the overall quality of your essay.
Lack of Authenticity
Be true to yourself in your personal statement. Don't try to present an image of yourself that is not authentic or that you think the admissions committee wants to see. Be honest and genuine in your writing.
In conclusion, crafting a winning medical school essay is a crucial step toward securing admission to the medical school of your dreams.
This blog has provided examples of essays along with tips to craft an excellent medical school personal statement. By avoiding mistakes, you can increase your chances of standing out from the crowd and impressing the admissions committee.
Struggling with your medical school essays or college papers? Look no further!
Our college paper writing service specializes in crafting exceptional papers tailored to your academic needs, including medical school essays. And for an extra boost in your writing tasks, don't forget to explore our AI essay generator .
Elevate your academic performance with our medical school essay writing service and unlock the potential of our AI essay tools.
Get started today!
Frequently Asked Question (FAQs)
What is the ideal med school personal statement word limit.
There is no set length for a medical school personal statement, but most schools typically require a personal statement of 500-800 words.
How do I choose a topic for my medical school essay?
Choose a topic that showcases your unique perspective and experiences, and illustrates your journey to medicine. Consider what makes you stand out and what you are passionate about.
Should I mention my grades and test scores in my medical school essay?
It is not necessary to mention your grades and test scores in your medical school essay as they are already included in your application. Instead, focus on showcasing your unique qualities, experiences, and perspective.
Can I get help with writing my medical school essay?
Yes, there are various resources available to help you with writing your medical school essay. Consider seeking help from a writing tutor, career services office, or professional writing service like ours.
Nova A. (Literature, Marketing)
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Paper Due? Why Suffer? That’s our Job!
Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.
ORDER YOUR PAPER
15% off today
from a verified trusted writer

Mastering the Art of Writing a Health Care Essay on a Good Topic
'A healthy nation is a wealthy nation' - this famous proverb inspires many young people to pursue a career in healthcare, becoming nurses, physicians, therapists, etc. However, some of them fail to realize the responsibility that comes with such occupations. This may bring about a situation whereby colleges and universities turn out unqualified healthcare and nursing experts. To prevent it from happening, professors who teach respective disciplines assign their students the task of writing a health care essay. Being either an essay or research paper, it presents the students with a choice: to examine the problem on their own using various tools and equipment or analyze all available sources on the given research question, offering some personal findings.
14 Amazing Health Care Essay Topics with Introduction Examples
In your essay about health care, you may either talk about various diseases, symptoms, diagnosis, treatment, or methods used by doctors to help their patients, as well as their roles in general. In most cases, students should criticize the modern healthcare system as it really is in need of improvement. It is necessary that they provide some vivid real-life examples if they wish to convince their audience of their point of view.
Approaches to healthcare in the US, UK, and Australia differ, so you may focus on discussing their pros and cons in the essays about health care.
To help you understand which issues to discuss, we have listed the best health care essay topics below. You can also find short answers to each question.
Why is Healthcare Important to Society?
"Healthcare and medicine is a broad term that refers to a system involving maintenance and enhancement of medical services to cater to the health demands of human beings and other living creatures. The quality of healthcare services is one of the most critical factors that predetermines a country's well-being. The system usually varies depending on the healthcare policies of the region. In highly industrialized countries (i.e.countries of the First World), the system is advanced, with almost every citizen having unrestricted access to healthcare services. The low economic level in underdeveloped countries exerts an adverse impact on the healthcare system of these nations."
Is Healthcare a Right or a Privilege
"In the countries of the Third World, healthcare and medicine are not developed enough to save the lives of all of their citizens. Most of them cannot afford quality services, and that is the main difference between developed and underdeveloped countries as far as healthcare is concerned. Unlike poor people, the rich should make health their priority. However, they often neglect to do so, wasting almost all their money on things that harm their body, such as tobacco, alcoholic beverages, drugs, etc. In other words, they tend to have more bad habits, and they value their health less."
Overweight is Putting Strain on the Health Care in the United States
"Childhood obesity in the United States has reached epidemic proportions. This type of disorder has adverse effects on both physical and mental health, as obese kids tend to fall victim to school bullies. The worst consequence of being overweight is Diabetes Type II, and, unfortunately, more and more US children are facing this problem. The pivotal role in the increase in fat intake is played by environmental factors, tastes and preferences, and culture. Highly stressful activities like homework assignments may cause the child to eat more sweets, while their parents do nothing to restrict their consumption of sugar-rich foods. And finally, the lack of physical exercises also takes its toll."
Is Healthcare a Human Right?
"According to NCBI, healthcare is not a human right. To understand why it is important to define both terms. 'Human right' refers to a moral right of great significance that each human being should be entitled to. Dictionaries define healthcare as 'the act of taking prevention or important procedures to make a person's well-being better.' Healthcare is even more complex and confusing to define. Its meaning is too broad to be considered a human right. So, is there a person ultimately responsible for providing healthcare to the entire world? Insisting that healthcare is a human right is, therefore, wrong and pointless."
Should the Government Provide Health Care Insurance?
"The US government is not the only one responsible for providing healthcare insurance to all its citizens. It is only typical of the representatives of the political left to believe that the government should do that. All parties agree that health care is a valuable service, but the government has other important things to take care of. Rather than take care of medicine and nursing, the government's main goal should be to monitor and control the political and economic situation in the country. In fact, each organization has its goals, and so does the government. The government may protect the customer's freedom to buy goods and services by putting in place the corresponding laws and regulations. That is the best thing the US government can do as far as healthcare is concerned."
Causes and Effects of Health Care Crisis in America
"While urban population is more or less OK with its healthcare system, the rural areas of the US keep on suffering from what they call an American healthcare crisis. Hospitals in these regions continue to close down, while those that remain operational provide services of increasingly poor quality. More than 80 rural hospitals have shuttered during the last eight years because their personnel lacked the qualifications to cure patients properly. More than 700 hospitals are at high risk of being closed down, as they lack qualified healthcare professionals. Therefore, emergency medical services are becoming very important, because this is the only way of providing help to patients suffering from strokes, heart attacks, and other heart-related conditions."
Professionalism in Healthcare
"Being a doctor is the most responsible job in the world. It is also the most in-demand one, even though not always properly remunerated. In the underdeveloped countries, the doctor's salaries are among the lowest. In the US, the situation is much better, but still needs improvement in many respects. Medical personnel in this country are granted a license to invest long hours in research and diligent evaluation. Licensure is the way to guarantee the doctor's excellent skills and rich experience in a specific field. It is their willingness to place personal needs after the needs of the patient."
What Has Been the Impact of Medicare on the Healthcare System?
"Quality medicare and teamwork are the essential prerequisites of professional attitude and behavior. The most essential qualities of any medical expert are integrity, accountability, motivation, altruism, and empathy. This way the crucial trust between the patient and professionals is developed. Advanced interpersonal and communication skills impact the quality of medicare as well. Over the past 20 years, we have been witnessing the resurgence of interest in professional training and fair evaluation in the US. It is, therefore, experienced doctors' job to support and guide young professionals on their way to success."
Why Do You Want to Pursue a Career in Healthcare?
"Several factors, the salary being probably the most important one, motivate a lot of young people to choose a career in healthcare. Everyone knows that good medical experts are valued extremely high in the United States. Jobs in healthcare guarantee great opportunities and full security. Quite a few students consider helping other people their priority because they lost their loved ones to fatal diseases. They want to contribute to the medical field by finding a cure to the most complicated disorders some day. And finally, a career in healthcare provides an excellent opportunity to live and work in different parts of the world."
Cultural Diversity in Healthcare
"The purpose of this research paper is to identify basic nuances and issues of cultural diversity in the context of medical treatment, as well as offer solutions aimed at preventing said issues. The main focus is on communication as a culture-based phenomenon, correlation between the patient's progress and expert's treatment, and possible communication characteristics that act as obstacles between healthcare staff and patients. Of the two theoretical approaches used in the study, the first one relates to the information processing, while the second one concerns changing behaviors and interpretation."
Healthcare in America
"Though considered one of the best in the world, the American health care system still has some catching up to do with other countries, including the US's closest neighbor Canada. The US lacks a uniform health system that could offer universal healthcare coverage. Its healthcare system can be referred to as hybrid as it is funded from different sources, such as private funds (48%), households funds (28%), and private businesses funds(20%). The majority of medical and nursing services in this country are privately-owned, even if they are financed by the government. What makes this system stand out from the rest of the world is its great professional staff."
Healthcare in Canada
"Canada has implemented one of the best healthcare reforms in the world. Over the past 4 decades, the country has introduced a number of improvements, making medical treatment affordable for almost every citizen. Urgent and essential health care services are provided based on the needs rather than financial opportunities. This fact alone shows how generous the Canadian government and its healthcare professionals are. When it comes to healthcare, they value fairness and equality more than other nations do. The local healthcare system keeps getting improved as the nation's population increases. It is also important to acknowledge that the very essence of healthcare is also undergoing change."
Public vs. Private Healthcare Sectors
"When comparing the public and private healthcare sectors, it is impossible to ignore the NHS or the National Health Service. The organization, whose staff is made up mostly of primary care nurses or emergency care nurses, provides free health care services to the UK population. That is the reason why the job of Registered Nurse is so prevalent in local healthcare institutions. Specialized caregivers account for another sizeable portion of the healthcare sector. Each young professional is provided with a lot of opportunities for professional development and further career growth.
Communication in Healthcare
"Communication is one of the most important factors in healthcare. Without knowing the details of the patient's conditions and their medical history, the doctor will not be able to make a proper diagnosis. The evidence obtained in the course of this study indicates that there's a direct correlation between the medical representative's communication skills and the patient's willingness to follow the doctor's advice. The doctor's duty is to help the patient control their chronic condition all by themselves, if needed, as well as acquire preventive behaviors. The doctor should not simply cure the patient, but rather teach them some significant lessons to help them remain healthy."
Hopefully, these samples of papers on medicine and nursing will help you choose the hottest topics and best introductions to your essays and research papers. Still having problems? We can offer affordably-priced assistance with any sort of academic writing, including an essay on health care! Try our services at any time, and you won't be disappointed!
- Stats & Feedback
Have your tasks done by our professionals to get the best possible results.
NO Billing information is kept with us. You pay through secure and verified payment systems.
All papers we provide are of the highest quality with a well-researched material, proper format and citation style.
Our 24/7 Support team is available to assist you at any time. You also can communicate with your writer during the whole process.
You are the single owner of the completed order. We DO NOT resell any papers written by our expert
All orders are done from scratch following your instructions. Also, papers are reviewed for plagiarism and grammar mistakes.
You can check the quality of our work by looking at various paper examples in the Samples section on our website.
Love reading, but my essays leave a lot to be desired. Ordering from you, I've actually improved my skills a bit, thanks a lot.
I could not expect that you would complete all calculations right, moreover your writer explained in details how he did it and he also guided me with all additional questions I had. Thank you for my writer!
- High School $11.23 page 14 days
- College $12.64 page 14 days
- Undergraduate $13.2 page 14 days
- Graduate $14.08 page 14 days
- PhD $14.59 page 14 days
Our service has received a swarm of positive reviews, around 596 testimonials proving our success rate to be 9.7 / 10 .
"Finance is one of my favorite courses, but that research paper was really tight. I'm so grateful my writer was attentive to all the requirements and did everything perfectly!"
"I hate writing any analysis-related papers. Your service is my salvation! Can relax without worries that my prof will be unsatisfied with my ideas. Also, one of the cheapest services I've used!"
"I don't have time to look through archives and all that just to find out who said what in what place that time in Spain. Thankfully, the writer assigned to me did all the job for me, and did it so well that I got an A! Thank you, definitely bookmarking your site."
"Referencing was weak. I liked the paper you wrote but I had to edit my paper to change some quotes. I would ask you to revise it but had no time. Next time I plan to use you, will for sure order in advance. "
"Thank you for the research paper on Saudi legal system. It was rather good and only some parts needed revision. The writer was attentive and fixed the paper when I requested. your support is amazing as well! "
"I would like to thank you with all my heart. It was a miracle that you managed to complete my huge thesis for such short period of time. What you've done was actually enough. Will need your help soon with my dissertation. See you!"
- Essay Writing
- Term Paper Writing
- Research Paper Writing
- Coursework Writing
- Case Study Writing
- Article Writing
- Article Critique
- Annotated Bibliography Writing
- Research Proposal
- Thesis Proposal
- Dissertation Writing
- Admission / Application Essay
- Editing and Proofreading
- Multiple Choice Questions
- Group Project
- Lab Report Help
- Statistics Project Help
- Math Problems Help
- Buy Term Paper
- Term Paper Help
- Case Study Help
- Complete Coursework for Me
- Dissertation Editing Services
- Marketing Paper
- Bestcustomwriting.com Coupons
- Edit My Paper
- Hire Essay Writers
- Buy College Essay
- Custom Essay Writing
- Culture Essay
- Argumentative Essay
- Citation Styles
- Cause and Effect Essay
- 5 Paragraph Essay
- Paper Writing Service
- Help Me Write An Essay
- Write My Paper
- Research Paper Help
- Term Papers for Sale
- Write My Research Paper
- Homework Help
- College Papers For Sale
- Write My Thesis
- Coursework Assistance
- Custom Term Paper Writing
- Buy An Article Critique
- College Essay Help
- Paper Writers Online
- Write My Lab Report
- Mathematics Paper
- Write My Essay
- Do My Homework
- Buy a PowerPoint Presentation
- Buy a Thesis Paper
- Buy an Essay
- Comparison Essay
- Buy Discussion Post
- Buy Assignment
- Deductive Essay
- Exploratory Essay
- Literature Essay
- Narrative Essay
- Opinion Essay
- Take My Online Class
- Reflective Essay
- Response Essay
- Custom Papers
- Dissertation Help
- Buy Research Paper
- Criminal Law And Justice Essay
- Political Science Essay
- Pay for Papers
- College Paper Help
- How to Write a College Essay
- High School Writing
- Personal Statement Help
- Book Report
- Report Writing
- Cheap Coursework Help
- Literary Research Paper
- Essay Assistance
- Academic Writing Services
- Coursework Help
- Thesis Papers for Sale
- Coursework Writing Service UK
2 Med School Essays That Admissions Officers Loved
Here are tips on writing a medical school personal statement and examples of essays that stood out.
2 Great Med School Personal Statements

