An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts


Measuring best practices for workplace safety, health and wellbeing: The Workplace Integrated Safety and Health Assessment
Glorian sorensen.
1 Dana-Farber Cancer Institute, Boston, MA
2 Harvard T.H. Chan School of Public Health, Boston, MA
Emily Sparer
Jessica a.r. williams.
3 University of Kansas School of Medicine, Kansas City, KS
Daniel Gundersen
Leslie i. boden.
4 Boston University School of Public Health, Boston, MA
Jack T. Dennerlein
5 Northeastern University, Boston, MA
Dean Hashimoto
6 Partners HealthCare, Inc., Boston, MA
7 Boston College Law School, Newton Centre, MA
Jeffrey N. Katz
8 Brigham and Women’s Hospital, Boston, MA
Deborah L. McLellan
Cassandra a. okechukwu, nicolaas p. pronk.
9 HealthPartners Institute, Minneapolis, MN
Anna Revette
Gregory r. wagner, associated data.
To present a measure of effective workplace organizational policies, programs and practices that focuses on working conditions and organizational facilitators of worker safety, health and wellbeing: the Workplace Integrated Safety and Health (WISH) Assessment.
Development of this assessment used an iterative process involving a modified Delphi method, extensive literature reviews, and systematic cognitive testing.
The assessment measures six core constructs identified as central to best practices for protecting and promoting worker safety, health and wellbeing: leadership commitment; participation; policies, programs and practices that foster supportive working conditions; comprehensive and collaborative strategies; adherence to federal and state regulations and ethical norms; and data-driven change.
Conclusions
The WISH Assessment holds promise as a tool that may inform organizational priority setting and guide research around causal pathways influencing implementation and outcomes related to these approaches.
INTRODUCTION
Efforts to protect and promote the safety, health, and wellbeing of workers have increasingly focused on integrating the complex and dynamic systems of the work organization and work environment. 1 – 3 The National Institute for Occupational Safety and Health (NIOSH) applies this integrated approach in the Total Worker Health ® (TWH) initiative by attending to “policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being.” 4 NIOSH has defined best practices as a set of essential elements for TWH that prioritizes a hazard-free work environment and recognizes the significant role of job-related factors in workers’ health and wellbeing. 5 , 6
Increasingly, others have also emphasized the importance of improvements in working conditions as central to best practice recommendations. 7 – 15 For example, the Robert Wood Johnson Foundation’s efforts have focused on building a culture of health in the workplace. 16 Continuous improvement systems have relied on employee participation as a means of shaping positive working conditions. 17 – 19 In Great Britain, continuous improvement processes are employed through a set of “management standards” that assess and address stressors in the workplace, including demands, control, support, relationships, role, and organizational change. 20 Researchers have reported benefits to this integrated systems approach, including reductions in pain and occupational injury and disability rates; 21 – 26 strengthened health and safety programs; 27 , 28 improvements in health behaviors; 29 – 38 enhanced rates of employee participation in programs; 39 and reduced costs. 28
Assessment of the extent to which a workplace adheres to best practice recommendations related to an integrated systems approach is important for several reasons. Understanding relationships between working conditions and worker safety and health outcomes can inform priority-setting and decision making for researchers, policy-makers, and employers alike, and may motivate employer actions to improve workplace conditions. 40 In turn, identifying the impact of worker health and safety on business-related outcomes, such as worker performance, productivity, and turnover, may help to demonstrate the importance of protecting and promoting worker health for the bottom line. 41 Baseline data with follow up assessments can also provide a means for tracking improvements in working conditions and related health outcomes over time. An important part of the process for evaluating workplace adherence to recommendations and understanding its relationship to worker and business outcomes is the creation of assessment tools that effectively capture implementation of best practice recommendations.
In 2013, the Harvard T.H. Chan School of Public Health Center for Work, Health and Wellbeing published a set of “Indicators of Integration” that were designed to assess the extent to which an organization has implemented an approach integrating occupational safety and health with worksite health promotion. 1 This instrument assessed four domains: organizational leadership and commitment; collaboration between health protection and worksite health promotion; supportive organizational policies and practices (including accountability and training, management and employee engagement, benefits and incentives to support workplace health promotion and protection, integrated evaluation and surveillance); and comprehensive program content. The instrument was validated in two samples, 42 , 43 and has played as useful role in the evolving dialogue around integrated approaches to worker safety, health and wellbeing. 44 , 45 There is a need, however, for building on this work toward assessment of more conceptually grounded and practical constructs that measure the implementation of systems approaches focusing on improving working conditions as a means of protecting and promoting worker safety, health and wellbeing.
This manuscript describes an improved measure that reflects the Center’s conceptual model, which articulates the central role of working conditions in shaping health and safety outcomes as well as enterprise outcomes such as absenteeism and turnover ( Figure 1 ). 2 Working conditions, placed centrally in the model as core determinants of worker health and safety, encompass the physical environment and the organization of work (i.e., psycho-social factors, job design and demands, health and safety climate). The model highlights the potential interactions across systems, guiding exploration of the shared effects of the physical environment and the organization of work. Working conditions serve as a pathway from enterprise and workforce characteristics and effective policies, programs, and practices, to worker safety and health outcomes, as well as to more proximal outcomes such as health-related behaviors. Effective policies, programs, and practices may also contribute to improvements in enterprise outcomes such as turnover and health care costs. Feedback loops underscore the complexity of the system of inter-relationships across multiple dimensions, and highlight the potential synergy of intervention effects.

Systems level conceptual model centered around working conditions.
The purpose of this paper is to present a new measure of effective workplace organizational policies, programs and practices that focuses on working conditions as well as organizational facilitators of worker safety, health and wellbeing: the Workplace Integrated Safety and Health (WISH) Assessment. The objective of the WISH Assessment is to evaluate the extent to which workplaces implement effective comprehensive approaches to protect and promote worker health, safety and wellbeing. The policies, programs and practices encompassed by these approaches include both those designed to prevent work-related injuries and illnesses, and those designed to enhance overall workforce health and wellbeing.
Like the Indicators of Integration, this assessment is designed to be completed at the organizational level by employer representatives, such as directors of human resources, occupational safety, or employee health. These representatives are likely to be knowledgeable of organizational priorities, as well as policies, programs and practices related to workplace safety and health. Moreover, these representatives are in the position to influence the cultural and structural re-alignment necessary for integrated approaches. These organizational assessments are increasingly being used by policymakers, organizational leadership, and health and safety committees to guide goal setting and decision making. Organizational assessments such as this one may additionally complement worker surveys that can effectively capture employee practices as well as their perceptions of working conditions.
The WISH Assessment differs from the Indicators of Integration in two important ways: it embraces an increased focus on the central role of working conditions (as illustrated in Figure 1 ), and it expands assessment of best practice systems approaches to include a broader definition of protecting and promoting worker safety, health and wellbeing. This paper also describes the methods used to develop this instrument.
Investigators from the Harvard Chan School Center for Work, Health and Wellbeing, a TWH Center for Excellence representing multiple institutions in the Boston area, developed the WISH Assessment. 46 This instrument measures workplace-level implementation of policies, programs and practices that protect and promote worker safety, health and wellbeing. Accordingly, the intended respondents are organizational representatives who are knowledgeable about existing policies, programs and practices at workplaces, such as executives at small businesses, or directors of human resources or safety departments. Development of the WISH Assessment relied on an iterative process involving a modified Delphi method, extensive literature reviews, and systematic cognitive testing.
Delphi method and literature review
The Center’s conceptual model 2 and related literature provided a guiding framework for the development of the WISH Assessment. As a starting point, we used constructs and related measures included in the Center’s published 1 and validated 42 , 43 Indicators of Integration tool. Based on an extensive review of literature, we expanded and revised the constructs captured by the instrument from four to seven. Next, we reviewed these constructs and their definitions using an iterative modified Delphi process 47 with an expert review panel, including Center investigators. We reviewed the literature to identify extant items for these and similar constructs, placing a priority on the inclusion of validated measures where feasible. To ensure content validity and adequate coverage across attributes for each construct, we reviewed working drafts of the instrument with the Center’s External Advisory Board, as well as members of other TWH Centers of Excellence. 48 Through repeated discussions, iterative review and revisions in six meetings over ten months, the Center members reached consensus related to a set of core domains and related measures. The working draft of the instrument was further reviewed by a survey methodologist, and prepared for cognitive testing. Following three rounds of cognitive testing and revision, as described below, Center investigators again reviewed and finalized this working version of the WISH Assessment.
Cognitive testing methods
The purpose of cognitive testing is to ensure that the items included on a survey effectively measure the intended constructs and are uniformly understood by potential respondents. The process focuses on the performance of each candidate item when used with members of the intended respondent group, and specifically assesses comprehension, information retrieval, judgment/estimation, and selection of response category. 49 , 50 In the development of the WISH Assessment, we tested the instrument through three rounds of interviews.
Data Collection
Participants were asked to fill out the self-administered paper (N=15) or web (N=4) survey and participate in a telephone-administered qualitative interview with a trained interviewer. Participants received the survey 48 hours prior to the interview, and were encouraged to complete the survey as close to the actual interview as possible. They were not explicitly encouraged to consult with others, nor were they told not to.
The semi-structured interviews were conducted using a structured interview guide and retrospective probing techniques. The first round focused on comprehension of key attributes for each item (e.g., concepts of integration and collaborative environments) and of key words or phrases in the context of the question and instrument. Items revised following round 1 were again tested in a second round using the same approach. The focus of round 2 was to assess the adequacy of revisions in addressing the problems identified in round 1. A third round of interviews was conducted to confirm there were no additional problems due to revisions based on round 2. Across all rounds, the interviews concluded with a series of questions about the participant’s overall experience in completing the survey. For example, participants could provide general feedback on the survey content and the time required to complete the survey, and could comment on questions that didn’t fit within the survey or were duplicative. Participants were compensated with a $20 Amazon gift card for their time.
Participants were selected using purposive sampling to ensure diversity across industries and organizational roles, and included directors of human resources, occupational health, safety, and similar positions from hospitals (n=9), risk management (n=2), technology (n=2), transportation (n=2), community health center (n=1), manufacturing (n=1), laboratory research and development (n=1), and emergency response (n=1). Participants were identified through the Center for Work, Health and Wellbeing, and included attendees at a continuing education course and former collaborators on other projects. New participants were included in subsequent rounds of testing in order to ensure that revisions to items from each round adequately addressed the limitations, and that items were appropriately and uniformly interpreted among respondents.
Following each round, feedback was summarized by item. Participant feedback was used to determine if the question wording needed modification. Each item was first considered on its own, and then assessed in terms of its fit in measuring its construct. A survey methodologist made suggested revisions which were then reviewed and discussed by the author team and interviewers to ensure that they retained substantive focus on the construct. We revised items when participants found terminology unclear or when participants’ answers did not map onto the intended construct. An item was removed if it was found to be redundant or did not adequately map onto the intended construct, and its deletion did not compromise content validity. We analyzed data across industry, and also assessed responses specific to the hospital industry, which included the most respondents.
Description of the constructs and measures
We identified six core constructs as central to best practices for protecting and promoting worker safety, health and wellbeing through the Delphi process and literature review. The items included in each construct with their response categories are included in Table 1 . Following the Indicators of Integration, this assessment was designed to be answered by one or more persons within an organization who are likely to be familiar with the organization’s policies, programs and practices related to worker safety, health and wellbeing. Below, we present each construct, including its definition, rationale for inclusion, and sources of the items included.
Workplace Integrated Safety and Health (WISH) Assessment
| This brief survey is designed to assess the extent to which organizations effectively implement integrated approaches to worker safety, health and wellbeing. The term “integrated approaches” refers to policies, programs, and practices that aim to prevent work-related injuries and illnesses and enhance overall workforce health and wellbeing. This survey is meant to be completed by health and safety representatives, either in human resources or in safety, at the middle management level. There are no right or wrong answers–Your responses are meant to reflect your understanding of policies, practices and programs currently implemented within your organization. |
| 1. The following questions refer to leadership commitment. We define the term “leadership commitment” to mean the following: An organization’s leadership makes worker safety, health, and well-being a clear priority for the entire organization. They drive accountability and provide the necessary resources and environment to create positive working conditions. Response Categories: Please indicate how often you feel your organization or its leaders do each of the following: Not all the time, some of the time, most of the time, all of the time. |
| a. The company’s leadership, such as senior leaders and middle managers, communicate their commitment to a work environment that supports employee safety, health, and wellbeing. |
| b. The organization allocates enough resources such as enough workers and money to implement policies or programs to protect and promote worker safety and health. |
| c. Our company’s leadership, such as senior leaders and managers, take responsibility for ensuring a safe and healthy work environment. |
| d. Worker health and safety are part of the organization’s mission, vision or business objectives. |
| e. The importance of health and safety is communicated across all levels of the organization, both formally and informally. |
| f. The importance of health and safety is consistently reflected in actions across all levels of the organization, both formally and informally. |
| 2. The following questions refer to participation. We define the term “participation” to mean the following: Stakeholders at every level of an organization, including organized labor or other worker organizations if present, help plan and carry out efforts to protect and promote worker safety and health. Response categories: For these collaborative activities or programs, please indicate how often you believe your organization implements each: not at all, some of the time, most of the time, all of the time. |
| a. Managers and employees work together in planning, implementing, and evaluating comprehensive safety and health programs, policies, and practices for employees. |
| b. This company has a joint worker-management committee that addresses efforts to protect and promote worker safety and health. |
| c. In this organization, managers across all levels consistently seek employee involvement and feedback in decision making. |
| d. Employees are encouraged to voice concerns about working conditions without fear of retaliation. |
| e. Leadership, such as supervisors and managers, initiate discussions with employees to identify hazards or other concerns in the work environment. |
| 3. The following questions refer to policies, programs, and practices focused on positive working conditions. We define this term to mean the following: The organization enhances worker safety, health, and well-being with policies and practices that improve working conditions. Response categories: For each of the following policies or practices, please indicate the degree to which they are implemented at your company: not at all, somewhat, mostly, completely. |
| a. The workplace is routinely evaluated by staff trained to identify potential health and safety hazards. |
| b. Supervisors are responsible for identifying unsafe working conditions on their units. |
| c. Supervisors are responsible for correcting unsafe working conditions on their units. |
| d. This workplace provides a supportive environment for safe and healthy behaviors, such as a tobacco-free policy, healthy food options, or facilities for physical activity. |
| e. Organizational policies or programs are in place to support employees when they are dealing with personal or family issues. |
| f. Leadership, such as supervisors and managers, make sure that workers are able to take their entitled breaks during work (e.g. meal breaks). |
| g. Supervisors and managers make sure workers are able to take their earned times away from work such as sick time, vacation, and parental leave. |
| h. This organization ensures that policies to prevent harm to employees from abuse, harassment, discrimination, and violence are followed. |
| i. This organization has trainings for workers and managers across all levels to prevent harm to employees from abuse, harassment, discrimination, and violence. |
| j. This workplace provides support to employees who are returning to work after time off due to work-related health conditions. |
| k. This workplace provides support to employees who are returning to work after time off due to non-work related health conditions. |
| l. This organization takes proactive measures to make sure that the employee’s workload is reasonable, for example, that employees can usually complete their assigned job tasks within their shift. |
| m. Employees have the resources such as equipment and training do their jobs safely and well. |
| n. All employees in this organization receive paid leave, including sick leave. |
| 4. The following questions refer to comprehensive and collaborative strategies. We define this term to mean the following: Employees from across the organization work together to develop comprehensive health and safety initiatives. Response categories: For the following collaborative or comprehensive policies, programs, or practices, please indicate the degree to which your company implements each: not at all, somewhat, mostly, completely. |
| a. This company has a comprehensive approach to promote and protect worker safety and health. This includes collaborative efforts across departments as well as education and programs for individuals and policies about the work environment. |
| b. This company has a comprehensive approach to worker wellbeing. This includes collaboration across departments in efforts to prevent work-related illness and injury and to promote worker health. |
| c. This company coordinates policies, programs, and practices for worker health safety, and wellbeing across departments. |
| d. Managers are held accountable for implementing best practices to protect worker safety, health, and wellbeing, for example through their performance reviews. |
| e. Managers are given resources, such as equipment and trainings, for implementing best practices to protect and promote worker safety, health, and wellbeing. |
| f. This company prioritizes protection and promotion of worker safety and health when selecting vendors and subcontractors. |
| 5. The following questions refer to adherence. We define the term “adherence” to mean the following: The organization adheres to federal and state regulations, as well as ethical norms, that advance worker safety, health, and well-being. Response categories: For each of the following statements, please indicate the degree to which you believe your company adheres to or prioritizes standards and regulations: not at all, somewhate, mostly, completely. |
| a. This organization complies with standards for legal conduct. |
| b. In this organization, people show sincere respect for others’ ideas, values, beliefs |
| c. This workplace complies with regulations aimed at eliminating or minimizing potential exposures to recognized hazards. |
| d. This company ensures that safeguards regarding worker confidentiality, privacy and non-retaliation protections are followed. |
| e. The wages for the lowest-paid employees in this organization seem to be enough to cover basic living expenses such as housing and food. |
| 6. The following questions refer to data-driven change. We define this term to mean the following: Regular evaluation guides an organization’s priority setting, decision making, and continuous improvement of worker safety, health, and well-being initiatives. Response categories: Please indicate the degree to which your company does each of the following: not at all, somewhat,mostly, completely. |
| a. The effects of policies and programs to promote worker safety and health are measured using data from multiple sources, such as injury data, employee feedback, and absence records |
| b. Data from multiple sources on health, safety, and wellbeing are integrated and presented to leadership on a regular basis. |
| c. Evaluations of policies, programs and practices to protect and promote worker health are used to improve future efforts. |
| d. Integrated data on employee safety and health outcomes are coordinated across all relevant departments. |
Leadership Commitment , defined as: “Leadership makes worker safety, health, and well-being a clear priority for the entire organization. They drive accountability and provide the necessary resources and environment to create positive working conditions.” This construct was included in our Indicators of Integration; items in the WISH Assessment were adapted from this prior measure, as well as from other sources. 1 , 41 , 51 , 52 Organizational leadership has been linked to an array of worker safety, health and wellbeing outcomes, 53 , 54 including organizational safety climate, 55 , 56 job-related wellbeing, 57 , 58 workplace injuries, 59 , 60 and health behaviors. 61 , 62 This element recognizes that top management is ultimately responsible for setting priorities that define worker and worksite safety and health as part of the organization’s vision and mission. 14 , 16 Leadership roles include providing the resources needed for implementing best practices related to worker safety, health and wellbeing; establishing accountability for implementation of relevant policies and practices; and effectively communicating these priorities through formal and informal channels. 51 , 52
Participation , defined as: “Stakeholders at every level of an organization, including labor unions or other worker organizations if present, help plan and carry out efforts to protect and promote worker safety and health.” Many organizations have mechanisms in place to engage employees and managers in decision making and planning. These mechanisms may be used in planning and implementing integrated policies and programs, for example through joint worker-management committees that combine efforts to protect and promote worker safety, health and wellbeing. 7 , 63 , 64 Employee participation in decision-making facilitates a broader organizational culture of health, safety and wellbeing. Participation also includes encouraging employees to identify and report threats to safety and health, without fear of retaliation and with the expectation that their concerns will be addressed. Items included were adapted from the Indicators of Integration 1 and a self-assessment checklist from the Center for the Promotion of Health in the New England Workplace. 65
Policies, programs and practices that foster supportive working conditions , defined as: “The organization enhances worker safety, health, and well-being with policies and practices that improve working conditions.” These policies, programs and practices are central to the conceptual model presented in Figure 1 . Items include measures of the physical work environment and the organization of work (i.e., psychosocial factors, job tasks, demands, and resources), and are drawn from multiple sources. 1 , 41 , 66 – 69 The focus on working conditions is based on principles of prevention articulated in a hierarchy of controls framework, which has been applied within TWH. 10 , 70 Eliminating or reducing recognized hazards, whether in the physical work environment or the organizational environment, provides the most effective means of reducing exposure to potential for hazards on the job. Policies and processes to protect workers from physical hazards include routine inspections of the work environment, with mechanisms in place for correction of identified hazards, as well as policies that support safe and healthy behaviors, such as tobacco control policies. A supportive work organization includes safeguards against job strain, work overload, and harassment, 7 , 71 – 74 as well as supports for workers as they address work-life balance, return to work after an illness or injury, and take entitled breaks, including meal breaks as well as sick and vacation time. 75 , 76
Comprehensive and collaborative strategies , defined as: “Employees from across the organization work together to develop comprehensive health and safety initiatives.” Measures were adapted from our Indicators of Integration 1 and also relied on recent recommendations from the American College of Occupational and Environmental Medicine. 41 Although efforts to protect and promote worker safety and health have traditionally functioned independently, this construct acknowledges the benefits derived from collaboration across departments within an organization to protect and promote worker safety and health, both through policies about the work environment as well as education for workers. These efforts carry through into the selection of subcontractors and vendors, recognizing their impact on working conditions.
