- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español

You are here
Nih…turning discovery into health ®.
Research for Healthy Living
Obesity and Nutrition

More than one-third of U.S. adults — and about 17 percent of U.S. children — are obese. Obesity puts people at risk for many health issues including heart disease, stroke, type 2 diabetes, arthritis, and certain types of cancer. Because these conditions are some of the top preventable causes of chronic illness and death, NIH has a considerable interest in addressing obesity.
The problem of obesity seems straightforward: When we eat more calories than we burn, our bodies store this extra energy as fat. Yet, we all know how hard it can be just to lose a few pounds. And solving this problem on a population-sized scale has proven to be tremendously difficult. That is because so many factors play a role: where we live and work, how much time we spend sitting – and the availability of safe spaces for exercise – and the fact that many people cannot choose alternatives. Access to nutritious food can be a major barrier for many with low incomes or mobility limitations.
Heredity also has an impact. For example, NIH research shows that certain gene variations that occur in one of six people of European descent translate into an extra 7 pounds, on average. Those discoveries are pointing to pathways involved in obesity that suggest potential ways to prevent undesirable weight gain. Research on the social factors contributing to obesity also offers ideas for intervention. When people are provided funds to buy food once a week, instead of monthly, they are more likely to buy fresh fruits and vegetables instead of pre-packaged (and often less-nutritious) goods. We also know that affordable housing programs lead to better nutrition, because people no longer must compromise on food in order to pay rent.
Did you know?
NIH research funding across the nation generated $65 billion in new economic activity in 2016.
« Previous: Research for Healthy Living Next: Arthritis »
This page last reviewed on November 16, 2023
Connect with Us
- More Social Media from NIH
Food and Diet

Beyond Willpower: Diet Quality and Quantity Matter
It’s no secret that the amount of calories people eat and drink has a direct impact on their weight: Consume the same number of calories that the body burns over time, and weight stays stable. Consume more than the body burns, weight goes up. Less, weight goes down. But what about the type of calories: Does it matter whether they come from specific nutrients-fat, protein, or carbohydrate? Specific foods-whole grains or potato chips? Specific diets-the Mediterranean diet or the “Twinkie” diet? And what about when or where people consume their calories: Does eating breakfast make it easier to control weight? Does eating at fast-food restaurants make it harder?
There’s ample research on foods and diet patterns that protect against heart disease, stroke, diabetes, and other chronic conditions. The good news is that many of the foods that help prevent disease also seem to help with weight control-foods like whole grains, vegetables, fruits, and nuts. And many of the foods that increase disease risk-chief among them, refined grains and sugary drinks-are also factors in weight gain.Conventional wisdom says that since a calorie is a calorie, regardless of its source, the best advice for weight control is simply to eat less and exercise more. Yet emerging research suggests that some foods and eating patterns may make it easier to keep calories in check, while others may make people more likely to overeat.
This article briefly reviews the research on dietary intake and weight control, highlighting diet strategies that also help prevent chronic disease.
Macronutrients and Weight: Do Carbs, Protein, or Fat Matter?
When people eat controlled diets in laboratory studies, the percentage of calories from fat, protein, and carbohydrate do not seem to matter for weight loss. In studies where people can freely choose what they eat, there may be some benefits to a higher protein, lower carbohydrate approach. For chronic disease prevention, though, the quality and food sources of these nutrients matters more than their relative quantity in the diet. And the latest research suggests that the same diet quality message applies for weight control.
Dietary Fat and Weight
Low-fat diets have long been touted as the key to a healthy weight and to good health. But the evidence just isn’t there: Over the past 30 years in the U.S., the percentage of calories from fat in people’s diets has gone down, but obesity rates have skyrocketed. ( 1 , 2 ) Carefully conducted clinical trials have found that following a low-fat diet does not make it any easier to lose weight than following a moderate- or high-fat diet. In fact, study volunteers who follow moderate- or high-fat diets lose just as much weight, and in some studies a bit more, as those who follow low-fat diets. ( 3 , 4 ) And when it comes to disease prevention, low-fat diets don’t appear to offer any special benefits. ( 5 )
Part of the problem with low-fat diets is that they are often high in carbohydrate, especially from rapidly digested sources, such as white bread and white rice. And diets high in such foods increase the risk of weight gain, diabetes, and heart disease. (See Carbohydrates and Weight , below.)
For good health, the type of fat people eat is far more important that the amount (see box), and there’s some evidence that the same may be true for weight control. ( 6 – 9 ) In the Nurses’ Health Study, for example, which followed 42,000 middle-age and older women for eight years, increased consumption of unhealthy fats-trans fats, especially, but also saturated fats-was linked to weight gain, but increased consumption of healthy fats-monounsaturated and polyunsaturated fat-was not. ( 6 )
Protein and Weight

Higher protein diets seem to have some advantages for weight loss, though more so in short-term trials; in longer term studies, high-protein diets seem to perform equally well as other types of diets. ( 3 , 4 ) High-protein diets tend to be low in carbohydrate and high in fat, so it is difficult to tease apart the benefits of eating lots of protein from those of eating more fat or less carbohydrate. But there are a few reasons why eating a higher percentage of calories from protein may help with weight control:
- More satiety: People tend to feel fuller, on fewer calories, after eating protein than they do after eating carbohydrate or fat. ( 10 )
- Greater thermic effect: It takes more energy to metabolize and store protein than other macronutrients, and this may help people increase the energy they burn each day. ( 10 , 11 )
- Improved body composition: Protein seems to help people hang on to lean muscle during weight loss, and this, too, can help boost the energy-burned side of the energy balance equation. ( 11 )
Higher protein, lower carbohydrate diets improve blood lipid profiles and other metabolic markers, so they may help prevent heart disease and diabetes. ( 4 , 12 , 13 ) But some high-protein foods are healthier than others: High intakes of red meat and processed meat are associated with an increased risk of heart disease, diabetes, and colon cancer. ( 14 – 16 )
Replacing red and processed meat with nuts, beans, fish, or poultry seems to lower the risk of heart disease and diabetes. ( 14 , 16 ) And this diet strategy may help with weight control, too, according to a recent study from the Harvard School of Public Health. Researchers tracked the diet and lifestyle habits of 120,000 men and women for up to 20 years, looking at how small changes contributed to weight gain over time. ( 9 ) People who ate more red and processed meat over the course of the study gained more weight-about a pound extra every four years. People who ate more nuts over the course of the study gained less weight-about a half pound less every four years.
Carbohydrates and Weight
Lower carbohydrate, higher protein diets may have some weight loss advantages in the short term. ( 3 , 4 ) Yet when it comes to preventing weight gain and chronic disease, carbohydrate quality is much more important than carbohydrate quantity.

Read more about carbohydrates on The Nutrition Source
Milled, refined grains and the foods made with them-white rice, white bread, white pasta, processed breakfast cereals, and the like-are rich in rapidly digested carbohydrate. So are potatoes and sugary drinks. The scientific term for this is that they have a high glycemic index and glycemic load. Such foods cause fast and furious increases in blood sugar and insulin that, in the short term, can cause hunger to spike and can lead to overeating-and over the long term, increase the risk of weight gain, diabetes, and heart disease. ( 17 – 19 )
For example, in the diet and lifestyle change study, people who increased their consumption of French fries, potatoes and potato chips, sugary drinks, and refined grains gained more weight over time-an extra 3.4, 1.3, 1.0, and 0.6 pounds every four years, respectively. ( 9 ) People who decreased their intake of these foods gained less weight.
Specific Foods that Make It Easier or Harder to Control Weight
There’s growing evidence that specific food choices may help with weight control. The good news is that many of the foods that are beneficial for weight control also help prevent heart disease, diabetes, and other chronic diseases. Conversely, foods and drinks that contribute to weight gain—chief among them, refined grains and sugary drinks—also contribute to chronic disease.
Whole Grains, Fruits and Vegetables, and Weight

Read more about whole grains on The Nutrition Source
Whole grains-whole wheat, brown rice, barley, and the like, especially in their less-processed forms-are digested more slowly than refined grains. So they have a gentler effect on blood sugar and insulin, which may help keep hunger at bay. The same is true for most vegetables and fruits. These “slow carb” foods have bountiful benefits for disease prevention, and there’s also evidence that they can help prevent weight gain.

Read more about vegetables and fruits on The Nutrition Source
The weight control evidence is stronger for whole grains than it is for fruits and vegetables. ( 20 – 22 ) The most recent support comes from the Harvard School of Public Health diet and lifestyle change study: People who increased their intake of whole grains, whole fruits (not fruit juice), and vegetables over the course of the 20-year study gained less weight-0.4, 0.5, and 0.2 pounds less every four years, respectively. ( 9 )
Of course, the calories from whole grains, whole fruits, and vegetables don’t disappear. What’s likely happening is that when people increase their intake of these foods, they cut back on calories from other foods. Fiber may be responsible for these foods’ weight control benefits, since fiber slows digestion, helping to curb hunger. Fruits and vegetables are also high in water, which may help people feel fuller on fewer calories.
Nuts and Weight

Read more about nuts on The Nutrition Source
Nuts pack a lot of calories into a small package and are high in fat, so they were once considered taboo for dieters. As it turns out, studies find that eating nuts does not lead to weight gain and may instead help with weight control, perhaps because nuts are rich in protein and fiber, both of which may help people feel fuller and less hungry. ( 9 , 23 – 25 ) People who regularly eat nuts are less likely to have heart attacks or die from heart disease than those who rarely eat them, which is another reason to include nuts in a healthy diet. ( 19 )
Dairy and Weight

Read more about calcium and milk on The Nutrition Source
The U.S. dairy industry has aggressively promoted the weight-loss benefits of milk and other dairy products, based largely on findings from short-term studies it has funded. ( 26 , 27 ) But a recent review of nearly 50 randomized trials finds little evidence that high dairy or calcium intakes help with weight loss. ( 28 ) Similarly, most long-term follow-up studies have not found that dairy or calcium protect against weight gain, ( 29 – 32 ) and one study in adolescents found high milk intakes to be associated with increased body mass index. ( 33 )
One exception is the recent dietary and lifestyle change study from the Harvard School of Public Health, which found that people who increased their yogurt intake gained less weight; increases in milk and cheese intake, however, did not appear to promote weight loss or gain. ( 9 ) It’s possible that the beneficial bacteria in yogurt may influence weight control, but more research is needed.
Sugar-Sweetened Beverages and Weight

Read more about healthy drinks on The Nutrition Source
There’s convincing evidence that sugary drinks increase the risk of weight gain, obesity, and diabetes: ( 34 – 36 ) A systematic review and meta-analysis of 88 studies found “clear associations of soft drink intake with increased caloric intake and body weight.” ( 34 ) In children and adolescents, a more recent meta analysis estimates that for every additional 12-ounce serving of sugary beverage consumed each day, body mass index increases by 0.08 units. ( 35 ) Another meta analysis finds that adults who regularly drink sugared beverages have a 26 percent higher risk of developing type 2 diabetes than people who rarely drink sugared beverages. ( 36 ) Emerging evidence also suggests that high sugary beverage intake increases the risk of heart disease. ( 37 )
Like refined grains and potatoes, sugary beverages are high in rapidly-digested carbohydrate. (See Carbohydrates and Weight , above.) Research suggests that when that carbohydrate is delivered in liquid form, rather than solid form, it is not as satiating, and people don’t eat less to compensate for the extra calories. ( 38 )
These findings on sugary drinks are alarming, given that children and adults are drinking ever-larger quantities of them: In the U.S., sugared beverages made up about 4 percent of daily calorie intake in the 1970s, but by 2001, represented about 9 percent of calories. ( 36 ) The most recent data find that on any given day, half of Americans consume some type of sugared beverage, 25 percent consume at least 200 calories from sugared drinks, and 5 percent of consume at least 567 calories-the equivalent of four cans of sugary soda. ( 39 )
The good news is that studies in children and adults have also shown that cutting back on sugary drinks can lead to weight loss. ( 40 , 41 ) Sugary drinks have become an important target for obesity prevention efforts, prompting discussions of policy initiatives such as taxing soda. ( 42 )
Fruit Juice and Weight
It’s important to note that fruit juices are not a better option for weight control than sugar-sweetened beverages. Ounce for ounce, fruit juices-even those that are 100 percent fruit juice, with no added sugar- are as high in sugar and calories as sugary sodas. So it’s no surprise that a recent Harvard School of Public Health study, which tracked the diet and lifestyle habits of 120,000 men and women for up to 20 years, found that people who increased their intake of fruit juice gained more weight over time than people who did not. ( 9 ) Pediatricians and public health advocates recommend that children and adults limit fruit juice to just a small glass a day, if they consume it at all.
Alcohol and Weight

