
- Learn /

Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.
How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com

Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
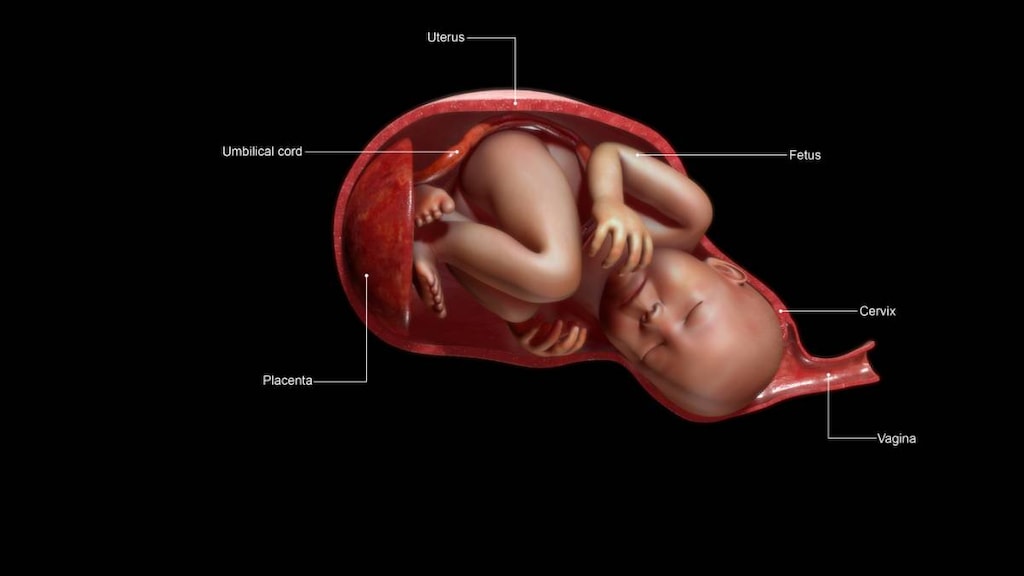
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

How your twins’ fetal positions affect labor and delivery

What happens to your baby right after birth

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.

Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.
What to know about baby’s position at birth
Having a baby is an exciting time, but it’s common to have some worries about labor and delivery. One thing that often causes mums-to-be concern is what position their baby will be in when the time comes for them to be born.
For a vaginal delivery, the baby must descend through the birth canal, passing through your pelvis to reach the vaginal opening. The position of the baby - or presentation of the fetus as it is also known - affects how quickly and easily the baby can be born. Some positions allow the baby to tuck their chin, and re-position and rotate their head to make their journey easier.
Here’s a guide to help you understand the language used to describe the position of babies and some tips for helping them into the ideal position for birth.
Position of the baby before birth
During pregnancy your baby has room to move about in your uterus or womb - twisting, turning, rolling, stretching and getting in some kicks. As your pregnancy progresses and they grow bigger there’s less room for them to move, but your baby should still move regularly until they are born, even during labor.
Sometime between 32 and 38 weeks of pregnancy, but usually around week 36, babies tend to move into a head down position. This allows their head to come out of your vagina first when they are born. Only about 3 to 4 percent of babies do not move into a head-first or cephalic presentation before birth.
What’s the ideal position of a baby for birth?
Occiput anterior is the ideal presentation for your baby to be in for a vaginal delivery.
Occiput anterior is a type of head-first or cephalic presentation for delivery of a baby. About 95 to 97 percent of babies position themselves in a cephalic presentation for delivery, often with the crown or top of their head - which is also known as the vertex - entering the birth canal first.
Usually when a baby is being born in a vertex presentation the back of the baby’s head, which is called the occiput, is towards the front or anterior of your pelvis and their back is towards your belly. Their chin is also typically in a flexed position, tucked into their chest.
Occiput anterior is the best and safest position for a baby to be born by a vaginal birth. It allows the smallest diameter of a baby’s head to descend into the birth canal first, making it easier for the baby to fit through your pelvis.
What other positions are babies born in?
Sometimes babies don’t position themselves in the ideal position for birth. These other positions are called abnormal positions. Listed below are the abnormal positions or presentations that some babies are born in.
Occiput posterior or back-to-back presentation
Occiput posterior position or back-to-back presentation occurs when the occiput - back of a baby’s head - is positioned towards your tailbone or back during delivery. Sometimes this presentation is also called “sunny side up” because babies born in this position enter the world facing up. About 5 percent of babies are delivered in the occiput posterior position.
Babies presenting in the occiput posterior position find it harder to make their way through the birth canal, which can lead to a longer labor. This presentation is three times more likely to end in a cesarean section (c-section) compared with babies presenting in the ideal, occiput anterior presentation.
Breech presentation
A breech presentation occurs when your baby’s buttock, feet or both are set to come out first at birth. About 3 to 4 percent of full-term babies are born in a breech position.
There are three types of breech presentation including:
- Frank breech. Frank breech is the most common breech presentation, occurring in 50 to 70 percent of breech births. Babies in the Frank breech position have their hips flexed and their knees extended so that their legs are folded flat against their head. Their bottom is closest to the birth canal.
- Footling or incomplete breech. Footling or incomplete breeches occur in 10 to 30 percent of breech births. An incomplete breech presentation is where just one of the baby’s knees is bent up. Their other foot and bottom are closest to the birth canal. In a footling breech presentation, one or both feet may be delivered first.
- Complete breech. A complete breech presentation is less common, occurring in 5 to 10 percent of breech births. Babies in a complete breech position have both knees bent and their feet and bottom are closest to the birth canal.
A breech delivery can result in the baby’s head or shoulders becoming stuck because opening to the uterus (cervix) may not be stretched enough by the baby’s body to allow the head and shoulders to pass through. Umbilical cord prolapse can also occur. This is when the cord slips into the vagina before the baby is delivered. If the cord is pinched then the flow of blood and oxygen to the baby can be reduced.
If an exam reveals your baby is sitting in a breech position and you’re past 36 weeks of pregnancy then external cephalic version (ECV) might be attempted to improve your chances of having a vaginal birth. ECV is performed by a qualified healthcare professional and it involves them pressing their hands on the outside of your belly to try and turn the baby.
Most babies found to be in a breech position are delivered by c-section because studies indicate that a vaginal delivery is about three times more likely to cause serious harm to the baby.
Brow and face presentations
Babies can also arrive brow- or face-first. A brow presentation results in the widest part of your baby’s head trying to fit through your pelvis first. This is a rare presentation, affecting about 1 in every 500 to 1400 births.
Instead of flexing and tucking their chin, babies presenting brow-first slightly extend their head and neck in the same way they would if they were looking up.
If your baby stays in a brow presentation it’s highly unlikely that they will be able to make their way through your pelvis. If your cervix is fully dilated then your doctor may be able to use their hand or ventouse - a vacuum cup - to move your baby’s head into a flexed position. If there are signs that your baby is becoming distressed or labor isn’t progressing then a c-section may be recommended.
More than half of the babies presenting brow-first, however, flex their head during early labor and move into a better position that allows labor to progress. Although, some babies tip their head back further and present face-first.
A face presentation is another rare position for a baby to be born in, occurring in only 1 in every 600 to 800 births.
Almost three quarters of babies presenting face-first can be delivered vaginally, especially if the baby’s chin is near your pubic bone, although labor may be prolonged.
Some baby’s presenting face-first may need to be delivered by c-section, particularly if their chin is near your tailbone, your labor is not progressing or your baby’s heart rate is causing concern.
Shoulder presentation
If your baby is lying sideways across your uterus - in a transverse lie - their shoulder can present first. Shoulder presentation occurs in less than 1 percent of deliveries. Virtually all babies in a shoulder presentation will need to be delivered by c-section. If labor begins while the baby is in this position then the shoulder will become stuck in the pelvis and the labor will not progress.
What factors can influence the position of my baby?
A number of factors can influence the position of your baby during labor and delivery, including:
- If you have been pregnant before
- The size and shape of your pelvis
- Having an abnormally shaped uterus
- Having growths in your uterus, such as fibroids
- Having placenta previa - the placenta covers some or all of the cervix
- A premature birth
- Having twins or multiple babies
- Having too much (polyhydramnios) or too little (oligohydramnios) amniotic fluid
- Abnormalities that prevent the baby tucking their chin to their chest
How do I tell what position my baby is in?
Your midwife or your obstetrician-gynecologist (OB-GYN) should be able to tell you the position of your baby by feeling your belly, using an ultrasound scan or conducting a pelvic exam.
You might also be able to tell the position of the baby from their movements.
If your baby is in a back-to-back position your belly may feel more squishy and their kicks are likely to be felt or seen around the middle of your belly. You may also notice that instead of your belly poking out there is a dip around your belly button.
If your baby is in the ideal occiput anterior presentation you’re likely to feel the firm, rounded surface of your baby’s back on one side of your belly and feel kicks up under your ribs.
How do I get my baby into the best position for birth?
Here are some tips to try to encourage your baby to engage in the ideal position for birth:
- Remain upright, but lean forward to create more space in your pelvis for your baby to turn.
- Sit with your back as straight as possible and your knees lower than your hips. Placing a cushion under your bottom and one behind your back may make this position more comfortable. Avoid sitting with your knees higher than your pelvis.
- When you read a book, sit on a dining room chair and rest your elbows on the table. Lean forward slightly with your knees apart. Avoid crossing your knees.
- If pelvic girdle pain is not an issue, try sitting facing backwards with your arms resting on the back of a chair.
- Watch TV kneeling on the floor leaning over a big bean bag.
- Go for a swim.
- Sit on a birth ball or swiss ball - they can be used both before and during labor.
- Lie down on your side rather than your back. Place a pillow between your knees for comfort.
- Try moving about on all fours. Try wiggling your hips or arching your back before straightening your spine again.
- During Braxton Hicks (practice contractions), use a forward leaning posture
- During contractions, stay on your feet, lean forwards and rock your hips from side to side and up and down to get your bottom wiggling as you walk
Remember to attend your antenatal appointments and contact your midwife or OB-GYN if you have any questions or concerns about the position of your baby.
Article references
- MedlinePlus . Your baby in the birth canal. Available at: https://medlineplus.gov/ency/article/002060.htm . [Accessed May 19, 2022].
- NHS Inform. How your baby lies in the womb. August 17, 2021. Available at: https://www.nhsinform.scot/ready-steady-baby/labour-and-birth/getting-ready-for-the-birth/how-your-baby-lies-in-the-womb . [Accessed May 19, 2022].
- The American College of Obstetricians and Gynecologists (ACOG). If Your Baby is Breech. November 2020. Available at: https://www.acog.org/womens-health/faqs/if-your-baby-is-breech . [Accessed May 19, 2022].
- MedlinePlus. Breech - series - Types of breech presentation. March 12, 2020. Available at: https://medlineplus.gov/ency/presentations/100193_3.htm . [Accessed May 19, 2022].
- Medscape . Breech Presentation. January 20, 2022. Available at: https://emedicine.medscape.com/article/262159-overview . [Accessed May 19, 2022].
- Physicians & Midwives. Which Way is Up? What Your Baby’s Position Means for Your Delivery. November 15, 2012. Available at: https://physiciansandmidwives.com/what-your-babys-position-means-for-delivery/ . [Accessed May 19, 2022].
- BabyCentre. What is brow presentation? Available at: https://www.babycentre.co.uk/x564026/what-is-brow-presentation . [Accessed May 19, 2022].
- NCT. Bay position in the womb before birth. Available at: https://www.nct.org.uk/labour-birth/getting-ready-for-birth/baby-positions-womb-birth . [Accessed May 19, 2022].
- NHS Forth Valley. Ante Natal Advice for Optimal Fetal Positioning. 2020. Available at: https://nhsforthvalley.com/wp-content/uploads/2014/01/Ante-Natal-Advice-for-Optimal-Fetal-Positioning.pdf . [Accessed May 19, 2022].
Read this next

What are the health benefits of tea?
Tea is a popular beverage consumed worldwide. Regularly drinking tea is thought to have many potential health benefits. Read on to find out how tea may help you

Healthy heart diet guide
Making simple changes to your diet is the first step to being heart-healthy. Add these foods to your everyday eating plan.