Adherence , defined as: “ The organization adheres to federal and state regulations, as well as ethical norms, that advance worker safety, health, and well-being.” The importance of this construct has been recognized by multiple organizations, whose contributions and metrics were incorporated in the measures included here. 7 , 77 – 79 Employers have a legal obligation to provide a safe and healthy work environment. 7 , 68 There is also significant agreement that any system that includes health and safety metrics must include safeguards for employee confidentiality and privacy. 7 , 41
Data-driven change , defined as: “Regular evaluation guides an organization’s priority setting, decision making, and continuous improvement of worker safety, health, and well-being initiatives.” Building health metrics into corporate reporting underscores the importance of worker health and safety as a business priority. 16 , 80 Feedback to leadership based on evaluation and monitoring of integrated programs, policies and practices can provide a basis for ongoing quality improvement. An integrated system that reports outcomes related both to occupational health as well as health behaviors and other health and wellbeing indicators can point to shared root causes within the conditions of work. 1 , 14
Cognitive testing results
We tested the WISH Assessment in three rounds of cognitive testing with a total of 19 participants. (See Appendix 1 for changes made to the items across the three rounds of testing.) On average, participants completed the self-administered survey in about 10–15 minutes, and the cognitive interviews took an average of 45 minutes. In the first round of cognitive testing, three participants completed a web version of the survey, and five, a paper-and-pencil version. Because we found no differences in concerns raised, the second round used only a paper survey, whereas the third included web respondents to confirm no differences in the final instrument. Changes made to the survey items were based on input from multiple respondents over the three rounds of interviews, and did not rely specifically on input from any one individual.
For items with uniform interpretation, revisions were made if respondents suggested a word or phrase that would clarify the question that investigators felt retained substantive focus. In addition, some items were dropped because they revealed multiple sources of problems, were too difficult to answer, or were identified as redundant. The first round of testing led to the removal of seven items and the modifying of 24 items. The second round of cognitive testing revealed that problems with the question wording remained with 15 questions in the context of the full survey. No additional questions were removed. These specific questions were updated and re-tested among three participants.
Throughout the cognitive testing process, we found several items to have either ambiguous terminology resulting in non-uniform or restrictive interpretation, inadequate framing of key terms and constructs, or lack of knowledge or perceived ability to provide an answer, resulting in poor information retrieval or mapping to the construct. Items measuring integration or collaboration within an organization were more often identified as problematic; to address this concern, we included a description of these constructs in the survey’s introduction to frame the survey for respondents. Although there was uniform interpretation of items asking about employee’s living wage, some respondents reported they did not have knowledge to provide an accurate answer. Most other items revealed uniform interpretation and no concerns regarding information retrieval or selecting response categories.
Looking at the items by construct, we identified particular concerns with items measuring two domains: “ policies, programs, and practices that foster supportive working conditions” and “adherence ” to norms and regulations. To address these concerns, we revised these items by improving the description of constructs or the terms in the respective sections’ introductions, using less ambiguous wording and integrating appropriate examples as necessary. We found commonalities across the responses in the remaining four domains, and describe our specific remediation process for each of these domains:
Leadership commitment
In round 1, we found a lack of clarity for the concept of “leadership.” For example, one respondent from the health care industry reported that: “[senior leaders and middle managers] should be distinguished and not conflated because there are several layers of management.” As a result, several respondents expressed difficulty retrieving accurate information due to level-specific answers. One respondent from a laboratory research and development company noted “[…] leadership communicate their commitment to safety and health through written policies. If you were to add supervisors – people closer to the front line – it would be different.” We addressed this concern by rewriting the introduction for this domain to clearly define “leadership commitment” and remove mention of leadership levels. However, we retained the wording “[…] such as senior leaders and middle managers, […]” in two items to reflect that organizations have channels through which commitment is communicated or enforced.
Participation
The questions for collaborative participation were largely identified as clear and uniformly interpreted. However, there was lack of clarity regarding who the key stakeholders were, particularly in the introduction. In addition, respondents reported that the introduction was too wordy and had a high literacy bar. Given these concerns and the suggestion that the use of the term “culture” was too academic, so we omitted use of this term. Some respondents expressed difficulty retrieving an appropriate answer due to this lack of clear framing of items in the introduction. We addressed this concern by rewriting the introduction to emphasize the definition of “participation” in the context of an organization’s activities that ensure worker safety and health. Feedback from round 2 found that this helped frame the item set more clearly. However, the word “encourage” in “In this organizational culture, managers encourage employees to get involved in making decisions” was identified as ambiguous. This was changed to “[…] seek employee involvement and feedback […]”.
Comprehensive and collaborative strategies
The most common feedback, expressed among several participants in multiple industries, for items in this domain was difficulty with the concept of “comprehensive,” i.e., that programming should address both prevention of illness and injury and promotion of worker health and safety. To a lesser extent, respondents also found difficulty with the “collaborative” concept. For example, some respondents including those from the hospital industry and in risk management, expressed difficulty responding to an item that included both “prevent” and “enhance,” which were perceived as “two different questions within this question.” We addressed these concerns by more clearly defining the two core constructs in a revised introduction. Moreover, we revised items to retain both “prevent and promote” while more clearly framing the question in context of collaboration. For example, the item “This company has a comprehensive approach to worker wellbeing that includes efforts to prevent work-related illness and injury as well as to enhance worker health” was revised to “This company has a comprehensive approach to worker wellbeing. This includes collaboration across departments in efforts to prevent work-related illness and injury and to promote worker health.”
Data-driven change
For this domain, we found evidence of poor cueing for the concepts of integration and coordination in the context of using data to produce organizational change. For example, several respondents from the hospital industry expressed that they did not understand what was meant by “integrated” in the context of “Summary reports on integrated policies and programs are presented to leadership on a regular basis, while also protecting employee confidentiality,” or “coordinated system” in context of “Data related to employee safety and health outcomes are integrated within a coordinated system.” Remediation focused on clarifying the context and definitions for integration and coordination. First, the introduction was revised to explicitly define data-driven change. Secondly, items were reworded to clarify integration and coordination. For example, “Summary reports on integrated policies and programs are presented to leadership on a regular basis, while also protecting employee confidentiality” was revised to “Data from multiple sources on health, safety, and wellbeing are integrated and presented to leadership on a regular basis.”
Our analyses also underscored commonalities across industries even when these issues seemed industry-specific. For example, comments from several participants suggested that a product-based mission may often dominate concerns about worker safety and health. In healthcare, this may be manifested by prioritizing patient care and safety over worker health and safety, or in other industries by a focus on production or timeline goals. Across industries, there was widespread agreement that Employee Assistant Programs was the primary resource for supporting employees dealing with personal or family issues.
Effective policies, programs and practices contribute to improvements in worker health, safety and wellbeing, as well as to enterprise outcomes such as improved employee morale, reduced absence and turnover, potentially reduced healthcare costs, and improved quality of services. 2 , 40 , 81 – 84 This manuscript presents the Workplace Integrated Safety and Health (WISH) Assessment, designed to evaluate the extent to which organizations implement best practice recommendations for an integrated, systems approach to protecting and promoting worker safety, health and wellbeing. This instrument builds on the Indicators of Integration, previously published and validated by the Center for Work, Health and Wellbeing. 1 , 42 , 43 We have expanded this tool based on the conceptual model presented in Figure 1 , 2 which prioritizes working conditions as determinants of worker safety, health and wellbeing. In addition, the WISH Assessment is designed to measure the extent to which an organization implements best practice recommendations. These constructs have also been used to inform in the Center’s guidelines for implementing best practice integrated approaches. 8
A growing range of metrics are available to assess organizational approaches to worker safety and health. The Integrated Health & Safety Index (IHS Index), created by the American College of Occupational and Environmental Medicine in collaboration with the Underwriters Laboratories, focuses on translating health and safety into value for businesses using three dimensions: economic, environmental and social standards. 41 By focusing on value, this measure has the potential to bolster the business case for health and safety. 41 , 85 The HERO Health and Well-being Best Practices Scorecard in Collaboration with Mercer is an online tool that allows employers to receive emailed feedback on their health and well-being practices. 86 Similarly, the American Heart Association’s Workplace Health Achievement Index provides an on-line self-assessment scorecard that includes comparisons with other companies. 87 The health metrics designed by the Vitality Institute include both a long and short form questionnaire, both with automatic scoring. 88 The Center for the Promotion of Health in the New England Workplace (CPH-NEW) has developed a tool to assess organizational readiness for implementing an integrated approach 11 and is developing a tool that focuses on participatory engagement of workers, with the goal of involving workers in the process of prioritizing health and safety issues and then developing and evaluating the proposed solutions. 89 Other measures of the work environment, such as the Health and Safety Executive Managements Standards Indicator Tool used in the United Kingdom, are designed to be taken by workers and so can provide detailed information on conditions as they are experienced by workers, but do not capture company-level policies and programs. 90 The WISH Assessment, designed to assess a company’s use of best practices for health and safety, is substantially shorter than the IHS Index and the HERO Scorecard, does not require the compilation of metrics and does not use individual employee data. In addition, in comparison to these other measures, the WISH Assessment can be used to guide organizations towards best practices and can be easily completed by organizations that might not have the resources to use the more extensive assessments.
Next steps in the development of the WISH Assessment include validation of the instrument across multiple samples, and design and testing of a scoring system. We validated the Indicators of Integration in two samples and found it to have convergent validity and high internal consistency, and to express one unified factor even when slight changes were made to adapt the measure. 42 , 43 We expect to follow a similar approach in validating this tool and assessing its dimensionality in large samples using factor analysis. Our goal is to design a scoring system that would be appropriate for both applied and research applications. As such, we expect the scoring algorithm to be simple enough for auto-calculation.
This tool may ultimately serve multiple purposes. As a research tool, it may provide a measure of workplace best practices that can be examined as determinants of worker safety and health outcomes. After being validated, the WISH Assessment may be used to explore organizational characteristics that may be associated with implementation of best practices. This instrument also responds to calls for practical tools for organizations implementing an integrated approach and focusing on working conditions. 41 The Center used the Indicators of Integration as part of a larger assessment process in three small-to-medium manufacturing businesses to inform organizations’ priority setting and decision making around the integration of occupational safety and health and health promotion. 91 In-person group discussions with key staff and executive leaders were used to rate each question on the scorecard, resulting in actionable steps based on identified gaps. Similarly, a validated WISH Assessment could be translated into a scorecard to be used to inform priority setting, decision making and to monitor changes over time in conditions of work and related health and safety outcomes. The Center has also applied the constructs defined in the WISH Assessment in its new best practice guidelines, 8 which include suggestions for formal and informal policies and practices ( Table 2 ).
Example Policies and Practices by each WISH construct.
| Construct | Formal Policies | Informal Practices |
|---|---|---|
| Physical environment Work organization Psychosocial environment | Physical environment Work organization Psychosocial environment | |
McLellan D, Moore W, Nagler E, Sorensen G. 2017. Implementing an integrated approach: Weaving worker health, safety, and well-being into the fabric of your organization. Dana-Farber Cancer Institute: Boston, MA. http://centerforworkhealth.sph.harvard.edu/
These indicators describe policies, programs and practices within the control of a specific organization or enterprise, and are most likely to apply to organizations that employ approximately 100 or more employees. The cognitive testing conducted to refine the items included in the WISH Assessment included representatives from organizations in selected settings; the generalizability of these results may therefore be restricted to similar types of organizations. There remains a need for exploring how this measure may function in different industries and across organizations of varying size. Although the purpose of the WISH instrument is to provide a measure that might be broadly useful across industries, we also recognize that each industry faces particular challenges due to the nature of what they do; supplementary questions may be needed to address these industry-specific concerns. Although this measure has not yet been validated, we believe it is important to share it and to explore opportunities for collaboration with other researchers interested in testing its psychometric properties and across populations and settings, in order to further develop this tool. It will ultimately be important as well to develop mechanisms for scoring this instrument, taking account potential weighting across the domains included.
Growing evidence clearly documents the benefits to be derived from integrated systems approaches for protecting and promoting worker safety, health and wellbeing. Practical, validated measures of best practices that are supported by existing evidence and do not place an undue burden on respondents are needed to support systematic study and organizational change. In cognitive testing, we demonstrated that the items included in this instrument effectively assess the defined constructs. Our goal was to create a measure that will be broadly useful and valid across industry, and might contribute to understanding differences and similarities by industry. Thus, the general applicability of this instrument is a strength in that it would allow for comparisons across industries, if so desired by substantive research. We also recognize the potential benefits of industry-specific versions of this instrument which may use this broader instrument as a base set of measures while also expanding on areas that are unique to a given industry. This may help increase understanding of industry-specific health and safety challenges. The WISH Assessment holds promise as a tool that may inform organizational priority setting and guide research around causal pathways influencing implementation and outcomes related to these approaches.
Supplementary Material
Supplemental digital content, acknowledgments.
This work was supported by a grant from the National Institute for Occupational Safety and Health (U19 OH008861) for the Harvard T.H. Chan School of Public Health Center for Work, Health and Well-being.
Conflict of Interest noted: None
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Systematic literature review on the effects of occupational safety and health (OSH) interventions at the workplace
Affiliation.
- 1 Johan Hviid Andersen, Professor, Department of Occupational Medicine, Danish Ramazzini Centre, Regional Hospital West Jutland - University Clinic, Gl. Landevej 61, 7400 Herning, Denmark. [email protected].
- PMID: 30370910
- DOI: 10.5271/sjweh.3775
Objectives The aim of this review was to assess the evidence that occupational safety and health (OSH) legislative and regulatory policy could improve the working environment in terms of reduced levels of industrial injuries and fatalities, musculoskeletal disorders, worker complaints, sick leave and adverse occupational exposures. Methods A systematic literature review covering the years 1966‒2017 (February) was undertaken to capture both published and gray literature studies of OSH work environment interventions with quantitative measures of intervention effects. Studies that met specified in- and exclusion criteria went through an assessment of methodological quality. Included studies were grouped into five thematic domains: (i) introduction of OHS legislation, (ii) inspection/enforcement activity, (iii) training, such as improving knowledge, (iv), campaigns, and (v) introduction of technical device, such as mechanical lifting aids. The evidence synthesis was based on meta-analysis and a modified Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach. Results The search for peer-reviewed literature identified 14 743 journal articles of which 45 fulfilled the inclusion criteria and were eligible for meta-analysis. We identified 5181 articles and reports in the gray literature, of which 16 were evaluated qualitatively. There was moderately strong evidence for improvement by OHS legislation and inspections with respect to injuries and compliance. Conclusions This review indicates that legislative and regulatory policy may reduce injuries and fatalities and improve compliance with OHS regulation. A major research gap was identified with respect to the effects of OSH regulation targeting psychological and musculoskeletal disorders.
PubMed Disclaimer
Similar articles
- Systematic review of qualitative literature on occupational health and safety legislation and regulatory enforcement planning and implementation. MacEachen E, Kosny A, Ståhl C, O'Hagan F, Redgrift L, Sanford S, Carrasco C, Tompa E, Mahood Q. MacEachen E, et al. Scand J Work Environ Health. 2016 Jan;42(1):3-16. doi: 10.5271/sjweh.3529. Epub 2015 Oct 13. Scand J Work Environ Health. 2016. PMID: 26460511 Review.
- A systematic literature review of the effectiveness of occupational health and safety regulatory enforcement. Tompa E, Kalcevich C, Foley M, McLeod C, Hogg-Johnson S, Cullen K, MacEachen E, Mahood Q, Irvin E. Tompa E, et al. Am J Ind Med. 2016 Nov;59(11):919-933. doi: 10.1002/ajim.22605. Epub 2016 Jun 7. Am J Ind Med. 2016. PMID: 27273383 Review.
