
- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons

Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

10.1: Weight Management intro
- Last updated
- Save as PDF
- Page ID 53421

- Garrett Rieck & Justin Lundin
- College of the Canyons
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Achieving and sustaining appropriate body weight across the lifespan is vital to maintaining good health and quality of life. Many behavioral, environmental, and genetic factors have been shown to affect a person’s body weight. Calorie balance over time is the key to weight management. Calorie balance refers to the relationship between calories consumed from foods and beverages and calories expended in normal body functions (i.e., metabolic processes) and through physical activity. People cannot control the calories expended in metabolic processes, but they can control what they eat and drink, as well as how many calories they use in physical activity.
Calories consumed must equal calories expended for a person to maintain the same body weight. Consuming more calories than expended will result in weight gain. Conversely, consuming fewer calories than expended will result in weight loss. This can be achieved over time by eating fewer calories, being more physically active, or, best of all, a combination of the two.
Maintaining a healthy body weight and preventing excess weight gain throughout the lifespan are highly preferable to losing weight after weight gain. Once a person becomes obese, reducing body weight back to a healthy range requires significant effort over a span of time, even years. People who are most successful at losing weight and keeping it off do so through continued attention to calorie balance.
The current high rates of overweight and obesity among virtually all subgroups of the population in the United States demonstrate that many Americans are in calorie imbalance—that is, they consume more calories than they expend. To curb the obesity epidemic and improve their health, Americans need to make significant efforts to decrease the total number of calories they consume from foods and beverages and increase calorie expenditure through physical activity. Achieving these goals will require Americans to select a healthy eating pattern that includes nutrient-dense foods and beverages they enjoy, meets nutrient requirements, and stays within calorie needs. In addition, Americans can choose from a variety of strategies to increase physical activity.
Key Recommendations
- Prevent and/or reduce overweight and obesity through improved eating and physical activity behaviors.
- Control total calorie intake to manage body weight. For people who are overweight or obese, this will mean consuming fewer calories from foods and beverages.
- Increase physical activity and reduce time spent in sedentary behaviors.
- Maintain appropriate calorie balance during each stage of life—childhood, adolescence, adulthood, pregnancy and breastfeeding, and older age.
An Epidemic of Overweight and Obesity
The prevalence of overweight and obesity in the United States is dramatically higher now than it was a few decades ago. This is true for all age groups, including children, adolescents, and adults. One of the largest changes has been an increase in the number of Americans in the obese category. As shown in the maps below, the prevalence of obesity has doubled and in some cases tripled between the 1990s and 2011.
Figure \(\PageIndex{1}\). Obesity Rates
The high prevalence of overweight and obesity across the population is of concern because individuals who are overweight obese, compared to those with a normal or healthy weight, are at increased risk for many serious diseases and health conditions, including the following:
- All-causes of death (mortality)
- High blood pressure (Hypertension)
- High LDL cholesterol, low HDL cholesterol, or high levels of triglycerides (Dyslipidemia)
- Type 2 diabetes
- Coronary heart disease
- Gallbladder disease
- Osteoarthritis (a breakdown of cartilage and bone within a joint)
- Sleep apnea and breathing problems
- Some cancers (endometrial, breast, colon, kidney, gallbladder, and liver)
- Low quality of life
- Mental illness such as clinical depression, anxiety, and other mental disorders
- Body pain and difficulty with physical functioning
Ultimately, obesity can increase the risk of premature death. These increased health risks are not limited to adults. Weight-associated diseases and conditions that were once diagnosed primarily in adults are now observed in children and adolescents with excess body fat. For example, cardiovascular disease risk factors, such as high blood cholesterol and hypertension, and type 2 diabetes are now increasing in children and adolescents. The adverse effects also tend to persist through the lifespan, as children and adolescents who are overweight and obese are at substantially increased risk of being overweight and obese as adults and developing weight-related chronic diseases later in life. Primary prevention of obesity, especially in childhood, is an important strategy for combating and reversing the obesity epidemic.
All Americans—children, adolescents, adults, and older adults—are encouraged to strive to achieve and maintain a healthy body weight. Adults who are obese should make changes in their eating and physical activity behaviors to prevent additional weight gain and promote weight loss. Adults who are overweight should not gain additional weight, and most, particularly those with cardiovascular disease risk factors, should make changes to their eating and physical activity behaviors to lose weight. Children and adolescents are encouraged to maintain calorie balance to support normal growth and development without promoting excess weight gain. Children and adolescents who are overweight or obese should change their eating and physical activity behaviors so that their BMI-for-age percentile does not increase over time. Further, a health care provider should be consulted to determine appropriate weight management for the child or adolescent. Families, schools, and communities play important roles in supporting changes in eating and physical activity behaviors for children and adolescents.
Maintaining a healthy weight also is important for certain subgroups of the population, including women who are capable of becoming pregnant, pregnant women, and older adults.
- Women are encouraged to achieve and maintain a healthy weight before becoming pregnant. This may reduce a woman’s risk of complications during pregnancy, increase the chances of a healthy infant birth weight, and improve the long-term health of both mother and infant.
- Pregnant women are encouraged to gain weight within the 2009 Institute of Medicine (IOM) gestational weight gain guidelines. Maternal weight gain during pregnancy outside the recommended range is associated with increased risks for maternal and child health.
- Adults ages 65 years and older who are overweight are encouraged to not gain additional weight. Among older adults who are obese, particularly those with cardiovascular disease risk factors, intentional weight loss can be beneficial and result in improved quality of life and reduced risk of chronic diseases and associated disabilities.
- Complications |
- Diagnosis |
- Treatment |
- Special Populations |
- Prognosis |
- Prevention |
- Key Points |
Obesity is a chronic, multifactorial, relapsing disorder characterized by excess body weight and defined as a body mass index (BMI) of ≥ 30 kg/m2. Complications include cardiovascular disorders (particularly in people with excess abdominal fat), diabetes mellitus, certain cancers, cholelithiasis, metabolic dysfunction-associated steatotic liver disease, cirrhosis, osteoarthritis, reproductive disorders in men and women, psychologic disorders, and, for people with BMI ≥ 35, premature death. Diagnosis is based on BMI. Treatment includes lifestyle modification (eg, diet, physical activity, behavior), anti-obesity medications, and bariatric (weight-loss) surgery.
(See also Obesity in Adolescents .)
Prevalence of obesity in the United States is high in all age groups (see table Changes in Prevalence of Obesity According to NHANES ) and has nearly doubled since the obesity epidemic began in the late 1970s. In 2017–2018, 42.4% of adults had obesity: prevalence was highest in men and women age 40 to 59 ( 1 , 2 ). Prevalence was lowest in non-Hispanic Asian adults (17.4%) compared with non-Hispanic Black (49.6%), Hispanic (44.8%), and non-Hispanic White (42.2%) adults. There were no significant differences in prevalence between men and women among non-Hispanic White, non-Hispanic Asian, or Hispanic adults; however, prevalence among non-Hispanic Black women (56.9%) was higher than all other groups.
In the United States, obesity and its complications cause as many as 300,000 premature deaths each year, making it second only to cigarette smoking as a preventable cause of death. Also, obesity is associated with greater job absenteeism, loss of productivity, and higher health care costs. The annual cost of health care in the United States related to obesity is estimated to be $150 billion.
The American Board of Obesity Medicine (ABOM) was established in 2011 to help train clinicians and standardize practices for managing obesity. ABOM diplomates come from a variety of specialties, including internal medicine, family medicine, pediatrics, surgery, and obstetrics and gynecology. Diplomates share a goal of providing compassionate, individualized, and evidence-based care and improving the overall health of the population. The ABOM stresses obesity be considered a chronic disorder that requires lifelong treatment and follow-up.
1. Hales CM, Carroll MD, Fryar CD, et al : Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics, 2020.
2. The State of Obesity 2022 . Trust for America's Health, 2022. Accessed 10/30/23.
Etiology of Obesity
Causes of obesity are multifactorial and include genetic predisposition and behavioral, metabolic, and hormonal influences. Ultimately, obesity results from a long-standing imbalance between energy intake and energy expenditure, including energy utilization for basic metabolic processes and energy expenditure from physical activity. However, many other factors appear to increase a person's predisposition to obesity, including endocrine disruptors (eg, bisphenol A [BPA]), gut microbiome, sleep/wake cycles, and environmental factors.
Genetic factors
Heritability of BMI is high across different age groups, ranging from 40 to 60% ( 1 , 2 ). With few exceptions, obesity does not follow a simple Mendelian pattern of inheritance but is rather a complex interplay of multiple loci. Genetic factors may affect the many signaling molecules and receptors used by parts of the hypothalamus and gastrointestinal tract to regulate food intake (see sidebar Pathways Regulating Food Intake ). Genome studies have helped define signaling pathways implicated in the predisposition to obesity. Differences in expression of signaling molecules within the leptin-melanocortin pathway (eg, the melanocortrin-4 receptor) have been particularly associated with central control of appetite. Genetic factors can be inherited or result from conditions in utero (called genetic imprinting). Environmental conditions such as nutrition, sleep patterns, and alcohol consumption alter gene expression in various metabolic pathways epigenetically; this effect suggests possible reversibility of environmental factors and refinement of therapeutic targets.
Pathways Regulating Food Intake
Genetic factors also regulate energy expenditure, including basal metabolic rate, diet-induced thermogenesis, and nonvoluntary activity–associated thermogenesis. Genetic factors may have a greater effect on the distribution of body fat, particularly abdominal fat (which increases the risk of metabolic syndrome ), than on the amount of body fat.
Lifestyle and behavioral factors
Weight is gained when caloric intake exceeds energy needs. Important determinants of energy intake include
Portion sizes
The energy density of the food
Systemic drivers of lifestyle and behavioral factors are rooted in community culture and economic systems. Communities which do not have access to fresh fruits and vegetables and which do not consume water as the main fluid consumed tend to have higher rates of obesity. High-calorie, energy-dense foods (eg, processed foods), diets high in refined carbohydrates, and consumption of soft drinks, fruit juices, and alcohol promote weight gain.
Access to safe recreational spaces (eg, pedestrian and biking infrastructure, parks) and availability of public transportation can encourage physical activity and help protect against obesity.
Regulatory factors
Prenatal maternal obesity, prenatal maternal smoking , excessive weight gain during pregnancy (see table Guidelines for Weight Gain During Pregnancy ), and intrauterine growth restriction can disturb weight regulation and contribute to weight gain during childhood and later. Obesity that persists beyond early childhood makes weight loss in later life more difficult.
The composition of the gut microbiome also appears to be an important factor; early use of antibiotics and other factors that alter the composition of the gut microbiome may promote weight gain and obesity later in life ( 3 ).
Early exposure to obesogens, a type of endocrine-disrupting chemical (eg, cigarette smoke, bisphenol A, air pollution, flame retardants, phthalates, polychlorinated biphenyls) can alter metabolic set points through epigenetics or nuclear activation, increasing the propensity of developing obesity ( 4 ).
Adverse childhood events or abuse in early childhood increase risk of several disorders, including obesity. The Centers for Disease Control and Prevention's adverse childhood events study demonstrated that childhood history of verbal, physical, or sexual abuse predicted an increase of 8% in risk of a BMI ≥ 30 and 17.3% in risk of a BMI ≥ 40. Certain types of abuse carried the strongest risk. For example, frequent verbal abuse had the largest increase in risk (88%) of a BMI > 40. Being often hit and injured increased the risk of BMI > 30 by 71% ( 5 ). Cited mechanisms for the association between abuse and obesity include neurobiologic and epigenetic phenomena ( 6 ).
Insufficient sleep (usually considered 7 )
Smoking cessation is associated with weight gain and can deter patients from quitting smoking.
Uncommonly, weight gain is caused by one of the following disorders:
Alternations in brain structure and function caused by a tumor (especially a craniopharyngioma) or an infection (particularly those affecting the hypothalamus), which can stimulate consumption of excess calories
Hyperinsulinism due to pancreatic tumors
Hypercortisolism due to Cushing syndrome , which causes predominantly abdominal obesity
Hypothyroidism (rarely a cause of substantial weight gain)
Hypogonadism
Eating disorders
At least 2 pathologic eating patterns may be associated with obesity:
Binge eating disorder is consumption of large amounts of food quickly with a subjective sense of loss of control during the binge and distress after it. This disorder does not include compensatory behaviors, such as vomiting. Binge eating disorder occurs in about 3.5% of women and 2% of men during their lifetime and in about 10 to 20% of people entering weight reduction programs. Obesity is usually severe, large amounts of weight are frequently gained or lost, and pronounced psychologic disturbances are present.
Night-eating syndrome
Similar but less extreme patterns probably contribute to excess weight gain in more people. For example, eating after the evening meal contributes to excess weight gain in many people who do not have night-eating syndrome.
Etiology references
1. Mahmoud AM : An overview of epigenetics in obesity: The role of lifestyle and therapeutic interventions. Int J Mol Sci 23 (3):1341. 2022. doi: 10.3390/ijms23031341
2. Nan C, Guo B, Claire Warner C, et al : Heritability of body mass index in pre-adolescence, young adulthood and late adulthood. Eur J Epidemiol 27 (4):247–253, 2012. doi: 10.1007/s10654-012-9678-6 Epub 2012 Mar 18.
3. Ajslev TA, Andersen CS, Gamborg M, et al : Childhood overweight after establishment of the gut microbiota: The role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes 35 (4): 522–529, 2011. doi: 10.1038/ijo.2011.27
4. Heindel JJ, Newbold R, Schug TT : Endocrine disruptors and obesity. Nat Rev Endocrinol 11 (11):653–661, 2015. doi: 10.1038/nrendo.2015.163
5. Williamson DF, Thompson TJ, Anda RF, et al : Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord 26 (8):1075–1082, 2002. doi: 10.1038/sj.ijo.0802038
6. Anda RF, Felitti VJ, Bremner JD, et al : The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 256 (3):174–186, 2006. doi: 10.1007/s00406-005-0624-4
7. Taheri S, Lin L, Austin D, et al : Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1 (3):e62, 2004. doi: 10.1371/journal.pmed.0010062 Epub 2004 Dec 7.
Complications of Obesity
Complications of obesity can affect almost every organ system; they include the following:
Metabolic syndrome
Diabetes mellitus
Cardiovascular disorders
Venous thromboembolism
Liver disorders ( metabolic dysfunction-associated fatty liver disease , which may lead to cirrhosis )
Gallbladder disease ( cholelithiasis )
Gastroesophageal reflux
Obstructive sleep apnea
Reproductive system disorders, including infertility in both sexes, a low serum testosterone level in men, and polycystic ovary syndrome in women
Many cancers (especially colon cancer and breast cancer )
Osteoarthritis
Tendon and fascial disorders
Skin disorders (eg, intertriginous infections )
Hypertension
Depression , anxiety , and body dysmorphic disorder
Fat tissue is an active endocrine organ that secretes adipokines and free fatty acids that increase systemic inflammation, resulting in conditions such as , atherosclerosis , and impaired immunity.
The pathogenesis of obesity-related hypertension is mediated largely by activation of the renin-angiotensin-aldosterone system via leptin and angiotensin directly released from visceral adipocytes. Increased sympathetic nervous system activity increases vasoconstriction.
, dyslipidemias , and hypertension (metabolic syndrome) can develop, often leading to diabetes mellitus and coronary artery disease . These complications are more likely in patients with fat that is concentrated abdominally (visceral fat), a high serum triglyceride level, a family history of type 2 diabetes mellitus or premature cardiovascular disease, or a combination of these risk factors.
Obstructive sleep apnea can result if excess fat in the neck compresses the airway during sleep. Breathing stops for moments, as often as hundreds of times a night. This disorder, often undiagnosed, can cause loud snoring and excessive daytime sleepiness and increases the risk of hypertension , cardiac arrhythmias , and metabolic syndrome .
Obesity may cause obesity-hypoventilation syndrome (Pickwickian syndrome). Impaired breathing leads to hypercapnia, reduced sensitivity to carbon dioxide in stimulating respiration, hypoxia, cor pulmonale , and risk of premature death. This syndrome may occur alone or secondary to obstructive sleep apnea.
Skin disorders are common; increased sweat and skin secretions, trapped in thick folds of skin, are conducive to fungal and bacterial growth, making intertriginous infections especially common.
Being overweight probably predisposes to gout , deep venous thrombosis , and pulmonary embolism .
Obesity leads to social, economic, and psychologic problems as a result of prejudice, discrimination, poor body image, and low self-esteem. For example, people may be underemployed or unemployed.
Diagnosis of Obesity
Body mass index (BMI)
Waist circumference
Body composition analysis
In adults, BMI, defined as weight (kg) divided by the square of the height (m 2 ), is used to screen for overweight or obesity:
Overweight = 25 to 29.9 kg/m2
Class I obesity = 30 to 34.9 kg/m2
Class II obesity = 35 to 39.9 kg/m2
Class II obesity = ≥ 40 kg/m2
BMI is a commonly used tool that can be easily calculated and correlates with metabolic and fat mass disease in human population studies. However, BMI is a crude screening tool and has limitations in many subpopulations. It tends to overdiagnose overweight and obesity in muscular patients and underdiagnose them in patients with sarcopenia. Some experts think that BMI cutoffs should vary based on ethnicity, sex, and age. The World Health Organization (WHO) and International Diabetes Federation suggest lower cutoff points for people of Asian descent compared with those of other ethnicities ( 1 ).
Waist circumference and the presence of metabolic syndrome appear to predict risk of metabolic and cardiovascular complications better than BMI does ( 2 ). The waist circumference that increases risk of complications due to obesity varies by ethnic group and sex ( 3 ).
Body composition—the percentage of body fat and muscle—is also considered when obesity is diagnosed. Although probably unnecessary in routine clinical practice, body composition analysis can be helpful if clinicians question whether elevated BMI is due to muscle or excessive fat.
Men are considered to have obesity when body fat levels are > 25%. In women, the cutoff is > 32%.
The percentage of body fat can be estimated by measuring skinfold thickness (usually over the triceps) or determining mid upper arm muscle area .
Bioelectrical impedance analysis (BIA) can estimate percentage of body fat simply and noninvasively. BIA estimates percentage of total body water directly; percentage of body fat is derived indirectly. BIA is most reliable in healthy people and in people with only a few chronic disorders that do not change the percentage of total body water (eg, moderate obesity, diabetes mellitus). Whether measuring BIA poses risks in people with implanted defibrillators is unclear.
Underwater (hydrostatic) weighing is the most accurate method for measuring percentage of body fat. Costly and time-consuming, it is used more often in research than in clinical care. To be weighed accurately while submerged, people must fully exhale beforehand.
Imaging procedures, including CT, MRI, and dual-energy x-ray absorptiometry (DXA), can also estimate the percentage and distribution of body fat but are usually used only for research.
Other testing
Patients with obesity should be screened for common comorbid disorders, such as obstructive sleep apnea , diabetes , dyslipidemia , hypertension , steatotic liver disease , and depression . Screening tools can help; for example, for obstructive sleep apnea, clinicians can use an instrument such as the STOP-BANG questionnaire (see table STOP-BANG Risk Score for Obstructive Sleep Apnea ) and often the apnea-hypopnea index (total number of apnea or hypopnea episodes occurring per hour of sleep). Obstructive sleep apnea is often underdiagnosed, and obesity increases the risk.
Diagnosis references
1. WHO Expert Consultation : Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet . 363 (9403):157–163, 2004. doi: 10.1016/S0140-6736(03)15268-3 Erratum in Lancet 363 (9412):902, 2004.
3. Ross R, Neeland IJ, Yamashita S, et al : Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS [International Atherosclerosis Society] and ICCR [International Chair on Cardiometabolic Risk] Working Group on Visceral Obesity. Nat Rev Endocrinol 16 (3):177–189, 2020. doi: 10.1038/s41574-019-0310-7 Epub 2020 Feb 4.
3. Luo J, Hendryx M, Laddu D, et al : Racial and ethnic differences in anthropometric measures as risk factors for diabetes. Diabetes Care 2019 42 (1):126–133. 2019. doi: 10.2337/dc18-1413 Epub 2018 Oct 23.
Treatment of Obesity
Dietary management
Physical activity
Behavioral interventions, anti-obesity medications.
Bariatric surgery
Weight loss of even 5 to 10% improves overall health, helps reduce risk of developing cardiovascular complications (eg, hypertension , dyslipidemia , ) and helps lessen their severity ( 1 ), and may lessen the severity of other complications and comorbid disorders such as obstructive sleep apnea , steatotic liver disease , infertility , and depression .
Support from health care practitioners, peers, and family members and various structured programs can help with weight loss and weight maintenance. Emphasizing obesity as a chronic disorder, rather than a cosmetic issue caused by lack of self-control, helps empower patients to seek sustainable care and clinicians to provide such care. Using people-first language, such as "people with obesity" rather than "obese people," helps avoid labeling patients by their disease and combats stigma.
Balanced eating is important for weight loss and maintenance.
Strategies include
Eating small meals and avoiding or carefully choosing snacks
Substituting fresh fruits and vegetables and salads for refined carbohydrates and processed food
Substituting water for soft drinks or juices
Limiting alcohol consumption to moderate levels
Including no- or low-fat dairy products, which are part of a healthy diet and help provide an adequate amount of vitamin D
Low-calorie, high-fiber diets that modestly restrict calories (by 600 kcal/day) and that incorporate lean protein appear to have the best long-term outcome. Foods with a low glycemic index (see table Glycemic Index of Some Foods ) and marine fish oils or monounsaturated fats derived from plants (eg, olive oil) reduce the risk of cardiovascular disorders and diabetes .
Use of meal replacements can help with weight loss and maintenance; these products can be used regularly or intermittently.
Diets that are overly restrictive are unlikely to be maintained or to result in long-term weight loss. Diets that limit caloric intake to basal energy expenditure (BEE), described as very low calorie diets, can have as few as 800 kcal/day.
Energy expenditure and metabolic rate vary with diet and activity. Restrictive dieting may produce short-term modest weight loss; however, levels of hormones such as leptin, insulin , gastric inhibitory polypeptide (GIP), and ghrelin change to favor weight regain. In a long-term analysis of low-calorie diets, between one- third and two thirds of dieters regained more weight than they lost initially ( 2 ).
Exercise increases energy expenditure, basal metabolic rate, and diet-induced thermogenesis. Exercise also seems to regulate appetite to more closely match caloric needs. Other benefits associated with physical activity include
Increased insulin sensitivity
Improved lipid profile
Lower blood pressure
Better aerobic fitness
Improved psychologic well-being
Decreased risk of breast and colon cancer
Increased life expectancy
Exercise, including strengthening (resistance) exercises, increases muscle mass. Because muscle tissue burns more calories at rest than does fat tissue, increasing muscle mass produces lasting increases in basal metabolic rate. Exercise that is interesting and enjoyable is more likely to be sustained. A combination of aerobic and resistance exercise is better than either alone. Guidelines suggest physical activity of 150 minutes/week for health benefits and 300 to 360 minutes/week for weight loss and maintenance. Developing a more physically active lifestyle can help with weight loss and maintenance.
Clinicians can recommend various behavioral interventions to help patients lose weight ( 3 ). They include
Self-monitoring
Stress management
Contingency management
Problem solving
Stimulus control
Support may come from a group, friends or family members. Participation in a support group can improve adherence to lifestyle changes and thus increase weight loss. The more frequently people attend group meetings, the greater the support, motivation, and supervision they receive and the greater their accountability, resulting in greater weight loss. Patients can get support by using social media to connect with each other and clinicians.
Self-monitoring may include keeping a food log (including the number of calories in foods), weighing regularly, and observing and recording behavioral patterns. Other useful information to record includes time and location of food consumption, the presence or absence of other people, and mood. Clinicians can provide feedback about how patients may improve their eating habits.
Stress management involves teaching patients to identify stressful situations and to develop strategies to manage stress that do not involve eating (eg, going for a walk, meditating, deep breathing).
Contingency management involves providing tangible rewards for positive behaviors (eg, for increasing time spent walking or reducing consumption of certain foods). Rewards may be given by other people (eg, from members of a support group or a health care practitioner) or by the person (eg, purchase of new clothing or tickets to a concert). Verbal rewards (praise) may also be useful.
Problem solving involves identifying and planning ahead for situations that increase the risk of unhealthy eating (eg, travelling, going out to dinner) or that reduce the opportunity for physical activity (eg, driving across country).
Stimulus control involves identifying obstacles to healthy eating and an active lifestyle and developing strategies to overcome them. For example, people may avoid going by a fast food restaurant or not keep sweets in the house. For a more active lifestyle, they may take up an active hobby (eg, gardening), enroll in scheduled group activities (eg, exercise classes, sports teams), walk more, make a habit of taking the stairs instead of elevators, and park at the far end of parking lots (resulting in a longer walk).
Technology-based resources such as applications for mobile devices, and other technological devices may also help with adherence to lifestyle changes and weight loss. Applications can help patients set a weight-loss goal, monitor their progress, track food consumption, and record physical activity.
Pharmacotherapy to treat obesity should be considered for people with a BMI of > 27 kg/m2 plus comorbidities or 30 kg/m2 without comorbidities ( 4 ). Before prescribing medications, clinicians must identify comorbidities that may be affected by medications (eg. diabetes , seizure disorders , opioid use disorder ), and concomitant medications that may promote weight gain.
Most anti-obesity medications are in one of the following classes:
glucagon -like peptide 1 [GLP-1] agonists)
Weight loss, effects on comorbidities, and adverse effect profiles differ widely among medications.
Patients must be warned that stopping long-term anti-obesity medications may result in weight regain.
Specific medications include:
inhibits pancreatic lipase, decreasing intestinal absorption of fat and improving blood glucose and lipids. Because orlistat orlistat difficult to tolerate. Orlistat is available over-the-counter.
The combination of (used to treat seizure disorders and migraines) is approved for long-term use. This combination medication results in weight loss for up to 2 years. Because birth defects are a risk, the combination should be given to women of reproductive age only if they are using contraception and are tested monthly for pregnancy. Other potential adverse effects include sleep problems, cognitive impairment, and increased heart rate. Long-term cardiovascular effects are unknown, and postmarketing studies are ongoing ( 5 ).
lorcaserin compared with those taking placebo. The most common adverse effects in patients without diabetes are headache, nausea, dizziness, fatigue, dry mouth, and constipation; these effects are usually self-limited. Lorcaserin serotonin syndrome is a risk. Lorcaserin was withdrawn from the United States market after an increased cancer risk was identified in a postmarketing trial ( 6 ).
bupropion include nausea, vomiting, headache, and mild increases in systolic and diastolic blood pressure. Contraindications to bupropion include uncontrolled hypertension and a history of or risk factors for seizures because bupropion reduces the seizure threshold.
7 insulin release from the pancreas to induce glycemic control; liraglutide also stimulates satiety and reduces food intake. Liraglutide is injected daily, and dose is titrated up over the course of 5 weeks. Adverse effects include nausea and vomiting; liraglutide has warnings that include acute pancreatitis and risk of thyroid C-cell tumors.
insulin release and reduces appetite and energy intake via effects on appetite centers in the hypothalamus. Semaglutide 2.4 mg subcutaneously has resulted in a mean body weight loss of 14.9% at 68 weeks versus 2.4% in patients treated with placebo ( 8 ). Patients taking semaglutide also had greater improvements in cardiovascular risk factors as well as patient-reported physical functioning. Like liraglutide , the most common adverse effects of semaglutide include nausea and diarrhea, which are usually transient and mild to moderate in severity. Warnings for semaglutide include thyroid tumors and pancreatitis.
is a novel gastric inhibitory polypeptide (GIP) and GLP-1 agonist used to treat type 2 diabetes. In a phase 3 trial, it resulted in substantial and sustained reductions in body weight in patients who did not have diabetes. Improvements in cardiometabolic disease were also observed. It can cause pancreatitis, hypoglycemia, and C-cell tumors of the thyroid and is contraindicated in patients with multiple endocrine neoplasia syndrome type 2 ( 9 ).
All GLP-1 agonists are associated with adverse effects such as nausea, vomiting, and delayed gastric emptying, which can increase the risk of aspiration. The American Society of Anesthesiologists Task Force on Preoperative Fasting recommends holding daily-dosed GLP-1 agonists the day of surgery and weekly-dosed medications 1 week before surgery ( 10 ).
Studies have shown that anti-obesity medications can be safe and effective for weight loss after bariatric surgery if weight is regained. Investigation into the use of anti-obesity medications (eg, GLP-1 receptor agonists) as a bridge t therapy to metabolic and bariatric surgery is ongoing ( 11 ).
Anti-obesity medications should be stopped or changed if patients do not have documented weight loss after 12 weeks of treatment.
Bariatric surgery is the most effective treatment for patients with severe obesity.
Treatment references
1. Arnett DK, Blumenthal RS, Albert, MA, et al : 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140 (11):e596-e646, 2019. doi: 10.1161/CIR.0000000000000678 Epub 2019 Mar 17.
2. Mann T, Tomiyama AJ, Westling E, et al : Medicare's search for effective obesity treatments: Diets are not the answer. Am Psychol 62 (3):220–233, 2007. doi: 10.1037/0003-066X.62.3.220
3. US Preventive Services Task Force : Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults. JAMA 320 (11):1163–1171, 2018, 2018. doi: 10.1001/jama.2018.13022
4. Garvey WT, Mechanick JI, Brett EM, et al American Association of Clinical Endocrinologists and the American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract 22 Suppl 3:1–203, 2016. doi: 10.4158/EP161365.GL Epub 2016 May 24.
5. Jordan J, Astrup A, Engeli S, et al J Hypertens 32 (6): 1178–1188, 2014. doi: 10.1097/HJH.0000000000000145 Published online 2014 Apr 30.
6. Mahase E M: Weight loss pill praised as "holy grail" is withdrawn from US market over cancer link. BMJ 20;368:m705, 2020. doi: 10.1136/bmj.m705 PMID: 32079611.
7. Mehta A, Marso SP, Neeland, IJ Obes Sci Pract 3 (1):3–14, 2017. doi: 10.1002/osp4.84 Epub 2016 Dec 19.
8. Wilding JPH, Batterham RL, Calanna S, et al N Engl J Med 18;384(11):989, 2021. doi: 10.1056/NEJMoa2032183
9. Jastreboff AM, Aronne LJ, Ahmad NN, et al N Engl J Med 21;387 (3):205–216, 2022. doi: 10.1056/NEJMoa2206038 Epub 2022 Jun 4.
10. Joshi GP, Abdelmalak BB, Weigel WA, et al
11. Mok J, Mariam OA, Brown A, et al JAMA Surg 158 (10):1003–1011, 2023. doi:10.1001/jamasurg.2023.2930
Special Populations in Obesity
Obesity is a particular concern in children and older adults.
Obesity in children is defined as BMI greater than the 95th percentile. For children with obesity, complications are more likely to develop because the duration of the disorder is longer. More than 25% of children and adolescents meet overweight or obesity criteria. (See also Obesity in Adolescents .) Similar to adults, complications related to obesity in children include hypertension, dyslipidemia, diabetes and joint problems.