How to keep cool and survive a heatwave
Heatwaves are on the rise worldwide putting you at risk of dehydration, heat exhaustion and heat stroke. Try these tips to help you stay cool

7 Lifestyle changes to help reduce obstructive sleep apnea
Some simple lifestyle changes can help you reduce your obstructive sleep apnea symptoms. Here are 7 tips you can try.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Geburtshilfe Frauenheilkd
- v.76(3); 2016 Mar
Language: English | German
Foetal Gender and Obstetric Outcome
Fetales geschlecht und geburtshilfliches outcome, b. schildberger.
1 FH Gesundheitsberufe OÖ, Linz, Österreich
2 Institut für klinische Epidemiologie der Tirol Kliniken, Innsbruck, Österreich
Associated Data
Introduction: Data on specific characteristics based on the gender of the unborn baby and their significance for obstetrics are limited. The aim of this study is to analyse selected parameters of obstetric relevance in the phases pregnancy, birth and postpartum period in dependence on the gender of the foetus. Materials and Methods: The selected study method comprised a retrospective data acquisition and evaluation from the Austrian birth register of the Department of Clinical Epidemiology of Tyrolean State Hospitals. For the analysis all inpatient singleton deliveries in Austria during the period from 2008 to 2013 were taken into account (live and stillbirths n = 444 685). The gender of the baby was correlated with previously defined, obstetrically relevant parameters. Results: In proportions, significantly more premature births and sub partu medical interventions (vaginal and abdominal surgical deliveries. episiotomies) were observed for male foetuses (p < 0.001). The neonatal outcome (5-min Apgar score, umbilical pH value less than 7.1, transfer to a neonatal special unit) is significantly poorer for boys (p < 0.001). Discussion: In view of the vulnerability of male foetuses and infants, further research is needed in order to be able to react appropriately to the differing gender-specific requirements in obstetrics.
Zusammenfassung
Einleitung: Die Studienlage über die vom Geschlecht des ungeborenen Kindes ausgehenden Spezifika und deren Bedeutung in der Geburtshilfe ist limitiert. Ziel der Arbeit ist, anhand ausgewählter, geburtshilflich relevanter Parameter die Phasen Schwangerschaft, Geburt und Wochenbett in Abhängigkeit zum fetalen Geschlecht zu analysieren. Material und Methoden: Als Methode wurde eine retrospektive Datenerhebung und -auswertung aus dem Geburtenregister Österreich des Instituts für klinische Epidemiologie der Tirol Kliniken gewählt. Zur Analyse wurden alle stationären Einlingsgeburten in Österreich im Zeitraum von 2008–2013 (Lebend- und Totgeburten n = 444 685) herangezogen. Das Geschlecht des Kindes wurde mit vorab definierten, geburtshilflich relevanten Variablen in Beziehung gesetzt. Ergebnisse: Im Verhältnis sind bei männlichen Feten signifikant mehr Frühgeburten und medizinische Interventionen sub partu (vaginal und abdominal operativer Entbindungsmodus, Episiotomie) zu verzeichnen (p < 0,001). Das neonatale Outcome (5-min-Apgar-Wert, Na-pH-Wert unter 7,1, Verlegung auf neonatologische Abteilung) ist bei Knaben signifikant schlechter (p < 0,001). Diskussion: Im Hinblick auf die Vulnerabilität von männlichen Feten und Neugeborenen ist weitere Forschung notwendig, um in der Geburtshilfe den geschlechtsspezifisch unterschiedlichen Bedarfen entsprechend agieren zu können.
Introduction
The available studies on foetal gender as a specific influencing variable during pregnancy and birth are limited. In comparison our knowledge on the progress of infantile growth is relatively certain. In 280 days the unborn baby achieves a length of ca. 50 centimetres, whereby infant boys have on average a body length 1 centimetre and a head circumference of ca. 5 millimetres more than infant girls. At all times during pregnancy female foetuses have larger length-weight and head circumference-weight ratios than males. Already in the second trimester girls exhibit a shorter femur length and a smaller biparietal head diameter. Although girls show a lower intrauterine growth in comparison to boys they exhibit an accelerated maturation of about 4–6 weeks 1 .
Various studies have shown that placental dysfunctions, especially severe pre-eclampsia and intrauterine growth retardation, occur significantly more frequently in pregnancies involving a male foetus. The placentas of male foetuses exhibit significantly higher rates of deciduitis and velamentous navel insertions as well as a significantly lower incidence of placental infarction than the placenta of female foetuses 2 , 3 , 4 , 5 , 6 .
In the mothers of male infants, in comparison to the mothers of female babies, higher incidences of premature rupture of membranes and premature births can be observed 7 . The rates of gestational diabetes mellitus, macrosomia, protracted opening and expulsion phases, umbilical cord prolapses, umbilical cord looping and genuine umbilical cord knots are significantly elevated. Furthermore, male babies are more frequently delivered by Caesarean section than female babies 7 , 8 , 9 .
Also, the rates of vaginal surgical deliveries are higher, and the indication for birth completion is more frequently given with the diagnosis of “threatening intrauterine asphyxia” in the case of male babies. The rate of sonographically diagnosed growth retardation, however, is higher for female infants 10 .
Several studies have recognised male gender as being a risk factor during pregnancy and birth. The biological mechanisms of this gender-specific difference are, however, still virtually unknown even though various theories discuss the influence of hormonal, physiological or genetic factors 8 , 11 , 12 , 13 , 14 .
Although new management strategies have led to better and better therapeutic results for very preterm infants, boys still exhibit higher mortality and morbidity than girls. For boys in the group of very preterm infants significant differences can be seen in the criteria higher birth weight, oxygen dependency, hospital stay, pulmonary bleeding, treatment with steroids, skull anomalies and mortality. These differences also remain significant in the subsequent course. The authors conclude that male gender per se represents a risk factor for the poor general condition of very premature babies as well as for their poorer developmental course 15 , 16 , 17 .
The accelerated maturation for girls is well known and, in the neonatal period and infancy, results in girls having a markedly greater ability to form a primary relationship, being emotional stable, easier to calm down and being less restless. The perception of social and other interactions starts earlier in girls. In boys, on the other hand, the early ability to form relationships and coping strategies, for example, in cases of pain and discomfort are influenced by the greater restlessness, the delayed development of sleep rhythm and the vulnerability. “In unfavourable circumstances this leads to a higher degree of psychophysical stress in the male child” 18 .
The consideration of gender-specific components already in the perinatal phase should, in the sense of the aims of gender medicine, help to optimise the preventative, diagnostic, therapeutic and rehabilitation processes of general and health care from the very beginning “to act as an important step and bridge towards personalised medicine” 19 .
The aim of this study is to consider with the help of selected obstetrically relevant parameters the phases pregnancy, birth and postpartum period in relation to foetal gender. On the basis of the above-mentioned considerations, we posed the following guiding question for our research: what influence does foetal gender have on selected obstetric parameters?
Materials and Methods
For this publication we have obtained a positive vote from the Ethics Commission of Upper Austria and permission for the data analysis from the board of the Austrian birth register at the Department of Clinical Epidemiology of Tyrolean State Hospitals in Innsbruck.
We have decided upon a retrospective data acquisition and evaluation from the Austrian birth register as method for this study. The Austrian birth register contains the results of all births occurring in hospitals in Austria since 2008 in an epidemiological data base.
Samples and variables
For the analysis, all inpatient singleton births in Austria in the period from 2008 to 2013 (n = 444 685 live births) were included. The gender of the baby was correlated with the following, previously defined and obstetrically relevant variables: parity, duration of pregnancy, birth weight, tocolysis, position of the baby at birth, drug-induced labour, micro blood gas analysis sub partu, peridural or spinal anaesthesia, delivery mode, delivery position, duration of delivery, performance of episiotomy, perineal trauma, 5-min Apgar score, umbilical cord pH, disorder of placenta separation, transfer of the infant post partum to neonatal department, perinatal mortality.
The parameters duration of delivery, episiotomy, 5-min Apgar score, umbilical cord pH under 7.1 and transfer of the baby to a neonatal department were additionally analysed with the specific sample “live birth at term” (gestational weeks 36 + 6–42 + 0) (n = 411 380), in order to enable a differentiated presentation of the results.
Statistical evaluation
The χ2 test was used for the statistical evaluation and presentation of the results. As a consequence of the large sample size statistically significant results are possible already for small differences and have to be considered for their clinical relevance.
Among the total number of all inpatient live births from singleton pregnancies in Austria in the period 2008–2013 (n = 444 685) 51.5 % were boys and 48.5 % were girls ( Table 1 ).
Table 1 Representation of the proportions of boys and girls arranged according to the obstetric parameters. The influence of the foetal gender on selected obstetric parameters.
