
- What is Strategy?
- Business Models
- Developing a Strategy
- Strategic Planning
- Competitive Advantage
- Growth Strategy
- Market Strategy
- Customer Strategy
- Geographic Strategy
- Product Strategy
- Service Strategy
- Pricing Strategy
- Distribution Strategy
- Sales Strategy
- Marketing Strategy
- Digital Marketing Strategy
- Organizational Strategy
- HR Strategy – Organizational Design
- HR Strategy – Employee Journey & Culture
- Process Strategy
- Procurement Strategy
- Cost and Capital Strategy
- Business Value
- Market Analysis
- Problem Solving Skills
- Strategic Options
- Business Analytics
- Strategic Decision Making
- Process Improvement
- Project Planning
- Team Leadership
- Personal Development
- Leadership Maturity Model
- Leadership Team Strategy
- The Leadership Team
- Leadership Mindset
- Communication & Collaboration
- Problem Solving
- Decision Making
- People Leadership
- Strategic Execution
- Executive Coaching
- Strategy Coaching
- Business Transformation
- Strategy Workshops
- Leadership Strategy Survey
- Leadership Training
- Who’s Joe?
“A fact is a simple statement that everyone believes. It is innocent, unless found guilty. A hypothesis is a novel suggestion that no one wants to believe. It is guilty until found effective.”
– Edward Teller, Nuclear Physicist
During my first brainstorming meeting on my first project at McKinsey, this very serious partner, who had a PhD in Physics, looked at me and said, “So, Joe, what are your main hypotheses.” I looked back at him, perplexed, and said, “Ummm, my what?” I was used to people simply asking, “what are your best ideas, opinions, thoughts, etc.” Over time, I began to understand the importance of hypotheses and how it plays an important role in McKinsey’s problem solving of separating ideas and opinions from facts.

What is a Hypothesis?
“Hypothesis” is probably one of the top 5 words used by McKinsey consultants. And, being hypothesis-driven was required to have any success at McKinsey. A hypothesis is an idea or theory, often based on limited data, which is typically the beginning of a thread of further investigation to prove, disprove or improve the hypothesis through facts and empirical data.
The first step in being hypothesis-driven is to focus on the highest potential ideas and theories of how to solve a problem or realize an opportunity.
Let’s go over an example of being hypothesis-driven.
Let’s say you own a website, and you brainstorm ten ideas to improve web traffic, but you don’t have the budget to execute all ten ideas. The first step in being hypothesis-driven is to prioritize the ten ideas based on how much impact you hypothesize they will create.

The second step in being hypothesis-driven is to apply the scientific method to your hypotheses by creating the fact base to prove or disprove your hypothesis, which then allows you to turn your hypothesis into fact and knowledge. Running with our example, you could prove or disprove your hypothesis on the ideas you think will drive the most impact by executing:
1. An analysis of previous research and the performance of the different ideas 2. A survey where customers rank order the ideas 3. An actual test of the ten ideas to create a fact base on click-through rates and cost
While there are many other ways to validate the hypothesis on your prioritization , I find most people do not take this critical step in validating a hypothesis. Instead, they apply bad logic to many important decisions . An idea pops into their head, and then somehow it just becomes a fact.
One of my favorite lousy logic moments was a CEO who stated,
“I’ve never heard our customers talk about price, so the price doesn’t matter with our products , and I’ve decided we’re going to raise prices.”
Luckily, his management team was able to do a survey to dig deeper into the hypothesis that customers weren’t price-sensitive. Well, of course, they were and through the survey, they built a fantastic fact base that proved and disproved many other important hypotheses.

Why is being hypothesis-driven so important?
Imagine if medicine never actually used the scientific method. We would probably still be living in a world of lobotomies and bleeding people. Many organizations are still stuck in the dark ages, having built a house of cards on opinions disguised as facts, because they don’t prove or disprove their hypotheses. Decisions made on top of decisions, made on top of opinions, steer organizations clear of reality and the facts necessary to objectively evolve their strategic understanding and knowledge. I’ve seen too many leadership teams led solely by gut and opinion. The problem with intuition and gut is if you don’t ever prove or disprove if your gut is right or wrong, you’re never going to improve your intuition. There is a reason why being hypothesis-driven is the cornerstone of problem solving at McKinsey and every other top strategy consulting firm.
How do you become hypothesis-driven?
Most people are idea-driven, and constantly have hypotheses on how the world works and what they or their organization should do to improve. Though, there is often a fatal flaw in that many people turn their hypotheses into false facts, without actually finding or creating the facts to prove or disprove their hypotheses. These people aren’t hypothesis-driven; they are gut-driven.
The conversation typically goes something like “doing this discount promotion will increase our profits” or “our customers need to have this feature” or “morale is in the toilet because we don’t pay well, so we need to increase pay.” These should all be hypotheses that need the appropriate fact base, but instead, they become false facts, often leading to unintended results and consequences. In each of these cases, to become hypothesis-driven necessitates a different framing.
• Instead of “doing this discount promotion will increase our profits,” a hypothesis-driven approach is to ask “what are the best marketing ideas to increase our profits?” and then conduct a marketing experiment to see which ideas increase profits the most.
• Instead of “our customers need to have this feature,” ask the question, “what features would our customers value most?” And, then conduct a simple survey having customers rank order the features based on value to them.
• Instead of “morale is in the toilet because we don’t pay well, so we need to increase pay,” conduct a survey asking, “what is the level of morale?” what are potential issues affecting morale?” and what are the best ideas to improve morale?”
Beyond, watching out for just following your gut, here are some of the other best practices in being hypothesis-driven:
Listen to Your Intuition
Your mind has taken the collision of your experiences and everything you’ve learned over the years to create your intuition, which are those ideas that pop into your head and those hunches that come from your gut. Your intuition is your wellspring of hypotheses. So listen to your intuition, build hypotheses from it, and then prove or disprove those hypotheses, which will, in turn, improve your intuition. Intuition without feedback will over time typically evolve into poor intuition, which leads to poor judgment, thinking, and decisions.
Constantly Be Curious
I’m always curious about cause and effect. At Sports Authority, I had a hypothesis that customers that received service and assistance as they shopped, were worth more than customers who didn’t receive assistance from an associate. We figured out how to prove or disprove this hypothesis by tying surveys to transactional data of customers, and we found the hypothesis was true, which led us to a broad initiative around improving service. The key is you have to be always curious about what you think does or will drive value, create hypotheses and then prove or disprove those hypotheses.
Validate Hypotheses
You need to validate and prove or disprove hypotheses. Don’t just chalk up an idea as fact. In most cases, you’re going to have to create a fact base utilizing logic, observation, testing (see the section on Experimentation ), surveys, and analysis.
Be a Learning Organization
The foundation of learning organizations is the testing of and learning from hypotheses. I remember my first strategy internship at Mercer Management Consulting when I spent a good part of the summer combing through the results, findings, and insights of thousands of experiments that a banking client had conducted. It was fascinating to see the vastness and depth of their collective knowledge base. And, in today’s world of knowledge portals, it is so easy to disseminate, learn from, and build upon the knowledge created by companies.
NEXT SECTION: DISAGGREGATION
DOWNLOAD STRATEGY PRESENTATION TEMPLATES
THE $150 VALUE PACK - 600 SLIDES 168-PAGE COMPENDIUM OF STRATEGY FRAMEWORKS & TEMPLATES 186-PAGE HR & ORG STRATEGY PRESENTATION 100-PAGE SALES PLAN PRESENTATION 121-PAGE STRATEGIC PLAN & COMPANY OVERVIEW PRESENTATION 114-PAGE MARKET & COMPETITIVE ANALYSIS PRESENTATION 18-PAGE BUSINESS MODEL TEMPLATE
JOE NEWSUM COACHING

EXECUTIVE COACHING STRATEGY COACHING ELEVATE360 BUSINESS TRANSFORMATION STRATEGY WORKSHOPS LEADERSHIP STRATEGY SURVEY & WORKSHOP STRATEGY & LEADERSHIP TRAINING
THE LEADERSHIP MATURITY MODEL
Explore other types of strategy.
BIG PICTURE WHAT IS STRATEGY? BUSINESS MODEL COMP. ADVANTAGE GROWTH
TARGETS MARKET CUSTOMER GEOGRAPHIC
VALUE PROPOSITION PRODUCT SERVICE PRICING
GO TO MARKET DISTRIBUTION SALES MARKETING
ORGANIZATIONAL ORG DESIGN HR & CULTURE PROCESS PARTNER
EXPLORE THE TOP 100 STRATEGIC LEADERSHIP COMPETENCIES
TYPES OF VALUE MARKET ANALYSIS PROBLEM SOLVING
OPTION CREATION ANALYTICS DECISION MAKING PROCESS TOOLS
PLANNING & PROJECTS PEOPLE LEADERSHIP PERSONAL DEVELOPMENT
Pursue the Next You in 2024 with 20% Tuition Reduction on September Courses!
An Overview of Management Theories: Classical, Behavioral, and Modern Approaches

Last Updated June 30, 2022
In both theory and practice, business management is at a crisis point . The world is changing — and changing quickly. There is no single management philosophy that answers every need. The best managers are flexible and blend methods. They adapt several management theories as needed to handle new situations.
Some people may believe in the Great Man Theory of Leadership . Others know that management is like anything else: Practice and education improve performance. Understanding different management theories help managers prioritize the processes, relationships and information that impact an organization’s success.
How should a leader set goals and guide their teams to realize them? Many heads are better than one, and this article covers three types of management approaches and many of the individual theories categorized within them.
Three Types of Management Theories
While ideas overlap between the categories, these three classifications differentiate management according to their focus and the era they came from:
- Classical management theory: emerged from the Industrial Revolution and revolves around maximizing efficiency and production.
- Behavioral management theory: started in the early 20 th century and addresses the organization’s human and social elements.
- Modern management theory: followed on the heels of World War II and combines mathematical principles with sociology to develop holistic approaches to management.
The origin of one movement doesn’t indicate the conclusion of the previous one. All three of these approaches still exist in contemporary practice.
Newer is not always better either. Each philosophy was born out of changing ideals and emerging possibilities, but today’s business world is complex. Different theories better suit different needs.
Classical Management Theory
Classical management theory prioritizes profit and assumes that personal gain motivates employees. It aims to streamline operations and increase productivity.
Major concepts include specialization, incentivization, and hierarchical structure. The first two contribute to employee efficiency and drive. Centralized leadership simplifies decision-making, and a meritocratic chain of commands provides order and oversight. At every level, standardization reduces waste and error.
There are many strengths to classical management theory. It provides clarity for both the organization and its personnel, and specialization and sound hiring practices place employees in positions they can handle and even master.
Shortcomings of classical management theory can include:
- The treatment of workers as machines without accounting for the role job satisfaction and workplace culture play in an organization’s success
- The difficulty of applying some of its principles outside a limited manufacturing context
- A top-down approach to communication that neglects employee input and prevents collaboration
- Failure to provide for creativity and innovation, which rigid structures and hyper specialization can stifle
The following management approaches belong to the overarching category of classical management theory:
Scientific Management Theory
Scientific management theory is sometimes called Taylorism after its founder Frederick Winslow Taylor, a mechanical engineer. Taylor employed scientific methods to develop organizational principles that suited mass production needs. After creating and proving his theory as a manager and consultant, he wrote ” The Principles of Scientific Management ” in 1911.
Taylor wanted to replace outdated, “rule-of-thumb” methods with more efficient processes. To this end, he identified four core principles of good management. The manager:
- Develops a science consisting of best practices for all elements of their employees’ work
- Selects and trains employees accordingly
- Works with employees to ensure that the science is followed
- Assumes half the responsibility for all work through process development, guidance, and maintenance
Today, many companies have adopted a version of the scientific management theory . By standardizing tools and procedures, they hope to increase productivity and reduce the reliance on individual talent and workers.
Bureaucratic Management Theory
Max Weber was one of the foremost scholars of the late 19 th and early 20 th century. He strongly influenced — and continues to influence — economic, religious, and political sociology. He explains bureaucratic management theory in “ Economy and Society ,” published posthumously in 1922.
Weber believed that standard rules and well-defined roles maximize the efficiency of an organization. Everyone should understand the responsibilities and expectations of their position, their place within a clear hierarchy and general corporate policies. Hiring decisions and the application of rules should be impersonal, guided only by reason and established codes.
Weber’s theory provides for orderly and scalable institutions. At least some element of bureaucracy informs most large organizations, whether they’re public, private, or profit driven.
Administrative Management Theory
Just as scientific management theory is sometimes called Taylorism, administrative management theory is sometimes called Fayolism.
Henri Fayol was a mining engineer who sought to codify the responsibilities of management and the principles of effective administration. He outlined these in “ General and Industrial Management ” in 1916.
His guide identifies 14 principles of management:
- Division of work: Divide work into tasks and between employees.
- Authority: Balance responsibility with commensurate authority.
- Unity of command: Give each employee one direct manager.
- Unity of direction: Align goals between employees.
- Equity: Treat all employees equally.
- Order: Maintain order through an organized workforce.
- Discipline: Establish and follow rules and regulations.
- Initiative: Encourage employees to show initiative.
- Remuneration: Pay employees fairly for the work they do.
- Stability: Ensure that employees feel secure in their positions.
- Scalar chain: Establish a clear hierarchy of command.
- Subordination of individual interest: Prioritize group needs.
- Esprit de corps: Inspire group unity and pride.
- A balance between centralization and delegation: Concentrate ultimate authority but delegate individual decisions.
According to Fayol, managers need to develop practices that foster each of the 14 principles.
Behavioral Management Theory
Behavioral management theory places the person rather than the process at the heart of business operations. It examines the business as a social system as well as a formal organization. Therefore, productivity depends on proper motivation, group dynamics, personal psychology, and efficient processes.
Behavioral management theory humanizes business. Feelings have a practical impact on operations. Team spirit, public recognition, and personal pride encourage employees to perform better. Individual relationships also play a role. Employees are more likely to go the extra mile for a boss they respect and who respects them.
Shortcomings of behavioral management theory include:
- The difficulty of balancing personal relationships with professional conduct
- An inclination toward socially motivated hiring practices that can be unjust
- The danger of assuming that all individuals respond the same way to the same situations and for the same reasons
Common behavioral management theories include the following:
Human Relations Theory
The fundamental texts on human relations theory evolved from an experiment following classical theory. Elton Mayo worked as part of a team evaluating the impact on the productivity of various workplace conditions at the Hawthorne Works, a large factory complex. Early results were self-contradicting; changes in opposite directions both improved productivity.
Mayo realized that the researchers’ attention to the workers was the common factor. It instilled pride and fulfilled particular social needs of the workers. This led to the development of the “Hawthorne effect,” a principle of research that suggests researcher attention affects the subjects in a study and impacts the results.
In business management, the Hawthorne studies led to articulating the role that human relations play in business operations. Mayo and later theorists developed several related conclusions, including:
- Group dynamics affect job performance.
- Communication between employees and employers must go in both directions.
- Production standards depend more on workplace culture than on official objectives.
- In addition to compensation, perceived value affects performance.
- Workers prefer to participate in the decision-making process.
- Integration between departments or groups positively impacts an organization.
In the modern workplace, sanctioned social activities and open, defined communication channels owe a debt to human relations theory.
Theory X and Theory Y
Douglas McGregor primarily investigated the way managers motivate their employees. The same tactics don’t work across the board, and individuals require different types of oversight or encouragement. In 1960, McGregor developed Theory X and Theory Y in response, laid out in “ The Human Side of Enterprise .”
This management theory divides workers into two camps that require two leadership styles. Theory X workers lack drive. Managers need to provide large amounts of structure and direction to get them to accomplish the necessary work. These workers demand an authoritarian style of management.
Theory Y workers are self-motivated individuals who enjoy their work and find it fulfilling. They benefit from a more participative environment that fosters growth and development.
McGregor’s theory of differentiated management practices remains relevant, but neither workers nor managers tend to exist at the extreme ends of what should be a more nuanced spectrum. The approach also neglects the reciprocal effect managers and workers can have on one another. A natural self-starter can have their ambition micromanaged out of them.
Modern Management Theory
Modern management theory adopts an approach to management that balances scientific methodology with humanistic psychology. It uses emerging technologies and statistical analysis to make decisions, streamline operations and quantify performance. At the same time, it values individual job satisfaction and a healthy corporate culture.
This category of theories is more holistic and flexible than its predecessors. Data-driven decisions can remove human bias while still accommodating employee health and happiness indicators. Modern management theory also allows organizations to adapt to complex, fluid situations with local solutions instead of positing a single, overriding principle to drive management.
Shortcomings of the modern management approach include:
- The prioritization of information that can be difficult, expensive, and time-consuming to collect
- The gap between theoretical flexibility and practical agility
- The tendency of some strains to be descriptive rather than prescriptive
Two popular strains of modern management theory are systems theory and contingency theory:
Systems Management Theory
It’s no surprise that Ludwig Von Bertalanffy, who developed systems management theory, was a biologist. This theory borrows heavily from that discourse. Systems theory proposes that each business is like a single living organism. Distinct elements play different roles but ultimately work together to support the business’s health. The role of management is to facilitate cooperation and holistic process flows.
Systems management theory sometimes leans more toward metaphorical description than prescriptive application. However, you can see evidence of the approach in technological architectures and tools that standardize services and open access to information. For example, innovations such as data fabric help break down departmental silos.
Contingency Management Theory
Contingency management theory addresses the complexity and variability of the modern work environment. Fred Fiedler realized that no one set of characteristics – no single approach – provided the best leadership in all situations. Success instead depended on the leader’s suitability to the situation in which they found themselves.
Fiedler focused on three factors that determine that situation:
- Task structure: How well defined is the job?
- Leader-member relations: How well does the leader work with team members?
- Leader position power: How much authority does the leader have? To what extent can they distribute punishments and rewards?
Managers can be classified as having a task-oriented or a people-oriented style. Task-oriented managers organize teams to accomplish projects quickly and effectively. People-oriented managers are good at handling team conflict, building relationships, and facilitating synergy. Task-oriented leaders thrive in both highly favorable and unfavorable conditions, but people-oriented leaders do better in more moderate configurations.
The least-preferred coworker (LPC) scale is a common management tool developed by Fiedler to help leaders pinpoint their style. The scale asks you to identify the coworker you have the hardest time working with and rate them. Relationship-oriented managers tend to score higher on the LPC scale than task-oriented managers.
What’s Next for Management Theory?
It’s time for a new category of management theory. The business world requires more than a single new idea, and it’s ripe for a constellation of new theories.
Ecology and technology continue to reshape our concerns, resources, and possibilities. Remote work physically distances coworkers, and worldwide health and climate concerns create fragile relationships with globalization. Equity is no longer “a nice idea” but an urgent imperative. Volatile conditions lead people to search for meaning at work and everywhere else.
No one truly knows what’s next. But it will likely build on and cherry-pick from the above management approaches, reorienting them around a new philosophical core. Familiarize yourself with predominant principles today and prepare yourself for a new movement tomorrow.
Related Articles

Take the next step in your career with a program guide!
By completing this form and clicking the button below, I consent to receiving calls, text messages and/or emails from BISK, its client institutions, and their representatives regarding educational services and programs. I understand calls and texts may be directed to the number I provide using automatic dialing technology. I understand that this consent is not required to purchase goods or services. If you would like more information relating to how we may use your data, please review our privacy policy .
- Business Essentials
- Leadership & Management
- Credential of Leadership, Impact, and Management in Business (CLIMB)
- Entrepreneurship & Innovation
- Digital Transformation
- Finance & Accounting
- Business in Society
- For Organizations
- Support Portal
- Media Coverage
- Founding Donors
- Leadership Team

- Harvard Business School →
- HBS Online →
- Business Insights →
Business Insights
Harvard Business School Online's Business Insights Blog provides the career insights you need to achieve your goals and gain confidence in your business skills.
- Career Development
- Communication
- Decision-Making
- Earning Your MBA
- Negotiation
- News & Events
- Productivity
- Staff Spotlight
- Student Profiles
- Work-Life Balance
- AI Essentials for Business
- Alternative Investments
- Business Analytics
- Business Strategy
- Business and Climate Change
- Creating Brand Value
- Design Thinking and Innovation
- Digital Marketing Strategy
- Disruptive Strategy
- Economics for Managers
- Entrepreneurship Essentials
- Financial Accounting
- Global Business
- Launching Tech Ventures
- Leadership Principles
- Leadership, Ethics, and Corporate Accountability
- Leading Change and Organizational Renewal
- Leading with Finance
- Management Essentials
- Negotiation Mastery
- Organizational Leadership
- Power and Influence for Positive Impact
- Strategy Execution
- Sustainable Business Strategy
- Sustainable Investing
- Winning with Digital Platforms
A Beginner’s Guide to Hypothesis Testing in Business

- 30 Mar 2021
Becoming a more data-driven decision-maker can bring several benefits to your organization, enabling you to identify new opportunities to pursue and threats to abate. Rather than allowing subjective thinking to guide your business strategy, backing your decisions with data can empower your company to become more innovative and, ultimately, profitable.
If you’re new to data-driven decision-making, you might be wondering how data translates into business strategy. The answer lies in generating a hypothesis and verifying or rejecting it based on what various forms of data tell you.
Below is a look at hypothesis testing and the role it plays in helping businesses become more data-driven.
Access your free e-book today.
What Is Hypothesis Testing?
To understand what hypothesis testing is, it’s important first to understand what a hypothesis is.
A hypothesis or hypothesis statement seeks to explain why something has happened, or what might happen, under certain conditions. It can also be used to understand how different variables relate to each other. Hypotheses are often written as if-then statements; for example, “If this happens, then this will happen.”
Hypothesis testing , then, is a statistical means of testing an assumption stated in a hypothesis. While the specific methodology leveraged depends on the nature of the hypothesis and data available, hypothesis testing typically uses sample data to extrapolate insights about a larger population.
Hypothesis Testing in Business
When it comes to data-driven decision-making, there’s a certain amount of risk that can mislead a professional. This could be due to flawed thinking or observations, incomplete or inaccurate data , or the presence of unknown variables. The danger in this is that, if major strategic decisions are made based on flawed insights, it can lead to wasted resources, missed opportunities, and catastrophic outcomes.
The real value of hypothesis testing in business is that it allows professionals to test their theories and assumptions before putting them into action. This essentially allows an organization to verify its analysis is correct before committing resources to implement a broader strategy.
As one example, consider a company that wishes to launch a new marketing campaign to revitalize sales during a slow period. Doing so could be an incredibly expensive endeavor, depending on the campaign’s size and complexity. The company, therefore, may wish to test the campaign on a smaller scale to understand how it will perform.
In this example, the hypothesis that’s being tested would fall along the lines of: “If the company launches a new marketing campaign, then it will translate into an increase in sales.” It may even be possible to quantify how much of a lift in sales the company expects to see from the effort. Pending the results of the pilot campaign, the business would then know whether it makes sense to roll it out more broadly.
Related: 9 Fundamental Data Science Skills for Business Professionals
Key Considerations for Hypothesis Testing
1. alternative hypothesis and null hypothesis.
In hypothesis testing, the hypothesis that’s being tested is known as the alternative hypothesis . Often, it’s expressed as a correlation or statistical relationship between variables. The null hypothesis , on the other hand, is a statement that’s meant to show there’s no statistical relationship between the variables being tested. It’s typically the exact opposite of whatever is stated in the alternative hypothesis.
For example, consider a company’s leadership team that historically and reliably sees $12 million in monthly revenue. They want to understand if reducing the price of their services will attract more customers and, in turn, increase revenue.
In this case, the alternative hypothesis may take the form of a statement such as: “If we reduce the price of our flagship service by five percent, then we’ll see an increase in sales and realize revenues greater than $12 million in the next month.”
The null hypothesis, on the other hand, would indicate that revenues wouldn’t increase from the base of $12 million, or might even decrease.
Check out the video below about the difference between an alternative and a null hypothesis, and subscribe to our YouTube channel for more explainer content.
2. Significance Level and P-Value
Statistically speaking, if you were to run the same scenario 100 times, you’d likely receive somewhat different results each time. If you were to plot these results in a distribution plot, you’d see the most likely outcome is at the tallest point in the graph, with less likely outcomes falling to the right and left of that point.

With this in mind, imagine you’ve completed your hypothesis test and have your results, which indicate there may be a correlation between the variables you were testing. To understand your results' significance, you’ll need to identify a p-value for the test, which helps note how confident you are in the test results.
In statistics, the p-value depicts the probability that, assuming the null hypothesis is correct, you might still observe results that are at least as extreme as the results of your hypothesis test. The smaller the p-value, the more likely the alternative hypothesis is correct, and the greater the significance of your results.
3. One-Sided vs. Two-Sided Testing
When it’s time to test your hypothesis, it’s important to leverage the correct testing method. The two most common hypothesis testing methods are one-sided and two-sided tests , or one-tailed and two-tailed tests, respectively.
Typically, you’d leverage a one-sided test when you have a strong conviction about the direction of change you expect to see due to your hypothesis test. You’d leverage a two-sided test when you’re less confident in the direction of change.

4. Sampling
To perform hypothesis testing in the first place, you need to collect a sample of data to be analyzed. Depending on the question you’re seeking to answer or investigate, you might collect samples through surveys, observational studies, or experiments.
A survey involves asking a series of questions to a random population sample and recording self-reported responses.
Observational studies involve a researcher observing a sample population and collecting data as it occurs naturally, without intervention.
Finally, an experiment involves dividing a sample into multiple groups, one of which acts as the control group. For each non-control group, the variable being studied is manipulated to determine how the data collected differs from that of the control group.

Learn How to Perform Hypothesis Testing
Hypothesis testing is a complex process involving different moving pieces that can allow an organization to effectively leverage its data and inform strategic decisions.
If you’re interested in better understanding hypothesis testing and the role it can play within your organization, one option is to complete a course that focuses on the process. Doing so can lay the statistical and analytical foundation you need to succeed.
Do you want to learn more about hypothesis testing? Explore Business Analytics —one of our online business essentials courses —and download our Beginner’s Guide to Data & Analytics .

About the Author
- Data, AI, & Machine Learning
- Managing Technology
- Social Responsibility
- Workplace, Teams, & Culture
- AI & Machine Learning
- Diversity & Inclusion
- Big ideas Research Projects
- Artificial Intelligence and Business Strategy
- Responsible AI
- Future of the Workforce
- Future of Leadership
- All Research Projects
- AI in Action
- Most Popular
- The Truth Behind the Nursing Crisis
- Coaching for the Future-Forward Leader
- Measuring Culture
Our summer 2024 issue highlights ways to better support customers, partners, and employees, while our special report shows how organizations can advance their AI practice.
- Past Issues
- Upcoming Events
- Video Archive
- Me, Myself, and AI
- Three Big Points

Why Hypotheses Beat Goals

- Developing Strategy
- Skills & Learning

Not long ago, it became fashionable to embrace failure as a sign of a company’s willingness to take risks. This trend lost favor as executives recognized that what they wanted was learning, not necessarily failure. Every failure can be attributed to a raft of missteps, and many failures do not automatically contribute to future success.
Certainly, if companies want to aggressively pursue learning, they must accept that failures will happen. But the practice of simply setting goals and then being nonchalant if they fail is inadequate.
Instead, companies should focus organizational energy on hypothesis generation and testing. Hypotheses force individuals to articulate in advance why they believe a given course of action will succeed. A failure then exposes an incorrect hypothesis — which can more reliably convert into organizational learning.
What Exactly Is a Hypothesis?
When my son was in second grade, his teacher regularly introduced topics by asking students to state some initial assumptions. For example, she introduced a unit on whales by asking: How big is a blue whale? The students all knew blue whales were big, but how big? Guesses ranged from the size of the classroom to the size of two elephants to the length of all the students in class lined up in a row. Students then set out to measure the classroom and the length of the row they formed, and they looked up the size of an elephant. They compared their results with the measurements of the whale and learned how close their estimates were.
Note that in this example, there is much more going on than just learning the size of a whale. Students were learning to recognize assumptions, make intelligent guesses based on those assumptions, determine how to test the accuracy of their guesses, and then assess the results.
This is the essence of hypothesis generation. A hypothesis emerges from a set of underlying assumptions. It is an articulation of how those assumptions are expected to play out in a given context. In short, a hypothesis is an intelligent, articulated guess that is the basis for taking action and assessing outcomes.
Get Updates on Transformative Leadership
Evidence-based resources that can help you lead your team more effectively, delivered to your inbox monthly.
Please enter a valid email address
Thank you for signing up
Privacy Policy
Hypothesis generation in companies becomes powerful if people are forced to articulate and justify their assumptions. It makes the path from hypothesis to expected outcomes clear enough that, should the anticipated outcomes fail to materialize, people will agree that the hypothesis was faulty.
Building a culture of effective hypothesizing can lead to more thoughtful actions and a better understanding of outcomes. Not only will failures be more likely to lead to future successes, but successes will foster future successes.
Why Is Hypothesis Generation Important?
Digital technologies are creating new business opportunities, but as I’ve noted in earlier columns , companies must experiment to learn both what is possible and what customers want. Most companies are relying on empowered, agile teams to conduct these experiments. That’s because teams can rapidly hypothesize, test, and learn.
Hypothesis generation contrasts starkly with more traditional management approaches designed for process optimization. Process optimization involves telling employees both what to do and how to do it. Process optimization is fine for stable business processes that have been standardized for consistency. (Standardized processes can usually be automated, specifically because they are stable.) Increasingly, however, companies need their people to steer efforts that involve uncertainty and change. That’s when organizational learning and hypothesis generation are particularly important.
Shifting to a culture that encourages empowered teams to hypothesize isn’t easy. Established hierarchies have developed managers accustomed to directing employees on how to accomplish their objectives. Those managers invariably rose to power by being the smartest person in the room. Such managers can struggle with the requirements for leading empowered teams. They may recognize the need to hold teams accountable for outcomes rather than specific tasks, but they may not be clear about how to guide team efforts.
Some newer companies have baked this concept into their organizational structure. Leaders at the Swedish digital music service Spotify note that it is essential to provide clear missions to teams . A clear mission sets up a team to articulate measurable goals. Teams can then hypothesize how they can best accomplish those goals. The role of leaders is to quiz teams about their hypotheses and challenge their logic if those hypotheses appear to lack support.
A leader at another company told me that accountability for outcomes starts with hypotheses. If a team cannot articulate what it intends to do and what outcomes it anticipates, it is unlikely that team will deliver on its mission. In short, the success of empowered teams depends upon management shifting from directing employees to guiding their development of hypotheses. This is how leaders hold their teams accountable for outcomes.
Members of empowered teams are not the only people who need to hone their ability to hypothesize. Leaders in companies that want to seize digital opportunities are learning through their experiments which strategies hold real promise for future success. They must, in effect, hypothesize about what will make the company successful in a digital economy. If they take the next step and articulate those hypotheses and establish metrics for assessing the outcomes of their actions, they will facilitate learning about the company’s long-term success. Hypothesis generation can become a critical competency throughout a company.
How Does a Company Become Proficient at Hypothesizing?
Most business leaders have embraced the importance of evidence-based decision-making. But developing a culture of evidence-based decision-making by promoting hypothesis generation is a new challenge.
For one thing, many hypotheses are sloppy. While many people naturally hypothesize and take actions based on their hypotheses, their underlying assumptions may go unexamined. Often, they don’t clearly articulate the premise itself. The better hypotheses are straightforward and succinctly written. They’re pointed about the suppositions they’re based on. And they’re shared, allowing an audience to examine the assumptions (are they accurate?) and the postulate itself (is it an intelligent, articulated guess that is the basis for taking action and assessing outcomes?).
Related Articles
Seven-Eleven Japan offers a case in how do to hypotheses right.
For over 30 years, Seven-Eleven Japan was the most profitable retailer in Japan. It achieved that stature by relying on each store’s salesclerks to decide what items to stock on that store’s shelves. Many of the salesclerks were part-time, but they were each responsible for maximizing turnover for one part of the store’s inventory, and they received detailed reports so they could monitor their own performance.
The language of hypothesis formulation was part of their process. Each week, Seven-Eleven Japan counselors visited the stores and asked salesclerks three questions:
- What did you hypothesize this week? (That is, what did you order?)
- How did you do? (That is, did you sell what you ordered?)
- How will you do better next week? (That is, how will you incorporate the learning?)
By repeatedly asking these questions and checking the data for results, counselors helped people throughout the company hypothesize, test, and learn. The result was consistently strong inventory turnover and profitability.
How can other companies get started on this path? Evidence-based decision-making requires data — good data, as the Seven-Eleven Japan example shows. But rather than get bogged down with the limits of a company’s data, I would argue that companies can start to change their culture by constantly exposing individual hypotheses. Those hypotheses will highlight what data matters most — and the need of teams to test hypotheses will help generate enthusiasm for cleaning up bad data. A sense of accountability for generating and testing hypotheses then fosters a culture of evidence-based decision-making.
The uncertainties and speed of change in the current business environment render traditional management approaches ineffective. To create the agile, evidence-based, learning culture your business needs to succeed in a digital economy, I suggest that instead of asking What is your goal? you make it a habit to ask What is your hypothesis?
About the Author
Jeanne Ross is principal research scientist for MIT’s Center for Information Systems Research . Follow CISR on Twitter @mit_cisr .
More Like This
Add a comment cancel reply.
You must sign in to post a comment. First time here? Sign up for a free account : Comment on articles and get access to many more articles.
Comment (1)
Richard jones.

What Is A Research (Scientific) Hypothesis? A plain-language explainer + examples
By: Derek Jansen (MBA) | Reviewed By: Dr Eunice Rautenbach | June 2020
If you’re new to the world of research, or it’s your first time writing a dissertation or thesis, you’re probably noticing that the words “research hypothesis” and “scientific hypothesis” are used quite a bit, and you’re wondering what they mean in a research context .
“Hypothesis” is one of those words that people use loosely, thinking they understand what it means. However, it has a very specific meaning within academic research. So, it’s important to understand the exact meaning before you start hypothesizing.
Research Hypothesis 101
- What is a hypothesis ?
- What is a research hypothesis (scientific hypothesis)?
- Requirements for a research hypothesis
- Definition of a research hypothesis
- The null hypothesis
What is a hypothesis?
Let’s start with the general definition of a hypothesis (not a research hypothesis or scientific hypothesis), according to the Cambridge Dictionary:
Hypothesis: an idea or explanation for something that is based on known facts but has not yet been proved.
In other words, it’s a statement that provides an explanation for why or how something works, based on facts (or some reasonable assumptions), but that has not yet been specifically tested . For example, a hypothesis might look something like this:
Hypothesis: sleep impacts academic performance.
This statement predicts that academic performance will be influenced by the amount and/or quality of sleep a student engages in – sounds reasonable, right? It’s based on reasonable assumptions , underpinned by what we currently know about sleep and health (from the existing literature). So, loosely speaking, we could call it a hypothesis, at least by the dictionary definition.
But that’s not good enough…
Unfortunately, that’s not quite sophisticated enough to describe a research hypothesis (also sometimes called a scientific hypothesis), and it wouldn’t be acceptable in a dissertation, thesis or research paper . In the world of academic research, a statement needs a few more criteria to constitute a true research hypothesis .
What is a research hypothesis?
A research hypothesis (also called a scientific hypothesis) is a statement about the expected outcome of a study (for example, a dissertation or thesis). To constitute a quality hypothesis, the statement needs to have three attributes – specificity , clarity and testability .
Let’s take a look at these more closely.
Need a helping hand?
Hypothesis Essential #1: Specificity & Clarity
A good research hypothesis needs to be extremely clear and articulate about both what’ s being assessed (who or what variables are involved ) and the expected outcome (for example, a difference between groups, a relationship between variables, etc.).
Let’s stick with our sleepy students example and look at how this statement could be more specific and clear.
Hypothesis: Students who sleep at least 8 hours per night will, on average, achieve higher grades in standardised tests than students who sleep less than 8 hours a night.
As you can see, the statement is very specific as it identifies the variables involved (sleep hours and test grades), the parties involved (two groups of students), as well as the predicted relationship type (a positive relationship). There’s no ambiguity or uncertainty about who or what is involved in the statement, and the expected outcome is clear.
Contrast that to the original hypothesis we looked at – “Sleep impacts academic performance” – and you can see the difference. “Sleep” and “academic performance” are both comparatively vague , and there’s no indication of what the expected relationship direction is (more sleep or less sleep). As you can see, specificity and clarity are key.
Hypothesis Essential #2: Testability (Provability)
A statement must be testable to qualify as a research hypothesis. In other words, there needs to be a way to prove (or disprove) the statement. If it’s not testable, it’s not a hypothesis – simple as that.
For example, consider the hypothesis we mentioned earlier:
Hypothesis: Students who sleep at least 8 hours per night will, on average, achieve higher grades in standardised tests than students who sleep less than 8 hours a night.
We could test this statement by undertaking a quantitative study involving two groups of students, one that gets 8 or more hours of sleep per night for a fixed period, and one that gets less. We could then compare the standardised test results for both groups to see if there’s a statistically significant difference.
Again, if you compare this to the original hypothesis we looked at – “Sleep impacts academic performance” – you can see that it would be quite difficult to test that statement, primarily because it isn’t specific enough. How much sleep? By who? What type of academic performance?
So, remember the mantra – if you can’t test it, it’s not a hypothesis 🙂
Defining A Research Hypothesis
You’re still with us? Great! Let’s recap and pin down a clear definition of a hypothesis.
A research hypothesis (or scientific hypothesis) is a statement about an expected relationship between variables, or explanation of an occurrence, that is clear, specific and testable.
So, when you write up hypotheses for your dissertation or thesis, make sure that they meet all these criteria. If you do, you’ll not only have rock-solid hypotheses but you’ll also ensure a clear focus for your entire research project.
What about the null hypothesis?
You may have also heard the terms null hypothesis , alternative hypothesis, or H-zero thrown around. At a simple level, the null hypothesis is the counter-proposal to the original hypothesis.
For example, if the hypothesis predicts that there is a relationship between two variables (for example, sleep and academic performance), the null hypothesis would predict that there is no relationship between those variables.
At a more technical level, the null hypothesis proposes that no statistical significance exists in a set of given observations and that any differences are due to chance alone.
And there you have it – hypotheses in a nutshell.
If you have any questions, be sure to leave a comment below and we’ll do our best to help you. If you need hands-on help developing and testing your hypotheses, consider our private coaching service , where we hold your hand through the research journey.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
17 Comments
Very useful information. I benefit more from getting more information in this regard.
Very great insight,educative and informative. Please give meet deep critics on many research data of public international Law like human rights, environment, natural resources, law of the sea etc
In a book I read a distinction is made between null, research, and alternative hypothesis. As far as I understand, alternative and research hypotheses are the same. Can you please elaborate? Best Afshin
This is a self explanatory, easy going site. I will recommend this to my friends and colleagues.
Very good definition. How can I cite your definition in my thesis? Thank you. Is nul hypothesis compulsory in a research?
It’s a counter-proposal to be proven as a rejection
Please what is the difference between alternate hypothesis and research hypothesis?
It is a very good explanation. However, it limits hypotheses to statistically tasteable ideas. What about for qualitative researches or other researches that involve quantitative data that don’t need statistical tests?
In qualitative research, one typically uses propositions, not hypotheses.
could you please elaborate it more
I’ve benefited greatly from these notes, thank you.
This is very helpful
well articulated ideas are presented here, thank you for being reliable sources of information
Excellent. Thanks for being clear and sound about the research methodology and hypothesis (quantitative research)
I have only a simple question regarding the null hypothesis. – Is the null hypothesis (Ho) known as the reversible hypothesis of the alternative hypothesis (H1? – How to test it in academic research?
this is very important note help me much more
Hi” best wishes to you and your very nice blog”
Trackbacks/Pingbacks
- What Is Research Methodology? Simple Definition (With Examples) - Grad Coach - […] Contrasted to this, a quantitative methodology is typically used when the research aims and objectives are confirmatory in nature. For example,…
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Module 1: Introduction to Organizational Behavior
History of management theory, learning outcomes.
- Describe the history of management theory
So what is management theory? First, let’s break down the term. Theories help us understand our experiences by using research and observable facts. Management is the act of supervising and directing people, tasks, and things [1] . So, simply put, management theory is a collection of understandings and findings that help managers best support their teams and goals.
The Importance of Management Theories
Management theories help organizations to focus, communicate, and evolve. Using management theory in the workplace allows leadership to focus on their main goals. When a management style or theory is implemented, it automatically streamlines the top priorities for the organization. Management theory also allows us to better communicate with people we work with which in turn allows us to work more efficiently. By understanding management theory, basic assumptions about management styles and goals can be assumed and can save time during daily interactions and meetings within an organization.
Theories can only reach so far, and management theories are no exception. There is no such thing as a one-size-fits-all management theory. What may work for one organization may not be relevant for another. Therefore, when one theory does not fit a particular situation, it is important to explore the option of developing a new theory that would lead in a new, more applicable direction. While some theories can stand the test of time, other theories may grow to be irrelevant and new theories will develop in their place.
The Evolution of Management Theory
While the next section will get into the nitty-gritty behind the history of different types of management theory, it is important to have a basic understanding as to why management theory was such an important and ground-breaking idea. The Industrial Revolution is at the center of management theory. From the late 1700s through the early 1900s, the Industrial Revolution brought extraordinary change to the workplace and forever transformed the way companies operate.

While productivity goals can be set easily, managing a team to meet productivity goals was not so simple. For the first time, managers had to find new and innovative ways to motivate a sizable number of employees to perform. Since this was a new concept, research, observations, experiments, and trial and error were all used to find new and better ways to manage employees. The Industrial Revolution gave birth to a variety of management theories and concepts, many of which are still relevant and essential in today’s workforce. In addition, many management theories have developed since the end of the Industrial Revolution as society continues to evolve. Each management theory plays a role in modern management theory and how it is implemented.
PRactice Question
Let’s take a look at some key management theories, explore their history and reasoning, and learn about the masterminds behind them.
- Taylor, F. W. (1914). The Principles of Scientific Management . Harper. ↵
- History of Management Theory. Authored by : Freedom Learning Group. Provided by : Lumen Learning. License : CC BY: Attribution
- Untitled. Authored by : Elevate. Provided by : Unsplash. Located at : https://unsplash.com/photos/rT1lK2GEVdg . License : CC0: No Rights Reserved . License Terms : Unsplash License

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How to Write a Great Hypothesis
Hypothesis Definition, Format, Examples, and Tips
Verywell / Alex Dos Diaz
- The Scientific Method
Hypothesis Format
Falsifiability of a hypothesis.
- Operationalization
Hypothesis Types
Hypotheses examples.
- Collecting Data
A hypothesis is a tentative statement about the relationship between two or more variables. It is a specific, testable prediction about what you expect to happen in a study. It is a preliminary answer to your question that helps guide the research process.
Consider a study designed to examine the relationship between sleep deprivation and test performance. The hypothesis might be: "This study is designed to assess the hypothesis that sleep-deprived people will perform worse on a test than individuals who are not sleep-deprived."
At a Glance
A hypothesis is crucial to scientific research because it offers a clear direction for what the researchers are looking to find. This allows them to design experiments to test their predictions and add to our scientific knowledge about the world. This article explores how a hypothesis is used in psychology research, how to write a good hypothesis, and the different types of hypotheses you might use.
The Hypothesis in the Scientific Method
In the scientific method , whether it involves research in psychology, biology, or some other area, a hypothesis represents what the researchers think will happen in an experiment. The scientific method involves the following steps:
- Forming a question
- Performing background research
- Creating a hypothesis
- Designing an experiment
- Collecting data
- Analyzing the results
- Drawing conclusions
- Communicating the results
The hypothesis is a prediction, but it involves more than a guess. Most of the time, the hypothesis begins with a question which is then explored through background research. At this point, researchers then begin to develop a testable hypothesis.
Unless you are creating an exploratory study, your hypothesis should always explain what you expect to happen.
In a study exploring the effects of a particular drug, the hypothesis might be that researchers expect the drug to have some type of effect on the symptoms of a specific illness. In psychology, the hypothesis might focus on how a certain aspect of the environment might influence a particular behavior.
Remember, a hypothesis does not have to be correct. While the hypothesis predicts what the researchers expect to see, the goal of the research is to determine whether this guess is right or wrong. When conducting an experiment, researchers might explore numerous factors to determine which ones might contribute to the ultimate outcome.
In many cases, researchers may find that the results of an experiment do not support the original hypothesis. When writing up these results, the researchers might suggest other options that should be explored in future studies.
In many cases, researchers might draw a hypothesis from a specific theory or build on previous research. For example, prior research has shown that stress can impact the immune system. So a researcher might hypothesize: "People with high-stress levels will be more likely to contract a common cold after being exposed to the virus than people who have low-stress levels."
In other instances, researchers might look at commonly held beliefs or folk wisdom. "Birds of a feather flock together" is one example of folk adage that a psychologist might try to investigate. The researcher might pose a specific hypothesis that "People tend to select romantic partners who are similar to them in interests and educational level."
Elements of a Good Hypothesis
So how do you write a good hypothesis? When trying to come up with a hypothesis for your research or experiments, ask yourself the following questions:
- Is your hypothesis based on your research on a topic?
- Can your hypothesis be tested?
- Does your hypothesis include independent and dependent variables?
Before you come up with a specific hypothesis, spend some time doing background research. Once you have completed a literature review, start thinking about potential questions you still have. Pay attention to the discussion section in the journal articles you read . Many authors will suggest questions that still need to be explored.
How to Formulate a Good Hypothesis
To form a hypothesis, you should take these steps:
- Collect as many observations about a topic or problem as you can.
- Evaluate these observations and look for possible causes of the problem.
- Create a list of possible explanations that you might want to explore.
- After you have developed some possible hypotheses, think of ways that you could confirm or disprove each hypothesis through experimentation. This is known as falsifiability.
In the scientific method , falsifiability is an important part of any valid hypothesis. In order to test a claim scientifically, it must be possible that the claim could be proven false.
Students sometimes confuse the idea of falsifiability with the idea that it means that something is false, which is not the case. What falsifiability means is that if something was false, then it is possible to demonstrate that it is false.
One of the hallmarks of pseudoscience is that it makes claims that cannot be refuted or proven false.
The Importance of Operational Definitions
A variable is a factor or element that can be changed and manipulated in ways that are observable and measurable. However, the researcher must also define how the variable will be manipulated and measured in the study.
Operational definitions are specific definitions for all relevant factors in a study. This process helps make vague or ambiguous concepts detailed and measurable.
For example, a researcher might operationally define the variable " test anxiety " as the results of a self-report measure of anxiety experienced during an exam. A "study habits" variable might be defined by the amount of studying that actually occurs as measured by time.
These precise descriptions are important because many things can be measured in various ways. Clearly defining these variables and how they are measured helps ensure that other researchers can replicate your results.
Replicability
One of the basic principles of any type of scientific research is that the results must be replicable.
Replication means repeating an experiment in the same way to produce the same results. By clearly detailing the specifics of how the variables were measured and manipulated, other researchers can better understand the results and repeat the study if needed.
Some variables are more difficult than others to define. For example, how would you operationally define a variable such as aggression ? For obvious ethical reasons, researchers cannot create a situation in which a person behaves aggressively toward others.
To measure this variable, the researcher must devise a measurement that assesses aggressive behavior without harming others. The researcher might utilize a simulated task to measure aggressiveness in this situation.
Hypothesis Checklist
- Does your hypothesis focus on something that you can actually test?
- Does your hypothesis include both an independent and dependent variable?
- Can you manipulate the variables?
- Can your hypothesis be tested without violating ethical standards?
The hypothesis you use will depend on what you are investigating and hoping to find. Some of the main types of hypotheses that you might use include:
- Simple hypothesis : This type of hypothesis suggests there is a relationship between one independent variable and one dependent variable.
- Complex hypothesis : This type suggests a relationship between three or more variables, such as two independent and dependent variables.
- Null hypothesis : This hypothesis suggests no relationship exists between two or more variables.
- Alternative hypothesis : This hypothesis states the opposite of the null hypothesis.
- Statistical hypothesis : This hypothesis uses statistical analysis to evaluate a representative population sample and then generalizes the findings to the larger group.
- Logical hypothesis : This hypothesis assumes a relationship between variables without collecting data or evidence.
A hypothesis often follows a basic format of "If {this happens} then {this will happen}." One way to structure your hypothesis is to describe what will happen to the dependent variable if you change the independent variable .
The basic format might be: "If {these changes are made to a certain independent variable}, then we will observe {a change in a specific dependent variable}."
A few examples of simple hypotheses:
- "Students who eat breakfast will perform better on a math exam than students who do not eat breakfast."
- "Students who experience test anxiety before an English exam will get lower scores than students who do not experience test anxiety."
- "Motorists who talk on the phone while driving will be more likely to make errors on a driving course than those who do not talk on the phone."
- "Children who receive a new reading intervention will have higher reading scores than students who do not receive the intervention."
Examples of a complex hypothesis include:
- "People with high-sugar diets and sedentary activity levels are more likely to develop depression."
- "Younger people who are regularly exposed to green, outdoor areas have better subjective well-being than older adults who have limited exposure to green spaces."
Examples of a null hypothesis include:
- "There is no difference in anxiety levels between people who take St. John's wort supplements and those who do not."
- "There is no difference in scores on a memory recall task between children and adults."
- "There is no difference in aggression levels between children who play first-person shooter games and those who do not."
Examples of an alternative hypothesis:
- "People who take St. John's wort supplements will have less anxiety than those who do not."
- "Adults will perform better on a memory task than children."
- "Children who play first-person shooter games will show higher levels of aggression than children who do not."
Collecting Data on Your Hypothesis
Once a researcher has formed a testable hypothesis, the next step is to select a research design and start collecting data. The research method depends largely on exactly what they are studying. There are two basic types of research methods: descriptive research and experimental research.
Descriptive Research Methods
Descriptive research such as case studies , naturalistic observations , and surveys are often used when conducting an experiment is difficult or impossible. These methods are best used to describe different aspects of a behavior or psychological phenomenon.
Once a researcher has collected data using descriptive methods, a correlational study can examine how the variables are related. This research method might be used to investigate a hypothesis that is difficult to test experimentally.
Experimental Research Methods
Experimental methods are used to demonstrate causal relationships between variables. In an experiment, the researcher systematically manipulates a variable of interest (known as the independent variable) and measures the effect on another variable (known as the dependent variable).
Unlike correlational studies, which can only be used to determine if there is a relationship between two variables, experimental methods can be used to determine the actual nature of the relationship—whether changes in one variable actually cause another to change.
The hypothesis is a critical part of any scientific exploration. It represents what researchers expect to find in a study or experiment. In situations where the hypothesis is unsupported by the research, the research still has value. Such research helps us better understand how different aspects of the natural world relate to one another. It also helps us develop new hypotheses that can then be tested in the future.
Thompson WH, Skau S. On the scope of scientific hypotheses . R Soc Open Sci . 2023;10(8):230607. doi:10.1098/rsos.230607
Taran S, Adhikari NKJ, Fan E. Falsifiability in medicine: what clinicians can learn from Karl Popper [published correction appears in Intensive Care Med. 2021 Jun 17;:]. Intensive Care Med . 2021;47(9):1054-1056. doi:10.1007/s00134-021-06432-z
Eyler AA. Research Methods for Public Health . 1st ed. Springer Publishing Company; 2020. doi:10.1891/9780826182067.0004
Nosek BA, Errington TM. What is replication ? PLoS Biol . 2020;18(3):e3000691. doi:10.1371/journal.pbio.3000691
Aggarwal R, Ranganathan P. Study designs: Part 2 - Descriptive studies . Perspect Clin Res . 2019;10(1):34-36. doi:10.4103/picr.PICR_154_18
Nevid J. Psychology: Concepts and Applications. Wadworth, 2013.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
- Resources Home 🏠
- Try SciSpace Copilot
- Search research papers
- Add Copilot Extension
- Try AI Detector
- Try Paraphraser
- Try Citation Generator
- April Papers
- June Papers
- July Papers

The Craft of Writing a Strong Hypothesis

Table of Contents
Writing a hypothesis is one of the essential elements of a scientific research paper. It needs to be to the point, clearly communicating what your research is trying to accomplish. A blurry, drawn-out, or complexly-structured hypothesis can confuse your readers. Or worse, the editor and peer reviewers.
A captivating hypothesis is not too intricate. This blog will take you through the process so that, by the end of it, you have a better idea of how to convey your research paper's intent in just one sentence.
What is a Hypothesis?
The first step in your scientific endeavor, a hypothesis, is a strong, concise statement that forms the basis of your research. It is not the same as a thesis statement , which is a brief summary of your research paper .
The sole purpose of a hypothesis is to predict your paper's findings, data, and conclusion. It comes from a place of curiosity and intuition . When you write a hypothesis, you're essentially making an educated guess based on scientific prejudices and evidence, which is further proven or disproven through the scientific method.
The reason for undertaking research is to observe a specific phenomenon. A hypothesis, therefore, lays out what the said phenomenon is. And it does so through two variables, an independent and dependent variable.
The independent variable is the cause behind the observation, while the dependent variable is the effect of the cause. A good example of this is “mixing red and blue forms purple.” In this hypothesis, mixing red and blue is the independent variable as you're combining the two colors at your own will. The formation of purple is the dependent variable as, in this case, it is conditional to the independent variable.
Different Types of Hypotheses

Types of hypotheses
Some would stand by the notion that there are only two types of hypotheses: a Null hypothesis and an Alternative hypothesis. While that may have some truth to it, it would be better to fully distinguish the most common forms as these terms come up so often, which might leave you out of context.
Apart from Null and Alternative, there are Complex, Simple, Directional, Non-Directional, Statistical, and Associative and casual hypotheses. They don't necessarily have to be exclusive, as one hypothesis can tick many boxes, but knowing the distinctions between them will make it easier for you to construct your own.
1. Null hypothesis
A null hypothesis proposes no relationship between two variables. Denoted by H 0 , it is a negative statement like “Attending physiotherapy sessions does not affect athletes' on-field performance.” Here, the author claims physiotherapy sessions have no effect on on-field performances. Even if there is, it's only a coincidence.
2. Alternative hypothesis
Considered to be the opposite of a null hypothesis, an alternative hypothesis is donated as H1 or Ha. It explicitly states that the dependent variable affects the independent variable. A good alternative hypothesis example is “Attending physiotherapy sessions improves athletes' on-field performance.” or “Water evaporates at 100 °C. ” The alternative hypothesis further branches into directional and non-directional.
- Directional hypothesis: A hypothesis that states the result would be either positive or negative is called directional hypothesis. It accompanies H1 with either the ‘<' or ‘>' sign.
- Non-directional hypothesis: A non-directional hypothesis only claims an effect on the dependent variable. It does not clarify whether the result would be positive or negative. The sign for a non-directional hypothesis is ‘≠.'
3. Simple hypothesis
A simple hypothesis is a statement made to reflect the relation between exactly two variables. One independent and one dependent. Consider the example, “Smoking is a prominent cause of lung cancer." The dependent variable, lung cancer, is dependent on the independent variable, smoking.
4. Complex hypothesis
In contrast to a simple hypothesis, a complex hypothesis implies the relationship between multiple independent and dependent variables. For instance, “Individuals who eat more fruits tend to have higher immunity, lesser cholesterol, and high metabolism.” The independent variable is eating more fruits, while the dependent variables are higher immunity, lesser cholesterol, and high metabolism.
5. Associative and casual hypothesis
Associative and casual hypotheses don't exhibit how many variables there will be. They define the relationship between the variables. In an associative hypothesis, changing any one variable, dependent or independent, affects others. In a casual hypothesis, the independent variable directly affects the dependent.
6. Empirical hypothesis
Also referred to as the working hypothesis, an empirical hypothesis claims a theory's validation via experiments and observation. This way, the statement appears justifiable and different from a wild guess.
Say, the hypothesis is “Women who take iron tablets face a lesser risk of anemia than those who take vitamin B12.” This is an example of an empirical hypothesis where the researcher the statement after assessing a group of women who take iron tablets and charting the findings.
7. Statistical hypothesis
The point of a statistical hypothesis is to test an already existing hypothesis by studying a population sample. Hypothesis like “44% of the Indian population belong in the age group of 22-27.” leverage evidence to prove or disprove a particular statement.
Characteristics of a Good Hypothesis
Writing a hypothesis is essential as it can make or break your research for you. That includes your chances of getting published in a journal. So when you're designing one, keep an eye out for these pointers:
- A research hypothesis has to be simple yet clear to look justifiable enough.
- It has to be testable — your research would be rendered pointless if too far-fetched into reality or limited by technology.
- It has to be precise about the results —what you are trying to do and achieve through it should come out in your hypothesis.
- A research hypothesis should be self-explanatory, leaving no doubt in the reader's mind.
- If you are developing a relational hypothesis, you need to include the variables and establish an appropriate relationship among them.
- A hypothesis must keep and reflect the scope for further investigations and experiments.
Separating a Hypothesis from a Prediction
Outside of academia, hypothesis and prediction are often used interchangeably. In research writing, this is not only confusing but also incorrect. And although a hypothesis and prediction are guesses at their core, there are many differences between them.
A hypothesis is an educated guess or even a testable prediction validated through research. It aims to analyze the gathered evidence and facts to define a relationship between variables and put forth a logical explanation behind the nature of events.
Predictions are assumptions or expected outcomes made without any backing evidence. They are more fictionally inclined regardless of where they originate from.
For this reason, a hypothesis holds much more weight than a prediction. It sticks to the scientific method rather than pure guesswork. "Planets revolve around the Sun." is an example of a hypothesis as it is previous knowledge and observed trends. Additionally, we can test it through the scientific method.
Whereas "COVID-19 will be eradicated by 2030." is a prediction. Even though it results from past trends, we can't prove or disprove it. So, the only way this gets validated is to wait and watch if COVID-19 cases end by 2030.
Finally, How to Write a Hypothesis
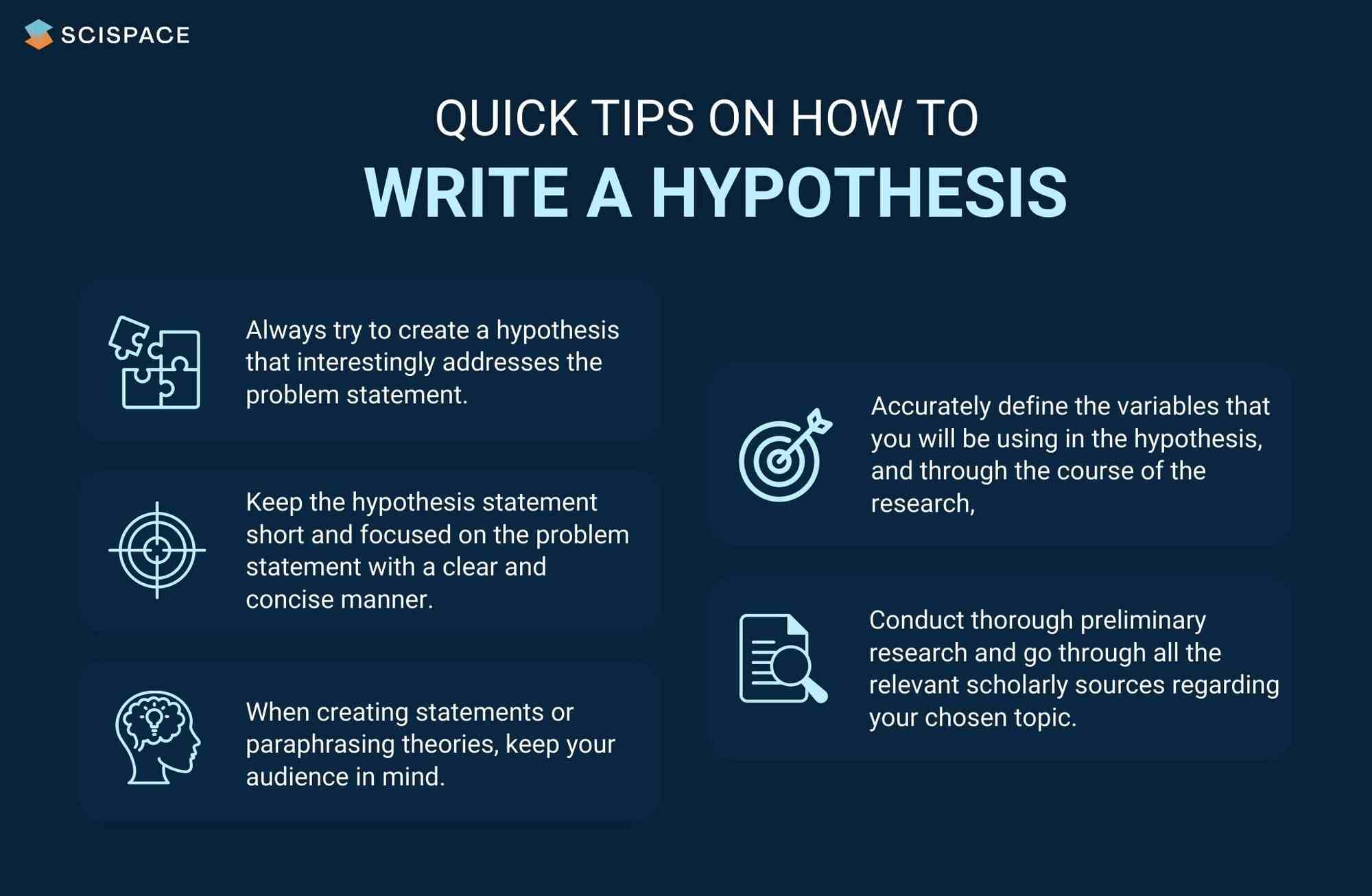
Quick tips on writing a hypothesis
1. Be clear about your research question
A hypothesis should instantly address the research question or the problem statement. To do so, you need to ask a question. Understand the constraints of your undertaken research topic and then formulate a simple and topic-centric problem. Only after that can you develop a hypothesis and further test for evidence.
2. Carry out a recce
Once you have your research's foundation laid out, it would be best to conduct preliminary research. Go through previous theories, academic papers, data, and experiments before you start curating your research hypothesis. It will give you an idea of your hypothesis's viability or originality.
Making use of references from relevant research papers helps draft a good research hypothesis. SciSpace Discover offers a repository of over 270 million research papers to browse through and gain a deeper understanding of related studies on a particular topic. Additionally, you can use SciSpace Copilot , your AI research assistant, for reading any lengthy research paper and getting a more summarized context of it. A hypothesis can be formed after evaluating many such summarized research papers. Copilot also offers explanations for theories and equations, explains paper in simplified version, allows you to highlight any text in the paper or clip math equations and tables and provides a deeper, clear understanding of what is being said. This can improve the hypothesis by helping you identify potential research gaps.
3. Create a 3-dimensional hypothesis
Variables are an essential part of any reasonable hypothesis. So, identify your independent and dependent variable(s) and form a correlation between them. The ideal way to do this is to write the hypothetical assumption in the ‘if-then' form. If you use this form, make sure that you state the predefined relationship between the variables.
In another way, you can choose to present your hypothesis as a comparison between two variables. Here, you must specify the difference you expect to observe in the results.
4. Write the first draft
Now that everything is in place, it's time to write your hypothesis. For starters, create the first draft. In this version, write what you expect to find from your research.
Clearly separate your independent and dependent variables and the link between them. Don't fixate on syntax at this stage. The goal is to ensure your hypothesis addresses the issue.
5. Proof your hypothesis
After preparing the first draft of your hypothesis, you need to inspect it thoroughly. It should tick all the boxes, like being concise, straightforward, relevant, and accurate. Your final hypothesis has to be well-structured as well.
Research projects are an exciting and crucial part of being a scholar. And once you have your research question, you need a great hypothesis to begin conducting research. Thus, knowing how to write a hypothesis is very important.
Now that you have a firmer grasp on what a good hypothesis constitutes, the different kinds there are, and what process to follow, you will find it much easier to write your hypothesis, which ultimately helps your research.
Now it's easier than ever to streamline your research workflow with SciSpace Discover . Its integrated, comprehensive end-to-end platform for research allows scholars to easily discover, write and publish their research and fosters collaboration.
It includes everything you need, including a repository of over 270 million research papers across disciplines, SEO-optimized summaries and public profiles to show your expertise and experience.
If you found these tips on writing a research hypothesis useful, head over to our blog on Statistical Hypothesis Testing to learn about the top researchers, papers, and institutions in this domain.
Frequently Asked Questions (FAQs)
1. what is the definition of hypothesis.
According to the Oxford dictionary, a hypothesis is defined as “An idea or explanation of something that is based on a few known facts, but that has not yet been proved to be true or correct”.
2. What is an example of hypothesis?
The hypothesis is a statement that proposes a relationship between two or more variables. An example: "If we increase the number of new users who join our platform by 25%, then we will see an increase in revenue."
3. What is an example of null hypothesis?
A null hypothesis is a statement that there is no relationship between two variables. The null hypothesis is written as H0. The null hypothesis states that there is no effect. For example, if you're studying whether or not a particular type of exercise increases strength, your null hypothesis will be "there is no difference in strength between people who exercise and people who don't."
4. What are the types of research?
• Fundamental research
• Applied research
• Qualitative research
• Quantitative research
• Mixed research
• Exploratory research
• Longitudinal research
• Cross-sectional research
• Field research
• Laboratory research
• Fixed research
• Flexible research
• Action research
• Policy research
• Classification research
• Comparative research
• Causal research
• Inductive research
• Deductive research
5. How to write a hypothesis?
• Your hypothesis should be able to predict the relationship and outcome.
• Avoid wordiness by keeping it simple and brief.
• Your hypothesis should contain observable and testable outcomes.
• Your hypothesis should be relevant to the research question.
6. What are the 2 types of hypothesis?
• Null hypotheses are used to test the claim that "there is no difference between two groups of data".
• Alternative hypotheses test the claim that "there is a difference between two data groups".
7. Difference between research question and research hypothesis?
A research question is a broad, open-ended question you will try to answer through your research. A hypothesis is a statement based on prior research or theory that you expect to be true due to your study. Example - Research question: What are the factors that influence the adoption of the new technology? Research hypothesis: There is a positive relationship between age, education and income level with the adoption of the new technology.
8. What is plural for hypothesis?
The plural of hypothesis is hypotheses. Here's an example of how it would be used in a statement, "Numerous well-considered hypotheses are presented in this part, and they are supported by tables and figures that are well-illustrated."
9. What is the red queen hypothesis?
The red queen hypothesis in evolutionary biology states that species must constantly evolve to avoid extinction because if they don't, they will be outcompeted by other species that are evolving. Leigh Van Valen first proposed it in 1973; since then, it has been tested and substantiated many times.
10. Who is known as the father of null hypothesis?
The father of the null hypothesis is Sir Ronald Fisher. He published a paper in 1925 that introduced the concept of null hypothesis testing, and he was also the first to use the term itself.
11. When to reject null hypothesis?
You need to find a significant difference between your two populations to reject the null hypothesis. You can determine that by running statistical tests such as an independent sample t-test or a dependent sample t-test. You should reject the null hypothesis if the p-value is less than 0.05.
You might also like

Consensus GPT vs. SciSpace GPT: Choose the Best GPT for Research

Literature Review and Theoretical Framework: Understanding the Differences

Types of Essays in Academic Writing - Quick Guide (2024)
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Your Strategy Should Be a Hypothesis You Constantly Adjust
- Amy C. Edmondson
- Paul J. Verdin

Too many leaders think it should be set in stone.
Strategies must be constantly adjusted to incorporate information from operations and the market. Research on recent dramatic cases of strategic failure in different industries and involving vastly different business models and strategies shows a common pattern: What started as small gaps in execution spiraled into business failures when initial strategies were not altered based on new information provided by experience. These companies’ strategies were viewed by their top executives as analytically sound; performance gaps were blamed on execution. An alternative perspective on strategy and execution — one that is more in tune with the nature of value creation in a world marked by volatility, uncertainty, complexity, and ambiguity — conceives of strategy as a hypothesis rather than a plan. Like all hypotheses, it starts with situation assessment and analysis — strategy’s classic tools. Also like all hypotheses, it must be tested through action. With this lens, encounters with customers provide data that is of ongoing interest to senior executives — vital inputs to dynamic strategy formulation. The authors call this approach strategy as learning , which contrasts sharply with the view of strategy as a stable, analytically rigorous plan for execution in the market. Strategy as learning is an executive activity characterized by ongoing cycles of testing and adjusting, fueled by data that can only be obtained through execution.
The widely accepted view that strategy and execution are separable activities sets companies up for failure in a fast-paced world.
- Amy C. Edmondson is the Novartis Professor of Leadership and Management at Harvard Business School. Her latest book is Right Kind of Wrong: The Science of Failing Well (Atria Books, 2023).
- Paul J. Verdin is the chair in strategy and organization at Solvay Brussels School of Economics and Management.
Partner Center
Definition of a Hypothesis
What it is and how it's used in sociology
- Key Concepts
- Major Sociologists
- News & Issues
- Research, Samples, and Statistics
- Recommended Reading
- Archaeology
A hypothesis is a prediction of what will be found at the outcome of a research project and is typically focused on the relationship between two different variables studied in the research. It is usually based on both theoretical expectations about how things work and already existing scientific evidence.
Within social science, a hypothesis can take two forms. It can predict that there is no relationship between two variables, in which case it is a null hypothesis . Or, it can predict the existence of a relationship between variables, which is known as an alternative hypothesis.
In either case, the variable that is thought to either affect or not affect the outcome is known as the independent variable, and the variable that is thought to either be affected or not is the dependent variable.
Researchers seek to determine whether or not their hypothesis, or hypotheses if they have more than one, will prove true. Sometimes they do, and sometimes they do not. Either way, the research is considered successful if one can conclude whether or not a hypothesis is true.
Null Hypothesis
A researcher has a null hypothesis when she or he believes, based on theory and existing scientific evidence, that there will not be a relationship between two variables. For example, when examining what factors influence a person's highest level of education within the U.S., a researcher might expect that place of birth, number of siblings, and religion would not have an impact on the level of education. This would mean the researcher has stated three null hypotheses.
Alternative Hypothesis
Taking the same example, a researcher might expect that the economic class and educational attainment of one's parents, and the race of the person in question are likely to have an effect on one's educational attainment. Existing evidence and social theories that recognize the connections between wealth and cultural resources , and how race affects access to rights and resources in the U.S. , would suggest that both economic class and educational attainment of the one's parents would have a positive effect on educational attainment. In this case, economic class and educational attainment of one's parents are independent variables, and one's educational attainment is the dependent variable—it is hypothesized to be dependent on the other two.
Conversely, an informed researcher would expect that being a race other than white in the U.S. is likely to have a negative impact on a person's educational attainment. This would be characterized as a negative relationship, wherein being a person of color has a negative effect on one's educational attainment. In reality, this hypothesis proves true, with the exception of Asian Americans , who go to college at a higher rate than whites do. However, Blacks and Hispanics and Latinos are far less likely than whites and Asian Americans to go to college.
Formulating a Hypothesis
Formulating a hypothesis can take place at the very beginning of a research project , or after a bit of research has already been done. Sometimes a researcher knows right from the start which variables she is interested in studying, and she may already have a hunch about their relationships. Other times, a researcher may have an interest in a particular topic, trend, or phenomenon, but he may not know enough about it to identify variables or formulate a hypothesis.
Whenever a hypothesis is formulated, the most important thing is to be precise about what one's variables are, what the nature of the relationship between them might be, and how one can go about conducting a study of them.
Updated by Nicki Lisa Cole, Ph.D
- What It Means When a Variable Is Spurious
- Understanding Path Analysis
- Pilot Study in Research
- Simple Random Sampling
- Exploitation
- What Is Multiculturalism? Definition, Theories, and Examples
- Convenience Samples for Research
- What Is Cultural Capital? Do I Have It?
- What Does Consumerism Mean?
- Visualizing Social Stratification in the U.S.
- What Is Symbolic Interactionism?
- What Is Cultural Hegemony?
- Understanding Stratified Samples and How to Make Them
- What Is Groupthink? Definition and Examples
- What Is a Reference Group?
- What Is Ethnography?
Educational resources and simple solutions for your research journey
What is a Research Hypothesis: How to Write it, Types, and Examples
Any research begins with a research question and a research hypothesis . A research question alone may not suffice to design the experiment(s) needed to answer it. A hypothesis is central to the scientific method. But what is a hypothesis ? A hypothesis is a testable statement that proposes a possible explanation to a phenomenon, and it may include a prediction. Next, you may ask what is a research hypothesis ? Simply put, a research hypothesis is a prediction or educated guess about the relationship between the variables that you want to investigate.
It is important to be thorough when developing your research hypothesis. Shortcomings in the framing of a hypothesis can affect the study design and the results. A better understanding of the research hypothesis definition and characteristics of a good hypothesis will make it easier for you to develop your own hypothesis for your research. Let’s dive in to know more about the types of research hypothesis , how to write a research hypothesis , and some research hypothesis examples .
Table of Contents
What is a hypothesis ?
A hypothesis is based on the existing body of knowledge in a study area. Framed before the data are collected, a hypothesis states the tentative relationship between independent and dependent variables, along with a prediction of the outcome.
What is a research hypothesis ?
Young researchers starting out their journey are usually brimming with questions like “ What is a hypothesis ?” “ What is a research hypothesis ?” “How can I write a good research hypothesis ?”
A research hypothesis is a statement that proposes a possible explanation for an observable phenomenon or pattern. It guides the direction of a study and predicts the outcome of the investigation. A research hypothesis is testable, i.e., it can be supported or disproven through experimentation or observation.

Characteristics of a good hypothesis
Here are the characteristics of a good hypothesis :
- Clearly formulated and free of language errors and ambiguity
- Concise and not unnecessarily verbose
- Has clearly defined variables
- Testable and stated in a way that allows for it to be disproven
- Can be tested using a research design that is feasible, ethical, and practical
- Specific and relevant to the research problem
- Rooted in a thorough literature search
- Can generate new knowledge or understanding.
How to create an effective research hypothesis
A study begins with the formulation of a research question. A researcher then performs background research. This background information forms the basis for building a good research hypothesis . The researcher then performs experiments, collects, and analyzes the data, interprets the findings, and ultimately, determines if the findings support or negate the original hypothesis.
Let’s look at each step for creating an effective, testable, and good research hypothesis :
- Identify a research problem or question: Start by identifying a specific research problem.
- Review the literature: Conduct an in-depth review of the existing literature related to the research problem to grasp the current knowledge and gaps in the field.
- Formulate a clear and testable hypothesis : Based on the research question, use existing knowledge to form a clear and testable hypothesis . The hypothesis should state a predicted relationship between two or more variables that can be measured and manipulated. Improve the original draft till it is clear and meaningful.
- State the null hypothesis: The null hypothesis is a statement that there is no relationship between the variables you are studying.
- Define the population and sample: Clearly define the population you are studying and the sample you will be using for your research.
- Select appropriate methods for testing the hypothesis: Select appropriate research methods, such as experiments, surveys, or observational studies, which will allow you to test your research hypothesis .
Remember that creating a research hypothesis is an iterative process, i.e., you might have to revise it based on the data you collect. You may need to test and reject several hypotheses before answering the research problem.
How to write a research hypothesis
When you start writing a research hypothesis , you use an “if–then” statement format, which states the predicted relationship between two or more variables. Clearly identify the independent variables (the variables being changed) and the dependent variables (the variables being measured), as well as the population you are studying. Review and revise your hypothesis as needed.
An example of a research hypothesis in this format is as follows:
“ If [athletes] follow [cold water showers daily], then their [endurance] increases.”
Population: athletes
Independent variable: daily cold water showers
Dependent variable: endurance
You may have understood the characteristics of a good hypothesis . But note that a research hypothesis is not always confirmed; a researcher should be prepared to accept or reject the hypothesis based on the study findings.
Research hypothesis checklist
Following from above, here is a 10-point checklist for a good research hypothesis :
- Testable: A research hypothesis should be able to be tested via experimentation or observation.
- Specific: A research hypothesis should clearly state the relationship between the variables being studied.
- Based on prior research: A research hypothesis should be based on existing knowledge and previous research in the field.
- Falsifiable: A research hypothesis should be able to be disproven through testing.
- Clear and concise: A research hypothesis should be stated in a clear and concise manner.
- Logical: A research hypothesis should be logical and consistent with current understanding of the subject.
- Relevant: A research hypothesis should be relevant to the research question and objectives.
- Feasible: A research hypothesis should be feasible to test within the scope of the study.
- Reflects the population: A research hypothesis should consider the population or sample being studied.
- Uncomplicated: A good research hypothesis is written in a way that is easy for the target audience to understand.
By following this research hypothesis checklist , you will be able to create a research hypothesis that is strong, well-constructed, and more likely to yield meaningful results.

Types of research hypothesis
Different types of research hypothesis are used in scientific research:
1. Null hypothesis:
A null hypothesis states that there is no change in the dependent variable due to changes to the independent variable. This means that the results are due to chance and are not significant. A null hypothesis is denoted as H0 and is stated as the opposite of what the alternative hypothesis states.
Example: “ The newly identified virus is not zoonotic .”
2. Alternative hypothesis:
This states that there is a significant difference or relationship between the variables being studied. It is denoted as H1 or Ha and is usually accepted or rejected in favor of the null hypothesis.
Example: “ The newly identified virus is zoonotic .”
3. Directional hypothesis :
This specifies the direction of the relationship or difference between variables; therefore, it tends to use terms like increase, decrease, positive, negative, more, or less.
Example: “ The inclusion of intervention X decreases infant mortality compared to the original treatment .”
4. Non-directional hypothesis:
While it does not predict the exact direction or nature of the relationship between the two variables, a non-directional hypothesis states the existence of a relationship or difference between variables but not the direction, nature, or magnitude of the relationship. A non-directional hypothesis may be used when there is no underlying theory or when findings contradict previous research.
Example, “ Cats and dogs differ in the amount of affection they express .”
5. Simple hypothesis :
A simple hypothesis only predicts the relationship between one independent and another independent variable.
Example: “ Applying sunscreen every day slows skin aging .”
6 . Complex hypothesis :
A complex hypothesis states the relationship or difference between two or more independent and dependent variables.
Example: “ Applying sunscreen every day slows skin aging, reduces sun burn, and reduces the chances of skin cancer .” (Here, the three dependent variables are slowing skin aging, reducing sun burn, and reducing the chances of skin cancer.)
7. Associative hypothesis:
An associative hypothesis states that a change in one variable results in the change of the other variable. The associative hypothesis defines interdependency between variables.
Example: “ There is a positive association between physical activity levels and overall health .”
8 . Causal hypothesis:
A causal hypothesis proposes a cause-and-effect interaction between variables.
Example: “ Long-term alcohol use causes liver damage .”
Note that some of the types of research hypothesis mentioned above might overlap. The types of hypothesis chosen will depend on the research question and the objective of the study.

Research hypothesis examples
Here are some good research hypothesis examples :
“The use of a specific type of therapy will lead to a reduction in symptoms of depression in individuals with a history of major depressive disorder.”
“Providing educational interventions on healthy eating habits will result in weight loss in overweight individuals.”
“Plants that are exposed to certain types of music will grow taller than those that are not exposed to music.”
“The use of the plant growth regulator X will lead to an increase in the number of flowers produced by plants.”
Characteristics that make a research hypothesis weak are unclear variables, unoriginality, being too general or too vague, and being untestable. A weak hypothesis leads to weak research and improper methods.
Some bad research hypothesis examples (and the reasons why they are “bad”) are as follows:
“This study will show that treatment X is better than any other treatment . ” (This statement is not testable, too broad, and does not consider other treatments that may be effective.)
“This study will prove that this type of therapy is effective for all mental disorders . ” (This statement is too broad and not testable as mental disorders are complex and different disorders may respond differently to different types of therapy.)
“Plants can communicate with each other through telepathy . ” (This statement is not testable and lacks a scientific basis.)
Importance of testable hypothesis
If a research hypothesis is not testable, the results will not prove or disprove anything meaningful. The conclusions will be vague at best. A testable hypothesis helps a researcher focus on the study outcome and understand the implication of the question and the different variables involved. A testable hypothesis helps a researcher make precise predictions based on prior research.
To be considered testable, there must be a way to prove that the hypothesis is true or false; further, the results of the hypothesis must be reproducible.
Frequently Asked Questions (FAQs) on research hypothesis
1. What is the difference between research question and research hypothesis ?
A research question defines the problem and helps outline the study objective(s). It is an open-ended statement that is exploratory or probing in nature. Therefore, it does not make predictions or assumptions. It helps a researcher identify what information to collect. A research hypothesis , however, is a specific, testable prediction about the relationship between variables. Accordingly, it guides the study design and data analysis approach.
2. When to reject null hypothesis ?
A null hypothesis should be rejected when the evidence from a statistical test shows that it is unlikely to be true. This happens when the test statistic (e.g., p -value) is less than the defined significance level (e.g., 0.05). Rejecting the null hypothesis does not necessarily mean that the alternative hypothesis is true; it simply means that the evidence found is not compatible with the null hypothesis.
3. How can I be sure my hypothesis is testable?
A testable hypothesis should be specific and measurable, and it should state a clear relationship between variables that can be tested with data. To ensure that your hypothesis is testable, consider the following:
- Clearly define the key variables in your hypothesis. You should be able to measure and manipulate these variables in a way that allows you to test the hypothesis.
- The hypothesis should predict a specific outcome or relationship between variables that can be measured or quantified.
- You should be able to collect the necessary data within the constraints of your study.
- It should be possible for other researchers to replicate your study, using the same methods and variables.
- Your hypothesis should be testable by using appropriate statistical analysis techniques, so you can draw conclusions, and make inferences about the population from the sample data.
- The hypothesis should be able to be disproven or rejected through the collection of data.
4. How do I revise my research hypothesis if my data does not support it?
If your data does not support your research hypothesis , you will need to revise it or develop a new one. You should examine your data carefully and identify any patterns or anomalies, re-examine your research question, and/or revisit your theory to look for any alternative explanations for your results. Based on your review of the data, literature, and theories, modify your research hypothesis to better align it with the results you obtained. Use your revised hypothesis to guide your research design and data collection. It is important to remain objective throughout the process.
5. I am performing exploratory research. Do I need to formulate a research hypothesis?
As opposed to “confirmatory” research, where a researcher has some idea about the relationship between the variables under investigation, exploratory research (or hypothesis-generating research) looks into a completely new topic about which limited information is available. Therefore, the researcher will not have any prior hypotheses. In such cases, a researcher will need to develop a post-hoc hypothesis. A post-hoc research hypothesis is generated after these results are known.
6. How is a research hypothesis different from a research question?
A research question is an inquiry about a specific topic or phenomenon, typically expressed as a question. It seeks to explore and understand a particular aspect of the research subject. In contrast, a research hypothesis is a specific statement or prediction that suggests an expected relationship between variables. It is formulated based on existing knowledge or theories and guides the research design and data analysis.
7. Can a research hypothesis change during the research process?
Yes, research hypotheses can change during the research process. As researchers collect and analyze data, new insights and information may emerge that require modification or refinement of the initial hypotheses. This can be due to unexpected findings, limitations in the original hypotheses, or the need to explore additional dimensions of the research topic. Flexibility is crucial in research, allowing for adaptation and adjustment of hypotheses to align with the evolving understanding of the subject matter.
8. How many hypotheses should be included in a research study?
The number of research hypotheses in a research study varies depending on the nature and scope of the research. It is not necessary to have multiple hypotheses in every study. Some studies may have only one primary hypothesis, while others may have several related hypotheses. The number of hypotheses should be determined based on the research objectives, research questions, and the complexity of the research topic. It is important to ensure that the hypotheses are focused, testable, and directly related to the research aims.
9. Can research hypotheses be used in qualitative research?
Yes, research hypotheses can be used in qualitative research, although they are more commonly associated with quantitative research. In qualitative research, hypotheses may be formulated as tentative or exploratory statements that guide the investigation. Instead of testing hypotheses through statistical analysis, qualitative researchers may use the hypotheses to guide data collection and analysis, seeking to uncover patterns, themes, or relationships within the qualitative data. The emphasis in qualitative research is often on generating insights and understanding rather than confirming or rejecting specific research hypotheses through statistical testing.
Editage All Access is a subscription-based platform that unifies the best AI tools and services designed to speed up, simplify, and streamline every step of a researcher’s journey. The Editage All Access Pack is a one-of-a-kind subscription that unlocks full access to an AI writing assistant, literature recommender, journal finder, scientific illustration tool, and exclusive discounts on professional publication services from Editage.
Based on 22+ years of experience in academia, Editage All Access empowers researchers to put their best research forward and move closer to success. Explore our top AI Tools pack, AI Tools + Publication Services pack, or Build Your Own Plan. Find everything a researcher needs to succeed, all in one place – Get All Access now starting at just $14 a month !
Related Posts

Back to School – Lock-in All Access Pack for a Year at the Best Price

Journal Turnaround Time: Researcher.Life and Scholarly Intelligence Join Hands to Empower Researchers with Publication Time Insights
Management Notes

Theories of Management – 5 Major Theories Explained in Detail | Principles of Management(POM)
Theories of management.
Table of Contents
A management theory provides insight and guidance into the principles and practices of effective management. In order to make informed decisions and improve their leadership abilities, managers need to understand these management theories in detail. They have evolved over time and offer different perspectives on managing people, resources, and organizations.
The following management theories are explained in detail:

A) Scientific Management:
Developed by Frederick Taylor, Scientific Management optimizes efficiency and productivity through scientific analysis and standardization of work processes. Key points of this theory include:
Time and Motion Studies: Taylor conducted studies to break down tasks into smaller, more efficient parts. The goal of his study was to identify the best way to perform tasks so that unnecessary movements would be eliminated and productivity would increase.
Division of Labor: The division of labor principle advocates assigning specialized tasks to workers based on their skills and abilities. The division of work can increase specialization and knowledge in organizations.
Standardization: Standardization of work methods, tools, and procedures helps achieve consistency and efficiency. By establishing standard procedures, organizations reduce variability and enhance efficiency.
Incentives: Scientific Management recommends providing financial rewards or incentives to motivate workers towards meeting productivity targets. Taylor believed that employees would be motivated by a fair and consistent rewards system.
B) Administrative Management Theory:
In Administrative Management theory, Henri Fayol is associated with the overall management of organizations. Its key principles include:
Unity of Command: This principle states that every employee must receive orders from one manager in order to avoid confusion and conflicts and to ensure that clear lines of authority and accountability are maintained.
Scalar Chain: This principle emphasizes the importance of clear lines of communication and coordination through the organizational hierarchy.
Division of Work: Organizations can maximize their strengths and skills by assigning tasks according to their specializations and expertise.
Unity of Direction: This principle emphasizes the importance of aligning efforts within an organization to achieve a common goal.
C) Behavioral Management Theory:
This theory focuses on understanding and improving the behavior of individuals within organizations. Key concepts include:
Hawthorne Effect: This finding illustrates the significance of social and psychological factors in the workplace by demonstrating that employee productivity is enhanced by being aware of being observed and valued for their work.
Human Needs and Motivation: According to behavioral theorists, employees have a variety of needs and motivations that influence their behavior. According to Maslow’s Hierarchy of Needs and Herzberg’s Two-Factor Theory, fulfilling employees’ needs enhances motivation and job satisfaction.
Leadership styles: Behavioral management theory explores different leadership styles and how they influence employee performance and behavior. A manager’s attitude toward employees can be influenced by a number of different styles, including autocratic, democratic, or laissez-faire leadership.
Group Dynamics: This approach to behavioral management emphasizes the influence of group dynamics on individual behavior and performance. Employee productivity and satisfaction are strongly influenced by factors such as team building, effective communication, and conflict resolution within groups.
D) Systems Management Theory:
Systems Management views organizations as complex systems comprised of interrelated and interdependent components. It focuses on a number of key concepts, such as:
Systems Thinking: The Systems Management theory emphasizes that organizations are made up of subsystems that interact with each other and with their external environment. By using this perspective, managers gain a better understanding of how organizations interconnect and depend on one another.
Synergy: Synergy refers to the belief that an organization is greater than the sum of its parts. Systems theorists believe that subsystems can be collaboratively interconnected to create value.
Feedback loops: Using feedback loops within organizations provides valuable information from internal and external sources, allows organizations to monitor and adjust their performance, among other things.
Contingency Approach: A contingency approach acknowledges that there is no universal management approach that is suitable for every situation. When making decisions, managers need to take into account factors such as organizational culture, technology, and the external environment. Management practices should be tailored to specific circumstances and contexts.
E) Theory of Contingency Management:
It emphasizes that management practices need to be tailored to the unique circumstances and context in which they are applied. Principles of this theory include:
Fit between Strategy and Environment : A contingency approach emphasizes the importance of aligning organizational strategies with the external environment. For organizations to succeed long-term, they need to understand and adapt to their industry’s specific conditions.
Contingency Factors: Management effectiveness is influenced by a number of contingency factors. These factors include an organization’s size, industry, technology, culture, and external market conditions. Adapting management practices to these factors increases the likelihood of success.
Flexible Management Approaches: Contingency Management theory recognizes the need for flexible management approaches. There is no “one size fits all” approach to management. Managers should be able to adapt and adjust their practices according to the specific needs and circumstances of the organization.
Problem-Solving Orientation: Contingency approaches promote a problem-solving mindset among management. Instead of relying on pre-determined solutions, managers should analyze problems and make decisions based on the unique situation they face. In finding solutions, this approach encourages adaptability and creativity.
It is possible for managers to gain insight into various aspects of organizational management if they understand and apply these management theories and choose appropriate approaches depending on their unique circumstances. The theories provide frameworks for guiding decision-making, enhancing leadership abilities, and improving organizational effectiveness.
- Contingency Theory – 4 Types of Contingencies Leadership Theories | Theories of Organization
- Recent Posts
- Frito Lay SWOT Analysis – Strengths, Weaknesses, Opportunities & Threats | SWOT Analysis - January 11, 2024
- Fox News SWOT Analysis – Strengths, Weaknesses, Opportunities & Threats | SWOT Analysis - January 5, 2024
- Freshly SWOT Analysis – Strengths, Weaknesses, Opportunities & Threats | SWOT Analysis - January 4, 2024
Share this:
Leave a comment cancel reply.
Notify me of follow-up comments by email.
Notify me of new posts by email.
- More from M-W
- To save this word, you'll need to log in. Log In
Definition of hypothesis
Did you know.
The Difference Between Hypothesis and Theory
A hypothesis is an assumption, an idea that is proposed for the sake of argument so that it can be tested to see if it might be true.
In the scientific method, the hypothesis is constructed before any applicable research has been done, apart from a basic background review. You ask a question, read up on what has been studied before, and then form a hypothesis.
A hypothesis is usually tentative; it's an assumption or suggestion made strictly for the objective of being tested.
A theory , in contrast, is a principle that has been formed as an attempt to explain things that have already been substantiated by data. It is used in the names of a number of principles accepted in the scientific community, such as the Big Bang Theory . Because of the rigors of experimentation and control, it is understood to be more likely to be true than a hypothesis is.
In non-scientific use, however, hypothesis and theory are often used interchangeably to mean simply an idea, speculation, or hunch, with theory being the more common choice.
Since this casual use does away with the distinctions upheld by the scientific community, hypothesis and theory are prone to being wrongly interpreted even when they are encountered in scientific contexts—or at least, contexts that allude to scientific study without making the critical distinction that scientists employ when weighing hypotheses and theories.
The most common occurrence is when theory is interpreted—and sometimes even gleefully seized upon—to mean something having less truth value than other scientific principles. (The word law applies to principles so firmly established that they are almost never questioned, such as the law of gravity.)
This mistake is one of projection: since we use theory in general to mean something lightly speculated, then it's implied that scientists must be talking about the same level of uncertainty when they use theory to refer to their well-tested and reasoned principles.
The distinction has come to the forefront particularly on occasions when the content of science curricula in schools has been challenged—notably, when a school board in Georgia put stickers on textbooks stating that evolution was "a theory, not a fact, regarding the origin of living things." As Kenneth R. Miller, a cell biologist at Brown University, has said , a theory "doesn’t mean a hunch or a guess. A theory is a system of explanations that ties together a whole bunch of facts. It not only explains those facts, but predicts what you ought to find from other observations and experiments.”
While theories are never completely infallible, they form the basis of scientific reasoning because, as Miller said "to the best of our ability, we’ve tested them, and they’ve held up."
- proposition
- supposition
hypothesis , theory , law mean a formula derived by inference from scientific data that explains a principle operating in nature.
hypothesis implies insufficient evidence to provide more than a tentative explanation.
theory implies a greater range of evidence and greater likelihood of truth.
law implies a statement of order and relation in nature that has been found to be invariable under the same conditions.
Examples of hypothesis in a Sentence
These examples are programmatically compiled from various online sources to illustrate current usage of the word 'hypothesis.' Any opinions expressed in the examples do not represent those of Merriam-Webster or its editors. Send us feedback about these examples.
Word History
Greek, from hypotithenai to put under, suppose, from hypo- + tithenai to put — more at do
1641, in the meaning defined at sense 1a
Phrases Containing hypothesis
- counter - hypothesis
- nebular hypothesis
- null hypothesis
- planetesimal hypothesis
- Whorfian hypothesis
Articles Related to hypothesis

This is the Difference Between a...
This is the Difference Between a Hypothesis and a Theory
In scientific reasoning, they're two completely different things
Dictionary Entries Near hypothesis
hypothermia
hypothesize
Cite this Entry
“Hypothesis.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/hypothesis. Accessed 2 Sep. 2024.
Kids Definition
Kids definition of hypothesis, medical definition, medical definition of hypothesis, more from merriam-webster on hypothesis.
Nglish: Translation of hypothesis for Spanish Speakers
Britannica English: Translation of hypothesis for Arabic Speakers
Britannica.com: Encyclopedia article about hypothesis
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day, incandescent.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
Plural and possessive names: a guide, 31 useful rhetorical devices, more commonly misspelled words, why does english have so many silent letters, your vs. you're: how to use them correctly, popular in wordplay, 8 words for lesser-known musical instruments, it's a scorcher words for the summer heat, 7 shakespearean insults to make life more interesting, birds say the darndest things, 10 words from taylor swift songs (merriam's version), games & quizzes.

