Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study
Contributed equally to this work with: Dominika Maison, Diana Jaworska, Dominika Adamczyk, Daria Affeltowicz
Roles Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Faculty of Psychology, University of Warsaw, Warsaw, Poland
Roles Formal analysis, Investigation, Writing – original draft, Writing – review & editing
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Roles Conceptualization, Formal analysis, Investigation, Methodology
- Dominika Maison,
- Diana Jaworska,
- Dominika Adamczyk,
- Daria Affeltowicz

- Published: October 11, 2021
- https://doi.org/10.1371/journal.pone.0258133
- Peer Review
- Reader Comments
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6 th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed that for all respondents the greatest challenges and the source of the greatest suffering were: a) limitation of direct contact with people; b) restrictions on movement and travel; c) necessary changes in active lifestyle; d) boredom and monotony; and e) uncertainty about the future.
Citation: Maison D, Jaworska D, Adamczyk D, Affeltowicz D (2021) The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study. PLoS ONE 16(10): e0258133. https://doi.org/10.1371/journal.pone.0258133
Editor: Shah Md Atiqul Haq, Shahjalal University of Science and Technology, BANGLADESH
Received: April 6, 2021; Accepted: September 18, 2021; Published: October 11, 2021
Copyright: © 2021 Maison et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files ( S1 Dataset ).
Funding: This work was supported by the Faculty of Psychology, University of Warsaw, Poland from the funds awarded by the Ministry of Science and Higher Education in the form of a subsidy for the maintenance and development of research potential in 2020 (501-D125-01-1250000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The coronavirus disease (COVID-19), discovered in December 2019 in China, has reached the level of a pandemic and, till June 2021, it has affected more than 171 million people worldwide and caused more than 3.5 million deaths all over the world [ 1 ]. The COVID-19 pandemic as a major health crisis has caught the attention of many researchers, which has led to the creation of a broad quantitative picture of human behavior during the coronavirus outbreak [ 2 – 4 ]. What has been established so far is, among others, the psychological symptoms that can occur as a result of lockdown [ 2 ], and the most common coping strategies [ 5 ]. However, what we still miss is an in-depth understanding of the changes in the ways of coping with challenges over different stages of the pandemic. In the following study, we used a longitudinal qualitative method to investigate the challenges during the different waves of the coronavirus pandemic as well as the coping mechanisms accompanying them.
In Poland, the first patient was diagnosed with COVID-19 on the 4 th March 2020. Since then, the number of confirmed cases has grown to more than 2.8 million and the number of deaths to more than 73,000 (June 2021) [ 1 ]. From mid-March 2020, the Polish government, similarly to many other countries, began to introduce a number of restrictions to limit the spread of the virus. These restrictions had been changing from week to week, causing diverse reactions in people [ 6 ]. It needs to be noted that the reactions to such a dynamic situation cannot be covered by a single study. Therefore, in our study we used qualitative longitudinal research in order to monitor changes in people’s emotions, attitudes, and behavior. So far, few longitudinal studies have been carried out that investigated the various issues related to the COVID-19 pandemic; however, all of them were quantitative [ 7 – 10 ]. The qualitative approach (and especially the use of enabling and projective techniques) allows for an in-depth exploration of respondents’ reactions that goes beyond respondents’ declarations and captures what they are less aware of or even unconscious of. This study consisted of six stages of interviews that were conducted at key moments for the development of the pandemic situation in Poland. The first stage of the study was carried out at the moment of the most severe lockdown and the biggest restrictions (March 2020) and was focused on exploration how did people react to the new uncertain situation. The second stage of the study was conducted at the time when restrictions were extended and the obligation to cover the mouth and nose everywhere outside the household were introduced (middle of April 2020) and was focused at the way how did people deal with the lack of family gatherings over Easter. The third stage of the study was conducted at the moment of announcing the four stages of lifting the restrictions (April 2020) and was focused on people’s reaction to an emerging vision of getting back to normalcy. The fourth stage of the study was carried out, after the introduction of the second stage of lifting the restrictions: shopping malls, hotels, and cultural institutions were gradually being opened (May 2020). The fifth stage of the study was conducted after all four stages of restriction lifting were in place (June 2020). Only the obligation to cover the mouth and nose in public spaces, an order to maintain social distance, as well as the functioning of public places under a sanitary regime were still in effect. During those 5 stages coping strategies with the changes in restrictions were explored. The sixth and last stage of the study was a return to the respondents after a longer break, at the turn of October and November 2020, when the number of coronavirus cases in Poland began to increase rapidly and the media declared “the second wave of the pandemic”. It was the moment when the restrictions were gradually being reintroduced. A full description of the changes occurring in Poland at the time of the study can be found in S1 Table .
The following study is the first qualitative longitudinal study investigating how people cope with the challenges arising from the COVID-19 pandemic at its different stages. The study, although conducted in Poland, shows the universal psychological relations between the challenges posed by the pandemic (and, even more, the restrictions resulting from the pandemic, which were very similar across different countries, not only European) and the ways of dealing with them.
Literature review
The COVID-19 pandemic has led to a global health crisis with severe economic [ 11 ], social [ 3 ], and psychological consequences [ 4 ]. Despite the fact that there were multiple crises in recent years, such as natural disasters, economic crises, and even epidemics, the coronavirus pandemic is the first in 100 years to severely affect the entire world. The economic effects of the COVID-19 pandemic concern an impending global recession caused by the lockdown of non-essential industries and the disruption of production and supply chains [ 11 ]. Social consequences may be visible in many areas, such as the rise in family violence [ 3 ], the ineffectiveness of remote education, and increased food insecurity among impoverished families due to school closures [ 12 ]. According to some experts, the psychological consequences of COVID-19 are the ones that may persist for the longest and lead to a global mental health crisis [ 13 ]. The coronavirus outbreak is generating increased depressive symptoms, stress, anxiety, insomnia, denial, fear, and anger all over the world [ 2 , 14 ]. The economic, social, and psychological problems that people are currently facing are the consequences of novel challenges that have been posed by the pandemic.
The coronavirus outbreak is a novel, uncharted situation that has shaken the world and completely changed the everyday lives of many individuals. Due to the social distancing policy, many people have switched to remote work—in Poland, almost 75% of white-collar workers were fully or partially working from home from mid-March until the end of May 2020 [ 15 ]. School closures and remote learning imposed a new obligation on parents of supervising education, especially with younger children [ 16 ]. What is more, the government order of self-isolation forced people to spend almost all their time at home and limit or completely abandon human encounters. In addition, the deteriorating economic situation was the cause of financial hardship for many people. All these difficulties and challenges arose in the aura of a new, contagious disease with unexplored, long-lasting health effects and not fully known infectivity and lethality [ 17 ]. Dealing with the situation was not facilitated by the phenomenon of global misinformation, called by some experts as the “infodemic”, which may be defined as an overabundance of information that makes it difficult for people to find trustworthy sources and reliable guidance [ 18 ]. Studies have shown that people have multiple ways of reacting to a crisis: from radical and even violent practices, towards individual solutions and depression [ 19 ]. Not only the challenges arising from the COVID-19 pandemic but also the ways of reacting to it and coping with it are issues of paramount importance that are worth investigating.
The reactions to unusual crisis situations may be dependent on dispositional factors, such as trait anxiety or perceived control [ 20 , 21 ]. A study on reactions to Hurricane Hugo has shown that people with higher trait anxiety are more likely to develop posttraumatic symptoms following a natural disaster [ 20 ]. Moreover, lack of perceived control was shown to be positively related to the level of distress during an earthquake in Turkey [ 21 ]. According to some researchers, the COVID-19 crisis and natural disasters have much in common, as the emotions and behavior they cause are based on the same primal human emotion—fear [ 22 ]. Both pandemics and natural disasters disrupt people’s everyday lives and may have severe economic, social and psychological consequences [ 23 ]. However, despite many similarities to natural disasters, COVID-19 is a unique situation—only in 2020, the current pandemic has taken more lives than the world’s combined natural disasters in any of the past twenty years [ 24 ]. It needs to be noted that natural disasters may pose different challenges than health crises and for this reason, they may provoke disparate reactions [ 25 ]. Research on the reactions to former epidemics has shown that avoidance and safety behaviors, such as avoiding going out, visiting crowded places, and visiting hospitals, are widespread at such times [ 26 ]. When it comes to the ways of dealing with the current COVID-19 pandemic, a substantial part of the quantitative research on this issue focuses on coping mechanisms. Studies have shown that the most prevalent coping strategies are highly problem-focused [ 5 ]. Most people tend to listen to expert advice and behave calmly and appropriately in the face of the coronavirus outbreak [ 5 ]. Problem-focused coping is particularly characteristic of healthcare professionals. A study on Chinese nurses has shown that the closer the problem is to the person and the more fear it evokes, the more problem-focused coping strategy is used to deal with it [ 27 ]. On the other hand, a negative coping style that entails risky or aggressive behaviors, such as drug or alcohol use, is also used to deal with the challenges arising from the COVID-19 pandemic [ 28 ]. The factors that are correlated with negative coping include coronavirus anxiety, impairment, and suicidal ideation [ 28 ]. It is worth emphasizing that social support is a very important component of dealing with crises [ 29 ].
Scientists have attempted to systematize the reactions to difficult and unusual situations. One such concept is the “3 Cs” model created by Reich [ 30 ]. It accounts for the general rules of resilience in situations of stress caused by crises, such as natural disasters. The 3 Cs stand for: control (a belief that personal resources can be accessed to achieve valued goals), coherence (the human desire to make meaning of the world), and connectedness (the need for human contact and support) [ 30 ]. Polizzi and colleagues [ 22 ] reviewed this model from the perspective of the current COVID-19 pandemic. The authors claim that natural disasters and COVID-19 pandemic have much in common and therefore, the principles of resilience in natural disaster situations can also be used in the situation of the current pandemic [ 22 ]. They propose a set of coping behaviors that could be useful in times of the coronavirus outbreak, which include control (e.g., planning activities for each day, getting adequate sleep, limiting exposure to the news, and helping others), coherence (e.g., mindfulness and developing a coherent narrative on the event), and connectedness (e.g., establishing new relationships and caring for existing social bonds) [ 22 ].
Current study
The issue of the challenges arising from the current COVID-19 pandemic and the ways of coping with them is complex and many feelings accompanying these experiences may be unconscious and difficult to verbalize. Therefore, in order to explore and understand it deeply, qualitative methodology was applied. Although there were few qualitative studies on the reaction to the pandemic [e.g., 31 – 33 ], they did not capture the perception of the challenges and their changes that arise as the pandemic develops. Since the situation with the COVID-19 pandemic is very dynamic, the reactions to the various restrictions, orders or bans are evolving. Therefore, it was decided to conduct a qualitative longitudinal study with multiple interviews with the same respondents [ 34 ].
The study investigates the challenges arising from the current pandemic and the way people deal with them. The main aim of the project was to capture people’s reactions to the unusual and unexpected situation of the COVID-19 pandemic. Therefore, the project was largely exploratory in nature. Interviews with the participants at different stages of the epidemic allowed us to see a wide spectrum of problems and ways of dealing with them. The conducted study had three main research questions:
- What are the biggest challenges connected to the COVID-19 pandemic and the resulting restrictions?
- How are people dealing with the pandemic challenges?
- What are the ways of coping with the restrictions resulting from a pandemic change as it continues and develops (perspective of first 6 months)?
The study was approved by the institutional review board of the Faculty of Psychology University of Warsaw, Poland. All participants were provided written and oral information about the study, which included that participation was voluntary, that it was possible to withdraw without any consequences at any time, and the precautions that would be taken to protect data confidentiality. Informed consent was obtained from all participants. To ensure confidentiality, quotes are presented only with gender, age, and family status.
The study was based on qualitative methodology: individual in-depth interviews, s which are the appropriate to approach a new and unknown and multithreaded topic which, at the beginning of 2020, was the COVID-19 pandemic. Due to the need to observe respondents’ reactions to the dynamically changing situation of the COVID-19 pandemic, longitudinal study was used where the moderator met on-line with the same respondent several times, at specific time intervals. A longitudinal study was used to capture the changes in opinions, emotions, and behaviors of the respondents resulting from the changes in the external circumstances (qualitative in-depth interview tracking–[ 34 ]).
The study took place from the end of March to October 2020. Due to the epidemiological situation in the country interviews took place online, using the Google Meets online video platform. The audio was recorded and then transcribed. Before taking part in the project, the respondents were informed about the purpose of the study, its course, and the fact that participation in the project is voluntary, and that they will be able to withdraw from participation at any time. The respondents were not paid for taking part in the project.
Participants.
In total, 115 interviews were conducted with 20 participants (6 interviews with the majority of respondents). Two participants (number 11 and 19, S2 Table ) dropped out of the last two interviews, and one (number 6) dropped out of the last interview. The study was based on a purposive sample and the respondents differed in gender, age, education, family status, and work situation (see S2 Table ). In addition to demographic criteria intended to ensure that the sample was as diverse as possible, an additional criterion was to have a permanent Internet connection and a computer capable of online video interviewing. Study participants were recruited using the snowball method. They were distant acquaintances of acquaintances of individuals involved in the study. None of the moderators knew their interviewees personally.
A total of 10 men and 10 women participated in the study; their age range was: 25–55; the majority had higher education (17 respondents), they were people with different professions and work status, and different family status (singles, couples without children, and families with children). Such diversity of respondents allowed us to obtain information from different life perspectives. A full description of characteristics of study participants can be found in S2 Table .
Each interview took 2 hours on average, which gives around 240 hours of interviews. Subsequent interviews with the same respondents conducted at different intervals resulted from the dynamics of the development of the pandemic and the restrictions introduced in Poland by the government.
The interviews scenario took a semi-structured form. This allowed interviewers freely modify the questions and topics depending on the dynamics of the conversation and adapt the subject matter of the interviews not only to the research purposes but also to the needs of a given respondent. The interview guides were modified from week to week, taking into account the development of the epidemiological situation, while at the same time maintaining certain constant parts that were repeated in each interview. The main parts of the interview topic guide consisted of: (a) experiences from the time of previous interviews: thoughts, feeling, fears, and hopes; (b) everyday life—organization of the day, work, free time, shopping, and eating, etc.; (c) changes—what had changed in the life of the respondent from the time of the last interview; (d) ways of coping with the situation; and (e) media—reception of information appearing in the media. Additionally, in each interview there were specific parts, such as the reactions to the beginning of the pandemic in the first interview or the reaction to the specific restrictions that were introduced.
The interviews were conducted by 5 female interviewers with experience in moderating qualitative interviews, all with a psychological background. After each series of interviews, all the members of the research teams took part in debriefing sessions, which consisted of discussing the information obtained from each respondent, exchanging general conclusions, deciding about the topics for the following interview stage, and adjusting them to the pandemic situation in the country.
Data analysis.
All the interviews were transcribed in Polish by the moderators and then double-checked (each moderator transcribed the interviews of another moderator, and then the interviewer checked the accuracy of the transcription). The whole process of analysis was conducted on the material in Polish (the native language of the authors of the study and respondents). The final page count of the transcript is approximately 1800 pages of text. The results presented below are only a portion of the total data collected during the interviews. While there are about 250 pages of the transcription directly related to the topic of the article, due to the fact that the interview was partly free-form, some themes merge with others and it is not possible to determine the exact number of pages devoted exclusively to analysis related to the topic of the article. Full dataset can be found in S1 Dataset .
Data was then processed into thematic analysis, which is defined as a method of developing qualitative data consisting of the identification, analysis, and description of the thematic areas [ 35 ]. In this type of analysis, a thematic unit is treated as an element related to the research problem that includes an important aspect of data. An important advantage of thematic analysis is its flexibility, which allows for the adoption of the most appropriate research strategy to the phenomenon under analysis. An inductive approach was used to avoid conceptual tunnel vision. Extracting themes from the raw data using an inductive approach precludes the researcher from imposing a predetermined outcome.
As a first step, each moderator reviewed the transcripts of the interviews they had conducted. Each transcript was thematically coded individually from this point during the second and the third reading. In the next step, one of the researchers reviewed the codes extracted by the other members of the research team. Then she made initial interpretations by generating themes that captured the essence of the previously identified codes. The researcher created a list of common themes present in all of the interviews. In the next step, the extracted themes were discussed again with all the moderators conducting the coding in order to achieve consistency. This collaborative process was repeated several times during the analysis. Here, further superordinate (challenges of COVID-19 pandemic) and subordinate (ways of dealing with challenges) themes were created, often by collapsing others together, and each theme listed under a superordinate and subordinate category was checked to ensure they were accurately represented. Through this process of repeated analysis and discussion of emerging themes, it was possible to agree on the final themes that are described below.
Main challenges of the COVID-19 pandemic.
Challenge 1 –limitation of direct contact with people . The first major challenge of the pandemic was that direct contact with other people was significantly reduced. The lockdown forced many people to work from home and limit contact not only with friends but also with close family (parents, children, and siblings). Limiting contact with other people was a big challenge for most of our respondents, especially those who were living alone and for those who previously led an active social life. Depending on their earlier lifestyle profile, for some, the bigger problem was the limitation of contact with the family, for others with friends, and for still others with co-workers.
I think that because I can’t meet up with anyone and that I’m not in a relationship , I miss having sex , and I think it will become even more difficult because it will be increasingly hard to meet anyone . (5 . 3_ M_39_single) . The number In the brackets at the end of the quotes marks the respondent’s number (according to Table 1 ) and the stage of the interview (after the dash), further is information about gender (F/M), age of the respondent and family status. Linguistic errors in the quotes reflect the spoken language of the respondents.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0258133.t001
Changes over time . Over the course of the 6 months of the study, an evolution in the attitudes to the restriction of face-to-face contact could be seen: from full acceptance, to later questioning its rationale. Initially (March and April), almost all the respondents understood the reasons for the isolation and were compliant. At the beginning, people were afraid of the unknown COVID-19. They were concerned that the tragic situation from Italy, which was intensively covered in the media, could repeat itself in Poland (stage 1–2 of the study). However, with time, the isolation started to bother them more and more, and they started to look for solutions to bypass the isolation guidelines (stage 3–4), both real (simply meeting each other) and mental (treating isolation only as a guideline and not as an order, perceiving the family as being less threatening than acquaintances or strangers in a store). The turning point was the long May weekend that, due to two public holidays (1 st and 3 rd May), has for many years been used as an opportunity to go away with family or friends. Many people broke their voluntary isolation during that time encouraged by information about the coming loosening of restrictions.
During the summer (stage 5 of the survey), practically no one was fully compliant with the isolation recommendations anymore. At that time, a growing familiarity could be observed with COVID-19 and an increasing tendency to talk about it as “one of many diseases”, and to convince oneself that one is not at risk and that COVID-19 is no more threatening than other viruses. Only a small group of people consciously failed to comply with the restrictions of contact with others from the very beginning of the pandemic. This behavior was mostly observed among people who were generally less anxious and less afraid of COVID-19.
I’ve had enough. I’ve had it with sitting at home. Okay, there’s some kind of virus, it’s as though it’s out there somewhere; it’s like I know 2 people who were infected but they’re still alive, nothing bad has happened to anyone. It’s just a tiny portion of people who are dying. And is it really such a tragedy that we have to be locked up at home? Surely there’s an alternative agenda there? (17.4_F_35_Adult and child)
Ways of dealing . In the initial phase, when almost everyone accepted this restriction and submitted to it, the use of communication platforms for social meetings increased (see Ways of dealing with challenges in Table 1 ) . Meetings on communication platforms were seen as an equivalent of the previous face-to-face contact and were often even accompanied by eating or drinking alcohol together. However, over time (at around stage 4–5 of the study) people began to feel that such contact was an insufficient substitute for face-to-face meetings and interest in online meetings began to wane. During this time, however, an interesting phenomenon could be seen, namely, that for many people the family was seen as a safer environment than friends, and definitely safer than strangers. The belief was that family members would be honest about being sick, while strangers not necessarily, and—on an unconscious level—the feeling was that the “family is safe”, and the “family can’t hurt them”.
When it became clear that online communication is an insufficient substitute for face-to-face contacts, people started to meet up in real life. However, a change in many behaviors associated with meeting people is clearly visible, e.g.: refraining from shaking hands, refraining from cheek kissing to greet one another, and keeping a distance during a conversation.
I can’t really say that I could ‘feel’ Good Friday or Holy Saturday. On Sunday, we had breakfast together with my husband’s family and his sister. We were in three different places but we connected over Skype. Later, at noon, we had some coffee with my parents, also over Skype. It’s obvious though that this doesn’t replace face-to-face contact but it’s always some form of conversation. (9.3_F_25_Couple, no children)
Challenge 2 –restrictions on movement and travel . In contrast to the restrictions on contact with other people, the restrictions on movement and the closing of borders were perceived more negatively and posed bigger challenges for some people (especially those who used to do a lot of travelling). In this case, it was less clear why these regulations were introduced (especially travel restrictions within the country). Moreover, travel restrictions, particularly in the case of international travels, were associated with a limitation of civil liberties. The limitation (or complete ban) on travelling abroad in the Polish situation evoked additional connotations with the communist times, that is, with the fact that there was no freedom of movement for Polish citizens (associations with totalitarianism and dictatorship). Interestingly, the lack of acceptance of this restriction was also manifested by people who did not travel much. Thus, it was not just a question of restricting travelling abroad but more of restricting the potential opportunity (“even if I’m not planning on going anywhere, I know I still can”).
Limitations on travelling around the country were particularly negatively felt by families with children, where parents believe that regular exercise and outings are necessary for the proper development of their children. For parents, it was problematic to accept the prohibition of leaving the house and going to the playground (which remained closed until mid-May). Being outdoors was perceived as important for maintaining immunity (exercise as part of a healthy lifestyle), therefore, people could not understand the reason underlying this restriction and, as a consequence, often did not accept it.
I was really bothered by the very awareness that I can’t just jump in my car or get on a plane whenever I want and go wherever I want. It’s not something that I have to do on a daily basis but freedom of movement and travelling are very important for me. (14.2_M_55_Two adults and children)
Changes over time . The travel and movement limitations, although objectively less severe for most people, aroused much greater anger than the restrictions on social contact. This was probably due to a greater sense of misunderstanding as to why these rules were being introduced in the first place. Moreover, they were often communicated inconsistently and chaotically (e.g., a ban on entering forests was introduced while, at the same time, shopping malls remained open and masses were allowed to attend church services). This anger grew over time—from interview to interview, the respondents’ irritation and lack of acceptance of this was evident (culminating in the 3 rd -4 th stage of the study). The limitation of mobility was also often associated with negative consequences for both health and the economy. Many people are convinced that being in the open air (especially accompanied by physical activity) strengthens immunity, therefore, limiting such activity may have negative health consequences. Some respondents pointed out that restricting travelling, the use of hotels and restaurants, especially during the holiday season, will have serious consequences for the existence of the tourism industry.
I can’t say I completely agree with these limitations because it’s treating everything selectively. It’s like the shopping mall is closed, I can’t buy any shoes but I can go to a home improvement store and buy some wallpaper for myself. So I don’t see the difference between encountering people in a home improvement store and a shopping mall. (18.2_F_48_Two adults and children)
Ways of dealing . Since the restriction of movement and travel was more often associated with pleasure-related behaviors than with activities necessary for living, the compensations for these restrictions were usually also from the area of hedonistic behaviors. In the statements of our respondents, terms such as “indulging” or “rewarding oneself” appeared, and behaviors such as throwing small parties at home, buying better alcohol, sweets, and new clothes were observed. There were also increased shopping behaviors related to hobbies (sometimes hobbies that could not be pursued at the given time)–a kind of “post-pandemic” shopping spree (e.g., a new bike or new skis).
Again, the reaction to this restriction also depended on the level of fear of the COVID-19 disease. People who were more afraid of being infected accepted these restrictions more easily as it gave them the feeling that they were doing something constructive to protect themselves from the infection. Conversely, people with less fears and concerns were more likely to rebel and break these bans and guidelines.
Another way of dealing with this challenge was making plans for interesting travel destinations for the post-pandemic period. This was especially salient in respondents with an active lifestyle in the past and especially visible during the 5 th stage of the study.
Today was the first day when I went to the store (due to being in quarantine after returning from abroad). I spent loads of money but I normally would have never spent so much on myself. I bought sweets and confectionery for Easter time, some Easter chocolates, too. I thought I’d do some more baking so I also bought some ingredients to do this. (1.2_ F_25_single)
Challenge 3 –necessary change in active lifestyle . Many of the limitations related to COVID-19 were a challenge for people with an active lifestyle who would regularly go to the cinema, theater, and gym, use restaurants, and do a lot of travelling. For those people, the time of the COVID constraints has brought about huge changes in their lifestyle. Most of their activities were drastically restricted overnight and they suddenly became domesticated by force, especially when it was additionally accompanied by a transition to remote work.
Compulsory spending time at home also had serious consequences for people with school-aged children who had to confront themselves with the distance learning situation of their children. The second challenge for families with children was also finding (or helping find) activities for their children to do in their free time without leaving the house.
I would love to go to a restaurant somewhere. We order food from the restaurant at least once a week, but I’d love to go to the restaurant. Spending time there is a different way of functioning. It is enjoyable and that is what I miss. I would also go to the cinema, to the theater. (13.3_M_46_Two adults and child.)
Changes over time . The nuisance of restrictions connected to an active lifestyle depended on the level of restrictions in place at a given time and the extent to which a given activity could be replaced by an alternative. Moreover, the response to these restrictions depended more on the individual differences in lifestyle rather than on the stage of the interview (except for the very beginning, when the changes in lifestyle and everyday activities were very sudden).
I miss that these restaurants are not open . And it’s not even that I would like to eat something specific . It is in all of this that I miss such freedom the most . It bothers me that I have no freedom . And I am able to get used to it , I can cook at home , I can order from home . But I just wish I had a choice . (2 . 6_F_27_single ).
Ways of dealing . In the initial phase of the pandemic (March-April—stage 1–3 of the study), when most people were afraid of the coronavirus, the acceptance of the restrictions was high. At the same time, efforts were made to find activities that could replace existing ones. Going to the gym was replaced by online exercise, and going to the cinema or theater by intensive use of streaming platforms. In the subsequent stages of the study, however, the respondents’ fatigue with these “substitutes” was noticeable. It was then that more irritation and greater non-acceptance of certain restrictions began to appear. On the other hand, the changes or restrictions introduced during the later stages of the pandemic were less sudden than the initial ones, so they were often easier to get used to.
I bought a small bike and even before that we ordered some resistance bands to work out at home, which replace certain gym equipment and devices. […] I’m considering learning a language. From the other online things, my girlfriend is having yoga classes, for instance. (7.2_M_28_Couple, no children)
Challenge 4 –boredom , monotony . As has already been shown, for many people, the beginning of the pandemic was a huge change in lifestyle, an absence of activities, and a resulting slowdown. It was sometimes associated with a feeling of weariness, monotony, and even of boredom, especially for people who worked remotely, whose days began to be similar to each other and whose working time merged with free time, weekdays with the weekends, and free time could not be filled with previous activities.
In some way, boredom. I can’t concentrate on what I’m reading. I’m trying to motivate myself to do such things as learning a language because I have so much time on my hands, or to do exercises. I don’t have this balance that I’m actually doing something for myself, like reading, working out, but also that I’m meeting up with friends. This balance has gone, so I’ve started to get bored with many things. Yesterday I felt that I was bored and something should start happening. (…) After some time, this lack of events and meetings leads to such immense boredom. (1.5_F_25_single)
Changes over time . The feeling of monotony and boredom was especially visible in stage 1 and 2 of the study when the lockdown was most restrictive and people were knocked out of their daily routines. As the pandemic continued, boredom was often replaced by irritation in some, and by stagnation in others (visible in stages 3 and 4 of the study) while, at the same time, enthusiasm for taking up new activities was waning. As most people were realizing that the pandemic was not going to end any time soon, a gradual adaptation to the new lifestyle (slower and less active) and the special pandemic demands (especially seen in stage 5 and 6 of the study) could be observed.
But I see that people around me , in fact , both family and friends , are slowly beginning to prepare themselves for more frequent stays at home . So actually more remote work , maybe everything will not be closed and we will not be locked in four walls , but this tendency towards isolation or self-isolation , such a deliberate one , appears . I guess we are used to the fact that it has to be this way . (15 . 6_M_43_Two adults and child) .
Ways of dealing . The answer to the monotony of everyday life and to finding different ways of separating work from free time was to stick to certain rituals, such as “getting dressed for work”, even when work was only by a computer at home or, if possible, setting a fixed meal time when the whole family would gather together. For some, the time of the beginning of the pandemic was treated as an extra vacation. This was especially true of people who could not carry out their work during the time of the most severe restrictions (e.g., hairdressers and doctors). For them, provided that they believed that everything would return to normal and that they would soon go back to work, a “vacation mode” was activated wherein they would sleep longer, watch a lot of movies, read books, and generally do pleasant things for which they previously had no time and which they could now enjoy without feeling guilty. Another way of dealing with the monotony and transition to a slower lifestyle was taking up various activities for which there was no time before, such as baking bread at home and cooking fancy dishes.
I generally do have a set schedule. I begin work at eight. Well, and what’s changed is that I can get up last minute, switch the computer on and be practically making my breakfast and coffee during this time. I do some work and then print out some materials for my younger daughter. You know, I have work till four, I keep on going up to the computer and checking my emails. (19.1_F_39_Two adults and children)
Challenge 5 –uncertainty about the future . Despite the difficulties arising from the circumstances and limitations described above, it seems that psychologically, the greatest challenge during a pandemic is the uncertainty of what will happen next. There was a lot of contradictory information in the media that caused a sense of confusion and heightened the feeling of anxiety.
I’m less bothered about the changes that were put in place and more about this concern about what will happen in the future. Right now, it’s like there’s these mood swings. […] Based on what’s going on, this will somehow affect every one of us. And that’s what I’m afraid of. The fact that someone will not survive and I have no way of knowing who this could be—whether it will be me or anyone else, or my dad, if somehow the coronavirus will sneak its way into our home. I simply don’t know. I’m simply afraid of this. (10.1_F_55_Couple, no children)
Changes over time . In the first phase of the pandemic (interviews 1–3), most people felt a strong sense of not being in control of the situation and of their own lives. Not only did the consequences of the pandemic include a change in lifestyle but also, very often, the suspension of plans altogether. In addition, many people felt a strong fear of the future, about what would happen, and even a sense of threat to their own or their loved ones’ lives. Gradually (interview 4), alongside anxiety, anger began to emerge about not knowing what would happen next. At the beginning of the summer (stage 5 of the study), most people had a hope of the pandemic soon ending. It was a period of easing restrictions and of opening up the economy. Life was starting to look more and more like it did before the pandemic, fleetingly giving an illusion that the end of the pandemic was “in sight” and the vision of a return to normal life. Unfortunately, autumn showed that more waves of the pandemic were approaching. In the interviews of the 6 th stage of the study, we could see more and more confusion and uncertainty, a loss of hope, and often a manifestation of disagreement with the restrictions that were introduced.
This is making me sad and angry. More angry, in fact. […] I don’t know what I should do. Up until now, there was nothing like this. Up until now, I was pretty certain of what I was doing in all the decisions I was making. (14.4_M_55_Two adults and children)
Ways of dealing . People reacted differently to the described feeling of insecurity. In order to reduce the emerging fears, some people searched (sometimes even compulsively) for any information that could help them “take control” of the situation. These people searched various sources, for example, information on the number of infected persons and the number of deaths. This knowledge gave them the illusion of control and helped them to somewhat reduce the anxiety evoked by the pandemic. The behavior of this group was often accompanied by very strict adherence to all guidelines and restrictions (e.g., frequent hand sanitization, wearing a face mask, and avoiding contact with others). This behavior increased the sense of control over the situation in these people.
A completely opposite strategy to reducing the feeling of uncertainty which we also observed in some respondents was cutting off information in the media about the scale of the disease and the resulting restrictions. These people, unable to keep up with the changing information and often inconsistent messages, in order to maintain cognitive coherence tried to cut off the media as much as possible, assuming that even if something really significant had happened, they would still find out.
I want to keep up to date with the current affairs. Even if it is an hour a day. How is the pandemic situation developing—is it increasing or decreasing. There’s a bit of propaganda there because I know that when they’re saying that they have the situation under control, they can’t control it anyway. Anyhow, it still has a somewhat calming effect that it’s dying down over here and that things aren’t that bad. And, apart from this, I listen to the news concerning restrictions, what we can and can’t do. (3.1_F_54_single)
Discussion and conclusions
The results of our study showed that the five greatest challenges resulting from the COVID-19 pandemic are: limitations of direct contact with people, restrictions on movement and travel, change in active lifestyle, boredom and monotony, and finally uncertainty about the future. As we can see the spectrum of problems resulting from the pandemic is very wide and some of them have an impact on everyday functioning and lifestyle, some other influence psychological functioning and well-being. Moreover, different people deal with these problems differently and different changes in everyday life are challenging for them. The first challenge of the pandemic COVID-19 problem is the consequence of the limitation of direct contact with others. This regulation has very strong psychological consequences in the sense of loneliness and lack of closeness. Initially, people tried to deal with this limitation through the use of internet communicators. It turned out, however, that this form of contact for the majority of people was definitely insufficient and feelings of deprivation quickly increased. As much data from psychological literature shows, contact with others can have great psychological healing properties [e.g., 29 ]. The need for closeness is a natural need in times of crisis and catastrophes [ 30 ]. Unfortunately, during the COVID-19 pandemic, the ability to meet this need was severely limited by regulations. This led to many people having serious problems with maintaining a good psychological condition.
Another troubling limitation found in our study were the restrictions on movement and travel, and the associated restrictions of most activities, which caused a huge change in lifestyle for many people. As shown in previous studies, travel and diverse leisure activities are important predictors of greater well-being [ 36 ]. Moreover, COVID-19 pandemic movement restrictions may be perceived by some people as a threat to human rights [ 37 ], which can contribute to people’s reluctance to accept lockdown rules.
The problem with accepting these restrictions was also related to the lack of understanding of the reasons behind them. Just as the limitation in contact with other people seemed understandable, the limitations related to physical activity and mobility were less so. Because of these limitations many people lost a sense of understanding of the rules and restrictions being imposed. Inconsistent communication in the media—called by some researchers the ‘infodemic’ [ 18 ], as well as discordant recommendations in different countries, causing an increasing sense of confusion in people.
Another huge challenge posed by the current pandemic is the feeling of uncertainty about the future. This feeling is caused by constant changes in the rules concerning daily functioning during the pandemic and what is prohibited and what is allowed. People lose their sense of being in control of the situation. From the psychological point of view, a long-lasting experience of lack of control can cause so-called learned helplessness, a permanent feeling of having no influence over the situation and no possibility of changing it [ 38 ], which can even result in depression and lower mental and physical wellbeing [ 39 ]. Control over live and the feeling that people have an influence on what happens in their lives is one of the basic rules of crisis situation resilience [ 30 ]. Unfortunately, also in this area, people have huge deficits caused by the pandemic. The obtained results are coherent with previous studies regarding the strategies harnessed to cope with the pandemic [e.g., 5 , 10 , 28 , 33 ]. For example, some studies showed that seeking social support is one of the most common strategies used to deal with the coronavirus pandemic [ 33 , 40 ]. Other ways to deal with this situation include distraction, active coping, and a positive appraisal of the situation [ 41 ]. Furthermore, research has shown that simple coping behaviors such as a healthy diet, not reading too much COVID-19 news, following a daily routine, and spending time outdoors may be protective factors against anxiety and depressive symptoms in times of the coronavirus pandemic [ 41 ].
This study showed that the acceptance of various limitations, and especially the feeling of discomfort associated with them, depended on the person’s earlier lifestyle. The more active and socializing a person was, the more restrictions were burdensome for him/her. The second factor, more of a psychological nature, was the fear of developing COVID-19. In this case, people who were more afraid of getting sick were more likely to submit to the imposed restrictions that, paradoxically, did not reduce their anxiety, and sometimes even heightened it.
Limitations of the study.
While the study shows interesting results, it also has some limitations. The purpose of the study was primarily to capture the first response to problems resulting from a pandemic, and as such its design is not ideal. First, the study participants are not diverse as much as would be desirable. They are mostly college-educated and relatively well off, which may influence how they perceive the pandemic situation. Furthermore, the recruitment was done by searching among the further acquaintances of the people involved in the study, so there is a risk that all the people interviewed come from a similar background. It would be necessary to conduct a study that also describes the reaction of people who are already in a more difficult life situation before the pandemic starts.
Moreover, it would also be worthwhile to pay attention to the interviewers themselves. All of the moderators were female, and although gender effects on the quality of the interviews and differences between the establishment of relationships between women and men were not observed during the debriefing process, the topic of gender effects on the results of qualitative research is frequently addressed in the literature [ 42 , 43 ]. Although the researchers approached the process with reflexivity and self-criticism at all stages, it would have seemed important to involve male moderators in the study to capture any differences in relationship dynamics.
Practical implications.
The study presented has many practical implications. Decision-makers in the state can analyze the COVID-19 pandemic crisis in a way that avoids a critical situation involving other infectious diseases in the future. The results of our study showing the most disruptive effects of the pandemic on people can serve as a basis for developing strategies to deal with the effects of the crisis so that it does not translate into a deterioration of the public’s mental health in the future.
The results of our study can also provide guidance on how to communicate information about restrictions in the future so that they are accepted and respected (for example by giving rational explanations of the reasons for introducing particular restrictions). In addition, the results of our study can also be a source of guidance on how to deal with the limitations that may arise in a recurrent COVID-19 pandemic, as well as other emergencies that could come.
The analysis of the results showed that the COVID-19 pandemic, and especially the lockdown periods, are a particular challenge for many people due to reduced social contact. On the other hand, it is social contacts that are at the same time a way of a smoother transition of crises. This knowledge should prompt decision-makers to devise ways to ensure pandemic safety without drastically limiting social contacts and to create solutions that give people a sense of control (instead of depriving it of). Providing such solutions can reduce the psychological problems associated with a pandemic and help people to cope better with it.
Conclusions
As more and more is said about the fact that the COVID-19 pandemic may not end soon and that we are likely to face more waves of this disease and related lockdowns, it is very important to understand how the different restrictions are perceived, what difficulties they cause and what are the biggest challenges resulting from them. For example, an important element of accepting the restrictions is understanding their sources, i.e., what they result from, what they are supposed to prevent, and what consequences they have for the fight against the pandemic. Moreover, we observed that the more incomprehensible the order was, the more it provoked to break it. This means that not only medical treatment is extremely important in an effective fight against a pandemic, but also appropriate communication.
The results of our study showed also that certain restrictions cause emotional deficits (e.g., loneliness, loss of sense of control) and, consequently, may cause serious problems with psychological functioning. From this perspective, it seems extremely important to understand which restrictions are causing emotional problems and how they can be dealt with in order to reduce the psychological discomfort associated with them.
Supporting information
S1 table. a full description of the changes occurring in poland at the time of the study..
https://doi.org/10.1371/journal.pone.0258133.s001
S2 Table. Characteristics of study participants.
https://doi.org/10.1371/journal.pone.0258133.s002
S1 Dataset. Transcriptions from the interviews.
https://doi.org/10.1371/journal.pone.0258133.s003
- 1. JHU CSEE. COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020 [cited 2021 Jun 1]. https://github.com/CSSEGISandData/COVID-19#covid-19-data-repository-by-the-center-for-systems-science-and-engineering-csse-at-johns-hopkins-university .
- View Article
- PubMed/NCBI
- Google Scholar
- 5. Gerhold L. COVID-19: Risk perception and coping strategies. Results from a survey in Germany. PsyArXiv [Preprint]. 2020 Mar 25.
- 6. Nowakowska K. Rok z koronawirusem: Od paniki, przez luz, do fatalizmu. [A year with coronavirus—from panic through chill to fatalism]. Dziennik Gazeta Prawna [Internet]. 2021 Mar 4 [cited 2021 Jun 1]. https://www.gazetaprawna.pl/wiadomosci/kraj/artykuly/8111858,szczepienia-maseczki-rok-z-koronawirusem-zycie-codzienne.html
- 11. Fernandes N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. IESE Business School Working Paper No. WP-1240-E. 2020 Mar 23.
- 15. ARC. Praca z domu w polskim wydaniu—badanie na zlecenie Gumtree.pl we współpracy z Randstat Polska [The Polish way of working from home—a study commissioned by Gumtree.pl in collaboration with Randstat Polska]. 2020 [cited 2021 Jun 1]. https://www.randstad.pl/strefa-pracownika/centrum-prasowe/badanie-gumtreepl-we-wspolpracy-z-randstad-potrafimy-sie-zorganizowac-choc-czasem-lubimy-sobie-poprzeszkadzac-praca-z-domu-w-polskim-wydaniu/
- 16. Sierpowska, I. O edukacji w czasie pandemii [On Education during pandemic]. Centrum Prasowe SWPS [Internet]. 2020 Sep 8. [cited 2021 Jun 1]. https://www.swps.pl/centrum-prasowe/informacje-prasowe/22390-o-edukacji-w-czasie-pandemii-2?dt=1622540060078
- 17. Polish Academy of Sciences. Understanding COVID-19. Report by the COVID-19 team at the President of the Polish Academy of Sciences. 2020 Sep 14. [Cited 2021 Jun 1]. https://informacje.pan.pl/images/2020/opracowanie-covid19-14-09-2020/ZrozumiecCovid19_opracowanie_PAN.pdf
- 25. Brown, K. The pandemic is not a natural disaster. The New Yorker [Internet]. 2020 Apr 13 [cited 2021 Jun 1]. https://www.newyorker.com/culture/annals-of-inquiry/the-pandemic-is-not-a-natural-disaster .
- 34. Maison D. Qualitative marketing research. Understanding consumer behaviour. London: Routledge; 2019.
- 36. Argyle M. Causes and correlates of happiness. In: Kahneman D, Diener E, Schwarz N, editors. Well-Being: The Foundations of Hedonic Psychology. New York: Russell Sage Foundation; 1999. p. 353–373.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 10, Issue 12
- Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0180-0213 Anam Shahil Feroz 1 , 2 ,
- Naureen Akber Ali 3 ,
- Noshaba Akber Ali 1 ,
- Ridah Feroz 4 ,
- Salima Nazim Meghani 1 ,
- Sarah Saleem 1
- 1 Community Health Sciences , Aga Khan University , Karachi , Pakistan
- 2 Institute of Health Policy, Management and Evaluation , University of Toronto , Toronto , Ontario , Canada
- 3 School of Nursing and Midwifery , Aga Khan University , Karachi , Pakistan
- 4 Aga Khan University Institute for Educational Development , Karachi , Pakistan
- Correspondence to Ms Anam Shahil Feroz; anam.sahyl{at}gmail.com
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours, myths and inaccurate information about the virus are spreading rapidly, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes of community members towards COVID-19 and its impact on their daily lives and mental well-being.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. The study will be conducted in the Karimabad Federal B Area and in the Garden (East and West) community settings in Karachi, Pakistan. The community members of these areas have been selected purposively for the interview. Study data will be analysed thematically using NVivo V.12 Plus software.
Ethics and dissemination Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The results of the study will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
- mental health
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-041641
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The mental health impact of the COVID-19 pandemic is likely to last much longer than the physical health impact, and this study is positioned well to explore the perceptions and attitudes of community members towards the pandemic and its impact on their daily lives and mental well-being.
This study will guide the development of context-specific innovative mental health programmes to support communities in the future.
One limitation is that to minimise the risk of infection all study respondents will be interviewed online over Zoom and hence the authors will not have the opportunity to build rapport with the respondents or obtain non-verbal cues during interviews.
The COVID-19 pandemic has affected almost 180 countries since it was first detected in Wuhan, China in December 2019. 1 2 The COVID-19 outbreak has been declared a public health emergency of international concern by the WHO. 3 The WHO estimates the global mortality to be about 3.4% 4 ; however, death rates vary between countries and across age groups. 5 In Pakistan, a total of 10 880 cases and 228 deaths due to COVID-19 infection have been reported to date. 6
The worldwide COVID-19 pandemic has not only incurred massive challenges to the global supply chains and healthcare systems but also has a detrimental effect on the overall health of individuals. 7 The pandemic has led to lockdowns and has created destructive impact on the societies at large. Most company employees, including daily wage workers, have been prohibited from going to their workplaces or have been asked to work from home, which has caused job-related insecurities and financial crises in the communities. 8 Educational institutions and training centres have also been closed, which resulted in children losing their routine of going to schools, studying and socialising with their peers. Delay in examinations is likewise a huge stressor for students. 8 Alongside this, parents have been struggling with creating a structured milieu for their children. 9 COVID-19 has hindered the normal routine life of every individual, be it children, teenagers, adults or the elderly. The crisis is engendering burden throughout populations and communities, particularly in developing countries such as Pakistan which face major challenges due to fragile healthcare systems and poor economic structures. 10
The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. 8 Further, the highly contagious nature of COVID-19 has also escalated confusion, fear and panic among community residents. Moreover, social distancing is often an unpleasant experience for community members and for patients as it adds to mental suffering, particularly in the local setting where get-togethers with friends and families are a major source of entertainment. 9 Recent studies also showed that individuals who are following social distancing rules experience loneliness, causing a substantial level of distress in the form of anxiety, stress, anger, misperception and post-traumatic stress symptoms. 8 11 Separation from family members, loss of autonomy, insecurity over disease status, inadequate supplies, inadequate information, financial loss, frustration, stigma and boredom are all major stressors that can create drastic impact on an individual’s life. 11 Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. 12 With the widespread use of social media, 13 rumours, myths and inaccurate information about COVID-19 are also spreading rapidly, not only among adults but are also carried on to children, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. 9 The psychological symptoms associated with COVID-19 at the community level are also manifested as anxiety-driven panic buying, resulting in exhaustion of resources from the market. 14 Some level of panic also dwells in the community due to the unavailability of essential protective equipment, particularly masks and sanitisers. 15 Similarly, mental health issues, including depression, anxiety, panic attacks, psychotic symptoms and even suicide, were reported during the early severe acute respiratory syndrome outbreak. 16 17 COVID-19 is likely posing a similar risk throughout the world. 12
The fear of transmitting the disease or a family member falling ill is a probable mental function of human nature, but at some point the psychological fear of the disease generates more anxiety than the disease itself. Therefore, mental health problems are likely to increase among community residents during an epidemic situation. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes towards COVID-19 among community residents and the impact of these perceptions and attitude on their daily lives and mental well-being.
Methods and analysis
Study design.