On analysis of the parity and its relationship to the gender of the baby, at first, no significant differences can be determined. Only after the motherʼs 7th delivery does a difference become visible: the relationship for boys of 56 % is significantly higher than that for girls with 44 %.
Duration of pregnancy and birth weight
The proportion of male infants is markedly higher than that for female infants not only for the extremely preterm births (weeks of gestation < 27 + 6) and the very preterm births (weeks of gestation 28 + 0–31 + 6) but also for the late preterm births (weeks of gestation 32 + 0–36 + 6) (55.1 : 44.9 %; 56.3 : 43.8 %; 55.2 : 44.8 %). For term births, the ratio of girls to boys is balanced. Significantly more boys (53.4 %) than girls (46.6 %) are born after completion of the 42nd week of pregnancy (p < 0.001).
For the birth weights of the babies, it is seen that in the category under 500 g the ratio of male infants with 47.1 % is markedly lower than that of female infants with 52.9 %. In the category between 500 g and 750 g the ratio of boys to girls is balanced. The ratio of male to female infants is significantly higher in the categories 750–999 g (55.3 % boys and 44.7 % girls) and 1000–1499 g (52.6 % boys and 47.4 % girls) (p < 0.001). In the category 1500–2499 g the ratio is reversed (46.5 % boys and 53.5 % girls), in the category 2500–3999 g it is balanced and in the category 4000–6500 g again markedly elevated in favour of boys (66.4 % boys and 33.6 % girls).
The proportion of pregnancies and births in which tocolysis was applied is markedly higher for male foetuses with 55.4 % as compared to females with 44.6 %.
Sub partu interventions and delivery mode
For the parameters position of the baby at delivery, the ratio of boys to girls is relatively balanced for the proper cephalic position. On the other hand, there are marked differences with higher proportions for boys in cases with anomalous cephalic presentation (52.7 % boys, 47.3 % girls) and transverse presentation (53.8 % boys, 46.2 % girls) and there are significantly more girls with breech presentations at birth (45.6 % boys, 54.4 % girls) (p < 0.001).
With regard to drug-induced labour and foetal gender no differences could be found.
Micro blood gas analyses during birth for evaluation of the general condition of the infant were employed significantly more often for boys (55 %) than for girls (45 %) (p < 0.001).
Use of peridural or, respectively, spinal anaesthesia as pain therapy during birth was requested similarly independent of the gender of the unborn baby.
With regard to the mode of delivery, there were no significant differences between the genders of the babies in the categories “spontaneous birth” and “primary Caesarean section”. The proportion of boys is markedly higher than that of girls in the vaginal surgical delivery modes (vacuum: 56.8 % boys, 43.2 % girls; forceps: 62.4 % boys, 37.6 % girls) and also in the category “secondary Caesarean section” (55.7 % boys, 44.3 % girls).
For the parameter position of the baby in vaginal deliveries, the Austrian birth register records the categories “delivery room bed”, “stool delivery”, “water birth” and “others”. In the context of these categories no relevant differences between the foetal genders could be demonstrated.
For the duration of delivery, no relationships with foetal gender could be derived. In the case of duration of delivery in excess of 24 hours, the proportion of girls is slightly elevated as compared to boys, and this is also the case in the sample of term births.
With 54.6 %, episiotomies are performed significantly more frequently in the births of boys than in the births of girls (p < 0.001). If we consider only the sample of term births (weeks of gestation 36 + 6 to 42 + 0), the result is very similar. In this subgroup the ratio is 54.4 % for the boys and 45.6 % for the girls.
Similarly, perineal traumata, especially severe perineal traumata are more frequent in the course of birth of boys than during the birth of girls.
Disorders of placental separation are significantly less frequent with 47.2 % in the placentas of male foetuses than in the placentas of female foetuses with 52.8 %.
Perinatal outcome
In the case of the 5-min Apgar score as instrument to evaluate the clinically identifiable general condition of the new born baby we find a significantly higher proportion especially of low scores for the boys. For all new born infants exhibiting an Apgar score of 9–10 after 5 minutes, the ratio between boys and girls is balanced.
This tendency can also be seen when the reduced sample of live births at term is used in the analysis (weeks of gestation 36 + 6–42 + 0).
The proportion of boys with an umbilical cord pH value of less than 7.1 is 53.9 % which is significantly higher than that for the girls with 46.1 %. Also in the sample of live births at term, boys show a significantly higher proportion of 53.6 % than girls with 46.4 % (p < 0.001).
Transfer of the new born baby to a neonatal department between birth and the 7th day after birth in all categories is significantly more frequently necessary for boys than for girls. The same result is found on evaluating the sample of live births at term.
The obstetric parameter mortality prior to birth (n = 2214) does not exhibit any differences with regard to the gender of the foetus. During delivery the relative proportion of male foetuses with 63.3 % as compared to 36.7 % for the female foetuses is markedly elevated as it is also after birth with 63.3 % for the boys and 36.7 % for the girls.
An analysis of selected, obstetrically relevant parameters in relation to the gender of the foetus provides a contribution to the gender-oriented optimisation of general and health-care management. Our results are, in principle, in accord with the results of studies by Di Renzo et al. (2007), Aibar et al. (2012) and Khalil (2013) and demonstrate that male foetuses have a higher vulnerability in the perinatal phase and a high obstetric risk 7 , 10 , 11 .
The high tendency towards premature births or, respectively, the higher rate of preterm births for boys revealed by these data confirms the results of previous studies 2 , 3 , 6 , 7 . Di Renzo et al. assumed that the higher incidences of premature rupture of membranes and preterm births among boys can be attributed to their relatively higher weights and lower gestational ages 7 . However, this assumption contradicts the results of Challis et al. (2013), who demonstrated in their study that chorionic trophoblast cells from pregnancies with a male foetus possess the potential to generate a pro-inflammatory environment by which the significantly higher rate of male preterm births than female preterm births can be explained 20 . This further substantiates the results of Zeitlin et al. (2004) that the tendency for preterm births among boys is significantly more frequently due to the spontaneous onset of contractions and less often due to a medically indicated and drug-induced completion of the pregnancy 21 . This generally high rate of preterm births requires more research initiatives on the pathophysiological processes. For this there is a need to acquire basic knowledge about the intrinsic and extrinsic triggers of the threatening preterm birth as a complex event under consideration of gender-specific characteristics.
We can also confirm the high rates of interventions among males foetuses sub partu (vaginal surgical conclusion of the birth process, Caesarean section) demonstrated in the studies of Di Renzo et al., Sheiner et al. and Dunn et al. 7 , 8 , 14 . The relatively higher rate of micro blood gas analyses (MBA) employed during the birth of boys allows the conclusion of a higher rate of at least suspected hypoxia in the foetal metabolism. In this context it is still not clear whether the physiological characteristics of boys lead more often to stress phases during birth or if the interpretation of findings (above all of CTG and MBA) require a gender-specific differentiation. In order to more exactly evaluate the foetal condition sub partu, we need a further specialisation of the possible monitoring and diagnostic options as well as their adaptation to gender-specific peculiarities.
The higher birth weight of boys may be a factor to help explain the higher rates of vaginal surgical deliveries and Caesarean sections. However, it has not been possible to confirm a relationship between higher birth weight and longer duration of birth. At duration of birth in excess of 24 hours the proportion of girls is even higher than that of boys.
As can be seen from the parameters 5-min Apgar score, umbilical pH value and transfer of the infant post partum, the higher intervention rate sub partu does not lead to a better neonatal outcome for boys in comparison to girls. Dunn et al. reported similar results where, in spite of a higher rate of interventions, lower Apgar scores, more reanimation procedures and a higher rate of respiratory distress were demonstrated for male babies 14 . Also in this context the question must be posed as to how reliable are the instruments used during birth to monitor the foetus and how valid is the interpretation of the so obtained data.
One limitation of this study is the lacking analysis of multifactorial events. This would have been suitable to more precisely describe indications, interventions and neonatal outcome in relation to foetal gender.
According to these results male foetuses and babies exhibit a vulnerable constitution not only in the prepartal phase but also sub partu and post partum. On the basis of this finding, it is essential to generate further basic knowledge about the physiological and pathophysiological processes during pregnancy and birth in dependence on the gender of the foetus.
Then it would be possible to derive preventative, diagnostic and therapeutic measures according to the foetal gender and to apply them accordingly. This knowledge could contribute to an optimisation of obstetric management, especially with regard to a reduction in the rates of preterm births and preterm interventions.
Conflict of Interest None.
Supporting Information