Getty Images
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality.
A personal statement is often a pivotal factor in medical school admissions decisions.
"The essay really can cause me to look more deeply at the entire application," Dr. Stephen Nicholas, former senior associate dean of admissions with the Columbia University Vagelos College of Physicians and Surgeons , told U.S. News in 2017. "So I do think it's pretty important."
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality, according to Dr. Barbara Kazmierczak, director of the M.D.-Ph.D. Program and a professor of medicine and microbial pathogenesis with the Yale School of Medicine.
“The passion that the writer is bringing to this topic tells us about the individual rather than the topic that they’re describing, and the essay is the place for us to learn about the applicant – who they are and what experiences have brought them to this point of applying to medical school,” she told U.S. News in 2017.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School , says personal statements help medical schools determine whether applicants have the character necessary to excel as a doctor. "Grit is something we really look for," she says.
Evidence of humility and empathy , Rudeen adds, are also pluses.
Why Medical Schools Care About Personal Statements
The purpose of a personal statement is to report the events that inspired and prepared a premed to apply to medical school, admissions experts say. This personal essay helps admissions officers figure out whether a premed is ready for med school, and it also clarifies whether a premed has a compelling rationale for attending med school, these experts explain.
When written well, a medical school personal statement conveys a student's commitment to medicine and injects humanity into an admissions process that might otherwise feel cold and impersonal, according to admissions experts.
Glen Fogerty, associate dean of admissions and recruitment with the medical school at the University of Arizona—Phoenix , put it this way in an email: "To me, the strongest personal statements are the ones that share a personal connection. One where a candidate shares a specific moment, the spark that ignited their passion to become a physician or reaffirmed why they chose medicine as a career."
Dr. Viveta Lobo, an emergency medicine physician with the Stanford University School of Medicine in California who often mentors premeds, says the key thing to know about a personal statement is that it must indeed be personal, so it needs to reveal something meaningful. The essay should not be a dry piece of writing; it should make the reader feel for the author, says Lobo, director of academic conferences and continuing medical education with the emergency medicine department at Stanford.
A great personal statement has an emotional impact and "will 'do' something, not just 'say' something," Lobo wrote in an email. Admissions officers "read hundreds of essays – so before you begin, think of how yours will stand out, be unique and different," Lobo suggests.
How to Write a Personal Statement for Medical School
Lobo notes that an outstanding personal statement typically includes all of the following ingredients:
- An intriguing introduction that gets admissions officers' attention.
- Anecdotes that illustrate what kind of person the applicant is.
- Reflections about the meaning and impact of various life experiences .
- A convincing narrative about why medical school is the logical next step.
- A satisfying and optimistic conclusion.
"You should sound excited, and that passion should come through in your writing," Lobo explains.
A personal statement should tie together an applicant's past, present and future by explaining how previous experiences have led to this point and outlining long-term plans to contribute to the medical profession, Lobo said during a phone interview. Medical school admissions officers want to understand not only where an applicant has been but also the direction he or she is going, Lobo added.
When premeds articulate a vision of how they might assist others and improve society through the practice of medicine, it suggests that they aren't self-serving or simply interested in the field because of its prestige, Lobo says. It's ideal when premeds can eloquently describe a noble mission, she explains.
Elisabeth Fassas, author of "Making Pre-Med Count: Everything I Wish I'd Known Before Applying (Successfully) to Medical School," says premeds should think about the doctors they admire and reflect on why they admire them. Fassas, a first-year medical student at the University of Maryland , suggests pondering the following questions:
- "Why can you really only see yourself being a physician?"
- "What is it about being a doctor that has turned you on to this field?"
- "What kind of doctor do you imagine yourself being?"
- "Who do you want to be for your patients?"
- "What are you going to do specifically for your patients that only you can do?"
Fassas notes that many of the possible essay topics a med school hopeful can choose are subjects that other premeds can also discuss, such as a love of science. However, aspiring doctors can make their personal statements unique by articulating the lessons they learned from their life experiences, she suggests.
Prospective medical students need to clarify why medicine is a more suitable calling for them than other caring professions, health care fields and science careers, Fassas notes. They should demonstrate awareness of the challenges inherent in medicine and explain why they want to become doctors despite those difficulties, she says.
Tips on Crafting an Excellent Medical School Personal Statement
The first step toward creating an outstanding personal statement, Fassas says, is to create a list of significant memories. Premeds should think about which moments in their lives mattered the most and then identify the two or three stories that are definitely worth sharing.
Dr. Demicha Rankin, associate dean for admissions at the Ohio State University College of Medicine , notes that a personal statement should offer a compelling portrait of a person and should not be "a regurgitation of their CV."
The most outstanding personal statements are the ones that present a multifaceted perspective of the applicant by presenting various aspects of his or her identity, says Rankin, an associate professor of anesthesiology.
For example, a premed who was a swimmer might explain how the discipline necessary for swimming is analogous to the work ethic required to become a physician, Rankin says. Likewise, a pianist or another type of musician applying to medical school could convey how the listening skills and instrument-tuning techniques cultivated in music could be applicable in medicine, she adds.
Rankin notes that it's apparent when a premed has taken a meticulous approach to his or her personal statement to ensure that it flows nicely, and she says a fine essay is akin to a "well-woven fabric." One sign that a personal statement has been polished is when a theme that was explored at the beginning of the essay is also mentioned at the end, Rankin says, explaining that symmetry between an essay's introduction and conclusion makes the essay seem complete.
Rankin notes that the author of an essay might not see flaws in his or her writing that are obvious to others, so it's important for premeds to show their personal statement to trusted advisers and get honest feedback. That's one reason it's important to begin the writing process early enough to give yourself sufficient time to organize your thoughts, Rankin says, adding that a minimum of four weeks is typically necessary.
Mistakes to Avoid in a Medical School Personal Statement
One thing premeds should never do in an admissions essay is beg, experts say. Rankin says requests of any type – including a plea for an admissions interview – do not belong in a personal statement. Another pitfall to avoid, Rankin says, is ranting about controversial political subjects such as the death penalty or abortion.
If premeds fail to closely proofread their personal statement, the essay could end up being submitted with careless errors such as misspellings and grammar mistakes that could easily have been fixed, according to experts. Crafting a compelling personal statement typically necessitates multiple revisions, so premeds who skimp on revising might wind up with sloppy essays, some experts say.
However, when fine-tuning their personal statements, premeds should not automatically change their essays based on what others say, Fogerty warns.
"A common mistake on personal statements is having too many people review your statement, they make recommendations, you accept all of the changes and then – in the end – the statement is no longer your voice," Fogerty wrote in an email. It's essential that a personal statement sound like the applicant and represent who he or she is as a person, Fogerty says.
Dr. Nicholas Jones, a Georgia-based plastic and reconstructive surgeon, says the worst error that someone can make in the personal statement is to be inauthentic or deceptive.
"Do not lie. Do not fabricate," he warns.
Jones adds that premeds should not include a story in their personal statement that they are not comfortable discussing in-depth during a med school admissions interview . "If it's something too personal or you're very emotional and you don't want to talk about that, then don't put it in a statement."
Medical School Personal Statement Examples
Here are two medical school admissions essays that made a strong, positive impression on admissions officers. The first is from Columbia and the second is from the University of Minnesota. These personal statements are annotated with comments from admissions officers explaining what made these essays stand out.
Searching for a medical school? Get our complete rankings of Best Medical Schools.
Tags: medical school , education , students , graduate schools
Popular Stories
Top Business Schools

