
Move fast, think slow: How financial services can strike a balance with GenAI

Take on Tomorrow @ the World Economic Forum in Davos: Energy demand

Perspectives from the Global Entertainment & Media Outlook 2024–2028

Climate risk, resilience and adaptation

Business transformation

Sustainability assurance

The Leadership Agenda

Global Workforce Hopes and Fears Survey 2024

S+b digital issue: Generative AI: The 21st-century power play

The New Equation

PwC’s Global Annual Review

Committing to Net Zero

The Solvers Challenge
Loading Results
No Match Found

Case studies
Demonstrating our purpose in our work.
PwC's purpose is to "build trust in society and solve important problems." Our Partners and staff demonstrate a commitment to this purpose every day in the work we do with our Health Services clients. We do so because of a deep and passionate recognition of the importance of health to society - because health matters. The following case studies are an example of just a few engagements that show our strong desire to make a difference.
Working with clients to make an impact
We work side by side with health organizations and community residents, to improve health and wellness. The stories featured here illustrate the importance of working together to solve the complex health challenges we face. When we collaborate, our strengths are amplified. See how we are working together to solve complex health challenges.
{{filterContent.facetedTitle}}
{{item.publishDate}}
{{item.title}}
{{item.text}}

Ron Chopoorian
US Deals Leader, Partner, PwC United States
© 2017 - 2024 PwC. All rights reserved. PwC refers to the PwC network and/or one or more of its member firms, each of which is a separate legal entity. Please see www.pwc.com/structure for further details.
- Legal notices
- Cookie policy
- Legal disclaimer
- Terms and conditions
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
How Digital Transformation Can Improve Hospitals’ Operational Decisions
- Song-Hee Kim

It can help with patient flow, staffing, scheduling, and supply-chain management.
The use of digital technologies in clinical decision-making has received the most attention. But they also have the potential to help hospitals make better decisions in many areas of operations. Research and hospitals’ experiences show that they can make a big difference in such areas as the management of the patient flow, staffing, scheduling, and the supply chain. The result can be improvements in the quality and efficiency of care and patients’ access to it.
Many companies are interested in digital transformation — using digital technologies to create or modify business processes, culture, and customer experiences — to grow and stay ahead of the competition, and hospitals are no exception.
- Song-Hee Kim is an associate professor of operations management at the SNU Business School at Seoul National University. Her research focuses on data-driven decision-making within health care systems, especially how to design human-algorithm interactions to improve quality, efficiency, and access to care in hospitals.
- Hummy Song is an assistant professor of operations, information, and decisions at the University of Pennsylvania’s Wharton School. Her research focuses on how operations can be designed to help health care providers work more efficiently and effectively.
Partner Center
Explore our case studies to gain insight into the latest healthcare technology trends, guidance, and perspectives from prominent industry experts.

Clinical Research as a Care Option with Clinical Trials Access Network
Learn how a provider community primary care group was able to offer the latest treatment options and diagnostics by using Clinical Trials Access Network.
Explore All Case Studies

Case Study: Goshen Health transforms patient experiences and revenue cycle
Learn how adding patient engagement solutions to their patient access suite helped Goshen Health with staffing, patient experience, and cash collections.

Self-Scheduling Boosts Access and Reduces Staff Burden
Learn how ProHealth Physicians used self-guided online scheduling to ease administrative burden and rebound patient volume after COVID-19.

Health system boosts reach with payer channel scheduling
St. Luke’s Health dramatically increased volumes and decreased costly no shows with Optum® Digital Scheduling. Learn how you can, too.

Cardiology IT Solutions Solve Workflow Issues
Learn how Change Healthcare Cardiology’s IT solutions helped one medical center develop faster workflows, turnaround time, and more.

Helping an Emergency Services Practice Streamline Accounting
Learn more about Change Healthcare’s physician management services.

Helping a Medicare Payer That Had Failed CMS Audits
Change Healthcare Consulting helped a midsize payer modernize and automate its care management system and pass CMS audits.

A Midsized Plan Achieved HEDIS Certification and NCQA Accreditation with Help From Change Healthcare Consulting
Change Healthcare Consulting helped a fast-growing plan build its HEDIS program. It completed its HEDIS audit on time and helped the plan with NCQA accreditation.

Anesthesiology Group Improves Thanks to RCM for Physician Practices
Learn how an anesthesiology group increased profitability, efficiency, and stability thanks to Change Healthcare RCM for physician practices.

Replacing a Core Administrative Processing Solution (CAPS)
Learn how Change Healthcare Consulting helped a regional health plan implement an enterprise architecture to reduce complexity and improve user productivity.

EHR Selection and Procurement Case Study
Discover how a medical provider engaged Change Healthcare consultants to oversee the selection and procurement process for a new electronic health record (EHR) system.

Coordination of Benefits Services Help Health Plan
Discover how a regional carrier generated 250%+ ROI and increased yearly collections by $500,000 with comprehensive coordination of benefits (COB) solutions.
- Research article
- Open access
- Published: 14 November 2019
Organisational change in hospitals: a qualitative case-study of staff perspectives
- Chiara Pomare ORCID: orcid.org/0000-0002-9118-7207 1 ,
- Kate Churruca 1 ,
- Janet C. Long 1 ,
- Louise A. Ellis 1 &
- Jeffrey Braithwaite 1
BMC Health Services Research volume 19 , Article number: 840 ( 2019 ) Cite this article
44k Accesses
22 Citations
8 Altmetric
Metrics details
Organisational change in health systems is common. Success is often tied to the actors involved, including their awareness of the change, personal engagement and ownership of it. In many health systems, one of the most common changes we are witnessing is the redevelopment of long-standing hospitals. However, we know little about how hospital staff understand and experience such potentially far-reaching organisational change. The purpose of this study is to explore the understanding and experiences of hospital staff in the early stages of organisational change, using a hospital redevelopment in Sydney, Australia as a case study.
Semi-structured interviews were conducted with 46 clinical and non-clinical staff working at a large metropolitan hospital. Hospital staff were moving into a new building, not moving, or had moved into a different building two years prior. Questions asked staff about their level of awareness of the upcoming redevelopment and their experiences in the early stage of this change. Qualitative data were analysed using thematic analysis.
Some staff expressed apprehension and held negative expectations regarding the organisational change. Concerns included inadequate staffing and potential for collaboration breakdown due to new layout of workspaces. These fears were compounded by current experiences of feeling uninformed about the change, as well as feelings of being fatigued and under-staffed in the constantly changing hospital environment. Nevertheless, balancing this, many staff reported positive expectations regarding the benefits to patients of the change and the potential for staff to adapt in the face of this change.
Conclusions
The results of this study suggest that it is important to understand prospectively how actors involved make sense of organisational change, in order to potentially assuage concerns and alleviate negative expectations. Throughout the processes of organisational change, such as a hospital redevelopment, staff need to be engaged, adequately informed, trained, and to feel supported by management. The use of champions of varying professions and lead departments, may be useful to address concerns, adequately inform, and promote a sense of engagement among staff.
Peer Review reports
Change is a common experience in complex health care systems. Staff, patients and visitors come and go [ 1 ]; leadership, models of care, workforce and governing structures are reshaped in response to policy and legislative change [ 2 ], and new technologies and equipment are introduced or retired [ 3 ]. In addition to these common changes experienced throughout health care, the acute sector in many countries is constantly undergoing major changes to the physical hospital infrastructure [ 4 , 5 ]. In New South Wales, Australia, several reports have described the increase in hospital redevelopment projects as a ‘hospital building boom’ [ 4 , 6 ], with approximately 100 major health capital projects (i.e., projects over AUD$10 million) currently in train [ 7 ]. In addition to meeting the needs of a growing and ageing population [ 8 ], the re-design and refurbishment of older hospital infrastructure is supported by a range of arguments and anecdotal evidence highlighting the positive relationship between the hospital physical environment and patient [ 9 ] and staff outcomes [ 10 ]. While there are many reasons why hospital redevelopments are taking place, we know little about how hospital staff prospectively perceive change, and their experiences, expectations, and concerns. Hospital staff encapsulates any employee working in the hospital context. This includes clinical and non-clinical staff who provide care, support, cleaning, catering, managerial and administrative duties to patients and the broader community.
One reason as to why little research has explored the perspectives of hospital staff during a redevelopment may be because hospital redevelopment is often considered a physical, rather than organisational change. Organisational change means that not only the physical environment is altered, but also the behavioural operations, structural relationships and roles, and the hospital organisational culture may transform. For example, changing the physical health care environment can affect job satisfaction, stress, intention to leave [ 11 ], and the way staff work together [ 12 ].
Redeveloping a hospital can be both an exciting and challenging time for staff. In a recent notable example of opening a new hospital building in Australia, staff attitudes shifted from appreciation and excitement in the early stages of change to frustration and angst as the development progressed [ 13 ]. Similar experiences have been reported elsewhere, such as in a study describing the consequences for staff of hospital change in South Africa [ 14 ]. However, these examples explored staff attitudes towards change retrospectively and considered the change as a physical redevelopment, rather than organisational change. Such retrospective reports may be limited in validity [ 15 ] as prospective experiences and understanding of change reported by staff may be conflated with the final outcome of the change. The hospital redevelopment literature has also prospectively assessed health impacts of proposed redevelopment plans as a means to predetermine the impact of a large change on the population [ 16 ]; while prospective, this research again considers redevelopment as a physical modification, rather than an organisational change. Thus, while the literature has reported retrospective accounts of staff experiences in large hospital change and prospective assessment of the impact of the change, there is little research examining the understanding and experiences of staff in the early stages of redevelopmental change in hospitals through a lens of organisational change.
Seminal research in the organisational change literature highlights that the role of frontline workers (in this case hospital staff) is crucial to implementation of any process or change [ 17 , 18 ]. Specifically, that the support of actors (understanding, owning, and engaging) can determine the success of a change [ 19 ]. This is consistent with complexity science accounts which suggest that any improvement and transformation of health systems is dependent upon the actors involved, and the extent and quality of their interactions, their emergent behaviours, and localised responses [ 1 , 20 ]. In health care, change can be resisted when it is imposed on actors (in this case, hospital staff), but may be better accepted when people are involved and adopt a sense of ownership of the changes that will affect them [ 21 ]. This may include being involved in the design process. For this reason, it is important to examine the understanding and experiences of actors involved in a change (i.e., hospital staff in a redevelopment), in order to understand and potentially address their concerns, alleviating negative expectations prior to the change.
This study is part of a larger project exploring how hospital redevelopment influences the organisation, staff and patients involved [ 22 ]. The present study aimed to explore the understanding and experiences of staff prior to moving into a new building as one stage in a multidimensional organisational change project. The research questions were: How do staff make sense of this organisational change? How well informed do they feel? What are their expectations and concerns? What are the implications for hospitals undergoing organisational change, particularly redevelopment?
The study protocol has been published elsewhere [ 22 ]. The Consolidated criteria for reporting qualitative research (COREQ) guidelines were used to ensure comprehensive reporting of the qualitative study results (Additional file 1 ) [ 23 ] .
Study setting and participants
This study was conducted at a large metropolitan, publicly-funded hospital in Sydney, Australia. The facility is undergoing a multimillion-dollar development project to meet the growing needs of the community. This hospital has undergone a number of other changes over the last two decades, including incremental increases in size. Since its opening in the mid 1990s (with approximately 150 beds), several buildings have been added over the years. The hospital now has multiple buildings and over 500 beds.
During the time of this study, the hospital was in the second stage of the multi-stage redevelopment. This stage included: the opening of a new acute services building, the relocation of several wards to this new building (e.g., Intensive care unit (ICU) and Maternity), increases in resources (e.g., equipment, staffing), and the adoption of new ways of working (e.g., activity-based workspaces for support staff). Essentially, the redevelopment involves the opening of a new state-of-the-art building which will include moving services (and staff) from the old to the new building, with some wards staying in the old building. For the wards moving into the new building, this change does not initially involve more patients in existing services, but is intended to increase the number of staff because there will be more physical space to cover and new models of care introduced (e.g., ICU changing to single-bed rooms, more staff needed to individually attend to patients). The current redevelopment includes space for future expansion to account for the growing population. In addition to the redevelopment of the physical infrastructure, the way staff work together is also planned to change. Hospital leadership is aiming to foster a cultural shift towards greater cohesion and unity; highlighting that the hospital redevelopment can be conceptualised as an organisational change of considerable importance and magnitude.
Participants were hospital staff (clinical and non-clinical) working at the hospital under investigation. Staff working on four wards were targeted for interviews, with the intention to capture diverse experiences of the redevelopment and the broader organisational change; two of these wards would be moving into the new building (ICU and Maternity), one ward was not moving (Surgical), and one ward had moved into a new building two years prior (Respiratory). Interviews were also conducted with staff who held responsibilities across wards (e.g., General Services Department: cleaners, porters). The hospital staff were purposively recruited by department heads and snowballed from participants. Fifty staff members were approached (until data saturation was met) with four refusing to participate because they did not have the time.
Semi-structured interviews
Semi-structured interviews were conducted in private settings at the participants’ place of work (e.g., ward interview rooms, private offices). In the event a participant was unable to meet the researcher in person, interviews were conducted over the phone. A semi-structured interview guide was created in collaboration with key stakeholders from the hospital under investigation and following a literature review. The guide (Additional file 2 ) included questions aimed at exploring participants’: (1) understanding of the hospital’s culture and current ways of working; (2) understanding of the redevelopment and other hospital changes; and (3) concerns or expectations about the organisational change. The interviews were audio-taped and transcribed verbatim by the first author who is trained and experienced in conducting semi-structured interviews. No field notes were made during the interview nor were transcripts returned to participants for comment or correction due to the time poor characteristics of the study participants (hospital staff). Participants were informed that the research was part of the first author’s doctoral studies.
Interview data were analysed via thematic analysis [ 24 ] using NVivo [ 25 ]. This approach followed Braun and Clarke’s (2006) six phases of thematic analysis: familiarise, generate initial codes, develop themes, review potential themes, define and name themes, produce the report. Data were initially read multiple times by the first author, then descriptively and iteratively coded according to semantic features. The analysis included the use of inductive coding to identify patterns driven by the data, together with deductive coding, keeping the research questions in mind. Through examination of codes and coded data, themes were developed. The broader research team (KC, LAE, JCL) were included throughout each stage of the analysis process, with frequent discussions concerning the categorization of codes and themes. This process of having one researcher responsible for the analysis while other researchers then checked and clarified emerging themes throughout contributes to the trustworthiness of the findings [ 26 ].
In presenting the results, extracts have been edited minimally to enhance readability, without altering meaning or inference. Where extracts are presented, staff are coded according to their department (G: General – works across several wards; ICU: Intensive care unit; MAT: Maternity ward; RES: Respiratory ward; SUR: Surgical ward) and profession (AD: Administrative staff; CHGTEAM: Change management team staff; DR: Medical staff; GS: General services staff; MW: Midwifery staff; N: Nursing staff; OTH: Other profession).
Forty-six staff members participated in the semi-structured interviews. Interviews were typically conducted face-to-face ( n = 41; 89.1%), with five interviews conducted over the phone. No differences were discerned in content between these different mediums. Hospital staff taking part in interviews included those from: nursing and midwifery, medical, general services, administrative, and change management (Table 1 ). Change management staff are external to the hospital staff, and do not report to hospital executives. Interviews ranged from seven to 33 min in length ( M = 17 min). Participating staff had worked at the hospital for on average 10.5 years (range 5 months and 30 years).
Five themes were identified related to hospital staff’s understanding and experiences (i.e., expectations and concerns) of the change: staffing; benefits to patients; collaboration; fatigue; and adaptability. These expectations and concerns are schematically presented in Fig. 1 , with shades of red indicating negative expectations and concerns associated with the theme, and green representing positive expectations. Intensity of the colour demonstrated the frequency of positivity or negativity associated with that theme (i.e., deeper shades of red indicate frequency of negative discussion of this theme by different hospital staff). This figure also highlights the complexity and interrelatedness of these themes (e.g., the concern of inadequate staffing for the new building was linked with concerns about patient care, which could possibly impede the way the team work together, leading to staff feeling overworked and worn out; these expectations were all mitigated by the staff member’s understanding and awareness of the change). Explanations and examples are presented below.
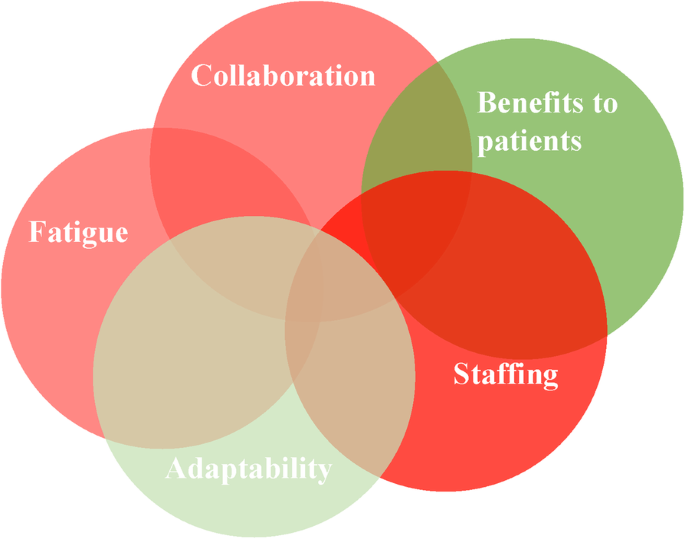
Thematic visualisation of staff understanding and expectations of the change
Hospital staff consistently held staffing to be a major concern in this redevelopment. To them, the opening of the new building, and with it the increase in physical size and addition of new services, meant that an increase in staff was crucial to successfully implement the change: “ My biggest uncertainty at the moment is the fact that I’m really concerned about whether I’m actually going to get enough staff ” (GS1). Many participants suggested that this issue would determine the success of the new hospital building. This was particularly important for staff moving into the new building with a bigger work space: “ We just need more staff. Yeah I think that’s the main issue - if we fix that then I believe everything should be smooth ” (ICUN4). For the most part, staff were unaware about how many new staff they would have in the new building. This uncertainty involved two related issues: (1) will we get the budget for new staff that we need? And if so, (2) where will we find all these new staff to employ?
On the first point, staff reported concerns that they would not have enough staff to cover the increased physical space and new ways of working within the new building. This lingering uncertainty was the result of external factors, specifically unresolved budget issues: “ But I suppose some of the issues stem from the fact that you never know how many beds we are able to open based on the funding from the government, and that is what is still up in the air ” (ICUDR1).
Regarding the second point, staff noted that even if budgetary issues were resolved, and there was enough money to hire new staff to fill the new building, a challenge would be finding the staff to recruit: “ I don’t know where these new staff are going to come from” (GN3). Some participants suggested that they already encountered difficulties with employing enough appropriately qualified staff and reported concerns that this issue would be compounded when they moved into the new building: “ Excitement will be way gone. It’s more to deal with that stress and the workload of other staff ” (ICUN4). Participants working on wards that were not moving into the new building also reported concerns about staffing. They noted that, despite not being directly involved in previous stages of the redevelopment, they had still been affected by these changes, because their colleagues were taken from their ward without consultation and moved into a new area. Hence, even staff not moving in the next stage of the redevelopment had concerns that their staffing levels would be affected: “ We have been told that we are not moving in there. And hopefully they don’t take our staff there ” (SURN5).
Benefits to patients
Many hospital staff expressed a positive expectation of the move related to benefits for patients. This was consistent across wards, departments and professions. Staff expected patients to experience benefits including reductions in infection rates and improved satisfaction, due to staying in a well-controlled and physically appealing environment with natural light: “ Any new place will give some joy or some happiness to people… The major change will be that because there are individual rooms, the infection rate will be lower and that I’m very pleased with” (ICUDR1).
Despite these participants reporting the improved physical environment was expected to positively affect patients, they also raised concerns that being in the new building might negatively affect patient safety because the increased physical space could introduce more room for error with the greater workload: “ Brings with it the fear, of how will we treat so many patients with nursing when you have one to one and the rooms are closed. That is a constant worry ” (ICUDR1). Participants indicated that this issue would be compounded if staffing levels were not increased.
Collaboration
Staff expressed multiple negative expectations or concerns about how their ways of working together would be affected by moving into the new building. Staff understood the change as more than just a physical expansion, but as an organisational change that would affect their ways of working. This understanding led to concern regarding how to work together in the new building. Specifically, staff moving into the new building were worried about the new layout of ICU, where nurses would be working alone in rooms with single patients. This would disrupt their ability to easily ask for support currently done by asking the nurse at an adjacent bed, or signalling to someone visible across the room: “ Single rooms are great for patients and everything but I think it becomes a bit more isolated for staffing ” (ICUOTH1). These concerns were also recognised among staff working in the change management team, who may not be directly affected by the change, but acknowledged that this is a major consequence of the move into the new building: “ All the beds, they were able to see each other all the time whereas now it’s a different work environment. They’re a bit more isolated… So that’s what we find is the challenge” (CHGTEAM2). Further, staff were concerned about working in open plan spaces that limit opportunity for private discussions, for example with other staff about workplace conflict or personal matters: “ I’m very concerned about insufficient space for private stuff ” (ICUAD1).
Staff reported negative expectations of collaboration breakdown not only within wards, but across the hospital. The organisational change will include far-flung staff and expanded infrastructure, which may decrease opportunity to collaborate directly. For several participants, the growing size of the hospital was seen as a fracturing of the positive, cohesive culture of what was once a smaller hospital—“ It used to be that the general manager would walk through and know everybody by name, the cleaner, maintenance crew, everybody knew everybody’s name ” (GN1)—into more disconnected, subunits: “ Now we’re very separate ” (ICUOTH1).
During interviews, many participants reported feeling over-worked and under-resourced. While some described being fatigued and unhappy at work, the redevelopment was, nevertheless, clearly a positive: “ We’re not happy because we’re under so much pressure and stress. But, you know, we are looking forward to the new build, it’ll be a beautiful building” (GN3). For others, there were concerns that their feelings of being over-worked would not subside with the opening of the new hospital building and that there was a lack of time to even consider the change. This was expressed by staff moving in to the new building, as well as those not moving:
Who has got the time to go and look at those decorative things ! (SURN5).
I can’t see how it will make a big difference to me… I don’t pay a lot of attention to the looks (MATDR1).
It doesn’t really matter… I could be providing it [patient care] in a tent or a building . (MATMW2).
Further, hospital staff expressed frustration in having to endure poor resourcing, which tempered their excitement for the new building: “We’ve all put up with whatever since whenever and I’m done, I’m so done” (ICUAD1). Some participants reported negative expectations related to the increase in physical space in the new building, as adding to the work load of clinical staff and requiring they travel further to get supplies and attend to patients: “They are worried about, hang on I’m going to have to do so many more laps” (ICUAD1). Similarly, an issue expressed on behalf of staff in the General Services Department was whether they will be able to adequately clean and cater for physically larger areas: “ I’m sitting here and looking at [a previous building that was opened] and seeing how filthy it is ” (CHGTEAM3). Concerns about being over-worked in the face of the redevelopment were further emphasised by some interviewees who discussed a problem with turnover: “ We’ve actually had a few people, I have had three people, which is unusual for us, who have looked for other jobs and are probably resigning. You know which is sort of the opposite of what we’d expect at this time, we’d expect they’d be excited for the new building ” (ICUN5). However, most staff in more junior positions had not seen the new building and thus were unaware of the layout and the degree to which it may impact their work: “ Because I have not seen the actual structure of the area, and I don’t know what they based it on and how they figured out a way to be friendly for both staff and patients at the same time ” (ICUN3). The unawareness and lack of understanding accentuated concerns and negative expectations among staff as they expected the worst.
Also contributing to reports of experiencing fatigue, staff described numerous other large changes taking place at the hospital over the years, in addition to the redevelopment: “ Basically for seven years we’ve been undergoing changes since I’ve been here. It is utterly exhausting having this many changes all the time ” (GS1). This highlights that while this study captures prospective insights to the change, change is constant in health care. While the move into the new building has not yet occurred, the move is part of a broader organisational change grander than the physical expansion of infrastructure. While this was a major concern for many staff, some of the senior medical staff dismissed this as being an issue, suggesting constant change is part of health care and should not lead to staff feeling worn out: “ I think once you get to my level you get good at kind of jumping through hoops… As you get more experienced, you just go with the flow a bit more” (SURDR2).
Adaptability
An additional theme involved staff’s positive expectation that they would be able to adapt to the changes brought about by the move into the new building. Reflecting on past experiences of organisational and infrastructure changes at the hospital, staff expressed that it could take time to adapt and see the benefits of the change: “ At the beginning, of course, everybody was scared of the changes and stuff like that, but eventually we got used to it. ” (SURN3). However, some staff reported that they saw adapting to the new building as a concern, potentially because of a lack of knowledge pertaining to what the new building entails: “ I just don’t know. I’m worried because I don’t know what we’re walking in to ” (ICUN2). In general, staff expressed an understanding of the change as one of physical growth (hospital redevelopment) and changes in ways of working (organisational change): “Getting bigger. So, basically taking all of our acute services and putting it in a brand spanking new building where they’re significantly expanding” (GN1); “ The biggest change is changing the way they work. Changing the way they deliver care .” (CHGTEAM2). When asked why the change was happening, hospital staff were consistent in attributing the need for redevelopment to population growth: “ To develop more resources to accommodate for the growing number of patients ” (SURDR3).
Feeling uninformed and uncertain about the change was expressed by staff of different professions and different levels throughout the hospital. In fact, even wards that were not moving to the new building were unsure if this was the case: “ There’s been no communication from anyone really. I hear from different people yes we are moving and then somebody says no we’re not. We’re staying here in the old building. So, I’m not sure exactly who’s going” (SURN1).
Our findings suggest that in the early stages of hospital redevelopment, staff experience both positive and negative expectations that are dependent upon the level of personal understanding, awareness of the change to come, and how well-resourced they already feel. Interviews with hospital staff highlighted a general understanding of the change as involving physical expansion of the hospital. However, participants also reported feeling inadequately informed about what is to come and described a range of sometimes differing expectations about the organisational effects of this change (e.g., on collaboration, for patients). This supports the conceptualisation of hospital redevelopment as not only a physical change, but an organisational one too.
The present study is the first to empirically explore the experiences and understanding of staff in the early stages of a hospital redevelopment, and conceptualised this as an organisational change. This conceptualisation is an important contribution to the organisational change literature because we show that change, even when based on the best evidence-based design, can be disappointing and bring about negative experiences for staff. The concerns and negative expectations of the change expressed by staff in the present study echo past research that retrospectively explored the experiences of staff during a hospital change, in Australia [ 13 ], and elsewhere [e.g., 14]. In the present study, staffing was a major concern reported by hospital staff. This is consistent with other reports of hospital redevelopment in the Australian context. For example, in a report into the opening of a new children’s hospital, staff were frustrated about the progression of the change and that a lack of staffing impacted on service planning. Staffing was also emphasised as an issue in another Australian hospital redevelopment project, where the building opened with insufficient staffing and resources [ 27 ]. Additionally, hospital staff in the present study indicated that they felt fatigued, so much so that excitement for the opening of the new building was diminishing. Reports of low staff morale in hospital redevelopment projects has also been documented in other Australian and international studies [ 13 , 14 ]. Further, participants in this study reported a lack of awareness of the redevelopment, something that appears to be common with a report of hospital revitalisation in the United States reporting a similar finding [ 28 ].
One source of many of the issues expressed by staff was uncertainty, a common and often inevitable experience in health care [ 29 ], for example, systems uncertainty about staffing levels and uncertainty about whether collaboration and support would break down as the hospital expands. While some types of uncertainty cannot be eradicated, it is important to manage uncertainty in times where information is available. One way to do this is to make sure front-line actors have a platform to seek information and ask questions during organisational change; having access to information is a predictor of success for organisational change in healthcare [ 30 ]. This may help alleviate stress associated with change and make the transition period less uncertain for staff, particularly in early stages where uncertainty may be greater. While it is not always possible for all the concerns and expectations of staff to be individually acknowledged and addressed by those coordinating the change (e.g., change management team or hospital executives), an alternative is through the use of ‘champions’ or ‘opinion leaders’. Opinion leaders are actors with a brokerage role; they carry information across social boundaries, such as between groups of professionals or different hospital wards [ 31 ]. Otherwise referred to as a ‘champion’, by virtue of their trustworthiness and connectedness, these actors are able to lead the opinions of others and are integral in the adoption and diffusion of new phenomena. Successful champions are enthusiastic and motivated about the change they are promoting [ 32 ]. In this case, a successful champion in a hospital undergoing organisational change is a staff member who can inform others and influence acceptance, and provide a positive frame for the change.
Implications
While findings may be localised to the hospital we researched, it is important to note that the hospital redevelopment under investigation is similar to other hospital redevelopments in metropolitan cities in Australia [ 7 ] and worldwide [ 5 ]. Specifically, the redevelopment is an expansion of infrastructure to meet the growing needs of the community which the hospital serves. The perceptions and experiences maintained by hospital staff will differ dependent on the state of the new facilities; these findings broadly generalise to any hospital redevelopment where a newer, larger building is opened. The implications of this study provide broad suggestions for other hospitals undergoing this type of hospital redevelopment.
Firstly, hospital redevelopment should be considered as more than physical change, but as an organisational change, in order to recognise the ripple effects of changing the infrastructure and how this may influence social and behavioural processes. From this study’s findings of the expectations and present experiences of organisational change, we recommend four strategies to aid in the early stages of hospital redevelopment: engage actors; plan and train; learn from the past; and increase managerial engagement (see Table 2 ). These recommendations correspond with suggestions from a past review examining transforming systems in health care [ 33 ]. Effort must be taken to ensure staff are informed of the change and rectify any confusions about who, what, when, and how the change is taking place. This is consistent with organisational change theory that maintains that large scale change requires significant effort and planning to ensure its success [ 19 ]. Therefore, an implication of this study lies in the importance of exploring the understanding and expectations of staff preceding a large organisational change in order to aid in the acceptance of, rather than resistance to, the change [ 21 ]. Further, this study also highlights the importance of studying the experiences of actors not directly involved in the organisational change but who are a part of the broader system (i.e., wards not moving implied they will be affected).
Strengths and limitations
A strength of this study lies in the number of participants and variability in the professions that contribute to the transferability of the study findings. Further, checking and clarifying themes with other researchers throughout the coding process increases the trustworthiness of the findings [ 26 ]. As to limitations, interviews were on average 17 min long, with the shortest interview lasting seven minutes. While this may be perceived as a short duration for collecting interview data it was appropriate for participants who were incredibly time poor (e.g., nurses on shift who could only get a 10 min break to talk to the researcher). It is important that the opinions of these busy staff are captured to reflect the true nature of a sample of varied hospital staff. Further, the findings may not be generalisable to other instances of organisational change and may be specific to the four wards and hospital examined in this study. Wards were purposively chosen rather than randomised. While findings may be specific to the hospital under investigation, the research has been designed to optimise research credibility in this qualitative analysis. Further, considerable context was provided to help readers infer relevance to different settings. This in-depth analysis of how staff understand and interpret organisational change in hospitals provides the opportunity to uncover theoretical insights into the processes of change in the health care system and the perspectives of staff during times of organisational change.
This study explored the prospective understanding and experiences of staff in organisational change in hospitals, using an Australian hospital redevelopment as a case exemplar. Findings indicated that staff were concerned about staffing levels, fatigue, and the potential for a breakdown of current collaborative working. These concerns are similar to past reports of redevelopment in hospitals. This paper presents recommendations for the early stages of organisational change in hospitals. For present and future hospital organisational change projects, it is important that staff concerns are addressed and that staff are informed adequately about the ongoing changes in order to improve their engagement and ownership of the change.
Availability of data and materials
The datasets analysed during the current study are not publicly available due to individual privacy, but are available from the corresponding author on reasonable request.
Abbreviations
Administrative staff
Change management team staff
Medical staff
General – works across several wards
General services staff
Intensive care unit
Maternity ward
Midwifery staff
Nursing staff
Other profession
Respiratory ward
Surgical ward
Braithwaite J, Churruca K, Ellis LA, Long JC, Clay-Williams R, Damen N, et al. Complexity science in healthcare-aspirations, approaches, applications and accomplishments: a white paper. Sydney, Australia: Macquarie University; 2017.
Google Scholar
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. Int J Qual Health Care. 2015;27(5):418–20.
Article Google Scholar
Malkin RA. Design of health care technologies for the developing world. Annu Rev Biomed Eng. 2007;9:567–87.
Article CAS Google Scholar
Ritchie E. NSW budget 2017: ‘hospital building boom’ at heart of $23bn deal. The Australian. 2017.
Carpenter D, Hoppszallern S. Hospital building report. The boom goes on. Hospitals Health Networks. 2006;80(3):48–50 2-4, 2.
PubMed Google Scholar
Aubusson K. Berejiklian government pledges $750 million for Sydney's RPA Hospital 2019 [5 Mar]. Available from: https://www.smh.com.au/national/nsw/berejiklian-government-pledges-750-million-for-sydney-s-rpa-hospital-20190304-p511n4.html .
NSW Government. Health Infrastructure 2018 [Available from: https://www.hinfra.health.nsw.gov.au/our-projects/project-search .
Australian Institute of Health and Welfare. Australia's health 2016. Canberra: AIHW; 2016.
Schweitzer M, Gilpin L, Frampton S. Healing spaces: elements of environmental design that make an impact on health. J Altern Complement Med. 2004;10:71–83.
Rechel B, Buchan J, McKee M. The impact of health facilities on healthcare workers’ well-being and performance. Int J Nurs Stud. 2009;46(7):1025–34.
Berry LL, Parish JT. The impact of facility improvements on hospital nurses. HERD. 2008;1(2):5–13.
Gharaveis A, Hamilton DK, Pati D. The impact of environmental design on teamwork and communication in healthcare facilities: a systematic literature review. HERD. 2018;11(1):119–37.
Children's Health Queensland Hospital and Health Service. Lady Cilento Children's Hospital clinical review. 2015.
Lourens G, Ballard H. The consequences of hospital revitalisation on staff safety and wellness. Occup Health Southern Africa. 2016;22(6):13–8.
Schwarz N, Sudman S. Autobiographical memory and the validity of retrospective reports. New York: Springer-Verlag; 2012.
Dannenberg AL, Bhatia R, Cole BL, Heaton SK, Feldman JD, Rutt CD. Use of health impact assessment in the US: 27 case studies, 1999–2007. Am J Prev Med. 2008;34(3):241–56.
Austin MJ, Ciaassen J. Impact of organizational change on organizational culture: implications for introducing evidence-based practice. J Evid Based Soc Work. 2008;5(1–2):321–59.
Fitzgerald L, McDermott A. Challenging perspectives on organizational change in health care: Taylor & Francis; 2017.
Book Google Scholar
Todnem BR. Organisational change management: a critical review. J Chang Manag. 2005;5(4):369–80.
Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. Br Med J. 2001;323(7313):625.
Braithwaite J. Changing how we think about healthcare improvement. Br Med J. 2018;361:k2014.
Pomare C, Churruca K, Long JC, Ellis LA, Gardiner B, Braithwaite J. Exploring the ripple effects of an Australian hospital redevelopment: a protocol for a longitudinal, mixed-methods study. BMJ Open. 2019;9(7):e027186.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Castleberry A. NVivo 10 [software program]. Version 10. QSR International; 2012. American journal of pharmaceutical education. 2014;78(1).
Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: a focus on trustworthiness. SAGE Open. 2014;4(1):2158244014522633.
Braithwaite J. How to fix a sick hospital: attend to its stressed health carers the Sydney morning herald; 2018.
Baker JG. The perspective of the staff regarding facility revitalization at Walter reed Army medical center. Army Medical Material Agency Fort Detrick MD; 2004.
Pomare C, Churruca K, Ellis LA, Long JC, Braithwaite J. A revised model of uncertainty in complex healthcare settings: a scoping review. J Eval Clin Pract. 2019;25(2):176–82.
Kash BA, Spaulding A, Johnson CE, Gamm L. Success factors for strategic change initiatives: a qualitative study of healthcare administrators' perspectives. J Healthc Manag. 2014;59(1):65–81.
Long JC, Cunningham FC, Braithwaite J. Bridges, brokers and boundary spanners in collaborative networks: a systematic review. BMC Health Serv Res. 2013;13(1):158.
Damschroder L, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein S. The role of the “champion” in infection prevention: results from a multisite qualitative study. BMJ Qual Saf. 2009;18(6):434–40.
Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q. 2012;90(3):421–56.
Download references
Acknowledgements
We thank the hospital executives, ward directors and nursing unit managers for their support in recruitment of interview participants. The authors also thank and acknowledge the interview participants.
CP was funded by the Australian Government Research Training Program (RTP) PhD Scholarship. JB is supported by multiple grants, including the National Health and Medical Research Council (NHMRC) Partnership Grant for Health Systems Sustainability (ID: 9100002). The funders had no role in the design, analysis and drafting of the manuscript.
Author information
Authors and affiliations.
Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Macquarie University, 75 Talavera Rd, Macquarie Park, Australia
Chiara Pomare, Kate Churruca, Janet C. Long, Louise A. Ellis & Jeffrey Braithwaite
You can also search for this author in PubMed Google Scholar
Contributions
CP and JB conceptualised the project. CP collected and analysed the data, and drafted the manuscript. KC, LAE and JCL assisted in the coding and interpretation of data. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chiara Pomare .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the relevant Ethics Committee in Sydney, New South Wales, Australia (no: 18/233). Due to ethical requirements, the committee cannot be named because it may lead to the identification of the study site. Informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Additional file 2.
Semi-structured interview guide.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Pomare, C., Churruca, K., Long, J.C. et al. Organisational change in hospitals: a qualitative case-study of staff perspectives. BMC Health Serv Res 19 , 840 (2019). https://doi.org/10.1186/s12913-019-4704-y
Download citation
Received : 23 May 2019
Accepted : 31 October 2019
Published : 14 November 2019
DOI : https://doi.org/10.1186/s12913-019-4704-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Organisational change
- Health systems change
- Hospital redevelopment
- Hospital expansion
- Staff expectations
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Insights on Healthcare
Read McKinsey’s latest insights on the changes that matter most for navigating the future of healthcare.
Provider Insights | Payer Insights | Healthcare Services & Technology Insights | Business Building in Healthcare | Consumer Health Insights | Behavioral Health Insights | Public Health Insights
Featured Insight

The future of Medicare Advantage
Featured article.