Cephalic presentation
October 14, 2016
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations) which are either more difficult to deliver or not deliverable by natural means.
The movement of the fetus to cephalic presentation is called head engagement. It occurs in the third trimester. In head engagement, the fetal head descends into the pelvic cavity so that only a small part (or none) of it can be felt abdominally. The perineum and cervix are further flattened and the head may be felt vaginally. Head engagement is known colloquially as the baby drop, and in natural medicine as the lightening because of the release of pressure on the upper abdomen and renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum, and the mother may experience the perpetual sensation that the fetus will “fall out” at any moment.
The vertex is the area of the vault bounded anteriorly by the anterior fontanelle and the coronal suture, posteriorly by the posterior fontanelle and the lambdoid suture and laterally by 2 lines passing through the parietal eminences.
In the vertex presentation the occiput typically is anterior and thus in an optimal position to negotiate the pelvic curve by extending the head. In an occiput posterior position, labor becomes prolonged and more operative interventions are deemed necessary. The prevalence of the persistent occiput posterior is given as 4.7 %
The vertex presentations are further classified according to the position of the occiput, it being right, left, or transverse, and anterior or posterior:
Left Occipito-Anterior (LOA), Left Occipito-Posterior (LOP), Left Occipito-Transverse (LOT); Right Occipito-Anterior (ROA), Right Occipito-Posterior (ROP), Right Occipito-Transverse (ROT);
By Mikael Häggström – Own work, Public Domain
Cephalic presentation. (2016, September 17). In Wikipedia, The Free Encyclopedia . Retrieved 05:18, September 17, 2016, from https://en.wikipedia.org/w/index.php?title=Cephalic_presentation&oldid=739815165
Insert/edit link
Enter the destination URL
Or link to existing content