Student Loans

Morse Code: Inside the College Rankings

Paying for College

You May Also Like
A guide to executive mba degrees.
Ilana Kowarski and Cole Claybourn May 24, 2024
How to Choose a Civil Rights Law School
Anayat Durrani May 22, 2024
Avoid Procrastinating in Medical School
Kathleen Franco, M.D., M.S. May 21, 2024

Good Law School Recommendation Letters
Gabriel Kuris May 20, 2024

Get Accepted to Multiple Top B-schools
Anayat Durrani May 16, 2024

Premeds and Emerging Medical Research
Zach Grimmett May 14, 2024

How to Get a Perfect Score on the LSAT
Gabriel Kuris May 13, 2024

Premeds Take 5 Public Health Courses
Rachel Rizal May 7, 2024

Fortune 500 CEOs With a Law Degree
Cole Claybourn May 7, 2024

Why It's Hard to Get Into Med School
A.R. Cabral May 6, 2024

The Benefits and Challenges of Socialized Medicine
This essay about socialized medicine examines its role in providing universal healthcare access, transcending wealth and privilege to ensure equitable health services for all. It highlights the benefits of health equity and cost control while addressing challenges such as funding, political opposition, and bureaucratic inefficiencies. The narrative explores both the promise and obstacles of socialized medicine, emphasizing its potential to transform the healthcare landscape despite the hurdles it faces.
How it works
In the complex framework of healthcare systems, socialized medicine stands out as a bold initiative, infusing the narrative of access with vibrant inclusivity while navigating the stormy seas of controversy. This intricate narrative intertwines numerous benefits and challenges, crafting a story of healthcare evolution marked by both admiration and apprehension.
At its essence, socialized medicine epitomizes the noble aspiration of universal healthcare, transcending the confines of wealth and privilege. By eliminating financial barriers, it heralds an era where medical facilities open their doors to all, embracing every individual with healthcare services.
In this egalitarian vision, the threat of financial catastrophe fades, replaced by the comforting assurance that one’s socioeconomic status will not determine the quality of care they receive.
In the grand orchestration of health equity, socialized medicine serves as a steadfast conductor, harmonizing a melody of accessibility for all. Marginalized communities are no longer relegated to the fringes of healthcare access, as the beacon of universal coverage shines brightly, guiding the way toward a more just and equitable healthcare landscape. In this radiant vision, the vast gap between privilege and poverty narrows, fostering a society where the right to health is upheld as an unalienable birthright.
Yet, amidst the chorus of praise, discordant notes of dissent resonate through the discourse. The call for fiscal responsibility echoes, its tone tinged with concern over the immense challenge of funding such a monumental endeavor. The shadow of taxation looms large, casting doubt on the feasibility of sustaining this lofty vision without straining the state’s finances.
Furthermore, the political arena becomes a battleground, where entrenched interests vie for dominance. Private insurers, pharmaceutical giants, and vested stakeholders act as defenders of the status quo, wary of the transformative potential that socialized medicine represents. Armed with the tools of lobbying and misinformation, they wage an unrelenting campaign to erode public support and maintain the existing order.
Yet, perhaps the most formidable challenge lies within the labyrinthine corridors of bureaucracy. Here, the machinery of governance grinds slowly, entangled in a web of red tape and administrative obstacles. Long wait times and bureaucratic inefficiencies threaten to undermine the very foundation of socialized medicine, casting doubt on its capacity to provide timely and effective care.
In the arena of innovation, socialized medicine faces another test. The swift advance of technological progress heralds a new era of healthcare delivery, where precision medicine and digital therapeutics promise to revolutionize patient care. Yet, amidst the excitement of progress, the risk of stagnation looms, threatening to stifle innovation and consign patients to outdated treatments and practices.
In conclusion, the narrative of socialized medicine is one of victory and challenge, a story of hope and difficulty woven into the fabric of healthcare discourse. Its benefits are numerous, offering the promise of universal access, health equity, and cost control. Yet, its journey is fraught with obstacles, from the bureaucratic maze to political opposition and the imperative of fiscal responsibility. Ultimately, the future of socialized medicine hangs in the balance, uncertain yet filled with the potential to transform the healthcare landscape for generations to come.
Cite this page
The Benefits and Challenges of Socialized Medicine. (2024, May 28). Retrieved from https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/
"The Benefits and Challenges of Socialized Medicine." PapersOwl.com , 28 May 2024, https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/
PapersOwl.com. (2024). The Benefits and Challenges of Socialized Medicine . [Online]. Available at: https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/ [Accessed: 29 May. 2024]
"The Benefits and Challenges of Socialized Medicine." PapersOwl.com, May 28, 2024. Accessed May 29, 2024. https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/
"The Benefits and Challenges of Socialized Medicine," PapersOwl.com , 28-May-2024. [Online]. Available: https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/. [Accessed: 29-May-2024]
PapersOwl.com. (2024). The Benefits and Challenges of Socialized Medicine . [Online]. Available at: https://papersowl.com/examples/the-benefits-and-challenges-of-socialized-medicine/ [Accessed: 29-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
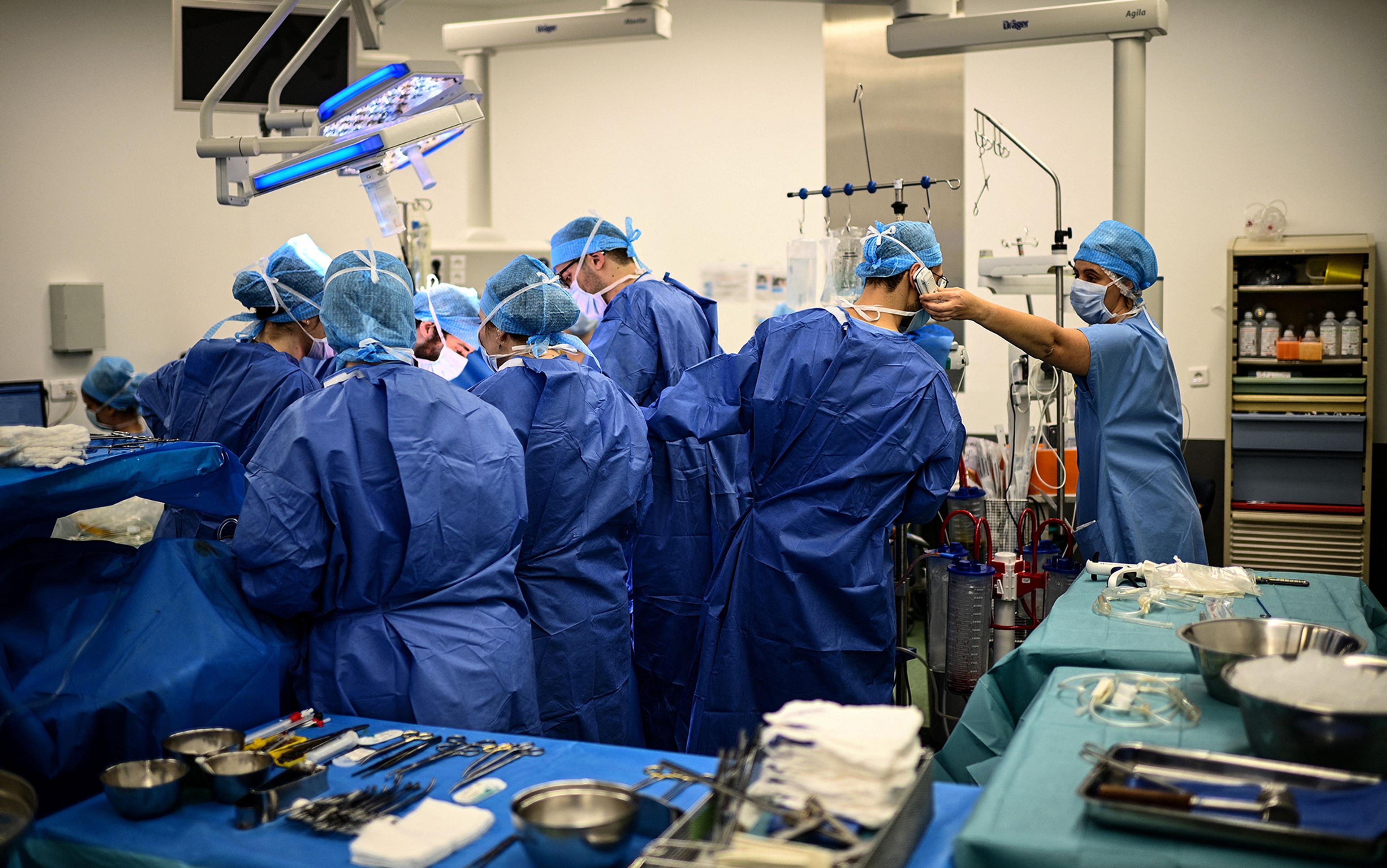
After assessing the lungs of a deceased patient, the thoracic surgeon Thomas Charrier (second from right) gives the green light for transplantation to his colleagues on the phone at the Foch hospital in Suresnes, Paris. This and all photos below taken on 9 December 2022 by Christophe Archambault/AFP. Courtesy Getty Images
Last hours of an organ donor
In the liminal time when the brain is dead but organs are kept alive, there is an urgent tenderness to medical care.
by Ronald W Dworkin + BIO
My patient was dead before I even saw her. She had been in a car accident. Now she was scheduled for organ donation.
