Hypertension: Introduction, Types, Causes, and Complications
Cite this chapter.
- Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO 4 ,
- Yoshio Iwashima MD, PhD, FAHA 5 &
- Kei Kamide MD, PhD, FAHA 6
8761 Accesses
4 Citations
Hypertension remains one of the most significant causes of mortality worldwide. It is preventable by medication and lifestyle modification. Office blood pressure (BP), out-of-office BP measurement with ambulatory BP monitoring, and self-BP measurement at home are reliable and important data for assessing hypertension. Primary hypertension can be defined as an elevated BP of unknown cause due to cardiovascular risk factors resulting from changes in environmental and lifestyle factors. Another type, secondary hypertension, is caused by various toxicities, iatrogenic disease, and congenital diseases. Complications of hypertension are the clinical outcomes of persistently high BP that result in cardiovascular disease (CVD), atherosclerosis, kidney disease, diabetes mellitus, metabolic syndrome, preeclampsia, erectile dysfunction, and eye disease. Treatment strategies for hypertension consist of lifestyle modifications (which include a diet rich in fruits, vegetables, and low-fat food or fish with a reduced content of saturated and total fat, salt restriction, appropriate body weight, regular exercise, moderate alcohol consumption, and smoking cessation) and drug therapies, although these vary somewhat according to different published hypertension treatment guidelines.
This is a preview of subscription content, log in via an institution to check access.

Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Changing concepts in hypertension management

Hypertension

Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Article PubMed Google Scholar
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Article CAS PubMed Google Scholar
National Clinical Guideline Centre (UK). Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34 [Internet]. London: Royal College of Physicians (UK); 2011 Aug. Available from http://www.ncbi.nlm.nih.gov/books/NBK83274 . PubMed PMID: 22855971.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15.
Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014;63:878–85.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–387.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham heart study: a cohort study. Lancet. 2001;358:1682–6.
Kokubo Y, Nakamura S, Watanabe M, Kamide K, Kawano Y, Kawanishi K, et al. Cardiovascular risk factors associated with incident hypertension according to blood pressure categories in non-hypertensive population in the Suita study: an Urban cohort study. Hypertension. 2011;58:E132.
Google Scholar
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
Kokubo Y. Traditional risk factor management for stroke: a never-ending challenge for health behaviors of diet and physical activity. Curr Opin Neurol. 2012;25:11–7.
Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754–832.
European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25:457–507.
Article Google Scholar
Guild SJ, McBryde FD, Malpas SC, Barrett CJ. High dietary salt and angiotensin II chronically increase renal sympathetic nerve activity: a direct telemetric study. Hypertension. 2012;59:614–20.
Mu S, Shimosawa T, Ogura S, Wang H, Uetake Y, Kawakami-Mori F, et al. Epigenetic modulation of the renal beta-adrenergic-WNK4 pathway in salt-sensitive hypertension. Nat Med. 2011;17:573–80.
WHO. Guideline: Sodium intake for adults and children. Geneva, World Health Organization (WHO), 2012. http://www.ncbi.nlm.nih.gov/books/NBK133309/pdf/TOC.pdf .
Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in westerners and east Asians. Hypertension. 2014;63:655–60.
Ascherio A, Rimm EB, Giovannucci EL, Colditz GA, Rosner B, Willett WC, et al. A prospective study of nutritional factors and hypertension among US men. Circulation. 1992;86:1475–84.
Ascherio A, Hennekens C, Willett WC, Sacks F, Rosner B, Manson J, et al. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension. 1996;27:1065–72.
Stamler J, Liu K, Ruth KJ, Pryer J, Greenland P. Eight-year blood pressure change in middle-aged men: relationship to multiple nutrients. Hypertension. 2002;39:1000–6.
Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric study. Am J Epidemiol. 2004;159:572–80.
Tsubota-Utsugi M, Ohkubo T, Kikuya M, Metoki H, Kurimoto A, Suzuki K, et al. High fruit intake is associated with a lower risk of future hypertension determined by home blood pressure measurement: the OHASAMA study. J Hum Hypertens. 2011;25:164–71.
Ueshima H, Stamler J, Elliott P, Chan Q, Brown IJ, Carnethon MR, et al. Food omega-3 fatty acid intake of individuals (total, linolenic acid, long-chain) and their blood pressure: INTERMAP study. Hypertension. 2007;50:313–9.
Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20:1493–9.
Kromhout D, Bosschieter EB, de Lezenne CC. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–9.
Yamori Y. Food factors for atherosclerosis prevention: Asian perspective derived from analyses of worldwide dietary biomarkers. Exp Clin Cardiol. 2006;11:94–8.
PubMed Central CAS PubMed Google Scholar
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Hamer M, Chida Y. Active commuting and cardiovascular risk: a meta-analytic review. Prev Med. 2008;46:9–13.
Hayashi T, Tsumura K, Suematsu C, Okada K, Fujii S, Endo G. Walking to work and the risk for hypertension in men: the Osaka Health Survey. Ann Intern Med. 1999;131:21–6.
Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296–304.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Groppelli A, Giorgi DM, Omboni S, Parati G, Mancia G. Persistent blood pressure increase induced by heavy smoking. J Hypertens. 1992;10:495–9.
Makris TK, Thomopoulos C, Papadopoulos DP, Bratsas A, Papazachou O, Massias S, et al. Association of passive smoking with masked hypertension in clinically normotensive nonsmokers. Am J Hypertens. 2009;22:853–9.
Zanchetti A. Intermediate endpoints for atherosclerosis in hypertension. Blood Press Suppl. 1997;2:97–102.
CAS PubMed Google Scholar
Iwashima Y, Kokubo Y, Ono T, Yoshimuta Y, Kida M, Kosaka T, et al. Additive interaction of oral health disorders on risk of hypertension in a Japanese urban population: the Suita study. Am J Hypertens. 2014;27:710–9.
Zelkha SA, Freilich RW, Amar S. Periodontal innate immune mechanisms relevant to atherosclerosis and obesity. Periodontol 2000. 2010;54:207–21.
Article PubMed Central PubMed Google Scholar
Tsioufis C, Kasiakogias A, Thomopoulos C, Stefanadis C. Periodontitis and blood pressure: the concept of dental hypertension. Atherosclerosis. 2011;219:1–9.
Kubo M, Hata J, Doi Y, Tanizaki Y, Iida M, Kiyohara Y. Secular trends in the incidence of and risk factors for ischemic stroke and its subtypes in Japanese population. Circulation. 2008;118:2672–8.
Sjol A, Thomsen KK, Schroll M. Secular trends in blood pressure levels in Denmark 1964–1991. Int J Epidemiol. 1998;27:614–22.
Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: the Suita study. Hypertension. 2008;52:652–9.
Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke. 2004;35:776–85.
Briasoulis A, Agarwal V, Tousoulis D, Stefanadis C. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studies. Heart. 2014;100:317–23.
Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, et al. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med. 2014;11:e1001591.
Bussemaker E, Hillebrand U, Hausberg M, Pavenstadt H, Oberleithner H. Pathogenesis of hypertension: interactions among sodium, potassium, and aldosterone. Am J Kidney Dis. 2010;55:1111–20.
Kokubo Y, Nakamura S, Okamura T, Yoshimasa Y, Makino H, Watanabe M, et al. Relationship between blood pressure category and incidence of stroke and myocardial infarction in an urban Japanese population with and without chronic kidney disease: the Suita study. Stroke. 2009;40:2674–9.
Kokubo Y. The mutual exacerbation of decreased kidney function and hypertension. J Hypertens. 2012;30:468–9.
Kokubo Y, Okamura T, Watanabe M, Higashiyama A, Ono Y, Miyamoto Y, et al. The combined impact of blood pressure category and glucose abnormality on the incidence of cardiovascular diseases in a Japanese urban cohort: the Suita study. Hypertens Res. 2010;33:1238–43.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301.
Aranda P, Ruilope LM, Calvo C, Luque M, Coca A, Gil de Miguel A. Erectile dysfunction in essential arterial hypertension and effects of sildenafil: results of a Spanish national study. Am J Hypertens. 2004;17:139–45.
Sharp SI, Aarsland D, Day S, Sonnesyn H, Alzheimer’s Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011;26:661–9.
Ninomiya T, Ohara T, Hirakawa Y, Yoshida D, Doi Y, Hata J, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58:22–8.
Thukkani AK, Bhatt DL. Renal denervation therapy for hypertension. Circulation. 2013;128:2251–4.
Myat A, Redwood SR, Qureshi AC, Thackray S, Cleland JG, Bhatt DL, et al. Renal sympathetic denervation therapy for resistant hypertension: a contemporary synopsis and future implications. Circ Cardiovasc Interv. 2013;6:184–97.
Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–401.
Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13.
Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med. 1994;330:877–84.
Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123:2799–810, 2799 p following 2810.
Steg PG, Bhatt DL, Wilson PW, D’Agostino Sr R, Ohman EM, Rother J, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–206.
Perry Jr HM, Davis BR, Price TR, Applegate WB, Fields WS, Guralnik JM, et al. Effect of treating isolated systolic hypertension on the risk of developing various types and subtypes of stroke: the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 2000;284:465–71.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350:757–64.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
American DA. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37 Suppl 1:S14–80.
Hollenberg NK, Price DA, Fisher ND, Lansang MC, Perkins B, Gordon MS, et al. Glomerular hemodynamics and the renin-angiotensin system in patients with type 1 diabetes mellitus. Kidney Int. 2003;63:172–8.
Mezzano S, Droguett A, Burgos ME, Ardiles LG, Flores CA, Aros CA, et al. Renin-angiotensin system activation and interstitial inflammation in human diabetic nephropathy. Kidney Int Suppl. 2003:(86);S64–70.
Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545–53.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417–28.
Bakris GL, Toto RD, McCullough PA, Rocha R, Purkayastha D, Davis P, et al. Effects of different ACE inhibitor combinations on albuminuria: results of the GUARD study. Kidney Int. 2008;73:1303–9.
ONTARGET Investigators, Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–59.
Download references
Sources of Funding
This study was supported by grants-in-aid from the Ministry of Education, Science, and Culture of Japan (Nos. 25293147 and 26670320), the Ministry of Health, Labor, and Welfare of Japan (H26-Junkankitou [Seisaku]-Ippan-001), the Rice Health Database Maintenance industry, Tojuro Iijima Memorial Food Science, the Intramural Research Fund of the National Cerebral and Cardiovascular Center (22-4-5).
Author information
Authors and affiliations.
Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, 5-7-1, Fujishiro-dai, Suita, Osaka, 565-8565, Japan
Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO
Divisions of Hypertension and Nephrology, National Cerebral and Cardiovascular Center, 5-7-1, Fujishiro-dai, Suita, Osaka, 565-8565, Japan
Yoshio Iwashima MD, PhD, FAHA
Division of Health Science, Osaka University Graduate School of Medicine, Suita, Osaka, Japan
Kei Kamide MD, PhD, FAHA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO .
Editor information
Editors and affiliations.
Center for Drug Evaluation and Research Division of Cardiovascular and Renal Products, US Food and Drug Administration, Silver Spring, Maryland, USA
Gowraganahalli Jagadeesh
Pharmacology Unit, AIMST University, Bedong, Malaysia
Pitchai Balakumar
Khin Maung-U
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Kokubo, Y., Iwashima, Y., Kamide, K. (2015). Hypertension: Introduction, Types, Causes, and Complications. In: Jagadeesh, G., Balakumar, P., Maung-U, K. (eds) Pathophysiology and Pharmacotherapy of Cardiovascular Disease. Adis, Cham. https://doi.org/10.1007/978-3-319-15961-4_30
Download citation
DOI : https://doi.org/10.1007/978-3-319-15961-4_30
Publisher Name : Adis, Cham
Print ISBN : 978-3-319-15960-7
Online ISBN : 978-3-319-15961-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Prevalence and risk factors of hypertension among adults: A community based study in Addis Ababa, Ethiopia
Meseret molla asemu.
1 School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia
Alemayehu Worku Yalew
Negussie deyessa kabeta, desalew mekonnen.
2 College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
Associated Data
All relevant data are within the manuscript and its Supporting Information files.
In all areas of the World Health Organization, the prevalence of hypertension was highest in Africa. High blood pressure is a significant risk factor for coronary and ischemic diseases, as well as hemorrhagic stroke. However, there were scarce data concerning the magnitude and risk factors of hypertension. Thus, this study aimed to identify the prevalence and associated factors of hypertension among adults in Addis Ababa city.
A community-based cross-sectional study was conducted from June to October 2018 in Addis Ababa city. Participants aged 18 years and older recruited using a multi-stage random sampling technique. Data were collected by face-to-face interview technique. All three WHO STEPS instruments were applied. Additionally, participants’ weight, height, waist, hip, and blood pressure (BP) were measured according to standard procedures.
Multiple logistic regressions were used and Odds ratios with 95% confidence intervals were also calculated to identify associated factors.
In this study, a total of 3560 participants were included.The median age was 32 years (IQR 25, 45). More than half (57.3%) of the respondents were females. Almost all (96.2%) of participants consumed vegetables and or fruits less than five times per day. Eight hundred and sixty-five (24.3%) of respondents were overweight, while 287 (8.1%) were obese. One thousand forty-one 29.24% (95% CI: 27.75–30.74) were hypertensive, of whom two-thirds (61.95%) did not know that they had hypertension.
Factors significantly associated with hypertension were age 30–49 and ≥50 years (AOR = 2.79, 95% CI: 1.39–5.56) and (AOR = 8.23, 95% CI: 4.09–16.55) respectively, being male (AOR = 1.88, 95% CI: 1.18–2.99), consumed vegetables less than or equal to 3 days per week (AOR = 2.44, 95% CI: 1.21–4.93), obesity (AOR = 2.05, 95%CI: 1.13–3.71), abdominal obesity (AOR = 1.70, 95% CI: 1.10–2.64) and high triglyceride level (AOR = 2.06, 95% CI: 1.38–3.07).