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
You and your baby at 32 weeks pregnant
Your baby at 32 weeks.
By about 32 weeks, the baby is usually lying with their head pointing downwards, ready for birth. This is known as cephalic presentation.
If your baby is not lying head down at this stage, it's not a cause for concern – there's still time for them to turn.
The amount of amniotic fluid in your uterus is increasing, and your baby is still swallowing fluid and passing it out as urine.
You at 32 weeks
Being active and fit during pregnancy will help you adapt to your changing shape and weight gain. It can also help you cope with labour and get back into shape after the birth.
Find out about exercise in pregnancy .
You may develop pelvic pain in pregnancy. This is not harmful to your baby, but it can cause severe pain and make it difficult for you to get around.
Find out about ways to tackle pelvic pain in pregnancy .
Read about the benefits of breastfeeding for you and your baby. It's never too early to start thinking about how you're going to feed your baby, and you do not have to make up your mind until your baby is born.
Things to think about
- how you might feel after the birth
Start4Life has more about you and your baby at 32 weeks pregnant .
You can sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Page last reviewed: 13 October 2021 Next review due: 13 October 2024
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 15: Abnormal Cephalic Presentations
Jessica Dy; Darine El-Chaar
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Malpresentations.
- TRANSVERSE POSITIONS OF THE OCCIPUT
- POSTERIOR POSITIONS OF THE OCCIPUT
- BROW PRESENTATIONS
- MEDIAN VERTEX PRESENTATIONS: MILITARY ATTITUDE
- FACE PRESENTATION
- SELECTED READING
- Full Chapter
- Supplementary Content
The fetus enters the pelvis in a cephalic presentation approximately 95 percent to 96 percent of the time. In these cephalic presentations, the occiput may be in the persistent transverse or posterior positions. In about 3 percent to 4 percent of pregnancies, there is a breech-presenting fetus (see Chapter 25 ). In the remaining 1 percent, the fetus may be either in a transverse or oblique lie (see Chapter 26 ), or the head may be extended with the face or brow presenting.
Predisposing Factors
Maternal and uterine factors.
Contracted pelvis: This is the most common and important factor
Pendulous maternal abdomen: If the uterus and fetus are allowed to fall forward, there may be difficulty in engagement
Neoplasms: Uterine fibromyomas or ovarian cysts can block the entry to the pelvis
Uterine anomalies: In a bicornuate uterus, the nonpregnant horn may obstruct labor in the pregnant one
Abnormalities of placental size or location: Conditions such as placenta previa are associated with unfavorable positions of the fetus
High parity
Fetal Factors
Errors in fetal polarity, such as breech presentation and transverse lie
Abnormal internal rotation: The occiput rotates posteriorly or fails to rotate at all
Fetal attitude: Extension in place of normal flexion
Multiple pregnancy
Fetal anomalies, including hydrocephaly and anencephaly
Polyhydramnios: An excessive amount of amniotic fluid allows the baby freedom of activity, and he or she may assume abnormal positions
Prematurity
Placenta and Membranes
Placenta previa
Cornual implantation
Premature rupture of membranes
Effects of Malpresentations
Effects on labor.
The less symmetrical adaptation of the presenting part to the cervix and to the pelvis plays a part in reducing the efficiency of labor.
The incidence of fetopelvic disproportion is higher
Inefficient uterine action is common. The contractions tend to be weak and irregular
Prolonged labor is seen frequently
Pathologic retraction rings can develop, and rupture of the lower uterine segment may be the end result
The cervix often dilates slowly and incompletely
The presenting part stays high
Premature rupture of the membranes occurs often
The need for operative delivery is increased
Effects on the Mother
Because greater uterine and intraabdominal muscular effort is required and because labor is often prolonged, maternal exhaustion is common
There is more stretching of the perineum and soft parts, and there are more lacerations
Tears of the uterus, cervix, and vagina
Uterine atony from prolonged labor
Early rupture of the membranes
Excessive blood loss
Tissue damage
Frequent rectal and vaginal examinations
Prolonged labor
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

Can placental location accurately predict fetal gender?
A baby’s gender is often detected via ultrasound around 20 weeks of pregnancy. What if there was a way to know sooner?
There are a multitude of reasons for parents to want to know the gender of their baby. Maybe they want to get started on the nursery or register for the baby shower.
A baby’s gender is often detected via ultrasound around 20 weeks of pregnancy. 1 What if there was a way to know sooner?
To answer the question, Dr. Saam Ramzi Ismali developed a theory (Ramzi’s method) that fetal sex could be determined as early as 6 weeks into pregnancy. The theory claims that the location of the placenta, or trophoblast, can define fetal gender as early as six weeks via ultrasound. If the placenta is developing on the left side, the sex is female. If it is developing on the right, the sex is male.
Unfortunately, Ramzi’s method has not been confirmed in any additional studies. There are no outward signs of sex until about 9 weeks of pregnancy. Differentiated genitalia cannot be seen clearly until about 15 weeks. 2 As a result, many ob/gyns dismiss the validity of Ramzi’s method entirely.
A gender prediction method that has been studied, however, is the use of cell-free DNA. Researchers used cell-free fetal DNA in plasma of pregnant women to determine early gender of the fetus with 96.7% accuracy. 3
- Fetal Development: Stages of Growth. Cleveland Clinic. Accessed October 21, 2020. https://my.clevelandclinic.org/health/articles/7247-fetal-development-stages-of-growth
- Santiago-Munoz P. Boy or girl? The difficulties of early gender prediction. diction. University of Texas Southwestern. December 20, 2016. Accessed October 21, 2020. https://utswmed.org/medblog/gender-prediction/
- Zargari M, Sadeghi MR, Shahhosseiny MH, et al. Fetal Sex Determination using Non-Invasive Method of Cell-free Fetal DNA in Maternal Plasma of Pregnant Women During 6(th)- 10(th) Weeks of Gestation. Avicenna J Med Biotechnol . 2011;3(4):201-206.