She was called an ‘ASA 6’. To estimate operative risk, the American Society of Anesthesiologists (ASA) has a classification system built around how sick a patient is, ranging from a healthy ASA 1 to a moribund ASA 5, the latter meaning someone is not expected to live 24 hours. When the system was created in the mid-20th century, a sixth class for dead people seemed pointless. Death was known to the dead only, and life to the living only, and between the two there had been no bridge. When the definition of death changed in the late 1960s, making it possible for a person to be ‘brain dead’ but with organs still very much alive and available for donation, a bridge appeared and a sixth class was created in the early 1980s. Since 1988, when officials started collecting organ transplant data, almost a million organ transplants have been performed in the United States. Most of the organs have come from brain-dead donors. In 2021 alone, the US had almost 10,000 such donors.
When told of my upcoming case, I had mixed feelings. On the one hand, being in perfect health, unaccustomed to suffering and therefore easily disconcerted by the thought of death, I was horrified. My attitude toward death was like that of a young person standing blindfolded and tied to a post, awaiting a volley from a firing squad. The whole concept made my blood run cold. Yet the case also aroused in me a feeling of relief. Simply put, there was no risk of malpractice, as my patient was already dead. Many anaesthesiologists have such self-centred thoughts when taking care of ASA 6 patients.
I n her early 30s, she had a youthful face, without the traces of severe illness that ICU patients typically have. With her hair wrapped inside a bright, polka-dotted kerchief, she gave off an expression of almost pleasant, good-humoured cheeriness.
Who was this young person whose life had been tragically snuffed out? I jabbed into every crack of her medical record to find out. But little had been written down. Both her life and death seemed simple enough to be chronicled in a few lines. Something had happened inside her brain with the car accident, and the end came.
We wheeled her toward the operating room. Before departing, I pulled the sheet over her exposed feet. Why? I had an objection to her being dead, but I had an even more serious objection to her being undignified. With my patient still partly in the world of the living, I wanted to keep a place for her in the part that pretends to be genteel.
Six hours she had been officially dead. Now she had re-entered the world of the living
When we arrived in the operating room, something turned over inside me, sank, and went cold. After all, she was dead. The day before, she was as whole as me – and now look. She would never rise again.
After we moved her from the gurney to the operating table, the doctors and nurses, so used to taking care of living patients, stared at one another stupidly, as if not knowing why they had come together or why they stood around the table. For a brief moment, each one of us likely had the same supernatural vision, how for the past six hours, after being declared brain dead, this woman had lain under the measureless power of death. Six hours she had been officially dead. Six times had the hour hand on the clock moved – and she had lain dead. Now she had re-entered the world of the living. I would support her blood pressure and pulse. I would make her blood bright red with oxygen. Indeed, she might even wake up and look at us, I fantasised. She might be raised from the dead.

Ghoulish thinking, yet I do not write about this case to be ghoulish. Nor am I trying to stake out a new position in the bioethics debate. My purpose is more practical. Today, artificial intelligence (AI) looms over medical practice. Although unlikely to replace doctors completely, AI makes some medical activities especially ripe targets for takeover, including the harvesting of organs from brain-dead donors. And why not? Bedside manner and the common touch cease to be concerns. Using AI machines rather than doctors to harvest organs also promises to save money.
Yet this impersonal, nonhuman method of organ retrieval may discourage people from becoming organ donors , or from letting dead relatives become so, thereby exacerbating the current organ shortage. People will see pictures of organ retrieval being carried on all around by inanimate machinery in a room completely abandoned by human beings. Bodies will be brought in and sent out, while the invisible, sleepless work of the machines goes on. ‘Please, tell me this is not my end,’ people will fret privately. And they will resist consenting to organ donation.
O rgan retrieval can take place at odd hours because the time between retrieval and transplantation must be minimised. A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day.
Although donors are dead, managing their anaesthesia can be tricky. To keep their organs healthy, their physiology must be carefully attended to, yet brain death affects each organ system differently. High intracranial pressure can lead to an enormous outpouring of adrenaline, which can injure the heart and other organs as circulation fails. Brain death can cause pulmonary oedema (fluid in the lungs), making it hard to oxygenate the blood, thereby damaging the organs by a second route. Brain death also wreaks havoc on the body’s endocrine system, causing vital hormone levels to fall and damaging organs by a third route.
My patient lay stretched out on the table. The room was silent, as I had not yet placed any vital sign monitors on her body. It was a sinister silence. The monitors typically emit sounds that resemble the unconcerned twitter of birds. In an operating room, they symbolise life. Their absence suggests that a patient is not alive. In fact, mine wasn’t.
Nature will never permit anyone to know the exact point where brain death becomes real death
Ready to cut, the surgeon spoke through his headphones to surgeons in other cities waiting for the organs. The rest of us said nothing as he gave them an estimated time of arrival. The team had a real need for a stout word in these last few moments before the operation began. Sensing the mood, the surgeon said some dignified things about how our patient was giving other people a chance to live. Everyone nodded in agreement. He seemed thankful and sincere, yet he had to be that way for, at such a moment, anyone with even a modicum of intelligence would have felt anything else as an affront.