- School Guide
- Mathematics
- Number System and Arithmetic
- Trigonometry
- Probability
- Mensuration
- Maths Formulas
- Class 8 Maths Notes
- Class 9 Maths Notes
- Class 10 Maths Notes
- Class 11 Maths Notes
- Class 12 Maths Notes
Hypothesis | Definition, Meaning and Examples
Hypothesis is a hypothesis is fundamental concept in the world of research and statistics. It is a testable statement that explains what is happening or observed. It proposes the relation between the various participating variables.
Hypothesis is also called Theory, Thesis, Guess, Assumption, or Suggestion . Hypothesis creates a structure that guides the search for knowledge.
In this article, we will learn what hypothesis is, its characteristics, types, and examples. We will also learn how hypothesis helps in scientific research.
Table of Content
What is Hypothesis?
Characteristics of hypothesis, sources of hypothesis, types of hypothesis, functions of hypothesis, how hypothesis help in scientific research.
Hypothesis is a suggested idea or an educated guess or a proposed explanation made based on limited evidence, serving as a starting point for further study. They are meant to lead to more investigation.
It’s mainly a smart guess or suggested answer to a problem that can be checked through study and trial. In science work, we make guesses called hypotheses to try and figure out what will happen in tests or watching. These are not sure things but rather ideas that can be proved or disproved based on real-life proofs. A good theory is clear and can be tested and found wrong if the proof doesn’t support it.
Hypothesis Meaning
A hypothesis is a proposed statement that is testable and is given for something that happens or observed.
- It is made using what we already know and have seen, and it’s the basis for scientific research.
- A clear guess tells us what we think will happen in an experiment or study.
- It’s a testable clue that can be proven true or wrong with real-life facts and checking it out carefully.
- It usually looks like a “if-then” rule, showing the expected cause and effect relationship between what’s being studied.
Here are some key characteristics of a hypothesis:
- Testable: An idea (hypothesis) should be made so it can be tested and proven true through doing experiments or watching. It should show a clear connection between things.
- Specific: It needs to be easy and on target, talking about a certain part or connection between things in a study.
- Falsifiable: A good guess should be able to show it’s wrong. This means there must be a chance for proof or seeing something that goes against the guess.
- Logical and Rational: It should be based on things we know now or have seen, giving a reasonable reason that fits with what we already know.
- Predictive: A guess often tells what to expect from an experiment or observation. It gives a guide for what someone might see if the guess is right.
- Concise: It should be short and clear, showing the suggested link or explanation simply without extra confusion.
- Grounded in Research: A guess is usually made from before studies, ideas or watching things. It comes from a deep understanding of what is already known in that area.
- Flexible: A guess helps in the research but it needs to change or fix when new information comes up.
- Relevant: It should be related to the question or problem being studied, helping to direct what the research is about.
- Empirical: Hypotheses come from observations and can be tested using methods based on real-world experiences.
Hypotheses can come from different places based on what you’re studying and the kind of research. Here are some common sources from which hypotheses may originate:
- Existing Theories: Often, guesses come from well-known science ideas. These ideas may show connections between things or occurrences that scientists can look into more.
- Observation and Experience: Watching something happen or having personal experiences can lead to guesses. We notice odd things or repeat events in everyday life and experiments. This can make us think of guesses called hypotheses.
- Previous Research: Using old studies or discoveries can help come up with new ideas. Scientists might try to expand or question current findings, making guesses that further study old results.
- Literature Review: Looking at books and research in a subject can help make guesses. Noticing missing parts or mismatches in previous studies might make researchers think up guesses to deal with these spots.
- Problem Statement or Research Question: Often, ideas come from questions or problems in the study. Making clear what needs to be looked into can help create ideas that tackle certain parts of the issue.
- Analogies or Comparisons: Making comparisons between similar things or finding connections from related areas can lead to theories. Understanding from other fields could create new guesses in a different situation.
- Hunches and Speculation: Sometimes, scientists might get a gut feeling or make guesses that help create ideas to test. Though these may not have proof at first, they can be a beginning for looking deeper.
- Technology and Innovations: New technology or tools might make guesses by letting us look at things that were hard to study before.
- Personal Interest and Curiosity: People’s curiosity and personal interests in a topic can help create guesses. Scientists could make guesses based on their own likes or love for a subject.
Here are some common types of hypotheses:
Simple Hypothesis
Complex hypothesis, directional hypothesis.
- Non-directional Hypothesis
Null Hypothesis (H0)
Alternative hypothesis (h1 or ha), statistical hypothesis, research hypothesis, associative hypothesis, causal hypothesis.
Simple Hypothesis guesses a connection between two things. It says that there is a connection or difference between variables, but it doesn’t tell us which way the relationship goes. Example: Studying more can help you do better on tests. Getting more sun makes people have higher amounts of vitamin D.
Complex Hypothesis tells us what will happen when more than two things are connected. It looks at how different things interact and may be linked together. Example: How rich you are, how easy it is to get education and healthcare greatly affects the number of years people live. A new medicine’s success relies on the amount used, how old a person is who takes it and their genes.
Directional Hypothesis says how one thing is related to another. For example, it guesses that one thing will help or hurt another thing. Example: Drinking more sweet drinks is linked to a higher body weight score. Too much stress makes people less productive at work.
Non-Directional Hypothesis
Non-Directional Hypothesis are the one that don’t say how the relationship between things will be. They just say that there is a connection, without telling which way it goes. Example: Drinking caffeine can affect how well you sleep. People often like different kinds of music based on their gender.
Null hypothesis is a statement that says there’s no connection or difference between different things. It implies that any seen impacts are because of luck or random changes in the information. Example: The average test scores of Group A and Group B are not much different. There is no connection between using a certain fertilizer and how much it helps crops grow.
Alternative Hypothesis is different from the null hypothesis and shows that there’s a big connection or gap between variables. Scientists want to say no to the null hypothesis and choose the alternative one. Example: Patients on Diet A have much different cholesterol levels than those following Diet B. Exposure to a certain type of light can change how plants grow compared to normal sunlight.
Statistical Hypothesis are used in math testing and include making ideas about what groups or bits of them look like. You aim to get information or test certain things using these top-level, common words only. Example: The average smarts score of kids in a certain school area is 100. The usual time it takes to finish a job using Method A is the same as with Method B.
Research Hypothesis comes from the research question and tells what link is expected between things or factors. It leads the study and chooses where to look more closely. Example: Having more kids go to early learning classes helps them do better in school when they get older. Using specific ways of talking affects how much customers get involved in marketing activities.
Associative Hypothesis guesses that there is a link or connection between things without really saying it caused them. It means that when one thing changes, it is connected to another thing changing. Example: Regular exercise helps to lower the chances of heart disease. Going to school more can help people make more money.
Causal Hypothesis are different from other ideas because they say that one thing causes another. This means there’s a cause and effect relationship between variables involved in the situation. They say that when one thing changes, it directly makes another thing change. Example: Playing violent video games makes teens more likely to act aggressively. Less clean air directly impacts breathing health in city populations.
Hypotheses have many important jobs in the process of scientific research. Here are the key functions of hypotheses:
- Guiding Research: Hypotheses give a clear and exact way for research. They act like guides, showing the predicted connections or results that scientists want to study.
- Formulating Research Questions: Research questions often create guesses. They assist in changing big questions into particular, checkable things. They guide what the study should be focused on.
- Setting Clear Objectives: Hypotheses set the goals of a study by saying what connections between variables should be found. They set the targets that scientists try to reach with their studies.
- Testing Predictions: Theories guess what will happen in experiments or observations. By doing tests in a planned way, scientists can check if what they see matches the guesses made by their ideas.
- Providing Structure: Theories give structure to the study process by arranging thoughts and ideas. They aid scientists in thinking about connections between things and plan experiments to match.
- Focusing Investigations: Hypotheses help scientists focus on certain parts of their study question by clearly saying what they expect links or results to be. This focus makes the study work better.
- Facilitating Communication: Theories help scientists talk to each other effectively. Clearly made guesses help scientists to tell others what they plan, how they will do it and the results expected. This explains things well with colleagues in a wide range of audiences.
- Generating Testable Statements: A good guess can be checked, which means it can be looked at carefully or tested by doing experiments. This feature makes sure that guesses add to the real information used in science knowledge.
- Promoting Objectivity: Guesses give a clear reason for study that helps guide the process while reducing personal bias. They motivate scientists to use facts and data as proofs or disprovals for their proposed answers.
- Driving Scientific Progress: Making, trying out and adjusting ideas is a cycle. Even if a guess is proven right or wrong, the information learned helps to grow knowledge in one specific area.
Researchers use hypotheses to put down their thoughts directing how the experiment would take place. Following are the steps that are involved in the scientific method:
- Initiating Investigations: Hypotheses are the beginning of science research. They come from watching, knowing what’s already known or asking questions. This makes scientists make certain explanations that need to be checked with tests.
- Formulating Research Questions: Ideas usually come from bigger questions in study. They help scientists make these questions more exact and testable, guiding the study’s main point.
- Setting Clear Objectives: Hypotheses set the goals of a study by stating what we think will happen between different things. They set the goals that scientists want to reach by doing their studies.
- Designing Experiments and Studies: Assumptions help plan experiments and watchful studies. They assist scientists in knowing what factors to measure, the techniques they will use and gather data for a proposed reason.
- Testing Predictions: Ideas guess what will happen in experiments or observations. By checking these guesses carefully, scientists can see if the seen results match up with what was predicted in each hypothesis.
- Analysis and Interpretation of Data: Hypotheses give us a way to study and make sense of information. Researchers look at what they found and see if it matches the guesses made in their theories. They decide if the proof backs up or disagrees with these suggested reasons why things are happening as expected.
- Encouraging Objectivity: Hypotheses help make things fair by making sure scientists use facts and information to either agree or disagree with their suggested reasons. They lessen personal preferences by needing proof from experience.
- Iterative Process: People either agree or disagree with guesses, but they still help the ongoing process of science. Findings from testing ideas make us ask new questions, improve those ideas and do more tests. It keeps going on in the work of science to keep learning things.
People Also View:
Mathematics Maths Formulas Branches of Mathematics
Hypothesis is a testable statement serving as an initial explanation for phenomena, based on observations, theories, or existing knowledge . It acts as a guiding light for scientific research, proposing potential relationships between variables that can be empirically tested through experiments and observations.
The hypothesis must be specific, testable, falsifiable, and grounded in prior research or observation, laying out a predictive, if-then scenario that details a cause-and-effect relationship. It originates from various sources including existing theories, observations, previous research, and even personal curiosity, leading to different types, such as simple, complex, directional, non-directional, null, and alternative hypotheses, each serving distinct roles in research methodology .
The hypothesis not only guides the research process by shaping objectives and designing experiments but also facilitates objective analysis and interpretation of data , ultimately driving scientific progress through a cycle of testing, validation, and refinement.
Hypothesis – FAQs
What is a hypothesis.
A guess is a possible explanation or forecast that can be checked by doing research and experiments.
What are Components of a Hypothesis?
The components of a Hypothesis are Independent Variable, Dependent Variable, Relationship between Variables, Directionality etc.
What makes a Good Hypothesis?
Testability, Falsifiability, Clarity and Precision, Relevance are some parameters that makes a Good Hypothesis
Can a Hypothesis be Proven True?
You cannot prove conclusively that most hypotheses are true because it’s generally impossible to examine all possible cases for exceptions that would disprove them.
How are Hypotheses Tested?
Hypothesis testing is used to assess the plausibility of a hypothesis by using sample data
Can Hypotheses change during Research?
Yes, you can change or improve your ideas based on new information discovered during the research process.
What is the Role of a Hypothesis in Scientific Research?
Hypotheses are used to support scientific research and bring about advancements in knowledge.

Please Login to comment...
Similar reads.
- Geeks Premier League
- School Learning
- Geeks Premier League 2023
- Maths-Class-12
- How to Delete Discord Servers: Step by Step Guide
- Google increases YouTube Premium price in India: Check our the latest plans
- California Lawmakers Pass Bill to Limit AI Replicas
- Best 10 IPTV Service Providers in Germany
- 15 Most Important Aptitude Topics For Placements [2024]
Improve your Coding Skills with Practice
What kind of Experience do you want to share?
What is Hypothesis? Definition, Meaning, Characteristics, Sources
- Post last modified: 10 January 2022
- Reading time: 18 mins read
- Post category: Research Methodology

- What is Hypothesis?
Hypothesis is a prediction of the outcome of a study. Hypotheses are drawn from theories and research questions or from direct observations. In fact, a research problem can be formulated as a hypothesis. To test the hypothesis we need to formulate it in terms that can actually be analysed with statistical tools.
As an example, if we want to explore whether using a specific teaching method at school will result in better school marks (research question), the hypothesis could be that the mean school marks of students being taught with that specific teaching method will be higher than of those being taught using other methods.
In this example, we stated a hypothesis about the expected differences between groups. Other hypotheses may refer to correlations between variables.
Table of Content
- 1 What is Hypothesis?
- 2 Hypothesis Definition
- 3 Meaning of Hypothesis
- 4.1 Conceptual Clarity
- 4.2 Need of empirical referents
- 4.3 Hypothesis should be specific
- 4.4 Hypothesis should be within the ambit of the available research techniques
- 4.5 Hypothesis should be consistent with the theory
- 4.6 Hypothesis should be concerned with observable facts and empirical events
- 4.7 Hypothesis should be simple
- 5.1 Observation
- 5.2 Analogies
- 5.4 State of Knowledge
- 5.5 Culture
- 5.6 Continuity of Research
- 6.1 Null Hypothesis
- 6.2 Alternative Hypothesis
Thus, to formulate a hypothesis, we need to refer to the descriptive statistics (such as the mean final marks), and specify a set of conditions about these statistics (such as a difference between the means, or in a different example, a positive or negative correlation). The hypothesis we formulate applies to the population of interest.
The null hypothesis makes a statement that no difference exists (see Pyrczak, 1995, pp. 75-84).
Hypothesis Definition
A hypothesis is ‘a guess or supposition as to the existence of some fact or law which will serve to explain a connection of facts already known to exist.’ – J. E. Creighton & H. R. Smart
Hypothesis is ‘a proposition not known to be definitely true or false, examined for the sake of determining the consequences which would follow from its truth.’ – Max Black
Hypothesis is ‘a proposition which can be put to a test to determine validity and is useful for further research.’ – W. J. Goode and P. K. Hatt
A hypothesis is a proposition, condition or principle which is assumed, perhaps without belief, in order to draw out its logical consequences and by this method to test its accord with facts which are known or may be determined. – Webster’s New International Dictionary of the English Language (1956)
Meaning of Hypothesis
From the above mentioned definitions of hypothesis, its meaning can be explained in the following ways.
- At the primary level, a hypothesis is the possible and probable explanation of the sequence of happenings or data.
- Sometimes, hypothesis may emerge from an imagination, common sense or a sudden event.
- Hypothesis can be a probable answer to the research problem undertaken for study. 4. Hypothesis may not always be true. It can get disproven. In other words, hypothesis need not always be a true proposition.
- Hypothesis, in a sense, is an attempt to present the interrelations that exist in the available data or information.
- Hypothesis is not an individual opinion or community thought. Instead, it is a philosophical means which is to be used for research purpose. Hypothesis is not to be considered as the ultimate objective; rather it is to be taken as the means of explaining scientifically the prevailing situation.
The concept of hypothesis can further be explained with the help of some examples. Lord Keynes, in his theory of national income determination, made a hypothesis about the consumption function. He stated that the consumption expenditure of an individual or an economy as a whole is dependent on the level of income and changes in a certain proportion.
Later, this proposition was proved in the statistical research carried out by Prof. Simon Kuznets. Matthus, while studying the population, formulated a hypothesis that population increases faster than the supply of food grains. Population studies of several countries revealed that this hypothesis is true.
Validation of the Malthus’ hypothesis turned it into a theory and when it was tested in many other countries it became the famous Malthus’ Law of Population. It thus emerges that when a hypothesis is tested and proven, it becomes a theory. The theory, when found true in different times and at different places, becomes the law. Having understood the concept of hypothesis, few hypotheses can be formulated in the areas of commerce and economics.
- Population growth moderates with the rise in per capita income.
- Sales growth is positively linked with the availability of credit.
- Commerce education increases the employability of the graduate students.
- High rates of direct taxes prompt people to evade taxes.
- Good working conditions improve the productivity of employees.
- Advertising is the most effecting way of promoting sales than any other scheme.
- Higher Debt-Equity Ratio increases the probability of insolvency.
- Economic reforms in India have made the public sector banks more efficient and competent.
- Foreign direct investment in India has moved in those sectors which offer higher rate of profit.
- There is no significant association between credit rating and investment of fund.
Characteristics of Hypothesis
Not all the hypotheses are good and useful from the point of view of research. It is only a few hypotheses satisfying certain criteria that are good, useful and directive in the research work undertaken. The characteristics of such a useful hypothesis can be listed as below:
Conceptual Clarity
Need of empirical referents, hypothesis should be specific, hypothesis should be within the ambit of the available research techniques, hypothesis should be consistent with the theory, hypothesis should be concerned with observable facts and empirical events, hypothesis should be simple.
The concepts used while framing hypothesis should be crystal clear and unambiguous. Such concepts must be clearly defined so that they become lucid and acceptable to everyone. How are the newly developed concepts interrelated and how are they linked with the old one is to be very clear so that the hypothesis framed on their basis also carries the same clarity.
A hypothesis embodying unclear and ambiguous concepts can to a great extent undermine the successful completion of the research work.
A hypothesis can be useful in the research work undertaken only when it has links with some empirical referents. Hypothesis based on moral values and ideals are useless as they cannot be tested. Similarly, hypothesis containing opinions as good and bad or expectation with respect to something are not testable and therefore useless.
For example, ‘current account deficit can be lowered if people change their attitude towards gold’ is a hypothesis encompassing expectation. In case of such a hypothesis, the attitude towards gold is something which cannot clearly be described and therefore a hypothesis which embodies such an unclean thing cannot be tested and proved or disproved. In short, the hypothesis should be linked with some testable referents.
For the successful conduction of research, it is necessary that the hypothesis is specific and presented in a precise manner. Hypothesis which is general, too ambitious and grandiose in scope is not to be made as such hypothesis cannot be easily put to test. A hypothesis is to be based on such concepts which are precise and empirical in nature. A hypothesis should give a clear idea about the indicators which are to be used.
For example, a hypothesis that economic power is increasingly getting concentrated in a few hands in India should enable us to define the concept of economic power. It should be explicated in terms of measurable indicator like income, wealth, etc. Such specificity in the formulation of a hypothesis ensures that the research is practicable and significant.
While framing the hypothesis, the researcher should be aware of the available research techniques and should see that the hypothesis framed is testable on the basis of them. In other words, a hypothesis should be researchable and for this it is important that a due thought has been given to the methods and techniques which can be used to measure the concepts and variables embodied in the hypothesis.
It does not however mean that hypotheses which are not testable with the available techniques of research are not to be made. If the problem is too significant and therefore the hypothesis framed becomes too ambitious and complex, it’s testing becomes possible with the development of new research techniques or the hypothesis itself leads to the development of new research techniques.
A hypothesis must be related to the existing theory or should have a theoretical orientation. The growth of knowledge takes place in the sequence of facts, hypothesis, theory and law or principles. It means the hypothesis should have a correspondence with the existing facts and theory.
If the hypothesis is related to some theory, the research work will enable us to support, modify or refute the existing theory. Theoretical orientation of the hypothesis ensures that it becomes scientifically useful. According to Prof. Goode and Prof. Hatt, research work can contribute to the existing knowledge only when the hypothesis is related with some theory.
This enables us to explain the observed facts and situations and also verify the framed hypothesis. In the words of Prof. Cohen and Prof. Nagel, “hypothesis must be formulated in such a manner that deduction can be made from it and that consequently a decision can be reached as to whether it does or does not explain the facts considered.”
If the research work based on a hypothesis is to be successful, it is necessary that the later is as simple and easy as possible. An ambition of finding out something new may lead the researcher to frame an unrealistic and unclear hypothesis. Such a temptation is to be avoided. Framing a simple, easy and testable hypothesis requires that the researcher is well acquainted with the related concepts.
Sources of Hypothesis
Hypotheses can be derived from various sources. Some of the sources is given below:
Observation
State of knowledge, continuity of research.
Hypotheses can be derived from observation from the observation of price behavior in a market. For example the relationship between the price and demand for an article is hypothesized.
Analogies are another source of useful hypotheses. Julian Huxley has pointed out that casual observations in nature or in the framework of another science may be a fertile source of hypotheses. For example, the hypotheses that similar human types or activities may be found in similar geophysical regions come from plant ecology.
This is one of the main sources of hypotheses. It gives direction to research by stating what is known logical deduction from theory lead to new hypotheses. For example, profit / wealth maximization is considered as the goal of private enterprises. From this assumption various hypotheses are derived’.
An important source of hypotheses is the state of knowledge in any particular science where formal theories exist hypotheses can be deduced. If the hypotheses are rejected theories are scarce hypotheses are generated from conception frameworks.
Another source of hypotheses is the culture on which the researcher was nurtured. Western culture has induced the emergence of sociology as an academic discipline over the past decade, a large part of the hypotheses on American society examined by researchers were connected with violence. This interest is related to the considerable increase in the level of violence in America.
The continuity of research in a field itself constitutes an important source of hypotheses. The rejection of some hypotheses leads to the formulation of new ones capable of explaining dependent variables in subsequent research on the same subject.
Null and Alternative Hypothesis
Null hypothesis.
The hypothesis that are proposed with the intent of receiving a rejection for them are called Null Hypothesis . This requires that we hypothesize the opposite of what is desired to be proved. For example, if we want to show that sales and advertisement expenditure are related, we formulate the null hypothesis that they are not related.
Similarly, if we want to conclude that the new sales training programme is effective, we formulate the null hypothesis that the new training programme is not effective, and if we want to prove that the average wages of skilled workers in town 1 is greater than that of town 2, we formulate the null hypotheses that there is no difference in the average wages of the skilled workers in both the towns.
Since we hypothesize that sales and advertisement are not related, new training programme is not effective and the average wages of skilled workers in both the towns are equal, we call such hypotheses null hypotheses and denote them as H 0 .
Alternative Hypothesis
Rejection of null hypotheses leads to the acceptance of alternative hypothesis . The rejection of null hypothesis indicates that the relationship between variables (e.g., sales and advertisement expenditure) or the difference between means (e.g., wages of skilled workers in town 1 and town 2) or the difference between proportions have statistical significance and the acceptance of the null hypotheses indicates that these differences are due to chance.
As already mentioned, the alternative hypotheses specify that values/relation which the researcher believes hold true. The alternative hypotheses can cover a whole range of values rather than a single point. The alternative hypotheses are denoted by H 1 .
Business Ethics
( Click on Topic to Read )
- What is Ethics?
- What is Business Ethics?
- Values, Norms, Beliefs and Standards in Business Ethics
- Indian Ethos in Management
- Ethical Issues in Marketing
- Ethical Issues in HRM
- Ethical Issues in IT
- Ethical Issues in Production and Operations Management
- Ethical Issues in Finance and Accounting
- What is Corporate Governance?
- What is Ownership Concentration?
- What is Ownership Composition?
- Types of Companies in India
- Internal Corporate Governance
- External Corporate Governance
- Corporate Governance in India
- What is Enterprise Risk Management (ERM)?
- What is Assessment of Risk?
- What is Risk Register?
- Risk Management Committee
Corporate social responsibility (CSR)
- Theories of CSR
- Arguments Against CSR
- Business Case for CSR
- Importance of CSR in India
- Drivers of Corporate Social Responsibility
- Developing a CSR Strategy
- Implement CSR Commitments
- CSR Marketplace
- CSR at Workplace
- Environmental CSR
- CSR with Communities and in Supply Chain
- Community Interventions
- CSR Monitoring
- CSR Reporting
- Voluntary Codes in CSR
- What is Corporate Ethics?
Lean Six Sigma
- What is Six Sigma?
- What is Lean Six Sigma?
- Value and Waste in Lean Six Sigma
- Six Sigma Team
- MAIC Six Sigma
- Six Sigma in Supply Chains
- What is Binomial, Poisson, Normal Distribution?
- What is Sigma Level?
- What is DMAIC in Six Sigma?
- What is DMADV in Six Sigma?
- Six Sigma Project Charter
- Project Decomposition in Six Sigma
- Critical to Quality (CTQ) Six Sigma
- Process Mapping Six Sigma
- Flowchart and SIPOC
- Gage Repeatability and Reproducibility
- Statistical Diagram
- Lean Techniques for Optimisation Flow
- Failure Modes and Effects Analysis (FMEA)
- What is Process Audits?
- Six Sigma Implementation at Ford
- IBM Uses Six Sigma to Drive Behaviour Change
- Research Methodology
- What is Research?
- Sampling Method
- Research Methods
- Data Collection in Research
Methods of Collecting Data
- Application of Business Research
- Levels of Measurement
- What is Sampling?
Hypothesis Testing
- Research Report
- What is Management?
- Planning in Management
- Decision Making in Management
- What is Controlling?
- What is Coordination?
- What is Staffing?
- Organization Structure
- What is Departmentation?
- Span of Control
- What is Authority?
- Centralization vs Decentralization
- Organizing in Management
- Schools of Management Thought
- Classical Management Approach
- Is Management an Art or Science?
- Who is a Manager?
Operations Research
- What is Operations Research?
- Operation Research Models
- Linear Programming
- Linear Programming Graphic Solution
- Linear Programming Simplex Method
- Linear Programming Artificial Variable Technique
- Duality in Linear Programming
- Transportation Problem Initial Basic Feasible Solution
- Transportation Problem Finding Optimal Solution
- Project Network Analysis with Critical Path Method
- Project Network Analysis Methods
- Project Evaluation and Review Technique (PERT)
- Simulation in Operation Research
- Replacement Models in Operation Research
Operation Management
- What is Strategy?
- What is Operations Strategy?
- Operations Competitive Dimensions
- Operations Strategy Formulation Process
- What is Strategic Fit?
- Strategic Design Process
- Focused Operations Strategy
- Corporate Level Strategy
- Expansion Strategies
- Stability Strategies
- Retrenchment Strategies
- Competitive Advantage
- Strategic Choice and Strategic Alternatives
- What is Production Process?
- What is Process Technology?
- What is Process Improvement?
- Strategic Capacity Management
- Production and Logistics Strategy
- Taxonomy of Supply Chain Strategies
- Factors Considered in Supply Chain Planning
- Operational and Strategic Issues in Global Logistics
- Logistics Outsourcing Strategy
- What is Supply Chain Mapping?
- Supply Chain Process Restructuring
- Points of Differentiation
- Re-engineering Improvement in SCM
- What is Supply Chain Drivers?
- Supply Chain Operations Reference (SCOR) Model
- Customer Service and Cost Trade Off
- Internal and External Performance Measures
- Linking Supply Chain and Business Performance
- Netflix’s Niche Focused Strategy
- Disney and Pixar Merger
- Process Planning at Mcdonald’s
Service Operations Management
- What is Service?
- What is Service Operations Management?
- What is Service Design?
- Service Design Process
- Service Delivery
- What is Service Quality?
- Gap Model of Service Quality
- Juran Trilogy
- Service Performance Measurement
- Service Decoupling
- IT Service Operation
- Service Operations Management in Different Sector
Procurement Management
- What is Procurement Management?
- Procurement Negotiation
- Types of Requisition
- RFX in Procurement
- What is Purchasing Cycle?
- Vendor Managed Inventory
- Internal Conflict During Purchasing Operation
- Spend Analysis in Procurement
- Sourcing in Procurement
- Supplier Evaluation and Selection in Procurement
- Blacklisting of Suppliers in Procurement
- Total Cost of Ownership in Procurement
- Incoterms in Procurement
- Documents Used in International Procurement
- Transportation and Logistics Strategy
- What is Capital Equipment?
- Procurement Process of Capital Equipment
- Acquisition of Technology in Procurement
- What is E-Procurement?
- E-marketplace and Online Catalogues
- Fixed Price and Cost Reimbursement Contracts
- Contract Cancellation in Procurement
- Ethics in Procurement
- Legal Aspects of Procurement
- Global Sourcing in Procurement
- Intermediaries and Countertrade in Procurement
Strategic Management
- What is Strategic Management?
- What is Value Chain Analysis?
- Mission Statement
- Business Level Strategy
- What is SWOT Analysis?
- What is Competitive Advantage?
- What is Vision?
- What is Ansoff Matrix?
- Prahalad and Gary Hammel
- Strategic Management In Global Environment
- Competitor Analysis Framework
- Competitive Rivalry Analysis
- Competitive Dynamics
- What is Competitive Rivalry?
- Five Competitive Forces That Shape Strategy
- What is PESTLE Analysis?
- Fragmentation and Consolidation Of Industries
- What is Technology Life Cycle?
- What is Diversification Strategy?
- What is Corporate Restructuring Strategy?
- Resources and Capabilities of Organization
- Role of Leaders In Functional-Level Strategic Management
- Functional Structure In Functional Level Strategy Formulation
- Information And Control System
- What is Strategy Gap Analysis?
- Issues In Strategy Implementation
- Matrix Organizational Structure
- What is Strategic Management Process?
Supply Chain
- What is Supply Chain Management?
- Supply Chain Planning and Measuring Strategy Performance
- What is Warehousing?
- What is Packaging?
- What is Inventory Management?
- What is Material Handling?
- What is Order Picking?
- Receiving and Dispatch, Processes
- What is Warehouse Design?
- What is Warehousing Costs?
You Might Also Like
What is descriptive research types, features, cross-sectional and longitudinal research, what is measure of dispersion, what is scaling techniques types, classifications, techniques, what is causal research advantages, disadvantages, how to perform, what is research problem components, identifying, formulating,, research process | types, what is literature review importance, functions, process,, what is measurement scales, types, criteria and developing measurement tools, what is research design types, leave a reply cancel reply.
You must be logged in to post a comment.
World's Best Online Courses at One Place
We’ve spent the time in finding, so you can spend your time in learning
Digital Marketing
Personal Growth
Development
- [email protected]
- Connecting and sharing with us

- Entrepreneurship
- Growth of firm
- Sales Management
- Retail Management
- Import – Export
- International Business
- Project Management
- Production Management
- Quality Management
- Logistics Management
- Supply Chain Management
- Human Resource Management
- Organizational Culture
- Information System Management
- Corporate Finance
- Stock Market
- Office Management
- Theory of the Firm
- Management Science
- Microeconomics
- Research Process
- Experimental Research
- Research Philosophy
- Management Research
- Writing a thesis
- Writing a paper
- Literature Review
- Action Research
- Qualitative Content Analysis
- Observation
- Phenomenology
- Statistics and Econometrics
- Questionnaire Survey
- Quantitative Content Analysis
- Meta Analysis
The definition of a hypothesis in management research
The second important consideration in the formulation of a research problem in quantitative research is the construction of a hypothesis. Hypotheses bring clarity, specificity and focus to a research problem, but are not essential for a study. You can conduct a valid investigation
without constructing a single formal hypothesis. On the other hand, within the context of a research study, you can construct as many hypotheses as you consider to be appropriate. Some believe that one must formulate a hypothesis to undertake an investigation; however, the author does not hold this opinion. Hypotheses primarily arise from a set of ‘hunches’ that are tested through a study and one can conduct a perfectly valid study without having these hunches or speculations. However, in epidemiological studies, to narrow the field of investigation, it is important to formulate hypotheses.
The importance of hypotheses lies in their ability to bring direction, specificity and focus to a research study. They tell a researcher what specific information to collect, and thereby provide greater focus.
Let us imagine you are at the races and you place a bet.You bet on a hunch that a particular horse will win. You will only know if your hunch was right after the race. Take another example. Suppose you have a hunch that there are more smokers than non-smokers in your class. To test your hunch, you ask either all or just some of the class if they are smokers. You can then conclude whether your hunch was right or wrong.
Now let us take a slightly different example. Suppose you work in the area of public health. Your clinical impression is that a higher rate of a particular condition prevails among people coming from a specific population subgroup. You want to find out the probable cause of this condition. There could be many causes. To explore every conceivable possibility would require an enormous amount of time and resources. Hence, to narrow the choice, based on your knowledge of the field, you could identify what you assume to be the most probable cause. You could then design a study to collect the information needed to verify your hunch. If on verification you were able to conclude that the assumed cause was the real cause of the condition, your assumption would have been right.
In these examples, you started with a superficial hunch or assumption. In one case (horse racing) you waited for the event to take place and in the other two instances you designed a study to assess the validity of your assumption, and only after careful investigation did you arrive at a conclusion about the validity of your assumptions.
Hypotheses are based upon similar logic. As a researcher you do not know about a phenomenon, a situation, the prevalence of a condition in a population or about the outcome of a programme, but you do have a hunch to form the basis of certain assumptions or guesses. You test these, mostly one by one, by collecting information that will enable you to conclude if your hunch was right. The verification process can have one of three outcomes. Your hunch may prove to be: right, partially right or wrong. Without this process of verification, you cannot conclude anything about the validity of your assumption.
Hence, a hypothesis is a hunch, assumption, suspicion, assertion or an idea about a phenomenon, relationship or situation, the reality or truth of which you do not know. A researcher calls these assumptions, assertions, statements or hunches hypotheses and they become the basis of an enquiry. In most studies the hypothesis will be based upon either previous studies or your own or someone else’s observations.
There are many definitions of a hypothesis. According to Kerlinger, ‘A hypothesis is a conjectural statement of the relationship between two or more variables’ (1986: 17). Webster’s Third New International Dictionary (1976) defines a hypothesis as:
a proposition, condition, or principle which is assumed, perhaps without belief, in order to draw out its logical consequences and by this method to test its accord with facts which are known or may be determined.
Black and Champion define a hypothesis as ‘a tentative statement about something, the validity of which is usually unknown’ (1976: 126). In another definition, Bailey defines a hypothesis as:
a proposition that is stated in a testable form and that predicts a particular relationship between two (or more) variables. In other words, if we think that a relationship exists, we first state it as a hypothesis and then test the hypothesis in the field. (1978: 35)
According to Grinnell:
A hypothesis is written in such a way that it can be proven or disproven by valid and reliable data — it is in order to obtain these data that we perform our study. (1988: 200)
From the above definitions it is apparent that a hypothesis has certain characteristics:
- It is a tentative proposition.
- its validity is unknown.
- In most cases, it specifies a relationship between two or more variables.
Source: Kumar Ranjit (2012), Research methodology: a step-by-step guide for beginners , SAGE Publications Ltd; Third edition.
29 Jul 2021
30 Jul 2021
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Username or email address *
Password *
Log in Remember me
Lost your password?
How to Generate and Validate Product Hypotheses
Every product owner knows that it takes effort to build something that'll cater to user needs. You'll have to make many tough calls if you wish to grow the company and evolve the product so it delivers more value. But how do you decide what to change in the product, your marketing strategy, or the overall direction to succeed? And how do you make a product that truly resonates with your target audience?
There are many unknowns in business, so many fundamental decisions start from a simple "what if?". But they can't be based on guesses, as you need some proof to fill in the blanks reasonably.
Because there's no universal recipe for successfully building a product, teams collect data, do research, study the dynamics, and generate hypotheses according to the given facts. They then take corresponding actions to find out whether they were right or wrong, make conclusions, and most likely restart the process again.
On this page, we thoroughly inspect product hypotheses. We'll go over what they are, how to create hypothesis statements and validate them, and what goes after this step.
What Is a Hypothesis in Product Management?
A hypothesis in product development and product management is a statement or assumption about the product, planned feature, market, or customer (e.g., their needs, behavior, or expectations) that you can put to the test, evaluate, and base your further decisions on . This may, for instance, regard the upcoming product changes as well as the impact they can result in.
A hypothesis implies that there is limited knowledge. Hence, the teams need to undergo testing activities to validate their ideas and confirm whether they are true or false.
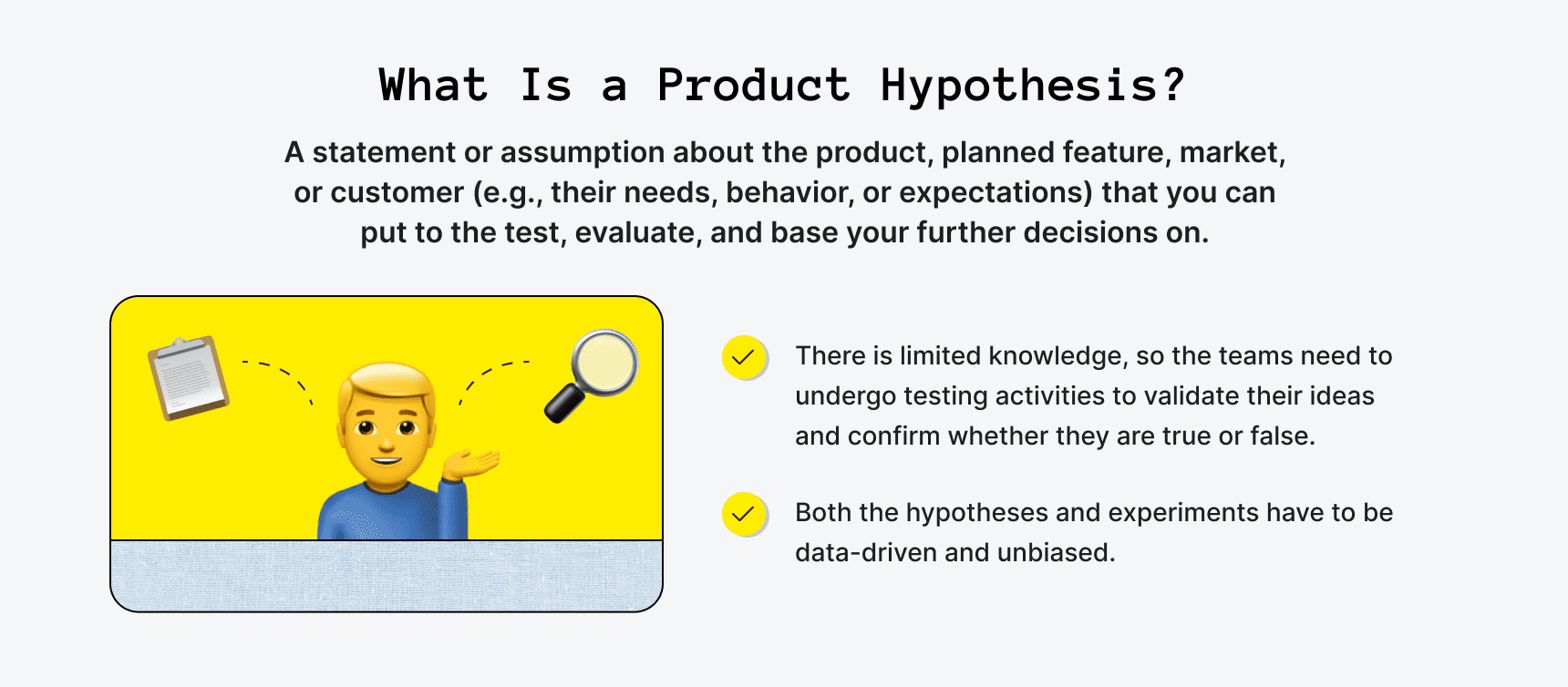
Hypotheses guide the product development process and may point at important findings to help build a better product that'll serve user needs. In essence, teams create hypothesis statements in an attempt to improve the offering, boost engagement, increase revenue, find product-market fit quicker, or for other business-related reasons.
It's sort of like an experiment with trial and error, yet, it is data-driven and should be unbiased . This means that teams don't make assumptions out of the blue. Instead, they turn to the collected data, conducted market research , and factual information, which helps avoid completely missing the mark. The obtained results are then carefully analyzed and may influence decision-making.
Such experiments backed by data and analysis are an integral aspect of successful product development and allow startups or businesses to dodge costly startup mistakes .
When do teams create hypothesis statements and validate them? To some extent, hypothesis testing is an ongoing process to work on constantly. It may occur during various product development life cycle stages, from early phases like initiation to late ones like scaling.
In any event, the key here is learning how to generate hypothesis statements and validate them effectively. We'll go over this in more detail later on.
Idea vs. Hypothesis Compared
You might be wondering whether ideas and hypotheses are the same thing. Well, there are a few distinctions.
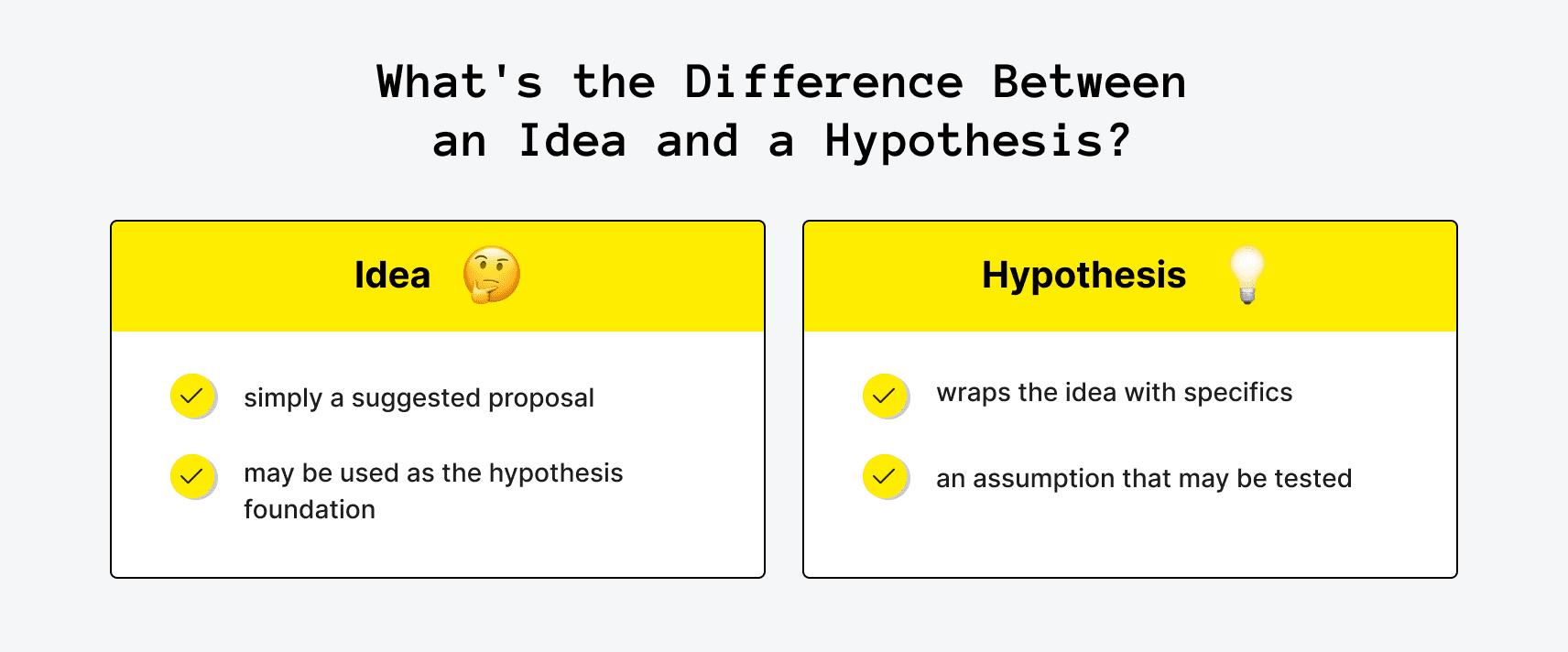
An idea is simply a suggested proposal. Say, a teammate comes up with something you can bring to life during a brainstorming session or pitches in a suggestion like "How about we shorten the checkout process?". You can jot down such ideas and then consider working on them if they'll truly make a difference and improve the product, strategy, or result in other business benefits. Ideas may thus be used as the hypothesis foundation when you decide to prove a concept.
A hypothesis is the next step, when an idea gets wrapped with specifics to become an assumption that may be tested. As such, you can refine the idea by adding details to it. The previously mentioned idea can be worded into a product hypothesis statement like: "The cart abandonment rate is high, and many users flee at checkout. But if we shorten the checkout process by cutting down the number of steps to only two and get rid of four excessive fields, we'll simplify the user journey, boost satisfaction, and may get up to 15% more completed orders".
A hypothesis is something you can test in an attempt to reach a certain goal. Testing isn't obligatory in this scenario, of course, but the idea may be tested if you weigh the pros and cons and decide that the required effort is worth a try. We'll explain how to create hypothesis statements next.

How to Generate a Hypothesis for a Product
The last thing those developing a product want is to invest time and effort into something that won't bring any visible results, fall short of customer expectations, or won't live up to their needs. Therefore, to increase the chances of achieving a successful outcome and product-led growth , teams may need to revisit their product development approach by optimizing one of the starting points of the process: learning to make reasonable product hypotheses.
If the entire procedure is structured, this may assist you during such stages as the discovery phase and raise the odds of reaching your product goals and setting your business up for success. Yet, what's the entire process like?
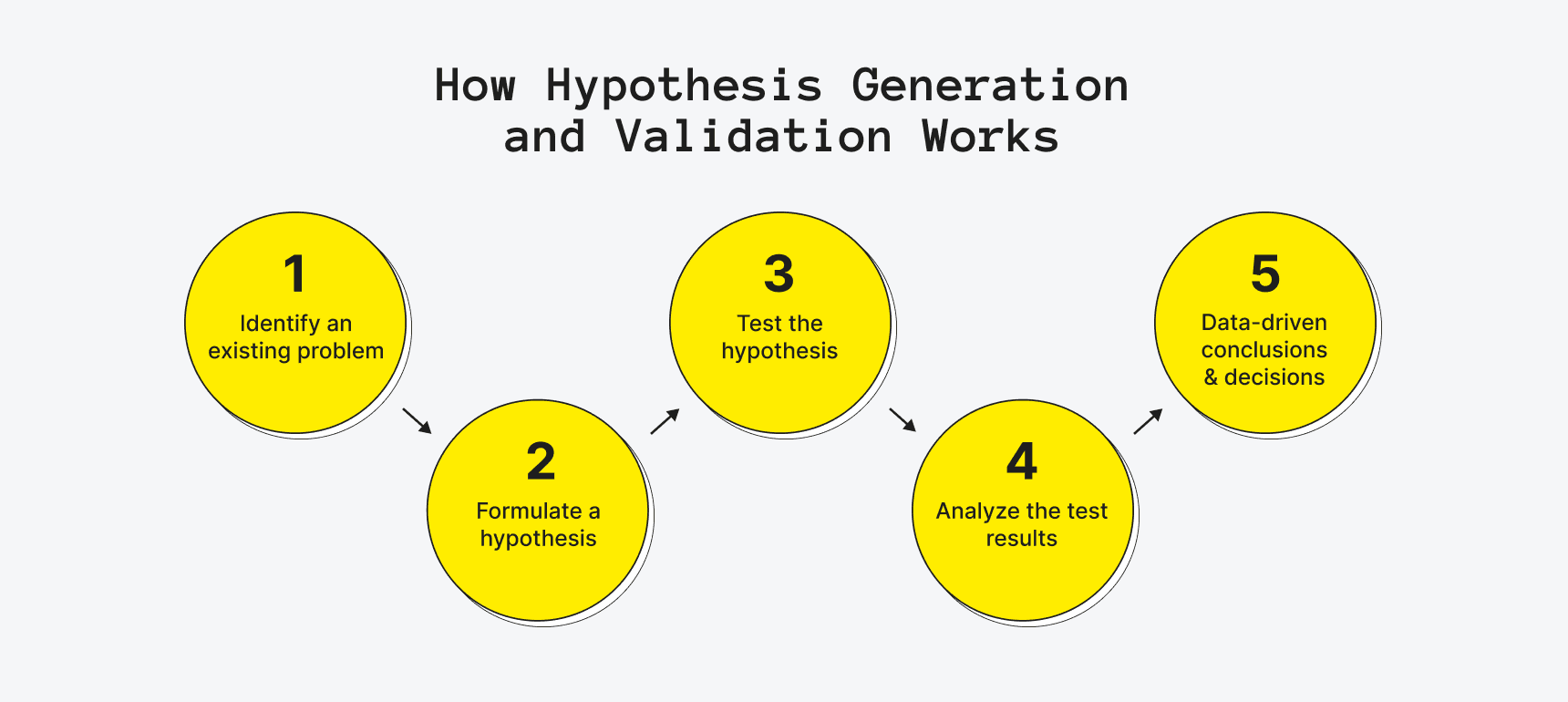
- It all starts with identifying an existing problem . Is there a product area that's experiencing a downfall, a visible trend, or a market gap? Are users often complaining about something in their feedback? Or is there something you're willing to change (say, if you aim to get more profit, increase engagement, optimize a process, expand to a new market, or reach your OKRs and KPIs faster)?
- Teams then need to work on formulating a hypothesis . They put the statement into concise and short wording that describes what is expected to achieve. Importantly, it has to be relevant, actionable, backed by data, and without generalizations.
- Next, they have to test the hypothesis by running experiments to validate it (for instance, via A/B or multivariate testing, prototyping, feedback collection, or other ways).
- Then, the obtained results of the test must be analyzed . Did one element or page version outperform the other? Depending on what you're testing, you can look into various merits or product performance metrics (such as the click rate, bounce rate, or the number of sign-ups) to assess whether your prediction was correct.
- Finally, the teams can make conclusions that could lead to data-driven decisions. For example, they can make corresponding changes or roll back a step.
How Else Can You Generate Product Hypotheses?
Such processes imply sharing ideas when a problem is spotted by digging deep into facts and studying the possible risks, goals, benefits, and outcomes. You may apply various MVP tools like (FigJam, Notion, or Miro) that were designed to simplify brainstorming sessions, systemize pitched suggestions, and keep everyone organized without losing any ideas.
Predictive product analysis can also be integrated into this process, leveraging data and insights to anticipate market trends and consumer preferences, thus enhancing decision-making and product development strategies. This approach fosters a more proactive and informed approach to innovation, ensuring products are not only relevant but also resonate with the target audience, ultimately increasing their chances of success in the market.
Besides, you can settle on one of the many frameworks that facilitate decision-making processes , ideation phases, or feature prioritization . Such frameworks are best applicable if you need to test your assumptions and structure the validation process. These are a few common ones if you're looking toward a systematic approach:
- Business Model Canvas (used to establish the foundation of the business model and helps find answers to vitals like your value proposition, finding the right customer segment, or the ways to make revenue);
- Lean Startup framework (the lean startup framework uses a diagram-like format for capturing major processes and can be handy for testing various hypotheses like how much value a product brings or assumptions on personas, the problem, growth, etc.);
- Design Thinking Process (is all about interactive learning and involves getting an in-depth understanding of the customer needs and pain points, which can be formulated into hypotheses followed by simple prototypes and tests).
Need a hand with product development?
Upsilon's team of pros is ready to share our expertise in building tech products.

How to Make a Hypothesis Statement for a Product
Once you've indicated the addressable problem or opportunity and broken down the issue in focus, you need to work on formulating the hypotheses and associated tasks. By the way, it works the same way if you want to prove that something will be false (a.k.a null hypothesis).
If you're unsure how to write a hypothesis statement, let's explore the essential steps that'll set you on the right track.
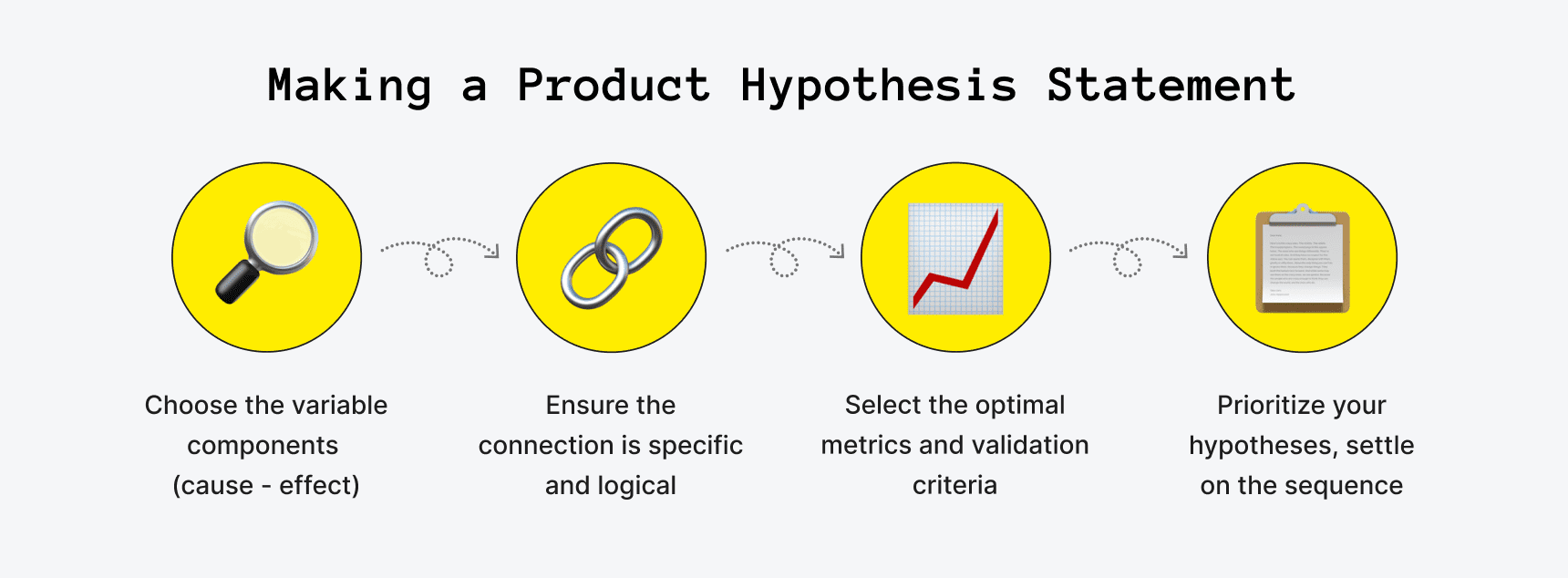
Step 1: Allocate the Variable Components
Product hypotheses are generally different for each case, so begin by pinpointing the major variables, i.e., the cause and effect . You'll need to outline what you think is supposed to happen if a change or action gets implemented.
Put simply, the "cause" is what you're planning to change, and the "effect" is what will indicate whether the change is bringing in the expected results. Falling back on the example we brought up earlier, the ineffective checkout process can be the cause, while the increased percentage of completed orders is the metric that'll show the effect.
Make sure to also note such vital points as:
- what the problem and solution are;
- what are the benefits or the expected impact/successful outcome;
- which user group is affected;
- what are the risks;
- what kind of experiments can help test the hypothesis;
- what can measure whether you were right or wrong.
Step 2: Ensure the Connection Is Specific and Logical
Mind that generic connections that lack specifics will get you nowhere. So if you're thinking about how to word a hypothesis statement, make sure that the cause and effect include clear reasons and a logical dependency .
Think about what can be the precise and link showing why A affects B. In our checkout example, it could be: fewer steps in the checkout and the removed excessive fields will speed up the process, help avoid confusion, irritate users less, and lead to more completed orders. That's much more explicit than just stating the fact that the checkout needs to be changed to get more completed orders.
Step 3: Decide on the Data You'll Collect
Certainly, multiple things can be used to measure the effect. Therefore, you need to choose the optimal metrics and validation criteria that'll best envision if you're moving in the right direction.
If you need a tip on how to create hypothesis statements that won't result in a waste of time, try to avoid vagueness and be as specific as you can when selecting what can best measure and assess the results of your hypothesis test. The criteria must be measurable and tied to the hypotheses . This can be a realistic percentage or number (say, you expect a 15% increase in completed orders or 2x fewer cart abandonment cases during the checkout phase).
Once again, if you're not realistic, then you might end up misinterpreting the results. Remember that sometimes an increase that's even as little as 2% can make a huge difference, so why make 50% the merit if it's not achievable in the first place?
Step 4: Settle on the Sequence
It's quite common that you'll end up with multiple product hypotheses. Some are more important than others, of course, and some will require more effort and input.
Therefore, just as with the features on your product development roadmap , prioritize your hypotheses according to their impact and importance. Then, group and order them, especially if the results of some hypotheses influence others on your list.
Product Hypothesis Examples
To demonstrate how to formulate your assumptions clearly, here are several more apart from the example of a hypothesis statement given above:
- Adding a wishlist feature to the cart with the possibility to send a gift hint to friends via email will increase the likelihood of making a sale and bring in additional sign-ups.
- Placing a limited-time promo code banner stripe on the home page will increase the number of sales in March.
- Moving up the call to action element on the landing page and changing the button text will increase the click-through rate twice.
- By highlighting a new way to use the product, we'll target a niche customer segment (i.e., single parents under 30) and acquire 5% more leads.

How to Validate Hypothesis Statements: The Process Explained
There are multiple options when it comes to validating hypothesis statements. To get appropriate results, you have to come up with the right experiment that'll help you test the hypothesis. You'll need a control group or people who represent your target audience segments or groups to participate (otherwise, your results might not be accurate).
What can serve as the experiment you may run? Experiments may take tons of different forms, and you'll need to choose the one that clicks best with your hypothesis goals (and your available resources, of course). The same goes for how long you'll have to carry out the test (say, a time period of two months or as little as two weeks). Here are several to get you started.
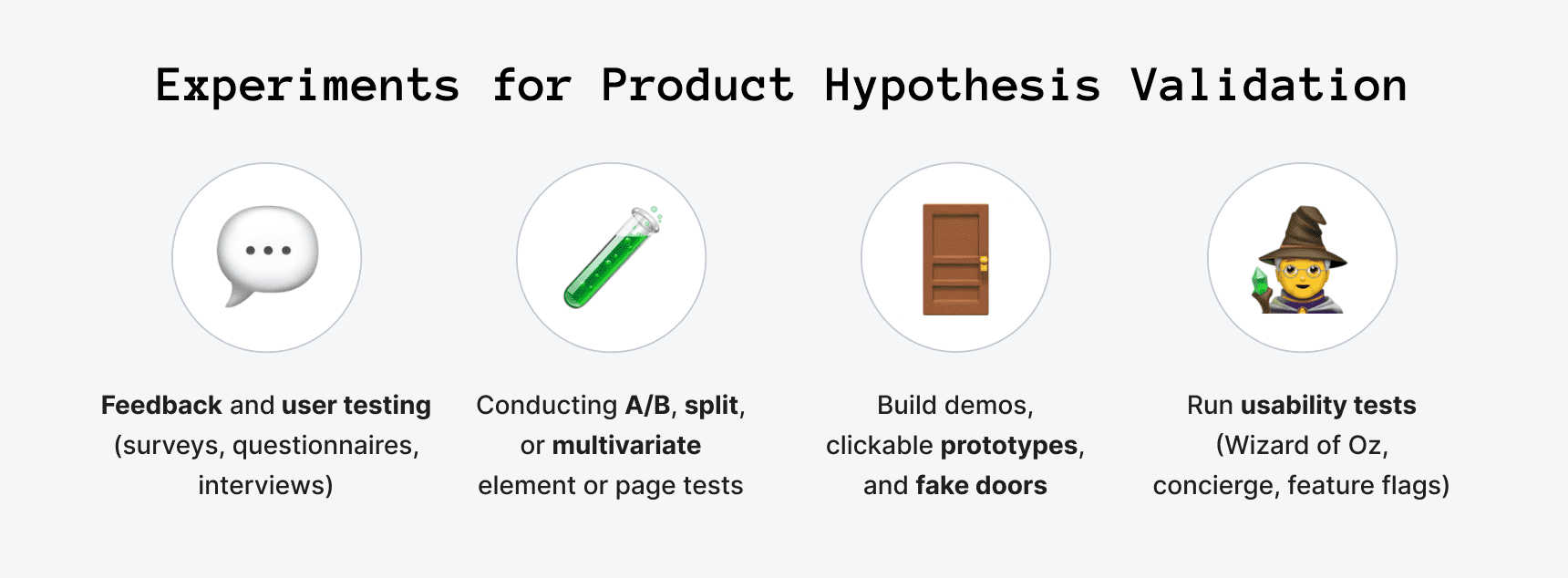
Feedback and User Testing
Talking to users, potential customers, or members of your own online startup community can be another way to test your hypotheses. You may use surveys, questionnaires, or opt for more extensive interviews to validate hypothesis statements and find out what people think. This assumption validation approach involves your existing or potential users and might require some additional time, but can bring you many insights.
Conduct A/B or Multivariate Tests
One of the experiments you may develop involves making more than one version of an element or page to see which option resonates with the users more. As such, you can have a call to action block with different wording or play around with the colors, imagery, visuals, and other things.
To run such split experiments, you can apply tools like VWO that allows to easily construct alternative designs and split what your users see (e.g., one half of the users will see version one, while the other half will see version two). You can track various metrics and apply heatmaps, click maps, and screen recordings to learn more about user response and behavior. Mind, though, that the key to such tests is to get as many users as you can give the tests time. Don't jump to conclusions too soon or if very few people participated in your experiment.
Build Prototypes and Fake Doors
Demos and clickable prototypes can be a great way to save time and money on costly feature or product development. A prototype also allows you to refine the design. However, they can also serve as experiments for validating hypotheses, collecting data, and getting feedback.
For instance, if you have a new feature in mind and want to ensure there is interest, you can utilize such MVP types as fake doors . Make a short demo recording of the feature and place it on your landing page to track interest or test how many people sign up.
Usability Testing
Similarly, you can run experiments to observe how users interact with the feature, page, product, etc. Usually, such experiments are held on prototype testing platforms with a focus group representing your target visitors. By showing a prototype or early version of the design to users, you can view how people use the solution, where they face problems, or what they don't understand. This may be very helpful if you have hypotheses regarding redesigns and user experience improvements before you move on from prototype to MVP development.
You can even take it a few steps further and build a barebone feature version that people can really interact with, yet you'll be the one behind the curtain to make it happen. There were many MVP examples when companies applied Wizard of Oz or concierge MVPs to validate their hypotheses.
Or you can actually develop some functionality but release it for only a limited number of people to see. This is referred to as a feature flag , which can show really specific results but is effort-intensive.
What Comes After Hypothesis Validation?
Analysis is what you move on to once you've run the experiment. This is the time to review the collected data, metrics, and feedback to validate (or invalidate) the hypothesis.
You have to evaluate the experiment's results to determine whether your product hypotheses were valid or not. For example, if you were testing two versions of an element design, color scheme, or copy, look into which one performed best.
It is crucial to be certain that you have enough data to draw conclusions, though, and that it's accurate and unbiased . Because if you don't, this may be a sign that your experiment needs to be run for some additional time, be altered, or held once again. You won't want to make a solid decision based on uncertain or misleading results, right?
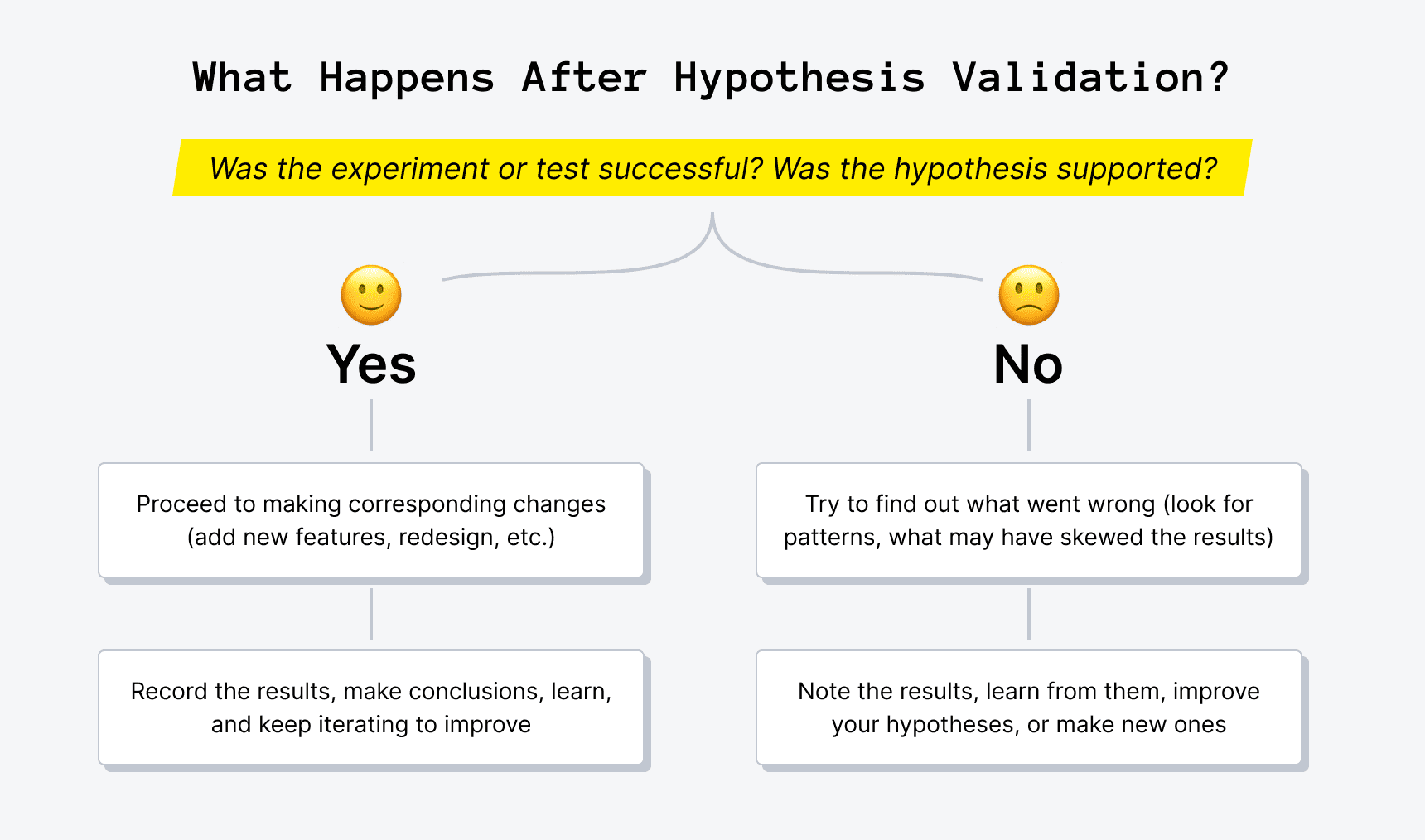
- If the hypothesis was supported , proceed to making corresponding changes (such as implementing a new feature, changing the design, rephrasing your copy, etc.). Remember that your aim was to learn and iterate to improve.
- If your hypothesis was proven false , think of it as a valuable learning experience. The main goal is to learn from the results and be able to adjust your processes accordingly. Dig deep to find out what went wrong, look for patterns and things that may have skewed the results. But if all signs show that you were wrong with your hypothesis, accept this outcome as a fact, and move on. This can help you make conclusions on how to better formulate your product hypotheses next time. Don't be too judgemental, though, as a failed experiment might only mean that you need to improve the current hypothesis, revise it, or create a new one based on the results of this experiment, and run the process once more.
On another note, make sure to record your hypotheses and experiment results . Some companies use CRMs to jot down the key findings, while others use something as simple as Google Docs. Either way, this can be your single source of truth that can help you avoid running the same experiments or allow you to compare results over time.
Have doubts about how to bring your product to life?
Upsilon's team of pros can help you build a product most optimally.
Final Thoughts on Product Hypotheses
The hypothesis-driven approach in product development is a great way to avoid uncalled-for risks and pricey mistakes. You can back up your assumptions with facts, observe your target audience's reactions, and be more certain that this move will deliver value.
However, this only makes sense if the validation of hypothesis statements is backed by relevant data that'll allow you to determine whether the hypothesis is valid or not. By doing so, you can be certain that you're developing and testing hypotheses to accelerate your product management and avoiding decisions based on guesswork.
Certainly, a failed experiment may bring you just as much knowledge and findings as one that succeeds. Teams have to learn from their mistakes, boost their hypothesis generation and testing knowledge , and make improvements according to the results of their experiments. This is an ongoing process, of course, as no product can grow if it isn't iterated and improved.
If you're only planning to or are currently building a product, Upsilon can lend you a helping hand. Our team has years of experience providing product development services for growth-stage startups and building MVPs for early-stage businesses , so you can use our expertise and knowledge to dodge many mistakes. Don't be shy to contact us to discuss your needs!
How Much Does It Cost to Build an AI Solution in 2024?

Top 30 Financial Terms for Startups

Writing a Winning SaaS Business Plan: A How-to Guide
Never miss an update.

Efficient Market Hypothesis (EMH)

Written by True Tamplin, BSc, CEPF®
Reviewed by subject matter experts.
Updated on July 12, 2023
Are You Retirement Ready?
Table of contents, efficient market hypothesis (emh) overview.
The Efficient Market Hypothesis (EMH) is a theory that suggests financial markets are efficient and incorporate all available information into asset prices.
According to the EMH, it is impossible to consistently outperform the market by employing strategies such as technical analysis or fundamental analysis.
The hypothesis argues that since all relevant information is already reflected in stock prices, it is not possible to gain an advantage and generate abnormal returns through stock picking or market timing.
The EMH comes in three forms: weak, semi-strong, and strong, each representing different levels of market efficiency.
While the EMH has faced criticisms and challenges, it remains a prominent theory in finance that has significant implications for investors and market participants.
Types of Efficient Market Hypothesis
The Efficient Market Hypothesis can be categorized into the following:
Weak Form EMH
The weak form of EMH posits that all past market prices and data are fully reflected in current stock prices.
Therefore, technical analysis methods, which rely on historical data, are deemed useless as they cannot provide investors with a competitive edge. However, this form doesn't deny the potential value of fundamental analysis.
Semi-strong Form EMH
The semi-strong form of EMH extends beyond historical prices and suggests that all publicly available information is instantly priced into the market.
This includes financial statements, news releases, economic indicators, and other public disclosures. Therefore, neither technical analysis nor fundamental analysis can yield superior returns consistently.
Strong Form EMH
The most extreme version of EMH, the strong form, asserts that all information, both public and private, is fully reflected in stock prices.
Even insiders with privileged information cannot consistently achieve higher-than-average market returns. This form, however, is widely criticized as it conflicts with securities regulations that prohibit insider trading .
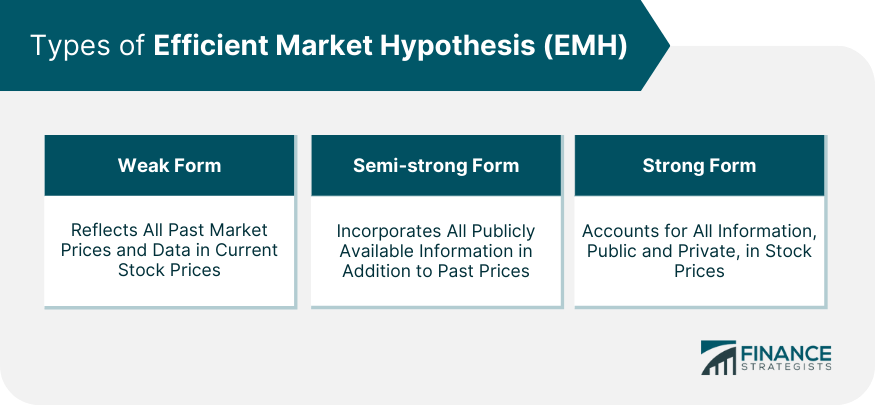
Assumptions of the Efficient Market Hypothesis
Three fundamental assumptions underpin the Efficient Market Hypothesis.
All Investors Have Access to All Publicly Available Information
This assumption holds that the dissemination of information is perfect and instantaneous. All market participants receive all relevant news and data about a security or market simultaneously, and no investor has privileged access to information.
All Investors Have a Rational Expectation
In EMH, it is assumed that investors collectively have a rational expectation about future market movements. This means that they will act in a way that maximizes their profits based on available information, and their collective actions will cause securities' prices to adjust appropriately.
Investors React Instantly to New Information
In an efficient market, investors instantaneously incorporate new information into their investment decisions. This immediate response to news and data leads to swift adjustments in securities' prices, rendering it impossible to "beat the market."
Implications of the Efficient Market Hypothesis
The EMH has several implications across different areas of finance.
Implications for Individual Investors
For individual investors, EMH suggests that "beating the market" consistently is virtually impossible. Instead, investors are advised to invest in a well-diversified portfolio that mirrors the market, such as index funds.
Implications for Portfolio Managers
For portfolio managers , EMH implies that active management strategies are unlikely to outperform passive strategies consistently. It discourages the pursuit of " undervalued " stocks or timing the market.
Implications for Corporate Finance
In corporate finance, EMH implies that a company's stock is always fairly priced, meaning it should be indifferent between issuing debt and equity . It also suggests that stock splits , dividends , and other financial decisions have no impact on a company's value.
Implications for Government Regulation
For regulators , EMH supports policies that promote transparency and information dissemination. It also justifies the prohibition of insider trading.
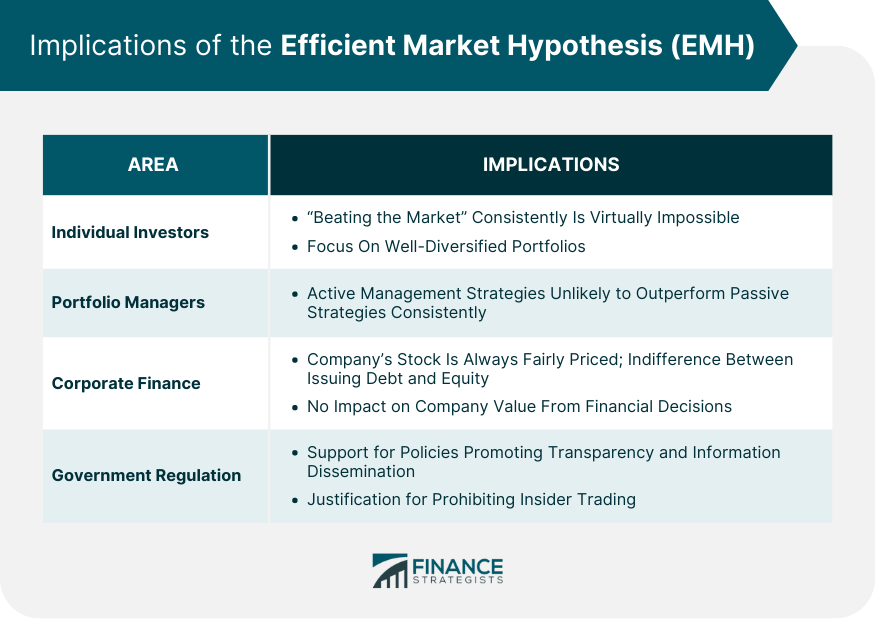
Criticisms and Controversies Surrounding the Efficient Market Hypothesis
Despite its widespread acceptance, the EMH has attracted significant criticism and controversy.
Behavioral Finance and the Challenge to EMH
Behavioral finance argues against the notion of investor rationality assumed by EMH. It suggests that cognitive biases often lead to irrational decisions, resulting in mispriced securities.
Examples include overconfidence, anchoring, loss aversion, and herd mentality, all of which can lead to market anomalies.
Market Anomalies and Inefficiencies
EMH struggles to explain various market anomalies and inefficiencies. For instance, the "January effect," where stocks tend to perform better in January, contradicts the EMH.
Similarly, the "momentum effect" suggests that stocks that have performed well recently tend to continue performing well, which also challenges EMH.
Financial Crises and the Question of Market Efficiency
The Global Financial Crisis of 2008 raised serious questions about market efficiency. The catastrophic market failure suggested that markets might not always price securities accurately, casting doubt on the validity of EMH.
Empirical Evidence of the Efficient Market Hypothesis
Empirical evidence on the EMH is mixed, with some studies supporting the hypothesis and others refuting it.
Evidence Supporting EMH
Several studies have found that professional fund managers, on average, do not outperform the market after accounting for fees and expenses.
This finding supports the semi-strong form of EMH. Similarly, numerous studies have shown that stock prices tend to follow a random walk, supporting the weak form of EMH.
Evidence Against EMH
Conversely, other studies have documented persistent market anomalies that contradict EMH.
The previously mentioned January and momentum effects are examples of such anomalies. Moreover, the occurrence of financial bubbles and crashes provides strong evidence against the strong form of EMH.
Efficient Market Hypothesis in Modern Finance
Despite criticisms, the EMH continues to shape modern finance in profound ways.
EMH and the Rise of Passive Investing
The EMH has been a driving force behind the rise of passive investing. If markets are efficient and all information is already priced into securities, then active management cannot consistently outperform the market.
As a result, many investors have turned to passive strategies, such as index funds and ETFs .
Impact of Technology on Market Efficiency
Advances in technology have significantly improved the speed and efficiency of information dissemination, arguably making markets more efficient. High-frequency trading and algorithmic trading are now commonplace, further reducing the possibility of beating the market.
Future of EMH in Light of Evolving Financial Markets
While the debate over market efficiency continues, the growing influence of machine learning and artificial intelligence in finance could further challenge the EMH.
These technologies have the potential to identify and exploit subtle patterns and relationships that human investors might miss, potentially leading to market inefficiencies.
The Efficient Market Hypothesis is a crucial financial theory positing that all available information is reflected in market prices, making it impossible to consistently outperform the market. It manifests in three forms, each with distinct implications.
The weak form asserts that all historical market information is accounted for in current prices, suggesting technical analysis is futile.
The semi-strong form extends this to all publicly available information, rendering both technical and fundamental analysis ineffective.
The strongest form includes even insider information, making all efforts to beat the market futile. EMH's implications are profound, affecting individual investors, portfolio managers, corporate finance decisions, and government regulations.
Despite criticisms and evidence of market inefficiencies, EMH remains a cornerstone of modern finance, shaping investment strategies and financial policies.
Efficient Market Hypothesis (EMH) FAQs
What is the efficient market hypothesis (emh), and why is it important.
The Efficient Market Hypothesis (EMH) is a theory suggesting that financial markets are perfectly efficient, meaning that all securities are fairly priced as their prices reflect all available public information. It's important because it forms the basis for many investment strategies and regulatory policies.

What are the three forms of the Efficient Market Hypothesis (EMH)?
The three forms of the EMH are the weak form, semi-strong form, and strong form. The weak form suggests that all past market prices are reflected in current prices. The semi-strong form posits that all publicly available information is instantly priced into the market. The strong form asserts that all information, both public and private, is fully reflected in stock prices.
How does the Efficient Market Hypothesis (EMH) impact individual investors and portfolio managers?
According to the EMH, consistently outperforming the market is virtually impossible because all available information is already factored into the prices of securities. Therefore, it suggests that individual investors and portfolio managers should focus on creating well-diversified portfolios that mirror the market rather than trying to beat the market.
What are some criticisms of the Efficient Market Hypothesis (EMH)?
Criticisms of the EMH often come from behavioral finance, which argues that cognitive biases can lead investors to make irrational decisions, resulting in mispriced securities. Additionally, the EMH has difficulty explaining certain market anomalies, such as the "January effect" or the "momentum effect." The occurrence of financial crises also raises questions about the validity of EMH.
How does the Efficient Market Hypothesis (EMH) influence modern finance and its future?
Despite criticisms, the EMH has profoundly shaped modern finance. It has driven the rise of passive investing and influenced the development of many financial regulations. With advances in technology, the speed and efficiency of information dissemination have increased, arguably making markets more efficient. Looking forward, the growing influence of artificial intelligence and machine learning could further challenge the EMH.
About the Author
True Tamplin, BSc, CEPF®
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide , a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University , where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon , Nasdaq and Forbes .
Related Topics
- AML Regulations for Cryptocurrencies
- Active vs Passive Investment Management
- Advantages and Disadvantages of Cryptocurrencies
- Aggressive Investing
- Asset Management vs Investment Management
- Becoming a Millionaire With Cryptocurrency
- Burning Cryptocurrency
- Cheapest Cryptocurrencies With High Returns
- Complete List of Cryptocurrencies & Their Market Capitalization
- Countries Using Cryptocurrency
- Countries Where Bitcoin Is Illegal
- Crypto Investor’s Guide to Form 1099-B
- Cryptocurrency Airdrop
- Cryptocurrency Alerting
- Cryptocurrency Analysis Tool
- Cryptocurrency Cloud Mining
- Cryptocurrency Risks
- Cryptocurrency Taxes
- Depth of Market
- Digital Currency vs Cryptocurrency
- Fundamental Analysis in Cryptocurrencies
- Global Macro Hedge Fund
- Gold-Backed Cryptocurrency
- How Much Does a Wealth Manager Make?
- How to Buy a House With Cryptocurrencies
- How to Cash Out Your Cryptocurrency
- Inventory Turnover Rate (ITR)
- Largest Cryptocurrencies by Market Cap
- Types of Fixed Income Investments
Ask a Financial Professional Any Question
Discover wealth management solutions near you, our recommended advisors.

Claudia Valladares
WHY WE RECOMMEND:
Fee-Only Financial Advisor Show explanation
Bilingual in english / spanish, founder of wisedollarmom.com, quoted in gobanking rates, yahoo finance & forbes.
IDEAL CLIENTS:
Retirees, Immigrants & Sudden Wealth / Inheritance
Retirement Planning, Personal finance, Goals-based Planning & Community Impact

Taylor Kovar, CFP®
Certified financial planner™, 3x investopedia top 100 advisor, author of the 5 money personalities & keynote speaker.
Business Owners, Executives & Medical Professionals
Strategic Planning, Alternative Investments, Stock Options & Wealth Preservation
We use cookies to ensure that we give you the best experience on our website. If you continue to use this site we will assume that you are happy with it.
Fact Checked
At Finance Strategists, we partner with financial experts to ensure the accuracy of our financial content.
Our team of reviewers are established professionals with decades of experience in areas of personal finance and hold many advanced degrees and certifications.
They regularly contribute to top tier financial publications, such as The Wall Street Journal, U.S. News & World Report, Reuters, Morning Star, Yahoo Finance, Bloomberg, Marketwatch, Investopedia, TheStreet.com, Motley Fool, CNBC, and many others.
This team of experts helps Finance Strategists maintain the highest level of accuracy and professionalism possible.
Why You Can Trust Finance Strategists
Finance Strategists is a leading financial education organization that connects people with financial professionals, priding itself on providing accurate and reliable financial information to millions of readers each year.
We follow strict ethical journalism practices, which includes presenting unbiased information and citing reliable, attributed resources.
Our goal is to deliver the most understandable and comprehensive explanations of financial topics using simple writing complemented by helpful graphics and animation videos.
Our writing and editorial staff are a team of experts holding advanced financial designations and have written for most major financial media publications. Our work has been directly cited by organizations including Entrepreneur, Business Insider, Investopedia, Forbes, CNBC, and many others.
Our mission is to empower readers with the most factual and reliable financial information possible to help them make informed decisions for their individual needs.
How It Works
Step 1 of 3, ask any financial question.
Ask a question about your financial situation providing as much detail as possible. Your information is kept secure and not shared unless you specify.

Step 2 of 3
Our team will connect you with a vetted, trusted professional.
Someone on our team will connect you with a financial professional in our network holding the correct designation and expertise.

Step 3 of 3
Get your questions answered and book a free call if necessary.
A financial professional will offer guidance based on the information provided and offer a no-obligation call to better understand your situation.
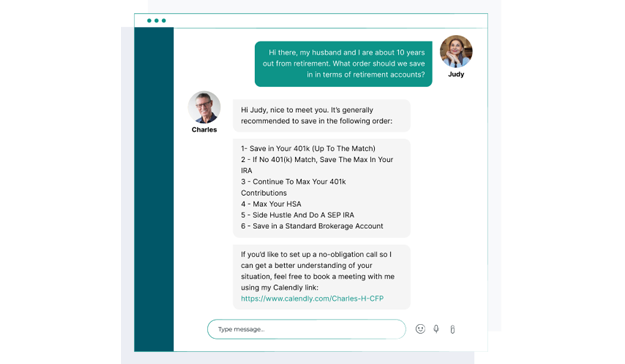
Where Should We Send Your Answer?

Just a Few More Details
We need just a bit more info from you to direct your question to the right person.
Tell Us More About Yourself
Is there any other context you can provide.
Pro tip: Professionals are more likely to answer questions when background and context is given. The more details you provide, the faster and more thorough reply you'll receive.
What is your age?
Are you married, do you own your home.
- Owned outright
- Owned with a mortgage
Do you have any children under 18?
- Yes, 3 or more
What is the approximate value of your cash savings and other investments?
- $50k - $250k
- $250k - $1m
Pro tip: A portfolio often becomes more complicated when it has more investable assets. Please answer this question to help us connect you with the right professional.
Would you prefer to work with a financial professional remotely or in-person?
- I would prefer remote (video call, etc.)
- I would prefer in-person
- I don't mind, either are fine
What's your zip code?
- I'm not in the U.S.
Submit to get your question answered.
A financial professional will be in touch to help you shortly.
Part 1: Tell Us More About Yourself
Do you own a business, which activity is most important to you during retirement.
- Giving back / charity
- Spending time with family and friends
- Pursuing hobbies
Part 2: Your Current Nest Egg
Part 3: confidence going into retirement, how comfortable are you with investing.
- Very comfortable
- Somewhat comfortable
- Not comfortable at all
How confident are you in your long term financial plan?
- Very confident
- Somewhat confident
- Not confident / I don't have a plan
What is your risk tolerance?
How much are you saving for retirement each month.
- None currently
- Minimal: $50 - $200
- Steady Saver: $200 - $500
- Serious Planner: $500 - $1,000
- Aggressive Saver: $1,000+
How much will you need each month during retirement?
- Bare Necessities: $1,500 - $2,500
- Moderate Comfort: $2,500 - $3,500
- Comfortable Lifestyle: $3,500 - $5,500
- Affluent Living: $5,500 - $8,000
- Luxury Lifestyle: $8,000+
Part 4: Getting Your Retirement Ready
What is your current financial priority.
- Getting out of debt
- Growing my wealth
- Protecting my wealth
Do you already work with a financial advisor?
Which of these is most important for your financial advisor to have.
- Tax planning expertise
- Investment management expertise
- Estate planning expertise
- None of the above
Where should we send your answer?
Submit to get your retirement-readiness report., get in touch with, great the financial professional will get back to you soon., where should we send the downloadable file, great hit “submit” and an advisor will send you the guide shortly., create a free account and ask any financial question, learn at your own pace with our free courses.
Take self-paced courses to master the fundamentals of finance and connect with like-minded individuals.
Get Started
To ensure one vote per person, please include the following info, great thank you for voting., get in touch with a financial advisor, submit your info below and someone will get back to you shortly..
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Null and Alternative Hypotheses | Definitions & Examples
Null & Alternative Hypotheses | Definitions, Templates & Examples
Published on May 6, 2022 by Shaun Turney . Revised on June 22, 2023.
The null and alternative hypotheses are two competing claims that researchers weigh evidence for and against using a statistical test :
- Null hypothesis ( H 0 ): There’s no effect in the population .
- Alternative hypothesis ( H a or H 1 ) : There’s an effect in the population.
Table of contents
Answering your research question with hypotheses, what is a null hypothesis, what is an alternative hypothesis, similarities and differences between null and alternative hypotheses, how to write null and alternative hypotheses, other interesting articles, frequently asked questions.
The null and alternative hypotheses offer competing answers to your research question . When the research question asks “Does the independent variable affect the dependent variable?”:
- The null hypothesis ( H 0 ) answers “No, there’s no effect in the population.”
- The alternative hypothesis ( H a ) answers “Yes, there is an effect in the population.”
The null and alternative are always claims about the population. That’s because the goal of hypothesis testing is to make inferences about a population based on a sample . Often, we infer whether there’s an effect in the population by looking at differences between groups or relationships between variables in the sample. It’s critical for your research to write strong hypotheses .
You can use a statistical test to decide whether the evidence favors the null or alternative hypothesis. Each type of statistical test comes with a specific way of phrasing the null and alternative hypothesis. However, the hypotheses can also be phrased in a general way that applies to any test.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

The null hypothesis is the claim that there’s no effect in the population.
If the sample provides enough evidence against the claim that there’s no effect in the population ( p ≤ α), then we can reject the null hypothesis . Otherwise, we fail to reject the null hypothesis.
Although “fail to reject” may sound awkward, it’s the only wording that statisticians accept . Be careful not to say you “prove” or “accept” the null hypothesis.
Null hypotheses often include phrases such as “no effect,” “no difference,” or “no relationship.” When written in mathematical terms, they always include an equality (usually =, but sometimes ≥ or ≤).
You can never know with complete certainty whether there is an effect in the population. Some percentage of the time, your inference about the population will be incorrect. When you incorrectly reject the null hypothesis, it’s called a type I error . When you incorrectly fail to reject it, it’s a type II error.
Examples of null hypotheses
The table below gives examples of research questions and null hypotheses. There’s always more than one way to answer a research question, but these null hypotheses can help you get started.
| ( ) | ||
| Does tooth flossing affect the number of cavities? | Tooth flossing has on the number of cavities. | test: The mean number of cavities per person does not differ between the flossing group (µ ) and the non-flossing group (µ ) in the population; µ = µ . |
| Does the amount of text highlighted in the textbook affect exam scores? | The amount of text highlighted in the textbook has on exam scores. | : There is no relationship between the amount of text highlighted and exam scores in the population; β = 0. |
| Does daily meditation decrease the incidence of depression? | Daily meditation the incidence of depression.* | test: The proportion of people with depression in the daily-meditation group ( ) is greater than or equal to the no-meditation group ( ) in the population; ≥ . |
*Note that some researchers prefer to always write the null hypothesis in terms of “no effect” and “=”. It would be fine to say that daily meditation has no effect on the incidence of depression and p 1 = p 2 .
The alternative hypothesis ( H a ) is the other answer to your research question . It claims that there’s an effect in the population.
Often, your alternative hypothesis is the same as your research hypothesis. In other words, it’s the claim that you expect or hope will be true.
The alternative hypothesis is the complement to the null hypothesis. Null and alternative hypotheses are exhaustive, meaning that together they cover every possible outcome. They are also mutually exclusive, meaning that only one can be true at a time.
Alternative hypotheses often include phrases such as “an effect,” “a difference,” or “a relationship.” When alternative hypotheses are written in mathematical terms, they always include an inequality (usually ≠, but sometimes < or >). As with null hypotheses, there are many acceptable ways to phrase an alternative hypothesis.
Examples of alternative hypotheses
The table below gives examples of research questions and alternative hypotheses to help you get started with formulating your own.
| Does tooth flossing affect the number of cavities? | Tooth flossing has an on the number of cavities. | test: The mean number of cavities per person differs between the flossing group (µ ) and the non-flossing group (µ ) in the population; µ ≠ µ . |
| Does the amount of text highlighted in a textbook affect exam scores? | The amount of text highlighted in the textbook has an on exam scores. | : There is a relationship between the amount of text highlighted and exam scores in the population; β ≠ 0. |
| Does daily meditation decrease the incidence of depression? | Daily meditation the incidence of depression. | test: The proportion of people with depression in the daily-meditation group ( ) is less than the no-meditation group ( ) in the population; < . |
Null and alternative hypotheses are similar in some ways:
- They’re both answers to the research question.
- They both make claims about the population.
- They’re both evaluated by statistical tests.
However, there are important differences between the two types of hypotheses, summarized in the following table.
| A claim that there is in the population. | A claim that there is in the population. | |
|
| ||
| Equality symbol (=, ≥, or ≤) | Inequality symbol (≠, <, or >) | |
| Rejected | Supported | |
| Failed to reject | Not supported |
Prevent plagiarism. Run a free check.
To help you write your hypotheses, you can use the template sentences below. If you know which statistical test you’re going to use, you can use the test-specific template sentences. Otherwise, you can use the general template sentences.
General template sentences
The only thing you need to know to use these general template sentences are your dependent and independent variables. To write your research question, null hypothesis, and alternative hypothesis, fill in the following sentences with your variables:
Does independent variable affect dependent variable ?
- Null hypothesis ( H 0 ): Independent variable does not affect dependent variable.
- Alternative hypothesis ( H a ): Independent variable affects dependent variable.
Test-specific template sentences
Once you know the statistical test you’ll be using, you can write your hypotheses in a more precise and mathematical way specific to the test you chose. The table below provides template sentences for common statistical tests.
| ( ) | ||
| test
with two groups | The mean dependent variable does not differ between group 1 (µ ) and group 2 (µ ) in the population; µ = µ . | The mean dependent variable differs between group 1 (µ ) and group 2 (µ ) in the population; µ ≠ µ . |
| with three groups | The mean dependent variable does not differ between group 1 (µ ), group 2 (µ ), and group 3 (µ ) in the population; µ = µ = µ . | The mean dependent variable of group 1 (µ ), group 2 (µ ), and group 3 (µ ) are not all equal in the population. |
| There is no correlation between independent variable and dependent variable in the population; ρ = 0. | There is a correlation between independent variable and dependent variable in the population; ρ ≠ 0. | |
| There is no relationship between independent variable and dependent variable in the population; β = 0. | There is a relationship between independent variable and dependent variable in the population; β ≠ 0. | |
| Two-proportions test | The dependent variable expressed as a proportion does not differ between group 1 ( ) and group 2 ( ) in the population; = . | The dependent variable expressed as a proportion differs between group 1 ( ) and group 2 ( ) in the population; ≠ . |
Note: The template sentences above assume that you’re performing one-tailed tests . One-tailed tests are appropriate for most studies.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Descriptive statistics
- Measures of central tendency
- Correlation coefficient
Methodology
- Cluster sampling
- Stratified sampling
- Types of interviews
- Cohort study
- Thematic analysis
Research bias
- Implicit bias
- Cognitive bias
- Survivorship bias
- Availability heuristic
- Nonresponse bias
- Regression to the mean
Hypothesis testing is a formal procedure for investigating our ideas about the world using statistics. It is used by scientists to test specific predictions, called hypotheses , by calculating how likely it is that a pattern or relationship between variables could have arisen by chance.
Null and alternative hypotheses are used in statistical hypothesis testing . The null hypothesis of a test always predicts no effect or no relationship between variables, while the alternative hypothesis states your research prediction of an effect or relationship.
The null hypothesis is often abbreviated as H 0 . When the null hypothesis is written using mathematical symbols, it always includes an equality symbol (usually =, but sometimes ≥ or ≤).
The alternative hypothesis is often abbreviated as H a or H 1 . When the alternative hypothesis is written using mathematical symbols, it always includes an inequality symbol (usually ≠, but sometimes < or >).
A research hypothesis is your proposed answer to your research question. The research hypothesis usually includes an explanation (“ x affects y because …”).
A statistical hypothesis, on the other hand, is a mathematical statement about a population parameter. Statistical hypotheses always come in pairs: the null and alternative hypotheses . In a well-designed study , the statistical hypotheses correspond logically to the research hypothesis.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Turney, S. (2023, June 22). Null & Alternative Hypotheses | Definitions, Templates & Examples. Scribbr. Retrieved September 2, 2024, from https://www.scribbr.com/statistics/null-and-alternative-hypotheses/
Is this article helpful?