In Addis Ababa, around one in three adults are hypertensive. With a large proportion, unaware of their condition. We recommend integrating regular community-based screening programs as integral parts of the health promotion and disease prevention strategies. Lifestyle interventions shall target the modifiable risk factors associated with hypertension, such as weight loss and increased vegetable consumption.
Introduction
Between 1980 and 2010, the proportion of the world’s population with high blood pressure (defined as systolic and or diastolic blood pressure ≥ 140/90 mmHg) or uncontrolled hypertension had dropped modestly. However, sharp rises due to population growth and aging have been recorded across the World Health Organization (WHO) regions over the past decade, with the largest rise in Africa at 30%. The lowest prevalence of raised blood pressure was noted in the Americas region, at 18%, while the global estimate among adults aged 18 years and above was around 22% in 2014. According to the WHO estimates,Ethiopia tops at 24.4% for all adults combined [ 1 – 3 ].
High blood pressure accounts for about 13.5% of annual deaths in the world. Moreover, hypertension directly accounts for 54% of all strokes and 47% of all coronary artery disease worldwide. At the same time, the most productive segment of the population is those aged 45 to 69, who make up more than half of this burden [ 4 ].
High blood pressure is a major risk factor for coronary and ischaemic diseases as well as bleeding stroke. It has been shown that blood pressure levels are positively associated with the risk of stroke and coronary heart disease [ 5 ]. One of the most modifiable risk factors for cardiovascular diseases is hypertension. However, awareness towards the treatment and control of hypertension is extremely low among the low and middle-income counties (LMICs), including Ethiopia.On top of this, the health care resources of the LMICs are overwhelmed by other priorities, including HIV/AIDS, tuberculosis, and malaria. As a result, many LMICs have not yet given due attention to its prevention and control [ 6 ].
In Ethiopia, non-communicable diseases such as hypertension and diabetes mellitus have begun to emerge as the leading causes of hospital admissions, morbidity, and mortality in health facilities located around the nation [ 7 ]. A 2016 report by the Ethiopian Public Health Institute (EPHI) found that 95% of Ethiopian adult populations have 1 to 2 risk factors for non-communicable diseases [ 8 , 9 ]. But there was little information on the extent and risk factors for hypertension at the community level in Ethiopia, including the Addis Ababa study area.
That little information was done by using the WHO stepwise tool step one and step two only [ 6 , 10 ]. And the study setting was at the facility level, though; there was a single study done at the national level using all the three World Health Organization stepwise tools [ 8 , 11 ]. Besides, the study area, Addis Ababa, is the largest urban center and capital of Ethiopia, providing approximately one-quarter of the urban population in Ethiopia [ 6 ]. This study aimed to determine the prevalence and associated factors of hypertension in the adult population of Addis Ababa using the three stepwise tools of the World Health Organization.
Study design and area
A cross-sectional community study was conducted from 1 June to 31 October 2018 in Addis Ababa City. Addis Ababa city is the capital city of Ethiopia. Administratively, Addis Ababa subdivided into ten sub-cities and 116 woredas [ 12 ]. According to the Central Statistical Agency of the Federal Democratic Republic of Ethiopia, the city was projected to inhabit 3,433,999 population by 2017 [ 13 ].
Sampling techniques and sample size determination
Multi-stage cluster sampling techniques were employed by first identifying seven of the ten sub-cities based on preset criteria, including the location of the area, population density, and socioeconomic status. Then, one woreda was randomly selected from each selected sub-cities. After that, two ’ketenas’ were randomly picked from the chosen woredas, which are the smallest geographical units within woredas. Finally, for each ketena, the first household was randomly selected, while subsequent households were selected based on proximity to the first and the preceding household.
A total of 3,724 eligible adults aged 18 and over were interviewed at the selected households. The required sample size was determined using the single population proportion formula by considering: prevalence of hypertension 31.5% from a previous study done in Addis Ababa, Ethiopia [ 6 ], α = 0.05 (z = 1.96), the margin of error 2%, design effect of 1.5 and 20% possible non-response rate. We also determined the sample size for the risk factors of hypertension by using two population proportion formula. But the maximum sample size was attained during the single population proportion formula. As well, the total sample size for each sub-city was determined using with probability proportional to size (PPS).
Data collection instruments and measurements
We used the adapted WHO STEPwise approach to surveillance tools. These tools have a sequential process and aim to serve as an entry point for low- and middle-income countries to monitor chronic diseases and their risk factors. All the three WHO STEPS instrument was applied to collect data on the selected information, including socio-demographic, behavioral, physical, and biochemical measurements as a part of the core and expanded modules [ 14 ]. The tools were first pretested among adults found outside the study area and, then modifications were made based on the findings.
The data were collected via face-to-face interview by trained baccalaureate nurse and laboratory technicians. Weighing scales and non stretch tape were used to measure body weight and height. Weight and height were measured as participants were standing without shoes and wearing lightweight clothing. Height was recorded to the nearest 0.5 cm; weight was recorded to the nearest 100g. Body Mass Index (BMI) was calculated as weight in kilograms divided by height in meters squared (weight (kg)/height (m 2 ) and classified as underweight (<18.5), normal (18.5–24.9), overweight (25–29.9) and obese (≥ 30.0).
Waist circumference was measured at the level of the iliac crest using a non stretch tape measure. Hip circumference measured at the maximum circumference of the hip and; waist-to-hip ratio (WHR) calculated as a ratio of waist and hip circumference.
Physical activity was measured using the Global Physical Activity Questionnaire (GPAQ) section of the STEPS instrument, and the total physical activity is presented in MET (metabolic equivalent) minutes per week. The instrument explores three main areas of day-to-day activities: work (including domestic work), transport, and recreational activities. The level of total physical activity was subsequently classified into high, moderate, or low using the GPAQ analysis guideline provided along with the STEPS instrument [ 14 ].
Using a standardized automated blood pressure monitor, blood pressure was measured on the left arm as per the WHO protocol by informing the participants to remain seated and relaxed.Three blood pressure measurements were taken with at least 3-minute intervals between them. The mean value of the 2 nd and 3 rd measurements was used for analysis [ 14 ]. Blood pressure (BP) classified according to the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) [ 3 ].
To ensure the quality of the data collection, data collectors were trained by the principal investigator; and later on, daily checks were carried out by field supervisors and the principal investigator. The weight of the participants, measured on a pre-calibrated electronic scale. Weighing scales checked and zero levels adjusted between measurements; we also placed the scale on a firm flat surface. The blood pressure was measured in a seated position by a digital device (OMRON M2 Eco). The instrument has been clinically approved and recommended by the World Health Organization. In addition, WHO’s STEPwise tools have been previously validated and implemented in mainly developing countries, including Ethiopia [ 6 , 8 ].
Operational definitions
Hypertension : defined as a mean measured blood pressure of ≥ 140 mmHg systolic and/or the mean measured diastolic blood pressure of ≥ 90 mmHg or self-reported history of hypertension.
Body Mass Index (BMI) : calculated as weight in kilograms divided by height in meters squared (weight (kg)/height (m 2 ). BMI was categorized as per the World Health Organization guidelines [ 14 ], underweight (BMI <18.5), normal (BMI ≥18.5 to ≤ 24.9), overweight (BMI ≥ 25.0 to ≤ 29.9) or obese (BMI ≥ 30.0).
Waist to hip ratio : calculated as waist circumference in cm divided by hip circumference in cm and it was used as a measure of abdominal obesity. Waist to hip ratio ≥ 0.90 m in men and ≥ 0.85m in women is defined as having abdominal obesity [ 15 ].
High physical activity: a person reaching any of the following criteria is classified in this category:
- Vigorous-intensity activity on at least 3 days achieving a minimum of at least 1,500 MET-minutes/week OR
- 7 or more days of any combination of walking, moderate- or vigorous intensity activities achieving a minimum of at least 3,000 MET-minutes per week.
Moderate physical activity: a person not meeting the criteria for the "high" category, but meeting any of the following criteria is classified in this category:
- 3 or more days of vigorous-intensity activity of at least 20 minutes per day
- 5 or more days of moderate-intensity activity or walking of at least 30 minutes per day OR
- 5 or more days of any combination of walking, moderate- or vigorous intensity activities achieving a minimum of at least 600 MET-minutes per week.
Low physical activity: a person not meeting any of the above mentioned criteria under moderate or high physical activities falls in this category.
Raised fasting blood glucose was defined as capillary whole blood value ≥110 mg/dl.
Raised total cholesterol was defined as total blood cholesterol level ≥190mg/dl.
Raised triglyceride was defined as raised triglyceride level ≥150 mg/dl.
Data analysis
Double data entry procedures were performed using the EpiData 3.1 statistical software, and analyses were performed using IBM SPSS software version23. Binary logistical regression was used to identify risk factors for hypertension. Initially, possible risk factors were assessed using bivariate analyses; then we did the multivariable logistic regression model to control confounding factors, and statistical significance was accepted when the P-value < 0.05. The Hosmer-Lemeshow goodness-of-fit statistic was used to evaluate whether or not the assumptions necessary for the application of multiple logistic regression are met. Odds ratios (OR) with 95% Confidence Intervals (CI) were computed.
Ethical clearance
Ethical clearance was obtained from the Addis Ababa University, College of Health Sciences Institutional Review Board (IRB), and the city government of Addis Ababa Health Bureau Ethical Review Committee (ERC). A letter of permission was obtained from the selected sub-city health offices. Respondents were fully informed about the purpose of the study and gave verbal and written consent. Participants having high blood pressure, high blood glucose level, and or abnormal lipid profiles during the study period were referred and informed to go to nearby health facilities for further diagnosis and management.
Results and discussion
Description of the study participants.
From the total 3724 sampled population, consent was given to the 3560 participants to involve in step one and two questionnaires, making an overall response rate of 95.59%. Using a random sampling technique, 582 (20%) of the study participants who participated in the interview and physical measurements were selected for the step three questionnaires (biochemical assessment).
Respondents were between 18 and 95 years old and, the median age was 32 years old (IQR 25, 45). More than half (57.3%) of the respondents were females. The majority (74.8%) were Orthodox Christians, followed by Muslims (14.9%). Above one-third (37%) of them were self-employed, while nearly a half (49.6%) were currently married ( Table 1 ).
| Characteristics | Frequency | Percent |
|---|---|---|
| Male | 1520 | 42.7 |
| Female | 2040 | 57.3 |
| Orthodox | 2664 | 74.8 |
| Muslim | 530 | 14.9 |
| Protestant | 333 | 9.4 |
| Catholic | 14 | 0.4 |
| Other | 19 | 0.6 |
| Government employee | 388 | 10.9 |
| Non-government employee | 257 | 7.2 |
| Self employed | 1316 | 37.0 |
| Student | 301 | 8.5 |
| House wife | 750 | 21.1 |
| Daily laborer | 83 | 2.3 |
| Merchant | 69 | 1.9 |
| Unemployed(able to work) | 173 | 4.9 |
| Unemployed(unable to work) | 47 | 1.3 |
| Retired (pensioner) | 176 | 5.0 |
| 18–29 | 1508 | 42.4 |
| 30–49 | 1304 | 36.6 |
| 50 and above (50–95) | 748 | 21.0 |
| 1–4 | 2178 | 61.2 |
| ≥5 | 1382 | 38.8 |
| Never married | 1331 | 37.4 |
| Currently married | 1767 | 49.6 |
| Separated | 49 | 1.4 |
| Divorced | 139 | 3.9 |
| Widowed | 271 | 7.6 |
| Non response | 3 | 0.1 |
| Primary | 1176 | 33.0 |
| Secondary | 719 | 20.2 |
| Preparatory | 464 | 13.0 |
| Technique | 67 | 1.9 |
| College and above | 539 | 15.1 |
| Not attended formal education | 595 | 16.7 |
Behavioral risk factors of the study participants
Tobacco use.
Tobacco use was assessed by interviewing respondents about their current smoking status, previous smoking experience, the age they started smoking, and exposure to second-hand smoke. Overall, about 4.2% (150) of survey respondents were current smokers (daily smokers and non-daily smokers) ( Table 2 ). Of these, a majority (88.66%) smoke cigarettes on daily basis, with an average of 10 cigarettes per day. More than three-fourth 136 (90.66%) of current smokers were male compared to female (p < 0.001). The average age at which smokers started smoking was 21 ± 6.58 years. Fifty-five (1.61 percent) have smoked cigarettes in the past. One hundred nineteen (3.4%) were passive smokers or second-hand smokers.
| Characteristics | Number | Percent | Hypertension (%, CI) |
|---|---|---|---|
| 18–29 | 1508 | 42.4 | 12.86 (11.17–14.56) |
| 30–49 | 1304 | 36.6 | 31.29 (28.77–33.81) |
| ≥50 | 748 | 21.0 | 58.69 (55.15–62.23) |
| Yes | 150 | 4.2 | 34.67 (26.96–42.37) |
| No | 3410 | 95.8 | 29.00 (27.48–30.53) |
| Yes | 330 | 9.3 | 31.2 (26.19–36.24) |
| No | 3229 | 90.7 | 29.0 (27.45–30.58) |
| Yes | 1162 | 32.6 | 32.79 (30.09–35.49) |
| No | 2397 | 67.4 | 27.53 (25.74–29.32) |
| None | 1107 | 31.1 | 34.24 (31.44–37.04) |
| 1–3 days | 2126 | 59.7 | 27.19 (25.29–29.08) |
| 4–7 days | 266 | 7.5 | 24.81 (19.59–30.04) |
| Don’t know | 61 | 1.7 | 29.51 (17.73–41.29) |
| None | 530 | 14.9 | 30.19 (26.27–34.11) |
| 1–3 days | 2549 | 71.6 | 29.23 (27.46–30.99) |
| 4–7 days | 448 | 12.6 | 28.57 (24.37–32.77) |
| Don’t know | 33 | 0.9 | 24.24 (8.81–39.67) |
| Yes | 542 | 15.2 | 21.77 (18.29–25.26) |
| No | 3018 | 84.8 | 30.58 (28.94–32.23) |
| Yes | 986 | 27.7 | 30.53 (27.65–33.41) |
| No | 2574 | 72.3 | 28.75 (27.00–30.50) |
| Yes | 51 | 8.5 | 58.82 (44.84–72.80) |
| No | 551 | 91.5 | 37.57 (33.51–41.62) |
| Yes | 255 | 43.8 | 49.80 (43.63–55.98) |
| No | 327 | 56.2 | 31.50 (26.44–36.56) |
| Yes | 241 | 41.4 | 54.36 (48.02–60.69) |
| No | 341 | 58.6 | 29.03 (24.19–33.87) |
| Yes | 718 | 20.2 | 38.30 (34.74–41.87) |
| No | 2714 | 76.2 | 26.46 (24.79–28.12) |
| Don’t know | 128 | 3.6 | 37.50 (29.00–46.00) |
Khat chewing
There were 330 (9.3%) participants who reported chewing khat ( Table 2 ). Over a third of the respondents, 105 (31.53%) and half, 172 (51.65%) chew khat on a daily and weekly basis, respectively. On the other hand, 153 participants (4.3%) had previously chewed khat.