The surgeon cut into the patient’s chest. Almost immediately the patient’s heart rate and blood pressure jumped. It resembled the powerful surge of life that comes during a period when a person’s very existence and survival are at stake. The jump originated in a spinal reflex that stimulated the woman’s sympathetic nervous system below the level of the brain. Still, it seemed a manifestation of her will to live. Even more so when her hand moved – a sure sign of life! But that, too, was mediated through a spinal reflex.
I gave the patient some anaesthetic gas. I also gave her some opioids. Why the latter? After all, a dead patient doesn’t feel pain. In part because opioids help to lower heart rate and blood pressure directly, but also, I must admit, because I thought my patient might still be a ‘little alive’, whatever that means, and therefore in pain. Irrational on my part, yes, but the secret of life, including the definition of life, still remains the deepest and most mysterious one. Here Nature permits no eavesdroppers; never will she permit anyone to know the exact point where brain death becomes real death. At this, she draws a veil. I wanted to hedge my bets.
The woman’s blood pressure soon dropped too low. I poured fluid into her intravenous line. In the meantime, the surgeon moved hurriedly to extract her heart, clamping the large blood vessels leading both to and from it. Our fast pace betrayed another incongruence. Speed is thought to be a bit unrefined in an operating room. True, it is needed to save money, but ideally the operating room is an ordered world with calm transitions, a world without haste, except during an emergency to save a patient’s life. The visibly hasty fashion in which I and the surgeon worked made it seem like one of those urgent situations. In fact, I was trying to keep her circulation going long enough for the surgeon to tear her heart out.
I transfused a unit of blood, as excessive blood clotting, common after brain death, had made her dangerously anaemic. I turned on the warming mattress lying underneath her to keep her body temperature from dropping below 36 degrees Celsius. Brain death interferes with the body’s ability to regulate temperature, and the resulting hypothermia poses a risk to the organs. Finally, I gave her insulin to control her blood sugar level, as brain death often causes blood sugar to rise. All of these are routine lifesaving measures. In the past, I had used them to fight off death in my sickest patients, but here I had to remind myself that my patient was already dead.
T he surgeon removed her heart. The irrevocable instant had come. It was as when a train starts with a violent jerk, as if to overcome a disinclination to change its state of inertia. For many in the operating room, this was the moment when the woman’s life really ended.
A minute before, I had heard the melodies of the electrocardiogram (EKG) and pulse oximeter without really thinking about them. An anaesthesiologist’s ear is so capable of adapting itself that a continuous din, like the noise of a street or the rushing sound of a river, adjusts itself completely to their consciousness. But the unexpected halt in the sounds startled me into listening – and looking. I stared over the ether screen into the woman’s now-vacant chest cavity. It was shameful and terrible to gaze upon. Part of me felt as if I had abetted a murder around the corner.
I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate
The surgeon injected the heart with cold preservative and put it in a box. His next target was the lungs. He asked me to manually give the woman one last deep breath so that he could confirm that all parts of her lungs had been expanded before their removal. The breath I gave her was slow and gentle, like a sigh. Indeed, medically speaking, it was a sigh. On ventilators, there is a function labelled ‘sigh’ which, when pressed, gives a patient a single sustained deep breath to open up the lung’s small air sacs. Almost proudly, I imagined the sigh I gave this woman to be more human than what a machine could give. Compressing the anaesthesia bag with my hand, I imagined how she might have sighed in the past, on her own, in the face of some bitter reality, some trick or force of fate, crushing her heart but also uplifting her. I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate, a deep breath that begins with disappointment, passes into resignation, and ends in acceptance. I crafted that last sigh as if it were the epilogue to a tragedy.
When the woman exhaled her last bit of sigh, I removed her breathing tube. The surgeon took out her lungs and stapled her windpipe shut. At this point, there was little for me to do, and my inactivity plunged me into a sense of nothingness. I felt I was going to gag on my thoughts if I didn’t do something. I walked away from my patient to look inside a cupboard. I opened a few drawers. Then I felt badly for doing so. Although one of us was dead, still there seemed to be two of us here. It’s as if the woman and I were friends and I didn’t want to leave my friend. I went back and stood by her head.
The surgical team removed the rest of her organs and the case finished. Here the woman and I reached a parting of the ways. I stared at her face seriously and fixedly as though I wanted to look my fill and imprint forever on my memory her image. I cannot recall for how long I looked. Great moments are always outside of time.
Our relationship proved significant. Nothing is more characteristic of the total lack of spiritual connection between myself and other patients than the fact that I have forgotten most of their names and faces. But this woman’s name and face I remember. And when I speak of memory, I do not mean something akin to a register kept in a well-ordered office, a place in which documents are laid away in store. I mean something submerged in the rushing stream of my blood, memory as a living organ in which every feeling experienced that day retains its natural essence, its original intensity, its primary historical form.

M y patient lived longer than what her death certificate says. She lived in my mind during the organ retrieval and continues to live in my memory because I do not want to forget her, and because I cannot forget her. Although I know only her general outlines, our connection satisfies some deep law of harmony underlying all life, in which every person must enter into communion with another person in order fully to live. By that standard, my patient lived past her official time of death.
When AI replaces the anaesthesiologist during organ retrievals, you, the organ donor, will not live any longer than what’s listed on your death certificate. The air inside the operating room is already cold, dry and unpleasant. Various monitors will sit on the top shelf of the anaesthesia machine, regulated by AI. Their special melodic rings will no longer be necessary, as their data will be sent along to AI in silence. Care will be delivered without the mediation of human minds, senses or hands.
Before your lungs are removed, the machine’s ventilator bellows will go up, down, up, down. Capable only of whooshing and not ringing, the bellows will seem to call sadly through the cold air to the monitors sitting above, waiting fruitlessly for a response. What a simple, insignificant movement: up, down, up, down, never getting away from the same place. It will be the only activity surrounding your head amid the metal machines, with their cold, menacing gleam. Nobody will be sitting next to you to wonder about what you were like, or about the things that distinguished your personality and made it special. A vision of the future arises: similarly deserted operating rooms with AI machines all moving automatically, while the people who used to work in them have gone off somewhere to sit dreamily on the grass beneath the sky.
Medicine has tapped a new source of organs in the form of donation after circulatory death
It seems a decidedly unpleasant environment in which to meet one’s end, and enough to discourage those on the fence from becoming potential organ donors. Rather than live a bit longer in the mind of another person, rather than have that person think about you and wonder about you, entertain irrational imaginary concerns about you, slip a little extra narcotic into your intravenous line ‘just in case’, engage in metaphysical speculations about your breathing pattern, and imagine you a friend, you will be alone on the table, and your surgery will more closely resemble a bandit raid. The machines will be determined to take everything, every organ. Reduced to financial terms, it will be as if you were left penniless.
Worse, a new danger will come to overlie the chilling sense of emptiness, scaring even more people away from becoming organ donors. Because there are already too few brain-dead donors – each year, more than 8,000 people in the US die while on the waiting list for organs – medicine has tapped a new source of organs in the form of donation after circulatory death (DCD). These organ donors are not brain dead, although many of them are unconscious. Instead, they lack circulatory or respiratory activity after being disconnected from artificial life-support systems. Without such activity after a few minutes of so-called ‘no touch’, they are declared dead, and their organs become available for donation. Their numbers have been growing over the past two decades. Today, they account for about 10 per cent of transplanted organs in the US.
The problem is that certain medicines necessarily given to these donors before death, but in expectation of death, may hasten their death. The medicines are given for the sole purpose of making their organs more viable for transplantation. Heparin, for example, prevents blood clotting, while phentolamine dilates blood vessels and improves blood flow to the organs. Yet heparin also increases the chances of bleeding into the brain, while phentolamine may lower blood pressure to the degree that a person goes into shock. Although these patients are near death for other reasons, the medicines may become their actual cause of death. This makes doctors uneasy; hence the rule not to give these medicines to donors prone to bleeding or with low blood pressure.
Y et the rule risks driving away potential donors, who will naturally think: ‘Doctors won’t give you these medicines to kill you; on the other hand, they won’t give you these medicines to help you. At some point, doctors aren’t really on your side. But when?’ As the number of brain-dead donors drops, medicine will increasingly rely on DCD donors to compensate. Already sensitised by the image of surrendering their organs to machines in a metallic desert, potential donors will fear being herded into the ‘imminent death’ category to meet some organ quota, a fear only heightened when word gets out that doctors are not always their advocates.
Currently, doctors in the US must get consent before declaring people DCD donors, but another model, called the ‘presumed consent model’, already operates in other countries and allows the recovery of organs without prior authorisation. A cascade of events threatens to turn organ retrieval into a kind of science-fiction nightmare, where organ shortages lead to medicines being given to people to preserve their organs while possibly hastening their death, all without telling them the plan or asking for their permission.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines
Whenever people start to think about becoming an organ donor, they immediately make a leap to their own precious person. Who am I, what am I, what am I without my organs, and so forth. It is part and parcel of being a human being. That some people are willing to surrender their organs after death suggests that, to feel oneself human, they need more than merely having a whole body; they also need an atmosphere of simple humanity. To feel human, people need to feel that they occupy space in the thoughts and feelings of others. It is why they consider becoming organ donors in the first place. They imagine helping others by giving up a part of themselves in the future. In exchange, they imagine the recipients thinking from time to time about what they, their donors, were like. In that way, the donors feel a connection with whomever those recipients might be, and feel somehow fulfilled.

I’d like to think that caring for my brain-dead patient satisfied some small part of this need to feel human, whether on the part of my patient before she died and who perhaps lived in expectation of becoming a donor one day, or on the part of her relatives who gave their consent to the procedure after she was declared brain dead. Either way, I connected with her or with her family.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines willy-nilly. You don’t satisfy people’s urge to feel human by making the bridge to the next world a totally inhuman one.
The lesson extends far beyond organ donation. AI promises to make healthcare quicker, more precise, and error-free. To the degree that it replaces doctors and nurses, it portends a massive shift in medicine that seems to come every 30 years, when people are so overwhelmed by the burden of their own technological creations, they need every iota of their strength to adjust. Once again, with the advent of AI, advancements promise to put healthcare on an entirely new footing and, once again, the inevitable backlash will be there. So it was in the 1960s, when new medical technologies and procedures, such as home dialysis machines and coronary artery bypass surgery, improved life, and yet, during this same period, the medical profession’s reputation plummeted, as patients complained that doctors had grown cold and impersonal. So it was in the 1990s, when the rise of managed care promised greater efficiency at less cost, and a ‘win-win’ strategy anchored in preventive medicine, led to a patient rebellion against being treated like cattle, including their inability to choose their own doctor, and rushed visits to practitioners ‘on the plan’.
Now, in the 2020s, the stage is set for outrage, yet again. AI promises to elevate healthcare; but, to the degree that it replaces doctors and nurses, it also threatens to depersonalise patients and to wash off their distinctive colours until everyone has the same drab tint. In the crucible that looms, patients are going to rebel. And it is in the arena of organ donation, where they face death by machine, that they are likely to baulk loudest, and first.

