A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services

Search form
Print this issue
Good Sleep for Good Health
Get the Rest You Need

Sometimes, the pace of modern life barely gives you time to stop and rest. It can make getting a good night’s sleep on a regular basis seem like a dream.
But sleep is as important for good health as diet and exercise. Good sleep improves your brain performance, mood, and health.
Not getting enough quality sleep regularly raises the risk of many diseases and disorders. These range from heart disease and stroke to obesity and dementia.
There’s more to good sleep than just the hours spent in bed, says Dr. Marishka Brown, a sleep expert at NIH. “Healthy sleep encompasses three major things,” she explains. “One is how much sleep you get. Another is sleep quality—that you get uninterrupted and refreshing sleep. The last is a consistent sleep schedule.”
People who work the night shift or irregular schedules may find getting quality sleep extra challenging. And times of great stress—like the current pandemic—can disrupt our normal sleep routines. But there are many things you can do to improve your sleep.
Sleep for Repair
Why do we need to sleep? People often think that sleep is just “down time,” when a tired brain gets to rest, says Dr. Maiken Nedergaard, who studies sleep at the University of Rochester.
“But that’s wrong,” she says. While you sleep, your brain is working. For example, sleep helps prepare your brain to learn, remember, and create.
Nedergaard and her colleagues discovered that the brain has a drainage system that removes toxins during sleep.
“When we sleep, the brain totally changes function,” she explains. “It becomes almost like a kidney, removing waste from the system.”
Her team found in mice that the drainage system removes some of the proteins linked with Alzheimer’s disease. These toxins were removed twice as fast from the brain during sleep.
Everything from blood vessels to the The system that protects your body from invading viruses, bacteria, and other microscopic threats. immune system uses sleep as a time for repair, says Dr. Kenneth Wright, Jr., a sleep researcher at the University of Colorado.
“There are certain repair processes that occur in the body mostly, or most effectively, during sleep,” he explains. “If you don’t get enough sleep, those processes are going to be disturbed.”
Sleep Myths and Truths
How much sleep you need changes with age. Experts recommend school-age children get at least nine hours a night and teens get between eight and 10. Most adults need at least seven hours or more of sleep each night.
There are many misunderstandings about sleep. One is that adults need less sleep as they get older. This isn’t true. Older adults still need the same amount. But sleep quality can get worse as you age. Older adults are also more likely to take medications that interfere with sleep.
Another sleep myth is that you can “catch up” on your days off. Researchers are finding that this largely isn’t the case.
“If you have one bad night’s sleep and take a nap, or sleep longer the next night, that can benefit you,” says Wright. “But if you have a week’s worth of getting too little sleep, the weekend isn’t sufficient for you to catch up. That’s not a healthy behavior.”
In a recent study, Wright and his team looked at people with consistently deficient sleep. They compared them to sleep-deprived people who got to sleep in on the weekend.
Both groups of people gained weight with lack of sleep. Their bodies’ ability to control blood sugar levels also got worse. The weekend catch-up sleep didn’t help.
On the flip side, more sleep isn’t always better, says Brown. For adults, “if you’re sleeping more than nine hours a night and you still don’t feel refreshed, there may be some underlying medical issue,” she explains.
Sleep Disorders
Some people have conditions that prevent them from getting enough quality sleep, no matter how hard they try. These problems are called sleep disorders.
The most common sleep disorder is insomnia. “Insomnia is when you have repeated difficulty getting to sleep and/or staying asleep,” says Brown. This happens despite having the time to sleep and a proper sleep environment. It can make you feel tired or unrested during the day.
Insomnia can be short-term, where people struggle to sleep for a few weeks or months. “Quite a few more people have been experiencing this during the pandemic,” Brown says. Long-term insomnia lasts for three months or longer.
Sleep apnea is another common sleep disorder. In sleep apnea, the upper airway becomes blocked during sleep. This reduces or stops airflow, which wakes people up during the night. The condition can be dangerous. If untreated, it may lead to other health problems.
If you regularly have problems sleeping, talk with your health care provider. They may have you keep a sleep diary to track your sleep for several weeks. They can also run tests, including sleep studies. These look for sleep disorders.
Getting Better Sleep
If you’re having trouble sleeping, hearing how important it is may be frustrating. But simple things can improve your odds of a good night’s sleep. See the Wise Choices box for tips to sleep better every day.
Treatments are available for many common sleep disorders. Cognitive behavioral therapy can help many people with insomnia get better sleep. Medications can also help some people.
Many people with sleep apnea benefit from using a device called a CPAP machine. These machines keep the airway open so that you can breathe. Other treatments can include special mouthguards and lifestyle changes.
For everyone, “as best you can, try to make sleep a priority,” Brown says. “Sleep is not a throwaway thing—it’s a biological necessity.”
Popular Stories

Tired, Achy Eyes?

Connective Tissue Disorders

Sound Check
When Cancer Spreads
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Healthy Aging / Sleep and longevity: How quality sleep impacts your life span
Sleep and longevity: How quality sleep impacts your life span
Please login to bookmark.
Username or Email Address
Remember Me

You may be able to sleep your way to a longer life.
According to recently published research involving 172,321 adults, men who get adequate sleep live about five years longer than men who don’t. For women, it’s two years.
However, about a third of adults cut sleep short, raising their risk of heart attack, dementia and diabetes, among other health conditions.
How does slumber protect health and extend life? Let’s take a closer look at what happens in your brain and body as you snooze.
What are the benefits of sleep?
“Sleep is restorative,” says Virend Somers, M.D., Ph.D., a cardiologist at Mayo Clinic who has extensively studied the impact of sleep on health. “During sleep, your brain and body perform many critical tasks important for overall health.”
While you’re asleep, the body heals and restores itself. The immune system repairs sore muscles and injured tissues. The spaces between brain cells widen, allowing fluid to flush away toxins. Memories are processed, consolidated and stored too.
Muscles relax, and glands and tissues secrete essential hormones, like growth hormone and testosterone.
“Sleep has multiple functions on every biological level.” Virend Somers, M.D., Ph.D.
Does lack of sleep cause health issues?
When you don’t sleep enough, you cut short those healing and restorative processes, increasing your risk of several health problems.
Belly fat accumulates. Lack of sleep interferes with hormones like leptin and ghrelin, which regulate hunger and appetite. In Mayo Clinic research , when healthy study participants slept only four hours a night, they consumed 350 more calories than usual the following day.
“Typically, when healthy people eat more than they need, the excess is stored in subcutaneous fat under the skin,” says Dr. Somers, one of the study authors. However, when the sleep-deprived participants overate, the excess was stored as inflammation-producing visceral fat deep in their abdomens.
Blood pressure rises. In other research done at Mayo Clinic , sleep deprivation led to rises in blood pressure, both during the day and during the night.
“That’s how powerful sleep deprivation can be,” says Dr. Somers. “Even when a sleep-deprived person is able to sleep deeply, blood pressure is still higher.
This may explain why other research shows that people who sleep fewer than seven hours tend to experience accelerated aging of their hearts and blood vessels.
Blood sugar goes up . Prolonged sleep deprivation has been linked with insulin resistance, poor glucose tolerance, and an increased risk of type 2 diabetes.
Brain function declines. When you don’t sleep enough, the brain doesn’t have enough time to thoroughly flush away toxic byproducts, raising your risk of neurological conditions like Alzheimer’s disease.
How much sleep do I need?
You’ve likely met someone who seems to thrive on five or so hours a night. “These natural short sleepers wake up completely rested and extremely functional. They are high-performing people,” says Dr. Somers. “They are not sleepy at all. They are doing fine, and they can live a long time.”
However, natural short sleepers are rare.
Most people need at least seven hours to wake refreshed, says Dr. Somers. Some need more.
How can you tell if you’re sleeping enough? Consider two questions:
- Do you wake naturally, without the help of an alarm clock?
- Do you feel rested and restored during the day?
If you answer yes to both questions, you’re likely getting enough sleep. On the other hand, “If an alarm clock wakes you, by definition, you could have slept longer,” Dr. Somers says. “If you feel sleepy, that also means you need to sleep more.”
Is it natural to sleep less as I age?
As you get older, your sleep changes.
Your pineal gland produces less melatonin, the hormone that rises at night to make you feel sleepy. Reduced melatonin levels lead to less deep sleep and more light sleep. On top of that, your 24-hour circadian sleep-wake cycle may shift, making you feel more tired earlier in the evening but awake earlier in the morning. You might nod off around 8 p.m. and feel wide awake at 4 or 5 a.m.
“It’s not that you need less sleep as you get older. You probably still need at least seven hours, like most people. It’s that your sleep architecture has changed,” says Dr. Somers.
Assuming you wake naturally and feel rested and restored during the day, those age-related changes aren’t necessarily a problem, he says.
How to get better sleep
These lifestyle changes can help improve your sleep quality.
Create a bedtime routine. Your brain picks up on your daily habits. As a result, by going through the same series of steps each night before bed, you tell your brain it’s time to wind down. Your bedtime routine doesn’t have to be elaborate, says Dr. Somers. Brushing your teeth, changing into your pj’s, and cuddling or saying good night to a partner or pet is likely all you need.
Keep your room dark. “Over thousands of years, our brains evolved to use light and darkness as cues for sleep,” says Dr. Somers. “Your pineal gland recognizes how much light is around you.” He says even the dim illumination of the LED light on a clock will tell the gland to shut down melatonin production. “The darker it is, the more likely you are to sleep.”
Exercise regularly. Moderate aerobic exercise like walking has been shown to improve sleep quality, especially the slow-wave sleep that’s key to tissue repair.
Pay attention to your medications. “Forty percent of older people are on five or more medications,” says Dr. Somers. “Some of those medications disrupt sleep.” For example, diuretics used to lower blood pressure can wake you with an urge to urinate. If you suspect that a medication might be disturbing your sleep, talk to your healthcare professional. Sometimes, taking the drug in the morning (instead of the afternoon) can clear up the problem.
Get a checkup. Various health conditions — ranging from arthritis to an enlarged prostate — can make it difficult to sleep. Talk to your healthcare professional about ways to manage pain, frequent urination and other problems that keep you awake.
Stick to a schedule. Try to wake up at the same time every day, even if you have nowhere to go. Similarly, keep your bedtime consistent, says Dr. Somers.
Learn more: 6 steps to better sleep .
Don’t drink. Alcohol can worsen sleep quality, says Dr. Somers. Though alcohol might initially make you feel drowsy, you’ll likely wake a few hours later and feel unrefreshed the following day, he says.
Many people stumble onto their sleep remedies over time, says Dr. Somers.
“If you’ve found a way that helps you — a way that no one else is talking about — that doesn’t mean you shouldn’t use it,” says Dr. Somers. “If it works for you, do it.”

Relevant reading
Heal Your Gut, Save Your Brain
Cognitive decline is not your destiny. You can improve your brain function through small steps taken every day. Heal Your Gut, Save Your Brain, by gastroenterologist and health advocate Dr. Partha Nandi, highlights the latest research on the gut-brain connection and gives you a clear protocol for maintaining brain health…

Discover more Healthy Aging content from articles, podcasts, to videos.
You May Also Enjoy

by Sophie J. Bakri, M.D.

by Craig L. Bowron, M.D.

by Nathan K. LeBrasseur, Ph.D., Christina Chen, M.D.

by Lynne S. Peterson, M.D.

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.
8 Health Benefits of Sleep

Staff Writer
Jay Summer is a health content writer and editor. She holds a B.S. in psychology and master's degrees in writing and public policy.
Want to read more about all our experts in the field?

Dr. Abhinav Singh
Sleep Medicine Physician
Dr. Singh is the Medical Director of the Indiana Sleep Center. His research and clinical practice focuses on the entire myriad of sleep disorders.
Sleep Foundation
Fact-Checking: Our Process
The Sleep Foundation editorial team is dedicated to providing content that meets the highest standards for accuracy and objectivity. Our editors and medical experts rigorously evaluate every article and guide to ensure the information is factual, up-to-date, and free of bias.
The Sleep Foundation fact-checking guidelines are as follows:
- We only cite reputable sources when researching our guides and articles. These include peer-reviewed journals, government reports, academic and medical associations, and interviews with credentialed medical experts and practitioners.
- All scientific data and information must be backed up by at least one reputable source. Each guide and article includes a comprehensive bibliography with full citations and links to the original sources.
- Some guides and articles feature links to other relevant Sleep Foundation pages. These internal links are intended to improve ease of navigation across the site, and are never used as original sources for scientific data or information.
- A member of our medical expert team provides a final review of the content and sources cited for every guide, article, and product review concerning medical- and health-related topics. Inaccurate or unverifiable information will be removed prior to publication.
- Plagiarism is never tolerated. Writers and editors caught stealing content or improperly citing sources are immediately terminated, and we will work to rectify the situation with the original publisher(s)
- Although Sleep Foundation maintains affiliate partnerships with brands and e-commerce portals, these relationships never have any bearing on our product reviews or recommendations. Read our full Advertising Disclosure for more information.
Table of Contents
Improved Mood
Healthy heart, regulated blood sugar, improved mental function, restored immune system, stress relief, athletic performance, maintaining healthy weight, tips for getting better sleep.
Like eating nutritious food, drinking water, and exercising regularly, getting quality sleep is an important component of overall health. Although the exact reasons humans need to sleep remain unknown, sleep experts agree there are numerous benefits to consistently getting a full night’s rest. Most adults should get at least seven hours of sleep each night.
While sleeping , the body performs a number of repairing and maintaining processes that affect nearly every part of the body. As a result, a good night’s sleep, or a lack of sleep, can impact the body both mentally and physically .
Sleep restores the body and improves energy levels , so waking up well-rested can have a positive impact on an individual’s mood Trusted Source UpToDate More than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights. View Source . In contrast, people who get inadequate sleep are at higher risk of experiencing mental distress Trusted Source Centers for Disease Control and Prevention (CDC) As the nation’s health protection agency, CDC saves lives and protects people from health threats. View Source . A chronic lack of sleep can lead to anxiety, depression, and irritability. However, developing a consistent sleep routine often resolves these symptoms.
Quality sleep promotes cardiac health. During sleep, heart rate slows down, and blood pressure decreases Trusted Source Centers for Disease Control and Prevention (CDC) As the nation’s health protection agency, CDC saves lives and protects people from health threats. View Source . This means that during sleep, the heart and vascular system are able to rest.
However, insufficient sleep is a risk factor for unwanted cardiovascular events. Lack of sleep causes blood pressure to remain high for an extended period of time, increasing the risk of heart disease , heart attack, and heart failure .
Sleep impacts the body’s relationship with the hormone insulin , which helps blood sugar, or glucose, enter the body’s cells . The cells then use glucose as energy. Sleeping seven hours or more each night helps ensure blood sugar is regulated in the body Trusted Source Centers for Disease Control and Prevention (CDC) As the nation’s health protection agency, CDC saves lives and protects people from health threats. View Source .
Adults who get less than seven hours of sleep at night are at increased risk for Type 2 diabetes. Without enough sleep, the body’s resistance to insulin increases because cells are not able to use insulin appropriately, which leads to too much sugar in the bloodstream.
Sleep is believed to help with memory and cognitive thinking. Brain plasticity theory, a major theory on why humans sleep, posits that sleep is necessary so the brain can grow, reorganize, restructure, and make new neural connections Trusted Source National Center for Biotechnology Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . These connections in the brain help individuals learn new information and form memories during sleep. In other words, a good night’s sleep can lead to better problem-solving and decision-making skills.
A lack of sleep can have a negative impact on the ability to think clearly, form memories, learn well, and function optimally during the day. The ability to think quickly slows down after only a week of insufficient sleep Trusted Source Medscape Reference Medscape is on online destination for healthcare professionals worldwide, offering expert perspectives, drug and disease information, and professional education. View Source . Accuracy on tasks also decreases after a week of getting five hours of sleep or less each night. Sleep-deprived people perform poorly in activities that require quick responses and attention to multiple tasks, such as driving.
Insufficient sleep also impacts judgment. Less than five hours of sleep at night is correlated with riskier behavior. A sleep-deprived person is at higher risk of making poor decisions because they only have the ability to focus on a desired outcome, not the consequences.
Restorative theories of sleep suggest that sleep restores and repairs the body, making people feel refreshed in the morning. During sleep, the body produces growth hormones necessary for development in children and adolescents. These growth hormones also repair tissues and cells in people of all ages. The body also produces cytokines during sleep, which support the immune system in fighting infections Trusted Source National Heart, Lung, and Blood Institute (NHLBI) The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders. View Source .
Inadequate sleep can impact the body’s immune response to infection. Chronic sleep loss can make individuals more susceptible to common infections, such as a cold, while insufficient sleep over time can lead to a greater risk for immunodeficiency.
Getting appropriate sleep each night can help manage stress . When people wake up refreshed, they avoid the stressors that come with functioning while sleep-deprived, such as poor performance, difficulty thinking clearly, and lack of energy. Quality sleep can also reduce anxiety, depression, and other mental health strains related to stress.
Sleep is a key element of athletic recovery Trusted Source UpToDate More than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights. View Source , and the body’s production of growth hormones is highest during sleep. These growth hormones are necessary for the repair of tissue and likely contribute to muscle growth. Most athletes require eight hours of sleep each night for restoration and to avoid overtraining and improve their performance.
Without sleep, athletes are at risk for lowered performance, fatigue, and changes in mood. Performing with less sleep also heightens the risk for injury Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source . The potential for injury rises even more when an athlete’s sleep time decreases and time spent training increases.
Quality sleep, in addition to exercise, stress management, and healthy eating choices, is an important part Trusted Source Centers for Disease Control and Prevention (CDC) As the nation’s health protection agency, CDC saves lives and protects people from health threats. View Source of maintaining a healthy weight. During sleep, the body naturally produces more of an appetite suppressor, called leptin, while reducing production of the appetite stimulant ghrelin. On nights of too-little sleep, however, production of ghrelin increases and leptin decreases. As a result, a lack of sleep can lead to a greater feeling of hunger.
To get better sleep, and the many health benefits that come along with it, we take a look at the healthy practices around sleep, known as sleep hygiene. A number of lifestyle adjustments can help improve sleep quality.
Create a Consistent Sleep Schedule
A regular sleep and wake routine helps the body keep a consistent internal clock Trusted Source National Heart, Lung, and Blood Institute (NHLBI) The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders. View Source . Sleep experts recommend going to bed and getting up at the same time each day, including weekends.
Some adults like to nap during the day to avoid sleepiness. Keeping naps to about 20 minutes lessens fatigue without impacting sleep schedules. Naps that are too long can reduce alertness and defeat the purpose of napping. Individuals who choose to nap should avoid napping too late in the afternoon so that they can still fall asleep at their usual bedtime.

Make a Quality Sleep Environment
Although individual preferences may vary, most people sleep best in a dark, quiet, and cool bedroom. Too much light or noise at night can keep people awake or interrupt sleep. An eye mask or blackout curtains can eliminate unwanted light, and earplugs and noise machines can reduce distracting noises. Additionally, a fan can cool the room and serve as a noise machine.
Replacing old, worn, or uncomfortable mattresses and pillows with new and supportive ones can help improve sleep quality. The best mattresses and pillows for sleep depend on an individual’s preferred sleep positions and physical needs.
Avoid Caffeine, Nicotine, and Alcohol Before Bedtime
Caffeine is a stimulant that provides a boost of energy and alertness . When taken in the afternoon or evening, caffeine can make it difficult to fall asleep at night. The use of nicotine, found in cigarettes, in the evening is associated with more time spent awake at night. While some people drink alcohol before bedtime intending to get to sleep faster, alcohol is associated with lighter, lower quality sleep.
Exercise During the Day
Daytime exercise can make it easier to fall asleep and daily exercise is associated with better sleep quality. Exercise may also help individuals fall asleep faster and increase the overall time spent sleeping. It can be beneficial to exercise outside, as sunlight exposure during the day also improves sleep. People should avoid exercising too late in the day so that their bodies can relax before bedtime.
Avoid Screens Before Bedtime
Setting electronic devices aside at least 30 minutes before bedtime can make it easier to fall asleep. Phones, tablets, computers, and other electronics with screens emit blue light, which can disrupt the body’s natural production of the sleep hormone melatonin and make it difficult to fall asleep.
Instead, sleep experts advise developing a relaxing routine in the hour before bedtime. During this period of winding down, choose a restful activity such as reading or taking a warm shower.
Talk to a Doctor About Sleep
Those concerned about their sleep quality should consult with a health care provider. It may be helpful to keep a sleep diary to record sleep experiences and other symptoms. Discussing these symptoms with a doctor can identify potential causes for insufficient or interrupted sleep. Doctors can also talk through personalized strategies for improving sleep and refer individuals for additional testing as necessary.
About Our Editorial Team

Jay Summer, Staff Writer

Medically Reviewed by
Dr. Abhinav Singh, Sleep Medicine Physician MD
References 11 sources.
Cirelli, C. (2022, March 13). Insufficient sleep: Definition, epidemiology, and adverse outcomes. In R. Benca (Ed.). UpToDate.
Blackwelder, A., Hoskins, M., & Huber, L. (2021). Effect of inadequate sleep on frequent mental distress. Preventing Chronic Disease, 18.
National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. (2021, January 4). How does sleep affect your heart health? Centers for Disease Control and Prevention.
Centers for Disease Control and Prevention. (2020, December 10) Sleep for a good cause. Centers for Disease Control and Prevention., Retrieved April 5, 2022, from
Puderbaugh, M. and Emmady, P. D. (2022, February 8). Neuroplasticity. In StatPearls. StatPearls Publishing.
Bollu, P. C. (2019, November 5). Normal sleep, sleep physiology, and sleep deprivation. Medscape.
National Heart, Lung, and Blood Institute. (n.d.). How sleep works.
Halson, S. (2020, May 1). Overtraining syndrome in athletes. In F. G. O’Connor (Ed.). UpToDate.
Watson, A. M. (2017). Sleep and athletic performance. Current Sports Medicine Reports, 16(6), 413–418.
Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. (2021, January 1). Healthy weight, nutrition, and physical activity. Centers for Disease Control and Prevention.
National Heart, Lung and Blood Institute. (2022, March 24). Healthy sleep habits.
Learn More About How Sleep Works

How to Become a Morning Person

How Much Sleep Do You Need?

How Memory and Sleep Are Connected

What Causes Excessive Sleepiness?

What Causes Restless Sleep?

Biphasic Sleep: What It Is And How It Works

Polyphasic Sleep: Benefits and Risks

Sleep Inertia: How to Combat Morning Grogginess

REM Rebound: Causes and Effects

Do Moon Phases Affect Your Sleep?

Why Do We Need Sleep?

Alpha Waves and Sleep

How Age Affects Your Circadian Rhythm

How Is Sleep Different For Men and Women?

Circadian Rhythm

Chronotypes: Definition, Types, & Effect on Sleep

Sleep Drive and Your Body Clock

Daylight Saving Time: Everything You Need to Know

How To Get a Good Night’s Sleep in a Hotel

Does Napping Impact Your Sleep at Night?

Does Daytime Tiredness Mean You Need More Sleep?

Why Do I Wake Up at 3 am?

Sleep Debt: The Hidden Cost of Insufficient Rest

Sleep Satisfaction and Energy Levels

How Sleep Works: Understanding the Science of Sleep

What Makes a Good Night's Sleep

What Happens When You Sleep?

Sleep and Social Media
Adenosine and Sleep: Understanding Your Sleep Drive

Oversleeping

Hypnagogic Hallucinations

Hypnopompic Hallucinations

What All-Nighters Do To Your Cognition

Long Sleepers

How to Wake Up Easier

Sleep Spindles

Does Your Oxygen Level Drop When You Sleep?

100+ Sleep Statistics

Short Sleepers

How Electronics Affect Sleep

Myths and Facts About Sleep

What’s the Connection Between Race and Sleep Disorders?

Sleep Latency

Microsleep: What Is It, What Causes It, and Is It Safe?

Light Sleeper: What It Means and What To Do About It
Other articles of interest, best mattresses, sleep testing and solutions, bedroom environment, sleep hygiene.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Sleep timing, sleep consistency, and health in adults: a systematic review
Affiliations.
- 1 Healthy Active Living and Obesity Research Group, Children's Hospital of Eastern Ontario Research Institute, Ottawa, ON K1H 8L1, Canada.
- 2 School of Kinesiology and Health Studies, Queen's University, Kingston, ON K7L 3N6, Canada.
- 3 Department of Kinesiology, University of Waterloo, Waterloo, ON N2L 3G1, Canada.
- 4 Department of Applied Human Sciences, University of Prince Edward Island, Charlottetown, PE C1A 4P3, Canada.
- 5 Independent Researcher, Kanata, ON K2K 0E5, Canada.
- 6 School of Rehabilitation Sciences, McMaster University, Hamilton, ON L8S 1C7, Canada.
- 7 Queen's University Library, Queen's University, Kingston, ON K7L 3N6, Canada.
- 8 Départment de psychologie, Université de Montréal, Montreal, QC H2V 2S9, Canada.
- PMID: 33054339
- DOI: 10.1139/apnm-2020-0032
The objective of this systematic review was to examine the associations between sleep timing (e.g., bedtime/wake-up time, midpoint of sleep), sleep consistency/regularity (e.g., intra-individual variability in sleep duration, social jetlag, catch-up sleep), and health outcomes in adults aged 18 years and older. Four electronic databases were searched in December 2018 for articles published in the previous 10 years. Fourteen health outcomes were examined. A total of 41 articles, including 92 340 unique participants from 14 countries, met inclusion criteria. Sleep was assessed objectively in 37% of studies and subjectively in 63% of studies. Findings suggest that later sleep timing and greater sleep variability were generally associated with adverse health outcomes. However, because most studies reported linear associations, it was not possible to identify thresholds for "late sleep timing" or "large sleep variability". In addition, social jetlag was associated with adverse health outcomes, while weekend catch-up sleep was associated with better health outcomes. The quality of evidence ranged from "very low" to "moderate" across study designs and health outcomes using GRADE. In conclusion, the available evidence supports that earlier sleep timing and regularity in sleep patterns with consistent bedtimes and wake-up times are favourably associated with health. (PROSPERO registration no.: CRD42019119534.) Novelty This is the first systematic review to examine the influence of sleep timing and sleep consistency on health outcomes. Later sleep timing and greater variability in sleep are both associated with adverse health outcomes in adults. Regularity in sleep patterns with consistent bedtimes and wake-up times should be encouraged.
Keywords: bedtime; catch-up sleep; directives; décalage horaire social; guidelines; heure du coucher; heure du réveil; midpoint of sleep; point médian du sommeil; public health; régularité du sommeil; santé publique; sleep regularity; sleep variability; social jetlag; sommeil de rattrapage; variabilité du sommeil; wake-up time.
PubMed Disclaimer
Similar articles
- A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Janssen I, Clarke AE, Carson V, Chaput JP, Giangregorio LM, Kho ME, Poitras VJ, Ross R, Saunders TJ, Ross-White A, Chastin SFM. Janssen I, et al. Appl Physiol Nutr Metab. 2020 Oct;45(10 (Suppl. 2)):S248-S257. doi: 10.1139/apnm-2020-0160. Appl Physiol Nutr Metab. 2020. PMID: 33054342
- Sleep duration and health in adults: an overview of systematic reviews. Chaput JP, Dutil C, Featherstone R, Ross R, Giangregorio L, Saunders TJ, Janssen I, Poitras VJ, Kho ME, Ross-White A, Carrier J. Chaput JP, et al. Appl Physiol Nutr Metab. 2020 Oct;45(10 (Suppl. 2)):S218-S231. doi: 10.1139/apnm-2020-0034. Appl Physiol Nutr Metab. 2020. PMID: 33054337
- Sedentary behaviour and health in adults: an overview of systematic reviews. Saunders TJ, McIsaac T, Douillette K, Gaulton N, Hunter S, Rhodes RE, Prince SA, Carson V, Chaput JP, Chastin S, Giangregorio L, Janssen I, Katzmarzyk PT, Kho ME, Poitras VJ, Powell KE, Ross R, Ross-White A, Tremblay MS, Healy GN. Saunders TJ, et al. Appl Physiol Nutr Metab. 2020 Oct;45(10 (Suppl. 2)):S197-S217. doi: 10.1139/apnm-2020-0272. Appl Physiol Nutr Metab. 2020. PMID: 33054341
- Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T, Weiss SK, Connor Gorber S, Kho ME, Sampson M, Belanger K, Eryuzlu S, Callender L, Tremblay MS. Chaput JP, et al. Appl Physiol Nutr Metab. 2016 Jun;41(6 Suppl 3):S266-82. doi: 10.1139/apnm-2015-0627. Appl Physiol Nutr Metab. 2016. PMID: 27306433 Review.
- Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Saunders TJ, Gray CE, Poitras VJ, Chaput JP, Janssen I, Katzmarzyk PT, Olds T, Connor Gorber S, Kho ME, Sampson M, Tremblay MS, Carson V. Saunders TJ, et al. Appl Physiol Nutr Metab. 2016 Jun;41(6 Suppl 3):S283-93. doi: 10.1139/apnm-2015-0626. Appl Physiol Nutr Metab. 2016. PMID: 27306434 Review.
- Association between sleep duration and cardiovascular risk: the EVasCu cross-sectional study. Martínez-García I, Saz-Lara A, Cavero-Redondo I, Otero-Luis I, Gómez-Guijarro MD, Moreno-Herraiz N, López-López S, Pascual-Morena C. Martínez-García I, et al. Front Physiol. 2024 Jul 26;15:1430821. doi: 10.3389/fphys.2024.1430821. eCollection 2024. Front Physiol. 2024. PMID: 39129755 Free PMC article.
- Changes in Sleep Duration and Sleep Timing in the General Population from before to during the First COVID-19 Lockdown: A Systematic Review and Meta-Analysis. Ceolin C, Limongi F, Siviero P, Trevisan C, Noale M, Catalani F, Conti S, Di Rosa E, Perdixi E, Remelli F, Prinelli F, Maggi S. Ceolin C, et al. Int J Environ Res Public Health. 2024 May 2;21(5):583. doi: 10.3390/ijerph21050583. Int J Environ Res Public Health. 2024. PMID: 38791798 Free PMC article. Review.
- Quality of sleep and excessive daytime sleepiness among medical students in a Brazilian private university. Souza AKR, Sandes RS, Vasco RFV, Albuquerque EVA. Souza AKR, et al. Rev Assoc Med Bras (1992). 2024 Apr 22;70(3):e20231141. doi: 10.1590/1806-9282.20231141. eCollection 2024. Rev Assoc Med Bras (1992). 2024. PMID: 38656002 Free PMC article.
- Association of sleep timing with all-cause and cardiovascular mortality: the Sleep Heart Health Study and the Osteoporotic Fractures in Men Study. Ma M, Fan Y, Peng Y, Ma Q, Jia M, Qi Z, Yang J, Wang W, Ma X, Yan B. Ma M, et al. J Clin Sleep Med. 2024 Apr 1;20(4):545-553. doi: 10.5664/jcsm.10926. J Clin Sleep Med. 2024. PMID: 38561941
- Independent and Joint Associations of Physical Activity and Sleep on Mental Health Among a Global Sample of 200,743 Adults. Brown DMY, Lerner I, Cairney J, Kwan MY. Brown DMY, et al. Int J Behav Med. 2024 Mar 26. doi: 10.1007/s12529-024-10280-8. Online ahead of print. Int J Behav Med. 2024. PMID: 38532194
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases & Disorders Education Program
- Publications and Resources
- Clinical Trials
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Ask a Scientist
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To How Sleep Works
- Why Is Sleep Important?
- How Sleep Works
- Your Sleep/Wake Cycle
- Sleep Phases and Stages
- How Much Sleep Is Enough?
MORE INFORMATION
How Sleep Works Why Is Sleep Important?
Language switcher.
Sleep plays a vital role in good health and well-being throughout your life. The way you feel while you are awake depends in part on what happens while you are sleeping. During sleep, your body is working to support healthy brain function and maintain your physical health.
In children and teens, sleep also helps support growth and development. Getting inadequate sleep over time can raise your risk for chronic (long-term) health problems. It can also affect how well you think, react, work, learn, and get along with others. Learn how sleep affects your heart and circulatory system, metabolism , respiratory system, and immune system and how much sleep is enough.

This brochure describes the differences between the types of sleep needed to feel awake and to be healthy and offers tips for getting a good night’s sleep.
Heart and circulatory system
When you fall asleep and enter non-REM sleep , your blood pressure and heart rate fall. During sleep, your parasympathetic system controls your body, and your heart does not work as hard as it does when you are awake. During REM sleep and when waking, your sympathetic system is activated, increasing your heart rate and blood pressure to the usual levels when you are awake and relaxed. A sharp increase in blood pressure and heart rate upon waking has been linked to angina, or chest pain, and heart attacks .
People who do not sleep enough or wake up often during the night may have a higher risk of:
- Coronary heart disease
- High blood pressure
Hormones and sleep
Your body makes different hormones at different times of day. This may be related to your sleep pattern or your circadian clocks. In the morning, your body releases hormones that promote alertness, such as cortisol, which helps you wake up. Other hormones have 24-hour patterns that vary throughout your life; for example, in children, the hormones that tell the glands to release testosterone, estrogen, and progesterone are made in pulses at night, and the pulses get bigger as puberty approaches.
Metabolism and sleep
The way your body handles fat varies according to various circadian clocks, including those in the liver, fat, and muscle. For example, the circadian clocks make sure that your liver is prepared to help digest fats at appropriate times. Your body may handle fat differently if you eat at unusual times.
Studies have shown that not getting enough quality sleep can lead to:
- Higher levels of the hormones that control hunger, including leptin and ghrelin, inside your body
- Decreased ability to respond to insulin
- Increased consumption of food, especially fatty, sweet, and salty foods
- Decreased physical activity
- Metabolic syndrome
All of these contribute to overweight and obesity .
Respiratory and immune systems
During sleep, you breathe less often and less deeply and take in less oxygen. These changes can cause problems in people who have health problems such as asthma or chronic obstructive pulmonary disease (COPD) . Asthma symptoms are usually worse during early morning sleep. Likewise, breathing problems in people who have lung diseases such as COPD can become worse during sleep.
Sleep also affects different parts of your immune system, which become more active at different times of day. For example, when you sleep, a particular type of immune cell works harder. That is why people who do not sleep enough may be more likely to get colds and other infections.

