- Brain & Nervous System

What to Know About Speech Impairment

A speech impairment affects people who have problems speaking in a regular tone of voice or tempo. Speech impairments make it hard for people to communicate properly, and they can happen in both children and adults.
These disorders can cause frustration and embarrassment to the person suffering from them.
What is Speech Impairment?
People who have speech impairments have a hard time pronouncing different speech sounds. They might distort the sounds of some words and leave other sounds out completely.
There are three general categories of speech impairment:
- Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production.
- Voice disorder. A voice disorder means you have an atypical tone of voice. It could be an unusual pitch, quality, resonance, or volume.
- Articulation disorder. If you have an articulation disorder, you might distort certain sounds. You could also fully omit sounds.
Stuttering , or stammering, is a common fluency disorder that affects about 3 million Americans. It usually affects young children who are just learning to speak, but it can continue on into adulthood.
Speech and language impairments are two words that are often used interchangeably, but they are two very different types of problems.
Speech means talking. It uses the jaw muscles, tongue, lips, and vocal chords. Language is a set of words and symbols made to communicate a message. Language and speech disorders can affect you separately, or both can happen at the same time.
Types of Speech Impairments
Speech impairments can begin in childhood and carry on through your adult years. Others can happen due to trauma, or after a medical event like a stroke.
The types of speech impairments are:
- Childhood apraxia of speech. This can happen to children when it’s time for them to start talking. The brain’s signals don’t communicate with the mouth, so the child can’t move their lips and tongue in the way they’re mean to.
- Dysarthria. This type of speech impairment happens when the muscles you use to talk are too weak, and can’t form words properly.
- Orofacial myofunctional disorders (OMD). OMDs are characterized by an abnormal pattern of facial muscle use. OMD interferes with how the facial muscles, including the tongue, are used. People who suffer from OMD might also struggle to breathe through their nose.
- Speech sound disorders. It’s normal for children to struggle to pronounce certain sounds as they learn to talk. But after ages four or five, constant mispronunciation might signal a problem. It can continue into adulthood, or some people get it after a stroke.
- Stuttering. Stuttering can mean repeating words or sounds like “uh” and “um” (disfluencies) involuntarily. Stuttering can be intensified by strong emotions or stress.
- Voice. A voice disorder can mean you “lost” your voice because you stressed it too much. It can also mean a chronic cough or paralysis of the vocal cords, among others.
Health Issues That Affect Speech Impairment
Other than childhood speech impairments, there are a range of reasons you could get one in your adult years. They can happen due to a traumatic event, illness, or surgery.
Dysarthria , aphasia, and voice disturbances can happen in adulthood, and are usually due to these medical events.
Aphasia. Aphasia is the loss of ability to understand words, spoken or written. There are many types of aphasia . It can happen after a stroke or if a tumor reaches the part of the brain where language is processed.
Medical issues that can cause aphasia:
- Head trauma
- Transient ischemic attack (TIA)
- Brain tumor
- Alzheimer’s disease
Dysarthria. Dysarthria is usually caused by a nerve problem. The person suffering from it loses the ability to make certain sounds or might have poor pronunciation. It can also affect your ability to control the tongue, larynx, lips, and vocal chords.
Medical issues that can cause dysarthria:
- Facial trauma
- Diseases that affect your nervous system
- Side effects of certain medication
- Alcoholic intoxication
- Dentures that don’t fit properly
- Transient ischemic attack (TIA)
Voice disturbances. Traumatic events or extreme stress placed on the vocal cords can cause you to “lose” your voice or have a vocal disturbance. Disease can also affect the way your voice sounds.
Cancerous or noncancerous growths or nodules on the vocal cords can make your voice sound different.
Understanding Speech Impairments
Having a speech impairment can be a very frustrating and embarrassing experience for the person experiencing it. It’s important to be patient and understanding when communicating.
Try the following tips to improve communication and foster an accepting environment with someone who has a speech impairment:
- Speak slowly and use hand gestures
- Keep a pen and paper handy in case it’s needed to communicate
- Maintain a calm environment free of stimulating sounds
- Use simple phrases when you speak
- Use your normal tone of voice
Consulting with a mental health care provider can help with feelings of anger and depression that can accompany speech impairments.

Top doctors in ,
Find more top doctors on, related links.
- Brain & Nervous System News & Features
- Brain & Nervous System Reference
- Brain & Nervous System Slideshows
- Brain & Nervous System Quizzes
- Brain & Nervous System Videos
- Find a Neurologist
- Living Better With MS
- Alzheimer's Disease
- Creutzfeldt-Jakob Disease
- Guillain-Barré Syndrome
- Lou Gehrig’s Disease (ALS)
- Multiple Sclerosis
- Parkinson's Disease
- Restless Legs Syndrome
- Spinal Muscular Atrophy
- More Related Topics
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
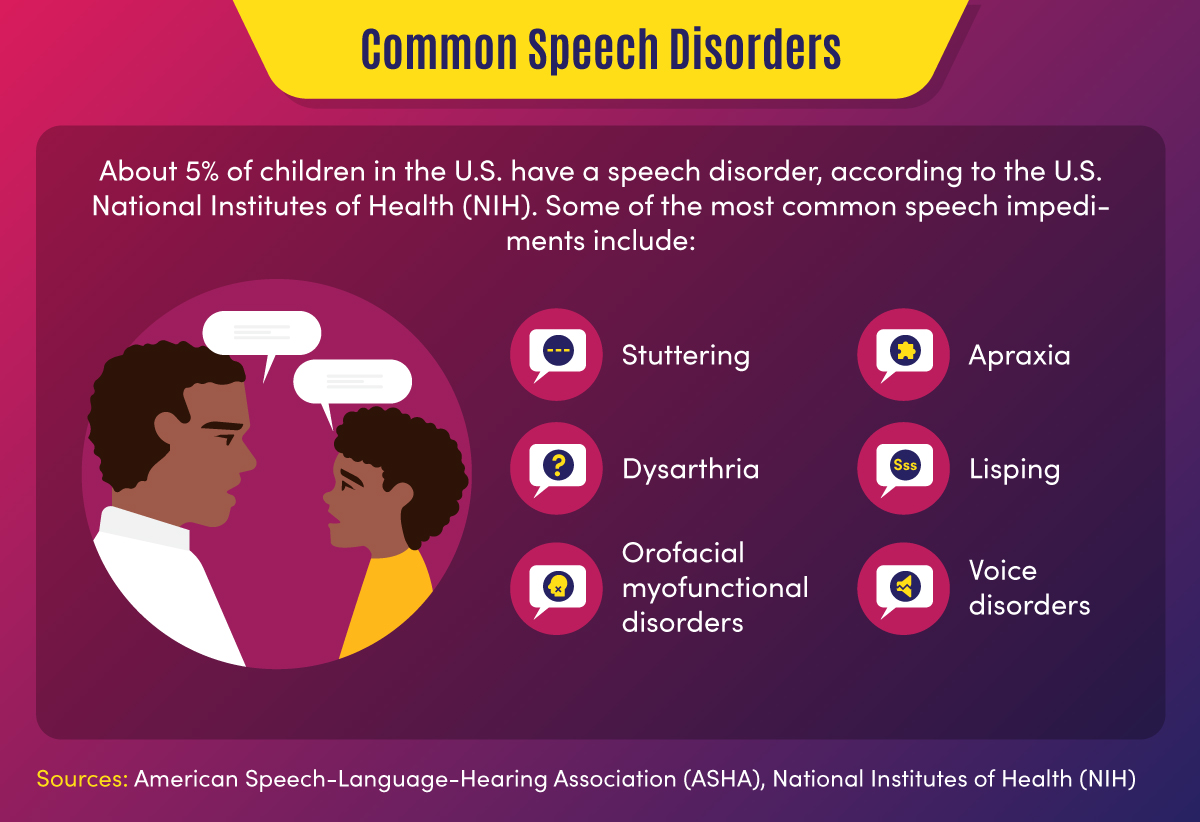
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.

- Bachelor’s Degrees
- Master’s Degrees
- Doctorate Degrees
- Certificate Programs
- Nursing Degrees
- Cybersecurity
- Human Services
- Science & Mathematics
- Communication
- Liberal Arts
- Social Sciences
- Computer Science
- Admissions Overview
- Tuition and Financial Aid
- Incoming Freshman and Graduate Students
- Transfer Students
- Military Students
- International Students
- Early Access Program
- About Maryville
- Our Faculty
- Our Approach
- Our History
- Accreditation
- Tales of the Brave
- Student Support Overview
- Online Learning Tools
- Infographics
Home / Blog
Speech Impediment Guide: Definition, Causes, and Resources
December 8, 2020

Tables of Contents
What Is a Speech Impediment?
Types of speech disorders, speech impediment causes, how to fix a speech impediment, making a difference in speech disorders.
Communication is a cornerstone of human relationships. When an individual struggles to verbalize information, thoughts, and feelings, it can cause major barriers in personal, learning, and business interactions.
Speech impediments, or speech disorders, can lead to feelings of insecurity and frustration. They can also cause worry for family members and friends who don’t know how to help their loved ones express themselves.
Fortunately, there are a number of ways that speech disorders can be treated, and in many cases, cured. Health professionals in fields including speech-language pathology and audiology can work with patients to overcome communication disorders, and individuals and families can learn techniques to help.

Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual’s ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
Some 7.7% of U.S. children — or 1 in 12 youths between the ages of 3 and 17 — have speech, voice, language, or swallowing disorders, according to the National Institute on Deafness and Other Communication Disorders (NIDCD). About 70 million people worldwide, including some 3 million Americans, experience stuttering difficulties, according to the Stuttering Foundation.
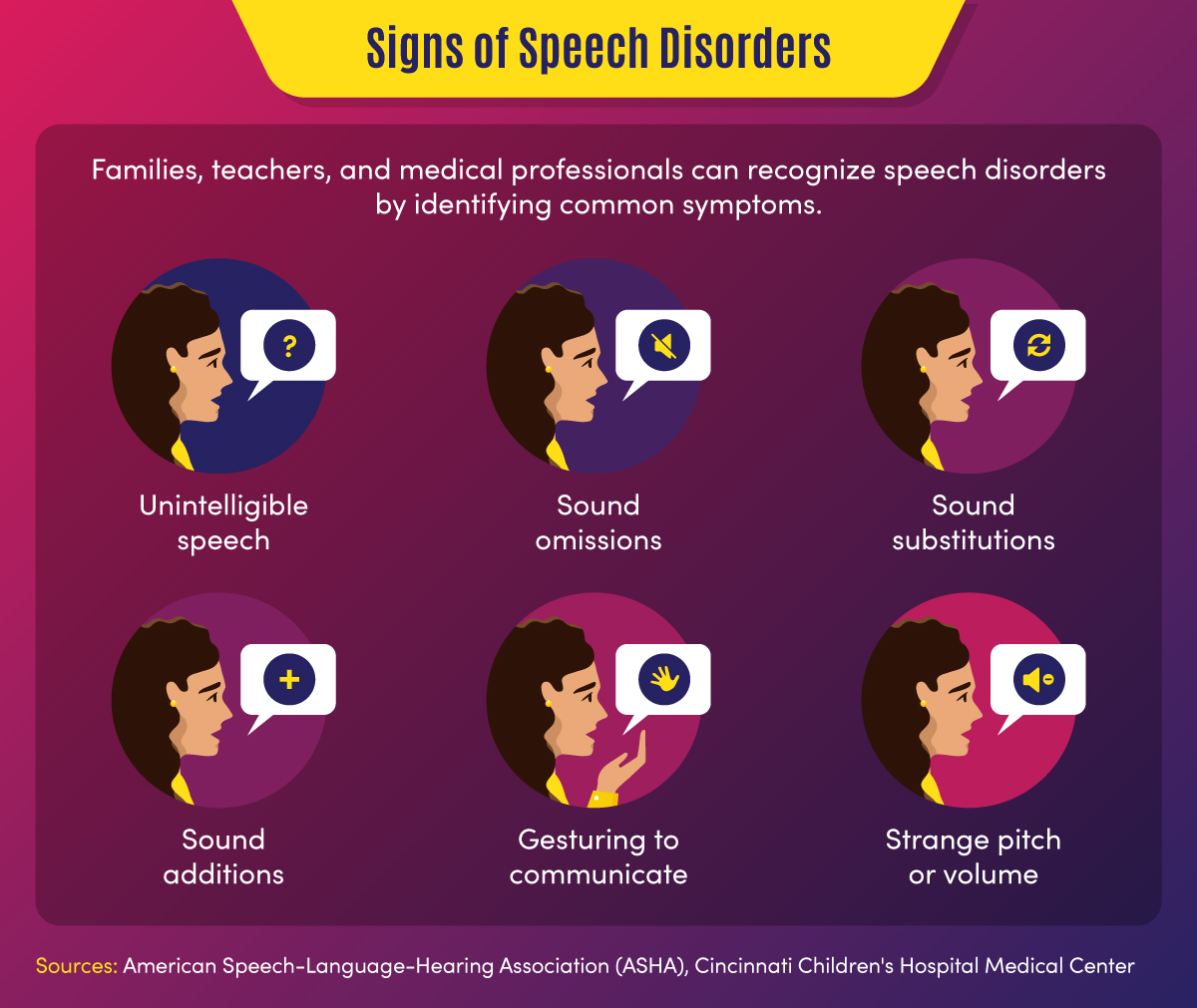
Common signs of a speech disorder
There are several symptoms and indicators that can point to a speech disorder.
- Unintelligible speech — A speech disorder may be present when others have difficulty understanding a person’s verbalizations.
- Omitted sounds — This symptom can include the omission of part of a word, such as saying “bo” instead of “boat,” and may include omission of consonants or syllables.
- Added sounds — This can involve adding extra sounds in a word, such as “buhlack” instead of “black,” or repeating sounds like “b-b-b-ball.”
- Substituted sounds — When sounds are substituted or distorted, such as saying “wabbit” instead of “rabbit,” it may indicate a speech disorder.
- Use of gestures — When individuals use gestures to communicate instead of words, a speech impediment may be the cause.
- Inappropriate pitch — This symptom is characterized by speaking with a strange pitch or volume.
In children, signs might also include a lack of babbling or making limited sounds. Symptoms may also include the incorrect use of specific sounds in words, according to the American Speech-Language-Hearing Association (ASHA). This may include the sounds p, m, b, w, and h among children aged 1-2, and k, f, g, d, n, and t for children aged 2-3.
Back To Top
Categories of Speech Impediments
Speech impediments can range from speech sound disorders (articulation and phonological disorders) to voice disorders. Speech sound disorders may be organic — resulting from a motor or sensory cause — or may be functional with no known cause. Voice disorders deal with physical problems that limit speech. The main categories of speech impediments include the following:
Fluency disorders occur when a patient has trouble with speech timing or rhythms. This can lead to hesitations, repetitions, or prolonged sounds. Fluency disorders include stuttering (repetition of sounds) or (rapid or irregular rate of speech).
Resonance disorders are related to voice quality that is impacted by the shape of the nose, throat, and/or mouth. Examples of resonance disorders include hyponasality and cul-de-sac resonance.
Articulation disorders occur when a patient has difficulty producing speech sounds. These disorders may stem from physical or anatomical limitations such as muscular, neuromuscular, or skeletal support. Examples of articulation speech impairments include sound omissions, substitutions, and distortions.
Phonological disorders result in the misuse of certain speech sounds to form words. Conditions include fronting, stopping, and the omission of final consonants.
Voice disorders are the result of problems in the larynx that harm the quality or use of an individual’s voice. This can impact pitch, resonance, and loudness.
Impact of Speech Disorders
Some speech disorders have little impact on socialization and daily activities, but other conditions can make some tasks difficult for individuals. Following are a few of the impacts of speech impediments.
- Poor communication — Children may be unable to participate in certain learning activities, such as answering questions or reading out loud, due to communication difficulties. Adults may avoid work or social activities such as giving speeches or attending parties.
- Mental health and confidence — Speech disorders may cause children or adults to feel different from peers, leading to a lack of self-confidence and, potentially, self-isolation.
Resources on Speech Disorders
The following resources may help those who are seeking more information about speech impediments.
Health Information : Information and statistics on common voice and speech disorders from the NIDCD
Speech Disorders : Information on childhood speech disorders from Cincinnati Children’s Hospital Medical Center
Speech, Language, and Swallowing : Resources about speech and language development from the ASHA
Children and adults can suffer from a variety of speech impairments that may have mild to severe impacts on their ability to communicate. The following 10 conditions are examples of specific types of speech disorders and voice disorders.
1. Stuttering
This condition is one of the most common speech disorders. Stuttering is the repetition of syllables or words, interruptions in speech, or prolonged use of a sound.
This organic speech disorder is a result of damage to the neural pathways that connect the brain to speech-producing muscles. This results in a person knowing what they want to say, but being unable to speak the words.
This consists of the lost ability to speak, understand, or write languages. It is common in stroke, brain tumor, or traumatic brain injury patients.
4. Dysarthria
This condition is an organic speech sound disorder that involves difficulty expressing certain noises. This may involve slurring, or poor pronunciation, and rhythm differences related to nerve or brain disorders.
The condition of lisping is the replacing of sounds in words, including “th” for “s.” Lisping is a functional speech impediment.
6. Hyponasality
This condition is a resonance disorder related to limited sound coming through the nose, causing a “stopped up” quality to speech.
7. Cul-de-sac resonance
This speech disorder is the result of blockage in the mouth, throat, or nose that results in quiet or muffled speech.
8. Orofacial myofunctional disorders
These conditions involve abnormal patterns of mouth and face movement. Conditions include tongue thrusting (fronting), where individuals push out their tongue while eating or talking.
9. Spasmodic Dysphonia
This condition is a voice disorder in which spasms in the vocal cords produce speech that is hoarse, strained, or jittery.
10. Other voice disorders
These conditions can include having a voice that sounds breathy, hoarse, or scratchy. Some disorders deal with vocal folds closing when they should open (paradoxical vocal fold movement) or the presence of polyps or nodules in the vocal folds.
Speech Disorders vs. Language Disorders
Speech disorders deal with difficulty in creating sounds due to articulation, fluency, phonology, and voice problems. These problems are typically related to physical, motor, sensory, neurological, or mental health issues.
Language disorders, on the other hand, occur when individuals have difficulty communicating the meaning of what they want to express. Common in children, these disorders may result in low vocabulary and difficulty saying complex sentences. Such a disorder may reflect difficulty in comprehending school lessons or adopting new words, or it may be related to a learning disability such as dyslexia. Language disorders can also involve receptive language difficulties, where individuals have trouble understanding the messages that others are trying to convey.
Resources on Types of Speech Disorders
The following resources may provide additional information on the types of speech impediments.
Common Speech Disorders: A guide to the most common speech impediments from GreatSpeech
Speech impairment in adults: Descriptions of common adult speech issues from MedlinePlus
Stuttering Facts: Information on stuttering indications and causes from the Stuttering Foundation
Speech disorders may be caused by a variety of factors related to physical features, neurological ailments, or mental health conditions. In children, they may be related to developmental issues or unknown causes and may go away naturally over time.
Physical and neurological issues. Speech impediment causes related to physical characteristics may include:
- Brain damage
- Nervous system damage
- Respiratory system damage
- Hearing difficulties
- Cancerous or noncancerous growths
- Muscle and bone problems such as dental issues or cleft palate
Mental health issues. Some speech disorders are related to clinical conditions such as:
- Autism spectrum disorder
- Down syndrome or other genetic syndromes
- Cerebral palsy or other neurological disorders
- Multiple sclerosis
Some speech impairments may also have to do with family history, such as when parents or siblings have experienced language or speech difficulties. Other causes may include premature birth, pregnancy complications, or delivery difficulties. Voice overuse and chronic coughs can also cause speech issues.
The most common way that speech disorders are treated involves seeking professional help. If patients and families feel that symptoms warrant therapy, health professionals can help determine how to fix a speech impediment. Early treatment is best to curb speech disorders, but impairments can also be treated later in life.
Professionals in the speech therapy field include speech-language pathologists (SLPs) . These practitioners assess, diagnose, and treat communication disorders including speech, language, social, cognitive, and swallowing disorders in both adults and children. They may have an SLP assistant to help with diagnostic and therapy activities.
Speech-language pathologists may also share a practice with audiologists and audiology assistants. Audiologists help identify and treat hearing, balance, and other auditory disorders.
How Are Speech Disorders Diagnosed?
Typically, a pediatrician, social worker, teacher, or other concerned party will recognize the symptoms of a speech disorder in children. These individuals, who frequently deal with speech and language conditions and are more familiar with symptoms, will recommend that parents have their child evaluated. Adults who struggle with speech problems may seek direct guidance from a physician or speech evaluation specialist.
When evaluating a patient for a potential speech impediment, a physician will:
- Conduct hearing and vision tests
- Evaluate patient records
- Observe patient symptoms
A speech-language pathologist will conduct an initial screening that might include:
- An evaluation of speech sounds in words and sentences
- An evaluation of oral motor function
- An orofacial examination
- An assessment of language comprehension
The initial screening might result in no action if speech symptoms are determined to be developmentally appropriate. If a disorder is suspected, the initial screening might result in a referral for a comprehensive speech sound assessment, comprehensive language assessment, audiology evaluation, or other medical services.
Initial assessments and more in-depth screenings might occur in a private speech therapy practice, rehabilitation center, school, childcare program, or early intervention center. For older adults, skilled nursing centers and nursing homes may assess patients for speech, hearing, and language disorders.
How Are Speech Impediments Treated?
Once an evaluation determines precisely what type of speech sound disorder is present, patients can begin treatment. Speech-language pathologists use a combination of therapy, exercise, and assistive devices to treat speech disorders.
Speech therapy might focus on motor production (articulation) or linguistic (phonological or language-based) elements of speech, according to ASHA. There are various types of speech therapy available to patients.
Contextual Utilization — This therapeutic approach teaches methods for producing sounds consistently in different syllable-based contexts, such as phonemic or phonetic contexts. These methods are helpful for patients who produce sounds inconsistently.
Phonological Contrast — This approach focuses on improving speech through emphasis of phonemic contrasts that serve to differentiate words. Examples might include minimal opposition words (pot vs. spot) or maximal oppositions (mall vs. call). These therapy methods can help patients who use phonological error patterns.
Distinctive Feature — In this category of therapy, SLPs focus on elements that are missing in speech, such as articulation or nasality. This helps patients who substitute sounds by teaching them to distinguish target sounds from substituted sounds.
Core Vocabulary — This therapeutic approach involves practicing whole words that are commonly used in a specific patient’s communications. It is effective for patients with inconsistent sound production.
Metaphon — In this type of therapy, patients are taught to identify phonological language structures. The technique focuses on contrasting sound elements, such as loud vs. quiet, and helps patients with unintelligible speech issues.
Oral-Motor — This approach uses non-speech exercises to supplement sound therapies. This helps patients gain oral-motor strength and control to improve articulation.
Other methods professionals may use to help fix speech impediments include relaxation, breathing, muscle strengthening, and voice exercises. They may also recommend assistive devices, which may include:
- Radio transmission systems
- Personal amplifiers
- Picture boards
- Touch screens
- Text displays
- Speech-generating devices
- Hearing aids
- Cochlear implants
Resources for Professionals on How to Fix a Speech Impediment
The following resources provide information for speech therapists and other health professionals.
Assistive Devices: Information on hearing and speech aids from the NIDCD
Information for Audiologists: Publications, news, and practice aids for audiologists from ASHA
Information for Speech-Language Pathologists: Publications, news, and practice aids for SLPs from ASHA
Speech Disorder Tips for Families
For parents who are concerned that their child might have a speech disorder — or who want to prevent the development of a disorder — there are a number of activities that can help. The following are tasks that parents can engage in on a regular basis to develop literacy and speech skills.
- Introducing new vocabulary words
- Reading picture and story books with various sounds and patterns
- Talking to children about objects and events
- Answering children’s questions during routine activities
- Encouraging drawing and scribbling
- Pointing to words while reading books
- Pointing out words and sentences in objects and signs
Parents can take the following steps to make sure that potential speech impediments are identified early on.
- Discussing concerns with physicians
- Asking for hearing, vision, and speech screenings from doctors
- Requesting special education assessments from school officials
- Requesting a referral to a speech-language pathologist, audiologist, or other specialist
When a child is engaged in speech therapy, speech-language pathologists will typically establish collaborative relationships with families, sharing information and encouraging parents to participate in therapy decisions and practices.
SLPs will work with patients and their families to set goals for therapy outcomes. In addition to therapy sessions, they may develop activities and exercises for families to work on at home. It is important that caregivers are encouraging and patient with children during therapy.
Resources for Parents on How to Fix a Speech Impediment
The following resources provide additional information on treatment options for speech disorders.
Speech, Language, and Swallowing Disorders Groups: Listing of self-help groups from ASHA
ProFind: Search tool for finding certified SLPs and audiologists from ASHA
Baby’s Hearing and Communication Development Checklist: Listing of milestones that children should meet by certain ages from the NIDCD
If identified during childhood, speech disorders can be corrected efficiently, giving children greater communication opportunities. If left untreated, speech impediments can cause a variety of problems in adulthood, and may be more difficult to diagnose and treat.
Parents, teachers, doctors, speech and language professionals, and other concerned parties all have unique responsibilities in recognizing and treating speech disorders. Through professional therapy, family engagement, positive encouragement and a strong support network, individuals with speech impediments can overcome their challenges and develop essential communication skills.
Additional Sources
American Speech-Language-Hearing Association, Speech Sound Disorders
Identify the Signs, Signs of Speech and Language Disorders
Intermountain Healthcare, Phonological Disorders
MedlinePlus, Speech disorders – children
National Institutes of Health, National Institutes on Deafness and Other Communication Disorders, “Quick Statistics About Voice, Speech, Language”
Bring us your ambition and we’ll guide you along a personalized path to a quality education that’s designed to change your life.
Take Your Next Brave Step
Receive information about the benefits of our programs, the courses you'll take, and what you need to apply.

10 Most Common Speech-Language Disorders & Impediments
As you get to know more about the field of speech-language pathology you’ll increasingly realize why SLPs are required to earn at least a master’s degree . This stuff is serious – and there’s nothing easy about it.
In 2016 the National Institute on Deafness and Other Communication Disorders reported that 7.7% of American children have been diagnosed with a speech or swallowing disorder. That comes out to nearly one in 12 children, and gets even bigger if you factor in adults.
Whether rooted in psycho-speech behavioral issues, muscular disorders, or brain damage, nearly all the diagnoses SLPs make fall within just 10 common categories…
Types of Speech Disorders & Impediments
Apraxia of speech (aos).
Apraxia of Speech (AOS) happens when the neural pathway between the brain and a person’s speech function (speech muscles) is lost or obscured. The person knows what they want to say – they can even write what they want to say on paper – however the brain is unable to send the correct messages so that speech muscles can articulate what they want to say, even though the speech muscles themselves work just fine. Many SLPs specialize in the treatment of Apraxia .
There are different levels of severity of AOS, ranging from mostly functional, to speech that is incoherent. And right now we know for certain it can be caused by brain damage, such as in an adult who has a stroke. This is called Acquired AOS.
However the scientific and medical community has been unable to detect brain damage – or even differences – in children who are born with this disorder, making the causes of Childhood AOS somewhat of a mystery. There is often a correlation present, with close family members suffering from learning or communication disorders, suggesting there may be a genetic link.
Mild cases might be harder to diagnose, especially in children where multiple unknown speech disorders may be present. Symptoms of mild forms of AOS are shared by a range of different speech disorders, and include mispronunciation of words and irregularities in tone, rhythm, or emphasis (prosody).
Stuttering – Stammering
Stuttering, also referred to as stammering, is so common that everyone knows what it sounds like and can easily recognize it. Everyone has probably had moments of stuttering at least once in their life. The National Institute on Deafness and Other Communication Disorders estimates that three million Americans stutter, and reports that of the up-to-10-percent of children who do stutter, three-quarters of them will outgrow it. It should not be confused with cluttering.
Most people don’t know that stuttering can also include non-verbal involuntary or semi-voluntary actions like blinking or abdominal tensing (tics). Speech language pathologists are trained to look for all the symptoms of stuttering , especially the non-verbal ones, and that is why an SLP is qualified to make a stuttering diagnosis.
The earliest this fluency disorder can become apparent is when a child is learning to talk. It may also surface later during childhood. Rarely if ever has it developed in adults, although many adults have kept a stutter from childhood.
Stuttering only becomes a problem when it has an impact on daily activities, or when it causes concern to parents or the child suffering from it. In some people, a stutter is triggered by certain events like talking on the phone. When people start to avoid specific activities so as not to trigger their stutter, this is a sure sign that the stutter has reached the level of a speech disorder.
The causes of stuttering are mostly a mystery. There is a correlation with family history indicating a genetic link. Another theory is that a stutter is a form of involuntary or semi-voluntary tic. Most studies of stuttering agree there are many factors involved.
Dysarthria is a symptom of nerve or muscle damage. It manifests itself as slurred speech, slowed speech, limited tongue, jaw, or lip movement, abnormal rhythm and pitch when speaking, changes in voice quality, difficulty articulating, labored speech, and other related symptoms.
It is caused by muscle damage, or nerve damage to the muscles involved in the process of speaking such as the diaphragm, lips, tongue, and vocal chords.
Because it is a symptom of nerve and/or muscle damage it can be caused by a wide range of phenomena that affect people of all ages. This can start during development in the womb or shortly after birth as a result of conditions like muscular dystrophy and cerebral palsy. In adults some of the most common causes of dysarthria are stroke, tumors, and MS.
A lay term, lisping can be recognized by anyone and is very common.
Speech language pathologists provide an extra level of expertise when treating patients with lisping disorders . They can make sure that a lisp is not being confused with another type of disorder such as apraxia, aphasia, impaired development of expressive language, or a speech impediment caused by hearing loss.
SLPs are also important in distinguishing between the five different types of lisps. Most laypersons can usually pick out the most common type, the interdental/dentalised lisp. This is when a speaker makes a “th” sound when trying to make the “s” sound. It is caused by the tongue reaching past or touching the front teeth.
Because lisps are functional speech disorders, SLPs can play a huge role in correcting these with results often being a complete elimination of the lisp. Treatment is particularly effective when implemented early, although adults can also benefit.
Experts recommend professional SLP intervention if a child has reached the age of four and still has an interdental/dentalised lisp. SLP intervention is recommended as soon as possible for all other types of lisps. Treatment includes pronunciation and annunciation coaching, re-teaching how a sound or word is supposed to be pronounced, practice in front of a mirror, and speech-muscle strengthening that can be as simple as drinking out of a straw.
Spasmodic Dysphonia
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably. Many SLPs specialize in the treatment of Spasmodic Dysphonia .
SLPs will most often encounter this disorder in adults, with the first symptoms usually occurring between the ages of 30 and 50. It can be caused by a range of things mostly related to aging, such as nervous system changes and muscle tone disorders.
It’s difficult to isolate vocal chord spasms as being responsible for a shaky or trembly voice, so diagnosing SD is a team effort for SLPs that also involves an ear, nose, and throat doctor (otolaryngologist) and a neurologist.
Have you ever heard people talking about how they are smart but also nervous in large groups of people, and then self-diagnose themselves as having Asperger’s? You might have heard a similar lay diagnosis for cluttering. This is an indication of how common this disorder is as well as how crucial SLPs are in making a proper cluttering diagnosis .
A fluency disorder, cluttering is characterized by a person’s speech being too rapid, too jerky, or both. To qualify as cluttering, the person’s speech must also have excessive amounts of “well,” “um,” “like,” “hmm,” or “so,” (speech disfluencies), an excessive exclusion or collapsing of syllables, or abnormal syllable stresses or rhythms.
The first symptoms of this disorder appear in childhood. Like other fluency disorders, SLPs can have a huge impact on improving or eliminating cluttering. Intervention is most effective early on in life, however adults can also benefit from working with an SLP.
Muteness – Selective Mutism
There are different kinds of mutism, and here we are talking about selective mutism. This used to be called elective mutism to emphasize its difference from disorders that caused mutism through damage to, or irregularities in, the speech process.
Selective mutism is when a person does not speak in some or most situations, however that person is physically capable of speaking. It most often occurs in children, and is commonly exemplified by a child speaking at home but not at school.
Selective mutism is related to psychology. It appears in children who are very shy, who have an anxiety disorder, or who are going through a period of social withdrawal or isolation. These psychological factors have their own origins and should be dealt with through counseling or another type of psychological intervention.
Diagnosing selective mutism involves a team of professionals including SLPs, pediatricians, psychologists, and psychiatrists. SLPs play an important role in this process because there are speech language disorders that can have the same effect as selective muteness – stuttering, aphasia, apraxia of speech, or dysarthria – and it’s important to eliminate these as possibilities.
And just because selective mutism is primarily a psychological phenomenon, that doesn’t mean SLPs can’t do anything. Quite the contrary.
The National Institute on Neurological Disorders and Stroke estimates that one million Americans have some form of aphasia.
Aphasia is a communication disorder caused by damage to the brain’s language capabilities. Aphasia differs from apraxia of speech and dysarthria in that it solely pertains to the brain’s speech and language center.
As such anyone can suffer from aphasia because brain damage can be caused by a number of factors. However SLPs are most likely to encounter aphasia in adults, especially those who have had a stroke. Other common causes of aphasia are brain tumors, traumatic brain injuries, and degenerative brain diseases.
In addition to neurologists, speech language pathologists have an important role in diagnosing aphasia. As an SLP you’ll assess factors such as a person’s reading and writing, functional communication, auditory comprehension, and verbal expression.
Speech Delay – Alalia
A speech delay, known to professionals as alalia, refers to the phenomenon when a child is not making normal attempts to verbally communicate. There can be a number of factors causing this to happen, and that’s why it’s critical for a speech language pathologist to be involved.
The are many potential reasons why a child would not be using age-appropriate communication. These can range anywhere from the child being a “late bloomer” – the child just takes a bit longer than average to speak – to the child having brain damage. It is the role of an SLP to go through a process of elimination, evaluating each possibility that could cause a speech delay, until an explanation is found.
Approaching a child with a speech delay starts by distinguishing among the two main categories an SLP will evaluate: speech and language.
Speech has a lot to do with the organs of speech – the tongue, mouth, and vocal chords – as well as the muscles and nerves that connect them with the brain. Disorders like apraxia of speech and dysarthria are two examples that affect the nerve connections and organs of speech. Other examples in this category could include a cleft palette or even hearing loss.
The other major category SLPs will evaluate is language. This relates more to the brain and can be affected by brain damage or developmental disorders like autism. There are many different types of brain damage that each manifest themselves differently, as well as developmental disorders, and the SLP will make evaluations for everything.
Issues Related to Autism
While the autism spectrum itself isn’t a speech disorder, it makes this list because the two go hand-in-hand more often than not.
The Centers for Disease Control and Prevention (CDC) reports that one out of every 68 children in our country have an autism spectrum disorder. And by definition, all children who have autism also have social communication problems.
Speech-language pathologists are often a critical voice on a team of professionals – also including pediatricians, occupational therapists, neurologists, developmental specialists, and physical therapists – who make an autism spectrum diagnosis .
In fact, the American Speech-Language Hearing Association reports that problems with communication are the first detectable signs of autism. That is why language disorders – specifically disordered verbal and nonverbal communication – are one of the primary diagnostic criteria for autism.
So what kinds of SLP disorders are you likely to encounter with someone on the autism spectrum?
A big one is apraxia of speech. A study that came out of Penn State in 2015 found that 64 percent of children who were diagnosed with autism also had childhood apraxia of speech.
This basic primer on the most common speech disorders offers little more than an interesting glimpse into the kind of issues that SLPs work with patients to resolve. But even knowing everything there is to know about communication science and speech disorders doesn’t tell the whole story of what this profession is all about. With every client in every therapy session, the goal is always to have the folks that come to you for help leave with a little more confidence than when they walked in the door that day. As a trusted SLP, you will build on those gains with every session, helping clients experience the joy and freedom that comes with the ability to express themselves freely. At the end of the day, this is what being an SLP is all about.
Ready to make a difference in speech pathology? Learn how to become a Speech-Language Pathologist today
- Emerson College - Master's in Speech-Language Pathology online - Prepare to become an SLP in as few as 20 months. No GRE required. Scholarships available.
- NYU Steinhardt - NYU Steinhardt's Master of Science in Communicative Sciences and Disorders online - ASHA-accredited. Bachelor's degree required. Graduate prepared to pursue licensure.
- Arizona State University - Online - Online Bachelor of Science in Speech and Hearing Science - Designed to prepare graduates to work in behavioral health settings or transition to graduate programs in speech-language pathology and audiology.
American Speech-Language-Hearing Association
- Certification
- Publications
- Continuing Education
- Practice Management
- Audiologists
- Speech-Language Pathologists
- Academic & Faculty
- Audiology & SLP Assistants
Speech Sound Disorders
On this page:
About Speech Sound Disorders
Signs and symptoms of speech sound disorders, causes of speech sound disorders, seeing a professional, other resources.
Children may say some sounds the wrong way as they learn to talk. They learn some sounds earlier, like p, m, or w. Other sounds take longer to learn, like z, v, or th. Most children can say almost all speech sounds correctly by 4 years old. A child who does not say sounds by the expected ages may have a speech sound disorder. You may hear the terms "articulation disorder" and "phonological disorder" to describe speech sound disorders like this.
To learn more about what you should expect your child to be able to say, see these two resources:
- ASHA's Communication and Feeding Milestones: Birth to 5 Years
- Your Child's Communication Development: Kindergarten Through Fifth Grade
Adults can also have speech sound disorders. Some adults have problems that started when they were children. Others may have speech problems after a stroke or traumatic brain injury . To learn more about adult speech disorders after a stroke or traumatic brain injury, see apraxia of speech in adults and dysarthria .
Your child may substitute one sound for another, leave sounds out, add sounds, or change a sound. It can be hard for others to understand them.
It is normal for young children to say the wrong sounds sometimes. For example, your child may make a "w" sound for an "r" and say "wabbit" for "rabbit." They may leave sounds out of words, such as "nana" for "banana." This is okay when they are young. It may be a problem if they keep making these mistakes as they get older.
You and your child may also sound different because you have an accent or dialect. This is not a speech sound disorder.
The chart below shows the ages when most English-speaking children develop sounds. Children learning more than one language may develop some sounds earlier or later.
| Makes cooing sounds | |
| Laughs and makes playful sounds | |
| Makes speech-like babbling sounds like | |
| Babbles longer strings of sounds like | |
| Says and in words Familiar people understand the child's speech | |
| Says and in words May still make mistakes on the and sounds Most people understand the child’s speech |
Many children learn to say speech sounds over time, but some do not. You may not know why your child has problems speaking.
Some children have speech problems because the brain has trouble sending messages to the speech muscles telling them how and when to move. This is called apraxia. Childhood apraxia of speech is not common but will cause speech problems.
Some children have speech problems because the muscles needed to make speech sounds are weak. This is called dysarthria .
Your child may have speech problems if he has
- a developmental disorder, like autism;
- a genetic syndrome, like Down syndrome;
- hearing loss, from ear infections or other causes; or
- brain damage, like cerebral palsy or a head injury.
Adults can also have speech sound disorders. Some adults have problems that started when they were children. Others may develop speech problems after a stroke or traumatic brain injury , or other trauma. To learn more about adult speech disorders, see apraxia of speech in adults , dysarthria , laryngeal cancer , and oral cancer .
Testing for Speech Sound Disorders
A speech-language pathologist, or SLP, can test your child's speech. The SLP will listen to your child to hear how they say sounds. The SLP also will look at how your child moves their lips, jaw, and tongue. The SLP may also test your child’s language skills. Many children with speech sound disorders also have language disorders. For example, your child may have trouble following directions or telling stories.
It is important to have your child’s hearing checked to make sure they do not have a hearing loss. A child with a hearing loss may have more trouble learning to talk.
The SLP can also help decide if you have a speech problem or speak with an accent. An accent is the unique way that groups of people sound. Accents are NOT a speech or language disorder.
Treatment for Speech Sound Disorders
SLPs can help you or your child say sounds correctly and clearly. Treatment may include the following:
- Learning the correct way to make sounds
- Learning to tell when sounds are right or wrong
- Practicing sounds in different words
- Practicing sounds in longer sentences
See ASHA information for professionals on the Practice Portal’s Speech Sound Disorders page.
- Identify the Signs
- Typical Speech and Language Development
In the Public Section
- Hearing & Balance
- Speech, Language & Swallowing
- About Health Insurance
- Adding Speech & Hearing Benefits
- Advocacy & Outreach
- Find a Professional
- Advertising Disclaimer
- Advertise with us
ASHA Corporate Partners
- Become A Corporate Partner

