- Undergraduate Admissions
- Graduate Admissions
- Teacher Certification Options
- International Admissions Information
- Financial Aid and Scholarships
- Undergraduate Majors and Minors
- Master’s Programs
- Certificates of Advanced Study
- Doctoral Programs
- Online, Hybrid, and Flexible Programs
- Career Services and Certification
- For Families and Supporters
- Learning Communities
- Student Organizations
- Undergraduate Peer Advisors
- Bridge to the City
- Engaged BIPOC Scholar-Practitioner Program
- Field Placements & Internships
- Orange Holmes Scholars
- Spector/Warren Fellowship
- Study Abroad
- Research News
- Faculty Bookshelf
- Faculty Publications
- Grants & Awards
- Doctoral Dissertations
- Research Resources and Support
- Office of Professional Research and Development
- Atrocity Studies Annual Lecture
- Antiracist Algebra Coalition
- Ganders Lecture Series
- InquiryU@Solvay
- Intergroup Dialogue Program
- Otto’s Fall Reading Kickoff
- Psycho-Educational Teaching Laboratory
- The Study Council
- Writing Our Lives
- Center for Academic Achievement and Student Development
- Center on Disability and Inclusion
- Center for Experiential Pedagogy and Practice
- Latest News
- Upcoming Events
- Education Exchange
- Get Involved
- Advisory Board
- Tolley Medal
- Administration
- From the Dean
- Convocation
- Accreditation
- Request Info
- Grants & Awards

Suicide Risk: Case Studies and Vignettes
Identifying warning signs case study.
Taken from Patterson, C. W. (1981). Suicide. In Basic Psychopathology: A Programmed Text.
Instructions: Underline all words and phrases in the following case history that are related to INCREASED suicidal risk. Then answer the questions at the end of the exercise.
History of Present Illness
The client is a 65-year-old white male, divorced, living alone, admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time.
A heavy drinker, he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia, anorexia, and a ten pound weight loss. He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed, states that, “nobody can help me” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities, “just drinking.”
Past Psychiatric History
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him. Treated with ECT, he did “pretty good, but only for about two years” thereafter.
Social History
An only child, his parents are deceased (father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years, usually quitting or being fired because of “my temper.” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources. He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times, he has no children or close friends.
Mental Status Examination
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information. Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile.
Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead. There were no thoughts about wishing to harm others.
Mood was one of depression. He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
Diagnostic Impression
- drug overdose (Valium and alcohol)
- Dysthymic Disorder (depression)
- Substance Use Disorder (alcohol)
Questions for Exercise
You have interviewed the client, obtained the above history, and now have to make some decisions about the client. He wants to leave the hospital.
- Is he a significant risk for suicide?
- discharging him as he wishes and with your concurrence?
- discharging him against medical advice (A.M.A.)?
- discharging him if he promises to see a therapist at a nearby mental health center within the next few days?
- holding him for purposes of getting his psychiatric in-client care even though he objects?
- Discuss briefly why you would not have chosen the other alternatives in question #2.
Identifying Warning Signs Case Study: Feedback/Answers
The client is a 65-year-old white male , divorced , living alone , admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time. A heavy drinker , he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia and a ten pound weight loss . He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed , states that, “ nobody can help me ” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities , “just drinking.”
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him . Treated with ECT, he did “pretty good, but only for about two years” thereafter.
An only child, his parents are deceased ( father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years , usually quitting or being fired because of “ my temper .” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources . He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times , he has no children or close friends .
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information . Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile. Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead . There were no thoughts about wishing to harm others. Mood was one of depression . He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
- Is he a significant risk for suicide? Yes. The client presents a considerable suicidal risk, with respect to demographic characteristics, psychiatric diagnosis and mental status findings.
- Discuss briefly why you would not have chosen the other alternatives in question #2. The client appears to be actively suicidal at the present time,and may act upon his feelings. Nothing about his life has changed because of his attempt. He still is lonely, with limited social resources. He feels no remorse for his suicidal behavior and his future remains unaltered. He must be hospitalized until some therapeutic progress can be made.
Short-Term Suicide Risk Vignettes
*Case study vignettes taken from Maris, R. W., Berman, A. L., Maltsberger, J. T., & Yufit, R. I. (Eds), (1992). Assessment and prediction of suicide. New York: Guilford. And originally cited in Stelmachers, Z. T., & Sherman, R. E. (1990). Use of case vignettes in suicide risk assessment. Suicide and Life-Threatening Behavior, 20, 65-84.
The assessment of suicide risk is a complicated process. The following vignettes are provided to promote discussion of suicide risk factors, assessment procedures, and intervention strategies. The “answers” are not provided, rather students are encouraged to discuss cases with each other and faculty. Two examples of how discussions may be facilitated are provided.
37-year-old white female, self-referred. Stated plan is to drive her car off a bridge. Precipitant seems to be verbal abuse by her boss; after talking to her nightly for hours, he suddenly refused to talk to her. As a result, patient feels angry and hurt, threatened to kill herself. She is also angry at her mother, who will not let patient smoke or bring men to their home. Current alcohol level is .15; patient is confused, repetitive, and ataxic. History reveals a previous suicide attempt (overdose) 7 years ago, which resulted in hospitalization. After spending the night at CIC and sobering, patient denies further suicidal intent.
16-year-old Native American female, self-referred following an overdose of 12 aspirins. Precipitant: could not tolerate rumors at school that she and another girl are sharing the same boyfriend. Denies being suicidal at this time (“I won’t do it again; I learned my lesson”). Reports that she has always had difficulty expressing her feelings. In the interview, is quiet, guarded, and initially quite reluctant to talk. Diagnostic impression: adjustment disorder.
49-year-old white female brought by police on a transportation hold following threats to overdose on aspirin (initially telephoned CIC and was willing to give her address). Patient feels trapped and abused, can’t cope at home with her schizophrenic sister. Wants to be in the hospital and continues to feel like killing herself. Husband indicates that the patient has been threatening to shoot him and her daughter but probably has no gun. Recent arrest for disorderly conduct (threatened police with a butcher knife). History of aspirin overdose 3 years ago. In the interview, patient is cooperative; appears depressed, anxious, helpless, and hopeless. Appetite and sleep are down, and so is her self-esteem. Is described as “anhedonic.” Alcohol level: .12.
23-year-od white male, self-referred. Patient bought a gun 2 months ago to kill himself and claims to have the gun and four shells in his car (police found the gun but no shells). Patient reports having planned time and place for suicide several times in the past. States that he cannot live any more with his “emotional pain” since his wife left him3 years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency, but has been sober for 20 months and currently goes to AA.
22-year-old black male referred to CIC from the Emergency Room on a transportation hold. He referred himself to the Emergency Room after making fairly deep cuts on his wrists requiring nine stitches. Current stress is recent breakup with his girlfriend and loss of job. Has developed depressive symptoms for the last 2 months, including social withdrawal, insomnia, anhedonia, and decreased appetite. Blames his sister for the breakup with girlfriend. Makes threats to sister (“I will slice up that bitch, she is dead when I get out”). Patient is an alcoholic who just completed court-ordered chemical dependency treatment lasting 3 weeks. He is also on parole for attempted rape. There is a history of previous suicide attempts and assaultive behavior, which led to the patient being jailed. In the interview, patient is vague regarding recent events and history. He denies intent to kill himself but admits to still being quite ambivalent about it. Diagnostic impression: antisocial personality.
19-year-old white male found by roommate in a “sluggish” state following the ingestion of 10 sleeping pills (Sominex) and one bottle of whiskey. Recently has been giving away his possessions and has written a suicide note. After being brought to the Emergency Room, declares that he will do it again. Blood alcohol level: .23. For the last 3 or 4 weeks there has been sleep and appetite disturbance, with a 15-pound weight loss and subjective feelings of depression. Diagnostic impression: adjustment disorder with depressed mood versus major depressive episode. Patient refused hospitalization.
30-year-old white male brought from his place of employment by a personnel representative. Patient has been thinking of suicide “all the time” because he “can’t cope.” Has a knot in his stomach; sleep and appetite are down (sleeps only 3 hours per night); and plans either to shoot himself, jump off a bridge, or drive recklessly. Precipitant: constant fighting with his wife leading to a recent breakup (there is a long history of mutual verbal/physical abuse). There is a history of a serious suicide attempt: patient jumped off a ledge and fractured both legs; the precipitant for that attempt was a previous divorce. There is a history of chemical dependency with two courses of treatment. There is no current problem with alcohol or drugs. Patient is tearful, shaking, frightened, feeling hopeless, and at high risk for impulsive acting out. He states that life isn’t worthwhile.
Vignette Discussion Examples
Vignette example 1.
Twenty-six year old white female phoned her counselor, stated that she might take pills, and then hung up and kept the phone off the hook. The counselor called the police and the patient was brought to the crisis intervention center on a transportation hold. Patient was angry, denied suicidal attempt, and refused evaluation; described as selectively mute, which means she wouldn’t answer any of the questions she didn’t like.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? Student Answer 1: Maybe moderate because the person is warning somebody, basically a plea for help. Facilitator: Okay, so we have suicidal talk. That’s one of our red flags. What else? She said she might take pills, so we didn’t know if she does have the pills. So she has a plan. The plan would be to take pills, but we don’t know if we have means. Student Answer 2: High. She’s also angry. I don’t know if she’s angry often. Facilitator: A person in this situation who is really thinking about killing themselves tends not to deny it. They tend not to deny it. There are exceptions to everything, but most of the time, for some reason, this is one of the things where people tend to mostly tell you the truth. If you ask people, they tend to tell you the truth. It’s a very funny thing about suicide that way. That’s certainly not true about most things. If you ask people how much they drink…But, “Are you thinking about killing yourself?” “Well, yes.” If you ask a question, you tend to get a more or less accurate, straight answer. Student question: Is that because it doesn’t matter anymore? If they’re going to die anyway, who’s going to care about what anybody thinks or what happens? Facilitator: My hypothesis would be, when someone is at that point, they’re talking about real, true things. They’re not into play. This is where they are. If they’re really looking at it, then they’re just at that place. What’s to hide at that point? You don’t have anything to lose. It’s a state of mind. And then if you’re not in that place—it’s like, how close are you to the edge of that cliff? “I’m not there. I know where that is, and I’m not there.” “If you get there, will you tell me?” “Yeah, I’m not there.” So, people have a sense—if they’ve gotten that close, they know where that line is, and they know about where they stand in regard to it, because it’s a very hard-edged, true thing.
Twenty-three year old white male, self-referred. Patient bought a gun two months ago to kill himself and claims to have the gun and four shells in his car. Police found the gun but no shells. Patient reports having planned time and place for suicide several times in the past. States that he cannot live anymore with his emotional pain since his wife left him three years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency but has been sober for 20 months and currently goes to AA.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? On a scale from 0 to 7 (7 being very high). Student Answer 1: High. On a scale of 0 to 7? Student Answer: Six. Student Answer 2: I would say three. I think it would be lower because if he’s already bought the gun two months ago and he’s self-referring himself to get help, he wants to live. He has not made peace with whatever, and he’s more likely not give away his things, and he’s going to AA meetings. I think it’s lower than really an extreme…I would say a three or four. Student Answer 3: I would say a four or five, moderate. Student Answer 4: About a five..several times and hasn’t followed through, tells me he doesn’t really want to follow through with it. Facilitator: And there are no shells, right? So we can see some of the red flags are there, but some of them aren’t. He’s still sober… Student: He has a support group. Student: He’s not using, though he bought a gun—so that’s a concern. There is a lot there. Student: He may not have the shells so he doesn’t have the opportunity to. So does that make him more…? Student 2: Think I’ll change mine to a five. Facilitator: So the mean was 4.68, so 5 was the mode. If we’re saying this is a moderate risk, what things would we look for that would make this a high risk? Student: Take away AA. Student: If he falls off the wagon, he goes right to the top. Student: And if he finds the shells. Facilitator: Because it probably is not that hard to find shells. All these stores around here, you can get shells quicker than you can get a gun, so he’s only a five-minute purchase away from having lethal—in contrast to not having the gun. Student: Could there be a difference in the time? Let’s say his wife left him just four to six months ago rather than three years. Would that be something that would be more serious? Facilitator: Yes, or if his wife just left him. So, say his wife left him a month ago that would bump it up. So that’s unresolved. That’s taking a person that was worried and that’s pushing him higher. Student: It also raises the homicide rate. Facilitator: Yes, because these tend to be murder-suicides. How often have we seen that? Murder-suicide is a big deal. If she won’t be with me, she won’t be with anybody.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Pract Cases Emerg Med
- v.3(1); 2019 Feb
A Single-session Crisis Intervention Therapy Model for Emergency Psychiatry
Associated data.
Presentations for anxiety and depression constitute the fastest growing category of mental health diagnoses seen in emergency departments (EDs). Even non-psychiatric clinicians must be prepared to provide psychotherapeutic interventions for these patients, just as they might provide motivational interviewing for a patient with substance use disorders. This case report of an 18-year-old woman with suicidal ideation illustrates the practicality and utility of a brief, single-session, crisis intervention model that facilitated discharge from the ED. This report will help practitioners to apply this model in their own practice and identify patients who may require psychiatric hospitalization.
INTRODUCTION
Symptoms of anxiety and depression are the most common reasons to present for emergency psychiatric care. 1 The broad differential for depressive and anxiety symptoms includes major depressive, post-traumatic stress, adjustment, substance-induced, and personality disorders. 2 Because medications are not indicated for some of these conditions, all emergency department (ED) clinicians must be prepared to provide brief, non-pharmacologic treatment. This case report demonstrates a single-session, crisis intervention model for ED patients presenting with anxiety and depression.
CASE REPORT
An 18-year-old woman was brought to the ED by ambulance. Paramedics reported that the patient was on the phone with her mother and said she wanted to be dead. Her mother lives in another country and called emergency services. The patient was tearful and “very stressed” on arrival. Vital signs, a routine urine toxicology screen, and pregnancy test were unremarkable. She reported suicidal thoughts for about a week attributed to poor grades in college, family conflict, and financial obligations. She had missed several appointments with her therapist and prescriber and had recently run out of sertraline (Zoloft). She declined to provide her mother’s phone number.
The patient described a history of abuse at a young age. She had one prior psychiatric hospitalization after walking into traffic in a suicide attempt at age 15. Other episodes of self-harm started at age 10 and were non-suicidal in nature. Her biological father had minimal contact with the patient. Her grandmother had been diagnosed with schizophrenia. The patient denied access to firearms.
Concerned about multiple suicide safety risk factors, the emergency psychiatrist began a structured, single-session psychotherapy. The psychiatrist and patient wrote a timeline of events preceding the presentation ( Figure 1 ). In so doing, she provided more details of her history. Ten months prior, she had to leave her apartment due to conflicts with roommates. Beginning college, she worried about tuition and found two jobs. Despite several attempts to re-schedule her therapy appointments around her work schedule, the therapist’s office did not return her calls. The patient also revealed that a supportive stepfather lived nearby. The morning of her ED visit, she received another reminder about her tuition bill. She was talking with a roommate about this bill; however, she felt her roommate did not fully appreciate her challenges, and she then called her mother.

A timeline of stressors preceding the patient’s emergency department visit.
The psychiatrist and patient agreed all this would be stressful for anyone. Her affect evolved from tearful to more composed, and she identified some immediate goals: find a new therapist; talk with her school about a tuition grant; identify a tutor; and spend more time doing things she enjoys ( Supplemental Figure ). She agreed to let the resident call her mother who could help complete these tasks. The patient’s mother corroborated the patient’s history. In fact, the mother had already spoken with the school about help with tuition and had begun searching for new outpatient providers.
To complete discharge planning, a nurse made an appointment for the patient with a new outpatient provider. The patient completed a written safety plan and was offered a follow-up call. The family was apprised of local crisis resources. Within an hour, the evaluating psychiatrist felt that this patient’s acute risk was significantly mitigated through safety planning, mobilization of social supports, connection to treatment, and acute de-escalation to justify discharge. After six months, she had persistent resolution of suicidal thoughts without recurrent self-harm or inpatient hospitalization.
This brief psychotherapy emphasizes active problem-solving and is adapted from a multi-session model built for integrated care settings. 3 Specialized single-session psychotherapies have been described for other psychiatric conditions including insomnia, 4 gambling, 5 agitation, 6 and suicidal ideation. 7 Therapy models described for ED settings are often applied by non-psychiatric staff, for example, motivational interviewing for substance use 8 and safety planning for suicidality. 9 , 10
This model uses the concept of crisis as a framework for assessment and treatment. A crisis occurs when a person’s usual coping skills are inadequate to a life stressor. 11 A crisis may be precipitated by medical illness or interpersonal conflicts. A patient’s ability to cope with stressors arises from individual temperament, life experiences, personal skills, and social network. When a crisis develops, individuals are unable to access these strengths to resolve the crisis. Anxiety, depression, a sense of feeling overwhelmed, or suicidal ideation ensues in a patient with perhaps little psychiatric treatment history and a high level of functioning that includes stable employment and relationships. Some patients manifest primitive coping skills such as somatization that precipitate an ED visit. A crisis may also relate to worsening symptoms in patients with chronic psychiatric illness, for example, increased suicidal ideation in a patient with borderline personality disorder. Crisis does not fit neatly into the Diagnostic and Statistical Manual of Mental Disorders , 5 th edition, (DSM-5) but is most closely related to the diagnosis of adjustment disorder. 12
Single-session therapy leverages the crisis model to help patients and providers understand the origins of the ED visit and begin actively resolving the crisis. This intervention may be delivered by emergency physicians or ED behavioral health consultants including social workers or nurses. Patients most likely to benefit from this therapy present in the context of a discrete life stressor and have a history of better psychological functioning and insight.
CPC-EM Capsule
What do we already know about this clinical entity?
Anxiety, depression, and adjustment reactions represent the fastest-growing category of reasons for psychiatric presentations to the emergency department (ED) .
What makes this presentation of disease reportable?
This case demonstrates how a single-session crisis therapy in the ED may avert hospitalization for a depressed, suicidal patient .
What is the major learning point?
ED clinicians should be prepared to recommend or deliver brief psychotherapy for these common psychiatric presentations .
How might this improve emergency medicine practice?
Most suicidal ED patients are hospitalized. However, most patients with depression or suicidality can be safely treated in the ED and discharged .
One-Session Crisis Intervention Psychotherapy
The goals of this intervention include ameliorating anxiety and depressive symptoms, initiating treatment, and identifying patients who may need referral for more intensive psychiatric treatment. These steps and their therapeutic benefits are summarized in Table .
Summary of working steps and therapeutic processes for one-session crisis intervention therapy.
| Stage | Working steps | Therapeutic process |
|---|---|---|
| 1. Recognize the crisis and identify the precipitant(s) | ) | |
| 2. Characterize the patient’s response | ||
| 3. Formulate together | ||
| 4. Identify behavioral goals and offer concrete support | ) | |
| 5. Engage social supports | ) |
DSM-5 , Diagnostic and Statistical Manual for Mental Disorders, 5th ed.; ED , emergency department.
1. Recognize the Crisis and Identify the Precipitant
Patients in crisis present to the ED with a range of psychiatric symptoms including anxiety, depression, fatigue, or poor sleep. After excluding a somatic etiology of psychiatric symptoms and ensuring acute safety, the clinician must elucidate the onset of the patient’s psychiatric symptoms. In the ED it is important to keep in mind that suicidality is often a symptom of underlying distress, does not necessarily indicate the presence of a severe psychiatric disorder, and can be treated in outpatient settings. 13
Writing a timeline with the patient helps identify life stressors driving the crisis. This technique is helpful for several reasons. First, many patients in crisis feel overwhelmed and are challenged to recall and reconstruct a helpful history. A structured framework focuses the interview on the acute presentation. A timeline is easy for both clinicians and patients to interpret. And, in the act of writing a timeline together, the clinician and patient build therapeutic rapport that itself is part of the healing process. Finally, the resulting product can be used to later formulate the crisis state with the patient.
2. Characterize the Patient’s Response
The patient’s emotional and behavioral responses to the crisis state should be considered in guiding treatment. 14
Validate the patient’s emotional response to the crisis. The emotional response is often readily described by the patient: stressed, overwhelmed, anxious, or alone. The clinician may validate the emotional state by noting it to be an understandable response to the clear stressors described in the timeline. A patient’s endorsement of depression is not synonymous with major depressive disorder (a specific diagnosis with precise diagnostic criteria).
Behavioral responses are characterized by immobility, avoidance, or adaptation. Immobility is a sense of feeling stuck and persistently unable to problem-solve, as this patient felt initially. Some patients avoid their problems entirely, thereby prolonging the crisis and exacerbating its consequences. Immobile and avoidant patients need help identifying the precipitant of the crisis and brainstorming possible solutions. Immobile or avoidant patients who cannot demonstrate more adaptive skills may require referral to specialty psychiatric care.
Patients who demonstrate adaptive responses to crisis are positioned to grow from their crisis and manage their lives more effectively. In this case, the patient moved from a more immobile stance to one characterized by greater initiative and adaptation.
3. Formulate Together
With a timeline of precipitants and a sense of the patient’s response styles, the clinician formulates the acute crisis aloud with the patient. What are the precipitants? How do these make the patient feel? What does the patient need to address the crisis? What choices are available?
The resulting conversation is both diagnostic and therapeutic. This patient experienced relief from an expert’s explanation of why she did not feel well. The clinician validated the severity of the patient’s stressors while offering optimism and active problem-solving.
A broad psychiatric differential should always be considered. Cognitive impairment related to severe depression or disorganization due to psychosis may be recognized in the course of therapy. Such symptoms complicate less-restrictive outpatient treatment and may alter disposition planning. Antidepressant discontinuation syndrome was considered less likely here given the timing and quality of her depressive symptoms.
4. Identify Behavioral Goals and Offer Concrete Support
The clinician helps the patient generate a to-do list of goals to resolve the crisis. This patient’s list is included as Supplemental Figure . Goals should be specific, realistic, and accomplishable in the near future. 15 Patients with more aspirational goals (e.g., feel better) should identify intermediate steps that are specific and accomplishable. Solutions-focused thinking can be introduced by asking, “If things were going well in your life, how would things look four weeks from now?” This conversation invites the patient to anticipate potential obstacles to resolution of the crisis—and also begin envisioning discharge from the ED.
Clinicians need to provide practical support for patients. For example, this patient needed help making an international phone call. Making an appointment for an outpatient provider improves outpatient adherence and reduces ED return rates. 16 , 17 Identifying triggers for suicidal thoughts, coping skills, and supportive contacts through a safety plan reduces the risk of subsequent self-harm and improves symptom burden. 9 , 18 , 19
5. Engage Social Supports
Patients in crisis are quick to say they have nobody to help them when, in fact, supportive friends or family are indeed available. This social network should be mobilized while the patient is in the ED.
A hub-and-spoke diagram helps the patient recognize persons who can help resolve the crisis ( Figure 2 ). The patient is in the middle hub. As many other persons as possible are written around the spokes of the wheel. Supportive persons are connected to the hub with a solid line, and less-supportive contacts are connected with a dashed line. The most important one or two persons are starred.

A hub-and-spoke diagram of the patient’s social supports.
The clinician should contact these supportive persons. Collateral information provides a stronger diagnostic and suicide safety assessment. 20 In this instance, that the patient’s mother described so many supportive actions already underway illustrates how the crisis state induces a perception of isolation and hopelessness. Social supports should be enlisted to help in treatment planning. For example, family may take the patient to a follow-up appointment. When collateral information introduces new data worrying for safety risk or a social network is truly unavailable, the clinician may more strongly consider more intensive treatment including hospitalization.
Most ED visits for suicidal ideation still result in hospitalization. 21 This single-session, crisis intervention complements the traditional expectations of emergency psychiatric evaluations by providing clinicians a way to treat symptoms of anxiety and depression in the ED. This model may also assist in the treatment of boarding psychiatric patients and encourage further studies of psychotherapy in the emergency setting.
Supplementary Information
Acknowledgments.
The author would like to thank Dr. Robert Feinstein, MD, for his mentorship and intellectual contributions to this model. Also, Dr. Jack Gende, DO, deserves thanks for his superb care of this patient. Dr. Simpson presented an earlier iteration of this model at the Academy of Psychosomatic Medicine Annual Meeting, November 9–12, 2016, in Austin, TX.
Section Editor: Shadi Lahham, MD
Full text available through open access at http://escholarship.org/uc/uciem_cpcem
Documented patient informed consent and/or Institutional Review Board approval has been obtained and filed for publication of this case report.
Conflicts of Interest : By the CPC-EM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Claire Malengret and Claire Dall'Osto
This chapter provides a foundation for understanding the nature of a crisis, how a person may be impacted by a crisis, and the models, processes, and strategies a crisis counsellor uses to assess and intervene when people in crisis seek help and support. With an emphasis on how crisis intervention differs from other counselling interventions, a case study is provided with the aim to help the reader reflect on and apply relevant crisis models of assessment and intervention learned in this chapter. Further differentiation is made between crisis stressors resulting in exposure to a traumatic event and ongoing traumatic stress responses requiring long-term counselling, psychiatric services, or specialised mental health intervention. Due to the nature of crisis work, there is a high prevalence of burnout and work-related stress in this field. As such, counsellors working in crisis work need to practice self-care, regular clinical supervision, and the continuing maintenance of the counsellor’s general health and wellbeing.
Learning Objectives
- Describe the nature of crisis.
- Identify the types of crisis.
- Recognise and understand common emotional, physical, behavioural, and cognitive reactions of people in crisis.
- Analyse the major theories underpinning crisis counselling interventions.
- Examine the importance and role of the therapeutic relationship within crisis counselling.
- Apprehend the ethical implications and professional issues of crisis intervention.
- Identify trauma definitions, assessment, and treatment approaches.
- Identify and reflect on your own personal history and experiences of crisis, including responses.
- Recognise and understand the impact of crisis counselling work on the counsellor and the need to implement self-care practices and stress management strategies.
Introduction
We live in a world where millions of people are confronted with crisis-provoking events each year that they cannot cope with or resolve on their own and, therefore, will often seek help from counsellors. Examples of crisis-inducing events include natural disasters such as bushfires, sexual assaults, terrorist attacks, the death of a loved one, a suicide attempt, domestic violence, relationship breakdown, retirement, promotion, and demotion, change in school status, pregnancy, divorce, physical illness, unemployment, and more recently, a world pandemic. These situations can be a turning point in a person’s life—either one of growth, strength, and opportunity or health decline, dysfunction, and emotional illness (Roberts & Dziegielewski, 1995; Roberts, 2005; Hoff et al., 2009). When people experience a crisis, it is the support they receive during and immediately after the crisis that often plays a crucial part in determining the impact of the crisis on their lives (France, 2014). Therefore, it is imperative crisis counsellors have the understanding, skills, and knowledge to offer a short-term intervention that assists people in crisis to cope, stabilise and receive the support and resources they need.
What is a crisis?
When a person experiences a crisis, they experience severe disruption of their psychological equilibrium and are unable to use their usual ways of coping. This then results in a state of disequilibrium and impaired functioning (Lewis & Roberts, 2001; Roberts, 2005). Because the person is unable to draw on their everyday problem-solving methods during a crisis, and there is a sense of diminished control over the events and limited options, they may experience confusion or bewilderment (Hendricks, 1985; Pollio, 1995).