Lung Health Basics: Sleep
People with lung disease often have trouble sleeping. Sleep is critical to overall health, so take the first step to sleeping better: learn these sleep terms, and find out about treatments that can help with sleep apnea.
Problems with thinking and memory
Sleep helps with learning and the formation of long-term memories. Not getting enough sleep or enough high-quality sleep can lead to problems focusing on tasks and thinking clearly. Read our Sleep Deprivation and Deficiency page for more information on how lack of sleep affects performance of daily activities, including driving and schoolwork.

Why sleep is important

Sleep is essential for a person’s health and wellbeing, according to the National Sleep Foundation (NSF). Yet millions of people do not get enough sleep and many suffer from lack of sleep. For example, surveys conducted by the NSF (1999-2004) reveal that at least 40 million Americans suffer from over 70 different sleep disorders and 60 percent of adults report having sleep problems a few nights a week or more. Most of those with these problems go undiagnosed and untreated. In addition, more than 40 percent of adults experience daytime sleepiness severe enough to interfere with their daily activities at least a few days each month — with 20 percent reporting problem sleepiness a few days a week or more. Furthermore, 69 percent of children experience one or more sleep problems a few nights or more during a week.
According to psychologist and sleep expert David F. Dinges, Ph.D., of the Division of Sleep and Chronobiology and Department of Psychiatry at the University of Pennsylvania School of Medicine, irritability, moodiness and disinhibition are some of the first signs a person experiences from lack of sleep . If a sleep-deprived person doesn’t sleep after the initial signs, said Dinges, the person may then start to experience apathy, slowed speech and flattened emotional responses, impaired memory and an inability to be novel or multitask. As a person gets to the point of falling asleep, he or she will fall into micro sleeps (5-10 seconds) that cause lapses in attention, nod off while doing an activity like driving or reading and then finally experience hypnagogic hallucinations, the beginning of REM sleep. (Dinges, Sleep, Sleepiness and Performance , 1991)
Everyone’s individual sleep needs vary. In general, most healthy adults are built for 16 hours of wakefulness and need an average of eight hours of sleep a night. However, some individuals are able to function without sleepiness or drowsiness after as little as six hours of sleep. Others can't perform at their peak unless they've slept ten hours. And, contrary to common myth, the need for sleep doesn't decline with age but the ability to sleep for six to eight hours at one time may be reduced. (Van Dongen & Dinges, Principles & Practice of Sleep Medicine , 2000)
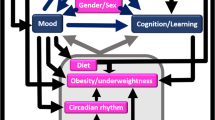
Psychologists and other scientists who study the causes of sleep disorders have shown that such problems can directly or indirectly be tied to abnormalities in the following systems:
Physiological systems
Brain and nervous system
Cardiovascular system
Metabolic functions
Immune system
Furthermore, unhealthy conditions, disorders and diseases can also cause sleep problems, including:
Pathological sleepiness, insomnia and accidents
Hypertension and elevated cardiovascular risks (MI, stroke)
Emotional disorders (depression, bipolar disorder)
Obesity; metabolic syndrome and diabetes
Alcohol and drug abuse (Dinges, 2004)
Groups that are at particular risk for sleep deprivation include night shift workers, physicians (average sleep = 6.5 hours a day; residents = 5 hours a day), truck drivers, parents and teenagers. (American Academy of Sleep Medicine and National Heart, Lung, and Blood Institute Working Group on Problem Sleepiness. 1997).
Stress is the number one cause of short-term sleeping difficulties , according to sleep experts. Common triggers include school- or job-related pressures, a family or marriage problem and a serious illness or death in the family. Usually the sleep problem disappears when the stressful situation passes. However, if short-term sleep problems such as insomnia aren't managed properly from the beginning, they can persist long after the original stress has passed.
Drinking alcohol or beverages containing caffeine in the afternoon or evening, exercising close to bedtime, following an irregular morning and nighttime schedule, and working or doing other mentally intense activities right before or after getting into bed can disrupt sleep.
If you are among the 20 percent of employees in the United States who are shift workers, sleep may be particularly elusive. Shift work forces you to try to sleep when activities around you — and your own "biological rhythms" — signal you to be awake. One study shows that shift workers are two to five times more likely than employees with regular, daytime hours to fall asleep on the job.
Traveling also disrupts sleep, especially jet lag and traveling across several time zones. This can upset your biological or “circadian” rhythms.
Environmental factors such as a room that's too hot or cold, too noisy or too brightly lit can be a barrier to sound sleep. And interruptions from children or other family members can also disrupt sleep. Other influences to pay attention to are the comfort and size of your bed and the habits of your sleep partner. If you have to lie beside someone who has different sleep preferences, snores, can't fall or stay asleep, or has other sleep difficulties, it often becomes your problem too!
Having a 24/7 lifestyle can also interrupt regular sleep patterns: the global economy that includes round the clock industries working to beat the competition; widespread use of nonstop automated systems to communicate and an increase in shift work makes for sleeping at regular times difficult.
A number of physical problems can interfere with your ability to fall or stay asleep. For example, arthritis and other conditions that cause pain, backache, or discomfort can make it difficult to sleep well.
Epidemiological studies suggest self-reported sleep complaints are associated with an increased relative risk of cardiovascular morbidity and mortality. For women, pregnancy and hormonal shifts including those that cause premenstrual syndrome (PMS) or menopause and its accompanying hot flashes can also intrude on sleep.
Finally, certain medications such as decongestants, steroids and some medicines for high blood pressure, asthma, or depression can cause sleeping difficulties as a side effect.
It is a good idea to talk to a physician or mental health provider about any sleeping problem that recurs or persists for longer than a few weeks.
According to the DSM, some psychiatric disorders have fatigue as a major symptom. Included are: major depressive disorder (includes postpartum blues), minor depression , dysthymia, mixed anxiety-depression, seasonal affective disorder and bipolar disorder .
According to a long-term study published in the 2004 April issue of Alcoholism: Clinical and Experimental Research , young teenagers whose preschool sleep habits were poor were more than twice as likely to use drugs, tobacco or alcohol. This finding was made by the University of Michigan Health System as part of a family health study that followed 257 boys and their parents for 10 years. The study found a significant connection between sleep problems in children and later drug use, even when other issues such as depression, aggression, attention problems and parental alcoholism were taken into account. Long-term data on girls isn't available yet. The researchers suggest that early sleep problems may be a "marker" for predicting later risk of early adolescent substance abuse — and that there may be a common biological factor underlying both traits. Although the relationship between sleep problems and the abuse of alcohol in adults is well known, this is the first study to look at the issue in children.
Nightmares are dreams with vivid and disturbing content. They are common in children during REM sleep. They usually involve an immediate awakening and good recall of the dream content.
Sleep terrors are often described as extreme nightmares. Like nightmares, they most often occur during childhood, however they typically take place during non-REM (NREM) sleep. Characteristics of a sleep terror include arousal, agitation, large pupils, sweating, and increased blood pressure. The child appears terrified, screams and is usually inconsolable for several minutes, after which he or she relaxes and returns to sleep. Sleep terrors usually take place early in the night and may be combined with sleepwalking. The child typically does not remember or has only a vague memory of the terrifying events.
In the August 2004 issue of the journal Sleep , Dr. Timothy Roehrs, the Director of research at the Sleep Disorders and Research Center at Henry Ford Hospital in Detroit published one of the first studies to measure the effect of sleepiness on decision making and risk taking. He found that sleepiness does take a toll on effective decision making.
Cited in the October 12, New York Times Science section, Dr. Roehrs and his colleagues paid sleepy and fully alert subjects to complete a series of computer tasks. At random times, they were given a choice to take their money and stop. Or they could forge ahead with the potential of either earning more money or losing it all if their work was not completed within an unknown remainder of time.
Dr. Roehrs found that the alert people were very sensitive to the amount of work they needed to do to finish the tasks and understood the risk of losing their money if they didn't. But the sleepy subjects chose to quit the tasks prematurely or they risked losing everything by trying to finish the task for more money even when it was 100 percent likely that they would be unable to finish, said Dr. Roehrs.
According to the National Commission on Sleep Disorders Research (1998) and reports from the National Highway Safety Administration (NHSA)(2002), high-profile accidents can partly be attributed to people suffering from a severe lack of sleep.
Each year the cost of sleep disorders, sleep deprivation and sleepiness, according to the NCSDR, is estimated to be $15.9 million in direct costs and $50 to $100 billion a year in indirect and related costs. And according to the NHSA, falling asleep while driving is responsible for at least 100,000 crashes, 71,000 injuries and 1,550 deaths each year in the United States. Young people in their teens and twenties, who are particularly susceptible to the effects of chronic sleep loss, are involved in more than half of the fall-asleep crashes on the nation's highways each year. Sleep loss also interferes with the learning of young people in our nation's schools, with 60 percent of grade school and high school children reporting that they are tired during the daytime and 15 percent of them admitting to falling asleep in class.
According to the Department of Transportation (DOT), one to four percent of all highway crashes are due to sleepiness, especially in rural areas and four percent of these crashes are fatal.
Risk factors for drowsy driving crashes:
Late night/early morning driving
Patients with untreated excessive sleepiness
People who obtain six or fewer hours of sleep per day
Young adult males
Commercial truck drivers
Night shift workers
Medical residents after their shift
According to sleep researchers, a night's sleep is divided into five continually shifting stages, defined by types of brain waves that reflect either lighter or deeper sleep. Toward morning, there is an increase in rapid eye movement, or REM sleep, when the muscles are relaxed and dreaming occurs, and recent memories may be consolidated in the brain. The experts say that hitting a snooze alarm over and over again to wake up is not the best way to feel rested. “The restorative value of rest is diminished, especially when the increments are short,” said psychologist Edward Stepanski, PhD who has studied sleep fragmentation at the Rush University Medical Center in Chicago. This on and off again effect of dozing and waking causes shifts in the brain-wave patterns. Sleep-deprived snooze-button addicts are likely to shorten their quota of REM sleep, impairing their mental functioning during the day. ( New York Times , October 12, 2004)
Certain therapies, like cognitive behavioral therapy teach people how to recognize and change patterns of thought and behavior to solve their problems. Recently this type of therapy has been shown to be very effective in getting people to fall asleep and conquer insomnia.
According to a study published in the October 2004 issue of The Archives of Internal Medicine , cognitive behavior therapy is more effective and lasts longer than a widely used sleeping pill, Ambien, in reducing insomnia. The study involved 63 healthy people with insomnia who were randomly assigned to receive Ambien, the cognitive behavior therapy, both or a placebo. The patients in the therapy group received five 30-minute sessions over six weeks. They were given daily exercises to “recognize, challenge and change stress-inducing” thoughts and were taught techniques, like delaying bedtime or getting up to read if they were unable to fall asleep after 20 minutes. The patients taking Ambien were on a full dose for a month and then were weaned off the drug. At three weeks, 44 percent of the patients receiving the therapy and those receiving the combination therapy and pills fell asleep faster compared to 29 percent of the patients taking only the sleeping pills. Two weeks after all the treatment was over, the patients receiving the therapy fell asleep in half the time it took before the study and only 17 percent of the patients taking the sleeping pills fell asleep in half the time. (New York Times, October 5, 2004)
According to leading sleep researchers, there are techniques to combat common sleep problems:
Keep a regular sleep/wake schedule
Don’t drink or eat caffeine four to six hours before bed and minimize daytime use
Don’t smoke, especially near bedtime or if you awake in the night
Avoid alcohol and heavy meals before sleep
Get regular exercise
Minimize noise, light and excessive hot and cold temperatures where you sleep
Develop a regular bed time and go to bed at the same time each night
Try and wake up without an alarm clock
Attempt to go to bed earlier every night for certain period; this will ensure that you’re getting enough sleep
In clinical settings, cognitive-behavior therapy (CBT) has a 70-80 percent success rate for helping those who suffer from chronic insomnia. Almost one third of people with insomnia achieve normal sleep and most reduce their symptoms by 50 percent and sleep an extra 45-60 minutes a night. When insomnia exists along with other psychological disorders like depression, say the experts, the initial treatment should address the underlying condition.
But sometimes even after resolving the underlying condition, the insomnia still exists, says psychologist Jack Edinger, PhD, of the VA Medical Center in Durham, North Carolina and Professor of Psychiatry and Behavioral Sciences at Duke University and cautions that treating the depression usually doesn’t resolve the sleep difficulties. From his clinical experience, he has found that most patients with insomnia should be examined for specific behaviors and thoughts that may perpetuate the sleep problems. When people develop insomnia, they try to compensate by engaging in activities to help them get more sleep. They sleep later in the mornings or spend excessive times in bed. These efforts usually backfire, said Edinger.
From his clinical work and research on sleep, psychologist Charles M. Morin, PhD, a Professor in the Psychology Department and Director of the Sleep Disorders Center at University Laval in Quebec, Canada says that ten percent of adults suffer from chronic insomnia. In a study released in the recent issue of Sleep Medicine Alert published by the NSF, Morin outlines how CBT helps people overcome insomnia. Clinicians use sleep diaries to get an accurate picture of someone’s sleep patterns. Bedtime, waking time, time to fall asleep, number and durations of awakening, actual sleep time and quality of sleep are documented by the person suffering from insomnia.
A person can develop poor sleep habits (i.e. watching TV in bed or eating too much before bedtime), irregular sleep patterns (sleeping too late, taking long naps during the day) to compensate for lost sleep at night. Some patients also develop a fear of not sleeping and a pattern of worrying about the consequences of not sleeping, said Morin. “Treatments that address the poor sleep habits and the faulty beliefs and attitudes about sleep work but sometimes,” said Morin, “medication may play a role in breaking the cycle of insomnia. But behavioral therapies are essential for patients to alter the conditions that perpetuate it.”
CBT attempts to change a patient’s dysfunctional beliefs and attitudes about sleep. “It restructure thoughts — like, ‘I’ve got to sleep eight hours tonight’ or ‘I’ve got to take medication to sleep’ or ‘I just can’t function or I’ll get sick if I don’t sleep.’ These thoughts focus too much on sleep, which can become something like performance anxiety — sleep will come around to you when you’re not chasing it,” said Edinger.
What works in many cases, said Morin and Edinger, is to standardize or restrict a person’s sleep to give a person more control over his or her sleep. A person can keep a sleep diary for a couple of weeks and a clinician can monitor the amount of time spent in bed to the actual amount of time sleeping. Then the clinician can instruct the patient to either go to bed later and get up earlier or visa versa. This procedure improves the length of sleeping time by imposing a mild sleep deprivation situation, which has the result of reducing the anxiety surrounding sleep. To keep from falling asleep during the day, patients are told not to restrict sleep to less than five hours.
Standardizing sleep actually helps a person adjust his or her homeostatic mechanism that balances sleep, said Edinger. “Therefore, if you lose sleep, your homeostatic mechanism will kick in and will work to increase the likelihood of sleeping longer and deeper to promote sleep recovery. This helps a person come back to their baseline and works for the majority.”
A person can also establish more stimulus control over his or her bedroom environment, said Morin. This could include: going to bed only when sleepy, getting out of bed when unable to sleep, prohibiting non-sleep activities in the bedroom, getting up at the same time every morning (including weekends) and avoiding daytime naps.
Finally, a person can incorporate relaxation techniques as part of his or her treatment. For example, a person can give herself or himself an extra hour before bed to relax and unwind and time to write down worries and plans for the following day.
In CBT, said Morin, breaking the thought process and anxiety over sleep is the goal. “After identifying the dysfunctional thought patterns, a clinician can offer alternative interpretations of what is getting the person anxious so a person can think about his or her insomnia in a different way.” Morin offers some techniques to restructure a person’s cognitions. “Keep realistic expectations, don’t blame insomnia for all daytime impairments, do not feel that losing a night’s sleep will bring horrible consequences, do not give too much importance to sleep and finally develop some tolerance to the effects of lost sleep.
According to Edinger, aging weakens a person’s homeostatic sleep drive after age 50. Interestingly, the length of the circadian cycle stays roughly the same over the lifespan but the amplitude of the circadian rhythm may decline somewhat with aging.
National Sleep Foundation http://www.thensf.org
American Academy of Sleep Medicine http://www.aasmnet.org/
American Insomnia Association http://www.americaninsomniaassociation.org/
Sleep Research Society http://www.sleepresearchsociety.org/
NIH National Center for Sleep Disorders Research http://www.nhlbi.nih.gov/sleep
The MayoClinic.com Sleep Center
(Blake, et al, Psychological Reports, 1998; National Heart, Lung and Blood Institute Working Group on Insomnia, 1998)
David F. Dinges, PhD , Professor of Psychology in Psychiatry, Chief, Division of Sleep and Chronobiology, University of Pennsylvania School of Medicine
Jack Edinger, PhD , of the VA Medical Center in Durham, North Carolina and Professor of Psychiatry and Behavioral Sciences at Duke University
Charles M. Morin, PhD , a Professor in the Psychology Department and Director of the Sleep Disorders Center at University Laval in Quebec, Canada
Timothy Roehrs, PhD , the Director of Research, Sleep Disorders and Research Center at Henry Ford Hospital
Edward Stepanski, PhD , who has studied sleep fragmentation at the Rush University Medical Center in Chicago
Related Reading
- Getting a good night’s sleep: How psychologists help with insomnia
- What to Do When You Dread Your Bed
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 01 October 2019
Sleep quality, duration, and consistency are associated with better academic performance in college students
- Kana Okano 1 ,
- Jakub R. Kaczmarzyk 1 ,
- Neha Dave 2 ,
- John D. E. Gabrieli 1 &
- Jeffrey C. Grossman ORCID: orcid.org/0000-0003-1281-2359 3
npj Science of Learning volume 4 , Article number: 16 ( 2019 ) Cite this article
453k Accesses
129 Citations
1741 Altmetric
Metrics details
Although numerous survey studies have reported connections between sleep and cognitive function, there remains a lack of quantitative data using objective measures to directly assess the association between sleep and academic performance. In this study, wearable activity trackers were distributed to 100 students in an introductory college chemistry class (88 of whom completed the study), allowing for multiple sleep measures to be correlated with in-class performance on quizzes and midterm examinations. Overall, better quality, longer duration, and greater consistency of sleep correlated with better grades. However, there was no relation between sleep measures on the single night before a test and test performance; instead, sleep duration and quality for the month and the week before a test correlated with better grades. Sleep measures accounted for nearly 25% of the variance in academic performance. These findings provide quantitative, objective evidence that better quality, longer duration, and greater consistency of sleep are strongly associated with better academic performance in college. Gender differences are discussed.
Similar content being viewed by others
Effect of sleep and mood on academic performance—at interface of physiology, psychology, and education
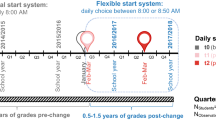
A 4-year longitudinal study investigating the relationship between flexible school starts and grades

Macro and micro sleep architecture and cognitive performance in older adults
Introduction.
The relationship between sleep and cognitive function has been a topic of interest for over a century. Well-controlled sleep studies conducted with healthy adults have shown that better sleep is associated with a myriad of superior cognitive functions, 1 , 2 , 3 , 4 , 5 , 6 including better learning and memory. 7 , 8 These effects have been found to extend beyond the laboratory setting such that self-reported sleep measures from students in the comfort of their own homes have also been found to be associated with academic performance. 9 , 10 , 11 , 12 , 13
Sleep is thought to play a crucial and specific role in memory consolidation. Although the exact mechanisms behind the relationship between sleep, memory, and neuro-plasticity are yet unknown, the general understanding is that specific synaptic connections that were active during awake-periods are strengthened during sleep, allowing for the consolidation of memory, and synaptic connections that were inactive are weakened. 5 , 14 , 15 Thus, sleep provides an essential function for memory consolidation (allowing us to remember what has been studied), which in turn is critical for successful academic performance.
Beyond the effects of sleep on memory consolidation, lack of sleep has been linked to poor attention and cognition. Well-controlled sleep deprivation studies have shown that lack of sleep not only increases fatigue and sleepiness but also worsens cognitive performance. 2 , 3 , 16 , 17 In fact, the cognitive performance of an individual who has been awake for 17 h is equivalent to that exhibited by one who has a blood alcohol concentration of 0.05%. 1 Outside of a laboratory setting, studies examining sleep in the comfort of peoples’ own homes via self-report surveys have found that persistently poor sleepers experience significantly more daytime difficulties in regards to fatigue, sleepiness, and poor cognition compared with persistently good sleepers. 18
Generally, sleep is associated with academic performance in school. Sleep deficit has been associated with lack of concentration and attention during class. 19 While a few studies report null effects, 20 , 21 most studies looking at the effects of sleep quality and duration on academic performance have linked longer and better-quality sleep with better academic performance such as school grades and study effort. 4 , 6 , 9 , 10 , 11 , 12 , 13 , 22 , 23 , 24 , 25 , 26 , 27 Similarly, sleep inconsistency plays a part in academic performance. Sleep inconsistency (sometimes called “social jet lag”) is defined by inconsistency in sleep schedule and/or duration from day to day. It is typically seen in the form of sleep debt during weekdays followed by oversleep on weekends. Sleep inconsistency tends to be greatest in adolescents and young adults who stay up late but are constrained by strict morning schedules. Adolescents who experience greater sleep inconsistency perform worse in school. 28 , 29 , 30 , 31
Although numerous studies have investigated the relationship between sleep and students’ academic performance, these studies utilized subjective measures of sleep duration and/or quality, typically in the form of self-report surveys; very few to date have used objective measures to quantify sleep duration and quality in students. One exception is a pair of linked studies that examined short-term benefits of sleep on academic performance in college. Students were incentivized with offers of extra credit if they averaged eight or more hours of sleep during final exams week in a psychology class 32 or five days leading up to the completion of a graphics studio final assignment. 33 Students who averaged eight or more hours of sleep, as measured by a wearable activity tracker, performed significantly better on their final psychology exams than students who chose not to participate or who slept less than eight hours. In contrast, for the graphics studio final assignments no difference was found in performance between students who averaged eight or more hours of sleep and those who did not get as much sleep, although sleep consistency in that case was found to be a factor.
Our aim in this study was to explore how sleep affects university students’ academic performance by objectively and ecologically tracking their sleep throughout an entire semester using Fitbit—a wearable activity tracker. Fitbit uses a combination of the wearer’s movement and heart-rate patterns to estimate the duration and quality of sleep. For instance, to determine sleep duration, the device measures the time in which the wearer has not moved, in combination with signature sleep movements such as rolling over. To determine sleep quality, the Fitbit device measures the wearer’s heart-rate variability which fluctuates during transitions between different stages of sleep. Although the specific algorithms that calculate these values are proprietary to Fitbit, they have been found to accurately estimate sleep duration and quality in normal adult sleepers without the use of research-grade sleep staging equipment. 34 By collecting quantitative sleep data over the course of the semester on nearly 100 students, we aimed to relate objective measures of sleep duration, quality, and consistency to academic performance from test to test and overall in the context of a real, large university college course.
A secondary aim was to understand gender differences in sleep and academic performance. Women outperform men in collegiate academic performance in most subjects 35 , 36 , 37 , 38 and even in online college courses. 39 Most of the research conducted to understand this female advantage in school grades has examined gender differences in self-discipline, 40 , 41 , 42 and none to date have considered gender differences in sleep as a mediating factor on school grades. There are inconsistencies in the literature on gender differences in sleep in young adults. While some studies report that females get more quantity 43 but worse quality sleep compared with males, 43 , 44 other studies report that females get better quality sleep. 45 , 46 In the current study, we aim to see whether we would observe a female advantage in grades and clarify how sleep contributes to gender differences.
Bedtime and wake-up times
On average, students went to bed at 1:54 a.m. (Median = 1:47 a.m., Standard Deviation (SD) of all bedtime samples = 2 h 11 min, SD of mean bedtime per participant = 1 h) and woke up at 9:17 a.m. (Median = 9:12 a.m., SD of all wake-up time samples = 2 h 2 min; SD of mean wake-up time per participant = 54 min). The data were confirmed to have Gaussian distribution using the Shapiro–Wilks normality test. We conducted an ANOVA with the overall score (sum of all grade-relevant quizzes and exams—see “Procedure”) as the dependent variable and bedtime (before or after median) and wake-up time (before or after median) as the independent variables. We found a main effect of bedtime ( F (1, 82) = 6.45, p = 0.01), such that participants who went to bed before median bedtime had significantly higher overall score ( X = 77.25%, SD = 13.71%) compared with participants who went to bed after median bedtime ( X = 70.68%, SD = 11.01%). We also found a main effect of wake-up time ( F (1, 82) = 6.43, p = 0.01), such that participants who woke up before median wake-up time had significantly higher overall score ( X = 78.28%, SD = 9.33%) compared with participants who woke up after median wake-up time ( X = 69.63%, SD = 14.38%), but found no interaction between bedtime and wake-up time ( F (1, 82) = 0.66, p = 0.42).
A Pearson’s product-moment correlation between average bedtime and overall score revealed a significant and negative correlation ( r (86) = −0.45, p < 0.0001), such that earlier average bedtime was associated with a higher overall score. There was a significant and negative correlation between average wake-up time and overall score ( r (86) = −0.35, p < 0.001), such that earlier average wake-up time was associated with a higher overall score. There was also a significant and positive correlation between average bedtime and average wake-up time (r (86) = 0.68, p < 0.0001), such that students who went to bed earlier tended to also wake up earlier.
Sleep duration, quality, and consistency in relation to academic performance
Overall, the mean duration of sleep for participants throughout the entire semester was 7 h 8 min (SD of all sleep samples = 1 h 48 min, SD of mean sleep duration per participant = 41 min). There was a significant positive correlation between mean sleep duration throughout the semester (sleep duration) and overall score ( r (86) = 0.38, p < 0.0005), indicating that a greater amount of sleep was associated with a higher overall score (Fig. 1a ). Similarly, there was a significant positive correlation between mean sleep quality throughout the semester (Sleep Quality) and Overall Score ( r (86) = 0.44, p < 0.00005). Sleep inconsistency was defined for each participant as the standard deviation of the participant’s daily sleep duration in minutes so that a larger standard deviation indicated greater sleep inconsistency. There was a significant negative correlation between sleep inconsistency and overall score ( r (86) = −0.36, p < 0.001), indicating that the greater inconsistency in sleep duration was associated with a lower overall score (Fig. 1b ).
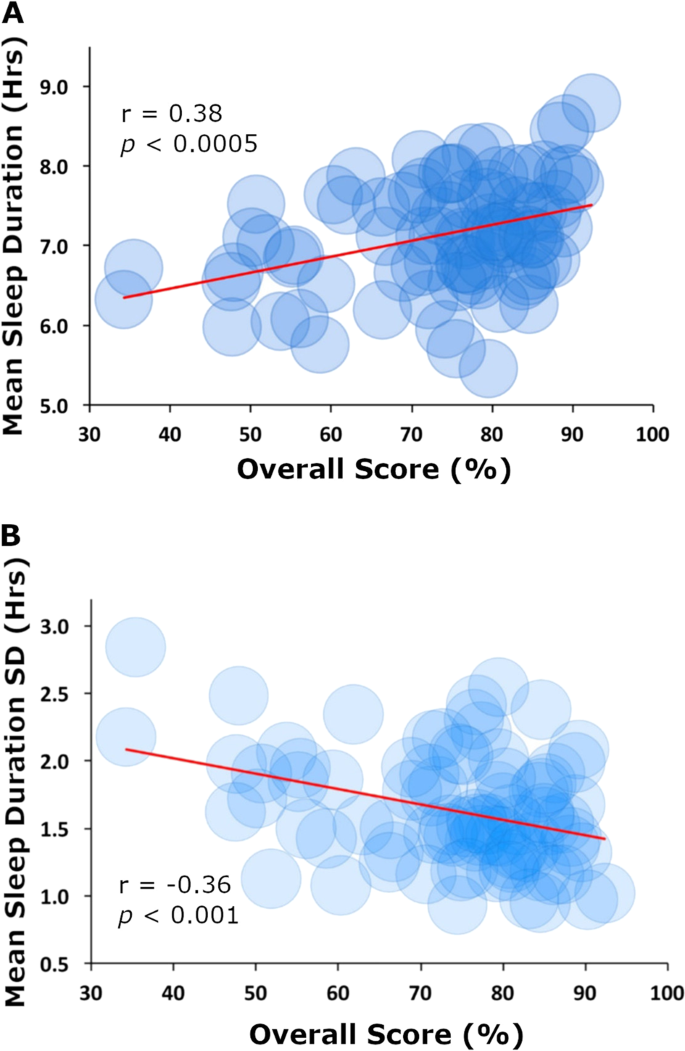
Correlations between sleep measures and overall score. a Average daily hours slept (sleep duration) vs. overall score for the semester. b Standard deviation of average daily hours of sleep (sleep inconsistency) vs. overall score in class
Timing of sleep and its relation to academic performance
To understand sleep and its potential role in memory consolidation, we examined the timing of sleep as it related to specific assessments. All Pearson correlations with three or more comparisons were corrected for multiple comparisons using false discovery rate. 47
Night before assessments
We conducted a correlation between sleep quality the night before a midterm and respective midterm scores as well as sleep duration the night before a midterm and respective scores. There were no significant correlations with sleep duration or sleep quality for all three midterms (all r s < 0.20, all p s > 0.05). Similar analyses for sleep duration and sleep quality the night before respective quizzes revealed no correlations ( r s from 0.01 to 0.26, all p s > 0.05).
Week and month leading up to assessments
To understand the effect of sleep across the time period while course content was learned for an assessment, we examined average sleep measures during the 1 month leading up to the midterms. We found a significant positive correlation between average sleep duration over the month leading up to scores on each midterm ( r s from 0.25 to 0.34, all p s < 0.02). Similar analyses for average sleep duration over one week leading up to respective quizzes were largely consistent with those of midterms, with significant correlations on 3 of 8 quizzes (rs from 0.3 to 0.4, all p s < 0.05) and marginal correlations on an additional 3 quizzes (rs from 0.25 to 0.27, all p s < 0.08).
There was a significant and positive correlation between sleep quality scores averaged over the month leading up to each midterm for all three midterms ( r s from 0.21 to 0.38, all p s < 0.05). Similar analyses for average Sleep Quality over one week leading up to respective quizzes revealed a significant correlation on 1 of 8 quizzes ( r (86) = 0.42, p < 0.005) and marginal correlations on 3 quizzes ( r s from 0.25 to 0.27, all p s < 0.08).
Variance of assessment performance accounted for by sleep measures
In order to calculate how much of the variance on assessment performance was accounted for by the sleep measures, we conducted a stepwise regression on overall score using three regressors: sleep duration, sleep quality, and sleep inconsistency. The relative importance of each variable was calculated using the relaimpo package in R 48 to understand individual regressor’s contribution to the model, which is not always clear from the breakdown of model R 2 when regressors are correlated. We found a significant regression ( F (3,84) = 8.95, p = .00003), with an R 2 of 0.24. Students’ predicted overall score was equal to 77.48 + 0.21 (sleep duration) + 19.59 (Sleep Quality) – 0.45 (sleep inconsistency). While sleep inconsistency was the only significant individual predictor of overall score ( p = 0.03) in this analysis, we found that 24.44% of variance was explained by the three regressors. The relative importance of these metrics were 7.16% sleep duration, 9.68% sleep quality, and 7.6% sleep inconsistency.
Gender differences
Females had better Sleep Quality ( t (88) = 2.63, p = 0.01), and less sleep inconsistency ( t (88) = 2.18, p = 0.03) throughout the semester compared with males, but the two groups experienced no significant difference in sleep duration ( t (88) = 1.03, p = 0.3). Sleep duration and sleep quality were significantly correlated in both males ( r (41) = 0.85, p < 0.00001) and females ( r (43) = 0.64, p < 0.00001), but this correlation was stronger in males ( Z = −2.25, p = 0.02) suggesting that it may be more important for males to get a long-duration sleep in order to get good quality sleep. In addition, sleep inconsistency and sleep quality were significantly negatively correlated in males ( r (41) = −0.51, p = 0.0005) but not in females ( r (43) = 0.29, p > 0.05), suggesting that it may be more important for males to stick to a regular daily sleep schedule in order to get good quality sleep.
Females scored higher on overall score compared with males ( t (88) = −2.48, p = 0.01), but a one-way analysis of covariance (ANCOVA) revealed that females and males did not perform significantly different on overall score when controlling for Sleep Quality, F (1, 85) = 2.22, p = 0.14. Sleep inconsistency and overall score were negatively correlated in males ( r (41) = −0.44, p = 0.003) but not in females ( r (43) = −0.13, p = 0.39), suggesting that it is important for males to stick to a regular sleep schedule in order to perform well in academic performance but less so for females. No other gender differences were detected between other sleep measures and overall score.
This study found that longer sleep duration, better sleep quality, and greater sleep consistency were associated with better academic performance. A multiple linear regression revealed that these three sleep measures accounted for 24.44% of the variance in overall grade performance. Thus, there was a substantial association between sleep and academic performance. The present results correlating overall sleep quality and duration with academic performance are well aligned with previous studies 6 , 11 , 12 , 24 , 25 on the role of sleep on cognitive performance. Similarly, this study compliments the two linked studies that found longer sleep duration during the week before final exams 47 and consistent sleep duration five days prior to a final assignment 48 enhanced students’ performance. The present study, however, significantly extends our understanding of the relation between sleep and academic performance by use of multiple objective measures of sleep throughout an entire semester and academic assessments completed along the way.
The present study also provides new insights about the timing of the relation between sleep and academic performance. Unlike a prior study, 23 we did not find that sleep duration the night before an exam was associated with better test performance. Instead we found that both longer sleep duration and better sleep quality over the full month before a midterm were more associated with better test performance. Rather than the night before a quiz or exam, it may be more important to sleep well for the duration of the time when the topics tested were taught. The implications of these findings are that, at least in the context of an academic assessment, the role of sleep is crucial during the time the content itself is learned, and simply getting good sleep the night before may not be as helpful. The outcome that better “content-relevant sleep” leads to improved performance is supported by previous controlled studies on the role of sleep in memory consolidation. 14 , 15
Consistent with some previous research 45 , 46 female students tended to experience better quality sleep and with more consistency than male students. In addition, we found that males required a longer and more regular daily sleep schedule in order to get good quality sleep. This female advantage in academic performance was eliminated once sleep patterns were statistically equated, suggesting that it may be especially important to encourage better sleep habits in male students (although such habits may be helpful for all students).
Several limitations of the present study may be noted. First, the sleep quality measures were made with proprietary algorithms. There is an evidence that the use of cardiac, respiratory, and movement information from Fitbit devices can accurately estimate sleep stages, 32 but there is no published evidence that Fitbit’s 1~10 sleep quality scores represent a valid assessment of sleep quality. Second, the relation between sleep and academic performance may be moderated by factors that can affect sleep, such as stress, anxiety, motivation, personality traits, and gender roles. Establishing a causal relation between sleep and academic performance will require experimental manipulations in randomized controlled trials, but these will be challenging to conduct in the context of real education in which students care about their grades. Third, these findings occurred for a particular student population at MIT enrolled in a particular course, and future studies will need to examine the generalizability of these findings to other types of student populations and other kinds of classes.
In sum, this study provides evidence for a strong relation between sleep and academic performance using a quantifiable and objective measures of sleep quality, duration, and consistency in the ecological context of a live classroom. Sleep quality, duration, and consistency together accounted for a substantial amount (about a quarter) of the overall variance in academic performance.
Participants
One hundred volunteers (47 females) were selected from a subset of students who volunteered among 370 students enrolled in Introduction to Solid State Chemistry at the Massachusetts Institute of Technology to participate in the study. Participants were informed of the study and gave written consent obtained in accordance with the guidelines of and approved by the MIT Committee on the Use of Humans as Experimental Subjects. Due to limitations in funding, we only had access to 100 Fitbit devices and could not enroll all students who volunteered; consequently, the first 100 participants to volunteer were selected. All participants were gifted a wearable activity tracker at the completion of the study in exchange for their participation. Seven participants were excluded from analysis because they failed to wear their activity tracker for more than 80% of the semester, three participants were excluded because they lost their wearable activity tracker, and another two participants were excluded because they completed less than 75% of the assessments in the class. Of the 88 participants who completed the study (45 females), 85 were freshmen, one was a junior and two were seniors (mean age = 18.19 years).
The Solid State Chemistry class is a single-semester class offered in the fall semester and geared toward freshmen students to satisfy MIT’s general chemistry requirement. The class consisted of weekly lectures by the professor and two weekly recitations led by 12 different teaching assistants (TAs). Each student was assigned to a specific recitation section that fit their schedule and was not allowed to attend other sections; therefore, each student had the same TA throughout the semester. Students took (1) weekly quizzes that tested knowledge on the content covered the week leading up to the quiz date, (2) three midterms that tested knowledge on the content covered in the 3–4 weeks leading up to the exam date, and (3) a final exam that tested content covered throughout the semester. Based on a one-way between subjects’ analysis of variance (ANOVA) to compare the effect of teaching assistants (TAs) on overall grade, we found no significant differences in overall grade across the TAs (F (10, 77) = 1.82, p = 0.07. (One TA was removed from the analysis because he only had one student who was participating in this study).
Participants were asked to wear an activity tracker for the entire duration of the semester without going below 80% usage each week. If 80% or more usage was not maintained, warning emails were sent at the end of that respective week. Participants were asked to return the device if they dipped below 80% usage more than three out of the 14 weeks of the semester. The average usage rate at the end of the semester for the 88 participants who completed the study was 89.4% (SD = 5.5%). The missing data appeared to be at random and were deleted prior to data analysis. As part of a separate research question, 22 of the 88 participants joined an intense cardiovascular exercise class for which they received separate physical education credit. These students performed similarly to the other 67 participants in terms of final class grade ( t (88) = 1.57, p = 0.12), exercise amount (total amount of moderately and very active minutes on the wearable device) (t (88) = 0.59, p = 0.56), sleep amount ( t (88) = 0.3, p = 0.77), and sleep quality ( t (88) = 0.14, p = 0.9), so they were included in all of the analyses.
Participants’ activities were tracked using a Fitbit Charge HR. Data from the device were recorded as follows: heart rate every 5 min; steps taken, distance traveled, floors climbed, calories burned and activity level measurements every 15 min; resting heart rate daily; and sleep duration and quality for every instance of sleep throughout the day. Sleep quality was determined using Fitbit’s proprietary algorithm that produces a value from 0 (poor quality) to 10 (good quality).
Assessments
Nine quizzes, three midterm examinations, and one final examination were administered throughout the 14-week class to assess the students’ academic achievement. The students’ cumulative class grade was made up of 25% for all nine quizzes (lowest quiz grade was dropped from the average), 15% for each midterm exam, and 30% for the final exam for a total of 100%.
At MIT, freshmen are graded on a Pass or No Record basis in all classes taken during their first semester. Therefore, all freshmen in this class needed a C- level or better (≥50%, no grading on a curve) to pass the class. A failing grade (a D or F grade) did not go on their academic record. All upperclassmen were given letter grades; A (≥85%), B (70–84%), C (50–69%), D (45–49%), F (≤44%). Because a large portion of the class had already effectively “passed” the class before taking Quiz 9 and the final exam, we excluded these two assessments from our analyses due to concerns about students’ motivation to perform their best. We calculated for each student an overall score defined as the sum of the eight quizzes and three midterms to summarize academic performance in the course.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
No custom codes were used in the analysis of this study
Dawson, D. & Reid, K. Fatigue, alcohol and performance impairment. Nature 388 , 540–545 (1997).
Article Google Scholar
Lim, J. & Dinges, D. F. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol. Bull. 136 , 375–389 (2010).
Harrison, Y. & Horne, J. A. The impact of sleep deprivation on decision making: a review. J. Exp. Psychol. Appl. 6 , 236–249 (2000).
Article CAS Google Scholar
Wagner, U., Gais, S., Haider, H., Verleger, R. & Born, J. Sleep inspires insight. Nature 427 , 352–355 (2004).
Walker, M. P. & Stickgold, R. Sleep, memory, and plasticity. Annu. Rev. Psychol. 57 , 139–166 (2006).
Wong, M. L. et al. The interplay between sleep and mood in predicting academic functioning, physical health and psychological health: a longitudinal study. J. Psychosom. Res. 74 , 271–277 (2013).
Diekelmann, S., Wilhelm, I. & Born, J. The whats and whens of sleep-dependent memory consolidation. Sleep. Med. Rev. 13 , 309–321 (2009).
Fogel, S. M., Smith, C. T. & Cote, K. A. Dissociable learning-dependent changes in REM and non-REM sleep in declarative and procedural memory systems. Behav. Brain Res. 180 , 48–61 (2007).
Eliasson, A. H. & Lettieri, C. J. Early to bed, early to rise! Sleep habits and academic performance in college students. Sleep. Breath. 14 , 71–75 (2010).
Gaultney, J. F. The prevalence of sleep disorders in college students: Impact on academic performance. J. Am. Coll. Health 59 , 91–97 (2010).
Gilbert, S. P. & Weaver, C. C. Sleep quality and academic performance in university students: A wake-up call for college psychologists. J. Coll. Stud. Psychother. 24 , 295–306 (2010).
Gomes, A. A., Tavares, J. & de Azevedo, M. H. P. Sleep and academic performance in undergraduates: A multi-measure, multi-predictor approach. Chronobiol. Int. 28 , 786–801 (2011).
Lemma, S., Berhane, Y., Worku, A., Gelaye, B. & Williams, M. A. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep. Breath. 18 , 257–263 (2014).
Gilestro, G. F., Tononi, G. & Cirelli, C. Widespread changes in synaptic markers as a function of sleep and wakefulness in drosophila. Science 324 , 109–112 (2009).
Rasch, B. & Born, J. About sleep’s role in memory. Physiol. Rev. 93 , 681–766 (2013).
Alhola, P. & Polo-Kantola, P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr. Dis. Treat. 3 , 553–567 (2007).
PubMed PubMed Central Google Scholar
Durmer, J. S. & Dinges, D. F. Neurocognitive consequences of sleep deprivation. Semin. Neurol. 25 , 117–129 (2005).
Alapin, I. et al. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? J. Psychosom. Res. 49 , 381–390 (2000).
Orzech, K. M., Salafsky, D. B. & Hamilton, L. A. The state of sleep among college students at a large public university. J. Am. Coll. Health 59 , 612–619 (2011).
Eliasson, A., Eliasson, A., King, J., Gould, B. & Eliasson, A. Association of sleep and academic performance. Sleep. Breath. 6 , 45–48 (2002).
Johns, M. W., Dudley, H. A. & Masterton, J. P. The sleep habits, personality and academic performance of medical students. Med. Educ. 10 , 158–162 (1976).
Merikanto, I., Lahti, T., Puusniekka, R. & Partonen, T. Late bedtimes weaken school performance and predispose adolescents to health hazards. Sleep. Med. 14 , 1105–1111 (2013).
Zeek, M. L. et al. Sleep duration and academic performance among student pharmacists. Am. J. Pharm. Educ. 79 , 5–12 (2015).
Hartmann, M. E. & Prichard, J. R. Calculating the contribution of sleep problems to undergraduates’ academic success. Sleep. Health 4 , 463–471 (2018).
Mirghani, H. O., Mohammed, O. S., Almurtadha, Y. M. & Ahmed, M. S. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res. Notes 8 , 706 (2015).
Onyper, S. V., Thacher, P. V., Gilbert, J. W. & Gradess, S. G. Class start times, Sleep, and academic performance in college: a path analysis. Chronobiol. Int. 29 , 318–335 (2012).
Ming, X. et al. Sleep insufficiency, sleep health problems and performance in high school students. Clin. Med. Insights Circ. Respir. Pulm. Med. 5 , 71–79 (2011).
Lee, Y. J., Park, J., Soohyun, K., Seong-jin, C. & Seog Ju, K. Academic performance among adolescents with behaviorally. J. Clin. Sleep. Med. 11 , 61–68 (2015).
Díaz-Morales, J. F. & Escribano, C. Social jetlag, academic achievement and cognitive performance: Understanding gender/sex differences. Chronobiol. Int. 32 , 822–831 (2015).
Raley, H., Naber, J., Cross, S. & Perlow, M. The impact of duration of sleep on academic performance in University students. Madr. J. Nurs. 1 , 11–18 (2016).
Haraszti, R. Á., Ella, K., Gyöngyösi, N., Roenneberg, T. & Káldi, K. Social jetlag negatively correlates with academic performance in undergraduates. Chronobiol. Int. 31 , 603–612 (2014).
Scullin, M. K. The eight hour sleep challenge during final exams week. Teach. Psychol. 46 , 55–63 (2018).
King, E., Mobley, C. & Scullin, M. K. The 8‐hour challenge: incentivizing sleep during end‐of‐term assessments. J. Inter. Des. 44 , 85–99 (2018).
PubMed Google Scholar
Beattie, Z. et al. Estimation of sleep stages using cardiac and accelerometer data from a wrist-worn device. Sleep 40 , A26–A26 (2017).
Clark, M. J. & Grandy, J. Sex differences in the academic performance of scholastic aptitude test takers. ETS Res. Rep. Ser. 2 , 1-27 (1984).
Google Scholar
Kimball, M. M. A new perspective on women’s math achievement. Psychol. Bull. 105 , 198–214 (1989).
Mau, W.-C. & Lynn, R. Gender differences on the scholastic aptitude test, the American college test and college grades. Educ. Psychol. 21 , 133–136 (2001).
Willingham, W. W. & Cole, N. S. Gender and fair assessment . (Mahwah, NJ, US, Lawrence Erlbaum Associates, 1997).
Volchok, E. Differences in the performance of male and female students in partially online courses at a community college. Community Coll . J . Res . Pract . 1–17, https://doi.org/10.1080/10668926.2018.1556134 (2018).
Duckworth, A. L. et al. Will not want: self-control rather than motivation explains the female advantage in report card grades. Learn. Individ. Differ. 39 , 13–23 (2015).
Carvalho, R. G. G. Gender differences in academic achievement: The mediating role of personality. Pers. Individ. Differ. 94 , 54–58 (2016).
Duckworth, A. L. & Seligman, M. E. P. Self-discipline gives girls the edge: gender in self-discipline, grades, and achievement test scores. J. Educ. Psychol. 98 , 198–208 (2006).
Tsai, L. L. & Li, S. P. Sleep patterns in college students: Gender and grade differences. J. Psychosom. Res. 56 , 231–237 (2004).
Becker, S. P. et al. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4 , 174–181 (2018).
Bixler, E. O. et al. Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J. Sleep. Res. 18 , 221–228 (2009).
Mallampalli, M. P. & Carter, C. L. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J. Women’s. Health 23 , 553–562 (2014).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodol.) 57 , 289–300 (1995).
Grömping, U. Relative importance for linear regression in R: The package relaimpo. J. Stat. Softw. 17 , 1–27 (2015).
Download references
Acknowledgements
This research was supported by a grant from the Horace A. Lubin Fund in the MIT Department of Materials Science and Engineering to J.C.G. and funding from MIT Integrated Learning Initiative to K.O. and J.R.K. The authors are grateful for many useful discussions with Carrie Moore and Matthew Breen at the Department of Athletics, Physical Education, and Recreation at MIT.
Author information
Authors and affiliations.
MIT Integrated Learning Initiative, Department of Brain and Cognitive Sciences, and McGovern Institute for Brain Research, Massachusetts Institute of Technology, Cambridge, MA, 02139, USA
Kana Okano, Jakub R. Kaczmarzyk & John D. E. Gabrieli
Harvard Business School, Boston, MA, 02163, USA
Department of Materials Science and Engineering Massachusetts Institute of Technology, Cambridge, MA, 02139, USA
Jeffrey C. Grossman
You can also search for this author in PubMed Google Scholar
Contributions
K.O. and J.C.G. conceived, designed, supervised, and analyzed the project. J.K. and N.D. helped analyze the data. The manuscript was written by K.O., J.D.E.G., and J.C.G.
Corresponding author
Correspondence to Jeffrey C. Grossman .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Okano, K., Kaczmarzyk, J.R., Dave, N. et al. Sleep quality, duration, and consistency are associated with better academic performance in college students. npj Sci. Learn. 4 , 16 (2019). https://doi.org/10.1038/s41539-019-0055-z
Download citation
Received : 20 March 2019
Accepted : 17 July 2019
Published : 01 October 2019
DOI : https://doi.org/10.1038/s41539-019-0055-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative

This article is cited by
Social isolation consequences: lessons from covid-19 pandemic in a context of dynamic lock-down in chile.
- Alessandra Patrono
- Stefano Renzetti
- Roberto G. Lucchini
BMC Public Health (2024)
Electrophysiological effects of Japanese cedarwood on sleep quality in humans
- Tsuyoshi Okamoto
- Taisuke Nakashima
- Kuniyoshi Shimizu
Journal of Wood Science (2024)
Ontogeny and social context regulate the circadian activity patterns of Lake Malawi cichlids
- Aakriti Rastogi
- Alex C. Keene
Journal of Comparative Physiology B (2024)
The Effects of Pre-bedtime Blue-Light Exposure on Subjective Sleep Quality, Attention, and Work Efficiency in Men Students: A Pilot Study
- Takuya Uchiumi
- Masao Ishizawa
- Toshiaki Sato
Sleep and Vigilance (2024)
Sleep duration associated with feelings but not with test scores: an observational study
- Kosha J. Mehta
Discover Psychology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Why Sleep Is Important for Brain Health

A neurologist and sleep medicine specialist explain how sleep impacts our brain health and how to regulate our circadian rhythms for optimal sleep.
It’s estimated that at least 50 million Americans suffer from a sleep disorder. But sleep—both the quantity and quality—is crucial to our brain health. Research has now shown a correlation between sleep disturbances and numerous neurological diseases. These include stroke, cognitive aging, dementia, Parkinson’s disease, and others.
The brain is complex and interconnected. The American Brain Foundation believes finding a cure for one brain disease will help find cures for others. Just as well, the association between sleep and brain health illustrates how one issue can be linked to multiple diseases.
In our recent webinar , Phyllis C. Zee, MD, PhD, Chief of the Division of Sleep Medicine at Northwestern University’s Feinberg School of Medicine, spoke about how sleep and our circadian rhythms play an important role in brain health.
The Role of Sleep and Circadian Rhythms
The “master clock” of the brain, the suprachiasmatic nucleus, controls many systems of the body exhibiting rhythmic activity patterns. Our body systems follow a cycle of rest and activity, synchronized with each other to help the body function. This means sleep is regulated by our bodies at the cellular and molecular level. “Similarly, the circadian rhythm, or these near 24-hour biological rhythms, have been shown to be genetically regulated and they exist in almost every cell of our body,” says Dr. Zee.
It’s a two-way relationship. Our brains and bodies regulate our sleep and circadian rhythms. Equally so, our sleep and circadian rhythms affect our brains and bodies. Sleep disturbances have a broad impact on our health and body functions. They’re also linked to an increased risk for disease, including neurodegenerative disorders like Alzheimer’s and Parkinson’s. Some data indicates that sleep and circadian rhythm dysfunction, such as fragmented sleep or night wakings, may be a risk factor for these types of brain disease.
More specifically, research shows that slow-wave sleep, or deep sleep, decreases with age. A lower amount of deep sleep is associated with an increase in beta amyloid. This is a protein that has been found to accumulate in people with Alzheimer’s. When we get quality sleep, the fluids between neurons are better able to flush out large molecules and prevent toxic buildup through a process called the glymphatic flow. Disrupted sleep could therefore increase the risk for neurodegenerative brain diseases.
Additionally, many people with Parkinson’s disease experience REM sleep behavior disorder (RBD), in which they physically act out their dreams, for years before their diagnosis. In this way, the sleep disorder could be considered a prodromal syndrome, or a sign that may precede Parkinson’s. People with RBD are also more likely to develop cognitive problems or dementia.
How to Improve Sleep and Circadian Rhythms to Preserve Brain Health
This connection between sleep and brain health shows us there is potential to prevent and treat brain diseases by improving sleep and circadian rhythms. Dr Zee asks, “If we can improve sleep and circadian rhythms, can they be these targets for disease modification and some of these age-related changes?”
For example, in one study, researchers used a sound that stimulates slow-wave sleep (acoustic stimulation) to improve deep sleep in older adults. The amount of improvement in slow-wave sleep was directly correlated to an improvement in memory. In another study of people with Parkinson’s, timed light therapy improved daytime sleepiness, sleep quality, daily physical activity levels, and Total Unified Parkinson’s Disease Rating Scale score, which measures the severity and progression of the disease.
For our bodies to function well, our internal rhythm needs to be in sync with our external exposure to light and darkness. The retinas in our eyes have receptors that take in different wavelengths of light, both sunlight and artificial, from across the whole spectrum. Matching your internal clock to that of the sun ensures you get the right types of light at the right times. These daily shifts in light and dark affect our sleep and wake cycles, circadian rhythms, metabolism, and energy levels. Our nutrition—when, what, and how much we eat—also provides information to our master clock.
In this way, our lifestyles can affect our sleep and circadian rhythms. That can mean external factors, like our daily schedule or cycles of light exposure, can negatively impact sleep. But it also means lifestyle changes have the power to positively impact sleep.
To start, Dr. Zee recommends setting a regular sleep-wake schedule that will provide 7 to 8 hours of sleep per night. However, she notes that it’s not only how much you sleep but also when you sleep—that is, staying in rhythm—that is important for brain health. Appropriately timed light exposure and eating, as well as regular exercise and activity levels during the day, will help your body stay in rhythm. Also, reduce or avoid alcohol, as it can disrupt your sleep and suppress REM and slow-wave sleep. This causes a rebound effect that awakens you in the early morning hours.
How Much Sleep Is Enough? How Do You Know You’re Getting Enough?
Regularity is key. We all have a bad night here and there. But if it’s chronic it can have a bigger impact on our health. The general recommendation is 7 to 8 hours for adults, possibly closer to 7 hours for older adults. But there are also individual differences based on our unique bodies and needs.
So how do you know you’re getting enough sleep? Consider how you feel during the day. Are you able to stay awake and attentive and carry out your daily activities? Since we can’t get regular imaging of our brains, these daytime indicators help us gauge how much sleep we need.
Can Medications or Supplements Help You Sleep?
Pharmaceuticals don’t typically provide deep sleep. In other cases, they can induce deep sleep all night long. But they also cause people to wake up feeling “hungover” or more tired. When it comes to deep sleep, more is not better. Timing is important: deep sleep is necessary earlier in the night and dissipates closer to morning.
Melatonin affects the circadian system and promotes sleep by decreasing the arousal, or alerting signal, from the circadian clock. With aging, our natural melatonin levels go down. If you choose to take melatonin, be sure to stick to small doses (between half a milligram to 3 milligrams) unless recommended otherwise by your doctor, as high doses can affect your vascular system.
Some people experience insomnia and feel like they can’t “shut down” their brains. In these cases, imaging shows that even while asleep there is a lot of metabolic activity in the brain, sometimes even more than during the daytime. This may account for the fatigue and decreased attention many of those with insomnia experience. Besides medication, cognitive behavioral therapy (CBT) can help address this issue and decrease that arousal.
What’s the Best Way to Measure Sleep?
Most consumer technology devices, like Fitbits, don’t measure the brain-wave sleep that is an indicator of brain health. However, they can still offer insights about your sleeping patterns and wakefulness during the course of the night. During slow-wave sleep or REM sleep, there are physical changes in your body. These include your heart rate, body temperature, and activity levels. Sensors that monitor those levels can use algorithms to predict when you’re asleep versus when you’re awake, and some newer algorithms can even distinguish light and deep sleep. One advantage to these sensors, as opposed to a formal overnight sleep study, is that they measure every day and can give a sense of your sleep regularity over time.
Is There Anything Wrong With Staying Up Late if You Can Still Get 7 to 8 Hours of Sleep?
As Dr. Zee says, “It’s better to live with your clock than against your clock.” The key is getting the right amount of quality sleep during your individual circadian time. For a “night owl,” living with your clock might translate to a later bedtime and wake time, as your schedule allows. But if you need to accommodate your work or social obligations, the use of light exposure and melatonin can help shift your clock.
Will a Nap Help?
Between 1 and 3 p.m., we may feel a natural “afternoon dip” in energy levels. Taking a nap during this time can refresh us, but it won’t make up for lost nighttime sleep. While we may not sleep for 7 to 8 hours straight every night, consolidated sleep is important. That’s because the extended time allows us to move through sleep cycles. You likely won’t hit all the necessary points in a sleep cycle during a nap.
If you have concerns about your sleep, be sure to speak to your doctor. They can recommend lifestyle changes, medications, or supplements that align with your unique biology and circumstances to help you get quality sleep—and ultimately improve your brain health.
The American Brain Foundation is committed to finding cures for all brain diseases. Donate today to make a difference . With your help, we won’t have to imagine a world without brain disease, we’ll be able to live in one.
- Your Name *
- Your Email *
- Your Message *
- Name This field is for validation purposes and should be left unchanged.
Don’t forget to join our email list to stay updated on the latest brain disease information, resources and events.
- ABOUT THE PROJECT
- ONGOING PROJECTS
- PUBLICATIONS
- SURVEY METHODS
- SPOTLIGHT ON:
- DRUGS AND ALCOHOL
- PHYSICAL ACTIVITY
- SEDENTARY BEHAVIOR
- SEE ALL FINDINGS
- WOMEN’S FINANCIAL SECURITY
- HOME OWNERSHIP
- EMERGENCY FUNDS
- HEALTH INSURANCE
- INVESTMENTS
- LIFE INSURANCE
- LONG TERM CARE
- VOLUNTEERISM
- CIVIC ENGAGEMENT
- RELIGIOUS ORGANIZATIONS
- WORKING FOR PAY
- AFFILIATE INTERVIEWS
- DIRECTORS’ BLOG POSTS
- EXPERT PERSPECTIVES
- PERSONAL PERSPECTIVES
- STANFORD CENTER ON LONGEVITY >
- Research Update on Diet
- Research Update on Sleep
Research Update 1
By Marie Conley Smith
I n a world full of opportunities, stressors, inequalities, and distractions, maintaining a healthy lifestyle can be challenging, and sleep is often the first habit to suffer. Good sleep hygiene is a huge commitment: it takes up about a third of the day, every day, and works best when kept on a consistent schedule. It does not help that the primary short-term symptoms of insufficient sleep can be self-medicated away with caffeine. However, the effects of sleep loss can range from inconvenient to downright dangerous; people have trouble learning and being productive, take risks more readily, and are more likely to get into accidents. These effects also last longer than it takes to get them, as recovering from each night of poor sleep takes multiple days. When it comes to sleep, every night counts. In this update, we will discuss what Stanford researchers have to say about sleep and why we need it, who is getting too little of it, and some of the latest findings that may help us sleep better.
We have not cracked the code on sleep
Despite this progress, scientists have not been able to crack the code of why sleep is critical to brain function. There is also little consensus about how sleep stages actually affect quality of sleep and how they affect us when we are awake.
Part of the challenge of cracking the code on sleep is how difficult it is to study. The gold standard of sleep study, polysomnography, developed by Dement in the 1960s, 1 is the most reliable tool for measuring many sleep characteristics and detecting sleep disorders such as obstructive sleep apnea and narcolepsy. However, it is expensive and time-consuming to run, which means that usually only a night or two is recorded. This snapshot of sleep may not reflect what normally occurs for a given person, and makes it difficult to draw conclusions about their behavior and performance in the days surrounding the sleep measurement.
The recent explosion in consumer wearable devices is a promising trend for researchers because of their potential to measure thousands of people’s sleep in their natural environments. They have not yet been widely adopted as measurement tools by scientists, however, as it is unclear if they provide the level of precision and measurement consistency required for a scientific study. Researchers at Stanford have called for these devices to be cleared by the FDA before using them to assign a diagnosis. 2 The “holy grail” would be a wearable device that could track sleep accurately while also providing performance information about the rest of the day, which would allow researchers to recognize more nuanced relationships between how people sleep and how it affects their lives.

The short- and long-term effects of insufficient sleep
We all know anecdotally what it is like to get too little sleep; it might be described with words and phrases like “tired,” “cranky,” “sluggish,” and “need caffeine.” Review of the scientific literature reveals how wide-ranging these effects can be. With too little sleep, people have a harder time learning 3 and concentrating, and are more likely to take risks. 4,5 The likelihood of getting into an auto accident increases. 6 Sleep deprivation has a bidirectional relationship with depression, 7,8 in that insomnia often both precedes and follows a depressive episode. Short sleep also interferes with other Healthy Living behaviors: people are more likely to crave sweet and fatty foods 9 and to choose foods that are calorically dense, 10 are more prone to injury during exercise, 11 and have an increased risk of obesity. 12
Sleep deprivation can even affect mundane daily activities. In 2017, then Stanford PhD candidate Tim Althoff and Professor Jamie Zeitzer of the Stanford Center for Sleep Sciences and Medicine took up the sleep measurement challenge by collaborating with Microsoft Research to examine the effects of sleep deprivation through a common daily activity: using an online search engine. 13 They paired users’ Microsoft Band sleep data with their Bing searches among users who had agreed to share their activity for study. By linking quantity and timing of sleep with typing speed during the searches, they were able to draw a number of conclusions about how sleep quality affects performance.
In this study, the researchers captured the sleep duration and search engine interactions of over 31,000 people. The researchers measured the amount of time between keystrokes as people typed their search engine entries, and used this as a measure of daily performance (that is, how well people did after a night of sleep). They were able to track the people who had multiple nights of insufficient sleep (defined as 6 hours of sleep or fewer) to see if their typing speed changed. They found that, on average, one night of insufficient sleep resulted in worse performance for three days, and two nights of insufficient sleep negatively impacted performance for six days. In other words, it took people almost an entire week to recover their performance after two consecutive nights of insufficient sleep. The implication is that the impact of sleep loss can persist for days.
Recent Stanford solutions for better sleep
Ongoing research at Stanford has led both to treatments for sleep disorders and to recommendations for best sleep practices for the public.

There are a few clinics and organizations that offer CBTI remotely in an effort to give more people access. There are apps such as SleepRate , which features content designed by Stanford researchers, Somryst , which was recently approved by the FDA, and Sleepio , which is offered by several large employers as an employee benefit. The Cleveland Sleep Clinic offers a 6-week online program called “ Go! to Sleep ,” and the U.S. Department of Veterans Affairs offers one of the same duration called “ Path to Better Sleep .” A physician should be consulted before starting any of these programs to ensure there are not any underlying disorders that need to be addressed.
Ultrashort light flash therapy Professor Jamie Zeitzer was interested in helping people who had a hard time sleeping because their circadian rhythm was not in sync with their desired sleep schedule. He discovered that ultrashort bursts of light directed into a person’s closed eyes while they were sleeping was very effective at shifting the time a person starts getting sleepy. Sleep doctors had already been using continuous light to help people reset their internal clock while they were awake; this new short-flash method shows great promise not only because of its effectiveness, but because it can be administered passively while people are sleeping. The approach involves wearing a sleep mask that emits the bright flashes and has been shown to only wake individuals who are particularly sensitive to light.