- Occupational safety and health enforcement tools for preventing occupational diseases and injuries. Mischke C, Verbeek JH, Job J, Morata TC, Alvesalo-Kuusi A, Neuvonen K, Clarke S, Pedlow RI. Mischke C, et al. Cochrane Database Syst Rev. 2013 Aug 30;(8):CD010183. doi: 10.1002/14651858.CD010183.pub2. Cochrane Database Syst Rev. 2013. PMID: 23996220 Review.
- Workplace health understandings and processes in small businesses: a systematic review of the qualitative literature. MacEachen E, Kosny A, Scott-Dixon K, Facey M, Chambers L, Breslin C, Kyle N, Irvin E, Mahood Q; Small Business Systematic Review Team. MacEachen E, et al. J Occup Rehabil. 2010 Jun;20(2):180-98. doi: 10.1007/s10926-009-9227-7. J Occup Rehabil. 2010. PMID: 20140483 Review.
- Exploratory Study on Occupational Health Hazards among Health Care Workers in the Philippines. Faller EM, Bin Miskam N, Pereira A. Faller EM, et al. Ann Glob Health. 2018 Aug 31;84(3):338-341. doi: 10.29024/aogh.2316. Ann Glob Health. 2018. PMID: 30835385 Free PMC article.
- Effectiveness of Occupational Safety and Health interventions: a long way to go. Vitrano G, Micheli GJL. Vitrano G, et al. Front Public Health. 2024 May 9;12:1292692. doi: 10.3389/fpubh.2024.1292692. eCollection 2024. Front Public Health. 2024. PMID: 38784580 Free PMC article. Review.
- Occupational health and safety regulatory interventions to improve the work environment: An evidence and gap map of effectiveness studies. Bondebjerg A, Filges T, Pejtersen JH, Kildemoes MW, Burr H, Hasle P, Tompa E, Bengtsen E. Bondebjerg A, et al. Campbell Syst Rev. 2023 Dec 11;19(4):e1371. doi: 10.1002/cl2.1371. eCollection 2023 Dec. Campbell Syst Rev. 2023. PMID: 38089568 Free PMC article.
- Effects of the Labor Inspection Authority's regulatory tools on physician-certified sick leave and employee health in Norwegian home-care services - a cluster randomized controlled trial. Finnanger Garshol B, Knardahl S, Emberland JS, Skare Ø, Johannessen HA. Finnanger Garshol B, et al. Scand J Work Environ Health. 2024 Jan 1;50(1):28-38. doi: 10.5271/sjweh.4126. Epub 2023 Oct 30. Scand J Work Environ Health. 2024. PMID: 37903341 Free PMC article. Clinical Trial.
- PROTOCOL: Occupational health and safety regulatory interventions to improve the work environment: An evidence and gap map of effectiveness studies. Bondebjerg A, Filges T, Pejtersen JH, Viinholt BCA, Burr H, Hasle P, Tompa E, Birkefoss K, Bengtsen E. Bondebjerg A, et al. Campbell Syst Rev. 2022 Apr 12;18(2):e1231. doi: 10.1002/cl2.1231. eCollection 2022 Jun. Campbell Syst Rev. 2022. PMID: 36911348 Free PMC article.
- Study of purchasing behavior evolution of work-safety-service based on hierarchical mixed supervision. Jingjing Z, Wei L. Jingjing Z, et al. Front Psychol. 2022 Nov 30;13:991539. doi: 10.3389/fpsyg.2022.991539. eCollection 2022. Front Psychol. 2022. PMID: 36532995 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Scandinavian Journal of Work, Environment & Health
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Health Safety & Wellbeing at Work: A review of the literature

In the changing world of work, health, safety and well-being are matters of continued and increasing concern for governments, employers and workers. The following document reviews the amassing body of literature in this field, focusing on topics and themes that are relevant to both local and global contexts. The key question guiding the review is a deceptively simple one: What makes for good health and safety at work? More specifically, the review is driven by the following questions: 1) What are the key factors of health, safety and well-being at work? 2) What can New Zealand learn from other jurisdictions? 3) What is the future of health, safety and well-being at work?
Related Papers
IOSH Research Report
Paul Almond
Work, Employment & Society
Clive Smallman
New Zealand Journal of Industrial Relations
Paul Duignan
Gerard Zwetsloot
There is growing attention in industry for the Vision Zero strategy, which in terms of work-related health and safety is often labelled as Zero Accident Vision or Zero Harm. The consequences of a genuine commitment to Vision Zero for addressing health, safety and well-being and their synergies are discussed. The Vision Zero for work-related health, safety and well-being is based on the assumption that all accidents, harm and work-related diseases are preventable. Vision Zero for health, safety and well-being is then the ambition and commitment to create and ensure safe and healthy work and to prevent all accidents, harm and work-related diseases in order to achieve excellence in health, safety and well-being. Implementation of Vision Zero is a process – rather than a target, and healthy organizations make use of a wide range of options to facilitate this process. There is sufficient evidence that fatigue, stress and work organization factors are important determinants of safety beha...
International journal of …
Chris Cunningham
Chief Hyginus Chika Onuegbu JP,LLM, MA,MSc, FCTI, FCA
When a worker leaves his residence to work for the upkeep of his family and contribute to the economy of his society and nation, he does so with a believe that he will come back to the warm embrace of his family at least the way he was when he left them. He does not expect that the work will howsoever lead to his death or disability or injury or ill health. There is therefore no gainsaying that he has a right to demand this from the society and the nation and that his employer, the society and nation have a duty to ensure that this right to safety and health at work is respected.
Cristina Leovaridis
3rd International Conference on Human Security, 4-5 November 2016, Belgrade, Serbia, ISBN 978-86-80144-09-2
Valentina Ranaldi
Safety Science
Maureen Dollard
Ciencia & Tecnología para la Salud Visual y Ocular
Ivonne Constanza Valero-Pacheco
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.

RELATED PAPERS
Oman Chapter of Arabian Journal of Business and Management Review
Vartikka Indermun
IZA Institute of Labor Economics Discussion Paper Series
Ioannis Theodossiou
Procedia Economics and Finance
Rares Munteanu
Isaac Mintah
Journal of Education and Practice
Rosemary Mbogo
Valentine Smith , Zaheer Rajack
International Journal for Research in Applied Science & Engineering Technology (IJRASET)
IJRASET Publication
Oxford Research Encyclopedia of Criminology
David Whyte
catherine grant
PsycEXTRA Dataset
Ala'a Shehabi
Muhammad Rafiqul Islam
Safety and Health for Workers - Research and Practical Perspective
Bankole Fasanya
Regulating Workplace Risks
Annie Thébaud-Mony
Elsa Underhill
Journal of Developing Country Studies, Vol 2, No.9, 2012. ISSN 2224-607X (Paper) ISSN 2225-0565 (Online)
Ruby Melody Agbola
Wesley McTernan
Frontiers in Psychology
Fabrizio Bracco
professor Tareq abdhulkadhum naser Alasadi
aditya jain
Risk Analysis VIII
Taleb Mounia
Doni Sutrisno
Mabelene Sim
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Open access
- Published: 20 June 2023
Impact assessment of e-trainings in occupational safety and health: a literature review
- Mohammad Mahdi Barati Jozan ORCID: orcid.org/0000-0002-5197-6260 1 ,
- Babak Daneshvar Ghorbani 2 ,
- Md Saifuddin Khalid ORCID: orcid.org/0000-0002-3731-2564 3 ,
- Aynaz Lotfata ORCID: orcid.org/0000-0002-7511-1755 4 &
- Hamed Tabesh ORCID: orcid.org/0000-0003-3081-0488 1
BMC Public Health volume 23 , Article number: 1187 ( 2023 ) Cite this article
6491 Accesses
4 Citations
Metrics details
Implementing workplace preventive interventions reduces occupational accidents and injuries, as well as the negative consequences of those accidents and injuries. Online occupational safety and health training is one of the most effective preventive interventions. This study aims to present current knowledge on e-training interventions, make recommendations on the flexibility, accessibility, and cost-effectiveness of online training, and identify research gaps and obstacles.
All studies that addressed occupational safety and health e-training interventions designed to address worker injuries, accidents, and diseases were chosen from PubMed and Scopus until 2021. Two independent reviewers conducted the screening process for titles, abstracts, and full texts, and disagreements on the inclusion or exclusion of an article were resolved by consensus and, if necessary, by a third reviewer. The included articles were analyzed and synthesized using the constant comparative analysis method.
The search identified 7,497 articles and 7,325 unique records. Following the title, abstract, and full-text screening, 25 studies met the review criteria. Of the 25 studies, 23 were conducted in developed and two in developing countries. The interventions were carried out on either the mobile platform, the website platform, or both. The study designs and the number of outcomes of the interventions varied significantly (multi-outcomes vs. single-outcome). Obesity, hypertension, neck/shoulder pain, office ergonomics issues, sedentary behaviors, heart disease, physical inactivity, dairy farm injuries, nutrition, respiratory problems, and diabetes were all addressed in the articles.
According to the findings of this literature study, e-trainings can significantly improve occupational safety and health. E-training is adaptable, affordable, and can increase workers’ knowledge and abilities, resulting in fewer workplace injuries and accidents. Furthermore, e-training platforms can assist businesses in tracking employee development and ensuring that training needs are completed. Overall, this analysis reveals that e-training has enormous promise in the field of occupational safety and health for both businesses and employees.
Peer Review reports
Introduction
Occupational injuries and diseases are among the most serious public health issues [ 1 ]. According to the most recent International Labor Organization report (2017), over 2.78 million workers die each year as a result of occupational accidents and work-related diseases [ 2 ]. The most serious negative consequences of occupational accidents and injuries are long-term disabilities [ 3 ] reduced ability to perform job duties [ 3 , 4 , 5 ], early retirement [ 3 ], medical care expenditure [ 4 , 5 ], absenteeism [ 4 , 5 , 6 ], presenteeism [ 4 , 5 ], and death [ 3 ]. These cost the global economy 3.94% of the global Gross Domestic Product (GDP) [ 2 ]. In various countries, these costs range from 1.8 to 6% of GDP [ 3 ].Treatment and preventive interventions are two types of interventions used to reduce occupational diseases and injuries, as well as the negative consequences of these events [ 7 ].
Preventive interventions in occupational health aim to change the work condition to prevent occupational accidents and reduce their harmful effects. There are three types of preventive interventions: primary preventive interventions, secondary preventive interventions, and tertiary preventive interventions [ 7 ]. Primary preventive interventions aim to create conditions that will help to prevent occupational disease and injury. In other words, these interventions aim to eliminate or reduce workers’ exposure to workplace hazards. Secondary and tertiary preventive interventions attempt to prevent disease or injury progression in the post-accident steps [ 7 ]. The primary preventive interventions are divided into three types: Environmental interventions, clinical interventions, and behavioral interventions are the first three [ 8 ]. Environmental interventions attempt to eliminate the causes of occupational accidents by altering work methods, equipment, and physical space [ 9 ]. Clinical interventions (for example, pre-employment medical examinations [ 10 ]) use therapeutic methods to prevent disease [ 8 ]. Behavioral interventions aim to change workers’ behavior in order for them to be safer at work [ 8 ].
Many developing and developed countries implement occupational safety and health programs (OSH) for workers due to the importance of safe behavior in reducing the costs of occupational accidents and their negative consequences [ 11 ]. The most important component of the OSH program has been introduced as education [ 12 , 13 , 14 , 15 , 16 ]. The World Health Organization (WHO) has also identified worker, employee, and occupational medicine specialist training as a key component in improving worker health [ 17 ].
The two main approaches in occupational education are class-based education and e-learning. Simple and low-cost solution [ 18 , 19 , 20 , 21 , 22 , 23 , 24 ], greater convenience [ 21 ], availability [ 18 , 21 , 22 , 24 ], high acceptance among the workforce [ 25 ], enhanced self-management and adherence in the target population [ 26 , 27 , 28 ], primary source for health-related information [ 29 , 30 ], internet availability for users [ 31 , 32 , 33 ], mobile phone availability for users [ 34 , 35 ], ability to use a personalized approach [ 23 ], flexibility to fit the users’ schedules [ 33 ], reach large numbers of participants [ 23 , 33 ] and prefer technology-enhanced educational programs [ 29 ] are the most important reasons that have made e-learning as a suitable alternative to traditional and class-based education.
In the last decade, studies [ 20 , 36 , 37 , 38 , 39 ] have been conducted to evaluate the provision of online and personalized occupational health and safety training content. Systematic reviews have been conducted on the impact of occupational health and safety e-training in limited cases [ 23 , 40 , 41 , 42 ], such as limiting studies to a geographical area [ 41 ], an occupational safety and health problem [ 23 , 40 , 42 ], a type of intervention [ 23 ], and etc. The limitations of systematic reviews did not have the comprehensive outlook on e-training role in the behavioral change and improve health. Given these relevant premises, the goal of this study is to conduct a systematic review of published studies that have used e-training to reduce occupational accidents through the end of 2021.
With the increasing use of technology in the delivery of training programs, e-learning has become a popular mode of training delivery with several potential benefits, such as flexibility, accessibility, and cost-effectiveness. This study seeks to evaluate the impact of e-trainings in occupational safety and health by conducting a comprehensive literature review. The findings of this study contribute to the ongoing discussions on how technology can be leveraged to improve workplace safety measures and reduce accidents and injuries. Moreover, it is essential to understand the effectiveness of e-training programs compared to traditional training methods and identify best practices for developing effective e-training programs. This study aims to fill this gap in current knowledge by providing a comprehensive analysis of the existing literature on e-trainings in occupational safety and health.
This study has two primary objectives: providing up-to-date details on online occupational health and safety training interventions and offering recommendations, discussing research gaps and challenges in online occupational health and safety training interventions.
Materials and methods
As a paper selection methodology, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 43 ] was utilized, which involves four phases: identification, screening, eligibility, and included. The first phase sets the search technique and databases used in the search. The title, abstract, and full text of the publications are assessed in the following steps, based on the inclusion-exclusion criteria set for the systematic review. The included articles are then determined. The qualitative synthesis is completed after the finalization of the included articles.
Identification phase: search strategy
A computer-based literature search in the PubMed and Scopus databases was carried out. These databases were searched until the end of 2021. The search used a combination of text terms and a hierarchically regulated vocabulary that was tailored to each database. The text terms were divided into workplace safety and health (Group 1) and e-training (Group 2). These groups were joined together with “AND.“ Group 1 terms included occupational health, occupational safety, workplace health, and workplace safety. e-Training, e-Education, online training, online learning, mobile training, and mobile education were all included in Group 2. The terms from each of the three categories were then joined together with “OR.“
Screening and eligibility phase
Determining the inclusion and exclusion criteria and the screening process are two important activities of this phase.
Inclusion/exclusion criteria
The inclusion criteria for this study involved educational interventions aimed at improving occupational safety and health among workers (Intervention) and published in English (Language) by the end of 2021 (Publication period). The interventions were designed for workers (Population) and delivered educational content through web or mobile-based platforms (Technology). The final inclusion criterion was that the interventions evaluate primarily outcomes related to occupational safety and health.
However, certain types of studies were excluded from the analysis. The interventions that were considered included those which examined multiple components or did not isolate the impact of training as a specific intervention component. The study population was also limited to excluding students, health professionals, disabled workers, military personnel, and drivers (Population). Outcome measures related to mental health, sleep, stress, and addiction were also excluded (Outcome). Similarly, studies utilizing 3D animation, Virtual Reality, Virtual game-based simulation, and 360-degree panoramas were excluded (Technology). Lastly, studies forced to use online education due to Coronavirus Disease 2019 (COVID-19) conditions were not considered.
Screening process
Two reviewers independently reviewed titles, abstracts, and full texts based on inclusion/exclusion criteria. Disagreements between the two reviewers on the inclusion/exclusion of an article were settled by consensus and, if required, by a third reviewer.
Included phase: analysis
A meta-analysis of the impact of e-training on enhancing occupational safety and health is impossible due to the different nature of the literature on the type of treatments, study design, primary and secondary outcomes, and evaluation approaches. As a result, this study explains the nature of the included studies’ implementation practice models in order to highlight the studies’ strengths and limitations and make recommendations for future research.
The comparative analysis method is used for the analysis and synthesis in order to extract the themes emerging from the evidence [ 44 ]. This method, like other qualitative data analysis methods, involved coding data into themes and then categorizing and drawing conclusions based on them. These codes contained a concept associated with that part of the article from which the code is extracted. To maintain consistency and create non-overlapping code sets, a clear definition was provided for each code [ 45 ]. The qualitative content analysis process includes eight steps: data preparation, reading the article carefully several times to obtain a sense of the whole, determining the critical information of each part of the article (transcripts), defining the unit of analysis using themes, development of coding scheme to organize data, coding the entire article based on the developed coding scheme, conclusion based on the coded data, and describing and interpreting the findings [ 45 ]. Two reviewers independently read the articles in-depth and coded them. The reviewers and the lead author compiled the obtained results, and if there were any differences, they tried to resolve them. The disagreements were resolved by discussion.
Each article was reviewed to extract methods, parameters, and the purpose of evaluating e-training. The following codes were extracted for each article: the purpose of study, study design, population study, the unit of allocation (workplace/individual), country, primary/secondary outcomes, platform, educational content structure, and evaluation of the study.
The computer-based literature search yielded 7,497 articles, of which 7,325 were identified after removing 172 duplicate papers. Six thousand four hundred articles were removed during the title review phase and 777 articles were removed during the abstract review phase. 64 articles were removed during the title review phase. Finally, 25 articles met the criteria for inclusion. Figure 1 depicts PRISMA flow diagram of this systematic review study. The articles included in this review are listed in Table 1 in appendix .