Risk factors for obesity in infants are low birth weight ( 1 ) and maternal weight, diabetes, and smoking .
After puberty, food intake increases; in boys, the extra calories are used to increase protein deposition, but in girls, fat storage is increased.
For children with obesity, psychologic complications (eg, poor self-esteem, social difficulties, depression) and musculoskeletal complications can develop early. Some musculoskeletal complications, such as slipped capital femoral epiphyses , are specific to children. Other early complications may include obstructive sleep apnea , , hyperlipidemia, and nonalcoholic steatohepatitis . Risk of cardiovascular, respiratory, metabolic, hepatic, and other obesity-related complications increases when these children become adults.
Risk of obesity persisting into adulthood depends partly on when obesity first develops. In a meta-analysis of several large cohort studies, 55% of children with obesity continued to have obesity in adolescence, and 70% continued to have obesity over the age of 30 ( 2 ).
Treatment of obesity in children and adolescents involves lifestyle modifications and, for children with severe obesity, metabolic and bariatric surgery .. Participating in physical activities during childhood may promote a lifelong physically active lifestyle. Limiting sedentary activities (eg, watching TV, using the computer or handheld devices) can also help. Medications and surgery are avoided but, if complications of obesity are life threatening, may be warranted.
Measures that control weight and prevent obesity in children may have the largest public health benefits. Such measures should be implemented in the family, schools, and primary care. However, lifestyle modifications often do not result in permanent weight loss.
The 2023 updated guidelines from the American Academy of Pediatrics (AAP) recommend that children and adolescents who have severe obesity (defined as BMI ≥ 40 or BMI > 35 with significant health complications related to obesity) should be treated with metabolic and bariatric surgery, and treatment should involve a multidisciplinary team. The major metabolic and bariatric surgical societies have similar recommendations; however, metabolic and bariatric surgery is not often used in children and adolescents. Barriers include stigma against bariatric surgery in this population and lack of available centers and clinicians trained to take care of children and adolescents with obesity ( 3 ).
Older adults
In the United States, the percentage of older people with obesity has been increasing.
With age, body fat increases and is redistributed to the abdomen, and muscle mass is lost, largely because of physical inactivity, but decreased androgens and growth hormone (which are anabolic) and inflammatory cytokines produced in obesity may also play a role.
Risk of complications depends on
Body fat distribution (increasing with a predominantly abdominal distribution)
Duration and severity of obesity
Associated sarcopenia
Increased waist circumference, suggesting abdominal fat distribution, predicts morbidity (eg, hypertension , diabetes mellitus , coronary artery disease ) and mortality risk better in older adults than does BMI. With aging, fat tends to accumulate more in the waist.
For older adults, physicians may recommend that caloric intake be reduced and physical activity be increased. However, if older patients wish to substantially reduce their caloric intake, their diet should be supervised by a physician. Physical activity also improves muscle strength, endurance, and overall well-being and reduces the risk of developing chronic disorders such as diabetes. Activity should include strengthening and endurance exercises.
Metabolic and bariatric surgery has historically been used less frequently in older patients. In a large retrospective study comparing outcomes in patients sleeve gastrectomy or gastric bypass , complication rates between the groups were similar. Although older patients tended to have higher American Society of Anesthesiologists (ASA) scores and more comorbidities at baseline, morbidity and mortality after surgery did not differ between groups. In the ≥ 65 group, the positive effect of bariatric surgery on weight loss and obesity-related comorbidities was present but less pronounced than in the 4 ).
Special populations references
1. Jornayvaz FR, Vollenweider P, Bochud M, et al : Low birth weight leads to obesity, diabetes and increased leptin levels in adults: The CoLaus study. Cardiovasc Diabetol 15:73, 2016. doi: 10.1186/s12933-016-0389-2
2. Simmonds M, Llewellyn A, Owen ACG, Woolacott N : Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes Rev 17 (2):95–107, 2016. doi: 10.1111/obr.12334 Epub 2015 Dec 23.
3. Elkhoury D, Elkhoury C, Gorantla VR . Improving access to child and adolescent weight loss surgery: A review of updated National and International Practice Guidelines. Cureus 15 (4):e38117, 2023. doi: 10.7759/cureus.38117
4. Iranmanesh P, Boudreau V, Ramji K, et al : Outcomes of bariatric surgery in elderly patients: A registry-based cohort study with 3-year follow-up. Int J Obes (Lond) 46 (3), 574–580 2022. https://doi.org/10.1038/s41366-021-01031-]]
Prognosis for Obesity
If untreated, obesity tends to progress. The probability and severity of complications are proportional to
The absolute amount of fat
The distribution of the fat
Absolute muscle mass
After weight loss, most people return to their pretreatment weight within 5 years, and accordingly, obesity requires a lifelong management program similar to that for any other chronic disorder. Also, when anti-obesity medications are stopped, patients tend to regain weight.
Prevention of Obesity
Regular physical activity and healthy eating improve general fitness, can control weight, and help prevent diabetes mellitus and obesity. Even without weight loss, exercise decreases the risk of cardiovascular disorders. Dietary fiber decreases the risk of colon cancer and cardiovascular disorders.
Sufficient and good-quality sleep, management of stress, and moderation of alcohol intake are also important. However, many biologic and socioeconomic factors are out of a person's control.
Obesity increases the risk of many common health problems and causes up to 300,000 premature deaths each year in the United States, making it second only to cigarette smoking as a preventable cause of death.
Excess caloric intake and too little physical activity contribute the most to obesity, but genetic susceptibility and various disorders (including eating disorders) may also contribute.
Screen patients using BMI and waist circumference and, when body composition analysis is indicated, by measuring skinfold thickness or using bioelectrical impedance analysis.
Screen patients with obesity for common comorbid disorders, such as obstructive sleep apnea, diabetes, dyslipidemia, hypertension, steatotic liver disease, and depression.
Encourage patients to lose even 5 to 10% of body weight by changing their diet, increasing physical activity, and using behavioral interventions if possible.
Consider anti-obesity medications if BMI is ≥ 30 or if BMI is ≥ 27 with complications (eg, hypertension, insulin resistance); however, for severe obesity, surgery is most effective.
Encourage all patients to exercise, to eat healthily, to get enough sleep, and to manage stress.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Weight Management
- Understanding Adult Overweight & Obesity
- Health Risks
- Español
Health Risks of Overweight & Obesity
In this section:
Type 2 diabetes
High blood pressure, heart disease, metabolic syndrome, fatty liver diseases, some cancers, breathing problems, osteoarthritis, diseases of the gallbladder and pancreas, kidney disease, pregnancy problems, fertility problems, sexual function problems, mental health problems.
Overweight and obesity may increase your risk for many health problems—especially if you carry extra fat around your waist. Reaching and staying at a healthy weight can help prevent these problems, stop them from getting worse, or even make them go away.
Type 2 diabetes is a disease that occurs when your blood glucose , also called blood sugar, is too high. Nearly 9 in 10 people with type 2 diabetes have overweight or obesity. 12 Over time, high blood glucose can lead to heart disease , stroke, kidney disease , eye problems , nerve damage , and other health problems .
If you are at risk for type 2 diabetes, you may be able to prevent or delay diabetes by losing at least 5% to 7% of your starting weight. 13,14 For instance, if you weigh 200 pounds, your goal would be to lose about 10 to 14 pounds.

High blood pressure , also called hypertension, is a condition in which blood flows through your blood vessels with a force greater than normal. Having a large body size may increase blood pressure because your heart needs to pump harder to supply blood to all your cells. Excess fat may also damage your kidneys , which help regulate blood pressure.
High blood pressure can strain your heart, damage blood vessels, and raise your risk of heart attack , stroke , kidney disease , and death. 10 Losing enough weight to reach a healthy body mass index range may lower high blood pressure and prevent or control related health problems.
Heart disease is a term used to describe several health problems that affect your heart, such as a heart attack , heart failure , angina , or an abnormal heart rhythm. Having overweight or obesity increases your risk of developing conditions that can lead to heart disease, such as high blood pressure, high blood cholesterol , and high blood glucose. In addition, excess weight can also make your heart have to work harder to send blood to all the cells in your body. Losing excess weight may help you lower these risk factors for heart disease.
A stroke happens when a blood vessel in your brain or neck is blocked or bursts, cutting off blood flow to a part of your brain. A stroke can damage brain tissue and make you unable to speak or move parts of your body.
Overweight and obesity are known to increase blood pressure—and high blood pressure is the leading cause of strokes. Losing weight may help you lower your blood pressure and other risk factors for stroke, including high blood glucose and high blood cholesterol.
Metabolic syndrome is a group of conditions that increase your risk for heart disease, diabetes , and stroke. To be diagnosed with metabolic syndrome, you must have at least three of the following conditions
- large waist size
- high level of triglycerides in your blood
- high blood pressure
- high level of blood glucose when fasting
- low level of HDL cholesterol —the “good” cholesterol—in your blood
Metabolic syndrome is closely linked to overweight and obesity and to a lack of physical activity. Healthy lifestyle changes that help you control your weight may help you prevent and reduce metabolic syndrome.
Fatty liver diseases develop when fat builds up in your liver , which can lead to severe liver damage, cirrhosis , or even liver failure . These diseases include nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) .
NAFLD and NASH most often affect people who have overweight or obesity. People who have insulin resistance , unhealthy levels of fat in the blood, metabolic syndrome , type 2 diabetes, and certain genes can also develop NAFLD and NASH.
If you have overweight or obesity, losing at least 3% to 5% of your body weight may reduce fat in the liver. 15
Cancer is a collection of related diseases. In all types of cancer, some of the body’s cells begin to grow abnormally or out of control. The cancerous cells sometimes spread to other parts of the body.
Overweight and obesity may raise your risk of developing certain types of cancer . Men with overweight or obesity are at a higher risk for developing cancers of the colon , rectum , and prostate . 10 Among women with overweight or obesity, cancers of the breast , lining of the uterus , and gallbladder are more common.

Adults who gain less weight as they get older have lower risks of many types of cancer, including colon, kidney , breast, and ovarian cancers . 16
Overweight and obesity can also affect how well your lungs work, and excess weight increases your risk for breathing problems. 17
Sleep apnea
Sleep apnea is a common problem that can happen while you are sleeping. If you have sleep apnea, your upper airway becomes blocked, causing you to breathe irregularly or even stop breathing altogether for short periods of time. Untreated sleep apnea may raise your risk for developing many health problems, including heart disease and diabetes.
Obesity is a common cause of sleep apnea in adults. 18 If you have overweight or obesity, you may have more fat stored around your neck, making the airway smaller. A smaller airway can make breathing difficult or cause snoring. If you have overweight or obesity, losing weight may help reduce sleep apnea or make it go away.
Asthma is a chronic, or long-term, condition that affects the airways in your lungs. The airways are tubes that carry air in and out of your lungs. If you have asthma, the airways can become inflamed and narrow at times. You may wheeze, cough, or feel tightness in your chest.
Obesity can increase your risk of developing asthma, experiencing worse symptoms, and having a harder time managing the condition. 19 Losing weight can make it easier for you to manage your asthma. For people who have severe obesity, weight-loss surgery—also called metabolic and bariatric surgery—may improve asthma symptoms. 17
Osteoarthritis is a common, long-lasting health problem that causes pain, swelling, stiffness, and reduced motion in your joints . Obesity is a leading risk factor for osteoarthritis in the knees, hips, and ankles. 20
Having overweight or obesity may raise your risk of getting osteoarthritis by putting extra pressure on your joints and cartilage. If you have excess body fat, your blood may have higher levels of substances that cause inflammation . Inflamed joints may raise your risk for osteoarthritis.

If you have overweight or obesity, losing weight may decrease stress on your knees, hips, and lower back and lessen inflammation in your body. If you have osteoarthritis, losing weight may improve your symptoms. Research shows that exercise is one of the best treatments for osteoarthritis. Exercise can improve mood, decrease pain, and increase flexibility.
Gout is a kind of arthritis that causes pain and swelling in your joints. Gout develops when crystals made of a substance called uric acid build up in your joints. Risk factors include having obesity, being male, having high blood pressure, and eating foods high in purines . 21 These foods include red meat, liver, and anchovies.
Gout is treated mainly with medicines. Losing weight may also help prevent and treat gout. 22
Overweight and obesity may raise your risk of getting gallbladder diseases, such as gallstones and cholecystitis . People who have obesity may have higher levels of cholesterol in their bile , which can cause gallstones. They may also have a large gallbladder that does not work well.
Having a large amount of fat around your waist may raise your risk for developing gallstones. But losing weight quickly also increases your risk. If you have obesity, talk with your health care professional about how to lose weight safely .
Obesity can also affect your pancreas , a large gland behind your stomach that makes insulin and enzymes to help you digest food. People who have obesity have a higher risk of developing inflammation of the pancreas, called pancreatitis . High levels of fat in your blood can also raise your risk of having pancreatitis. You can lower your chances of getting pancreatitis by sticking with a low-fat, healthy eating plan.
Kidney disease means your kidneys are damaged and can’t filter your blood as they should. Obesity raises the risk of developing diabetes and high blood pressure, which are the most common causes of chronic kidney disease (CKD). Even if you don’t have diabetes or high blood pressure, having obesity may increase your risk of developing CKD and speed up its progress. 23
If you have overweight or obesity, losing weight may help you prevent or delay CKD. If you are in the early stages of CKD, consuming healthy foods and beverages , being active, and losing excess weight may slow the progress of the disease and keep your kidneys healthier longer. 24

Overweight and obesity raise the risk of developing health problems during pregnancy that can affect the pregnancy and the baby’s health. Pregnant people who have obesity may have a greater chance of 10
- developing gestational diabetes , or diabetes that occurs during pregnancy
- having preeclampsia , or high blood pressure during pregnancy, which can cause severe health problems for the pregnant person and baby if left untreated
- needing a caesarean delivery —or c-section—and, as a result, taking longer to recover after giving birth
- having complications from surgery and anesthesia , especially if they have severe obesity
- gaining more weight or continuing to have overweight or obesity after the baby is born
Having obesity or gaining too much weight during pregnancy can also increase health risks for the baby, including 25
- being born larger than expected based on the sex of the baby or the duration of the pregnancy
- developing chronic diseases as adults, including type 2 diabetes, obesity, heart disease, and asthma
Talk with your health care professional about how to
- reach a healthy weight before pregnancy
- gain a healthy amount of weight during pregnancy
- safely lose weight after your baby is born
Obesity increases the risk of developing infertility . Infertility in women means not being able to get pregnant after a year of trying, or getting pregnant but not being able to carry a pregnancy to term. For men, it means not being able to get a woman pregnant. 26
Obesity is linked to lower sperm count and sperm quality in men. 27 In women, obesity is linked to problems with the menstrual cycle and ovulation . 26 Obesity can also make it harder to become pregnant with the help of certain infertility treatments or procedures. 26
Women with obesity who lose 5% of their body weight may increase their chances of having regular menstrual periods, ovulating, and becoming pregnant. 28
Obesity may also increase the risk of developing sexual function problems. 29 Having overweight or obesity increase the risk of developing erectile dysfunction (ED) , a condition in which males are unable to get or keep an erection firm enough for satisfactory sexual intercourse.
Few studies have looked at how obesity may affect female sexual function by contributing to problems such as loss of sexual desire, being unable to become or stay aroused, being unable to have an orgasm, or having pain during sex. 30 But research suggests that healthy eating, increased physical activity, and weight loss may help reduce sexual function problems in people with obesity. 29,30
In addition to increasing the risk for developing physical health problems, obesity can also affect mental health, increasing the risk for developing 31
- long-term stress
- body image problems
- low self-esteem
- eating disorders
Studies show that people with overweight or obesity are also likely to face weight-related bias at school and work, which may cause long-term harm to their quality of life. 31 Losing excess weight has been found to improve body image and self-esteem and reduce symptoms of depression. 32
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.2(4); Oct-Dec 2014

