Instant insights, infinite possibilities

55 research questions about mental health
Last updated
11 March 2024
Reviewed by
Brittany Ferri, PhD, OTR/L
Short on time? Get an AI generated summary of this article instead
Research in the mental health space helps fill knowledge gaps and create a fuller picture for patients, healthcare professionals, and policymakers. Over time, these efforts result in better quality care and more accessible treatment options for those who need them.
Use this list of mental health research questions to kickstart your next project or assignment and give yourself the best chance of producing successful and fulfilling research.
- Why does mental health research matter?
Mental health research is an essential area of study. It includes any research that focuses on topics related to people’s mental and emotional well-being.
As a complex health topic that, despite the prevalence of mental health conditions, still has an unending number of unanswered questions, the need for thorough research into causes, triggers, and treatment options is clear.
Research into this heavily stigmatized and often misunderstood topic is needed to find better ways to support people struggling with mental health conditions. Understanding what causes them is another crucial area of study, as it enables individuals, companies, and policymakers to make well-informed choices that can help prevent illnesses like anxiety and depression.
- How to choose a strong mental health research topic
As one of the most important parts of beginning a new research project, picking a topic that is intriguing, unique, and in demand is a great way to get the best results from your efforts.
Mental health is a blanket term with many niches and specific areas to explore. But, no matter which direction you choose, follow the tips below to ensure you pick the right topic.
Prioritize your interests and skills
While a big part of research is exploring a new and exciting topic, this exploration is best done within a topic or niche in which you are interested and experienced.
Research is tough, even at the best of times. To combat fatigue and increase your chances of pushing through to the finish line, we recommend choosing a topic that aligns with your personal interests, training, or skill set.
Consider emerging trends
Topical and current research questions are hot commodities because they offer solutions and insights into culturally and socially relevant problems.
Depending on the scope and level of freedom you have with your upcoming research project, choosing a topic that’s trending in your area of study is one way to get support and funding (if you need it).
Not every study can be based on a cutting-edge topic, but this can be a great way to explore a new space and create baseline research data for future studies.
Assess your resources and timeline
Before choosing a super ambitious and exciting research topic, consider your project restrictions.
You’ll need to think about things like your research timeline, access to resources and funding, and expected project scope when deciding how broad your research topic will be. In most cases, it’s better to start small and focus on a specific area of study.
Broad research projects are expensive and labor and resource-intensive. They can take years or even decades to complete. Before biting off more than you can chew, consider your scope and find a research question that fits within it.
Read up on the latest research
Finally, once you have narrowed in on a specific topic, you need to read up on the latest studies and published research. A thorough research assessment is a great way to gain some background context on your chosen topic and stops you from repeating a study design. Using the existing work as your guide, you can explore more specific and niche questions to provide highly beneficial answers and insights.
- Trending research questions for post-secondary students
As a post-secondary student, finding interesting research questions that fit within the scope of your classes or resources can be challenging. But, with a little bit of effort and pre-planning, you can find unique mental health research topics that will meet your class or project requirements.
Examples of research topics for post-secondary students include the following:
How does school-related stress impact a person’s mental health?
To what extent does burnout impact mental health in medical students?
How does chronic school stress impact a student’s physical health?
How does exam season affect the severity of mental health symptoms?
Is mental health counseling effective for students in an acute mental crisis?
- Research questions about anxiety and depression
Anxiety and depression are two of the most commonly spoken about mental health conditions. You might assume that research about these conditions has already been exhausted or that it’s no longer in demand. That’s not the case at all.
According to a 2022 survey by Centers for Disease Control and Prevention (CDC), 12.5% of American adults struggle with regular feelings of worry, nervousness, and anxiety, and 5% struggle with regular feelings of depression. These percentages amount to millions of lives affected, meaning new research into these conditions is essential.
If either of these topics interests you, here are a few trending research questions you could consider:
Does gender play a role in the early diagnosis of anxiety?
How does untreated anxiety impact quality of life?
What are the most common symptoms of anxiety in working professionals aged 20–29?
To what extent do treatment delays impact quality of life in patients with undiagnosed anxiety?
To what extent does stigma affect the quality of care received by people with anxiety?
Here are some examples of research questions about depression:
Does diet play a role in the severity of depression symptoms?
Can people have a genetic predisposition to developing depression?
How common is depression in work-from-home employees?
Does mood journaling help manage depression symptoms?
What role does exercise play in the management of depression symptoms?
- Research questions about personality disorders
Personality disorders are complex mental health conditions tied to a person’s behaviors, sense of self, and how they interact with the world around them. Without a diagnosis and treatment, people with personality disorders are more likely to develop negative coping strategies during periods of stress and adversity, which can impact their quality of life and relationships.
There’s no shortage of specific research questions in this category. Here are some examples of research questions about personality disorders that you could explore:
What environments are more likely to trigger the development of a personality disorder?
What barriers impact access to care for people with personality disorders?
To what extent does undiagnosed borderline personality disorder impact a person’s ability to build relationships?
How does group therapy impact symptom severity in people with schizotypal personality disorder?
What is the treatment compliance rate of people with paranoid personality disorder?
- Research questions about substance use disorders
“Substance use disorders” is a blanket term for treatable behaviors and patterns within a person’s brain that lead them to become dependent on illicit drugs, alcohol, or prescription medications. It’s one of the most stigmatized mental health categories.
The severity of a person’s symptoms and how they impact their ability to participate in their regular daily life can vary significantly from person to person. But, even in less severe cases, people with a substance use disorder display some level of loss of control due to their need to use the substance they are dependent on.
This is an ever-evolving topic where research is in hot demand. Here are some example research questions:
To what extent do meditation practices help with craving management?
How effective are detox centers in treating acute substance use disorder?
Are there genetic factors that increase a person’s chances of developing a substance use disorder?
How prevalent are substance use disorders in immigrant populations?
To what extent do prescription medications play a role in developing substance use disorders?
- Research questions about mental health treatments
Treatments for mental health, pharmaceutical therapies in particular, are a common topic for research and exploration in this space.
Besides the clinical trials required for a drug to receive FDA approval, studies into the efficacy, risks, and patient experiences are essential to better understand mental health therapies.
These types of studies can easily become large in scope, but it’s possible to conduct small cohort research on mental health therapies that can provide helpful insights into the actual experiences of the people receiving these treatments.
Here are some questions you might consider:
What are the long-term effects of electroconvulsive therapy (ECT) for patients with severe depression?
How common is insomnia as a side effect of oral mental health medications?
What are the most common causes of non-compliance for mental health treatments?
How long does it take for patients to report noticeable changes in symptom severity after starting injectable mental health medications?
What issues are most common when weaning a patient off of an anxiety medication?
- Controversial mental health research questions
If you’re interested in exploring more cutting-edge research topics, you might consider one that’s “controversial.”
Depending on your own personal values, you might not think many of these topics are controversial. In the context of the research environment, this depends on the perspectives of your project lead and the desires of your sponsors. These topics may not align with the preferred subject matter.
That being said, that doesn’t make them any less worth exploring. In many cases, it makes them more worthwhile, as they encourage people to ask questions and think critically.
Here are just a few examples of “controversial” mental health research questions:
To what extent do financial crises impact mental health in young adults?
How have climate concerns impacted anxiety levels in young adults?
To what extent do psychotropic drugs help patients struggling with anxiety and depression?
To what extent does political reform impact the mental health of LGBTQ+ people?
What mental health supports should be available for the families of people who opt for medically assisted dying?
- Research questions about socioeconomic factors & mental health
Socioeconomic factors—like where a person grew up, their annual income, the communities they are exposed to, and the amount, type, and quality of mental health resources they have access to—significantly impact overall health.
This is a complex and multifaceted issue. Choosing a research question that addresses these topics can help researchers, experts, and policymakers provide more equitable and accessible care over time.
Examples of questions that tackle socioeconomic factors and mental health include the following:
How does sliding scale pricing for therapy increase retention rates?
What is the average cost to access acute mental health crisis care in [a specific region]?
To what extent does a person’s environment impact their risk of developing a mental health condition?
How does mental health stigma impact early detection of mental health conditions?
To what extent does discrimination affect the mental health of LGBTQ+ people?
- Research questions about the benefits of therapy
Therapy, whether that’s in groups or one-to-one sessions, is one of the most commonly utilized resources for managing mental health conditions. It can help support long-term healing and the development of coping mechanisms.
Yet, despite its popularity, more research is needed to properly understand its benefits and limitations.
Here are some therapy-based questions you could consider to inspire your own research:
In what instances does group therapy benefit people more than solo sessions?
How effective is cognitive behavioral therapy for patients with severe anxiety?
After how many therapy sessions do people report feeling a better sense of self?
Does including meditation reminders during therapy improve patient outcomes?
To what extent has virtual therapy improved access to mental health resources in rural areas?
- Research questions about mental health trends in teens
Adolescents are a particularly interesting group for mental health research due to the prevalence of early-onset mental health symptoms in this age group.
As a time of self-discovery and change, puberty brings plenty of stress, anxiety, and hardships, all of which can contribute to worsening mental health symptoms.
If you’re looking to learn more about how to support this age group with mental health, here are some examples of questions you could explore:
Does parenting style impact anxiety rates in teens?
How early should teenagers receive mental health treatment?
To what extent does cyberbullying impact adolescent mental health?
What are the most common harmful coping mechanisms explored by teens?
How have smartphones affected teenagers’ self-worth and sense of self?
- Research questions about social media and mental health
Social media platforms like TikTok, Instagram, YouTube, Facebook, and X (formerly Twitter) have significantly impacted day-to-day communication. However, despite their numerous benefits and uses, they have also become a significant source of stress, anxiety, and self-worth issues for those who use them.
These platforms have been around for a while now, but research on their impact is still in its infancy. Are you interested in building knowledge about this ever-changing topic? Here are some examples of social media research questions you could consider:
To what extent does TikTok’s mental health content impact people’s perception of their health?
How much non-professional mental health content is created on social media platforms?
How has social media content increased the likelihood of a teen self-identifying themselves with ADHD or autism?
To what extent do social media photoshopped images impact body image and self-worth?
Has social media access increased feelings of anxiety and dread in young adults?
- Mental health research is incredibly important
As you have seen, there are so many unique mental health research questions worth exploring. Which options are piquing your interest?
Whether you are a university student considering your next paper topic or a professional looking to explore a new area of study, mental health is an exciting and ever-changing area of research to get involved with.
Your research will be valuable, no matter how big or small. As a niche area of healthcare still shrouded in stigma, any insights you gain into new ways to support, treat, or identify mental health triggers and trends are a net positive for millions of people worldwide.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 18 April 2023
Last updated: 27 February 2023
Last updated: 22 August 2024
Last updated: 5 February 2023
Last updated: 16 August 2024
Last updated: 9 March 2023
Last updated: 30 April 2024
Last updated: 12 December 2023
Last updated: 11 March 2024
Last updated: 4 July 2024
Last updated: 6 March 2024
Last updated: 5 March 2024
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next, log in or sign up.
Get started for free

Research Topics & Ideas: Mental Health
100+ Mental Health Research Topic Ideas To Fast-Track Your Project
If you’re just starting out exploring mental health topics for your dissertation, thesis or research project, you’ve come to the right place. In this post, we’ll help kickstart your research topic ideation process by providing a hearty list of mental health-related research topics and ideas.
PS – This is just the start…
We know it’s exciting to run through a list of research topics, but please keep in mind that this list is just a starting point . To develop a suitable education-related research topic, you’ll need to identify a clear and convincing research gap , and a viable plan of action to fill that gap.
If this sounds foreign to you, check out our free research topic webinar that explores how to find and refine a high-quality research topic, from scratch. Alternatively, if you’d like hands-on help, consider our 1-on-1 coaching service .
Overview: Mental Health Topic Ideas
- Mood disorders
- Anxiety disorders
- Psychotic disorders
- Personality disorders
- Obsessive-compulsive disorders
- Post-traumatic stress disorder (PTSD)
- Neurodevelopmental disorders
- Eating disorders
- Substance-related disorders

Mood Disorders
Research in mood disorders can help understand their causes and improve treatment methods. Here are a few ideas to get you started.