Alcohol consumption
One thousand one hundred sixty-two (32.6%) participants consumed alcohol and of that 783 (22.0%) consumed alcohol during the last month ( Table 2 ). Binge drinking is defined; as consuming alcohol for men five and above, or women four and above drink on one occasion and, the result showed that 269 (7.6%) of men and 81 (2.3%) of women binge drunker.
Dietary habits of the study participants
Two thousand three hundred ninety-two (67.2%) consumed fruits, at least one time per week, and the mean fruit consumption per week was 2.12 (±1.48) days, as well, the majority 2268 (94.77%) ate fruit 1–2 serving per day with a mean of 1.36 (±0.58) times per day. Similarly, more than three forth 2997 (84.2%) of the participants ate vegetables at least one time per week with a mean of 2.46 (± 1.46) per week, and most of them 2827 (94.33%) ate it 1–2 times per day with mean serving time per day was 1.55 (±0.61). Nearly three fourth 2511 (70.6%) of respondents reported that they usually use vegetable oils like Nug (Guizotia Abyssinica), Sesame, and Sunflower oil for meal preparation, while nearly one-fourth 839 (23.6%) use a vegetable oil which was solid at room temperature. Nearly all 3423 participants (96.2%) consumed vegetables and fruits less than five times a day.
Physical activity
The total median physical activity of the respondents was 7440 (IQR 2888, 12240) and, the median total physical activity (TPA, in MET-minutes per week) was estimated to be 7800 (IQR 3000, 14280) in males and 7200 (2880, 11320) in females. Approximately 29.5% of males and 4.6% of females were; categorized as having a high (vigorous) level of TPA. However, significantly more women (36.4%) than men (16.0%) classified as having low levels of TPA (P < 0.001). In addition, most of the study participants, 3198 (89.8%), walked or cycled for a minimum of 10 minutes per day.
Physiological characteristics of the study participants
Body mass index and waist to hip ratio.
Weight and height measured in all participants at 3560; the average BMI for respondents was 23.54 (±4.39 kg/m 2 ). Eight hundred and sixty-five (24.3%) were overweight, while 287 (8.1%) were obese. Moreover, the average hip-waist ratio was 0.88 (±0.086 m 2 )) with 0.89 (± 0.086 m 2 ) and 0.87 (±0.085 m 2 ) for men and women, respectively. Over two-thirds of females (67.06%) and 32.9% of males had abdominal obesity.
Biochemical measurements of the respondents
Of the total number of participants, the blood sample was collected from 582 participants (20 percent). The average FBS was 86.7 (±36.2 mg/dl), and the prevalence of high blood sugar, high cholesterol, and triglycerides was 8.5%, 43.8%, and 41.4%, respectively ( Table 2 ).

Prevalence of hypertension
Three consecutive blood pressure measurements took from 3,560 respondents (95.16%) and; an average of the second and third measurements used for blood pressure analysis. The mean systolic and diastolic blood pressure of the respondents was 125.03 (95% CI: 124.39–125.62) mm Hg and 79.58 (95% CI: 79.8–79.97) mm Hg, respectively. The mean SBP was 126.95 (95% CI: 126.03–127.87) mmHg among males and 123.59 (95% CI: 122.72–124.47) mmHg among females. Likewise, the mean DBP was 80.76 (95% CI: 80.14–81.38) mm Hg in males and 78.69 (95% CI: 78.17–79.21) mm Hg in females. Both mean SBP (P < 0.001) and DBP (P < 0.001) were significantly higher in men compared to women.
The overall prevalence of hypertension was 29.24% (95% CI: 27.75–30.74), slightly higher among men 30.13 (95% CI: 27.82–32.44) than women 28.58 (95% CI: 26.66–30.54). Of the 1041 hypertensive respondents, 645 (61.95%) had just been diagnosed in the survey (new screening).
Factors associated with hypertension
Multivariable logistic regression analysis found that of several non-modifiable factors, age and gender were associated with hypertension. The odds of hypertension increased with increased age. The odds of hypertension increased almost three times AOR = 2.79 (95% CI: 1.39–5.56) among respondents aged 30–49 years, and it was eight times AOR = 8.23 (95% CI: 4.09–16.55) higher among respondents aged 50 years and above as compared to those 18–22 years old. The odds of hypertension were almost twice as high AOR = 1.88 (95% CI: 1.18–2.99) in men compared with women.
From modifiable and other factors, eating fewer vegetables per week, body mass index, abdominal obesity, and high triglycerides levels were associated with hypertension. The odds of hypertension increased more than two times AOR = 2.44 (95% CI: 1.21–4.93) among respondents who consumed vegetable less than or equal to three days per week compared to those who ate more than three days per week.
The chance of hypertension reduced by 73% among underweight participants AOR = 0.27 (95% CI: 0.07–0.97), but the odds were two times higher AOR = 2.05 (95%CI: 1.13–3.71) among obese participants as compared to those having normal BMI. Moreover, the odds of hypertension was almost two times higher AOR = 1.70 (95% CI: 1.10–2.64) among participants with abdominal obesity as compared to their counterparts.
The odds of hypertension was also increased by two AOR = 2.06 (95% CI: 1.38–3.07) among participants who had high triglyceride level as compared to their counterparts.
The odds of hypertension was also increased by two AOR = 2.06 (95% CI: 1.38–3.07) in participants with high triglyceride level compared to their counterparts. In this particular study, risky behaviors, including alcohol use, vigorous physical activity, family history of hypertension or diabetes, high blood sugar, and high cholesterol level not significantly associated with hypertension ( Table 3 ).
| Variable | Hypertension | Crude OR (95% CI) | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| 18–29 | 194 | 1314 | 1.00 | 1.00 | |
| 30–49 | 408 | 896 | 3.08 (2.55–3.73) | 2.79 (1.39–5.56)* | 0.003 |
| ≥50 | 439 | 309 | 9.62(7.80–11.87) | 8.23 (4.09–16.55)** | < 0.001 |
| Female | 538 | 1457 | 1.00 | 1.00 | |
| Male | 458 | 1062 | 1.08 (0.93–1.25) | 1.88 (1.18–2.99)* | 0.004 |
| Primary | 334 | 842 | 1.00 | 1.00 | |
| 2 & preparatory | 304 | 879 | 0.87 (0.73–1.05) | 1.03 (0.58–1.80) | 0.66 |
| Technique & college | 142 | 464 | 0.77 (0.62–0.97) | 0.97 (0.49–1.89) | 0.94 |
| Unable to read & write | 261 | 334 | 1.97 (1.60–2.42) | 1.10 (0.64–1.88) | 0.65 |
| No | 660 | 1737 | 1.00 | 1.00 | |
| Yes | 381 | 781 | 1.28 (1.10–1.49) | 1.35 (0.87–2.09) | 0.34 |
| No | 923 | 2095 | 1.00 | 1.00 | |
| Yes | 118 | 424 | 0.62 (0.51–0.79) | 1.05 (0.51–2.15) | 0.88 |
| Yes | 848 | 2142 | 1.00 | 1.00 | |
| No | 169 | 300 | 0.70 (0.57–0.86) | 1.02 (0.59–1.78) | 0.93 |
| Yes | 718 | 1996 | 1.00 | 1.00 | |
| No | 275 | 443 | 0.58 (0.48–0.69) | 0.73 (0.45–1.19) | 0.34 |
| 18.5–24.9 | 504 | 1539 | 1.00 | 1.00 | |
| <18.5 | 48 | 319 | 0.46 (0.33–0.63) | 0.27 (0.07–0.97)* | 0.036 |
| 25–29.9 | 341 | 519 | 2.01 (1.69–2.34) | 1.48 (0.95–2.32) | 0.072 |
| ≥ 30 | 145 | 139 | 3.19 (2.47–4.10) | 2.05 (1.13–3.71)* | 0.011 |
| No | 350 | 1308 | 1.00 | 1.00 | |
| Yes | 691 | 1211 | 2.13 (1.84–2.48) | 1.70 (1.10–2.64)* | 0.026 |
| No (< 110 mg/dL) | 207 | 344 | 1.00 | 1.00 | |
| Yes (≥ 110 mg/dL) | 30 | 21 | 2.37 (1.32–4.27) | 0.943 (0.35–2.54) | 0.74 |
| No (<190 mg/dL) | 103 | 224 | 1.00 | 1.00 | |
| Yes (≥ 190 mg/dL) | 127 | 128 | 2.158 (1.54–3.03) | 0.92 (0.46–1.86) | 0.48 |
| No (<150 mg/dL) | 99 | 242 | 1.00 | 1.00 | |
| Yes (≥ 150 mg/dL) | 131 | 110 | 2.91 (2.06–4.11) | 2.06 (1.38–3.07)** | < 0.001 |
| >3 days | 128 | 320 | 1.00 | 1.00 | |
| ≤ 3 days | 905 | 2174 | 1.04 (0.84–1.29) | 2.44 (1.21–4.93)* | 0.009 |
P-value < 0.05 * and <0.000**, (backward logistic regression method was employed).
The study found that approximately one in three adults aged 18 and over is hypertensive. During childhood, there are modest facts about a gender change in blood pressure. However, beginning with youth, males tend to have a higher average level. But later in life, the difference gets smaller, and the pattern can even be changed [ 16 ]. The prevalence of hypertension in the current study is slightly higher among men than women, which is comparable; a community-based study conducted in Addis Ababa, Ethiopia, reported prevalence of hypertension was 31.5% and 28.9% among males and females, respectively [ 6 ]. Moreover, this study is also comparable with other community-based studies conducted in Jalalabad, Afghanistan (28.4), Kenya (29.4%), Uganda (30.5%), and Gondar city (28.3%) [ 10 , 17 – 19 ].
The prevalence of hypertension in this study is considerably higher as compared to other studies Bangladesh (16.0%), Eritrea (16.4%), Addis Ababa (25%), Bahir Dar (25.1%), Durame Southern Ethiopia (22.4%), Gilgel Gibe South West Ethiopia (5.8%) and Mekelle (20.1%) [ 11 , 20 – 25 ]. The difference may be explained by the age differences of the surveyed populations (18 years and above in our case, whereas in the other studies, the age of the participants varies between 15 and 64 years). Differences may also be attributed to the diversity of sociodemographic characteristics, sample size, lifestyle, and dietary patterns of the study participants.
On the contrary, the prevalence of hypertension in our study is lower than other similar community-based studies conducted in South Africa (38.9%), Sudan (35.7%), Nigeria (33.1%) and Cameroon (47.5%) [ 26 – 29 ]. This disparity can be due to variations in race, genetics, and prevalence of obesity (higher among others), all of which are likely to influence blood pressure.
From non-modifiable risk factors, age is one of the risk factors of hypertension proved by many studies; there is a positive association between age and hypertension when age increases, the odds of hypertension also increases [ 6 , 10 , 11 , 17 , 18 , 21 , 24 , 26 ]. It is primarily due to the increase in systolic blood pressure with age, mainly due to the reduction in elasticity (increased stiffness) of large duct arteries [ 30 ]. Inthe same vein, this study, this study found out that respondents aged 30–49 years had 3 times higher odds of hypertension, and 8 fold higher odds among participants aged 50 and above. In terms of gender, the prevalence of hypertension was almost two times higher in males compared to females in the current study, which is consistent with other study findings [ 11 , 22 , 25 , 28 ].
According to the World Health Organization, overweight and obesity are a major risk factor for heart disease, including high blood pressure, which is the number one cause of death [ 31 ]. In our study, the odds of hypertension were two times higher among obese participants compared to those with normal body mass index; however, the chances of hypertension were reduced by 73% among underweight participants. This finding (especially the obese category) was in line with previous reports from Ethiopia, Kenya, Uganda, Sudan, Bangladesh, and Cameroon [ 10 , 18 , 21 , 22 , 24 , 25 , 27 , 28 , 32 ], and this showed that obesity is one of the risk factor associated with hypertension almost all studies. Moreover, the odds of hypertension were two times higher among abdominally obese respondents compared to their counterparts, the result is also consistent with other studies [ 27 , 28 , 33 , 34 ].
Hypertriglyceridemia is a powerful predictor of cardiovascular disease, which causes endothelial damage, and loss of physiological vasomotor activity that results from endothelial damage can occur in the form of high blood pressure [ 35 ]. In our study, having a high triglyceride level was independently associated with hypertension. The odds of hypertension increased by two among participants with high triglyceride levels relative to their counterparts; our findings are consistent with those of others [ 33 , 36 ].