Prevention of overweight and obesity in adult populations: a systematic review
Leslea peirson.
1 McMaster Evidence Review and Synthesis Centre, Hamilton, Ont.
James Douketis
2 Department of Medicine, McMaster University, Hamilton, Ont.
3 St. Joseph’s HealthCare Hamilton, Hamilton, Ont.
Donna Ciliska
Donna fitzpatrick-lewis, muhammad usman ali, parminder raina, associated data.
The prevalence of normal-weight adults is decreasing, and the proportion in excessive weight categories (body mass index ≥ 25) is increasing. In this review, we sought to identify interventions to prevent weight gain in normal-weight adults.
We searched multiple databases from January 1980 to June 2013. We included randomized trials of primary care–relevant behavioural, complementary or alternative interventions for preventing weight gain in normal-weight adults that reported weight change at least 12 months after baseline. We included any studies reporting harms. We planned to extract and pool data for 4 weight outcomes, 6 secondary health outcomes and 5 adverse events categories.
One small study provided moderate-quality evidence. The 12-month program, which used education and financial strategies and was offered more than 25 years ago in the United States, was successful in stabilizing weight and producing weight loss. More intervention participants maintained their baseline weight or lost weight than controls (82% v. 56%, p < 0.0001), and program participants maintained their weight better than controls by showing greater weight reduction by the end of the intervention (mean difference adjusted for height –0.82, 95% confidence interval –1.57 to –0.06, kg). No evidence was available for sustained effects or for any other weight outcomes, secondary outcomes or harms.
Interpretation
We were unable to determine whether behavioural interventions led to weight-gain prevention and improved health outcomes in normal-weight adults. Given the importance of primary prevention, and the difficulty of losing weight and maintaining weight loss, this paucity of evidence is surprising and leaves clinicians and public health practitioners with unclear direction. Registration: PROSPERO no. CRD42012002753
Overweight and obesity (body mass index [BMI] 25–29.9 and ≥ 30, respectively), are global problems with increasing prevalence in most countries. 1 Excess adiposity is related to a considerable increase in morbidity 2 – 4 and premature mortality. 5 , 6 The natural history of weight changes in adults has not been well studied, but data were collected on Canadian adults and analyzed for changes between 1996/97 and 2004/05. 7 The overall change was average gain of 4 kg for men and 3.4 kg for women. 7 Similarly, a large cohort study in the United States found that nonobese adults gain, on average, 0.8 lb (about 0.36 kg) annually. 8 Another Canadian-based study showed that the prevalence of normal-weight adults decreased by almost 7% between 2000/01 and 2011, and the authors predicted a continued decline in this weight category, estimating that more than 55% of the adult population would be overweight or obese by 2019. 9
Although a number of groups have produced clinical guidelines for overweight and obesity, there is an identified gap in knowledge regarding interventions that help maintain normal weight (BMI 18.5–24.9). 10 – 15 Prevention is ideal, but it is not clear whether interventions for normal-weight people can prevent weight gain. We conducted a systematic review to address whether primary care–relevant interventions for normal-weight adults led to short-term or sustained weight-gain prevention or improved health outcomes.
The protocol was registered with PROSPERO (no. CRD42012002753) ( www.crd.york.ac.uk/prospero ).
Search strategy
We searched Embase, MEDLINE, Cochrane Central Register of Controlled Trials and PsycINFO from January 1980 to June 2013. The MEDLINE search strategy is provided as an example in Appendix 1 (available at http://www.cmajopen.ca/content/2/4/E268/suppl/DC1 ). References of primary studies included in this review and related systematic reviews were searched for studies not captured by our search.
PICOS statement
The PICOS (population, intervention, comparator, outcome, setting) framework was as follows: (P) normal-weight adults aged 18 years or older; (I) behavioural, complementary or alternative interventions for weight-gain prevention; (C) no intervention, usual care or minimal component; (O) change in weight, BMI, waist circumference or total body fat percentage, change in secondary health outcomes (lipids, glucose, blood pressure), and harms of interventions; and (S) generalizable to Canadian primary care settings. Additional details are provided in Box 1 .
Population, intervention, comparator, outcomes and setting
• Normal-weight (BMI 18.5–24.9) adults aged ≥ 18 yr
Interventions
• Behavioural (diet, exercise and/or lifestyle), complementary or alternative (e.g., acupuncture, chiropractic, herbal supplements) interventions for preventing weight gain
Intervention effectiveness
• No intervention, usual care or minimal intervention (e.g., newsletter or single information session on healthy living)
Intervention harms
• Any type of comparison group or no comparison group
• Primary weight outcomes: change in weight (kg), BMI and waist circumference; total body fat percentage; secondary health outcomes: change in total cholesterol, low-density lipoprotein cholesterol, fasting blood glucose, incidence of type 2 diabetes, and systolic and diastolic blood pressure
• Labelling; disordered eating; psychological distress, such as anxiety, depression and stigma; nutritional deficits; cost burden
• Generalizable to Canadian primary care settings, or feasible for conducting in or referral from primary care; interventions should be initiated through (or feasible within) a primary care setting and (could be) delivered by a health care professional (e.g., physician, psychologist, nurse, dietician)
Note: BMI = body mass index.
Inclusion and exclusion criteria
The inclusion and exclusion criteria are provided in Box 2 .
Studies were included if they met the following criteria:
• Intervention involved a behavioural, complementary and/or alternative strategy for weight-gain prevention; behavioural interventions could include diet, exercise and/or lifestyle strategies (lifestyle strategies were typically referred to as such by study authors and often included counselling, education or support, and environmental changes in addition to diet and/or exercise); complementary and alternative interventions included strategies such as acupuncture, chiropractic treatment and herbal supplements
• Intervention targeted adults aged ≥ 18 yr with normal weight (BMI 18.5–24.9)
• Population was unselected, selected for low cardiovascular disease risk, or selected for increased risk for cardiovascular disease, hypertension, dyslipidemia or type 2 diabetes; population could include some (but not all) people with cardiovascular disease
• Randomized controlled trial with no intervention, usual care or minimal component (e.g., single newsletter or information session on general health) comparison group (condition applied only to studies assessing intervention effectiveness)
• Sample included at least 30 participants per arm at both baseline and the minimum outcome assessment point
• Reported data for 1 or more specified weight outcomes [i.e., change in weight (kg), BMI, waist circumference, total body fat percentage]
• Reported data for outcomes of interest at least 12 mo after baseline assessment
• No restrictions on study design, comparison group, number of participants, weight outcome reporting or timing of assessment were applied to studies that reported data for harms
• Results were published in English or French
Studies were excluded for the following reasons:
• Intervention involved a faith-based approach, a pharmacologic strategy or a surgical procedure
• Intervention targeted people who were underweight (BMI < 18.5), or overweight or obese (BMI ≥ 25)
• Population was limited to participants with cardiovascular disease, or specifically enrolled participants who were pregnant, had an eating disorder or a condition that predisposes weight gain (e.g., metabolic syndrome, polycystic ovary syndrome)
• Intervention was conducted in an in-patient hospital, institutional, school or occupational setting, or any setting deemed not generalizable to primary care, such as those with existing social networks among participants or the ability to offer intervention elements that could not be replicated in a primary health care setting; clinical institutions (hospital, metabolic units) were excluded because we believed these were unlikely to be primary prevention programs and would mostly include overweight or obese people
• Design was a case report, case series or chart review
• Only available results were published in a language other than English or French
Study selection, quality assessment and data abstraction
Titles and abstracts of papers were reviewed independently in duplicate. Any citation marked for inclusion by either team member went to full-text screening, which was also done independently in duplicate. Randomized trials were assessed using the Cochrane risk-of-bias tool. 16 Overall, strength of the evidence (assessed as high, moderate, low or very low quality) was determined using the Grading of Recommendations Assessment, Development and Evaluation framework (GRADEpro version 3.2). One team member completed full data abstraction and a second verified all extractions. All data were re-verified before analyses. Interrater disagreements were resolved through discussion.
Data analysis plan
For meta-analyses, we planned to use posttreatment means and standard deviations (SDs) for continuous outcomes (e.g., weight in kg) and number-of-events data for binary outcomes (e.g., incidence of type 2 diabetes). We intended to use the DerSimonian and Laird random-effects model with inverse variance method to generate summary measures of effect as mean difference for continuous outcomes and risk ratio for binary outcomes. 17 For studies that did not report SDs, we planned to calculate this value from the reported standard error (SE) of the mean, or from the 95% confidence intervals (CIs). 18 For studies that provided neither SDs nor SEs for follow-up data, we would impute the SD from baseline values or included studies of similar sample size and for the same outcome. For studies with more than one intervention arm (e.g., 2 diet plus exercise arms, one community-based group and one correspondence course), we planned to pool the data to do a pair-wise comparison with the control group. Alternatively, if groups were substantively different (e.g., low-calorie diet, high-intensity aerobic exercise), we intended to include the data for each arm compared with the control group but split the sample size for the control group to avoid a unit-of-analysis error and double counting. 16 Weight reported in pounds was to be converted to kilograms. Similarly, if total cholesterol, low-density lipoproteins and fasting glucose were reported in mg/dL, they would be converted to Canadian standard units (i.e., mmol/L). We planned to use the Cochran Q (α = 0.10) and I 2 statistic to quantify heterogeneity within and between subgroups. If sufficient data were available, sensitivity analyses would be performed to evaluate statistical stability and effect on statistical heterogeneity. Subanalyses were to be based on the following: type of intervention (diet, exercise, diet plus exercise, lifestyle), intervention duration (≤□12 mo, > 12 mo), sex, baseline cardiovascular disease risk status (high risk: identified risk factors and/or diagnosis of type 2 diabetes, hypertension, dyslipidemia; low risk; unselected population; or not specified) and the study’s risk-of-bias rating (high, unclear, low).
The database search located 31 974 unique studies. Manual searches and reviews of reference lists from recent (published 2012–2013) relevant systematic reviews located 15 additional studies. After full-text screening, only one study was located that met the inclusion criteria for this review ( Figure 1 ).

Selection of studies on interventions to prevent weight gain in normal-weight adults.
Included study
We found one trial that met the inclusion criteria for a normal-weight population. 19 Twenty-five other studies were excluded because of samples of mixed-weight populations; this indirect evidence is reported in the adult overweight and obesity prevention review we prepared for the Canadian Task Force on Preventive Health Care. 20 The included pilot study was a randomized controlled trial of a 12-month education- and incentive-based intervention conducted in the US state of Minnesota in the 1980s. The study involved collaboration between researchers in the School of Public Health at the University of Minnesota and staff at a local health department. A staged recruitment strategy began with mailed invitations to a random sample of 3000 adults out of about 6000 who attended a centre for cardiovascular risk factor screening in the previous 18 months and whose weight was recorded as normal (i.e., < 115% ideal weight as per 1983 Metropolitan Life Insurance Company tables). Because of study limitations, only 61% of those who indicated interest (422/690) were invited to attend an orientation session, and 219 people were enrolled (110 assigned to the intervention group; 109 assigned to the control group). Based on measures taken at the screening visit, the sample was 71% female, mean age was 45.9 years, mean BMI was 23.1, mean systolic blood pressure was 114.1 mm Hg, mean diastolic blood pressure was 69.8 mm Hg, mean serum cholesterol level was 4.9 mmol/L and 8% of the participants smoked. The only significant baseline difference between intervention and control groups was the percentage of participants with prior involvement in formal weight-control programs (18% intervention, 30% control).
To raise awareness, participants in the Pound of Prevention pilot program ( n = 110) were mailed monthly newsletters containing information about weight-related issues (e.g., diet, exercise, psychology of weight management, association between weight and health). To encourage regular self-monitoring, on a monthly basis they were asked to mail a record of their weight and a description of any weight-control strategies they were using. To increase motivation, a financial incentive system was set up to withdraw $10 per month from each intervention participant’s personal bank account. The accumulated money was reimbursed with interest at any time on request or at the end of the 1-year study, on the condition that the participant’s weight did not increase from baseline. Finally, about 6 months into the program a 4-session mini-course was offered to provide more extensive information and assistance on managing and losing weight through diet and exercise. Although open to all intervention participants, these sessions were primarily intended for those who experienced weight gain or who were unhappy about the amount of weight they gained during the first half of the program. Control participants ( n = 109) had no contact with the program other than attending the orientation session when baseline measures were collected before group assignment and attending a follow-up visit for the 1-year outcome assessment.
There were insufficient trials to perform meta-analyses for any outcomes.
The included study 19 reported only weight change in pounds (converted here to kilograms). All but 9 participants were included in the analysis. Five program participants dropped out because they moved and 2 discontinued their involvement for unspecified reasons. Two control participants were excluded from the analysis because medical conditions prevented taking weight measurements. More intervention participants ( n = 103) maintained their baseline weight or lost weight during the 12-month intervention than control participants ( n = 108) (82% v. 56%, p < 0.0001). Although both groups showed an overall reduction in weight from the baseline to postintervention assessments, our calculations show that program participants had a greater reduction in weight by the end of the intervention (mean difference adjusted for height –0.82, 95% CI –1.57 to –0.06, kg). No data were available to assess maintenance of weight-gain prevention, intervention effects on any other weight-related or secondary health outcomes, or adverse effects of program participation.
The available evidence was rated as moderate quality; downgrading occurred only for methodologic concerns identified through our assessment of the study’s risk of bias. 16 An overall unclear risk-of-bias rating was assigned because of the following: methods for generating the allocation sequence and concealing allocation were not described; it was not clear whether staff performing measures were unaware of group status; owing to the nature of behavioural interventions, participants and personnel were aware of group status; there was no mention of sample size calculations or power analyses; and those who expressed interest in participating may not have been representative of the general population (only 8% of those invited took part, and those who took part were more likely to be women, to not smoke and to have lower systolic blood pressure; they may have been more weight conscious than the general population and some may have been interested in losing weight).
We found only one trial of weight-gain prevention in normal-weight participants. 19 This is surprising considering the excess morbidity and mortality associated with overweight and obesity, the importance placed on prevention, the persistence of weight once gained and the difficulty in maintaining weight loss after any intervention. The paucity of evidence leaves clinicians and public health practitioners with unclear direction.
The included pilot study involving normal-weight participants reported moderate-quality evidence that educational strategies and financial incentives contributed to stabilized weight in the intervention group by the end of the 1-year program. Some adults in both groups lost weight, but fewer lost weight in the control group than in the intervention group. An increase in weight of less than 0.5 kg over one year may not appear clinically meaningful, but this should be considered with regard to weight gain that typically occurs in adults (3–4 kg in 8 yr) 7 and obesity-related health problems. 2 – 6 It is interesting that the later full trial of this intervention with more than 1000 participants (mean baseline BMI in overweight category) found no difference in weight gain at 3 years. 21
This review was unable to address whether weight gain prevention is sustained or if preventing weight gain in normal-weight adults leads to other health improvements. Furthermore, no harms of interest to this review and no adverse effects of any kind were reported; therefore, we cannot comment on the likelihood of normal-weight adults experiencing adverse events as a result of participating in interventions for prevention of weight gain.
Data are still lacking regarding interventions that help normal-weight adults maintain their normal weight. A review of trials (26 studies) of mixed-weight populations provided indirect evidence that programs were successful in stabilizing weight and producing some weight loss by the end of the interventions. 20 Intervention participants lost 0.73 (95% CI –0.93 to –0.54) kg more, lowered their BMI by 0.24 (95% CI –0.34 to –0.15) more, reduced their waist circumference by an additional 0.95 (95% CI –1.27 to –0.63) cm and lost 1.27% (95% CI –1.93% to –0.61%) more total body fat than the control group. 20 Similarly, a review of lifestyle interventions for preventing weight gain in young adults showed better weight maintenance among program participants than controls; intervention participants showed a modest mean decrease in body weight (–0.87, 95% CI –1.56 to –0.18, kg), whereas controls showed a modest mean increase (0.86, 95% CI 0.14 to 1.57, kg). 22 A slightly older review found 9 behaviourally based interventions that focused on weight-gain prevention among adults; 5 showed small but significant benefits in favour of the intervention groups whereas the remaining trials showed no effect. 23 Another review with broader inclusion criteria found 11 trials and 11 observational studies that indicated there may be effective strategies to prevent weight gain, such as low-fat diets, eating fewer meals out of the home, consuming more fruits and vegetables, monitoring heart rate during exercise and participation in group lifestyle sessions with reminder text messages. 24 Reviews that include studies with mixed-weight populations 22 – 24 have critiques of the evidence that also apply to our findings: there is a small number of programs for weight-gain prevention, fewer still of high quality; substantial heterogeneity across strategies makes it difficult to comment on effective program features; the interventions and studies are typically of short duration so sustainability is unknown; and small samples means there may be insufficient power to detect change.
Limitations
This review found only one study reporting on the effectiveness of interventions to prevent weight gain in normal-weight adults. 19 This single study was assessed as having unclear risk of bias, primarily due to the lack of information about sequence generation, allocation and blinding of outcome assessment, as well as concerns regarding study power and a high potential for selection bias. Also, results were available for only one specified weight outcome and none of the secondary outcomes or adverse effects of interest.
A language filter was applied in the original search because of limited resources available to appropriately handle papers in multiple languages (e.g., screening, translation and interpretation); including only publications in English or French meant papers about relevant interventions available only in other languages were not captured.
This review did not examine evidence for how long it takes a normal-weight person to become overweight or obese; this remains an unanswered question that may be the focus of future clinical research.
Because of very limited and dated evidence, we were unable to conclusively determine whether behaviourally based, primary care–relevant prevention programs lead to short-term or sustained weight-gain prevention and improved health outcomes in normal-weight adults. Despite increasing prevalence of overweight and obesity, and the enormity of the social, emotional, physical and economic sequelae, there are few upstream measures in place for true primary prevention (directed at the normal-weight population). Contemporary intervention research involving normal-weight samples with long-term follow-up is required to effectively answer this question.
In this review, people who were motivated to join a program for weight-gain prevention not only did not gain weight, but actually lost a small amount of weight. For adults with normal weight at baseline, this small weight loss may not be clinically meaningful, but it may offer protection against the health risks generally associated with weight gain. Interpreting these results is challenging, and it is difficult to know how normal-weight adults might be motivated to consider participating in such interventions.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see http://www.cmajopen.ca/content/2/4/E268/suppl/DC1
Supplementary Material
Acknowledgements.
Parminder Raina holds a Tier 1 Canada Research Chair in Geroscience, and the Raymond and Margaret Labarge Chair in Research and Knowledge Application for Optimal Aging. Rachel Warren, Meghan Kenny, Eva Tsakonas and Mary Gauld contributed to the relevance and quality assessment, and data extraction phases. We are grateful to Maureen Rice for the literature search, and to Sharon Peck-Reid for database management and formatting of the report. The Public Health Agency of Canada Scientific Officers Sarah Connor Gorber and Amanda Shane contributed to the original protocol development and review of drafts of the technical report. Similarly, the Adult Obesity Working Group of the Canadian Task Force on Preventive Health Care members Paula Brauer, Maria Bacchus, Neil Bell, Elizabeth Shaw and Harminder Singh provided comments on the protocol and initial analyses.

Introduction
Research design and methods, conclusions, article information, effect of 5:2 regimens: energy-restricted diet or low-volume high-intensity interval training combined with resistance exercise on glycemic control and cardiometabolic health in adults with overweight/obesity and type 2 diabetes: a three-arm randomized controlled trial.
M.Li, J.Li, Y.X., J.G., Q.C., and Y.D. contributed equally to this work.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Mian Li , Jie Li , Yu Xu , Jinli Gao , Qiuyu Cao , Yi Ding , Zhuojun Xin , Ming Lu , Xiaoting Li , Haihong Song , Jue Shen , Tianzhichao Hou , Ruixin He , Ling Li , Zhiyun Zhao , Min Xu , Jieli Lu , Tiange Wang , Shuangyuan Wang , Hong Lin , Ruizhi Zheng , Jie Zheng , Callum John Baker , Shenghan Lai , Nathan Anthony Johnson , Guang Ning , Stephen Morris Twigg , Weiqing Wang , Yan Liu , Yufang Bi; Effect of 5:2 Regimens: Energy-Restricted Diet or Low-Volume High-Intensity Interval Training Combined With Resistance Exercise on Glycemic Control and Cardiometabolic Health in Adults With Overweight/Obesity and Type 2 Diabetes: A Three-Arm Randomized Controlled Trial. Diabetes Care 20 May 2024; 47 (6): 1074–1083. https://doi.org/10.2337/dc24-0241
Download citation file:
- Ris (Zotero)
- Reference Manager
We aimed to examine the effects of a 5:2 diet (2 days per week of energy restriction by formula diet) or an exercise (2 days per week of high-intensity interval training and resistance training) intervention compared with routine lifestyle education (control) on glycemic control and cardiometabolic health among adults with overweight/obesity and type 2 diabetes.
This two-center, open-label, three-arm, parallel-group, randomized controlled trial recruited 326 participants with overweight/obesity and type 2 diabetes and randomized them into 12 weeks of diet intervention ( n = 109), exercise intervention ( n = 108), or lifestyle education (control) ( n = 109). The primary outcome was the change of glycemic control measured as glycated hemoglobin (HbA 1c ) between the diet or exercise intervention groups and the control group after the 12-week intervention.
The diet intervention significantly reduced HbA 1c level (%) after the 12-week intervention (−0.72, 95% CI −0.95 to −0.48) compared with the control group (−0.37, 95% CI −0.60 to −0.15) (diet vs. control −0.34, 95% CI −0.58 to −0.11, P = 0.007). The reduction in HbA 1c level in the exercise intervention group (−0.46, 95% CI −0.70 to −0.23) did not significantly differ from the control group (exercise vs. control −0.09, 95% CI −0.32 to 0.15, P = 0.47). The exercise intervention group was superior in maintaining lean body mass. Both diet and exercise interventions induced improvements in adiposity and hepatic steatosis.
These findings suggest that the medically supervised 5:2 energy-restricted diet could provide an alternative strategy for improving glycemic control and that the exercise regimen could improve body composition, although it inadequately improved glycemic control.
Graphical Abstract