Generative AI in healthcare: Adoption trends and what’s next
Most recent articles.

German healthcare in the postpandemic era: Physician insights

Digital transformation: Health systems’ investment priorities

The AI opportunity: How payers can capture it now

Scaling national e-health: Best practices from around the world
Featured collections.

The Future of Nursing: McKinsey’s Frontline Insights

McKinsey on Healthcare: Innovate to thrive

McKinsey Insights on Healthcare Consumerism: Trends and Perspectives

McKinsey on Healthcare Podcast
Our conversations.

Unlocking the power of price transparency data

Speaking to hearts and minds in healthcare

Beyond the numbers: Creating a more diverse future for health

Meeting the member where they are: What is the future of health equity?
Provider insights.

How to bridge the experience gap by supporting nurses of all tenures

Payment integrity in the age of AI and value-based care
Payer insights.

How price transparency could affect US healthcare markets

2024 payers outlook: Opportunities abound
Healthcare services & technology insights.

The potential benefits of AI for healthcare in Canada

2024 healthcare services outlook: Challenges and opportunities
Want to learn more about how we help clients in healthcare practice, business building in healthcare.

Value creation through business model innovation in US healthcare

Leadership rundown: How US healthcare leaders are scaling innovation and transformation
Consumer health insights.

Consumers rule: Driving healthcare growth with a consumer-led strategy

Healthcare in Latin America: What are consumers looking for?

Consumers’ perceptions of their health-related social needs

Meeting changing consumer needs: The US retail pharmacy of the future
Behavioral health insights.

Working nine to thrive

Understanding and prioritizing nurses’ mental health and well-being

Reframing employee health: Moving beyond burnout to holistic health

Gen Z mental health: The impact of tech and social media
Public health insights.

Public health’s inflection point with generative AI

Future-proofing health systems for climate risks and pandemics

The end of the COVID-19 public health emergency: What’s next?

Virtual health for all: Closing the digital divide to expand access
More insights.

Liquid biopsy: Charting innovation in early cancer screening

The state of US women’s heart health: A path to improved health and financial outcomes

Netherlands advanced: Building a future labor market that works

Bridging the women’s health gap: A country-level exploration

Early adoption of generative AI in commercial life sciences

Ensuring the financial sustainability of academic medical centers

Redesigning for speed: Addressing life cycle compression in biopharma

The business of healthcare: ‘I’m always optimistic about what’s possible’

‘We need to invest in health workers between major pandemics—not just when we have a pandemic’

What to expect in US healthcare in 2024 and beyond
Related practice.
- Life Sciences
- Public & Social Sector
Connect with our Healthcare Practice
- Digital Marketing
- Facebook Marketing
- Instagram Marketing
- Ecommerce Marketing
- Content Marketing
- Data Science Certification
- Machine Learning
- Artificial Intelligence
- Data Analytics
- Graphic Design
- Adobe Illustrator
- Web Designing
- UX UI Design
- Interior Design
- Front End Development
- Back End Development Courses
- Business Analytics
- Entrepreneurship
- Supply Chain
- Financial Modeling
- Corporate Finance
- Project Finance
- Harvard University
- Stanford University
- Yale University
- Princeton University
- Duke University
- UC Berkeley
- Harvard University Executive Programs
- MIT Executive Programs
- Stanford University Executive Programs
- Oxford University Executive Programs
- Cambridge University Executive Programs
- Yale University Executive Programs
- Kellog Executive Programs
- CMU Executive Programs
- 45000+ Free Courses
- Free Certification Courses
- Free DigitalDefynd Certificate
- Free Harvard University Courses
- Free MIT Courses
- Free Excel Courses
- Free Google Courses
- Free Finance Courses
- Free Coding Courses
- Free Digital Marketing Courses
10 AI in Healthcare Case Studies [2024]
Artificial intelligence (AI) stands as the beacon of hope in a rapidly evolving healthcare landscape, with healthcare data doubling every two years and medical knowledge expanding exponentially, promising to revolutionize patient care and transform healthcare outcomes.
AI is transforming healthcare by introducing innovative solutions that enhance patient care, elevate clinical outcomes, and refine healthcare delivery processes. One significant impact area is AI-powered diagnostics, where algorithms analyze medical images, genetic data, and patient records to assist healthcare providers in accurate and timely diagnoses. This enhances the speed of diagnostics, reduces errors, and refines treatment planning.
Moreover, AI-powered predictive analytics facilitate proactive interventions by predicting patient outcomes, identifying high-risk individuals, and tailoring treatment plans. This proactive strategy contributes to improved chronic condition management, lowering hospital readmissions, and overall enhanced patient well-being.
AI’s involvement in drug discovery and development expedites the identification of potential drug candidates, optimizes clinical trials, and enables precision medicine strategies. Additionally, AI-driven robotic systems enhance surgical precision, minimize invasiveness, and accelerate patient recovery times.
These case studies highlight the immense potential of AI in transforming healthcare delivery, enhancing patient outcomes, and optimizing operational efficiency.
Case Study 1: AI-Powered Diagnostics in Radiology
The integration of AI into healthcare has heralded transformative changes, particularly within medical imaging. A notable collaboration between Massachusetts General Hospital (MGH) and the Massachusetts Institute of Technology (MIT) is an exemplary effort to develop AI algorithms tailored for radiology applications.
Implementation
The project aimed to harness the power of AI to aid radiologists in detecting and diagnosing diseases through medical images, such as X-rays and CT scans. Utilizing deep learning techniques, the AI system was trained on extensive datasets comprising annotated images to recognize patterns indicative of various conditions, including but not limited to cancers, fractures, and organ abnormalities.
The AI system’s performance exceeded expectations, demonstrating exceptional accuracy in identifying abnormalities and anomalies. In a published study in the Journal of the American Medical Association (JAMA), the AI system achieved a diagnostic accuracy rate of 94% in detecting lung nodules, significantly outperforming human radiologists, who scored 65% accuracy in the same task.
This implementation of AI in radiology has significantly influenced healthcare delivery. Firstly, it has relieved radiologists of mundane tasks through automation, enabling them to dedicate more time to interpreting intricate cases and delivering personalized patient care. Secondly, AI-driven diagnostics have streamlined the diagnostic process, resulting in expedited treatment initiation and enhanced patient outcomes. The success of this project has not only demonstrated the potential of AI in enhancing medical imaging but also paved the way for the widespread adoption of AI-powered diagnostic tools in healthcare institutions globally.
Related: Famous Female Healthcare Leaders
Case Study 2: Personalized Medicine with AI
Personalized medicine represents a groundbreaking shift in healthcare, focusing on tailoring treatment plans to individual patient traits. This paradigm shift from traditional one-size-fits-all medicine to tailored interventions has been made possible by AI and data analytics advancements.
One of the most notable implementations of AI in personalized medicine is the collaboration between the Mayo Clinic and IBM Watson Health. This collaboration utilized Watson’s cognitive computing prowess to create AI-driven tools that analyze extensive patient data, encompassing genetic profiles, medical records, treatment histories, and pertinent scientific studies. Subsequently, the AI system formulates personalized treatment suggestions derived from this comprehensive analysis.
The outcomes of implementing AI in personalized medicine have been highly promising, particularly in oncology. By factoring in each patient’s distinct genetic composition and medical background, AI facilitates the recommendation of targeted therapies with enhanced efficacy and reduced adverse effects. Clinical trials and real-world applications have demonstrated that patients receiving AI-recommended treatments experience higher response rates, longer progression-free survival, and improved overall outcomes compared to standard treatments.
The impact of AI in personalized medicine extends far beyond oncology, with potential applications in various disease areas. The utilization of AI’s analytical capabilities empowers healthcare providers to extract valuable insights from intricate datasets, enabling the delivery of precise and efficient treatments to patients. This methodology not only amplifies clinical outcomes but also boosts patient contentment while curbing healthcare expenses by mitigating redundant procedures and medications. As AI continues to evolve and integrate into healthcare workflows, personalized medicine is poised to become the cornerstone of modern healthcare delivery, offering patients tailored interventions that are truly transformative.
Case Study 3: AI-Powered Electronic Health Records (EHR) Optimization
Electronic Health Records (EHR) have evolved into a fundamental component of contemporary healthcare, consolidating patient data and streamlining care delivery processes. However, managing and leveraging the vast amounts of data within EHR systems can pose significant challenges. To address this, healthcare organizations are turning to AI to streamline EHR processes and unlock valuable insights.
A prime example of AI-powered EHR optimization is the collaboration between Cerner Corporation, a prominent EHR provider, and the University of Missouri Health Care (MU Health Care). By integrating AI algorithms into their EHR systems, they aimed to automate routine tasks, enhance data analytics capabilities, and improve overall healthcare efficiency.
The implementation of AI in EHR optimization yielded tangible benefits for healthcare providers and patients alike. The AI-powered system automated administrative tasks such as documentation and billing, reducing the burden on healthcare staff and allowing them to allocate more time to patient care. Furthermore, AI-driven analytics equip healthcare teams with the tools to pinpoint trends, anticipate patient outcomes, and customize treatment strategies grounded in data-driven insights. This fosters improved clinical decision-making and fosters enhanced healthcare outcomes.
The impact of AI in EHR optimization extends beyond operational efficiency. It has a profound impact on patient safety, as AI algorithms can flag potential errors and inconsistencies in medical records, reducing the risk of medical errors. Additionally, AI-driven EHR systems facilitate data-driven healthcare delivery, enabling personalized care experiences for patients based on their unique medical histories and needs. The success of this implementation has catalyzed the adoption of AI-driven EHR solutions worldwide, revolutionizing the way healthcare institutions manage and leverage patient data to improve care quality and outcomes.
Related: How Can Healthcare Leaders Use AI?
Case Study 4: AI-Assisted Surgical Robotics
The fusion of AI technologies with surgical robotics has ushered in a new era in the field of surgery, offering unprecedented levels of precision, safety, and efficiency. These advancements have significantly improved patient outcomes and revolutionized surgical practices worldwide.
A standout illustration of AI-assisted surgical robotics is the da Vinci Surgical System, pioneered by Intuitive Surgical. This cutting-edge platform seamlessly integrates AI algorithms to augment surgical capabilities, including image recognition, tissue analysis, and instrument control. The incorporation of AI into surgical procedures offers surgeons real-time feedback and support, thereby refining their surgical expertise and decision-making capabilities during operations.
The integration of AI in surgical robotics has yielded remarkable outcomes across various surgical specialties. Improved surgical accuracy enables the performance of intricate procedures with minimal damage to surrounding tissues, resulting in accelerated recovery periods and reduced post-operative complications. Patients undergoing AI-assisted surgeries encounter decreased pain levels, shorter hospital stays, and enhanced long-term recovery prospects.
The impact of AI-assisted surgical robotics is multifaceted and transformative. Patients benefit from minimally invasive procedures, reduced risks, and faster recovery, ultimately improving their quality of life. Healthcare providers witness improved surgical outcomes, increased operational efficiency, and reduced healthcare costs. Moreover, AI-driven surgical robotics enable remote surgeries, empowering expert surgeons to perform procedures from distant locations, thereby enhancing access to specialized care and expertise globally.
Case Study 5: AI-Driven Predictive Analytics for Patient Outcomes
Accurate prediction of patient outcomes holds paramount importance for healthcare providers, enabling them to make well-informed decisions and optimize the delivery of care. AI-driven predictive analytics have emerged as a powerful tool in healthcare, enabling proactive interventions and personalized treatment plans.
A notable implementation is the collaboration between Johns Hopkins Hospital and Microsoft Azure AI. Leveraging vast amounts of patient data, including electronic health records, medical imaging, and genomic information, AI algorithms were trained to predict patient outcomes, such as disease progression, readmission risks, and response to treatments.
The implementation of AI-driven predictive analytics has significantly improved patient care and healthcare outcomes. By analyzing historical data and identifying patterns, AI algorithms can forecast patient trajectories with high accuracy, enabling healthcare providers to intervene early, prevent complications, and tailor treatments based on individual patient profiles.
The impact of AI-driven predictive analytics in healthcare is profound. It enables proactive and personalized care, leading to better patient outcomes, reduced hospital readmissions, and optimized resource utilization. Healthcare providers can allocate resources more efficiently, prioritize high-risk patients, and deliver targeted interventions, ultimately improving patient satisfaction and healthcare quality.
Related: Role of CDO in the Healthcare Sector
Case Study 6: AI in Epidemic Outbreak Prediction
Timely prediction of epidemic outbreaks is crucial for preventing health crises. Traditional methods often lag, hindering effective responses to infectious disease threats.
AI models were developed using machine learning to analyze diverse datasets, including historical outbreak records, climate conditions, and global travel patterns. These models aimed to identify early indicators of potential outbreaks, integrating real-time data to refine predictions continually.
The AI models have been instrumental in predicting outbreaks of diseases like influenza and dengue. For instance, they were able to predict regional outbreaks several weeks in advance with a high degree of accuracy, enabling preemptive actions.
The use of AI in predicting epidemic outbreaks has revolutionized public health responses, enabling governments and health organizations to allocate resources efficiently and implement targeted interventions. This proactive strategy has substantially lessened the effects of infectious diseases, showcasing how AI can bolster public health monitoring and crisis response.
Case Study 7: AI for Mental Health Monitoring
Stigma and scarce resources for early detection frequently result in mental health issues remaining unidentified. Effective monitoring and timely intervention are crucial for managing these conditions.
Applications powered by AI were crafted to scrutinize individual behavior and social media interactions. Employing natural language processing and machine learning, these applications detect language and behavioral signals that could suggest mental health conditions like depression or anxiety.
The AI systems have successfully identified patterns that correlate with mental health conditions, leading to early interventions. In trials, these tools demonstrated a high level of accuracy in detecting depressive behavior based on text analysis and activity patterns.
This AI-driven approach has significantly improved the support for mental health by enabling early diagnosis and intervention, thereby helping to reduce the overall burden of mental health issues. It has also facilitated a greater awareness and understanding of mental health conditions, promoting a proactive approach to mental health care.
Related: Healthcare Administration Interview Questions
Case Study 8: Robot-Assisted Surgery for Pediatric Patients
The diminutive size and fragility of young patients pose unique challenges in pediatric surgery, necessitating unparalleled precision and control.
AI-driven robotic systems, such as the da Vinci Surgical System, were employed to assist surgeons in performing complex pediatric surgeries. These systems offer superior visualization, precision, and control that surpass human abilities, enabling extremely delicate procedures to be carried out with minimal invasiveness.
The use of AI-assisted robotic systems in pediatric surgeries has led to improved surgical accuracy and success rates. Notably, these surgeries have seen reductions in complications, quicker recovery times, and minimized surgical trauma, which are crucial for pediatric patients.
The introduction of robotic systems in pediatric surgery has transformed surgical practices in children’s healthcare. Patients experience advantages from minimally invasive surgeries, including reduced pain, shorter stays in the hospital, and faster recovery to routine activities. Additionally, surgeons can conduct intricate surgeries with greater confidence and precision, improving both the quality of treatment and patient safety.
Case Study 9: AI in Sleep Study and Therapy
Sleep disorders significantly impact quality of life but are often challenging to diagnose and treat effectively due to their complex nature and variability among individuals.
AI was integrated into wearable devices and mobile apps to monitor and analyze sleep patterns continuously. These tools utilized algorithms to assess sleep quality, duration, disturbances, and cycles. The AI models were trained using vast datasets of sleep behavior to predict disorders and personalize therapeutic recommendations.
The AI-enhanced tools provided accurate assessments of sleep quality and identified specific disorders like insomnia or sleep apnea in their early stages. Users received personalized insights and recommendations for improving sleep hygiene based on the analysis, leading to noticeable improvements in sleep quality.
The adoption of AI in sleep studies and therapy has revolutionized the management of sleep disorders. It has empowered individuals with actionable data to improve their sleep, leading to better overall health and well-being. Furthermore, healthcare providers can offer more precise and effective treatments, enhancing patient care and reducing the need for invasive diagnostic procedures.
Related: Effective Leadership in Healthcare Management
Case Study 10: AI for Chronic Disease Management
Managing chronic diseases such as diabetes and heart disease is a major public health challenge, requiring continuous monitoring and personalized care to effectively manage and prevent complications.
AI technology has been incorporated into wearable devices and mobile applications to continuously monitor and analyze sleep patterns. The AI systems analyzed this data to detect trends and predict potential health events. These platforms were designed to provide real-time feedback to patients and healthcare providers, facilitating timely interventions and adjustments in treatment plans.
The implementation of these AI systems has led to more proactive management of chronic conditions. Patients experienced improved control over their diseases with fewer episodes of acute exacerbations. Healthcare providers were able to tailor treatments more effectively, based on the data-driven insights provided by AI, leading to better overall health outcomes.
The use of AI in managing chronic diseases has greatly improved patient involvement and compliance with treatment protocols. It has also reduced the burden on healthcare systems by decreasing the frequency of hospital visits and the need for emergency care. Overall, this technology has contributed to a higher quality of life for patients and more efficient resource utilization in healthcare settings.
AI is revolutionizing healthcare by offering innovative solutions across various domains, from diagnostics and personalized medicine to EHR optimization, surgical robotics, and predictive analytics. Its impact on improving patient outcomes, enhancing healthcare delivery, and optimizing resource utilization underscores its importance as a transformative technology in modern healthcare.
- Is EdTech a bubble? [10 Factors that Matter] [2024]
- Detailed History of Oxford University [2024]
Team DigitalDefynd
We help you find the best courses, certifications, and tutorials online. Hundreds of experts come together to handpick these recommendations based on decades of collective experience. So far we have served 4 Million+ satisfied learners and counting.
30 Incredible Generative AI Statistics [2024]

How can HR teams make use of Artificial Intelligence? [2024]

15 Ways AI Is Helping Humanity [2024]

Intersection of AI and Quantum Computing [2024]

Artificial Intelligence in eSports [5 Case Studies]

How to effectively manage a Healthcare Team [2024]
- Health Care Services
- Public Health
- Delivery of Health Care
Collaborative innovation in healthcare: a case study of hospitals as innovation platforms
- January 2020
- International Journal of Value Chain Management 11(1):24

- University of Oulu

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Denise Rahal

- Erno Marjakangas
- Jukka Majava
- Kaisa Hyvärinen

- HEALTH POLICY PLANN

- Maryam Bigdeli
- Aniss Lakhal
- Sanaa Belabbes

- Int J Innovat Learn

- Maria R.A. Moreira
- Mãdãlina Gherman

- Kathleen M. Eisenhardt
- A.M. Huberman

- Creativ Innovat Manag

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplements
- French Abstracts
- Portuguese Abstracts
- Spanish Abstracts
- Author Guidelines
- Submission Site
- Open Access
- About International Journal for Quality in Health Care
- About the International Society for Quality in Health Care
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Contact ISQua
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, acknowledgements, data availability.
- < Previous
Case study: international healthcare service quality, building a model for cultivating cultural sensitivity
- Article contents
- Figures & tables
- Supplementary Data
Ya-Ting Yang, Yi-Hsin Elsa Hsu, Kung-Pei Tang, Christine Wang, Stephen Timmon, Wen-Ta Chiu, Saileela Annavajjula, Jan-Show Chu, Case study: international healthcare service quality, building a model for cultivating cultural sensitivity, International Journal for Quality in Health Care , Volume 32, Issue 9, November 2020, Pages 639–642, https://doi.org/10.1093/intqhc/mzaa097
- Permissions Icon Permissions
In the context of medical tourism, cultural differences and language barriers are unneglectable factors, which compromise the shared decision-making between doctor and patients.
This study constructs a cultural sensitivity cultivation (CSC) model that could be used to train medical professionals in the sector of medical tourism.
Since 2016, there have been explorations in new strategies to offer better services. A critical step added is to include clients’ perspectives in the re-examining process as a way to cultivate cultural sensitivity among the service providers. This practice expands to the sector of medical tourism. In our case study, we are able to conclude a new model that could yield quality international healthcare services.
The steps of our CSC model include (i) ‘Promote Awareness’ for shifting mindset, (ii) ‘Share Scenarios’ for developing empathy and compassion, (iii) ‘Review Process’ for collecting detail feedback, (iv) ‘Identify Gaps’ for targeting areas for improvement and (v) ‘Improve Systems,’ for changing standard operation procedures (SOPs) based on the strategies through Assmann’s theory with a cultural–anthropological approach.
After Kuang Tien General Hospital (KTGH) implemented the new model for 1 year, the number of international patients has increased by 64%. More research could be done in the future to cover all the important aspects of providing international medical services and could apply the CSC model to different healthcare settings.
To optimize the shared decision-making between the doctor and medical traveler patients, healthcare providers should not only overcome language and cultural barriers but also should avoid unnecessary gestures in terms of status respect. Inviting patients to be co-investigator for quality improvement is a viable solution.
In the context of medical tourism, cultural differences and language barriers are unneglectable factors, which compromise the shared decision-making between doctor and patients. This situation has raised the demand for cultural competency training for medical providers. In recent years, Taiwan is gradually being recognized as a destination of choice for high-quality and affordable healthcare [ 1 ].
Therefore, there is an immediate need to rectify the problem. This study aims to construct a cultural sensitivity cultivation (CSC) model to train Taiwanese medical professionals to enhance shared decision-making and healthcare service for medical tourists.
The study was conducted at Kuang Tien General Hospital (KTGH), a regional hospital founded more than a decade ago in Taiwan. In order to develop the CSC model using a systematic approach, a combination of literature studies, case report analyses, in-depth interviews and statistical comparisons was applied. In addition to the literature studies, we undertook an exploratory qualitative study to investigate the concept of international healthcare service quality focusing on cultural sensitivity cultivating. Adopting multiple qualitative and quantitative approaches provides a sound foundation for generating empirical conceptual frameworks of complex concepts. There are three experienced researchers reviewed applied this concept of respect when reviewing five extensive case reports provided by the KTGH. The reports include detailed information such as patients’ previsit, visit, and postvisit information (follow-up and testimonials). Also, the Chief Strategy Officer and members of the hospital participated in in-person interviews. The results of literature reviews have indicated a lack of standardization in medical tourism regulation. This has led to difficulties relating to ethical issues such as informed consent and health equity control [ 2 ]. On the other hand, the healthcare providers’ commitment to improving their cultural sensitivities is the essential component to ensure high quality of medical tourism services [ 3 ]. However, there are very few studies that address the basic theories needed in order to establish the ideal relationship between international medical seekers and healthcare providers. Hence, a cultural–anthropological approach by Assmann [ 4 ] is adopted to develop this CSC model. This is because Assmann’s theory can transcend the economic colonialist globalization framework. Assmann’s theory addresses five forms of respect: (i) Status respect ‘respect due to the position and office,’ (ii) Respect for achievement ‘respect that distinguishes individual according to their ability and achievements,’ (iii) Social respect ‘raising emotional temperature of society surplus personal appearance, abilities or possessions, which is focusing of recognition and admiration,’ (iv) Cultural respect ‘affirmative action on a global level of intercultural communication and digital self-expression within a larger political framework of decolonization’ (v) Civil respect ‘multicultural and multiethnic society stimulate new forms of social perception, interaction and empathy.’
Findings and Results
From the interviews and analysis, we discovered several fundamental strategies that KTGH employs in improving their staff’s ability to care for international patients by based on the strategies through Assmann’s theory with a cultural–anthropological approach between medical professionals and international patients such as they include practicing ‘social respect’ and ‘civil respect’ through the improvement of verbal and nonverbal communication skills; embodying the ‘cultural respect’ through sharing experience among different ethnic groups and hosting international holiday promotional events to promote mutual understandings among global citizens and also applied the Assmann’s respect theory with the international patients’ visit journey from promote awareness, share scenarios, review process, identify gaps and improve system to connected with CSC model. Since 2016, KTGH has started the efforts of exploring new strategies to offer better services, and they have especially paid attention to cultivating staffs’ intercultural competencies. During each service delivery to an international patient, staff records details on patient–doctor interactions. They use the recordings to create case studies or scenarios to develop hospital-wide training to cultivate empathy for all. To decrease the conventional ‘status respect’ between the doctor-patient relationship, the research team invited ‘the clients,’ the international healthcare seekers, to work as the ‘co-investigators.’ The goal is to include patients’ perspectives when examining behaviors occurred during the healthcare-seeking process.
After implementing these new strategies for 1 year, KTGH received testimonials from international patients on the high quality of their healthcare services. In addition, the number of international patients increased by 64% in the following year. Witnessing KTGH process and success in cultivating cultural awareness, we have used its practice to form the CSC model in our study, as shown in Figure 1 .

The stage of ‘Promoting Awareness’ emphasizes the importance of educating and introducing staff to cultural differences and characteristics. The ‘Share Scenarios’ stage promotes empathy and compassion through sharing through the previous experiences and lessons learned between one and another. The ‘Review Process’ stage consists of collecting service feedback from teams and discussing step-by-step experiences with patients. The ‘Identify Gaps’ stage is to target areas for improvement in each step: pre-, during- and postvisit experiences with patients. Lastly, under ‘Improve Systems,’ the model emphasizes the point in shaping patients’ experiences systemically through discussions with involved departments to enhance standard operation procedures (SOPs).
The proposed CSC model provides a conceptual framework and a systematic application process in the area where little research was conducted previously. According to the research analyzing publications in the IJQHC over the past 3 years, one of the leading keywords is ‘quality improvement’ [ 5 ]. There are various approaches to quality improvement, with different levels, from quality indicators to systematic monitoring [ 6 ]. The CSC model indicates that besides the apparent reason of language abilities that contribute to quality service, other important elements such as creating cultural awareness and using previous experiences to develop training materials are also crucial to improve service quality and experience for international patients. Although the CSC model is developed based on experiences in a single healthcare facility that offers international healthcare, we have made valuable observations that could lead to quality healthcare service in this specific facility. Attention to data can itself significantly improve data quality [ 7 ]; we have observed in this case that focusing on the internal process of delivering healthcare services could also improve the quality of the service itself. Based on the CSC model, we encourage more research that could be done in the future to cover all aspects of providing international medical services and consider applying the CSC model in different healthcare settings. Further implementation and investigation of the effects of the CSC model are suggested.
The authors thank CSF and staff members of KTGH who assisted in providing the data for this study.
We have interviewed subjects, and all data are available upon request to reviewers and editors. No new data were generated or analyzed.
Stephano RM . Health & Wellness Destination Guide . Taiwan : Global Health Insurance Publications , 2014 . http://taiwan.medicaltourism.com/online-view/document.pdf
Google Scholar
Google Preview
Foley BM , Haglin JM , Tanzer JR et al. Patient care without borders: a systematic review of medical and surgical tourism . J Travel Med 2019 ; 26 :6.
Rokni L , Park S-H , Avci T . Improving medical tourism services through human behaviour and cultural competence . Iran J Public Health 2019 ; 48 : 1988 – 96 .
Assmann A . Civilizing societies: recognition and respect in a global world . New Lit Hist 2013 ; 44 : 69 – 91 .
Iqbal U , Yu CY , Li J . What are the leading keywords of IJQHC in last 3 years? Int J Qual Health Care 2015 ; 27 : 163 – 4 .
Geboers H , Mokkink H , Montfort P et al. . Continuous quality improvement in small general medical practices: the attitudes of general practitioners and other practice staff . Int J Qual Health Care 2001 ; 13 : 391 – 7 .
Mate KS , Bennett B , Mphatswe W et al. Challenges for routine health system data management in a large public programme to prevent mother-to-child HIV transmission in South Africa . PLos One 2009 ; 4 :e5483.
Author notes
# Equal Contribution.
- health personnel
- central serous chorioretinopathy
- cultural differences
- quality improvement
- language barriers
- medical tourism
- shared decision making
- standard operating procedure
- cultural sensitivity
| Month: | Total Views: |
|---|---|
| August 2020 | 6 |
| September 2020 | 9 |
| October 2020 | 5 |
| November 2020 | 49 |
| December 2020 | 32 |
| January 2021 | 8 |
| February 2021 | 23 |
| March 2021 | 45 |
| April 2021 | 32 |
| May 2021 | 57 |
| June 2021 | 38 |
| July 2021 | 27 |
| August 2021 | 33 |
| September 2021 | 12 |
| October 2021 | 34 |
| November 2021 | 37 |
| December 2021 | 24 |
| January 2022 | 46 |
| February 2022 | 33 |
| March 2022 | 48 |
| April 2022 | 66 |
| May 2022 | 40 |
| June 2022 | 42 |
| July 2022 | 21 |
| August 2022 | 31 |
| September 2022 | 34 |
| October 2022 | 58 |
| November 2022 | 28 |
| December 2022 | 31 |
| January 2023 | 42 |
| February 2023 | 29 |
| March 2023 | 28 |
| April 2023 | 52 |
| May 2023 | 26 |
| June 2023 | 28 |
| July 2023 | 27 |
| August 2023 | 31 |
| September 2023 | 27 |
| October 2023 | 29 |
| November 2023 | 44 |
| December 2023 | 19 |
| January 2024 | 27 |
| February 2024 | 43 |
| March 2024 | 50 |
| April 2024 | 36 |
| May 2024 | 84 |
| June 2024 | 40 |
| July 2024 | 45 |
| August 2024 | 54 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1464-3677
- Print ISSN 1353-4505
- Copyright © 2024 International Society for Quality in Health Care and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Manage communications
- Mutual Fund & 529 accounts
I invest on behalf of my clients.
I consult or invest on behalf of a financial institution.
I want to learn more about BlackRock.
To reach a different BlackRock site directly, please update your user type .
Where it pays to get choosy: A case study in stock selection
- Ibrahim Kanan
- Tony DeSpirito
The healthcare sector offers a compelling mix of defensive characteristics and growth potential driven by innovation. It also features ample dispersion that presents stock pickers with an opportunity to parse potential leaders and laggards in pursuit of above-market return.
As active equity investors , we’re not content to accept what the market has to offer. Our mission is to assess companies on their underlying fundamentals to target those stocks that we believe have the potential to outperform the broad market over a three- to five-year time horizon.
This mission takes on greater significance in what we see as a new era of more normalized interest rates and volatility ― an environment in which a rising tide no longer lifts all boats and stock selection becomes more important to portfolio outcomes.
While attractive opportunities are on offer across all sectors and industries, our daily work as stock pickers has revealed that the opportunity for selectivity is more prominent in some areas of the market ― a function of greater dispersion and industry-level nuance that can be concealed at the broad index level. Case in point: The tech sector led the market in the first half of this year, but the lion’s share of that return came from semiconductors ― the not-so-secret sauce to enabling AI.
More surprising may be the importance of selection in the healthcare sector. As shown in the chart below, healthcare ranks among the top three sectors for return differentiation across individual stocks. This suggests greater opportunity to apply fundamental research to parse potential winners and losers in pursuit of index-beating returns.
Healthy stock-picking opportunities Average return dispersion across selected sectors, 2003-2023

Source: BlackRock Fundamental Equities, with data from Refinitiv, Dec. 31, 2003-Dec. 31, 2023. Chart shows the average dispersion of annual return across the noted sectors in the Russell 1000 Index. Dispersion is defined as interdecile range, or the difference between the 10th (top) and 90th percentile of stock returns within each sector. “Remaining sectors” include energy, comms services, financials, materials, industrials, consumer staples, real estate and utilities.
We have felt this firsthand in our work analyzing stocks for inclusion in the BlackRock Equity Dividend Fund and BlackRock Large Cap Value ETF , where healthcare was the second-largest sector exposure and a top contributor to return despite relatively muted performance at the index level in 2023. (Healthcare returned 2% in 2023 versus an S&P 500 return of 26%.)
Parsing the opportunity in healthcare
The big picture around healthcare makes it an appealing sector for long-term investors. It tends to do relatively well no matter the economic backdrop, given that healthcare needs do not change with GDP. It benefits from the secular tailwind of aging populations, as age begets greater healthcare needs and associated increases in health-related spending. It’s also a diverse sector that is rife with innovation. And despite all of this, the healthcare sector has been trading at an attractive valuation that is below the broad market average.
Importantly, however, not all healthcare stocks offer the same appeal, and investing at the index level could expose portfolios to big risk. The reason: U.S. healthcare benchmarks include heavy weightings in mature pharmaceutical companies ― and these face an onslaught of revenue-busting patent expirations that could weigh on their performance, as well as that of the healthcare indexes.
What’s ailing U.S. pharma
When drug patents expire and cheaper generics come to market, drug maker revenues inevitably decline. Our analysis shows several major U.S. pharma companies losing patent protection on up to 70% of their revenue by 2030.
These companies’ profits are also at risk of disproportionate decline, as it’s usually the oldest and highest-margin products that are losing patent protection. This is because drug makers tend to increase prices incrementally each year after a new product launch. Their manufacturing costs, however, remain stable ― allowing gross margins to rise. Companies also spend less on marketing as a drug matures and gains popular recognition. By the time these drugs hit patent expiration and fall off a company’s line-up, they typically have grown to become the highest-margin products.
Another complicating factor: When a drug patent expires, the same sales force is selling one less product, rendering the business less productive. Companies must find something new to sell to justify the fixed cost of their sales force, or otherwise shrink their business. The options here are limited:
1) Spend more on research and development (R&D) of new products. The rub: Returns on R&D have been declining and the process requires substantial time.
2) Negotiate a deal to buy a (hopefully) blockbuster drug. The rub: Companies typically overpay on high expectations for an essentially unknown, never-marketed product.
At the same time, the Inflation Reduction Act (IRA) imposes further price pressure by giving Medicare the authority to negotiate prices on select drugs. That process is underway, with results (and potential price reductions) due in September.
Given all of the above, valuations of many U.S. pharma companies require close scrutiny. Pricing that underestimates the pending impact of the patent cliff can make some of these stocks “value traps” ― sporting a low price-to-earnings multiple that is actually much higher when accounting for their patent expirations and the associated earnings impact.
A “remedy” in active selection
Active stock pickers can seek to avert much of the risk at the index level by avoiding those companies most exposed and directing their investments to more interesting pockets of healthcare. Among them:
European pharmaceutical companies. In general, these companies face a much less severe patent issue and have better drug pipelines, offering greater return potential and quality on a par with U.S. counterparts.
Makers of GLP-1 “diabesity” drugs. GLP-1s are a notable exception to our U.S. pharma aversion. We believe these promising new therapies for diabetes and weight loss have ample runway as they just begin their success journey.
Drug distributors. The patent cliff can be a boon for drug distributors in that they are able to distribute generic alternatives, which usually offer higher profit margins than branded products. Plus, volumes are higher as more generics become available once patent protection lapses.
The above case study is just one example of how active stock selection can help to achieve alpha, or above-market return, through a deep understanding of sector-level dynamics. We believe the ability to parse potential winners and losers based on underlying company fundamentals and observations of the industry environment should bring increasing value to portfolios, especially against a backdrop of heightened market dispersion.