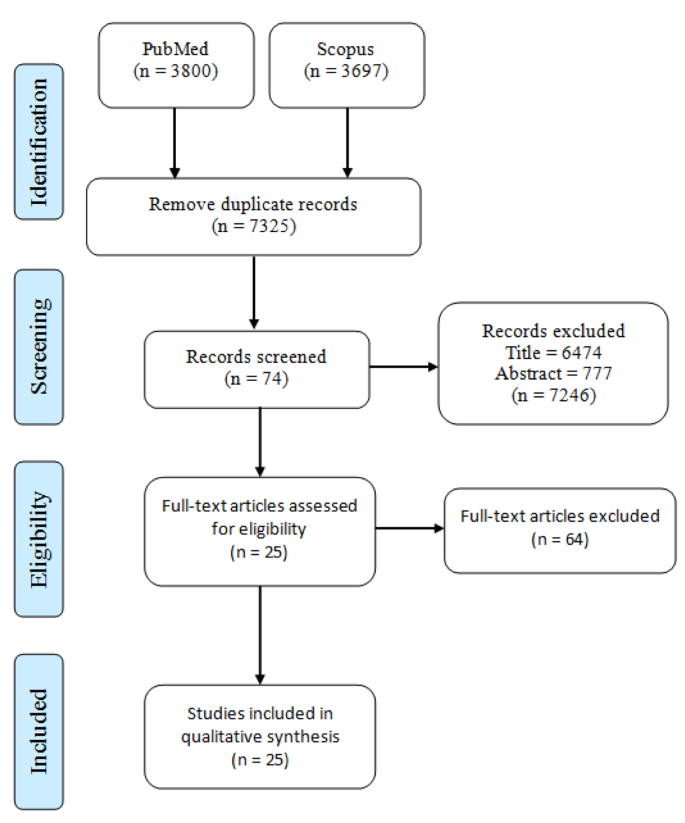
PRISMA flow diagram
The summary of the evaluation of the articles is shown in Table 1 . E-training has been used in 9 areas of occupational safety and health: sedentary behaviors, obesity, neck/shoulder pain/stiffness and Low Back Pain (LBP), physical inactivity, office ergonomics, hypertension, nutrition, respiratory, and multi-topic. The number of the included studies based on the year of publication, topic and country is given in Figs. 2 and 3 , and Fig. 4 respectively.
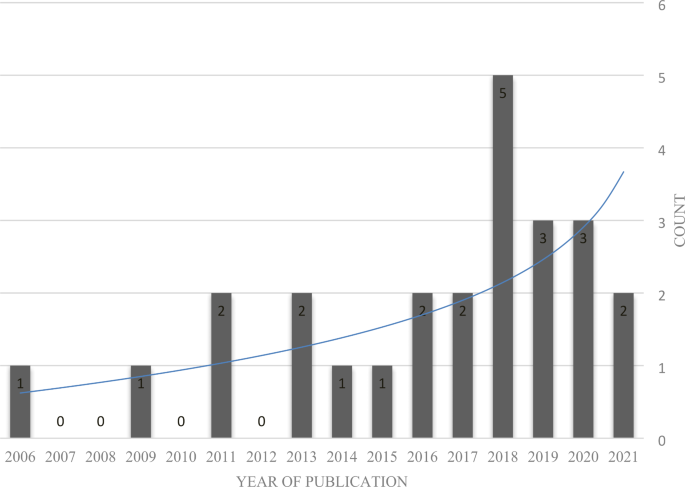
The number of the included studies based on the publication year
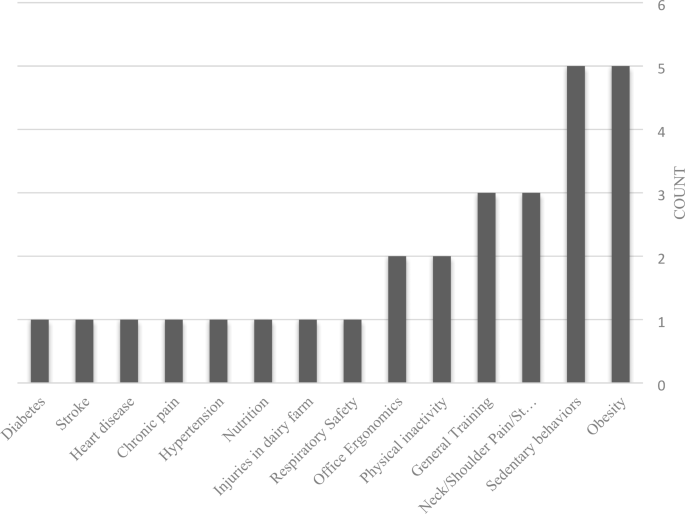
The number of the included studies based on the topic
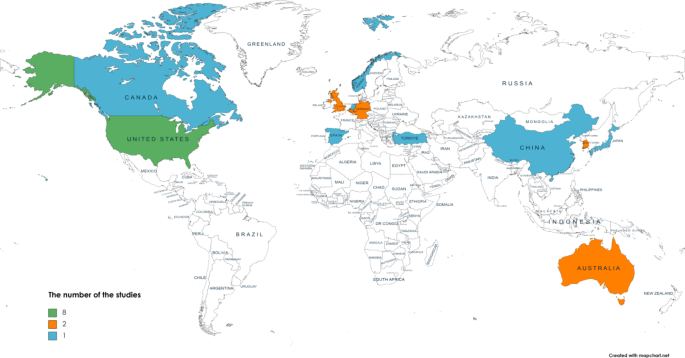
The number of the included studies based on each country. USA (n = 8); Australia, South Korea, UK, Germany, Belgium (n = 2), Japan, Turkey, Norway, Canada, Spain, China, Netherlands (n = 1)
Sedentary behaviors
A sedentary lifestyle is a significant public health concern in modern society [ 32 , 35 , 46 , 47 ], as it can lead to poor physical and mental health [ 48 , 49 , 50 ] and the development of serious diseases such as cancer, obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease [ 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 ]. Sedentary behavior is defined as any waking behavior (sitting, reclining, or lying posture) that consumes 1.5 metabolic equivalents of energy [ 52 ] and is prevalent in office settings [ 60 , 61 , 62 , 63 , 64 ]. Inactive activities account for nearly 65–82% of working time in industrialized countries [ 64 , 65 , 66 ], and 54–77% of office workers sit all day [ 66 , 67 , 68 ]. To address the negative consequences of sedentary behavior in the workplace, effective interventions must be designed, including encouraging desk-based employees to spend at least 2–4 h standing or doing light activity, taking regular breaks from sitting [ 69 ], considering environmental factors [ 70 , 71 ]., addressing concerns about productivity [ 72 ], and increasing awareness among employees and employers through training programs [ 73 ]. E-training has been used in [ 36 , 73 , 74 , 75 , 76 ] to reduce sedentary behavior and address the mentioned challenges.
A theory-driven, web-based, computer-tailored application called Start to Stand has been developed to reduce sedentary behavior at work [ 36 ]. The application includes both mandatory and optional components. In the mandatory component, personalized advice on how to interrupt and reduce sitting was provided, and the optional component has five non-committal sections: interruptions in sedentary behaviors, replacing sedentary behaviors with standing, sedentary behaviors during commuting, sedentary behaviors during work breaks (e.g., lunch), and developing a sedentary behavior change action plan that motivates participants to achieve their objectives by creating an action plan. The application uses various theories, such as the Theory of Planned Behavior [ 77 ], self-determination theory [ 78 , 79 ], and self-regulation theory [ 80 ], to provide recommendations to users. In order to evaluate the implemented application, the accessibility of participants and the acceptability were reported. One hundred and twelve employees from public city service were invited to participate in the study. The feasibility test showed that education, employment status, level of breaks at work, and attitudes towards interrupting sitting at work were influential in requesting advice, and 39% of participants requested at least one non-committal section from the optional component. The acceptability test revealed that most participants found the advice interesting, relevant, and motivating. The majority of participants (98.0%) reported that they had reduced their sedentary behavior or intended to do so.
The effects of the Start to Stand application [ 36 ] have been evaluated among Flemish employees in a field-based approach [ 75 ]. In order to assess a Randomized Controlled Trial (RCT) study designed with three groups; tailored group: the participants received the Start to Stand application, generic group: participants received a web-based application that provided general information on reducing or interrupting workplace sitting, and control group: participants did not receive any intervention. Two hundred thirteen employees participated in the intervention (tailored group n = 78, generic group n = 84, and control group n = 51). Outcomes were measured at baseline, one month, and three months after the intervention (follow-ups). Results showed a statistically significant difference in total workday sitting, sitting at work, other leisure time sitting, and break at work in the intervention group compared to the other two groups over time.
The dissemination evaluation of the Start to Stand application [ 36 ] in the Finnish population was done by [ 73 ]. The Reach, Effectiveness, Adoption, Implementation, and Maintenance framework (RE-AIM framework) [ 81 , 82 ] has been used for this proposal, which evaluates the potential public health impact of behavioral interventions from five perspectives ‘reach’, ‘efficacy/effectiveness,’ ‘adoption,’ ‘implementation,’ and ‘maintenance.’ The main dissemination methods used were partner websites, emails, newsletters, and social media. Over the evaluation period (12 October 2016 until 6 February 2018), 6,906 unique users visited the site. The evaluation results of the RE-AIM framework components are reported as follows. Firstly, Reach, which compares the characteristics of the study population with the target population (population in Flanders), showed that participants significantly differed from the target population in terms of age, gender, Body Mass Index (BMI), and Physical Activity (PA). Secondly, Efficacy/Effectiveness refers to the application’s positive and negative consequences in optimal and real-world conditions, respectively. The results of this section are presented in [ 75 ]. Thirdly, Maintenance refers to a continuous effort to make the software available to the target audience. In this case, the website was available to the public from 12 to 2016 to 6 February 2018. Fourthly, Adoption assesses delivery staff and setting variables. This item is outside the scope of this article [ 74 ]. Lastly, Implementation refers to intervention fidelity and resources (cost and time) to be used to implement the system in a real-world setting. The time spent on the dissemination activities was about 25.6 h, and the cost paid to the staff to perform these activities was 845 EUR.
The effect of the action plan section of the Start to Stand application [ 36 ] on changing sedentary behavior was evaluated in [ 76 ]. Creating an action plan was a non-committal section of the optional component of the application. The study had two goals: to examine the characteristics of users who made action plans (Goal 1) and the content of those action plans (Goal 2). The action plans consisted of four parts: what behavior to change when the action plan is triggered, where the action plan takes place, how long/frequent the breaks from sitting, and the purpose of the action plan. Participants in this study (n = 1,701) were divided into two groups, participants who had made at least one action plan (Group 1, n = 231) and those who had not made any action plans (Group 2). The study found significant differences between the two groups in terms of age, sedentary behavior at work, and awareness of health risks related to prolonged sitting. The participants in Group 1 were older, more sedentary at work, and more aware of the negative consequences of prolonged sitting (Goal 1). Most generated action plans focused on breaks from sitting every 30 min and replacing sitting with periods of standing (Goal 2).
A mobile-based application has been developed by [ 73 ]; the study aims to investigate the feasibility of implementing the application to reduce sedentary behavior in desk-based office workers. The application provides feedback on prolonged sitting, educational facts, setting goals to reduce sitting and reminders to achieve these goals, and self-monitoring features. The intervention was designed for eight weeks, and a feasibility cluster randomized controlled study with three groups has been designed to evaluate the application: Mobile Application Group (MA Group): the participants received the application, Mobile Application and Sit-Stand Work Desk Group (MA + SSWD Group): in addition to the application, a sit-stand work desk (SSWD) also provided for the participants and control group. Fifty-six workers participated in the study that 20, 20, and 16 participants were allocated in the MA, MA + SSWD, and control group, respectively. The feasibility of the application was assessed using several measures, including recruitment and retention, engagement, intervention delivery, and acceptability. The recruitment of companies to participate in the study was challenging; however, the retention rate was high among the recruited groups. Regarding engagement, the MA group showed better response time than the MA + SSWD group, and they acknowledged the reminders more. However, technical issues and diminishing user engagement have compromised the delivery of the intervention. In terms of acceptability, most participants in both MA and MA + SSWD groups found the intervention appropriate. Nonetheless, the MA group reported higher satisfaction levels than the MA + SSWD group.
Obesity is a major risk factor for non-communicable diseases such as diabetes, cardiovascular diseases, and some cancers [ 83 , 84 ]. Over 1.9 billion adults were overweight, and over 600 million were obese in 2014 [ 85 ]. Obesity is a significant global health challenge [ 86 , 87 , 88 , 89 ] and requires considerable healthcare resources to manage and prevent associated complications [ 90 , 91 , 92 , 93 ]. However, it is a modifiable disease [ 94 , 95 ], and multicomponent behavioral interventions have been shown to significantly affect weight loss and obesity-related complications in adults [ 96 , 97 , 98 , 99 ]. E-training has been used as a behavioral intervention for weight loss in the workforce [ 37 , 100 , 101 , 102 ]. An integrated and personalized mobile application for weight loss in work environments has been developed and evaluated by [ 37 ]. It includes a personalized diet prescription algorithm, a PA prescription algorithm, a convenient method of tracking daily diet and PA, and behavior change strategies for encouraging weight reduction to maximize user adherence. Weight reduction was the primary outcome. Thirty obese participants used the application for 12 weeks. They experienced a statistically significant mean weight reduction of 5.8%, along with improvements in secondary outputs such as anthropometric measures, metabolic profiles, fat measures, and bioimpedance measurements.
An online weight loss program for weight loss in work environments has been developed and evaluated by [ 100 ]. The percent weight loss and the achievement of clinical cut-points by class attendance were the primary and secondary outcomes, respectively. The intervention included a 10-week intervention focusing on the modification of eating habits (mindful eating, healthy eating, and stop-eating cues), medical considerations, weight loss, PA, weight maintenance, and self-monitoring. Data from 140,445 employees of different companies in the U.S. who used the program were analyzed, and class attendance and education level were found to be significantly correlated with percent weight loss. Evaluation of secondary outcomes determined that 71% of participants lost less than 3% of their starting weight, 16% achieved clinically beneficial weight loss (3-4% weight loss), and 13% achieved clinically significant weight loss (more than or equal to 5% weight loss).
The effectiveness of a weight loss mobile app based on WeChat is evaluated by [ 101 ] in a 6-month cohort study with 15,310 employees who worked in government agencies and enterprises in the Shunyi District of Beijing. The application was sent to the participants through messages on WeChat and allowed Participants to interact with others and receive expert feedback. Additionally, a weight loss unit rankings component was developed to motivate and encourage participants. Three thousand four hundred sixty-seven participants were in the control group, and 11,843 participants were in the intervention group. Those in the intervention group lost significantly more weight than those in the control group, with weight loss varying based on age (< 40 and ≥ 40) and educational level. The more active the intervention group members were, the more weight they lost.
An online lifestyle-intensive behavioral therapy-based intervention for weight loss and weight management for workers has been evaluated by [ 102 ]. The intervention was designed for 52 weeks, which included weekly 30-minute sessions that focused on education about PA, healthy eating, savvy food shopping, managing stress, sleep, and motivation. The content was based on the Centers for Disease Control and Prevention (CDC) DPP curriculum [ 103 ]. An entertaining television-like series was also shown during the classes to introduce a healthy lifestyle. In addition, personalized PA, meal plans, and exercise aids were provided for the first 16 weeks. In addition to the training section, there is a dashboard based on self-reported information and information on exercise. Sixty-nine thousand five hundred ninety-eight workers from 96 companies in the United States participated in this intent-to-treat cohort study. Participants were divided into three categories based on their attendance: those who attended at least one session, those who attended at least four active sessions (active participants), and those who completed the entire program (program completers). The participants who attended at least one session lost an average of 2.8% body weight, with 23% achieving 5% weight loss. The active participants lost an average of 3.5% body weight, with 29% achieving 5% weight loss. The program completers lost an average of 4.3% body weight, with 36% achieving 5% weight loss. Based on the results, gender, number of classes attended, obesity, and age are predictors of 5% and higher weight loss.
Neck/shoulder pain/stiffness and low back pain
Musculoskeletal pain is one of the common medical complaints in the working population [ 104 , 105 ]. Neck pain, shoulder pain, neck stiffness, shoulder stiffness, and LBP are the most important musculoskeletal pains in the workplace [ 25 , 34 ]. Factors that contribute to the increase in work-related musculoskeletal pains can be divided into three categories: sedentary lifestyle in work factors [ 106 , 107 , 108 ], physical factors such as poor posture or muscle weakness [ 106 ], and psychological factors [ 109 ].
Based on moderate-to-strong evidence, exercise therapy can significantly relieve pain and improve musculoskeletal disease function [ 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 ]; however, adherence to prescribed exercises is a significant challenge [ 120 , 121 ]. The lower the adherence to the exercise, the lower the effect of the treatment [ 122 ]. Therefore, adherence to the exercise should be considered in the design of interventions [ 123 ]. The attractiveness of the programs [ 122 ], expert feedback and interaction [ 124 , 40 , 122 , 125 , 126 , 127 , 128 , 129 ], performance evaluation [ 122 ], support by experts [ 122 , 123 ], and review sessions [ 123 ] are strategies that affect increasing adherence. In all three papers in this Sects. [ 25 , 34 , 130 ], interventions have been designed to improve commitment to the prescribed exercises.
An exercise-based artificial intelligence (AI)–assisted Chatbot on the LINE application has been implemented and evaluated by [ 25 ]. LINE is the most popular social media application in Japan [ 131 ]. The Chatbot included interactive features to improve participants’ adherence to the exercise program. The degree of pain and the improvement of pain were the primary outcomes. A RCT was designed to evaluate the application, and 121 participants with either neck/shoulder stiffness/pain or LBP or both were randomly assigned to intervention (n = 61) and control (n = 62) groups. The intervention group received exercise and educational instructions for 12 weeks. The result showed that the intervention group had statistically significant improvements in pain levels and exercise adherence compared to the control group. The adherence rate in the intervention group was 92% during the intervention.
A smartphone-based exercise program has been implemented and evaluated by [ 34 ]. This program divided the office workers into four categories based on the type of neck pain and offered corresponding exercise programs for each category. For this purpose, an algorithm has been implemented to help the user determine the kind of neck pain using simple tests. A single-group repeated-measures study was designed to evaluate the application. The developed program was given to 23 office workers suffering from neck pain to follow an exercise program for 10–12 min per day, three days per week, for eight weeks. The primary outcomes evaluated in the study were pain intensity and functional disability, both of which showed significant improvements after the intervention. Some secondary outcomes were also evaluated in the study. Quality of life also improved significantly, while fear avoidance and cervical spine ranges of motion (cervical ROM) did not show significant changes. The patient satisfaction was 3.91 (5.0). The adherence rate was 91.85%. The average time duration per exercise session was 16.86 ± 7.38 min.