Ecology and environmental sciences
To take care of the Earth, humans must recognise that we are both a part of the animal kingdom and its dominant power
Hugh Desmond
Quantum theory
Quantum dialectics
When quantum mechanics posed a threat to the Marxist doctrine of materialism, communist physicists sought to reconcile the two
Jim Baggott

Nations and empires
A United States of Europe
A free and unified Europe was first imagined by Italian radicals in the 19th century. Could we yet see their dream made real?
Fernanda Gallo

Stories and literature
On Jewish revenge
What might a people, subjected to unspeakable historical suffering, think about the ethics of vengeance once in power?
Shachar Pinsker

Building embryos
For 3,000 years, humans have struggled to understand the embryo. Now there is a revolution underway
John Wallingford

Design and fashion
Sitting on the art
Given its intimacy with the body and deep play on form and function, furniture is a ripely ambiguous artform of its own
Emma Crichton Miller
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Three Stories About the Value of Advance Care Planning
- 1 Cambia Palliative Care Center of Excellence at UW Medicine, University of Washington, Seattle
- 2 Division of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Harborview Medical Center, University of Washington, Seattle
- Original Investigation Intervention to Promote Communication About Goals of Care for Hospitalized Patients With Serious Illness J. Randall Curtis, MD, MPH; Robert Y. Lee, MD, MS; Lyndia C. Brumback, PhD; Erin K. Kross, MD; Lois Downey, MA; Janaki Torrence, MS; Nicole LeDuc, BS; Kasey Mallon Andrews, MS; Jennifer Im, MSc; Joanna Heywood, BS; Crystal E. Brown, MD, MA; James Sibley, BS; William B. Lober, MD, MS; Trevor Cohen, MBChB, PhD; Bryan J. Weiner, PhD; Nita Khandelwal, MD, MS; Nauzley C. Abedini, MD, MSc; Ruth A. Engelberg, PhD JAMA
There is an ongoing debate among the palliative care community about the value of advance care planning and whether current evidence suggests that advance care planning is inherently ineffective. I’m not writing this essay to take a side in this debate—I believe both sides have merit. Rather, I write to tell 3 personal stories of the role advance care planning has played for my family and in my own life. My entire career has focused on developing and evaluating ways to improve communication with patients and families about serious illness care. These 3 stories are informed by that experience and yet are told not from the perspective of a physician and researcher, but from the perspective of a son-in-law, son, and patient.
Thank you. I am retired and rather old. When working, one of my many small town primary care practice functions was to serve as hospice director. Your contribution to advance planning means more to me than just about anything I ever read or tried to learn in those years of caring.
Your three anecdotes are extraordinary exemplifications of value.
My best wishes in your difficult journey ahead. You have my admiration and highest respect.
Read More About
Curtis JR. Three Stories About the Value of Advance Care Planning. JAMA. 2021;326(21):2133–2134. doi:10.1001/jama.2021.21075
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Nice To E-Meet You!
What marketing services do you need for your project.
- Company About us Clients
- Services Content Marketing ICO & STO Marketing PR & Distribution Social Media Marketing AI Copy Editing SEO & Link Building PPC Management Design Services Email Marketing
- Portfolio Articles Design White Papers Case Studies
- Blog All posts Guest posting
- Top Choices Top companies Submit your company
- Services Content Marketing ICO & STO Marketing PR & Distribution Social Media Marketing SEO & Link Building PPC Management Design Services Email Marketing AI Copy Editing
- Top Choice Top companies Submit your company
How Virtual Medical Assistants Can Transform Patient Care

Haley Osborne Freelance Writer
Are administrative tasks like appointment scheduling, prescription refills, and medical billing eating into your practice time?
You’re not alone. Managing these tasks can be quite complex and time-consuming. Fortunately, a virtual medical assistant (VMA) can streamline these processes, allowing you to focus more on what truly matters – patient care.
Boosting Efficiency And Saving Time
VMAs handle a wide array of administrative tasks that typically consume a lot of valuable time. Imagine not having to spend countless hours scheduling appointments or deciphering complicated insurance statements. A VMA can efficiently manage these tasks, freeing you up to spend more time meeting and talking with your patients.
Appointment scheduling
Need to streamline your scheduling process? A VMA can efficiently handle appointment bookings, finding times that work for both you and your patients. They can also send reminders to ensure patients don’t miss their visits, which helps reduce no-shows.
Prescription refills
Managing prescription refills can be extremely time-consuming. Your VMA can easily request refills and ensure patients have the medications they need without unnecessary delays. This can improve patient satisfaction and adherence to treatment plans.
Medical billing
Medical billing can be a headache for many practices. A VMA can assist with understanding and processing bills, identifying errors, and communicating with insurance companies to ensure accurate payments. This can greatly help in reducing billing errors and improve revenue cycle management.
Enhancing Patient Care And Communication
Beyond administrative tasks, VMAs can significantly enhance the overall patient care experience.
Proactive patient communication
VMAs can improve communication between healthcare providers and patients. They can send appointment reminders, answer basic questions, and schedule follow-up appointments, keeping patients informed about their care plans. This proactive approach can lead to better patient engagement and adherence.
Remote patient monitoring
For patients with chronic conditions, VMAs can be incredibly invaluable. They can monitor vital signs, track medication adherence, and report any changes to healthcare providers, helping to catch health issues early. This approach in monitoring can lead to better patient outcomes and reduce hospital readmissions.
Improved accessibility
For patients with limited mobility or transportation issues, VMAs can facilitate virtual consultations, reducing the need for in-person visits and making healthcare more accessible. This can be especially beneficial for elderly or disabled patients.
Empowering Providers To Manage Patient Care
VMAs can help providers take a more proactive role in managing patient care.
Health information management
VMAs can organize and manage patient health information, keeping track of medical histories, medications, allergies, and immunizations, ensuring this information is readily available when needed. This can improve the accuracy and efficiency of patient care.
Preventative care reminders
Ensure patients don’t miss important screenings or vaccinations. A VMA can send reminders for preventive care appointments, helping patients stay on top of their health. This can lead to better long-term health outcomes.
Research and resource assistance
Need to find a specialist or learn more about a condition? Your VMA can help navigate credible medical resources and provide answers to your questions. This can save you time and ensure you have the information you need to provide the best care.
Integrating Technology In Healthcare
Telehealth appointments.
VMAs can help set up and manage telehealth appointments, ensuring a smooth process for both providers and patients.This can increase access to care and improve patient satisfaction.
Electronic health records
VMAs can manage EHRs, helping to keep patient records organized and easily accessible. This can improve the efficiency and accuracy of patient care.
The Future Of Healthcare
Virtual medical assistants are transforming how we interact with the healthcare system. By handling administrative tasks, improving communication, and providing tools to manage patient care, VMAs enable providers to focus more on delivering quality healthcare. If you’re looking to streamline your practice and enhance patient care, consider integrating a virtual medical assistant.
Care coordination
VMAs provide personalized care coordination. Whether it’s arranging specialist consultations, managing follow-up care, or coordinating between different healthcare providers, VMAs ensure your patient care is seamless and well-organized. This can improve the continuity and quality of care.
Educational support
VMAs can assist with educating patients about their health conditions and treatment options. They can direct patients to reliable health information and resources, making it easier for them to make informed decisions about their care. This can empower patients and improve their health literacy.
Virtual medical assistants are more than just a convenience—they’re changing the landscape of healthcare. By handling administrative burdens, enhancing patient care, and providing the tools and knowledge to manage patient health, VMAs are paving the way for a more efficient, accessible, and patient-centered healthcare system. Embrace the future of healthcare with a virtual medical assistant and enhance your practice today.
Once a week you will get the latest articles delivered right to your inbox
You can also read, top 10 places to hire book publishing services in 2024.
The Crucial Role Of AML And KYC Compliance In Cryptocurrency

iGaming SEO Tips: What Bonuses Bring The Most Traffic

Ergonomic Excellence: Choosing The Right Office Chair For Productivity And Comfort