Read more about alcohol on The Nutrition Source
Even though most alcoholic beverages have more calories per ounce than sugar-sweetened beverages, there’s no clear-cut evidence that moderate drinking contributes to weight gain. While the recent diet and lifestyle change study found that people who increased their alcohol intake gained more weight over time, the findings varied by type of alcohol. ( 9 ) In most previous prospective studies, there was no difference in weight gain over time between light-to-moderate drinkers and nondrinkers, or the light-to-moderate drinkers gained less weight than nondrinkers. ( 43 – 47 )
Diet Patterns, Portion Size, and Weight
People don’t eat nutrients or foods in isolation. They eat meals that fall into an overall eating pattern, and researchers have begun exploring whether particular diet or meal patterns help with weight control or contribute to weight gain. Portion sizes have also increased dramatically over the past three decades, as has consumption of fast food-U.S. children, for example, consume a greater percentage of calories from fast food than they do from school food ( 48 )-and these trends are also thought to be contributors to the obesity epidemic.
Dietary Patterns and Weight
So-called “prudent” dietary patterns-diets that feature whole grains, vegetables, and fruits-seem to protect against weight gain, whereas “Western-style” dietary patterns-with more red meat or processed meat, sugared drinks, sweets, refined carbohydrates, or potatoes-have been linked to obesity. ( 49 – 52 ) The Western-style dietary pattern is also linked to increased risk of heart disease, diabetes, and other chronic conditions.
Following a Mediterranean-style diet, well-documented to protect against chronic disease, ( 53 ) appears to be promising for weight control, too. The traditional Mediterranean-style diet is higher in fat (about 40 percent of calories) than the typical American diet (34 percent of calories ( 54 )), but most of the fat comes from olive oil and other plant sources. The diet is also rich in fruits, vegetables, nuts, beans, and fish. A 2008 systematic review found that in most (but not all) studies, people who followed a Mediterranean-style diet had lower rates of obesity or more weight loss. ( 55 ) There is no single “Mediterranean” diet, however, and studies often use different definitions, so more research is needed.
Breakfast, Meal Frequency, Snacking, and Weight
There is some evidence that skipping breakfast increases the risk of weight gain and obesity, though the evidence is stronger in children, especially teens, than it is in adults. ( 56 ) Meal frequency and snacking have increased over the past 30 years in the U.S. ( 57 )-on average, children get 27 percent of their daily calories from snacks, primarily from desserts and sugary drinks, and increasingly from salty snacks and candy. But there have been conflicting findings on the relationship between meal frequency, snacking, and weight control, and more research is needed. ( 56 )
Portion Sizes and Weight
Since the 1970s, portion sizes have increased both for food eaten at home and for food eaten away from home, in adults and children. ( 58 , 59 ) Short-term studies clearly demonstrate that when people are served larger portions, they eat more. One study, for example, gave moviegoers containers of stale popcorn in either large or medium-sized buckets; people reported that they did not like the taste of the popcorn-and even so, those who received large containers ate about 30 percent more popcorn than those who received medium-sized containers. ( 60 ) Another study showed that people given larger beverages tended to drink significantly more, but did not decrease their subsequent food consumption . ( 67 ) An additional study provided evidence that when provided with larger portion sizes, people tended to eat more, with no decrease in later food intake. ( 68 ) There is an intuitive appeal to the idea that portion sizes increase obesity, but long-term prospective studies would help to strengthen this hypothesis.
Fast Food and Weight
Fast food is known for its large portions, low prices, high palatability, and high sugar content, and there’s evidence from studies in teens and adults that frequent fast-food consumption contributes to overeating and weight gain. ( 61 – 66 ) The CARDIA study, for example, followed 3,000 young adults for 13 years. People who had higher fast-food-intake levels at the start of the study weighed an average of about 13 pounds more than people who had the lowest fast-food-intake levels. They also had larger waist circumferences and greater increases in triglycercides, and double the odds of developing metabolic syndrome. ( 62 ) More research is needed to tease apart the effect of eating fast food itself from the effect of the neighborhood people live in, or other individual traits that may make people more likely to eat fast food.
The Bottom Line: Healthy Diet Can Prevent Weight Gain and Chronic Disease
Weight gain in adulthood is often gradual, about a pound a year ( 9 )-too slow of a gain for most people to notice, but one that can add up, over time, to a weighty personal and public health problem. There’s increasing evidence that the same healthful food choices and diet patterns that help prevent heart disease, diabetes, and other chronic conditions may also help to prevent weight gain:
- Choose minimally processed, whole foods-whole grains, vegetables, fruits, nuts, healthful sources of protein (fish, poultry, beans), and plant oils.
- Limit sugared beverages, refined grains, potatoes, red and processed meats, and other highly processed foods, such as fast food.
Though the contribution of any one diet change to weight control may be small, together, the changes could add up to a considerable effect, over time and across the whole society. ( 9 ) Since people’s food choices are shaped by their surroundings, it’s imperative for governments to promote policy and environmental changes that make healthy foods more accessible and decrease the availability and marketing of unhealthful foods.
1. Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med . 2002;113 Suppl 9B:47S-59S.
2. Melanson EL, Astrup A, Donahoo WT. The relationship between dietary fat and fatty acid intake and body weight, diabetes, and the metabolic syndrome. Ann Nutr Metab . 2009;55:229-43.
3. Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med . 2009;360:859-73.
4. Shai I, Schwarzfuchs D, Henkin Y, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med . 2008;359:229-41.
5. Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial. JAMA . 2006;295:39-49.
6. Field AE, Willett WC, Lissner L, Colditz GA. Dietary fat and weight gain among women in the Nurses’ Health Study. Obesity (Silver Spring) . 2007;15:967-76.
7. Koh-Banerjee P, Chu NF, Spiegelman D, et al. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr . 2003;78:719-27.
8. Thompson AK, Minihane AM, Williams CM. Trans fatty acids and weight gain. Int J Obes (Lond) . 2011;35:315-24.
9. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med . 2011;364:2392-404.
10. Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr . 2004;23:373-85.
11. Westerterp-Plantenga MS, Nieuwenhuizen A, Tome D, Soenen S, Westerterp KR. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr . 2009;29:21-41.
12. Furtado JD, Campos H, Appel LJ, et al. Effect of protein, unsaturated fat, and carbohydrate intakes on plasma apolipoprotein B and VLDL and LDL containing apolipoprotein C-III: results from the OmniHeart Trial. Am J Clin Nutr . 2008;87:1623-30.
13. Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA . 2005;294:2455-64.
14. Bernstein AM, Sun Q, Hu FB, Stampfer MJ, Manson JE, Willett WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation . 2010;122:876-83.
15. Aune D, Ursin G, Veierod MB. Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia . 2009;52:2277-87.
16. Pan A, Sun Q, Bernstein AM, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr . 2011;94(4):1088-96.
17. Abete I, Astrup A, Martinez JA, Thorsdottir I, Zulet MA. Obesity and the metabolic syndrome: role of different dietary macronutrient distribution patterns and specific nutritional components on weight loss and maintenance. Nutr Rev . 2010;68:214-31.
18. Barclay AW, Petocz P, McMillan-Price J, et al. Glycemic index, glycemic load, and chronic disease risk—a meta-analysis of observational studies. Am J Clin Nutr . 2008;87:627-37.
19. Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med . 2009;169:659-69.
20. Koh-Banerjee P, Franz M, Sampson L, et al. Changes in whole-grain, bran, and cereal fiber consumption in relation to 8-y weight gain among men. Am J Clin Nutr . 2004;80:1237-45.
21. Liu S, Willett WC, Manson JE, Hu FB, Rosner B, Colditz G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr . 2003;78:920-7.
22. Ledoux TA, Hingle MD, Baranowski T. Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev . 2011;12:e143-50.
23. Mattes RD, Kris-Etherton PM, Foster GD. Impact of peanuts and tree nuts on body weight and healthy weight loss in adults. J Nutr . 2008;138:1741S-5S.
24. Bes-Rastrollo M, Sabate J, Gomez-Gracia E, Alonso A, Martinez JA, Martinez-Gonzalez MA. Nut consumption and weight gain in a Mediterranean cohort: The SUN study. Obesity (Silver Spring) . 2007;15:107-16.
25. Bes-Rastrollo M, Wedick NM, Martinez-Gonzalez MA, Li TY, Sampson L, Hu FB. Prospective study of nut consumption, long-term weight change, and obesity risk in women. Am J Clin Nutr . 2009;89:1913-19.
26. Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J . 2000;14:1132-8.
27. Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res . 2004;12:582-90.
28. Lanou AJ, Barnard ND. Dairy and weight loss hypothesis: an evaluation of the clinical trials. Nutr Rev . 2008;66:272-9.
29. Phillips SM, Bandini LG, Cyr H, Colclough-Douglas S, Naumova E, Must A. Dairy food consumption and body weight and fatness studied longitudinally over the adolescent period. Int J Obes Relat Metab Disord . 2003;27:1106-13.
30. Rajpathak SN, Rimm EB, Rosner B, Willett WC, Hu FB. Calcium and dairy intakes in relation to long-term weight gain in US men. Am J Clin Nutr . 2006;83:559-66.
31. Snijder MB, van Dam RM, Stehouwer CD, Hiddink GJ, Heine RJ, Dekker JM. A prospective study of dairy consumption in relation to changes in metabolic risk factors: the Hoorn Study. Obesity (Silver Spring) . 2008;16:706-9.
32. Boon N, Koppes LL, Saris WH, Van Mechelen W. The relation between calcium intake and body composition in a Dutch population: The Amsterdam Growth and Health Longitudinal Study. Am J Epidemiol . 2005;162:27-32.
33. Berkey CS, Rockett HR, Willett WC, Colditz GA. Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Arch Pediatr Adolesc Med . 2005;159:543-50.
34. Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health . 2007;97:667-75.
35. Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr . 2009;89:438-9; author reply 9-40.
36. Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav . 2010;100:47-54.
37. Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care . 2010;33:2477-83.
38. Pan A, Hu FB. Effects of carbohydrates on satiety: differences between liquid and solid food. Curr Opin Clin Nutr Metab Care . 2011;14:385-90.
39. Ogden CL KB, Carroll MD, Park S. Consumption of sugar drinks in the United States , 2005-2008. Hyattsville, MD: National Center for Health Statistics; 2011.
40. Chen L, Appel LJ, Loria C, et al. Reduction in consumption of sugar-sweetened beverages is associated with weight loss: the PREMIER trial. Am J Clin Nutr . 2009;89:1299-306.
41. Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics . 2006;117:673-80.
42. Brownell KD, Farley T, Willett WC, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med . 2009;361:1599-605.
43. Wang L, Lee IM, Manson JE, Buring JE, Sesso HD. Alcohol consumption, weight gain, and risk of becoming overweight in middle-aged and older women. Arch Intern Med . 2010;170:453-61.
44. Liu S, Serdula MK, Williamson DF, Mokdad AH, Byers T. A prospective study of alcohol intake and change in body weight among US adults. Am J Epidemiol . 1994;140:912-20.
45. Wannamethee SG, Field AE, Colditz GA, Rimm EB. Alcohol intake and 8-year weight gain in women: a prospective study. Obes Res . 2004;12:1386-96.
46. Lewis CE, Smith DE, Wallace DD, Williams OD, Bild DE, Jacobs DR, Jr. Seven-year trends in body weight and associations with lifestyle and behavioral characteristics in black and white young adults: the CARDIA study. Am J Public Health . 1997;87:635-42.
47. Bes-Rastrollo M, Sanchez-Villegas A, Gomez-Gracia E, Martinez JA, Pajares RM, Martinez-Gonzalez MA. Predictors of weight gain in a Mediterranean cohort: the Seguimiento Universidad de Navarra Study 1. Am J Clin Nutr . 2006;83:362-70; quiz 94-5.
48. Poti JM, Popkin BM. Trends in Energy Intake among US Children by Eating Location and Food Source, 1977-2006. J Am Diet Assoc . 2011;111:1156-64.
49. Schulze MB, Fung TT, Manson JE, Willett WC, Hu FB. Dietary patterns and changes in body weight in women. Obesity (Silver Spring) . 2006;14:1444-53.
50. Newby PK, Muller D, Hallfrisch J, Andres R, Tucker KL. Food patterns measured by factor analysis and anthropometric changes in adults. Am J Clin Nutr . 2004;80:504-13.
51. Schulz M, Nothlings U, Hoffmann K, Bergmann MM, Boeing H. Identification of a food pattern characterized by high-fiber and low-fat food choices associated with low prospective weight change in the EPIC-Potsdam cohort. J Nutr . 2005;135:1183-9.
52. Newby PK, Muller D, Hallfrisch J, Qiao N, Andres R, Tucker KL. Dietary patterns and changes in body mass index and waist circumference in adults. Am J Clin Nutr . 2003;77:1417-25.
53. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr . 2010;92:1189-96.
54. Wright JD WC-Y. Trends in intake of energy and macronutrients in adults from 1999-2000 through 2007-2008 . Hyattsville, MD: National Center for Health Statistics; 2010.
55. Buckland G, Bach A, Serra-Majem L. Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev . 2008;9:582-93.
56. Dietary Guidelines for Americans Advisory Committee. Report of the DGAC on the Dietary Guidelines for Americans , 2010 ; 2010.
57. Popkin BM, Duffey KJ. Does hunger and satiety drive eating anymore? Increasing eating occasions and decreasing time between eating occasions in the United States. Am J Clin Nutr . 2010;91:1342-7.
58. Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977-1998. JAMA . 2003;289:450-3.
59. Piernas C, Popkin BM. Food portion patterns and trends among U.S. children and the relationship to total eating occasion size, 1977-2006. J Nutr . 2011;141:1159-64.
60. Wansink B, Kim J. Bad popcorn in big buckets: portion size can influence intake as much as taste. J Nutr Educ Behav . 2005;37:242-5.
61. Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr., Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr . 2007;85:201-8.
62. Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR, Jr., Popkin BM. Regular consumption from fast food establishments relative to other restaurants is differentially associated with metabolic outcomes in young adults. J Nutr . 2009;139:2113-8.
63. Taveras EM, Berkey CS, Rifas-Shiman SL, et al. Association of consumption of fried food away from home with body mass index and diet quality in older children and adolescents. Pediatrics . 2005;116:e518-24.
64. French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention study: dietary, behavioral and demographic correlates. Int J Obes Relat Metab Disord . 2000;24:1353-9.
65. Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet . 2005;365:36-42.
66. Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev . 2008;9:535-47.
67. Rolls, B. J., L. S. Roe, et al. (2007). “The effect of large portion sizes on energy intake is sustained for 11 days.” Obesity (Silver Spring) 15(6): 1535-1543.
68. Ello-Martin, J. A., J. H. Ledikwe, et al. (2005). “The influence of food portion size and energy density on energy intake: implications for weight management.” Am J Clin Nutr 82(1 Suppl): 236S-241S.
Obesity Essay
Last updated on: Feb 9, 2023
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- how to write a movie review
- how to write a research methodology
- how to write a conclusion
- scholarship essay writing
- 10essential essay writing techniques for students
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved
- About Project
- Testimonials
Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
- Entertainment
- Environment
- Information Science and Technology
- Social Issues
Home Essay Samples Health
Essay Samples on Obesity
How important is the role of genetics in common obesity.
Frequently characterised by a body mass index greater than 30kg/m^2, obesity is rapidly becoming a serious problem for not just high-income countries, but also middle-income countries, with trends predicting that by 2025, 21% of women and 18% of men will be obese. Even in lower-income...
Childhood Obesity: Will Children Live Long Enough To Make a Difference
The late 1940’s brought on a radical and drastic new change to the American culture when McDonald’s first opened its doors and started introducing the public to quick, easy, and convenient new ways to consume their food. McDonald’s prided themselves on being able to easily...
- Childhood Obesity
Effects of Sleep and on Childhood Obesity and Multiple Studies
Around the world there are very large numbers of obesity in children. Obesity is one factor that will carry on into your adulthood if not treated or prevented from happening. The International Journal of Obesity recognized this and decided to do a study on the...
Unhealthy Eating Habits and Childhood Obesity
Obesity in children is a growing public health concern (Memedi, Tasic, Nikolic, Jancevska, Gucev, 2013). According to the report of (WHO2018) “in just 40 years the number of school-age children and adolescents with obesity has risen more than 10-fold, from 11 million to 124 million...
Spread Of Obesity In Large Social Network: Birds Of A Feather Flock Together
In 2007 July, Nicholas Christakis, a professor of public health at Harvard Medical School, and James Fowler, an associate professor of political science at UC San Diego, published a cover article in medicine's most prestigious journal, the New England Journal of Medicine, complete with a...
Stressed out with your paper?
Consider using writing assistance:
- 100% unique papers
- 3 hrs deadline option
Obesity Is A Disease: Social Problem Of Being Overweight
Nowadays obesity and overweight become a major social problem. They not only have high correlation with many serious and chronic diseases but also cause economic impact. The definition of obesity and overweight is deviant or excessive fat accumulation may impair health. Body mass index (BMI),...
Considering Obesity A Disease: The Spreading Condition
What is Obesity? Obesity is a medical condition in both children and adults that occurs when someone is extremely overweight which can give rise to medical conditions such as heart disease and high blood pressure. It is measured using a BMI scale which takes sex,...
Childhood Obesity: A Realistic Solution
According to the Britannica Encyclopedia, Obesity is classified as having a BMI, also known as body mass index, of forty or higher (Encyclopaedia Britannica, 2019). A person’s body mass index is meant to be an indicator of high body fatness and, although it does not...
The Rates Of Childhood Obesity
The number of children experiencing childhood obesity continues to remain too high and poses health threats. Although childhood obesity is multifactorial, research has shown over and over again the impact physical activity has on decreasing this risk, as well as reducing many other health risks....
An Attempt To End Obesity With Junk And Healthy Food
In an article published by The Atlantic magazine David H Freedman poses the statement “How junk food can end obesity.” the article focuses on how the media, and Health Food enthusiasts have been demonizing industrialized, and processed foods. When I came across David’s article, the...
- Healthy Food
The Crucial Issue Of Child Obesity In The World And Methods Of Its Prevention
Abstract Child obesity is a condition of excessive body fat that results from a chronic energy imbalance whereby intake exceeds expenditure. There was telephone survey conducted among the selected minorities that have the history of child obesity. There were 10,000 respondents to the survey. Aged...
- Healthy Lifestyle
Deadly Consequences Of Sugar And Glucose Epidemic In The United States
Questions Obesity rate in the United States have been increased since the past 20 years because of the amount of food we eat which contains a lot of sugar. In addition to the obesity rate, studies have shown a connection between to large amounts of...
- High Fructose Corn Syrup
Link Between the Beverage Consumption and Body Fat in U.S Children
Abstract Soft drinks have become a major contribution to obesity and other health related problems in America. The soft drink epidemic provides many calories with added sugar. it has been linked to overall diet quality and meeting nutrient requirements. Additional eighty-five empty calories or five...
My Personal Opinion on the 'Supersize Me'
My personal opinion on the 'Supersize Me' video is Americans and everyone else on this earth is responsible for their personal choices. I don’t think restaurants should be held accountable for people gaining weight because humans have the choice if they should eat out or...
- Documentary
- Super Size Me
Obesity Epidemic in America In Documentary 'Supersize Me'
14 years ago award winning director Morgan Spurlock flamboyantly demonstrated the consequences of trying to sustain yourself on a calorie filled diet. Over a 30-day period, the producer and star of the documentary ate nothing but McDonalds for his daily three meals. He also travels...
The Vitro Meat: Meat Gone Wrong
In the United States the rate of obesity was 39.8% and affected 93.3 million US adults in 2015 and 2016, according to the Center for Disease Control and Prevention data (“Adult Obesity Facts”). The rate of obesity is up due to technology that is constantly...
The Occurrences of Child Obesity in U.S and Canada
Abstract This paper I will be summarizing four different articles from four different sources that’s associated with Child Obesity. Topic includes: (1) Prevalence of Obesity and Severe Obesity in US Children,1999-2014. (2) Canadian kids aren’t playing outside enough, experts say, and it’s harming their health....
The Various Causes of Child Obesity
Why is there's a big epidemic of child and adolescent obesity? Obesity is a condition that is associated with having an excess amount of body fat, defined by genetic and environmental factors that are difficult to control when dieting. The state of Ohio has the...
Child Obesity Situation in Oklahoma
On September 18, 2018, an article in Metro News written by Tanveer Mann was published about a child whose name is unknown for privacy reasons who died from a heart disease caused by obesity. The child was only 13 years old and had a body...
The Problem of Child Obesity Abuse
A rhetorical analysis on child obesity abuse, over Childhood Obesity: Is it Abuse? By Abigail Darwin is an informative article on Childhood Obesity being inhibited, she describes to us what our country as a whole is doing to fight against obesity in children. She also...
Physical Activity: Learning the Outcomes and Benefits
Physical activity can be a broad spectrum which can including all forms of activity, stated by Davies (2011) “walking, cycling, active play, working out at a gym, dancing, gardening and competitive sport” (Davies et al., 2011: 1e61) (Active, 2011). Regular activity (leisure-time physical activity, workouts,...
- Physical Exercise
The Economics of Weight Loss Under Condition of Obesity
Abstract Obesity is now being considered one of the biggest health concerns globally. Ironically, while India records the largest no. of underweight population in the world along with China, it has also been placed in the top 5 countries in terms of obesity as per...
- Weight Loss
Childhood Bedtime On Adolescent Obesity
Introduction Obesity is one of the largest growing incidences in today’s society however, your sleep as a child can impact your weight as an adolescent and into adulthood. Many individuals know the importance of eating healthy and exercising, but don’t know as much about the...
- Adolescence
The Role of Evolution on Food and Eating Habits
Evolution is always happening and will always be as long as there is life to carry it out. We must admit that evolution is happening today all around us. Evolution shapes every human’s day to day life. Our knowledge of how things change, specifically how...
- Eating Habits
Popularity Of Nas And Obesity/Diabetes Spike
Non-caloric artificial sweeteners (NAS) are a popular food additive used among people of different body types. Initially, NAS were marketed to be “healthy” and a lower calorie option than for example sucrose, common table sugar. NAS are commonly found in an array of food items...
Coca-Cola In Global Fight Towards Obesity
Coca-Cola is one of the most popular brand in the world. It is also the highest selling soft drink in history. Coca-Cola is developing its business future plan is to become a total beverage company by giving people more of the drinks they demand which...
Obesity – A Multifactorial Disorder With A Genetic Basis
In past times, the genetic makeup of an individual has been said to be the main link of inheriting diseases. For some diseases, this claim may be true, however some diseases differ in the aspect as environmental factors now contribute widely to a person’s health....
Obesity – Extremely Fast Rising Public Health Problem In The United States
Obesity is currently considered the most significant public health problem in the United States that continues to rise at high levels in our world today. Unfortunately, with the struggles to manage obesity once recognized, there is still not a long-term preventative policy that exists. The...
- Public Health
Obesity As An Epidemic In America
Obesity is a condition where one has so much body fat that it could potentially affect their health negatively. A person is considered obese if their BMI (Body mass Index) is 30 kg/m2 or more. Obesity in an epidemic in the United States. Obese people...
The Problem Of High Level Of Obesity In Malaysia
Overview of Obesity According to NHMS studies from 1996-2015, the rate of obesity in Malaysia had significantly increased within these year. In term of states in Malaysia, Putrajaya recorded as the highest state that has prevalence of obesity which is 25.8% compare to Sabah that...
An Epidemic Of Obesity In Papua New Guinea
OBESITY IN PAPUA NEW GUINEA Obesity is one of the immense problem of lifestyle disease as far as health is concerned. What is obesity? Medically obesity is simply defined as the build-up or accumulation of excessive fats in the adipose tissue of the human body....
- Cultural Identity
The Policy Against Obesity In Canada
With Canada being labeled as one of countries with the most overweight population in OECD’s 2017 Obesity Calendar, there is a rising concern among policy makers to battle this epidemic. At least 25.8% of Canada’s population above the age of 15 is considered obese. (Ferreras)...
Best topics on Obesity
1. How Important is the Role of Genetics in Common Obesity
2. Childhood Obesity: Will Children Live Long Enough To Make a Difference
3. Effects of Sleep and on Childhood Obesity and Multiple Studies
4. Unhealthy Eating Habits and Childhood Obesity
5. Spread Of Obesity In Large Social Network: Birds Of A Feather Flock Together
6. Obesity Is A Disease: Social Problem Of Being Overweight
7. Considering Obesity A Disease: The Spreading Condition
8. Childhood Obesity: A Realistic Solution
9. The Rates Of Childhood Obesity
10. An Attempt To End Obesity With Junk And Healthy Food
11. The Crucial Issue Of Child Obesity In The World And Methods Of Its Prevention
12. Deadly Consequences Of Sugar And Glucose Epidemic In The United States
13. Link Between the Beverage Consumption and Body Fat in U.S Children
14. My Personal Opinion on the ‘Super Size Me’
15. Obesity Epidemic in America In Documentary ‘Super Size Me’
- Mental Illness
- Chronic Pain
- Nursing Home
- Borderline Personality Disorder
- Universal Health Care
Need writing help?
You can always rely on us no matter what type of paper you need
*No hidden charges
100% Unique Essays
Absolutely Confidential
Money Back Guarantee
By clicking “Send Essay”, you agree to our Terms of service and Privacy statement. We will occasionally send you account related emails
You can also get a UNIQUE essay on this or any other topic
Thank you! We’ll contact you as soon as possible.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Journal Menu
- Nutrients Home
- Aims & Scope
Editorial Board
- Reviewer Board
Topical Advisory Panel
- Instructions for Authors
Special Issues
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
- arrow_forward_ios Forthcoming issue arrow_forward_ios Current issue
- Vol. 16 (2024)
- Vol. 15 (2023)
- Vol. 14 (2022)
- Vol. 13 (2021)
- Vol. 12 (2020)
- Vol. 11 (2019)
- Vol. 10 (2018)
- Vol. 9 (2017)
- Vol. 8 (2016)
- Vol. 7 (2015)
- Vol. 6 (2014)
- Vol. 5 (2013)
- Vol. 4 (2012)
- Vol. 3 (2011)
- Vol. 2 (2010)
- Vol. 1 (2009)
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
Nutrition and Obesity
A section of Nutrients (ISSN 2072-6643).
Section Information
Over the last few decades, obesity has become the most prevalent metabolic disorder worldwide. Excess adiposity increases the risk for the development of cardiometabolic alterations such as type 2 diabetes, cardiovascular disease, dyslipidemia, non-alcoholic fatty liver disease and cancer, among others. In the last few years, our knowledge of obesity has greatly improved, but more research is needed to better understand the mechanisms underlying the development of this metabolic condition and its pathophysiology, and to optimize its management.
We welcome original research articles describing basic, clinical and applied studies representing novel and significant advances in all areas relevant to obesity and related disorders, as well as reviews. The areas of research covered by this section relate to all aspects of obesity diagnosis, pathophysiology and treatment.
Topics include, but are not limited to:
- Adipose tissue pathophysiology;
- Biomarkers;
- Physical activity;
- Adipokines;
- Pediatric obesity;
- Obesity phenotyping;
- Omic studies;
- Regulation of appetite;
- Body composition;
- Energy expenditure;
- Cardiometabolic risk factors;
- Nutritional epidemiology;
- Animal models;
- New technologies (for phenotyping or treatment);
- In vitro models, including organoids;
- Psychological aspects;
- Metabolic syndrome;
- Type 2 diabetes;
- Non-alcoholic fatty liver disease;
- Other obesity-related metabolic disturbances;
- Dietary treatment;
- Lifestyle intervention;
- Pharmacological treatment;
- Metabolic surgery;
- Intermittent fasting;
- Cardiometabolic risk improvement after weight loss;
- Body composition changes;
- Weight regain;
- Predictors of treatment success;
- Use of apps for weight loss;
- Novel targets;
- Transgenerational effects;
- Treatment of children and adolescents.
Following special issues within this section are currently open for submissions:
- Diet, Inflammation and Metabolic Complications (Deadline: 5 July 2024 )
- Dietary Patterns and Lifestyle Promoting Healthy Weight Strategies in Children and Adolescents–2nd Edition (Deadline: 15 July 2024 )
- Featured Articles on Nutrition and Obesity Management (2nd Edition) (Deadline: 25 July 2024 )
- Prevention of Obesity in the Lifecycle: Risks and Determinants (Deadline: 25 July 2024 )
- Nutrition, Diet Components and Healthy Weight (Deadline: 5 August 2024 )
- Effect of Diet Quality and Physical Activity on Childhood Obesity (Deadline: 5 August 2024 )
- Community-Based Strategies for Obesity Prevention: A Nutritional Perspective (Deadline: 5 August 2024 )
- Dietary Strategies for Obesity (Deadline: 15 August 2024 )
- The Role of Dietary Patterns in Malnutrition – Relevance of Body Weight upon Non-communicable Diseases (Deadline: 20 August 2024 )
- The Effect of Lifestyle and Eating Habits on Obesity (Deadline: 15 September 2024 )
- Dietary Behaviors and Obesity Predisposition (Deadline: 25 September 2024 )
- From Obesity to Eating Disorders: Scaling Up the Evidence (Deadline: 30 September 2024 )
- Diet and Nutrition Approaches in Obesity Treatment (Deadline: 5 October 2024 )
- The Effect of Eating Habits and Physical Activity on Childhood Obesity (Deadline: 25 November 2024 )
- The Adipose-Nutrition Axis: Implications for Obesity, Inflammation, and Chronic Disease (Deadline: 25 November 2024 )
- Nutritional Strategies for Preserving Fat-Free Mass during Intentional Weight Loss (Deadline: 25 November 2024 )
- Dietary Approaches and Exercise in the Management of Overweight and Obesity (Deadline: 15 December 2024 )
- Nutritional and Metabolic Changes Affecting Adipose Tissue Biology (Deadline: 15 January 2025 )
- Nutritional Involvement in Psychopathology and Lifestyle of the Population with Severe Obesity Undergoing Bariatric Surgery or Other Interventional Approaches (Deadline: 15 January 2025 )
- Nutritional Intervention and Physical Activity in Obese Adolescents and Children (Deadline: 25 March 2025 )
- Hot topics on Nutrition and Obesity 2024 (Deadline: 31 March 2025 )
Papers Published
Further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Data, Statistics, and Research
- Healthy People 2030
- Healthy Eating and Active Living Survey (CBS HEAL)
- Interactive Database
- DNPAO Published Research
Related Topics:
- Physical Activity
Healthy People 2030 Related to Physical Activity, Nutrition, and Obesity
Healthy People 2030 sets data-driven national objectives to improve health and well-being over the next decade. Healthy People 2030 includes 359 core — or measurable — objectives as well as developmental and research objectives. Below are the indicators and objectives that align with the work of CDC's Division of Nutrition, Physical Activity, and Obesity (DNPAO).