Shaun Turney
Other students also liked, inferential statistics | an easy introduction & examples, hypothesis testing | a step-by-step guide with easy examples, type i & type ii errors | differences, examples, visualizations, what is your plagiarism score.
- Search Search Please fill out this field.
What Is Strategic Management?
- How It Worls
- The 5 Phases
Why Is Strategic Management Important?
- Strategic Management FAQs
The Bottom Line
- Business Essentials
:max_bytes(150000):strip_icc():format(webp)/wk_headshot_aug_2018_02__william_kenton-5bfc261446e0fb005118afc9.jpg)
Yarilet Perez is an experienced multimedia journalist and fact-checker with a Master of Science in Journalism. She has worked in multiple cities covering breaking news, politics, education, and more. Her expertise is in personal finance and investing, and real estate.
:max_bytes(150000):strip_icc():format(webp)/YariletPerez-d2289cb01c3c4f2aabf79ce6057e5078.jpg)
Investopedia / Alex Dos Diaz
Strategic management is an approach to the management of an organization’s resources in order to achieve its goals and objectives.
Strategic management involves setting objectives, analyzing the competitive environment, analyzing the internal organization, evaluating strategies, and ensuring that management rolls out the strategies across the organization .
Key Takeaways
- Companies, universities, nonprofits, and other organizations can use strategic management as a way to set goals and meet objectives.
- Flexible companies may find it easier to make changes to their structure and plans, while inflexible companies may chafe at a changing environment.
- A strategic manager may oversee strategic management plans and devise ways for organizations to meet their benchmark goals.
Understanding Strategic Management
Strategic management is divided into several schools of thought. A prescriptive approach to strategic management outlines how strategies should be developed, while a descriptive approach focuses on how strategies should be put into practice. These schools differ on whether strategies are developed through an analytic process, in which all threats and opportunities are accounted for, or are more like general guiding principles to be applied.
Business culture , the skills and competencies of employees, and organizational structure are all important factors that influence how an organization can achieve its stated objectives. Inflexible companies may find it difficult to succeed in a changing business environment. Creating a barrier between the development of strategies and their implementation can make it difficult for managers to determine whether objectives have been efficiently met.
While an organization’s upper management is ultimately responsible for its strategy , the strategies are often sparked by actions and ideas from lower-level managers and employees. An organization may have several employees devoted to strategy, rather than relying solely on the chief executive officer ( CEO ) for guidance.
Because of this reality, organizational leaders focus on learning from past strategies and examining the environment at large. The collective knowledge is then used to develop future strategies and to guide the behavior of employees to ensure that the entire organization is moving forward. For these reasons, effective strategic management requires both an inward and outward perspective.
Strategic management extends to internal and external communication practices as well as to tracking, which ensures that the company meets goals as defined in its strategic management plan.
The 5 Phases of Strategic Management
Strategic management involves managing an organization's resources, analyzing internal and external forces, and developing strategies to realize goals and objectives. There are five key phases that can help businesses execute their strategies.
- An organization must first establish clear, realistic goals. Its goals should answer what the company wants to achieve and why. Once set, a company can then identify the objectives, or how the goals will be reached. During this phase, a company can articulate its vision and long- and short-term goals.
- Organizations must then be able to examine, understand, and codify what internal and external forces affect their business and goals, as well as what they need to remain competitive. Analytical tools, such as SWOT analysis , are helpful during this phase.
- Based on the results of the analysis, a company can then develop its strategy, outlining how it will achieve its goals. In this phase, the company will identify the people, technology, and other resources it needs; how these resources will be allocated to fulfill tasks; and what performance metrics are needed to measure success. It is also critical to gain buy-in from stakeholders and business leaders.
- Once the strategies are defined, it is time for execution. The strategy is taken from planning to implementation. During this phase, the allocated resources are placed into action based on their roles and responsibilities.
- The final stage of strategic management is to evaluate the effectiveness of implemented strategies using defined metrics. The company will also determine whether ineffective strategies should be replaced with more viable ones. It should continue to monitor the business landscape and internal operations, as well as maintain strategies that have proven effective.
Example of Strategic Management
Let's say a for-profit technical college wishes to increase new student enrollment and enrolled student graduation rates over the next three years. The purpose is to make the college known as the best buy for a student's money among five for-profit technical colleges in the region, with a goal of increasing revenue.
In that case, strategic management means ensuring the school has funds to create high-tech classrooms and hire the most qualified instructors. The college also invests in marketing and recruitment and implements student retention strategies. The college’s leadership assesses whether its goals have been achieved on a periodic basis.
The purpose of strategic management is to help a company find ways to be more competitive. To that end, putting strategic management plans into practice is the most important aspect of this approach. Some action steps that companies may take to execute their strategic management plans include identifying benchmarks, realigning resources (financial and human), and putting leadership resources in place to oversee the creation, sale, and deployment of products and services.
Strategic management allows a company to analyze areas for operational improvement. In many cases, it may follow an analytical process—identifying specific threats and specific opportunities—unique to the company.
Or a company may choose to just abide by general strategic management guidelines that are applicable to any company.
Strategic management is the process of setting goals, procedures, and objectives in order to make a company or organization more competitive. Typically, strategic management looks at effectively deploying staff and resources to achieve company goals. Often, strategic management includes strategy evaluation, internal organization analysis, and strategy execution throughout the company.
What Is an Example of Strategic Management?
Consider a large company that wants to achieve more ambitious online sales rates. To meet this goal, the company will develop a strategy, communicate the strategy, apply it across various units and departments in the organization, integrate it with employee goals, and execute accordingly. If an effective strategy is applied, ideally, it will help the company achieve its targets through a single, coordinated process.
What Are the Key Elements of Strategic Management?
Strategic management is not a one-size-fits-all strategy. However, there are key elements that are found to be critical. These include goal setting, industry and organizational analyses, strategy formation, strategy implementation; and the measurement, monitoring, and controlling of strategies.
Strategic management is the assembling and management of resources to achieve a company's goals and objectives. Strategic management helps companies set goals, gain a competitive edge, better manage their resources, and more. There is not one prescription for all. Companies must create and adapt a strategic management process that works best for the firm and those they serve. Strategic management does not end with the successful implementation of strategies; it continues for the life of the business.
:max_bytes(150000):strip_icc():format(webp)/GettyImages-1027438182-6962f1838c764e54b86be72a2bbaf78f.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Work & Careers
- Life & Arts
Economist Eugene Fama: ‘Efficient markets is a hypothesis. It’s not reality’
To read this article for free, register now.
Once registered, you can: • Read free articles • Get our Editor's Digest and other newsletters • Follow topics and set up personalised events • Access Alphaville: our popular markets and finance blog
Explore more offers.
Then $75 per month. Complete digital access to quality FT journalism. Cancel anytime during your trial.
FT Digital Edition
Today's FT newspaper for easy reading on any device. This does not include ft.com or FT App access.
- Global news & analysis
- Expert opinion
Standard Digital
Essential digital access to quality FT journalism on any device. Pay a year upfront and save 20%.
- FT App on Android & iOS
- FT Edit app
- FirstFT: the day's biggest stories
- 20+ curated newsletters
- Follow topics & set alerts with myFT
- FT Videos & Podcasts
Terms & Conditions apply
Explore our full range of subscriptions.
Why the ft.
See why over a million readers pay to read the Financial Times.

- Project Management
Home » Free Resources » »
What is Quality Management? A Complete Guide
- Written by Contributing Writer
- Updated on August 27, 2024

The importance of quality cannot be overstated when it comes to businesses, their success and their longevity. When there is quality, it translates to value for customers, streamlined processes, and continual growth.
We often hear the term “quality control” in the context of how a business produces goods or services to the satisfaction of its customers consistently. However, there’s a larger concept at play, which covers quality control and other quality-related strategies. It’s called quality management.
So, what is quality management?
If you’re a project manager or aspiring to be one, you’ll want to understand how quality management works. This article comprehensively examines what it is, how it works, the methods, and everything you need to know about quality management.
We’ll also discuss how you can better understand quality and other project management concepts through a Lean Six Sigma course .
Quality Management: Definition & Examples
In short, it involves management tasks and roles focused on defining and executing quality policies through strategies like quality planning, assurance, and control.
Let’s understand this through an example.
Consider running a bakery on your street. Sales are good, but you notice some areas for enhancement. The nearby shop has fresher flour, and your oven isn’t heating evenly. You decide to upgrade. You monitor the results and plan further refinements.
In essence, this illustrates quality management (QM). It’s the act of assessing and refining quality throughout an organization. It is the act of combining quality assurance (QA) with process enhancement.
QM sets objectives, identifies shortcomings, and makes necessary adjustments. In short, it’s the strategy to improve operations and bridge experience gaps.
Also Read: What Is Lean Management, and Why Is It Worth Mastering?
History of Quality Management in a Nutshell
Quality Management started with Walter Shewhart at Bell Laboratories in the early 20th century. He introduced statistical quality control (SQC), focusing on process improvement over the end product.
During World War II, the U.S. applied SQC for military production. However, post-war civilian manufacturers lagged in adopting these improvements. Then, engineers Deming and Juran traveled to war-torn Japan. Their approach emphasized ‘Total Quality,’ a holistic approach to improvement. Their efforts transformed Japan into a manufacturing titan.
By the 1980s, recognizing Japan’s success and shortcomings, the U.S. adopted Total Quality Management (TQM). 1987, the ISO 9000 standard was introduced, becoming a global quality benchmark.
As the 21st century rolled in, with globalization and technology at the forefront, approaches like Motorola’s Six Sigma emerged, emphasizing near-perfect outputs.
Today, quality management isn’t limited to manufacturing; it’s a universal pursuit, spanning sectors from healthcare to cutting-edge technologies like Blockchain.
What is Quality Management: Four Stages
The four Quality Management (QM) stages are often described as part of the Plan-Do-Check-Act (PDCA) cycle, also known as the Deming Cycle or Shewhart Cycle.
Here’s a brief overview:
This is the initial stage where you identify an opportunity and plan for change. This involves setting objectives, defining processes to meet the objectives, and determining the resources needed.
In this stage, you implement the plan on a small scale, ideally in a controlled environment. This is where the changes are tested, and data is collected for the next step.
Here, you assess your test results, comparing them against the expected outcomes to determine any differences. You’ll analyze the data collected during the “Do” phase to understand whether the change has led to improvements.
You take corrective action Based on the “Check” phase results. If the implemented change leads to the desired improvement, you can scale up the implementation. If not, you must revisit the “Plan” phase to identify new or refined solutions.
This cycle keeps repeating, always aiming to make things better. When one cycle finishes, it helps set up the next, ensuring we’re always checking and improving our methods for the best results.
Also Read: What Is Process Mapping & How to Create It?
Most Popular Quality Management Methods
Four essential quality management methods stand out. Each offers unique benefits and challenges; the best fit depends on a company’s structure, needs, and goals.
Standardized Systems
Set by the government, these standards, like ISO certifications, are mandatory for certain products (e.g., baby car seats). Some firms adopt these standards voluntarily to enhance their reputation or align with their vision.
Total Quality Management (TQM)
This aims to boost quality throughout a company. It assesses the firm’s overarching quality goals and then evaluates every process and factor affecting quality for improvement.
A detailed, data-centered approach, Six Sigma focuses on defining, measuring, analyzing, enhancing, and maintaining quality. Predominantly used by large manufacturers, it necessitates thorough training. For deeper insights, consider enrolling in a boot camp.
Continuous Quality Improvement (CQI)
As the name suggests, the enhancement never stops. Recognizing perfection is a journey, CQI prioritizes people over processes, using the Plan, Do, Check, Act framework to improve quality.
What are the Main Quality Management Principles?
Quality management revolves around several guiding principles. Adopted by the International Standard for Quality Management, these principles enable organizations to refine their processes for optimal results:
Prioritizing Customers
Every organization’s main goal should be to understand and surpass the needs and expectations of its customers. By recognizing and fulfilling both current and future customer needs, businesses ensure customer loyalty, leading to increased revenue. Effective and efficient processes enhance quality, satisfying more customers.
Importance of Leadership
The success of any organization is directly linked to its leadership. Effective leaders foster unity, setting clear goals that engage employees and stakeholders. A positive organizational culture helps employees achieve their potential and work towards company goals. Engaging employees in goal-setting often leads to heightened productivity and commitment.
Engaging Employees
Active employee involvement is crucial. All staff should be empowered to contribute value regardless of their employment status or role. Constant skill improvement and consistent performance should be promoted. Empowerment, decision-making involvement, and recognition motivate employees, ensuring they feel valued and responsible for their contributions.
Adopting a Process-Centric Mindset
Organizational performance hinges on efficient and effective processes. Recognizing that superior processes lead to consistency, efficiency, and ongoing improvement is vital. Organizations thrive when they can effectively manage inputs and the processes that yield outputs.
Commitment to Ongoing Improvement
An enduring focus on improvement can transform organizations, enhancing flexibility, performance, and adaptability. A proactive stance on creating and evolving processes is crucial to stay competitive.
Data-Driven Decision Making
Grounding decisions in analyzed and validated data offers a clearer understanding of the market dynamics. Such a factual approach ensures businesses can execute strategies that yield desired outcomes while providing a basis for past decisions. It aids in understanding the interconnected nature of actions and their consequences.
Building Strong Relationships
Effective relationship management, especially with suppliers and stakeholders, is paramount. Recognizing that various parties can influence an organization’s trajectory ensures better supply chain management. By cultivating and maintaining these relationships, businesses enhance their chances of long-term success and collaboration.
Also Read: What Is Lean Six Sigma? A Comprehensive Guide to Understanding the Methodology
What is a Quality Management System (QMS)?
Let us look at how the principles of quality management are implemented through the QMS or Quality Management System.
A Quality Management System (QMS) ensures that products are made to meet quality standards. It monitors products from start to finish, ensuring they align with industry and regulatory norms.
QMS can be manual or software-driven and comprises two main parts: quality assurance and quality control.
While quality assurance focuses on inspecting processes during production, quality control evaluates the end products using customer feedback and on-site inspections. Quality assurance maintains consistent quality during production, and quality control verifies the final product’s quality.
The Importance of Quality Management Systems in Business
Why do businesses need QMS? Here is a breakdown of what it means to the business processes:
Product Oversight
The QMS constantly monitors products, beginning with acquiring raw materials and continuing to ship finished goods. It’s vigilant about tracking the quantity of products made and promptly identifying faulty ones.
Vendor Product Evaluation
This aspect of the QMS ensures that products sourced from vendors align with predetermined quality benchmarks. Vendor products can be quickly identified and returned if they fall short of these standards.
Scheduled Evaluations
Regular assessments are scheduled for staff, products, and equipment, ensuring ongoing quality compliance.
Error Tracking and Rectification
One vital feature of a QMS is its ability to spot and record current errors within the system. Beyond identifying them, it establishes strategies to both rectify present issues and devise mechanisms to prevent similar problems in the future.
Supplier Performance Assessment
A QMS employs key performance indicators (KPIs) to evaluate suppliers’ efficiency and reliability critically.
Policy and Procedure Updates
An effective QMS stays updated with any changes to company policies and procedures.
Moreover, it provides detailed and actionable reports on all facets of the quality management process.
Things to Remember When Choosing a Quality Management System
When choosing a QMS, numerous options can be overwhelming. Here’s a condensed guide to making an informed decision.
Industry Experience
It’s essential to check if the QMS provider has experience in your sector. They should have worked with similar businesses and be conversant with your specific quality requirements. Moreover, they should offer reliable references and display deep industry knowledge in software, installation, and training.
Functionality Needs
Determine if the software aligns with your business requirements. Key functionalities to consider include:
- Meeting industry-specific quality compliance standards
- Integration capabilities with other systems
- Tracking non-conformities and offering a comprehensive audit trail
- Features like Correct and Preventative Action (CAPA) management to address root causes
- AQL and RQL sampling throughout processes
- Efficient document control to log all quality endeavors
- Display of KPIs for supplier performance evaluation
- Flexibility to gather data from various sources, including mobile devices or the web
Real-time visibility into quality events is crucial. A robust QMS provides insights across the enterprise, allowing proactive issue resolution. It should offer the ability to monitor vendors and employees for compliance and training needs.
Master Quality Management for Better Project Outcomes
Quality management is paramount in every industry. For project managers, it’s critical to ensure streamlined processes that lead to the desired level of quality and performance.
If you want formal training in quality management, enrolling in a professional Lean Six Sigma certification can be a great starting point.
You might also like to read:
Six Sigma Principles: A Comprehensive Guide to Implementing and Optimizing Your Processes
Six Sigma vs. Lean Six Sigma: Which Methodology Is Right for Your Business?
What is Lean Methodology?
Six Sigma in Healthcare: Concept, Benefits and Examples
The Top 24 Lean Six Sigma Interview Questions for 2023
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Recommended Articles

Career Tips: How to Handle Project Failures?
Understanding why projects fail is the key to preventing future setbacks. Learn how to handle project failures and turn them into valuable learning experiences.

Ensuring Project Success: What is the Critical Path Method in Project Management?
The critical path method in project management helps identify tasks that affect a project’s timeline. Learn its basics and how to apply it to keep complex projects on track.

What is a Stakeholder in Project Management?
Understand the role of stakeholders in project management. This guide explains who they are, why they matter, and how to manage them for successful project delivery.

WBS in Project Management: What It Is and How You Use It?
Discover the significance of Work Breakdown Structure (WBS) in project management on the UMass Amherst Boot Camps blog. Learn what WBS is and how it can streamline your project planning and execution process.

Project Management Qualifications: Here’s What You Need to Know
This article provides an in-depth look at project management qualifications, including what it entails, eligibility, requirements, a solid career path, and why certification is a good idea.

How to Ace the PMP Exam in 2024-25? A Comprehensive Guide
Looking for help with PMP exam preparation? Our comprehensive guide is the ultimate resource for your PMP exam-related tips and strategies.
Lean Six Sigma Certification
Learning Format
Online Bootcamp
Program benefits.
- Green and Black Belt exam training material included
- Aligned with IASSC-Lean Six Sigma
- Masterclasses from top faculty of UMass Amherst
- UMass Amherst Alumni Association membership
2024 Theses Doctoral
Towards a Computational Theory of the Brain: The Simplest Neural Models, and a Hypothesis for Language
Mitropolsky, Daniel
Obtaining a computational understanding of the brain is one of the most important problems in basic science. However, the brain is an incredibly complex organ, and neurobiological research has uncovered enormous amounts of detail at almost every level of analysis (the synapse, the neuron, other brain cells, brain circuits, areas, and so on); it is unclear which of these details are conceptually significant to the basic way in which the brain computes. An essential approach to the eventual resolution of this problem is the definition and study of theoretical computational models, based on varying abstractions and inclusions of such details. This thesis defines and studies a family of models, called NEMO, based on a particular set of well-established facts or well-founded assumptions in neuroscience: atomic neural firing, random connectivity, inhibition as a local dynamic firing threshold, and fully local plasticity. This thesis asks: what sort of algorithms are possible in these computational models? To the extent possible, what seem to be the simplest assumptions where interesting computation becomes possible? Additionally, can we find algorithms for cognitive phenomena that, in addition to serving as a "proof of capacity" of the computational model, otherwise reflect what is known about these processes in the brain? The major contributions of this thesis include: 1. The formal definition of the basic-NEMO and NEMO models, with an explication of their neurobiological underpinnings (that is, realism as abstractions of the brain). 2. Algorithms for the creation of neural \emph{assemblies}, or highly dense interconnected subsets of neurons, and various operations manipulating such assemblies, including reciprocal projection, merge, association, disassociation, and pattern completion, all in the basic-NEMO model. Using these operations, we show the Turing-completeness of the NEMO model (with some specific additional assumptions). 3. An algorithm for parsing a small but non-trivial subset of English and Russian (and more generally any regular language) in the NEMO model, with meta-features of the algorithm broadly in line with what is known about language in the brain. 4. An algorithm for parsing a much larger subset of English (and other languages), in particular handling dependent (embedded) clauses, in the NEMO model with some additional memory assumptions. We prove that an abstraction of this algorithm yields a new characterization of the context-free languages. 5. Algorithms for the blocks-world planning task, which involves outputting a sequence of steps to rearrange a stack of cubes in one order into another target order, in the NEMO model. A side consequence of this work is an algorithm for a chaining operation in basic-NEMO. 6. Algorithms for several of the most basic and initial steps in language acquisition in the baby brain. This includes an algorithm for the learning of the simplest, concrete nouns and action verbs (words like "cat" and "jump") from whole sentences in basic-NEMO with a novel representation of word and contextual inputs. Extending the same model, we present an algorithm for an elementary component of syntax, namely learning the word order of 2-constituent intransitive and 3-constituent transitive sentences. These algorithms are very broadly in line with what is known about language in the brain.
- Computer science
- Neurosciences
- Brain--Physiology
- Language acquisition
- Computational linguistics
- Computational neuroscience
- English language
- Russian language

More About This Work
- DOI Copy DOI to clipboard
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Braunwald's Corner
- ESC Guidelines
- EHJ Dialogues
- Issue @ a Glance Podcasts
- CardioPulse
- Weekly Journal Scan
- European Heart Journal Supplements
- Year in Cardiovascular Medicine
- Asia in EHJ
- Most Cited Articles
- ESC Content Collections
- Author Guidelines
- Submission Site
- Why publish with EHJ?
- Open Access Options
- Submit from medRxiv or bioRxiv
- Author Resources
- Self-Archiving Policy
- Read & Publish
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About European Heart Journal
- Editorial Board
- About the European Society of Cardiology
- ESC Publications
- War in Ukraine
- ESC Membership
- ESC Journals App
- Developing Countries Initiative
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Table of contents, tables of recommendations, list of tables, list of figures, abbreviations and acronyms, 1. preamble, 2. introduction, 3. pathophysiology of elevated blood pressure and hypertension, 4. clinical consequences of elevated blood pressure and hypertension, 5. measuring blood pressure, 6. definition and classification of elevated blood pressure and hypertension, and cardiovascular disease risk assessment, 7. diagnosing hypertension and investigating underlying causes, 8. preventing and treating elevated blood pressure and hypertension, 9. managing specific patient groups or circumstances, 10. acute and short-term lowering of blood pressure, 11. patient-centred care in hypertension, 12. key messages, 13. gaps in the evidence, 14. ‘what to do’ and ‘what not to do’ messages from the guidelines, 15. evidence tables, 16. data availability statement, 17. author information, 18. appendix, 19. references, 2024 esc guidelines for the management of elevated blood pressure and hypertension: developed by the task force on the management of elevated blood pressure and hypertension of the european society of cardiology (esc) and endorsed by the european society of endocrinology (ese) and the european stroke organisation (eso).
John William McEvoy and Rhian M Touyz Chairpersons contributed equally to the document and are joint corresponding authors.
Cian P McCarthy and Rosa Maria Bruno Task Force Co-ordinators contributed equally to the document.
Author/Task Force Member affiliations are listed in author information.
1 Representing the European Renal Association (ERA), 2 Representing the European Society of Endocrinology (ESE), 3 Representing the European Stroke Organisation (ESO), 4 Representing the European Geriatric Medicine Society (EuGMS).
ESC Clinical Practice Guidelines (CPG) Committee: listed in the Appendix.
ESC subspecialty communities having participated in the development of this document:
Associations: Association of Cardiovascular Nursing & Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Association of Percutaneous Cardiovascular Interventions (EAPCI), Heart Failure Association (HFA).
Councils: Council for Cardiology Practice, Council on Hypertension, Council on Stroke.
Working Groups: Aorta and Peripheral Vascular Diseases, Cardiovascular Pharmacotherapy, E-Cardiology.
Patient Forum
Disclaimer. The ESC Guidelines represent the views of the ESC and were produced after careful consideration of the scientific and medical knowledge and the evidence available at the time of their publication. The ESC is not responsible in the event of any contradiction, discrepancy and/or ambiguity between the ESC Guidelines and any other official recommendations or guidelines issued by the relevant public health authorities, in particular in relation to good use of healthcare or therapeutic strategies. Health professionals are encouraged to take the ESC Guidelines fully into account when exercising their clinical judgment, as well as in the determination and the implementation of preventive, diagnostic or therapeutic medical strategies; however, the ESC Guidelines do not override, in any way whatsoever, the individual responsibility of health professionals to make appropriate and accurate decisions in consideration of each patient’s health condition and in consultation with that patient and, where appropriate and/or necessary, the patient’s caregiver. Nor do the ESC Guidelines exempt health professionals from taking into full and careful consideration the relevant official updated recommendations or guidelines issued by the competent public health authorities, in order to manage each patient’s case in light of the scientifically accepted data pursuant to their respective ethical and professional obligations. It is also the health professional’s responsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of prescription. The ESC warns readers that the technical language may be misinterpreted and declines any responsibility in this respect.
Permissions. The content of these European Society of Cardiology (ESC) Guidelines has been published for personal and educational use only. No commercial use is authorized. No part of the ESC Guidelines may be translated or reproduced in any form without written permission from the ESC. Permissions can be obtained upon submission of a written request to Oxford University Press, the publisher of the European Heart Journal and the party authorized to handle such permissions on behalf of the ESC ( [email protected] ).

- Article contents
- Figures & tables
- Supplementary Data
John William McEvoy, Cian P McCarthy, Rosa Maria Bruno, Sofie Brouwers, Michelle D Canavan, Claudio Ceconi, Ruxandra Maria Christodorescu, Stella S Daskalopoulou, Charles J Ferro, Eva Gerdts, Henner Hanssen, Julie Harris, Lucas Lauder, Richard J McManus, Gerard J Molloy, Kazem Rahimi, Vera Regitz-Zagrosek, Gian Paolo Rossi, Else Charlotte Sandset, Bart Scheenaerts, Jan A Staessen, Izabella Uchmanowicz, Maurizio Volterrani, Rhian M Touyz, ESC Scientific Document Group , 2024 ESC Guidelines for the management of elevated blood pressure and hypertension: Developed by the task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO) , European Heart Journal , 2024;, ehae178, https://doi.org/10.1093/eurheartj/ehae178
- Permissions Icon Permissions
1. Preamble 7
2. Introduction 8
2.1. What is new 9
3. Pathophysiology of elevated blood pressure and hypertension 17
4. Clinical consequences of elevated blood pressure and hypertension 17
5. Measuring blood pressure 18
5.1. Introduction and pertinent definitions 18
5.2. Practical recommendations for measuring blood pressure 19
5.2.1. Clinical validation of equipment for measuring blood pressure 19
5.2.2. Office blood pressure measurement 19
5.2.3. Home blood pressure measurement 20
5.2.4. Ambulatory blood pressure measurement 22
5.2.5. Comparison of home and ambulatory blood pressure monitoring 23
5.3. What is the best method for measuring blood pressure to diagnose hypertension? 23
5.3.1. Blood pressure measurement for hypertension screening 23
5.3.2. Blood pressure measurement for diagnosing hypertension 23
5.4. What is the best method for measuring blood pressure for long-term management of hypertension? 23
5.4.1. Home monitoring 23
5.4.2. Ambulatory monitoring 23
5.5. Measuring blood pressure in selected groups 24
5.5.1. Pregnancy 24
5.5.2. Atrial fibrillation 24
5.5.3. Orthostatic hypotension 24
5.6. Novel methods of measuring blood pressure 24
6. Definition and classification of elevated blood pressure and hypertension, and cardiovascular disease risk assessment 25
6.1. Definition and classification of elevated blood pressure and hypertension 25
6.2. Principles of a risk-based approach for managing blood pressure and preventing cardiovascular disease 25
6.2.1. Role of cardiovascular disease risk assessment 25
6.3. Predicting cardiovascular disease risk 26
6.3.1. 10-year cardiovascular disease risk-prediction models 27
6.4. Refining cardiovascular disease risk estimation beyond risk models 28
6.4.1. Sex-specific non-traditional cardiovascular disease risk modifiers 28
6.4.2. Non-traditional cardiovascular disease risk modifiers shared by men and women 29
6.4.3. Additional risk decision tests 30
6.5. Summary of the cardiovascular disease risk stratification approach for allocating blood pressure treatment 30
7. Diagnosing hypertension and investigating underlying causes 32
7.1. Screening for hypertension 32
7.2. Confirming the diagnosis of hypertension 32
7.3. Communicating the diagnosis 33
7.4. Baseline assessment and diagnostic approach 33
7.4.1. Medical history, medication history, and physical examination 33
7.4.2. Drug adherence and persistence with treatment 34
7.4.3. Routine and optional tests 34
7.4.3.1. The kidneys 36
7.4.3.2. The heart 36
7.4.3.3. The arteries 37
7.4.4. Genetic testing 37
7.5. Resistant hypertension: definition and diagnosis 37
7.6. Secondary hypertension: when to screen/further investigations 39
7.6.1. General considerations 39
7.6.2. Primary aldosteronism 39
7.6.3. Renovascular hypertension 40
7.6.4. Obstructive sleep apnoea syndrome 40
7.6.5. Phaeochromocytoma/paraganglioma 43
8. Preventing and treating elevated blood pressure and hypertension 43
8.1. Prevention strategies in early life 43
8.2. Non-pharmacological interventions 43
8.2.1. Dietary sodium and potassium intake 43
8.2.1.1. Sodium 43
8.2.1.2. Potassium 44
8.2.2. Physical activity and exercise 45
8.2.3. Weight reduction and diet 46
8.2.4. Alcohol, coffee, and soft drinks 46
8.2.5. Smoking 46
8.3. Pharmacological interventions 47
8.3.1. Treatment strategy to reduce adverse cardiovascular disease outcomes 47
8.3.2. Drug classes with evidence on clinical outcomes in the target population 47
8.3.3. New therapies with blood pressure-lowering properties that await supportive evidence from cardiovascular outcomes trials prior to guideline endorsement and routine use in hypertension 48
8.3.4. Drug combinations and up-titrating strategies 48
8.3.5. A practical algorithm for intensive, effective, and tolerable blood pressure lowering with drug therapy, including considerations around single-pill combinations 48
8.3.6. Timing of blood pressure-lowering drug treatment 51
8.4. Selecting patients for pharmacological blood pressurelowering treatment 51
8.5. Intensity of blood pressure-lowering therapy and ideal treatment targets 53
8.5.1. Expected degree of blood pressure reduction with approved drugs 53
8.5.2. The ideal target of blood pressure-lowering treatment 53
8.5.3. Personalizing treatment strategies 54
8.5.4. Duration and monitoring of drug therapy 55
8.6. Device-based blood pressure lowering 55
8.6.1. Catheter-based renal denervation 55
8.6.2. Other devices 57
8.7. Unintended and potentially harmful consequences of blood pressure lowering and implications for treatment targets 57
8.7.1. Adverse effects of blood pressure-lowering medications 57
8.7.1.1. Symptomatic adverse effects 57
8.7.1.2. Renal effects 57
8.7.1.3. Erectile dysfunction 57
8.7.2. Pill burden and non-adherence 57
8.7.3. Potentially harmful consequences of blood pressure lowering for frail older people 57
8.7.4. Clinical inertia in blood pressure lowering 57
9. Managing specific patient groups or circumstances 58
9.1. Young adulthood (18–40 years) 58
9.1.1. Definition and epidemiology 58
9.1.2. Secondary hypertension in young adulthood 58
9.1.3. Measurement and management of blood pressure in young adults 58
9.2. Pregnancy 58
9.2.1. Definition and epidemiology 58
9.2.2. Classifying hypertension in pregnancy 58
9.2.3. Measuring blood pressure in pregnancy 59
9.2.4. Investigating hypertension in pregnancy 59
9.2.5. Preventing hypertension and pre-eclampsia 59
9.2.6. Treatment initiation and blood pressure targets 59
9.2.7. Managing mild hypertension in pregnancy (office blood pressure 140–159/90–109 mmHg) 59
9.2.8. Managing severe hypertension in pregnancy (>160/110 mmHg) 60
9.2.9. Managing blood pressure post-partum 60
9.2.10. Risk of recurrence of hypertensive disorders in a subsequent pregnancy 60
9.3. Very old age (≥85 years), frailty, multimorbidity, and polypharmacy 60
9.3.1. Definition of frailty 60
9.3.2. Randomized controlled trials of blood pressure lowering in frail older patients 61
9.3.3. Starting blood pressure-lowering treatment in very old or frail patients 62
9.3.4. Maintaining blood pressure lowering in very old or frail patients 62
9.4. Isolated systolic and diastolic hypertension 62
9.4.1. Definition of isolated systolic hypertension 62
9.4.2. Isolated systolic hypertension, risk factors, and ageing 62
9.4.3. Isolated systolic hypertension in young adults 63
9.4.4. Isolated diastolic hypertension 63
9.5. Orthostatic hypotension with supine hypertension 63
9.6. Diabetes 64
9.6.1. Diabetes and elevated blood pressure/hypertension 64
9.6.2. J-shaped curve of blood pressure and risk of cardiovascular disease in patients with diabetes 64
9.6.3. Managing blood pressure in diabetes 64
9.7. Chronic kidney disease 64
9.7.1. Relationship between hypertension and chronic kidney disease 64
9.7.2. Blood pressure lowering in chronic kidney disease 65
9.7.3. Managing blood pressure in chronic kidney disease 65
9.7.4. Blood pressure targets in chronic kidney disease 65
9.8. Cardiac disease 65
9.8.1. Blood pressure thresholds and targets in patients with cardiac disease 65
9.8.2. Coronary artery disease with particular reference to the blood pressure J-curve 66
9.8.3. Valvular heart disease 66
9.8.4. Heart failure 66
9.8.5. Heart rhythm disease (including AF) 67
9.9. Chronic cerebrovascular disease and/or cognitive impairment 67
9.9.1. Role of hypertension in chronic cerebrovascular disease 67
9.9.2. Treatment in patients with history of prior stroke or transient ischaemic attack 67
9.9.3. Treatment in patients with chronic cerebrovascular disease and cognitive impairment 67
9.10. Aortopathy 68
9.10.1. Coarctation of the aorta 68
9.10.2. Bicuspid aortic valve-related aortopathy 68
9.10.3. Preventing aortic dilation and dissection in high-risk patients 68
9.11. Different ethnic groups 68
9.12. Nocturnal hypertension 68
9.12.1. Definition 68
9.12.2. Epidemiology 69
9.12.3. Night-time blood pressure as a cardiovascular disease risk factor 69
9.12.4. Treatment of nocturnal hypertension 69
9.13. Resistant hypertension 69
9.13.1. Definition of resistant hypertension 69
9.13.2. Non-pharmacological interventions 69
9.13.3. Pharmacological interventions 69
9.13.4. Devices for blood pressure lowering 70
9.14. Management of specific causes of secondary hypertension 71
9.14.1. General considerations 71
9.14.2. Primary aldosteronism 71
9.14.3. Renovascular hypertension 71
9.14.4. Phaeochromocytoma/paraganglioma 72
9.14.5. Obstructive sleep apnoea syndrome 72
9.14.6. Drug-induced hypertension 72
9.14.6.1. Anticancer drug-induced hypertension 72
9.14.7. Other forms of secondary hypertension 72
10. Acute and short-term lowering of blood pressure 72
10.1. Acute blood pressure management in hypertensive emergencies 72
10.1.1. Definition and characteristics of hypertensive emergencies 72
10.1.2. Acute management of hypertensive emergencies 73
10.1.3. Prognosis and follow-up 73
10.2. Acute blood pressure management in acute intracerebral haemorrhage 73
10.3. Acute blood pressure management in acute ischaemic stroke 73
10.4. Acute blood pressure management in pre-eclampsia and severe hypertension in pregnancy 74
10.4.1. Pre-eclampsia 74
10.4.2. Severe acute hypertension in pregnancy 74
10.5. Peri-operative acute management of elevated blood pressure 74
10.5.1. Blood pressure-lowering drugs in the peri-operative phase 74
11. Patient-centred care in hypertension 75
11.1. Definition 75
11.2. Communicating consequences of treatment 75
11.3. Self-measuring and monitoring 76
11.4. Facilitating medication adherence and persistence 76
11.5. Multidisciplinary management 76
12. Key messages 77
13. Gaps in the evidence 78
14. ‘What to do’ and ‘what not to do’ messages from the guidelines 78
15. Evidence tables 82
16. Data availability statement 82
17. Author information 82
18. Appendix 82
19. References 83
Recommendation Table 1 — Recommendations for measuring blood pressure (see Evidence Tables 1–8) 24
Recommendation Table 2 — Recommendations for categorizing blood pressure (see Evidence Table 9) 25
Recommendation Table 3 — Recommendations for assessing cardiovascular disease risk among individuals with elevated blood pressure (office systolic blood pressure 120–139 mmHg or diastolic blood pressure 70–89 mmHg) (see Evidence Tables 10 and 11) 28
Recommendation Table 4 — Recommendations for refining cardiovascular disease risk (see Evidence Tables 12–14) 30
Recommendation Table 5 — Recommendations for blood pressure screening (see Evidence Table 15) 32
Recommendation Table 6 — Recommendations for confirming hypertension diagnosis 32
Recommendation Table 7 — Recommendations for assessing adherence and persistence with treatment (see Evidence Table 16) 34
Recommendation Table 8 — Recommendations for assessing renal hypertension-mediated organ damage 36
Recommendation Table 9 — Recommendations for assessing cardiac hypertension-mediated organ damage 36
Recommendation Table 10 — Recommendations for assessing vascular hypertension-mediated organ damage (see Evidence Table 17) 37
Recommendation Table 11 — Recommendations for genetic testing in hypertension management 37
Recommendation Table 12 — Recommendations for resistant hypertension work-up (see Evidence Table 18) 39
Recommendation Table 13 — Recommendations for screening for secondary hypertension (see Evidence Tables 19 and 20) 43
Recommendation Table 14 — Recommendations for screening for hypertension in children and adolescents (see Evidence Table 21) 43
Recommendation Table 15 — Recommendations for non-pharmacological treatment of blood pressure and cardiovascular risk reduction (see Evidence Tables 22–26) 47
Recommendation Table 16 — Recommendations for pharmacological treatment of hypertension (see Evidence Tables 27, 28, and 29) 51
Recommendation Table 17 — Recommendations for initiating blood pressure-lowering treatment (see Evidence Tables 30–32) 52
Recommendation Table 18 — Recommendations for blood pressure targets with treatment (see Evidence Table 34) 55
Recommendation Table 19 — Recommendations for follow-up in patients with treated hypertension (see Evidence Table 33) 55
Recommendation Table 20 — Recommendations for device-based treatment of hypertension (see Evidence Table 35) 56
Recommendation Table 21 — Recommendations for managing hypertension in young adults (see Evidence Tables 36 and 37) 58
Recommendation Table 22 — Recommendations for managing hypertension in pregnancy (see Evidence Tables 38–40) 60
Recommendation Table 23 — Recommendations for managing hypertension in patients who are very old or frail (see Evidence Table 41) 62
Recommendation Table 24 — Recommendations for managing hypertension in patients with orthostatic hypotension 64
Recommendation Table 25 — Recommendations for managing hypertension in patients with diabetes 64
Recommendation Table 26 — Recommendations for managing hypertension in patients with chronic kidney disease 65
Recommendation Table 27 — Recommendations for managing hypertension in patients with cardiac disease 67
Recommendation Table 28 — Recommendations for managing hypertension in patients with chronic cerebrovascular disease and cognitive impairment 68
Recommendation Table 29 — Recommendations for managing hypertension in different ethnic groups 68
Recommendation Table 30 — Recommendations for treating resistant hypertension (see Evidence Tables 42 and 43) 70
Recommendation Table 31 — Recommendations for managing hypertension in patients with renovascular hypertension (see Evidence Tables 44 and 45) 71
Recommendation Table 32 — Recommendations for acutely managing blood pressure in patients with intracerebral haemorrhage or acute ischaemic stroke 73
Recommendation Table 33 — Recommendations for acutely managing blood pressure in patients with severe hypertension in pregnancy and pre-eclampsia (see Evidence Table 46) 74
Recommendation Table 34 — Recommendations for communicating consequences of treatment (see Evidence Table 47) 76
Recommendation Table 35 — Recommendations for self-measuring and monitoring blood pressure (see Evidence Table 48) 76
Recommendation Table 36 — Recommendations for multi/interdisciplinary blood pressure management (see Evidence Table 49) 76
Table 1 Classes of recommendations 7
Table 2 Levels of evidence 8
Table 3 New recommendations 9
Table 4 Revised recommendations 12
Table 5 Comparison of office, home, and ambulatory blood pressure measurement thresholds for elevated blood pressure and hypertension 22
Table 6 Comparison of ambulatory and home blood pressure monitoring 23
Table 7 Key illness representations and treatment beliefs: how these apply to communicating a hypertension diagnosis to the patient (note that gender influences these representations) 34
Table 8 Routine tests recommended in the initial work-up of a patient with elevated blood pressure or hypertension 35
Table 9 Optional tests that may be used as clinically indicated in the initial work-up of a patient with elevated blood pressure or hypertension to assess hypertension-mediated organ damage or established cardiovascular disease 36
Table 10 Current definition of resistant hypertension 39
Table 11 Conditions found to cause pseudo-resistance or resistance to blood pressure-lowering treatment 39
Table 12 Drugs and conditions that affect aldosterone, renin, and aldosterone-to-renin ratio 40
Table 13 Optional tests that should be used to screen for secondary hypertension in the presence of suggestive signs, symptoms, or medical history 41
Table 14 Initiation of blood pressure-lowering treatment based on confirmed blood pressure category and cardiovascular disease risk 52
Table 15 What to do and what not to do 78
Figure 1 Pathophysiology of elevated blood pressure and hypertension 17
Figure 2 Persistently elevated blood pressure and hypertension lead to hypertension-mediated organ damage and cardiovascular disease 18
Figure 3 Summary of office blood pressure measurement 20
Figure 4 Summary of home blood pressure measurement 21
Figure 5 Summary of ambulatory blood pressure measurement 22
Figure 6 Blood pressure categories 26
Figure 7 Sufficiently high cardiovascular risk conditions that warrant blood pressure-lowering treatment among adults with elevated blood pressure 27
Figure 8 Cardiovascular disease risk modifiers to consider for up-classification of risk 29
Figure 9 Summary of cardiovascular disease risk-stratification approach for blood pressure treatment in adults with elevated blood pressure 31
Figure 10 Protocol for confirming hypertension diagnosis 33
Figure 11 Definitions, assessments, and potential interventions for the three phases of adherence to BP-lowering medications 35
Figure 12 Tests and criteria for defining hypertension-mediated organ damage and considerations for their use in clinical practice 38
Figure 13 Summary of primary aldosteronism as a common form of secondary hypertension 41
Figure 14 Summary of renovascular disease as a common form of secondary hypertension 42
Figure 15 Summary of obstructive sleep apnoea as a common form of secondary hypertension 42
Figure 16 Physical activity according to different types of exercise and reduction of blood pressure and overall cardiovascular disease risk 44
Figure 17 Effects of main lifestyle factors on blood pressure and cardiovascular risk reduction 45
Figure 18 Practical algorithm for pharmacological blood pressure lowering 49
Figure 19 Central Illustration 50
Figure 20 Systolic blood pressure categories and treatment target range 54
Figure 21 Frailty assessment in the management of blood pressure 61
Figure 22 Management of resistant hypertension 70
Figure 23 Patient-centred care 75
Figure 24 The five dimensions of adherence (WHO, 2003) applied to hypertension 77
Ankle–brachial index
Ambulatory blood pressure monitoring
Action to Control Cardiovascular Risk in Diabetes
Angiotensin-converting enzyme
Albumin:creatinine ratio
Atrial fibrillation
Apnoea–hypopnoea index
As low as reasonably achievable
Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack
Automated office blood pressure (measurement)
Angiotensin receptor blocker
Angiotensin receptor-neprilysin inhibitor
Aldosterone-to-renin ratio
Atherosclerotic cardiovascular disease
Body mass index
Blood pressure
Body surface area
Coronary artery calcium
Coronary artery disease
Calcium channel blocker
Chronic Hypertension and Pregnancy
Confidence interval
Chronic kidney disease
Chronic Kidney Disease Epidemiology Collaboration
Coronavirus disease 2019
Continuous positive airway pressure
Clinical Practice Guidelines
Computed tomography
Cardiovascular disease
Dietary Approaches to Stop Hypertension
Diastolic blood pressure
Diet, ExerCIse and carDiovascular hEalth–Salt
European Association for Cardio-Thoracic Surgery
Electrocardiogram
Estimated glomerular filtration rate
European Prospective Investigation into Cancer and Nutrition
European Society of Cardiology
European Society of Hypertension
Effects of intensive Systolic blood Pressure lowering treatment in reducing RIsk of vascular evenTs
Fibromuscular dysplasia-induced renovascular hypertension
Glomerular filtration rate
Glucagon-like peptide-1
General practitioner
Glycated haemoglobin
Home blood pressure monitoring
High-density lipoprotein
Heart failure with preserved ejection fraction
Heart failure with (mildly) reduced ejection fraction
Human immunodeficiency virus
Hypertension-mediated organ damage
Intramuscular
Intravenous
Kidney Disease: Improving Global Outcomes
Left atrial
Low-density lipoprotein
Left ventricular
Left ventricular hypertrophy
Mineralocorticoid receptor antagonist
Magnetic resonance imaging
Number needed to treat
N-terminal pro-brain natriuretic peptide
Obstructive sleep apnoea syndrome
Phaeochromocytoma/paraganglioma
Prospective Randomized Evaluation of Preoperative Angiotensin-Converting Enzyme Inhibition
Patient-Reported Experience Measures
Patient-Reported Outcome Measures
Percutaneous transluminal renal angioplasty
Pulse wave velocity
Renin-angiotensin-aldosterone system
A Study of the Recor Medical Paradise System in Clinical Hypertension
Renin–angiotensin system
Randomized controlled trial
Renovascular hypertension
Relative wall thickness
Systolic blood pressure
Systematic COronary Risk Evaluation 2
Systematic COronary Risk Evaluation 2–Older Persons
Sodium–glucose co-transporter 2
Single-nucleotide polymorphism
Sympathetic nervous system
Single-pill combination
Systolic Blood Pressure Intervention Trial
Salt Substitute and Stroke Study
Strategy of Blood Pressure Intervention in Elderly Hypertensive Patients
Semaglutide Treatment Effect in People with Obesity
Transient ischaemic attack
Treating Resistant Hypertension Using Lifestyle Modification to Promote Health
Thyroid-stimulating hormone
World Health Organization
White matter lesion
Guidelines evaluate and summarize available evidence with the aim of assisting health professionals in proposing the best diagnostic or therapeutic approach for an individual patient with a given condition. Guidelines are intended for use by health professionals and the European Society of Cardiology (ESC) makes its guidelines freely available.
ESC Guidelines do not override the individual responsibility of health professionals to make appropriate and accurate decisions in consideration of each patient’s health condition and in consultation with that patient or the patient’s caregiver where appropriate and/or necessary. It is also the health professional’s responsibility to verify the rules and regulations applicable in each country to drugs and devices at the time of prescription and to respect the ethical rules of their profession.
ESC Guidelines represent the official position of the ESC on a given topic and are regularly updated when warranted by new evidence. ESC Policies and Procedures for formulating and issuing ESC Guidelines can be found on the ESC website ( https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Guidelines-development/Writing-ESC-Guidelines ). This guideline version updates and replaces the previous version from 2018.
The Members of this task force were selected by the ESC to include professionals involved in the medical care of patients with this pathology, as well as patient representatives and methodologists. The selection procedure included an open call for authors and aimed to include members from across the whole of the ESC region and from relevant ESC Subspecialty Communities. Consideration was given to diversity and inclusion, notably with respect to gender and country of origin. The task force performed a critical review and evaluation of the published literature on diagnostic and therapeutic approaches including assessment of the risk-benefit ratio. The strength of every recommendation and the level of evidence supporting them were weighed and scored according to predefined scales as outlined in Tables 1 and 2 below. Patient-Reported Outcome Measures (PROMs) and Patient-Reported Experience Measures (PREMs) were also evaluated as the basis for recommendations and/or discussion in these guidelines. The task force followed ESC voting procedures and all approved recommendations were subject to a vote and achieved at least 75% agreement among voting members. Members of the task force with declared interests on specific topics were asked to abstain from voting on related recommendations.
Classes of recommendations

Levels of evidence

The experts of the writing and reviewing panels provided declaration of interest forms for all relationships that might be perceived as real or potential sources of conflicts of interest. Their declarations of interest were reviewed according to the ESC declaration of interest rules, which can be found on the ESC website ( http://www.escardio.org/guidelines ) and have been compiled in a report published in a supplementary document with the guidelines. Funding for the development of ESC Guidelines is derived entirely from the ESC with no involvement of the healthcare industry.
The ESC Clinical Practice Guidelines (CPG) Committee supervises and co-ordinates the preparation of new guidelines and is responsible for the approval process. In addition to review by the CPG Committee, ESC Guidelines undergo multiple rounds of double-blind peer review by external experts, including members from across the whole of the ESC region, all National Cardiac Societies of the ESC and from relevant ESC Subspecialty Communities. After appropriate revisions, the guidelines are signed off by all the experts in the task force. The finalized document is signed off by the CPG Committee for publication in the European Heart Journal .
ESC Guidelines are based on analyses of published evidence, chiefly on clinical trials and meta-analyses of trials, but potentially including other types of studies. Evidence tables summarizing key information from relevant studies are generated early in the guideline development process to facilitate the formulation of recommendations, to enhance comprehension of recommendations after publication, and reinforce transparency in the guidelines development process. The tables are published in their own section of ESC Guidelines and reference specific recommendation tables.
Off-label use of medication may be presented in these guidelines if a sufficient level of evidence shows that it can be considered medically appropriate for a given condition. However, the final decisions concerning an individual patient must be made by the responsible health professional giving special consideration to:
The specific situation of the patient. Unless otherwise provided for by national regulations, off-label use of medication should be limited to situations where it is in the patient’s interest with regard to the quality, safety, and efficacy of care, and only after the patient has been informed and has provided consent;
Country-specific health regulations, indications by governmental drug regulatory agencies, and the ethical rules to which health professionals are subject, where applicable.
This 2024 document updates the 2018 ESC/European Society of Hypertension (ESH) Guidelines on the management of arterial hypertension. 1 While the current document builds on prior guidelines, it also incorporates important updates and new recommendations based on current evidence. For example:
The title has changed from ‘Guidelines on the management of arterial hypertension’ to ‘Guidelines on the management of elevated blood pressure and hypertension’. This is based on evidence that the risk for cardiovascular disease (CVD) attributable to blood pressure (BP) is on a continuous exposure scale, not a binary scale of normotension vs. hypertension. 2 , 3 Updated evidence also increasingly demonstrates the benefit on CVD outcomes of BP-lowering medications among persons with high CVD risk and BP levels that are elevated but that do not meet traditional thresholds used to define hypertension. The term ‘arterial’ is removed from the title of the 2024 Guidelines, as arterial hypertension can also occur in the pulmonary arteries, which is not a focus here.
The 2024 Guidelines continue to define hypertension as office systolic BP of ≥140 mmHg or diastolic BP of ≥90 mmHg. However, a new BP category called ‘Elevated BP’ is introduced. Elevated BP is defined as an office systolic BP of 120–139 mmHg or diastolic BP of 70–89 mmHg.
A major, evidence-based change in the 2024 Guidelines is the recommendation to pursue a target systolic BP of 120–129 mmHg among adults receiving BP-lowering medications. There are several important caveats to this recommendation, including: (i) the requirement that treatment to this BP target is well tolerated by the patient, (ii) the fact that more lenient BP targets can be considered in persons with symptomatic orthostatic hypotension, those aged 85 years or over, or those with moderate-to-severe frailty or limited life expectancy, and (iii) a strong emphasis on out-of-office BP measurement to confirm the systolic BP target of 120–129 mmHg is achieved. For those selected individual cases where a target systolic BP of 120–129 mmHg is not pursued, either due to intolerance or the existence of conditions that favour a more lenient BP target, we recommend targeting a BP that is as low as reasonably achievable. Personalized clinical decision-making and shared decisions with the patient are also emphasized.
Another important change in the 2024 Guidelines compared with earlier versions is the increased focus on evidence related to fatal and non-fatal CVD outcomes rather than surrogate outcomes such as BP lowering alone. Except for lifestyle interventions and low-risk non-pharmacological interventions aimed at implementation or care delivery, the current guidelines require that, for a Class I recommendation to be made for a drug or procedural intervention, the evidence must show benefit on CVD outcomes and not only BP lowering.
The task force comprised of a balanced representation of males and females.
The present guidelines consider sex and gender as an integral component throughout the document, rather than in a separate section at the end. In this document, sex is the biological condition of being female or male from conception, based on genes, and gender is the socio-cultural dimension of being a woman or a man in a given society, based on gender roles, gender norms, gender identity, and gender relations valid in the respective society at a given timepoint. 4 , 5

The task force recognized that a major challenge in guideline usage is poor implementation. This likely contributes to suboptimal control of hypertension. 7–9 To address this, a dedicated section on implementation is included in the Supplementary data online . Moreover, through a new initiative, we include information from national societies following a survey on guideline implementation completed during the national society peer review of the guidelines document. It is hoped this information may help inform national societies about potential barriers to implementation.
2.1. What is new
These 2024 Guidelines contain a number of new and revised recommendations, which are summarized in Tables 3 and 4 , respectively.
New recommendations

Revised recommendations

Persistently high BP in systemic arteries is the hallmark of hypertension, which is the most important modifiable risk factor for all-cause and CVD morbidity and mortality globally. 2 Most patients with hypertension have essential or primary hypertension, where the exact cause remains unknown, while an estimated 10% have secondary hypertension, with an identifiable cause (notably some studies indicate that the prevalence of secondary hypertension may be substantially higher, with modern systematic screening). 10
The pathophysiology of hypertension involves complex interactions between environmental and behavioural factors, genes, hormonal networks, and multiple organ systems (renal, cardiovascular, and central nervous system 11 ) ( Figure 1 ). In addition, vascular and immune mechanisms are involved. 12 Dysregulation of these processes leads to hypertension, which if uncontrolled, can lead to hypertension-mediated organ damage (HMOD) and adverse CVD outcomes.

Pathophysiology of elevated blood pressure and hypertension.
BP, blood pressure; PNS, parasympathetic nervous system; RAAS, renin-angiotensin-aldosterone system; SNP, single-nucleotide polymorphism; SNS, sympathetic nervous system. Complex interplay between genes, environmental, and behavioural factors, organs, physiological systems, and neurohumoral processes contribute to BP regulation. Dysfunction of these processes leads to hypertension. The contribution of these factors to elevated BP and hypertension may differ among males and females.
Details on the pathophysiological processes, molecular mechanisms, and environmental and psychosocial elements that underlie hypertension are provided in the Supplementary text ( Supplementary data online ).
Longstanding hypertension causes organ damage and ultimately leads to cardiovascular, cerebrovascular, and clinical renal disease, which are all major contributors to the global burden of chronic disease ( Figure 2 ). 2 , 13–22 Organs adversely affected by elevated BP and hypertension include the heart, brain, kidneys, eyes, and vessels (macrocirculation and microcirculation in organs with low resistance, such as the brain or kidney 23 ), which undergo structural and functional changes. Although factors besides BP can contribute to these changes (i.e. dyslipidaemia, hyperglycaemia), we use the term ‘hypertension-mediated organ damage’ to indicate the presence of subclinical complications of hypertension that indicate high risk for subsequent clinical events. HMOD may have different profiles in men and women; for instance, left ventricular hypertrophy (LVH) and left atrial dilatation are more frequent in women. 24–28

Persistently elevated blood pressure and hypertension lead to hypertension-mediated organ damage and cardiovascular disease.
AF, atrial fibrillation; CAD, coronary artery disease; GFR, glomerular filtration rate; LA, left atrial; LV, left ventricular; LVH, left ventricular hypertrophy. See the supplementary data online for detailed information on sex differences.
Evidence of HMOD usually indicates long-standing elevated BP and/or hypertension and confers incremental prognostic information regarding CVD risk in all BP categories. 29–31 Unless treated, HMOD can progress from asymptomatic to symptomatic, ultimately resulting in overt CVD events. 31
The pathophysiological mechanisms underlying HMOD in the heart, brain, kidneys, vessels, and eyes are detailed in the Supplementary text ( Supplementary data online ). The clinical consequences of HMOD, especially cerebrovascular disease (stroke and cognitive decline), kidney disease (acute and chronic), and heart disease [heart failure, atrial fibrillation (AF), ischaemic heart disease, and valvular disease] are also discussed in the Supplementary text ( Supplementary data online ). In addition, the Supplement highlights the impact of different measures of BP on CVD risk, including systolic BP, diastolic BP, pulse pressure, and BP variability. 22 , 32–36
5.1. Introduction and pertinent definitions
This section reviews practical aspects of BP measurement, including technique and clinical validation of devices. It also reviews the evidence for the most appropriate BP measurement methods when screening populations for hypertension, diagnosing hypertension, and managing patients receiving BP-lowering interventions. The current guidelines promote use of out-of-office measurement for diagnosis and ongoing management of hypertension, reflecting increasing evidence for the stronger relationship of home and ambulatory monitoring with outcomes, the ability to detect white-coat and masked hypertension, new BP treatment targets as low as 120–129 mmHg systolic ( Table 5 ), and evidence supporting enabling patient involvement and shared decision-making.
Comparison of office, home, and ambulatory blood pressure measurement thresholds for elevated blood pressure and hypertension
| . | Office BP (mmHg) . | Home BP (mmHg) . | Daytime ABPM (mmHg) . | 24 h ABPM (mmHg) . | Night-time ABPM (mmHg) . |
|---|---|---|---|---|---|
| Non-elevated BP | <120/70 | <120/70 | <120/70 | <115/65 | <110/60 |
| Elevated BP | 120/70–<140/90 | 120/70–<135/85 | 120/70–<135/85 | 115/65–<130/80 | 110/60–<120/70 |
| Hypertension | ≥140/90 | ≥135/85 | ≥135/85 | ≥130/80 | ≥120/70 |
| . | Office BP (mmHg) . | Home BP (mmHg) . | Daytime ABPM (mmHg) . | 24 h ABPM (mmHg) . | Night-time ABPM (mmHg) . |
|---|---|---|---|---|---|
| Non-elevated BP | <120/70 | <120/70 | <120/70 | <115/65 | <110/60 |
| Elevated BP | 120/70–<140/90 | 120/70–<135/85 | 120/70–<135/85 | 115/65–<130/80 | 110/60–<120/70 |
| Hypertension | ≥140/90 | ≥135/85 | ≥135/85 | ≥130/80 | ≥120/70 |
ABPM, ambulatory blood pressure monitoring; BP, blood pressure.
a The BP thresholds provided assume that a standardized approach to office BP measurement is performed ( Figure 3 ). However, evidence indicates that office BP measurement in routine clinical settings is often not done using a standardized approach and, in this case, the routine office BP value may be 5–10 mmHg higher than it would have been if measured using the recommended standardized approach. 65 , 66
Definitions:
Systolic BP: arterial BP during systole (maximum arterial pulsatile pressure). This is measured using an auscultatory device at the onset of the first Korotkoff sound. Oscillometric devices estimate systole using an algorithm that imputes from mean arterial pressure. 37
Diastolic BP: arterial BP during diastole (minimum arterial pulsatile pressure). This is measured using an auscultatory device at the time of complete disappearance of the Korotkoff sounds (fifth sound). If there is no disappearance of sounds (no fifth sound) then the fourth Korotkoff sound (muffling) is used to estimate diastolic BP. Oscillometric devices estimate diastole using an algorithm that imputes from mean arterial pressure. 37
Inter-arm difference: systolic BP difference of >10 mmHg when BP is measured sequentially in each arm. 38
Postural/orthostatic hypotension: decrement of ≥20 mmHg in systolic BP and/or ≥10 mmHg in diastolic BP when BP is measured in the standing position at 1 and/or 3 min after standing following a 5-min period in the sitting or lying position.
White-coat hypertension: BP that is above the threshold for diagnosing hypertension in the office but below the threshold in home/ambulatory settings, e.g. ≥140/90 mmHg in office but <135/85 mmHg at home/ambulatory daytime (or 24-h BP < 130/80 mmHg).
Masked hypertension: BP that is below the hypertension diagnostic threshold in the office but above the hypertension diagnostic threshold in home/ambulatory settings, e.g. <140/90 mmHg in clinic but ≥135/85 mmHg at home/ambulatory daytime (or 24-h BP ≥130/80 mmHg).
Office BP: also known as clinic BP. The two terms are interchangeable. This guidelines document uses ‘office BP’ preferentially. Of note, office BP can be measured manually or using an automated device. In addition, automated office BP (AOBP) can be conducted in a setting attended by a healthcare professional or in an unattended fashion. Finally, not all office BP measurements are equal, with some facilities using a standardized method (which is recommended and outlined below) and others unfortunately using suboptimal approaches to office BP measurement.
Home BP measurement (HBPM): an out-of-office approach to measuring BP when the patient measures their own BP at home using a validated monitor (usually an upper-arm oscillometric cuff device).
Ambulatory BP measurement (ABPM): an out-of-office BP measurement that uses a fully automated oscillometric device, usually for a 24-h period, and measures BP at set intervals.
5.2. Practical recommendations for measuring blood pressure
5.2.1. clinical validation of equipment for measuring blood pressure.
A prerequisite of BP measurement is that it must be undertaken using a device that has been clinically validated and confirmed to be accurate. Of the commercially available oscillometric BP measurement devices, as few as 6% have been adequately tested. 39–41 National and international organizations provide lists of validated monitors (e.g. www.stridebp.org , www.validatebp.org ).
Since the 2018 ESC/ESH Guidelines on the management of arterial hypertension, three arbiters of device accuracy (the Association for the Advancement of Medical Instrumentation, the ESH, and the International Organization for Standardization) have published a universal standard for validating devices for measuring BP. 42 This standard will likely become widely adopted. Validation standards and methodology need to be developed and implemented for novel BP measurement devices that are non-occlusive and ‘cuffless’. 43 , 44
5.2.2. Office blood pressure measurement
All BP measurements can be influenced by circumstances of measurement, including position, ambient temperature, the technique of measurement, accuracy of equipment, and physical condition of the patient. 45 For BP measurements in the office, we recommend following a standardized method ( Figure 3 ).

Summary of office blood pressure measurement.
BP, blood pressure.
Patient preparation: BP should be measured with the patient seated comfortably after 5 min of rest. Patients should avoid exercising and stimulants (caffeine, tobacco) for at least 30 min before measurement. The patient’s bladder should be emptied if needed. 46 Patients should be seated with their legs unfolded and their back supported at the time of measurement. The arm should be supported (to avoid isometric exercise-induced increases in BP). Clothing at the location of the cuff placement should be removed; rolling up of shirt sleeves should be avoided as this can result in a tourniquet effect.
BP measurement technique: auscultatory or oscillometric techniques can be used to measure BP non-invasively. The manual auscultatory approach is the traditional method of measuring systolic and diastolic BP at the brachial artery site using a stethoscope. In contrast, oscillometric devices compute mean arterial BP using the oscillation amplitude with cuff deflation (or inflation) and then estimate systolic and diastolic BP. Oscillometric devices can be semi-automated (taking one reading per activation) or fully automated (obtaining multiple readings before averaging them). Oscillometric devices are not typically validated for use in AF, and the manual auscultatory method is preferred in these circumstances when feasible. 47–49
BP cuff selection and positioning: an appropriately sized cuff should be used, as an under-sized or over-sized cuff will artificially elevate or reduce BP, respectively. 50 The bladder length should be 75%–100% and the width 35%–50% of the arm circumference. The arm circumference can be measured at the mid-point of the olecranon and the acromion but many cuffs include sizing indicators. The cuff should be positioned on the patient’s upper arm at the level of the heart with the lower edge of the cuff a few centimetres above the antecubital fossa. The stethoscope should not be placed under the cuff. In those with significant obesity where a correctly fitting upper arm cuff is not available, measurement at the lower arm or wrist can be considered as an alternative. 51
BP measurement by manual auscultation: three BP measurements should be taken, each 1–2 min apart, and additional measurements only if the readings differ by >10 mmHg (e.g. this may occur with arrhythmias or white-coat effects). The BP recorded should be the average of the last two BP readings.
BP measurement using AOBP measurement: as noted above, AOBP using oscillometric devices may be obtained with (attended) or without (unattended) clinicians or staff present. Clear evidence regarding superiority of unattended vs. attended AOBP in managing BP to reduce rates of CVD is lacking; however, because BP readings may differ for unattended vs. attended measurements, 52 we advise that a consistent approach be used depending on local resource and preference. AOBP monitors typically make three or six readings at 1-min intervals and provide an average. AOBP correlates more closely with mean ABPM than with the manual auscultatory technique and may reduce measurement error and white-coat effects. 53
Inter-arm BP difference: at the initial visit, BP should be measured in both arms to detect an inter-arm difference. Though devices allowing simultaneous measurement in both arms exist, sequential arm measurement is considered sufficiently reliable. 54 , 55 Measurement in the contralateral arm should be undertaken once the three measurements in the index arm have been taken, and if a difference is detected, further measurement in the original arm is indicated to ensure the difference is consistent. If systolic BP differs by >10 mmHg between arms, subsequent measurements are obtained using the arm with the higher BP value. Significant inter-arm BP differences may reflect arterial stenosis or coarctation of the aorta, which may require investigation. Also, of note, in some patients one arm is preferred to the other for routine BP measurement (e.g. to avoid measurement of BP in an arm with an arteriovenous fistula or an arm where axillary lymph node dissection has occurred).
Postural/orthostatic hypotension: patients should be assessed for orthostatic hypotension at the initial visit and if concerning symptoms arise. After 5 min of rest in the sitting or lying position, BP should be measured at 1 min and/or 3 min after standing, with a threshold for orthostatic hypotension of ≥20/10 mmHg (systolic BP/diastolic BP) drop. Measurement after lying may be more sensitive for detecting orthostatic hypotension and may better predict falls but may be less feasible than measurement after sitting in clinical practice. 56
Pulse assessment: heart rate should be recorded at the initial visit and arrhythmia excluded.
5.2.3. Home blood pressure measurement
HBPM is an out-of-office approach to measuring BP when the patient measures their own BP at home using a validated monitor (usually an upper-arm oscillometric cuff device). 57 , 58 A consistent approach to HBPM should be used ( Figure 4 ). Patients should be counselled to follow the same preparation steps as used in clinics, which are outlined in Section 5.2.2 . Two measurements should be taken at each measurement session, performed 1–2 min apart. Measurements should be made twice a day (morning and evening) at the same time for a minimum of 3 days and up to 7 days. 59 At the end of the measurement period, all readings are averaged. If the average after 3 days is close to the treatment threshold, then measurement should continue for the full 7 days. Patients should be informed to keep a record of their home BP values and to ask their healthcare provider that the device accuracy be intermittently checked. Devices older than 4 years may be inaccurate and, if inaccurate, should be replaced. 60

Summary of home blood pressure measurement.
BP, blood pressure; HBPM, home blood pressure measurement. a Morning HBPM readings should be obtained before breakfast and before intake of medication but not immediately after awakening.
An average HBPM of ≥135/85 mmHg (equivalent to an office BP of ≥140/90 mmHg) should be used to diagnose hypertension and an average systolic BP of 120–134 mmHg or diastolic BP of 70–84 mmHg should be used to diagnose elevated BP. Of note, we use the same lower BP threshold (120/70 mmHg) for both office and HBPM in defining elevated BP. 61
5.2.4. Ambulatory blood pressure measurement
ABPM (summarized in Figure 5 ) is an out-of-office BP measurement that uses a fully automated device, usually for a 24-h period. The devices measure BP by the oscillometric method and are programmed to measure BP at set intervals. Readings are usually obtained at 15–30 min intervals during the day (typically 7 a.m. to 11 p.m.) and 30–60 min intervals at night (typically 11 p.m. to 7 a.m.). The software usually provides average BP measurements for daytime, night-time, and 24 h. A minimum of 70% useable BP recordings is required for a valid measurement session, typically numbering ≥27 measurements over 24 h. Preferably, seven nocturnal readings should also be obtained. 62 However, emerging data indicate that ≥8/≥4 wake/sleep readings may be adequate if more cannot be obtained. 63 Prior to using mean ABPM values (either 24 h, daytime, or night-time) the raw BP values at each measurement should be reviewed for possible outlier or erroneous values. A diary should record activities (e.g. meals and exercise) and sleep time to assist interpretation. The diagnostic thresholds for elevated BP and hypertension using ABPM, and comparison with office BP and HBPM, are provided in Table 5 . 61 , 64

Summary of ambulatory blood pressure measurement.
ABPM, ambulatory blood pressure measurement; BP, blood pressure.
5.2.5. Comparison of home and ambulatory blood pressure monitoring
There is overlap between home and ambulatory monitoring in terms of differentiating between hypertensive phenotypes. However, around 15% of people will have diagnostic disagreement, of whom approximately 50% will represent clinically significant differences of >5 mmHg. 67 The advantages and disadvantages of home and ambulatory monitoring are outlined in Table 6 .
Comparison of ambulatory and home blood pressure monitoring
| |
| |
| |
| |
5.3. What is the best method for measuring blood pressure to diagnose hypertension?
5.3.1. blood pressure measurement for hypertension screening.
Opportunistic screening is typically performed using office BP measurement and is key in detecting possible hypertension. However, a single screening office BP alone does not typically have sufficient diagnostic test performance to establish a diagnosis, especially for BP values close to diagnostic thresholds. Therefore, a single screening office BP requires some form of repeat BP assessment to confirm a diagnosis (preferably out-of-office or repeat office if out-of-office is not available). Relatedly, the BP threshold for acting on a screening office BP by conducting repeat BP assessments should also be lower than the office BP threshold used for diagnosing hypertension. This latter consideration is particularly relevant in the presence of increased CVD risk or markers of HMOD. Also of note, populations where masked hypertension is more prevalent include men, those who smoke, those with excessive alcohol intake, or those with diabetes or obesity. 68 , 69 While a screening office BP of >160/100 mmHg is almost always consistent with a diagnosis of hypertension, a small proportion of patients will have extreme white-coat effects that motivate prompt repeat BP assessment. 68 Hypertension screening approaches are discussed further in Section 7.1 .
5.3.2. Blood pressure measurement for diagnosing hypertension
After detecting high BP in the office, subsequent BP measurement for diagnosing hypertension depends on the clinical circumstances. Office BP has lower specificity than ABPM for detecting hypertension, so diagnosis based on office BP alone is less desirable unless resources do not allow out-of-office measurements. 70 For screening BP of 160–179 mmHg systolic or 100–109 mmHg diastolic, prompt confirmation (within 1 month) using either office or out-of-office methods is recommended, as delays in treatment are associated with increased CVD event rates. 71 For BP of ≥180/110 mmHg, assessment for hypertensive emergency is recommended. In the setting of hypertensive emergency, immediately commencing BP-lowering treatment is recommended, otherwise, prompt confirmation (preferably within a week) can be considered prior to commencing treatment ( Sections 7 and 10 ).
For screening BP of 140–159/90–99 mmHg, out-of-office BP should be measured to confirm the diagnosis. 72 When treatment of elevated BP is being considered (e.g. 120–139/70–89 mmHg) for individuals with high risk CVD conditions or sufficiently high 10-year predicted CVD risk, out-of-office BP measurement is recommended, both to confirm BP and to assess for masked hypertension. Out-of-office measurements may also be helpful for individuals with office BP of 130–139/85–89 mmHg to diagnose masked hypertension. Further details on the diagnostic evaluation of hypertension are provided in Section 7.2 .
5.4. What is the best method for measuring blood pressure for long-term management of hypertension?
While repeat office measurement of BP remains the commonest approach to long-term management of hypertension, several lines of investigation support augmenting office BP measurements with out-of-office assessment.
5.4.1. Home monitoring
There are over 50 trials of different self-monitoring-based interventions. 73 Self-monitoring is associated with lower mean systolic BP at 12 months [−3.2 mmHg; 95% confidence interval (CI) −4.9 to −1.6 mmHg]. 74 Furthermore, there are known benefits of telemonitoring, digital interventions, and mobile health in managing BP. 75–78 Self-monitoring is also likely to be cost-effective. 79 Unfortunately, in clinical practice, some patients may not provide reliable information on their home BP, and both their device and measurement technique need to be checked.
5.4.2. Ambulatory monitoring
ABPM provides a reference BP measurement but repeat ABPM testing is sometimes not practical due to resource constraints and, uncommonly, low patient acceptability. 80 There is a paucity of data on treatment guided by ABPM vs. that of office or HBPM measurements. A trial of treatment guided by HBPM vs. clinic and ambulatory monitoring found equivalence in BP control and HMOD. 81 Other studies reported a non-significant trend to worse BP control with ambulatory vs. office BP monitoring, though the ambulatory group also received fewer medications. 82 Potential advantages of ABPM over HBPM include diagnosing nocturnal hypertension or symptomatic transient hypotension or hypertension with exertion. As such, ABPM and HBPM should be considered complementary and additive, rather than competing approaches to long-term BP management. 83
5.5. Measuring blood pressure in selected groups
5.5.1. pregnancy.
Monitoring BP during pregnancy is typically done at antenatal visits, which vary dependent on trimester (with increasing frequency towards term). BP tends to reach a nadir at 20–30 weeks of pregnancy before increasing towards term at 40 weeks. 84 Only a small number of automated oscillometric BP monitors have been adequately validated in pregnancy and several have failed, usually due to providing BP values that are erroneously high. 85 Auscultatory measurement with sphygmomanometry is consequently the clinical standard in pregnancy. 85 Self-monitoring at home is not yet proven to be effective in gestational hypertension. 86 , 87 While norms for BP during pregnancy remain unclear, the 2022 Chronic Hypertension and Pregnancy (CHAP) trial indicated benefit of targeting clinic BP below 140/90 mmHg. 88 Consideration of secondary causes of hypertension is important in young women with gestational hypertension. Further details are provided in Section 9.2 and the 2018 ESC Guideline for the management of cardiovascular disease during pregnancy. 89
5.5.2. Atrial fibrillation
Hypertension is a risk factor for AF. 90 , 91 Oscillometric BP monitors are not always accurate in the presence of AF, due to the greater variability of BP beat to beat, so multiple auscultatory measurements are recommended. 48 , 92 , 93 Some oscillometric BP monitors include an algorithm for detecting AF, but an electrocardiogram (ECG) is still required to confirm the diagnosis. 49 , 94
5.5.3. Orthostatic hypotension
Postural or orthostatic hypotension is common, 95 , 96 present in approximately 10% of all hypertensive adults and up to 50% of older institutionalized adults. 97 , 98 Orthostatic hypotension is defined as a BP drop of ≥20/10 mmHg 1 and/or 3 min after standing following a 5-min period in the seated or lying position. 99–101 Diagnosis is made in the office. Routine ABPM is not currently suitable for formally assessing orthostatic hypotension, 102 though it may help in some cases, particularly when accompanied by a patient symptom diary. 103
5.6. Novel methods of measuring blood pressure
New methods to measure BP are under development. Continuous office and out-of-office BP recordings and ABPM and HBPM have been developed that derive beat-to-beat, reading-to-reading, and day-to-day BP variability. However, there is no agreement on the optimum approach to measuring variability, and there is no trial evidence that reducing BP variability specifically can reduce CVD events. 104 Other emerging technologies include wearable, wrist-based BP measurement devices, devices evaluating central BP, and cuffless devices implementing plethysmographic or other technologies. 105 , 106 However, there is at present insufficient scientific consensus on the accuracy standards and validation procedures that these cuffless devices must comply with prior to commercialization. 43 , 44 , 107–109
In view of these issues, none of these cuffless measurement modalities are currently recommended for routine clinical use.
Recommendations for measuring blood pressure (see Evidence Tables 1–8)

6.1. Definition and classification of elevated blood pressure and hypertension
Epidemiological studies demonstrate a continuous and log-linear association between BP and adverse CVD outcomes. 22 , 32 , 33 , 114 , 115 Starting at levels as low as 90 mmHg systolic, the higher the BP the higher the relative risk of CVD including atherosclerosis. 32 , 114 These observational data are complemented by randomized clinical trials (RCTs), 116 which have provided experimental evidence regarding the BP range for which BP lowering with treatment is proven to reduce CVD events. Of note, some studies suggest a stronger relative risk for CVD for a given BP among females compared with males. 117 , 118
A healthy lifestyle should be encouraged for all adults to prevent an increase in BP and development of hypertension. 119 , 120 To aid pharmacological treatment decisions, the 2024 ESC Guidelines recommend a simplified categorization of adults according to their BP ( Figure 6 ). In compiling this categorization, priority was given to evidence from randomized trials over observational data. However, it is important to reiterate that the risk of CVD attributable to BP is continuous and that interpreting randomized trial data is an iterative process involving an element of subjectivity. As such, no categorization of BP can be considered immutable or flawless.

Blood pressure categories.
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; DBP, diastolic blood pressure; HBPM, home blood pressure monitoring; SBP, systolic blood pressure. We note that the respective non-daytime ABPM thresholds for elevated BP and hypertension diagnosis are listed in Section 5 ( Table 5 ).
The 2024 Guidelines define hypertension as a confirmed office systolic BP of ≥140 mmHg or diastolic BP of ≥90 mmHg. For this diagnosis to be made, confirmation is recommended with out-of-office measurements (HBPM or ABPM) or at least one repeat office measurement at a subsequent visit, as detailed in Section 5 and Section 7.2 . This definition is based on several factors. First, meta-analyses of randomized trials provide evidence among all adults and across various settings for the benefit of BP-lowering therapy among patients with BP above this threshold. 116 , 121 , 122 Second, most adults with BP above this threshold are at increased CVD risk, typically with 10-year risk estimates of ≥10% for fatal and non-fatal CVD events. 123–125 The higher the patient’s baseline absolute risk for CVD, the greater the net benefit from BP-lowering treatment and, at the population level, the lower the estimated number needed to treat (NNT). 126–128 Third, this more traditional BP threshold for hypertension is already widely used by policymakers to define a disease state, and maintaining this BP threshold to define hypertension (vs. lowering it) does not require most adults to be labelled with what is widely considered a disease. 129
Here, we introduce a new BP category called ‘elevated BP’, which is defined as an office systolic BP of 120–139 mmHg or diastolic BP of 70–89 mmHg. Within this BP range, the efficacy of BP-lowering therapy has been established in meta-analyses of RCTs, 116 but average CVD risk in the elevated BP group is not sufficiently high to merit drug treatment in all patients. 123 , 124 , 130 Pharmacological treatment initiation is, however, suggested for a subgroup of patients within this BP range who are at increased global risk of CVD as identified by the risk stratification approach outlined in Sections 6.3 , 6.4 , and 8 .
Non-elevated BP is defined as a systolic BP of <120 mmHg and a diastolic BP of <70 mmHg. Fewer individuals within this BP range are at increased risk of CVD, 124 and evidence for CVD benefit with BP-lowering pharmacological treatment is lacking due to an absence of trials. We use the term ‘non-elevated BP’ to define this BP category in recognition that these are treatment categories and not prognostic categories. Because the relative risk for CVD starts to increase at BP below this threshold (even as low as 90 mmHg systolic BP), particularly among women, 117 , 118 we avoid terms like ‘normal BP’, ‘optimal BP’, or ‘normotension’ in defining this category.
Recommendations for categorizing blood pressure (see Evidence Table 9)

6.2. Principles of a risk-based approach for managing blood pressure and preventing cardiovascular disease
In the context of BP-lowering interventions, randomized trials demonstrate a consistent relative risk reduction in adverse CVD outcomes per unit reduction in BP. 131 , 139 However, many medical interventions incur costs and have side effects. Therefore, guidance is needed on selecting patients most likely to benefit from BP-lowering treatment. This is especially true among adults with elevated BP (office systolic BP of 120–139 mmHg and/or diastolic BP of 70–89 mmHg). Practical aspects for implementing a risk-based approach are further discussed in Section 8 .
6.2.1. Role of cardiovascular disease risk assessment
The risk of adverse CVD outcomes increases log-linearly with constant increments in systolic BP and diastolic BP. 22 , 32 , 33 , 114 , 140 Concurrently, at higher BP, there is clustering of additional CVD risk factors. 141 , 142 Consequently, many patients with hypertension will have an estimated 10-year risk for CVD events of ≥10%, 116 , 121 , 122 which, for the purposes of these guidelines, is considered sufficiently high risk to merit consideration of BP-lowering treatment in the setting of elevated BP. 143
Using BP thresholds for hypertension alone for allocating treatment would lead to under-treatment of many high-risk patients. 144 , 145 , 115 A substantial proportion of excess CVD events attributable to BP occur in patients with BP levels below the traditional threshold for hypertension diagnosis. As the efficacy of BP lowering on preventing CVD events extends down to a systolic BP of 120 mmHg and a diastolic BP of 70 mmHg, 116 , 135 , 136 , 146 patients with elevated BP and increased CVD risk can also derive benefit from BP-lowering treatment. 124 , 145
The heterogeneity in CVD risk among adults with elevated BP is larger than in those with hypertension, as such patients tend to be younger, and their absolute CVD risk depends more on the prevalence of concomitant CVD risk factors. 123 , 147 Consequently, formally estimating the patient’s CVD risk, encapsulating demographics and other CVD risk factors, is recommended to guide BP-lowering treatment decisions among patients with elevated BP. 148–151
6.3. Predicting cardiovascular disease risk
Certain conditions on their own are associated with sufficient CVD risk such that patients with elevated BP alongside these conditions can be considered for BP-lowering therapy ( Figure 7 ). These include moderate or severe chronic kidney disease (CKD), 152 established clinical CVD (coronary heart disease, cerebrovascular disease, peripheral arterial disease, or heart failure) 153–158 concomitant HMOD (see Figure 7 ; Section 7 ; Supplementary data online , Table S1 ), 31 , 159 diabetes mellitus, and familial hypercholesterolaemia (probable or definite). 160–163 Regarding diabetes, some adults aged <60 years with type 2 diabetes and elevated BP have 10-year CVD risk of <10%. Accordingly, the diabetes-specific Systematic COronary Risk Evaluation 2 (SCORE2)-Diabetes risk-prediction model should be considered to confirm CVD risk is sufficiently high (≥10%) among individuals with type 2 diabetes mellitus who are aged <60 years. 164

Sufficiently high cardiovascular risk conditions that warrant blood pressure-lowering treatment among adults with elevated blood pressure.
CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate. a Coronary heart disease, cerebrovascular disease, peripheral arterial disease. b See Section 7 . c SCORE2-Diabetes should be considered to identify lower-risk individuals (<10% 10-year CVD risk), who may not require BP-lowering medication, particularly in individuals <60 years.
In the absence of these sufficiently high-risk conditions, risk-prediction models (SCORE2 and SCORE-OP) have been developed in the general population to predict 10-year risk of CVD. 165 , 166 In adults with elevated BP without the above sufficiently high-risk conditions, risk-prediction models are recommended to inform BP-lowering treatment decisions. Risk-prediction models are more accurate than clinical judgment or tallying of individual risk factors. 167–169
6.3.1. 10-year cardiovascular disease risk-prediction models
Prediction models differ in their input variables, predicted endpoints (outputs), and populations in which they were derived and validated. We endorse the use of SCORE2 for individuals aged 40–69 years and SCORE2–Older Persons (SCORE2-OP) for individuals aged ≥70 years for predicting 10-year global risk of fatal and non-fatal CVD events (stroke or myocardial infarction). 165 , 166 The management of adults aged <40 years is discussed in Section 9.1 . The SCORE2 and SCORE2-OP models are preferred over other 10-year risk-prediction models, as they predict both fatal and non-fatal CVD events, have been validated and recalibrated to European populations, and because SCORE2-OP is adjusted for the competing risk of non-cardiovascular mortality. Calculating SCORE2 or SCORE2-OP is recommended for individuals with elevated BP who are not already at sufficiently high CVD risk due to established CVD, moderate or severe CKD, probable or definite familial hypercholesterolaemia, diabetes mellitus, or HMOD. 165 , 166 , 170
For the purpose of BP-lowering treatment decisions, individuals with elevated BP and a predicted 10-year CVD risk of ≥10% by SCORE2 or SCORE2-OP are considered in these guidelines to be sufficiently high risk, with details on the choice of lifestyle or drugs to facilitate BP-lowering treatment in this setting provided in Section 8 . 171 , 172 A number of considerations influenced our choice to recommend a single risk threshold of ≥10%, vs. the alternative option of using age-specific risk thresholds, such as those provided in the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. 170 For example, contemporary data indicate the heightened importance of BP control in older adults due to their higher absolute CVD risk (resulting in a lower NNT) and concomitantly to reduce age-dependent adverse outcomes attributable to increased BP, such as dementia. Recent treat-to-target trials (testing systolic BP targets of approximately 120 mmHg) used a single CVD risk inclusion threshold and were also enriched with older adults. 135 , 136 , 146 In addition, the average CVD event rate in the control arm of a landmark meta-analysis showing the benefits of more intensive BP-lowering treatment was approximately equivalent to a 10% 10-year risk. 116 Finally, the task force, which included patient members, felt that age-specific risk thresholds could result in BP treatment decisions being made solely based on age, which is difficult to support scientifically or otherwise. To try to avoid any confusion with the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice, we use the terms ‘sufficiently high risk’ or ‘increased risk’ to describe a person with 10-year CVD risk of ≥10% (rather than the terms ‘high risk’ or ‘very high risk’).
Recommendations for assessing cardiovascular disease risk among individuals with elevated blood pressure (office systolic blood pressure 120–139 mmHg or diastolic blood pressure 70–89 mmHg) (see Evidence Tables 10 and 11)

6.4. Refining cardiovascular disease risk estimation beyond risk models
The SCORE2 and SCORE2-OP risk-prediction models incorporate traditional risk factors such as age, sex, systolic BP, cholesterol values, and smoking status to predict 10-year risk of CVD. 165 , 166 However, they do not include ‘non-traditional’ CVD risk factors (detailed below and hereafter termed 'risk modifiers’). Non-traditional CVD risk modifiers can improve the predictive performance (i.e. discrimination) of other CVD risk-prediction models, and may also apply to SCORE2 or SCORE2-OP. 173 For example, among individuals with elevated BP and borderline increased 10-year predicted CVD risk by SCORE2 or SCORE2-OP (estimates of 5% to <10%), these non-traditional CVD risk modifiers may help up-classify the patient's risk and thereby prompt BP-lowering treatment ( Figure 8 ).

Cardiovascular disease risk modifiers to consider for up-classification of risk.
ASCVD, atherosclerotic cardiovascular disease; HIV, human immunodeficiency virus.
6.4.1. Sex-specific non-traditional cardiovascular disease risk modifiers
Sex differences in the distribution of traditional and non-traditional CVD risk factors have been documented among patients with hypertension. 174 Although sex itself is included as an input variable in the SCORE2 and SCORE2-OP, and though these models were derived separately in men and women, some sex-specific, non-traditional risk modifiers were not included, and their associated impact on CVD risk may not be fully captured by SCORE2, SCORE2-OP, or SCORE2-Diabetes.
The relationship between BP and overall CVD risk is similar in both sexes, though some studies even suggest a stronger relative risk for CVD for a given BP level among females compared with males. 117 Female-specific, non-traditional CVD risk modifiers often arise at specific times throughout the life course, especially during pregnancy and the peri-partum period. Women with a history of hypertensive disorders of pregnancy, including gestational hypertension and pre-eclampsia, have a two-fold higher long-term risk of CVD vs. women without these pregnancy conditions. 175–177 The relative long-term CVD risk associated with hypertensive disorders of pregnancy may also be higher in younger vs. older pregnant women. 178 , 179 Most, but not all, of the excess CVD risk associated with hypertensive disorders of pregnancy is captured by conventional CVD risk factors. 176 , 178 Gestational diabetes is independently associated with an approximately two-fold increase in the long-term relative risk of CVD events. 180 Other complications such as pre-term delivery, recurrent miscarriage, and one or more stillbirths are associated with a 40% relative increase in long-term CVD risk. 181–185 Accordingly, a history of specific pregnancy complications, including gestational hypertension, pre-eclampsia, gestational diabetes, pre-term delivery, one or more stillbirths, and recurrent miscarriage, can be considered as non-traditional CVD risk modifiers to up-classify women with elevated BP and borderline increased 10-year predicted CVD risk (5% to <10%) to sufficiently high risk, thereby influencing the risk-based management of their elevated BP.
Evidence whether other female-specific conditions (infertility, polycystic ovary syndrome, and premature menopause) and male-specific conditions (androgenic alopecia and erectile dysfunction) improve prediction of CVD sufficiently to inform risk-based BP-lowering treatment decisions is inconclusive at present.
6.4.2. Non-traditional cardiovascular disease risk modifiers shared by men and women
In addition to sex-specific risk modifiers, several other non-traditional risk factors are associated with an increased risk of CVD, but few have been shown to improve risk prediction or discrimination beyond traditional CVD risk factors.
We advise considering high-CVD-risk race/ethnicity (e.g. South Asian), 186–188 family history of premature onset atherosclerotic CVD (CVD event in males aged <55 years and/or females <65 years), 189 , 190 socio-economic deprivation, 191 inflammatory conditions (e.g. systemic lupus erythematosus, rheumatoid arthritis, and psoriasis affecting 10% or more of body surface area or requiring systemic therapy), 192–202 HIV, 203–205 and severe mental illness (major depressive disorder, bipolar disorder, and schizophrenia) 206–208 as shared non-traditional risk modifiers to up-classify the risk of individuals with a borderline increased 10-year predicted risk using SCORE2/SCORE2-OP (5% to <10%) to sufficiently high CVD risk.
6.4.3. Additional risk decision tests
Coronary artery calcium (CAC) scoring improves CVD risk prediction and reclassifies risk when added to conventional CVD risk factor-based estimation models. 209 , 210 A CAC score of >100 Agatston units or ≥75th percentile for age, sex, and ethnicity favours up-classification of CVD risk. 127 Internal or external carotid plaque may also improve CVD risk prediction. 211 Similarly, femoral artery plaque detection may improve CVD risk prediction. 212–214 Arterial stiffness, as assessed by pulse wave velocity (PWV), is associated with increased risk of CVD events and improves CVD risk stratification. 215–218 Common arterial stiffness thresholds for increased risk include carotid–femoral PWV of >10 m/s and brachial–ankle PWV of >14 m/s. After assessing 10-year predicted CVD risk and non-traditional risk factors, if a risk-based treatment decision remains uncertain for patients with elevated BP, it is reasonable to measure a CAC score or, alternatively, carotid or femoral plaque, or arterial stiffness; most especially after shared decision-making with the patient and after considering cost (see Section 7 for more details on these tests). There is also evidence that elevated cardiac biomarker levels (specifically high-sensitivity cardiac troponin and B-type natriuretic peptide/N-terminus B-type natriuretic peptide) are significant and effective risk modifiers, 219 , 220 with further supportive data from hypertensive participants. 159 , 221 , 222 Of note, these cardiac biomarkers can be considered markers of HMOD ( Section 7 ); however, we focus on them in this risk modifier section because they may be elevated due to other reasons besides high BP (such as atherosclerosis or heart rhythm disease).
Recommendations for refining cardiovascular disease risk (see Evidence Tables 12–14)

6.5. Summary of the cardiovascular disease risk stratification approach for allocating blood pressure treatment
Measured BP combined with 10-year CVD risk-prediction models and non-traditional risk modifiers should be used for stratifying risk when allocating BP-lowering treatment for persons with elevated BP ( Figure 9 ). It is important to stress here that patients with confirmed hypertension are recommended to receive BP-lowering treatment and no further risk stratification is needed.

Summary of cardiovascular disease risk-stratification approach for blood pressure treatment in adults with elevated blood pressure.
ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CAC, coronary artery calcium; CKD, chronic kidney disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; DM, diabetes mellitus; FH, familial hypercholesterolaemia; HMOD, hypertension-mediated organ damage; NT-proBNP, N-terminal pro-brain natriuretic peptide; SBP, systolic blood pressure; SCORE2, Systematic COronary Risk Evaluation 2; SCORE2-OP, Systematic COronary Risk Evaluation 2–Older Persons.
For patients with elevated BP, the presence of diabetes, familial hypercholesterolaemia, established CVD (defined as prior acute or chronic coronary syndrome, cerebrovascular disease, symptomatic peripheral arterial disease, or heart failure), moderate or severe CKD, or HMOD confers increased CVD risk. One caveat is that, specifically for individuals with elevated BP and type 2 diabetes mellitus only aged <60 years, SCORE2-Diabetes should be considered to identify lower CVD risk individuals (<10% over 10 years).
Otherwise, for patients without these high-risk conditions, 10-year risk of CVD should be calculated using SCORE2 (if aged 40–69 years) and SCORE2-OP (if aged ≥70 years). Patients with elevated BP and a 10-year predicted risk of CVD events ≥10% are considered sufficiently high risk to warrant BP-lowering treatment (either by lifestyle or drug treatment, see Section 8 ). For patients with elevated BP and borderline increased predicted CVD risk by SCORE2/SCORE2-OP (5% to <10% over 10 years), up-classification of risk may be considered in the presence of sex-specific or shared non-traditional risk modifiers. After considering sex-specific and shared non-traditional risk modifiers, if a risk-based BP-lowering treatment decision remains uncertain, it may be reasonable to measure CAC score, carotid or femoral plaque, high-sensitivity cardiac troponin or B-type natriuretic peptide biomarkers, or arterial stiffness.
Risk stratification for patients with non-elevated BP (systolic BP of <120 mmHg and diastolic BP of <70 mmHg) is not required for the purpose of allocating BP-lowering treatment, as the safety and efficacy of commencing BP-lowering treatment below this threshold is uncertain. Risk assessment may nonetheless be needed in this setting when considering other prevention therapies (e.g. lipid lowering).
7.1. Screening for hypertension
Hypertension is predominantly an asymptomatic condition that is typically detected by systematic or opportunistic screening in a healthcare setting. Systematic screening refers to any process where individuals are identified and invited to a healthcare setting solely to measure their BP and CVD risk profile. Opportunistic screening refers to BP being measured when the patient presents to a healthcare setting for any reason, such as a routine check-up or the treatment of an acute or chronic condition. Self-screening and non-physician screening are also increasingly used. 227–230
Few data are available on the effectiveness of different hypertension screening strategies to reduce the morbidity and mortality associated with hypertension. 231–233 More evidence is needed before systematic screening programmes with BP measurement can be recommended in all adults to reduce CVD events. 231
Opportunistic BP screening in a primary care setting appears effective, with an estimated 90% of all adults aged >40 years in the UK having a BP check within a 5-year time period, 234 though these findings may not extrapolate to other countries. When patients provide HBPM recordings, these can also be used as part of an opportunistic screening programme (see Section 5.2 ). 235
Despite ongoing uncertainty about the effect of hypertension screening programmes on CVD outcomes, many studies have demonstrated that screening (mostly opportunistic screening) increases hypertension detection, and that the benefits of screening likely outweigh harms. 70 Global initiatives to raise BP awareness, such as the May Measurement Month, 228 or targeted initiatives, such as the barbershop health outreach programmes, 229 are successful examples of BP screening campaigns.
Screening for hypertension, like for global CVD risk assessment, should be intermittently repeated, e.g. every 3 years. Considering the rate of progression to hypertension in European population samples, 236 it is reasonable to measure BP at least every 3 years in the case of non-elevated BP and low–moderate CVD risk (i.e. individuals aged <40 years). More frequent BP checks (i.e. yearly) should be considered in individuals 40 years or older and individuals with elevated BP not currently meeting indications for treatment 170 ( Figure 10 ).