Crisis states are temporary, lasting from hours through to an estimated six weeks, as the body cannot sustain being ‘off balance’ or in a state of disequilibrium, indefinitely. Resolving a crisis effectively may take some months, and this may involve learning new skills, reappraising the situation differently, or adapting to the new situation. Because people may resolve the crisis in a maladaptive or adaptive manner, some may be impacted by various mental health conditions such as depression, substance abuse, or post-traumatic stress disorder (PTSD) (Roberts, 2005).
There are four types of crises that a person may experience and include:
- developmental crisis or crisis in the life cycle (adjustments to transitions such as ageing, parenting)
- situational crisis (sexual assault, natural disaster, car accident)
- existential crisis (inner turmoil or conflicts in relation to the way a person lives their life, and views of their meaning and purpose)
- systemic crisis (the impact of colonisation on our First nations’ people or the 2009 Victorian ‘Black Saturday’ bushfires) (James & Myer, 2008).
Crisis is in the eye of the beholder
It is important to note the difficult task of defining a crisis. This is due to the subjectivity of the concept. Although the main reason for a crisis is usually preceded by a traumatic or hazardous event, it is imperative to realise that the individual’s perception of the event and their inability to cope with the event are two other conditions to consider. Focusing only on the event itself also suggests that one can categorise a crisis but that all people may respond in the same manner to a particular event. Thus, it is not the actual event that activates a crisis state, but how a person interprets or perceives these events, how they cope, and the degree to which they have access to social resources, that determine how they respond. In other words, crisis is in the eye of the beholder (Hoff et al., 2009; Hoffer & Martin, 2020).
This perception is influenced by several factors in a person’s life, such as personal characteristics, biological, gender, culture, attachment style, previous life experiences, social context, personal values, level of resilience, influences, availability of social support, previous trauma, and history of major mental illness (Loughran, 2011; Roberts & Ottens, 2005). It is also important to understand that people who are reacting to a crisis are not necessarily showing pathological responses but normal crisis responses to an abnormal event (Bateman, 2010; Hobfoll et al., 2007; James, 2008).
Principles and characteristics of crisis
The following principles and characteristics help to create an understanding of the nature of a crisis, and emphasise not only the important work of a crisis counsellor but the values and philosophical assumptions that need to guide their practice:
- crisis embodies both danger and opportunity for the person experiencing the crisis
- crisis contains the seeds of growth and impetus for change
- crisis is usually time limited but may develop into a prolonged crisis if the person experiences a series of stressful situations after the crisis
- crisis is often complex and difficult to resolve
- a crisis counsellor’s experiences of crisis in their personal life may greatly enhance their effectiveness in crisis intervention
- quick fixes may not be applicable to many crisis situations
- crisis confronts people with choices
- emotional disequilibrium or disorganization accompany crisis
- the resolution of crisis and the personhood of crisis workers interrelate (James, 2008, p. 19).
Learning activity 1
- How do you think your previous life experiences of crisis may increase your effectiveness as a crisis counsellor?
- What personal qualities do you possess that may enhance an intervention that you use with a person who has experienced a crisis?
- What are the risks of having unresolved crisis experiences as a counsellor, and how might this impact your effectiveness in crisis work?
Common reactions to a crisis
Listed here are some of the common reactions a person might experience, which are normal responses given the abnormality of the event they have experienced.
| Emotional
| Physical |
| Behavioural | Cognitive
|
Table content sourced from Massazza et al ., (2021) used under a CC BY licence and Wahlström et al ., (2013) used under a CC BY-NC licence.
Learning activity 2
Imagine your life on a timeline from when you were born up until today. On this timeline, plot the most important or critical events (positive or negative) in your life that were turning points or changed you in some way.
- Looking at the critical events on your timeline, which events would you see as a crisis?
- How did those events change you?
What is crisis counselling?
Crisis counselling is an immediate response to people experiencing overwhelming events and may prevent the potential negative impact of psychological trauma. It focuses on the here and now, dealing with the immediate presenting needs at the point of crisis, and providing emergency psychological care to assist in helping the person return to an adaptive level of functioning (Flannery & Everly, 2000; Hobfoll et al., 2007).
The key goals that underpin crisis counselling frameworks and models are:
- meeting the person who is experiencing a crisis where they are at
- assessing and monitoring the person’s level of risk
- assisting them in mobilising of resources
- stabilising (by reducing distress
- improved or restored adaptive functioning (where possible) (Roberts & Ottens, 2005).
The difference between crisis counselling and other counselling interventions
Crisis counselling is different to the provision of ongoing therapeutic support. Because crisis counselling offers short-term strategies to prevent damage during and immediately after the person has experienced a crisis or devastating event, it requires that the counsellor be more active and directive than usual (James, 2008). Ongoing counselling may follow on from crisis to ensure the long-term improvement of a person’s mental health and wellbeing, but this is not the goal of crisis counselling. Instead, the goal is to provide a responsive and timely intervention to return a person to previous levels of functioning through the implementation of mobilising necessary resources, including the facilitation of links to these resources (Flannery & Everly, 2000). Given crisis counselling is the implementation of a short-term measure of support, it is often referred to as brief intervention or brief therapy. The timeframe for crisis counselling is between six to ten weeks and is guided by specific relevant models, guiding principles, and actions (Hendricks, 1985).
Case study: A bushfire crisis
You are part of a mobile service team who travels to a fire-affected area to provide support to individuals, families and emergency services workers affected by the recent bushfires. You arrive at a regional town that has just been devastated by catastrophic bushfires. A recovery centre has been set up at the local town hall and 700 individuals and families are presently seeking support at this recovery centre. You are assigned to Brett (35), a cattle farmer whose property, livestock, and beloved dog were lost in the fires. Brett is a third-generation cattle farmer on his family property. Within the first few minutes of meeting him, you observe that recalling these events for him results in constant tearfulness, and a questioning of what he could have done to be more prepared to have a different outcome. Brett explains that he has not slept in several days, and if he does sleep, he has nightmares. He also expresses to you that he does not know what the future holds for him now. Brett explains that he cannot focus for very long because he finds it difficult to believe this has happened to him. You observe that Brett appears to be numb and detached and unable to articulate his narrative in a linear and clear manner. Brett explains that he feels concerned for his ten employees who are no longer able to support their families. He also mentions that recently he went through a divorce which he felt devastated by at the time.
Learning activity 3
- From Brett’s reactions, what suggests that he is experiencing a crisis?
- What is the contributing factor that disrupts Brett’s equilibrium most? Is it the nature of the crisis event itself or the way Brett responds?
- Are there any risk factors to consider in Brett’s case?
Traumatic stress, crisis, and trauma
The term crisis is not interchangeable with traumatic stress and trauma. Dulmus and Hilarski (2003) explain a person is in a crisis state when they have experienced a situation or event and they have been unable to cope with it by utilising their usual coping mechanisms to lessen the impact of the event. This results in the person entering a state of disequilibrium (Roberts & Ottens, 2005).
Traumatic stress is when a crisis or event, such as child abuse, rape, combat trauma, and catastrophic natural disasters, overwhelms normal coping skills and is perceived as life-threatening (Behrman & Reid, 2002). Trauma can be defined as ‘… an experience of extreme stress or shock that is/or was, at some point, part of life’ (Gomes, 2014).
It is adaptive and normal for a person who has been exposed to a traumatic event to exhibit some anxiety in the early stages as this enables them to maintain vigilance as a way to increase safety. Others may feel numb after being exposed to a traumatic event. This is also an adaptive and normal response as much-needed insulation is provided to a person’s psychological system after the traumatic event (McNally et al., 2003). Those who do experience a traumatic injury can suffer from long-lasting consequences that impact them physically, cognitively, emotionally, and financially (Herrera-Escobar et al., 2021).
It is common for acute stress symptoms to be experienced after a traumatic event. When a person is exposed to a threat, neurotransmitters and hormones inform a physical response. The sympathetic nervous system is activated through a series of interconnected neurons that initiate a fight or flight response. The body releases glucose and adrenalin, increases heart rate and respiration, and remains in a state of high alert to manage any additional threat. At this point in time, the person is trying to make sense of their experience and is often feeling afraid and vulnerable as they attempt to rationalise what just occurred. Anxiety, loss of appetite, irritability, sleep difficulties, concentration difficulties, and hypervigilance can occur whilst in this physiological state. Warchal and Graham (2011) further explain that a person can have recurrent and involuntary memories of the traumatic event. A heightened state of arousal makes it difficult for them to respond normally, make decisions, and complete paperwork to link them to resources. Walsh (2007) explains that most people adapt and cope and therefore do not suffer long-term disturbance.
Post-traumatic stress disorder
Ongoing therapeutic support is required if a person continues to experience feelings of helplessness, intense fear or horror, re-living the traumatic event, hypervigilance, or emotional numbness. Norris et al. (2002) identified ongoing support to include long-term counselling or psychiatric services, or specialised mental health intervention. People generally possess enough resilience to circumvent the development of trauma symptoms that inform a formal trauma diagnosis, such as post-traumatic stress disorder. The DSM5-TR classifies PTSD as an anxiety disorder that can develop after exposure to a traumatic event (American Psychiatric Association [APA], 2022). Rosenman (2002) reported that 57% of the Australian population reported a lifetime experience of a specified trauma. There are four different categories PTSD can be clustered into: (1) recurrent re-experiences of the traumatic event in the form of intrusive thoughts, nightmares, or flashbacks; (2) numbing and avoidance of trauma-related stimuli; (3) hyperarousal and reactivity; and (4) alterations in cognitions and mood (APA, 2022).
The origins and development of crisis counselling interventions
The research and development of crisis intervention originates in the 1940’s when the reactions of people whose loved ones had died in a fire at a nightclub in Boston in 1943 were recorded and studied by psychiatrist Erich Lindemann and his colleagues (Lindemann, 1944). Another psychiatrist, Gerald Caplan, expanded on this work and developed a four-stage model of crisis reactions (or phases of reactions that a person in a crisis may experience) which have formed the foundation for later contributions from theorists in crisis counselling. Caplan (1961, 1964) describes these phases as follows:
Phase 1 : increase in tension and distress from the crisis-inducing event
Phase 2 : there is an escalation in the disruption of the person’s life as they are stuck and cannot resolve the crisis quickly
Phase 3 : the person cannot resolve the crisis through their usual problem-solving methods
Phase 4 : the person resolves the crisis by mental collapse or deterioration, or they partially resolve it by adopting new ways of coping.
Erikson’s (1963) stage model of developmental crises and Roberts’ (1995) seven-stage crisis intervention model have led to the development of numerous crisis intervention models, particularly in the last two decades. Erikson’s focus was on World War II veterans’ disconnect from their culture together with the confusion associated with the traumatic war experiences rather than focusing on men suffering from repressed conflicts. Erikson assessed that veterans were experiencing confusion of identity about what they were and who they were in direct opposition to the lens of repressed conflict being used during this time period.
Characteristics of the crisis counsellor
The crisis counsellor’s ability to remain calm and simultaneously avoid subjective involvement in the crisis is crucial. This means that crisis counselling may not be suitable for every counsellor (Shapiro & Koocher, 1996). A crisis counsellor should communicate in a manner that is patient, sensitive, self-aware, and compassionate. Other characteristics and behaviours include warmth, understanding and acceptance, being available but not intrusive or controlling, trustworthy, empathic, caring, displaying effective listening skills, encouraging the person seeking appropriate referrals and support, and being able to maintain confidentiality (Bateman, 2010; Rainer & Brown, 2011; Westefeld & Heckman-Stone, 2003).
The crisis counsellor aims to establish a therapeutic relationship as they do in general counselling, however in crisis counselling, they do so in a shorter time-frame period. Other crisis intervention skills include encouragement, basic attending and listening skills, reflection of emotions, and instilling hope (cf. Ivey & Ivey, 2007; James, 2008).
Key crisis interventions
As mentioned previously, crisis intervention provides the opportunity for the crisis counsellor to help facilitate an independent decision-making process with the client by promoting them as the agent of change in their life and assisting them to identify and utilise their own resources (France, 2014).
When determining if crisis intervention is the most relevant intervention, several categories are to be considered. These include:
- a cumulative effect
- the impact on a person
- their family and community
- the unexpectedness and duration of the event or situation; and
- a person’s level of control over the event or situation (Hendricks, 1985).
Critical incident stress debriefing
Developed in 1974 by Jeffrey T. Mitchell, critical incident stress debriefing (CISD) or psychological debriefing is a seven-phase supportive crisis intervention process that was initially used with small groups of first responders such as firefighters, paramedics, and police officers to help them manage their reactions and distress following their exposure to a traumatic event (Mitchell, 1983). Over time, CISD became an intervention used with groups outside of emergency services, such as hospitals, businesses, schools, community groups and churches. However, although CISD is used extensively, current research shows mixed results for the use of this intervention with some findings suggesting that it is ineffective in preventing post-traumatic stress disorder (PTSD) symptoms and even contributing to the worsening of stress-related symptoms in individuals who received this type of intervention (Bledsoe, 2003).
The next section will address assessment in crisis intervention followed by an outline of two key crisis interventions, Roberts’ seven-stage model of crisis intervention and psychological first aid, and an application of these interventions to Brett’s case.
Assessment in crisis intervention
The responsibility of the crisis counsellor is to conduct a structured assessment in a timely and responsive manner to assess whether psychological homeostasis has been disrupted, there is evidence of dysfunction and distress, and usual coping mechanisms are not able to be utilised. Assessment is ongoing throughout the intervention process and allows the crisis counsellor to evaluate the person’s affective and cognitive state, and behavioural functioning. By assessing these three areas, the crisis counsellor can evaluate and monitor how adaptively or maladaptively the person is functioning, including whether they are a danger to themselves or others, and then apply the most appropriate intervention (James, 2008).
Listed below are examples of what a crisis counsellor is looking for across the three domains when assessing people who have experienced a crisis:
- Do they appear to be emotionally overwhelmed or severely withdrawn?
- Is what they are saying coherent and logical or are they not making sense?
- When observing their behaviours, are they pacing? Are they having difficulty breathing?
- Are they able to sit calmly?
- Are they unresponsive?
When people express suicidal ideation or have a plan to suicide, it is crucial to conduct a rapid suicide risk assessment which includes gathering information by inquiring about the following:
- How long they have been having suicidal thoughts?
- Have they made any suicide attempts in the past?
- Have they recently sought help?
- Do they have a plan to suicide?
- If they do have a plan, do they have access to the means to carry out this plan?
Further information and guidelines on suicide risk assessment can be found at the end of this chapter in the Recommended referral and resources list section. There is also a specific chapter in this book related to suicide.
Helplines – phone counselling and support
There is a range of organisations in Australia that provide support for people who are in crisis and need to talk to someone about their distress. Due to their convenience, accessibility, affordability, and relative anonymity, these helplines are a common form of crisis support.
Lifeline Australia 13 11 14
beyondblue 1300 22 4636
Mensline Australia 1300 78 99 78
Kids Help Line 1800 55 1800
1800RESPECT 1800 737 732
Roberts’ seven-stage crisis model
Roberts’ (1995, 2005) seven-stage model of crisis intervention is a cognitive-behaviourally based, systematic, and structured model used for crisis assessment and intervention. It is a common model used by crisis counsellors to help people build and restore their ways of coping and improve their problem-solving skills that a crisis may evoke.
With a focus on strengths and resiliency, these sequential stages can be applied to a broad range of crisis situations and are as follows:
- plan and conduct a thorough assessment including, danger to self and others, imminent danger, lethality
- make psychological contact, establish rapport and rapidly establish the collaborative relationship by showing genuine respect for the individual and having a non-judgmental attitude
- identify major problems or the dimensions of the problems including the precipitating event
- encourage exploration of feelings and emotions including active listening, reassurance and validation
- generate and explore alternatives including untapped resources and new coping strategies
- develop and formulate an action plan
- plan follow-up and leave the door open for booster sessions which may occur three to six months later (Roberts, 2005, p. 21).
Psychological first aid
Identified as the first level of post-incident short-term care, psychological first aid is an evidenced-based model that provides emotional and practical support to individuals, groups, and communities impacted by a natural disaster, catastrophic event, traumatic or terrorist event, or another emergency situation (Australian Red Cross & Australian Psychological Society, 2010; Ruzek et al., 2007). The aim of psychological first aid is to help people reduce their initial symptoms, have their current needs met, and support them in implementing adaptive coping strategies.
Psychological first aid meets the following four basic standards:
- Consistent with evidence and research on risk and resilience following trauma (that is, evidence-informed)
- Applicable and practical in field settings (compared with a medical/health professional office somewhere)
- Appropriate for developmental levels across the lifespan (e.g., there are different techniques available for supporting children, adolescents, and adults)
- Culturally informed and delivered in a flexible manner, as it is often offered by members of the same community as the supported individuals (Ruzek et al., 2007).
Psychological first aid is based on the understanding that, just as natural disasters, catastrophic events, traumatic or terrorist events, or other emergency situation differ vastly from each other, so do the psychological reactions of individuals, groups and communities experiencing them. Because some of these reactions can interfere with an individual’s ability to cope and manage the crisis, psychological first aid can help in their recovery. Psychological first aid has five basic elements that are to promote:
- self-efficacy (self-empowerment)
- connectedness
- hope (Hobfoll et al., 2007).
Case study: Crisis intervention
Roberts’ seven-stage model of crisis intervention
Using Roberts’ (2005) seven-stage model as an intervention with Brett, your first step is to conduct a psychosocial and lethality assessment. As he tells his story to you, you need to gather information such as whether he has any emotional support, any medical needs, how he is coping, and whether he is currently using any drugs and/or alcohol. Assessing any imminent danger and ascertaining whether Brett may be at risk of suicide is also a priority in this initial stage. Although in this case, Brett may not talk about having suicidal thoughts (i.e., suicidal ideation) or have a suicide plan, he does say, “I don’t know what the future holds for me now”, which at this point would prompt a probing question in checking what he means. It would be important to consider other risk factors, such as previous mental health issues, being socially isolated, or recently experienced a significant loss (for example, Brett has recently divorced which may be a risk factor in his case).
The second stage is about building rapport with Brett which you may have established already from taking the time to be present and hear his story in the assessment stage. This stage is crucial in developing a therapeutic relationship with Brett and, therefore, it is important you show a genuine interest in his story, respect and accept him, and also display fundamental qualities and characteristics of a crisis counsellor as discussed earlier in the chapter.
Crisis intervention is focused on the major problems, so in this next stage, you are wanting to find out why Brett has sought help now. This might seem obvious as you might assume it is the devastation of the fire. This may not be the priority issue, therefore, at this point you are not only finding out about the event that ‘was the last straw’ but you are also helping Brett prioritise the problems to work through. It is important that you gain an understanding of why those problems make it a crisis for him.
In stage four of this model (i.e., encourage exploration of feelings and emotions) you are actively listening to Brett’s story, allowing him to express and vent his feelings, and giving him the opportunity to articulate what it is about the situation that is making it difficult for him to cope. You may challenge some of his responses by giving him correct information and reframing his statements and interpretations about the situation.
Generating and exploring alternatives (stage 5) can be ‘tricky’ as the timing needs to be appropriate to help Brett explore options in moving forward to resolve the crisis. If you have established rapport, listened to his story, and Brett feels heard and understood, he may be more open to this. A strategy may include asking Brett, “How have you coped in the past when you’ve been through a crisis and felt the same way you do now?”.
Stage six includes implementing an action plan to address some of the problems he has identified, for example, making an appointment with his general practitioner regarding the poor sleep patterns he is experiencing. This stage also involves asking questions that may help Brett make meaning from the crisis such as, “Why did this happen?”, “What does it mean?”, “What are the alternatives that could have been put in place to prevent the event?”, “Who was involved?”, and “What responses to the crisis potentially made it worse (cognitively and behaviourally)?” (Roberts & Ottens, 2005).
The final stage is planning to follow up with Brett two to six weeks later in order to evaluate if the crisis is being resolved, and to also check his physical and cognitive state, how his overall functioning is, any stressors and how he is handling them, and any referrals to external agencies such as housing, medical, legal etc. You may also schedule a ‘booster’ session a month after this crisis intervention has been completed.
The application of psychological first aid to the case study requires an expansion of the five core principles of psychological first aid. In your immediate work with Brett, the intervention includes efforts to:
- reduce his distress by modelling calm, and making Brett feel safe and secure
- identify and assist Brett with his current needs
- establish a human connection with Brett
- facilitate Brett’s social support
- help Brett understand the disaster and its context
- help Brett identify his own strengths and abilities to cope
- foster belief in Brett’s ability to cope
- give Brett hope
- assist with early screening for Brett needing further or specialised help
- promote adaptive functioning in Brett
- get Brett through the first period of high-intensity and uncertainty
- set Brett up to be able to naturally recover from an event
- reduce the chance of post-traumatic stress disorder for Brett (Australian Red Cross & Australian Psychological Society, 2010, p. 11).
Brett is a 35-year-old independent Australian male farmer who may believe that expressing emotions or feelings is a sign of weakness. Bleich et al. (2003) explain that when an individual believes they are weak, “going crazy” or believes there is “something wrong with me”, an effective strategy in the intervention is to normalise and reassure Brett “you are neither sick nor crazy; you are going through a crisis, and having a normal reaction to an abnormal situation”. It is important to remind Brett that he is safe in order to minimise his vigilance. Promoting calm for Brett, immediately after his rural town was devastated by catastrophic bush fires, can assist Brett to foster positive emotions. It is advisable to intervene and limit Brett’s exposure to media coverage as this may trigger negative emotional states. The challenge for you is to convince Brett that he does not need to be as vigilant and limit media exposure as all day exposure is too much (Fredrickson, 2001).
The crisis counsellor and self-care
In their book, The Resilient Practitioner, Skovholt and Trotter-Mathison (2016) offer their insights and research on burnout and compassion fatigue for those in the helping profession and emphasise the importance of implementing self-care strategies in its prevention. Given the demands of the work of a crisis counsellor and the risk of vicarious traumatisation, protective and proactive approaches are imperative in the sustainability and vitality of a career where one is working intensely with human suffering and adversity. Tools and approaches, such as frequent supervision, high commitment to self-care, creating a personal balance of caring for self and caring for others, proactively and directly confronting stressors at work and at home, and ensuring that one has enriching relationships and activities outside of the work environment, are essential components in professional wellness and in the prevention of burnout and compassion fatigue (Adamson et al., 2014; Skovholt & Trotter-Mathison, 2016).
Learning activity 4
The development of a self-care plan can assist the crisis counsellor in supporting their wellbeing, reducing stress, and sustaining positive mental health in the long-term.
List five self-care strategies that you might use to promote and enhance your mental health and wellbeing
Counsellor reflections
Due to the nature and intensity of the role, crisis counselling may not be a suitable specialisation of counselling for every counsellor. Based on my experience, this type of work requires a counsellor to have the ability to remain calm and operate in a systematic and rational manner whilst assessing a client’s level of instability and distress. Building rapport quickly with a client facing a crisis is vital to the effectiveness of the intervention, which highlights again how important it is for the crisis counsellor to show acceptance, empathy, and genuineness to the client.
Working as a frontline crisis counsellor is demanding, and, therefore, it is imperative that ongoing support and clinical supervision are received to minimise and manage compassion fatigue and vicarious trauma. Additionally, I have found that a strong commitment to self-practices such as mindfulness, yoga, and muscle relaxation have reduced work-related stress and burnout over the years.
This chapter has provided a brief foundation for intervening with people who have experienced a crisis. With a primary focus on psychological first aid and Roberts’ seven-stage model of crisis intervention, and an application of these models to a case study, this chapter has covered the essentials in understanding the nature and types of crisis, the common reactions of a person who has experienced a crisis, and the impact of ongoing traumatic stress responses that require long-term counselling intervention. A list of other supports available, referrals and resources are included at the end of this chapter for your information and further reading.
Recommended referral and resources list
Australian Psychological Society: Psychological first aid . This resource is a useful guide to supporting people affected by a disaster. The guide provides an overview of the implementation of best practices in psychological first aid as an immediate intervention following a traumatic event or disaster.
Suicide risk assessment . Working with the suicidal person Clinical practice guidelines for emergency departments and mental health services (Department of Health, Melbourne, Victoria, 2010).
Guidelines for integrated suicide-related crisis and follow-up care in emergency departments and other acute settings (2017).
Other Resources for telephone and online crisis support:
- Life in Mind : Australian suicide prevention services.
- Standby : Support after suicide. Face-to-face and telephone support.
Other counselling resources
Psychological first aid : This video [11:07] provides information on the application of psychological first aid to assist individuals to reduce stress symptoms and assist in meeting an individual’s basic needs and identify resources to aid in a healthy recovery, immediately following a crisis, such as a personal crisis, natural disaster, traumatic event or natural disaster.
Glossary of terms
compassion fatigue— a state of feeling emotional and physically exhausted from helping people who are distressed or traumatised resulting in a diminished ability to show compassion or empathise
crisis — a time of intense difficulty or danger
hypervigilance — being in a state of increased alertness where one is sensitive to surroundings
intervention — the action or process of intervening
model — describes how counsellors can implement theories
stress — a state of mental or emotional strain or tension resulting from adverse or demanding circumstances
principles — a fundamental truth or proposition that serves as the foundation for a system of belief or behaviour or for a chain of reasoning
reaction — something done, felt, or thought in response to a situation or event
suicidal ideation — thoughts of wanting to take one’s own life or suicide
theory — a plausible or scientifically acceptable general principle offered to explain a hypothesis or belief
therapeutic relationship — refers to the consistent and close association that exists between the counsellor and client. This is also known as a therapeutic alliance.
trauma — a deeply distressing or disturbing experience
vicarious trauma — trauma symptoms that a counsellor may experience as a result of the ongoing exposure to trauma stories from their clients
Reference List
Adamson, C., Beddoe, L., & Davys, A. (2014). Building resilient practitioners: Definitions and practitioner understandings. The British Journal of Social Work, 44 (3), 522-541. https://doi.org/10.1093/bjsw/bcs142
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders. Text revised (5th ed.). https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425787
Australian Red Cross and Australian Psychological Society. (2010). Psychological first aid: An Australian guide .
Bateman, V. L. (2010) The interface between trauma and grief following the Victorian bushfires: Clinical interventions beyond the crisis, Grief Matters: The Australian Journal of Grief and Bereavement, 13 (2), 43- 48.
Behrman, G., & Reid, W. J. (2002). Post trauma intervention: Basic tasks. Brief Treatment and Crisis Intervention, 2 , 39-47.
Bledsoe, B. E. (2003). Critical incident stress management (CISM): Benefit or risk for emergency services. Prehospital Emergency Care, 7 (2), 272-279.
Bleich, A., Gelkopf, M., & Solomon, Z. (2003). Exposure to terrorism, stress-related mental health symptoms, and coping behaviors among a nationally representative sample in Israel. Journal of the American Medical Association, 290 (5) 612-616.
Caplan, G. (1961). An approach to community mental health. Grune and Stratton.
Caplan, G. (1964). Principles of preventative psychiatry. Basic Books.
Department of Health, Melbourne, Victoria (2010). Working with the suicidal person: Clinical practice guidelines for emergency departments and mental health services . www.health.vic.gov.au/mentalhealth
Dulmus, C. N., & Hilarski, C. (2003). When stress constitutes trauma and trauma constitutes crisis. The stress–trauma-crisis continuum. Brief Treatment and Crisis Intervention, 3 , 27-35.
Erikson, E. (1963). Childhood and Anxiety (2nd ed.). Norton.