A tailored web-based exercise intervention for physically untrained office workers with sub-acute non-specific LBP has been evaluated by [ 130 ]. This study aimed to assess: the impact of an intervention on exercise-related behavior to improve LBP and its correlation with functional disability improvement. For the first purpose, participants’ health status was categorized into five categories (pre-contemplation, contemplation, preparation, decision/ action, and maintenance), and their behavior change was evaluated and updated after the intervention. Participants were then classified into three categories based on their behavioral changes: no change, negative behavioral change, or positive behavioral change. One hundred participants in the RCT study were equally divided into two intervention groups (intervention and standard care) and control groups (usual care only). The intervention group received educational content and exercises via the Internet, and after nine months, most participants were in maintenance status and willing to continue the program (first objective). For the second purpose, the intervention group’s positive behavioral change was statistically significant, and there was a strong correlation between the stage of change and functional disability levels.
Physical inactivity
Physical inactivity is another occupational problem related to exercise that increases the risk of cardiovascular disease [ 132 ], cancer [ 133 ], musculoskeletal disorders [ 134 ], mental disorders and health conditions [ 135 ], and mortality [ 136 ]. It also leads to decreased quality of life [ 137 ] and daily activity performance [ 138 , 139 ]. Therefore, the low level of PA in the workplace is a crucial health challenge [ 140 ], causing about 3.2 million deaths per year globally [ 136 ]. Based on the data collected from 122 countries, almost one-third of the adult population of these countries had a low level of PA [ 141 ]. Adherence to prescribed exercises is a challenge for promoting PA interventions in the workplace. Only 40–45% of studies reported positive effects [ 142 , 143 ]. E-training has improved PA in the work environment [ 144 , 145 ].
The impact of a pedometer-based intervention for the promotion of PA has been evaluated by [ 130 ]. This 6-week intervention is designed based on the socio-cognitive learning theory [ 146 ], the theory of planned behavior [ 147 ], and the Health Action Process Approach (HAPA) model [ 148 ]. The intervention incorporated gamification features such as quizzes that aim to improve participants’ knowledge on PA and general health, the ability for each participant to select up to three health goals per week from a pool of 60 predetermined options, and the participants can determine the number of steps as step goals. Participants can join the weekly team or even individually challenge and compare themselves with others based on the results of game elements. One hundred seventy-six workers participated in the RCT study, with 99 in the intervention group and 77 in the control group. Direct health promotion outcomes, such as PA-related knowledge, intentions, and self-efficacy, and intermediate health outcomes including, Time spent on vigorous PA per week, Time spent on moderate PA per week, and Time spent walking per week, were measured. The results showed significant differences in all direct health promotion outcomes and only in Time spent walking per week among intermediate health outcomes between the control and intervention groups.
The feasibility and effectiveness of a web-based program to increase PA have been evaluated by [ 145 ]. The intervention used a PA monitor (PAM) and a website to provide personalized PA recommendations. Participants could upload their scores on the PAM to the website and plan and evaluate their recommendations based on earned scores, preferences, and PA goals. A RCT study was designed with the participation of 102 workers from eight work sites in Amsterdam to evaluate the intervention. Participants were randomly assigned into control groups (n = 51) and intervention groups (n = 51). The intervention group received a PAM and Web-based tailored PA advice for three months. The control group received a brochure on increasing PA and brief general PA recommendations. Primary outcomes included time spent on light-intensity, moderate-intensity, and vigorous-intensity activity. Several secondary outcomes were also evaluated through measurements (body weight, body height, waist and hip circumference, BMI, etc.) or questionnaires (attitude, social influences, self-efficacy, etc.). The outcomes were evaluated before the intervention (Baseline), immediately after the intervention (Post-Test), and five months after the intervention (Follow-up). Results showed no significant differences in primary and secondary outcomes between the intervention and control groups at post-test and follow-up. Some process measures were also measured in the study. Most intervention group participants reported wearing the PAM regularly and setting personal goals on the website, but some found the advice unappealing, not personal enough, or impractical.
Office ergonomics
Long-term computer use is crucial in office work [ 149 ] due to the increasing reliance on data-based technologies, which has made many office tasks heavily reliant on computers [ 150 ]. In the European Union, 50% of men and 45% of women use computers at work every day [ 151 ]. However, this prolonged computer use can lead to [ 152 , 153 , 154 , 155 , 156 ], eye strain [ 157 , 158 , 159 , 160 , 161 ], and psychosocial stress [ 162 , 163 , 164 ]. To mitigate these adverse effects, interventions at work fall into four categories: ergonomic workplace design, employee selection and placement, aggressive medical management, and employee training and education [ 165 ]. When the first three options are not always available, providing educational materials is a viable option [ 166 , 167 , 168 ]. E-training is used to reduce office ergonomics issues [ 38 , 169 ].
Online office ergonomics training has been implemented and evaluated by [ 169 ]. The educational content includes six animated and interactive modules: Introducing office ergonomics, ergonomics awareness, ergonomics assessment/self-assessment, healthy work behaviors and Environment, how to Set up a Workstation, and Exercise at Work. Three hundred programmers or typists participated in this study, 250 of which were in the study group, and 50 were in the pilot group. The participants were assessed before training and immediately after training using knowledge and behavior assessments. A workplace interaction questionnaire and Rapid Upper Limb Assessment (RULA) were used to assess the behavior. Based on the score obtained from the questionnaire, the risk level of the participants was divided into four categories: Low, Mild, Moderate, High, and Very High. The RULA assesses working posture and identifies risks associated with the shoulder, hand, and wrist postures. Results showed statistically significant improvements in knowledge assessment scores, workplace interaction scores, RULA scores, and a decrease in complaints of health-related pains (Pain, Aching, Burning, Numbness, Tingling, Tenderness, Stiffness, and Cramp).
The position of the computer monitor relative to the eyes is an important factor in eye strain [ 158 , 169 ], especially for those who wear glasses, particularly for presbyopic users [ 170 ]. Adjusting chairs can also reduce visual symptoms [ 171 , 172 , 173 ]. Therefore, the ergonomic design of a computer workplace has been introduced as an effective intervention [ 174 ].
A website has been evaluated by [ 38 ] to help employees adjust their computers in the work environment without expert support. The content presented on the website is divided into two parts: sitting position, table, keyboard and lighting, and the adjustment of the monitor in dependence on the kind of eyewear. Three categories of data were collected to evaluate the intervention: the table height, depth, width, and the height and width of the monitor and its inclination relative to vertical, the posture of participants during their natural working, gaze inclination, viewing distance, head inclination, and complaints (eye strain, headache symptoms, and musculoskeletal strain). Data were collected before the study and one week and five weeks after the intervention from 24 workers using computers. Participants were divided into two groups: those who were not presbyopic and those who were. The intervention lasted six weeks, and 23 of the 24 participants modified their computer workstations (6, 6, and 11 participants adjusted the monitor positioning, the chair, and both the monitor and the chair, respectively). The relationship between changes in ergonomics settings and complaints was investigated based on the reported complaints. The chair adjustment had a statistically significant effect on reducing musculoskeletal complaints. Lowering one’s gaze resulted in fewer visual complaints, which was statistically significant.
Hypertension
Hypertension is a major risk factor for various cardiovascular diseases [ 175 ], and only a small percentage of people follow blood pressure treatment [ 176 ]. Worse cardiovascular outcomes and increase in treatment costs are negative consequences of poorly controlled hypertension [ 177 , 178 ]. Interventions like weight loss [ 179 , 180 ], exercise [ 181 , 182 ], workplace health programs [ 183 , 184 , 185 ], and community education [ 186 ] are the most important category of interventions to reduce hypertension. Only one intervention [ 187 ] evaluated e-training in controlling hypertension in workers.
The effect of using a digital health intervention to control blood pressure has been investigated by [ 187 ] on 3,330 workers throughout the U.S. for more than a year. Participants were given educational and motivational materials and individualized care plans to help them manage their hypertension. Participants were divided into two categories: users: participants who visited the application five times or more during a year, and nonusers: participants who visited the application less than five times. Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DSP), weight, and BMI were the primary outcomes in this study. Based on the reported result, the decrease in SBP, DSP, and BMI in users was significant compared to nonusers. Increasing login frequency was significantly associated with reducing SBP, DSP, weight, and BMI.
A nutrient-poor diet is a major health risk for the workforce [ 188 ], leading to obesity, diabetes, and heart disease [ 189 ], harming work productivity [ 190 , 191 , 192 , 193 ], and absenteeism [ 191 , 192 , 193 ]. Therefore, investing in nutrition improves the health of society and national economies [ 190 , 194 ]. Only one intervention [ 195 ] evaluated e-training in improving diets in the workplace.
Online self-paced training to improve knowledge and increase the healthy behaviors of construction workers has been developed and evaluated by [ 195 ]. The topics covered in this intervention are the importance of nutrition in occupational performance and health, obstacles to healthy eating, and solutions to promote healthy eating. It takes about 50 min to complete the training content. A pre-test and post-test design has been used to evaluate the intervention. Changes in knowledge and behavior were the primary outcomes. The changes were evaluated before the intervention (Baseline), immediately after the intervention (Post-training), and 12 weeks after the intervention (Follow-up). This intervention involved 62 apprentices from ten highway construction trades that were divided into two control and intervention groups. The intervention group provided online nutrition training, and the control group provided online content about positive thinking. The participants in the intervention group showed improvements in knowledge and positive behavior (reducing the consuming sugary snacks, reducing sugary beverages such as soda and coffee, reducing the eating of fast food, and increasing the consumption of fruits and vegetables) changes compared to the control group from baseline to post-training. However, these improvements were not maintained at the follow-up evaluation. In addition to the primary outcomes, accessibility was also evaluated. According to the published results, 70% of the participants in the intervention group reported they would highly recommend the training for others, and 75% believed that more training for occupational health and safety issues should be provided to the workforce.
Respiratory
Occupational respiratory illnesses are one of the most important diseases of workers. Working conditions cause 15% of chronic obstructive lung diseases [ 196 ] and 15-23% of new-onset asthma in adults [ 197 ]. Education plays an important role in reducing these negative consequences. Only one intervention [ 198 ] evaluated e-training in respiratory safety.
A computer-based multimedia respiratory safety training has been evaluated by [ 198 ]. The content was prepared for two groups, young and old workers, according to working memory constraints and cognitive load theory [ 209 , 210 , 211 , 212 ] and the levels of learning. The educational content was designed in three formats: text (TXT), text with pictures/animations (TAP), and text with pictures/animations and audio narration (NAP). The educational content of all three types was the same and included: the employer’s responsibilities, how to clean respirators, how respirators work, etc. This intervention included 81 factory workers randomly assigned to one of three groups. The participants’ knowledge and ability to solve tasks relevant to the delivered information were examined immediately following the intervention. According to the findings, knowledge acquired by young and old participants is the same, regardless of educational content format. Still, the NAP group had the most significant effect on applying knowledge to the real world for both age groups. Additionally, the NAP group had a significant difference in problem-solving ability between young and old groups.
Multi-topic
Training in previous studies was limited to one topic. Some studies cover various aspects of occupational safety and health and provide educational content on various topics. E-training has been used to learn several topics in [ 18 , 199 , 200 , 201 , 202 ].
The effect of web-based health promotion programs on improving the productivity of employees has been assessed by [ 199 ], including weight management, chronic pain management, overcoming depression, and overcoming insomnia. The review did not include depression and sleep programs. There was no restriction on how many programs could be run concurrently. However, the reported results included employees who only participated in one program. Weight loss was the primary outcome of the weight management program, and pain intensity and pain unpleasantness were the primary outcomes of the chronic pain management program. Work productivity and activity impairment were assessed in addition to the primary outcome. The program included over 200,000 employees (weight: 218,081, pain: 7,145) and assessed primary outcomes at 30, 60, and 180 days following the interventions. Results showed that more than half of the participants experienced improved health status (reduction of pain and weight) compared to baseline, and work productivity and activity impairment scores were significantly lower than baseline at all time points. Furthermore, the findings revealed that improved worker health had a significant relationship with reduced productivity impairment.
Education and awareness, early detection, and disease management intervention have been evaluated by [ 200 ]. This workplace intervention aims to reduce the risk factors associated with metabolic syndrome. This multifaceted workplace intervention focuses on metabolic syndrome risk factors. The intervention is designed in the form of a website that comprises several sections. Firstly, the health risk assessment tool @live [ 203 ] is available to help users identify their risk factors. Secondly, on-site screening and clinical visits with registered nurses are offered. Thirdly, call-back interviews are conducted to address disease management, one of the most critical topics discussed during the phone calls. Finally, on-site educational programs are organized to enhance participants’ knowledge and awareness about the risk factors associated with metabolic diseases. The four risk factors for MetS (blood pressure, blood glucose, total cholesterol, and waist circumference) were primary clinical outcomes. Disease management was the secondary clinical outcome. The study involved 2,000 employees from over 30 worksites in British Columbia, and data was collected and analyzed over one year. The results showed a significant reduction in blood pressure and cholesterol levels, as well as a 15% reduction in the number of risk factors between baseline and six months after the intervention. The most important changes in disease management were medication changes, lifestyle changes, and visits to a family doctor.
A mobile-based educational intervention for U.S. dairy farm workers has been evaluated by [ 39 ], which aimed to address difficulties in providing occupational safety and health training due to an increase in the number of workers on the job, as well as immigrant workers with limited English proficiency. Providing a multilingual personalized learning environment based on the characteristics above is the solution presented in this study. The educational content consisted of general training on safety and health issues and specific training for three job categories in dairy farms: general and outside jobs, milker and calf caretaker, and feeder. After completing the first part, the participants followed the second part according to their job category. Kirkpatrick’s Four-Level Training Evaluation Model is used to evaluate training effectiveness [ 199 ], and 1,432 dairy workers from 40 farms participated in this study. The study found that participants reported good learning experiences (Level 1), and there was a statistically significant increase in their occupational health and safety knowledge before and after the training (Level 2). To evaluate Level 3, 3 months after the training, 9 out of 40 farms were randomly evaluated. 95% and participants applied the safety techniques learned in the workplace and stated they do their job more safely.
An online safety and health training intervention to increase knowledge and promote safe behavior of the young workforce has been evaluated by [ 198 ]. Promoting U through Safety and Health (PUSH) training is used in this study. PUSH training expands the content of Youth@Work [ 204 , 205 ], a classroom-based curriculum to address the safety needs of young workers. PUSH develops this curriculum, including protection from workplace hazards, promoting health, and improving communication in the workplace. In addition to expanding the content, the format has changed from classroom-based to online format [ 206 , 207 ]. One of the most important advantages of this course is covering a wide range of industries [ 208 , 209 , 210 , 211 ]. To evaluate this study, the knowledge of participants is measured before the intervention (Baseline), after the intervention (Post-training), and three months after the intervention (Follow-up). One hundred and twenty-four young workers participated in the pretest-posttest study. Based on the results, the increase in knowledge score in the post-training had a statistically significant difference from the baseline. The decrease in knowledge score after three months was significant compared to the post-training. In addition, the website’s likeability and acceptability, applying workplace training and changing behaviors was assessed. Participants reported that the training was interactive and informative, which improved their ability to identify and control hazards in the workplace, communicate with managers, and behave more safely.
The Massive Open Online Course (MOOC) Occupational Health that launched in 2015 and developed for Low- and Middle-Income Countries (LMIC) has been introduced by [ 201 ] to share knowledge on occupational safety and health. This study aims to explain the different characteristics of LMIC participants in MOOCs. Because there were no restrictions on using the MOOC, people from any country could register in the MOOC. The educational content included six modules, one module per week. The educational content includes: Module (1) basic concepts, Module (2) chemical and biological safety, Module (3) physical safety, Module (4) work-related diseases, Module (5) psychosocial safety, and Module (6) Care of the Worker. Each module contains 24–28 sections and takes approximately 4 h to complete. In addition, a discussion and feedback environment has been created for the participants. Of the 5,866 people who registered, 72.4% were from an LMIC, only 5% of the participants completed the training courses, and 23,547 comments were posted. 46.7% of the participants were females. Age is divided into 7 categories: <18, 18–25, 26–35, 36–45, 46–55, 56–65, and > 65 years. 0.3%, 12.1%, 38.3%, 26.7%, 11.1%, 7.8%, and 3% of participants were in the stated age groups, respectively. In terms of the employment sector, most participants (50.9%) were employed in the health and social sector. Regarding employment status, 57.8% reported that they are employed full-time, and 91.2% of the participants reported having education above secondary level. Improving career prospects, learning new things, and adding a fresh perspective to current work were the most important motivations for participating in this training course. The satisfaction of different parts of the MOOC (design and content) was 83–95%.
A digital toolkit to facilitate employees’ understanding of health screening at the workplace has been developed and evaluated by [ 18 ]. The development of this toolkit involved four stages: an online survey to examine employees’ views on health checks in the workplace and identify educational content and tool usage guide; stakeholder consultation to gather feedback and improve the guidance materials created in the first step; toolkit development and expert peer review to evaluate relevance, utility, and accessibility of the toolkit; and toolkit fidelity testing to evaluate the user experience, content relevance, utility, and accessibility of the implemented toolkit. The most important content suggested by stakeholders and experts is the business case for workplace health initiatives, the employer’s responsibility to provide a safe workplace, and providing information about occupational diseases and health. The implemented toolkit was given to 20 pilot employers, and fidelity (delivery and engagement) and implementation qualities (practicability, resource challenges, attitudes toward the toolkit, acceptability, usability, and cost) were assessed. The extent to which the intervention was delivered in accordance with the protocol (fidelity of delivery) and the extent to which the user engages with the content (fidelity of engagement) are measured in the fidelity assessment. According to the reported results, the toolkit had high fidelity of delivery and engagement. Based on the results of the evaluation of implementation qualities, a score is calculated for each item in implementation qualities, and the toolkit achieved the predetermined success rate in all items except the cost.
Educational program implementation necessitates both financial and human resources. Due to limited resources and infrastructure in developing countries, allocating resources for training is not a priority for managers, making providing effective training difficult. These constraints are less severe in developed countries, but because of the competitive environment and rising costs, managers must prioritize resource optimization to reduce costs.
Because of its benefits, e-training has been introduced as an alternative method of traditional learning in a variety of fields. E-training has been considered as an alternative to classroom-based occupational health and safety training methods in the last decade [ 20 , 36 , 37 , 38 , 39 ]. As illustrated in Fig. 2 , e-training has received a lot of attention since 2013, and the number of published studies has almost always increased.