Leading health indicators
Of the core Healthy People 2030 objectives, there is a subset of 23 leading health indicators . This subset helps organizations, communities, and states focus their resources and efforts to improve the health and well-being of all people. Four leading health indicators are directly related to DNPAO's work:
- Reduce consumption of added sugars by people 2 and older—NWS–10 .
- Reduce household food insecurity and hunger—NWS–01 .
- Increase the proportion of adults who do enough aerobic and muscle-strengthening activity—PA–05 .
- Reduce the proportion of children and adolescents with obesity—NWS–04.
In addition to the leading health indicators, the objectives below are related to DNPAO's work.
Healthy eating
For people 2 and older :
- Increase fruit consumption—NWS–06 .
- Increase vegetable consumption—NWS–07 .
- Increase consumption of dark green vegetables, red and orange vegetables, and beans and peas—NWS–08 .
- Increase whole grain consumption—NWS–09 .
- Reduce consumption of saturated fat—NWS–11 .
- Reduce consumption of sodium—NWS–12 .
Vitamins and minerals
- Increase calcium consumption—NWS–13 .
- Increase potassium consumption—NWS–14 .
- Increase vitamin D consumption—NWS–15 .
For other population groups :
- Reduce iron deficiency in children 1 to 2 years—NWS–16 .
- Reduce iron deficiency in females 12 to 49—NWS–17 .
- Increase the proportion of women of childbearing age who get enough folic acid—MICH–12 .
Breastfeeding
- Increase the proportion of infants who are breastfed exclusively through age 6 months—MICH–15 .
- Increase the proportion of infants who are breastfed at 1 year—MICH–16 .
Healthy food environment
- Increase the proportion of students participating in the School Breakfast Program—AH–04 .
- Eliminate very low food security in children—NWS–02 .
Physical activity for children and adolescents
Increase the proportion of:
- Children who do enough aerobic physical activity—PA–09 .
- Children aged 2 to 5 years who get no more than one hour of screen time a day—PA–13 .
- Children and adolescents who play sports—PA–12 .
- Adolescents who do enough aerobic physical activity—PA–06 .
- Adolescents who do enough muscle–strengthening activity—PA–07 .
- Adolescents who do enough aerobic and muscle-strengthening activity—PA–08 .
- Adolescents who participate in daily school physical education—ECPB–01 .
Physical activity for adults
- Reduce the proportion of adults who do no physical activity in their free time—PA–01 .
Increase the proportion of adults:
- Who do enough aerobic physical activity for substantial health benefits—PA–02 .
- Who do enough aerobic physical activity for extensive health benefits—PA–03 .
- Who do enough muscle–strengthening activity—PA–04 .
- With arthritis who get counseling for physical activity—A–04 .
Physical activity for older adults
- Increase the proportion of older adults with physical or cognitive health problems who get physical activity—OA–01 .
- Reduce the rate of emergency department visits due to falls among older adults—OA–03 .
Neighborhood and built environment
- Adults who walk or bike to get places—PA–10 .
- Adolescents who walk or bike to get places—PA–11 .
Healthy weight for adults
- Reduce the proportion of adults with obesity—NWS–03 .
- Increase the proportion of health care visits by adults with obesity that include counseling on weight loss, nutrition, or physical activity—NWS–05 .
- Increase the proportion of women who had a healthy weight before pregnancy—MICH–13 .
- Children who get sufficient sleep—EMC–03 .
- High school students who get enough sleep—SH–04 .
- Adults who get enough sleep—SH–03 .
Developmental objectives
In addition to core objectives, developmental objectives represent specific high-priority public health issues. These public health issues are associated with evidence-based interventions but do not yet have reliable baseline data.
The developmental objectives related to DNPAO are to increase the proportion of:
- Children who participate in high–quality early childhood education programs—EMC-D03 .
- Schools that don't sell less healthy foods and drinks—ECBP-D02 .
- Worksites that offer an employee physical activity program—ECBP-D04 .
- Worksites that offer an employee nutrition program—ECBP-D05 .
Research objectives
Research objectives represent public health issues with a high health or economic burden. These public health issues can also have significant disparities between population groups. These public health issues are not yet associated with evidence-based interventions.
Objectives are to increase the proportion of:
- Childcare centers where children aged 3 to 5 years do at least 60 minutes of physical activity a day—PA–RO1 .
- Eligible students participating in the Summer Food Service Program—AH-R03 .
Overall health and well-being measures
Overall health and well-being measures are broad outcome measures intended to assess the Healthy People 2030 vision . This vision is of a society where all people can achieve their full potential for health and well-being across the lifespan. Unlike the leading health indicators and core objectives, these measures do not have targets.
- Overall well-being—OHM-1
Healthy life expectancy
- Life expectancy at birth—free of activity limitation—OHM-2 .
- Life expectancy at birth—free of disability—OHM-3 .
- Life expectancy at birth—in good or better health—OHM-4 .