Flannery, R. B., & Everly, G. S. (2000). Crisis intervention: A review . International Journal of Emergency Mental Health, 2 (2), 119-125.
France, K. (2014). Crisis intervention: A handbook of immediate person-to- person help (6th ed.). Charles Thomas Pub.
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broader-and-build theory of positive emotions. American Psychologist , 56 , 218-226.
Hendricks, J. E. (1985). Crisis intervention: Contemporary issues for on-site interveners . Charles C Thomas.
Herrera-Escobar, J., Osman, S., Das, S. Toppo, A, Orlas, C., Castillo-Angeles, M., Rosario, A., Janjua, M., Arain, M., Reidy, E., Jarman, M., Nehra, D., Price, M., Bulger, E., & Haider, A. (2021). Long-term patient-reported outcomes and patient-reported outcome measures after injury: the National Trauma Research Action Plan (NTRAP) scoping review. Journal of Trauma and Acute Care Surgery , 90 (5), 891–900. https://doi.org/10.1097/TA.0000000000003108
Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J., Friedman, M., Gersons, B. P. R., de Jong, J. T. V. M., Layne, C. M., Maguen, S., Neria, Y., Norwood, A. E., Pynoos, R. S., Reissman, D., Ruzek, J. I., Shalev, A. Y., Solomon, Z., Steinberg, A. M., & Ursano, R. J. (2007). Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry, 70 (4), 283-315.
Hoff, L. A., Hallisey, B. J., & Hoff, M. (2009). People in crisis: Clinical and diversity perspectives (6th ed.). Routledge.
Hoffer, K., & Martin, T. (2020). Prepare for recovery: Approaches for psychosocial response and recovery. Journal of Business Continuity & Emergency Planning , 13 (4), 340–351.
Ivey, A. E. & Ivey, M. B. (2007). Intentional interviewing and counseling: Facilitating client development in a multicultural society (6th ed.). Thomson.
James, R. K. (2008). Crisis intervention strategies (6th ed.). Thomson.
James, R. K., & Myer, R. A. (2008). Crisis counseling. In F. T. L. Leong, E. M. Altmaier, & B. D. Johnson (Eds.), Encyclopedia of counseling (Vol. 2, pp. 544-548). Sage.
Lindemann, E. (1944). Symptomology and management of acute grief. American Journal of Psychiatry, 101 , 141-148.
Loughran, H. (2011). Understanding crisis therapies: An integrated approach to crisis intervention and post-traumatic stress. Jessica Kingsley Publishers.
Lewis, S., & Roberts, A. R. (2001). Crisis assessment tools: The good, the bad and the available. Brief Treatment and Crisis Intervention, 1 , 17-28.
Massazza, A., Brewin, C. R., & Joffe, H. (2021). Feelings, thoughts, and behaviors during disaster. Qualitative Health Research, 31 (2), 323-337. https://doi.org/10.1177/1049732320968791
McNally, R., Bryant, R., & Ehlers, A. (2003). Does early psychological intervention promote recovery from posttraumatic stress? Psychological Science in the Public Interest, 4 , 45–79.
Mitchell J. (1983). When disaster strikes…the critical incident stress debriefing procedure. Journal of Emergency Medical Services , 8 (1),36–39.
Myer, R. A. (2001). Assessment for crisis intervention: A triage assessment model. Brooks/Cole.
Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry , 65 (3), 207–239. https://doi.org/10.1521/psyc.65.3.207.20173
Pollio, D. E. (1995). Use of humour in crisis intervention. Families in Society: The Journal of Contemporary Human Services , 76 (6), 376-384.
Rainer, J., & Brown, B. (2011). Crisis counseling and therapy. Routledge.
Roberts, A. R. (Ed.), (1995). Crisis intervention and time-limited cognitive treatment . Sage.
Roberts, A. R. (2005). Bridging the past and present to the future of crisis intervention and crisis management. In A. R. Roberts (Ed.), Crisis intervention handbook: Assessment, treatment, and research (3rd ed., pp. 3–34). Oxford University Press.
Roberts, A. R., & Dziegielewski, S. F. (1995). Foundation skills and applications of crisis intervention and cognitive therapy. In A. R. Roberts (Ed.), Crisis intervention and time-limited cognitive treatment (pp. 3–27). Sage.
Roberts, A. R. & Ottens, A. J. (2005). The seven-stage crisis intervention model: A road map to goal attainment, problem solving and crisis resolution. Brief Treatment and Crisis Intervention, 1, 17-28.
Rosenman, S. (2002). Trauma and posttraumatic stress disorder in Australia: Findings in the population sample of the Australian National Survey of Mental Health and Wellbeing. Australian & New Zealand Journal of Psychiatry, 36 (4), 515-520. https://doi.org/10.1046/j.1440-1614.2002.01039.x
Ruzek, J., Brymer, M., Jacobs, A. K., Layne, C., Vernberg, E. M., & Watson, P. J. (2007). Psychological first aid. Journal of Mental Health Counseling , 29 (1), 17–49.
Shapiro, D. E., & Koocher, G. P. (1996). Goals and practical considerations in outpatient medical crises intervention. Professional Psychology: Research and Practice, 27 (2), 109-120. https://doi.org/10.1037/0735-7028.27.2.109
Silva, S. M. G. (2014). Engaging touch & movement in somatic experiencing trauma resolution approach. International University for Graduate Studies. https://www.stiftung-traumatherapie.com/fileadmin/stiftung/information/forschung/Punkt1_Punkt2_engaging-touch-and-movement-in-se-trama-resolution-approach-dissertation-bySoniaGomes-2014.pdf
Skovholt, T. M., & Trotter-Mathison, M. (2016). The resilient practitioner: Burnout and compassion fatigue prevention and self-care strategies for the helping professions . Routledge.
Wahlström, L., Michélsen, H., Schulman, A., Backheden, H., & Keskinen-Rosenqvist, R. (2013). Longitudinal course of physical and psychological symptoms after a natural disaster. European Journal of Psychotraumatology, 4 (1), Article 21892. https://doi.org/10.3402/ejpt.v4i0.21892
Walsh, F. (2007). Traumatic loss and major disasters: Strengthening family and community resilience. Family Process, 46 (2), 207-227.
Warchal, L. R., & Graham, L. B. (2011). Promoting positive adaptation in adult survivors of natural disasters. Adultspan Journal , 10 (1), 34–51.
Westefeld, J. J., & Heckman-Stone, C. (2003). The integrated problem-solving model of crisis intervention: Overview and application. The Counselling Psychologist, 31 (2), 221- 239.
Author Information
Claire Malengret FDRP, B.Ed.,M.Couns., GDM, Family Dispute Resolution, Cert IV TAE, PACFA Reg. (Clin.), MHE prac. 21971, Accredited Supervisor (PACFA, AAOS)
Claire is currently the National Clinical Advisor at an Australian non-for-profit organisation that supports young people and their families who have been impacted by chronic illness. With over 15 years experience in education, counselling and organisational development roles, Claire is passionate about coming alongside people, building trust and transparency, and supporting them to grow their skills and build capability. She is a clinical counsellor, accredited supervisor, an endorsed mental health practitioner, and certified family dispute resolution practitioner who holds a Master of Counselling, a Graduate Diploma in Management, and a Bachelor of Education.
Claire Dall’Osto BSocSc (with Distinction), GradCertPrac(Client assessment & Case management), GradCertPrac(Statutory child protection), Dip(Couns), Dip(Just), CertIV(Train&Assess)
Claire has been working in the child protection industry within the government and NGO sector for 15 years, and has gained expert experience, knowledge, and skills in the child protection and foster care systems. She has worked with biological parents, foster and kinship carers, and children who have experienced harm, abuse, trauma, grief and loss, attachment disruptions, mental health issues, and behaviour and conduct problems. Claire has provided crisis intervention in refuges, providing specialist support, and safe and secure accommodation for women and children escaping domestic and family violence, as well as providing specialist trauma counselling for people who have experienced domestic and family violence, and sexual assault.
Common Client Issues in Counselling: An Australian Perspective Copyright © 2023 by Claire Malengret and Claire Dall'Osto is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Writing a Counselling Case Study
As a counselling student, you may feel daunted when faced with writing your first counselling case study. Most training courses that qualify you as a counsellor or psychotherapist require you to complete case studies.
Before You Start Writing a Case Study

However good your case study, you won’t pass if you don’t meet the criteria set by your awarding body. So before you start writing, always check this, making sure that you have understood what is required.
For example, the ABC Level 4 Diploma in Therapeutic Counselling requires you to write two case studies as part of your external portfolio, to meet the following criteria:
- 4.2 Analyse the application of your own theoretical approach to your work with one client over a minimum of six sessions.
- 4.3 Evaluate the application of your own theoretical approach to your work with this client over a minimum of six sessions.
- 5.1 Analyse the learning gained from a minimum of two supervision sessions in relation to your work with one client.
- 5.2 Evaluate how this learning informed your work with this client over a minimum of two counselling sessions.
If you don’t meet these criteria exactly – for example, if you didn’t choose a client who you’d seen for enough sessions, if you described only one (rather than two) supervision sessions, or if you used the same client for both case studies – then you would get referred.
Check whether any more information is available on what your awarding body is looking for – e.g. ABC publishes regular ‘counselling exam summaries’ on its website; these provide valuable information on where recent students have gone wrong.
Selecting the Client
When you reflect on all the clients you have seen during training, you will no doubt realise that some clients are better suited to specific case studies than others. For example, you might have a client to whom you could easily apply your theoretical approach, and another where you gained real breakthroughs following your learning in supervision. These are good ones to choose.
Opening the Case Study
It’s usual to start your case study with a ‘pen portrait’ of the client – e.g. giving their age, gender and presenting issue. You might also like to describe how they seemed (in terms of both what they said and their body language) as they first entered the counselling room and during contracting.

If your agency uses assessment tools (e.g. CORE-10, WEMWBS, GAD-7, PHQ-9 etc.), you could say what your client scored at the start of therapy.
Free Handout Download
Writing a Case Study: 5 Tips
Describing the Client’s Counselling Journey
This is the part of the case study that varies greatly depending on what is required by the awarding body. Two common types of case study look at application of theory, and application of learning from supervision. Other possible types might examine ethics or self-awareness.
Theory-Based Case Studies
If you were doing the ABC Diploma mentioned above, then 4.1 would require you to break down the key concepts of the theoretical approach and examine each part in detail as it relates to practice. For example, in the case of congruence, you would need to explain why and how you used it with the client, and the result of this.
Meanwhile, 4.2 – the second part of this theory-based case study – would require you to assess the value and effectiveness of all the key concepts as you applied them to the same client, substantiating this with specific reasons. For example, you would continue with how effective and important congruence was in terms of the theoretical approach in practice, supporting this with reasoning.
In both, it would be important to structure the case study chronologically – that is, showing the flow of the counselling through at least six sessions rather than using the key concepts as headings.
Supervision-Based Case Studies
When writing supervision-based case studies (as required by ABC in their criteria 5.1 and 5.2, for example), it can be useful to use David Kolb’s learning cycle, which breaks down learning into four elements: concrete experience, reflective observation, abstract conceptualisation and active experimentation.
Rory Lees-Oakes has written a detailed guide on writing supervision case studies – entitled How to Analyse Supervision Case Studies. This is available to members of the Counselling Study Resource (CSR).
Closing Your Case Study
In conclusion, you could explain how the course of sessions ended, giving the client’s closing score (if applicable). You could also reflect on your own learning, and how you might approach things differently in future.

Sign up for your FREE e-newsletter
You’ll regularly recieve powerful strategies for personal development, tips to improve the growth of your counselling practice, the latest industry news and much more.
We’ll keep your information private and never sell, rent, trade or share it with any other organisation. And you can cancel anytime.
Case Studies
Case studies, case studies and more case studies!
A Counselling Case Study Exploring Loss
Sue and Tom lost their child Jill to leukaemia approximately one year ago. Tom suggested that Sue attend Professional Counselling because she still doesn’t seem to be able to cope with everyday living. For ease of writing the Professional Counsellor is abbreviated to C. A précis of the session is as follows In the first […]
- September 17, 2010
- Case Studies , Relationship & Families
A Counselling Case Study Using CBT
Jocelyn works as a Human Resources Manager for a large international organisation. She is becoming more and more stressed at work as the company is constantly changing and evolving. It is a requirement of her job that she keeps up with this change by implementing new strategies as well as ensuring focus is kept on […]
- March 18, 2010
- Case Studies , Counselling Therapies , Workplace Issues
Drug Addictions and Group Work
A Support Group had been advertised on the display board of the local Drug and Alcohol Treatment Centre in the City where the Counsellor had been seeing each of the members for private counselling prior to the start of the programme. Ten clients enrolled in the group but by 7:15pm only 5 of the ten […]
- September 29, 2009
- Addictions , Case Studies , Group Work
Counselling Case Study: Using REBT
Thomas is a 33 year old married man, who has recently become a father. He explains that he feels his self-esteem has been gradually deteriorating ever since he was married. He says that he can’t find reasons to enjoy life with his wife due to feelings of inadequacy as a husband. In his new role […]
- September 7, 2009
Counselling Case Study: Managing Anxiety
Leah is a 24 year old woman who was recently discharged from the Army on medical grounds. During her four years in the Army, Leah experienced high levels of stress and anxiety which she coped with by drinking heavily. When she presented for counselling, Leah had been sober for 55 days and was seeking strategies […]
- June 5, 2009
- Addictions , Case Studies , Stress Management
Counselling Case Study: Learning to Let Go
Elizabeth came to counselling because she was experiencing intense anger, and was not coping with her life. She complained of failed relationships with her ex-husband, and with another man whom she left her husband to be with. Elizabeth cannot move on from the anger she feels about her failed relationships and she is feeling isolated […]
- June 26, 2008
Counselling Case Study: Social Anxiety
Sasha is a 60 year old woman who has recently retired from a career in teaching. Working for many years in a secondary school environment, Sasha was confident, motivated and dedicated to her work, but at the same time looking forward to retirement so she and her husband could travel and spend more time with […]
- February 11, 2008
- Case Studies , Clinical Mental Health , Stress Management
A Case of Using Logical Consequences
Richard is a 41-year-old plant operator in a heavy machinery company. He works long hours and must start very early each day. Twelve months ago he accepted a transfer from a country location to a capital city 250 kilometres away from his family. Due to financial obligations this was seen as a necessity. He travelled […]
- January 23, 2008
A Case of Using a Person-Centred and Cognitive-Behavioural Approach to Burnout
Brett is a 36 year old man who works as an accountant for a small family business. The business is failing and Brett will probably have to begin the process of “winding it up” in the near future. His commitment to the business and his friends, the business owners, has intensified the level of stress […]
- June 26, 2007
- Case Studies , Clinical Mental Health , Relationship & Families , Workplace Issues
Counselling Case Study: An Overwhelmed Client
Chris came to counselling because he was experiencing increasing feelings of being stressed, overwhelmed and weighed down by his commitments in life. He has been particularly concerned about his negative thoughts and attitude at work and at home and would like to change this. Chris has been seeing a Professional Counsellor for three sessions and […]
- June 1, 2007
- Case Studies , Relationship & Families , Stress Management
A Case of Mid-Life Difficulties
Fritz is 42 years of age and has been in Australia for the past 25 years. He migrated from Germany with his immediate family, comprising of his mother, father and two sisters. At the age of 17 Fritz was filled with great dreams and aspirations for his new life in a new country and until […]
- May 14, 2007
- Case Studies , Lifespan Development , Multicultural Issues , Relationship & Families
A Case of Stressful Life Change
Author: Jane Barry A précis of the sessions is as follows. For ease of writing the Professional Counsellor is abbreviated to “C”. In the first session, “C” asked some open questions to prompt Mary to start discussing her dilemmas. Mary was able to convey the events leading up to her problems clearly, although was reduced […]
- April 23, 2007
- Case Studies , Children & Adolescents , Disability Issues , Relationship & Families , Trauma & Disaster Mental Health
Counselling Case Study: Relationship Problems
Mark is 28 and has been married to Sarah for six years. He works for his uncle and they regularly stay back after work to chat. Sarah has threatened to leave him if he does not spend more time with her, but when they are together, they spend most of the time arguing, so he […]
- April 16, 2007
Counselling Case Study: Domestic Violence
The client, Gary, called to make his first appointment and said he was persuaded by “a mate” to attend counselling to control his anger. In short Gary was a perpetrator of physical abuse against his intimate female partner, Julie, who is 22 years of age. The couple have no children but his partner has recently […]
- March 27, 2007
A Case of Loss and Grief
Jim had come to counselling to seek help with dealing with the sale of his late mother’s estate. He was experiencing a lot of anger with the issue and also with his brother, Frank, who was joint inheritor. Frank was facing bankruptcy and needed the proceeds of the sale of the family home to save […]
- March 23, 2007
- Case Studies , Loss & Grief , Relationship & Families
- Research article
- Open access
- Published: 01 April 2021
Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters
- Tamar Wyte-Lake ORCID: orcid.org/0000-0001-8449-7701 1 , 2 ,
- Susan Schmitz 1 ,
- Reginald J. Kornegay 3 ,
- Felix Acevedo 4 &
- Aram Dobalian 1 , 5
BMC Public Health volume 21 , Article number: 639 ( 2021 ) Cite this article
2429 Accesses
2 Citations
Metrics details
Community disaster resilience is comprised of a multitude of factors, including the capacity of citizens to psychologically recover. There is growing recognition of the need for public health departments to prioritize a communitywide mental health response strategy to facilitate access to behavioral health services and reduce potential psychological impacts. Due to the US Department of Veterans Affairs’ (VA) extensive experience providing trauma-informed behavioral healthcare to its Veterans, and the fact that VA Medical Centers (VAMCs) are located throughout the United States, the VA is well situated to be a key partner in local communities’ response plans. In this study we examined the role the VA can play in a community’s behavioral health response using case studies from three disasters.
This study investigated experiences of VA employees in critical emergency response positions ( N = 17) in communities where disasters occurred between 2017 and 2019. All respondents were interviewed March–July 2019. Data were collected via semi-structured interviews exploring participants’ experiences and knowledge about VA activities provided to communities following the regional disasters. Data were analyzed using thematic and grounded theory coding methods.
Respondents underscored VA’s primary mission after a disaster was to maintain continuity of care to Veterans. The majority also described the VA supporting community recovery. Specifically, three recent events provided key examples of VA’s involvement in disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships as well as prioritization from VA leadership to engage in humanitarian missions. The behavioral health interventions were provided by behavioral health teams integrated into disaster assistance centers and non-VA hospitals, VA mobile units deployed into the community, and VA telehealth services.
Conclusions
Recent disasters have revealed that coordinated efforts between multidisciplinary agencies can strengthen communities’ capacity to respond to mental health needs, thereby fostering resilience. Building relationships with local VAMCs can help expedite how VA can be incorporated into emergency management strategies. In considering the strengths community partners can bring to bear, a coordinated disaster mental health response would benefit from involving VA as a partner during planning.
Peer Review reports
Disaster behavioral health
The current COVID-19 pandemic, while still underway, has already demonstrated the need for psychological interventions to manage the isolation, stress, and trauma stemming from the ongoing disaster [ 1 , 2 , 3 , 4 , 5 ]. While the scale of the event is unprecedented, interest in understanding the psychological consequences of disasters is not unique to the pandemic [ 6 , 7 , 8 , 9 , 10 ]. Generally, studies exploring the impacts of disasters on behavioral health have found increases in psychological distress in the short term, with the potential for some individuals to experience long-term psychiatric disorders such as posttraumatic stress disorder, depression, and anxiety [ 6 , 7 , 8 , 9 , 10 ].
To ameliorate the potential negative health effects to impacted populations, numerous early interventions have been explored [ 7 , 11 , 12 , 13 , 14 ]. Some countries such as the Netherlands and Iceland use federally structured plans to implement disaster behavioral health interventions [ 12 , 15 ]. And countries like New Zealand have invested heavily in developing extensive mental health programs in response to large scale disaster events [ 16 , 17 ]. In the United States, federal entities strive to create resources and guidance on implementing behavioral health services after disaster, however, interventions are generally managed and delivered by state, territory, and local agencies [ 14 , 18 , 19 ]. Often, after federally declared disasters, the US Federal Government additionally provides funding through the Crisis Counseling Assistance and Training Program (CCP) to community behavioral health programs [ 8 , 13 , 20 ]. Yet the structure and content of interventions are left to the discretion of the implementing agency.
Regardless of the services provided, having a plan in place prior to a disaster can facilitate implementation [ 8 , 11 , 12 , 13 , 19 , 21 , 22 ]. Few publications detail the creation of a local disaster behavioral health response plans [ 15 , 18 , 20 ] or describe the process in which interventions were deployed following an incident [ 7 , 10 , 15 , 20 , 23 , 24 ]. Common themes arising in studies exploring disaster behavioral health plans or interventions are the need for interdisciplinary teams and interagency collaboration [ 8 , 12 , 18 , 19 , 20 ] and strong community response [ 16 ].
The United States Department of Veterans Affairs
One interagency partner often overlooked in the United States is the U.S. Department of Veterans Affairs (VA) Veterans Health Administration (VHA). Previous publications on VHA’s participation in collaborative disaster planning and preparedness efforts with local communities identified barriers to its involvement [ 25 , 26 ]. One such barrier is that the community, and sometime even VHA employees, are unaware that VHA is tasked with planning for and acting to support “national, state, and local emergency management, public health, safety and homeland security efforts” [ 9 , 27 ]. This responsibility to contribute to community efforts is called the VA’s Fourth Mission and is in addition to VHA’s duty to ensure continuity of services to veterans after a disaster.
The expertise of VHA’s 322,030 healthcare professionals and support staff who provide a range of services at its 1255 healthcare facilities spread throughout the U.S. and its territories makes VHA a valuable potential partner in disaster response [ 28 ]. In addition to inpatient and ambulatory medical care, VHA provides a variety of reintegration programs including trauma recovery and behavioral health services for Veterans and their families at its facilities and through community-based care at Vet Centers, Mobile Vet Centers, and college and university campuses [ 29 ]. How these services are applied in community response efforts has been detailed in the grey literature [ 28 , 30 , 31 , 32 ].
This study highlights the potential role of local VA facilities in supporting local behavioral health activities after a disaster, and specifically, presents three exemplars of VHA integrating into communities’ disaster behavioral health response and providing behavioral health support to non-Veterans. The three VA facilities and the events they responded to are: (1) VA Pacific Island Healthcare System (VAPIHC), which is based in Honolulu, Hawaii but provides care to Veterans throughout numerous Pacific Islands. On October 24th, 2018, Super Typhoon Yutu made direct landfall on the Mariana Islands, a US Commonwealth with a nascent established VA tele-mental health clinic on the island of Tinian. This was the strongest typhoon ever recorded to strike the area, severely damaging or destroying many buildings and much of the critical infrastructure of Tinian [ 33 ]; (2) Orlando VA Healthcare System, which serves east central Florida, and encompasses 7 counties. On June 12, 2016, a domestic terrorist attack [ 34 ], targeted hate crime, and one of the deadliest mass shootings in the U.S. occurred at a local establishment, Pulse Nightclub. In a matter of hours, 49 people were killed and 53 were wounded before law enforcement breached the building and ended the violence [ 35 ]; and (3) VA Southern Nevada HCS (VASNHCS), located in and providing care throughout Las Vegas, Nevada. On October 1, 2017, the worst mass shooting in modern history took place at the Route 91 Harvest Music Festival on the downtown Las Vegas Strip. A gunman opened fire on a crowd of more than 22,000, killing 58 people and wounding 413 [ 36 ]. These cases provide examples of interagency partnerships and the implementation of collaborative responses for communities developing their own plans to address the behavioral health needs of their citizens during disasters, including the ongoing COVID-19 pandemic.
Study design
The results presented in this paper stem from a larger study broadly examining the role of local VA facilities in responding to regional large-scale disasters. This study used qualitative interview methods to elicit study participants’ experiences during disasters impacting the U.S. between 2016 and 2018 (see Table 1 for the full list of the disasters covered in the study, the impacted US states and territories, and VA entities affiliated with the impacted areas). Findings on disaster behavioral health functions were pulled as a subset of data and analyzed. The VA Greater Los Angeles Healthcare System Institutional Review Board (Los Angeles, California USA) approved this study.
Setting and sample
The full study sample was purposively chosen to represent individuals with emergency response roles critical to coordinating VA’s local response to disasters. Emergency management personnel at various levels of the VA were the first point of contact and, when applicable, identified additional individuals with critical response roles to interview. Additional respondents were recruited independently by the project team These facilities made up the broad recruitment sample. Due to some respondents covering multiple disasters or being deployed to disasters outside their normal service region, not all entities were included in the final sample.

Data collection methods
Data were collected through semi-structured, 60-min telephone interviews between March–August 2019, using an interview guide developed for this study (see Additional file 1 ). Interviews were conducted individually with each respondent and led jointly by at least two of the authors. Interviews explored participants’ experiences and knowledge about VA activities in the community, specifically focusing on how VA networked and coordinated with non-VA community agencies. Interviews were audio-recorded, although one respondent declined to be recorded.
Analysis plan
A total of 17 individuals were interviewed. However, five interviews did not indicate collaborating with non-VA entities and were therefore not included in the analysis. Due to their involvement in multiple disasters, two respondents were interviewed twice. At completion of the interviews, this resulted in 13 interview recordings being transcribed, and one set of interview notes (due to interviewee declining to be recorded), resulting in a total of 14 interviews that were analyzed with Atlas.ti (v.7) using a grounded theory approach. In phase one of analysis, one author reviewed all 14 interviews, using inductive coding to identify emergent themes in the data, and informed by extensive conversations about project findings held by the project team at the conclusion of each interview [ 37 ]. As a product of this process, a significant emergent theme [ 37 ] was the presence of interagency partnerships implementing collaborative responses to address the behavioral health needs of local citizens during disasters. A decision was made by the project team to narrow the focused coding analyses [ 37 ] to the way local VA facilities engaged in a behavioral response within their local community, in response to their respective large-scale disaster events.
In phase two of the analysis, the initial codes identified by SS were reviewed by TWL for consistency and agreement. Codes not deemed consistent to the focus topic were dropped. Additional grounded themes were confirmed by the team and applied to the data set [ 37 ]. Consensus on final codes was achieved, and one code list was finalized. In phase three of the analysis, the final code list was applied across all relevant interviews. The final code list had a focus on behavioral health response, including behavioral health activities, method of delivery, reactions of staff, and types of impacted community populations, but also included an identification of high level themes across all disasters, including VA expertise, integrating into local, established response activities, identification of local needs, and logistical challenges. Authors TWL and SS then independently coded each interview and resolved discrepancies by consensus.
All respondents played a substantial role in VA’s activities following the respective disasters. However, only 12 participants indicated the VAMC they supported collaborated with non-VA partners during the event in question. Included disasters ranged from widespread to geographically contained; weather-related to acts of violence; and direct impact on VA facilities ranged from none to significant. Though not all respondents described intensive engagement with the community following the event, all respondents described the importance of integrating into local, established response activities. This translated into involvement in community-wide drills and planning committees and following the lead of local incident command. Respondents indicated one of the areas where the VA could provide support to the community was in disaster behavioral health relief operations.