- The impact of genetics on the susceptibility to depression
- Efficacy of antidepressants vs. cognitive behavioural therapy
- The role of gut microbiota in mood regulation
- Cultural variations in the experience and diagnosis of bipolar disorder
- Seasonal Affective Disorder: Environmental factors and treatment
- The link between depression and chronic illnesses
- Exercise as an adjunct treatment for mood disorders
- Hormonal changes and mood swings in postpartum women
- Stigma around mood disorders in the workplace
- Suicidal tendencies among patients with severe mood disorders
Anxiety Disorders
Research topics in this category can potentially explore the triggers, coping mechanisms, or treatment efficacy for anxiety disorders.
- The relationship between social media and anxiety
- Exposure therapy effectiveness in treating phobias
- Generalised Anxiety Disorder in children: Early signs and interventions
- The role of mindfulness in treating anxiety
- Genetics and heritability of anxiety disorders
- The link between anxiety disorders and heart disease
- Anxiety prevalence in LGBTQ+ communities
- Caffeine consumption and its impact on anxiety levels
- The economic cost of untreated anxiety disorders
- Virtual Reality as a treatment method for anxiety disorders
Psychotic Disorders
Within this space, your research topic could potentially aim to investigate the underlying factors and treatment possibilities for psychotic disorders.
- Early signs and interventions in adolescent psychosis
- Brain imaging techniques for diagnosing psychotic disorders
- The efficacy of antipsychotic medication
- The role of family history in psychotic disorders
- Misdiagnosis and delayed treatment of psychotic disorders
- Co-morbidity of psychotic and mood disorders
- The relationship between substance abuse and psychotic disorders
- Art therapy as a treatment for schizophrenia
- Public perception and stigma around psychotic disorders
- Hospital vs. community-based care for psychotic disorders

Personality Disorders
Research topics within in this area could delve into the identification, management, and social implications of personality disorders.
- Long-term outcomes of borderline personality disorder
- Antisocial personality disorder and criminal behaviour
- The role of early life experiences in developing personality disorders
- Narcissistic personality disorder in corporate leaders
- Gender differences in personality disorders
- Diagnosis challenges for Cluster A personality disorders
- Emotional intelligence and its role in treating personality disorders
- Psychotherapy methods for treating personality disorders
- Personality disorders in the elderly population
- Stigma and misconceptions about personality disorders
Obsessive-Compulsive Disorders
Within this space, research topics could focus on the causes, symptoms, or treatment of disorders like OCD and hoarding.
- OCD and its relationship with anxiety disorders
- Cognitive mechanisms behind hoarding behaviour
- Deep Brain Stimulation as a treatment for severe OCD
- The impact of OCD on academic performance in students
- Role of family and social networks in treating OCD
- Alternative treatments for hoarding disorder
- Childhood onset OCD: Diagnosis and treatment
- OCD and religious obsessions
- The impact of OCD on family dynamics
- Body Dysmorphic Disorder: Causes and treatment
Post-Traumatic Stress Disorder (PTSD)
Research topics in this area could explore the triggers, symptoms, and treatments for PTSD. Here are some thought starters to get you moving.
- PTSD in military veterans: Coping mechanisms and treatment
- Childhood trauma and adult onset PTSD
- Eye Movement Desensitisation and Reprocessing (EMDR) efficacy
- Role of emotional support animals in treating PTSD
- Gender differences in PTSD occurrence and treatment
- Effectiveness of group therapy for PTSD patients
- PTSD and substance abuse: A dual diagnosis
- First responders and rates of PTSD
- Domestic violence as a cause of PTSD
- The neurobiology of PTSD
Neurodevelopmental Disorders
This category of mental health aims to better understand disorders like Autism and ADHD and their impact on day-to-day life.
- Early diagnosis and interventions for Autism Spectrum Disorder
- ADHD medication and its impact on academic performance
- Parental coping strategies for children with neurodevelopmental disorders
- Autism and gender: Diagnosis disparities
- The role of diet in managing ADHD symptoms
- Neurodevelopmental disorders in the criminal justice system
- Genetic factors influencing Autism
- ADHD and its relationship with sleep disorders
- Educational adaptations for children with neurodevelopmental disorders
- Neurodevelopmental disorders and stigma in schools
Eating Disorders
Research topics within this space can explore the psychological, social, and biological aspects of eating disorders.
- The role of social media in promoting eating disorders
- Family dynamics and their impact on anorexia
- Biological basis of binge-eating disorder
- Treatment outcomes for bulimia nervosa
- Eating disorders in athletes
- Media portrayal of body image and its impact
- Eating disorders and gender: Are men underdiagnosed?
- Cultural variations in eating disorders
- The relationship between obesity and eating disorders
- Eating disorders in the LGBTQ+ community
Substance-Related Disorders
Research topics in this category can focus on addiction mechanisms, treatment options, and social implications.
- Efficacy of rehabilitation centres for alcohol addiction
- The role of genetics in substance abuse
- Substance abuse and its impact on family dynamics
- Prescription drug abuse among the elderly
- Legalisation of marijuana and its impact on substance abuse rates
- Alcoholism and its relationship with liver diseases
- Opioid crisis: Causes and solutions
- Substance abuse education in schools: Is it effective?
- Harm reduction strategies for drug abuse
- Co-occurring mental health disorders in substance abusers
Choosing A Research Topic
These research topic ideas we’ve covered here serve as thought starters to help you explore different areas within mental health. They are intentionally very broad and open-ended. By engaging with the currently literature in your field of interest, you’ll be able to narrow down your focus to a specific research gap .
It’s important to consider a variety of factors when choosing a topic for your dissertation or thesis . Think about the relevance of the topic, its feasibility , and the resources available to you, including time, data, and academic guidance. Also, consider your own interest and expertise in the subject, as this will sustain you through the research process.
Always consult with your academic advisor to ensure that your chosen topic aligns with academic requirements and offers a meaningful contribution to the field. If you need help choosing a topic, consider our private coaching service.
Good morning everyone. This are very patent topics for research in neuroscience. Thank you for guidance
What if everything is important, original and intresting? as in Neuroscience. I find myself overwhelmd with tens of relveant areas and within each area many optional topics. I ask myself if importance (for example – able to treat people suffering) is more relevant than what intrest me, and on the other hand if what advance me further in my career should not also be a consideration?
This information is really helpful and have learnt alot
Phd research topics on implementation of mental health policy in Nigeria :the prospects, challenges and way forward.
This info is indeed help for someone to formulate a dissertation topic. I have already got my path from here.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 July 2023
Assessment of depression and anxiety in young and old with a question-based computational language approach
- Sverker Sikström 1 ,
- Bleona Kelmendi 2 &
- Ninni Persson 3 , 4
npj Mental Health Research volume 2 , Article number: 11 ( 2023 ) Cite this article
8003 Accesses
8 Citations
2 Altmetric
Metrics details
- Health care
- Human behaviour
Middle aged adults experience depression and anxiety differently than younger adults. Age may affect life circumstances, depending on accessibility of social connections, jobs, physical health, etc, as these factors influence the prevalence and symptomatology. Depression and anxiety are typically measured using rating scales; however, recent research suggests that such symptoms can be assessed by open-ended questions that are analysed by question-based computational language assessments (QCLA). Here, we study middle aged and younger adults’ responses about their mental health using open-ended questions and rating scales about their mental health. We then analyse their responses with computational methods based on natural language processing (NLP). The results demonstrate that: (1) middle aged adults describe their mental health differently compared to younger adults; (2) where, for example, middle aged adults emphasise depression and loneliness whereas young adults list anxiety and financial concerns; (3) different semantic models are warranted for younger and middle aged adults; (4) compared to young participants, the middle aged participants described their mental health more accurately with words; (5) middle-aged adults have better mental health than younger adults as measured by semantic measures. In conclusion, NLP combined with machine learning methods may provide new opportunities to identify, model, and describe mental health in middle aged and younger adults and could possibly be applied to the older adults in future research. These semantic measures may provide ecological validity and aid the assessment of mental health.
Introduction
Depression and anxiety disorders are global phenomena and create widespread and growing problems in healthcare 1 . Untreated depression can be disabling 2 , 3 , 4 , 5 and have financial consequences 6 . In 2000, the economic burden of depression in the US was an estimated USD 83.1 billion, of which USD 51.5 billion were workplace costs 7 . Early and efficient diagnostic methods are essential for applying effective and appropriate treatment. The development of more precise diagnostic instruments and accessible treatment methods is warranted. One important aspect is how such disorders vary across the lifespan. Rating scales have typically been used to quantify levels of depression and anxiety. In contrast, language is a natural way for people to communicate their mental states, and language ability is preserved or even improves as people age 8 . Recent advancements in computational language models (CLA) allow for quantitative assessment of depression and anxiety using words generated from open questions related to mental health 9 . This unique study aims to assess age differences in the reporting of mental health issues using question based computational language assessments (QCLA), which to the best of our knowledge has not been done previously.The prevalence of depression and anxiety varies across the lifespan 10 , 11 , therefore the age dependent differences in the word responses and description of mental health using the QCLA approach is of interest. Studies have identified age differences in the prevalence of depression and anxiety. Younger adults (16–29 years) were more likely to be affected by depression and severe anxiety than the older adults 10 . Contrary to this report, Lenze et al. 12 , found a relatively high rate of both current and lifetime anxiety disorders in the elderly, where 35% of the older participants had received an anxiety disorder diagnosis at least once, and 23% had been diagnosed recently. In summary, the prevalence of depression and anxiety disorders varies across the lifespan.
In the following, we will provide a current review of the literature on the differences in terms of mental health between younger, middle age and old adults.
Young adults
Younger adults (16–29 years) are more likely to be affected by depression and severe anxiety than older adults 10 . In 2022, the young age group was most affected by severe anxiety at 16% and in Sweden 13 ; 4% was diagnosed with depression 13 . There is emerging evidence, that the prevalence of anxiety disorders is associated with young age, but also female gender and given chronic diseases 14 . In terms of aetiology, different subtypes of childhood maltreatment, child–parent bonding, stressful life events, as well as a genetic liability predict subsequent depression 15 , 16 . Depression is a risk factor for all-cause mortality, with greater risk for greater severity 17 . Thus, suicide is the most common cause of death in young men in the United Kingdom aged between 25 and 34 years 18 . Life changes and stress because of the Covid-19 pandemic are mirrored in an increase of depression and anxiety in the young 19 . Younger adults who struggle financially are at higher risk of mental health problems 20 .
Middle-aged adults
In Sweden, approximately 7% of middle-aged adults (30–59 years) are diagnosed with depression 13 , while only very few are affected by severe anxiety 13 . Regarding the period prevalence of 1 year, one in seven middle-aged participants (45–64 years) experienced symptoms consistent with ICD-10 anxiety or affective disorder in the preceding 12 months 21 . Anxiety disorders are most prevalent in the lifespan of 25–44 years 13 . In comparison to the prevalence of 1 in 16 of the older age group (60–75 and older), middle-aged adults were more likely to be affected by anxiety and affective disorders 21 . Major depressive disorder (MDD) is a common mental illness that may occur at any age during the lifespan. However, the highest risk period for onset is from mid to late adolescence to early 40s 22 . The presence of a physical disorder is significantly associated with the presence of mental disorders for middle-aged people 21 . Depression may even worsen health conditions, as it is associated with macrovascular complications and all-cause mortality in a patient cohort with diabetes 23 . For anxiety disorders among middle-aged and older adults, physical health, socioeconomic status, immigrant status and nutritional factors are associated with its occurrence 24 . Perceived stress interacts with age during the development of depression and anxiety disorders 25 , 26 . Employment and marital status may function as an important predictor of mental disorders in middle-aged groups 21 . Middle-aged participants were more likely to be affected by a mental disorder 12 months after experiencing separation, divorce, or death of a partner 13 , 21 .
Regarding the point and lifetime prevalence of anxiety disorders in the elderly, Lenze et al. 12 found a relatively high rate of both current and lifetime anxiety disorders in the elderly, where 35% of the older participants had received an anxiety disorder diagnosis at least once, and 24% had been diagnosed recently. Depression late in life displays a clinical phenomenon 27 ; there is a greater likelihood of comorbidities, differing aetiology and symptom expression compared to depression in younger adults. The aetiology of depression in the elderly is more heterogeneous than in younger adults 28 . Age-related changes in the brain, neurodegenerative and cardiovascular diseases may be of importance for the development of depression in later life 27 , 28 . Studies have shown that comorbidity between clinically significant depression and anxiety may be as high as 48.3% 29 . The risk of mortality due to depression and anxiety disorders is higher in older adults 30 , while suicide risk is particularly high in older men 31 . For the elderly (75 years or older), the likelihood for a suicide attempt rises by three times in comparison to younger age groups 32 . Anxiety-related disorders are also correlated with a higher level of suicidality 12 . The elderly showed higher levels of loneliness, as well as higher levels of distress and exhaustion during the Covid-19 pandemic, with anxiety influencing the emergence of depression 33 . Bergdahl and Bergdahl 25 observed perceived stress to be impacting the development of depression and anxiety disorders among high age groups (60–69 years) in Sweden. Elderly are more likely to be widowed and in poor health compared to younger adults, which can aggravate the risk of depression 34 , 35 . In contrast, social capital (i.e., resources from social networks) may function as a source of mental wellbeing in the elderly 36 .