This study will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews (IDIs) with community members. The IDIs aim to explore perceptions of community members towards COVID-19 and its impact on their mental well-being.
Study setting and study participants
The study will be conducted in two communities in Karachi City: Karimabad Federal B Area Block 3 Gulberg Town, and Garden East and Garden West. Karimabad is a neighbourhood in the Karachi Central District of Karachi, Pakistan, situated in the south of Gulberg Town bordering Liaquatabad, Gharibabad and Federal B Area. The population of this neighbourhood is predominantly Ismailis. People living here belong mostly to the middle class to the lower middle class. It is also known for its wholesale market of sports goods and stationery. Garden is an upmarket neighbourhood in the Karachi South District of Karachi, Pakistan, subdivided into two neighbourhoods: Garden East and Garden West. It is the residential area around the Karachi Zoological Gardens; hence, it is popularly known as the ‘Garden’ area. The population of Garden used to be primarily Ismailis and Goan Catholics but has seen an increasing number of Memons, Pashtuns and Baloch. These areas have been selected purposively because the few members of these communities are already known to one of the coinvestigators. The coinvestigator will serve as a gatekeeper for providing entrance to the community for the purpose of this study. Adult community members of different ages and both genders will be interviewed from both sites, as mentioned in table 1 . Interview participants will be selected following the eligibility criteria.
- View inline
Study participants for indepth interviews
IDIs with community members
We will conduct IDIs with community members to explore the perceptions and attitudes of community members towards COVID-19 and its effects on their daily lives and mental well-being. IDI participants will be identified via the community WhatsApp group, and will be invited for an interview via a WhatsApp message or email. Consent will be taken over email or WhatsApp before the interview begins, where they will agree that the interview can be audio-recorded and that written notes can be taken. The interviews will be conducted either in Urdu or in English language, and each interview will last around 40–50 min. Study participants will be assured that their information will remain confidential and that no identifying features will be mentioned on the transcript. The major themes will include a general discussion about participants’ knowledge and perceptions about the COVID-19 pandemic, perceptions on safety measures, and perceived challenges in the current situation and its impact on their mental well-being. We anticipate that 24–30 interviews will be conducted, but we will cease interviews once data saturation has been achieved. Data saturation is the point when no new themes emerge from the additional interviews. Data collection will occur concurrently with data analysis to determine data saturation point. The audio recordings will be transcribed by a transcriptionist within 24 hours of the interviews.
An interview guide for IDIs is shown in online supplemental annex 1 .
Supplemental material
Eligibility criteria.
The following are the criteria for inclusion and exclusion of study participants:
Inclusion criteria
Residents of Garden (East and West) and Karimabad Federal B Area of Karachi who have not contracted the disease.
Exclusion criteria
Those who refuse to participate in the study.
Those who have experienced COVID-19 and are undergoing treatment.
Those who are suspected for COVID-19 and have been isolated/quarantined.
Family members of COVID-19-positive cases.
Data collection procedure
A semistructured interview guide has been developed for community members. The initial questions on the guide will help to explore participants’ perceptions and attitudes towards COVID-19. Additional questions on the guide will assess the impact of these perceptions and attitude on the daily lives and mental health and well-being of community residents. All semistructured interviews will be conducted online via Zoom or WhatsApp. Interviews will be scheduled at the participant’s convenient day and time. Interviews are anticipated to begin on 1 December 2020.
Patient and public involvement
No patients were involved.
Data analysis
We will transcribe and translate collected data into English language by listening to the audio recordings in order to conduct a thematic analysis. NVivo V.12 Plus software will be used to import, organise and explore data for analysis. Two independent researchers will read the transcripts at various times to develop familiarity and clarification with the data. We will employ an iterative process which will help us to label data and generate new categories to identify emergent themes. The recorded text will be divided into shortened units and labelled as a ‘code’ without losing the main essence of the research study. Subsequently, codes will be analysed and merged into comparable categories. Lastly, the same categories will be grouped into subthemes and final themes. To ensure inter-rater reliability, two independent investigators will perform the coding, category creation and thematic analyses. Discrepancies between the two investigators will be resolved through consensus meetings to reduce researcher bias.
Ethics and dissemination
Study participants will be asked to provide informed, written consent prior to participation in the study. The informed consent form can be submitted by the participant via WhatsApp or email. Participants who are unable to write their names will be asked to provide a thumbprint to symbolise their consent to participate. Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The study results will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
The findings of this study will help us to explore the perceptions and attitudes towards the COVID-19 pandemic and its impact on the daily lives and mental well-being of individuals in the community. Besides, an indepth understanding of the needs of the community will be identified, which will help us develop context-specific innovative mental health programmes to support communities in the future. The study will provide insights into how communities are managing their lives under such a difficult situation.
- World Health Organization
- Nielsen-Saines K , et al
- Worldometer
- Ebrahim SH ,
- Gozzer E , et al
- Snoswell CL ,
- Harding LE , et al
- Nargis Asad
- van Weel C ,
- Qidwai W , et al
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Tripathy S ,
- Kar SK , et al
- Schwartz J ,
- Maunder R ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
ASF and NAA are joint first authors.
Contributors ASF and NAA conceived the study. ASF, NAA, RF, NA, SNM and SS contributed to the development of the study design and final protocols for sample selection and interviews. ASF and NAA contributed to writing the manuscript. All authors reviewed and approved the final version of the paper.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 06 June 2024
“The genie is out of the bottle”: a qualitative study on the impact of COVID-19 on continuing professional development
- Sophie Soklaridis 1 , 2 , 3 , 4 , 11 ,
- Rowen Shier 1 ,
- Rabia Zaheer 1 ,
- Michelle Scully 1 ,
- Betsy Williams 5 , 6 , 7 ,
- Sam J. Daniel 8 , 10 ,
- Sanjeev Sockalingam 1 , 2 , 4 ,
- Linda Dang 9 &
- Martin Tremblay 10
BMC Medical Education volume 24 , Article number: 631 ( 2024 ) Cite this article
262 Accesses
Metrics details
The onset of the COVID-19 pandemic catalysed a monumental shift in the field of continuing professional development (CPD). Prior to this, the majority of CPD group-learning activities were offered in-person. However, the pandemic forced the field to quickly pivot towards more novel methods of learning and teaching in view of social distancing regulations. The purpose of this study was to obtain the perspectives of CPD leaders on the impact of the pandemic to elucidate trends, innovations, and potential future directions in the field.
Semi-structured interviews were conducted between April-September 2022 with 23 CPD leaders from Canada and the USA. Interviews were audio-recorded, transcribed, and de-identified. A thematic analysis approach was used to analyse the data and generate themes.
Participants characterised COVID-19 as compelling widespread change in the field of CPD. From the interviews, researchers generated six themes pertaining to the impact of the pandemic on CPD: (1) necessity is the mother of innovation, (2) the paradox of flexibility and accessibility, (3) we’re not going to unring the bell, (4) reimagining design and delivery, (5) creating an evaluative culture, and (6) a lifeline in times of turmoil.
This qualitative study discusses the impact of the pandemic on the field of CPD and leaders’ vision for the future. Despite innumerable challenges, the pandemic created opportunities to reform design and delivery. Our findings indicate a necessity to maintain an innovative culture to best support learners, to improve the healthcare system, and to prepare for future emergencies.
Peer Review reports
Continuing professional development (CPD) in the health professions comprises education activities which serve to maintain, develop, and/or increase health professionals’ competence and performance [ 1 , 2 ]. Research suggests that CPD is integral to safe and effective practice, and that a lack of engagement in CPD activities results in risks to patients, staff, and organisations [ 3 ].
With the global onset of the Coronavirus disease 2019 (COVID-19) pandemic in March 2020, the field of CPD was met with unprecedented disruption, echoing the turmoil felt across society. Prior to this, formal CPD opportunities were predominantly provided in person, through conferences, courses, seminars, workshops, and grand rounds [ 4 ]. Similarly, informal CPD activities traditionally took place through person-to-person mentoring, coaching [ 5 ], or membership in a community of practice [ 6 ]. Despite an abundance of promising digital technology pre-pandemic, CPD organisations largely exhibited resistance towards embracing novel delivery methods [ 7 ]. However, with the advent of COVID-19, ushering in an era of self-isolation and physical-distancing measures [ 8 ], CPD providers were compelled to adapt their approach to delivery and accreditation [ 9 ]. The urgency of this transformation was further elevated by the centrality of CPD in equipping clinicians with credible information and the necessary skills to navigate the evolving health crisis [ 10 ]. In this qualitative study, we conducted semi-structured interviews with leaders in the field of CPD across Canada and the USA to understand the trends and innovations in teaching and learning that emerged from the pandemic and to explore how leaders imagine the future of CPD education. We discuss shifting attitudes and the emergence of new priority areas. This work contributes significantly to the literature by illuminating the field’s own standpoint on its successes and shortcomings during the pandemic and ambitions for the future. We note that at the time of writing of this article the World Health Organization has declared an end to COVID-19 as a Public Health Emergency of International Concern [ 11 ], likewise there appears to be a prevailing trend to downplay the pandemic as a past tense phenomenon in an effort to return to a semblance of normalcy [ 12 ]. However, the implications of the pandemic for CPD continue to reshape the landscape, necessitating ongoing adaptations and an enduring commitment to address the evolving needs of clinician learners.
Given the exploratory nature of our study, a qualitative research design was chosen as the most appropriate method for eliciting the perspectives of CPD leaders.
Participants and recruitment
To meet the inclusion criteria, participants had to be: (1) CPD leaders, (2) work in Canada or the USA, and (3) be fluent in written and verbal English. Our criteria for a “CPD leader” included involvement in CPD scholarship (discovery, integration, application, and/or teaching) [ 13 ], while holding a formal leadership position or having 10 + years of experience in the field.
A total of 23 participants were recruited using purposive and convenience sampling [ 14 ]. This combined approach allowed us to specifically recruit individuals with expertise in CPD leadership and the knowledge needed to answer our research question. It also provided an opportunity to ask individuals within our professional network to suggest colleagues who might be interested in participating in our study. To capture variability and diversity in perspectives, participants were selected from a range of institutions (universities, colleges, and academic health centres) and geographical regions from Canada (British Columbia, Manitoba, Nova Scotia, Ontario, Quebec) and the USA (California, Illinois, Kentucky, Maryland, Ohio, Tennessee, Wisconsin). Participants’ experience in the field ranged from 2 to 35 years, and multiple participants ( n = 12) held dual roles as CPD professionals and medical doctors.
Prospective participants were contacted by the principal investigator (SSok) through email to inform them about the study. Interested participants were thereupon forwarded to a member of the research team (RS, RZ), who was not known to them and had no affiliation with any of the CPD offices, to recruit and initiate the consent and interview process.
Data collection
Interviews, approximately 60 min in length, were conducted between April and September 2022 by two members of the research team (RS, RZ) via WebEx video conferencing [ 15 ]. Research Electronic Data Capture (REDCap), a secure web-based software platform, was used to obtain e-consent from participants [ 16 , 17 ]. Interviews were audio-recorded, transcribed, and de-identified. Quotes included in this article convey key messages from the wider data set and have been lightly edited for clarity. Open-ended interview questions covered topics including: (1) How has COVID-19 disrupted CPD? (2) How are CPD organisations adapting to the new reality? and (3) Potential future directions in CPD? (See Additional file 1 for the complete set of interview questions).
Data analysis
We conducted a thematic analysis using the six-step process detailed by Braun and Clarke [ 18 ]. After a familiarisation period, authors (RS, RZ, SSok) independently reviewed a subset of transcripts before collaboratively generating an initial codebook. Subsequently, all 23 transcripts were uploaded into Dedoose 9.0.54 qualitative-analysis software [ 19 ] and coded by authors LD, MS, and RS. Authors (LD, MS, RS, RZ, SSok) met routinely to discuss coding, reflexive memos, and to identify recurring patterns in the data. Next, authors (BW, LD, MS, MT, RS, RZ, SSok) organised codes into preliminary themes, ensuring that all codes captured under one theme were interrelated. Iterative re-coding and analysis were performed to refine themes until they were reflective of the complete data set. This article presents a subset of the data gathered during the study. A portion of the data was separately published in consideration of its distinctive thematic elements warranting detailed examination [ 20 ].
Trustworthiness
In this study we employed intercoder reliability [ 21 ], negative case analysis [ 22 ], and reflexivity [ 23 ] to enhance the trustworthiness of our analysis. Double-coding was implemented for the first three transcripts until coder consensus was established. Throughout coding and analysis, authors (LD, MS, RS, RZ) engaged in reflexive memoing to extract meaning from the data, promote critical thinking, and enhance team dialogue [ 24 ]. Furthermore, given our diverse personal and professional identities, we frequently engaged in discussion to determine appropriate research paradigms for our research objectives and to investigate our collective subjectivity [ 25 ].
Research Ethics Board approval was obtained from the Centre for Addiction and Mental Health (REB 023/2021).
From the data, we generated six themes related to the impact of the pandemic on CPD organisations: (1) necessity is the mother of innovation, (2) the paradox of flexibility and accessibility, (3) we’re not going to unring the bell, (4) reimagining design and delivery, (5) creating an evaluative culture, and (6) a lifeline in times of turmoil (See Table 1 ).
Theme 1: necessity is the mother of innovation
According to our participants, prior to the pandemic, there was widespread reluctance within CPD to deviate from ‘traditional’ ways of delivery, namely in-person education. The field showed little inclination towards the integration of emerging technologies or alternative educational approaches, holding firm in a ‘don’t fix what isn’t broken’ mentality.
“Healthcare providers are initially very resistant to new technology; we don’t want to play with new technology. We only want ‘safe’ stuff.” – P015.
The disruptions of the pandemic engendered a need for adaptation within CPD organisations. Many participants commented that change was long overdue, specifying that the required tools and technologies already existed, however, implementation had been limited. Against this setting, the pandemic brought forth an opportunity to leverage these preexisting innovations.
“Technology was already disrupting but people had a choice […] COVID took those choices away. It accelerated the use of technologies that already existed which people were struggling to get deployed.” – P008. “I guess if you say, necessity is the mother of invention, we innovated. But it’s not so much innovation as it was in some cases, we were just forced to use the tools that were there in order to connect and interact.” – P013.
Participants noted that the pandemic fundamentally shifted decision-making mechanisms within their organisations. For CPD course developers this comprised the implementation of rapid knowledge dissemination strategies and swift determinations regarding modalities and formats. Similarly, CPD accreditors created rapid response teams to expedite their procedures. Thus, previously arduous hierarchical processes were replaced with rapid and targeted decision-making approaches.
“We didn’t have the luxury of saying, okay, we can work three months with a planning committee. Everything we did in terms of identifying subject matter experts, how we engage them, the frequency we engage them, all of our processes that were tried and true for so many years, we just had to stop and re-design given this environment. I think that’s innovation.” – P002.
However, as illustrated by one participant, as the health crisis has waned, some of the conventional hierarchical practices in CPD have begun to resurface:
“In the beginning I think there was more space for innovation because a lot of the hierarchy that goes along with decision making within any institution was taken away because people realised that you had to do things, and you had to do things quickly. Some of that hierarchy has come back now.” – P007.
Nevertheless, participants determined that the pandemic imposed a much-needed shift in prevailing attitudes towards innovation:
“In the past when you brought those [technologies] up, people’s eyes glazed over […] Now they’re like, oh really, I could do that? I can operate an anaesthesia machine remotely? Tell me more! Before it was, you’ve got to be kidding me, that’s dangerous.” – P008.
Theme 2: the paradox of flexibility and accessibility
The response to virtual learning was mixed. CPD providers faced many challenges as they navigated unfamiliar technology, striving to make the content both meaningful and engaging. Additionally, concerns emerged about the potential loss of ‘hands-on’ experience, prompting questions about pedagogical quality and transferability:
“Some of it we have noticed from the residents that have been coming through, and certainly from the course that I developed, I think people are missing out on some of the hands-on training that virtual CPD cannot provide.” – P023.
Despite pedagogical uncertainties, there appeared to be a marked rise in CPD programming attendance, with many attributing this to increased accessibility and flexibility. The pivot towards virtual CPD offerings enabled participation from a broader community of clinicians in ways that were not possible pre-pandemic. Notably, some participants described how virtual platforms enhanced accessibility.
“The good thing has been the reach. Many of the providers are saying that they’ve been able to reach individual learners and audiences, including those internationally and in more rural areas that we were not able to reach before.” – P002. “For example, in India, women emergency physicians are never resourced to go to international conferences. The guys go, and the women stay behind and man the fort. Having something remote can provide access to education.” – P016. “For our young membership it’s good because they can attend even if they have a baby at home.” – P012.
Furthermore, one participant highlighted the utility of virtual CPD for learners with diverse learning needs:
“There are people that have hearing disabilities that really appreciate being online, as it’s a controlled environment […] They can really focus and concentrate on what is being said, and with the addition of subtitles, it’s really reducing some accessibility challenges.” – P019.
In contrast, some participants were less optimistic about virtual education. Although women were cited as potential benefactors of virtual CPD, they were also asymmetrically burdened by household and parental obligations during the pandemic, thus limiting their capacity to meaningfully engage in CPD.
“Women’s work was impacted significantly for clinicians and non-clinicians, because even though we talk about equality and we’re working outside our homes, we still do far more at home. I could give you examples of two or three PhD researchers in CPD who I had meetings with, and their partner got the good computer, the office, the quiet space in the basement, and they were in the TV room with SpongeBob playing […] I suspect when we look at the literature we’ll discover that a lot of guys wrote papers during COVID, and a lot of women just didn’t have the bandwidth.” – P016.
Moreover, participants signalled the challenges that older clinicians experienced with the rapid introduction of new technologies:
“A lot of our senior members closed their practices, and retired either because of the lack of patients, or the lack of their ability to acquire the technology that they needed to see their patients virtually and confidently. It really put such a burden on them.” – P023.
Similarly, several participants cautioned against adding superfluous virtual education to a busy clinician’s life. Given the inordinate rate of burnout associated with the pandemic, participants felt that an overabundance of programming compromised both clinicians’ task attention and their work/life boundaries.
“I think added flexibility for people is something that’s really important. A “7 a.m. Grand Rounds” where half of your female faculty couldn’t attend because they were dropping children off at school, but now they’re online and can actually participate. But I also think it really needs to be tempered because just because you can put something online and ask that a clinician do it in their spare time, it just erodes into the time that they’re not supposed to be doing work.” – P003. “Normally [clinicians] would book off their practice and would go to a conference for two days. That was no longer possible. So, moving online, even though there was greater flexibility, there was still that sense that I might have to stop at any moment and take a call.” – P009.
Theme 3: we’re not going to unring the bell
As pandemic restrictions eased, many organisations moved towards a “hybrid,” “blended,” or “hyflex” model of delivery. Footnote 1 Despite the lack of clarity around these terms, there was widespread expectation that this model will remain prominent.
“I foresee us living in a hybrid environment for a long time and having that extra flexibility for people to determine how they want to participate.” – P020. “The definitions are constantly changing because we haven’t really defined what it’s going to look like after the pandemic. There are all of these words that we’re using like hyflex, hybrid, but there’s no concrete definition. And there are ways of collaborative learning with technology that haven’t even been defined yet.” – P017.
Conversely, several participants acknowledged that virtual delivery may not always be preferred. While some learners appreciated this new mode of delivery, many lamented the loss of networking and social connection, as well as the Zoom fatigue associated with videoconferencing. Participants substantiated this through examples such as clinicians’ eagerness to resume in-person events despite the presence of tangible barriers, including travel time:
“We offered [a conference] virtually and in-person. The virtual numbers were so low that we cancelled the virtual. We have about 260 mostly rural doctors coming down to a location in the province because networking and getting out of the communities was so important.” – P010. “The number one complaint is we can’t break bread. We can’t talk with one another. We can’t meet our future employers. Maybe they want to speak with somebody on the east coast or the west coast. How are the programs different? We can have these conversations, but it’s limited.” – P017.
Additional considerations pertaining to hybrid events can act as deterrents. For instance, these events can be more cost prohibitive, requiring additional staffing and information technology infrastructure. This can make hybrid delivery especially challenging to implement in smaller scale contexts.
“Many [organisations] were doing hybrid [events]. We tried to do that, but we had such low numbers that it wasn’t worth the cost. It costs so much more to do both.” – P010. “The biggest problem we have right now is the smaller teams cannot do hybrid CPD. We tried to help them, but it was not a success […] They are now starting to do face-to-face CPD, and they did virtual CPD during the pandemic, but the hybrid one is really, really difficult to implement.” – P004.
Hybrid events were also described as more challenging to host than exclusively virtual or in-person events. During the initial transition to virtual delivery, both learners and educators had to navigate unfamiliar technology. Educators had to adapt their content and find ways to meaningfully engage the audience in the absence of body language and the inclination of learners to multitask. These challenges are compounded in a hybrid environment where educators must decipher how to effectively engage both audiences simultaneously.
“But if we do the two together, that’s where I think the challenge is going to be. How do you integrate both an in-person and a virtual component, and be able to satisfy both audiences, and have everyone feel included in a meaningful way?” – P010.
Despite these concerns, most participants concurred that the field has changed forever:
“What it’s going to look like after the pandemic is really hard to say because everything is changing so quickly right now, but we’re not going to unring the bell. You’re not going to get to a point where we’re going to go back to the way things were before the pandemic as far as teaching and CPD goes. We’re on a very steep learning curve right now.” – P017.
Theme 4: reimagining design and delivery
In addition to the longevity of hybrid education, participants shared how CPD could further refine delivery methods to maximise learning and drive practice change. They commented on anticipated learning model trends which included: micro and practice-based learning; learner-centric and personalised learning; workplace-based and in situ learning; collaborative learning (team-based and interprofessional education); longitudinal learning; and mentoring/coaching. Further research is needed to determine optimal learning environments, approaches, and design.
“I think CPD going forward is no longer the kind of didactic, bums in seats […] I think CPD needs to be workplace-based, practice-based, able to do where you are at, when you have time to do it, with the space and tools that you have.” – P009. “The future of CPD really has to be flexible, individualised, point in time, work integrated, leveraging people’s experiences. That sounds almost impossible today. How do you do that? Other than having a one-to-one educator learner structure. That’s my immediate thought. But that’s because we haven’t figured it out yet.” – P005.
Participants similarly contemplated the use of technology to enhance CPD education, including social media, electronic medical records, virtual reality, and artificial intelligence (AI).
“I have a feeling long-term-wise there are a lot of activities that AI could replace. For example, instead of speaking to a coach about a problem, you could get that basic interaction with AI, and you could go back to it as often as you needed as opposed to using those human resources, which is often where we run out of steam. I see [AI] as a potential significant addition that would make the delivery of CPD easier, but still effective and impactful.” – P018.
In tandem with reimagined tools and methods for education, a few participants underscored the importance of involving key stakeholders in education design, emphasising the importance of these voices in the conception, implementation, and delivery of CPD.
“Scholarship in innovation without ensuring that the end user is at the table with the implementation in the design of what you’re trying to create, I think it is potentially an oversight. Because the best designed, best intended education, with the most robust outcomes, if it cannot be adopted and integrated into the workflow of your target audience, it’s not going to matter.” – P003. “I think one way to improve things would be to have a patient, somebody who is using the health services, to have them in our meetings, and to have them take a look at the evaluation that we do of our program.” – P004.
Theme 5: creating an evaluative culture
Participants called for improved evaluation strategies to assess the quality of CPD education as well as learner and, ultimately, patient outcomes. Historically, evaluation has been insufficient and under-resourced, however, post-COVID, there appears to be increasing momentum towards a data-driven approach to improving service delivery.
“As leaders in CPD, we need to create a culture of finding new ways. We need to test what we’re actually doing and gather data and show whether or not it’s working.” – P013. “Is the quality of what is produced virtually of higher quality, lesser quality, or the same quality as in-person CPD? – P023. “We need to have some evaluations that really do reflect likelihood to change. It no longer cuts the mustard to say we served ‘x’ number of people, and they liked it.” – P011.
Furthermore, evaluations should be multipronged, longitudinal, and demonstrate tangible outcomes:
“All education should be designed around outcomes; improved patient outcomes, improved environment for people to practise in, increased value, decreased cost; there are a million.” – P003.
However, some participants noted that barriers such as limited resources, including time and money, continue to hinder meaningful evaluation initiatives.
“I think that resources don’t exist to measure outcomes and design activities in a meaningful way. Pushing on [CPD] offices to create education that leads to meaningful outcomes, again without providing the resources to measure the patient outcomes or collect and analyse the data is unfair.” – P003.
Evaluation is integral to demonstrating the value of CPD. Despite the increasing recognition of its importance, much work remains to ensure it is ingrained within the field.
“If we can’t show our value to decreasing costs and improving patient outcomes in the long-term, I do believe there is a significant threat to CPD education.” – P002. “Evaluation culture is starting, but we still have so much teaching to do to make sure that it’s something that is well accepted.” – P004.
Theme 6: a lifeline in times of turmoil
Finally, participants remarked that the value of CPD became heightened during the pandemic among medical professionals and the public. Amid chaos and confusion, it became a trusted source of information providing life-saving education about the virus, ultimately, becoming a lifeline for those working in medicine.
“It has impressed me how much CPD can do to be of value and a change in what is happening to the population. CPD plays a critical role in not only just delivering education […] We are a trusted source.” – P010. “I think the value of CPD has been significantly elevated. It became a very important, valued, sought after solution to a complex problem. And so, it has elevated its position in health professions.” – P005.
Moreover, CPD attained an indispensable status in the reorganisation of the healthcare system, expanding their mandate and facilitating interprofessional and cross-organisational collaboration to manage the crisis.
“CPD became a forum to manage this health crisis. This has shown the power of education and bringing the leaders together in helping to manage a health crisis or anything healthcare related.” – P010. “We helped our colleagues organise themselves. We reorganised the healthcare system. The nurses were gone, so what do you do in the clinics now? How can we help them? So CPD now includes management. That is something that we didn’t do before. We needed to do CPD for team leaders. They needed that. They needed the help to manage their team. All the organisation of the clinic, of the hospital, how can we be there for them, and teach them how to do it? The subjects of CPD exploded with the pandemic.” – P004.
To best prepare for the next emergency, participants extracted key lessons from COVID-19, which included adaptability, rapid decision-making, and collaboration.
“Today it’s COVID. Tomorrow it may be something else. So, educators need to find that adaptability.” – P005.
“I think we need to think about how CPD can help institutions prepare for the next pandemic. We’re going to have another pandemic at some point, how do we learn from this so that we’re better prepared to help our institutions, and how can we be strategic players in that so we can ramp up much more efficiently and less chaotically the next time we have to deal with an emergency like this.” – P014.
However, some participants expressed concern that the lessons from this pandemic may lose traction. Notably, one participant positioned this apprehension in the context of the 2002–2004 severe acute respiratory syndrome (SARS) outbreak, highlighting that much of the knowledge gained from that crisis was overlooked. This led to inadequate emergency preparedness resulting in the reactionary approach to innovation during COVID-19.
“[An author] wrote an article about SARS1 in which he outlined all of the things that CPD should become because of SARS1. It included using technology more, more longitudinal, more networking. SARS1 was quite short lived, although it was still very impactful. But there we were ten years later reading the article and it told us exactly what we should have been doing, and we would have been very prepared […] Most people will probably say that CPD has changed forever. I think it’s changed given that we’ve been in this pandemic for quite a long time. I’m still not convinced CPD has changed forever. I don’t know if we’ve changed our mindset enough as a group of professionals. I think we’re still thinking about knowledge transfer in a very traditional way. I probably sit on the side of, we will go back to as it was, more than we will hold on to the changes.” – P013.
Irrespective of participants’ viewpoints on the lasting impact of COVID-19 on CPD, there was widespread agreement that a comprehensive examination of both the failures and successes of the field’s response to the crisis is essential.
“Let’s say we get another pandemic, how can CPD be more effective in rolling out information? It’s hard to teach when information is not reliable and is ever-changing. How can CPD offices in the future, using COVID as an example, find out what went wrong, what went right?” – P011. “By the time something like a crisis happens it’s too late. It’s too late to innovate. You just respond.” – P013.
To our knowledge, this is the first study exploring the perspectives of CPD leaders regarding the impact of COVID-19 on CPD and potential directions post-pandemic. We found that the pandemic incited a long-awaited transformation in teaching and delivery, although some CPD leaders expressed reservations about the endurance of these changes. Historical evidence attests that periods of turmoil act as powerful catalysts for innovation. Our participants substantiated that the pandemic acted as an inflection point for CPD. McMahon [ 10 ] highlights that the urgent demand for new solutions prompted CPD organisations to adopt a more decentralised approach to decision-making, thus fostering an environment ripe for innovation. In alignment with the broader literature, our findings indicate that the most prominent change experienced within CPD was the transition to virtual education which was associated with a significant surge in CPD attendance at the beginning of the pandemic [ 10 , 29 , 30 , 31 ].
Increased flexibility and accessibility have been touted as the primary advantages of online learning [ 29 , 32 ]; however, there exists a duality of sentiments regarding the implications for historically excluded groups. Some scholars contend that the flexibility offered by virtual delivery has the potential to eliminate systemic barriers for equity-denied groups [ 29 , 32 ]. In particular, COVID-19 may have increased access to medical education content for women [ 29 ], parents of young children [ 33 ], individuals from remote communities [ 29 , 34 ], and international audiences [ 35 ] who may face barriers to in-person attendance. Conversely, we found that in certain instances, virtual delivery impeded clinicians’ ability to meaningfully engage in CPD, particularly for women and senior clinicians. This duality is recognized in the literature which cautions that virtual CPD may inadvertently reinforce gender disparities. There is evidence that women were disproportionately burdened by household and childcare duties during the pandemic, thereby potentially reducing their capacity to engage in virtual CPD [ 33 , 36 ]. While additional research on this topic is warranted, in light of these nascent findings, CPD program developers should consider the divergent experiences that exist among different populations when assessing content delivery modalities.
Despite the challenges listed above, our findings suggest a prevailing interest in retaining the virtual component of medical education which may significantly alter the nature of CPD delivery moving forward. In fact, some scholars argue that learning preferences have been permanently altered by the pandemic [ 31 ]. Given undergraduate and graduate medical education students also pivoted to virtual learning, with research indicating a high degree of acceptance [ 37 ], this may further reinforce the enduring nature of the virtual component. While the wider literature indicates a preference towards “hybrid” education [ 31 , 32 ], there remains gaps in knowledge regarding this modality. Our research indicates a foremost need to obtain definitional clarity regarding what constitutes “hybrid,” “hyflex,” and/or “blended” education. In addition, there remains a paucity of literature on the unique considerations associated with meaningful engagement during hybrid events. Preliminary research has begun to contribute to this gap, for example, Gottlieb et al. [ 35 ] found that using multiple mediums can introduce challenges with synchrony that dilute the quality of experience for both in-person and virtual audiences. The authors suggest that enlisting technology specialists, creating opportunities for interactivity and engagement, and ensuring that content is appropriate for digital format are crucial to enhancing hybrid events. In proceeding forward, the creation of best practices in hybrid CPD is imperative.
In conjunction with this pivot towards virtual formats, our participants asserted that greater change is needed in CPD to sustain relevance in the face of evolving societal circumstances. These calls to reform CPD predate the pandemic [ 38 ]. Our participants exhorted the investigation and adoption of innovative learning models such as team-based, workplace, and practice-based learning, which gained momentum during the pandemic. These approaches are crucial for thinking and moving beyond professional silos [ 39 ], enhancing knowledge translation through practice [ 40 ], and ensuring learned skills and knowledge are relevant to patient care [ 41 ], respectively. Moreover, several of our participants expressed a keen interest in expanding the use of innovative technology which they experimented with during COVID-19, albeit with varying degrees of success. This included the use of trending digital tools such as social media [ 42 ], podcasting [ 43 ], and AI [ 44 ], which have been explored by other scholars.
Our participants further voiced the need for CPD to be informed by systematic evaluation to measure learning and clinical outcomes. Scholars have long advocated for robust evaluation and assessment practices in CPD, contending that the development of effective learning interventions requires evidence-based content with well-defined, attainable, and measurable learning outcomes [ 45 ]. This can help bolster the value of CPD by providing objective indicators that demonstrate how CPD activities improve clinician performance, augment healthcare quality, and improve cost effectiveness [ 46 ]. While outcome evaluation is crucial, a recent scoping review [ 47 ] examining CPD evaluation techniques revealed major gaps; the authors argue for comprehensive approaches that integrate process evaluation and that are guided by theoretical frameworks. We contend that this endeavour is not possible without meaningful support from CPD offices, through both increased financial and human resources.
As a final consideration, our participants underscored the need for CPD to adopt a proactive stance in preparation for future crises. However, in light of CPD’s failure to implement lessons from previous emergencies, participants expressed concerns that takeaways from COVID-19 may not be internalised and applied moving forward. For example, in their article on CPD delivery after the 2003 Toronto SARS outbreak, Davis et al. [ 48 ] urged providers to develop a “flexible” emergency preparedness plan outlining the role of technology in achieving those aims. Moreover, the authors stressed the importance of transitioning CPD from “a passive, reactive model toward a multimodal, proactive, and systemic vehicle” to facilitate the dissemination of up-to-date information. These recommendations resonated with our participants, who felt that had these been effectuated, the field would have been better prepared for COVID-19. Drawing on lessons from the past with an eye to the future, three paramount COVID-19 takeaways were proposed: (1) the importance of fostering a culture of innovation, (2) promoting interprofessional and patient collaborations, and (3) demonstrating the value proposition of CPD as a lifeline for clinicians.
Limitations
We note that because the study sample was restricted to participants from Canada and the USA, the findings should be interpreted within this specific contextual milieu and may not necessarily be transferable to other settings. While we made efforts to recruit a diverse sample (including professional backgrounds and years of experience), we did not formally collect demographic data. Finally, given this research captured perspectives during a determinate timeframe, we acknowledge that attitudes, perspectives, and experiences may have evolved as the COVID-19 situation has progressed.
The pandemic presented profound implications for CPD, compelling a culture of adaptability and innovation. The challenges generated opportunities for the field to reimagine CPD design and delivery to reflect evolving societal conditions and preferences. Moreover, this allowed the field to build resilience and demonstrate its value to healthcare and greater society. We caution that while the public health emergency appears to have subsided, our research underscores the need to sustain progress made during the crisis to ensure a better “new normal.” As we move forward, we call for the CPD community to leverage this momentum and internalise lessons learned to avoid perpetuating past mistakes during inevitable future crises.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
It is important to note that terms such as “hybrid,” “blended,” and “hyflex” remain ambiguous with limited understanding of their precise definitions [ 26 ]. Our participants further noted there is a prevailing trend to use the above terms interchangeably in the field of CPD. As such, for the purposes of this article, we can only offer a loose definition of “hybrid,” “blended,” and “hyflex” learning as incorporating both in-person and online components [ 26 , 27 , 28 ]. Further research is needed to establish comprehensive definitions in the CPD context.
Abbreviations
- Continuing professional development
Coronavirus disease 2019
Artificial intelligence
Severe acute respiratory syndrome
Campbell C, Silver I, Sherbino J, Ten Cate O, Holmboe ES. Competency-based continuing professional development. Med Teach. 2010;32(8):657–62.
Article Google Scholar
Samuel A, Cervero RM, Durning SJ, Maggio LA. Effect of Continuing Professional Development on Health professionals’ performance and patient outcomes: a scoping review of knowledge syntheses. Acad Med J Assoc Am Med Coll. 2021;96(6):913–23.
Cervero RM, Gaines JK. The impact of CME on Physician Performance and Patient Health outcomes: an updated synthesis of systematic reviews. J Contin Educ Health Prof. 2015;35(2):131–8.
Ng V, Gupta A, Erlich D. Brought about by necessity: how the pandemic accelerated a transformation of continuing professional development. Educ Prim Care. 2022;33(1):2–5.
Hansman CA. Mentoring and Informal Learning as Continuing Professional Education. New Dir Adult Contin Educ. 2016;2016(151):31–41.
Wenger E, McDermott R, Snyder WM. Cultivating communities of Practice: a guide to managing knowledge. Boston: Harvard Business Review; 2002.
Google Scholar
Headleand C. Online CPD is one pandemic innovation worth fighting for. Times Higher Education [Internet]. 2021 Sept 24 [cited 2023 Jul 17]. https://www.timeshighereducation.com/campus/online-cpd-one-pandemic-innovation-worth-fighting .
Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368(6493):860–8.
Kawczak S, Fernandez A, Frampton B, Mooney M, Nowacki A, Yako M, et al. Observations from transforming a Continuing Education programme in the COVID-19 era and preparing for the future. J Eur CME. 2021;10(1):1964315.
McMahon GT. Facilitating flexibility: the role of CPD regulators and accreditors during a Crisis. J Eur CME. 2021;10(1):1993432.
World Health Organization. WHO Director-General’s opening remarks at the media briefing – 5 May 2023 [Internet]. 2023 May 5 [cited 2023 Oct 31]. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing---5-may-2023 .
Mooallem J, Gilbertson P. by A. Three Years Into Covid, We Still Don’t Know How to Talk About It. The New York Times [Internet]. 2023 Feb 22 [cited 2023 Jun 9]; https://www.nytimes.com/interactive/2023/02/22/magazine/covid-pandemic-oral-history.html .
Boyer EL. Scholarship reconsidered: priorities of the professoriate. Expanded edition. San Francisco, CA: Jossey-Bass; 2016. xxv + 198.
Etikan I. Comparison of Convenience Sampling and Purposive Sampling. Am J Theor Appl Stat. 2016;5(1):1–4.
Webex. Webex by Cisco [Internet]. 2022 [cited 2023 Oct 9]. https://www.webex.com/ .
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Dedoose. Dedoose [Internet]. Los Angeles. CA: SocioCultural Research Consultants, LLC; 2022. Available from: www.dedoose.com.
Soklaridis S, Zaheer R, Scully M, Shier R, Williams B, Dang L et al. ‘We are in for a culture change’: continuing professional development leaders’ perspectives on COVID-19, burn-out and structural inequities. BMJ Lead. 2023;leader.
O’Connor C, Joffe H. Intercoder Reliability in Qualitative Research: debates and practical guidelines. Nternational J Qual Methods. 2020;19:1–13.
Johnson JL, Adkins D, Chauvin S. A review of the Quality indicators of Rigor in qualitative research. Am J Pharm Educ. 2020;84(1):7120.
Darawsheh W. Reflexivity in research: promoting rigour, reliability and validity in qualitative research. Int J Ther Rehabil. 2014;21(12):560–8.
Birks M, Chapman Y, Francis K. Memoing in qualitative research: probing data and processes. J Res Nurs. 2008;13(1):68–75.
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–52.
Saichaie K. Blended, flipped, and Hybrid Learning: definitions, developments, and directions. New Dir Teach Learn. 2020;2020(164):95–104.
Kusters IS, Gregory ME, Bryan JL, Hysong SJ, Woodard LD, Naik AD, et al. Development of a hybrid, Interprofessional, interactive quality improvement curriculum as a Model for Continuing Professional Development. J Med Educ Curric Dev. 2020;7:2382120520930778.
Bernson-Leung ME, MacNeill H. Big Assumptions in Online and Blended Continuing Professional Development: Finding Our Way Forward Together. J Contin Educ Health Prof. 2022;10.1097/CEH.0000000000000528.
Kisilevsky E, Margolin E, Kohly RP. Access, an unintended consequence of virtual continuing medical education during COVID-19: a department’s experience at the University of Toronto. Can J Ophthalmol J Can Ophtalmol. 2021;56(1):e18–9.
Windrim RC, Gan E, Kingdom JC. The impact of COVID-19 on Continuing Professional Development: go Green and Go Home? J Obstet Gynaecol Can. 2022;44(3):231–3.
McMahon GT. Effect of the COVID-19 pandemic on Accredited Continuing Medical Education in the United States. J Contin Educ Health Prof. 2022;42(4):e125–7.
MacNeill H, Paton M, Schneeweiss S, Wiljer D. Perceived Advantages and Disadvantages of Online Continuing Professional Development (CPD) During COVID-19: CPD Providers’ Perspectives. J Contin Educ Health Prof [Internet]. 2023 May 17 [cited 2023 Jun 8];Publish Ahead of Print. https://journals.lww.com/ https://doi.org/10.1097/CEH.0000000000000512 .
Cheng C, Papadakos J, Umakanthan B, Fazelzad R, Martimianakis MA (Tina), Ugas M On the advantages and disadvantages of virtual continuing medical education, et al. editors. a scoping review. Can Med Educ J. 2023;14(3):41–74.
Cassidy D, Edwards G, Bruen C, Kelly H, Arnett R, Illing J. Are we ever going back? Exploring the views of Health professionals on Postpandemic Continuing Professional Development modalities. J Contin Educ Health Prof. 2023 Summer;43(3):172.
Gottlieb M, Sebok-Syer SS, Bawden A, Shah M, Jordan J. Faces on a screen: a qualitative study of the virtual and in-person conference experience. AEM Educ Train. 2022;6(6):e10827.
Soklaridis S, Black G, LeBlanc C, MacKinnon KR, Holroyd-Leduc J, Clement F, et al. Academic Productivity of Equity-Deserving Physician scholars during COVID-19: a scoping review. Acad Med. 2023;98(1):123–35.
Wilcha RJ. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963.
Lockyer J, Bursey F, Richardson D, Frank JR, Snell L, Campbell C, et al. Competency-based medical education and continuing professional development: a conceptualization for change. Med Teach. 2017;39(6):617–22.
Sklar D, Yilmaz Y, Chan TM. What the COVID-19 pandemic can teach Health professionals about Continuing Professional Development. Acad Med. 2021;96(10):1379–82.
Manley K, Martin A, Jackson C, Wright T. A realist synthesis of effective continuing professional development (CPD): a case study of healthcare practitioners’ CPD. Nurse Educ Today. 2018;69:134–41.
Institute of Medicine (US) Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in the Health Professions [Internet]. Washington (DC): National Academies Press (US); 2010 [cited 2023 Jul 13]. https://www.ncbi.nlm.nih.gov/books/NBK219797/ .
Hall E, Kreuter JD, Sörö T, Dzara K, Gooding HC. Harnessing the Power of Social Media to support a Professional Learning Network during the COVID-19 pandemic. J Contin Educ Health Prof. 2021;41(1):10–2.
Tarchichi TR, Szymusiak J. Continuing Medical Education in the time of Social Distancing: the case for expanding podcast usage for Continuing Education. J Contin Educ Health Prof. 2021;41(1):70–4.
Kung TH, Cheatham M, Medenilla A, Sillos C, Leon LD, Elepaño C, et al. Performance of ChatGPT on USMLE: potential for AI-assisted medical education using large language models. PLOS Digit Health. 2023;2(2):e0000198.
Filipe HP, Silva ED, Stulting AA, Golnik KC. Continuing Professional Development: best practices. Middle East Afr J Ophthalmol. 2014;21(2):134–41.
Moore DEJ. A framework for outcomes evaluation in the continuing professional development of physicians. In: Davis DA, Barnes BE, Fox RD, editors. The continuing professional development of physicians: from research to practice. Chicago: AMA; 2003. pp. 249–74.
Hosseini S, Allen L, Khalid F, Li D, Stellrecht E, Howard M et al. Evaluation of Continuing Professional Development for Physicians – Time for Change: a scoping review. Perspect Med Educ 12(1):198–207.
Davis D, Ryan D, Sibbald G, Rachlis A, Davies S, Manchul L, et al. Severe acute respiratory syndrome and the delivery of continuing medical education: case study from Toronto. J Contin Educ Health Prof. 2004;24(2):76–81.
Download references
Acknowledgements
The authors thank the Fédération des médecins spécialistes du Québec for providing financial support for this work.
This study was funded by the Fédération des médecins spécialistes du Québec Collaborative Research Grant (grant number N/A).
Author information
Authors and affiliations.
Department of Education Services, Centre for Addiction and Mental Health, Toronto, ON, Canada
Sophie Soklaridis, Rowen Shier, Rabia Zaheer, Michelle Scully & Sanjeev Sockalingam
Department of Psychiatry, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
Sophie Soklaridis & Sanjeev Sockalingam
Department of Family and Community Medicine, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
Sophie Soklaridis
The Wilson Centre, University Health Network, University of Toronto, Toronto, ON, Canada
Professional Renewal Centre, Lawrence, KS, USA
Betsy Williams
Wales Behavioral Assessment, Lawrence, KS, USA
Department of Psychiatry, School of Medicine, University of Kansas, Lawrence, KS, USA
Department of Pediatric Surgery, McGill University, Montréal, Québec, Canada
Sam J. Daniel
Slaight Family Centre for Youth in Transition, Centre for Addiction and Mental Health, Toronto, ON, Canada
Continuing Professional Development Department, Fédération des médecins spécialistes du Québec, Montréal, Québec, Canada
Sam J. Daniel & Martin Tremblay
Centre for Addiction and Mental Health, 1025 Queen Street West B1 – 2nd Floor, Room 2300, Toronto, ON, M6J 1H4, Canada
You can also search for this author in PubMed Google Scholar
Contributions
SSok was involved in the conception of the project, the design, data acquisition, data analysis, data interpretation, and the writing of the manuscript. RS contributed to the data acquisition, data analysis, data interpretation, and writing of the manuscript. RZ contributed to the data acquisition, data analysis, data interpretation, and writing of the manuscript. MS contributed to the data analysis, data interpretation, and writing of the manuscript. BW contributed to the data analysis, data interpretation, and writing of the manuscript. SJD was involved in the conception of the project, the design, and writing of the manuscript. SS contributed to the data acquisition and writing of the manuscript. LD contributed to the data analysis, data interpretation, and writing of the manuscript. MT was involved in the conception of the project, the design, data analysis, data interpretation, and writing of the manuscript.
Corresponding author
Correspondence to Sophie Soklaridis .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Research Ethics Board of the Centre for Addiction and Mental Health (REB 023/2021). Participation in this study was voluntary and participants provided electronic informed consent.
Consent for publication
Authors’ information.