You Can Also Read
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Health Effects of Cigarette Smoking
- Secondhand Smoke
- E-cigarettes (Vapes)
- Menthol Tobacco Products
- Morbidity and Mortality Weekly Reports (MMWR)
- About Surveys
- Other Tobacco Products
- Smoking and Tobacco Use Features
- Patient Care Settings and Smoking Cessation
- Patient Care
- Funding Opportunity Announcements
- State and Community Work
- National and State Tobacco Control Program
- Multimedia and Tools
- Tobacco - Health Equity
- Tobacco - Surgeon General's Reports
- State Tobacco Activities Tracking and Evaluation (STATE) System
- Global Tobacco Control
Health Effects of Vaping
At a glance.
Learn more about the health effects of vaping.
- No tobacco products, including e-cigarettes, are safe.
- Most e-cigarettes contain nicotine, which is highly addictive and is a health danger for pregnant people, developing fetuses, and youth. 1
- Aerosol from e-cigarettes can also contain harmful and potentially harmful substances. These include cancer-causing chemicals and tiny particles that can be inhaled deep into lungs. 1
- E-cigarettes should not be used by youth, young adults, or people who are pregnant. E-cigarettes may have the potential to benefit adults who smoke and are not pregnant if used as a complete substitute for all smoked tobacco products. 2 3 4
- Scientists still have a lot to learn about the short- and long-term health effects of using e-cigarettes.
Most e-cigarettes, or vapes, contain nicotine, which has known adverse health effects. 1
- Nicotine is highly addictive. 1
- Nicotine is toxic to developing fetuses and is a health danger for pregnant people. 1
- Acute nicotine exposure can be toxic. Children and adults have been poisoned by swallowing, breathing, or absorbing vaping liquid through their skin or eyes. More than 80% of calls to U.S. poison control centers for e-cigarettes are for children less than 5 years old. 5
Nicotine poses unique dangers to youth because their brains are still developing.
- Nicotine can harm brain development which continues until about age 25. 1
- Youth can start showing signs of nicotine addiction quickly, sometimes before the start of regular or daily use. 1
- Using nicotine during adolescence can harm the parts of the brain that control attention, learning, mood, and impulse control. 1
- Adolescents who use nicotine may be at increased risk for future addiction to other drugs. 1 6
- Youth who vape may also be more likely to smoke cigarettes in the future. 7 8 9 10 11 12
Other potential harms of e-cigarettes
E-cigarette aerosol can contain substances that can be harmful or potentially harmful to the body. These include: 1
- Nicotine, a highly addictive chemical that can harm adolescent brain development
- Cancer-causing chemicals
- Heavy metals such as nickel, tin, and lead
- Tiny particles that can be inhaled deep into the lungs
- Volatile organic compounds
- Flavorings such as diacetyl, a chemical linked to a serious lung disease. Some flavorings used in e-cigarettes may be safe to eat but not to inhale because the lungs process substances differently than the gut.
E-cigarette aerosol generally contains fewer harmful chemicals than the deadly mix of 7,000 chemicals in smoke from cigarettes. 7 13 14 However, this does not make e-cigarettes safe. Scientists are still learning about the immediate and long-term health effects of using e-cigarettes.
Dual use refers to the use of both e-cigarettes and regular cigarettes. Dual use is not an effective way to safeguard health. It may result in greater exposure to toxins and worse respiratory health outcomes than using either product alone. 2 3 4 15
Some people who use e-cigarettes have experienced seizures. Most reports to the Food and Drug Administration (FDA ) have involved youth or young adults. 16 17
E-cigarettes can cause unintended injuries. Defective e-cigarette batteries have caused fires and explosions, some of which have resulted in serious injuries. Most explosions happened when the batteries were being charged.
Anyone can report health or safety issues with tobacco products, including e-cigarettes, through the FDA Safety Reporting Portal .
Health effects of vaping for pregnant people
The use of any tobacco product, including e-cigarettes, is not safe during pregnancy. 1 14 Scientists are still learning about the health effects of vaping on pregnancy and pregnancy outcomes. Here's what we know now:
- Most e-cigarettes, or vapes, contain nicotine—the addictive substance in cigarettes, cigars, and other tobacco products. 18
- Nicotine is a health danger for pregnant people and is toxic to developing fetuses. 1 14
- Nicotine can damage a fetus's developing brain and lungs. 13
- E-cigarette use during pregnancy has been associated with low birth weight and pre-term birth. 19 20
Nicotine addiction and withdrawal
Nicotine is the main addictive substance in tobacco products, including e-cigarettes. With repeated use, a person's brain gets used to having nicotine. This can make them think they need nicotine just to feel okay. This is part of nicotine addiction.
Signs of nicotine addiction include craving nicotine, being unable to stop using it, and developing a tolerance (needing to use more to feel the same). Nicotine addiction can also affect relationships with family and friends and performance in school, at work, or other activities.
When someone addicted to nicotine stops using it, their body and brain have to adjust. This can result in temporary symptoms of nicotine withdrawal which may include:
- Feeling irritable, jumpy, restless, or anxious
- Feeling sad or down
- Having trouble sleeping
- Having a hard time concentrating
- Feeling hungry
- Craving nicotine
Withdrawal symptoms fade over time as the brain gets used to not having nicotine.
Nicotine addiction and mental health
Nicotine addiction can harm mental health and be a source of stress. 21 22 23 24 More research is needed to understand the connection between vaping and mental health, but studies show people who quit smoking cigarettes experience: 25
- Lower levels of anxiety, depression, and stress
- Improved positive mood and quality of life
Mental health is a growing concern among youth. 26 27 Youth vaping and cigarette use are associated with mental health symptoms such as depression. 22 28
The most common reason middle and high school students give for currently using e-cigarettes is, "I am feeling anxious, stressed, or depressed." 29 Nicotine addiction or withdrawal can contribute to these feelings or make them worse. Youth may use tobacco products to relieve their symptoms, which can lead to a cycle of nicotine addiction.
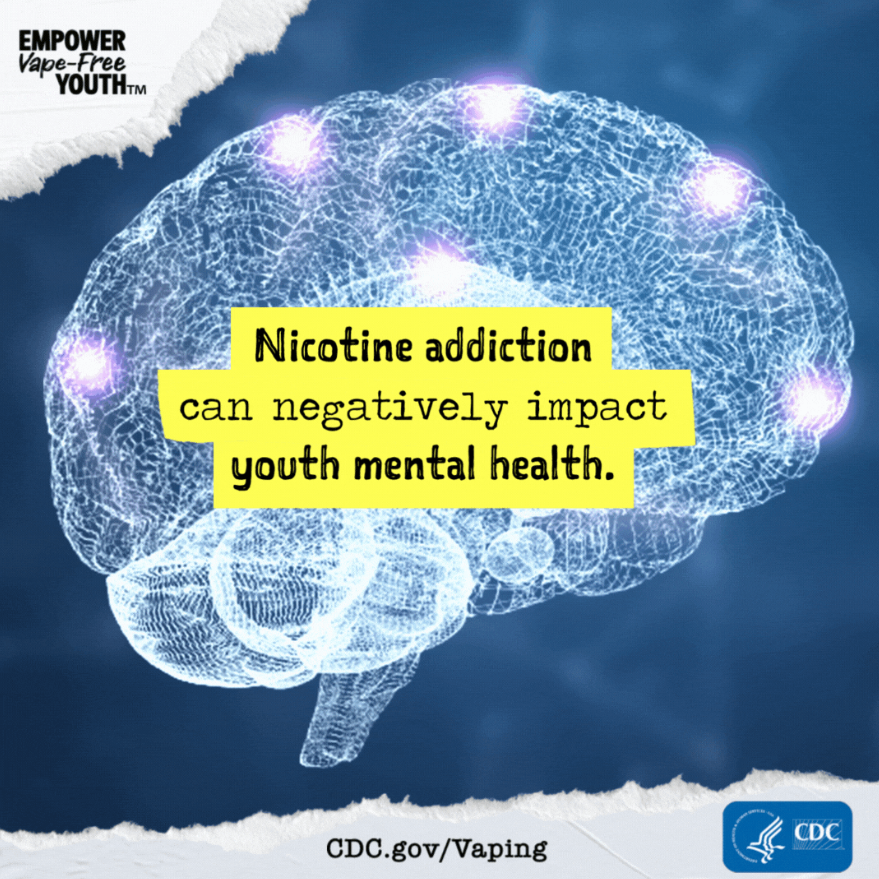
- U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General . Centers for Disease Control and Prevention; 2016. Accessed Feb 14, 2024.
- Goniewicz ML, Smith DM, Edwards KC, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes . JAMA Netw Open. 2018;1(8):e185937.
- Reddy KP, Schwamm E, Kalkhoran S, et al. Respiratory symptom incidence among people using electronic cigarettes, combustible tobacco, or both . Am J Respir Crit Care Med. 2021;204(2):231–234.
- Smith DM, Christensen C, van Bemmel D, et al. Exposure to nicotine and toxicants among dual users of tobacco cigarettes and e-cigarettes: Population Assessment of Tobacco and Health (PATH) Study, 2013-2014 . Nicotine Tob Res. 2021;23(5):790–797.
- Tashakkori NA, Rostron BL, Christensen CH, Cullen KA. Notes from the field: e-cigarette–associated cases reported to poison centers — United States, April 1, 2022–March 31, 2023 . MMWR Morb Mortal Wkly Rep. 2023;72:694–695.
- Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain . J Physiol. 2015;593(16):3397–3412.
- National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes . The National Academies Press; 2018.
- Barrington-Trimis JL, Kong G, Leventhal AM, et al. E-cigarette use and subsequent smoking frequency among adolescents . Pediatrics. 2018;142(6):e20180486.
- Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use . Pediatrics. 2016;138(1):e20160379.
- Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013 . Nicotine Tob Res. 2015;17(2):228–235.
- Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis . JAMA Pediatr. 2017;171(8):788–797.
- Sun R, Méndez D, Warner KE. Association of electronic cigarette use by U.S. adolescents with subsequent persistent cigarette smoking . JAMA Netw Open. 2023;6(3):e234885.
- U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease . Centers for Disease Control and Prevention; 2010. Accessed Feb 13, 2024.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General . Centers for Disease Control and Prevention; 2014. Accessed Feb 12, 2024.
- Mukerjee R, Hirschtick JL, LZ Arciniega, et al. ENDS, cigarettes, and respiratory illness: longitudinal associations among U.S. youth . AJPM. Published online Dec 2023.
- Faulcon LM, Rudy S, Limpert J, Wang B, Murphy I. Adverse experience reports of seizures in youth and young adult electronic nicotine delivery systems users . J Adolesc Health . 2020;66(1):15–17.
- U.S. Food and Drug Administration. E-cigarette: Safety Communication - Related to Seizures Reported Following E-cigarette Use, Particularly in Youth and Young Adults . U.S. Department of Health and Human Services; 2019. Accessed Feb 14, 2024.
- Marynak KL, Gammon DG, Rogers T, et al. Sales of nicotine-containing electronic cigarette products: United States, 2015 . Am J Public Health . 2017;107(5):702-705.
- Regan AK, Bombard JM, O'Hegarty MM, Smith RA, Tong VT. Adverse birth outcomes associated with prepregnancy and prenatal electronic cigarette use . Obstet Gynecol. 2021;138(1):85–94.
- Regan AK, Pereira G. Patterns of combustible and electronic cigarette use during pregnancy and associated pregnancy outcomes . Sci Rep. 2021;11(1):13508.
- Kutlu MG, Parikh V, Gould TJ. Nicotine addiction and psychiatric disorders . Int Rev Neurobiol. 2015;124:171–208.
- Obisesan OH, Mirbolouk M, Osei AD, et al. Association between e-cigarette use and depression in the Behavioral Risk Factor Surveillance System, 2016-2017 . JAMA Netw Open. 2019;2(12):e1916800.
- Prochaska JJ, Das S, Young-Wolff KC. Smoking, mental illness, and public health . Annu Rev Public Health. 2017;38:165–185.
- Wootton RE, Richmond RC, Stuijfzand BG, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study . Psychol Med. 2020;50(14):2435–2443.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis . BMJ. 2014;348:g1151.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2011–2021 . U.S. Department of Health and Human Services; 2023. Accessed Dec 15, 2023.
- U.S. Department of Health and Human Services. Protecting Youth Mental Health: The U.S. Surgeon General's Advisory . Office of the Surgeon General; 2021. Accessed Jan 5, 2024.
- Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents . Prev Med. 2017;96:73–78.
- Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021 . MMWR Surveill Summ. 2022;71(No. SS-5):1–29.
Smoking and Tobacco Use
Commercial tobacco use is the leading cause of preventable disease, disability, and death in the United States.
For Everyone
Health care providers, public health.