Previous studies done so far suggested that use of alcohol, cigarette smoking, Khat use, literacy level, physical activity, raised fasting glucose level, family history of hypertension, family history of diabetes, and excessive salt use were significantly associated with hypertension. In contradiction, in this study, the above variables were not significantly associated with hypertension [ 4 , 17 , 18 , 24 , 25 , 27 , 37 ]. A contradicting finding was noted in this current study where all the above variables showed no significant association with hypertension.The inconsistency in these results may be due to the variation of sample size, study settings, and population characteristics. These variations may also be explained by the research design issues (as a cross-sectional design can’t distinguish the sequences of explanatory variables and the outcome). The other element of this study included adults 18 years of age or older, but different studies used a different age class, which should make comparisons difficult. Additionally, the respondents might not know whether they had a family history of hypertension or not due to the silent killer and asymptomatic nature of the diseases this may underestimate the risk factors of the disease. Though, we use the standardized WHO STEPs risk factor questionnaire allows for comparability on the presence of risk factors between various communities, regions, and countries.
There was a high prevalence of hypertension among adults in the city of Addis Ababa, which may indicate a hidden epidemic in the population. Even though the study was conducted in the capital city, there was a large proportion of hypertensive respondents (61.95%) were unaware of having the condition and newly screened for the first time by the current study. Increasing age, gender being male, obesity and abdominal obesity, consumption of low vegetables, and raised triglyceride levels were significantly associated with hypertension.
As a result, lifestyle changes and the introduction of obesity and hypertension screening programs are recommended. These programs should focus on lifestyle changes, including eating fruits and vegetables, maintaining a normal weight, and weight loss intervention. The findings also underscore the vital need for community-based screening programs for the early detection of hypertension and obesity.
Supporting information
Acknowledgments.
The authors would like to express their appreciation to the following organizations and individuals for contributing to the success of this study: The authors wish to extend their most sincere thanks to all participants in the study. We thank the data collectors and supervisors. We also want to convey our deepest gratitude to Armed Forces Comprehensive Specialized Hospital because they allowed us to do all the lipid profiles with their laboratory technicians.
Funding Statement
This work was funded by Addis Ababa University, Addis Ababa, Ethiopia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2021; 16(4): e0248934.
Decision Letter 0
21 Dec 2020
PONE-D-20-26679
Prevalence and risk factors of hypertension among adults: a Community Based Study in Addis Ababa, Ethiopia
Dear Dr. MESERET MOLLA ASEMU,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
As you will recognize from the comments of the reviewers both raised major points of critique, especially regarding design of the study and presentation of data.
Please submit your revised manuscript within 2 months. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Rudolf Kirchmair
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. We suggest you thoroughly copyedit your manuscript for language usage, spelling, and grammar. If you do not know anyone who can help you do this, you may wish to consider employing a professional scientific editing service.
Whilst you may use any professional scientific editing service of your choice, PLOS has partnered with both American Journal Experts (AJE) and Editage to provide discounted services to PLOS authors. Both organizations have experience helping authors meet PLOS guidelines and can provide language editing, translation, manuscript formatting, and figure formatting to ensure your manuscript meets our submission guidelines. To take advantage of our partnership with AJE, visit the AJE website ( http://learn.aje.com/plos/ ) for a 15% discount off AJE services. To take advantage of our partnership with Editage, visit the Editage website ( www.editage.com ) and enter referral code PLOSEDIT for a 15% discount off Editage services. If the PLOS editorial team finds any language issues in text that either AJE or Editage has edited, the service provider will re-edit the text for free.
Upon resubmission, please provide the following:
- The name of the colleague or the details of the professional service that edited your manuscript
- A copy of your manuscript showing your changes by either highlighting them or using track changes (uploaded as a *supporting information* file)
- A clean copy of the edited manuscript (uploaded as the new *manuscript* file)
3. Please include additional information regarding the survey or questionnaire used in the study and ensure that you have provided sufficient details that others could replicate the analyses. For instance, if you developed a questionnaire as part of this study and it is not under a copyright more restrictive than CC-BY, please include a copy, in both the original language and English, as Supporting Information.
4. In the Methods, please discuss whether and how the questionnaire was validated and/or pre-tested. If this did not occur, please provide the rationale for not doing so.
5. We note that you have stated that you will provide repository information for your data at acceptance. Should your manuscript be accepted for publication, we will hold it until you provide the relevant accession numbers or DOIs necessary to access your data. If you wish to make changes to your Data Availability statement, please describe these changes in your cover letter and we will update your Data Availability statement to reflect the information you provide.
6. PLOS requires an ORCID iD for the corresponding author in Editorial Manager on papers submitted after December 6th, 2016. Please ensure that you have an ORCID iD and that it is validated in Editorial Manager. To do this, go to ‘Update my Information’ (in the upper left-hand corner of the main menu), and click on the Fetch/Validate link next to the ORCID field. This will take you to the ORCID site and allow you to create a new iD or authenticate a pre-existing iD in Editorial Manager. Please see the following video for instructions on linking an ORCID iD to your Editorial Manager account: https://www.youtube.com/watch?v=_xcclfuvtxQ
7. Thank you for submitting the above manuscript to PLOS ONE. During our internal evaluation of the manuscript, we found significant text overlap between your submission and the following previously published works, some of which you are an author.
https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/1471-2261-12-113
https://ejcm.journals.ekb.eg/article_11046_f56232e3d004cc38fe78b7b616f2799e.pdf
https://www.scribd.com/doc/115910728/Ncd-Report-Full-en-English
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2736927/
https://link.springer.com/article/10.1186/s12889-015-2610-8?code=241bf12b-10c4-493b-805c-c06d7a2cbf80
We would like to make you aware that copying extracts from previous publications, especially outside the methods section, word-for-word is unacceptable. In addition, the reproduction of text from published reports has implications for the copyright that may apply to the publications.
Please revise the manuscript to rephrase the duplicated text, cite your sources, and provide details as to how the current manuscript advances on previous work. Please note that further consideration is dependent on the submission of a manuscript that addresses these concerns about the overlap in text with published work.
We will carefully review your manuscript upon resubmission, so please ensure that your revision is thorough.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Partly
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: No
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: Yes
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Line 71- Which are the "Non Communicable Diseases risk factors?
Line 164- Why p-value of < 0.20 was used as criteria to include it in the multivariable logistic
regression model?
Quite a small group of the study population were smokers in this study- can you explain why?
It is recommended that the diagnosis of hypertension should be based on:
repeated office BP measurements on more than one visit in the ESC-guidelines from 2018-
in this study the definition hypertension was defined on just one visit. Is the definition of hypertension chooses too weakly in this study?
Reviewer #2: Manuscript ID number:
Title of paper:
Despite careful approach to investigate Prevalence and risk factors of hypertension, manuscript needs minor revisions to make it easy to understand before being published.
General comments:
1. Language editing strongly recommended
2. The body of the text suffers from several spelling and grammatical errors. Please consider a professional language edit. Example: scare (page 3 first paragraph),
3. Standardized your tables by removing the boarders and include P values in table 3
4. In the abstract result section, almost all (96.2%) of participants consume vegetables and or fruits less than five times per day.
Is that feasible consuming vegetable & fruits five times per day in Ethiopian context? Or you mean five times per week? Make it clear
Page 3 & 4
5. Moreover, in Ethiopia non-communicable diseases such as hypertension and diabetes mellitus appear on the list of leading causes of morbidity and mortality in the hospitals and regional health bureaus across the country. A report by Ethiopian Public Health Institute (EPHI) in 2016 showed that 95% of the Ethiopian adult populations have 1-2 Non-Communicable Diseases risk factors (6, 7). But, there were scare data with regard to the magnitude and risk factors of common non communicable disease at the community level in Ethiopia including the study area Addis Ababa. Moreover, the study area represents the largest urban center in Ethiopia, hosting about 25% of the urban population in the country (5).
Since you are not intended to study all types of non-communicable diseases better to focus on hypertension). Paragraph 4, page 3 needs both language & grammatical edition.
6. The method section, selection of the study participant,
the last paragraph a total of 3724 all needs to reconsider again
7. A community based cross-sectional study was conducted from June to October 2018 in Addis.
Please provide more precise date of study begin and termination
8. Multi-stage cluster sampling techniques was employed. Seven of the ten sub-cities were selected purposefully by considering the area that was found, the population density and the economic activities.
You didn’t say anything about how you determine the sample size. How you calculate your sample size, what assumptions you used to calculate your sample size both for the magnitude & factors. Also, important you should show us how you allocate the number of participants to Sub-cities or Woreda Or Kebeles, Ketenas & households?
9. One of the methods of maintaining the quality of data is keeping the data collection instrument valid & reliable (in you case weight scale & BP apparatus, the STEPS Questionnaire). In this regard you didn’t say anything.
How you maintain the reliability & validity of this instruments? We need more clarification on this issue
10. In the description of the study participants, result section, you calculate both the mean with SD and Median with IQR for the respondents’ age.
What was the reason and which one was appropriate for your data? Need clarification
11. In Tobacco use section to told us about 4.2% (150), of the survey participants were current smokers (daily and non-daily smokers) again in the last two sentence of the same section you presented, fifty-five (1.61%) were ever smoked cigarettes and One hundred nineteen (3.4%) were passive smoking or second-hand smoke.
What does this imply? Are these 55 peoples being among 150 who currently smoke? Needs to be clarified.
12. Weight and height measurement were taken from all participants 3560 and the BMI was calculated for those participants. But you didn’t show how you calculate the BMI (only you defined BMI in the operational definition).
It is important to show how was the BMI calculated in the methods section. The procedure you used needs to be clearly kept in the method section
13. You told us that blood sample was collected from 20% of the total study participants.
It is not sufficient to write 20% of total you need to write the actual number of participants you collect blood sample.
14. In the result section, prevalence of hypertensin, you presented the overall prevalence of hypertension was 29.24% (95% CI: 27.75-30.74), slightly higher among men 30.13 (95% CI: 27.82-32.44), than women 28.58 (95% CI: 26.66-30.54) even though the difference was not statistically significant (χ2=1.015, P= 0.314).
But in the factors associated with you stated that sex had significant association with hypertension (The odds of hypertension was almost two times higher AOR= 1.88 (95% CI: 1.18-2.99) among males as compared to females). Needs clarification and reconsideration.
Page 19 discussion section
15. Hypertension is an important modifiable risk factor for cardiovascular disease (CVD). It currently accounts for about 13.5% of annual global deaths. Hypertension is directly responsible for 54% of all strokes and 47% of all coronary heart disease worldwide. Moreover, over half of this burden occurs in individuals aged 45–69 years, which is the most productive segment of the population (31).
Better to start your discussion by summary of your results and good if you use this in the introduction section
16. …………. So, the prevalence of hypertension in the current study is slightly higher among men than women which is comparable with a community based study conducted in Addis Ababa, Ethiopia which reported the prevalence of hypertension was 31.5% and 28.9% among males and females, respectively (5). Moreover, this study is also comparable with other community-based studies conducted in Jalalabad, Afghanistan (28.4), Kenya (29.4%), Uganda 375 (30.5%), and Gondar city (28.3%) (12-15).
Here first you talk about the association between hypertension and gender or sex and on the next paragraph back to compare the prevalence with other studies. I see some confusion here I think you would want to change the order of the paragraph?
17. ……… which the risk of hypertension increases with age. This is mainly due to systolic blood pressure increase with age, mainly because of reduced elasticity (increased stiffness) of the large conduit arteries (26). In this study respondents aged 30-49 years; had 3 times higher risk of hypertension and even moreover, it is 8 times higher risk among participants aged 50 years and above.
What is your message here for the patients and health care providers you provide? Is there anything that recommend to tackle this problem or age? You should better to emphasize on modifiable factors than non-modifiable like age & sex. Need your consideration
18. This finding (especially obese category) was in line with previous reports from Ethiopia, Kenya, Uganda, Sudan, Bangladesh, and Cameroon (13, 15, 17, 18, 21, 22, 24, 25, 27). Moreover, the risk of hypertension was 2 times higher among abdominally obese respondents and this finding is in line with other studies (24, 25, 28, 29) and the same to the level of triglyceride also.
Since this is the most important area that your recommendation is focused, comparing the findings is not sufficient. Better to find the reason of similarity or differences and give your recommendation or message based on that. Therefore, you need to work on it and put your recommendation.
Page 21, first paragraph
19. In contradiction, in this study the above variables were not significantly associated with hypertension. The inconsistency of these findings may be due to the low prevalence of these factors in the community especially among females.
What does it mean? I don’t think your reason for differences is correct. May you need to find tangible reason for this difference.
20. Additionally, the respondents might not know whether they had a family history of hypertension or diabetes due to the silent killer nature of the diseases this may underestimate the prevalence of the diseases.
How the silent killer nature of the disease affects the prevalence of hypertension since the prevalence was determined by measuring their blood pressure? Or you want to say the severity of the disease? Not clear
Do you think diabetes is a silent killer? Since your objectives did not include diabetes why you include here?
21. The other reason should since some of the information was based on self-report and is subjected to social desirability and recall biases.
These issues are very critical in research. How you manage this social desirability and recall biases since this can affect severely your findings? You have to show us either in the discussion or method section how you control theses biases clearly? In addition, with all these short comings or limitations do think your research could be eligible for publication? Better to avoid those limitations that can be controlled methodologically
22. In the conclusion section …. There was a high prevalence of hypertension among adults in the Addis Ababa city and this may show a hidden epidemic in the population. What is your reference to say high prevalence or to conclude this is a hidden epidemic? You have to show here
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #2: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: Manuscript ID number.docx
Author response to Decision Letter 0
A rebuttal letter
Manuscript PONE-D-20-26679
Response to Reviewers
Dear Rudolf Kirchmair,
Thank you for the opportunity to provide a revised version of the manuscript. “Prevalence and risk factors of hypertension among adults: a Community Based Study in Addis Ababa, Ethiopia” for publication in PLOS ONE Journal. We appreciate the time and effort you and the examiners put into providing comments on our manuscript. We have incorporated the suggestions and comments made by the reviewers. These changes are highlighted in the manuscript. A point-by-point response to the reviewers’ comments and concerns is provided below in blue.