The first (SSok), second (RS), third (RZ), fourth (MS), sixth (SJD), seventh (SS), eighth (LD), and ninth (MT) are Canadian, while the fifth (BW) is American. SSok, RS, RZ, and MS are qualitative critical social science researchers. BW, SJD, SS, and MT conduct clinical outcomes research using both quantitative and qualitative methodologies. At the time of the study, LD was a student. Five authors (SSok, BW, SJD, SS, and MT) are actively engaged in North American continuing professional development initiatives, whereas four authors (RS, RZ, MS, and LD) maintain a peripheral role in the field through research contributions. Three of the authors (BW, SJD, and SS) provide clinical care.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Soklaridis, S., Shier, R., Zaheer, R. et al. “The genie is out of the bottle”: a qualitative study on the impact of COVID-19 on continuing professional development. BMC Med Educ 24 , 631 (2024). https://doi.org/10.1186/s12909-024-05498-9
Download citation
Received : 09 November 2023
Accepted : 30 April 2024
Published : 06 June 2024
DOI : https://doi.org/10.1186/s12909-024-05498-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Delivery modalities
- Accessibility
- Emergency preparedness
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy.
Hide this message
You are using an outdated browser. Please upgrade your browser to improve your experience and security.
The Directory of Open Access Journals
Quick search.
Majallah-i Dānishgāh-i ’Ulūm-i Pizishkī-i Shahīd Ṣadūqī Yazd (Apr 2021)
Qualitative Research in COVID 19 Pandemic
- Abdolghani Abdollahi Mohammad,
- Mohammad Reza Firouzkouhi
Affiliations
Read online
Introduction: Quantitative research is not suitable for COVID pandemic research because it does not cover the social consequences of qualitative research. COVID 19 is a social event that is important because of the disruption of the natural order of society. To defeat the disease, social interaction is needed, so qualitative research is appropriate to find the challenges and experiences of society. Therefore, due to the inconsistency of peoplechr('39')s health behaviors with epidemiological models, peoplechr('39')s vulnerability in epidemics, unexpected consequences or surprising results, extracting participantschr('39') experiences from medical procedures and revealing flexibility in the face of social problems, the use of qualitative research in this pandemic that will be important..
- qualitative research
- quantitative research
WeChat QR code

- Open access
- Published: 05 June 2024
Differential impacts of health systems and sociocultural environment on vulnerable populations during the COVID-19 pandemic: lessons from four Asia-Pacific countries
- Jakyung Lee 1 , 2 na1 ,
- Susan Park 1 , 3 na1 ,
- Soong-nang Jang 1 , 4 ,
- Katherine Ann Reyes 5 ,
- Fernando Garcia Jr. 6 ,
- Carmelita Canila 6 ,
- Joseph Oraño 5 ,
- Alfredo Jose Ballesteros 5 ,
- Tri Muhartini 7 ,
- Sandra Frans 7 ,
- Tiara Marthias 7 ,
- Likke Prawidya Putri 7 ,
- Yodi Mahendradhata 7 &
- Chuan De Foo 8 , 9
BMC Public Health volume 24 , Article number: 1501 ( 2024 ) Cite this article
353 Accesses
1 Altmetric
Metrics details
This study aims to evaluate healthcare systems and pandemic responses in relation to marginalized and vulnerable groups, identify populations requiring urgent care, and assess the differential impacts on their health during the pandemic.
Data were collected by the Asia-Pacific Observatory on Health Systems and Policies (APO)–National University of Singapore and APO–International Health Policy Program consortium members: Korea, Indonesia, Philippines, and Singapore. Data were collected through a combination of semi-structured interviews, policy document reviews, and analysis of secondary data.
Our findings reveal that the pandemic exacerbated existing health disparities, particularly affecting older adults, women, and children. Additionally, the study identified LGBTI individuals, healthcare workers, slum dwellers, and migrant workers as groups that faced particularly severe challenges during the pandemic. LGBTI individuals encountered heightened discrimination and limited access to health services tailored to their needs. Healthcare workers suffered from immense stress and risk due to prolonged exposure to the virus and critical working conditions. Slum dwellers struggled with healthcare access and social distancing due to high population density and inadequate sanitation. Migrant workers were particularly hard hit by high risks of virus transmission and stringent, often discriminatory, isolation measures that compounded their vulnerability. The study highlights the variation in the extent and nature of vulnerabilities, which were influenced by each country’s specific social environment and healthcare infrastructure. It was observed that public health interventions often lacked the specificity required to effectively address the needs of all vulnerable groups, suggesting a gap in policy and implementation.
Conclusions
The study underscores that vulnerabilities vary greatly depending on the social environment and context of each country, affecting the degree and types of vulnerable groups. It is critical that measures to ensure universal health coverage and equal accessibility to healthcare are specifically designed to address the needs of the most vulnerable. Despite commonalities among groups across different societies, these interventions must be adapted to reflect the unique characteristics of each group within their specific social contexts to effectively mitigate the impact of health disparities.
Peer Review reports
The 2019 coronavirus disease (COVID-19) pandemic exacerbated pre-existing inequalities in social, economic, and health systems, amplifying the harmful effects of COVID-19 [ 1 , 2 , 3 ]. Although researchers generally agreed on who were considered vulnerable to the COVID-19 threat, different interpretations emerged across different national contexts. These vulnerable groups’ health needs are complex and closely related to their socioeconomic conditions. Each country’s healthcare system and social resilience may impact vulnerability characteristics [ 4 ] and the outcome of the COVID-19 pandemic [ 5 , 6 ]. Hence, we must redefine at-risk populations in the context of COVID-19 threats based on the healthcare system of each country and the socioeconomic situation in preparation for emerging infectious diseases [ 7 ].
Assessing the healthcare systems and social resilience of different countries may provide insight into the development of effective policies to better respond to public health emergencies. For example, a review of COVID-19 responses in 28 countries suggested that highly effective countries activated comprehensive responses, adapted the health system’s capacity, and preserved functions and resources for both COVID-19-related and non-COVID-19-related care, thus reducing vulnerability in health and well-being [ 8 ]. Another study comparing nine high-income countries in the Asia-Pacific region (e.g., Singapore and South Korea) and Europe (e.g., Germany and the UK) showed that interventions in Asian countries were implemented with higher speed, scale, and intensity, leading to early success in the control of COVID-19 [ 9 ]. Han et al. [ 9 ] suggested that Asian countries’ previous experiences with epidemics, such as Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome, contributed to high investment in public health infrastructure and public compliance with government restrictions and preventive measures.
However, research on COVID-19 responses in the Asia-Pacific region has been limited. Moreover, comparative studies of COVID-19 responses that included Asia-Pacific countries focused on disease control measures rather than the impact of such policies on vulnerable populations [ 10 , 11 ]. Southeast Asian countries faced severe challenges to COVID-19, but their unique interventions, such as the use of community health volunteers, may provide insights for other countries [ 12 ]. Asia-Pacific countries share several cultural and environmental features: livestock and poultry rearing methods, high population density, high population migration rates, and changes in their ecological environment due to climate change. However, cooperation in health security among Asia-Pacific countries is stalling. Therefore, comparing and considering the policy responses in Asia-Pacific countries is necessary to improve the response levels to the epidemic and promote health justice through international cooperation.
We chose four Asia-Pacific countries that are members of the Asia-Pacific Observatory on Health Systems and Policies (APO)–National University of Singapore (NUS) and APO–International Health Policy Program (IHPP) consortium for this study: South Korea, Indonesia, the Philippines, and Singapore. The countries varied in the levels of epidemiological outcomes, including confirmed cases and death rates, as well as in the strategies to respond to the pandemic. The country selection is also based on the differences in healthcare systems, and the selected countries represent a range of income levels. We assumed that the differences in socioeconomic and environmental factors would affect COVID-19 response policies and the health outcomes of vulnerable populations in the four countries. We investigated the characterization of marginalized and vulnerable populations in the four countries and collected country-specific data, such as specific healthcare policies, and their applications.
The goals of this study are to (1) evaluate the healthcare systems and COVID-19 responses focused on marginalized and vulnerable populations during the pandemic; (2) identify the marginalized and vulnerable populations who required urgent care during the COVID-19 pandemic; and (3) assess the differential impact of the COVID-19 pandemic on health and well-being in vulnerable populations. We aim to provide new perspectives on a country’s pandemic preparedness while also highlighting effective management methods for improving response plans for other emerging infectious diseases.
Data were collected from the APO–NUS and APO–IHPP consortium members from Korea, Indonesia, the Philippines, and Singapore, over the course of February 2022. This study triangulates qualitative methods, including semi-structured interviews, discussions with relevant experts through workshops, and reviews of national policy documents. The authors from each country determined the vulnerable and marginalized groups within their nations and complete semi-structured interview questionnaires regarding national responses to these groups. The interview items were based on the Global Health Security (GHS) index and the Joint External Evaluation (JEE) tool, both validated by previous studies [ 13 , 14 ]. Table 1 lists interview items and the full interview questionnaires is available in Supplementary Material 1 . To complete the questionnaires, the authors for each country analyzed policy documents and secondary data, and sought expert opinions to complement the collected data. Relevant experts from each country included members of international organizations, university professors specialized in related fields, and government officials from departments dedicated to infectious disease response. Subsequently, discussions were held among the authors from each country to reach a consensus.
The data from each country were integrated by the Korean research team in March 2023. Two researchers separately analyzed initially, then they cross-examined each other’s analysis. The part of results which were the same interpretations by two researchers were accepted, but when the interpretations differed, it went through a process of reaching agreement though discussion. All content analysis processes and results were reviewed for agreement by another researcher who are PhD in Public Health. Finally, all participating researchers reviewed the analysis results and reached an agreement.
Table 2 summarizes the priorities of vulnerable populations in four countries, as determined by policy documents, secondary data, and expert opinions.
Common vulnerable populations in four countries
Older adults.
As a common vulnerable group in the four countries, older adults were considered a priority target group. The older population (generally 60 years and above) is deemed a vulnerable group for many reasons. First, they are a population more predisposed to severe conditions due to pre-existing medical conditions. Due to the restricted access to healthcare services and chronic disease diagnosis services during the pandemic, this population may suffer from further complications and deterioration from pre-existing comorbidities. Comorbidities also predispose older people to more severe symptoms and outcomes if they are infected with the virus [ 15 ].
Furthermore, cluster infections have focused on long-term care facilities, resulting in more deaths due to the health vulnerabilities of the subjects [ 16 ]. Nursing home residents were reported to comprise 25% of the deaths due to COVID-19 in the US and 50% in European countries (e.g., France and Ireland) [ 17 ]. Nursing homes and assisted living facilities in many countries have failed to prevent the virus from spreading among older residents and staff timely. In addition to the chronic shortage of care workers, the devaluation of older adults in facilities and their caregivers during the COVID-19 pandemic exacerbated the care crisis in long-term care facilities [ 18 ]. To mitigate such damage, measures to restrict visitors to senior care facilities caused additional problems, such as emotional distress or victim abuse.
Women have been prioritized as one of the most vulnerable groups during the pandemic, as they bear most of the burden at home (performing both work and caregiving tasks), which is further intensified when work-from-home setting and home-based learning arrangements for their children were implemented during tightened movement restrictions. During the COVID-19 pandemic, many family caregivers, who are women, experienced anxiety, loneliness, and workplace disruptions, such as loss of jobs and wage reduction [ 19 ]. Domestic violence against women also increased. In Singapore, the Association of Women for Action and Research reported an exponential increase in calls to its helplines from women since the beginning of 2020.
Furthermore, women’s sexual, reproductive, and maternal health were affected by the disruptions in essential health services. A review of 95 studies showed that pregnant women with COVID-19 were more likely to experience adverse health outcomes, including preeclampsia, preterm birth, maternal mental health issues, and even deaths [ 20 ]. There was also a lack of clear and evidence-based guidelines for COVID-19 patients on delivery and breastfeeding, which may potentially harm pregnant women’s health [ 21 ]. Pregnant women were reported to be excluded from most COVID-19 treatment and vaccination programs., hindering the development of effective treatments for them [ 22 ].
However, there is little (if any) policy specifically addressing women’s heightened needs during this health emergency. Most of the initiatives are created from the ground up and through the lens of civil society. Despite the gendered impact of the COVID-19 pandemic on health, public health research and policy development that consider gender differences are limited [ 23 ].
Children and youth
Children with mild symptoms may act as the sources of COVID-19 transmission in schools and community settings [ 24 ]. More importantly, the health and well-being of the children were negatively affected by school closures and social distancing measures [ 25 ]. Young children experienced high levels of stress, anxiety, and disturbance of sleep, especially those with low socioeconomic status or pre-existing mental health issues [ 26 ]. The disruption of essential health services affected the health of children and adolescents, particularly those living in vulnerable conditions [ 25 ]. Restrictions during the COVID-19 pandemic also decreased physical activity among young people under the age of 18 [ 27 ]. These unfavorable conditions for the growth of young children during the COVID-19 pandemic may have a long-term impact on their physical and mental health. Because previous COVID-19 studies primarily focused on adults, more research is needed to understand the long-term health effects of COVID-19 on the younger population and identify ways to mitigate its negative impact on them.
Other vulnerable populations by country
Lgbti people.
In May 2020, over 200 infected cases were linked to an outbreak in a nightclub in Seoul’s Itaewon district [ 28 ]. A news report that a person with a confirmed infection visited a gay club sparked homophobia [ 29 ]. In response, LGBTI people were reluctant to test for COVID-19, revealing the privacy invasion issue in the current testing system. LGBTI organizations advocated for local governments to implement anonymous testing to reduce LGBTI people’s fear of retaliation. A large body of prior research has shown that LGBTI people face significant health inequalities due to heteronormativity, minority stress, victimization, discrimination, and stigma [ 30 ]. The case of Itaewon in Korea demonstrated that the LGBTI population’s health inequalities were exacerbated in the country’s response to COVID-19. Health inequality occurs in situations where heterosexuality is the norm [ 31 ]. In Korea, conversion therapy that infringes human rights continues, despite international organizations, such as the United Nations, urging to cease the practice [ 32 ]. This social environment contributes to high rates of drinking, smoking, depression, and suicidal ideation among LGBTI people in Korea [ 33 , 34 , 35 ]. Nevertheless, same-sex couples in Korea do not receive the same spousal health insurance coverage as heterosexual couples [ 36 ].
Homeless people
Homeless people were a blind spot for Korean national strategies against COVID-19. Due to unclear residences, the health authorities had difficulty conducting epidemiological investigations. Seoul’s government operated temporary shelters, but the lack of adequate space for physical distancing made them vulnerable to infection. Moreover, homeless people experienced various challenges in their daily lives during the COVID-19 pandemic, including employment and the use of social welfare services [ 37 ]. Due to the closures of local soup kitchens and healthcare organizations, homeless people on the streets and shelter dwellers were also deprived of free meals and health services during the COVID-19 pandemic [ 38 ]. Furthermore, since the government designated public hospitals as specialized facilities for COVID-19 patients, many homeless people had restricted access to medical services.
Healthcare workers
High infection risks and mortality among healthcare workers have been reported in Indonesia [ 39 ]. A significant number of caseloads resulted in a high workload of healthcare workers, which was aggravated by a lack of personal protective equipment (PPE) and medical supplies [ 39 , 40 ]. During the early stages of the COVID-19 pandemic, the PPE shortage was a commonly mentioned cause of death for healthcare professionals worldwide [ 41 ]. Moreover, the number of healthcare workers in Indonesia dealing with the demands of COVID-19 cases was insufficient. As the number of COVID-19 patients in Indonesia increased, so did the workload of medical workers, resulting in long and irregular working hours. These working conditions caused psychological distress for healthcare workers [ 42 ]. A lack of staff, uncertainty about COVID-19 control, and inadequate protection measures were identified as key stressors among Indonesian healthcare workers [ 43 ].
Religious leaders
Although Indonesia is a religious country with many denominations, most of the population is Muslim. Massive religious gatherings in Indonesia aided the spread of the COVID-19 virus. The public saw government gathering restrictions and social distancing measures as threats to religious traditions [ 44 ]. Similarly, in South Korea, gatherings of the “Shincheonji” Church were a source of outbreaks in the early phase of the COVID-19 pandemic. These examples highlight the importance of comprehending the effects of religion, culture, and social factors on people’s perceptions and behaviors during pandemics. People of different faiths may react differently when it comes to following preventive health measures.
Philippines
Slum dwellers and people in informal settlements.
With 42,857 people per square kilometer, Manila is the world’s most densely populated city. COVID-19 ripped through high-density slum dwellings in Metro Manila [ 45 ]. According to World Bank data, approximately half of the urban population lives in slums [ 46 ]. People living in high-density areas are more vulnerable to the negative effects of community quarantine, such as economic difficulties, food insecurity, and domestic violence. Furthermore, in 2020, typhoons Vamco (Rolly) and Goni (Ulysses) wreaked havoc on homes. Consequently, at least 30,000 people in Manila have been displaced and forced to live in communal shelters, making it difficult to follow the recommended social distancing and self-quarantine measures.
Migrant workers
The spotlight was on migrant workers in Singapore, in part due to social factors and the existing policy climate [ 47 ]. Most COVID-19 cases in Singapore occurred during the initial wave among migrant workers, following several large outbreaks in migrant worker dormitories [ 48 ]. Independent observers and local nongovernmental organizations (NGOs) pointed to deficiencies in workers’ dormitories regarding the provision and quality of basic necessities. As of May 6, 2020, there were 17,758 confirmed cases of COVID-19 among dormitory workers (88% of 20,198 nationally confirmed cases) [ 48 ]. Due to their poor living conditions, migrant workers could not effectively practice public health measures, such as social distancing. Migrant workers in Singapore are generally low-skilled, young blue-collar workers from Bangladesh, India, China, Thailand, and Myanmar. During the early stages of the outbreak, the government isolated all dormitories and established medical units of doctors and nurses stationed at the dormitories to care for the workers [ 49 ]. Complete movement restrictions increase depression and stress symptoms [ 50 ]. Additionally, several migrant workers attempted suicide at their dormitories [ 51 ]. The government also prioritized testing for migrant workers, and as of December 2020, 54,505 dormitory residents had tested positive [ 49 ]. Although Singapore implemented adequate measures to control COVID-19 in community settings, delayed responses for the migrant worker population led to rapid increases in the number of COVID-19 cases that partially triggered a circuit breaker lockdown early in the pandemic to reduce community transmission [ 52 ].
Even before COVID-19, migrant workers were more likely to be employed in low-wage jobs with long working hours and hazardous working conditions [ 53 ]. Previous research has shown that immigrants are more likely to be exposed to pesticides and chemicals and often have higher workloads than non-migrant workers [ 53 , 54 , 55 ]. However, it is difficult for migrant workers to access adequate healthcare due to inadequate labor protection measures, limited access to health insurance and limited eligibility for legal healthcare [ 56 ].
National response against COVID-19 focused on vulnerable populations
Table 3 shows the national response to COVID-19 and the effectiveness of national policies and implementation for marginalized and vulnerable populations. The authors assessed the effectiveness of health policy and implementation for vulnerable populations.
In Korea, large-scale rapid testing was freely available throughout the country. Korea’s reaction to COVID-19, represented by the “3T” approach (testing, tracking, and treatment), was recognized as a successful response early in the pandemic [ 57 ]. Tracing involved an epidemiologic investigation of all people who had had contact with confirmed cases for 14 days using various data sources, such as mobile phone location data, CCTV, and credit card usage history. In the early stage of the pandemic, the routes of movement and patients’ personal information were revealed. Although the information disclosed was anonymous, there were concerns that it could be used to identify patients’ identities. As a result, guidelines were revised several times, and the extensive tracking system for confirmed cases was suspended beginning in April 2022. Based on the tracing results of confirmed cases and their close contacts, quarantine was the primary measure to combat COVID-19. In the early stages of the pandemic, confirmed cases were isolated in healthcare facilities. Except for patients with high-risk health conditions, patients were allowed to be isolated at home once the patient population exploded. Vaccination and treatment were top priorities for older adults and those suffering from underlying diseases.
Korea had the highest response capacity to infectious disease threats of the four countries studied based on the GHS score. However, public disclosure of the tracking results represented serious violations of personal privacy and resulted in the social stigma of individuals with confirmed COVID-19 cases. Risk communication strengthened community awareness of COVID-19 status and helps to mitigate economic losses. However, there was a lack of response to protect vulnerable populations, particularly victims of discrimination and violence [ 58 ]. People with COVID-19 symptoms may have avoided testing for fear of exposing personal information.
During the first and second waves of the pandemic, Indonesia experienced a shortage of human resources in hospitals and primary care settings. Many health workers contracted COVID-19, disrupting the health service. Surveillance in Indonesia was passive due to the weak implementation of contact tracing. The government would bear the costs if the public primary health center and the health office carried out the tracking. On the contrary, if private health facilities conducted the contact tracing, the costs were paid.
Indonesia implemented policies specific to disabled people. These included ensuring easy access to COVID-19 testing, free health services, health protection, psychosocial support, home visit services for public health consultations and those related to COVID-19. It also includes providing relevant information about disabilities to healthcare workers in order for them to understand the specific needs of people with disabilities. However, the instructions were less specific; their content was more in the form of messages and considerations for facilitators and assisting institutions for people with disabilities rather than in the form of concrete action proposals that were easy to implement.
The government used the “Vulnerable Populations as Identified in the Demographic Vulnerability Tool” to prioritize contact tracing. This tool considers the risk of infection by age and population density of the environment. The Department of Health issued Department Memorandum No. 2020 − 0189, which specified the close contacts prioritized in contact tracing, including “vulnerable populations as identified in the demographic vulnerabilities tool.” The tool was developed based on epidemiological investigation evidence of COVID-19 cases in urban areas like Manila in the early stages of the pandemic. This tool considers demographic vulnerability based on three conditions: (1) more than four household members living in a housing unit 20 m 2 or smaller; (2) the total number of people 60 years old and over living in a housing unit larger than 20 m 2 ; and (3) the total number of people 60 years old and over living alone in a housing unit larger than 10 m 2 .
The government imposed a lockdown policy for Metro Manila, which included school closures, a ban on large gatherings, community quarantine, a series of stay-at-home orders, and movement restrictions in designated areas. Furthermore, the Philippine government provided continuous social and economic support to those affected by the response to the pandemic, such as the Republic Act (RA) 11,469, which provided emergency subsidies to low-income households. Despite economic assistance policies, the amount provided by RA 11,469 was insufficient to meet the needs of families during prolonged periods of lockdown or unemployment.
Extensive testing was conducted with migrant workers in focus. The Ministry of Manpower (MOM) prioritized PCR testing for migrant workers in essential services to work safely during Singapore’s circuit breaker period. In August 2020, Fast and Easy Testing–Rostered Routine Testing (RRT) was implemented in this population, with each migrant worker receiving a nose swab every 14 days. Unvaccinated workers were required to test on the 3rd, 7th, and 11th days following each RRT date. Once a high proportion of migrant workers had been fully vaccinated, the MOM announced that the RRT criteria would be waived for certain groups of migrant workers, including those who had been fully vaccinated; construction, marine and process sector workers; front-line workers in dormitories and onboarding centers; and migrant workers’ recreation centers. However, unvaccinated workers would still be required to undergo RRT every three days. Through effective social distance measures, Singapore successfully suppressed the number of COVID-19 infections and deaths. Quarantine measures for migrant workers were a major factor that suppressed community transmission. However, physical and emotional sequelae after isolation revealed the vulnerability of migrant workers in Singapore.
This study explored the effects of four Asian-Pacific countries’ national COVID-19 responses and social factors on the most vulnerable population groups. We reviewed the vulnerable groups commonly identified in the four countries: older adults, women, children, and adolescents. The results also identified vulnerable groups in each country’s sociocultural environment. For example, in Korea, LGBTI and homeless people were identified as vulnerable populations in Korea. Meanwhile, healthcare workers in lower-middle-income countries, such as Indonesia, were shown to be extremely vulnerable during the COVID-19 pandemic. Housing vulnerability was identified in high-density cities in the Philippines, whereas in Singapore, high-intensity tests and quarantine policies for migrant workers were found to have unintended consequences.
All reviewed countries implemented vaccination and testing policies that took into account their vulnerable populations, including older adults, women, children, and healthcare workers. Due to restricted access to health services during the pandemic, the health of older people may have deteriorated due to pre-existing comorbidities. Moreover, wide range of women with various situations can be categorized as vulnerable population in each country. Women bear most of the burden at multiple roles including work, house chores and caregiving tasks, which is further intensified when work-from-home setting and home-based learning arrangements for their children were implemented during tightened movement restrictions [ 19 ]. Many female family caregivers experienced anxiety, loneliness, and employment disruptions [ 19 ]. Increased domestic violence against women and disruptions to essential health services affected women’s sexual, reproductive, and maternal health [ 20 , 21 ]. The struggle of healthcare workers due to increased workloads and a lack of resources was a problem experienced in both high-income and low- or middle-income countries [ 59 ]. Furthermore, a large portion of healthcare workers around the globe are women, which doubled the burden and hazards for them. The disruption of essential health services also adversely affected the health of children and adolescents, especially those living in vulnerable conditions [ 25 ].
However, this study revealed insufficient targeted responses for socially vulnerable groups in many countries. The results showed that gaps in health inequality can be exacerbated when decisions are made without considering vulnerable groups in the population. For example, three countries considered vulnerable populations without adequate housing. People in informal settlements often face many challenges that can undermine health equity, ranging from poverty, inadequate infrastructure, and housing insecurity [ 60 , 61 ]. As a result, slum dwellers are at a higher risk of infectious and noncommunicable diseases, mental health effects, and injuries from violence and traffic accidents [ 60 , 61 ]. In addition, urban slum dwellers face conditions that significantly impact health inequity, such as spatial, political, and economic exclusion, compared to city dwellers [ 62 ].
The implementation of social policies by the government also had unintended consequences. For instance, physical distancing measures, such as stay-at-home policies, school closures, bans on social gatherings, and limited contact for certain populations, may have shown health benefits in slowing COVID-19 transmission. However, it also resulted in limited access to health and social services and social isolation. The significant increase in older adult abuse and adolescent suicide rate [ 63 , 64 ] during these periods could be attributed to COVID-19 restrictions [ 65 ]. The response to COVID-19 revealed limitations in reaching those with low access to the healthcare system. Continuous research is needed to understand the long-term health effects of COVID-19 on vulnerable populations.
Our study showed the importance of equity in health and basic needs in protecting human rights. A comprehensive approach is required to protect vulnerable populations during and after pandemics. Governments must understand that the policies for public health responses may have varying effects on different populations, particularly on the marginalized ones. Therefore, it is essential to consider the various social factors that may mediate the impact of the COVID-19 pandemic. When developing public health strategies, the government must prioritize identifying and protecting vulnerable populations. Clear risk communication and support measures for vulnerable populations should be implemented immediately. More information transparency is needed to minimize public confusion and stigmatization of marginalized community members. When a quarantine is necessary, public health authorities should provide adequate information about protocols and basic supplies to minimize the negative consequences of isolation. Although proactive disease prevention strategies are effective, ethical considerations should also be emphasized. Privacy protection, for example, should be considered during contact tracing. It is also critical for each nation to invest in its public health sector to increase capacity and access to healthcare services and to develop a sustainable healthcare system.
The analysis of the four countries provides important insights for mitigating current challenges and preparing for the post-pandemic era. The COVID-19 response policies towards LGBTI individuals and migrant workers in Korea and Singapore suggest implementing anti-discrimination policies in conjunction with public health strategies and incorporating more detailed human rights considerations. The case of disease transmission among slum dwellers in the Philippines highlights the impact of housing conditions on health, underscoring the importance of improving housing and providing economic support. Additionally, the healthcare crisis in Indonesia due to a lack of medical resources reveals the need for strengthening healthcare infrastructure and supporting healthcare workers. The differences in vulnerable populations across countries offer information on which health issues should be prioritized for improvement in epidemic crisis responses specific to each nation.
Furthermore, our comparative analysis highlights the importance of cooperation between nations to combat the pandemic by illustrating similarities and differences in public health strategies between countries and their impact on vulnerable populations. A previous study reported that despite the initial variations in public health measures’ speediness, strictness, and resourcefulness during the COVID-19 pandemic, the measures became similar in most countries over time [ 13 ]. As time passed, the lessons learned from various countries may have provided practical guidelines for controlling the pandemic. Beyond knowledge sharing, international solidarity is critical for recovery. Moreover, global governance and increased collaboration in surveillance, research, and best practices are critical for resilient responses [ 66 ]. Such a collaborative approach would aid in identifying effective ways to protect vulnerable populations and improve health equity during the pandemic.
This study had several limitations. First, this study may not capture all policy changes over time due to the rapid changes in policies and support measures during the COVID-19 pandemic. Many policy measures may have changed since the time this article was written. Second, this may lead to biases in rating priority levels due to the subjective nature of the experts’ opinions. This study involved relevant experts who are representative members from each country in international organizations, aiming to reflect the situation of their respective countries accurately. These experts used their social and academic networks to collect advice that would help identify the objective characteristics of each nation. It was anticipated that objective prioritization of issues would be feasible through the involvement of these experts and the interviewees they selected. However, there are inherent limitations to this method, primarily because it relies heavily on the perspectives of selected experts. Third, while detailing the characteristics of the vulnerable populations would aid in targeting policy interventions toward specific groups, this was not done in the current study. Consequently, because the level of vulnerability was not assessed in detail to identify high-risk subgroups, the definition of vulnerable groups relied largely on the opinions of individual researchers, potentially limiting the applicability of the findings to broader or different contexts. Fourth, this study is grounded within interpretative approach; thus, we did not gather demographic information of interviewees because the study did not only use data from interviews but also multiple resources for each item.
The COVID-19 pandemic challenged health systems worldwide. Understanding the impact of healthcare systems and social resilience on vulnerable populations during the COVID-19 pandemic is critical. Our findings revealed that COVID-19 exacerbated existing inequalities in social conditions, gender, and healthcare. Across the four countries, vulnerable groups were consistently identified as older adults, women, children, and adolescents. Meanwhile, LGBTI people, healthcare workers, slum dwellers, and migrant workers were also highlighted as highly vulnerable. Depending on the social environment and context of a country, the degree and types of vulnerable groups might be various in each country.
The results suggest the importance of emphasizing equity in healthcare and human rights protection to mitigate the pandemic’s negative impact. Most importantly, measures to ensure universal health coverage and equal accessibility to health care must be specified based on the most vulnerable groups even though there are the common and unique features among vulnerable groups in each society.
Data availability
Data will be made available from the corresponding author, SJ, on reasonable request.
Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. 2021;8:732–42.
Article PubMed Google Scholar
Czymara CS, Langenkamp A, Cano T. Cause for concerns: gender inequality in experiencing the COVID-19 lockdown in Germany. Eur Soc. 2021;23(sup1):S68–81.
Article Google Scholar
Patel JA, Nielsen FBH, Badiani AA, Assi S, Unadkat VA, Patel B, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020;183:110–1.
Article CAS PubMed Google Scholar
Alizadeh H, Sharifi A. Analysis of the state of social resilience among different socio-demographic groups during the COVID- 19 pandemic. Int J Disaster Risk Reduct. 2021;64:102514.
Article PubMed PubMed Central Google Scholar
Kumru S, Yiğit P, Hayran O. Demography, inequalities and global health security index as correlates of COVID-19 morbidity and mortality. Int J Health Plann Manage. 2022;37:944–62.
Rose SM, Paterra M, Isaac C, Bell J, Stucke A, Hagens A et al. Analysing COVID-19 outcomes in the context of the 2019 global health security (GHS) index. BMJ Glob Health. 2021;6.
The L. Redefining vulnerability in the era of COVID-19. Lancet. 2020;395:1089.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27:964–80.
Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525–34.
Article CAS PubMed PubMed Central Google Scholar
Wu S, Neill R, De Foo C, Chua AQ, Jung AS, Haldane V, et al. Aggressive containment, suppression, and mitigation of Covid-19: lessons learnt from eight countries. BMJ. 2021;375:e067508.
Wang D, Mao Z. A comparative study of public health and social measures of COVID-19 advocated in different countries. Health Policy. 2021;125:957–71.
Bezbaruah S, Wallace P, Zakoji M, Padmini Perera WS, Kato M. Roles of community health workers in advancing health security and resilient health systems: emerging lessons from the COVID-19 response in the South-East Asia region. WHO S East. Asia J Public Health. 2021;10:41–8.
Google Scholar
Garfield R, Bartee M, Mayigane LN. Validating Joint External evaluation reports with the quality of outbreak response in Ethiopia, Nigeria and Madagascar. BMJ Glob Health. 2019;4(6):e001655.
Rose SM, Paterra M, Isaac C, Bell J, Stucke A, Hagens A, Tyrrell S, Guterbock M, Nuzzo JB. Analysing COVID-19 outcomes in the context of the 2019 Global Health Security (GHS) Index. BMJ Glob Health. 2021;6(12):e007581.
Bigdelou B, Sepand MR, Najafikhoshnoo S, Negrete JAT, Sharaf M, Ho JQ, et al. COVID-19 and preexisting comorbidities: risks, synergies, and clinical outcomes. Front Immunol. 2022;13:890517.
Lee SW, Yuh WT, Yang JM, Cho YS, Yoo IK, Koh HY, et al. Nationwide results of COVID-19 contact tracing in South Korea: individual participant data from an epidemiological survey. JMIR Med Inf. 2020;8:e20992.
Grabowski DC, Mor V. Nursing home care in crisis in the wake of COVID-19. JAMA. 2020;324:23–4.
McGilton KS, Escrig-Pinol A, Gordon A, Chu CH, Zúñiga F, Sanchez MG, et al. Uncovering the devaluation of nursing home staff during COVID-19: are we fuelling the next health care crisis? J Am Med Dir Assoc. 2020;21:962–5.
Truskinovsky Y, Finlay JM, Kobayashi LC. Caregiving in a pandemic: COVID-19 and the well-being of family caregivers 55 + in the United States. Med Care Res Rev. 2022;79:663–75.
Jamieson DJ, Rasmussen SA. An update on COVID-19 and pregnancy. Am J Obstet Gynecol. 2022;226:177–86.
Kotlar B, Gerson EM, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 2021;18:10.
Taylor MM, Kobeissi L, Kim C, Amin A, Thorson AE, Bellare NB, et al. Inclusion of pregnant women in COVID-19 treatment trials: a review and global call to action. Lancet Glob Health. 2021;9:e366–71.
Connor J, Madhavan S, Mokashi M, Amanuel H, Johnson NR, Pace LE, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Soc Sci Med. 2020;266:113364.
Li X, Xu W, Dozier M, He Y, Kirolos A, Theodoratou E, et al. The role of children in transmission of SARS-CoV-2: a rapid review. J Glob Health. 2020;10:011101.
World Health Organization. Considering the impact of COVID-19 on children. Geneva: WHO; 2022.
Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293:113429.
Neville RD, Lakes KD, Hopkins WG, Tarantino G, Draper CE, Beck R, et al. Global changes in child and adolescent physical activity during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. 2022;176:886–94.
PubMed PubMed Central Google Scholar
Kang CR, Lee JY, Park Y, Huh IS, Ham HJ, Han JK, et al. Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg Infect Dis. 2020;26:2499–501.
Chung E, Yi J. Pandemic priorities: the impact of South Korea’s COVID-19 policies on vulnerable populations. Int J Public Admin. 2021;44:1028–38.
Zeeman L, Sherriff N, Browne K, McGlynn N, Mirandola M, Gios L, et al. A review of lesbian, gay, bisexual, trans and intersex (LGBTI) health and healthcare inequalities. Eur J Public Health. 2019;29:974–80.
Utamsingh PD, Richman LS, Martin JL, Lattanner MR, Chaikind JR. Heteronormativity and practitioner-patient interaction. Health Commun. 2016;31:566–74.
Watch HR, [annual review]. Human rights situation of LGBTI in South Korea. 2016. https://www.hrw.org/news/2018/12/18/submission-human-rights-watch-committee-rights-child-south-korea . Accessed 2018-12-18.
Kim S, Yang E. Suicidal ideation in gay men and lesbians in South Korea: a test of the interpersonal-psychological model. Suicide Life Threat Behav. 2015;45:98–110.
Kwak Y, Kim JS. Associations between Korean adolescents’ sexual orientation and suicidal ideation, plans, attempts, and medically serious attempts. Iran J Public Health. 2017;46:475–84.
Lee DY, Kim SH, Woo SY, Yoon BK, Choi D. Associations of health-risk behaviors and health cognition with sexual orientation among adolescents in school: analysis of pooled data from Korean nationwide survey from 2008 to 2012. Med (Baltim). 2016;95:e3746.
Jarrell Z. South Korean gay couple denied health care benefits in court. 2022. https://www.losangelesblade.com/2022/01/07/south-korean-gay-couple-denied-health-care-benefits-in-court/ . Accessed August 15 2022.
Welfare M. National survey of homeless people. South Korea: Ministry of Health and Welfare; 2021.
Lim D, Hong S. The impact of Covid-19 on homeless persons and Jjokbahng dwellers and its policy implications. Res Brief. 2022;90:13.
Yunus F, Andarini S. Letter from Indonesia. Respirology. 2020;25:1328–9.
Mahendradhata Y, Andayani NLPE, Hasri ET, Arifi MD, Siahaan RGM, Solikha DA, et al. The capacity of the Indonesian healthcare system to respond to COVID-19. Front Public Health. 2021;9:649819.
Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from corona virus (COVID-19) disease. Occup Med (Lond). 2020;70:370–4.
Margaretha SEPM, Effendy C, Kusnanto H, Hasinuddin M. Determinants psychological distress of Indonesian health care providers during COVID-19 pandemic. Syst Rev Pharm. 2020;11:1052–60.
CAS Google Scholar
Windarwati HD, Ati NAL, Paraswati MD, Ilmy SK, Supianto AA, Rizzal AF, et al. Stressor, coping mechanism, and motivation among health care workers in dealing with stress due to the COVID-19 pandemic in Indonesia. Asian J Psychiatry. 2021;56:102470.
Djalante R, Lassa J, Setiamarga D, Sudjatma A, Indrawan M, Haryanto B, et al. Review and analysis of current responses to COVID-19 in Indonesia: period of January to March 2020. Prog Disaster Sci. 2020;6:100091.
Villarama EPS, Lopez EB, Sayo AR, Seposo X, Ariyoshi K, Smith C. COVID-19 is moving to high-density, poor residential areas in Metropolitan Manila, Philippines. Western Pac Surveill Response J. 2021;12:53–5.
The World Bank. Population living in slums (% of urban population) - Philippines. 2018. https://data.worldbank.org/indicator/EN.POP.SLUM.UR.ZS?locations=PH&most_recent_value_desc=true . Accessed 20 Dec 2022.
Vochelet R. Who gets to speak for migrant workers in Singapore? Diplomat. 2022.
Koh D. Migrant workers and COVID-19. Occup Environ Med. 2020;77:634–6.
Singapore MoH. Measures to contain the COVID-19 outbreak in migrant workers dormitories. 2020. https://www.moh.gov.sg/news-highlights/details/measures-to-contain-the-covid-19-outbreak-in-migrant-worker-dormitories . Accessed August 15 2022.
Saw YE, Tan EY, Buvanaswari P, Doshi K, Liu JC. Mental health of international migrant workers amidst large-scale dormitory outbreaks of COVID-19: a population survey in Singapore. J Migr Health. 2021;4:100062.
Geddie J, Aravindan A. Spate of suicides among migrant workers in Singapore raises concern. Michigan, US: Reuters; 2020.
Ngiam JN, Chew N, Tham SM, Beh DL, Lim ZY, Li TYW, et al. Demographic shift in COVID-19 patients in Singapore from an aged, at-risk population to young migrant workers with reduced risk of severe disease. Int J Infect Dis. 2021;103:329–35.
Moyce SC, Schenker M. Migrant workers and their Occupational Health and safety. Annu Rev Public Health. 2018;39:351–65.
Hansen E, Donohoe M. Health issues of migrant and seasonal farmworkers. J Health Care Poor Underserved. 2003;14:153–64.
Malhotra R, Arambepola C, Tarun S, de Silva V, Kishore J, Østbye T. Health issues of female foreign domestic workers: a systematic review of the scientific and gray literature. Int J Occup Environ Health. 2013;19:261–77.
Schenker MB. A global perspective of migration and occupational health. Am J Ind Med. 2010;53:329–37.
Asian Development Bank. Assessment of COVID-19 response in the Republic of Korea. Manila: Asian Development Bank; 2021.
Book Google Scholar
Park D, Ha J. Comparison of COVID-19 and MERS risk communication in Korea: a case study of TV public service advertisements. Risk Manag Healthc Policy. 2020;13:2469–82.
Hennein R, Lowe S. A hybrid inductive-abductive analysis of health workers’ experiences and wellbeing during the COVID-19 pandemic in the United States. PLoS ONE. 2020;15:e0240646.
Unger A, Riley LW. Slum health: from understanding to action. PLOS Med. 2007;4:1561–6.
Harpham T. Urban health in developing countries: what do we know and where do we go? Health Place. 2009;15:107–16.
de Snyder VN, Friel S, Fotso JC, Khadr Z, Meresman S, Monge P, et al. Social conditions and urban health inequities: realities, challenges and opportunities to transform the urban landscape through research and action. J Urban Health. 2011;88:1183–93.
Cloutier RL, Marshaall R. A dangerous pandemic pair: Covid19 and adolescent mental health emergencies. Am J Emerg Med. 2021;46:776–7.
Korea times. Rising youth suicide. 2021. https://www.koreatimes.co.kr/www/opinion/2021/10/202_316449.html . Accessed August 08 2021.
Han SD, Mosqueda L. Elder abuse in the COVID-19 era. J Am Geriatr Soc. 2020;68:1386–7.
Sagan A, Thomas S, McKee M, Karanikolos M, Azzopardi-Muscat N, de la Mata I, et al. COVID-19 and health systems resilience: lessons going forwards. Eurohealth. 2020;26:20–4.
Download references
Acknowledgements
Not applicable.
The study’s funder had no role in study design, data collection, analysis, interpretation, or report writing.
Author information
Jakyung Lee and Susan Park contributed equally to this work.
Authors and Affiliations
Institute for Community Care and Health Equity, Chung-Ang University, Seoul, Republic of Korea
Jakyung Lee, Susan Park & Soong-nang Jang
Hyo-tree nursing home, Incheon, Republic of Korea
Jakyung Lee
Seoul National University, Seoul, Republic of Korea
Red Cross College of Nursing, Chung-Ang University, 84 Heukseok-ro, Dongjak-gu, Seoul, 06974, Republic of Korea
Soong-nang Jang
Alliance for Improving Health Outcomes, Quezon City, Philippines
Katherine Ann Reyes, Joseph Oraño & Alfredo Jose Ballesteros
College of Public Health, University of the Philippines Manila, Manila, Philippines
Fernando Garcia Jr. & Carmelita Canila
Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Depok, Indonesia
Tri Muhartini, Sandra Frans, Tiara Marthias, Likke Prawidya Putri & Yodi Mahendradhata
NUS Saw Swee Hock School of Public Health and National University Health System, Singapore, Singapore
Chuan De Foo
Duke NUS Graduate Medical School, Singapore, Singapore
You can also search for this author in PubMed Google Scholar
Contributions
JL, SP, and SJ conceptualized the study. SJ and SP designed the methodology. JL and SP were responsible for writing the first draft of the manuscript. JL, SP, SJ, KAR, FG, CC, JO, AJB, TM, SF, TM, LPP, YM, and CDF contributed to data analysis and interpretation of the results. All authors reviewed the manuscript. JL and SP were considered contributing equally to this work.
Corresponding author
Correspondence to Soong-nang Jang .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval and consent to participate in this study were not required since the quantitative data is secondary and is available in the public domain, and interviews were conducted through advisory meetings. Data was fully anonymized for analysis.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lee, J., Park, S., Jang, Sn. et al. Differential impacts of health systems and sociocultural environment on vulnerable populations during the COVID-19 pandemic: lessons from four Asia-Pacific countries. BMC Public Health 24 , 1501 (2024). https://doi.org/10.1186/s12889-024-18949-1
Download citation
Received : 05 December 2023
Accepted : 24 May 2024
Published : 05 June 2024
DOI : https://doi.org/10.1186/s12889-024-18949-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health equity
- Vulnerable population
- Health policy
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 24 April 2024
Trauma-Informed Healthcare Leadership? Evidence and opportunities from interviews with leaders during COVID-19
- Sonia Rose Harris ORCID: orcid.org/0000-0002-4599-5684 1 ,
- Alexis Amano ORCID: orcid.org/0000-0001-7136-2197 2 ,
- Marcy Winget ORCID: orcid.org/0000-0002-5893-280X 3 ,
- Kelley M Skeff 3 &
- Cati G Brown-Johnson ORCID: orcid.org/0000-0002-5415-3665 3
BMC Health Services Research volume 24 , Article number: 515 ( 2024 ) Cite this article
634 Accesses
Metrics details
COVID-19 impacted the mental health of healthcare workers, who endured pressures as they provided care during a prolonged crisis. We aimed to explore whether and how a Trauma-Informed Care (TIC) approach was reflected in qualitative perspectives from healthcare leaders of their experience during COVID-19 (2020–2021).
Semi-structured interviews with healthcare leaders from four institutions were conducted. Data analysis consisted of four stages informed by interpretative phenomenological analysis: 1) deductive coding using TIC assumptions, 2) inductive thematic analysis of coded excerpts, 3) keyword-in-context coding of full transcripts for 6 TIC principles with integration into prior inductive themes, and 4) interpretation of themes through 6 TIC principles (safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and awareness of cultural, historical, and gender issues).
The actions of leaders ( n = 28) that were reported as successful and supportive responses to the COVID-19 pandemic or else missed opportunities reflected core principles of Trauma-Informed Care. To promote safety , leaders reported affirmative efforts to protect staff by providing appropriate physical protection, and enhanced psychological safety by providing channels for communication about emotional well-being. To promote trustworthiness and transparency, leaders listened to their staff, shared current COVID-19 information, and increased frequency of meetings to disseminate accurate information. To promote mutual support , strategies included wellness check-ins, sharing uplifting stories, affirming common goals, articulating fears, and leading by example. Examples of empowerment included: making time and adjusting modalities for flexible communication; naming challenges outside of the hospital; and functioning as a channel for complaints.
Reported missed opportunities included needing more dedicated time and space for healthcare employees to process emotions, failures in leadership managing their own anxiety, and needing better support for middle managers. Awareness of the TIC principle of cultural, historical, and gender issues was largely absent. Results informed the nascent Trauma-Informed Healthcare Leadership (TIHL) framework.
Conclusions
We propose the Trauma-Informed Healthcare Leadership framework as a useful schema for action and analysis. This approach yields recommendations for healthcare leaders including creating designated spaces for emotional processing, and establishing consistent check-ins that reference personal and professional well-being.