Diabetes poses a significant public health issue that needs effective and cost-efficient glycemic control strategies ( 1 ). Lifestyle intervention involving dietary modification and enhanced physical activity serves as a first-line treatment for type 2 diabetes. Daily calorie restriction leading to substantial weight loss has been proven to improve glycemic control and induce diabetes remission ( 2 , 3 ). However, these approaches typically involve a rigorous continuous caloric restriction, which significantly impacts daily life and proves challenging to adhere to, particularly for the working-age population without severe obesity ( 4 ). Lifestyle interventions that are flexible to work-life rhythms could enhance compliance.
The 5:2 diet, a periodic fasting regimen involving a very-low-calorie diet for 2 days per week and a regular diet for the remaining 5 days ( 5 ), has presented a comparable effect to continuous energy restriction on the reduction of glycated hemoglobin (HbA 1c ) in type 2 diabetes, although results were inconsistent and limited by small sample sizes ( 6–9 ). The efficacy of the 5:2 diet challenges the existing paradigm of lifestyle intervention where sustained behavior change is required. Approaches where people are required to modify their behaviors intensely but intermittently may allow a more convenient and efficacious way to achieve metabolic benefits.
Similarly, observational studies demonstrated the benefits of a weekend warrior physical activity pattern characterized as doing all exercise on 1 or 2 days of the week ( 10 ). Since lack of time is one of the most cited barriers to regular physical activity, the amount of aerobic and resistance training (RT) recommended by guidelines may be burdensome for individuals with not a lot of free time ( 11 , 12 ). Early evidence from small-scale studies suggests that as little as 4 min of high-intensity interval training (HIIT) at a low volume may reduce HbA 1c ( 13–16 ), although others have not corroborated these findings ( 17 , 18 ). The combined approach of low-volume HIIT and RT could offer a comprehensive, time-efficient exercise strategy ( 19 ); nonetheless, its efficacy for glycemic control has rarely been studied.
Both the 5:2 diet and low-volume HIIT combined with RT have shown potential as practical strategies, which are time efficient and flexible to work-life rhythms. Thus, we designed a study, the first of its kind as a randomized controlled trial, to examine the effects of 2 days per week energy-restricted diet or low-volume HIIT combined with RT intervention undertaken on 2 days of the week (5:2 regimen) compared with routine lifestyle education (control) on glycemic control, as well as body composition, liver fat content, and cardiometabolic parameters, among adults with overweight/obesity and type 2 diabetes.
Study Design and Participants
The Intermittent Intensive Diet and Enhanced Physical Activity on Glycemic Control in Newly Diagnosed Type 2 Diabetes Study (IDEATE) was a two-center, open-label, three-arm, parallel-group, randomized controlled trial. Participants were randomized 1:1:1 to one of three arms: diet intervention (2 days per week energy-restricted diet), exercise intervention (2 days per week low-volume HIIT combined with RT), and control (routine lifestyle education). The study consisted of a 12-week intervention and a 36-week postintervention follow-up observation. The primary outcome was the difference in the change of glycemic control measured as HbA 1c between the diet or exercise intervention groups and the control group after a 12-week intervention. The secondary outcomes included changes in other glycemic metrics, body weight, body composition, liver fat content, serum lipids, and blood pressure (BP). The study was approved by the ethical review committee of Ruijin Hospital (Ruijin-2018-174) and registered prospectively at ClinicalTrials.gov (NCT03839667).
The prescreening of potential participants started in January 2019 at the Third People’s Hospital of Datong and Shanghai Songnan Health Community Center. Potentially eligible participants were identified by the clinical primary care team from electronic medical records or were referred by medical clinics. Participants were initially asked about their age, disease history, etc., via a simple categorical questionnaire, and once written consent was provided, the final eligibility of participants was established before randomization. Eligible participants were aged 40–70 years, reported a diagnosis of type 2 diabetes within the prior 2 years, and had a BMI of 25.0–39.9 kg/m 2 and an HbA 1c ranging from 7.0 to 8.9%. Individuals were excluded if they had type 1 diabetes or received insulin treatment; had a cardiovascular event in the previous 6 months; had uncontrolled hypertension; reported currently completing >75 min of high-intensity exercise or 150 min of moderate-intensity exercise per week; reported a high alcohol intake; had an active foot ulcer; had impaired liver function or renal function; had a history of food allergies or bariatric surgery; were currently pregnant, breastfeeding, or planning a pregnancy; or had other conditions not eligible for the trial. The study’s design is described in detail in the study protocol ( Supplementary Material ).
Intervention
Diet intervention.
The diet intervention group received 12 weeks of a 5:2 diet comprising a restricted energy intake of 790 kcal per day on 2 days per week (mostly consecutive) and a regular diet on the remaining 5 days. Energy restriction was induced with a total diet replacement phase using a low-energy formula diet (∼25% of energy from protein, ∼55% from carbohydrates, and ∼20% from fat; Chiatai Qingchunbao Pharmaceutical Co., Ltd., Hangzhou, China). The dietitian evaluated adherence and discussed the improvement plan with participants through telephone or WeChat instant messaging weekly, together with face-to-face education monthly. Consumption of food besides the formula diet was defined as having less adherence.
Exercise Intervention
The exercise intervention group completed 12 weeks of twice-weekly (mostly nonconsecutive) supervised exercise at the health care centers, consisting of a single bout of 4 min of HIIT at 85–90% of age-predicted heart rate maximum with a 5-min warm-up and 5-min cooldown and four machine-based resistance exercises involving two sets of 8–12 repetitions at 80% of 1-repetition maximum. HIIT was undertaken using a cycle ergometer, and resistance exercise was undertaken using a comprehensive strength machine. Heart rate was monitored with a Bluetooth heart rate chest strap (GEONAUTE), and the intensity of RT was recorded for each region (shoulders, chest, back, and anterior chain [thigh]). Adherence to the exercise intervention protocol was defined as completing sessions with HIIT at ≥85% heart rate maximum and RT at 80% of one-repetition maximum. During the coronavirus disease 2019 (COVID-19) pandemic, participants allocated to the exercise intervention completed HIIT or RT sessions at home, including cycle ergometer, treadmill, or running in place and strength training without equipment, with supervision by physicians through real-time audio or video meetings.
Lifestyle Education
Routine lifestyle education was performed in the same manner for all intervention and control groups by physicians masked to the randomization and consisted of instructions on healthy diet and exercise per the Guidelines for the Prevention and Treatment of Type 2 Diabetes in China ( 20 ). The physicians offered lifestyle advice to the participants through telephone or WeChat weekly, together with face-to-face education monthly.
Antihyperglycemic Medication Management
During the 12-week intervention, participants were asked to maintain their medication type, dosage, or frequency, unless certain conditions arose. Sulfonylureas were omitted on days of energy restriction. If any glucose readings were <4 mmol/L or >20 mmol/L or fasting blood glucose levels >10 mmol/L, participants were advised to contact physicians for potential medication changes. During the intervention and follow-up phases, physicians who were masked to the study group made decisions about patients’ antihyperglycemic medication. Medication dosages were recorded at every visit, and the medication effect score (MES) was used to quantify changes ( 21 ).
Glycemic Control
We evaluated glycemic control by blood sampling at all visits, including baseline (before intervention) and weeks 4, 12 (after intervention, assessment of primary outcome), 24, 36, and 48. All fasting blood collection was performed at the physical examination center, refraining from the intervention for at least 48 h to avoid the interference of acute response to energy restriction or exercise. Then, participants underwent a standard oral glucose tolerance test (OGTT), and blood was sampled at 30 min and 120 min for postload plasma glucose (PPG). Plasma glucose concentrations were analyzed using a glucose oxidase or hexokinase method, and HbA 1c was determined through high-performance liquid chromatography (Bio-Rad, Hercules, CA) within 2 h after blood sample collection. Glucose area under the curve (AUC) was calculated as 1/2 (fasting plasma glucose [FPG] + 30-min PPG) × 30 min/h + 1/2 (30-min PPG + 120-min PPG) × 90 min/h ( 22 , 23 ). Fasting serum samples were shipped by air on dry ice to the study central laboratory at the Shanghai Institute of Endocrine and Metabolic Disease to measure the lipids profile and insulin (Atellica Solution; Siemens Healthineers). Insulin resistance (IR) was calculated using the HOMA method: HOMA-IR = fasting insulin (μIU/mL) × fasting glucose (mmol/L) / 22.5.
Body Composition
Trained study nurses measured body weight, height, and waist circumference. BMI was calculated as body weight in kilograms divided by height in meters squared. Waist circumference was measured at the level of the umbilicus with the patient in the standing position. We used bioelectrical impedance analysis (H-Key350, Beijing Seehigher Technology Co., Ltd., Beijing, China) to estimate body fat mass, body fat percentage, and lean body mass.
Liver Fat Content
Liver fat content was measured and quantified by abdominal MRI-proton density fat fraction (PDFF) examination using a 3.0-T MRI scanner (Ingenia; Philips Healthcare). Fat-water separation images of the liver were acquired using a mDIXON-Quant sequence. The mDIXON-Quant is a 3-dimensional fast field echo sequence and uses multiple acquired echoes to generate water, fat, T2*, and fat fraction images synthesized from the water-fat images. Nine circular regions of interest (ROIs) corresponding to the Couinaud liver segments on the MRI-PDFF maps were analyzed. Each ROI had an area of 3 cm 2 and was placed near the center of each segment while avoiding major vessels, liver edges, and artifacts. The PDFF in each of the nine ROIs was recorded, and the PDFF value across the entire liver was reported as the mean of the PDFF values of all nine ROIs. The technician performing the MRI-PDFF measurements was masked to participant group assignment.
Cardiometabolic Parameters
BP measurements were obtained using an automated electronic device (Omron Model HEM-752 Fuzzy; Omron, Tokyo, Japan). HDL cholesterol, LDL cholesterol, and triglycerides were measured at the central laboratory using enzymatic methods with an autoanalyzer (cobas c 701; Roche, Mannheim, Germany).
Statistical Analysis
We calculated that 324 participants (108 per group) would provide 90% power to detect a significant difference of −0.5% in HbA 1c (SD 1.0%) between the diet or exercise intervention and control group, which was based on a two-tailed independent-samples t test with a significance level of 0.05 and a predicted dropout rate of 20%. The estimations were derived from the effect estimated by previous studies of the 5:2 diet or structured exercise training for 12 weeks in participants with type 2 diabetes, which were also in line with a clinically significant change in HbA 1c recommended by the American Diabetes Association ( 6 , 24 , 25 ). Finally, 326 participants were recruited. Randomization was conducted with a 1:1:1 ratio on the stratification of three factors: study center, sex (men vs. women), and age-group (<65 vs. ≥65 years). Block randomization was done with block sizes of six using an independent online computerized randomization system. The staff responsible for allocation were masked to the block sizes.
Data were analyzed according to participants’ randomization assignment (intention to treat). Multiple imputations for missing data in the multivariable analyses were conducted using the Markov chain Monte Carlo method. Supplementary Table 1 shows the number (percent) of missing data for multiple imputation. A linear mixed model was conducted to assess time, group, and time × group effects for each continuous outcome using PROC MIXED of SAS statistical software to obtain point estimates and 95% CIs of the treatment effects and to test for differences between the diet or exercise intervention and control intervention by the interaction terms (time × group), with adjustments for study center, sex, and age, which are the stratification factors in the randomization. MES, HOMA-IR, liver fat content, and triglyceride outcomes were log-transformed for the analysis and reported on the original scale using the equation (10^β − 1) × x0, where ^β is the estimate or interval limit and x0 is the baseline sample mean. The categorical outcomes, including the proportion of diabetes remission and incidence of severe adverse events or adverse events across groups, were analyzed using χ 2 test and logistic regression analysis. Bonferroni adjustment was applied for the primary outcome to protect against false-positive findings due to multiple comparisons of three groups. No multiple test adjustments were performed for secondary outcomes, so such analyses should be interpreted as exploratory. We used SAS 9.4 and R version 4.1.1 software for statistical analyses. All reported P values were nominal. Statistical significance was set as a two-tailed P < 0.05.
As shown in Fig. 1 , a total of 440 individuals were initially enrolled for prescreening. Of these participants, 114 were excluded for not meeting eligibility criteria, declining participation, or withdrawing their consent. Consequently, 326 participants were randomized to the diet intervention group ( n = 109), exercise intervention group ( n = 108), or control group ( n = 109). Finally, 301 (92.33%) completed the intervention and the 12-week assessment of primary outcome until June 2021. Baseline characteristics were similar between participants who completed the interventions and those who dropped out ( Supplementary Table 2 ). Supplementary Table 3 summarizes the baseline sample characteristics: 116 women and 210 men, mean (SD) age 52.65 (8.13) years, mean (SD) HbA 1c level 7.63% (0.85%) (59.88 [9.27] mmol/mol), and mean (SD) BMI 27.71 (2.61) kg/m 2 . No significant differences existed across groups for baseline characteristics, including the proportion of participants taking antihyperglycemic medication and the level of MES ( Supplementary Tables 3 and 4 ). Figure 2A presents the proportion of participants who were considered adherent to their intervention per week. After the 12-week intervention period, 98 diet group participants and 81 exercise group participants were adherent for ≥80% of the whole intervention, and 105 control group participants completed the education session; these participants were considered compliant and included in the per-protocol population.

Study participant flowchart.

Adherence to intervention, body weight change, and glycemic control during the 12-week intervention period. A : Proportion of participants who were considered adherent to the diet and exercise intervention protocol per week. B : Absolute change of self-monitored body weight per week. Bars indicate mean ± SE. C : Individual data of relative HbA 1c change (%) from baseline after intervention among participants who underwent randomization and had a 12-week assessment. D : Proportion of diabetes remissions after the 12-week intervention and the multivariable-adjusted odds ratios of diabetes remission for the diet or exercise intervention compared with the control group among patients who underwent randomization and had a 12-week assessment. Odds ratios were adjusted for age at recruitment, sex, study center, baseline HbA 1c , and baseline MES of antihyperglycemic medication.
Primary Outcome
Following the intention-to-treat principle, all randomized individuals were included. Participants in the diet intervention group experienced a greater decrease in HbA 1c level (%) after the 12-week intervention (−0.72, 95% CI −0.95 to −0.48) compared with the control group (−0.37, 95% CI −0.60 to −0.15) (diet vs. control −0.34, 95% CI −0.58 to −0.11, P = 0.007). The reduction in HbA 1c level in the exercise intervention group (−0.46, 95% CI −0.70 to −0.23) did not significantly differ from the control group (exercise vs. control −0.09, 95% CI −0.32 to 0.15, P = 0.47) ( Table 1 ). Among the 301 patients who underwent the 12-week assessment, the proportion and degree of reduction in HbA 1c were more significant in the diet intervention group than in the control group ( Fig. 2C ).
Intention-to-treat analysis for the effects of intervention on primary and secondary outcomes
Data are included for 326 participants according to the intention-to-treat principle after multiple imputations and presented as the estimates and corresponding 95% CIs for within-group changes and between-group differences after intervention. P values for the difference between intervention and control group (group × time) were analyzed for the diet intervention group and exercise intervention group, respectively. Data were analyzed using a linear mixed model with repeated measures to test intervention effects, adjusting for age at recruitment, sex, and study center.
Secondary Outcome
Diabetes was in remission in 20 (19.42%) participants in the diet intervention group, 11 (11.83%) in the exercise intervention group, and 11 (10.48%) in the control group, which was defined as HbA 1c <6.5% without antihyperglycemic medication after the intervention. Compared with the control group, the diet intervention, but not the exercise intervention, increased the likelihood of diabetes remission (diet vs. control adjusted odds ratio 3.60 [95% CI 1.40–9.25, P = 0.008]; exercise vs. control adjusted odds ratio 1.42 [95% CI 0.51–3.95, P = 0.52]) ( Fig. 2D ).
In the intention-to-treat analysis for other glycemic metrics, glucose AUC during OGTT and OGTT 30-min PPG improved in the diet intervention group compared with the control group (diet vs. control: glucose AUC [mmol ⋅ min/L] −84.77 [95% CI −160.13 to −9.42, P = 0.028]; OGTT 30-min PPG [mmol/L] −1.16 [95% CI −1.74 to −0.57, P = 0.0001]), but not in the exercise intervention group. There were no significant differences between interventions and control in MES, FPG, OGTT 120-min PPG, and HOMA-IR ( P > 0.05) ( Table 1 ).
During the 12-week intervention, significant reductions in self-monitoring body weight were observed across all three groups, with the diet intervention group showing the most pronounced effect ( Fig. 2B ). A reduction in body weight became evident after 4 weeks of intervention in the diet group ( Fig. 3B ). After the 12-week intervention, the diet intervention achieved significantly greater reductions in body weight (kg) compared with the control group (diet vs. control −1.94 [95% CI −2.70 to −1.19, P < 0.0001], exercise vs. control −0.48 [95% CI −1.24 to 0.28, P = 0.21]), which was also observed for BMI and waist circumference. The exercise intervention exhibited a superior effect on preserving lean body mass (kg) compared with the control group (diet vs. control 0.29 [95% CI −0.70 to 1.27, P = 0.57], exercise vs. control 1.08 [95% CI 0.05 to 2.10, P = 0.039]). Both diet and exercise interventions induced greater reduction in body fat mass and fat-to-lean mass ratio compared with the control group. There were notable reductions in liver fat content (%) after diet and exercise interventions (diet vs. control −2.31 [95% CI −3.07 to −1.47, P < 0.0001], exercise vs. control −1.27 [95% CI −2.14 to −0.30, P = 0.012]). Favorable changes in HDL cholesterol were observed in the diet intervention group but not in the exercise group. Both diet and exercise interventions significantly reduced diastolic BP. No significant alterations were detected in LDL cholesterol, triglycerides, or systolic BP ( Table 1 ).

Intention-to-treat analysis for the changes of HbA 1c and body weight according to groups during the 12-week intervention and 36-week postintervention follow-up period. Data were included for 326 participants according to the intention-to-treat principle after multiple imputations. A : HbA 1c . B : Body weight. Bars indicated mean ± SE from baseline to each visit for each group. The shaded area represents the intervention period. P values for the difference between the intervention and the control group (group × time) were analyzed for the diet intervention group and exercise intervention group, respectively. Data were analyzed using a linear mixed model with repeated measures to test intervention effects, adjusting for age at recruitment, sex, and study center.
Supplementary Table 5 shows that no serious adverse events occurred in the diet or exercise intervention groups, with only one serious event reported in the control group (hospitalization due to a nasal polypectomy). The occurrence of serious adverse events or adverse events was evenly distributed across all groups.
Sensitivity Analysis
We excluded 16 participants who changed their antihyperglycemic medication during the intervention ( Supplementary Table 6 ), and similar results were obtained ( Supplementary Table 7 ). We confirmed the results in the per-protocol population and further detected a significantly reduced FPG, OGTT 120-min PPG, and HOMA-IR in the diet intervention group ( Supplementary Table 8 ). After excluding 15 participants who received modified exercise intervention and 1 who withdrew because of an inability to train at home during the COVID-19 pandemic, the effect of the exercise intervention was not substantially changed ( Supplementary Table 9 ).
Postintervention Follow-up Assessment
After the intervention, we continued to monitor the HbA 1c and body weight every 12 weeks to identify the sustainability of the intervention effects. Compared with baseline, the diet and exercise interventions continued to significantly enhance glycemic control and body weight during the postintervention follow-up period. However, no significant differences in HbA 1c were detected between the interventions and control ( Fig. 3A ). The diet intervention continued to show sustained weight loss until week 36, after which the trend converged ( Fig. 3B ). Similar trends were obtained in the per-protocol population ( Supplementary Fig. 1 ). After excluding participants who altered their antihyperglycemic medication, the effects on body weight caused by the diet intervention were sustained by week 48 ( Supplementary Fig. 2 ).
To our knowledge, this randomized controlled trial is the first to investigate the effects of energy-restricted diet or low-volume HIIT combined with RT (5:2 regimen) on glycemic control in adults with overweight/obesity and type 2 diabetes. Our findings suggest that the 5:2 energy-restricted diet intervention improved glycemic control, body composition, and cardiometabolic parameters compared with routine lifestyle education. Despite observing favorable effects on body composition, including significant reductions in adiposity and liver fat content and superior maintenance of lean body mass, the exercise intervention did not significantly decrease HbA 1c compared with routine lifestyle education.
The current study is the largest trial to date to examine the effect of a 5:2 diet on glycemic control in patients with type 2 diabetes, aligning with prior smaller-scale studies ( 6–8 , 26 , 27 ). For instance, Corley et al. ( 26 ) reported a 0.6–0.7% absolute reduction of HbA 1c from baseline after 12 weeks of a 5:2 diet. Furthermore, our study identified a significant decrease in peak glucose after 30 min of OGTT following the diet intervention, suggesting potential improvements in early-phase β-cell responsiveness ( 22 ), which also led to a significant reduction in glucose AUC during the 120-min OGTT, thereby reducing the overall blood glucose burden ( 23 ). Participants in the diet intervention were significantly more likely to achieve diabetes remission, with a prevalence rate of 19.42% compared with the control group at 10.48%. Although the remission rate induced by the 5:2 diet intervention was relatively lower than that of other studies implementing rigorous and continuous caloric restriction and greater weight losses, such as the Diabetes Remission Clinical Trial (DiRECT) with a prevalence of 46% ( 2 ), it was comparable to the prevalence of 11.5% observed in the Look AHEAD (Action for Health in Diabetes) study, which also implemented a combined physical activity and diet program ( 28 ). It is worth noting that previous trials were predominantly conducted in western populations with severe obesity, most of which had a mean BMI >35 kg/m 2 . Our study distinguishes itself by extending the evidence for the equivalent effectiveness of a 5:2 diet in improving glycemic control in diabetes with overweight or mild obesity, a nonnegligible proportion of the people with diabetes in Asia ( 29 ). As conducted in our study, it should be emphasized that the 5:2 diet be performed under medical supervision regarding appropriate adjustment of hypoglycemic drugs and monitoring of blood glucose.
On the other hand, the low-volume HIIT and RT intervention failed to induce improvements in glycemic control compared with routine lifestyle education. Among previous trials, only one study involving 80 patients investigated the effects of combined HIIT and RT, reporting no appreciable benefits in HbA 1c levels ( 30 ). According to a meta-analysis involving 32 randomized controlled trials, HIIT intervention reduced HbA 1c by 0.34% ( 31 ). In the current study, participants experienced a −0.46% (95% CI −0.70% to −0.23%) absolute decrease in HbA 1c after a 12-week low-volume HIIT combined with RT. It is worth noting that participants in the control group also made substantial improvements in glycemic control, possibly because of their participation in exercise and diet guidance as part of routine lifestyle education. Our results aligned with a prior meta-analysis involving 47 trials evaluating the efficacy of structured exercise training or physical activity advice to lower HbA 1c levels, which showed that aerobic exercise plus RT and only physical activity plus dietary advice resulted in HbA 1c reductions of 0.51% and 0.58%, respectively ( 24 ).
Even so, our study suggests that both a 5:2 diet regimen and low-volume HIIT combined with RT intervention could induce improvements in body composition and hepatic steatosis for type 2 diabetes. Our low-volume exercise intervention did not induce significant weight loss, which was consistent with the literature, but showed a superior effect of maintaining lean body mass compared with the control intervention ( 32 ). Currently, the efficacy of HIIT on body composition remains controversial. HIIT was reported to reduce body fat, visceral fat, or liver fat in several small-scale studies ( 13 , 18 , 33 ) but not in other studies ( 34 , 35 ). A meta-analysis involving 47 trials concluded that low-volume HIIT is not superior to nonexercise control for improving body composition measures of body fat mass ( 36 ). Our study is the first to detect the effect of low-volume HIIT combined with RT on reducing body adiposity and liver fat content, as well as its unique benefits on maintaining lean body mass during fat loss compared with the control intervention.
In essence, while the 5:2 diet and exercise interventions can lead to positive changes in body composition, exercise training alone only resulted in a slight increase in weekly energy expenditure. Conversely, the diet intervention group experienced a greater energy deficit with a more pronounced metabolic benefit ( 37 ). In addition, since we observed a higher compliance of the supervised home exercise during the COVID-19 pandemic (93%), it might be deduced that the exercise intervention requiring individuals to travel to a supervised exercise center and possibly creating scheduling conflicts resulted in lower compliance, limiting its effectiveness to some extent. Recently, randomized controlled trials investigating the effect of an intermittent fasting diet, HIIT, or combined intervention on glycemic control and body composition in adults with normal glucose demonstrated that only combined diet and exercise interventions resulted in improved glycemic control or liver fat content, not isolated diet or exercise interventions alone ( 18 , 35 ). A recent four-arm randomized trial in 82 patients with newly diagnosed type 2 diabetes also found that adding an exercise intervention to diet-induced weight loss improves glucose-stimulated β-cell function ( 38 ). In our study, we chose not to combine interventions because of concerns about the potential safety issues of simultaneous calorie restriction and exercise training on intervention days based on the 5:2 regimen design. Given the benefits of exercise in maintaining lean body mass detected in our study, future trials are warranted to explore whether aperiodic fasting combined with low-volume HIIT and RT is an effective and safe option for people with diabetes under continuous blood glucose monitoring.
We also found that the diet intervention failed to show significant durability in improving HbA 1c compared with routine lifestyle education, despite significant within-group improvements from baseline to the 1-year mark. In contrast, the effect on body weight was significantly maintained after the intervention, suggesting the potential for sustained benefits on body weight from short-term interventions. This pattern aligns with a previous meta-analysis that found that long-term interventions are associated with significant diabetes risk reduction, while short-term interventions are more effective in weight loss because of metabolic adaptation and poor compliance with long-term interventions ( 39 , 40 ).
Our trial does have several limitations. First, our study population only included type 2 diabetes diagnosed within the past 2 years with an HbA 1c ranging from 7.0 to 8.9%, limiting the application to patients with a longer duration and poorer glycemic control. Because of safety concerns, our study focused on newly diagnosed type 2 diabetes with relatively preserved β-cell function and did not include patients with insulin treatment or with an HbA 1c ≥9.0% who would be recommended to consider insulin treatment by several leading guidelines ( 41 ). Second, we assessed body composition using bioelectrical impedance analysis, which is less accurate than DEXA. Third, we relied on finger-prick tests to monitor blood glucose levels, potentially underestimating both hyperglycemic and hypoglycemic episodes. Finally, we did not collect information on whether the participants maintained the diet or exercise regimen in the postintervention follow-up period.
In conclusion, our study demonstrates that a short-term 5:2 energy-restricted diet could significantly improve glycemic control, body composition, and several cardiometabolic parameters. Despite no significant benefit on glycemic control, the exercise protocol improved body adiposity and hepatic steatosis and showed superior effects in maintaining lean body mass. These findings challenge the current paradigm of lifestyle intervention in which frequent behavioral change is required to see improvements in metabolic health. Our study suggests that a medically supervised 5:2 energy-restricted diet could serve as an alternative strategy for improving glycemic control. Further research is warranted to explore the effect of the 5:2 regimen with a combination of diet and exercise.
Acknowledgments. The authors thank the study participants for participating in the IDEATE study. The authors also thank Di Zhang, Wenzhong Zhou, and Wei Miao from Shanghai Institute of Endocrine and Metabolic Diseases for support in performing laboratory analyses and all students for invaluable contributions to the execution of the study. The authors thank Fuhua Yan and Xinxin Xu from Ruijin Hospital for support with the MRI scanning and analysis. The authors also thank Shanghai Ashermed Medical Technology Co., Ltd. for providing the contract research organization services. The authors thank Danqing Min and Xiaoyu Wang from University of Sydney for support in the discussion on exercise intervention strategies. Finally, the authors are grateful to the Chiatai Qingchunbao Pharmaceutical Co., Ltd. for donating the low-energy formula diet used in the diet intervention.
Funding. Support for this research was obtained from National Key Research and Development Program of China grants 2022ZD0162102, 2023YFC2506700, and 2021YFA1301103; National Natural Science Foundation of China grants 81561128019, 82088102, 91857205, 82022011, 81970728, and 81930021; Shanghai Rising-Star Program grant 21QA1408100; the Innovative Research Team of High-Level Local Universities in Shanghai, Shanghai Clinical Research Center for Metabolic Diseases grant 19MC1910100; and Shanghai Municipal Government grant 22Y31900300.
The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors declare no competing interests.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.Li, J.Li, Y.X., and J.G., wrote the original draft of the manuscript. M.Li, Y.X., G.N., W.W., and Y.B. acquired funding. M.Li, C.J.B., N.A.J., S.M.T., Y.L., and Y.B. contributed to the methodology. M.Li, G.N., W.W., Y.L., and Y.B. contributed to the conceptualization of the study. J.Li, J.G., M.Lu, X.L., H.S., J.S., T.H., R.H., L.L., and Y.L. contributed to the investigation. Q.C., Y.D., Z.X., and R.Z. contributed to the formal analysis. Z.Z., M.X., J.Lu, T.W., S.W., H.L., and J.Z. contributed to the data curation. C.J.B., S.L., N.A.J., G.N., S.M.T., W.W., Y.L., and Y.B. reviewed and edited the manuscript. G.N., W.W., Y.L., and Y.B. provided supervision. All authors revised the manuscript for critical content and approved the final draft for publication. Y.B. is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Handling Editors. The journal editors responsible for overseeing the review of the manuscript were Elizabeth Selvin and Stephanie L. Fitzpatrick.
Clinical trials reg. no. NCT03839667, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.25501816 .
Email alerts
- Online ISSN 1935-5548
- Print ISSN 0149-5992
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