In summary, the prevalence of depression and anxiety disorders varies across the lifespan. While there are no age of onset (AOO) specific guidelines for treating depression, the treatment of pre-adult or late-life depression should be considered individually depending on the patient 22 , as age-specific differences in life circumstances may influence the onset. Therefore specialised diagnostic methods should be considered for younger and older adults implementing each reality of life and language for patients affected by depression and anxiety disorders.
Artificial intelligence (AI) technologies have shown beneficial effects in clinical decision-making, treatments, managing healthcare and research 37 , 38 , 39 . AI technologies can help quantify mental health in electronic health records, mood rating scales, brain imaging data, novel monitoring systems, smartphone or video data and social media platforms. AI has demonstrated great accuracy in predicting and classifying depression, anxiety and other psychiatric illnesses or suicide ideation 40 , 41 . AI methods have been used to analyse social media posts for depression, providing an opportunity for studying a large population 42 , 43 using probabilistic models, crowdsourcing technology 44 , 45 and computational language assessments (CLA) (Eichstaedt et al. 6 ). These findings suggest the significance and value of words when describing mental health.
A natural language processing method called latent semantic analysis (LSA) 46 , where open-ended questions about mental health are applied, may facilitate registration of information closer to individual behaviour in a real-world setting. The LSA has been validated against several traditional rating scales, and demonstrated good statistical properties with competitive, or even higher reliability 9 .
The QCLA can be applied to semantic data (i.e., words and sentences), where the assessment is based on high-dimensional word embeddings from a large language corpus 47 ). Kjell et al. 48 investigated word response relating to the symptoms of major depressive disorder (MDD) and generalised anxiety disorders (GAD) as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The results of the QCLA showed that all primary and secondary language responses correlated significantly with the depression scale Patient Health Questionnaire 9-item (PHQ-9 49 ). Together, these findings suggest that QCLA may be helpful in clinical assessment of mental health.
Machine learning (ML) and (AI) methods demonstrate potential, as subjective descriptions of mental health can be monitored and to facilitate the diagnostic process 50 , 51 , 52 , 53 . Advances in ML and AI could provide more personalised care for patients to aid decisions on the best suitable treatments and interventions 54 . While text offers a rich source of unstructured information for ML models, there is risk that this learning will also pick up the human biases that ML is based on ref. 54 . An example of such bias is that old and young people may be assessed on the same criteria, whereas symptoms may differ with age, which emphasises that more research is required.
Currently, there is a large gap in knowledge about how people of different ages describe their mental health in their own words. An age-specific application of machine learning and artificial intelligence methods may allow for personalised assessment and treatment of mental health 55 , 56 .
Our research question addresses differences in descriptive word responses related to mental health in younger and middle-aged adults. The aim is to investigate potential differences in the semantic representation across the lifespan.
We hypothesise that the semantic representations of mental health differ for younger (i.e., young) and older (i.e., middle-aged) adults (H1), and that these differences are expressed in specific semantic attributes (H2). Given H1 is supported, we hypothesise that different prediction models are required for predicting mental health in younger and older adults (H3). Due to language skills improving with age, we hypothesise that the prediction models may be more accurate for older (H4). Given previous reports on rating scales for measuring mental health in younger and older adults, we hypothesise that the language-based prediction models of older individuals show better mental health than for the younger (H5).
Participants
The study consisted of 883 participants with English as a first language. Seven participants were removed from the analysis as they either failed to follow the instructions, or did not respond to the control questions correctly (e.g., choose the option on the left hand side). The final analysis included 876 participants. 457 participants were recruited from the Mechanical Turk ( www.mturk.com ) platform, and 419 from the Prolific Academic ( https://prolific.co/ ) platform. Half the participants were recruited by screening for MDD or GAD as assessed by using the self-reported depression and anxiety symptoms (SDAS) (Sikström et al., 57 in revision), which is an online version of the Mini International Neuropsychiatric Interview (MINI). The SDAS has been validated by clinicians for MDD (Kappa = 0.76) and for GAD (Kappa = 0.52), for details of this see the Supplementary Information. The other half of participants were recruited without screening; however, they were also assessed by SDAS. Using this measure, 61 (34 younger) participants had MDD alone, 137 (70 younger) had GAD alone, and 259 (139 younger) had both MDD and GAD. Participants younger than the median age of 32.5 were categorised as younger. The age in the given sample ranged from 18 to 70 years ( M = 35.5, SD = 11.9). 538 participants identified as female, 327 as male and 11 as “other gender”. The study lasted approximately 20 min, and participants received USD 4 for their time.
Semantic open-ended questions—Word responses
In total, the participants were asked 11 open-end questions and five rating scales. The open-ended questions can roughly be categorised into topics of; mental health, causes of mental health, positive psychology, and symptoms of mental health. Three open-ended questions were about mental health: “Describe your mental health with descriptive words”, “During the last two weeks, describe in words whether you felt depressed or not”, “During the last two weeks, describe in words whether you have felt worry or not”. They were also asked three questions about the underlying causes of their mental health, depression, and anxiety (“Describe the reason for your mental health/depression/worry in descriptive words). There were two open-ended questions for positive psychology, one on satisfaction (“Overall in your life, describe in words whether you are satisfied or not?”) and harmony (“Overall in your life, describe in words whether you are in harmony with your life or not?”). Eight questions were asked about symptoms (“Describe your sleep/concentration/appetite/energy/self/movement/behaviour/interest with descriptive words)”. The participants were asked to respond using five words for the mental health questions (general, depression, anxiety), three words for the reason questions (general reason, depression reason, anxiety reason), three words for the positive psychology questions (satisfaction, harmony), and two words for the symptom questions. The participants were asked to write one word in each text box, thus the number of boxes matched the number words they were asked to write.
Rating scales
The following rating scales were used to measure depression PHQ-9 49 , anxiety Generalised Anxiety Disorder 7-item scale (GAD-7 58 )), satisfaction with life (SWILS 59 , 60 ), and harmony in life (HILS 48 ). SDAS was used to validate the participants’ MDD and GAD diagnoses.
Control items
One control item per rating scale was included, for example “Answer ‘disagree’ on this question”. If the participant failed to answer all the control questions correctly, they were excluded from the analysis. These control questions were essential for ensuring the quality of the dataset by guaranteeing the participant’s focus on the task and to improve the statistical reliability 61 , 62 , 63 .
Demographic inventory
A demographic survey was included, in which the participants were asked about their age and gender. They were also asked to provide their country of origin and first language, as well as a description of their estimated household income. In order to measure the estimated household income, the participants responded to the question “Does the total income of your household allow you to cover your needs?” with either, “Our income does not cover our needs, there are great difficulties” (1) to “Our income covers our needs, we can save” (7).
To participate in the study, a declaration of informed written consent was required. Participants were told that their responses would be anonymised before analysis, and that they could withdraw from the study at any time without needing to give a reason. The questions and rating scales were presented in a random order. Finally, demographic information was collected, and a debrief on the purpose of the study was provided.
The study was reviewed by the Swedish Ethical Review Authority (EPN), who determined no ethical approval was needed, as the participants were anonymously recruited and tested (reg. no.: 2020-00730).
Data analyses
The primary aim of the analysis was to study age differences in mental health by looking at the differences in the semantic representations of the descriptive words dependent on their age. The machine learning was trained to the continuous value of age. Methods proposed by Kjell et al. 9 were used and the words were quantified using a latent semantic analysis (LSA) trained to predict the participants’ age with machine learning.
The data analysis was conducted using the online software for statistical analysis of text, SemanticExcel.com. This software includes pre-programmed semantic representations that are generated by the LSA method based on the English version of Google N-gram data ( N = 5). In this method, a co-occurrence matrix is generated first, where each cell includes the frequency of a word in the N-gram. The content of the cells is then normalised by taking the logarithm of the frequency plus one. A semantic representation is then generated by applying a data compression algorithm known as the singular value decomposition (SVD). This generates vectors describing the words in the corpus. Each vector consists of 512 dimensions and is normalised to a length of one. The word responses were added together, and the length was again normalised to one, so that each response to a word question was described by one vector (see Kjell et al. 9 for details). The semantic similarity between two semantic representations can be measured using the cosine of the angle between the vectors, which is calculated as the inner product of the two vectors divided by the product of their magnitudes.
We investigated whether semantic representation depends on age by predicted age from the semantic representation. A variable, called “All texts”, were generated that included the text responses from all the questions for each participant. Age was predicted based on this variable, using the method described in the “Data analysis” section.
Given that the semantic representation differs depending on age, we are interested in studying what attributes are indicative of younger and older people’s description of their mental health (where participants younger than the median age of 32.5 were categorised as young). We used the model generated for the concatenation of all the text that was generated in the analysis of H1, and applied this model to words in the dataset. Then we used two-sided t tests to investigate whether each word was indicative of young or old participants.
We applied the linguist inquire word count (LIWC), a method to assess the how related texts are to certain predefined and manually generated word list 64 . These word lists ( N = 63) represent psychologically relevant categories of words (e.g., emotions, work, stress). The LIWC measures is based on word frequency, and not on word embeddings, and is calculated by counting the percentage of words in each text that is also is presented in each LIWC word list.
Machine learning was used to study whether the semantic representation depended on the age of the participants (for methodological details, see Kjell et al. 9 ). Multiple linear regression ( y = c × x ) was used to predict the age ( y ) using the semantic representation ( x ) as input. The training and test data set was separated by using a 10% leave-out cross-validation procedure. The number of dimensions used in the regression was optimised using a nested cross-validation procedure. The predicted values of age were compared with the empirical data using Pearson correlation ( r ), and the proportion of explained variance ( r 2 ).
Basic statistics
The dataset consisted of a total of 36,396 words, with 4010 unique words. Participants on average generated 42 words (standard deviation 1.4). The mean natural word frequency, as measured by Google N-grams, was 0.00011. The frequency of the words, nor the log frequency of the words, did not correlate with age.
H1: does the semantic representation depend on age?
The results showed that this semantic representation from the All texts variable predicted age (Pearson correlation between predict and empirical age; r = 0.31, r 2 = 0.10, p < 0.0001). Furthermore, prediction models were generated separately for each text variable. The results showed that seven variables were significant, following Bonferroni correction for multiple comparison (sleep, self, affective behaviour, general, energy, harmony, depression), gender without correction for multiple comparison (movement, worry, depression reason, worry reason). Three questions did not correlate with age (appetite general, and interest) (see Table 1 ).
H2: word indicative of younger and older adults
Figure 1 shows a word cloud that summarise the words for all participants (see the footnote for details). Figure 2 shows word clouds indicative of young (left) and old (right) participants and follows the Bonferroni correction for multiple comparisons. These words were manually classified by the authors into ten semantic categories in Table 2A .
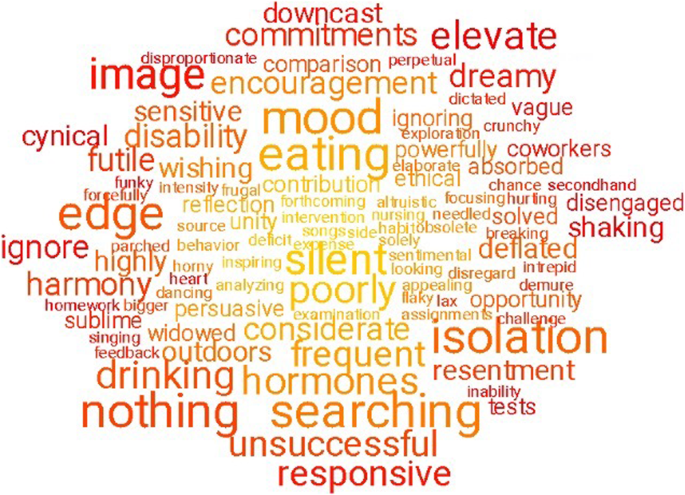
Note: The word clouds show 100 words that are the most indicative of the text data compared with a random sample of words in Google N-gram. The words were taken from the concatenation of all text questions “Text all” and compared with a random sample of words in Google N-gram, using the multiple linear regression as specified in the text. All words showed significant Pearson correlations with age following the Bonferroni correction for multiple comparisons, where the colour coding represent the p values. The font size represents the frequency of the words in the data set.