Insights from our Global CIO
Taking Stock: U.S. Equity Market Outlook
What’s next for markets? Tony DeSpirito, Global CIO of Fundamental Equities, shares insights on U.S. equities with a quarterly market recap and look ahead.
Equity investing for a new era: The return of alpha
When it comes to stocks, a rising tide is no longer lifting all boats. The era of easy money has ended, and the age of selectivity is on. Tony DeSpirito discusses how alpha, or above-market return, is poised to become a bigger driver of outcomes.
Why BlackRock Fundamental Equities?
With decades of experience and a local presence around the world, our fundamental equity investors bring unique expertise to their discipline and deep, bottom-up insight that powers our mission to generate alpha for our clients.
- Mutual funds
- iShares ETFs
- Closed-end funds
- Cash alternatives
- Commodity funds
- Stock funds
- Multi-asset funds
- Real estate funds
- Science and Technology Trust
- Resources & Commodities Strategy Trust
- Global Allocation Fund
- LifePath Index Retirement Fund
- Technology Opportunities Fund
- iShares Core S&P 500 ETF
- All funds All funds
- 529 College Savings Plan 529 College Savings Plan
- BlackRock Impact Opportunities
- Fixed Income
- Fundamental Equities
- Multi-Asset Strategies & Solutions
- Systematic Investing
- Cash management
- Factor-based investing
- Investing for retirement
- LifePath® target date funds
- All active investment strategies All active investment strategies
- Weekly commentary
- Global investment outlook
- BlackRock Investment Institute
- Investment stewardship
- Our approach to sustainability
- Portfolio management views
- Education center
- Retirement volatility strategies
- Planning for retirement
- What is a 401(K)?
- Document library
- Shareholder reports
- Regulatory documents
- Share classes and loads
- Tax information
- Forms & Applications
- 529 Forms & Applications
- LifePath spending tool
- LifePath selector tool
- iShares core builder
- College saving estimator
- All insights All insights
- The Bid podcast The Bid podcast
- About BlackRock
- BlackRock retirement
- Customer service
- Digital service
As a global investment manager and fiduciary to our clients, our purpose at BlackRock is to help everyone experience financial well-being. Since 1999, we've been a leading provider of financial technology, and our clients turn to us for the solutions they need when planning for their most important goals.
Investing involves risk, including possible loss of principal. Investment in a specific sector can entail greater volatility given the narrower focus of the investment universe and concentration in sector-specific risks. Investments in health services industries may be affected by changes in regulations, advancing technological developments and product liability lawsuits.
This material is not intended to be relied upon as a forecast, research or investment advice, and is not a recommendation, offer or solicitation to buy or sell any securities or to adopt any investment strategy. The opinions expressed are as of August 2024 and may change as subsequent conditions vary. The information and opinions contained in this post are derived from proprietary and nonproprietary sources deemed by BlackRock to be reliable, are not necessarily all-inclusive and are not guaranteed as to accuracy. As such, no warranty of accuracy or reliability is given and no responsibility arising in any other way for errors and omissions (including responsibility to any person by reason of negligence) is accepted by BlackRock, its officers, employees or agents. This post may contain “forward-looking” information that is not purely historical in nature. Such information may include, among other things, projections and forecasts. There is no guarantee that any forecasts made will come to pass. Reliance upon information in this post is at the sole discretion of the reader. Past performance is no guarantee of future results.
BlackRock Large Cap Value ETF The Fund is actively managed and does not seek to replicate the performance of a specified index. The Fund may have a higher portfolio turnover than funds that seek to replicate the performance of an index.
Convertible securities are subject to the market and issuer risks that apply to the underlying common stock.
International investing involves risks, including risks related to foreign currency, limited liquidity, less government regulation and the possibility of substantial volatility due to adverse political, economic or other developments. These risks often are heightened for investments in emerging/ developing markets or in concentrations of single countries.
Carefully consider the Funds' investment objectives, risk factors, and charges and expenses before investing. This and other information can be found in the Funds' prospectuses or, if available, the summary prospectuses, which may be obtained by visiting the iShares Fund and BlackRock Fund prospectus pages. Read the prospectus carefully before investing.
Prepared by BlackRock Investments, LLC, member FINRA.
© 2024 BlackRock, Inc or its affiliates. All Rights Reserved. BLACKROCK and iSHARES are trademarks of BlackRock, Inc., or its affiliates . All other trademarks are those of their respective owners.
USRRMH0824U/S-3798496
Success Stories

Harmonizing Customer Support with AI-Powered Semantic Search for a Payer Contact Center
- a.prlst-para')[this.getAttribute('data-index')].href, encodeURIComponent(this.getAttribute('data-title')));" class="share">

Chronicles of Harmony

Cloud-hosted automated platform boosts care management at payor enterprise

Leading payer organization implements cloud ecosystem to drive operational excellence

Healthcare insurer accelerates sales with cloud enrollment platform

Multi-state Blue reduces production defects by 30% through streamlined application testing

Healthcare insurance portal enhances the user experience

Attaining 99% claims processing accuracy for a health plan with a diverse application landscape

Refreshing a personalized communication platform for a leading pathologist organization

A healthcare firm’s journey towards achieving 96% precision in monthly claims reserve forecasts

Elevating care management for a health plan covering 4.7 million members

Tackling data security and access challenges for a multi-state health insurer

Achieving Lightning-Fast Case Resolution In Under A Minute For A Leading Managed Care Company

Multi-state managed care organization expands strategically with a playbook-driven growth approach

Resolving grievances and appeals for a leading managed healthcare company

Ramping up data operations efficiency for the cloud journey ahead

Leading managed care organization conducts enhanced operations through streamlined processes

Empowering a Managed Care Organization To Implement Playbook-Based

Modernizing legacy systems to elevate operational efficiency and member engagement for a health plan provider

A leading health insurer bolsters cybersecurity to minimize vulnerabilities

Breaking barriers to patient wellness through hyper-personalization and collaboration

Leading Medicaid MCO successfully navigates market changes through lean operations

Empowering A Health Tech Company to Diagnose Disease Onset Faster and Improve Treatment Pathways

Empowering Actionable Insights for a Leading Health Insurer by Facilitating Flawless Data Migration


Ensuring Harmonized Onboarding; Provider Data Access for a Regional Medicaid Payer

Leading Healthcare Provider Cultivates Customer-centricity through Automated Enrollment

Composing the melody for smoother operations for a leading health tech company

How we helped a leading health insurer hit high notes through auto-adjudication of claims

American Insurer Modernizes Data Platform for Better Service Delivery and Customer Engagement

Embarking Large Scale Operations Transformation Journey to Optimize Cost and Sustain Business Growth for a Fortune 500 US Healthcare Payer

Improving Constituent Experience via Contact Center Transformation

Building resilience through Azure transformation for a large Health Care payer

58 Tons of CO2 Emission Reduction by Reimagining Registration and Login Process

Expedited Execution for Acquisition and Expansion Programs for a Leading Health Plan

Infosys Helps Molina accelerate Time-to-Market of Government sponsored Health Plan for Puerto Rico
Aetna streamlines communications and improves speed-to-market with Infosys and HP Exstream solution

Infosys partners with a Government department for implementation of Electronic Health records.

Infosys Enables Health Insurer To Engage Patients in Their Healthcare Through Personal Health Record Model

Infosys' Integration and Collaboration Solution Helps Mercy Health Plans Enhance Customer Satisfaction

Portal Strategy and Technology Architecture Enhancement for a Pharmacy Benefit Manager (PBM)

Infosys - Aetna's Trusted IT Partner for more than a Decade

Long Term Care Partners Modernizes Core Systems to Optimize Operations and Support Growth

Infosys developed an Enterprise Data Warehouse for a Commercial Health Benefits Company

Establishing a Testing Center of Excellence for a Commercial Health Benefits Company

Healthcare Major Accelerates Time-to-Market by 9 months using Service-Oriented Architecture

Leveraging Service-Oriented Architecture for Competitive Advantage
Trending @infosys.
- Survey paper
- Open access
- Published: 19 June 2019
Big data in healthcare: management, analysis and future prospects
- Sabyasachi Dash 1 na1 ,
- Sushil Kumar Shakyawar 2 , 3 na1 ,
- Mohit Sharma 4 , 5 &
- Sandeep Kaushik 6
Journal of Big Data volume 6 , Article number: 54 ( 2019 ) Cite this article
472k Accesses
799 Citations
103 Altmetric
Metrics details
‘Big data’ is massive amounts of information that can work wonders. It has become a topic of special interest for the past two decades because of a great potential that is hidden in it. Various public and private sector industries generate, store, and analyze big data with an aim to improve the services they provide. In the healthcare industry, various sources for big data include hospital records, medical records of patients, results of medical examinations, and devices that are a part of internet of things. Biomedical research also generates a significant portion of big data relevant to public healthcare. This data requires proper management and analysis in order to derive meaningful information. Otherwise, seeking solution by analyzing big data quickly becomes comparable to finding a needle in the haystack. There are various challenges associated with each step of handling big data which can only be surpassed by using high-end computing solutions for big data analysis. That is why, to provide relevant solutions for improving public health, healthcare providers are required to be fully equipped with appropriate infrastructure to systematically generate and analyze big data. An efficient management, analysis, and interpretation of big data can change the game by opening new avenues for modern healthcare. That is exactly why various industries, including the healthcare industry, are taking vigorous steps to convert this potential into better services and financial advantages. With a strong integration of biomedical and healthcare data, modern healthcare organizations can possibly revolutionize the medical therapies and personalized medicine.
Introduction
Information has been the key to a better organization and new developments. The more information we have, the more optimally we can organize ourselves to deliver the best outcomes. That is why data collection is an important part for every organization. We can also use this data for the prediction of current trends of certain parameters and future events. As we are becoming more and more aware of this, we have started producing and collecting more data about almost everything by introducing technological developments in this direction. Today, we are facing a situation wherein we are flooded with tons of data from every aspect of our life such as social activities, science, work, health, etc. In a way, we can compare the present situation to a data deluge. The technological advances have helped us in generating more and more data, even to a level where it has become unmanageable with currently available technologies. This has led to the creation of the term ‘big data’ to describe data that is large and unmanageable. In order to meet our present and future social needs, we need to develop new strategies to organize this data and derive meaningful information. One such special social need is healthcare. Like every other industry, healthcare organizations are producing data at a tremendous rate that presents many advantages and challenges at the same time. In this review, we discuss about the basics of big data including its management, analysis and future prospects especially in healthcare sector.
The data overload
Every day, people working with various organizations around the world are generating a massive amount of data. The term “digital universe” quantitatively defines such massive amounts of data created, replicated, and consumed in a single year. International Data Corporation (IDC) estimated the approximate size of the digital universe in 2005 to be 130 exabytes (EB). The digital universe in 2017 expanded to about 16,000 EB or 16 zettabytes (ZB). IDC predicted that the digital universe would expand to 40,000 EB by the year 2020. To imagine this size, we would have to assign about 5200 gigabytes (GB) of data to all individuals. This exemplifies the phenomenal speed at which the digital universe is expanding. The internet giants, like Google and Facebook, have been collecting and storing massive amounts of data. For instance, depending on our preferences, Google may store a variety of information including user location, advertisement preferences, list of applications used, internet browsing history, contacts, bookmarks, emails, and other necessary information associated with the user. Similarly, Facebook stores and analyzes more than about 30 petabytes (PB) of user-generated data. Such large amounts of data constitute ‘ big data ’. Over the past decade, big data has been successfully used by the IT industry to generate critical information that can generate significant revenue.
These observations have become so conspicuous that has eventually led to the birth of a new field of science termed ‘ Data Science ’. Data science deals with various aspects including data management and analysis, to extract deeper insights for improving the functionality or services of a system (for example, healthcare and transport system). Additionally, with the availability of some of the most creative and meaningful ways to visualize big data post-analysis, it has become easier to understand the functioning of any complex system. As a large section of society is becoming aware of, and involved in generating big data, it has become necessary to define what big data is. Therefore, in this review, we attempt to provide details on the impact of big data in the transformation of global healthcare sector and its impact on our daily lives.
Defining big data
As the name suggests, ‘big data’ represents large amounts of data that is unmanageable using traditional software or internet-based platforms. It surpasses the traditionally used amount of storage, processing and analytical power. Even though a number of definitions for big data exist, the most popular and well-accepted definition was given by Douglas Laney. Laney observed that (big) data was growing in three different dimensions namely, volume, velocity and variety (known as the 3 Vs) [ 1 ]. The ‘big’ part of big data is indicative of its large volume. In addition to volume, the big data description also includes velocity and variety. Velocity indicates the speed or rate of data collection and making it accessible for further analysis; while, variety remarks on the different types of organized and unorganized data that any firm or system can collect, such as transaction-level data, video, audio, text or log files. These three Vs have become the standard definition of big data. Although, other people have added several other Vs to this definition [ 2 ], the most accepted 4th V remains ‘veracity’.
The term “ big data ” has become extremely popular across the globe in recent years. Almost every sector of research, whether it relates to industry or academics, is generating and analyzing big data for various purposes. The most challenging task regarding this huge heap of data that can be organized and unorganized, is its management. Given the fact that big data is unmanageable using the traditional software, we need technically advanced applications and software that can utilize fast and cost-efficient high-end computational power for such tasks. Implementation of artificial intelligence (AI) algorithms and novel fusion algorithms would be necessary to make sense from this large amount of data. Indeed, it would be a great feat to achieve automated decision-making by the implementation of machine learning (ML) methods like neural networks and other AI techniques. However, in absence of appropriate software and hardware support, big data can be quite hazy. We need to develop better techniques to handle this ‘endless sea’ of data and smart web applications for efficient analysis to gain workable insights. With proper storage and analytical tools in hand, the information and insights derived from big data can make the critical social infrastructure components and services (like healthcare, safety or transportation) more aware, interactive and efficient [ 3 ]. In addition, visualization of big data in a user-friendly manner will be a critical factor for societal development.
Healthcare as a big-data repository
Healthcare is a multi-dimensional system established with the sole aim for the prevention, diagnosis, and treatment of health-related issues or impairments in human beings. The major components of a healthcare system are the health professionals (physicians or nurses), health facilities (clinics, hospitals for delivering medicines and other diagnosis or treatment technologies), and a financing institution supporting the former two. The health professionals belong to various health sectors like dentistry, medicine, midwifery, nursing, psychology, physiotherapy, and many others. Healthcare is required at several levels depending on the urgency of situation. Professionals serve it as the first point of consultation (for primary care), acute care requiring skilled professionals (secondary care), advanced medical investigation and treatment (tertiary care) and highly uncommon diagnostic or surgical procedures (quaternary care). At all these levels, the health professionals are responsible for different kinds of information such as patient’s medical history (diagnosis and prescriptions related data), medical and clinical data (like data from imaging and laboratory examinations), and other private or personal medical data. Previously, the common practice to store such medical records for a patient was in the form of either handwritten notes or typed reports [ 4 ]. Even the results from a medical examination were stored in a paper file system. In fact, this practice is really old, with the oldest case reports existing on a papyrus text from Egypt that dates back to 1600 BC [ 5 ]. In Stanley Reiser’s words, the clinical case records freeze the episode of illness as a story in which patient, family and the doctor are a part of the plot” [ 6 ].
With the advent of computer systems and its potential, the digitization of all clinical exams and medical records in the healthcare systems has become a standard and widely adopted practice nowadays. In 2003, a division of the National Academies of Sciences, Engineering, and Medicine known as Institute of Medicine chose the term “ electronic health records ” to represent records maintained for improving the health care sector towards the benefit of patients and clinicians. Electronic health records (EHR) as defined by Murphy, Hanken and Waters are computerized medical records for patients any information relating to the past, present or future physical/mental health or condition of an individual which resides in electronic system(s) used to capture, transmit, receive, store, retrieve, link and manipulate multimedia data for the primary purpose of providing healthcare and health-related services” [ 7 ].
Electronic health records
It is important to note that the National Institutes of Health (NIH) recently announced the “All of Us” initiative ( https://allofus.nih.gov/ ) that aims to collect one million or more patients’ data such as EHR, including medical imaging, socio-behavioral, and environmental data over the next few years. EHRs have introduced many advantages for handling modern healthcare related data. Below, we describe some of the characteristic advantages of using EHRs. The first advantage of EHRs is that healthcare professionals have an improved access to the entire medical history of a patient. The information includes medical diagnoses, prescriptions, data related to known allergies, demographics, clinical narratives, and the results obtained from various laboratory tests. The recognition and treatment of medical conditions thus is time efficient due to a reduction in the lag time of previous test results. With time we have observed a significant decrease in the redundant and additional examinations, lost orders and ambiguities caused by illegible handwriting, and an improved care coordination between multiple healthcare providers. Overcoming such logistical errors has led to reduction in the number of drug allergies by reducing errors in medication dose and frequency. Healthcare professionals have also found access over web based and electronic platforms to improve their medical practices significantly using automatic reminders and prompts regarding vaccinations, abnormal laboratory results, cancer screening, and other periodic checkups. There would be a greater continuity of care and timely interventions by facilitating communication among multiple healthcare providers and patients. They can be associated to electronic authorization and immediate insurance approvals due to less paperwork. EHRs enable faster data retrieval and facilitate reporting of key healthcare quality indicators to the organizations, and also improve public health surveillance by immediate reporting of disease outbreaks. EHRs also provide relevant data regarding the quality of care for the beneficiaries of employee health insurance programs and can help control the increasing costs of health insurance benefits. Finally, EHRs can reduce or absolutely eliminate delays and confusion in the billing and claims management area. The EHRs and internet together help provide access to millions of health-related medical information critical for patient life.
Digitization of healthcare and big data
Similar to EHR, an electronic medical record (EMR) stores the standard medical and clinical data gathered from the patients. EHRs, EMRs, personal health record (PHR), medical practice management software (MPM), and many other healthcare data components collectively have the potential to improve the quality, service efficiency, and costs of healthcare along with the reduction of medical errors. The big data in healthcare includes the healthcare payer-provider data (such as EMRs, pharmacy prescription, and insurance records) along with the genomics-driven experiments (such as genotyping, gene expression data) and other data acquired from the smart web of internet of things (IoT) (Fig. 1 ). The adoption of EHRs was slow at the beginning of the 21st century however it has grown substantially after 2009 [ 7 , 8 ]. The management and usage of such healthcare data has been increasingly dependent on information technology. The development and usage of wellness monitoring devices and related software that can generate alerts and share the health related data of a patient with the respective health care providers has gained momentum, especially in establishing a real-time biomedical and health monitoring system. These devices are generating a huge amount of data that can be analyzed to provide real-time clinical or medical care [ 9 ]. The use of big data from healthcare shows promise for improving health outcomes and controlling costs.
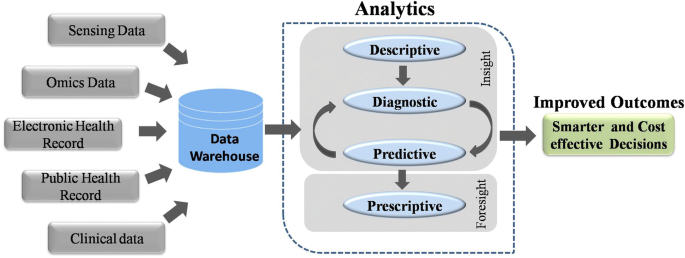
Workflow of Big data Analytics. Data warehouses store massive amounts of data generated from various sources. This data is processed using analytic pipelines to obtain smarter and affordable healthcare options
Big data in biomedical research
A biological system, such as a human cell, exhibits molecular and physical events of complex interplay. In order to understand interdependencies of various components and events of such a complex system, a biomedical or biological experiment usually gathers data on a smaller and/or simpler component. Consequently, it requires multiple simplified experiments to generate a wide map of a given biological phenomenon of interest. This indicates that more the data we have, the better we understand the biological processes. With this idea, modern techniques have evolved at a great pace. For instance, one can imagine the amount of data generated since the integration of efficient technologies like next-generation sequencing (NGS) and Genome wide association studies (GWAS) to decode human genetics. NGS-based data provides information at depths that were previously inaccessible and takes the experimental scenario to a completely new dimension. It has increased the resolution at which we observe or record biological events associated with specific diseases in a real time manner. The idea that large amounts of data can provide us a good amount of information that often remains unidentified or hidden in smaller experimental methods has ushered-in the ‘- omics ’ era. The ‘ omics ’ discipline has witnessed significant progress as instead of studying a single ‘ gene ’ scientists can now study the whole ‘ genome ’ of an organism in ‘ genomics ’ studies within a given amount of time. Similarly, instead of studying the expression or ‘ transcription ’ of single gene, we can now study the expression of all the genes or the entire ‘ transcriptome ’ of an organism under ‘ transcriptomics ’ studies. Each of these individual experiments generate a large amount of data with more depth of information than ever before. Yet, this depth and resolution might be insufficient to provide all the details required to explain a particular mechanism or event. Therefore, one usually finds oneself analyzing a large amount of data obtained from multiple experiments to gain novel insights. This fact is supported by a continuous rise in the number of publications regarding big data in healthcare (Fig. 2 ). Analysis of such big data from medical and healthcare systems can be of immense help in providing novel strategies for healthcare. The latest technological developments in data generation, collection and analysis, have raised expectations towards a revolution in the field of personalized medicine in near future.
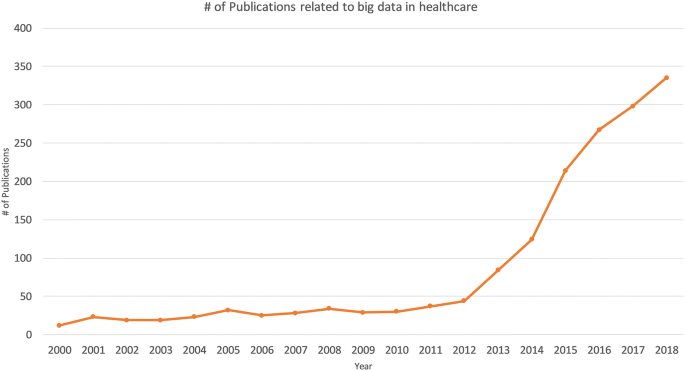
Publications associated with big data in healthcare. The numbers of publications in PubMed are plotted by year
Big data from omics studies
NGS has greatly simplified the sequencing and decreased the costs for generating whole genome sequence data. The cost of complete genome sequencing has fallen from millions to a couple of thousand dollars [ 10 ]. NGS technology has resulted in an increased volume of biomedical data that comes from genomic and transcriptomic studies. According to an estimate, the number of human genomes sequenced by 2025 could be between 100 million to 2 billion [ 11 ]. Combining the genomic and transcriptomic data with proteomic and metabolomic data can greatly enhance our knowledge about the individual profile of a patient—an approach often ascribed as “individual, personalized or precision health care”. Systematic and integrative analysis of omics data in conjugation with healthcare analytics can help design better treatment strategies towards precision and personalized medicine (Fig. 3 ). The genomics-driven experiments e.g., genotyping, gene expression, and NGS-based studies are the major source of big data in biomedical healthcare along with EMRs, pharmacy prescription information, and insurance records. Healthcare requires a strong integration of such biomedical data from various sources to provide better treatments and patient care. These prospects are so exciting that even though genomic data from patients would have many variables to be accounted, yet commercial organizations are already using human genome data to help the providers in making personalized medical decisions. This might turn out to be a game-changer in future medicine and health.
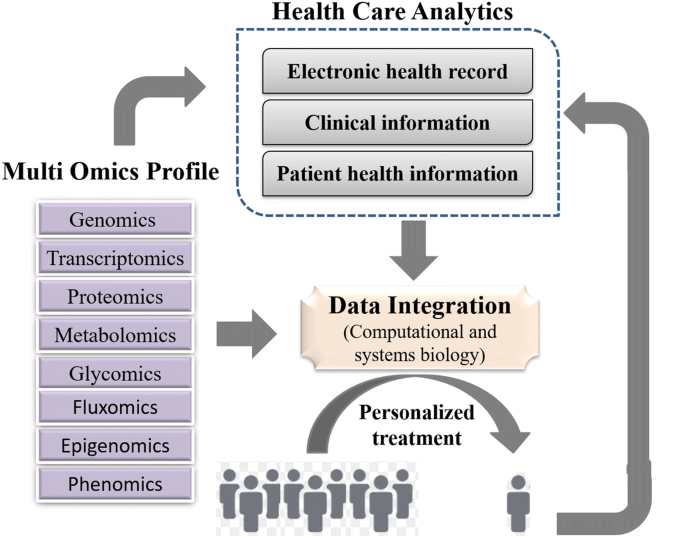
A framework for integrating omics data and health care analytics to promote personalized treatment
Internet of Things (IOT)
Healthcare industry has not been quick enough to adapt to the big data movement compared to other industries. Therefore, big data usage in the healthcare sector is still in its infancy. For example, healthcare and biomedical big data have not yet converged to enhance healthcare data with molecular pathology. Such convergence can help unravel various mechanisms of action or other aspects of predictive biology. Therefore, to assess an individual’s health status, biomolecular and clinical datasets need to be married. One such source of clinical data in healthcare is ‘internet of things’ (IoT).
In fact, IoT is another big player implemented in a number of other industries including healthcare. Until recently, the objects of common use such as cars, watches, refrigerators and health-monitoring devices, did not usually produce or handle data and lacked internet connectivity. However, furnishing such objects with computer chips and sensors that enable data collection and transmission over internet has opened new avenues. The device technologies such as Radio Frequency IDentification (RFID) tags and readers, and Near Field Communication (NFC) devices, that can not only gather information but interact physically, are being increasingly used as the information and communication systems [ 3 ]. This enables objects with RFID or NFC to communicate and function as a web of smart things. The analysis of data collected from these chips or sensors may reveal critical information that might be beneficial in improving lifestyle, establishing measures for energy conservation, improving transportation, and healthcare. In fact, IoT has become a rising movement in the field of healthcare. IoT devices create a continuous stream of data while monitoring the health of people (or patients) which makes these devices a major contributor to big data in healthcare. Such resources can interconnect various devices to provide a reliable, effective and smart healthcare service to the elderly and patients with a chronic illness [ 12 ].
Advantages of IoT in healthcare
Using the web of IoT devices, a doctor can measure and monitor various parameters from his/her clients in their respective locations for example, home or office. Therefore, through early intervention and treatment, a patient might not need hospitalization or even visit the doctor resulting in significant cost reduction in healthcare expenses. Some examples of IoT devices used in healthcare include fitness or health-tracking wearable devices, biosensors, clinical devices for monitoring vital signs, and others types of devices or clinical instruments. Such IoT devices generate a large amount of health related data. If we can integrate this data with other existing healthcare data like EMRs or PHRs, we can predict a patients’ health status and its progression from subclinical to pathological state [ 9 ]. In fact, big data generated from IoT has been quiet advantageous in several areas in offering better investigation and predictions. On a larger scale, the data from such devices can help in personnel health monitoring, modelling the spread of a disease and finding ways to contain a particular disease outbreak.
The analysis of data from IoT would require an updated operating software because of its specific nature along with advanced hardware and software applications. We would need to manage data inflow from IoT instruments in real-time and analyze it by the minute. Associates in the healthcare system are trying to trim down the cost and ameliorate the quality of care by applying advanced analytics to both internally and externally generated data.
Mobile computing and mobile health (mHealth)
In today’s digital world, every individual seems to be obsessed to track their fitness and health statistics using the in-built pedometer of their portable and wearable devices such as, smartphones, smartwatches, fitness dashboards or tablets. With an increasingly mobile society in almost all aspects of life, the healthcare infrastructure needs remodeling to accommodate mobile devices [ 13 ]. The practice of medicine and public health using mobile devices, known as mHealth or mobile health, pervades different degrees of health care especially for chronic diseases, such as diabetes and cancer [ 14 ]. Healthcare organizations are increasingly using mobile health and wellness services for implementing novel and innovative ways to provide care and coordinate health as well as wellness. Mobile platforms can improve healthcare by accelerating interactive communication between patients and healthcare providers. In fact, Apple and Google have developed devoted platforms like Apple’s ResearchKit and Google Fit for developing research applications for fitness and health statistics [ 15 ]. These applications support seamless interaction with various consumer devices and embedded sensors for data integration. These apps help the doctors to have direct access to your overall health data. Both the user and their doctors get to know the real-time status of your body. These apps and smart devices also help by improving our wellness planning and encouraging healthy lifestyles. The users or patients can become advocates for their own health.
Nature of the big data in healthcare
EHRs can enable advanced analytics and help clinical decision-making by providing enormous data. However, a large proportion of this data is currently unstructured in nature. An unstructured data is the information that does not adhere to a pre-defined model or organizational framework. The reason for this choice may simply be that we can record it in a myriad of formats. Another reason for opting unstructured format is that often the structured input options (drop-down menus, radio buttons, and check boxes) can fall short for capturing data of complex nature. For example, we cannot record the non-standard data regarding a patient’s clinical suspicions, socioeconomic data, patient preferences, key lifestyle factors, and other related information in any other way but an unstructured format. It is difficult to group such varied, yet critical, sources of information into an intuitive or unified data format for further analysis using algorithms to understand and leverage the patients care. Nonetheless, the healthcare industry is required to utilize the full potential of these rich streams of information to enhance the patient experience. In the healthcare sector, it could materialize in terms of better management, care and low-cost treatments. We are miles away from realizing the benefits of big data in a meaningful way and harnessing the insights that come from it. In order to achieve these goals, we need to manage and analyze the big data in a systematic manner.
Management and analysis of big data
Big data is the huge amounts of a variety of data generated at a rapid rate. The data gathered from various sources is mostly required for optimizing consumer services rather than consumer consumption. This is also true for big data from the biomedical research and healthcare. The major challenge with big data is how to handle this large volume of information. To make it available for scientific community, the data is required to be stored in a file format that is easily accessible and readable for an efficient analysis. In the context of healthcare data, another major challenge is the implementation of high-end computing tools, protocols and high-end hardware in the clinical setting. Experts from diverse backgrounds including biology, information technology, statistics, and mathematics are required to work together to achieve this goal. The data collected using the sensors can be made available on a storage cloud with pre-installed software tools developed by analytic tool developers. These tools would have data mining and ML functions developed by AI experts to convert the information stored as data into knowledge. Upon implementation, it would enhance the efficiency of acquiring, storing, analyzing, and visualization of big data from healthcare. The main task is to annotate, integrate, and present this complex data in an appropriate manner for a better understanding. In absence of such relevant information, the (healthcare) data remains quite cloudy and may not lead the biomedical researchers any further. Finally, visualization tools developed by computer graphics designers can efficiently display this newly gained knowledge.
Heterogeneity of data is another challenge in big data analysis. The huge size and highly heterogeneous nature of big data in healthcare renders it relatively less informative using the conventional technologies. The most common platforms for operating the software framework that assists big data analysis are high power computing clusters accessed via grid computing infrastructures. Cloud computing is such a system that has virtualized storage technologies and provides reliable services. It offers high reliability, scalability and autonomy along with ubiquitous access, dynamic resource discovery and composability. Such platforms can act as a receiver of data from the ubiquitous sensors, as a computer to analyze and interpret the data, as well as providing the user with easy to understand web-based visualization. In IoT, the big data processing and analytics can be performed closer to data source using the services of mobile edge computing cloudlets and fog computing. Advanced algorithms are required to implement ML and AI approaches for big data analysis on computing clusters. A programming language suitable for working on big data (e.g. Python, R or other languages) could be used to write such algorithms or software. Therefore, a good knowledge of biology and IT is required to handle the big data from biomedical research. Such a combination of both the trades usually fits for bioinformaticians. The most common among various platforms used for working with big data include Hadoop and Apache Spark. We briefly introduce these platforms below.
Loading large amounts of (big) data into the memory of even the most powerful of computing clusters is not an efficient way to work with big data. Therefore, the best logical approach for analyzing huge volumes of complex big data is to distribute and process it in parallel on multiple nodes. However, the size of data is usually so large that thousands of computing machines are required to distribute and finish processing in a reasonable amount of time. When working with hundreds or thousands of nodes, one has to handle issues like how to parallelize the computation, distribute the data, and handle failures. One of most popular open-source distributed application for this purpose is Hadoop [ 16 ]. Hadoop implements MapReduce algorithm for processing and generating large datasets. MapReduce uses map and reduce primitives to map each logical record’ in the input into a set of intermediate key/value pairs, and reduce operation combines all the values that shared the same key [ 17 ]. It efficiently parallelizes the computation, handles failures, and schedules inter-machine communication across large-scale clusters of machines. Hadoop Distributed File System (HDFS) is the file system component that provides a scalable, efficient, and replica based storage of data at various nodes that form a part of a cluster [ 16 ]. Hadoop has other tools that enhance the storage and processing components therefore many large companies like Yahoo, Facebook, and others have rapidly adopted it. Hadoop has enabled researchers to use data sets otherwise impossible to handle. Many large projects, like the determination of a correlation between the air quality data and asthma admissions, drug development using genomic and proteomic data, and other such aspects of healthcare are implementing Hadoop. Therefore, with the implementation of Hadoop system, the healthcare analytics will not be held back.
Apache Spark
Apache Spark is another open source alternative to Hadoop. It is a unified engine for distributed data processing that includes higher-level libraries for supporting SQL queries ( Spark SQL ), streaming data ( Spark Streaming ), machine learning ( MLlib ) and graph processing ( GraphX ) [ 18 ]. These libraries help in increasing developer productivity because the programming interface requires lesser coding efforts and can be seamlessly combined to create more types of complex computations. By implementing Resilient distributed Datasets (RDDs), in-memory processing of data is supported that can make Spark about 100× faster than Hadoop in multi-pass analytics (on smaller datasets) [ 19 , 20 ]. This is more true when the data size is smaller than the available memory [ 21 ]. This indicates that processing of really big data with Apache Spark would require a large amount of memory. Since, the cost of memory is higher than the hard drive, MapReduce is expected to be more cost effective for large datasets compared to Apache Spark. Similarly, Apache Storm was developed to provide a real-time framework for data stream processing. This platform supports most of the programming languages. Additionally, it offers good horizontal scalability and built-in-fault-tolerance capability for big data analysis.
Machine learning for information extraction, data analysis and predictions
In healthcare, patient data contains recorded signals for instance, electrocardiogram (ECG), images, and videos. Healthcare providers have barely managed to convert such healthcare data into EHRs. Efforts are underway to digitize patient-histories from pre-EHR era notes and supplement the standardization process by turning static images into machine-readable text. For example, optical character recognition (OCR) software is one such approach that can recognize handwriting as well as computer fonts and push digitization. Such unstructured and structured healthcare datasets have untapped wealth of information that can be harnessed using advanced AI programs to draw critical actionable insights in the context of patient care. In fact, AI has emerged as the method of choice for big data applications in medicine. This smart system has quickly found its niche in decision making process for the diagnosis of diseases. Healthcare professionals analyze such data for targeted abnormalities using appropriate ML approaches. ML can filter out structured information from such raw data.
Extracting information from EHR datasets
Emerging ML or AI based strategies are helping to refine healthcare industry’s information processing capabilities. For example, natural language processing (NLP) is a rapidly developing area of machine learning that can identify key syntactic structures in free text, help in speech recognition and extract the meaning behind a narrative. NLP tools can help generate new documents, like a clinical visit summary, or to dictate clinical notes. The unique content and complexity of clinical documentation can be challenging for many NLP developers. Nonetheless, we should be able to extract relevant information from healthcare data using such approaches as NLP.
AI has also been used to provide predictive capabilities to healthcare big data. For example, ML algorithms can convert the diagnostic system of medical images into automated decision-making. Though it is apparent that healthcare professionals may not be replaced by machines in the near future, yet AI can definitely assist physicians to make better clinical decisions or even replace human judgment in certain functional areas of healthcare.
Image analytics
Some of the most widely used imaging techniques in healthcare include computed tomography (CT), magnetic resonance imaging (MRI), X-ray, molecular imaging, ultrasound, photo-acoustic imaging, functional MRI (fMRI), positron emission tomography (PET), electroencephalography (EEG), and mammograms. These techniques capture high definition medical images (patient data) of large sizes. Healthcare professionals like radiologists, doctors and others do an excellent job in analyzing medical data in the form of these files for targeted abnormalities. However, it is also important to acknowledge the lack of specialized professionals for many diseases. In order to compensate for this dearth of professionals, efficient systems like Picture Archiving and Communication System (PACS) have been developed for storing and convenient access to medical image and reports data [ 22 ]. PACSs are popular for delivering images to local workstations, accomplished by protocols such as digital image communication in medicine (DICOM). However, data exchange with a PACS relies on using structured data to retrieve medical images. This by nature misses out on the unstructured information contained in some of the biomedical images. Moreover, it is possible to miss an additional information about a patient’s health status that is present in these images or similar data. A professional focused on diagnosing an unrelated condition might not observe it, especially when the condition is still emerging. To help in such situations, image analytics is making an impact on healthcare by actively extracting disease biomarkers from biomedical images. This approach uses ML and pattern recognition techniques to draw insights from massive volumes of clinical image data to transform the diagnosis, treatment and monitoring of patients. It focuses on enhancing the diagnostic capability of medical imaging for clinical decision-making.
A number of software tools have been developed based on functionalities such as generic, registration, segmentation, visualization, reconstruction, simulation and diffusion to perform medical image analysis in order to dig out the hidden information. For example, Visualization Toolkit is a freely available software which allows powerful processing and analysis of 3D images from medical tests [ 23 ], while SPM can process and analyze 5 different types of brain images (e.g. MRI, fMRI, PET, CT-Scan and EEG) [ 24 ]. Other software like GIMIAS, Elastix, and MITK support all types of images. Various other widely used tools and their features in this domain are listed in Table 1 . Such bioinformatics-based big data analysis may extract greater insights and value from imaging data to boost and support precision medicine projects, clinical decision support tools, and other modes of healthcare. For example, we can also use it to monitor new targeted-treatments for cancer.
Big data from omics
The big data from “omics” studies is a new kind of challenge for the bioinformaticians. Robust algorithms are required to analyze such complex data from biological systems. The ultimate goal is to convert this huge data into an informative knowledge base. The application of bioinformatics approaches to transform the biomedical and genomics data into predictive and preventive health is known as translational bioinformatics. It is at the forefront of data-driven healthcare. Various kinds of quantitative data in healthcare, for example from laboratory measurements, medication data and genomic profiles, can be combined and used to identify new meta-data that can help precision therapies [ 25 ]. This is why emerging new technologies are required to help in analyzing this digital wealth. In fact, highly ambitious multimillion-dollar projects like “ Big Data Research and Development Initiative ” have been launched that aim to enhance the quality of big data tools and techniques for a better organization, efficient access and smart analysis of big data. There are many advantages anticipated from the processing of ‘ omics’ data from large-scale Human Genome Project and other population sequencing projects. In the population sequencing projects like 1000 genomes, the researchers will have access to a marvelous amount of raw data. Similarly, Human Genome Project based Encyclopedia of DNA Elements (ENCODE) project aimed to determine all functional elements in the human genome using bioinformatics approaches. Here, we list some of the widely used bioinformatics-based tools for big data analytics on omics data.
SparkSeq is an efficient and cloud-ready platform based on Apache Spark framework and Hadoop library that is used for analyses of genomic data for interactive genomic data analysis with nucleotide precision
SAMQA identifies errors and ensures the quality of large-scale genomic data. This tool was originally built for the National Institutes of Health Cancer Genome Atlas project to identify and report errors including sequence alignment/map [SAM] format error and empty reads.
ART can simulate profiles of read errors and read lengths for data obtained using high throughput sequencing platforms including SOLiD and Illumina platforms.
DistMap is another toolkit used for distributed short-read mapping based on Hadoop cluster that aims to cover a wider range of sequencing applications. For instance, one of its applications namely the BWA mapper can perform 500 million read pairs in about 6 h, approximately 13 times faster than a conventional single-node mapper.
SeqWare is a query engine based on Apache HBase database system that enables access for large-scale whole-genome datasets by integrating genome browsers and tools.
CloudBurst is a parallel computing model utilized in genome mapping experiments to improve the scalability of reading large sequencing data.
Hydra uses the Hadoop-distributed computing framework for processing large peptide and spectra databases for proteomics datasets. This specific tool is capable of performing 27 billion peptide scorings in less than 60 min on a Hadoop cluster.
BlueSNP is an R package based on Hadoop platform used for genome-wide association studies (GWAS) analysis, primarily aiming on the statistical readouts to obtain significant associations between genotype–phenotype datasets. The efficiency of this tool is estimated to analyze 1000 phenotypes on 10 6 SNPs in 10 4 individuals in a duration of half-an-hour.
Myrna the cloud-based pipeline, provides information on the expression level differences of genes, including read alignments, data normalization, and statistical modeling.
The past few years have witnessed a tremendous increase in disease specific datasets from omics platforms. For example, the ArrayExpress Archive of Functional Genomics data repository contains information from approximately 30,000 experiments and more than one million functional assays. The growing amount of data demands for better and efficient bioinformatics driven packages to analyze and interpret the information obtained. This has also led to the birth of specific tools to analyze such massive amounts of data. Below, we mention some of the most popular commercial platforms for big data analytics.
Commercial platforms for healthcare data analytics
In order to tackle big data challenges and perform smoother analytics, various companies have implemented AI to analyze published results, textual data, and image data to obtain meaningful outcomes. IBM Corporation is one of the biggest and experienced players in this sector to provide healthcare analytics services commercially. IBM’s Watson Health is an AI platform to share and analyze health data among hospitals, providers and researchers. Similarly, Flatiron Health provides technology-oriented services in healthcare analytics specially focused in cancer research. Other big companies such as Oracle Corporation and Google Inc. are also focusing to develop cloud-based storage and distributed computing power platforms. Interestingly, in the recent few years, several companies and start-ups have also emerged to provide health care-based analytics and solutions. Some of the vendors in healthcare sector are provided in Table 2 . Below we discuss a few of these commercial solutions.
Ayasdi is one such big vendor which focuses on ML based methodologies to primarily provide machine intelligence platform along with an application framework with tried & tested enterprise scalability. It provides various applications for healthcare analytics, for example, to understand and manage clinical variation, and to transform clinical care costs. It is also capable of analyzing and managing how hospitals are organized, conversation between doctors, risk-oriented decisions by doctors for treatment, and the care they deliver to patients. It also provides an application for the assessment and management of population health, a proactive strategy that goes beyond traditional risk analysis methodologies. It uses ML intelligence for predicting future risk trajectories, identifying risk drivers, and providing solutions for best outcomes. A strategic illustration of the company’s methodology for analytics is provided in Fig. 4 .