Similar delivery times between misoprostol dosages among obese patients reported
A recent study found that obese patients undergoing induction of labor experienced similar delivery times regardless of whether they received 50 μg or 25 μg of vaginal misoprostol, though multiparous patients showed faster delivery with the higher dosage.
S1E4: Dr. Kristina Adams-Waldorf: Pandemics, pathogens and perseverance
This episode of Pap Talk by Contemporary OB/GYN features an interview with Dr. Kristina Adams-Waldorf, Professor in the Department of Obstetrics and Gynecology and Adjunct Professor in Global Health at the University of Washington (UW) School of Medicine in Seattle.

Buprenorphine use in pregnancy linked to decreased fetal breathing movements
According to a poster presented at ACOG 2024, use of the synthetic opioid buprenorphine depressed fetal breathing in biophysical profile assessments, but had no significant impact on other factors like amniotic fluid index or fetal tone.
S1E3: Dr. Emily S. Miller: Placental pathology and MVM evidence
This episode of Pap Talk by Contemporary OB/GYN features an interview with Dr. Emily S. Miller, with Northwestern Medicine in Chicago.

Identifying gaps in syphilis treatment and prenatal care among pregnant individuals
Preventing congenital syphilis comes down to quick diagnosis and treatment of the infection in pregnancy, and the number of missed opportunities to do so in the United States continues to grow.

Exploring the impact of maternal asthma on placental hormones and placental weight
In a poster presented at ACOG 2024, investigators found that mean placental weight was higher in patients with asthma, and that pregnancy hormone levels do differ based on asthma status.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
- Second Opinion
Cephalic Disorders
(Disorders of Head Size)
Cephalic disorders affect the central nervous system as it develops. They may also affect the brain and the growth of the skull. These disorders can cause a variety of developmental delays, physical disabilities, and threats to a child’s life. Cephalic disorders begin during pregnancy early in a baby’s development. They are also called neurodevelopmental disorders.
One of the most visible signs of a cephalic disorder is the unusual size or shape of a baby’s head. Problems from these disorders are most likely when a baby’s head is much smaller or larger than the average for their age.
Facts about cephalic disorders
These disorders may range from mild to severe. This depends on the parts of the brain and central nervous system affected. Many people with cephalic disorders live relatively normal lives. But some cephalic disorders are so severe that a baby will die within weeks or months of birth.
Types of cephalic disorders
There are many different cephalic disorders, including:
Anencephaly. This condition happens when the top of the neural tube doesn’t close as the baby develops during pregnancy. A major part of the brain, skull, and scalp are missing. The brain tissue that remains is often exposed. These babies are born unconscious, deaf, and blind. Babies with this condition often die within hours or days of birth.
Colpocephaly. The back part of the chambers of the brain (the occipital horns) are abnormally large. Babies with this condition have an unusually small head and an intellectual disability. Other symptoms may include muscle spasms, motor abnormalities, and seizures.
Holoprosencephaly. As the baby develops during pregnancy, the brain grows into one single lobe instead of two. There are different grades of severity. A baby may have very mild abnormalities and be able to lead a relatively normal life. Or there may be severe abnormalities and limited function. Many babies with the severe form of this disorder die before or soon after birth. Others may live, but may have severely deformed faces and severe cognitive and neurological impairment.
Hydranencephaly. With this rare condition, the cerebral hemispheres of the brain are missing. They are replaced by pockets of cerebrospinal fluid. These babies may seem normal at birth. But within a few months they become irritable. They don’t develop along a normal timeline. Most of these children have severe neurological and cognitive impairment. They usually die within several years.
Hydrocephalus. This is not really a cephalic disorder, but it can cause a large head size in infants. With this condition, cerebrospinal fluid builds up in the ventricles of the brain. Children usually need a tube (shunt) to drain the excess fluid. The outcome depends on the cause of the hydrocephalus and how early therapy is started.
Iniencephaly. This disorder combines the extreme backward bending of the baby’s head with severe spinal defects. The baby's distorted body may also put the mother’s life in danger. Babies with this disorder rarely live more than a few hours.
Lissencephaly. In normal brain development, nerve cells (neurons) travel to the correct part of the nervous system and connect to each other. This and other related disorders happen when the brain neurons don’t end up in the correct place during development. This causes an unusual brain formation and an extremely small head. There is a range of neurological disability, from mild developmental delay to severe neurologic dysfunction and even death.
Microcephaly. With this condition, a baby’s head is much smaller than normal. Many children with smaller than average heads have normal intelligence and develop correctly. But this condition is common in many known disorders such as Down syndrome. Many children with microcephaly may have an intellectual disability, as well as cerebral palsy, sensory disorders including vision problems, poor motor skills, lack of balance and coordination, and trouble thinking and learning as expected for the child’s age. Microcephaly is also a symptom of other birth defects such as lissencephaly and porencephaly.
Macrencephaly (also called megalencephaly). With this disorder, a baby’s head is much larger than normal. This may be because the brain grows unusually large. Experts believe this disorder may occur because normal cell production in the brain is disrupted. Children may have seizures, developmental delays, and other motor problems. (This disorder is different than macrocephaly, an enlargement of the head without related brain defects. It is usually inherited and has no symptoms.)
Porencephaly. This disorder occurs when a pocket of cerebrospinal fluid forms in the baby’s brain during development. It is believed to be related to an infection or stroke, either during pregnancy or the newborn stage. Some children with this disorder have normal intelligence and few if any developmental problems. Others have motor or cognitive difficulties of varying degrees. The severity depends on the size of the cerebrospinal fluid-filled pockets, and where they are in the brain.
Schizencephaly. This rare disorder happens when slits (clefts) form in one or both hemispheres of the brain. Symptoms will vary depending on how many clefts a child has, and if they are on one or both sides of the brain. Some people with this disorder lead relatively normal lives. Others may have severe developmental delays, motor delays or even paralysis, or seizures.
Symptoms vary depending on the type of cephalic disorder, but may include:
Unusually large or small head
Trouble swallowing or eating
Poor muscle tone
Deformed fingers or toes
Deformed face
Delays in the development of physical abilities or language
Delayed growth
To make a diagnosis, the healthcare provider may consider symptoms and health history, and do a physical exam of the skull and body. You will often be referred to a specialist, such as a geneticist to help make a diagnosis. The healthcare provider may also order tests:
Blood tests
CT scan or MRI scans (MRI scans often show more detail)
Head size is often considered during diagnosis. A healthcare provider will use a measuring tape to measure the distance around your baby’s head (circumference). The tape is usually placed just above the eyebrows and around the widest part of the head. This number is compared with standard growth charts.
Head size can change as a baby grows into a toddler or young child. A child’s head size may be measured at every well visit or office visit to see if the head is changing shape. This usually continues until age 3, unless there is a reason to keep track past that age.
When to call your child's healthcare provider
Some cephalic disorders are clearly present from birth. Others are not. Call the healthcare provider if you have concerns about your child’s ability to meet developmental milestones. These include starting to roll over, crawl, walk, or speak at the expected age. Also call if you are concerned about the shape of your child’s face or head.
Treatment for cephalic disorders depends on the type of disorder. Treatments may include:
Physical therapy for motion
Speech therapy for language
Medicines, such as antiseizure medicine, for symptoms
Shunts to drain excess fluid off the brain
Surgery to help correct a deformed skull or face
Comfort care
The true cause of cephalic disorders is not fully known. Experts believe that genes may be a factor. Things that happen during a woman’s pregnancy may also play a role. These can include having an infection or being exposed to toxic chemicals.
The best way to try to prevent cephalic disorders is to be as healthy as possible during pregnancy. This means staying away from alcohol, cigarettes, and illegal drugs. It’s also important to eat a varied, healthy diet. Getting enough folic acid has been shown to reduce the risk for certain birth defects, including some cephalic disorders. But many women take good care of themselves during pregnancy and still give birth to a child with a cephalic disorder. Some of these disorders may be caused by intrauterine infection or an injury. Hereditary conditions may also be a factor. Genetic counseling may help you understand your risks in future pregnancies.
- Stanford Medicine Children’s Health Pediatrics – Monterey
- Bass Center for Childhood Cancer and Blood Diseases
- Children's Orthopedic and Sports Medicine Center
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health