The most important features in reducing costs in e-training programs are the ability to create content once and reuse it multiple times, access to content at any time and from any location, and the presence of infrastructures to simulate classroom-based training activities such as discussion forums [ 18 , 33 ]. In addition, personalization of educational content based on needs, preferences and concerns, which are expensive to provide in class-based training, can increase the richness of educational content [ 20 , 36 , 37 , 38 , 39 ].
In addition to affecting workforce health, effective classroom-based training fosters a sense of usefulness and importance in the workforce. As a result, it can boost work productivity, which is one of the most effective competitive advantages in industries. Concerning the distinction between classroom-based training and e-training, few studies examined the relationship between e-training and work productivity; more studies should be designed to investigate this relationship.
The difference in the number of studies conducted in developing and developed countries is significant. Out of 25 studies, 23 studies were conducted in developed countries (USA, Australia, Korea, UK, Germany, Belgium, Japan, Norway, Canada, Spain, and Netherlands) and only 2 studies were conducted in developing countries (Turkey and China). Due to the contextual differences, the results obtained in developed countries are not valid for developing countries. Therefore, there is a need for developing countries to conduct more research.
Occupational health and safety training covers a wide range of topics: chemical safety, electrical safety, fire safety, machine guarding safety, noise safety, lighting safety, etc. But educational interventions support a limited range of these topics. Although sedentary behaviors, obesity and physical inactivity, and office ergonomics problems are very important, interventions should also be designed to evaluate the impact of e-training on other topics.
Paying attention to the limited occupational safety and health topics has caused the effect of e-training to be investigated only in a narrow category of jobs. For example, sedentary behaviors and office ergonomics interventions focus on office workers. On the contrary, the audience of chemical safety or machine guarding safety training includes mostly workers who work in production lines and non-office environments. Considering the significant differences in the work environment, work activities, and capabilities of workers in different jobs, there is a need to design interventions to evaluate the impact of e-training in all topics. The lack of balance in the coverage of occupational health and safety topics prevents providing a big picture of the impact of e-training.
One of the most significant benefits of e-training is the ability to personalize content based on the needs, preferences, and concerns of the learners [ 20 , 36 , 37 , 38 , 39 ]. One of the most difficult challenges for content personalization is the high diversity of learner characteristics in occupational safety and health training compared to other environments (such as university education). The most important differences are age, education level, work activities and work environments, language, ethnicity, race, familiarity with information technology, and prior knowledge. Often, workers, from newly hired young workers to older people nearing retirement, work alongside each other. Additionally, the workforce may have differing levels of education, ranging from elementary to higher education. Work activities and work environments vary greatly, from heavy manual work in high-risk environments to light office activities in low-risk environments. The responsibility for injury also differs among workers. In countries with a large immigrant workforce, language proficiency, ethnic differences, and racial differences can present significant challenges when providing educational programs. Familiarity with information technology is another area where there are differences among workers, as the degree of mastery and availability of tools such as phones, tablets, and internet access varies. Finally, workers’ prior knowledge may differ widely due to variations in completed occupational and health training programs. Due to the high diversity of learner characteristics, there is a need for occupational health and safety trainings to provide higher degrees of personalization.
The cost of implementation plays a significant role in managers’ decisions to implement interventions, particularly in developing countries. Educational interventions can increase costs in two ways: by producing educational content with complex and expensive technologies such as virtual reality [ 212 , 213 , 214 ] and augmented reality [ 215 , 216 , 217 ], and by using expensive intervention design tools such as ActivPAL [ 80 ], PAM [ 145 ], and SSWD [ 73 ]. ActivPAL recorded total sitting time awake, sitting at work, standing at work, and breaks at work. It is an inclinometer that can distinguish periods of sitting or lying from standing and assess breaks from sitting in adults [ 80 ]. The PAM is a device for recording PA (pedometer, accelerometer and etc.) automatically [ 145 ]. When these interventions are implemented in real-world settings, the costs rise exponentially. Because rising costs are a major impediment to implementing interventions in the real world, effective low-cost interventions should be developed. According to the reviewed interventions, simple content creation methods are also highly effective.
Some workers with special circumstances, such as the elderly [ 218 , 219 , 220 ], those with physical disabilities [ 221 ], immigrants [ 222 , 223 , 224 ], and others [ 225 ], have received less attention in studies. Because a number of workers are usually working in a shared working environment, the error of one worker may result in injury to other workers. As a result, there is a need to provide occupational health and safety training to all workers while taking into account their individual and social differences.
The use of social networks to implement educational interventions has received a lot of attention. Interventions based on WeChat [ 101 ], WhatsApp [ 33 ], and LINE [ 131 ] were designed for this review. Accessibility and the absence of the need to install additional software are two significant advantages of using social networks in educational interventions. Because these tools are intended for public discussions, they are not ideal for educational interventions. Of course, they can meet many of the needs of researchers.
Because confidential information about learners may be transferred during health education interventions, the use of social networks should be used with greater caution. Creating infrastructure, such as designing questionnaires, developing follow-up capabilities, and implementing structures to protect personal data, can greatly assist researchers in designing educational interventions. These features are also available on other websites, such as YouTube.
Two important aspects that receive little attention in studies are cost-effectiveness analysis and examining interventions in real-world settings. Real environments differ greatly from controlled environments. These distinctions can be seen in areas such as cost management. The difference in evaluation measures between the interventions performed in the controlled environment and the real environment can be seen in this review. Although lessons learned in controlled environments can increase the percentage of success in real-world situations, evaluating interventions in real-world situations provided a more complete picture of their effectiveness.
Occupational diseases and injuries typically involve multiple risk factors. For example, extensive research has been conducted to identify the risk factors of obesity. Some common risk factors for obesity include physical inactivity [ 226 , 227 , 228 , 229 ], unhealthy diet [ 230 , 231 ], education level [ 232 , 233 , 234 , 235 , 236 ], length of sleep time [ 227 , 228 , 237 ], and stress/depression [ 230 , 232 , 234 , 237 ]. As part of some research studies, efforts have been made toward categorizing risk factors. For instance, in [ 232 ], the authors have classified risk factors into four distinct categories: individual factors such as genetic factors (e.g., sex, ethnicity), depression, etc., social factors including family influences (e.g., marriage), peer influences, etc., lifestyle/behavioral such as food consumption (e.g., energy intake), PA, etc., environmental factors including community characteristics (e.g., rural-urban, access to unhealthy food options, crime), state policies, marketing, etc.
Limitations
To effectively address health issues in educational interventions, it is necessary to take a comprehensive and holistic approach that considers all relevant factors. For example, studies surrounding obesity tend to prioritize low activity levels as a risk factor, while other areas may go unaddressed. We need to broaden our perspective and include a wider range of factors when designing and implementing occupational safety and health education interventions.
Because our search was confined to two databases and articles written in English, it is probable that some relevant articles were overlooked. This systematic review also omitted studies that employed e-training for Corona epidemic research. Second, we removed interventions related to psychological risk variables from our analysis. Taking these aspects into account can provide a complete picture of the success of occupational health and safety training interventions, in future studies. Finally, the studies in this systematic review used various assessment methodologies and outcomes, making comparison impossible.
In this study, the literature review focuses on the possible impact of e-trainings on occupational safety and health. Technology has transformed how we approach training programs, and e-training has been proven to have various advantages in terms of flexibility, accessibility, and cost-effectiveness. The findings have demonstrated that e-trainings can be an effective tool for improving knowledge and skills among workers, which can ultimately lead to a reduction in workplace accidents and injuries. Additionally, e-training platforms can allow employers to track employee progress and ensure that training requirements are met. Further research is needed to explore this topic in greater depth and to identify best practices for implementing e-training programs in various industries.
Data Availability
The datasets used and/or analyzed during the current study are available from the first author on reasonable request.
Konijn AM, Lay AM, Boot CRL, Smith PM. The effect of active and passive occupational health and safety (OHS) training on OHS awareness and empowerment to participate in injury prevention among workers in Ontario and British Columbia (Canada). Saf Sci. 2018;108:286–91.
Article Google Scholar
International Labour Organization. Safety and Health at Work. International Labour Organization, Geneva, Switzerland.
Takala J, Hämäläinen P, Saarela KL, Yun LY, Manickam K, Jin TW, et al. Global estimates of the burden of injury and illness at work in 2012. J Occup Environ Hyg. 2014;11(5):326–37.
Article PubMed PubMed Central Google Scholar
Boles M, Pelletier B, Lynch W. The relationship between health risks and work productivity. J Occup Environ Med. 2004;737–45.
Nagata T, Mori K, Ohtani M, Nagata M, Kajiki S, Fujino Y, et al. Total health-related costs due to absenteeism, presenteeism, and medical and pharmaceutical expenses in japanese employers. J Occup Environ Med. 2018;60(5):e273.
Macedo AC, Trindade CS, Brito AP, Socorro Dantas M. On the effects of a workplace fitness program upon pain perception: a case study encompassing office workers in a portuguese context. J Occup Rehabil. 2011;21(2):228–33.
Article PubMed Google Scholar
Verbeek J, Ivanov I. Essential occupational safety and health interventions for low-and middle-income countries: an overview of the evidence. Saf Health Work. 2013;4(2):77–83.
Centers for Disease Control and Prevention. Assessing the effectiveness of disease and injury prevention programs: costs and consequences. MMWR: recommendations and reports: morbidity and mortality weekly report. Recommendations and reports/Centers for Disease Control. 1995;44(RR–10):1–0.
Google Scholar
Creely KS, Cowie H, Van Tongeren M, Kromhout H, Tickner J, Cherrie JW. Trends in inhalation exposure—a review of the data in the published scientific literature. Ann Occup Hyg. 2007;51(8):665–78.
PubMed Google Scholar
Mahmud N, Schonstein E, Schaafsma F, Lehtola MM, Fassier J-B, Reneman MF et al. Pre-employment examinations for preventing occupational injury and disease in workers. Cochrane database Syst Rev. 2010;(12).
Burke MJ, Sarpy SA, Smith-Crowe K, Chan-Serafin S, Salvador RO, Islam G. Relative effectiveness of worker safety and health training methods. Am J Public Health. 2006;96(2):315–24.
Caffaro F, Cremasco MM, Bagagiolo G, Vigoroso L, Cavallo E. Effectiveness of occupational safety and health training for migrant farmworkers: a scoping review. Public Health. 2018;160:10–7.
Article CAS PubMed Google Scholar
Field WE, Tormoehlen RL. Education and training as intervention strategies. Agricultural medicine. Springer; 2006. 42–52.
Burke MJ, Salvador RO, Smith-Crowe K, Chan-Serafin S, Smith A, Sonesh S. The Dread Factor: How Hazards and Safety Training Influence Learning and Performance. J Appl Psychol [Internet]. 2011;96(1):46–70. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-79251514631 &doi=10.1037%2Fa0021838&partnerID=40&md5=daa99afa59973c67ab8be77f877bca2a.
Taylor MA, Wirth O, Olvina M, Alvero AM. Experimental analysis of using examples and non-examples in safety training. J Safety Res [Internet]. 2016;59:97–104. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84993990712&doi=10 .1016%2Fj.jsr.2016.10.002&partnerID=40&md5=5fd1153274412d21580ffa8c80d82350.
Redinger CF, Levine SP. Development and evaluation of the Michigan Occupational Health and Safety Management System Assessment Instrument: a universal OHSMS performance measurement tool. Am Ind Hyg Assoc J. 1998;59(8):572–81.
World Health Organization. WHO Global Plan of Action on Workers Health (2008–2017). InWHO Global Plan of Action on Workers Health (2008–2017) 2013.
Blake H, Somerset S, Evans C. Development and Fidelity Testing of the Test@Work Digital Toolkit for employers on Workplace Health checks and Opt-In HIV Testing. Int J Environ Res Public Health. 2020 Jan;17(1).
Schriver R, Giles S. Real ROI numbers. Train \& Dev. 1999;53(8):51–3.
Rucker NP. Efficacy of office ergonomics training: an evaluation and comparison of instructor and Web-based* training. Texas A\&M University; 2004.
Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Others. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. 2006;8(2):e498.
de Vries H, Brug J. Computer-tailored interventions motivating people to adopt health promoting behaviours: introduction to a new approach. 1999.
Broekhuizen K, Kroeze W, van Poppel MNM, Oenema A, Brug J. A systematic review of randomized controlled trials on the effectiveness of computer-tailored physical activity and dietary behavior promotion programs: an update. Ann Behav Med. 2012;44(2):259–86.
IWS, Internet World Stats. World Internet usage and population statistics June 30, 2014 - Mid-Year Update. http://www.internetworldstats.com/stats.htm . Archived at: http://www.webcitation.org/6Vv7gMvJn . Access date: January, 28 2015.
Anan T, Kajiki S, Oka H, Fujii T, Kawamata K, Mori K et al. Effects of an Artificial intelligence-assisted Health Program on Workers with Neck/Shoulder Pain/Stiffness and Low Back Pain: Randomized Controlled Trial. JMIR mHealth uHealth. 2021 Sep;9(9):e27535.
Patel N, Jones P, Adamson V, Spiteri M, Kinmond K. Chronic obstructive pulmonary disease patients’ experiences of an enhanced self-management model of care. Qual Health Res. 2016;26(4):568–77.
Morrison D, Mair FS, Chaudhuri R, McGee-Lennon M, Thomas M, Thomson NC, et al. Details of development of the resource for adults with asthma in the RAISIN (randomized trial of an asthma internet self-management intervention) study. BMC Med Inform Decis Mak. 2015;15(1):1–16.
Wakefield BJ, Holman JE, Ray A, Scherubel M, Adams MR, Hillis SL, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed e-Health. 2011;17(4):254–61.
Holman DM, White MC. Dietary behaviors related to cancer prevention among pre-adolescents and adolescents: the gap between recommendations and reality. Nutr J. 2011;10(1):1–8.
Fotheringham MJ, Wonnacott RL, Owen N. Computer use and physical inactivity in young adults: public health perils and potentials of new information technologies. Ann Behav Med. 2000;22(4):269–75.
Members WG, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Executive Summary: Heart Disease and Stroke Statistics–2016 update: a Report from the American Heart Association. Circulation. 2016;133(4):447–54.
Spittaels H, Van Cauwenberghe E, Verbestel V, De Meester F, Van Dyck D, Verloigne M, et al. Objectively measured sedentary time and physical activity time across the lifespan: a cross-sectional study in four age groups. Int J Behav Nutr Phys Act. 2012;9(1):1–12.
Ng WM, Cheung K. A feasibility study of a WhatsApp-delivered Transtheoretical Model-based intervention to promote healthy eating habits for firefighters in Hong Kong: A cluster randomized controlled trial. Trials [Internet]. 2020;21(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0 -85086604022&doi=10.1186%2Fs13063-020-04258-6&partnerID=40&md5=30943819bbec3b303322a7e835ec6c93.
Lee M, Lee SH, Kim T, Yoo H-J, Kim SH, Suh D-W, et al. Feasibility of a smartphone-based Exercise Program for Office Workers with Neck Pain: an Individualized Approach using a self-classification algorithm. Arch Phys Med Rehabil. 2017 Jan;98(1):80–7.
Bennie JA, Chau JY, van der Ploeg HP, Stamatakis E, Do A, Bauman A. The prevalence and correlates of sitting in european adults-a comparison of 32 eurobarometer-participating countries. Int J Behav Nutr Phys Act. 2013;10(1):1–13.
De Cocker K, De Bourdeaudhuij I, Cardon G, Vandelanotte C. Theory-driven, web-based, computer-tailored advice to reduce and interrupt sitting at work: development, feasibility and acceptability testing among employees. BMC Public Health. 2015 Sep;15:959.
Han MK, Cho B, Kwon H, Son KY, Lee H, Lee JK et al. A Mobile-Based Comprehensive Weight Reduction Program for the Workplace (Health-On): Development and Pilot Study. JMIR mHealth uHealth. 2019 Nov;7(11):e11158.
Meinert M, König M, Jaschinski W. Web-based office ergonomics intervention on work-related complaints: a field study. Ergonomics [Internet]. 2013;56(11):1658–68. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0 -84888008244&doi=10.1080%2F00140139.2013.835872&partnerID=40&md5=548826d7d57c455deaca74d7e8d86658.
Rodriguez A, Hagevoort GR, Leal D, Pompeii L, Douphrate DI. Using mobile technology to increase safety awareness among dairy workers in the United States. J Agromedicine. 2018;23(4):315–26.
Hewitt S, Sephton R, Yeowell G. Others. The effectiveness of digital health interventions in the management of musculoskeletal conditions: systematic literature review. J Med Internet Res. 2020;22(6):e15617.
Booth A, et al. Applying findings from a systematic review of workplace-based e‐learning: implications for health information professionals. Health Inform Libr J. 2009;26(1):4–21.
Zerguine H, et al. Online office ergonomics training programs: a scoping review examining design and user-related outcomes. Saf Sci. 2023;158:106000.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow,C. D., … Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic reviews, 10(1), 1–11.
Hewitt-Taylor J. Use of constant comparative analysis in qualitative research. Nurs Stand (through 2013). 2001;15(42):39.
Article CAS Google Scholar
Renz SM, Carrington JM, Badger TA. Two strategies for qualitative content analysis: an intramethod approach to triangulation. Qual Health Res. 2018;28(5):824–31.
Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the australian diabetes, obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369–71.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81.
de Rezende LFM, Rodrigues Lopes M, Rey-López JP, Matsudo VKR. Luiz O do C. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS ONE. 2014;9(8):e105620.
Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–905.
Saunders TJ, McIsaac T, Douillette K, Gaulton N, Hunter S, Rhodes RE, et al. Sedentary behaviour and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10):197–S217.
Lynch BM. Sedentary behavior and Cancer: a systematic review of the literature and proposed Biological MechanismsSedentary Behavior and Cancer. Cancer Epidemiol Biomarkers \& Prev. 2010;19(11):2691–709.
Shen D, Mao W, Liu T, Lin Q, Lu X, Wang Q, et al. Sedentary behavior and incident cancer: a meta-analysis of prospective studies. PLoS ONE. 2014;9(8):e105709.
Lynch BM, Leitzmann MF. An evaluation of the evidence relating to physical inactivity, sedentary behavior, and cancer incidence and mortality. Curr Epidemiol Reports. 2017;4(3):221–31.