Peer Review reports
In the early years (2020–2021) of the COVID-19 pandemic, the incidence of depression and anxiety increased in the United States (US), and overall psychological well-being decreased [ 1 , 2 , 3 ]. The mental health of healthcare workers was particularly negatively impacted as they endured unrelenting challenges in providing patient care during the prolonged crisis [ 3 , 4 , 5 ]. Negative contributors to mental health for these healthcare workers included: feeling stressed and stretched too thin, concern about exposing family/network to illness, emotional and physical exhaustion, a lack of appropriate emotional support from colleagues and supervisors, and struggles with managing home responsibilities and isolation caused by work requirements [ 6 ]. In response to these negative impacts on healthcare personnel, the US Department of Health and Human Services issued recommendations to transform workplace culture, with goals to 1) empower through reduced administrative tasks, 2) eliminate punitive policies for seeking mental health care, and 3) prioritize social connection by increasing flexibility in scheduling and building peer- and team-based care models [ 7 ]. Healthcare personnel were still expected to continue performing their duties and deliver quality healthcare, often without time for recovery or restoration [ 6 , 7 ].
Previous disaster management reports (e.g., after the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak [ 8 ], 9/11 attack on the United States, and Hurricane Katrina in New Orleans) include lessons learned about the impacts of traumatic events on healthcare workers, such as need for resources that facilitate reflection on new stressors, for systems that mitigate the impact of interpersonal isolation, and for mental health resources without financial barriers for healthcare workers [ 9 , 10 , 11 ]. Analyses of the impact of COVID-19 on healthcare workers showed similar themes [ 3 , 6 , 7 , 10 ], and emphasized the need for hospital- and health system preparedness [ 12 ].
Trauma-informed care (TIC) is considered a gold standard for effective care to support patient mental health [ 13 , 14 , 15 , 16 ]. The TIC framework emphasizes a shift from asking “what’s wrong with you” to “what happened to you,” emphasizing the need for a complete understanding of a person’s lived experience in accounting for and understanding their actions [ 17 ]. This perspective underscores the need to understand a person’s behavior in the context of their life experience [ 17 ]. In medical centers, the application of TIC involves changing organizational culture through policies and procedures and incorporating an understanding of the impact on trauma into routine care [ 18 ]. The US Substance Abuse and Mental Health Services Administration (SAMHSA) outlines four key assumptions (four R’s) in TIC [ 19 ]: 1) Realize the impact of trauma on individuals, families, and groups; 2) Recognize signs of trauma; 3) Respond by applying major TIC principles; 4) avoid Re-traumatization. In addition to these four assumptions, TIC is built on 6 principles [ 19 ]: safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and awareness of cultural, historical, and gender issues and oppression. TIC has been widely applied, for instance in schools, social work practices, treatment of domestic violence, juvenile justice, homelessness services, and child welfare agencies [ 15 , 16 , 18 , 20 , 21 ]. Within the last decade, TIC principles have also been applied in healthcare settings; reports in healthcare indicate that TIC can improve patient care outcomes [ 13 , 22 ].
We aimed to explore whether and how a Trauma-Informed Care (TIC) approach was reflected in qualitative perspectives from healthcare leaders of their experience during COVID-19 (2020–2021). Our hope was that this analysis could inform leaders in healthcare about how to support teams and avoid pitfalls during ongoing and future crises.
Participating Institutions and Sampling: Administrative and medical leaders at four healthcare organizations across the United States (from Colorado, Michigan, and Northern California) were invited to participate in a qualitative study. Eligibility included Vice Presidents, Directors, Division Chiefs, and other high-level leadership, with goal of a sample balanced across levels of leadership and also subject matter expertise (e.g., Nursing, IT, Finance.) Institutions represented a convenience sample including three academic medicine centers and one community institution.
Interview Questions/Guide: The interview guide (Additional File 1 ) was developed based on our team’s previous study [ 23 ], and focused on understanding healthcare leader feelings of joy and distress during COVID-19. The guide aimed to identify both gratifying and distressing professional experiences prior to and during the COVID-19 pandemic. We received pilot feedback from a high-level administrator with expertise in wellness.
Recruitment Strategy: Per methods outlined in Skeff et al. [ 23 ], we recruited in a multi-step process to protect the confidentiality of participants. Once a site contact was in place at each institution, the research team furnished them with IRB-approved introduction emails, which underscored research goals and purpose. These emails were sent to potential participants directly from the site contacts. Subsequently, the research team (AA/CBJ) responded directly to potential participants, without cc’ing connecting site contacts. We contacted potential participants no more than three times by email; site contacts were not informed as to who did or did not choose to participate.
Interviews: Two women researchers, with PhD and Master’s level training and expertise in qualitative research (CBJ, AA) conducted phone and video interviews (Zoom, Zoom Video Communications, San Jose, USA); Site A and B interviews were collected August to September 2021, Site C interviews October to November 2021, and Site D interviews in November 2021. Interviews were in-depth and semi-structured, each interview (one per participant) lasted between 30–60 min. One interviewer was additionally a subject matter expert in a related topic area: physician wellness and burnout (CBJ).
Participants provided written consent to participate and verbal consent to record interviews and were assured of the anonymity of interview reporting. Interviews were professionally transcribed (Rev, Rev.com, Inc, San Francisco, USA); any identifying information was deleted.
Qualitative analysis method and rigor: Data analysis for this study used an interpretative phenomenological analysis with theme clustering using TIC Framework [ 24 ]. Data analysis was conducted in four phases: 1) a priori coding using the four TIC assumptions; 2) inductive thematic coding of those excerpts; 3) keyword assisted coding of the full transcripts for elements of the six TIC Principles, and subsequent integration of those excerpts into prior inductive themes; and 4) interpretation of themes through the six TIC Principles. First, we used a priori coding with the deductive framework of TIC assumptions: realize, recognize, respond, and resist re-traumatization . Two qualitative researchers (AA and SRH) consecutively reviewed all transcripts and coded the excerpts to the four assumptions. We identified significant overlap between the four assumptions within the data set; multiple excerpts were coded for all four TIC assumptions. While this addressed our objective of whether TIC elements could be observed in leadership experiences of gratification and distress, it did not address our subsequent question of how TIC might be evidenced in interviews.
Thus, as a second phase, SRH and CBJ used consensus coding approaches to organize TIC excerpts into inductive themes (e.g., listening) using twice-weekly meetings to come to consensus through an iterative process. We simultaneously reviewed literature for other Trauma-Informed Care organizing frameworks to help understand the data.
A third phase of analysis involved mapping inductive themes from the TIC excerpts to the 6 principles of Trauma-Informed Care : 1. Safety; 2. Trustworthiness and transparency; 3. Collaboration and mutuality; 4. Peer support; 5. Empowerment, voice, and choice; and 6. Awareness of cultural, historical, and gender issues . Safety was defined as all people within the organization feeling physically and psychologically safe. Trustworthiness and transparency were defined as organizational activities conducted transparently with a goal of increasing trust. Peer support refers to mutual self-help. Collaboration and mutuality were defined as emphasizing teamwork and power sharing. Empowerment, voice, and choice refer to building on individual strengths and shared decision making and choice. Finally, awareness of cultural, historical, and gender issues was defined as awareness of oppression with efforts to move away from prejudice and bias. These definitions were adapted from the Substance Abuse and Mental Health Service Administration [ 19 ]. Two authors (SRH and CBJ) met weekly to come to consensus over a two-month period [ 25 ]. In addition to this focused consensus analysis, all co-authors reviewed developing organizational patterns of the results during monthly research team meetings.
To ensure a comprehensive account of healthcare leaders’ experiences with this trauma-informed lens, one researcher (SRH) conducted additional coding using a modified keyword-in context approach [ 26 ]. SRH used keywords to search the data set for TIC principles and close synonyms using qualitative software (NVivo 12, QSR International, Melbourne, AUS). Passages containing a keyword were reviewed by two authors (SRH and CBJ) and incorporated into the analysis when the passage included a term used in a way that matched the definitions of the TIC principles used in this dataset. Final structure for the data was organized by the TIC principles.
This project was presented for discussion and feedback in a lecture format and small group sessions to over 40 healthcare leaders interested in clinician wellness and healthcare worker burnout in February and March 2024. This project was approved by our Institutional Review Board (Protocol # 39948).
Participants
Twenty-eight interviews were conducted via phone or Zoom with participants from four healthcare institutions across the United States (in Colorado, Michigan, and Northern California). These institutions represented both academic medical centers and community hospitals. Participants included healthcare leadership in finance, service lines, operations, and education. They filled specific roles of Chief Financial Officer, Chief Nursing Officer, Chief Medical Officer, Executive Director, or Director. Participants were 61% women ( n = 17/28) and included ages across deciles from 30 to 70. 75% were white ( n = 21/28) and all had 10 + years of experience in the field of health care administration. All participants who consented for an interview completed their interview. To maintain anonymity, participants have been assigned a random participant number (1–28). We use the term “leaders” throughout our results to highlight their role as leaders in their setting.
Overall, the actions of leaders that were reported as either successful responses to the COVID-19 pandemic or missed opportunities to alleviate distress mapped to core principles of trauma-informed care. Safety; trustworthiness and transparency; and empowerment, voice, and choice were reflected in our data. Principles of peer support and collaboration and mutuality were combined in our analysis as “mutual support” because while we saw examples of teamwork and power-sharing (collaboration and mutuality), there were not distinct elements of mutual self-help (peer support) perhaps due to power differentials between staff and leadership. The sixth assumption, awareness of cultural, historical, and gender issues, was largely absent from our data set. Leaders’ supportive actions and strategies are presented by TIC principle below. Table 1 provides further qualitative examples, organized first by TIC principle, then by theme. Table 1 also includes recommended future actions based on our data.
Safety . Healthcare leaders employed the principle of safety, which is defined as all members of the organization feeling both physically and psychologically safe, by (1) promoting protection to ensure physical health and (2) by not taking complaints personally. Leaders reported a missed opportunity for supporting psychological safety by not providing more attention, space, and time for emotional processing.
Promoting physical protection . Healthcare leaders reported that addressing staff concerns about physical safety—including the limited supply of personal protective equipment (PPE)—was paramount to supporting staff wellness during COVID-19. Some department’s PPE allotment was lower than staff needs. The disparity in resources raised staff fears and anxiety. In response, leaders reported feeling successful when they increased communication and specifically identified best practices vs. realistic approaches in the current environment.
Even though you know that [reusing masks with different patients, washing masks] is not best practice, it’s better than nothing—but it’s not best practice…. It was hard conversations about what is appropriate and what was the best we could do versus best practice. (Participant 2)
One leader reported using extension intravenous (IV) tubing so that nursing staff could monitor the IVs of patients from outside the intensive care unit (ICU) room. While the participant reported receiving complaints from system executives, there were no negative patient outcomes and staff were extremely satisfied.
In the end, we had absolutely zero negative patient outcomes, and our patients got better care. And the nursing staff was extremely satisfied with that, because they were able to not have to sit in that room with a patient shedding the virus. (Participant 4)
Not taking complaints personally . In best-case scenarios, interviewed healthcare leaders managed to not take complaints personally or respond in anger when they received complaints from staff for situations beyond leadership control. This spirit of acceptance created space for venting frustration without retaliation, supporting psychological safety. When leaders found themselves the target of anger, effective managers worked to let it go. “The anger of the staff that’s directed towards you, even though it’s probably not personal, but you’re the punching bag about not keeping [staff] safe” (Participant 1). In best circumstances leaders looked for potential root causes of the frustration: fear, concern for their team, lack of control:
I’d get an angry email from the head of the department and he’s just looking… out for their staff right? And, and their nurses and their other employees. So I totally get it, right. Cause I’m doing the same for mine… (Participant 8)
Missed opportunity- Not providing more attention, space, and time for emotional processing . Interviewed healthcare leaders reported that they recognized a responsibility as team leads to create space for staff to process emotions by encouraging staff to speak freely without concerns of minimization or retaliation. They reported that not dealing with the emotions of staff during the crisis setting of COVID-19 had a lasting impact:
Even now, we continue to see that and how people are very short with one another, and they don’t allow mistakes in other people and there’s a lot of unneeded hysteria, and I think that it stems back to us not really dealing with all of these emotions that we went through last year. And how do you deal with that on an administrative level, in a hospital when you have hundreds of people reporting to you? I don’t really know the answer to that, but if there was anything that I could have done better, that would’ve been anything. (Participant 7)
Trustworthiness and Transparency . To promote trustworthiness and transparency, defined as organizational activities conducted transparently to increase trust, leaders reported: (1) listening; (2) increasing frequency of information dissemination; and (3) making decisions transparently. Missed opportunities to establish trustworthiness and transparency included: (4) overcommunicating on time off and (5) not containing leadership anxiety.
Listening . Intentional listening in one-on-one interactions worked well to identify specific concerns. Leaders recognized their responsibility to “hear people out, because they need to feel like they've been heard” (Participant 4). Listening with patience established two levels of trust: “So what helps... What I need to do is give myself time to listen and to let people know what we're doing for them. So, both those things take time… one kind of helps establish understanding, trust, and the other helps establish … the next level of trust where, ‘oh, he is acting on some of the things I expressed earlier'” (Participant 4). By listening, one participant learned that staff valued hearing that managers may not have an answer but were making efforts to address staff concerns:
I think that there's a value in just listening and acknowledging and we may not have an answer, and no one does. I feel that to recognize that [transparency] exists, I think goes such a long way and I think that's why we've developed such a great rapport with many of our frontline teams, because they feel, and they see that we hear them. (Participant 5)
Increasing frequency of information dissemination. Healthcare leaders increased the frequency and modality of information dissemination about COVID-19 in response to the changing environment. Specific examples included: increasing team meetings; weekly huddles; and frequent actionable information-sharing. Leaders increased the frequency of communication to address the constant flux of COVID-19 information. A participant recalled increasing meetings to twice a month. Frequent communication in established settings created opportunities to address changing circumstances.
Leaders recognized that timely sharing of information about decision-making and the availability of resources increased trust among staff members and inhibited the spread of rumors.
When communication breaks down, that’s when rumor control starts. So, I think just being fully transparent with where you’re at, whether you had PPE, whether you didn’t. Whether you had to a process together to reuse N-95s…. [The staff] can trust you. Because it comes down to trust, it really does, it comes down to trust. (Participant 25)
Making decisions transparently . When leaders were transparent about their decision-making processes, they could communicate effectively that they were acting in the best interest of staff and patients. When they lacked information due to changing guidelines or circumstances, they reported discomfort.
I think also not always being able to answer questions or give our teams the most. Part of it is we don’t know the answers. And so not being able to provide direction to our team sometimes just because the information was changing. I felt a little bit not powerless, but I felt I always wanted to try to do more, and I couldn’t. So, I think that doesn’t feel great. (Participant 18)
Missed Opportunity- Overcommunicating on time off. Healthcare leaders noted that too much communication, specifically on weekends, sent a message that staff should continue to work even on their days off, which could undermine trust.
When we have the command center set up and there’s these things going, and we say, "Hey, it’s the weekend. You don’t need to do this." And then yet on the weekend, we’re sending them texts or emails and all these pieces... I have definitely heard from quite a few of them for feeling like... They tell us to try and work on... taking care of ourselves and resting and removing ourselves. And then yet these emails come in and it definitely comes across as we expect you to respond to these. (Participant 13)
Missed Opportunity- Containing leadership anxiety . Leaders reported missed opportunities that centered on failures to manage their own anxiety and contain it within their leadership team. Interviewees shared that they failed to protect staff from leadership anxiety, which created more chaos:
The major leadership failure here was that leaders didn’t contain anxiety within their teams. They let that anxiety fuel their own anxiety and threw it out for the organization. So we just all run and collided into each other. It was really damaging, and it took a lot of time to manage… (Participant 17)
Empowerment, Voice, and Choice (Empowerment) . Leaders communicated with staff with flexible times and modalities to promote individual empowerment defined as sharing decision making and choice. Leaders reported that they gave staff options for how and when to connect. Building pathways of support required leaders “to flex our hours, be on our emails constantly, circle back with the staff” (Participant 4). Leaders also added communication modalities - frequent emails, in-person and virtual huddle meetings, personal cell phone communications, texting options, and in-person meetings - to increase accessibility:
I gave my personal cell phone out in addition to my work cell phone, so that the staff could text or call me at any point in time. And they did, and I answered them back and went down and listened to them and their fears…Very difficult time. (Participant 4)
Mutual Support . To promote mutual support, defined as mutual self-help and teamwork, leaders reported: (1) checking on staff wellness and creating personal touch points to foster connection, particularly in virtual settings; (2) leading by example; and (3) sharing positive messages. Leaders reported a missed opportunity for mutual support by not supporting middle managers.
Checking on wellness and creating personal touch points . Leaders strengthened individual relationships with staff through developing or expanding wellness check-ins and personal touch points. These conversations set precedents to communicate about emotional well-being. For example, one leader shared that, in response to work-from-home requirements, they transitioned to “good morning” (Participant 22) emails, increased touch points with staff, and articulated interest in the impact of (home) stressors outside of work. These efforts opened pathways of communication and supported staff well-being:
We established this routine of almost good morning type emails... almost akin to if you were walking down the hallway and going in somebody’s door and just saying good morning. …it was also good from a wellness perspective, just from the standpoint of “we got to just talk” . (Participant 22)
Leading by Example . Leaders led by example, modeling desired behaviors while working to understand the unique needs of staff members. One leader noted that it was the responsibility of the leader to step in when no one else would:
I remember this one time my team doesn’t want to come in back to work, I have a patient I need to discharge. He’s homeless, he refused to wear a mask. He’s coming out to the nursing station, nursing staff [and] doctors freaked out. I remember, I wear a mask ... At that time, we also didn’t have all the PPE that we have, right? I physically went into the room and I have to push the patient’s belongings out, so he can go to a hotel. Somebody has to do the job and at the end, someone has to do it. If nobody does it, a leader has to step in and do it. (Participant 3)
Identifying a common goal . Identifying a common goal motivated teams and set universal expectations for how to respond to the new environment. One participant reported that a shared goal equipped teams to respond cohesively to the crisis.
I think it was obviously a very scary time, a lot of uncertainty surrounding when the pandemic first became, I guess, an outbreak. And one of those things that I felt like went really well as a hospital administrator is the team got together very quickly. The common goal was definitely our motivator to be able to kind of think things through. (Participant 5)
One leader spoke specifically about the common goal of “getting the job done” (Participant 5) . This participant saw team members pivot from their own responsibilities to working collaboratively for team success.
Sharing positive messages. Healthcare leaders reported that positive messages motivated the team and alleviated stress and fear during the early crisis of COVID-19. They reflected awareness that the challenges would impact each person differently recognizing that individual circumstances and prior experiences influence reactions, articulating both the recognize and realize assumption in TIC. In times of crisis, people will experience highs and lows at different times. The responsibility to engage in uplifting communication shifted by day and mood among team members. Positive messages served to “motivate” and to help people “feel better” (Participant 25).
Additionally, sharing positive moments and uplifting stories helped people “rise to the occasion” (Participant 25). To boost morale and positive messaging, leaders focused team messages to emphasize that no two people were having identical experiences during the pandemic, whether at work or at home.
Supporting everybody who was in a different situation. Some people had babies at home, some people had elementary school kids that you can’t just sit in front of a computer and think they’re going to work. There was no two people experiencing the same environment or anxiety, whether it was work-related or not. (Participant 28)
Positive communication unified and strengthened teams to respond to the crisis:
What I really appreciated about our team was it was as though different people were at a high on different days. And so, those people who were feeling better did a really nice job of just building up the team and supporting us and helping us feel good. (Participant 22)
Even in a shared experience, people react differently; however, leaders emphasized unequivocal support for the team, regardless of where they might be.
Missed Opportunity- Supporting middle management . Finally, one leader noted that the demands on middle management coming from front-line teams as well as executive and higher-level leadership were extreme. These leaders could have been better supported by higher-level leadership.
I think the first thing that comes to my mind is trying to figure out the best way to support middle management. Those people that are sort of in between trying to keep the team of frontline people together, but then also have the demands coming down from them, and trying to figure out with the current situation, how do we support that group, so they don’t feel like they’re supposed to be working 24 hours a day, seven days a week, and help them address their own burnout. (Participant 13)
Cultural, Historical, and Gender Issues . One leader reported naming and addressing oppression and racism occurring outside the hospital, acknowledging that there would be an impact on staff. As team leads, participants were also responsible for addressing challenges that could impact staff function, even when they occurred outside of the hospital system and outside of leadership control. For example, one leader described using their leadership platform to talk about George Floyd’s murder and the potential impact of racism on staff:
And I think the one that was really scary, but I felt like I had to do it, was to just talk about race. … I could not let that moment in time go by us without acknowledging how much pain many people… were feeling. (Participant 15)
The Trauma-Informed Healthcare Leadership approach
Our reported results informed the nascent Trauma-Informed Healthcare Leadership (TIHL) approach. The TIHL approach (Fig. 1 & Table 2 ) highlights successful actions and missed opportunities by leaders in different relationships/settings: one-on-one management, team participation and leadership, and at the system level. To promote safety , leaders reported affirmative efforts to protect staff by providing appropriate physical protection (e.g., PPE), and enhanced psychological safety by providing channels for communication about emotional well-being. To promote trustworthiness and transparency, leaders listened to their staff, shared up to date COVID-19 information, and increased frequency of huddles and meetings to disseminate accurate information. To promote mutual support , strategies included wellness check-ins, sharing uplifting stories, affirming common goals, articulating fears; and leading by example. Examples of empowerment included: making time and adjusting modalities for flexible communication; naming challenges outside of the hospital; and functioning as a channel for complaints.
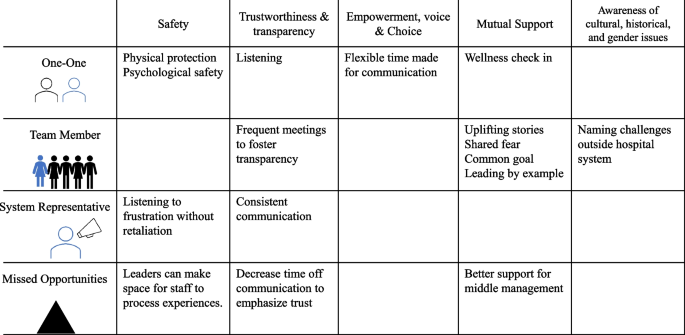
Trauma-Informed Healthcare Leadership: Successful actions and missed opportunities by leaders in one-on-one, team, and system relationships during COVID, mapped to principles of Trauma-Informed Care
This study documents evidence of hospital administrator actions reflecting principles of trauma-informed care (TIC) during the crisis setting of the COVID-19 pandemic. Leaders reported successful actions and missed opportunities to support staff that mapped to core principles of trauma-informed care: safety; trustworthiness and transparency; peer support/collaboration and mutuality; and empowerment, voice, and choice. Awareness of the TIC principle of cultural, historical, and gender issues was largely absent.
Traumatic events, whether experienced at work or outside of employment, can manifest in behaviors or feelings that may not be related to the original stressor [ 27 ]. Through this work, we identified core behaviors to seed the proposed Trauma-Informed Healthcare Leadership (TIHL) framework (Fig. 1 and Table 2 ). These behaviors, which are mapped to the 6 key principles of TIC, suggest actions leaders can take to prevent distress and/or mitigate trauma at different levels of relationships. Based on our data and evidence in the literature, we believe that the application of the Trauma-Informed Healthcare Leadership approach may establish some of the necessary supports to alleviate stress and anxiety related to traumatic events in healthcare—that can manifest as other behaviors or contribute to burnout. Like the Sanctuary Model or other trauma-informed organizational practices [ 28 , 29 , 30 , 31 ], the proposed Trauma-Informed Healthcare Leadership framework could support leaders and staff during healthcare system strain. The Trauma-Informed Healthcare Leadership framework, however, might be more accessible to a broader set of healthcare systems due to its concise approach and strong origin in the well-established Trauma-Informed Care principles. Perhaps a best-case scenario for a system interested in addressing healthcare worker needs during and after crisis would be to start with the Trauma-Informed Healthcare Leadership approach and extend into the Sanctuary Model as time and resources allow [ 28 ].
Addressing Gaps: Supporting mental health, providing dedicated time and space for emotions, elevating needs of middle managers
Notably, leaders reported missed opportunities in the areas of safety, trust, and mutual support , pointing to an underlying gap in leadership awareness and tools to support health care worker emotional experience and mental health. Leaders noted a range of failures related to mental health supports, from a lack of dedicated space for healthcare employees to process emotions related to stressors, to limitations in managing leadership anxiety. Successes exist in the behavioral health sphere in the form of trauma-informed supervision, which we posit could be applied to remedy these gaps. Behavioral health supervision works to prevent and mitigate vicarious trauma and serves as a protective factor against anxiety and depression [ 14 ]. This practice combines knowledge of trauma with supervision and emphasizes that the relationship between supervisor and supervisees must be built on trust, with clear expectations regarding boundaries, listening, and the open exchange of feedback [ 14 ]. Additionally, emotional processing may look different for each individual and change on any given day [ 32 ]. Creating space for emotional processing could be designated spaces for verbal communication about feelings or creating time in the day for rest, exercise, or preparing nutritious food [ 32 ].
While trauma-informed supervision is useful to address gaps, it manifests in a one-to-one relationship; further research is needed to address the application of trauma-informed supervision in a one-to-many or system-mediated relationship. To support teams of health care workers, individuals must have access to a variety of psychological supports—not only through resources such as Employee Assistance Programs, but also by the allocation of time and space for individual processing, as well as with their administrators and managers. Previous literature indicates that providing dedicated spaces through restorative circles (i.e., structured times and space to discuss emotions and perception) to process emotions and self-reflect could increase self-awareness, compassion, and tolerance of stress for all involved.[ 33 ]
Lastly, with respect to leadership-identified gaps, this study also validates the need for targeted support for middle management and frontline managers. Middle managers are essential to the success of the healthcare system because these leaders provide direct support to staff [ 34 ], and this direct manager relationship is more predictive of retention than any other relationship in a work environment [ 35 , 36 , 37 ]. Additionally, previous work indicates that leadership qualities of supervisors impact staff well-being and predict burnout [ 38 ]. However, despite their importance, middle and front line managers may be limited by HR and system constraints [ 39 , 40 ]. Therefore, leveraging resources to support middle level managers may enhance both safety and mutual support (TIC Principles)—and be protective against burnout and attrition. Application of trauma-informed care in elementary school settings that trained administrators in trauma-informed approaches (to apply to students) reduced administrator burnout [ 41 ]. It stands to reason that trauma-informed training for leadership and middle managers with the first goal of supporting their staff may similarly have additional benefits of reducing leadership burnout and fatigue.
Addressing (Lack of) Awareness of Cultural, Historical, and Gender Issues
To address observed blind spot of cultural, historical, and gender issues , system level anti-oppression work is needed. Responses that mapped to the final TIC principle, awareness of cultural, historical, and gender issues , were very rarely discussed by our participants, suggesting that leaders are further hindered in their ability to address the intersection of traumatic experiences. Historically marginalized healthcare workers may be at greater risk for burnout at work[ 42 , 43 ] and poorer mental health in general [ 44 ], in addition to potentially being more vulnerable, as a population, to the impacts of trauma [ 45 , 46 ]. Previous research on racism experienced by physicians of color in health-care settings reports that physicians frequently face overt racism as well as microaggressions in their workplace [ 47 ].
Creating recognition of societal, community, and organizational oppression among healthcare leaders and staff may be the first step in addressing cultural, historical, and gender issues , but naming these issues is only the very first step. Healthcare system leadership may look to anti-racist actions in healthcare delivery to address racism and oppression in the hospital system, such as The Healing ARC or Presence 5 for Racial Justice [ 48 , 49 ]. The Healing ARC, a race-conscious approach developed by two physicians at Brigham and Women’s Hospital, calls for a shift towards holding healthcare institutions accountable for actions that result in racial inequities in health [ 50 , 51 , 52 ]. The Healing ARC is built on three components: 1) acknowledgement, meaning acknowledging how racism has added to inequities in health; 2) redress, meaning putting in place compensatory actions to account for actions; and 3) closure, meaning institutions work collaboratively with the community that has been harmed to affirm that harm has been addressed and repaid [ 50 , 51 , 52 ]. These components are similar to other restorative justice approaches emphasizing acknowledgement of harm [ 33 , 48 ]. Leaders can look to establish this or a similar model within their own system to address institutionalized racism and oppression [ 33 , 53 ].
Limitations
This study has limitations in terms of data collection and analysis. First, the focus of the interviews was not trauma-informed care. Had we asked about TIC principles, participants may have provided more focused responses, particularly regarding awareness of oppression. However, the open nature of interviews can also be seen as a strength of this study. Additionally, we only conducted one interview with each participant. Given the sensitive nature (asking about moments of joy and distress and role during the pandemic) of our interviews, a longitudinal approach may have supported greater relationship rapport and trust, which could have provided more robust examples. Finally, we cannot speak to motivation of behaviors, i.e., were their responses intentionally or unintentionally brought out of trauma-informed care. In terms of participants, our sample only includes leadership. To strengthen the Trauma-Informed Healthcare Leadership approach, it will need validation across staff. Finally, trauma-informed care does not inform a strict adoptions model; instead, this approach offers principles and assumptions. Adapting to TIHL will include defining TIC in the healthcare leadership space while offering recommendations. We hope this work is a first step in that direction.
Healthcare leaders demonstrated application of principles of trauma-informed care during the early crisis of COVID-19, specifically supporting safety, trust, mutual support, and empowerment for staff. They also reported gaps and missed opportunities related to: 1) providing more dedicated time and space for healthcare employees to process emotions related to stressors, 2) failures in managing leadership anxiety, and 3) the need for better support for middle managers. Notably, few participants addressed the principle of cultural, historical, and gender issues, indicating that efforts to promote anti-racist and anti-oppression inclusive work cultures that actively work to address continued discrimination and oppressive practices may be needed. Based on our results and corroborating literature, we propose the Trauma-Informed Healthcare Leadership framework, a straightforward approach with specific recommendations for leadership. Future research can validate and query this emerging approach and expand to middle managers and non-administrator leaders within the healthcare system.
Availability of data and materials
The data that supports these findings are available from the corresponding author, CBJ, upon reasonable request.
Abbreviations
Trauma-Informed Care
Trauma-Informed Healthcare Leadership
United States
Severe Acute Respiratory Syndrome
Substance Abuse and Mental Health Services Administration
Institutional Review Board
Personal protective equipment
Intravenous
Intensive care unit
Coiro MJ, Watson KH, Ciriegio A, et al. Coping with COVID-19 stress: Associations with depression and anxiety in a diverse sample of U.S. adults. Curr Psychol. Published online November 4, 2021. https://doi.org/10.1007/s12144-021-02444-6 .
Kujawa A, Green H, Compas BE, Dickey L, Pegg S. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37(12):1280–8.
Article CAS PubMed Google Scholar
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;1(89):531–42.
Article Google Scholar
Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;1(290): 113130.
Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE. 2021;16(3): e0246454.
Article CAS PubMed PubMed Central Google Scholar
De Kock JH, Latham HA, Cowden RG. The mental health of healthcare workers during the COVID-19 pandemic: a narrative review. Curr Opin Psychiatry. 2022;35(5):311–6.
Article PubMed Google Scholar
Mental Health America. [cited 2022 Oct 24]. The Mental Health of Healthcare Workers in COVID-19. Available from: https://mhanational.org/mental-health-healthcare-workers-covid-19
SARS | Basics Factsheet | CDC. [cited 2022 Dec 9]. Available from: https://www.cdc.gov/sars/about/fs-sars.html
Iwai Y, Holdren S, Rosen LT, Hu NY. Narrative trajectories of disaster response: ethical preparedness from Katrina to COVID-19. Med Humanit. 2022;48(2):e8–e8.
DePierro J, Lowe S, Katz C. Lessons learned from 9/11: Mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;1(288): 113024.
Zhong S, Clark M, Hou XY, Zang YL, Fitzgerald G. Development of hospital disaster resilience: conceptual framework and potential measurement. Emerg Med J. 2014;31(11):930–8.
Hendel S, d’Arville A. Reimagining health preparedness in the aftermath of COVID-19. Br J Anaesth. 2022;128(2):e100–3.
King S, Chen KLD, Chokshi B. Becoming Trauma Informed: Validating a Tool to Assess Health Professional’s Knowledge, Attitude, and Practice. Pediatr Qual Saf. 2019;4(5): e215.
Article PubMed PubMed Central Google Scholar
Berger R, Quiros L. Best practices for training trauma-informed practitioners: Supervisors’ voice. Traumatology. 2016;22(2):145–54.
Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma Informed Care in Medicine: Current Knowledge and Future Research Directions. Fam Community Health. 2015;38(3):216–26.
Reeves E. A Synthesis of the Literature on Trauma-Informed Care. Issues Ment Health Nurs. 2015;36(9):698–709.
Winfrey O, Perry BD. What Happened to You?: Conversations on Trauma, Resilience, and Healing. 1st ed. An Oprah Book: Flatiron Books; 2021. p. 304.
Google Scholar
Marsac ML, Kassam-Adams N, Hildenbrand AK, Nicholls E, Winston FK, Leff SS, et al. Implementing a Trauma-Informed Approach in Pediatric Health Care Networks. JAMA Pediatr. 2016;170(1):70–7.
Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Rockville, MD: : Substance Abuse and Mental Health Services Administration; 2014. Report No.: HHS Publication No. (SMA) 14–4884. Available from: https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf
Knight C. Trauma Informed Practice and Care: Implications for Field Instruction. Clin Soc Work J. 2019;47(1):79–89.
Koetting C. Trauma-Informed Care: Helping Patients with a Painful Past. J Christ Nurs Q Publ Nurses Christ Fellowsh. 2016;33(4):206–13.
Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits LM. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatr Serv Wash DC. 2005;56(10):1213–22.
Skeff KM, Brown-Johnson CG, Asch SM, Zionts DL, Winget M, Kerem Y. Professional Behavior and Value Erosion: A Qualitative Study of Physicians and the Electronic Health Record. J Healthc Manag Am Coll Healthc Exec. 2022;67(5):339–52.
Smith J. https://www.apa.org . [cited 2023 Dec 5]. Essentials of Interpretative Phenomenological Analysis. Available from: https://www.apa.org/pubs/books/essentials-interpretative-phenomenological-analysis
Creswell JW, Miller DL. Determining Validity in Qualitative Inquiry. Theory Pract. 2000;39(3):124–30.
Seale C, Charteris-Black J. The SAGE Handbook of Qualitative Methods in Health Research. In London: SAGE Publications Ltd; 2022. Available from: https://methods.sagepub.com/book/sage-hdbk-qualitative-methods-in-health-research
Van der Kolk BA. The Body keeps the score: brain, mind and body in the healing of trauma. New York, NY: Penguin Books; 2015. p. 445.
Esaki N, Benamati J, Yanosy S, Middleton JS, Hopson LM, Hummer VL, et al. The Sanctuary Model: Theoretical Framework. Fam Soc J Contemp Soc Serv. 2013;94(2):87–95.
Bloom S. Caring for the Caregiver: Avoiding and Treating Vicarious Trauma. In 2003. p. 459–70.
Galvin E, O’Donnell R, Avery J, Morris H, Mousa A, Halfpenny N, et al. Residential Out-of-Home Care Staff Perceptions of Implementing a Trauma-Informed Approach: The Sanctuary Model. J Child Adolesc Trauma. 2022;15(3):653–67.
Unick GJ, Bassuk EL, Richard MK, Paquette K. Organizational trauma-informed care: Associations with individual and agency factors. Psychol Serv. 2019;16(1):134–42.
Dr. Lisa Feldman Barrett: How to Understand Emotions | Huberman Lab Podcast. 2023 [cited 2023 Nov 9]. Available from: https://www.youtube.com/watch?v=FeRgqJVALMQ
Lauridsen MB, Munkejord MC. Creating Conditions for Professional Development through a Trauma-Informed and Restorative Practice. Soc Work. 2022;67(2):135–44.
Embertson MK. The importance of middle managers in healthcare organizations. J Healthc Manag Am Coll Healthc Exec. 2006;51(4):223–32.
Naz S, Li C, Nisar QA, Khan MAS, Ahmad N, Anwar F. A Study in the Relationship Between Supportive Work Environment and Employee Retention: Role of Organizational Commitment and Person-Organization Fit as Mediators. SAGE Open. 2020;10(2):2158244020924694.
Allen DG, Bryant PC, Vardaman JM. Retaining Talent: Replacing Misconceptions With Evidence-Based Strategies. Acad Manag Perspect. 2010;24(2):48–64.
Mackenzie ML, Wallach DF. "The Boss-Employee Relationship: Influence on Job Retention" (2012). Faculty Works: Business (1973-2022). 11. https://digitalcommons.molloy.edu/bus_fac/11 .
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet. 2016;388(10057):2272–81.
Kilroy J, Townsend K, Dundon T. Embedding reciprocity in human resource management: A social exchange theory of the role of frontline managers. [cited 2022 Dec 19]. Available from: https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/1748-8583.12468
Townsend K, Wilkinson A, Bamber G, Allan C. Accidental, unprepared, and unsupported: clinical nurses becoming managers. Int J Hum Resour Manag. 2012;23(1):204–20.
Kim S, Crooks CV, Bax K, Shokoohi M. Impact of Trauma-Informed Training and Mindfulness-Based Social-Emotional Learning Program on Teacher Attitudes and Burnout: A Mixed-Methods Study. School Ment Health. 2021;13(1):55–68.
Joseph MM, Ahasic AM, Clark J, Templeton K. State of Women in Medicine: History, Challenges, and the Benefits of a Diverse Workforce. Pediatrics. 2021;148(Suppl 2):e2021051440C.
Harvey SB, Epstein RM, Glozier N, Petrie K, Strudwick J, Gayed A, et al. Mental illness and suicide among physicians. Lancet Lond Engl. 2021;398(10303):920–30.
Article CAS Google Scholar
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS ONE. 2015;10(9): e0138511.
Anderson M. For black Americans, experiences of racial discrimination vary by education level, gender. Pew Research Center. [cited 2022 Dec 12]. Available from: https://www.pewresearch.org/fact-tank/2019/05/02/for-black-americans-experiences-of-racial-discrimination-vary-by-education-level-gender/
Williams MT, Metzger IW, Leins C, DeLapp C. Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Pract Innov. 2018;3:242–60.
Serafini K, Coyer C, Speights JB, Donovan D, Guh J, Washington J, et al. Racism as Experienced by Physicians of Color in the Health Care Setting. Fam Med. 2020;52(4):282–7.
Brown-Johnson C, Cox J, Shankar M, Baratta J, De Leon G, Garcia R, et al. The Presence 5 for Racial Justice Framework for anti-racist communication with Black patients. Health Serv Res. [cited 2022 Sep 21];n/a(n/a). Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/1475-6773.14015
Shankar M, Henderson K, Garcia R, Li G, Titer K, Acholonu RG, et al. Presence 5 for Racial Justice Workshop: Fostering Dialogue Across Medical Education to Disrupt Anti-Black Racism in Clinical Encounters. MedEdPORTAL J Teach Learn Resour. 2022;18:11227.
Ansell DA, James B, De Maio FG. A Call for Antiracist Action. N Engl J Med. 2022;387(1): e1.
Boston Review. [cited 2022 Dec 13]. An Antiracist Agenda for Medicine. Available from: https://www.bostonreview.net/articles/michelle-morsebram-wispelwey-what-we-owe-patients-case-medical-reparations/
P W, H M, WilsonMichael, MazimbaSula, K H, P A, et al. Leveraging Clinical Decision Support for Racial Equity: A Sociotechnical Innovation. NEJM Catal Innov Care Deliv. 2022 Jul 25 [cited 2022 Dec 13]; Available from: https://catalyst.nejm.org/doi/full/ https://doi.org/10.1056/CAT.22.0076
Coates R, Umbreit M, Vos B. Restorative justice circles: An exploratory study. Contemp Justice Rev. 2003;6(3):265–78.
Download references
Acknowledgements
Not applicable
This study was funded by Stanford University School of Medicine.
Author information
Authors and affiliations.
School of Social Work, University of Minnesota, St. Paul, MN, USA
Sonia Rose Harris
UCLA Fielding School of Public Health, Los Angeles, CA, USA
Alexis Amano
Stanford University School of Medicine, Palo Alto, CA, USA
Marcy Winget, Kelley M Skeff & Cati G Brown-Johnson
You can also search for this author in PubMed Google Scholar
Contributions
CBJ, SRH, AA, MW, and KS contributed to conception and design. SRH and CBJ wrote the main manuscript text. AA and CBJ conducted data collection. SRH, AA, and CBJ conducted data analysis, which was reviewed in monthly meetings by MW and KS. All authors reviewed the manuscript.
Corresponding author
Correspondence to Cati G Brown-Johnson .
Ethics declarations
Ethics approval and consent to participate.
This project was approved by our Stanford University Institutional Review Board (Protocol # 39948). All the methods and procedures carried out in this study were in accordance with relevant guidelines and regulation. Written consent was obtained from all participants to participate. Verbal informed consent was obtained from all participants at the beginning of the interview to record and transcribe interviews. This was approved by the Stanford University Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview Protocol
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Harris, S., Amano, A., Winget, M. et al. Trauma-Informed Healthcare Leadership? Evidence and opportunities from interviews with leaders during COVID-19. BMC Health Serv Res 24 , 515 (2024). https://doi.org/10.1186/s12913-024-10946-9
Download citation
Received : 15 May 2023
Accepted : 02 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12913-024-10946-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Administrators
- Qualitative methods
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
COVID-19: Qualitative Research With Vulnerable Populations
Affiliation.
- 1 DePaul University, Chicago, IL, USA.
- PMID: 33349176
- DOI: 10.1177/0894318420965225
With COVID-19 affecting all types of research, the authors of this article contribute to the discussions on how COVID-19 affects the world of qualitative nursing research in irrefutable ways. Underrepresented and vulnerable populations are faced with higher rates and severity of COVID-19, heightening the need to better address their health needs, which require their voices to be heard. Moreover, nurses' perspectives on practicing during COVID-19 are needed. These nurses are vulnerable and their voices must be heard. Qualitative research methodology is advantageous to bringing attention to the lived experience of others as they unfold. Thus, we offer suggestions to aid in the collection and interpretation of qualitative data among vulnerable populations. We also provide practical tips for qualitative researchers, including an exemplar of conducting qualitative research among vulnerable nurses in light of COVID-19.
Keywords: COVID-19; qualitative research; vulnerable populations.
PubMed Disclaimer

Similar articles
- Qualitative review of promising practices for testing vulnerable populations at off-site COVID-19 testing centers. Winterbauer E, Levy PD, Calhoun D, Elwell T, Fishbein E, Donohue S, Little J. Winterbauer E, et al. Healthc (Amst). 2021 Mar;9(1):100519. doi: 10.1016/j.hjdsi.2021.100519. Epub 2021 Jan 9. Healthc (Amst). 2021. PMID: 33454583 Free PMC article.
- Narrative research methods with vulnerable people: sharing insights. Catherine Framp A, McAllister M, Dwyer T. Catherine Framp A, et al. Nurse Res. 2019 Dec 16;27(4):42-47. doi: 10.7748/nr.2019.e1671. Epub 2019 Oct 5. Nurse Res. 2019. PMID: 31802652
- Using internet-based approaches to collect qualitative data from vulnerable groups: reflections from the field. Neville S, Adams J, Cook C. Neville S, et al. Contemp Nurse. 2016 Dec;52(6):657-668. doi: 10.1080/10376178.2015.1095056. Epub 2015 Oct 21. Contemp Nurse. 2016. PMID: 26394073
- Nurses' use of qualitative research approaches to investigate tobacco use and control. Schultz AS, Bottorff JL, McKeown SB. Schultz AS, et al. Annu Rev Nurs Res. 2009;27:115-44. doi: 10.1891/0739-6686.27.115. Annu Rev Nurs Res. 2009. PMID: 20192102 Review.
- The ethics of conducting research with mental health service users. Keogh B, Daly L. Keogh B, et al. Br J Nurs. 2009 Mar 12-25;18(5):277-8, 280--1. doi: 10.12968/bjon.2009.18.5.40539. Br J Nurs. 2009. PMID: 19273987 Review.
- Reflections on the process, challenges, and lessons learned conducting remote qualitative research on Violence against women during COVID-19 pandemic lockdown in South Africa. Mahlangu P, Machisa MT, Jewkes R, Gibbs A, Shai N, Sikweyiya Y. Mahlangu P, et al. BMC Public Health. 2024 Jan 2;24(1):33. doi: 10.1186/s12889-023-17480-z. BMC Public Health. 2024. PMID: 38166875 Free PMC article.
- Informing efforts beyond tailored promotional campaigns by understanding contextual factors shaping vaccine hesitancy among equity-deserving populations in Canada: an exploratory qualitative study. Nascimento LG, Dubé È, Burns KE, Brown P, Calnan M, Ward PR, Filice E, Herati H, Ike NAU, Rotolo B, Meyer SB. Nascimento LG, et al. Int J Equity Health. 2023 Oct 7;22(1):209. doi: 10.1186/s12939-023-02025-y. Int J Equity Health. 2023. PMID: 37805472 Free PMC article.
- Nurse managers' experience during the COVID-19 pandemic in China: A qualitative study. Chen Y, Jiang H, Shen Y, Gu H, Zhou P. Chen Y, et al. Nurs Open. 2023 Nov;10(11):7255-7265. doi: 10.1002/nop2.1978. Epub 2023 Aug 21. Nurs Open. 2023. PMID: 37605492 Free PMC article.
- Publication Trends in Reablement - A Scoping Review. Guadaña J, Oyeneyin B, Moe CF, Tuntland H. Guadaña J, et al. J Multidiscip Healthc. 2023 Jun 13;16:1641-1660. doi: 10.2147/JMDH.S407802. eCollection 2023. J Multidiscip Healthc. 2023. PMID: 37333025 Free PMC article. Review.