29 terrible fad diets that did more harm than good
Posted: 21 January 2024 | Last updated: 22 January 2024

Diets to avoid at all costs!
Throughout the centuries, people have tried just about every diet going in the quest for a slimmer waistline and better health. However, fad diets are notoriously difficult to sustain – and, in some cases, they can be dangerous and even deadly. Here, nutritionist Angela Dowden rounds up some of the most eccentric, weird and dangerous diets from the 1500s to the present day.
1558: the starvation diet
We've all heard about calorie counting, but this restrictive diet was around long before calories were a thing. Written by Italian nobleman Luigi Cornaro, La Vita Sobra (The Sober Life) advocated extreme starvation as a way to lose weight and boost health. The author himself lost weight and reportedly lived to the age of 102 by eating just 12oz (342g) of food and drinking 14oz (400ml) of wine per day. Evidence suggests mice live longer when fed starvation rations, but it's not been proven in humans.

1727: the 'move away from the swamp' diet
In 1727 writer Thomas Short observed that overweight people often lived near swamps. He published a treatise entitled The Causes and Effects of Corpulence , outlining that the only logical way to lose weight was to move further away from any swamps. Obviously, no connection between swamps and weight actually exists, but there is some evidence that people living in rural areas have a higher risk of obesity.

1700s: hot sand to 'sweat out fat'

Early 1800s: the Lord Byron vinegar diet
British poet and politician Lord Byron apparently lost a signficant amount of weight between 1806-11, surviving on a diet of biscuits, soda water and large quantities of vinegar. Apple cider vinegar is still held up as a weight loss aid, but there's no evidence it works. In fact, drinking large doses of vinegar can be dangerous; Byron swigged so much he had stomach problems.

1830s: the 'chastity' diet
Wholewheat Graham flour is named after Reverend Sylvester Graham, who was an advocate of temperance and vegetarianism. He also believed that white sugar, refined flour and spices promoted sinful sexual urges and were best avoided. It's likely, then, he would be a bit upset that his legacy lives on in the s’more – a traditional US campfire favourite in which two Graham crackers are sandwiched together with a layer of melted marshmallow and chocolate.

Mid 1800s: rubber underwear
Rubber underwear was the Spanx of the 19th century, with people hoping to hold in their wobbly bits and lose weight, thanks to the sweating caused by wearing such garments. Unfortunately, the fluid loss only caused temporary weight loss, and the sweaty rubber undies made skin more vulnerable to infection.

1800s: diet pills with arsenic
Most nutritionists agree that diet pills are not a healthy way to manage your weight. Popping pills to speed up metabolism became a diet trend back in the 19th century, but shockingly many of these seemingly miracle tablets contained small amounts of strychnine and arsenic, which consumers might not have been aware of. Chronic arsenic poisoning leads to cancer and liver disease.

1894: the corn flakes diet


Early 1900s: the tapeworm diet

1903: chewing and spitting
American dietician Horace Fletcher became known as the 'Great Masticator' thanks to his belief that chewing food for 100 bites per minute would result in weight loss, making a person stronger as well as limiting the amount of food consumed. Followers were also encouraged to spit out whatever was left in their mouths that hadn’t turned to liquid when the chewing was done. Gross!

1920s: smoke to 'reduce'
If ever there was a diet that should come with a health warning, it's this. In 1928, American cigarette brand Lucky Strike coined the slogan 'reach for a Lucky instead of a sweet', encouraging people to suppress their hunger pangs by smoking instead. (This photo shows a surviving billboard from the 1930s.) It went on to advise people to 'avoid harmful methods to reduce' and enjoy the delicious toasted flavour of Luckies as 'a delightful alternative to the things that make you fat' instead. Oh, the benefits of hindsight…

1923: the milk diet
Bernarr Macfadden was an American body builder who advocated consuming nothing but eight to 12 pints of milk per day for peak fitness. He went on to say that, while he realised sticking to such a stringent diet based on milk would hinder people taking part in many activities, it was essential to stick to the regime if you wanted to see results. While of course milk is nutritious, it lacks vitamin C and fibre, and can cause digestive problems in people with lactose intolerance.

1930s: the Inuit diet
Swedish Artic explorer Vilhjalmur Stefansson belived that a high calorie diet of whale blubber, caribou and raw fish was the best, because the Inuit who lived on this diet were slim and healthy. While this diet is high in heart-healthy omega-3 fats, it lacks fruit and vegetables, and ignores the fact the Inuit are genetically adapted to their diet and burn a lot of calories due to their active lifestyles.

1940s: master cleanse diet
The master cleanse diet – a liquid only, 10-day diet where you drink a lemonade-like beverage, salt-water drink and a herbal laxative tea – started in the 1940s but, incredibly, it's still used by people who want fast results. In an interview with Oprah, Beyoncé revealed that she did the cleanse to lose weight for her role in 2006 movie Dreamgirls . It will likely lead to weight loss because it's so low in calories. But it’s short on nutrients, and impossible to sustain in the long term.

1950s: the cabbage soup diet
The cabbage soup diet became popular among 1950s housewives who wanted to lose weight quickly, and it's been in and out of fashion ever since. Dieters eat three to four servings of cabbage soup a day, which fills your stomach, but side effects like fatigue, light-headedness and flatulence are common. The diet is very low in calories, so of course you will lose weight but eating cabbage soup alone doesn’t provide enough protein or energy to maintain good health.

1962: the drinking man’s diet
Shaping up while enjoying steak and red wine might sound like a great idea, but there are plenty of associated health problems. In The Drinking Man’s Diet , Robert Cameron advocated a diet of meat paired with alcohol – and this became one of the first low-carbohydrate diet trends. However, experts soon branded the diet unhealthy, as more than one or two alcoholic drinks daily is linked with cancer, heart disease, strokes and accidents.

1960s: the sleeping beauty diet
It's believed the origins of the bizarre and dangerous Sleeping Beauty Diet – which, in the simplest terms, involves sleeping to avoid eating – are found in Jacqueline Susan's 1960s bestseller Valley of the Dolls , which saw one character going to a Swiss sleep clinic in order to lose weight. Worringly, this was a more recent trend involving taking sleeping tablets and sleeping a lot to avoid hunger and eating. It's a diet that was reportedly used by Elvis Presley, who even went as far to be put into an induced coma to lose weight.
1960s: amphetamines
During the 1960s, taking stimulants to speed up the metabolism was prevalent, and in 1970-71 it was revealed 5% of adults in the US had used amphetamines in the past 12 months. Diet clinics, where poorly qualified 'diet doctors' dished out the highly addictive medication like sweets, were everywhere. Side effects of amphetamines include anxiety, headaches and a dry mouth.

Early 1970s: the grapefruit diet
Obviously, replacing a meal with a piece of fruit is going to reduce your calorie intake and help you lose weight, but surviving on so little energy isn't the healthiest of solutions. Popular in the 1970s, the grapefruit diet involves eating a grapefruit at every meal, sometimes with nothing else. Interestingly, though, research has since found that components in grapefruit may have a beneficial effect on blood glucose and insulin levels, at least in mice, and that could help prevent obesity.

1974: the Hollywood cookie diet
The Hollywood cookie diet still exists but launched in 1974. The meal replacement diet involves eating up to four high-protein cookies in place of breakfast, lunch and snacks. Sadly, it’s not as fun as it sounds – the cookies aren’t as tasty as proper biscuits, and it's hard to get enough fruit, veg and other nutrients into your diet when you're mainly eating processed cookies. You may lose weight but you won't have a balanced, healthy diet.

1981: Beverley Hills diet
A fad diet devised by author Judy Mazel in the 1980s, the Beverley Hills eating plan allows only fruit for the first 10 days, carbohydrates from day 11 and finally protein on day 19. It’s based on the unscientific notion that blending certain foods inhibits digestion, and that undigested food is what makes people gain fat. It’s complete nonsense and potentially dangerous too, with just 800-1,000 calories a day and a lack of nutrients.

Early 1990s: the Hallelujah Diet
US Reverend George Malkmus created this biblical diet based on only consuming things that Adam and Eve might have eaten in the Garden of Eden. The diet, which is mainly based on eating fruit and vegetables, also combines using supplements from his company, which is a sure sign of a fad diet. Apart from anything else, we're pretty sure Adam and Eve wouldn't have had access to any local health food stores to get their hands on tablets.

2007: the Kimkins diet
Heidi Kimberly 'Kimmer' Diaz faked a 200lb (91kg) weight loss and made money from this scam diet plan, which promotes an extremely low-carb diet, eating as few as 500 calories a day and taking laxatives. The dangerous diet attracted attention in 2007 when it was featured in Woman’s World magazine, which subsequently apologised.

2010: the baby food diet
The baby food diet hit the headlines when it was linked to a celebrity trainer and a host of Hollywood stars. The rumoured diet plan involves eating 14 portions of puréed fruit and vegetables, plus an 'adult' meal in the evening. You'll lose weight quickly on this low-calorie diet but you won't get all of the nutrients an adult needs.

2013: eating cotton wool balls

2018: celery juice
The diet fad of fresh celery juice was kicked off by Anthony William, an LA-based wellness influencer who calls himself the Medical Medium and the 'originator of a global celery juice movement'. It's claimed drinking a pint or more of celery juice a day helps boost weight loss, tackle skin problems, raise energy levels, and more. In fact, though, there’s absolutely no evidence that it's more or less healthy than any other vegetable juice.

2019: the sirtfood diet
The sirtfood diet sees you eat a selection of foods including kale, walnuts, strawberries, onions, chilli, chocolate and red wine, which are meant to boost the 'SIRT' proteins in the body that raise metabolism levels and reduce inflammation. The plan, which was created by by two UK-based nutritionists, Aidan Goggins and Glen Matten, involves drinking a green juice every day and following a calorie-restricted diet. The diet gained popularity when it was linked to Adele, who has since said she has never followed the plan, and experts say there is no specific research proving sirtfoods are beneficial.

Early 2020s: the carnivore diet
The carnivore diet, cutting out all plant products and only eating animal produce (red and white meat, fish, eggs and dairy) has steadily gained popularity. Hugh Jackman reportedly used the diet to get in shape for his role in Wolverine , while other celebrities linked to the diet include Heidi Montag, Joe Rogan and James Blunt (the latter reportedly developed scurvy after two months on an all-meat diet). This eating plan misses out all of the important vitamins and nutrients from fruits and vegetables, as well as being dangerously low in fibre. These factors could lead to a higher risk of colon cancer, type 2 diabetes and cardiovascular disease.