Mortality and health summary
- Life expectancy at birth—OHM-5 .
- Free of activity limitation (all ages)—OHM-6 .
- Free of disability (ages 1 and older)—OHM-7 .
- Respondent-assessed health status — in good or better health (all ages)—OHM-8 .
Objective code abbreviations
- A—Arthritis
- DO—Developmental Objective
- ECBP—Educational and Community-Based Programs
- EMC—Early and Middle Childhood
- MICH—Maternal, Infant, and Child Health
- NWS—Nutrition and Weight Status
- OA—Older Adults
- OHM—Overall Health and Well–Being Measures
- PA—Physical Activity
- RO—Research Objective
- SH—Sleep Health
Data, Trends, Maps
An interactive database plus lists of published research about nutrition, physical activity, and obesity.
- Introduction
- Conclusions
- Article Information
A, Violin plots show the distribution of essential amino acid and protein intake relative to body mass. Dots indicate medians; whiskers, 95% CIs; red dashed lines, respective recommendations. B, Nutrient mean adequacy ratios (presented as ratios, ranging from 0-1, left axis) and the proportion of individuals above and below recommendations for essential amino acids and protein (presented as percentages, ranging from 0%-100%, right axis) are shown.
A, Violin plots show the distribution of relative caloric contribution of each food processing category. Dashed lines indicate reference values from the Brazilian population living in metropolitan areas. B, The relative contribution of each food processing category to protein intake is shown. Dots indicate medians; whiskers, 95% CIs.
A, The association between binary variables (consuming protein supplements and consuming textured soy protein) with inadequate protein intake is shown. B, The association between quartiles of continuous variables and inadequate protein intake is shown. Results are presented as odds ratio coefficients and 95% CIs for having inadequate protein intake given the variable in comparison with the reference level. NA indicates not applicable.
eTable 1. Examples of common vegan foods and their classification according to Nova system
eTable 2. Comparison of subsets with available and missing data across variables
eTable 3. Micronutrients intake
eTable 4. Nutrient adequacy ratios of protein and essential amino acids
eTable 5. Intake of nonessential amino acids
eTable 6. Caloric contribution and protein intake according to Nova food processing category and amino acid intake considering textured soy protein as unprocessed and minimally processed food
eTable 7. Coefficients from adjusted logistic regression models estimating protein inadequacy (complete case analysis, n=558)
eTable 8. Coefficients from adjusted logistic regression models estimating protein inadequacy (imputed dataset, n=774)
eFigure 1. Study flowchart
eFigure 2. Caloric and protein intake according to Nova food processing categories considering textured soy protein as unprocessed and minimally processed
eFigure 3. Main food sources of protein and essential amino acids
eFigure 4. Protein and essential amino acids intake, nutrient adequacy ratios and proportion of individuals meeting recommended intakes in the imputed (n=774) dataset
eFigure 5. Exploratory logistic regression models estimating the probability of protein inadequacy according to protein supplement intake or texturized soy protein intake as continuous variables
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Leitão AE , Esteves GP , Mazzolani BC, et al. Protein and Amino Acid Adequacy and Food Consumption by Processing Level in Vegans in Brazil. JAMA Netw Open. 2024;7(6):e2418226. doi:10.1001/jamanetworkopen.2024.18226
Manage citations:
© 2024
- Permissions
Protein and Amino Acid Adequacy and Food Consumption by Processing Level in Vegans in Brazil
- 1 Applied Physiology and Nutrition Research Group–School of Physical Education and Sport and Faculdade de Medicina, Universidade de Sao Paulo, São Paulo, São Paulo, Brazil
- 2 Center of Lifestyle Medicine; Laboratory of Assessment and Conditioning in Rheumatology, Hospital das Clínicas, Faculdade de Medicina, Universidade de Sao Paulo, São Paulo, São Paulo, Brazil
- 3 Food Research Center, University of São Paulo, São Paulo, Brazil
- 4 School of Applied Sciences, State University of Campinas, Limeira, Brazil
Question Do individuals who adhere to a vegan diet meet protein and essential amino acid needs, and are they reliant on ultraprocessed foods?
Findings In this cross-sectional survey study of responses to a 1-day food diary from 774 adults who adhered to a vegan diet, including 558 participants with body weight data, the mean protein and amino acid adequacy ratio comparing nutrient intake vs recommendations was 0.95; unprocessed or minimally processed and ultraprocessed foods accounted for 66.5% and 13.2% of energy intake, respectively. Protein supplements, textured soy protein, and ultraprocessed food were associated with decreased odds of protein inadequacy and unprocessed and minimally processed protein with increased odds of protein inadequacy.
Meaning This study found that most individuals who adhered to a vegan diet attained protein recommendations but were less likely to do so when consuming less ultraprocessed food.
Importance Major concerns regarding individuals who adhere to a vegan diet are whether they meet protein and essential amino acid recommendations and how reliant they are on ultraprocessed foods.
Objectives To investigate whether individuals who adhere to a vegan diet meet protein and essential amino acid recommendations and, as secondary objectives, to determine ultraprocessed food intake and potential factors associated with inadequate protein intake in this population.
Design, Setting, and Participants This cross-sectional survey study was conducted between September 2021 and January 2023 in Brazil among male and female adults (aged 18 years or older) who adhered to a vegan diet recruited from social media platforms.
Exposure Adherence to a vegan diet and unprocessed and minimally processed foods and ultraprocessed food consumption.
Main Outcomes and Measures Protein and essential amino acid intake and food consumption by processing level were assessed using a 1-day food diary. Nutrient adequacy ratios were calculated by dividing nutrient intake by its recommendation (using scores truncated at 1) for each participant and then finding the mean across participants for each nutrient. The mean adequacy ratio was the mean of all nutrient adequacy ratios.
Results Of 1014 participants who completed the survey, 774 individuals (median [IQR] age, 29 [24-35] years; 637 female [82.3%]) were confirmed as adhering to a vegan diet and provided adequate food recalls, among whom 558 individuals reported body weight and so had relative protein and amino acid intake values available. The median (IQR) body mass index (calculated as weight in kilograms divided by height in meters squared) of participants was 22.6 (20.3-24.8). The nutrient adequacy ratio of protein was 0.93 (95% CI, 0.91-0.94); for essential amino acids, ratios ranged from 0.90 (95% CI, 0.89-0.92) for lysine to 0.98 (95% CI, 0.97-0.99) for phenylalanine and tyrosine. The mean adequacy ratio for protein and all amino acids was 0.95 (95% CI, 0.94-0.96). The median intake level was 66.5% (95% CI, 65.0%-67.9%) of total energy intake for unprocessed and minimally processed food and 13.2% (95% CI, 12.4%-14.4%) of total energy intake for ultraprocessed food. Adjusted logistic regression models showed that consuming protein supplements (odds ratio [OR], 0.06 [95% CI 0.02-0.14]; P < .001) or textured soy protein (OR, 0.32 [95% CI, 0.17-0.59]; P < .001) was associated with decreased odds of inadequate protein intake. Higher ultraprocessed food intake levels were also associated with decreased odds of inadequate protein intake (eg, fourth vs first quartile of intake: OR, 0.16 [95% CI, 0.07-0.33]; P < .001), and higher unprocessed and minimally processed protein intake levels were associated with increased odds of inadequate protein intake (eg, fourth vs first quartile of intake: OR, 12.42 [95% CI, 5.56-29.51]; P < .001).
Conclusions and Relevance In this study, most individuals who adhered to a vegan diet attained protein and essential amino acid intake recommendations, largely based their diet of unprocessed and minimally processed food, and had a significantly lower proportion of ultraprocessed food intake compared with previous reports. Participants consuming less ultraprocessed food were more likely to have inadequate protein intake, suggesting a significant reliance on ultraprocessed proteins for this population.
Veganism is a lifestyle increasing in popularity worldwide that supports abstaining from the use of animal products. This leads to a dietary pattern that excludes meat, fish, poultry, dairy, eggs, and honey, among other animal-derived foods (henceforth, vegan diet ). 1 , 2
Refraining from protein-rich animal foods has generated ongoing controversy as to whether individuals who adhere to a vegan diet can adequately meet protein requirements. 3 Although studies show that these individuals can have borderline-adequate protein intake, albeit slightly reduced vs individuals consuming omnivorous diets, 4 it is unknown whether protein sources habitually consumed by vegans allow for adequate essential amino acid intake.
A range of plant-based meat and dairy substitutes have been formulated with the claim of being practical, protein-rich complements to a vegan diet. However, overconsumption of these products may disrupt the alimentary basis of vegan diets (unprocessed and minimally processed plant-based foods, such as fruits, vegetables, and whole grains) and lead to an increase in ultraprocessed food intake. 5 , 6 The association of ultraprocessed food intake with overall health has been widely debated, 7 - 9 warranting the investigation of food consumption as a function of processing level in the vegan population. Therefore, the primary aim of this study was to describe protein and essential amino acid intake in a survey of Brazilian individuals who follow a vegan diet. The secondary aim was assessing food intake by processing level according to the Nova classification system and investigating potential factors associated with protein inadequacy.
This cross-sectional survey study was approved by the Centro Universitário Estácio de Sá de Santa Catarina ethical committee and conducted according to the Helsinki declaration. All participants signed a digital informed consent form. This manuscript adheres to the Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology ( STROBE-nut ) reporting guideline and American Association for Public Opinion Research ( AAPOR ) reporting guideline for surveys. 10
Data in this study derive from the Vegan Eating Habits and Nutritional Evaluation Survey (VEGAN-EATS), a cross-sectional survey conducted between September 2021 and January 2023. We previously published an analysis of disordered eating attitudes and food choice motives in this population stemming from this survey. 11 This study expands on the topic by investigating the dietary profile of Brazilian vegan diets, with the topical issue of protein, essential amino acid intake, and food processing in this population.
Participants were recruited through advertisements on social media platforms and included males and females aged 18 years or older currently living in Brazil with internet access and the ability to read. Participants completed an online survey using the Google Forms platform (Google LLC).
The survey included questions regarding participant general characteristics, self-reported anthropometric data, and vegan lifestyle. General characteristics included educational level (elementary school, high school, college, or postgraduate education), income (categorized according to the Brazilian Institute of Geography and Statistics in levels of A [≥US $4200], B [US $1350-$4200], C [US $550-$1350], and D or E [≤US $550]), 12 smoking (yes or no) and drinking status (none, 1-2 times/mo, 2-4 times/mo, 2-3 times/wk, or ≥ 4 times/wk), and exercise habits (does not exercise, 1-2 h/wk, 3-4 h/wk, 5-6 h/wk, or ≥7 h/wk). Vegan lifestyle–related questions were the duration of adherence to a vegan diet (< 1 y, 1-2 y, 2-3 y, 3-4 years, and >5 y) and main motivation to shift toward a vegan diet (ethics, health reasons, environment, politics, life philosophy, medical restrictions, religion, or sports performance). Macronutrient and micronutrient, amino acid, and food intake by processing level were assessed by a self-administered 1-day food diary. This tool has been previously shown to perform adequately compared with the typical three 24-hour recalls, 13 and it was selected due to the impossibility of implementing repeated 24-hour recalls within our study. Participants received an instructional video on how to fulfil the diary and fully report quantity and type of foods and beverages consumed within the previous 24 hours, including a precise level of detail on food preparation and ingredients, allowing best practices for Nova food classification. 14 , 15 Total energy (kilocalories), macronutrient amounts (grams), and relative contributions of each Nova food processing category to the total energy intake were calculated. We also calculated the relative contribution stemming from proteins by food processing category. Examples of commonly reported foods and their classification are available in eTable 1 in Supplement 1 .
Food diaries were quantified with Nutritionist Pro software version 7.3 (Axxya Systems) using the US Department of Agriculture database. When nutritional information was not available, we searched the literature or directly contacted food companies. Amino acid composition was available for most consumed proteins (94.2%).
Due to missingness in body weight and height (available in 558 individuals), individuals with and without these data were compared and analyzed for potential associations between missingness and variables (eTable 2 in Supplement 1 ). There were only subtle differences between subgroups across all variables. Given that protein and amino acid intake adequacy requires assessing intake relative to body weight, observations with missing variables were excluded and complete cases were used for the main analysis. We also provided a complementary analysis in which missing body weight was imputed through multiple imputation 16 using the mice package 17 in R statistical software set to 5 iterations and the classification and regression trees method. A matrix of factors associated with body weight within the dataset was selected (age, sex, income class, exercise habits, motivation to shift to a vegan diet, total energy intake, and protein intake). The mean body weight from these 5 imputed datasets was used for descriptive statistics and model adjustment.
Descriptive data are presented as median and IQR for continuous variables and absolute and relative frequency (number and percentage) for categorical variables. We calculated 95% CIs surrounding the median using the bootstrap method through the boot package in R statistical software set to 10 000 iterations.
Protein and amino acid intake (milligrams per kilogram body weight per·day) were compared with Recommended Dietary Allowances from Dietary Reference Intakes. 18 Nutrient adequacy ratios were calculated by dividing nutrient intake by its recommendation (with scores being truncated at 1) for each participant and then finding the mean of values across the entire sample for each nutrient. 19 The mean adequacy ratio was calculated by taking the mean of all nutrient adequacy ratios. 19 We obtained 95% CIs via bootstrapping (see previous description).
The median protein and amino acid contribution of individual food items was calculated, and the top 30 or 10 food items for protein and essential amino acids, respectively, were plotted. To further assess potential factors associated with inadequate protein intake, participants were classified as having inadequate (<0.8 g/kg) or adequate (≥0.8 g/kg) protein intake, 18 and logistic regression models with Firth penalization 20 were used considering protein intake status as the outcome variable. Protein supplements or texturized soy protein consumption were used as binary variables (yes or no) in the main analysis. Quartiles were calculated for continuous variables (eg, unprocessed and minimally processed food, ultraprocessed food, and unprocessed and ultraprocessed protein intake) and used as categorical variables. Models were adjusted for age, sex, body weight, and energy intake relative to body weight. The α level was set at .05 for all analyses, and all P values assume a 2-sided test. All data cleaning, exploration, and visualization was performed using R statistical software version 4.2.2 (R Project for Statistical Computing) and RStudio (Posit Software, PBC) with dplyr and ggplot2 packages.
Among 1014 participants who completed the survey, 43 individuals were excluded for not fully adhering to a vegan diet and 197 individuals were excluded due to insufficient report on foods and portions, resulting in 774 individuals (median [IQR] age, 29 [24-35] years; 637 female [82.3%]) who completed the survey, were confirmed as adhering to a vegan diet, and provided adequate food recalls. The median body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) was 22.6 (20.3-24.8). Most participants were from the Southeast region of Brazil (491 participants [63.4%]), had a high educational level (280 participants with postgraduate education [36.2%]), were within socioeconomic class B (296 participants [38.2%]), reported no alcohol consumption (324 participants [41.9%]) or smoking habits (706 participants [91.2%]), exercised from 5 to 6 hr/wk (176 participants [22.7%]), and had adhered to a vegan diet for 5 years or longer (219 participants [28.3%]) ( Table 1 ). Because 216 participants did not report body weight, relative protein and amino acid intakes were available for 558 individuals (complete case population; median [IQR] age, 29 [24-37] years; 459 female [82.3%]) (see eFigure 1 in Supplement 1 for study flowchart and eTable 2 in Supplement 1 for all demographic information).
In the 1-day food diary among all participants, the median (IQR) intake was 1782 (1.385-2.227) kilocalories, with a distribution of 58.9% (52.3%-64.7%) carbohydrates, 14.9% (12.3%-18.8%) proteins, and 24.7% (18.8%-30.8%) fat. The median protein intake among the complete case population was 1.12 g/kg/d (95% CI, 1.05-1.16 g/kg/d) ( Figure 1 , A), whereas the median (IQR) dietary fiber intake was 44 (31-61) g/d ( Table 1 ). Other micronutrient intake levels can be found in eTable 3 in Supplement 1 .
Among the complete case population, the nutrient adequacy ratio for protein intake was 0.93 (95% CI, 0.921-0.94). Median intake levels of all essential amino acids were greater than recommended levels ( Figure 1 , B; see eTable 4 in Supplement 1 for numerical values). Nutrient adequacy ratios were higher than 0.90 for all essential amino acids. Lysine presented the lowest (0.90 [95% CI, 0.89-0.92]), and phenylalanine and tyrosine the highest (0.98 [95% CI, 0.97-0.99]) adequacy ratios ( Table 2 ; Figure 1 , B). The mean adequacy ratio across protein and all essential amino acids was 0.95 (95% CI, 0.94-0.96). Median intake levels of nonessential amino acids are available in eTable 5 in Supplement 1 .
Among the full study population, there was a high intake level of unprocessed and minimally processed food (66.5% [95% CI, 65.0%-67.9%] of total energy intake), which was higher than values reported for metropolitan areas in Brazil. 21 They had a low intake level as a percentage of total energy intake of processed culinary ingredients (8.3% [95% CI, 7.6%-8.8%]), processed food (6.2% [95% CI, 5.1%-6.8%]), and ultraprocessed food (13.2% [95% CI, 12.4%-14.4%]), all lower than values reported in metropolitan areas in Brazil ( Table 2 ; Figure 2 ). 21 Unprocessed and minimally processed food were also the main source of protein as the percentage of total energy from proteins (61.8% [95% CI, 59.4%-64.0%]), followed by ultraprocessed (23.6% [95% CI, 21.0%-26.3%]) and processed (7.4% [95% CI, 6.1%-8.7%]) foods. In a sensitivity analysis considering textured soy protein as unprocessed and minimally processed rather than ultraprocessed food, there was a decrease in the contribution of ultraprocessed food to total calories from 13.2% to 10.7% (95% CI, 9.4%-11.7%) and energy intake from proteins from 23.6% to 14.3% (95% CI, 12.2%-16.0%) (eTable 6 and eFigure 2 in Supplement 1 ). Individual food analyses for the main sources of protein and essential amino acids are available in eFigure 3 in Supplement 1 .
Adjusted logistic regression models among the complete case population showed that consuming protein supplements (odds ratio [OR], 0.06 [95% CI, 0.02-0.14]; P < .001) and textured soy protein (OR, 0.32 [95% CI, 0.17-0.59]; P < .001) compared with not consuming those products was associated with reduced odds of displaying inadequate protein intake ( Figure 3 A). The second, third, and fourth quartiles of ultraprocessed food intake (eg, fourth vs first quartile of intake: OR, 0.16 [95% CI, 0.07-0.33]; P < .001) and the third and fourth quartiles of ultraprocessed protein intake were associated with reduced odds of displaying inadequate protein intake, while the second, third, and fourth quartiles of unprocessed protein intake (eg, fourth vs first quartile of intake: OR, 12.42 [95% CI, 5.56-29.51]; P < .001) was associated with increased odds of displaying inadequate protein intake compared with the respective first quartile (see Figure 3 B for model coefficients and eTable 7 in Supplement 1 for quartiles). Results remained virtually unchanged in analyses performed with the imputed dataset (774 participants), not altering the original interpretation of our results (eTable 8 and eFigure 4 in Supplement 1 ). An exploratory analysis considering protein supplement and texturized soy protein intake as continuous rather than binary variables showed a negative association of protein supplement and texturized soy protein intake with the probability of displaying protein inadequacy (eFigure 5 in Supplement 1 ), which is in agreement with our main analysis.
This cross-sectional survey study analyzed self-reported data from 1-day food diaries on protein and amino acid intake and food processing level among individuals who adhered to a vegan diet. The main findings were that the mean adequacy ratio for protein and essential amino acids was high, participants had a high level of consumption of unprocessed and minimally processed food and a low level of consumption of processed and ultraprocessed food, and consumption of ultraprocessed protein sources was associated with decreased odds of showing inadequate protein intake, while the opposite was true for unprocessed and minimally processed protein sources.
Although previous evidence from smaller samples indicated that vegan diets may provide adequate protein, albeit lower than that of omnivorous diets, 4 it was still unclear whether they delivered enough essential amino acids. In our sample, a high mean adequacy for protein and essential amino acids was observed. To the best of our knowledge, the largest previous study to address amino acid intake in vegans was a cross-sectional analysis of the European Prospective Investigation into Cancer and Nutrition (EPIC)–Oxford cohort (98 individuals). 22 The authors found lower amino acid intake among individuals who adhered to a vegan diet compared with meat-eaters; however, whether this difference was associated with relevant deficiencies was unknown. 22 Based on a much larger sample and using a higher-resolution instrument, our study offers novel evidence that the most vegans can meet essential amino acid recommendations.
However, a considerable segment of participants did not meet recommendations for particular essential amino acids. For instance, lysine and the combination of methionine and cystine showed the lowest nutrient adequacy in our sample. Indeed, these amino acids are generally lower in plant- vs animal-based proteins. 23 , 24 Importantly, all amino acids are needed in adequate amounts to support de novo tissue protein synthesis, 25 reinforcing the need for properly planned, well-balanced combinations of different plant-based protein sources to attain an optimal essential amino acid profile.
Mounting evidence shows that increased ultraprocessed food consumption favors several negative health-related outcomes, such as higher energy intake and weight gain, higher prevalence of nontransmissible chronic diseases, and an overall increased mortality rate. 26 - 31 Although vegan diets are traditionally based on fresh and in natura foods, there has been a tendency of increased ultraprocessed food consumption in vegans due to the proliferation of plant-based meat and dairy substitutes, possibly compromising the quality of vegan diets. 5 A previous study in a French cohort 6 found ultraprocessed food consumption to be 39.5% of total energy intake among individuals who adhered to a vegan diet vs 33% in meat-eaters. In our study, unprocessed and minimally processed foods represented the highest caloric contribution in vegan diets, with a smaller presence of ultraprocessed foods. One may argue that compared with other countries, the plant-based meat and dairy substitute industry in Brazil may be less active, providing fewer or less attractive options. Considering the global trend in the protein market toward an increasing popularity of plant-based protein and the growing demand for high-quality, natural, and sustainable protein sources, 32 an increase in consumption of ultraprocessed foods among Brazilian individuals who adhere to a vegan diet may be expected in the future, warranting follow-up surveys to monitor possible health outcomes.
Recently, the discussion on whether all subgroups of ultraprocessed foods are equally harmful compared with one another has gained traction. Indeed, a 2023 study 33 found that distinct subgroups of ultraprocessed foods were differently associated with type 2 diabetes risk; subgroups, such as fruit- and dairy-based ultraprocessed desserts, had a risk reduction. Another study 34 found that although ultraprocessed food consumption was associated with multimorbidity related to cancer and cardiometabolic diseases, this association was not seen in the subgroup of plant-based ultraprocessed foods, suggesting that Nova may not capture possible nuance in quality among ultraprocessed items. In our study, textured soy protein was an important contributor to ultraprocessed food consumption. This is a challenging food item to classify given that there is significant variability in formulations considering the presence of food additives and cosmetics. This prompted us to use a more conservative approach of classifying this food as ultraprocessed, which is in accordance with previous research. 6 In a sensitivity analysis considering textured soy protein as unprocessed and minimally processed, the energy contribution from ultraprocessed food decreased greatly. The reduction in relative contribution of ultraprocessed food to protein intake was even more pronounced, clearly suggesting that reclassification of individual foods may be associated with impactful changes in the contribution of ultraprocessed foods to vegan diets.
We found that protein supplement, textured soy protein, ultraprocessed food, and ultraprocessed protein intake were associated with reduced probabilities of protein inadequacy. Conversely, unprocessed and minimally processed protein intake was associated with an increased probability of protein inadequacy. This may be partially explained by the lower energy and protein density in plant- vs animal-derived foods, 35 suggesting that it may be challenging for vegans fully avoiding ultraprocessed foods to reach higher levels of protein intake without substantially increasing food (and perhaps calorie) intake. While these findings do not imply that ultraprocessed foods are essential for individuals who adhere to a vegan diet to meet protein recommendations, it reveals a significant reliance on these foods to attend protein requirements. One may suggest that certain ultraprocessed foods, such as textured soy protein, may be recommended for this population. Despite convincing data associating the broad category of ultraprocessed with poor outcomes, it is hard to reconcile textured soy protein as having detrimental health outcomes, with ample evidence suggesting otherwise. 36 - 38 This holds true for protein supplements, an evidence-based strategy to support muscle health 39 also associated with protein adequacy in this study. At least regarding individuals who adhere to a vegan diet, unrestricted advice to avoid ultraprocessed foods may have unintended consequences, such as protein intake inadequacies, that warrant further investigation. This also suggests that vegans may benefit from public policies aimed to facilitate access to more natural and healthy foods and amplify nutritional support and education for adequacy of overall food intake. Simultaneously, our data reinforce the urgent need for the development of affordable, healthier, better-quality, cleaner-label, and protein-rich plant-based food options by the industry.
Strengths of this study include the large sample size and use of food diaries to quantify food intake. 40 The study also has several limitations, including the cross-sectional design, self-reporting of information, and use of a 1-day food diary instead of repeated measurements of food intake. Our study features a convenience sample, predominantly composed of females, with eutrophic BMI and a high educational level. While this may limit the generalizability of our findings, epidemiological studies confirm that this as the typical sociodemographic profile of vegans. 41 - 43 Nonetheless, our conclusions cannot be extrapolated to more population samples with a lower socioeconomical status or with different dietary patterns. Further studies are warranted to answer such questions.
In this cross-sectional survey study including a 1-day dietary assessment, individuals who adhered to a vegan diet mostly attained protein and essential amino acid intake recommendations and had a lower intake of ultraprocessed food compared with previous reports on vegans and the overall Brazilian population. Importantly, ultraprocessed protein sources were associated with a decreased likelihood of inadequate protein intake, while the opposite was true for unprocessed protein sources. The role of ultraprocessed foods in vegan diets needs to be further investigated given that common protein sources in the vegan diet may not be associated with the same detrimental health outcomes as other ultraprocessed foods, while contributing to protein requirements in this population.
Accepted for Publication: April 21, 2024.
Published: June 24, 2024. doi:10.1001/jamanetworkopen.2024.18226
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Leitão AE et al. JAMA Network Open .
Corresponding Author: Hamilton Roschel, PhD, Center of Lifestyle Medicine; Laboratory of Assessment and Conditioning in Rheumatology, Hospital das Clínicas, Faculdade de Medicina, Universidade de Sao Paulo, Av Dr Arnaldo, 455, Third Floor, 01246-903, São Paulo, São Paulo, Brazil ( [email protected] ).
Author Contributions: Dr Roschel and Mr Esteves had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Ms Leitão and Mr Esteves have contributed equally to this work and share first authorship.
Concept and design: Leitão, Esteves, Mazzolani, Roschel.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Leitão, Esteves, Roschel.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Leitão, Esteves.
Obtained funding: Mazzolani, Roschel.
Administrative, technical, or material support: Leitão, Santini, Santo André, Gualano, Roschel.
Supervision: Leitão, Mazzolani, Gualano, Roschel.
Conflict of Interest Disclosures: Drs Gualano and Roschel reported receiving research grants and supplement donations for scientific studies from AlzChem, Natural Alternatives International, DuPont, JBS, and NotCompany. Dr Gualano reported receiving support for participation in scientific conferences and honorarium for speaking at lectures from AlzChem and serving as a member of the Scientific Advisory Board for AlzChem. No other disclosures were reported.
Funding/Support: Mr Esteves, Ms Mazzolani, Ms Smaira, Ms Santo André, Dr Gualano, and Dr Roschel were supported by grants 2019/14820-6, 2019/14819-8, 2020/07860-9, 2022/02229-4, and 2017/13552-2 from the São Paulo Research Foundation. Ms Leitão and Mr Santini were supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil-Finance Code 001. Drs Gualano and Roschel were supported by grants 308307/2021-6 and 301914/2017-6 from the National Council for Scientific and Technological Development.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Share full article
Advertisement
Supported by
Guest Essay
A Year on Ozempic Taught Me We’re Thinking About Obesity All Wrong

By Johann Hari
Mr. Hari is a British journalist and the author of “Magic Pill: The Extraordinary Benefits — and Disturbing Risks — of the New Weight Loss Drugs.”
Ever since I was a teenager, I have dreamed of shedding a lot of weight. So when I shrank from 203 pounds to 161 in a year, I was baffled by my feelings. I was taking Ozempic, and I was haunted by the sense that I was cheating and doing something immoral.
I’m not the only one. In the United States (where I now split my time), over 70 percent of people are overweight or obese, and according to one poll, 47 percent of respondents said they were willing to pay to take the new weight-loss drugs. It’s not hard to see why. They cause users to lose an average of 10 to 20 percent of their body weight, and clinical trials suggest that the next generation of drugs (probably available soon) leads to a 24 percent loss, on average. Yet as more and more people take drugs like Ozempic, Wegovy and Mounjaro, we get more confused as a culture, bombarding anyone in the public eye who takes them with brutal shaming.
This is happening because we are trapped in a set of old stories about what obesity is and the morally acceptable ways to overcome it. But the fact that so many of us are turning to the new weight-loss drugs can be an opportunity to find a way out of that trap of shame and stigma — and to a more truthful story.
In my lifetime, obesity has exploded, from being rare to almost being the norm. I was born in 1979, and by the time I was 21, obesity rates in the United States had more than doubled . They have skyrocketed since. The obvious question is, why? And how do these new weight-loss drugs work? The answer to both lies in one word: satiety. It’s a concept that we don’t use much in everyday life but that we’ve all experienced at some point. It describes the sensation of having had enough and not wanting any more.
The primary reason we have gained weight at a pace unprecedented in human history is that our diets have radically changed in ways that have deeply undermined our ability to feel sated. My father grew up in a village in the Swiss mountains, where he ate fresh, whole foods that had been cooked from scratch and prepared on the day they were eaten. But in the 30 years between his childhood and mine, in the suburbs of London, the nature of food transformed across the Western world. He was horrified to see that almost everything I ate was reheated and heavily processed. The evidence is clear that the kind of food my father grew up eating quickly makes you feel full. But the kind of food I grew up eating, much of which is made in factories, often with artificial chemicals, left me feeling empty and as if I had a hole in my stomach. In a recent study of what American children eat, ultraprocessed food was found to make up 67 percent of their daily diet. This kind of food makes you want to eat more and more. Satiety comes late, if at all.
One scientific experiment — which I have nicknamed Cheesecake Park — seemed to me to crystallize this effect. Paul Kenny, a neuroscientist at Mount Sinai Hospital in New York, grew up in Ireland. After he moved in 2000 to the United States, when he was in his 20s, he gained 30 pounds in two years. He began to wonder if the American diet has some kind of strange effect on our brains and our cravings, so he designed an experiment to test it. He and his colleague Paul Johnson raised a group of rats in a cage and gave them an abundant supply of healthy, balanced rat chow made out of the kind of food rats had been eating for a very long time. The rats would eat it when they were hungry, and then they seemed to feel sated and stopped. They did not become fat.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Contributors
- Newsletters
1 Trending: Trump’s Biggest Debate Opponents Are The Media, Not Biden
2 trending: exclusive: biden admin ‘ignored’ vaccine safety protocols to fast-track its covid shot mandates, 3 trending: there’s a charlottesville every week, and most democrats are fine with it, 4 trending: democrats love ‘democracy’ so much, they’re trying to keep rfk jr. off the 2024 ballot, is america’s trillion-dollar obesity problem here to stay.