The American Speech-Language-Hearing Association (ASHA) is the national professional, scientific, and credentialing association for 234,000 members, certificate holders, and affiliates who are audiologists; speech-language pathologists; speech, language, and hearing scientists; audiology and speech-language pathology assistants; and students.
- All ASHA Websites
- Work at ASHA
- Marketing Solutions
Information For
Get involved.
- ASHA Community
- Become a Mentor
- Become a Volunteer
- Special Interest Groups (SIGs)
Connect With ASHA
American Speech-Language-Hearing Association 2200 Research Blvd., Rockville, MD 20850 Members: 800-498-2071 Non-Member: 800-638-8255
MORE WAYS TO CONNECT
Media Resources
- Press Queries
Site Help | A–Z Topic Index | Privacy Statement | Terms of Use © 1997- American Speech-Language-Hearing Association

- Games & Quizzes
- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
- Prevalence of speech disorders
- Classification of speech disorders
- Treatment and rehabilitation
- Development of speech correction
Voice disorders
Disorders of language development.
- Stuttering, or stammering
Dysphasia and aphasia
Shaking palsy, intellectual disability, language and mental disorder, speech of the hard of hearing, loss of tongue, nasal speech, cleft palate speech.

Major types of speech disorders
Our editors will review what you’ve submitted and determine whether to revise the article.
- Table Of Contents
In international terminology, disorders of the voice are described as dysphonia . Depending on the underlying cause, the various types of dysphonia are subdivided by the specifying adjective. Thus, a vocal disorder stemming from paralysis of the larynx is a paralytic dysphonia; injury (trauma) of the larynx may produce traumatic dysphonia; endocrine dysphonia reflects the voice changes resulting from disease of the various endocrine glands such as the pituitary. The various dysphonias of clearly organic origin from systemic disease (e.g., muscular, nervous, or degenerative disease afflicting the entire body) or from local laryngeal changes differ in their visible symptomatology, as well as in the perceptual impression produced by the abnormal voice. Nevertheless, it has not yet been possible to define the acoustical alterations in the vocal spectrum that would allow a clear and objective differentiation among the subjective graduations of an abnormal voice as hoarse, harsh, husky, breathy, grating, gravelly, or gritty.
Because a large group of dysphonias have no visible laryngeal causes, they are grouped as nonorganic. Two main types of these so-called functional voice disorders may be distinguished: the habitual dysphonias that arise from faulty speaking habits and the psychogenic dysphonias that stem from emotional causes. Both of these types of dysphonia again occur in two basic subtypes, the hyperkinetic (overactive) and the hypokinetic (underactive) since emotional disorders interfere with voluntary vocal function by causing either excessive or depressed physiological activity. In the hyperkinetic disorders, the highly coordinated patterns of phonation regress to the primitive , forceful, and exaggerated sphincter action of the larynx as seen during gagging. The result is hyperkinetic dysphonia, the gratingly harsh vocal disorder due to excessive muscular action in a constricted larynx. In the second subtype, the movements for phonation regress even more deeply to the original function of respiration; the sluggish larynx remains more or less open, and the glottis is incompletely closed for phonation, leading to hypokinetic dysphonia with subdued, breathy huskiness.
The most frequent speech disorders are those that disturb the child’s acquisition or learning of language. Studies of large numbers of children with developmental language disorders have shown that at least two chief classes of these disorders may be distinguished: general language disability from genetic factors with a familial (inherited) pattern chiefly from the paternal side, and acquired language disorders due to damage sustained before, during, or shortly after birth (i.e., perinatally).
These latter perinatal damages encompass the gamut of toxic, infectious, traumatic, nutritional, hormonal, and other damages that may hurt the growing fetus or young infant. Major and minor birth injury is not an infrequent factor. Hereditary factors also encompass a great variety of genetically predetermined influences, including familial tendency to exhibit slow language development, lesser endowment in the brain area for language, inferior function in the highest brain areas of auditory performance without organic damage to the ears, slow maturation of motor function (including clumsiness and deviation from normal cerebral dominance), and other signs of delayed cerebral growth. Additional environmental causes include poor language patterns used by the family, parental neglect, emotional maladjustment, general weakness from prolonged disease, as well as various socioeconomic, cultural, and other psychological influences.
While some otherwise perfectly normal children, particularly boys, may not elect to begin talking until age three, making good progress in every respect from then on, the absence of speech after age two may be caused by any of the conditions mentioned thus far and would appear to merit prompt investigation. If an organic cause can be detected, the symptomatic description of delayed language development then yields to a specific etiologic (causal) diagnosis . Although it is best to describe the absence of speech in early childhood as simply delayed language development, some investigators tend to refer to this condition as congenital (present at birth) aphasia.
Many children encounter unusual difficulties in mastering the patterns of articulation of their mother tongue and are said to manifest articulatory immaturity (infantile dyslalia). If no organic cause can be found, the probable cause may be delayed maturation of psychomotor skills.
Marked delays of language development are often followed by a period of inability to learn the rules of grammar and syntax at the usual age ( dysgrammatism). Though this is often a sign of inherited language disability, it may reflect intellectual disability or other types of brain damage.
Some children who have suffered such laboured language development may then go through a period of retarded reading and writing disability, a condition often defined as dyslexia . Again, there are two chief varieties: the primary or developmental reading and writing disability due to constitutional (organic) and hereditary factors, and a large secondary group of symptomatic reading disorders acquired through any of the influences that retard language development in general, including troubles with vision . Practically all investigators agree that primary or developmental dyslexia shows a marked hereditary tendency (is familial) and is typically associated with other disorders of psychomotor development and poor function in the auditory area in the brain. Primary dyslexia is significantly associated with other developmental speech disorders.
Articulatory disorders
A peculiar impediment of speech, cluttering (or tachyphemia) is characterized by hasty, sloppy, erratic, stumbling, jerky, and poorly intelligible speech that may somewhat resemble stuttering but differs from it markedly in that the clutterer is usually unaware of it, remains unconcerned, and does not seem to fear speaking situations. Its association with other past or persistent signs of subnormal language development differentiates congenital cluttering from emotional stuttering. Experts are strikingly unanimous in stressing the hereditary nature of cluttering.
Although lisping belongs among the articulatory disorders and usually has the same causes as articulatory disorders (dyslalia) in general, it differs from other disorders of articulation in several respects. For one, lisping occurs in various varieties: with the tongue tip protruding between the front teeth, with a slurping noise in the cheek pouch, with the tongue too far back along the palatal midline, with excessive tongue pressure against the teeth; in several snorting and nasal subtypes, as well as through substitute hissing deep in the throat or even within the larynx, such as in cleft-palate speech. Moreover, the causes of lisping include a diverse group of particular conditions: abnormal number or position of teeth; imitation of other lispers; deficiency of palatal closure; slight hearing loss in the high frequencies; as well as several psychologic causes, such as effeminate affectation, infantile mannerisms, or mental disturbance. Lisping is less easily outgrown than the other infantile dyslalias and may persist into adult life if not corrected.

Stuttering , or stammering
Academically known as dysphemia, what is called stuttering in the United States is usually named stammering in the United Kingdom. While everyone seems to know what stuttering sounds like, experts do not agree about what really causes it. In the age groups after puberty, stuttering is the most frequent and conspicuous type of disturbed speech encountered. This is one reason why among the studies dealing with speech pathology in the world literature those devoted to stuttering are the largest single group. Despite numerous and intensive studies of the problem, findings and conclusions are far from unanimous. A great number of theories have been proposed to explain the origin and nature of stuttering, which range from the premise that subtle physical disturbances in the nervous system (so-called neurogenic asynchronies) are responsible to the opinion that psychological maladjustment alone is to blame.
Research findings indicate (as is the case with many developmental speech disorders, particularly language disability, articulatory disorders, reading disability, and cluttering) that trouble with stuttering affects the male sex two to four times more frequently than the female. Hereditary predisposition has been noted in many studies of large groups of stutterers, with evidence for an inherited tendency found among as many as 40 percent of the stutterers studied. Some experts insist that stuttering is not a single disease entity but that it comprises several types of the disorder with different causes. According to such views, the familial occurrence of stuttering represents a combination of the stuttering symptom with a cluttering tendency that is inherited. Although imitation of another stutterer may form the basis for acquiring the habit, purely psychological explanations that stress parental attitudes in training their children fail to reveal why many stutterers have siblings (brothers or sisters) with perfectly normal speech.
The treatment of stuttering is difficult and often demands much skill and responsibility on the part of the therapist. There is no medical cure for stuttering. For a time it was hoped that new psychopharmacological drugs (e.g., tranquilizers) might facilitate and accelerate recovery from stuttering. Although these efforts have not produced a pharmacological treatment thus far, several therapeutic approaches have been developed that can improve an affected individual’s speech. The typical approach in this disorder is a strict program of psychotherapy (talking freely with a psychiatrist or psychologist so as to reduce emotional problems) supported by various applications of learning theory or behavioral theory (in retraining the stutterer) and other techniques depending on the therapist’s position. It is widely agreed that the patient must acquire a better adjustment to the problems of his or her life and that he or she needs to develop a technique for controlling symptoms and fears. Prognosis (predicted outcome of treatment) thus is held to depend greatly on the patient’s motivation and perseverance. It is interesting to note that experienced investigators no longer aspire to a “cure” of stuttering through an etiologic (causal) approach. Instead of focusing on underlying causes, they aim at making the patient “symptom-free” via symptomatic therapy.
Prevention of stuttering may be aided through parent counseling . The normal, immature speech of many children is characterized by various nonfluencies; these include hesitations, syllable repetition, groping for the right word, and vocalizations between words such as “ah-ah.” Some misguided parents castigate these normal signs of developing speech with various admonitions and, even worse, try to forbid the nonfluencies by mislabeling them as stuttering. In some children, this parental interference associates normal nonfluency with feelings of insecurity and fear, tending to make the child become a real stutterer. Much research has been devoted to this probable etiology for one type of stuttering; its elimination through parental guidance indeed has been reported to help in reducing the number of stutterers.