- Positive and negative experiences with the COVID-19 pandemic among lonely and non-lonely populations in Germany. Wegner L, Liu S. Wegner L, et al. Front Public Health. 2023 Mar 2;10:1067038. doi: 10.3389/fpubh.2022.1067038. eCollection 2022. Front Public Health. 2023. PMID: 36937827 Free PMC article.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 11 June 2024
Understanding contextual and practical factors to inform WHO recommendations on using chest imaging to monitor COVID-19 pulmonary sequelae: a qualitative study exploring stakeholders’ perspective
- Gladys Honein-AbouHaidar 1 ,
- Cynthia Rizkallah 1 ,
- Imad Bou Akl 2 ,
- Gian Paolo Morgano 3 ,
- Tereza Vrbová 4 ,
- Emilie van Deventer 5 ,
- Maria del Rosario Perez 5 &
- Elie A. Akl ORCID: orcid.org/0000-0002-3444-8618 6
Health Research Policy and Systems volume 22 , Article number: 67 ( 2024 ) Cite this article
115 Accesses
5 Altmetric
Metrics details
A recommendation by the World Health Organization (WHO) was issued about the use of chest imaging to monitor pulmonary sequelae following recovery from COVID-19. This qualitative study aimed to explore the perspective of key stakeholders to understand their valuation of the outcome of the proposition, preferences for the modalities of chest imaging, acceptability, feasibility, impact on equity and practical considerations influencing the implementation of using chest imaging.
A qualitative descriptive design using in-depth interviews approach. Key stakeholders included adult patients who recovered from the acute illness of COVID-19, and providers caring for those patients. The Evidence to Decision (EtD) conceptual framework was used to guide data collection of contextual and practical factors related to monitoring using imaging. Data analysis was based on the framework thematic analysis approach.
33 respondents, including providers and patients, were recruited from 15 different countries. Participants highly valued the ability to monitor progression and resolution of long-term sequelae but recommended the avoidance of overuse of imaging. Their preferences for the imaging modalities were recorded along with pros and cons. Equity concerns were reported across countries (e.g., access to resources) and within countries (e.g., disadvantaged groups lacked access to insurance). Both providers and patients accepted the use of imaging, some patients were concerned about affordability of the test. Facilitators included post- recovery units and protocols. Barriers to feasibility included low number of specialists in some countries, access to imaging tests among elderly living in nursing homes, experience of poor coordination of care, emotional exhaustion, and transportation challenges driving to a monitoring site.
We were able to demonstrate that there is a high value and acceptability using imaging but there were factors influencing feasibility, equity and some practical considerations associated with implementation. We had a few suggestions to be considered by the expert panel in the formulation of the guideline to facilitate its implementation such as using validated risk score predictive tools for lung complications to recommend the appropriate imaging modality and complementary pulmonary function test.
Peer Review reports
The novel coronavirus disease (COVID-19) first emerged in December 2019 in the city of Wuhan in China and became a pandemic as of March 2020. As of December 4, 2022 it had infected more than 611 million individuals and claimed the lives of almost 6.6 million individuals globally [ 40 ]. Ever since the first cases started to appear, the scientific community generated evidence related to the epidemiology of the virus, the clinical management of the disease, and its sequelae among survivors.
A systematic review of data from November 2021 till April 2022 showed that 32% of individuals affected by COVID-19 were asymptomatic [ 31 ]. A report from the Chinese Center for Disease Control and Prevention in 2020 showed that among those who developed symptoms, 40% had mild symptoms (fever, cough, fatigue, and headache) [ 41 ], mostly treated at home unless they developed complications that required short-term hospitalization. The remaining cases were treated in hospitals and encompassed moderate symptoms leading to pneumonia reported by 40%; severe symptoms that required oxygen therapy reported by 15% of the cases [ 39 ]. Finally, 5% develop complications leading to organ failure, mainly respiratory failure. Most of these complications increase in the presence of pre-existing risk factors [ 36 ].
Since December 2019 till November 2022, COVID-19 survivors account for more than 635 million individuals thus far. Many survivors experience sequelae of the illness that can linger for months, and are often referred to as “long-haulers” or sufferers of long-COVID syndrome [ 22 , 25 , 36 ]. Among those who recover from moderate or severe illness, long term pulmonary sequelae may be expected. The damage incurred by the virus during the acute and post-acute phase, causes the lung tissue to become fibrotic [ 4 ]. Other long-term consequences have been reported, including psychological [ 37 ], neurological, cardiovascular, and musculoskeletal, among others. Nalbandian et al. use the term “post-acute COVID-1” for long-term complications and/or symptoms present beyond four weeks from the beginning of the symptoms, i.e. after the acute phase of the disease [ 24 ]. The term “Post COVID-19 condition” has been initially proposed by WHO [ 6 ] and its clinical case definition was published [ 33 ].
Given the magnitude of this pandemic, the epidemiological studies that show the sequelae of the infection are important [ 22 , 25 , 36 ], but equally important is to know how to monitor those patients for those sequelae. The World Health Organization (WHO) has regularly updated guidance for clinical management of COVID-19, proposing a multidisciplinary approach to patient care after acute illness [ 39 ]. Early on in this pandemic, WHO issued a rapid advice guide on the use of chest imaging in acute care for COVID-19 patients considering three imaging modalities: radiography, computed tomography and ultrasound [ 1 ]. WHO conducted new systematic reviews [ 42 ] to update this rapid guidance and included a new research question on the use of chest imaging in patients who recovered from COVID-19. Persistence of pulmonary sequelae among COVID-19 patients are important to consider. Long-term physical, functional and neuropsychological complications resulting from the lung injury have been reported six to 12 months after discharge from hospital using chest imaging [ 8 ]. All severe cases admitted to intensive care units and 21% of moderate cases admitted to regular units had persistent pulmonary sequelae, which were detected using chest radiography imaging 8 weeks after discharge. 7% of patients showed glass opacities, defined as an area of haziness through which vessels and bronchial structures may still be seen, using computed tomography 18 weeks post-discharge [ 28 ]. One year after discharge, the prevalence of ground glass opacities dropped significantly but 95% of COVID-19 patients admitted to ICU had abnormal CT scans [ 8 ]. Hence, the importance of monitoring the sequelae of the infection. However, monitoring and compliance can be influenced by several other factors including availability of resources, transportation, co-morbidities, and other practical factors [ 15 ].
To optimally inform the development of this recommendation, it was considered important to explore qualitatively the relevant contextual factors influencing its implementation. WHO recommends using evidence from qualitative research to understand the valuation of the recommendations, their acceptability to stakeholders, their feasibility and equity, and the practical considerations influencing their implementation [ 38 ].
Thus, the aim of this study was to explore the perspective of key stakeholders, including providers and patients from the global community, to understand their valuation of the outcome of the proposition (i.e., monitoring pulmonary sequelae), their preferences for the modalities of chest imaging, and the acceptability, feasibility, impact on equity, and practical considerations influencing the implementation of using chest imaging.
Methods and materials
Design and approach.
This study draws on a descriptive qualitative design [ 30 ] using an in-depth interview with key stakeholder informants.
We secured ethical approval from the American University of Beirut Institutional Ethics Board before starting the study. All participants provided a verbal informed consent to participate and record the discussion. We ensured confidentiality by anonymizing transcripts, assigning each participant a codename that starts with the country name followed by P for health care professionals and Pa for patients.
Conceptual frameworks
We structured the study based on the GRADE Evidence to Decision (EtD) framework (see Table 1 ) [ 3 ], and on Heen et al. practical issues framework (see Table 2 ) [ 14 ]. We judged some practical issues to be already captured by the EtD framework (e.g., medical routine, procedure and device, recovery and adaptation, adverse effects, overall physical well-being, and costs and access). We judged other practical issues to be irrelevant (e.g., food and drinks, exercise and activities, social life and relationships, and work and education). Consequently, we deemed the following five practical issues as relevant: tests and visits, coordination of care, emotional well-being, pregnancy and nursing, and travel and driving.
Sample and recruitment
We used the purposeful sampling approach. Our key informant group included adult patients (18 years of age or older) who have recovered from acute COVID-19 illness. We also targeted health practitioners, specifically radiologists and pulmonologists caring for those patients. We excluded providers not involved in the care of COVID-19 patients.
We aimed to adopt a maximum variation sampling approach in terms of severity of disease for patients (mild, moderate, or severe) and job title for practitioners across all regions of the world.
At first, we identified health care professionals in each of the six WHO regions (Africa, Americas, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) through health care providers on the research team (known sponsor sampling approach). [MQ, 1988. #27] Then, we asked the identified providers to invite patients from their practice to participate in the study (snowball sampling). We also asked patient advocates from different countries to identify potential participants, who were invited by email until saturation was reached. (MQ., 1988).
Data collection
We used a semi-structured approach for interviews using both predetermined open-ended and probing questions (Additional file 1 : Appendix 1: KI interview guide for providers and Additional file 2 : Appendix 2: KI interview guide for patients) [ 7 ]
The interviewer (GHA), an experienced qualitative researcher who had no prior relationship with the participants, conducted the virtual interviews using WebEx. Interviews lasted on average 60 min (range 30–90 min). The discussions were in English, except for one interview conducted in Italian and translated by GPM.
We recruited between October 27, 2020, and December 26, 2020, a total of 33 participants, including 10 patients and 23 providers (of which 11 pulmonologists, 5 radiologists, 3 nephrologists, 2 intensivists, 1 family physician and 1 general practitioner) (Additional file 3 : Appendix 3: Participants’ list: providers and patients).
The first author conducted all interviews virtually using WebEx, Zoom or WhatsApp applications. Participants chose the location at the time of their preference. Recruitment and data collection occurred between October 27 and December 26, 2020.
Data analysis
GHA and CR conducted the analysis using the framework thematic analytical approach. This analytical approach consisted of 7 stages [ 12 ]. In stage 1, CR transcribed the audio-recordings verbatim. In Stage 2, GHA and CR familiarized themselves with the content of the discussion by reading each transcript and taking notes. In stage 3, CR indexed the data based on the GRADE EtD construct and Heen et al. practical issues. She provided a label for each meaningful datum. In stage 4, after indexing a few transcripts, GHA and CR met to discuss their labels and merge them into categories. In stage 5, CR applied those categories to the remaining transcripts. In stage 6, GHA and CR charted all opinions and views indexed under each category. In stage 7, they compared and contrasted the categories, and mapped connections between them. Finally, a complete narrative of the findings was created. These findings were supported by quotations triangulated between health care professionals and patients.
We ensured credibility, reflexivity, and confirmability throughout this process. For credibility and confirmability we used transcribed audio-recorded interviews as the main data repository maximum variation sampling, and a semi-structured interview approach. For reflexivity, the interviewer had no prior relationship with participants and two individuals were involved in the analysis to avoid bias interpretation of the results.
The reporting of this study followed the Consolidated criteria for Reporting Qualitative research (COREQ) Checklist [ 35 ] (Additional file 4 : Appendix 4: COREQ checklist).
Table 3 provides a summary of results for the perceptions of stakeholders of the contextual factors, based on the GRADE EtD framework and Heen et al. practical issues.
In the following text, we present a detailed narrative of themes illustrated by selected quotes from participants. In Additional file 5 : Appendices 5–10, we provide exemplary quotes from both providers and patients for each theme.
Monitoring progression is highly valued when chosen wisely and acceptable.
All patients thought if their providers asked them to do chest imaging post-recovery, they would not question its value and they “ would do whatever they [providers] wanted” US-Pa01.
Similarly providers perceived imaging post-COVID-19 as highly valuable when there is clinical indication. Mild cases ‘ patients don’t routinely need any kind of follow up imaging ’. US-P03.
While moderate and severe cases as well as those with underlying chronic diseases such as human immunodeficiency virus (HIV) infection and tuberculosis coinfection, it will be highly valued, as this participant indicated:
India-P13: So it depends on the severity of the disease during the hospitalization, and the condition of the patient on discharge.
Further, COVID-19 patients, particularly those who were hospitalized might end up with potential multi-organ dysfunction, and the stay in the intensive care unit might expose them to various diseases, such as pneumonia. Hence, for many providers monitoring them post-recovery would be an opportunity to screen and intervene on time to avoid further complications. For example, this provider pointed to low-immunity and co-infection and the importance of frequent monitoring on the treatment.
Nigeria- P06: The follow up is major. Some of them have a low immunity and if we do not catch the bacterial infection on time yes, we lost them. I think the follow up is very crucial.
Interestingly, one provider indicated that, given that this is a new disease, monitoring patients post-recovery can help the scientific understanding of the long-term sequelae of the infection and eventually improve the care.
US-P08 : mostly to understand the disease more. You see what they have findings on the imaging initially they have been improving. Also mostly to kind of look at long term sequela of the condition. But mostly to understand the disease itself, which is kind of relatively had been new.
On the other hand, a few provider participants cautioned against over-testing. First, it would be unnecessary since it will not add “to the decision making in terms of therapy…[and] you don’t want them to be having unnecessary exposure to radiation with multiples radiographs or multiple CT scans. India-P09.
Further, over-testing might end up detecting indolent findings, which would add to their psychological stress, hence unethical from the perspective of one participant:
Swiss-P02: “I think so, and then you might have a problem that you start to find incidental findings. And then you’re going to have to deal with following up on other things that you might see on the X ray that may not be even real, you know, and that’s another ethical problem. If they don’t need the radiography, you’re exposing them to radiation This psychological stress to wait yet for other results depleted patients’ tolerance. Who indicated that they “ would be very anxious because... my lung function might be deteriorating, I might have long term sequela. Ethiopia-Pa03.
Monitoring and follow-up are a reasonable clinical practice.
Among providers, we found that monitoring using imaging to follow-up on the patient’s resolution, or any potential sequelae of the disease was an acceptable practice, in fact it has been already a common practice among almost all participants except for one participant who indicated that due to poor resources in the country, monitoring was never an option.
Cameroon-P11 : No monitoring whatsoever ... Okay so I would think it’s very important to do radiological follow up on them specially to see how much damage has occurred in their lungs and also to see if some damages are still continuing after discharge. In essence our potentials in treating COVID- 19 does not lay so much emphasis on radiological findings and I understand that this is a limitation of our treatment.
Providers also indicated that since some COVID-19 patients were already accustomed to monitoring for other underlying diseases, such as for dialysis or cardiac matters, adding chest imaging monitoring would be acceptable for them. However, the downside is that often times patients may need to spend longer time for the visit, which can be beyond their ability to tolerate.
Swiss-P02: Well, I have to say if a patient is on dialysis, and they have to come 3 times a week. So, we see them and …we try to do a radiography at the baseline… we do another radiography or a CT or whatever but basically for us we get to see them pretty routinely... I think for the dialysis patients again, for them, it’s a burden because either they must come earlier to go to the radiography before the dialysis, or then go after dialysis and then it delays them going home. And then it complicates the transport.
Patients found monitoring a reasonable process, however the cost of the test would matter.
Africa-Pa02: No because it [test] is very expensive, both CT scan and treatment
Preferences for each chest imaging modality are driven by indication and the pros and cons of each.
Preferences for the different imaging modalities were mainly voiced by providers. The clinical indication and the pros and cons for each test dictate the type of test to be done.
Chest radiography is the preferred option for the following conditions: mild cases still complaining of chest pain to monitor clearance of the lungs, and for dialysis patients to detect water retention as one nephrologist indicated:
Swiss-P02: I think honestly, for our patients, sometimes the X rays actually helpful. Because sometimes they lose a lot of weight, and we need to know how much water we need to remove from the patient in a dialysis treatment. And occasionally you don’t know how quickly the patient has lost weight with COVID. So, sometimes you do the X Ray with an excuse of COVID, but you’re actually looking to see, are they filling up with water, are they’re going to develop heart failure. So, for us, sometimes there’s another extra added value.
There were a few pros for using X-rays including ‘ reducing the radiation from CT [which] is so large that if you do so frequently, it may not be good or ethical’ US-P07. It is available in local clinics as one provider indicated: ‘a lot of family doctors can do X rays. It’s amazing. They have an X ray thing in their clinic in their little office’ USP02. At times the choice of the test is driven by the cost of the test, therefore providers would choose whatever is affordable for patients as this provider indicated: ‘ The common is Chest X ray… but in some cases we do high resolution CT because CT is expensive so we do it for only those who can afford it, not for all of them’ US-P06.
The cons are not being sensitive enough and may miss significant pathology.
‘The chest X Ray, it’s not sensitive enough to show you a significant pathology. And so we have seen it with COVID, you know the chest X Ray misses a proportion, like, 40% or something’ US-P07.
Providers gave several indications for choosing chest CT scan. Chest CT scan is very sensitive to ground glass, consolidation, and fluid retention. It is also recommended for patients still depending on oxygen long after discharge. Often, it is used in cases where providers are anticipating persistent interstitial manifestations like non-specific interstitial pneumonia (NSIP). It can identify fibrotic changes and detect additional diseases, if any.
India- P05: as far as the CT scan is concerned, it is basically, it gives you a fuller picture of the chest. I mean, what is happening inside the lungs, right from the trachea to the lung parenchyma. So generally, the mindset for patients out here is better go for a CT scan because, uh, it gives a good resolution.
The cons included higher radiation exposure, lack of accessibility in local clinics and affordability for various populations.
‘If you want a CT, then the patient has to go to a hospital or a private place and then definitely for some of them it involves travel and sometimes it’s even hours of travel’ US-P02 .
The nursing and pregnant women population was of concern for radiologists, as extra precautions are needed to avoid any harm when doing the imaging.
South Africa- P16: So, high radiation risk or high radiation dose to the breasts. And reasonably achievable. So, we try to take it down to the minimum.
Finally, for the lung ultrasound, it is the preferred option to assess peripheral consolidation. It is considered an easy modality test as it is portable, accessible in local clinics, and affordable.
US-P08: … We’ve been relying a lot on it and they’re criteria to follow with the ultrasound. It’s a very easy modality. Yes, we’re using it. And now it’s like, you have those small portable ones. It’s very easy to clean it from room after room, way better than cleaning the whole chest X Ray machine.
The potential for missing central consolidation and significant pathology were cited as the major cons.
‘I mean, scanned by ultrasound, we are only able to see the peripheral one third, which are involved in COVID, but it is not only the peripheral. So central areas, we are not able to visualize using ultrasound’ US-P05.
Equity concerns across countries and within countries.
The availability of resources and health insurance coverage across and within countries impacted equity. Access to resources varied between developed such as USA and developing countries such as African countries.
One provider from the USA said:
US-P08: We have 2 big centers. CT scan is available very widely. Any issues that need any further care, again, we have video system, so if they need further evaluation, they go to their closest hospital, they get stabilized and they get transferred to one of the biggest centers, which is not too far. And either they get transferred by ground, or they’re sick, they get transferred by air, which is really fast, like talking 10 to 15 minutes by helicopter or a plane. So, the CT scan is widely available if it needs, like, a little bit of more advanced things the biggest centers, definitely, the patients get referred to them, but mostly when they get sick and need admission. For outpatient, like, imaging, scans, pulmonary function test, ultrasounds, these things are very widely available.
Compared with what providers in Africa said:
Cameroon-P11: Okay so I would think it’s very important to do radiological follow up…Most of our district health facilities will not have radiology equipment. So normally we would just do auscultations, and manage them as such, and when they go, we do not follow up. Ethiopia-P07: We have only one CT scan room, so we don’t want to contaminate that. We have a lot of patients, so we only order chest radiography using a machine which is dedicated for that purpose. So definitely if you ask the people to take CT scan for all those who have COVID, it will definitely it would put a burden to the imaging service we have and also to the health professionals, and they think that they can also have COVID-19.
One patient said when the cost of the test is fully covered, everyone would comply.
Czech-Pa06: it’s covered by the health insurance. Okay. So everyone is covered, everybody in the Czech Republic
But when there is no insurance coverage, then patients would more likely opt out.
Pakistan-Pa04: I am a teacher, so my insurance company is taking care of my entire cost of stay in hospital and all expenses…Not the case for everyone... We are a third world country. For example, Remdesivir many cannot afford it. CT scan is slightly expensive. 75% will not be able to afford those expenses.
Other factors impacting equity include the quality chasm between public and private within a country. Often, the non-insured have to rely on public services, which are typically described as crowded, under-resourced, and generally of poorer quality compared to private ones. Similarly, patients living in urban areas have better accessibility to services as compared to patients living in rural areas.
India- P09: So, CT scan facilities are most of the time available in, at least 2 or 3 cities like ours. Public sector it is a few. It is difficult to access. In private sectors, there are lots of CT scans, but again, the out of expenditure really goes high. India- P05: Yeah, that can be a problem because the means of travel are, you know, buses and trains in our country for traveling from one area to another and areas who have radiological imaging modalities are mostly located in urban areas and suburban areas.
Finally, non-COVID patients were perceived to be at disadvantage during the pandemic. Despite their needs for follow-up, many were either avoiding health care institutions (out of fear of getting the disease) or were being deferred by their providers to avoid exposing them to the infection. In either case, their follow-up care was being jeopardized by the pandemic.
India-P09: Yeah, so definitely COVID patients are still able to access healthcare in an appropriate period. And it is most unfortunate, those patients who have non-COVID illness, they are much more neglected, uh, because of this whole crisis.
Barriers and facilitators for feasibility.
Providers reported three facilitators of feasibility. Having a post-recovery COVID-19 unit with protocols was the main lever for providers to act. A provider from Ethiopia said:
‘We have a clinic, which is, uh, you know, we have a head nurse. We have a few. 6 to 7 nurses and because we have limited number of nurses, this group of nurses, half of the time they spend it with the chest team… When they come to the clinic, and we see like, 45 to 50 patients and that divided to like on average 5 residents, 1 fellow and 1 senior. We have to go through each CT scan of each patient’ Ethiopia-P07.
Second, many health centers had already established monitoring systems for other diseases, e.g., kidney disease requiring dialysis. Having the infrastructure already in place made it easier for them to build on it by adding the monitoring process for COVID-19.
‘It will actually be going to be easily integrated because a lot of these patients [oncology patients] they end up getting CT scans and, you know, pet scans routinely. Yeah, because as part of their, you know, follow up and as part of their staging, so I don’t think it will be a problem at all… What we can do, and we’ve been doing that is to try and combine these tests together so that if they have 1 appointment, they can get the rest of it together’ Jordan- P04.
The third facilitating factor was the ability to scale up team efforts. Dedicated teams were able to provide optimal services despite the multiple challenges as illustrated in this quote:
India-P05: Daily, we are able to see around 75 to 100 patients…what we have done in our Institute, that we have a hand, picked a few consultants from my department myself included. So, every other day, and, I mean, every alternate day, we are having emergency duties. So we are having dedicated duties for reporting COVID patients, on CT scan and we do it, uh, every alternate day…I mean, it has increased the burden for sure. But then we are doing it.
But the reported challenges were numerous too.
Most providers from low- and middle-income countries indicated that their human and non-human resources were limited. They did not have enough specialists in the country to do the monitoring, including pulmonologists and radiologists.
‘The lack of specialists to follow these patients. I mean, South Africa is a country of 65M people, and we’ve got 70 pulmonologists’ South Africa-P14.
For both developing and developed countries, the number of support staff available to do the tracing did not commensurate with the need, given the large number of patients.
I think the biggest challenge, obviously there’s a huge number of patients. It is overwhelming like, we’ve created a small group of doctors to, like, call patients and tell them they’re COVID positive and discuss the results. But eventually we were overwhelmed because there just so many positive patients. And so the solution was to then just say, well, you should talk to your ordering provider, your primary provider. The hard part there is as much as everyone is trying to keep up with, things changed so quickly with COVID recommendations, that primary care providers who are giving the right advice 6 weeks ago are no longer giving you the right advice US-P03.
The back log in imaging appointments due to limited number of equipment (e.g., CT scan) challenged the feasibility in developing countries.
‘ Yeah, we have a back log. We have a lot of back logs [radiology tests]. Even for admitted patients, it is difficult sometimes’ Ethiopia-P11
Some providers indicated that for elderly population, especially those living in nursing homes, access to imaging would be a challenge due to imposed COVID-19 restrictions.
US-P03: The patient population, that’s a little harder to get imaging on actually patients who go to, like, nursing homes. Because many skilled nursing facilities, they don’t have radiology services there and the ability to get the patient with medical transport from the skilled nursing facility to wherever the radiology is in back or the doctor’s appointment, or whatever, that too is also actually very difficult. So I think that population, that group where they have both mobility and transportation issues is a big one .
Patients reported different feasibility challenges.
One patient who was a severe case indicated that he was extremely deconditioned after discharge. If it was not for the rehabilitation, he would not be able to do any further testing.
US-Pa01 : I had to be lying in bed for 3 weeks. So after that, I literally could not stand up. I wasn’t able to sort of get out of the bed into a wheelchair to go to the bathroom for a week. We’re talking about a severe case.
Coordination between health care providers was lacking. For example, one patient reported receiving phone calls from the primary care provider, from their pulmonologist and another from the health center, related to the same issue.
Ethiopia-Pa03: Yeah, I think so. From my side, I was communicating with the social worker from the hospital because I was a staff there, so they call me, and they put me in contact with the psych department…. Things are very decentralized so a lot of guys might call them. The follow up is not organized so this might cause people to avoid seeking health care.
For some, it was too much to bear, too many calls, too many follow-ups.
Swiss-P02 : I think they get frustrated because they’re being phoned by a lot of different people. There’s quite a lot of phone calls also by people from the community checking on them and the officials checking that they’re at home and not outside when they should be at home, you know, these things. So I think they get a lot of phone calls. And I know for some of them, it’s definitely quite burdensome yeah, yeah.
This study highlighted important factors that informed the development of the WHO recommendation about the use of chest imaging for monitoring patients who recovered from COVID-19. While WHO suggests not systematically scheduling chest imaging follow-up at the time of hospital discharge, it identifies patient groups who might benefit from periodic follow-up imaging. This study showed that providers from 15 countries highly valued this recommendation and that patients did not question its value if it was requested by their providers. Some feasibility challenges related to availability of human and non-human resources (e.g. lack of specialists, supporting staff and/or radiological equipment), represented major challenges for implementation and likely led to inequities between high and low resource countries. Lack of specialists, support staff and radiological equipment were the major challenges for implementation.
Using chest imaging to assess lung sequelae evolution and early detection of complications such is unquestioned [ 17 ]. We know by now that COVID-19 survivors’ number is in the hundreds of millions worldwide, and the figures continue to rise. We also know that residual lung complications including lung fibrosis, bronchiectasis, or other structural abnormalities [ 18 , 19 ] are expected to remain months post-discharge among three quarters of patients [ 43 ]. Those sequelae affect lung functioning, exercise capacity and health related quality of life [ 18 , 19 ].
However, we anticipate that the monitoring using imaging on this gigantic number of survivors is far from being a simple one size fits all approach. As noted in this study, variation in resources mattered. Thus, we propose a few suggestions to facilitate the implementation of the recommended guideline, and we discuss them below. First, clinicians can include risk stratification based on validated risk score predictive tools for lung complications to recognize the patients who might benefit from follow-up imaging and identify the appropriate imaging modality, hence reducing unnecessary tests and avoiding unjustified radiation exposure, at times unethical as suggested by our participants. In low-resource settings where CT scans are scarce, effective evidence-based alternatives for imaging can be used. Third, complementary lung function tests can be concurrently considered to reduce unnecessary use of imaging. Fourth, rehabilitation programs for COVID-19 survivors are needed for monitoring patients.
Triaging patients into average and high risk for lung complications can be done using several tools from as simple as a risk score predictive tool, [ 17 , 21 ] imaging scoring to a more sophisticated artificial intelligence tool [ 10 , 11 ]. In either case, those tools are often based on key indicators that are meant to predict lung complications and to aid clinicians in their decision-making [ 13 , 21 ]. In this study, most providers were already stratifying patients based on the severity of the case during the acute phase. It is possible that their decision-making was arbitrary thus running into the risk of introducing algorithmic bias. To alleviate those systemic errors, the validated predictive risk score, imaging scores, or AI tools are meant to alleviate these bias and systemic errors. Examples of tools are numerous. Liang et al. as an example of predictive risk score, encompassed age (more than 65), co-morbidities, and Lactate dehydrogenase, blood urea nitrogen, D-dimer, procalcitonin, and ferritin levels provided an efficient risk evaluation system, and the model had an excellent discrimination and calibration during internal validation [ 21 ]. Chest radiography scoring systems and High Resolution CT scan categorization and quantification have also been used to stratify patients’ severity. [ 17 ] Alexander et al. reported a number of AI algorithms (more than 75) related to pulmonary medicine that received US Food and Drug Administration and Conformité Européenne approval [ 2 ]. It is warranted to increase awareness and adoption of those tools among providers in this specialty [ 2 ].
The role of the different modalities of imaging in the acute phase is more commonly reported in the literature than in the post-recovery phase [ 5 , 16 , 17 ]. Given the insufficient historic data on the sequelae of COVID-19, it is understandable that the evidence is still scattered and scant around the capabilities and limitations of each imaging modality in monitoring sequelae post-recovery. Shaw et al. indicated that chest radiography can be used for follow-up imaging despite the limitations in detecting subtle parenchymal changes, while chest CT is a more sensitive modality [ 32 ]. Lung ultrasound is also another option to evaluate sequelae [ 5 ]. Peng et al. found that US findings correlate with typical CT findings specifically useful to identify peripheral distribution of lung involvement [ 27 ]. Hence, the choice of modality needs to be carefully considered based on the clinical presentations and the availability of resources. However, more longitudinal studies are needed to refine this evidence and guide the practice (Rubin A, 2012) and systematic reviews of the literature are also needed.
The sequelae of COVID-19 need also to be assessed using complementary testing. Despite being asymptomatic, residual abnormalities in pulmonary function tests are expected weeks and months after discharge. Patients with persistent, new, or changing symptoms should have access to follow-up care including screening, assessment and rehabilitation interventions comprising pulmonary function tests when resources permit [ 39 ]. Zhao et al. found that the diffusion capacity of the lung for carbon monoxide (DLCO) measured by means of breath spirometry test can detect abnormal lung function among survivors. Urea nitrogen is another parameter to detect residual changes after discharge. D-Dimer elevation was an independent predictor for abnormal DLCO, thus patients with raised D-Dimer require pulmonary rehabilitation and need to be followed-up for sequelae [ 43 ].
Potential diagnostic testing strategies to inform clinical care and prognosis in the Post COVID-19 condition are numerous. New insights on the multidisciplinary nature of this condition suggest that several imaging modalities—in addition to chest imaging—might be considered subject to the clinical condition [ 26 ].
A few of our providers reported having rehabilitation centers for COVID-19 patients. Two of the severe cases we interviewed reported being severely deconditioning after spending on average three weeks in the intensive care unit, one reported being transferred to a rehabilitation center. Thornton indicates that despite the severity of their illnesses, COVID-19 patients unlike heart attack, trauma, and stroke, leave hospitals with the least support. Further, an estimated 45% of patients may require low level of rehabilitation interventions, while 4% will require more intensive rehabilitation for their neurological, respiratory and mental sequelae [ 34 ]. When asked about the feasibility of doing the imaging, some said they were too tired to go out of their homes. Hence, the need for rehabilitation programs in each country is a necessity.
The findings of this qualitative study were presented to the expert panel developing the WHO recommendation on the use of chest imaging to monitor COVID-19 pulmonary sequelae. The expert panel did consider the important contextual and practical factors influencing the implementation of the recommendation when issuing their recommendation.
Strengths and limitations
There are areas of strengths and a few limitations to be acknowledged. The most important strength is the qualitative approach adopted to delve into the details influencing the implementation of the guideline from the perspective of the stakeholders. Primary qualitative studies or systematic reviews, called qualitative evidence syntheses (QES), are becoming more commonly used in guideline development [ 20 ]. To our knowledge, no previous study examined the providers nor patients’ perspectives on monitoring using imaging post-recovery. Thus, the evidence we brought in this primary qualitative study provided a wealth of knowledge in great breadth and depth that would have not been possible otherwise. Further, we made every effort to maximize representation from different parts of the world. We included providers and patients from most continents, hence capturing a global perspective on the contextual factors influencing the implementation of monitoring using imaging. We conducted this qualitative research using at most considerations for trustworthiness including credibility, reflexivity, and confirmability. More importantly, the findings of this study were presented alongside evidence on the interventions’ benefits and harms to the guideline development guide and eventually incorporated into the COVID-19 living catalogue of guidelines [ 9 ].
Challenges encountered included our ability to recruit more patients. Most providers indicated that they needed ethical approval from their own health institutions to refer patients to us. Those patients who were referred by providers were mainly health care providers themselves. However, we relied on a patient support group to refer patients to be interviewed in order to maximize participation. In a few cases, language used during the interview was a challenge. Not all individuals were fluent in English. In one case, the patient had to call in the sister to translate the views. The vast majority were able to articulate freely.
Another challenge was recruiting providers from all specialties. For example, our sample did not include oncologists nor cardiologists. Perhaps, their perspectives would have concurred with our findings but also expanded.
This study explored the different contextual factors influencing the use of chest imaging in COVID-19 patients for post-recovery monitoring using the evidence to practice framework. This study demonstrated that there is a high value and acceptability using imaging but there were factors influencing feasibility, equity and some practical considerations associated with implementation. We suggested several measures to improve the feasibility of the guideline such as using validated risk score predictive tools for lung complications to recommend the appropriate imaging modality and complementary pulmonary function test.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on request.
Abbreviations
Coronavirus disease
World Health Organization
Intensive care unit
Computed tomography scan
GRADE evidence to decision
Diffusing capacity of lung for carbon monoxide
Akl EA, Blazic I, Yaacoub S, Frija G, Chou R, Appiah JA, Fatehi M, Flor N, Hitti E, Jafri H, Jin ZY, Kauczor HU, Kawooya M, Kazerooni EA, Ko JP, Mahfouz R, Muglia V, Nyabanda R, Sanchez M, et al. Use of chest imaging in the diagnosis and management of COVID-19: a WHO rapid advice guide. Radiology. 2021;298(2):E63–9. https://doi.org/10.1148/radiol.2020203173 .
Article PubMed Google Scholar
Alexander A, Jiang A, Ferreira C, Zurkiya D. An intelligent future for medical imaging: a market outlook on artificial intelligence for medical imaging. J Am Coll Radiol. 2020;17(1):165–70. https://doi.org/10.1016/j.jacr.2019.07.019 .
Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD, Group GW. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices 1: Introduction. BMJ. 2016;353:i2016. https://doi.org/10.1136/bmj.i2016 .
Bazdyrev E, Rusina P, Panova M, Novikov F, Grishagin I, Nebolsin V. Lung fibrosis after COVID-19: treatment prospects. Pharmaceuticals (Basel). 2021. https://doi.org/10.3390/ph14080807 .
Czawlytko C, Hossain R, White CS. COVID-19 diagnostic imaging recommendations. Appl Radiol. 2020;49:10–5.
Article Google Scholar
Diaz JV, Herridge M, Bertagnolio S, Davis HE, Dua T, Kaushic C, Marshall JC, Del Rosario Perez M, Strub-Wourgaft N, Soriano JB. Towards a universal understanding of post COVID-19 condition. Bull World Health Organ. 2021;99(12):901–3. https://doi.org/10.2471/BLT.21.286249 .
Article PubMed PubMed Central Google Scholar
Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40(4):314–21. https://doi.org/10.1111/j.1365-2929.2006.02418.x .
Eberst G, Claude F, Laurent L, Meurisse A, Roux-Claude P, Barnig C, Vernerey D, Paget-Bailly S, Bouiller K, Chirouze C, Behr J, Grillet F, Ritter O, Karaer S, Pili-Floury S, Winiszewski H, Samain E, Decavel P, Capellier G, Westeel V. Result of one-year, prospective follow-up of intensive care unit survivors after SARS-CoV-2 pneumonia. Ann Intensive Care. 2022;12(1):23. https://doi.org/10.1186/s13613-022-00997-8 .
Article CAS PubMed PubMed Central Google Scholar
eCOVID-19RecMap. COVID19 Recommendations and Gateway to Contextualization. 2021. Retrieved September 24 from https://covid19.recmap.org/ .
Ferrari D, Milic J, Tonelli R, Ghinelli F, Meschiari M, Volpi S, Faltoni M, Franceschi G, Iadisernia V, Yaacoub D, Ciusa G, Bacca E, Rogati C, Tutone M, Burastero G, Raimondi A, Menozzi M, Franceschini E, Cuomo G, et al. Machine learning in predicting respiratory failure in patients with COVID-19 pneumonia-challenges, strengths, and opportunities in a global health emergency. PLoS ONE. 2020;15(11): e0239172. https://doi.org/10.1371/journal.pone.0239172 .
Fields BKK, Demirjian NL, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19) diagnostic technologies: a country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic. Clin Imaging. 2020;67:219–25. https://doi.org/10.1016/j.clinimag.2020.08.014 .
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. https://doi.org/10.1186/1471-2288-13-117 .
Halalau A, Imam Z, Karabon P, Mankuzhy N, Shaheen A, Tu J, Carpenter C. External validation of a clinical risk score to predict hospital admission and in-hospital mortality in COVID-19 patients. Ann Med. 2021;53(1):78–86. https://doi.org/10.1080/07853890.2020.1828616 .
Article CAS PubMed Google Scholar
Heen AF, Vandvik PO, Brandt L, Montori VM, Lytvyn L, Guyatt G, Quinlan C, Agoritsas T. A framework for practical issues was developed to inform shared decision-making tools and clinical guidelines. J Clin Epidemiol. 2021;129:104–13. https://doi.org/10.1016/j.jclinepi.2020.10.002 .
Jiang DH, Roy DJ, Gu BJ, Hassett LC, McCoy RG. Postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection: a state-of-the-art review. JACC Basic Transl Sci. 2021;6(9):796–811. https://doi.org/10.1016/j.jacbts.2021.07.002 .
Jiang ZZ, He C, Wang DQ, Shen HL, Sun JL, Gan WN, Lu JY, Liu XT. The role of imaging techniques in management of COVID-19 in China: from diagnosis to monitoring and follow-up. Med Sci Monit. 2020;26:e924582. https://doi.org/10.12659/MSM.924582 .
Larici AR, Cicchetti G, Marano R, Merlino B, Elia L, Calandriello L, Del Ciello A, Farchione A, Savino G, Infante A, Larosa L, Colosimo C, Manfredi R, Natale L. Multimodality imaging of COVID-19 pneumonia: from diagnosis to follow-up. A comprehensive review. Eur J Radiol. 2020;131: 109217. https://doi.org/10.1016/j.ejrad.2020.109217 .
Leung T, Chan A, Chan E, Chan V, Chui C, Cowling B, Gao L, Ge M, Hung I, Ipa M. Short-and potential long-term adverse health outcomes of COVID-19: a rapid review. Emerg Microbes Infect. 2020;9(1):2190–9. https://doi.org/10.1080/22221751.2020.1825914 .
Leung TYM, Chan AYL, Chan EW, Chan VKY, Chui CSL, Cowling BJ, Gao L, Ge MQ, Hung IFN, Ip MSM, Ip P, Lau KK, Lau CS, Lau LKW, Leung WK, Li X, Luo H, Man KKC, Ng VWS, et al. Short- and potential long-term adverse health outcomes of COVID-19: a rapid review. Emerg Microbes Infect. 2020;9(1):2190–9. https://doi.org/10.1080/22221751.2020.1825914 .
Lewin S, Glenton C. Are we entering a new era for qualitative research? Using qualitative evidence to support guidance and guideline development by the World Health Organization. Int J Equity Health. 2018;17(1):126. https://doi.org/10.1186/s12939-018-0841-x .
Liang W, Liang H, Ou L, Chen B, Chen A, Li C, Li Y, Guan W, Sang L, Lu J, Xu Y, Chen G, Guo H, Guo J, Chen Z, Zhao Y, Li S, Zhang N, Zhong N, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180(8):1081–9. https://doi.org/10.1001/jamainternmed.2020.2033 .
Mendelson M, Nel J, Blumberg L, Madhi SA, Dryden M, Stevens W, Venter FWD. Long-COVID: an evolving problem with an extensive impact. S Afr Med J. 2020;111(1):10–2. https://doi.org/10.7196/SAMJ.2020.v111i11.15433 .
MQ, P. Qualitative evaluation methods. 1988.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, Ahluwalia N, Bikdeli B, Dietz D, Der-Nigoghossian C, Liyanage-Don N, Rosner GF, Bernstein EJ, Mohan S, Beckley AA, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15. https://doi.org/10.1038/s41591-021-01283-z .
Nath A, Smith B. Neurological issues during COVID-19: an overview. Neurosci Lett. 2021;742: 135533. https://doi.org/10.1016/j.neulet.2020.135533 .
Organization WH. Clinical Management of COVID-19—Interim Guidance. 2020. Retrieved October 27, 2020 from https://www.who.int/publications/i/item/clinical-management-ofcovid-19 .
Peng QY, Wang XT, Zhang LN. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46(5):849–50. https://doi.org/10.1007/s00134-020-05996-6 .
Robey RC, Kemp K, Hayton P, Mudawi D, Wang R, Greaves M, Yioe V, Rivera-Ortega P, Avram C, Chaudhuri N. Pulmonary sequelae at 4 months after COVID-19 infection: a single-centre experience of a COVID follow-up service. Adv Ther. 2021;38(8):4505–19. https://doi.org/10.1007/s12325-021-01833-4 .
Rubin A, Bellamy J. Practitioner’s guide to using research for evidence-based practice. 2012.
Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40. https://doi.org/10.1002/1098-240x(200008)23:4%3c334::aid-nur9%3e3.0.co;2-g .
Shang W, Kang L, Cao G, Wang Y, Gao P, Liu J, Liu M. Percentage of asymptomatic infections among SARS-CoV-2 omicron variant-positive individuals: a systematic review and meta-analysis. Vaccines (Basel). 2022. https://doi.org/10.3390/vaccines10071049 .
Shaw JA, Smit DP, Griffith-Richards S, Koegelenberg CFN. Utility of routine chest radiography in ocular tuberculosis and sarcoidosis. Int J Tuberc Lung Dis. 2018;22(11):1374–7. https://doi.org/10.5588/ijtld.18.0013 .
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–7. https://doi.org/10.1016/S1473-3099(21)00703-9 .
Thornton J. Covid-19: the challenge of patient rehabilitation after intensive care. BMJ. 2020;369: m1787. https://doi.org/10.1136/bmj.m1787 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Vehar S, Boushra M, Ntiamoah P, Biehl M. Post-acute sequelae of SARS-CoV-2 infection: caring for the ‘long-haulers.’ Cleve Clin J Med. 2021;88(5):267–72. https://doi.org/10.3949/ccjm.88a.21010 .
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42. https://doi.org/10.1016/j.bbi.2020.05.048 .
WHO. Using evidence from qualitative research to develop WHO guidelines. 2014.
WHO. Living guidance for clinical management of COVID-19 . 2021. [Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 ].
WHO. WHO Coronavirus (COVID-19) Dashboard: World Health Organization . 2021. [Available from: https://covid19.who.int/ .
WHO. Infection prevention and control in the context of coronavirus disease 2019 (COVID-19): a living guideline. In. 2022. https://www.ncbi.nlm.nih.gov/pubmed/35767666 .
WHO. WHO guidelines on the use of chest imaging in COVID-19. 2022.
Zhao YM, Shang YM, Song WB, Li QQ, Xie H, Xu QF, Jia JL, Li LM, Mao HL, Zhou XM, Luo H, Gao YF, Xu AG. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine. 2020;25: 100463. https://doi.org/10.1016/j.eclinm.2020.100463 .
Download references
Acknowledgements
We would like to acknowledge Mr. Hussain Jafri, patient advocate, for his contribution in recruiting participants. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the WHO, its representatives, or the countries they represent.
This study received funding from the World Health Organization/International. All co-authors assisted in the drafting of the manuscript and read and approved the final version.
Author information
Authors and affiliations.
Hariri School of Nursing, American University of Beirut, Beirut, Lebanon
Gladys Honein-AbouHaidar & Cynthia Rizkallah
Department of Internal Medicine, American University of Beirut, Beirut, Lebanon
Imad Bou Akl
Department of Health Research Methods, Evidence and Impact McMaster University, 1280 Main Street West, Hamilton, Canada
Gian Paolo Morgano
Czech National Centre for Evidence-Based Healthcare and Knowledge Translation (CEBHC-KT), Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno, Czech Republic
Tereza Vrbová
Radiation and Health Unit, Department of Environment, Climate Change and Health, World Health Organization, Geneva, Switzerland
Emilie van Deventer & Maria del Rosario Perez
Department of Medicine, American University of Beirut, Riad-El-Solh, P.O. Box 11-0236, Beirut, 1107 2020, Lebanon
Elie A. Akl
You can also search for this author in PubMed Google Scholar
Contributions
GHA has led the data collection, analysis, and interpretation, and wrote the first draft of the manuscript. CR has contributed to data collection. EAA and GHA have led the conceptualization and design of the study. EAA, EvD, MdRP and GHA critically reviewed the manuscript. IBA, MdRP, GPM and TV contributed to the data collection. All authors have revised and provided comments and contributions to the manuscript. All authors have read and given final approval of the version to be published.
Corresponding authors
Correspondence to Emilie van Deventer or Elie A. Akl .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the institutional review board of the American University of Beirut (SBS-2020-0206). Informed consent in verbal form was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Appendix 1. KI interview guide for providers.
Additional file 2:
Appendix 2. KI interview guide for patients.
Additional file 3:
Appendix 3. Participants’ list: providers and patients.
Additional file 4:
Appendix 4. COREQ checklist.
Additional file 5:
Appendix 5. Valuation of outcomes associated with using chest imaging to monitor COVID-19 pulmonary sequelae, with exemplary quotes. Appendix 6. Preferences for each chest imaging modality used to monitor COVID-19 pulmonary sequelae, by indication, pros and cons, with exemplary quotes. Appendix 7. Acceptability of using chest imaging to monitor COVID-19 pulmonary sequelae, by providers and patients respectively, its determinants, with exemplary quotes. Appendix 8. Determinants of equity of using chest imaging to monitor COVID-19 pulmonary sequelae and exemplary quotes. Appendix 9. Feasibility of using chest imaging to monitor COVID-19 pulmonary sequelae by facilitators and barriers, with exemplary quotes. Appendix 10. Practical issues that patients might consider when using chest imaging to monitor COVID-19 pulmonary sequelae, with exemplary quotes.
Rights and permissions
Open Access This article is licensed under the terms of the Creative Commons Attribution 3.0 IGO License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the WHO, provide a link to the Creative Commons licence and indicate if changes were made. The use of the WHO’s name, except in reference to the article, and the use of the WHO’s logo, is not authorized as part of this licence. The link provided below includes additional terms and conditions of the licence. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/3.0/igo/ .
Reprints and permissions
About this article
Cite this article.