Dempsey PC, Biddle SJH, Buman MP, Chastin S, Ekelund U, Friedenreich CM, et al. New global guidelines on sedentary behaviour and health for adults: broadening the behavioural targets. Int J Behav Nutr Phys Act. 2020;17(1):1–12.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32.
Van Uffelen JGZ, Wong J, Chau JY, Van Der Ploeg HP, Riphagen I, Gilson ND, et al. Occupational sitting and health risks: a systematic review. Am J Prev Med. 2010;39(4):379–88.
Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41(2):207–15.
Proper KI, Singh AS, Van Mechelen W, Chinapaw MJM. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40(2):174–82.
Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in US occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6(5):e19657.
Article CAS PubMed PubMed Central Google Scholar
Tudor-Locke C, Leonardi C, Johnson WD, Katzmarzyk PT. Time spent in physical activity and sedentary behaviors on the working day: the american time use survey. J Occup Environ Med. 2011;1382–7.
Clark BK, Thorp AA, Winkler EAH, Gardiner PA, Healy GN, Owen N, et al. Validity of self-reported measures of workplace sitting time and breaks in sitting time. Med Sci Sports Exerc. 2011;43(10):1907–12.
De Cocker K, Duncan MJ, Short C, van Uffelen JGZ, Vandelanotte C. Understanding occupational sitting: prevalence, correlates and moderating effects in australian employees. Prev Med (Baltim). 2014 Oct;67:288–94.
Parry S, Straker L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health. 2013;13(1):1–10.
Hadgraft NT, Healy GN, Owen N, Winkler EAH, Lynch BM, Sethi P, et al. Office workers’ objectively assessed total and prolonged sitting time: individual-level correlates and worksite variations. Prev Med reports. 2016;4:184–91.
Kazi A, Duncan M, Clemes S, Haslam C. A survey of sitting time among UK employees. Occup Med (Chic Ill). 2014;64(7):497–502.
Waters CN, Ling EP, Chu AHY, Ng SHX, Chia A, Lim YW, et al. Assessing and understanding sedentary behaviour in office-based working adults: a mixed-method approach. BMC Public Health. 2016;16(1):1–11.
Loh R, Stamatakis E, Folkerts D, Allgrove JE, Moir HJ. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: a systematic review and meta-analysis. Sport Med. 2020;50(2):295–330.
Healy GN, Eakin EG, LaMontagne AD, Owen N, Winkler EAH, Wiesner G, et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med (Baltim). 2013;57(1):43–8.
Neuhaus M, Healy GN, Dunstan DW, Owen N, Eakin EG. Workplace sitting and height-adjustable workstations: a randomized controlled trial. Am J Prev Med. 2014;46(1):30–40.
Stephenson A, McDonough SM, Murphy MH, Nugent CD, Wilson IM, Mair JL. Exploring the views of desk-based office workers and their employers’ beliefs regarding strategies to reduce occupational sitting time, with an emphasis on technology-supported approaches. J Occup Environ Med. 2020;62(2):149–55.
Stephenson A, Garcia-Constantino M, Murphy MH, McDonough SM, Nugent CD, Mair JL. The “Worktivity” mHealth intervention to reduce sedentary behaviour in the workplace: a feasibility cluster randomised controlled pilot study. BMC Public Health. 2021 Jul;21(1):1416.
Cocker K, De, Cardon G, Bennie JA, Kolbe-Alexander T, Meester F, De VC. From evidence-based research to practice-based evidence: disseminating a web-based computer-tailored workplace sitting intervention through a Health Promotion Organisation. Int J Environ Res Public Health. 2018 May;15(5).
De Cocker K, De Bourdeaudhuij I, Cardon G, Vandelanotte C. others. The effectiveness of a web-based computer-tailored intervention on workplace sitting: a randomized controlled trial. J Med Internet Res. 2016;18(5):e5266.
De Cocker K, Cardon G, Vergeer I, Radtke T, Vandelanotte C. Who uses Action Planning in a web-based computer-tailored intervention to reduce workplace sitting and what do action plans look like? Analyses of the start to stand intervention among flemish employees. Appl Psychol Health Well Being. 2019 Nov;11(3):543–61.
Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50(2):179–211.
RYAN DECIEL, Richard M. Intrinsic motivation and self-determination in human behavior. Springer Science & Business Media; 2013.
Deci EL, Ryan RM, editors. Handbook of self-determination research. University Rochester Press; 2004.
Maes S, Karoly P. Self-regulation assessment and intervention in physical health and illness: a review. Appl Psychol. 2005;54(2):267–99.
Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sport Exerc. 2011;43(8):1561–7.
Harden SM, Gaglio B, Shoup JA, Kinney KA, Johnson SB, Brito F, et al. Fidelity to and comparative results across behavioral interventions evaluated through the RE-AIM framework: a systematic review. Syst Rev. 2015;4(1):1–13.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7.
Hruby A, Hu FB. The epidemiology of obesity: a big picture. PharmacoEconomics. 2015;33(7):673–89.
World Health Organization. 2016 Jun. Obesity and overweight URL: http://www.who.int/mediacentre/factsheets/fs311/en/ [accessed 2016-09-24] [WebCite Cache ID 6tiKjrL03].
Obesity. : preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:i-xii, 1. [Medline: 11234459].
Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Guidelines (2013) for managing overweight and obesity in adults. Obesity. 2014;22(S2):1–S410.
Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes, Metab Syndr Obes targets Ther. 2010;285–95.
Tsai AG, Williamson DF, Glick HA. Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes Rev. 2011;12(1):50–61.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
Clemes SA, Patel R, Mahon C, Griffiths PL. Sitting time and step counts in office workers. Occup Med (Chic Ill). 2014;64(3):188–92.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25.
Wilson PWF, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162(16):1867–72.
Specchia ML, Veneziano MA, Cadeddu C, Ferriero AM, Mancuso A, Ianuale C, et al. Economic impact of adult obesity on health systems: a systematic review. Eur J Public Health. 2015;25(2):255–62.
Pi-Sunyer FX, Becker DM, Bouchard C, Carleton RA, Colditz GA, Dietz WH, et al. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. J Am Diet Assoc. 1998;98(10):1178–91.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth. United States; 2017. pp. 2015–6.
Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(11):1163–71.
Williamson DA, Bray GA, Ryan DH. Is 5\% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity. 2015;23(12):2319.
Apovian CM, Aronne LJ. The 2013 American Heart Association/American College of Cardiology/The obesity society guideline for the management of overweight and obesity in adults: what is new about diet, drugs, and surgery for obesity? Circulation. 2015;132(16):1586–91.
Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–6.
Earnest CP, Church TS. A retrospective analysis of Employee Education Level on Weight loss following participation in an online, Corporately Sponsored, Weight loss program. J Occup Environ Med. 2020 Oct;62(10):e573–80.
He C, Wu S, Zhao Y, Li Z, Zhang Y, Le J, et al. Social media-promoted weight loss among an Occupational Population: Cohort Study using a WeChat Mobile phone app-based campaign. J Med Internet Res. 2017 Oct;19(10):e357.
Horstman C, Aronne L, Wing R, Ryan DH, Johnson WD. Implementing an Online weight-management intervention to an Employee Population: initial experience with real appeal. Obesity (silver spring). 2018 Nov;26(11):1704–8.
Centers for Disease Control and Prevention. Centers for Disease Control and Prevention Diabetes Prevention Recognition Program standards and operating procedures. https://www.cdc.gov/diabetes/prevention/pdf/dprp_standards_09-02-2011.pdf . Published January 1, 2015. Accessed December 18, 2017.
Development and Evaluation of an Online. Toolkit for managers of 9-1-1 Emergency Communications Centers to reduce occupational stress.
Bureau of Labor Statistics. Labor force statistics from the Current Population Survey: Employment status of the civilian noninstitutional population, 1947 to date. 2018.
Verhagen AP, Bierma-Zeinstra SMA, Burdorf A, Stynes SM, de Vet HCW, Koes BW. Conservative interventions for treating work-related complaints of the arm, neck or shoulder in adults. Cochrane Database Syst Rev. 2013;(12).
Kleinman N, Patel AA, Benson C, Macario A, Kim M, Biondi DM. Economic burden of back and neck pain: effect of a neuropathic component. Popul Health Manag. 2014;17(4):224–32.
Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–64.
Eriksen W. Linking work factors to neck myalgia: the nitric oxide/oxygen ratio hypothesis. Med Hypotheses. 2004;62(5):721–6.
Babatunde OO, Jordan JL, der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. PLoS ONE. 2017;12(6):e0178621.
Green S, Buchbinder R, Hetrick SE. Physiotherapy interventions for shoulder pain. Cochrane database Syst Rev. 2003;(2).
Hayden J, Van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane database Syst Rev. 2005;(3).
Bell JA, Burnett A. Exercise for the primary, secondary and tertiary prevention of low back pain in the workplace: a systematic review. J Occup Rehabil. 2009;19(1):8–24.
Shariat A, Cleland JA, Danaee M, Kargarfard M, Sangelaji B, Tamrin SBM. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Brazilian J Phys Ther. 2018;22(2):144–53.
Tunwattanapong P, Kongkasuwan R, Kuptniratsaikul V. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: a randomized controlled trial. Clin Rehabil. 2016;30(1):64–72.
Ylinen J, Kautiainen H, Wirén K, Häkkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross-over trial. J Rehabil Med. 2007;39(2):126–32.
Louw S, Makwela S, Manas L, Meyer L, Terblanche D, Brink Y. Effectiveness of exercise in office workers with neck pain: a systematic review and meta-analysis. South Afr J Physiother. 2017;73(1).
de Campos TF, Maher CG, Steffens D, Fuller JT, Hancock MJ. Exercise programs may be effective in preventing a new episode of neck pain: a systematic review and meta-analysis. J Physiother. 2018;64(3):159–65.
Shiravi S, Letafatkar A, Bertozzi L, Pillastrini P, Khaleghi Tazji M. Efficacy of abdominal control feedback and scapula stabilization exercises in participants with forward head, round shoulder postures and neck movement impairment. Sports Health. 2019;11(3):272–9.
Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J. 2013;13(12):1940–50.
Essery R, Geraghty AWA, Kirby S, Yardley L. Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil. 2017;39(6):519–34.
Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, et al. Barriers to home-based exercise program adherence with chronic low back pain: patient expectations regarding new technologies. Ann Phys Rehabil Med. 2016;59(2):107–13.
Jordan JL, Holden MA, Mason EEJ, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010;(1).
Argent R, Daly A, Caulfield B, editors. others. Patient involvement with home-based exercise programs: can connected health interventions influence adherence? JMIR mHealth uHealth. 2018;6(3):e8518.
Buhrman M, Nilsson-Ihrfeldt E, Jannert M, Ström L, Andersson G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med. 2011;43(6):500.
del Pozo-Cruz B, Parraca JA, del Pozo-Cruz J, Adsuar JC, Hill J, Gusi N. An occupational, internet-based intervention to prevent chronicity in subacute lower back pain: a randomised controlled trial. J Rehabil Med. 2012 Jun;44(7):581–7.
del Pozo-Cruz B, Adsuar JC, Parraca J, del Pozo-Cruz J, Moreno A, Gusi N. A web-based intervention to improve and prevent low back pain among office workers: a randomized controlled trial. J Orthop \& Sport Phys Ther. 2012;42(10):831–D6.
Irvine AB, Russell H, Manocchia M, Mino DE, Glassen TC, Morgan R, et al. Mobile-web app to self-manage low back pain: randomized controlled trial. J Med Internet Res. 2015;17(1):e3130.
Petrozzi MJ, Leaver A, Ferreira PH, Rubinstein SM, Jones MK, Mackey MG. Addition of MoodGYM to physical treatments for chronic low back pain: a randomized controlled trial. Chiropr \& Man Ther. 2019;27(1):1–12.
del Pozo-Cruz B, del Pozo-Cruz J, Adsuar JC, Parraca J, Gusi N. Reanalysis of a tailored web-based exercise programme for office workers with sub-acute low back pain: assessing the stage of change in behaviour. Psychol Health Med. 2013;18(6):687–97.
https://www.statista.com/topics/1999/line/#dossierContents__outerWrapper .
Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: an update. Cardiovasc Res. 2007;73(2):326–40.
Stewart BWKP, Wild CP, editors. World cancer report 2014. World Health Organization. Lyon. Geneva: International Agency for Research on Cancer; 2015.
Humphreys BR, McLeod L, Ruseski JE. Physical activity and health outcomes: evidence from Canada. Health Econ. 2014;23(1):33–54.
Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–93.
Kokkinos P, Sheriff H, Kheirbek R. Physical inactivity and mortality risk. Cardiol Res Pract. 2011;2011.
Payne N, Gledhill N, Katzmarzyk PT, Jamnik V. Health-related fitness, physical activity, and history of back pain. Can J Appl Physiol. 2000;25(4):236–49.
Kovacs FM, Abraira V, Zamora J, del Real MTG, Llobera J, Fernández C, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine (Phila Pa 1976). 2004;29(2):206–10.
Van Der Roer N, Ostelo RWJG, Bekkering GE, Van Tulder MW, De Vet HCW. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine (Phila Pa 1976). 2006;31(5):578–82.
Wilkerson GB, Boer NF, Smith CB, Heath GW. Health-related factors associated with the healthcare costs of office workers. J Occup Environ Med. 2008;593–601.
Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–57.
To QG, Chen TTL, Magnussen CG, To KG. Workplace physical activity interventions: a systematic review. Am J Heal Promot. 2013;27(6):e113–23.
Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19(1):149–80.
Dadaczynski K, Schiemann S, Backhaus O. Promoting physical activity in worksite settings: results of a german pilot study of the online intervention Healingo fit. BMC Public Health. 2017 Sep;17(1):696.
Slootmaker SM, Chinapaw MJM, Schuit AJ, Seidell JC, Van Mechelen W. Feasibility and effectiveness of online physical activity advice based on a personal activity monitor: randomized controlled trial. J Med Internet Res. 2009 Jul;11(3):e27.
Trommsdorff G, Bandura. Albert: Sozial-kognitive Lerntheorie. Soziol Rev Besprechungen neuer Lit. 1981;4:102–3.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Schwarzer R, Luszczynska A. How to overcome health-compromising behaviors: the health action process approach. Eur Psychol. 2008;13(2):141.
Andries F, Smulders PGW, Dhondt S. The use of computers among the workers in the European Union and its impact on the quality of work. Behav \& Inf Technol. 2002;21(6):441–7.
Jensen C, Finsen L, Søgaard K, Christensen H. Musculoskeletal symptoms and duration of computer and mouse use. Int J Ind Ergon. 2002;30(4–5):265–75.
Eurofound (European Foundation for the Improvement of Living and Working Conditions). Fourth european Working Conditions Survey. Luxembourg: Office for Official Publications of the European Communities; 2007.
Luttmann A, Jager M, Griefahn B, Caffier G, Liebers F, Organization WH et al. Preventing musculoskeletal disorders in the workplace. 2003.
Fang S, Dropkin J, Herbert R, Triola D, Landsbergis P. Workers’ compensation experiences of computer users with musculoskeletal disorders. Am J Ind Med. 2007;50(7):512–8.
Levanon Y, Gefen A, Lerman Y, Givon U, Ratzon NZ. Reducing musculoskeletal disorders among computer operators: comparison between ergonomics interventions at the workplace. Ergonomics. 2012;55(12):1571–85.
Robertson MM. Health and performance consequences of office ergonomic interventions among computer workers. In: International Conference on Ergonomics and Health Aspects of Work with Computers. 2007. p. 135–43.
Taieb-Maimon M, Cwikel J, Shapira B, Orenstein I. The effectiveness of a training method using self-modeling webcam photos for reducing musculoskeletal risk among office workers using computers. Appl Ergon. 2012;43(2):376–85.
Aarås A, Horgen G, Helland M. Can visual discomfort influence on muscle pain and muscle load for visual display unit (VDU) workers? In: International Conference on Ergonomics and Health Aspects of Work with Computers. 2007. p. 3–9.
Jainta S, Jaschinski W. Fixation disparity: binocular vergence accuracy for a visual display at different positions relative to the eyes. Hum Factors. 2002;44(3):443–50.
Rempel D, Willms K, Anshel J, Jaschinski W, Sheedy J. The effects of visual display distance on eye accommodation, head posture, and vision and neck symptoms. Hum Factors. 2007;49(5):830–8.
Robertson MM, Ciriello VM, Garabet AM. Office ergonomics training and a sit-stand workstation: Effects on musculoskeletal and visual symptoms and performance of office workers. Appl Ergon. 2013;44(1):73–85.
Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31(5):502–15.
Gilbert-Ouimet M, Brisson C, Vézina M, Trudel L, Bourbonnais R, Masse B, et al. Intervention study on psychosocial work factors and mental health and musculoskeletal outcomes. Heal Pap. 2011;11:47–66.
Huang Y-H, Robertson MM, Chang K-I. The role of environmental control on environmental satisfaction, communication, and psychological stress: effects of office ergonomics training. Environ Behav. 2004;36(5):617–37.
BAuA (Federal Institute for Occupational Safety and Health). Research on Health and Safety at Work. Research and Development Programme. 1st ed. Dortmund, Germany: Federal Institute for Occupational Safety and Health (BAuA); 2011.
Saunders RL, Stultz MR. Education and training. Sourcebook of Occupational Rehabilitation. Springer; 1998. 109–26.
King PM. A program planning model for injury prevention education. Occup Ther Pract. 1993;4(4):47.
Rempel D. Ergonomics–prevention of work-related musculoskeletal disorders. West J Med. 1992;156(4):409.
CAS PubMed PubMed Central Google Scholar
Stokols D, Pelletier KR, Fielding JE. The ecology of work and health: research and policy directions for the promotion of employee health. Health Educ Q. 1996;23(2):137–58.
Dalk\il\inç M, Kayihan H. Efficacy of web-based [e-learning] office ergonomics training: a test study. J Musculoskelet Pain. 2014;22(3):275–85.
Jaschinski W, Heuer H, Kylian H. Preferred position of visual displays relative to the eyes: a field study of visual strain and individual differences. Ergonomics. 1998;41(7):1034–49.
Allie P, Bartha MC, Kokot D, Purvis C. A field observation of display placement requirements for presbyopic and prepresbyopic computer users. In: Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2010. p. 709–13.