Illustration of application of “Intelligent Application Suite” provided by AYASDI for various analyses such as clinical variation, population health, and risk management in healthcare sector
Linguamatics
It is an NLP based algorithm that relies on an interactive text mining algorithm (I2E). I2E can extract and analyze a wide array of information. Results obtained using this technique are tenfold faster than other tools and does not require expert knowledge for data interpretation. This approach can provide information on genetic relationships and facts from unstructured data. Classical, ML requires well-curated data as input to generate clean and filtered results. However, NLP when integrated in EHR or clinical records per se facilitates the extraction of clean and structured information that often remains hidden in unstructured input data (Fig. 5 ).
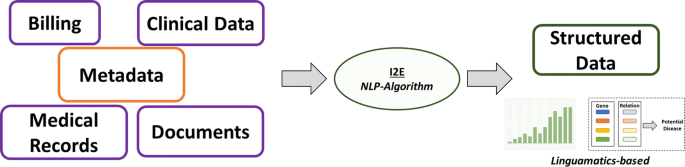
Schematic representation for the working principle of NLP-based AI system used in massive data retention and analysis in Linguamatics
This is one of the unique ideas of the tech-giant IBM that targets big data analytics in almost every professional sector. This platform utilizes ML and AI based algorithms extensively to extract the maximum information from minimal input. IBM Watson enforces the regimen of integrating a wide array of healthcare domains to provide meaningful and structured data (Fig. 6 ). In an attempt to uncover novel drug targets specifically in cancer disease model, IBM Watson and Pfizer have formed a productive collaboration to accelerate the discovery of novel immune-oncology combinations. Combining Watson’s deep learning modules integrated with AI technologies allows the researchers to interpret complex genomic data sets. IBM Watson has been used to predict specific types of cancer based on the gene expression profiles obtained from various large data sets providing signs of multiple druggable targets. IBM Watson is also used in drug discovery programs by integrating curated literature and forming network maps to provide a detailed overview of the molecular landscape in a specific disease model.
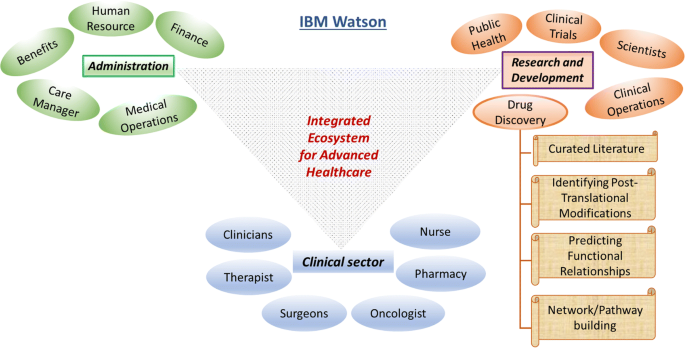
IBM Watson in healthcare data analytics. Schematic representation of the various functional modules in IBM Watson’s big-data healthcare package. For instance, the drug discovery domain involves network of highly coordinated data acquisition and analysis within the spectrum of curating database to building meaningful pathways towards elucidating novel druggable targets
In order to analyze the diversified medical data, healthcare domain, describes analytics in four categories: descriptive, diagnostic, predictive, and prescriptive analytics. Descriptive analytics refers for describing the current medical situations and commenting on that whereas diagnostic analysis explains reasons and factors behind occurrence of certain events, for example, choosing treatment option for a patient based on clustering and decision trees. Predictive analytics focuses on predictive ability of the future outcomes by determining trends and probabilities. These methods are mainly built up of machine leaning techniques and are helpful in the context of understanding complications that a patient can develop. Prescriptive analytics is to perform analysis to propose an action towards optimal decision making. For example, decision of avoiding a given treatment to the patient based on observed side effects and predicted complications. In order to improve performance of the current medical systems integration of big data into healthcare analytics can be a major factor; however, sophisticated strategies need to be developed. An architecture of best practices of different analytics in healthcare domain is required for integrating big data technologies to improve the outcomes. However, there are many challenges associated with the implementation of such strategies.
Challenges associated with healthcare big data
Methods for big data management and analysis are being continuously developed especially for real-time data streaming, capture, aggregation, analytics (using ML and predictive), and visualization solutions that can help integrate a better utilization of EMRs with the healthcare. For example, the EHR adoption rate of federally tested and certified EHR programs in the healthcare sector in the U.S.A. is nearly complete [ 7 ]. However, the availability of hundreds of EHR products certified by the government, each with different clinical terminologies, technical specifications, and functional capabilities has led to difficulties in the interoperability and sharing of data. Nonetheless, we can safely say that the healthcare industry has entered into a ‘post-EMR’ deployment phase. Now, the main objective is to gain actionable insights from these vast amounts of data collected as EMRs. Here, we discuss some of these challenges in brief.
Storing large volume of data is one of the primary challenges, but many organizations are comfortable with data storage on their own premises. It has several advantages like control over security, access, and up-time. However, an on-site server network can be expensive to scale and difficult to maintain. It appears that with decreasing costs and increasing reliability, the cloud-based storage using IT infrastructure is a better option which most of the healthcare organizations have opted for. Organizations must choose cloud-partners that understand the importance of healthcare-specific compliance and security issues. Additionally, cloud storage offers lower up-front costs, nimble disaster recovery, and easier expansion. Organizations can also have a hybrid approach to their data storage programs, which may be the most flexible and workable approach for providers with varying data access and storage needs.
The data needs to cleansed or scrubbed to ensure the accuracy, correctness, consistency, relevancy, and purity after acquisition. This cleaning process can be manual or automatized using logic rules to ensure high levels of accuracy and integrity. More sophisticated and precise tools use machine-learning techniques to reduce time and expenses and to stop foul data from derailing big data projects.
Unified format
Patients produce a huge volume of data that is not easy to capture with traditional EHR format, as it is knotty and not easily manageable. It is too difficult to handle big data especially when it comes without a perfect data organization to the healthcare providers. A need to codify all the clinically relevant information surfaced for the purpose of claims, billing purposes, and clinical analytics. Therefore, medical coding systems like Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) code sets were developed to represent the core clinical concepts. However, these code sets have their own limitations.
Some studies have observed that the reporting of patient data into EMRs or EHRs is not entirely accurate yet [ 26 , 27 , 28 , 29 ], probably because of poor EHR utility, complex workflows, and a broken understanding of why big data is all-important to capture well. All these factors can contribute to the quality issues for big data all along its lifecycle. The EHRs intend to improve the quality and communication of data in clinical workflows though reports indicate discrepancies in these contexts. The documentation quality might improve by using self-report questionnaires from patients for their symptoms.
Image pre-processing
Studies have observed various physical factors that can lead to altered data quality and misinterpretations from existing medical records [ 30 ]. Medical images often suffer technical barriers that involve multiple types of noise and artifacts. Improper handling of medical images can also cause tampering of images for instance might lead to delineation of anatomical structures such as veins which is non-correlative with real case scenario. Reduction of noise, clearing artifacts, adjusting contrast of acquired images and image quality adjustment post mishandling are some of the measures that can be implemented to benefit the purpose.
There have been many security breaches, hackings, phishing attacks, and ransomware episodes that data security is a priority for healthcare organizations. After noticing an array of vulnerabilities, a list of technical safeguards was developed for the protected health information (PHI). These rules, termed as HIPAA Security Rules, help guide organizations with storing, transmission, authentication protocols, and controls over access, integrity, and auditing. Common security measures like using up-to-date anti-virus software, firewalls, encrypting sensitive data, and multi-factor authentication can save a lot of trouble.
To have a successful data governance plan, it would be mandatory to have complete, accurate, and up-to-date metadata regarding all the stored data. The metadata would be composed of information like time of creation, purpose and person responsible for the data, previous usage (by who, why, how, and when) for researchers and data analysts. This would allow analysts to replicate previous queries and help later scientific studies and accurate benchmarking. This increases the usefulness of data and prevents creation of “data dumpsters” of low or no use.
Metadata would make it easier for organizations to query their data and get some answers. However, in absence of proper interoperability between datasets the query tools may not access an entire repository of data. Also, different components of a dataset should be well interconnected or linked and easily accessible otherwise a complete portrait of an individual patient’s health may not be generated. Medical coding systems like ICD-10, SNOMED-CT, or LOINC must be implemented to reduce free-form concepts into a shared ontology. If the accuracy, completeness, and standardization of the data are not in question, then Structured Query Language (SQL) can be used to query large datasets and relational databases.
Visualization
A clean and engaging visualization of data with charts, heat maps, and histograms to illustrate contrasting figures and correct labeling of information to reduce potential confusion, can make it much easier for us to absorb information and use it appropriately. Other examples include bar charts, pie charts, and scatterplots with their own specific ways to convey the data.
Data sharing
Patients may or may not receive their care at multiple locations. In the former case, sharing data with other healthcare organizations would be essential. During such sharing, if the data is not interoperable then data movement between disparate organizations could be severely curtailed. This could be due to technical and organizational barriers. This may leave clinicians without key information for making decisions regarding follow-ups and treatment strategies for patients. Solutions like Fast Healthcare Interoperability Resource (FHIR) and public APIs, CommonWell (a not-for-profit trade association) and Carequality (a consensus-built, common interoperability framework) are making data interoperability and sharing easy and secure. The biggest roadblock for data sharing is the treatment of data as a commodity that can provide a competitive advantage. Therefore, sometimes both providers and vendors intentionally interfere with the flow of information to block the information flow between different EHR systems [ 31 ].
The healthcare providers will need to overcome every challenge on this list and more to develop a big data exchange ecosystem that provides trustworthy, timely, and meaningful information by connecting all members of the care continuum. Time, commitment, funding, and communication would be required before these challenges are overcome.
Big data analytics for cutting costs
To develop a healthcare system based on big data that can exchange big data and provides us with trustworthy, timely, and meaningful information, we need to overcome every challenge mentioned above. Overcoming these challenges would require investment in terms of time, funding, and commitment. However, like other technological advances, the success of these ambitious steps would apparently ease the present burdens on healthcare especially in terms of costs. It is believed that the implementation of big data analytics by healthcare organizations might lead to a saving of over 25% in annual costs in the coming years. Better diagnosis and disease predictions by big data analytics can enable cost reduction by decreasing the hospital readmission rate. The healthcare firms do not understand the variables responsible for readmissions well enough. It would be easier for healthcare organizations to improve their protocols for dealing with patients and prevent readmission by determining these relationships well. Big data analytics can also help in optimizing staffing, forecasting operating room demands, streamlining patient care, and improving the pharmaceutical supply chain. All of these factors will lead to an ultimate reduction in the healthcare costs by the organizations.
Quantum mechanics and big data analysis
Big data sets can be staggering in size. Therefore, its analysis remains daunting even with the most powerful modern computers. For most of the analysis, the bottleneck lies in the computer’s ability to access its memory and not in the processor [ 32 , 33 ]. The capacity, bandwidth or latency requirements of memory hierarchy outweigh the computational requirements so much that supercomputers are increasingly used for big data analysis [ 34 , 35 ]. An additional solution is the application of quantum approach for big data analysis.
Quantum computing and its advantages
The common digital computing uses binary digits to code for the data whereas quantum computation uses quantum bits or qubits [ 36 ]. A qubit is a quantum version of the classical binary bits that can represent a zero, a one, or any linear combination of states (called superpositions ) of those two qubit states [ 37 ]. Therefore, qubits allow computer bits to operate in three states compared to two states in the classical computation. This allows quantum computers to work thousands of times faster than regular computers. For example, a conventional analysis of a dataset with n points would require 2 n processing units whereas it would require just n quantum bits using a quantum computer. Quantum computers use quantum mechanical phenomena like superposition and quantum entanglement to perform computations [ 38 , 39 ].
Quantum algorithms can speed-up the big data analysis exponentially [ 40 ]. Some complex problems, believed to be unsolvable using conventional computing, can be solved by quantum approaches. For example, the current encryption techniques such as RSA, public-key (PK) and Data Encryption Standard (DES) which are thought to be impassable now would be irrelevant in future because quantum computers will quickly get through them [ 41 ]. Quantum approaches can dramatically reduce the information required for big data analysis. For example, quantum theory can maximize the distinguishability between a multilayer network using a minimum number of layers [ 42 ]. In addition, quantum approaches require a relatively small dataset to obtain a maximally sensitive data analysis compared to the conventional (machine-learning) techniques. Therefore, quantum approaches can drastically reduce the amount of computational power required to analyze big data. Even though, quantum computing is still in its infancy and presents many open challenges, it is being implemented for healthcare data.
Applications in big data analysis
Quantum computing is picking up and seems to be a potential solution for big data analysis. For example, identification of rare events, such as the production of Higgs bosons at the Large Hadron Collider (LHC) can now be performed using quantum approaches [ 43 ]. At LHC, huge amounts of collision data (1PB/s) is generated that needs to be filtered and analyzed. One such approach, the quantum annealing for ML (QAML) that implements a combination of ML and quantum computing with a programmable quantum annealer, helps reduce human intervention and increase the accuracy of assessing particle-collision data. In another example, the quantum support vector machine was implemented for both training and classification stages to classify new data [ 44 ]. Such quantum approaches could find applications in many areas of science [ 43 ]. Indeed, recurrent quantum neural network (RQNN) was implemented to increase signal separability in electroencephalogram (EEG) signals [ 45 ]. Similarly, quantum annealing was applied to intensity modulated radiotherapy (IMRT) beamlet intensity optimization [ 46 ]. Similarly, there exist more applications of quantum approaches regarding healthcare e.g. quantum sensors and quantum microscopes [ 47 ].
Conclusions and future prospects
Nowadays, various biomedical and healthcare tools such as genomics, mobile biometric sensors, and smartphone apps generate a big amount of data. Therefore, it is mandatory for us to know about and assess that can be achieved using this data. For example, the analysis of such data can provide further insights in terms of procedural, technical, medical and other types of improvements in healthcare. After a review of these healthcare procedures, it appears that the full potential of patient-specific medical specialty or personalized medicine is under way. The collective big data analysis of EHRs, EMRs and other medical data is continuously helping build a better prognostic framework. The companies providing service for healthcare analytics and clinical transformation are indeed contributing towards better and effective outcome. Common goals of these companies include reducing cost of analytics, developing effective Clinical Decision Support (CDS) systems, providing platforms for better treatment strategies, and identifying and preventing fraud associated with big data. Though, almost all of them face challenges on federal issues like how private data is handled, shared and kept safe. The combined pool of data from healthcare organizations and biomedical researchers have resulted in a better outlook, determination, and treatment of various diseases. This has also helped in building a better and healthier personalized healthcare framework. Modern healthcare fraternity has realized the potential of big data and therefore, have implemented big data analytics in healthcare and clinical practices. Supercomputers to quantum computers are helping in extracting meaningful information from big data in dramatically reduced time periods. With high hopes of extracting new and actionable knowledge that can improve the present status of healthcare services, researchers are plunging into biomedical big data despite the infrastructure challenges. Clinical trials, analysis of pharmacy and insurance claims together, discovery of biomarkers is a part of a novel and creative way to analyze healthcare big data.
Big data analytics leverage the gap within structured and unstructured data sources. The shift to an integrated data environment is a well-known hurdle to overcome. Interesting enough, the principle of big data heavily relies on the idea of the more the information, the more insights one can gain from this information and can make predictions for future events. It is rightfully projected by various reliable consulting firms and health care companies that the big data healthcare market is poised to grow at an exponential rate. However, in a short span we have witnessed a spectrum of analytics currently in use that have shown significant impacts on the decision making and performance of healthcare industry. The exponential growth of medical data from various domains has forced computational experts to design innovative strategies to analyze and interpret such enormous amount of data within a given timeframe. The integration of computational systems for signal processing from both research and practicing medical professionals has witnessed growth. Thus, developing a detailed model of a human body by combining physiological data and “-omics” techniques can be the next big target. This unique idea can enhance our knowledge of disease conditions and possibly help in the development of novel diagnostic tools. The continuous rise in available genomic data including inherent hidden errors from experiment and analytical practices need further attention. However, there are opportunities in each step of this extensive process to introduce systemic improvements within the healthcare research.
High volume of medical data collected across heterogeneous platforms has put a challenge to data scientists for careful integration and implementation. It is therefore suggested that revolution in healthcare is further needed to group together bioinformatics, health informatics and analytics to promote personalized and more effective treatments. Furthermore, new strategies and technologies should be developed to understand the nature (structured, semi-structured, unstructured), complexity (dimensions and attributes) and volume of the data to derive meaningful information. The greatest asset of big data lies in its limitless possibilities. The birth and integration of big data within the past few years has brought substantial advancements in the health care sector ranging from medical data management to drug discovery programs for complex human diseases including cancer and neurodegenerative disorders. To quote a simple example supporting the stated idea, since the late 2000′s the healthcare market has witnessed advancements in the EHR system in the context of data collection, management and usability. We believe that big data will add-on and bolster the existing pipeline of healthcare advances instead of replacing skilled manpower, subject knowledge experts and intellectuals, a notion argued by many. One can clearly see the transitions of health care market from a wider volume base to personalized or individual specific domain. Therefore, it is essential for technologists and professionals to understand this evolving situation. In the coming year it can be projected that big data analytics will march towards a predictive system. This would mean prediction of futuristic outcomes in an individual’s health state based on current or existing data (such as EHR-based and Omics-based). Similarly, it can also be presumed that structured information obtained from a certain geography might lead to generation of population health information. Taken together, big data will facilitate healthcare by introducing prediction of epidemics (in relation to population health), providing early warnings of disease conditions, and helping in the discovery of novel biomarkers and intelligent therapeutic intervention strategies for an improved quality of life.
Availability of data and materials
Not applicable.
Laney D. 3D data management: controlling data volume, velocity, and variety, Application delivery strategies. Stamford: META Group Inc; 2001.
Google Scholar
Mauro AD, Greco M, Grimaldi M. A formal definition of big data based on its essential features. Libr Rev. 2016;65(3):122–35.
Article Google Scholar
Gubbi J, et al. Internet of Things (IoT): a vision, architectural elements, and future directions. Future Gener Comput Syst. 2013;29(7):1645–60.
Doyle-Lindrud S. The evolution of the electronic health record. Clin J Oncol Nurs. 2015;19(2):153–4.
Gillum RF. From papyrus to the electronic tablet: a brief history of the clinical medical record with lessons for the digital Age. Am J Med. 2013;126(10):853–7.
Reiser SJ. The clinical record in medicine part 1: learning from cases*. Ann Intern Med. 1991;114(10):902–7.
Reisman M. EHRs: the challenge of making electronic data usable and interoperable. Pharm Ther. 2017;42(9):572–5.
Murphy G, Hanken MA, Waters K. Electronic health records: changing the vision. Philadelphia: Saunders W B Co; 1999. p. 627.
Shameer K, et al. Translational bioinformatics in the era of real-time biomedical, health care and wellness data streams. Brief Bioinform. 2017;18(1):105–24.
Service, R.F. The race for the $1000 genome. Science. 2006;311(5767):1544–6.
Stephens ZD, et al. Big data: astronomical or genomical? PLoS Biol. 2015;13(7):e1002195.
Yin Y, et al. The internet of things in healthcare: an overview. J Ind Inf Integr. 2016;1:3–13.
Moore SK. Unhooking medicine [wireless networking]. IEEE Spectr 2001; 38(1): 107–8, 110.
MathSciNet Google Scholar
Nasi G, Cucciniello M, Guerrazzi C. The role of mobile technologies in health care processes: the case of cancer supportive care. J Med Internet Res. 2015;17(2):e26.
Apple, ResearchKit/ResearchKit: ResearchKit 1.5.3. 2017.
Shvachko K, et al. The hadoop distributed file system. In: Proceedings of the 2010 IEEE 26th symposium on mass storage systems and technologies (MSST). New York: IEEE Computer Society; 2010. p. 1–10.
Dean J, Ghemawat S. MapReduce: simplified data processing on large clusters. Commun ACM. 2008;51(1):107–13.
Zaharia M, et al. Apache Spark: a unified engine for big data processing. Commun ACM. 2016;59(11):56–65.
Gopalani S, Arora R. Comparing Apache Spark and Map Reduce with performance analysis using K-means; 2015.
Ahmed H, et al. Performance comparison of spark clusters configured conventionally and a cloud servicE. Procedia Comput Sci. 2016;82:99–106.
Saouabi M, Ezzati A. A comparative between hadoop mapreduce and apache Spark on HDFS. In: Proceedings of the 1st international conference on internet of things and machine learning. Liverpool: ACM; 2017. p. 1–4.
Strickland NH. PACS (picture archiving and communication systems): filmless radiology. Arch Dis Child. 2000;83(1):82–6.
Article MathSciNet Google Scholar
Schroeder W, Martin K, Lorensen B. The visualization toolkit. 4th ed. Clifton Park: Kitware; 2006.
Friston K, et al. Statistical parametric mapping. London: Academic Press; 2007. p. vii.
Li L, et al. Identification of type 2 diabetes subgroups through topological analysis of patient similarity. Sci Transl Med. 2015;7(311):311ra174.
Valikodath NG, et al. Agreement of ocular symptom reporting between patient-reported outcomes and medical records. JAMA Ophthalmol. 2017;135(3):225–31.
Fromme EK, et al. How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J Clin Oncol. 2004;22(17):3485–90.
Beckles GL, et al. Agreement between self-reports and medical records was only fair in a cross-sectional study of performance of annual eye examinations among adults with diabetes in managed care. Med Care. 2007;45(9):876–83.
Echaiz JF, et al. Low correlation between self-report and medical record documentation of urinary tract infection symptoms. Am J Infect Control. 2015;43(9):983–6.
Belle A, et al. Big data analytics in healthcare. Biomed Res Int. 2015;2015:370194.
Adler-Milstein J, Pfeifer E. Information blocking: is it occurring and what policy strategies can address it? Milbank Q. 2017;95(1):117–35.
Or-Bach, Z. A 1,000x improvement in computer systems by bridging the processor-memory gap. In: 2017 IEEE SOI-3D-subthreshold microelectronics technology unified conference (S3S). 2017.
Mahapatra NR, Venkatrao B. The processor-memory bottleneck: problems and solutions. XRDS. 1999;5(3es):2.
Voronin AA, Panchenko VY, Zheltikov AM. Supercomputations and big-data analysis in strong-field ultrafast optical physics: filamentation of high-peak-power ultrashort laser pulses. Laser Phys Lett. 2016;13(6):065403.
Dollas, A. Big data processing with FPGA supercomputers: opportunities and challenges. In: 2014 IEEE computer society annual symposium on VLSI; 2014.
Saffman M. Quantum computing with atomic qubits and Rydberg interactions: progress and challenges. J Phys B: At Mol Opt Phys. 2016;49(20):202001.
Nielsen MA, Chuang IL. Quantum computation and quantum information. 10th anniversary ed. Cambridge: Cambridge University Press; 2011. p. 708.
Raychev N. Quantum computing models for algebraic applications. Int J Scientific Eng Res. 2015;6(8):1281–8.
Harrow A. Why now is the right time to study quantum computing. XRDS. 2012;18(3):32–7.
Lloyd S, Garnerone S, Zanardi P. Quantum algorithms for topological and geometric analysis of data. Nat Commun. 2016;7:10138.
Buchanan W, Woodward A. Will quantum computers be the end of public key encryption? J Cyber Secur Technol. 2017;1(1):1–22.
De Domenico M, et al. Structural reducibility of multilayer networks. Nat Commun. 2015;6:6864.
Mott A, et al. Solving a Higgs optimization problem with quantum annealing for machine learning. Nature. 2017;550:375.
Rebentrost P, Mohseni M, Lloyd S. Quantum support vector machine for big data classification. Phys Rev Lett. 2014;113(13):130503.
Gandhi V, et al. Quantum neural network-based EEG filtering for a brain-computer interface. IEEE Trans Neural Netw Learn Syst. 2014;25(2):278–88.
Nazareth DP, Spaans JD. First application of quantum annealing to IMRT beamlet intensity optimization. Phys Med Biol. 2015;60(10):4137–48.
Reardon S. Quantum microscope offers MRI for molecules. Nature. 2017;543(7644):162.
Download references
Acknowledgements
Author information.
Sabyasachi Dash and Sushil Kumar Shakyawar contributed equally to this work
Authors and Affiliations
Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, 10065, NY, USA
Sabyasachi Dash
Center of Biological Engineering, University of Minho, Campus de Gualtar, 4710-057, Braga, Portugal
Sushil Kumar Shakyawar
SilicoLife Lda, Rua do Canastreiro 15, 4715-387, Braga, Portugal
Postgraduate School for Molecular Medicine, Warszawskiego Uniwersytetu Medycznego, Warsaw, Poland
Mohit Sharma
Małopolska Centre for Biotechnology, Jagiellonian University, Kraków, Poland
3B’s Research Group, Headquarters of the European Institute of Excellence on Tissue Engineering and Regenerative Medicine, AvePark - Parque de Ciência e Tecnologia, Zona Industrial da Gandra, Barco, 4805-017, Guimarães, Portugal
Sandeep Kaushik
You can also search for this author in PubMed Google Scholar
Contributions
MS wrote the manuscript. SD and SKS further added significant discussion that highly improved the quality of manuscript. SK designed the content sequence, guided SD, SS and MS in writing and revising the manuscript and checked the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sandeep Kaushik .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Dash, S., Shakyawar, S.K., Sharma, M. et al. Big data in healthcare: management, analysis and future prospects. J Big Data 6 , 54 (2019). https://doi.org/10.1186/s40537-019-0217-0
Download citation
Received : 17 January 2019
Accepted : 06 June 2019
Published : 19 June 2019
DOI : https://doi.org/10.1186/s40537-019-0217-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biomedical research
- Big data analytics
- Internet of things
- Personalized medicine
- Quantum computing
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Public Health Res
- v.12(3); 2023 Jul
- PMC10345816