Dysphasia means the partial or total loss of language as a result of lesions in those parts of the brain that are directly related to language function. Stroke in elderly patients and head injury in younger ones are typical causes. Aphasia is seen most frequently when the left side of the brain is afflicted, as evidenced by paralysis of the right arm and leg. Evidence indicates that the left hemisphere is dominant in all right-handed individuals and in some left-handers as well. Some experts even believe that the left brain hemisphere is dominant for language in most individuals regardless of handedness and that dominance of the right brain is exceptional in some left-handers. According to other opinions, dominance for language is more evenly distributed in both hemispheres in left-handed persons. The two major brain areas recognized as intimately associated with language function are Broca’s area , in the third frontal convolution, and Wernicke’s area , in the posterior third of the upper temporal convolution. The angular gyrus at the junction of the temporal (side), parietal (top), and occipital (back) lobes of the brain is believed to be related to graphic language as used for reading and writing.
Aphasiology, the science of aphasic language loss, is studied by neurologists, neurosurgeons, some phoniatrists, certain speech pathologists, as well as some psychologists and linguists. This diversity of research background accounts, in part, for the great diversity in theoretical approaches to aphasia. Numerous classification schemes that have been proposed vary from simple groupings into a few main types of aphasia to complicated systems with many forms and subtypes of aphasic disturbances. Similar to research in stuttering, the literature on aphasia is exceptionally large and growing.
The essence of aphasia is the loss of memory for the meaning of language and its production. Thus, in the predominantly expressive or motor forms, the patient can no longer remember the intricate patterns for articulation; a patient can no longer form a word in speaking or writing , even though the patient may know what he or she wants to express. In the predominantly receptive or sensory forms, the patient can talk freely, sometimes excessively and incessantly ( logorrhea), although with numerous errors and meaningless clichés, but no longer comprehends what is said to him or her or what he or she tries to read. Those who recover from receptive forms of the disorder are likely to explain that during their aphasia spoken language sounded like an unintelligible, alien tongue. The degree to which there is combination of expressive and receptive symptoms varies greatly with the type and extent of brain lesion. There may be total loss of all language functions (global aphasia) to slight residual errors or misunderstandings when the brain damage is only slight or temporary. A major complication of aphasia is the frequent association with right hemiplegia , in which the paralyzed hand is no longer serviceable for writing. Retraining of the left hand for writing may then become necessary.
Management of aphasia has two goals: one, the physical recovery of the patient through treatment by the internist, neurologist, and possibly brain surgeon, and two, the reeducation of the brain functions that are still present, the aim of which is to help the patient relearn some use of language under the guidance of the speech pathologist. The better the patient’s recovery from the brain lesion, the more chances there are of prompt and complete return of language. When the brain losses are permanent, the patient must relearn each word, sentence, and phrase like the young child, albeit in a more cumbersome manner, apparently using parts of the brain that still function. He or she is repeatedly shown the picture of an object along with its printed name; these words are spoken by his or her teacher over and over in the hope that the patient will learn to repeat the word or phrase until he or she can say it spontaneously. Words that are relevant to the patient’s everyday life are emphasized first with due consideration for his or her interests and past occupation; later the patient may advance to the use of abstract concepts and of higher levels of language. Various types of automated training programs are available, which enable the patient to practice at his or her own pace.
Symptomatic speech disorders
Under this heading may be summarized various types of communication disorders that develop on the basis of known structural lesions or metabolic disturbances. Etiologic classifications group these impediments according to the types of organic diseases, as well as in respect to the afflicted effector organs (such as the tongue). Disturbed speech from lesions in the various parts of the nervous system is known as dysarthria. Intellectual disability usually limits the development of linguistic ability to the same extent as it does intellectual capacity; this language disorder has been described as dyslogia. Mental disturbances can also manifest themselves in linguistic symptoms, such as in the peculiar ( dysphrenic) mode of speech among sufferers of schizophrenia. Hearing loss dating from early childhood leads to a typical distortion of the speech pattern for which various names have been coined, such as audiogenic dyslalia. Visible defects in oral articulators such as the lips and teeth limit the mechanics of articulation and thus reduce the quality and intelligibility of speech; such speech problems are known collectively as dysglossia.
Damage to those parts of the nervous system that regulate the actions of voice and speech cause distinctive alterations of the speech pattern. The most important disorder of this type is cerebral palsy from brain injury before, during, or soon after birth. The majority of cerebral palsy victims retain normal intelligence but are handicapped by distortions of voluntary movements, including those for speaking. Just as walking may be stilted and jerky and arm movements crude and uncontrolled, the patterns of voice and speech will reflect the same distortions. Great advances in rehabilitation have been achieved in the recent past, such as with the well-known Bobath method, which is based on learned suppression of primitive reflexes.
Another type of dysarthria is observed in cases of Parkinson disease . This affliction of the nervous system makes body movements either excessively rigid or tremulously repetitive, such as with the so-called “pill-rolling” sign of hand tremor. Voice and speech reflect the same patterns, sometimes appearing as the first obvious symptoms of the disease. Brain surgery is used in an attempt to improve these abnormal body movements, often with good general results, although speech may be little improved or even made worse. An example of a surgical procedure used to treat Parkinson disease is deep brain stimulation , in which an electrode is implanted into a specific area of the brain to alleviate symptoms of disordered movement. Certain drugs, such as l -dopa (levodopa), can also lessen the severity of involuntary movement.
When a neurologic disease damages the bulbar nuclei (in the brain stem) of the nerves innervating the organs for speech, the effect of bulbar dysarthria is heard. In severe cases, the voice may be reduced to a faint grunting, while articulation deteriorates into mumbling or total muteness. Chorea , another neural disorder manifested in sudden jerky movements of the entire body, may be associated with bizarre, explosive disruptions of the speech flow. Cerebellar dysarthria results from disease of the brain part called the cerebellum (which regulates fine motor coordination), leading to various disorganizations of speech including a “drunken” (ataxic) quality.
Major advances in the science of inheritance (genetics) and in biochemistry have clarified a number of inborn metabolic causes of many types of intellectual disability. Some of these impairments can be avoided through genetic counseling of prospective parents or prevented by prompt treatment following early diagnosis. (In some cases a change in diet is effective.) Improved prenatal care may reduce the size of another group of intellectually disabled individuals whose problem stems from brain damage sustained during fetal life. However, the number of unknown causes in other cases of intellectual disability is still considerable.
The total management of the intellectually disabled child concerns a large group of specialists: pediatrician, geneticist, clinical psychologist, audiologist and speech pathologist, and special educators in institutions for such children. Following classification on the basis of a level of educability, the child undergoes a composite training program geared to his or her capabilities. Intensive training in language usage not only tends to improve the individual’s communication skills but also forms a bridge to increased general learning. In some instances, intellectual disability occurs in combination with hearing loss; in such cases, the audiologist prescribes a hearing aid and auditory training to improve the receptive aspects of communication.
Expert analysis of the bizarre speech patterns associated with certain psychiatric disturbances is of primary diagnostic significance. If a mute child persists in stereotyped rituals and strange behaviour, a diagnosis of childhood autism is likely to be made. This is distinguished from a similar disorder called childhood schizophrenia, in which previously good general and linguistic development falls apart in association with similarly bizarre behaviour. In adolescence, a sudden change of voice to a shrill falsetto or weird chanting may herald the outbreak of juvenile schizophrenic disease. Infantile lisping, strange distortions of articulation, and various eccentricities in verbal expression are other signs of schizophrasic speech in the adult schizophrenic. Linguistic study may help the psychiatrist in analyzing the patient’s ways of thinking and to provide a measure of the sufferer’s progress under therapy. Great therapeutic stress is placed on establishing contact with the autistic child by eliciting from him or her some sort of communication. Language is felt to be one of the best bridges to break open the closed inner world of such children.
Hearing loss that dates from childhood hinders the normal development of language because the most important sensory portal for speech learning remains deficient. Such children learn to say the sounds of speech as they hear them—in a muffled, distorted, or even inaudible fashion. The articulatory disorder (audiogenic dyslalia) usually reflects the measured (audiometric) pattern of hearing loss. If sound waves at high frequencies cannot be heard, speech sounds with formants in that high-frequency region will be affected. The hissing sibilants contain the highest formants and are therefore most typically disturbed by high-frequency hearing loss. The lower frequencies that can still be heard limit the audible formants to this residual range, which transposes the normal formant patterns into the abnormally lowered frequency band. As a result, a sharp hissing S is spoken as a muted Sh, and the light vowels are transformed into their darker counterparts (for example, the word “set” may be pronounced as “shot” or “shöd” as if it were German).
The voice reflects analogous changes. In the case of conductive hearing loss (in which neural structures for hearing are intact), the patient hears himself or herself well through the bones of the skull but cannot hear others. Because bone conduction remains good, the individual will perceive his or her own voice as being loud and hence tends to keep it subdued. The opposite occurs with neural (or perceptive) hearing loss in which there is nerve dysfunction. In this case, the patient hears his or her own voice as poorly as that of others and tends to talk in an overloud and screeching voice.
Correction of audiogenic dyslalia may be possible through early fitting of a suitable hearing aid, intensive auditory training, and speech exercises aided by audiovisual playback devices (auditory trainers, tape recorders, visible speech devices, etc.).
Profound or total deafness going back to early childhood without special training inevitably leads to the absence of oral language development. Deaf children have traditionally been educated in special schools for the deaf, where the oral method (showing how to shape the oral structures for each speech sound) of teaching speech has competed with the older manual method of allowing the deaf to communicate through their own gestural or finger spelling. Advances in training include the liberal use of amplification devices (e.g., group hearing aids) in all school situations as well as the earliest possible fitting of hearing aids following definite diagnosis. Through methods such as recording brain-wave patterns in response to measured sound stimulation (EEG response audiometry), this can be accomplished even when the patient cannot communicate that he or she hears (e.g., in very young babies).
Speech impediments from defective articulators
Dysglossic (from defective oral structures) disorders in articulation have interested humankind for the longest time; the biblical and poetical interchange of the words for “tongue” and “speech” in many languages has kept alive the assumption that speech originates within the fleshy tongue . For the same reason, the popular term tongue-tied still persists to refer to an abnormally immobile tongue and some assumed resulting limitation of linguistic ability. Even the academic designation of the science of languages as “linguistic” is traditionally based on the Latin word lingua for tongue.
In practice, the condition of a true tongue-tie (ankyloglossia) occurs only rarely and is quite easily corrected through a simple operation. Even when the shortened band beneath the tongue tip is permitted to persist, very little speech disturbance, if any, is audible in such persons. The only limitation of articulation to be expected is the decreased ability to protrude the tongue tip between the teeth for the English Th and the trilling lingual R in southern German, Latin, and Slavic languages . In any event, a true tongue-tie never causes stuttering, lisping, or any other of the major speech disorders.
Major defects of the tongue from paralysis, injury, or surgery reduce the articulation of the lingual sounds to the same extent that the tongue’s mobility is visibly limited. Spontaneous compensation is usually quite prompt, depending on the patient’s general linguistic talent. One exception is complete bilateral (both sides) paralysis of the tongue, which causes a very severe disorder of chewing and swallowing as well as severe limitation of speech intelligibility. The total loss of the tongue (true aglossia) from injury or surgery is often amazingly well compensated. Patients can learn to use residual portions of a tongue stump as well as other oral structures to substitute for the missing tongue; indeed, some persons without a tongue have relearned to speak so well that the listener would not suspect its absence.
Several types of nasal speech are not easily diagnosed; even specialized physicians are often not fully aware of the differences.
Increased nasal resonance leads to open nasality (hypernasal speech), affecting all oral speech sounds that should not be nasal. Organic causes impair the accuracy of palatal occlusion during emission of the nonnasal sounds. Among these are paralysis, congenital malformation , injury, or defects of the palate. The functional causes of palatal sluggishness include imitation, faulty speech habits, dialectal influences, hearing loss, intellectual disability, or psychiatric disorders.
Decreased nasal resonance produces closed nasality (hyponasal speech), which muffles the three nasal resonants (M, N, and Ng). The best known organic causes are an acute cold, hay fever , large adenoids, and all other nasal diseases that obstruct the airway . Functional causes are less frequent, in the form of a rare, faulty speech habit; occasionally the problem comes from intellectual disability or from severe language disability.
Mixed nasality poses a serious problem; it stems from the combination of one cause of open nasality with another of closed nasality (one may be of organic type and the other functional, or both may be organic). A typical combination is the open nasality from paralysis (paresis) of the palate (or its congenital deficiency) combined with closed nasality from obstruction of the nasopharynx by adenoids. The resulting mixed nasality causes the nasal resonants to sound muffled and subdued, while careful testing reveals slight open nasality on all oral sounds.
Treatment of nasal speech is unlikely to be successful without prudent balancing of all factors involved. This responsibility rests primarily with the diagnosing otolaryngologist or phoniatrist. The complaint of “talking through the nose” should never warrant a tonsil and adenoid operation without complete evaluation. If this were done in the example cited just above, removal of the obstructing adenoids would alleviate only the closed nasality, while making the open component more severe with marked deterioration of the patient’s speech. This dilemma is often present when adenoids cause chronic middle-ear disease with hearing loss, while the palate is incompetent, as from a slight congenital malformation or paresis. In such case, the patient’s general health and hearing must be weighed against the possibility of making his or her speech worse.
This type of organic dysglossia has also been named rhinoglossia (Greek rhin , rhis : “nose”) because it is an organic cause of excessively nasal speech. Clefts of the lip, upper jaw, and hard and soft palate occur in various types and combinations. Cleft palate is a congenital (present at birth) malformation that develops for various reasons during the early weeks of embryonic life. The causes may be grouped as follows: inheritance in some cases; embryonal damage from various environmental causes in others; while still other cases of cleft palate are part of a syndrome of general or multiple malformation, which may again be hereditary, the result of chromosomal aberrations , or of environmental origin. Genetic influences are inferred from evidence that North American Indians (Montana) show a high incidence of cleft palate, but blacks (as on the island of Jamaica) show an unusually low incidence.
The speech disorder in cleft palate cases is complex. As a direct, mechanical result of the absent velopharyngeal (soft palate-pharynx) closure, voiced sounds assume an abnormal nasal quality from the unusual resonance of the nasal chambers. The influence of nasality on the perceptual and acoustic characteristics of the speech sounds has been discussed earlier. A second component is a mechanical limitation in articulating plosive sounds (e.g., P) because the necessary intraoral pressure cannot be achieved. For the same reason, the sibilant sounds (e.g., S) are greatly distorted because the articulating air escapes through the nose before it can produce the characteristic hissing noise at one of the places of constriction. The child with an unrepaired cleft palate seems unconsciously to attempt to overcome these mechanical limitations in several ways. He or she tries to constrict the nostrils through facial grimaces and attempts to increase the expiratory air pressure. The child also succumbs to the “law of centripetal regression of articulation”—he or she shifts the articulation of the oral sounds below the point of deficient palatal occlusion, down into the pharynx or even the larynx. It is easy to demonstrate by X-ray fluoroscopy how the larynx becomes constricted during each plosive or sibilant sound in such cases.
These mechanical limitations of articulation in cleft palate lead to secondary modifications of behaviour. Linguistic ability is retarded through general limitation of speech learning; emotional reactions to the handicap may complicate the clinical picture; a vicious circle is thus established, which in turn impedes the sufferer’s general intellectual and special linguistic development.
Other coincidental disorders complicate the pattern of cleft-palate speech. Many cleft-palate patients also suffer from middle-ear infection , and the resulting hearing loss may add the component of audiogenic dyslalia. In other cases, the structural malformation may be complicated by intellectual disability. Coincidental genetic factors may aggravate the speech problem when the syndrome of familial (neurally inherited) language disability is superimposed. In such cases, the mechanical speech disorder of rhinoglossia becomes complicated by the additional signs of delayed speech development, articulatory dyspraxia, dysgrammatism, and reading and writing disability. This combination is evident in some cases following the successful surgical correction of the palatal deficiency . Although the nasality is promptly alleviated in such cases, the various speech disorders from language disability may persist, since they have nothing directly to do with the previous cleft palate.
Management of cleft palate is the task of a well-coordinated team. The plastic surgeon closes the palatal deficiency, the psychologist analyzes the intellectual endowment, the speech pathologist corrects the various components of disordered speech, the audiologist determines coincidental hearing loss, and the otolaryngologist cares for the health of nose and ears. Tonsils and adenoids may be diseased, leading to the frequent complication of middle-ear infection with hearing loss. This condition may require removal of tonsils and adenoids to preserve hearing. A dilemma is then created; removal of tonsils and adenoids is generally contraindicated in cases of deficient palatal closure because this operation increases the degree of open nasality. The child’s welfare then should be carefully considered in order to avoid any harm.
When surgical repair is not feasible , the palatal defect may be covered by a special prosthetic plate ( obturator) similar to false dental appliances. This technique has been known for many centuries, and various models of obturators have been constructed in the course of time. Cleft-palate care therefore includes the services of a prosthodontist (who makes false teeth) for the optimal construction of such appliances. If worn by children, obturators should be regularly altered to maintain continuous fit as the patient grows.
Well-organized centres for the management of cleft palate are able to offer excellent care so that the speech impediment can be ideally or almost completely corrected in many cases. The problem of cleft palate thus demonstrates once more that human speech requires complex detailed study of its normal functions and manifold approaches for the correction of its imperfections.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medscape J Med
- v.10(6); 2008
Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood
Patricia a. prelock.
Department of Communication Sciences, University of Vermont, Burlington, Vermont
Tiffany Hutchins
Frances p. glascoe.
Department of Pediatrics, Vanderbilt University, Nashville, Tennessee
Disclosure: Tiffany Hutchins, PhD, has disclosed no relevant financial relationships in addition to her employment.
Disclosure: Frances P. Glascoe, PhD, has disclosed no relevant financial relationships in addition to her employment.
Abstract and Introduction
Speech-language problems are the most common disability of childhood yet they are the least well detected, particularly in primary care settings. The goal of this article is to: (1) define the nature of speech-language problems, their causes, and consequences; (2) facilitate early recognition by healthcare providers via accurate screening and surveillance measures suitable for busy clinics; and (3) describe the referral and intervention process.
Introduction
Speech-language deficits are the most common of childhood disabilities and affect about 1 in 12 children or 5% to 8% of preschool children. [1] The consequences of untreated speech-language problems are significant and lead to behavioral challenges, mental health problems, reading difficulties, [2] and academic failure including in-grade retention and high school dropout. [3] Yet, such problems are ones that are least well detected in primary care, [4] even though intervention is available and plentiful.
Speech-language impairments embrace a wide range of conditions that have, at their core, challenges in effective communication. As the term implies, they include speech disorders which refer to impairment in the articulation of speech sounds, fluency, and voice as well as language disorders which refer to impairments in the use of the spoken (or signed or written) system and may involve the form of language (grammar and phonology), the content of language (semantics), and the function of language (pragmatics). [5] These may also be described more generally as communication disorders which are typically classified by their impact on a child's receptive skills (ie, the ability to understand what is said or to decode, integrate, and organize what is heard) and expressive skills (ie, the ability to articulate sounds, use appropriate rate and rhythm during speech, exhibit appropriate vocal tone and resonance, and use sounds, words, and sentences in meaningful contexts). There are common conditions in infants, toddlers, and preschoolers that are associated with receptive and expressive communication challenges as presented in Table 1 . [6 – 17]
Disorders in Young Children Commonly Associated With Receptive and Expressive Communication Problems
| Condition & Cause | Receptive Communication Problems | Expressive Communication Problems |
|---|---|---|
| Psychosocial risk, abuse and neglect | Less talkative and fewer conversational skills than expected; seldom volunteer ideas or discuss feelings; utterances shorter than peers | |
| Autism spectrum disorder | Difficulty analyzing, integrating, and processing information; misinterpretation of social cues | Variability in speech production from functionally nonverbal to echolalic speech to nearly typical speech; use of language in social situations is more challenging than producing language forms (eg, articulating speech sounds, using sentence structure) ; tendency to use verbal scripts; difficulty selecting the right words to represent intended meaning; often mechanical voice quality |
| Brain injury | Difficulty making connections, inferences and using information to solve problems; challenges in attention and memory which affect linguistic processing; challenges in understanding figurative language and multiple meaning words | Greatest difficulty is commonly inpragmatics – using language appropriately across contexts, especially narratives and conversations |
| Cerebral palsy | Speech sound discrimination, information processing and attention can be areas of challenge; language comprehension is affected by cognitive status | Dysarthric speech – slower rate, with shorter phrases or prolonged pauses; articulation is often imprecise with distorted vowel productions; voice quality can be breathy or harsh, hypernasal with a low or monotone pitch; apraxic speech – sound substitutions that can be inconsistent, groping for sound production and nonfluent volitional speech with more fluent automatic speech ; language production is affected by breath support as well as cognitive status |
| Fetal drug or alcohol exposure | Difficulty comprehending verbal information, especially understanding abstract concepts, multiple word meanings, and words indicating time and space | Fewer vocalizations in infancy, poor use of gestures and delays in oral language ; poor word retrieval, shorter sentences, and less well-developed conversational skills |
| Fluency disorders | Difficulty with the rate and rhythm of speech; false starts; repetitions of sounds, syllables and words; may or may not be accompanied by atypical physical behaviors (eg, grimacing, head bobbing) | |
| Hearing impairment | Difficulty with sound perception and discrimination, voice recognition, and understanding of speech, especially under adverse hearing conditions | Sound productions made until about 6 months; limited oral output depending on degree of hearing loss; for oral communicators, vocal resonance, speech sound accuracy, and syntactic structure often affected |
| Intellectual Disability | Comprehension of language is often below cognitive ability ; difficulty organizing and categorizing information heard for later retrieval; difficulty with abstract concepts; difficulty interpreting information presented auditorily | Production is often below cognitive ability ; similar but slower developmental path than typical peers; tendency to use more immature language forms; tendency to produce shorter and less elaborated utterances |
| Specific language impairment | Slower and less efficient information processing , ; limited capacity for understanding language , | Shorter, less elaborated sentences than typical peers; difficulty in rule formulation for speech sound, word, and sentence productions ; ineffective use of language forms in social contexts sometimes leading to inappropriate utterances ; poorly developed vocabulary |
It is important to distinguish speech and language impairment from language delay and language difference. Language delay is characterized by the emergence of language that is relatively late albeit typical in its pattern of development. In contrast to an impairment or a delay, a language difference is associated with systematic variation in vocabulary, grammar, or sound structures. Such variation is “used by a group of individuals [and] reflects and is determined by shared regional, social, or cultural and ethnic factors” and is not considered a disorder. [18]
Unfortunately, non-native speakers of English, speakers of various dialects (whose language also varies within dialect), and bilingual or multilingual speakers are frequently classified as language delayed or disordered when, in fact, they are language different [18 , 19] –although problems of underidentification also occur. This is particularly important in an increasingly pluralistic society such as ours in which 1 of 4 people identify as other than white non-Hispanic, approximately 17% of the population is bilingual (mostly speaking Spanish and English), and where minorities represent more than 50% of the population in several cities and counties. [20]
The overidentification of culturally and linguistically diverse populations commonly occurs when a mismatch is observed and incorrectly interpreted between a language used in a particular community and that of the majority culture. This may be seen most clearly in the improper use of formal tests of speech and language to assess the competencies of speakers who are dissimilar to the sample upon which the test was normed and developed. [21] Similar errors also occur during informal evaluations of language and literacy as when the sound structure of the language influences the spelling or grammatical conventions used in written discourse. [22] With regard to bilingualism, it is commonly assumed that children's acquisition of 1 or both languages is delayed; however, the effects of bilingualism are more complex and differ with the age of the child, the nature of the linguistic input, and the manner and timing of language acquisition. What is clear is that equivalent proficiency in each language should not be expected or assumed as this has the potential to lead to misidentification of a speech and language impairment. (For more information on the effects of bilingualism on language learning, see http://asha.org/public/speech/development/BilingualChildren.htm and http://asha.org/public/speech/development/second.htm ) In the case of culturally and linguistically diverse individuals, decisions to intervene and bring language use in line with that of the majority culture or promote proficiency in the dominant language are not inappropriate; however, such decisions must be seen as separate from the language difference vs disorder question.
In your experience, which of the following is the most important barrier to the effective assessment of speech and language impairment in young children? (Select only 1 answer.)
- ○ Variability in the development of speech and language in young children
- ○ Lack of effective screening tools that discriminate children with and without speech and language impairment
- ○ Lack of accurate parent interview tools that identify clear concerns in speech and language development
- ○ Insufficient time with young children in the clinical setting to observe speech and language skills
- ○ Inadequate understanding of milestones for speech and language development
How confident are you that you are up-to-date in the diagnosis and management of speech and language impairment in young children? (Select only 1 answer.)
- ○ Not at all confident
- ○ Somewhat confident
- ○ Confident
- ○ Very confident
All of the following statements about young children with speech and language impairment are true except :
- ○ Young children tend to produce words with sounds that are consistent with the words they already know
- ○ Young children are able to communicate intent before speaking their first words
- ○ Disfluency is a common occurrence in a young child's early speech
- ○ Children usually begin to put 2 words together at 30 months
Answer: Children usually begin to put 2 words together at 30 months. Children usually begin to put 2 words together at 18 months.
Etiology, Neurobiology, and Prevalence of Speech-Language Impairments
The etiology of most cases of speech-language impairments is unknown but diverse causes are suspected. The range of causes or origins includes anatomical abnormalities, cognitive deficits, faulty learning, genetic differences, hearing impairments, neurologic impairments, or physiologic abnormalities. [6] As noted above, language differences as revealed in the communication output associated with diverse cultural, ethnic, regional or social dialects are not considered disorders. [5] Speech and language impairments may be acquired (ie, result from illness, injury or environmental factors) or congenital (ie, present at birth).
Children with speech and language impairment are an under-representation of the broader occurrence of communication disorders, [23] especially considering the co-occurrence of communication disorders with other disabilities (eg, learning disabilities). Approximately 8% to 12% of preschool populations exhibit language impairments. [6] Among children enrolled in early intervention programs, 46% have communication impairments while 26% have developmental delays in multiple areas, usually including language skills. [24] These findings indicate that the most common presentation of disability in preschoolers involves problems with language.
In a family with a child with a speech and language impairment, which of the following would be clinically appropriate?
- ○ Reassure the parents that the child is just a late talker and will catch up
- ○ Urge the parents to have their child undergo genetic testing
- ○ Discourage the child's parents and sibling(s) from talking for the child as this may be a primary cause of a speech and language impairment
- ○ Advise the parent to have the child's hearing tested
Answer: Advise the parent to have the child's hearing tested. This is appropriate because hearing would be the first condition to rule out as a potential cause of a speech and language delay.
Course and Prognosis
Speech-language impairment sometimes emerges during infancy with challenges in response to sound, atypical birth cries, or limited response to others and progresses through the toddler and preschool age with limited comprehension of spoken language and difficult interactions with peers and others as well as delays in producing first words and word combinations. Speech and language difficulties often persist in school age with difficulties following directions, attending and comprehending oral and written language, and problems producing narratives and using language appropriately in social contexts. Parents are often the first to notice difficulties as they encounter other children with more advanced speech-language skills and thus often wonder if their child is behind. [25] Although many parents raise concerns to primary care providers, many do not. In turn, primary care providers who do not use quality screening tools often dismiss parental concerns with panaceas such as, “He's a boy. Boys talk later.” Or, “Let's give this some time and see if it continues.” Yet, parental concerns about speech and language are associated with developmental disabilities [26] and, thus, careful screening with accurate tools is the requisite response. [27]