Activities described by respondents were often centered around tasks where the VA could reduce the caseload of other community agencies by identifying Veterans obtaining services in the community and meeting their needs regardless if they were previously enrolled in VA benefits. One key activity described by several respondents included outreach into local shelters. As one respondent explained, VA staff at shelters “[distribute] fliers [that] outline that our counselors are experts in trauma, loss, and in readjustment. They also provide referrals to Veterans for a variety of services, including housing and employment. We also offered free counseling for all community members impacted .”
Identifying where shelters were established and receiving authorization to deploy VA assets to those locations required coordination with local authorities. Multiple respondents mentioned connecting with emergency management running relief efforts to describe available VA resources and detail the services available to both Veterans and the community at large. In some of the events explored in this study, the non-VA authorities were unaware of what the VA could offer while others had pre-existing relationships that allowed for more transparent understanding of how the VA could support response efforts. One respondent went on to describe how the disaster that impacted their VAMC led to additional outreach to local jurisdictions and shelter coordinating agencies (e.g., the American Red Cross) to build relationships and understanding specifically of the behavioral health services the VA could deploy, if needed and approved.
Respondents noted there were specific benefits to conducting outreach in locations where other agencies provided services to the people impacted such as shelters and Local Assistance Centers. They noted that VA staff could more easily reach Veterans to enroll them, if eligible, into VA services and offer care to those who usually used non-VA health and mental health facilities, thereby supporting local agencies by reducing potential patient loads elsewhere. Additionally, by positioning resources at a central location, VA could more readily offer community members services as an extension of their work with Veterans. One specific resource identified as useful for Veteran and community support was Mobile Vet Centers, which have the primary goal of providing social work and mental health services to Veterans. In cases where respondents mentioned this resource, they underscored that non-Veteran community members who requested services in the first days after the disaster were never turned away.
Three community profiles
Three disaster events described by respondents distinctly highlighted cases where the VA was deeply involved in the local community’s disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships, as well as prioritization from VA leadership to engage in humanitarian missions to support the community.
Telehealth in Tinian, Mariana Islands
Prior to Super Typhoon Yutu impacting the Mariana Islands, the VA Pacific Island Healthcare System (VAPIHC) established tele-mental health services on the island of Tinian. These services were located at a non-VA owned healthcare clinic using pre-positioned VA telemedicine equipment and coordinated with the clinic director and staff. Typhoon Yutu devastated the island and led to many Tinian healthcare clinic employees losing their homes. The clinic with VA tele-mental health equipment became a temporary housing site for staff as it was undamaged by the storm. The clinic director realized that in addition to sheltering needs, employees also experienced significant trauma. However, there were limited mental health resources on the island. Once VA became aware of the need, it worked with other federal agencies to manage the logistics of implementing services that took advantage of pre-positioned VA resources.
“… it was a relationship that we had with [the US Department of Health and Human Services] (HHS) and a relationship that we had with the folks on Guam and Saipan … we have a lot of relationships going on. So, we knew that we had that telehealth equipment. We also knew that Tinian was … hit pretty hard. And that there was a lot of grief. And so I can’t say how it totally emerged, but there’s so many relationships and there’s so much communication during an emergency.”
Respondents reported it was initially challenging to identify whether VA could provide mental health services in the community and how the services would be funded. Staff at all levels of the VA worked with the Federal Emergency Management Agency (FEMA) and HHS to get official authorization as well as receive federal funding for VAPIHC to provide time limited tele-mental health interventions to clinic staff on Tinian. VAPIHC Tele-mental Health Hub coordinated with the local clinic director to inform employees about available services and utilized technology onsite to provide weekly support groups for 13 health center employees.
Director’s 50 in Orlando, Florida and the pulse nightclub shooting
The Orlando VA Healthcare System (OVAHCS) houses a unique emergency response team “The Director’s 50.” Made up of multi-disciplinary VA healthcare workers, including mental health professionals (i.e. psychologists, psychiatrists, mental health nurses), the Director’s 50 can deploy a team of up to 50 volunteers within 2 hours to areas throughout the region when authorized by the Orlando VAMC Director. As described by one respondent, the mission of the team is,
“to provide an immediate gap fill to an emergency before VA can get its assets organized and into a formal support and response role. So the team is multi-disciplinary and multi-functional with its capabilities, so that it can immediately address the needs of the emergency response until VA can formalize how it’s going to provide their support to the community.”
The Director’s 50 includes interdisciplinary clinical and service support training for all members such as triage and treatment services, mental health intervention, peer counseling, and psychological support to trauma. Through participation in community-wide exercises and drills, the Director’s 50 has built versatile capabilities and strong relationships with local emergency management agencies and area hospitals.
In response to the Pulse Nightclub Shooting, VA Central Office requested OVAHCS to deploy the Director’s 50 to provide VA resources and support the community’s response. The team activated their mass notification system to alert their nearly 100 volunteer members and quickly assembled an initial response team of about 15 clinical, mental health, and support professionals within 1 hour. Respondents noted having internal approval can speed up the process of deploying teams. In general, to distribute VA resources into the community, a federal disaster declaration is required to initiate the Robert T. Stafford Disaster Relief and Emergency Assistance Act or where the HHS Secretary has activated the National Disaster Medical System, both of which grant VA the ability to provide assistance. Therefore, respondents noted a need to balance expectations of leadership to help quickly, while also ensuring VA resources were legally allowed to be used in the response.
One thing that facilitated OVAHCS’s integration into the local response system was a pre-existing relationship with the City of Orlando’s Office of Emergency Management and the Central Florida Medical Disaster Coalition, which facilitated the Director’s 50 integration into the city’s response and allowed them to report to the victim reunification center. The team was tasked.
“to be the initial communication to the family members for those victims that actually passed away. So, 49 victims, our team was assigned to go ahead and be the initial contact to let them know that their loved ones had passed, and to begin the coordination for services, grief counseling and victim advocacy, you know, to help them prepare the initial points of piecing together their lives after being notified of such tragic events.”
Accordingly, the initial multi-disciplinary team narrowed its focus to mainly members with mental health expertise. Over the next 2 weeks, the team worked with the community, helping to manage vigils and gatherings for the public, and continuing grief counseling and mental health support for the whole community, including providing peer behavioral health support to municipal first responders. Since this act of violence targeted people who were Lesbian Gay Bisexual Transgender Queer (LGBTQ) frequenting Pulse Nightclub, not only were relatives of victims or survivors from inside the building affected, but the entire LGBTQ community felt the traumatic impact of the shooting. One respondent described the importance of providing mental health support from multiple community agencies when a disaster of this magnitude occurs,
“And they [the people who were at the shooting] truly needed a place, and this is why we were there for greater than just the 24-48 hours of initially identifying the people who was killed during the shooting, you had everyone that was inside of the club who were seeking a place where they could go and receive the care and support that they needed as well. And obviously, you know, this is something that is an endemic issue with healthcare as a whole, is the access to mental health counseling and services. So VA, as well as some other partnering mental health organizations were able to supply that need right there at the site where they were doing victim notification or victim reunification and family support. We were able to do that.”
One respondent noted a key point to remember about the Director’s 50, “they are all volunteers...And these people will go—you know, 24 hours a day, day in and day out, to execute that mission. And we have to think about team resiliency.” This included caring for team member’s well-being by rotating staff and providing and attending to the mental heath of one another. As described by one respondent,
“Because when it was all said and done, the team was very affected by what they had to do. You know, just imagine hearing—you know, overwhelming grief for every one of the 49 victims’ families that would show up. And the team took that burden on … and I will tell you, to this day, it still affects the people who went and supported that mission. And they really—those who supported that mission have a greater reverence for what we do now, as a team. So you’d never have to ask them to—whether they are going to support anything related to the Director’s 50. That comradery that’s there, they won’t let their own kind of—go into the bowels of despair like that, alone.”
Integrating into community response in Las Vegas, Nevada after the route 91 harvest festival shooting
As a large city with many national and international visitors, respondents described Las Vegas as having a very centralized emergency response structure. Relationships between VA Southern Nevada HCS (VASNHCS) and local response agencies and area hospitals were described as “tightknit” with great working relationships where organizations plan and prepare for disasters together. As one respondent put it,
“what I do know is my community. I know my community partners. I know what they have, what they don’t have, they know what I have, what I don’t have. And that’s what makes us so resilient. That’s community.”
Although located too far away from the Las Vegas Strip to actively receive injured victims when the shooting occurred at the Route 91 Harvest Music Festival, VASNHCS activated its Hospital Incident Command System so it could actively participate in the community’s response and organize efforts. A Multi-Agency Coordination Center (MACC) organized the response activities, and respondents underscored the value of both pre-existing relationships and an understanding of the county’s emergency response structure. As explained by a respondent,
“You can’t wait for your community to ask you. You have to be on the forefront and know what they need. And you only do that by knowing your community. You know, I spent probably as much time in my community as I do in my medical center. A lot of the time, it’s my own time, but again, it builds that relationship that when they’re updating their mass casualty plan, one of the people they’re calling is [me].”
This previous collaboration, as well as being present at the MACC, allowed VASNHCS to identify community needs that it could address.
As news of the shooting spread, VA leadership tasked VASNHCS with deploying staff into the community. However, it was challenging to balance the push from VA to deploy with continuing to respect established local coordination structures. VASNHCS maintained a presence within the Medical Area Surge Command of the MACC to offer resources and expertise, waiting for requests, instead of directly deploying assets outside of the established system.
In the immediate response, VASNHCS assisted with managing fatalities. It offered morgue space to the county and initiated the mass fatality plan to increase morgue capacity. This provided the county and partner hospitals space for victims until they could be processed, and families could claim them. Additionally, VASNHC offered a Psychological First Aid (PFA) team.
Initially, VASNHCS deployed their PFA team to the community’s family reunification center. The team was composed of social workers, psychologists, psychiatrists, administrators (as support staff), canteen services (for water and snacks to sustain clients and staff), and the medical center’s Chief of Staff. As the situation evolved, the MACC received requests from local agencies for psychological assistance and VASNHCS transitioned to directly integrating into area hospitals.
Three Las Vegas hospitals received the bulk of the injured or dead and recognized the need for psychological interventions with their staff. Due to their close relationships with other hospitals, one respondent explained that they were familiar with the Employee Assistance Program (EAP) at these hospitals. The respondent knew it would take time for the EAP to arrive onsite and they would most likely focus on clinical staff involved in directly treating the injured. Therefore, VASNHCS developed a three-pronged approach to complement EAP services at the receiving hospitals. Firstly, the PFA team provided what one respondent called “ trauma therapy ” to hospital staff, regardless whether they worked the night of the shooting. The assistance extended beyond clinical staff to non-clinical departments, such as environmental services/housekeeping, whose staff were also impacted through their response roles.
Respondents reported one of the reasons their response in the hospitals was so successful was that the team was multidisciplinary, allowing staff from different departments to talk to people in similar positions, which was valued by the recipients.
“So for example, we have a nurse that’s trained in trauma, psychological first aid. So they want the nurses at [the hospital with a patient surge], they want to talk to our team. They were still processing. But when we brought our nurse into the ward, they were more than willing to open up to her, because she was one of them. She was part of their tribe. So we try to match our tribe to their tribe, and that’s why we were successful.”
Secondly, the VASNHCS team worked with victims of the shooting, providing PFA and social work services. Thirdly, they integrated with family members of patients at the hospitals and provided them items that they did not otherwise have because they were visitors to Las Vegas. Examples included coordinating free transportation to and from hospitals and hotels, connecting them to local mortuary services, and providing information about how to access services when they returned home.
The PFA team ran for 24 h a day, for 7 days in those three impacted hospitals. To balance VA patient care with the community response mission, VASNHCS staff volunteered shifts outside of their normal work hours. One respondent described the overwhelming desire of VA staff to help their community.
“And while it didn’t impact our staff or our clinics, or our patients, it impacted our community. I think another thing that still amazes me to this day, was the outpour of our staff and what I mean by that is they were coming out of the woodwork to support. We had more volunteers working an eight-hour shift and then coming in [to volunteer] at five o’clock or four o’clock and working to midnight to two in the morning and not go home until four or five in the morning, and then go to work the next day, because we didn’t want to impact our patient care. And they were doing this out of their—you know, because they care. They care about the community, they care about the event, they care about the people. And then at the end of the day, you know, we had more volunteers than we had placements, because we did not want to overwhelm the health systems with all of these VA personnel.”
However, with new volunteers each shift, a key lesson learned was to have a daily team debrief. As people changed daily, a debrief provided key information and a running tally of support being provided to save time and avoid reinventing the wheel identifying contacts or systems already developed.
Another lesson was that preparedness requires ongoing maintenance. The importance of ongoing preparedness was underscored when VASNHCS realized that leading up to the shooting, they had reduced their focus on PFA training. As described by one respondent, “ We noticed that we need that continuous [psychological first aid] training, that we need continuous exercising, and it’s not an easy fit, to send a bunch of people to someone else’s hospital or an area to do that kind of service .” They also realized the first wave of personnel went into community hospitals without basic supplies they needed to provide services, including basic items such as pens, PFA guides, and informational brochures.
Three months following the shooting, the VASNHCS Emergency Manager, working with the Chief of Social Work hosted a lunch for staff who volunteered to thank them for their involvement. During that event, they realized volunteers were not only impacted by the event itself, but also by their time providing support in the community. They therefore created a forum to again gather staff who had deployed at the 6 month and 9 month marks to eat and talk about the impact of the event on the healthcare system and themselves. On the 1 year anniversary, management had a special event for the volunteers,
“we actually had people from the community that we supported coming in and they broke bread with our team and what they did was, they talked about what the impact of the VA Southern Nevada Healthcare System was going into that event, and how we helped them bridge the gap [of mental health support] that was crucial at that time, and how appreciative they were to our cause and our Clark County Office of Emergency Management gave all our staff that responded T-shirts that said Vegas Strong, because they wanted them to know that we—they appreciated the work that we did for them to support our community.”
The need for attention to the psychological well-being of individuals during and after a disaster has been well proven as disasters have been found to be associated with both short and long-term symptoms and disorders [ 6 , 7 , 8 , 9 , 10 , 38 ]. Although in some parts of the world there are federally structured plans to implement disaster behavioral health interventions, in the United States there is a patchwork system that often relies on support and resource allocation from a multitude of agencies [ 8 , 13 , 14 , 18 , 19 , 20 ]. In this study we examined the role the VA can play in a community’s disaster relief effort and highlighted the opportunity for VA to support behavioral health response focusing specifically on case studies from three disasters.
Essential to effective emergency management is an understanding of, and engagement with, available resources in a local community. This is of particular importance when considering complex individual and group needs such as behavioral health support. VA Medical Centers can be seen as challenging partners to work with because they are both a federal entity and a local healthcare facility [ 26 ]. However, in the case of Super Typhoon Yutu, the federal positioning of the VA and its connection with HHS and FEMA facilitated the deployment of VAPIHC virtual resources. The regional respondents who supported the VA disaster mission in Tinian described how preexisting relationships with federal partners facilitated authorization and funding.
Another potential challenge to incorporating the VA into response efforts is that prior to offering services, VA leadership must balance the mission of the agency with community needs, without contradicting the restrictions of the Stafford Act. In all three presented cases, VA’s behavioral health support was not formally included in a city or county response plan, and yet pre-existing relationships between key stakeholders facilitated the provision of VA behavioral health services to support identified community needs. Respondents also described participating in interagency coordinating groups, response trainings, and exercises before the disaster. These activities aided in a deeper understanding of the response structures each partner operated under and encouraged strong rapport between agencies.
Relationships between VA emergency management and local emergency management proved invaluable as VA staff understood that services should not be provided without first engaging local response coordinators. All VA facility leadership and emergency managers are required to be trained in the Incident Command System (ICS) and National Incident Management System (NIMS), which are the coordinating structures all U.S. response agencies work within [ 39 ]. As a health care provider at a national level, VHA falls within the operations section Essential Support Function (ESF) 8: Public Health and Medical Services to support the Department of Health and Human Services [ 40 ]. Local jurisdictions may also connect with VAMCs through ESF 8 representation. For example, the VA has provided significant support to communities impacted by COVID-19. As of July 8, 2020, VA provided more than 330,000 pieces of Personal Protective Equipment (PPE) in support of the Fourth Mission, as well as hand sanitizer, laundry support, test kits and testing support, and webcams for use with existing equipment to state and local facilities. In addition, VA has admitted 279 non-Veterans to VA Medical Centers because of the pandemic [ 27 ]. Much of this coordination was done through ESF 8 coordination at a local or national level.
While respondents did not go into detail about their participation in the emergency management structure, some participants described their VA’s roles within emergency operations as liaisons. Groups such as this could report to either the planning, operations, or command sections within the ICS. Group supervisors would most commonly report to the operations section chief, likely through branch directors, given that the focus of the work would be more on specialized functions as needed for tactical operations. Regardless of where they fit, their presence at emergency operations centers and command posts facilitated communication to allow for VA’s integration into incident action plans. Particularly during the response to mass casualty events in Orlando and Las Vegas, understanding the local response network and then proffering available services was essential to avoid confusion or duplication of activities. By working within the established coordination centers, VA’s efforts were effectively integrated into the greater community behavioral health response and were deployed to points of greatest need. Although a detailed understanding of the integration of VA activities into ICS structures fell outside of the scope of this work, future assessment of the integration of VA representatives into local, state, and/or regional ICS structures could help clarify roles and identify which section liaisons best support (e.g., operations, planning, logistics) [ 40 ].
VA is increasingly strengthening partnerships with agencies that provide behavioral health services to Veterans and their families who use non-VA community-based care [ 41 ]. In each case example, the primary support provided by VA to the community was the provision of behavioral health services in response to an identified need. Respondents described this as being due, in large part, to the recognition of VA’s expertise in trauma and post-trauma treatment, thereby allowing these resources to come to the forefront. While not mentioned by the respondents, an additional value that VA providers add to disaster behavioral health responses is their exposure to and understanding of the unique needs of various populations throughout their communities. In addition to ensuring care is culturally competent to the unique identity of being a Veteran, VA staff must respect the diversity of Veterans themselves. Just like the U.S. population at large, Veterans represent a range of ages, races, genders, sexual orientations, socioeconomic statuses, etc. and mental health services must be considerate of this diversity. The VA recognizes this and offers training to providers to understand and respect their patients’ unique needs [ 42 ]. Working with a variety of populations preposition VA staff to have a deeper understanding of the post-disaster needs of the wider community.
Two of the case examples described in this study especially bring to the forefront the importance of disaster behavioral health response planning and implementation teams understanding unique experiences of community members. Super Typhoon Yutu directly impacted an archipelago housing a majority Asian and/or Pacific Island population. The Pulse Nightclub shooting, while a terrorist event, was a targeted hate crime intended to inflict violence on the LGBTQ community. Disaster behavioral health interventions for these affected groups not only need to take into consideration the importance of cultural competency but also the potential of re-traumatization and distinct population mental health needs.
In the Northern Mariana Islands, while there is a mix of ethnic groups (Filipino, Chamorro, Chinese, Carolinian, Korean, Palauan, etc.), many either identify as or are categorized more broadly as Asian and/or Pacific Islanders. Although there are more than 1.4 million people who are considered Pacific Islanders living the in the U.S., there is a dearth of information on the mental health of this population [ 43 ]. Similarly, the prevalence and incidence rates of mental illness in the Mariana Islands is not well studied [ 44 ]. Some sources attribute this lack of understanding to a disproportionate underuse of mental health services [ 43 ]. However, Asian and Pacific Islanders within the U.S. and those territories affiliated with it often experience transgenerational trauma, discrimination, continued loss from colonization, historical trauma, and mental health stigma which can impact psychological wellbeing and help seeking behavior. Additionally, cultural elements (collectivism, reverence for the past, hierarchical social order, etc.) of this population are important to understand when providing behavioral health services [ 43 , 45 ]. One of the reasons respondents indicated that the VA was asked to provide assistance following Typhoon Yutu was the lack of availability of mental health services in Tinian. The established VA telehealth technology increased accessibility to behavioral practitioners from VAPIHC who most likely were experienced working with Asian and Pacific Island populations since more than 55,000 Veterans who identify as this ethnicity live in Island Areas or Hawaii [ 46 , 47 ].
The Pulse Nightclub Shooting was a terrorist driven hate crime targeting individuals who identified as LGBTQ. Members of this group often experience discrimination, stigma, and trauma throughout their lives. Discrimination and heterocentric health and mental health practices can marginalize this population and impact help seeking behavior [ 48 , 49 ]. This is of particular concern as individuals who are LGBTQ face numerous mental health disparities with a higher likelihood of experiencing depression, anxiety, substance misuse, and suicide attempts. The shooting not only targeted LGBTQ people but it also took place during Latin Pride Night meaning many of the victims and casualties were LGBTQ Latinx. The resulting psychological impacts of the Pulse Nightclub shooting on those directly impacted, people who are LGBTQ Latinx, and individuals in the wider LGBTQ community have been investigated and show experiences of trauma and impacts on perceived safety [ 50 ]. At the time of the shooting, the Orlando VAMC had established relationships with LGBTQ local mental health services and had staff knowledgeable in the needs of this community [ 51 ]. In fact, in the recent past, the VA has increased its efforts to ensure Veterans who are LGBTQ receive the highest quality patient-centered care possible [ 52 ]. Mental health services in particular have bolstered recognition of the complex needs of these Veterans [ 52 ].
All three cases demonstrate innovative ways VA can provide behavioral health support outside of their facilities, i.e., via telehealth capabilities across an ocean and into a healthcare clinic, teams of mobile units reaching directly into the community to support victims, victims’ families, and the community at large, and finally by incorporating PFA teams directly into hospitals to support staff, patients, and patients’ families. This flexibility across sites to address different needs and populations while using varying available infrastructure support, is paramount to any local jurisdiction’s ability to meet on the ground needs following a disaster. It demonstrates the variability between VAMCs and the importance of local disaster behavioral health planning teams to pre-identify resources to assess local capacity. Plans can then be developed that access and deploy the tools/skills of interdisciplinary and interagency teams. Building processes to deploy local health and mental health practitioners can lead to more rapid implementation of interventions and help ensure the diversity of the impacted community is recognized and respected. Additional studies focused on how communities develop disaster behavioral health plans could provide insight into which agencies are involved and how they collaborate. It may also be useful to assess whether and how these plans are implemented to identify best practices.
In addition to the people directly impacted by disasters, respondents underscored the importance of offering support to responders as well. There is growing recognition that health care workers are themselves front-line response workers who may be psychologically impacted when caring for others, leading to a growing emphasis on the importance of selfcare and employee wellbeing [ 39 , 40 , 41 , 42 ]. In all three case studies, behavioral health support was, at least in part, directed toward healthcare workers. In the case of Las Vegas, a respondent highlighted the advantage of having behavioral health support come from individuals who understood the culture of the population they were helping, e.g., nurses supporting nurses. Further, respondents in Las Vegas and Orlando highlighted the importance of supporting deployed behavioral health team members. They detailed actions to maintain staff well-being by having rotating shifts, encouraging peer support, and facilitating gatherings for staff to publicly thank them for their efforts and allow them to address their experiences together as a group. Understanding the needs of healthcare and behavioral health personnel and building support networks into response frameworks can help better sustain and strengthen the overall response process.
A primary limitation of this study is that interviews were conducted up to one and a half years after the disasters described, potentially impacting recall. However, multiple interviewees corroborated the information presented for each of the case studies. Another limitation is that this study focused exclusively on the experiences of VA employees fulfilling mission requirements and their description of instances where VA acted in support of the Fourth Mission. Very few of the respondents directly provided the behavioral health interventions. These perspectives could provide deeper understanding of the interventions themselves as well as the impacts they may have on practitioners. Neither community members nor coalition partners were interviewed in this study. Future research would benefit from both interviewing non-VA participants to explore additional perspectives and gain greater insight on how local jurisdictions experienced collaborating with VA representatives and exploring alternative approaches to mental health units within and outside VA to examine whether and when different approaches may be preferable.
As the largest integrated healthcare system in the United States, VA can play an important role in disaster response across the country. As recognition of VA’s expertise in behavioral health grows, particularly around trauma and post-trauma treatment, VA should be considered a strong potential partner in behavioral health responses. Local VAMC staff are part of the community in which they live and the Veterans they serve are a microcosm of the larger population of the U.S. As the respondents in this study showed, there is a deep desire by VA staff to provide support following a disaster if they are able. Anticipating potential behavioral health concerns, and having a plan to address them, can foster community disaster resilience. While these plans may be different for each jurisdiction, they can be strengthened by identifying and incorporating a range of partners. Having preexisting relationships where VA’s capabilities are known before a disaster occurs can facilitate the rapid deployment of VA resources into identified areas of community need. The case studies presented demonstrate the flexible nature of these resources. By extending knowledge about innovative ways to share behavioral health and other resources in a disaster response, communities and healthcare coalitions can be better prepared to engage collectively and rapidly mobilize essential assets to support the wellbeing of those who need it most.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Crisis Counseling Assistance and Training Program
U.S. Department of Veterans Affairs
Veterans Health Administration
VA Medical Center
VA Pacific Island Healthcare System
VA Southern Nevada HCS
Veterans Health Administration Health Care System
Veterans Integrated Service Network
Office of Emergency Management
US Department of Health and Human Services
Federal Emergency Management Agency
Lesbian Gay Bisexual Transgender Queer
Multi-Agency Coordination Center
Psychological First Aid
Employee Assistance Program
Personal Protective Equipment
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Article CAS PubMed PubMed Central Google Scholar
Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. https://doi.org/10.1192/j.eurpsy.2020.35 .
Article CAS PubMed Google Scholar
Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510–2. https://doi.org/10.1056/NEJMp2008017 .
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 .
Article PubMed PubMed Central Google Scholar
Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatr. 2020. https://doi.org/10.1177/0706743720926676 .
Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716–22. https://doi.org/10.1192/bjp.2018.210 .
Article PubMed Google Scholar
Beinecke R, Raymond A, Cisse M, Renna K, Khan S, Fuller A, et al. The mental health response to the Boston bombing: a three-year review. Int J Ment Health. 2017;46(2):89–124. https://doi.org/10.1080/00207411.2017.1294969 .
Article Google Scholar
Beinecke RH. Addressing the mental health needs of victims and responders to the Boston Marathon bombings. Int J Ment Health. 2014;43(2):17–34. https://doi.org/10.2753/IMH0020-7411430202 .
Dobalian A, Callis R, Davey VJ. Evolution of the Veterans Health Administration’s role in emergency management since September 11, 2001. Disaster Med Public Health Prep. 2011;5(S2):S182–4. https://doi.org/10.1001/dmp.2011.61 .
Heslin KC, Stein JA, Dobalian A, Simon B, Lanto AB, Yano EM, et al. Alcohol problems as a risk factor for postdisaster depressed mood among U.S. veterans. Psychol Addict Behav. 2013;27(1):207–13. https://doi.org/10.1037/a0030637 .
Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70(4):283–337. https://doi.org/10.1521/psyc.2007.70.4.283 .
Jacobs J, Oosterbeek M, Tummers LG, Noordegraaf M, Yzermans CJ, Duckers MLA. The organization of post-disaster psychosocial support in the Netherlands: a meta-synthesis. Eur J Psychotraumatol. 2019;10(1):1544024. https://doi.org/10.1080/20008198.2018.1544024 .
North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–18. https://doi.org/10.1001/jama.2013.107799 .
Watson PJ, Ruzek JI. Academic/state/federal collaborations and the improvement of practices in disaster mental health services and evaluation. Admin Pol Ment Health. 2009;36(3):215–20. https://doi.org/10.1007/s10488-009-0212-4 .