Protocol for confirming hypertension diagnosis.
BP, blood pressure; CVD, cardiovascular disease; SCORE2, Systematic COronary Risk Evaluation 2; SCORE2-OP, Systematic COronary Risk Evaluation 2–Older Persons.
Recommendations for blood pressure screening (see Evidence Table 15)

7.2. Confirming the diagnosis of hypertension
As noted in Section 5 , assessment at a single visit by office BP has lower specificity compared with ABPM for diagnosing hypertension. 70 , 238–241 Accordingly, a protocol for confirming the diagnosis of hypertension is proposed ( Figure 10 ), with out-of-office BP measurement as the preferred method for confirming cases of elevated BP or hypertension. For initial screening systolic BP of >160 mmHg and/or diastolic BP of >100 mmHg, a prompt re-evaluation (within days to weeks but not >1 month) preferably with ABPM or HBPM is advisable. 71 BP of >180/110 mmHg at screening requires exclusion of hypertensive emergencies, which should be managed as appropriate (see 242 and Section 10 ) with prompt treatment. For individuals with BP of >180/110 mmHg at screening but without hypertensive emergency, prompt confirmation (preferably within a week) can be considered prior to commencing treatment.
Recommendations for confirming hypertension diagnosis

7.3. Communicating the diagnosis
Behavioural responses to health-related threats are strongly influenced by five core themes (termed ‘illness representations’), which are identity, timeline, cause, consequences, and control/cure. 243 , 244 These illness representations form the basis of how patients understand a diagnosis, and can influence their responses after being diagnosed with hypertension. 243 This conceptual framework can help guide the clinical communication of a diagnosis of hypertension. For example, patients’ understanding of the chronic nature of hypertension (i.e. timeline theme) is key for ensuring long-term engagement with medical treatment. 245 Prior to commencing treatment, it is helpful to understand the extent to which patients believe that medications are necessary and ascertain if they have concerns. 246 The core illness representations and beliefs about medicines for clinicians to consider are included in Table 7 .
Key illness representations and treatment beliefs: how these apply to communicating a hypertension diagnosis to the patient (note that gender influences these representations)
| Illness representation . | Example patient question . | Application to a hypertension diagnosis conversation . |
|---|---|---|
| Identity | What is the disease/illness label and the related symptoms? | The condition where your systolic BP is ≥140 and/or diastolic BP ≥90 mmHg is called hypertension. We classify systolic BP 120–139 or diastolic BP 70–89 mmHg as elevated BP. For most people, this has no noticeable signs or symptoms, therefore, we need to monitor your BP to assess how medications and behavioural changes are working. |
| Control | Is the illness controllable through medical intervention or behavioural change? | Hypertension can usually be controlled with medication and behavioural changes such as dietary changes and regular physical activity. For some people we need to try a few different options before we get BP under control. |
| Timeline | Is this an acute or chronic problem? | This is a serious long-term or chronic condition condition that will require long-term management. This means that it may need to be managed throughout life. |
| Consequences | What are the physical and psychosocial consequences? | If hypertension is not controlled, then there is a risk of a serious acute cardiovascular disease event such as a stroke or heart attack; however, if it is managed through the right medical intervention and behavioural changes, then this risk can be reduced and the condition will have less consequences for your life. |
| Causes | What caused the condition? | Multiple factors contribute to someone developing hypertension. These include both non-modifiable factors (e.g. genetics and age) and modifiable factors (e.g. diet, weight, and physical activity). We are best focusing on those things that we can control to reduce your BP. |
| Illness representation . | Example patient question . | Application to a hypertension diagnosis conversation . |
|---|---|---|
| Identity | What is the disease/illness label and the related symptoms? | The condition where your systolic BP is ≥140 and/or diastolic BP ≥90 mmHg is called hypertension. We classify systolic BP 120–139 or diastolic BP 70–89 mmHg as elevated BP. For most people, this has no noticeable signs or symptoms, therefore, we need to monitor your BP to assess how medications and behavioural changes are working. |
| Control | Is the illness controllable through medical intervention or behavioural change? | Hypertension can usually be controlled with medication and behavioural changes such as dietary changes and regular physical activity. For some people we need to try a few different options before we get BP under control. |
| Timeline | Is this an acute or chronic problem? | This is a serious long-term or chronic condition condition that will require long-term management. This means that it may need to be managed throughout life. |
| Consequences | What are the physical and psychosocial consequences? | If hypertension is not controlled, then there is a risk of a serious acute cardiovascular disease event such as a stroke or heart attack; however, if it is managed through the right medical intervention and behavioural changes, then this risk can be reduced and the condition will have less consequences for your life. |
| Causes | What caused the condition? | Multiple factors contribute to someone developing hypertension. These include both non-modifiable factors (e.g. genetics and age) and modifiable factors (e.g. diet, weight, and physical activity). We are best focusing on those things that we can control to reduce your BP. |
| Treatment beliefs . | Example patient question . | Application to a hypertension diagnosis communication . |
|---|---|---|
| Necessity | To what extent is treatment necessary? | Taking BP-lowering medication every day is necessary to keep your BP under control and to help prevent a more serious health problem developing. Do you think that these medicines will help you? |
| Concerns | To what extent does treatment cause concern? | Some patients have concerns about taking daily medications throughout their life, e.g. about side effects. Do you have any concerns about taking your BP medications every day? |
| Treatment beliefs . | Example patient question . | Application to a hypertension diagnosis communication . |
|---|---|---|
| Necessity | To what extent is treatment necessary? | Taking BP-lowering medication every day is necessary to keep your BP under control and to help prevent a more serious health problem developing. Do you think that these medicines will help you? |
| Concerns | To what extent does treatment cause concern? | Some patients have concerns about taking daily medications throughout their life, e.g. about side effects. Do you have any concerns about taking your BP medications every day? |
The 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice recommend “an informed discussion about CVD risk and treatment benefits—tailored to the needs of a patient” as part of a diagnosis communication in hypertension. 170 This can be facilitated using an interdisciplinary healthcare-provided approach (see Section 11 ) and by visual information or other more accessible material that might optimally communicate hypertension-related risk. 128 Visualizing risk by medical imaging to motivate risk-reducing behaviour changes may also be beneficial. 247
7.4. Baseline assessment and diagnostic approach
7.4.1. medical history, medication history, and physical examination.
The purpose of clinical evaluation is to diagnose hypertension, delineate factors potentially contributing to hypertension, identify other CVD risk factors, define relevant comorbidities, screen for potential secondary causes of hypertension (where indicated), and establish whether there is evidence of HMOD or existing cardiac, cerebrovascular, or renal disease.
Details on medical history and physical examination steps are summarized in the supplement (see Supplementary data online , Tables S2 and S3 ), as well as drugs or substances that may increase BP (see Supplementary data online , Table S4 ).
7.4.2. Drug adherence and persistence with treatment
Adherence is defined as the extent to which a patient’s behaviour, e.g. with respect to taking medication, coincides with agreed recommendations from a healthcare provider. Persistence represents the amount of time from initiation to discontinuation of therapy. 248 Adherence to medical therapies is especially suboptimal in asymptomatic conditions such as hypertension. 249–254 Non-adherence to BP-lowering therapy correlates with a higher risk of CVD events. 255 , 256 Objective methods to assess adherence, such as detecting prescribed drugs in blood or urine samples and directly observed treatment (witnessed pill intake during ABPM), have demonstrated their potential usefulness, particularly in the setting of apparently resistant hypertension. 257 However, all methods for testing drug adherence have limitations.
Non-adherence to BP-lowering therapy depends on many factors ( Figure 11 ). 253 Effective patient–physician communication is crucial to improve adherence. 258 , 259 Single-pill combinations improve persistence in BP-lowering treatment and are associated with lower all-cause mortality. 260

Definitions, assessments, and potential interventions for the three phases of adherence to BP-lowering medications.
Recommendations for assessing adherence and persistence with treatment (see Evidence Table 16)

7.4.3. Routine and optional tests
Routine tests include laboratory and clinical tests to detect increased CVD risk and relevant comorbidities (e.g. hyperlipidaemia and diabetes) ( Table 8 ).
Routine tests recommended in the initial work-up of a patient with elevated blood pressure or hypertension
| Routine test . | Clinical utility . |
|---|---|
| Fasting blood glucose (and HbA1c if fasting blood glucose is elevated) | Assessing CVD risk and comorbidities |
| Serum lipids: total cholesterol, LDL cholesterol, HDL and non-HDL cholesterol, triglycerides | Assessing CVD risk |
| Blood sodium and potassium, haemoglobin and/or haematocrit, calcium, and TSH | Screening secondary hypertension (primary aldosteronism, Cushing’s disease, polycythaemia, hyperparathyroidism, and hyperthyroidism) |
| Blood creatinine and eGFR; urinalysis and urinary albumin-to-creatinine ratio | Assessing CVD risk and HMOD Guiding treatment choice Screening secondary hypertension (renoparenchymal and renovascular) |
| 12-lead ECG | Assessing HMOD (left atrial enlargement, left ventricular hypertrophy) Assessing irregular pulse and other comorbidities (AF, previous acute myocardial infarction) |
| Routine test . | Clinical utility . |
|---|---|
| Fasting blood glucose (and HbA1c if fasting blood glucose is elevated) | Assessing CVD risk and comorbidities |
| Serum lipids: total cholesterol, LDL cholesterol, HDL and non-HDL cholesterol, triglycerides | Assessing CVD risk |
| Blood sodium and potassium, haemoglobin and/or haematocrit, calcium, and TSH | Screening secondary hypertension (primary aldosteronism, Cushing’s disease, polycythaemia, hyperparathyroidism, and hyperthyroidism) |
| Blood creatinine and eGFR; urinalysis and urinary albumin-to-creatinine ratio | Assessing CVD risk and HMOD Guiding treatment choice Screening secondary hypertension (renoparenchymal and renovascular) |
| 12-lead ECG | Assessing HMOD (left atrial enlargement, left ventricular hypertrophy) Assessing irregular pulse and other comorbidities (AF, previous acute myocardial infarction) |
AF, atrial fibrillation; CVD, cardiovascular disease; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; HbA1c, glycated haemoglobin; HDL, high-density lipoprotein; HMOD, hypertension-mediated organ damage; LDL, low-density lipoprotein; TSH, thyroid-stimulating hormone.
Optional tests should be considered in the initial assessment if they are likely to change patient management, with the main rationale being to improve CVD risk stratification. 170 As highlighted in Section 6 , for adults with elevated BP who also have a 10-year estimated CVD risk of 5% to <10%, optional tests including those for HMOD may be considered if up-classification of risk on the basis of an abnormal test result could prompt initiation of BP-lowering therapy. 31 , 170 Evidence of subclinical microvascular neurodegeneration and/or lacunar brain disease due to small-vessel pathology may also indicate HMOD. 264
While the role of optional tests for HMOD ( Table 9 ) in the management of elevated BP is emphasized in these guidelines, we also note that these tests may help to optimize treatment in hypertensive adults with BP of >140/90 mmHg who are prescribed BP-lowering therapy (e.g. by facilitating patient adherence and overcoming clinician inertia in achieving an intensive BP treatment target of as low as 120 mmHg systolic). The role of visualizing HMOD in helping motivate risk-reducing changes in patients and overcome physician inertia has been tested in interventional trials ( Section 7.3 ). 247 , 265–267
Optional tests that may be used as clinically indicated in the initial work-up of a patient with elevated blood pressure or hypertension to assess hypertension-mediated organ damage or established cardiovascular disease
| Optional test . | Clinical utility . |
|---|---|
| Echocardiography | Assessing HMOD (hypertensive heart disease) Assessing established CVD (previous acute myocardial infarction, heart failure) Assessing thoracic aorta dilation |
| CAC by cardiac CT or carotid or femoral artery ultrasound imaging | Assessing HMOD (atherosclerotic plaque) |
| Large artery stiffness (carotid–femoral or brachial–ankle PWV) | Assessing HMOD (arterial stiffness) |
| High-sensitivity cardiac troponin and/or NT-proBNP | Assessing HMOD |
| Ankle–brachial index | Assessing established CVD (lower-extremity arterial disease) |
| Abdominal ultrasound | Assessing established CVD (abdominal aneurysm) |
| Fundoscopy | Assessing HMOD (hypertensive retinopathy) Diagnosing hypertensive emergency/malignant hypertension (haemorrhages and exudates, papilloedema) |
| Optional test . | Clinical utility . |
|---|---|
| Echocardiography | Assessing HMOD (hypertensive heart disease) Assessing established CVD (previous acute myocardial infarction, heart failure) Assessing thoracic aorta dilation |
| CAC by cardiac CT or carotid or femoral artery ultrasound imaging | Assessing HMOD (atherosclerotic plaque) |
| Large artery stiffness (carotid–femoral or brachial–ankle PWV) | Assessing HMOD (arterial stiffness) |
| High-sensitivity cardiac troponin and/or NT-proBNP | Assessing HMOD |
| Ankle–brachial index | Assessing established CVD (lower-extremity arterial disease) |
| Abdominal ultrasound | Assessing established CVD (abdominal aneurysm) |
| Fundoscopy | Assessing HMOD (hypertensive retinopathy) Diagnosing hypertensive emergency/malignant hypertension (haemorrhages and exudates, papilloedema) |
CAC, coronary artery calcium; CT, computed tomography; CVD, cardiovascular disease; HMOD, hypertension-mediated organ damage; NT-proBNP, N-terminal pro-brain natriuretic peptide; PWV, pulse wave velocity.
HMOD assessment is also an important way to identify young adults <40 years old who have increased CVD risk, since 10-year estimated CVD risk by SCORE2 cannot be calculated in this age group (see Section 8.1 ). More details on diagnostic thresholds for HMOD by the various assessment options, including important sex differences, are provided in Supplementary data online , Tables S1 and S5 and Figure 12 .

Tests and criteria for defining hypertension-mediated organ damage and considerations for their use in clinical practice.
ACR, albumin:creatinine ratio; BP, blood pressure; BSA, body surface area; CT, computed tomography; CVD, cardiovascular disease; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; HMOD, hypertension-mediated organ damage; hs-cTnT, high-sensitivity cardiac troponin T; LA, left atrial; LV, left ventricular; LVH, left ventricular hypertrophy; NT-proBNP, N-terminal pro-brain natriuretic peptide; PWV, pulse wave velocity; RWT, relative wall thickness; SCORE2, Systematic COronary Risk Evaluation 2; SCORE2-OP, Systematic COronary Risk Evaluation 2–Older Persons. More details and references can be found in the Supplementary data online , Tables S1 and S5 .
Finally, some individuals may be at heightened risk for CVD events when cardiac and vascular HMOD measurements like LVH and increased PWV do not regress over time with appropriate treatment and BP control. 14 , 268–271
Investigations aimed at screening for secondary hypertension are additional optional tests and are detailed in Section 7.6 . Of note, patients with an incidental adrenal nodule or nodules (typically detected on imaging of the abdomen done for other clinical reasons) warrant screening for elevated BP and hypertension. Those with adrenal incidentalomas and hypertension warrant a basic work-up for secondary hypertension to include screening for primary aldosteronism, Cushing's syndrome and phaeochromocytoma.
7.4.3.1. The kidneys
CKD is defined as abnormalities of kidney structure or function, present for at least 3 months with implications for health. 272 Renal function is evaluated initially using serum creatinine and an estimated glomerular filtration rate (eGFR) equation (preferably race-free CKD-EPI) and typically for proteinuria. 273 Our definition of moderate-to-severe CKD requires an eGFR of <60 mL/min/1.73 m 2 or albuminuria of ≥30 mg/g (≥3 mg/mmol). Intensive BP control in patients with CKD reduces rates of CVD events. 274 , 275 CKD can influence the choice of BP-lowering treatment ( Sections 8 and 9 ), as well as newer drugs for cardiovascular prevention, such as sodium–glucose co-transporter 2 (SGLT2) inhibitors and finerenone.
We recommend repeat measurement of eGFR and urine albumin:creatinine ratio (ACR) at least annually if clinically significant CKD is diagnosed. Renal ultrasound and Doppler examination to evaluate causes of CKD and to exclude renoparenchymal and renovascular hypertension (RVH) should also be considered. 276 , 277
Recommendations for assessing renal hypertension-mediated organ damage

7.4.3.2. The heart
A 12-lead ECG is a part of the initial routine work-up for all patients with hypertension and should be repeated whenever patients present with an irregular pulse or cardiac symptoms. The ECG should be analysed for LVH ( Supplementary data online , Table S1 ) and AF. 31 , 278–282
Echocardiography is recommended in patients with hypertension when the ECG is abnormal, murmurs are detected, or there are cardiac symptoms. A full, standardized, two-dimensional echocardiogram should be performed, preferably with tissue Doppler and strain assessment. Echocardiography can be considered for all patients with newly diagnosed hypertension, if local resources and reimbursement policies allow. Over 5 years of follow-up, subclinical left ventricular diastolic dysfunction predicts the incidence of CVD. 283–285 In addition, LVH detected by echocardiography predicts total and cardiovascular mortality and CVD events in the general population, 286 , 287 including in young adults. 26 , 268 , 288 , 289 Data on the associations with CVD of other metrics for detecting HMOD in the heart are also available. 26 , 268 , 290 Since cardiac size and function differ by sex, sex-specific thresholds for detecting HMOD in the heart are used to avoid under-diagnosis in women. 25 , 174 , 291
Recommendations for assessing cardiac hypertension-mediated organ damage

7.4.3.3. The arteries
Cardiac computed tomography (CT) may be used to measure CAC and, if intravascular contrast is administered, fully visualize coronary artery disease to improve risk stratification. 211 , 293 As noted in Section 6 , CAC scoring can reclassify CVD risk upwards or downwards in addition to conventional risk factors. 127 , 170 , 211 , 233 , 294 Carotid ultrasound detects presence or absence of carotid plaque (wall thickness ≥ 1.5 mm) and stenosis. Presence of plaque in the carotid or femoral arteries improves risk prediction for CVD events in asymptomatic patients on top of conventional risk-factor assessment. 211 , 247 , 265 , 267 , 295 , 296 Systematic use of intima media thickness does not appear to consistently improve prediction of future CVD events. 297 Arterial stiffness is measured as carotid–femoral PWV or brachial–ankle PWV, and can contribute to predictive value and risk reclassification. 28 , 31 , 215 , 216 PWV is currently used mostly for research purposes or in specialist referral centres. Checking for inter-arm BP difference may identify a subclavian stenosis as vascular HMOD. 38 Other tests assessing the vasculature [such as abdominal ultrasound or ankle–brachial index (ABI)] should also be considered in patients with hypertension, when specific cardiovascular complications (abdominal aneurysm, peripheral artery disease) are clinically suspected. Finally, microvascular HMOD can be assessed by fundoscopy. A simplified classification has been proposed and validated. 298 In hypertensive individuals, the presence of mild or moderate hypertensive retinopathy is associated with an increased risk of CVD events. 299 Fundoscopy is recommended also in hypertensive diabetic patients and in the work-up of malignant hypertension and hypertensive emergencies.
Recommendations for assessing vascular hypertension-mediated organ damage (see Evidence Table 17)

7.4.4. Genetic testing
Hypertension is considered a complex polygenic disorder, because many genes or gene combinations influence BP. 300 , 301 However, some well-defined phenotypes relating to single-gene mutations (i.e. monogenic forms of hypertension) have been identified (see Supplementary data online , Table S6 ). These are rare, but knowledge of the genetic defect may allow targeted treatment of the proband and also proper management of the patient’s siblings. 302 , 303 As such, genetic testing should be considered only for those with a high prior probability of having a monogenic condition and such patients should be referred to specialized centres. In most patients with elevated BP or hypertension, routine genetic testing is not recommended. Family history and a pedigree analysis can help to find a heritable pattern of hypertension or hypotension. 304
Recommendations for genetic testing in hypertension management

7.5. Resistant hypertension: definition and diagnosis
Despite availability and use of multiple BP-lowering medications, many patients worldwide have uncontrolled hypertension. 306–308 Considering this, societies have introduced the term ‘drug-resistant hypertension’, or ‘treatment-resistant hypertension’, or ‘resistant hypertension’, 309 which has been reported in 10%–20% of patients with hypertension. 310 , 311
Resistant hypertension is not a disease per se . Compared with treated patients who achieve BP control, patients with resistant hypertension (by any definition) have a worse prognosis: risk of myocardial infarction, stroke, end-stage renal disease, and death in these adults may be two- to six-fold higher. 309 Secondary causes of hypertension are also more likely in the presence of resistant hypertension. 312
All resistant hypertension definitions require a diuretic in the prescribed multiple-drug regimen, because excess salt intake and salt and water retention are key players in resistance to BP-lowering treatments ( Table 10 ). 309 In addition, excluding pseudo-resistance is a prerequisite. Specifically, pseudo-resistance indicates poor adherence to BP-lowering treatment, which should be verified by careful questioning of the patient in the first instance ( Section 7.4.3 ). 257 In addition, white-coat hypertension must be excluded. 263 Contributors to pseudo-resistance are listed in Table 11 . Objective evaluation of adherence (either directly observed treatment or detecting prescribed drugs in blood or urine samples) should also be considered, if resources allow.
Current definition of resistant hypertension
| Definition of resistant hypertension . |
|---|
| Hypertension is defined as resistant when a treatment strategy including appropriate lifestyle measures and treatment with maximum or maximally tolerated doses of a diuretic (thiazide or thiazide-like), a RAS blocker, and a calcium channel blocker fail to lower office systolic and diastolic BP values to <140 mmHg and/or <90 mmHg, respectively. These uncontrolled BP values must be confirmed by out-of-office BP measurements (HBPM or ABPM— for relevant BP thresholds). |
| Definition of resistant hypertension . |
|---|
| Hypertension is defined as resistant when a treatment strategy including appropriate lifestyle measures and treatment with maximum or maximally tolerated doses of a diuretic (thiazide or thiazide-like), a RAS blocker, and a calcium channel blocker fail to lower office systolic and diastolic BP values to <140 mmHg and/or <90 mmHg, respectively. These uncontrolled BP values must be confirmed by out-of-office BP measurements (HBPM or ABPM— for relevant BP thresholds). |
| Key considerations . |
|---|
| ) an adequately up-titrated loop diuretic is necessary to define resistant hypertension; |
| Key considerations . |
|---|
| ) an adequately up-titrated loop diuretic is necessary to define resistant hypertension; |
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; HBPM, home blood pressure monitoring; RAS, renin–angiotensin system.
Conditions found to cause pseudo-resistance or resistance to blood pressure-lowering treatment
| Causes of pseudo-resistant hypertension . |
|---|
| Poor adherence to and persistence with treatment White-coat phenomenon Poor BP measurement method Marked brachial artery calcification (Osler phenomenon) Clinician inertia (inadequate doses, inappropriate combinations of BP-lowering drugs) Munchausen syndrome (rare) |
| Causes of pseudo-resistant hypertension . |
|---|
| Poor adherence to and persistence with treatment White-coat phenomenon Poor BP measurement method Marked brachial artery calcification (Osler phenomenon) Clinician inertia (inadequate doses, inappropriate combinations of BP-lowering drugs) Munchausen syndrome (rare) |
| Causes of resistant hypertension . |
|---|
| Overweight/obesity Physical inactivity Excess daily dietary sodium Excess habitual alcohol consumption |
| See , |
| See |
| Causes of resistant hypertension . |
|---|
| Overweight/obesity Physical inactivity Excess daily dietary sodium Excess habitual alcohol consumption |
| See , |
| See |
The work-up of patients presumed to have resistant hypertension is complex and often requires technologies that are not available to GPs. 257 , 309 Accordingly, we recommend these patients are referred to specialized centres.
Recommendations for resistant hypertension work-up (see Evidence Table 18)

7.6. Secondary hypertension: when to screen/further investigations
7.6.1. general considerations.
Secondary hypertension is more prevalent than previously thought ( Figures 13 – 15 ). 312–317 Depending on the definition used and the cohort studied, the prevalence of secondary hypertension is 10%–35% in all hypertensive patients 318 , 319 and up to 50% of patients with resistant hypertension (though the latter prevalence estimate included persons with eGFR < 40 mL/min/1.73 m 2 ). 312 Primary aldosteronism is a common cause, 315 , 320 with, e.g. a high prevalence of hyperaldosteronism (up to 12%) observed in patients with BP of >180/110 mmHg. 316 Despite these numbers, screening rates for primary aldosteronism, even in high-risk groups such as those with resistant hypertension 321 and hypokalaemia, 322 are low (around 2% and 4% of eligible patients, respectively). In most healthcare systems, GPs are typically the ‘gatekeeper’ of access to specialized care and should be involved in screening patients for common causes of secondary hypertension, especially sleep apnoea and primary aldosteronism ( Supplementary data online , Tables S2 and S3 ). Primary aldosteronism is associated with an increased risk of CVD events, which may be partly independent of BP. 323 , 324

Summary of primary aldosteronism as a common form of secondary hypertension.
AF, atrial fibrillation; HMOD, hypertension-mediated organ damage.

Summary of renovascular disease as a common form of secondary hypertension.
CT-Angio, computed tomography angiography; CV, cardiovascular; FMD, fibromuscular dysplasia; GFR, glomerular filtration rate; MRI, magnetic resonance imaging; RAS, renin–angiotensin system.

Summary of obstructive sleep apnoea as a common form of secondary hypertension.
AF, atrial fibrillation; ABPM, ambulatory blood pressure monitor; CPAP, continuous positive airway pressure.
7.6.2. Primary aldosteronism
Though spontaneous or diuretic-induced hypokalaemia are strongly suggestive of primary aldosteronism, a history of hypokalaemia is not present in most patients diagnosed with this condition. The aldosterone-to-renin ratio (ARR) is thus recommended for primary aldosteronism screening (see Figure 13 ). 325 This test can easily be done in treatment-naïve patients, though it is far more common for the ARR test to be considered when patients are already being treated for elevated BP or hypertension. This is relevant because ARR can be influenced by the drugs being taken at the time of testing. Accordingly, there are 2 approaches to screen for aldosteronism among patients who are already undergoing treatment for elevated BP or hypertension:
The first is to conduct ARR testing in treated patients with an indication for aldosteronism screening as efficiently as possible and without changing or stopping their baseline BP-lowering medications, simply to facilitate such testing. The ARR result then needs to be interpreted in the context of the specific medication(s) the patient is taking. Advantages of this approach include reducing barriers to screening and no change in medication in these patients, many of whom do not have BP controlled and in whom further deterioration in their BP control by stopping or changing medication may increase risk of CVD. Disadvantages include the interpretation of the ARR result, which depends on the specific medications taken at the time of testing. 326 Input from a hypertension specialist or endocrinologist may be necessary.
To reliably estimate renin and aldosterone status (and therefore ARR), and to facilitate a ‘clean’ screen for aldosteronism, a second approach is to discontinue drugs that affect these variables whenever feasible before ARR testing ( Table 12 ). Such interfering drugs include, beta-blockers, centrally acting drugs (e.g., clonidine and alpha-methyldopa) renin-angiotensin system (RAS) blockers and diuretics. 326 Long-acting calcium channel blockers (CCBs), either dihydropyridine or non-dihydropyridine, and alpha-receptor antagonists do not interfere with the ARR and can be used instead of interfering medications before ARR testing. Should drugs that do not interfere with the ARR be contraindicated or insufficient to control BP, centrally acting sympatholytic drugs can also then be used, but at the risk of slightly more false positives (by renin suppression). Furthermore, when mineralocorticoid receptor antagonists (MRAs) cannot be stopped for safety reasons (i.e. severe hypokalaemia or severe hypertension among patients with severe hyperaldosteronism), recent evidence suggests that the accuracy of ARR testing under this treatment is only marginally impacted, particularly in the presence of florid primary aldosteronism. 327
Assessing sodium intake (preferably 24 h urinary sodium, or sodium-to-creatinine ratio in the morning urine sample) is also important for interpreting the ARR, as is time in menstrual cycle for females. ARR cut-offs vary depending on unit of measurement and by local laboratory. For detailed information, readers are referred to the latest primary aldosteronism guidelines. 328 , 329
Drugs and conditions that affect aldosterone, renin, and aldosterone-to-renin ratio
| Factor . | Effect on plasma aldosterone levels . | Effect on renin levels . | Effect on ARR . |
|---|---|---|---|
| Hypokalaemia | |||
| Potassium loading | |||
| Sodium restriction | |||
| Sodium loading | |||
| Beta-adrenergic blockers | |||
| Calcium channel blockers (DHPs) | with short-acting DHPs | ||
| ACE inhibitors | |||
| ARBs | |||
| Potassium-sparing diuretics | |||
| Potassium-wasting diuretics | |||
| Alpha-2 agonists (clonidine, methyldopa) | |||
| NSAIDs | |||
| Steroids | |||
| Contraceptive agents (drospirenone) | |||
| Factor . | Effect on plasma aldosterone levels . | Effect on renin levels . | Effect on ARR . |
|---|---|---|---|
| Hypokalaemia | |||
| Potassium loading | |||
| Sodium restriction | |||
| Sodium loading | |||
| Beta-adrenergic blockers | |||
| Calcium channel blockers (DHPs) | with short-acting DHPs | ||
| ACE inhibitors | |||
| ARBs | |||
| Potassium-sparing diuretics | |||
| Potassium-wasting diuretics | |||
| Alpha-2 agonists (clonidine, methyldopa) | |||
| NSAIDs | |||
| Steroids | |||
| Contraceptive agents (drospirenone) | |||
↑, raised; ↓, lowered; →, no effect; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; ARR, aldosterone-to-renin ratio; DHPs, dihydropyridines; FN, false negative; FP, false positive; NSAID, non-steroidal anti-inflammatory drug.
7.6.3. Renovascular hypertension
Renovascular hypertension (RVH) defines a condition where renal artery occlusion or stenosis decreases renal perfusion pressure to a level that activates the renin–angiotensin–aldosterone system (RAAS), thereby raising BP. Major causes are atherosclerosis and fibromuscular dysplasia ( Figure 14 and Supplementary data online , Tables S1 and S2 ). Atherosclerosis is the most common form of RVH, especially in older adults. 318 Fibromuscular dysplasia is a systemic non-atherosclerotic vascular disease involving medium-sized muscular arteries. When renal arteries are involved, fibromuscular dysplasia may induce RVH (FMD-RVH), especially in children and younger women. 330–332
Though not highly sensitive, very elevated renin levels raise the suspicion for RVH. The work-up of RVH ( Table 13 ) is based on imaging tests, such as renal artery Doppler ultrasound, with bilateral assessment of renal arterial resistive index, or abdominal CT angiography, or magnetic resonance imaging (MRI), in line with current ESC Guidelines on the diagnosis and treatment of peripheral arterial diseases, 277 which will be updated in 2024. Of note, bystander renal artery stenosis may be present in patients with essential hypertension, without causing secondary hypertension due to RVH. Since fibromuscular dysplasia is a systemic disease, CT or MRI angiography from head to pelvis is recommended in patients with FMD-RVH. 277 , 332
Optional tests that should be used to screen for secondary hypertension in the presence of suggestive signs, symptoms, or medical history
| Cause of secondary hypertension . | Screening test . |
|---|---|
| Primary aldosteronism | Aldosterone-to-renin ratio Helpful information can also be provided by reviewing prior potassium levels (hypokalaemia increases the likelihood of coexistent primary hyperaldosteronism) |
| Renovascular hypertension | Renal doppler ultrasound Abdominal CT angiogram or MRI |
| Phaeochromocytoma/paraganglioma | 24 h urinary and/or plasma metanephrine and normetanephrine |
| Obstructive sleep apnoea syndrome | Overnight ambulatory polysomnography |
| Renal parenchymal disease | Plasma creatinine, sodium, and potassium eGFR Urine dipstick for blood and protein Urinary albumin-to-creatinine ratio Renal ultrasound |
| Cushing’s syndrome | 24 h urinary free cortisol Low-dose dexamethasone suppression test |
| Thyroid disease (hyper- or hypothyroidism) | TSH |
| Hyperparathyroidism | Parathyroid hormone Calcium and phosphate |
| Coarctation of the aorta | Echocardiogram Aortic CT angiogram |
| Cause of secondary hypertension . | Screening test . |
|---|---|
| Primary aldosteronism | Aldosterone-to-renin ratio Helpful information can also be provided by reviewing prior potassium levels (hypokalaemia increases the likelihood of coexistent primary hyperaldosteronism) |
| Renovascular hypertension | Renal doppler ultrasound Abdominal CT angiogram or MRI |
| Phaeochromocytoma/paraganglioma | 24 h urinary and/or plasma metanephrine and normetanephrine |
| Obstructive sleep apnoea syndrome | Overnight ambulatory polysomnography |
| Renal parenchymal disease | Plasma creatinine, sodium, and potassium eGFR Urine dipstick for blood and protein Urinary albumin-to-creatinine ratio Renal ultrasound |
| Cushing’s syndrome | 24 h urinary free cortisol Low-dose dexamethasone suppression test |
| Thyroid disease (hyper- or hypothyroidism) | TSH |
| Hyperparathyroidism | Parathyroid hormone Calcium and phosphate |
| Coarctation of the aorta | Echocardiogram Aortic CT angiogram |
CT, computed tomography; eGFR, estimated glomerular filtration rate; MRI, magnetic resonance imaging; TSH, thyroid-stimulating hormone.
7.6.4. Obstructive sleep apnoea syndrome
Obstructive sleep apnoea syndrome (OSAS) is prevalent in hypertension and particularly in resistant hypertension, with studies indicating that up to 60% of patients with resistant hypertension have features of OSAS. 314 OSAS should be suspected in patients with hypertension and suggestive symptoms (see Supplementary data online , Table S2 ), in all patients with resistant hypertension, and in patients with non-dipping or reverse-dipping pattern at 24 h BP monitoring, especially if obese ( Figure 15 ). Using validated questionnaires may help identify patients at high risk of OSAS. 333 Lack of suggestive symptoms does not rule out OSAS. A simplified polysomnogram confirms the diagnosis [apnoea–hypopnoea index (AHI) > 5] and can quantify the severity of OSAS (mild: AHI < 15; moderate: AHI of 15–30; severe: AHI > 30). 334
7.6.5. Phaeochromocytoma/paraganglioma
Phaeochromocytomas/paragangliomas (PPGLs) are a rare form of secondary hypertension characterized by a highly heterogeneous clinical presentation. 335 , 336 PPGLs are usually discovered incidentally. 337
A PPGL should be suspected in the presence of signs and symptoms of catecholamine excess or in syndromic PPGL, in patients with a family history of PPGL, and in carriers of a germline mutation in one of the PPGL-causing genes. 338 Since normetanephrine and metanephrine are secreted constitutively, as opposed to the highly variable nature of catecholamine secretion, they are preferred as screening tests for PPGL ( Table 13 ).
Recommendations for screening for secondary hypertension (see Evidence Tables 19 and 20)

The ultimate goal of preventing and treating elevated BP and hypertension is to reduce CVD, to improve quality of life, and to prevent premature death. Crucially, besides BP, other CVD risk factors need to be comprehensively addressed (e.g. smoking, glucose, dyslipidaemia) as detailed in the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. 170 Indeed, it is worth emphasizing that, when combined, these CVD risk factors have multiplicative (not additive) effects on CVD risk. 340
8.1. Prevention strategies in early life
Detailed information on this topic is provided in the Supplementary data online . High BP tracks from childhood to adulthood. 341 , 342 Hypertension in childhood was redefined in a 2022 ESC Consensus Document. 343
Recommendations for screening for hypertension in children and adolescents (see Evidence Table 21)

8.2. Non-pharmacological interventions
A major underlying contributor to elevated BP and hypertension in the general adult population is unhealthy lifestyle, with severe consequences for all-cause and CVD mortality. As such, we give lifestyle interventions to reduce BP a special status in our recommendations throughout these guidelines ( Figures 16 and 17 ). This is reflected by a modified approach to the class of recommendations for lifestyle interventions compared with medical interventions (pharmacological or procedural). Given the salutary benefits of healthy lifestyle on a range of outcomes that extend well beyond BP-lowering effects, 347 including broad mental and physical health benefits, we do not require lifestyle interventions to have RCT evidence for efficacy in reducing CVD events through BP lowering to achieve a Class I recommendation. In deciding to give lifestyle interventions this status, the task force also recognizes that: (i) lifestyle interventions are less likely to be subjected to clinical outcomes trials (e.g. due to funding limitations and lack of interest from industry), and (ii) the risks of adverse effects and toxicity relating to healthy lifestyle interventions are low. In contrast, in these guidelines, to achieve a Class I recommendation (irrespective of level of evidence) there needs to be evidence that medical interventions that reduce BP also decrease CVD events by BP lowering.

Physical activity according to different types of exercise and reduction of blood pressure and overall cardiovascular disease risk.
Priority is given to aerobic exercise training (green). BP, blood pressure; CVD, cardiovascular disease.

Effects of main lifestyle factors on blood pressure and cardiovascular risk reduction.
BP, blood pressure; CV, cardiovascular. Smoking cessation reduces overall cardiovascular risk but not BP (long arrow). Salt reduction reduces BP and (for persons with high baseline intake) reduces cardiovascular risk. Increased potassium intake and higher physical activity, as well as optimized weight management, reduce BP and are associated with lower overall cardiovascular risk (short arrows).
8.2.1. Dietary sodium and potassium intake
8.2.1.1. sodium.
Reducing dietary salt (sodium chloride) intake in individuals with high baseline intake lowers CVD event rates. 348 Extensive observational studies have reported dose–response associations between high dietary sodium intake and CVD events. 349–351 The potential impact of salt reduction on population health is significant, particularly in countries where the population’s average salt intake is high. Pooled data from long-term follow-up salt-reduction trials demonstrate that reducing salt by 2.5 g/day is associated with an approximately 20% reduction in CVD events at the population level. 349
The health benefits of salt reduction are likely mediated, largely, by BP-lowering effects. 352–354 An almost linear relationship has been described in a dose–response meta-analysis between sodium intake ranging from 0.4 to 7.6 g/day and reduction of systolic and diastolic BP is independent of baseline BP. 355 , 356 Women appear to be, on average, more sodium sensitive than men, 357 and may have greater outcome benefits when receiving comparable sodium-restricted diets. 358 Trial evidence for the BP-lowering benefits of salt reduction extend down to daily sodium intakes of <1.5 g/day. 356 , 358–361
The task force acknowledges that the observational data linking sodium intake to CVD outcomes are mixed and that some studies have not found a link between salt intake and CVD. 362 , 363 In addition, a potential J-curve exists between sodium intake and CVD events (whereby some analyses suggest that sodium reduction to very low levels could be harmful). 363 , 364 While there are differences of opinion, the task force agreed that, on balance, (i) observational J-curve data are often due to reverse causality or confounding, 114 , 348 , 365 , 366 (ii) the relationship between dietary sodium and stroke is typically linear in shape, without any J-curve, (iii) if the J-curve were causal, the adverse effect of very low sodium on CVD would have to be mediated by some harmful mechanism that overcomes the expected benefit mediated by BP lowering (which is unlikely), and (iv) estimation of sodium intake using spot-urine sodium testing (which was commonly done in studies reporting a J-curve) may not be as valid as other methods. 367 For example, most (but not all) 362 reports measuring 24 h urine sodium excretion (a surrogate measure of sodium intake) have not reported a J-curve association with CVD. 350 , 364 Furthermore the causal evidence demonstrating reduced CVD with sodium restriction (using potassium-enriched salt substitutes) in the Salt Substitute and Stroke Study (SSaSS) and Diet, ExerCIse and carDiovascular hEalth-Salt (DECIDE-Salt) trials was compelling, 348 , 368 even though sodium restriction in these trials was not below 2 g/day.
It is recommended to restrict total dietary sodium intake to approximately 2 g/day or less (equivalent to approximately 5 g or about a teaspoon of salt per day). This includes added salt and salt already contained in food. While the feasibility of this sodium target can be debated, the evidence for the benefits of this sodium target among patients with elevated BP or hypertension is sufficient, particularly in terms of lowering BP. The optimal sodium intake in the general population with non-elevated BP is less clear (noting also that the BP-lowering effect of salt reduction among patients with non-elevated BP appears lower). 353 , 354 A more feasible compromise in the general population might be a target sodium intake range of 2–4 g/day. 369 , 370 It needs to be emphasized that large parts of daily sodium intake occur by means of sodium consumption contained in processed foods.
8.2.1.2. Potassium
Optimal dietary potassium intake, e.g. by consuming diets rich in fruits and vegetables, has BP-lowering effects and may be associated with lower CVD risk. 348 , 364 , 368 , 371–373 The association between potassium intake, systolic BP, and CVD events may be sex-specific, being stronger in women. 374 The World Health Organization (WHO) recommends over 3.5 g/day (∼90 mmol/day) of dietary potassium. 375 Excessive potassium supplementation should, however, be avoided 374 and CKD guidelines recommend dietary potassium restriction to <2.4 g/day in persons with advanced CKD (see Supplementary data online ). 376
A lower urinary sodium-to-potassium ratio (Na + /K + ratio; a surrogate for reduced dietary sodium intake complemented by increased potassium intake) has been associated with a greater reduction in systolic and diastolic BP than with a higher ratio. 348 , 377
In patients with hypertension and high dietary sodium, increased dietary intake of potassium (in addition to lower dietary sodium) should be considered. 348 , 350 , 378 In patients with persistently high sodium intake (>5 g/day) and without moderate-to-advanced CKD, particularly women, an increase in potassium intake by 0.5–1.0 g/day may be considered to achieve a favourable Na + /K + ratio of 1.5–2.0 and to reduce CVD risk. Potassium supplementation can be achieved by substituting sodium using potassium enriched salts (75% sodium chloride and 25% potassium chloride) 368 , 379 , 380 or by increasing dietary potassium intake [e.g. a 125 g (medium) banana contains about 450 mg potassium, or unsalted boiled spinach (840 mg/cup) or mashed avocado (710 mg/cup)]. In patients with CKD and/or those taking potassium-sparing medication, such as some diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs) or spironolactone, serum levels of potassium should be monitored (noting that phlebotomy recommendations to avoid spuriously high potassium results should be followed).
8.2.2. Physical activity and exercise
In a systematic review and meta-analyses, aerobic (endurance) exercise was suggested as the first-line exercise therapy for reducing BP in patients with elevated BP and hypertension vs. alternative forms of exercise, such as dynamic or isometric resistance training. 381 In patients with hypertension, regular aerobic exercise substantially lowers systolic BP by up to 7–8 mmHg and diastolic BP by up to 4–5 mmHg. 381 , 382 For non-white patients with hypertension, dynamic resistance training elicits BP reductions that appear comparable to aerobic exercise. 383 Isometric resistance training also achieves clinically relevant BP reductions in patients with hypertension, but results are inconsistent and more data from more high-quality intervention trials are required (see Supplementary data online ). 381 , 384 , 385 With respect to mode and intensity of aerobic exercise, high-intensity interval training elicits comparable BP reductions to moderate continuous exercise, with high-intensity interval training achieving greater improvement in physical fitness. 386
In patients with known hypertension, engaging in physical activity is associated with reduced CVD mortality risk vs. sedentary patients with hypertension. 387
An exaggerated BP response to exercise may yield diagnostic merits for predicting incident hypertension and CVD. In a meta-analysis, an exaggerated BP response to exercise was associated with an increased risk for masked hypertension. 388 The risk of coronary heart disease also increases with higher systolic BP during exercise, independent of systolic BP at rest. 389
Prior recommendations for at least 150 min/week of moderate intensity aerobic exercise (≥30 min, 5–7 days/week) can be maintained. 1 , 390 Alternatively, 75 min of vigorous-intensity exercise per week over 3 days may be performed, with additional benefits derived by achieving 300 min of moderate-intensity or 150 min of vigorous-intensity aerobic physical activity per week. 390 , 391 As acute aerobic exercise induces intensity-dependent short-term reductions in ambulatory BP after exercise, patients with elevated BP and hypertension may benefit from daily exercise to improve their 24 h BP profile and avoid BP peaks on sedentary days. 392 Aerobic exercise should be complemented by low- or moderate-intensity resistance training (2–3 times per week), e.g. dynamic resistance, starting at 2–3 sets of 10–15 repetitions at 40%–60% of one-repetition maximum 393 or isometric resistance training with three sets of 1–2 min contractions, such as hand-grip, plank, or wall sit ( Figure 16 ). 381 , 394
In uncontrolled hypertension at rest, high-intensity exercise should be applied with caution, with resting systolic BP of >200 mmHg and diastolic BP of >110 mmHg indicating relative contraindications. 395 Age, sex, gender, 396 ethnicity, and comorbidities, as well as individual preferences, should be considered for individual exercise prescription. Detailed information on exercise prescription in terms of frequency, intensity, time (duration) and type and progression are available in the 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease, 390 which include recommendations for pre-participation screening and cardiopulmonary exercise testing. 390
8.2.3. Weight reduction and diet
Visceral obesity is common and associated with incident hypertension. 397 , 398 An average weight loss of 5 kg has been associated with an average systolic and diastolic BP reduction of 4.4 and 3.6 mmHg, respectively. 399 Data show that, starting at an index body mass index (BMI) of 40 kg/m 2 , a median weight loss of 13% is associated with a 22% lower risk for hypertension. 400 , 401 Maintaining even moderate weight loss of 5%–10% of initial body weight can improve not only BP, but also glucose and lipid metabolism, and potentially reduce premature all-cause mortality. 402–404 However, achieving long-term effects in patients with hypertension via weight loss is challenging and the magnitude of these effects remains unclear. 405 , 406 Weight stabilization during middle-age appears to be an important and attainable goal to prevent obesity-related increase in BP later in life. 407
Evidence-based diets, such as the Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet, are established interventions in patients with hypertension to reduce their BP and CVD risk. 408 , 409 Additional information on healthy dietary patterns is provided in the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice and Supplementary data online . 170
In combination with weight-loss and exercise interventions 410 and low sodium intake, 411 the DASH diet has added effect on BP reduction. 412 Pharmacological treatment of obesity with orlistat achieved a slight reduction of 2.6 mmHg in systolic BP. 413 The greatest BP-lowering effects of weight-loss medications may be achieved with the glucagon-like peptide 1 (GLP-1) receptor agonists. 414–416 For example, in the Semaglutide Treatment Effect in People with Obesity (STEP-1) trial, the GLP-1 analogue semaglutide resulted in a mean weight reduction of 12.4% and a 5.1 mmHg reduction in systolic BP. 415
8.2.4. Alcohol, coffee, and soft drinks
In a 2020 Cochrane review, the short-term effects of alcohol on BP were dose dependent; low-dose alcohol (<14 g) did not affect BP within 6 h, medium-dose (14–28 g) decreased both systolic and diastolic BP, and high-dose alcohol (>30 g) first decreased BP up to 12 h and then increased BP following >13 h of consumption by 3.7 mmHg systolic and 2.4 mmHg diastolic. 417 The trials in this Cochrane review included small numbers of women. In the longer term, no evidence has been found for a protective effect of chronic alcohol consumption on hypertension, for either sex. In contrast, even low-dose alcohol consumption (10 g/day) increases chronic risk of hypertension by 14% in men, but not in women. 418 As per the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice, men and women are recommended to stay within the upper limit of drinking alcoholic beverages (100 g/week of pure alcohol). Defining number of drinks depends on portion size, the standards of which differ per country, but translates to 8–14 g/drink. 170 Emerging data indicate it is likely healthiest to avoid all alcohol, where possible. 419
Coffee intake is not associated with a higher risk of hypertension in the general population; in fact, higher coffee consumption may be associated with a lower risk for incident hypertension. 420 Data regarding the association between tea drinking and CVD are inconclusive, though mechanistic trials have suggested benefits on BP lowering. 421 In contrast, energy drinks with high concentrations of ingredients such as taurine and caffeine increase BP and may lead to acute or chronic cardiovascular complications in young adults. 422–424
Consuming two or more servings per day of sugar-sweetened beverages was associated with a 35% higher risk of coronary artery disease in women in the Nurses’ Health Study. 425 In the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort, both sugar- and artificially sweetened soft drinks were associated with higher all-cause mortality. 426 In children and adolescents, sugar-sweetened beverages increased systolic BP and the risk for incident hypertension. 427 It is recommended to restrict free sugar consumption, in particular sugar-sweetened beverages, to a maximum of 10% of energy intake.
8.2.5. Smoking
To stop smoking is arguably the most effective measure in preventing major CVD events at the individual level, likely through improved vascular health. 428–431 Estimated health benefits will be even more substantial looking at all-cause morbidity and mortality, e.g. including smoking cessation for cancer prevention.
The effects of electronic cigarettes (e-cigarettes) on BP remain unclear and to date there are no robust outcomes data. However, growing evidence suggests that e-cigarettes can increase BP (see Supplementary data online ). 432 , 433
Among adults, smoking affects ambulatory BP by raising daily BP, 434 but effects of chronic smoking on office BP appear to be small. 435 Smoking cessation advice helps, but more intensive interventions are superior. 436 , 437 As recommended by previous ESC Guidelines, smoking cessation is recommended to reduce CVD risk and improve non-CVD health. 1 , 170
Recommendations for non-pharmacological treatment of blood pressure and cardiovascular risk reduction (see Evidence Tables 22–26)

8.3. Pharmacological interventions
8.3.1. treatment strategy to reduce adverse cardiovascular disease outcomes.
The main goal of reducing BP is to prevent adverse CVD outcomes. The relative risk reduction afforded by a fixed degree of BP reduction is largely independent of pre-treatment BP. 116 There is a clear relationship between the intensity of BP lowering and the relative and absolute reduction in risk of CVD events for all adults, regardless of age (at least up to 85 years), sex, prior CVD, diabetes, or AF. 116 , 131 , 443–445 With this strong evidence for the ‘the lower the better, but within reason’ paradigm, decision rules are required for selecting patients most likely to benefit from treatment. 172 In this section, a summary of evidence for BP-lowering drug treatment is provided, followed by strategies for their use for preventing CVD.
8.3.2. Drug classes with evidence on clinical outcomes in the target population
The major drug classes with robust evidence for BP-mediated reduction in CVD events are ACE inhibitors, ARBs, dihydropyridine CCBs, diuretics (thiazides and thiazide-like diuretics such as hydrochlorothiazide, chlorthalidone, and indapamide), and beta-blockers (see Supplementary data online , Tables S7 and S8 ). 122 , 446 , 447 The first four are recommended as first-line options for starting hypertension treatment in the general population. Beta-blockers can be added preferentially in circumstances such as in the presence of angina or heart failure, after myocardial infarction, or for controlling heart rate, where they are the cornerstone of therapy. 122 , 448 , 449 In such settings, second-generation (cardioselective) and, specifically, third-generation (vasodilating) beta-blockers are preferred. 450 However, beta-blockers are less effective than ACE inhibitors, ARBs, CCBs, or diuretics at preventing stroke, and have a higher discontinuation rate due to side effects. 451 , 452 Beta-blockers and diuretics, especially when combined, are associated with an increased risk of new-onset diabetes in predisposed patients. 453 , 454 The effect of RAS blockers and CCBs on preventing progression of HMOD also appears to be superior to beta-blockers. 455–458 Beta-blockers should also be avoided in patients with isolated systolic hypertension or more generally with arterial stiffness, as they increase stroke volume (given the lower heart rate). 218
When therapy and adherence with the above-mentioned drug classes is optimized but insufficient to reach BP goals, other drug classes can be used for treating hypertension. Of these, spironolactone, an MRA, appears to be the most effective at further lowering BP in resistant hypertension; however, more evidence of CVD risk-lowering effects with MRAs among all hypertensive populations, especially those without resistant hypertension, is needed. 459 Specifically, while use of MRAs in patients with heart failure has provided clinical evidence on the effectiveness of MRAs for preventing CVD events, dedicated outcome trials in patients with primary hypertension without heart failure are lacking. Because the present guidelines require trial evidence for CVD outcome benefit for a BP-lowering drug or procedure to achieve a Class I recommendation, and given no outcome trials of MRAs have been conducted in general samples of patients with primary hypertension, we have given MRAs a Class IIa recommendation (see below). We acknowledge that spironolactone was provided a Class I recommendation in the 2018 ESC/ESH Guidelines on the management of arterial hypertension. However, to be consistent with our requirement for trial evidence for CVD outcomes benefit in patients with hypertension, the task force agreed to provide a Class IIa recommendation for spironolactone in these 2024 Guidelines. Importantly, it was also agreed that a Class IIa recommendation (i.e. should be considered) is an endorsement of MRAs for treating resistant hypertension but one that acknowledges some uncertainty of outcomes benefit. Future outcome trials of MRAs, perhaps including finerenone, 460–462 are encouraged in patients with hypertension.
Clinical outcome evidence from trials for other BP-lowering drug classes, such as alpha-blockers, hydralazine, minoxidil, other potassium-sparing diuretics, and centrally acting agents, is less compelling and caution regarding adverse effects is warranted. However, they may be a final addition if all other therapeutic efforts are insufficient to decrease BP. Of note, in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack (ALLHAT) trial, the alpha-blocker arm was stopped early due to futility of benefit for the CVD outcome. 463
8.3.3. New therapies with blood pressure-lowering properties that await supportive evidence from cardiovascular outcomes trials prior to guideline endorsement and routine use in hypertension
A few other drug classes with indication in heart failure have emerged that also have BP-lowering properties. For example, the angiotensin receptor–neprilysin inhibitor (ARNi) sacubitril/valsartan, which was initially developed for hypertension, 464 reduces CVD mortality and morbidity in patients with heart failure, an effect that may have been mediated, in part, by superior BP lowering compared with enalapril alone. 465 , 466 In a post hoc subgroup analysis, sacubitril/valsartan lowered BP in adults with both heart failure with preserved ejection fraction (HFpEF) and resistant hypertension. 467 In the context of research studies, sacubitril/valsartan has been used in higher doses (200 mg or 400 mg once daily) for treating hypertension. 464 , 466 , 468 , 469
SGLT2 inhibitors have shown favourable effects on CVD events and renal haemodynamics in patients with and without type 2 diabetes, and in heart failure trials. 470 In these trials, SGLT2 inhibitors did lower BP, though only modestly. 471 Small trials among adults with hypertension have confirmed the potential for BP lowering with this drug class. 472 , 473
Other new drugs with preliminary data include GLP-1 agonists and the new non-steroidal MRAs, e.g. finerenone, in managing hypertension. 415 , 460 , 461 In addition, novel aldosterone synthase inhibitors (baxdrostat and lorundrostat) have significantly lowered BP in patients with uncontrolled hypertension in phase 2 trials. 474 , 475
The dual endothelin-A and -B receptor antagonist aprocitentan also reduced office and 24 h BP compared with placebo at 4 weeks in patients with resistant hypertension in a phase 3 trial. 476 Zilebesiran, an investigational RNA interference agent administered subcutaneously, inhibits hepatic angiotensinogen synthesis and a single dose reduced 24 h BP over approximately 6 months. 477
8.3.4. Drug combinations and up-titrating strategies
To treat hypertension, many patients will require more than one BP-lowering medication. Combining drugs from different drug classes can have additive or synergistic effects and lead to greater BP reduction than increasing the dose of one drug. 478–483 The superior BP-lowering efficacy of combination therapy is mediated, at least in part, by the potential of combination therapy to target multiple pathophysiological pathways contributing to perturbed BP in each patient. 484 A further benefit of combination therapy is the potential to use lower doses of each individual BP-lowering agent, which may reduce side effects and improve adherence and persistence, 485 though the evidence for this hypothesis has been questioned. 486
Upfront low-dose combination therapy is therefore recommended in persons with hypertension, with the potential advantages of fewer side effects and swifter BP control being important for long-term adherence. 487–489 If combination BP-lowering therapy is pursued, single-pill combinations are preferred. For those with elevated BP who have an indication for BP-lowering treatment, monotherapy is recommended in the first instance.
One caveat to combination therapy in hypertension is that patient-level response to individual BP-lowering drug classes can be heterogeneous (suggesting some patients may benefit from more personalized treatment compared with routine combinations). 490 This is relevant also with respect to race/ethnicity (see Section 9 ). Another caveat is that the evidence for reduced CVD outcomes with BP-lowering drugs in combination therapy is based on observational studies. 491–493 There are no outcomes data from prospective trials that prove superiority of upfront combination therapy (either as single-pill combinations or as separate pills) over upfront monotherapy in the isolated treatment of hypertension. 486 Therefore, we considered giving upfront combination therapy (either as separate pills or as single-pill combinations) a Class IIa recommendation in these guidelines. However, given the totality of evidence for outcomes benefit in observational studies, randomized trial data for better BP control and adherence, and importantly, also given CVD outcomes benefit for polypills (a form of single-pill combination) in randomized trials, 494–496 we chose to provide a Class I recommendation for upfront combination therapy in adults with confirmed hypertension, in agreement with 2018 ESC recommendations.
The major four drug classes (ACE inhibitors, ARBs, dihydropyridine CCBs, and thiazide or thiazide-like diuretics) are recommended as first-line BP-lowering medications, either alone or in combination. 122 , 447 , 484 , 497 An exception is the combination of two RAS blockers, which is not recommended. 498–500 For most hypertensive patients, a single-pill combination, initially containing two of these major drug classes, and initially at low dose, is recommended. 489 , 501 , 502 Doses of BP-lowering drugs are presented in the Supplementary data online , Tables S7 and S8 .
When BP is still uncontrolled under maximally tolerated triple-combination (RAS blocker, CCB, and diuretic) therapy, and after adherence is assessed, the patient should be considered resistant and referred to an expert centre for appropriate work-up (see Section 7.5 ). At the same time, the addition of spironolactone should be considered. 459 If spironolactone is not tolerated, eplerenone or other MRA, or beta-blockers (if not already indicated), should be considered. Eplerenone may need to be dosed higher (50–200 mg) for effective BP lowering. In a meta-analysis, eplerenone 25 mg did not lower BP. 503 Due to the shorter time of action than spironolactone, eplerenone may need to be administered twice daily for treating hypertension. An alternative to MRA as fourth-line treatment for BP lowering is the use of beta-blockers for persons who do not already have a compelling indication. A vasodilating beta-blocker (e.g. labetalol, carvedilol, or nebivolol) is preferred when a beta-blocker is chosen. 504 However, we note that the BP-lowering effects of beta-blockade appears to be less potent than spironolactone in the setting of resistant hypertension. 459
Only thereafter should hydralazine, other potassium-sparing diuretics (amiloride and triamterene), centrally acting BP-lowering medications, or alpha-blockers be considered. Given multiple side-effects, minoxidil should only be considered if all other pharmacological agents prove ineffective in resistant hypertension. 505
As noted above, polypills combining fixed doses of BP-lowering treatment, lipid-lowering therapy and, if indicated, aspirin are effective in more general CVD prevention. 496 , 506–509 However, the polypill is not available for routine clinical use in many European countries.
8.3.5. A practical algorithm for intensive, effective, and tolerable blood pressure lowering with drug therapy, including considerations around single-pill combinations
The aim of the algorithm in Figure 18 is to introduce a low-dose double- and then triple-combination strategy while monitoring tolerance among patients with hypertension, and only afterwards to start up-titrating doses to maximum amounts.

Practical algorithm for pharmacological blood pressure lowering.
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BP, blood pressure; CCB, calcium channel blocker; FU, follow-up.
Initiation with monotherapy, slower up-titration, and lower dosing should be considered in the setting of elevated BP and increased CVD risk, or in moderate-to-severe frailty, limited life expectancy, symptomatic orthostatic hypotension, or older people (aged ≥85 years). Ideally, BP should be treated to target within 3 months to retain the confidence of the patient, to ensure long-term adherence, and to reduce CVD risk. 71
An overview of the recommended approach to BP management in all adult patients is provided in Figure 19 (Central Illustration). Also, of note, teleconsultation, multidisciplinary or nurse-led care, or patient self-monitoring can help with achieving BP control in certain healthcare systems. 75 , 510 , 511

Central Illustration.
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CVD, cardiovascular disease; CKD, chronic kidney disease; DBP, diastolic blood pressure; HBPM, home blood pressure monitoring; OH, orthostatic hypotension; SBP, systolic blood pressure; SCORE2, Systematic COronary Risk Evaluation 2; SCORE2-OP, Systematic COronary Risk Evaluation 2–Older Persons. Summary algorithm for BP classification and management. See Section 5 for recommendations on out-of-office confirmation of the three BP categories. a Adults with type 2 diabetes mellitus only and younger than 60 years should be considered for SCORE2-Diabetes assessment. b Though scientific data demonstrate that, under research conditions, the optimal target BP is ≤120/70 mmHg, the target BP recommended by these guidelines in routine practice is 120–129/70–79 mmHg. If achieving this target is not possible, or if treatment is not well tolerated, then BP should be treated to as low as reasonably achievable. For persons with elevated BP, treatment with lifestyle measures for 3 months is first recommended, prior to considering medications.
8.3.6. Timing of blood pressure-lowering drug treatment
Current evidence does not show benefit of diurnal timing of BP-lowering drug administration on major CVD outcomes. 512 It is important that medication is taken at the most convenient time of day to improve adherence. Patients should also be encouraged to take medications at the same time each day and in a consistent setting, to help ensure adherence. 246 , 513
Recommendations for pharmacological treatment of hypertension (see Evidence Tables 27, 28, and 29)

8.4. Selecting patients for pharmacological blood pressure-lowering treatment
Commencement of BP-lowering treatment is often decided based on office BP measurements but, where possible, the present guidelines strongly recommend using out-of-office BP measurement for confirming elevated BP and hypertension (see Section 5 ) . As detailed in Section 6 , an office BP of <120/70 mmHg is categorized in these guidelines as non-elevated BP.
When a patient is diagnosed with confirmed hypertension (sustained BP ≥ 140/90 mmHg), starting BP-lowering treatment is recommended irrespective of CVD risk, which should consist of a simultaneous combination of lifestyle interventions and pharmacological therapy. Lifestyle interventions are crucial as an initial treatment step, and must be strongly emphasized with the patient, but concurrent pharmacological therapy is recommended. This concurrent initiation of lifestyle and pharmacological therapy should not give patients the impression that lifestyle changes are of lesser importance, and the patient should be counselled that these lifestyle changes may allow subsequent discontinuation or down-titration of medication, which can be used as motivation to persist with lifestyle changes. After treatment initiation, the patient should be seen frequently (e.g. every 1–3 months with a GP or specialist) until BP is controlled. BP should be controlled, preferably within 3 months (see also Section 6 and algorithm Figure 18 ). If lifestyle changes are effective in BP lowering, pharmacological treatments may subsequently be down-titrated or stopped as appropriate.
When office BP is 120–139/70–89 mmHg, the patient is considered as having elevated BP, and further CVD risk stratification is recommended to guide therapy ( Table 14 ).
In patients with elevated BP who are not at increased risk for CVD (10-year CVD risk <10%) and do not have other high-risk conditions or risk modifiers, BP-lowering lifestyle measures are recommended. While there are not enough outcomes data for a drug recommendation in lower CVD risk adults with elevated BP, there is some evidence to suggest that relative treatment effects of BP lowering are similar across a wide range of predicted risk categories, including among those with a <10% risk. 518 Therefore, while we do not provide a formal recommendation for this, if initial lifestyle measures are not successful after 6–12 months, drug treatment might be discussed on an individual basis among lower CVD-risk adults when BP is between 130/80 and <140/90 mmHg. 518
In patients with elevated BP (office BP of 120–139/70–89 mmHg) who are at sufficiently high risk for CVD (e.g. 10-year CVD risk ≥ 10%) or in the presence of high-risk conditions or borderline 10-year CVD risk (5% - <10%) combined with risk modifiers or abnormal risk tool tests, BP-lowering lifestyle measures should be initiated for 3 months. Following this, pharmacological therapy is recommended for persons with confirmed BP of ≥130/80 mmHg, when these lifestyle changes have not worked or are not being implemented ( Section 8.2 ) Prompt addition of pharmacological therapy, if needed by 3 months, should be emphasized, to avoid therapeutic inertia. 519 For those with BP of 120–129/70–79 mmHg, ongoing and intensified lifestyle intervention is preferred.
The above recommendations apply to all individuals with elevated BP, irrespective of age. However, recognizing the lack of conclusive evidence and added risk of side effects among certain subgroups, the task force also recommends that, among patients with elevated BP, BP-lowering treatment should always be started based on individual clinical judgment and shared decision-making.
Initiation of blood pressure-lowering treatment based on confirmed blood pressure category and cardiovascular disease risk
| Blood pressure (mmHg) . | Non-elevated BP (<120/70) . | Elevated BP (120/70 to 139/89) . | Hypertension (≥140/90) . | |
|---|---|---|---|---|
| Assumed all at sufficiently high risk to benefit from pharmacological treatment | ||||
| Lifestyle measures for prevention Screen BP and CVD risk opportunistically | Lifestyle measures for treatment Monitor BP and CVD risk yearly | Lifestyle measures and pharmacological treatment (after 3-month delay). Monitor BP yearly once treatment control is established | Lifestyle measures and pharmacological treatment (immediate) Monitor BP yearly once treatment control is established | |
| Blood pressure (mmHg) . | Non-elevated BP (<120/70) . | Elevated BP (120/70 to 139/89) . | Hypertension (≥140/90) . | |
|---|---|---|---|---|
| Assumed all at sufficiently high risk to benefit from pharmacological treatment | ||||
| Lifestyle measures for prevention Screen BP and CVD risk opportunistically | Lifestyle measures for treatment Monitor BP and CVD risk yearly | Lifestyle measures and pharmacological treatment (after 3-month delay). Monitor BP yearly once treatment control is established | Lifestyle measures and pharmacological treatment (immediate) Monitor BP yearly once treatment control is established | |
BP, blood pressure; CKD, chronic kidney disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; FH, familial hypercholesterolaemia; HMOD, hypertension-mediated organ damage; SBP, systolic blood pressure.
a Caution in adults with orthostatic hypotension, moderate-to-severe frailty, limited life expectancy, and older patients (aged ≥85 years).
In addition, consideration of BP-lowering drug treatment should be deferred until BP is >140/90 mmHg in the following settings: pre-treatment symptomatic orthostatic hypotension, age ≥85 years, clinically significant moderate-to-severe frailty, and/or limited predicted lifespan (<3 years) due to high competing risk (including eGFR < 30 mL/min/1.73 m 2 ). Patients with elevated BP in these settings are less likely to obtain sufficient net benefit from BP-lowering drug therapy or to tolerate intensive drug therapy. Section 9 contains more information on the treatment of specific subgroups, including older and frail adults.
Recommendations for initiating blood pressure-lowering treatment (see Evidence Tables 30–32)

8.5. Intensity of blood pressure-lowering therapy and ideal treatment targets
8.5.1. expected degree of blood pressure reduction with approved drugs.
The magnitude of BP reduction achieved with the main classes of BP-lowering medications (ACE inhibitors, ARBs, dihydropyridine CCBs, diuretics, and beta-blockers) as monotherapy is similar overall. 528 , 529 BP reduction with standard doses of any of these five classes can be expected to be approximately 9/5 mmHg with office BP and 5/3 mmHg with ABPM. 478 These BP-lowering effects may attenuate over time. 530 Combination therapy (e.g. with three drugs at half standard dose) over the short term can lower office BP by up to 20/11 mmHg. 478 , 531 The reason why beta-blockers are not considered first-line BP-lowering medications (outside of compelling indications) is not because of inferior BP-lowering properties (particularly for vasodilating beta-blockers), 532 but because of inferior efficacy in reducing CVD events (particularly stroke) among patients with hypertension, and tolerance issues. 533–536
The BP-lowering effect of each BP medication class generally increases with the dose administered, though this relationship is not linear. 537 Effects of each medication can also vary at the individual level, sometimes requiring personalization by matching the patient with the best medication for them. 490 The magnitude of BP reduction for any BP-lowering medication may increase as a function of the pre-treatment BP, which is also known as Wilders principle. 538 , 539
The BP-lowering effect of pharmacological therapy is typically evident after 1–2 weeks of treatment, 540 but the maximum effect might take longer to manifest. Therefore, the advised follow-up after 1–3 months (1 month preferred with a GP or specialist) allows for assessment of tolerance/safety, but also allows enough time to gauge the full BP-lowering effect of each drug titration (see Section 8.3.4 ).
8.5.2. The ideal target of blood pressure-lowering treatment
As discussed in Section 6 , optimal control of BP translates into CVD risk reduction, thereby reducing morbidity and mortality in the population. 116 , 478 , 541
BP threshold is defined as the BP at which BP-lowering treatment is initiated, while BP target is the BP goal with treatment.
The BP threshold to initiate BP-lowering therapy is not necessarily the same as the recommended BP target once therapy is commenced (in other words, treatment threshold and treatment target may not be the same for a given patient). Specifically, for hypertensive patients in whom BP-lowering treatment is recommended above a baseline BP of ≥140/90 mmHg, the recommended target of BP-lowering therapy is 120–129/70–79 mmHg, provided treatment is well tolerated (see Supplementary data online ). Persons with elevated BP who receive treatment are also recommended to achieve a target of 120–129/70–79 mmHg.
Therefore, the treatment target in the 2024 Guidelines is always 120–129/70–79 mmHg (but only if treatment is tolerated and with certain exceptions where more lenient targets are advised). In contrast, the treatment threshold may differ based on CVD risk, specifically in the elevated BP category. For example, in addition to hypertensive adults with BP ≥140/90 mmHg, there are individuals with an office systolic BP of 130–139 mmHg and/or diastolic BP of 80–89 mmHg who have sufficiently high CVD risk to recommend BP-lowering drug treatment.
The BP target range of 120–129/70–79 mmHg recommended in these guidelines reflects the most current evidence from contemporaneous RCTs 135 , 136 , 146 , 542–545 and from meta-analyses of RCTs. 131 Of note, this treatment target reduces CVD events in older adults 136 , 523 with evidence for efficacy of more intensive BP-lowering treatment targets established up to age 85 years. 131 Furthermore, research data indicate that, to optimally reduce CVD risk, achieving an on-treatment BP of 120/70 mmHg is the best point on the BP target range provided in our guideline recommendations ( Figure 20 ). However, while we strongly considered recommending a treatment target of exactly 120/70 mmHg with out-of-office BP confirmation, we instead chose a target range of 120–129/70–79 mmHg (preferably with out-of-office BP confirmation but also allowing for office BP) for the following reasons: providing flexibility to patients and clinicians; feedback from external peer review; feedback from patients that lifestyle is preferred to medication unless BP is in the hypertensive range; the knowledge that contemporary treat-to-target intensive BP trials included only persons with baseline systolic BP of ≥130 mmHg; and a recognition that the BP values recorded under research conditions using systematic approaches to measurement (while strongly recommended by these guidelines) are not always the same as BP values recorded under routine clinical care, which can be 5–10 mmHg higher. 65 , 66

Systolic blood pressure categories and treatment target range.
BP, blood pressure; SBP, systolic blood pressure.
In addition, the trial data confirming efficacy for our recommended treatment target of 120–129/70–79 mmHg do not necessarily apply to moderately-to-severely frail adults who were generally excluded from trials. Furthermore, the data supporting this BP target among adults aged >85 years are inconclusive. 131 Frailty can occur at different ages and is, together with tolerability of BP-lowering treatment, an important characteristic when considering the BP target for a given patient. Accordingly, personalized BP-lowering treatment should be instituted in people aged ≥85 years and/or those with significant frailty. Recommended indicators of frailty in guiding BP-lowering treatment are given in Section 9 .
Several important nuances are highlighted and warrant consideration prior to implementing the new BP target of 120–129/70–79 mmHg among patients receiving BP-lowering therapy:
Evidence for a systolic BP-lowering treatment target of 120–129 mmHg is strong (Class I, level of evidence A).
Evidence for a specific diastolic BP-lowering treatment target is less strong in those who are treated to a systolic target of 120–129 mmHg. While most adults treated to a systolic BP target of 120–129 mmHg will also achieve a diastolic BP of 70–79 mmHg, not all will. 543 , 546 Furthermore, adults who achieve systolic BP control are generally at low relative risk for CVD, even when diastolic BP is 70–90 mmHg. 547 , 548 Nonetheless, due in part to the known higher risk of isolated diastolic hypertension among younger adults, 549 the task force agreed that it is reasonable to target an on-treatment diastolic BP of 70–79 mmHg among patients with diastolic BP of ≥80 mmHg who are already at the systolic BP target of 120–129 mmHg (Class IIb, level of evidence C).
The task force acknowledges the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice, 170 which take a stepwise approach to their recommendations for BP-lowering treatment. The 2021 Guidelines recommended an on-treatment systolic BP target of 130–139 mmHg as the first step and then—based on patient preferences, risk, and frailty—to aim for a target on-treatment systolic BP of <130 mmHg as the second step. While we recognize the potential value of this two-step approach, which many clinicians may choose to follow, the current guidelines emphasize one on-treatment BP target (120–129/70–79 mmHg, provided treatment is tolerated). This one-step approach is based on the evidence, and motivated to discourage therapeutic inertia around BP lowering. As an illustrative example of the latter concern for therapeutic inertia, an on-treatment systolic BP of 135 mmHg (office) may be considered reasonable when reviewing the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice but, we hope, will not be considered reasonable to those who follow the updated 2024 ESC Guidelines presented here. Specifically, it is well established that an on-treatment systolic BP of 135 mmHg is not optimal relative to more intensive control. 116 , 131 , 135 , 136 , 445 , 542 , 543 , 545
We acknowledge that the results from RCTs cannot always be extrapolated to routine clinical care. In addition, we recognize the increased risk of side effects among patients receiving more intensive BP-lowering treatments, compared with traditional BP targets. 545 , 550 Accordingly, an important caveat to our treatment target of 120–129/70–79 mmHg is the recommendation to pursue this target only when treatment is well tolerated. In cases where BP-lowering treatment is not well tolerated and a target of 120–129/70–79 mmHg is not possible, it is recommended to follow the ‘as low as reasonably achievable’ (ALARA) principle, by targeting treatment to a BP that is as low as reasonably achievable.
In addition to adults with significant frailty and/or who are ≥85 years of age, the evidence for a BP-lowering treatment target of 120–129/70–79 mmHg may also not generalize to patients with: (i) pre-treatment symptomatic orthostatic hypotension, (ii) limited predicted lifespan (e.g. <3 years), 527 and/or (iii) high levels of competing risk for non-CVD death including CKD with eGFR < 30 mL/min/1.73 m 2 ) (see Section 9 ).
Finally, as outlined in Section 5 , these guidelines endorse a ‘trust but verify’ approach to office BP measurements, and, where possible, confirming BP with accurate out-of-office BP measurements (ABPM, HBPM) is recommended prior to starting treatment, to monitor the treatment effect of BP-lowering medication.
Recommendations for blood pressure targets with treatment (see Evidence Table 34)

8.5.3. Personalizing treatment strategies
Though promising, there is little to no evidence to date from CVD outcome trials to use novel biomarkers for individualizing BP-lowering treatment. 551 , 552 Nonetheless, different patient groups can be identified, and medication initiation can be tailored to pre-existing conditions, such as diabetes mellitus, CKD, AF, post-myocardial infarction, heart failure, metabolic syndrome, and proteinuria/albuminuria ( Section 9 ). History of previous side effects and possible and compelling indications also need to be considered when selecting treatment (see Supplementary data online , Tables S9 and S10 ). Cardioselective beta-blockers may be used in low dose in chronic asthma, 553 , 554 in line with their use in patients with heart failure with chronic asthma.
For considerations of BP-lowering treatment among specific patient populations of interest, including different racial/ethnic populations, see Section 9 .
8.5.4. Duration and monitoring of drug therapy
BP-lowering treatment is usually chronic, often lifelong. This raises the question of long-term efficiency, long-term side effects, adherence, and persistence with therapy. While BP-lowering therapies typically provide an overall durable effect, some attenuation of effect may be seen over time. 66 , 530 First-line BP-lowering medication classes appear to be safe for long-term use. 555–557 Once BP is controlled, at least a yearly follow-up is advised. Because of the known temporal variability in BP 558 , 559 and medication efficacy in the long term, 530 medication changes may be necessary over time (see Supplementary data online ).
Recommendations for follow-up in patients with treated hypertension (see Evidence Table 33)

8.6. Device-based blood pressure lowering
Several device-based therapies designed to lower BP have been investigated. 560 , 561 To date, the best evidence exists for catheter-based renal denervation.
8.6.1. Catheter-based renal denervation
Sympathetic nervous system overactivity contributes to the development and progression of hypertension. 562 Renal denervation aims to interrupt afferent and efferent sympathetic nerves in the adventitia and perivascular tissue of the renal arteries. 563 The 2018 ESC/ESH Guidelines on the management of arterial hypertension did not recommend the use of device-based therapies for routine treatment of hypertension, unless in the context of clinical studies and RCTs. 1 This was based on negative data using first-generation radiofrequency catheters (see Supplementary data online ).
More recent data from sham-controlled trials investigating second-generation radiofrequency and ultrasound catheters demonstrated a BP-lowering efficacy in a broad range of patients, with and without concomitant BP-lowering medications, including those with resistant hypertension. 564–568 Long-term, non-randomized, follow-up data from the Global Symplicity Registry, 569 Symplicity HTN-3 trial, 570 Spyral HTN-ON MED pilot trial, 571 and A Study of the Recor Medical Paradise System in Clinical Hypertension (RADIANCE-HTN) SOLO trial 572 indicate a sustained BP-lowering effect for up to 3 years. A single-centre open-label study suggested sustained BP reductions up to 10 years. 573 These data also highlight a potentially important advantage of renal denervation, namely that the BP-lowering effect of this intervention might be ‘always on’, making this approach attractive for patients with suboptimal medication adherence. 254 Some patients may prefer a one-off procedure rather than taking daily medications chronically and may request renal denervation.
Of significance, there are no reported procedure-related serious safety signals in the first- and second-generation trials beyond the usual risk of femoral arterial access procedures (noting that most trials to date were not powered for safety outcomes and that the task force could find no published meta-analysis data on exact rates of major bleeding and major femoral artery vascular access complications after renal denervation procedures). However, the rate of major bleeding and major femoral artery vascular access complications for coronary angiography using a femoral approach is typically reported as 1%–4% 574 , 575 but has been reported as 5%–10% in some studies. 575 Trials investigating radial access for renal denervation are currently ongoing ( ClinicalTrials.gov identifier: NCT05234788). After renal denervation, there is a 0.25%–0.5% rate of renal artery stenosis/dissection requiring stenting. 576 Long-term follow-up data up to 3 years have not suggested worsening of renal function beyond the expected rates in patients with hypertension with mildly-to-moderately reduced renal function. 569 , 577 Of note, sham-controlled trials to date excluded patients with severely reduced kidney function at baseline. 564 , 566–568
Despite the clear promise of renal denervation in reducing BP, there are some concerns that warrant consideration, as we indicate in the recommendations. First, the effect of current renal denervation catheter technologies on BP lowering is relatively modest for an invasive procedure (meta-analyses report placebo-corrected systolic BP lowering of approximately 6 mmHg on office BP assessment and 4 mmHg on 24 h ABPM). 578 As such, the average BP-lowering effect of renal denervation appears no more than for one standard BP-lowering medication. Accordingly, many adults undergoing renal denervation will likely require ongoing, post-procedural, BP-lowering drugs.
Second, the cost-effectiveness of renal denervation has not been fully established. Since effects of current renal denervation technologies are similar to that of one standard BP-lowering medication, most of which are generic, it is difficult to see a scenario where renal denervation could be proven cost-effective for most patients. An exception might be patients who are at very high risk of CVD events and who have uncontrolled BP due to resistant hypertension (with or without non-adherence). 579 , 580
Third, there are no adequately powered outcomes trials demonstrating that renal denervation reduces CVD events and is safe in the long term. While observational reports have suggested associations between renal denervation and reduced risk for CVD events, 581 , 582 these observational data have major inferential limitations including a significant potential for confounding. While BP lowering is typically a good surrogate for CVD benefit, there is no guarantee that this is true with renal denervation and, furthermore, off-target effects independent of BP could influence CVD and other adverse-event rates after the procedure. Because of the lack of outcomes trials, renal denervation cannot reach the Class I indication threshold set by this task force. Arguments that outcomes trials will not be funded are insufficient to influence guideline recommendations. However, it is hoped that the position of these guidelines will motivate industry to sponsor the necessary renal denervation outcomes trials.
Fourth, related to the lack of outcomes data, the potentially ‘always on’ effect of renal denervation could backfire if late complications emerge. Medications causing complications or side effects can simply be stopped and replaced with alternative medications when such problems emerge; this is not true with renal denervation.
Fifth, the impact of scaling up renal denervation on usual cardiac department catheterization laboratory workflows is of some concern. Specifically, it is important that renal denervation procedures do not delay timely access to other elective procedures with proven efficacy in reducing CVD outcomes. 583
Sixth, there is still no direct evidence to gauge whether renal denervation procedures are successful and that the kidneys are denervated and do not reinnervate over time. 584 Relatedly, the concept of responders and non-responders to renal denervation (and the hypothesis that predictors of response might be found to help identify patients most suitable for the procedure) is questioned. Medical interventions, including drugs, are naturally subject to inter-individual variability in response. 567 Additionally, there are few examples in medicine of consistent and clinically useful predictors of treatment response for medical conditions that have complex genetic and environmental underpinnings (i.e. conditions like hypertension).
A multidisciplinary hypertension team, including experts in hypertension and percutaneous cardiovascular interventions, is recommended to evaluate the indication and to perform the procedure. 585 Based on the available evidence, renal denervation may be considered for patients who have uncontrolled, true resistant hypertension with a three-drug combination and who express a preference to undergo renal denervation. 566 , 568 , 585 This recommendation is informed, in part, by the higher risk of CVD events in this subgroup, which represents a major unmet clinical need and which also means that cost-effectiveness considerations are likely to be optimal in this setting. In patients who are non-adherent or intolerant to multiple BP-lowering medications, particularly first-line agents, and who have high predicted CVD risk and a BP that is not at target, renal denervation may, for the same reasons, be considered if the patients express a preference to undergo renal denervation after a tailored shared decision-making process. The shared decision-making process requires that the patients are fully informed about the benefits, limitations, and risks associated with renal denervation.
Recommendations for device-based treatment of hypertension (see Evidence Table 35)

8.6.2. Other devices
Most device-based therapies investigated for BP-lowering therapy in hypertension have been aimed at modulating the autonomic nervous system activity (baroreflex activation therapy, endovascular baroreflex amplification therapy, and carotid body ablation). 560 Cardiac neuromodulation therapy aims to lower left ventricular preload by variably altering the atrioventricular interval using a dual-chamber, rate-responsive, implantable pulse generator in patients indicated for implantation or replacement of a dual-chamber pacemaker. 591 , 592 Some, though not all, of these devices have shown promising results in non-randomized, single-arm studies. A sham-controlled trial investigating central iliac arteriovenous stent anastomosis was terminated early after longer-term follow-up data indicated an increase in heart failure in the stent group. 561 Therefore, the use of these device-based therapies is not recommended for routinely treating hypertension until further evidence regarding their safety and efficacy becomes available (see Supplementary data online ).
8.7. Unintended and potentially harmful consequences of blood pressure lowering and implications for treatment targets
8.7.1. adverse effects of blood pressure-lowering medications, 8.7.1.1. symptomatic adverse effects.
BP-lowering medications have multiple side effects, which may be more common in females. 536 , 593 , 594 Although generally well tolerated, common side effects include headaches, cough, dizziness or light-headedness, diarrhoea or constipation, fatigue, ankle swelling, and erectile problems, depending on the drug class (see Supplementary data online , Table S9 ). 536 , 550 , 593–597
In randomized trials of adults aged >60 years, the overall rate of symptomatic BP-lowering drug withdrawal was higher than the rate of placebo withdrawal (approximately 15% vs. 5%). 593 A systematic review, which included 280 638 participants in 58 RCTs, reported no evidence for an increased relative risk of falls in those taking BP-lowering drugs. 550 There was, however, an increased relative risk of mild hyperkalaemia, acute kidney injury, hypotension, and syncope. Furthermore, very frail adults were excluded from BP-lowering trials, which is relevant because such patients are more prone to adverse effects and polypharmacy (see Supplementary data online ). 596
8.7.1.2. Renal effects
A systematic review reported an increased risk of acute kidney injury and hyperkalaemia associated with BP-lowering treatment. 550 Analyses of outcomes by specific drug class showed that drugs affecting the RAAS were more likely to be associated with acute kidney injury and hyperkalaemia. 550
Patients with significant CKD tend to be excluded from RCTs. 137 , 545 , 598 It is important to remember these exclusion criteria, and that patients with CKD are more likely to suffer from resistant hypertension, when extrapolating the results of more intensive BP lowering to patients with moderate-to-severe CKD (see Section 9 ). 599
8.7.1.3. Erectile dysfunction
Older classes of BP-lowering drugs (including diuretics, beta-blockers, and centrally acting medications) are associated with erectile dysfunction. 600 However, newer classes have neutral effects. 601 Angiotensin receptor antagonists may have beneficial effect on erectile function. 602
8.7.2. Pill burden and non-adherence
More intensive treatment of elevated BP and hypertension may be associated with an increased risk of polypharmacy and pill burden, which are themselves associated with non-adherence. 603 , 604 Single-pill, fixed-dose drug combinations can help to reduce pill burden and are recommended to improve adherence (refer to Section 8.3.4 ).
Increased intensity of BP lowering (while ultimately cost reducing in terms of CVD reduction) 605 can also result in higher upfront direct and indirect healthcare costs, with more people requiring medication and higher demand for technology-based adherence strategies, which can be challenging to implement, especially in resource-poor settings. 604
8.7.3. Potentially harmful consequences of blood pressure lowering for frail older people
Unintended consequences of BP lowering (hypotension, syncope, falls) can be hazardous for frail older people in particular. 606 Retrospective studies have shown that adults aged >75 years from the general population, who would have met the criteria for inclusion in the Systolic Blood Pressure Intervention Trial (SPRINT), had a rate of injurious falls and syncope that was nearly five times that of the standard care group in the trial. This suggests that healthy participant bias may have contributed to the findings of SPRINT and other similar BP-lowering trials, and that the results may not fully generalize to older adults in more routine clinical care. 607
Patients’ functional ability should be considered in addition to age to help negate any unintended consequences of BP lowering in a frailer cohort. Despite their chronological age, older patients with hypertension who are fit and can independently carry out activities of daily living will benefit from guideline-directed treatment similar to younger cohorts. 131 However, tailoring treatment targets and treatment plans for frail older patients is necessary to avoid unintended consequences. This should include assessing frailty, including cognitive status, risk of falls, propensity for symptomatic orthostatic hypotension, polypharmacy, and other comorbid conditions. 608 , 609 Of note, and as detailed in Section 9 , some data indicate a benefit of more intensive BP-lowering on cognitive function. 523 , 610 , 611 For those with loss of function but preserved activities of daily living, a more detailed geriatric assessment is required to explore the risks and benefits of treatment, as well as considerations for tailoring therapeutic strategies where appropriate. For patients who are both functionally impaired and unable to carry out activities of daily living, the therapeutic goals of hypertension treatment should be personalized, and medications discontinued where appropriate (see Section 9.3 ). 596
8.7.4. Clinical inertia in blood pressure lowering
The fear of serious adverse events with BP-lowering medications is often cited as a reason for clinical inertia, although the evidence to date from meta-analyses of RCTs suggests these side-effect concerns may be exaggerated. 550 , 612 However, RCTs often select populations with less frailty and multimorbidity who are more likely to tolerate treatment. 613 Consequently, fewer adverse effects might be reported than would be expected in the general population. It remains up to individual clinicians to initiate shared decision-making with each patient, especially patients in vulnerable groups and those who have experienced previous adverse events, weighing up potential benefits against risks of treatment. 614 , 615
9.1. Young adulthood (18–40 years)
9.1.1. definition and epidemiology.
In the present guidelines ‘young adulthood’ is defined as age 18–40 years. The prevalence of hypertension in young adults is increasing in men and women. 616–618 Unhealthy lifestyle, gender, obesity, and socio-economic factors contribute. 617 , 619–621 Hypertension-attributable CVD burden in young adults, evaluated as mortality or years of living with disability, has increased in the last decades, especially in low- and middle-income countries and in men. 622 Hypertension awareness, treatment, and control in young adults is lower than in other age categories, a result driven by worse control in young men. 623
Systolic and diastolic hypertension and isolated diastolic hypertension are associated with increased CVD risk in the young (see Supplementary data online ). 624 Isolated systolic hypertension in the young is discussed in Section 9.4 .
9.1.2. Secondary hypertension in young adulthood
Secondary hypertension is more frequent in younger than in later-onset hypertension, with a prevalence of 15%–30% in hypertensive young adults reported from some referral centres. 625 , 626 Major causes of secondary hypertension include drug-induced hypertension (e.g. oestrogen-progesterone oral contraceptives; cold medication) and primary aldosteronism. The use of recreational drugs/substances, as well as supplements and energy drinks should be investigated (see Section 7 ).
Combined oestrogen-progesterone contraceptives are among the most common causes of drug-induced hypertension in young women, 627 , 628 and should not be used in hypertensive women unless there is no other method available or acceptable to the patient. 629 Conversely, progestin-only contraceptives are generally considered safe in women with hypertension. 89 , 630 , 631 Fibromuscular dysplasia should be considered as a cause of secondary hypertension in young women, 626 , 632 whereas primary aldosteronism, the most common form of secondary hypertension, is equally common in different age classes. 316 Screening for secondary hypertension is thus recommended in young adults with hypertension. However, in obese young adults, primary hypertension is more common, though OSAS should also be considered in this instance. 633
9.1.3. Measurement and management of blood pressure in young adults
Out-of-office BP measurement is recommended in young adults for confirming diagnosis, since the white-coat phenomenon occurs in the young. 634 Because of the lower absolute CVD risk in this age category compared with older adults, hard-endpoint randomized trials of BP lowering in young adults have not been performed. However, since relative risk reduction by BP-lowering treatment is homogeneous in any age group, including those <55 years old, 131 young adults with suitable indications are also expected to benefit from BP-lowering therapy. The hypertension management algorithm based on CVD risk proposed in Section 6 is not fully applicable in young adults, since SCORE2 has not been validated for individuals <40 years old. Even risk stratification based on lifetime risk assessment does not apply to very young adults (e.g. 20–30 years of age). 128 In the absence of established CVD, diabetes mellitus, familial hypercholesterolaemia, and moderate or severe CKD a BP-lowering treatment initiation threshold of office 140/90 mmHg is appropriate in most young adults. However, HMOD assessment may be considered in patients aged <40 years to stratify individuals with elevated BP into a higher risk category. For example, arterial stiffness better reclassifies CVD risk in individuals aged <50 years than in older individuals. 28 , 215 Echocardiographic left ventricular mass also maintains its added reclassification and discrimination on top of risk scores in young adults (see Section 6 for discussion of risk modifiers). 289
Irrespective of cardiovascular risk, all young adults with elevated BP are recommended to follow lifestyle guidance for BP lowering. A discussion about family planning should be taken with young women of childbearing potential at each visit. 635 , 636
Adherence to treatment is low in young adults, <50% in some studies. 251 Therefore, communicating the importance of adherence, education, and follow-up clinics is important. (see Sections 7 and 11 ).
Recommendations for managing hypertension in young adults (see Evidence Tables 36 and 37)

9.2. Pregnancy
9.2.1. definition and epidemiology.
Hypertension in pregnancy is typically defined as systolic BP of ≥140 mmHg and/or diastolic BP of ≥90 mmHg, measured using repeated BP readings in the office or hospital on two separate occasions or ≥15 min apart in severe hypertension (≥160/110 mmHg). 1 , 637 , 638
Hypertension in pregnancy is the second leading cause of maternal death after maternal peri-partum haemorrhage. 639 Approximately 7% of pregnancies are complicated by hypertension, of which 3% are due to pre-eclampsia and around 1% are chronic or pre-existing hypertension. 640 Women with a history of hypertensive disorders during pregnancy are at increased risk of subsequent hypertension and CVD. 640–642
9.2.2. Classifying hypertension in pregnancy
Hypertension in pregnancy includes:
Chronic hypertension: precedes pregnancy, develops before 20 weeks of gestation, persists for >6 weeks post-partum, and may be associated with proteinuria.
Gestational hypertension: develops after 20 weeks of gestation and usually resolves within 6 weeks post-partum.
Antenatally unclassifiable hypertension: BP is first recorded after 20 weeks of gestation, and hypertension is diagnosed but it is unclear if chronic or not; reassessment is necessary 6 weeks post-partum.
Pre-eclampsia: gestational hypertension accompanied by new-onset: (i) proteinuria (>0.3 g/day or ≥30 mg/mmol ACR), (ii) other maternal organ dysfunction, including acute kidney injury (serum creatinine ≥ 1 mg/dL), liver dysfunction (elevated transaminases > 40 UI/L with or without right upper quadrant or epigastric abdominal pain), neurological complications (convulsions, altered mental status, blindness, stroke, severe headaches, and persistent visual scotomata), or haematological complications (platelet count < 150 000/µL, disseminated intravascular coagulation, haemolysis), or (iii) uteroplacental dysfunction (such as foetal growth restriction, abnormal umbilical artery Doppler waveform analysis, or stillbirth). 643 The only cure for pre-eclampsia is delivery, which is recommended at 37 weeks’ gestation, or earlier in high-risk cases. Of note, proteinuria is not mandatory for diagnosing pre-eclampsia but is present in about 70% of cases. 644 Also, as proteinuria may be a late manifestation of pre-eclampsia, it should be suspected when de novo hypertension is accompanied by headache, visual disturbances, abdominal pain, or abnormal laboratory tests, specifically low platelets and/or abnormal liver function.
Other potential causes for high BP, including pain and anxiety, must be excluded when treating hypertension during pregnancy.
9.2.3. Measuring blood pressure in pregnancy
See Section 5.5.1 for information on BP measurement approaches in pregnancy. 645 It is important to restate here that oscillometric devices tend to under-estimate the true BP and are unreliable in severe pre-eclampsia; only a few have been validated in pregnancy. Importantly, only the relatively few devices validated for measuring BP in pregnancy and pre-eclampsia should be used ( https://stridebp.org ).
9.2.4. Investigating hypertension in pregnancy
Basic laboratory investigations include urinalysis, blood count, haematocrit, liver enzymes, serum creatinine, and serum uric acid. Serum uric acid is increased in pre-eclampsia and identifies women at increased risk of adverse maternal and foetal outcomes in hypertensive pregnancies. 646
All pregnant women should be assessed for proteinuria in early pregnancy (e.g. 11–14 weeks’ gestation). 647 A dipstick test of ≥1+ should prompt further investigations, including ACR, which can be quickly determined in a single spot-urine sample. 648 An ACR of <30 mg/mmol (<0.3 mg/mg) can rule out proteinuria. 649 Higher values should prompt 24 h urine collection.
In one study, 10% of pregnant women with chronic hypertension had secondary hypertension (estimated to affect 0.24% of all pregnancies). 650 Secondary hypertension during pregnancy is associated with an increased risk of adverse outcomes. 650 The most common cause of secondary hypertension during pregnancy is CKD. The onset of hypertension during the first trimester, at the peak of human chorionic gonadotropin (HCG) secretion, should prompt consideration of primary aldosteronism. 651 Phaeochromocytoma in pregnant women is rare (0.002% of all pregnancies) but highly morbid. 652 , 653
9.2.5. Preventing hypertension and pre-eclampsia
Low-to-moderate-intensity exercise, especially if supervised and initiated during the first trimester of pregnancy, decreases the incidence of developing gestational hypertension. 654 As such, after consultation with their obstetrician, all pregnant women should participate in physical activity, unless contraindicated. 655 Factors indicating risk of pre-eclampsia are discussed in the Supplementary data online .
Women at high or moderate risk of pre-eclampsia should be advised to take 100–150 mg of aspirin daily at bedtime from gestational weeks 12–36. 647 , 656 , 657
Oral calcium supplementation of 0.5–2 g daily is recommended for preventing pre-eclampsia in women with low dietary intake of calcium (<600 mg daily). 658 , 659
9.2.6. Treatment initiation and blood pressure targets
Acute management of BP in pre-eclampsia and eclampsia is detailed in Section 10.4 .
Meta-analyses have found no evidence for an increased risk for delivering small-for-gestational-age babies in pregnant women with mild hypertension receiving BP-lowering medications. 660 Despite a historical paucity of trial data, previous European guidelines 1 , 89 recommended initiating BP-lowering drug treatment (i) in all women with persistently elevated office BP of ≥150/90 mmHg, and (ii) in women with gestational hypertension (with or without proteinuria), pre-existing hypertension with superimposed gestational hypertension, or hypertension with subclinical HMOD, when office BP is >140/90 mmHg.
In the CHAP trial, treating pregnant women with chronic hypertension and BP of ≥140/90 mmHg reduced the occurrence of pre-eclampsia with severe features, and reduced medically indicated pre-term birth <35 weeks, compared with only treating severe hypertension (BP ≥ 160/105 mmHg). 88 Tight BP control (target diastolic BP < 85 mmHg) compared with less-tight BP control (target diastolic BP < 100 mmHg) reduces the incidence of subsequent severe maternal hypertension (BP ≥ 160/110 mmHg), but not foetal or other maternal outcomes in women with mild hypertension at baseline (diastolic BP of 85–105 mmHg). 661
Treatment with BP-lowering drugs in all pregnant women with confirmed BP of ≥140/90 mmHg is recommended to reduce the progression to severe hypertension and the related risks for adverse pregnancy outcomes. 660 , 661 In women with pre-existing and gestational hypertension with and without pre-eclampsia, we recommend lowering BP below 140 mmHg for systolic and to 80–90 mmHg for diastolic BP. 661 Evidence to support a BP target as low as 120–129/70–79 mmHg is lacking in pregnancy, though such evidence exists for non-pregnant patients receiving BP-lowering medication.
9.2.7. Managing mild hypertension in pregnancy (office blood pressure 140–159/90–109 mmHg)
RAS inhibitors are not recommended in pregnancy due to adverse foetal and neonatal outcomes. The BP-lowering drugs of choice are: beta-blockers (most data are available for labetalol, a non-selective beta-blocker that also acts as an alpha-blocker in higher doses; metoprolol and bisoprolol are also considered safe), dihydropyridine CCBs (most data are available for nifedipine, which is generally considered first choice, also felodipine, nitrendipine, amlodipine, and isradipine can be used), and methyldopa. 662 , 663 A meta-analysis suggests that beta-blockers and CCBs are more effective than methyldopa in preventing severe hypertension. 660 Of note, however, atenolol should be avoided, as it is associated with foetal growth restriction. 664 , 665 Methyldopa has been associated with an increased risk of post-partum depression and caution is therefore advised both intra-partum and post-partum. 637 Hydralazine can be particularly effective for severe hypertension in pregnancy and can be administered intravenously in hypertensive admissions ( Section 10 ). 666–668 While thiazide diuretics in pregnancy have limited safety data and should be used with caution, other diuretics such as furosemide are not contraindicated and may be necessary in some situations (see Supplementary data online ). 669
9.2.8. Managing severe hypertension in pregnancy (>160/110 mmHg)
Acute onset of severe hypertension persisting for more than 15 min is considered a hypertensive emergency in pregnancy and is covered in Section 10.4.2 .
9.2.9. Managing blood pressure post-partum
For women with hypertension during pregnancy, BP should be measured within 6 h of delivery and, if possible, daily for at least a week after discharge from the hospital. 637 Post-partum hypertension is common in the first week and associated with prolonged hospitalization. 670
Women with hypertension in pregnancy are at increased risk of chronic hypertension, 671 CKD, 672 and CVD. 177 , 223 , 640 The relative risk of chronic hypertension is highest in the first 6 months following delivery, motivating regular screening in these women. 673 Women with gestational hypertension, especially those with pre-eclampsia, have higher risk of masked hypertension. 674 BP measurements, ideally including out-of-office measurements, urine analyses, and CVD risk assessment, should at least be performed 6–12 weeks, 6 months, and 12 months post-partum and, after that, annually. Recent data indicate the potential utility of self-monitoring of BP during the busy early post-partum period. 675
All BP-lowering drugs are excreted into breast milk. 637 Except for propranolol, atenolol, acebutolol, and nifedipine, most drugs are excreted in very low concentrations in breast milk (see Supplementary data online , Table S11 ). 637
9.2.10. Risk of recurrence of hypertensive disorders in a subsequent pregnancy
About 20%–30% of women with hypertensive disorders in a previous pregnancy will experience recurrence in a subsequent pregnancy. 676 , 677 The earlier the onset of hypertension in the first pregnancy, the higher the risk of recurrence in a subsequent pregnancy. 677
Further details on managing hypertension and other cardiovascular disorders in pregnancy are available elsewhere. 89 , 637
Recommendations for managing hypertension in pregnancy (see Evidence Tables 38–40)