Lumos Sleep Mask
Professor Zeitzer and his team administered these ultrashort light flashes to teenagers, whose natural circadian systems have shifted so that their sleep and wake times are considerably later than children or adults. The time structure of our society, and schools in particular, does not take this into account. Professor Zeitzer administered the light flashes to see if it would help teens go to bed earlier. 20 They found that, while the teenagers were getting sleepy earlier, the light flashes alone were not enough to get the teenagers to bed earlier. With a second group of teens, they combined the light therapy with cognitive behavioral therapy (CBT) sessions. The CBT sessions served to inform the teens about sleep health and hygiene and helped them schedule their activities to allow for their desired sleep hours. After this combined therapy trial, the teens went to bed an average of 50 minutes earlier, getting an average of 43 more minutes of sleep per night. The researchers found the CBT component to be integral to behavior change – without the added education and support, the teens were not motivated enough to change their behavior and would simply push past their sleepiness.
This ultrashort light flash therapy can be used by anyone who may want to shift their sleep schedule; for example, to rebound from jet lag or to cope with a consistent graveyard shift at work. There is no evidence that other groups would require accompanying CBT like the teens, as long as they are self-motivated to change their sleep schedule. Zeitzer plans to test this technology next with older adults who wish to push their sleep time later. A company has spun out of this work, which Zeitzer advises but in which he has no financial interest, called Lumos . They are currently developing their product, and are hoping to make this intervention widely available.
Data Spotlight on: Black Americans

While most Americans have seen improvements in sleep over the past decade, Black Americans continue to sleep significantly less than other groups. This trend has been examined both by researchers and the popular press. 21,22 Researchers have found that Black Americans, in addition to getting shorter sleep, are also more likely to get poor quality sleep – spending less time in the most restorative stages of sleep 23,24 – and to develop obstructive sleep apnea. 25 Black Americans are also disproportionately affected by diseases that have been associated with poor sleep, such as obesity, diabetes, 26 and cardiovascular disease. 25
The exact reason(s) for Black Americans’ poor sleep is still unclear, though researchers have proposed potential contributing factors, largely related to the social inequality Black Americans face in the U.S.:
Experiences of discrimination : the stress of racial discrimination has been associated with spending lesstime in deep sleep and more time in light sleep among Black Americans. 24
Living environment : neighborhood quality has been linked to sleep quality, 27 and Stanford researchersfound that racial and income disparities persist in neighborhoods. 28 They found that while middle-income white families are more likely to live in resource-rich neighborhoods with other middle-income families, middle-income black families tend to live in markedly lower-income, resource-poorneighborhoods.
Work and income inequality : for example, shift work can cause irregular working hours. This leadspeople to suffer “social jetlag,”; a discrepancy in sleep hours between work and free days, 29 leading tosymptoms of sleep deprivation.
Lack of access to resources : particularly sleep-related healthcare and education.
Some of these factors are being addressed directly. Professor Girardin Jean-Louis from New York University and his team have devoted themselves to addressing the access to healthcare and education issue among local black communities in New York by tailoring online materials about obstructive sleep apnea to the culture, language, and barriers of specific communities. 30 Professor Jamie Zeitzer and his team at Stanford recently completed an initial clinical trial of a drug (suvorexant), which was found to help people who work at night get three more hours of sleep during the day. 31 Professor Zeitzer’s ultrashort light flash therapy (discussed above) may also help with shift work. These interventions could help to improve sleep for Black Americans, but they may not make up the whole picture; it could be that the underlying social inequality needs to be addressed in order to fully close the sleep gap.
Thanks to Jamie Zeitzer and Ken Smith for their insights and edits on this report.
- Deak, M., & Epstein, L. J. (2009). The history of polysomnography. Sleep Medicine Clinics , 4 (3), 313–321.
- Cheung, J., Zeitzer, J. M., Lu, H., & Mignot, E. (2018). Validation of minute-to-minute scoring for sleep and wake periods in a consumer wearable device compared to an actigraphy device. Sleep Science and Practice , 2 (1), 11. https://doi.org/10.1186/s41606-018-0029-8
- Gao, C., Terlizzese, T., & Scullin, M. K. (2019). Short sleep and late bedtimes are detrimental to educational learning and knowledge transfer: An investigation of individual differences in susceptibility. Chronobiology International , 36 (3), 307–318. https://doi.org/10.1080/07420528.2018.1539401
- O’Brien, E. M., & Mindell, J. A. (2005). Sleep and risk-taking behavior in adolescents. Behavioral Sleep Medicine , 3 (3), 113–133. https://doi.org/10.1207/s15402010bsm0303_1
- Rusnac, N., Spitzenstetter, F., & Tassi, P. (2019). Chronic sleep loss and risk-taking behavior: Does the origin of sleep loss matter? Behavioral Sleep Medicine , 17 (6), 729–739. https://doi.org/10.1080/15402002.2018.1483368
- Bioulac, S., Micoulaud-Franchi, J.-A., Arnaud, M., Sagaspe, P., Moore, N., Salvo, F., & Philip, P. (2017). Risk of motor vehicle accidents related to sleepiness at the wheel: A systematic review and meta-analysis. Sleep , 40 (10). https://doi.org/10.1093/sleep/zsx134
- Franzen, P. L., & Buysse, D. J. (2008). Sleep disturbances and depression: Risk relationships for subsequent depression and therapeutic implications. Dialogues in Clinical Neuroscience , 10 (4), 473–481.
- Tsuno, N., & Ritchie, K. (2005). Sleep and Depression. The Journal of Clinical Psychiatry , 16.
- Lv, W., Finlayson, G., & Dando, R. (2018). Sleep, food cravings and taste. Appetite , 125 , 210–216. https://doi.org/10.1016/j.appet.2018.02.013
- Pardi, D., Buman, M., Black, J., Lammers, G. J., & Zeitzer, J. M. (2017). Eating decisions based on alertness levels after a single night of sleep manipulation: A randomized clinical trial. Sleep , 40 (2). https://doi.org/10.1093/sleep/zsw039
- Chennaoui, M., Arnal, P. J., Sauvet, F., & Léger, D. (2015). Sleep and exercise: A reciprocal issue? Sleep Medicine Reviews , 20 , 59–72. https://doi.org/10.1016/j.smrv.2014.06.008
- Cappuccio, F. P., Taggart, F. M., Kandala, N. B., Currie, A., Peile, E., Stranges, S., & Miller, M. A. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep , 31 (5), 619-626.
- Althoff, T., Horvitz, E., White, R. W., & Zeitzer, J. (2017, April). Harnessing the web for population-scale physiological sensing: A case study of sleep and performance. In Proceedings of the 26th international conference on World Wide Web (pp. 113-122).
- Roth, T. (2007). Insomnia: Definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine , 3 (5 Suppl), S7–S10.
- Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine , 165 (2), 125–133. https://doi.org/10.7326/M15-2175
- Jacobs, G. D., Pace-Schott, E. F., Stickgold, R., & Otto, M. W. (2004). Cognitive behavior therapy and pharmacotherapy for insomnia: A randomized controlled trial and direct comparison. Archives of Internal Medicine , 164 (17), 1888–1896. https://doi.org/10.1001/archinte.164.17.1888
- Manber, R., Bei, B., Simpson, N., Asarnow, L., Rangel, E., Sit, A., & Lyell, D. (2019). Cognitive behavioral therapy for prenatal insomnia: A randomized controlled trial. Obstetrics & Gynecology , 133 (5), 911–919. https://doi.org/10.1097/AOG.0000000000003216
- Ong, J. C., Crawford, M. R., Dawson, S. C., Fogg, L. F., Turner, A. D., Wyatt, J. K., Crisostomo, M. I., Chhangani, B. S., Kushida, C. A., Edinger, J. D., Abbott, S. M., Malkani, R. G., Attarian, H. P., & Zee, P. C. (2020). A randomized controlled trial of CBT-I and PAP for obstructive sleep apnea and comorbid insomnia: Main outcomes from the MATRICS study. Sleep . https://doi.org/10.1093/sleep/zsaa041
- Karlin, B. E., Trockel, M., Taylor, C. B., Gimeno, J., & Manber, R. (20130415). National dissemination of cognitive behavioral therapy for insomnia in veterans: Therapist- and patient-level outcomes. Journal of Consulting and Clinical Psychology , 81 (5), 912. https://doi.org/10.1037/a0032554
- Kaplan, K. A., Mashash, M., Williams, R., Batchelder, H., Starr-Glass, L., & Zeitzer, J. M. (2019). Effect of light flashes vs sham therapy during sleep with adjunct cognitive behavioral therapy on sleep quality among adolescents: A randomized clinical trial. JAMA Network Open , 2 (9), e1911944. https://doi.org/10.1001/jamanetworkopen.2019.11944
- Resnick, B. (2015, October 27). The Racial Inequality of Sleep . The Atlantic. https://www.theatlantic.com/health/archive/2015/10/the-sleep-gap-and-racial-inequality/412405/
- Resnick, B., & Barton, G. (2018, April 12). Black Americans don’t sleep as well as white Americans. That’s a problem. Vox. https://www.vox.com/science-and-health/2018/4/12/17224328/sleep-gap-black-white-minority-america-health-consequences
- Beatty, D. L., Hall, M. H., Kamarck, T. A., Buysse, D. J., Owens, J. F., Reis, S. E., Mezick, E. J., Strollo, P. J., & Matthews, K. A. (2011). Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology , 30 (3), 351–359. https://doi.org/10.1037/a0022976
- Tomfohr, L., Pung, M. A., Edwards, K. M., & Dimsdale, J. E. (2012). Racial differences in sleep architecture: The role of ethnic discrimination. Biological Psychology , 89 (1), 34–38. https://doi.org/10.1016/j.biopsycho.2011.09.002
- Olafiranye, O., Akinboboye, O., Mitchell, J., Ogedegbe, G., & Jean-Louis, G. (2013). Obstructive sleep apnea and cardiovascular disease in blacks: A call to action from association of black cardiologists. American Heart Journal , 165 (4), 468–476. https://doi.org/10.1016/j.ahj.2012.12.018
- Jackson, C. L., Redline, S., Kawachi, I., & Hu, F. B. (2013). Association between sleep duration and diabetes in black and white adults. Diabetes Care , 36 (11), 3557–3565. https://doi.org/10.2337/dc13-0777
- Hale, L., Hill, T. D., & Burdette, A. M. (2010). Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Preventive Medicine , 51 (3–4), 275–278. https://doi.org/10.1016/j.ypmed.2010.06.017
- Reardon, S. F., Fox, L., & Townsend, J. (2015). Neighborhood income composition by household race and income, 1990–2009. The ANNALS of the American Academy of Political and Social Science , 660 (1), 78–97. https://doi.org/10.1177/0002716215576104
- Wittmann, M., Dinich, J., Merrow, M., & Roenneberg, T. (2006). Social jetlag: Misalignment of biological and social time. Chronobiology International , 23 (1–2), 497–509. https://doi.org/10.1080/07420520500545979
- Jean-Louis, G., Robbins, R., Williams, N. J., Allegrante, J. P., Rapoport, D. M., Cohall, A., & Ogedegbe, G. (2020). Tailored Approach to Sleep Health Education (TASHE): A randomized controlled trial of a web-based application. Journal of Clinical Sleep Medicine . https://doi.org/10.5664/jcsm.8510
- Zeitzer, J. M., Joyce, D. S., McBean, A., Quevedo, Y. L., Hernandez, B., & Holty, J.-E. (2020). Effect of suvorexant vs placebo on total daytime sleep hours in shift workers: A randomized clinical trial. JAMA Network Open , 3 (6), e206614. https://doi.org/10.1001/jamanetworkopen.2020.6614
- Sleep Disorders
- Good Sleep Habits
- Other Sleep Problems
- What Affects Sleep
- Tests & Treatment
- View Full Guide
Surprising Reasons to Get More Sleep

A lack of sleep at night can make you cranky the next day. And over time, skimping on sleep can mess up more than just your morning mood. Studies show getting quality sleep on a regular basis can help improve all sorts of issues, from your blood sugar to your workouts.
Here's why you should give your body the ZZZs it needs.
Sharper Brain
When you're running low on sleep, you'll probably have trouble holding onto and recalling details. That's because sleep plays a big part in both learning and memory. Without enough sleep, it's tough to focus and take in new information. Your brain also doesn't have enough time to properly store memories so you can pull them up later.
Sleep lets your brain catch up so you're ready for what's next.
Another thing that your brain does while you sleep is process your emotions. Your mind needs this time in order to recognize and react the right way. When you cut that short, you tend to have more negative emotional reactions and fewer positive ones.
Chronic lack of sleep can also raise the chance of having a mood disorder. One large study showed that when you have insomnia, you're five times more likely to develop depression, and your odds of anxiety or panic disorders are even greater.
Refreshing slumber helps you hit the reset button on a bad day, improve your outlook on life, and be better prepared to meet challenges.
Healthier Heart
While you sleep, your blood pressure goes down, giving your heart and blood vessels a bit of a rest. The less sleep you get, the longer your blood pressure stays up during a 24-hour cycle. High blood pressure can lead to heart disease, including stroke.
Short-term down time can have long-term payoffs.
Athletic Achievement
If your sport requires quick bursts of energy , like wrestling or weightlifting, sleep loss may not affect you as much as with endurance sports like running, swimming, and biking. But you're not doing yourself any favors.
Besides robbing you of energy and time for muscle repair, lack of sleep saps your motivation, which is what gets you to the finish line. You'll face a harder mental and physical challenge -- and see slower reaction times.
Proper rest sets you up for your best performance.
Steadier Blood Sugar
During the deep, slow-wave part of your sleep cycle, the amount of glucose in your blood drops. Not enough time in this deepest stage means you don't get that break to allow a reset -- like leaving the volume turned up. Your body will have a harder time responding to your cells' needs and blood sugar levels.
Allow yourself to reach and remain in this deep sleep, and you're less likely to get type 2 diabetes.
Germ Fighting
To help you ward off illnesses, your immune system identifies harmful bacteria and viruses in your body and destroys them. Ongoing lack of sleep changes the way your immune cells work. They may not attack as quickly, and you could get sick more often.
Good nightly rest now can help you avoid that tired, worn-out feeling, as well as spending days in bed as your body tries to recover.
Weight Control
When you're well-rested, you're less hungry. Being sleep-deprived messes with the hormones in your brain -- leptin and ghrelin -- that control appetite.
With those out of balance, your resistance to the temptation of unhealthy foods goes way down. And when you're tired, you're less likely to want to get up and move your body. Together, it's a recipe for putting on pounds.
The time you spend in bed goes hand-in-hand with the time you spend at the table and at the gym to help you manage your weight.
Too Much of a Good Thing?
Sleep needs vary, but on average, regularly sleeping more than 9 hours a night may do more harm than good. Research found that people who slept longer had more calcium buildup in their heart arteries and less flexible leg arteries, too.
Your best bet is to shoot for 7-8 hours of slumber each night for peak health benefits.
- Benefits of Sleep
- How Much Sleep Is Enough?

Top doctors in ,
Find more top doctors on, related links.
- Healthy Sleep News
- Healthy Sleep Reference
- Healthy Sleep Slideshows
- Healthy Sleep Quizzes
- Healthy Sleep Blogs
- Healthy Sleep Videos
- Sleep Medications
- Find a Neurologist
- Find a Sleep Specialist
- Circadian Rhythm
- Drug Interaction Checker
- Restless Legs Syndrome
- Sleep Apnea
- Teeth Grinding
- Track Your Sleep
- More Related Topics
- How It Works
- Testimonials
- Know Your Risk
- Book Your Scan
The Incredible Benefits of Sleep: Why a Good Night’s Rest Is Essential for Your Health

Sleep is a fundamental pillar of self-care , alongside nutrition and exercise. As awareness grows about its vital role, more people recognize that quality sleep is not a luxury but a necessity for optimal physical and mental functioning.
Sleep promotes growth and cellular repair, supports heart health, helps maintain a healthy weight, and strengthens the immune system, among other things. Many people struggle to achieve sufficient sleep. However, ongoing research highlights the far-reaching impacts of sleep deprivation, prompting a shift in focus toward sleep quality and overall well-being.
This article will explore the science behind sleep, the benefits of getting enough sleep, and how sleep deprivation can negatively impact health.
The Benefits of Sleep: Unlocking the Power of Rest for Better Health
The science behind sleep: understanding its importance.
Sleep is a complex biological process that occurs in cycles through the night, consisting of both non-rapid eye movement (NREM) and rapid eye movement (REM) stages. Each cycle typically lasts 90-120 minutes, with 4-5 cycles occurring during a full night’s sleep.
This is divided into four stages :
- Stage N1: Light sleep lasting 5-10 minutes.
- Stage N2: Deeper sleep lasting 10-25 minutes, characterized by sleep spindles and K-complexes.
- Stage N3 and N4: Deep sleep, also known as slow-wave sleep, lasting 20-40 minutes.
During deep NREM sleep, the body repairs tissues, builds bone and muscle, and strengthens the immune system. Stage N2 of NREM sleep is particularly important for memory consolidation.
REM sleep occurs about 90 minutes after falling asleep and is characterized by rapid eye movements, increased brain activity, and vivid dreams. Like N2 NREM sleep, REM also helps transfer short-term memories to long-term storage.
Sleep also helps regulate hormones, controlling appetite, stress, and growth.
Sleep and Physical Health
Adequate sleep is crucial for maintaining optimal physical health. It supports immune function by enhancing the production and effectiveness of T-cells, which fight infections and regulate immune responses.
For heart health, sleep allows the cardiovascular system to rest, reducing blood pressure and heart rate, which helps prevent heart disease and stroke. Sleep also plays a vital role in weight management by regulating hunger hormones like ghrelin and leptin, helping to control appetite and metabolism.
Proper sleep also improves insulin sensitivity, aiding blood sugar regulation and reducing the risk of type 2 diabetes . Overall, consistent quality sleep is essential for bodily repair, restoration, and maintenance of various physiological functions.
Sleep and Mental Health
Sleep significantly impacts mood, stress levels, and cognitive function. Adequate sleep promotes emotional regulation, reducing the risk of depression and anxiety . Conversely, sleep deprivation can amplify negative emotions and stress reactivity.
Quality sleep enhances cognitive abilities, including attention, memory consolidation, and decision-making. Poor sleep is associated with increased stress hormone levels, while sufficient sleep helps regulate the stress response .
Moreover, sleep is vital for brain function, clearing waste products and supporting neuroplasticity . The relationship between sleep and mental health is bidirectional ; improving sleep quality can lead to better mental health outcomes and vice versa, highlighting the importance of prioritizing good sleep habits for overall well-being.
Sleep and Longevity
Regular quality sleep is crucial for promoting longevity and reducing the risk of chronic disease.
Studies have shown that individuals with good sleep quality tend to live longer and have fewer chronic diseases than those with poor sleep quality. For example, older adults with high affective well-being (which includes good sleep quality) can expect to live more years free of disability and chronic disease.
Higher sleep regularity is associated with significantly lower risks of all-cause, cancer, and cardiometabolic mortality, suggesting that maintaining a consistent sleep schedule may be more beneficial for health and longevity than focusing solely on sleep duration.
The Specific Benefits of Getting Enough Sleep
Enhanced cognitive function.
Sleep enhances memory consolidation , stabilizing and integrating new memories into long-term storage. This is achieved through the reactivation and stabilization of memory representations during sleep.
Furthermore, sleep, especially when it follows closely after learning, significantly boosts declarative memory , which includes facts and knowledge. Short sleep periods, even naps, can enhance memory consolidation, although longer sleep durations provide better outcomes.
Sleep also promotes consolidating complex cognitive skills, including strategic thinking and problem-solving . It enhances the ability to integrate new information with existing knowledge, facilitating the discovery of underlying rules and associations.
Better Emotional Regulation
Sleep plays a crucial role in managing stress, anxiety, and mood swings, leading to better emotional health. REM sleep is critical for consolidating emotional memories . It creates a neurochemically safe environment that allows for reprocessing emotional memories without interfering with stress-related chemicals.
Improving sleep quality positively impacts mental health . Effective management of sleep disorders can alleviate depressive symptoms and restore optimal mental functioning .
Sleep and stress have a cyclical relationship. Stress can lead to sleep problems , increasing stress responses and decreasing the ability to regulate emotions, creating a feedback loop that affects overall emotional health.
Physical Restoration and Healing
Sleep is important for muscle recovery, tissue repair, and physical rejuvenation. Adequate sleep helps control local inflammation , which is essential for muscle repair. Sleep extension can manage inflammation, aiding recovery from exercise-induced muscle injuries. Furthermore, deep sleep stages, particularly slow-wave sleep, are associated with releasing growth hormone , which is crucial for protein synthesis and muscle recovery.
The Consequences of Sleep Deprivation
Short-term effects.
The immediate effects of lack of sleep are multifaceted. It impairs judgment, leading to poor decision-making and increased risk-taking behaviors. Reduced alertness is a primary effect, resulting in slower reaction times and decreased vigilance, which can be particularly dangerous when driving or operating machinery.
Sleep loss also negatively impacts mood, causing irritability, emotional volatility, and increased stress responses . These effects can manifest after even one night of insufficient sleep, highlighting the role of maintaining optimal mental and emotional functioning.
Long-Term Health Risks
Chronic sleep deprivation poses significant long-term health risks, particularly in relation to heart disease, obesity, and diabetes .
- Heart disease: Individuals who consistently get less than 7 hours of sleep per night have a 48 percent higher risk of developing coronary heart disease.
- Obesity: Research indicates that people who chronically sleep less than 6 hours per night have about a 55 percent higher risk of becoming obese.
- Diabetes: Individuals with chronic sleep deprivation have a 28 percent higher risk of developing type 2 diabetes.
Sleep deprivation not only affects daily functioning but also significantly increases the likelihood of developing serious chronic diseases that can impact overall health and longevity.

Impact on Daily Life
Insufficient sleep can significantly negatively impact work performance, relationships, and quality of life. It leads to decreased focus, impaired cognitive function, lower productivity, and increased errors.
Relationships suffer due to increased irritability, reduced emotional regulation, and decreased empathy. Chronic sleep deprivation negatively affects overall well-being, increasing risks of mental health issues, physical health problems, and reduced immune function. It also decreases motivation for healthy habits and lowers life satisfaction.
Poor sleep creates cognitive and emotional impairments that create a cycle of reduced performance and increased stress that affects all areas of life. Prioritizing adequate quality sleep is crucial for maintaining optimal work performance, nurturing relationships, and supporting overall health and life satisfaction.
Summary: The Benefits of Sleep
Sleep is vital to overall health, contributing to physical restoration, cognitive function, and emotional well-being. Consistently getting enough quality sleep reduces the risk of chronic diseases, supports heart health, and enhances daily performance.
Conversely, sleep deprivation poses serious risks, including heightened susceptibility to mental health issues, obesity, and diabetes. Prioritizing sleep as an essential part of a healthy lifestyle is crucial. Adopting good sleep practices and seeking professional help if sleep issues persist can significantly affect long-term health and quality of life. Make sleep a priority today for a healthier tomorrow.
If you want to continue caring for your overall health, why not book an Ezra full body scan today? Detect any issues early and put yourself on the road to long-term health. Our yearly scan screens for potential cancers early, using AI to enhance the process, making it more efficient and affordable.
- [email protected]
- 888 402 3972
- Our Tech Blog
- Our Mission
- Our Advisors
- Our Care Team
- Full Body MRI Scan
- Conditions We Scan For
- Prostate AI
- Terms & Conditions
- Privacy Policy
- Telehealth Authorization
- For Providers
- For Employers
- For Imaging Partners
© 2024 Ezra
Here’s how you know
- U.S. Department of Health and Human Services
- National Institutes of Health
Meditation and Mindfulness: Effectiveness and Safety

.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What are meditation and mindfulness?
Meditation has a history that goes back thousands of years, and many meditative techniques began in Eastern traditions. The term “meditation” refers to a variety of practices that focus on mind and body integration and are used to calm the mind and enhance overall well-being. Some types of meditation involve maintaining mental focus on a particular sensation, such as breathing, a sound, a visual image, or a mantra, which is a repeated word or phrase. Other forms of meditation include the practice of mindfulness, which involves maintaining attention or awareness on the present moment without making judgments.
Programs that teach meditation or mindfulness may combine the practices with other activities. For example, mindfulness-based stress reduction is a program that teaches mindful meditation, but it also includes discussion sessions and other strategies to help people apply what they have learned to stressful experiences. Mindfulness-based cognitive therapy integrates mindfulness practices with aspects of cognitive behavioral therapy.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Are meditation and mindfulness practices safe?
Meditation and mindfulness practices usually are considered to have few risks. However, few studies have examined these practices for potentially harmful effects, so it isn’t possible to make definite statements about safety.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} More
A 2020 review examined 83 studies (a total of 6,703 participants) and found that 55 of those studies reported negative experiences related to meditation practices. The researchers concluded that about 8 percent of participants had a negative effect from practicing meditation, which is similar to the percentage reported for psychological therapies. The most commonly reported negative effects were anxiety and depression. In an analysis limited to 3 studies (521 participants) of mindfulness-based stress reduction programs, investigators found that the mindfulness practices were not more harmful than receiving no treatment.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} How popular are meditation and mindfulness?
According to the National Health Interview Survey, an annual nationally representative survey, the percentage of U.S. adults who practiced meditation more than doubled between 2002 and 2022, from 7.5 to 17.3 percent. Of seven complementary health approaches for which data were collected in the 2022 survey, meditation was the most popular, beating out yoga (used by 15.8 percent of adults), chiropractic care (11.0 percent), massage therapy (10.9 percent), guided imagery/progressive muscle relaxation (6.4 percent), acupuncture (2.2 percent), and naturopathy (1.3 percent).
For children aged 4 to 17 years, data are available for 2017; in that year, 5.4 percent of U.S. children used meditation.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Why do people practice mindfulness meditation?
In a 2012 U.S. survey, 1.9 percent of 34,525 adults reported that they had practiced mindfulness meditation in the past 12 months. Among those responders who practiced mindfulness meditation exclusively, 73 percent reported that they meditated for their general wellness and to prevent diseases, and most of them (approximately 92 percent) reported that they meditated to relax or reduce stress. In more than half of the responses, a desire for better sleep was a reason for practicing mindfulness meditation.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What are the health benefits of meditation and mindfulness?
Meditation and mindfulness practices may have a variety of health benefits and may help people improve the quality of their lives. Recent studies have investigated if meditation or mindfulness helps people manage anxiety, stress, depression, pain, or symptoms related to withdrawal from nicotine, alcohol, or opioids.
Other studies have looked at the effects of meditation or mindfulness on weight control or sleep quality.
However, much of the research on these topics has been preliminary or not scientifically rigorous. Because the studies examined many different types of meditation and mindfulness practices, and the effects of those practices are hard to measure, results from the studies have been difficult to analyze and may have been interpreted too optimistically.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Stress, Anxiety, and Depression
- A 2018 NCCIH-supported analysis of 142 groups of participants with diagnosed psychiatric disorders such as anxiety or depression examined mindfulness meditation approaches compared with no treatment and with established evidence-based treatments such as cognitive behavioral therapy and antidepressant medications. The analysis included more than 12,000 participants, and the researchers found that for treating anxiety and depression, mindfulness-based approaches were better than no treatment at all, and they worked as well as the evidence-based therapies.
- A 2021 analysis of 23 studies (1,815 participants) examined mindfulness-based practices used as treatment for adults with diagnosed anxiety disorders. The studies included in the analysis compared the mindfulness-based interventions (alone or in combination with usual treatments) with other treatments such cognitive behavioral therapy, psychoeducation, and relaxation. The analysis showed mixed results for the short-term effectiveness of the different mindfulness-based approaches. Overall, they were more effective than the usual treatments at reducing the severity of anxiety and depression symptoms, but only some types of mindfulness approaches were as effective as cognitive behavioral therapy. However, these results should be interpreted with caution because the risk of bias for all of the studies was unclear. Also, the few studies that followed up with participants for periods longer than 2 months found no long-term effects of the mindfulness-based practices.
- A 2019 analysis of 23 studies that included a total of 1,373 college and university students looked at the effects of yoga, mindfulness, and meditation practices on symptoms of stress, anxiety, and depression. Although the results showed that all the practices had some effect, most of the studies included in the review were of poor quality and had a high risk of bias.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} High Blood Pressure
Few high-quality studies have examined the effects of meditation and mindfulness on blood pressure. According to a 2017 statement from the American Heart Association, the practice of meditation may have a possible benefit, but its specific effects on blood pressure have not been determined.
- A 2020 review of 14 studies (including more than 1,100 participants) examined the effects of mindfulness practices on the blood pressure of people who had health conditions such as hypertension, diabetes, or cancer. The analysis showed that for people with these health conditions, practicing mindfulness-based stress reduction was associated with a significant reduction in blood pressure.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Pain
Studies examining the effects of mindfulness or meditation on acute and chronic pain have produced mixed results.
- A 2020 report by the Agency for Healthcare Research and Quality concluded that mindfulness-based stress reduction was associated with short-term (less than 6 months) improvement in low-back pain but not fibromyalgia pain.
- A 2020 NCCIH-supported analysis of five studies of adults using opioids for acute or chronic pain (with a total of 514 participants) found that meditation practices were strongly associated with pain reduction.
- Acute pain, such as pain from surgery, traumatic injuries, or childbirth, occurs suddenly and lasts only a short time. A 2020 analysis of 19 studies examined the effects of mindfulness-based therapies for acute pain and found no evidence of reduced pain severity. However, the same analysis found some evidence that the therapies could improve a person’s tolerance for pain.
- A 2017 analysis of 30 studies (2,561 participants) found that mindfulness meditation was more effective at decreasing chronic pain than several other forms of treatment. However, the studies examined were of low quality.
- A 2019 comparison of treatments for chronic pain did an overall analysis of 11 studies (697 participants) that evaluated cognitive behavioral therapy, which is the usual psychological intervention for chronic pain; 4 studies (280 participants) that evaluated mindfulness-based stress reduction; and 1 study (341 participants) of both therapies. The comparison found that both approaches were more effective at reducing pain intensity than no treatment, but there was no evidence of any important difference between the two approaches.
- A 2019 review found that mindfulness-based approaches did not reduce the frequency, length, or pain intensity of headaches. However, the authors of this review noted that their results are likely imprecise because only five studies (a total of 185 participants) were included in the analysis, and any conclusions made from the analysis should be considered preliminary.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Insomnia and Sleep Quality
Mindfulness meditation practices may help reduce insomnia and improve sleep quality.
- A 2019 analysis of 18 studies (1,654 total participants) found that mindfulness meditation practices improved sleep quality more than education-based treatments. However, the effects of mindfulness meditation approaches on sleep quality were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Substance Use Disorder
Several clinical trials have investigated if mindfulness-based approaches such as mindfulness-based relapse prevention (MBRP) might help people recover from substance use disorders. These approaches have been used to help people increase their awareness of the thoughts and feelings that trigger cravings and learn ways to reduce their automatic reactions to those cravings.
- A 2018 review of 37 studies (3,531 total participants) evaluated the effectiveness of several mindfulness-based approaches to substance use disorder treatment and found that they significantly decreased participants’ craving levels. The mindfulness-based practices were slightly better than other therapies at promoting abstinence from substance use.
- A 2017 analysis specifically focused on MBRP examined 9 studies (901 total participants) of this approach. The analysis concluded that MBRP was not more effective at preventing substance use relapses than other treatments such as health education and cognitive behavioral therapy. However, MBRP did slightly reduce cravings and symptoms of withdrawal associated with alcohol use disorders.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Post-Traumatic Stress Disorder
Studies have suggested that meditation and mindfulness may help reduce symptoms of post-traumatic stress disorder (PTSD).
- A 2018 review supported by NCCIH examined the effects of meditation (in 2 studies, 179 total participants) and other mindfulness-based practices (in 6 studies, 332 total participants) on symptoms of PTSD. Study participants included veterans, nurses, and people who experienced interpersonal violence. Six of the eight studies reported that participants had a reduction of PTSD symptoms after receiving some form of mindfulness-based treatment.
- A 2018 clinical trial funded by the U.S. Department of Defense compared the effectiveness of meditation, health education, and prolonged exposure therapy, a widely accepted treatment for PTSD recommended by the American Psychological Association. Prolonged exposure therapy helps people reduce their PTSD symptoms by teaching them to gradually remember traumatic memories, feelings, and situations. The study included 203 veterans with PTSD as a result of their active military service. The results of the study showed that meditation was as effective as prolonged exposure therapy at reducing PTSD symptoms and depression, and it was more effective than PTSD health education. The veterans who used meditation also showed improvement in mood and overall quality of life.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Cancer
Mindfulness-based approaches may improve the mental health of people with cancer.
- A 2019 analysis of 29 studies (3,274 total participants) of mindfulness-based practices showed that use of mindfulness practices among people with cancer significantly reduced psychological distress, fatigue, sleep disturbance, pain, and symptoms of anxiety and depression. However, most of the participants were women with breast cancer, so the effects may not be similar for other populations or other types of cancer.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Weight Control and Eating Behavior
Studies have suggested possible benefits of meditation and mindfulness programs for losing weight and managing eating behaviors.
- A 2017 review of 15 studies (560 total participants) looked at the effects of mindfulness-based practices on the mental and physical health of adults with obesity or who were overweight. The review found that these practices were very effective methods for managing eating behaviors but less effective at helping people lose weight. Mindfulness-based approaches also helped participants manage symptoms of anxiety and depression.
- A 2018 analysis of 19 studies (1,160 total participants) found that mindfulness programs helped people lose weight and manage eating-related behaviors such as binge, emotional, and restrained eating. The results of the analysis showed that treatment programs, such as mindfulness-based stress reduction and mindfulness-based cognitive therapy, that combine formal meditation and mindfulness practices with informal mindfulness exercises were especially effective methods for losing weight and managing eating.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Attention-Deficit Hyperactivity Disorder
Several studies have been done on using meditation and mindfulness practices to improve symptoms of attention-deficit hyperactivity disorder (ADHD). However, the studies have not been of high quality and the results have been mixed, so evidence that meditation or mindfulness approaches will help people manage symptoms of ADHD is not conclusive.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} How do meditation and mindfulness work?
Some research suggests that meditation and mindfulness practices may affect the functioning or structure of the brain. Studies have used various methods of measuring brain activity to look for measurable differences in the brains of people engaged in mindfulness-based practices. Other studies have theorized that training in meditation and mindfulness practices can change brain activity. However, the results of these studies are difficult to interpret, and the practical implications are not clear.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} NCCIH-Funded Research
NCCIH supports a variety of meditation and mindfulness studies, including:
- An evaluation of how the brain responds to the use of mindfulness meditation as part of a combined treatment for migraine pain.
- A study of the effectiveness of mindfulness therapy and medication (buprenorphine) as a treatment for opioid use disorder.
- A study of a mindfulness training program designed to help law enforcement officers improve their mental health by managing stress and increasing resilience.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Tips To Consider
- Don’t use meditation or mindfulness to replace conventional care or as a reason to postpone seeing a health care provider about a medical problem.
- Ask about the training and experience of the instructor of the meditation or mindfulness practice you are considering.
- Take charge of your health—talk with your health care providers about any complementary health approaches you use. Together, you can make shared, well-informed decisions
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} For More Information
Nccih clearinghouse.
The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature. The Clearinghouse does not provide medical advice, treatment recommendations, or referrals to practitioners.
Toll-free in the U.S.: 1-888-644-6226
Telecommunications relay service (TRS): 7-1-1
Website: https://www.nccih.nih.gov
Email: [email protected] (link sends email)
Know the Science
NCCIH and the National Institutes of Health (NIH) provide tools to help you understand the basics and terminology of scientific research so you can make well-informed decisions about your health. Know the Science features a variety of materials, including interactive modules, quizzes, and videos, as well as links to informative content from Federal resources designed to help consumers make sense of health information.
Explaining How Research Works (NIH)
Know the Science: How To Make Sense of a Scientific Journal Article
Understanding Clinical Studies (NIH)
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed .
Website: https://pubmed.ncbi.nlm.nih.gov/
NIH Clinical Research Trials and You
The National Institutes of Health (NIH) has created a website, NIH Clinical Research Trials and You, to help people learn about clinical trials, why they matter, and how to participate. The site includes questions and answers about clinical trials, guidance on how to find clinical trials through ClinicalTrials.gov and other resources, and stories about the personal experiences of clinical trial participants. Clinical trials are necessary to find better ways to prevent, diagnose, and treat diseases.
Website: https://www.nih.gov/health-information/nih-clinical-research-trials-you
Research Portfolio Online Reporting Tools Expenditures & Results (RePORTER)
RePORTER is a database of information on federally funded scientific and medical research projects being conducted at research institutions.
Website: https://reporter.nih.gov
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Key References
- Anheyer D, Leach MJ, Klose P, et al. Mindfulness-based stress reduction for treating chronic headache: a systematic review and meta-analysis . Cephalalgia . 2019;39(4):544-555.
- Black LI, Barnes PM, Clarke TC, Stussman BA, Nahin RL. Use of yoga, meditation, and chiropractors among U.S. children aged 4–17 years . NCHS Data Brief, no 324. Hyattsville, MD: National Center for Health Statistics. 2018.
- Breedvelt JJF, Amanvermez Y, Harrer M, et al. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: a meta-analysis . Frontiers in Psychiatry . 2019;10:193.
- Burke A, Lam CN, Stussman B, et al. Prevalence and patterns of use of mantra, mindfulness and spiritual meditation among adults in the United States . BMC Complementary and Alternative Medicine. 2017;17(1):316.
- Carrière K, Khoury B, Günak MM, et al. Mindfulness‐based interventions for weight loss: a systematic review and meta‐analysis . Obesity Reviews . 2018;19(2):164-177.
- Cavicchioli M, Movalli M, Maffei C. The clinical efficacy of mindfulness-based treatments for alcohol and drugs use disorders: a meta-analytic review of randomized and nonrandomized controlled trials . European Addiction Research . 2018;24(3):137-162.
- Cillessen L, Johannsen M, Speckens AEM, et al. Mindfulness‐based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta‐analysis of randomized controlled trials . Psychooncology . 2019;28(12):2257-2269.
- Creswell JD. Mindfulness interventions . Annual Review of Psychology. 2017;68:491-516.
- Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation . American Psychologist. 2015;70(7):581-592.
- Farias M, Maraldi E, Wallenkampf KC, et al. Adverse events in meditation practices and meditation-based therapies: a systematic review . Acta Psychiatrica Scandinavica. 2020;142(5):374-393.
- Garland EL, Brintz CE, Hanley AW, et al. Mind-body therapies for opioid-treated pain: a systematic review and meta-analysis . JAMA Internal Medicine . 2020;180(1):91-105.
- Goldberg SB, Tucker RP, Greene PA, et al. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis . Clinical Psychology Review . 2018;59:52-60.
- Grant S, Colaiaco B, Motala A, et al. Mindfulness-based relapse prevention for substance use disorders: a systematic review and meta-analysis . Journal of Addiction Medicine . 2017;11(5):386-396.
- Haller H, Breilmann P, Schröter M et al. A systematic review and meta‑analysis of acceptance and mindfulness‑based interventions for DSM‑5 anxiety disorders . Scientific Reports . 2021;11(1):20385.
- Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis . Annals of Behavioral Medicine. 2017;51(2):199-213.
- Hirshberg MJ, Goldberg SB, Rosenkranz M, et al. Prevalence of harm in mindfulness-based stress reduction . Psychological Medicine. August 18, 2020. [Epub ahead of print].
- Intarakamhang U, Macaskill A, Prasittichok P. Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: a systematic review and meta-analysis . Heliyon. 2020;6(4):e03834.
- Khoo E-L, Small R, Cheng W, et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis . Evidence-Based Mental Health. 2019;22(1):26-35.
- Levine GN, Lange RA, Bairey-Merz CN, et al. Meditation and cardiovascular risk reduction: a scientific statement from the American Heart Association . Journal of the American Heart Association. 2017;6(10):e002218.
- Nidich S, Mills PJ, Rainforth M, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial . Lancet Psychiatry . 2018;5(12):975-986.
- Niles BL, Mori DL, Polizzi C, et al. A systematic review of randomized trials of mind-body interventions for PTSD . Journal of Clinical Psychology . 2018;74(9):1485-1508.
- Rogers JM, Ferrari M, Mosely K, et al. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes . Obesity Reviews . 2017;18(1):51-67.
- Rosenkranz MA, Dunne JD, Davidson RJ. The next generation of mindfulness-based intervention research: what have we learned and where are we headed? Current Opinion in Psychology. 2019;28:179-183.
- Rusch HL, Rosario M, Levison LM, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials . Annals of the New York Academy of Sciences . 2019;1445(1):5-16.
- Schell LK, Monsef I, Wöckel A, et al. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database of Systematic Reviews. 2019;3(3):CD011518. Accessed at cochranelibrary.com on June 3, 2022.
- Semple RJ, Droutman V, Reid BA. Mindfulness goes to school: things learned (so far) from research and real-world experiences . Psychology in the Schools. 2017;54(1):29-52.
- Shires A, Sharpe L, Davies JN, et al. The efficacy of mindfulness-based interventions in acute pain: a systematic review and meta-analysis . Pain . 2020;161(8):1698-1707.
- Van Dam NT, van Vugt MK, Vago DR, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation . Perspectives on Psychological Science. 2018;13(1):36-61.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Other References
- American Academy of Pediatrics Section on Integrative Medicine. Mind-body therapies in children and youth. Pediatrics . 2016;138(3):e20161896.
- Coronado-Montoya S, Levis AW, Kwakkenbos L, et al. Reporting of positive results in randomized controlled trials of mindfulness-based mental health interventions. PLoS One . 2016;11(4):e0153220.
- Dakwar E, Levin FR. The emerging role of meditation in addressing psychiatric illness, with a focus on substance use disorders. Harvard Review of Psychiatry . 2009;17(4):254-267.
- Goyal M, Singh S, Sibinga EMS, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine. 2014;174(3):357-368.
- Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research . Washington, DC: National Academies Press; 2011.
- Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149(7):936-943.
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350-1352.
- McKeering P, Hwang Y-S. A systematic review of mindfulness-based school interventions with early adolescents. Mindfulness . 2019;10:593-610.
- Muratori P, Conversano C, Levantini V, et al. Exploring the efficacy of a mindfulness program for boys with attention-deficit hyperactivity disorder and oppositional defiant disorder. Journal of Attention Disorders . 2021;25(11):1544-1553.
- Nahin RL, Rhee A, Stussman B. Use of complementary health approaches overall and for pain management by US adults. JAMA. 2024;331(7):613-615.
- Poissant H, Mendrek A, Talbot N, et al. Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: a systematic review. Behavioural Neurology . 2019;2019:5682050.
- Skelly AC, Chou R, Dettori JR, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Comparative Effectiveness Review no. 227. Rockville, MD: Agency for Healthcare Research and Quality; 2020. AHRQ publication no. 20-EHC009.
- Stieger JR, Engel S, Jiang H, et al. Mindfulness improves brain–computer interface performance by increasing control over neural activity in the alpha band. Cerebral Cortex . 2021;31(1):426-438.
- Teasdale JD, Segal ZV, Williams JMG, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology . 2000;68(4):615-623.
- Weng HY, Lewis-Peacock JA, Hecht FM, et al. Focus on the breath: brain decoding reveals internal states of attention during meditation. Frontiers in Human Neuroscience . 2020;14:336.
- Yoshida K, Takeda K, Kasai T, et al. Focused attention meditation training modifies neural activity and attention: longitudinal EEG data in non-meditators. Social Cognitive and Affective Neuroscience . 2020;15(2):215-223.
- Yuan JP, Connolly CG, Henje E, et al. Gray matter changes in adolescents participating in a meditation training. Frontiers in Human Neuroscience . 2020;14:319.
- Zhang J, Díaz-Román A, Cortese S. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: a systematic review and meta-analysis. Evidence-Based Mental Health . 2018;21(3):87-94.
Acknowledgments
Thanks to Elizabeth Ginexi, Ph.D., Erin Burke Quinlan, Ph.D., and David Shurtleff, Ph.D., NCCIH, for their review of this 2022 publication.
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your health care provider(s). We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.
Related Topics
Pain: Considering Complementary Approaches (eBook)
For Consumers
8 Things to Know About Meditation and Mindfulness
For Health Care Providers
Use of Yoga, Meditation, and Chiropractic by Adults and Children
Mind and Body Approaches for Chronic Pain
Meditation - Systematic Reviews/Reviews/Meta-analyses (PubMed®)
Meditation - Randomized Controlled Trials (PubMed®)
Research Results
National Survey Reveals Increased Use of Yoga, Meditation, and Chiropractic Care Among U.S. Adults
National Survey Reveals Increased Use of Yoga and Meditation Among U.S. Children
Mindfulness-Based Stress Reduction, Cognitive-Behavioral Therapy Shown To Be Cost Effective for Chronic Low-Back Pain
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Trusted Health Information from the National Institutes of Health
4 discoveries beyond the brain
Nih research explores early signs of brain disorders.