Thordardottir EB, Gudmundsdottir B, Petursdottir G, Valdimarsdottir UA, Hauksdottir A. Psychosocial support after natural disasters in Iceland-implementation and utilization. Int J Disaster Risk Reduction. 2018;27:642–8. https://doi.org/10.1016/j.ijdrr.2017.11.006 .
Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71(9):1025–31. https://doi.org/10.1001/jamapsychiatry.2014.652 .
Gray L, MacDonald C, Mackie B, Paton D, Johnston D, Baker MG. Community responses to communication campaigns for influenza A (H1N1): a focus group study. BMC Public Health. 2012;12(1):1–12.
Compton MT, Cibulas BK, Gard B, Kaslow NJ, Kotwicki RJ, Reissman DB, et al. Incorporating community mental health into local bioterrorism response planning: experiences from the DeKalb County Board of Health. Community Ment Health J. 2005;41(6):647–63. https://doi.org/10.1007/s10597-005-8846-5 .
Pfefferbaum B, Flynn BW, Schonfeld D, Brown LM, Jacobs GA, Dodgen D, et al. The integration of mental and behavioral health into disaster preparedness, response, and recovery. Disaster Med Public Health Prep. 2012;6(1):60–6. https://doi.org/10.1001/dmp.2012.1 .
Elrod CL, Hamblen JL, Norris FH. Challenges in implementing disaster mental health programs: state program directors’ perspectives. Ann Am Acad Pol Soc Sci. 2016;604(1):152–70.
Gil-Rivas V, Kilmer RP. Building community capacity and fostering disaster resilience. J Clin Psychol. 2016;72(12):1318–32. https://doi.org/10.1002/jclp.22281 .
Melmer P, Carlin M, Castater CA, Koganti D, Hurst SD, Tracy BM, et al. Mass casualty shootings and emergency preparedness: a multidisciplinary approach for an unpredictable event. J Multidiscip Healthc. 2019;12:1013–21. https://doi.org/10.2147/JMDH.S219021 .
Naturale A, Lowney LT, Brito CS. Lessons learned from the Boston Marathon bombing victim services program. Clin Soc Work J. 2017;45(2):111–23. https://doi.org/10.1007/s10615-017-0624-7 .
Reifels L, Pietrantoni L, Prati G, Kim Y, Kilpatrick DG, Dyb G, et al. Lessons learned about psychosocial responses to disaster and mass trauma: an international perspective. Eur J Psychotraumatol. 2013;4.
Dobalian A. The US Department of veterans affairs and sustainable health care coalitions. Disaster Med Public Health Prep. 2015;9(6):726–7. https://doi.org/10.1017/dmp.2015.136 .
Schmitz S, Wyte-Lake T, Dobalian A. Facilitators and barriers to preparedness partnerships: a veterans affairs medical center perspective. Disaster Med Public Health Prep. 2018;12(4):431–6. https://doi.org/10.1017/dmp.2017.92 .
VA Fourth Mission Summary [ https://www.va.gov/health/coronavirus/statesupport.asp ].
Office of Public and Intergovernmental Affairs [ https://www.va.gov/opa/pressrel/searchResults.cfm ].
Affairs USDoV: VA Office of mental health and suicide prevention guidebook. 2018.
Google Scholar
Lawrence Q. VA secretary Wilkie: ‘We are the surge force’. In: The coronavirus crisis: NPR. NPR.org ; 2020.
Services UDoHH. HHS, FEMA, DOD and VA continue to provide sustained and critical medical care support for Puerto Rico as part of Trump Administration response to Hurricane Maria. In . HHS.gov News: US Department of Health & Human Services; 2017.
Steinhauer J. The V.A. Prepares to back up a health care system threatened by coronavirus: The New York Times; 2020.
Agency FEM. Super typhoon Yutu: one year later: FEMA; 2019.
Foundation NP: After-action review of the orlando fire department response to the attack at pulse nightclub. 2018.
Investigation FBo: Active shooter incidents in the United States in 2016 an 2017. 2018.
Department LVMP: 1 October after action review. 2018.
Charmaz K, Belgrave LL. Grounded theory: The Blackwell Encyclopedia of Sociology; 2007. https://doi.org/10.1002/9781405165518.wbeosg070 .
Lowe SR, Galea S. The mental health consequences of mass shootings. Trauma Violence Abuse. 2017;18(1):62–82. https://doi.org/10.1177/1524838015591572 .
Department of Veterans Affairs. National incident management system compliance: VHA Directive 0320.12(1): Administration VH. Washington, DC; 2021.
Veterans Health Administration. COVID-19 response plan: Management OoE; 2020.
US Department of Defense DoVA, Department of Health & Human Services. Interagency task force on military and veterans mental health; 2017. p. 1–31.
National Academies of Sciences E, and Medicine, Health and Medicine Division, Board on Health Care Services, Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies Press (US); 2018.
Subica AM, Aitaoto N, Link BG, Yamada AM, Henwood BF, Sullivan G. Mental health status, need, and unmet need for mental health services among U.S. Pacific islanders. Psychiatr Serv. 2019;70(7):578–85. https://doi.org/10.1176/appi.ps.201800455 .
Buettner K, Sablan J, Funk M, Arriola, J, Price, S, Sugiura, K, Diminic S, Drew N. WHO profile on mental health in development (WHO proMIND): Commonwealth of the Northern Mariana Islands. Geneva, World Health Organization; 2013. https://apps.who.int/iris/bitstream/handle/10665/85304/9789241505741_eng.pdf;jsessionid=A222F532F705877A650948706A437484 . Accessed 26 Mar 2021.
Mental health in the Asian Americans/Pacific Islander Community [ https://www.amsa.org/2020/09/04/mental-health-in-the-asian-americans-pacific-islander-community/#:~:text=Mental%20Health%20of%20Pacific%20Islanders&text=According%20to%20a%202019%20study%20for%20the%20general%20US%20population ].
Alessi EJ. Acknowledging the impact of social forces on sexual minority clients: introduction to the special issue on clinical practice with LGBTQ populations: Springer; 2013.
Veteran Population [ https://www.va.gov/vetdata/veteran_population.asp ].
Ussher JM. Heterocentric practices in health research and health care: implications for mental health and subjectivity of LGBTQ individuals. Fem Psychol. 2009;19(4):561–7. https://doi.org/10.1177/0959353509342933 .
LGBTQI [ https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI ].
Stults CB, Kupprat SA, Krause KD, Kapadia F, Halkitis PN. Perceptions of safety among LGBTQ people following the 2016 pulse nightclub shooting. Psychol Sex Orientat Gend Divers. 2017;4(3):251–6. https://doi.org/10.1037/sgd0000240 .
Lesbian, Gay, Bisexual and Transgender Veteran Care [ https://www.orlando.va.gov/services/lgbt/index.asp ].
National Academies of Sciences E, and Medicine. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies of Sciences E, and Medicine; 2018.
Download references
Acknowledgements
Not applicable.
This work was supported by the US Department of Veterans Affairs, Veterans Health Administration, Office of Emergency Management and the Office of Population Health. The views expressed in this presentation are those of the author and do not necessarily reflect the position or policy of the VA or the US government.
Author information
Authors and affiliations.
Department of Veterans Affairs, Veterans Emergency Management Evaluation Center (VEMEC), 16111 Plummer St. MS-152, North Hills, CA, 91343, USA
Tamar Wyte-Lake, Susan Schmitz & Aram Dobalian
Department of Family Medicine, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR, 97239, USA
Tamar Wyte-Lake
Orlando VA Medical Center, 13800 Veterans Way, Orlando, FL, 32728, USA
Reginald J. Kornegay
VA Southern Nevada Healthcare System, 6900 N. Pecos Road, North Las Vegas, NV, 89086, USA
Felix Acevedo
Division of Health Systems Management and Policy, University of Memphis School of Public Health, Memphis, TN, USA
Aram Dobalian
You can also search for this author in PubMed Google Scholar
Contributions
TWL and SS planned the study, including instrumentation, conducted the data analysis, and wrote the paper. RJK and FA supported the qualitative analysis and contributed to revising the paper. AD helped to plan the study and contributed to revising the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Tamar Wyte-Lake .
Ethics declarations
Ethics approval and consent to participate.
The Greater Los Angeles VA Healthcare System Institutional Review Board (Los Angeles, CA USA) approved this study. As the research presented no more than minimal risk of harm to subjects and involved no procedures for which written consent would be normally required outside of the research context, the study received a waiver for documentation of consent from the Institutional Review Board, and verbal, recorded audio consent was approved.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
2017 Disaster Qualitative Study: Collaboration Project Interview Guide. Interview guide utilized during project’s semi-structured interviews.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wyte-Lake, T., Schmitz, S., Kornegay, R.J. et al. Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters. BMC Public Health 21 , 639 (2021). https://doi.org/10.1186/s12889-021-10650-x
Download citation
Received : 05 August 2020
Accepted : 18 March 2021
Published : 01 April 2021
DOI : https://doi.org/10.1186/s12889-021-10650-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency preparedness
- Behavioral health; disaster response
- US Department of Veterans Affairs
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Crisis Counseling Case Study Assignment (Mine)

Case study of Mine, a 67-year old woman, who served as a nurse during the 1980 Iran-Iraq war. Models used BASIC-Ph, Continuities and Psychological Debriefing.
Related Papers
ekstensi 2017
LA ACADEMIA DE LA FLUIDEZ Y ELOCUENCIA (EST. 1738) , Edgar Durakhanyan , ANTHONY BASHFORD, Ph.D.
Jan Wallcraft
Beatriz Isabel Zendron Range
Rohmatus Naini
Motherhood, Mental Illness and Recovery
Nancy Erickson
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
The Most Useful Crisis Management Examples: The Good, Bad, and Ugly
By Andy Marker | August 19, 2020
- Share on Facebook
- Share on LinkedIn
Link copied
Review crisis management examples to learn from others’ experiences with this comprehensive collection of case studies. Examples are organized by theme, and include crisis management successes and failures.
In this article, find crisis management examples organized by best practice , five of the costliest crises ever (and what was learned) , and examples of companies that have built the world’s most valuable brands by safeguarding their reputations.
What Is Crisis Management?
Crisis management refers to the practice of preparing for negative incidents, minimizing their damage and disruption, and getting an organization back on track as quickly as possible. Crisis managers anticipate likely threats and develop strategies to cope with their impact. To read more about crisis management please visit our "The Essential Guide to Crisis Management" article.
Effective Crisis Management Examples
Effective crisis management occurs when an organization employs skillful planning and a proactive response to avert a crisis entirely, limit its severity and duration, or turn it into an opportunity. These examples feature organizations that responded with transparency and agility.
CPG Product Crisis Management Example: Tylenol Product Tampering
In 1982, seven people in the Chicago area died after taking Tylenol capsules poisoned with cyanide. The tampering was believed to have occurred when someone injected the chemical into capsules and returned them to store shelves. The deaths remain unsolved, but the way Johnson & Johnson handled the episode has become a teaching case study for effective crisis management at Harvard Business School and elsewhere. In 2003, Fortune magazine named James Burke, the company’s CEO at the time, as one of history’s greatest CEOs for the way he handled the scare.
Below are some highlights of Johnson & Johnson’s handling of the crisis:
- Fast and Decisive Action: According to a book on the case by Harvard Professor Richard Tedlow, on the afternoon of the first two deaths, the company halted all product advertising, sent 450,000 messages to hospitals, doctors’ offices, and other stakeholders, and established toll-free hotlines for consumers. At a cost of more than $100 million, the company recalled all products from store shelves — one of the first nationwide recalls — even though government officials felt that doing so was excessive. Additionally, Johnson & Johnson issued warnings to consumers not to take its pain reliever.
- Honesty and Integrity: Despite evidence that the poison was introduced via store shelves, Johnson & Johnson did not try to evade blame. As a result, Burke was praised for his honesty. His integrity stood out in the context of the post-Nixon era and the unforthright handling of the Three Mile Island nuclear disaster. The company became a pioneer in developing tamper-proof packaging, and eventually moved away from capsules to a more tamper-resistant caplet. Burke was candid in expressing regret that the company had not done so right away.
In less than a year, Tylenol regained its market share and sales leadership, and according to a BrandSpark study, it continues to rank highly for consumer trust.
For a comprehensive look at crisis management in the Tylenol deaths, see this profile of Burke’s leadership and analysis of Johnson & Johnson communications .
Healthcare Crisis Management Example: Global Pandemic
While the global pandemic that began in late 2019 challenged many organizations, the calamity also highlighted examples of strong crisis management.
The Cleveland Clinic Abu Dhabi operates as a U.S. medical center in the United Arab Emirates. The hospital faced COVID-19 early in its migration beyond China. The clinic responded quickly in order to both expand its emergency capacity and continue providing care for cancer and transplant patients, as well as for those with other complex needs.
Dr. Rakesh Suri, CEO of Cleveland Clinic Abu Dhabi, says that forming a crisis management team (that included individuals from all levels of the organization) was a critical step, as doing so enabled the hospital to act with agility. The medical center also coordinated with other local hospitals to maximize resources and play to each institution’s strengths.
The executive team took extra steps to take care of staff, including talking honestly about their emotional challenges and providing sleeping rooms, meditation space, online workouts, nutritious food, counseling, and childcare.
An in-depth case study on the hospital surfaced several lessons, including the importance of preparing for worst-case scenarios, leaders empowering their teams to solve problems innovatively, encouraging candor, proactively engaging all stakeholders, and taking care of physical and mental well-being.
In business, companies had to pivot quickly as the pandemic changed the marketplace. A 2020 Harvard Business School study of 350 senior executives in China who faced the crisis early found some key commonalities among those who managed effectively, including the following:
- Improve decision-making by moving away from the hierarchical model.
- Collaborate in new ways with customers, suppliers, regulators, and even competitors.
- Support remote work by changing company culture to prioritize trust and results over command-and-control and physical presence.
- Ask employees to self-select for challenging assignments in order to get maximum ownership and motivation.
- Embed new learning and innovative digital strategies that arise in a crisis into your organization’s muscle memory.
Examples of Bad Crisis Management (and What They Teach Us)
In contrast, examples of poor crisis management are usually marked by fundamental errors in preparation or execution of an emergency plan — and sometimes both. Often, these problems compound, which only multiplies the scale of the crisis.
This is especially true in so-called black swan events — incidents that are extremely rare, have severe consequences, and are generally perceived in hindsight to have been obvious to happen. Since the likelihood of a black swan event occurring is low, leaders may dismiss the risk (if they are even conscious of it). But, the grave consequences of black swan events can pose a much larger threat.
Following are real-world examples of weak crisis management and the lessons crisis managers can take from them.
Natural Disaster Crisis Management Example: Hurricane Katrina
In August 2005, Hurricane Katrina hit the U.S. Gulf Coast and flooded New Orleans, causing more than $100 billion in property damage and killing more than 1,800 people. Even though the hurricane began as a natural disaster, the scale of the catastrophe was man-made. Various analyses of the response, including a report by Congress, focused on weak aspects of the crisis management and highlighted the following important lessons:
- Preparation Is Key: In 2006, a study by the Army Corps of Engineers found that the levees built to protect New Orleans from flooding were incorrectly engineered, poorly built, and insufficiently funded. Additionally, government officials who were aware of the storm forecast did not make provisions to evacuate residents who did not have cars or could not afford bus fare, which left tens of thousands of vulnerable people stuck in the city. The government also didn’t position enough emergency supplies in New Orleans ahead of the storm.
- Train Your Crisis Team: The Federal Emergency Management Agency (FEMA) was led by officials who were political appointees and had no experience in disaster management. A congressional review found that agencies handling the response were unsure of their roles and responsibilities. Government agencies failed to learn from a drill of a similar hurricane hitting New Orleans the previous year.
- Simplify Communications and Decision Making: Federal and local crisis managers struggled to communicate due to equipment failure and incompatible technologies. Confusion among different levels of government paralyzed decision making. Ultimately, the crisis plan was too complex — with 29 federal agencies playing a role, duties were unclear and too much red tape hampered efforts.
- Act Quickly but Not Rashly: About $2 billion spent by FEMA in Hurricane Katrina was wasted or fraudulently claimed, according to a New York Times analysis. In many ways, this was a symptom of a poorly planned and executed crisis response. For example, FEMA ordered $100 million in excess ice that truckers shuttled around the country for weeks while the agency tried to figure out where it should go (after storing it for two years, the government melted the ice). Additionally, the agency spent $7.9 million to renovate a former army base as a shelter in Alabama that only 10 people stayed at (the shelter closed within a month). Half of the mobile homes ordered as temporary housing — at a cost of $430 million — went unused.
For in-depth case study of Hurricane Katrina crisis management, see “Katrina and the Federal Emergency Management Agency: A Case Study in Organizational Failure. ”
Industrial Disaster Crisis Management Example: Bhopal Gas Leak
In 1984, a toxic gas leak from a Union Carbide India pesticide plant in Bhopal, India killed up to 30,000 people from immediate and long-term effects (according to estimates) and injured about 575,000. The accident is one of the world’s worst industrial disasters.
The leak was caused by the introduction of water into a chemical tank, which resulted in a heat-generating, runaway reaction. Several inquiries found evidence of company negligence, but an internal analysis blamed employee sabotage.
Researchers have written extensively about the accident, and some of the lessons cited are universally helpful in crisis management, including the following:
- Rehearse Emergency Procedures: The plant did not have an emergency plan, and plant operators did not know how to handle an emergency. No effective public warning system or public education about the risks were in place.
- Prioritize Crisis Readiness: The company reduced training and staffing at the plant to save costs. Supplies of gas masks were inadequate, and several plant safety mechanisms were either deactivated or faulty. Additionally, several experts found that there weren’t enough operators for the unit to function safely. On the night of the accident, the supervisor delayed investigating an initial small leak until after a crew break, rather than being proactive.
- Share Information: A U.S. Union Carbide plant found earlier in the year that a runaway reaction in the chemical tank could happen, but they didn’t communicate it to the India plant. When the leak occurred, plant staff did not inform senior managers or local authorities. Most of the information on the chemical involved, including how to treat exposure, was proprietary and was not disclosed. So, public health authorities and hospitals in Bhopal did not know immediately what victims had been exposed to (and therefore couldn’t provide the best antidotes).
For in-depth case studies on the Bhopal accident, see Union Carbide Corp.’s site dedicated to the tragedy, as well as “ An Analysis of the Bhopal Accident” and “ The Bhopal Disaster and Its Aftermath .”
Five of the Most Costly Corporate Crises and Their Lessons
In addition to the human toll, a crisis can also be financially devastating for a company and its shareholders. Aside from direct costs, businesses may face fines, damage claims, legal settlements, damage to brand value, exodus of key revenue-generating staff, competitive disadvantages, and stock price declines.
Social media has compounded these effects. A study by Pentland Analytics that compared corporate crises in 2000 and 2018 found that social media amplified damage, doubling the loss of shareholder value (from a 15 percent to a 30 percent decline in the first year after a crisis).
The most costly crises have multi-dimensional financial impacts. Following are some examples of calamities that caused extensive financial damage to the companies.
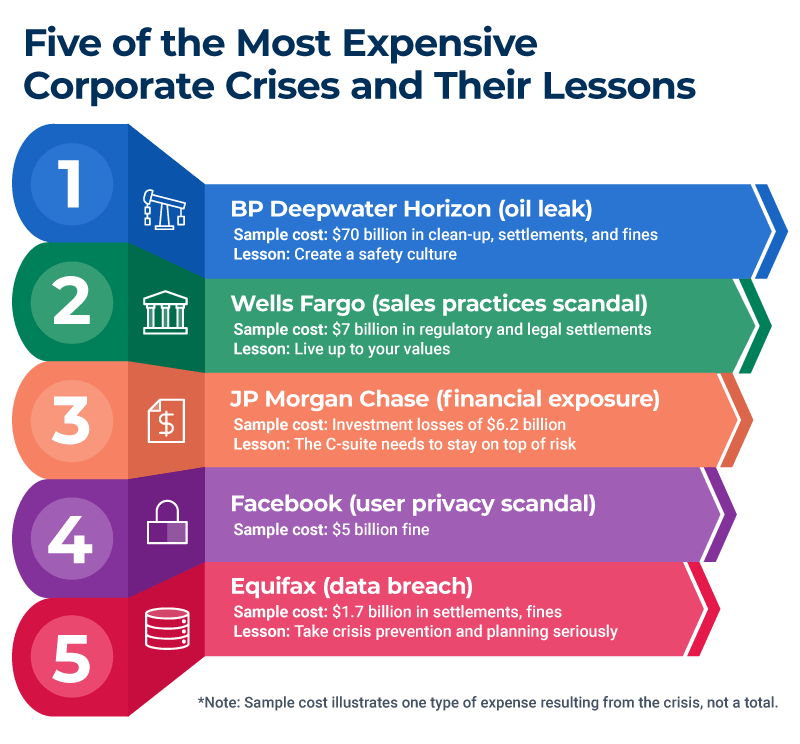
1. Example: BP Deepwater Horizon
In 2010, BP’s Deepwater Horizon oil-drilling rig in the Gulf of Mexico exploded, killing 11 employees and causing an oil leak that lasted for three months. This is the biggest oil spill in U.S. history.
The oil spill devastated the environment and tourism. Damage to the environment has been long-lasting — one study valued the impact at $17.2 billion . The spill also caused billions of dollars in negative economic impact on tourism in the region. Meanwhile, the financial toll for the company included the following costs:
- Through early 2020, BP paid about $70 billion in clean-up costs, legal settlements, and fines.
- In the two months after the spill, the company’s shareholders lost $105 billion as its stock price plummeted.
- For a time, the company’s survival was in question. Its bonds crashed in value, and the company had to stop paying dividends for three quarters.
- In the United States, the BP brand faced a backlash from consumers, and BP gas stations saw sales drop 10 to 40 percent in the immediate aftermath of the spill.
- BP had to reduce its business spending for years, which analysis said put it behind competitors such as Shell, whose brand value rose 24 percent that year, according to Interbrand. BP dropped from the second-largest global oil company in 2010 to fourth, where it has remained.
Crisis Management Lesson: Create a Safety Culture Studies have attributed the accident to a series of human mistakes and technical failures in the context of a high-risk corporate culture and weak regulatory supervision . The studies noted overconfidence on the part of BP, based on many years of not having an offshore well blowout in deep water. They also cite a lack of planning for low-probability, high-impact oil spills.
Operators and managers grew accustomed to normalizing signs of potential trouble and ignored weak signals of looming disaster. Alarm systems on the rig were suppressed, and crucial equipment was not properly maintained. The Center for Catastrophic Risk Management at the University of California Berkeley blamed the absence of a safety culture and shortsighted prioritization of the bottom line. According to the center’s report, BP “forgot to be afraid.”
2. Example: Wells Fargo
For 14 years, until the practice was exposed in 2016, hundreds of thousands of Wells Fargo employees opened customer accounts without consent to meet sales targets and generate fees for the bank. The financial consequences included the following:
- The bank paid more than $7 billion to settle government investigations and private lawsuits.
- Wells Fargo lost business from the state governments of California and Illinois, as well as from the cities of Chicago, Philadelphia, and Seattle, among others who cited the illegal behavior as the reason.
- In response to the scandal, in 2018, the Federal Reserve imposed a limit on the bank’s growth, putting Wells Fargo at a competitive disadvantage and costing it an unknown amount of potential increase in customers and loans.
- The company lost $220 billion in stock market value in the two and a half years after the enforcement action. The stock hit a 10-year low in May 2020, faring far worse than its peers.
- The bank has racked up heavy expenses related to the crisis, including legal fees, investigation costs, and spending on an ad campaign aimed at restoring consumer trust.
Crisis Management Lesson: Live Up to Your Company Values to Avoid Scandals According to the government, Wells Fargo executives were aware of the abuses as early as 2002, but failed to act despite espousing a culture of integrity. The executives imposed such aggressive sales targets for staff that many employees said they felt they had no choice but to engage in the illegal practices. The government is pursuing some individual executives for their roles.
For an in-depth discussion, you can read the full report issued by the U.S. House of Representatives .
3. Example: Equifax
In 2017, Equifax, a credit reporting bureau, suffered a data breach that gave hackers access to sensitive personal information for 147 million consumers. The incident was the most expensive data security breach to date. In 2020, four members of China’s People’s Liberation Army were indicted in the United States in the breach.
- The company had $1.7 billion in legal settlements, fines, fees for consultants, lawyers, and investigators, and the cost of providing credit monitoring and identity protection to consumers.
- In the week after Equifax disclosed the breach, the company lost $5.3 billion in market valuation as its stock price declined 31 percent.
- For the first time ever, a credit rating agency downgraded its outlook on a company over cybersecurity concerns. A credit rating downgrade increases a company’s borrowing costs. Moody’s dropped its rating on Equifax to negative from stable in 2019, two years after the breach, citing continued high costs related to the hack. Moody’s further projected that the spending would continue to hurt Equifax’s profitability.
Crisis Management Lesson: Take Crisis Prevention and Planning Seriously A congressional investigation found that relatively basic mistakes at Equifax led to the breach. For example, the attack occurred through a server vulnerability that was a known issue. Equifax had previously notified its system administrators to patch the issue, but the person responsible for the point of entry did not get the message because Equifax’s email list was out of date.
An expired digital certificate allowed malicious network activity to stay hidden. Proper data governance protocols, which limit user access to sensitive information, were not in place — this allowed the attackers to run about 9,000 queries to find the consumer data. The attack lasted about 76 days before it was discovered.
The company’s public response contained many missteps (including directing consumers to a website that had bugs, according to IT experts) and as such, did not inspire confidence. For example, the site asked consumers, who had just had personal information stolen via Equifax, to enter most of their Social Security numbers to find out if they were included in the hack. The company mistakenly tweeted a phishing link for the response website four times instead of the correct URL, according to Wired magazine.
Crisis management experts said Equifax lacked comprehensive prevention and response plans and faulted the company’s slow disclosure. (Equifax discovered the breach in July 2017 but did not reveal it until September 2017.) Given the sensitivity of the information in their database, Equifax should have had much more robust preparation, experts said.
For details on crisis management planning, see “ Step-by-Step Guide to Writing a Crisis Management Plan .” You can also use one of these free disaster recovery planning templates to help get your business back on track.
4. Example: JP Morgan Chase
In 2012, a trader in JP Morgan Chase’s London office, nicknamed the London Whale, ran a portfolio of esoteric derivative investments. The trader was part of a team whose mandate was to hedge the bank’s operating risks. But, the whale’s investment strategies turned out to be flawed, and the size of these transactions was so great that they affected world credit markets. The whale’s trades ultimately lost money on a massive scale, and the company sustained the following financial impacts:
- Investment losses of $6.2 billion.
- JP Morgan Chase received fines of more than $1 billion by U.S. and British regulators.
- Senior executives were stripped of $75 million in compensation after an internal investigation.
- The company had to pay one hundred and fifty million to settle a shareholder class action lawsuit.
- A loss in stock market value of $14.4 billion in the two days after disclosing the problem.
- The company’s reputation as a careful risk manager was also damaged. In 2012, research company Interbrand found that the value of JP Morgan’s brand had dropped 8 percent, to $11.5 billion.
Crisis Management Lesson: The C-Suite Needs to Stay on Top of Risk When he realized the full potential for disaster, the London Whale, whose real name is Bruno Iksil, suggested that the company immediately take a loss on the positions. This move would have resulted in much less financial damage.