Honein-AbouHaidar, G., Rizkallah, C., Bou Akl, I. et al. Understanding contextual and practical factors to inform WHO recommendations on using chest imaging to monitor COVID-19 pulmonary sequelae: a qualitative study exploring stakeholders’ perspective. Health Res Policy Sys 22 , 67 (2024). https://doi.org/10.1186/s12961-023-01088-1
Download citation
Received : 15 December 2022
Accepted : 02 December 2023
Published : 11 June 2024
DOI : https://doi.org/10.1186/s12961-023-01088-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chest imaging
- Practice guidelines
- Qualitative research
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Open Access Kent State (OAKS)
- Open Access Kent State
- Nurse Reports of Moral Distress During the COVID-19 Pandemic
| Author(s) | |
|---|---|
| Abstract | COVID-19 was devastating for many frontline nurses embroiled in health care's response. Most media outlets reported from several large metropolitan areas in New York, California, and Florida, leaving other regions to wonder about the extent to which their nurses were suffering. |
| Format | |
| Identifier(s) | |
| Publication Date | |
| Publication Title | |
| Publisher | |
| Volume | |
| Keywords | |
| Subject | |
| Rights | |
| License | |
| Community | |
| Permalink |
- Chicago/Turabian
Street Address
Mailing address.
- oaks [at] kent [dot] edu
Quick Links
- Frequently Asked Questions
- Rights and Reuse
Information
- Accessibility
- Annual Security Reports
- Emergency Information
- For Our Alumni
- For the Media
- Health Services
- Jobs & Employment
- May 4th, 50th Commemoration
- Privacy Statement
- Website Feedback
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Sociol

Conducting rapid qualitative interview research during the COVID-19 pandemic—Reflections on methodological choices
Marta wanat.
1 Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, United Kingdom
Aleksandra J. Borek
Caitlin pilbeam, sibyl anthierens.
2 Department of Family Medicine and Population Health, University of Antwerp, Antwerp, Belgium
Sarah Tonkin-Crine
3 National Institute for Health Research Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance, Oxford, United Kingdom
Associated Data
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
As the COVID-19 pandemic has shown, setting up studies in time to gather relevant, real-world data enables researchers to capture current views and experiences, focus on practicalities on the ground, and deliver actionable results. Delivering high quality rapid studies in healthcare poses several challenges even in non-emergency situations. There is an expanding literature discussing benefits and challenges of conducting rapid research, yet there are relatively few examples related to methodological dilemmas and decisions that researchers may face when conducting rapid studies. In rapidly-changing emergency contexts, some of these challenges may be more easily overcome, while others may be unique to the emergency, magnified, or emerge in different ways. In this manuscript, we discuss our reflections and lessons learnt across the research process when conducting rapid qualitative interview studies in the context of a healthcare emergency, focusing on methodological issues. By this we mean the challenging considerations and pragmatic choices we made, and their downstream impacts, that shaped our studies. We draw on our extensive combined experience of delivering several projects during the COVID-19 pandemic in both single and multi-country settings, where we implemented rapid studies, or rapidly adapted an existing study. In the context of these studies, we discuss two main considerations, with a particular focus on the complexities, multiple facets, and trade-offs involved in: (i) team-based approaches to qualitative studies; and (ii) timely and rapid data collection, analysis and dissemination. We contribute a transparent discussion of these issues, describing them, what helped us to deal with them, and which issues have been difficult to overcome. We situate our discussion of arising issues in relation to existing literature, to offer broader recommendations while also identifying gaps in current understandings of how to deal with these methodological challenges. We thus identify key considerations, lessons, and possibilities for researchers implementing rapid studies in healthcare emergencies and beyond. We aim to promote transparency in reporting, assist other researchers in making informed choices, and consequently contribute to the development of the rapid qualitative research.
Introduction
The field of rapid qualitative research has a long-standing history in social sciences (Vindrola-Padros, 2021a ). It has origins in the movement to involve local communities in identifying their own needs (Murray, 1999 ; McNall and Foster-Fishman, 2007 ), which then spread to the area of public health and social sciences (Richardson et al., 2021 ). Rapid research may take many forms (Richardson et al., 2021 ) and indeed researchers have delineated over 15 distinctive approaches in rapid qualitative research (Vindrola-Padros, 2021a ). The diversity in approaches has also been reflected in somewhat heterogeneous definitions, based on the type of rapid approach (e.g., McNall and Foster-Fishman, 2007 ; Beebe, 2014 ; Vindrola-Padros, 2021a ), with some authors highlighting key differences between them (McNall and Foster-Fishman, 2007 ). Nevertheless, features that seem to be common (but not essential) across these diverse approaches have been identified, including: rapid timeframes; team-based approach; use of multiple methods; iterative nature (e.g., simultaneous data collection and analysis); and a participatory focus, including engagement with relevant stakeholders to set research priorities and facilitate dissemination of actionable findings (Beebe, 2001 ; McNall and Foster-Fishman, 2007 ; Vindrola-Padros, 2021a ). Indeed, some have urged researchers to think about these features on a continuum rather than as essential for all rapid qualitative studies (Vindrola-Padros, 2021a ). For example, while a team-based approach may be beneficial for some studies, for others it may not be possible or useful (Vindrola-Padros, 2021a ). It is also worth noting that, alongside the development of rapid approaches, we have also seen researchers creating rapid techniques with the aim of speeding up the process of data collection (through, e.g., mind-mapping, note-taking, or real time transcription) or analysis (through, e.g., omitting transcription, using voice recognition software for transcription, mind mapping, or direct coding from the audio-recordings) (Vindrola-Padros and Johnson, 2020 ). These techniques, in contrast to rapid qualitative research approaches, can be also used as part of longer-term studies (Vindrola-Padros and Johnson, 2020 ).
As qualitative researchers wanted to produce meaningful yet rapid research findings during the COVID-19 pandemic, the use of rapid qualitative research methods has seen an increase. This has been noted previously, with researchers turning to rapid approaches in other pandemics such as Ebola (Johnson and Vindrola-Padros, 2017 ). The COVID-19 pandemic has thus ignited further interest in rapid qualitative approaches, and created a particular opportunity to move the field forward. Successful setup and implementation of rapid qualitative studies in healthcare pose several challenges even in non-emergency situations. There may be unique challenges to conducting qualitative studies in extraordinary circumstances, such as a pandemic (Graetz et al., 2022 ). In rapidly-changing emergency contexts, some of these challenges may be novel, magnified, or emerge in different ways and at different stages of the research process, whilst others may be more easily overcome. Understanding these challenges as well as successful ingredients is important. Discussions of such methodological choices are still limited, although they are needed to assist researchers interested in rapid approaches to make informed research design decisions (Vindrola-Padros, 2021a ), and there have been calls to compare the reliability of rapid techniques to identify their strengths and weaknesses (Johnson and Vindrola-Padros, 2017 ; Vindrola-Padros and Johnson, 2020 ). In this manuscript, we reflect on the methodological decisions and their consequences in the context of implementing rapid qualitative studies. The aim of our discussion is to identify key considerations, lessons, and possibilities for researchers implementing rapid studies in healthcare emergencies and beyond. This offers transparent guidance for researchers to make informed choices, and is an important part of preparedness in responding to pandemics and other urgent healthcare needs.
Materials and methods
This article draws on our experiences with six studies that we conducted during (and which related to) the COVID-19 pandemic. Throughout the process of data collection, analysis, and writing up these studies (between April 2020 and December 2021), all authors met on a regular basis to discuss their reflections on methodological choices within, and between study teams. These meetings provided the groundwork for this manuscript, as they allowed us to reflect on methodological dilemmas in each study. With time, the meetings enabled cross-study reflections and more theoretically-informed discussions around the suitability and feasibility of using rapid methods in our studies at the time and in the future, leading us to identify key points of comparison and learning. We further interrogated our understandings through repeated rounds of writing and reviewing related manuscripts. As our discussions and meetings continued, we identified a number of challenges and issues. Two issues were particularly important to our studies, which related to two of four commonly described features of rapid qualitative research, namely the process of implementing a team-based approach and ensuring rapid data collection (McNall and Foster-Fishman, 2007 ; Vindrola-Padros, 2021a ). Within these two key features, we identified a number of issues which we kept coming back to and became the focus of this manuscript. We use our six studies to demonstrate to the reader how these methodological choices and challenges have played out. The key features of these studies are summarized in Table 1 ; in brief:
Overview of conducted rapid studies.
| Sample | 146 interviews with 66 patients and 80 HCPs, from eight countries | 18 interviews with 10 university staff members and eight students | 21 interviews with scientists from five countries | 24 interviews with 18 HCPs | 105 interviews with 14 HCPs | 18 interviews with household members from two countries |
| Design | Stand-alone qualitative study | Mixed-methods study embedded within a cohort study | Stand-alone qualitative study | Longitudinal qualitative study (cross-sectional—most participants were interviewed twice), adapted from a standard pre-planned study | Longitudinal qualitative study (trajectory—participants were interviewed multiple times over a year) | Mixed-methods study |
| Data collection period | April to July 2020 | December 2020 to January 2021 | December 2020 to April 2021 | Two time-points: November 2020, and May 2021 | February 2020 to February 2021 | May to July 2020 |
| Setting and countries | England, Belgium, the Netherlands, Ireland, Greece, Poland, Sweden and Germany | England | England, Belgium, the Netherlands, Sweden and Germany | England | England and Scotland | Belgium and the Netherlands |
| Data collection methods and techniques | Semi-structured interviews | Semi-structured interviews | Semi-structured interviews | Semi-structured interviews | Semi-structured interviews | Semi-structured interviews |
| Transcription | Fully transcribed | Not transcribed | Fully transcribed | Fully transcribed | Partially transcribed | Not transcribed |
| Analysis | Deductive and inductive thematic analysis | Deductive framework analysis | Deductive and inductive thematic analysis | Inductive thematic analysis | Framework and narrative analysis | Deductive and inductive thematic analysis |
- RECOVER-QUAL (Wanat et al., 2021a , b , 2022 ) was a qualitative study in eight European countries investigating patients' and healthcare professionals' (HCPs') experiences of receiving/delivering care for respiratory symptoms in primary care during 2020.
- FACTS (Hirst et al., 2021 ; Wanat et al., 2021c ) was a mixed-methods study embedded within a cohort study exploring university students' and staff' experiences of using Lateral Flow Tests for COVID-19.
- SCIENTIST (Colman et al., 2021 ) was a qualitative study exploring views and experiences of scientists working on government advisory boards during the COVID-19 pandemic.
- STEP-UP (Borek et al., 2021 ) was a qualitative study with primary care HCPs about the impact of COVID-19 on antibiotic prescribing and stewardship, conducted as part of a larger program of research.
- HCP Policy and Experiences study (Borek et al., 2022 ; Pilbeam et al., 2022 ) was a longitudinal qualitative study exploring the dynamics of policy development and HCPs' experiences of working in the COVID-19 pandemic.
- HOUSEHOLD (Verberk et al., 2021 ) was a mixed-method study in Belgium and the Netherlands investigating how household members navigated COVID-19 recommendations to prevent the spread of infection within the home.
We discuss and reflect on two main considerations, which we identified as core features shaping and shaped by the methodological choices we made in the studies we conducted, namely:
- 1. Team-based approach to rapid qualitative studies.
- Team readiness and expertise.
- Sharing data collection.
- Transcription, summaries, and consequences for analysis.
- 2. Timely and rapid data collection and analysis.
- Multiple facets of timely data collection.
- Diversity in “rapid” study timeframes.
Team-based approach to rapid qualitative studies
One of the key features of rapid qualitative approaches is the extent to which a team-based approach is adopted. As highlighted by Vindrola-Padros, there is a continuum on which rapid approaches can be placed when it comes to teamwork, ranging from lone researchers to large teams (Vindrola-Padros, 2021a ). We discuss here the importance of team readiness and expertise, the practicalities of sharing data collection between different researchers, and what this means for data analysis.
Team readiness and expertise
First, the readiness of the team, and familiarity of team members are important to start and conduct a new, or add-on, study rapidly. We found that teams that were already established, or where members already knew each other, were more easily able to rapidly set up and conduct their study. For example, the STEP-UP study was conducted within a larger multi-workstream research program which had started about 4 years before this qualitative study. The team was well-established and familiar, having worked together on different studies, sub-studies, and journal articles. There were several benefits to this, in particular: there was no extra time or effort needed to get to know each person's approach and working style; team roles and responsibilities were already established, meaning that everyone immediately knew what to do and what others were doing; processes for, and approaches to, study set-up and conduct, data collection and analysis, data management and team meetings were already established, allowing a quick and smooth execution.
In contrast, new teams were rapidly assembled in our other studies. For example, in the “HCP Policy and Experiences” study, a new team was set-up including collaborators who had not worked together before, and were from different institutions and research traditions/backgrounds (e.g., health psychology, anthropology, history, clinical medicine). This interdisciplinary collaboration provided much-needed breadth in perspectives on the health crisis, enabling us to identify unique insights and speak to wider audiences. Further, collaborating across institutions meant pooling resources and expertise, and established important new links and relationships. This also enabled producing different types of outputs, including academic journal articles, written evidence submissions to public inquiries, and disseminating findings to policymakers. Nevertheless, our newly-formed interdisciplinary and inter-institutional collaboration also posed some challenges. For example, the rapid and urgent nature of this study meant that, in the initial stages, there was little time for the team to come together to fully figure out how to leverage the benefits of interdisciplinary working more fully, which was consolidated more as the study progressed.
Second, an important part of the team readiness is whether the wider (institutional) infrastructure supports the rapid set-up of studies, with ethical approvals being a key element. For example, in the STEP-UP and SCIENTIST studies, we applied for ethics approvals to amend existing study protocols to address additional research questions and include additional participants. As opposed to designing and approving a completely new study, adapting an existing study enabled a quicker study set-up, participant recruitment, and utilized the resources that were already in place (such as staff/time, funds). In contrast, in the RECOVER-QUAL study, we were able to obtain very rapid ethical approval in some countries but the time to obtain local approvals varied considerably (7–67 days).
Finally, the expertise of team members in terms of qualitative methods is important. In four of our studies, data collection was done by experienced qualitative researchers who each had expertise in conducting interviews with various participant groups. For these projects, we therefore did not often face the task of having to train junior researchers in the basic principles of qualitative research. However, in the RECOVER-QUAL and HOUSEHOLD studies, data collection was shared between interviewers from different countries. Each country led their own data collection, but with the same topic guide being implemented. Due to time pressures, the RECOVER-QUAL core research team prioritized training to all interviewers which focused on understanding the study aims and the topic guide, rather than how to conduct interviews. However, this was complemented by on-demand support for each, depending how much experience they had previously had with qualitative research. In the HOUSEHOLD study, we had one senior colleague providing significant hands-on support and training to an inexperienced qualitative researcher, both in relation to the study aims and the interviewing technique. This was challenging given the tight timelines for the study but the one-on-one training was personalized to meet the needs of the less experienced researcher.
In contrast, across the majority of studies we had limited opportunity to involve other researchers, including more junior colleagues. We therefore did not have a chance to share the workload or speed up the data collection process. This was mainly related to how our research team, consisting of a few experienced qualitative researchers, operated before the pandemic.
Whilst our study teams had extensive expertise in qualitative methods, we were relatively new to the rapid qualitative methods. Rapid approaches were determined by the research questions being answered and, as such, we learned more about them through training, engagement with literature and extensive experience when conducting the studies. This involved not only learning the practicalities of conducting rapid data collection or analysis, but also being pushed to quickly examine our own assumptions of whether we believed rapid techniques were credible to us. While for some of the studies, wider study teams included members who have used rapid approaches before, we were not able to fully benefit from their expertise because of rapid timelines. Applying a rapid approach became easier, or more natural, the more studies we worked on, as we started becoming more confident in making, and assessing the consequences of, methodological decisions.
Sharing data collection
The fieldwork across all six studies was conducted by teams ranging in size; three studies had the fieldwork conducted by solo researchers, and three studies shared data collection between two or more researchers. In the SCIENTIST, HOUSEHOLD and RECOVER-QUAL studies data collection was shared between two or more interviewers, each conducting interviews in their native language. Sharing data collection had several advantages. First, it allowed sharing workload between the researchers, which in the context of rapid timelines was particularly beneficial. Secondly, using teams in multiple countries allowed us to access participants we would not be able to recruit otherwise. In addition, it enabled us to collect data in participants' native language, thus allowing them to express their thoughts more freely. Thirdly, given the specific context of the COVID-19 pandemic, it was useful to have researchers not only speaking the native language but also understanding the context of each country, specifically relevant COVID-19 policies, current affairs and legislation (e.g., related to quarantines).
In contrast, in the STEP-UP, FACTS and (vast majority of) “HCP Policy and Experiences” studies data was collected by solo researchers. Having a single researcher collecting data was beneficial in particular for the “HCP Policy and Experiences” study, as it enabled the same researcher to build relationships with participants over time. This was important in retaining participants and collecting consistent data across the course of the study. Given that the researcher knew the participants and data so well, this also facilitated rapid analysis and dissemination of findings via journal articles led by the same researcher.
Transcription, summaries, and consequences for analysis
One of the strategies used in rapid qualitative research to speed-up the analysis and/or save cost is to not transcribe the audio recordings of interviews or focus groups, and analyse fieldnotes and/or recordings directly. Out of our six studies, the data were fully transcribed in three, not transcribed in two, and partially transcribed in one. The decision to transcribe or not was dependent on the study aims, timescale and resources, and had important downstream impacts on sharing workloads and the kinds of analysis possible.
For example, in the SCIENTIST, RECOVER-QUAL and STEP-UP studies we were able to secure the resources to transcribe all interviews and rely on transcription to analyse data. The reasons for transcription were slightly different across these studies; the datasets for the RECOVER-QUAL and STEP-UP studies were always planned to be transcribed as the studies were not initially planned to be rapid. In the STEP-UP study, having all transcripts and interview notes also helped another researcher contribute to the rapid analysis as they could quickly and easily familiarize themselves with and code the data. Conversely, in the SCIENTIST study, once we started collecting the data, it became apparent that transcription would be very beneficial as the research team had limited experience of the study topic and data was richer than we initially expected. Here, having access to transcripts allowed us to get a greater understanding of the issues faced by the participants in a shorter amount of time than if we had only had recordings, while also allowing the in-depth analysis to be achieved more quickly.
In the SCIENTIST and RECOVER-QUAL studies, data was charted against a priori categories identified based on the topic guide (deductive analysis) to shorten the time needed for the analysis. However, data within each category was then coded inductively line-by-line to create sub-categories, and identify themes while ensuring that our analysis was grounded in data. Prior to transcription both RECOVER-QUAL and the SCIENTIST study collected interview summaries after each interview or batch of interviews. This enabled the research team to access data quickly prior to it being transcribed and translated into English but also enabled each interviewer to highlight key points from interviews to inform analysis from an early stage. Interview summaries were complemented by discussions within the whole research team to allow interviewers to explain the data collected in the context of what was happening with the COVID pandemic in their own country.
In contrast, the HOUSEHOLD study was set up from the beginning to rapidly inform policy. Similarly, the FACTS study aimed to provide rapid qualitative results to support quantitative findings. As such, these two studies were the most rapid in our portfolio. Transcription was not carried out and this was seen as crucial in speeding up the analysis and the dissemination of results. This impacted the analysis; after each interview, we charted the data onto an a priori framework, including relevant quotes, and discussed the data with other researchers (if applicable). This was a very structured approach, allowing the team to quickly have an overview of the whole dataset. It was also possible as the studies had clear and contained research questions, with datasets analyzed with this lens in mind. This approach contrasted with the interview summaries collected in the studies above which were unstructured and led by each interviewer identifying what they thought was the key information. We felt that the less-structured initial approach was possible as we could still rely on more “traditional” qualitative analysis as a result of access to the transcripts, while the lack of transcripts in the latter studies “forced” us to be more driven by the pre-existing categories to ensure systematic approach to analysis.
Finally, in the “HCP Policy and Experiences” study, notes from all 105 interviews were made by the interviewer summarizing the key points discussed, and case summaries were produced giving an overview of each participants' longitudinal experiences and narrative. Due to resource constraints, only a sub-set (73) of interviews were transcribed. The interviews which were considered particularly important or detailed were selected for transcription. This pragmatic approach had benefits as well as challenges. While transcripts are important, they are not the only source of data in an interview study. Keeping fieldnotes alongside interviews was helpful in capturing aspects of the interviews that were not necessarily captured by transcribing what was said; they also allowed capturing communication occurring before or after the recorder was turned on/off, or through other mediums (e.g., email). On the other hand, the verbatim transcripts provided a detailed record of the content of the interviews, and thus allowed for thematic coding and analysis of the data. Unstructured notes were helpful to inform interpretation, whereas time pressure meant that re-listening to all recordings was often unfeasible. These considerations became particularly pertinent when a new researcher joined the team to conduct further analysis of these data. This second researcher was less familiar with the interviews that were not transcribed, and while the notes helped give a rapid introduction and overview of the dataset, they found the verbatim transcripts particularly helpful. Therefore, when working with transcribed and non-transcribed data, and sharing data analysis with a researcher who did not collect the data themselves, there was a tendency to give more attention to transcribed interviews because they could be more easily coded and quoted.
Timely and rapid data collection
Timely and rapid data collection are two important features of rapid research; data needs to be collected quickly and at informative timepoint(s). We discuss here ways in which timeliness and rapidity became pertinent to our studies.
Multiple facets of timely data collection
Rapid research is often considered as research conducted within a short time, although the duration of the rapid studies also differs largely. Rather than focusing just on the overall timeline or duration of the study, we found considering the timeliness of the data collection a key and helpful aspect of rapid research. When conducting our studies, we became aware of the multidimensionality of the concept of timeliness. Here we discuss three aspects related to timeliness of data collection: (i) capturing the phenomena of interest in real time; (ii) complexities of mixed-methods studies; and (iii) ever-changing context of pandemics.
Capturing the phenomena of interest in real time
Perhaps the most obvious dimension of timeliness is whether the data is being collected in a way that allows researchers to capture phenomena of interest in real time. Although the benefit of “hindsight” can be of particular significance, gathering data as things are happening, rather than retrospectively, has great advantages especially when needed to inform policy and emergency responses. It allows exploration of issues as events unfold, and uniquely captures participants' insights, views, and sense making in the midst of their experiences prior to subsequent reflections and reinterpretations.
In the RECOVER-QUAL study, we were able to interview HCPs in the first few weeks of the pandemic (the first lockdown). As we were interested in how they were adjusting to the changes in care delivery, they could describe these changes almost as they were happening. Some participants commented how even a week could make a difference in how they felt about the situation, as it was changing very rapidly on the ground. In contrast, we interviewed some participants in later months, but still within the period of the first lockdown. This “delay” was due to ethical approvals taking longer in some countries. These later interviews were slightly different as participants had more time to adjust to the changes in primary care and, importantly, to process what was happening and how they felt about it. This meant that the interviews were to some extent retrospective and participants often described how they felt initially and how they felt at the time of the interview.
In addition, the aim of the “HCP Policy and Experiences” study was to explore the experiences of HCPs during the COVID-19 pandemic, and how they changed over time. The first pilot interviews were conducted in February 2020 at the very start of the pandemic in the UK. To rapidly start the study and capture experiences “in real time,” participants were recruited through contacts/networks of the research team members. While this strategy enabled a prompt start and recruitment, recruiting a wider range of participants and purposeful sampling were more difficult. In this longitudinal study, participants were interviewed between 4 and 10 times throughout the first year of the COVID-19 pandemic. Interviews were scheduled depending on participants' availability and the pace of changes in their work (e.g., roles and responsibilities), guidelines and the pandemic's impact on healthcare services. This allowed us to collect timely (“real-time”) data, which could identify trajectories of how HCPs' experiences changed over time throughout a rapidly-changing context.
In contrast, in our STEP-UP study, we wanted to capture the impact of the pandemic on antibiotic prescribing and stewardship. However, we were reluctant to add burden and additional pressure on HCPs to participate in the study early in the pandemic when clinicians had other priorities. When we conducted the interviews in autumn 2020, we found that HCPs perceived their antibiotic prescribing as elevated early in the pandemic, and then returning to more usual in autumn. Although conducting the interviews later in the pandemic meant that we did not capture the perceived impact in “real time,” we were able to explore HCPs' reflections of the few months at the time when they seemed in a better position to reflect and share their experiences.
Complexities of mixed-methods studies
Mixed methods research often poses challenges in integrating datasets. In the context of rapid research, this alignment between the timeliness of data collection and integrating datasets became even more important. Two of our studies, the FACTS and HOUSEHOLD studies, were qualitative studies conducted alongside quantitative components, thus making timeliness of data collection of the two components closely related.
The FACTS study was a cohort study with a qualitative sub-study. The cohort study ran from October 2020 to January 2021, and aimed to examine the feasibility of regular self-testing for SARS-CoV-2 using LFTs in a university setting (Hirst et al., 2021 ). To complement this work, we conducted a qualitative study looking at acceptability of the testing, by doing interviews with university students and staff. To ensure consistency in timeframes for both studies, data collection for the qualitative study had to be completed within the timeframe of the cohort study. Specifically, we wanted to avoid interviewing people about their experiences of using LFTs beyond the period of the cohort study to ensure that interview participants had not had significantly greater experience of self-testing. Similarly, in the HOUSEHOLD study it was crucial that we were able to conduct interviews with participants while they were still in quarantine to capture how their experiences of adhering to infection control measures unfolded. We conducted interviews 7–15 days after the COVID-19 diagnosis of the index case, but this required a great time commitment by both researchers working on the project and close collaboration with the team recruiting patients in practice.
Ever changing context of pandemics
Finally, the context of the pandemic became very important in examining whether data was collected and disseminated in a timely manner. This context—shaped by local guidance and (inter)national public health policies such as those related to testing, quarantine requirements, and models of delivery in and access to primary and secondary care—became central for us to understand in order to interpret participants' experiences.
In the HOUSEHOLD study, context became particularly pertinent to timely data collection. Specifically, as the study was conducted in Belgium and the Netherlands, we became acutely aware of the significance of the policy changes relevant to the study aims. Even though the study was being conducted at the same time in the two countries, the COVID-19 restrictions and regulations related to quarantine requirements in both countries were changing rapidly. This influenced interpretations of participants' views on quarantine and infection control measures. As a result, we allocated extra resources to collect data in both countries as closely as possible to each other. We also closely monitored changing guidelines to be ready to consider, albeit often at short notice, what it might mean for the data collection.
In the “HCPs Policy and Experiences” study, we faced similar issues, especially as one of the aims of the study was to explore the impact of the changing COVID-19-related policies and guidelines for HCPs. We also included participants from different settings (general practice, emergency care, different hospital departments) where policies and practices often differed, and changed frequently, so we had to keep track of a vast number of contextual and policy shifts. We did this through linking policy or guidance documents to international monitoring of key policy and guidelines available online, and keeping a record of guideline documents and announcements (including clinical practice, infection prevention and control, public health, and occupational health and safety guidelines); particularly those related to any changes mentioned by participants in interviews. Although this added a large amount of additional work, this was especially helpful in informing our analysis. We could contextualize our year-long longitudinal data against a policy timeline of relevant guidelines and guideline changes that we constructed from tracking these in real-time.
Finally, working with policy colleagues also allowed dissemination of findings in a timely manner, in relation to the ever-changing policy landscape. Therefore, in addition to traditional dissemination channels such as scientific publications, for three of the projects (HCP Policy and Experiences, HOUSEHOLD and RECOVER-QUAL) we worked closely with policy partners to disseminate the findings in the form of policy briefs, summaries, or regular updates to policymakers (e.g., European Centre for Disease Prevention Control, 2020 ; World Health Organisation, 2020 ). Regardless of the overall study timeframes, we were thus able to rapidly disseminate findings to different audiences as data collection was still ongoing.
Diversity of “Rapid” study timeframes
Our studies ranged in timeframes, from days to a few months, with the longest, a longitudinal study, conducted over a year. Drawing on terminology from longitudinal research, we consider the study timeframe (period over which the data is collected) and the tempo (intensity) of data collection in tandem, to reflect on what “rapid” meant in our studies.
Rapid timeframe and intensive tempo
In our FACTS study, we faced a particularly rapid timeframe, which was planned for only 2 months (December 2020–January 2021). However, the study frame was shortened even more as the study had to pause for 2 weeks when university students and staff went on their Christmas break. This meant that recruitment and data collection had to be particularly condensed which resulted in 18 interviews being conducted across just 13 days, with many instances of interviews being conducted one after another. While we successfully completed data collection within this timeframe, it required significant re-organization of workload within the team related to other studies being conducted at the same time. The data collection and analysis were conducted by one person which put a particular pressure on the timely delivery. A team-based approach to data collection might have been particularly useful here to share this intense fieldwork.
In contrast, the SCIENTIST study and the RECOVER-QUAL studies had different timeframes and tempos. The data collection timeframe for the SCIENTIST study was 5 months, with 21 participants. While we collected and analyzed data simultaneously, thus allowing for a rapid dissemination, the tempo of data collection was slower as it largely depended on access to and availability of the participants (scientists working on the COVID-19 advisory boards). Similarly, the RECOVER-QUAL study had a 4-month data collection timeframe, but the tempo of data collection in each country was more intense (2–6 weeks) to reduce diversity in experience within countries.
Longitudinal design: The case for a longer timeframe with intensive tempo
Although a longitudinal design might at first seem contradictory to rapid research, based on our reflections from conducting two longitudinal studies (STEP-UP and “HCP Policy and Experiences” study), we examine how a longer timeframe may be employed together with a more intensive tempo of data collection, analysis and dissemination.
The “HCP Policy and Experiences” study was designed from the outset as a longitudinal qualitative study that aimed to follow HCPs over a year and explore how the context (e.g., policies, guidelines) and their experiences changed over time during the pandemic. The value of a longitudinal design is that it allows researchers to explore what changes, or does not change, over time through multiple data collection points with (usually) a smaller sample of participants. The timeframe (in our example—a year) might not as such match the typical shorter timeframes of rapid research. However, the tempo of data collection and analysis was intensified and enabled by using some rapid research techniques. The time for approvals, set-up and recruitment were shortened and intensified (compared to standard qualitative studies) by prioritizing resources and the study for approvals, and by recruiting participants through existing networks. Data collection was also intensified as we started collecting interviews as soon as participants were identified in the early stages of the emerging pandemic, and we arranged frequent interviews (depending on each participant's availability) over the first months of the pandemic when policy changes occurred rapidly. Finally, data was analyzed alongside data collection, with ongoing dissemination of the emerging findings on a weekly basis in the form of updates to policymakers, and preparing academic publications at points throughout data collection.
In this manuscript, we described the most salient methodological issues that we faced when setting up and implementing six rapid qualitative studies during the COVID-19 pandemic. As others have highlighted, there is a need to openly discuss methodological choices in rapid research, to promote transparency in reporting, assist other researchers in making informed choices, and consequently move the field forward (Vindrola-Padros, 2021a ). Here, we reflected on two interconnected issues, often central to rapid qualitative approaches. We also provide a summary of key considerations in relation to discussed methodological dilemmas in Table 2 .
Summary of key considerations in relation to methodological choices.
| Implementing a team-based approach vs. a solo researcher approach | • The breath of the research question (narrow or broad, exploratory questions) • The need to maintain rapport and minimize sample attrition (e.g., in a longitudinal study) • The tempo of data collection and analysis (e.g., more or less intensive) • Complexity of data collection (e.g., involving multiple settings, countries, or topics) • The need to invest time and training in larger teams, bringing together divergent viewpoints and methodological expertise • The novelty of the topic to the research team • Structure of the research team and ways of working (e.g., clear roles and responsibilities, regular meetings and updates) |
| Transcription of data | • The type of analytic approach (e.g., structured/deductive analysis or inductive analysis) • Priorities, and constraints of the research project (e.g., money, time, policy relevance, engagement with local stakeholders) • The size of the research team and which researchers are analyzing the data • The extent to which researchers use field notes, summaries and group discussions to support the process of making sense of the data |
| Conducting timely research | • (Changing) external context of the study • The need to invest resources to be able to collect data in time • Complexity of design (stand-alone or mixed methods studies) • Workloads of potential participants and ethical responsibility in collecting and not collecting data in time |
| Conducting rapid research | • The required timeframe (period of data collection) and tempo (intensity of data collection) • Availability of staff to ensure rapid data collection and share workload |
Considering how to ensure a suitable and successful team-based approach to rapid research
A team-based approach is one of the key features of rapid qualitative research. While some consider it essential (McNall and Foster-Fishman, 2007 ), others suggest considering a team-based approach on a continuum from solo researchers to larger teams, depending on the study design (Vindrola-Padros, 2021a ). In our studies, we utilized both a solo-researcher and a team-based approach to data collection and analysis. It is important to reflect which of these may be most suitable for a study, and researchers may want to take into account a number of factors. Firstly, one of the key considerations might be the tempo and complexity of data collection and analysis. We found a team-based approach most beneficial in studies with a more intense tempo and more complex data collection (e.g., involving multiple countries, settings, topics/research questions). As also discussed by others, larger research groups were hugely valuable in enabling workload-sharing, better access to participants, faster data collection, collection of data in local languages, and allowing the team to benefit from insights related to local contexts when collecting and interpreting the data (Graetz et al., 2022 ). However, as others highlighted as well (Vindrola-Padros et al., 2020 ), larger research groups pose the challenge of ensuring a shared understanding of the methodological approach to qualitative research being undertaken. Related to that, it may be difficult to bring together potentially divergent viewpoints of researchers coming from different disciplines and traditions (Vindrola-Padros and Johnson, 2020 ). While this can be offset by investing time in appropriate training and collaborative team meetings, the larger the team, the more difficult it may be to do that. The challenges of interdisciplinary research are well-established (Larsen, 2018 ; Bardosh et al., 2020 ), but working under tight timelines, in newly established teams can magnify these challenges (Baxter et al., 2021 ; Colman et al., 2021 ). Given the great value of interdisciplinary working, especially in healthcare emergencies, practical strategies may help to manage some of the challenges we experienced; for example, using Rapid Assessment Process (RAP) sheets to facilitate more systematic updates, summaries of data and a more systemic approach to building infrastructure for cross-country and/or interdisciplinary research (Vindrola-Padros, 2021a ). Secondly, the team readiness, and related to that, the novelty of the topic to the study team, may also be important. In some of our studies we benefited from being able to work with researchers who we knew well and had experience of using qualitative methods. We also found that when the topic was new to (some of) the research team, it was also useful to adopt a team-based approach to share insights, and leverage individuals' expertise. Others have also highlighted that a team-based approach can be a good way of sharing existing expertise and having a lead researcher familiar with the topic, can be useful in ensuring that the rest of the team can contribute to the analysis (Vindrola-Padros et al., 2020 ). Thirdly, the scope of the study and breath of research questions can also be an important consideration. We found that a solo researcher approach was most beneficial for studies with narrower research questions (i.e., rather than broader, more exploratory ones), which rely less on team input for data collection and analysis. Finally, for the longitudinal studies, in line with other researchers (Worth et al., 2009 ), we found that one person collecting all data facilitated rapport and relationship-building with the participants. While in the rapid studies, this may not always be seen as a priority, it is an important consideration to ensure low sample attrition. Thus, we would urge researchers to carefully consider the suitability and implications of team-based vs. solo approaches. Particularly, the potential trade-offs involved as well as the provisions necessary to support the approach taken, make it an effective use of resources, and derive the most benefit from it.
Considering benefits and challenges related to transcribing data
The traditional approach in qualitative research often involves audio recordings and transcription, with the aim of using the transcripts for analysis (Greenwood et al., 2017 ). Transcription has often been thought of as a non-negotiable part of qualitative interview research, and challenging this can be difficult (Vindrola-Padros and Johnson, 2020 ). However, some have highlighted the importance of considering the diversity of qualitative traditions and schools, and that while transcription can be of great value to some qualitative approaches, for others it may not be essential (Halcomb and Davidson, 2006 ). Rapid studies may in particular eliminate transcription of data, and thus it is important to consider both the suitability of (lack) of transcription in this context, as well as the downstream consequences including workloads and the type of analysis that is possible. Firstly, as highlighted by others, transcription decisions need to be closely linked, and appropriate, to the study aims and analytic approach (Tessier, 2012 ). In line with others (Gravois et al., 1992 ; Halcomb and Davidson, 2006 ), we felt that transcription provided more flexibility during thematic analysis as it facilitated making conceptual links between categories. Transcription may be even more important and beneficial for qualitative approaches which rely on making these conceptual links in order to develop theory, for example in grounded theory (Walker and Myrick, 2006 ). There is a paucity of rapid qualitative research involving such qualitative methodologies, and the studies published during the pandemic using grounded theory seem to rely on transcribed data to be able to create conceptual frameworks based on the results (e.g., Rees et al., 2021 ; Hörold et al., 2022 ). This is perhaps not surprising as conceptual analysis or drawing on theory takes time which may not be always compatible with rapid research timeframes (Vindrola et al., 2021a). Thus, while it may be difficult to implement a grounded theory methodology in a rapid study, it is important to highlight that researchers using such methodologies, may choose to adopt a discrete rapid technique at different stages of data collection or analysis, if their aim is to reduce the time required for data collection or analysis for these parts of the research process. It is also worth noting though that even when having access to transcripts, fieldnotes collected during or after interviews, and interview summaries, are also greatly beneficial in making sense of the data. Fieldnotes have a long standing place in qualitative research and can add an important layer to the analysis (Phillippi and Lauderdale, 2017 ), as transcripts cannot be assumed to be the only source of data in an interview. In contrast, in our studies which relied on more descriptive analysis, the lack of transcription was not disadvantageous. Thus, more descriptive analysis was possible based on recordings only, but the availability of transcripts further facilitated making links between categories. Secondly, the researchers may want to reflect on whether their motivation for omitting transcription is to save time or money. Specifically, researchers seeking to save money may want to omit transcription but then aim to “counterbalance” the lack of it by committing (significant) time to formulating codes and themes based on extensive listening to audio recordings (Gravois et al., 1992 ; Greenwood et al., 2017 ), or introduce an additional step in data collection where researchers create a mind map with participants in a focus group, which would be an equivalent of generating of “codes” or “categories” (Burgess-Allen and Owen-Smith, 2010 ). In the context of the healthcare emergency such as the COVID-19 pandemic, saving time and rapidly analyzing data, may be the most important motivator (Johnson and Vindrola-Padros, 2017 ; Vindrola-Padros et al., 2020 ; Hoernke et al., 2021 ). In this instance, researchers may omit the transcripts and analyse the data directly from the recording, which may involve producing a list of initial issues (themes) after each focus group/research encounter that are then ranked later on (Joe et al., 2015 ), or using RAP sheets (Vindrola-Padros, 2021a ) in order to speed up the process. In our studies we were often focused on producing actionable results, and were motivated by the aim of influencing policy based on incoming data. Thus, regardless of whether the transcription was possible or not, we relied on more descriptive and structured analysis to formulate a reply to a focused research question. Thirdly, it is worth considering who will conduct the analysis and how transcription may affect this process. In our studies, transcription of data allowed researchers who did not collect the data to more quickly familiarize themselves with the data and contribute to the analysis, and it made it easier to select supporting/illustrative quotes when writing up. Related to that, it is worth reflecting on the need for a transparent and permanent record of the data collected and analysis, particularly for studies with richer datasets and/or with additional research questions for future secondary analyses. Overall, given the variety of approaches possible with and without transcripts, we urge researchers to be clear about their priorities (e.g., time, cost, impact) as these have important implications for the type of analysis possible and/or appropriate. To support researchers in making such informed choices and ensuring study quality, sufficient training and expertise specifically in employing rapid qualitative approaches should also be sought (Vindrola-Padros, 2021a ).
Considering how to ensure timely research
Rapid research is often motivated by the need to be responsive to changing priorities, thus ensuring its timeliness (Vindrola-Padros, 2021b ; Vindrola-Padros et al., 2021 ). Timeliness of research has been somewhat discussed in the literature, mainly in relation to evaluations, with authors highlighting that when the research is conducted is as important as whether it addresses the “right” issues (Grasso, 2003 ; McNall et al., 2004 ). For healthcare research to be useful, its findings need to be rapid, responsive, and relevant (Riley et al., 2013 ). In the context of health emergencies, Vindrola-Padros et al. ( 2020 ) also highlighted the importance of research timeliness and its ability to deliver timely and actionable findings, which can inform evidence-based public health response. However, for social scientists, including qualitative researchers, an important aspect of timeliness is that it is partially dependent on whether these researchers are invited to contribute to the pandemic response early enough (Vindrola-Padros et al., 2020 ). Thus, the discussion around timelines has been focused mainly around whether the study findings are produced in timely way, so they could inform the policy decisions, or at least contribute to the evidence being considered (Grasso, 2003 ; McNall et al., 2004 ). While these are essential features of rapid research, the COVID-19 pandemic has brought out another aspect of timeliness related to when the data was collected, rather than only to when it was used. Specifically, in the rapidly changing context of COVID-19, our studies highlighted the importance of three additional aspects of timeliness: collecting data in real time (rather than retrospectively), carefully considering the changing external context, and the complexities of mixed methods studies. These aspects have been discussed to a lesser extent in the methodology-focused literature.
Timeliness of findings is of course closely linked to timely data collection, but it perhaps has not been acknowledged to the same extent (with some exceptions, e.g., Vindrola-Padros et al., 2020 ). We have illustrated here that timeliness is a distinctive feature of rapid research. Thus, it is possible to have timely findings, for example through simultaneous data collection and analysis, but still not collect data in real time. Hoernke et al. ( 2021 ) also highlighted this issue as they collected interviews with HCPs before, during and after the first peak of the pandemic, with authors noting that this approach allowed them to capture HCPs' experiences as the situation was unfolding. When attempting to collect data in real time, researchers may want to consider the feasibility of such an approach. In our studies, we have discussed the importance of considering the extent of heterogeneity between the countries collecting data within the same study. In studies conducted in multiple settings or countries, it is important to reflect on and identify the key differences between these settings or countries which may impact how researchers interpret the data, especially if the periods of data collection are not aligned. Others have acknowledged the complexities of implementing studies in multiple countries during the COVID-19 pandemic, and the limitations of not gathering comparable data (Ding et al., 2021 ; Kilian et al., 2021 , 2022 ); however, these aspects have not been highlighted as an important dimension of timelines in rapid qualitative research across multiple sites. Nevertheless, there remains the need to consider the burden and additional pressure on participants taking part in the studies in real time (Vindrola-Padros et al., 2021 ). Our study highlights that researchers should reflect on the opportunities and costs offered by gathering data in real time, and its impact on participants. Finally, the diversity of designs of qualitative and mixed methods approaches have been highlighted before (Vindrola-Padros, 2021a ), including conducting (i) a rapid study to inform longer-term research, (ii) a shorter study exploring remaining questions after a longer study has been completed, or (iii) a parallel rapid study to a longer program of work. Conducting mixed methods research is challenging as it requires an integration of research teams conducting each sub-study, as well as a clear strategy for triangulating the data (Tashakkori and Creswell, 2007 ; O'Cathain et al., 2010 ). Our studies conducted during the COVID-19 pandemic also highlight an additional challenge for certain mixed-methods designs, namely the need to align the data collection timelines to ensure that the data is comparable and can be truly triangulated. This also requires careful planning and appropriate resources.
Considering how to ensure rapid data collection
Rapid timeframes, understandably, are considered a key feature in rapid qualitative approaches. We have found that a useful way of considering the extent to which the study can be considered rapid is not only timeframe of data collection but also its tempo. Both terms have a long-standing use in longitudinal qualitative research. While a timeframe can be understood as the length of data collection, tempo can be defined as the number, length and frequency of visits to the field (Neale, 2021 ). While the frequency of visits is of course a unique feature of the longitudinal design, the number and length can be particularly useful when considering the rapid qualitative research as well. This has implications for how we define what rapid is; while it may be difficult to define the study length for the study to be classed as rapid because the extent of rapidness will depend on the aims, research question, context and other factors, there are also attempts to create a boundary with some suggesting that data collection should not exceed 6 months. This is on the basis that data collection longer than that will start resemble a non-rapid study (Vindrola-Padros, 2021a ). Interestingly, similar arguments have been expressed in relation to longitudinal qualitative research, highlighting that there is no universal length of data collection period, as this will greatly depend on the study objectives. For example, Saldana coined the term “shortitudinal,” to describe studies which combine intensive data collection periods with shorter time frames (starting from several months) (Saldaña, 2003 ). On a practical level, the researchers may want to consider the tempo of their data collection. For example, a 4-month study with 80 interviews (as for example in the RECOVER-QUAL study) may demand different approaches and resources than a 5-month study with 21 interviews (as was the case with our SCIENTIST study). Thus, the required resources, staff workloads and competing priorities across multiple projects, and the type of analysis will have to be considered. Studies utilizing more intense tempo, may benefit from a team-based approach to manage workloads. However, even a team-based approach may not allow a more conceptual analysis in short periods of time, and thus more structured approach may need to be considered.
A particular example of the tension and importance of considering both timeframe and tempo might be a longitudinal design in the context of rapid research. At first glance, longitudinal design and rapid research seem incompatible. As highlighted earlier, this closely links with an idea that rapid studies are conducted over relatively shorter periods of time, and thus not allowing space (and time) for dealing with challenges related to more complex designs. In the field of rapid qualitative research, longer timeframes have been somewhat indirectly discussed in relation to some rapid qualitative approaches such as Rapid Feedback Evaluation or Rapid Cycle Evaluation. These approaches are considered as either having short study timeframes or having longer timeframes with built-in feedback loops/cycles for the continuous sharing of findings (Vindrola-Padros et al., 2021 ), with the latter potentially making the studies longer overall. The context of the pandemic also puts these “traditional” timeframes in spotlight. Despite a great number of qualitative studies examining experiences of patients and HCPs during the pandemic, longitudinal rapid qualitative design has been utilized less frequently. This is not surprising; longitudinal design is still underutilized in applied healthcare research (Wanat et al., 2021d ). However, there are notable examples of combining longitudinal design and rapid research; for example a study by Turner and colleagues who examined how GP practices maintained face to face contact by conducting four interviews between May and June 2020 through combining rapid timeframes and timely dissemination, with longitudinal design (Turner et al., 2021 ). It is also worth noting that, similarly to grounded theory studies conducted during the pandemic discussed earlier, the studies which used longitudinal designs and were conducted over a short period of time have not always been classified as rapid by the authors themselves (e.g., Maison et al., 2021 ). This highlights that short data collection period does not automatically lead to a study being called “rapid.” It also shows the complexities in defining the key characteristics of rapid studies, and applying these when designing and implementing rapid qualitative approaches. Based on the recent examples, there seems to be a scope for innovation in rapid qualitative researchers by adopting more complex designs with both shorter and longer study timeframes.