• A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
• A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
• An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
Authors’ response: Dear academic editor, thank you for providing the link. We carefully read and edited our manuscript as per the guidelines.
2. We suggest you thoroughly copyedit your manuscript for language usage, spelling, and grammar. If you do not know anyone who can help you do this, you may wish to consider employing a professional scientific editing service.
Whilst you may use any professional scientific editing service of your choice, PLOS has partnered with both American Journal Experts (AJE) and Editage to provide discounted services to PLOS authors. Both organizations have experience helping authors meet PLOS guidelines and can provide language editing, translation, manuscript formatting, and figure formatting to ensure your manuscript meets our submission guidelines. To take advantage of our partnership with AJE, visit the AJE website ( http://learn.aje.com/plos/ ) for a 15% discount off AJE services. To take advantage of our partnership with Editage, visit the Editage website ( www.editage.com ) and enter referral code PLOSEDIT for a 15% discount off Editage services. If the PLOS editorial team finds any language issues in text that either AJE or Editage has edited, the service provider will re-edit the text for free.
• The name of the colleague or the details of the professional service that edited your manuscript
• A copy of your manuscript showing your changes by either highlighting them or using track changes (uploaded as a *supporting information* file)
• A clean copy of the edited manuscript (uploaded as the new *manuscript* file)
Authors’ response: Thank you for your feedback and suggestion. We accepted the comments on language usage, spelling, and grammar, based on the comments we edited our manuscript as much as possible by using online grammar and language checkers (Grammarly) and with my friend speaks fluent English at our university. We have prepared and attached our manuscript highlighting the changes and uploaded it as a *supporting information* file. We have also prepared and attached the edited manuscript and uploaded it as the new *manuscript* file.
Authors’ response: Thank you for your comment. We have attached the questionnaires we used for the current survey in both the original (Amharic) and English language as Supporting Information.
Authors’ response: Thank you for your feedback. This was incorporated into the method portion of our manuscript. The questionnaire was also adapted from the World Health Organization and validated in various previous studies in Ethiopia. However, pretesting took place.
Authors’ response: Thank you for your comment. The current study is part of a large study with multiple objectives to assess Epidemiology of common non communicable diseases, among adults in Addis Ababa, Ethiopia. Further publication is expected from the dataset which prevents us from making it publicly right now. So, we made changes in our cover letter and we have included in the updated Data Availability statement part.
Authors’ response: Thank you for your comment. We ensured that we have an ORCID iD.
Authors’ response: Thank you for your comment. We have redrafted the entire duplicate text into the manuscript based on your recommendation.
[Note: HTML mark up is below. Please do not edit.]
Reviewer #1: Partly
Reviewer #2: Yes
________________________________________
Authors’ response: Thank you for your comment. The manuscript is revised accordingly to improve its scientific writing. The conclusions are revised as well to reflect the data presented.
Reviewer #1: No
Authors’ response: Thank you for your comment. We accepted your comment, and we have incorporated it into the result part of our manuscript. We have included the p value in table 3, as suggested by the reviewer. Moreover, we also incorporated other comments from the reviewers.
Reviewer #1: Yes
Authors’ response: Thank you for your comments. The current study is part of a large study with multiple objectives to assess Epidemiology of common non communicable diseases, among adults in Addis Ababa, Ethiopia. Although additional publications are planned based on the dataset, we have included the raw data in SPSS format in the data availability section.
Authors’ response: Thank you for your comments. The manuscript has been reassessed and all grammatical mistakes have been corrected.
Reviewer #1: Line 71- Which are the "Non Communicable Diseases risk factors?
Authors’ response: Thank you for your question. The 1-2 non communicable risk factors were over-weight (BMI ≥ 25 kg/m2), consumption of fruit and vegetables less than 5 servings per day and raised BP (SBP≥140 and/or DBP ≥ 90 mmHg or currently on medication for raise blood pressure and insufficient physical activities.
Authors’ response: Thank you for your question. We read different articles and as a rule of thumb, they selected all the variables whose p-value < 0.2 on binary logistic regression for multivariable logistic regression. But we could not obtain from the standard biostatistics books, so corrected by entering all the variables we used in binary logistics analysis into multivariable logistic regression.
Authors’ response: Thank you for your question. As we have seen from different studies conducted in Ethiopia, including the study area, Addis Ababa, the prevalence of smoking was low; the possible reason may be the number of smokers in the study setting was low.
Authors’ response: Thank you for your comment. We have measured the blood pressure of study participants three times, and we took the mean of the second and the third records because mostly the first record became high. The World Health Organization; and the American Health Association recommends one visit three times measurements to define hypertension during a community survey. The definition is not weak because we measured three times; moreover, we measured their blood pressure in their home; this also minimizes the white coat false records of high blood pressure. Also, the literature that we used in the discussion part used this method.
Reviewer #2: Manuscript ID number:
Authors’ response: Thank you for your feedback and suggestion. We accepted the comments and strongly recommended issues on language editing and based on the comments we thoroughly edited our manuscript as much as possible by using online grammar and language checkers (Grammarly) and with my friend speaks fluent English in our university.
Authors’ response: Thank you for your feedback and suggestion. We accepted the comment and made corrections.
Authors’ response: Thank you for your feedback and suggestion. The comment was accepted and the p-values were added to Table 3.
Authors’ response: Thank you for your clarification question. Healthy eating, including an adequate intake of fruits and vegetables (five servings a day), is one of the key public health measures to prevent NCDs. Eating fruits and vegetables five times daily is recommended by the World Health Organization in developed and developing countries, including Ethiopia. But, in many countries worldwide, the vast majority of the population consumes less than the recommended amount of five servings of fruit and vegetables per day, though low intake of fruits and vegetables was estimated to cause 4.7% of the global disease burden – as estimated in DALYs. And in our study, as we mentioned in the method part we used the WHO STEPS instrument and one of the major core questions was to assess the dietary habit, including the fruits and vegetables of participants whether they are in line with the WHO recommendation or not.
Authors’ response: Thank you for your comments. We accepted the comment and made corrections.
Authors’ response: Thank you for your comment. We accepted the comment and made corrections.
Authors’ response: Thank you for your comment. We accepted the comment and incorporated and re-wrote the exact start and end date of the study.
Authors’ response: Thank you for your comment. We accept the comment, and we have incorporated the sample size determination. We also explained how we allocate the number of participants in the selected sub-cities in the method part of our manuscript.
Authors’ response: Thank you for your questions. We agree with the question and have responded to it in the method portion of our manuscript.
Authors’ response: Thank you for your comment. We accepted the comment. Because our variable age was skewed, we chose the median as a measure of central tendency rather than as a mean. We have corrected in the result part of our manuscript.
Authors’ response: Thank you for your clarification question. From the total participants, 150 (4.2%) of them was currently a smoker. But if they were not current smokers, we asked them whether they smoke cigarettes or not by saying, “In the past, did you ever smoke any tobacco products?” If they said yes to the above question, we considered them as previous smokers or Ex-smoker. So, from the total current non-smokers, we got 55 participants, classified under the previous smoker; this number is not included in the 150 current smokers.
Authors’ response: Thank you for your comment. We accepted your comment, and we have incorporated it into the method part of our manuscript.
Authors’ response: Thank you for your comment. We accepted your comment, and we have incorporated it into the result part of our manuscript.
Authors’ response: Thank you for your comment. We accepted your comment, and we have corrected it into the result part of our manuscript.
Authors’ response: Thank you for your comment. We accepted your comment, and we have corrected it.
Authors’ response: Thank you for your comment. Your feedback is accepted and corrected.
Authors’ response: Thank you for your comment. Our message for the patients was to be screened and get treatment. So, they can prevent complications associated with untreated hypertension. For the health providers, especially the Health Extension Workers (in our country, they went to each community house to deliver contraception, vaccine), we told them to take blood pressure whether they have a symptom or not for those aged peoples. The other thing we give more emphasis on modifiable factors since they can modify them.
Authors’ response: Thank you for your comment. Your feedback is accepted and corrected. Additionally, the respondents might not know whether they had a family history of hypertension due to the silent killer nature of the diseases this may underestimate the risk factors of the diseases. Since family history of hypertension is one of the risk factors of hypertension.
We used different mechanisms to avoid biases. To avoid social desirability bias, first, we explained the aim of the survey for each participant and during data collection; we kept it anonymous and confidential. After data collection, the information is kept in a safe and secured place. Moreover, to avoid recall bias we asked timeline timeliness of the information and standard questionnaires prepared by the World Health Organization. So, since we did all the activities that help us to minimize the biases we excluded the sentence included as a limitation
Authors’ response: Thank you for your question. Our finding showed that 30% of study participants had hypertension but a study conducted in one of the urban areas of Ethiopia showed that the prevalence of hypertension was 20%; moreover, a large proportion, 62% of them unaware of having the problem; that is why we would like to say this showed the hidden epidemic of the disease among adults aged 18 year and above. Moreover, hypertension is a chronic disease if it is not diagnosed and treated early may end up with life-threatening complication and death.
6. PLOS authors have the option to publish the peer review history of their article (what does this mean?). If published, this will include your full peer review and any attached files.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy.
Reviewer #2: No
Authors’ response:Thank you. We agreed and corrected that comment.
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Authors’ response:Thank you. We have registered with PACE and all the tables do fit with PLOS. We downloaded from the PACE and uploaded as Table 1, Table 2 and Table 3 in TIF format.
Submitted filename: Point by point response re.docx
Decision Letter 1
PONE-D-20-26679R1
Dear Dr. ASEMU,
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #2: The Author tried to address More or less the comments given by me. It can be published on your journal
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Reviewer #2: Yes: Daniel G/Tsadik W/giorgis
Acceptance letter
11 Mar 2021
Dear Dr. Asemu:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Prof Rudolf Kirchmair
- Research article
- Open access
- Published: 12 May 2020
Awareness, treatment, and control of hypertension and related factors in adult Iranian population
- Mohsen Mirzaei ORCID: orcid.org/0000-0002-4153-5023 1 ,
- Masoud Mirzaei ORCID: orcid.org/0000-0001-6455-0747 1 ,
- Behnam Bagheri ORCID: orcid.org/0000-0001-8482-0038 2 &
- Ali Dehghani ORCID: orcid.org/0000-0001-9355-8035 3
BMC Public Health volume 20 , Article number: 667 ( 2020 ) Cite this article
22k Accesses
35 Citations
Metrics details
Hypertension, known as the silent killer, is a major risk factor for cardiovascular disease. Awareness and treatment of hypertension is not appropriate in the world, and this has led to an increase in mortality and morbidity caused by uncontrolled hypertension. This study aims to estimate awareness, treated, and controlled hypertensive and relevant predictors in an adult Iranian population.
This cross-sectional study was conducted on 10,000 adults aged 20–69 years in Yazd, Iran. They were selected through multi-stage random cluster sampling in 2015–2016. Blood pressure was measured three-time with standard protocol by trained health workers. Those with a positive history of hypertension and using anti-hypertensive drugs, prescribed by a physician, were considered hypertensive. Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic BP of ≥90 mmHg. Uncontrolled hypertension was defined in accordance with recommended treatment targets by the Joint National Committee (JNC7). Logistic regression was used to assess the predictors of hypertension awareness, treatment and control.
The prevalence of hypertension was 37.3%, and the prevalence of pre-hypertension was 46.4%. 49.7% of People with hypertension were aware of their disease, and 71.5% of them were using antihypertensive drugs prescribed by physicians. Blood pressure was controlled in 38.9% of the treated patients. In the adjusted model, older age, female sex, and history of diabetes mellitus were positively associated with higher awareness. High physical activity, tobacco smoking, and diabetes are the only predictors of treated high blood pressure. Younger age, female sex, and higher education were determinants of controlled hypertension. Having health insurance was significantly correlated with awareness and control of hypertension.
Hypertension is a public health problem in this population, which is not well controlled. Half of the patients were unaware. Intervention for increased screening coverage is needed. It should plan to raise public awareness about hypertension and improve hypertension control under the supervision of physicians. Implement a family physician program is recommended in the health system.
Peer Review reports
High blood pressure is an important risk factor for cardiovascular disease and causes 7.5 million deaths per year (12.8% of all deaths) annually [ 1 ]. The global burden of disease study suggests that systolic blood pressure is accountable for the highest proportion of lost years of life due to premature death, with 212 million years lost [ 2 ]. The high blood pressure rank in the world increased from the fourth in 1990 to the second in men and first in women in 2017 [ 3 ]. The prevalence of hypertension (HTN) in various regions of the world has been reported from 4 to 78%. In the Eastern Mediterranean region, it is on average 29.5% and in Iran 22% [ 4 , 5 , 6 ].
Among the known risk factors for non-communicable diseases, hypertension after high Body Mass Index (BMI), unhealthy diet, and high blood glucose is the fourth risk factor, which has increased by 6.7% from 2005 to 2016 [ 7 ]. Yazd Healthy Heart Project reported the prevalence of HTN 25.6% in Yazd [ 8 ]. The number of people with HTN in low-middle income countries (1.04 billion) is higher than in developed countries (694 million), which shows an increasing trend from 2000 to 2010(7.7%). However, it decreased by 2.6% in high-income countries [ 9 , 10 , 11 ].
Despite the high prevalence, studies have shown that in the world, the percentage of unawareness, untreated, and even uncontrolled HTN is significantly high [ 9 ]. In general, 50–75% of patients with hypertension do not receive proper treatment [ 12 ]. In Iran (2011), 43.2% of patients are aware of their illness, 34.8% of hypertensive persons are treated, and 38.6% of them are controlled which vary across provinces.