But, according to a U.S. Senate report, his managers began to conceal the magnitude of losses. They produced a shadow spreadsheet and hoped the investment positions would turn around, which resulted in mounting losses.
Reviews of the episode found that risk-management practices for the division were less rigorous than for other areas of the bank. First, the bank ignored warning signs from its risk metrics and then changed the risk standards (so the warning signs went away), according to a company report.
Although people internally realized the potential extent of losses, bank management downplayed them in public. In 2012, CEO Jamie Dimon dismissed the incident as a “complete tempest in a teapot,” the Senate report said, a position he would later reverse.
The bank‘s investigation found that there was too little scrutiny of the London activities by its top management. In the aftermath, the bank strengthened risk management and made the review team more independent to address the group-think mentality that limited questioning of the investment strategy, JP Morgan said. The episode sparked calls for tougher regulation.
5. Example: Facebook
In March 2018, a whistleblower told two newspapers that a British firm called Cambridge Analytica had bought data about 87 million users and their friends without their consent from Facebook. The company used the data to build voter profiles that Cambridge sold to election campaigns, including Donald Trump’s presidential run.
The episode sparked a scandal over user privacy at Facebook, the biggest of many. CEO Mark Zuckerberg was called to testify before Congress. The company faced investigations by regulators in the United States and Britain, as well as lawsuits from several jurisdictions.
The financial repercussions included the following:
- The U.S. Federal Trade Commission imposed a $5 billion fine against the company — the largest ever. The FTC said Facebook’s behavior violated a previous consent decree with the agency. The Securities and Exchange Commision fined the company $100 million and British regulators fined 500,000 pounds.
- Engagement on Facebook dropped by 20 percent in the months after the scandal, a metric that affects the company’s ad revenue.
- Facebook users’ confidence in the company dropped 66 percent in the weeks after the scandal broke and Zuckerberg testified before Congress, according to a Ponemon Institute survey. Some users quit Facebook (including 3 million Europeans) in the subsequent months over privacy abuses. The hashtag #DeleteFacebook began trending on social media, and public support for tighter regulation of social media grew.
- Growth in Facebook revenue and users dropped in the quarter after the Cambridge Analytica affair. The company’s stock valuation lost $130 billion in two hours after the news, weakening the social network’s forecast further.
- Facebook sustained a drop in brand value of 6 percent (about $2.9 billion) for the year to $45.2 billion, according to Interbrand.
Crisis Management Lesson: Apologize When You are Wrong U.S. investigators found that Facebook violated consumer trust by allowing a third party to collect users’ personal data without their knowledge. The data collectors also violated Facebook policies that required deleting the data.
Facebook CEO Zuckerberg was silent for five days before issuing a statement acknowledging that mistakes had been made. Facebook users heavily criticized the response, prompting Zuckerberg later to say, “I’m sorry” in media interviews. IT experts said the response was slow and underwhelming.
Critics faulted Facebook for technical decisions that resulted in app developers being able to access information about users’ friends, saying safeguards were inadequate. Commentators such as Tufts University cybersecurity expert Susan Landau also criticized Facebook for not taking legal action against Cambridge Analytica and for failing to inform users whose data was taken until well after the news broke.
The company placed full-page newspaper ads, made changes to data-handling practices, and implemented other reforms, but consumer trust remained damaged. Analysts said Facebook’s gestures, including its lack of apology, rang hollow and came too late.
Best Crisis Managers Safeguard Their Brands
Protecting your reputation is an important aspect of crisis management, and conveying authenticity and empathy is paramount when anyone is harmed.
Reputation research firm RepTrak found in a 2020 survey of 80,000 consumers globally that corporate responsibility (made up of workplace quality, governance, and corporate citizenship) accounts for 41 percent of its reputation. (For details on how and when to apologize, see “ Models and Theories to Improve Crisis Management .”)
Corporate reputation is an important influence on consumer behavior. RepTrak data shows a company with an excellent reputation activates willingness to buy among 79 percent of consumers, compared to 9 percent for companies with poor reputations.
Companies that maintain strong reputations through the decades are typically examples of strong risk and crisis management. But that is not to say they have necessarily avoided all calamities: sometimes, these organizations have faced a pivotal crisis and turned it into an opportunity to achieve long-term reputation strength.
Reputation is the primary determiner of brand value, which is a company asset that can be worth billions. Interbrand found that the value of the top 10 global brands in 2019 was collectively almost $1 trillion.
Top 10 Most Valuable Global Brands*
- Apple: $234.2 billion
- Google: $167.7 billion
- Amazon: $125.3 billion
- Microsoft: $108.9 billion
- Coca-Cola: $63.4 billion
- Samsung: $61.1 billion
- Toyota: $56.2 billion
- Mercedes: $50.1 billion
- McDonald’s: $45.3 billion
- Disney: $44.4 billion
*Source: Interbrand, 2019
Crisis Management Examples by Best Practice
Crisis case studies help illustrate best practices and how companies apply them. The following examples show how crisis management leaders and laggards performed on fundamental best practices in specific situations.
Crisis Management Best Practice: Form a Crisis Team
While you should have a designated crisis management team, you may also need smaller teams focused on particular issues. Cross-functional teams are often especially effective. Free team members from their normal duties while they are handling the crisis, remove constraints, and give them the resources they need, such as specialized external experts. When the crisis is over, review the team’s performance. (For more about crisis management teams, see “How to Build and Effective Crisis Management Team.”
Example: When Volkswagen faced a crisis over its diesel-emissions scandal, Oliver Larkin, group head of investor relations, told IR Magazine that the company “immediately put in place a task force team, with representatives from the communication side but also from the technical side and the legal side evaluating the information as it was coming through – and those people were working 24/7.” The group’s focus was on messaging, VW’s reputation, and relationships with major investors, and other responsibilities were put aside. Specialists, who were situation consultants, also joined the effort.
Crisis Management Best Practice: Have a Plan
Hopefully, your crisis management plan includes a communications plan that you’ve detailed in advance. But if not, or if you overlooked anything relevant to the crisis at hand, do some quick planning at the beginning of the crisis. Make sure to plan for social media, and draft holding statements. To learn how to write a plan, read “ Step-by-Step Guide to Writing a Crisis Management Plan .”
Examples: In a case study of what not to do, Amazon faced negative attention around its 2019 Prime Day shopping promotion. Staff around the world protested over alleged poor working conditions and abusive company policies. Actions leading up to and on the day sparked media coverage, calls for legislative action, and late-night TV segments. Amazon did not comment publicly, defying public relations best practices. PR experts speculated the company did not have a crisis communications plan to mitigate the damage.
As an example of strong crisis communications, the American Federation of Government Employees, the union representing 700,000 employees of the U.S. federal government, responded to the coronavirus crisis with a multi-pronged communications plan. The goal was to draw attention to concerns over a shortage of protective gear and testing, policies, and short-staffing.
The union sued the federal government for hazard pay, and then targeted individual agencies by publicizing the plights of their staff to the media with press releases, TV appearances, and a daily newsletter. Internally, the union sent daily email alerts and digital campaigns to local leaders, weekly updates to members, mass texts, and memes to get the word out.
Crisis Management Best Practice: Pick the Right Spokesperson
Choose an individual who has the knowledge and training to address the crisis and is in a position of authority. You can coach the right person on working with the media, but putting a representative who lacks expertise in front of the cameras will backfire: your organization will come across uninformed or incompetent.
Example: During the coronavirus pandemic, Dr. Anthony Fauci, Director of the National Institute of Allergy and Infection Diseases for more than 30 years, brought expertise to his role as explainer in chief to the American public.
He conveyed the importance of citizens staying home with clear and consistent messaging, and he deftly handled complex questions about science from the media. He gave interviews on social media, podcasts, sports shows, digital news sites, as well as traditional media, to reach all demographics, including teenagers.
Crisis Management Best Practice: Be Present
In a serious crisis, leaders should always be on site, either at headquarters or the location that makes the most sense. Cancel business trips, and return from vacations.
Example: In early 2020, wildfires burned more than 20 percent of Australia’s forests and killed 26 people. During the disaster, Australian Prime Minister Scott Morrison faced an outpouring of anger from citizens and intense media criticism after secretly taking a Hawaiian vacation and having his staff deny it.
The prime minister’s representatives refused to disclose his location, igniting a social media storm and dominating media coverage. Then, an Australian tourist shared a photo he snapped with the leader on a Hawaiian beach. The government had to backtrack, which caused huge embarrassment and a scandal about the cover-up.
Crisis Management Best Practice: Respond Quickly
Issue a statement within the first hour of a crisis and publish frequent updates. Keep customers and other stakeholders informed about progress. If you’re unsure about frequency, err on the side of too much communication, rather than too little.
Example: In 2018, after switching delivery companies, Kentucky Fried Chicken (KFC) suffered supply problems that caused a shortage of chicken at its U.K. restaurants. The company was forced to close more than two-thirds of its locations.
Even though the crisis response group initially had little information about the problem, the team quickly acknowledged the issue publicly. Within hours the team explained what had happened, how it was being addressed, and when it would be solved.
“Our instinct was that we had to face the issue head on: a chicken restaurant without chicken. Not ideal,” a spokeswoman for KFC told Raconteur at the time. “We were responding live as we received new information. We acted fast in assessing the issue and working out the best approach.”
In a negative case study, General Motors in 2014 did a series of vehicle recalls due to faulty ignition switches that affected 30 million cars. The company ultimately paid about $4.1 billion in repair costs, victim compensation, and fines.
But perhaps even more damaging was the revelation that the automaker had known about the problem for at least a decade , at one point blaming the fault on short drivers and heavy key chains. The resulting publicity and congressional hearings harmed GM’s reputation, and one senator described the company as having a “culture of cover-up.”
Use a crisis communications strategy template to help you assign important responsibilities and build a process and response plan in the early stages of a crisis. For all other crisis management templates please visit our template article . You can also learn about step-by-step instructions on how to build a strong crisis management strategy , including free templates and tips from experts.
Crisis Management Best Practice: Be Compassionate
Respond empathetically to show that your organization cares about people. Fear of lawsuits often causes companies to resort to carefully parsed legal language or circumspection. While minimizing liability is important, showing your human side goes a long way to winning goodwill and defusing anger, which often is a motivating factor in lawsuits.
Example: In 2019, Boeing responded to news that its 737 MAX airplane had caused two crashes and killed 346 people due to faulty software by insisting the aircraft was safe and that there was no engineering or technical problem.
The CEO blamed poor pilot training. Governments around the world grounded all the planes. Crisis communications experts criticized Boeing’s handling as slow, legalistic, and lacking empathy. Moreover, they noted that Boeing’s stated values include acting with the highest ethical standards, taking personal responsibility, and valuing human life above all else, and that these should have guided its response.
Crisis Management Best Practice: Speak the Truth
Be upfront and transparent, and don’t hide behind euphemisms or jargon. The truth will eventually become clear, and obfuscating will only cause further mistrust and resentment.
Example: In a negative case study, United Airlines forcibly removed a 69-year-old doctor from an overbooked flight leaving Chicago in 2017. Security officers dragged him off the plane. A passenger captured the scene on video and bystanders reported the officers threw the man against an armrest. The doctor later said he lost two teeth and had a concussion and broken nose.
United CEO Oscar Munoz told employees by email the passenger had been “disruptive and belligerent.” In a public statement, he said the airline had to “re-accommodate” the man, a euphemism for the procedure of removing a paying passenger from the flight so an airline employee could have the seat.
The video of the doctor’s rough treatment went viral on social media and showed that the doctor had not acted out as Munoz claimed. United faced a wave of public anger, and its stock lost $1.4 billion in value. Munoz later apologized and promised the incident would not happen again, but his planned promotion to United’s chairman was canceled.
Crisis Management Best Practice: Focus and Move Ahead
Give the crisis full attention, but do not lose sight of your future. Whenever possible, align your crisis response actions with the long-term vision and overarching goals of your organization.
Example: In early 2020, Delta Air Lines (like all carriers) faced a catastrophe as a global pandemic virtually eliminated demand for airline travel. While challenges persisted, the airline began working toward regaining financial stability.
CFO Paul Jacobson, who crafted and led Delta’s financial crisis response to the Sept. 11, 2001 attacks, canceled his announced retirement to help rebuild the airline. To accomplish this task, Jacobson used strategies such as securing emergency government aid and deferring long-term capital spending.
Crisis Management Best Practice: Communicate Clearly
Present information openly and in a way that others can understand. Recognize that personal perspective influences how everyone interprets information. Don’t hide from bad news.
Example: In 1986, the Space Shuttle Challenger disintegrated little more than a minute into flight, killing all seven crew members. Investigations found the cause was the failure of an o-ring seal in a solid rocket booster that allowed pressurized burning gas to escape and cause structural disintegration.
Poor communication and decision-making were determined to be major contributing causes to the disaster. The investigating commission found the launch should not have been approved. They cited a lack of effective communication between the decision-makers and the engineers, the absence of a formal communications channel which isolated management, and selective listening. The panel found the decision to proceed with the launch was based on incomplete and misleading information.
Crisis Management Examples by Type: Social Media, Product Problems, and More
Crisis management case studies are especially instructive when you compare how two organizations coped with relatively similar problems. The following examples are organized around crisis type, including social media crises.
Examples of Social Media and PR Crisis Management
Social media has enabled users to spread negative or embarrassing information about a brand in a nanosecond. Companies need to monitor social media actively and act quickly to address public relations problems. Unflattering episodes can go viral, severely damaging a company’s reputation.
Examples of Good Social Media Crisis Management
The most effective uses of social media to address company crises are typically characterized by speed and, when appropriate, humor — although companies should also address underlying issues.
- Example: Popeye’s In 2019, Popeye’s debuted a fried chicken sandwich that consumers praised on Twitter, comparing it favorably to rival Chick-fil-A’s offering. Chick-fil-A responded with a tweet promoting its sandwich as “the original.” Popeye’s shot back cheekily, “Y’all good?” The retort ignited the so-called “chicken-sandwich wars,” which Popeye’s won as Americans flocked to its stores.
- Example: Red Cross In 2011, the American Red Cross defused a crisis over a rogue tweet with humor. A staff member mistakenly sent a personal tweet to the organization’s account: “When we drink we do it right #gettngslizzerd.” As the tweet started to spread, Red Cross defused the PR nightmare with this tweet acknowledging the error: “We’ve deleted the rogue tweet but rest assured the Red Cross is sober and we’ve confiscated the keys.” A beer brand mentioned in the original tweet responded by asking its fans to donate to the Red Cross.
- Example: Tide In 2018, teenagers uploaded to social media videos of themselves eating Tide laundry detergent pods, which are poisonous, in the “Tide Pod Challenge.” Rather than trying to ignore the controversy, manufacturer Procter & Gamble swung into action by lobbying social media platforms to remove the videos, mounting a communications campaign, and placing its own video of NFL player Rob Gronkowski urging people not to swallow the pods on social media and broadcast television.
Examples of Bad Social Media Crisis Management
Crises can start or worsen on social media when brands display insensitivity or are slow to react to growing negative engagement. Following are some examples of companies that mishandled social media.
- Example: Gillette In 2019, razor maker Gillette sought to promote the values of the #MeToo anti-sexual harassment movement with a video that it placed on YouTube and in ads. After a century of promoting men who use its products as alpha males and virile, the company in the video first showed men bullying and mansplaining, and then contrasted them with empathetic men who stop others from bad behavior toward women. Despite some scattered praise, the video got twice as many dislikes as likes on YouTube, and calls for a Gillette boycott arose. Twitter users bashed the company for negatively stereotyping men and shaming its customers.
- Example: Tinder In 2015, dating app Tinder responded to a negative article about it in Vanity Fair magazine with a 31-tweet rant. The tweets were defensive, included profanity, and a claim that the app had helped people in North Korea meet dates. The overreaction made Tinder the butt of jokes and drew negative attention to the company.
- Example: Applebee’s In 2013, a waitress at restaurant chain Applebee’s posted a customer’s receipt on Reddit (with the name visible). The customer had written a critical comment about an automatic 18 percent tip added to the bill for a big party. Applebee’s said on Facebook, “We wish this situation hadn’t happened.” Thousands of negative comments flooded in every hour. The story went viral, and Applebee’s response was panned by PR experts as pouring gasoline on the fire. The company’s social media team answered Twitter comments by copying and pasting its corporate policy statement, which users perceived as a snarky response. Then, failing to keep up with the flood of reaction, the company disabled user posts on its Facebook page. Next, the team posted an update with the corporate statement, hiding the previous statement and more than 20,000 comments. Users perceived the tactic as deleting their posts, which enraged them.
Examples of Crisis Management Involving Product Problems
Product crises can be especially damaging for companies because their sales and brand are likely to suffer. Effective crisis management can ensure that the fallout is minimized. Poor crisis management can make it worse.
Examples of Good Crisis Management of Product Problems
Companies that manage crises caused by faulty products well show concern for customers, take responsibility for the issues, and respond decisively with improvements.
- Example: Mattel In 2017, toy maker Mattel recalled nearly 2 million toys that were tainted with outlawed lead paint. The act angered parents and attracted regulator attention. The problem stemmed from a contract manufacturer that used paint not authorized by Mattel. Within a few days, Mattel identified the factory, halted production, and launched an investigation. The company voluntarily expanded its review and made two more product recalls, even adding an unrelated problem. The company imposed stringent new tests on products before they could be sold, changed suppliers, and put its own staff in contract manufacturing plants. Mattel communicated consistently and repeatedly apologized. The company won praise for its swift and honest response, and the company now enjoys a reputation of trustworthiness.
- Example: Samsung In 2016, Korean electronics company Samsung faced a crisis when its Galaxy Note 7 smartphones exploded due to a battery problem. Sales slumped as airlines banned passengers from carrying the phone on board. Samsung responded by immediately taking accountability, being transparent about not immediately knowing the cause, and vowing to determine the problem. The company put 700 engineers on the problem and opened the research to third parties. When the problem was identified, the company communicated the issue clearly and introduced quality assurance and safety features. Samsung also launched a campaign aimed at tying its brand image to a larger purpose and improving its culture. In the next year, Samsung’s brand value rose 9 percent, according to Interbrand, and its Galaxy S8 yielded record profits the following year.
Examples of Bad Crisis Management for Product Problems
Examples of poor crisis management by companies over product issues are often marked by slow acknowledgement or even denial.
- Example: Takata Japanese auto parts maker Takata produced car airbags that exploded and were linked to at least 14 deaths. Governments recalled some 70 million airbags by 2017. Studies of the problem found design and engineering flaws. Before the extent of the problem became clear, Takata did not want to face embarrassment or prosecution. A senate report found that the company manipulated test data and did not adequately address safety concerns. The report concluded the company’s safety culture was broken. Takata ultimately went bankrupt with an estimated $15 billion in liabilities for recall and other costs.
- Example: Nike In 2019, U.S. star college basketball player Zion Williamson sprained his knee when his Nike shoe broke, little more than 30 seconds into a highly anticipated game. The crisis quickly gained the name “shoegate” in the media. The company’s stock dropped $1.1 billion the next day, social media buzzed with jokes and jabs, and commentators described the incident as a brand failure. While the incident did not inflict long-lasting damage on the company, Nike was panned for waiting for three hours to issue a response. They stumbled by minimizing it as an “isolated incident,” while media reports pointed out four other recent similar shoe malfunctions.
Improve Your Crisis Management Tactics with Real-Time Work Management in Smartsheet
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team — and adapt as those needs change.
The Smartsheet platform makes it easy to plan, capture, manage, and report on work from anywhere, helping your team be more effective and get more done. Report on key metrics and get real-time visibility into work as it happens with roll-up reports, dashboards, and automated workflows built to keep your team connected and informed.
When teams have clarity into the work getting done, there’s no telling how much more they can accomplish in the same amount of time. Try Smartsheet for free, today.
Discover why over 90% of Fortune 100 companies trust Smartsheet to get work done.

About Features Online Exclusives From the President Career Consultation Knowledge Share Explore
Crisis counseling: A blend of safety and compassion
By Bethany Bray

W hen crisis strikes, clients need a counselor who can listen and share their heartbreak without inserting themselves into the situation, says Amanda DiLorenzo-Garcia, an American Counseling Association member and mobile response coordinator for the Alachua County Crisis Center in Gainesville, Florida. She describes crisis counseling as a short-term intervention to an acute situation with a singular purpose: ensuring that the client is safe and feels seen and heard.
Clients need someone who is “willing to be there, be present and be uncomfortable,” she explains. “We can’t help to fix the situation; all we can do is help the client to withstand it, to survive it — and often that’s heartbreaking. It challenges our humanity. … We have to stretch ourselves to be able to hold space for the immense emotions of despair, grief, hopelessness and helplessness, and that can be really uncomfortable to do.”
Part of life
Crisis counseling is a specialty within the counseling profession, but it’s also a skill that all counselors need to master because crises will pop up in everyday life for clients in all settings.
Thelma Duffey and Shane Haberstroh, in the ACA-published book Introduction to Crisis and Trauma Counseling , explain that crisis “is often an immediate, unpredictable event that occurs in people’s lives — such as receiving a threatening medical diagnosis, experiencing a miscarriage or undergoing a divorce — that can overwhelm the ways that they naturally cope.”
Crisis can also occur when multiple stressors are present simultaneously in a client’s life and a seemingly small incident, such as losing their keys and getting locked out of the house, pushes them to “the end of their rope” and sends them into a tailspin, says Ruth Ouzts Moore, an associate professor in the Counselor Education Department at the Chicago School of Professional Psychology.
Shock, denial and disbelief are often the first emotions that clients experience in crisis situations, along with hopelessness and helplessness, says DiLorenzo-Garcia, who co-presented on “Breaking Through Barriers to Provide Effective Crisis Support” at ACA’s Virtual Conference Experience this past spring with Jessica L. Tinstman Jones and Amber Haley. A vast range of physical, mental, emotional and behavioral symptoms can indicate that a client is in crisis, she notes. (See list below.)
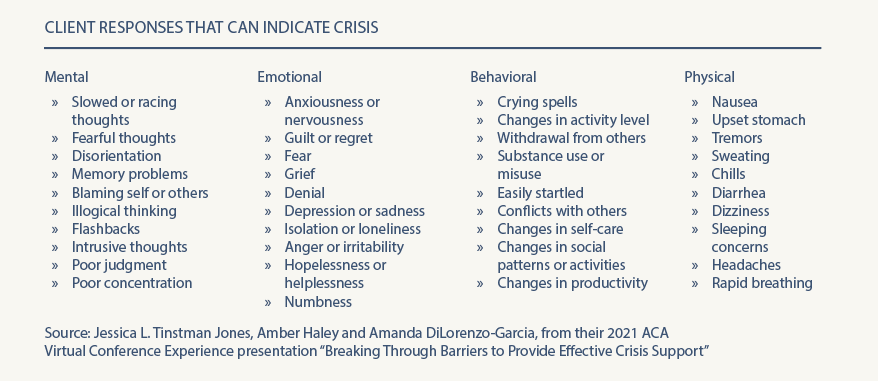
Moore defines crisis as the presence of a “risk of foreseeable harm” in a client’s life, either immediately or in the short term. The client may not automatically disclose this risk factor in counseling, however. Instead, their presenting concern can often be a “Band-Aid” or something more benign, she says, and it’s up to the counselor to “peel away the layers” to assess for risk. This can especially be the case with children, who may be referred to counseling for behavioral issues or because they’re falling behind at school. Sometimes, a crisis — such as abuse at home — may be the root cause of these struggles, notes Moore, an ACA member who specializes in working with children and adolescents who have experienced crisis and trauma.
Ali Martinez is a licensed marriage and family therapist and director of the Alachua County Crisis Center (where DiLorenzo-Garcia also works). In addition to mobile crisis response and in-person counseling services, the center operates a local 24/7 crisis hotline and responds to calls from their area of Florida to the National Suicide Prevention Lifeline. Most of the more than 45,000 calls the agency answers each year are from people who are feeling utterly alone as they face something that feels threatening to them, Martinez says. This includes losses that involve the death of a loved one as well as relational, financial and other losses.
“Most [callers] are not suicidal but are in some level of pain — experiencing something big that hasn’t been fully expressed, and they’re seeking space to do that,” Martinez explains. “They either are truly alone in what they are facing or feel alone in what they’re facing. They’re desperate for some sense of connection. They often know we can’t fix what’s happening — and that’s not usually what they’re seeking. …The struggle with crisis, what creates the danger and the true pain around a crisis, is the sense of how it disconnects us from people. The chaos, lack of control and strong emotions can make us feel alone. On the hotline, so often it’s trying to manage that chaos and find validation and connection — that what they’re feeling is a normal response to an abnormal situation. People often need someone outside their own world to let them know that what they’re feeling is OK and give them permission to express it.”
Crisis is self-defined
People can express their feeling of being in crisis very differently, but one common way that it manifests is tunnel vision, according to Martinez. In counseling, practitioners may hear a client who is experiencing a crisis speak with a narrowed scope or train of thought, returning to a singular experience or feeling over and over again.
Clients in crisis may feel like they’re drowning in emotions and that the issue that sent them into crisis is all-encompassing. Counselors may get the sense that their words are not getting through to the client because the client’s anger or despair is “filling the room,” Martinez says. Attending to the pain a client experiences during a crisis forces counselors to slow down their approach.
If counselors are “trying to get [the client] to look at the long term or take a bigger perspective and they can’t seem to do that and they keep coming back to that one painful thing, then we must change our approach and realize that this is the most important thing for them right now — and we have to listen for that,” Martinez says.
Above all, counselors must remember that “a crisis is defined by the person in it,” Martinez stresses. “For them, if it’s a crisis, it’s a crisis, and we have to honor that. Be aware that in that moment, we might have a much broader perspective on the possibilities [in the client’s life] and we might have good ideas about what could happen, but they may not be ready to hear it.” One of the most powerful things a counselor can say to a client in crisis is “tell me what this means to you,” she adds.
Martinez gives an example of a 12-year-old adolescent who is devastated after their first romantic relationship ends in heartbreak. As an adult, it would be easy for a counselor to tell the preteen client that this is the first of many heartbreaks life will bring. However, the client won’t be ready to focus on larger lessons about relationships and self until the counselor has helped them attend to their initial pain and despair over the breakup.
“For them, this is everything — feeling rejection and shame, sadness and despair. It doesn’t make it any less of a crisis experience for them,” Martinez says. “We [counselors] have to go in understanding it from their thinking.”
Josh Larson, a licensed professional counselor (LPC) in private practice in Denver, agrees that crisis must be self-defined by the client. He previously worked as a crisis clinician and operations and quality assurance specialist at Rocky Mountain Crisis Partners, a nonprofit organization that answers calls around the clock for several crisis hotlines, including the National Suicide Prevention Lifeline.
“We would always assure the caller that what they feel is a crisis, is a crisis. For one person, it could be that their cat got outside and they haven’t seen [the cat] for two hours and they’re feeling suicidal. For someone else, it’s something much bigger or more layered,” says Larson, an ACA member. “As a practitioner, even if what the client is telling us wouldn’t be a crisis for us, if they identify it as a crisis, then we need to treat it as such.”
Freedom to speak authentically
There is no shortage of crisis counseling models and assessment tools in the professional literature for practitioners to draw from in their work with clients. The counselors interviewed for this article did not recommend any one particular model or framework over another. They instead encouraged practitioners to research and select the counseling approach that works best for their style and client population.