9.3. Very old age (≥85 years), frailty, multimorbidity, and polypharmacy
9.3.1. definition of frailty.
The most common definition of frailty is an age-associated, biological syndrome characterized by decreased biological reserves, due to dysregulation of several physiological systems. 682 This puts an individual at risk when facing physiological stressors, and is associated with poor outcomes, such as disability, hospitalization, and death. 683 The estimated prevalence of frailty in people aged >65 years is 7%–16% and is greater in women than in men. 684 , 685 Although the main determinant of frailty is age, chronological age must be differentiated from biological age. 686 An older patient can be fit and robust while a multimorbid young patient can be frail. Using multiple drugs may have more unpredictable effects on BP in older patients, because of increased competition for underlying mechanisms responsible for their degradation and elimination, and because the ability of the baro- 687 and chemo-reflex 688 systems in maintaining a steady treated BP level can decline with ageing.
With respect to BP, two issues compound interpretation of the frailty literature. First, frailty on its own is a strong predictor of mortality and cardiovascular complications 689 and is accompanied by a decrease in systolic BP. 690 This raises the issue of the so-called BP J-curve (see Section 9.8 ) and reverse causality, with frailty rather than excessive BP lowering being the root cause of adverse health outcomes. Only properly randomized and controlled clinical trials can differentiate between the effects of frailty vs. overly intensive BP-lowering treatment, but unfortunately, few BP-lowering trials have included a substantial proportion of frail patients. Second, there is no consensus on how to grade frailty in day-to-day clinical practice. 606 Complex frailty scales exist for application in research, 523 , 691 but unless they are electronically generated, 692 they are typically not practical in routine clinical care. Nonetheless, the clinical frailty scale ( Figure 21 ) is intuitive and easy to administer and has been validated against 5-year risk of death. 596 , 693

Frailty assessment in the management of blood pressure.
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CV, cardiovascular; CVD, cardiovascular disease; HBPM, home blood pressure monitoring; IADLs, independent activities of daily living; OH, orthostatic hypotension. Adapted from Rockwood et al . 693
9.3.2. Randomized controlled trials of blood pressure lowering in frail older patients
Few adults aged ≥85 years have been included in trials. 131 In addition, generalizing data from RCTs to very frail patients may not be possible. 692 , 694–697 However, the currently available evidence from RCTs has not demonstrated weakening of the benefits of BP-lowering treatment (i.e. no effect modification) among frailer patients enrolled in these trials, although these participants likely had no more than mild frailty (see Supplementary data online ). 523 , 694 , 698
In the absence of robust randomized evidence, several observational studies have suggested that lowering BP might not be warranted or even be harmful in patients with significant frailty or multimorbidity, particularly when BP is not very high. For instance, a systematic review and meta-analysis of non-randomized studies that investigated associations between BP and risk of mortality in older patients found evidence for interaction by frailty status, suggesting that lowering BP might be harmful in this patient group. 699 However, as noted above and in Section 9.8 , these observational J-curve findings are unreliable when guiding clinical care, as unidentified biases potentially confound the results. For instance, in addition to reverse causality, stiffness of the large arteries is associated with both low diastolic BP and increased mortality. 697 In addition, absolute CVD risk increases with age, indicating that fewer older than younger patients with hypertension may need to be treated to prevent one adverse health outcome. 700
Therefore, given the totality of evidence from clinical trials, 523 , 694 , 701 , 702 very old and frail patients with hypertension should not be denied the potential benefits of BP-lowering treatment down to a target of 120–129/70–79 mmHg. However, personalized decision-making should be a priority in the very old and frail. Together with management of BP, a major consideration should also be whether reversible causes of frailty can be addressed, 609 e.g. by treating underlying comorbidities or undergoing supervised muscle-strengthening physiotherapy or supervised exercise and co-ordination and balance training. 703
9.3.3. Starting blood pressure-lowering treatment in very old or frail patients
All patients must be fully informed about the benefits and risks of starting BP-lowering treatment, so that their preference is considered. Among 34 hypertension guidelines, 18 recommended 150 mmHg as the systolic goal in frailer and/or older patients, but four endorsed systolic targets <130 mmHg or <120 mmHg. 704 Treatment can be started with a long-acting dihydropyridine calcium channel antagonist. 596 , 705 To achieve BP control, an ACE inhibitor, or if contraindicated, an ARB, can also be used. Thereafter, low-dose thiazides or thiazide-like diuretics are preferred unless there is a specific contraindication, such as gout, orthostatic hypotension, or disturbed micturition (including micturition syncope). 596 , 705 Beta-blockers are less desirable as they reduce heart rate, cause fatigue, and increase the systolic pulse wave amplitude, which is insufficiently buffered in stiff central elastic arteries. Vasodilating beta-blockers and direct vasodilators (e.g. hydralazine and minoxidil) are associated with increased risk of orthostasis. Though data are conflicting, 706 alpha-blockers are also considered less desirable as they appear to be associated with an increased risk of orthostasis and falls in very old patients (aged ≥85 years). 707 , 708 Alpha-1 blockers, such as doxazosin, prazosin, terazosin (also used to treat prostate symptoms), are particularly prone to causing orthostasis. 98 Once the appropriate combination is found, a combination tablet with variable composition of two agents may optimize adherence. Starting with combination therapy is not advised in most very old and/or frail patients, unless BP is very high.
9.3.4. Maintaining blood pressure lowering in very old or frail patients
If very old and frail patients tolerate BP-lowering treatment well, there is no automatic need to deprescribe or discontinue treatment; however, this should be kept under review. In the case of progressive frailty, systolic BP tends to drop, 709 such that deprescription of a BP-lowering drug might become necessary. To identify candidate drugs for deprescribing, a patient’s current medications should be reviewed to identify BP-lowering drugs that may have become contraindicated due to concomitant prescriptions or newly developed comorbidities. 705 To help guide deprescription of BP-lowering agents, ABPM can be used to detect orthostatic hypotension or a highly variable BP not buffered by autonomic nervous reflexes. 687 , 688
Recommendations for managing hypertension in patients who are very old or frail (see Evidence Table 41)

9.4. Isolated systolic and diastolic hypertension
9.4.1. definition of isolated systolic hypertension.
Isolated systolic hypertension is typically defined as systolic BP of ≥140 mmHg with a diastolic BP of <90 mmHg. While isolated systolic hypertension is uncommon in younger patients, 713 it is the most common type of hypertension in older patients; >80% of untreated patients with hypertension aged >60 years have isolated systolic hypertension. 714
9.4.2. Isolated systolic hypertension, risk factors, and ageing
Systolic BP increases with age in men and women until the eighth decade of life, while diastolic BP gradually increases up until the fifth or sixth decade of life, after which it either plateaus or decreases. As a result, the pulse pressure (the difference between the systolic and diastolic BP) gradually widens from middle age. 34 These BP changes are related to increased aortic stiffening with age. 715 , 716
Since most older patients with hypertension have isolated systolic hypertension, and since with advancing age, risk of CVD events is driven by systolic rather than diastolic BP, 717 management of isolated systolic hypertension in older adults is broadly in line with that of combined systolic-diastolic hypertension seen in younger adults. 718 Early isolated systolic hypertension studies used systolic BP treatment targets of 160 or 150 mmHg. 718 However, results from the SPRINT and the Strategy of Blood Pressure Intervention in Elderly Hypertensive Patients (STEP) trials (mean BP at study entry of 140/78 mmHg and 146/82 mmHg, respectively, indicating that many of the patients had isolated systolic hypertension) confirm that lower systolic BP targets are effective in reducing CVD events in patients with isolated systolic hypertension (see Supplementary data online ). 135 , 136
Since relative risk reduction by BP-lowering treatment is homogeneous in any age group, whereas absolute risk reduction is larger with advancing age, 131 therapeutic inertia in older patients with isolated systolic hypertension should be avoided (see Section 9.3 ). As noted earlier, beta-blockers should be avoided in patients with isolated systolic hypertension or more generally with arterial stiffness, as they increase stroke volume (given the lower heart rate). 218
9.4.3. Isolated systolic hypertension in young adults
In young adults (<40 years old), the presence of isolated systolic hypertension poses different pathophysiological and clinical considerations. In young patients with isolated systolic hypertension, arterial stiffness 713 and relative risk of CVD events 624 appear to be similar to those without isolated systolic hypertension and lower than young adults with combined systolic-diastolic hypertension and isolated diastolic hypertension. Indeed, younger patients with isolated systolic hypertension appear to comprise a heterogeneous group. 719 For these reasons, it might be reasonable to assess central BP and arterial stiffness in these individuals, as recommended by other scientific societies. 720 , 721 Out-of-office BP measurement is recommended to exclude white-coat hypertension, which is often associated with isolated systolic hypertension in the young. 634
9.4.4. Isolated diastolic hypertension
Isolated diastolic hypertension is defined as a systolic BP of <140 mmHg with a diastolic BP of ≥90 mmHg. The isolated diastolic hypertension phenotype is more commonly seen in younger adults and, particularly, younger adults with obesity or other metabolic derangements. 722 , 723 In older adults with this phenotype, consideration should be given to whether the diastolic BP was accurately measured. 724
Patients with isolated diastolic hypertension appear to have a slightly increased relative risk for CVD of 5%–30%. 548 , 723 , 725 However, because patients with isolated diastolic hypertension are younger, they tend to have few events, and very large samples are required to show this association. Furthermore, because the absolute risk for CVD among these individuals is low (typically <10% over 10 years), it is less clear if isolated diastolic hypertension should prompt initiation of BP-lowering medication, particularly among persons in whom baseline systolic BP is already at the target of 120–129 mmHg. 723 Irrespective, patients with isolated diastolic hypertension should be followed up, as they are at increased risk for systolic hypertension. 723
Finally, it is also worth noting that when a patient achieves a target systolic BP of 120–129 mmHg with BP-lowering treatment, there is little to no high-quality trial evidence that further intensifying BP-lowering medication to achieve both systolic BP of <120 mmHg and also diastolic BP of <70 mmHg improves CVD prognosis. 547 , 723
9.5. Orthostatic hypotension with supine hypertension
Patients with orthostatic hypotension need not be hypotensive and indeed, many have supine elevated BP or supine hypertension. Furthermore, many patients with orthostatic hypotension are asymptomatic. Orthostatic hypotension is present in around 10% of all adults with hypertension and is defined as a drop in BP of ≥20/10 mmHg after rising from either a sitting or lying position to a standing position (see Section 5.5.3 ). 97 , 99 Assessment for orthostatic hypotension should be timed to occur at 1 and/or 3 min after standing. Because seated to standing assessment can lead to under-detection of orthostatic hypotension, it is preferable, where possible, to test for orthostatic hypotension using a supine (lying) to standing assessment (see Section 5 ). 56 , 98 , 726
Assessing for orthostatic hypotension is important in managing adults with elevated BP or hypertension for several reasons. First, findings of trials linking more intensive BP control to improved outcomes may not generalize to patients with orthostatic hypotension, particularly when it is severe in magnitude (standing systolic BP < 110 mmHg 97 ) and/or symptomatic. Second, orthostatic hypotension may be associated with symptoms that may limit the patient’s tolerability of more intensive BP-lowering approaches. Third, orthostatic hypotension may be associated with an increased risk of adverse effects commonly co-attributed to pharmacological BP lowering (such as hospitalizations for hypotension). 727 Fourth, orthostatic hypotension is associated with increased risk for CVD. 728
However, the frequency of orthostatic hypotension is not increased in the more intensive BP-lowering arms of randomized trials compared with the less intensive BP-lowering arms. 726 , 727 , 729 , 730 As such, and in contrast to common belief, it does not appear that more intensive treatment of BP (which almost always requires more BP-lowering medication) worsens orthostatic hypotension. In contrast, there is some evidence that more intensive treatment of hypertension may actually reduce the risk of orthostatic hypotension. 730 , 731
The aetiology of orthostatic hypotension may be considered as neurogenic or non-neurogenic, with the latter being far more common. 99 Patients with orthostatic hypotension may have underlying neurodegenerative diseases, diabetes, B12 deficiency, 732 renal failure, dehydration, prolonged recumbency, deconditioning, and triggering medications (like alpha-blockers, beta-blockers, diuretics, nitrates, antidepressants, and antipsychotics). Of note, ACE inhibitors, ARBs, and dihydropyridine CCBs are examples of BP-lowering medications that appear to have less impact on orthostatic hypotension, and their adverse impact, if any, on orthostatic hypotension typically occurs in the first 2 weeks or so after starting or intensifying treatment. 733
Managing patients with supine hypertension and orthostatic hypotension is a common clinical conundrum. More detailed reviews on this topic are available elsewhere. 98 , 99 The approach to managing orthostatic hypotension should be non-pharmacological at first. Patients with orthostatic hypotension should be asked to change position slowly, maintain adequate hydration, and avoid alcohol and large meals. Compression stockings, crossing legs while standing, and abdominal binders may also help and should be trialled. 734 , 735 Abdominal heating pads and a head-up bed position can reduce supine (typically nocturnal) hypertension, which may reduce nocturnal diuresis and daytime orthostatic hypotension. 736
The treatment of orthostatic hypotension among those with supine hypertension is not to automatically down-titrate BP-lowering medications. Rather, reversible causes should be sought and treated (including discontinuation of offending medications), and patients requiring BP-lowering medication should be switched to BP-lowering medications that are less likely to cause orthostatic hypotension. When symptoms are disabling and the above interventions do not help, particularly in neurogenic orthostatic hypotension, the best evidence exists for midodrine to reverse orthostatic hypotension, and this may be given in conjunction with ongoing BP-lowering medications when supine hypertension exists. 99 An alternative option to midodrine is droxidopa, though this is less readily available. Specialist referral is prudent when persons with supine hypertension are prescribed these orthostatic hypotension treatments, as these agents can increase supine BP more than standing BP.
Recommendations for managing hypertension in patients with orthostatic hypotension

9.6. Diabetes
9.6.1. diabetes and elevated blood pressure/hypertension.
Patients with diabetes (both type 1 and type 2) often have elevated BP or hypertension, and are about twice as likely to suffer a major CVD event over the medium to long term compared with those without diabetes. 737 Diabetes is also a major cause of microvascular events, such as retinopathy and nephropathy. 738 , 739 Although the risk of CVD in patients with diabetes varies by screening and diagnostic methods, 740 , 741 as well as with the presence of other CVD risk factors, 740 , 742 on average, patients with diabetes are at ≥10% 10-year risk for CVD. However, formal risk estimation with the use of SCORE2-Diabetes among type 2 diabetes mellitus patients should be considered if they are aged <60 years (see Section 6 ). 164 , 739
9.6.2. J-shaped curve of blood pressure and risk of cardiovascular disease in patients with diabetes
Evidence on the BP threshold and target for treatment in patients with diabetes has been subject to debate. Reports of a J-shaped association between BP and risk of CVD in diabetes, 743 and the lack of a clear benefit of treatment on cardiac outcomes at lower BP in some meta-analyses, 744–746 has led to some cautious recommendations for intensive treatment in this patient population.
An individual patient data meta-analysis by the Blood Pressure Lowering Treatment Trialists’ Collaboration tested treatment effects in 103 325 patients with diabetes and provided evidence against effect modification by categories of baseline BP down to a systolic BP of 120 mmHg. 445 BP reduction in patients with diabetes is expected to reduce the risk of diabetes-associated complications including retinopathy, vasculopathy, and nephropathy (albuminuria and end-stage renal disease), which adds weight to the importance of reducing BP in these patients (see Supplementary data online ). 745–747 This task force also considered the fact that a proportion of patients with diabetes have orthostatic hypotension due to diabetic neuropathy, 748 which might affect the tolerability of BP lowering.
9.6.3. Managing blood pressure in diabetes
We recommend that all patients with diabetes are offered pharmacological BP-lowering treatment with a BP target of 120–129/70–79 mmHg, if feasible and tolerated. 136 , 146 , 445 , 747 , 749–752 The task force further sees no strong evidence for a differential BP treatment targets in patients with diabetes and those without. 136 , 146 , 445 , 746 , 747 While the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial reported a null primary endpoint for more intensive BP targets in diabetes, stroke was marginally reduced. 137 Furthermore, extended follow-up of ACCORD, 750 as well as analyses of intensive BP reduction in those randomized to the standard glycaemic arm, 749 provide evidence suggesting benefit consistent with the SPRINT, STEP, and Effects of intensive Systolic blood Pressure lowering treatment in reducing RIsk of vascular evenTs (ESPRIT) trials. 136 , 146 , 545 Overall, all major BP-lowering medication classes are effective in preventing CVD in people with or without diabetes. Of note, however, albuminuria is more common in diabetes and, for this reason, ACE inhibitors and ARBs have potential advantages that may warrant consideration for BP-lowering in patients with diabetes (see Supplementary data online , Table S10 ). 753
Evidence for modifying BP-lowering treatment in patients with pre-diabetes is somewhat limited. Furthermore, the relative effect of BP lowering is relatively consistent across different categories of BMI as a measure of obesity. 754 , 755 It is also noteworthy that elevated BP itself may increase the risk of diabetes, 755 emphasizing the potential role of BP lowering in preventing diabetes in addition to preventing CVD. Among the major classes of BP-lowering drugs, ACE inhibitors and ARBs are effective in preventing new-onset diabetes and can be considered in patients at risk of diabetes and who are indicated for BP-lowering therapy. 164 , 755
Recommendations for managing hypertension in patients with diabetes

9.7. Chronic kidney disease
9.7.1. relationship between hypertension and chronic kidney disease.
Approximately 850 million people worldwide have CKD, with >80% of them hypertensive, and the prevalence is expected to rise to 1.56 billion by 2025. 756–759 The pathogeneses of hypertension and CKD are closely entwined. 760 Resistant hypertension, masked hypertension, HMOD, and higher night-time BP are common in patients with CKD. 761 CVD is one of the largest contributors to mortality in patients with CKD, with hypertension being a major risk factor. 760 , 762
For the purposes of these guidelines, adults with moderate-to-severe CKD and elevated BP are at sufficiently high risk to be considered for BP-lowering drug therapy as outlined in Section 8 and the Central Illustration ( Figure 19 ). We use Kidney Disease: Improving Global Outcomes (KDIGO) categories to define CKD-based risk, and our definition of moderate-to-severe CKD comprises persons with an eGFR of <60 mL/min/1.73 m 2 and/or albuminuria of ≥30 mg/g (≥3 mg/mmol). 19 For persons with mild CKD and elevated BP, a CVD risk assessment should be conducted before deciding on BP-lowering treatment.
9.7.2. Blood pressure lowering in chronic kidney disease
BP lowering in patients with CKD is associated with beneficial effect on CVD events and mortality. 275 , 763–766 BP lowering reduces progression of CKD and the incidence of end-stage renal disease, but this tends to be only in those with significant proteinuria at baseline. 766 , 767
9.7.3. Managing blood pressure in chronic kidney disease
Patients with CKD should receive lifestyle advice, especially regarding reducing sodium intake. Dietary potassium supplementation recommendations are provided in Section 8 , with caution required among persons with moderate-to-severe CKD. While exercise appears to have little effect on improving BP in patients with CKD 768 or patients on dialysis, 769 those with CKD on ACE inhibitor monotherapy have protection against adverse kidney outcomes, CVD events, cardiovascular death, and all-cause death. 770 , 771 Both ACE inhibitors and ARBs reduce the risk of CVD events and kidney failure compared with placebo; however, ACE inhibitors appear to do so with higher probability than ARBs. 772 , 773 Patients with CKD usually require combination therapy, and this should be initiated as a combination of a RAS inhibitor and a CCB or diuretic. In patients with eGFR < 30 mL/min/1.73 m 2 , an adequately up-titrated loop diuretic is necessary to define resistant hypertension. Chlorthalidone, typically added to a loop diuretic, also effectively lowers BP and reduces microalbuminuria in patients with resistant hypertension with stage 4 CKD (eGFR of 15–30 mL/min/1.73 m 2 ). 774 The combination of an ACE inhibitor and an ARB is not recommended in CKD or any other BP-treatment scenario.
9.7.4. Blood pressure targets in chronic kidney disease
Evidence regarding BP targets in patients with CKD is complex and controversial. The 2021 KDIGO Guideline suggested that adults with elevated BP and CKD be treated to a target systolic BP of <120 mmHg, when tolerated, using standardized office BP measurement (Class of Recommendation IIb). 19 This suggestion was based, in part, on the SPRINT trial. 545 It should be noted that patients with 24 h urine protein excretion ≥ 1 g/day or eGFR < 20 mL/min/1.73 m 2 were excluded from SPRINT. In patients with CKD, after a median follow-up of 3.3 years, the hazard ratio for the primary composite cardiovascular outcome was 0.81 (95% CI 0.63–1.05) and for all-cause death it was 0.72 (95% CI 0.53–0.99). Although intensive BP lowering in SPRINT resulted in greater early decline in eGFR, there was no evidence that this reduction in eGFR attenuated the beneficial effects of the SPRINT intervention on CVD events or death. 775
Several systematic reviews have examined the benefit of intensive BP control in patients with CKD (see Supplementary data online ). Some have shown no benefit of intensive BP control on renal outcomes, 764 , 767 while others showed lower mortality in intensively treated vs. non-intensively treated patients. 275 Highlighting the beneficial effects of SGLT2 inhibitors in persons with CKD 776 , 777 and finerenone in persons with CKD and diabetes 460–462 , 778 is relevant, though these drugs are not currently marketed for BP-lowering effects alone.
Recommendations for managing hypertension in patients with chronic kidney disease

9.8. Cardiac disease
9.8.1. blood pressure thresholds and targets in patients with cardiac disease.
Recommended BP thresholds for initiating BP-lowering therapy and recommended BP targets in patients receiving therapy are provided in Sections 6 and 8 . All patients with a history of CVD (including coronary artery disease) are at increased risk of recurrent CVD. As such, these patients are recommended to be treated with BP-lowering therapy for confirmed baseline BP of ≥130/80 mmHg and the recommended treatment target BP of 120–129/70–79 mmHg, provided treatment is tolerated (see Sections 6 and 8 ). As stated in Section 8 , it should be remembered that a systolic BP of 120 mmHg (especially by out-of-office assessment) is likely the optimal point in the target range recommended in these guidelines. In addition to considering patients with known CVD at sufficiently high risk for more intensive BP treatment targets, the task force considers patients with both severe valvular heart disease and symptomatic heart failure to also be at sufficiently high risk. We also note that, whether used for angina control or BP control, a beta-blocker should not be combined with a non-dihydropyridine CCB.
9.8.2. Coronary artery disease with particular reference to the blood pressure J-curve
Important considerations in patients with coronary artery disease are: (i) the BP J-curve (an observation suggesting that over-intensive BP lowering may increase CVD risk in some patients), and (ii) compelling indications for specific classes of BP-lowering medications.
The J-curve phenomenon describes increased risk for CVD observed among patients with the lowest and highest BP in the dataset, with the best CVD outcome rates typically observed among those with BP in the normal range (e.g. systolic BP of 100–120 mmHg and diastolic BP of 60–80 mmHg). For this reason, the J-curve is sometimes also called the U-curve, with both terms typically used interchangeably. 697 , 783 , 784
However, observational data do not consistently demonstrate a BP J-curve with CVD risk. 697 It is more commonly observed among patients with established clinical CVD, such as those with coronary artery disease, or in secondary prevention cohorts. 785 , 786 Furthermore, the J-curve is more commonly observed when analysing diastolic BP values vs. systolic BP values, though it has been described for both. 114 , 697 This stronger relationship with diastolic BP has informed the hypothesis that the J-curve may be caused by reduced perfusion of major organs at low BP, which is particularly operative for diastolic BP in the coronary vasculature when considering ischaemic heart disease events (since coronary blood flow is largely confined to diastole). 786 , 787
If excessive lowering of BP causes CVD events, this needs to be addressed in treatment recommendations provided by BP management guidelines. The 2018 ESC/ESH Guidelines on the management of arterial hypertension introduced, for the first time, lower bounds of BP-lowering treatment targets, implying that treatment be de-intensified for patients with on-treatment BP below these bounds (i.e. <120 mmHg systolic or <70 mmHg diastolic). 1 The 2023 ESH document also makes this argument. 788
However, since 2018, compelling evidence has demonstrated that the BP J-curve evident in observational datasets is highly unlikely to reflect a causal process and can instead be attributed to residual confounding and/or reverse causation. 33 , 114 , 115 , 546 , 697 , 789–793
Accordingly, while low BP can indicate a high-risk state, particularly among older adults and those with comorbidities, there is no evidence that this is a causal phenomenon. Indeed, if there is another indication for BP-lowering therapy (e.g. in a patient with wide pulse pressure and a baseline systolic BP of >140 mmHg but diastolic BP of <60 mmHg), the evidence suggests that such therapy should be provided if tolerated to reduce CVD risk.
There is a limit to how low BP can be treated without potentially tipping the scales in favour of CVD harm vs. CVD benefit. However, it is not clear what that limit is and how much it differs based on comorbidities. Currently, the data do not suggest that risk for CVD can be causally increased by treating any patient to the recommended intensive BP target outlined in these guidelines of as low as 120/70 mmHg. We also do not recommend stopping or de-intensifying BP-lowering medication among asymptomatic patients with on-treatment BP of <120/70 mmHg. It should be recognized, though, that there are no robust data demonstrating that an on-treatment systolic BP of <90 mmHg or an on-treatment diastolic BP of <50 mmHg is safe from a CVD perspective and there is clear potential for harm. Furthermore, it must be emphasized that the above discussion of the BP J-curve relates solely to CVD risk and does not consider the known non-CVD side effects of BP-lowering drugs, like, e.g. orthostatic hypotension, syncope, and renal injury. We do know that patients treated to a more intensive BP target of 120/70 mmHg are at increased risk for these side effects, 550 which is why these guidelines stress that this more intensive target should only be pursued among those in whom treatment is being tolerated ( Section 8 ).
The second consideration in managing BP in patients with coronary artery disease is the recommended use of BP-lowering medications with compelling indications based on outcomes trials that demonstrated CVD outcomes benefits in the setting of coronary artery disease. These recommendations are provided in the recommendation table below.
9.8.3. Valvular heart disease
Most patients with both severe heart valve disease and heart failure, defined by the 2021 ESC/European Association for Cardio-Thoracic Surgery (EACTS) Guidelines for the management of valvular heart disease, 794 can be considered at increased risk of CVD. Accordingly, it is recommended they are treated with BP-lowering therapy for confirmed baseline BP of >130/80 mmHg, and their recommended target of treatment is BP of 120–129/70–79 mmHg, provided treatment is tolerated. Persons with mild-to-moderate heart valve disease should have a CVD risk assessment prior to deciding their BP-lowering treatment threshold and target.
Vasodilating ARBs/ACE inhibitors are preferable over vasodilating dihydropyridine CCBs because of the link between valvular heart disease and subsequent heart failure and given the stronger efficacy evidence for ARBs/ACE inhibitors in the setting of heart failure once manifested. 795 In aortic valve stenosis, concomitant hypertension influences both the aortic root, the aortic valve, and the left ventricular structure and function. 796 In this subgroup, treatment preferably with ARBs/ACE inhibitors should be considered. A beta-blocker may be added if BP remains >140/90 mmHg. 796 , 797
9.8.4. Heart failure
Patients with symptomatic heart failure are at increased risk of CVD. Therefore, it is recommended that these patients are treated with BP-lowering therapy for confirmed baseline BP of >130/80 mmHg and their recommended treatment target is BP of 120–129/70–79 mmHg, provided treatment is tolerated and with out-of-office confirmation of on-treatment BP. Of note, many patients with systolic heart failure on maximal heart failure therapies have BP of <120/70 mmHg, and we do not recommend de-intensifying such treatment unless indicated by symptomatic side effects. Besides referencing the new evidence for ARNi and SGLT2 inhibitor therapies, 795 our 2024 recommendations for heart failure are largely unchanged from the 2018 ESC/ESH Guidelines on the management of arterial hypertension. Non-dihydropyridine CCBs should not be used in heart failure. Frailty and hypotension risk should be assessed in older heart failure patients being considered for ARNi and SGLT2 inhibitor therapies, and older patients should be closely followed to ensure they are tolerating such treatments. For more information on the management of heart failure, we direct readers to the latest ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. 798
Recommendations for managing hypertension in patients with cardiac disease

9.8.5. Heart rhythm disease (including AF)
Not all patients with heart rhythm disease, including those with AF, are at increased risk for CVD and, as such, the management of BP among patients with heart rhythm disease should be the same as for the general adult population. 443 However, there is a close relationship between increased BP and AF risk, hence, ensuring good BP control is important. 801 , 802 Management of heart rhythm disorders should follow recommendations in guidelines specific to these conditions. 803
9.9. Chronic cerebrovascular disease and/or cognitive impairment
9.9.1. role of hypertension in chronic cerebrovascular disease.
Hypertension is a risk factor for chronic cerebrovascular disease through its direct effects on brain structure and microvasculature. This manifests as transient ischaemic attack (TIA) and stroke in the acute setting, but chronic hypertension can lead to covert stroke and white-matter ischaemic change over time, resulting in cognitive decline and progressive vascular dementia. 804–808 Hypertension is also associated with increased risk of Alzheimer’s disease, 809 and is a risk factor for developing AF, heart failure, and CKD, all of which are associated with increased risk of developing cognitive impairment and dementia. 810–813 For the purposes of these guidelines, adults with a history of stroke or TIA and elevated BP are considered at sufficiently high risk to be considered for BP-lowering drug therapy as outlined in Section 8 and the Central Illustration ( Figure 19 ).
9.9.2. Treatment in patients with history of prior stroke or transient ischaemic attack
In patients with a prior history of TIA and ischaemic stroke, BP-lowering treatment reduces the risk of any recurrent stroke by 20%. 814–817 The aetiology of stroke can affect the degree of risk reduction with pharmacological treatment, with greater reductions observed for intracerebral haemorrhage and lacunar ischaemic stroke syndromes. 818–820
Most prior guidelines recommend an intensive BP target in patients with a prior history of stroke, typically using combination treatment (ACE inhibitor/ARB plus either a calcium channel antagonist or a thiazide/thiazide-like diuretic), with therapy commencing immediately after TIA and within a few days of ischaemic stroke (see Supplementary data online and see Section 10.3 for acute BP management during hospitalization for stroke). 814 , 815 , 821–824
Regimens containing an ACE inhibitor and thiazide/thiazide-like diuretic may be superior to beta-blockers in terms of stroke risk reduction. 825 , 826 Regarding intensive BP control after stroke, typically targeting a systolic BP of <130 mmHg, individual trials were somewhat inconclusive, but a meta-analysis showed a reduced risk of recurrent stroke of 22% in the intensive treatment group randomized to a target systolic BP as low as 120 mmHg. 543 , 824 , 827 , 828 Caveats to this recommendation would be for frail patients, who have a much higher rate of stroke and recurrent stroke than the general population, and who are more sensitive to adverse effects of BP-lowering agents (see Section 9.3 ). 596 , 606 , 607 , 829
9.9.3. Treatment in patients with chronic cerebrovascular disease and cognitive impairment
Treatment of hypertension represents a key mechanism for reducing the global burden of dementia at the population level. 830 Epidemiological studies have reported associations between mid-life hypertension and development of cognitive decline in later life, with, e.g. mid-life hypertension increasing relative risk of lifetime dementia by 20%–54%. 831–837 In one observational meta-analysis, an increased risk for dementia emerged with systolic BP of >130 mmHg. 831
Evidence for lowering BP to reduce the risk of dementia is limited due to heterogeneity in populations studied, cognitive testing methods used, and the varied use of dementia or cognitive impairment or both as a primary outcome. 838 , 839 Findings from individual studies have mixed results (see Supplementary data online ). 264 , 839–843 Studies on effects of BP-lowering treatment on white-matter intensities concluded that patients in the intensive-control arm had less white-matter intensity accumulation than in the standard-treatment arm. 841 , 844 Studies in which people with stroke and TIA were included reported a reduced risk of dementia and cognitive decline for the active-treatment group, but a mixed signal for dementia alone. 841 , 845 However, individual studies may have been under-powered and more recent meta-analyses do convincingly support efficacy in reducing dementia with BP-lowering treatment. 610 , 611 Indeed, these meta-analyses reported a reduced risk of incident dementia or cognitive impairment with BP lowering of 7%–13%. 610 , 611 While one trial suggested superiority of long-acting CCBs, 264 it is unclear if any first-line BP-lowering agent is preferable for preventing dementia and cognitive impairment. 846 , 847
The role of competing risk mechanisms including orthostatic hypotension 848 and BP variability 849 may be important factors in treatment decisions for people with frailty, multimorbidity, and/or chronic cerebrovascular disease.
Recommendations for managing hypertension in patients with chronic cerebrovascular disease and cognitive impairment

9.10. Aortopathy
9.10.1. coarctation of the aorta.
Aortic coarctation is associated with CVD in the long term, even following early surgical or percutaneous treatment. The most common complications are associated with hypertension, which is common in aortic coarctation. When aortic coarctation is not treated, patients often develop severe hypertension and HMOD (especially LVH and left ventricular dysfunction, aortopathy, and cerebrovascular complications). 850–852 No formal RCTs to define optimal medical treatment of hypertension in aortic coarctation have been conducted, therefore, patients not suitable for, or having undergone, intervention should be treated for hypertension following the core algorithm for the general population.
9.10.2. Bicuspid aortic valve-related aortopathy
Bicuspid aortic valve is the most common congenital heart disease and is sometimes associated with aortopathy or aortic coarctation. Bicuspid aortic valve disease is associated with an increased risk of valve malfunction and adverse aortic events. 853 , 854 This risk is exacerbated by hypertension.
Beyond aortic dilation and aneurysm formation, bicuspid aortic valve disease is also a risk factor for aortic dissection and rupture. 855 Blood pressure should be carefully monitored and controlled. 856
9.10.3. Preventing aortic dilation and dissection in high-risk patients
A modest dilatation of the ascending aorta or aortic root is often associated with chronic hypertension and HMOD. An additional cause of aortopathy (bicuspid valve, coarctation, Marfan or other syndromes) should be considered in more severe cases. 857 Patients with aortic dilatation should have their BP optimally controlled following the core algorithm for the general hypertension population.
In patients with Marfan syndrome, prophylactic use of ARBs, ACE inhibitors, or beta-blockers may reduce complications or progression of aortic dilation. 857–860 More information is available in the 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. 861
9.11. Different ethnic groups
Influx and settlement of migrant populations in Europe have contributed to regional population growth and changes in its composition. 862 Ethnic minority populations are disproportionally affected by hypertension and hypertension-mediated complications, compared with historically native Europeans, with data suggesting migrant women are particularly vulnerable. 536 , 863 In particular, hypertension is more prevalent in those of African descent. 863 , 864 The predominant group of European black ethnicity originates from sub-Saharan Africa, 863 but specific studies on the management and control of hypertension in this population are lacking, and data are often extrapolated from studies in the African American population. 864 This assumption requires caution, as differences likely exist between these populations in terms of CVD risk, economic, and sociological status, 865 , 866 as well as responses to BP-lowering drugs. 867
Black patients have a greater prevalence of low-renin, salt-sensitive hypertension and may be more predisposed to HMOD than white patients, possibly in part due to increased vascular stiffness. 864 , 868 , 869 Salt restriction, thiazide or thiazide-like diuretics, and CCBs appear particularly useful in black patients with hypertension, whereas RAS blocker monotherapy may be less effective. 870–873 If combination therapy is needed, in a recent RCT conducted in sub-Saharan African countries, amlodipine plus either hydrochlorothiazide or perindopril proved to be equally effective and superior, respectively, to hydrochlorothiazide plus perindopril. 874 When RAS blockers are used in combination therapy, ARBs may be preferable to ACE inhibitors, as angioedema appears more common with ACE inhibitors in black patients.
Despite some recent progress, 875 data on hypertension epidemiology and management in European immigrant patients are still lacking. 863 , 875–877
Recommendations for managing hypertension in different ethnic groups

9.12. Nocturnal hypertension
9.12.1. definition.
Nocturnal hypertension is defined as night-time BP of >120 mmHg systolic and/or >70 mmHg diastolic by 24 h ABPM. Nocturnal hypertension can occur as day–night sustained hypertension or isolated nocturnal hypertension (daytime BP < 135/85 mmHg on 24 h ABPM). Physiologically, BP is expected to decrease during sleep by 10%–20% relative to daytime BP. 878 Night-time dipping patterns are classified into four groups: 879 , 880
Inverse dipping (riser): nocturnal increase in BP (night-to-day ratio of >1.0).
Non-dipper: reduced night-time BP dip of <10% (or night-to-day ratio of >0.9 and ≤1.0).
Normal dipping: fall in night-time BP of >10% and <20% (or night-to-day ratio of 0.8 to 0.9).
Extreme dipping: marked fall in night-time BP of >20% (or night-to-day ratio of <0.8).
Patients with nocturnal hypertension may be dippers or non-dippers. Of note, the long-term reproducibility of dipping patterns appears to be low. 881 , 882
9.12.2. Epidemiology
Nocturnal hypertension has been observed in up to half of patients with hypertension, 883–886 and is associated with increased HMOD, 883 impaired renal function, and diabetes mellitus. 887 Nocturnal hypertension appears to be more prevalent in black 888–890 and Asian 891 , 892 populations. Masked uncontrolled hypertension, which occurs in 30% of patients treated for hypertension, is more often due to poorly controlled nocturnal BP than daytime BP on ABPM. 893
Environmental factors, including sleep duration and higher humidity, 894 nocturia, 895 OSAS, 896 obesity, high salt intake in salt-sensitive patients, 897 orthostatic hypotension, autonomic dysfunction, CKD, 898–900 diabetic neuropathy/diabetes, 901 and old age 62 are associated with non-dipping. Moreover, nocturnal hypertension and absent night-time dipping pattern are more common in secondary hypertension. 902 , 903
9.12.3. Night-time blood pressure as a cardiovascular disease risk factor
Nocturnal hypertension is a risk factor for adverse CVD events, 904 cerebrovascular disease, including stroke, 905 and cardiovascular mortality. 891 , 906 , 907 Night-time BP may provide more prognostic information than daytime BP, perhaps as it is less dependent on physical activities. Non-dipping 908–910 and reverse dipping (nocturnal rise in BP) may also be associated with increased CVD risk. 62 , 910–913 A nocturnal rise in BP is associated with an increased risk of dementia and Alzheimer’s disease in older men. 914 There is also some evidence that extreme dipping, particularly in untreated patients, is associated with an increased risk for CVD events. 35 , 886
9.12.4. Treatment of nocturnal hypertension
There is no reliable evidence that BP-lowering medication should be routinely dosed at bedtime. The diurnal timing of drug administration is discussed in Section 8.3.4 . In patients with secondary hypertension, the underlying cause (OSAS, primary aldosteronism) should be treated as discussed in Section 9.14 .
9.13. Resistant hypertension
9.13.1. definition of resistant hypertension.
Resistant hypertension is defined as BP remaining above goal despite three or more BP-lowering drugs of different classes at maximally tolerated doses, of which one is a diuretic ( Table 11 ). 915 Resistant hypertension should be managed at specialized centres with the expertise and resources to exclude pseudo-resistant hypertension (adherence testing) and causes of secondary hypertension. 916
9.13.2. Non-pharmacological interventions
The Treating Resistant Hypertension Using Lifestyle Modification to Promote Health (TRIUMPH) trial demonstrated significant clinic and ambulatory BP reductions in patients with resistant hypertension participating in a 4-month lifestyle intervention comprising diet and exercise interventions delivered within a cardiac rehabilitation programme. 917
9.13.3. Pharmacological interventions
BP-lowering treatment of resistant hypertension with single-pill combinations is recommended to reduce the pill burden, thereby increasing drug adherence and persistence. 492
As resistant hypertension often, and especially in CKD, 918 represents a state of salt retention and volume expansion secondary to relative aldosterone excess, 516 , 919 , 920 BP control may be improved by switching hydrochlorothiazide to long-acting thiazide-like diuretics, such as chlorthalidone. 921 , 922 However, a recent trial of chlorthalidone vs. hydrochlorothiazide—which probably included a sizeable proportion of adults with resistant hypertension—did not demonstrate any difference in systolic BP or CVD outcomes between the two medications. In the subgroup of patients with prior CVD, there was a strong trend of benefit with chlorthalidone on CVD outcomes. 447 Of note, the risk of hypokalaemia was higher in the chlorthalidone group than in the hydrochlorothiazide group. 447 In patients with eGFR < 30 mL/min/1.73 m 2 , an adequately up-titrated loop diuretic is necessary to define resistant hypertension.
Most patients with resistant hypertension require the addition of non-first-line BP-lowering drugs ( Figure 22 ). Of these, low-dose spironolactone (25–50 mg daily) should be considered first. 459 , 515 , 923–925 In patients with resistant hypertension and type 2 diabetes, spironolactone (25–50 mg daily) reduced BP and albuminuria. 926 The use of spironolactone can be precluded by limited tolerability due to anti-androgenic side effects resulting in breast tenderness or gynaecomastia (in about 6%), impotence in men, and menstrual irregularities in women. 927 The efficacy and safety of spironolactone for treating resistant hypertension have not yet been established in patients with significant renal impairment. Moreover, spironolactone, especially in addition to RAS inhibitors, increases the risk of hyperkalaemia. 927 , 928 Therefore, spironolactone should be restricted to patients with an eGFR of ≥30 mL/min/1.73 m 2 and a plasma potassium concentration of ≤4.5 mmol/L. 459 Steroidal MRAs are contraindicated in patients with an eGFR of <30 mL/min/1.73 m 2 . Serum electrolytes and kidney function should be monitored soon after initiation and frequently thereafter. In patients with resistant hypertension and CKD (eGFR of 25–45 mL/min/1.73 m 2 ), the oral potassium binder patiromer enabled more patients to continue treatment with spironolactone. 929

Management of resistant hypertension.
BP, blood pressure; K + , potassium; SPC, single-pill combination.
If spironolactone is not tolerated due to anti-androgen side effects, eplerenone may be used. If eplerenone is used, higher doses (i.e. 50–200 mg daily) and twice-daily dosing may be necessary to achieve a BP-lowering effect. 503 Of note, eplerenone is not licensed for hypertension treatment in many countries.
When not already prescribed for a compelling indication, beta-blockers should be considered in the treatment of resistant hypertension, though their BP-lowering effects appear to be less potent than spironolactone in the setting of resistant hypertension. 459
Amiloride and clonidine have data suggesting they are as effective as spironolactone for BP lowering, though they lack outcomes data. A non-exhaustive list of additional medications sometimes used for BP-lowering purposes includes other centrally acting BP-lowering medications (e.g. methyldopa), hydralazine, aliskiren, minoxidil, triamterene, and loop diuretics ( Figure 22 ). 515 , 516 As noted earlier, minoxidil use is often limited by side effects.
9.13.4. Devices for blood pressure lowering
Several devices have been investigated for treating resistant hypertension. Of these, the most evidence is available for catheter-based renal denervation. As discussed in Section 8.6.1 , several randomized, sham-controlled trials have been published, demonstrating a BP-lowering efficacy over 24 h for radiofrequency and ultrasound renal denervation in a broad spectrum of hypertension, including resistant hypertension. 568 , 585 Other devices are still under investigation and are not recommended for routine use in clinical practice ( Section 8.6.2 ).
Recommendations for treating resistant hypertension (see Evidence Tables 42 and 43)

9.14. Management of specific causes of secondary hypertension
9.14.1. general considerations.
These guidelines will describe only the general principles of managing the most common forms of secondary hypertension. For the rarer forms of secondary hypertension, patients should be referred to specialized hypertension centres.
By definition, secondary hypertension should be, for the most part, cured when the underlying cause has been unambiguously identified and removed. However, in clinical practice, this is not always the case. Vascular remodelling, a common feature of a delayed diagnosis of secondary hypertension, affects renal function and can account for residual high BP in some patients with secondary hypertension. The rate of cure is higher when the diagnosis is made early in the course of the disease. Most common forms of secondary hypertension are listed in Table 13 .
9.14.2. Primary aldosteronism
Primary aldosteronism (Conn syndrome) is the most common form of secondary hypertension. The management of primary aldosteronism depends on its subtype, particularly on adrenal lesions being unilateral or bilateral, because the unilateral forms are amenable to surgical treatment while the latter require lifelong medical treatment. In sporadic forms, unilateral primary aldosteronism is distinguished from bilateral primary aldosteronism by adrenal vein sampling or functional imaging with radiolabelled tracers. 930–932 In the much less common familial forms (necessitating a family history be taken), genetic testing for germline mutations is necessary. 933
For unilateral primary aldosteronism, surgical removal of the offending adrenal gland is typically considered, unless the patient is older or has comorbidities of concern. Surgery is not an option for bilateral primary aldosteronism. Medical treatment is currently based on MRAs. Among MRAs, spironolactone is the most widely available. The effective dose, usually 50–100 mg once daily, can be titrated up to 300–400 mg once daily, if necessary. Eplerenone is also used and, despite being less potent than spironolactone and requiring twice-daily administration, it has the advantage of causing less gynaecomastia and erectile dysfunction in men. 934 Newer agents, such as the non-steroidal MRAs finerenone and exarenone, and the aldosterone synthase inhibitor baxdrostat, which lower BP in resistant hypertension, 326 , 474 are also being tested for treating primary aldosteronism. Of the familial forms, only glucocorticoid-remediable primary aldosteronism, now reclassified as familial hyperaldosteronism type 1, can be corrected with dexamethasone, 935 usually with low doses that are free of glucocorticoid effects and can be safely used during pregnancy. 936 For detailed information, readers are referred to the latest primary aldosteronism guidelines. 328 , 329
9.14.3. Renovascular hypertension
Patients with RVH should receive medical therapy to reduce BP in the first instance. Percutaneous transluminal renal angioplasty (PTRA) without stenting is the treatment of choice for fibromuscular dysplasia, and can restore renal perfusion pressure and lower BP. 937 When this is not feasible, RAS blockers are the drugs of choice for treatment, but they require careful monitoring of renal function over time, as they can cause acute renal failure in those with tight bilateral stenoses or a stenosed solitary functioning kidney. Possible involvement of the carotid, coronary, and other major arteries, possibly leading to dissection if BP is not controlled, should also be considered, as fibromuscular dysplasia is now recognized as a systemic disease affecting multiple vascular beds.
Patients with significant atherosclerotic renal artery stenosis are at very high risk of CVD and renal events. It is recommended that PTRA and stenting are performed in experienced centres due to the high risk of restenosis. Unfortunately, though these studies did not solely recruit patients with true significant atherosclerotic RVH, publication of some null trials 938 , 939 have decreased the enthusiasm for investigating atherosclerotic renal artery stenosis. This could result in more uncontrolled hypertension, recurrent flash pulmonary oedema (Pickering syndrome), and worsening renal function ultimately leading to end-stage renal disease. 940
Recommendations for managing hypertension in patients with renovascular hypertension (see Evidence Tables 44 and 45)

9.14.4. Phaeochromocytoma/paraganglioma
Phaeochromocytomas are rare adrenal tumours that secrete catecholamines and are present in <0.2% of patients with hypertension. A small percentage (<10%) of catecholamine-producing tumours are extra-adrenal and are derived from sympathetic and non-sympathetic nerves. More than 35% of the non-syndromic PPGLs are due to germline mutations. 338 These mutations should be screened for because, when found, they can drive management of the proband and the family and also inform the choice of functional imaging. Moreover, some germline mutations, such as those involving succinate dehydrogenase B, carry a risk of malignant adrenal tumours. 301 , 336
Sympathetic PPGLs are usually secreting and present with chronic, episodic, or labile hypertension. Adrenergic crises cause hypertensive emergencies and should be treated with an intravenous (i.v.) alpha-1-blocker, such as phentolamine, doxazosin or terazosin, or labetalol. When given i.v. (1–2 mg/kg) twice weekly as a bolus over 1 min followed by a continuous infusion, labetalol also has alpha-blocker properties and has the advantage of allowing titration of the infusion based on the BP response, and avoids tachycardia via beta-blockade.
Identifying a single tumour mandates surgical excision after adequate pharmacological preparation, because secreting PPGLs can cause fatal events with no warning. Administering doxazosin or terazosin, followed by a beta-blocker, usually controls BP and adrenergic crises. As PPGLs are associated with a redistribution of volume from the periphery to the cardiopulmonary system, 944 patients with PPGLs have peripheral hypovolaemia that exposes them to the risk of profound hypotension, particularly right after tumour excision. Therefore, adequate fluid administration should be carefully managed.
9.14.5. Obstructive sleep apnoea syndrome
The management of this prevalent condition should be driven by the result of a polysomnography study, which should provide the value of the AHI (the average number of episodes per hour) and the sleep position in which apnoeic–hypopnoeic episodes occur. For mild OSAS (AHI < 15), weight loss and advice on sleep hygiene are usually sufficient. For moderate (AHI of 15–30) and severe (AHI > 30) OSAS, continuous positive airway pressure (CPAP) is indicated and usually improves BP control and helps to resolve resistant hypertension. If CPAP is not tolerated, the site of upper airway obstruction should be determined by an Ear, Nose, and Throat evaluation with drug-induced sleep endoscopy as a potential step to corrective surgery.
9.14.6. Drug-induced hypertension
Over-the-counter medications, prescribed drugs, and drug abuse (recreational substances and misuse of drugs) can cause hypertension ( Supplementary data online , Table S4 ).
9.14.6.1. Anticancer drug-induced hypertension
Growing evidence indicates that, while contemporary anticancer and anti-angiogenic drugs improve cancer survival, they can also cause hypertension ( Supplementary data online , Table S4 ). This is especially evident in patients treated with vascular endothelial growth factor inhibitors, in whom BP increases in 80%–90%. 945 Tyrosine kinase inhibitors and proteasome inhibitors also increase BP, as do adjuvant therapies (corticosteroids, calcineurin inhibitors, non-steroidal anti-inflammatory drugs, and anti-androgen hormone therapy). Hypertension caused by anticancer drugs is often dose limiting and may be reversible after therapy interruption or discontinuation. Evidence-based clinical trials specifically addressing patients who develop hypertension due to cancer therapy are lacking. It is recommended that management of hypertension in these patients follows that for the general population. 945 , 946 Managing these complex patients requires multidisciplinary healthcare involving oncologists, hypertension specialists, cardiologists, and nephrologists, 945 , 946 as highlighted in the 2022 ESC Guidelines on cardio-oncology. 946
9.14.7. Other forms of secondary hypertension
Other forms of secondary hypertension, such as genetic causes of hypertension (Liddle’s syndrome, glucocorticoid-remediable aldosteronism), excess liquorice, Cushing’s syndrome, thyroid disease, hyperparathyroidism, aortic coarctation, and acromegaly are rare. Affected patients should be referred to specialized centres for treatment.
10.1. Acute blood pressure management in hypertensive emergencies
10.1.1. definition and characteristics of hypertensive emergencies.
Hypertensive emergency is defined as BP of ≥180/110 mmHg (see Figure 10 ) associated with acute HMOD, often in the presence of symptoms. Hypertensive emergencies are potentially life-threatening and require immediate and careful intervention to reduce BP, often with i.v. therapy.
Symptoms of hypertensive emergency depend on the organs affected but may include headache, visual disturbances, chest pain, shortness of breath, dizziness, and other neurological deficits. In patients with hypertensive encephalopathy, somnolence, lethargy, tonic–clonic seizures, and cortical blindness may precede a loss of consciousness; however, focal neurological lesions are rare and should raise the suspicion of stroke.
As outlined in Section 7 , we define HMOD among patients with chronically elevated BP or hypertension as the presence of specific cardiac, vascular, and renal alterations. 31 , 159 However, in the setting of hypertensive emergency, more acute manifestations of organ damage are relevant for management.
Acute manifestations of organ damage include:
Patients with severe acute hypertension associated with other clinical conditions likely to require urgent reduction in BP, e.g. acute onset of aortic dissection, myocardial ischaemia, eclampsia, or heart failure.
Malignant hypertension, defined as extreme BP elevations and acute microvascular damage (microangiopathy) affecting various organs. 947 The hallmark of this condition is small-artery fibrinoid necrosis in the kidneys, retina, and brain. The acute microangiopathy is typically characterized clinically by retinopathy (flame haemorrhages, cotton wool spots, and/or papilloedema). Other manifestations of microangiopathy include disseminated intravascular coagulation, encephalopathy (in about 15% of cases), acute heart failure, and acute deterioration in renal function.
Patients with sudden severe hypertension due to phaeochromocytoma, which can result in severe acute organ damage.
The term ‘hypertension urgency’ describes severe hypertension in patients without clinical evidence of acute organ damage. While these patients require BP reduction, they do not usually require admission to hospital, and BP reduction is best achieved with oral medication according to the drug treatment algorithm presented in Section 8 . However, these patients may require more urgent outpatient review to ensure that their BP is controlled.
Acute and severe increases in BP can sometimes be precipitated by sympathomimetics such as methamphetamine or cocaine, when caution around beta-blocker use is also needed. Many patients in an emergency department with acute pain or distress may have acutely elevated BP that will normalize when the pain and distress are relieved, rather than requiring any specific intervention to lower BP.
A diagnostic work-up is necessary for patients with a suspected hypertensive emergency (see Supplementary data online , Table S12 ).
10.1.2. Acute management of hypertensive emergencies
Key considerations in defining treatment are:
Establishing the affected target organ(s) and whether they require any specific interventions other than BP lowering.
Determining whether there is a precipitating cause for the acute rise in BP and/or another concomitant health condition present that might affect the treatment plan (e.g. pregnancy).
The recommended timing and magnitude of BP lowering required for safe BP reduction.
These considerations will inform the type of BP-lowering treatment required. Regarding BP-lowering drugs, i.v. treatment using a short half-life drug is typically ideal to allow careful titration of the BP response to treatment. This requires a higher dependency clinical area with facilities for continuous or near-continuous haemodynamic monitoring. Recommended drug treatments for specific hypertensive emergencies are provided in the Supplementary data online , Table S13 .
Rapid and uncontrolled or excessive BP lowering is not recommended in hypertensive emergency as this can lead to further complications. Although i.v. drug administration is recommended for most hypertensive emergencies, oral therapy with ACE inhibitors, ARBs, or beta-blockers (shorter-acting formulations like captopril or metoprolol) can also be effective. However, low initial doses should be used because these patients can be very sensitive to these agents, and treatment should take place in hospital. Further comprehensive details on the clinical management of hypertensive emergencies are available elsewhere. 242
10.1.3. Prognosis and follow-up
The survival of patients with hypertensive emergencies has improved over the past few decades, but these patients remain at high risk and should be screened for secondary hypertension.
10.2. Acute blood pressure management in acute intracerebral haemorrhage
In acute intracerebral haemorrhage, an increased BP is common and is associated with a greater risk of haematoma expansion and death, and a worse prognosis for neurological recovery. In trials testing immediate BP lowering (within <6 h) to a systolic target of <140 mmHg, the achieved systolic BP in the intervention group was typically 140–160 mmHg and was reported to reduce the risk of haematoma expansion. 948 , 949 Excessive acute drops in systolic BP (>70 mmHg) may be associated with acute renal injury and early neurological deterioration and should be avoided. 950 , 951
10.3. Acute blood pressure management in acute ischaemic stroke
The beneficial effects of BP reduction in acute ischaemic stroke remain unclear. In patients not receiving i.v. thrombolysis or mechanical thrombectomy, there is no evidence for actively lowering BP unless it is extremely high (e.g. >220/120 mmHg). If BP is extremely high, an initial moderate relative reduction of 10%–15% over a period of hours may be considered. 952 The reason for a more conservative approach to acute BP management is that cerebral autoregulation may be impaired in acute stroke, and maintaining cerebral perfusion relies on systemic BP.
In contrast, patients who are treated with i.v. thrombolysis or mechanical thrombectomy (or both) should have more proactive management of severe hypertension, because they have an increased risk of reperfusion injury and intracranial haemorrhage. In patients undergoing treatment with i.v. thrombolysis, BP should be lowered to <185/110 mmHg prior to thrombolysis and then maintained at <180/105 mmHg over the following 24 h. 953 In patients undergoing treatment with mechanical thrombectomy (with or without i.v. thrombolysis) there is limited evidence from clinical trials, but BP should also be lowered to <180/105 mmHg prior to thrombectomy and maintained over the next 24 h. 953 , 954 Therefore, patients with acute ischaemic stroke and a BP of <180/105 mmHg in the first 72 h after stroke do not seem to benefit from the introduction or reintroduction of BP-lowering medication. 955 For stable patients who remain hypertensive (≥140/90 mmHg) ≥3 days after an acute ischaemic stroke, initiation or reintroduction of BP-lowering medication is recommended.
Recommendations for acutely managing blood pressure in patients with intracerebral haemorrhage or acute ischaemic stroke

10.4. Acute blood pressure management in pre-eclampsia and severe hypertension in pregnancy
10.4.1. pre-eclampsia.
Pre-eclampsia is discussed in Section 9 . Here we focus on its management in the acute setting. Pre-eclampsia is cured by delivery. Most international societies, including the ESC, recommend an intensive approach to BP lowering in pre-eclampsia. 89 , 964 , 965 In women with pre-eclampsia and severe hypertension, immediately reducing systolic BP to <160 mmHg and diastolic BP to <105 mmHg using i.v. labetalol or nicardipine (with administration of magnesium sulfate if appropriate and consideration of delivery if appropriate) was recommended in the 2018 ESC/ESH Guidelines on the management of arterial hypertension and the 2022 ESC Guidelines for management of cardiovascular disease in pregnancy. 1 , 89 The objective of treatment is to lower BP within 150–180 min.
Magnesium sulfate [4 g i.v. over 5 min, then 1 g/h i.v.; or 5 g intramuscularly (i.m.) into each buttock, then 5 g i.m. every 4 h] is recommended for eclampsia treatment but also for women with pre-eclampsia who have severe hypertension and proteinuria or hypertension and neurological symptoms or signs. 966 There is a risk of hypotension when magnesium is given concomitantly with nifedipine. 967 If BP control is not achieved by 360 min despite two medications, consulting critical care is recommended for intensive care unit admission, stabilization, and delivery (if appropriate). 966 Since plasma volume is reduced in pre-eclampsia, diuretic therapy should be avoided.
10.4.2. Severe acute hypertension in pregnancy
Severe hypertension in pregnancy (without pre-eclampsia) may necessitate acute BP-lowering therapies. Severe hypertension in pregnancy is defined in general as systolic BP of >160 mmHg and diastolic BP of >110 mmHg and is associated with adverse maternal and peri-natal outcomes independent of pre-eclampsia and potentially of the same magnitude as eclampsia itself. 89 , 968
There are differences in rate of BP control between i.v. labetalol and i.v. hydralazine in severe hypertension in pregnancy. 969 While evidence is conflicting, 667 , 668 hydralazine may be associated with more peri-natal adverse events than other drugs. 970 Nifedipine seems to provide lower BP with lower rates of neonatal complications than labetalol. 971
Recommendations for acutely managing blood pressure in patients with severe hypertension in pregnancy and pre-eclampsia (see Evidence Table 46)

10.5. Peri-operative acute management of elevated blood pressure
Details are provided in the ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. 972 Peri-operative hypertension, hypotension, and BP variability are associated with haemodynamic instability and poor clinical outcomes for patients undergoing surgery. 973 Pre-operative risk assessment for BP management, therefore, should involve assessing for underlying end-organ damage and comorbidities. 974 Postponing necessary non-cardiac surgery is not usually warranted for patients with minor or moderate elevations in BP, as they are not at higher CVD risk. 130 , 975
Avoiding large fluctuations in BP in the peri-operative course is important, and planning a strategy for a patient should account for the baseline office BP. 974–977
There is insufficient evidence for reduced or increased peri-operative BP targets compared to usual care BP targets to lower peri-operative events. 978 No specific measure of BP appears better than any other for predicting risk of peri-operative events. 975
10.5.1. Blood pressure-lowering drugs in the peri-operative phase
Routine initiation of a beta-blocker peri-operatively is not necessary. 979
Pre-operative initiation of beta-blockers in advance of high-risk, non-cardiac surgery may be considered in patients who have known coronary artery disease or myocardial ischaemia 980 or two or more significantly elevated clinical risk factors in order to reduce the incidence of peri-operative myocardial infarction. 979 Peri-operative continuation of beta-blockers is recommended for patients currently taking beta-blockers. 981
Some studies suggest that continued use of ACE inhibitors is associated with a higher risk of peri-operative hypotension and subsequent end-organ damage including kidney injury, myocardial infarction, and stroke. 982 In the Prospective Randomized Evaluation of Preoperative Angiotensin-Converting Enzyme Inhibition (PREOP-ACEI) trial, transient pre-operative interruption of ACE inhibitor therapy was associated with a decreased risk of intra-operative hypotension. 983 A subsequent systematic review also showed a decreased risk of intra-operative hypotension with withholding ACE inhibitors/ARBs before surgery, but no association with decreased mortality or CVD outcomes. 984 On the other hand, vigilance is needed because withholding ACE inhibitors has also been shown to increase post-operative hypertension. 985 In patients with heart failure, loop diuretics can be continued in patients prone to volume overload. 986 CCBs are generally considered safe pre-operatively.
11.1. Definition
Patient-centred care is defined as an attitude of the healthcare professional that closely aligns with the patient’s preferences and needs. 987 In the patient-centred approach ( Figure 23 ), patients are viewed as active participants in health services, who work as partners alongside healthcare professionals. A patient-centred approach is associated with higher satisfaction rates, better adherence to recommendations and prescriptions, and better treatment, particularly in the management of chronic illness, such as hypertension. 988 While there is limited evidence for the efficacy and effectiveness of specific shared decision-making intervention strategies in hypertension care, 989 it is viewed as an ethical imperative in healthcare practice and health policy, and in clinical guidelines. 130

Patient-centred care.
11.2. Communicating consequences of treatment
In line with patient-centred care, it is important to assess whether patients understand their hypertension-related risk, the rationale for any hypertension treatment, the benefits and harms of hypertension treatment, and that the treatment plan is also centrally guided by what matters most to the patient. Risk communication is challenging, and providers need to be led by the individual’s preferences when presenting more detailed numeric and visual representations of risk and the likely benefits and harms of hypertension treatment. Socio-demographic differences in healthcare need to be considered in patient–provider communication. 990 , 991
Standard approaches to communicate consequences of treatment can involve 10-year risk of a CVD event with SCORE2 or SCORE2-OP. Alternatively, individual risk and risk reduction can be communicated in terms of ‘risk age’ or ‘heart age’ ( Section 7.3 ).
Recommendations for communicating consequences of treatment (see Evidence Table 47)

11.3. Self-measuring and monitoring
Self-care refers to individual responsibility for healthy lifestyle behaviours, as well as the actions required to cope with health conditions. 996 , 997 In the context of hypertension, it also includes self-management and self-measurement of BP.
Self-management includes lifestyle behaviour (diet, exercise, smoking, alcohol), co-management of medical treatments, and support for adhering to prescribed medication. 998 Self-monitoring allows high BP to be detected early, 999 and enables patients to co-manage medications with their healthcare provider. 1000 , 1001 Suitably validated and correctly used digital devices have the potential to support co-management, 1002 , 1003 and facilitate remote monitoring of BP. 76 , 81 , 1004
Recommendations for self-measuring and monitoring blood pressure (see Evidence Table 48)

11.4. Facilitating medication adherence and persistence
Adherence ( Figure 24 ) to BP-lowering drug regimens in clinical practice is almost always lower than seen in clinical trials. 1007 Most apparent treatment-resistant hypertension is accounted for by non-adherence. 1008 Adherence should always be assessed with a no-blame approach. Various methods are available to assess adherence and, along with details on barriers to adherence, are described in the Supplementary data online and Table S14 . 1009

The five dimensions of adherence (WHO, 2003) applied to hypertension.
Adherence may also be facilitated by an optimal therapeutic regimen, which can be achieved by medication reviews carried out at appropriate intervals. Several factors should be considered: (i) identifying drug-related adverse events and appropriate dosing levels, (ii) using long-acting drugs that require once-daily dosing (preferably drugs that are long-acting due to pharmacokinetic properties rather than galenic formulation), (iii) avoiding complex dosing schedules, (iv) using single-pill combinations whenever feasible, (v) taking into account the financial capacity of the patient to pay for a given regimen in the longer term, if relevant, or other pertinent aspects of the local or national healthcare systems, and (vi) enlisting support of a family member or other social support to facilitate medication adherence and persistence (see Supplementary data online , Table S15 ). 1010
While there have been advancements in digital tools to support self-management of chronic illness including hypertension, there is little efficacy evidence evaluating these interventions. Therefore, it is premature to make recommendations about specific digital tools.
11.5. Multidisciplinary management
A collaborative approach to managing hypertension, using team-based care among physicians, nurses, pharmacists, dietitians, and physiotherapists, offers significant benefits over physician-only care. Multidisciplinary care is intended to be collaborative and complementary to regular medical care 1011 and is associated with lower systolic and diastolic BP 227 , 229 , 1012 , 1013 and improved outcomes. 230 , 1014 Task-shifting away from physicians is necessary to meet the huge need for the management of elevated BP and hypertension in the population. 1015 Prescribing remains a physician duty, but prescribing can be conducted under collaborative practice agreements with the multidisciplinary team in many countries.
Further details on patient-centred care in hypertension is provided in the Supplementary data online .
Recommendations for multi/interdisciplinary blood pressure management (see Evidence Table 49)

Given the demographic transition and the worldwide ageing of populations, the number of individuals with elevated BP or hypertension is increasing worldwide.
The trajectory of BP control appears to be worsening in North America, in some (but not all) European countries, and elsewhere around the world.
The risk for CVD attributable to BP is on a continuous log-linear exposure variable scale, not a binary scale of normotension vs. hypertension.
BP-lowering drugs can reduce CVD risk even among individuals not traditionally classified as hypertensive. Accordingly, a new BP category called ‘elevated BP’ is introduced. Elevated BP is defined as an office systolic BP of 120–139 mmHg or diastolic BP of 70–89 mmHg. Hypertension remains defined as office BP of ≥140/90 mmHg.
Hypertension in women is under-studied in basic, clinical, and population research.
HMOD suggests long-standing or severe hypertension and is associated with increased CVD risk.
Absolute CVD risk must be considered when assessing and managing elevated BP.
Despite the growing number of hypertension guidelines, the rates of diagnosis, treatment, and control of hypertension (and elevated BP) remain suboptimal. A major factor underlying this is poor implementation of evidence-based guidelines in real-world clinical practice.
One of the most important changes in the 2024 Guidelines is the focus on evidence related to CVD outcomes of BP-lowering interventions rather than BP lowering alone.
Irrespective of the threshold BP above which BP-lowering treatment (lifestyle or pharmacological or other treatment) is recommended, the on-treatment BP target is 120–129/70–79 mmHg for all adults, provided this treatment is well tolerated. There are several important exceptions to these targets and individualized decision-making is always the most important priority.
Drivers of worsening trajectories of BP control in women and men.
Need for sex-specific data on epidemiology, risk factors, and pathophysiology of hypertension. Need for more prospective studies to assess women’s and men’s specific CVD risk factors pertinent to adults with elevated BP and hypertension, due to biological and socio-cultural conditions. This includes sex-specific weighting of traditional risk factors, as well as inclusion of sex-dependent, non-traditional, vascular risk factors such as stress, socio-economic conditions, and others. 1017 , 1018 We are also lacking data on sex-specific hormonal and genetic mechanisms and pathophysiology in the human. 1019 Another important area in need of investigation is a better understanding of the role of gender in the management of elevated BP and hypertension (including gender-driven barriers in accessing medical care and adherence).
More widespread validation of home BP measuring devices. Validation protocols for cuffless BP measurement devices have just recently been proposed and need to be tested.
Clinical effectiveness of HMOD in directing intensity of care and personalized approaches in managing elevated BP and hypertension.
Best practice to screen and manage primary aldosteronism.
Clinical benefits of treating low CVD-risk individuals with elevated BP and further data strengthening the use of BP-lowering medication among high-risk persons with baseline systolic BP of 120–129 mmHg.
Need for more data on the sex-specific optimal dosing, effects, and adverse effects of BP-lowering drugs, 1020 in particular from specifically planned prospective randomized trials.
More consideration for overall CVD outcomes of BP-lowering interventions.
More European data (RCTs, real life) about the beneficial effect of treating patients with elevated BP and hypertension with polypills (inclusive of non-BP lowering medications).
CVD outcomes-based data on MRAs as add-on therapy solely for resistant hypertension.
Trials on the BP-lowering effects of newer antidiabetic drugs (such as SGLT2 inhibitors and GLP-1 receptor agonists) or drugs that now have indications for other conditions, such as finerenone or sacubitril-valsartan.
Beneficial BP and CVD effects of increasing dietary potassium intake and other lifestyle interventions. Studies to disentangle the effect of sodium reduction vs. the effect of potassium supplementation on BP control and CVD outcomes.
RCTs comparing single-pill combination therapy with fixed doses vs. multiple monotherapies and their effects on CVD outcomes.
Cardiovascular outcomes trials of renal denervation.
BP-lowering treatment RCTs on different ethnic and migrant groups established in Europe.
Pharmacological BP management in young adults (aged <40 years) and better data on the efficacy of a life-course approach for the drug management of BP. 1021
CVD outcomes in moderately to severely frail and/or very elderly persons where BP medications have been deprescribed, and the impact of competing risks.
Management of renal artery disease with haemodynamically stable but severe stenosis (i.e. without high-risk features).
Need for clinical trials on managing hypertension in patients treated with anticancer drugs or anti-rejection drugs in recipients of an allograft transplant.
Hypertension management in the setting of climate changes, global warming, air and other forms of pollution, pandemics, war zones, and in the context of drug restrictions experienced in some low-to-middle-income countries.
Need to improve implementation of guidelines by healthcare providers.
How to develop sustainable hypertension care at the intersection of growing numbers of patients and limited resources.
Treat-to-target trials specifically testing BP-lowering drugs among drug-naïve persons with baseline BP of 120–129 mmHg and increased CVD risk.
A selected sample of the main messages from these guidelines are provided in Table 15 .
What to do and what not to do