We know the answer is healthy nutrition and exercise habits. The question is do we have the political willpower to embrace the solutions?

- Share Article on Facebook
- Share Article on Twitter
- Share Article on Truth Social
- Copy Article Link
- Share Article via Email
According to an exclusive Washington Examiner report last week, the House GOP warned that obesity will cost Americans up to $9.1 trillion in medical costs over the next decade. This is over double last year’s estimate and an increase of over $7 billion per year.
A report from 2021 called obesity a major public health crisis, and it’s only gotten worse since then. One in five children is reportedly obese, and one in four adults tips the scale with a body mass index (BMI) of 30 or over. Granted, BMI is not a perfect measurement and its merits can be debated, but one doesn’t really need exacting science to see that America is fat. Really fat.
And while the report includes both direct and indirect costs such as treatments for asthma, cardiovascular disease, and cancer, they are likely missing other veiled costs.
Whole Person Health
The report’s numbers, while staggering, don’t include the number of people seeking treatment for mental health conditions that many doctors won’t link to obesity. Western medicine is famous for addressing health care, like government, in silos of “expertise” without looking at the person as a holistic, symbiotic organism with a body, mind, and soul. Traditional medical training encourages students to choose areas of “expertise” like the heart or the brain or the gut without a single consideration that all these things are connected.
For example, a study from 2018 was partly responsible for discovering what has become known as “hope molecules” or mytokines that are secreted during exercise due to muscular contraction. These hope molecules cross the blood-brain barrier to positively affect mental health by reducing symptoms of depression or trauma and increasing resilience to stress.
Stanford doctor Shebani Sethi founded the first academic Metabolic Psychiatry Clinical program in 2015 to address the connection between metabolic and mental health. Dr. Sethi’s research demonstrated the success of a ketogenic diet as a metabolic treatment for mental illness including bipolar disorder, depression, and even schizophrenia.
In short, healthy people are generally happier people.
As the report also points out, the societal costs of obesity go well beyond medical payments. The obesity epidemic cuts into the overall size of the U.S. economy because of reductions in labor supply and labor productivity. The economy is expected to be between $13.5 trillion and $14.7 trillion smaller over the next decade because of obesity.
The costs to national security may not yet have been quantified monetarily, but there has been no shortage of headlines about America being “too fat to fight.” A 2020 Pentagon study demonstrated Americans aged 17-24 did not meet the military’s sign-up requirements due to being overweight, using drugs, or having mental and physical health problems.
Do Americans Have the Will to Change?
“Failure to address this growing health crisis is immoral,” stated David Schweikert, R-Ariz., vice chairman of the Joint Economic Committee that published the report. “Society has the tools at our disposal to address this crisis,” he continued.
Schweikert is right. It is immoral, and we do have the tools. We’ve always had the tools (Hint: It’s not Ozempic). It’s called healthy nutrition and exercise habits. The question is do we have the willpower and the political will to embrace the solutions?
Are the bureaucrats at the HHS, the FDA, and the USDA willing to embrace and promote the most cutting-edge nutritional science instead of bending the knee to the multibillion-dollar agriculture and pharmaceutical lobbyists? Will they change the food pyramid? Will they stop subsidizing the production of corn, wheat, and soy, and help farmers return to a sustainable form of agriculture? Will they stop insisting on sacrificing human health for some unscientific green agenda?
Are our politicians willing to put restrictions on what can be purchased with WIC and SNAP payments? Will the Department of Education instill rigorous physical education requirements for all children in public and private schools rather than insisting tampons be put in boys’ bathrooms?
Are educators and parents willing to move beyond radical gender ideology to reinstate home economic classes to teach children how to garden and cook for themselves? Are they willing to spend some more time cooking themselves?
Do parents have the resilience to endure endless tantrums when they insist their children get off their screens and get outside? Will they go out and play with them?
Clearly, there is a lot of good information out there. Dr. Sethi’s study was published in 2020, and her clinic was opened in 2015. Dr. Casey Means just published a book last month called Good Energy addressing the need to reevaluate how we look at metabolic health. Other experts such as Dr. Mark Hyman, Dr. Andrew Weil, and Dr. Kelly Brogan, just to name a few, have been touting the benefits of using food, exercise, and lifestyle as medicine for decades, even if they may have slightly different takes on the best approach.
Many of these doctors are known among the intellectual and economic elite, but their remedies are not mainstream because good health demands less dependence on a trillion-dollar sick care system and the businesses that profit from it. That includes everything from pharmaceutical companies to food corporations to the huge hospital conglomerates.
Solving the obesity epidemic is simple. But it won’t be easy and requires will, discipline, and courage — virtues that are, unfortunately, in short supply these days.
More from Health
Pharmaceutical Industry Is Bankrolling Obesity Group That Promotes ‘Body Positivity’
Fauci Admits There Was No Scientific Evidence For Six-Foot Social Distancing Rule

‘Love Yourself,’ Preach Celebrities Embracing Weight-Loss Drugs

There’s Nothing Pro-Life About Ted Cruz And Katie Britt’s IVF Bill

The War On Nicotine Is A War On Vitality

British Nurse Lucy Letby’s Murder Trials Illustrate Deadly Consequences Of Socialized Medicine

New York Primary Voters Send ‘Squad’ Member Jamaal Bowman To The Unemployment Line

DoD Report Hides How Many Taxpayer Dollars It Sends To Communist Chinese Labs
Introducing
The Federalist Community
Join now to unlock comments, browse ad-free, and access exclusive content from your favorite FDRLST writers
Start your FREE TRIAL
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The Epidemiology of Obesity: A Big Picture
The epidemic of overweight and obesity presents a major challenge to chronic disease prevention and health across the life course around the world. Fueled by economic growth, industrialization, mechanized transport, urbanization, an increasingly sedentary lifestyle, and a nutritional transition to processed foods and high calorie diets over the last 30 years, many countries have witnessed the prevalence of obesity in its citizens double, and even quadruple. Rising prevalence of childhood obesity, in particular, forebodes a staggering burden of disease in individuals and healthcare systems in the decades to come. A complex, multifactorial disease, with genetic, behavioral, socioeconomic, and environmental origins, obesity raises risk of debilitating morbidity and mortality. Relying primarily on epidemiologic evidence published within the last decade, this non-exhaustive review discusses the extent of the obesity epidemic, its risk factors—known and novel—, sequelae, and economic impact across the globe.
1. Introduction
Obesity is a complex, multifactorial, and largely preventable disease ( 1 ), affecting, along with overweight, over a third of the world’s population today ( 2 , 3 ). If secular trends continue, by 2030 an estimated 38% of the world’s adult population will be overweight and another 20% will be obese ( 4 ). In the USA, the most dire projections based on earlier secular trends point to over 85% of adults being overweight or obese by 2030 ( 5 ). While growth trends in overall obesity in most developed countries seem to have leveled off ( 2 ), morbid obesity in many of these countries continues to climb, including among children. In addition, obesity prevalence in developing countries continues to trend upwards toward US levels.
Obesity is typically defined quite simply as excess body weight for height, but this simple definition belies an etiologically complex phenotype primarily associated with excess adiposity, or body fatness, that can manifest metabolically and not just in terms of body size ( 6 ). Obesity greatly increases risk of chronic disease morbidity—namely disability, depression, type 2 diabetes, cardiovascular disease, certain cancers—and mortality. Childhood obesity results in the same conditions, with premature onset, or with greater likelihood in adulthood ( 6 ). Thus, the economic and psychosocial costs of obesity alone, as well as when coupled with these comorbidities and sequealae, are striking.
In this article, we outline the prevalence and trends of obesity, then review the myriad risk factors to which a preventive eye must be turned, and finally present the costs of obesity in terms of its morbidity, mortality, and economic burden.
2. Classification of Body Weight in Adults
The current most widely used criteria for classifying obesity is the body mass index (BMI; body weight in kilograms, divided by height in meters squared, Table 1 ), which ranges from underweight or wasting (<18.5 kg/m 2 ) to severe or morbid obesity (≥40 kg/m 2 ). In both clinical and research settings, waist circumference, a measure of abdominal adiposity, has become an increasingly important and discriminating measure of overweight/obesity ( 7 ). Abdominal adiposity is thought to be primarily visceral, metabolically active fat surrounding the organs, and is associated with metabolic dysregulation, predisposing individuals to cardiovascular disease and related conditions ( 8 ). Per internationally used guidelines of metabolic syndrome—a cluster of dysmetabolic conditions that predispose individuals to cardiovascular disease of which abdominal adiposity is one component—a waist circumference resulting in increased cardiovascular risk is defined as ≥94 cm in European men, and ≥80 cm in European women, with different cut points recommended in other races and ethnicities (e.g., ≥90 and ≥80 cm in men and women, respectively, in South Asians, Chinese, and Japanese) ( 8 , 9 ).
Common Classifications of Body Weight in Adults and Children
| ≥20 years | BMI (kg/m ) | 18.50 to 24.99 | ≥25.00 : 25.00 to | ≥30.00 | |
| WHO 2006 | 0-60 months | BMI Z or WH Z | >−2 to ≤2 SD | to ≤3 SD | >3 SD |
| WHO 2007 | 5-19 years | BMI Z | >−2 to ≤1 SD | >1 to ≤2 SD | >2 SD |
| IOTF | 2-18 years | Growth curve for BMI at age 18 | BMI = 25 | BMI = 30 | |
| 2-19 years | BMI percentile | ≥5th to <85th | ≥85th to <95th | ≥95th |
Abbreviations used: BMI, body mass index; IOTF, International Obesity Task Force; SD, standard deviation; WHO, World Health Organization; WH weight-for-height; Z, z score.
3. Classification of Body Weight in Children
In children, body weight classifications ( Table 1 ) differ from those of adults because body composition varies greatly as a child develops, and further varies between boys and girls primarily owing to differences in sexual development and maturation. The World Health Organization (WHO) Child Growth Standards are the most widely currently used classification system of weight and height status for children from birth to 5 years old, based on data from children in six regions across the globe born and raised in optimal conditions ( 10 ). In 2007, the WHO published updated growth references combining the 1977 National Center for Health Statistics (NCHS)/WHO growth reference and the 2006 WHO Child Growth Standards to create the most recent BMI-for-age references for individuals aged 5–19 years ( 11 ). Thus, the latest WHO guidelines are designed to represent relatively seamless standards and references from birth all the way into late adolescence/early adulthood.
In the USA, the Centers for Disease Control and Prevention (CDC) currently use the 2000 CDC growth references based on 1963–1994 US children’s data, to determine age- and sex-specific BMI percentiles for children aged 2–19 years ( 12 ). Overweight is defined in US children as age- and sex-specific BMI ≥85th and <95th percentile, while obesity is ≥95th percentile ( 13 ). Cut points for severe obesity in childhood have been proposed in recognition of the alarming growing prevalence of this extreme condition, defined as the 99th BMI percentile ( 13 ) or 120% of the 95th percentile ( 14 ). For US children <2 years old, the CDC currently uses the 2006 WHO Child Growth Standards, described above ( 15 ).
4. Prevalence and Trends
4.1. adult obesity—us and europe.
The first indications that obesity was taking on epidemic proportions originated in the USA and Europe. With few restrictions on access to or availability of food, the prevalence of overweight and obesity in the USA climbed virtually unmitigated over the last 50 years. Today, those who are overweight (BMI 25–<30 kg/m 2 ) or obese (BMI ≥30 kg/m 2 ) in the USA eclipse two-fold the numbers of those who are normal weight ( 16 ). In US adults, 1960–1994 trends showed that while levels of overweight hovered at approximately 31% over the time period, in contrast, age-adjusted obesity jumped from 13 to 23%, bringing the crude prevalence of overweight or obesity to 55% of the American population ( 17 ). Unfortunately, 1994 did not represent the endpoint of the upward trend, as the following decade saw adult obesity rise from 23 to 32% by 2003–2004 ( 16 ). In the last 10 years, national estimates of obesity seem to indicate that the steady upward trend of obesity in Americans has leveled off at a prevalence of about 35% ( 16 ) ( Figure 1 ), perhaps having reached some “Malthusian” obesity limit. However, certain subpopulations are faring worse than others, as 2011–2012 obesity rates in Hispanics and non-Hispanic blacks were 43 and 48%, respectively, pointing to a disproportionate burden in differing racial/ethnic and/or socioeconomic status (SES) groups. Gender also plays a role, with women being disproportionately affected by extreme obesity (classes 2–3, BMI ≥35 kg/m 2 ) than men, regardless of age or race/ethnicity ( 16 ).

Trends in age-adjusted prevalence of overweight, obesity, and extreme obesity in US adults, aged 20–74 years, 1960–2012. Trends in prevalence of overweight as BMI 25–<30 kg/m 2 (circles), and upward trends in obesity as BMI ≥30 kg/m 2 (squares), and extreme obesity as BMI ≥40 kg/m 2 (diamonds) in adult males (closed points) and females (open points). The figure is based on data from NHES I (1960–1962), NHANES I (1971–1974), NHANES II (1976–1980), NHANES III (1988–1994), and NHANES (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012). Data derived are derived from Ogden, et al ., and Fryar, et al . ( 16 , 141 ). BMI, body mass index; NHANES, National Health and Nutrition Examination Survey; NHES, National Health Examination Survey.
Meanwhile, in Europe, longitudinal data (1992–1998 to 1998–2005) from participants in five countries involved in the European Prospective Investigation into Cancer and Nutrition (EPIC) study (Italy, the United Kingdom, the Netherlands, Germany, and Denmark), indicate that adult obesity increased modestly from 13 to 17% in that time period ( 18 ). However, were such linear trends were to continue, the overall obesity prevalence in these populations could reach 30% by 2015, paralleling US rates. A more conservative projection suggests a prevalence of just 20% obesity in these populations by 2015, if public awareness and public health measures take hold ( 18 ).
European studies including populations beyond EPIC indicate there is considerable disparity in overweight/obesity between European countries. A systematic review of national and regional surveys conducted between 1990 and 2008 points to obesity rates as low as 4.0 and 6.2% in French men and women, respectively (regional survey, 1994–1996), and as high as 30.0 and 32.0% in Czech men and women, respectively (national survey, 2002–2005) ( 19 ). Regional trends within Europe are apparent, with southern Italy and southern Spain, and Eastern European countries showing higher prevalence of obesity than countries in Western and Northern Europe ( 19 ). As in the USA, these data suggest that socioeconomic disparities and relatively recent/ongoing economic transitions are playing a considerable role in apparent differences across and within countries with respect to obesity risk.
4.2. Child Obesity—USA and Europe
US children may be faring better than their adult counterparts in some ways ( 16 ), potentially offsetting earlier dire predictions of rampant obesity by 2030 ( 5 ). In national surveys, levels of overweight in children, as in adults, seem to have leveled off (or even declined) at approximately 30% of US children aged 2–19 years ( 16 , 20 ). However, this belies a potentially disturbing long-term trend in the rising prevalence of extreme obesity (equivalent to adult class 2 obesity and higher, BMI ≥35 kg/m 2 ). Since 1999–2000, the prevalence of class 2 obesity in children (BMI ≥120% of the 95th percentile) has risen from 3.8 to 5.9% and class 3 obesity (BMI ≥140% of the 95th percentile) has doubled from 0.9 to 2.1%, the latter category jumping 30% since 2009–2010 alone ( 20 ). Again, as in their adult counterparts, certain sub-populations appear to be faring worse than others, notably Hispanic girls and Black boys, in whom overweight, obesity, and class 2 obesity have increased significantly ( 20 ).
Childhood obesity prevalence varies considerably between and within countries as well. Relatively recent estimates based on 2007–2008 data of children aged 6–9-years collected in 12 European countries as a part of the WHO European Childhood Obesity Surveillance Initiative observed overweight/obesity (BMI z score >+1 standard deviation [SD]) prevalence of 19.3–49.0% of boys and 18.4–42.5% of girls, while obesity (BMI z score >+2 SD) affected 6.0–26.6% of boys and 4.6–17.3% of girls. Researchers continued to observe the trend of north-south and west-east gradients evident in adults, with the highest levels of overweight in southern European countries ( 21 ).
4.3. Obesity Beyond North America and Europe
The data discussed above focus on the USA and European countries, many with robust national health surveillance programs. While historical data tends to be scarcer outside of these regions, an alarming picture has emerged over the last decades in low- and middle-income countries around the globe, complicated by rapidly changing socioeconomic environments. While country-specific trends are not discussed in this article, regional and national estimates of long-term changes in child (<20 years old) and adult (>20 years old) overweight and obesity have increased in nearly all countries and regions since 1980 ( Figure 2 ) ( 2 , 3 ). While the USA still may boast the largest absolute numbers of overweight and obese individuals, several other nations exceed the USA in terms of overall prevalence and, moreover, the rate of growth in certain countries is disheartening. For example, the prevalence of overweight and obesity in nationally representative Mexican adults was estimated to be 71.3% overweight/obese, with overweight at 38.8% and obesity at 32.4% ( 22 ). This prevalence represents an increase of 15% since 2000, placing this population among the most rapidly accelerating in terms of obesity prevalence over the last decade. Further, while rates of overweight remained relatively stable since 2000 at approximately 38% overall, extreme obesity (class 3, BMI ≥40 kg/m 2 ) increased by an estimated 76.5% from 2000 to 2012. These trends are also evident in countries outside of the Americas. In China, for example, between 1993 and 2009, overweight (BMI 25 to <27.5 kg/m 2 ) doubled in men (8 to 17%) and increased from 11 to 14% in women. Meanwhile, obesity (BMI ≥27.5 kg/m 2 ) nearly quadrupled in men, from 3 to 11%, and doubled in women, from 5 to 10%. Chinese children are faring as badly as their adult counterparts: overweight/obesity doubled from 6 to 13% in children aged 6–17 years over the same time period, suggesting that the obesity epidemic will continue to deepen in this country ( 23 ).