The use of a “wait and see” approach underscores the difficulty in distinguishing children who are language delayed from those who have a speech and language impairment. Although most children who have aspeech and language impairment have a history of language delay, only one quarter to one half of late-talkers are eventually diagnosed with a language disorder. [19] In advocating for a more aggressive response for late-talking children, some have argued for careful scrutiny of other risk factors that may guide decisions to refer and intervene. [19] Predictors of a true speech and language impairment that should be considered include poor receptive language skills, [28] limited expressive language skills (eg, small vocabulary, few verbs), and limited development in the sound structure of a language (eg, limited number of consonants, limited variety in babbling structure, vowel errors). [26] Additional predictors include nonspeech (eg, behavioral problems, few gestures, little imitation or symbolic play), environmental (eg, low socioeconomic status, parental use of a directive rather than sensitive and responsive interactional style), and hereditary factors (eg, family history). [26] As a general recommendation, professionals are urged to consider a larger number of risk factors with greater concern. [26]
Often speech-language impairments can be difficult to distinguish from what is considered typical variations in speech and language. For example, disfluencies in speech may be either normal or abnormal. In the nonstuttering child, the most common disfluencies include 1-unit word repetitions (eg, “I… I want that”), interjections (eg, “I saw a… um… picture”), and revisions (eg, “I don't know where… Mommy, help me find my doll”) and, when combined, comprise no more than 10% of words spoken. [29] In the stuttering child, the fluency disorder typically emerges between the ages of 2 and 5 years, is more common among males than females, and is characterized by more than 10% disfluencies in speech, multi-unit syllable (eg, “s-s-s-s-s-September”) and word (eg, “That's my-my-my ball”) repetitions, and may be accompanied by secondary behaviors such as eye-blinking, head-bobbing, or grimacing, as well as feelings of frustration or embarrassment surrounding the stuttering event. [29]
Identification of speech and language impairments is further complicated by the fact that they often masquerade as other diagnostic conditions. For example, children with a diagnosis of attention-deficit/hyperactivity disorder (ADHD) may in fact have an underlying language disorder. Differential diagnosis is challenged by the diagnostic criteria shared between the 2 conditions. Specifically, the diagnostic criteria for ADHD share several characteristics with language disorders including difficulty listening when spoken to, following instructions, talking excessively, blurting out answers, interrupting, and waiting for turns in conversation. [30] Similarly, 50% of preschoolers presenting for psychiatric services were found in several studies to have undiagnosed language impairment. [31 , 32]
The diagnostic criteria for speech-language impairments are defined both by the Diagnostic and Statistical Manual of Mental Disorders , 4th edition (DSM-IV) [33 , 34] and by the Individuals with Disabilities Education Act (IDEA) through the US Department of Education. Table 2 specifies the criteria for communication disorders as described in the DSM-IV. As an example of eligibility criteria for speech-language impairment in response to IDEA guidelines, Vermont indicates that children must demonstrate significant deficits greater than 2 standard deviations below the mean in listening comprehension (eg, measures of auditory (language) processing or comprehension of connected speech including semantics, syntax, phonology, recalling information, following directions and pragmatics) and/or oral expression (eg, measures of oral discourse-syntax, semantics, phonology and pragmatics; voice; fluency; articulation) to qualify as speech or language impaired. [35]
Characteristics of Communication Disorders as Described in the DSM-IV [33 , 34]
| Characteristics | Expressive Language Disorder | Mixed Receptive-Expressive Language Disorder |
|---|---|---|
| Standardized tests indicate skill area is substantially below what is expected considering chronological age (CA), IQ, and education | Expressive language development (eg, vocabulary, tense errors, word recall, sentence length, and complexity) is below nonverbal IQ and receptive language | Battery of measures of receptive and expressive languagedevelopment (eg, understanding words, sentences, or specific word types-spatial terms) is below nonverbal IQ |
| Difficulties interfere with academic or occupational achievement or with social communication | X | X |
| If mental retardation, environmental deprivation, sensory or speech motor deficit is present, difficulties are greater than what is expected | X | X |
| Criteria not met for mixed receptive-expressive language disorder | X | |
| Criteria not met for pervasive developmental disorder | X | X |
Distinguishing children with speech-language deficits from those with other disabilities is often a challenging task as several disabilities share characteristics and have similar diagnostic criteria. For example, an intellectual disability is one in which a child's performance falls at or below 1.5 standard deviations from the mean on a test of intellectual ability with concurrent deficits in adaptive behavior. Children with intellectual disabilities, however, often have significant challenges in receptive and expressive communication as is typical of children with speech and language impairments. Children with learning disabilities have deficits in 1 or more basic skill areas including oral expression and listening comprehension, challenges characteristic of children with speech-language impairments. Children with pervasive developmental disorders/autism exhibit marked impairments in communication and social interaction and restricted and repetitive stereotyped patterns of behavior. Although social impairment is a defining feature of autism, communication impairments are similar to those with a speech-language impairment.
Which of the following is not true of speech-language impairment?
- ○ Early intervention is critical as speech-language impairments place children at risk for later academic difficulties
- ○ Most children with speech-language impairments have intellectual deficits
- ○ Communication disorders may manifest themselves at different stages of life
- ○ Children with learning disabilities are likely to have speech and language impairments
Answer: Most children with speech-language impairments have intellectual deficits. Although many children who have mental retardation have speech-language impairments, most children with specific speech-language impairments have nonverbal intelligence within normal limits.
Screening and Early Assessment of Speech-Language Disorders
The American Academy of Pediatrics recommends ongoing surveillance and periodic use of broad-band screening measures at all well-visits. Table 3 provides information on a number of tools that have high levels of accuracy in detecting speech-language problems and other disabilities. All included measures were standardized on national samples, proven to be reliable, and validated against a range of measures. When used, referral rates to early intervention programs rise to meet prevalence. [36] In the absence of accurate measures, most providers rely on informal milestone checklists. These lack criteria and are probably the leading reason why only about 1 in 4 children with disabilities of any kind are referred for needed assistance.
Accurate Developmental, Mental Health/Behavioral, and Academic Screens Suitable for Primary Care *
| Developmental-Behavioral Screens for Young Children | Age Range | Description | Scoring | Accuracy | Time Frame/Costs |
|---|---|---|---|---|---|
| (2002), Ellsworth & Vandermeer Press, Ltd., 1013 Austin Court, Nolensville TN 37135; phone: 615-776-4121 fax: 615-776-4119; ($30.00)PEDS is also available online together with the Modified Checklist of Autism in Toddlers for electronic records: contact. | Birth to 8 years | 10 questions eliciting parents' concerns in English, Spanish, Vietnamese, Somali, Arabic, and many other languages. Written at the 5th grade level. Determines when to refer, provide a second screen, provide patient education, or monitor development, behavior/emotional, and academic progress. Provides longitudinal surveillance and triage. | Identifies children as low, moderate, or high risk for various kinds of disabilities and delays | Sensitivity ranges from 74% to 79% and specificity ranges from 70% to 80% across age levels | About 2 minutes (if interview needed) Print materials = ∼$0.31 Admin. = ∼$0.88 Total = ∼$1.19 |
| (formerly Infant Monitoring System) (2004), Paul H. Brookes Publishing, Inc., PO Box 10624, Baltimore, MD 21285; phone: 1-800-638-3775 ($199) For screening mental/health/behavioral problems, there is also the , which works like the ASQ. | 4–60 months | Parents indicate children's developmental skills on 25–35 items (4–5 pages) using a different form for each well visit. Reading level varies across items from 3rd to 12th grade. Can be used in mass mail-outs for child-find programs. Available in English, Spanish, French, and Korean. | Single pass/fail score for developmental status | Sensitivity ranges from 70% to 90% at all ages except the 4-month level. Specificity ranges from 76% to 91% | About 15 minutes (if interview needed) Materials = ∼$0.40 Admin. = ∼$4.20 Total = ∼$4.60 |
| (1998). Paul H. Brookes Publishing, Inc., P.O. Box 10624, Baltimore, MD, 21285; phone 1-800-638-3775. (Part of CSBS-DP, ) ($99.95 w/CD-ROM) | 6–24 months | Parents complete the Checklist's 24 multiple-choice questions in English. Reading level is 6th grade. Based on screening for delays in language development as the first evident symptom that a child is not developing typically. Does not screen for motor milestones. The Checklist is copyrighted but remains free for use at the Brookes Web site although the factor scoring system is complicated and requires purchase of the CD-ROM. | Manual table of cut-off scores at 1.25 standard deviations below the mean O0052, an optional scoring CD-ROM | Sensitivity is 78%; specificity is 84%. | About 5 to 10 minutes Materials = ∼$0.20 Admin. = ∼$3.40 Total = ∼$3.60 |
| (2007), Ellsworth & Vandermeer Press, Ltd., 1013 Austin Court, Nolensville TN 37135; phone: 615-776-4121; fax: 615-776-4119 ($275) | 0–8 years | PEDS-DM consists of 6–8 items at each age level (spanning the well visit schedule). Each item taps a different domain (fine/gross motor, self-help, academics, expressive/receptive language, social-emotional). Items are administered by parents or professionals. Forms are laminated and marked with a grease pencil. It can be used to complement PEDS or stand alone. Administered by parent report or directly. Written at the 2nd grade level. A longitudinal score form tracks performance. Supplemental measures also include the M-CHAT, Family Psychosocial Screen, PSC-17, the SWILS, the Vanderbilt, and a measure of parent-child interactions. An Assessment Level version is available for NICU follow-up and early intervention programs. | Cutoffs tied to performance above and below the 16th percentile for each item and its domain. On the Assessment Level, age equivalent scores are produced and enable users to compute percentage of delays. | Sensitivity ranges from 75% to 87%; specificity ranges from 71% to 88% for performance in each domain. Sensitivity ranges from 70% to 94%; specificity ranges from 77% to 93% across age levels. | About 3–5 minutes Materials = ∼.$0.02 Admin. = ∼$1.00 Total = ∼$1.02 |
| . Jellinek MS, Murphy JM, Robinson J, et al. Pediatric Symptom Checklist: Screening school age children for academic and psychosocial dysfunction. , 1988;112:201-209 (the test is included in the article). Also can be freely downloaded at or with factor scores at . The Pictorial PSC, useful with low-income Spanish speaking families, is included in PEDS: Developmental Milestones ( ). | 4–16 years | 35 short statements of problem behaviors including both externalizing (conduct) and internalizing (depression, anxiety, adjustment, etc.) Ratings of never, sometimes, or often are assigned a value of 0,1, or 2. Scores totaling 28 or more suggest referrals. Factor scores identify attentional, internalizing, and externalizing problems. Factor scoring is available for download at: | Single refer/nonrefer score | All but one study showed high sensitivity (80% to 95%) but somewhat scattered specificity (68% – 100%). | About 7 minutes (if interview needed) Materials = ∼$0.10 Admin. = ∼$2.38 Total = ∼$2.48 |
| Glascoe FP. , 2002. Items courtesy of Curriculum Associates, Inc. The SWILS can be freely downloaded at: and is included in PEDS: Developmental Milestones | 6–14 years | Children are asked to read 29 common safety words (eg, High Voltage, Wait, Poison) aloud. The number of correctly read words is compared to a cutoff score. Results predict performance in math, written language, and a range of reading skills. Test content may serve as a springboard to injury prevention counseling. | Single cutoff score indicating the need for a referral | 78% to 84% sensitivity and specificity across all ages | About 7 minutes (if interview needed) Materials = ∼$0.30 Admin. = ∼$2.38 Total = ∼$2.68 |
| Kemper KJ, Kelleher KJ. Family psychosocial screening: instruments and techniques. . 1996;4:325-339. The measures are included in the article and downloadable at (included in the PEDS: Developmental Milestones). | Screens parents and best used along with the above screens | A 2-page clinic intake form that identifies psychosocial risk factors associated with developmental problems including: a 4-item measure of parental history of physical abuse as a child; (2) a 6-item measure of parental substance abuse; and (3) a 3-item measure of maternal depression. | Refer/nonrefer scores for each risk factor. Also has guides to referring and resource lists. | All studies showed sensitivity and specificity to larger inventories greater than 90% | About 15 minutes (if interview needed) Materials = ∼$0.20 Admin. = ∼$4.20 Total = ∼$4.40 |
© 2007, Glascoe FP. PEDS: Developmental Milestones Professionals Manual. Nashville, Tennessee: Ellsworth & Vandermeer Press, Ltd. Permission is given to reproduce this table.
The first column in Table 3 provides publication information and the cost of purchasing a specimen set. The “Description” column provides information on alternative ways, if available, to administer measures (eg, waiting rooms). The “Accuracy” column shows the percentage of patients with and without problems identified correctly. The “Time Frame/Costs” column shows the costs of materials per visit along with the costs of professional time (using an average salary of $50 per hour) needed to administer and interpret each measure. Time/cost estimates do not include expenses associated with referring. For parent report tools, administration time reflects not only scoring of test results, but also the relationship between each test's reading level and the percentage of parents with less than a high school education (who may or may not be able to complete measures in waiting rooms due to literacy problems and will need interview administrations).
Even when screens are deployed, it is nevertheless helpful to complement these brief measures with clinical observation. The brevity of screens useful for primary care means that some skills may not be captured. For example, at any given age range, a brief screen may not present articulation items, measure ability to repeat a story, describe daily events, ask questions, or engage in conversation, etc. The value in routinely administering validated, accurate screening tools, however, is essential to improving currently problematic and extremely low rates of early detection on the part of primary healthcare providers.
Table 4 describes some major language developmental milestones in the prelinguistic (birth to 1 year) and linguistic period (1 year and beyond). [37 , 38] It is important to note that there are wide variations in the speed (and style) with which typically developing children acquire language skills.
Average Age and Range of Ages for Achievement for Important Language Developmental Milestones * [37 , 38]
| Prelinguistic Period (birth – 1 year) | Language Precursors |
|---|---|
| 2–4 months | |
| 6–7 months | |
| 9–10 months | |
| 12–14 months | |
| 15–24 months (average = 18 months) | |
| 18–24 months | |
| 18–27 months | |
| 27–36 months | |
| 30–48 months |
Providers are reminded that these indicators are an aid to early detection but do not substitute for quality measurement. See Table 3 for a list of screening measures with proven accuracy.
Screening for Other Potential Contributors to Speech-Language Deficits
Another critical avenue for exploration into possible contributors to speech-language deficits is psychosocial risk. Parents who are depressed and/or have housing or food instability have children more likely to have language problems, perhaps because parents lack the energy and freedom from preoccupations to engage in the kinds of language-mediated social interactions known to support optimal child language development. Some parents are not aware of positive parenting practices that promote development, especially language skills (eg, talking with and reading to their child, creating opportunities for sustained dialogue, responding contingently to a child's initiations). Detecting and intervening when psychosocial risk factors, including abuse and neglect, are present has the potential to prevent language problems from developing. Screens for psychosocial risk factors including depression and parent-child interactions are widely available and include the Family Psychosocial Screen and the Brigance Parent-Child Interactions Scale . Both are included in PEDS: Developmental Milestones [39] as supplementary measures helpful for surveillance and offer evidence-based compliance with recommendations in early detection from the American Academy of Pediatrics. [40] , Many other screens, such as the Ages and Stages Questionnaire , include a background information questionnaire that captures common psychosocial risk factors. [41]
Screening Older Children
With school-age children, obtaining and reviewing group achievement test scores can help reveal undiagnosed language deficits. Such children typically have weaknesses in general information (eg, science, social studies knowledge), problems with reading comprehension, and sometimes also problems with math concepts. Table 3 also includes screens suitable for primary care professionals working with children aged 8 years and older.
For both preschoolers and school-age children, broad-band screens (or review of group achievement test results) should be deployed first and serve as a guide to the selection of narrow-band instruments. For example, attentional deficits can be due to a range of conditions such as language impairment, learning disabilities, and mental health problems such as depression. The optimal approach is to administer a broad developmental or academic screen along with a measure such as the Pediatric Symptom Checklist (which discriminates mental health from attentional difficulties). Only afterward and as suggested by the results of broad-band measures should a narrowly focused tool such as the Vanderbilt ADHD Diagnostic Rating Scale be administered. Making sure that other conditions are treated first or at least concomitantly with ADHD is essential.
Billing and Coding for Screening
Primary care providers can use the – 25 modifier to their preventive service code (to indicate that stand-alone services were offered and then use 96110 times the number of screens administered, eg, 96110 X 2. For insurers not accepting units, the distinct procedural service of each screen is best represented with the – 59 modifier appended to each additional unit of 96110.
In 2005, the Centers for Medicare and Medicaid Services published a total relative value unit (RVU) of 0.36 for 96110, which amounts to a Medicare payment of $13.64. None of this can guarantee that a valid claim will be accepted, so the American Academy of Pediatrics is willing to help with denied claims via their Coding Hotline: 800-433-9016, x4022, or at .gro.paa@eniltohgnidocpaa RVUs do not cover physician time, so making use of office staff and parent-report tools is essential.
Referrals and Other Interventions
Once suspicion exists that a child may have a speech-language impairment, referral to early intervention or to the public schools (depending on age) is the first step. These programs offer intervention by speech-language pathologists. If sufficient quantity is not available, referrals can also be made to private therapy services, which may be covered by the patients' insurance. If there appear to be underlying medical conditions, assessment by other disciplines, such as developmental-behavioral or neurodevelopmental pediatrics, is important.
For families with psychosocial risk factors, developmental promotion is essential as is careful monitoring of progress. If brief advice and information handouts are not effective and particularly if children have delays not sufficiently great as to qualify for services, then parent training, quality day care, Head Start, after-school tutoring, and private speech-language therapy should be recommended. Table 5 shows a list of professional development and referral resources. Table 6 provides a list of resources and information for parents.
Professional Development and Referral Resources
| Links to State, regional, and local early intervention and testing services provided without charge to families whose children have known or suspected disabilities through the Individuals with Disabilities Act (IDEA) | |
| Provides help finding Head Start programs | |
| , | Provides assistance locating quality preschool and day care programs |
| Supplies information about parent training classes | |
| Official Web site of The American Academy of Pediatrics' Section on Developmental and Behavioral Pediatrics. The site offers tutorials in early detection and information on the management of children with a range of conditions. | |
| Provides training slide shows on early detection and offers an early detection discussion list focused on primary care | |
Resources and Information for Parents
| ASHA Websites | Content |
|---|---|
| Typical speech and language development | |
| What is language? What is speech? | |
| How does your child hear and talk? | |
| Communication Development: Kindergarten-5th grade | |
| Reading and writing (literacy) | |
| Social language use (pragmatics) | |
| Learning more than 1 language | |
| Late blooming or language problem? | |
| Apel K, Masterson J (2001). . American Speech and Language Association. | This book is designed to answer parents' questions about their child's speech and language development and describes speech and language development during infancy and the toddler and preschool years. |
Components of a Diagnostic Evaluation of Speech-Language Impairment and the Nature of Interventions
Although screening tools for speech-language often identify those children who have speech-language impairments, a screening is not a diagnostic evaluation and only suggests a child requires a more comprehensive assessment. There are several goals in a diagnostic assessment, including verifying that a speech-language impairment exists, describing the strengths and challenges of the child's speech and language, evaluating the severity of the problem, ascertaining the etiology, determining recommendations for a treatment plan, and providing a prognosis. [6] Assessment requires obtaining a sample of communication skills across settings through a number of procedures. It is critical to collect information not only from standardized, formal tools but also to gather more authentic, real-life information to facilitate meaningful and accurate decisions. Typically, case history information, parent interviews, checklists from other providers, systematic observation, hearing screening, and examination of the speech mechanism is included. [6] Formal norm-referenced tests are used to assess articulation, phonology, grammatical understanding and production, and pragmatic language use. The collection of data from the authentic assessment tools and the formal measures provide a comprehensive picture of the speech-language needs of a young child with a communication impairment.
All of the following are true in the assessment of a young child with speech-language impairments except :
- ○ Obtaining information from multiple sources across settings is necessary to specify communication strengths and challenges
- ○ Speech-language pathologists (SLPs) make diagnoses of specific speech-language impairment, identify probable causes, determine severity, describe the likely prognosis, and provide recommendations
- ○ Clinical judgment is most appropriate for determining the severity of a child's speech-language impairment
- ○ During assessment, speech, language, hearing, and processing abilities should be probed
Answer: Clinical judgment is most appropriate for determining the severity of a child's speech-language impairment. Objective criteria are important to ensure consistency in the assessment of severity.
To determine the prognosis for a young child with a speech-language impairment, which of the following is true?
- ○ A clinician should avoid providing prognostic information, as questions like “Will my son outgrow his speech-language impairment?” cannot be answered
- ○ Trial therapy during an assessment period is an appropriate strategy to inform prognosis
- ○ Families and clinicians have little difficulty making decisions about whether or not a young child with early expressive language delay will benefit from therapy
- ○ Single evaluation measures can be used to determine the severity of a young child's speech-language impairment and the prognosis for successful outcomes
Answer: Trial therapy during an assessment period is an appropriate strategy to inform prognosis. Clinicians often probe a child's response to intervention strategies to determine responsiveness to treatment and to inform the development of the treatment plan.
Intervention Approaches and Outcomes
The complexity of impairments in speech and language requires a variety of intervention approaches that can address deficits in language form (syntax, phonology, morphology), language content (semantics), and language use (pragmatics) as well as speech and voice production. Further, intervention for young children may involve not just the speech-language pathologist but also care providers and peers.
The ultimate goal of intervention is to increase a child's success in using language to communicate his or her intent, respond to the intent of others, and participate in reciprocal interactions. The speech and language targets vary for each child depending on the context and aspects of communication affected. Targets may or may not follow a strict developmental approach. Sometimes a more functional approach is appropriate, supporting communication at the point of frustration and breakdown. [6] Intervention targets should consider the family's desired outcomes for their child's communication. Targets should be developmentally appropriate and meaningful to the child.
Several teaching methods are used to support the speech and language of children. Modeling is a typical intervention strategy that provides focused stimulation on the speech or language targets selected for an individual child. Cueing is another frequently used technique that includes direct and indirect verbal cues (eg, asking a child to imitate a sound, word, or utterance) or nonverbal cues (eg, giving a child a jar with a desired item that can't be opened without help). In addition, responding to a child's communication efforts through reinforcement or corrective feedback (eg, “Remember to say the ending sound /t/ so we know you mean the word ‘boat’”) is frequently used to facilitate effective communication. [6]
Case Studies
Bobby [pseudonym] is a 7-year-old boy whom you have seen in your office for a number of years. He comes to you today for his annual check-up. Bobby is enrolled in the second grade. His mother is concerned because Bobby's teachers have noted difficulties in his ability to learn to read. Specifically, Bobby's teachers say that he has difficulties with word recognition and reading comprehension. Bobby's mother indicates that this is consistent with her own observations that he seems to have trouble with understanding what is being said (eg, directions, questions) and storytelling. Moreover, she suspects that Bobby's vocabulary is less well developed compared with his peers. She also describes frequent errors in how he formulates sentences such as omitting possessives (eg, “Sam dog” instead of “Sam's dog”) and verbs (eg, “He cooking” instead of “He is cooking”) that she fears are atypical. Bobby's nonverbal IQ is in the typical range.
The difficulties described above are most consistent with a possible diagnosis of:
- ○ Autism spectrum disorder
- ○ Intellectual disability
- ○ Specific language impairment
- ○ Language delay
Answer: Specific language impairment.
Darius [pseudonym] is a 5-year-old African American boy whom you are meeting today for the first time. He and his mother have recently moved to your area and she has brought him to you because he seems to be developing a nasty cough. When talking with Darius, you notice that he is extremely difficult to understand. Darius is a speaker of African American English; however, even with young speakers of this dialect, you have never had such difficulty understanding and communicating effectively. You learn that he and his parents have just moved from an impoverished community in South Carolina where he attended an age-appropriate class in a school in which approximately 85% of his classmates were black, to a school district in your area that almost entirely comprises white administrators, staff, and students. His mother further reports that Darius's new teachers have expressed concerns about his language. They say he is hard to understand, has a limited vocabulary, cannot master letter-sound correspondences, and has trouble listening to and understanding others.
Which of the following additional patient characteristics obtained from the mother would increase your suspicion of a diagnosis of speech and language impairment? (Select all that apply.)
- ▪ Darius's mother reports that he has always talked differently compared with his parents, siblings, and peers
- ▪ Darius's scores on a test of articulation of standard English are in the 10th percentile
- ▪ Darius becomes frustrated when you ask him to repeat himself
- ▪ Even though they are consistent with the sound structure of African American English, errors in Darius's spelling are quite common (eg, he writes "nes" instead of “nest”)
Answer: Darius's mother reports that he has always talked differently compared with his parents, siblings, and peers.
Which of the following additional patient or parent characteristics would increase your suspicion that Darius is exhibiting a language difference as opposed to a speech and language impairment? (Select all that apply.)
- ▪ Not only do you find Darius difficult to understand, but his mother is equally difficult to understand; both seem to be using a variation of African American English dialect that, although not commonly heard in your area, is characteristic of their native community
- ▪ Darius's scores on a test of vocabulary standardized on a cross-section of North American native English speakers are in the 35th percentile
- ▪ Darius's mother has no trouble understanding him
- ▪ Darius's mother does not share these concerns and considers him competent in all aspects of his language development
Answer: Not only do you find Darius difficult to understand, but his mother is equally difficult to understand; both seem to be using a variation of African American English dialect that, although not commonly heard in your area, is characteristic of their native community. Darius's mother does not share these concerns and considers him competent in all aspects of his language development.
You have been Sam's [pseudonym] primary care physician since he was born. He is now 18 months old and comes to you for his annual flu shot. During this visit, his mother expresses concerns about his speech and language development. More specifically, she reports he is “not talking like other kids his age” and uses repeated vocalizations (eg, “eh eh eh eh” while pointing) to communicate. Very recently, Sam has begun to use some words which are often paired with a gesture (eg, “Daddy” while pointing or “up” while raising hands to be picked up). You notice during your visit that Sam is a social and attentive child. He looks at other people and follows their eye gaze to distal objects. He also seems to understand the speech that his mother directs to him and he can easily carry out 2-step commands (eg, “Pick up the cup and sit next to me, please”). Sam's mother is aware of no immediate or extended family members who have ever had a speech or language impairment. Sam has no history of ear infection, and a recent hearing screen indicated hearing in the normal range.
- ▪ Limited imitation
- ▪ Limited pretend play
- ▪ Limited facial expressiveness
- ▪ Excessive use of nonverbal communicative gestures (eg, reaching, pointing, looking)
Answer: Limited imitation. Limited pretend play.
What should the mother expect with time if her child does not have a speech and language impairment but is rather a late-talker? (Select all that apply.)
- ▪ The child will begin to engage in unusual repetitive behaviors
- ▪ The child will steadily albeit slowly add new words and begin to combine them into 2-word utterances
- ▪ Any new words that the child utters are likely to be distorted and difficult to understand
- ▪ The child may develop aggressive behaviors to cope with his inability to communicate effectively
Answer: The child will steadily albeit slowly add new words and begin to combine them into 2-word utterances.
Theresa [pseudonym] is a 3-year-old female whom you have seen in your office regularly since her birth. She comes to you today for her annual check-up. During her visit, you observe that Theresa is precocious in her language development. Indeed, her mother reports that she has always been a “great talker” and that she began to speak in well-formed utterances at age 18 months. During this visit, you notice a number of disfluencies in Theresa's speech. At one point, she repeats a word 3 times before getting the rest of the sentence out (ie, “I see… see… see a book with a clown”). Theresa's mother states that these kinds of disfluencies began about 1 month ago and, although she characterizes them as relatively infrequent, she has questions about whether this kind of speech is normal.
Which of the following additional patient characteristics obtained from your observation of Theresa would increase your suspicion of a diagnosis of a fluency disorder? (Select all that apply.)
- ▪ Theresa seems aware of and perturbed by her disfluencies
- ▪ Theresa sometimes jerks her head when hesitating to utter her next word
- ▪ Approximately 20% of Theresa's words appear to constitute disfluencies
- ▪ Theresa produces multi-unit syllable repetitions (eg, “t-t-t-time”)
- ▪ All of the above
Answer: All of the above.
Reader Comments on: Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood See reader comments on this article and provide your own.
Readers are encouraged to respond to the author at [email protected] or to George Lundberg, MD, Editor in Chief of The Medscape Journal of Medicine , for the editor's eyes only or for possible publication as an actual Letter in the Medscape Journal via email: ten.epacsdem@grebdnulg
Contributor Information
Patricia A. Prelock, Department of Communication Sciences, University of Vermont, Burlington, Vermont.
Tiffany Hutchins, Department of Communication Sciences, University of Vermont, Burlington, Vermont.
Frances P. Glascoe, Department of Pediatrics, Vanderbilt University, Nashville, Tennessee.
A Review on Speech Disorders and Processing of Disordered Speech
- Published: 14 June 2022
- Volume 126 , pages 1621–1631, ( 2022 )
Cite this article