Evidence tables are available at European Heart Journal online.
No new data were generated or analysed in support of this research.
Author/task force Member Affiliations: Cian P. McCarthy , Cardiovascular Division Massachusetts General Hospital and Harvard Medical School Boston, MA, United States of America; Rosa Maria Bruno , PARCC, Université Paris Cité, Inserm, Paris, France, and Pharmacology & Hypertension, AP-HP, Hôpital Européen Georges Pompidou, Paris, France; Sofie Brouwers , Cardiovascular Center Aalst, Department of Cardiology, OLV Clinic Aalst, Aalst, Belgium, and Department of Experimental Pharmacology, Faculty of Medicine and Pharmacy, Vrije Universiteit Brussel, Brussels, Belgium; Michelle D. Canavan , School of Medicine, College of Medicine, Nursing and Health Sciences, University of Galway, Galway, Ireland, and Department of Geriatric Medicine, University Hospital Galway, Saolta Hospitals Group, Galway, Ireland; Claudio Ceconi , Motusmed Clinic, Brescia, Italy; Ruxandra Maria Christodorescu , Department V Internal Medicine, University of Medicine and Pharmacy V Babes, Timisoara, Romania, and Research Center, Institute of Cardiovascular Diseases, Timisoara, Romania; Stella S. Daskalopoulou , Medicine Research Institute of the McGill University Health Centre, McGill University, Montreal, Canada; Charles J. Ferro , Department of Renal Medicine, University Hospitals Birmingham, Birmingham, United Kingdom, and Institute of Cardiovascular Sciences University of Birmingham, Birmingham, United Kingdom; Eva Gerdts , Department of Clinical Science, University of Bergen, Bergen, Norway, and Department of Heart Disease, Haukeland University Hospital, Bergen, Norway; Henner Hanssen , Department Sport, Exercise and Health, Medical Faculty, University of Basel, Basel, Switzerland; Julie Harris (United Kingdom), ESC Patient Forum, Sophia Antipolis, France; Lucas Lauder , Department of cardiology, University hospital Basel, Basel, Switzerland, and Department of internal medicine III, Cardiology, Angiology, and Intensive Care Medicine, Saarland university medical center, Homburg, Germany; Richard J. McManus , Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, United Kingdom; Gerard J. Molloy , School of Psychology, University of Galway, Galway, Ireland; Kazem Rahimi , Deep Medicine, Nuffield Department of Women’s and Reproductive Health, University of Oxford, Oxford, United Kingdom; Vera Regitz-Zagrosek , Charite, University Medicine Berlin, Gender in Medicine, Berlin, Germany; Gian Paolo Rossi , Department of Medicine, DIMED, University of Padua, Padua, Italy; Else Charlotte Sandset , Department of Neurology, Oslo University Hospital, Oslo, Norway, The Norwegian Air Ambulance Foundation, Oslo, Norway, and Institute of Clinical Medicine University of Oslo, Oslo, Norway; Bart Scheenaerts (Belgium), ESC Patient Forum, Sophia Antipolis, France; Jan A. Staessen , Non-Profit Research Association Alliance for the Promotion of Preventive Medicine, Mechelen, Belgium, and Biomedical Research Group, Faculty of Medicine, University of Leuven, Leuven, Belgium; Izabella Uchmanowicz , Department of Nursing and Obstetrics, Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland; and Maurizio Volterrani , Exercise Science and Medicine San Raffaele Open University, Rome, Italy, and Cardiopulmonary Department, IRCCS San Raffaele, Rome, Italy.
ESC Scientific Document Group
Includes Document Reviewers and ESC National Cardiac Societies.
Document Reviewers: Ana Abreu (CPG Review Co-ordinator) (Portugal), Michael Hecht Olsen (CPG Review Co-ordinator) (Denmark), Marco Ambrosetti (Italy), Emmanuel Androulakis (United Kingdom), Lia Evi Bang (Denmark), Jesper Nørgaard Bech (Denmark), Michael A. Borger (Germany), Pierre Boutouyrie (France), Luís Bronze (Portugal), Sergio Buccheri (Sweden), Regina Dalmau (Spain), Maria Carmen De Pablo Zarzosa (Spain), Christian Delles (United Kingdom), Maria Manuela Fiuza (Portugal), Rahima Gabulova (Azerbaijan), Bjørn Olav Haugen (Norway), Christian Heiss (United Kingdom), Borja Ibanez (Spain), Stefan James (Sweden), Vikas Kapil (United Kingdom), Meral Kayikçioglu (Turkey), Lars Køber (Denmark), Konstantinos C. Koskinas (Switzerland), Emanuela Teresa Locati (Italy), Sharon MacDonald (United Kingdom), Anastasia S. Mihailidou (Australia), Borislava Mihaylova (United Kingdom), Richard Mindham (United Kingdom) Martin Bodtker Mortensen (Denmark), Sandor Nardai (Hungary), Lis Neubeck (United Kingdom), Jens Cosedis Nielsen (Denmark), Peter M. Nilsson (Sweden), Agnes A. Pasquet (Belgium), Mónica Mendes Pedro (Portugal), Eva Prescott (Denmark), Amina Rakisheva (Kazakhstan), Ernst Rietzschel (Belgium), Bianca Rocca (Italy), Xavier Rossello (Spain), Jean-Paul Schmid (Switzerland), Eduard Shantsila (United Kingdom), Isabella Sudano (Switzerland), Ana Teresa Timóteo (Portugal), Georgios Tsivgoulis (Greece), Andrea Ungar (Italy), Ilonca Vaartjes (Netherlands), Frank Visseren (Netherlands), Heinz Voeller (Germany), Christiaan Vrints (Belgium), Adam Witkowski (Poland), Maria-Christina Zennaro (France), and Katja Zeppenfeld (Netherlands).
ESC National Cardiac Societies actively involved in the review process of the 2024 ESC Guidelines for the management of elevated blood pressure and hypertension:
Albania: Albanian Society of Cardiology, Naltin Shuka; Algeria: Algerian Society of Cardiology, Nadia Laredj; Austria: Austrian Society of Cardiology, Noemi Pavo; Azerbaijan: Azerbaijan Society of Cardiology, Ulvi Mirzoyev; Belgium: Belgian Society of Cardiology, Philippe van de Borne; Bosnia and Herzegovina: Association of Cardiologists of Bosnia and Herzegovina, Šekib Sokolović; Bulgaria: Bulgarian Society of Cardiology, Arman Postadzhiyan; Croatia: Croatian Cardiac Society, Jure Samardzic; Cyprus: Cyprus Society of Cardiology, Petros Agathangelou; Czechia: Czech Society of Cardiology, Jiri Widimsky; Denmark: Danish Society of Cardiology, Michael Hecht Olsen; Egypt: Egyptian Society of Cardiology, Wael M. El-Kilany; Estonia: Estonian Society of Cardiology, Priit Pauklin; Finland: Finnish Cardiac Society, Jari A. Laukkanen; France: French Society of Cardiology, Romain Boulestreau; Georgia: Georgian Society of Cardiology, Bezhan Tsinamdzgvrishvili; Germany: German Cardiac Society, Ulrich Kintscher; Greece: Hellenic Society of Cardiology, Maria Marketou; Hungary: Hungarian Society of Cardiology, Dénes Páll; Iceland: Icelandic Society of Cardiology, Þórdís Jóna Hrafnkelsdóttir; Ireland: Irish Cardiac Society, Eamon Dolan; Israel: Israel Heart Society, Talya Wolak; Italy: Italian Federation of Cardiology, Grzegorz Bilo; Kazakhstan: Association of Cardiologists of Kazakhstan, Meiramgul Kapsimetovna Tundybayeva; Kyrgyzstan: Kyrgyz Society of Cardiology, Erkin Mirrakhimov, Latvia: Latvian Society of Cardiology, Karlis Trusinskis; Lebanon: Lebanese Society of Cardiology, Ghassan Kiwan; Libya: Libyan Cardiac Society, Omar Msalem; Lithuania: Lithuanian Society of Cardiology, Jolita Badarienė; Luxembourg: Luxembourg Society of Cardiology, Cristiana-Astra Banu; Malta: Maltese Cardiac Society, Matthew Mercieca Balbi; Moldova (Republic of): Moldavian Society of Cardiology, Alexandru Caraus; Montenegro: Montenegro Society of Cardiology, Aneta Boskovic; Morocco: Moroccan Society of Cardiology, Najat Mouine; Netherlands: Netherlands Society of Cardiology, Tom Vromen; North Macedonia: National Society of Cardiology of North Macedonia, Marijan Bosevski; Norway: Norwegian Society of Cardiology, Helga B. Midtbø; Poland: Polish Cardiac Society, Adrian Doroszko; Portugal: Portuguese Society of Cardiology, Hélder Dores; Romania: Romanian Society of Cardiology, Elisabeta Badila; San Marino: San Marino Society of Cardiology, Roberto Bini; Serbia: Cardiology Society of Serbia, Dragan Vojislav Simić; Slovenia: Slovenian Society of Cardiology, Zlatko Fras; Spain: Spanish Society of Cardiology, Pilar Mazón; Sweden: Swedish Society of Cardiology, Jonas Spaak; Switzerland: Swiss Society of Cardiology, Thilo Burkard; Syrian Arab Republic: Syrian Cardiovascular Association, Elias Barakat; Tunisia: Tunisian Society of Cardiology and Cardiovascular Surgery, Salem Abdessalem; Türkiye: Turkish Society of Cardiology, Yilmaz Gunes; Ukraine: Ukrainian Association of Cardiology, Yurij M. Sirenko; United Kingdom of Great Britain and Northern Ireland: British Cardiovascular Society, Adrian J. B. Brady; and Uzbekistan: Association of Cardiologists of Uzbekistan, Gulnoz Abdusattarovna Khamidullaeva.
ESC Clinical Practice Guidelines (CPG) Committee: Eva Prescott (Chairperson) (Denmark), Stefan James (Co-Chairperson) (Sweden), Elena Arbelo (Spain), Colin Baigent (United Kingdom), Michael A. Borger (Germany), Sergio Buccheri (Sweden), Borja Ibanez (Spain), Lars Køber (Denmark), Konstantinos C. Koskinas (Switzerland), John William McEvoy (Ireland), Borislava Mihaylova (United Kingdom), Richard Mindham (United Kingdom), Lis Neubeck (United Kingdom), Jens Cosedis Nielsen (Denmark), Agnes A. Pasquet (Belgium), Amina Rakisheva (Kazakhstan), Bianca Rocca (Italy), Xavier Rossello (Spain), Ilonca Vaartjes (Netherlands), Christiaan Vrints (Belgium), Adam Witkowski (Poland), and Katja Zeppenfeld (Netherlands).
Williams B , Mancia G , Spiering W , Rosei EA , Azizi M , Burnier M , et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension . Eur Heart J 2018 ; 39 : 3021 – 104 . https://doi.org/10.1093/eurheartj/ehy339
Google Scholar
Murray CJL , Aravkin AY , Zheng P , Abbafati C , Abbas KM , Abbasi-Kangevari M , et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 . Lancet 2020 ; 396 : 1223 – 49 . https://doi.org/10.1016/S0140-6736(20)30752-2
Mensah GA , Fuster V , Murray CJL , Roth GA , Mensah GA , Abate YH , et al. Global burden of cardiovascular diseases and risks, 1990–2022 . J Am Coll Cardiol 2023 ; 82 : 2350 – 473 . https://doi.org/10.1016/j.jacc.2023.11.007
Johnson JL , Greaves L , Repta R . Better science with sex and gender: facilitating the use of a sex and gender-based analysis in health research . Int J Equity Health 2009 ; 8 : 14 . https://doi.org/10.1186/1475-9276-8-14
Mauvais-Jarvis F , Bairey Merz N , Barnes PJ , Brinton RD , Carrero J-J , DeMeo DL , et al. Sex and gender: modifiers of health, disease, and medicine . Lancet 2020 ; 396 : 565 – 82 . https://doi.org/10.1016/s0140-6736(20)31561-0
Camm AJ , Lüscher TF , Maurer G , Serruys PW (eds). The ESC Textbook of Cardiovascular Medicine . Oxford University Press , 2018 .
Google Preview
Mayfield SK , Foti K , Moran AE , Blakeman DE , Frieden TR . Hypertension call to action: will we respond to the call with action? Am J Hypertens 2022 ; 35 : 214 – 6 . https://doi.org/10.1093/ajh/hpab191
Muntner P . The continuing challenge of low rates of blood pressure control among US adults . Am J Hypertens 2022 ; 35 : 839 – 41 . https://doi.org/10.1093/ajh/hpac075
Reuter H , Jordan J . Status of hypertension in Europe . Curr Opin Cardiol 2019 ; 34 : 342 – 9 . https://doi.org/10.1097/hco.0000000000000642
Brown JM , Siddiqui M , Calhoun DA , Carey RM , Hopkins PN , Williams GH , et al. The unrecognized prevalence of primary aldosteronism: a cross-sectional study . Ann Intern Med 2020 ; 173 : 10 – 20 . https://doi.org/10.7326/m20-0065
Oparil S , Acelajado MC , Bakris GL , Berlowitz DR , Cífková R , Dominiczak AF , et al. Hypertension . Nat Rev Dis Primers 2018 ; 4 : 18014 . https://doi.org/10.1038/nrdp.2018.14
Navaneethabalakrishnan S , Smith HL , Arenaz CM , Goodlett BL , McDermott JG , Mitchell BM . Update on immune mechanisms in hypertension . Am J Hypertens 2022 ; 35 : 842 – 51 . https://doi.org/10.1093/ajh/hpac077
Levy D , Garrison RJ , Savage DD , Kannel WB , Castelli WP . Prognostic implications of echocardiographically determined left ventricular mass in the Framingham heart study . N Engl J Med 1990 ; 322 : 1561 – 6 . https://doi.org/10.1056/nejm199005313222203
Devereux RB , Wachtell K , Gerdts E , Boman K , Nieminen MS , Papademetriou V , et al. Prognostic significance of left ventricular mass change during treatment of hypertension . JAMA 2004 ; 292 : 2350 – 6 . https://doi.org/10.1001/jama.292.19.2350
de Simone G , Gottdiener JS , Chinali M , Maurer MS . Left ventricular mass predicts heart failure not related to previous myocardial infarction: the cardiovascular health study . Eur Heart J 2008 ; 29 : 741 – 7 . https://doi.org/10.1093/eurheartj/ehm605
Verdecchia P , Porcellati C , Reboldi G , Gattobigio R , Borgioni C , Pearson TA , et al. Left ventricular hypertrophy as an independent predictor of acute cerebrovascular events in essential hypertension . Circulation 2001 ; 104 : 2039 – 44 . https://doi.org/10.1161/hc4201.097944
Hijazi Z , Verdecchia P , Oldgren J , Andersson U , Reboldi G , Di Pasquale G , et al. Cardiac biomarkers and left ventricular hypertrophy in relation to outcomes in patients with atrial fibrillation: experiences from the RE-LY trial . J Am Heart Assoc 2019 ; 8 : e010107 . https://doi.org/10.1161/jaha.118.010107
Siedlinski M , Carnevale L , Xu X , Carnevale D , Evangelou E , Caulfield MJ , et al. Genetic analyses identify brain structures related to cognitive impairment associated with elevated blood pressure . Eur Heart J 2023 ; 44 : 2114 – 25 . https://doi.org/10.1093/eurheartj/ehad101
Cheung AK , Chang TI , Cushman WC , Furth SL , Hou FF , Ix JH , et al. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease . Kidney International 2021 ; 99 : S1 – 87 . https://doi.org/10.1016/j.kint.2020.11.003
Subbiah A , Bhowmik D . KDIGO recommendations on blood pressure management in chronic kidney disease . Kidney Int 2022 ; 101 : 1299 . https://doi.org/10.1016/j.kint.2022.02.036
Cheung CY , Biousse V , Keane PA , Schiffrin EL , Wong TY . Hypertensive eye disease . Nat Rev Dis Primers 2022 ; 8 : 14 . https://doi.org/10.1038/s41572-022-00342-0
Lewington S , Clarke R , Qizilbash N , Peto R , Collins R . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies . Lancet 2002 ; 360 : 1903 – 13 . https://doi.org/10.1016/s0140-6736(02)11911-8
O’Rourke MF , Safar ME . Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy . Hypertension 2005 ; 46 : 200 – 4 . https://doi.org/10.1161/01.Hyp.0000168052.00426.65
Gerdts E , Izzo R , Mancusi C , Losi MA , Manzi MV , Canciello G , et al. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk (the Campania Salute Network) . Int J Cardiol 2018 ; 258 : 257 – 61 . https://doi.org/10.1016/j.ijcard.2017.12.086
Gerdts E , Okin PM , de Simone G , Cramariuc D , Wachtell K , Boman K , et al. Gender differences in left ventricular structure and function during antihypertensive treatment: the Losartan intervention for endpoint reduction in hypertension study . Hypertension 2008 ; 51 : 1109 – 14 . https://doi.org/10.1161/hypertensionaha.107.107474
Gerdts E , Wachtell K , Omvik P , Otterstad JE , Oikarinen L , Boman K , et al. Left atrial size and risk of major cardiovascular events during antihypertensive treatment: Losartan Intervention for Endpoint Reduction in Hypertension Trial . Hypertension 2007 ; 49 : 311 – 6 . https://doi.org/10.1161/01.Hyp.0000254322.96189.85
Park JB , Schiffrin EL . Small artery remodeling is the most prevalent (earliest?) form of target organ damage in mild essential hypertension . J Hypertens 2001 ; 19 : 921 – 30 . https://doi.org/10.1097/00004872-200105000-00013
Vasan RS , Pan S , Xanthakis V , Beiser A , Larson MG , Seshadri S , et al. Arterial stiffness and long-term risk of health outcomes: the Framingham heart study . Hypertension 2022 ; 79 : 1045 – 56 . https://doi.org/10.1161/hypertensionaha.121.18776
Piskorz D . Hypertensive mediated organ damage and hypertension management. How to assess beneficial effects of antihypertensive treatments? High Blood Press Cardiovasc Prev 2020 ; 27 : 9 – 17 . https://doi.org/10.1007/s40292-020-00361-6
Vallelonga F , Cesareo M , Menon L , Airale L , Leone D , Astarita A , et al. Cardiovascular hypertension-mediated organ damage in hypertensive urgencies and hypertensive outpatients . Front Cardiovasc Med 2022 ; 9 : 889554 . https://doi.org/10.3389/fcvm.2022.889554
Vasan RS , Song RJ , Xanthakis V , Beiser A , DeCarli C , Mitchell GF , et al. Hypertension-mediated organ damage: prevalence, correlates, and prognosis in the community . Hypertension 2022 ; 79 : 505 – 15 . https://doi.org/10.1161/hypertensionaha.121.18502
Rapsomaniki E , Timmis A , George J , Pujades-Rodriguez M , Shah AD , Denaxas S , et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people . Lancet 2014 ; 383 : 1899 – 911 . https://doi.org/10.1016/s0140-6736(14)60685-1
Malik R , Georgakis MK , Vujkovic M , Damrauer SM , Elliott P , Karhunen V , et al. Relationship between blood pressure and incident cardiovascular disease: linear and nonlinear Mendelian randomization analyses . Hypertension 2021 ; 77 : 2004 – 13 . https://doi.org/10.1161/hypertensionaha.120.16534
Ji H , Kim A , Ebinger JE , Niiranen TJ , Claggett BL , Bairey Merz CN , et al. Sex differences in blood pressure trajectories over the life course . JAMA Cardiol 2020 ; 5 : 19 – 26 . https://doi.org/10.1001/jamacardio.2019.5306
Salles GF , Reboldi G , Fagard RH , Cardoso CRL , Pierdomenico SD , Verdecchia P , et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis . Hypertension 2016 ; 67 : 693 – 700 . https://doi.org/10.1161/hypertensionaha.115.06981
Verdecchia P . Prognostic value of ambulatory blood pressure: current evidence and clinical implications . Hypertension 2000 ; 35 : 844 – 51 . https://doi.org/10.1161/01.hyp.35.3.844
Mauck GW , Smith CR , Geddes LA , Bourland JD . The meaning of the point of maximum oscillations in cuff pressure in the indirect measurement of blood pressure—part ii . J Biomech Eng 1980 ; 102 : 28 – 33 . https://doi.org/10.1115/1.3138195
Clark CE , Warren FC , Boddy K , McDonagh STJ , Moore SF , Goddard J , et al. Associations between systolic interarm differences in blood pressure and cardiovascular disease outcomes and mortality: individual participant data meta-analysis, development and validation of a prognostic algorithm: the INTERPRESS-IPD collaboration . Hypertension 2021 ; 77 : 650 – 61 . https://doi.org/10.1161/hypertensionaha.120.15997
Picone DS , Deshpande RA , Schultz MG , Fonseca R , Campbell NRC , Delles C , et al. Nonvalidated home blood pressure devices dominate the online marketplace in Australia: major implications for cardiovascular risk management . Hypertension 2020 ; 75 : 1593 – 9 . https://doi.org/10.1161/hypertensionaha.120.14719
Picone DS , Campbell NRC , Schutte AE , Olsen MH , Ordunez P , Whelton PK , et al. Validation status of blood pressure measuring devices sold globally . JAMA 2022 ; 327 : 680 – 1 . https://doi.org/10.1001/jama.2021.24464
Stergiou GS , O’Brien E , Myers M , Palatini P , Parati G , Kollias A , et al. STRIDE BP international initiative for accurate blood pressure measurement: systematic review of published validation studies of blood pressure measuring devices . J Clin Hypertens (Greenwich) 2019 ; 21 : 1616 – 22 . https://doi.org/10.1111/jch.13710
Stergiou GS , Alpert B , Mieke S , Asmar R , Atkins N , Eckert S , et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) collaboration statement . Hypertension 2018 ; 71 : 368 – 74 . https://doi.org/10.1161/hypertensionaha.117.10237
Stergiou GS , Mukkamala R , Avolio A , Kyriakoulis KG , Mieke S , Murray A , et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension working group on blood pressure monitoring and cardiovascular variability . J Hypertens 2022 ; 40 : 1449 – 60 . https://doi.org/10.1097/hjh.0000000000003224
Stergiou GS , Avolio AP , Palatini P , Kyriakoulis KG , Schutte AE , Mieke S , et al. European Society of Hypertension recommendations for the validation of cuffless blood pressure measuring devices: European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability . J Hypertens 2023 ; 41 : 2074 – 87 . https://doi.org/10.1097/hjh.0000000000003483
McAlister FA , Straus SE . Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review . BMJ 2001 ; 322 : 908 – 11 . https://doi.org/10.1136/bmj.322.7291.908
Fagius J , Karhuvaara S . Sympathetic activity and blood pressure increases with bladder distension in humans . Hypertension 1989 ; 14 : 511 – 7 . https://doi.org/10.1161/01.hyp.14.5.511
Stergiou GS , Kyriakoulis KG , Stambolliu E , Destounis A , Karpettas N , Kalogeropoulos P , et al. Blood pressure measurement in atrial fibrillation: review and meta-analysis of evidence on accuracy and clinical relevance . J Hypertens 2019 ; 37 : 2430 – 41 . https://doi.org/10.1097/hjh.0000000000002201
Clark CE , McDonagh STJ , McManus RJ . Accuracy of automated blood pressure measurements in the presence of atrial fibrillation: systematic review and meta-analysis . J Hum Hypertens 2019 ; 33 : 352 – 64 . https://doi.org/10.1038/s41371-018-0153-z
Verberk WJ , Omboni S , Kollias A , Stergiou GS . Screening for atrial fibrillation with automated blood pressure measurement: research evidence and practice recommendations . Int J Cardiol 2016 ; 203 : 465 – 73 . https://doi.org/10.1016/j.ijcard.2015.10.182
Manning DM , Kuchirka C , Kaminski J . Miscuffing: inappropriate blood pressure cuff application . Circulation 1983 ; 68 : 763 – 6 . https://doi.org/10.1161/01.cir.68.4.763
Irving G , Holden J , Stevens R , McManus RJ . Which cuff should I use? Indirect blood pressure measurement for the diagnosis of hypertension in patients with obesity: a diagnostic accuracy review . BMJ Open 2016 ; 6 : e012429 . https://doi.org/10.1136/bmjopen-2016-012429
Keeley EC , Villanueva M , Chen YE , Gong Y , Handberg EM , Smith SM , et al. Attended vs unattended systolic blood pressure measurement: a randomized comparison in patients with cardiovascular disease . J Clin Hypertens (Greenwich) 2020 ; 22 : 1987 – 92 . https://doi.org/10.1111/jch.14037
Myers MG , Godwin M , Dawes M , Kiss A , Tobe SW , Grant FC , et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial . BMJ 2011 ; 342 : d286 . https://doi.org/10.1136/bmj.d286
Clark CE . Inter-arm blood pressure difference, when is it a useful risk marker for cardiovascular events? J Hum Hypertens 2022 ; 36 : 117 – 9 . https://doi.org/10.1038/s41371-021-00629-x
Clark CE , Steele AM , Taylor RS , Shore AC , Ukoumunne OC , Campbell JL . Interarm blood pressure difference in people with diabetes: measurement and vascular and mortality implications: a cohort study . Diabetes Care 2014 ; 37 : 1613 – 20 . https://doi.org/10.2337/dc13-1576
Juraschek SP , Appel LJ , Mitchell CM , Mukamal KJ , Lipsitz LA , Blackford AL , et al. Comparison of supine and seated orthostatic hypotension assessments and their association with falls and orthostatic symptoms . J Am Geriatr Soc 2022 ; 70 : 2310 – 9 . https://doi.org/10.1111/jgs.17804
Stergiou GS , Palatini P , Parati G , O’Brien E , Januszewicz A , Lurbe E , et al. European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement . J Hypertens 2021 ; 39 : 1293 – 302 . https://doi.org/10.1097/hjh.0000000000002843
Parati G , Stergiou GS , Bilo G , Kollias A , Pengo M , Ochoa J , et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the working group on blood pressure monitoring and cardiovascular variability of the European Society of Hypertension . J Hypertens 2021 ; 39 : 1742 – 67 . https://doi.org/10.1097/hjh.0000000000002922
Bradley CK , Choi E , Abdalla M , Mizuno H , Lam M , Cepeda M , et al. Use of different blood pressure thresholds to reduce the number of home blood pressure monitoring days needed for detecting hypertension . Hypertension 2023 ; 80 : 2169 – 77 . https://doi.org/10.1161/hypertensionaha.123.21118
Hodgkinson JA , Lee MM , Milner S , Bradburn P , Stevens R , Hobbs FDR , et al. Accuracy of blood-pressure monitors owned by patients with hypertension (ACCU-RATE study): a cross-sectional, observational study in central England . Br J Gen Pract 2020 ; 70 : e548 – 54 . https://doi.org/10.3399/bjgp20X710381
Niiranen TJ , Asayama K , Thijs L , Johansson JK , Ohkubo T , Kikuya M , et al. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome . Hypertension 2013 ; 61 : 27 – 34 . https://doi.org/10.1161/hypertensionaha.111.00100
Parati G , Stergiou G , O’Brien E , Asmar R , Beilin L , Bilo G , et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring . J Hypertens 2014 ; 32 : 1359 – 66 . https://doi.org/10.1097/hjh.0000000000000221
Yang WY , Thijs L , Zhang ZY , Asayama K , Boggia J , Hansen TW , et al. Evidence-based proposal for the number of ambulatory readings required for assessing blood pressure level in research settings: an analysis of the IDACO database . Blood Press 2018 ; 27 : 341 – 50 . https://doi.org/10.1080/08037051.2018.1476057
Asayama K , Stolarz-Skrzypek K , Yang WY , Hansen TW , Brguljan-Hitij J , Odili AN , et al. What did we learn from the international databases on ambulatory and home blood pressure in relation to cardiovascular outcome? Hypertens Res 2023 ; 46 : 934 – 49 . https://doi.org/10.1038/s41440-023-01191-4
Drawz PE , Agarwal A , Dwyer JP , Horwitz E , Lash J , Lenoir K , et al. Concordance between blood pressure in the systolic blood pressure intervention trial and in routine clinical practice . JAMA Intern Med 2020 ; 180 : 1655 – 63 . https://doi.org/10.1001/jamainternmed.2020.5028
Jaeger BC , Bress AP , Bundy JD , Cheung AK , Cushman WC , Drawz PE , et al. Longer-term all-cause and cardiovascular mortality with intensive blood pressure control: a secondary analysis of a randomized clinical trial . JAMA Cardiol 2022 ; 7 : 1138 – 46 . https://doi.org/10.1001/jamacardio.2022.3345
Ntineri A , Niiranen TJ , McManus RJ , Lindroos A , Jula A , Schwartz C , et al. Ambulatory versus home blood pressure monitoring: frequency and determinants of blood pressure difference and diagnostic disagreement . J Hypertens 2019 ; 37 : 1974 – 81 . https://doi.org/10.1097/hjh.0000000000002148
Sheppard JP , Fletcher B , Gill P , Martin U , Roberts N , McManus RJ . Predictors of the home-clinic blood pressure difference: a systematic review and meta-analysis . Am J Hypertens 2016 ; 29 : 614 – 25 . https://doi.org/10.1093/ajh/hpv157
Franklin SS , Thijs L , Li Y , Hansen TW , Boggia J , Liu Y , et al. Masked hypertension in diabetes mellitus: treatment implications for clinical practice . Hypertension 2013 ; 61 : 964 – 71 . https://doi.org/10.1161/hypertensionaha.111.00289
Guirguis-Blake JM , Evans CV , Webber EM , Coppola EL , Perdue LA , Weyrich MS . Screening for hypertension in adults: updated evidence report and systematic review for the US preventive services task force . JAMA 2021 ; 325 : 1657 – 69 . https://doi.org/10.1001/jama.2020.21669
Xu W , Goldberg SI , Shubina M , Turchin A . Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study . BMJ 2015 ; 350 : h158 . https://doi.org/10.1136/bmj.h158
Antza C , Farmakis I , Doundoulakis I , Akrivos E , Stalikas N , Zafeiropoulos S , et al. Reproducibility of masked hypertension and office-based hypertension: a systematic review and meta-analysis . J Hypertens 2022 ; 40 : 1053 – 9 . https://doi.org/10.1097/hjh.0000000000003111
Uhlig K , Patel K , Ip S , Kitsios GD , Balk EM . Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis . Ann Intern Med 2013 ; 159 : 185 – 94 . https://doi.org/10.7326/0003-4819-159-3-201308060-00008
Tucker KL , Sheppard JP , Stevens R , Bosworth HB , Bove A , Bray EP , et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis . PLoS Med 2017 ; 14 : e1002389 . https://doi.org/10.1371/journal.pmed.1002389
McManus RJ , Mant J , Franssen M , Nickless A , Schwartz C , Hodgkinson J , et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial . Lancet 2018 ; 391 : 949 – 59 . https://doi.org/10.1016/s0140-6736(18)30309-x
McManus RJ , Little P , Stuart B , Morton K , Raftery J , Kelly J , et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial . BMJ 2021 ; 372 : m4858 . https://doi.org/10.1136/bmj.m4858
Li R , Liang N , Bu F , Hesketh T . The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis . JMIR Mhealth Uhealth 2020 ; 8 : e17776 . https://doi.org/10.2196/17776
Acharya S , Neupane G , Seals A , Madhav KC , Giustini D , Sharma S , et al. Self-measured blood pressure-guided pharmacotherapy: a systematic review and meta-analysis of US-based telemedicine trials . Hypertension 2024 ; 81 : 648 – 57 . https://doi.org/10.1161/hypertensionaha.123.22109
Monahan M , Jowett S , Nickless A , Franssen M , Grant S , Greenfield S , et al. Cost-effectiveness of telemonitoring and self-monitoring of blood pressure for antihypertensive titration in primary care (TASMINH4) . Hypertension 2019 ; 73 : 1231 – 9 . https://doi.org/10.1161/hypertensionaha.118.12415
Wood S , Greenfield SM , Sayeed Haque M , Martin U , Gill PS , Mant J , et al. Influence of ethnicity on acceptability of method of blood pressure monitoring: a cross-sectional study in primary care . Br J Gen Pract 2016 ; 66 : e577 – 586 . https://doi.org/10.3399/bjgp16X685717
Stergiou GS , Karpettas N , Destounis A , Tzamouranis D , Nasothimiou E , Kollias A , et al. Home blood pressure monitoring alone vs. combined clinic and ambulatory measurements in following treatment-induced changes in blood pressure and organ damage . Am J Hypertens 2014 ; 27 : 184 – 92 . https://doi.org/10.1093/ajh/hpt206
Staessen JA , Byttebier G , Buntinx F , Celis H , O’Brien ET , Fagard R . Antihypertensive treatment based on conventional or ambulatory blood pressure measurement. A randomized controlled trial. Ambulatory blood pressure monitoring and treatment of hypertension investigators . JAMA 1997 ; 278 : 1065 – 72 . https://doi.org/10.1001/jama.1997.03550130039034
McEvoy JW , Leahy N , Parati G . The apples and oranges of blood pressure variability . Hypertension 2023 ; 80 : 2556 – 8 . https://doi.org/10.1161/hypertensionaha.123.21927
Ishikuro M , Obara T , Metoki H , Ohkubo T , Yamamoto M , Akutsu K , et al. Blood pressure measured in the clinic and at home during pregnancy among nulliparous and multiparous women: the BOSHI study . Am J Hypertens 2013 ; 26 : 141 – 8 . https://doi.org/10.1093/ajh/hps002
Bello NA , Woolley JJ , Cleary KL , Falzon L , Alpert BS , Oparil S , et al. Accuracy of blood pressure measurement devices in pregnancy: a systematic review of validation studies . Hypertension 2018 ; 71 : 326 – 35 . https://doi.org/10.1161/hypertensionaha.117.10295
Tucker KL , Mort S , Yu LM , Campbell H , Rivero-Arias O , Wilson HM , et al. Effect of self-monitoring of blood pressure on diagnosis of hypertension during higher-risk pregnancy: the BUMP 1 randomized clinical trial . JAMA 2022 ; 327 : 1656 – 65 . https://doi.org/10.1001/jama.2022.4712
Chappell LC , Tucker KL , Galal U , Yu L-M , Campbell H , Rivero-Arias O , et al. Effect of self-monitoring of blood pressure on blood pressure control in pregnant individuals with chronic or gestational hypertension: the BUMP 2 randomized clinical trial . JAMA 2022 ; 327 : 1666 – 78 . https://doi.org/10.1001/jama.2022.4726
Tita AT , Szychowski JM , Boggess K , Dugoff L , Sibai B , Lawrence K , et al. Treatment for mild chronic hypertension during pregnancy . N Engl J Med 2022 ; 386 : 1781 – 92 . https://doi.org/10.1056/NEJMoa2201295
Regitz-Zagrosek V , Roos-Hesselink JW , Bauersachs J , Blomström-Lundqvist C , Cífková R , De Bonis M , et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy . Eur Heart J 2018 ; 39 : 3165 – 241 . https://doi.org/10.1093/eurheartj/ehy340
Tikhonoff V , Kuznetsova T , Thijs L , Cauwenberghs N , Stolarz-Skrzypek K , Seidlerová J , et al. Ambulatory blood pressure and long-term risk for atrial fibrillation . Heart 2018 ; 104 : 1263 – 70 . https://doi.org/10.1136/heartjnl-2017-312488
Lip GYH , Coca A , Kahan T , Boriani G , Manolis AS , Olsen MH , et al. Hypertension and cardiac arrhythmias: a consensus document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE) . Europace 2017 ; 19 : 891 – 911 . https://doi.org/10.1093/europace/eux091
Šelmytė-Besusparė A , Barysienė J , Petrikonytė D , Aidietis A , Marinskis G , Laucevičius A . Auscultatory versus oscillometric blood pressure measurement in patients with atrial fibrillation and arterial hypertension . BMC Cardiovasc Disord 2017 ; 17 : 87 . https://doi.org/10.1186/s12872-017-0521-6
Omboni S , Ballatore T , Rizzi F , Tomassini F , Campolo L , Panzeri E , et al. 24-Hour ambulatory blood pressure telemonitoring in patients at risk of atrial fibrillation: results from the TEMPLAR project . Hypertens Res 2022 ; 45 : 1486 – 95 . https://doi.org/10.1038/s41440-022-00932-1
Seccia TM , Letizia C , Muiesan ML , Lerco S , Cesari M , Bisogni V , et al. Atrial fibrillation as presenting sign of primary aldosteronism: results of the prospective appraisal on the prevalence of primary aldosteronism in hypertensive (PAPPHY) study . J Hypertens 2020 ; 38 : 332 – 9 . https://doi.org/10.1097/hjh.0000000000002250
McDonagh STJ , Mejzner N , Clark CE . Prevalence of postural hypotension in primary, community and institutional care: a systematic review and meta-analysis . BMC Fam Pract 2021 ; 22 : 1 . https://doi.org/10.1186/s12875-020-01313-8
Tran J , Hillebrand SL , Meskers CGM , Iseli RK , Maier AB . Prevalence of initial orthostatic hypotension in older adults: a systematic review and meta-analysis . Age Ageing 2021 ; 50 : 1520 – 8 . https://doi.org/10.1093/ageing/afab090
Juraschek SP , Hu JR , Cluett JL , Ishak AM , Mita C , Lipsitz LA , et al. Orthostatic hypotension, hypertension treatment, and cardiovascular disease: an individual participant meta-analysis . JAMA 2023 ; 330 : 1459 – 71 . https://doi.org/10.1001/jama.2023.18497
Juraschek SP , Cortez MM , Flack JM , Ghazi L , Kenny RA , Rahman M , et al. Orthostatic hypotension in adults with hypertension: a scientific statement from the American Heart Association . Hypertension 2024 ; 81 : e16 – 30 . https://doi.org/10.1161/hyp.0000000000000236
Raber I , Belanger MJ , Farahmand R , Aggarwal R , Chiu N , Al Rifai M , et al. Orthostatic hypotension in hypertensive adults: Harry Goldblatt award for early career investigators 2021 . Hypertension 2022 ; 79 : 2388 – 96 . https://doi.org/10.1161/hypertensionaha.122.18557
Wieling W , Kaufmann H , Claydon VE , van Wijnen VK , Harms MPM , Juraschek SP , et al. Diagnosis and treatment of orthostatic hypotension . Lancet Neurol 2022 ; 21 : 735 – 46 . https://doi.org/10.1016/s1474-4422(22)00169-7
Juraschek SP , Daya N , Rawlings AM , Appel LJ , Miller ER , Windham BG , et al. Association of history of dizziness and long-term adverse outcomes with early vs later orthostatic hypotension assessment times in middle-aged adults . JAMA Intern Med 2017 ; 177 : 1316 – 23 . https://doi.org/10.1001/jamainternmed.2017.2937
Brignole M , Moya A , de Lange FJ , Deharo J-C , Elliott PM , Fanciulli A , et al. Practical instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope . Eur Heart J 2018 ; 39 : e43 – 80 . https://doi.org/10.1093/eurheartj/ehy071
Rivasi G , Groppelli A , Brignole M , Soranna D , Zambon A , Bilo G , et al. Association between hypotension during 24 h ambulatory blood pressure monitoring and reflex syncope: the SynABPM 1 study . Eur Heart J 2022 ; 43 : 3765 – 76 . https://doi.org/10.1093/eurheartj/ehac347
Smith TO , Sillito JA , Goh CH , Abdel-Fattah A-R , Einarsson A , Soiza RL , et al. Association between different methods of assessing blood pressure variability and incident cardiovascular disease, cardiovascular mortality and all-cause mortality: a systematic review . Age Ageing 2020 ; 49 : 184 – 92 . https://doi.org/10.1093/ageing/afz178
Kim S , Xiao X , Chen J . Advances in photoplethysmography for personalized cardiovascular monitoring . Biosensors (Basel) 2022 ; 12 : 863 . https://doi.org/10.3390/bios12100863
Dagamseh A , Qananwah Q , Al Quran H , Shaker Ibrahim K . Towards a portable-noninvasive blood pressure monitoring system utilizing the photoplethysmogram signal . Biomed Opt Express 2021 ; 12 : 7732 – 51 . https://doi.org/10.1364/boe.444535
Sharman JE , Avolio AP , Baulmann J , Benetos A , Blacher J , Blizzard CL , et al. Validation of non-invasive central blood pressure devices: ARTERY Society task force consensus statement on protocol standardization . Eur Heart J 2017 ; 38 : 2805 – 12 . https://doi.org/10.1093/eurheartj/ehw632
Sharman JE , O’Brien E , Alpert B , Schutte AE , Delles C , Hecht Olsen M , et al. Lancet Commission on Hypertension group position statement on the global improvement of accuracy standards for devices that measure blood pressure . J Hypertens 2020 ; 38 : 21 – 9 . https://doi.org/10.1097/hjh.0000000000002246
Lunardi M , Muhammad F , Shahzad A , Nadeem A , Combe L , Simpkin AJ , et al. Performance of wearable watch-type home blood pressure measurement devices in a real-world clinical sample . Clin Res Cardiol . 2023 . https://doi.org/10.1007/s00392-023-02353-7
Clark CE , Warren FC , Boddy K , McDonagh STJ , Moore SF , Teresa Alzamora M , et al. Higher arm versus lower arm systolic blood pressure and cardiovascular outcomes: a meta-analysis of individual participant data from the INTERPRESS-IPD collaboration . Hypertension 2022 ; 79 : 2328 – 35 . https://doi.org/10.1161/hypertensionaha.121.18921
Margolis KL , Dehmer SP , Sperl-Hillen J , O’Connor PJ , Asche SE , Bergdall AR , et al. Cardiovascular events and costs with home blood pressure telemonitoring and pharmacist management for uncontrolled hypertension . Hypertension 2020 ; 76 : 1097 – 103 . https://doi.org/10.1161/hypertensionaha.120.15492
Sheppard JP , Tucker KL , Davison WJ , Stevens R , Aekplakorn W , Bosworth H B , et al. Self-monitoring of blood pressure in patients with hypertension-related multi-morbidity: systematic review and individual patient data meta-analysis . Am J Hypertens 2020 ; 33 : 243 – 51 . https://doi.org/10.1093/ajh/hpz182
Cooke G , Doust J , Sanders S . Is pulse palpation helpful in detecting atrial fibrillation? A systematic review . J Fam Pract 2006 ; 55 : 130 – 4 .
Arvanitis M , Qi G , Bhatt DL , Post WS , Chatterjee N , Battle A , et al. Linear and nonlinear Mendelian randomization analyses of the association between diastolic blood pressure and cardiovascular events: the J-curve revisited . Circulation 2021 ; 143 : 895 – 906 . https://doi.org/10.1161/circulationaha.120.049819
Whelton SP , McEvoy JW , Shaw L , Psaty BM , Lima JAC , Budoff M , et al. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors . JAMA Cardiol 2020 ; 5 : 1011 – 8 . https://doi.org/10.1001/jamacardio.2020.1731
Rahimi K , Bidel Z , Nazarzadeh M , Copland E , Canoy D , Ramakrishnan R , et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis . Lancet 2021 ; 397 : 1625 – 36 . https://doi.org/10.1016/S0140-6736(21)00590-0
Ji H , Niiranen TJ , Rader F , Henglin M , Kim A , Ebinger JE , et al. Sex differences in blood pressure associations with cardiovascular outcomes . Circulation 2021 ; 143 : 761 – 3 . https://doi.org/10.1161/circulationaha.120.049360
Kringeland E , Tell GS , Midtbø H , Igland J , Haugsgjerd TR , Gerdts E . Stage 1 hypertension, sex, and acute coronary syndromes during midlife: the Hordaland health study . Eur J Prev Cardiol 2022 ; 29 : 147 – 54 . https://doi.org/10.1093/eurjpc/zwab068
Appel LJ , Moore TJ , Obarzanek E , Vollmer WM , Svetkey LP , Sacks FM , et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group . N Engl J Med 1997 ; 336 : 1117 – 24 . https://doi.org/10.1056/nejm199704173361601
Toledo E , Hu FB , Estruch R , Buil-Cosiales P , Corella D , Salas-Salvadó J , et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial . BMC Med 2013 ; 11 : 207 . https://doi.org/10.1186/1741-7015-11-207
Sundström J , Arima H , Jackson R , Turnbull F , Rahimi K , Chalmers J , et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis . Ann Intern Med 2015 ; 162 : 184 – 91 . https://doi.org/10.7326/m14-0773
Ettehad D , Emdin CA , Kiran A , Anderson SG , Callender T , Emberson J , et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis . Lancet 2016 ; 387 : 957 – 67 . https://doi.org/10.1016/s0140-6736(15)01225-8
Muntner P , Whelton PK . Using predicted cardiovascular disease risk in conjunction with blood pressure to guide antihypertensive medication treatment . J Am Coll Cardiol 2017 ; 69 : 2446 – 56 . https://doi.org/10.1016/j.jacc.2017.02.066
Herrett E , Strongman H , Gadd S , Tomlinson L , Nitsch D , Bhaskaran K , et al. The importance of blood pressure thresholds versus predicted cardiovascular risk on subsequent rates of cardiovascular disease: a cohort study in English primary care . Lancet Healthy Longev 2022 ; 3 : e22 – 30 . https://doi.org/10.1016/s2666-7568(21)00281-6
Navar AM , Pencina MJ , Peterson ED . Assessing cardiovascular risk to guide hypertension diagnosis and treatment . JAMA Cardiol 2016 ; 1 : 864 – 71 . https://doi.org/10.1001/jamacardio.2016.2861
Kovell LC , Ahmed HM , Misra S , Whelton SP , Prokopowicz GP , Blumenthal RS , et al. US hypertension management guidelines: a review of the recent past and recommendations for the future . J Am Heart Assoc 2015 ; 4 : e002315 . https://doi.org/10.1161/jaha.115.002315
McEvoy JW , Martin SS , Dardari ZA , Miedema MD , Sandfort V , Yeboah J , et al. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy . Circulation 2017 ; 135 : 153 – 65 . https://doi.org/10.1161/circulationaha.116.025471
Rossello X , Dorresteijn JA , Janssen A , Lambrinou E , Scherrenberg M , Bonnefoy-Cudraz E , et al. Risk prediction tools in cardiovascular disease prevention: a report from the ESC Prevention of CVD Programme led by the European Association of Preventive Cardiology (EAPC) in collaboration with the Acute Cardiovascular Care Association (ACCA) and the Association of Cardiovascular Nursing and Allied Professions (ACNAP) . Eur J Prev Cardiol 2019 ; 26 : 1534 – 44 . https://doi.org/10.1177/2047487319846715
Ioannidis JPA . Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world . JAMA 2018 ; 319 : 115 – 6 . https://doi.org/10.1001/jama.2017.19672
Whelton PK , Carey RM , Aronow WS , Casey DE , Collins KJ , Dennison Himmelfarb C , et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines . Circulation 2018 ; 138 : e484 – 594 . https://doi.org/10.1161/cir.0000000000000596
Rahimi K , Bidel Z , Nazarzadeh M , Copland E , Canoy D , Wamil M , et al. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis . Lancet 2021 ; 398 : 1053 – 64 . https://doi.org/10.1016/S0140-6736(21)01921-8
Brunström M , Carlberg B . Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis . JAMA Intern Med 2018 ; 178 : 28 – 36 . https://doi.org/10.1001/jamainternmed.2017.6015
Arguedas JA , Leiva V , Wright JM . Blood pressure targets in adults with hypertension . Cochrane Database Syst Rev 2020 ; 12 : CD004349 . https://doi.org/10.1002/14651858.CD004349.pub3
Saiz LC , Gorricho J , Garjón J , Celaya MC , Erviti J , Leache L . Blood pressure targets for the treatment of people with hypertension and cardiovascular disease . Cochrane Database Syst Rev 2022 ; 11 : CD010315 . https://doi.org/10.1002/14651858.CD010315.pub5
Wright JT Jr , Williamson JD , Whelton PK , Snyder JK , Sink KM , Rocco MV , et al. A randomized trial of intensive versus standard blood-pressure control . N Engl J Med 2015 ; 373 : 2103 – 16 . https://doi.org/10.1056/NEJMoa1511939
Zhang W , Zhang S , Deng Y , Wu S , Ren J , Sun G , et al. Trial of intensive blood-pressure control in older patients with hypertension . N Engl J Med 2021 ; 385 : 1268 – 79 . https://doi.org/10.1056/NEJMoa2111437
Cushman WC , Evans GW , Byington RP , Goff DC Jr , Grimm RH Jr , Cutler JA , et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus . N Engl J Med 2010 ; 362 : 1575 – 85 . https://doi.org/10.1056/NEJMoa1001286
Ferrucci L , Furberg CD , Penninx BW , DiBari M , Williamson JD , Guralnik JM , et al. Treatment of isolated systolic hypertension is most effective in older patients with high-risk profile . Circulation 2001 ; 104 : 1923 – 6 . https://doi.org/10.1161/hc4101.097520
Leening MJ , Ferket BS , Steyerberg EW , Kavousi M , Deckers JW , Nieboer D , et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study . BMJ 2014 ; 349 : g5992 . https://doi.org/10.1136/bmj.g5992
Ference BA , Bhatt DL , Catapano AL , Packard CJ , Graham I , Kaptoge S , et al. Association of genetic variants related to combined exposure to lower low-density lipoproteins and lower systolic blood pressure with lifetime risk of cardiovascular disease . JAMA 2019 ; 322 : 1381 – 91 . https://doi.org/10.1001/jama.2019.14120
Kannel WB . Risk stratification in hypertension: new insights from the Framingham study . Am J Hypertens 2000 ; 13 : S3 – 10 . https://doi.org/10.1016/s0895-7061(99)00252-6
Weycker D , Nichols GA , O’Keeffe-Rosetti M , Edelsberg J , Khan Z , Kaura S , et al. Risk-factor clustering and cardiovascular disease risk in hypertensive patients . Am J Hypertens 2007 ; 20 : 599 – 607 . https://doi.org/10.1016/j.amjhyper.2006.10.013
Constanti M , Floyd CN , Glover M , Boffa R , Wierzbicki AS , McManus RJ . Cost-effectiveness of initiating pharmacological treatment in stage one hypertension based on 10-year cardiovascular disease risk: a Markov modeling study . Hypertension 2021 ; 77 : 682 – 91 . https://doi.org/10.1161/hypertensionaha.120.14913
Forouzanfar MH , Liu P , Roth GA , Ng M , Biryukov S , Marczak L , et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015 . JAMA 2017 ; 317 : 165 – 82 . https://doi.org/10.1001/jama.2016.19043
Karmali KN , Ning H , Goff DC , Lloyd-Jones DM . Identifying individuals at risk for cardiovascular events across the spectrum of blood pressure levels . J Am Heart Assoc 2015 ; 4 : e002126 . https://doi.org/10.1161/jaha.115.002126
Liu J , Li Y , Ge J , Yan X , Zhang H , Zheng X , et al . Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial . Lancet 2024 ; 404 : 245 – 55 . https://doi.org/10.1016/S0140-6736(24)01028-6
Wilson PW , D’Agostino RB , Levy D , Belanger AM , Silbershatz H , Kannel WB . Prediction of coronary heart disease using risk factor categories . Circulation 1998 ; 97 : 1837 – 47 . https://doi.org/10.1161/01.cir.97.18.1837
Sussman J , Vijan S , Hayward R . Using benefit-based tailored treatment to improve the use of antihypertensive medications . Circulation 2013 ; 128 : 2309 – 17 . https://doi.org/10.1161/circulationaha.113.002290
Karmali KN , Lloyd-Jones DM , van der Leeuw J , Goff DC , Yusuf S , Zanchetti A , et al. Blood pressure-lowering treatment strategies based on cardiovascular risk versus blood pressure: a meta-analysis of individual participant data . PLoS Med 2018 ; 15 : e1002538 . https://doi.org/10.1371/journal.pmed.1002538
Gaziano TA , Steyn K , Cohen DJ , Weinstein MC , Opie LH . Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level . Circulation 2005 ; 112 : 3569 – 76 . https://doi.org/10.1161/circulationaha.105.535922
Basu S , Sussman JB , Hayward RA . Black-white cardiovascular disease disparities after target-based versus personalized benefit-based lipid and blood pressure treatment . MDM Policy Pract 2017 ; 2 :2381468317725741. https://doi.org/10.1177/2381468317725741
Go AS , Chertow GM , Fan D , McCulloch CE , Hsu CY . Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization . N Engl J Med 2004 ; 351 : 1296 – 305 . https://doi.org/10.1056/NEJMoa041031
Klooster CCV , Bhatt DL , Steg PG , Massaro JM , Dorresteijn JAN , Westerink J , et al. Predicting 10-year risk of recurrent cardiovascular events andcardiovascular interventions in patients with established cardiovascular disease: results from UCC-SMART and REACH . Int J Cardiol 2021 ; 325 : 140 – 8 . https://doi.org/10.1016/j.ijcard.2020.09.053
Kaasenbrood L , Boekholdt SM , van der Graaf Y , Ray KK , Peters RJG , Kastelein JJP , et al. Distribution of estimated 10-year risk of recurrent vascular events and residual risk in a secondary prevention population . Circulation 2016 ; 134 : 1419 – 29 . https://doi.org/10.1161/circulationaha.116.021314
Eisen A , Bhatt DL , Steg PG , Eagle KA , Goto S , Guo J , et al. Angina and future cardiovascular events in stable patients with coronary artery disease: insights from the Reduction of Atherothrombosis for Continued Health (REACH) registry . J Am Heart Assoc 2016 ; 5 : e004080 . https://doi.org/10.1161/jaha.116.004080
Taylor CJ , Roalfe AK , Iles R , Hobbs FD . Ten-year prognosis of heart failure in the community: follow-up data from the Echocardiographic Heart of England Screening (ECHOES) study . Eur J Heart Fail 2012 ; 14 : 176 – 84 . https://doi.org/10.1093/eurjhf/hfr170
Shah KS , Xu H , Matsouaka RA , Bhatt DL , Heidenreich PA , Hernandez AF , et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5–year outcomes . J Am Coll Cardiol 2017 ; 70 : 2476 – 86 . https://doi.org/10.1016/j.jacc.2017.08.074
Benjamin EJ , Wolf PA , D’Agostino RB , Silbershatz H , Kannel WB , Levy D . Impact of atrial fibrillation on the risk of death: the Framingham heart study . Circulation 1998 ; 98 : 946 – 52 . https://doi.org/10.1161/01.cir.98.10.946
Pandey A , Patel KV , Vongpatanasin W , Ayers C , Berry JD , Mentz RJ , et al. Incorporation of biomarkers into risk assessment for allocation of antihypertensive medication according to the 2017 ACC/AHA high blood pressure guideline: a pooled cohort analysis . Circulation 2019 ; 140 : 2076 – 88 . https://doi.org/10.1161/circulationaha.119.043337
Mulnier HE , Seaman HE , Raleigh VS , Soedamah-Muthu SS , Colhoun HM , Lawrenson RA , et al. Risk of myocardial infarction in men and women with type 2 diabetes in the UK: a cohort study using the general practice research database . Diabetologia 2008 ; 51 : 1639 – 45 . https://doi.org/10.1007/s00125-008-1076-y
Soedamah-Muthu SS , Fuller JH , Mulnier HE , Raleigh VS , Lawrenson RA , Colhoun HM . High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: a cohort study using the general practice research database . Diabetes Care 2006 ; 29 : 798 – 804 . https://doi.org/10.2337/diacare.29.04.06.dc05-1433
Wong ND , Glovaci D , Wong K , Malik S , Franklin SS , Wygant G , et al. Global cardiovascular disease risk assessment in United States adults with diabetes . Diab Vasc Dis Res 2012 ; 9 : 146 – 52 . https://doi.org/10.1177/1479164112436403
Paquette M , Bernard S , Cariou B , Hegele RA , Genest J , Trinder M , et al. Familial hypercholesterolemia-risk-score: a new score predicting cardiovascular events and cardiovascular mortality in familial hypercholesterolemia . Arterioscler Thromb Vasc Biol 2021 ; 41 : 2632 – 40 . https://doi.org/10.1161/atvbaha.121.316106
SCORE2-Diabetes Working Group and the ESC Cardiovascular Risk Collaboration . SCORE2-Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Europe . Eur Heart J 2023 ; 44 : 2544 – 56 . https://doi.org/10.1093/eurheartj/ehad260
SCORE Working Group and the ESC Cardiovascular Risk Collaboration . SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe . Eur Heart J 2021 ; 42 : 2439 – 54 . https://doi.org/10.1093/eurheartj/ehab309
SCORE OP working group and ESC Cardiovascular Risk Collaboration . SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions . Eur Heart J 2021 ; 42 : 2455 – 67 . https://doi.org/10.1093/eurheartj/ehab312
Pignone M , Phillips CJ , Elasy TA , Fernandez A . Physicians’ ability to predict the risk of coronary heart disease . BMC Health Serv Res 2003 ; 3 : 13 . https://doi.org/10.1186/1472-6963-3-13
Grover SA , Lowensteyn I , Esrey KL , Steinert Y , Joseph L , Abrahamowicz M . Do doctors accurately assess coronary risk in their patients? Preliminary results of the coronary health assessment study . BMJ 1995 ; 310 : 975 – 8 . https://doi.org/10.1136/bmj.310.6985.975
Friedmann PD , Brett AS , Mayo-Smith MF . Differences in generalists’ and cardiologists’ perceptions of cardiovascular risk and the outcomes of preventive therapy in cardiovascular disease . Ann Intern Med 1996 ; 124 : 414 – 21 . https://doi.org/10.7326/0003-4819-124-4-199602150-00005
Visseren FLJ , Mach F , Smulders YM , Carballo D , Koskinas KC , Bäck M , et al. ESC guidelines on cardiovascular disease prevention in clinical practice . Eur Heart J 2021 ; 42 : 3227 – 337 . https://doi.org/10.1093/eurheartj/ehab484
Xie X , Atkins E , Lv J , Bennett A , Neal B , Ninomiya T , et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis . Lancet 2016 ; 387 : 435 – 43 . https://doi.org/10.1016/s0140-6736(15)00805-3
Herrett E , Gadd S , Jackson R , Bhaskaran K , Williamson E , van Staa T , et al. Eligibility and subsequent burden of cardiovascular disease of four strategies for blood pressure-lowering treatment: a retrospective cohort study . Lancet 2019 ; 394 : 663 – 71 . https://doi.org/10.1016/s0140-6736(19)31359-5
Matsushita K , Kaptoge S , Hageman SHJ , Sang Y , Ballew SH , Grams ME , et al. Including measures of chronic kidney disease to improve cardiovascular risk prediction by SCORE2 and SCORE2-OP . Eur J Prev Cardiol 2023 ; 30 : 8 – 16 . https://doi.org/10.1093/eurjpc/zwac176
Gerdts E , Sudano I , Brouwers S , Borghi C , Bruno RM , Ceconi C , et al. Sex differences in arterial hypertension . Eur Heart J 2022 ; 43 : 4777 – 88 . https://doi.org/10.1093/eurheartj/ehac470
Brown MC , Best KE , Pearce MS , Waugh J , Robson SC , Bell R . Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis . Eur J Epidemiol 2013 ; 28 : 1 – 19 . https://doi.org/10.1007/s10654-013-9762-6
Honigberg MC , Zekavat SM , Aragam K , Klarin D , Bhatt DL , Scott NS , et al. Long-term cardiovascular risk in women with hypertension during pregnancy . J Am Coll Cardiol 2019 ; 74 : 2743 – 54 . https://doi.org/10.1016/j.jacc.2019.09.052
Leon LJ , McCarthy FP , Direk K , Gonzalez-Izquierdo A , Prieto-Merino D , Casas JP , et al. Preeclampsia and cardiovascular disease in a large UK pregnancy cohort of linked electronic health records: a CALIBER study . Circulation 2019 ; 140 : 1050 – 60 . https://doi.org/10.1161/circulationaha.118.038080
Haug EB , Horn J , Markovitz AR , Fraser A , Klykken B , Dalen H , et al. Association of conventional cardiovascular risk factors with cardiovascular disease after hypertensive disorders of pregnancy: analysis of the Nord-Trøndelag health study . JAMA Cardiol 2019 ; 4 : 628 – 35 . https://doi.org/10.1001/jamacardio.2019.1746
Wu P , Haththotuwa R , Kwok CS , Babu A , Kotronias RA , Rushton C , et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis . Circ Cardiovasc Qual Outcomes 2017 ; 10 : e003497 . https://doi.org/10.1161/circoutcomes.116.003497
Kramer CK , Campbell S , Retnakaran R . Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis . Diabetologia 2019 ; 62 : 905 – 14 . https://doi.org/10.1007/s00125-019-4840-2
Kyriacou H , Al-Mohammad A , Muehlschlegel C , Foster-Davies L , Bruco MEF , Legard C , et al. The risk of cardiovascular diseases after miscarriage, stillbirth, and induced abortion: a systematic review and meta-analysis . Eur Heart J Open 2022 ; 2 : oeac065 . https://doi.org/10.1093/ehjopen/oeac065
Kessous R , Shoham-Vardi I , Pariente G , Holcberg G , Sheiner E . An association between preterm delivery and long-term maternal cardiovascular morbidity . Am J Obstet Gynecol 2013 ; 209 : 368.e1 – 8 . https://doi.org/10.1016/j.ajog.2013.05.041
Markovitz AR , Stuart JJ , Horn J , Williams PL , Rimm EB , Missmer SA , et al. Does pregnancy complication history improve cardiovascular disease risk prediction? Findings from the HUNT study in Norway . Eur Heart J 2019 ; 40 : 1113 – 20 . https://doi.org/10.1093/eurheartj/ehy863
Saei Ghare Naz M , Sheidaei A , Aflatounian A , Azizi F , Ramezani Tehrani F . Does adding adverse pregnancy outcomes improve the Framingham cardiovascular risk score in women? Data from the Tehran Lipid and Glucose Study . J Am Heart Assoc 2022 ; 11 : e022349 . https://doi.org/10.1161/jaha.121.022349
Gladstone RA , Pudwell J , Nerenberg KA , Grover SA , Smith GN . Cardiovascular risk assessment and follow-up of women after hypertensive disorders of pregnancy: a prospective cohort study . J Obstet Gynaecol Can 2019 ; 41 : 1157 – 67.e1 . https://doi.org/10.1016/j.jogc.2018.10.024
Patel AP , Wang M , Kartoun U , Ng K , Khera AV . Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asian individuals: results from the UK Biobank prospective cohort study . Circulation 2021 ; 144 : 410 – 22 . https://doi.org/10.1161/circulationaha.120.052430
Tillin T , Hughes AD , Whincup P , Mayet J , Sattar N , McKeigue PM , et al. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri-ethnic prospective cohort study (SABRE—Southall And Brent REvisited) . Heart 2014 ; 100 : 60 – 7 . https://doi.org/10.1136/heartjnl-2013-304474
Rabanal KS , Igland J , Tell GS , Jenum AK , Klemsdal TO , Ariansen I , et al. Validation of the cardiovascular risk model NORRISK 2 in South Asians and people with diabetes . Scand Cardiovasc J 2021 ; 55 : 56 – 62 . https://doi.org/10.1080/14017431.2020.1821909
Veronesi G , Gianfagna F , Giampaoli S , Chambless LE , Mancia G , Cesana G , et al. Improving long-term prediction of first cardiovascular event: the contribution of family history of coronary heart disease and social status . Prev Med 2014 ; 64 : 75 – 80 . https://doi.org/10.1016/j.ypmed.2014.04.007
Sivapalaratnam S , Boekholdt SM , Trip MD , Sandhu MS , Luben R , Kastelein JJP , et al. Family history of premature coronary heart disease and risk prediction in the EPIC-Norfolk prospective population study . Heart 2010 ; 96 : 1985 – 9 . https://doi.org/10.1136/hrt.2010.210740
Kimenai DM , Pirondini L , Gregson J , Prieto D , Pocock SJ , Perel P , et al. Socioeconomic deprivation: an important, largely unrecognized risk factor in primary prevention of cardiovascular disease . Circulation 2022 ; 146 : 240 – 8 . https://doi.org/10.1161/circulationaha.122.060042
Avina-Zubieta JA , Thomas J , Sadatsafavi M , Lehman AJ , Lacaille D . Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies . Ann Rheum Dis 2012 ; 71 : 1524 – 9 . https://doi.org/10.1136/annrheumdis-2011-200726
Crowson CS , Matteson EL , Roger VL , Therneau TM , Gabriel SE . Usefulness of risk scores to estimate the risk of cardiovascular disease in patients with rheumatoid arthritis . Am J Cardiol 2012 ; 110 : 420 – 4 . https://doi.org/10.1016/j.amjcard.2012.03.044
Arts EE , Popa C , Den Broeder AA , Semb A G , Toms T , Kitas G D , et al. Performance of four current risk algorithms in predicting cardiovascular events in patients with early rheumatoid arthritis . Ann Rheum Dis 2015 ; 74 : 668 – 74 . https://doi.org/10.1136/annrheumdis-2013-204024
Arts EE , Popa CD , Den Broeder AA , Donders R , Sandoo A , Toms T , et al. Prediction of cardiovascular risk in rheumatoid arthritis: performance of original and adapted SCORE algorithms . Ann Rheum Dis 2016 ; 75 : 674 – 80 . https://doi.org/10.1136/annrheumdis-2014-206879
Gelfand JM , Neimann AL , Shin DB , Wang X , Margolis DJ , Troxel AB . Risk of myocardial infarction in patients with psoriasis . JAMA 2006 ; 296 : 1735 – 41 . https://doi.org/10.1001/jama.296.14.1735
Miller IM , Ellervik C , Yazdanyar S , Jemec GB . Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors . J Am Acad Dermatol 2013 ; 69 : 1014 – 24 . https://doi.org/10.1016/j.jaad.2013.06.053
Eder L , Chandran V , Gladman DD . The Framingham risk score underestimates the extent of subclinical atherosclerosis in patients with psoriatic disease . Ann Rheum Dis 2014 ; 73 : 1990 – 6 . https://doi.org/10.1136/annrheumdis-2013-203433
Armstrong EJ , Harskamp CT , Armstrong AW . Psoriasis and major adverse cardiovascular events: a systematic review and meta-analysis of observational studies . J Am Heart Assoc 2013 ; 2 : e000062 . https://doi.org/10.1161/jaha.113.000062
Elmets CA , Leonardi CL , Davis DMR , Gelfand JM , Lichten J , Mehta NN , et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities . J Am Acad Dermatol 2019 ; 80 : 1073 – 113 . https://doi.org/10.1016/j.jaad.2018.11.058
Lu X , Wang Y , Zhang J , Pu D , Hu N , Luo J , et al. Patients with systemic lupus erythematosus face a high risk of cardiovascular disease: a systematic review and meta-analysis . Int Immunopharmacol 2021 ; 94 : 107466 . https://doi.org/10.1016/j.intimp.2021.107466
Drosos GC , Konstantonis G , Sfikakis PP , Tektonidou MG . Underperformance of clinical risk scores in identifying vascular ultrasound-based high cardiovascular risk in systemic lupus erythematosus . Eur J Prev Cardiol . 2020 . https://doi.org/10.1177/2047487320906650
Shah ASV , Stelzle D , Lee KK , Beck EJ , Alam S , Clifford S , et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis . Circulation 2018 ; 138 : 1100 – 12 . https://doi.org/10.1161/circulationaha.117.033369
Triant VA , Perez J , Regan S , Massaro JM , Meigs JB , Grinspoon SK , et al. Cardiovascular risk prediction functions underestimate risk in HIV infection . Circulation 2018 ; 137 : 2203 – 14 . https://doi.org/10.1161/circulationaha.117.028975
Triant VA, Lyass A, Hurley LB, Borowsky LH, Ehrbar RQ, H W , et al. Cardiovascular Risk Estimation Is Suboptimal in People With HIV . J Am Heart Assoc. 2024 ; 13 : e029228 . https://doi.org/10.1161/JAHA.123.029228
Correll CU , Solmi M , Veronese N , Bortolato B , Rosson S , Santonastaso P , et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls . World Psychiatry 2017 ; 16 : 163 – 80 . https://doi.org/10.1002/wps.20420
Lambert AM , Parretti HM , Pearce E , Price MJ , Riley M , Ryan R , et al. Temporal trends in associations between severe mental illness and risk of cardiovascular disease: a systematic review and meta-analysis . PLoS Med 2022 ; 19 : e1003960 . https://doi.org/10.1371/journal.pmed.1003960
Cunningham R , Poppe K , Peterson D , Every-Palmer S , Soosay I , Jackson R . Prediction of cardiovascular disease risk among people with severe mental illness: a cohort study . PLoS One 2019 ; 14 : e0221521 . https://doi.org/10.1371/journal.pone.0221521
Yeboah J , Young R , McClelland RL , Delaney JC , Polonsky TS , Dawood FZ , et al. Utility of nontraditional risk markers in atherosclerotic cardiovascular disease risk assessment . J Am Coll Cardiol 2016 ; 67 : 139 – 47 . https://doi.org/10.1016/j.jacc.2015.10.058
Akintoye E , Afonso L , Bengaluru Jayanna M , Bao W , Briasoulis A , Robinson J , et al. Prognostic utility of risk enhancers and coronary artery calcium score recommended in the 2018 ACC/AHA multisociety cholesterol treatment guidelines over the pooled cohort equation: insights from 3 large prospective cohorts . J Am Heart Assoc 2021 ; 10 : e019589 . https://doi.org/10.1161/jaha.120.019589
Peters SA , den Ruijter HM , Bots ML , Moons KG . Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: a systematic review . Heart 2012 ; 98 : 177 – 84 . https://doi.org/10.1136/heartjnl-2011-300747
Nicolaides AN , Panayiotou AG , Griffin M , Tyllis T , Bond D , Georgiou N , et al. Arterial ultrasound testing to predict atherosclerotic cardiovascular events . J Am Coll Cardiol 2022 ; 79 : 1969 – 82 . https://doi.org/10.1016/j.jacc.2022.03.352
Laclaustra M , Casasnovas JA , Fernández-Ortiz A , Fuster V , León-Latre M , Jiménez-Borreguero LJ , et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium: the AWHS study . J Am Coll Cardiol 2016 ; 67 : 1263 – 74 . https://doi.org/10.1016/j.jacc.2015.12.056
López-Melgar B , Fernández-Friera L , Oliva B , García-Ruiz JM , Peñalvo JL , Gómez-Talavera S , et al. Subclinical atherosclerosis burden by 3D ultrasound in mid-life: the PESA study . J Am Coll Cardiol 2017 ; 70 : 301 – 13 . https://doi.org/10.1016/j.jacc.2017.05.033
Ben-Shlomo Y , Spears M , Boustred C , May M , Anderson SG , Benjamin EJ , et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects . J Am Coll Cardiol 2014 ; 63 : 636 – 46 . https://doi.org/10.1016/j.jacc.2013.09.063
Ohkuma T , Ninomiya T , Tomiyama H , Kario K , Hoshide S , Kita Y , et al. Brachial-Ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis . Hypertension 2017 ; 69 : 1045 – 52 . https://doi.org/10.1161/hypertensionaha.117.09097
Stone K , Veerasingam D , Meyer ML , Heffernan KS , Higgins S , Maria Bruno R , et al. Reimagining the value of brachial-ankle pulse wave velocity as a biomarker of cardiovascular disease risk-a call to action on behalf of VascAgeNet . Hypertension 2023 ; 80 : 1980 – 92 . https://doi.org/10.1161/hypertensionaha.123.21314
An DW , Hansen TW , Aparicio LS , Chori B , Huang Q-F , Wei F-F , et al. Derivation of an outcome-driven threshold for aortic pulse wave velocity: an individual-participant meta-analysis . Hypertension 2023 ; 80 : 1949 – 59 . https://doi.org/10.1161/hypertensionaha.123.21318
de Lemos JA , Ayers CR , Levine BD , deFilippi CR , Wang TJ , Hundley W , et al. Multimodality strategy for cardiovascular risk assessment: performance in 2 population-based cohorts . Circulation 2017 ; 135 : 2119 – 32 . https://doi.org/10.1161/circulationaha.117.027272
Hageman SHJ , Petitjean C , Pennells L , Kaptoge S , Pajouheshnia R , Tillmann T , et al. Improving 10-year cardiovascular risk prediction in apparently healthy people: flexible addition of risk modifiers on top of SCORE2 . Eur J Prev Cardiol 2023 ; 30 : 1705 – 14 . https://doi.org/10.1093/eurjpc/zwad187
McEvoy JW , Chen Y , Nambi V , Ballantyne CM , Sharrett AR , Appel LJ , et al. High-sensitivity cardiac troponin T and risk of hypertension . Circulation 2015 ; 132 : 825 – 33 . https://doi.org/10.1161/circulationaha.114.014364
Hussain A , Sun W , Deswal A , de Lemos JA , McEvoy JW , Hoogeveen RC , et al. Association of NT-ProBNP, blood pressure, and cardiovascular events: the ARIC study . J Am Coll Cardiol 2021 ; 77 : 559 – 71 . https://doi.org/10.1016/j.jacc.2020.11.063
Stuart JJ , Tanz LJ , Cook NR , Spiegelman D , Missmer SA , Rimm EB , et al. Hypertensive disorders of pregnancy and 10-year cardiovascular risk prediction . J Am Coll Cardiol 2018 ; 72 : 1252 – 63 . https://doi.org/10.1016/j.jacc.2018.05.077
Timpka S , Fraser A , Schyman T , Stuart JJ , Åsvold BO , Mogren I , et al. The value of pregnancy complication history for 10-year cardiovascular disease risk prediction in middle-aged women . Eur J Epidemiol 2018 ; 33 : 1003 – 10 . https://doi.org/10.1007/s10654-018-0429-1
Blankenberg S , Salomaa V , Makarova N , Ojeda F , Wild P , Lackner KJ , et al. Troponin I and cardiovascular risk prediction in the general population: the BiomarCaRE consortium . Eur Heart J 2016 ; 37 : 2428 – 37 . https://doi.org/10.1093/eurheartj/ehw172
Zeller T , Tunstall-Pedoe H , Saarela O , Ojeda F , Schnabel RB , Tuovinen T , et al. High population prevalence of cardiac troponin I measured by a high-sensitivity assay and cardiovascular risk estimation: the MORGAM biomarker project Scottish cohort . Eur Heart J 2014 ; 35 : 271 – 81 . https://doi.org/10.1093/eurheartj/eht406
Schoenthaler AM , Lancaster KJ , Chaplin W , Butler M , Forsyth J , Ogedegbe G , et al. Cluster randomized clinical trial of FAITH (faith-based approaches in the treatment of hypertension) in blacks . Circ Cardiovasc Qual Outcomes 2018 ; 11 : e004691 . https://doi.org/10.1161/circoutcomes.118.004691
Beaney T , Schutte AE , Stergiou GS , Borghi C , Burger D , Charchar F , et al. May Measurement Month 2019: the global blood pressure screening campaign of the international society of Hypertension . Hypertension 2020 ; 76 : 333 – 41 . https://doi.org/10.1161/hypertensionaha.120.14874
Victor RG , Lynch K , Li N , Blyler C , Muhammad E , Handler J , et al. A cluster-randomized trial of blood-pressure reduction in black barbershops . N Engl J Med 2018 ; 378 : 1291 – 301 . https://doi.org/10.1056/NEJMoa1717250
Sun Y , Mu J , Wang DW , Ouyang N , Xing L , Guo X , et al. A village doctor-led multifaceted intervention for blood pressure control in rural China: an open, cluster randomised trial . Lancet 2022 ; 399 : 1964 – 75 . https://doi.org/10.1016/s0140-6736(22)00325-7
Schmidt BM , Durao S , Toews I , Bavuma CM , Hohlfeld A , Nury E , et al. Screening strategies for hypertension . Cochrane Database Syst Rev 2020 ; 5 : CD013212 . https://doi.org/10.1002/14651858.CD013212.pub2
Kaczorowski J , Chambers LW , Dolovich L , Paterson JM , Karwalajtys T , Gierman T , et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP) . BMJ 2011 ; 342 : d442 . https://doi.org/10.1136/bmj.d442
Lindholt JS , Søgaard R , Rasmussen LM , Mejldal A , Lambrechtsen J , Steffensen FH , et al. Five-year outcomes of the Danish cardiovascular screening (DANCAVAS) trial . N Engl J Med 2022 ; 387 : 1385 – 94 . https://doi.org/10.1056/NEJMoa2208681
Sheppard JP , Schwartz CL , Tucker KL , McManus RJ . Modern management and diagnosis of hypertension in the United Kingdom: home care and self-care . Ann Glob Health 2016 ; 82 : 274 – 87 . https://doi.org/10.1016/j.aogh.2016.02.005
Andersson H , Hedström L , Bergman S , Bergh H . The outcome of two-step blood pressure screening in dental healthcare . Scand J Public Health 2018 ; 46 : 623 – 9 . https://doi.org/10.1177/1403494818759840
Zhang H , Thijs L , Kuznetsova T , Fagard RH , Li X , Staessen JA . Progression to hypertension in the non-hypertensive participants in the Flemish study on environment, genes and health outcomes . J Hypertens 2006 ; 24 : 1719 – 27 . https://doi.org/10.1097/01.hjh.0000242395.07473.92
Conen D , Aeschbacher S , Thijs L , Li Y , Boggia J , Asayama K , et al. Age-specific differences between conventional and ambulatory daytime blood pressure values . Hypertension 2014 ; 64 : 1073 – 9 . https://doi.org/10.1161/hypertensionaha.114.03957
Karnjanapiboonwong A , Anothaisintawee T , Chaikledkaew U , Dejthevaporn C , Attia J , Thakkinstian A . Diagnostic performance of clinic and home blood pressure measurements compared with ambulatory blood pressure: a systematic review and meta-analysis . BMC Cardiovasc Disord 2020 ; 20 : 491 . https://doi.org/10.1186/s12872-020-01736-2
Viera AJ , Yano Y , Lin FC , Simel DL , Yun J , Dave G , et al. Does this adult patient have hypertension?: The rational clinical examination systematic review . JAMA 2021 ; 326 : 339 – 47 . https://doi.org/10.1001/jama.2021.4533
Green BB , Anderson ML , Cook AJ , Ehrlich K , Hall YN , Hsu C , et al. Clinic, home, and kiosk blood pressure measurements for diagnosing hypertension: a randomized diagnostic study . J Gen Intern Med 2022 ; 37 : 2948 – 56 . https://doi.org/10.1007/s11606-022-07400-z
Kim JS , Rhee MY , Kim CH , Kim YR , Do U , Kim J-H , et al. Algorithm for diagnosing hypertension using out-of-office blood pressure measurements . J Clin Hypertens (Greenwich) 2021 ; 23 : 1965 – 74 . https://doi.org/10.1111/jch.14382
van den Born BH , Lip GYH , Brguljan-Hitij J , Cremer A , Segura J , Morales E , et al. ESC Council on Hypertension position document on the management of hypertensive emergencies . Eur Heart J Cardiovasc Pharmacother 2019 ; 5 : 37 – 46 . https://doi.org/10.1093/ehjcvp/pvy032
Ross S , Walker A , MacLeod MJ . Patient compliance in hypertension: role of illness perceptions and treatment beliefs . J Hum Hypertens 2004 ; 18 : 607 – 13 . https://doi.org/10.1038/sj.jhh.1001721
Hagger MS , Koch S , Chatzisarantis NLD , Orbell S . The common sense model of self-regulation: meta-analysis and test of a process model . Psychol Bull 2017 ; 143 : 1117 – 54 . https://doi.org/10.1037/bul0000118
Meyer D , Leventhal H , Gutmann M . Common-sense models of illness: the example of hypertension . Health Psychol 1985 ; 4 : 115 – 35 . https://doi.org/10.1037//0278-6133.4.2.115
O’Carroll RE , Chambers JA , Dennis M , Sudlow C , Johnston M . Improving adherence to medication in stroke survivors: a pilot randomised controlled trial . Ann Behav Med 2013 ; 46 : 358 – 68 . https://doi.org/10.1007/s12160-013-9515-5
Hollands GJ , Usher-Smith JA , Hasan R , Alexander F , Clarke N , Griffin SJ . Visualising health risks with medical imaging for changing recipients’ health behaviours and risk factors: systematic review with meta-analysis . PLoS Med 2022 ; 19 : e1003920 . https://doi.org/10.1371/journal.pmed.1003920
Burnier M . Medication adherence and persistence as the cornerstone of effective antihypertensive therapy . Am J Hypertens 2006 ; 19 : 1190 – 6 . https://doi.org/10.1016/j.amjhyper.2006.04.006
Parati G , Goncalves A , Soergel D , Bruno RM , Caiani EG , Gerdts E . New perspectives for hypertension management: progress in methodological and technological developments . Eur J Prev Cardiol 2023 ; 30 : 48 – 60 . https://doi.org/10.1093/eurjpc/zwac203
Naderi SH , Bestwick JP , Wald DS . Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients . Am J Med 2012 ; 125 : 882 – 7.e1 . https://doi.org/10.1016/j.amjmed.2011.12.013
Chang TE , Ritchey MD , Park S , Chang A , Odom EC , Durthaler J , et al. National rates of nonadherence to antihypertensive medications among insured adults with hypertension, 2015 . Hypertension 2019 ; 74 : 1324 – 32 . https://doi.org/10.1161/hypertensionaha.119.13616
Qvarnström M , Kahan T , Kieler H , Brandt L , Hasselström J , Bengtsson Boström K , et al. Persistence to antihypertensive drug treatment in Swedish primary healthcare . Eur J Clin Pharmacol 2013 ; 69 : 1955 – 64 . https://doi.org/10.1007/s00228-013-1555-z
Burnier M , Egan BM . Adherence in hypertension . Circ Res 2019 ; 124 : 1124 – 40 . https://doi.org/10.1161/circresaha.118.313220
Curneen JMG , Rabbitt L , Browne D , O’Donoghue DF , Alansari Y , Harhen B , et al. Major disparities in patient-reported adherence compared to objective assessment of adherence using mass spectrometry: a prospective study in a tertiary-referral hypertension clinic . Br J Clin Pharmacol 2022 ; 89 : 1948 – 55 . https://doi.org/10.1111/bcp.15292
Corrao G , Parodi A , Nicotra F , Zambon A , Merlino L , Cesana G , et al. Better compliance to antihypertensive medications reduces cardiovascular risk . J Hypertens 2011 ; 29 : 610 – 8 . https://doi.org/10.1097/HJH.0b013e328342ca97
Kim S , Shin DW , Yun JM , Hwang Y , Park SK , Ko Y-J , et al. Medication adherence and the risk of cardiovascular mortality and hospitalization among patients with newly prescribed antihypertensive medications . Hypertension 2016 ; 67 : 506 – 12 . https://doi.org/10.1161/hypertensionaha.115.06731
Lane D , Lawson A , Burns A , Azizi M , Burnier M , Jones DJL , et al. Nonadherence in hypertension: how to develop and implement chemical adherence testing . Hypertension 2022 ; 79 : 12 – 23 . https://doi.org/10.1161/hypertensionaha.121.17596
Marshall IJ , Wolfe CD , McKevitt C . Lay perspectives on hypertension and drug adherence: systematic review of qualitative research . BMJ 2012 ; 345 : e3953 . https://doi.org/10.1136/bmj.e3953
Schoenthaler A , Knafl GJ , Fiscella K , Ogedegbe G . Addressing the social needs of hypertensive patients: the role of patient–provider communication as a predictor of medication adherence . Circ Cardiovasc Qual Outcomes 2017 ; 10 : e003659 . https://doi.org/10.1161/circoutcomes.117.003659
Schmieder RE , Wassmann S , Predel HG , Weisser B , Blettenberg J , Gillessen A , et al. Improved persistence to medication, decreased cardiovascular events and reduced all-cause mortality in hypertensive patients with use of single-pill combinations: results from the START-study . Hypertension 2023 ; 80 : 1127 – 35 . https://doi.org/10.1161/hypertensionaha.122.20810
Ruzicka M , Leenen FHH , Ramsay T , Bugeja A , Edwards C , McCormick B , et al. Use of directly observed therapy to assess treatment adherence in patients with apparent treatment-resistant hypertension . JAMA Intern Med 2019 ; 179 : 1433 – 4 . https://doi.org/10.1001/jamainternmed.2019.1455
Pio-Abreu A , Trani-Ferreira F , Silva GV , Bortolotto LA , Drager LF . Directly observed therapy for resistant/refractory hypertension diagnosis and blood pressure control . Heart 2022 ; 108 : 1952 – 6 . https://doi.org/10.1136/heartjnl-2022-320802
Tomaszewski M , White C , Patel P , Masca N , Damani R , Hepworth J , et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis . Heart 2014 ; 100 : 855 – 61 . https://doi.org/10.1136/heartjnl-2013-305063
Forette F , Seux ML , Staessen JA , et al. The prevention of dementia with antihypertensive treatment: new evidence from the systolic hypertension in Europe (Syst-Eur) study . Arch Intern Med 2002 ; 162 : 2046 – 52 . https://doi.org/10.1001/archinte.162.18.2046
Näslund U , Ng N , Lundgren A , Fhärm E , Grönlund C , Johansson H , et al. Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomised controlled trial . Lancet 2019 ; 393 : 133 – 42 . https://doi.org/10.1016/s0140-6736(18)32818-6
Bengtsson A , Norberg M , Ng N , Carlberg B , Grönlund C , Hultdin J , et al. The beneficial effect over 3 years by pictorial information to patients and their physician about subclinical atherosclerosis and cardiovascular risk: results from the VIPVIZA randomized clinical trial . Am J Prev Cardiol 2021 ; 7 : 100199 . https://doi.org/10.1016/j.ajpc.2021.100199
Sjölander M , Carlberg B , Norberg M , Näslund U , Ng N . Prescription of lipid-lowering and antihypertensive drugs following pictorial information about subclinical atherosclerosis: a secondary outcome of a randomized clinical trial . JAMA Netw Open 2021 ; 4 : e2121683 . https://doi.org/10.1001/jamanetworkopen.2021.21683
Muiesan ML , Salvetti M , Monteduro C , Bonzi B , Paini A , Viola S , et al. Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients . Hypertension 2004 ; 43 : 731 – 8 . https://doi.org/10.1161/01.HYP.0000121223.44837.de
Guerin AP , Blacher J , Pannier B , Marchais SJ , Safar ME , London GM , et al. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure . Circulation 2001 ; 103 : 987 – 92 . https://doi.org/10.1161/01.cir.103.7.987
Cardoso CRL , Salles GF . Prognostic value of changes in aortic stiffness for cardiovascular outcomes and mortality in resistant hypertension: a cohort study . Hypertension 2022 ; 79 : 447 – 56 . https://doi.org/10.1161/hypertensionaha.121.18498
Laurent S , Chatellier G , Azizi M , Calvet D , Choukroun G , Danchin N , et al. SPARTE study: normalization of arterial stiffness and cardiovascular events in patients with hypertension at medium to very high risk . Hypertension 2021 ; 78 : 983 – 95 . https://doi.org/10.1161/hypertensionaha.121.17579
Levin A , Stevens PE , Bilous RW , Coresh J , De Francisco ALM , De Jong PE , et al. Summary of recommendation statements . Kidney Int Suppl (2011) 2013 ; 3 : 5 – 14 . https://doi.org/10.1038/kisup.2012.77
Matsushita K , Coresh J , Sang Y , Chalmers J , Fox C , Guallar E , et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data . Lancet Diabetes Endocrinol 2015 ; 3 : 514 – 25 . https://doi.org/10.1016/s2213-8587(15)00040-6
Cheung AK , Rahman M , Reboussin DM , Craven TE , Greene T , Kimmel PL , et al. Effects of intensive BP control in CKD . J Am Soc Nephrol 2017 ; 28 : 2812 – 23 . https://doi.org/10.1681/asn.2017020148
Malhotra R , Nguyen HA , Benavente O , Mete M , Howard BV , Mant J , et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis . JAMA Intern Med 2017 ; 177 : 1498 – 505 . https://doi.org/10.1001/jamainternmed.2017.4377
Stevens PE , Levin A . Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline . Ann Intern Med 2013 ; 158 : 825 – 30 . https://doi.org/10.7326/0003-4819-158-11-201306040-00007
Aboyans V , Ricco JB , Bartelink MEL , Björck M , Brodmann M , Cohnert T , et al. 2017 ESC Guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) . Eur Heart J 2018 ; 39 : 763 – 816 . https://doi.org/10.1093/eurheartj/ehx095
Iribarren C , Round AD , Lu M , Okin PM , McNulty EJ . Cohort study of ECG left ventricular hypertrophy trajectories: ethnic disparities, associations with cardiovascular outcomes, and clinical utility . J Am Heart Assoc 2017 ; 6 : e004954 . https://doi.org/10.1161/jaha.116.004954
Okin PM , Devereux RB , Jern S , Kjeldsen SE , Julius S , Dahlöf B . Baseline characteristics in relation to electrocardiographic left ventricular hypertrophy in hypertensive patients: the Losartan Intervention For Endpoint reduction (LIFE) in hypertension study . Hypertension 2000 ; 36 : 766 – 73 . https://doi.org/10.1161/01.hyp.36.5.766
Okin PM , Oikarinen L , Viitasalo M , Toivonen L , Kjeldsen SE , Nieminen MS , et al. Prognostic value of changes in the electrocardiographic strain pattern during antihypertensive treatment: the Losartan Intervention for End-point reduction in hypertension study (LIFE) . Circulation 2009 ; 119 : 1883 – 91 . https://doi.org/10.1161/circulationaha.108.812313
Lehtonen AO , Puukka P , Varis J , Porthan K , Tikkanen JT , Nieminen MS , et al. Prevalence and prognosis of ECG abnormalities in normotensive and hypertensive individuals . J Hypertens 2016 ; 34 : 959 – 66 . https://doi.org/10.1097/hjh.0000000000000882
Pewsner D , Jüni P , Egger M , Battaglia M , Sundström J , Bachmann LM . Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: systematic review . BMJ 2007 ; 335 : 711 . https://doi.org/10.1136/bmj.39276.636354.AE
Kuznetsova T , Thijs L , Knez J , Cauwenberghs N , Petit T , Gu Y-M . Longitudinal changes in left ventricular diastolic function in a general population . Circ Cardiovasc Imaging 2015 ; 8 : e002882 . https://doi.org/10.1161/circimaging.114.002882
Zhao L , Zierath R , Claggett B , Dorbala P , Matsushita K , Kitzman D . Longitudinal changes in left ventricular diastolic function in late life: the ARIC study . JACC Cardiovasc Imaging 2023 ; 16 : 1133 – 45 . https://doi.org/10.1016/j.jcmg.2023.02.022
Redfield MM , Jacobsen SJ , Burnett JC Jr , Mahoney DW , Bailey KR , Rodeheffer RJ . Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic . JAMA 2003 ; 289 : 194 – 202 . https://doi.org/10.1001/jama.289.2.194
Sundström J , Lind L , Arnlöv J , Zethelius B , Andrén B , Lithell HO . Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men . Circulation 2001 ; 103 : 2346 – 51 . https://doi.org/10.1161/01.cir.103.19.2346
Seko Y , Kato T , Yamaji Y , Haruna Y , Nakane E , Haruna T , et al. Discrepancy between left ventricular hypertrophy by echocardiography and electrocardiographic hypertrophy: clinical characteristics and outcomes . Open Heart 2021 ; 8 : e001765 . https://doi.org/10.1136/openhrt-2021-001765
Modin D , Biering-Sørensen SR , Mogelvang R , Landler N , Jensen JS , Biering-Sørensen T . Prognostic value of echocardiography in hypertensive versus nonhypertensive participants from the general population . Hypertension 2018 ; 71 : 742 – 51 . https://doi.org/10.1161/hypertensionaha.117.10674
Armstrong AC , Jacobs DR Jr , Gidding SS , Colangelo LA , Gjesdal O , Lewis CE , et al. Framingham score and LV mass predict events in young adults: CARDIA study . Int J Cardiol 2014 ; 172 : 350 – 5 . https://doi.org/10.1016/j.ijcard.2014.01.003
Kuznetsova T , Thijs L , Knez J , Herbots L , Zhang Z , Staessen JA . Prognostic value of left ventricular diastolic dysfunction in a general population . J Am Heart Assoc 2014 ; 3 : e000789 . https://doi.org/10.1161/jaha.114.000789
Marwick TH , Gillebert TC , Aurigemma G , et al. Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) . Eur Heart J Cardiovasc Imaging 2015 ; 16 : 577 – 605 . https://doi.org/10.1093/ehjci/jev076
Douglas PS , Garcia MJ , Haines DE , Lai WW , Manning WJ , Patel AR , et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography. A report of the American College of Cardiology Foundation appropriate use criteria task force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance American College of Chest Physicians . J Am Soc Echocardiogr 2011 ; 24 : 229 – 67 . https://doi.org/10.1016/j.echo.2010.12.008
van Rosendael AR , Bax AM , Smit JM , van den Hoogen IJ , Ma X , Al’Aref S , et al. Clinical risk factors and atherosclerotic plaque extent to define risk for major events in patients without obstructive coronary artery disease: the long-term coronary computed tomography angiography CONFIRM registry . Eur Heart J Cardiovasc Imaging 2020 ; 21 : 479 – 88 . https://doi.org/10.1093/ehjci/jez322
Mehta A , Pandey A , Ayers CR , Khera A , Sperling LS , Szklo M , et al. Predictive value of coronary artery calcium score categories for coronary events versus strokes: impact of sex and race: MESA and DHS . Circ Cardiovasc Imaging 2020 ; 13 : e010153 . https://doi.org/10.1161/circimaging.119.010153
Bengtsson A , Lindvall K , Norberg M , Fhärm E . Increased knowledge makes a difference!—general practitioners’ experiences of pictorial information about subclinical atherosclerosis for primary prevention: an interview study from the VIPVIZA trial . Scand J Prim Health Care 2021 ; 39 : 77 – 84 . https://doi.org/10.1080/02813432.2021.1882083
Ibanez B , Fernández-Ortiz A , Fernández-Friera L , García-Lunar I , Andrés V , Fuster V . Progression of early subclinical atherosclerosis (PESA) study: JACC focus seminar 7/8 . J Am Coll Cardiol 2021 ; 78 : 156 – 79 . https://doi.org/10.1016/j.jacc.2021.05.011
Den Ruijter HM , Peters SA , Anderson TJ , Britton AR , Dekker JM , Eijkemans MJ . Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis . JAMA 2012 ; 308 : 796 – 803 . https://doi.org/10.1001/jama.2012.9630
Downie LE , Hodgson LA , DSylva C , McIntosh RL , Rogers SL , Connell P , et al. Hypertensive retinopathy: comparing the Keith-Wagener-Barker to a simplified classification . J Hypertens 2013 ; 31 : 960 – 5 . https://doi.org/10.1097/HJH.0b013e32835efea3
Liew G , Xie J , Nguyen H , Keay L , Kamran Ikram M , McGeechan K , et al. Hypertensive retinopathy and cardiovascular disease risk: 6 population-based cohorts meta-analysis . Int J Cardiol Cardiovasc Risk Prev 2023 ; 17 : 200180 . https://doi.org/10.1016/j.ijcrp.2023.200180
Padmanabhan S , Caulfield M , Dominiczak AF . Genetic and molecular aspects of hypertension . Circ Res 2015 ; 116 : 937 – 59 . https://doi.org/10.1161/circresaha.116.303647
Casey R , Neumann HPH , Maher ER . Genetic stratification of inherited and sporadic phaeochromocytoma and paraganglioma: implications for precision medicine . Hum Mol Genet 2020 ; 29 : R128 – 137 . https://doi.org/10.1093/hmg/ddaa201
Rossi GP , Ceolotto G , Caroccia B , Lenzini L . Genetic screening in arterial hypertension . Nat Rev Endocrinol 2017 ; 13 : 289 – 98 . https://doi.org/10.1038/nrendo.2016.196
Cascón A , Calsina B , Monteagudo M , Mellid S , Díaz-Talavera A , Currás-Freixes M , et al. Genetic bases of pheochromocytoma and paraganglioma . J Mol Endocrinol 2023 ; 70 : e220167 . https://doi.org/10.1530/jme-22-0167
Staessen JA , Wang J , Bianchi G , Birkenhäger WH . Essential hypertension . Lancet 2003 ; 361 : 1629 – 41 . https://doi.org/10.1016/s0140-6736(03)13302-8
Lenders JW , Duh QY , Eisenhofer G , Gimenez-Roqueplo A-P , Grebe SKG , Murad MH , et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline . J Clin Endocrinol Metab 2014 ; 99 : 1915 – 42 . https://doi.org/10.1210/jc.2014-1498
Poulter NR , Prabhakaran D , Caulfield M . Hypertension . Lancet 2015 ; 386 : 801 – 12 . https://doi.org/10.1016/s0140-6736(14)61468-9
Mills KT , Bundy JD , Kelly TN , Reed JE , Kearney PM , Reynolds K , et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries . Circulation 2016 ; 134 : 441 – 50 . https://doi.org/10.1161/circulationaha.115.018912
Wei FF , Zhang ZY , Huang QF , Staessen JA . Diagnosis and management of resistant hypertension: state of the art . Nat Rev Nephrol 2018 ; 14 : 428 – 41 . https://doi.org/10.1038/s41581-018-0006-6
Carey RM , Calhoun DA , Bakris GL , Brook RD , Daugherty SL , Dennison-Himmelfarb Cheryl R , et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association . Hypertension 2018 ; 72 : e53 – 90 . https://doi.org/10.1161/hyp.0000000000000084
Carey RM , Sakhuja S , Calhoun DA , Whelton PK , Muntner P . Prevalence of apparent treatment-resistant hypertension in the United States . Hypertension 2019 ; 73 : 424 – 31 . https://doi.org/10.1161/hypertensionaha.118.12191
Vongpatanasin W . Resistant hypertension: a review of diagnosis and management . JAMA 2014 ; 311 : 2216 – 24 . https://doi.org/10.1001/jama.2014.5180
Azizi M , Sapoval M , Gosse P , Monge M , Bobrie G , Delsart P , et al. Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial . Lancet 2015 ; 385 : 1957 – 65 . https://doi.org/10.1016/s0140-6736(14)61942-5
Rossi GP , Bernini G , Caliumi C , Desideri G , Fabris B , Ferri C , et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients . J Am Coll Cardiol 2006 ; 48 : 2293 – 300 . https://doi.org/10.1016/j.jacc.2006.07.059
Pedrosa RP , Drager LF , Gonzaga CC , Sousa MG , de Paula LKG , Amaro ACS , et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension . Hypertension 2011 ; 58 : 811 – 7 . https://doi.org/10.1161/hypertensionaha.111.179788
Douma S , Petidis K , Doumas M , Papaefthimiou P , Triantafyllou A , Kartali N , et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study . Lancet 2008 ; 371 : 1921 – 6 . https://doi.org/10.1016/s0140-6736(08)60834-x
Monticone S , Burrello J , Tizzani D , Bertello C , Viola A , Buffolo F , et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice . J Am Coll Cardiol 2017 ; 69 : 1811 – 20 . https://doi.org/10.1016/j.jacc.2017.01.052
Käyser SC , Deinum J , de Grauw WJ , Schalk BWM , Bor HJHJ , Lenders JWM , et al. Prevalence of primary aldosteronism in primary care: a cross-sectional study . Br J Gen Pract 2018 ; 68 : e114 – 22 . https://doi.org/10.3399/bjgp18X694589
Rimoldi SF , Scherrer U , Messerli FH . Secondary arterial hypertension: when, who, and how to screen? Eur Heart J 2014 ; 35 : 1245 – 54 . https://doi.org/10.1093/eurheartj/eht534
Rossi GP , Bisogni V , Rossitto G , Maiolino G , Cesari M , Zhu R , et al. Practice recommendations for diagnosis and treatment of the most common forms of secondary hypertension . High Blood Press Cardiovasc Prev 2020 ; 27 : 547 – 60 . https://doi.org/10.1007/s40292-020-00415-9
Calhoun DA , Nishizaka MK , Zaman MA , Thakkar RB , Weissmann P . Hyperaldosteronism among black and white subjects with resistant hypertension . Hypertension 2002 ; 40 : 892 – 6 . https://doi.org/10.1161/01.hyp.0000040261.30455.b6
Jaffe G , Gray Z , Krishnan G , Stedman M , Zheng Y , Han J , et al. Screening rates for primary aldosteronism in resistant hypertension: a cohort study . Hypertension 2020 ; 75 : 650 – 9 . https://doi.org/10.1161/hypertensionaha.119.14359
Hundemer GL , Imsirovic H , Vaidya A , Yozamp N , Goupil R , Madore F , et al. Screening rates for primary aldosteronism among individuals with hypertension plus hypokalemia: a population-based retrospective cohort study . Hypertension 2022 ; 79 : 178 – 86 . https://doi.org/10.1161/hypertensionaha.121.18118
Monticone S , D’Ascenzo F , Moretti C , Williams TA , Veglio F , Gaita F , et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis . Lancet Diabetes Endocrinol 2018 ; 6 : 41 – 50 . https://doi.org/10.1016/s2213-8587(17)30319-4
Savard S , Amar L , Plouin PF , Steichen O . Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study . Hypertension 2013 ; 62 : 331 – 6 . https://doi.org/10.1161/hypertensionaha.113.01060
Hiramatsu K , Yamada T , Yukimura Y , Komiya I , Ichikawa K , Ishihara M , et al. A screening test to identify aldosterone-producing adenoma by measuring plasma renin activity. Results in hypertensive patients . Arch Intern Med 1981 ; 141 : 1589 – 93 . https://doi.org/10.1001/archinte.1981.00340130033011
Rossi GP . Primary aldosteronism: JACC state-of-the-art review . J Am Coll Cardiol 2019 ; 74 : 2799 – 811 . https://doi.org/10.1016/j.jacc.2019.09.057
Rossi GP , Ceolotto G , Rossitto G , Maiolino G , Cesari M , Seccia TM . Effects of mineralocorticoid and AT1 receptor antagonism on the aldosterone-renin ratio in primary aldosteronism—the EMIRA study . J Clin Endocrinol Metab 2020 ; 105 : 2060 – 7 . https://doi.org/10.1210/clinem/dgaa080
Rossi GP , Bisogni V , Bacca AV , Bacca AV , Belfiore A , Cesari M , et al. The 2020 Italian Society of Arterial Hypertension (SIIA) practical guidelines for the management of primary aldosteronism . Int J Cardiol Hypertens 2020 ; 5 : 100029 . https://doi.org/10.1016/j.ijchy.2020.100029
Faconti L , Kulkarni S , Delles C , Kapil V , Lewis P , Glover M , et al. Diagnosis and management of primary hyperaldosteronism in patients with hypertension: a practical approach endorsed by the British and Irish Hypertension Society . J Hum Hypertens 2024 ; 38 : 8 – 18 . https://doi.org/10.1038/s41371-023-00875-1
Olin JW , Gornik HL , Bacharach JM , Biller J , Fine LJ , Gray BH , et al. Fibromuscular dysplasia: state of the science and critical unanswered questions: a scientific statement from the American Heart Association . Circulation 2014 ; 129 : 1048 – 78 . https://doi.org/10.1161/01.cir.0000442577.96802.8c
Faconti L , Morselli F , Sinha M , Chrysochou C , Chowienczyk PJ . Fibromuscular dysplasia and hypertension—a statement on behalf of the British and Irish Hypertension Society . J Hum Hypertens 2021 ; 35 : 1051 – 3 . https://doi.org/10.1038/s41371-020-00456-6
Gornik HL , Persu A , Adlam D , Aparicio LS , Azizi M , Boulanger M , et al. First international consensus on the diagnosis and management of fibromuscular dysplasia . J Hypertens 2019 ; 37 : 229 – 52 . https://doi.org/10.1097/hjh.0000000000002019
Abrishami A , Khajehdehi A , Chung F . A systematic review of screening questionnaires for obstructive sleep apnea . Can J Anaesth 2010 ; 57 : 423 – 38 . https://doi.org/10.1007/s12630-010-9280-x
Chai-Coetzer CL , Antic NA , Hamilton GS , McArdle N , Wong K , Yee BJ , et al. Physician decision making and clinical outcomes with laboratory polysomnography or limited-channel sleep studies for obstructive sleep apnea: a randomized trial . Ann Intern Med 2017 ; 166 : 332 – 40 . https://doi.org/10.7326/m16-1301
Lenders JW , Eisenhofer G , Mannelli M , Pacak K . Phaeochromocytoma . Lancet 2005 ; 366 : 665 – 75 . https://doi.org/10.1016/s0140-6736(05)67139-5
Lenders JWM , Kerstens MN , Amar L , Prejbisz A , Robledo M , Taieb D , et al. Genetics, diagnosis, management and future directions of research of phaeochromocytoma and paraganglioma: a position statement and consensus of the Working Group on Endocrine Hypertension of the European Society of Hypertension . J Hypertens 2020 ; 38 : 1443 – 56 . https://doi.org/10.1097/hjh.0000000000002438
Mannelli M , Ianni L , Cilotti A , Conti A . Pheochromocytoma in Italy: a multicentric retrospective study . Eur J Endocrinol 1999 ; 141 : 619 – 24 . https://doi.org/10.1530/eje.0.1410619
Neumann HPH , Young WF Jr , Eng C . Pheochromocytoma and paraganglioma . N Engl J Med 2019 ; 381 : 552 – 65 . https://doi.org/10.1056/NEJMra1806651
Hundemer GL , Curhan GC , Yozamp N , Wang M , Vaidya A . Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study . Lancet Diabetes Endocrinol 2018 ; 6 : 51 – 9 . https://doi.org/10.1016/s2213-8587(17)30367-4
Jackson R , Lawes CM , Bennett DA , Milne RJ , Rodgers A . Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk . Lancet 2005 ; 365 : 434 – 41 .
Yang L , Sun J , Zhao M , Liang Y , Bovet P , Xi B . Elevated blood pressure in childhood and hypertension risk in adulthood: a systematic review and meta-analysis . J Hypertens 2020 ; 38 : 2346 – 55 . https://doi.org/10.1097/hjh.0000000000002550
Allen NB , Krefman AE , Labarthe D , Greenland P , Juonala M , Kähönen M , et al. Cardiovascular health trajectories from childhood through middle age and their association with subclinical atherosclerosis . JAMA Cardiol 2020 ; 5 : 557 – 66 . https://doi.org/10.1001/jamacardio.2020.0140
de Simone G , Mancusi C , Hanssen H , Genovesi S , Lurbe E , Parati G , et al. Hypertension in children and adolescents . Eur Heart J 2022 ; 43 : 3290 – 301 . https://doi.org/10.1093/eurheartj/ehac328
Falkstedt D , Koupil I , Hemmingsson T . Blood pressure in late adolescence and early incidence of coronary heart disease and stroke in the Swedish 1969 conscription cohort . J Hypertens 2008 ; 26 : 1313 – 20 . https://doi.org/10.1097/HJH.0b013e3282ffb17e
Jacobs DR Jr , Woo JG , Sinaiko AR , Daniels SR , Ikonen J , Juonala M , et al. Childhood cardiovascular risk factors and adult cardiovascular events . N Engl J Med 2022 ; 386 : 1877 – 88 . https://doi.org/10.1056/NEJMoa2109191
Oikonen M , Nuotio J , Magnussen CG , Viikari JSA , Taittonen L , Laitinen T , et al. Repeated blood pressure measurements in childhood in prediction of hypertension in adulthood . Hypertension 2016 ; 67 : 41 – 7 . https://doi.org/10.1161/hypertensionaha.115.06395
Garcia-Lunar I , van der Ploeg HP , Fernández Alvira JM , van Nassau F , Castellano Vázquez JM , van der Beek AJ , et al. Effects of a comprehensive lifestyle intervention on cardiovascular health: the TANSNIP-PESA trial . Eur Heart J 2022 ; 43 : 3732 – 45 . https://doi.org/10.1093/eurheartj/ehac378
Neal B , Wu Y , Feng X , Zhang R , Zhang Y , Shi J , et al. Effect of salt substitution on cardiovascular events and death . N Engl J Med 2021 ; 385 : 1067 – 77 . https://doi.org/10.1056/NEJMoa2105675
He FJ , Tan M , Ma Y , MacGregor GA . Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review . J Am Coll Cardiol 2020 ; 75 : 632 – 47 . https://doi.org/10.1016/j.jacc.2019.11.055
Ma Y , He FJ , Sun Q , Yuan C , Kieneker LM , Curhan GC , et al. 24-Hour urinary sodium and potassium excretion and cardiovascular risk . N Engl J Med 2022 ; 386 : 252 – 63 . https://doi.org/10.1056/NEJMoa2109794
Ma H , Xue Q , Wang X , Li X , Franco OH , Li Y , et al. Adding salt to foods and hazard of premature mortality . Eur Heart J 2022 ; 43 : 2878 – 88 . https://doi.org/10.1093/eurheartj/ehac208
Huang L , Trieu K , Yoshimura S , M Woodward , N Campbell , D Lackland , et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials . BMJ 2020 ; 368 : m315 . https://doi.org/10.1136/bmj.m315
Graudal N , Hubeck-Graudal T , Jürgens G , Taylor RS . Dose-response relation between dietary sodium and blood pressure: a meta-regression analysis of 133 randomized controlled trials . Am J Clin Nutr 2019 ; 109 : 1273 – 8 . https://doi.org/10.1093/ajcn/nqy384
Graudal NA , Hubeck-Graudal T , Jurgens G . Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride . Cochrane Database Syst Rev 2020 ; 12 : CD004022 . https://doi.org/10.1002/14651858.CD004022.pub5
Filippini T , Malavolti M , Whelton PK , Naska A , Orsini N , Vinceti M . Blood pressure effects of sodium reduction: dose–response meta-analysis of experimental studies . Circulation 2021 ; 143 : 1542 – 67 . https://doi.org/10.1161/circulationaha.120.050371
Gupta DK , Lewis CE , Varady KA , Su YR , Madhur MS , Lackland DT , et al. Effect of dietary sodium on blood pressure: a crossover trial . JAMA 2023 ; 330 : 2258 . https://doi.org/10.1001/jama.2023.23651
He J , Gu D , Chen J , Jaquish CE , Rao DC , Hixson JE , et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study . J Hypertens 2009 ; 27 : 48 – 54 . https://doi.org/10.1097/hjh.0b013e328316bb87
Sacks FM , Svetkey LP , Vollmer WM , Appel LJ , Bray GA , Harsha D , et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet . N Engl J Med 2001 ; 344 : 3 – 10 . https://doi.org/10.1056/nejm200101043440101
MacGregor GA , Markandu ND , Sagnella GA , Singer DR , Cappuccio FP . Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension . Lancet 1989 ; 2 : 1244 – 7 . https://doi.org/10.1016/s0140-6736(89)91852-7
Whelton PK , Appel LJ , Espeland MA , Applegate WB , Ettinger WH Jr , Kostis JB , et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE) . JAMA 1998 ; 279 : 839 – 46 . https://doi.org/10.1001/jama.279.11.839
He FJ , Li J , Macgregor GA . Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials . BMJ 2013 ; 346 : f1325 . https://doi.org/10.1136/bmj.f1325
Stolarz-Skrzypek K , Kuznetsova T , Thijs L , Tikhonoff V , Seidlerová J , Richart T , et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion . JAMA 2011 ; 305 : 1777 – 85 . https://doi.org/10.1001/jama.2011.574
Messerli FH , Hofstetter L , Syrogiannouli L , Rexhaj E , Siontis GCM , Seiler C , et al. Sodium intake, life expectancy, and all-cause mortality . Eur Heart J 2021 ; 42 : 2103 – 12 . https://doi.org/10.1093/eurheartj/ehaa947
Mente A , O’Donnell M , Rangarajan S , McQueen M , Dagenais G , Wielgosz A , et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study . Lancet 2018 ; 392 : 496 – 506 . https://doi.org/10.1016/s0140-6736(18)31376-x
Au Yeung SL , Schooling CM . Impact of urinary sodium on cardiovascular disease and risk factors: a 2 sample Mendelian randomization study . Clin Nutr 2021 ; 40 : 1990 – 6 . https://doi.org/10.1016/j.clnu.2020.09.018
Zanetti D , Bergman H , Burgess S , Assimes TL , Bhalla V , Ingelsson E . Urinary albumin, sodium, and potassium and cardiovascular outcomes in the UK Biobank: observational and Mendelian randomization analyses . Hypertension 2020 ; 75 : 714 – 22 . https://doi.org/10.1161/hypertensionaha.119.14028
Nolan P , McEvoy JW . Salt restriction for treatment of hypertension—current state and future directions . Curr Opin Cardiol 2024 ; 39 : 61 – 7 . https://doi.org/10.1097/hco.0000000000001098
Yuan Y , Jin A , Neal B , Feng X , Qiao Q , Wang H , et al. Salt substitution and salt-supply restriction for lowering blood pressure in elderly care facilities: a cluster-randomized trial . Nat Med 2023 ; 29 : 973 – 81 . https://doi.org/10.1038/s41591-023-02286-8
Lechner K , Schunkert H . Recommendations on sodium intake for cardiovascular health: conviction or evidence? Eur Heart J 2020 ; 41 : 3374 – 5 . https://doi.org/10.1093/eurheartj/ehaa545
O’Donnell M , Mente A , Alderman MH , Brady AJB , Diaz R , Gupta R , et al. Salt and cardiovascular disease: insufficient evidence to recommend low sodium intake . Eur Heart J 2020 ; 41 : 3363 – 73 . https://doi.org/10.1093/eurheartj/ehaa586
Aburto NJ , Hanson S , Gutierrez H , Hooper L , Elliott P , Cappuccio FP . Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses . BMJ 2013 ; 346 : f1378 . https://doi.org/10.1136/bmj.f1378
O’Donnell M , Mente A , Rangarajan S , McQueen MJ , Wang X , Liu L , et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events . N Engl J Med 2014 ; 371 : 612 – 23 . https://doi.org/10.1056/NEJMoa1311889
Wouda RD , Boekholdt SM , Khaw KT , Wareham NJ , de Borst MH , Hoorn EJ , et al. Sex-specific associations between potassium intake, blood pressure, and cardiovascular outcomes: the EPIC-Norfolk study . Eur Heart J 2022 ; 43 : 2867 – 75 . https://doi.org/10.1093/eurheartj/ehac313
Filippini T , Naska A , Kasdagli MI , Torres D , Lopes C , Carvalho C , et al. Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials . J Am Heart Assoc 2020 ; 9 : e015719 . https://doi.org/10.1161/jaha.119.015719
O’Donnell M , Yusuf S , Vogt L , Mente A , Messerli FH . Potassium intake: the Cinderella electrolyte . Eur Heart J 2023 ; 44 : 4925 – 34 . https://doi.org/10.1093/eurheartj/ehad628
Kidney Disease Outcomes Quality Initiative (K/DOQI) . K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease . Am J Kidney Dis 2004 ; 43 : S1 – 290 . https://doi.org/10.1053/j.ajkd.2004.03.006
Ndanuko RN , Ibrahim R , Hapsari RA , Neale EP , Raubenheimer D , Charlton KE . Association between the urinary sodium to potassium ratio and blood pressure in adults: a systematic review and meta-analysis . Adv Nutr 2021 ; 12 : 1751 – 67 . https://doi.org/10.1093/advances/nmab036
Messerli FH , O’Donnell M , Mente A , Yusuf S . Settling the controversy of salt substitutes and stroke: sodium reduction or potassium increase? Eur Heart J 2022 ; 43 : 3365 – 7 . https://doi.org/10.1093/eurheartj/ehac160
Yin X , Paige E , Tian M , Li Q , Huang L , Yu J , et al. The proportion of dietary salt replaced with potassium-enriched salt in the SSaSS: implications for scale-up . Hypertension 2023 ; 80 : 956 – 65 . https://doi.org/10.1161/hypertensionaha.122.20115
Xu X , Zeng L , Jha V , Cobb LK , Shibuya K , Appel LJ , et al. Potassium-enriched salt substitutes: a review of recommendations in clinical management guidelines . Hypertension 2024 ; 81 : 400 – 14 . https://doi.org/10.1161/hypertensionaha.123.21343
Hanssen H , Boardman H , Deiseroth A , Moholdt T , Simonenko M , Kränkel N , et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: a consensus document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension . Eur J Prev Cardiol 2022 ; 29 : 205 – 15 . https://doi.org/10.1093/eurjpc/zwaa141
Van Hoof R , Hespel P , Fagard R , Lijnen P , Staessen J , Amery A . Effect of endurance training on blood pressure at rest, during exercise and during 24 hours in sedentary men . Am J Cardiol 1989 ; 63 : 945 – 9 . https://doi.org/10.1016/0002-9149(89)90145-8
MacDonald HV , Johnson BT , Huedo-Medina TB , Livingston J , Forsyth KC , Kraemer WJ , et al. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: a meta-analysis . J Am Heart Assoc 2016 ; 5 : e003231 . https://doi.org/10.1161/jaha.116.003231
Hansford HJ , Parmenter BJ , McLeod KA , Wewege MA , Smart NA , Schutte AE , et al. The effectiveness and safety of isometric resistance training for adults with high blood pressure: a systematic review and meta-analysis . Hypertens Res 2021 ; 44 : 1373 – 84 . https://doi.org/10.1038/s41440-021-00720-3
Van Hoof R , Macor F , Lijnen P , Staessen J , Thijs L , Vanhees L , et al. Effect of strength training on blood pressure measured in various conditions in sedentary men . Int J Sports Med 1996 ; 17 : 415 – 22 . https://doi.org/10.1055/s-2007-972871
Leal JM , Galliano LM , Del Vecchio FB . Effectiveness of high-intensity interval training versus moderate-intensity continuous training in hypertensive patients: a systematic review and meta-analysis . Curr Hypertens Rep 2020 ; 22 : 26 . https://doi.org/10.1007/s11906-020-1030-z
Rossi A , Dikareva A , Bacon SL , Daskalopoulou SS . The impact of physical activity on mortality in patients with high blood pressure: a systematic review . J Hypertens 2012 ; 30 : 1277 – 88 . https://doi.org/10.1097/HJH.0b013e3283544669
Cuspidi C , Gherbesi E , Faggiano A , Sala C , Carugo S , Grassi G , et al. Masked hypertension and exaggerated blood pressure response to exercise: a review and meta-analysis . Diagnostics (Basel) 2023 ; 13 : 1005 . https://doi.org/10.3390/diagnostics13061005
Mariampillai JE , Liestøl K , Kjeldsen SE , Prestgaard EE , Engeseth K , Bodegard J , et al. Exercise systolic blood pressure at moderate workload is linearly associated with coronary disease risk in healthy men . Hypertension 2020 ; 75 : 44 – 50 . https://doi.org/10.1161/hypertensionaha.119.13528
Pelliccia A , Sharma S , Gati S , Bäck M , Börjesson M , Caselli S . 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease . Eur Heart J 2021 ; 42 : 17 – 96 . https://doi.org/10.1093/eurheartj/ehaa605
Bull FC , Al-Ansari SS , Biddle S , Borodulin K , Buman MP , Cardon G , et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour . Br J Sports Med 2020 ; 54 : 1451 – 62 . https://doi.org/10.1136/bjsports-2020-102955
Saco-Ledo G , Valenzuela PL , Ramírez-Jiménez M , Morales JS , Castillo-García A , Blumenthal JA , et al. Acute aerobic exercise induces short-term reductions in ambulatory blood pressure in patients with hypertension: a systematic review and meta-analysis . Hypertension 2021 ; 78 : 1844 – 58 . https://doi.org/10.1161/hypertensionaha.121.18099
Garber CE , Blissmer B , Deschenes MR , Franklin BA , Lamonte MJ , Lee I-M , et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise . Med Sci Sports Exerc 2011 ; 43 : 1334 – 59 . https://doi.org/10.1249/MSS.0b013e318213fefb
Edwards JJ , Deenmamode AHP , Griffiths M , Arnold O , Cooper NJ , Wiles JD , et al. Exercise training and resting blood pressure: a large-scale pairwise and network meta-analysis of randomised controlled trials . Br J Sports Med 2023 ; 57 : 1317 – 26 . https://doi.org/10.1136/bjsports-2022-106503
Fletcher GF , Ades PA , Kligfield P , Arena R , Balady GJ , Bittner VA , et al. Exercise standards for testing and training: a scientific statement from the American Heart Association . Circulation 2013 ; 128 : 873 – 934 . https://doi.org/10.1161/CIR.0b013e31829b5b44
Craft BB , Carroll HA , Lustyk MK . Gender differences in exercise habits and quality of life reports: assessing the moderating effects of reasons for exercise . Int J Lib Arts Soc Sci 2014 ; 2 : 65 – 76 .
Mathieu P , Poirier P , Pibarot P , Lemieux I , Després JP . Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease . Hypertension 2009 ; 53 : 577 – 84 . https://doi.org/10.1161/hypertensionaha.108.110320
Chandra A , Neeland IJ , Berry JD , Ayers CR , Rohatgi A , Das SR , et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas heart study . J Am Coll Cardiol 2014 ; 64 : 997 – 1002 . https://doi.org/10.1016/j.jacc.2014.05.057
Neter JE , Stam BE , Kok FJ , Grobbee DE , Geleijnse JM . Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials . Hypertension 2003 ; 42 : 878 – 84 . https://doi.org/10.1161/01.Hyp.0000094221.86888.Ae
Haase CL , Lopes S , Olsen AH , Satylganova A , Schnecke V , McEwan P . Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database . Int J Obes (Lond) 2021 ; 45 : 1249 – 58 . https://doi.org/10.1038/s41366-021-00788-4
Moore LL , Visioni AJ , Qureshi MM , Bradlee ML , Ellison RC , D’Agostino R . Weight loss in overweight adults and the long-term risk of hypertension: the Framingham study . Arch Intern Med 2005 ; 165 : 1298 – 303 . https://doi.org/10.1001/archinte.165.11.1298
Zomer E , Gurusamy K , Leach R , Trimmer C , Lobstein T , Morris S , et al. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis . Obes Rev 2016 ; 17 : 1001 – 11 . https://doi.org/10.1111/obr.12433
Wing RR , Espeland MA , Clark JM , Hazuda HP , Knowler WC , Pownall HJ , et al. Association of weight loss maintenance and weight regain on 4-year changes in CVD risk factors: the action for health in diabetes (Look AHEAD) clinical trial . Diabetes Care 2016 ; 39 : 1345 – 55 . https://doi.org/10.2337/dc16-0509
Ma C , Avenell A , Bolland M , Hudson J , Stewart F , Robertson C , et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis . BMJ 2017 ; 359 : j4849 . https://doi.org/10.1136/bmj.j4849
Semlitsch T , Krenn C , Jeitler K , Berghold A , Horvath K , Siebenhofer A . Long-term effects of weight-reducing diets in people with hypertension . Cochrane Database Syst Rev 2021 ; 2 : CD008274 . https://doi.org/10.1002/14651858.CD008274.pub4
Wing RR , Bolin P , Brancati FL , Bray GA , Clark JM , Coday M , et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes . N Engl J Med 2013 ; 369 : 145 – 54 . https://doi.org/10.1056/NEJMoa1212914
Pagidipati NJ , Phelan M , Page C , Clowse M , Henao R , Peterson ED , et al. The importance of weight stabilization amongst those with overweight or obesity: results from a large health care system . Prev Med Rep 2021 ; 24 : 101615 . https://doi.org/10.1016/j.pmedr.2021.101615
Estruch R , Ros E , Salas-Salvadó J , Covas M-I , Corella D , Arós F , et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts . N Engl J Med 2018 ; 378 : e34 . https://doi.org/10.1056/NEJMoa1800389
Delgado-Lista J , Alcala-Diaz JF , Torres-Peña JD , Quintana-Navarro GM , Fuentes F , Garcia-Rios A , et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): a randomised controlled trial . Lancet 2022 ; 399 : 1876 – 85 . https://doi.org/10.1016/s0140-6736(22)00122-2
Blumenthal JA , Babyak MA , Hinderliter A , Watkins LL , Craighead L , Lin P-H , et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study . Arch Intern Med 2010 ; 170 : 126 – 35 . https://doi.org/10.1001/archinternmed.2009.470
Juraschek SP , Miller ER III , Weaver CM , Appel LJ . Effects of sodium reduction and the DASH diet in relation to baseline blood pressure . J Am Coll Cardiol 2017 ; 70 : 2841 – 8 . https://doi.org/10.1016/j.jacc.2017.10.011
Gay HC , Rao SG , Vaccarino V , Ali MK . Effects of different dietary interventions on blood pressure: systematic review and meta-analysis of randomized controlled trials . Hypertension 2016 ; 67 : 733 – 9 . https://doi.org/10.1161/hypertensionaha.115.06853
Siebenhofer A , Winterholer S , Jeitler K , Horvath K , Berghold A , Krenn C , et al. Long-term effects of weight-reducing drugs in people with hypertension . Cochrane Database Syst Rev 2021 ; 1 : CD007654 . https://doi.org/10.1002/14651858.CD007654.pub5
Müller TD , Blüher M , Tschöp MH , DiMarchi RD . Anti-obesity drug discovery: advances and challenges . Nat Rev Drug Discov 2022 ; 21 : 201 – 23 . https://doi.org/10.1038/s41573-021-00337-8
Wilding JPH , Batterham RL , Calanna S , Davies M , Van Gaal LF , Lingvay I , et al. Once-weekly semaglutide in adults with overweight or obesity . N Engl J Med 2021 ; 384 : 989 – 1002 . https://doi.org/10.1056/NEJMoa2032183
Davies M , Færch L , Jeppesen OK , Pakseresht A , Pedersen SD , Perreault L , et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial . Lancet 2021 ; 397 : 971 – 84 . https://doi.org/10.1016/s0140-6736(21)00213-0
Tasnim S , Tang C , Musini VM , Wright JM . Effect of alcohol on blood pressure . Cochrane Database Syst Rev 2020 ; 7 : CD012787 . https://doi.org/10.1002/14651858.CD012787.pub2
Liu F , Liu Y , Sun X , Yin Z , Li H , Deng K , et al. Race- and sex-specific association between alcohol consumption and hypertension in 22 cohort studies: a systematic review and meta-analysis . Nutr Metab Cardiovasc Dis 2020 ; 30 : 1249 – 59 . https://doi.org/10.1016/j.numecd.2020.03.018
Griswold MG , Fullman N , Hawley C , Arian N , Zimsen SRM , Tymeson HD , et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 . Lancet 2018 ; 392 : 1015 – 35 . https://doi.org/10.1016/s0140-6736(18)31310-2
D’Elia L , La Fata E , Galletti F , Scalfi L , Strazzullo P . Coffee consumption and risk of hypertension: a dose–response meta-analysis of prospective studies . Eur J Nutr 2019 ; 58 : 271 – 80 . https://doi.org/10.1007/s00394-017-1591-z
Hodgson JM , Puddey IB , Woodman RJ , Mulder TPJ , Fuchs D , Scott K , et al. Effects of black tea on blood pressure: a randomized controlled trial . Arch Intern Med 2012 ; 172 : 186 – 8 . https://doi.org/10.1001/archinte.172.2.186
Shah SA , Chu BW , Lacey CS , Riddock IC , Lee M , Dargush AE . Impact of acute energy drink consumption on blood pressure parameters: a meta-analysis . Ann Pharmacother 2016 ; 50 : 808 – 15 . https://doi.org/10.1177/1060028016656433
Shah SA , Szeto AH , Farewell R , Shek A , Fan D , Quach KN , et al. Impact of high volume energy drink consumption on electrocardiographic and blood pressure parameters: a randomized trial . J Am Heart Assoc 2019 ; 8 : e011318 . https://doi.org/10.1161/jaha.118.011318
Basrai M , Schweinlin A , Menzel J , Mielke H , Weikert C , Dusemund B , et al. Energy drinks induce acute cardiovascular and metabolic changes pointing to potential risks for young adults: a randomized controlled trial . J Nutr 2019 ; 149 : 441 – 50 . https://doi.org/10.1093/jn/nxy303
Fung TT , Malik V , Rexrode KM , Manson JE , Willett WC , Hu FB . Sweetened beverage consumption and risk of coronary heart disease in women . Am J Clin Nutr 2009 ; 89 : 1037 – 42 . https://doi.org/10.3945/ajcn.2008.27140
Mullee A , Romaguera D , Pearson-Stuttard J , Viallon V , Stepien M , Freisling H , et al. Association between soft drink consumption and mortality in 10 European countries . JAMA Intern Med 2019 ; 179 : 1479 – 90 . https://doi.org/10.1001/jamainternmed.2019.2478
Farhangi MA , Nikniaz L , Khodarahmi M . Sugar-sweetened beverages increases the risk of hypertension among children and adolescence: a systematic review and dose–response meta-analysis . J Transl Med 2020 ; 18 : 344 . https://doi.org/10.1186/s12967-020-02511-9
Critchley JA , Capewell S . Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review . JAMA 2003 ; 290 : 86 – 97 . https://doi.org/10.1001/jama.290.1.86
Anthonisen NR , Skeans MA , Wise RA , Manfreda J , Kanner RE , Connett JE . The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial . Ann Intern Med 2005 ; 142 : 233 – 9 . https://doi.org/10.7326/0003-4819-142-4-200502150-00005
Thomson B , Emberson J , Lacey B , Lewington S , Peto R , Jemal A . Association between smoking, smoking cessation, and mortality by race, ethnicity, and sex among US adults . JAMA Netw Open 2022 ; 5 : e2231480 . https://doi.org/10.1001/jamanetworkopen.2022.31480
Yang JJ , Yu D , Shu XO , Wen W , Rahman S , Abe S . Reduction in total and major cause-specific mortality from tobacco smoking cessation: a pooled analysis of 16 population-based cohort studies in Asia . Int J Epidemiol 2022 ; 50 : 2070 – 81 . https://doi.org/10.1093/ije/dyab087
Martinez-Morata I , Sanchez TR , Shimbo D , Navas-Acien A . Electronic cigarette use and blood pressure endpoints: a systematic review . Curr Hypertens Rep 2020 ; 23 : 2 . https://doi.org/10.1007/s11906-020-01119-0
Kim SY , Jeong SH , Joo HJ , Park M , Park E-C , Kim JH , et al. High prevalence of hypertension among smokers of conventional and e-cigarette: using the nationally representative community dwelling survey . Front Public Health 2022 ; 10 : 919585 . https://doi.org/10.3389/fpubh.2022.919585
Groppelli A , Giorgi DM , Omboni S , Parati G , Mancia G . Persistent blood pressure increase induced by heavy smoking . J Hypertens 1992 ; 10 : 495 – 9 . https://doi.org/10.1097/00004872-199205000-00014
Primatesta P , Falaschetti E , Gupta S , Marmot MG , Poulter NR . Association between smoking and blood pressure: evidence from the health survey for England . Hypertension 2001 ; 37 : 187 – 93 . https://doi.org/10.1161/01.hyp.37.2.187
Stead LF , Buitrago D , Preciado N , Sanchez G , Hartmann-Boyce J , Lancaster T . Physician advice for smoking cessation . Cochrane Database Syst Rev 2013 ; 2013 : CD000165 . https://doi.org/10.1002/14651858.CD000165.pub4
Rasmussen M , Lauridsen SV , Pedersen B , Backer V , Tønnesen H . Intensive versus short face-to-face smoking cessation interventions: a meta-analysis . Eur Respir Rev 2022 ; 31 : 220063 . https://doi.org/10.1183/16000617.0063-2022
Filippou CD , Thomopoulos CG , Kouremeti MM , Sotiropoulou LI , Nihoyannopoulos PI , Tousoulis DM , et al. Mediterranean diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials . Clin Nutr 2021 ; 40 : 3191 – 200 . https://doi.org/10.1016/j.clnu.2021.01.030
Cowell OR , Mistry N , Deighton K , Matu J , Griffiths A , Minihane AM , et al. Effects of a Mediterranean diet on blood pressure: a systematic review and meta-analysis of randomized controlled trials and observational studies . J Hypertens 2021 ; 39 : 729 – 39 . https://doi.org/10.1097/hjh.0000000000002667
Roerecke M , Tobe SW , Kaczorowski J , Bacon SL , Vafaei A , Hasan OSM , et al. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies . J Am Heart Assoc 2018 ; 7 : e008202 . https://doi.org/10.1161/jaha.117.008202
Ding C , O’Neill D , Bell S , Stamatakis E , Britton A . Association of alcohol consumption with morbidity and mortality in patients with cardiovascular disease: original data and meta-analysis of 48,423 men and women . BMC Med 2021 ; 19 : 167 . https://doi.org/10.1186/s12916-021-02040-2
Marklund M , Singh G , Greer R , Cudhea F , Matsushita K , Micha R , et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: modelling study . BMJ 2020 ; 369 : m824 . https://doi.org/10.1136/bmj.m824
Pinho-Gomes AC , Azevedo L , Copland E , Canoy D , Nazarzadeh M , Ramakrishnan R , et al. Blood pressure-lowering treatment for the prevention of cardiovascular events in patients with atrial fibrillation: an individual participant data meta-analysis . PLoS Med 2021 ; 18 : e1003599 . https://doi.org/10.1371/journal.pmed.1003599
Bidel Z , Nazarzadeh M , Canoy D , Copland E , Gerdts E , Woodward M , et al. Sex-specific effects of blood pressure lowering pharmacotherapy for the prevention of cardiovascular disease: an individual participant-level data meta-analysis . Hypertension 2023 ; 80 : 2293 – 302 . https://doi.org/10.1161/hypertensionaha.123.21496
Nazarzadeh M , Bidel Z , Canoy D , Copland E , Bennett DA , Dehghan A , et al. Blood pressure-lowering treatment for prevention of major cardiovascular diseases in people with and without type 2 diabetes: an individual participant-level data meta-analysis . Lancet Diabetes Endocrinol 2022 ; 10 : 645 – 54 . https://doi.org/10.1016/s2213-8587(22)00172-3
Thomopoulos C , Parati G , Zanchetti A . Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs—overview and meta-analyses . J Hypertens 2015 ; 33 : 195 – 211 . https://doi.org/10.1097/hjh.0000000000000447
Ishani A , Cushman WC , Leatherman SM , Lew RA , Woods P , Glassman PA , et al. Chlorthalidone vs. hydrochlorothiazide for hypertension-cardiovascular events . N Engl J Med 2022 ; 387 : 2401 – 10 . https://doi.org/10.1056/NEJMoa2212270
Ziff OJ , Samra M , Howard JP , Bromage DI , Ruschitzka F , Francis DP , et al. Beta-blocker efficacy across different cardiovascular indications: an umbrella review and meta-analytic assessment . BMC Med 2020 ; 18 : 103 . https://doi.org/10.1186/s12916-020-01564-3
Thomopoulos C , Bazoukis G , Tsioufis C , Mancia G . Beta-blockers in hypertension: overview and meta-analysis of randomized outcome trials . J Hypertens 2020 ; 38 : 1669 – 81 . https://doi.org/10.1097/hjh.0000000000002523
Mancia G , Kjeldsen SE , Kreutz R , Pathak A , Grassi G , Esler M . Individualized beta-blocker treatment for high blood pressure dictated by medical comorbidities: indications beyond the 2018 European Society of Cardiology/European Society of Hypertension Guidelines . Hypertension 2022 ; 79 : 1153 – 66 . https://doi.org/10.1161/hypertensionaha.122.19020
Bradley HA , Wiysonge CS , Volmink JA , Mayosi BM , Opie LH . How strong is the evidence for use of beta-blockers as first-line therapy for hypertension? Systematic review and meta-analysis . J Hypertens 2006 ; 24 : 2131 – 41 . https://doi.org/10.1097/01.hjh.0000249685.58370.28
Wiysonge CS , Bradley HA , Volmink J , Mayosi BM , Opie LH . Beta-blockers for hypertension . Cochrane Database Syst Rev 2017 ; 1 : CD002003 . https://doi.org/10.1002/14651858.CD002003.pub5
Elliott WJ , Meyer PM . Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis . Lancet 2007 ; 369 : 201 – 7 . https://doi.org/10.1016/s0140-6736(07)60108-1
Bangalore S , Parkar S , Grossman E , Messerli FH . A meta-analysis of 94,492 patients with hypertension treated with beta blockers to determine the risk of new-onset diabetes mellitus . Am J Cardiol 2007 ; 100 : 1254 – 62 . https://doi.org/10.1016/j.amjcard.2007.05.057
Laurent S , Briet M , Boutouyrie P . Large and small artery cross-talk and recent morbidity-mortality trials in hypertension . Hypertension 2009 ; 54 : 388 – 92 . https://doi.org/10.1161/hypertensionaha.109.133116
Klingbeil AU , Schneider M , Martus P , Messerli FH , Schmieder RE . A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension . Am J Med 2003 ; 115 : 41 – 6 . https://doi.org/10.1016/s0002-9343(03)00158-x
Zanchetti A , Bond MG , Hennig M , Neiss A , Mancia G , Dal Palù C , et al. Calcium antagonist lacidipine slows down progression of asymptomatic carotid atherosclerosis: principal results of the European Lacidipine Study on Atherosclerosis (ELSA), a randomized, double-blind, long-term trial . Circulation 2002 ; 106 : 2422 – 7 . https://doi.org/10.1161/01.cir.0000039288.86470.dd
Schiffrin EL , Deng LY . Comparison of effects of angiotensin I-converting enzyme inhibition and beta-blockade for 2 years on function of small arteries from hypertensive patients . Hypertension 1995 ; 25 : 699 – 703 . https://doi.org/10.1161/01.hyp.25.4.699
Williams B , MacDonald TM , Morant S , Webb DJ , Sever P , McInnes G , et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial . Lancet 2015 ; 386 : 2059 – 68 . https://doi.org/10.1016/s0140-6736(15)00257-3
Agarwal R , Filippatos G , Pitt B , Anker SD , Rossing P , Joseph A , et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis . Eur Heart J 2022 ; 43 : 474 – 84 . https://doi.org/10.1093/eurheartj/ehab777
Agarwal R , Ruilope LM , Ruiz-Hurtado G , Haller H , Schmieder RE , Anker SD , et al. Effect of finerenone on ambulatory blood pressure in chronic kidney disease in type 2 diabetes . J Hypertens 2023 ; 41 : 295 – 302 . https://doi.org/10.1097/hjh.0000000000003330
Bakris GL , Agarwal R , Anker SD , Pitt B , Ruilope LM , Rossing P , et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes . N Engl J Med 2020 ; 383 : 2219 – 29 . https://doi.org/10.1056/NEJMoa2025845
The ALLHAT Officers Coordinators for the ALLHAT Collaborative Research Group . Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) . JAMA 2000 ; 283 : 1967 – 75 . https://doi.org/10.1001/jama.283.15.1967
Ruilope LM , Dukat A , Böhm M , Lacourcière Y , Gong J , Lefkowitz MP . Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study . Lancet 2010 ; 375 : 1255 – 66 . https://doi.org/10.1016/s0140-6736(09)61966-8
McMurray JJ , Packer M , Desai AS , Gong J , Lefkowitz MP , Rizkala AR , et al. Angiotensin – neprilysin inhibition versus enalapril in heart failure . N Engl J Med 2014 ; 371 : 993 – 1004 . https://doi.org/10.1056/NEJMoa1409077
Rakugi H , Kario K , Yamaguchi M , Sasajima T , Gotou H , Zhang J . Efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertension: a randomized, double-blind, multicenter study . Hypertens Res 2022 ; 45 : 824 – 33 . https://doi.org/10.1038/s41440-021-00819-7
Jackson AM , Jhund PS , Anand IS , Düngen H-D , Lam CSP , Lefkowitz MP , et al. Sacubitril-valsartan as a treatment for apparent resistant hypertension in patients with heart failure and preserved ejection fraction . Eur Heart J 2021 ; 42 : 3741 – 52 . https://doi.org/10.1093/eurheartj/ehab499
Kario K , Sun N , Chiang FT , Supasyndh O , Baek SH , Inubushi-Molessa A , et al. Efficacy and safety of LCZ696, a first-in-class angiotensin receptor neprilysin inhibitor, in Asian patients with hypertension: a randomized, double-blind, placebo-controlled study . Hypertension 2014 ; 63 : 698 – 705 . https://doi.org/10.1161/hypertensionaha.113.02002
Williams B , Cockcroft JR , Kario K , Zappe DH , Brunel PC , Wang Q , et al. Effects of sacubitril/valsartan versus olmesartan on central hemodynamics in the elderly with systolic hypertension: the PARAMETER study . Hypertension 2017 ; 69 : 411 – 20 . https://doi.org/10.1161/hypertensionaha.116.08556
Herrington WG , Savarese G , Haynes R , Marx N , Mellbin L , Lund LH , et al. Cardiac, renal, and metabolic effects of sodium-glucose co-transporter 2 inhibitors: a position paper from the European Society of Cardiology ad-hoc task force on sodium-glucose co-transporter 2 inhibitors . Eur J Heart Fail 2021 ; 23 : 1260 – 75 . https://doi.org/10.1002/ejhf.2286
Gupta R , Maitz T , Egeler D , Mehta A , Nyaeme M , Hajra A , et al. SGLT2 inhibitors in hypertension: role beyond diabetes and heart failure . Trends Cardiovasc Med 2022 ; 33 : 479 – 86 . https://doi.org/10.1016/j.tcm.2022.05.005
Kario K , Ferdinand KC , Vongpatanasin W . Are SGLT2 inhibitors new hypertension drugs? Circulation 2021 ; 143 : 1750 – 3 . https://doi.org/10.1161/circulationaha.121.053709
Yan C , Thijs L , Cao Y , Trenson S , Zhang Z-Y , Janssens S , et al. Opportunities of antidiabetic drugs in cardiovascular medicine: a meta-analysis and perspectives for trial design . Hypertension 2020 ; 76 : 420 – 31 . https://doi.org/10.1161/hypertensionaha.120.14791
Freeman MW , Halvorsen YD , Marshall W , Pater M , Isaacsohn J , Pearce C , et al. Phase 2 trial of baxdrostat for treatment-resistant hypertension . N Engl J Med 2023 ; 388 : 395 – 405 . https://doi.org/10.1056/NEJMoa2213169
Laffin LJ , Rodman D , Luther JM , Vaidya A , Weir MR , Rajicic N , et al. Aldosterone synthase inhibition with lorundrostat for uncontrolled hypertension: the target-HTN randomized clinical trial . JAMA 2023 ; 330 : 1140 – 50 . https://doi.org/10.1001/jama.2023.16029
Schlaich MP , Bellet M , Weber MA , Danaietash P , Bakris GL , Flack JM , et al. Dual endothelin antagonist aprocitentan for resistant hypertension (PRECISION): a multicentre, blinded, randomised, parallel-group, phase 3 trial . Lancet 2022 ; 400 : 1927 – 37 . https://doi.org/10.1016/s0140-6736(22)02034-7
Desai AS , Webb DJ , Taubel J , Casey S , Cheng Y , Robbie GJ , et al. Zilebesiran, an RNA interference therapeutic agent for hypertension . N Engl J Med 2023 ; 389 : 228 – 38 . https://doi.org/10.1056/NEJMoa2208391
Law MR , Wald NJ , Morris JK , Jordan RE . Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials . BMJ 2003 ; 326 : 1427 . https://doi.org/10.1136/bmj.326.7404.1427
Mahmud A , Feely J . Low-dose quadruple antihypertensive combination: more efficacious than individual agents—a preliminary report . Hypertension 2007 ; 49 : 272 – 5 . https://doi.org/10.1161/01.HYP.0000254479.66645.a3
Wald DS , Law M , Morris JK , Bestwick JP , Wald NJ . Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials . Am J Med 2009 ; 122 : 290 – 300 . https://doi.org/10.1016/j.amjmed.2008.09.038
Chow CK , Thakkar J , Bennett A , Hillis G , Burke M , Usherwood T , et al. Quarter-dose quadruple combination therapy for initial treatment of hypertension: placebo-controlled, crossover, randomised trial and systematic review . Lancet 2017 ; 389 : 1035 – 42 . https://doi.org/10.1016/s0140-6736(17)30260-x
Chow CK , Atkins ER , Hillis GS , Nelson MR , Reid CM , Schlaich MP , et al. Initial treatment with a single pill containing quadruple combination of quarter doses of blood pressure medicines versus standard dose monotherapy in patients with hypertension (QUARTET): a phase 3, randomised, double-blind, active-controlled trial . Lancet 2021 ; 398 : 1043 – 52 . https://doi.org/10.1016/s0140-6736(21)01922-x
Webster R , Salam A , de Silva HA , Selak V , Stepien S , Rajapakse S , et al. Fixed low-dose triple combination antihypertensive medication vs usual care for blood pressure control in patients with mild to moderate hypertension in Sri Lanka: a randomized clinical trial . JAMA 2018 ; 320 : 566 – 79 . https://doi.org/10.1001/jama.2018.10359
MacDonald TM , Williams B , Webb DJ , Morant S , Caulfield M , Cruickshank JK , et al. Combination therapy is superior to sequential monotherapy for the initial treatment of hypertension: a double-blind randomized controlled trial . J Am Heart Assoc 2017 ; 6 : e006986 . https://doi.org/10.1161/jaha.117.006986
Salam A , Kanukula R , Atkins E , Wang X , Islam S , Kishore SP , et al. Efficacy and safety of dual combination therapy of blood pressure-lowering drugs as initial treatment for hypertension: a systematic review and meta-analysis of randomized controlled trials . J Hypertens 2019 ; 37 : 1768 – 74 . https://doi.org/10.1097/hjh.0000000000002096
Zhang ZY , Yu YL , Asayama K , Hansen TW , Maestre GE , Staessen JA . Starting antihypertensive drug treatment with combination therapy: controversies in hypertension—con side of the argument . Hypertension 2021 ; 77 : 788 – 98 . https://doi.org/10.1161/hypertensionaha.120.12858
Kahan T . Low-dose combination of blood pressure-lowering medicines . Lancet 2021 ; 398 : 1022 – 3 . https://doi.org/10.1016/s0140-6736(21)01964-4
Rea F , Corrao G , Merlino L , Mancia G . Initial antihypertensive treatment strategies and therapeutic inertia . Hypertension 2018 ; 72 : 846 – 53 . https://doi.org/10.1161/hypertensionaha.118.11308
Egan BM , Bandyopadhyay D , Shaftman SR , Wagner CS , Zhao Y , Yu-Isenberg KS . Initial monotherapy and combination therapy and hypertension control the first year . Hypertension 2012 ; 59 : 1124 – 31 . https://doi.org/10.1161/hypertensionaha.112.194167
Sundström J , Lind L , Nowrouzi S , Hagström E , Held C , Lytsy P , et al. Heterogeneity in blood pressure response to 4 antihypertensive drugs: a randomized clinical trial . JAMA 2023 ; 329 : 1160 – 9 . https://doi.org/10.1001/jama.2023.3322
Tsioufis K , Kreutz R , Sykara G , van Vugt J , Hassan T . Impact of single-pill combination therapy on adherence, blood pressure control, and clinical outcomes: a rapid evidence assessment of recent literature . J Hypertens 2020 ; 38 : 1016 – 28 . https://doi.org/10.1097/hjh.0000000000002381
Parati G , Kjeldsen S , Coca A , Cushman WC , Wang J . Adherence to single-pill versus free-equivalent combination therapy in hypertension: a systematic review and meta-analysis . Hypertension 2021 ; 77 : 692 – 705 . https://doi.org/10.1161/hypertensionaha.120.15781