Impact of COVID-19 on healthcare system in India: A systematic review
Megha kapoor.
1 Laboratory of Disease Dynamics & Molecular Epidemiology, Amity Institute of Public Health, Amity University, Noida, Uttar Pradesh, India
Karuna Nidhi Kaur
Shazina saeed.
2 Amity Institute of Public Health, Amity University, Uttar Pradesh, Noida, India
Mohd Shannawaz
Amrish chandra.
Despite an extensive healthcare system in India, the COVID-19 Pandemic created havoc upon the existing Indian healthcare system by disrupting the supply of essential healthcare services to patients. It has also highlighted the significant-quality discrepancies of healthcare facilities between the rural-urban areas and between public and private healthcare providers. The not so advanced healthcare system of India was exposed through the lack of oxygen and essential drugs required for the treatment of COVID-19. Additionally, during the pandemic period there was a drastic decline in seeking non-COVID-19 disease related healthcare services. The objective of this systematic review is to determine whether COVID-19 has impacted the healthcare system in India.
Introduction
India, the second most populous country in the world has been severely impacted by the ongoing COVID-19 pandemic since it’s emergence. COVID-19 has impacted every sector in the country including healthcare. Indian healthcare system crumbled under the massive burden of the global pandemic highlighting the gaps and challenges in the existing health delivery system.
COVID-19 or Coronavirus is an upper respiratory tract infection of high virulence. It was formerly known as ‘2019-nCoV’ and is caused by the SARS-CoV-2 virus. 1 It first originated from Wuhan city, Central Hubei province of China in December 2019. Several clusters of patients with viral pneumonia of unknown origin were reported to be epidemiologically associated with the Hunan seafood market, Wuhan, China. 2 Soon, cases of pneumonia were reported in other parts of the world as it spread rapidly crossing the borders of China. A massive number of people started losing their lives in China and following its spread to other countries; it was declared a public health emergency of international concern on 30th January 2020 by World Health Organization (WHO). After more than 118,000 cases in 114 countries, and 4291 people lost their lives, COVID-19 was declared as a pandemic by World Health Organization (WHO) on 11th march 2020. 3 As the countries continued to struggle with a lack of resources and capacity the viral outbreak spread rapidly worldwide, infecting millions of people all across the globe including India.
Those infected with Coronavirus disease (COVID-19) exhibit a varying range of symptoms ranging from mild to moderate. It affects people of all ages; however, the risk of serious infection increases with advancing age. Patients infected with coronavirus disease and presenting with pre-existing co-morbidities such as diabetes, asthma and cardiovascular diseases (CVDs) are more vulnerable to experiencing unfavourable outcomes or experiencing death.
A healthy individual can acquire COVID-19 infection directly by coming in close contact with an infected individual through the droplets emitted during sneezing or coughing. It can also be transmitted indirectly after coming in contact with contaminated surfaces such as door knobs. It affects every individual differently with cough, fever, sore throat, tiredness and lethargy being the most common symptoms of the illness. Individuals can also develop few lesser common symptoms such as loss of taste, diarrhoea, irritation of the eyes and rash on the skin among others. An individual can develop shortness of breath or experience difficulty in breathing and requires urgent medical attention. These symptoms may take 4–5 days to appear after coming in contact with a virus or as long as 14 days and can also be asymptomatic.
The first wave
In India, the first case of COVID-19 infection was reported on 27TH January 2020, when a 20 year old female with a travel history of China presented with a sore throat and dry cough in the emergency department of General Hospital, Thrissur, Kerala. 4 Since then, COVID-19 has taken a serious toll in India and worldwide. To prevent the spread of COVID-19 infection, the Government of India announced a nationwide lockdown for 21 days on 24 March 2020, which was further extended. It was not until 30th May, that the government uplifted the restrictions in an ‘unlock’ phase-wise manner. Throughout, national advisories were generated and the norm of ‘social distancing’ and ‘work from home was introduced. People were advised to practise social distancing, wear masks and avoid going out unnecessarily and only people of ‘essential services such as doctors, nurses, police and home services were exempted. These preventive measures allowed the Indian Healthcare delivery system to prepare for the pandemic. These measures stopped the further spread of COVID-19 infection and the efforts of the Indian Government to contain the viral spread were applauded internationally. India has experienced three COVID-19 pandemic waves till now with a massive surge during the second wave in March 2021. 5
The second wave and Indian healthcare system
The first wave had a low infectivity rate since the lockdown was imposed and individuals practised social distancing. Therefore, it largely affected the economy and livelihoods of Indians without any serious implications on the healthcare system. However, during march 2021, the country witnessed the most dangerous second wave that created havoc as individuals started taking preventive measures more casually due to ‘pandemic fatigue’. This was characterized by an increasing number of cases between 25 and 50 years of age, a shortage of essential medicine and equipment, and medical professionals. 6 Indian healthcare system failed to meet daily oxygen demand, Intensive Care Units (ICU) beds and oxygen beds due to which many hospitals had to turn the patients away, resulting in higher mortality rates. This lead to the disruption of routine immunization procedures, and treatment of Non-communicable and communicable diseases. 7 This revealed the overstretched and overburdened existing Indian Healthcare system. This also highlighted the failing healthcare management system and lacking public health system and efficient healthcare models in India. The Indian government failed to respond to the second wave effectively unlike the first wave.
The third wave of COVID-19 in India
With the emergence of the new Omicron variant of SARS-CoV2, the cases increased in January 2022. 8 The majority of the cases were asymptomatic or mildly symptomatic. With increased administration of the COVID-19 vaccine, the patients admitted in ICU were mostly unvaccinated or with pre-existing co-morbidities. The demand for hospital beds, oxygen beds and ventilators were low and mostly remained unoccupied.
The third wave was different from the first two waves due to various factors such as low virulence of the omicron variant despite high transmissibility and administration of either single or both doses of COVID—19 vaccine to the adult population, authenticating the effectiveness of the vaccine.
Therefore, the COVID-19 pandemic has significantly disrupted the healthcare systems in India. Hence, this review aims to describe the impact of COVID-19 on the healthcare system concerning the patient visit and reception of treatment, diagnostic tests done and referral services in India. It is necessary to conduct this review as it will aid in developing new healthcare models in order to manage the COVID-19 pandemic at present and prevent any further waves from arising in the future.
Health care system in India
A sound and effective healthcare system enable the country to respond to a pandemic efficiently by overcoming the challenges and barriers encountered in providing healthcare.
The Indian healthcare system is a mixed framework, including both public and private healthcare service providers. However, a large proportion of private healthcare providers are present in urban India, providing, secondary and tertiary healthcare services. 9
The objective of this systematic review is to determine the impact of the COVID-19 pandemic on the healthcare system in India.
Rationale: The rationale for this study is to investigate the impact of the COVID-19 pandemic on the healthcare system in India, considering the challenges, gaps and disruptions experienced during this global health crisis.
Material and methods
Study design.
This systematic review was conducted on the available online published studies in high-quality journals related to COVID-19 impact on healthcare services in India.
Search strategy
A thorough extensive literature search was conducted between 14 February 2022 and 20 February 2022 on the electronic database ‘PubMed’ for quality studies published between time period 2019 and 2022 using the search strategy (impact) AND (COVID-19) AND (healthcare system) OR (Primary Health centre)) OR (secondary health centre)) OR (community health centre)) OR (tertiary health centre))) OR (hospital)) OR (government)) OR (private)) AND (India).
The following keywords and Medical Subject Headings (MeSH) entries were used:
COVID-19, healthcare system, India.
Studies that met the eligibility criteria were selected based on the inclusion and exclusion criteria after screening the database for this systematic review.
Inclusion and exclusion criteria
This systematic review included the studies conducted in the English language during the COVID-19 Pandemic assessing the healthcare system in India. Studies involving outpatient clinics visit, hospital admissions, diagnostic tests done, minor and major surgeries and case referrals were also included.
Studies which were conducted in private clinics & not involving government, primary, secondary and tertiary centres, along with the studies conducted on the physical & mental health status of healthcare providers through surveys were excluded as shown in Table 1 .
Summary of excluded studies.
| S No. | Criteria for exclusion | Authors | Study summary |
|---|---|---|---|
| 1 | Study determining the experience of teleconsultations in Indian hospital during COVID-19 lockdown. | Ravindran et al., 2021 | This study provided 977 free of cost teleconsultation to the patients ensuring continuity of treatment and medicinal prescriptions were provided to the patients and WhatsApp was preferred modality for communication. |
| 2 | Study to determine effects of COVID-19 on maternal health and complications due to delayed obstetric care. | Goyal et al., 2020 | This study was conducted on pregnant women to determine various complications due to delay in seeking obstetric care. |
| 3. | Study to determine impact of COVID-19 lockdown on health services, physical, mental and social well-being of population | Raman et al., 2021 | This study concluded negative impact between health variables, depression, depression, social loneliness with various lockdown stages. |
| 4. | Study to determine association between psychological association and physical symptoms among healthcare workers during COVID-19 breakout. | Chew et al., 2020 | 906 healthcare workers were evaluated, and significant association was found between physical symptoms and psychological outcomes of depression, anxiety, stress, post-traumatic stress disorder (PTSD) during COVID-19 outbreak. |
| 5. | Study to determine stress levels among healthcare workers during COVID-19 | Wadasadawala et al., 2021 | A survey conducted on 758 healthcare workers during COVID-19 Pandemic revealed significant levels of anxiety, depression and stress among them. |
| 6. | Study to determine mental health and quality of life among Indian healthcare professionals during Covid-19 pandemic. | Suryavanshi et al., 2020 | This study was conducted on 197 Indian Healthcare Professionals during COVID −19 pandemic and concluded a high prevalence of symptoms of depression and anxiety and low Quality of life among them. |
| 7. | Study to determine mental health status of healthcare workers during COVID-19 outbreak. | Sil et al., 2020 | This study was conducted through online semi structured questionnaire on front line dermatologists during COVID-19 outbreak and concluded significant prevalence of symptoms of depression and stress among them. |
| 8. | Study to evaluate mental health status of Indian front-line doctors during COVID −19 pandemic. | Das et al., 2020 | This study evaluated 422 responses and concluded significant prevalence of symptoms of depression and stress among frontline COVID-19 doctors. |
| 9. | Study to determine health status of healthcare workers due to long working hours, repeated exposure to COVID-19 infection, stress and fatigue. | Banerjee et al., 2020 | This study concluded that out of 274 healthcare workers, 75 were found to be positive for SARS-CoV2, and they are at higher risk for being to COVID-19 infection. |
Data extraction
After completion of the initial screening process, a total of seven articles were selected to be included in this systematic review. The study selection process is illustrated in Figure 1 , representing the PRISMA (Preferred reporting items for systematic reviews and meta-analysis) flow diagram for this systematic review.

PRISMA flow diagram of the systematic search.
From the selected articles following data was extracted by preparing an MS Excel spreadsheet: title of the study, study objectives, study methodology and conclusion.
Table 2 shows the summary of all the included articles in this systematic review.
Summary of included studies.
| S. No. | Title of the study | Link of the study | Objective of the study | Study design | Major findings | Conclusion |
|---|---|---|---|---|---|---|
| Impact of COVID-19 on cancer care in India: a cohort study | To determine how COVID-19 has impacted cancer care in India | Ambidirectional cohort study | Reduction in new patient registration, follow up visits, chemotherapy, major surgeries, radiotherapy, reduction in pathological and radiological diagnostic tests, palliative care referrals between March 1 and 31 may 2020. | The cancer care services have been affected in India during pandemic when compared from between March 1 and May 2020 with 2019. | ||
| The Impact of COVID-19 Pandemic on Nephrology and Transplant Services and Clinical Training in India | to determine the effects of the COVID-19 on nephrology and transplant services and clinical training at the Institute of Kidney Disease and Research Centre (Ahmedabad, India) | Prospective observational study | • There was reduction in the number of outpatients and inpatients in 2020 during pandemic compared with data from 2019. • Reduction in patients undergoing following-haemodialysis, renal transplant, nonelective procedures | Pandemic has affected the nephrology and transplant services | ||
| Impact of nationwide lockdown on cancer care during COVID-19 pandemic: A retrospective analysis from western India | Impact of nationwide lockdown on cancer care during COVID-19 pandemic: A retrospective analysis from western India – ScienceDirect | To determine the effects of COVID-19 pandemic on Cancer patients in receiving treatment and patient visits for cancer care at Gujarat Cancer and Research Institute | Retrospective observational study | • Conducted pre-lockdown and during lockdown (from January to May 2020) • Reduced patient visits of patients during lockdown. • Chemotherapy was most received treatment by the patients. • Reduction in overall treatment received by the patients. | During the pandemic lockdown negatively impacted the care of cancer patients in terms of visits and treatment received. | |
| Impact of COVID-19 pandemic, national lockdown and unlocking on an apex tertiary care ophthalmic institute | | Determine the impact of COVID-19 pandemic, national lockdown, and unlocking on ophthalmic care provided by the government-funded apex health institute of India in March 23, 2020, to July 15, 2020, compared with that from March 23, 2019, to July 15, 2019. | Retrospective observational study | • During the lockdown period routine outpatient flow reduced, Emergency services decreased, • Mechanical trauma, microbial keratitis, and conjunctivitis were the most common reported presentations, • The number of donor corneas collected and emergency therapeutic keratoplasties performed also reduced routine patient consultations were significantly lower than of last year during unlocking phase. | • COVID-19 pandemic and national lockdown impacted the delivery of ophthalmic care by the apex-ophthalmic institute severely. • lifting of pandemic associated lockdown did not improve patient inflow. | |
| Impact of COVID-19 on the practice of orthopaedics and trauma – an epidemiological study of the full pandemic year of a tertiary care centre of New Delhi | To Determine the impact of COVID-19 pandemic on the clinical practice of trauma and orthopaedics, in a tertiary care hospital of New Delhi, by collecting the hospital data for 2019 and 2020 and analysing it after comparing. | Observational study | • Reduction in outpatient attendance, admission, surgery procedures. • Reduction in arthroplasty surgery, paediatric orthopaedic cases, and spinal surgery | during the lockdown period, orthopaedics and trauma’s clinical practice saw a reduction in the outpatients, admissions, and surgery. | ||
| Impact of COVID-19-related lockdown-I on a network of rural eye centres in Southern India | To define the demographic profile and ocular disorders from 20 rural eye centres during lockdown-I and its comparison with the pre-lockdown period in the era of pandemic. | A retrospective cross-sectional observational study | • As compared to the pre-lockdown, during lockdown-I, the patient visits were higher in cornea and anterior segment • During lockdown-I, the number of patients reduced compared to pre-pandemic period. | Lockdown-I severely impacted the eye patient care in rural areas. | ||
| Impact of COVID-19 pandemic and national lockdown on ocular trauma at a tertiary eye care institute | To determine the impact of COVID-19 pandemic and national lockdown on the demographic profile and clinical profile of patients presenting with ocular trauma in a tertiary eye care institute. | A retrospective, hospital-based, comparative study | After the lockdown was announced, no patient presented to the emergency department in the initial 1-week period. But, the no of patients increased gradually over months. | During the COVID-19 pandemic, there was a decline in the number of patients with ocular trauma. |
According to the objective of this systematic review the results described based upon the Impact of the COVID-19 Pandemic on the health care system in India on various parameters – number of outpatients, number of inpatients, number of patients undergoing minor and major surgeries, emergency trauma cases, patients undergoing nonurgent elective procedures.
Impact of COVID-19 on cancer care in India
From the seven included articles in this review, two articles described the disrupted oncology services in India by comparing these before and during the pandemic. A cohort study to describe the impact of COVID-19 on cancer care in India compared the oncology services provisions by cancer patients between 01 March 2020 and 01 March 2020 with similar duration for 2019 and concluded that there was a 54% reduction in new patient registration, 46% reduction in patient follow-up visit, 36% reduction in hospital admissions, 37% reduction in outpatient chemotherapy, 49% reduction in number of major surgeries, 52% reduction in minor surgeries, 23% reduction in patients accessing radiotherapy, 38% reduction in pathological diagnostic testing, 43% reduction in radiological diagnostic tests and 29% reduction in palliative care referrals. It also found that there was more reduction of oncology services for larger metro cities than smaller cities. 10 Another study, A retrospective analysis from western India determining the impact of the COVID-19 lockdown on Cancer care stated reduced patient visits and number of treatments received during the lockdown with chemotherapy being the most common treatment received. 11
Impact of COVID-19 on nephrology services in India
Only one study out of the seven included studies described the impact of the COVID-19 pandemic on nephrology and transplant services at a tertiary care centre, in Ahmedabad, India. The study concluded that there was significant reduction in a number of outpatients and inpatients between April 2020 and June 2020 when compared with a similar duration in 2019 almost by 50%. There was also a reduction in donor transplants, haemodialysis and nonelective procedures such as renal biopsies and arteriovenous fistulas during March 2020. 12
Impact of COVID-19 on ophthalmic care in India
Three out of seven included studies reported the impact of COVID-19 on ophthalmic care in India. A study conducted at a tertiary care ophthalmic institute in India reported a decrease of 97.14% in the routine patient visit, a decline of 35.25% in emergency outpatient visits, a decrease in routine and emergency ward admissions by 95.18% and 61.66% respectively, a reduction of elective surgeries by 98.18%, decrease of 58.81% in emergency surgeries, reduction of 99.61% in the number of donor corneas collected between 25 March 2020 and 15 July 2020 with comparison on previous year data of the same duration. 13 A study conducted in rural eye centres of Southern India reported that between 23 March 2020 and 19 April 2020, the total number of patients reduced during the lockdown-I period versus pre-lockdown. Only essential procedures were performed and most of the patients were treated for conjunctivitis. 14 A third study, which was conducted in a tertiary eye care Institute reported that there was a reduction in the number of patients presenting with ocular trauma in their emergency department during the lockdown as compared to the previous year. 15
Impact of the COVID-19 pandemic on the clinical practice of trauma and orthopaedics
A single epidemiology study out of seven studies included in this article, which was conducted at a tertiary care centre in New Delhi, explained various outcomes of the COVID-19 pandemic on the practice of orthopaedics and trauma through comparison between the pandemic period and pre-lockdown. It stated a reduction by 71.93% in outpatient attendance, a reduction of 59.35% in inpatient admissions, 55.78% reduction in surgical procedures including arthroplasty surgery, trauma and arthroscopic surgery during the pandemic period. 16
This study is being conducted to investigate the impact of the COVID-19 pandemic on the health care system in India by a systematic review approach based upon the eligibility criteria, seven articles related to the purpose of the study were screened after inclusion and the final analysis was prepared. The included studies defined various parameters – number of outpatients, number of inpatients, number of patients undergoing minor and major surgeries, emergency trauma cases, patients undergoing nonurgent elective procedures, follow-up visits for assessment of the impact of the COVID-19 pandemic on overstretched and overburdened health care system Of India. The studies included in this article reported that the COVID-19 pandemic has sharply affected the health care services in India including cancer care, nephrology services, ophthalmic care, trauma practice and orthopaedics care.
The COVID-19 Pandemic has led to a disrupted healthcare system which has subsequently impacted non-COVID disease conditions. The observed reduction in the number of new patient registrations, hospital registrations, major and minor surgeries, and transplant procedures as summarized in various studies during March 2020–April 2020 could be due to fear of infection among patients. The patients residing in rural parts of India found it difficult to access health services in metro cities due to travel restrictions during the lockdown period and this has led to delays in early screening, correct diagnosis and appropriate treatment which is of grave concern. These patients may present with advanced stages of the disease and create a backlog of patients by overloading the healthcare system.
Hospitals faced certain challenges that inhibited them from providing appropriate care to the patient such as- many hospitals being converted to COVID-19 dedicated treatment facilities and as result, they faced a widespread shortage of Personal Protective Equipment (PPE) supplies. Hospitals reported a shortage of adequate staff as they were themselves exposed to the virus. Various hospitals reported lack of necessary medical equipments such as ICU beds and Ventilators which was a major threat.
Despite the lockdown and various challenges encountered, hospitals realized the need of improving the accessibility of healthcare through teleconsultation along with in-person visits during these challenging times. In the absence of direct consultations to the patients, telemedicine was conducted to address the concerns of outpatients and therefore, reduce their need to visit the hospital.
In general, the COVID-19 Pandemic has posed a serious threat to all aspects of the healthcare system in India by affecting the activities of hospitals that provide treatment services to patients for non-COVID-19 diseases.
The results of this study show that Indian Healthcare System during the COVID-19 pandemic has suffered serious challenges, which can be a wake-up call because due to delayed diagnosis, a large number of patients will present with advanced stages of the non- covid-19 disease such as cancers, which may require emergency treatment. Strengthening of the Indian healthcare system is required so that it does not crumble under future pandemics if any. Need of the hour is a robust healthcare model and effective healthcare policies with regular updates to manage the current pandemic along with more emphasis on telemedicine as this is not the last pandemic that India will face. In conclusion, the COVID-19 pandemic has significantly impacted the healthcare system in India.
Limitations of the study: This study has limitation regarding language inclusion, as the researchers’ proficiency was limited to English, resulting in the exclusion of articles written in other languages. Another major limitation is the bias as the he papers relies on available online published studies in high-quality journals, which may introduce a bias towards studies that have been published and accessible. There may be relevant studies that have not been included in the review, potentially leading to a skewed representation of the impact of COVID-19 on the healthcare system in India.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement: No Ethical approval is needed.
4 Design Thinking Case Studies in Healthcare: Nursing
The 4 case studies by Penn Nursing illustrate how nurses can be really powerful collaborators and generators of solutions within Healthcare. The videos describe the main attributes that nurses bring to the problem solving table
- Empathy. A big part of a nurses role is to be able to empathize with their patients, so it comes naturally to nurses.
- Problem solving skills. Nurses have to solve problems on a daily basis during their shifts. They are really good at problem solving.
- Nurses see the actual problems first hand on a daily basis. They know better than anyone what issues need to be addressed.
- Nurses care for patients. They see the issues and problem solve on the fly. They are used to working with rough prototypes and iterating fast to improve.
- In general as the last video points out, nurses are unaware of the ideas and solutions that could be applied to their problems. Inclusion in the problem solving process and an understanding of the options and solutions being proposed could help to speed up the innovation process.
Visit Penn Nursing website Design Thinking for Health to watch videos on the following case studies
- Cathy Bowles, Co-Founder of Rightcare Solutions, Penn Nursing Innovators: D2S2 Decision Support Tool for Discharge Planning
- Ernesto Holgiun, Penn Nursing Innovators: Drying Inspection Apparatus for Diabetes - Patented the first ever foot care telehealth system.
- Sarah Szanton: Johns Hopkins Hospital, Capable Program: Helping elderly community members live more safely at home. CAPABLE is a client-centered home-based intervention to increase mobility, functionality, and capacity to “age in place” for low-income older adults. Read more...
- Rachel Walker, UMass Amerhurst College of Nursing: IV Fluid System. Co-creating support strategies for cancer survivorship
For a full index of all The Design Thinking Association articles on Design Thinking in Healthcare, visit our vertical markets - Healthcare page .
To read this content please select one of the options below:
Please note you do not have access to teaching notes, lean six sigma for the healthcare sector: a multiple case study analysis from the indian context.
International Journal of Quality & Reliability Management
ISSN : 0265-671X
Article publication date: 2 October 2019
The purpose of this paper is to explore the voice of the customer, key performance indicators, critical to quality characteristics, critical success factors, and commonly used tools and techniques for deploying the Lean Six Sigma (LSS) strategy in Indian private hospitals, with special attention to the medical records.
Design/methodology/approach
The study utilizes the action research methodology to obtain a greater understanding of the use of LSS in the Indian healthcare sector. Multiple case studies were designed and successfully deployed to understand and ascertain challenges in LSS implementation. Five case studies were carried out in the Medical Records Departments (MRD) of four private hospitals in India.
Patients perceive that waiting in queue harms their health, which can be rectified by addressing the cycle time of the system. The research also found that effective leadership, availability of data, involvement of cross-functional team and effective communication are critical to the success of LSS projects. In addition, control charts, cause and effect diagram, 5S, gemba, two-sample t -test, standardization, waste analysis and value stream mapping are some of the common tools used to improve healthcare systems.
Research limitations/implications
The research was restricted to studying the impact of LSS on the workflow and resource consumption of the MRD in Indian allopathic hospitals only. The validity of the results can be improved by including more hospitals and more case studies from the healthcare sector in different countries.
Originality/value
The findings will enable researchers, academicians and practitioners to incorporate the results of the study in LSS implementation within the healthcare system to increase the likelihood of successful deployment. This will provide greater stimulus across other departments in the hospital sector for wider and broader application of LSS for creating and sustaining process improvements.
- Lean Six Sigma
- Medical records
Bhat, S. , Antony, J. , Gijo, E.V. and Cudney, E.A. (2020), "Lean Six Sigma for the healthcare sector: a multiple case study analysis from the Indian context", International Journal of Quality & Reliability Management , Vol. 37 No. 1, pp. 90-111. https://doi.org/10.1108/IJQRM-07-2018-0193
Emerald Publishing Limited
Copyright © 2019, Emerald Publishing Limited
Related articles
All feedback is valuable.
Please share your general feedback
Report an issue or find answers to frequently asked questions
Contact Customer Support

“Case Studies in Healthcare: Success Stories and Lessons Learned”

Table of Contents
The healthcare industry is an ever-evolving field with innovations and improvements happening daily. As healthcare providers strive to deliver the best care possible, case studies have become a valuable resource for learning and growth. In this article, we will explore various case studies in healthcare, highlighting both success stories and the lessons learned along the way. By analyzing what works and why, we can gain insight into the practices that lead to triumphs in healthcare and potentially replicate these successes in our own organizations.
Case Studies in Healthcare: A Closer Look at Triumphs and Takeaways
Healthcare case studies provide a unique opportunity to dissect real-world scenarios, understand the decisions made, and measure the outcomes of those choices. One notable success story is the implementation of telemedicine in rural areas. By leveraging technology, healthcare providers have successfully expanded access to care for patients who would otherwise have to travel long distances for treatment. Lessons learned include the importance of investing in reliable technology and training staff to effectively use telemedicine platforms.
Another critical case study involves the management of electronic health records (EHRs). When a large hospital system transitioned to a new EHR system, they faced significant resistance from physicians who were accustomed to the old way of doing things. However, by involving physicians in the planning and implementation process, the hospital successfully integrated the new system, leading to improved efficiency and patient care. This case study highlights the value of stakeholder engagement and effective change management.
In the fight against infectious diseases, case studies have shown the significance of swift and coordinated responses. An example of this is the containment of Ebola in West Africa. Through international collaboration and the rapid deployment of healthcare resources, the spread of the virus was effectively limited. This case study underscores the importance of preparedness, communication, and teamwork in tackling healthcare crises.
Success Stories in Healthcare: Analyzing What Works and Why
Understanding why certain strategies succeed is crucial for replicating positive results in the healthcare industry. For instance, one hospital’s initiative to reduce patient readmissions focused on comprehensive discharge planning and follow-up care. By ensuring patients had clear instructions and support after leaving the hospital, readmission rates dropped significantly. This case study emphasizes the role of thorough patient education and post-discharge care in improving outcomes.
In the realm of preventive care, a primary care clinic introduced a program to increase vaccination rates among its patient population. By actively reaching out to patients due for immunizations and offering flexible scheduling options, the clinic saw a dramatic increase in vaccination rates. The takeaway from this case study is the impact of proactive patient engagement and removing barriers to care.
Lastly, a healthcare organization’s embrace of continuous quality improvement (CQI) led to enhanced patient safety and satisfaction. By fostering a culture of open communication and ongoing learning, the organization identified areas for improvement and systematically implemented changes. This case study demonstrates the power of a commitment to CQI as a driver for excellence in healthcare.
The healthcare industry is rich with case studies that provide valuable insights and lessons learned. By analyzing and understanding these success stories, healthcare providers can apply similar strategies to achieve positive outcomes in their own organizations. Whether it’s through technology, stakeholder engagement, or quality improvement initiatives, these case studies offer a blueprint for triumph and provide a roadmap for future success in the ever-changing landscape of healthcare.
Why are case studies valuable in the healthcare industry, and how do they provide insights into successful decision-making and problem-solving within healthcare organizations?
Case studies are valuable as they offer real-world examples of challenges and solutions in healthcare. They provide insights into successful decision-making, problem-solving, and strategies that can be applied by healthcare professionals and organizations facing similar scenarios.
How does the article select and present case studies, and what criteria are considered to ensure the relevance and applicability of the showcased success stories to a diverse audience?
The article discusses the criteria for selecting case studies, such as their impact on healthcare outcomes, innovation, or overcoming significant challenges. It highlights the diversity of cases to ensure relevance to a broad audience, considering different healthcare settings, specialties, and contexts.
Can you provide examples of healthcare case studies featured in the article, and how do these stories illustrate successful decision-making or lessons learned that can benefit readers in the healthcare field?
Certainly! Examples may include cases where innovative technologies improved patient outcomes, or instances where strategic decisions enhanced operational efficiency. The article presents these stories to illustrate valuable lessons learned and best practices that readers can apply in their own healthcare settings.
In what ways do case studies contribute to professional development and learning opportunities for healthcare professionals, and how can organizations leverage these stories for continuous improvement and staff training?
The article explores how case studies offer learning opportunities, allowing healthcare professionals to gain insights from others’ experiences. Organizations can leverage these stories for staff training, fostering a culture of continuous improvement and encouraging employees to apply lessons learned to their daily practices.
For healthcare leaders seeking to implement successful strategies within their organizations, what recommendations and actionable insights does the article provide based on the analysis of the showcased case studies?
The article offers recommendations based on the case studies, such as the importance of collaboration, data-driven decision-making, and embracing innovation. It provides actionable insights that healthcare leaders can use to inform their decision-making processes and drive positive outcomes within their organizations.
Leave a comment Cancel reply
You must be logged in to post a comment.
+1 (800) 782 1768