Scientists developed a simple skin biopsy that could identify people with certain disorders, including Parkinson’s disease.
Neurodegenerative diseases—such as Alzheimer’s disease , Parkinson’s disease (PD), Lewy body dementia (LBD), and amyotrophic lateral sclerosis (also known as ALS or Lou Gehrig’s disease)—affect millions of people around the world. These conditions progressively damage nerve cells in the brain and nervous system. Over time, this can lead to problems with movement, thinking, memory, and more.
A century ago, many neurological conditions could only be diagnosed through an autopsy (after the person had died). Fortunately, today’s doctors and scientists have more ways to examine the brains and nervous systems of living patients. But these disorders can still be challenging to detect. Current diagnostic tools often identify these diseases after they have already started to damage the brain.
The National Institute of Neurological Disorders and Stroke (NINDS) leads research to help better understand, diagnose, and treat these conditions. Here are four recent discoveries that may help doctors and scientists spot early signs of damage, develop and test new treatments, and figure out who might benefit most from specific therapies.
Heart imaging reveals early signs
NINDS researchers at the NIH Clinical Center used a new method to identify early signs of PD and LBD . This team used a special type of PET scan to look at the hearts of people at high risk for these diseases. They found that people who later developed PD or LBD had levels of a chemical called norepinephrine in their hearts that were much lower than is typical, years before they showed any symptoms.
These findings suggest that PD or LBD might start in the part of the nervous system that controls automatic body functions (like heart rate and blood pressure) even before they affect the brain. Being able to spot these early signs could change how doctors understand and treat these diseases.
Blood tests for mitochondrial damage
NIH-funded researchers are developing a blood test that measures the level of damage to the DNA inside mitochondria —the cell’s energy producers. Previous research suggests that mitochondrial damage may be linked to some cases of PD, so focusing on this damage may help identify and diagnose PD early on. In this study, blood samples from people with PD showed more cell damage compared to samples from healthy volunteers. Some people with PD also had more damage than others.
Researchers still need to show that the test works in larger and more diverse populations. If successful, the test could help identify treatments that target mitochondria, learn which patients are most likely to respond to certain treatments, and determine whether a treatment is working.
Artificial intelligence analyzes sleep breathing patterns
In another innovative study, NINDS-funded researchers used an artificial intelligence (AI) program to identify PD by analyzing breathing patterns during sleep . The researchers tested the AI program using two types of sleep data: breathing patterns and brain activity.
By looking at 12 nights of sleep test data from people with and without PD, the program was able to identify those with PD with a high degree of accuracy. It also detected small changes in PD symptoms over a longer period of time more accurately than traditional clinical assessments.
This program could help both doctors and researchers. By using this tool, doctors may find PD earlier, and researchers may develop new treatments easier and faster. However researchers need to test it with more people from diverse backgrounds first. They also think it could be especially helpful for people who live in remote areas or have trouble leaving home.
Top: A participant wearing a chest belt during a sleep study to measure breathing patterns. Bottom: A wireless sensor uses radio signals to monitor breathing patterns without physical contact during sleep.
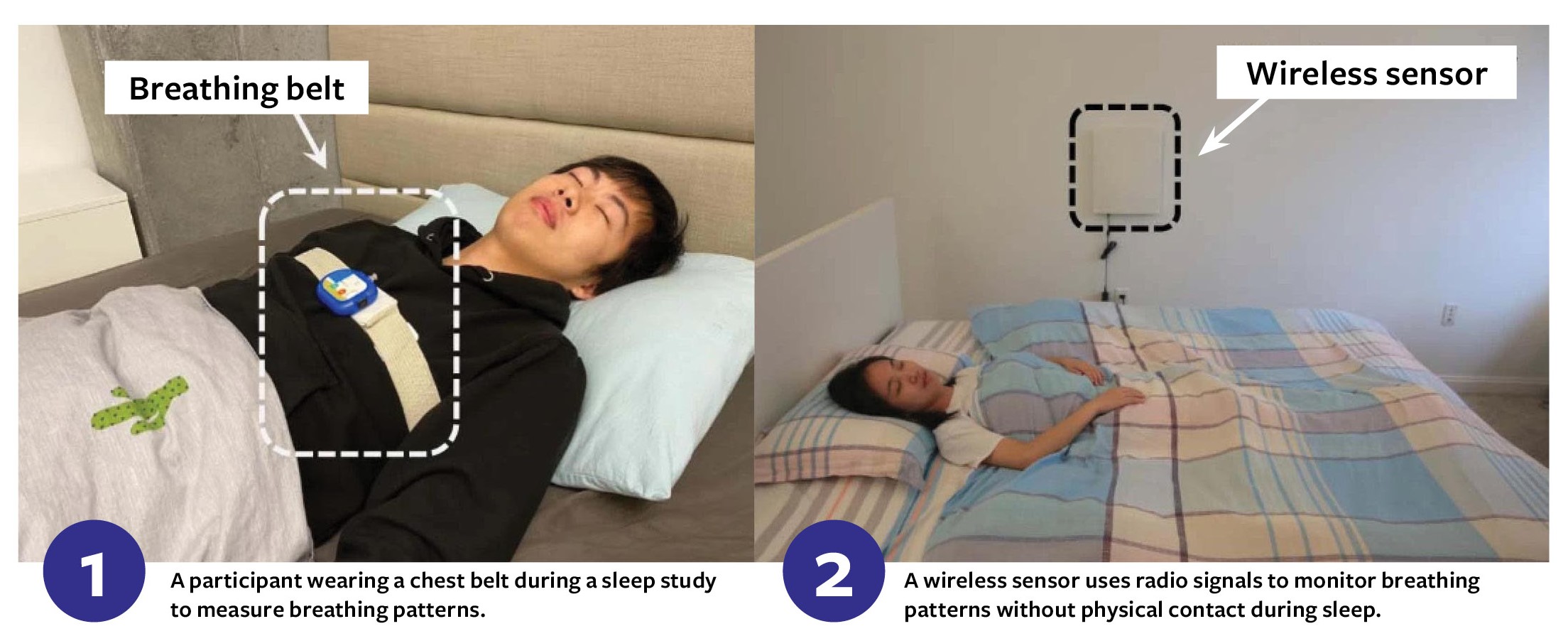
Image 1: A participant wearing a chest belt during a sleep study to measure breathing patterns. Image 2: A wireless sensor uses radio signals to monitor breathing patterns without physical contact during sleep.
Skin biopsy for neurodegenerative diseases
NIH-funded researchers developed a simple skin biopsy that may identify people with PD, LBD, and related disorders. This quick, nearly painless test looks for phosphorylated alpha-synuclein, a specific protein that’s associated with certain neurodegenerative diseases.
In this study, researchers looked at small skin samples from people diagnosed with one of these conditions and people without any history of neurodegenerative diseases. The test found this protein in more than 90% of people with a diagnosis compared to only 3% of individuals without one. This could lead to faster, more accurate diagnoses and earlier treatments for patients.
Sources: NIH Research Matters , National Institute of Neurological Disorders and Stroke , MedlinePlus
August 29, 2024
You May Also Like

Meet Walter J. Koroshetz, M.D., Director of the National Institute of Neurological Disorders and Stroke
Dr. Walter J. Koroshetz has been fascinated by the brain and how it works from a young age. This curiosity,...

Lewy body dementia: What you need to know
Lewy body dementia (LBD) is one of the most common types of dementia—but also one of the least well-known. The...
Trusted health information delivered to your inbox
Enter your email below
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Memory and Sleep: How Sleep Cognition Can Change the Waking Mind for the Better
The memories that we retain can serve many functions. They guide our future actions, form a scaffold for constructing the self, and continue to shape both the self and the way we perceive the world. Although most memories we acquire each day are forgotten, those integrated within the structure of multiple prior memories tend to endure. A rapidly growing body of research is steadily elucidating how the consolidation of memories depends on their reactivation during sleep. Processing memories during sleep not only helps counteract their weakening but also supports problem solving, creativity, and emotional regulation. Yet, sleep-based processing might become maladaptive, such as when worries are excessively revisited. Advances in research on memory and sleep can thus shed light on how this processing influences our waking life, which can further inspire the development of novel strategies for decreasing detrimental rumination-like activity during sleep and for promoting beneficial sleep cognition.
MEMORY AND THE MAGIC TOOLBOX
People acquire and maintain an immense amount of information during their lifetimes, but how that happens is hard to fathom. Whereas memory research has focused heavily on acquisition and retrieval as the two most essential steps for memories to be of use, in this article we emphasize the additional processing that memories undergo during offline periods.
New knowledge is not assimilated instantaneously; rather, memory storage changes over time. Forgetting may be the usual fate of newly acquired information, unless memory consolidation can counter forgetting, producing enduring memories that are less susceptible to decay or interference ( Paller 2009 ). Although consolidation may include many mechanisms operative over long periods of time ( Dudai 2012 ), a crucial part of the consolidation process may occur over periods of sleep. In this article, we elaborate on how memory reactivation during sleep contributes to memory stability and memory use. We also consider how sleep-based processing can contribute to creative insights and psychological well-being.
As a nightly ritual, some people like to document each day’s highlights by writing a diary entry. Indeed, before going to sleep at night, each of us (diary writer or not) is capable of remembering a great deal about the day’s happenings, including activities, thoughts, emotions, and interactions with others. These are fully viable memories; however, most do not remain so easy to remember. On subsequent days, forgetting and interference take their toll. It would be much more challenging to retrospectively produce a complete diary entry after a few days have passed, and extremely difficult to remember the experiences of a random and not especially eventful day from the past. 1
How is it that some memories can be recalled in detail years later? Forgetting and interference can apparently be avoided when memory storage is modified through consolidation mechanisms, considered in detail below. Still, memory storage falls short of providing us with a verbatim readout or a complete diary entry of the various events, thoughts, and emotions we experience each day. The information that we do maintain serves an arguably more important role than mere documentation: These memories shape our personalities, our perspectives, and our decision making. The human brain controls a remarkable capacity to adaptively learn from our experiences, thereby improving the way we cope with life’s challenges.
As a fanciful analogy, imagine a handyman’s magic toolbox, replete with tools that gradually adjust their functionality in accordance with the jobs they are given. The tools thus evolve to become optimized for jobs they are likely to encounter in the future. Likewise, the brain’s plasticity enables it to change its functionality in accordance with how it is used. Thanks to continual changes in memory storage, we not only have new knowledge that we can use, but we also have the ability to use our brains in different ways.
We postulate here that consolidation largely transpires without us knowing about it—because we are asleep at the time. Moreover, understanding the neurophysiology of memory processing during sleep may be the key to understanding how the memories formed while we are awake are preserved and transformed, and how they transform us. Ultimately, changes in memory storage during sleep may shape not only what we can remember but also who we are.
MEMORY CONSOLIDATION AT A SYSTEMS LEVEL
Declarative memories encompass many things that “we know that we know.” This knowledge is used in the decisions we make and forms the basis of a life story that we can tell ourselves. We also acquire nondeclarative memories, and therefore we have knowledge that “we don’t know that we know.” Nondeclarative knowledge is often used without concomitant remembering of where and when it was acquired. Memories in both categories, declarative and nondeclarative, do not necessarily function in isolation; they can interact with each other and with working memory (which functions to maintain and manipulate information online). Importantly, multiple types of memory commonly affect the way we think and the decisions we make.
A guiding principle in contemporary memory research is that we cannot rely on a single mechanism to explain all human memory phenomena. The challenge of understanding a given type of memory thus includes detailing how a specified brain system operates to support memory function and how that operation is or is not different from that of other brain systems. Despite this guiding principle, some concepts may apply in basically the same way for many types of memory. For example, sleep could be universally relevant—for perceptual learning ( Karni et al. 1994 ), skill learning ( Walker et al. 2002 ), paired-associate learning ( Plihal & Born 1997 ), and maybe all types of learning. The jury is still out on this idea, but it seems clear at this point that many types of memory are subject to change in one way or another during sleep ( Rasch & Born 2013 ).
Declarative memories depend on specific parts of the neocortex, each specializing in certain types of information processing. Memories for facts and events invariably depend on links among these cortically based pieces of a memory, such as different sensory qualities or conceptual attributes. Accordingly, declarative memories are characterized by their reliance on novel cross-cortical connections ( Paller 2002 ). Plasticity in connections across brain regions, including multiple cortical regions and other brain structures, can be key to consolidation—or, more specifically, to systems consolidation, in contrast to synaptic consolidation, which concerns cellular and molecular facets of consolidation. Here we focus on the former type of consolidation.
The neocortex, on its own, is not well-equipped for transforming entire experiences into lasting memory traces. The apparatus of the medial temporal lobe, centrally including the hippocampus, provides the neocortex with the capacity for storing declarative memories in an enduring way. In keeping with this idea, damage to the medial temporal lobe can lead to a profound impairment in learning, or anterograde amnesia. The hippocampus presumably helps fulfill the need to rapidly acquire declarative memories ( Marr 1971 , McClelland et al. 1995 , Norman et al. 2005 ), which is not the forte of the cortex working by itself (perhaps with some exceptions; see Hebscher et al. 2019 ). Declarative memories can be gradually stabilized via a slower process whereby cortical networks are altered under hippocampal guidance. In this way, some declarative memories can become independent of the hippocampus; memories may become schematic, may lose details including various contextual features concerning the circumstances of their acquisition, and may be transformed to only hold the bare facts, general outlines, or a portion of the information acquired. In addition, the hippocampus may continue to be involved in retrieval for some memories with regard to specific episodic details ( Nadel & Moscovitch 1997 , Miller et al. 2020 ). Although this scenario provides a sketch of the gradual memory changes of consolidation, the contributions of hippocampal–neocortical interactions to memory change are not fully understood.
The idea that memory stabilization is a gradual process that takes place after an initial encoding stage has its roots in the work of Müller & Pilzecker (1900) . On the basis of their studies of learning nonsense syllables, they inferred that there are “certain physiological processes, which serve to strengthen the associations … [that] continue with increasing intensity for a period of time” (cited in Lechner et al. 1999 , p. 81). Decades later, retrograde amnesia was observed in rodents given an electroconvulsive shock 15 minutes after learning ( Duncan 1949 ). In contrast, memory remained intact when the shocks were delivered 1 hour after learning. This pattern of experimentally induced retrograde amnesia substantiates the notion of post-learning consolidation. For different types of memory and different animal species, the amount of time required for a memory to become immune to an amnestic insult may differ. The proposal that human declarative memories undergo consolidation for many months after learning, initially regarded by researchers as surprising, is now widely accepted ( Squire 1992 , Squire & Wixted 2011 ). There is certainly still room for alternative views and for debate on many aspects of consolidation (e.g., Yonelinas et al. 2019 ), including how to characterize the hippocampal contribution (e.g., Murray et al. 2007 , Aly & Ranganath 2018 ). The path to ascribing a major role to the hippocampus in memory consolidation followed from reports of severe memory impairments in patient H.M., who received a medial temporal lobectomy as treatment for intractable epilepsy ( Scoville & Milner 1957 ). Damage to this brain region generally produces not only anterograde amnesia, but also temporally graded retrograde amnesia, which spares remote but not recent declarative memories. Evidence from retrograde memory deficits thus fits with the notion that there can be a protracted time period following initial acquisition, as consolidation progresses, when declarative memories depend on a hippocampal–neocortical dialogue. What does this dialogue entail?
A putative mechanism for declarative memory consolidation involves the offline engagement of the same neural circuits involved in learning, thereby reinstating the learning-related activity in the service of memory reactivation. This reactivation may support consolidation whether or not there is a concurrent experience of conscious retrieval. A relevant sort of physiological reactivation was first observed in the activity of rodent hippocampal place neurons, which fire selectively when the animal occupies a specific patch of space. Rodent hippocampal place cells with fields used in recent exploration fired more frequently during sleep compared to cells with fields not encountered during pre-sleep exploration ( Pavlides & Winson 1989 ). In a seminal study on memory consolidation, Wilson & McNaughton (1994) found that coordinated place cell activity in the hippocampus was likely to reoccur again during sleep. This finding was later extended to show that the temporal patterns of action potentials exhibited during wake are repeated during sleep, constituting memory replay ( Skaggs & McNaughton 1996 ). These results brought forward the hypothesis that memory is strengthened via replay within the hippocampus. Additional studies in rodents showing coordinated replay between the hippocampus and the neocortex during sleep suggest that replay is an essential aspect of the hippocampal–neocortical dialogue that can stabilize cortical representations ( Foster 2017 ). Many findings now support the idea that memory reactivation during both waking rest periods and sleep is relevant for the modification, integration, and stabilization of memories.
Memory processing may be particularly effective during sleep due to its unique physiological and neurochemical properties (see the sidebar titled Sleep Physiology). Of course, memories can readily be modified or updated during wake in light of new experiences (for a review of wake reactivation and consolidation, see Tambini & Davachi 2019 ). During sleep, as a consequence of increased sensory gating and environmental factors—when sleeping in a secluded space that is quiet and dark—there is usually far less incoming sensory information (nevertheless, sensory processing continues; see below). Consolidation may indeed be more effective, and less subject to interference or contamination, when memories are reactivated during sleep.
PHYSIOLOGY OF MEMORY CONSOLIDATION DURING SLEEP
Behavioral studies of memory consolidation during sleep have produced ample evidence of superior retrieval of various types of information after a period of sleep compared to a period of wake (e.g., Karni et al. 1994 , Plihal & Born 1997 , Walker et al. 2002 , Tucker et al. 2006 ). In rodents, consistent evidence has suggested a causal role for rapid eye movement (REM) sleep in memory consolidation ( Smith 1995 , Rasch & Born 2013 , Klinzing et al. 2019 ). Historically, there have been many attempts to tie human REM sleep to memory (e.g., Crick & Mitchison 1983 , Winson 1985 , Paller & Voss 2004 ), and diverse ideas about its role in consolidation are still debated. Here we emphasize the better understood role of non-REM (NREM) sleep.
A prominent account of sleep-based consolidation, sometimes termed the active systems consolidation hypothesis, suggests that memory reactivation in the hippocampus during NREM sleep dictates changes in cortical networks ( Buzsáki 1998 , Born et al. 2006 ). This proposed mechanism embraces selectivity, as some memories are reactivated and others not. An alternative account, the synaptic homeostasis hypothesis, instead attributes the memory benefits of sleep to widespread downscaling of synaptic strength, thereby increasing the signal-to-noise ratio for memory retrieval ( Tononi & Cirelli 2014 ). Importantly, synaptic downscaling and active consolidation are not mutually exclusive. Recent accounts emphasize the critical contributions of both reactivation and synaptic downscaling for retaining old memories and for encoding new ones ( Klinzing et al. 2019 ).
The implementation of sleep-related consolidation through reactivation appears to be intimately related to certain physiological features of sleep characterized as field-potential oscillations, particularly during slow-wave sleep (SWS). These oscillations appear to be orchestrated together in the form of nested oscillations (e.g., Staresina et al. 2015 ), as described below and depicted in Figure 1 . Sharp-wave/ripple complexes (SWRs), found locally in the hippocampus, are nested in the troughs of thalamo-cortical sleep spindles, which, in turn, ride on the peaks (or up-states) of cortical slow oscillations (SOs). Accordingly, consolidation is enabled by a synchronized temporal frame for communication among brain areas ( Diekelmann & Born 2010 ).

The consolidation of declarative memories during slow-wave sleep is thought to involve multiple brain regions and neuronal interactions, reflected in the set of brain oscillations pictured here. The slowest of these are neocortical slow oscillations ( red ). The so-called up-states of these oscillations coincide with high levels of neuronal activity across many regions of the cortex, which makes the up-states conducive to cross-cortical interactions. The synchronization of thalamo-cortical spindles ( blue ) with slow-oscillation up-states facilitates memory processing. Sharp-wave/ripple complexes ( green , shown at a larger scale) can be generated in the hippocampus and are also synchronized with spindles. Ripples coincide with hippocampal replay and are causally associated with memory processing. Figure adapted from Born & Wilhelm (2012) .
Sharp-Wave/Ripple Complexes
SWRs are commonly observed in recordings from area CA1 of the rodent hippocampus. Somewhat similar observations have been made in human intracranial recordings. The high-frequency ripples (70–110 Hz in humans, 150–200 Hz in rodents) coincide with a characteristic high-amplitude wave (i.e., a sharp wave). Hippocampal-place-cell replay patterns are predominantly observed contemporaneously with SWRs, during both sleep ( Wilson & McNaughton 1994 ) and wake ( Nádasdy et al. 1999 ). Furthermore, disruption of SWRs during sleep negatively affects memory ( Girardeau et al. 2009 ), whereas their artificial extension benefits memory during wake ( Fernández-Ruiz et al. 2019 ). In fact, the causal role of SWRs in memory consolidation has received more support than that of hippocampal replay ( Laventure & Benchenane 2020 ).
SWRs likely contribute to memory consolidation in conjunction with other physiological events. Rodent SWRs take place predominantly within the time frame of thalamo-cortical spindles, and their propagation from the hippocampus may add to the excitation of spindles ( Sirota et al. 2003 ). Human findings are also consistent with the idea that SWRs are nested within SOs and spindles ( Helfrich et al. 2018 , Staresina et al. 2015 ). Indeed, SWRs have been considered to coincide with hippocampal output that can eventually reach various cortical zones. In support of this idea, SWRs in human hippocampal recordings precede activity in adjacent cortex ( Axmacher et al. 2008 , Nir et al. 2011 ). Notably, coupling between SWRs in the hippocampus and ripple-like activity in the neocortex was strengthened by sleep that followed learning ( Khodagholy et al. 2017 ). Additional evidence linking wake SWRs to memory includes their timing, anticipating recollection in both free-recall tests ( Norman et al. 2019 ) and cued-recall tests ( Vaz et al. 2019 ).
SWRs and simultaneous neocortical ripple-like activity could reflect the aforementioned hippocampal–neocortical dialogue. Sleep spindles could play a synchronizing role for this mechanism ( Ngo et al. 2020 ). Complicating this story, however, Axmacher et al. (2008) reported that memory performance correlated with ripples in the human rhinal cortex but not the hippocampus, and that more ripples occurred during quiet wake than sleep in both the hippocampus and the rhinal cortex. How exactly is memory processing different during wake and during sleep? Differences between SWRs may provide clues. In rodents, wake SWRs coincide with high-fidelity replay and remain local, whereas sleep SWRs coincide with noisier replay and, as described below, are coordinated with widespread cortical SOs ( Roumis & Frank 2015 ). Accordingly, high-fidelity reactivation may support memory-guided planning during wake, whereas noisier, distributed reactivations may support generalization during sleep.
Hippocampal SWRs seem to be triggered by SOs and spindles from the neocortex ( Sirota et al. 2003 , Nir et al. 2011 ). A cortical-to-hippocampal trajectory is also consonant with replay in the visual cortex preceding replay in the hippocampus ( Ji & Wilson 2007 ). Moreover, replay in these two brain regions tends to occur during distinct temporal frames, such that both replay and SWRs may be synchronized by SO timing.
Slow Oscillations
SOs (≤1 Hz), observed in the scalp electroencephalogram (EEG) or in local field potentials, reflect coordinated neural activity of large areas of the cortex and typically serve to coordinate higher-frequency local activity ( Varela et al. 2001 ). During the SO trough (or down-state), pyramidal neurons and interneurons are silenced, whereas during the SO peak (or up-state), neuronal burst-like activity predominates ( Volgushev et al. 2006 ). SOs during sleep do not occur simultaneously throughout cortex; they typically appear frontally first and travel posteriorly ( Massimini et al. 2004 ). Intracranial recordings of SO propagation documented various paths, such as from neocortex to parahippocampal gyrus to entorhinal cortex to hippocampus ( Nir et al. 2011 ). Whereas many SOs follow such cortical trajectories, many other SOs occur locally. Different types of information processing may thus correspond to different types of SO patterns, particularly in relation to cortical origin and trajectory. Indeed, SO activity over a specific cortical area can reflect previous learning dependent on that area ( Huber et al. 2004 ).
SOs are the hallmark of SWS. Both low-frequency EEG power and SWS duration have repeatedly been found to be correlated with memory improvement over sleep, primarily for declarative memory (e.g., Backhaus et al. 2007 , Westerberg et al. 2012 ). More directly, SOs have been linked with consolidation in studies using transcranial direct current stimulation or auditory stimulation to entrain SOs. Many such studies have shown enhanced SOs and a concurrent improvement in retention over sleep ( Marshall et al. 2006 , Ngo et al. 2013 , Westerberg et al. 2015 , Papalambros et al. 2017 ). However, SO enhancement has also occurred in the absence of observed memory improvements ( Cox et al. 2014 , Weigenand et al. 2016 , Henin et al. 2019 , Papalambros et al. 2019 ). One possible explanation for the mixed memory results in these studies is that the word-pair recall measures used often had low test-retest reliability, which would not be conducive to producing consistent results in repeated-measure designs comparing stimulation and sham stimulation. Studies with improved memory measures or more powerful experimental designs are needed to clarify this discrepancy in the literature. Nevertheless, the existing results offer considerable support for the notion that SOs function as a driving mechanism for strengthening memories during sleep.
Sleep Spindles
A sleep spindle is defined as a waxing-and-waning oscillation at 11–16 Hz with a duration between 0.5 s and 3 s. Spindles originate in the thalamus and propagate to different neocortical sites ( Fernandez & Luthi 2020 ). Although models explaining spindles’ contribution to memory focus on their interaction with SOs, they are most frequent in N2, when SOs are less common than during SWS ( Purcell et al. 2017 ). However, given findings that memory changes after a nap correlated with SWS spindle activity but not with N2 spindle activity ( Antony et al. 2012 , Cox et al. 2012 ), spindles during SWS may be particularly important for consolidation.
The importance of the link between SOs and spindles is underscored by the finding that their coupling predicts the degree of memory strengthening over sleep (e.g., Latchoumane et al. 2017 ). Furthermore, manipulating SOs during sleep also increases sleep spindles (e.g., Marshall et al. 2006 ). Phase-amplitude coupling between SOs and spindles is often observed, as spindles are prevalent during the SO up-state (e.g., Steriade et al. 1993 , Mölle et al. 2002 ). Yet, spindles and SOs in human intracranial recordings often do not coincide ( Nir et al. 2011 ). Analyses of spindle-SO coupling patterns must take into account ( a ) that spindles are highly variable across individuals ( Cox et al. 2019 ) and ( b ) that there may be multiple spindle subtypes. Spindles have been distinguished based on their spatial distribution in the brain, their frequency, and their behavioral relevance. For example, slow spindles (≤13 Hz) tend to be nested in the down-state of the SO, whereas fast spindles (>13 Hz) are nested in the up-state ( Mölle et al. 2011 , Cox et al. 2014 ).
Increasing empirical support has convincingly linked spindles with memory consolidation ( Antony et al. 2018 , Cairney et al. 2018 ), though the literature on spindles historically emphasized many other functions, such as sensory processing and intelligence ( Fernandez & Luthi 2020 ). Higher spindle density has been associated with better memory in word-pair learning ( Gais et al. 2002 ), visuospatial learning ( Clemens et al. 2006 ), episodic learning ( Cox et al. 2012 ), and procedural learning ( Milner et al. 2006 , Nishida & Walker 2007 ). In a pharmacological study, the GABA A agonist zolpidem (Ambien®) was found to increase sleep spindles and to improve word-pair recall but not motor-sequence learning ( Mednick et al. 2013 ).
Further insights about spindles and their role in memory consolidation may be obtained using methods to manipulate spindles. For example, auditory entrainment produced an increase in spindles with characteristics resembling those of endogenous spindles ( Antony & Paller 2017 ). Similarly, electrical stimulation with transcranial alternating current was used to boost spindle activity, also benefiting motor memory consolidation ( Lustenberger et al. 2016 ). Future studies should investigate the functional relevance of cross-frequency coupling via conjoint manipulations, such as manipulations of spindles and SOs, combined with extensive memory testing.
Nested Oscillations and Hippocampal-Cortical Communication
Given that systems consolidation of a declarative memory entails coordinated memory processing across cortex and hippocampus, cross-frequency coupling across regions may be a critical ingredient. Because thalamo-cortical SOs can propagate throughout large parts of the cortex, a plurality of cortical regions participating in a declarative memory can be primed to interact. Hippocampal projections can then precisely engage the relevant cortical circuits, as coordination between spindles and ripples could allow SWRs to dictate replay in those specific circuits ( Geva-Sagiv & Nir 2019 ).
A rapid flow of information engaging a cortical-hippocampal-cortical loop can thus be described ( Rothschild et al. 2017 , Lewis & Bendor 2019 , Rothschild 2019 ). The initial cortical activity, corresponding to an incomplete memory trace, determines which memory will be reactivated. For example, the first step could be that one or more pieces of a recent experience might come to be reactivated cortically. Second, this information would be projected to the hippocampal networks that were also activated during the original experience, via the same anatomical pathways from cortex to hippocampus. Then, wider cortical involvement would unfold in the third step, based on hippocampal replay accompanied by SWRs, instantiating pattern completion to recruit other pieces of that recent experience. Consequently, the multimodal and multidimensional components initially encoded across the cortex could be fully reactivated.
In this way, an interaction between hippocampal networks and cortical networks could enhance cortico-cortical connections to solidify a complete declarative memory trace. While this cortical-hippocampal-cortical loop is steadily being characterized in more anatomical detail, specific functional consequences can also be investigated by manipulating the content of the memory reactivation, as described below.
Toward a Causal Link Between Reactivation and Consolidation
Neural evidence that could causally link reactivation with consolidation faces several interpretive challenges. When a person reactivates a memory in the normal course of remembering, it can be difficult to disentangle neural signatures of reactivation from new learning. Hippocampal activation observed using neuroimaging during recall, for example, could signify that the hippocampus is enabling reactivation or, alternatively, that the hippocampus is contributing to learning the novel experience of the recall episode itself (which could then be remembered later). Both types of processing are likely to occur concurrently. Similarly, we cannot easily dissociate acquisition from retrieval: If a certain oscillation is observed in the hippocampus during acquisition, it could be because old semantic information must be retrieved to make sense of the new information in context.
During sleep, some of these same interpretive issues may be in play but to a lesser extent, as new episodic memories are not readily formed as they are during wake. Importantly, plasticity can still be operative in neural circuits, though various views on the cellular mechanisms of plasticity during sleep have been controversial. Although this literature is beyond the scope of this review, we note that some views emphasize a facilitation of cortical plasticity during SWS (e.g., Timofeev & Chauvette 2017 ).
How can mechanisms of reactivation, and the function of reactivation in the service of consolidation, be studied in humans? Here we advocate for using sensory stimulation methods. Although the sleeping brain suppresses sensory input during sleep, some sensory processing nevertheless persists, perhaps in order to monitor the surroundings ( Andrillon & Kouider 2019 ). We can leverage this standby mode of stimulus processing in two different ways. First, as described above, we can use stimuli to manipulate brain physiology, as in entraining SOs and spindles. Second, as described below, we can use learning-related stimulation to systematically manipulate memory processing.
TARGETED MEMORY REACTIVATION
Targeted memory reactivation (TMR) is a technique for probing memory reactivation during sleep ( Oudiette & Paller 2013 , Schouten et al. 2017 ). TMR can also be used during wake, although the term has most often been used in the context of sleep studies. First, stimuli such as sounds or scents are associated with specific newly learned information ( Figure 2a ). Then, the same sensory stimuli are unobtrusively presented during sleep. To avoid awakenings, sounds are often presented at a low intensity. The chief finding from recent TMR studies was confirmed by a meta-analysis that included results from over 90 experiments ( Hu et al. 2020 ): When TMR was applied during SWS or N2, memory was selectively improved for the associated information compared to comparable information for which TMR was not applied.