In Northern Iran, about one-third of the treated patients have controlled hypertension [ 13 ]. In Azar’s cohort, 60% of the participants are aware of their illness, and 68% have controlled blood pressure. In Shiraz, 69% have controlled blood pressure [ 13 , 14 , 15 ]. The 2010 study in Yazd showed that the rate of awareness for hypertension was 43.7% of the patients. 77.1% of them were treated, and only 12.4%, who treated, had controlled blood pressure [ 16 ]. This difference between the prevalence, awareness, and control of high blood pressure among countries as well as among different regions of a country in other studies is also reported [ 17 ]. The most important complication of uncontrolled blood pressure is morbidity and mortality of cardiovascular diseases (51% of stroke and 45% of deaths due to myocardial infarction) [ 18 ]. Inappropriate management of HTN can be the result of socioeconomic factors such as poor health literacy, lack of access to health care providers due to lack of centers, or inability to pay for health costs, and so on. Identifying these factors may help to design more effective health interventions. The purpose of this study is to estimate the prevalence of awareness, treatment, and control of hypertension and relevant predicting factors in an adult Iranian population.
This study is a cross-sectional analysis of the data from the recruitment phase of the Yazd Health Study (YaHS), which is a population-based longitudinal study designed to determine the prevalence of non-communicable diseases and their risk factors in Yazd Greater Area. The maximum sample size was calculated according to 50% prevalence and significance level of 99%, for all the NCD and their risk factors. The initial sample size was calculated 538. It was corrected based on ten strata of five participants in each age group (20–29, 30–39, 40–49, 50–59, 60–69 years) by each sex in clusters. The design effect of 1.5 was considered, it was predicted that 5% would not respond in the recruitment phase ( n = 8494) and 15% attrition rate or loss to follow-up was predicted and added to the number which was reached to 9768 in the second wave. Thus, we decided to enroll 10,000 persons in the study. Blocks of urban-rural neighborhoods were considered as clusters. The blocks were randomly selected. According to tossing the cluster random sampling method, 10,000 residents of Yazd (20–69 years old) were selected from 200 clusters in years 2015–2016. Of each age group of ten, five were selected in clusters of 50 (25 men and 25 women). A completed method of study was published elsewhere [ 19 ]. Informed consent was given to participate in the study. According to the protocol, the questionnaire is repeated every five years to provide longitudinal information for determining the risk factors for health and the incidence of disease.
The interviewers completed a valid questionnaire and measured anthropometric and blood pressure at a home visit. See Additional file for the YaHS questionnaire (s1). The overall response rate was 98% ( n = 9800). Demographic characteristics, history of cardiovascular disease, and the relevant risk factors were recorded. Trained people in a sitting position measured physical examination and after rest, using a standard and appropriate cuff size for the participant’s arm [ 20 ]. The pressure measurement was carried out three times at five-minute intervals by calibrated Reichter electronic sphygmomanometers (Model N-Champion, Reister GMBH, Germany), which were calibrated regularly. The mean of second and third measurements was recorded as blood pressure and used for analysis. People with the following characteristics were classified hypertensive case: a) Self-reported previous diagnosis of hypertension by the physician, and b) systolic BP ≥140 or diastolic BP ≥90 mmHg according to the Joint National Committee JNC7 classification [ 21 ].
Awareness of hypertension was defined as a self-reported previous diagnosis of hypertension by a physician among the participants with hypertension. Unawareness of hypertension was defined by blood pressure ≥ 140/90 mmHg without a prior diagnosis by a physician or the use of any antihypertensive drugs.
The participants who were aware of their hypertension, who answered the question: “When was the last time you referred to a doctor for your high blood pressure?”, “over the past three months,” were categorized in the treated group.
Controlled hypertension was defined for those taking antihypertensive medication for the management of high BP at the time of the interview. It had systolic BP < 140 mmHg and diastolic BP < 90 mmHg. Uncontrolled hypertension was defined following recommended treatment targets of systolic BP ≥140 mmHg and diastolic BP ≥90 mmHg (Including those who were aware). SBP/DBP goals recommended for Specific disease (diabetes mellitus) was < 130/80 mmHg [ 22 ].
Physical activity was assessed by the International Physical Activity Questionnaire ( IPAQ ), short-form (SF). It examines the intensity of physical activity over the last week for different levels, individually. Metabolic equivalent (MET; multiples of resting energy expenditure) by minutes per week estimated by self-reported duration (in minutes) and number of days for types of activity in the past seven days. Finally, participants were classified into three levels of “low”, “moderate” and “high” physical activity [ 23 ]. Body Mass Index (BMI) calculated as weight/height 2 in kg/m 2 and was classified to underweight < 18.5, normal = 18.5–24.5, overweight = 25.0–29.9, and obese ≥30.00 [ 24 ]. Those who answered “Yes” to the question “Do you smoke cigarettes or hookah?” were considered current smokers [ 19 ].
The study was approved by the ethics committee of Shahid Sadoughi University of Medical Science, Yazd, Iran (IR.SSU.MEDICINE.REC.1396.311). The study was explained to all respondents willing to participate. All participants had the right to withdraw from the study at any time. Informed consent was obtained from each participant before data collection. Participants with a new diagnosis of hypertension were advised to refer to their health center or physician for the follow-up.
Descriptive statistics were reported, and age-standardized prevalence rates were calculated using the direct method based on Yazd and Iran population in the national census 2011 [ 25 ]. Awareness, treatment, and control of hypertension were presented as percentages. A chi-square test was used for categorical variables to analyze the differences in demographic variables between the groups. Binary logistic regression was fitted. For binary logistic regression, two groups were defined; aware and unaware, treated and untreated and controlled and uncontrolled. It performed to ascertain the effects of age, gender, education, health insurance, place of residence, BMI & physical activity, smoking and history of diabetes mellitus (as independent variables) on the likelihood that participants who are aware of their illness, those who are being treated and whose blood pressure is controlled. Multivariable logistic regression analyses (enter method) were performed to assess the association between dependent (awareness, treated, and controlled hypertension) and independent variables. Crude differences in proportions were presented by using χ 2 -tests. Association of independent factors with awareness, treatment and control of hypertension (dependent variables) were reported as odds ratios with 95% confidence intervals (CI) after adjustment. All statistical analyses were performed using SPSS version 16 software. A p -value of less than 0.05 was considered statistically significant.
Of the total respondents, 49.2% of participants were men and 4.1% were from the rural areas; 25.7% had primary or less education; 15.7% of the participants had BSc, MSc. or doctorate degrees; 94.5% of the participants had universal health insurance. Most participants (84%) were married; 68.9% of men and 11.7% of women were employed and 74.4% of women were housewives.
Of the total 9800 participants, 1817 (18.5%) had a history of hypertension, 45.6% of those between 60 and 69 years old. Hypertension was more prevalent in women (21.9 vs. 15.2%, P < 0.0001) than men. The age-standardized prevalence of hypertension in this population was 10.5%. age and sex standardized prevalence rates of hypertension was 12.03 according to the national population census (Male: 9.2%, female: 14.2%) [ 25 ]. To enable comparison across regions, we used the World Health Organization (WHO) ‘world’ population for age and sex standardization [ 26 ]. According to WHO population, the prevalence of hypertension was14.04% (male: 11.6%, female: 16.5%).
The frequency of high blood pressure was higher in people with less education. Hypertension is more common in the indigenous population compared to migrants from other provinces (19.5% vs. 13.1%, P < 0.0001). A history of two years or more of hypertension has been reported in 72.4% of patients. 28.8% of patients did not refer to the doctor for the treatment of their high blood pressure for four months or more. Socioeconomic factors and family history of common disease associated with self-reported hypertension in Yazd greater area was shown in Table 1 .
Overall, half of the adults with hypertension were aware of their disease (49.7%). This proportion increased with age, from 11.9% at the age of 20 to 29 years to 67.0% at the age of 60 to 69 years ( P < 0.0001). Women were more aware of their disease ( P < 0.0001). Hypertension was more common in overweight and obese patients, less educated, those with low physical activity, and patients with a positive family history of cardiovascular disease and diabetes ( P < 0.0001).
The age and sex standardized prevalence of newly diagnosed hypertension (unaware patients) in this population was 16.2%. The mean age of newly diagnosed hypertension cases were nine years lower than known cases (47.4 vs.56.9) ( P < 0.0001). Most newly diagnosed hypertension patients were male (62.5%), 70.7% of these patients were found to be in the stage I of hypertension. The prevalence of diastolic hypertension was higher in this group compared to systolic hypertension (67.4% vs. 59.5%). The mean systolic blood pressure of this sub-group was slightly lower than known cases (140.3 mmHg vs. 141.9) ( p = 0.017). However, the mean diastolic blood pressure in this group was higher (93.1 mmHg vs. 85.8) ( P < 0.0001).
71.3% of the aware patients (33.0% of all participants with high blood pressure) were referred to physicians during the past 3 months. Younger and more educated people are less likely to go to treatment by physicians, compared to older people ( P = 0.015) and illiterate ( P = 0.024). The control of hypertension among males was significantly lower than females; also, uncontrolled hypertension increased with age ( P < 0.0001). There was no significant difference in terms of the treatment and control of hypertension between those with and without health insurance, physical activity, place of residence, or abnormal BMI (Table 2 ). Figure 1 shows a summary finding of prevalence, its unawareness and uncontrolled hypertension among adult participants.
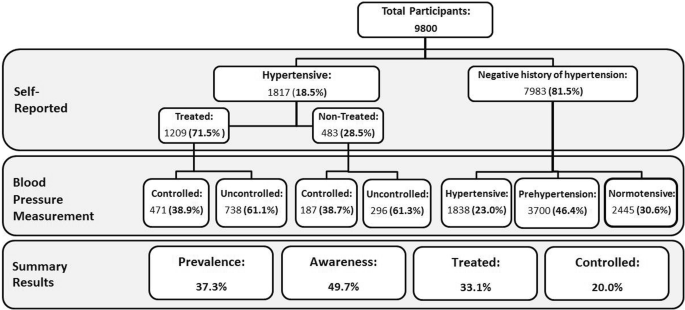
Hypertension, its awareness, and control among adults 20–69 years in Yazd Greater Area- Iran
logistic regression analysis ascertained the effects of predictors of awareness, treatment, and control of hypertension. Age, sex, BMI, physical activity, insurance, and diabetes history are able to predict changes in awareness. (χ 2 (9) = 776.154, p < 0.0001). It correctly classified 69.7% of cases. The logistic regression model was statistically significant for treatment (χ 2 = 40.748, p = 0.001) with correct classification of 71.6% cases. Physical activity, smoking, and a history of diabetes can predict changes in treatment. The model for control of hypertension classified 62.4% of cases, correctly. Age, sex, and insurance are predictors of change to control hypertension (χ 2 (9) = 66.724, p < 0.0001). Table 3 shows the contribution of each independent variable to the model and its statistical significance.
The prevalence of hypertension is high among the Yazd adult population with inappropriate awareness and controlled hypertension rates. Less than half of aware patients, who were treated, had controlled blood pressure.
The results indicate that Yazd is among the areas with high blood pressure prevalence compared to similar studies in Iran and the world [ 12 ]. The prevalence of hypertension in the world has also been reported 28.8% in high and 31.5% in low-income countries [ 27 ], indicating a worsening situation in Yazd. This might be justified by the different prevalence of risk factors due to ethnicity and lifestyle changes, or different age groups in the study. Having screening intervention programs in place, may increase the difference in the prevalence of diagnosed and treated patients across regions, as well as in one area over different years.
Almost 50% of Yazdi adults are aware of their hypertension, which is lower than in high-income countries (67%) but higher than low/middle-income countries (37.9%) [ 27 ]. In different countries this awareness has been reported from 25 to 75% [ 28 ]. Awareness in Yazd is lower compared to most studies in Iran (69.2% in Isfahan, [ 9 ] 60.5% in Tabriz [ 12 ],, and 57% in Kerman [ 29 ]. It is slightly higher than Golestan’s (46.2%) and a previous study in Yazd (43.7%) [ 12 , 16 ]. Over the past decade, the 5% awareness increase in Yazd was not satisfactory, considering increased access to health centers and increase in the number of health insured.
The study shows that about three-quarters of patients (71.5%), who were aware of their disease, had visited by the physician during the past three months. Although the treated hypertension in Yazd is higher than the world average (36.9%), [ 27 ] it is more inadequate than other studies in Iran [ 9 , 12 ]. The availability and affordability (low cost) of health care services have made this index more favorable in Iran than in the world - even in high-income countries (55.6%) [ 16 , 27 ]. Un-prescribed drug use and differences in the definition of treated people may be other reasons for this difference. Despite treatment, only 39% of the participants had controlled hypertension, which is close to the worldwide statistics (37.1%), although it was less than high-income countries (50.4%) [ 27 ]. Although the difference between treated and controlled hypertension was reported in all studies, in Iran, Isfahan (59.1%) and Tabriz (68.5%) reported a better-controlled situation [ 9 , 12 ] suggesting poor control of hypertension in Yazd. In Yazd, 71.5% of those who were aware of their hypertension was visited by a physician for receiving medication. However, in both treated and untreated groups, blood pressure control did not differ (38.9% vs. 38.7%). This was lower than the result of several studies including some from developed countries, [ 30 ] and was similar to another multinational study (32.5%) [ 12 ]. Controlled hypertension was higher among females, younger age groups; health insured and educated participants which were in line with other studies [ 12 , 31 ]. More physicians’ visits (by women), lack of other underlying diseases in young population, and low-cost access to health care for the insured, explain these predictors for better control of hypertension according to the regression analysis. A comparison of blood pressure control status in Yazd in this study with the previous study shows threefold growth. Since awareness and treatment of the disease have not changed, improved quality of treatment by physicians has been effective. The high awareness and uncontrolled hypertension may justify irregular follow-up by family physicians and primary health centers, especially in the urban areas.