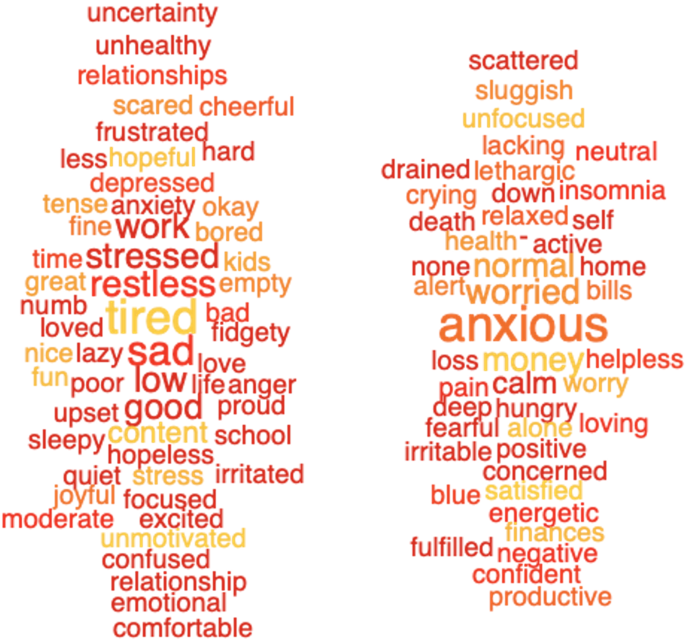
Note: The word clouds show 100 words that are the most indicative of the younger adults (left cloud) and older adults (right cloud) ages. See also footnote to Fig. 1 .
The results show that older people relate their mental health to words related to anxiety (“anxious”, “worry”, etc.), whereas young individuals focus on words related to depression and stress (“sad”, “stressed”, “restless”, “depressed” etc.). Furthermore, younger adults mention issues related to their main activities (e.g., “work”, “school”, “relationships”), whereas the older population uses words more focused on feelings and body states (i.e., “hunger”, “health”, “death”, “crying”, “insomnia”).
Here we used LIWC to investigate which categories are indicative of the younger and the older groups by using the “All text” variable. The LIWC scores in the 63 categories was correlated with age. Table 2B shows the LIWC categories with Pearson correlation coefficients that were significantly different from zero. The “insight” and “cognitive processes” categories correlated positively with age, following the Bonferroni correction for multiple comparisons. The “family”, “money”, “discrepancy” and “positive emotion” categories also correlated positively, but without correction for multiple comparisons. The “anxiety”, “friends”, “function words”, “adverbs”, “space”, “assent”, “negative emotion”, “feeling” and “relativity” categories correlated negatively with age, without correction for multiple comparisons.
H3: do younger and older adults require different semantic prediction models?
Here we investigate whether a prediction model of mental health trained on older or younger adults differs from a prediction model applied to younger or and older groups. Two hypotheses are tested here. If the prediction models that are trained and tested on the older group are better at predicting mental health scores than the prediction models that are trained and tested on the younger group, then this supports the idea that the data quality of the old group is better than the younger group (H3). Furthermore, if there is an interaction effect between whether the training and test is made on the same versus different groups, and the older versus younger group, then this supports the hypothesis that different prediction models are required for older versus the younger groups (H2).
Hypothesis 3 is evaluated as follows: the data set was divided using median split criteria, where young participants were aged below 32.5, and an older group equal to or larger than this age. The cross-validation procedure was applied separately to each of the 17 semantic representations (listed in Table 1 ). These semantic representations were trained on each of the four mental health rating scales (i.e., related to depression (PHQ-9), anxiety (GAD-7), harmony (HILS) and satisfaction (SWLS)). 68 prediction models were generated for each of the four groups and the results were evaluated using Pearson correlations between predicted and empirical rating for each of these models.
A repeated measure ANOVA was used to analyse the correlation coefficients, where the factors were age (younger versus older) and testing-training (same versus opposite data). There was a significant age by test–training interaction ( F (1, 67) = 22.2, p < 0.001, Fig. 3 ), indicating that models generated older and younger people depending on whether they were tested on the younger and older participants. This suggests that the different prediction models are required for the younger and older study groups, and Hypothesis 3 is supported.

Note: The y-axis shows the Pearson correlation ( a ) and mean squared error (MSE) ( b ) between predicted and empirical rating scales averaged over all the semantic representations and the rating scales. The training data is divided into younger (left) and older participants (right), using either models trained on the same data set that they were applied on (blue) or trained on the opposite dataset (red).
H4: do older people generate better semantic prediction models?
The ANOVA also shows a significant main effect on age ( F (1, 67) = 196.3, p < 0.001) indicating that ratings scales are better predicted from the semantic representations for the older compared to the younger participants (Fig. 3 ), supporting Hypothesis 4. Thus, accuracy was higher for older participants both when they were evaluated on the older participants and when they were evaluated on the younger participants.
H5: mental health in younger and older adults
Word clouds show words indicative of young and old people (on the x-axis) with low or high for depression (on the y -axis for Fig. 4 ) and low or high anxiety (on the y-axis for Fig. 5 ). Rating scales and semantic measures of mental health were correlated with age (Table 3 ). Rating scales of depression (PHQ-9) and anxiety (GAD-7) correlated negatively with age following the Bonferroni correction of multiple comparisons. Similar results were found for the corresponding semantic measures, based on training of these rating scales. Finally, we correlated the semantic measures, using the rating scales as covariates. The results show that the semantic measures of depression and anxiety still correlated with age following the corresponding rating scales as covariates.

Note. The word clouds on the left are represent young people and those in the right old people ( r = 0.28). The upper word clouds represent high PHQ-9 scores and the lower word clouds low PHQ-9 scores ( r = 0.76). See also footnote to Fig. 1 .

Note. Same as Fig. 4 , however, the upper word clouds represent high GAD-7 and the lower word clouds low GAD-7 ( r = 0.71).
The aim of this article has been to investigate age differences in mental health using semantic representations generated from descriptive keyword responses to mental health questions. Indeed, the results demonstrated age differences; (1) middle-aged adults describe their mental health differently compared to younger adults; (2) for example, middle-aged adults emphasise depression and loneliness, whereas young adults list anxiety and money; (3) different semantic models are warranted for younger and middle-aged adults; (4) middle-aged participants described their mental health more accurately compared to young participants; (5) middle-aged adults have better mental health than younger adults as measured using semantic measures.
The first and second hypotheses addressed age differences to be found in the semantic representation. The age differences found in specifically semantic open-ended mental health questions is a novel discovery. Our data provides the possibility to summarise age-related themes linked to young and old people, using indicative words (see word cloud in Figs. 1 , 2 , 4 , and 5 ). The young population lists words linking to aspects of social relationships, suggesting these are important for their mental health, while the older adults use words related to health, disease, death, insomnia, sadness and appetite.
Previous reports using more traditional rating scales have found that geriatric depression may emerge from neuronal age-related changes, and sometimes even neurodegenerative disease and cardiovascular changes in the brain 28 . This has given rise to selective rating scales for the elderly, such as the Geriatric Depression Scale 65 . Age differences in reported symptoms may, in part, be the result of generational differences regarding environmental factors such as personal circumstances (e.g., refs. 19 , 20 , 33 , 66 , 67 , 68 ). This explanation could be of particular importance as genetic factors potentially play a greater role in the emergence of depression and anxiety among younger adults 27 , 28 . The semantic open-ended question tool used in the current report may aid, speed up and facilitate proper diagnostic process regardless of a patient’s age in primary care context where expertise in geriatrics is less common.
The third hypothesis assumes that younger and older people may require different semantic prediction models. The present findings suggest that different prediction models are needed for younger and older adults. However, the model most appropriate for middle-aged adults was also better fitted to the data from the younger participants. We propose that the semantic data contains sufficient information for generating reasonable predictions in data from both younger and middle-aged adults. Middle-aged adults often out-perform younger adults in language skills 69 . The elderly has more advanced semantic networks as life experience may, in part, mediate such effects. Future studies focussing on an elderly sample may benefit from the assessment of language skills as a potential moderator of the effects reported herein.
The fourth hypothesis examined how well the semantic representation could predict rating scales depended both on whether the prediction models were based on younger or older adults. The prediction model of several ratings scales yielded higher accuracy when training was based on the older participants. A possible interpretation of this is that middle-aged adults are better at expressing their mental health in free words than younger adults. This finding was true, both when the data was evaluated on the younger and the middle-aged groups. This suggests that the finding cannot be easily explained with the notion that younger adults are less careful when responding to surveys. Sloppy answers would have generated less accurate rating scales, leading to the poorest predictability when applying the young model to the young dataset. In contrast, we found an interaction effect between the age group that the model was trained on and the age group that it was evaluated on, possibly suggesting a difference in semantic models for young and old. Overall, this suggests an interpretation that the older adults generated more informative descriptive keywords of their mental health than their younger counterparts.
Hypothesis 5 states that mental health varies in younger and older adults. According to the present study, older age was associated with lower levels of depression, which aligns with previously reported findings (18–29 years) in Villarroel et al. 70 , who discovered this was the case for both the rating scales and the semantic measures. Interestingly, these findings remain significant for the semantic measures, even after controlling for the effect of more traditional rating scales such as PHQ-9. This may indicate that the semantic measure of depression and anxiety provides additional information to the results of the rating scales.
Language is the natural way for people to communicate their mental state. Nevertheless, the dominating method of measuring psychological constructs are rating scales. A possible reason for this is that language has been difficult to quantify. Recent developments in natural language processing provide unprecedented opportunities for measuring language, with the possible application to mental health and ageing. There are several advantages with QCLA:
Language is the natural way for people to communicate their mental state. Sikström et al. 71 showed that people prefer to describe their mental health using written language responses, as they found this method to be more precise and they are able to elaborate on their responses. Additionally, it was the preferred way to communicate with mental health professionals compared to rating scales. However, when rating scales were preferred, this was due to their ease and speed of use.
Language base measure of mental health has high validity . When mental health is measured using computational methods using words generated to describe mental health, there is evidence of a high correlation with validated scales of depression and anxiety 9 . Furthermore, combining free text and word responses about harmony and satisfaction using transformer-based models demonstrate, to our knowledge, the highest correlation yet between language responses and rating scales, which rivals the theoretical limits based on test–retest data ( r = 0.84, r 2 = 66).
Language can be used to describe mental health constructs . Rating scales are defined by researchers and provide a fixed measure of scale. In contrast, the QCLA approach allows for a data-driven measure of constructs, where data from a specific group of participants (i.e., culture, age, etc.) can be used to describe constructs. This definition can subsequently be visualised in a word cloud. We believe that this provides a more dynamic and natural way of thinking about mental constructs, as the scales of constructs are generated from data in a particular context.
Computational analysis of language can be used for clinical assessments . In combination with machine learning, the semantic mental health constructs can estimate age-specific mental health trajectories. Such algorithms may contribute to more efficient healthcare treatments, or may even serve as a means for notifying healthcare personnel or family members about how to act on subclinical symptoms and how to best support individuals with mental health problems.
Personal assessment . One major strength of the open-ended measure of mental health is that the participants describe their mental health status in their own words. This measure promotes ecological validity to a greater extent, as the responses are closer to their personal communication style and real-life context when compared to traditional rating tools, such as Likert scales, based on fixed items. Furthermore, open-ended questions can counteract the effect of reporting bias when assessing mental health. Self-reported information from traditional questionnaires may contain social desirability biases 72 , which can escalate or underestimate the studied effects of mental health.
The present results should be interpreted in the context of some limitations of QCLA. First, the study suffers from limited generalisability due to the non-random recruitment procedure. Second, another limitation is the associative nature of the current study, which precludes making direct inference about causality due to the lack of experimental control. Third, the sample consisted of a small proportion of old adults. There is a demand for future studies to focus on this age group in order to conclude differences of language usage and AI models to describe mental health in the elderly. Therefore, our results would benefit from future replications to increase the generalisability.