Egan BM , Kjeldsen SE , Narkiewicz K , Kreutz R , Burnier M . Single-pill combinations, hypertension control and clinical outcomes: potential, pitfalls and solutions . Blood Press 2022 ; 31 : 164 – 8 . https://doi.org/10.1080/08037051.2022.2095254
Yusuf S , Joseph P , Dans A , Gao P , Teo K , Xavier D , et al. Polypill with or without aspirin in persons without cardiovascular disease . N Engl J Med 2021 ; 384 : 216 – 28 . https://doi.org/10.1056/NEJMoa2028220
Roshandel G , Khoshnia M , Poustchi H , Hemming K , Kamangar F , Gharavi A , et al. Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): a pragmatic, cluster-randomised trial . Lancet 2019 ; 394 : 672 – 83 . https://doi.org/10.1016/s0140-6736(19)31791-x
Joseph P , Roshandel G , Gao P , Pais P , Lonn E , Xavier D , et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis . Lancet 2021 ; 398 : 1133 – 46 . https://doi.org/10.1016/s0140-6736(21)01827-4
van Vark LC , Bertrand M , Akkerhuis KM , Brugts JJ , Fox K , Mourad J-J , et al. Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin–angiotensin–aldosterone system inhibitors involving 158 998 patients . Eur Heart J 2012 ; 33 : 2088 – 97 . https://doi.org/10.1093/eurheartj/ehs075
Parving HH , Brenner BM , McMurray JJ , de Zeeuw D , Haffner SM , Solomon SD , et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes . N Engl J Med 2012 ; 367 : 2204 – 13 . https://doi.org/10.1056/NEJMoa1208799
Fried LF , Emanuele N , Zhang JH , Brophy M , Conner TA , Duckworth W , et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy . N Engl J Med 2013 ; 369 : 1892 – 903 . https://doi.org/10.1056/NEJMoa1303154
Yusuf S , Teo KK , Pogue J , Dyal L , Copland I , Schumacher H , et al. Telmisartan, ramipril, or both in patients at high risk for vascular events . N Engl J Med 2008 ; 358 : 1547 – 59 . https://doi.org/10.1056/NEJMoa0801317
Gupta AK , Arshad S , Poulter NR . Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis . Hypertension 2010 ; 55 : 399 – 407 . https://doi.org/10.1161/hypertensionaha.109.139816
Gnanenthiran SR , Wang N , Di Tanna GL , Salam A , Webster R , de Silva HA , et al. Association of low-dose triple combination therapy vs usual care with time at target blood pressure: a secondary analysis of the TRIUMPH randomized clinical trial . JAMA Cardiol 2022 ; 7 : 645 – 50 . https://doi.org/10.1001/jamacardio.2022.0471
Tam TS , Wu MH , Masson SC , Tsang MP , Stabler SN , Kinkade A , et al. Eplerenone for hypertension . Cochrane Database Syst Rev 2017 ; 2 : CD008996 . https://doi.org/10.1002/14651858.CD008996.pub2
Pedersen ME , Cockcroft JR . The vasodilatory beta-blockers . Curr Hypertens Rep 2007 ; 9 : 269 – 77 . https://doi.org/10.1007/s11906-007-0050-2
Sica DA . Minoxidil: an underused vasodilator for resistant or severe hypertension . J Clin Hypertens (Greenwich) 2004 ; 6 : 283 – 7 . https://doi.org/10.1111/j.1524-6175.2004.03585.x
Muñoz D , Uzoije P , Reynolds C , Miller R , Walkley D , Pappalardo S , et al. Polypill for cardiovascular disease prevention in an underserved population . N Engl J Med 2019 ; 381 : 1114 – 23 . https://doi.org/10.1056/NEJMoa1815359
Castellano JM , Pocock SJ , Bhatt DL , Quesada AJ , Owen R , Fernandez-Ortiz A , et al. Polypill strategy in secondary cardiovascular prevention . N Engl J Med 2022 ; 387 : 967 – 77 . https://doi.org/10.1056/NEJMoa2208275
González-Juanatey JR , Cordero A , Castellano JM , Masana L , Dalmau R , Ruiz E , et al. The CNIC-polypill reduces recurrent major cardiovascular events in real-life secondary prevention patients in Spain: the NEPTUNO study . Int J Cardiol 2022 ; 361 : 116 – 23 . https://doi.org/10.1016/j.ijcard.2022.05.015
Jowett S , Barton P , Roalfe A , Fletcher K , Hobbs FDR , McManus RJ , et al. Cost-effectiveness analysis of use of a polypill versus usual care or best practice for primary prevention in people at high risk of cardiovascular disease . PLoS One 2017 ; 12 : e0182625 . https://doi.org/10.1371/journal.pone.0182625
McManus RJ , Mant J , Bray EP , Holder R , Jones MI , Greenfield S , et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial . Lancet 2010 ; 376 : 163 – 72 . https://doi.org/10.1016/s0140-6736(10)60964-6
Clark CE , Smith LF , Taylor RS , Campbell JL . Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis . BMJ 2010 ; 341 : c3995 . https://doi.org/10.1136/bmj.c3995
Mackenzie IS , Rogers A , Poulter NR , Williams B , Brown MJ , Webb DJ , et al. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial . Lancet 2022 ; 400 : 1417 – 25 . https://doi.org/10.1016/s0140-6736(22)01786-x
Conn VS , Ruppar TM , Chase JA , Enriquez M , Cooper PS . Interventions to improve medication adherence in hypertensive patients: systematic review and meta-analysis . Curr Hypertens Rep 2015 ; 17 : 94 . https://doi.org/10.1007/s11906-015-0606-5
Corrao G , Parodi A , Zambon A , Heiman F , Filippi A , Cricelli C , et al. Reduced discontinuation of antihypertensive treatment by two-drug combination as first step. Evidence from daily life practice . J Hypertens 2010 ; 28 : 1584 – 90 . https://doi.org/10.1097/HJH.0b013e328339f9fa
Krieger EM , Drager LF , Giorgi DMA , Pereira AC , Barreto-Filho JAS , Nogueira AR , et al. Spironolactone versus clonidine as a fourth-drug therapy for resistant hypertension: the ReHOT randomized study (resistant hypertension optimal treatment) . Hypertension 2018 ; 71 : 681 – 90 . https://doi.org/10.1161/hypertensionaha.117.10662
Williams B , MacDonald TM , Morant SV , Webb DJ , Sever P , McInnes GT , et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies . Lancet Diabetes Endocrinol 2018 ; 6 : 464 – 75 . https://doi.org/10.1016/s2213-8587(18)30071-8
Mann JF , Schmieder RE , McQueen M , Dyal L , Schumacher H , Pogue J , et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial . Lancet 2008 ; 372 : 547 – 53 . https://doi.org/10.1016/s0140-6736(08)61236-2
Jones DW , Whelton PK , Allen N , Clark D III , Gidding SS , Muntner P , et al. Management of stage 1 hypertension in adults with a low 10-year risk for cardiovascular disease: filling a guidance gap: a scientific statement from the American Heart Association . Hypertension 2021 ; 77 : e58 – 67 . https://doi.org/10.1161/hyp.0000000000000195
Ali DH , Kiliç B , Hart HE , Bots ML , Biermans MCJ , Spiering W , et al. Therapeutic inertia in the management of hypertension in primary care . J Hypertens 2021 ; 39 : 1238 – 45 . https://doi.org/10.1097/hjh.0000000000002783
Appel LJ , Champagne CM , Harsha DW , Cooper LS , Obarzanek E , Elmer PJ , et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial . JAMA 2003 ; 289 : 2083 – 93 . https://doi.org/10.1001/jama.289.16.2083
Appel LJ , Sacks FM , Carey VJ , Obarzanek E , Swain JF , Miller ER , et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial . JAMA 2005 ; 294 : 2455 – 64 . https://doi.org/10.1001/jama.294.19.2455
Thomopoulos C , Parati G , Zanchetti A . Effects of blood-pressure-lowering treatment on outcome incidence. 12. Effects in individuals with high-normal and normal blood pressure: overview and meta-analyses of randomized trials . J Hypertens 2017 ; 35 : 2150 – 60 . https://doi.org/10.1097/hjh.0000000000001547
Williamson JD , Supiano MA , Applegate WB , Berlowitz DR , Campbell RC , Chertow GM , et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial . JAMA 2016 ; 315 : 2673 – 82 . https://doi.org/10.1001/jama.2016.7050
Beckett N , Peters R , Leonetti G , Duggan J , Fagard R , Thijs L , et al. Subgroup and per-protocol analyses from the hypertension in the very elderly trial . J Hypertens 2014 ; 32 : 1478 – 87 ; discussion 1487. https://doi.org/10.1097/hjh.0000000000000195
Jowett S , Kodabuckus S , Ford GA , Hobbs FDR , Lown M , Mant J , et al. Cost-effectiveness of antihypertensive deprescribing in primary care: a Markov modelling study using data from the OPTiMISE trial . Hypertension 2022 ; 79 : 1122 – 31 . https://doi.org/10.1161/hypertensionaha.121.18726
Odden MC , McClure LA , Sawaya BP , White CL , Peralta CA , Field TS , et al. Achieved blood pressure and outcomes in the secondary prevention of small subcortical strokes trial . Hypertension 2016 ; 67 : 63 – 9 . https://doi.org/10.1161/hypertensionaha.115.06480
Chen T , Shao F , Chen K , Wang Y , Wu Z , Wang Y , et al. Time to clinical benefit of intensive blood pressure lowering in patients 60 years and older with hypertension: a secondary analysis of randomized clinical trials . JAMA Intern Med 2022 ; 182 : 660 – 7 . https://doi.org/10.1001/jamainternmed.2022.1657
Neaton JD , Grimm RH Jr , Prineas RJ , Stamler J , Grandits GA , Elmer PJ , et al. Treatment of mild hypertension study. Final results. Treatment of mild hypertension study research group . JAMA 1993 ; 270 : 713 – 24 . https://doi.org/10.1001/jama.1993.03510060059034
Wu J , Kraja AT , Oberman A , Lewis C , Ellison R , Arnett D , et al. A summary of the effects of antihypertensive medications on measured blood pressure . Am J Hypertens 2005 ; 18 : 935 – 42 . https://doi.org/10.1016/j.amjhyper.2005.01.011
Canoy D , Copland E , Nazarzadeh M , Ramakrishnan R , Pinho-Gomes A-C , Salam A , et al. Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials . Heart 2022 ; 108 : 1281 – 9 . https://doi.org/10.1136/heartjnl-2021-320171
Paz MA , de-La-Sierra A , Sáez M , Barceló MA , Rodríguez JJ , Castro S , et al. Treatment efficacy of anti-hypertensive drugs in monotherapy or combination: ATOM systematic review and meta-analysis of randomized clinical trials according to PRISMA statement . Medicine (Baltimore) 2016 ; 95 : e4071 . https://doi.org/10.1097/md.0000000000004071
Morales-Salinas A , Kones R . Concerning the degradation of β-blocker use in the 2018 ESC/ESH hypertension guidelines . Eur Heart J 2019 ; 40 : 2091 . https://doi.org/10.1093/eurheartj/ehz125
Lindholm LH , Carlberg B , Samuelsson O . Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis . Lancet 2005 ; 366 : 1545 – 53 . https://doi.org/10.1016/s0140-6736(05)67573-3
Larochelle P , Tobe SW , Lacourcière Y . β-Blockers in hypertension: studies and meta-analyses over the years . Can J Cardiol 2014 ; 30 : S16 – 22 . https://doi.org/10.1016/j.cjca.2014.02.012
Reboussin DM , Allen NB , Griswold ME , Guallar E , Hong Y , Lackland DT , et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines . Hypertension 2018 ; 71 : e116 – 35 . https://doi.org/10.1161/hyp.0000000000000067
Wright JM , Musini VM , Gill R . First-line drugs for hypertension . Cochrane Database Syst Rev 2018 ; 4 : CD001841 . https://doi.org/10.1002/14651858.CD001841.pub3
Johnston GD . Dose-response relationships with antihypertensive drugs . Pharmacol Ther 1992 ; 55 : 53 – 93 . https://doi.org/10.1016/0163-7258(92)90029-y
Law MR , Morris JK , Wald NJ . Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies . BMJ 2009 ; 338 : b1665 . https://doi.org/10.1136/bmj.b1665
Messerli FH , Bangalore S , Schmieder RE . Wilder’s principle: pre-treatment value determines post-treatment response . Eur Heart J 2015 ; 36 : 576 – 9 . https://doi.org/10.1093/eurheartj/ehu467
Lasserson DS , Buclin T , Glasziou P . How quickly should we titrate antihypertensive medication? Systematic review modelling blood pressure response from trial data . Heart 2011 ; 97 : 1771 – 5 . https://doi.org/10.1136/hrt.2010.221473
Thomopoulos C , Parati G , Zanchetti A . Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials . J Hypertens 2014 ; 32 : 2285 – 95 . https://doi.org/10.1097/hjh.0000000000000378
Verdecchia P , Staessen JA , Angeli F , de Simone G , Achilli A , Ganau A , et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial . Lancet 2009 ; 374 : 525 – 33 . https://doi.org/10.1016/s0140-6736(09)61340-4
Benavente OR , Coffey CS , Conwit R , Hart RG , McClure LA , Pearce LA , et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial . Lancet 2013 ; 382 : 507 – 15 . https://doi.org/10.1016/s0140-6736(13)60852-1
Vaduganathan M , Claggett BL , Juraschek SP , Solomon SD . Assessment of long-term benefit of intensive blood pressure control on residual life span: secondary analysis of the Systolic Blood Pressure Intervention Trial (SPRINT) . JAMA Cardiol 2020 ; 5 : 576 – 81 . https://doi.org/10.1001/jamacardio.2019.6192
Lewis CE , Fine LJ , Beddhu S , Cheung AK , Cushman WC , Cutler JA , et al. Final report of a trial of intensive versus standard blood-pressure control . N Engl J Med 2021 ; 384 : 1921 – 30 . https://doi.org/10.1056/NEJMoa1901281
Beddhu S , Chertow GM , Cheung AK , Cushman WC , Rahman M , Greene T , et al. Influence of baseline diastolic blood pressure on effects of intensive compared with standard blood pressure control . Circulation 2018 ; 137 : 134 – 43 . https://doi.org/10.1161/circulationaha.117.030848
McEvoy JW , Daya N , Rahman F , Hoogeveen RC , Blumenthal RS , Shah AM , et al. Association of isolated diastolic hypertension as defined by the 2017 ACC/AHA blood pressure guideline with incident cardiovascular outcomes . JAMA 2020 ; 323 : 329 – 38 . https://doi.org/10.1001/jama.2019.21402
Jacobsen AP , Al Rifai M , Arps K , Whelton SP , Budoff MJ , Nasir K , et al. A cohort study and meta-analysis of isolated diastolic hypertension: searching for a threshold to guide treatment . Eur Heart J 2021 ; 42 : 2119 – 29 . https://doi.org/10.1093/eurheartj/ehab111
McEvoy JW , Yang WY , Thijs L , Zhang Z-Y , Melgarejo JD , Boggia J , et al. Isolated diastolic hypertension in the IDACO study: an age-stratified analysis using 24-hour ambulatory blood pressure measurements . Hypertension 2021 ; 78 : 1222 – 31 . https://doi.org/10.1161/hypertensionaha.121.17766
Albasri A , Hattle M , Koshiaris C , Dunnigan A , Paxton B , Fox SE , et al. Association between antihypertensive treatment and adverse events: systematic review and meta-analysis . BMJ 2021 ; 372 : n189 . https://doi.org/10.1136/bmj.n189
Savoia C , Volpe M , Grassi G , Borghi C , Agabiti Rosei E , Touyz RM , et al. Personalized medicine-a modern approach for the diagnosis and management of hypertension . Clin Sci (Lond) 2017 ; 131 : 2671 – 85 . https://doi.org/10.1042/cs20160407
Egan BM , Basile JN , Rehman SU , Davis PB , Grob CH 3rd , Riehle JF , et al. Plasma renin test–guided drug treatment algorithm for correcting patients with treated but uncontrolled hypertension: a randomized controlled trial . Am J Hypertens 2009 ; 22 : 792 – 801 . https://doi.org/10.1038/ajh.2009.63
Huang KY , Tseng PT , Wu YC , Tu Y-K , Stubbs B , Su K-P , et al. Do beta-adrenergic blocking agents increase asthma exacerbation? A network meta-analysis of randomized controlled trials . Sci Rep 2021 ; 11 : 452 . https://doi.org/10.1038/s41598-020-79837-3
Bennett M , Chang CL , Tatley M , Savage R , Hancox RJ . The safety of cardioselective β 1 - blockers in asthma: literature review and search of global pharmacovigilance safety reports . ERJ Open Res 2021 ; 7 : 00801-2020 . https://doi.org/10.1183/23120541.00801-2020
Assimes TL , Elstein E , Langleben A , Suissa S . Long-term use of antihypertensive drugs and risk of cancer . Pharmacoepidemiol Drug Saf 2008 ; 17 : 1039 – 49 . https://doi.org/10.1002/pds.1656
Zhang Y , Song M , Chan AT , Meyerhardt JA , Willett WC , Giovannucci EL . Long-term use of antihypertensive medications, hypertension and colorectal cancer risk and mortality: a prospective cohort study . Br J Cancer 2022 ; 127 : 1974 – 82 . https://doi.org/10.1038/s41416-022-01975-4
Grossman E , Messerli FH . Long-term safety of antihypertensive therapy . Prog Cardiovasc Dis 2006 ; 49 : 16 – 25 . https://doi.org/10.1016/j.pcad.2006.06.002
Parati G , Stergiou GS , Dolan E , Bilo G . Blood pressure variability: clinical relevance and application . J Clin Hypertens (Greenwich) 2018 ; 20 : 1133 – 7 . https://doi.org/10.1111/jch.13304
Schutte AE , Kollias A , Stergiou GS . Blood pressure and its variability: classic and novel measurement techniques . Nat Rev Cardiol 2022 ; 19 : 643 – 54 . https://doi.org/10.1038/s41569-022-00690-0
Lauder L , Azizi M , Kirtane AJ , Böhm M , Mahfoud F . Device-based therapies for arterial hypertension . Nat Rev Cardiol 2020 ; 17 : 614 – 28 . https://doi.org/10.1038/s41569-020-0364-1
Mahfoud F , Schlaich MP , Lobo MD . Device therapy of hypertension . Circ Res 2021 ; 128 : 1080 – 99 . https://doi.org/10.1161/circresaha.121.318091
DiBona GF . Sympathetic nervous system and hypertension . Hypertension 2013 ; 61 : 556 – 60 . https://doi.org/10.1161/hypertensionaha.111.00633
DiBona GF , Esler M . Translational medicine: the antihypertensive effect of renal denervation . Am J Physiol Regul Integr Comp Physiol 2010 ; 298 : R245 – 253 . https://doi.org/10.1152/ajpregu.00647.2009
Böhm M , Kario K , Kandzari DE , Mahfoud F , Weber MA , Schmieder RE , et al. Efficacy of catheter-based renal denervation in the absence of antihypertensive medications (SPYRAL HTN-OFF MED Pivotal): a multicentre, randomised, sham-controlled trial . Lancet 2020 ; 395 : 1444 – 51 . https://doi.org/10.1016/s0140-6736(20)30554-7
Weber MA , Kirtane AJ , Weir MR , Radhakrishnan J , Das T , Berk M , et al. The REDUCE HTN: R EINFORCE: randomized, sham-controlled trial of bipolar radiofrequency renal denervation for the treatment of hypertension . JACC Cardiovasc Interv 2020 ; 13 : 461 – 70 . https://doi.org/10.1016/j.jcin.2019.10.061
Kandzari DE , Böhm M , Mahfoud F , Townsend RR , Weber MA , Pocock S , et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial . Lancet 2018 ; 391 : 2346 – 55 . https://doi.org/10.1016/s0140-6736(18)30951-6
Azizi M , Schmieder RE , Mahfoud F , Weber MA , Daemen J , Davies J , et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial . Lancet 2018 ; 391 : 2335 – 45 . https://doi.org/10.1016/s0140-6736(18)31082-1
Azizi M , Sanghvi K , Saxena M , Gosse P , Reilly JP , Levy T , et al. Ultrasound renal denervation for hypertension resistant to a triple medication pill (RADIANCE-HTN TRIO): a randomised, multicentre, single-blind, sham-controlled trial . Lancet 2021 ; 397 : 2476 – 86 . https://doi.org/10.1016/s0140-6736(21)00788-1
Mahfoud F , Böhm M , Schmieder R , Narkiewicz K , Ewen S , Ruilope L , et al. Effects of renal denervation on kidney function and long-term outcomes: 3-year follow-up from the global SYMPLICITY registry . Eur Heart J 2019 ; 40 : 3474 – 82 . https://doi.org/10.1093/eurheartj/ehz118
Bhatt DL , Vaduganathan M , Kandzari DE , Leon MB , Rocha-Singh K , Townsend RR , et al. Long-term outcomes after catheter-based renal artery denervation for resistant hypertension: final follow-up of the randomised SYMPLICITY HTN-3 trial . Lancet 2022 ; 400 : 1405 – 16 . https://doi.org/10.1016/s0140-6736(22)01787-1
Mahfoud F , Kandzari DE , Kario K , Townsend RR , Weber MA , Schmieder RE , et al. Long-term efficacy and safety of renal denervation in the presence of antihypertensive drugs (SPYRAL HTN-ON MED): a randomised, sham-controlled trial . Lancet 2022 ; 399 : 1401 – 10 . https://doi.org/10.1016/s0140-6736(22)00455-x
Rader F , Kirtane AJ , Wang Y , Daemen J , Lurz P , Sayer J , et al. Durability of blood pressure reduction after ultrasound renal denervation: three-year follow-up of the treatment arm of the randomised RADIANCE-HTN SOLO trial . EuroIntervention 2022 ; 18 : e677 – 85 . https://doi.org/10.4244/eij-d-22-00305
Al Ghorani H , Kulenthiran S , Recktenwald MJM , Lauder L , Kunz M , Götzinger F , et al. 10-year outcomes of catheter-based renal denervation in patients with resistant hypertension . J Am Coll Cardiol 2023 ; 81 : 517 – 9 . https://doi.org/10.1016/j.jacc.2022.11.038
Stone P , Campbell J , Thompson S , Walker J . A prospective, randomized study comparing ultrasound versus fluoroscopic guided femoral arterial access in noncardiac vascular patients . J Vasc Surg 2020 ; 72 : 259 – 67 . https://doi.org/10.1016/j.jvs.2019.09.051
Jolly SS , Yusuf S , Cairns J , Niemelä K , Xavier D , Widimsky P , et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial . Lancet 2011 ; 377 : 1409 – 20 . https://doi.org/10.1016/s0140-6736(11)60404-2
Townsend RR , Walton A , Hettrick DA , Hickey GL , Weil J , Sharp ASP , et al. Review and meta-analysis of renal artery damage following percutaneous renal denervation with radiofrequency renal artery ablation . EuroIntervention 2020 ; 16 : 89 – 96 . https://doi.org/10.4244/eij-d-19-00902
Sanders MF , Reitsma JB , Morpey M , Gremmels H , Bots ML , Pisano A , et al. Renal safety of catheter-based renal denervation: systematic review and meta-analysis . Nephrol Dial Transplant 2017 ; 32 : 1440 – 7 . https://doi.org/10.1093/ndt/gfx088
Ahmad Y , Francis DP , Bhatt DL , Howard JP . Renal denervation for hypertension: a systematic review and meta-analysis of randomized, blinded, placebo-controlled trials . JACC Cardiovasc Interv 2021 ; 14 : 2614 – 24 . https://doi.org/10.1016/j.jcin.2021.09.020
Chowdhury EK , Reid CM , Zomer E , Kelly DJ , Liew D . Cost-effectiveness of renal denervation therapy for treatment-resistant hypertension: a best case scenario . Am J Hypertens 2018 ; 31 : 1156 – 63 . https://doi.org/10.1093/ajh/hpy108
Sharp ASP , Cao KN , Esler MD , Kandzari DE , Lobo MD , Schmieder RE , et al. Cost-effectiveness of catheter-based radiofrequency renal denervation for the treatment of uncontrolled hypertension: an analysis for the UK based on recent clinical evidence . Eur Heart J Qual Care Clin Outcomes 2024 : qcae001 . https://doi.org/10.1093/ehjqcco/qcae001
Fengler K , Reimann P , Rommel KP , Kresoja K-P , Blazek S , Unterhuber M , et al. Comparison of long-term outcomes for responders versus non-responders following renal denervation in resistant hypertension . J Am Heart Assoc 2021 ; 10 : e022429 . https://doi.org/10.1161/jaha.121.022429
Mahfoud F , Mancia G , Schmieder RE , Ruilope L , Narkiewicz K , Schlaich M , et al. Cardiovascular risk reduction after renal denervation according to time in therapeutic systolic blood pressure range . J Am Coll Cardiol 2022 ; 80 : 1871 – 80 . https://doi.org/10.1016/j.jacc.2022.08.802
Byrne RA , Rossello X , Coughlan JJ , Barbato E , Berry C , Chieffo A , et al. ESC guidelines for the management of acute coronary syndromes . Eur Heart J 2023 ; 44 : 3720 – 826 . https://doi.org/10.1093/eurheartj/ehad191
Singh RR , Denton KM . Renal denervation . Hypertension 2018 ; 72 : 528 – 36 . https://doi.org/10.1161/hypertensionaha.118.10265
Barbato E , Azizi M , Schmieder RE , Lauder L , Böhm M , Brouwers S , et al. Renal denervation in the management of hypertension in adults. A clinical consensus statement of the ESC Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) . Eur Heart J 2023 ; 44 : 1313 – 30 . https://doi.org/10.1093/eurheartj/ehad054
Bhatt DL , Kandzari DE , O’Neill WW , D’Agostino R , Flack JM , Katzen BT , et al. A controlled trial of renal denervation for resistant hypertension . N Engl J Med 2014 ; 370 : 1393 – 401 . https://doi.org/10.1056/NEJMoa1402670
Desch S , Okon T , Heinemann D , Kulle K , Röhnert K , Sonnabend M , et al. Randomized sham-controlled trial of renal sympathetic denervation in mild resistant hypertension . Hypertension 2015 ; 65 : 1202 – 8 . https://doi.org/10.1161/hypertensionaha.115.05283
Mathiassen ON , Vase H , Bech JN , Christensen KL , Buus NH , Schroeder AP , et al. Renal denervation in treatment-resistant essential hypertension. A randomized, SHAM-controlled, double-blinded 24–h blood pressure-based trial . J Hypertens 2016 ; 34 : 1639 – 47 . https://doi.org/10.1097/hjh.0000000000000977
Townsend RR , Mahfoud F , Kandzari DE , Kario K , Pocock S , Weber MA , et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial . Lancet 2017 ; 390 : 2160 – 70 . https://doi.org/10.1016/s0140-6736(17)32281-x
Kario K , Yokoi Y , Okamura K , Fujihara M , Ogoyama Y , Yamamoto E , et al. Catheter-based ultrasound renal denervation in patients with resistant hypertension: the randomized, controlled REQUIRE trial . Hypertens Res 2022 ; 45 : 221 – 31 . https://doi.org/10.1038/s41440-021-00754-7
Neuzil P , Merkely B , Erglis A , Marinskis G , de Groot JR , Schmidinger H , et al. Pacemaker-mediated programmable hypertension control therapy . J Am Heart Assoc 2017 ; 6 : e006974 . https://doi.org/10.1161/jaha.117.006974
Kalarus Z , Merkely B , Neužil P , Grabowski M , Mitkowski P , Marinskis G , et al. Pacemaker-based cardiac neuromodulation therapy in patients with hypertension: a pilot study . J Am Heart Assoc 2021 ; 10 : e020492 . https://doi.org/10.1161/jaha.120.020492
Musini VM , Tejani AM , Bassett K , Puil L , Wright JM . Pharmacotherapy for hypertension in adults 60 years or older . Cochrane Database Syst Rev 2019 ; 6 : CD000028 . https://doi.org/10.1002/14651858.CD000028.pub3
Musini VM , Gueyffier F , Puil L , Salzwedel DM , Wright JM . Pharmacotherapy for hypertension in adults aged 18 to 59 years . Cochrane Database Syst Rev 2017 ; 8 : CD008276 . https://doi.org/10.1002/14651858.CD008276.pub2
Thomopoulos C , Parati G , Zanchetti A . Effects of blood-pressure-lowering treatment in hypertension: 9. Discontinuations for adverse events attributed to different classes of antihypertensive drugs: meta-analyses of randomized trials . J Hypertens 2016 ; 34 : 1921 – 32 . https://doi.org/10.1097/hjh.0000000000001052
Benetos A , Petrovic M , Strandberg T . Hypertension management in older and frail older patients . Circ Res 2019 ; 124 : 1045 – 60 . https://doi.org/10.1161/circresaha.118.313236
Frey L , Gravestock I , Pichierri G , Steurer J , Burgstaller JM . Serious adverse events in patients with target-oriented blood pressure management: a systematic review . J Hypertens 2019 ; 37 : 2135 – 44 . https://doi.org/10.1097/hjh.0000000000002176
Palmer SC , Sciancalepore M , Strippoli GF . Trial quality in nephrology: how are we measuring up? Am J Kidney Dis 2011 ; 58 : 335 – 7 . https://doi.org/10.1053/j.ajkd.2011.06.006
Carriazo S , Sarafidis P , Ferro CJ , Ortiz A . Blood pressure targets in CKD 2021: the never-ending guidelines debacle . Clin Kidney J 2022 ; 15 : 845 – 51 . https://doi.org/10.1093/ckj/sfac014
Kessler A , Sollie S , Challacombe B , Briggs K , Van Hemelrijck M . The global prevalence of erectile dysfunction: a review . BJU Int 2019 ; 124 : 587 – 99 . https://doi.org/10.1111/bju.14813
Doumas M , Douma S . The effect of antihypertensive drugs on erectile function: a proposed management algorithm . J Clin Hypertens (Greenwich) 2006 ; 8 : 359 – 64 . https://doi.org/10.1111/j.1524-6175.2005.05285.x
Ismail SB , Noor NM , Hussain NHN , Sulaiman Z , Shamsudin MA , Irfan M . Angiotensin receptor blockers for erectile dysfunction in hypertensive men: a brief meta-analysis of randomized control trials . Am J Mens Health 2019 ; 13 :1557988319892735. https://doi.org/10.1177/1557988319892735
Lawson AJ , Hameed MA , Brown R , Cappuccio FP , George S , Hinton T , et al. Nonadherence to antihypertensive medications is related to pill burden in apparent treatment-resistant hypertensive individuals . J Hypertens 2020 ; 38 : 1165 – 73 . https://doi.org/10.1097/hjh.0000000000002398
Choudhry NK , Kronish IM , Vongpatanasin W , Ferdinand KC , Pavlik VN , Egan BM , et al. Medication adherence and blood pressure control: a scientific statement from the American heart association . Hypertension 2022 ; 79 : e1 – 14 . https://doi.org/10.1161/hyp.0000000000000203
Liao CT , Toh HS , Sun L , Yang C-T , Hu A , Wei D , et al. Cost-effectiveness of intensive vs standard blood pressure control among older patients with hypertension . JAMA Netw Open 2023 ; 6 : e230708 . https://doi.org/10.1001/jamanetworkopen.2023.0708
O’Donoghue P , O’Halloran AM , Kenny RA , Romero-Ortuno R . Do the frail experience more adverse events from intensive blood pressure control? A 2-year prospective study in the Irish Longitudinal Study on Ageing (TILDA) . EClinicalMedicine 2022 ; 45 : 101304 . https://doi.org/10.1016/j.eclinm.2022.101304
Sexton DJ , Canney M , O’Connell MDL , Moore P , Little MA , O’Seaghdha CM , et al. Injurious falls and syncope in older community-dwelling adults meeting inclusion criteria for SPRINT . JAMA Intern Med 2017 ; 177 : 1385 – 7 . https://doi.org/10.1001/jamainternmed.2017.2924
Masoli JAH , Sheppard JP , Rajkumar C . Hypertension management in older patients-are the guideline blood pressure targets appropriate? Age Ageing 2022 ; 51 : afab226 . https://doi.org/10.1093/ageing/afab226
Richter D , Guasti L , Walker D , Lambrinou E , Lionis C , Abreu A , et al. Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute Cardio Vascular Care (ACVC), Association of Cardiovascular Nursing and Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG) Aorta and Peripheral Vascular Diseases, WG e-Cardiology, WG Thrombosis, of the European Society of Cardiology, European Primary Care Cardiology Society (EPCCS) . Eur J Prev Cardiol 2022 ; 29 : 216 – 27 . https://doi.org/10.1093/eurjpc/zwaa167
Hughes D , Judge C , Murphy R , Loughlin E , Costello M , Whiteley W , et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta-analysis . JAMA 2020 ; 323 : 1934 – 44 . https://doi.org/10.1001/jama.2020.4249
Peters R , Xu Y , Fitzgerald O , Aung HL , Beckett N , Bulpitt C , et al. Blood pressure lowering and prevention of dementia: an individual patient data meta-analysis . Eur Heart J 2022 ; 43 : 4980 – 90 . https://doi.org/10.1093/eurheartj/ehac584
Pathak A , Poulter NR , Kavanagh M , Kreutz R , Burnier M . Improving the management of hypertension by tackling awareness, adherence, and clinical inertia: a symposium report . Am J Cardiovasc Drugs 2022 ; 22 : 251 – 61 . https://doi.org/10.1007/s40256-021-00505-6
Sheppard JP , Lown M , Burt J , Temple E , Lowe R , Ashby H , et al. Generalizability of blood pressure lowering trials to older patients: cross-sectional analysis . J Am Geriatr Soc 2020 ; 68 : 2508 – 15 . https://doi.org/10.1111/jgs.16749
Thomopoulos C , Parati G , Zanchetti A . Effects of blood pressure lowering treatment in hypertension: 8. Outcome reductions vs. discontinuations because of adverse drug events—meta-analyses of randomized trials . J Hypertens 2016 ; 34 : 1451 – 63 . https://doi.org/10.1097/hjh.0000000000000972
Jordan J , Tank J , Reuter H . Risk-benefit assessment of intense blood pressure lowering . Hypertension 2019 ; 74 : 1302 – 4 . https://doi.org/10.1161/hypertensionaha.119.13835
Rietz H , Pennlert J , Nordström P , Brunström M . Prevalence, time-trends and clinical characteristics of hypertension in young adults: nationwide cross-sectional study of 1.7 million Swedish 18-year-olds, 1969–2010 . J Hypertens 2022 ; 40 : 1231 – 8 . https://doi.org/10.1097/hjh.0000000000003141
Ostchega Y , Fryar CD , Nwankwo T , Nguyen DT . Hypertension prevalence among adults aged 18 and over: United States, 2017–2018 . NCHS Data Brief 2020 ; 364 : 1 – 8 .
O’Neil A , Scovelle AJ , Milner AJ , Kavanagh A . Gender/sex as a social determinant of cardiovascular risk . Circulation 2018 ; 137 : 854 – 64 . https://doi.org/10.1161/circulationaha.117.028595
Bruno RM , Pucci G , Rosticci M , Guarino L , Guglielmo C , Agabiti Rosei C , et al. Association between lifestyle and systemic arterial hypertension in young adults: a national, survey-based, cross-sectional study . High Blood Press Cardiovasc Prev 2016 ; 23 : 31 – 40 . https://doi.org/10.1007/s40292-016-0135-6
Suzuki Y , Kaneko H , Yano Y , Okada A , Itoh H , Matsuoka S , et al. Association of cardiovascular health metrics with risk of transition to hypertension in non-hypertensive young adults . Am J Hypertens 2022 ; 35 : 858 – 66 . https://doi.org/10.1093/ajh/hpac057
Haggart RC , Bartels CM , Smith MA , Johnson HM . Sociodemographics and hypertension control among young adults with incident hypertension: a multidisciplinary group practice observational study . J Hypertens 2018 ; 36 : 2425 – 33 . https://doi.org/10.1097/hjh.0000000000001872
Liu J , Bu X , Wei L , Wang X , Lai L , Dong C , et al. Global burden of cardiovascular diseases attributable to hypertension in young adults from 1990 to 2019 . J Hypertens 2021 ; 39 : 2488 – 96 . https://doi.org/10.1097/hjh.0000000000002958
Zhang Y , Moran AE . Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014 . Hypertension 2017 ; 70 : 736 – 42 . https://doi.org/10.1161/hypertensionaha.117.09801
Yano Y , Stamler J , Garside DB , Daviglus ML , Franklin SS , Carnethon MR , et al. Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality: the Chicago Heart Association Detection Project in Industry study . J Am Coll Cardiol 2015 ; 65 : 327 – 35 . https://doi.org/10.1016/j.jacc.2014.10.060
Noilhan C , Barigou M , Bieler L , Amar J , Chamontin B , Bouhanick B , et al. Causes of secondary hypertension in the young population: a monocentric study . Ann Cardiol Angeiol (Paris) 2016 ; 65 : 159 – 64 . https://doi.org/10.1016/j.ancard.2016.04.016
Jones ESW , Esack I , Mangena P , Rayner BL . Hypertension in adolescents and young adults referred to a tertiary hypertension clinic in Cape Town, South Africa . Medicine (Baltimore) 2020 ; 99 : e23137 . https://doi.org/10.1097/md.0000000000023137
Chasan-Taber L , Willett WC , Manson JE , Spiegelman D , Hunter DJ , Curhan G , et al. Prospective study of oral contraceptives and hypertension among women in the United States . Circulation 1996 ; 94 : 483 – 9 . https://doi.org/10.1161/01.cir.94.3.483
Lubianca JN , Faccin CS , Fuchs FD . Oral contraceptives: a risk factor for uncontrolled blood pressure among hypertensive women . Contraception 2003 ; 67 : 19 – 24 . https://doi.org/10.1016/s0010-7824(02)00429-8
The American College of Obstetricians and Gynecologists . ACOG practice bulletin No. 206: use of hormonal contraception in women with coexisting medical conditions . Obstet Gynecol 2019 ; 133 : e128 – 50 . https://doi.org/10.1097/aog.0000000000003072
Glisic M , Shahzad S , Tsoli S , Chadni M , Asllanaj E , Rojas LZ , et al. Association between progestin-only contraceptive use and cardiometabolic outcomes: a systematic review and meta-analysis . Eur J Prev Cardiol 2018 ; 25 : 1042 – 52 . https://doi.org/10.1177/2047487318774847
Archer DF , Ahrendt HJ , Drouin D . Drospirenone-only oral contraceptive: results from a multicenter noncomparative trial of efficacy, safety and tolerability . Contraception 2015 ; 92 : 439 – 44 . https://doi.org/10.1016/j.contraception.2015.07.014
Pappaccogli M , Di Monaco S , Warchoł-Celińska E , Lorthioir A , Amar L , Aparicio LS , et al. The European/International Fibromuscular Dysplasia Registry and Initiative (FEIRI)—clinical phenotypes and their predictors based on a cohort of 1000 patients . Cardiovasc Res 2021 ; 117 : 950 – 9 . https://doi.org/10.1093/cvr/cvaa102
Thompson P , Logan I , Tomson C , Sheerin N , Ellam T . Obesity, sex, race, and early onset hypertension: implications for a refined investigation strategy . Hypertension 2020 ; 76 : 859 – 65 . https://doi.org/10.1161/hypertensionaha.120.15557
Saladini F , Fania C , Mos L , Mazzer A , Casiglia E , Palatini P . Office pulse pressure is a predictor of favorable outcome in young- to middle-aged subjects with stage 1 hypertension . Hypertension 2017 ; 70 : 537 – 42 . https://doi.org/10.1161/hypertensionaha.117.09516
Hoeltzenbein M , Tissen-Diabaté T , Fietz AK , Zinke S , Kayser A , Meister R , et al. Increased rate of birth defects after first trimester use of angiotensin converting enzyme inhibitors—treatment or hypertension related? An observational cohort study . Pregnancy Hypertens 2018 ; 13 : 65 – 71 . https://doi.org/10.1016/j.preghy.2018.04.022
Ahmed B , Tran DT , Zoega H , Kennedy SE , Jorm LR , Havard A . Maternal and perinatal outcomes associated with the use of renin-angiotensin system (RAS) blockers for chronic hypertension in early pregnancy . Pregnancy Hypertens 2018 ; 14 : 156 – 61 . https://doi.org/10.1016/j.preghy.2018.09.010
Cífková R , Johnson MR , Kahan T , Brguljan J , Williams B , Coca A , et al. Peripartum management of hypertension: a position paper of the ESC Council on Hypertension and the European Society of Hypertension . Eur Heart J Cardiovasc Pharmacother 2020 ; 6 : 384 – 93 . https://doi.org/10.1093/ehjcvp/pvz082
Magee LA , Brown MA , Hall DR , Gupte S , Hennessy A , Karumanchi SA , et al. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice . Pregnancy Hypertens 2022 ; 27 : 148 – 69 . https://doi.org/10.1016/j.preghy.2021.09.008
Kassebaum NJ , Barber RM , Bhutta ZA , Dandona L , Gething PW , Hay SI , et al. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015 . The Lancet 2016 ; 388 : 1775 – 812 . https://doi.org/10.1016/S0140-6736(16)31470-2
Garovic VD , White WM , Vaughan L , Saiki M , Parashuram S , Garcia-Valencia O , et al. Incidence and long-term outcomes of hypertensive disorders of pregnancy . J Am Coll Cardiol 2020 ; 75 : 2323 – 34 . https://doi.org/10.1016/j.jacc.2020.03.028
Heida KY , Franx A , van Rijn BB , Eijkemans MJC , Boer JMA , Verschuren MWM , et al. Earlier age of onset of chronic hypertension and type 2 diabetes mellitus after a hypertensive disorder of pregnancy or gestational diabetes mellitus . Hypertension 2015 ; 66 : 1116 – 22 . https://doi.org/10.1161/hypertensionaha.115.06005
Garovic VD , Bailey KR , Boerwinkle E , Hunt SC , Weder AB , Curb D , et al. Hypertension in pregnancy as a risk factor for cardiovascular disease later in life . J Hypertens 2010 ; 28 : 826 – 33 . https://doi.org/10.1097/HJH.0b013e328335c29a
Brown MA , Magee LA , Kenny LC , Karumanchi SA , McCarthy FP , Saito S , et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice . Hypertension 2018 ; 72 : 24 – 43 . https://doi.org/10.1161/hypertensionaha.117.10803
Homer CS , Brown MA , Mangos G , Davis GK . Non-proteinuric pre-eclampsia: a novel risk indicator in women with gestational hypertension . J Hypertens 2008 ; 26 : 295 – 302 . https://doi.org/10.1097/HJH.0b013e3282f1a953
Davis GK , Roberts LM , Mangos GJ , Brown MA . Comparisons of auscultatory hybrid and automated sphygmomanometers with mercury sphygmomanometry in hypertensive and normotensive pregnant women: parallel validation studies . J Hypertens 2015 ; 33 : 499 – 505 ; discussion 505–496. https://doi.org/10.1097/hjh.0000000000000420
Schmella MJ , Clifton RG , Althouse AD , Roberts JM . Uric acid determination in gestational hypertension: is it as effective a delineator of risk as proteinuria in high-risk women? Reprod Sci 2015 ; 22 : 1212 – 9 . https://doi.org/10.1177/1933719115572477
Rolnik DL , Wright D , Poon LC , O’Gorman N , Syngelaki A , de Paco Matallana C , et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia . N Engl J Med 2017 ; 377 : 613 – 22 . https://doi.org/10.1056/NEJMoa1704559
Chappell LC , Shennan AH . Assessment of proteinuria in pregnancy . BMJ 2008 ; 336 : 968 – 9 . https://doi.org/10.1136/bmj.39540.657928.BE
Jeon HR , Jeong DH , Lee JY , Woo EY , Shin GT , Kim S-Y . sFlt-1/PlGF ratio as a predictive and prognostic marker for preeclampsia . J Obstet Gynaecol Res 2021 ; 47 : 2318 – 23 . https://doi.org/10.1111/jog.14815
Bateman BT , Bansil P , Hernandez-Diaz S , Mhyre JM , Callaghan WM , Kuklina EV . Prevalence, trends, and outcomes of chronic hypertension: a nationwide sample of delivery admissions . Am J Obstet Gynecol 2012 ; 206 : 134.e1 – 8 . https://doi.org/10.1016/j.ajog.2011.10.878
Zhou J , Azizan EAB , Cabrera CP , Fernandes-Rosa FL , Boulkroun S , Argentesi G , et al. Somatic mutations of GNA11 and GNAQ in CTNNB1-mutant aldosterone-producing adenomas presenting in puberty, pregnancy or menopause . Nat Genet 2021 ; 53 : 1360 – 72 . https://doi.org/10.1038/s41588-021-00906-y
Lenders JWM , Langton K , Langenhuijsen JF , Eisenhofer G . Pheochromocytoma and pregnancy . Endocrinol Metab Clin North Am 2019 ; 48 : 605 – 17 . https://doi.org/10.1016/j.ecl.2019.05.006
Bancos I , Atkinson E , Eng C , Young WF Jr , Neumann HPH , Yukina M , et al. Maternal and fetal outcomes in phaeochromocytoma and pregnancy: a multicentre retrospective cohort study and systematic review of literature . Lancet Diabetes Endocrinol 2021 ; 9 : 13 – 21 . https://doi.org/10.1016/s2213-8587(20)30363-6
Martínez-Vizcaíno V , Sanabria-Martínez G , Fernández-Rodríguez R , Cavero-Redondo I , Pascual-Morena C , Álvarez-Bueno C , et al. Exercise during pregnancy for preventing gestational diabetes mellitus and hypertensive disorders: an umbrella review of randomised controlled trials and an updated meta-analysis . Bjog 2023 ; 130 : 264 – 75 . https://doi.org/10.1111/1471-0528.17304
Mottola MF , Davenport MH , Ruchat SM , Davies GA , Poitras VJ , Gray CE , et al. 2019 Canadian guideline for physical activity throughout pregnancy . Br J Sports Med 2018 ; 52 : 1339 – 46 . https://doi.org/10.1136/bjsports-2018-100056
Askie LM , Duley L , Henderson-Smart DJ , Stewart LA . Antiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient data . Lancet 2007 ; 369 : 1791 – 8 . https://doi.org/10.1016/s0140-6736(07)60712-0
Duley L , Meher S , Hunter KE , Seidler AL , Askie LM . Antiplatelet agents for preventing pre-eclampsia and its complications . Cochrane Database Syst Rev 2019 ; 2019 : CD004659 . https://doi.org/10.1002/14651858.CD004659.pub3
Hofmeyr GJ , Lawrie TA , Atallah ÁN , Torloni MR . Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems . Cochrane Database Syst Rev 2018 ; 10 : CD001059 . https://doi.org/10.1002/14651858.CD001059.pub5
Dwarkanath P , Muhihi A , Sudfeld CR , Wylie BJ , Wang M , Perumal N , et al. Two randomized trials of low-dose calcium supplementation in pregnancy . N Engl J Med 2024 ; 390 : 143 – 53 . https://doi.org/10.1056/NEJMoa2307212
Abalos E , Duley L , Steyn DW , Gialdini C . Antihypertensive drug therapy for mild to moderate hypertension during pregnancy . Cochrane Database Syst Rev 2018 ; 10 : CD002252 . https://doi.org/10.1002/14651858.CD002252.pub4
Magee LA , von Dadelszen P , Rey E , Ross S , Asztalos E , Murphy KE , et al. Less-tight versus tight control of hypertension in pregnancy . N Engl J Med 2015 ; 372 : 407 – 17 . https://doi.org/10.1056/NEJMoa1404595
Redman CW . Fetal outcome in trial of antihypertensive treatment in pregnancy . Lancet 1976 ; 2 : 753 – 6 . https://doi.org/10.1016/s0140-6736(76)90597-3
Cockburn J , Moar VA , Ounsted M , Redman CW . Final report of study on hypertension during pregnancy: the effects of specific treatment on the growth and development of the children . Lancet 1982 ; 1 : 647 – 9 . https://doi.org/10.1016/s0140-6736(82)92202-4
Bellos I , Pergialiotis V , Papapanagiotou A , Loutradis D , Daskalakis G . Comparative efficacy and safety of oral antihypertensive agents in pregnant women with chronic hypertension: a network metaanalysis . Am J Obstet Gynecol 2020 ; 223 : 525 – 37 . https://doi.org/10.1016/j.ajog.2020.03.016
Lydakis C , Lip GY , Beevers M , Beevers DG . Atenolol and fetal growth in pregnancies complicated by hypertension . Am J Hypertens 1999 ; 12 : 541 – 7 . https://doi.org/10.1016/s0895-7061(99)00031-x
Sridharan K , Sequeira RP . Drugs for treating severe hypertension in pregnancy: a network meta-analysis and trial sequential analysis of randomized clinical trials . Br J Clin Pharmacol 2018 ; 84 : 1906 – 16 . https://doi.org/10.1111/bcp.13649
Bhat AD , Keasler PM , Kolluru L , Dombrowski MM , Palanisamy A , Singh PM , et al. Treatment of acute-onset hypertension in pregnancy: a network meta-analysis of randomized controlled trials comparing anti-hypertensives and route of administration . Pregnancy Hypertens 2023 ; 34 : 74 – 82 . https://doi.org/10.1016/j.preghy.2023.10.005
Ehikioya E , Okobi OE , Beeko MAE , Abanga R , Abah NNI , Briggs L , et al. Comparing intravenous labetalol and intravenous hydralazine for managing severe gestational hypertension . Cureus 2023 ; 15 : e42332 . https://doi.org/10.7759/cureus.42332
Halpern DG , Weinberg CR , Pinnelas R , Mehta-Lee S , Economy KE , Valente AM , et al. Use of medication for cardiovascular disease during pregnancy: JACC state-of-the-art review . J Am Coll Cardiol 2019 ; 73 : 457 – 76 . https://doi.org/10.1016/j.jacc.2018.10.075
Goel A , Maski MR , Bajracharya S , Wenger JB , Zhang D , Salahuddin S , et al. Epidemiology and mechanisms of de novo and persistent hypertension in the postpartum period . Circulation 2015 ; 132 : 1726 – 33 . https://doi.org/10.1161/circulationaha.115.015721
Behrens I , Basit S , Melbye M , Lykke JA , Wohlfahrt J , Bundgaard H , et al. Risk of post-pregnancy hypertension in women with a history of hypertensive disorders of pregnancy: nationwide cohort study . BMJ 2017 ; 358 : j3078 . https://doi.org/10.1136/bmj.j3078
Barrett PM , McCarthy FP , Evans M , Kublickas M , Perry IJ , Stenvinkel P , et al. Hypertensive disorders of pregnancy and the risk of chronic kidney disease: a Swedish registry-based cohort study . PLoS Med 2020 ; 17 : e1003255 . https://doi.org/10.1371/journal.pmed.1003255
Giorgione V , Ridder A , Kalafat E , Khalil A , Thilaganathan B . Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis . BJOG 2021 ; 128 : 495 – 503 . https://doi.org/10.1111/1471-0528.16545
Benschop L , Duvekot JJ , Versmissen J , van Broekhoven V , Steegers EAP , Roeters van Lennep JE , et al. Blood pressure profile 1 year after severe preeclampsia . Hypertension 2018 ; 71 : 491 – 8 . https://doi.org/10.1161/hypertensionaha.117.10338
Kitt J , Fox R , Frost A , Shanyinde M , Tucker K , Bateman PA , et al. Long-term blood pressure control after hypertensive pregnancy following physician-optimized self-management: the POP-HT randomized clinical trial . JAMA 2023 ; 330 : 1991 – 9 . https://doi.org/10.1001/jama.2023.21523
van Oostwaard MF , Langenveld J , Schuit E , Papatsonis DNM , Brown MA , Byaruhanga RN , et al. Recurrence of hypertensive disorders of pregnancy: an individual patient data metaanalysis . Am J Obstet Gynecol 2015 ; 212 : 624.e1 – 17 . https://doi.org/10.1016/j.ajog.2015.01.009
Brown MA , Mackenzie C , Dunsmuir W , Roberts L , Ikin K , Matthews J , et al. Can we predict recurrence of pre-eclampsia or gestational hypertension? BJOG 2007 ; 114 : 984 – 93 . https://doi.org/10.1111/j.1471-0528.2007.01376.x
Heimberger S , Perdigao JL , Mueller A , Shahul S , Naseem H , Minhas R , et al. Effect of blood pressure control in early pregnancy and clinical outcomes in African American women with chronic hypertension . Pregnancy Hypertens 2020 ; 20 : 102 – 7 . https://doi.org/10.1016/j.preghy.2020.03.008
Salazar MR , Espeche WG , Balbín E , Leiva Sisnieguez CE , Leiva Sisnieguez BC , Stavile RN , et al. Office blood pressure values and the necessity of out-of-office measurements in high-risk pregnancies . J Hypertens 2019 ; 37 : 1838 – 44 . https://doi.org/10.1097/hjh.0000000000002140
Buawangpong N , Teekachunhatean S , Koonrungsesomboon N . Adverse pregnancy outcomes associated with first-trimester exposure to angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers: a systematic review and meta-analysis . Pharmacol Res Perspect 2020 ; 8 : e00644 . https://doi.org/10.1002/prp2.644
Weber-Schoendorfer C , Kayser A , Tissen-Diabaté T , Winterfeld U , Eleftheriou G , Te Winkel B , et al. Fetotoxic risk of AT1 blockers exceeds that of angiotensin-converting enzyme inhibitors: an observational study . J Hypertens 2020 ; 38 : 133 – 41 . https://doi.org/10.1097/hjh.0000000000002233
Chen X , Mao G , Leng SX . Frailty syndrome: an overview . Clin Interv Aging 2014 ; 9 : 433 – 41 . https://doi.org/10.2147/cia.S45300
Rodriguez-Mañas L , Fried LP . Frailty in the clinical scenario . Lancet 2015 ; 385 : e7 – 9 . https://doi.org/10.1016/s0140-6736(14)61595-6
Fried LP , Tangen CM , Walston J , Newman AB , Hirsch C , Gottdiener J , et al. Frailty in older adults: evidence for a phenotype . J Gerontol A Biol Sci Med Sci 2001 ; 56 : M146 – 156 . https://doi.org/10.1093/gerona/56.3.m146
Fried LP , Kronmal RA , Newman AB , Bild DE , Mittelmark MB , Polak JF , et al. Risk factors for 5-year mortality in older adults: the cardiovascular health study . JAMA 1998 ; 279 : 585 – 92 . https://doi.org/10.1001/jama.279.8.585
Martens DS , Thijs L , Latosinska A , Trenson S , Siwy J , Zhang Z-Y , et al. Urinary peptidomic profiles to address age-related disabilities: a prospective population study . Lancet Healthy Longev 2021 ; 2 : e690 – 703 . https://doi.org/10.1016/s2666-7568(21)00226-9
Monahan KD . Effect of aging on baroreflex function in humans . Am J Physiol Regul Integr Comp Physiol 2007 ; 293 : R3 – r12 . https://doi.org/10.1152/ajpregu.00031.2007
Paleczny B , Niewiński P , Rydlewska A , Piepoli MF , Borodulin-Nadzieja L , Jankowska EA , et al. Age-related reflex responses from peripheral and central chemoreceptors in healthy men . Clin Auton Res 2014 ; 24 : 285 – 96 . https://doi.org/10.1007/s10286-014-0263-9
Anker D , Santos-Eggimann B , Zwahlen M , Santschi V , Rodondi N , Wolfson C , et al. Blood pressure in relation to frailty in older adults: a population-based study . J Clin Hypertens (Greenwich) 2019 ; 21 : 1895 – 904 . https://doi.org/10.1111/jch.13722
Ravindrarajah R , Hazra NC , Hamada S , Charlton J , Jackson SHD , Dregan A , et al. Systolic blood pressure trajectory, frailty, and all-cause mortality >80 years of age: cohort study using electronic health records . Circulation 2017 ; 135 : 2357 – 68 . https://doi.org/10.1161/circulationaha.116.026687
Searle SD , Mitnitski A , Gahbauer EA , Gill TM , Rockwood K . A standard procedure for creating a frailty index . BMC Geriatr 2008 ; 8 : 24 . https://doi.org/10.1186/1471-2318-8-24
Clegg A , Bates C , Young J , Ryan R , Nichols L , Ann Teale E , et al. Development and validation of an electronic frailty index using routine primary care electronic health record data . Age Ageing 2016 ; 45 : 353 – 60 . https://doi.org/10.1093/ageing/afw039
Rockwood K , Song X , MacKnight C , Bergman H , Hogan DB , McDowell I , et al. A global clinical measure of fitness and frailty in elderly people . CMAJ 2005 ; 173 : 489 – 95 . https://doi.org/10.1503/cmaj.050051
Nguyen TN , Harris K , Woodward M , Chalmers J , Cooper M , Hamet P , et al. The impact of frailty on the effectiveness and safety of intensive glucose control and blood pressure-lowering therapy for people with type 2 diabetes: results from the ADVANCE trial . Diabetes Care 2021 ; 44 : 1622 – 9 . https://doi.org/10.2337/dc20-2664
Masoli JAH , Delgado J , Pilling L , Strain D , Melzer D . Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality . Age Ageing 2020 ; 49 : 807 – 13 . https://doi.org/10.1093/ageing/afaa028
Aparicio LS , Thijs L , Boggia J , Jacobs L , Barochiner J , Odili AN , et al. Defining thresholds for home blood pressure monitoring in octogenarians . Hypertension 2015 ; 66 : 865 – 73 . https://doi.org/10.1161/hypertensionaha.115.05800
Gaffney B , Jacobsen AP , Pallippattu AW , Leahy N , McEvoy JW . The diastolic blood pressure J-curve in hypertension management: links and risk for cardiovascular disease . Integr Blood Press Control 2021 ; 14 : 179 – 87 . https://doi.org/10.2147/ibpc.S286957
Warwick J , Falaschetti E , Rockwood K , Mitnitski A , Thijs L , Beckett N , et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over . BMC Med 2015 ; 13 : 78 . https://doi.org/10.1186/s12916-015-0328-1
Todd OM , Wilkinson C , Hale M , Wong NL , Hall M , Sheppard JP , et al. Is the association between blood pressure and mortality in older adults different with frailty? A systematic review and meta-analysis . Age Ageing 2019 ; 48 : 627 – 35 . https://doi.org/10.1093/ageing/afz072
Li Y , Thijs L , Zhang ZY , Asayama K , Hansen TW , Boggia J , et al. Opposing age-related trends in absolute and relative risk of adverse health outcomes associated with out-of-office blood pressure . Hypertension 2019 ; 74 : 1333 – 42 . https://doi.org/10.1161/hypertensionaha.119.12958
Beckett NS , Peters R , Fletcher AE , Staessen JA , Liu L , Dumitrascu D , et al. Treatment of hypertension in patients 80 years of age or older . N Engl J Med 2008 ; 358 : 1887 – 98 . https://doi.org/10.1056/NEJMoa0801369
Peters R , Beckett N , McCormack T , Fagard R , Fletcher A , Bulpitt C . Treating hypertension in the very elderly-benefits, risks, and future directions, a focus on the hypertension in the very elderly trial . Eur Heart J 2014 ; 35 : 1712 – 8 . https://doi.org/10.1093/eurheartj/eht464
Travers J , Romero-Ortuno R , Bailey J , Cooney MT . Delaying and reversing frailty: a systematic review of primary care interventions . Br J Gen Pract 2019 ; 69 : e61 – 9 . https://doi.org/10.3399/bjgp18X700241
Bogaerts JMK , von Ballmoos LM , Achterberg WP , Gussekloo J , Streit S , van der Ploeg MA , et al. Do we AGREE on the targets of antihypertensive drug treatment in older adults: a systematic review of guidelines on primary prevention of cardiovascular diseases . Age Ageing 2022 ; 51 : afab192 . https://doi.org/10.1093/ageing/afab192
Sheppard JP , Benetos A , McManus RJ . Antihypertensive deprescribing in older adults: a practical guide . Curr Hypertens Rep 2022 ; 24 : 571 – 80 . https://doi.org/10.1007/s11906-022-01215-3
McDonnell CC , Rogers KC , Regen SM , Finks SW . The Fall Risk with Alpha blockers Given InitiaL dose or Elderly status (FRAGILE) study . Ann Pharmacother 2020 ; 54 : 226 – 31 . https://doi.org/10.1177/1060028019880305
Hiremath S , Ruzicka M , Petrcich W , McCallum MK , Hundemer GL , Tanuseputro P , et al. Alpha-blocker use and the risk of hypotension and hypotension-related clinical events in women of advanced age . Hypertension 2019 ; 74 : 645 – 51 . https://doi.org/10.1161/hypertensionaha.119.13289
Li H , Xu TY , Li Y , Chia Y-C , Buranakitjaroen P , Cheng H-M , et al. Role of α1-blockers in the current management of hypertension . J Clin Hypertens (Greenwich) 2022 ; 24 : 1180 – 6 . https://doi.org/10.1111/jch.14556
Ravindrarajah R , Dregan A , Hazra NC , Hamada S , Jackson SHD , Gulliford MC , et al. Declining blood pressure and intensification of blood pressure management among people over 80 years: cohort study using electronic health records . J Hypertens 2017 ; 35 : 1276 – 82 . https://doi.org/10.1097/hjh.0000000000001291
Chun S , Han K , Lee S , Cho M-H , Jeong S-M , Jung H-W , et al. Impact of frailty on the relationship between blood pressure and cardiovascular diseases and mortality in young-old adults . J Pers Med 2022 ; 12 : 418 . https://doi.org/10.3390/jpm12030418
Khan N , McAlister FA . Re-examining the efficacy of beta-blockers for the treatment of hypertension: a meta-analysis . CMAJ 2006 ; 174 : 1737 – 42 . https://doi.org/10.1503/cmaj.060110
Lavan AH , Gallagher P , Parsons C , O’Mahony D . STOPPFrail (Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy): consensus validation . Age Ageing 2017 ; 46 : 600 – 7 . https://doi.org/10.1093/ageing/afx005
Eeftinck Schattenkerk DW , van Gorp J , Vogt L , Peters RJ , van den Born BH . Isolated systolic hypertension of the young and its association with central blood pressure in a large multi-ethnic population. The HELIUS study . Eur J Prev Cardiol 2018 ; 25 : 1351 – 9 . https://doi.org/10.1177/2047487318777430
Franklin SS , Jacobs MJ , Wong ND , L’Italien GJ , Lapuerta P . Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III . Hypertension 2001 ; 37 : 869 – 74 . https://doi.org/10.1161/01.hyp.37.3.869
Van Bortel LM , Laurent S , Boutouyrie P , Chowienczyk P , Cruickshank JK , De Backer T , et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity . J Hypertens 2012 ; 30 : 445 – 8 . https://doi.org/10.1097/HJH.0b013e32834fa8b0
The Reference Values for Arterial Stiffness Collaboration . Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’ . Eur Heart J 2010 ; 31 : 2338 – 50 . https://doi.org/10.1093/eurheartj/ehq165
Li Y , Wei FF , Thijs L , Boggia J , Asayama K , Hansen TW , et al. Ambulatory hypertension subtypes and 24-hour systolic and diastolic blood pressure as distinct outcome predictors in 8341 untreated people recruited from 12 populations . Circulation 2014 ; 130 : 466 – 74 . https://doi.org/10.1161/circulationaha.113.004876
Staessen JA , Gasowski J , Wang JG , Thijs L , Hond ED , Boissel J-P , et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials . Lancet 2000 ; 355 : 865 – 72 . https://doi.org/10.1016/s0140-6736(99)07330-4
McEniery CM , Yasmin , Wallace S , Maki-Petaja K , McDonnell B , Sharman JE , et al. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults . Hypertension 2005 ; 46 : 221 – 6 . https://doi.org/10.1161/01.HYP.0000165310.84801.e0
Palatini P , Rosei EA , Avolio A , Bilo G , Casiglia E , Ghiadoni L , et al. Isolated systolic hypertension in the young: a position paper endorsed by the European Society of Hypertension . J Hypertens 2018 ; 36 : 1222 – 36 . https://doi.org/10.1097/hjh.0000000000001726
Unger T , Borghi C , Charchar F , Khan NA , Poulter NR , Prabhakaran D , et al. 2020 International Society of Hypertension global hypertension practice guidelines . Hypertension 2020 ; 75 : 1334 – 57 . https://doi.org/10.1161/hypertensionaha.120.15026
Yano Y , Chang Kim H , Lee H , Azahar N , Ahmed S , Kitaoka K , et al. Response to isolated diastolic hypertension and risk of cardiovascular disease: controversies in hypertension—con side of the argument . Hypertension 2022 ; 79 : 1579 . https://doi.org/10.1161/hypertensionaha.122.19493
Jacobsen AP , McKittrick M , Daya N , Al Rifai M , McEvoy JW . Isolated diastolic hypertension and risk of cardiovascular disease: controversies in hypertension—con side of the argument . Hypertension 2022 ; 79 : 1571 – 8 . https://doi.org/10.1161/hypertensionaha.122.18458
Blank SG , Mann SJ , James GD , West JE , Pickering TG . Isolated elevation of diastolic blood pressure. Real or artifactual? Hypertension 1995 ; 26 : 383 – 9 . https://doi.org/10.1161/01.hyp.26.3.383
Cho SMJ , Lee H , Koyama S , Zou RS , Schuermans A , Ganesh S , et al. Cumulative diastolic blood pressure burden in normal systolic blood pressure and cardiovascular disease . Hypertension 2024 ; 81 : 273 – 81 . https://doi.org/10.1161/hypertensionaha.123.22160
Grobman B , Turkson-Ocran RN , Staessen JA , Yu Y-L , Lipsitz LA , Mukamal KJ , et al. Body position and orthostatic hypotension in hypertensive adults: results from the Syst-Eur trial . Hypertension 2023 ; 80 : 820 – 7 . https://doi.org/10.1161/hypertensionaha.122.20602
Juraschek SP , Taylor AA , Wright JT Jr , Evans GW , Miller ER , Plante TB , et al. Orthostatic hypotension, cardiovascular outcomes, and adverse events: results from SPRINT . Hypertension 2020 ; 75 : 660 – 7 . https://doi.org/10.1161/hypertensionaha.119.14309
Juraschek SP , Daya N , Appel LJ , Miller ER , McEvoy JW , Matsushita K , et al. Orthostatic hypotension and risk of clinical and subclinical cardiovascular disease in middle-aged adults . J Am Heart Assoc 2018 ; 7 : e008884 . https://doi.org/10.1161/jaha.118.008884
Fleg JL , Evans GW , Margolis KL , Barzilay J , Basile JN , Bigger JT , et al. Orthostatic hypotension in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) blood pressure trial: prevalence, incidence, and prognostic significance . Hypertension 2016 ; 68 : 888 – 95 . https://doi.org/10.1161/hypertensionaha.116.07474
Juraschek SP , Hu JR , Cluett JL , Ishak A , Mita C , Lipsitz LA , et al. Effects of intensive blood pressure treatment on orthostatic hypotension : a systematic review and individual participant-based meta-analysis . Ann Intern Med 2021 ; 174 : 58 – 68 . https://doi.org/10.7326/m20-4298
Ylitalo A , Airaksinen KE , Sellin L , Huikuri HV . Effects of combination antihypertensive therapy on baroreflex sensitivity and heart rate variability in systemic hypertension . Am J Cardiol 1999 ; 83 : 885 – 9 . https://doi.org/10.1016/s0002-9149(98)01067-4
Ganjehei L , Massumi A , Razavi M , Wilson JM . Orthostatic hypotension as a manifestation of vitamin B12 deficiency . Tex Heart Inst J 2012 ; 39 : 722 – 3 .
Shimbo D , Barrett Bowling C , Levitan EB , Deng L , Sim JJ , Huang L , et al. Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication . Circ Cardiovasc Qual Outcomes 2016 ; 9 : 222 – 9 . https://doi.org/10.1161/circoutcomes.115.002524
Krediet CT , van Lieshout JJ , Bogert LW , Immink RV , Kim Y-S , Wieling W , et al. Leg crossing improves orthostatic tolerance in healthy subjects: a placebo-controlled crossover study . Am J Physiol Heart Circ Physiol 2006 ; 291 : H1768 – 72 . https://doi.org/10.1152/ajpheart.00287.2006
Okamoto LE , Diedrich A , Baudenbacher FJ , Harder R , Whitfield JS , Iqbal F , et al. Efficacy of servo-controlled splanchnic venous compression in the treatment of orthostatic hypotension: a randomized comparison with midodrine . Hypertension 2016 ; 68 : 418 – 26 . https://doi.org/10.1161/hypertensionaha.116.07199
Okamoto LE , Celedonio JE , Smith EC , Gamboa A , Shibao CA , Diedrich A , et al. Local passive heat for the treatment of hypertension in autonomic failure . J Am Heart Assoc 2021 ; 10 : e018979 . https://doi.org/10.1161/jaha.120.018979
Buyken AE , von Eckardstein A , Schulte H , Cullen P , Assmann G . Type 2 diabetes mellitus and risk of coronary heart disease: results of the 10-year follow-up of the PROCAM study . Eur J Cardiovasc Prev Rehabil 2007 ; 14 : 230 – 6 . https://doi.org/10.1097/HJR.0b013e3280142037
Nathan DM . Long-term complications of diabetes mellitus . N Engl J Med 1993 ; 328 : 1676 – 85 . https://doi.org/10.1056/nejm199306103282306
Marx N , Federici M , Schütt K , Müller-Wieland D , Ajjan RA , Antunes MJ , et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes . Eur Heart J 2023 ; 44 : 4043 – 140 . https://doi.org/10.1093/eurheartj/ehad192
Pylypchuk R , Wells S , Kerr A , Poppe K , Harwood M , Mehta S , et al. Cardiovascular risk prediction in type 2 diabetes before and after widespread screening: a derivation and validation study . Lancet 2021 ; 397 : 2264 – 74 . https://doi.org/10.1016/s0140-6736(21)00572-9
Danaei G , Fahimi S , Lu Y , Zhou B , Hajifathalian K , Di Cesare M , et al. Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis: a pooled analysis of 96 population-based studies with 331288 participants . Lancet Diabetes Endocrinol 2015 ; 3 : 624 – 37 . https://doi.org/10.1016/S2213-8587(15)00129-1
Wright AK , Suarez-Ortegon MF , Read SH , Kontopantelis E , Buchan I , Emsley R , et al. Risk factor control and cardiovascular event risk in people with type 2 diabetes in primary and secondary prevention settings . Circulation 2020 ; 142 : 1925 – 36 . https://doi.org/10.1161/circulationaha.120.046783
Adamsson Eryd S , Gudbjörnsdottir S , Manhem K , Rosengren A , Svensson A-M , Miftaraj M , et al. Blood pressure and complications in individuals with type 2 diabetes and no previous cardiovascular disease: national population based cohort study . BMJ 2016 ; 354 : i4070 . https://doi.org/10.1136/bmj.i4070
Brunström M , Carlberg B . Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses . BMJ 2016 ; 352 : i717 . https://doi.org/10.1136/bmj.i717
Emdin CA , Rahimi K , Neal B , Callender T , Perkovic V , Patel A . Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis . JAMA 2015 ; 313 : 603 – 15 . https://doi.org/10.1001/jama.2014.18574
Thomopoulos C , Parati G , Zanchetti A . Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 – Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials . J Hypertens 2017 ; 35 : 922 – 44 . https://doi.org/10.1097/hjh.0000000000001276
Rahman F , McEvoy JW , Ohkuma T , Marre M , Hamet P , Harrap S , et al. Effects of blood pressure lowering on clinical outcomes according to baseline blood pressure and cardiovascular risk in patients with type 2 diabetes mellitus . Hypertension 2019 ; 73 : 1291 – 9 . https://doi.org/10.1161/hypertensionaha.118.12414
Agashe S , Petak S . Cardiac autonomic neuropathy in diabetes mellitus . Methodist Debakey Cardiovasc J 2018 ; 14 : 251 – 6 . https://doi.org/10.14797/mdcj-14-4-251
Beddhu S , Chertow GM , Greene T , Whelton PK , Ambrosius WT , Cheung AK , et al. Effects of intensive systolic blood pressure lowering on cardiovascular events and mortality in patients with type 2 diabetes mellitus on standard glycemic control and in those without diabetes mellitus: reconciling results from ACCORD BP and SPRINT . J Am Heart Assoc 2018 ; 7 : e009326 . https://doi.org/10.1161/jaha.118.009326
Buckley LF , Dixon DL , Wohlford GF , Wijesinghe DS , Baker WL , Van Tassell BW . Intensive versus standard blood pressure control in SPRINT-eligible participants of ACCORD-BP . Diabetes Care 2017 ; 40 : 1733 – 8 . https://doi.org/10.2337/dc17-1366
Brouwer TF , Vehmeijer JT , Kalkman DN , Berger WR , van den Born B-JH , Peters RJ , et al. Intensive blood pressure lowering in patients with and patients without type 2 diabetes: a pooled analysis from two randomized trials . Diabetes Care 2018 ; 41 : 1142 – 8 . https://doi.org/10.2337/dc17-1722
Shi S , Gouskova N , Najafzadeh M , Wei LJ , Kim DH . Intensive versus standard blood pressure control in type 2 diabetes: a restricted mean survival time analysis of a randomised controlled trial . BMJ Open 2021 ; 11 : e050335 . https://doi.org/10.1136/bmjopen-2021-050335
Palmer SC , Mavridis D , Navarese E , Craig JC , Tonelli M , Salanti G , et al. Comparative efficacy and safety of blood pressure-lowering agents in adults with diabetes and kidney disease: a network meta-analysis . Lancet 2015 ; 385 : 2047 – 56 . https://doi.org/10.1016/s0140-6736(14)62459-4
Ying A , Arima H , Czernichow S , Woodward M , Huxley R , Turnbull F , et al. Effects of blood pressure lowering on cardiovascular risk according to baseline body-mass index: a meta-analysis of randomised trials . Lancet 2015 ; 385 : 867 – 74 . https://doi.org/10.1016/s0140-6736(14)61171-5
Nazarzadeh M , Bidel Z , Canoy D , Copland E , Wamil M , Majert J , et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis . Lancet 2021 ; 398 : 1803 – 10 . https://doi.org/10.1016/s0140-6736(21)01920-6
Kearney PM , Whelton M , Reynolds K , Muntner P , Whelton PK , He J , et al. Global burden of hypertension: analysis of worldwide data . Lancet 2005 ; 365 : 217 – 23 . https://doi.org/10.1016/s0140-6736(05)17741-1
Jager KJ , Kovesdy C , Langham R , Rosenberg M , Jha V , Zoccali C , et al. A single number for advocacy and communication—worldwide more than 850 million individuals have kidney diseases . Kidney Int 2019 ; 96 : 1048 – 50 . https://doi.org/10.1016/j.kint.2019.07.012
Foreman KJ , Marquez N , Dolgert A , Fukutaki K , Fullman N , McGaughey M , et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories . Lancet 2018 ; 392 : 2052 – 90 . https://doi.org/10.1016/s0140-6736(18)31694-5
Ortiz A , Sanchez-Niño MD , Crespo-Barrio M , De-Sequera-Ortiz P , Fernández-Giráldez E , García-Maset R , et al. The Spanish Society of Nephrology (SENEFRO) commentary to the Spain GBD 2016 report: keeping chronic kidney disease out of sight of health authorities will only magnify the problem . Nefrologia (Engl Ed) 2019 ; 39 : 29 – 34 . https://doi.org/10.1016/j.nefro.2018.09.002
Law JP , Pickup L , Pavlovic D , Townend JN , Ferro CJ . Hypertension and cardiomyopathy associated with chronic kidney disease: epidemiology, pathogenesis and treatment considerations . J Hum Hypertens 2023 ; 37 : 1 – 19 . https://doi.org/10.1038/s41371-022-00751-4
Fay KS , Cohen DL . Resistant hypertension in people with CKD: a review . Am J Kidney Dis 2021 ; 77 : 110 – 21 . https://doi.org/10.1053/j.ajkd.2020.04.017
Webster AC , Nagler EV , Morton RL , Masson P . Chronic kidney disease . Lancet 2017 ; 389 : 1238 – 52 . https://doi.org/10.1016/s0140-6736(16)32064-5
Ninomiya T , Perkovic V , Turnbull F , Neal B , Barzi F , Cass A , et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials . BMJ 2013 ; 347 : f5680 . https://doi.org/10.1136/bmj.f5680
Aggarwal R , Petrie B , Bala W , Chiu N . Mortality outcomes with intensive blood pressure targets in chronic kidney disease patients . Hypertension 2019 ; 73 : 1275 – 82 . https://doi.org/10.1161/hypertensionaha.119.12697
Bangalore S , Toklu B , Gianos E , Schwartzbard A , Weintraub H , Ogedegbe G , et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials . Am J Med 2017 ; 130 : 707 – 19.e8 . https://doi.org/10.1016/j.amjmed.2017.01.004
Lv J , Ehteshami P , Sarnak MJ , Tighiouart H , Jun M , Ninomiya T , et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis . CMAJ 2013 ; 185 : 949 – 57 . https://doi.org/10.1503/cmaj.121468
Tsai WC , Wu HY , Peng YS , Yang J-Y , Chen H-Y , Chiu Y-L , et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis . JAMA Intern Med 2017 ; 177 : 792 – 9 . https://doi.org/10.1001/jamainternmed.2017.0197
Thompson S , Wiebe N , Padwal RS , Gyenes G , Headley SAE , Radhakrishnan J , et al. The effect of exercise on blood pressure in chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials . PLoS One 2019 ; 14 : e0211032 . https://doi.org/10.1371/journal.pone.0211032
Huang M , Lv A , Wang J , Xu N , Ma G , Zhai Z , et al. Exercise training and outcomes in hemodialysis patients: systematic review and meta-analysis . Am J Nephrol 2019 ; 50 : 240 – 54 . https://doi.org/10.1159/000502447
Zhang Y , He D , Zhang W , Xing Y , Guo Y , Wang F , et al. ACE inhibitor benefit to kidney and cardiovascular outcomes for patients with non-dialysis chronic kidney disease stages 3–5: a network meta-analysis of randomised clinical trials . Drugs 2020 ; 80 : 797 – 811 . https://doi.org/10.1007/s40265-020-01290-3
Jafar TH , Stark PC , Schmid CH , Landa M , Maschio G , de Jong PE , et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis . Ann Intern Med 2003 ; 139 : 244 – 52 . https://doi.org/10.7326/0003-4819-139-4-200308190-00006
Xie X , Liu Y , Perkovic V , Li X , Ninomiya T , Hou W , et al. Renin-angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a Bayesian network meta-analysis of randomized clinical trials . Am J Kidney Dis 2016 ; 67 : 728 – 41 . https://doi.org/10.1053/j.ajkd.2015.10.011
Wu HY , Huang JW , Lin HJ , Liao W-C , Peng Y-S , Hung K-Y , et al. Comparative effectiveness of renin-angiotensin system blockers and other antihypertensive drugs in patients with diabetes: systematic review and Bayesian network meta-analysis . BMJ 2013 ; 347 : f6008 . https://doi.org/10.1136/bmj.f6008
Agarwal R , Sinha AD , Cramer AE , Balmes-Fenwick M , Dickinson JH , Ouyang F , et al. Chlorthalidone for hypertension in advanced chronic kidney disease . N Engl J Med 2021 ; 385 : 2507 – 19 . https://doi.org/10.1056/NEJMoa2110730
Beddhu S , Shen J , Cheung AK , Kimmel PL , Chertow GM , Wei G , et al. Implications of early decline in eGFR due to intensive BP control for cardiovascular outcomes in SPRINT . J Am Soc Nephrol 2019 ; 30 : 1523 – 33 . https://doi.org/10.1681/asn.2018121261
Herrington WG , Staplin N , Wanner C , Green JB , Hauske SJ , Emberson JR , et al. Empagliflozin in patients with chronic kidney disease . N Engl J Med 2023 ; 388 : 117 – 27 . https://doi.org/10.1056/NEJMoa2204233
Heerspink HJL , Stefánsson BV , Correa-Rotter R , Chertow GM , Greene T , Hou F-F , et al. Dapagliflozin in patients with chronic kidney disease . N Engl J Med 2020 ; 383 : 1436 – 46 . https://doi.org/10.1056/NEJMoa2024816
Pitt B , Filippatos G , Agarwal R , Anker SD , Bakris GL , Rossing P , et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes . N Engl J Med 2021 ; 385 : 2252 – 63 . https://doi.org/10.1056/NEJMoa2110956
Ku E , McCulloch CE , Inker LA , Tighiouart H , Schaefer F , Wühl E , et al. Intensive BP control in patients with CKD and risk for adverse outcomes . J Am Soc Nephrol 2023 ; 34 : 385 – 93 . https://doi.org/10.1681/asn.0000000000000072
Lewis EJ , Hunsicker LG , Clarke WR , Berl T , Pohl MA , Lewis JB , et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes . N Engl J Med 2001 ; 345 : 851 – 60 . https://doi.org/10.1056/NEJMoa011303
Brenner BM , Cooper ME , de Zeeuw D , Keane WF , Mitch WE , Parving H-H , et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy . N Engl J Med 2001 ; 345 : 861 – 9 . https://doi.org/10.1056/NEJMoa011161
The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) . Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy . Lancet 1997 ; 349 : 1857 – 63 . https://doi.org/10.1016/S0140-6736(96)11445-8
Cruickshank JM , Thorp JM , Zacharias FJ . Benefits and potential harm of lowering high blood pressure . Lancet 1987 ; 1 : 581 – 4 . https://doi.org/10.1016/s0140-6736(87)90231-5
Staessen J , Bulpitt C , Clement D , De Leeuw P , Fagard R , Fletcher A , et al. Relation between mortality and treated blood pressure in elderly patients with hypertension: report of the European working party on high blood pressure in the elderly . BMJ 1989 ; 298 : 1552 – 6 . https://doi.org/10.1136/bmj.298.6687.1552
Böhm M , Schumacher H , Teo KK , Lonn EM , Mahfoud F , Mann JFE , et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials . Lancet 2017 ; 389 : 2226 – 37 . https://doi.org/10.1016/s0140-6736(17)30754-7
Böhm M , Ferreira JP , Mahfoud F , Duarte K , Pitt B , Zannad F , et al. Myocardial reperfusion reverses the J-curve association of cardiovascular risk and diastolic blood pressure in patients with left ventricular dysfunction and heart failure after myocardial infarction: insights from the EPHESUS trial . Eur Heart J 2020 ; 41 : 1673 – 83 . https://doi.org/10.1093/eurheartj/ehaa132
McEvoy JW , Chen Y , Rawlings A , Hoogeveen RC , Ballantyne CM , Blumenthal RS , et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control . J Am Coll Cardiol 2016 ; 68 : 1713 – 22 . https://doi.org/10.1016/j.jacc.2016.07.754
Mancia G , Kreutz R , Brunström M , Burnier M , Grassi G , Januszewicz A , et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA) . J Hypertens 2023 ; 41 : 1874 – 2071 . https://doi.org/10.1097/hjh.0000000000003480
Carvalho JJ , Baruzzi RG , Howard PF , Poulter N , Alpers M P , Franco L J , et al. Blood pressure in four remote populations in the INTERSALT study . Hypertension 1989 ; 14 : 238 – 46 . https://doi.org/10.1161/01.hyp.14.3.238
Birrane JP , Foschi M , Sacco S , McEvoy JW . Another nail in the coffin of causality for the diastolic blood pressure J curve . Hypertension 2022 ; 79 : 794 – 7 . https://doi.org/10.1161/hypertensionaha.122.18997
Mueller NT , Noya-Alarcon O , Contreras M , Appel LJ , Dominguez-Bello MG . Association of age with blood pressure across the lifespan in isolated Yanomami and Yekwana villages . JAMA Cardiol 2018 ; 3 : 1247 – 9 . https://doi.org/10.1001/jamacardio.2018.3676
Ilkun OL , Greene T , Cheung AK , Whelton PK , Wei G , Boucher RE , et al. The influence of baseline diastolic blood pressure on the effects of intensive blood pressure lowering on cardiovascular outcomes and all-cause mortality in type 2 diabetes . Diabetes Care 2020 ; 43 : 1878 – 84 . https://doi.org/10.2337/dc19-2047
Shihab S , Boucher RE , Abraham N , Wei G , Beddhu S . Influence of baseline diastolic blood pressure on the effects of intensive systolic blood pressure lowering on the risk of stroke . Hypertension 2022 ; 79 : 785 – 93 . https://doi.org/10.1161/hypertensionaha.121.18172
Vahanian A , Beyersdorf F , Praz F , Milojevic M , Baldus S , Bauersachs J , et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease . Eur Heart J 2022 ; 43 : 561 – 632 . https://doi.org/10.1093/eurheartj/ehab395
McDonagh TA , Metra M , Adamo M , Gardner RS , Baumbach A , Böhm M , et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure . Eur Heart J 2021 ; 42 : 3599 – 726 . https://doi.org/10.1093/eurheartj/ehab368
Mancusi C , de Simone G , Brguljan Hitij J , Sudano I , Mahfoud F , Parati G , et al. Management of patients with combined arterial hypertension and aortic valve stenosis: a consensus document from the Council on Hypertension and Council on Valvular Heart Disease of the European Society of Cardiology, the European Association of Cardiovascular Imaging (EACVI), and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) . Eur Heart J Cardiovasc Pharmacother 2021 ; 7 : 242 – 50 . https://doi.org/10.1093/ehjcvp/pvaa040
Nielsen OW , Sajadieh A , Sabbah M , Greve AM , Olsen MH , Boman K , et al. Assessing optimal blood pressure in patients with asymptomatic aortic valve stenosis: the simvastatin ezetimibe in aortic stenosis study (SEAS) . Circulation 2016 ; 134 : 455 – 68 . https://doi.org/10.1161/circulationaha.115.021213
McDonagh TA , Metra M , Adamo M , Gardner RS , Baumbach A , Böhm M , et al. 2023 focused update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure . Eur Heart J 2023 ; 44 : 3627 – 39 . https://doi.org/10.1093/eurheartj/ehad195
Yusuf S , Pfeffer MA , Swedberg K , Granger CB , Held P , McMurray JJV , et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial . Lancet 2003 ; 362 : 777 – 81 . https://doi.org/10.1016/s0140-6736(03)14285-7
Pitt B , Pfeffer MA , Assmann SF , Boineau R , Anand IS , Claggett B , et al. Spironolactone for heart failure with preserved ejection fraction . N Engl J Med 2014 ; 370 : 1383 – 92 . https://doi.org/10.1056/NEJMoa1313731
Nazarzadeh M , Pinho-Gomes AC , Bidel Z , Canoy D , Dehghan A , Byrne KS , et al. Genetic susceptibility, elevated blood pressure, and risk of atrial fibrillation: a Mendelian randomization study . Genome Med 2021 ; 13 : 38 . https://doi.org/10.1186/s13073-021-00849-3
Emdin CA , Anderson SG , Salimi-Khorshidi G , Woodward M , MacMahon S , Dwyer T , et al. Usual blood pressure, atrial fibrillation and vascular risk: evidence from 4.3 million adults . Int J Epidemiol 2017 ; 46 : 162 – 72 . https://doi.org/10.1093/ije/dyw053
Hindricks G , Potpara T , Dagres N , Arbelo E , Bax JJ , Blomström-Lundqvist C , et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC . Eur Heart J 2021 ; 42 : 373 – 498 . https://doi.org/10.1093/eurheartj/ehaa612
Alber J , Alladi S , Bae HJ , Barton DA , Beckett LA , Bell JM , et al. White matter hyperintensities in vascular contributions to cognitive impairment and dementia (VCID): knowledge gaps and opportunities . Alzheimers Dement (N Y) 2019 ; 5 : 107 – 17 . https://doi.org/10.1016/j.trci.2019.02.001
Georgakis MK , Duering M , Wardlaw JM , Dichgans M . WMH and long-term outcomes in ischemic stroke: a systematic review and meta-analysis . Neurology 2019 ; 92 : e1298 – 308 . https://doi.org/10.1212/wnl.0000000000007142
Jokinen H , Koikkalainen J , Laakso HM , Melkas S , Nieminen T , Brander A , et al. Global burden of small vessel disease-related brain changes on MRI predicts cognitive and functional decline . Stroke 2020 ; 51 : 170 – 8 . https://doi.org/10.1161/strokeaha.119.026170
Potter T , Lioutas VA , Tano M , Pan A , Meeks J , Woo D , et al. Cognitive impairment after intracerebral hemorrhage: a systematic review of current evidence and knowledge gaps . Front Neurol 2021 ; 12 : 716632 . https://doi.org/10.3389/fneur.2021.716632
Wang F , Hua S , Zhang Y , Zhu J , Liu R , Jiang Z . Association between small vessel disease markers, medial temporal lobe atrophy and cognitive impairment after stroke: a systematic review and meta-analysis . J Stroke Cerebrovasc Dis 2021 ; 30 : 105460 . https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105460
Ungvari Z , Toth P , Tarantini S , Prodan CI , Sorond F , Merkely B , et al. Hypertension-induced cognitive impairment: from pathophysiology to public health . Nat Rev Nephrol 2021 ; 17 : 639 – 54 . https://doi.org/10.1038/s41581-021-00430-6
Kelly D , Rothwell PM . Disentangling the multiple links between renal dysfunction and cerebrovascular disease . J Neurol Neurosurg Psychiatry 2020 ; 91 : 88 – 97 . https://doi.org/10.1136/jnnp-2019-320526
Papanastasiou CA , Theochari CA , Zareifopoulos N , Arfaras-Melainis A , Giannakoulas G , Karamitsos TD , et al. Atrial fibrillation is associated with cognitive impairment, all-cause dementia, vascular dementia, and Alzheimer’s disease: a systematic review and meta-analysis . J Gen Intern Med 2021 ; 36 : 3122 – 35 . https://doi.org/10.1007/s11606-021-06954-8
Li J , Wu Y , Zhang D , Nie J . Associations between heart failure and risk of dementia: a PRISMA-compliant meta-analysis . Medicine (Baltimore) 2020 ; 99 : e18492 . https://doi.org/10.1097/md.0000000000018492
Canavan M , O’Donnell MJ . Hypertension and cognitive impairment: a review of mechanisms and key concepts . Front Neurol 2022 ; 13 : 821135 . https://doi.org/10.3389/fneur.2022.821135
Dawson J , Béjot Y , Christensen LM , De Marchis GM , Dichgans M , Hagberg G , et al. European Stroke Organisation (ESO) guideline on pharmacological interventions for long-term secondary prevention after ischaemic stroke or transient ischaemic attack . Eur Stroke J 2022 ; 7 : I – XLI . https://doi.org/10.1177/23969873221100032
Kleindorfer DO , Towfighi A , Chaturvedi S , Cockroft KM , Gutierrez J , Lombardi-Hill D , et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association . Stroke 2021 ; 52 : e364 – 467 . https://doi.org/10.1161/str.0000000000000375
Zonneveld TP , Richard E , Vergouwen MD , Nederkoorn PJ , de Haan RJ , Roos YB , et al. Blood pressure-lowering treatment for preventing recurrent stroke, major vascular events, and dementia in patients with a history of stroke or transient ischaemic attack . Cochrane Database Syst Rev 2018 ; 7 : CD007858 . https://doi.org/10.1002/14651858.CD007858.pub2
Boncoraglio GB , Del Giovane C , Tramacere I . Antihypertensive drugs for secondary prevention after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis . Stroke 2021 ; 52 : 1974 – 82 . https://doi.org/10.1161/strokeaha.120.031945
Fischer U , Cooney MT , Bull LM , Silver LE , Chalmers J , Anderson CS , et al. Acute post-stroke blood pressure relative to premorbid levels in intracerebral haemorrhage versus major ischaemic stroke: a population-based study . Lancet Neurol 2014 ; 13 : 374 – 84 . https://doi.org/10.1016/s1474-4422(14)70031-6
Yusuf S , Diener HC , Sacco RL , Cotton D , Ôunpuu S , Lawton WA , et al. Telmisartan to prevent recurrent stroke and cardiovascular events . N Engl J Med 2008 ; 359 : 1225 – 37 . https://doi.org/10.1056/NEJMoa0804593
PROGRESS Collaborative Group . Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack . Lancet 2001 ; 358 : 1033 – 41 . https://doi.org/10.1016/s0140-6736(01)06178-5
McGurgan IJ , Kelly PJ , Turan TN , Rothwell PM . Long-term secondary prevention: management of blood pressure after a transient ischemic attack or stroke . Stroke 2022 ; 53 : 1085 – 103 . https://doi.org/10.1161/strokeaha.121.035851
Rudd AG , Bowen A , Young GR , James MA . The latest national clinical guideline for stroke . Clin Med (Lond) 2017 ; 17 : 154 – 5 . https://doi.org/10.7861/clinmedicine.17-2-154
Arima H , Chalmers J , Woodward M , Anderson C , Rodgers A , Davis S , et al. Lower target blood pressures are safe and effective for the prevention of recurrent stroke: the PROGRESS trial . J Hypertens 2006 ; 24 : 1201 – 8 . https://doi.org/10.1097/01.hjh.0000226212.34055.86
Kitagawa K , Yamamoto Y , Arima H , Maeda T , Sunami N , Kanzawa T , et al. Effect of standard vs intensive blood pressure control on the risk of recurrent stroke: a randomized clinical trial and meta-analysis . JAMA Neurol 2019 ; 76 : 1309 – 18 . https://doi.org/10.1001/jamaneurol.2019.2167
Suchard MA , Schuemie MJ , Krumholz HM , You SC , Chen R , Pratt N , et al. Comprehensive comparative effectiveness and safety of first-line antihypertensive drug classes: a systematic, multinational, large-scale analysis . Lancet 2019 ; 394 : 1816 – 26 . https://doi.org/10.1016/s0140-6736(19)32317-7
Wang WT , You LK , Chiang CE , Sung S-H , Chuang S-Y , Cheng H-M , et al. Comparative effectiveness of blood pressure-lowering drugs in patients who have already suffered from stroke: traditional and Bayesian network meta-analysis of randomized trials . Medicine (Baltimore) 2016 ; 95 : e3302 . https://doi.org/10.1097/md.0000000000003302
Bath PM , Scutt P , Blackburn DJ , Ankolekar S , Krishnan K , Ballard C , et al. Intensive versus guideline blood pressure and lipid lowering in patients with previous stroke: main results from the pilot ‘Prevention of Decline in Cognition after Stroke Trial’ (PODCAST) randomised controlled trial . PLoS One 2017 ; 12 : e0164608 . https://doi.org/10.1371/journal.pone.0164608
Mant J , McManus RJ , Roalfe A , Fletcher K , Taylor CJ , Martin U , et al. Different systolic blood pressure targets for people with history of stroke or transient ischaemic attack: PAST-BP (Prevention After Stroke—Blood Pressure) randomised controlled trial . BMJ 2016 ; 352 : i708 . https://doi.org/10.1136/bmj.i708
Kolmos M , Christoffersen L , Kruuse C . Recurrent ischemic stroke—a systematic review and meta-analysis . J Stroke Cerebrovasc Dis 2021 ; 30 : 105935 . https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.105935
Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission . Lancet 2020 ; 396 : 413 – 46 . https://doi.org/10.1016/s0140-6736(20)30367-6
Ou YN , Tan CC , Shen XN , Xu W , Hou X-H , Dong Q , et al. Blood pressure and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 209 prospective studies . Hypertension 2020 ; 76 : 217 – 25 . https://doi.org/10.1161/hypertensionaha.120.14993
Abell JG , Kivimäki M , Dugravot A , Tabak AG , Fayosse A , Shipley M , et al. Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertension . Eur Heart J 2018 ; 39 : 3119 – 25 . https://doi.org/10.1093/eurheartj/ehy288
Alpérovitch A , Blachier M , Soumaré A , Ritchie K , Dartigues J-F , Richard-Harston S , et al. Blood pressure variability and risk of dementia in an elderly cohort, the Three-City study . Alzheimers Dement 2014 ; 10 : S330 – 337 . https://doi.org/10.1016/j.jalz.2013.05.1777
McGrath ER , Beiser AS , DeCarli C , Plourde KL , Vasan RS , Greenberg S , et al. Blood pressure from mid- to late life and risk of incident dementia . Neurology 2017 ; 89 : 2447 – 54 . https://doi.org/10.1212/wnl.0000000000004741
Skoog I , Nilsson L , Persson G , Lernfelt B , Landahl S , Palmertz B , et al. 15-year longitudinal study of blood pressure and dementia . Lancet 1996 ; 347 : 1141 – 5 . https://doi.org/10.1016/s0140-6736(96)90608-x
Launer LJ , Masaki K , Petrovitch H , Foley D , Havlik RJ . The association between midlife blood pressure levels and late-life cognitive function. The Honolulu-Asia aging study . JAMA 1995 ; 274 : 1846 – 51 . https://doi.org/10.1001/jama.1995.03530230032026
Gottesman RF , Albert MS , Alonso A , Coker LH , Coresh J , Davis SM , et al. Associations between midlife vascular risk factors and 25-year incident dementia in the atherosclerosis risk in Communities (ARIC) cohort . JAMA Neurol 2017 ; 74 : 1246 – 54 . https://doi.org/10.1001/jamaneurol.2017.1658
Levine DA , Springer MV , Brodtmann A . Blood pressure and vascular cognitive impairment . Stroke 2022 ; 53 : 1104 – 13 . https://doi.org/10.1161/strokeaha.121.036140
Bosch J , O’Donnell M , Swaminathan B , Lonn EM , Sharma M , Dagenais G , et al. Effects of blood pressure and lipid lowering on cognition: results from the HOPE-3 study . Neurology 2019 ; 92 : e1435 – 46 . https://doi.org/10.1212/wnl.0000000000007174
Applegate WB , Pressel S , Wittes J , Luhr J , Shekelle RB , Camel GH , et al. Impact of the treatment of isolated systolic hypertension on behavioral variables. Results from the systolic hypertension in the elderly program . Arch Intern Med 1994 ; 154 : 2154 – 60 . https://doi.org/10.1001/archinte.1994.00420190047006
Williamson JD , Pajewski NM , Auchus AP , Bryan RN , Chelune G , Cheung AK , et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial . JAMA 2019 ; 321 : 553 – 61 . https://doi.org/10.1001/jama.2018.21442
Peters R , Beckett N , Forette F , Tuomilehto J , Clarke R , Ritchie C , et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial . Lancet Neurol 2008 ; 7 : 683 – 9 . https://doi.org/10.1016/s1474-4422(08)70143-1
Lithell H , Hansson L , Skoog I , Elmfeldt D , Hofman A , Olofsson B , et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial . J Hypertens 2003 ; 21 : 875 – 86 . https://doi.org/10.1097/00004872-200305000-00011
White WB , Wakefield DB , Moscufo N , Guttmann CRG , Kaplan RF , Bohannon RW , et al. Effects of intensive versus standard ambulatory blood pressure control on cerebrovascular outcomes in older people (INFINITY) . Circulation 2019 ; 140 : 1626 – 35 . https://doi.org/10.1161/circulationaha.119.041603
Tzourio C , Anderson C , Chapman N , Woodward M , Neal B , MacMahon S , et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease . Arch Intern Med 2003 ; 163 : 1069 – 75 . https://doi.org/10.1001/archinte.163.9.1069
Peters R , Yasar S , Anderson CS , Andrews S , Antikainen R , Arima H , et al. Investigation of antihypertensive class, dementia, and cognitive decline: a meta-analysis . Neurology 2020 ; 94 : e267 – 81 . https://doi.org/10.1212/wnl.0000000000008732
Yang W , Luo H , Ma Y , Si S , Zhao H . Effects of antihypertensive drugs on cognitive function in elderly patients with hypertension: a review . Aging Dis 2021 ; 12 : 841 – 51 . https://doi.org/10.14336/ad.2020.1111
Iseli R , Nguyen VTV , Sharmin S , Reijnierse EM , Lim WK , Maier AB , et al. Orthostatic hypotension and cognition in older adults: a systematic review and meta-analysis . Exp Gerontol 2019 ; 120 : 40 – 9 . https://doi.org/10.1016/j.exger.2019.02.017
Ernst ME , Ryan J , Chowdhury EK , Margolis KL , Beilin LJ , Reid CM , et al. Long-term blood pressure variability and risk of cognitive decline and dementia among older adults . J Am Heart Assoc 2021 ; 10 : e019613 . https://doi.org/10.1161/jaha.120.019613
Nakamura K , Stefanescu Schmidt A . Treatment of hypertension in coarctation of the aorta . Curr Treat Options Cardiovasc Med 2016 ; 18 : 40 . https://doi.org/10.1007/s11936-016-0462-x
Dijkema EJ , Leiner T , Grotenhuis HB . Diagnosis, imaging and clinical management of aortic coarctation . Heart 2017 ; 103 : 1148 – 55 . https://doi.org/10.1136/heartjnl-2017-311173
Panzer J , Bové T , Vandekerckhove K , De Wolf D . Hypertension after coarctation repair-a systematic review . Transl Pediatr 2022 ; 11 : 270 – 9 . https://doi.org/10.21037/tp-21-418
Schaefer BM , Lewin MB , Stout KK , Gill E , Prueitt A , Byers P H , et al. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape . Heart 2008 ; 94 : 1634 – 8 . https://doi.org/10.1136/hrt.2007.132092
Wang J , Deng W , Lv Q , Li Y , Liu T , Xie M , et al. Aortic dilatation in patients with bicuspid aortic valve . Front Physiol 2021 ; 12 : 615175 . https://doi.org/10.3389/fphys.2021.615175
Davies RR , Kaple RK , Mandapati D , Gallo A , Botta DM , Elefteriades JA , et al. Natural history of ascending aortic aneurysms in the setting of an unreplaced bicuspid aortic valve . Ann Thorac Surg 2007 ; 83 : 1338 – 44 . https://doi.org/10.1016/j.athoracsur.2006.10.074
Lindman BR , Otto CM . Time to treat hypertension in patients with aortic stenosis . Circulation 2013 ; 128 : 1281 – 3 . https://doi.org/10.1161/circulationaha.113.005275
Erbel R , Aboyans V , Boileau C , Bossone E , Di Bartolomeo R , Eggebrecht H , et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC) . Eur Heart J 2014 ; 35 : 2873 – 926 . https://doi.org/10.1093/eurheartj/ehu281
Shores J , Berger KR , Murphy EA , Pyeritz RE . Progression of aortic dilatation and the benefit of long-term beta-adrenergic blockade in Marfan’s syndrome . N Engl J Med 1994 ; 330 : 1335 – 41 . https://doi.org/10.1056/nejm199405123301902
Groenink M , den Hartog AW , Franken R , Radonic T , de Waard V , Timmermans J , et al. Losartan reduces aortic dilatation rate in adults with Marfan syndrome: a randomized controlled trial . Eur Heart J 2013 ; 34 : 3491 – 500 . https://doi.org/10.1093/eurheartj/eht334
Pitcher A , Spata E , Emberson J , Davies K , Halls H , Holland L , et al. Angiotensin receptor blockers and β blockers in Marfan syndrome: an individual patient data meta-analysis of randomised trials . Lancet 2022 ; 400 : 822 – 31 . https://doi.org/10.1016/s0140-6736(22)01534-3
Mazzolai L , Rodriguez-Palomares JF , Teixido-Tura G , Lanzi S , Boc V , Bossone E , et al. 2024 ESC Guidelines for the management peripheral arterial and aortic diseases . Eur Heart J 2024 . https://doi.org/10.1093/eurheartj/ehae179
Rechel B , Mladovsky P , Ingleby D , Mackenbach JP , McKee M . Migration and health in an increasingly diverse Europe . Lancet 2013 ; 381 : 1235 – 45 . https://doi.org/10.1016/s0140-6736(12)62086-8
Modesti PA , Reboldi G , Cappuccio FP , Agyemang C , Remuzzi G , Rapi S , et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis . PLoS One 2016 ; 11 : e0147601 . https://doi.org/10.1371/journal.pone.0147601
Whelton PK , Einhorn PT , Muntner P , Appel LJ , Cushman WC , Diez Roux AV , et al. Research needs to improve hypertension treatment and control in African Americans . Hypertension 2016 ; 68 : 1066 – 72 . https://doi.org/10.1161/hypertensionaha.116.07905
Kaufman JS , Cooper RS , McGee DL . Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race . Epidemiology 1997 ; 8 : 621 – 8 .
Agyemang C , van Oeffelen AA , Norredam M , Kappelle LJ , Klijn CJM , Bots ML , et al. Socioeconomic inequalities in stroke incidence among migrant groups: analysis of nationwide data . Stroke 2014 ; 45 : 2397 – 403 . https://doi.org/10.1161/strokeaha.114.005505
Mehanna M , Gong Y , McDonough CW , Beitelshees AL , Gums JG , Chapman AB , et al. Blood pressure response to metoprolol and chlorthalidone in European and African Americans with hypertension . J Clin Hypertens (Greenwich) 2017 ; 19 : 1301 – 8 . https://doi.org/10.1111/jch.13094
Faconti L , McNally RJ , Farukh B , Adeyemi O , Cruickshank JK , Wilkinson IB , et al. Differences in hypertension phenotypes between Africans and Europeans: role of environment . J Hypertens 2020 ; 38 : 1278 – 85 . https://doi.org/10.1097/hjh.0000000000002403
Schutte AE , Kruger R , Gafane-Matemane LF , Breet Y , Strauss-Kruger M , Cruickshank JK , et al. Ethnicity and arterial stiffness . Arterioscler Thromb Vasc Biol 2020 ; 40 : 1044 – 54 . https://doi.org/10.1161/atvbaha.120.313133
Erlinger TP , Vollmer WM , Svetkey LP , Appel LJ . The potential impact of nonpharmacologic population-wide blood pressure reduction on coronary heart disease events: pronounced benefits in African-Americans and hypertensives . Prev Med 2003 ; 37 : 327 – 33 . https://doi.org/10.1016/s0091-7435(03)00140-3
The ALLHAT Officers Coordinators for the ALLHAT Collaborative Research Group . Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) . JAMA 2002 ; 288 : 2981 – 97 . https://doi.org/10.1001/jama.288.23.2981
Wright JT Jr , Dunn JK , Cutler JA , Davis BR , Cushman WC , Ford CE , et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril . JAMA 2005 ; 293 : 1595 – 608 . https://doi.org/10.1001/jama.293.13.1595
Wright JT Jr , Harris-Haywood S , Pressel S , Barzilay J , Baimbridge C , Bareis CJ , et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) . Arch Intern Med 2008 ; 168 : 207 – 17 . https://doi.org/10.1001/archinternmed.2007.66
Ojji DB , Mayosi B , Francis V , Badri M , Cornelius V , Smythe W , et al. Comparison of dual therapies for lowering blood pressure in Black Africans . N Engl J Med 2019 ; 380 : 2429 – 39 . https://doi.org/10.1056/NEJMoa1901113
van der Linden EL , Couwenhoven BN , Beune E , Daams JG , van den Born B-JH , Agyemang C . Hypertension awareness, treatment and control among ethnic minority populations in Europe: a systematic review and meta-analysis . J Hypertens 2021 ; 39 : 202 – 13 . https://doi.org/10.1097/hjh.0000000000002651
Agyemang C , Nyaaba G , Beune E , Meeks K , Owusu-Dabo E , Addo J , et al. Variations in hypertension awareness, treatment, and control among Ghanaian migrants living in Amsterdam, Berlin, London, and nonmigrant Ghanaians living in rural and urban Ghana—the RODAM study . J Hypertens 2018 ; 36 : 169 – 77 . https://doi.org/10.1097/hjh.0000000000001520
van Laer SD , Snijder MB , Agyemang C , Peters RJ , van den Born BH . Ethnic differences in hypertension prevalence and contributing determinants – the HELIUS study . Eur J Prev Cardiol 2018 ; 25 : 1914 – 22 . https://doi.org/10.1177/2047487318803241
Costello HM , Gumz ML . Circadian rhythm, clock genes, and hypertension: recent advances in hypertension . Hypertension 2021 ; 78 : 1185 – 96 . https://doi.org/10.1161/hypertensionaha.121.14519
O’Brien E , Sheridan J , O’Malley K . Dippers and non-dippers . Lancet 1988 ; 2 : 397 . https://doi.org/10.1016/s0140-6736(88)92867-x
Pickering TG , Shimbo D , Haas D . Ambulatory blood-pressure monitoring . N Engl J Med 2006 ; 354 : 2368 – 74 . https://doi.org/10.1056/NEJMra060433
Abdalla M , Goldsmith J , Muntner P , Diaz KM , Reynolds K , Schwartz JE , et al. Is isolated nocturnal hypertension a reproducible phenotype? Am J Hypertens 2016 ; 29 : 33 – 8 . https://doi.org/10.1093/ajh/hpv058
Mancia G , Facchetti R , Bombelli M , Quarti-Trevano F , Cuspidi C , Grassi G . Short- and long-term reproducibility of nighttime blood pressure phenotypes and nocturnal blood pressure reduction . Hypertension 2021 ; 77 : 1745 – 55 . https://doi.org/10.1161/hypertensionaha.120.16827
Nolde JM , Kiuchi MG , Lugo-Gavidia LM , Ho JK , Chan J , Matthews VB , et al. Nocturnal hypertension: a common phenotype in a tertiary clinical setting associated with increased arterial stiffness and central blood pressure . J Hypertens 2021 ; 39 : 250 – 8 . https://doi.org/10.1097/hjh.0000000000002620
Thomas SJ , Booth JN III , Jaeger BC , Hubbard D , Sakhuja S , Abdalla M , et al. Association of sleep characteristics with nocturnal hypertension and nondipping blood pressure in the CARDIA study . J Am Heart Assoc 2020 ; 9 : e015062 . https://doi.org/10.1161/jaha.119.015062
Kario K , Hoshide S , Haimoto H , Yamagiwa K , Uchiba K , Nagasaka S , et al. Sleep blood pressure self-measured at home as a novel determinant of organ damage: Japan morning surge home blood pressure (J-HOP) study . J Clin Hypertens (Greenwich) 2015 ; 17 : 340 – 8 . https://doi.org/10.1111/jch.12500
de la Sierra A , Gorostidi M , Banegas JR , Segura J , de la Cruz JJ , Ruilope LM , et al. Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens 2014 ; 27 : 680 – 7 . https://doi.org/10.1093/ajh/hpt175
Wijkman M , Länne T , Engvall J , Lindström T , Östgren CJ , Nystrom FH , et al. Masked nocturnal hypertension—a novel marker of risk in type 2 diabetes . Diabetologia 2009 ; 52 : 1258 – 64 . https://doi.org/10.1007/s00125-009-1369-9
Muntner P , Lewis CE , Diaz KM , Carson AP , Kim Y , Calhoun D , et al. Racial differences in abnormal ambulatory blood pressure monitoring measures: results from the coronary artery risk development in young adults (CARDIA) study . Am J Hypertens 2015 ; 28 : 640 – 8 . https://doi.org/10.1093/ajh/hpu193
Thomas SJ , Booth JN III , Bromfield SG , Seals SR , Spruill TM , Ogedegbe G , et al. Clinic and ambulatory blood pressure in a population-based sample of African Americans: the Jackson heart study . J Am Soc Hypertens 2017 ; 11 : 204 – 212.e205 . https://doi.org/10.1016/j.jash.2017.02.001
Husain A , Lin FC , Tuttle LA , Olsson E , Viera AJ . The reproducibility of racial differences in ambulatory blood pressure phenotypes and measurements . Am J Hypertens 2017 ; 30 : 961 – 7 . https://doi.org/10.1093/ajh/hpx079
Li Y , Wang JG . Isolated nocturnal hypertension: a disease masked in the dark . Hypertension 2013 ; 61 : 278 – 83 . https://doi.org/10.1161/hypertensionaha.111.00217
Hoshide S , Kario K , de la Sierra A , Bilo G , Schillaci G , Banegas JR , et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study . Hypertension 2015 ; 66 : 750 – 6 . https://doi.org/10.1161/hypertensionaha.115.05958
Banegas JR , Ruilope LM , de la Sierra A , Gorostidi M , Segura J , Martell N , et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension . Eur Heart J 2014 ; 35 : 3304 – 12 . https://doi.org/10.1093/eurheartj/ehu016
Huang JF , Zhang DY , Sheng CS , An D-W , Li M , Cheng Y-B , et al. Isolated nocturnal hypertension in relation to host and environmental factors and clock genes . J Clin Hypertens (Greenwich) 2022 ; 24 : 1255 – 62 . https://doi.org/10.1111/jch.14532
Matsumoto T , Tabara Y , Murase K , Setoh K , Kawaguchi T , Nagashima S , et al. Nocturia and increase in nocturnal blood pressure: the Nagahama study . J Hypertens 2018 ; 36 : 2185 – 92 . https://doi.org/10.1097/hjh.0000000000001802
Seif F , Patel SR , Walia HK , Rueschman M , Bhatt DL , Blumenthal RS , et al. Obstructive sleep apnea and diurnal nondipping hemodynamic indices in patients at increased cardiovascular risk . J Hypertens 2014 ; 32 : 267 – 75 . https://doi.org/10.1097/hjh.0000000000000011
Kimura G , Dohi Y , Fukuda M . Salt sensitivity and circadian rhythm of blood pressure: the keys to connect CKD with cardiovascular events . Hypertens Res 2010 ; 33 : 515 – 20 . https://doi.org/10.1038/hr.2010.47
Drawz PE , Alper AB , Anderson AH , Brecklin CS , Charleston J , Chen J , et al. Masked hypertension and elevated nighttime blood pressure in CKD: prevalence and association with target organ damage . Clin J Am Soc Nephrol 2016 ; 11 : 642 – 52 . https://doi.org/10.2215/cjn.08530815
Kanno A , Metoki H , Kikuya M , Terawaki H , Hara A , Hashimoto T , et al. Usefulness of assessing masked and white-coat hypertension by ambulatory blood pressure monitoring for determining prevalent risk of chronic kidney disease: the Ohasama study . Hypertens Res 2010 ; 33 : 1192 – 8 . https://doi.org/10.1038/hr.2010.139
Kushiro T , Kario K , Saito I , Teramukai S , Sato Y , Okuda Y , et al. Increased cardiovascular risk of treated white coat and masked hypertension in patients with diabetes and chronic kidney disease: the HONEST study . Hypertens Res 2017 ; 40 : 87 – 95 . https://doi.org/10.1038/hr.2016.87
Lurbe E , Redon J , Kesani A , Pascual JM , Tacons J , Alvarez V , et al. Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes . N Engl J Med 2002 ; 347 : 797 – 805 . https://doi.org/10.1056/NEJMoa013410
Cuspidi C , Sala C , Tadic M , Gherbesi E , De Giorgi A , Grassi G , et al. Clinical and prognostic significance of a reverse dipping pattern on ambulatory monitoring: an updated review . J Clin Hypertens (Greenwich) 2017 ; 19 : 713 – 21 . https://doi.org/10.1111/jch.13023
Wu Q , Hong M , Xu J , Tang X , Zhu L , Gao P , et al. Diurnal blood pressure pattern and cardiac damage in hypertensive patients with primary aldosteronism . Endocrine 2021 ; 72 : 835 – 43 . https://doi.org/10.1007/s12020-021-02606-3
Kario K , Hoshide S , Mizuno H , Kabutoya T , Nishizawa M , Yoshida T , et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP study . Circulation 2020 ; 142 : 1810 – 20 . https://doi.org/10.1161/circulationaha.120.049730
Kario K , Hoshide S , Nagai M , Okawara Y , Kanegae H . Sleep and cardiovascular outcomes in relation to nocturnal hypertension: the J-HOP nocturnal blood pressure study . Hypertens Res 2021 ; 44 : 1589 – 96 . https://doi.org/10.1038/s41440-021-00709-y
Wang Q , Wang Y , Wang J , Zhang L , Zhao MH . Nocturnal systolic hypertension and adverse prognosis in patients with CKD . Clin J Am Soc Nephrol 2021 ; 16 : 356 – 64 . https://doi.org/10.2215/cjn.14420920
Hansen TW , Li Y , Boggia J , Thijs L , Richart T , Staessen JA . Predictive role of the nighttime blood pressure . Hypertension 2011 ; 57 : 3 – 10 . https://doi.org/10.1161/hypertensionaha.109.133900
Staessen JA , Thijs L , Fagard R , O’Brien ET , Clement D , de Leeuw PW , et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension . JAMA 1999 ; 282 : 539 – 46 . https://doi.org/10.1001/jama.282.6.539
Verdecchia P , Porcellati C , Schillaci G , Borgioni C , Ciucci A , Battistelli M , et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension . Hypertension 1994 ; 24 : 793 – 801 . https://doi.org/10.1161/01.hyp.24.6.793
Ohkubo T , Hozawa A , Yamaguchi J , Kikuya M , Ohmori K , Michimata M , et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study . J Hypertens 2002 ; 20 : 2183 – 9 . https://doi.org/10.1097/00004872-200211000-00017
Nagai M , Hoshide S , Ishikawa J , Shimada K , Kario K . Ambulatory blood pressure as an independent determinant of brain atrophy and cognitive function in elderly hypertension . J Hypertens 2008 ; 26 : 1636 – 41 . https://doi.org/10.1097/HJH.0b013e3283018333
Staessen JA , Thijs L , Ohkubo T , Kikuya M , Richart T , Boggia J , et al. Thirty years of research on diagnostic and therapeutic thresholds for the self-measured blood pressure at home . Blood Press Monit 2008 ; 13 : 352 – 65 . https://doi.org/10.1097/MBP.0b013e3283108f93
Kario K , Shimada K . Risers and extreme-dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure . Clin Exp Hypertens 2004 ; 26 : 177 – 89 . https://doi.org/10.1081/ceh-120028556
Tan X , Sundström J , Lind L , Franzon K , Kilander L , Benedict C , et al. Reverse dipping of systolic blood pressure is associated with increased dementia risk in older men: a longitudinal study over 24 years . Hypertension 2021 ; 77 : 1383 – 90 . https://doi.org/10.1161/hypertensionaha.120.16711
Judd E , Calhoun DA . Apparent and true resistant hypertension: definition, prevalence and outcomes . J Hum Hypertens 2014 ; 28 : 463 – 8 . https://doi.org/10.1038/jhh.2013.140
Denker MG , Haddad DB , Townsend RR , Cohen DL . Blood pressure control 1 year after referral to a hypertension specialist . J Clin Hypertens (Greenwich) 2013 ; 15 : 624 – 9 . https://doi.org/10.1111/jch.12146
Blumenthal JA , Hinderliter AL , Smith PJ , Mabe S , Watkins LL , Craighead L , et al. Effects of lifestyle modification on patients with resistant hypertension: results of the TRIUMPH randomized clinical trial . Circulation 2021 ; 144 : 1212 – 26 . https://doi.org/10.1161/circulationaha.121.055329
Hung SC , Kuo KL , Peng CH , Wu C-H , Lien Y-C , Wang Y-C , et al. Volume overload correlates with cardiovascular risk factors in patients with chronic kidney disease . Kidney Int 2014 ; 85 : 703 – 9 . https://doi.org/10.1038/ki.2013.336
Taler SJ , Textor SC , Augustine JE . Resistant hypertension: comparing hemodynamic management to specialist care . Hypertension 2002 ; 39 : 982 – 8 . https://doi.org/10.1161/01.hyp.0000016176.16042.2f
Gaddam KK , Nishizaka MK , Pratt-Ubunama MN , Pimenta E , Aban I , Oparil S , et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion . Arch Intern Med 2008 ; 168 : 1159 – 64 . https://doi.org/10.1001/archinte.168.11.1159
Roush GC , Ernst ME , Kostis JB , Tandon S , Sica DA . Head-to-head comparisons of hydrochlorothiazide with indapamide and chlorthalidone: antihypertensive and metabolic effects . Hypertension 2015 ; 65 : 1041 – 6 . https://doi.org/10.1161/hypertensionaha.114.05021
Peterzan MA , Hardy R , Chaturvedi N , Hughes AD . Meta-analysis of dose-response relationships for hydrochlorothiazide, chlorthalidone, and bendroflumethiazide on blood pressure, serum potassium, and urate . Hypertension 2012 ; 59 : 1104 – 9 . https://doi.org/10.1161/hypertensionaha.111.190637
Chen C , Zhu XY , Li D , Lin Q , Zhou K . Clinical efficacy and safety of spironolactone in patients with resistant hypertension: a systematic review and meta-analysis . Medicine (Baltimore) 2020 ; 99 : e21694 . https://doi.org/10.1097/md.0000000000021694
Zhao D , Liu H , Dong P , Zhao J . A meta-analysis of add-on use of spironolactone in patients with resistant hypertension . Int J Cardiol 2017 ; 233 : 113 – 7 . https://doi.org/10.1016/j.ijcard.2016.12.158
Bazoukis G , Thomopoulos C , Tsioufis C . Effect of mineralocorticoid antagonists on blood pressure lowering: overview and meta-analysis of randomized controlled trials in hypertension . J Hypertens 2018 ; 36 : 987 – 94 . https://doi.org/10.1097/hjh.0000000000001671
Oxlund CS , Henriksen JE , Tarnow L , Schousboe K , Gram J , Jacobsen IA . Low dose spironolactone reduces blood pressure in patients with resistant hypertension and type 2 diabetes mellitus: a double blind randomized clinical trial . J Hypertens 2013 ; 31 : 2094 – 102 . https://doi.org/10.1097/HJH.0b013e3283638b1a
Desai R , Park H , Brown JD , Mohandas R , Pepine CJ , Smith SM . Comparative safety and effectiveness of aldosterone antagonists versus beta-blockers as fourth agents in patients with apparent resistant hypertension . Hypertension 2022 ; 79 : 2305 – 15 . https://doi.org/10.1161/hypertensionaha.122.19280
Juurlink DN , Mamdani MM , Lee DS , Kopp A , Austin PC , Laupacis A , et al. Rates of hyperkalemia after publication of the randomized aldactone evaluation study . N Engl J Med 2004 ; 351 : 543 – 51 . https://doi.org/10.1056/NEJMoa040135
Agarwal R , Rossignol P , Romero A , Garza D , Mayo MR , Warren S , et al. Patiromer versus placebo to enable spironolactone use in patients with resistant hypertension and chronic kidney disease (AMBER): a phase 2, randomised, double-blind, placebo-controlled trial . Lancet 2019 ; 394 : 1540 – 50 . https://doi.org/10.1016/s0140-6736(19)32135-x
Burton TJ , Mackenzie IS , Balan K , Koo B , Bird N , Soloviev DV , et al. Evaluation of the sensitivity and specificity of (11)C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn’s adenomas . J Clin Endocrinol Metab 2012 ; 97 : 100 – 9 . https://doi.org/10.1210/jc.2011-1537
Rossi GP , Maiolino G , Seccia TM . Adrenal venous sampling: where do we stand? Endocrinol Metab Clin North Am 2019 ; 48 : 843 – 58 . https://doi.org/10.1016/j.ecl.2019.08.012
Wu X , Senanayake R , Goodchild E , Bashari WA , Salsbury J , Cabrera CP , et al. [(11)C]metomidate PET-CT versus adrenal vein sampling for diagnosing surgically curable primary aldosteronism: a prospective, within-patient trial . Nat Med 2023 ; 29 : 190 – 202 . https://doi.org/10.1038/s41591-022-02114-5
Lenzini L , Prisco S , Caroccia B , Rossi GP . Saga of familial hyperaldosteronism: yet a new channel . Hypertension 2018 ; 71 : 1010 – 4 . https://doi.org/10.1161/hypertensionaha.118.11150
Parthasarathy HK , Ménard J , White WB , Young WF , Williams GH , Williams B , et al. A double-blind, randomized study comparing the antihypertensive effect of eplerenone and spironolactone in patients with hypertension and evidence of primary aldosteronism . J Hypertens 2011 ; 29 : 980 – 90 . https://doi.org/10.1097/HJH.0b013e3283455ca5
Shagjaa T , Sanga V , Rossi GP . Skin hyperpigmentation due to post-surgical adrenal insufficiency regressed with the dexamethasone treatment . J Clin Med 2022 ; 11 : 5379 . https://doi.org/10.3390/jcm11185379
Sanga V , Lenzini L , Seccia TM , Rossi GP . Familial hyperaldosteronism type 1 and pregnancy: successful treatment with low dose dexamethasone . Blood Press 2021 ; 30 : 133 – 7 . https://doi.org/10.1080/08037051.2020.1863771
Persu A , Touzé E , Mousseaux E , Barral X , Joffre F , Plouin P-F . Diagnosis and management of fibromuscular dysplasia: an expert consensus . Eur J Clin Invest 2012 ; 42 : 338 – 47 . https://doi.org/10.1111/j.1365-2362.2011.02577.x
Wheatley K , Ives N , Gray R , Kalra PA , Moss JG , Baigent C , et al. Revascularization versus medical therapy for renal-artery stenosis . N Engl J Med 2009 ; 361 : 1953 – 62 . https://doi.org/10.1056/NEJMoa0905368
Cooper CJ , Murphy TP , Cutlip DE , Jamerson K , Henrich W , Reid DM , et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis . N Engl J Med 2014 ; 370 : 13 – 22 . https://doi.org/10.1056/NEJMoa1310753
Bailey SR , Beckman JA , Dao TD , Misra S , Sobieszczyk PS , White CJ , et al. ACC/AHA/SCAI/SIR/SVM 2018 appropriate use criteria for peripheral artery intervention: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Heart Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, and Society for Vascular Medicine . J Am Coll Cardiol 2019 ; 73 : 214 – 37 . https://doi.org/10.1016/j.jacc.2018.10.002
Trinquart L , Mounier-Vehier C , Sapoval M , Gagnon N , Plouin PF . Efficacy of revascularization for renal artery stenosis caused by fibromuscular dysplasia: a systematic review and meta-analysis . Hypertension 2010 ; 56 : 525 – 32 . https://doi.org/10.1161/hypertensionaha.110.152918
Sanga V , Bertoli E , Crimì F , Barbiero G , Battistel M , Teresa Seccia M , et al. Pickering syndrome: an overlooked renovascular cause of recurrent heart failure . J Am Heart Assoc 2023 ; 12 : e030474 . https://doi.org/10.1161/jaha.123.030474
Bhalla V , Textor SC , Beckman JA , Casanegra AI , Cooper CJ , Kim ESH , et al. Revascularization for renovascular disease: a scientific statement from the American Heart Association . Hypertension 2022 ; 79 : e128 – 43 . https://doi.org/10.1161/hyp.0000000000000217
Bravo E , Fouad-Tarazi F , Rossi G , Imamura M , Lin WW , Madkour MA , et al. A reevaluation of the hemodynamics of pheochromocytoma . Hypertension 1990 ; 15 : I128 – 131 . https://doi.org/10.1161/01.hyp.15.2_suppl.i128
Cohen JB , Brown NJ , Brown SA , Dent S , van Dorst DCH , Herrmann SM , et al. Cancer therapy-related hypertension: a scientific statement from the American Heart Association . Hypertension 2023 ; 80 : e46 – 57 . https://doi.org/10.1161/hyp.0000000000000224
Lyon AR , López-Fernández T , Couch LS , Asteggiano R , Aznar MC , Bergler-Klein J , et al. ESC guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) . Eur Heart J 2022 ; 43 : 4229 – 361 . https://doi.org/10.1093/eurheartj/ehac244
Boulestreau R , van den Born BH , Lip GYH , Gupta A . Malignant hypertension: current perspectives and challenges . J Am Heart Assoc 2022 ; 11 : e023397 . https://doi.org/10.1161/jaha.121.023397
Ma L , Hu X , Song L , Chen X , Ouyang M , Billot L , et al. The third intensive care bundle with blood pressure reduction in acute cerebral haemorrhage trial (INTERACT3): an international, stepped wedge cluster randomised controlled trial . Lancet 2023 ; 402 : 27 – 40 . https://doi.org/10.1016/s0140-6736(23)00806-1
Moullaali TJ , Wang X , Sandset EC , Woodhouse LJ , Law ZK , Arima H , et al. Early lowering of blood pressure after acute intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data . J Neurol Neurosurg Psychiatry 2022 ; 93 : 6 – 13 . https://doi.org/10.1136/jnnp-2021-327195
Wang X , Di Tanna GL , Moullaali TJ , Martin R’ H , Shipes VB , Robinson TG , et al. J-shape relation of blood pressure reduction and outcome in acute intracerebral hemorrhage: a pooled analysis of INTERACT2 and ATACH-II individual participant data . Int J Stroke 2022 ; 17 : 1129 – 36 . https://doi.org/10.1177/17474930211064076
Qureshi AI , Huang W , Lobanova I , Barsan WG , Hanley DF , Hsu CY , et al. Outcomes of intensive systolic blood pressure reduction in patients with intracerebral hemorrhage and excessively high initial systolic blood pressure: post hoc analysis of a randomized clinical trial . JAMA Neurol 2020 ; 77 : 1355 – 65 . https://doi.org/10.1001/jamaneurol.2020.3075
Bath PM , Krishnan K . Interventions for deliberately altering blood pressure in acute stroke . Cochrane Database Syst Rev 2014 ; 2014 : CD000039 . https://doi.org/10.1002/14651858.CD000039.pub3
Berge E , Whiteley W , Audebert H , De Marchis GM , Fonseca AC , Padiglioni C , et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke . Eur Stroke J 2021 ; 6 : I – LXII . https://doi.org/10.1177/2396987321989865
LeCouffe NE , Kappelhof M , Treurniet KM , Lingsma HF , Zhang G , van den Wijngaard IR , et al. 2B, 2C, or 3: what should be the angiographic target for endovascular treatment in ischemic stroke? Stroke 2020 ; 51 : 1790 – 6 . https://doi.org/10.1161/strokeaha.119.028891
Mistry EA , Hart KW , Davis LT , Gao Y , Prestigiacomo CJ , Mittal S , et al. Blood pressure management after endovascular therapy for acute ischemic stroke: the BEST-II randomized clinical trial . JAMA 2023 ; 330 : 821 – 31 . https://doi.org/10.1001/jama.2023.14330
Lee M , Ovbiagele B , Hong KS , Wu Y-L , Lee J-E , Rao NM , et al. Effect of blood pressure lowering in early ischemic stroke: meta-analysis . Stroke 2015 ; 46 : 1883 – 9 . https://doi.org/10.1161/strokeaha.115.009552
Anderson CS , Huang Y , Lindley RI , Chen X , Arima H , Chen G , et al. Intensive blood pressure reduction with intravenous thrombolysis therapy for acute ischaemic stroke (ENCHANTED): an international, randomised, open-label, blinded-endpoint, phase 3 trial . Lancet 2019 ; 393 : 877 – 88 . https://doi.org/10.1016/s0140-6736(19)30038-8
Mazighi M , Richard S , Lapergue B , Sibon I , Gory B , Berge J , et al. Safety and efficacy of intensive blood pressure lowering after successful endovascular therapy in acute ischaemic stroke (BP-TARGET): a multicentre, open-label, randomised controlled trial . Lancet Neurol 2021 ; 20 : 265 – 74 . https://doi.org/10.1016/s1474-4422(20)30483-x
Yang P , Song L , Zhang Y , Zhang X , Chen X , Li Y , et al. Intensive blood pressure control after endovascular thrombectomy for acute ischaemic stroke (ENCHANTED2/MT): a multicentre, open-label, blinded-endpoint, randomised controlled trial . Lancet 2022 ; 400 : 1585 – 96 . https://doi.org/10.1016/s0140-6736(22)01882-7
Sandset EC , Anderson CS , Bath PM , Christensen H , Fischer U , Gąsecki D , et al. European Stroke Organisation (ESO) guidelines on blood pressure management in acute ischaemic stroke and intracerebral haemorrhage . Eur Stroke J 2021 ; 6 : Xlviii – lxxxix . https://doi.org/10.1177/23969873211012133
Anderson CS , Heeley E , Huang Y , Wang J , Stapf C , Delcourt C , et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage . N Engl J Med 2013 ; 368 : 2355 – 65 . https://doi.org/10.1056/NEJMoa1214609
Qureshi AI , Palesch YY , Barsan WG , Hanley DF , Hsu CY , Martin RL , et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage . N Engl J Med 2016 ; 375 : 1033 – 43 . https://doi.org/10.1056/NEJMoa1603460
Moullaali TJ , Wang X , Woodhouse LJ , Law ZK , Delcourt C , Sprigg N , et al. Lowering blood pressure after acute intracerebral haemorrhage: protocol for a systematic review and meta-analysis using individual patient data from randomised controlled trials participating in the blood pressure in acute stroke collaboration (BASC) . BMJ Open 2019 ; 9 : e030121 . https://doi.org/10.1136/bmjopen-2019-030121
American College of Obstetricians and Gynecologists . Gestational hypertension and preeclampsia: ACOG practice bulletin, number 222 . Obstet Gynecol 2020 ; 135 : e237 – 60 . https://doi.org/10.1097/aog.0000000000003891
Garovic VD , Dechend R , Easterling T , Karumanchi SA , Baird SM , Magee LA , et al. Hypertension in pregnancy: diagnosis, blood pressure goals, and pharmacotherapy: a scientific statement from the American Heart Association . Hypertension 2022 ; 79 : e21 – 41 . https://doi.org/10.1161/hyp.0000000000000208
Magee LA , Nicolaides KH , von Dadelszen P . Preeclampsia . N Engl J Med 2022 ; 386 : 1817 – 32 . https://doi.org/10.1056/NEJMra2109523
Altman D , Carroli G , Duley L , Farrell B , Moodley J , Neilson J , et al. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie trial: a randomised placebo-controlled trial . Lancet 2002 ; 359 : 1877 – 90 . https://doi.org/10.1016/s0140-6736(02)08778-0
Poon LC , Magee LA , Verlohren S , Shennan A , von Dadelszen P , Sheiner E , et al. A literature review and best practice advice for second and third trimester risk stratification, monitoring, and management of pre-eclampsia: compiled by the pregnancy and non-communicable diseases committee of FIGO (the International Federation of Gynecology and Obstetrics) . Int J Gynaecol Obstet 2021 ; 154 Suppl 1 : 3 – 31 . https://doi.org/10.1002/ijgo.13763
Muhammad S , Usman H , Dawha YM , Yahya A , Yekeen A , Bako B . Comparison of intravenous labetalol and hydralazine for severe hypertension in pregnancy in Northeastern Nigeria: a randomized controlled trial . Pregnancy Hypertens 2022 ; 29 : 1 – 6 . https://doi.org/10.1016/j.preghy.2022.05.001
Magee LA , Cham C , Waterman EJ , Ohlsson A , von Dadelszen P . Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis . BMJ 2003 ; 327 : 955 – 60 . https://doi.org/10.1136/bmj.327.7421.955
Wu HZ , Cheng Y , Yu D , Li J-B , Jiang Y-F , Zhu Z-N . Different dosage regimens of nifedipine, labetalol, and hydralazine for the treatment of severe hypertension during pregnancy: a network meta-analysis of randomized controlled trials . Hypertens Pregnancy 2022 ; 41 : 126 – 38 . https://doi.org/10.1080/10641955.2022.2056196
Halvorsen S , Mehilli J , Cassese S , Hall TS , Abdelhamid M , Barbato E , et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery . Eur Heart J 2022 ; 43 : 3826 – 924 . https://doi.org/10.1093/eurheartj/ehac270
Lizano-Díez I , Poteet S , Burniol-Garcia A , Cerezales M . The burden of perioperative hypertension/hypotension: a systematic review . PLoS One 2022 ; 17 : e0263737 . https://doi.org/10.1371/journal.pone.0263737
Futier E , Lefrant JY , Guinot PG , Godet T , Lorne E , Cuvillon P , et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial . JAMA 2017 ; 318 : 1346 – 57 . https://doi.org/10.1001/jama.2017.14172
Sanders RD , Hughes F , Shaw A , Thompson A , Bader A , Hoeft A , et al. Perioperative quality initiative consensus statement on preoperative blood pressure, risk and outcomes for elective surgery . Br J Anaesth 2019 ; 122 : 552 – 62 . https://doi.org/10.1016/j.bja.2019.01.018
Messina A , Robba C , Calabrò L , Zambelli D , Iannuzzi F , Molinari E , et al. Association between perioperative fluid administration and postoperative outcomes: a 20-year systematic review and a meta-analysis of randomized goal-directed trials in major visceral/noncardiac surgery . Crit Care 2021 ; 25 : 43 . https://doi.org/10.1186/s13054-021-03464-1
Meng L , Yu W , Wang T , Zhang L , Heerdt PM , Gelb AW . Blood pressure targets in perioperative care . Hypertension 2018 ; 72 : 806 – 17 . https://doi.org/10.1161/hypertensionaha.118.11688
Wanner PM , Wulff DU , Djurdjevic M , Korte W , Schnider TW , Filipovic M . Targeting higher intraoperative blood pressures does not reduce adverse cardiovascular events following noncardiac surgery . J Am Coll Cardiol 2021 ; 78 : 1753 – 64 . https://doi.org/10.1016/j.jacc.2021.08.048
Blessberger H , Lewis SR , Pritchard MW , Fawcett LJ , Domanovits H , Schlager O , et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing non-cardiac surgery . Cochrane Database Syst Rev 2019 ; 9 : CD013438 . https://doi.org/10.1002/14651858.CD013438
McGory ML , Maggard MA , Ko CY . A meta-analysis of perioperative beta blockade: what is the actual risk reduction? Surgery 2005 ; 138 : 171 – 9 . https://doi.org/10.1016/j.surg.2005.03.022
Kertai MD , Cooter M , Pollard RJ , Buhrman W , Aronson S , Mathew JP , et al. Is compliance with surgical care improvement project cardiac (SCIP-Card-2) measures for perioperative β-blockers associated with reduced incidence of mortality and cardiovascular-related critical quality indicators after noncardiac surgery? Anesth Analg 2018 ; 126 : 1829 – 38 . https://doi.org/10.1213/ane.0000000000002577
Roshanov PS , Rochwerg B , Patel A , Salehian O , Duceppe E , Belley-Côté EP , et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the vascular events in noncardiac surgery patIents cOhort evaluatioN prospective cohort . Anesthesiology 2017 ; 126 : 16 – 27 . https://doi.org/10.1097/aln.0000000000001404
Shiffermiller JF , Monson BJ , Vokoun CW , Beachy MW , Smith MP , Sullivan JN , et al. Prospective randomized evaluation of preoperative angiotensin-converting enzyme inhibition (PREOP-ACEI) . J Hosp Med 2018 ; 13 : 661 – 7 . https://doi.org/10.12788/jhm.3036
Hollmann C , Fernandes NL , Biccard BM . A systematic review of outcomes associated with withholding or continuing angiotensin-converting enzyme inhibitors and angiotensin receptor blockers before noncardiac surgery . Anesth Analg 2018 ; 127 : 678 – 87 . https://doi.org/10.1213/ane.0000000000002837
Ackland GL , Patel A , Abbott TEF , Begum S , Dias P , Crane DR , et al. Discontinuation vs. continuation of renin–angiotensin system inhibition before non-cardiac surgery: the SPACE trial . Eur Heart J 2024 ; 45 : 1146 – 55 . https://doi.org/10.1093/eurheartj/ehad716
McEvoy MD , Gupta R , Koepke EJ , Feldheiser A , Michard F , Levett D , et al. Perioperative quality initiative consensus statement on postoperative blood pressure, risk and outcomes for elective surgery . Br J Anaesth 2019 ; 122 : 575 – 86 . https://doi.org/10.1016/j.bja.2019.01.019
Ekman I , Swedberg K , Taft C , Lindseth A , Norberg A , Brink E , et al. Person-centered care—ready for prime time . Eur J Cardiovasc Nurs 2011 ; 10 : 248 – 51 . https://doi.org/10.1016/j.ejcnurse.2011.06.008
Krist AH , Tong ST , Aycock RA , Longo DR . Engaging patients in decision-making and behavior change to promote prevention . Stud Health Technol Inform 2017 ; 240 : 284 – 302 . https://doi.org/10.3233/ISU-170826
Johnson RA , Huntley A , Hughes RA , Hughes RA , Cramer H , Turner KM , et al. Interventions to support shared decision making for hypertension: a systematic review of controlled studies . Health Expect 2018 ; 21 : 1191 – 207 . https://doi.org/10.1111/hex.12826
Johnson RL , Roter D , Powe NR , Cooper LA . Patient race/ethnicity and quality of patient–physician communication during medical visits . Am J Public Health 2004 ; 94 : 2084 – 90 . https://doi.org/10.2105/ajph.94.12.2084
Williams MV , Davis T , Parker RM , Weiss BD . The role of health literacy in patient-physician communication . Fam Med 2002 ; 34 : 383 – 9 .
Karmali KN , Persell SD , Perel P , Lloyd-Jones DM , Berendsen MA , Huffman MD . Risk scoring for the primary prevention of cardiovascular disease . Cochrane Database Syst Rev 2017 ; 3 : CD006887 . https://doi.org/10.1002/14651858.CD006887.pub4
Ma C , Zhou Y , Zhou W , Huang C . Evaluation of the effect of motivational interviewing counselling on hypertension care . Patient Educ Couns 2014 ; 95 : 231 – 7 . https://doi.org/10.1016/j.pec.2014.01.011
Huang X , Xu N , Wang Y , Sun Y , Guo A . The effects of motivational interviewing on hypertension management: a systematic review and meta-analysis . Patient Educ Couns 2023 ; 112 : 107760 . https://doi.org/10.1016/j.pec.2023.107760
Glaser E , Richard C , Lussier MT . The impact of a patient web communication intervention on reaching treatment suggested guidelines for chronic diseases: a randomized controlled trial . Patient Educ Couns 2017 ; 100 : 2062 – 70 . https://doi.org/10.1016/j.pec.2017.05.022
Richard AA , Shea K . Delineation of self-care and associated concepts . J Nurs Scholarsh 2011 ; 43 : 255 – 64 . https://doi.org/10.1111/j.1547-5069.2011.01404.x
Wilkinson A , Whitehead L . Evolution of the concept of self-care and implications for nurses: a literature review . Int J Nurs Stud 2009 ; 46 : 1143 – 7 . https://doi.org/10.1016/j.ijnurstu.2008.12.011
Bodenheimer T , Lorig K , Holman H , Grumbach K . Patient self-management of chronic disease in primary care . JAMA 2002 ; 288 : 2469 – 75 . https://doi.org/10.1001/jama.288.19.2469
Barlow J , Wright C , Sheasby J , Turner A , Hainsworth J . Self-management approaches for people with chronic conditions: a review . Patient Educ Couns 2002 ; 48 : 177 – 87 . https://doi.org/10.1016/s0738-3991(02)00032-0
Hallberg I , Ranerup A , Kjellgren K . Supporting the self-management of hypertension: patients’ experiences of using a mobile phone-based system . J Hum Hypertens 2016 ; 30 : 141 – 6 . https://doi.org/10.1038/jhh.2015.37
Almeida GO , Aidar FJ , Matos DG , Almeida-Neto PF , Melo EV , Barreto Filho JAS , et al. Non-targeted self-measurement of blood pressure: association with self-medication, unscheduled emergency visits and anxiety . Medicina (Kaunas) 2021 ; 57 : 75 . https://doi.org/10.3390/medicina57010075
Greaves F , Joshi I , Campbell M , Roberts S , Patel N , Powell J , et al. What is an appropriate level of evidence for a digital health intervention? Lancet 2019 ; 392 : 2665 – 7 . https://doi.org/10.1016/s0140-6736(18)33129-5
Morton K , Dennison L , May C , Murray E , Little P , McManus RJ , et al. Using digital interventions for self-management of chronic physical health conditions: a meta-ethnography review of published studies . Patient Educ Couns 2017 ; 100 : 616 – 35 . https://doi.org/10.1016/j.pec.2016.10.019
McKinstry B , Hanley J , Wild S , Pagliari C , Paterson M , Lewis S , et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial . BMJ 2013 ; 346 : f3030 . https://doi.org/10.1136/bmj.f3030
Persell SD , Peprah YA , Lipiszko D , Lee JY , Li JJ , Ciolino JD , et al. Effect of home blood pressure monitoring via a smartphone hypertension coaching application or tracking application on adults with uncontrolled hypertension: a randomized clinical trial . JAMA Netw Open 2020 ; 3 : e200255 . https://doi.org/10.1001/jamanetworkopen.2020.0255
Andersson U , Nilsson PM , Kjellgren K , Hoffmann M , Wennersten A , Midlöv P , et al. PERson-centredness in Hypertension management using Information Technology: a randomized controlled trial in primary care . J Hypertens 2023 ; 41 : 246 – 53 . https://doi.org/10.1097/hjh.0000000000003322
Bergland OU , Halvorsen LV , Søraas CL , Hjørnholm U , Kjær VN , Rognstad S , et al. Detection of nonadherence to antihypertensive treatment by measurements of serum drug concentrations . Hypertension 2021 ; 78 : 617 – 28 . https://doi.org/10.1161/hypertensionaha.121.17514
Durand H , Hayes P , Morrissey EC , Newell J , Casey M , Murphy AW , et al. Medication adherence among patients with apparent treatment-resistant hypertension: systematic review and meta-analysis . J Hypertens 2017 ; 35 : 2346 – 57 . https://doi.org/10.1097/hjh.0000000000001502
Kronish IM , Thorpe CT , Voils CI . Measuring the multiple domains of medication nonadherence: findings from a Delphi survey of adherence experts . Transl Behav Med 2021 ; 11 : 104 – 13 . https://doi.org/10.1093/tbm/ibz133
DiMatteo MR . Social support and patient adherence to medical treatment: a meta-analysis . Health Psychol 2004 ; 23 : 207 – 18 . https://doi.org/10.1037/0278-6133.23.2.207
Houle SK , Chatterley T , Tsuyuki RT . Multidisciplinary approaches to the management of high blood pressure . Curr Opin Cardiol 2014 ; 29 : 344 – 53 . https://doi.org/10.1097/hco.0000000000000071
Woodham NS , Taneepanichskul S , Somrongthong R , Kitsanapun A , Sompakdee B . Effectiveness of a multidisciplinary approach intervention to improve blood pressure control among elderly hypertensive patients in rural Thailand: a quasi-experimental study . J Multidiscip Healthc 2020 ; 13 : 571 – 80 . https://doi.org/10.2147/jmdh.S254286
Mattei da Silva ÂT , de Fátima Mantovani M , Castanho Moreira R , Perez Arthur J , Molina de Souza R . Nursing case management for people with hypertension in primary health care: a randomized controlled trial . Res Nurs Health 2020 ; 43 : 68 – 78 . https://doi.org/10.1002/nur.21994
He J , Ouyang N , Guo X , Sun G , Li Z , Mu J , et al. Effectiveness of a non-physician community health-care provider-led intensive blood pressure intervention versus usual care on cardiovascular disease (CRHCP): an open-label, blinded-endpoint, cluster-randomised trial . Lancet 2023 ; 401 : 928 – 38 . https://doi.org/10.1016/s0140-6736(22)02603-4
Creegan D , McEvoy JW . Selected highlights in the updated treatment of hypertension . Trends Cardiovasc Med https://doi.org/10.1016/j.tcm.2023.11.001
Jaffe MG , Lee GA , Young JD , Sidney S , Go AS . Improved blood pressure control associated with a large-scale hypertension program . JAMA 2013 ; 310 : 699 – 705 . https://doi.org/10.1001/jama.2013.108769
Hänsel M , Steigmiller K , Luft AR , Gebhard C , Held U , Wegener S , et al. Neurovascular disease in Switzerland: 10-year trends show non-traditional risk factors on the rise and higher exposure in women . Eur J Neurol 2022 ; 29 : 2851 – 60 . https://doi.org/10.1111/ene.15434
de Ruiter SC , Schmidt AF , Grobbee DE , den Ruijter HM , Peters SAE . Sex-specific Mendelian randomisation to assess the causality of sex differences in the effects of risk factors and treatment: spotlight on hypertension . J Hum Hypertens 2023 ; 37 : 602 – 8 . https://doi.org/10.1038/s41371-023-00821-1
Chapman N , Ching SM , Konradi AO , Nuyt AM , Khan T , Twumasi-Ankrah B , et al. Arterial hypertension in women: state of the art and knowledge gaps . Hypertension 2023 ; 80 : 1140 – 9 . https://doi.org/10.1161/hypertensionaha.122.20448
Tamargo J , Caballero R , Mosquera ED . Sex and gender differences in the treatment of arterial hypertension . Expert Rev Clin Pharmacol 2023 ; 16 : 329 – 47 . https://doi.org/10.1080/17512433.2023.2189585
Olsen MH , Angell SY , Asma S , Boutouyrie P , Burger D , Chirinos JA , et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension . Lancet 2016 ; 388 : 2665 – 712 . https://doi.org/10.1016/s0140-6736(16)31134-5
Author notes