Respiratory syncytial virus (RSV) case study: Avery
- Immunisations
Description
Part of our collection of RSV resources for professionals .
RSV case study Avery
Media enquiries.
If you have a media enquiry relating to this publication, please contact the Communications and Engagement team .
Requesting other formats and reporting issues
If you require publications or documents in other formats, please email [email protected] .
To report any issues with a publication, please email [email protected] .
Share this page
We use cookies on this website which are essential for it to work. We also use non-essential cookies to help us improve our websites, which you can opt out of in cookie settings. Any data collected is anonymised. By continuing to use this site, you agree to our use of cookies.
- Open access
- Published: 02 September 2024
Public service motivation, public sector preference and employment of Kenyan medical doctor interns: a cross-sectional and prospective study
- Daniel Mbuthia 1 na1 ,
- Yingxi Zhao 2 na1 ,
- David Gathara 1 , 3 ,
- Catia Nicodemo 4 , 5 ,
- Gerry McGivern 6 ,
- Jacinta Nzinga 1 &
- Mike English 1 , 2
Human Resources for Health volume 22 , Article number: 61 ( 2024 ) Cite this article
Metrics details
Kenya grapples with a paradox; severe public sector workforce shortages co-exist with rising unemployment among healthcare professionals. Medical schools have increased trainee outputs, but only 45% of newly qualified/registered doctors were absorbed by the public sector during 2015–2018. In such a context, we explore what influences doctors’ career choices at labour market entry, specifically understanding the role of public service motivation (PSM).
We conducted a cross-sectional and prospective study of interns and recently graduated doctors to examine PSM, their intention to work in the public sector and their final employment sector and status. We surveyed them on their PSM and job intentions and conducted a prospective follow-up survey of the interns, around one year later, to understand their employment status.
We recruited 356 baseline participants and followed up 76 out of 129 eligible interns. The overall PSM score was high among all participants (rated 4.50/5.00) irrespective of sector preferences. 48% (171/356) of the participants preferred to work in the public sector immediately after internship, alongside 16% (57/356) preferring direct entry into specialist training—commonly in the public sector. Only 13% (46/356) and 7% (25/365) preferred to work in the private or faith-based sector. Despite the high proportion of interns preferring public sector jobs, only 17% (13/76) were employed in the public sector at follow-up and 13% (10/76) were unemployed, due to lack of job availability.
High PSM scores irrespective of sector preferences suggest that doctors are generally committed to serving the ‘public good’. Many intended to work in the public sector but were unable to due to lack of job opportunities. Policymakers have an opportunity to tackle workforce gaps in the public sector as young doctors continue to express a preference for such work. To do this they should prioritise creating adequate and sustainable job opportunities.
Peer Review reports
Introduction
Public administration scholars have long been inquiring about what motivates people to join/work for the public sector and the value of this motivation to public organisations. Perry and Wise (1990) introduced the concept of public service motivation (PSM), which they defined as “an individual’s predisposition to respond to motives grounded primarily or uniquely in public institutions and organizations” [ 1 ]. Perry also later developed a PSM measure from a US population sample which includes four conceptual dimensions of PSM: attraction to public policy making, commitment to public interest, compassion, and self-sacrifice [ 2 ]. The critique of Perry’s scale over its cross-cultural and international application led to a revision of the scale by Kim and colleagues, who adapted the PSM dimensions and the measure to make it suitable across diverse cultures and languages [ 3 ].
Work examining PSM has consistently demonstrated the consequences of PSM in relationship to person–organisation fit, job satisfaction, commitment [ 4 , 5 , 6 ], and retention. Studies have also focused on whether PSM is associated with individuals’ sector choices, and whether PSM could form the basis of recruiting candidates for public organisations [ 7 , 8 ]. A number of studies have established that measures of PSM among public servants are greater than for those working in private organisations [ 6 , 9 ]. Other studies have examined whether PSM exists prior to job entry and whether it could predict public sector preference [ 4 , 9 , 10 , 11 , 12 ]. However, PSM has only been studied in a narrow range of national contexts, mostly in high-income countries, and very few studies have used Kim’s PSM scale, especially in low- and middle-income country (LMIC) settings. Our study therefore extends PSM research by using Kim’s scale, and investigating its association with the career decisions of Kenyan medical doctors who are in their internship and expected, after one year, to transition to independent clinical practice as fully licensed medical practitioners. We suggest this pre-licensure phase is critical in shaping individuals’ career trajectories, and of great interest considering the workforce shortages of medical doctors, especially in the public sector in LMIC contexts.
The Kenyan context
The public sector provides the largest share of healthcare in Kenya. Approximately 46% of health facilities are run by the government in 2022, 44% by the private sector and the rest by faith-based and non-governmental organisations [ 13 ]. However, the public sector provides a greater proportion of inpatient hospital care, particularly to the poor and those in rural areas [ 14 ], as the costs of utilising public hospital services are lower. Additionally, a large number of private sector facilities are small clinics and dispensaries [ 15 ].
Kenya grapples with a shortage of medical workforce, with an estimated density of 0.23 per 1000 population in 2020. This is significantly lower than the average for LMICs (1.4 per 1000 in 2017) [ 16 ]. Medical doctors are typically trained in universities through a Bachelor of Medicine & Bachelor of Surgery (MBChB) programme that lasts six years with an additional internship year. As with other African countries, medical schools in Kenya are expanding to meet health workforce gaps. Now 11 medical schools are providing undergraduate medical training with a combined annual output of 628 in 2019 [ 17 ], nearly double that of only a few years previously (287 in 2006, 320 in 2016) [ 18 , 19 , 20 ].
Before 2013, when Kenya devolved responsibility for health systems to 47 semi-autonomous county governments, medical doctors were automatically employed and deployed by the national government after their internship. Since devolution, counties have managed health workforce recruitment and management [ 21 , 22 ], and automatic employment of medical doctors post-internship ended. This means that medical doctors now must apply for jobs after internship, but whether they are employed is contingent on vacancies advertised by county/national government(s) and other organisations. Most doctors who completed their internship would initially be employed as medical doctors in public, private or faith-based health facilities. Public sector roles in the Ministry of Health or County Health Department or parastatal organisations typically require some prior working experience with entry into specialist training also requiring 2–3 years’ work experience.
Recent data from the Kenyan Ministry of Health suggested between 2015 and 2018, only 45% (825/1,800) of newly qualified and registered doctors were employed in the public sector [ 19 ]. Such low absorption could be due to the lack of job opportunities provided by governments (“demand side”) [ 23 ], or medical doctors’ preferring alternatives to public sector jobs (“supply side”), potentially due to the poor conditions they face as interns in public hospitals [ 24 ]. Understanding what influences medical doctors’ employment choices is crucial for shaping effective healthcare policies and workforce planning, especially as the majority of hospital care provided to the population is still through the public sector [ 14 ]. Several studies in Kenya have investigated healthcare professionals’ public sector preferences [ 25 , 26 ]. However, to the best of our knowledge, no previous study has examined the concept of PSM and its relations with Kenyan medical interns’ career preferences. Our study fills this gap.
We used a combined cross-sectional and a prospective study design to examine PSM, intention to work in the public sector and final employment sector among medical interns and recently graduated medical doctors in Kenya. This study is embedded in a larger project that focuses on the internship training experiences of Kenyan doctors [ 24 ].
From Nov 2021 to May 2022, we conducted a cross-sectional survey of Kenyan medical interns and medical doctors who completed their internship within 3 years. We used a mix of convenience and snowball sampling approaches [ 27 ] to include survey participants. We worked with different stakeholders and asked them to share the survey through their respective platforms such as WhatsApp or short message service (SMS). Our approach included working with (a) the Kenyan Medical Practitioners and Dentists Council, which shared the survey with all eligible medical officers on their registry through SMS; (b) the Kenya Medical Association Young Doctor Network and Kenya Young Doctor Caucus that shared within their respective WhatsApp groups; (c) three major medical schools based in or near Nairobi that shared within recent graduate class representative; and (d) selected facilities in the Clinical Information Network operated by KEMRI-Wellcome Trust Research Programme [ 28 , 29 ], which shared the survey within facilities’ own WhatsApp groups. The survey was online and self-administered through REDCap, and one GB of data (worth 250 KES or 1.8 GBP) were given to respondents who fully completed the survey. Out of an estimated 2,400 eligible participants (estimated 600 graduates per year), 498 started the survey and 356 fully completed the survey and so were included for analysis. Out of the 356 sample, 227 were medical doctors who completed their internship within 3 years and 129 were current interns.
The cross-sectional survey questionnaire focuses on PSM and public sector intention. It includes questions on (1) demographics and medical training (name of medical school and internship hospital as well as funding for medical training); (2) preferred job roles immediately after internship and five years after internship (one of seven options listed in Table 3 , or others). Medical doctors who had already completed internship and were already in the labour market were required to indicate the year of internship completion, and what was their most preferred option when they finished internship; and (3) PSM evaluation using the scale developed by Kim et al. [ 3 ]. The scale has 16 items grouped into four factors and domains, i.e. attraction to public participation, commitment to public values, compassion, and self-sacrifice. The questionnaire was developed as part of a broader medical internship experience project and questions were pre-tested including the use of cognitive interviews [ 30 , 31 ] to ensure that all questions were relevant and that respondents could fully understand the questions.
We further conducted a prospective telephone follow-up of the 129 medical interns from March to May 2023, around one year later, to understand their final employment status. We only followed up participants who had consented to a follow-up interview at baseline, and who provided us with their phone numbers. The follow-up survey included five questions on their current role, locations, employment terms, and also an open-ended question on reasons for current employment.
Data were managed and analysed using STATA (Stata V.17). Descriptive statistics on frequencies, percentages and means were used to describe the demographics, PSM and public sector intention of all baseline participants as well as and final employment status of follow-up participants. For example, we calculated the mean score (out of 5) across four PSM domains and the aggregated PSM score. We also conducted a confirmatory factor analysis to examine the performance of PSM in the sample and the degree to which items are related to the underlying dimension as proposed by Kim et al. [ 3 ].
Ethical approval for the study is issued by Oxford Tropical Research Ethics Committee (OxTREC 563-20 and OxTREC 518-21) and Kenya Medical Research Institute (KEMRI) (SERU 4071). Electronic consents or written consents were obtained for all survey participants.
Participant characteristics
Basic sociodemographic and medical training characteristics of baseline participants are presented in Table 1 . 36% (129/356) of the survey population were interns at the time of the survey, having completed 6.5 months of internship training on average; the rest were post-internship doctors that mostly completed their internship from 2020 to 2022. The University of Nairobi contributed to 57% (201/356) of the survey population, it is also the largest medical school in Kenya graduating nearly half of the doctors. Most participants undertook their internship in public facilities (78%, 276/356), whereas 73% of internship training centres are public hospitals [ 32 ]. As for follow-up, 116 out of 129 interns agreed to be followed up through telephone calls. We successfully followed up 77 of them with complete data (66%). The time from baseline to follow-up is on average 14 months.
- Public service motivation
As shown in Table 2 in the item- and factor-specific means. Self-sacrifice, which is the foundational concept representing the altruistic or pro-social origins of PSM, was rated slightly lower in our sample (factor mean 3.88 out of 5). For example, Q16 “I would agree to a good plan to make a better life for the poor, even if it costs me money” was rated 4.04 out of 5. Nonetheless, despite overall lower average compared to other domains, some factors under self-sacrifice, i.e. Q13 “I am prepared to make sacrifices for the good of society” were rated quite highly indicating substantial commitment and inherent value to serving public good being integral to medical doctors’ professional identity and could therefore explain the overall high PSM among medical doctors. Other factors and the overall PSM score (4.50 out of 5) were relatively high, suggesting that most respondents had high motivation for public service. Also shown in Additional fle 1 , older participants and those who received scholarships during medical training had higher PSM scores.
Indices of the PSM developed by Kim et al. [ 3 ], which has not been previously tested in the Kenyan sample, showed a moderate fit according to the confirmatory factor analysis (comparative fit index [CFI] = 0.92, root mean square error of approximation [RMSEA] = 0.08, standardised root mean squared residual [SRMR] = 0.06). When removing item Q2, as Kim and colleagues suggest [ 33 ], there was a slight improvement in RMSEA but still a moderate fit. The reliability coefficient (Cronbach’s alpha) for the overall scale was 0.88 and the coefficients for the four factors ranged from 0.76 to 0.88 (Table 2 ).
Intention to work in the public sector
Baseline participants ( n = 356) were asked about their preferred job roles immediately after internship and five years after internship (Table 3 ). Most participants (48%, 171/356) stated a preference to work in the public sector as medical doctors immediately after internship, followed by direct entry into specialist training (16%, 57/356)—which is also predominantly undertaken in the public sector. Preference for entry into the private sector (13%, 46/356) or faith-based sector (7%, 27/356) immediately after internship were low. As for job sector preference five years after internship, low preference for the private and faith-based sectors (10%, 36/356 and 4%, 14/356) persisted. At 5 years slightly fewer respondents intended to remain working in the public sector (21%, 75/356) and more stated a preference to go into specialist medical training (42%, 150/356). These trends are similar between the 129 interns and the post-internship doctors (Table 4 ).
We also compared PSM scores between baseline participants with different career intentions (Additional File 2 ). We found that participants with different intentions for career sector all had high PSM with minimal variations. For example, those who preferred to work in the public sector as medical doctors had an average PSM score of 4.45 out of 5, whereas those preferring to work in the private sector and faith-based sector had scores of 4.53 and 4.70 out of 5, respectively. Therefore, our findings suggest that PSM is not a useful discriminator for career intention, but instead other factors such as pay and working arrangement might influence career intention more.
Employment in the public sector at follow-up
Table 4 presents the career intention and final employment of medical interns. Out of 129 interns recruited at baseline, we successfully followed up 76 participants who completed their internship and hereby focused on these participants. While 49% (37/76) of these participants indicated intention to work in the public sector as medical doctors at baseline, only 17% (13/76) indicated actual employment in the public sector one year after internship. Most respondents (65%, 49/76) ended up working in the private sector or faith-based hospitals despite not being the preferred job choice. Around one year after internship, no respondents were employed in the Ministry of Health/County Health Department or parastatal organisations, not-for-profit technical assistance organisations or enrolled in specialist trainings.
Additionally, 13% (10/76) of respondents suggested that they were unemployed at the time of follow-up. Of those who were employed, only 8% (5/66) were employed on a permanent contract, and more commonly they were employed on contract (52%, 34/66) or on a locum basis (41%, 27/66) especially for private-sector jobs. When asked reasons for choosing their current employment as an open-ended question, nearly 60% of respondents stated that these were the only available jobs for them, oftentimes only temporary job contracts available in private sectors.
Our cross-sectional and prospective study of Kenyan medical doctors and interns provided insights into their PSM, intention to work for the public sector and their final employment. Our findings show that the majority of the respondents generally had high motivation for public service. Most (48%) respondents stated a preference to work as medical doctors in the public sector, rather than the private or faith-based sector immediately after internship, but only 17% indicated actual employment in the public sector at one-year follow-up, with 65% working in private health care, and 13% unemployed.
There were also minimal variations between their PSM scores, which suggests that public sector job preference is not linked to PSM. We found that while all the other items/domains of PSM were rated high, the pro-social aspect of PSM, i.e. self-sacrifice, was rated relatively lower among the respondents. These findings are similar to Harris et al.’s study of Ugandan public servants, where Kim et al.’s scale suggested an overall high public service, commitment to public values, and compassion, and low willingness to self-sacrifice in favour of the common good [ 34 ]. Some studies reported that self-sacrifice is the most impactful and stable PSM dimension and is associated with a preference for public sector employment [ 35 ]. However, a recent review of PSM literature in Africa highlighted contradictory findings regarding the linkage between self-sacrifice and inclination towards public service, highlighting the possible differences in culture and value that could explain PSM and motives [ 6 ].
The minimal variations of PSM between participants with different career intentions also suggested that PSM is measuring a set of attitudes towards ‘public service’, not necessarily ‘public sector’ [ 36 ]. The concept of public sector could be interpreted differently in different cultures and settings [ 37 ]. In the Kenyan setting, working in faith-based not-for-profit organisations could also be considered as working for the ‘semi-public sector’. Because a medical doctor’s job is serving people and saving lives, regardless of the sectors they work, all respondents may believe they were working in the public interest and helping society. Our findings therefore indicated that PSM might not be the primary reason for the low absorption of medical doctors into the public sector in the Kenyan setting.
As noted, nearly half of the medical doctors surveyed indicated intention to work in public hospitals immediately after internship, but only 17% were employed in the public sector at follow-up. This finding is similar to previous qualitative work with medical doctors in Kenya and Uganda [ 23 , 38 ]. The preference for the public sector could be due to various reasons beyond PSM and ‘serving the public’. For example, this may be due to better pay and job security, the public sector being “easier to work in” or linked enabling with dual practices, and culturally ingrained appreciation for public sector jobs [ 38 , 39 , 40 ]. In comparison, jobs in the private sector were perceived to have poorer contractual terms and involve higher workloads in the Kenyan setting. This contrasts with high-income settings, where private medical work is better paid [ 23 , 38 ].
Kenya has boosted its supply of medical professionals through the expansion of medical training, although this has still not yet reached the country’s goal listed under its norms and standards [ 20 ]. However, demand for public sector doctors has increased more slowly, despite a shortage of doctors in the public sector. This is mostly due to the lack of sustained financial commitments for the health workforce and preference for other healthcare cadres [ 23 ]. Consequently, despite public sector preference many doctors remain unemployed, underemployed, or work in the private sector, often on temporary contracts, [ 23 , 38 ]. Many doctors “just want a job anywhere (they) could find”, even if it is not the role they would have ideally chosen [ 38 ].
The findings of this study have implications for policy and practice. First on the positive side, our data support evidence that, for certain professions, the nature of the job serves some public good and therefore is perceived as ‘public service’, as evidenced by the high PSM scores regardless of sector preference. Given this, policymakers and healthcare managers therefore need to worry less about medical doctors’ public service values and motivations, but need to remain attentive to other factors that might influence doctors' career choices, satisfaction and retention.
Second, considering the mismatch between public sector intention and employment of doctors, and the high level of health worker unemployment, Kenya needs to prioritise workforce planning. This proactive approach could ensure that the training and development of medical doctors is aligned with national healthcare needs and employment capacities, therefore reducing the risk of unemployment among newly trained doctors. Additionally, many African countries have been conducting health labour market analysis [ 20 , 41 ] and there exists an opportunity to integrate PSM into this analysis to better contextualise planning efforts as well as inform recruitment, retention, and motivation of healthcare workers. Significantly, LMICs need to re-think the causes of health workforce shortages in the public sector, as many are witnessing growing health workforce underutilisation and unemployment [ 42 ]. More in-depth, country-specific research evidence on the supply/demand mismatch dilemma is needed to draw policymakers’ attention to this issue.
Finally, our study adds to the global PSM literature by first using the PSM scale developed by Kim et al. in the Kenyan healthcare setting [ 3 ]. While Kim et al.’s scale was developed in 2013, with an international sample across 12 countries in response to criticisms of the American focus of the scale developed by Perry in 1996 [ 2 ], the majority of PSM scholarship still largely used the Perry scale when measuring PSM [ 4 , 6 , 43 ]. The use of Kim et al.’s scale is still limited in LMICs especially African countries, and many studies did not report on its psychometric performances. One exception is the work by Mikkelsen and colleagues which tested Kim et al. scale in four world regions including three countries in Africa (Ghana, Malawi and Uganda). Mikkelsen and colleagues suggested the scale’s partial metric invariance and scale non-invariance, i.e. causes and consequences of PSM are comparable across most countries but not means and its dimension. Our study suggested a moderate-to-good fit according to the confirmatory factor analysis and reliability coefficient, future studies should consider testing the scale’s performance in different populations and contexts.
Limitations
There are some limitations that should be considered when interpreting our results. First, this work was conducted during the Covid-19 pandemic, which presented logistics challenges for data collection. We therefore used a mix of convenience and snowballing approaches to sample baseline respondents. The 356 responses came from all medical schools and 65 out of 74 internship hospitals. The sample is roughly 15% of the eligible population but not representative. Covid-19 might have also impacted the broad labour market dynamic. For example, high PSM among study participants and financial constraints of the government.
Second, at baseline, we included respondents who were interns and also those who already completed internships. While data in Appendix 1 suggested no significant differences between these participants, we acknowledge that responses from post-internship medical doctors could be subject to recall biases. Furthermore, we also did not survey these graduated doctors of their current sector of employment, and further comparing PSM scores between doctors in different sectors could help us further understand the role of PSM.
Third, while the risk of loss to follow-up is low considering the similar trends of job intention between baseline and follow-up intern respondents (Table 4 ), it is possible that people who did not respond to our baseline survey had different career intentions and employment outcomes. Moreover, we were only able to follow up interns on average 14 months after internship, and their career outcomes may be changing due to the emerging labour market dynamic in Kenya. Nonetheless, we still believe it provided a good description of the medical doctor and intern population.
Finally, we also acknowledge our self-administered survey, including PSM could be influenced by social desirability biases. This might be true for the relatively lower self-sacrifice domain. Considering the possible differences in culture and value that explain PSM but also respondents’ response patterns, future studies should continue testing PSM in diverse populations and contexts.
We investigated PSM, public sector employment intention, and the actual employment of Kenyan medical doctors and interns. Our study found high scores of PSM among doctors irrespective of their sector preferences. These findings indicated an innate desire to serve the public good as a common trait among medical doctors in Kenya. PSM was not necessarily linked with sector preference due to contextual factors such as job stability and better pay which attracted medical doctors to public sector jobs. Many doctors stated their intention to work in the public sector but few were able to do so, due to a lack of job opportunities. Policymakers should focus on creating job opportunities to ensure medical doctors are recruited and retained in the public sector.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Perry JL, Wise LR. The motivational bases of public service. Public Admin Rev. 1990;50:367–73.
Article Google Scholar
Perry JL. Measuring public service motivation: an assessment of construct reliability and validity. J Public Admin Res Theory. 1996;6(1):5–22.
Kim S, Vandenabeele W, Wright BE, Andersen LB, Cerase FP, Christensen RK. Investigating the structure and meaning of public service motivation across populations: developing an international instrument and addressing issues of measurement invariance. J Public Admin Res Theory. 2013;23(1):79–102.
Ritz A, Brewer GA, Neumann O. Public service motivation: a systematic literature review and outlook. Public Adm Rev. 2016;76(3):414–26.
Vandenabeele W, Brewer GA, Ritz A. Past, present, and future of public service motivation research. Public Administration. 2014;92(4):779–89.
Bawole JN, Mensah JK, Amegavi GB. Public service motivation scholarship in Africa: a systematic review and research agenda. Int J Public Adm. 2019;42(6):497–508.
Houston DJ. Walking the walk” of public service motivation: public employees and charitable gifts of time, blood, and money. J Public Admin Res Theory. 2006;16(1):67–86.
Kjeldsen AM, Jacobsen CB. Public service motivation and employment sector: attraction or socialization? J Public Admin Res Theory. 2013;23(4):899–926.
Clerkin RM, Coggburn JD. The dimensions of public service motivation and sector work preferences. Rev Public Personnel Admin. 2012;32(3):209–35.
Google Scholar
Vandenabeele W. Government calling: public service motivation as an element in selecting government as an employer of choice. Public Admin. 2008;86(4):1089–105.
Lewis GB, Frank SA. Who wants to work for the government? Public Adm Rev. 2002;62(4):395–404.
Christensen RK, Wright BE. The effects of public service motivation on job choice decisions: disentangling the contributions of person-organization fit and person-job fit. J Public Admin Res Theory. 2011;21(4):723–43.
Kenya Master Health Facility List: Find all the health facilities in Kenya [Internet]. http://kmhfl.health.go.ke/#/home . Accessed 9 Mar 2021.
Irimu G, Ogero M, Mbevi G, Kariuki C, Gathara D, Akech S, et al. Tackling health professionals’ strikes: an essential part of health system strengthening in Kenya. BMJ Glob Health. 2018;3(6): e001136.
Article PubMed PubMed Central Google Scholar
Putzeist L. TFHC. Kenya Healthcare Sector Report 2016. https://www.tfhc.nl/publication/kenyan-healthcare-sector-report-2016/ . Accessed 28 Feb 2023.
World Bank. Physicians (per 1,000 people) - Low & middle income [Internet]. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=XO . Accessed 19 Jan 2023.
English M, Strachan B, Esamai F, Ngwiri T, Warfa O, Mburugu P, et al. The paediatrician workforce and its role in addressing neonatal, child and adolescent healthcare in Kenya. Arch Dis Child. 2020;105(10):927–31.
Article PubMed Google Scholar
Kenya Ministry of Health. Kenya Health Workforce Report: The Status of Healthcare Professionals in Kenya, 2015. [Internet]. 2017. https://taskforce.org/wp-content/uploads/2019/09/KHWF_2017Report_Fullreport_042317-MR-comments.pdf . Accessed 23 Jan 2020.
Kenya Ministry of Health. Kenya Human Resource for Health Strategic Plan 2019–2023 (Final draft). 2019.
Okoroafor SC, Kwesiga B, Ogato J, Gura Z, Gondi J, Jumba N, et al. Investing in the health workforce in Kenya: trends in size, composition and distribution from a descriptive health labour market analysis. BMJ Glob Health. 2022;7(Suppl 1): e009748.
USAID, PEPFAR, Health Policy Plus. Kenya Health System Assessment [Internet]. 2019. http://www.healthpolicyplus.com/ns/pubs/11328-11600_KenyaHSAReport.pdf
Tsofa B, Goodman C, Gilson L, Molyneux S. Devolution and its effects on health workforce and commodities management—early implementation experiences in Kilifi County, Kenya. Int J Equity Health. 2017;16(1):169.
Zhao Y, Mbuthia D, Munywoki J, Gathara D, Nicodemo C, Nzinga J, et al. Examining the absorption of post-internship medical officers into the public sector at county-level in devolved Kenya: a qualitative case study. BMC Health Serv Res. 2023;23(1):875.
Zhao Y, Mbuthia D, Gathara D, Nzinga J, Tweheyo R, English M, et al. ‘We were treated like we are nobody’: a mixed-methods study of medical doctors’ internship experiences in Kenya and Uganda. BMJ Glob Health. 2023;8(11): e013398.
Takemura T, Kielmann K, Blaauw D. Job preferences among clinical officers in public sector facilities in rural Kenya: a discrete choice experiment. Hum Resour Health. 2016;8(14):1.
Muthuri RNDK, Senkubuge F, Hongoro C. An investigation of healthcare professionals’ motivation in public and mission hospitals in Meru County, Kenya. Healthcare (Basel). 2020;8(4):530.
Parker C, Scott S, Geddes A. Snowball Sampling. SAGE Research Methods Foundations [Internet]. 2019. http://methods.sagepub.com/foundations/snowball-sampling . Accessed 17 Jan 2023.
English M, Irimu G, Akech S, Aluvaala J, Ogero M, Isaaka L, et al. Employing learning health system principles to advance research on severe neonatal and paediatric illness in Kenya. BMJ Glob Health. 2021;6(3): e005300.
Gathara D, Malla L, Ayieko P, Karuri S, Nyamai R, Irimu G, et al. Variation in and risk factors for paediatric inpatient all-cause mortality in a low income setting: data from an emerging clinical information network. BMC Pediatr. 2017;17(1):99.
Scott K, Ummer O, LeFevre AE. The devil is in the detail: reflections on the value and application of cognitive interviewing to strengthen quantitative surveys in global health. Health Policy Plan. 2021;36(6):982–95.
Article CAS PubMed PubMed Central Google Scholar
Willis GB, Artino AR. What do our respondents think we’re asking? Using cognitive interviewing to improve medical education surveys. J Grad Med Educ. 2013;5(3):353–6.
Kenya Medical Practitioners and Dentists Council. Approved Internship Centres [Internet]. https://medicalboard.co.ke/functions/approved-internship-centres/ . Accessed 12 Feb 2020.
Kim S. Partial metric invariance of the international measure of public service motivation among twelve countries: a research note. Int J Public Adm. 2022;45(15):1103–9.
Harris A, Apio Ayado I, Schuster C, Meyer-Sahling J, Mikkelsen KS. Civil service management practices for a more motivated, committed and ethical public service in Uganda [Internet]. University College London: Kampala, Uganda. Kampala, Uganda: University College London; 2018 https://christianschuster.net/Ghana_report_final_fordistribution.pdf . Accessed 12 Jan 2024.
Meyer-Sahling J, Mikkelsen KS, Schuster C. Merit recruitment, tenure protections and public service motivation: evidence from a conjoint experiment with 7,300 public servants in Latin America. Afr Eastern Eur Public Admin. 2021;99(4):740–57.
Vandenabeele W, Walle S. International difference in public service motivation: Comparing regions across the world. 2008. https://www.semanticscholar.org/paper/International-difference-in-public-service-regions-Vandenabeele-Walle/901c3e0f1b66b5e0b30d51211f393b8e8085a06f . Accessed 13 Jan 2024.
Mikkelsen KS, Schuster C, Meyer-Sahling JH. A cross-cultural basis for public service? Public service motivation measurement invariance in an original survey of 23,000 public servants in ten countries and four world regions. Int Public Manag J. 2021;24(6):739–61.
Zhao Y, Mbuthia D, Ankomisyani DS, Blacklock C, Gathara D, Molyneux S, et al. The influence of internship training experience on Kenyan and Ugandan doctors’ career intentions and decisions: a qualitative study. Glob Health Action. 2023;16(1):2272390.
Barsoum G. The public sector as the employer of choice among youth in Egypt: the relevance of public service motivation theory. Int J Public Adm. 2015;23(39):1–11.
Tweheyo R, Daker-White G, Reed C, Davies L, Kiwanuka S, Campbell S. ‘Nobody is after you; it is your initiative to start work’: a qualitative study of health workforce absenteeism in rural Uganda. BMJ Glob Health. 2017;2(4): e000455.
Ahmat A, Okoroafor SC, Kazanga I, Asamani JA, Millogo JJS, Illou MMA, et al. The health workforce status in the WHO African Region: findings of a cross-sectional study. BMJ Glob Health. 2022;7(Suppl 1): e008317.
Siankam Tankwanchi A, N’simbo A, Hagopian A. Health worker unemployment in LMICs with shortage: a policy brief prepared for the 2nd review of the relevance and effectiveness of the WHO Global Code of Practice on the International Recruitment of Health Personnel. 2019.
Marques TMG. Research on public service motivation and leadership: a bibliometric study. Int J Public Adm. 2021;44(7):591–606.
Download references
This work is supported by an Africa Oxford travel grant (AfOx-209). YZ is supported by the University of Oxford Clarendon Fund Scholarship, an Oxford Travel Abroad Bursary and a Keble Association grant. DG and ME are supported by the National Institute for Health Research, Learning to Harness Innovation in Global Health for Quality Care (HIGH-Q) using UK aid from the UK Government to support global health research [NIHR130812]. ME is supported by a Wellcome Trust Senior Research Fellowship (#207522). CN receives funding from the Economic and Social Research Council [grant number ES/T008415/1]. National Institute for Health Research Applied Research Collaboration Oxford and Thames Valley at Oxford Health NHS Foundation Trust. Consortium iNEST (Interconnected North-Est Innovation Ecosystem) funded by the European Union NextGenerationEU (Piano Nazionale di Ripresa e Resilienza (PNRR)—Missione 4 Componente 2, Investimento 1.5—D.D. 1058 23/06/2022, ECS_00000043). The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government.
Author information
Daniel Mbuthia and Yingxi Zhao contributed equally to this manuscript as joint first authors.
Authors and Affiliations
KEMRI-Wellcome Trust Research Programme, Nairobi, Kenya
Daniel Mbuthia, David Gathara, Jacinta Nzinga & Mike English
NDM Centre for Global Health Research, Nuffield Department of Medicine, University of Oxford, S Parks Rd, Oxford, OX1 3SY, UK
Yingxi Zhao & Mike English
MARCH Centre, London School of Hygiene and Tropical Medicine, London, UK
David Gathara
Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK
Catia Nicodemo
Department of Economics, Verona University, Verona, Italy
King’s Business School, King’s College London, London, UK
Gerry McGivern
You can also search for this author in PubMed Google Scholar
Contributions
DM, YZ, DG, CN, JN and ME designed the study. DM and YZ contributed to data collections. YZ conducted analysis. DM and YZ wrote the first draft of the manuscript. All authors provided critical feedback on the first draft of the manuscript, read and approved the final manuscript.
Corresponding author
Correspondence to Yingxi Zhao .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1. correlation analysis between psm scores and other characteristics., supplementary material 2. comparison of psm scores between different career intentions., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mbuthia, D., Zhao, Y., Gathara, D. et al. Public service motivation, public sector preference and employment of Kenyan medical doctor interns: a cross-sectional and prospective study. Hum Resour Health 22 , 61 (2024). https://doi.org/10.1186/s12960-024-00945-6
Download citation
Received : 19 March 2024
Accepted : 22 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12960-024-00945-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Public sector
- Labour market
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- All health topics
Popular topics
- Communicable Diseases Department
- Vaccine preventable disease
- Department of Healthier Populations and Noncommunicable Diseases (HPN)
- Universal health coverage
- Research and Innovation
- Planning, Monitoring and Evaluation
- Publications
- News releases
- Media Statements
- Feature stories
- Opinion Editorials
- World Health Day 2024
- Emergency Operations
- Country Health Emergency Preparedness & IHR
- Infectious Hazard Management
- Health Emergency Information & Risk Assessment
- Public health Laboratory services
- Regional Strategic Roadmap for Health Security (2023-2027) endorsed by the Regional Committee
- Nepal Earthquake
- Thailand becomes first in SEAR with WHO classified emergency medical team
- Where we work
- Country Strategy and Support
- Regional Director
- Regional Committee
- Seventy-sixth Session of the Regional Committee
- Collaborating Centers
Health officials, partners, and experts meet to strategize scale-up of regional innovations for improving quality integrated primary health care
Health officials, development partners, and experts met this week to strategize scaling up of innovations to improve quality integrated primary health care at a Regional Workshop here. Participants reviewed successful models from across the WHO South-East Asia Region, specifically explored innovations related to National PHC Integration in Indonesia, and collectively identified steps forward for improving both quality and integration in healthcare delivery.
“Poor quality care is today, a greater barrier to reducing mortality in low-and middle-income countries than insufficient access,” said Saima Wazed, Regional Director, WHO South-East Asia, in her inaugural address at the ‘Regional Workshop on Innovations for Quality Integrated Primary Health Care.’ She emphasized that as a key aspect of quality, the integration of primary health services is crucial for providing seamless care throughout an individual’s life.
“Integration through ensuring service continuity and people-centredness is a key determinant of quality,” the Regional Director added.

(Photo credit: WHO Indonesia)
The World Health Organization is urging countries in the WHO South-East Asia Region to expand the adoption of cutting-edge policies, practices, and technologies that provide comprehensive, quality care throughout all stages of life. This call-to-action highlights successful models from across the Region, aimed at tackling the increasing challenges of noncommunicable diseases (NCDs), mental health, public health emergencies, and climate effects alongside traditional priorities in service delivery.
The WHO South-East Asia Region has long recognized primary health care as the foundation of robust health systems and broader development goals. In 2023, health ministers from the Region reaffirmed their commitment to prioritizing investments in primary health care. The South-East Asia Region Primary Health Care Strategy 2022-2030 outlines key actions to transform health systems through a primary health care approach.
The recently launched WHO South-East Asia Regional Roadmap for Results and Resilience, underscores WHO’s commitment to building a learning health system that prioritises innovations, equity, and sustainability . The holistic approach aims to ensure health and well-being for all in a comprehensive manner. With WHO serving as a key enabler , the roadmap seeks to forge partnerships across governments, development agencies, philanthropic organizations, academia, the private sector, and civil society to achieve universal health coverage.
According to the Lancet Commission, nearly 60% of the 8.6 million annual deaths from treatable conditions are linked to poor quality care. During the COVID-19 pandemic, the lack of integration of public health functions in primary health care posed a significant bottleneck, in prevention, preparedness, and response. It also underscored the urgent need to strengthen primary health care systems while integrating essential public health functions in the Region for better preparedness and resilience against future health crises.
Addressing the diverse challenges in delivering quality integrated primary health care to the Region’s two billion people, the Regional Director said, “We stand at a historic moment in time. A remarkable transformation is taking place across our countries in our Region: a transformation from a focus on a few select diseases to that of the full human condition, across the life course.”A compilation of “Positive Practice Case Stories” was launched, featuring a set of 20 case studies from across the Region that highlight innovative approaches and solutions in various countries.

“My vision for our Region is where people have access to quality healthcare, regardless of where they live, and regardless of their income or social status. I would like us to be a Region which takes a holistic approach to health and well-being; where people are empowered - both physically and mentally - to achieve their full potential. I would like to shape a Region which cares for all and strengthens and protects the most vulnerable who live in it.” the Regional Director said.
To read more about the ‘ Positive practices in developing primary healthcare-oriented health systems’ scan the QR code below or click the link here