In conclusion, combining latent semantic estimates with machine learning methods may provide new opportunities to discriminate, model, and describe mental health in older and younger adults. Together, these methodologies may provide greater accuracy and precision in the evaluation of mental health across the adult lifespan.
Data availability
The data is not publicly available as it includes sensitive text data; however, requests for the data can be submitted to the corresponding author.
Code availability
The data analysis was conducted using the online software for statistical analysis of text, SemanticExcel that can be accessed on semanticexcel.com 73 . For code, see https://github.com/sverkersikstrom/semanticCode .
WHO. Mental health. https://www.who.int/health-topics/mental-health#tab=tab_1 (2021).
McCracken, L. M., Badinlou, F., Buhrman, M. & Brocki, K. C. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatry 63 , e81 (2020).
Article PubMed Google Scholar
Mihalopoulos, C. & Vos, T. Cost–effectiveness of preventive interventions for depressive disorders: an overview. Expert Rev. Pharmacoecon. Outcomes Res. 13 , 237–242 (2013).
Moreira-Almeida, A., Lotufo Neto, F. & Koenig, H. G. Religiousness and mental health: a review. Rev. Bras. Psiquiatr. 28 , 242–250 (2006).
Murray, C. J. L. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 , 2197–2223 (2012).
Eichstaedt, J. C. et al. Facebook language predicts depression in medical records. Proc. Natl Acad. Sci. USA 115 , 11203–11208 (2018).
Article CAS PubMed PubMed Central Google Scholar
Greenberg, P. E. et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J. Clin. Psychiatry 64 , 1465–1475 (2003).
Kemper, S., Kynette, D. & Norman, S. in Everyday Memory and Aging (eds West, R. L. & Sinnott, J. D.) 138–152 (Springer, 1992).
Kjell, O. N. E., Kjell, K., Garcia, D. & Sikström, S. Semantic measures: using natural language processing to measure, differentiate, and describe psychological constructs. Psychol. Methods 24 , 92–115 (2019).
Statista. Sweden: share of people with depression, by age 2020. https://www.statista.com/statistics/960041/share-of-people-diagnosed-with-depression-in-sweden-by-age/ (2021).
Statista. Sweden: share of people with severe anxiety, by age 2020. https://www.statista.com/statistics/961442/share-of-people-with-severe-anxiety-in-sweden-by-age/ (2021).
Lenze, E. J. et al. Comorbid anxiety disorders in depressed elderly patients. Am. J. Psychiatry 157 , 722–728 (2000).
Article CAS PubMed Google Scholar
Statista. Share of people diagnosed with depression in Sweden 2022, by age. https://www.statista.com/statistics/961442/share-of-people-with-severe-anxiety-in-sweden-by-age/ (2023).
Remes, O., Brayne, C., Van Der Linde, R. & Lafortune, L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 6 , e00497 (2016).
Article PubMed PubMed Central Google Scholar
Su, Y. et al. Specific and cumulative lifetime stressors in the aetiology of major depression: a longitudinal community-based population study. Epidemiol. Psychiatr. Sci. 31 , E3 (2022).
Tausczik, Y. R. & Pennebaker, J. W. The psychological meaning of words: LIWC and computerized text analysis methods. J. Lang. Soc. Psychol. 29 , 24–54 (2010).
Article Google Scholar
Xia, W. et al. Association between self-reported depression and risk of all-cause mortality and cause-specific mortality. J. Affect. Disord. 299 , 353–358 (2022).
Agerbo, E., Nordentoft, M. & Mortensen, P. B. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. BMJ 325 , 74 (2002).
Hawes, M. T., Szenczy, A. K., Klein, D. N., Hajcak, G. & Nelson, B. D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 52 , 3222–3230 (2021).
Eisenberg, D., Gollust, S. E., Golberstein, E. & Hefner, J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 77 , 534–542 (2007).
Trollor, J. N., Anderson, T. M., Sachdev, P. S., Brodaty, H. & Andrews, G. Age shall not weary them: mental health in the middle-aged and the elderly. Aust. NZ J. Psychiatry 41 , 581–589 (2007).
Yalin, N., Young, A. H. in Age of Onset of Mental Disorders (eds de Girolamo, G., McGorry, P. & Sartorius, N.) 111–124 (Springer, 2019).
Wu, C., Hsu, L. & Wang, S. Association of depression and diabetes complications and mortality: a population-based cohort study. Epidemiol. Psychiatr. Sci. 29 , E96 (2020).
Davison, K. M. et al. Nutritional factors, physical health and immigrant status are associated with anxiety disorders among middle-aged and older adults: findings from baseline data of the Canadian longitudinal study on aging (CLSA). Int. J. Environ. Res. Public Health 17 , 1493 (2020).
Bergdahl, J. & Bergdahl, M. Perceived stress in adults: prevalence and association of depression, anxiety and medication in a Swedish population. Stress Health 18 , 235–241 (2002).
Cattan, M., White, M., Bond, J. & Learmouth, A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc. 25 , 41–67 (2005).
Gottfries, C. G. Late life depression. Eur. Arch. Psychiatry Clin. Neurosci. 251 (Suppl. 2), II57–II61 (2001).
Gottfries, C. G. Is there a difference between elderly and younger patients with regard to the symptomatology and aetiology of depression? Int. Clin. Psychopharmacol. 13 , S13–S18 (1998).
Johansson, R., Carlbring, P., Heedman, Å., Paxling, B. & Andersson, G. Depression, anxiety and their comorbidity in the Swedish general population: point prevalence and the effect on health-related quality of life. PeerJ 1 , e98 (2013).
Rapp, M. A., Gerstorf, D., Helmchen, H. & Smith, J. Depression predicts mortality in the young old, but not in the oldest old: results from the Berlin Aging Study. Am. J. Geriatr. Psychiatry 16 , 844–852 (2008).
De Leo, D. Late-life suicide in an aging world. Nat. Aging 2 , 7–12 (2022).
Ojagbemi, A., Oladeji, B., Abiona, T. & Gureje, O. Suicidal behaviour in old age-results from the Ibadan Study of Ageing. BMC Psychiatry 13 , 1–7 (2013).
Yildirim, H., Işik, K. & Aylaz, R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Soc. Work Public Health 36 , 194–204 (2021).
Fischer, L. R., Wei, F., Solberg, L. I., Rush, W. A. & Heinrich, R. L. Treatment of elderly and other adult patients for depression in primary care. J. Am. Geriatr. Soc. 51 , 1554–1562 (2003).
Gorska-Ciebiada, M., Saryusz-Wolska, M., Ciebiada, M. & Loba, J. Mild cognitive impairment and depressive symptoms in elderly patients with diabetes: prevalence, risk factors, and comorbidity. J. Diabet. Res. 2014 , 179648 (2014).
Nyqvist, F., Forsman, A. K., Giuntoli, G. & Cattan, M. Social capital as a resource for mental well-being in older people: a systematic review. Aging Mental Health 17 , 394–410 (2013).
Luxton, D. D. in Artificial Intelligence in Behavioral and Mental Health Care (ed. Luxton, D. D.) 1–26 (Academic Press, 2016).
Mathers, C. D. & Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 3 , e442 (2006).
Mazure, C. M. & Maciejewski, P. K. A model of risk for major depression: effects of life stress and cognitive style vary by age. Depress. Anxiety 17 , 26–33 (2003).
Graham, S. et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr. Psychiatry Rep. 21 , 116 (2019).
Graham, S. A. & Depp, C. A. Artificial intelligence and risk prediction in geriatric mental health: what happens next? Int. Psychogeriatr. 31 , 921–923 (2019).
Lin, L. Y. et al. Association between social media use and depression among U.S. young adults. Depress. Anxiety 33 , 323–331 (2016).
Lindwall, M., Rennemark, M., Halling, A., Berglund, J. & Hassmén, P. Depression and exercise in elderly men and women: findings from the Swedish national study on aging and care. J. Aging Phys. Activity 15 , 41–55 (2007).
Choudhury, M. de, Counts, S. & Horvitz, E. Social media as a measurement tool of depression in populations. In Proceedings of the 5th Annual ACM Web Science Conference 47–56 (ACM, 2013).
D’Alfonso, S. et al. Artificial intelligence-assisted online social therapy for youth mental health. Front. Psychol. 8 , 796 (2017).
Landauer, T. K. & Dumais, S. T. A solution to Plato’s problem: the latent semantic analysis theory of acquisition, induction, and representation of knowledge. Psychol. Rev. 104 , 211–240 (1997).
Kjell, K., Johnsson, P. & Sikström, S. Freely generated word responses analyzed with artificial intelligence predict self-reported symptoms of depression, anxiety, and worry. Front. Psychol. 12 , 602581 (2021).
Kjell, O. N. E., Daukantaitė, D., Hefferon, K. & Sikström, S. The harmony in life scale complements the satisfaction with life scale: expanding the conceptualization of the cognitive component of subjective well-being. Soc. Indic. Res. 126 , 893–919 (2016).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16 , 606–613 (2001).
Lovejoy, C. A., Buch, V. & Maruthappu, M. Technology and mental health: the role of artificial intelligence. Eur. Psychiatry 55 , 1–3 (2019).
Löwe, B., Unützer, J., Callahan, C. M., Perkins, A. J. & Kroenke, K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med. Care 42 , 1194–1201 (2004).
Löwe, B. et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 46 , 266–274 (2008).
Lu, G. et al. Tough times, extraordinary care: a critical assessment of chatbot-based digital mental healthcare solutions for older persons to fight against pandemics like COVID-19. In Proceedings of Sixth International Congress on Information and Communication Technology 735–743 (Springer, 2022).
Chen, I. Y., Szolovits, P. & Ghassemi, M. Can AI help reduce disparities in general medical and mental health care? AMA J. Ethics 21 , E167–E179 (2019).
Horn, R. L. & Weisz, J. R. Can artificial intelligence improve psychotherapy research and practice? Adm. Policy Ment. Health 47 , 852–855 (2020).
Jha, I. P., Awasthi, R., Kumar, A., Kumar, V. & Sethi, T. Learning the mental health impact of COVID-19 in the United States with explainable artificial intelligence. JMIR Ment. Health 8 , e25097 (2021).
Sikström S., Kjell O. (in revision). Language Analyzed by Computational Methods Predicts Depression Episodes More Accurately than Rating Scales Alone.
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Diener, E., Emmons, R. A., Larsen, R. J. & Griffin, S. The satisfaction with life scale. J. Pers. Assess. 49 , 71–75 (1985).
Erickson, K. I., Leckie, R. L. & Weinstein, A. M. Physical activity, fitness, and gray matter volume. Neurobiol. Aging 35 (Suppl. 2), S20–S28 (2014).
Oppenheimer, D. M., Meyvis, T. & Davidenko, N. Instructional manipulation checks: detecting satisficing to increase statistical power. J. Exp. Social Psychol. 45 , 867–872 (2009).
O’Riley, A. A. & Fiske, A. Emphasis on autonomy and propensity for suicidal behavior in younger and older adults. Suicide Life-threatening Behav. 42 , 394–404 (2012).
Pearson, S. et al. Depression and insulin resistance: cross-sectional associations in young adults. Diabetes Care 33 , 1128–1133 (2010).
Pennebaker, J. W. Using computer analyses to identify language style and aggressive intent: the secret life of function words. Dyn. Asymmetric Conflict 4 , 92–102 (2011).
Yesavage, J. A. et al. Development and validation of a geriatric depression screening scale: a preliminary report. J. Psychiatr. Res . 17 , 37–49 (1982).
Virgincar, A., Doherty, S. & Siriwardhana, C. The impact of forced migration on the mental health of the elderly: a scoping review. Int. Psychogeriatr. 28 , 889–896 (2016).
Williams, J. W. et al. Treatment of dysthymia and minor depression in primary care: a randomized controlled trial in older adults. JAMA 284 , 1519–1526 (2000).
Williamson, V., Stevelink, S. A. M., Greenberg, K. & Greenberg, N. Prevalence of mental health disorders in elderly U.S. military veterans: a meta-analysis and systematic review. Am. J. Geriatr. Psychiatry 26 , 534–545 (2018).
Horn, J. L. & Cattell, R. B. Age differences in fluid and crystallized intelligence. Acta Psychol. 26 , 107–129 (1967).
Article CAS Google Scholar
Villarroel, M. A. & Terlizzi, E. P. Symptoms of depression among adults: United States, 2019. NCHS Data Brief . 1–8 (2020).