No matter the model — or even if no model is used at all — a competent crisis counselor should shape a session into an arc that begins with rapport building and ends with connecting the person with resources. This last step ensures that the client has a safety plan (if needed) and is aware of options for follow-up care, such as local counseling services, walk-in crisis clinics and emergency hotline numbers. In the middle of this arc, at the core and heart of the therapeutic interaction, counselors create a nonjudgmental and empathetic space for the client to talk about their situation and share their burden.
The client does most of the talking in crisis counseling sessions, with the majority of the time spent simply “letting them tell their story,” DiLorenzo-Garcia explains.
Given that some clients may experience suicidal ideation during a crisis, an important part of this work is becoming well-versed in suicide assessment. DiLorenzo-Garcia and the other counselors interviewed for this article recommend that practitioners weave questions about a client’s safety, including those focused on suicide assessment benchmarks and protective factors, throughout the conversation.
In some situations, crisis counseling can offer clients the much-needed freedom to make strong statements without feeling judged or censored, Moore notes. This includes the freedom to talk about feelings such as anger or thoughts of harming oneself that can have shame or stigma attached to them.
This was the case for a 15-year-old client Moore once counseled who had turned to drinking, taking drugs and other risky behaviors to deal with turmoil at home, including feeling powerless when his father was abusive toward his mother. In session, the teen, referring back to an invective his father had directed at him, asserted, “I want to be an asshole.” Moore didn’t flinch at the client’s use of profanity. Instead, she responded, “You’re not an asshole.” When she repeated her statement, the teen began to cry, releasing emotions that had been pent-up.
“He had a deep, deep level of anger, resentment and betrayal that we needed to talk through. He found freedom in being able to say those things in a safe environment,” Moore recalls. “It was freeing that he could speak so strongly and hear his counselor repeat it back.”
Many of the crisis calls DiLorenzo-Garcia’s team responds to are in the public schools. Sometimes they respond because a student has called the county hotline themselves, but most often it’s because a school staff member (a school counselor, principal, school resource officer or administrator) has called to request their help.
In such cases, DiLorenzo-Garcia often begins a one-on-one session with a student by explaining the context of why the school asked her to come and speak with them. She assures the student that they are not in trouble and that she’s there because people are concerned about them. For example, she may say, “This is what I’ve heard from your school counselor, but I’m curious what your perspective is. What’s going on for you?”
“That’s the door opener. I reassure them, ‘I don’t want to make any assumptions about you. Your experience is your own, and I want to understand,’” says DiLorenzo-Garcia, a postdoctoral scholar at the University of Central Florida whose dissertation was on the loss and growth experience of mass shooting survivors and their families.
If the client’s experience includes thoughts of suicide, allowing them to talk through how they truly feel can help both the client and counselor realize how serious those thoughts are, DiLorenzo-Garcia adds. Sometimes a client has thoughts of suicide but doesn’t want to die, which can be accompanied by feelings of shame or isolation. If a client has a concrete plan to end their life, talking that through can help determine whether or how soon the client might act on that plan — and the necessity for follow-up care.
Assessing client needs
Larson notes that a majority of the callers during his time at Rocky Mountain Crisis Partners were not suicidal. However, some callers would say at the start of the call that they were not suicidal, but as the conversation went on and they began to unpack the depth of their emotions, it would become clear they were in fact experiencing suicidal ideation, he says.
This aspect of crisis counseling is why it’s imperative for counselors to be familiar with and proficient in suicide assessment . A counselor should be able to assess for preparatory behaviors, substance use problems, a client’s internal and external coping mechanisms, and other benchmarks to determine next steps, including safety planning or follow-up counseling, DiLorenzo-Garcia says.
Moore says it is important to be knowledgeable about assessing for not only suicidal ideation but also homicidal ideation when clients are in crisis. She acknowledges that asking questions about homicidal intent can be uncomfortable for practitioners. However, counselors must keep in mind that when in crisis, clients could have thoughts about harming others as well as themselves, she says.
“Be comfortable asking those difficult questions: ‘Are you having thoughts of killing yourself or harming anyone else?’ Don’t sugarcoat it,” says Moore, who presented the session “One Size Doesn’t Fit All: Creative Strategies for Counseling Diverse Families in Crisis” at ACA’s Virtual Conference Experience.
Larson points out that, along with active listening, validation of a client’s concerns and assurance of safety, de-escalation is a large part of crisis counseling. This can include mini versions of deep breathing and other grounding skills that clinicians might use in long-term counseling sessions with clients.
It can be helpful to match the person’s affect level, Larson says. For example, a counselor shouldn’t respond to a person who is hysterical with a flat, monotone voice. Instead, mirror them with a tone that is slightly calmer to gradually de-escalate the situation, he advises. Similarly, a crisis counselor shouldn’t respond to a client who is monotone or expressionless with a bright, bubbly demeanor. Instead, mirror their tone at a slightly more expressive level to gradually lift their affect, he says.
In crisis counseling, de-escalation and being presented with the opportunity to talk through what they are feeling will be enough for some clients, Larson continues. Others will be looking for help with problem-solving, such as conflict resolution or next steps to take after receiving a crushing health diagnosis. But Larson finds that clients in crisis are usually looking for one or the other, not both. Therefore, he advises counselors to be upfront and ask those in crisis, “What do you need? Do you want someone to listen or [someone to] help you problem-solve?”
“If you offer solutions to someone who is not wanting them, it can escalate them further into crisis,” Larson adds. Instead, he may tell clients, “I’m listening, and I’m willing to offer solutions if that’s what you’re looking for.”
In cases of suicidal ideation, DiLorenzo-Garcia finds it helpful to focus on the short term with clients. For example, she may say, “It’s a lot to ask you to live forever or live until next year, but right now, let’s talk about if you can live to tomorrow. What might that look like? Can you withstand the pain you’re going through just for tonight? What would it look like to survive and come back to school tomorrow?”
The counselors interviewed for this article emphasize that it is critical to arrange for follow-up support after crisis sessions but say that involving law enforcement to conduct welfare checks on a person in crisis should be done only as a last resort.
“ Always follow up with a person who is in crisis, even if your session ends well and it sounds like things are going to work out,” DiLorenzo-Garcia stresses. Her agency contacts each client within three days after the initial crisis counseling session to make sure they are supported and doing well. In school settings, she also debriefs the adults involved in the student’s care (e.g., parents, school counselor) to ensure they are aware of the student’s needs and any next steps after a crisis counseling session.
Client safety
Meredith McNiel, an LPC who co-wrote the chapter “Crisis and Trauma Counseling With Couples and Families” in Introduction to Crisis and Trauma Counseling , notes that during crisis counseling, practitioners should focus on client safety through three lenses:
- Feeling safe to express themselves fully in the crisis counseling session
- Feeling safe at home and in the world outside of the counseling session
- Feeling safe within their life, including protective factors and social connections
An important part of this focus, she says, is reminding clients (multiple times if needed) that the counseling session is a safe and confidential space to speak freely about what they are experiencing.
Clients may disclose dark and powerful thoughts, such as suicidal or homicidal ideation, during crisis counseling, and McNiel acknowledges that many counselors’ first instinct may be to refer these clients for more intensive care. However, practitioners need to push through this initial reaction to keep from breaking clients’ trust.
“If a counselor is worried or nervous or scared about handling a situation, the client will feel that,” McNiel says. “We need to be comfortable asking hard questions while keeping the client comfortable.” The counselor should allow the client to say what they need to in session and “hold that space” without trying to fix their situation, she stresses.
“In a suicide crisis session, many professionals might [automatically] think, ‘Where can we send you?’ and in my experience, that is an absolute last resort. If a client hears that they’re going to be hospitalized or referred out to someone they don’t know or trust, they can instantly lose trust with a counselor,” says McNiel, an ACA member with a private counseling practice in Austin, Texas. Instead, “allow the session to happen fully in the way the client needs to share or release and process, and go from there,” she advises. “I assure [the client] that if anything further needs to happen, we will decide that together. I will not take control of what’s going to happen. I remind them that they are in control of their circumstances.” (See more about the ethical guidelines regarding protecting clients from “serious and foreseeable harm” in Standard B.2.a. of the 2014 ACA Code of Ethics at counseling.org/ethics .)
Crisis counseling is “less clinical and more relational” than long-term counseling, explains McNiel, who was a crisis counselor at the University of Texas at San Antonio Academy for Crisis and Trauma Counseling during her LPC internship. Practitioners need to let clients share and talk through their experience “until it feels complete” — whatever that looks like for them.
To ensure that a client’s safety and comfort are the primary focus in crisis counseling, practitioners must be so familiar with assessment tools that they don’t need to read the questions off a piece of paper or computer screen, says McNiel, whose doctoral research was on college counseling work with students who were suicidal. “[Instead of] saying, ‘Hold on, I’m going to grab this checklist and ask you some questions’ … ask questions in a relational way and fill out the assessment afterward rather than stopping the flow of a session,” she says. Counselors should be “getting answers [from the client] through conversation rather than interrogation.”
For example, an assessment tool might prompt a counselor to ask the client, “Are you thinking about killing yourself?” Practitioners still need to ask direct questions about suicidal ideation, but couching those questions in a more conversational way aids in maintaining trust, McNiel notes. Alternatively, the counselor could say, “I can see and hear that you are really struggling with this situation. You’ve shared with me that you have thoughts about killing yourself, and that makes sense considering what you’ve been through. I’m wondering how close you are to doing that? How close are you to going home and following through [on those feelings]?”
“The difference [in phrasing it this way] is the compassion in the language surrounding those really heavy questions,” she notes.
At the conclusion of a crisis session, counselors should talk through next steps with the client, including addressing what the client would do if things became worse and a crisis resurfaced after the session, McNiel says. If the individual is a long-term client, she advises scheduling their next session and letting them know how and when to reach the counselor during nonbusiness hours, as well as providing crisis hotline numbers.
Martinez agrees that in crisis counseling, practitioners should resist the urge to “fix” the situation the client is facing. In addition, counselors should avoid viewing it as a linear cause and effect. This includes thinking of suicidal ideation in binary terms of yes or no.
“We have to think of suicide in a much broader continuum, a range of pain and despair,” Martinez says. “[Society’s] fear and the stigma around suicidality makes us think about it as an on-or-off switch, but it’s more complicated than that.”
By definition, crisis is chaotic and messy, and the goal of a crisis counseling session is to de-escalate and share that burden, rather than organize or reorder it. Martinez illustrates this with a metaphor of a jumbled pile of sticks on the ground. A counselor’s instinct might be to gather the sticks and assemble a neat structure for the client, she says. Instead, crisis counseling involves allowing the client to pick up the sticks, one by one, and assemble them however they need to — even if it’s just into another pile on the ground that, to an outsider, looks equally as messy. “That’s much more powerful than us trying to figure out where the sticks belong,” Martinez says.
If a counselor approaches a crisis counseling session with the goal of tracking a client’s story in context, the counselor will miss the client’s full range of emotions — and the chance to connect and help the client bear that pain, Martinez says. “We can get caught up in [feeling that] ‘I need to make sense of the story.’ But that’s our need, our desire. The client may not need that or be ready for that. … When they talk and are listened to, they often begin to make sense of it themselves.”
Take Care of Yourself
The counselors interviewed for this article agree that it is imperative for practitioners who engage in crisis counseling to take steps to avoid burnout. In addition to regular self-care, this can include ongoing supervision or consultation with colleagues as well as other methods to combat feelings of isolation and empathy fatigue that can easily overwhelm practitioners whose clients share such heavy and troubling topics.
Moore suggests counselors take steps to maintain a balanced caseload and stay aware of how stress and burnout manifest for them personally. “Doing trauma and crisis work is heavy stuff. It can be super rewarding but super draining,” Moore says. “We carry [clients’] trauma with us, so it’s important to take care of ourselves. … Sadly, we need more and more counselors to do crisis work, and if you don’t take care of yourself, that’s one less counselor to help people who need it.”
It’s also important to remember that sharing the burden of crisis with clients is a gift, Larson says. A crisis counselor may be the only person the client feels they can talk to during their lowest moments.
“It takes a lot of courage to pick up a phone and tell a stranger [a crisis counselor] that you want to die,” Larson says. “Always remember that it’s an honor and privilege to hear people’s hardest stuff — their deepest, darkest secrets.”

- Amanda DiLorenzo-Garcia: [email protected]
- Josh Larson: [email protected]
- Ali Martinez: [email protected]
- Meredith McNiel: [email protected]
- Ruth Ouzts Moore: [email protected]
- Assessment, Diagnosis & Treatment
- Trauma & Stress-Related Disorders
Search CT Articles
Current Issue
VIEW ISSUE ARCHIVE
Sign Up for Updates

2461 Eisenhower Avenue, Suite 300, Alexandria, Va. 22314 | 800-347-6647 | (fax) 800-473-2329
My ACA Join Now Contact Us Privacy Policy Terms of Use © All Rights Reserved.
- Search Menu
- Sign in through your institution
- Advance articles
- Author Guidelines
- Submission Site
- About Children & Schools
- About the National Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Literature review, alive program, implications for school social work practice.
- < Previous
Trauma and Early Adolescent Development: Case Examples from a Trauma-Informed Public Health Middle School Program
- Article contents
- Figures & tables
- Supplementary Data
Jason Scott Frydman, Christine Mayor, Trauma and Early Adolescent Development: Case Examples from a Trauma-Informed Public Health Middle School Program, Children & Schools , Volume 39, Issue 4, October 2017, Pages 238–247, https://doi.org/10.1093/cs/cdx017
- Permissions Icon Permissions
Middle-school-age children are faced with a variety of developmental tasks, including the beginning phases of individuation from the family, building peer groups, social and emotional transitions, and cognitive shifts associated with the maturation process. This article summarizes how traumatic events impair and complicate these developmental tasks, which can lead to disruptive behaviors in the school setting. Following the call by Walkley and Cox for more attention to be given to trauma-informed schools, this article provides detailed information about the Animating Learning by Integrating and Validating Experience program: a school-based, trauma-informed intervention for middle school students. This public health model uses psychoeducation, cognitive differentiation, and brief stress reduction counseling sessions to facilitate socioemotional development and academic progress. Case examples from the authors’ clinical work in the New Haven, Connecticut, urban public school system are provided.
Within the U.S. school system there is growing awareness of how traumatic experience negatively affects early adolescent development and functioning ( Chanmugam & Teasley, 2014 ; Perfect, Turley, Carlson, Yohannan, & Gilles, 2016 ; Porche, Costello, & Rosen-Reynoso, 2016 ; Sibinga, Webb, Ghazarian, & Ellen, 2016 ; Turner, Shattuck, Finkelhor, & Hamby, 2017 ; Woodbridge et al., 2016 ). The manifested trauma symptoms of these students have been widely documented and include self-isolation, aggression, and attentional deficit and hyperactivity, producing individual and schoolwide difficulties ( Cook et al., 2005 ; Iachini, Petiwala, & DeHart, 2016 ; Oehlberg, 2008 ; Sajnani, Jewers-Dailley, Brillante, Puglisi, & Johnson, 2014 ). To address this vulnerability, school social workers should be aware of public health models promoting prevention, data-driven investigation, and broad-based trauma interventions ( Chafouleas, Johnson, Overstreet, & Santos, 2016 ; Johnson, 2012 ; Moon, Williford, & Mendenhall, 2017 ; Overstreet & Chafouleas, 2016 ; Overstreet & Matthews, 2011 ). Without comprehensive and effective interventions in the school setting, seminal adolescent developmental tasks are at risk.
This article follows the twofold call by Walkley and Cox (2013) for school social workers to develop a heightened awareness of trauma exposure's impact on childhood development and to highlight trauma-informed practices in the school setting. In reference to the former, this article will not focus on the general impact of toxic stress, or chronic trauma, on early adolescents in the school setting, as this work has been widely documented. Rather, it begins with a synthesis of how exposure to trauma impairs early adolescent developmental tasks. As to the latter, we will outline and discuss the Animating Learning by Integrating and Validating Experience (ALIVE) program, a school-based, trauma-informed intervention that is grounded in a public health framework. The model uses psychoeducation, cognitive differentiation, and brief stress reduction sessions to promote socioemotional development and academic progress. We present two clinical cases as examples of trauma-informed, school-based practice, and then apply their experience working in an urban, public middle school to explicate intervention theory and practice for school social workers.
Impact of Trauma Exposure on Early Adolescent Developmental Tasks
Social development.
Impact of Trauma on Early Adolescent Development
| Developmental Task . | Impact . | Citations . |
|---|---|---|
| Social development | ||
| Forming and maintaining healthy relationships | ; ; ; | |
| Mentalization and increased cognitive discrimination | ; | |
| Moving from family to peers as primary relationships | ||
| Cognitive development and emotional regulation | ||
| Increasing impulse control and affect regulation | ; ; | |
| Coordinating dynamic between cognition and affect | ; ; ; | |
| Developmental Task . | Impact . | Citations . |
|---|---|---|
| Social development | ||
| Forming and maintaining healthy relationships | ; ; ; | |
| Mentalization and increased cognitive discrimination | ; | |
| Moving from family to peers as primary relationships | ||
| Cognitive development and emotional regulation | ||
| Increasing impulse control and affect regulation | ; ; | |
| Coordinating dynamic between cognition and affect | ; ; ; | |
Traumatic experiences may create difficulty with developing and differentiating another person's point of view (that is, mentalization) due to the formation of rigid cognitive schemas that dictate notions of self, others, and the external world ( Frydman & McLellan, 2014 ). For early adolescents, the ability to diversify a single perspective with complexity is central to modulating affective experience. Without the capacity to diversify one's perspective, there is often difficulty differentiating between a nonthreatening current situation that may harbor reminders of the traumatic experience and actual traumatic events. Incumbent on the school social worker is the need to help students understand how these conflicts may trigger a memory of harm, abandonment, or loss and how to differentiate these past memories from the present conflict. This is of particular concern when these reactions are conflated with more common middle school behaviors such as withdrawing, blaming, criticizing, and gossiping ( Card, Stucky, Sawalani, & Little, 2008 ).
Encouraging cognitive discrimination is particularly meaningful given that the second social developmental task for early adolescents is the re-orientation of their primary relationships with family toward peers ( Henderson & Thompson, 2010 ). This shift may become complicated for students facing traumatic stress, resulting in a stunted movement away from familiar connections or a displacement of dysfunctional family relationships onto peers. For example, in the former, a student who has witnessed and intervened to protect his mother from severe domestic violence might believe he needs to sacrifice himself and be available to his mother, forgoing typical peer interactions. In the latter, a student who was beaten when a loud, intoxicated family member came home might become enraged, anxious, or anticipate violence when other students raise their voices.
Cognitive Development and Emotional Regulation
During normative early adolescent development, the prefrontal cortex undergoes maturational shifts in cognitive and emotional functioning, including increased impulse control and affect regulation ( Wigfield, Lutz, & Wagner, 2005 ). However, these developmental tasks can be negatively affected by chronic exposure to traumatic events. Stressful situations often evoke a fear response, which inhibits executive functioning and commonly results in a fight-flight-freeze reaction. If a student does not possess strong anxiety management skills to cope with reminders of the trauma, the student is prone to further emotional dysregulation, lowered frustration tolerance, and increased behavioral problems and depressive symptoms ( Iachini et al., 2016 ; Saltzman, Steinberg, Layne, Aisenberg, & Pynoos, 2001 ).
Typical cognitive development in early adolescence is defined by the ambiguity of a transitional stage between childhood remedial capacity and adult refinement ( Casey & Caudle, 2013 ; Van Duijvenvoorde & Crone, 2013 ). Casey and Caudle (2013) found that although adolescents performed equally as well as, if not better than, adults on a self-control task when no emotional information was present, the introduction of affectively laden social cues resulted in diminished performance. The developmental challenge for the early adolescent then is to facilitate the coordination of this ever-shifting dynamic between cognition and affect. Although early adolescents may display efficient and logically informed behaviors, they may struggle to sustain these behaviors, especially in the presence of emotional stimuli ( Casey & Caudle, 2013 ; Van Duijvenvoorde & Crone, 2013 ). Because trauma often evokes an emotional response ( Johnson & Lubin, 2015 ), these findings insinuate that those early adolescents who are chronically exposed will have ongoing regulation difficulties. Further empirical findings considering the cognitive effects of trauma exposure on the adolescent brain have highlighted detriments in working memory, inhibition, memory, and planning ability ( Moradi, Neshat Doost, Taghavi, Yule, & Dalgleish, 1999 ).
Using a Public Health Framework for School-Based, Trauma-Informed Services
The need for a more informed and comprehensive approach to addressing trauma within the schools has been widely articulated ( Chafouleas et al., 2016 ; Durlak, Weissberg, Dymnicki, Taylor, & Schellinger, 2011 ; Jaycox, Kataoka, Stein, Langley, & Wong, 2012 ; Overstreet & Chafouleas, 2016 ; Perry & Daniels, 2016 ). Overstreet and Matthews (2011) suggested that using a public health model to address trauma in schools will promote prevention, early identification, and data-driven investigation and yield broad-based intervention on a policy and communitywide level. A public health approach focuses on developing interventions that address the underlying causal processes that lead to social, emotional, and cognitive maladjustment. Opening the dialogue to the entire student body, as well as teachers and administrators, promotes inclusion and provides a comprehensive foundation for psychoeducation, assessment, and prevention.
ALIVE: A Comprehensive Public Health Intervention for Middle School Students
| Psychoeducation . | Assessment . | Individualized Support . |
|---|---|---|
| Conduct psychoeducational conversations with all students on the impact of traumatic exposure across developmental domains: social, emotional, cognitive, and academic | Informal process accompanying psychoeducation that leads to the identification of students requiring further, more intensive support | One-on-one counseling related to student's adverse experience Engagement occurs as traumatic stress influences school-based behaviors |
| Psychoeducation . | Assessment . | Individualized Support . |
|---|---|---|
| Conduct psychoeducational conversations with all students on the impact of traumatic exposure across developmental domains: social, emotional, cognitive, and academic | Informal process accompanying psychoeducation that leads to the identification of students requiring further, more intensive support | One-on-one counseling related to student's adverse experience Engagement occurs as traumatic stress influences school-based behaviors |
Note: ALIVE = Animating Learning by Integrating and Validating Experience.
Psychoeducation
The classroom is a place traditionally dedicated to academic pursuits; however, it also serves as an indicator of trauma's impact on cognitive functioning evidenced by poor grades, behavioral dysregulation, and social turbulence. ALIVE practitioners conduct weekly trauma-focused dialogues in the classroom to normalize conversations addressing trauma, to recruit and rehearse more adaptive cognitive skills, and to engage in an insight-oriented process ( Sajnani et al., 2014 ).
Using a parable as a projective tool for identification and connection, the model helps students tolerate direct discussions about adverse experiences. The ALIVE practitioner begins each academic year by telling the parable of a woman named Miss Kendra, who struggled to cope with the loss of her 10-year-old child. Miss Kendra is able to make meaning out of her loss by providing support for schoolchildren who have encountered adverse experiences, serving as a reminder of the strength it takes to press forward after a traumatic event. The intention of this parable is to establish a metaphor for survival and strength to fortify the coping skills already held by trauma-exposed middle school students. Furthermore, Miss Kendra offers early adolescents an opportunity to project their own needs onto the story, creating a personalized figure who embodies support for socioemotional growth.
Following this parable, the students’ attention is directed toward Miss Kendra's List, a poster that is permanently displayed in the classroom. The list includes a series of statements against adolescent maltreatment, comprehensively identifying various traumatic stressors such as witnessing domestic violence; being physically, verbally, or sexually abused; and losing a loved one to neighborhood violence. The second section of the list identifies what may happen to early adolescents when they experience trauma from emotional, social, and academic perspectives. The practitioner uses this list to provide information about the nature and impact of trauma, while modeling for students and staff the ability to discuss difficult experiences as a way of connecting with one another with a sense of hope and strength.
Furthermore, creating a dialogue about these issues with early adolescents facilitates a culture of acceptance, tolerance, and understanding, engendering empathy and identification among students. This fostering of interpersonal connection provides a reparative and differentiated experience to trauma ( Hartling & Sparks, 2008 ; Henderson & Thompson, 2010 ; Johnson & Lubin, 2015 ) and is particularly important given the peer-focused developmental tasks of early adolescence. The positive feelings evoked through classroom-based conversation are predicated on empathic identification among the students and an accompanying sense of relief in understanding the scope of trauma's impact. Furthermore, the consistent appearance of and engagement by the ALIVE practitioner, and the continual presence of Miss Kendra's list, effectively counters traumatically informed expectations of abandonment and loss while aligning with a public health model that attends to the impact of trauma on a regular, systemwide basis.
Participatory and Somatic Indicators for Informal Assessment during the Psychoeducation Component of the ALIVE Intervention
| Participatory . | Somatic . |
|---|---|
| Attempting to the conversation | A disposition |
| Subtle forms of | Bodily of somatic activation |
| A in specific dialogue around certain trauma types | Physical displays of or |
| , functions as a physical form of avoidance | |
| Participatory . | Somatic . |
|---|---|
| Attempting to the conversation | A disposition |
| Subtle forms of | Bodily of somatic activation |
| A in specific dialogue around certain trauma types | Physical displays of or |
| , functions as a physical form of avoidance | |
Notes: ALIVE = Animating Learning by Integrating and Validating Experience. Examples are derived from authors’ clinical experiences.
In addition to behavioral symptoms, the content of conversation is considered. All practitioners in the ALIVE program are mandated reporters, and any content presented that meets criteria for suspicion of child maltreatment is brought to the attention of the school leadership and ALIVE director. According to Johnson (2012) , reports of child maltreatment to the Connecticut Department of Child and Family Services have actually decreased in the schools where the program has been implemented “because [the ALIVE program is] catching problems well before they have risen to the severity that would require reporting” (p. 17).
Case Example 1
The following demonstrates a middle school classroom psychoeducation session and assessment facilitated by an ALIVE practitioner (the first author). All names and identifying characteristics have been changed to protect confidentiality.
Ms. Skylar's seventh grade class comprised many students living in low-income housing or in a neighborhood characterized by high poverty and frequent criminal activity. During the second week of school, I introduced myself as a practitioner who was here to speak directly about difficult experiences and how these instances might affect academic functioning and students’ thoughts about themselves, others, and their environment.
After sharing the Miss Kendra parable and list, I invited the students to share their thoughts about Miss Kendra and her journey. Tyreke began the conversation by wondering whether Miss Kendra lost her child to gun violence, exploring the connection between the list and the story and his own frequent exposure to neighborhood shootings. To transition a singular connection to a communal one, I asked the students if this was a shared experience. The majority of students nodded in agreement. I referred the students back to the list and asked them to identify how someone's school functioning or mood may be affected by ongoing neighborhood gun violence. While the students read the list, I actively monitored reactions and scanned for inattention and active avoidance. Performing both active facilitation of discussion and monitoring students’ reactions is critical in accomplishing the goals of providing quality psychoeducation and identifying at-risk students for intervention.
After inspection, Cleo remarked that, contrary to a listed outcome on Miss Kendra's list, neighborhood gun violence does not make him feel lonely; rather, he “doesn't care about it.” Slumped down in his chair, head resting on his crossed arms on the desk in front of him, Cleo's body language suggested a somatized disengagement. I invited other students to share their individual reactions. Tyreke agreed that loneliness is not the identified affective experience; rather, for him, it's feeling “mad or scared.” Immediately, Greg concurred, expressing that “it makes me more mad, and I think about my family.”