2023: the lion diet
The lion diet, now a massive TikTok trend, takes the carnivore diet a step further, allowing only red meat, salt and water. The elimination diet, which claims to help heal the gut, body and brain, was originally created by podcaster Mikhaila Fuller, who says following it has helped ease her many health problems. Experts warn against it, though, saying the diet lacks nutrients and fibre, is high in saturated fat, and could lead to health problems including high cholesterol and haemorrhoids.
Now discover the diet advice you should definitely ignore, according to experts
More for You
10 warning signs of high cholesterol you shouldn't ignore
'Congress Ran An Underground Business Of Weapons Import': PM Modi On ABP Report On BrahMos
Will Elon Musk Accept Nag Ashwin's Invitation To Test Drive The 6 Ton Beast Bujji, The High-End Car From Kalki 2898 AD?
ECI Recommends Suspension of IPS Officer DS Kutey, Sends Another For Medical Examination
Key rules changing from June 1: From Driving License to Aadhar Card, and more
Hookah vs Vape vs Cigarette: Which is more harmful? | Do Flavoring Agents make them more addictive?
10 silliest animals in the wild (though we find them cute)
PM Modi Exclusive: 'Don't Have Cordial Relations, But I Call Them When...': NaMo On Ties With Gandhis
'Rohit Sharma, Ishan Kishan Will Not Be Playing For MI', Ex India Batter Makes Bold Predictions For IPL 2025
Clash Of The Mighty Cruisers - Kawasaki Eliminator vs RE Shotgun 650
Soaked Kishmish: 10 benefits of consuming them every morning
UP Board Class 10 topper Prachi Nigam, trolled for facial hair, says this to women in glow-up video: ‘Never try to…’
6 signs that indicate heart problems
'They are slowly killing us...' Zerodha's Nithin Kamath's SOSs
Porsche case: NCP MLA Sunil Tingre's role under Pune police scanner, CM Shinde breaks silence — 5 points
How to use castor oil for hair growth? A complete guide
Master Blaster Sachin Tendulkar And Son Arjun Tendulkar Set Off! | N18S #sachintendulkar #shorts
Top 10 career options in AI, Data Science
Yamaha's YZF-R15M Sportbike Could Be the Perfect Beginner Sportbike
Weight loss story: Man loses 60 kg, shares his diet and fitness plan
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Exercise and Insulin Resistance Markers in Children and Adolescents With Excess Weight : A Systematic Review and Network Meta-Analysis
- 1 Navarrabiomed, Instituto de Investigación Sanitaria de Navarra, Hospital Universitario de Navarra, Universidad Pública de Navarra, Pamplona, Spain
- 2 One Health Research Group, Universidad de Las Américas, Quito, Ecuador
- 3 Centro de Investigación Biomédica en Red Sobre Fragilidad y Envejecimiento Saludable, Instituto de Salud Carlos III, Madrid, Spain
- 4 Department of Nursing, Universitat de València, Valencia, Spain
- Correction Error in Affiliations JAMA Pediatrics
Question Which type of exercise is most effective in reducing insulin resistance markers, and what is the dose-response association between exercise dose and these markers in children and adolescents with overweight and obesity?
Findings In this systematic review and network meta-analysis of 55 studies with a total of 3051 children and adolescents, high-intensity interval training alone or combined with resistance training exerted the greatest reduction in insulin resistance markers. In addition, the minimum exercise dosage required to yield clinically meaningful improvements in fasting insulin and homeostatic model assessment for insulin resistance (HOMA-IR) was approximately 900 to 1200 metabolic equivalent of task minutes per week; however, the certainty of evidence varied from low to moderate.
Meaning These findings suggest that youths with excess weight who engage in a minimum of two to three 60-minute sessions of moderate to vigorous activity per week, preferably through high-intensity interval training alone or combined with resistance training, achieve substantial improvements in fasting insulin and HOMA-IR.
Importance Although benefits have been reported for most exercise modalities, the most effective exercise approaches for reducing insulin resistance in children and adolescents with excess weight and the optimal exercise dose remain unknown.
Objective To compare exercise training modalities and their association with changes in insulin resistance markers among children and adolescents with excess weight and to establish the optimal exercise dose.
Data Sources For this systematic review and network meta-analysis, 6 electronic databases (PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Scopus, Web of Science, and CINAHL) were searched for studies from inception to April 1, 2023.
Study Selection Randomized clinical trials (ie, randomized controlled trials and randomized trials without a control group) were included if they reported outcomes associated with aerobic training, resistance training, high-intensity interval training (HIIT), or a combination of these interventions.
Data Extraction and Synthesis Data extraction for this systematic review was conducted following a network meta-analysis extension of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guideline. Effect sizes were calculated as the mean difference (MD) with 95% CI using random-effects inverse-variance models with the Hartung-Knapp-Sidik-Jonkman method. The hierarchy of competing interventions was defined using the surface under the cumulative ranking curve. The Cochrane Risk-of-Bias tool, version 2 (RoB2), was used to independently assess the risk of bias of the included studies. The certainty of evidence in consistent networks was assessed using the Grading of Recommendation, Assessment, Development and Evaluation approach. The study protocol was prospectively registered with PROSPERO. Data analyses were conducted between May and June 2023.
Main Outcomes and Measures The primary outcomes were fasting glucose, insulin, and homeostatic model assessment for insulin resistance (HOMA-IR).
Results This analysis included 55 studies with a total of 3051 children and adolescents (mean [SD] age, 13.5 [2.3] years; 1537 girls [50.4%] and 1514 boys [49.6%]). Exercise was associated with reductions in fasting insulin (MD, −4.38 μU/mL [95% CI, −5.94 to −2.82 μU/mL]) and HOMA-IR (MD, –0.87 [95% CI, –1.20 to –0.53]). A nonlinear association in both markers was observed, with a required minimal exercise dosage of approximately 900 to 1200 metabolic equivalent of task minutes per week, especially in children and adolescents with insulin resistance at baseline. Combination HIIT and resistance training and concurrent training were the most effective approaches for reducing insulin resistance markers. On average, the certainty of evidence varied from low to moderate.
Conclusions and Relevance These findings underscore the role of exercise interventions in enhancing insulin resistance markers among children and adolescents with overweight and obesity. It is advisable to include resistance exercises alongside aerobic and HIIT programs for a minimum of two to three 60-minute sessions per week.
Read More About
García-Hermoso A , López-Gil JF , Izquierdo M , Ramírez-Vélez R , Ezzatvar Y. Exercise and Insulin Resistance Markers in Children and Adolescents With Excess Weight : A Systematic Review and Network Meta-Analysis . JAMA Pediatr. 2023;177(12):1276–1284. doi:10.1001/jamapediatrics.2023.4038
Manage citations:
© 2024
Artificial Intelligence Resource Center
Pediatrics in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 28 May 2024
Sleep quality mediates the effect of medical social support on depression symptoms in patients with HIV/AIDS
- Ziqi Chen 1 , 2 na1 ,
- Kailian He 1 , 3 na1 ,
- Yulu Chen 1 , 2 ,
- Xiashuang Zhang 1 , 2 ,
- Zeyan Ye 1 , 2 ,
- Chaofan Xie 1 , 2 ,
- Tingyu Luo 1 , 2 ,
- Xiaofeng Fu 4 ,
- Wuxiang Shi 5 ,
- Zhiyong Zhang 1 , 2 ,
- Liang Cao 1 , 6 &
- You Li 1 , 2
BMC Public Health volume 24 , Article number: 1429 ( 2024 ) Cite this article
Metrics details
The purpose of our study is to further understanding of the depression symptoms of HIV/AIDS patients in Guilin, Guangxi via exploring whether there is a mediating effect of sleep quality on medical-social support and depression symptoms and therefore provide a theoretical basis for application of medical-social support to alleviate depression symptoms of HIV/AIDS patients.
A convenience sampling method was used to select 200 HIV/AIDS patients for the study. Depression symptoms, sleep quality, and medical-social support of the study participants were investigated using The Center for Epidemiological Studies Depression Scale (CES-D), The Pittsburg Sleep Quality Index (PSQI), and The Medical Outcomes Study Social Support Survey (MOS-SSS), respectively. Predictors of depression symptoms were explored by multiple linear regression, and Pearson correlation was used to analyze the relationship between sleep quality, medical-social support, and depression symptoms. Mediating effect analysis was performed by nonparametric Bootstrap test.
In this study, the incidence of depression symptoms was 54.4%. Multiple linear regression analysis showed that leanness (β = 0.161, P = 0.008), obesity (β = 0.186, P = 0.002), sleep quality score > 7 (β = 0.331, P < 0.001), and medical-social support score > 56 (β = -0.247, P < 0.001) could influence depression symptoms of HIV and Pearson’s correlation analysis demonstrated that there was a two-way correlation between sleep quality, medical social support and depression symptoms ( P < 0.05). In addition, Bootstrap tests showed that medical-social support might affect depression symptoms not only directly but also indirectly through the mediating effect of sleep quality with the direct and mediating effects accounting for 77.25% and 22.75% of the total effect, respectively.
The prevalence of depression symptoms is high among HIV/AIDS patients in Guilin City. The depressive symptoms of PLWHs(people living with HIV) are related to their sleep quality and medical-social support, and sleep quality partially mediates the relationship between medical-social support and depression symptoms. Therefore, interventions to improve sleep quality and medical-social support have the potential to allay the depression symptoms of HIV/AIDS patients.
Peer Review reports
Introduction
According to a survey conducted by UNAIDS in 2020, about 37.6 million people worldwide have been infected with HIV/AIDS by 2020, and about 480,000 to 1 million people may die from AIDS-related illnesses [ 1 ]. The Chinese Health Care Commission also showed that in 2021a total of 60,154 AIDS cases were reported nationwide, of which 19,623 died [ 2 ]. Suffice it to say that AIDS has become a serious global public health and social problem which imposes an enormous physical and economic burden on both individuals, health care systems and society. HIV patients may suffer from physical diseases as well as several mental problems, among which depression is the most common-seen mental health challenge,with clinical manifestations as low mood, loss of pleasure, reduced motivation and energy, guilt or low self-esteem, problems with sleep or appetite, suicidal attempt and concentration difficulties [ 3 ]. Globally, more than 350 million people currently suffer from depression, and its lifetime prevalence in the general population is estimated around 3 to 17%. Studies had shown that depression was three times more prevalence in the HIV-positive population than in the general population, and its lifetime prevalence this population was estimated to be between 22% and 45% [ 4 ]. Predicted by WHO, by the end of 2030, depression and HIV/AIDS will be the leading causes of disability around the world [ 1 ].A variety of factors may contribute to the development of depressive symptoms in PLWH, such as age, gender, marital status, monthly income, occupational status, opportunistic infections, adverse reactions to medications, the presence of other chronic diseases, social stigma, occupational disability, low social support, and chronic physical discomfort and illness [ 5 ]. Antidepressants are an effective way to treat depression, however, PLWH patients are more likely to receive psychotherapy than medication.
It's held that medical-social support may strengthen the belief and will of HIV patients to survive and have a positive impact on their physical health. A multitude of previous studies had shown that PLWHs often had to endure severe illness-related stress, including stigma, discrimination, financial difficulties, side effects of antiretroviral therapy (ART) treatment, unemployment, etc., any of which could lead to depression, anxiety, suicidality [ 6 ]. Studies had shown that adult PLWHs with poor social support were 31% more likely to develop depression than those with more social support. Less social support may result in irregular medication which in turn aggravates the infected status and therefore, causes social isolation, and eventual depression [ 7 ]. Another study confirmed a significant negative association between medical-social support and poor sleep quality, with older adults with low levels of medical-social support having a 1.40 times higher risk of poor sleep quality compared to those with high levels of social support [ 8 ]. Having positive social relationships can promote healthier sleep by encouraging positive emotions, reducing stress, and preventing social isolation [ 9 ]. Social isolation can lead to greater stress and damage mental health [ 10 ]. Sufficient medical-social support may enable PLWHs to cope with the negative effects of stress more actively [ 6 ].
Sleep disturbance is an often-heard complaint in patients with chronic illnesses, including those with HIV infection. It may occur at any stages of HIV infection, but is more common at the advanced stage of HIV. A meta-analysis showed that the global prevalence of PLWH sleep disorders in adults was 58 percent [ 11 ]. Better sleep quality in HIV patients is closely related to the indicators of quality of life, such as overall well-being, anxiety, reduced depressive symptoms, and reduced symptom severity, whereas co-occurrence of poor sleep quality and HIV infection complicates clinical management. Poor sleep quality has been reported commonplace in PLWHs. Studies conducted in the United States and China [ 12 , 13 ] had shown, the symptom most closely correlating with poor sleep quality was depression. Depression leads to hyperfunction of the hypothalamic-pituitary-adrenal axis, increased sympathetic excitability, and elevated circulating levels of norepinephrine and cortisol, resulting in an enhanced state of arousal in the patient, which in turn affects sleep quality [ 14 ]. At the same time, sleep problems can precede and precipitate depressive episodes, which in turn contribute to the development of depression. Even after depressive symptoms have resolved, sleep problems remain a residual symptom that needs to be treated [ 15 ]. Thus, there is a strong link between sleep and depressive symptoms, and sleep may even play an important role in the etiology and maintenance of depressive symptoms.
In the specific population of HIV/AIDS patients, the relationship between both sleep quality, medical-social support and depression has been studied more [ 12 , 15 , 16 ], while the mediating role of sleep quality between medical-social support and depression has rarely been examined. The present study aimed to fill this research gap and provide evidence for effective prevention and treatment of depressive symptoms in HIV/AIDS patients in the future. Therefore, we analyzed the possible influences on depressive symptoms among HIV patients in Guilin City, focusing on the relationship between sleep quality, medical-social support and depressive symptoms, and proposed the hypothesis that sleep quality has a mediating effect between medical-social support and depressive symptoms.
Objects and methods
Study population.
Convenience sampling was adopted in cross-sectional study to select 200 patients with HIV/AIDS in Guilin City from January 2022 to July 2022 for the current study. Inclusion criteria were as follows: (1) Age ≥ 18 years. (2) Those who were tested positive for HIV antibody. (3) Full ability to comprehend and complete the questionnaire independently. Exclusion Criteria were the following: (1) serious visual and hearing impairment or insufficient reading and comprehension ability. (2) serious acute or chronic physical illnesses which resulted in functional impairment. (3) Unwillingness to participate in this survey. This study was conducted by the investigators (all of whom were trained in standardized procedures professional staff engaged in the follow-up of HIV/AIDS patients in Guilin City and various counties and districts) who carried out the questionnaire survey on the selected participants through interviews. Recruitment of participants was limited to those who were followed up in the department of AIDS control and prevention and the confidentiality of the subjects was ensured. All subjects signed an informed consent form prior to the survey, and the survey was conducted under the approval of the Ethics Committee of Guilin Medical College(GYLL2021078).
Estimation of sample size
According to relevant studies [ 17 ], the prevalence of depressive symptoms in HIV-infected patients was about 41.0%, with a permissible error of 0.1 and a Zα of 1.96, which was calculated using the formula n=(Zα 2 × pq)/d 2 , yielding a sample size of 95. Considering a 10% failure rate and the design effect of the survey (m = 1.5), N = n×(1 + 0.1)×1.5 = 154(persons).
Data collection
We collected demographic, including the following: (a) General demographic characteristics: basic personal information such as gender, age, ethnicity, height, weight, household location, health status, education level, monthly household income, occupation, marital status, etc.; (b) Clinical information: level of CD4 + T-lymphocyte (referred to as CD4 + cells) counts, HIV viral loads, diagnosis time and infection, antiretroviral treatment, etc.; (c) Other information: route of infection, HIV testing of last year, sexual life within 6 months, history of chronic illness, etc. [ 16 , 18 ]. According to the Guidelines for the Prevention and Control of Overweight and Obesity in Chinese Adults [ 19 ], Body Mass Index (BMI) < 18.5 kg/m 2 indicates lean, BMI between 18.5 and 23.9 kg/m 2 indicates normal weight, BMI between 24.0 and 27.9 kg/m 2 indicates overweight, and BMI ≥ 28.0 kg/m 2 indicates obesity.
Depression was measured using The Center for Epidemiological Studies Depression Scale (CES-D) [ 20 ], designed by the National Institute of Mental Health and widely used in general population for screening and assess depressive symptoms, which was primarily used to measure the degree of depression of the recent week in the study population. The scale is set up from four dimensions which are Depressed Mood, Positive Mood, Somatic Symptoms and Activity Latency. The CES-D scale is scored on a 0–3 Likert 4-point scale, with total scores ranging from 0 to 60. There is no specific and definite score for depression. A score of ≥ 16 is generally considered to display a potential tendency for depression and the higher scores may show a higher likelihood of being depressive.
The Pittsburg Sleep Quality Index (PSQI), compiled by Buysse et al. [ 21 ] in 1989 and translated into Chinese by Liu Xianchen et al. [ 22 ] in 1996, was verified to have a reliability of 0.85 and a validity of 0.83, which is suitable for measuring sleep condition of the latest month in Chinese population. The PSQI scale consists of seven factors: subjective sleep quality, sleep latency, duration of sleep, habitual sleep efficiency, sleep disorders, medication for sleep, and daytime dysfunction. Each factor is scored from 0 to 3, and the total score of the scale ranges from 0 to 21, with a score of “0” indicating no difficulty and a score of “21” indicating great difficulty in all areas. In Chinese population, a total PSQI score of > 7 indicates presence of sleep disorders [ 22 ].
The Medical Outcomes Study Social Support Survey (MOS-SSS), developed by Sherbourne & Stewart [ 23 ], consists of four dimensions: practical support, message and emotional support, interactive social cooperation, and emotional support. A score of 1 to 5 is recorded depending on the number of occurrence and the degree of severity, with 1 indicating no support at all, 2 indicating scanty support, 3 indicating support available for some time, 4 indicating support available for most of the time, and 5 indicating constant support. The total score ranges from 19 to 95, and the higher the score is, the higher the level of medical social support patients may receive. Some Chinese scholars proposed that 56 points might be used as a cutoff and ≤ 56 points representing low medical social support while > 56 points might indicate high medical social support [ 2 ].
Statistical analysis
Data were entered in double parallel using EpiData 3.1 software and statistically analyzed by SPSS28.0. Summarized as mean ± standard deviation (‾χ ± s) and categorical variables as frequency (percentage). One-way test, Kolmogorov-Smirnov test was used to assess normal continuous variables, and data conforming to normal distribution were analyzed using t-test or chi-square test. Following the one-way analysis, multiple linear regression was used to further investigate the relationship between the variables of interest and depressive symptoms. Pearson correlations were analyzed for the relationship between sleep quality, medical-social support, and depression symptoms, followed by mediated effects analyses via nonparametric Bootstrap using the SPSS28.0 macro program PROCESS4.1 component. The Bootstrap methodology was developed from the 5000 replicate samples to generate 95% bias-corrected confidence intervals, with intervals excluding 0 indicating a significant mediating effect. Finally, mediation effect plots were further demonstrated by graphing with AMOS 24.0 software. P < 0.05 was considered statistically significant.
Demographic characteristics
A total of 200 questionnaires were distributed in this study and all 200 questionnaires were retrieved. Among them, 129 (64.50%) were made on male and 71 (35.5%) were on female. The age distribution ranged from 21 to 85 years with a mean age of 51.53 ± 13.44 years. The participants were mainly Han (76.00%), followed by Yao (19.50%), 59.00% had a partner in their marital status. In terms of educational attainment, 39.50% were in elementary school and below, 41.50% in junior high school, and 19.00% in high school and above, and by occupation, 74.00% were farmers. The mean score of depression scale in HIV/AIDS patients was 18.33±9.72 and the incidence of depressive symptoms was 54.40%.The results of univariate analysis showed statistically significant differences in depression across health status, BMI, antiretroviral treatment status, sleep quality and medical-social support (all P < 0.05) (Table 1 ).
Multiple linear regression analysis of depression symptoms in HIV/AIDS patients
The results of multiple linear regression analysis showed that among the relevant factors affecting the depressive symptoms of HIV/AIDS patients, the four variables, namely, thinness, obesity, sleep quality, and medical-social support, entered the regression model, and the results suggested that thinness (β = 0.161, P = 0.008), obesity (β = 0.186, P = 0.002), and sleep quality scores > 7 (Beta = 0.331, P < 0.001) all elevated depression scores and predisposed HIV/AIDS patients to depression symptoms. A medical social support score > 56 (β = -0.247, P < 0.001) decreased depression scores in HIV/AIDS patients and made them less prone to depression symptoms. These four variables explained 35.9% of the variance in depression scores. As for the correlation of antiretroviral treatment status on depression symptoms, the difference was not statistically significant ( P > 0.05). From the standardized regression coefficients, the importance of the effects of the four variants ondepressive status was, in descending order, obesity, sleep quality score > 7, medical-social support score > 56, and thinness (Tables 2 and 3 ).
Correlation analysis of medical-social support, sleep quality and depression symptoms in HIV/AIDS patients
Pearson correlation analysis was used to measure the correlation between the variables. The correlation matrix of the variables is shown in Table 4 , which showed that there was a two-by-two correlation between sleep quality, medical social support and depression symptoms in HIV/AIDS patients, with negative correlation between sleep quality and medical social support, medical social support and depression symptoms in HIV/AIDS patients ( P < 0.05) and positive correlation between sleep quality and depression symptoms ( P < 0.05).
The mediating role of sleep quality
The results showed that medical-social support was negatively correlated with the effect of depression symptoms(β = -0.357, T = -5.378, P < 0.05), and when the mediating variable was added, medical-social support remained negatively correlated with depression symptoms (β = -0.250, T = -4.380, P < 0.05). Medical-social support was negatively correlated with sleep quality (β = -0.206, T = -2.963, P < 0.05), and sleep quality had a positive effect on depression symptoms (β = 0.519, T = 9.084, P < 0.05). (Table 5 ; Fig. 1 )
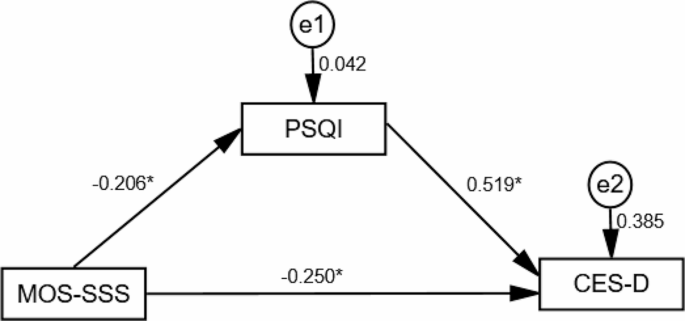
Schematic representation of the mediating effects of sleep quality
Using Bootstrap resampling (5000 samples), the results showed a statistically significant difference in the direct effect of medical social support on depression symptoms as well as the indirect effect of depression symptoms( P < 0.05), suggesting that medical social support may affect depression not only directly, but also indirectly through the mediating effect of sleep quality. Adjusting the model by including BMI, health status and antiviral treatment status as covariates similarly showed the same results as above. Before adjustment, the direct and indirect mediating effects accounted for 69.90% and 30.10% of the total effect, respectively. After adjustment for the inclusion of covariates, the direct and indirect mediating effects accounted for 77.25% and 22.75% of the total effect, respectively (Table 6 ).
Table 6 Analysis of the mediating role of sleep quality in the relationship between medical social support and depressive symptoms Effect se T P LLCI ULCI relative effect value Model 1a Total effect -0.206 0.038 -5.378 <0.001 -0.282 -0.131 \Direct effect -0.144 0.033 -4.380 <0.001 -0.209 -0.079 69.90% Indirect effect -0.062 0.022 \\ -0.106 -0.022 30.10% Model 2b Total effect -0.189 0.036 -5.207 <0.001 -0.261 -0.118 \Direct effect -0.146 0.033 -4.485 <0.001 -0.210 -0.082 77.25% Indirect effect -0.043 0.017 \\ -0.078 -0.013 22.75% Note: a, no adjustment; b, adjusted for inclusion of BMI, health status, and antiviral treatment as covariates.
As the most common mental health challenge associated with HIV/AIDS patients, depression may even aggravate the disease [ 24 ]. In our study population, the mean depression score of HIV/AIDS patients was 18.33 ± 9.72, and the prevalence of depression sympyoms was 54.5%, which was higher than the global prevalence (31%) [ 25 ], and what was reported by Kim Madundo et al. (41%) [ 26 ] and Wang (47.7%) [ 27 ]. Possible reasons for this discrepancy may be related to timing, sample size, and differences in response to HIV infection around China, which influenced our subjects socially.
It has been shown that both leanness and obesity might have a negative impact on development of depression symptoms in HIV/AIDS patients. It’s widely acceptable that BMI is an important indicator of body nutritional status and a simple and cost-effective tool for monitoring the clinical response of HIV patients after initiation of ART [ 28 ]. Martinez [ 29 ] showed that higher BMI and adiposity slowed HIV disease progression and higher baseline BMI was associated with a lower risk of developing AIDS. In line with these previous studies mentioned above, our study also demonstrated that both malnutrition and obesity may contribute to the vulnerability of HIV/AIDS patients to depression symptoms [ 30 , 31 ]. In contrast to Luo et al. [ 32 ], who found that obesity reduced the prevalence of depression in middle-aged and older men, Crisp [ 33 ] found a positive correlation between severe obesity and low levels of depression in men in their study. On the other hand, no association between obesity and depression or obesity increasing risk of depression were also reported [ 34 , 35 ]. Therefore, more research is required to unvail the mystery of the relationship between obesity and depression. Low body weight and low BMI associated with disease wasting [ 36 ] may result in not only impaired immune recovery and increased mortality in the early stages of ART [ 37 ], but also the prevalence of menstrual disorders in PLWHs [ 38 ]. As a matter of fact, women are more likely to be depressive than men due to their physical hormonal fluctuations, such as hypersensitivity and hormonal changes during menopause [ 39 ]. In conclusion, there may be a strong association between obesity status and depression symptoms. BMI, as a tool to explore the relationship between obesity and depression symptoms, easily to be detected, may alert healthcare providers to the alteration in subject’s mood status at early stage.
In the present study, high medical-social support alleviated depression, similar to the study by Mohamud et al [ 40 ], where those with poor medical-social support were more likely to develop depression than those with moderate medical-social support. Though negative social behaviors may result in depression, it's still more likely that people with HIV try to avoid seeking help from others due to social stigma, which inevidently increases their loneliness, isolation, and depression. Data suggests that 41.7% of the people with HIV have experienced HIV-related discrimination, and more than 76% report that their family members are even been discriminated against [ 41 ]. Moreover, increased emotional, financial, and physical burden of stigmatization were observed [ 42 ]. Despite legal access to health care, employment and education, discrimination still persists in both medical and non-medical resources [ 12 , 42 ]. Stigmatization, fatigue feelings, worthlessness, shame, and fear of HIV exposure, isolation, and hopelessness may further exacerbate depression which in turn may lead to ultimate treatment failure. In China, where most activities are culturally family-centered, it's much easier for most patients to receive or solicit support from their families. Hence, a supportive and active family environment may positively affect the mood of patients, prevent social isolation, and promote healthy sleep habits [ 11 ]. Good social support may enable PLWH to better cope with the negative effects of stress and modulate themselves to physical discomfort [ 43 ]. To summarize, adequate and ready medical-social support may play a critical role in assisting the patients in building up their confidence to live optimistically, maintaining a good psychological state, and ultimately improving treatment outcomes.
PLWH frequently claimed sleep disturbances. In our study, sleep quality was not only a positive predictor of depressive symptoms, but also had a mediating effect in medical social support and depressive symptoms. This suggests that medical social support can both directly and indirectly influence depressive symptoms in HIV/AIDS patients by affecting sleep quality. In China, where AIDS is still a highly stigmatized disease, the impact of HIV infection on psychological status, as well as the prejudice and social stigma followed, may place PLWH at a higher risk of depression which may subsequently induce sleep disorders [ 44 ]. Sleep disorders may, in turn, lead to aggravation of depressive symptoms in PLWH, which was consistent with that participants suffering from depression were 4.44 times more likely to experience poor sleep quality compared to those without depression [ 11 ]. The possible reason for this is that PLWH are more psychologically stressed after HIV infection and mostly reluctant to resort to others, which lead to depression and other adverse emotions and poor sleep quality. Whereas high medical social support may alleviate depressive symptoms by increasing positive emotions in HIV/AIDS patients, thereby improving sleep quality, it may provide a new way of thinking about alleviating depressive symptoms in HIV/AIDS patients in Guilin. Thus, addressing sleep disorders may alleviate mental illness, and treating depressive symptoms may improve sleep quality, while increasing the level of medical-social support in PLWH is needed.
Our study described the current status of depression among people living with HIV/AIDS (PLWH) in Guilin and the mediating role of sleep quality in medical-social support and depressive symptoms. And the results suggested that there were two ways to reduce the depressive symptoms of PLWH: (1) Taking measures to improve the sleep quality of PLWH, such as promoting a more regular lifestyle. (2) Improving medical-social support for PLWH, such as increasing more daily social contacts. PLWHs often have difficulty in obtaining social support directly from friends and relatives, which highlights the psychological support and care provided by health care providers for PLWHs. It is very feasible for health service staff, especially those for PLWH, to utilize their professional knowledge and exclusive channels to provide adequate and sustainable services.
Limitation.
Although our study provides some valuable insights into the beneficial effects of medical-social support on depression symptoms, there are still some limitations worth being taken into account when the current results were interpreted. First, because this was a cross-sectional study, it was not possible to determine causality. Second, the reliance on self-reported data for certain variables may introduce potential recall bias, which may affect the accuracy and completeness of the data collected. Third, the application of convenience sampling methods may also lead to sample selection bias, limiting the generalizability of our findings on other populations. Fourth, depressive symptoms are conceptualized differently from depression, and research on depressive symptoms may not fully guide interventions for depression. Therefore, in future studies, more sound research design and sampling methods to increase the sample size of the study are required to obtain more reliable and generalizable results. Secondly, clinical diagnosis with the aim that the results can better guide interventions for depression may be considered to introduce. Finally, the results of this study need to be further confirmed by prospective follow-up studies with large samples.
In summary, the prevalence of depression symptoms is high among HIV/AIDS patients in Guilin City. The depressive symptoms of PLWHs may be related to sleep quality and medical-social support. In addition, sleep quality may partially mediate the relationship between medical-social support and depressive symptoms. Therefore, interventions to improve sleep quality and medical-social support may have the potential to reduce severity of the depressive symptomsof HIV/AIDS patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Junaid K, Afzal S, Daood M, Siddiqui M. Substance abuse and mental health issues among HIV/AIDS patients. Jcpsp-J Coll Physici. 2023;33:325–34.
Google Scholar
He K, Zhang X, Yang D, Fu X, Chen Y, Chen Z, et al. Analysis of factors influencing depression in elderly people living with HIV/AIDS based on structural equation model: A Cross-Sectional Study in Guangxi, China. J Multidiscip Health. 2023;16:1491–501.
Necho M, Belete A, Tsehay M. Depressive symptoms and their determinants in patients who are on antiretroviral therapy in the case of a low-income country, Ethiopia: A systematic review and meta-analysis. Int J Ment Health SY. 2021;15:3.
Article Google Scholar
Zhu W, Gao J, Guo J, Wang L, Li W. Anxiety, depression, and sleep quality among breast cancer patients in North China: Mediating roles of hope and medical social support. Support Care Cancer. 2023;31:514.
Abdisa E, Tolesa T, Abadiga M. Prevalence of depressive symptoms and its associated factors among people living with HIV attending public hospitals of Nekemte Town, Western Ethiopia, 2021. Behav Neurol. 2021;2021:8854791.
Yu Y, Luo B, Qin L, Gong H, Chen Y. Suicidal ideation of people living with HIV and its relations to depression, anxiety and social support. BMC Psychol. 2023;11:159.
Article PubMed PubMed Central Google Scholar
Weldesenbet AB, Kebede SA, Tusa BS. The effect of poor social support on depression among HIV/AIDS patients in Ethiopia: A systematic review and meta-analysis. Depress Res Treat. 2020;2020:6633686.
PubMed PubMed Central Google Scholar
Salehi Z, Pasha H, Hosseini SR, Kheirkhah F, Bijani A. The impact of social support, physical and psychological performance on sleep outcomes in Iranian older adults: A case-control study. BMC Geriatr. 2023;23:791.
Fekete EM, Seay J, Antoni MH, Mendez AJ, Fletcher MA, Szeto A, et al. Oxytocin, social support, and sleep quality in low-income minority women living with HIV. Behav Sleep Med. 2014;12:207–21.
Article PubMed Google Scholar
Zewudie BT, Geze S, Mesfin Y, Argaw M, Abebe H, Mekonnen Z, et al. A systematic review and meta-analysis on depression and associated factors among adult HIV/AIDS-Positive patients attending ART clinics of Ethiopia: 2021. Depress Res Treat. 2021;2021:8545934.
GebreEyesus FA, Degu FS, Yohanes YB, Azagew AW. Sleep quality and associated factors among adult people living with HIV on follow-up at Dessie Town Governmental Health Facilities Antiretroviral Therapy Clinics, Northeast, Ethiopia, 2020, a multicenter cross-sectional study. BMC Psychiatry. 2023;23:132.
Huang X, Li H, Meyers K, Xia W, Meng Z, Li C, et al. Burden of sleep disturbances and associated risk factors: A cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep-UK. 2017;7:3657.
Crum-Cianflone NF, Roediger MP, Moore DJ, Hale B, Weintrob A, Ganesan A, et al. Prevalence and factors associated with sleep disturbances among early-treated HIV-infected persons. Clin Infect Dis. 2012;54:1485–94.
Pruessner M, Hellhammer DH, Pruessner JC, Lupien SJ. Self-reported depressive symptoms and stress levels in healthy young men: Associations with the cortisol response to awakening. Psychosom Med. 2003;65:92–9.
Rogers BG, Lee JS, Bainter SA, Bedoya CA, Pinkston M, Safren SA. A multilevel examination of sleep, depression, and quality of life in people living with HIV/AIDS. J Health Psychol. 2020;25:1556–66.
Mao Y, Qiao S, Li X, Zhao Q, Zhou Y, Shen Z. Depression, social support, and adherence to antiretroviral therapy among people living with HIV in Guangxi, China: A longitudinal study. Aids Educ Prev. 2019;31:38–50.
Sun W, Lu H, Huang F, Shiu CS, Zhang L, Chen WT. Longitudinal trajectory of the association between quality of life and depression among people living with HIV in China: A mixed effects model. AIDS Care. 2022;34:966–73.
Liu L, Pang R, Sun W, Wu M, Qu P, Lu C, et al. Functional social support, psychological capital, and depressive and anxiety symptoms among people living with HIV/AIDS employed full-time. BMC Psychiatry. 2013;13:324.
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17 Suppl:1–36.
PubMed Google Scholar
Rooney AS, Moore RC, Paolillo EW, Gouaux B, Umlauf A, Letendre SL, et al. Depression and aging with HIV: Associations with health-related quality of life and positive psychological factors. J Affect Disorders. 2019;251:1–7.
Buysse DJ, Reynolds CR, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiat Res. 1989;28:193–213.
Xian Chen L, Mao Qin T, Lei H, Ai Zheng W, Hong Xin W, Gui Fang Z. Reliability and validity of the pittsburgh sleep quality index. Chin J Psychiatry. 1996:103–7.
Sherbourne CD, Stewart AL. The Mos social support survey. Soc Sci Med. 1991;32:705–14
Li S, Yu S, Yang Q, Yin J, Zhu H, Jiang Y, et al. Prevalence of suicide ideation among HIV/AIDS patients in China: A systematic review and meta-analysis. Front Public Health. 2023;11:1082521.
Rezaei S, Ahmadi S, Rahmati J, Hosseinifard H, Dehnad A, Aryankhesal A, et al. Global prevalence of depression in HIV/AIDS: A systematic review and meta-analysis. BMJ Support Palliat. 2019;9:404–12.
Madundo K, Knettel BA, Knippler E, Mbwambo J. Prevalence, severity, and associated factors of depression in newly diagnosed people living with HIV in Kilimanjaro, Tanzania: A cross-sectional study. BMC Psychiatry. 2023;23:83.
Wang D, Deng Q, Chen H, Wang M, Liu Z, Wang H, et al. Profiles of depressive symptoms and influential factors among people living with HIV in China. BMC Public Health. 2023;23:151.
Alebel A, Sibbritt D, Petrucka P, Demant D. Association between body mass index variation and early mortality among 834 ethiopian adults living with HIV on ART: A joint modelling approach. Infect Dis Ther. 2023;12:227–44.
Martinez SS, Campa A, Bussmann H, Moyo S, Makhema J, Huffman FG, et al. Effect of BMI and fat mass on HIV disease progression in HIV-infected, antiretroviral treatment-naive adults in Botswana. Brit J Nutr. 2016;115:2114–21.
Article CAS PubMed Google Scholar
Camara A, Sow MS, Toure A, Sako FB, Camara I, Soumaoro K, et al. Anxiety and depression among HIV patients of the infectious disease department of Conakry University Hospital in 2018. Epidemiol Infect. 2020;148:e8.
Article CAS PubMed PubMed Central Google Scholar
Zoungrana J, Dembele JP, Sako FB, Siranyan S, Traore J, Sawadogo A, et al. Depression and HIV: Epidemiological and clinical aspects at the Bamako University Hospital (Mali). Med Sante Trop. 2017;27:186–9.
CAS PubMed Google Scholar
Luo H, Li J, Zhang Q, Cao P, Ren X, Fang A, et al. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: Evidence from the Charls. BMC Public Health. 2018;18:909.
Crisp AH, McGuiness B. Jolly fat: relation between obesity and psychoneurosis in general population. Br Med J. 1976;1:7–9.
Faith MS, Matz PE, Jorge MA. Obesity-depression associations in the population. J Psychosom Res. 2002;53:935–42.
Roberts RE, Duong HT. Does major depression affect risk for adolescent obesity? J Affect Disorders. 2015;186:162–7.
Zhong H, Wei F, Song Y, Chen H, Ni Z. Health-related quality of life and associated factors among people living with HIV/AIDS in Sichuan, China: A cross-sectional study. Front Public Health. 2023;11:1133657.
Fuseini H, Gyan BA, Kyei GB, Heimburger DC, Koethe JR. Undernutrition and HIV infection in Sub-Saharan Africa: Health outcomes and therapeutic interventions. Curr HIV-AIDS Rep. 2021;18:87–97.
King EM, Albert AY, Murray M. HIV and amenorrhea: A meta-analysis. AIDS. 2019;33:483–91.
Qian J, Li N, Ren X. Obesity and depressive symptoms among Chinese people aged 45 and over. Sci Rep-UK. 2017;7:45637.
Mohamud AK, Ahmed OA, Mohamud AA, Dirie NI. Prevalence of and factors associated with depression among adult patients living with HIV/AIDs undergoing ART unit in Banadir hospital, Mogadishu Somalia. BMC Psychiatry. 2023;23:232.
Wu X, Chen J, Huang H, Liu Z, Li X, Wang H. Perceived stigma, medical social support and quality of life among people living with HIV/AIDS in Hunan, China. Appl Nurs Res. 2015;28:169–74.
Zhang C, Li X, Liu Y, Qiao S, Zhang L, Zhou Y, et al. Emotional, physical and financial burdens of stigma against people living with HIV/AIDS in China. AIDS Care. 2016;28 Suppl 1:124–31.
Chen WT, Huang F, Sun W, Zhang L. Fear of COVID and physical health among people living with HIV in China: Mediation effects of HIV stigma, social support, and substance use. AIDS Behav. 2023:1–8.
Chen CC, Liu HY, Chen YC, Ko NY. Relationships among trajectories of sleep disturbance, depression, and antiretroviral therapy in persons newly diagnosed with HIV: A One-and-a-half-year observational longitudinal study. Nat Sci Sleep. 2022;14:2133–42.
Download references
Acknowledgements
The authors would like to express their gratitude to the Guilin CDC and pay their respects to them. The authors acknowledge the efforts of the study team and extend special thanks to the patients who participated in this study.
This work was funded by Innovation Platform and Talent Plan in Guilin (20220120-2), the Major Science and Technology Projects in Guangxi (GKAA22096026).
Author information
Ziqi Chen and Kailian He contributed equally to this manuscript.
Authors and Affiliations
Department of Environmental Health and Occupational Medicine, School of Public Health, Guilin Medical University, Guilin, Guangxi, 541199, People’s Republic of China
Ziqi Chen, Kailian He, Yulu Chen, Xiashuang Zhang, Zeyan Ye, Chaofan Xie, Tingyu Luo, Zhiyong Zhang, Liang Cao & You Li
Guangxi Health Commission Key Laboratory of Entire Lifecycle Health and Care, Guilin Medical University), Guilin, Guangxi, 541199, People’s Republic of China
Ziqi Chen, Yulu Chen, Xiashuang Zhang, Zeyan Ye, Chaofan Xie, Tingyu Luo, Zhiyong Zhang & You Li
Health and Wellness Section, Yibin Center for Disease Control and Prevention, Yibin, Sichuan, 644600, People’s Republic of China
Department of AIDS Control and Prevention, Guilin Center for Disease Control and Prevention, Guilin, Guangxi, 541000, People’s Republic of China
Xiaofeng Fu
Health Management Unit, Faculty of Humanities and Management, Guilin Medical University, Guilin, Guangxi, 541199, People’s Republic of China
Wuxiang Shi
Department of Experimental Teaching Center, School of Public Health, Guilin Medical University, Guilin, Guangxi, 541199, People’s Republic of China
You can also search for this author in PubMed Google Scholar
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas. They took part in drafting, revising or critically reviewing the article. They gave final approval of the version to be published. All authors have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Corresponding authors
Correspondence to Liang Cao or You Li .
Ethics declarations
Ethics approval and consent to participate.
Our research protocol was approved by the Ethics Committee of Guilin Medical University (GYLL2021078). All subjects signed an informed consent form prior to the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, Z., He, K., Chen, Y. et al. Sleep quality mediates the effect of medical social support on depression symptoms in patients with HIV/AIDS. BMC Public Health 24 , 1429 (2024). https://doi.org/10.1186/s12889-024-18174-w
Download citation
Received : 09 August 2023
Accepted : 21 February 2024
Published : 28 May 2024
DOI : https://doi.org/10.1186/s12889-024-18174-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep quality
- Depression symptoms
- Mediating effect
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Etiologies underlying subtypes of long-standing type 2 diabetes
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation College of Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, UAE
Roles Data curation, Investigation, Methodology
Affiliation Dubai Diabetes Center, Dubai Health, Dubai, UAE
Affiliation Endocrinology Department, Dubai Hospital, Dubai Health, Dubai, UAE
Roles Data curation, Formal analysis, Methodology
Roles Data curation, Formal analysis, Investigation, Methodology
Roles Formal analysis, Methodology, Software, Supervision
Roles Data curation, Formal analysis, Methodology, Supervision
Roles Formal analysis, Methodology, Resources
Roles Formal analysis, Investigation, Methodology, Project administration
Roles Data curation, Methodology
Roles Formal analysis, Investigation, Methodology
Affiliation Pathology Department, Dubai Hospital, Dubai Health, Dubai, UAE
Roles Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing
- Riad Bayoumi,
- Muhammad Farooqi,
- Fatheya Alawadi,
- Mohamed Hassanein,
- Aya Osama,
- Debasmita Mukhopadhyay,
- Fatima Abdul,
- Fatima Sulaiman,
- Stafny Dsouza,