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 02 September 2024
Green spaces provide substantial but unequal urban cooling globally
- Yuxiang Li 1 ,
- Jens-Christian Svenning ORCID: orcid.org/0000-0002-3415-0862 2 ,
- Weiqi Zhou ORCID: orcid.org/0000-0001-7323-4906 3 , 4 , 5 ,
- Kai Zhu ORCID: orcid.org/0000-0003-1587-3317 6 ,
- Jesse F. Abrams ORCID: orcid.org/0000-0003-0411-8519 7 ,
- Timothy M. Lenton ORCID: orcid.org/0000-0002-6725-7498 7 ,
- William J. Ripple 8 ,
- Zhaowu Yu ORCID: orcid.org/0000-0003-4576-4541 9 ,
- Shuqing N. Teng 1 ,
- Robert R. Dunn 10 &
- Chi Xu ORCID: orcid.org/0000-0002-1841-9032 1
Nature Communications volume 15 , Article number: 7108 ( 2024 ) Cite this article
28 Altmetric
Metrics details
- Climate-change mitigation
- Urban ecology
Climate warming disproportionately impacts countries in the Global South by increasing extreme heat exposure. However, geographic disparities in adaptation capacity are unclear. Here, we assess global inequality in green spaces, which urban residents critically rely on to mitigate outdoor heat stress. We use remote sensing data to quantify daytime cooling by urban greenery in the warm seasons across the ~500 largest cities globally. We show a striking contrast, with Global South cities having ~70% of the cooling capacity of cities in the Global North (2.5 ± 1.0 °C vs. 3.6 ± 1.7 °C). A similar gap occurs for the cooling adaptation benefits received by an average resident in these cities (2.2 ± 0.9 °C vs. 3.4 ± 1.7 °C). This cooling adaptation inequality is due to discrepancies in green space quantity and quality between cities in the Global North and South, shaped by socioeconomic and natural factors. Our analyses further suggest a vast potential for enhancing cooling adaptation while reducing global inequality.
Similar content being viewed by others
Global climate-driven trade-offs between the water retention and cooling benefits of urban greening
Water, energy and climate benefits of urban greening throughout Europe under different climatic scenarios
Magnitude of urban heat islands largely explained by climate and population
Introduction.
Heat extremes are projected to be substantially intensified by global warming 1 , 2 , imposing a major threat to human mortality and morbidity in the coming decades 3 , 4 , 5 , 6 . This threat is particularly concerning as a majority of people now live in cities 7 , including those cities suffering some of the hottest climate extremes. Cities face two forms of warming: warming due to climate change and warming due to the urban heat island effect 8 , 9 , 10 . These two forms of warming have the potential to be additive, or even multiplicative. Climate change in itself is projected to result in rising maximum temperatures above 50 °C for a considerable fraction of the world if 2 °C global warming is exceeded 2 ; the urban heat island effect will cause up to >10 °C additional (surface) warming 11 . Exposures to temperatures above 35 °C with high humidity or above 40 °C with low humidity can lead to lethal heat stress for humans 12 . Even before such lethal temperatures are reached, worker productivity 13 and general health and well-being 14 can suffer. Heat extremes are especially risky for people living in the Global South 15 , 16 due to warmer climates at low latitudes. Climate models project that the lethal temperature thresholds will be exceeded with increasing frequencies and durations, and such extreme conditions will be concentrated in low-latitude regions 17 , 18 , 19 . These low-latitude regions overlap with the major parts of the Global South where population densities are already high and where population growth rates are also high. Consequently, the number of people exposed to extreme heat will likely increase even further, all things being equal 16 , 20 . That population growth will be accompanied by expanded urbanization and intensified urban heat island effects 21 , 22 , potentially exacerbating future Global North-Global South heat stress exposure inequalities.
Fortunately, we know that heat stress can be buffered, in part, by urban vegetation 23 . Urban green spaces, and especially urban forests, have proven an effective means through which to ameliorate heat stress through shading 24 , 25 and transpirational cooling 26 , 27 . The buffering effect of urban green spaces is influenced by their area (relative to the area of the city) and their spatial configuration 28 . In this context, green spaces become a kind of infrastructure that can and should be actively managed. At broad spatial scales, the effect of this urban green infrastructure is also mediated by differences among regions, whether in their background climate 29 , composition of green spaces 30 , or other factors 31 , 32 , 33 , 34 . The geographic patterns of the buffering effects of green spaces, whether due to geographic patterns in their areal extent or region-specific effects, have so far been poorly characterized.
On their own, the effects of climate change and urban heat islands on human health are likely to become severe. However, these effects will become even worse if they fall disproportionately in cities or countries with less economic ability to invest in green space 35 or in other forms of cooling 36 , 37 . A number of studies have now documented the so-called ‘luxury effect,’ wherein lower-income parts of cities tend to have less green space and, as a result, reduced biodiversity 38 , 39 . Where the luxury effect exists, green space and its benefits become, in essence, a luxury good 40 . If the luxury effect holds among cities, and lower-income cities also have smaller green spaces, the Global South may have the least potential to mitigate the combined effects of climate warming and urban heat islands, leading to exacerbated and rising inequalities in heat exposure 41 .
Here, we assess the global inequalities in the cooling capability of existing urban green infrastructure across urban areas worldwide. To this end, we use remotely sensed data to quantify three key variables, i.e., (1) cooling efficiency, (2) cooling capacity, and (3) cooling benefit of existing urban green infrastructure for ~500 major cities across the world. Urban green infrastructure and temperature are generally negatively and relatively linearly correlated at landscape scales, i.e., higher quantities of urban green infrastructure yield lower temperatures 42 , 43 . Cooling efficiency is widely used as a measure of the extent to which a given proportional increase in the area of urban green infrastructure leads to a decrease in temperature, i.e., the slope of the urban green infrastructure-temperature relationship 42 , 44 , 45 (see Methods for details). This simple metric allows quantifying the quality of urban green infrastructure in terms of ameliorating the urban heat island effect. Meanwhile, the extent to which existing urban green infrastructure cools down an entire city’s surface temperatures (compared to the non-vegetated built-up areas) is referred to as cooling capacity. Hence, cooling capacity is a function of the total quantity of urban green infrastructure and its cooling efficiency (see Methods).
As a third step, we account for the spatial distributions of urban green infrastructure and populations to quantify the benefit of cooling mitigation received by an average urban inhabitant in each city given their location. This cooling benefit is a more direct measure of the cooling realized by people, after accounting for the within-city geography of urban green infrastructure and population density. We focus on cooling capacity and cooling benefit as the measures of the cooling capability of individual cities for assessing their global inequalities. We are particularly interested in linking cooling adaptation inequality with income inequality 40 , 46 . While this can be achieved using existing income metrics for country classifications 47 , here we use the traditional Global North/South classification due to its historical ties to geography which is influential in climate research.
Results and discussion
Our analyses indicate that existing green infrastructure of an average city has a capability of cooling down surface temperatures by ~3 °C during warm seasons. However, a concerning disparity is evident; on average Global South cities have only two-thirds the cooling capacity and cooling benefit compared to Global North cities. This inequality is attributable to the differences in both quantity and quality of existing urban green infrastructure among cities. Importantly, we find that there exists considerable potential for many cities to enhance the cooling capability of their green infrastructure; achieving this potential could dramatically reduce global inequalities in adaptation to outdoor heat stress.
Quantifying cooling inequality
Our analyses showed that both the quantity and quality of the existing urban green infrastructure vary greatly among the world’s ~500 most populated cities (see Methods for details, and Fig. 1 for examples). The quantity of urban green infrastructure measured based on remotely sensed indicators of spectral greenness (Normalized Difference Vegetation Index, NDVI, see Methods) had a coefficient of variation (CV) of 35%. Similarly, the quality of urban green infrastructure in terms of cooling efficiency (daytime land surface temperatures during peak summer) had a CV of 37% (Supplementary Figs. 1 , 2 ). The global mean value of cooling capacity is 2.9 °C; existing urban green infrastructure ameliorates warm-season heat stress by 2.9 °C of surface temperature in an average city. In truth, however, the variation in cooling capacity was great (global CV in cooling capacity as large as ~50%), such that few cities were average. This variation is strongly geographically structured. Cities closer to the equator - tropical and subtropical cities - tend to have relatively weak cooling capacities (Fig. 2a, b ). As Global South countries are predominantly located at low latitudes, this pattern leads to a situation in which Global South cities, which tend to be hotter and relatively lower-income, have, on average, approximately two-thirds the cooling capacity of the Global North cities (2.5 ± 1.0 vs. 3.6 ± 1.7°C, Wilcoxon test, p = 2.7e-12; Fig. 2c ). The cities that most need to rely on green infrastructure are, at present, those that are least able to do so.
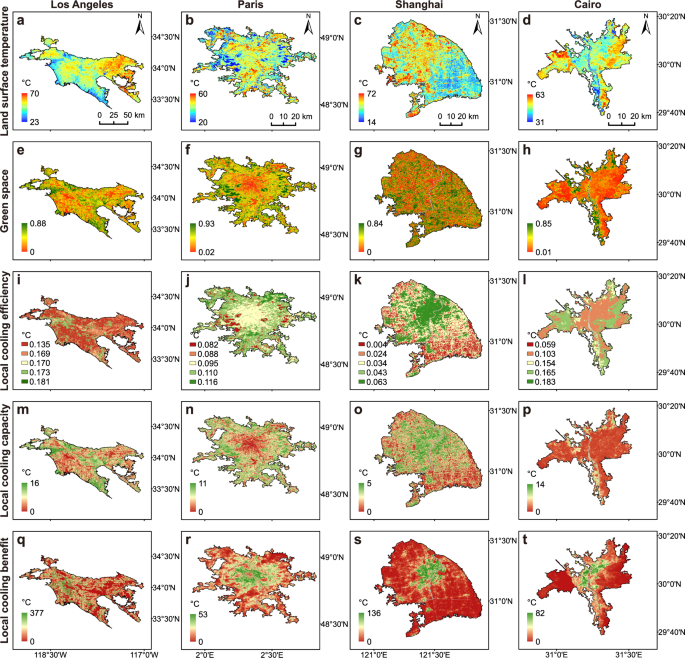
a , e , i , m , q Los Angeles, US. b , f , j , n , r Paris, France. c , g , k , o , s Shanghai, China. d , h , l , p , t Cairo, Egypt. Local cooling efficiency is calculated for different local climate zone types to account for within-city heterogeneity. In densely populated parts of cities, local cooling capacity tends to be lower due to reduced green space area, whereas local cooling benefit (local cooling capacity multiplied by a weight term of local population density relative to city mean) tends to be higher as more urban residents can receive cooling amelioration.
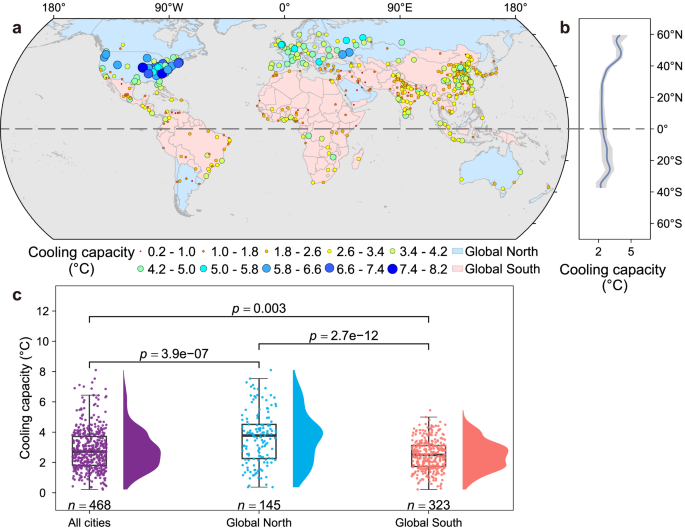
a Global distribution of cooling capacity for the 468 major urbanized areas. b Latitudinal pattern of cooling capacity. c Cooling capacity difference between the Global North and South cities. The cooling capacity offered by urban green infrastructure evinces a latitudinal pattern wherein lower-latitude cities have weaker cooling capacity ( b , cubic-spline fitting of cooling capacity with 95% confidence interval is shown), representing a significant inequality between Global North and South countries: city-level cooling capacity for Global North cities are about 1.5-fold higher than in Global South cities ( c ). Data are presented as box plots, where median values (center black lines), 25th percentiles (box lower bounds), 75th percentiles (box upper bounds), whiskers extending to 1.5-fold of the interquartile range (IQR), and outliers are shown. The tails of the cooling capacity distributions are truncated at zero as all cities have positive values of cooling capacity. Notice that no cities in the Global South have a cooling capacity greater than 5.5 °C ( c ). This is because no cities in the Global South have proportional green space areas as great as those seen in the Global North (see also Fig. 4b ). A similar pattern is found for cooling benefit (Supplementary Fig. 3 ). The two-sided non-parametric Wilcoxon test was used for statistical comparisons.
When we account for the locations of urban green infrastructure relative to humans within cities, the cooling benefit of urban green infrastructure realized by an average urban resident generally becomes slightly lower than suggested by cooling capacity (see Methods; Supplementary Fig. 3 ). Urban residents tend to be densest in the parts of cities with less green infrastructure. As a result, the average urban resident experiences less cooling amelioration than expected. However, this heterogeneity has only a minor effect on global-scale inequality. As a result, the geographic trends in cooling capacity and cooling benefit are similar: mean cooling benefit for an average urban resident also presents a 1.5-fold gap between Global South and North cities (2.2 ± 0.9 vs. 3.4 ± 1.7 °C, Wilcoxon test, p = 3.2e-13; Supplementary Fig. 3c ). Urban green infrastructure is a public good that has the potential to help even the most marginalized populations stay cool; unfortunately, this public benefit is least available in the Global South. When walking outdoors, the average person in an average Global South city receives only two-thirds the cooling amelioration from urban green infrastructure experienced by a person in an average Global North city. The high cooling amelioration capacity and benefit of the Global North cities is heavily influenced by North America (specifically, Canada and the US), which have both the highest cooling efficiency and the largest area of green infrastructure, followed by Europe (Supplementary Fig. 4 ).
One way to illustrate the global inequality of cooling capacity or benefit is to separately look at the cities that are most and least effective in ameliorating outdoor heat stress. Our results showed that ~85% of the 50 most effective cities (with highest cooling capacity or cooling benefit) are located in the Global North, while ~80% of the 50 least effective are Global South cities (Fig. 3 , Supplementary Fig. 5 ). This is true without taking into account the differences in the background temperatures and climate warming of these cities, which will exacerbate the effects on human health; cities in the Global South are likely to be closer to the limits of human thermal comfort and even, increasingly, the limits of the temperatures and humidities (wet-bulb temperatures) at which humans can safely work or even walk, such that the ineffectiveness of green spaces in those cities in cooling will lead to greater negative effects on human health 48 , work 14 , and gross domestic product (GDP) 49 . In addition, Global South cities commonly have higher population densities (Fig. 3 , Supplementary Fig. 5 ) and are projected to have faster population growth 50 . This situation will plausibly intensify the urban heat island effect because of the need of those populations for housing (and hence tensions between the need for buildings and the need for green spaces). It will also increase the number of people exposed to extreme urban heat island effects. Therefore, it is critical to increase cooling benefit via expanding urban green spaces, so that more people can receive the cooling mitigation from a given new neighboring green space if they live closer to each other. Doing so will require policies that incentivize urban green spaces as well as architectural innovations that make innovations such as plant-covered buildings easier and cheaper to implement.
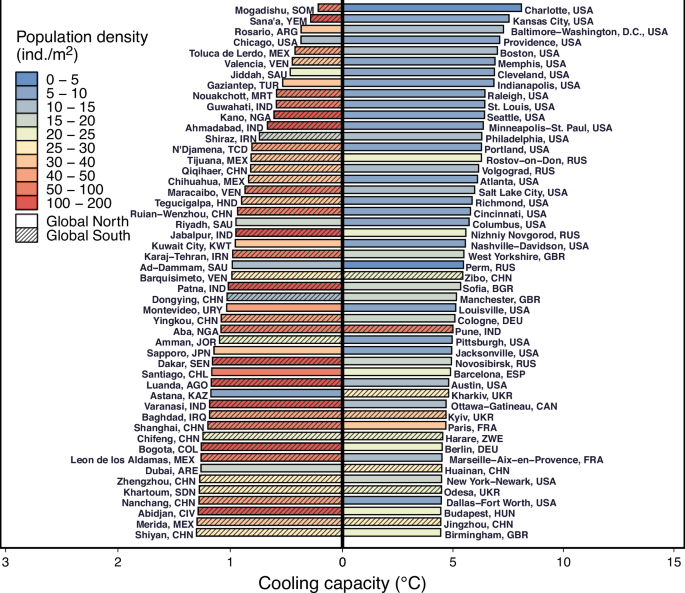
The axes on the right are an order of magnitude greater than those on the left, such that the cooling capacity of Charlotte in the United States is about 37-fold greater than that of Mogadishu (Somalia) and 29-fold greater than that of Sana’a (Yemen). The cities presenting lowest cooling capacities are most associated with Global South cities at higher population densities.
Of course, cities differ even within the Global North or within the Global South. For example, some Global South cities have high green space areas (or relatively high cooling efficiency in combination with moderate green space areas) and hence high cooling capacity. These cities, such as Pune (India), will be important to study in more detail, to shed light on the mechanistic details of their cooling abilities as well as the sociopolitical and other factors that facilitated their high green area coverage and cooling capabilities (Supplementary Figs. 6 , 7 ).
We conducted our primary analyses using a spatial grain of 100-m grid cells and Landsat NDVI data for quantifying spectral greenness. Our results, however, were robust at the coarser spatial grain of 1 km. We find a slightly larger global cooling inequality (~2-fold gap between Global South and North cities) at the 1-km grain using MODIS data (see Methods and Supplementary Fig. 17 ). MODIS data have been frequently used for quantifying urban heat island effects and cooling mitigation 44 , 45 , 51 . Our results reinforce its robustness for comparing urban thermal environments between cities across broad scales.
Influencing factors
The global inequality of cooling amelioration could have a number of proximate causes. To understand their relative influence, we first separately examined the effects of quality (cooling efficiency) and quantity (NDVI as a proxy indicator of urban green space area) of urban green infrastructure. The simplest null model is one in which cooling capacity (at the city scale) and cooling benefit (at the human scale) are driven primarily by the proportional area in a city dedicated to green spaces. Indeed, we found that both cooling capacity and cooling benefit were strongly correlated with urban green space area (Fig. 4 , Supplementary Fig. 8 ). This finding is useful with regards to practical interventions. In general, cities that invest in saving or restoring more green spaces will receive more cooling benefits from those green spaces. By contrast, differences among cities in cooling efficiency played a more minor role in determining the cooling capacity and benefit of cities (Fig. 4 , Supplementary Fig. 8 ).
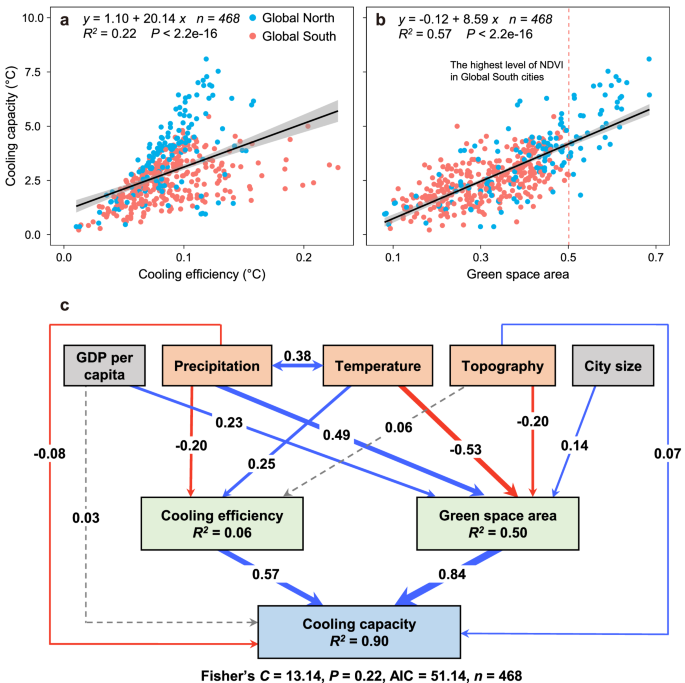
a Relationship between cooling efficiency and cooling capacity. b Relationship between green space area (measured by mean Landsat NDVI in the hottest month of 2018) and cooling capacity. Note that the highest level of urban green space area in the Global South cities is much lower than that in the Global North (dashed line in b ). Gray bands indicate 95% confidence intervals. Two-sided t-tests were conducted. c A piecewise structural equation model based on assumed direct and indirect (through influencing cooling efficiency and urban green space area) effects of essential natural and socioeconomic factors on cooling capacity. Mean annual temperature and precipitation, and topographic variation (elevation range) are selected to represent basic background natural conditions; GDP per capita is selected to represent basic socioeconomic conditions. The spatial extent of built-up areas is included to correct for city size. A bi-directional relationship (correlation) is fitted between mean annual temperature and precipitation. Red and blue solid arrows indicate significantly negative and positive coefficients with p ≤ 0.05, respectively. Gray dashed arrows indicate p > 0.05. The arrow width illustrates the effect size. Similar relationships are found for cooling benefits realized by an average urban resident (see Supplementary Fig. 8 ).
A further question is what shapes the quality and quantity of urban green infrastructure (which in turn are driving cooling capacity)? Many inter-correlated factors are possibly operating at multiple scales, making it difficult to disentangle their effects, especially since experiment-based causal inference is usually not feasible for large-scale urban systems. From a macroscopic perspective, we test the simple hypothesis that the background natural and socioeconomic conditions of cities jointly affect their cooling capacity and benefit in both direct and indirect ways. To this end, we constructed a minimal structural equation model including only the most essential variables reflecting background climate (mean annual temperature and precipitation), topographic variation (elevation range), as well as gross domestic product (GDP) per capita and city area (see Methods; Fig. 4c ).
We found that the quantity of green spaces in a city (again, in proportion to its size) was positively correlated with GDP per capita and city area; wealthier cities have more green spaces. It is well known that wealth and green spaces are positively correlated within cities (the luxury effect) 40 , 46 ; our analysis shows that a similar luxury effect occurs among them at a global scale. In addition, larger cities often have proportionally more green spaces, an effect that may be due to the tendency for large cities (particularly in the US and Canada) to have lower population densities. Cities that were hotter and had more topographic variation tended to have fewer green spaces and those that were more humid tended to have more green spaces. Given that temperature and humidity are highly correlated with the geography of the Global South and Global North, it is difficult to know whether these effects are due to the direct effects of temperature and precipitation, for example, on the growth rate of vegetation and hence the transition of abandoned lots into green spaces, or are associated with historical, cultural and political differences that via various mechanisms correlate to climate. Our structural equation model explained only a small fraction of variation among cities in their cooling efficiency, which is to say the quality of their green space. Cooling efficiency was modestly influenced by background temperature and precipitation—the warmer a city, the greater the cooling efficiency in that city; conversely, the more humid a city the less the cooling efficiency of that city.
Our analyses suggested that the lower cooling adaptation capabilities of Global South cities can be explained by their lower quantity of green infrastructure and, to a much lesser extent, their weaker cooling efficiency (quality; Supplementary Fig. 2 ). These patterns appear to be in part structured by GDP, but are also associated with climatic conditions 39 , and other factors. A key question, unresolved by our work, is whether the climatic correlates of the size of green spaces in cities are due to the effects of climate per se or if they, instead, reflect correlates between contemporary climate and the social, cultural, and political histories of cities in the Global South 52 . Since urban planning has much inertia, especially in big cities, those choices might be correlated with climate because of the climatic correlates of political histories. It is also possible that these dynamics relate, in part, to the ways in which climate influences vegetation structure. However, this seems less likely given that under non-urban conditions vegetation cover (and hence cooling capacity) is normally positively correlated with mean annual temperature across the globe, opposite to our observed negative relationships for urban systems (Supplementary Fig. 9g ). Still, it is possible that increased temperatures in cities due to the urban heat island effects may lead to temperature-vegetation cover-cooling capacity relationships that differ from those in natural environments 53 , 54 . Indeed, a recent study found that climate warming will put urban forests at risk, and the risk is disproportionately higher in the Global South 55 .
Our model serves as a starting point for unraveling the mechanisms underlying global cooling inequality. We cannot rule out the possibility that other unconsidered factors correlated with the studied variables play important roles. We invite systematic studies incorporating detailed sociocultural and ecological variables to address this question across scales.
Potential of enhancing cooling and reducing inequality
Can we reduce the inequality in cooling capacity and benefits that we have discovered among the world’s largest cities? Nuanced assessments of the potential to improve cooling mitigation require comprehensive considerations of socioeconomic, cultural, and technological aspects of urban management and policy. It is likely that cities differ greatly in their capacity to implement cooling through green infrastructure, whether as a function of culture, governance, policy or some mix thereof. However, any practical attempts to achieve greater cooling will occur in the context of the realities of climate and existing land use. To understand these realities, we modeled the maximum additional cooling capacity that is possible in cities, given existing constraints. We assume that this capacity depends on the quality (cooling efficiency) and quantity of urban green infrastructure. Our approach provides a straightforward metric of the cooling that could be achieved if all parts of a city’s green infrastructure were to be enhanced systematically.
The positive outlook is that our analyses suggest a considerable potential of improving cooling capacity by optimizing urban green infrastructure. An obvious way is through increases in urban green infrastructure quantity. We employ an approach in which we consider each local climate zone 56 to have a maximum NDVI and cooling efficiency (see Methods). For a given local climate zone, the city with the largest NDVI values or cooling efficiency sets the regional upper bounds for urban green infrastructure quantities or quality that can be achieved. Notably, these maxima are below the maxima for forests or other non-urban spaces for the simple reason that, as currently imagined, cities must contain gray (non-green) spaces in the form of roads and buildings. In this context, we conduct a thought experiment. What if we could systematically increase NDVI of all grid cells in each city, per local climate zone type, to a level corresponding to the median NDVI of grid cells in that upper bound city while keeping cooling efficiency unchanged (see Methods). If we were able to achieve this goal, the cooling capacity of cities would increase by ~2.4 °C worldwide. The increase would be even greater, ~3.8°C, if the 90th percentile (within the reference maximum city) was reached (Fig. 5a ). The potential for cooling benefit to the average urban resident is similar to that of cooling capacity (Supplementary Fig. 10a ). There is also potential to reduce urban temperatures if we can enhance cooling efficiency. However, the benefits of increases in cooling efficiency are modest (~1.5 °C increases at the 90th percentile of regional upper bounds) when holding urban green infrastructure quantity constant. In theory, if we could maximize both quantity and cooling efficiency of urban green infrastructure (to 90th percentiles of their regional upper bounds respectively), we would yield increases in cooling capacity and benefit up to ~10 °C, much higher than enhancing green space area or cooling efficiency alone (Fig. 5a , Supplementary Fig. 10a ). Notably, such co-maximization of green space area and cooling efficiency would substantially reduce global inequality to Gini <0.1 (Fig. 5b , Supplementary Fig. 10b ). Our analyses thus provide an important suggestion that enhancing both green space quantity and quality can yield a synergistic effect leading to much larger gains than any single aspect alone.
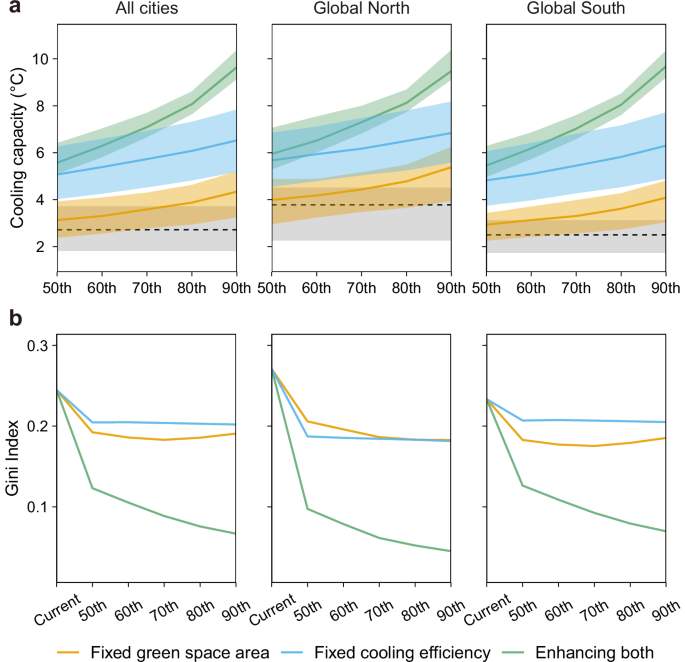
a The potential of enhancing cooling capacity via either enhancing urban green infrastructure quality (i.e., cooling efficiency) while holding quantity (i.e., green space area) fixed (yellow), or enhancing quantity while holding quality fixed (blue) is much lower than that of enhancing both quantity and quality (green). The x-axis indicates the targets of enhancing urban green infrastructure quantity and/or quality relative to the 50–90th percentiles of NDVI or cooling efficiency, see Methods). The dashed horizontal lines indicate the median cooling capacity of current cities. Data are presented as median values with the colored bands corresponding to 25–75th percentiles. b The potential of reducing cooling capacity inequality is also higher when enhancing both urban green infrastructure quantity and quality. The Gini index weighted by population density is used to measure inequality. Similar results were found for cooling benefit (Supplementary Fig. 10 ).
Different estimates of cooling capacity potential may be reached based on varying estimates and assumptions regarding the maximum possible quantity and quality of urban green infrastructure. There is no single, simple way to make these estimates, especially considering the huge between-city differences in society, culture, and structure across the globe. Our example case (above) begins from the upper bound city’s median NDVI, taking into account different local climate zone types and background climate regions (regional upper bounds). This is based on the assumption that for cities within the same climate regions, their average green space quantity may serve as an attainable target. Still, urban planning is often made at the level of individual cities, often only implemented to a limited extent and made with limited consideration of cities in other regions and countries. A potentially more realistic reference may be taken from the existing green infrastructure (again, per local climate zone type) within each particular city itself (see Methods): if a city’s sparsely vegetated areas was systematically elevated to the levels of 50–90th percentiles of NDVI within their corresponding local climate zones within the city, cooling capacity would still increase, but only by 0.5–1.5 °C and with only slightly reduced inequalities among cities (Supplementary Fig. 11 ). This highlights that ambitious policies, inspired by the greener cities worldwide, are necessary to realize the large cooling potential in urban green infrastructure.
In summary, our results demonstrate clear inequality in the extent to which urban green infrastructure cools cities and their denizens between the Global North and South. Much attention has been paid to the global inequality of indoor heat adaptation arising from the inequality of resources (e.g., less affordable air conditioning and more frequent power shortages in the Global South) 36 , 57 , 58 , 59 . Our results suggest that the inequality in outdoor adaptation is particularly concerning, especially as urban populations in the Global South are growing rapidly and are likely to face the most severe future temperature extremes 60 .
Previous studies have been focusing on characterizing urban heat island effects, urban vegetation patterns, resident exposure, and cooling effects in particular cities 26 , 28 , 34 , 61 , regions 22 , 25 , 62 , or continents 32 , 44 , 63 . Recent studies start looking at global patterns with respect to cooling efficiency or green space exposure 35 , 45 , 64 , 65 . Our approach is one drawn from the fields of large-scale ecology and macroecology. This approach is complementary to and, indeed, can, in the future, be combined with (1) mechanism driven biophysical models 66 , 67 to predict the influence of the composition and climate of green spaces on their cooling efficiency, (2) social theory aimed at understanding the factors that govern the amount of green space in cities as well as the disparity among cities 68 , (3) economic models of the effects of policy changes on the amount of greenspace and even (4) artist-driven projects that seek to understand the ways in which we might reimagine future cities 69 . Our simple explanatory model is, ultimately, one lens on a complex, global phenomenon.
Our results convey some positive outlook in that there is considerable potential to strengthen the cooling capability of cities and to reduce inequalities in cooling capacities at the same time. Realizing this nature-based solution, however, will be challenging. First, enhancing urban green infrastructure requires massive investments, which are more difficult to achieve in Global South cities. Second, it also requires smart planning strategies and advanced urban design and greening technologies 37 , 70 , 71 , 72 . Spatial planning of urban green spaces needs to consider not only the cooling amelioration effect, but also their multifunctional aspects that involve multiple ecosystem services, mental health benefits, accessibility, and security 73 . In theory, a city can maximize its cooling while also maximizing density through the combination of high-density living, ground-level green spaces, and vertical and rooftop gardens (or even forests). In practice, the current cities with the most green spaces tend to be lower-density cities 74 (Supplementary Fig. 12 ). Still, innovation and implementation of new technologies that allow green spaces and high-density living to be combined have the potential to reduce or disconnect the negative relationship between green space area and population density 71 , 75 . However, this development has yet to be realized. Another dimension of green spaces that deserves more attention is the geography of green spaces relative to where people are concentrated within cities. A critical question is how best should we distribute green spaces within cities to maximize cooling efficiency 76 and minimize within-city cooling inequality towards social equity 77 ? Last but not least, it is crucial to design and manage urban green spaces to be as resilient as possible to future climate stress 78 . For many cities, green infrastructure is likely to remain the primary means people will have to rely on to mitigate the escalating urban outdoor heat stress in the coming decades 79 .
We used the world population data from the World’s Cities in 2018 Data Booklet 80 to select 502 major cities with population over 1 million people (see Supplementary Data 1 for the complete list of the studied cities). Cities are divided into the Global North and Global South based on the Human Development Index (HDI) from the Human Development Report 2019 81 . For each selected city, we used the 2018 Global Artificial Impervious Area (GAIA) data at 30 m resolution 82 to determine its geographic extent. The derived urban boundary polygons thus encompass a majority of the built-up areas and urban residents. In using this approach, rather than urban administrative boundaries, we can focus on the relatively densely populated areas where cooling mitigation is most needed, and exclude areas dominated by (semi) natural landscapes that may bias the subsequent quantifications of the cooling effect. Our analyses on the cooling effect were conducted at the 100 m spatial resolution using Landsat data and WorldPop Global Project Population Data of 2018 83 . In order to test for the robustness of the results to coarser spatial scales, we also repeated the analyses at 1 km resolution using MODIS data, which have been extensively used for quantifying urban heat island effects and cooling mitigation 44 , 45 , 51 . We discarded the five cities with sizes <30 km 2 as they were too small for us to estimate their cooling efficiency based on linear regression (see section below for details). We combined closely located cities that form contiguous urban areas or urban agglomerations, if their urban boundary polygons from GAIA merged (e.g., Phoenix and Mesa in the United States were combined). Our approach yielded 468 polygons, each representing a major urbanized area that were the basis for all subsequent analyses. Because large water bodies can exert substantial and confounding cooling effects, we excluded permanent water bodies including lakes, reservoirs, rivers, and oceans using the Copernicus Global Land Service (CGLS) Land Cover data for 2018 at 10 m resolution 84 .
Quantifying the cooling effect
As a first step, we calculated cooling efficiency for each studied city within the GAIA-derived urban boundary. Cooling efficiency quantifies the extent to which a given area of green spaces in a city can reduce temperatures. It is a measure of the effectiveness (quality) of urban green spaces in terms of heat amelioration. Cooling efficiency is typically measured by calculating the slope of the relationship between remotely-sensed land surface temperature (LST) and vegetation cover through ordinary least square regression 42 , 44 , 45 . It is known that cooling efficiency varies between cities. Influencing factors might include background climate 29 , species composition 30 , 85 , landscape configuration 28 , topography 86 , proximity to large water bodies 33 , 87 , urban morphology 88 , and city management practices 31 . However, the mechanism underlying the global pattern of cooling efficiency remains unclear.
We used Landsat satellite data provided by the United States Geological Survey (USGS) to calculate the cooling efficiency of each studied city. We used the cloud-free Landsat 8 Level 2 LST and NDVI data. For each city we calculated the mean LST in each month of 2018 to identify the hottest month, and then derived the hottest month LST; we used the cloud-free Landsat 8 data to calculate the mean NDVI for the hottest month correspondingly.
We quantified cooling efficiency for different local climate zones 56 separately for each city, to account for within-city variability of thermal environments. To this end, we used the Copernicus Global Land Service data (CGLS) 84 and Global Human Settlement Layers (GHSL) Built-up height data 89 of 2018 at the 100 m resolution to identify five types of local climate zones: non-tree vegetation (shrubs, herbaceous vegetation, and cultivated vegetation according to the CGLS classification system), low-rise buildings (built up and bare according to the CGLS classification system, with building heights ≤10 m according to the GHSL data), medium-high-rise buildings (built up and bare areas with building heights >10 m), open tree cover (open forest with tree cover 15–70% according to the CGLS system), and closed tree cover (closed forest with tree cover >70%).
For each local climate zone type in each city, we constructed a regression model with NDVI as the predictor variable and LST as the response variable (using the ordinary least square method). We took into account the potential confounding factors including topographic elevation (derived from MERIT DEM dataset 90 ), building height (derived from the GHSL dataset 89 ), and distance to water bodies (derived from the GSHHG dataset 91 ), the model thus became: LST ~ NDVI + topography + building height + distance to water. Cooling efficiency was calculated as the absolute value of the regression coefficient of NDVI, after correcting for those confounding factors. To account for the multi-collinearity issue, we conducted variable selection based on the variance inflation factor (VIF) to achieve VIF < 5. Before the analysis, we discarded low-quality Landsat pixels, and filtered out the pixels with NDVI < 0 (normally less than 1% in a single city). Cooling efficiency is known to be influenced by within-city heterogeneity 92 , 93 , and, as a result, might sometimes better fit non-linear relationships at local scales 65 , 76 . However, our central aim is to assess global cooling inequality based on generalized relationships that fit the majority of global cities. Previous studies have shown that linear relationships can do this job 42 , 44 , 45 , therefore, here we used linear models to assess cooling efficiency.
As a second step, we calculated the cooling capacity of each city. Cooling capacity is a positive function of the magnitude of cooling efficiency and the proportional area of green spaces in a city and is calculated based on NDVI and the derived cooling efficiency (Eq. 1 , Supplementary Fig. 13 ):
where CC lcz and CE lcz are the cooling capacity and cooling efficiency for a given local climate zone type in a city, respectively; NDVI i is the mean NDVI for 100-m grid cell i ; NDVI min is the minimum NDVI across the city; and n is the total number of grid cells within the local climate zone. Local cooling capacity for each grid cell i (Fig. 1 , Supplementary Fig. 7 ) can be derived in this way as well (Supplementary Fig. 13 ). For a particular city, cooling capacity may be dependent on the spatial configuration of its land use/cover 28 , 94 , but here we condensed cooling capacity to city average (Eq. 2 ), thus did not take into account these local-scale factors.
where CC is the average cooling capacity of a city; n lcz is the number of grid cells of the local climate zone; m is the total number of grid cells within the whole city.
As a third step, we calculated the cooling benefit realized by an average urban resident (cooling benefit in short) in each city. Cooling benefit depends not only on the cooling capacity of a city, but also on where people live within a city relative to greener or grayer areas of the city. For example, cooling benefits in a city might be low even if the cooling capacity is high if the green parts and the dense-population parts of a city are inversely correlated. Here, we are calculating these averages while aware that in any particular city the exposure of a particular person will depend on the distribution of green spaces in a city, and the occupation, movement trajectories of a person, etc. On the scale of a city, we calculated cooling benefit following a previous study 35 , that is, simply adding a weight term of population size per 100-m grid cell into cooling capacity in Eq. ( 1 ):
Where CB lcz is the cooling benefit of a given local climate zone type in a specific city, pop i is the number of people within grid cell i , \(\overline{{pop}}\) is the mean population of the city.
Where CB is the average cooling benefit of a city. The population data were obtained from the 100-m resolution WorldPop Global Project Population Data of 2018 83 . Local cooling benefit for a given grid cell i can be calculated in a similar way, i.e., local cooling capacity multiplied by a weight term of local population density relative to mean population density. Local cooling benefits were mapped for example cities for the purpose of illustrating the effect of population spatial distribution (Fig. 1 , Supplementary Fig. 7 ), but their patterns were not examined here.
Based on the aforementioned three key variables quantified at 100 m grid cells, we conducted multivariate analyses to examine if and to what extent cooling efficiency and cooling benefit are shaped by essential natural and socioeconomic factors, including background climate (mean annual temperature from ECMWF ERA5 dataset 95 and precipitation from TerraClimate dataset 96 ), topography (elevation range 90 ), and GDP per capita 97 , with city size (geographic extent) corrected for. We did not include humidity because it is strongly correlated with temperature and precipitation, causing serious multi-collinearity problems. We used piecewise structural equation modeling to test the direct effects of these factors and indirect effects via influencing cooling efficiency and vegetation cover (Fig. 4c , Supplementary Fig. 8c ). To account for the potential influence of spatial autocorrelation, we used spatially autoregressive models (SAR) to test for the robustness of the observed effects of natural and socioeconomic factors on cooling capacity and benefit (Supplementary Fig. 14 ).
Testing for robustness
We conducted the following additional analyses to test for robustness. We obtained consistent results from these robustness analyses.
(1) We looked at the mean hottest-month LST and NDVI within 3 years (2017-2019) to check the consistency between the results based on relatively short (1 year) vs. long (3-year average) time periods (Supplementary Fig. 15 ).
(2) We carried out the approach at a coarser spatial scale of 1 km, using MODIS-derived NDVI and LST, as well as the population data 83 in the hottest month of 2018. In line with our finer-scale analysis of Landsat data, we selected the hottest month and excluded low-quality grids affected by cloud cover and water bodies 98 (water cover > 20% in 1 × 1 km 2 grid cells) of MODIS LST, and calculated the mean NDVI for the hottest month. We ultimately obtained 441 cities (or urban agglomerations) for analysis. At the 1 km resolution, some local climate zone types would yield insufficient samples for constructing cooling efficiency models. Therefore, instead of identifying local climate zone explicitly, we took an indirect approach to account for local climate confounding factors, that is, we constructed a multiple regression model for a whole city incorporating the hottest-month local temperature 95 , precipitation 96 , and humidity (based on NASA FLDAS dataset 99 ), albedo (derived from the MODIS MCD43A3 product 100 ), aerosol loading (derived from the MODIS MCD19A2 product 101 ), wind speed (based on TerraClimate dataset 96 ), topography elevation 90 , distance to water 91 , urban morphology (building height 102 ), and human activity intensity (VIIRS nighttime light data as a proxy indicator 103 ). We used the absolute value of the linear regression coefficient of NDVI as the cooling efficiency of the whole city (model: LST ~ NDVI + temperature + precipitation + humidity + distance to water + topography + building height + albedo + aerosol + wind speed + nighttime light), and calculated cooling capacity and cooling benefit based on the same method. Variable selection was conducted using the criterion of VIF < 5.
Our results indicated that MODIS-based cooling capacity and cooling benefit are significantly correlated with the Landsat-based counterparts (Supplementary Fig. 16 ); importantly, the gap between the Global South and North cities is around two-fold, close to the result from the Landsat-based result (Supplementary Fig. 17 ).
(3) For the calculation of cooling benefit, we considered different spatial scales of human accessibility to green spaces: assuming the population in each 100 × 100 m 2 grid cell could access to green spaces within neighborhoods of certain extents, we calculated cooling benefit by replacing NDVI i in Eq. ( 3 ) with mean NDVI within the 300 × 300 m 2 and 500 × 500 m 2 extents centered at the focal grid cell (Supplementary Fig. 18 ).
(4) Considering cities may vary in minimum NDVI, we assessed if this variation could affect resulting cooling capacity patterns. To this end, we calculated the cooling capacity for each studied city using NDVI = 0 as the reference (i.e., using NDVI = 0 instead of minimum NDVI in Supplementary Fig. 13b ), and correlated it with that using minimum NDVI as the reference (Supplementary Fig. 19 ).
Quantifying between-city inequality
Inequalities in access to the benefits of green spaces in cities exist within cities, as is increasingly well-documented 104 . Here, we focus instead on the inequalities among cities. We used the Gini coefficient to measure the inequality in cooling capacity and cooling benefit between all studied cities across the globe as well as between Global North or South cities. We calculated Gini using the population-density weighted method (Fig. 5b ), as well as the unweighted and population-size weighted methods (Supplementary Fig. 20 ).
Estimating the potential for more effective and equal cooling amelioration
We estimated the potential of enhancing cooling amelioration based on the assumptions that urban green space quality (cooling efficiency) and quantity (NDVI) can be increased to different levels, and that relative spatial distributions of green spaces and population can be idealized (so that their spatial matches can maximize cooling benefit). We assumed that macro-climate conditions act as the constraints of vegetation cover and cooling efficiency. We calculated the 50th, 60th, 70th, 80th, and 90th percentiles of NDVI within each type of local climate zone of each city. For a given local climate zone type, we obtained the city with the highest NDVI per percentile value as the regional upper bounds of urban green infrastructure quantity. The regional upper bounds of cooling efficiency are derived in a similar way. For each local climate zone in a city, we generated a potential NDVI distribution where all grid cells reach the regional upper bound values for the 50th, 60th, 70th, 80th, or 90th percentile of urban green space quantity or quality, respectively. NDVI values below these percentiles were increased, whereas those above these percentiles remained unchanged. The potential estimates are essentially dependent on the references, i.e., the optimal cooling efficiency and NDVI that a given city can reach. However, such references are obviously difficult to determine, because complex natural and socioeconomic conditions could play important roles in determining those cooling optima, and the dominant factors are unknown at a global scale. We employed the simplifying assumption that background climate could act as an essential constraint according to our results. We therefore used the Köppen climate classification system 105 to determine the reference separately in each climate region (tropical, arid, temperate, and continental climate regions were involved for all studied cities).
We calculated potential cooling capacity and cooling benefit based on these potential NDVI maps (Fixed cooling efficiency in Fig. 5 ). We then calculated the potentials if cooling efficiency of each city can be enhanced to 50–90th percentile across all urban local climate zones within the corresponding biogeographic region (Fixed green space area in Fig. 5 ). We also calculated the potentials if both NDVI and cooling efficiency were enhanced (Enhancing both in Fig. 5) to a certain corresponding level (i.e., i th percentile NDVI + i th percentile cooling efficiency). We examined if there are additional effects of idealizing relative spatial distributions of urban green spaces and humans on cooling benefits. To this end, the pixel values of NDVI or population amount remained unchanged, but their one-to-one correspondences were based on their ranking: the largest population corresponds to the highest NDVI, and so forth. Under each scenario, we calculated cooling capacity and cooling benefit for each city, and the between-city inequality was measured by the Gini coefficient.
We used the Google Earth Engine to process the spatial data. The statistical analyses were conducted using R v4.3.3 106 , with car v3.1-2 107 , piecewiseSEM v2.1.2 108 , and ineq v0.2-13 109 packages. The global maps of cooling were created using the ArcGIS v10.3 software.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
City population statistics data is collected from the Population Division of the Department of Economic and Social Affairs of the United Nations ( https://www.un.org/development/desa/pd/content/worlds-cities-2018-data-booklet ). Global North-South division is based on Human Development Report 2019 which from United Nations Development Programme ( https://hdr.undp.org/content/human-development-report-2019 ). Global urban boundaries from GAIA data are available from Star Cloud Data Service Platform ( https://data-starcloud.pcl.ac.cn/resource/14 ) . Global water data is derived from 2018 Copernicus Global Land Service (CGLS 100-m) data ( https://developers.google.com/earth-engine/datasets/catalog/COPERNICUS_Landcover_100m_Proba-V-C3_Global ), European Space Agency (ESA) WorldCover 10 m 2020 product ( https://developers.google.com/earth-engine/datasets/catalog/ESA_WorldCover_v100 ), and GSHHG (A Global Self-consistent, Hierarchical, High-resolution Geography Database) at https://www.soest.hawaii.edu/pwessel/gshhg/ . Landsat 8 LST and NDVI data with 30 m resolution are available at https://developers.google.com/earth-engine/datasets/catalog/LANDSAT_LC08_C02_T1_L2 . Land surface temperature (LST) data with 1 km from MODIS Aqua product (MYD11A1) is available at https://developers.google.com/earth-engine/datasets/catalog/MODIS_061_MYD11A1 . NDVI (1 km) dataset from MYD13A2 is available at https://developers.google.com/earth-engine/datasets/catalog/MODIS_061_MYD13A2 . Population data (100 m) is derived from WorldPop ( https://developers.google.com/earth-engine/datasets/catalog/WorldPop_GP_100m_pop ). Local climate zones are also based on 2018 CGLS data ( https://developers.google.com/earth-engine/datasets/catalog/COPERNICUS_Landcover_100m_Proba-V-C3_Global ), and built-up height data is available from Global Human Settlement Layers (GHSL, 100 m) ( https://developers.google.com/earth-engine/datasets/catalog/JRC_GHSL_P2023A_GHS_BUILT_H ). Temperature data is calculated from ERA5-Land Monthly Aggregated dataset ( https://developers.google.com/earth-engine/datasets/catalog/ECMWF_ERA5_LAND_MONTHLY_AGGR ). Precipitation and wind data are calculated from TerraClimate (Monthly Climate and Climatic Water Balance for Global Terrestrial Surfaces, University of Idaho) ( https://developers.google.com/earth-engine/datasets/catalog/IDAHO_EPSCOR_TERRACLIMATE ). Humidity data is calculated from Famine Early Warning Systems Network (FEWS NET) Land Data Assimilation System ( https://developers.google.com/earth-engine/datasets/catalog/NASA_FLDAS_NOAH01_C_GL_M_V001 ). Topography data from MERIT DEM (Multi-Error-Removed Improved-Terrain DEM) product is available at https://developers.google.com/earth-engine/datasets/catalog/MERIT_DEM_v1_0_3 . GDP from Gross Domestic Product and Human Development Index dataset is available at https://doi.org/10.5061/dryad.dk1j0 . VIIRS nighttime light data is available at https://developers.google.com/earth-engine/datasets/catalog/NOAA_VIIRS_DNB_MONTHLY_V1_VCMSLCFG . City building volume data from Global 3D Building Structure (1 km) is available at https://doi.org/10.34894/4QAGYL . Albedo data is derived from the MODIS MCD43A3 product ( https://developers.google.com/earth-engine/datasets/catalog/MODIS_061_MCD43A3 ), and aerosol data is derived from the MODIS MCD19A2 product ( https://developers.google.com/earth-engine/datasets/catalog/MODIS_061_MCD19A2_GRANULES ). All data used for generating the results are publicly available at https://doi.org/10.6084/m9.figshare.26340592.v1 .
Code availability
The codes used for data collection and analyses are publicly available at https://doi.org/10.6084/m9.figshare.26340592.v1 .
Dosio, A., Mentaschi, L., Fischer, E. M. & Wyser, K. Extreme heat waves under 1.5 °C and 2 °C global warming. Environ. Res. Lett. 13 , 054006 (2018).
Article ADS Google Scholar
Suarez-Gutierrez, L., Müller, W. A., Li, C. & Marotzke, J. Hotspots of extreme heat under global warming. Clim. Dyn. 55 , 429–447 (2020).
Article Google Scholar
Guo, Y. et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology 25 , 781–789 (2014).
Article PubMed PubMed Central Google Scholar
Mora, C. et al. Global risk of deadly heat. Nat. Clim. Chang. 7 , 501–506 (2017).
Ebi, K. L. et al. Hot weather and heat extremes: health risks. Lancet 398 , 698–708 (2021).
Article PubMed Google Scholar
Lüthi, S. et al. Rapid increase in the risk of heat-related mortality. Nat. Commun. 14 , 4894 (2023).
Article ADS PubMed PubMed Central Google Scholar
United Nations Department of Economic Social Affairs, Population Division. in World Population Prospects 2022: Summary of Results (United Nations Fund for Population Activities, 2022).
Sachindra, D., Ng, A., Muthukumaran, S. & Perera, B. Impact of climate change on urban heat island effect and extreme temperatures: a case‐study. Q. J. R. Meteorol. Soc. 142 , 172–186 (2016).
Guo, L. et al. Evaluating contributions of urbanization and global climate change to urban land surface temperature change: a case study in Lagos, Nigeria. Sci. Rep. 12 , 14168 (2022).
Article ADS CAS PubMed PubMed Central Google Scholar
Liu, Z. et al. Surface warming in global cities is substantially more rapid than in rural background areas. Commun. Earth Environ. 3 , 219 (2022).
Mentaschi, L. et al. Global long-term mapping of surface temperature shows intensified intra-city urban heat island extremes. Glob. Environ. Change 72 , 102441 (2022).
Asseng, S., Spänkuch, D., Hernandez-Ochoa, I. M. & Laporta, J. The upper temperature thresholds of life. Lancet Planet. Health 5 , e378–e385 (2021).
Zander, K. K., Botzen, W. J., Oppermann, E., Kjellstrom, T. & Garnett, S. T. Heat stress causes substantial labour productivity loss in Australia. Nat. Clim. Chang. 5 , 647–651 (2015).
Flouris, A. D. et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet. Health 2 , e521–e531 (2018).
Xu, C., Kohler, T. A., Lenton, T. M., Svenning, J.-C. & Scheffer, M. Future of the human climate niche. Proc. Natl Acad. Sci. USA 117 , 11350–11355 (2020).
Lenton, T. M. et al. Quantifying the human cost of global warming. Nat. Sustain. 6 , 1237–1247 (2023).
Harrington, L. J. et al. Poorest countries experience earlier anthropogenic emergence of daily temperature extremes. Environ. Res. Lett. 11 , 055007 (2016).
Bathiany, S., Dakos, V., Scheffer, M. & Lenton, T. M. Climate models predict increasing temperature variability in poor countries. Sci. Adv. 4 , eaar5809 (2018).
Alizadeh, M. R. et al. Increasing heat‐stress inequality in a warming climate. Earth Future 10 , e2021EF002488 (2022).
Tuholske, C. et al. Global urban population exposure to extreme heat. Proc. Natl Acad. Sci. USA 118 , e2024792118 (2021).
Article CAS PubMed PubMed Central Google Scholar
Manoli, G. et al. Magnitude of urban heat islands largely explained by climate and population. Nature 573 , 55–60 (2019).
Article ADS CAS PubMed Google Scholar
Wang, J. et al. Anthropogenic emissions and urbanization increase risk of compound hot extremes in cities. Nat. Clim. Chang. 11 , 1084–1089 (2021).
Article ADS CAS Google Scholar
Bowler, D. E., Buyung-Ali, L., Knight, T. M. & Pullin, A. S. Urban greening to cool towns and cities: a systematic review of the empirical evidence. Landsc. Urban Plan. 97 , 147–155 (2010).
Armson, D., Stringer, P. & Ennos, A. The effect of tree shade and grass on surface and globe temperatures in an urban area. Urban For. Urban Green. 11 , 245–255 (2012).
Wang, C., Wang, Z. H. & Yang, J. Cooling effect of urban trees on the built environment of contiguous United States. Earth Future 6 , 1066–1081 (2018).
Pataki, D. E., McCarthy, H. R., Litvak, E. & Pincetl, S. Transpiration of urban forests in the Los Angeles metropolitan area. Ecol. Appl. 21 , 661–677 (2011).
Konarska, J. et al. Transpiration of urban trees and its cooling effect in a high latitude city. Int. J. Biometeorol. 60 , 159–172 (2016).
Article ADS PubMed Google Scholar
Li, X., Zhou, W., Ouyang, Z., Xu, W. & Zheng, H. Spatial pattern of greenspace affects land surface temperature: evidence from the heavily urbanized Beijing metropolitan area, China. Landsc. Ecol. 27 , 887–898 (2012).
Yu, Z., Xu, S., Zhang, Y., Jørgensen, G. & Vejre, H. Strong contributions of local background climate to the cooling effect of urban green vegetation. Sci. Rep. 8 , 6798 (2018).
Richards, D. R., Fung, T. K., Belcher, R. & Edwards, P. J. Differential air temperature cooling performance of urban vegetation types in the tropics. Urban For. Urban Green. 50 , 126651 (2020).
Winbourne, J. B. et al. Tree transpiration and urban temperatures: current understanding, implications, and future research directions. BioScience 70 , 576–588 (2020).
Schwaab, J. et al. The role of urban trees in reducing land surface temperatures in European cities. Nat. Commun. 12 , 6763 (2021).
Vo, T. T. & Hu, L. Diurnal evolution of urban tree temperature at a city scale. Sci. Rep. 11 , 10491 (2021).
Wang, J. et al. Comparing relationships between urban heat exposure, ecological structure, and socio-economic patterns in Beijing and New York City. Landsc. Urban Plan. 235 , 104750 (2023).
Chen, B. et al. Contrasting inequality in human exposure to greenspace between cities of Global North and Global South. Nat. Commun. 13 , 4636 (2022).
Pavanello, F. et al. Air-conditioning and the adaptation cooling deficit in emerging economies. Nat. Commun. 12 , 6460 (2021).
Turner, V. K., Middel, A. & Vanos, J. K. Shade is an essential solution for hotter cities. Nature 619 , 694–697 (2023).
Hope, D. et al. Socioeconomics drive urban plant diversity. Proc. Natl Acad. Sci. USA 100 , 8788–8792 (2003).
Leong, M., Dunn, R. R. & Trautwein, M. D. Biodiversity and socioeconomics in the city: a review of the luxury effect. Biol. Lett. 14 , 20180082 (2018).
Schwarz, K. et al. Trees grow on money: urban tree canopy cover and environmental justice. PloS ONE 10 , e0122051 (2015).
Chakraborty, T., Hsu, A., Manya, D. & Sheriff, G. Disproportionately higher exposure to urban heat in lower-income neighborhoods: a multi-city perspective. Environ. Res. Lett. 14 , 105003 (2019).
Wang, J. et al. Significant effects of ecological context on urban trees’ cooling efficiency. ISPRS J. Photogramm. Remote Sens. 159 , 78–89 (2020).
Marando, F. et al. Urban heat island mitigation by green infrastructure in European Functional Urban Areas. Sust. Cities Soc. 77 , 103564 (2022).
Cheng, X., Peng, J., Dong, J., Liu, Y. & Wang, Y. Non-linear effects of meteorological variables on cooling efficiency of African urban trees. Environ. Int. 169 , 107489 (2022).
Yang, Q. et al. Global assessment of urban trees’ cooling efficiency based on satellite observations. Environ. Res. Lett. 17 , 034029 (2022).
Yin, Y., He, L., Wennberg, P. O. & Frankenberg, C. Unequal exposure to heatwaves in Los Angeles: Impact of uneven green spaces. Sci. Adv. 9 , eade8501 (2023).
Fantom N., Serajuddin U. The World Bank’s Classification of Countries by Income (The World Bank, 2016).
Iungman, T. et al. Cooling cities through urban green infrastructure: a health impact assessment of European cities. Lancet 401 , 577–589 (2023).
He, C. et al. The inequality labor loss risk from future urban warming and adaptation strategies. Nat. Commun. 13 , 3847 (2022).
Kii, M. Projecting future populations of urban agglomerations around the world and through the 21st century. npj Urban Sustain 1 , 10 (2021).
Paschalis, A., Chakraborty, T., Fatichi, S., Meili, N. & Manoli, G. Urban forests as main regulator of the evaporative cooling effect in cities. AGU Adv. 2 , e2020AV000303 (2021).
Hunte, N., Roopsind, A., Ansari, A. A. & Caughlin, T. T. Colonial history impacts urban tree species distribution in a tropical city. Urban For. Urban Green. 41 , 313–322 (2019).
Kabano, P., Harris, A. & Lindley, S. Sensitivity of canopy phenology to local urban environmental characteristics in a tropical city. Ecosystems 24 , 1110–1124 (2021).
Frank, S. D. & Backe, K. M. Effects of urban heat islands on temperate forest trees and arthropods. Curr. Rep. 9 , 48–57 (2023).
Esperon-Rodriguez, M. et al. Climate change increases global risk to urban forests. Nat. Clim. Chang. 12 , 950–955 (2022).
Stewart, I. D. & Oke, T. R. Local climate zones for urban temperature studies. Bull. Am. Meteorol. Soc. 93 , 1879–1900 (2012).
Biardeau, L. T., Davis, L. W., Gertler, P. & Wolfram, C. Heat exposure and global air conditioning. Nat. Sustain. 3 , 25–28 (2020).
Davis, L., Gertler, P., Jarvis, S. & Wolfram, C. Air conditioning and global inequality. Glob. Environ. Change 69 , 102299 (2021).
Colelli, F. P., Wing, I. S. & Cian, E. D. Air-conditioning adoption and electricity demand highlight climate change mitigation–adaptation tradeoffs. Sci. Rep. 13 , 4413 (2023).
Sun, L., Chen, J., Li, Q. & Huang, D. Dramatic uneven urbanization of large cities throughout the world in recent decades. Nat. Commun. 11 , 5366 (2020).
Liu, D., Kwan, M.-P. & Kan, Z. Analysis of urban green space accessibility and distribution inequity in the City of Chicago. Urban For. Urban Green. 59 , 127029 (2021).
Hsu, A., Sheriff, G., Chakraborty, T. & Manya, D. Disproportionate exposure to urban heat island intensity across major US cities. Nat. Commun. 12 , 2721 (2021).
Zhao, L., Lee, X., Smith, R. B. & Oleson, K. Strong contributions of local background climate to urban heat islands. Nature 511 , 216–219 (2014).
Wu, S., Chen, B., Webster, C., Xu, B. & Gong, P. Improved human greenspace exposure equality during 21st century urbanization. Nat. Commun. 14 , 6460 (2023).
Zhao, J., Zhao, X., Wu, D., Meili, N. & Fatichi, S. Satellite-based evidence highlights a considerable increase of urban tree cooling benefits from 2000 to 2015. Glob. Chang. Biol. 29 , 3085–3097 (2023).
Article CAS PubMed Google Scholar
Nice, K. A., Coutts, A. M. & Tapper, N. J. Development of the VTUF-3D v1. 0 urban micro-climate model to support assessment of urban vegetation influences on human thermal comfort. Urban Clim. 24 , 1052–1076 (2018).
Meili, N. et al. An urban ecohydrological model to quantify the effect of vegetation on urban climate and hydrology (UT&C v1. 0). Geosci. Model Dev. 13 , 335–362 (2020).
Nesbitt, L., Meitner, M. J., Sheppard, S. R. & Girling, C. The dimensions of urban green equity: a framework for analysis. Urban For. Urban Green. 34 , 240–248 (2018).
Hedblom, M., Prévot, A.-C. & Grégoire, A. Science fiction blockbuster movies—a problem or a path to urban greenery? Urban For. Urban Green. 74 , 127661 (2022).
Norton, B. A. et al. Planning for cooler cities: a framework to prioritise green infrastructure to mitigate high temperatures in urban landscapes. Landsc. Urban Plan 134 , 127–138 (2015).
Medl, A., Stangl, R. & Florineth, F. Vertical greening systems—a review on recent technologies and research advancement. Build. Environ. 125 , 227–239 (2017).
Chen, B., Lin, C., Gong, P. & An, J. Optimize urban shade using digital twins of cities. Nature 622 , 242–242 (2023).
Pamukcu-Albers, P. et al. Building green infrastructure to enhance urban resilience to climate change and pandemics. Landsc. Ecol. 36 , 665–673 (2021).
Haaland, C. & van Den Bosch, C. K. Challenges and strategies for urban green-space planning in cities undergoing densification: a review. Urban For. Urban Green. 14 , 760–771 (2015).
Shafique, M., Kim, R. & Rafiq, M. Green roof benefits, opportunities and challenges—a review. Renew. Sust. Energ. Rev. 90 , 757–773 (2018).
Wang, J., Zhou, W. & Jiao, M. Location matters: planting urban trees in the right places improves cooling. Front. Ecol. Environ. 20 , 147–151 (2022).
Lan, T., Liu, Y., Huang, G., Corcoran, J. & Peng, J. Urban green space and cooling services: opposing changes of integrated accessibility and social equity along with urbanization. Sust. Cities Soc. 84 , 104005 (2022).
Wood, S. & Dupras, J. Increasing functional diversity of the urban canopy for climate resilience: Potential tradeoffs with ecosystem services? Urban For. Urban Green. 58 , 126972 (2021).
Wong, N. H., Tan, C. L., Kolokotsa, D. D. & Takebayashi, H. Greenery as a mitigation and adaptation strategy to urban heat. Nat. Rev. Earth Environ. 2 , 166–181 (2021).
United Nations. Department of economic and social affairs, population division. in The World’s Cities in 2018—Data Booklet (UN, 2018).
United Nations Development Programme (UNDP). Human Development Report 2019: Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human Development in the 21st Century (United Nations Development Programme (UNDP), 2019)
Li, X. et al. Mapping global urban boundaries from the global artificial impervious area (GAIA) data. Environ. Res. Lett. 15 , 094044 (2020).
Stevens, F. R., Gaughan, A. E., Linard, C. & Tatem, A. J. Disaggregating census data for population mapping using random forests with remotely-sensed and ancillary data. PloS ONE 10 , e0107042 (2015).
Buchhorn, M. et al. Copernicus global land cover layers—collection 2. Remote Sens 12 , 1044 (2020).
Gillerot, L. et al. Forest structure and composition alleviate human thermal stress. Glob. Change Biol. 28 , 7340–7352 (2022).
Article CAS Google Scholar
Hamada, S., Tanaka, T. & Ohta, T. Impacts of land use and topography on the cooling effect of green areas on surrounding urban areas. Urban For. Urban Green. 12 , 426–434 (2013).
Sun, X. et al. Quantifying landscape-metrics impacts on urban green-spaces and water-bodies cooling effect: the study of Nanjing, China. Urban For . Urban Green. 55 , 126838 (2020).
Zhang, Q., Zhou, D., Xu, D. & Rogora, A. Correlation between cooling effect of green space and surrounding urban spatial form: Evidence from 36 urban green spaces. Build. Environ. 222 , 109375 (2022).
Pesaresi, M., Politis, P. GHS-BUILT-H R2023A - GHS building height, derived from AW3D30, SRTM30, and Sentinel2 composite (2018) . European Commission, Joint Research Centre (JRC) https://doi.org/10.2905/85005901-3A49-48DD-9D19-6261354F56FE (2023).
Yamazaki, D. et al. A high‐accuracy map of global terrain elevations. Geophys. Res. Lett. 44 , 5844–5853 (2017).
Wessel, P. & Smith, W. H. A global, self‐consistent, hierarchical, high‐resolution shoreline database. J. Geophys. Res. Solid Earth 101 , 8741–8743 (1996).
Ren et al. climatic map studies: a review. Int. J. Climatol. 31 , 2213–2233 (2011).
Zhou, X. et al. Evaluation of urban heat islands using local climate zones and the influence of sea-land breeze. Sust. Cities Soc. 55 , 102060 (2020).
Zhou, W., Huang, G. & Cadenasso, M. L. Does spatial configuration matter? Understanding the effects of land cover pattern on land surface temperature in urban landscapes. Landsc. Urban Plan 102 , 54–63 (2011).
Muñoz Sabater, J. ERA5-Land monthly averaged data from 1981 to present . Copernicus Climate Change Service (C3S) Climate Data Store (CDS) https://doi.org/10.24381/cds.68d2bb30 (2019).
Abatzoglou, J. T., Dobrowski, S. Z., Parks, S. A. & Hegewisch, K. C. TerraClimate, a high-resolution global dataset of monthly climate and climatic water balance from 1958–2015. Sci. Data 5 , 1–12 (2018).
Kummu, M., Taka, M. & Guillaume, J. H. Gridded global datasets for gross domestic product and Human Development Index over 1990–2015. Sci. Data 5 , 1–15 (2018).
Zanaga, D. et al. ESA WorldCover 10 m 2020 v100. https://doi.org/10.5281/zenodo.5571936 (2021).
McNally, A. et al. A land data assimilation system for sub-Saharan Africa food and water security applications. Sci. Data 4 , 1–19 (2017).
Schaaf C., & Wang Z. MODIS/Terra+Aqua BRDF/Albedo Daily L3 Global - 500m V061 . NASA EOSDIS Land Processes Distributed Active Archive Center. https://doi.org/10.5067/MODIS/MCD43A3.061 (2021).
Lyapustin A., & Wang Y. MODIS/Terra+Aqua Land Aerosol Optical Depth Daily L2G Global 1km SIN Grid V061 . NASA EOSDIS Land Processes Distributed Active Archive Center. https://doi.org/10.5067/MODIS/MCD19A2.061 (2022).
Li, M., Wang, Y., Rosier, J. F., Verburg, P. H. & Vliet, J. V. Global maps of 3D built-up patterns for urban morphological analysis. Int. J. Appl. Earth Obs. Geoinf. 114 , 103048 (2022).
Google Scholar
Elvidge, C. D., Baugh, K., Zhizhin, M., Hsu, F. C. & Ghosh, T. VIIRS night-time lights. Int. J. Remote Sens. 38 , 5860–5879 (2017).
Zhou, W. et al. Urban tree canopy has greater cooling effects in socially vulnerable communities in the US. One Earth 4 , 1764–1775 (2021).
Beck, H. E. et al. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci. Data 5 , 1–12 (2018).
R. Core Team. R: A Language and Environment for Statistical Computing . R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/ (2023).
Fox J., & Weisberg S. An R Companion to Applied Regression 3rd edn (Sage, 2019). https://socialsciences.mcmaster.ca/jfox/Books/Companion/ .
Lefcheck, J. S. piecewiseSEM: Piecewise structural equation modelling in r for ecology, evolution, and systematics. Methods Ecol. Evol. 7 , 573–579 (2016).
Zeileis, A. _ineq: Measuring Inequality, Concentration, and Poverty_ . R package version 0.2-13. https://CRAN.R-project.org/package=ineq (2014).
Download references
Acknowledgements
We thank all the data providers. We thank Marten Scheffer for valuable discussion. C.X. is supported by the National Natural Science Foundation of China (Grant No. 32061143014). J.-C.S. was supported by Center for Ecological Dynamics in a Novel Biosphere (ECONOVO), funded by Danish National Research Foundation (grant DNRF173), and his VILLUM Investigator project “Biodiversity Dynamics in a Changing World”, funded by VILLUM FONDEN (grant 16549). W.Z. was supported by the National Science Foundation of China through Grant No. 42225104. T.M.L. and J.F.A. are supported by the Open Society Foundations (OR2021-82956). W.J.R. is supported by the funding received from Roger Worthington.
Author information
Authors and affiliations.
School of Life Sciences, Nanjing University, Nanjing, China
Yuxiang Li, Shuqing N. Teng & Chi Xu
Center for Ecological Dynamics in a Novel Biosphere (ECONOVO), Department of Biology, Aarhus University, Aarhus, Denmark
Jens-Christian Svenning
State Key Laboratory of Urban and Regional Ecology, Research Center for Eco-Environmental Sciences, Chinese Academy of Sciences, Beijing, China
University of Chinese Academy of Sciences, Beijing, China
Beijing Urban Ecosystem Research Station, Research Center for Eco-Environmental Sciences, Chinese Academy of Sciences, Beijing, China
School for Environment and Sustainability, University of Michigan, Ann Arbor, MI, USA
Global Systems Institute, University of Exeter, Exeter, UK
Jesse F. Abrams & Timothy M. Lenton
Department of Forest Ecosystems and Society, Oregon State University, Corvallis, OR, USA
William J. Ripple
Department of Environmental Science and Engineering, Fudan University, Shanghai, China
Department of Applied Ecology, North Carolina State University, Raleigh, NC, USA
Robert R. Dunn
You can also search for this author in PubMed Google Scholar
Contributions
Y.L., S.N.T., R.R.D., and C.X. designed the study. Y.L. collected the data, generated the code, performed the analyses, and produced the figures with inputs from J.-C.S., W.Z., K.Z., J.F.A., T.M.L., W.J.R., Z.Y., S.N.T., R.R.D. and C.X. Y.L., S.N.T., R.R.D. and C.X. wrote the first draft with inputs from J.-C.S., W.Z., K.Z., J.F.A., T.M.L., W.J.R., and Z.Y. All coauthors interpreted the results and revised the manuscript.
Corresponding authors
Correspondence to Shuqing N. Teng , Robert R. Dunn or Chi Xu .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Communications thanks Chris Webster and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, peer review file, description of additional supplementary files, supplementary data 1, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Li, Y., Svenning, JC., Zhou, W. et al. Green spaces provide substantial but unequal urban cooling globally. Nat Commun 15 , 7108 (2024). https://doi.org/10.1038/s41467-024-51355-0
Download citation
Received : 06 December 2023
Accepted : 05 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1038/s41467-024-51355-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