Prevalence of overweight and obesity in adults aged ≥20 years by global region, 1980–2008. From left to right, each column represents the estimated regional prevalence of overweight and obesity for 1980, 1985, 1990, 1995, 2000, 2005, and 2008. For a given region, a dark gray column indicates the lowest estimated prevalence in the trend, while the highest estimated prevalence is indicated by a black column. As is evident, the vast majority of regions demonstrate the lowest estimated prevalence of overweight and obesity in 1980, and the highest in 2008, demonstrating the global reach of obesity. The scale shows 25, 50, and 100% prevalence columns, for reference. Asterisks denotes high income. Data are sourced from Stevens, et al . ( 3 ).
5. Risk Factors for Obesity
Currently, our greatest gap in knowledge is not regarding the numbers of risk factors, nor in their independent impact on risk, but rather in how they interact with one another—their confluence—to produce today’s aptly if unfortunately named “globesity” epidemic. Obesity arises as the result of an energy imbalance between calories consumed and the calories expended, creating an energy surplus and a state of positive energy balance resulting in excess body weight. This energy imbalance is partially a result of profound social and economic changes at levels well beyond the control of any single individual. These “obesogenic” changes—economic growth, growing availability of abundant, inexpensive, and often nutrient-poor food, industrialization, mechanized transportation, urbanization—have been occurring in high-income countries since the early 20th century, and today these forces are accelerating in low- and middle-income countries. And yet, not all of us living in obesogenic environments experience the same growth in our waistlines. Hereditary factors—genetics, family history, racial/ethnic differences—and our particular socioeconomic and sociocultural milieus have been shown to affect risk of obesity ( Table 2 ) even in ostensibly similar obesogenic environments. So while body weight regulation is and should be viewed as a complex interaction between environmental, socioeconomic, and genetic factors, ultimately, personal behaviors in response to these conditions continue to play a dominant role in preventing obesity. Importantly, apart from genetics, every risk factor discussed below is modifiable .
Risk Factors, Comorbidities, and Sequelae of Obesity
5.1. Genetics of Obesity
To date, over 60 relatively common genetic markers 1 have been implicated in elevated susceptibility to obesity ( 24 , 25 ); however, the 32 most common genetic variants are thought to account for <1.5% of the overall inter-individual variation in BMI ( 24 ). When these 32 “top” genetic hits are combined into a genetic risk of obesity score, those with the highest genetic risk (i.e., carriers of over 38 risk alleles), have just a 2.7 kg/m 2 higher BMI on average than those with a low genetic risk. This translates into about a 15-lb (7-kg) weight difference between two 5’3” (160 cm) individuals with high versus low genetic risk ( 24 ). Although genetics undoubtedly play a role, this relatively small difference in BMI, coupled with the dramatic rise in obesity over the last half century in developed and developing nations alike point to obesity risk factors beyond genetics. A concomitant and rich area of research has therefore evolved investigating gene-environment interaction based on the idea that underlying genetic risk predisposes individuals to particularly adverse (or beneficial) effects of behavioral or environmental exposures such as diet and exercise, a concept scientifically popularized in, for example, the “thrifty gene” hypothesis ( 26 ). In many ways, these types of gene-environment interactions are playing out in population research: for example, a variant in FTO (rs9939609)—the strongest obesity susceptibility locus—increases odds of obesity in risk allele carriers by an estimated 23% per allele; however, this risk is modified by physical activity in adults ( 27 , 28 ) and children ( 29 ), among other factors. Nevertheless, these types of interactions have so far been investigated in relatively few genetic risk loci out of millions, and with just a handful of environmental factors, raising important questions of how to aggregate this complexity for public health and ultimately personalized medicine.
In addition, parental diet, lifestyle, and other exposures have been implicated in subsequent offspring obesity risk, including famine exposure ( 30 ), parental obesity ( 31 – 33 ), smoking ( 34 ), endocrine-disrupting and other chemicals ( 35 , 36 ), and weight gain during gestation and gestational diabetes ( 33 , 37 ). These and other studies point to lasting effects of fetal programming that via differing mechanisms, likely epigenetic, result in substantial repercussions in life course health, with implications across the socioeconomic/food availability spectrum. Careful management of diet and lifestyle in pre- and perinatal periods could exert a considerable impact on the obesity epidemic for generations to come ( 37 ).
5.2. Individual Behaviors
5.2.1. diet.
In the decades preceding the 21st century, the vast majority of research on obesity risk factors focused on individual-level, largely modifiable behaviors. The role of diet and physical activity in mitigating obesity risk and reducing prevalent obesity have received the most attention, and with good reason: 15% of deaths in 2000 in the USA were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Caloric intake and expenditure needed for weight maintenance or healthy growth has historically taken center stage ( 39 ), and caloric restriction remains today a primary focus of most popular and clinical weight-management and weight-loss approaches.
Beyond overall caloric intake to regulate body weight, a tremendous amount of research has attempted to resolve the roles of diet quality and dietary patterns, including those specifying combinations of macronutrients ( 40 ). Evidence from clinical trials have almost universally shown that caloric restriction, regardless of dietary pattern, is associated with better weight outcomes ( 40 ). Although the metabolic nuances and relative merits of the differing dietary patterns for various comorbid conditions are still being investigated, the evidence seems to suggest that merely adhering to a diet—nearly irrespective of what type of healthy diet it is—has an impact on weight loss/control ( 41 – 43 ).
For long-term maintenance of healthy weight, evidence from observational cohorts indicate that diets that are considered “healthier” lead to better long-term weight maintenance, or at least mitigate weight gain typically associated with aging through middle age. For example, research in US health professionals pointed to averaged 4-year weight gain throughout middle age as being strongly associated with increasing intake of potato chips and potatoes, sugar-sweetened beverages, and processed and unprocessed red meats, but inversely associated with the intake of vegetables, fruits, whole grains, nuts, and yogurt ( 44 ). Specific food groups, such as sugar-sweetened beverages, have received considerable attention largely because added sugar consumption (primarily as sugar-sweetened beverages) has been rising concomitantly with prevalent obesity ( 45 ). Indeed, the weight of the evidence about the role of sugar-sweetened beverages in obesity ( 46 , 47 ) is a strong impetus for public health interventions and policies, such as limiting advertising on these beverages as in Mexico ( 48 ), attempts to limit beverage sizes permitted for sale as in New York City ( 49 ), taxation, eliminating sale in schools, etc.
5.2.2. Physical Activity, Sedentary Behaviors, and Sleep
Personal behaviors beyond diet (physical activity, sleep, sedentary and screen time, and stress) have also been independently associated with weight change and maintenance in adulthood. Combined with diet, these elements have synergistic and likely cumulative effects on an individual’s ability to maintain or obtain a healthy body weight over the life course. Recently reviewed evidence from randomized trials and observational studies support 2008 US recommendations for weight management ( 50 ), consistently showing that in general, 150–250 minutes per week of moderate intensity activity is required to prevent weight gain, or aid in weight loss when accompanied by dietary restriction ( 51 ). Activity (>250 minutes per week) is associated with weight loss and weight maintenance after weight loss ( 51 ). Leisure-time activities involving sitting, but which are not truly restful behaviors, such as getting <6 or >8 hours of sleep in adults and adolescents ( 44 , 52 – 55 ) or <10–11 hours of sleep in children ( 52 ), television viewing or screen time ( 44 , 56 , 57 ), and other leisure-time sitting ( 58 ) are also associated with weight gain.
5.3. Socioeconomic Risk Factors: Income and Education
Income has had a shifting role in obesity risk over the last century. As late as the mid-20th century, the USA and Europe could link wealth directly with obesity—the wealthier an individual, the more likely to be overweight. Over the last few decades, however, perhaps owing to the abundance of cheap and highly available food, coupled with changing sociocultural norms, this link has flipped. Today, wealth in the USA tends to be inversely correlated with obesity, and it is those who are at or below the level of poverty who appear to have the highest rates of obesity ( 59 ). Indeed, in US cities where the homeless are surveyed, the prevalence of overweight and obesity parallels that of non-homeless populations, contrary to our typical beliefs about thinness accompanying food insecurity or homelessness ( 60 , 61 ).
More broadly, across 11 Organisation for Economic Co-Operation and Development (OECD) countries, SES, whether defined by household income or occupation-based social class, showed an inverse relationship with obesity: women, in particular, had consistently higher prevalence of overweight/obesity the less affluent they were ( 62 ). In men, too, those in low income strata tended to have higher prevalence of obesity, but the gradient for overweight reversed in about half of the countries surveyed. That is, in some countries, poverty was associated with more prevalent overweight than wealth, but in others, lower income was associated with more favorable weight status. The differences between sexes in terms of income status and obesity, in particular the trend reversal in men, may be in part due to low-paying jobs typically involving more physically demanding work performed by men more than by women ( 62 ). Adding complexity to this picture is the role of education: in the 11 OECD countries discussed above, education showed a strong inverse relationship with overweight/obesity, particularly in women, who had consistently higher prevalence of overweight/obesity the less educated they were ( 62 ).
As wealth rises in low- and middle-income countries, it is expected for poverty-obesity patterns to begin more closely mimicking those of high-income countries. Evidence of this transition is already accumulating. In explorations of the role of education and wealth in women and weight status in four middle-income countries (Colombia, Peru, Jordan, and Egypt), authors observed a significant interaction between education and wealth: in women with little or no education, higher income was associated with 9–40% higher odds of obesity, while in those with higher levels of education, the association with income was either not present (Egypt, Peru) or associated with 14–16% lower odds of obesity (Jordan, Colombia) ( 63 ). This suggests that in currently transitioning economies, education may offset the apparently negative effects of increasing purchasing power in emerging obesogenic environments. However, the protective effect of education has yet to be seen in the poorer countries, such as India, Nigeria, and Benin, where both education and wealth were directly associated with increased odds of obesity ( 63 ).This is perhaps unsurprising, as obesity was relatively rare at <6.0% of women in these countries, and >50% of women had little or no education.
The glimmer of hope, then, is that in the context of a paradigm of diseases of affluence, in which the transition to wealth seem to invariably lead to higher obesity and thus greater chronic disease burden, higher education levels may yet offset some of the frightening challenges that lay before us.
5.4. Environmental 2 Risk Factors
5.4.1. the built environment.
Research on the built environment tends to focus on a few measurable characteristics of neighborhoods as they relate to weight status, while holding sociodemographic and other person-level characteristics constant. Such neighborhood characteristics range from more concrete factors (e.g., fast food restaurants, supermarkets, parks, transportation, etc.) to more variably scored factors (e.g., walkability, neighborhood healthiness). Most studies of the built environment have been cross-sectional, tending to focus on one or two characteristics; thus, findings on the relative importance or effects of given characteristics on obesity have been inconsistent ( 66 – 72 ), revealing the fundamental challenge of teasing out whether neighborhood characteristics play a causal role in weight status, or whether health-minded folks inhabit health-friendly areas to begin with (residential selection bias) ( 73 ). However, the emerging picture points to the primacy of diet-related built environments over those associated with physical activity. While presence of neighborhood physical activity or recreational spaces has been associated with increased physical activity levels or energy expenditure ( 71 , 72 ), healthy food environments, characterized by availability of produce or presence of supermarkets over convenience stores or fast food restaurants, play a potentially more important role ( 68 , 70 , 74 , 75 ).
Research on the causality of the built environment as obesity-inducing or health-promoting is critical for municipalities and public health authorities to justify potentially costly improvements to public spaces and/or zoning regulations. There is an unmet need for standardized measures, definitions, and criteria, established residential and occupational geographic radii relevant to health, and research methodologies that can take into account the complexity of something as seemingly simple as a neighborhood.
5.4.2. Environmental “Pathogens”: Viruses, Microbiomes, and Social Networks
Growing evidence from animal and human studies indicates that obesity may be attributable to infection, or that obesity itself may be a contagion. Infectious agents include viruses, the trillions of microbiota inhabiting the human gut, and, of course, obese humans as infectious agents themselves.
Although several viruses have been identified as potentially having a causal role in obesity ( 76 ), Ad-36 is among the most studied, being causally associated with adiposity in animals. Studies in diverse human populations generally support greater Ad-36 viral loads as probably causal of obesity in both children and adults ( 76 – 79 ), with links to other metabolic traits ( 77 , 79 ).
Ground-breaking research in the last decade has emerged on the role of trillions of gut bacteria—the human microbiome—in relation to obesity, energy metabolism, and carbohydrate and lipid digestion, opening promising therapeutic avenues for obesity and disease ( 80 ). Two primary phyla of bacteria differ in their proportions in lean vs. obese populations; these proportions change as obese individuals lose weight and correlate highly with the percentage of body weight lost ( 81 ). Broad and sometimes dramatic changes in microbiome populations have been catalogued following gastric bypass surgery ( 80 ), and in both the short- ( 82 , 83 ) and long-term ( 81 , 83 ) in response to changes in dietary composition ( 80 ). Research in mice indicates that increased adiposity is a transmissible trait via microbiome transplantation ( 84 ), and has prompted similar experimental fecal transplantation research in humans for the promotion of weight loss ( 85 ). In addition, other research has examined the feeding of pre- and probiotics as therapeutic modalities designed to manipulate the gut microbiome; these strategies also show promise for a range of conditions ( 85 ).
Finally, the importance of social networks—real and virtual—in obesity is a fascinating, relatively new area of research that capitalizes on known characteristics of infectious disease transmission. In a landmark 2007 study examining the spread of obesity due to social ties using 32-year prospective data from the Framingham Heart Study, Christakis and Fowler ( 86 ) showed that an individual’s chances of becoming obese increased by 57% if he or she had a friend who became obese in a given 4-year interval. This was a stronger risk ratio than that observed between pairs of adult siblings or even between spouses. Conversely, it may be possible to capitalize on the social contagion of obesity in the reverse direction, that is, in the promotion of healthy weight and behavior. Intervention studies of weight loss often include a social-relational component, although the evidence supporting any single approach or its efficacy is relatively scarce ( 87 ). In theory, a supportive network, community, or coaching relationship is supposed to improve weight loss; despite a lack of strong evidence, it is a key component of many popular commercial (e.g., Weight Watchers), trial/intervention, and online approaches.
6. Costs of Obesity: Co-Morbidities, Mortality, and Economic Burden
Obesity is associated with concomitant or increased risk of nearly every chronic condition, from diabetes, to dyslipidemia, to poor mental health. Its impacts on risk of stroke and cardiovascular disease, certain cancers, and osteoarthritis are significant.
6.1. Overall Mortality
In the year 2000 in the USA, 15% of deaths were attributable to excess weight, owing to poor diet and physical inactivity ( 38 ). Overweight/obesity in middle age shortens life expectancy by an estimated 4–7 years ( 88 ). Many long-term cohort studies, as well as three recent major syntheses of pooled data from established cohorts ( 89 – 91 ), which adequately accounted for history of smoking and chronic disease status, unequivocally show that overweight and obesity over the life course is associated with excess risk of total mortality, death from cardiovascular disease, diabetes, cancer, or accidental death ( 89 – 97 ).
Some studies suggest that excess body weight may be protective against mortality from certain chronic conditions—resulting in a so-called “obesity paradox.” However, most studies that have shown an obesity paradox, or no association between obesity and mortality, have been conducted in groups of older (>65) or elderly patients or in those with chronic conditions, or have inadequately accounted for smoking. Indeed, the role of excess adiposity in old age is unclear. While the protective effects of overweight in specific instances of diseased older populations may be real, these observations are fraught with methodological problems, especially reverse causation, and belie the limitations of generalizing excess adiposity’s supposed benefits to younger populations over the life course, not least because excess body weight leads to higher disease incidence to begin with ( 7 ).
6.2. Diabetes
Excess weight and diabetes are so tightly linked that the American Diabetes Association recommends physicians test for type 2 diabetes and assess risk of future diabetes in asymptomatic people ≥45 years old simply if they are overweight/obese, and regardless of age if they are severely obese ( 98 ). Overweight raises risk of developing type 2 diabetes by a factor of three, and obesity by a factor of seven, compared to normal weight ( 99 ). Excess weight in childhood and in young adulthood, and weight gain through early to mid-adulthood are strong risk factors for diabetes ( 100 – 102 ). While not every overweight/obese individual has diabetes, some 80% of those with diabetes are overweight/obese ( 103 ). Obesity itself raises diabetes risk even in the absence of other metabolic dysregulation (insulin resistance, poor glycemic control, hypertension, dyslipidemia). While metabolically healthy obese individuals are estimated to have half the risk of their metabolically unhealthy counterparts, they still have four times the risk of those who are normal weight and metabolically healthy ( 104 ).
6.3. Heart and Vascular Diseases
Ischemic heart disease and stroke are the leading causes of death in the USA and globally ( 105 ). Excess body weight is a well-known risk factor for heart disease and ischemic stroke, including their typical antecedents—dyslipidemia and hypertension. Recent studies have consistently shown that benign obesity appears to be a myth ( 106 – 108 ); overweight clearly adds to risk of heart disease and stroke beyond its implications for hypertension, dyslipidemia, and dysglycemia.
Given childhood obesity rates, research has lately focused on the role of obesity in early life and subsequent adulthood disease. Obesity in childhood or adolescence has been associated with twofold or higher risk of adult hypertension, coronary heart disease, and stroke ( 100 ). A recent study pooling data from four child cohorts (aged 11 years at baseline with average 23-year follow-up), observed that, compared with individuals who were normal weight in childhood and non-obese as adults, those who were normal weight or overweight but became obese as adults, or who were obese and stayed obese into adulthood, had considerably higher risk of high-risk dyslipidemia, hypertension, and higher carotid intima-media thickness. Notably, those individuals who were overweight/obese as children, but non-obese as adults, had similar risk profiles to those individuals who were never obese, indicating that the potential health effects of childhood obesity can be offset by weight loss prior to or while entering into adulthood ( 109 ).
6.4. Cancer
An estimated 6% of all cancers (4% in men, 7% in women) diagnosed in 2007 were attributable to obesity ( 110 ). Beyond being a major risk factor for diabetes, which itself is a risk factor for most cancers, obesity has long been understood to be associated with increased risk of esophageal, colon, pancreatic, postmenopausal breast, endometrial, and renal cancers ( 111 ). More recently, evidence has accumulated that overweight and/or obesity raise risk of cancers of the gallbladder ( 112 ), liver ( 113 ), ovaries (epithelial) ( 114 ), and advanced cancer of the prostate ( 115 ), as well as leukemia ( 116 ).
6.5. Trauma and Infection
A study in Pennsylvania (USA) trauma centers (2000–2009) showed that in-hospital mortality and risk of major complications of surgery were increased in obese patients as compared to non-obese patients. Severely obese patients had upwards of 30% increased risk of mortality from their trauma than non-obese patients, and double the risk of major complications. Severely obese females also had more than double the risk of developing wound complications, and quadruple the risk of developing decubitus ulcers ( 117 ). A recent meta-analysis of obesity in trauma care concluded that obesity was associated with 45% increased odds of mortality, longer stays in the intensive care unit, and higher rates of complications, and tended to associate with longer durations of mechanical ventilation and longer stays in the hospital overall, compared to non-obese patients, despite equivalent injury severity ( 118 ).
While elevated risk of chronic disease is a seemingly obvious consequence of obesity, increasing attention is being given to increased risk of infection and infectious disease in obesity, including surgical-site, intensive care unit (ICU)-acquired catheter, blood, nosocomial, urinary tract, and cellulitis and other skin infections ( 119 ), community-acquired infections, and poorer recovery outcomes owing to higher risk of influenza, pneumonia, bacteremia, and sepsis ( 119 ). Impaired immunological response may be an underlying mechanism; recent research has demonstrated lower vaccine efficacy and serological response to vaccination in the obese. For example, a recent study estimated an eightfold increase in the odds of non-responsiveness to hepatitis-B vaccination in obese versus normal-weight women ( 120 ).
The consequences of a global obesity epidemic may not merely be greater chronic and infectious disease burden for the obese, but also a greater global burden of infectious disease owing to obesity. Greater infectious disease vigilance may be required in populations with high levels of overweight/obesity, and there is a clear need for better clinical practice guidelines (e.g., use and dosage of antimicrobials, vaccines, other pharmaceuticals) for obese individuals.
6.6. Mental Health