- hypertension
- cardiovascular diseases
- heart disease risk factors
- blood pressure
- blood pressure determination
Supplementary data
| Month: | Total Views: |
|---|---|
| August 2024 | 22,734 |
Email alerts
Related articles in pubmed, citing articles via, looking for your next opportunity, affiliations.
- Online ISSN 1522-9645
- Print ISSN 0195-668X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
2024 ESC Clinical Practice Guidelines for the Management of Chronic Coronary Syndromes

As explained by Professor Christiaan Vrints (University of Antwerp - Antwerp, Belgium) and Professor Felicita Andreotti (Fondazione Policlinico Universitario Gemelli IRCCS and Catholic University Medical School - Rome, Italy), Chairs of the Guidelines Task Force, the first main change to the ESC Guidelines on chronic coronary syndromes (CCS) is its definition. 1
The guidelines were developed by 28 task force members, including 26 experts and 2 patients. Patients’ input contributed greatly by keeping the focus on patient perspectives and on clear, understandable content. Additionally, involving patients aims to empower them to participate in decision-making and, as a result, to stimulate adherence to healthy lifestyles and appropriate therapies.
“The term CCS was first introduced in the 2019 guidelines but, based on expanded pathophysiological concepts, a new more comprehensive definition has been developed,” explains Prof. Vrints, continuing: “There is a shift in our understanding away from the simple concept of inducible myocardial ischaemia caused by fixed, focal, flow-limiting atherosclerotic stenosis of a large or medium coronary artery. Today’s more complex and dynamic model embraces structural and functional abnormalities in both the macro- and microvascular compartments of the coronary tree, which may be focal or diffuse.”
A stepwise approach to managing suspected CCS is advocated in the 2024 guidelines, beginning with STEP 1, a general clinical evaluation to differentiate the patient’s signs and symptoms from non-cardiac causes of chest pain and rule out acute coronary syndrome. STEP 2 is a cardiac specialist examination, including an echocardiography at rest to rule out left ventricular dysfunction and valvular heart disease. A new Class I recommendation endorses estimating the pre-test likelihood of obstructive epicardial coronary artery disease (CAD) using the Risk Factor-weighted Clinical Likelihood model.
STEP 3 involves testing to establish the CCS diagnosis and determine the patient's risk of future events. It is now recommended that coronary computed tomography angiography is used to diagnose obstructive CAD and to estimate the risk of major adverse cardiovascular events (MACE) in individuals with suspected CCS and low or moderate (>5%–50%) pre-test likelihood of obstructive CAD. In those with moderate or high (>15%–85%) pre-test likelihood of obstructive CAD, there are new Class I recommendations regarding the use of stress echocardiography, positron emission tomography and cardiac magnetic resonance perfusion imaging, if available.
Invasive coronary angiography (ICA) is recommended to diagnose obstructive CAD in individuals with a high pre- or post-test likelihood of disease, severe symptoms refractory to medical therapy, angina at a low level of exercise, and/or high event risk. When ICA is indicated, it is recommended that the functional severity of ‘intermediate’ stenoses is evaluated by invasive functional testing (fractional flow reserve and instantaneous wave-free ratio) before revascularisation.
STEP 4 includes lifestyle and risk-factor modification combined with disease-modifying medications, with coronary revascularisation if symptoms are refractory to medical treatment or if high-risk CAD is present. “Shared decision-making between patients and healthcare professionals, based on patient-centred care, is paramount in defining the appropriate therapeutic pathway for CCS patients,” states Prof. Andreotti. “And where needed, the most appropriate revascularisation modality should be selected based on the patient’s profile, coronary anatomy, procedural factors, patient preference and outcome expectations.” The 2024 guidelines confirm the findings of the 2022 ESC/EACTS Task Force that coronary artery bypass grafting (CABG) is recommended as the overall preferred revascularisation mode over percutaneous coronary intervention (PCI) for left main CAD in low-risk surgical patients given the lower risk of spontaneous myocardial infarction and repeat revascularisation. It is also acknowledged that in patients with significant left main CAD of low complexity (SYNTAX score ≤ 22), in whom PCI can provide equivalent completeness of revascularisation to that of CABG, PCI is recommended as an alternative to CABG.
The high prevalence of angina with nonobstructive coronary arteries (ANOCA) and ischaemia with nonobstructive coronary arteries (INOCA) and its associated MACE rate is noted in the guidelines. It is recommended that symptomatic patients with suspected ANOCA/INOCA who do not respond to guideline-derived medical therapy should undergo invasive coronary functional testing to determine underlying endotypes to guide appropriate medical therapy.
The final section concerns long-term follow-up and care, with new recommendations on the use of simplified medication regimens, along with mobile health interventions to improve adherence to healthy lifestyles and medical therapy.
Want to know more about what’s new? 2024 ESC Guidelines are now published in the European Heart Journal and are available on the ESC Pocket Guidelines app .
- Vrints C, et al. 2024 ESC Guidelines on the management of chronic coronary syndromes. Eur Heart J. 2024. doi:10.1093/eurheartj/ehae177.


COMMENTS
Hypothesis Definition. In the context of a consulting interview, a hypothesis definition is "a testable statement that needs further data for verification". In other words, the meaning of a hypothesis is that it's an educated guess that you think could be the answer to your client's problem. A hypothesis is therefore not always true.
And, being hypothesis-driven was required to have any success at McKinsey. A hypothesis is an idea or theory, often based on limited data, which is typically the beginning of a thread of further investigation to prove, disprove or improve the hypothesis through facts and empirical data. The first step in being hypothesis-driven is to focus on ...
An Overview of Management Theories: Classical, Behavioral, and Modern Approaches. In both theory and practice, business management is at a crisis point. The world is changing — and changing quickly. There is no single management philosophy that answers every need. The best managers are flexible and blend methods.
Critical management authors are thus justified in directing attention to the constraining and possibly alienating role of language. The construct of management theory is here a case in point: Such theory embodies, indeed requires, a deterministic picture of human existence that is typically unacknowledged, presumably because it is unrecognized.
3. One-Sided vs. Two-Sided Testing. When it's time to test your hypothesis, it's important to leverage the correct testing method. The two most common hypothesis testing methods are one-sided and two-sided tests, or one-tailed and two-tailed tests, respectively. Typically, you'd leverage a one-sided test when you have a strong conviction ...
Hypothesis generation contrasts starkly with more traditional management approaches designed for process optimization. Process optimization involves telling employees both what to do and how to do it. Process optimization is fine for stable business processes that have been standardized for consistency.
A research hypothesis (also called a scientific hypothesis) is a statement about the expected outcome of a study (for example, a dissertation or thesis). To constitute a quality hypothesis, the statement needs to have three attributes - specificity, clarity and testability. Let's take a look at these more closely.
Management theories help organizations to focus, communicate, and evolve. Using management theory in the workplace allows leadership to focus on their main goals. When a management style or theory is implemented, it automatically streamlines the top priorities for the organization. Management theory also allows us to better communicate with ...
Developing a hypothesis (with example) Step 1. Ask a question. Writing a hypothesis begins with a research question that you want to answer. The question should be focused, specific, and researchable within the constraints of your project. Example: Research question.
A hypothesis is a tentative statement about the relationship between two or more variables. It is a specific, testable prediction about what you expect to happen in a study. It is a preliminary answer to your question that helps guide the research process. Consider a study designed to examine the relationship between sleep deprivation and test ...
Simple hypothesis. A simple hypothesis is a statement made to reflect the relation between exactly two variables. One independent and one dependent. Consider the example, "Smoking is a prominent cause of lung cancer." The dependent variable, lung cancer, is dependent on the independent variable, smoking. 4.
Summary. Strategies must be constantly adjusted to incorporate information from operations and the market. Research on recent dramatic cases of strategic failure in different industries and ...
A hypothesis is a prediction of what will be found at the outcome of a research project and is typically focused on the relationship between two different variables studied in the research. It is usually based on both theoretical expectations about how things work and already existing scientific evidence. Within social science, a hypothesis can ...
It seeks to explore and understand a particular aspect of the research subject. In contrast, a research hypothesis is a specific statement or prediction that suggests an expected relationship between variables. It is formulated based on existing knowledge or theories and guides the research design and data analysis. 7.
Incentives: Scientific Management recommends providing financial rewards or incentives to motivate workers towards meeting productivity targets. Taylor believed that employees would be motivated by a fair and consistent rewards system. B) Administrative Management Theory: In Administrative Management theory, Henri Fayol is associated with the overall management of organizations.
The meaning of HYPOTHESIS is an assumption or concession made for the sake of argument. How to use hypothesis in a sentence. The Difference Between Hypothesis and Theory Synonym Discussion of Hypothesis.
Hypothesis is a hypothesis isfundamental concept in the world of research and statistics. It is a testable statement that explains what is happening or observed. It proposes the relation between the various participating variables. Hypothesis is also called Theory, Thesis, Guess, Assumption, or Suggestion. Hypothesis creates a structure that ...
Hypothesis is a prediction of the outcome of a study. Hypotheses are drawn from theories and research questions or from direct observations. In fact, a research problem can be formulated as a hypothesis. To test the hypothesis we need to formulate it in terms that can actually be analysed with statistical tools.
Hence, a hypothesis is a hunch, assumption, suspicion, assertion or an idea about a phenomenon, relationship or situation, the reality or truth of which you do not know. A researcher calls these assumptions, assertions, statements or hunches hypotheses and they become the basis of an enquiry.
A hypothesis in product development and product management is a statement or assumption about the product, planned feature, market, or customer (e.g., their needs, behavior, or expectations) that you can put to the test, evaluate, and base your further decisions on. This may, for instance, regard the upcoming product changes as well as the ...
The Efficient Market Hypothesis is a crucial financial theory positing that all available information is reflected in market prices, making it impossible to consistently outperform the market. It manifests in three forms, each with distinct implications. The weak form asserts that all historical market information is accounted for in current ...
The null hypothesis (H0) answers "No, there's no effect in the population.". The alternative hypothesis (Ha) answers "Yes, there is an effect in the population.". The null and alternative are always claims about the population. That's because the goal of hypothesis testing is to make inferences about a population based on a sample.
Strategic management is the assembling and management of resources to achieve a company's goals and objectives. Strategic management helps companies set goals, gain a competitive edge, better ...
The efficient market hypothesis is just "a model", Fama stresses. "It's got to be wrong to some extent." "The question is whether it is efficient for your purpose.
Quality Management: Definition & Examples. So, what is quality management? In short, it involves management tasks and roles focused on defining and executing quality policies through strategies like quality planning, assurance, and control. Let's understand this through an example. Consider running a bakery on your street.
Obtaining a computational understanding of the brain is one of the most important problems in basic science. However, the brain is an incredibly complex organ, and neurobiological research has uncovered enormous amounts of detail at almost every level of analysis (the synapse, the neuron, other brain cells, brain circuits, areas, and so on); it is unclear which of these details are ...
18In the context of the Malaysian construction industry, effective leadership remains pivotal for navigating the complexities inherent in engineering projects. Past studies have consistently identified leadership as one of the critical factors in ensuring the success of construction projects. Effective leadership has been linked to project performance, timely completion, and team coordination.
Guidelines evaluate and summarize available evidence with the aim of assisting health professionals in proposing the best diagnostic or therapeutic approac
"The term CCS was first introduced in the 2019 guidelines but, based on expanded pathophysiological concepts, a new more comprehensive definition has been developed," explains Prof. Vrints, continuing: "There is a shift in our understanding away from the simple concept of inducible myocardial ischaemia caused by fixed, focal, flow ...
SAN ANTONIO — Recently updated practice parameters will help clinicians better recognize and treat anaphylaxis, Jeffrey Demain, MD, FAAAAI, FACAAI, FAAP, told Healio at the 16th Annual Allergy ...