Conclusions
Rapid qualitative research can be successfully set up and implemented in the context of a healthcare emergency, but can pose methodological dilemmas and challenges for researchers. In this manuscript, we have focused on two methodological issues, which became pertinent to our studies, namely implementing a team-based approach, and conducting timely and rapid research. By sharing our experiences and reflections, we hope to contribute to the transparency in conducting and reporting rapid studies and help other researchers to make better informed methodological choices. We also encourage other researchers in engaging with such methodological discussions to help move the field of rapid qualitative research forward.
Data availability statement
Ethics statement.
The studies involving human participants were reviewed and approved by relevant Ethics Committees. RECOVER-QUAL—Ethical approval for the whole project was granted in England by the South Central Berkshire Research Ethics Committee (reference number: 20/SC/0175). The seven research sites outside of the UK also obtained ethical approval from their local organizations. FACTS—The study was approved by the University of Oxford Research Ethics Committee in October 2020 (CUREC ethics reference {"type":"entrez-nucleotide","attrs":{"text":"R72896","term_id":"846928"}} R72896 /RE001). SCIENTIST—The study received ethical approval from the Ethics Committee of Antwerp University Hospital (20/13/150). HOUSEHOLD—The study received ethical approval from the Medical Ethical Committee Utrecht (NL) and Medical Ethics Committee UZA Antwerp (BE) (Reference number 20-185/D and 20/14/ 177 respectively). STEP-UP—The study was reviewed and approved by the University of Oxford Medical Sciences Inter-Divisional Research Ethics Committee (ref. {"type":"entrez-nucleotide","attrs":{"text":"R59812","term_id":"830507"}} R59812 ) and the NHS Health Research Authority (ref. 19/HRA/0434). HCP Policy and Experiences—The study was approved by the University of Oxford's Medical Sciences Interdivisional Research Ethics Committee (ref. {"type":"entrez-nucleotide","attrs":{"text":"R69302","term_id":"842819"}} R69302 ). Participants in all studies gave informed consent to participate in the research, and their consent was documented.
Author contributions
MW led the writing of the first draft. All authors contributed to writing the first draft of the manuscript. All authors contributed to conception and design of the study, manuscript revision, read, and approved the submitted version.
The RECOVER-QUAL, HOUSEHOLD, and SCIENTIST studies were part of the RECOVER (Rapid European COVID-19 Emergency Response research). RECOVER was funded by the EU Horizon 2020 research and innovation program under (Grant Agreement No. 101003589). FACTS study did not receive external funding. STEP-UP study was funded by the Economic and Social Research Council (ESRC) through the Antimicrobial Resistance Cross Council Initiative supported by the seven research councils in partnership with other funders (Grant No. ES/P008232/1). It was also supported by the NIHR HPRU in Healthcare Associated Infections and Antimicrobial Resistance at the University of Oxford and Imperial College London in partnership with UK Health Security Agency, the NIHR Oxford Biomedical Research Centre, and the NIHR under the Applied Health Research (ARC) program for North West London. HCP Policy and Experiences study was funded by the UKRI/NIHR 2019 nCoV Rapid Response Call through a grant (Grant No. NIHR200907) which supported AB and CP, with support from the NIHR HPRU in Emerging and Zoonotic Infections at University of Liverpool in partnership with UK Health Security Agency, and in collaboration with Liverpool School of Tropical Medicine and the University of Oxford. ST-C is funded by the NIHR HPRU in Healthcare Associated Infections and Antimicrobial Resistance at the University of Oxford in partnership with UK Health Security Agency.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Bardosh K. L., de Vries D. H., Abramowitz S., Thorlie A., Cremers L., Kinsman J., et al.. (2020). Integrating the social sciences in epidemic preparedness and response: a strategic framework to strengthen capacities and improve global health security . Glob. Health 16 , 1–18. 10.1186/s12992-020-00652-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baxter R., Jemberie W. B., Li X., Naseer M., Pauelsen M., Shebehe J., et al.. (2021). COVID-19: Opportunities for interdisciplinary research to improve care for older people in Sweden . Scand. J. Public Health 49 , 29–32. 10.1177/1403494820969544 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beebe J. (2001). Rapid Assessment Process: An Introduction . Walnut Creek, CA: Altra Mira Press. [ Google Scholar ]
- Beebe J. (2014). Rapid Qualitative Inquiry: A Field Guide to Team-based Assessment . Lanham, MD: Rowman and Littlefield. [ Google Scholar ]
- Borek A. J., Maitland K., McLeod M., Campbell A., Hayhoe B., Butler C. C., et al.. (2021). Impact of the COVID-19 pandemic on community antibiotic prescribing and stewardship: a qualitative interview study with general practitioners in England . Antibiotics 10 , 1531. 10.3390/antibiotics10121531 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Borek A. J., Pilbeam C., Mableson H., Wanat M., Atkinson P., Sheard S., et al.. (2022). Experiences and concerns of health workers throughout the first year of the COVID-19 pandemic in the UK: a longitudinal qualitative interview study . PLoS ONE 17 , e0264906. 10.1371/journal.pone.0264906 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Burgess-Allen J., Owen-Smith V. (2010). Using mind mapping techniques for rapid qualitative data analysis in public participation processes . Health Expect. 13 , 406–415. 10.1111/j.1369-7625.2010.00594.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Colman E., Wanat M., Goossens H., Tonkin-Crine S., Anthierens S. (2021). Following the science? Views from scientists on government advisory boards during the COVID-19 pandemic: a qualitative interview study in five European countries . BMJ Glob. Health 6 , e006928. 10.1136/bmjgh-2021-006928 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ding K., Yang J., Chin M.-K., Sullivan L., Demirhan G., Violant-Holz V., et al.. (2021). Mental health among adults during the COVID-19 pandemic lockdown: a cross-sectional multi-country comparison . Int. J. Environ. Res. 18 , 2686. 10.3390/ijerph18052686 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- European Centre for Disease Prevention and Control. (2020). Rapid risk assessment: Novel coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK – sixth update . Retrieved from Solna, Sweden: https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-update-Outbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf (accessed July 27, 2022).
- Graetz D. E., Sniderman E., Villegas C., Ragab I., Laptsevich A., et al.. (2022). Utilizing multilingual methods and rapid analysis for global qualitative research during a pandemic . Glob. Qual. Nurs. Res . 9 , 23333936221080969. 10.1177/23333936221080969 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grasso P. G. (2003). What makes an evaluation useful? Reflections from experience in large organizations . Am. J. Eval. 24 , 507–514. 10.1177/109821400302400408 [ CrossRef ] [ Google Scholar ]
- Gravois T., Rosenfield S., Greenberg B. (1992). Establishing reliability for coding implementation concerns of school-based teams from audiotapes . Eval. Rev. 16 , 562–569. 10.1177/0193841X9201600507 [ CrossRef ] [ Google Scholar ]
- Greenwood M., Kendrick T., Davies H., Gill F. J. (2017). Hearing voices: comparing two methods for analysis of focus group data . Appl. Nurs. Res. 35 , 90–93. 10.1016/j.apnr.2017.02.024 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Halcomb E. J., Davidson P. M. (2006). Is verbatim transcription of interview data always necessary? Appl. Nurs. Res 19 , 38–42. 10.1016/j.apnr.2005.06.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hirst J. A., Logan M., Fanshawe T. R., Mwandigha L., Wanat M., Vicary C., et al.. (2021). Feasibility and acceptability of community coronavirus disease 2019 testing strategies (FACTS) in a university setting . Open Forum Infect. Dis. 8 , ofab495. 10.1093/ofid/ofab495 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoernke K., Djellouli N., Andrews L., Lewis-Jackson S., Manby L., Martin S., et al.. (2021). Frontline healthcare workers' experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal . BMJ Open 11 , e046199. 10.1136/bmjopen-2020-046199 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hörold M., Drewitz K. P., Piel J., Hrudey I., Rohr M., Brunnthaler V., et al.. (2022). Intensive care units healthcare professionals' experiences and negotiations at the beginning of the COVID-19 pandemic in Germany: a grounded theory study . INQUIRY:J. Health Car. 59 , 469580221081059, 10.1177/00469580221081059 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joe J., Chaudhuri S., Le T., Thompson H., Demiris G. (2015). The use of think-aloud and instant data analysis in evaluation research: exemplar and lessons learned . J. Biomed. Inform. 56 , 284–291. 10.1016/j.jbi.2015.06.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson G. A., Vindrola-Padros C. (2017). Rapid qualitative research methods during complex health emergencies: a systematic review of the literature . Soc. Sci. Med. 189 , 63–75. 10.1016/j.socscimed.2017.07.029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kilian C., Neufeld M., Manthey J., Alavidze S., Bobrova A., Baron-Epel O., et al.. (2022). Self-reported changes in alcohol and tobacco use during COVID-19: findings from the eastern part of WHO European Region . Eur. J. Public Health 32 , 474–480. 10.1093/eurpub/ckac011 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kilian C., Rehm J., Allebeck P., Barták M., Braddick F., Gual A., et al.. (2021). Conducting a multi-country online alcohol survey in the time of the COVID-19 pandemic: opportunities and challenges . Int. J. Methods Psychiatr. Res. 30 , e1875. 10.1002/mpr.1875 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Larsen S. E. (2018). Interdisciplinarity, history and cultural encounters . Eur. Rev. 26 , 354–367. 10.1017/S1062798717000734 [ CrossRef ] [ Google Scholar ]
- Maison D., Jaworska D., Adamczyk D., Affeltowicz D. (2021). The challenges arising from the COVID-19 pandemic and the way people deal with them. A qualitative longitudinal study . PLoS ONE 16 e0258133. 10.1371/journal.pone.0258133 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McNall M., Foster-Fishman P. G. (2007). Methods of rapid evaluation, assessment, and appraisal . Am. J. Eval. 28 , 151–168. 10.1177/1098214007300895 [ CrossRef ] [ Google Scholar ]
- McNall M. A., Welch V. E., Ruh K. L., Mildner C. A., Soto T. (2004). The use of rapid-feedback evaluation methods to improve the retention rates of an HIV/AIDS healthcare intervention . Eval. Program Plann. 27 , 287–294. 10.1016/j.evalprogplan.2004.04.003 [ CrossRef ] [ Google Scholar ]
- Murray S. A. (1999). Experiences with “rapid appraisal” in primary care: involving the public in assessing health needs, orientating staff, and educating medical students . BMJ 318 , 440–444. 10.1136/bmj.318.7181.440 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Neale B. (2021). The Craft of Qualitative Longitudinal Research: The Craft of Researching Lives Through Time . Newcastle upon Tyne: SAGE. [ Google Scholar ]
- O'Cathain A., Murphy E., Nicholl J. (2010). Three techniques for integrating data in mixed methods studies . BMJ 341 , c4587. 10.1136/bmj.c4587 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Phillippi J., Lauderdale J. (2017). A guide to field notes for qualitative research: context and conversation . Qual. Health Res. 28 , 381–388. 10.1177/1049732317697102 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pilbeam C., Tonkin-Crine S., Martindale A.-M., Atkinson P., Mableson H., Lant S., et al.. (2022). How do healthcare workers ‘Do' guidelines? Exploring how policy decisions impacted UK Healthcare Workers during the first phase of the COVID-19 pandemic . Qual. Health Res. 32 , 729–743. 10.1177/10497323211067772 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rees S., Farley H., Moloney C. (2021). How registered nurses balance limited resources in order to maintain competence: a grounded theory study . BMC Nurs . 20 , 176. 10.1186/s12912-021-00672-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Richardson J., Godfrey B., Walklate S. (2021). Rapid, remote and responsive research during COVID-19 . Methodol. Innov. 14 , 1–9. 10.1177/20597991211008581 [ CrossRef ] [ Google Scholar ]
- Riley W. T., Glasgow R. E., Etheredge L., Abernethy A. P. (2013). Rapid, responsive, relevant (R3) research: a call for a rapid learning health research enterprise . Clin. Transl. Med. 2 , 1–6. 10.1186/2001-1326-2-10 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saldaña J. (2003). Longitudinal Qualitative Research: Analyzing Change Through Time . Lanham, MD: Rowman Altamira. [ Google Scholar ]
- Tashakkori A., Creswell J. W. (2007). The new era of mixed methods . J. Mix. Methods Res . 1 , 3–7. 10.1177/2345678906293042 [ CrossRef ] [ Google Scholar ]
- Tessier S. (2012). From field notes, to transcripts, to tape recordings: evolution or combination? Int. J. Qual. Methods 11 , 446–460. 10.1177/160940691201100410 [ CrossRef ] [ Google Scholar ]
- Turner A., Scott A., Horwood J., Salisbury C., Denholm R., Scott L. (2021). Maintaining face-to-face contact during the COVID-19 pandemic: a longitudinal qualitative investigation in UK primary care . Br. J.Gen. Pract.Open. 5 , BJGPO.2021.0036. 10.3399/BJGPO.2021.0036 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Verberk J. D., Anthierens S. A., Tonkin-Crine S., Goossens H., Kinsman J., de Hoog M. L., et al.. (2021). Experiences and needs of persons living with a household member infected with SARS-CoV-2: a mixed method study . PLoS ONE 16 , e0249391. 10.1371/journal.pone.0249391 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vindrola-Padros C. (2021a). Doing Rapid Qualitative Research . Newcastle upon Tyne: SAGE. [ Google Scholar ]
- Vindrola-Padros C. (2021b). Can we re-imagine research so it is timely, relevant and responsive? Comment on “Experience of Health Leadership in Partnering with University-Based Researchers in Canada: A Call to ‘Re-Imagine' Research.” Int. J. Health Policy Manag . 10 , 172. 10.34172/ijhpm.2020.43 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vindrola-Padros C., Brage E., Johnson G. A. (2021). Rapid, responsive, and relevant?: a systematic review of rapid evaluations in health care . Am. J. Eval. 42 , 13–27. 10.1177/1098214019886914 [ CrossRef ] [ Google Scholar ]
- Vindrola-Padros C., Chisnall G., Cooper S., Dowrick A., Djellouli N., Symmons S. M., et al.. (2020). Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19 . Qual. Health Res. 30 , 2192–2204. 10.1177/1049732320951526 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vindrola-Padros C., Johnson G. A. (2020). Rapid techniques in qualitative research: a critical review of the literature . Qual. Health Res 30 , 1596–1604. 10.1177/1049732320921835 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walker D., Myrick F. (2006). Grounded theory: an exploration of process and procedure . Qual. Health Res. 16 , 547–559. 10.1177/1049732305285972 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wanat M., Boylan A.-M., Borek A. J. (2021d). Value, challenges and practical considerations when designing, conducting and analysing a longitudinal qualitative study in family medicine . BMJ Fam. Med. Commun. Health 9 ( Suppl. 1 ), e001283. 10.1136/fmch-2021-001283 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wanat M., Hoste M., Gobat N., Anastasaki M., Böhmer F., Chlabicz S., et al.. (2021a). Transformation of primary care during the COVID-19 pandemic: experiences of healthcare professionals in eight European countries . Br. J. Gen. Pract. 71 , e634–e642. 10.3399/BJGP.2020.1112 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wanat M., Hoste M., Gobat N., Anastasaki M., Böhmer F., Chlabicz S., et al.. (2021b). Supporting primary care professionals to stay in work during the COVID-19 pandemic: views on personal risk and access to testing during the first wave of pandemic in Europe . Front. Med. 8 , 726319. 10.3389/fmed.2021.726319 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wanat M., Hoste M. E., Gobat N. H., Anastasaki M., Böhmer F., Chlabicz S., et al.. (2022). Patients' and clinicians' perspectives on the primary care consultations for acute respiratory infections during the first wave of the COVID-19 pandemic: an eight-country qualitative study in Europe . Br. J. Gen. Pract. Open . 1–12. 10.3399/BJGPO.2021.0172 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wanat M., Logan M., Hirst J. A., Vicary C., Lee J. J., Perera R., et al.. (2021c). Perceptions on undertaking regular asymptomatic self-testing for COVID-19 using lateral flow tests: a qualitative study of university students and staff . BMJ Open 11 , e053850. 10.1136/bmjopen-2021-053850 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organisation (2020). Home Care for Patients With Suspected or Confirmed COVID-19 and Management of Their Contacts. Interim Guidance . Geneva: WHO Worldwide. Retrieved from: Home care for patients with suspected or confirmed COVID-19 and management of their contacts (who.int). Available online at: https://www.who.int/publications/i/item/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts [ Google Scholar ]
- Worth A., Irshad T., Bhopal R., Brown D., Lawton J., et al.. (2009). Vulnerability and access to care for South Asian Sikh and Muslim patients with life limiting illness in Scotland: prospective longitudinal qualitative study . BMJ 338 , b183. 10.1136/bmj.b183 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
This paper is in the following e-collection/theme issue:
Published on 28.5.2024 in Vol 8 (2024)
Health Care Professionals’ Experiences With Using Information and Communication Technologies in Patient Care During the COVID-19 Pandemic: Qualitative Study
Authors of this article:

Original Paper
- Carly A Cermak 1, 2 , MClSc, PhD ;
- Heather Read 1 , PhD ;
- Lianne Jeffs 1, 2, 3 , RN, PhD
1 Science of Care Institute, Sinai Health, Toronto, ON, Canada
2 Lunenfeld-Tanenbaum Research Institute, Sinai Health, Toronto, ON, Canada
3 Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada
Corresponding Author:
Carly A Cermak, MClSc, PhD
Science of Care Institute
Sinai Health
1 Bridgepoint Drive
Toronto, ON, M4M 2B5
Phone: 1 4165864800
Email: [email protected]
Background: The COVID-19 pandemic acted as a catalyst for the use of information and communication technology (ICT) in inpatient and outpatient health care settings. Digital tools were used to connect patients, families, and providers amid visitor restrictions, while web-based platforms were used to continue care amid COVID-19 lockdowns. What we have yet to learn is the experiences of health care providers (HCPs) regarding the use of ICT that supported changes to clinical care during the COVID-19 pandemic.
Objective: The aim of this paper was to describe the experiences of HCPs in using ICT to support clinical care changes during the COVID-19 pandemic. This paper is reporting on a subset of a larger body of data that examined changes to models of care during the pandemic.
Methods: This study used a qualitative, descriptive study design. In total, 30 HCPs were recruited from 3 hospitals in Canada. One-on-one semistructured interviews were conducted between December 2022 and June 2023. Qualitative data were analyzed using an inductive thematic approach to identify themes across participants.
Results: A total of 30 interviews with HCPs revealed 3 themes related to their experiences using ICT to support changes to clinical care during the COVID-19 pandemic. These included the use of ICT (1) to support in-person communication with patients, (2) to facilitate connection between provider to patient and patient to family, and (3) to provide continuity of care.
Conclusions: HCP narratives revealed the benefits of digital tools to support in-person communication between patient and provider, the need for thoughtful consideration for the use of ICT at end-of-life care, and the decision-making that is needed when choosing service delivery modality (eg, web based or in person). Moving forward, organizations are encouraged to provide education and training on how to support patient-provider communication, find ways to meet patient and family wishes at end-of-life care, and continue to give autonomy to HCPs in their clinical decision-making regarding service delivery modality.
Introduction
The health care workforce had to quickly adapt to the COVID-19 pandemic, with health systems grappling with the provision of COVID-19 care at the same time as non-COVID-19 care. Restrictions to reduce the spread of COVID-19 put an additional strain on the health care system. Health care providers (HCPs) were left to problem-solve how to continue providing compassionate, connected care among layers of personal protective equipment and visitor restrictions. Fortunately, the COVID-19 pandemic was a catalyst for digital health to support the ongoing response to the COVID-19 pandemic, with web-based care emerging as the primary innovation of information and communication technology (ICT) used in medical care [ 1 , 2 ]. Uses of ICT in medical care include remote consultations, digital noninvasive care, and digital platforms for data sharing [ 3 ].
ICT played an important role in supporting changes to clinical care within inpatient and outpatient health care settings. Within inpatient settings, ICT was integral in maintaining connectivity between patients, families, and providers when changes to visitor policies were implemented [ 4 ]. For example, the use of mobile devices and tablets allowed for connection between patient and family and supported knowledge transfer between provider and family [ 5 ]. Within outpatient settings, ICT was integral in continuing care when COVID-19 lockdown restrictions limited in-person visits [ 1 ]. For example, videoconference and telemedicine services (ie, web-based care) emerged as a platform for providers to use to allow for remote care [ 1 ]. In both facets, ICT facilitated connection, acting as an essential link between patients, families, and providers. However, we have yet to learn of HCPs’ experiences in using ICT to support clinical care.
Learning from the experiences of HCPs’ use of ICT will offer valuable insights into how innovative uses of ICT might continue to be used in inpatient and outpatient health care settings moving forward. From here, uses of ICT can inform organizational leadership of the systems or processes that may require further investigation to support ICT use in clinical care in a postpandemic world. The main objective of the study was to examine changes to models of care during the pandemic from the perspectives of HCPs, implementation team members, and leaders across 3 Canadian hospitals. For this paper, we report on a storyline that emerged from this work to describe the experiences of HCPs’ use of ICT that supported changes to clinical care during the COVID-19 pandemic.
Study Design
This qualitative descriptive study was undertaken from March 2022 to June 2023 to understand changes to models of care during the COVID-19 pandemic through the experiences of HCPs, implementation team members, and leaders across 3 hospitals in Canada. This paper is reporting on a subset of data related to HCPs’ experiences of using ICT in supporting changes to clinical care, drawn from the larger study that explored changes to models of care that took place during the COVID-19 pandemic. The reporting of this study was guided by the Standards for Reporting Qualitative Research [ 6 ].
Sampling and Participant Recruitment
In total, 30 HCPs were recruited from critical care, inpatient, and ambulatory services across 3 hospitals in Canada. A purposeful sampling strategy was used where recruiting took place in organizations that were known to have been affected by COVID-19 restrictions and policies. Site leads at participating institutions disseminated study information to HCPs (eg, nurses, physicians, and allied health disciplines) working within their respective health care organizations. From here, interview participants self-referred to this study. Inclusion criteria included current employment as an HCP working at the health care organization over the course of the pandemic and postpandemic recovery.
Data Collection
One-on-one, semistructured interviews were conducted by members of the research team (Kang Kang Margolese, Marina Morris, Lily Zeng, Marie Oliveira, Adebisi Akande, HR, Frances Bruno, or CAC) between December 2022 and June 2023. Demographic information, including age, gender, ethnicity, health discipline, time in profession, time in organization, and time in current role, was collected from all participants before the interview to ensure diversity within the sample. An interview guide was developed by the research team that explored the following five areas: (1) changes to care (eg, “What was your role like before the pandemic? How did care change over the course of the last 3 years?”), (2) provisions of care (eg, “What did you/your team start/stop doing? How did you prioritize care?”), (3) emotions (eg, “How did care change feel for you/your team? What supports were available to you?”), (4) implementation and evaluation (eg, “How were changes implemented and evaluated?”), and (5) lessons that were learned or future recommendations.
Data collection was completed by nonclinical research staff (Kang Kang Margolese, Marina Morris, Lily Zeng, Adebisi Akande, and HR) and clinical research staff (Marie Oliveira, Frances Bruno, and CAC). Data collection was concluded when saturation of themes was reached, meaning that limited new insights emerged from existing themes with the collected data sample [ 7 ]. The interviews were conducted via either a videoconferencing platform or in person and were approximately 45 to 60 minutes in length.
Ethical Considerations
Ethics was formally reviewed and approved by Sinai Health’s Research Ethics Board (REB# 22-0153-E), as well as at each participating site: Sunnybrook Health Sciences Centre (REB# 5571) and Providence Health Care (REB# H22-02792). Participants were informed that participation in this study was completely voluntary and that they could withdraw from the study at any time without penalty. Verbal informed consent was obtained before the start of the interviews, and participants were given an electronic gift card in recognition of their time. The honorarium for participants was CAD $20 (US $26.4). Demographic information was collected from all participants before the interview. These data were anonymized and stored separately from the transcripts, which were deidentified and stored on a secure server.
Data Analysis
The research design was conceived within an interpretivist paradigm, where the researchers’ purpose was to gather insight into how clinical care changed during the COVID-19 pandemic through the learning of the experiences of participants [ 8 ]. Interviews were analyzed using an inductive thematic analysis approach, which included openly coding line by line to organize data in a meaningful, systematic way; examining the codes to identify themes; and reviewing the themes [ 9 ]. Specifically, the entire research team openly coded a small group of interviews (n=3) independently, line by line, and then met as a group to review codes, discuss themes, and develop an initial codebook through consensus. From here, the research team coded the bulk of the interviews in pairs, meeting as needed to ensure the reliability of coding, using the primary investigator (LJ) to triangulate and resolve any discrepancies as needed.
Reflexivity was demonstrated through regular debriefs of interviews and a review of the codebook at 1- to 2-week intervals during the coding process. Primary adjustments were additions of new codes as interviews were collected from new participant subgroups. For example, the initial codebook was derived from nurse interviews, and new codes were required as the project expanded into allied health disciplines. Codes that related to HCPs’ experiences of ICT included disciplinary changes, technical changes and innovations, improvisation, problem-solving, tools, and technology recommendations. NVivo software (QSR International) was used to facilitate the cross-synthesis analysis. As a final step of analysis to ensure saturation and methodological rigor, the primary investigator for the study (LJ) reviewed the emergent coding schema with the original transcripts.
Participant Characteristics
A total of 30 participants (site A: n=4, site B: n=14, and site C: n=12) described their experiences of how ICT supported changes to clinical care. Table 1 presents the demographic characteristics. Themes generated from participants included the use of ICT (1) for supporting in-person communication with patients; (2) for enabling connection between patients, providers, and families; and (3) for providing continuity of care amid COVID-19 restrictions.
| Characteristic | Values | |
| 26-30 | 3 (10) | |
| 31-35 | 3 (10) | |
| 36-40 | 3 (10) | |
| 41-45 | 9 (30) | |
| 46-50 | 3 (10) | |
| 51-55 | 6 (20) | |
| 56-60 | 1 (3) | |
| 61+ | 2 (7) | |
| Female | 30 (100) | |
| Male | 0 (0) | |
| , n (%) | ||
| Asian | 4 (13) | |
| Canadian | 6 (20) | |
| European | 2 (7) | |
| Hispanic | 1 (3) | |
| White | 15 (50) | |
| Mixed | 2 (7) | |
| Nursing | 6 (20) | |
| Social work | 8 (27) | |
| Music therapy | 2 (7) | |
| Physiotherapy | 3 (10) | |
| Recreation therapy | 2 (7) | |
| Occupational therapy | 2 (7) | |
| Spiritual care | 3 (10) | |
| Dietetics | 3 (10) | |
| Psychology | 1 (3) | |
| In profession | 16.84 (8.59) | |
| At organization | 14.23 (8.82) | |
| In current role | 10.95 (8.20) | |
a HCP: health care provider.
b Participant self-identified; categories were not provided.
Supporting In-Person Communication With Patients
Participants described how tablets supported in-person communication to mitigate the impact that personal protective equipment (PPE) had on verbal interactions with patients. PPE such as masks, Plexiglas, and visors posed challenges in communicating effectively, particularly for patients who were hard of hearing or who had difficulties with comprehension. Efforts to support communication were essential as communication breakdowns created confusion for the patients with detrimental consequences:
And so when talking to elderly people, when they can’t read your lips or when they can’t really hear you through three layers of protective equipment, they get very confused and multiple confusing events leads to possible more agitation and agitation leads to an automatic write-off from a lot of health care providers as to a reason why not to provide a certain person with care. [Site B, 01, physiotherapist]
Participants described coming up with innovative ways to facilitate communication amid the layers of PPE, with tablets and phones used to break down communication barriers. Applications such as speech to text allowed live transcription of providers’ speech, which can be used as a tool to support comprehension for patients who were hearing impaired. Further, speech-to-text applications provided patients and families a model of how this tool can be used to support communication outside of the hospital setting:
And so, this [iPads] has been a huge help...it helps people, patients who haven’t heard of this...they go home with a brand-new strategy that makes their daily life so much easier. [Site C, 08, social worker]
In addition to using tablets to support communication with patients who were hard of hearing, participants also expressed the value of using tablets for translation services for patients who did not speak English. Benefits included the convenience of dialing translation services from an iPad:
We have translation services on them [iPads]...which has been so, so wonderful to have to just go into someone’s room who doesn’t speak English...And just call up this interpretation service, have a human being there and that was really a key. [Site C, 29, spiritual health practitioner]
Challenges surfaced when both a videoconferencing platform and translation services were required—specifically, the difficulties in handling 2 ICT tools simultaneously and the need to prioritize videoconferencing all the while hoping that family members were relaying information correctly:
...you can’t hold a Zoom, you know, iPad and then hold a translator phone to it, you know what I mean? So then it became family trying to find someone at their end who could relay information. [Site B, 13, occupational therapist]
Enabling Connection Between Patients, Providers, and Families
Participants described how digital devices facilitated the connection between provider to family and provider to patient during visitor restrictions. This included using phones and iPads to connect families to their loved ones in hospitals, especially at end-of-life care. Participants also described that providing a digital connection to families at end-of-life care was a service that could help families move through the grief process.
...we facilitated a FaceTime and all kinds of video calls for people to be able to talk to their loved ones. And even to their religious leaders in certain cases...Families were not able to be with a loved one when they were dying…we were a bridge between them. [Site B, 07, spiritual care]
...we recorded a memorial service that was generic and was put up on YouTube and we could send the link...And so many people just didn’t have the needed ritual to move through grief. And that was something that we could give them and that was—we received so much good feedback and gratitude for that. [Site C, 29, spiritual health practitioner]
While there were benefits of tablet use to connect families to patients at end-of-life care, a digital connection created an internal struggle for HCPs as they witnessed the lack of physical touch and difficulties in accommodating end-of-life rituals:
I feel like I struggled when I had to use an iPad to connect patients to family members and it could be in a very vulnerable situation, like a patient was dying, he doesn’t speak English, the daughter’s on the iPad, she’s crying, she can’t hold her dad, can’t hold his hand...I think we have to recognize that...there is a rite of passage before somebody dies. There are certain steps for religious people and families that need to happen to honour a dying body for them to move on to wherever that place is...So anointing, communion, confession. Those are not things that are amenable to a Zoom method. [Site B, 12, nursing]
Further, participants expressed the challenges with navigating the frequency of communication between patient and family, such as balancing family requests with staffing resources within the hospital:
...when you had multiple family members who each wanted their turn to visit once a week. Well, you know, you don’t have staff to be able to support five Facetimes per resident. So, we started to have to limit it and say...like two Facetimes a week for a family, or for a resident...So, that was a challenge. [Site B, 05, social worker]
Providing Continuity of Care
Participants described how the use of videoconferencing platforms such as Zoom (Zoom Video Communications) enhanced communication between providers and families, such as when needing to provide medical updates or discharge recommendations. Zoom provided accessible options for patients with hearing or comprehension challenges using closed captioning. Furthermore, Zoom enabled more efficient and faster communication between the care team and family, rather than being faced with the complexities of coordinating schedules of team members and families who may be coming in from out of town:
It [Zoom] optimized our efficiency for delivering family meetings...the specialist physicians were able to attend more of these family meetings than in the past, because of the ability to attend virtually. And then, more family were able to attend than...in the past. And it was able to happen faster because we could do it virtually versus waiting several days for a family member to arrive from another city. [Site B, 13, occupational therapist]
Participants also expressed the benefits of web-based care for patient access, particularly for patients with mobility challenges or lack of transportation:
I can actually say that shift [to virtual] was very positive because...it actually eliminated some of the concerns my patients have about transportation, or ways that they’re able to get out there, be it because of their physical impairment post-operation. Or simply just because they don’t have the resources to get transit for whatever reason. [Site A, 23, social worker]
Further, some participants expressed how web-based care positively changed clinical practice for counseling services:
And from all the patients I’ve intervened with...I’d say .01% want to come in person...I find that on Zoom you can sort of see the environment they’re in...I think that COVID has revolutionized social work intervention...I only have good things to say about it. COVID has opened up a whole new world for counseling. [Site B, 15, social worker]
Web-based care was not without its challenges. Clinicians described that greater access to care increased referrals from patients who would historically not come for in-person treatment, particularly for mental health services:
...we found that we were getting more referrals from ... all these different patients who would have not been able to come to hospital to do in-person groups...people with anxiety disorders, like agoraphobia. People who had not seen—have difficulty going outside the house. [Site A, 16, nursing]
...the workload increased enormously, and was impossible to keep up with because before people had to come in to [the hospital] to see me so that actually restricted the number of people that I could see to people who lived in [the city], or in some neighbouring communities. At times, people would come in and come drive like 90 to 120 minutes to come and see me but due to Covid, when we shifted to online therapy...now, everybody in [the province] had access to me who were part of these programs...many people wanted to see the psychologist because they wouldn’t have to drive in. [Site C, 16, psychologist]
Consequently, participants described that more visits over Zoom led to greater fatigue as a result of having to simultaneously navigate Zoom and in-person teaching, resulting in a reduction in group therapy frequency:
We noticed for us clinicians we were just getting so fatigued that it was just too much. Because running a group in-person, and running it over Zoom is very, very different. You’re staring at a screen, you’re looking at all the faces in the room. You’re trying to navigate the PowerPoint, there’s a lot of things happening simultaneously, that when we were doing four groups a week we just noticed this is not sustainable for us. So we had to shift it to three groups. So one less group a week. So I think that’s a huge change in terms of provision of care. [Site A, 16, nursing]
In terms of providing clinical care, clinicians described the challenges of conducting a physical assessment or providing counseling treatment via Zoom or by phone:
We do some physical examination. So it’s hard just to understand the status just by phone, even if you ask them “Any swelling?” Then they say no but actually they have, so the knowledge may not be there. [Site C, 10, registered dietician]
...in Zoom it’s very limited and you mostly see the face. Right? You don’t see what the person is doing with their hands, arms, with their legs, with their feet. [Site B, 07, spiritual care practitioner]
It’s just something about being in the same room with someone when their emotions are high that you don’t actually have to do anything in particular, but just the calming presence makes a difference. I think that people get some of that on Zoom...I don’t know how similar or different, but I’m just assuming that it’s probably a bit watered down...Whereas if I was just in the room, I think just being quiet with the person would be enough and might be even better at times. [Site C, 16, psychologist]
Finally, clinicians described the challenges of using web-based care when working with older patients due to limited experiences with technology or cognitive impairments. Interestingly, some participants felt that the reliance on web-based care reduced the attendance of older populations who were not familiar with the technology.
...our average age is 97, they’re not tech savvy, they’re not necessarily understanding, comprehending, you know, that, you know, as we would understand that you can actually talk to someone who’s not present here, but it’s in the same time...So, I would call it, you’re having a video call. I try and explain it’s that, you’re having a video telephone call. And then, they just think they’re looking at a television, you know, and they’re just watching kind of a show and stuff. [Site B, 10, recreation therapist]
Some of our clients—some people with dementia don’t understand...either they don’t recognize themselves, or they get agitated by the sight of themselves—so having the person facilitating the Zoom understand how to turn off the view that you can see yourself, was important...I think I lost a number of older spouses that used to come to the group, because they...had difficulty understanding the technology, or just their digital literacy, or access to technology wasn’t that great. So currently...and interestingly, that has changed the demographic of people who are coming in my Caregiver Group. [Site B, 08, social worker]
Principal Findings
The aim of this qualitative descriptive study was to describe the experiences of HCPs in how ICT supported changes to clinical care during the COVID-19 pandemic. Participant narratives revealed 3 key findings: the benefits of digital tools to support in-person communication between patient and provider, the need for thoughtful consideration for the use of ICT at end-of-life care, and the support for the continued use of web-based care, when appropriate. We discuss HCPs’ experiences as they relate to the literature and provide recommendations for health care organizations that can make use of ICT in a more collaborative way while reflecting on patient and family values.
Communication between patients and providers is essential for quality care and for reducing preventable adverse medical events [ 10 ]. Patients who have been appropriately supported in their communication have reported to be more satisfied in their hospital stay [ 11 ]. Devices to assist with communication, more commonly referred to as alternative augmentative communication (AAC), have existed in health care for decades. AAC is an intervention approach for individuals who require added support (augmentative) or a replacement (alternative) for their communication [ 12 ]. AAC can be low technology such as communication boards or pictures or high technology such as communication systems on iPads and speech-generation devices and can be used for a short or long period of time depending on the individual’s communication needs [ 12 ].
The COVID-19 pandemic spawned a rapid adoption of digital tools such as tablets, which became an available tool to reduce communication barriers experienced with mask-wearing when speaking to patients and families and allow for participation in conversation. Additionally, tablets enabled access to video language interpretation for patients who were mechanically ventilated and awake [ 13 ], a unique example of reducing language barriers when families were not able to be present for interpretation. However, participant narratives using digital tools within acute care and rehabilitation contrast the literature describing the experiences of patients and families in the intensive care unit. In the intensive care unit, HCPs and families reported barriers to the implementation of communication supports, particularly for patients who were mechanically ventilated and awake [ 14 ]. Nurses reported feeling inadequate and frustrated in trying to support patients [ 14 ], whereas families reported frustration with communication breakdowns, inconsistent availability of tools, and insufficient training by the HCP [ 15 ]. Patients described being mechanically ventilated as a vulnerable, lonely, and fearful experience [ 15 ], particularly as verbal communication was not an option.
The collective experiences of nurses, families, and patients emphasize the impact that a lack of communication supports can have at the bedside. Further, the experiences of nurses, families, and patients shed light on the education and training that is needed for successful patient-provider communication to support participation in conversation, particularly for patients on mechanical ventilation. Reports from speech-language pathologists working with patients who are critically ill revealed positive patient-provider communication outcomes when there was nurse collaboration and readily available communication supports at the bedside [ 13 ]. Thus, the experiences of patients, families, and HCPs highlight the integral role that leadership and hospital policies play in prioritizing communication access, tool availability, and organizational-wide training [ 13 , 16 ]. For system-level change, it is recommended that hospital leaders develop regular staff training on communication supports led by professionals with expertise in this area such as speech-language pathologists [ 14 ]. For increased awareness on the importance of communication supports in health care, it is recommended that education on patient-provider communication starts as early as the undergraduate and postgraduate level for health discipline (ie, clinical) programs [ 14 ].
Videoconferencing tools have been used to connect loved ones for over a decade and have been shown to have positive psychosocial outcomes for nursing home residents when used as an addition to in-person family visits [ 17 ]. Specifically, older residents in nursing homes who received videoconferencing visits with family in addition to in-person family visits had a greater mean change in baseline depressive symptoms and feelings of loneliness when compared to older residents who had in-person visits only [ 17 ]. During the pandemic, however, videoconferencing tools and digital devices were used as a substitute for in-person visits due to visitor restrictions imposed by the COVID-19 pandemic. Although this enabled a connection between patient and family, the reduced frequency of family connections created tensions between both HCPs and family members.
Similar tensions were described by HCPs in the United Kingdom including communicating devastating news to relatives without having ever met them in person and the moral dilemma of what is “best” end-of-life care versus what could be offered given the COVID-19 restrictions [ 18 ]. Further, clinicians in Canada reported that web-based visits at end-of-life care prevented meaningful conversations typically had between family members at the bedside [ 19 ]. One physician described the importance of family connection in end-of-life care: “I’m now convinced that family members at the bedside improves patients’ ability to get better” [ 19 ]. The experiences of bereaved relatives aligned with the internal conflicts of HCPs in the United Kingdom: families wanted frequent communication that was easy to understand, one last chance to say goodbye through physical touch, and speaking to their loved one at bedside [ 20 ]. Similarly in Canada, HCPs, patients, and families all felt that restrictive acute care visitor policies impacted the safety and quality of care, mental health of everyone involved, families as partners in care, and communication and advocacy [ 4 ].
Although COVID-19 visitor restrictions have lifted, the experiences described by clinicians and families highlight the considerations needed for a positive, meaningful, end-of-life experience. One example of an organizational-wide intervention for end-of-life care includes the 3 Wishes Project (3WP), an intervention that gathers 3 wishes from the patient and family to help personalize and humanize end-of-life care [ 21 ]. The 3WP has demonstrated a positive impact on families and clinicians; families had a significantly higher rating of emotional and spiritual support than families who did not receive the 3WP [ 22 ], while clinicians reported greater morale and collaboration in helping families move toward acceptance [ 23 ]. Further, the 3WP has shown to build capacity for compassion at the organization level by facilitating collective noticing, feeling, and responding [ 24 ]. In other words, the implementation of 3WP creates system-level processes and structures to facilitate compassionate care while promoting the connection between patients, families, and HCPs [ 24 ]. Thus, while the use of digital devices will likely continue to be a complement to care [ 25 ], it is important that organizations encourage collective, compassionate care to meet the wishes of patients and families.
Literature describing the benefits and challenges of web-based care aligned with participant narratives. Benefits included faster access to care, greater efficiency, and improved convenience for patients [ 26 ]; challenges included conducting assessments without the ability to complete in-person physical examinations [ 26 ] and offering web-based care to patients with poor digital literacy [ 27 - 29 ]. What was unique to this study’s findings was the increase in referral rates with the implementation of web-based care. Two reasons for an increase in referrals as described by participants included greater access for patients with significant mental health needs who otherwise would not come in for services and greater access for patients living far away from the hospital. Consequently, more referrals increased the workload of HCPs, demonstrating the dichotomy between patient access to care and provider workload. This emphasizes the considerations needed to balance clinician workload with patient preference of service modality as organizations move toward hybrid models of care [ 25 ].
A recent US study examined patient preference for service modality for nonurgent care and found that when out-of-pocket costs were not a factor, slightly more than half of the sample (53%) preferred in-person visits to web-based care, while one-fifth (21%) preferred web-based and one-quarter (26%) had no preference or did not know what they preferred [ 30 ]. For individuals who had video visit experience, this was associated with their preference for video visits [ 30 ]. A closer look at demographic factors revealed that those who did not feel that video calls had a role in their medical care were generally older people, who lived rurally, and who had a lower income and educational level [ 30 ]. Conversely, patients who were younger and had a higher income and education were more likely to choose a video visit over in-person care [ 30 ]. While choice of service modality may be an option for nonurgent care moving forward, some populations may not have the same ability to choose. Rather, it is up to the HCP to decide whether web-based care is appropriate.
HCPs, such as psychiatrists, who work with patients with significant mental health disorders have described the role that contextual factors contribute to decision-making of service modality [ 31 ]. Contextual factors in decision-making included if an in-person visit provided greater therapeutic benefit than a web-based visit, if a general examination was needed, if there were caregivers nearby who could provide information, if insight into the living environment was necessary, and if safety resources were required for in-person visits [ 31 ]. There was no consensus among psychiatrists on the mental health conditions that would best be served, as some respondents felt web-based care offered unique benefits such as improved patient safety and reduced likelihood of escalation [ 31 ]. Taken together, a combination of factors will need to continue to be considered for service delivery modality moving forward, such as patient preference, nature of service provided, and technology literacy. Furthermore, thoughtful planning for the accessibility of technology use for underserved populations will likely be an element of consideration for the field of health care [ 32 ].
Limitations
First, this study is limited to the experiences of the HCP from urban hospitals in Ontario and British Columbia and may not be transferable to the full scope of pandemic hospital worker experiences across the globe. Consequently, there may have been uses of ICT that happened during the pandemic that were particularly novel or interesting but may not have been captured due to the nature of this qualitative study. Second, participants were given an electronic gift card after the interview in recognition of their time, which may have impacted self-referral into the study. Third, there were several research team members involved in interviews, which may have impacted the depth of information provided by the participants across interviews.
Conclusions
Experiences from HCP highlight the uses of ICT to support changes to clinical care during the pandemic. The use of digital tools supported patient-provider communication, enabled a connection between patients and families at end-of-life care, and provided continuity of care amid COVID-19 lockdowns. Moving forward, organizations are encouraged to provide education and training on how to support patient-provider communication in clinical care; find ways to implement collaborative, compassionate, end-of-life care; and continue to give autonomy to HCPs in their clinical decision-making regarding service delivery modality.
Acknowledgments
This study was funded by a grant from the Canadian Institutes of Health Research (W12179927). The authors would like to thank the participants who took time to reflect on the difficult experiences they and their colleagues faced during the COVID-19 pandemic. The authors would also like to thank the research team of Kang Kang Margolese, Marina Morris, Lily Zeng, Marie Oliveira, Adebisi Akande, and Frances Bruno who contributed to the data collection and analysis.
Data Availability
An aggregate summary of data generated and analyzed during this study are included in this published manuscript. Individual data transcripts cannot be publicly shared because of confidentiality.
Authors' Contributions
LJ conceived and designed the study and assisted with data analysis. CAC and HR assisted with data collection and data analysis. CAC drafted the manuscript, and all authors critically reviewed it as well as read and approved the final manuscript.
Conflicts of Interest
None declared.
- Liaw ST, Kuziemsky C, Schreiber R, Jonnagaddala J, Liyanage H, Chittalia A, et al. Primary care informatics response to Covid-19 pandemic: adaptation, progress, and lessons from four countries with high ICT development. Yearb Med Inform. 2021;30(1):44-55. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wu TC, Ho CTB. A narrative review of innovative responses during the COVID-19 pandemic in 2020. Int J Public Health. 2022;67:1604652. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tonetto LM, Saurin TA, Fogliatto FS, Tortorella GL, Narayanamurthy G, da Rosa VM, et al. Information and communication technologies in emergency care services for patients with COVID-19: a multi-national study. Int J Prod Res. 2023;61:8384-8400. [ CrossRef ]
- Montesanti S, MacKean G, Fitzpatrick KM, Fancott C. Family caregivers as essential partners in care: examining the impacts of restrictive acute care visiting policies during the COVID-19 pandemic in Canada. BMC Health Serv Res. 2023;23(1):320. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Levido A, Clement P, Gregory B, Morrey H, Kirrane M, Stott A, et al. Virtual engagement of families in the intensive care unit during COVID-19: a descriptive survey of family members of patients and health care workers. Telemed J E Health. 2023;29(3):466-472. [ CrossRef ] [ Medline ]
- O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245-1251. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893-1907. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Thanh NC, Thanh TTL. The interconnection between interpretivist paradigm and qualitative methods in education. Am J Educ Sci. 2015;1(2):24-27. [ FREE Full text ]
- Braun V, Clarke V. Thematic Analysis: A Practical Guide. London. SAGE Publications Ltd; 2022.
- Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rodriguez CS, Rowe M, Thomas L, Shuster J, Koeppel B, Cairns P. Enhancing the communication of suddenly speechless critical care patients. Am J Crit Care. 2016;25(3):e40-e47. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Beukelman DR, Mirenda P. Augmentative and Alternative Communication: Supporting Children and Adults with Complex Communication Needs. Baltimore MD. Paul H. Brookes Pub; 2013.
- Scibilia SJ, Gendreau SK, Towbin RT, Happ MB. Impact of COVID-19 on patient-provider communication in critical care: case reports. Crit Care Nurse. 2022;42(4):38-46. [ CrossRef ] [ Medline ]
- Kyranou M, Cheta C, Pampoulou E. Communicating with mechanically ventilated patients who are awake. A qualitative study on the experience of critical care nurses in Cyprus during the COVID-19 pandemic. PLoS One. 2022;17(12):e0278195. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Istanboulian L, Rose L, Yunusova Y, Dale C. Barriers to and facilitators for supporting patient communication in the adult ICU during the COVID-19 pandemic: a qualitative study. J Adv Nurs. 2022;78(8):2548-2560. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Santiago R, Gormley J, Altschuler T, Howard M, Pressman H, Blackstone S. Promoting system change for communication access in acute care hospitals. Assist Technol Outcomes Benefits. 2021;15(1):100-118. [ FREE Full text ]
- Tsai HH, Tsai YF. Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month videoconference program for older nursing home residents. J Med Internet Res. Nov 15, 2011;13(4):e93. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hanna JR, Rapa E, Dalton LJ, Hughes R, Quarmby LM, McGlinchey T, et al. Health and social care professionals' experiences of providing end of life care during the COVID-19 pandemic: a qualitative study. Palliat Med. 2021;35(7):1249-1257. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Elma A, Cook D, Howard M, Takaoka A, Hoad N, Swinton M, et al. Use of video technology in end-of-life care for hospitalized patients during the COVID-19 pandemic. Am J Crit Care. 2022;31(3):240-248. [ CrossRef ] [ Medline ]
- Hanna JR, Rapa E, Dalton LJ, Hughes R, McGlinchey T, Bennett KM, et al. A qualitative study of bereaved relatives' end of life experiences during the COVID-19 pandemic. Palliat Med. 2021;35(5):843-851. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cook D, Swinton M, Toledo F, Clarke F, Rose T, Hand-Breckenridge T, et al. Personalizing death in the intensive care unit: the 3 Wishes Project: a mixed-methods study. Ann Intern Med. 2015;163(4):271-279. [ CrossRef ] [ Medline ]
- Neville TH, Taich Z, Walling AM, Bear D, Cook DJ, Tseng CH, et al. The 3 Wishes Program improves families' experience of emotional and spiritual support at the end of life. J Gen Intern Med. 2023;38(1):115-121. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Neville TH, Agarwal N, Swinton M, Phung P, Xu X, Kao Y, et al. Improving end-of-life care in the intensive care unit: clinicians' experiences with the 3 Wishes Project. J Palliat Med. 2019;22(12):1561-1567. [ CrossRef ] [ Medline ]
- Vanstone M, Sadik M, Smith O, Neville TH, LeBlanc A, Boyle A, et al. Building organizational compassion among teams delivering end-of-life care in the intensive care unit: the 3 Wishes Project. Palliat Med. 2020;34(9):1263-1273. [ CrossRef ] [ Medline ]
- Ng G, Desai C, Gagliardi L, Donaghy S, Di Prospero L. Implementing digital devices to maintain family connections during the COVID-19 pandemic: experience of a large academic urban hospital. J Med Imaging Radiat Sci. 2023:1-6. [ CrossRef ] [ Medline ]
- Li E, Tsopra R, Jimenez G, Serafini A, Gusso G, Lingner H, et al. General practitioners' perceptions of using virtual primary care during the COVID-19 pandemic: an international cross-sectional survey study. PLOS Digit Health. 2022;1(5):e0000029. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Curran VR, Hollett A, Peddle E. Patient experiences with virtual care during the COVID-19 pandemic: phenomenological focus group study. JMIR Form Res. 2023;7:e42966. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chan-Nguyen S, Ritsma B, Nguyen L, Srivastava S, Shukla G, Appireddy R. Virtual care access and health equity during the COVID-19 pandemic, a qualitative study of patients with chronic diseases from Canada. Digit Health. 2022;8:20552076221074486. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kim J, Linos E, Fishman DA, Dove MS, Hoch JS, Keegan TH. Factors associated with online patient-provider communications among cancer survivors in the United States during COVID-19: cross-sectional study. JMIR Cancer. 2023;9:e44339. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open. 2021;4(12):e2136405. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Uscher-Pines L, Parks AM, Sousa J, Raja P, Mehrotra A, Huskamp HA, et al. Appropriateness of telemedicine versus in-person care: a qualitative exploration of psychiatrists' decision making. Psychiatr Serv. 2022;73(8):849-855. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Budhwani S, Fujioka J, Thomas-Jacques T, De Vera K, Challa P, De Silva R, et al. Challenges and strategies for promoting health equity in virtual care: findings and policy directions from a scoping review of reviews. J Am Med Inform Assoc. Apr 13, 2022;29(5):990-999. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| 3 Wishes Project |
| alternative augmentative communication |
| health care provider |
| information and communication technology |
| personal protective equipment |
Edited by A Mavragani; submitted 24.09.23; peer-reviewed by A Ševčíková, H Pilabré, A Olsson; comments to author 02.12.23; revised version received 06.03.24; accepted 21.03.24; published 28.05.24.
©Carly A Cermak, Heather Read, Lianne Jeffs. Originally published in JMIR Formative Research (https://formative.jmir.org), 28.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Formative Research, is properly cited. The complete bibliographic information, a link to the original publication on https://formative.jmir.org, as well as this copyright and license information must be included.
- Open access
- Published: 04 June 2024
Migraine self-management at work: a qualitative study
- Clara Knauf 1 ,
- Katherina Heinrichs 2 ,
- Rolf Süllwold 3 ,
- Andrea Icks 4 &
- Adrian Loerbroks 1
Journal of Occupational Medicine and Toxicology volume 19 , Article number: 22 ( 2024 ) Cite this article
207 Accesses
Metrics details
Migraine is common and can be highly disabling. Adequate migraine self-management (SM) can mitigate the potentially adverse health effects of migraine. However, adequate SM can be challenging to implement in everyday life, for instance, at the workplace. We aimed to explore how migraine SM is carried out at work and which occupational factors may determine effective implementation according to employees with migraine. We also explored the potential impact of the COVID-19 pandemic and the associated re-arrangement of working conditions on migraine SM at work.
We conducted semi-structured qualitative interviews (08/2020–01/2021). Participants were eligible if they have worked for at least six months with a minimum of twenty hours per week and with a migraine diagnosis. The interviews were transcribed and content-analyzed using MAXQDA.
Migraine SM was perceived to be influenced by social interactions at work (e.g., in terms of understanding vs. stigmatization), the level of job decision latitude (JDL, i.e., the extent to which one is able to influence work processes, e.g., when working from home), and workplace design (e.g., in terms of opportunities to withdraw from work). During the COVID-19 pandemic, especially increased JDL appeared to favorably influence migraine SM.
Conclusions
Migraine SM at work is fostered or complicated by various psychosocial working conditions. By considering these facilitators and barriers, more migraine-friendly workplaces can be created.
Migraine is associated with a considerable burden in terms of its prevalence, related disability, and cost. The prevalence is especially high among people between the age of 36 and 46, who are in the midst of their occupational life [ 1 ]. It has been estimated that the European Union loses € 111 billion annually due to migraine [ 2 ]. As much as 93% of this amount is considered to be attributable to indirect cost, i.e., cost resulting from lost and reduced productivity at work [ 2 ].
To successfully manage their condition, individuals with migraine need to acquire and apply various skills (i.e., self-management [SM]). Five major areas of migraine self-management activities have been identified in prior studies: (1) utilizing the healthcare system, (2) taking medication adequately, (3) using alternative therapies (such as osteopathy, herbal, and homeopathic remedies), (4) requesting social support, and (5) self-care (e.g., trigger detection and avoidance, stress management, and a healthy lifestyle) [ 3 , 4 , 5 ].
Migraine SM can be hampered or facilitated by external factors in everyday life, for instance, at the workplace. With regard to the latter, the European Federation of Neurological Associations (EFNA) conducted a survey in 2020 inquiring individuals with migraine or other types of headaches ( n = 167) from 20 European countries what their company should do to help them cope better with the effects of their health condition [ 6 ]. Proposed areas of improvement included (but were not limited to): more understanding by managers, more opportunities to work from home, private workspace, less social interaction, part-time work, and noise-cancelling headphones [ 6 ]. In the same vein, Scaratti et al. [ 7 ] used an online questionnaire to examine the needs of headache patients in Europe ( n = 103) related to staying at or returning to work. Here, too, physical environment adaptions (such as single offices, rest rooms), work-related aspects (e.g., longer, and flexible breaks), and support at work (among other things, social support by supervisors and human resources) were mentioned [ 7 ].
While there is thus confirmatory preliminary evidence regarding headache SM, there is still a need to examine in depth if and how working conditions may affect successful implementation of specifically migraine SM (rather than headache management in general) at work. Migraine cannot be equated with headache, as headache is only one symptom of migraine, which is also usually accompanied by other symptoms such as nausea, vomiting, or sensitivity to light, and thus likely to lead to more impairment. We aimed to gain detailed insights into the types of working conditions that may facilitate or hamper the ability to self-manage migraine. Work arrangements have changed swiftly and dramatically for many employees during the COVID-19 pandemic and we therefore also sought to explore the potential effects of these re-arrangements on SM strategies.
We conducted a qualitative study using semi-structured interviews. Our report adheres to the Consolidated Criteria for Reporting Qualitative Research (COREQ) statement [ 8 ].
The primary researcher (CK) was a medical student at the time of our study. Qualitative research skills are usually not acquired during medical studies in Germany. CK conducted the study to obtain a German Doctor of Medicine (Dr. med.) degree, which is comparable (in terms of its scope and quality) with a master thesis rather than with a PhD degree. The general choice of self-management at work as the research topic was due to the foci of the research group headed by AL, who acted as CK’s thesis supervisor. It was CK’s wish to relate her research project to migraine, as she had several migraine patients in her personal environment. CK familiarized herself extensively with the methodology of qualitative research (especially through self-studies and online tutorials) and in particular with the coding process. Prior to the interviews and the analysis, CK was trained (e.g., in interviewing techniques) by KH who is an experienced qualitative researcher [ 9 , 10 ] (female, degrees in psychology and public health). Also, detailed feedback and opportunities for reflection were provided during the actual interviewing and subsequent analysis (see below).
Study population
We sought to recruit participants who met the following inclusion criteria: (1) participant-report that migraine has ever been diagnosed by a physician and (2) employment with the migraine diagnosis for at least six months with a minimum of 20 working hours per week. Study participants were recruited via three different pathways: an inpatient rehabilitation clinic for headache disorders (Berolina Klinik, Löhne, Germany), migraine self-help groups from different regions in Germany, and private contacts of members of the study team. In the run-up to the interviews all potential participants received information on the objectives of the study, the professional background of the interviewer (CK) and the inclusion criteria (either via a flyer or from CK in person). This information was presented again later at the start of the interviews. It was also ensured at the beginning of the interviews that the inclusion criteria were met. All participants provided written informed consent prior to the interviews. In line with participants’ preferences, interviews were either conducted face-to-face or by telephone. Face-to-face interviews took place in the clinic or at the participants’ homes. We did not gather any information from non-participants, that is, from those who were exposed to our recruitment efforts (e.g., members of the self-help groups), but decided not to participate. Our study was approved by the Institutional Review Board of the Faculty of Medicine of the University of Düsseldorf, Germany (# 2019 − 627).
Data collection
Based on previous qualitative research by our group [ 9 , 11 ], we designed a topic guide [see Additional File 1 ]. After three interviews, the topic guide was discussed and adjusted by the study team. In particular, we then decided to add one question about migraine SM at work specifically during the COVID-19 pandemic, as this was an issue frequently referred to in the first interviews. Prior to the interviews, participants were asked to complete a standardized questionnaire collecting information on socio-demographics and the health status (see Results – Table 1 ).
Data collection took place from August 2020 to January 2021. All interviews were conducted in German by one researcher (CK), who took field notes during the interviews. Besides the interviewer and the participant, no one was present. Follow-up interviews were not conducted. All interviews were digitally recorded and transcribed. CK received detailed feedback on the way she conducted the interviews after three interviews from AL, who is an experienced qualitative researcher [ 9 , 10 , 11 , 13 ] (male, degrees in epidemiology and health sciences). These three interviews were initially supposed to serve as test interviews, but as they contained valuable information we decided to include these interviews in the analysis. There were also no major concerns from AL regarding CK’s interview style except that CK should be even more careful not to ask too closed questions. Data collection was terminated when thematic saturation was reached, which implies that no new information was expected to be delivered by additional interviews [ 14 ]. To verify that saturation had been reached, the data analysis already started during data collection. As the interviews and the analysis were carried out by the same person (CK), she was able to pay close attention to when no new aspects were mentioned in the interviews. The interviews were then terminated after consultation with AL. Study participants were not given access to the transcripts, nor could they provide feedback on the findings.
Qualitative data analysis
Transcripts were content-analyzed [ 15 ] using the software MAXQDA 2020. The coding was based closely on the topic guide and the research questions of the study. Consequently, the questions of our topic guide [see Additional File 1 ] served as main categories (deductive coding). For example, the question ‘Are there conditions at work that help you deal with your migraine?’ served as one main category, labelled ‘Facilitators of migraine self-management’. Subcategories were then developed based on the interview content (inductive coding). After CK had coded five interviews, the coding framework was carefully reviewed by two experienced qualitative researchers (KH and AL). Once everyone approved the initial coding framework, CK applied the code system to all interviews and expanded it by adding further categories. After this first round of coding was completed, AL reviewed the codes again. For instance, AL checked the structure of the coding tree level by level to see whether the codes may be overlapping or seemed ordered logically (e.g., according to the same criteria) within each level. He read all text passages included into each code to explore whether the respective text passages relate to the same phenomenon (and thus can be grouped into a single code) or whether codes may be merged or could be further sub-divided. Based on this, he suggested changes and other inductive categories and discussed them with CK. Based on this discussion, CK re-coded all interviews. Afterwards, the codes were re-discussed with AL and the framework was marginally adjusted. Finally, CK carried out a third and final round of coding. The analysis was carried out using German-language transcripts. The quotes presented in this paper were translated from German into English by a researcher who is familiar with health research and has a Master’s degree in English studies (see acknowledgments).
Description of the sample
In total, 24 interviews were conducted with a mean duration of 31.8 min (range: 17.6–55.3, standard deviation [SD] = 11.4). Twelve interviews were carried out face-to-face and twelve by telephone. Ten participants were recruited in the rehabilitation clinic, nine through self-help groups, and five were private contacts of study team members. Table 1 shows characteristics of our sample: our study population was mainly female (88%), and the mean age was 49.5 years (SD = 9.0). More than half of the participants ( n = 14) were classified as having a job that was mainly characterized by cognitive or psychosocial demands (e.g., librarian, social worker, pastoral counsellor). The remainder of participants had jobs with mixed requirements (e.g., teacher, nurse, shop assistant). The mean time since the diagnosis of migraine was 20.6 years and varied from five to 40 years (SD = 8.5). On average, participants reported to have had 10.0 days of migraine during the last month, but the variation was considerable (range: 2–26, SD = 6.6).
Qualitative interviews
A broad range of psychosocial facilitators and barriers of migraine SM at work emerged from our data which are described in the following. Our results indicated that the COVID-19 pandemic affected workplace SM both favorably and adversely.
All quotes referenced below can be found in the appendix [see Additional File 2 ]. If there is an interest in the shared migraine self-management strategies at work, a description of these can also be found in the appendix [see Additional File 3 ]. These are not explained in more detail below however, as the specification of the strategies is beyond the scope of our main research questions.
Which psychosocial working conditions influence migraine self-management at work?
Facilitators : The following working conditions were perceived to be helpful in managing migraine at work: (1) high social support, (2) high job decision latitude (JDL; i.e., the degree of an employee’s control over tasks and how and when they are addressed), and (3) a suitable workplace design.
Receiving social support at work from colleagues, supervisors, or in form of company or government policies was reported. Support by colleagues included the understanding for the illness, especially from colleagues with the same disease. It was frequently expressed that some colleagues could – without words – sense when the individual with migraine was not feeling well. Relevant support-related activities by colleagues that made migraine SM easier included support in avoiding triggers (e.g., by ensuring a good air supply), encouragement to withdraw during acute migraine attacks, and taking over tasks (quote 1). According to the participants, social support by supervisors was effective by creating flexible arrangements regarding tasks, working times, and locations, for example the option to work from home (quote 2). Overall, it seemed that understanding for the disease and the social support from colleagues and supervisors facilitated the SM strategy communication. In Germany, people with chronic illness (including migraine) can apply for a so-called “degree of disability”. This entails entitlement to – amongst other things – more holidays and better protection against dismissal from the job. This legal possibility was perceived as helpful, also in the way that these official degrees simplified the justification of the disease and certified its seriousness (quote 3). Furthermore, one participant shared that she has approached the staff council (in her case the teachers’ council). By disclosing her migraine in front of the council, she gained the understanding of her colleagues (quote 4).
In addition to social support, the study participants described a high JDL – that is, a high degree of control over their tasks – as beneficial. Influence on the order of tasks was perceived as allowing for flexibility in planning and carrying out SM during migraine attacks. Control over the type and number of tasks (e.g., working independently instead of attending meetings [quote 5] or the possibility to avoid screen work during the acute attack [quote 6]) were relevant in managing migraine attacks. Another important factor in terms of JDL was the possibility of working from home. The latter provided the opportunity to organize the working day according to one’s own preferences and to take flexible breaks. For example, one participant reported that one had the option of starting one’s working day later at home if one had a headache in the morning (quote 7). The improved opportunities of stopping work at home was also considered to be beneficial because, according to one participant, the threshold to stop working when experiencing complaints is lower when one works at home than at the workplace (quote 8).
A suitable workplace design, which referred mainly to a single rather than a multi-person office, was also experienced as helpful. In a single office, one had the opportunity to retreat and control air supply and light. As many individuals with migraine are sensitive to light during an attack, this can be beneficial (quote 9). In addition to the office situation, the provision of appropriate work equipment such as flicker-free screens, noise-cancelling headphones, and height-adjustable desks was also reported to have a positive effect on one’s migraine. The latter had been reported to reduce cramping in the shoulders and neck and thereby easing headaches (quote 10).
Barriers : The reported barriers represented in certain respects the opposites of the above-mentioned facilitators. Yet as these were explored separately and several aspects were not overlapping, they are described independently. The following aspects were mentioned: (1) poor social interactions, (2) unfavorable working time arrangements, (3) unfavorable workplace arrangements, and (4) other working conditions.
Poor social interactions included interactions with colleagues, supervisors, and service users. Several participants felt that migraine as a disease was often not taken seriously by others and stigmatized at their workplace. For example, this led to migraine being dismissed as a trifle or lack of understanding for staying at home in case of complaints (quote 11). One participant also emphasized the lack of empathy at the workplace: if one was present at work, one was expected to be fully functioning (quote 12). In this context, participants also found it bothering that migraine is “an invisible condition” (quote 13). During contact with service users (e.g., customers, patients, clients), it was reported to be disturbing that there were often high expectations that could not be met during a migraine attack and the associated impairments (quote 14).
Some workplace and working time arrangements were also considered as detrimental. In workplaces where migraine triggers were present (such as heavy noise, little air supply, bright light), migraine SM and especially the preventive strategy of trigger avoidance was reported to be negatively affected. For example, one participant reported the problem of sharing an office and not being able to adapt it to one’s own need, for example not having control over room temperature (quote 15). Visual display unit (VDU) work was also described to be a migraine trigger (quote 16). Another mentioned problem in workplace design was the lack of opportunities to retreat – physically (e.g., due to lack of break rooms, open-plan offices) and mentally (in terms of being permanently approachable). One participant, for example, shared that it was very difficult to deal with migraine if one always had to be approachable on business trips and thus has no possibility to retreat (quote 17). The lack of opportunities to retreat from challenging situations was believed to worsen symptoms and delay recovery from an attack. In terms of unfavorable working time arrangements, irregularity was mentioned as it implies an interruption of one’s usual circadian rhythm, which may trigger a migraine attack. This could be unscheduled client appointments due to public traffic (quote 18), shift work or exceptional weekend work (quote 19), but also business trips (including school trips as a teacher), missing or insufficient breaks, and time pressure at work (quote 20).
Other working conditions that were considered as barriers included, for example, a lack of staff and therefore a lack of replacement hampering one to go home when experiencing an acute migraine attack (quote 21) as well as poor contract conditions. Regarding the latter, one participant shared that she did not call in sick despite symptoms because then she did not get paid (quote 22).
It should also be mentioned that one study participant did not see any connection between migraine and the workplace and thus could not name any facilitators or barriers to SM (quote 23).
How was migraine self-management at work affected by the COVID-19 pandemic?
In Germany, the first two COVID-19-related lockdowns began in March 2020 (until May 2020) and in December 2020. As we gathered our data between August 2020 and January 2021, experiences during the COVID-19 pandemic were an important topic in the interviews.
One positive aspect for migraine SM during the pandemic was reported to be increased JDL. This was mainly due to new opportunities (and in some cases the obligation) to work remotely (quote 24) providing the advantage of more flexibility (e.g., the arrangement of breaks), a lower noise level, and an elimination of travel times. The fact that many employees took the opportunity to work from home also meant that the office was less busy and therefore more quiet (quote 25). This increased quietness also seemed to be beneficial for employees with migraine. One study participant reported that it was easier to close the office door to do a few stretching exercises (quote 26). The increased structuring of the working day and thus increased regularity as a facilitator for migraine SM (e.g., through stricter appointment policy [quote 27]), and the partial reduction of the workload also appeared to be positive. Furthermore, one study participant had more of a feeling of being needed in one’s work at a nursing home. The increased job satisfaction was reported to lower the frequency of migraine complaints (quote 28).
The stress caused by the additional hygienic measures, the mouth-to-nose covering, and the increased amount of screen work were perceived as negative for migraine SM. Coming in contact with COVID-19-positive people often necessitated use of additional stressful measures such as the application of hygiene or personal protective measures. This was, for example, reported by a study participant that worked as a nurse in a hospital (quote 29). The mouth-to-nose covering seemed to make it difficult not only to breathe but also to speak, which in turn was perceived to trigger migraine (quote 30). A final migraine trigger in the pandemic was the fear of the end of the pandemic and thus the loss of the possibility to work from home (quote 31).
Summary of main findings
According to our participants migraine SM at work is affected by social interactions (e.g., understanding as a facilitator vs. stigmatization as a barrier), the extent of JDL (e.g., in terms of working hours and localization) as well as the workplace design (e.g., regarding opportunities to retreat or to avoid VDU work). During the COVID-19 pandemic, it was considered positive for migraine SM that the daily structure was associated with more predictability and planning (e.g., through stricter appointment scheduling). It was also emphasized that there were more opportunities to work from home and thus better conditions for appropriate migraine SM through more JDL. A negative aspect associated with the COVID-19 pandemic was increased work-related screen time. Participants also shared that the novel hygiene measures (e.g., after contact with a COVID-19-positive person) and the mouth-to-nose covering triggered migraine complaints.
Findings in light of earlier research
In terms of barriers and facilitators, our findings are in line with prior research. A qualitative study on migraine and chronic daily headache management by Peters et al. [ 4 ] highlighted the importance of social support. The authors concluded that social support, especially from peers with the same conditions, can lead to better understanding from colleagues. The lack of social support and the feeling of stigmatization was an important aspect in another qualitative study by Heidari et al. [ 16 ], focusing on common themes of migraine patients. In that study one participant reported going to work despite migraine, because the supervisor seemed not to take migraine seriously [ 16 ]. One study – in accordance with our findings – linked stigmatization to migraine being an invisible disease, limiting the understanding for the condition [ 17 ]. Other factors influencing migraine SM that emerged from our study were factors related to workplace design. This is in keeping with findings from a cross-sectional study on the burden and impact of migraine on work productivity and quality of life that also addressed job-related migraine triggers and coping strategies: Looking at computer screens for too long was one of the two most frequently mentioned migraine triggers at the workplace [ 18 ]. Having control of light, noise and smells was under the top five coping strategies [ 18 ].
In the context of the EFNA study [ 6 ], individuals with migraine and other headache type patients were asked what their company should do to help them cope better with their condition. The wishes mentioned included a greater understanding for the disease, less social interaction, the possibility to work from home, flexible working hours, and more opportunities to withdraw if needed [ 6 ]. These aspects overlap with the facilitators that emerged from our study, in particular regarding social support and JDL.
Regarding the COVID-19 pandemic, our results are consistent with findings from other studies that found a link between personal protective equipment, especially the wearing of masks, and a worsening of migraine [ 19 , 20 , 21 ]. There is also further evidence that the increased screen time, for example due to remote working or online lessons during the pandemic, served as a trigger for migraine, in particular in young adults and adolescents [ 22 , 23 ]. However, remote working during the pandemic was generally considered to have a positive impact on migraine (e.g., reduced migraine attack duration) [ 24 ]. In a qualitative study by Buse et al. [ 20 ], examining the general impact of the COVID-19 pandemic on patients with migraine, participants reported that working from home was associated with more control, e.g., over the work environment. This reflects the importance of JDL for migraine SM. Notably, some factors that were mentioned to influence SM in general (e.g., social support) played little or no role in the COVID-19 pandemic and associated SM. The pandemic served as a kind of natural experiment elucidating which factors – when modified – influence migraine and its SM. Based on this, it can be hypothesized that the facilitator “JDL,” which played an important role in general and during the pandemic, has the utmost relevance on migraine SM at work. To our knowledge, no previous qualitative study on migraine or chronic headache has yet highlighted the high relevance of JDL for SM.
Methodological considerations
The interviews were conducted face-to-face or by telephone, depending on the preference of the participants. This provided us with the opportunity to include participants nationwide and despite restrictions due to COVID-19. We did not notice considerable differences regarding the contents between the two interview modes, which is supported by earlier research [ 25 ]. To reduce a potential healthy worker bias (i.e., the assumption that the working population is healthier than the non-working population), we recruited migraine patients who had ever worked for six months with a diagnosis of migraine and not only patients who were currently working. This allowed us to include patients who might have had to leave their job due to severe migraine or who attempted to regain their workability through rehabilitation.
We relied on the patients’ report of being diagnosed with migraine by a physician, and we did not apply the International Classification of Headache Disease [ 26 ] for diagnoses. However, those participants who were recruited from the rehabilitation clinic for migraine ( n = 10) had received a medical diagnosis of migraine and their condition was severe enough to threaten their employment status. Further, as we interviewed mainly patients from this rehabilitation clinic and from self-help groups, however, we cannot exclude the possibility of a selection bias: those patients interact with other individuals with migraine, a are usually well-informed about their condition, and their experiences and perspectives may differ to some extent from the broader patient population. Moreover, only three out of 24 participants were male. This may have limited the scope of views that emerged from male participants regarding migraine SM. Also, our study especially included patients who worked in a job with mainly cognitive and social demands. It is well conceivable that their experiences differ from that of migraine patients who work in a job with mainly physical demands (e.g., individuals working in transportation or farming). We were able to cover a broad distribution regarding the average number of migraine days per month (mean = 10.0, SD = 6.6, range: 2–26 days). These observations increase the confidence that we covered a large range of potential views and experiences.
Another methodological weakness is that the coding was carried out by only one single person who had no previous experience in coding (CK). The intense involvement of additional individuals in the coding process (e.g., more experienced coders, people with migraine, occupational physicians, and/or neurologists), would likely have led to a richer analysis and additional insights, but this was beyond the resources of our study (i.e., time and financial means).
Finally, due to the limited experience with qualitative research methods of the first author, who was also the primary analyst, and due to the fact that it was not feasible to substantially involve additional analysists in the coding, the depth of our analyses may have been limited. Accordingly, our study may be classified as a ‘topical survey’ with aspects of a ‘thematic survey’ – according to the classification of findings in qualitative studies suggested by Sandelowski & Barroso [ 27 ]. A topical survey stays close to the data collected and is primarily a description of it, whereas a thematic survey provides a higher level of transformation of data [ 27 ]. The purpose of thematic surveys were only achieved to a limited extent. However, Sandelowski & Barroso state that a topical survey is not necessarily inferior in terms of the quality of its value [ 27 ].
Implications for practice and research
Based on our findings, interventions could be devised to improve migraine SM at work. Regarding social support, it is important to reduce stigma of migraine to create a working environment in which patients feel comfortable to talk openly about their migraine without it being dismissed as a trifle. Our study thus calls attention to the fact that migraine healthcare professionals should offer support for improving patients’ social communication skills in the workplace leading to greater acceptance of the condition. One health care sector that seems particularly suitable for this endeavor is rehabilitation. Treatment in rehabilitation clinics in Germany involves patient education, which can help to raise awareness among migraine patients for the potential influence of their working conditions on their opportunities to manage their migraine at work. Also, patients can be empowered (e.g., by improving knowledge about legal frameworks and practicing communication skills) to modify their working conditions to some extent. Similar concepts are currently tested for other conditions than migraine [ 28 ].
To increase JDL, employers should try to give migraine patients as much freedom as possible. For example, for office jobs the possibility of expanding remote working should be explored. Here, the experience gained during the COVID-19 pandemic can be used. If working from home is not possible, care can be taken to create a migraine-friendly workplace, for example by providing single offices, noise-cancelling headphones, height-adjustable desks, and places of retreat. VDU work could also be designed to be as gentle as possible, e.g., by using flicker-free screens. If available and needed, occupational physicians should support all these interventions by educating workers with migraine and by serving as mediators between supervisors and employees with migraine.
All these interventions should be carefully developed and evaluated prior to their implementation in routine care. We believe that more preparatory research is needed. Firstly, as mentioned above, our analysis may be limited in depth. It therefore seems promising to carry out additional qualitative studies that involve analysts with more diverse professional backgrounds and employees with migraine as co-researchers. In the next step, the scope of the problem could be confirmed, and possible interventions may be explored. Quantitative research (e.g., surveys) would be suitable to examine, amongst others, the proportion of workers with migraine that find self-management at work to be challenging, to prioritize areas for intervention, and to examine what types of interventions would be acceptable to those receiving them and those potentially delivering them. Also, working life in the post-COVID-19 era has further evolved since our study to arrive at a “new normal” (e.g., allowing for more home office working hours than in the pre-COVID-era), which our study does not reflect, and which follow-up qualitative studies could explore. Furthermore, quantitative studies could test hypotheses that can be deduced from our qualitative study (e.g., “The ability to perform migraine SM at work is associated with the level of experienced JDL”). Such research could move beyond self-management as an outcome to include symptoms and occupational outcomes (e.g. workability, presenteeism and absenteeism) and may explore whether improved migraine SM at work curtails the considerable cost associated with migraine-related impairment.
Migraine SM at work is influenced positively and negatively by various occupational factors. By considering these facilitators and barriers, a more migraine-friendly workplace can be created to reduce a burden not only for patients but also for society. Further research is needed before interventions can be implemented.
Data availability
Data cannot be shared publicly because the transcripts may contain sensitive information. The data may be obtained from the corresponding author upon reasonable request and provided that legal frameworks are not violated and that responsibilities and confidentially have been clarified.
Abbreviations
Chronic migraine
- Self-management
Job decision latitude
European Federation of Neurological Associations
Visual display unit
Headache disorders. World Health Organization. 2016. https://www.who.int/news-room/fact-sheets/detail/headache-disorders . Accessed February 13, 2024.
Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, de la Ruiz E, Tassorelli C, Andrée C. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–11.
Article CAS PubMed Google Scholar
Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–41.
Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Migraine and chronic daily headache management: a qualitative study of patients’ perceptions. Scand J Caring Sci. 2004;18(3):294–303.
Article PubMed Google Scholar
Peters M, Abu-Saad HH, Robbins I, Vydelingum V, Dowson A, Murphy M. Patients’ management of migraine and chronic daily headache: a study of the members of the Migraine Action Association (United Kingdom). Headache. 2005;45(5):571–81.
Results of EFNA’s survey on stigma and neurological disorder. European Federation of Neurological Associations. 2020. https://www.efna.net/survey2020/ . Accessed January 13, 2023.
Scaratti C, Foitzek N, Grignani E, Leonardi M, Raggi A, Coenen M. The employment needs and the factors having a negative or positive impact on work of people with chronic diseases in Europe: the case of headache. Neurol Sci. 2018;39(Suppl 1):121–3.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Heinrichs K, Vu-Eickmann P, Hummel S, Gholami J, Loerbroks A. What are the perceived influences on asthma self-management at the workplace? A qualitative study. BMJ Open. 2018;8(8):e022126.
Article PubMed PubMed Central Google Scholar
Heinrichs K, Hermülheim V, Pilz González L, Loerbroks A. When in doubt … Career Indecision,Mental Wellbeing, and Consultation-seeking Behaviour-A qualitative interview study among students and counsellors. Int J Environ Res Public Health. 2021;18(23):12604.
Loerbroks A, Nguyen XQ, Vu-Eickmann P, Krichbaum M, Kulzer B, Icks A, Angerer P. Psychosocial working conditions and diabetes self-management at work: a qualitative study. Diabetes Res Clin Pract. 2018;140:129–38.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–21.
PubMed Google Scholar
Scharf J, Angerer P, Müting G, Loerbroks A. Return to work after Common Mental disorders: a qualitative study exploring the expectations of the involved stakeholders. Int J Environ Res Public Health. 2020;17(18):6635.
Corbin JM, Strauss AL. Basics of qualitative research: Techniques and procedures for developing grounded theory. Fourth edition. SAGE Publications. 2014.
Mayring P. Qualitative Content Analysis [Qualitative Inhaltsanalyse: Grundlagen und Techniken. 12., überarb. Aufl.]. Weinheim, Beltz. 2015.
Heidari E, Rao D, Pfalzgraf AR, Lobo C, Giannetti V. An explorative study of common themes of patient experiences with migraine. Prim Care Companion CNS Disord. 2022;24(2):21m02939.
Basoglu Koseahmet F, Polat B, Gozubatik-Celik RG, Baytekin I, Soylu MG, Ceyhan Dirican A, Ozturk M. An invisible cause of disability: stigma in migraine and epilepsy. Neurol Sci. 2022;43(6):3831–8.
Haw NJ, Cabaluna IT, Kaw GE, Cortez JF, Chua MP, Guce K. A cross-sectional study on the burden and impact of migraine on work productivity and quality of life in selected workplaces in the Philippines. J Headache Pain. 2020;21(1):125.
Yuksel H, Kenar SG, Gursoy GT, Bektas H. The impacts of masks and disinfectants on migraine patients in the COVID-19 pandemic. J Clin Neurosci. 2022;97:87–92.
Article CAS PubMed PubMed Central Google Scholar
Buse DC, Gerstein MT, Houts CR, McGinley JS, Uzumcu AA, McCarrier KP, Cooke A, Touba NM, Nishida TK, Wirth RJ, Lipton RB. Impact of the COVID-19 pandemic on people living with migraine: results of the MiCOAS qualitative study. Headache. 2022;62(3):284–93.
Ong JJY, Bharatendu C, Goh Y, Tang JZY, Sooi KWX, Tan YL, Tan BYQ, Teoh HL, Ong ST, Allen DM, Sharma VK. Headaches Associated with Personal Protective Equipment - A cross-sectional study among Frontline Healthcare workers during COVID-19. Headache. 2020;60(5):864–77.
Wehbe AT, Costa TE, Abbas SA, Costa JE, Costa GE, Wehbe TW. The effects of the COVID-19 confinement on screen time, headaches, stress and Sleep disorders among adolescents: A Cross Sectional Study. Chronic Stress (Thousand Oaks). 2022;6:24705470221099836.
Abou Hashish EA, Baatiah NY, Bashaweeh AH, Kattan AM. The online learning experience and reported headaches associated with screen exposure time among Saudi health sciences students during the COVID-19 pandemic. BMC Med Educ. 2022;22(1):226.
Currò CT, Ciacciarelli A, Vitale C, Vinci ES, Toscano A, Vita G, Trimarchi G, Silvestri R, Autunno M. Chronic migraine in the first COVID-19 lockdown: the impact of sleep, remote working, and other life/psychological changes. Neurol Sci. 2021;42(11):4403–18.
Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qualitative Res. 2004;4(1):107–18.
Article Google Scholar
IHS Classification ICHD-3. International Headache Society. https://ichd-3.org/classification-outline/ . Accessed February 13, 2024.
Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qual Health Res. 2003;13(7):905–23.
Salandi J, Hayden MC, Heinrichs K, Limbach M, Schultz K, Schwarzl G, Neumeister W, Loerbroks A. Can an educational intervention in the context of inpatient pulmonary rehabilitation improve asthma self-management at work? A study protocol of a randomized controlled trial. BMC Pulm Med. 2024;24(1):40.
Download references
Acknowledgements
The authors would like to thank Prof. Dr. Scott Stock Gissendanner for his support related to participant recruitment (Berolina Klinik, Löhne). For her translation of the quotes, we are grateful to Lisa Guthardt (Institute of Occupational, Social and Environmental Medicine, Faculty of Medicine, University of Düsseldorf). The authors would also like to thank the participants for taking their time to share their experiences with respect to working with migraine.
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any funding.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Institute of Occupational, Social and Environmental Medicine, Centre for Health and Society, Faculty of Medicine, University of Düsseldorf, Moorenstr. 5, Düsseldorf, 40225, Germany
Clara Knauf & Adrian Loerbroks
Institute of Health and Nursing Science, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany
Katherina Heinrichs
Berolina Klinik, Löhne, Germany
Rolf Süllwold
Institute of Health Services Research and Health Economics, Centre for Health and Society, Faculty of Medicine, University of Düsseldorf, Düsseldorf, Germany
Andrea Icks
You can also search for this author in PubMed Google Scholar
Contributions
C.K., K.H., A.I. and A.L. contributed to the conception and design of the study. C.K. and R.S. contributed to the acquisition of the data. The interviews were conducted by C.K. C.K. performed the analysis and interpretation of the data supported by K.H. and A.L. C.K. drafted the manuscript and all authors revised it for intellectual content. All authors read and approved the final version of the manuscript. All authors agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Adrian Loerbroks .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board of the Faculty of Medicine of the University of Düsseldorf, Germany (no 2019 − 627). All participants provided written informed consent prior to the interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Knauf, C., Heinrichs, K., Süllwold, R. et al. Migraine self-management at work: a qualitative study. J Occup Med Toxicol 19 , 22 (2024). https://doi.org/10.1186/s12995-024-00421-w
Download citation
Received : 26 February 2024
Accepted : 22 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1186/s12995-024-00421-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- COVID-19 pandemic
Journal of Occupational Medicine and Toxicology
ISSN: 1745-6673
- General enquiries: [email protected]
A Qualitative Assessment Of Tourism Research Amidst COVID-19 Pandemic In Pakistan
- 30(05/06/2024):1411-1427

- Riphah International University
- This person is not on ResearchGate, or hasn't claimed this research yet.

- British University in Dubai
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Yanchao Feng

- Congcong Zhang

- Latief Fitriani
- Andi Widiawati
- Nur Haeda Zaeni
- ENVIRON SCI POLLUT R
- Qadar Bakhsh Baloch
- Sourath Maher
- Syed Naseeb Shah

- Jawad Iqbal

- J CLEAN PROD

- Kashif Abbass

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

IMAGES
VIDEO
COMMENTS
The global response to mitigate the spread of the COVID-19 pandemic brought about massive health, social and economic impacts. Based on the pressing need to respond to the crisis, clinical trials a...
The purpose of this article is to reflect on our experience of carrying out three research studies (a rapid appraisal, a qualitative study based on interviews, and a mixed-methods survey) aimed at exploring health care delivery in the context of COVID-19. We highlight the importance of qualitative data to inform evidence-based public health ...
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. ... Introduction The COVID-19 pandemic has certainly resulted in an ...
This becomes a great step forward and helps international attempts regarding the COVID-19 pandemic outbreak. This may help to reduce the number of infected individuals from the disease and to prevent the coronavirus more widely in the community.
It is imperative to study psychosocial data related to the entire population, vulnerable groups, and COVID-19 patients to improve intervention measures and address the psychological impact of the COVID-19 pandemic (Holmes et al., 2020).
The purpose of this article is to reflect on our experience of carrying out three research studies (a rapid appraisal, a qualitative study based on interviews, and a mixed-methods survey) aimed at exploring health care delivery in the context of COVID-19. We highlight the importance of qualitative data to inform evidence-based public health ...
The COVID-19 pandemic has forced both quantitative and qualitative health researchers to adapt and strategize data collection strategies without causing any harm to the participants or researchers.
The COVID-19 pandemic has affected all aspects of human society, including education, culture, and the economy, and has also introduced changes in people's health behaviors such as drinking alcohol, nutrition intake, and practicing healthy living. This study conducted qualitative research in the Korean context to examine the changes in the smoking behavior of smokers and secondhand smoke ...
Our analysis offers methodological, ethical, and practical guidance in the COVID-19 pandemic and considerations for research conducted amid future pandemics and emergency situations. Keywords research ethics, online research methods, COVID-19, qualitative research, data collection, social media, informed consent, marginalized populations ...
As the COVID-19 pandemic has shown, setting up studies in time to gather relevant, real-world data enables researchers to capture current views and experiences, focus on practicalities on the ground, and deliver actionable results. ... and consequently contribute to the development of the rapid qualitative research.
The onset of the COVID-19 pandemic catalysed a monumental shift in the field of continuing professional development (CPD). Prior to this, the majority of CPD group-learning activities were offered in-person. However, the pandemic forced the field to quickly pivot towards more novel methods of learning and teaching in view of social distancing regulations.
Background: Methodological guidelines are required to ensure both the rigor and feasibility of just-in-time, qualitative research addressing the human experience and response to the COVID-19 pandemic and major public health crises. Objectives: This article presents methodological guidelines for just-in-time qualitative research based on our current, pandemic-relevant research.
In South Africa, public perceptions of the COVID-19 pandemic and risk mitigation measures remain mixed. To better understand health behaviours in the context of COVID-19, a qualitative study was conducted, which aimed to investigate perceptions relating to the COVID-19 pandemic among the South African adult population. Twelve online focus groups were conducted across the following age groups ...
Large gaps exist in the literature on COVID-19 pandemic-related mental health outcomes and after-effects specific to adolescents and young adults. The aim was to explore adolescents' and young adults' experiences of well-being, health and loneliness during the COVID-19 pandemic. A qualitative exploratory design with qualitative content analysis was used.
Abstract. The COVID-19 pandemic has forced both quantitative and qualitative health researchers to adapt and strategize data collection strategies without causing any harm to the participants or researchers. This has resulted in utilizing various types of strategies such as online surveys and synchronous virtual platforms such as Zoom and Webex.
The COVID-19 pandemic has been impacting the need, utilization, and delivery of mental health services with greater challenges being faced by clients and providers. With many clients facing reduced access to services and social isolation, a focus on suicide risk assessment and prevention is critical. Concern is particularly increased for clients with schizophrenia spectrum disorders given data ...
Introduction: Quantitative research is not suitable for COVID pandemic research because it does not cover the social consequences of qualitative research. COVID 19 is a social event that is important because of the disruption of the natural order of society. To defeat the disease, social interaction is needed, so qualitative research is ...
The 2019 coronavirus disease (COVID-19) pandemic exacerbated pre-existing inequalities in social, economic, and health systems, amplifying the harmful effects of COVID-19 [1,2,3].Although researchers generally agreed on who were considered vulnerable to the COVID-19 threat, different interpretations emerged across different national contexts.
Although the threat and uncertainty of the COVID-19 pandemic has become a significant source of distress, using religion to cope may be associated with more positive health. Given the severity and chronicity of the pandemic, religious individuals may also have relied on a variety of non-religious coping methods. Much of the existing COVID-19 research overlooks the role of religious group ...
Qualitative research is integral to the pandemic response. Qualitative methods are ideally suited to generating evidence to inform tailored, culturally appropriate approaches to COVID-19, and to me...
The COVID-19 pandemic generated an unprecedented global health crisis, affecting millions of individuals worldwide, including healthcare professionals. ... We relied on the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist . Throughout the research process, we adhered to the rigorous criteria proposed by Guba and ...
The actions of leaders (n = 28) that were reported as successful and supportive responses to the COVID-19 pandemic or else missed opportunities reflected core principles of Trauma-Informed Care. To promote safety, leaders reported affirmative efforts to protect staff by providing appropriate physical protection, and enhanced psychological ...
With COVID-19 affecting all types of research, the authors of this article contribute to the discussions on how COVID-19 affects the world of qualitative nursing research in irrefutable ways. Underrepresented and vulnerable populations are faced with higher rates and severity of COVID-19, heightenin …
A recommendation by the World Health Organization (WHO) was issued about the use of chest imaging to monitor pulmonary sequelae following recovery from COVID-19. This qualitative study aimed to explore the perspective of key stakeholders to understand their valuation of the outcome of the proposition, preferences for the modalities of chest imaging, acceptability, feasibility, impact on equity ...
Conclusions The long-term effects of moral distress have been discussed routinely in recent literature and are further complicated by the effects of the COVID-19 pandemic. Threats to the shrinking workforce of nurses must be taken seriously and interventions to improve the mental health and morale of frontline nurses must be prioritized and tested.
As the COVID-19 pandemic has shown, setting up studies in time to gather relevant, real-world data enables researchers to capture current views and experiences, focus on practicalities on the ground, and deliver actionable results. Delivering high quality ...
Background: The COVID-19 pandemic acted as a catalyst for the use of information and communication technology (ICT) in inpatient and outpatient health care settings. Digital tools were used to connect patients, families, and providers amid visitor restrictions, while web-based platforms were used to continue care amid COVID-19 lockdowns.
We also explored the potential impact of the COVID-19 pandemic and the associated re-arrangement of working conditions on migraine SM at work. We conducted semi-structured qualitative interviews (08/2020-01/2021).
The COVID-19 pandemic presents a substantial threat to Pakistan's tourism industry, precipitated by diverse factors. Scholars have shown considerable interest in researching the developments ...