- Audre Arlene Anthony 1 ,
- Chandreshekar Mohan Patil 1 &
- Jagadeesh Basavaiah ORCID: orcid.org/0000-0001-8457-5618 1
623 Accesses
Explore all metrics
Speech disorder refers to the situation that affects the ability of a person to produce sounds that generates words. People of any age can be affected by speech disorders. Speech disorders symptoms varies broadly contingent on the cause and the disorder severity. Multiple speech disorders can be developed in the people with different symptoms. Approximately one-fifth of theworld’s population suffer or have suffered from voice and speech production disorders due to diseases or some other dysfunction. Thus, there is a clear need for objective ways to evaluate the quality of voice and speech as well as its link to vocal fold activity, to evaluate the complex interaction between the larynx and voluntary movements of the articulators (i.e., lips, teeth, tongue, velum, jaw, etc.), or to evaluate disfluencies at the language level. With advances in speech signal processing and natural language processing, there has been recent interest in developing tools to detect more subtle changes in cognitive-linguistic function. This paper discusses on various speech disorders in children and adults such as apraxia, stuttering, voice disorders involving the larynx, Aphasia and dysarthria. This paper also presents a survey on different methods used for processing speech disorders.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
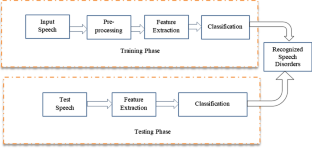
Similar content being viewed by others