VIDEO
COMMENTS
Healthcare sector. Follow this topic. ... but how health care providers should use them isn't quite so clear. ... The GSK Consumer Healthcare (GSK CH) case study deals with building a community ...
Figure 1 offers a geographic snapshot of the featured case studies. Health care of the future will be different from the health care of today. ... With extensive experience in research methodology and data analysis, Elsner conducts cross-sector research at the Center. [email protected] +1 215 282 1087 ...
Health System Innovation in Lesotho: Design and early operations of the Maseru Public Private Integrated Partnership. This PwC case study details the design and launch of an innovative partnership to dramatically improve delivery of healthcare in Lesotho in southern Africa. 07 Jun 2012.
January 18, 2022. Andrew Brookes/Getty Images. Summary. The use of digital technologies in clinical decision-making has received the most attention. But they also have the potential to help ...
Coordination of Benefits Services Help Health Plan. Discover how a regional carrier generated 250%+ ROI and increased yearly collections by $500,000 with comprehensive coordination of ... Explore our case studies to gain insight into the latest healthcare technology trends, guidance, and perspectives from prominent industry experts.
Change is a common experience in complex health care systems. Staff, patients and visitors come and go []; leadership, models of care, workforce and governing structures are reshaped in response to policy and legislative change [], and new technologies and equipment are introduced or retired [].In addition to these common changes experienced throughout health care, the acute sector in many ...
In our book 'Health Systems Improvement Across the Globe: Success Stories from 60 Countries', we gathered case-study accomplishments from 60 countries. A unique feature of the collection is the diversity of included countries, from the wealthiest and most politically stable such as Japan, Qatar and Canada, to some of the poorest, most ...
Health systems also need a larger workforce, but although the global economy could create 40 million new health-sector jobs by 2030, there is still a projected shortfall of 9.9 million physicians, ... this report looked at 23 applications in use today and provides case studies of 14 applications already in use. These illustrate the full range ...
1. Introduction. Artificial intelligence (AI) is defined as the intelligence of machines, as opposed to the intelligence of humans or other living species [1], [2].AI can also be defined as the study of "intelligent agents"—that is, any agent or device that can perceive and understand its surroundings and accordingly take appropriate action to maximize its chances of achieving its ...
July 25, 2024 - Surveyed healthcare leaders say their organizations are eager to use generative AI to help enhance how healthcare stakeholders work and operate, ... December 19, 2023 - The healthcare services sector has seen rapid growth over recent years. Despite the challenges organizations may face in 2024,...
2024 Global Health Care Sector Outlook. 6 MB PDF. Lingering COVID-19 effects are still contributing to widespread labor shortages and escalating costs, while the adoption of artificial intelligence (AI) presents possible solutions. Predicted to play a pivotal role in streamlining health care processes, AI promises precision and efficiency from ...
Healthcare providers can allocate resources more efficiently, prioritize high-risk patients, and deliver targeted interventions, ultimately improving patient satisfaction and healthcare quality. Related: Role of CDO in the Healthcare Sector . Case Study 6: AI in Epidemic Outbreak Prediction Background
innovation in healthcare: A case study of hospitals as innovation platforms ' presented. at MakeLearn and TIIM International Conference, Piran, Slovenia, 15- 17 May 2019. 1 Introduction. Cost ...
A case study approach [ 47, 48] was adopted here to understand the deployment of a whole system change in the acute hospital along the four dimensions of STS outlined above. A case study is an approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context [ 49 ].
Ya-Ting Yang, Yi-Hsin Elsa Hsu, Kung-Pei Tang, Christine Wang, Stephen Timmon, Wen-Ta Chiu, Saileela Annavajjula, Jan-Show Chu, Case study: international healthcare service quality, building a model for cultivating cultural sensitivity, International Journal for Quality in Health Care, Volume 32, Issue 9, November 2020, Pages 639-642, https ...
The healthcare sector offers a compelling mix of defensive characteristics and growth potential driven by innovation. It also features ample dispersion that presents stock pickers with an opportunity to parse potential leaders and laggards in pursuit of above-market return. ... The above case study is just one example of how active stock ...
Each case study takes a single telemedicine project or service as a unit of analysis. 3.2. The selected case studies. When selecting the case studies, it was important that the "appropriateness and the adequacy" (Shakir, 2002) to the research was maintained. In other words, we needed to ensure that the criteria were met to ensure the ...
A healthcare firm's journey towards achieving 96% precision in monthly claims reserve forecasts. Elevating care management for a health plan covering 4.7 million members. Tackling data security and access challenges for a multi-state health insurer. Achieving Lightning-Fast Case Resolution In Under A Minute For A Leading Managed Care Company.
'Big data' is massive amounts of information that can work wonders. It has become a topic of special interest for the past two decades because of a great potential that is hidden in it. Various public and private sector industries generate, store, and analyze big data with an aim to improve the services they provide. In the healthcare industry, various sources for big data include hospital ...
The first wave. In India, the first case of COVID-19 infection was reported on 27TH January 2020, when a 20 year old female with a travel history of China presented with a sore throat and dry cough in the emergency department of General Hospital, Thrissur, Kerala. 4 Since then, COVID-19 has taken a serious toll in India and worldwide. To prevent the spread of COVID-19 infection, the Government ...
The 4 case studies by Penn Nursing illustrate how nurses can be really powerful collaborators and generators of solutions within Healthcare. The videos describe the main attributes that nurses bring to the problem solving table. Empathy. A big part of a nurses role is to be able to empathize with their patients, so it comes naturally to nurses.
The validity of the results can be improved by including more hospitals and more case studies from the healthcare sector in different countries.,The findings will enable researchers, academicians and practitioners to incorporate the results of the study in LSS implementation within the healthcare system to increase the likelihood of successful ...
This case study demonstrates the power of a commitment to CQI as a driver for excellence in healthcare. The healthcare industry is rich with case studies that provide valuable insights and lessons learned. By analyzing and understanding these success stories, healthcare providers can apply similar strategies to achieve positive outcomes in ...
Requesting other formats and reporting issues. If you require publications or documents in other formats, please email [email protected].. To report any issues with a publication, please email [email protected].
When conducting QLR, time is the lens used to inform the overall study design and processes of data collection and analysis. While QLR is an evolving methodology, spanning diverse disciplines (Holland et al., 2006), a key feature is the collection of data on more than one occasion, often described as waves (Neale, 2021).Thus, researchers embarking on designing a new study need to consider ...
Background Kenya grapples with a paradox; severe public sector workforce shortages co-exist with rising unemployment among healthcare professionals. Medical schools have increased trainee outputs, but only 45% of newly qualified/registered doctors were absorbed by the public sector during 2015-2018. In such a context, we explore what influences doctors' career choices at labour market ...
Case study - Ahmed Making a difference to people's health and wellbing Find out about Ahmed Abukar's role as a Brent Health Matters Community Champion. Ahmed joined BHM as a volunteer Community Champion in May 2022, before being employed as a Community Coordinator in September 2023. ... Ahmed works in the Harlesden area, where he applies his ...
The South-East Asia Region Primary Health Care Strategy 2022-2030 outlines key actions to transform health systems through a primary health care approach. ... the private sector, and civil society to achieve universal health coverage. According to the Lancet Commission, nearly 60% of the 8.6 million annual deaths from treatable conditions are ...
The study uses the concept of habitus to understand whether the changing design of traditional rondavels has influenced their utilisation, based on a case study of the Mbhashe Local Municipality ...
Even before such lethal temperatures are reached, worker productivity 13 and general health and well-being 14 can suffer. ... a case study in Lagos, Nigeria. Sci. Rep. 12, 14168 (2022).