( a ) Targeted memory reactivation experiments generally include three phases. In the first phase (pre-sleep), participants acquire some new information. This information is coupled with stimuli that are included either as background context or as part of the learning (e.g., a meow sound paired with the spatial location of a cat image). In the second phase (sleep), these stimuli are unobtrusively presented during sleep. In the third phase (post-sleep), memory is tested after sleep. ( b ) In the experiment of Rasch et al. (2007) , spatial learning of 15 objects, each shown in two locations on a 5 × 6 grid, was accomplished while a rose odor was present. Next, during an overnight sleep session with polysomnographic monitoring, the odor or an odorless vehicle was presented during sleep. Finally, spatial memory was assessed the next morning. The results showed relatively better recall when the odor had been presented during slow-wave sleep compared to when it had not. This memory effect was not observed when odors were presented during rapid eye movement (REM) sleep or when the memory test was one of motor learning instead. ( c ) In the experiment of Rudoy et al. (2009) , spatial learning of 50 objects shown in random locations on a grid was accomplished while sounds were presented. For each object, a matching sound was used. Next, during an afternoon nap with polysomnographic monitoring, half of the sounds were presented at a low intensity. Finally, spatial memory was assessed when participants attempted to place each object at precisely the correct screen location. The results showed relatively better memory performance for objects if corresponding sounds had been presented during slow-wave sleep than if not. Error bars represent standard error of the mean.
Many older studies paved the way for the recent proliferation of TMR experiments. The earliest studies seldom used polysomnographic methods [i.e., continuous EEG, electrooculogram (EOG), and electromyogram (EMG) recordings] to ensure that individuals were asleep at the time of stimulation and to determine sleep stage. TMR experiments lacking polysomnography leave room for doubt about what happened during sleep. Also, some studies were ignored because they did not fit with the Zeitgeist on memory and sleep. For example, a study by Tilley (1979) did not have a large impact because sounds played during REM did not enhance memory performance, and at the time REM was the central focus of questions about consolidation during sleep. However, Tilley also reported a TMR effect for sounds presented during N2.
This research approach began to gain widespread interest following a study by Rasch et al. (2007) , wherein a spatial-learning improvement was produced using a rose odor during learning and again during SWS ( Figure 2b ). In a subsequent TMR study by Rudoy et al. (2009) , spatial learning was similarly improved but using sounds ( Figure 2c ): The results showed less forgetting for object locations that were cued by a sound during sleep compared to those that were not cued. In this and many subsequent experiments, half of the sounds were selected for presentation during sleep using a form of stratified sampling (i.e., matching the two sets on pre-sleep recall accuracy). Within-subject comparisons then allowed nonspecific effects of sleep, such as alertness and interference, to be ruled out. The relative benefit in recall accuracy for cued compared to uncued conditions, as now observed in many TMR studies ( Hu et al. 2020 ), demonstrates that stimuli presented during sleep can function to reactivate specific memories.
Memory changes observed in studies comparing post-sleep to pre-sleep performance are commonly used to support the inference that memories are indeed reactivated by TMR during sleep. This estimate of memory change is often subject to the proviso that the act itself of testing memory before sleep changes storage, as predicted by the testing effect ( Roediger & Karpicke 2006 ). Yet, sound experimental designs in typical TMR studies still allow for valid comparisons between two conditions, one with and one without TMR cues presented during sleep, using either between-subjects or within-subjects comparisons. A further advantage of this type of design is that participants commonly exhibit no knowledge of whether cues were presented or which cues were presented, so no demand characteristics or strategic confounds are operative during post-sleep memory testing. Although factors such as testing effects, forgetting, interference, and consolidation may all affect retrieval after a delay, and potentially confound memory comparisons between a retention period with sleep and one without sleep, differential memory changes due to a TMR manipulation can be firmly attributed to differential consolidation for cued relative to uncued memories.
These methods for manipulating reactivation of specific memories complement other methods of studying sleep-related memory consolidation and provide a valuable tool for deciphering the neural mechanisms whereby reactivation engages memory consolidation. Sound delivery, in particular, provides a marker for specifying a time frame during which reactivation may be more likely.
To establish TMR as an effective tool for investigating consolidation, and to better understand its boundary conditions, it is essential to determine what types of learned material can be reactivated, what methods produce reactivation, and which brain mechanisms are engaged. TMR can improve many other types of learning in addition to spatial learning, including many examples of both declarative and nondeclarative memory [ Hu et al. (2020) provide a comprehensive list as of mid-2019]. For example, TMR studies have shown a benefit for skill learning ( Antony et al. 2012 ), vocabulary learning ( Schreiner & Rasch 2015 ), and word recall ( Fuentemilla et al. 2013 ). TMR studies have used multiple types of auditory stimulation during sleep, including pure tones, frequency-modulated tones, segments of popular music, environmental sounds, and spoken words.
In rodents, TMR was used to directly link memory reactivation with hippocampal replay: When tones associated with spatial learning on a two-arm maze were played during NREM sleep, corresponding hippocampal place cells were preferentially reactivated over the next few seconds ( Bendor & Wilson 2012 ). Two tones were used in this experiment, one associated with a leftward response and the other with a rightward response, and both were presented during sleep. Therefore, unlike in most human TMR studies, there was no opportunity to determine whether memory changed due to the TMR procedure. In a subsequent study in rodents, Rothschild et al. (2017) found that a sound cue associated with pre-sleep learning biased auditory cortex activity, which predicted hippocampal SWR activity. These results were thus used to support the cortical-hippocampal-cortical loop theory of reactivation-dependent memory consolidation outlined above.
Neuroimaging has provided additional anatomical perspectives. For example, Cousins et al. (2016) used functional magnetic resonance imaging (fMRI) to reveal post-sleep changes due to TMR in brain activity associated with motor learning. Time in SWS correlated with greater hippocampal and caudate activity for cued versus uncued sequences in subsequent wake. Also, time in REM correlated with an increase in cerebellar and cortical motor activity for cued versus uncued sequences, suggesting that the effects of TMR during NREM sleep may depend on subsequent REM sleep as well. In an fMRI study of spatial learning using an auditory TMR procedure, the degree of memory benefit was found to be correlated with activity in the medial temporal lobe and the cerebellum, as well as with the degree of parahippocampal-precuneus connectivity, thus identifying several candidate measures of brain activity associated with sound-cued memory reactivation ( van Dongen et al. 2012 ; see also Berkers et al. 2018 ). An fMRI study using an olfactory TMR procedure found that scents associated with prior learning elicited learning-related patterns of brain activity during sleep, and this activity was correlated with post-sleep spatial memory improvement ( Shanahan et al. 2018 ). Complementing these neuroimaging findings, results from a study in epileptic patients suggested that one requirement for TMR is a relatively intact medial temporal region ( Fuentemilla et al. 2013 ). Word recall benefits from TMR were found for individuals in a healthy control group and for patients who had brain damage due to hippocampal sclerosis, but not if there was bilateral damage. Furthermore, across all patients the degree of benefit correlated with the volume of spared hippocampus.
The efficacy of TMR cues undoubtedly depends on many factors. Four such factors are as follows: ( a ) The cue must gain sufficient sensory processing but not produce awakening; ( b ) the association between the cue and the learned information must be sufficiently strong and specific, so that the cue preferentially reactivates the intended information; ( c ) memory measures must be highly sensitive and reliable; and ( d ) at the time of TMR, memories must be sufficiently strong for veridical memory reactivation to occur, but not so strong that there is no possibility for improvement ( Creery et al. 2015 , Cairney et al. 2016 ). Also, the improvement must be sufficient to produce superior performance compared to the uncued condition, which can be difficult to evaluate with a binary memory measure (correct/incorrect) that may be relatively insensitive to gradations of memory strength. The testing procedures, including the delay, must be selected with these requirements in mind, and in consideration of possible floor or ceiling effects.
Whereas TMR can selectively improve memory, we do not know whether the reactivation it produces is the same as spontaneous reactivation. To answer this question, neural signals could be compared for TMR-induced and spontaneous reactivation during sleep. Encouragingly, recent TMR studies have made progress in monitoring reactivation. Reinstatement of memory-specific neural signatures following cues has been observed using both EEG and fMRI ( Belal et al. 2018 , Cairney et al. 2018 , Schreiner et al. 2018 , Shanahan et al. 2018 , Wang et al. 2018 ). Two of these studies showed that this reactivation coincided with spindle activity ( Cairney et al. 2018 , Wang et al. 2018 ), converging with the aforementioned evidence implicating spindles. These results from TMR studies also converge with findings from studies of spontaneous reactivation that have also implicated spindles as a crucial component in decoding reactivated content ( Bergmann et al. 2012 , Schönauer et al. 2017 ).
Antony et al. (2018) used TMR to directly investigate the relevance of spindles. Their results showed that memory reactivation was most effective when a spindle occurred shortly after a TMR cue. Spindles are unlikely to occur in close succession and are typically separated by 3–6 s. Accordingly, an optimal time for cue presentation is at the end of this refractory period. Timing cue presentations accordingly was indeed found to favor memory benefits. Speculatively, the gap between sleep spindles may be helpful for segregating reactivation events during sleep ( Antony et al. 2018 ).
Going beyond research strategies that focus on solidifying prior learning during sleep, a different approach considers the potential to learn new things during sleep. Such efforts have achieved limited success in the circumscribed territory of associative learning ( Arzi et al. 2012 ) and perceptual learning ( Andrillon et al. 2017 ). Also, Arzi et al. (2014) showed that sleep conditioning changed waking behavior in participants who wished to quit smoking. Conditioned pairing of a noxious odor with the odor of smoking during stage N2 and REM reduced the number of cigarettes smoked compared to various control conditions. New learning during sleep may be limited to simple types of memory. On the other hand, new procedures derived from TMR studies may open up other opportunities. For example, new learning may be possible during lucid dreaming ( Konkoly et al. 2020 ). In another study, TMR was accomplished using a sound associated with learning to suppress a memory ( Simon et al. 2018 ). The results showed that new associations were formed during sleep when this suppression-related sound was presented along with sounds related to other memories. Because this TMR procedure apparently weakened those memories, we can infer that those memories became associated with the suppression action. Accordingly, a wide range of strategies should be pursued to map out the potential for TMR to change memories.
In summary, TMR methods provide a powerful tool for probing sleep-related memory consolidation and its consequences. Future studies using novel variations of these methods hold promise for providing additional insights into the relevant neurocognitive mechanisms. Furthermore, applying TMR methods outside the laboratory has potential for shaping sleep consolidation to improve memory and various other aspects of life.
SLEEP AS A CONTRIBUTOR TO CREATIVE INSIGHT AND EMOTIONAL REGULATION
Processing memories during sleep can lead not only to the strengthening of particular memories but also to other sorts of memory modification. For example, two distinct memories may become associated, such as when a connection emerges between a recent event and a remote event. Such connections can also be the basis for creativity and problem solving. The time-honored belief that a difficult decision can be dealt with more effectively after sleeping on it calls attention to the role of sleep in creativity and problem solving. Historically, creative insight has routinely been linked with dreaming, as in the anecdotes of August Kekulé’s discovery of the structure of benzene, Otto Loewi’s discovery of chemical transmission, Dmitry Mendeleev’s discovery of the periodic table of elements, and Paul McCartney’s creation of the melody for Yesterday .
Problem Solving and Creativity
A TMR study by Sanders et al. (2019) strongly corroborates the relevance of sleep for problem solving. In this study, participants were stumped by a set of puzzles, each of which was accompanied by a repeating musical theme ( Figure 3 ). Overnight, half of the themes were presented during SWS, which functioned to selectively increase the likelihood of producing solutions for those puzzles compared to the remaining puzzles.

Experimental design and results from Sanders et al. (2019) . ( a ) The participants attempted to solve a set of challenging puzzles (including matchstick, spatial, verbal, and rebus puzzles). Each puzzle was presented together with an arbitrary musical theme or sound, and participants were required to master these associations. The pre-sleep learning phase of the experiment ended when there were six puzzles that could not be solved in the 2 minutes allotted for working on each one. Participants slept in their own homes using a wireless sleep-monitoring device linked to a computer, which covertly presented sounds when slow-wave sleep (SWS) was detected. In this way, three of the six unsolved puzzles were reactivated using the corresponding sounds. The matchstick puzzle shown as an example came with instructions to move three matchsticks to create four equilateral triangles. ( b ) The results obtained the next day confirmed that memory reactivation had the predicted effect: When participants attempted to solve the same six puzzles, solving rates were higher for cued puzzles than for uncued puzzles. In the left panel, each orange circle represents a single participant’s success rate for one type of puzzle. The blue circles represent the average for each condition. Error bars represent 95% confidence intervals. The right panel shows the difference between the two conditions similarly. Figure adapted from Sanders et al. (2019) .
Even though puzzle memories were presumably reactivated during SWS in this experiment, the investigators could not exclude the possibility that REM was also important for the observed effect on problem solving. Other evidence supports the idea that REM sleep may be an optimal time for broad semantic associations that are perhaps indicative of creativity ( Stickgold et al. 1999 ). REM has also been empirically associated with solving word problems using solution hints from an ostensibly unrelated task ( Cai et al. 2009 ). Yet, some studies failed to find sleep benefits for problem solving ( Brodt et al. 2018 , Schönauer et al. 2018 ). Another example of problem solving was examined using a tedious numerical task that could instead be completed on the basis of a hidden shortcut. Following an 8-hour break including either sleep or wake, only 35% of the participants made this discovery. Participants who slept, compared to those who did not, were more likely to discover the shortcut, presumably by restructuring their memories of the task ( Wagner et al. 2004 ). A follow-up study showed that EEG activity during SWS in the form of power in the beta band (17–25 Hz) and perhaps part of the spindle band (10–11 Hz) predicted which participants would discover the shortcut ( Verleger et al. 2013 ).
Although creativity is inherently connected with problem solving, very few studies have directly addressed the relevance of sleep for creativity. Only one study adopted the TMR methodology in this context. This study used a creativity task that required participants to generate ways to motivate other people to do volunteer work ( Ritter et al. 2012 ). Instructions were given at night and the test was taken the next morning. Impartial raters scored the degree of creativity in the responses. Higher creativity was found when task-related odors were presented overnight compared to different-odor and no-odor control conditions in other participants. Additionally, participants in the task-related odor condition performed better than controls in selecting their most creative idea. However, the design did not allow the investigators to connect any specific sleep stage to this benefit. Odors presumably reactivated the task instructions and prompted ideas for creative solutions, just as musical sounds helped participants in the study of Sanders et al. (2019) reach solutions.
The available evidence is broadly consistent with the supposition that memory processing during sleep can be useful for various cognitive challenges that arguably share some properties with creativity. For example, reprocessing of recent episodic memories during sleep can support gist abstraction and generalization, which are useful modes of memory transformation ( Lewis & Durrant 2011 , Lutz et al. 2017 , Schapiro et al. 2017 , Tamminen et al. 2017 ). Ideally, sleep could support creative ways to relate recent experiences to current goals ( Paller & Voss 2004 ). Indeed, Winson’s (1985 , 2004 ) prescient proposal emphasized that offline memory processing engaged in the sleeping brain would help in dealing with ongoing issues encountered during the waking state. Cartwright (2010) conducted many studies of dreaming that led her to also emphasize this view. Earlier dreams in the night are generally based on recent memory fragments, whereas later dreams incorporate memory fragments from an increasingly farther past ( Roffwarg et al. 1978 ). Cartwright (1990) found that dreams during a single night sometimes all relate to a common theme, drawing on relevant knowledge from progressively further back in time. She identified systematic relationships between the dreams of recently divorced individuals and their postdivorce coping strategies, and critically, she found better emotional adjustment the more dreaming was used in this fashion.
A reasonable speculation, then, is that in dreams, and perhaps in sleep more generally, emotional issues can be worked through and behavioral strategies can be adjusted with reference to very recent experiences, older experiences, and their relationships. Strikingly, this use of memory processing during sleep is in keeping with the conception of consolidation described above, whereby recent memories are integrated with older ones to facilitate storage. Two benefits of sleep can thus be described as ( a ) reactivating and reorganizing memories and ( b ) creatively fine-tuning strategies in the service of solving current problems. These two benefits correspond roughly to modifying declarative memories and nondeclarative memories, respectively.
Emotional Memories and Emotional Regulation
How might sleep zero in on the specific memory processing that would be optimal for guiding problem solving? Ideally, the specific memories reactivated should be those relevant in some way for important upcoming challenges. It is thus sensible that emotional factors should enter into this computation.
Various findings support the claim that emotional memories are preferentially consolidated during sleep. Emotional memories likely benefit from arousal-related tagging during encoding ( Payne & Kensinger 2018 ). TMR was used in one study that compared results for negative emotional pictures and neutral pictures ( Cairney et al. 2014 ). The participants first learned picture-location associations as in many other TMR experiments, in this case with just six locations. Half of the pictures were cued during SWS using semantically related sounds. After sleep, an interesting pattern of results was revealed: Total time spent in SWS predicted faster spatial recall responses for cued pictures, but only in the negative emotion condition. Cuing did not influence spatial recall accuracy. The number of spindles during SWS also predicted the speed of recall responses, suggesting that sleep spindles mediate a selective enhancement of reactivated emotional memories.
REM may be particularly important for processing emotional memories, but the evidence is mixed. Although amygdala activity is increased during REM sleep ( Maquet et al. 1996 ), TMR cues improved emotional memories not when presented during REM but rather when presented during NREM ( Lehmann et al. 2016 ). Of course, both NREM and REM may be relevant. The evidence on whether memory processing during sleep increases or decreases arousal regulation for emotional memories in also unclear ( Tempesta et al. 2018 ). In one study, women exposed to a traumatic movie followed by a period of sleep experienced fewer traumatic memories when compared with women exposed to the traumatic movie followed by a neutral movie ( Kleim et al. 2016 ). In another study, sleep preserved the autonomic response to emotional stimuli after sleep, but it reduced the autonomic response as well as valence ratings to emotional stimuli one week later ( Bolinger et al. 2019 ). That is, sleep may be helpful for arousal regulation not on the next day but after some number of days. Although more research is certainly needed in this area, multiple investigators have championed the view that sleep aids the overnight resolution of emotional distress (e.g., Walker & van der Helm 2009 ). Notably, emotional benefits from sleep may be secondary to memory reorganization ( Vanderheyden et al. 2015 ).
Lack of sleep can certainly contribute, perhaps indirectly, to emotional dysregulation (as may be particularly evident, anecdotally, in cranky children in need of sleep). In an fMRI study, reduced top-down cognitive control was evident in sleep-deprived compared to control participants ( Yoo et al. 2007 ). Decreased connectivity between the medial prefrontal cortex and the amygdala was presumed to have caused greater amygdala activation and thus to have increased emotional reactivity.
Going beyond the commonsense idea that an insufficient quantity of sleep can make someone grumpy, we should also consider both the quality of sleep and the quality of the memory processing that transpires during sleep. How memories are processed during sleep could determine whether there are negative or positive consequences for psychological well-being. In the next section we explore the negative consequences more broadly.
SLEEP AND PSYCHOLOGICAL WELL-BEING
Bringing together the critical role of sleep in memory consolidation with the fact that memory is used for many cognitive functions leads to the following further inference: Sleep disturbances may have far-reaching cognitive consequences. Certainly drowsiness can affect cognition in many ways, but there’s more to it than simply the quantity of sleep. Memory processing during sleep might not be working properly. Even if there is sufficient sleep and plenty of time for overnight memory processing, that processing may become dysfunctional. A flaw could develop in the way memories are selected for reactivation or in the way they are processed, with the consequence that the normal progress of nightly consolidation could go awry. If so, the outcome may extend to pervasive problems for one’s well-being and mental health. Speculatively, some affective disorders may have at their core a dysfunction in memory processing during sleep.
Major depressive disorder (MDD), for example, is characterized by impaired sleep continuity, lower-than-normal density of NREM sleep, and higher-than-normal density of REM sleep ( Steiger & Pawlowski 2019 ). Additionally, slow-wave activity (conventionally defined as EEG power at 0.5–4 Hz), which includes the SOs described above, is abnormal in two ways. First, patients suffering from MDD exhibit reduced slow-wave activity relative to healthy controls ( Borbély et al. 1984 ). Second, the dynamics of this activity is altered. A decline in slow-wave activity over the course of a night of sleep is the typical pattern, thought to be a sign of normal sleep physiology. This decline is disrupted in depression ( Kupfer et al. 1986 ) and restored upon effective treatment ( Jindal et al. 2003 ). Moreover, insomnia is common in patients with depression ( Buysse et al. 2008 , Manber et al. 2008 ). Relatedly, bright-light therapy can be helpful in depression, in conjunction with its effects on circadian rhythms and sleep ( Pail et al. 2011 ). Memory symptoms noted in depression, particularly overgeneral autobiographical retrieval ( Williams et al. 2007 ), may also fit with the dependence of memory function on sleep and the alteration of sleep in depression.
A persistent controversy in depression research has concerned whether sleep abnormalities are a result of depressive illness or a contributing factor to it. The latter direction of causality has received considerable support, including evidence that sleep abnormalities often precede depressive episodes ( Ohayon & Roth 2003 ). Importantly, however, these do not need to be mutually exclusive alternatives. A bidirectional relationship is likely, as sleep and affective symptoms may reinforce each other throughout the progression of MDD ( Bao et al. 2017 ).
To further understand the mechanisms whereby sleep abnormalities may be operative in producing or exacerbating mood disorders such as MDD, research is needed to relate measures of sleep physiology in patients to cognition and mood. In particular, we concern ourselves here with the memory functions of sleep and the contribution of memory to MDD progression. Some of the most debilitating symptoms of MDD are tied to memory. By one account, patients suffering from MDD hold and empower negative representations about the self that serve to bias memory processing toward negative experiences ( Everaert et al. 2012 ). Consonant with this idea, depressed patients tend to recall negative memories better than healthy individuals do ( Fattahi Asl et al. 2015 ). It is therefore tempting to hypothesize that sleep disturbance and MDD are mediated by biasing effects of memory consolidation. Multiple investigators thinking along these lines have emphasized the role of REM sleep, suggesting that its prominence in MDD serves to overemphasize the consolidation of negative memories ( Walker & van der Helm 2009 , Harrington et al. 2018 ). Correspondingly, the three major classes of antidepressant drugs all profoundly suppress REM sleep ( Vertes & Eastman 2000 ). SWS has garnered far less attention in research on depression and related disorders, but given the wealth of evidence supporting the role of SWS in memory consolidation, it may be more relevant in this context than commonly assumed.
Insights into other psychiatric disorders beyond depression may also emerge through investigations of the relevance of memory consolidation during SWS. For example, other mood disorders such as social anxiety disorder can involve a negative memory bias as in depression ( Glazier & Alden 2019 ), and the bias may be operative during sleep. Supporting sleep’s suggested role in overemphasizing the consolidation of negative memories, one TMR study found that cueing negative memories resulted in more negative ratings one week later in socially anxious adolescents but not in healthy ones ( Groch et al. 2017 ).
Sleep disturbances are reported in 50–80% of people with psychiatric disorders ( Franzen & Buysse 2017 ). In posttraumatic stress disorder (PTSD), memory issues are particularly prominent, as are sleep-related symptoms, and some PTSD symptoms have been attributed to an excessive consolidation of negative memories ( Pitman et al. 2000 ). Sleep disturbances immediately following traumatic experiences may serve as a protective mechanism to prevent the consolidation of traumatic memories, though consolidation of emotional memories may span many nights ( Bolinger et al. 2019 ).
An excess of arousals during REM sleep may be one sign of maladaptive sleep in relation to emotional distress. This type of unstable or disrupted REM sleep has been observed in PTSD ( Germain et al. 2008 ) and in insomnia ( Riemann et al. 2012 ). To examine the association between this sign of low-quality sleep and emotional coping, Wassing and colleagues (2019) subjected healthy individuals to an episode of self-focused distress, and they found that sleep with abundant spindles followed by uninterrupted REM sleep predicted a healthier orientation the next day, as reflected by an adaptation in amygdala fMRI activity ( Figure 4 ). If we extend ideas from this experiment to patients, it could be that individuals who suffer the most persistent distress following trauma or emotional insult are those plagued by maladaptive memory processing during sleep; REM sleep punctuated by signs of arousal, presumably mediated by ascending noradrenergic systems, could be a sign of this specific type of maladaptive sleep-thinking. A fruitful direction for future research would be to flesh out the connections among REM stability, spindles prior to REM, and memory processing during sleep in relation to distressing memories.