Sikström, S., Pålsson Höök, A. & Kjell O. Precise language responses versus easy rating scales-Comparing respondents' views with clinicians’ belief of the respondent’s views. PLoS ONE 18 , e0267995 (2023).
Brenner, P. S. & DeLamater, J. D. Social desirability bias in self-reports of physical activity: is an exercise identity the culprit? Soc. Indic. Res. 117 , 489–504 (2014).
Sikström, S., Kjell, O. N. E. & Kjell, K. in Statistical Semantics: Methods and Applications (eds Sikström, S. & Garcia, D.) 87–103 (Springer, 2020).
Download references
Acknowledgements
This research was founded by the Kamprad Foundation (grant number 20180281) and Marianne och Marcus Wallenbergs Stiftelse (MMW-2021.0058).
Open access funding provided by Lund University.
Author information
Authors and affiliations.
Department of Psychology, Lund University, Lund, Sweden
Sverker Sikström
Department of Psychology, Potsdam University, Potsdam, Germany
Bleona Kelmendi
Department of Psychology, Uppsala University, Uppsala, Sweden
Ninni Persson
Institute for Globally Distributed Open Research and Education (IGDORE), Gothenburg, Sweden
You can also search for this author in PubMed Google Scholar
Contributions
S.S., B.K. and N.P. wrote the manuscript. S.S. and B.K. conducted the analysis and generated the research questions.
Corresponding author
Correspondence to Sverker Sikström .
Ethics declarations
Competing interests.
S.S. declares no non-financial interests and competing financial interest as a founder and shareholder of Ablemind.co AB. B.K. and N.P. declare no competing financial or non-financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary materials, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sikström, S., Kelmendi, B. & Persson, N. Assessment of depression and anxiety in young and old with a question-based computational language approach. npj Mental Health Res 2 , 11 (2023). https://doi.org/10.1038/s44184-023-00032-z
Download citation
Received : 22 November 2022
Accepted : 11 July 2023
Published : 24 July 2023
DOI : https://doi.org/10.1038/s44184-023-00032-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
1 km of living area: age differences in the association between neighborhood environment perception and self-rated health among chinese people.
BMC Public Health (2024)
Validation of the difficulties in emotion regulation scale (ders-28) in spanish young adult substance users
- Alba González-Roz
- Álvaro Postigo
- Elena Gervilla
Current Psychology (2024)
Life satisfaction after stroke and the associated factors across age groups in China: A cross-sectional study
- Yulong Wang
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Our systems are now restored following recent technical disruption, and we’re working hard to catch up on publishing. We apologise for the inconvenience caused. Find out more: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert
- > Journals
- > BJPsych Open
- > Volume 8 Issue 3
- > Key questions: research priorities for student mental...

Article contents
- Conclusions
Data availability
Key questions: research priorities for student mental health.
Published online by Cambridge University Press: 10 May 2022
The high prevalence of mental distress among university students is gaining academic, policy and public attention. As the volume of research into student mental health increases, it is important to involve students to ensure that the evidence produced can translate into meaningful improvements.
For the first time, we consult UK students about their research priorities on student mental health.
This priority setting exercise involved current UK university students who were asked to submit three research questions relating to student mental health. Responses were aggregated into themes through content analysis and considered in the context of existing research. Students were involved throughout the project, including inception, design, recruitment, analysis and dissemination.
UK university students ( N = 385) submitted 991 questions, categorised into seven themes: epidemiology, causes and risk factors, academic factors and work–life balance, sense of belonging, intervention and services, mental health literacy and consequences. Across themes, respondents highlighted the importance of understanding the experience of minority groups.
Students are interested in understanding the causes and consequences of poor mental health at university, across academic and social domains. They would like to improve staff and students’ knowledge about mental health, and have access to evidence-based support. Future research should take a broad lens to evaluate interventions; considering how services are designed and delivered, and investigating institutional and behavioural barriers to accessibility, including how this varies across different groups within the student population.
In the context of increasing prevalence of youth and young adult mental health problems, Reference McManus 1 , Reference Tabor, Patalay and Bann 2 including university students, Reference Auerbach, Mortier, Bruffaerts, Alonso, Benjet and Cuijpers 3 concern about mental health in the university setting is mounting and gaining media and public attention. Reference Gyimah 4 Increasing demand for services on campus has been observed internationally. Reference Tabor, Patalay and Bann 2 , Reference Auerbach, Mortier, Bruffaerts, Alonso, Benjet and Cuijpers 3 However, current approaches lack a solid evidence base, Reference Fernandez, Howse, Rubio-Valera, Thorncraft, Noone and Luu 5 , Reference Worsley, Pennington and Corcoran 6 and students have voiced concerns that existing services do not meet their needs. Reference Priestley, Broglia, Hughes and Spanner 7 In the UK, representatives of university leadership and students are urging the sector to adopt a whole-institution approach. 8 , Reference Hughes and Spanner 9 However, questions about how to achieve this remain unanswered. Eliciting student perspectives and experiences has been highlighted as an enabling strategy for the sector to develop effective and targeted initiatives attuned to diverse student needs and situated within a whole-university approach. Reference Hughes and Spanner 9 As research efforts mount, Reference Hernández-Torrano, Ibrayeva, Sparks, Lim, Clementi and Almukhambetova 10 it is important to involve students to ensure that work in this field translates into meaningful improvements attuned to students’ lived experiences. Reference Chalmers, Bracken, Djulbegovic, Garattini, Grant and Gülmezoglu 11 This project set out to consult students in the UK on their priorities for future research into student mental health. Our aim is to ensure that the student voice is influential in shaping the direction of future research.
Lived experience involvement
The project was initiated through the UK Research and Innovation funded Student Mental Health Research Network (SMaRteN), with a steering group developed from the SMaRteN leadership team. The group recruited diverse stakeholders, including students (both with and without lived experience of mental health difficulties at university), clinical psychologists, tutors and academic researchers. Co-creation was central to this project. This is distinguished from student consultation and participation, by the active involvement of students as equal stakeholders, Reference Braun and Clarke 12 reciprocally sharing knowledge and networks as part of a strengths and asset-based approach. Reference Bengtsson 13 Students were operating in a ‘peer researcher’ context, and worked with academic researchers to design the methodology, recruit a diverse student sample, analyse data and write up the findings. Several student peer researchers are authors on this paper.
Participants
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants were approved by the university ethics board (approval number LRS-19/20-14288). All participants were provided with information about the study and the opportunity to contact the researchers to ask questions before providing informed consent through an online form.
Our sample included 385 UK university students, who responded to advertisements publicised by SMaRteN and the student mental health charity, Student Minds. Advertisements were circulated through newsletters, Facebook, Twitter and Instagram. We did not provide any monetary incentive for participation. Adverts and the study information sheet reminded participants that the survey would provide an opportunity to help shape the future of research in this area, with SMaRteN funding being allocated to address the top priority questions.
Our sample was primarily under 25 years old ( n = 285, 74%) and mostly comprised women ( n = 251, 65%). Our sample included UK domiciled ( n = 279, 72%) and international ( n = 106, 28%) students and was 72% White, 15% Asian and 6% Black. A substantial minority of respondents identified as a sexual or romantic minority ( n = 118, 31%) and/or reported having a disability ( n = 95, 25%). Students represented all years and levels of study (undergraduate, 66%; taught postgraduate, 17%; postgraduate research, 15%), and represented most subject areas (see Table 1 ).
Table 1 Sample representation across academic areas, compared with UK representation, as reported in Higher Education Statistics Agency data
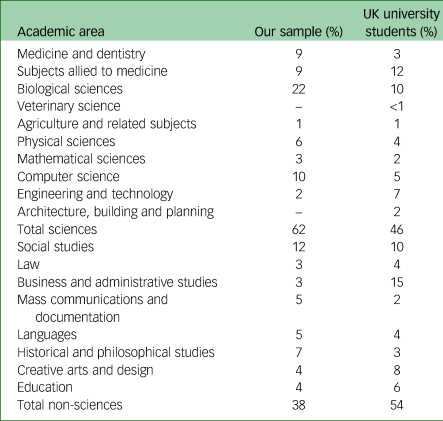
Data collection was carried out via an online survey hosted on Qualtrics (Seattle, WA, USA; see https://www.qualtrics.com/uk/ ) between October 2019 and February 2020. The survey was designed to be as short and simple as possible to make participation as easy. Respondents submitted up to three questions in response to the prompt: ‘In terms of student mental health, what do you think are the priority issues for researchers to explore?’. There was no word limit for the respondents’ submissions. After submitting questions, respondents were asked to complete demographic details.
Data analysis
The objective of our analysis was to understand respondents’ recommendations for future research and categorise these to create a shortlist of research priorities. We sought to capture student recommendations without passing judgement regarding the value of the research topic or whether the question had already been addressed.
A team of 26 students were involved in analysing the data, supported by experienced researchers. The student team were recruited through SMaRteN from universities across the UK. Selection focused on bringing together a diverse team. SMaRteN hosted a 2-day workshop, covering expenses to bring students together for training and co-creation activities.
To facilitate reflexivity, Reference Downe-Wamboldt 14 we followed an iterative approach, with themes developed and refined through consultation with all members of the team. This improves the reliability of analysis, minimising biases arising from individual researchers’ preconceptions. As respondents were invited to provide single sentence questions, without explaining their rationale, it was important not to overanalyse the data. In this context, content analysis was appropriate. As summarised in Fig. 1 , we followed four steps of content analysis, embedding the principles of co-creation in each step. Reference Burnard 15
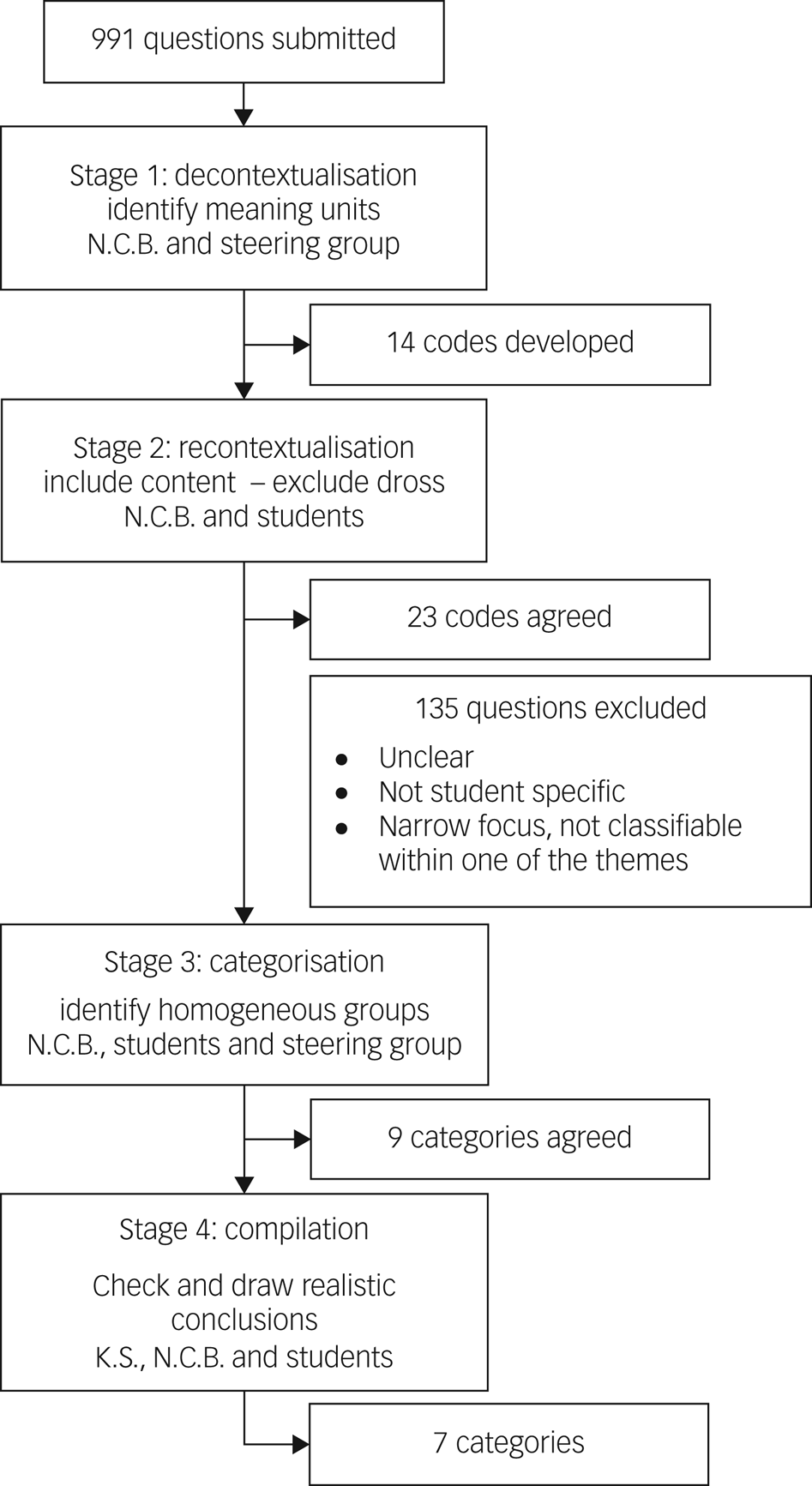
Fig. 1 Content analysis process.