IMAGES
VIDEO
COMMENTS
There are many ways of approaching an essay such as this one. Here are some methods that we find useful, and we hope they will be helpful to you as well. The most powerful essays are those which could not be written by anyone other than yourself. Keep this in mind as you begin your brainstorm.
View our collection of healthcare essays. Find inspiration for topics, titles, outlines, & craft impactful healthcare papers. Read our healthcare papers today! Homework Help; Essay Examples ... In 1990s the main concepts was that physicians were to be trained in numbers that were much greater than the demand for medical care in the U.S. could ...
Parker's essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school.
This essay discusses health policies, the determinants of health, and the connections between the two. The determinants of health are individual and environmental factors that affect people's physical and mental well-being and the ability to […] Artificial Intelligence in Healthcare and Medicine.
Think of type II diabetes, cardiovascular illness, breast cancer, and cirrhosis. These are topics you don't want to cover for the simple reason that they are too common. In this post, we give you a list of 30+ medical argumentative essay topics that aren't too obvious. These topic ideas should enable you to add a new spin to your work, so ...
Part 3: The medical school adversity essay Example adversity essay prompts. Example 1: "Share with us a difficult or challenging situation you have encountered and how you dealt with it.In your response, identify both the coping skills you called upon to resolve the dilemma, and the support person(s) from whom you sought advice." (University of Chicago Pritzker School of Medicine)
339 essay samples found. Health care encompasses a range of services provided by medical professionals to maintain or improve people's health. Essays on health care could explore the different health care systems across countries, challenges in healthcare delivery, ethical concerns, or the impact of technology and policy on healthcare services.
StudyCorgi has prepared an extensive list of health care topics to write about! Here, you'll find title ideas for various healthcare fields, including healthcare management, ethics, administration, leadership, policy, finance, care quality, and issues faced by healthcare workers. Our topics are suitable for both high school students and ...
Absolutely FREE essays on Health Care. All examples of topics, summaries were provided by straight-A students. Get an idea for your paper. search. Essay Samples ... It is known for its world-class medical care and cutting-edge research in various fields of medicine. The institution's mission statement is a reflection of its commitment to ...
The world's most dangerous drug. Write an essay on why integrating CHWs in health care settings is good for patients. Week 5. Strategic Communications for Effective Communications World Health Organization (WHO) Ethical dilemma in dental profession. Euthanasia: Ethics Versus the Right to Die.
Jehn also shares the following valuable writing tips to help you create a compelling final product: Tip #1. Before you begin writing your first draft, try imagining your audience so you can determine what they care about and how to frame your information in a way that will resonate with them. "I imagine a worst-case scenario for my readers.
Conclusion. The Healthcare system is one of the most important components of the U.S. social system since full productivity cannot be achieved without good health. This paper has argued that a free health care system would be the most effective system for America. To reinforce this assertion, the paper has articulated the benefits that the ...
Hospital patient care vs at-home patient care. Tips for Writing a Good Medical Essay Vary the length of the sentences! Long sentences can be monotonous and lull readers to sleep. It is important to mix your essay with short sentences to make the readers feel like they are reading natural speech. This will persuade readers to stay invested in ...
220+ medical school personal statement examples, plus a step-by-step guide to writing a unique essay and an analysis of a top-5 medical school personal statement. Part 1: Introduction to the medical school personal statement ... the human side of care provision. My experience with a tiny three-year-old boy and his mother in genetics clinic ...
Writing as a Veterinary Technician. The intention of this section is to provide veterinary technicians with guidelines for writing the patient care plan portion of the veterinary medical record. As there is no standardized format for writing a veterinary care plan, the following principles are only one example of how a care plan may be formulated.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
B. Final thoughts on why you are a strong candidate for medical school. C. Call-to-action or next steps. (Note: This is just one example of a potential outline for a medical school personal statement. The specific content and structure may vary based on individual experiences and preferences.)
14 Amazing Health Care Essay Topics with Introduction Examples. In your essay about health care, you may either talk about various diseases, symptoms, diagnosis, treatment, or methods used by doctors to help their patients, as well as their roles in general. In most cases, students should criticize the modern healthcare system as it really is ...
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School, says personal statements help medical schools determine whether applicants have the character necessary ...
784 essay samples found. Medicine and Health encompass the science and practice of diagnosing, treating, and preventing diseases. An essay could explore advancements in medical research, discuss ethical considerations in medical practice, or examine the societal impacts of healthcare policies and accessibility.
Rated as one of the top ten journals in healthcare administration, Medical Care is devoted to all aspects of the administration and delivery of healthcare. This scholarly journal publishes original, peer-reviewed papers documenting the most current developments in the rapidly changing field of healthcare. This timely journal reports on the findings of original investigations into issues ...
Essay Example: In the complex framework of healthcare systems, socialized medicine stands out as a bold initiative, infusing the narrative of access with vibrant inclusivity while navigating the stormy seas of controversy. This intricate narrative intertwines numerous benefits and challenges
A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day. Although donors are dead, managing their anaesthesia can be tricky.
In this narrative medicine essay, a critical care palliative care physician shares how 2 family members could not communicate their end of life wishes but ... 2 Division of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, Harborview Medical Center, University of Washington, Seattle. JAMA. 2021;326(21):2133-2134. doi:10.1001 ...
Last modified: 6th Aug 2021. Parkinson's disease (PD) is a progressive neurological disorder. PD occurs when the brain's substantia nigra neurons of the basal ganglia begin to die; therefore, decreasing dopamine in the body. The onset of PD can occur at a young age, but the most common diagnosis is after 60 years old....
Since their release, the medical community has been actively exploring large language models' (LLMs) capabilities, which show promise in providing accurate medical knowledge. One potential application is as a patient resource. This study analyzes and compares the ability of the currently available LLMs, ChatGPT-3.5, GPT-4, and Gemini, to provide postoperative care recommendations to plastic ...
This important reanalysis shows that continuous use of N95 respirators compared to medical masks in health-care settings was significantly protective against CRI (RR 0.48, 95%CI 0.35-0.65). Rates of ILI, laboratory (PCR)-confirmed respiratory viruses, and laboratory (PCR)-confirmed influenza were also lower in the continuous N95 arm, but ...
Medical billing. Medical billing can be a headache for many practices. A VMA can assist with understanding and processing bills, identifying errors, and communicating with insurance companies to ensure accurate payments. This can greatly help in reducing billing errors and improve revenue cycle management. Enhancing Patient Care And Communication
Am J Respir Crit Care Med. 2021;204(2):231-234. Smith DM, Christensen C, van Bemmel D, et al. Exposure to nicotine and toxicants among dual users of tobacco cigarettes and e-cigarettes: Population Assessment of Tobacco and Health (PATH) Study, 2013-2014. Nicotine Tob Res. 2021;23(5):790-797. Tashakkori NA, Rostron BL, Christensen CH, Cullen KA.
Jump to essay-10 42 United States Code, Section 1395dd(b)(1). Jump to essay-11 Response in Opposition to Applications for a Stay at 1, Moyle v. United States, 144 S.Ct. 540 (2024). Jump to essay-12 Id. at 2. Jump to essay-13 Idaho Code Ann. § 18-622. Jump to essay-14 Response in Opposition to Applications for a Stay at 2, Moyle v.