A Review on Automatic Assessment and Detection of Pathological Speech

Toward Explainable Automatic Classification of Children’s Speech Disorders

Articulatory Analysis and Classification of Pathological Speech
Data availability.
The data used to support the finding of this study are included within the article.
Shahin, M., Zafar, U., & Ahmed, B. (2020). The Automatic Detection of Speech Disorders in Children: Challenges, Opportunities, and Preliminary Results. IEEE Journal of Selected Topics in Signal Processing, 14 (2), 400–412. https://doi.org/10.1109/JSTSP.2019.2959393
Article Google Scholar
Alharbi S., Hasan M., Simons A.J.H., Brumfitt S., Green P. (2017) Detecting Stuttering Events in Transcripts of Children’s Speech. In: Camelin N., Estève Y., Martín-Vide C. (eds) Statistical Language and Speech Processing. SLSP 2017. Lecture Notes in Computer Science, vol 10583. Springer, Cham
Sadeen,A, Hasan, M, Simons, A, Brumfitt, S, Green, P (2018). A Lightly Supervised Approach to Detect Stuttering in Children's Speech. 3433–3437. https://doi.org/10.21437/Interspeech.2018-2155 .
Smith, D, Sneddon, A, Ward, L, Duenser, A, Freyne, J, Silvera-Tawil, D, Morgan, A (2017). Improving Child Speech Disorder Assessment by Incorporating Out-of-Domain Adult Speech. 2690–2694. https://doi.org/10.21437/Interspeech.2017-455 .
Kothalkar, P. V., Rudolph, J., Dollaghan, C., McGlothlin, J., Campbell, T. F., Hansen, J. H. L., Automatic Screening to Detect ’At Risk’ Child Speech Samples using a Clinical Group Verification framework*. (2018). 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). Honolulu, HI, 2018 , 4909–4913.
Google Scholar
Hanani, A., Attari, M., Farakhna, A., Joma'A, A., Hussein, M., Taylor, S. (2016) Automatic Identification of Articulation Disorders for Arabic Children Speakers. Proc. Workshop on Child Computer Interaction, 35–39.
Vikram, C., Tripathi, A., Kalita, S., Prasanna,SM. (2018) "Estimation of hypernasality scores from cleft lip and palate speech", Proc. Interspeech, 1701–1705
Sell, Gregory & Garcia-Romero, Daniel. (2015). Speaker diarization with plda i-vector scoring and unsupervised calibration. 2014 IEEE Workshop on Spoken Language Technology, SLT 2014 - Proceedings. 413–417. https://doi.org/10.1109/SLT.2014.7078610 .
Wang, X., Du, J., Sun, L., Wang, Q., Lee, C., A Progressive Deep Learning Approach to Child Speech Separation. (2018). 11th International Symposium on Chinese Spoken Language Processing (ISCSLP). Taipei City, Taiwan, 2018 , 76–80.
Shahin, M., Gutierrez-Osuna, R., Ahmed, B. 2016 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), Shanghai, 2016 6480–6484.
Teshaboyeva, G. (2020). Speech defects in young children and ways to overcome them. ACADEMICIA International Multidisciplinary Research Journal, 10 (6), 1761–1767.
Ruksenaite, J., Volkmer, A., Jiang, J., Johnson, J. C., Marshall, C. R., Warren, J. D., & Hardy, C. J. (2021). Primary progressive Aphasia: Toward a pathophysiological synthesis. Current Neurology and Neuroscience Reports, 21 (3), 1–2.
Zhang, Z., Xu, Q., Joshi, R.M. (2020) A meta‐analysis on the effectiveness of intervention in children with primary speech and language delays/disorders: focusing on China and the United States. Clin. Psychol. Psychother
Horton, R (2020) Systems-based approaches to speech-language pathology service delivery for school age children. In: Cases on Communication Disorders in Culturally Diverse Populations, pp. 113–136. IGI Global
Rumbach, A. F., Clayton, N. A., Muller, M. J., & Maitz, P. K. (2016). The speech-language pathologist’s role in multidisciplinary burn care: An international perspective. Burns, 42 (4), 863–871.
Jothi, K., Sivaraju, S., Yawalkar, P (2021) AI-based speech-language therapy using speech quality parameters for aphasia person: a comprehensive review. In: 4th International Conference on Electronics, Communication and Aerospace Technology (ICECA), 5382 -5392
Kohlschein, C., Schmitt, M., Schuller, B., Jeschke, S., Werner, C (2017) A machine learning-based system for the automatic evaluation of aphasia speech. In: IEEE 19th International Conference on e-Health Networking, Applications and Services (Healthcom)
Gasparetti, F., De Medio, C., Limongelli, C., Sciarrone, F., & Temperini, M. (2018). Prerequisites between learning objects: Automatic extraction based on a machine learning approach. Telematics and Informatics, 35 (3), 595–610.
Aishwarya, J., Kundapur, P., Kumar, S., Hareesha, K.S (2018) Kannada speech recognition system for Aphasic people. In: International Conference on Advances in Computing, Communications, and Informatics (ICACCI), 1753–1756
Briffa, C., & Porter, J. (2013). A systematic review of the collaborative clinical education model to inform speech-language pathology practice. International Journal of Speech-Language Pathology, 15 (6), 564–574.
Download references
Acknowledgements
We, the authors of the paper titled “A Review on Speech Disorders and Processing of Disordered Speech” hereby declare that the work included in the above paper is original and is an outcome of the research carried out by the authors indicated in it. Further, we declare that the work submitted has not been published already or under consideration for publication in any Journals/Conferences/Symposia/Seminars. We also declare that the work does not infringe on any copyrights, property rights of others including licences and it is free from plagiarism. The authors hereby assign all copyright rights of the paper to Springer.
This work is not funded by any governmental or non-governmental funding agencies.
Author information
Authors and affiliations.
Department of Electronics and Communication Engineering, Vidyavardhaka College of Engineering, Mysuru, India
Audre Arlene Anthony, Chandreshekar Mohan Patil & Jagadeesh Basavaiah
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jagadeesh Basavaiah .
Ethics declarations
Conflict of interest.
The authors declare that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Anthony, A.A., Patil, C.M. & Basavaiah, J. A Review on Speech Disorders and Processing of Disordered Speech. Wireless Pers Commun 126 , 1621–1631 (2022). https://doi.org/10.1007/s11277-022-09812-w
Download citation
Accepted : 28 May 2022
Published : 14 June 2022
Issue Date : September 2022
DOI : https://doi.org/10.1007/s11277-022-09812-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Speech disorder
- peech processing
- Find a journal
- Publish with us
- Track your research

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Speech disorders - children
A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the person's speech difficult to understand.
Common speech disorders are:
- Articulation disorders
- Phonological disorders
- Voice disorders or resonance disorders
Speech disorders are different from language disorders in children . Language disorders refer to someone having difficulty with:
- Getting their meaning or message across to others (expressive language)
- Understanding the message coming from others (receptive language)
Speech is one of the main ways in which we communicate with those around us. It develops naturally, along with other signs of normal growth and development . Disorders of speech and language are common in preschool age children.
Disfluencies are disorders in which a person repeats a sound, word, or phrase. Stuttering may be the most serious disfluency. It may be caused by:
- Genetic abnormalities
- Emotional stress
- Any trauma to the brain or infection
Articulation and phonological disorders may occur in other family members. Other causes include:
- Problems or changes in the structure or shape of the muscles and bones used to make speech sounds. These changes may include cleft palate and tooth problems.
- Damage to parts of the brain or the nerves (such as from cerebral palsy ) that control how the muscles work together to create speech.
- Hearing loss.
Voice disorders are caused by problems when air passes from the lungs, through the vocal cords, and then through the throat, nose, mouth, and lips. A voice disorder may be due to:
- Acid from the stomach moving upward ( GERD )
- Cancer of the throat
- Cleft palate or other problems with the palate
- Conditions that damage the nerves that supply the muscles of the vocal cords
- Laryngeal webs or clefts (a birth defect in which a thin layer of tissue is between the vocal cords)
- Noncancerous growths (polyps, nodules, cysts, granulomas, papillomas, or ulcers) on the vocal cords
- Overuse of the vocal cords from screaming, constantly clearing the throat, or singing
- Hearing loss
Stuttering is the most common type of disfluency.
Symptoms of disfluency can include:
- Repetition of sounds, words, or parts of words or phrases after age 4 (I want...I want my doll. I...I see you.)
- Putting in (interjecting) extra sounds or words (We went to the...uh...store.)
- Making words longer (I am Boooobbby Jones.)
- Pausing during a sentence or words, often with the lips together
- Tension in the voice or sounds
- Frustration with attempts to communicate
- Head jerking while talking
- Eye blinking while talking
- Embarrassment with speech
ARTICULATION DISORDER
The child is not able to produce speech sounds clearly, such as saying "coo" instead of "school."
- Certain sounds (like "r", "l", or "s") may be consistently distorted or changed (such as making the 's' sound with a whistle).
- Errors may make it hard for people to understand the person (only family members may be able to understand a child).
PHONOLOGICAL DISORDER
The child does not use some or all of the speech sounds to form words as expected for their age.
- The last or first sound of words (most often consonants) may be left out or changed.
- The child may have no problem pronouncing the same sound in other words (a child may say "boo" for "book" and "pi" for "pig", but may have no problem saying "key" or "go").
VOICE DISORDERS
Other speech problems include:
- Hoarseness or raspiness to the voice
- Voice may break in or out
- Pitch of the voice may change suddenly
- Voice may be too loud or too soft
- Person may run out of air during a sentence
- Speech may sound odd because too much air is escaping through the nose (hypernasality) or too little air is coming out through the nose (hyponasality)
Exams and Tests
Your health care provider will ask about your child's developmental and family history. The provider will do some neurological screening and check for:
- Fluency of speech
- Any emotional stress
- Any underlying condition
- Effect of speech disorder on daily life
Some other evaluation tools used to identify and diagnose speech disorders are:
- Denver Articulation Screening Examination.
- Leiter International Performance scale-3.
- Goldman-Fristoe Test of Articulation 3 (GFTA-3).
- Arizona Articulation and Phonology Scale 4th Revision (Arizona-4).
- Prosody-voice screening profile.
A hearing test may also be done to check for hearing loss as a cause of the speech disorder.
Children may outgrow milder forms of speech disorders. The type of treatment will depend on the severity of the speech disorder and its cause.
Speech therapy may help with more severe symptoms or any speech problems that do not improve.
In therapy, the therapist may teach your child how to use their tongue to create certain sounds.
If a child has a speech disorder, parents are encouraged to:
- Avoid expressing too much concern about the problem, which can make matters worse by making the child more self-conscious.
- Avoid stressful social situations whenever possible.
- Listen patiently to the child, make eye contact, don't interrupt, and show love and acceptance. Avoid finishing sentences for them.
- Set aside time for talking.
Support Groups
More information and support for people with stuttering and their families can be found at:
- American Institute for Stuttering -- stutteringtreatment.org
- American Speech-Language-Hearing Association (ASHA) -- www.asha.org/
- The Stuttering Foundation -- www.stutteringhelp.org
- National Stuttering Association (NSA) -- westutter.org
Outlook (Prognosis)
The outlook depends on the cause of the disorder. Speech can often be improved with speech therapy. Early treatment is likely to have better results.
Possible Complications
Speech disorders may lead to challenges with social interactions due to difficulty communicating.
When to Contact a Medical Professional
Contact your provider if:
- Your child's speech is not developing according to normal milestones.
- You think your child is in a high-risk group.
- Your child is showing signs of a speech disorder.
Hearing loss is a risk factor for speech disorders. At-risk infants should be referred to an audiologist for a hearing test. Hearing and speech therapy can then be started, if necessary.
As young children begin to speak, some disfluency is common, and most of the time, it goes away without treatment. If you place too much attention on the disfluency, a stuttering pattern may develop.
Alternative Names
Articulation deficiency; Articulation disorder; Phonological disorder; Voice disorders; Vocal disorders; Disfluency; Communication disorder - speech disorder; Speech disorder - stuttering; Cluttering; Stammering; Childhood onset fluency disorder
American Speech-Language-Hearing Association website. Voice disorders. www.asha.org/Practice-Portal/Clinical-Topics/Voice-Disorders/ . Accessed February 22, 2024.
Driver LE, Nelson ME. Pediatric speech disorders. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery . 7th ed. Philadelphia, PA: Elsevier; 2021:chap 183.
Simms MD. Language development and communication disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics . 21st ed. Philadelphia, PA: Elsevier; 2020:chap 52.
Trauner DA, Nass RD. Developmental language disorders. In: Swaiman KF, Ashwal S, Ferriero DM, et al, eds. Swaiman's Pediatric Neurology: Principles and Practice . 6th ed. Philadelphia, PA: Elsevier; 2017:chap 53.
Zajac DJ. Evaluation and management of speech disorders for the patient with cleft palate. In: Fonseca RJ, ed. Oral and Maxillofacial Surgery . 3rd ed. St Louis, MO: Elsevier; 2018:chap 32.
Review Date 2/17/2024
Updated by: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Speech and Language Problems in Children