In stage 1, codes were generated inductively, working with the questions provided rather than bringing in any preconceived ideas of the research questions that might be important. This approach was adopted to ensure we think carefully about the questions students were asking, as opposed to trying to fit their questions into the existing research framework. This process was completed independently by members of the steering group, before in-depth discussion, through which a single list of codes was agreed. Reference Downe-Wamboldt 14
At stage 2, students checked that all aspects of the content had been covered by revisiting the original questions, determining what should be included and excluded, and developing more detailed codes. Reference Burnard 15 For example, although the initial list of codes had included ‘academic pressure’, student analysis here clarified that this should include all questions related academic grades, success, workload, deadline and course-specific challenges.
In stage 3, the lead researcher (N.C.B.) worked iteratively with small groups of students to create categories around the codes, with the goal of reducing the categories without losing the content of units. Reference Graneheim and Lundman 16 Returning to the example of academic pressure, we identified parallels between the questions that had been grouped into this code and questions relating to the university extenuating/mitigating circumstances process. Students agreed it was hard to consider the impact of extenuating circumstances without considering these in the wider context of academic culture and assessment practice. Further, most questions relating to work–life balance focused on managing workload, and hence had clear relationship to the questions grouped under academic pressure. As such, we reduced the number of categories by grouping questions together into the category of ‘academic factors’. This process was continuously appraised to ensure categories were internally homogenous and externally heterogenous. Reference Krippendorff 17 For instance, although the questions around academic pressure and extenuating circumstances align, questions relating to academics’ appreciation for the pressure students experienced aligned more clearly with other questions about mental health literacy and academics’ understanding of mental health. In the final stage, categories were checked, named and described.
Across the analysis, although we primarily followed a manifest analysis, describing respondents’ questions as they were presented, at times a more latent approach was necessary to interpret questions that were phrased less clearly. Reference Bengtsson 13 For example, the question ‘What is the effect of workload on students’ mental health?’ can be simply described as asking about student workload, and thus grouped with other questions around workload and academic pressure. In contrast, we received a question reading ‘the amount of work?’. We chose to retain this question and place it within the category of ‘academic factors and work–life balance’. However, here we have assumed the respondent is referring to the work students have to do, rather than the amount of work universities might have to put in to improve student mental health.
In total, 991 questions were submitted and arranged into seven categories. In Table 2 , these categories are set out in descending order of frequency based on the number of questions asked in that category. We discuss each of these categories below.
Table 2 Summary of key priorities in context of existing research
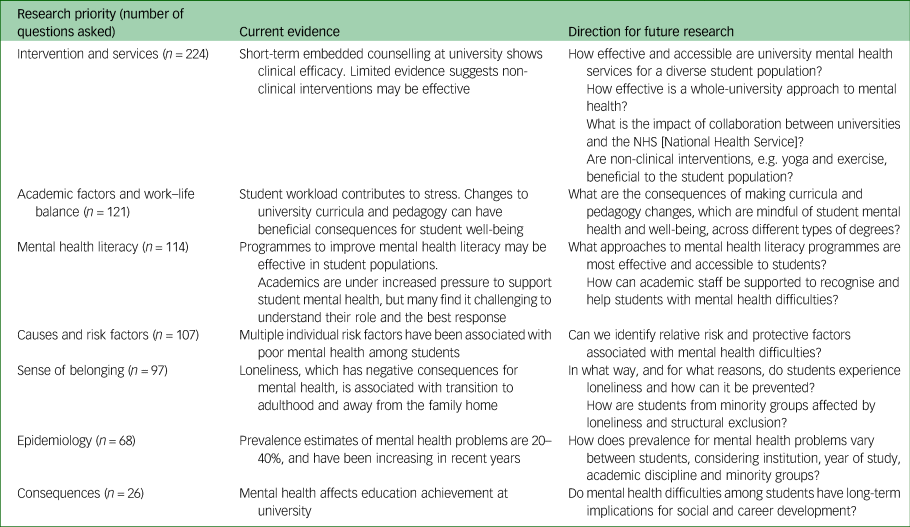
Intervention and services
The efficacy of existing services (including counselling, workshops and drop-in services) was raised, including whether these services meet the needs of a diverse student population. Respondents suggested the potential effects of a broad range of specific and sometimes novel interventions, including physical activity, yoga, mindfulness, social activities and events, and sleeping pods on campus. Questions considered cost-efficacy as well as how to increase funding.
Respondents questioned the appropriate balance between preventative work and responsive treatment, and how university support services should be designed to meet needs ranging from well-being through to complex and enduring mental health problems: ‘How can the support for student well-being versus chronic/severe mental illness be differentiated and acknowledged as separate issues?’
Respondents identified a need to clarify where the boundaries of responsibility between the National Health Service (NHS) and university services should lie and how these services should be better integrated, especially with the split between home and term-time addresses: ‘What is the role of universities in treating, preventing, helping with mental health? Where do they fit in with the NHS, charities and family/social structures?’ Questions asked whether there is adequate provision of professional mental health support for students, whether this is suitably accessible and what steps can be taken to improve availability and accessibility.
Academic factors and work–life balance
Respondents queried how academic pressure, including challenging content, high workload and a pressure to succeed, contribute to mental health problems. This pressure also included how academic success affects self-worth and how to overcome feelings of shame or embarrassment when struggling academically. Pressure was raised in relation to postgraduate students, with a focus on the relationship between mental health, performance and output. Respondents asked what steps can be taken to help those studying at university to cope with pressure: ‘How can students’ resilience and coping be increased so they are best equipped to deal with HE [higher education] study?’
Participants questions indicated that methods of assessment at university may affect mental health and asked whether changes to assessment design could reduce negative effects. Respondents were interested in examinations versus coursework, as well as how deadlines affect stress. A few questions considered the accessibility and efficacy of university extenuating circumstances: ‘Are universities able/willing to make the more flexible adjustments needed for students with long-term mental health conditions to engage?’
University teaching, including module organisation and structure, number of contact hours and online versus in-person teaching, were raised as potentially affecting mental health. Teaching style changes between school and university were also flagged as possibly problematic: ‘I feel like a lot of people are struggling with the first year. How can we make the gap between uni and high school smaller?’ These questions were raised by students across academic disciplines. Healthcare students uniquely also questioned how placements affect mental health.
Respondents asked about the challenge of time management and maintaining balance in their lives. Questions considered how to balance academic work with a social life and part-time job, and postulated whether trying to achieve this places strain on relationships and well-being. Although there were comparatively few questions relating to balance, students involved in the analysis requested that this theme be highlighted because of its relevance and importance.
Mental health literacy
Questions included whether, and in what ways, a culture of increased awareness, education and conversation would affect student mental health: ‘How is the growing awareness of mental health impacting student's mental health?’ Students were concerned about to identify mental health problems in themselves and their peers, and asked for more knowledge about how to respond to and help someone struggling with mental health problems. The importance of providing support to those who are helping friends with mental health problems was also highlighted. Students wanted knowledge of self-help strategies, and questioned how best to manage and cope with their own mental health problems at university: ‘What steps can students take to minimise their risk of adverse mental health issues?’ This theme also included whether students know what support and advice is available at university, and how they can access it, including how comfortable people feel reaching out for support, the role of stigma and shame, and how to encourage help-seeking behaviour.
Academic staff also play a part in creating a culture around mental health, and so respondents were interested in their mental health literacy and suggested providing resources, training programmes or policy implementation to help staff recognise and support students with mental health problems. Some questions considered whether students feel they are treated as individuals or in a more depersonalised and anonymous manner, and what impact this has on student mental health: ‘Would students suffering with poor mental health be able to work better with more consideration from teachers?’
Causes and risk factors
Identifying potential risk and protective factors for poor mental health was highlighted: ‘Which students are most at risk of poor mental health/well-being and why? And most likely to have good mental health and why – protective factors?’ Respondents posed questions about underlying reasons, triggers or drivers for problems, with some assuming that university has a negative impact on mental health: ‘What is causing mental illness at university, and is it a systemic problem?’ Specific possible contributing factors included student finances, living arrangements, drug and alcohol use, unhealthy lifestyles and concerns for future career prospects. Questions about living arrangements considered the impact of living away from home, transitioning between home and term-time addresses, communal versus solitary living and how living in halls of residence affects mental health. Respondents queried how a sense of belonging and academic factors, including the challenge of finding a work–life balance, might contribute to mental health problems. These questions have not been included here because there was sufficient interest to create independent categories.
Sense of belonging
Respondents wanted to know whether all students feel valued, included and appreciated within their university community, and how to improve this: ‘How can students feel more ‘at home’ and comfortable in their universities?’ Loneliness and isolation were raised, particularly the reasons why students are lonely, how this affects mental health and what can be done to reduce it. Respondents questioned how to make meaningful connections, and why students may feel alone despite being surrounded by people. Respondents considered how student social life affects mental health, including the role of societies and sports groups as well as negative experiences such as peer pressure, elitism and bullying.
Questions considered these problems from the perspective of minority or vulnerable groups, with issues surrounding loneliness being raised specifically for international, mature and commuter students. Respondents queried whether the university environment is inclusive for neurodiverse, minority ethnic, LGBTQ+, working class and disabled students, and how a lack of representation may accentuate loneliness. Victimisation and discrimination, including racism and sexual assault, were identified as potentially contributing to mental health problems at university: ‘How safe do you feel on your campus? Specifically, relevant for minoritized groups, i.e. BAME, LGBTQ, non-neurotypical students, etc. and women’.
Epidemiology
Questions falling into this category considered the prevalence of mental health problems among university students, including identifying the most common conditions, how the incidence of these problems is changing in universities and how prevalence differs between students and non-students. Many questions revealed underlying presumptions that student mental health is declining, and that students are more vulnerable to mental health problems than their peers: ‘Why has the prevalence of mental health problems in university students increased?’ They also questioned when mental health problems develop, whether this is before or after coming to university and how the move to university changes peoples’ experiences.
Consequences
A small number of questions asked about the consequences of mental health problems at university, and particularly the impact on academic achievement and social life. Respondents asked about drop-out rates in relation to mental health, and consequences for career development. Respondents were interested in the prognosis for those who struggle with mental health problems at university, including rates of recovery.
The aim of this co-creation project was to identify the mental health research priorities of university students and enable the student voice to shape the direction of future research. Our study identified seven key areas for future research. Many themes overlapped, reflecting the interconnectedness of different facets of student life. As summarised in Table 2 , we have positioned the students’ priorities in the context of the existing research, which is often small scale and narrowly focused, with limited consideration of racial, ethnic and sexual minorities. The project was undertaken before the COVID-19 pandemic, which has resulted in substantial disruption to students’ lives and rapid changes to university practices, and highlights the long-term challenges facing student mental health. It is important that student priorities are considered as the higher education sector transitions to a post-pandemic world.
Although the data available suggest that short-term embedded counselling at university is clinically effective, Reference Broglia, Ryan, Williams, Fudge, Knowles and Turner 18 evaluation of the efficacy of university mental health services has been minimal. Reference Barkham, Broglia, Dufour, Fudge, Knowles and Percy 19 There has been limited evaluation of interventions and services as part of a whole-university approach, Reference Fernandez, Howse, Rubio-Valera, Thorncraft, Noone and Luu 5 , Reference Worsley, Pennington and Corcoran 6 and to our knowledge, no published evaluation of the impact of collaboration between universities and the NHS. Although there has been some consideration of non-clinical interventions such as yoga and exercise, most studies are of poor quality, and it is not possible to rank which interventions work best, where and for whom. Reference Worsley, Pennington and Corcoran 6 Future studies must take a broader lens to evaluate interventions for students, especially how they are designed, delivered and made accessible, and should employ robust evaluation of service efficacy. In line with student priorities, it is vital that future research considers the efficacy of services for the diverse student population.