Misuse of medication or lack of regular patient care, as well as inadequate medication administration, can be a cause of the disease poor control.
After adjustment, patients with older age, history of diabetes, female sex, and health insured were more likely to aware of their hypertension. More elderly referrals to physicians and health centers for treatment and periodic care justify older people’s awareness of their blood pressure compared to younger adults. In this study, less awareness of men than women can be due to lower access to health centers, employment, and less attention to their health. This association between age and sex has been confirmed in other studies [ 9 , 12 , 16 ]. However, the odds ratios between sex-age groups in geographic regions vary depending on the level of education, availability, and cost of health services.
In this study, adult education did not correlate with their awareness, which is consistent with the findings of Katibeh et al. findings in Yazd [ 32 ]. However, most studies have reported a relationship between their education and awareness of hypertension [ 33 , 34 ]. Also, there was no relationship between high education and treated hypertension, as well as the control of hypertension. Higher education in people has no effect on the management of the disease, unlike the results of others, so it requires further investigation. Individuals’ health literacy appears to be more important than education for health care.
Although health insurance was not associated with patients being treated, insurance was a predictor of hypertension awareness and control. The positive effect of health insurance was also reported in other studies [ 35 ]. This can be due to the reduced cost of receiving services in continuing care.
In our study, having a history of diabetes is a predictor for awareness and treatment of hypertension. Others have confirmed that having another medical condition (diabetes, hyperlipidemia, etc.) is associated with the awareness and treatment of hypertension [ 9 , 34 , 36 ]. It will cause people to go to health centers; as a result, hypertension will be diagnosed sooner, and medication will be started. However, having diabetes was not a predictor for blood pressure control. Different goals in defining blood pressure control and various guidelines in diabetic patients have made blood pressure control more difficult in this group [ 37 ].
Strengths and limitations
The strengths of this study are the large sample size with random multi-stage cluster sampling from different urban and rural areas, 95% participation rate, and, most importantly the three measurements of blood pressure at home according to the standard protocol by trained health care providers. Investigating the relationship between tobacco smoking, obesity, physical activity, and diabetes history with hypertension awareness and control are among the other advantages of this study. This study, however, had some limitations. This cross-sectional study and cannot investigate the causality. Hypertensive risk factors such as stress, dietary habits, and alcohol use have not been analyzed. Tobacco smoking, physical activity, and diabetes were self-reported which may produce bias. The details of drug adherence are an important variable for the control of hypertension, which was not recorded in this study. Also, it was not considered the relationship between economic factors and health services utilization with awareness and control of hypertension.
Hypertension is a public health problem in Yazd, which is not well controlled. Half of the patients were undiagnosed, and more than half of known cases of hypertension were not controlled. It can lead to high-cost cardiovascular complications. This study represents a warning message for cardiovascular health in Yazdi adults. Health policymakers must consider new strategies for prevention. Intervention for increased screening coverage is needed, especially for men. Public awareness should be raised about hypertension and improved hypertension control under the supervision of physicians should be promoted. Implementation of family physician program for health insured persons may accelerate reaching these goals.
Availability of data and materials
The data collected by Yazd Health Study are not open access but can be shared under conditions of collaboration and endowment. Data are available from the authors upon reasonable request and with the permission of the principal investigator. For further information, please visit YaHS website at www.yahs-ziba.com
Abbreviations
Blood Pressure
Joint National Committee
- Hypertension
Body Mass Index
Confidence Interval
World Health Organization
Mouhtadi BB, Kanaan RMN, Iskandarani M, Rahal MK, Halat DH. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in Lebanese adults: a cross-sectional study. Glob Cardiol Sci Pract 2018;2018(1):6. http://doi.org/ https://doi.org/10.21542/gcsp.2018.6 .
Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1659–1724. http://doi.org/ https://doi.org/10.1016/S0140-6736(16)31679-8 .
Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, et al. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1345–1422. http://doi.org/ https://doi.org/10.1016/S0140-6736(17)32366-8 .
Salem H, Hasan DM, Eameash A, El-Mageed HA, Hasan S, Ali R. Worldwide prevalence of hypertension: A pooled meta-analysis of 1670 studies in 71 countries with 29.5 million participants. J Am Coll Cardiol. 2018;71. 11_Suppl: A1819. http://doi.org/ https://doi.org/10.1016/S0735-1097(18)32360-X .
Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci 2014;16(1):126–130. http://doi.org/ https://doi.org/10.1111/nhs.12060 .
Mirzaei M, Moayedallaie S, Jabbari L, Mohammadi M. Prevalence of hypertension in Iran 1980–2012: a systematic review. J Tehran Heart Cent. 2016;11(4):159–67.
PubMed PubMed Central Google Scholar
Institute for Health Metrics and Evaluation (IHME). Iran profile. Seattle: IHME, University of Washington. Available from http://www.healthdata.org/iran . Accessed 22.11.2017.
Kazemi T, Hajihosseini M, Mashreghimoghadam H, Azdaki N, Ziaee M. Prevalence and determinants of hypertension among Iranian adults, Birjand. Iran Int J Prev Med. 2017;8:36. http://doi.org/ . https://doi.org/10.4103/ijpvm.IJPVM_103_16 .
Article PubMed Google Scholar
Eghbali M, Khosravi A, Feizi A, Mansouri A, Mahaki B, Sarrafzadegan N. Prevalence, awareness, treatment, control, and risk factors of hypertension among adults: a cross-sectional study in Iran. Epidemiol Health 2018;40:e2018020. https://doi.org/ https://doi.org/10.4178/epih.e2018020 .
Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment, and control: data from the China health and retirement longitudinal study. Bull World Health Organ 2013;92:29–41. http://doi.org/ https://doi.org/10.2471/BLT.13.124495 .
Bloch MJ. The worldwide prevalence of hypertension exceeds 1.3 billion. J Am Soc Hypertens: JASH 2016;10(10):753–754 http://doi.org/ https://doi.org/10.1016/j.jash.2016.08.006 .
Ghorbani Z, Shamshirgaran SM, Ghaffari S, Sarbakhsh P, Najafipour F, Aminisani N. Hypertension prevalence, awareness, treatment and its correlates among people 35 years and older: Result from the pilot phase of the Azar cohort study. J Educ Health Promot. 2018;7. 45. http://doi.org/ https://doi.org/10.4103/jehp.jehp_118_17 .
Esteghamati A, Etemad K, Koohpayehzadeh J, Abbasi M, Meysamie A, Khajeh E, et al. Awareness, treatment and control of pre-hypertension and hypertension among adults in Iran. Arch Iran Med. 2016;19(7):456–64 http://doi.org/0161907/AIM.003 .
PubMed Google Scholar
Shirani S, Kelishadi R, Sarrafzadegan N, Khosravi A, Sadri G, Amani A, et al. Awareness, treatment and control of hypertension, dyslipidemia and diabetes mellitus in an Iranian population: the IHHP study. East Mediterr Health J. 2009;15(6):1455–63.
CAS PubMed Google Scholar
Gandomkar A, Poustchi H, Malekzadeh F, Malekzadeh MM, Moini M, Moghadami M, et al. Prevalence, awareness, treatment, control, and correlates of hypertension in the pars cohort study. Arch Iran Med. 2018;21(8):335–43.
Kalani Z, Abdi H, Shahbazi L, Salimi T, Amini PM. Hypertension in the Yazd adult population. Payesh. 2011;10(1):101–7.
Google Scholar
Mohamed SF MM, Wamai R, Wekesah F, Haregu T,Juma P, et al. Prevalence, awareness, treatment, and control of hypertension and their determinants: results from a national survey in Kenya. BMC Public Health. 2018;18 Suppl 3:1219. http://doi.org/ https://doi.org/10.1186/s12889-018-6052-y .
Tesfaye B, Haile D, Lake B, Belachew T, Tesfaye T, Abera H. Uncontrolled hypertension and associated factors among adult hypertensive patients on follow-up at Jimma University teaching and specialized hospital: a cross-sectional study. Res Rep Clin Cardiol 2017;8:21–29. http://doi.org/ https://doi.org/10.2147/RRCC.S132126 .
Mirzaei M, Salehi-Abargouei A, Mirzaei M, Mohsenpour MA. Cohort Profile: The Yazd Health Study (YaHS): a population-based study of adults aged 20–70 years (study design and baseline population data). Int J Epidemiol. 2017;47(3):697-68h. http://doi.org/ https://doi.org/10.1093/ije/dyx231 .
Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardio Clin 2010;28(4):571–586. http://doi.org/ https://doi.org/10.1016/j.ccl.2010.07.006 .
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2571. http://doi.org/ https://doi.org/10.1001/jama.289.19.2560 .
Tran TM, Giang NM. Changes in blood pressure classification, blood pressure goals, and pharmacological treatment of essential hypertension in medical guidelines from 2003 to 2013. IJC Metabolic & Endocrine 2014;2:1–10. http://doi.org/ https://doi.org/10.1016/j.ijcme.2014.01.001 .
Moghaddam MB, Aghdam FB, Jafarabadi MA, Allahverdipour H, Nikookheslat SD, Safarpour S. The Iranian version of international physical activity questionnaire (IPAQ) in Iran: content and construct validity, factor structure, internal consistency and stability. World Appl Sci J. 2012;18(8):1073–80.
Expert Consultation WHO. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Article Google Scholar
Statistical Centre of Iran. General Population and Housing Census (2016). Iran and Yazd profile. Available from: http://amarorgir Accessed 20 December 2016.
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization 2001;9(10).
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. http://doi.org/ https://doi.org/10.1161/CIRCULATIONAHA.115.018912 .
Devi P, Rao M, Sigamani A, Faruqui A, Jose M, Gupta R, et al. Prevalence, risk factors and awareness of hypertension in India: a systematic review. J Hum Hypertens. 2013;27(5):281–7. http://doi.org/ . https://doi.org/10.1038/jhh.2012.33 .
Article CAS PubMed Google Scholar
Najafipour H, Nasri HR, Afshari M, Moazenzadeh M, Shokoohi M, Foroud A, et al. Hypertension: diagnosis, control status, and its predictors in general population aged between 15 and 75 years: a community-based study in southeastern Iran. Int J Public Health 2014;59(6):999–1009. http://doi.org/ https://doi.org/10.1007/s00038-014-0602-6 .
Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, McAlister FA, Johansen H, Baclic O, Campbell N. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open 2013;3(8): e003423. http://doi.org/ https://doi.org/10.1136/bmjopen-2013-003423 .
Babiker FA, Elkhalifa Lamia A, Moukhyer ME. Awareness of hypertension and factors associated with uncontrolled hypertension in Sudanese adults. Cardiovasc J Afr 2013;24(6):208–212. http://doi.org/ https://doi.org/10.5830/CVJA-2013-035 .
Katibeh M, Sanjari Moghaddam A, Yaseri M, Neupane D, Kallestrup P, Ahmadieh H. Hypertension and associated factors in the Islamic Republic of Iran: a population-based study. East Mediterr Health J 2020;26(3):301–311. http://doi.org/ https://doi.org/10.26719/EMHJ.19.042 .
Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001–2009. PLoS One 2013;8(4):e60308. http://doi.org/ https://doi.org/10.1371/journal.pone.0060308 .
Malekzadeh MM, Etemadi A, Kamangar F, Khademi H, Golozar A, Islami F, et al. Prevalence, awareness and risk factors of hypertension in a large cohort of Iranian adult population. J Hypertens 2013;31(7):1364–1371. http://doi.org/ https://doi.org/10.1097/HJH.0b013e3283613053 .
Maimaris W, Paty J, Perel P, Legido-Quigley H, Balabanova D, Nieuwlaat R, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med 2013;10(7):e1001490. http://doi.org/ https://doi.org/10.1371/journal.pmed.1001490 .
Ware LJ, Chidumwa G, Charlton K, Schutte AE, Kowal P. Predictors of hypertension awareness, treatment, and control in South Africa: results from the WHO-SAGE population survey (wave 2). J Hum Hypertens 2019;33(2):157–166. http://doi.org/ https://doi.org/10.1038/s41371-018-0125-3 .
Grossman A, Grossman E. Blood pressure control in type 2 diabetic patients. Cardiovasc Diabetol2017;16(1):3. http://doi.org/ https://doi.org/10.1186/s12933-016-0485-3 .
Download references
Acknowledgments
We thank the people of Yazd for giving their time to Yazd health study. We acknowledge Shahid Sadoughi University of medical sciences for funding the study.
We express our gratitude to all those who helped us in this study, especially the good people of Yazd, the health workers.
This study was funded by Shahid Sadoughi University of Medical Sciences. Funding bodies had no role in data collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Yazd Cardiovascular Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Mohsen Mirzaei & Masoud Mirzaei
Shahediah Cohort Study, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Behnam Bagheri
Department of Epidemiology and Biostatistics, School of Public Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran
Ali Dehghani
You can also search for this author in PubMed Google Scholar
Contributions
The conception of the research idea was conducted by Mohsen Mirzaei (MM1) and Masoud Mirzaei (MM2) designed the study. BB conducted the study under the supervision of MM2. MM1 and BB analyzed the data and wrote the draught of the manuscript. AD reviewed and critically revised the manuscript. All authors read and approved the final manuscript. MM2 finalized the manuscript.
Corresponding author
Correspondence to Behnam Bagheri .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in this study were approved by the ethics committee of Shahid Sadoughi University of Medical Science, Yazd, Iran (IR.SSU.MEDICINE.REC.1396.311). During the training of interviewers, principal investigator emphasis was placed on the importance of obtaining informed consent that informed that participants can choose not to answer any questions. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was funded by Shahid Sadoughi University of Medical Sciences.