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

On this page:
What is stuttering?
Who stutters, how is speech normally produced, what are the causes and types of stuttering, how is stuttering diagnosed, how is stuttering treated, what research is being conducted on stuttering, where can i find additional information about stuttering.
Stuttering is a speech disorder characterized by repetition of sounds, syllables, or words; prolongation of sounds; and interruptions in speech known as blocks. An individual who stutters exactly knows what he or she would like to say but has trouble producing a normal flow of speech. These speech disruptions may be accompanied by struggle behaviors, such as rapid eye blinks or tremors of the lips. Stuttering can make it difficult to communicate with other people, which often affects a person’s quality of life and interpersonal relationships. Stuttering can also negatively influence job performance and opportunities, and treatment can come at a high financial cost.
Symptoms of stuttering can vary significantly throughout a person’s day. In general, speaking before a group or talking on the telephone may make a person’s stuttering more severe, while singing, reading, or speaking in unison may temporarily reduce stuttering.
Stuttering is sometimes referred to as stammering and by a broader term, disfluent speech .
Roughly 3 million Americans stutter. Stuttering affects people of all ages. It occurs most often in children between the ages of 2 and 6 as they are developing their language skills. Approximately 5 to 10 percent of all children will stutter for some period in their life, lasting from a few weeks to several years. Boys are 2 to 3 times as likely to stutter as girls and as they get older this gender difference increases; the number of boys who continue to stutter is three to four times larger than the number of girls. Most children outgrow stuttering. Approximately 75 percent of children recover from stuttering. For the remaining 25 percent who continue to stutter, stuttering can persist as a lifelong communication disorder.
We make speech sounds through a series of precisely coordinated muscle movements involving breathing, phonation (voice production), and articulation (movement of the throat, palate, tongue, and lips). Muscle movements are controlled by the brain and monitored through our senses of hearing and touch.
The precise mechanisms that cause stuttering are not understood. Stuttering is commonly grouped into two types termed developmental and neurogenic.
Developmental stuttering
Developmental stuttering occurs in young children while they are still learning speech and language skills. It is the most common form of stuttering. Some scientists and clinicians believe that developmental stuttering occurs when children’s speech and language abilities are unable to meet the child’s verbal demands. Most scientists and clinicians believe that developmental stuttering stems from complex interactions of multiple factors. Recent brain imaging studies have shown consistent differences in those who stutter compared to nonstuttering peers. Developmental stuttering may also run in families and research has shown that genetic factors contribute to this type of stuttering. Starting in 2010, researchers at the National Institute on Deafness and Other Communication Disorders (NIDCD) have identified four different genes in which mutations are associated with stuttering. More information on the genetics of stuttering can be found in the research section of this fact sheet.
Neurogenic stuttering
Neurogenic stuttering may occur after a stroke, head trauma, or other type of brain injury. With neurogenic stuttering, the brain has difficulty coordinating the different brain regions involved in speaking, resulting in problems in production of clear, fluent speech.
At one time, all stuttering was believed to be psychogenic, caused by emotional trauma, but today we know that psychogenic stuttering is rare.
Stuttering is usually diagnosed by a speech-language pathologist, a health professional who is trained to test and treat individuals with voice, speech, and language disorders. The speech-language pathologist will consider a variety of factors, including the child’s case history (such as when the stuttering was first noticed and under what circumstances), an analysis of the child’s stuttering behaviors, and an evaluation of the child’s speech and language abilities and the impact of stuttering on his or her life.
When evaluating a young child for stuttering, a speech-language pathologist will try to determine if the child is likely to continue his or her stuttering behavior or outgrow it. To determine this difference, the speech-language pathologist will consider such factors as the family’s history of stuttering, whether the child’s stuttering has lasted 6 months or longer, and whether the child exhibits other speech or language problems.
Although there is currently no cure for stuttering, there are a variety of treatments available. The nature of the treatment will differ, based upon a person’s age, communication goals, and other factors. If you or your child stutters, it is important to work with a speech-language pathologist to determine the best treatment options.
Therapy for children
For very young children, early treatment may prevent developmental stuttering from becoming a lifelong problem. Certain strategies can help children learn to improve their speech fluency while developing positive attitudes toward communication. Health professionals generally recommend that a child be evaluated if he or she has stuttered for 3 to 6 months, exhibits struggle behaviors associated with stuttering, or has a family history of stuttering or related communication disorders. Some researchers recommend that a child be evaluated every 3 months to determine if the stuttering is increasing or decreasing. Treatment often involves teaching parents about ways to support their child’s production of fluent speech. Parents may be encouraged to:
- Provide a relaxed home environment that allows many opportunities for the child to speak. This includes setting aside time to talk to one another, especially when the child is excited and has a lot to say.
- Listen attentively when the child speaks and focus on the content of the message, rather than responding to how it is said or interruptng the child.
- Speak in a slightly slowed and relaxed manner. This can help reduce time pressures the child may be experiencing.
- Listen attentively when the child speaks and wait for him or her to say the intended word. Don't try to complete the child’s sentences. Also, help the child learn that a person can communicate successfully even when stuttering occurs.
- Talk openly and honestly to the child about stuttering if he or she brings up the subject. Let the child know that it is okay for some disruptions to occur.
Stuttering therapy
Many of the current therapies for teens and adults who stutter focus on helping them learn ways to minimize stuttering when they speak, such as by speaking more slowly, regulating their breathing, or gradually progressing from single-syllable responses to longer words and more complex sentences. Most of these therapies also help address the anxiety a person who stutters may feel in certain speaking situations.
Drug therapy
The U.S. Food and Drug Administration has not approved any drug for the treatment of stuttering. However, some drugs that are approved to treat other health problems—such as epilepsy, anxiety, or depression—have been used to treat stuttering. These drugs often have side effects that make them difficult to use over a long period of time.
Electronic devices
Some people who stutter use electronic devices to help control fluency. For example, one type of device fits into the ear canal, much like a hearing aid, and digitally replays a slightly altered version of the wearer’s voice into the ear so that it sounds as if he or she is speaking in unison with another person. In some people, electronic devices may help improve fluency in a relatively short period of time. Additional research is needed to determine how long such effects may last and whether people are able to easily use and benefit from these devices in real-world situations. For these reasons, researchers are continuing to study the long-term effectiveness of these devices.
Self-help groups
Many people find that they achieve their greatest success through a combination of self-study and therapy. Self-help groups provide a way for people who stutter to find resources and support as they face the challenges of stuttering.
Researchers around the world are exploring ways to improve the early identification and treatment of stuttering and to identify its causes. For example, scientists have been working to identify the possible genes responsible for stuttering that tend to run in families. NIDCD scientists have now identified variants in four such genes that account for some cases of stuttering in many populations around the world, including the United States and Europe. All of these genes encode proteins that direct traffic within cells, ensuring that various cell components get to their proper location within the cell. Such deficits in cellular trafficking are a newly recognized cause of many neurological disorders. Researchers are now studying how this defect in cellular trafficking leads to specific deficits in speech fluency.
Researchers are also working to help speech-language pathologists determine which children are most likely to outgrow their stuttering and which children are at risk for continuing to stutter into adulthood. In addition, researchers are examining ways to identify groups of individuals who exhibit similar stuttering patterns and behaviors that may be associated with a common cause.
Scientists are using brain imaging tools such as PET (positron emission tomography) and functional MRI (magnetic resonance imaging) scans to investigate brain activity in people who stutter. NIDCD-funded researchers are also using brain imaging to examine brain structure and functional changes that occur during childhood that differentiate children who continue to stutter from those who recover from stuttering. Brain imaging may be used in the future as a way to help treat people who stutter. Researchers are studying whether volunteer patients who stutter can learn to recognize, with the help of a computer program, specific speech patterns that are linked to stuttering and to avoid using those patterns when speaking.
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
Use the following keywords to help you find organizations that can answer questions and provide information on stuttering:
- Speech-language pathologists
- Physician/practitioner referrals
For more information, contact us at:
NIDCD Information Clearinghouse 1 Communication Avenue Bethesda, MD 20892-3456 Toll-free voice: (800) 241-1044 Toll-free TTY: (800) 241-1055 Email: [email protected]
NIH Pub. No. 97-4232 February 2016
* Note: PDF files require a viewer such as the free Adobe Reader .
- To save this word, you'll need to log in. Log In
speech defect
Definition of speech defect
Love words.
You must — there are over 200,000 words in our free online dictionary, but you are looking for one that’s only in the Merriam-Webster Unabridged Dictionary.
Start your free trial today and get unlimited access to America's largest dictionary, with:
- More than 250,000 words that aren't in our free dictionary
- Expanded definitions, etymologies, and usage notes
- Advanced search features
Dictionary Entries Near speech defect
speech form
Cite this Entry
“Speech defect.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/speech%20defect. Accessed 1 Jul. 2024.
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
Plural and possessive names: a guide, commonly misspelled words, how to use em dashes (—), en dashes (–) , and hyphens (-), absent letters that are heard anyway, how to use accents and diacritical marks, popular in wordplay, it's a scorcher words for the summer heat, flower etymologies for your spring garden, 12 star wars words, 'swash', 'praya', and 12 more beachy words, 8 words for lesser-known musical instruments, games & quizzes.

Look up a word, learn it forever.
Defect of speech.
Other forms: defects of speech
- noun a disorder of oral speech synonyms: speech defect , speech disorder see more see less types: show 10 types... hide 10 types... anarthria partial or total loss of articulate speech resulting from lesions of the central nervous system aphonia , voicelessness a disorder of the vocal organs that results in the loss of voice cataphasia a speech disorder in which the same word is repeated several times in succession dysarthria impaired articulatory ability resulting from defects in the peripheral motor nerves or in the speech musculature dyslogia impaired ability to express ideas verbally; usually resulting from difficulties of reasoning (as in feeblemindedness or certain psychoses) dysphonia speech disorder attributable to a disorder of phonation lallation defective articulation of the `l' phoneme or the phoneme `r' is pronounced as `l' lambdacism speech defect involving excessive use or unusual pronunciation of the phoneme `l' lisp a speech defect that involves pronouncing `s' like voiceless `th' and `z' like voiced `th' stammer , stutter a speech disorder involving hesitations and involuntary repetitions of certain sounds type of: disorder , upset a physical condition in which there is a disturbance of normal functioning
Sign up now (it’s free!)
Whether you’re a teacher or a learner, vocabulary.com can put you or your class on the path to systematic vocabulary improvement..
Advertisement
One by One, Biden’s Closest Media Allies Defect After the Debate
The MSNBC host Joe Scarborough urged him to consider dropping out. So did other pundits the president had long viewed as his strongest allies in the news media.
- Share full article

By Michael M. Grynbaum
Reporting from Atlanta
- June 28, 2024
Joe Scarborough pursed his lips and jotted down a few notes at his desk. It was 6 a.m. on Friday, seven and a half hours after a diminished President Biden had gingerly stepped off the debate stage, and the host of “Morning Joe” on MSNBC was about to deliver a painful message to viewers of television’s most reliable redoubt of Biden support.
“I love Joe Biden,” Mr. Scarborough began as the cameras flipped on in his home studio in Maine. “I think his presidency has been an unqualified success.”
“He spent much of the night with his mouth agape and his eyes darting back and forth,” the anchor said. “He couldn’t fact-check anything Donald Trump said. He missed one layup after another after another.” Now, he concluded, “is the last chance for Democrats to decide whether this man we’ve known and loved for a very long time is up to the task of running for president of the United States.”
This was no mere act of punditry. Mr. Biden, 81, is a skeptic of the news media, but Mr. Scarborough is among a tiny group of commentators who have his ear. The president regularly speaks with the anchor and is a devoted watcher of “Morning Joe,” a show that has defended him against all manner of attacks.
No more. And Mr. Scarborough’s defection mirrored that of other longtime Biden media allies who, often in elegiac and pained tones, urged the president to consider dropping out in the wake of his shaky performance in Thursday’s debate against former President Donald J. Trump.
Thomas L. Friedman, a columnist for The New York Times who speaks frequently with Mr. Biden, wrote that he had wept watching the president. “Joe Biden, a good man and a good president, has no business running for re-election,” he said. Evan Osnos, Mr. Biden’s biographer and one of the few journalists granted extensive access to him, called the president “clearly a person who was diminished from where he was” four years ago. And on CNN, the Democratic analyst Van Jones delivered a soliloquy brimming with emotion, full of poignancy, defiance and regret.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
Dysarthria occurs when damage to the brain causes muscle weakness in a person's face, lips, tongue, throat, or chest. Muscle weakness in these parts of the body can make speaking very difficult ...
Speech disorders affect roughly 11.5% of the US population, and 5% of the primary school population. Speech is a complex process that requires precise timing, nerve and muscle control, and as a result is susceptible to impairments. A person who has a stroke, an accident or birth defect may have speech and language problems.
Definition. A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the child's speech difficult to understand. ... Laryngeal webs or clefts (a birth defect in which a thin layer of tissue is between the vocal cords) Noncancerous growths (polyps ...
There are three general categories of speech impairment: Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production. Voice disorder. A voice ...
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual's ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
Speech and Language Disorders. Speech is how we say sounds and words. People with speech problems may: not say sounds clearly. have a hoarse or raspy voice. repeat sounds or pause when speaking, called stuttering. Language is the words we use to share ideas and get what we want. A person with a language disorder may have problems:
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably.
speech disorder, any of the disorders that impair human speech. Human communication relies largely on the faculty of speech, supplemented by the production of certain sounds, each of which is unique in meaning. Human speech is extraordinarily complex, consisting of sound waves of a diverse range of frequencies, intensities, and amplitudes that ...
Signs and Symptoms of Speech Sound Disorders. Your child may substitute one sound for another, leave sounds out, add sounds, or change a sound. It can be hard for others to understand them. It is normal for young children to say the wrong sounds sometimes. For example, your child may make a "w" sound for an "r" and say "wabbit" for "rabbit."
Speech disorder - Major types of speech disorders: In international terminology, disorders of the voice are described as dysphonia. Depending on the underlying cause, the various types of dysphonia are subdivided by the specifying adjective. Thus, a vocal disorder stemming from paralysis of the larynx is a paralytic dysphonia; injury (trauma) of the larynx may produce traumatic dysphonia ...
Introduction. Speech-language deficits are the most common of childhood disabilities and affect about 1 in 12 children or 5% to 8% of preschool children. The consequences of untreated speech-language problems are significant and lead to behavioral challenges, mental health problems, reading difficulties, and academic failure including in-grade retention and high school dropout.
Speech disorder refers to the situation that affects the ability of a person to produce sounds that generates words. People of any age can be affected by speech disorders. Speech disorders symptoms varies broadly contingent on the cause and the disorder severity. Multiple speech disorders can be developed in the people with different symptoms. Approximately one-fifth of theworld's population ...
Speech Disorder: any defect or abnormality that prevents an individual from communicating by means of spoken words. Speech disorders may develop from nerve injury to the brain, muscular paralysis, structural defects, hysteria, or mental retardation.
Disorders of speech and language are common in preschool age children. Disfluencies are disorders in which a person repeats a sound, word, or phrase. Stuttering may be the most serious disfluency. It may be caused by: Genetic abnormalities. Emotional stress. Any trauma to the brain or infection.
Defect. Imperfection, flaw, or deficiency. That which is subject to a defect is missing a requisite element and, therefore, is not legally binding. Defective Service of Process, f
Stuttering is a speech disorder characterized by repetition of sounds, syllables, or words; prolongation of sounds; and interruptions in speech known as blocks. An individual who stutters exactly knows what he or she would like to say but has trouble producing a normal flow of speech. These speech disruptions may be accompanied by struggle ...
The meaning of SPEECH DEFECT is a defect in oral speech (such as lisping or stuttering).
explosive speech loud, sudden enunciation, occurring in certain brain diseases. speech and language in the omaha system, a client problem in the physiologic domain, defined as articulated vocal sounds, symbols, signs, or gestures used for communication. mirror speech speech in which the order of syllables is reversed.
defect of speech: 1 n a disorder of oral speech Synonyms: speech defect , speech disorder Types: show 10 types... hide 10 types... anarthria partial or total loss of articulate speech resulting from lesions of the central nervous system aphonia , voicelessness a disorder of the vocal organs that results in the loss of voice cataphasia a speech ...
Joe Scarborough pursed his lips and jotted down a few notes at his desk. It was 6 a.m. on Friday, seven and a half hours after a diminished President Biden had gingerly stepped off the debate ...
Nigel Farage, the Reform leader, joked about the incident in his own speech later on. TikTok confirmed the stream was suspended but put it down to a moderation error, saying access was restored ...