Wassing et al. (2019) used a variant of the targeted memory reactivation (TMR) procedure to examine how participants responded to a distressing episode. Before sleep, participants listened to a recording of their own off-key singing, which elicited a strong amygdala response. During sleep, odors linked with the stressful episode (and a control odor) were presented over multiple stages of sleep. Regardless of the TMR manipulation, two patterns of sleep were observed: sleep with undisturbed rapid eye movement (REM) periods ( top ) or REM interrupted by brief arousals ( bottom ). Amygdala responses the next day were reduced to the extent that REM was uninterrupted and also to the extent that spindles were frequent in the non-REM (NREM) period prior to REM. TMR with the stress-associated odor was found to enhance these effects. These findings demonstrate a specific connection between sleep after a stressful experience and future emotional responses. Figure adapted with permission from Wassing et al. (2019) .
Overall, this conceptualization of the interactions among maladaptive consolidation, sleep problems, and memory-related emotional problems may prove to be fruitful for understanding mental disorders. The memory work accomplished during sleep ideally supports adaptive memory function, but it can become maladaptive instead. In depression and anxiety, a patient’s day may be filled with excessive rumination and worry. Negative thoughts may be recirculated to the detriment of the person’s well-being. Harmful thinking may pervade sleep as well, producing further negative consequences. In this sense, optimal memory processing during sleep may elude psychiatric patients—and by extension, perhaps the same applies to those who experience less extreme psychological difficulties. Further investigation of sleep-related memory consolidation mechanisms could thus lead to new insights into sleep that apply whether an individual has clinical symptoms or not.
HARNESSING SLEEP TO IMPROVE PSYCHOLOGICAL WELL-BEING
The cumulative research using TMR shows that sleep-based consolidation is modifiable. Although much remains to be understood about this memory processing—including its neural substrates, its consequences, and the factors that dictate which memories are reactivated during sleep—at this point we can suggest some possible strategies for promoting beneficial sleep cognition. Efforts to optimize memory processing during sleep could have ramifications not only for memory but also for improving quality of life.
The importance of one’s quality of sleep is widely recognized. Standard ideas about sleep hygiene are now promoted widely (e.g., Walker 2017 ). Good sleep habits include endeavoring to obtain a sufficient quantity of sleep every night; arranging a dark, quiet, and cool sleep environment; avoiding alcohol, caffeine, and late-night screen use; and adopting a consistent bedtime and wake-up time seven days a week.
But what constitutes good-quality sleep? Our view is that the definition of sleep quality should be widened. It should not be limited to standard sleep physiology metrics such as the total time asleep, the continuity of sleep, or the density of slow waves and spindles. Such measures might be insensitive to subtle memory transactions. The importance of how memories are processed during sleep, and of the specific sorts of memories that are reactivated, must also be considered. Ultimately, functional measures should be developed to assess sleep’s contribution to memory, which means taking into account the degree of beneficial or detrimental memory reactivation.
A major factor that may influence sleep quality is the reemergence of negative memories. Much as waking rumination can be harmful, a proliferation of negative memories may also occur during sleep and may likewise have negative psychological consequences. Sleep-based rumination might be quite prevalent, regardless of clinical diagnosis. If rumination while awake can take a toll on well-being and reinforce a preoccupation with negative concerns, then the same may be true for sleep—harmful thoughts may pervade one’s sleep cognition, with harmful consequences. One’s remembered dream content might occasionally reflect these negative thoughts. Indeed, recurring nightmares or recurring stressful dreams could be a symptom of more pervasive suboptimal sleep. With reference to the literature reviewed above, memory processing during SWS could be very important, whether or not negative dreams are recalled after awakening.
Broadening this idea, rumination may be just one variant of a larger category of maladaptive memory processing during sleep. To take an extreme example, if the mind is excessively agitated during sleep, incessantly revisiting negative thoughts and memories, one consequence could be objectively poor sleep. This poor sleep could include a difficulty staying asleep or maintaining certain sleep stages, as in the arousal-filled REM periods noted above. Alternatively, sleep could look fairly normal electrophysiologically, but the nature of the memory processing could still have unwanted consequences for the individual after sleep. Intuitively, many individuals experience waking up “on the wrong side of the bed” after a full night of sleep, feeling unrested and ill-tempered. In both cases—maladaptive sleep with or without obvious signs of sleep disruption—there could be harmful ramifications for the waking mind.
A key empirical question is whether cultivating calm sleep can produce benefits for the waking mind. A worthy future goal for TMR research would be to test various methods to calm the mind during sleep. Exploring new strategies in this direction requires departing from the orthodox assumption that nothing can be done about the paths our minds take while we are asleep.
Such exploration must proceed together with research aimed at advancing our understanding of sleep, given that sleep may help with adaptive processing of traumatic memories. It could be that overnight emotional turmoil is the price we pay for subsequent waking benefits. If so, this sort of sleep-work should be perpetuated, not eliminated. This possibility deserves to be investigated further, but here we present an opposing line of thought: We suggest that sleep with maladaptive memory processing can be detrimental, in which case it could be helpful to change it, for instance through the counter-reactivation or inception of positive memories, feelings, or concepts.
Given that memory processing during sleep is modifiable, sleep-based consolidation affords the opportunity not just for improving memory function but also for restructuring the self. It may be possible to adjust the memories that we emphasize and maintain at the forefront of our psyche in an intentional and strategic way, in order to reach one’s goals of self-improvement. For example, if one values a reduction in self-centeredness and an increase in compassion for others, this intention can lead one to prioritize certain memories for reactivation and subsequent consolidation. Such an approach does not require something as unrealistic as drastically altering one’s set of autobiographical memories or starting all over by forgetting them, as in psychogenic amnesia. Rather, one might seek to gradually adjust both one’s declarative knowledge and one’s habits in a prosocial direction. In this sense, changing for the better concerns both declarative and nondeclarative memories. Change is possible based on what information we emphasize and recapitulate while awake, which is subject to further memory processing during sleep.
The natural, daily course of intentional wake memory processing followed by sleep memory processing may be sufficient to put into play this scenario of change for the better. A TMR protocol could also be adapted for use in conjunction with wake training to encourage positive changes. One example of such an application is in the context of the social biases that can implicitly affect our decisions and behavior toward others. Counter-stereotype training is one method to attempt to adjust such biases. In one study, TMR during sleep following such training was found to enhance bias changes, as indexed by performance measures from the Implicit Association Test ( Hu et al. 2015 ). These measures, however, are not high in test-retest reliability and are poor predictors of discriminatory behavior ( Oswald et al. 2013 ). Also, one attempt to closely replicate these TMR results failed to do so ( Humiston & Wamsley 2019 ). Ingrained attitudes may be difficult to change and also difficult to measure. Yet, various sorts of efforts along related lines might be worth pursuing in the interest of developing stronger cognitive control—for example, to increase prosocial tendencies.
Aside from TMR, there may be other ways to change the specific processing engaged by the sleeping brain. One tactic would be to control pre-sleep mental activity, in that positive waking thoughts could produce positive sleeping thoughts. Mental content during the last few minutes before falling asleep might be particularly influential. Indeed, a pre-sleep hypnosis procedure has been shown in several studies to increase sleep physiology measures of SWS in highly hypnotizable young subjects (e.g., Cordi et al. 2020 ). Adding TMR might extend these benefits further. More research should examine the consequences of tactics such as holding the pre-sleep intention to fill one’s sleep with positive thoughts. Dream control provides a further demonstration that we are not helplessly at the mercy of whatever happens during sleep. In the context of a lucid dream, for example, an individual can engage the intention to change what happens next. Changing a dream can be accomplished by using pre-sleep intentions and by using a variant of the TMR procedure to prompt particular dream content ( Konkoly et al. 2020 ).
The TMR research summarized above could be extended in many ways to attempt to instill particular thoughts during sleep. TMR procedures begin with pre-sleep learning, which in this case could involve a positive cognitive-affective orientation. Various tasks can be used to increase calm and peaceful states. Another option would be to decrease negative thinking, engaging strategies to dampen or reframe anxious, stressful, or otherwise maladaptive thoughts. Innovative TMR strategies could take aim at both of these goals to determine whether such changes are possible. Whereas Wassing and colleagues (2019) used TMR to reinstate the context of a particularly stressful and negative affect-laden experience, a variation on their design could instead reinstate positive experiences or invoke strategies that effectively reduce the unfortunate impact of negative experiences.
Finally, we acknowledge that the link between sleep and waking cognition is bidirectional. The quality of sleep reflects cognitive activity recently engaged while awake; the quality of wakefulness, in turn, reflects consolidation and other cognitive activity engaged while asleep; the quality of life reflects both. We may tend to ignore the portion of our lives occupied by sleep because it is predominantly out of view (like the dark side of the moon), but we do so at our peril. By understanding the mutual relationships between sleep and wake, and by embracing innovative ways to improve sleep, we can change the waking mind for the better.
SLEEP PHYSIOLOGY
Sleep is classically divided into stages characterized by distinct neural and bodily functions. Although future advances in sleep research and neural decoding may lead to refinements in our thinking about sleep physiology, contemporary schemes distinguish rapid eye movement (REM) sleep from three stages of non-REM (NREM) sleep. Each stage has characteristic electrophysiological features evident in the electroencephalogram, electrooculogram, and electromyogram. NREM includes stage 1 (N1), stage 2 (N2), and stage 3 (N3). Sleep progresses from light sleep to deeper sleep across these three stages as the ease of arousability decreases. N3 (formerly divided into N3 and N4) is also termed slow-wave sleep due to the high-amplitude slow waves (0.5–4 Hz) observed in the EEG. Nocturnal sleep consists of multiple cycles, typically 90 minutes in duration, including light sleep, slow-wave sleep, REM, and then a return to NREM. The majority of sleep is usually spent in N2 and slow-wave sleep, the stages most strongly implicated in memory consolidation to date.
ACKNOWLEDGMENTS
We thank our colleagues for many fruitful discussions, including Jessica Payne, Marcia Grabowecky, Bjorn Rasch, Ken Norman, Phyllis Zee, John Wixted, and members of Ken Paller’s lab group. We are also grateful for funding from the Human Frontier Science Program (to E.S.) and from the Mind Science Foundation, the McKnight Foundation, DARPA, NIH (R01-NS112942, T32-NS047987, and T32-HL007909), and NSF (BCS-1921678 and BCS-1829414).
| Memory consolidation | changes in memory storage following initial acquisition that stabilize new information and can include integration, transformation, and generalization |
| Memory reactivation | reemergence of information stored in brain networks during a previous experience, with or without the conscious experience of retrieving the memory |
| Declarative memories | the memories we rely on for the recall and recognition of factual and event information |
| Nondeclarative memories | an umbrella term for skills, habits, conditioning, priming, and other types of implicit learning, all typically exhibited without conscious retrieval |
| Anterograde amnesia | a memory disorder of impaired learning of new facts and events |
| Retrograde amnesia | a memory disorder of impaired retrieval of facts and events acquired prior to the onset of the disorder |
| Active systems consolidation hypothesis | the hypothesis that cortical traces of declarative memories are shaped during slow-wave sleep through hippocampal reactivation, facilitated by synchronized oscillations in different brain regions |
| Slow-wave sleep (SWS) | the deepest stage of sleep, dominated by cortical slow waves (0.5–4 Hz) that are observed in the electroencephalogram |
| Nested oscillations | oscillations at one frequency coinciding with features (e.g., peak or trough) of another, lower-frequency oscillation |
| Hippocampal replay | neuronal activity recapitulating that at learning, thought to constitute a readout of stored information as a sequence of place-cell action potentials |
| Targeted memory reactivation (TMR) | a method involving the unobtrusive presentation of learning-related stimuli during sleep, thereby biasing reactivation and impacting consolidation |
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
1 A remarkable exception to this rule has been documented in people with so-called highly superior autobiographical memory. Fewer than 100 individuals have been reported to have this capability. Their superior abilities have yet to be explained, but they are limited to autobiographical events and certain facts that are personally meaningful ( LePort et al. 2012 ). Instead of forgetting most days, they seem to remember nearly every day. They can recall events from long ago with the same ease that most of us recall what happened yesterday. Sleep may contribute to this capability. Our preliminary finding of a high density of sleep spindles in several of these individuals ( Westerberg et al. 2020 ) suggests that their sleep may be particularly beneficial, but additional evidence is needed to confirm this possibility.
LITERATURE CITED
- Aly M, Ranganath C. 2018. New perspectives on the hippocampus and memory . Neurosci. Lett . 680 :1–3 [ PubMed ] [ Google Scholar ]
- Andrillon T, Kouider S. 2019. The vigilant sleeper: neural mechanisms of sensory (de)coupling during sleep . Curr. Opin. Physiol . 15 :47–59 [ Google Scholar ]
- Andrillon T, Pressnitzer D, Léger D, Kouider S. 2017. Formation and suppression of acoustic memories during human sleep . Nat. Commun . 8 ( 1 ):179. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Antony JW, Gobel EW, O’Hare JK, Reber PJ, Paller KA. 2012. Cued memory reactivation during sleep influences skill learning . Nat. Neurosci . 15 ( 8 ):1114–16 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Antony JW, Paller KA. 2017. Using oscillating sounds to manipulate sleep spindles . Sleep 40 ( 3 ):zsw068 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Antony JW, Piloto L, Wang M, Pacheco P, Norman KA, Paller KA. 2018. Sleep spindle refractoriness segregates periods of memory reactivation . Curr. Biol . 28 ( 11 ):1736–43.e4 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Arzi A, Holtzman Y, Samnon P, Eshel N, Harel E, Sobel N. 2014. Olfactory aversive conditioning during sleep reduces cigarette-smoking behavior . J. Neurosci . 34 ( 46 ):15382–93 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Arzi A, Shedlesky L, Ben-Shaul M, Nasser K, Oksenberg A, et al. 2012. Humans can learn new information during sleep . Nat. Neurosci . 15 ( 10 ):1460–65 [ PubMed ] [ Google Scholar ]
- Axmacher N, Elger CE, Fell J. 2008. Ripples in the medial temporal lobe are relevant for human memory consolidation . Brain 131 ( 7 ):1806–17 [ PubMed ] [ Google Scholar ]
- Backhaus J, Born J, Hoeckesfeld R, Fokuhl S, Hohagen F,Junghanns K. 2007. Midlife decline in declarative memory consolidation is correlated with a decline in slow wave sleep . Learn. Mem . 14 ( 5 ):336–41 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bao Y-P, Han Y, Ma J, Wang R-J, Shi L, et al. 2017. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: meta-analysis and systematic review . Neurosci. Biobehav. Rev . 75 :257–73 [ PubMed ] [ Google Scholar ]
- Belal S, Cousins J, El-Deredy W, Parkes L, Schneider J, et al. 2018. Identification of memory reactivation during sleep by EEG classification . NeuroImage 176 :203–14 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bendor D, Wilson MA. 2012. Biasing the content of hippocampal replay during sleep . Nat. Neurosci . 15 ( 10 ):1439–44 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bergmann TO, Mölle M, Diedrichs J, Born J, Siebner HR. 2012. Sleep spindle-related reactivation of category-specific cortical regions after learning face-scene associations . Neuroimage 59 ( 3 ):2733–42 [ PubMed ] [ Google Scholar ]
- Berkers RMWJ, Ekman M, van Dongen EV, Takashima A, Paller KA, Fernández G. 2018. Cued reactivation during slow-wave sleep induces connectivity changes related to memory stabilization . Sci. Rep . 8 :16958. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bolinger E, Cunningham TJ, Payne JD, Bowman MA, Bulca E, et al. 2019. Sleep’s benefits to emotional processing emerge in the long term . Cortex 120 :457–70 [ PubMed ] [ Google Scholar ]
- Borbély AA, Tobler I, Loepfe M, Kupfer DJ, Ulrich RF, et al. 1984. All-night spectral analysis of the sleep EEG in untreated depressives and normal controls . Psychiatry Res . 12 ( 1 ):27–33 [ PubMed ] [ Google Scholar ]
- Born J, Rasch B, Gais S. 2006. Sleep to remember . Neuroscientist 12 ( 5 ):410–24 [ PubMed ] [ Google Scholar ]
- Born J, Wilhelm I. 2012. System consolidation of memory during sleep . Psychol. Res . 76 ( 2 ):192–203 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brodt S, Pöhlchen D, Táumer E, Gais S, Schönauer M. 2018. Incubation, not sleep, aids problem-solving . Sleep 41 ( 10 ):155 [ PubMed ] [ Google Scholar ]
- Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. 2008. Prevalence, course, and comorbidity of insomnia and depression in young adults . Sleep 31 ( 4 ):473–80 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Buzsáki G 1998. Memory consolidation during sleep: a neurophysiological perspective . J. Sleep Res . 7 ( S1 ):17–23 [ PubMed ] [ Google Scholar ]
- Cai DJ, Mednick SA, Harrison EM, Kanady JC, Mednick SC. 2009. REM, not incubation, improves creativity by priming associative networks . PNAS 106 ( 25 ):10130–34 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cairney SA, Durrant SJ, Hulleman J, Lewis PA. 2014. Targeted memory reactivation during slow wave sleep facilitates emotional memory consolidation . Sleep 37 ( 4 ):701–7 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cairney SA, Guttesen AÁV, El Marj N, Staresina BP. 2018. Memory consolidation is linked to spindle-mediated information processing during sleep . Curr. Biol . 28 ( 6 ):948–954.e4 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cairney SA, Lindsay S, Sobczak JM, Paller KA, Gaskell MG. 2016. The benefits of targeted memory reactivation for consolidation in sleep are contingent on memory accuracy and direct cue-memory associations . Sleep 39 ( 5 ):1139–50 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cartwright R 1990. A network model of dreams. In Sleep and Cognition, ed . Bootzin RR, Kihlstrom JF, Schacter DL, pp. 179–89. Washington, DC: Am. Psychol. Assoc. [ Google Scholar ]
- Cartwright RD. 2010. The Twenty-Four Hour Mind: The Role of Sleep and Dreaming in Our Emotional Lives . Oxford, UK: Oxford Univ. Press [ Google Scholar ]
- Clemens Z, Fabó D, Halász P. 2006. Twenty-four hours retention of visuospatial memory correlates with the number of parietal sleep spindles . Neurosci. Lett . 403 ( 1 ):52–56 [ PubMed ] [ Google Scholar ]
- Cordi MJ, Rossier L, Rasch B. 2020. Hypnotic suggestions given before nighttime sleep extend slow-wave sleep as compared to a control text in highly hypnotizable subjects . Int. J. Clin. Exp. Hypn . 68 ( 1 ):105–29 [ PubMed ] [ Google Scholar ]
- Cousins JN, El-Deredy W, Parkes LM, Hennies N, Lewis PA. 2016. Cued reactivation of motor learning during sleep leads to overnight changes in functional brain activity and connectivity . PLOS Biol . 14 ( 5 ):e1002451. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cox R, Hofman WF, Talamini LM. 2012. Involvement of spindles in memory consolidation is slow wave sleep-specific . Learn. Mem . 19 ( 7 ):264–67 [ PubMed ] [ Google Scholar ]
- Cox R, Rüber T, Staresina BP, Fell J. 2019. Heterogeneous profiles of coupled sleep oscillations in human hippocampus . Neuroimage 202 :116178. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cox R, van Driel J, de Boer M, Talamini LM. 2014. Slow oscillations during sleep coordinate interregional communication in cortical networks . J. Neurosci . 34 ( 50 ):16890–901 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Creery JD, Oudiette D, Antony JW, Paller KA. 2015. Targeted memory reactivation during sleep depends on prior learning . Sleep 38 ( 5 ):755–63 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crick F,Mitchison G. 1983. The function of dream sleep . Nature 304 :111–14 [ PubMed ] [ Google Scholar ]
- Diekelmann S, Born J. 2010. The memory function of sleep . Nat. Rev. Neurosci . 11 ( 2 ):114–26 [ PubMed ] [ Google Scholar ]
- Dudai Y 2012. The restless engram: Consolidations never end . Annu. Rev. Neurosci . 35 :227–47 [ PubMed ] [ Google Scholar ]
- Duncan CP. 1949. The retroactive effect of electroshock on learning . J. Cotnp. Physiol. Psychol . 42 ( 1 ):32–44 [ PubMed ] [ Google Scholar ]
- Everaert J, Koster EHW, Derakshan N. 2012. The combined cognitive bias hypothesis in depression . Clin. Psychol. Rev . 32 ( 5 ):413–24 [ PubMed ] [ Google Scholar ]
- Fattahi Asl A, Ghanizadeh A, Mollazade J, Aflakseir A. 2015. Differences of biased recall memory for emotional information among children and adolescents of mothers with MDD, children and adolescents with MDD, and normal controls . Psychiatry Res . 228 ( 2 ):223–27 [ PubMed ] [ Google Scholar ]
- Fernandez LMJ, Luthi A. 2020. Sleep spindles: mechanisms and functions . Physiol. Rev . 100 :805–68 [ PubMed ] [ Google Scholar ]
- Fernández-Ruiz A, Oliva A, de Oliveira EF, Rocha-Almeida F, Tingley D, Buzsaki G. 2019. Long-duration hippocampal sharp wave ripples improve memory . Science 364 ( 6445 ):1082–86 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Foster DJ. 2017. Replay comes of age . Annu. Rev. Neurosci . 40 :581–602 [ PubMed ] [ Google Scholar ]
- Franzen PL, Buysse DJ. 2017. Sleep in psychiatric disorders. In Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects , ed. Chokroverty S, pp. 977–96. New York: Springer [ Google Scholar ]
- Fuentemilla L,Miró J, Ripollás P, Vilà-Balló A,Juncadella M, et al. 2013. Hippocampus-dependent strengthening of targeted memories via reactivation during sleep in humans . Curr. Biol . 23 ( 18 ):1769–75 [ PubMed ] [ Google Scholar ]
- Gais S, Mölle M, Helms K, Born J. 2002. Learning-dependent increases in sleep spindle density . J. Neurosci . 22 ( 15 ):6830–34 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Germain A, Buysse DJ, Nofzinger E. 2008. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses . Sleep Med. Rev . 12 ( 3 ):185–95 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Geva-Sagiv M, Nir Y. 2019. Local sleep oscillations: implications for memory consolidation . Front. Neurosci . 13 :813. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Girardeau G, Benchenane K, Wiener SI, Buzsáki G, Zugaro MB. 2009. Selective suppression of hippocampal ripples impairs spatial memory . Nat. Neurosci . 12 ( 10 ):1222–23 [ PubMed ] [ Google Scholar ]
- Glazier BL, Alden LE. 2019. Social anxiety disorder and memory for positive feedback . J. Abnorm. Psychol . 128 ( 3 ):228–33 [ PubMed ] [ Google Scholar ]
- Groch S, Preiss A, McMakin DL, Rasch B, Walitza S, et al. 2017. Targeted reactivation during sleep differentially affects negative memories in socially anxious and healthy children and adolescents . J. Neurosci . 37 ( 9 ):2425–34 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harrington MO, Johnson JM, Croom HE, Pennington K, Durrant SJ. 2018. The influence of REM sleep and SWS on emotional memory consolidation in participants reporting depressive symptoms . Cortex 99 :281–95 [ PubMed ] [ Google Scholar ]
- Hebscher M, Wing E, Ryan J, Gilboa A. 2019. Rapid cortical plasticitysupports long-term memory formation . Trends Cogn. Sci . 23 ( 12 ):989–1002 [ PubMed ] [ Google Scholar ]
- Helfrich RF, Mander BA,Jagust WJ, Knight RT, Walker MP. 2018. Old brains come uncoupled in sleep: slow wave-spindle synchrony, brain atrophy, and forgetting . Neuron 97 ( 1 ):221–30.e4 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Henin S, Borges H, Shankar A, Sarac C, Melloni L, et al. 2019. Closed-loop acoustic stimulation enhances sleep oscillations but not memory performance . eNeuro 6 ( 6 ):0306–19.2019 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hu X, Antony JW, Creery JD, Vargas IM, Bodenhausen GV, Paller KA. 2015. Unlearning implicit social biases during sleep . Science 348 ( 6238 ):1013–15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hu X, Cheng L, Chiu MH, Paller KA. 2020. Promoting memory consolidation during sleep: a meta-analysis of targeted memory reactivation . Psychol. Bull . 146 :218–44 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huber R, Felice Ghilardi M, Massimini M, Tononi G. 2004. Local sleep and learning . Nature 430 ( 6995 ):78–81 [ PubMed ] [ Google Scholar ]
- Humiston GB, Wamsley EJ. 2019. Unlearning implicit social biases during sleep: a failure to replicate . PLOS ONE 14 ( 1 ):e0211416. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ji D, Wilson MA. 2007. Coordinated memory replay in the visual cortex and hippocampus during sleep . Nat. Neurosci . 10 ( 1 ):100–7 [ PubMed ] [ Google Scholar ]
- Jindal RD, Friedman ES, Berman SR, Fasiczka AL, Howland RH, Thase ME. 2003. Effects of sertraline on sleep architecture in patients with depression . J. Clin. Psychopharmacol . 23 ( 6 ):540–48 [ PubMed ] [ Google Scholar ]
- Karni A, Tanne D, Rubenstein BS, Askenasy JJ, Sagi D. 1994. Dependence on REM sleep of overnight improvement of a perceptual skill . Science 265 ( 5172 ):679–82 [ PubMed ] [ Google Scholar ]
- Khodagholy D, Gelinas JN, Buzsáki G. 2017. Learning-enhanced coupling between ripple oscillations in as-sociation cortices and hippocampus . Science 358 ( 6361 ):369–72 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kleim B, Wysokowsky J, Schmid N, Seifritz E, Rasch B. 2016. Effects of sleep after experimental trauma on intrusive emotional memories . Sleep 39 ( 12 ):2125–32 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Klinzing JG, Niethard N, Born J. 2019. Mechanisms of systems memory consolidation during sleep . Nat. Neurosci . 22 ( 10 ):1598–610 [ PubMed ] [ Google Scholar ]
- Konkoly KR, Appel K, Chabani E, Mangiaruga A, Gott J, et al. 2020. Real-time dialogue between experimenters and dreamers during REM sleep . Work. Pap., Northwestern Univ., Evanston, IL [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kupfer DJ, Reynolds CF, Ulrich RF, Grochocinski VJ. 1986. Comparison of automated REM and slow-wave sleep analysis in young and middle-aged depressed subjects . Biol. Psychiatry 21 ( 2 ):189–200 [ PubMed ] [ Google Scholar ]
- Latchoumane C-FV, Ngo H-VV, Born J, Shin H-S. 2017. Thalamic spindles promote memory formation during sleep through triple phase-locking of cortical, thalamic, and hippocampal rhythms . Neuron 95 ( 2 ):424–35.e6 [ PubMed ] [ Google Scholar ]
- Laventure S, Benchenane K. 2020. Validating the theoretical bases of sleep reactivation during sharp-wave ripples and their association with emotional valence . Hippocampus 30 ( 1 ):19–27 [ PubMed ] [ Google Scholar ]
- Lechner HA, Squire LR, Byrne JH. 1999. 100 years of consolidation—remembering Muller and Pilzecker . Learn. Mem . 6 ( 2 ):77–87 [ PubMed ] [ Google Scholar ]
- Lehmann M, Schreiner T, Seifritz E, Rasch B. 2016. Emotional arousal modulates oscillatory correlates of targeted memory reactivation during NREM, but not REM sleep . Sci. Rep . 6 ( 1 ):39229. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LePort AKR, Mattfeld AT, Dickinson-Anson H, Fallon JH, Stark CEL, et al. 2012. Behavioral and neuroanatomical investigation of Highly Superior Autobiographical Memory (HSAM) . Neurobiol. Learn. Mem . 98 ( 1 ):78–92 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lewis PA, Bendor D.2019. How targeted memory reactivation promotes the selective strengthening of memories in sleep . Curr. Biol . 29 ( 18 ):R906–12 [ PubMed ] [ Google Scholar ]
- Lewis PA, Durrant SJ. 2011. Overlapping memory replay during sleep builds cognitive schemata . Trends Cogn. Sci . 15 ( 8 ):343–51 [ PubMed ] [ Google Scholar ]
- Lustenberger C, Boyle MR, Alagapan S, Mellin JM, Vaughn BV, Fröhlich F. 2016. Feedback-controlled transcranial alternating current stimulation reveals a functional role of sleep spindles in motor memory consolidation . Curr. Biol . 26 ( 16 ):2127–36 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lutz ND, Diekelmann S, Hinse-Stern P, Born J, Rauss K. 2017. Sleep supports the slow abstraction of gist from visual perceptual memories . Sci. Rep . 7 :42950. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Manber R, Edinger JD, Gress JL, Pedro-Salcedo MGS, Kuo TF, Kalista T. 2008. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia . Sleep 31 ( 4 ):489–95 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maquet P, Péters J-M, Aerts J, Delfiore G, Degueldre C, et al. 1996. Functional neuroanatomy of human rapid-eye-movement sleep and dreaming . Nature 383 ( 6596 ):163–66 [ PubMed ] [ Google Scholar ]
- Marr D 1971. Simple memory: a theory for archicortex . Philos. Trans. R. Soc. B 262 ( 841 ):23–81 [ PubMed ] [ Google Scholar ]
- Marshall L, Helgadóttir H, Mölle M, Born J. 2006. Boosting slow oscillations during sleep potentiates memory . Nature 444 ( 7119 ):610–13 [ PubMed ] [ Google Scholar ]
- Massimini M, Huber R, Ferrarelli F, Hill S, Tononi G. 2004. The sleep slow oscillation as a traveling wave . J. Neurosci . 24 ( 31 ):6862–70 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McClelland JL,McNaughton BL, O’Reilly RC. 1995. Why there are complementary learning systems in the hippocampus and neocortex: insights from the successes and failures of connectionist models of learning and memory . Psychol. Rev . 102 ( 3 ):419–57 [ PubMed ] [ Google Scholar ]
- Mednick SC, McDevitt EA, Walsh JK, Wamsley E, Paulus M, et al. 2013. The critical role of sleep spindles in hippocampal-dependent memory: a pharmacology study . J. Neurosci . 33 ( 10 ):4494–504 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller TD, Chong TT-J, Aimola Davies AM, Johnson MR, Irani SR, et al. 2020. Human hippocampal CA3 damage disrupts both recent and remote episodic memories . eLife 9 :e41836. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Milner CE, Fogel SM, Cote KA. 2006. Habitual napping moderates motor performance improvements following a short daytime nap . Biol. Psychol . 73 ( 2 ):141–56 [ PubMed ] [ Google Scholar ]
- Mölle M, Bergmann TO, Marshall L, Born J. 2011. Fast and slow spindles during the sleep slow oscillation: disparate coalescence and engagement in memory processing . Sleep 34 ( 10 ):1411–21 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mölle M, Marshall L, Gais S, Born J. 2002. Grouping of spindle activity during slow oscillations in human non-rapid eye movement sleep . J. Neurosci . 22 ( 24 ):10941–47 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Müller G, Pilzecker A. 1900. Experimented Beiträge zur Lehre vom Gedächtnis [Experimental contributions to the theory of memory] . Leipzig, Ger: Verlag von Johann Ambrosius Barth [ Google Scholar ]
- Murray EA, Bussey TJ, Saksida LM. 2007. Visual perception and memory: a new view of medial temporal lobe function in primates and rodents . Annu. Rev. Neurosci . 30 :99–122 [ PubMed ] [ Google Scholar ]
- Nádasdy Z, Hirase H, Czurkó A, Csicsvari J, Buzsáki G. 1999. Replay and time compression of recurring spike sequences in the hippocampus . J. Neurosci . 19 ( 21 ):9497–507 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nadel L, Moscovitch M. 1997. Memory consolidation, retrograde amnesia and the hippocampal complex . Curr. Opin. Neurobiol . 7 ( 2 ):217–27 [ PubMed ] [ Google Scholar ]
- Ngo H-VV, Fell J, Staresina BP. 2020. Sleep spindles mediate hippocampal-neocortical coupling during sharp-wave ripples . eLife 9 :e57011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ngo H-VV,Martinetz T, Born J, Mölle M. 2013. Auditory closed-loop stimulation of the sleep slow oscillation enhances memory . Neuron 78 ( 3 ):545–53 [ PubMed ] [ Google Scholar ]
- Nir Y, Staba RJ, Andrillon T, Vyazovskiy VV, Cirelli C, et al. 2011. Regional slow waves and spindles in human sleep . Neuron 70 ( 1 ):153–69 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nishida M, Walker MP 2007. Daytime naps, motor memory consolidation and regionally specific sleep spin-dles . PLOS ONE 2 ( 4 ):e341. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Norman KA,Newman EL,Perotte AJ. 2005. Methods for reducing interference in the Complementary Learn-ing Systems model: oscillating inhibition and autonomous memory rehearsal . Neural Netw . 18 ( 9 ):1212–28 [ PubMed ] [ Google Scholar ]
- Norman Y, Yeagle EM, Khuvis S, Harel M, Mehta AD, Malach R. 2019. Hippocampal sharp-wave ripples linked to visual episodic recollection in humans . Science 365 ( 6454 ):eaax1030. [ PubMed ] [ Google Scholar ]
- Ohayon MM, Roth T. 2003. Place of chronic insomnia in the course of depressive and anxiety disorders . J. Psychiatr. Res . 37 ( 1 ):9–15 [ PubMed ] [ Google Scholar ]
- Oswald FL,Mitchell G, Blanton H,Jaccard J, Tetlock PE. 2013. Predicting ethnic and racial discrimination: a meta-analysis of IAT criterion studies . J. Pers. Soc. PsychoO . 105 ( 2 ):171–92 [ PubMed ] [ Google Scholar ]
- Oudiette D, Paller KA. 2013. Upgrading the sleeping brain with targeted memory reactivation . Trends Cogn. Sci . 17 ( 3 ):142–49 [ PubMed ] [ Google Scholar ]
- Pail G, Huf W, Pjrek E, Winkler D, Willeit M, et al. 2011. Bright-light therapy in the treatment of mood disorders . Neuro psychobiology 64 ( 3 ):152–62 [ PubMed ] [ Google Scholar ]
- Paller KA. 2002. Cross-cortical consolidation as the core defect in amnesia: prospects for hypothesis testing with neuropsychology and neuroimaging. In The Neuropsychology of Memory , ed. Squire LR, Schacter DL, pp. 73–87. New York: Guilford. 3rd ed. [ Google Scholar ]
- Paller KA. 2009. Memory consolidation: systems. In Encyclopedia of Neuroscience , ed. Squire LR, pp. 741–49. Oxford, UK: Academic [ Google Scholar ]
- Paller KA, Voss JL. 2004. Memory reactivation and consolidation during sleep . Learn. Mem . 11 ( 6 ):664–70 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Papalambros NA, Santostasi G, Malkani RG, Braun R, Weintraub S, et al.2017. Acoustic enhancement of sleep slow oscillations and concomitant memory improvement in older adults . Front. Hum. Neurosci . 11 :109. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Papalambros NA, Weintraub S, Chen T, Grimaldi D, Santostasi G, et al. 2019. Acoustic enhancement of sleep slow oscillations in mild cognitive impairment . Ann. Clin. Transl. Neurol . 6 ( 7 ):1191–201 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pavlides C, Winson J. 1989. Influences of hippocampal place cell firing in the awake state on the activity of these cells during subsequent sleep episodes . J. Neurosci . 9 ( 8 ):2907–18 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Payne JD, Kensinger EA. 2018. Stress, sleep, and the selective consolidation of emotional memories . Curr. Opin. Behav. Sci . 19 :36–43 [ Google Scholar ]
- Pitman RK, Shalev AY, Orr SP. 2000. Posttraumatic stress disorder: emotion, conditioning, and memory. In The New Cognitive Neurosciences , ed. Gazzaniga MS, pp. 1133–47. Cambridge, MA: MIT Press. 2nd ed. [ Google Scholar ]
- Plihal W, Born J. 1997. Effects of early and late nocturnal sleep on declarative and procedural memory . J. Cogn. Neurosci . 9 ( 4 ):534–47 [ PubMed ] [ Google Scholar ]
- Purcell SM, Manoach DS, Demanuele C, Cade BE, Mariani S, et al. 2017. Characterizing sleep spindles in 11,630 individuals from the National Sleep Research Resource . Nat. Commun . 8 :15930. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rasch B, Born J. 2013. About sleep’s role in memory . Physiol. Rev . 93 ( 2 ):681–766 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rasch B, Büchel C, Gais S, Born J. 2007. Odor cues during slow-wave sleep prompt declarative memory consolidation . Science 315 ( 5817 ):1426–29 [ PubMed ] [ Google Scholar ]
- Riemann D, Spiegelhalder K, Nissen C, Hirscher V, Baglioni C, Feige B. 2012. REM sleep instability—a new pathway for insomnia? Pharmacopsychiatry 45 ( 5 ):167–76 [ PubMed ] [ Google Scholar ]
- Ritter SM, Strick M, Bos MW, Baaren RBV, Dijksterhuis A. 2012. Good morning creativity: task reactivation during sleep enhances beneficial effect of sleep on creative performance . J. Sleep Res . 21 ( 6 ):643–47 [ PubMed ] [ Google Scholar ]
- Roediger HL, Karpicke JD. 2006. Test-enhanced learning: taking memory tests improves long-term retention . Psychol. Sci . 17 ( 3 ):249–55 [ PubMed ] [ Google Scholar ]
- Roffwarg HP, Herman JH, Bowe-Anders C, Tauber ES. 1978. The effects of sustained alterations of waking visual input on dream content. In The Mind in Sleep: Psychology and Psychophysiology , ed. Arkin AM, Antrobus JS, Ellman SJ, pp. 295–349. Hillsdale, NJ: Erlbaum [ Google Scholar ]
- Rothschild G 2019. The transformation of multi-sensory experiences into memories during sleep . Neurobiol. Learn. Mem . 160 :58–66 [ PubMed ] [ Google Scholar ]
- Rothschild G, Eban E, Frank LM. 2017. A cortical-hippocampal-cortical loop of information processing dur-ing memory consolidation . Nat. Neurosci . 20 ( 2 ):251–59 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Roumis DK, Frank LM. 2015. Hippocampal sharp-wave ripples in waking and sleeping states . Curr. Opin. Neurobiol . 35 :6–12 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rudoy JD, Voss JL, Westerberg CE, Paller KA. 2009. Strengthening individual memories by reactivating them during sleep . Science 326 ( 5956 ):1079. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sanders KEG, Osburn S, Paller KA, Beeman M. 2019. Targeted memory reactivation during sleep improves next-day problem solving . Psychol. Sci . 30 ( 11 ):1616–24. Corrigendum. 2020. Psychol. Sci. 31(8):1048 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schapiro AC, McDevitt EA, Chen L, Norman KA, Mednick SC, Rogers TT. 2017. Sleep benefits memory for semantic category structure while preserving exemplar-specific information . Sci. Rep . 7 ( 1 ):14869. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schönauer M, Alizadeh S, Jamalabadi H, Abraham A, Pawlizki A, Gais S. 2017. Decoding material-specific memory reprocessing during sleep in humans . Nat. Commun . 8 :15404. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schönauer M, Brodt S, Pöhlchen D, Breßmer A, Danek AH, Gais S. 2018. Sleep does not promote solving classical insight problems and magic tricks . Front. Hum. Neurosci . 12 :72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schouten DI, Pereira SIR, Tops M, Louzada FM. 2017. State of the art on targeted memory reactivation: Sleep your way to enhanced cognition . Sleep Med. Rev . 32 :123–31 [ PubMed ] [ Google Scholar ]
- Schreiner T, Doeller CF,Jensen O, Rasch B, Staudigl T. 2018. Theta phase-coordinated memory reactivation reoccurs in a slow-oscillatory rhythm during NREM sleep . Cell Rep . 25 ( 2 ):296–301 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schreiner T, Rasch B. 2015. Boosting vocabulary learning by verbal cueing during sleep . Cereb. Cortex 25 ( 11 ):4169–79 [ PubMed ] [ Google Scholar ]
- Scoville WB, Milner B. 1957. Loss of recent memory after bilateral hippocampal lesions . J. Neurol. Neurosurg. Psychiatry 20 ( 1 ):11–21 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shanahan LK, Gjorgieva E, Paller KA, Kahnt T, Gottfried JA. 2018. Odor-evoked category reactivation in human ventromedial prefrontal cortex during sleep promotes memory consolidation . eLife 7 :e39681. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simon KCNS, Gómez RL, Nadel L. 2018. Losing memories during sleep after targeted memory reactivation . Neurobiol. Learn. Mem . 151 :10–17 [ PubMed ] [ Google Scholar ]
- Sirota A, Csicsvari J, Buhl D, Buzsáki G. 2003. Communication between neocortex and hippocampus during sleep in rodents . PNAS 100 ( 4 ):2065–69 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Skaggs WE, McNaughton BL. 1996. Replay of neuronal firing sequences in rat hippocampus during sleep following spatial experience . Science 271 ( 5257 ):1870–73 [ PubMed ] [ Google Scholar ]
- Smith C 1995. Sleep states and memory processes . Behav. Brain Res . 69 ( 1–2 ):137–45 [ PubMed ] [ Google Scholar ]
- Squire LR. 1992. Declarative and nondeclarative memory: multiple brain systems supporting learning and memory . J. Cogn. Neurosci . 4 ( 3 ):232–43 [ PubMed ] [ Google Scholar ]
- Squire LR, Wixted JT. 2011. The cognitive neuroscience of human memory since H.M . Annu. Rev. Neurosci . 34 :259–88 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Staresina BP, Bergmann TO, Bonnefond M, van derMeij R, Jensen O, et al. 2015. Hierarchical nesting of slow oscillations, spindles and ripples in the human hippocampus during sleep . Nat. Neurosci . 18 ( 11 ):1679–86 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Steiger A, Pawlowski M. 2019. Depression and sleep . Int. J. Mol. Sci . 20 ( 3 ):607 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Steriade M, Nunez A, Amzica F. 1993. A novel slow (<1 Hz) oscillation of neocortical neurons in vivo: depolarizing and hyperpolarizing components . J. Neurosci . 13 ( 8 ):3252–65 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stickgold R, Scott L, Rittenhouse C, Hobson JA. 1999. Sleep-induced changes in associative memory . J. Cogn. Neurosci . 11 ( 2 ):182–93 [ PubMed ] [ Google Scholar ]
- Tambini A, Davachi L. 2019. Awake reactivation of prior experiences consolidates memories and biases cognition . Trends Cogn. Sci . 23 ( 10 ):876–90 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tamminen J, Lambon Ralph MA, Lewis PA. 2017. Targeted memory reactivation of newly learned words during sleep triggers REM-mediated integration of new memories and existing knowledge . Neurobiol. Learn. Mem . 137 :77–82 [ PubMed ] [ Google Scholar ]
- Tempesta D, Socci V, De Gennaro L, Ferrara M. 2018. Sleep and emotional processing . Sleep Med. Rev . 40 :183–95 [ PubMed ] [ Google Scholar ]
- Tilley AJ. 1979. Sleep learning during stage 2 and REM sleep . Biol. Psychol . 9 ( 3 ):155–61 [ PubMed ] [ Google Scholar ]
- Timofeev I, Chauvette S. 2017. Sleep slow oscillation and plasticity . Curr. Opin. Neurobiol . 44 :116–26 [ PubMed ] [ Google Scholar ]
- Tononi G, Cirelli C. 2014. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration . Neuron 81 ( 1 ):12–34 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tucker MA, Hirota Y, Wamsley EJ, Lau H, Chaklader A, Fishbein W. 2006. A daytime nap containing solely non-REM sleep enhances declarative but not procedural memory . Neurobiol. Learn. Mem . 86 ( 2 ):241–47 [ PubMed ] [ Google Scholar ]
- van Dongen EV, Takashima A, Barth M, Zapp J, Schad LR, et al. 2012. Memory stabilization with targeted reactivation during human slow-wave sleep . PNAS 109 ( 26 ):10575–80 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vanderheyden WM, George SA, Urpa L, Kehoe M, Liberzon I, Poe GR. 2015. Sleep alterations following exposure to stress predict fear-associated memory impairments in a rodent model of PTSD . Exp. Brain Res . 233 ( 8 ):2335–46 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Varela F, Lachaux J-P, Rodriguez E,Martinerie J. 2001. The brainweb: phase synchronization and large-scale integration . Nat. Rev. Neurosci . 2 ( 4 ):229–39 [ PubMed ] [ Google Scholar ]
- Vaz AP, Inati SK, Brunel N, Zaghloul KA. 2019. Coupled ripple oscillations between the medial temporal lobe and neocortex retrieve human memory . Science 363 ( 6430 ):975–78 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Verleger R, Rose M, Wagner U, Yordanova J, Kolev V. 2013. Insights into sleep’s role for insight: studies with the number reduction task . Adv. Cogn. Psychol . 9 ( 4 ):160–72 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vertes RP, Eastman KE. 2000. The case against memory consolidation in REM sleep . Behav. Brain Sci . 23 ( 6 ):867–76 [ PubMed ] [ Google Scholar ]
- Volgushev M, Chauvette S, Mukovski M, Timofeev I. 2006. Precise long-range synchronization of activity and silence in neocortical neurons during slow-wave sleep . J. Neurosci . 26 ( 21 ):5665–72 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wagner U, Gais S, Haider H, Verleger R, Born J. 2004. Sleep inspires insight . Nature 427 ( 6972 ):352–55 [ PubMed ] [ Google Scholar ]
- Walker MP. 2017. Why We Sleep: Unlocking the Power of Sleep and Dreams . New York: Simon & Schuster [ Google Scholar ]
- Walker MP, Brakefield T,Morgan A, Hobson JA, Stickgold R. 2002. Practice with sleep makes perfect: sleep-dependent motor skill learning . Neuron 35 ( 1 ):205–11 [ PubMed ] [ Google Scholar ]
- Walker MP, van der Helm E. 2009. Overnight therapy? The role of sleep in emotional brain processing . Psychol. Bull . 135 ( 5 ):731–48 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang D, Clouter A, Chen Q, Shapiro KL, Hanslmayr S. 2018. Single-trial phase entrainment of theta oscillations in sensory regions predicts human associative memory performance . J. Neurosci . 38 ( 28 ):6299–309 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wassing R, Lakbila-Kamal O, Ramautar JR, Stoffers D, Schalkwijk F, Van Someren EJW. 2019. Restless REM sleep impedes overnight amygdala adaptation . Curr. Biol . 29 ( 14 ):2351–58.e4 [ PubMed ] [ Google Scholar ]
- Weigenand A, Mölle M, Werner F, Martinetz T, Marshall L. 2016. Timing matters: Open-loop stimulation does not improve overnight consolidation of word pairs in humans . Eur. J. Neurosci . 44 ( 6 ):2357–68 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westerberg CE, Florczak SM, Weintraub S, Mesulam M-M, Marshall L, et al. 2015. Memory improvement via slow-oscillatory stimulation during sleep in older adults . Neurobiol. Aging 36 ( 9 ):2577–86 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westerberg CE,Mander BA, Florczak SM, Weintraub S, Mesulam M-M, et al. 2012. Concurrent impairments in sleep and memory in amnestic mild cognitive impairment . J. Int. Neuropsychol. Soc . 18 ( 3 ):490–500 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westerberg CE, Paller KA, McGaugh JL, Zee PC, Warby SC, et al. 2020. Highly superior autobiographical memory is associated with superior sleep physiology . Paper presented at the 61st Annual Meeting of the Psychonomic Society, online, Nov. 19–21 [ Google Scholar ]
- Williams JMG, Barnhofer T, Crane C, Herman D, Raes F, et al. 2007. Autobiographical memory specificity and emotional disorder . Psychol. Bull . 133 ( 1 ):122–48 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wilson MA, McNaughton BL. 1994. Reactivation of hippocampal ensemble memories during sleep . Science 265 ( 5172 ):676–79 [ PubMed ] [ Google Scholar ]
- Winson J 1985. Brain and Psyche: The Biology of the Unconscious . New York: Doubleday [ Google Scholar ]
- Winson J. 2004. To sleep, perchance to dream . Learn. Mem . 11 ( 6 ):659 [ Google Scholar ]
- Yonelinas AP, Ranganath C, Ekstrom AD, Wiltgen BJ. 2019. A contextual binding theory of episodic memory: systems consolidation reconsidered . Nat. Rev. Neurosci . 20 ( 6 ):364–75 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yoo S-S, Gujar N, Hu P, Jolesz FA, Walker MP. 2007. The human emotional brain without sleep—a prefrontal amygdala disconnect . Curr. Biol . 17 ( 20 ):R877–78 [ PubMed ] [ Google Scholar ]