Amick BC III, Menéndez CC, Bazzani L, Robertson M, DeRango K, Rooney T, et al. A field intervention examining the impact of an office ergonomics training and a highly adjustable chair on visual symptoms in a public sector organization. Appl Ergon. 2012;43(3):625–31.
Menéndez CC, Amick BC III, Robertson M, Bazzani L, DeRango K, Rooney T, et al. A replicated field intervention study evaluating the impact of a highly adjustable chair and office ergonomics training on visual symptoms. Appl Ergon. 2012;43(4):639–44.
Jaschinski W, Heuer H. Vision and eyes. Working postures and movements. CRC Press; 2004. 95–108.
Members WG, Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220.
Members WG, Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, et al. Executive summary: heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):188–97.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. Joint National Committee on Prevention DE, treatment of high blood pressure. National Heart L, blood I, National High blood pressure education program coordinating C. Seventh Rep Jt Natl Comm Prev Detect Eval treat high blood press Hypertens. 2003;42(6):1206–52.
Kovell LC, Ahmed HM, Misra S, Whelton SP, Prokopowicz GP, Blumenthal RS, et al. US hypertension management guidelines: a review of the recent past and recommendations for the future. J Am Heart Assoc. 2015;4(12):e002315.
Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, et al. Weight loss intervention in phase 1 of the trials of Hypertension Prevention. Arch Intern Med. 1993;153(7):849–58.
Tuck ML, Sowers J, Dornfeld L, Kledzik G, Maxwell M. The effect of weight reduction on blood pressure, plasma renin activity, and plasma aldosterone levels in obese patients. N Engl J Med. 1981;304(16):930–3.
Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503.
Duncan JJ, Farr JE, Upton SJ, Hagan RD, Oglesby ME, Blair SN. The effects of aerobic exercise on plasma catecholamines and blood pressure in patients with mild essential hypertension. JAMA. 1985;254(18):2609–13.
O’Donnell M. Does workplace health promotion work or not? Are you sure you really want to know the truth? Am J Heal Promot AJHP. 2013;28(1):iv–vi.
Widmer RJ, Allison TG, Keane B, Dallas A, Bailey KR, Lerman LO, et al. Workplace Digital Health is Associated with Improved Cardiovascular Risk factors in a frequency-dependent fashion: a large prospective observational cohort study. PLoS ONE. 2016;11(4):e0152657.
Pearson TA, Palaniappan LP, Artinian NT, Carnethon MR, Criqui MH, Daniels SR, et al. American Heart Association Guide for improving Cardiovascular Health at the Community Level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730–53.
Lu C-H, Tang S-T, Lei Y-X, Zhang M-Q, Lin W-Q, Ding S-H, et al. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health. 2015;15(1):1–9.
Senecal C, Widmer RJ, Johnson MP, Lerman LO, Lerman A. Digital health intervention as an adjunct to a workplace health program in hypertension. J Am Soc Hypertens. 2018 Oct;12(10):695–702.
Burton J. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices. Geneva, Switzerland: World Health Organization. http://www.who.int/iris/handle/10665/113144 . Published 2010. Accessed June 18, 2019.
World Health OrganizationDiet. Nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser. 2003;916:i–viii.
World Bank. Repositioning nutrition as central to development: a strategy for large-scale action. Washington, DC: The World Bank. http://documents.worldbank.org/curated/en/185651468175733998/Repositioning-nutrition-as-central-to-development-a-strategy-for-large-scale-action-overview . Published 2006. Accessed May 1, 2019.
Ferrie JE, Head J, Shipley MJ, Vahtera J, Marmot MG, Kivimäki M. BMI, obesity, and sickness absence in the Whitehall II study. Obesity. 2007;15(6):1554–64.
Berghöfer A, Pischon T, Reinhold T, Apovian CM, Sharma AM, Willich SN. Obesity prevalence from a european perspective: a systematic review. BMC Public Health. 2008;8(1):1–10.
IOTFIncreasing obesity rates in. Europe 1985–2005 London 2007. Available at: www.iotf.org/database/TrendsEuropeanadultsthroughtimev3.htm (10 April 2009, date last accessed).
Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S. The economic rationale for investing in stunting reduction. Matern \& child Nutr. 2013;9:69–82.
Rohlman DS, Parish MA, Hanson GC, Williams LS. Building a healthier workforce: an evaluation of an Online Nutrition Training for Apprentices. J Nutr Educ Behav. 2018 Oct;50(9):913–917e1.
Balmes J, Becklake M, Blanc P, Henneberger P. Others. American thoracic Society Statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167(5):787.
NIOSH. Worker Health Chartbook. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institutes of Health; 2004.
Wallen ES, Mulloy KB. Computer-based training for safety: Comparing methods with older and younger workers. J Safety Res [Internet]. 2006;37(5):461–7. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-33845331789 &doi=10.1016%2Fj.jsr.2006.08.003&partnerID=40&md5=615512d8b5132a1984149333b6e6eb37.
Silberman J, Schwartz S, Giuseffi DL, Wang C, Nevedal D, Bedrosian R. Reductions in employee productivity impairment observed after implementation of web-based worksite health promotion programs. J Occup Environ Med. 2011 Dec;53(12):1404–12.
Tarride JE, Harrington K, Balfour R, Simpson P, Foord L, Anderson L, et al. Partnership in employee health. A workplace health program for British Columbia Public Service Agency (Canada). Work. 2011;40(4):459–71.
Aryal A, Parish M, Rohlman DS. Generalizability of total Worker Health(®) online training for Young Workers. Int J Environ Res Public Health. 2019 Feb;16(4).
Tronstad T. Occupational health in developing countries - a massive open online course. Arch Environ Occup Health. 2021;76(5):291–300.
@live Health Risk Assessment. Vancouver: PBC Health Benefits Society. ; 2010. Available: http://www.pbchbs.com/Corp/group/group-Alive.aspx (accessed 2010 Feb 8).
Elliot DL, Goldberg L, Moe EL, DeFrancesco CA, Durham MB, Hix-Small H. Preventing substance use and disordered eating: initial outcomes of the ATHENA (athletes targeting healthy exercise and nutrition alternatives) program. Arch Pediatr \& Adolesc Med. 2004;158(11):1043–9.
Goldberg L, MacKinnon DP, Elliot DL, Moe EL, Clarke G, Cheong J. The adolescents training and learning to avoid steroids program: preventing drug use and promoting health behaviors. Arch Pediatr \& Adolesc Med. 2000;154(4):332–8.
O’Connor T, Loomis D, Runyan C, dal Santo JA, Schulman M. Adequacy of health and safety training among young latino construction workers. J Occup Environ Med. 2005;272–7.
Rohlman DS, Parish M, Elliot DL, Montgomery D, Hanson G. Characterizing the needs of a young working population: making the case for total worker health in an emerging workforce. J Occup Environ Med. 2013 Dec;55(12 Suppl):69–72.
Anger WK, Rohlman DS, Kirkpatrick J, Reed RR, Lundeen CA, Eckerman DA. cTRAIN: A computer-aided training system developed in SuperCard for teaching skills using behavioral education principles. Behav Res Methods, Instruments, \& Comput. 2001;33(2):277–81.
Anger WK, Tamulinas A, Uribe A, Ayala C. Computer-based training for immigrant latinos with limited formal education. Hisp J Behav Sci [Internet]. 2004;26(3):373–89. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-3543049442 &doi=10.1177%2F0739986304267735&partnerID=40&md5=f8f178c2207de7eb8cc57ad174956faf.
Eckerman DA, Abrahamson K, Ammerman T, Fercho H, Rohlman DS, Anger WK. Computer-based training for food services workers at a hospital. J Saf Res. 2004;35(3):317–27.
Eckerman DA, Lundeen CA, Steele A, Fercho HL, Ammerman TA, Anger WK. Interactive training versus reading to teach respiratory protection. J Occup Health Psychol. 2002;7(4):313.
Norris MW, Spicer K, Byrd T. Virtual reality: the new pathway for effective safety training. Prof Saf. 2019;64(06):36–9.
Lacko J. (2020, January). Health safety training for industry in virtual reality. In 2020 Cybernetics & Informatics (K&I) (pp. 1–5). IEEE.
Shamsudin NM, Mahmood NHN, Rahim ARA, Mohamad SF, Masrom M. Virtual reality training approach for occupational safety and health: a pilot study. Adv Sci Lett. 2018;24(4):2447–50.
Pereira RE, Gheisari M, Esmaeili B. (2018). Using panoramic augmented reality to develop a virtual safety training environment. In Construction Research Congress 2018 (pp. 29–39).
Kamal AA, Junaini SN, Hashim AH, Sukor FS, Said MF. (2021). The enhancement of OSH training with an augmented reality-based app. Int J Online Biomedical Eng, 17(13).
Placencio-Hidalgo D, Álvarez-Marín A, Castillo-Vergara M, Sukno R. Augmented reality for virtual training in the construction industry. Work. 2022;71(1):165–75.
Crawford JO, Graveling RA, Cowie HA, Dixon K. The health safety and health promotion needs of older workers. Occup Med. 2010;60(3):184–92.
Varianou-Mikellidou C, Boustras G, Dimopoulos C, Wybo JL, Guldenmund FW, Nicolaidou O, Anyfantis I. Occupational health and safety management in the context of an ageing workforce. Saf Sci. 2019;116:231–44.
Choi JD, Lee SJ. Study on improving the basic occupational safety and health training of the older workers in the construction industry. J Korea Academia-Industrial cooperation Soc. 2019;20(12):176–81.
Dewey R. Promoting job safety for workers with intellectual disabilities: the staying safe at work training curriculum. New solutions: a journal of environmental and occupational health policy. 2012;21(4):591–601.
Menger LM, Rosecrance J, Stallones L, Roman-Muniz IN. A guide to the design of occupational safety and health training for immigrant, Latino/a dairy workers. Front public health. 2016;4:282.
PubMed PubMed Central Google Scholar
Juárez-Carrillo PM, Liebman AK, Reyes IAC, Sánchez N, Y. V., Keifer MC. Applying learning theory to safety and health training for hispanic immigrant dairy workers. Health Promot Pract. 2017;18(4):505–15.
O’Connor T, Loomis D, Runyan C, dal, Santo JA, Schulman M. (2005). Adequacy of health and safety training among young Latino construction workers. Journal of occupational and environmental medicine, 272–277.
Arcury TA, Estrada JM, Quandt SA. Overcoming language and literacy barriers in safety and health training of agricultural workers. J Agromed. 2010;15(3):236–48.
Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001;38(3):789–95.
Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J. 1988;115(4):869–75.
Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288(14):1723–7.
Lavie CJ, Osman AF, Milani RV, Mehra MR. Body composition and prognosis in chronic systolic heart failure: the obesity paradox. Am J Cardiol. 2003;91(7):891–4.
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43(8):1439–44.
Lavie CJ, Mehra MR, Milani RV. Obesity and heart failure prognosis: paradox or reverse epidemiology? Eur Heart J. 2005;26(1):5–7.
Shamsuzzaman AS, Winnicki M, Lanfranchi P, Wolk R, Kara T, Accurso V, Somers VK. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002;105(21):2462–4.
Kenchaiah, S., Evans, J. C., Levy, D., Wilson, P. W., Benjamin, E. J., Larson, M.G., … Vasan, R. S. (2002). Obesity and the risk of heart failure. New England Journal of Medicine, 347(5), 305–313.
Lavie CJ, Ventura HO, Milani RV. The “obesity paradox”: is smoking/lung disease the explanation? Chest. 2008;134(5):896–8.
McAuley P, Myers J, Abella J, Froelicher V. Body mass, fitness and survival in veteran patients: another obesity paradox? Am J Med. 2007;120(6):518–24.
Lavie CJ, Milani RV, Ventura HO. Obesity, heart disease, and favorable prognosis—truth or paradox? Am J Med. 2007;120(10):825–6.
Download references
Acknowledgements
We thank the editor and the anonymous reviewers for their excellent suggestions to improve the original draft of the manuscript.
No funding was received.
Author information
Authors and affiliations.
Department of Medical Informatics, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Mohammad Mahdi Barati Jozan & Hamed Tabesh
Department of Foreign Languages, Iran University of Science and Technology, Tehran, Iran
Babak Daneshvar Ghorbani
Department of Applied Mathematics and Computer Science, Technical University of Denmark, Kongens Lyngby, Denmark
Md Saifuddin Khalid
School Of Veterinary Medicine, Department Of Veterinary Pathology, University of California, Davis, USA
Aynaz Lotfata
You can also search for this author in PubMed Google Scholar
Contributions
MMBJ: developed search strategy, conducted literature search, identified and selected studies, extracted data and assessed functionalities, drafted and revised manuscript. BDG: identified and selected studies, extracted data and assessed functionalities, drafted and revised manuscript. MSD, AL, and HT: provided guidance and supervised the research project, revised manuscript for important intellectual context. All authors reviewed and approved manuscript.
Corresponding author
Correspondence to Hamed Tabesh .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Barati Jozan, M.M., Ghorbani, B.D., Khalid, M.S. et al. Impact assessment of e-trainings in occupational safety and health: a literature review. BMC Public Health 23 , 1187 (2023). https://doi.org/10.1186/s12889-023-16114-8
Download citation
Received : 25 January 2023
Accepted : 13 June 2023
Published : 20 June 2023
DOI : https://doi.org/10.1186/s12889-023-16114-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Occupational injuries and accidents
- Preventive occupational health interventions
- Online occupational safety and health training
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

IMAGES
COMMENTS
Abstract and Figures. This literature review focuses on researches undertaken since 1980s onwards. The purpose of the study is to identify existing gaps on workplace safety and health management ...
Aligned with an E/HF approach, this systematic literature review sought to examine interventions reported within the scholarly and grey literature that aimed to reduce the risk of physical and psychological injury amongst older workers through changes to the organisation of work, work design, and the work environment.
This systematic literature review applied the matrix method to examine major literature in safety management practices and occupational health and safety performance.
Systematic literature review on the effects of occupational safety and health (OSH) interventions at the workplace October 2018 Scandinavian Journal of Work, Environment & Health 45(2)
According to the World Health and Organization (WHO), the occupational health and safety (OHS) is a multidisciplinary activity with the aim to: (1) protect and promote the health of workers by taking precautions against occupational accidents and diseases; (2) develop and promote healthy and safe work, work environment, and work organizations ...
First, the authors provide a formal definition of workplace safety and then create an integrated safety model (ISM) based on existing theory to summarize current theoretical expectations with regard to workplace safety. Second, the authors conduct a targeted review of the safety literature and compare extant empirical findings with the ISM.
INTRODUCTION. Efforts to protect and promote the safety, health, and wellbeing of workers have increasingly focused on integrating the complex and dynamic systems of the work organization and work environment. 1-3 The National Institute for Occupational Safety and Health (NIOSH) applies this integrated approach in the Total Worker Health ® (TWH) initiative by attending to "policies ...
This literature review focuses on researches undertaken since 1980s onwards. The purpose of the study is to identify existing gaps on workplace safety and health management and propose future research areas. The review adds value to existing
Summary. This chapter provides a comprehensive review of how occupational health and safety (OHS) can be adequately managed to enhance workers' physical well-being (safety/health and injury/illness) and protect them from being exposed to health and safety hazards at work. OHS serves as a major pillar of healthy workplace, where workers are able ...
Methods A systematic literature review covering the years 1966‒2017 (February) was undertaken to capture both published and gray literature studies of OSH work environment interventions with quantitative measures of intervention effects. Studies that met specified in- and exclusion criteria went through an assessment of methodological quality.
Objectives The aim of this review was to assess the evidence that occupational safety and health (OSH) legisla - tive and regulatory policy could improve the working environment in terms of reduced levels of industrial injuries and fatalities, musculoskeletal disorders, worker complaints, sick leave, and adverse occupational exposures. Methods ...
The Vision Zero for work-related health, safety and well-being is based on the assumption that all accidents, harm and work-related diseases are preventable. Vision Zero for health, safety and well-being is then the ambition and commitment to create and ensure safe and healthy work and to prevent all accidents, harm and work-related diseases in ...
Improving compliance with occupational safety and health regulations: an overarching review - Literature review . European Agency for Safety and Health at Work —- EU-OSHA 2 Authors: David Walters, Scientific Project Leader, Emeritus Professor, School of Social Sciences, Cardiff University, United Kingdom
Although we do maintain that available perspectives are cumulatively useful in improving safety knowledge and practice, we sought to integrate the abovementioned arguments into a single, guiding framework to advance the workplace safety literature and ease the process of a systematic review. The proposed comprehensive frame is depicted in Fig ...
Introduction. Employee health and safety programs should be a major priority for management because they safe lives, increase productivity, and reduce costs. These health and safety programs should stress employee involvement, continued monitoring, and an overall wellness component (Anthony et al., 2007).
This paper begins with background of safety issues and safety culture in construction industry. The objectives of this research are: To identify factors involved in the development of safety culture through searching and reviewing previous research. To present the findings of the literature review as a guide to understand the issues and ...
According to the World Health Organization (WHO), 1 an estimated 59 million people work in healthcare facilities globally, accounting for roughly 12% of the working population. The WHO 2 also reports that all healthcare workers, including healthcare professionals, are exposed to occupational hazards. The International Labour Organization (ILO) 3 reported that millions of healthcare workers ...
1. Toward an effective occupational heal th and safety culture: A multiple. stakeholder perspective. Abstract. This paper uses an extensive review of the sa fety culture literature to identify ...
Implementing workplace preventive interventions reduces occupational accidents and injuries, as well as the negative consequences of those accidents and injuries. Online occupational safety and health training is one of the most effective preventive interventions. This study aims to present current knowledge on e-training interventions, make recommendations on the flexibility, accessibility ...
A concept known as safety leadership (SL) emerged in the literature as a. way for a leader to encourage work place safety. SL, according to Zuofa and Ocheing (2017), is the use of a. leader's ...
The literature review identified that safety awareness might improve employees' productivity by saving work time. The study revealed that safety training was conducted well in the firm. ... These empirical results have confirmed a statement in a report by the European Agency for Safety and Health at Work ... (web pdf) https://www.ilo.org ...
Prioritize health and safety practices In today's fiercely competitive work environment, excessive job demands can cause stress and strain when they surpass the resources available to employees ...
Background: Work safety performance assessment is one part of the Occupational Health and Safety Management System activity, which aims to ensure workers' right to safety and health in the ...