IMAGES
VIDEO
COMMENTS
Benefits of Cephalic Presentation in Pregnancy. Cephalic presentation is one of the most ideal birth positions, and has the following benefits: It is the safest way to give birth as your baby's position is head-down and prevents the risk of any injuries. It can help your baby move through the delivery canal as safely and easily as possible.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Head Down, Facing Down (Cephalic Presentation) This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone ...
Head first (called vertex or cephalic presentation) Facing backward (occiput anterior position) Spine parallel to mother's spine (longitudinal lie) Neck bent forward with chin tucked. Arms folded across the chest . If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not ...
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... This is called an external cephalic version, and it has a 58 percent success rate for turning breech babies. For more information, ...
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy.
An incomplete breech presentation is where just one of the baby's knees is bent up. Their other foot and bottom are closest to the birth canal. In a footling breech presentation, one or both feet may be delivered first. Complete breech. A complete breech presentation is less common, occurring in 5 to 10 percent of breech births.
On the other hand, there are marked differences with higher proportions for boys in cases with anomalous cephalic presentation (52.7 % boys, 47.3 % girls) and transverse presentation (53.8 % boys, 46.2 % girls) and there are significantly more girls with breech presentations at birth (45.6 % boys, 54.4 % girls) (p < 0.001). With regard to drug ...
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Cephalic presentation occurs when the fetal head is positioned downward, with the occiput (the back of the head) closest to the mother's cervix and birth can...
Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). If your baby is in any position other than head down, your doctor may recommend a cesarean delivery. Breech presentation is when the baby's bottom is down ...
What is cephalic presentation? Flexi Says: Cephalic presentation is the position of the baby's head pointing downwards, facing your back. Discuss further with Flexi. Ask your own question!
By about 32 weeks, the baby is usually lying with their head pointing downwards, ready for birth. This is known as cephalic presentation. If your baby is not lying head down at this stage, it's not a cause for concern - there's still time for them to turn. The amount of amniotic fluid in your uterus is increasing, and your baby is still ...
Vertex presentation is when a fetus is headfirst in your vagina before delivery. Vertex presentation is the ideal position for a vaginal delivery. Locations: Abu Dhabi ... Yes, they essentially mean the same thing. Cephalic presentation means a fetus is in a head-down position. Vertex refers to the fetus's neck being tucked in. There are ...
The fetus enters the pelvis in a cephalic presentation approximately 95 percent to 96 percent of the time. In these cephalic presentations, the occiput may be in the persistent transverse or posterior positions. In about 3 percent to 4 percent of pregnancies, there is a breech-presenting fetus (see Chapter 25).
Right occiput anterior: The position is the same as that above, but the fetus is in the womb's right side. Posterior: The head is down, and the back is in line with the pregnant person's ...
The theory claims that the location of the placenta, or trophoblast, can define fetal gender as early as six weeks via ultrasound. If the placenta is developing on the left side, the sex is female. If it is developing on the right, the sex is male. Unfortunately, Ramzi's method has not been confirmed in any additional studies.
Differences between boy and girl pregnancy symptoms and signs. Product. Tracking cycle. Getting pregnant. Pregnancy. Help Center. Flo for Partners New. Anonymous Mode New. Health Library.
Cephalic disorders begin during pregnancy early in a baby's development. They are also called neurodevelopmental disorders. One of the most visible signs of a cephalic disorder is the unusual size or shape of a baby's head. Problems from these disorders are most likely when a baby's head is much smaller or larger than the average for ...