- CERTIFICATES
- SHOP BY CATEGORY EDIBLES TINCTURES & OILS TOPICALS SPA & WELLNESS SMOKEABLES PET PRODUCT
- SHOP BY HEALTH GOAL ANXIETY & STRESS PAIN RELIEF RELAX SLEEP ENERGY LIBIDO & INTIMACY APPETITE CONTROLL BEAUTY & SKIN SPA & WELLNESS
Your cart is empty
Continue Shopping
Choose where you'd like to continue shopping:
Shop by Collection
Shop by category.
- TINCTURES & OILS
- SPA & WELLNESS
- PET PRODUCT
SHOP BY HEALTH GOAL
- ANXIETY & STRESS
- PAIN RELIEF
- LIBIDO & INTIMACY
- APPETITE CONTROLL
- BEAUTY & SKIN
Article: CBD for sleep: Benefits, Side Effects, and Treatment

CBD for sleep: Benefits, Side Effects, and Treatment
Cannabidiol — also known as CBD — is one of the main cannabinoids in the cannabis plant. Cannabinoids interact with your endocannabinoid system , which helps your body maintain a state of balance and stability, or homeostasis.
Unlike tetrahydrocannabinol (THC) , CBD isn’t psychoactive, meaning it won’t get you “high.” Instead, it has a range of health applications, like reducing seizures in people with epilepsy and pain relief from various conditions .
Here’s what you need to know about using CBD for sleep.
To understand whether CBD can improve sleep, we first have to understand what causes poor sleep.
Possible causes of insomnia include:
- mental health disorders, such as depression and anxiety
- symptoms of chronic conditions, such as pain
- eating a large meal or consuming caffeine , especially toward bedtime
- environmental factors, such as distracting devices or an uncomfortable bed
If your insomnia is due to external factors or related conditions, CBD may help by treating the causes of sleeplessness.
While research on CBD is still in its infancy, a 2022 review Trusted Source suggests that CBD may help relieve insomnia, either alone or mixed with equal quantities of THC.
Some ways in which it might do this are by:
- reducing Trusted Source anxiety levels
- soothing Trusted Source chronic pain
- improving symptoms Trusted Source of REM sleep behavior disorder in people with Parkinson’s disease
- reducing daytime sleepiness
Can CBD can treat anxiety?
While some studies suggest that CBD can improve sleep, it is not always clear why. More research is needed Trusted Source .
There are a number of ways to take CBD , such as:
- vape concentrates
- oils and tinctures
- pills and capsules
- edibles, like gummies
Vaping usually gets CBD into your system faster than other forms. However, there’s not much research on vaping CBD, and vaping may pose Trusted Source respiratory and other risks.
Your weight, personal body chemistry, the nature of your sleep problems , and the product you use will affect how CBD works. They will also affect how much you should use and when to take it.
People who use CBD for anxiety and sleep problems may not notice an immediate effect. A 2019 study Trusted Source on sleep and anxiety pointed out that people noticed a difference after about a month.
What forms of CBD can help with sleep?
Oils, pills, and gummies are all options. Vaping enables the active ingredients to enter the bloodstream more quickly, but vaping may pose Trusted Source other health risks.
What more is there to know about CBD?
CBD products may help people sleep. Experts don’t know exactly why this happens, but research has suggested that they can help manage pain, anxiety, and daytime sleepiness, factors that can interfere with sleep.
Written by lea tuohy

Are you looking for a natural way to support your overall well-being? Look no further than our CBD gummies. Packed with the power of cannabidiol (CBD), these gummies offer a convenient and deliciou...
Lab-Grade Quality
Ensuring Purity and Potency in Every Product
Top-Notch Customer Support
Dedicated to Serving You with Excellence
Fast & Reliable Shipping
Get Your CBD Products Delivered Quickly and Securely
Organic & Non-GMO Ingredients
Committed to Natural and Sustainable Practices
Best Exercises for Health and Weight Loss
How to start exercising and stick to it, how to exercise with limited mobility, home workout and fitness tips: exercising without the gym, walking: an easy way to get fit, how to build an exercise plan, dog walking: the health benefits of walks with your dog, senior exercise and fitness tips.
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Alzheimer’s Disease & Dementia
- End of Life
- Meet Our Team
What are the mental health benefits of exercise?
Other mental health benefits of exercise, reaping the mental health benefits of exercise is easier than you think, overcoming obstacles to exercise, getting started with exercise when you have a mental health issue.
- Easy ways to move more that don't involve the gym
The Mental Health Benefits of Exercise
You already know that exercise is good for your body. But did you know it can also boost your mood, improve your sleep, and help you deal with depression, anxiety, stress, and more?

Exercise is not just about aerobic capacity and muscle size. Sure, exercise can improve your physical health and your physique, trim your waistline, improve your sex life, and even add years to your life. But that’s not what motivates most people to stay active.
People who exercise regularly tend to do so because it gives them an enormous sense of well-being. They feel more energetic throughout the day, sleep better at night, have sharper memories, and feel more relaxed and positive about themselves and their lives. And it’s also a powerful medicine for many common mental health challenges.
Regular exercise can have a profoundly positive impact on depression, anxiety, and ADHD. It also relieves stress, improves memory, helps you sleep better, and boosts your overall mood. And you don’t have to be a fitness fanatic to reap the benefits. Research indicates that modest amounts of exercise can make a real difference. No matter your age or fitness level, you can learn to use exercise as a powerful tool to deal with mental health problems, improve your energy and outlook, and get more out of life.
Exercise and depression
Studies show that exercise can treat mild to moderate depression as effectively as antidepressant medication—but without the side-effects, of course. As one example, a recent study done by the Harvard T.H. Chan School of Public Health found that running for 15 minutes a day or walking for an hour reduces the risk of major depression by 26%. In addition to relieving depression symptoms , research also shows that maintaining an exercise schedule can prevent you from relapsing.
Exercise is a powerful depression fighter for several reasons. Most importantly, it promotes all kinds of changes in the brain, including neural growth, reduced inflammation, and new activity patterns that promote feelings of calm and well-being. It also releases endorphins, powerful chemicals in your brain that energize your spirits and make you feel good. Finally, exercise can also serve as a distraction, allowing you to find some quiet time to break out of the cycle of negative thoughts that feed depression.
Exercise and anxiety
Exercise is a natural and effective anti-anxiety treatment . It relieves tension and stress, boosts physical and mental energy, and enhances well-being through the release of endorphins. Anything that gets you moving can help, but you’ll get a bigger benefit if you pay attention instead of zoning out.
Try to notice the sensation of your feet hitting the ground, for example, or the rhythm of your breathing, or the feeling of the wind on your skin. By adding this mindfulness element—really focusing on your body and how it feels as you exercise—you’ll not only improve your physical condition faster, but you may also be able to interrupt the flow of constant worries running through your head.
Exercise and stress
Ever noticed how your body feels when you’re under stress ? Your muscles may be tense, especially in your face, neck, and shoulders, leaving you with back or neck pain, or painful headaches. You may feel a tightness in your chest, a pounding pulse, or muscle cramps. You may also experience problems such as insomnia, heartburn, stomachache, diarrhea, or frequent urination. The worry and discomfort of all these physical symptoms can in turn lead to even more stress, creating a vicious cycle between your mind and body.
Exercising is an effective way to break this cycle. As well as releasing endorphins in the brain, physical activity helps to relax the muscles and relieve tension in the body. Since the body and mind are so closely linked, when your body feels better so, too, will your mind.
Exercise and ADHD
Exercising regularly is one of the easiest and most effective ways to reduce the symptoms of ADHD and improve concentration, motivation, memory, and mood. Physical activity immediately boosts the brain’s dopamine, norepinephrine, and serotonin levels—all of which affect focus and attention. In this way, exercise works in much the same way as ADHD medications such as Ritalin and Adderall.
Exercise and PTSD and trauma
Evidence suggests that by really focusing on your body and how it feels as you exercise, you can actually help your nervous system become “unstuck” and begin to move out of the immobilization stress response that characterizes PTSD or trauma. Instead of allowing your mind to wander, pay close attention to the physical sensations in your joints and muscles, even your insides as your body moves. Exercises that involve cross movement and that engage both arms and legs—such as walking (especially in sand), running, swimming, weight training, or dancing—are some of your best choices.
Outdoor activities like hiking, sailing, mountain biking, rock climbing, whitewater rafting, and skiing (downhill and cross-country) have also been shown to reduce the symptoms of PTSD.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
Even if you’re not suffering from a mental health problem, regular physical activity can still offer a welcome boost to your mood, outlook, and mental well-being.
Exercise can help provide:
Sharper memory and thinking. The same endorphins that make you feel better also help you concentrate and feel mentally sharp for tasks at hand. Exercise also stimulates the growth of new brain cells and helps prevent age-related decline .
Higher self-esteem. Regular activity is an investment in your mind, body, and soul. When it becomes habit, it can foster your sense of self-worth and make you feel strong and powerful. You’ll feel better about your appearance and, by meeting even small exercise goals, you’ll feel a sense of achievement.
Better sleep. Even short bursts of exercise in the morning or afternoon can help regulate your sleep patterns . If you prefer to exercise at night, relaxing exercises such as yoga or gentle stretching can help promote sleep.
More energy. Increasing your heart rate several times a week will give you more get-up-and-go. Start off with just a few minutes of exercise per day, and increase your workout as you feel more energized.
Stronger resilience. When faced with mental or emotional challenges in life, exercise can help you build resilience and cope in a healthy way, instead of resorting to alcohol, drugs, or other negative behaviors that ultimately only make your symptoms worse. Regular exercise can also help boost your immune system and reduce the impact of stress.
You don’t need to devote hours out of your busy day to train at the gym, sweat buckets, or run mile after monotonous mile to reap all the physical and mental health benefits of exercise. Just 30-minutes of moderate exercise five times a week is enough. And even that can be broken down into two 15-minute or even three 10-minute exercise sessions if that’s easier.
Even a little bit of activity is better than nothing
If you don’t have time for 15 or 30 minutes of exercise, or if your body tells you to take a break after 5 or 10 minutes, for example, that’s okay, too. Start with 5- or 10-minute sessions and slowly increase your time. The more you exercise, the more energy you’ll have, so eventually you’ll feel ready for a little more. The key is to commit to some moderate physical activity—however little—on most days. As exercising becomes a habit, you can slowly add extra minutes or try different types of activities. If you keep at it, the benefits of exercise will begin to pay off.
You don’t have to suffer to get results
Research shows that moderate levels of exercise are best for most people . Moderate means:
- That you breathe a little heavier than normal, but are not out of breath. For example, you should be able to chat with your walking partner, but not easily sing a song.
- That your body feels warmer as you move, but not overheated or very sweaty.
Can’t find time to exercise during the week? Be a weekend warrior
A recent study in the United Kingdom found that people who squeeze their exercise routines into one or two sessions during the weekend experience almost as many health benefits as those who work out more often. So don’t let a busy schedule at work, home, or school be an excuse to avoid activity. Get moving whenever you can find the time—your mind and body will thank you!
Even when you know that exercise will help you feel better, taking that first step is still easier said than done. Obstacles to exercising are very real—particularly when you’re also struggling with a mental health issue.
Here are some common barriers and how you can get past them.
Feeling exhausted. When you’re tired, depressed, or stressed, it seems that working out will just make you feel worse. But the truth is that physical activity is a powerful energizer. Studies show that regular exercise can dramatically reduce fatigue and increase your energy levels. If you are really feeling tired, promise yourself a quick, 5-minute walk. Chances are, once you get moving you’ll have more energy and be able to walk for longer.
Feeling overwhelmed. When you’re stressed or depressed, the thought of adding another obligation to your busy daily schedule can seem overwhelming. Working out just doesn’t seem practical. If you have children, finding childcare while you exercise can also be a big hurdle. However, if you begin thinking of physical activity as a priority (a necessity for your mental well-being), you’ll soon find ways to fit small amounts of exercise into even the busiest schedule.
Feeling hopeless. Even if you’ve never exercised before, you can still find ways to comfortably get active. Start slow with easy, low-impact activities a few minutes each day, such as walking or dancing.
Feeling bad about yourself. Are you your own worst critic? It’s time to try a new way of thinking about your body. No matter your weight, age or fitness level, there are plenty of others in the same boat. Ask a friend to exercise with you. Accomplishing even the smallest fitness goals will help you gain body confidence and improve how you think about yourself.
Feeling pain. If you have a disability, severe weight problem, arthritis, or any injury or illness that limits your mobility, talk to your doctor about ways to safely exercise . You shouldn’t ignore pain, but rather do what you can, when you can. Divide your exercise into shorter, more frequent chunks of time if that helps, or try exercising in water to reduce joint or muscle discomfort.
Many of us find it hard enough to motivate ourselves to exercise at the best of times. But when you feel depressed, anxious, stressed or have another mental health problem, it can seem doubly difficult. This is especially true of depression and anxiety, which can leave you feeling trapped in a catch-22 situation. You know exercise will make you feel better, but depression has robbed you of the energy and motivation you need to work out, or your social anxiety means you can’t bear the thought of being seen at an exercise class or running through the park.
Start small. When you’re under the cloud of anxiety or depression and haven’t exercised for a long time, setting extravagant goals like completing a marathon or working out for an hour every morning will only leave you more despondent if you fall short. Better to set achievable goals and build up from there.
Schedule workouts when your energy is highest. Perhaps you have most energy first thing in the morning before work or school or at lunchtime before the mid-afternoon lull hits? Or maybe you do better exercising for longer at the weekends. If depression or anxiety has you feeling tired and unmotivated all day long, try dancing to some music or simply going for a walk. Even a short, 15-minute walk can help clear your mind, improve your mood, and boost your energy level. As you move and start to feel a little better, you’ll often boost your energy enough to exercise more vigorously—by walking further, breaking into a run, or adding a bike ride, for example.
Focus on activities you enjoy. Any activity that gets you moving counts. That could include throwing a Frisbee with a dog or friend, walking laps of a mall window shopping, or cycling to the grocery store. If you’ve never exercised before or don’t know what you might enjoy, try a few different things. Activities such as gardening or tackling a home improvement project can be great ways to start moving more when you have a mood disorder—as well as helping you become more active, they can also leave you with a sense of purpose and accomplishment.
Be comfortable. Wear clothing that’s comfortable and choose a setting that you find calming or energizing. That may be a quiet corner of your home, a scenic path, or your favorite city park.
Reward yourself. Part of the reward of completing an activity is how much better you’ll feel afterwards, but it always helps your motivation to promise yourself an extra treat for exercising. Reward yourself with a hot bubble bath after a workout, a delicious smoothie, or with an extra episode of your favorite TV show, for example.
Make exercise a social activity. Exercising with a friend or loved one, or even your kids, will not only make exercising more fun and enjoyable, it can also help motivate you to stick to a workout routine. You’ll also feel better than if you were exercising alone. In fact, when you’re suffering from a mood disorder such as depression, the companionship can be just as important as the exercise.
Easy ways to move more that don’t involve the gym
Don’t have a 30-minute block of time to dedicate to yoga or a bike ride? Don’t worry. Think about physical activity as a lifestyle rather than just a single task to check off your to-do list. Look at your daily routine and consider ways to sneak in activity here, there, and everywhere.
Move in and around your home. Clean the house, wash the car, tend to the yard and garden, mow the lawn with a push mower, sweep the sidewalk or patio with a broom.
Sneak activity in at work or on the go. Bike or walk to an appointment rather than drive, use stairs instead of elevators, briskly walk to the bus stop then get off one stop early, park at the back of the lot and walk into the store or office, or take a vigorous walk during your coffee break.
Get active with the family. Jog around the soccer field during your kid’s practice, make a neighborhood bike ride part of your weekend routine, play tag with your children in the yard, go canoeing at a lake, walk the dog in a new place.
Get creative with exercise ideas. Pick fruit at an orchard, boogie to music, go to the beach or take a hike, gently stretch while watching television, organize an office bowling team, take a class in martial arts, dance, or yoga.
Make exercise a fun part of your everyday life
You don’t have to spend hours in a gym or force yourself into long, monotonous workouts to experience the many benefits of exercise. These tips can help you find activities you enjoy and start to feel better, look better, and get more out of life.
More Information
- Greer, T. L., Trombello, J. M., Rethorst, C. D., Carmody, T. J., Jha, M. K., Liao, A., Grannemann, B. D., Chambliss, H. O., Church, T. S., & Trivedi, M. H. (2016). Improvements in psychosocial functioning and health-related quality of life following exercise augmentation in patients with treatment response but non-remitted major depressive disorder: Results from the TREAD study. Depression and Anxiety, 33(9), 870–881. Link
- Kandola, A., Vancampfort, D., Herring, M., Rebar, A., Hallgren, M., Firth, J., & Stubbs, B. (2018). Moving to Beat Anxiety: Epidemiology and Therapeutic Issues with Physical Activity for Anxiety. Current Psychiatry Reports, 20(8), 63. Link
- Aylett, E., Small, N., & Bower, P. (2018). Exercise in the treatment of clinical anxiety in general practice – a systematic review and meta-analysis. BMC Health Services Research, 18(1), 559. Link
- Stubbs, B., Vancampfort, D., Rosenbaum, S., Firth, J., Cosco, T., Veronese, N., Salum, G. A., & Schuch, F. B. (2017). An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Research, 249, 102–108. Link
- Kandola, A. A., Osborn, D. P. J., Stubbs, B., Choi, K. W., & Hayes, J. F. (2020). Individual and combined associations between cardiorespiratory fitness and grip strength with common mental disorders: A prospective cohort study in the UK Biobank. BMC Medicine, 18(1), 303. Link
More in Exercise & Fitness
Tips for building a fitness plan, and finding the best exercises for you

How to make exercise a part of your everyday life

Chair exercises and fitness tips for people with injuries or disabilities

Even when your schedule changes, you can stay physically fit

How to reap the health benefits of walking

A guide to getting started and developing a balanced plan

Here’s how walking with your pooch can benefit you as well

No matter your age, it’s never too late to get started

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.

IMAGES
VIDEO
COMMENTS
In the inaugural issue of the Journal of Clinical Sleep Medicine (2005), a feature article 1 traced early milestones in the developing field of sleep medicine, which slowly emerged from the older field of sleep research during the 1970s and 1980s. Sleep medicine, the article noted, was closely linked with and made possible by the discovery of electrical activity in the brain.
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
There's more to good sleep than just the hours spent in bed, says Dr. Marishka Brown, a sleep expert at NIH. "Healthy sleep encompasses three major things," she explains. "One is how much sleep you get. Another is sleep quality—that you get uninterrupted and refreshing sleep. The last is a consistent sleep schedule.".
You may be able to sleep your way to a longer life. According to recently published research involving 172,321 adults, men who get adequate sleep live about five years longer than men who don't. For women, it's two years. However, about a third of adults cut sleep short, raising their risk of heart attack, dementia and diabetes, among other ...
benefits.9-12 Healthy sleep requires adequate sleep duration, appropriate ... and expand sleep health research. K Ramar, RK Malhotra, KA Carden, et al. Position statement: sleep is essential to health Journal of Clinical Sleep Medicine, Vol. 17, No. 10 2117 October 1, 2021.
Scientists have gone to great lengths to fully understand sleep's benefits. In studies of humans and other animals, they have discovered that sleep plays a critical role in immune function, metabolism, memory, learning, and other vital functions. ... Research suggests that sleep helps learning and memory in two distinct ways. First, a sleep ...
Introduction. Sleep is a universal behavior occupying a significant fraction of the 24-hour day,1,2 but its regulation and function(s) are far from being understood.3-5 There is an extensive amount of data and many theories, which suggest that sleep plays an active role in processes such as synaptic plasticity and memory functions,6-8 emotional regulation,9-11 metabolic functions and ...
Since the seminal research by Ebbinghaus and then, Jenkins and Dallenbach , dozens of studies have reported that sleep benefits consolidation of memories about our daily experiences, termed episodic memory, known to be dependent on the hippocampus (e.g., ref. 7)—especially when compared with a period of wake (refs. 7 -9 have reviews).
Improved Mood. Sleep restores the body and improves energy levels, so waking up well-rested can have a positive impact on an individual's mood . In contrast, people who get inadequate sleep are at higher risk of experiencing mental distress . A chronic lack of sleep can lead to anxiety, depression, and irritability.
Novelty This is the first systematic review to examine the influence of sleep timing and sleep consistency on health outcomes. Later sleep timing and greater variability in sleep are both associated with adverse health outcomes in adults. Regularity in sleep patterns with consistent bedtimes and wake-up times should be encouraged.
During sleep, your body is working to support healthy brain function and maintain your physical health. In children and teens, sleep also helps support growth and development. Getting inadequate sleep over time can raise your risk for chronic (long-term) health problems. It can also affect how well you think, react, work, learn, and get along ...
Sleep is essential for a person's health and wellbeing, according to the National Sleep Foundation (NSF). Yet millions of people do not get enough sleep and many suffer from lack of sleep. For example, surveys conducted by the NSF (1999-2004) reveal that at least 40 million Americans suffer from over 70 different sleep disorders and 60 percent of adults report having sleep problems a few ...
Before the 1950s, most people believed sleep was a passive activity during which the body and brain were dormant. "But it turns out that sleep is a period during which the brain is engaged in a number of activities necessary to life—which are closely linked to quality of life," says Johns Hopkins sleep expert and neurologist Mark Wu, M.D., Ph.D. Researchers like Wu are spending many of ...
Sleep measures accounted for nearly 25% of the variance in academic performance. ... One exception is a pair of linked studies that examined short-term benefits of sleep on academic performance in ...
It's estimated that at least 50 million Americans suffer from a sleep disorder. But sleep—both the quantity and quality—is crucial to our brain health. Research has now shown a correlation between sleep disturbances and numerous neurological diseases. These include stroke, cognitive aging, dementia, Parkinson's disease, and others.
This article tells you 9 reasons why you need to get more sleep. 1. May help you maintain or lose weight. Numerous studies have associated short sleep — defined as sleeping fewer than 7 hours ...
Research Update on Sleep; RESOURCES; Research Update 1. Sleep. By Marie Conley Smith. I n a world full of opportunities, stressors, inequalities, and distractions, maintaining a healthy lifestyle can be challenging, and sleep is often the first habit to suffer. Good sleep hygiene is a huge commitment: it takes up about a third of the day, every ...
Research efforts of medical and allied professions like nursing have resulted in a broader conceptualization of sleep (Hale et al., 2020), and sleep is considered a multidimensional entity.The contemporary concept of "sleep health" moves beyond individual symptoms and disorders, and integrates issues related to how individual behavioral factors (e.g., sleep habits), sociodemographic ...
Sharper Brain. Mood Boost. Healthier Heart. Athletic Achievement. 3 min read. A lack of sleep at night can make you cranky the next day. And over time, skimping on sleep can mess up more than just ...
Consequently, it is important that the benefits of improving sleep on mental health occur even in the presence of comorbid health complaints, as was reported in the present research. ... the timing of sleep is particularly important in circadian rhythm disorders and daytime sleepiness is a key outcome in sleep apnoea research. Future research ...
Getting extra sleep on the weekends to compensate for lost rest during the week may benefit your heart health, new research suggests.
Many people struggle to achieve sufficient sleep. However, ongoing research highlights the far-reaching impacts of sleep deprivation, prompting a shift in focus toward sleep quality and overall well-being. This article will explore the science behind sleep, the benefits of getting enough sleep, and how sleep deprivation can negatively impact ...
Naturally, catching up on sleep over the weekend is often the solution. New research suggests doing so may even benefit your heart health, amounting to a 19% lower risk of developing heart disease ...
A 2019 analysis of 18 studies (1,654 total participants) found that mindfulness meditation practices improved sleep quality more than education-based treatments. However, the effects of mindfulness meditation approaches on sleep quality were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise.
Artificial intelligence analyzes sleep breathing patterns. In another innovative study, NINDS-funded researchers used an artificial intelligence (AI) program to identify PD by analyzing breathing patterns during sleep. The researchers tested the AI program using two types of sleep data: breathing patterns and brain activity.
Although future advances in sleep research and neural decoding may lead to refinements in our thinking about sleep physiology, contemporary schemes distinguish rapid eye movement (REM) sleep from three stages of non-REM (NREM) sleep. ... Sleep benefits memory for semantic category structure while preserving exemplar-specific information. Sci ...
There are a number of ways to take CBD, such as:. vape concentrates; oils and tinctures; pills and capsules; edibles, like gummies; Vaping usually gets CBD into your system faster than other forms. However, there's not much research on vaping CBD, and vaping may pose Trusted Source respiratory and other risks.. Your weight, personal body chemistry, the nature of your sleep problems, and the ...
3. Yoga Can Improve Sleep. We all know how cranky we can feel after a bad night's sleep. Poor sleep can really ramp up stress levels. Research in the Journal of Clinical Sleep Medicine showed that seniors who did yoga regularly slept better and had fewer issues with insomnia than older adults who don't do yoga. The gentle movements and ...
Regular exercise can have a profoundly positive impact on depression, anxiety, and ADHD. It also relieves stress, improves memory, helps you sleep better, and boosts your overall mood. And you don't have to be a fitness fanatic to reap the benefits. Research indicates that modest amounts of exercise can make a real difference.
However, if they did get COVID, they were less likely to die from the disease if they had been taking semaglutide, the research showed. Another study presented at the ESC meeting and published in the JACC focused on a major killer, heart failure. This time, researchers looked at data from the FLOW trial, published in May and also funded by Novo ...