- Published: May 28, 2024
- https://doi.org/10.1371/journal.pone.0304036
- Reader Comments
Attempts to subtype, type 2 diabetes (T2D) have mostly focused on newly diagnosed European patients. In this study, our aim was to subtype T2D in a non-white Emirati ethnic population with long-standing disease, using unsupervised soft clustering, based on etiological determinants.
The Auto Cluster model in the IBM SPSS Modeler was used to cluster data from 348 Emirati patients with long-standing T2D. Five predictor variables (fasting blood glucose (FBG), fasting serum insulin (FSI), body mass index (BMI), hemoglobin A1c (HbA1c) and age at diagnosis) were used to determine the appropriate number of clusters and their clinical characteristics. Multinomial logistic regression was used to validate clustering results.
Five clusters were identified; the first four matched Ahlqvist et al subgroups: severe insulin-resistant diabetes (SIRD), severe insulin-deficient diabetes (SIDD), mild age-related diabetes (MARD), mild obesity-related diabetes (MOD), and a fifth new subtype of mild early onset diabetes (MEOD). The Modeler algorithm allows for soft assignments, in which a data point can be assigned to multiple clusters with different probabilities. There were 151 patients (43%) with membership in cluster peaks with no overlap. The remaining 197 patients (57%) showed extensive overlap between clusters at the base of distributions.
Conclusions
Despite the complex picture of long-standing T2D with comorbidities and complications, our study demonstrates the feasibility of identifying subtypes and their underlying causes. While clustering provides valuable insights into the architecture of T2D subtypes, its application to individual patient management would remain limited due to overlapping characteristics. Therefore, integrating simplified, personalized metabolic profiles with clustering holds greater promise for guiding clinical decisions than subtyping alone.
Citation: Bayoumi R, Farooqi M, Alawadi F, Hassanein M, Osama A, Mukhopadhyay D, et al. (2024) Etiologies underlying subtypes of long-standing type 2 diabetes. PLoS ONE 19(5): e0304036. https://doi.org/10.1371/journal.pone.0304036
Editor: Yee Gary Ang, National Healthcare Group, SINGAPORE
Received: November 9, 2023; Accepted: May 5, 2024; Published: May 28, 2024
Copyright: © 2024 Bayoumi et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Anonymized, primary databases will be available on request. But all patients’ confidential information will not be shared.
Funding: This study was supported by an internal grant [MBRU-CM-RG2019-06] awarded on May 29, 2019, by the College of Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, UAE. Further support was obtained from Sandooq Al Watan, Grant Number: SWARD-F22-013 awarded on August 30, 2022. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: All authors declare that they do not have any financial support or relationships that might have posed conflict of interest in this study.
1 Introduction
Diabetes is a heterogenous disease [ 1 , 2 ], with well-defined categories such as type 1 diabetes (T1D), latent autoimmune diabetes in adults (LADA), and monogenic types. The remaining patients are pooled together under T2D. However, patients with T2D present with a wide spectrum of clinical symptoms, and a range of variables that have a direct impact on glucose homeostasis. Patients may develop T2D at an early age or late in life [ 3 ]. They may be lean, overweight, obese, or morbidly obese [ 4 – 6 ]. The disease may be characterized by failure of insulin secretion or insulin resistance or both; may progress either rapidly or slowly and may be mild or severe. It may lead to one or more complications with a variety of outcomes [ 2 ]. Consequently, the clinical paradigm of one-size-fits-all leads to management and treatment failures in many patients [ 7 ]. Thus, there is a need to subtype T2D into distinct, well-defined groups [ 8 ] to better understand the underlying mechanisms, treatment responses, and prognoses associated with the disease. Several studies have attempted to identify T2D subtypes in patients of white European origin using various approaches, such as statistical clustering algorithms, clinical characteristics, genetics, and biomarkers [ 9 – 17 ]. T2D clustering was also replicated in other ethnic groups [ 18 – 22 ]. In most of these studies, subtyping of T2D was based on newly diagnosed patients [ 9 – 17 ] with a few exceptions where the temporal stability of clusters was tested in patients with short-term disease [ 13 , 16 , 23 ]. Few studies have attempted T2D subtyping in long-standing disease [ 3 , 21 – 24 ] to avoid the different rates of disease progression and the impact of complications [ 3 , 25 – 29 ].
Most studies have also used unsupervised K-means hard clustering methods with definitive assignment of data points to single clusters and reported distinct subtypes [ 9 , 11 – 13 , 18 – 22 ]. However, some other studies employed unsupervised soft clustering methods with the likelihood of data points belonging to more than one cluster and reported T2D subtypes with considerable overlap [ 14 – 17 ]. In this study, we continue to investigate the heterogeneity of T2D by cluster analysis of Emirati Arab T2D patients with long-standing disease, using unsupervised soft clustering algorithms.
2.1 Study design
This retrospective, cross-sectional, non-interventional study was conducted at the Dubai Diabetes Centre and Dubai Hospital of Dubai Health, Dubai, UAE. Dubai Diabetes Centre is dedicated to the specialized care of patients with diabetes. Dubai Hospital is a specialty hospital equipped with 600 beds and provides surgical and medical facilities. Both follow the American Diabetes Association Standards of Medical Care for Diabetes [ 2 ].
This study was approved by the Dubai Scientific Research Ethics Committee of Dubai Health Authority. Approval No. DSREC-12/2019-05 was issued on January 23, 2020. Further IRB extensions were granted by DSREC on 28 th April 2021 and 10 th May 2022. Written informed consent was obtained from patients during the face-to-face interviews. All relevant clinical and laboratory data were obtained from the Dubai Health Information System “SALAMA”. Information gathered was anonymized to maintain patient privacy and confidentiality. Clinical management and treatment protocols, all laboratory methods, radiographic imaging, and data obtained from the “SALAMA” hospital information system adhered to relevant Dubai Health regulations and guidelines and conformed to the provisions of the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013).
2.2 Patients
We aimed to collect enough data to identify genuine underlying disease clusters and avoid creating random ones. We anticipated our analysis to yield 4–5 subgroups, each containing a minimum of 20–30 observations. This ensured sufficient data points to effectively define the characteristics of each cluster.
A cohort of 348 Emirati patients with T2D were recruited from a database of 620 patients who underwent random screening between January 24th, 2020 and December 31st, 2022, at the outpatient departments of the Dubai Diabetes Centre and Dubai Hospital. The selected patients had complete data for all clustering parameters. Patients were tested for GAD antibodies (ELISA Test Kit; Demeditec Diagnostics, GmbH, Germany) to exclude T1D and LADA. The selected patients ranged in age from 18 to 87 years and included 167 men and 181 women. They had an average T2D duration of 14 years and at least two co-morbidities or complications. Each patient had been on two or more medications (metformin, thiazolidines, SGLT2 inhibitors, and GLP-1 agonists) for a minimum of two years. Patients with conditions causing secondary diabetes were excluded. For each patient, the clinical and laboratory data were obtained from the SALAMA electronic health record system used by all health facilities affiliated to Dubai Health. The recorded medical history, comorbidities, and complications of the disease were confirmed through face-to-face interviews with the patients.
2.3 Statistics
2.3.1 cluster analysis..
IBM SPSS Modeler (IBM North America, New York, USA) was used for clustering analysis. The software provides several machine-learning algorithms that can be used for classification, regression, clustering, and anomaly detection. These algorithms are based on artificial neural networks and deep learning.
The Auto Cluster model in IBM SPSS Modeler was utilized in the exploratory phase to determine the optimal clustering solution for the dataset comprising 348 Emirati patients with long-standing T2D. Five T2D variables (FBG, FSI, BMI, HbA1c and age at diagnosis) were standardized and employed as predictors to identify the suitable number of clusters and their characteristics. To mitigate the influence of confounding factors, such as comorbidities and complications associated with the long-standing T2D phenotype, the predictor variables were limited to those five parameters that directly or indirectly influence the disease’s pathophysiology. FBG and FSI levels are two crucial etiological factors that directly reflect the underlying pathophysiology of T2D. We used them in the initial exploratory technique for grouping the data. Furthermore, FBG and FSI were used in the explanatory process to assess peripheral insulin resistance (HOMA-IR) and/or impaired insulin secretion (HOMA-B), that served as descriptors of the clusters, not as part of the clustering process itself.
The BMI is used as a predictor for T2D because it is strongly linked to insulin resistance, a key factor in T2D pathophysiology. While HbA1c isn’t strictly an etiological variable for T2D, it plays a pivotal role in its diagnosis, monitoring, and prognosis. It is a valuable tool for providing long-term insights into glycemic control and the risk of developing long-term complications. Age at diagnosis of T2D reflects the cumulative effect on metabolic dysfunction and the duration of risk factors for complications. Early-onset T2D is associated with a more aggressive course and higher risk of complications, while late-onset disease is usually more benign.
The Auto Cluster model operates as a Bayesian Network Model for classification purposes. It sequentially employs three unsupervised soft clustering algorithms:
- A two-steps process: The initial step involves a single pass through the data to condense the raw input into a manageable set of subclusters. Subsequently, a hierarchical clustering method is utilized in the second step to progressively merge these subclusters into larger clusters. The two-step approach offers the advantage of automatically estimating the optimal number of clusters.
- The K-means clustering algorithm: This method defines a fixed number of clusters and iteratively assigns records to clusters while adjusting the cluster centers until further refinement does not enhance the model. Unlike predictive modelling, k-means employs unsupervised learning to uncover patterns within the input fields.
- The Kohonen algorithm: This generates a neural network capable of clustering the dataset into distinct groups. Once fully trained, similar records should be closed together on the output map, while dissimilar records will be positioned farther apart. This process also aids in determining an appropriate number of clusters.
Following sufficient iteration for each model, the Auto Cluster will produce a Silhouette index, with the model exhibiting the highest index being selected. The Auto Cluster node prioritizes algorithms and allocates data points into the relevant clusters accordingly. For both the two-steps and the K-means algorithms the same Silhouette Index of 0.64 was generated.
The Bayesian network assigns probabilities of membership to the participants in the five identified clusters. Each participant is represented as a node in the network by predictor variables and becomes an additional node that influences the main cluster assignment node. Conditional probability distributions model probabilistic dependencies, allowing computation of the likelihood of a participant belonging to a specific cluster, given their observed variables. Conditional probability distributions enable accurate inferences and yield probabilities of membership for each participant in one or more clusters. Therefore, the model computes the overlap of an individual within multiple clusters, as displayed in a heatmap [ S1 Table ].
The model also assigns membership and measures the degree of overlap between clusters using the silhouette coefficient. A high silhouette coefficient indicates that the data point is well-matched to its own cluster and poorly matched to neighboring clusters, with less overlap between the clusters. The silhouette coefficient ranges from -1 to 1. A value of 1 indicates that the data point fits perfectly into a single cluster, while a value of -1 indicates that the data point does not fit into any cluster. A value of 0 indicates that the data point is equally suited for two or more clusters. To highlight the clinical characteristics of clusters, data for individuals with a silhouette coefficient of 1.0, and/or probability of 1.0, on the Bayesian Network were selected, as they sat in the non-overlapping apices of clusters. They exhibited the highest degree of dysfunction in the etiological processes governing cluster membership. As one lowers the silhouette coefficient values in a sliding scale below 1.0, the degree of overlap decreases and the number of individuals in the non-overlapping apices of clusters increases but their clinical homogeneity and discreetness drops.
Principal component analysis was used to identify the linear combinations of the original variables that explained most of the variance in the data and to extract the features that were most correlated with the clustering variables. Principal component analysis has also been used to visualize the dataset and help in identifying clusters, as it transforms the dataset into a lower-dimensional space where the clusters are more easily separated.
2.3.2 Multinomial logistic regression.
Multinomial logistic regression in SPSS 29 was used in the explanatory phase of the study to validate the results of clustering performed by the Auto Cluster model in IBM SPSS Modeler and predict the probability of categorical dependent variables (Clusters 1–5), given a set of the five independent predictor variables (FBG, FSI, BMI, HbA1c, and age at diagnosis). The model was refined using a maximum likelihood procedure to determine the values of the model parameters that maximized the likelihood of the observed data. The relationship between the predictors and category of the dependent variable was modelled using the log-odds of each category relative to a reference category (Cluster 5). The outcome of the multinomial logistic regression model was a set of regression coefficients (B) for each predictor variable. The coefficients were then used to rank the importance of the predictors in each cluster. The odds ratio (OR) is a measure of the association between a predictor variable and a cluster, calculated by exponentiating the B value. The larger the B value, the stronger the association. An OR > 1 indicated that the predictor variable was associated with an increased risk of the outcome falling into a particular cluster relative to the reference category (Cluster 5).
2.3.3 HOMA assessment.
The higher the HOMA-IR, the greater the peripheral resistance to insulin, while the lower the HOMA-B, the greater the β-cell dysfunction. Generally, a HOMA-IR value < 1 indicates optimal insulin sensitivity. Levels above 1.9 indicate early resistance; levels above 2.9 indicate significant resistance. A HOMA-B value < 100 indicates β-cell dysfunction.
3.1 Demographics
The mean age of the 348 Emirati patients with T2D was 56 years, and the mean duration of diabetes was 14 years. The mean BMI was 31 and the mean age at diagnosis was 42 years. Gender-wise demographic characteristics are shown in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0304036.t001
Owing to the long duration and chronicity of T2D, considerable deterioration in the metabolic profiles of selected patients was observed. Of all patients, 90 (26%) had HOMA-IR > 3.0, indicating peripheral insulin resistance, while 140 (40%) had HOMA-B < 100, indicating pancreatic secretion dysfunction. The remaining 118 (34%) exhibited both pathophysiological dysfunctions. The prevalence of comorbidities and complications observed were also high, with hypertension at 62%, peripheral neuropathy at 53%, retinopathy at 33%, and coronary artery disease at 15% ( Table 2 ). In most patients, at least two comorbidities or complications of diabetes were observed.
https://doi.org/10.1371/journal.pone.0304036.t002
3.2 Cluster analysis
Results of the cluster analysis of the cohort of 348 Emirati patients with T2D with long-standing disease, are shown in Table 3 . No significant differences in cluster results were observed between male and female T2D patients. Therefore, results were reported for the total cohort throughout the manuscript. Five Clusters were identified in this study. The first four matched Ahlqvist et al [ 11 ] subgroups. Cluster 1 had severe insulin-resistant diabetes (SIRD) in 8% of patients. Cluster 2 had severe insulin deficient diabetes (SIDD) in 16%. Cluster 3 had mild age-related diabetes (MARD) in 25%. Cluster 4 had mild obesity-related diabetes (MOD) in 21%. A fifth new subtype of mild early onset diabetes (MEOD) was identified in 30% of mostly lean patients.
https://doi.org/10.1371/journal.pone.0304036.t003
However, there was extensive overlap between clusters. Cluster 1 (SIRD), with a positive average silhouette score, did not significantly overlap with any of the other clusters. The other four clusters, with negative average silhouette scores, seemed to overlap extensively. There were 151 patients (43%) with membership in cluster peaks with no overlap, as confirmed by a Silhouette Index and Bayesian probability of 1.0 ( Table 3 ). The remaining 197 patients (57%) showed extensive overlap between clusters confirmed by a Silhouette Index and Bayesian probability of <1.0 ( S1 Table ) with individuals appearing in two or more clusters ( Fig 1 ).
https://doi.org/10.1371/journal.pone.0304036.g001
Principal component analysis (PCA) was used to visualize the dataset and identify the five T2D clusters, as it transformed the dataset into a lower-dimensional space where the clusters were more easily separated ( Fig 2 ). Multinomial logistic regression was used to explain the relationship between predictor variables and categorical outcomes (clusters) and validate clustering results. We identified predictor variables that were significantly associated with the clusters and quantified the strength of these associations. The higher the regression coefficients (B) and the odds ratio (OR), the stronger the contribution to the cluster ( Table 4 ). The model coefficients ranked the importance of the predictor variables in each cluster [ S2 Table ].
The colors represent each cluster as light blue (Cluster 1- SIRD), red (Cluster 2- SIDD), dark blue (Cluster 3- MARD), green (Cluster 4- MOD), and yellow (Cluster 5- MEOD).
https://doi.org/10.1371/journal.pone.0304036.g002
https://doi.org/10.1371/journal.pone.0304036.t004
3.3 Cluster characteristics
The pathophysiological characteristics, and laboratory data of the five clusters identified in the cohort of 348 Emirati patients with long-standing T2D is shown in Table 5 . Characteristics of 4 clusters matched that of Ahlqvist et al [ 11 ] subgroups. Cluster 5 patients had a novel subtype of mild early-onset diabetes (MEOD) in mostly lean patients.
https://doi.org/10.1371/journal.pone.0304036.t005
3.4 Etiological processes governing T2D subtypes
To highlight the major etiological processes governing membership of subtypes, we selected data of patients at the non-overlapping apices of cluster distributions (N = 151), confirmed by a Silhouette Index ≥ 1.0 ( Table 6 ).
https://doi.org/10.1371/journal.pone.0304036.t006
In Cluster 1 (SIRD), the primary dysfunction was a markedly increased insulin resistance associated with moderate obesity. The patients had a normal insulin secretory capacity and moderately abnormal glucose homeostasis. Most of the patients had peripheral neuropathy ( Table 7 ).
https://doi.org/10.1371/journal.pone.0304036.t007
In Cluster 2 (SIDD), the primary dysfunction was severe insulin secretory deficiency accompanied by high insulin resistance and the highest level of HbA1c. Patients were obese, with the most severe uncontrolled glucose homeostasis and a higher frequency of complications such as retinopathy, peripheral neuropathy, and ischemic heart disease ( Table 7 ).
Cluster 3 (MARD) patients developed diabetes late in life and had the highest mean age at diagnosis. They were overweight and characterized by moderate insulin resistance, normal insulin secretory capacity, and mildly abnormal glucose homeostasis. However, these patients also had nephropathy, peripheral neuropathy, and ischemic heart disease ( Table 7 ).
Patients in Cluster 4 (MOD) had the highest BMI and developed diabetes early in life. They were characterized by moderate insulin resistance but normal insulin secretory capacity, with mildly abnormal glucose homeostasis. However, these patients also had retinopathy and nephropathy ( Table 7 ).
In Cluster 5 (MEOD), a novel T2D subtype, the patients were lean/overweight and developed the disease early in life. They had moderate insulin secretory dysfunction and mild insulin resistance with mildly abnormal glucose homeostasis ( Table 5 ). These patients had retinopathy, peripheral neuropathy, and ischemic heart disease ( Table 7 ).
4 Discussion
We attempted subtyping T2D in 348 Emirati patients using unsupervised soft cluster analysis by Auto Cluster IBM Modeler in the SPSS software, employing five etiological predictor variables: FBG, FSI, BMI, HbA1c and age at diagnosis. Multinomial logistic regression was used to validate the clustering process and to rank the importance of the predictor variables in each cluster. Five clusters were identified; the first four matched Ahlqvist et al [ 11 ] subgroups: SIRD, SIDD, MARD, and MOD. A fifth new subtype MEOD was identified in our dataset.
However, there was extensive overlap between clusters. Individuals in the non-overlapping apices of distribution of clusters were identified in only 151/348 patients (43%), with individuals appearing only once in a single cluster. The remaining 197/348 patients (57%) showed varying degrees of overlap, with individuals appearing in two or more clusters. As one lowers the silhouette coefficient values in a sliding scale below 1.0, the degree of overlap decreases and the number of individuals in the non-overlapping apices of clusters increases but their clinical homogeneity and discreetness drops. This extensive degree of overlap has been previously reported by different study groups: the Broad Institute of MIT [ 14 , 17 ]; the Oxford Center of Diabetes, UK [ 15 ] and the Exeter Research Group, UK [ 16 ].
Ahlqvist et al. [ 11 ] employed a data-driven, unsupervised hard clustering method to identify mutually exclusive patient subgroups within large, newly diagnosed T2D cohorts. Their subtyping scheme, although replicated in multiple studies [ 9 – 13 , 18 – 24 ]; including our current investigation, has been challenged by soft, unsupervised clustering techniques that revealed overlapping and alternative subgroupings [ 14 – 17 ]. Both approaches rely on continuous (non-discrete) clinical characteristics. Unlike discrete data with distinct categories, continuous data exists on a spectrum, hindering the definition of clear-cut cluster boundaries. Overlapping clusters inherently arise with such data, challenging the traditional concept of distinct, well-separated patient groups. Fuzzy boundaries further complicate cluster interpretation and labeling [ 14 – 17 ]. Hard unsupervised methods like Ahlqvist’s, rely on pre-defined subtypes, potentially overlooking unseen biological variations or dynamic processes. Conversely, soft unsupervised clustering avoids preconceived notions, potentially uncovering the true underlying data structure and heterogeneity. But, overlapping clusters, as observed in healthcare domains, can impede clinical decision-making due to ambiguous patient group assignment [ 31 – 33 ].
Previously, most T2D subtyping studies recruited newly diagnosed patients [ 9 – 17 ]. In contrast, in the present study, we tested the feasibility of clinical subtyping in T2D patients with long standing disease. The mean age of the patients was 56 years with mean diabetes duration exceeding 14 years. They were mostly obese, had various premorbid conditions, and had developed various complications of diabetes. In all five subtypes, the combination of the basic etiological dysfunction could still be identified despite co-morbidities and complications of the disease with advancing age. Our results agree with several studies where subtyping of T2D in long-standing disease have been successfully performed [ 3 , 21 – 23 , 26 ]. Despite temporal changes in lifestyle and environmental exposure causing decline in β-cell function and/or worsening of insulin resistance with increased frequency of complications, subtyping of long standing T2D is not obscured [ 21 , 22 , 24 – 26 ]. This is probably due to genetically determined factors that do not change over a lifetime.
To highlight the major etiological processes governing T2D subtypes, individuals in the non-overlapping apices of the cluster distribution (151/348) were selected to identify the major etiological determinants of a subtype. The four T2D subtypes, SIRD, SIDD, MARD, and MOD, which were identified in this cohort with long-standing disease, were mapped back to the four subtypes of newly diagnosed diabetes patients by Ahlqvist et al [ 11 ] in the Scania (ANDIS) study. Patients with SIRD and SIDD suffered severe abnormal glucose homeostasis, whereas patients with MARD and MOD had mild disease. The fifth type is a novel subtype of mild early onset T2D (MEOD) in mostly lean individuals.
In patients with SIRD (Cluster 1), the identified etiological dysfunction was severe peripheral insulin resistance. This is similar to the SIRD in the ANDIS study [ 11 ] and Group C in the IMI DIRECT study [ 15 ]. In patients with SIDD (Cluster 2), the identified etiological dysfunction was severe β-cell dysfunction, heightened by moderate/severe insulin resistance [ 29 ]. This subtype is similar to the SIDD described in the ANDIS Study (11) and the global archetype D, which had the worst glucose control, in the IMI-DIRECT study (15). In previous studies some patients with early-onset T2D had worse clinical outcomes and are at higher risk of stroke and myocardial infarction [ 34 ]. Patients with SIDD had early-onset and displayed characteristics of severe diabetes. Interestingly, the average age of onset for this subgroup (37.9 years) was comparable to the mild early-onset diabetes (MEOD) subgroup (36.5 years). However, the MEOD subgroup exhibited a distinctly milder clinical profile compared to the SIDD subgroup.
In patients with MARD (Cluster 3), the identified etiological dysfunction appeared to be mild peripheral resistance to insulin owing to advancing age. This subtype is similar to the MARD described in the ANDIS Study [ 11 ] and archetype A described in the IMI-DIRECT study [ 15 ]. In patients with MOD (Cluster 4), the identified etiological dysfunction was an obesity-driven peripheral resistance to insulin. This subtype is similar to the MOD described in the ANDIS Study [ 11 ] and archetype C described in the IMI-DIRECT study [ 15 ]. MEOD (Cluster 5) is a novel subtype that has not been previously reported in earlier studies. The patients were mostly lean, had early onset disease, mild/moderate β-cell dysfunction, and mild insulin resistance. This subtype of T2D has been previously identified in non-Caucasian ethnic groups in developing countries [ 35 – 37 ]. It is not surprising, therefore, that this cluster was identified among the Emiratis.
In summary, only the severe SIRD subtype appeared to be an independent disease entity. The statistical properties and clinical characteristics of the patients are distinct. Membership of most patients is restricted to this subtype and does not overlap with that of other subtypes. The next highest probability of being a distinct entity is the severe SIDD subtype. The other three mild subtypes, MARD, MORD, and MEOD did not qualify as independent disease entities. They exhibited an extensive overlap in subtype membership and high heterogeneity in their clinical characteristics.
The main aim of clustering is to identify patient subtypes with similar characteristics within a larger group of individuals with T2D, to enable clinicians to gain insights into the mechanisms of disease development and progression. This can potentially lead to personalized clinical management and improved patient outcomes. However, in our study, as in some other subtyping studies, it has been recognized that clustering based on continuous variables does not result in mutually exclusive subtypes [ 14 – 17 , 32 ]. Therefore, integrating simplified, personalized metabolic profiles with clustering holds greater promise for guiding clinical decisions than subtyping alone [ 8 , 32 ]. As per our results, the T2D specific phenotype profile: age at diagnosis, BMI, FBG, HbA1c, HOMA-B, and HOMA-IR could predict specific outcome for individual patients:
- Age at T2D diagnosis: Young age indicates a strong genetic predisposition. The younger the age at diagnosis, the more severe the disease and the higher the risk of complications. The older the age at diagnosis, the milder the disease [ 3 ].
- BMI: The higher the BMI, the higher the peripheral resistance to insulin, the more severe the disease, and the higher the risk of complications [ 38 ].
- FBG: The higher the Impaired Fasting Glucose level, the higher the hepatic insulin resistance and hepatic glucose production [ 1 , 39 – 42 ].
- HbA1c: The higher the HbA1c, the greater the disease severity (2).
- HOMA-B: The lower the HOMA-B score, the more severe the β-cell dysfunction [ 30 ].
- HOMA-IR: The higher the HOMA-IR, the higher the whole-body peripheral resistance to insulin [ 30 ].
Our study has some limitations. We used FBG and FSI in the exploratory phase where cluster analysis was performed and HOMA indices in the explanatory phase where cluster outcomes and characteristics were identified. We acknowledge the presence of moderate collinearity between the HOMA indices used in the explanatory phase. This can lead to difficulty in separating the true effect of insulin resistance from the effect of insulin secretion. To mitigate these effects, we used principal component analysis introducing new uncorrelated variables from the original set. It is also important to note that the computer models generating these indices incorporate additional parameters such as glucagon secretion and liver glucose production. Furthermore, these indices continue to be used in diabetes research for the lack of perfect alternatives. We used them only for broader trends and cluster identification and not for precise rigorous measurements.
We also used FBG and FSI in the exploratory phase of analysis which is less concerned with individual variable effects. It focuses on pattern identification and data relationships without trying to isolate the impact of specific variables on an outcome. They are about finding the underlying structure, not establishing causal links. It does not suffer from collinearity of the variables used. Therefore, while the same parameters were used in both exploratory and explanatory techniques, collinearity is only a concern within the explanatory models and not between the two phases of analysis.
The strength of this study is in confirming that T2D subtyping can be performed at any stage of the disease. This provides insight into the stability and evolution of clusters. Although the number of patients is small, the study provided proof-of-principle that soft, unsupervised clustering techniques reveal overlapping subgroupings of T2D and uncover further aspects of heterogeneity of T2D [ 43 ]. Because this was a retrospective study, we relied on existing data collected from medical records and patient interviews, leading to a potential recall bias or missing information. The small number of participants, broad inclusion criteria, and potential bias in data selection may limit the generalizability of the findings. The long duration of illness and unmeasured or unknown confounders, such as diabetes complications and drug responses, make it difficult to establish a clear temporal relationship between exposure and outcome. Yet, despite all that noise, clusters of T2D could be identified.
5 Conclusions
Despite the complex picture of long-standing T2D with comorbidities, complications and varied therapy, our study demonstrates the feasibility of identifying subtypes and their underlying causes. Five clusters were identified: the first four matched Ahlqvist et al [ 11 ] subgroups. Two subtypes were characterized by severe disease and two by mild disease. A fifth novel subtype, identified among mostly lean individuals is usually seen in non-white populations. While clustering provides valuable insights into the architecture of T2D subtypes, its application to individual patient management would remain limited due to overlapping characteristics. Therefore, integrating simplified, personalized metabolic profiles with clustering holds greater promise for guiding clinical decisions than subtyping alone. Future studies on the pathogenesis of subtypes and the prognosis of drug therapy are needed. Further longitudinal investigations are also required to clarify subtype stability over time, elucidate the factors influencing transitions between subtypes, and translate these findings into concrete clinical applications.
Supporting information
S1 checklist. human participants research checklist..
https://doi.org/10.1371/journal.pone.0304036.s001
S1 Table. Heat map of probabilities of cluster membership showing overlap between clusters.
A Silhouette Index of 1.0 indicates no overlap and <1.0 indicates overlap between clusters.
https://doi.org/10.1371/journal.pone.0304036.s002
S2 Table. The contribution of the five primary independent variables (Age at diagnosis, BMI, fasting insulin, Fasting Blood Glucose (FBG) and HbA1c) as predictors for T2D clusters using multinomial logistic regression.
https://doi.org/10.1371/journal.pone.0304036.s003
S1 File. SPSS_T2D_Database-Bayoumi.
https://doi.org/10.1371/journal.pone.0304036.s004
Acknowledgments
We are indebted to the Mohammed Bin Rashid University of Medicine and Health Sciences for their support of our research and to Dubai Academic Health Corporation for granting access to patients and their records. The contributions of the medical and nursing staff at Dubai Diabetes Centre and Dubai Hospital are highly appreciated.
- View Article
- PubMed/NCBI
- Google Scholar