Encouraging a variety of viewpoints, I stated, “It sounds like it might make you mad, scared, and may even bring up thoughts about your family. I wonder why people have different reactions?” Doing so moved the conversation into a phase of deeper reflection, simultaneously honoring the students’ voiced experience while encouraging critical thinking. A number of students responded by offering connections to their lives, some indicating they had difficulty identifying feelings. I reflected back, “Sometimes people feel something, but can't really put their finger on it, and sometimes they know exactly how they feel or who it makes them think about.”
I followed with a question: “How do you think it affects your schoolwork or feelings when you're in school?” Greg and Natalia both offered that sometimes difficult or confusing thoughts can consume their whole day, even while in class. Sharon began to offer a related comment when Cleo interrupted by speaking at an elevated volume to his desk partner, Tyreke. The two began to snicker and pull focus. By the time they gained the class's full attention, Cleo was openly laughing and pushing his chair back, stating, “No way! She DID!? That's crazy”; he began to stand up, enlisting Tyreke in the process. While this disruption may be viewed as a challenge to the discussion, it is essential to understand all behavior in context of the session's trauma content. Therefore, Cleo's outburst was interpreted as a potential avenue for further exploration of the topic regarding gun violence and difficulties concentrating. In turn, I posed this question to the class: “Should we talk about this stuff? I wonder if sometimes people have a hard time tolerating it. Can anybody think of why it might be important? Sharon, I think you were saying something about this.” While Sharon continued to share, Cleo and Tyreke gradually shifted their attention back to the conversation. I noted the importance of an individual follow-up with Cleo.
Natalia jumped back in the conversation, stating, “I think we talk about stuff like this so we know about it and can help people with it.” I checked in with the rest of the class about this strategy for coping with the impact of trauma exposure on school functioning: “So it sounds like these thoughts have a pretty big impact on your day. If that's the case, how do you feel less worried or mad or scared?” Marta quickly responded, “You could talk to someone.” I responded, “Part of my job here is to be a person to talk to one-on-one about these things. Hopefully, it will help you feel better to get some of that stuff off your chest.” The students nodded, acknowledging that I would return to discuss other items on the list and that there would be opportunities to check in with me individually if needed.
On reflection, Cleo's disruption in the discussion may be attributed to his personal difficulty emotionally managing intrusive thoughts while in school. This clinical assumption was not explicitly named in the moment, but was noted as information for further individual follow-up. When I met individually with Cleo, Cleo reported that his cousin had been shot a month ago, causing him to feel confused and angry. I continued to work with him individually, which resulted in a reduction of behavioral disruptions in the classroom.
In the preceding case example, the practitioner performed a variety of public health tasks. Foremost was the introduction of how traumatic experience may affect individuals and their relationships with others and their role as a student. Second, the practitioner used Miss Kendra and her list as a foundational mechanism to ground the conversation and serve as a reference point for the students’ experience. Finally, the practitioner actively monitored individual responses to the material as a means of identifying students who may require more support. All three of these processes are supported within the public health framework as a means toward assessment and early intervention for early adolescents who may be exposed to trauma.
Individualized Stress Reduction Intervention
Students are seen for individualized support if they display significant externalizing or internalizing trauma-related behavior. Students are either self-referred; referred by a teacher, administrator, or staff member; or identified by an ALIVE practitioner. Following the principle of immediate engagement based on emergent traumatic material, individual sessions are brief, lasting only 15 to 20 minutes. Using trauma-centered psychotherapy ( Johnson & Lubin, 2015 ), a brief inquiry addressing the current problem is conducted to identify the trauma trigger connected to the original harm, fostering cognitive discrimination. Conversation about the adverse experience proceeds in a calm, direct way focusing on differentiating between intrusive memories and the current situation at school ( Sajnani et al., 2014 ). Once the student exhibits greater emotional regulation, the ALIVE practitioner returns the student to the classroom in a timely manner and may provide either brief follow-up sessions for preventive purposes or, when appropriate, refer the student to more regular, clinical support in or out of the school.
Case Example 2
The following case example is representative of the brief, immediate, and open engagement with traumatic material and encouragement of cognitive discrimination. This intervention was conducted with a sixth grade student, Jacob (name and identifying information changed to ensure confidentiality), by an ALIVE practitioner (the second author).
I found Jacob in the hallway violently shaking a trash can, kicking the classroom door, and slamming his hands into the wall and locker. His teacher was standing at the door, distressed, stating, “Jacob, you need to calm down and go to the office, or I'm calling home!” Jacob yelled, “It's not fair, it was him, not me! I'm gonna fight him!” As I approached, I asked what was making him so angry, but he said, “I don't want to talk about it.” Rather than asking him to calm down or stop slamming objects, I instead approached the potential memory agitating him, stating, “My guess is that you are angry for a very good reason.” Upon this simple connection, he sighed and stopped kicking the trash can and slamming the wall. Jacob continued to demonstrate physical and emotional activation, pacing the hallway and making a fist; however, he was able to recount putting trash in the trash can when a peer pushed him from behind, causing him to yell. Jacob explained that his teacher heard him yelling and scolded him, making him more mad. Jacob stated, “She didn't even know what happened and she blamed me. I was trying to help her by taking out all of our breakfast trash. It's not fair.”
The ALIVE practitioner listens to students’ complaints with two ears, one for the current complaint and one for affect-laden details that may be connected to the original trauma to inquire further into the source of the trigger. Affect-laden details in case example 2 include Jacob's anger about being blamed (rather than toward the student who pushed him), his original intention to help, and his repetition of the phrase “it's not fair.” Having met with Jacob previously, I was aware that his mother suffers from physical and mental health difficulties. When his mother is not doing well, he (as the parentified child) typically takes care of the household, performing tasks like cooking, cleaning, and helping with his two younger siblings and older autistic brother. In the past, Jacob has discussed both idealizing his mother and holding internalized anger that he rarely expresses at home because he worries his anger will “make her sick.”
I know sometimes when you are trying to help mom, there are times she gets upset with you for not doing it exactly right, or when your brothers start something, she will blame you. What just happened sounds familiar—you were trying to help your teacher by taking out the garbage when another student pushed you, and then you were the one who got in trouble.
Jacob nodded his head and explained that he was simply trying to help.
I moved into a more detailed inquiry, to see if there was a more recent stressor I was unaware of. When I asked how his mother was doing this week, Jacob revealed that his mother's health had deteriorated and his aunt had temporarily moved in. Jacob told me that he had been yelled at by both his mother and his aunt that morning, when his younger brother was not ready for school. I asked, “I wonder if when the student pushed you it reminded you of getting into trouble because of something your little brother did this morning?” Jacob nodded. The displacement was clear: He had been reminded of this incident at school and was reacting with anger based on his family dynamic, and worries connected to his mother.
My guess is that you were a mix of both worried and angry by the time you got to school, with what's happening at home. You were trying to help with the garbage like you try to help mom when she isn't doing well, so when you got pushed it was like your brother being late, and then when you got blamed by your teacher it was like your mom and aunt yelling, and it all came flooding back in. The problem is, you let out those feelings here. Even though there are some similar things, it's not totally the same, right? Can you tell me what is different?
Jacob nodded and was able to explain that the other student was probably just playing and did not mean to get him into trouble, and that his teacher did not usually yell at him or make him worried. Highlighting this important differentiation, I replied, “Right—and fighting the student or yelling at the teacher isn't going to solve this, but more importantly, it isn't going to make your mom better or have your family go any easier on you either.” Jacob stated that he knew this was true.
I reassured Jacob that I could help him let out those feelings of worry and anger connected to home so they did not explode out at school and planned to meet again. Jacob confirmed that he was willing to do that. He was able to return to the classroom without incident, with the entire intervention lasting less than 15 minutes.
In case example 2, the practitioner was available for an immediate engagement with disturbing behaviors as they were happening by listening for similarities between the current incident and traumatic stressors; asking for specific details to more effectively help Jacob understand how he was being triggered in school; providing psychoeducation about how these two events had become confused and aiding him in cognitively differentiating between the two; and, last, offering to provide further support to reduce future incidents.
Germane to the practice of school social work is the ability to work flexibly within a public health model to attend to trauma within the school setting. First, we suggest that a primary implication for school social workers is not to wait for explicit problems related to known traumatic experiences to emerge before addressing trauma in the school, but, rather, to follow a model of prevention-assessment-intervention. School social workers are in a unique position within the school system to disseminate trauma-informed material to both students and staff in a preventive capacity. Facilitating this implementation will help to establish a tone and sharpened focus within the school community, norming the process of articulating and engaging with traumatic material. In the aforementioned classroom case example, we have provided a sample of how school social workers might work with entire classrooms on a preventive basis regarding trauma, rather than waiting for individual referrals.
Second, in addition to functional behavior assessments and behavior intervention plans, school social workers maintain a keen eye for qualitative behavioral assessment ( National Association of Social Workers, 2012 ). Using this skill set within a trauma-informed model will help to identify those students in need who may be reluctant or resistant to explicitly ask for help. As called for by Walkley and Cox (2013) , we suggest that using the information presented in Table 1 will help school social workers understand, identify, and assess the impact of trauma on early adolescent developmental tasks. If school social workers engage on a classroom level in trauma psychoeducation and conversations, the information in Table 3 may assist with assessment of children and provide a basis for checking in individually with students as warranted.
Third, school social workers are well positioned to provide individual targeted, trauma-informed interventions based on previous knowledge of individual trauma and through widespread assessment ( Walkley & Cox, 2013 ). The individual case example provides one way of immediately engaging with students who are demonstrating trauma-based behaviors. In this model, school social workers engage in a brief inquiry addressing the current trauma to identify the trauma trigger, discuss the adverse experience in a calm but direct way, and help to differentiate between intrusive memories and the current situation at school. For this latter component, the focus is on cognitive discrimination and emotional regulation so that students can reengage in the classroom within a short time frame.
Fourth, given social work's roots in collaboration and community work, school social workers are encouraged to use a systems-based approach in partnering with allied practitioners and institutions ( D'Agostino, 2013 ), thus supporting the public health tenet of establishing and maintaining a link to the wider community. This may include referring students to regular clinical support in or out of the school. Although the implementation of a trauma-informed program will vary across schools, we suggest that school social workers have the capacity to use a public health school intervention model to ecologically address the psychosocial and behavioral issues stemming from trauma exposure.
As increasing attention is being given to adverse childhood experiences, a tiered approach that uses a public health framework in the schools is necessitated. Nevertheless, there are some limitations to this approach. First, although the interventions outlined here are rooted in prevention and early intervention, there are times when formal, intensive treatment outside of the school setting is warranted. Second, the ALIVE program has primarily been implemented by ALIVE practitioners; the results from piloting this public health framework in other school settings with existing school personnel, such as school social workers, will be necessary before widespread replication.
The public health framework of prevention-assessment-intervention promotes continual engagement with middle school students’ chronic exposure to traumatic stress. There is a need to provide both broad-based and individualized support that seeks to comprehensively ameliorate the social, emotional, and cognitive consequences on early adolescent developmental milestones associated with traumatic experiences. We contend that school social workers are well positioned to address this critical public health issue through proactive and widespread psychoeducation and assessment in the schools, and we have provided case examples to demonstrate one model of doing this work within the school day. We hope that this article inspires future writing about how school social workers individually and systemically address trauma in the school system. In alignment with Walkley and Cox (2013) , we encourage others to highlight their practice in incorporating trauma-informed, school-based programming in an effort to increase awareness of effective interventions.
Card , N. A. , Stucky , B. D. , Sawalani , G. M. , & Little , T. D. ( 2008 ). Direct and indirect aggression during childhood and adolescence: A meta-analytic review of gender difference, intercorrelations, and relations to maladjustment . Child Development, 79 , 1185 – 1229 .
Google Scholar
Casey , B. J. , & Caudle , K. ( 2013 ). The teenage brain: Self control . Current Directions in Psychological Science, 22 ( 2 ), 82 – 87 .
Chafouleas , S. M. , Johnson , A. H. , Overstreet , S. , & Santos , N. M. ( 2016 ). Toward a blueprint for trauma-informed service delivery in schools . School Mental Health, 8 ( 1 ), 144 – 162 .
Chanmugam , A. , & Teasley , M. L. ( 2014 ). What should school social workers know about children exposed to intimate partner violence? [Editorial]. Children & Schools, 36 , 195 – 198 .
Cook , A. , Spinazzola , J. , Ford , J. , Lanktree , C. , Blaustein , M. , Cloitre , M. , et al. . ( 2005 ). Complex trauma in children and adolescents . Psychiatric Annals, 35 , 390 – 398 .
D'Agostino , C. ( 2013 ). Collaboration as an essential social work skill [Resources for Practice] . Children & Schools, 35 , 248 – 251 .
Durlak , J. A. , Weissberg , R. P. , Dymnicki , A. B. , Taylor , R. D. , & Schellinger , K. B. ( 2011 ). The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions . Child Development, 82 , 405 – 432 .
Frydman , J. S. , & McLellan , L. ( 2014 ). Complex trauma and executive functioning: Envisioning a cognitive-based, trauma-informed approach to drama therapy. In N. Sajnani & D. R. Johnson (Eds.), Trauma-informed drama therapy: Transforming clinics, classrooms, and communities (pp. 179 – 205 ). Springfield, IL : Charles C Thomas .
Google Preview
Hartling , L. , & Sparks , J. ( 2008 ). Relational-cultural practice: Working in a nonrelational world . Women & Therapy, 31 , 165 – 188 .
Henderson , D. , & Thompson , C. ( 2010 ). Counseling children (8th ed.). Belmont, CA : Brooks-Cole .
Iachini , A. L. , Petiwala , A. F. , & DeHart , D. D. ( 2016 ). Examining adverse childhood experiences among students repeating the ninth grade: Implications for school dropout prevention . Children & Schools, 38 , 218 – 227 .
Jaycox , L. H. , Kataoka , S. H. , Stein , B. D. , Langley , A. K. , & Wong , M. ( 2012 ). Cognitive behavioral intervention for trauma in schools . Journal of Applied School Psychology, 28 , 239 – 255 .
Johnson , D. R. ( 2012 ). Ask every child: A public health initiative addressing child maltreatment [White paper]. Retrieved from http://www.traumainformedschools.org/publications.html
Johnson , D. R. , & Lubin , H. ( 2015 ). Principles and techniques of trauma-centered psychotherapy . Arlington, VA : American Psychiatric Publishing .
Moon , J. , Williford , A. , & Mendenhall , A. ( 2017 ). Educators’ perceptions of youth mental health: Implications for training and the promotion of mental health services in schools . Child and Youth Services Review, 73 , 384 – 391 .
Moradi , A. R. , Neshat Doost , H. T. , Taghavi , M. R. , Yule , W. , & Dalgleish , T. ( 1999 ). Everyday memory deficits in children and adolescents with PTSD: Performance on the Rivermead Behavioural Memory Test . Journal of Child Psychology and Psychiatry, 40 , 357 – 361 .
National Association of Social Workers . ( 2012 ). NASW standards for school social work services . Retrieved from http://www.naswdc.org/practice/standards/NASWSchoolSocialWorkStandards.pdf
Oehlberg , B. ( 2008 ). Why schools need to be trauma informed . Trauma and Loss: Research and Interventions, 8 ( 2 ), 1 – 4 .
Overstreet , S. , & Chafouleas , S. M. ( 2016 ). Trauma-informed schools: Introduction to the special issue . School Mental Health, 8 ( 1 ), 1 – 6 .
Overstreet , S. , & Matthews , T. ( 2011 ). Challenges associated with exposure to chronic trauma: Using a public health framework to foster resilient outcomes among youth . Psychology in the Schools, 48 , 738 – 754 .
Perfect , M. , Turley , M. , Carlson , J. S. , Yohannan , J. , & Gilles , M. S. ( 2016 ). School-related outcomes of traumatic event exposure and traumatic stress symptoms in students: A systematic review of research from 1990 to 2015 . School Mental Health, 8 ( 1 ), 7 – 43 .
Perry , D. L. , & Daniels , M. L. ( 2016 ). Implementing trauma-informed practices in the school setting: A pilot study . School Mental Health, 8 ( 1 ), 177 – 188 .
Porche , M. V. , Costello , D. M. , & Rosen-Reynoso , M. ( 2016 ). Adverse family experiences, child mental health, and educational outcomes for a national sample of students . School Mental Health, 8 ( 1 ), 44 – 60 .
Sajnani , N. , Jewers-Dailley , K. , Brillante , A. , Puglisi , J. , & Johnson , D. R. ( 2014 ). Animating Learning by Integrating and Validating Experience. In N. Sajnani & D. R. Johnson (Eds.), Trauma-informed drama therapy: Transforming clinics, classrooms, and communities (pp. 206 – 242 ). Springfield, IL : Charles C Thomas .
Saltzman , W. R. , Steinberg , A. M. , Layne , C. M. , Aisenberg , E. , & Pynoos , R. S. ( 2001 ). A developmental approach to school-based treatment of adolescents exposed to trauma and traumatic loss . Journal of Child and Adolescent Group Therapy, 11 ( 2–3 ), 43 – 56 .
Sibinga , E. M. , Webb , L. , Ghazarian , S. R. , & Ellen , J. M. ( 2016 ). School-based mindfulness instruction: An RCT . Pediatrics, 137 ( 1 ), e20152532 .
Tucker , C. , Smith-Adcock , S. , & Trepal , H. C. ( 2011 ). Relational-cultural theory for middle school counselors . Professional School Counseling, 14 , 310 – 316 .
Turner , H. A. , Shattuck , A. , Finkelhor , D. , & Hamby , S. ( 2017 ). Effects of poly-victimization on adolescent social support, self-concept, and psychological distress . Journal of Interpersonal Violence, 32 , 755 – 780 .
van der Kolk , B. A. ( 2005 ). Developmental trauma disorder: Toward a rational diagnosis for children with complex trauma histories . Psychiatric Annals, 35 , 401 – 408 .
Van Duijvenvoorde , A.C.K. , & Crone , E. A. ( 2013 ). The teenage brain: A neuroeconomic approach to adolescent decision making . Current Directions in Psychological Science, 22 ( 2 ), 114 – 120 .
Walkley , M. , & Cox , T. L. ( 2013 ). Building trauma-informed schools and communities [Trends & Resources] . Children & Schools, 35 , 123 – 126 .
Wigfield , A. W. , Lutz , S. L. , & Wagner , L. ( 2005 ). Early adolescents’ development across the middle school years: Implications for school counselors . Professional School Counseling, 9 ( 2 ), 112 – 119 .
Woodbridge , M. W. , Sumi , W. C. , Thornton , S. P. , Fabrikant , N. , Rouspil , K. M. , Langley , A. K. , & Kataoka , S. H. ( 2016 ). Screening for trauma in early adolescence: Findings from a diverse school district . School Mental Health, 8 ( 1 ), 89 – 105 .
| Month: | Total Views: |
|---|---|
| August 2017 | 5 |
| September 2017 | 34 |
| October 2017 | 112 |
| November 2017 | 163 |
| December 2017 | 85 |
| January 2018 | 75 |
| February 2018 | 83 |
| March 2018 | 115 |
| April 2018 | 160 |
| May 2018 | 76 |
| June 2018 | 83 |
| July 2018 | 105 |
| August 2018 | 342 |
| September 2018 | 273 |
| October 2018 | 339 |
| November 2018 | 307 |
| December 2018 | 308 |
| January 2019 | 52 |
| February 2019 | 67 |
| March 2019 | 86 |
| April 2019 | 97 |
| May 2019 | 67 |
| June 2019 | 116 |
| July 2019 | 220 |
| August 2019 | 213 |
| September 2019 | 299 |
| October 2019 | 312 |
| November 2019 | 387 |
| December 2019 | 222 |
| January 2020 | 235 |
| February 2020 | 389 |
| March 2020 | 291 |
| April 2020 | 488 |
| May 2020 | 154 |
| June 2020 | 337 |
| July 2020 | 298 |
| August 2020 | 283 |
| September 2020 | 494 |
| October 2020 | 583 |
| November 2020 | 535 |
| December 2020 | 385 |
| January 2021 | 332 |
| February 2021 | 543 |
| March 2021 | 582 |
| April 2021 | 617 |
| May 2021 | 401 |
| June 2021 | 361 |
| July 2021 | 342 |
| August 2021 | 314 |
| September 2021 | 388 |
| October 2021 | 468 |
| November 2021 | 396 |
| December 2021 | 310 |
| January 2022 | 244 |
| February 2022 | 349 |
| March 2022 | 362 |
| April 2022 | 441 |
| May 2022 | 236 |
| June 2022 | 264 |
| July 2022 | 240 |
| August 2022 | 202 |
| September 2022 | 258 |
| October 2022 | 355 |
| November 2022 | 345 |
| December 2022 | 276 |
| January 2023 | 228 |
| February 2023 | 358 |
| March 2023 | 408 |
| April 2023 | 436 |
| May 2023 | 292 |
| June 2023 | 248 |
| July 2023 | 226 |
| August 2023 | 203 |
| September 2023 | 248 |
| October 2023 | 304 |
| November 2023 | 429 |
| December 2023 | 333 |
| January 2024 | 189 |
| February 2024 | 264 |
| March 2024 | 362 |
| April 2024 | 563 |
| May 2024 | 315 |
| June 2024 | 267 |
Email alerts
Citing articles via.
- About Children & Schools
- Recommend to your Library
Affiliations

- Online ISSN 1545-682X
- Print ISSN 1532-8759
- Copyright © 2024 National Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.

IMAGES
VIDEO
COMMENTS
Social Distancing is Lonely, But Our Online Therapists Are Here to Talk Day and Night. The Future Can Be Scary, But You're Not Alone. Stay Home and Speak to a Therapist Today
Awesome Counseling Textbooks & High Quality Here On Temu. New Users Enjoy Free Return. Enjoy Counseling Textbooks of Temu's best price, superior quality & full range of services.
ted as you have just joined the team. Intervention As discussed in this chapt. r, there is no one single model of crisis intervention. For the purpose of this example Roberts and Ottens' (2005) seven stage model will be made use o. o assist you to move from assessment to intervention. Stage 1: Assessment of Jean's stressors, enviro.
Vignette Discussion Examples Vignette Example 1. Twenty-six year old white female phoned her counselor, stated that she might take pills, and then hung up and kept the phone off the hook. The counselor called the police and the patient was brought to the crisis intervention center on a transportation hold.
Identify a case(s) for student to read and review. Provide specific prompts that you would like the student to address as a part of the assignment. Include prompts that have the student address the case from a clinical and macro viewpoint as well as consider some ethical considerations.
This case report of an 18-year-old woman with suicidal ideation illustrates the practicality and utility of a brief, single-session, crisis intervention model that facilitated discharge from the ED. This report will help practitioners to apply this model in their own practice and identify patients who may require psychiatric hospitalization.
A Case of Using Logical Consequences to Help a Client to Make Difficult Decisions 6 Section Two: Counselling Therapies A Case for Gestalt Therapy 12 A Case Using Behaviour Therapy 18 A Case Using Rational Emotive Behaviour Therapy (REBT) 24 A Case Demonstrating Person Centred Therapy 30 Section Three: Family Counselling
With an emphasis on how crisis intervention differs from other counselling interventions, a case study is provided with the aim to help the reader reflect on and apply relevant crisis models of assessment and intervention learned in this chapter. ... Examples of crisis-inducing events include natural disasters such as bushfires, sexual assaults ...
NCMHCE Sample Case Study. You are a licensed mental health counselor working in a community agency. Your client self-referred for services because "my mother won't stop bugging me for staying in bed all day. I can't help it. I am in a rut and cannot find a way out.".
tive stability. Client scores provide a guide for how directive the crisis counselor needs to be. The TAF: CIR is used throughout the case studies to help you learn to evaluate clients' reactions and stability across these three domains. Social locations are a way of looking at a person's idiosyncratic
The following case studies are representative of families that are experiencing a crisis and are based on a composite of issues the authors have encountered when working with families. Case Study 1 illustrates the impact of a job loss resulting in an economic crisis for a blended family.
this book are described and illustrated through the case studies. Each case study is unique and distinctive, with each offering a rare opportunity for mental health prac-titioners to get a bird's-eye view of what happens around the world. Therefore, the study of these cases individually and collectively will yield a wealth of information
One Canadian initiative, Gerstein Crisis Centre, stood out as a case study for mental health crisis support rooted in community and human rights. For more than 30 years, this community-based ...
For example, the ABC Level 4 Diploma in Therapeutic Counselling requires you to write two case studies as part of your external portfolio, to meet the following criteria: 4.2 Analyse the application of your own theoretical approach to your work with one client over a minimum of six sessions. 4.3 Evaluate the application of your own theoretical ...
Counselling Case Study: Using REBT. Thomas is a 33 year old married man, who has recently become a father. He explains that he feels his self-esteem has been gradually deteriorating ever since he was married. He says that he can't find reasons to enjoy life with his wife due to feelings of inadequacy as a husband.
In this study we examined the role the VA can play in a community's behavioral health response using case studies from three disasters. ... the US Federal Government additionally provides funding through the Crisis Counseling Assistance and Training ... Two of the case examples described in this study especially bring to the forefront the ...
Date: 25th November 2017 Student Name: Soraya Raeispour Student Number: 1700881 CNG5116: CRISIS COUNSELING CASE STUDY ASSIGNMENT Client Background Mine is a 67-year old retired nurse. She has been living in Abadan, a city in the south of Iran, her entire life. She was born to an Iranian mother and Indian father, and is the second youngest child ...
2 An individual in crisis requires their counselor to employ specific strategies to aid the client toward regaining equilibrium. Empathetic techniques rooted in listening and a goal to put the client in the driver's seat will facilitate a sense of control in the client and show them their own ability to find hope in the situation. In this example, Walter Taylor has just lost his home to a ...
This counseling tool kit offers a new operational approach for integrating ethical decision-making in crisis intervention. Following detailed discussions of crisis intervention within the framework of relational-cultural theory, a triage assessment system, and an original ethical decision-making protocol, nine diverse case studies in hospital ...
The deaths remain unsolved, but the way Johnson & Johnson handled the episode has become a teaching case study for effective crisis management at Harvard Business School and elsewhere. In 2003, Fortune magazine named James Burke, the company's CEO at the time, as one of history's greatest CEOs for the way he handled the scare.
Crisis counseling is a specialty within the counseling profession, but it's also a skill that all counselors need to master because crises will pop up in everyday life for clients in all settings. ... This was the case for a 15-year-old client Moore once counseled who had turned to drinking, taking drugs and other risky behaviors to deal with ...
The individual case example provides one way of immediately engaging with students who are demonstrating trauma-based behaviors. In this model, school social workers engage in a brief inquiry addressing the current trauma to identify the trauma trigger, discuss the adverse experience in a calm but direct way, and help to differentiate between ...
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
The crisis intervention model utilized at a counseling center on a major university campus (CCMUC) was qualitatively analyzed for effectiveness. In this case study, each clinician was interviewed to determine their professional perspective of the definition of crisis, how the clinician implemented crisis management, and the specific techniques and methods utilized during the crisis counseling ...
An unavoidable and unfortunate consequence of working in healthcare, and specifically in pediatric healthcare, is the potential exposure to high stress patient-related events that can cause emotional distress. An online, open access, multidisciplinary journal published quarterly by the International Critical Incident Stress Foundation, Inc.