The role of weight in mental health faces causal challenges, but what is clear is that obesity and adiposity are associated with anatomical as well as functional changes in the human brain. Studies in older populations have shown that BMI is inversely correlated with brain volume, and that obese older adults, compared to normal weight counterparts, show atrophy in the frontal lobes, anterior cingulate gyrus, hippocampus, and thalamus ( 121 ). In addition, obesity in children and adolescents (aged >9 years) has been associated with smaller orbitofrontal cortex gray matter volume, along with poorer performance in certain domains of executive function (e.g., inhibitory control) ( 122 ). Being overweight in midlife increases risk of Alzheimer's disease, vascular dementia, or any type of dementia by 35, 33, and 26%, respectively; even higher risk is observed for obesity ( 123 ). Importantly, physical activity, even among overweight individuals, may stave off poor mental functioning: moderately active or highly active adult overweight Finns did not have significantly increased risk of poor mental functioning at a 7-year follow-up compared to those who were normal weight and highly active, but inactive and overweight patients presented a nearly 40% increased risk of poor mental functioning ( 124 ). Thus, exercise may play an important mediating role in the relationship between excess body weight and age-related cognitive decline.
6.7. Economic Burden of Obesity
In the USA, recent estimates indicate that obese men are thought to incur an additional US$1,152 per year in medical spending, particularly due to hospitalizations and prescription drugs, compared to their non-obese counterparts, while obese women incur over double that of obese men, an additional US$3,613 per year in medical spending (year 2005 values). Extrapolating these costs to the national level, authors estimate some US$190 billion per year of healthcare spending, approximately 21% of US healthcare expenditures, is due to treating obesity and obesity-related conditions ( 125 ).
Total hospital costs account for a part of this: another author group studied non-bariatric, non-obstetric hospital procedures for obese patients, finding they were US$648 higher (year 2009 values) per capita than for non-obese patients. The estimated national hospital expenditures for the largest volume surgical procedures was US$160 million higher per year for obese than for their non-obese counterparts ( 126 ).
Employers bear a substantial brunt of obesity-related costs in the USA. Data from the Human Capital Management Services Research Reference Database (2001–2012) on employees and their dependents was used to compare medical, drug, sick leave, short-term disability, and workers’ compensation costs as well as absent days across three BMI strata: <27, ≥27–<30, and ≥30 kg/m 2 . Each of the costs was incrementally higher in ascending BMI categories. For example, total annual costs and total days absent in the highest vs. lowest BMI strata were US$6,313 versus US$4,258 (year 2012 values), and 7.5 versus 4.5 days. In addition, productivity was lowest in the obese group ( 127 ).
Finally, lifetime direct incremental medical costs of obesity in childhood in the USA were estimated to range from US$12,660 to US$19,630 (year 2012 values) for an obese 10-year old compared to a normal-weight 10-year old, if expected weight gain through adulthood among the normal weight child occurs ( 128 ). If normal weight children were to not continue on the typical weight gain trajectory into overweight/obesity, estimated incremental medical costs for today’s 10-year old obese child ranges between US$16,310 and US$39,080. Putting these figures into perspective, multiplying the lifetime medical cost estimate of US$19,000 by the number of obese 10-year-olds today generates a total direct medical cost of obesity of roughly US$14 billion for this 10-year old age group alone. In terms of big picture savings, the upper estimate of US$39,000 per case represents two years of public college tuition for that child ( 128 ).
In Europe, a 2008 review of 13 studies in ten Western European countries estimated the obesity-related healthcare burden had a relatively conservative upper limit of €10.4 billion annually (in Germany, in 1995 € equivalent), and ranging between <0.1 to 0.61% of each country’s gross domestic product (GDP). The review relied on study data from as early as the 1980s in the Netherlands, through 2002 in most of the remaining countries surveyed ( 129 ). A more recent review focused on 19 studies published in 2007–2010 in eight Western European countries (predominantly Germany, Denmark, and the United Kingdom). Excess health care costs of obesity or derivations of excess health care costs by comparisons of mean costs between normal weight and obese individuals in seven of the reviewed studies were between €117 and €1,873 per person (based on the € valuation given in each study year). Excess costs increased particularly due to severe obesity. Approximately 23% of medication costs and 6.9% of out-of-pocket costs were attributable to overweight or obesity. Health economic models estimated that 2.1–4.7% of total health care costs and 2.8% of total hospital costs were due to overweight and obesity. Total (direct and indirect) costs were generally unchanged from the 2008 estimate of the earlier review, accounting for 0.47–0.61% of GDP in these countries ( 130 ).
In the context of the Brazilian Unified Health System (i.e., public hospitals), estimated direct costs of diseases related to overweight/obesity in outpatient and inpatient care based on 2008–2010 data were US$2.1 billion annually (year 2010 values), 68.4% of which was attributable to hospitalizations, and the remainder due to ambulatory procedures ( 131 ). The largest costs of outpatient and inpatient care in both sexes were due to cardiovascular disease (US$747 million) followed by overweight- and obesity-related neoplasms (US$299.8 million), asthma (US$34 million), type 2 diabetes (US$3.7 million), and osteoarthritis (US$3.9 million). Authors estimated that these direct costs were a considerable underestimate of the true burden of overweight/obesity in Brazil, which would include private health care expenditures, as well as indirect costs due to lost productivity, premature death, and home care ( 131 ).
Given the predicted rise in obesity in Brazil, coronary heart disease, stroke, hypertension, cancers, osteoarthritis, and diabetes are projected to at least double by 2050, with concomitant doubling in health care costs, from US$5.8 billion in 2010 to US$10.1 billion per year—totaling US$330 billion over 40 years (year 2010 values). It is estimated that a 5% reduction in mean BMI across the population could save Brazil some US$57 billion over that time frame ( 132 ). A similar analytic approach that substituted Mexican prevalence and trends for the Brazilian ones estimated 2010 costs of obesity at US$806 million (year 2000 values), which were projected to increase to US$1.7 billion by 2050, at which point a mere 1% reduction in BMI prevalence in Mexico could save an estimated US$85 million per year ( 133 ).
Of course, none of these estimates include dollars spent on the weight-loss industry, which is estimated to be over US$60 billion dollars in 2014 in the USA alone ( 134 ), and includes non-prescription drugs and supplements, diet plans, gym memberships, workout videos, and an endless stream of money-making schemes.
7. Touching on Solutions, and Some Conclusions
Obesity is a major contributor to preventable disease and death across the globe, and poses a nearly unprecedented challenge not just to those tasked with addressing it at the public health level, or at the healthcare provider level, but to each of us as individuals, for none of us are immune. Increasing ease of life, owing to reduced physical labor and automated transportation, an increasingly sedentary lifestyle, and liberal access to calorie-dense food, driven by dramatic economic growth in many parts of the world in the last century, have turned a once rare disease of the affluent into one of the most common diseases—increasingly of the poor. That barely one in three people in the USA today are normal weight portends, quite simply, an astounding and frightening future. Significant reductions in public health and healthcare expenditures could occur around the world if we were able to stem the tide of childhood obesity trends, and if young and middle-aged overweight and obese adults lost approximately10% of their body weight, as recommended for a considerably reduced risk of debilitating chronic conditions ( 135 ).
Obesity is complex. Although its risk factors are myriad and compounding, there is an urgent need for deeper understanding of the way risk factors interact with each other, and the potential solutions to the epidemic are as multi-leveled and complex as its causes. There are calls for applying systems-level ( 136 ) and systems epidemiology ( 137 ) approaches to this and related nutrition and metabolic diseases, approaches which attempt to comprehensively address biological, behavioral, and environmental contributors to disease as well as their intricate feedback loops. Additional research on solutions to this epidemic would include, for example, examining the relative cost/benefit to individuals and populations of individual versus systemic policies and/or interventions, concurrently or independently, particularly when individuals and communities must decide between approaches given limited resources, and moreover, with the currently limited evidence in the case of broad industry, agricultural, or public health policies. For example, we could attempt to limit national production and import of sugar-sweetened beverages, tax sugar-sweetened beverages, or restrict fast food restaurant zoning. These largely political acts seem relatively inexpensive, but may have economic impacts in communities and regions beyond what we currently understand. We may push for the increasing medicalization of obesity, including developing an obesity vaccine. While such a “cure” may someday arise, the medicalization of a condition typically improves its treatment rather than its prevention, and prevention is key in the case of obesity. However, preventing and remediating obesity in children and adults—e.g., via health and wellness incorporation into curricula at every educational level from kindergarten through medical school—requires vast resources allocated to educators, as well as earlier diagnosis and treatment of overweight (education, counseling, drug treatment, etc.). Given these resource costs, perhaps greater attention should be given to pregnancy, a condition which is already highly medicalized and which may be an ideal preventive avenue for the provision of nutrition education and intensive monitoring of weight gain, to ensure that children have the most optimal start with respect to their future obesity risk. Clearly, no single approach is optimal, but with limited resources, an evidence base supporting one or more approaches or their combination is needed, as is tenacity and perhaps some audacity by local government and public health authorities in testing some of these approaches within their populations. However, an epidemic of this magnitude needs, quite simply, more resources. One of the reasons why the American Medical Association opted to declare obesity a “disease” was to give obesity the label it needs for greater allocation of resources for research, prevention, and treatment ( 1 ).
Despite the many unknowns, we can be cautiously optimistic about our ability to address the obesity epidemic. Indeed, we have relatively successfully faced similarly daunting public health challenges before: smoking, to name just one. While tobacco can loosely be thought of as a single product, and our food culture is infinitely more complex, as a case study in how to approach obesity, it provides numerous lessons in multi-level solutions to a major health threat in terms of both mitigation and prevention. We began by developing an understanding of smoking’s epidemiological impact and the healthcare costs borne by society, uncovered its biological basis, learned about and applied behavior change, and initiated and carried out vast public health, public policy, political, and economic strategies that ultimately affected whole environments as well as sociocultural norms.
It took over half a century to achieve the immense success we have with regard to smoking in the USA and still we are not yet tobacco-free ( 138 ); other parts of the world continue to wrestle with it to a greater degree. It has only been a couple decades since we first deeply appreciated that obesity was epidemic. We clearly still have a long way to go.
Key Points for Decision Makers
- In 2013, an estimated one in three adults worldwide was overweight or obese, and adult obesity exceeded 50% in several countries around the globe. While the prevalence of adult obesity in the developed world seems to have stabilized, the prevalence of obesity in children and adolescents globally, as well as adults obesity in developing countries, is still increasing. In addition, some developed countries continue to observe increasing prevalence of extreme classes of obesity.
- Overweight and obesity—defined as excess body weight for height—have genetic, behavioral, socioeconomic, and environmental origins.
- Obesity increases risk of major chronic diseases, including heart disease, diabetes, depression, and many cancers, as well as premature death.
- Estimates of annual healthcare costs attributable to obesity are US$190 billion per year in the USA, approximately 21% of US healthcare expenditures.
- Given its complexity, the obesity epidemic requires multilevel and integrated solutions, from individual intervention, to broad food policy, industry, and agriculture initiatives.
Acknowledgements
The authors declare no conflict of interest. AH is supported by an American Diabetes Association Mentor-Based Postdoctoral Fellowship award. FH is supported by NIH grants DK51158, HL60712, P30 DK46200, and U54CA155626. The authors broadly thank the researchers in this field for their consistent and tireless work in illuminating the etiology, sequelae, and solutions to this complex condition.
1 See also http://www.genome.gov/gwastudies/
2 We do not review the impact of food, agriculture, trade, and nutrition policy on obesity in the present paper, but refer interested readers to a recent review ( 64 ). Further, we do not address the body of growing evidence on the role of environmental pollutants–“obesogens”–in obesity, specifically those known as endocrine-disrupting chemicals. We refer readers to recent reviews on the topic ( 35 , 36 , 65 ).
Author Contributions
AH wrote the first draft of the paper. AH and FH contributed to writing, revised, and edited the paper. AH is the final guarantor of this work and takes full responsibility for its contents. Both authors read and approved the final manuscript.
Nutrition Essay Examples and Topics
Why you should not eat pork, digestion of a cheeseburger.
- Words: 1170
Coffee and Why It Is Good for You
Argument for removing vending machines in schools, coffee: benefits and disadvantages, the bread making process: main steps.
- Words: 1161
Why Is Pizza Popular?
- Words: 1687
Health Effects of Junk Food Intake
- Words: 2472
Dieting: Losing Weight Without Losing Your Mind
- Words: 1424
Carbohydrate Consumption and Its Importance
The disadvantages of canned food.
- Words: 1136
Obesity and Healthy Eating
Chocolate ice-cream: food product case, fats, carbohydrates, and proteins, an onion: an important vegetable, the common factors that causes bad eating habits, parental responsibility for childhood obesity, importance of health diet for modern person, child malnutrition: term definition, intermittent fasting: a path to improved well-being, health benefits of dark chocolate, the egyptian diet: sociology of food and nutrition.
- Words: 1576
Food: How Technology Has Changed the Way We Eat?
- Words: 1159
Using Food Preservatives Ethical
- Words: 5120
Rational Nutrition: The Key Elements
Vegetarian and non vegetarian healthier diet.
- Words: 2023
The Gluten-Free Diet: Advantages and Disadvantages
Importance of vitamin c for the human body.
- Words: 1116
Vegetarianism and Its Causes
Nutritional status of students: anthropometric data.
- Words: 1149
Ketogenic Diet: Potential Health Benefits and Risks
Nutrition education: its importance and promotion, dietary record of seven days of food intake, the world’s food problems’ solving.
- Words: 1156
The 24-Hour Dietary Recall Interview
- Words: 1668
Nutrition and Its Impact on the Environment
- Words: 1129
Food Security: Sustainable Development
Nutrition: a day’s dietary intake of carbohydrates, proteins, and fats.
- Words: 1072
Body Image and Advertising
Obesity: an american epidemy, impacts of fast food on childhood eating habits, vitamins and dietary supplement, does healthy food prevent obesity, how can societal marketing concept be used to influence children to eat a healthier diet, the fast-food industry and legal accountability for obesity, fast foods more harm than good.
- Words: 1898
Minerals’ Importance for Human Health
Sports nutrition: term definition.
- Words: 1904
Chocolate’s Positive and Negative Effects
- Words: 1195
Food Choices in the United States
Analysis of childhood obesity problem, nutrition and hydration, types of nutrition, analysis of breakfast for school children in usa, uk, finland and singapore, the role of food for sustainability in the built environment, the role of carbohydrates for human body, introducing infants to semi-solid food, cheese: process of making and different sorts.
- Words: 1384
Vegetarian or Meat Eaters
- Words: 1608
Unhealthy Lifestyle Among the Singapore Youth
- Words: 1061
Rice: Food Ingredient as a Currency
- Words: 1727
Influence of Modelling in Teenager’s Eating Disorders
- Words: 2326
Hibiscus Macaroon: Chemical and Microbiological Analysis
- Words: 1995
“Quit Meat” Vegetarian Diet: Pros and Cons
Moist and dry heat cookery.
- Words: 1586
Snacking: Positive and Negative Health Effects
Bread: origin, usage, and preservation, food diary: nutrition opportunities and challenges, the importance of carbohydrates, nutritional needs of an older adult: lifecycle nutrition and fitness, a universal maximum calorie intake for an adult.
- Words: 2207
Comprehensive Analysis of Diet
- Words: 1120
Nutritional Information on Restaurant Menus
- Words: 1244
Food and Taste Process Issues
- Words: 1517
The Food Impact on Health
Food insecurity among students, what kind of diet do you prefer, the dining out culture in america, you are what you eat: how does food become an addiction.
- Words: 3053
Dietary Habits in the United States
Field trip reflection: the smithsonian national museum of american history, carbohydrates: a dietary perspective, the concept of carbohydrates, optimum nutrition is needed for optimum health.
- Words: 1179
Diet and Water as an Overlooked Essential Nutrient
- Words: 1189
Benefits of Energy Drinks
Nutrition: chemical composition of the food, food texture in packaging of cakes, pastries and sweets, nutrition effects on human health, popular diets: the ketogenic diet, importance of healthy diet for immunity.
- Words: 1497
Food Processing and Farming Methods
Supplemental nutrition assistant program.
- Words: 1243
The Ketogenic Diet: Positive and Negative Influences
Creating specific nutrition analysis, fallacy analysis: the harm of meat consumption, food security: environmental impact, malaysian malnutrition problems.
- Words: 1484
India Pale Ale: The Beer Style History
Diverse insights on diabetes diets, dietary diversity and childhood obesity, mediterranean diet and its effect on the cardiovascular system.
- Words: 1439
Symptom Management, Nutrition, and Hydration at End-of-Life
- Words: 1259
Healthy Eating: Menu for a Preschooler
The pleasures of eating: food and consumer culture, human diet and its historical background, “scientific” assertions on the paleo diet, industrial meat business and environmental issues, should we start eating insects, main reasons for establishing food banks, mindful eating: searching for information, the “in defense of food” book by michael pollan, a nutrition guide for early childhood, the bowl of oatmeal components inspection, adding molasses in the dairy cow diet.
- Words: 1151
Analyzing Personal Diet and Intake Pattern
Dietary intake aspects analysis, the aspects of the ketogenic diet, role of nutritional genetics in health.
- Words: 1132
Pollo Guisado and Arroz con Leche
- Words: 2190
Analysis of Health Diet Benefits
Novo Nordisk presents key findings from semaglutide trials at ADA scientific sessions 2024
- Download PDF Copy
Novo Nordisk today announced the presentation of 34 abstracts highlighting the breadth of its portfolio at the upcoming 84 th Scientific Sessions of the American Diabetes Association (ADA). The conference will be held in-person and virtually from 21–24 June 2024 in Orlando, US.
Additional data from three landmark trials with semaglutide will also be presented in dedicated scientific sessions. The trials assess additional potential benefits of semaglutide, including evaluation of kidney and cardiovascular endpoints in people with type 2 diabetes and chronic kidney disease (FLOW, semaglutide 1.0 mg) and cardiovascular and glucose-related endpoints in people with obesity and CVD, with and without diabetes (SELECT and STEP HFpEF, semaglutide 2.4 mg).
We recognize that cardiometabolic conditions like cardiovascular disease, chronic kidney disease, obesity and type 2 diabetes are often interlinked and might occur in the same patient. We need to develop medicines that address multiple facets of the diseases. The broad data being presented this year at ADA reflect this goal. In particular, data from FLOW and SELECT look at ways to treat common comorbidities of diabetes and obesity, such as kidney disease and cardiovascular disease.” Stephen Gough, senior vice president and global chief medical officer, Novo Nordisk
All abstracts will be published on the website of the journal Diabetes ® . Data from the scientific sessions will be made available after their presentation.
Summary of presentations
Scientific sessions.
The following data will be presented in the dedicated scientific sessions as a part of the scientific agenda of the congress:
| The first dedicated kidney outcome trial with a GLP1-RA once-weekly semaglutide – FLOW trial results (scientific session; 24 June, 13:30–15:00 EST) |
| SELECT trial – New looks at glycemia, inflammation, and heart failure (scientific session; 22 June, 08:00–09:00 EST) |
| The STEP-HFpEF and STEP-HFpEF-DM trials – Targeting obesity to treat heart failure (scientific session; 23 June, 16:30–18:00 EST) |
Poster and oral presentations
The following abstracts were submitted by Novo Nordisk and are accepted for presentation at the congress:
| outcomes in type 2 diabetes: an observational study (PAUSE) (857-P) |
| oral semaglutide in Chinese patients with T2D by baseline characteristics: post hoc analysis of PIONEER 11 and 12 (752-P) |
| : A novel population-level system dynamics approach (1040-P) |
| and branded antiobesity medication for medical weight management: a retrospective analysis (1684-P) |
About Ozempic ®
Once-weekly subcutaneous semaglutide is approved in 0.5 mg, 1.0 mg and 2.0 mg doses under the brand name Ozempic ® and indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes and to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction or non-fatal stroke) in adults with type 2 diabetes and established cardiovascular disease.
About Rybelsus ®
Oral semaglutide is administered once daily and is approved for use in three therapeutic doses, 3 mg, 7 mg and 14 mg under the brand name Rybelsus ® . It is indicated for the treatment of adults with insufficiently controlled type 2 diabetes mellitus to improve glycemic control as an adjunct to diet and exercise.
About Wegovy ®
Once-weekly subcutaneous semaglutide 2.4 mg is approved under the brand name Wegovy ® and is indicated in combination with a reduced calorie diet and increased physical activity to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) in adults with established cardiovascular disease and either obesity or overweight, as well as to reduce excess body weight and maintain weight reduction long term in adults and pediatric patients aged 12 years and older with obesity and in adults with overweight in the presence of at least one weight-related comorbid condition.
Posted in: Drug Trial News | Medical Condition News
Tags: Agonist , Cardiometabolic , Cardiovascular Disease , Chronic , Chronic Kidney Disease , Clinical Trial , Diabetes , Diabetes Mellitus , Diet , Efficacy , Exercise , Fasting , GLP1 , GLP-1 , Glucagon , Glucagon-like Peptide-1 , Glucose , Glycemia , HbA1c , Health Care , Healthcare , Heart , Heart Failure , Hypoglycemia , in vivo , Inflammation , Insulin , Insulin Glargine , Kidney , Kidney Disease , Myocardial Infarction , Obesity , Peripheral Arterial Disease , Physical Activity , Receptor , Semaglutide , Stroke , Telemedicine , Type 2 Diabetes
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