IMAGES
VIDEO
COMMENTS
1. Target a minimal reduction in body weight of at least 5%-10% of initial body weight over a 3-6 month period. 2. Incorporate opportunities to enhance communication between healthcare professionals, dietitians, and exercise professionals and people with overweight and obesity following the initial weight-loss periods. 3.
a sweetener derived from corn through a mechanical process; the sweetener is blamed, in part, for the increasing weight of people in the United States. obesogenic environment. an environment that, by design, makes us fat; there is typically little physical activity and a plentiful assortment of high-calorie, high-fat, and high-sodium foods.
overweight. has extra body weight that is contributed by bone, muscle, body fat and/or water. - so, overweight can be all muscle. obesity. - excessive body fat. Prevalence in the US. - 70% of adults over the age of 20 were overweight or obese 2013-2014. - 1/3 are overweight. - more than 1/3 are obese.
Study with Quizlet and memorize flashcards containing terms like Obesity is the second leading cause of preventable _____ in the United States., Which of the following defines obesogenic environment?, Scientists now think high-fructose corn syrup may disrupt appetite control, making people _____ more often. and more.
Study with Quizlet and memorize flashcards containing terms like Fat cells develop by increasing in number and size. 9.1 Overweight and Obesity, Preventing obesity depends on maintaining a reasonable number of fat cells., The body regulates its body weight and defends it set point in a complex system that detects signals, integrates information, influences eating behavior, and adjusts energy ...
1. leptin protein. 2. ghrelin. 3. uncoupling proteins. 4. adiponectin. produced in fat cells, acts on the hypothalamus. -suppresses appetite and increases energy expenditure. -"satiety hormone". -obese people have increased levels of leptin. -cells may just not recognize it.
We have an expert-written solution to this problem! Metabolic syndrome is a cluster of symptoms that are predictive of CVD and diabetes risk. Which of the following factors is NOT among the risk cluster of symptoms? high blood HDL. Nutrition and Chronic Disease Learn with flashcards, games, and more — for free.
A lack of sleep increases it and decreases the satiety hormone leptin, therefore explaining the association between lack of sleep and overweight. Uncoupling proteins. Influence basal metabolic rate (BMR) & oppose the development of obesity. Cause of Overweight & Obesity: Overeating. -Abundance of high calorie, high-fat foods that are readily ...
What are the leading causes of overweight and obesity. -Excess energy intake. -Physical inactivity. What are some problems of being underweight. -Minimal body fat stores. -At a disadvantage in situations where energy reserves are needed. -May experience menstrual irregularity, infertility, and osteoporosis.
c. they are resistant to leptin. The effect of lipoprotein lipase (LPL) with respect to fat cell metabolism: a. is triggered by weight gain. b. explains why people who experience weight loss are more likely to gain weight. c. is responsible for the rate of fat breakdown being lower in men than women. d.
Obesity is defined as a body mass index (BMI) that exceeds 30 kg/m2 in adults and a BMI greater than or equal to the age- and sex-specific 95th percentile of the 2000 Centers for Disease Control and Prevention growth charts in children. Three leading causes of death in the United States are associated with obesity: cardiovascular disease, type ...
Worldwide adult obesity has more than doubled since 1990, and adolescent obesity has quadrupled. In 2022, 2.5 billion adults (18 years and older) were overweight. Of these, 890 million were living with obesity. In 2022, 43% of adults aged 18 years and over were overweight and 16% were living with obesity. In 2022, 37 million children under the ...
Being overweight or obese can have a serious impact on health. Carrying extra fat leads to serious health consequences such as cardiovascular disease (mainly heart disease and stroke), type 2 diabetes, musculoskeletal disorders like osteoarthritis, and some cancers (endometrial, breast and colon). These conditions cause premature death and ...
Key Takeaways. Overweight and obesity increase the risk for certain health problems including heart disease, Type 2 diabetes, high blood pressure, sleep apnea, certain cancers, and osteoarthritis. Being underweight is linked to nutritional deficiencies, delayed wound healing, hormonal abnormalities, increased susceptibility to infection, and ...
Genetic Influences. Obesity is a complex multifactorial chronic disease developing from interactive influences of numerous factors—social, behavioral, physiological, metabolic, cellular, and molecular. Genetic influences are difficult to explain and identification of the genes is not easily achieved through studies.
Figure \(\PageIndex{1}\). Obesity Rates. The high prevalence of overweight and obesity across the population is of concern because individuals who are overweight obese, compared to those with a normal or healthy weight, are at increased risk for many serious diseases and health conditions, including the following: All-causes of death (mortality)
Obesity is a chronic, multifactorial, relapsing disorder characterized by excess body weight and defined as a body mass index (BMI) of ≥ 30 kg/m2. Complications include cardiovascular disorders (particularly in people with excess abdominal fat), diabetes mellitus, certain cancers, cholelithiasis, metabolic dysfunction-associated steatotic ...
Obesity is a common cause of sleep apnea in adults. 18 If you have overweight or obesity, you may have more fat stored around your neck, making the airway smaller. A smaller airway can make breathing difficult or cause snoring. If you have overweight or obesity, losing weight may help reduce sleep apnea or make it go away. Asthma
Obesity is a multifactorial disease with a complex pathogenesis related to biological, 1 psychosocial, 2 socioeconomic, 3 and environmental 4,5 factors and heterogeneity in the pathways and mechanisms by which it leads to adverse health outcomes. 6-8 The "2013 AHA [American Heart Association]/ACC [American College of Cardiology]/TOS [The Obesity Society] Guideline for the Management of ...
1560 Wilson Blvd Suite 1000. Arlington, VA 22209-2442 US. +1 800-843-8114. Back to top. This resource provides information into the causes of weight gain, overweight, and obesity, and how said causes are linked to cancer risk.
Overweight women have a higher incidence of menstrual dysfunction and anovulation. Overweight and obese women are at a high risk for reproductive health. The risk of subfecundity and infertility, conception rates, miscarriage rates, and pregnancy complications are increased in these women. They have poor reproductive outcomes in natural as well ...
Causes of obesity and overweight - 7% Discount - For Reorder. Drugs made in Germany - Quality certificates, guarantee of the client's health We are Online 24*7 - The best service from the best Online pharmacy ... causes and effects of obesity essay 500 words; hill's metabolic weight loss and maintenance; Coy's Pizza Shop diabetes mellitus ...
Overweight and obesity (body mass index [BMI] 25-29.9 and ≥ 30, respectively), are global problems with increasing prevalence in most countries. 1 Excess adiposity is related to a considerable increase in morbidity 2 - 4 and premature mortality. 5, 6 The natural history of weight changes in adults has not been well studied, but data were collected on Canadian adults and analyzed for ...
This two-center, open-label, three-arm, parallel-group, randomized controlled trial recruited 326 participants with overweight/obesity and type 2 diabetes and randomized them into 12 weeks of diet intervention (n = 109), exercise intervention (n = 108), or lifestyle education (control) (n = 109).The primary outcome was the change of glycemic control measured as glycated hemoglobin (HbA 1c ...
In 1727 writer Thomas Short observed that overweight people often lived near swamps. He published a treatise entitled The Causes and Effects of Corpulence, outlining that the only logical way to ...
In both developed and developing countries, childhood obesity remains a major public health challenge in the 21st century. 1,2 The exact causes of childhood obesity are unclear but are believed to involve genetics, physical inactivity, unhealthy eating habits, and psychological factors. 3 In children and adolescents, obesity-related insulin ...
The purpose of our study is to further understanding of the depression symptoms of HIV/AIDS patients in Guilin, Guangxi via exploring whether there is a mediating effect of sleep quality on medical-social support and depression symptoms and therefore provide a theoretical basis for application of medical-social support to alleviate depression symptoms of HIV/AIDS patients.
Background Attempts to subtype, type 2 diabetes (T2D) have mostly focused on newly diagnosed European patients. In this study, our aim was to subtype T2D in a non-white Emirati ethnic population with long-standing disease, using unsupervised soft clustering, based on etiological determinants. Methods The Auto Cluster model in the IBM SPSS Modeler was used to cluster data from 348 Emirati ...
To investigate whether supplementation with iodine-reduced kelp (Laminaria japonica) powder decreases body fat composition in overweight Japanese subjects, a randomized, double-blind, placebo-controlled intervention study was conducted in 50 Japanese subjects with body mass index (BMI) ≥25 and <30 kg/m2. Subjects were randomly assigned to consume thirty tablets/d (10 tablets orally, 3 times ...
We examined the prevalence of obesity in two types of schools—a comprehensive school and a grammar school—in a rural German region of Brandenburg. Methods: In a cross-sectional study, BMI values were measured in 114 students in grades 5, 7, and 10. In addition to the demographic data, data on nutrition, physical activity, and mental well-being were collected using a questionnaire. Results ...