Supplementary information
Additional file 1..
YaHS questionnaire (English version)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mirzaei, M., Mirzaei, M., Bagheri, B. et al. Awareness, treatment, and control of hypertension and related factors in adult Iranian population. BMC Public Health 20 , 667 (2020). https://doi.org/10.1186/s12889-020-08831-1
Download citation
Received : 22 January 2020
Accepted : 01 May 2020
Published : 12 May 2020
DOI : https://doi.org/10.1186/s12889-020-08831-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- An estimated 1.28 billion adults aged 30–79 years worldwide have hypertension, most (two-thirds) living in low- and middle-income countries
- An estimated 46% of adults with hypertension are unaware that they have the condition.
- Less than half of adults (42%) with hypertension are diagnosed and treated.
- Approximately 1 in 5 adults (21%) with hypertension have it under control.
- Hypertension is a major cause of premature death worldwide.
- One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 33% between 2010 and 2030.
Hypertension (high blood pressure) is when the pressure in your blood vessels is too high (140/90 mmHg or higher). It is common but can be serious if not treated.
People with high blood pressure may not feel symptoms. The only way to know is to get your blood pressure checked.
Things that increase the risk of having high blood pressure include:
- older age
- being overweight or obese
- not being physically active
- high-salt diet
- drinking too much alcohol
Lifestyle changes like eating a healthier diet, quitting tobacco and being more active can help lower blood pressure. Some people may still need to take medicines.
Blood pressure is written as two numbers. The first (systolic) number represents the pressure in blood vessels when the heart contracts or beats. The second (diastolic) number represents the pressure in the vessels when the heart rests between beats. Hypertension is diagnosed if, when it is measured on two different days, the systolic blood pressure readings on both days is ≥140 mmHg and/or the diastolic blood pressure readings on both days is ≥90 mmHg.
Risk factors
Modifiable risk factors include unhealthy diets (excessive salt consumption, a diet high in saturated fat and trans fats, low intake of fruits and vegetables), physical inactivity, consumption of tobacco and alcohol, and being overweight or obese. In addition, there are environmental risk factors for hypertension and associated diseases, where air pollution is the most significant. Non-modifiable risk factors include a family history of hypertension, age over 65 years and co-existing diseases such as diabetes or kidney disease.
Most people with hypertension don’t feel any symptoms. Very high blood pressures can cause headaches, blurred vision, chest pain and other symptoms.
Checking your blood pressure is the best way to know if you have high blood pressure. If hypertension isn’t treated, it can cause other health conditions like kidney disease, heart disease and stroke.
People with very high blood pressure (usually 180/120 or higher) can experience symptoms including:
- severe headaches
- difficulty breathing
- blurred vision or other vision changes
- buzzing in the ears
- abnormal heart rhythm
If you are experiencing any of these symptoms and a high blood pressure, seek care immediately.
The only way to detect hypertension is to have a health professional measure blood pressure. Having blood pressure measured is quick and painless. Although individuals can measure their own blood pressure using automated devices, an evaluation by a health professional is important for assessment of risk and associated conditions.
Lifestyle changes can help lower high blood pressure. These include:
- eating a healthy, low-salt diet
- losing weight
- being physically active
- quitting tobacco.
If you have high blood pressure, your doctor may recommend one or more medicines. Your recommended blood pressure goal may depend on what other health conditions you have.
Blood pressure goal is less than 130/80 if you have:
- cardiovascular disease (heart disease or stroke)
- diabetes (high blood sugar)
- chronic kidney disease
- high risk for cardiovascular disease.
For most people, the goal is to have a blood pressure less than 140/90.
There are several common blood pressure medicines:
- ACE inhibitors including enalapril and lisinopril relax blood vessels and prevent kidney damage.
- Angiotensin-2 receptor blockers (ARBs) including losartan and telmisartan relax blood vessels and prevent kidney damage.
- Calcium channel blockers including amlodipine and felodipine relax blood vessels.
- Diuretics including hydrochlorothiazide and chlorthalidone eliminate extra water from the body, lowering blood pressure.
Lifestyle changes can help lower high blood pressure and can help anyone with hypertension. Many who make these changes will still need to take medicine.
These lifestyle changes can help prevent and lower high blood pressure.
- Eat more vegetables and fruits.
- Get at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous aerobic activity.
- Do strength building exercises 2 or more days each week.
- Lose weight if you’re overweight or obese.
- Take medicines as prescribed by your health care professional.
- Keep appointments with your health care professional.
Don’t:
- eat too much salty food (try to stay under 2 grams per day)
- eat foods high in saturated or trans fats
- smoke or use tobacco
- drink too much alcohol (1 drink daily max for women, 2 for men)
- miss or share medication.
Reducing hypertension prevents heart attack, stroke and kidney damage, as well as other health problems.
Reduce the risks of hypertension by:
- reducing and managing stress
- regularly checking blood pressure
- treating high blood pressure
- managing other medical conditions
- reducing exposure to polluted air.
Complications of uncontrolled hypertension
Among other complications, hypertension can cause serious damage to the heart. Excessive pressure can harden arteries, decreasing the flow of blood and oxygen to the heart. This elevated pressure and reduced blood flow can cause:
- chest pain, also called angina;
- heart attack, which occurs when the blood supply to the heart is blocked and heart muscle cells die from lack of oxygen. The longer the blood flow is blocked, the greater the damage to the heart;
- heart failure, which occurs when the heart cannot pump enough blood and oxygen to other vital body organs; and
- irregular heart beat which can lead to a sudden death.
Hypertension can also burst or block arteries that supply blood and oxygen to the brain, causing a stroke.
In addition, hypertension can cause kidney damage, leading to kidney failure.
Hypertension in low- and middle-income countries
The prevalence of hypertension varies across regions and country income groups. The WHO African Region has the highest prevalence of hypertension (27%) while the WHO Region of the Americas has the lowest prevalence of hypertension (18%).
The number of adults with hypertension increased from 594 million in 1975 to 1.13 billion in 2015, with the increase seen largely in low- and middle-income countries. This increase is due mainly to a rise in hypertension risk factors in those populations.
WHO response
The World Health Organization (WHO) supports countries to reduce hypertension as a public health problem.
In 2021, WHO released a new guideline for on the pharmacological treatment of hypertension in adults. The publication provides evidence-based recommendations for the initiation of treatment of hypertension, and recommended intervals for follow-up. The document also includes target blood pressure to be achieved for control, and information on who, in the health-care system, can initiate treatment.
To support governments in strengthening the prevention and control of cardiovascular disease, WHO and the United States Centers for Disease Control and Prevention (U.S. CDC) launched the Global Hearts Initiative in September 2016, which includes the HEARTS technical package. The six modules of the HEARTS technical package (Healthy-lifestyle counselling, Evidence-based treatment protocols, Access to essential medicines and technology, Risk-based management, Team-based care, and Systems for monitoring) provide a strategic approach to improve cardiovascular health in countries across the world.
In September 2017, WHO began a partnership with Resolve to Save Lives, an initiative of Vital Strategies, to support national governments to implement the Global Hearts Initiative. Other partners contributing to the Global Hearts Initiative are the CDC Foundation, the Global Health Advocacy Incubator, the Johns Hopkins Bloomberg School of Public Health, the Pan American Health Organization (PAHO) and the U.S. CDC. Since implementation of the programme in 2017 in 31 countries low- and middle-income countries, 7.5 million people have been put on protocol-based hypertension treatment through person-centred models of care. These programmes demonstrate the feasibility and effectiveness of standardized hypertension control programmes.
- More on hypertension
Hypertension: A Case Study
- January 2022
- 8(7):379 - 381

- Eternal University

- Akal College of Nursing Eternal University Baru Sahib.

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Muthu Kumaran

- Suzanne Oparil
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

IMAGES
VIDEO
COMMENTS
1. Introduction. Hypertension is a major public health problem due to its high prevalence all around the globe [1-4].Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [].It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [].Raised blood pressure is a major risk factor for chronic heart disease, stroke ...
1 Introduction. Hypertension is defined as a persistence increase in blood pressure above the normal range of 120/80 mmHg. The prevalence of hypertension increases with advancing age. The persistent and chronic elevated arterial pressure causes marked pathological changes in the vasculature and heart.
Thesis CENTRAL OSTROBOTHNIA UNIVERSITY OF APPLIED SCIENCES Degree Programme in Nursing September 2011 . ... 1 INTRODUCTION 1 2 MAIN CONCEPTS 3 2.1 Hypertension 3 ... Hypertension is a public health problem and a term used to describe HBP. It is a . of hypertension? 20 - , .
Introduction. Between 1980 and 2010, the proportion of the world's population with high blood pressure (defined as systolic and or diastolic blood pressure ≥ 140/90 mmHg) or uncontrolled hypertension had dropped modestly. ... Hypertension: defined as a mean measured blood pressure of ≥ 140 mmHg systolic and/or the mean measured diastolic ...
Introduction. Essential or primary hypertension, ... Hypertension control was rarely achieved and in fact worsened from 7.1% to 4.5% (p<0.01). Over the study period, mean body mass index, systolic and diastolic blood pressure, and mean waist circumference all significantly increased (p<0.01).
Results: Among adults aged 20 to 79 years, 24% of males and 23% of females had hypertension, de ned as measured BP ≥140/90 mm Hg or past-month use. of antihypertensive medication. Hyper tension ...
Introduction. Hypertension (HTN), defined as systolic blood pressure (SBP) > 140 mmHg or diastolic blood pressure (DBP) > 90 mmHg, is a major growing health problem across the globe [1-5]. It is the most common risk factor for cardiovascular disease and affects nearly two-thirds of adults aged 60 years or older [1,2].
393. HYPERTENSION: AN OVERVIEW. Aditya Dixit [a]* and Prashant Kumar Dhakad [a] Keywords: Systolic, diastolic, cardiovascular, cerebrovascular, angiotensin. Hypertension is a serious challenge ...
stroke across people with hypertension was 3.59% for Thai older men and 2.80% for older Thai women (Suwanwela, 2014). Hypertension is a chronic disease that puts an individual at risk for long-term health problems. Research on patients' knowledge about their hypertension suggests that patients perceived hypertension as a chronic lifelong ...
An Honors Thesis submitted in partial fulfillment of the requirements for Honors in . Waters College of Health Professions. By . Sarah Hogg. ... Introduction . Hypertension is a global public health crisis. It is the largest risk factor for cardiovascular disease, which is the leading cause of death globally. ...
CHAPTER ONE. INTRODUCTION Problem Description Approximately one in three American adults have hypertension (HTN) (Arnett et al., 2019). HTN is defined as a blood pressure greater than or equal to 140/90 mmHg. There is a 90% lifetime risk of developing HTN among those aged 55 and older who currently have normal blood pressure.
Background Hypertension, known as the silent killer, is a major risk factor for cardiovascular disease. Awareness and treatment of hypertension is not appropriate in the world, and this has led to an increase in mortality and morbidity caused by uncontrolled hypertension. This study aims to estimate awareness, treated, and controlled hypertensive and relevant predictors in an adult Iranian ...
Hypertension is a leading cause of cardiovascular and cerebrovascular morbidity and mortality worldwide. Treatment-resistant hypertension represents a cohort of patients with treated hypertension with at least 3 antihypertensives. In this thesis the important role of adherence testing, and prevalence of non-adherence is
1 INTRODUCTION This thesis focuses on lifestyle modification and patient empowerment on preven-tion of hypertension. Hypertension affects about 40% adults worldwide and it's known to be one of cardiovascular risk factors. Blood pressure tends to elevate due to several risk factors such as aging, lifestyle and medications. Lifestyle modification
Microsoft Word - Thesis_CHAPTER 1.doc. CHAPTER 1. INTRODUCTION. Hypertension is defined as high blood pressure (Hock et al., 1995). It is. known as a worldwide problem as 15-20% of all adults are affected by this condition. (Wang et al., 2008). Being one of the major risk factors for coronary heart disease,
analysis. The results revealed that overall self-management among patients with. hypertension was at a moderate level (M = 2.55, SD = 0.47). For five sub-dimensions. of self-management, the means of self-integration, self-regulation, interaction, self-. monitoring, and adherence, were also at the moderate level.
Background: Hypertension exerts a substantial public health burden on cardiovascular health and healthcare systems in India. Decision support systems (DSS), defined as tools that help clinicians ...
Robert M. Carey. Resistant hypertension is defined as failure to achieve goal blood pressure (BP) <140/90 mm Hg (or <130/80 mm Hg in patients with diabetes mellitus or chronic kidney disease) in patients with hypertension who are compliant with maxi-mum tolerated doses of an appropriate antihypertensive drug regimen consisting of a minimum of 3 ...
aware of hypertension and less than 42% of the adult are diagnosed and treated for hyperten-sion. Hypertension is a leading cause of premature death all over the world. The world health organization's targets for this disease is to prevent its prevalence worldwide by 33% between 2010 to 2030. (WHO 2021.)
Overview. Hypertension (high blood pressure) is when the pressure in your blood vessels is too high (140/90 mmHg or higher). It is common but can be serious if not treated. People with high blood pressure may not feel symptoms. The only way to know is to get your blood pressure checked.
1) Distance from the heart and 2) Nature of the blood vessel. Blood pressure is more in blood vessels close to the heart. Blood pressure is more in arterial system than in the venous system. This is because walls of arteries are thicker and less elastic; the walls of the veins are thinner and more elastic.
Hypertension is a medical condition in which blood pressure is chronically elevated. According to WHO World Health Report 2002, there are approximately 600 million people suffering from ...
Complete Thesis of Hypertension (2) - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. This document appears to be a thesis submitted by Abdul Ahad to fulfill requirements for a Pharm-D degree at the University of Balochistan in Quetta, Pakistan. The thesis assesses awareness and knowledge of hypertension among students at the University of ...