Revolutionizing Life Science: An Interview with SCIEX on ASMS, the SCIEX 7500+ System, and AI-Driven Quantitation
Jose Castro-Perez and Chris Lock, SCIEX
In our latest interview, News Medical speaks with SCIEX, a global leader in life science analytical technologies, about their exciting announcements at ASMS, the SCIEX 7500+ System, and how they utilize AI quantitation software to streamline solutions.

From Discovery Biology to ELRIG Chair
Melanie Leveridge
In this interview, we speak with Melanie Leveridge, Vice President of Discovery Biology at AstraZeneca and Chair of the Board for ELRIG UK, to discuss her extensive career in the pharmaceutical industry, her role in fostering scientific innovation, and her vision for ELRIG's future.

Breathing New Life into Diagnostics: Plasmion's SICRIT Technology
Revolutionizing Non-Invasive Diagnostics with Plasmion’s SICRIT Breath Analysis.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

Home — Essay Samples — Nursing & Health — Nutrition — The Importance Of Proper Nutrition And Healthy Diet
The Importance of Proper Nutrition and Healthy Diet
- Categories: Nutrition Obesity
About this sample

Words: 972 |
Published: Feb 8, 2022
Words: 972 | Pages: 2 | 5 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1617 words
2 pages / 1075 words
6 pages / 2912 words
1 pages / 2391 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nutrition
National Institutes of Health. (2021, March 24). Calcium. Office of Dietary Supplements. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256
Diet analysis is a crucial aspect of maintaining a healthy lifestyle. It involves the assessment of an individual's dietary intake and the subsequent evaluation of its impact on their overall health. In this essay, I will [...]
Healthy carob bars have gained attention as a potential substitute for traditional chocolate products. As a college student studying marketing, it is important to recognize the potential of healthy carob bars and develop a [...]
Pruvit Keto OS is a popular supplement in the health and wellness industry that claims to help individuals achieve ketosis faster and more effectively. This case study will examine the effectiveness of Pruvit Keto OS in helping [...]
In today’s fast-paced world, the importance of eating healthy has become more crucial than ever. With the rise in fast food and processed snacks, the need for a balanced and nutritious diet is often overlooked. The consequences [...]
The topic of school lunches has been a source of debate and controversy for many years. While some argue that they are not nutritious enough and others claim they are too expensive, there are positive aspects to consider as [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
More From Forbes
England’s kids are getting shorter amid poverty and poor nutrition.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
In this photo illustration a school student eats a hamburger in London, England.
The average height of England’s 5-year-olds has fallen over the last eleven years, while rates of obesity and type 2 diabetes have increased, a charity report shows.
The Food Foundation argues that calorie-dense but nutrient-poor diets are worsening health outcomes for younger generations. Behind these diets, the organization stats, are poverty-driven food insecurity, unhealthy environments that make it hard to provide good meals and the “agressive promotion of cheap junk food.”
Obesity has risen by almost a third since 2006 in kids aged 10 to 11, and diagnoses of Type 2 diabetes among under-25s have gone up by 22% over the last 5 years, the report found.
England’s newborns can expect to spend a year less in good health than those born 10 years ago, it states.
The Food Foundation used government data to produce the report, which it argues paints “a worrying picture” of the current state of child health and reveals “the worsening trajectory that they are facing.”
Sir Michael Marmot, who leads the University College London’s Institute of Health Equity said in a statement : “We used to think of the combination of undernutrition and obesity as a feature of low and middle income countries. We are now seeing it in Britain in 2024.”
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
Marmot, who is a Food Foundation trustee, previously authored two landmark reviews into the health impacts of England’s growing inequalities.
The Food Foundation argues the public is at a “crucial juncture” for child health, with the opportunity to “we evaluate our national priorities” around the corner.
The public are widely expected to install a Labour government when they head to the polls for a general election on July 4th. Various polls predict the Conservatives, who have been in power four 14 years, will lose hundreds of seats. Some even predict the Liberal Democrats, a much smaller party, may overtake them .
The Labour party are considered centre-left, while the Conservatives are traditionally centre-right. But the party has arguably lent further right as smaller rival right-wing parties — like Nigel Farage’s United Kingdom Indepence Party and, now, Reform U.K. — have gained steam. The Liberal Democrats are traditionally a centrist party with socially liberal ideals.
Both the Lib Dems and the Labour party have pledged to address inequality in some form if they make it to government. The Conservative party manifesto promises to increase regulation on advertising unhealthy food to kids and better research the effects of ultra-processed food. It does not contain the word “inequality,” and it mentions “poverty” only once, in the context of international development.
You can read my summary of the three main party’s health policy pledges here .
Henry Dimbleby, who performed an independent review into national food strategy said in response to the Food Foundation report: “The decline in children’s health shown clearly in this report is a shocking and deeply sad result of the failures of the food system in the UK. We need the next Government to take decisive action to make healthy and sustainable food affordable, stop the junk food escalation and to realise that investing in children’s health is an investment in the future of the country.”

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.
FDA expected to propose a label change to packaged foods: Nutrition info on the front

The Food and Drug Administration is expected to propose a change to prepackaged food sold in America: a requirement that the front of the packages display key nutrient information in addition to the nutrition label that’s already on the back.
The concept, designed to quickly convey health ramifications to busy consumers about the food and beverages they are considering purchasing, is not novel: Worldwide, dozens of countries already have front-of-package nutrition labels that come in various designs. In Chile, for example, a stop sign symbol on the front of an item indicates if it has high sugar, saturated fat, sodium or calories. In Israel, there’s a red warning label on such food and drinks. And in Singapore, beverages display a letter grade based on how nutritious they are.

Advocates have been asking the FDA for nearly two decades to require front-of-pack labels, which they say help people make healthier choices and prod food manufacturers to reformulate their recipes so they have fewer warnings on their products. The FDA stayed largely silent on the issue until it announced intentions to explore front-of-pack labels as part of a national health strategy released during a landmark White House Conference on Hunger, Nutrition, and Health in 2022. Since then, it has reviewed literature on front-of-pack labeling and conducted focus groups to test designs for labels.
But the idea faces opposition from trade associations representing America’s food and beverage makers, who created their own voluntary system for highlighting certain nutrients on the front of packages over a decade ago. And some of the label designs being considered by the FDA could be challenged on First Amendment grounds.
“The U.S. does interpret free speech much broader and more inclusive of corporate speech than any other country in the world,” said Jennifer Pomeranz, an associate professor at the New York University School of Global Public Health who has researched First Amendment obstacles to mandating front-of-package food labels.
Designs that are purely factual — stating the number of grams of added sugars, for example — are more likely to be considered constitutional than interpretive designs that have shapes or colors that characterize a product as unhealthy, her research found.
“It starts to get more iffy when you go into subjective,” Pomeranz said.
Among the multiple label options tested by the FDA, some used traffic light colors to indicate whether there was a high (red), medium (yellow) or low (green) amount of saturated fat, sodium or added sugars; others stated if a product was “high in” those nutrients, sometimes adding the percentage of the recommended daily value that a serving size contains.
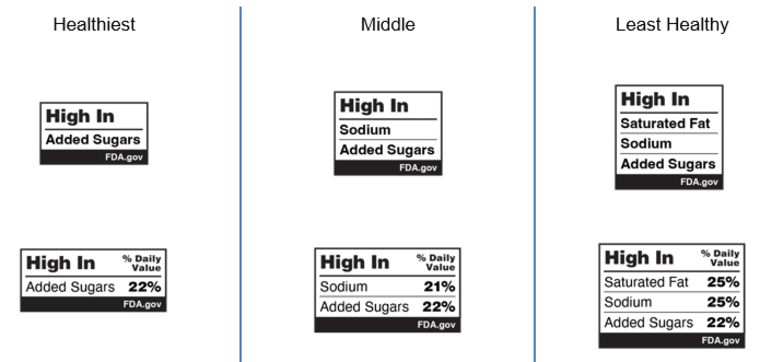
A spokesperson for the FDA declined to disclose to NBC News which label design it will use and did not say exactly when the agency will release its proposed rule, other than to say “it is targeting for this summer,” despite previously setting a deadline of this month.
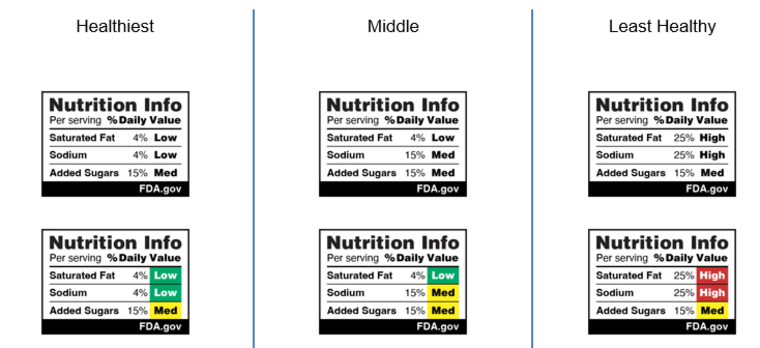
The Consumer Brands Association and the food industry association FMI, which created a voluntary label system for the food and beverage industry called Facts up Front that launched in 2011, have made clear they are against mandatory interpretive designs such as a red light/green light system. Interpretive labels “will raise unnecessary fear in consumers based on a single limiter nutrient without providing meaningful information as to how that food item might fit into overall healthy eating patterns,” they wrote in a public comment to the FDA in 2022.
They also say their voluntary system addresses the needs of consumers. Facts up Front uses up to four icons on the front of packages to highlight calories, saturated fat, sodium and added sugars per serving size. Manufacturers can also include nutrition information for up to two “nutrients to encourage,” such as potassium or fiber. The Consumer Brands Association says hundreds of thousands of products carry Facts up Front: 207,000 foods and beverages displayed them as of 2021, according to the most recent data available from the group.

“It’s really giving consumers a quick, consistent and holistic look at what the nutrition composition is of whatever they’re purchasing, and then helping those consumers make informed decisions,” said Sarah Gallo, the association’s vice president of product policy.
Advocates for mandatory front-of-package labeling disagree, arguing that the Facts up Front campaign is not used enough: By contrast, the nutrition facts label that is federally mandated to be on the backs or sides of packages appears on billions of products .
“Front-of-pack labeling is only reliable for consumers if it appears across the entire food supply, not only on the products of a handful of manufacturers who opt into a voluntary program,” said Eva Greenthal, a senior policy scientist at the food and health advocacy group Center for Science in the Public Interest, which first petitioned the FDA in 2006 to implement front-of-pack labels.
She also said Facts up Front does not give enough context to be helpful.
“Facts up Front does not provide any additional tools to help the consumer interpret that information,” she said. “We need something like the word ‘high in.’”
Courtney Gaine, president and CEO for the Sugar Association, the trade association for the U.S. sugar industry, said her group supports transparency but questions whether mandatory front-of-pack labeling will improve Americans’ diets.
“It just doesn’t seem like this has the evidence to show that this will make a difference,” she said.
But Greenthal and other advocates say there’s data from around the world to support it. In Chile, which in 2016 became the first country to apply front-of-package nutrition information, studies show people have made healthier consumer purchases and are choosing from healthier product reformulations .
“I think it’s a very classic food industry, anti-regulatory tactic to deny the science supporting a new policy that might be difficult to implement but is beneficial for society,” Greenthal said.
In its own review of scientific literature on front-of-pack labels, the FDA concluded that the labels “can help consumers identify healthy foods” and “appear helpful for those with lower nutrition knowledge and busy shoppers.”
The discussion comes as the percentage of Americans who are considered overweight or obese has risen , with obesity affecting about 42% of U.S. adults . More than 1 million Americans die from diet-related diseases such as cardiovascular disease, diabetes and certain cancers annually, according to the FDA.
The statistics don’t mean that the nutrition facts box that became required on the backs or sides of food packaging three decades ago has been a failure, said Xaq Frohlich, an associate professor of history at Auburn University and the author of the book “From Label to Table: Regulating Food in America in the Information Age.”
“Every time there’s been a change in the label, the food industry has reformulated its foods,” he said. “So even if you’re not reading the label, the food is changing, and it’s having that kind of impact.”
Greenthal said there are many people who would benefit from more nutritional information on the front of packages: busy parents rushing through the supermarket, people with low levels of nutrition literacy, and anyone else with limited time and energy to invest in their food choices.
“Policies like front-of-package labeling couldn’t come any sooner,” she said. “Diet-related chronic disease is one of the most important problems facing our country and hindering our population’s health.”
Elizabeth Chuck is a reporter for NBC News who focuses on health and mental health, particularly issues that affect women and children.

IMAGES
VIDEO
COMMENTS
Many people will think of corruption, racism and poverty. However, the rate at which obesity cases have grown in the modern society has made obesity one of the major... Obesity. Topics: Adipose tissue, Appetite, Body shape, Childhood obesity, Malnutrition, Nutrition, Obesity. 25.
Obesity and Nutrition. More than one-third of U.S. adults — and about 17 percent of U.S. children — are obese. Obesity puts people at risk for many health issues including heart disease, stroke, type 2 diabetes, arthritis, and certain types of cancer. Because these conditions are some of the top preventable causes of chronic illness and ...
This essay therefore analysis the different formations of obesity, the causes and in particular the significance of inheritance in the occurrence of obesity. Obesity Research: Hypothesis Testing and Statistics. The bar chart deals with the changes in the weight of five pilots suffering from obesity during three months.
Argumentative Essay on Obesity. Obesity is a growing epidemic that has plagued societies around the world. With the rise of fast food chains, sedentary lifestyles, and a lack of education on proper nutrition, obesity rates have skyrocketed in recent years. While some argue that obesity is a personal choice and should not be seen as a public ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Conclusion. In conclusion, obesity is a complex issue with multiple causes and significant effects on individuals and society. Poor dietary habits, sedentary lifestyles, and genetic factors contribute to its prevalence. The health consequences, economic costs, and social and psychological effects of obesity are profound and demand attention.
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities ...
The weight control evidence is stronger for whole grains than it is for fruits and vegetables. (20-22) The most recent support comes from the Harvard School of Public Health diet and lifestyle change study: People who increased their intake of whole grains, whole fruits (not fruit juice), and vegetables over the course of the 20-year study gained less weight-0.4, 0.5, and 0.2 pounds less ...
Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat. If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the ...
Get a custom Essay on Nutrition and Obesity: Management and Prevention. The rising cases of lifestyle diseases and weight problems compelled states and governments to institute policies that govern the quality of food offered by various food joints and restaurants. One of the regulations produced by governments like the United States is the ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
1. Obesity: Prevalence and Magnitude. The obesity epidemic is one of the most predominant public health challenges of the century and its prevalence continues to rise globally with now more than 500 billion obese individuals around the world [].Being associated with over 60 comorbid conditions and at least 12 different types of cancers, obesity poses significant health and economic burdens on ...
This narrative review is divided into two sections: the first examines the integrative impact of nutrition and physical exercise on managing obesity and type 2 diabetes (T2D), and the second addresses the fundamental biological targets implicated in nutritional and exercise-based interventions for obesity and T2D intervention.
Essay on obesity! Find high quality essays on 'Obesity' especially written for school, college, science and medical students. These essays will also guide you to learn about the causes, factors, treatment, management and complications related to obesity. Obesity is a chronic health condition in which the body fat reaches abnormal level.
Essay Samples on Obesity. Essay Examples. ... Nutrition; Obesity; Public Health; 530 Words | 1 Page. The Problem Of High Level Of Obesity In Malaysia. Overview of Obesity According to NHMS studies from 1996-2015, the rate of obesity in Malaysia had significantly increased within these year. In term of states in Malaysia, Putrajaya recorded as ...
At the time this essay was conceived, Mr. Siddiqi was with the Applied Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Maryland. Top. References. Institute of Medicine of the National Academies, Committee on Accelerating Progress in Obesity Prevention, Food and Nutrition Board.
Section Information. Over the last few decades, obesity has become the most prevalent metabolic disorder worldwide. Excess adiposity increases the risk for the development of cardiometabolic alterations such as type 2 diabetes, cardiovascular disease, dyslipidemia, non-alcoholic fatty liver disease and cancer, among others.
How obesity affects in nursing. Nursing practitioners offer certain basic functions for obese routine care. When attending the severely obese patient, basic factions such as bathing and dressing usually becomes a problem. The current trend in nurse shortage worsens the situation (Kovner, & Salsberg, 2002).
The Role of Nutrition in Obesity. This Special Issue of Nutrients, "Nutrients, Foods, Dietary Patterns and Obesity", includes nine original articles that explore the role of eating behaviors, diet quality and dietary interventions in obesity and its potential mechanisms. It also contains one systematic review and meta-analysis investigating ...
Reduce the proportion of adults with obesity—NWS-03. Increase the proportion of health care visits by adults with obesity that include counseling on weight loss, nutrition, or physical activity—NWS-05. Increase the proportion of women who had a healthy weight before pregnancy—MICH-13.
Introduction. Obesity is defined as having a body mass index (BMI) of 30 or higher. In America, the prevalence of obesity has been steadily increasing over the past few decades, with currently around 42% of the population being classified as obese. Addressing this issue is significant as it has far-reaching impacts on both individual and ...
To the best of our knowledge, the largest previous study to address amino acid intake in vegans was a cross-sectional analysis of the European Prospective Investigation into Cancer and Nutrition (EPIC)-Oxford cohort (98 individuals). 22 The authors found lower amino acid intake among individuals who adhered to a vegan diet compared with meat ...
In my lifetime, obesity has exploded, from being rare to almost being the norm. I was born in 1979, and by the time I was 21, obesity rates in the United States had more than doubled. They have ...
A report from 2021 called obesity a major public health crisis, and it's only gotten worse since then. One in five children is reportedly obese, and one in four adults tips the scale with a body ...
1. Introduction. Obesity is a complex, multifactorial, and largely preventable disease (), affecting, along with overweight, over a third of the world's population today (2,3).If secular trends continue, by 2030 an estimated 38% of the world's adult population will be overweight and another 20% will be obese ().In the USA, the most dire projections based on earlier secular trends point to ...
Check our 100% free nutrition essay, research paper examples. Find inspiration and ideas Best topics Daily updates. ... Obesity is considered a malnutrition because the extended consumption of nutrients can still lead to the lack macro- and microelements. Overweight and obesity are serious disorders affecting a substantial part of the current ...
About Ozempic ®. Once-weekly subcutaneous semaglutide is approved in 0.5 mg, 1.0 mg and 2.0 mg doses under the brand name Ozempic ® and indicated as an adjunct to diet and exercise to improve ...
Published: Feb 8, 2022. Nutrition is the process of providing your body nourishment in the form of food which is necessary for your health. The food choices you make every day can affect your health and your mood in a drastic way. Good nutrition is an important part of living a healthy lifestyle because it ultimately boils down to life and death.
Obesity has risen by almost a third since 2006 in kids aged 10 to 11, and diagnoses of Type 2 diabetes among under-25s have gone up by 22% over the last 5 years, the report found.
Manufacturers can also include nutrition information for up to two "nutrients to encourage," such as potassium or fiber. The Consumer Brands Association says hundreds of thousands of products ...