International research indicates that student workload is a major factor contributing to stress and can result in prolonged study times or drop-out. Reference Bowyer 20 , Reference Dyrbye, Thomas, Harper, Massie, Power and Eacker 21 However, despite growing research interest in a ‘whole of curriculum approach’, knowledge about how to support student mental health through curricula and pedagogy is lacking. Preliminary evidence from the USA demonstrated that a multidimensional curricula intervention involving reduction in contact time, a change in grading system, collaborative and practical learning initiatives, and an embedded resilience and mindfulness intervention, resulted in significant decreases in depressive and anxiety symptoms among medical students, with corresponding increases in quality of life, group cohesion, student satisfaction and examination scores. Reference Slavin, Schindler and Chibnall 22 This suggests that there is a promising way forward that could be adopted in the UK context across different types of degrees, in keeping with the many student questions on this topic.
Mental health literacy is defined as ‘knowledge and belief about mental disorders which aid their recognition, management or prevention’. Reference Jorm, Korten and Jacomb 23 Within this, understanding how to look after your own mental health and support peers is fundamental. Reference Jorm 24 Preliminary research has demonstrated potential efficacy and acceptability of peer support programmes Reference Byrom 25 and programmes to improve student mental health literacy among students. Reference Lo, Gupta and Keating 26 However, further research is needed to evaluate these more thoroughly and compare different approaches. Academics are under increased pressure to support student mental health, but many find it challenging to understand their role and the best response. Reference Hughes and Byrom 27 Research findings around mental health literacy are varied, with some studies identifying knowledge gaps Reference Redpath, Kearney, Nicholl, Mulvenna, Wallace and Martin 28 and others noting good levels of literacy among students and staff. Reference Gulliver, Farrer, Bennett and Griffiths 29 Exploring how staff and students can support themselves and others with mental health difficulties is an important priority for future research.
Research has only focused on whether a specific factor, in isolation, is relevant to mental health. For example, there is strong evidence of relationships between mental health problems and financial stress, Reference Andrews and Wilding 30 , Reference Richardson, Elliott and Roberts 31 drug and alcohol consumption, Reference Tembo, Burns and Kalembo 32 , Reference Walters, Bulmer, Troiano, Obiaka and Bonhomme 33 isolation and loneliness, Reference McIntyre, Worsley, Corcoran, Harrison Woods and Bentall 34 and sleep disruption Reference Peach, Gaultney and Gray 35 , Reference Di Benedetto, Towt and Jackson 36 among students, as well as experiences of adverse events before and during university. Reference Karatekin 37 Although studies have increasingly explored the link between factors such as accommodation environments, Reference Worsley, Harrison and Corcoran 38 , Reference Worsley, Harrison and Corcoran 39 and physical activity Reference Dogra, MacIntosh, O'Neill, D'Silva, Shearer and Smith 40 and student mental health, investigating general and comparative risk, protective and causal factors associated with mental health problems among students remains a high priority.
The repeated use of the word ‘loneliness’ within submitted questions was striking. There are strong links between loneliness and mental health problems, Reference Hawkley and Cacioppo 41 and loneliness is particularly associated with the transition from adolescence to adulthood. 42 Loneliness appears to be accentuated by the significant upheaval in social networks that occurs when young adults leave the family home. Reference Matthews, Odgers, Danese, Fisher, Newbury and Caspi 43 Research focusing on loneliness and student and postgraduate mental health is developing, Reference McIntyre, Worsley, Corcoran, Harrison Woods and Bentall 34 , Reference Vasileiou, Barnett, Barreto, Vines, Atkinson and Long 44 but studies to establish how student friendship groups form, how and why students experience loneliness at university and how student loneliness can be prevented should continue, particularly with student input. The COVID-19 pandemic caused further disruption to students’ social networks, with public concern for students missing the university experience. Reference Blackall and Mistlin 45 , Reference Montacute and Culliane 46 It will be important for research exploring the impact of COVID-19 to recognise that challenges around sense of belonging on the university campus predate the pandemic.
A sense of belonging is unique to the individual. As recognised by the students in our study, it is vital for issue of belonging and loneliness to be investigated among minority groups. Although there is a substantive body of research on attainment gaps for students from minority ethnic backgrounds in UK higher education, Reference Mountford-Zimdars, Sanders, Jones, Sabri and Moore 47 there are evidence gaps related to how structural exclusion affects mental health. Reference Alharbi and Smith 48
Existing evidence suggests 20–40% of university students are likely to meet criteria for mental health problems, and prevalence rates have been increasing over recent years. Reference Tabor, Patalay and Bann 2 , Reference Auerbach, Mortier, Bruffaerts, Alonso, Benjet and Cuijpers 3 Analysis of large population data-sets provides conflicting evidence about the relative prevalence of mental health problems between university students and peers not in higher education. Reference Tabor, Patalay and Bann 2 , Reference Lewis, McCloud and Callender 49 With notable exceptions, Reference Bewick, Koutsopoulou, Miles, Slaa and Barkham 50 , Reference Macaskill 51 there has been limited work within the UK identifying how mental health problems might vary across years of study, academic disciplines and universities, although this has been explored extensively within the USA. Reference Dyrbye, Thomas, Harper, Massie, Power and Eacker 21 Current data around the prevalence of mental health problems for minority student groups also remains limited.
In line with student priorities, future research must provide more precise estimates of the prevalence of student mental health problems, and identify how these vary across the student population. This will have important implications for service planning and provision. Given many students have pre-existing beliefs regarding prevalence and trends of mental health problems at university, clear communication of existing data and future findings is imperative.
In keeping with students’ concerns, research suggests mental health does affect educational achievement at university. Reference Eisenberg, Hunt and Speer 52 – Reference Allan, McKenna and Dominey 54 However longitudinal studies assessing long-term consequences across a wider breadth of domains, including social life and future career development, are lacking.
Strengths and limitations
Student involvement in every stage of the study increased the likelihood that the project would be responsive to students’ needs and research priorities. Our sample was broadly representative of the student population, although it overrepresented women, underrepresented undergraduate students and overrepresented students studying sciences, primarily because of a large representation of students studying medicine and dentistry, biological sciences (including psychology) and computer science (see Table 1 ). Given the widespread underrepresentation of men in research into student mental health, it will remain important for future research to develop specific strategies to consult and engage male students in research design. As a self-selective sample, it is important to recognise that the voices of students who care passionately about student mental health are likely to have been overrepresented in this project.
In conclusion, this project identifies seven key priorities for future research into student mental health from the perspective of UK university students. Students’ questions are mostly unmet in the existing literature, with less research into the mental health of racial, ethnic and sexual minority student communities. Research is needed in each of these seven areas, and Table 2 highlights key questions to be answered. However, three areas stand out as particularly important. ‘Interventions and services’ was the largest category of questions. This is also an area where there are research gaps. We do not need more research evaluating whether one-to-one clinical interventions are effective. Rather, research needs to assess the whole-university approach, understand the range of needs across a diverse student population and consider the broad student experience of services, from initial help-seeking through identifying appropriate support, triaging, waiting lists and using the service. In contrast to the attention students have given to academic factors, the research in this area is sparce. We need robust, large-scale evaluations of the impact of curricula and pedagogy on student mental health. Finally, there is a stark gap between student interest and research exploring sense of belonging. Future research must address the university social experience, to enhance our understanding of how this relates to student mental health and how it might be leveraged to improve mental health.
Our results have important implications for future funding to ensure research produces knowledge that is useful, relevant and meaningful to diverse student populations, as well as ensuring that knowledge can be translated into positive and practical changes within the higher education sector.
The fully anonymised data that support the findings of this study are available online from figshare at https://doi.org/10.6084/m9.figshare.15124908 .
Acknowledgements
The research was supported by the project steering group and the SMaRteN student team, including Oskar Kaleta, Aleks Saunders, Connor Gayle, Kwan Lui Cheng, Joshua Melwani, Eadie Simons, Sania Deshpande, Lesley Turner, Elizabeth James, Isabel De Castro, Megan Lawrence, Kirellos Miseih, Paulina Pawlak, Samuel Chu, Andrea Prisecaru, Keerthi Ramesh, Wangjingyi Liao, Reihannah Mahmoud, Emily Wielezynski, Chloe Casey, Nuvera Mukaty, Anusha Ramji, Oliver Anderson, Anna Ambwene, Ka Wai Li, Elizabeta Farys and Kristyana Taneva.
Author contributions
K.S. contributed to data analysis and interpretation, including checking, naming and describing categories from students’ questions, and contributed to the write-up and editing of the final paper. M.P. contributed to the design/procedure as a student in the steering group, by recruiting students to submit key questions, through analysing/thematising submitted questions and in editing the manuscript. A.L.D. contributed to the initial design of the priority setting exercise, supported student recruitment and made critical revisions to several drafts of the manuscript. E.B. advised in her role on the SMaRteN leadership team and contributed to the preparation of this manuscript. T.W. contributed to the design of the priority setting exercise, advised on the analysis and contributed to the writing up of the manuscript. D.R. helped to develop and support the priority setting exercise, helped with analysis and suggested comments on the final paper. K.T. contributed to the conceptualisation and development of study materials, project administration and writing (reviewing and editing) of the manuscript. M.O.V. contributed as a steering group member for the research, reviewing initial responses and providing feedback on themes. N.C.B. is Principal Investigator, and therefore took the lead on designing and implementing the priority setting exercise, analysing data and writing the manuscript. All authors had access to the data, and K.S., M.P., D.R. and N.C.B. in particular can verify the underlying data. All authors approved the final manuscript.
This project was funded by the Economic and Social Research Council (grant number ES/S00324X/1) awarded to N.C.B., A.L.D., E.B., T.W. and D.R. The funder had no involvement in the design, implementation or dissemination of this study.
Declaration of interest
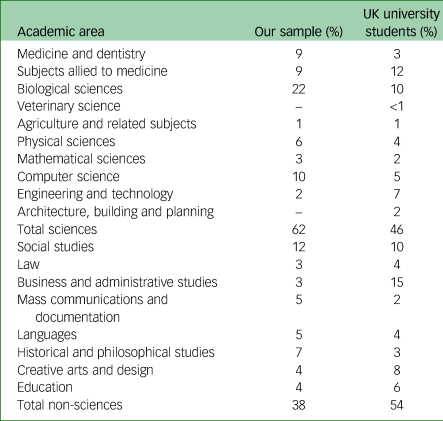
This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 8, Issue 3
- Katie Sampson (a1) , Michael Priestley (a2) , Alyson L. Dodd (a3) , Emma Broglia (a4) , Til Wykes (a1) , Dan Robotham (a5) , Katie Tyrrell (a6) , Marta Ortega Vega (a7) and Nicola C. Byrom (a8)
- DOI: https://doi.org/10.1192/bjo.2022.61
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
- How It Works
- PhD thesis writing
- Master thesis writing
- Bachelor thesis writing
- Dissertation writing service
- Dissertation abstract writing
- Thesis proposal writing
- Thesis editing service
- Thesis proofreading service
- Thesis formatting service
- Coursework writing service
- Research paper writing service
- Architecture thesis writing
- Computer science thesis writing
- Engineering thesis writing
- History thesis writing
- MBA thesis writing
- Nursing dissertation writing
- Psychology dissertation writing
- Sociology thesis writing
- Statistics dissertation writing
- Buy dissertation online
- Write my dissertation
- Cheap thesis
- Cheap dissertation
- Custom dissertation
- Dissertation help
- Pay for thesis
- Pay for dissertation
- Senior thesis
- Write my thesis
207 Mental Health Research Topics For Top Students

College and university students pursuing psychology studies must write research papers on mental health in their studies. It is not always an exciting moment for the students since getting quality mental health topics is tedious. However, this article presents expert ideas and writing tips for students in this field. Enjoy!
What Is Mental Health?
It is an integral component of health that deals with the feeling of well-being when one realizes his or her abilities, cope with the pressures of life, and productively work. Mental health also incorporates how humans interact with each other, emote, or think. It is a vital concern of any human life that cannot be neglected.
How To Write Mental Health Research Topics
One should approach the subject of mental health with utmost preciseness. If handled carelessly, cases such as depression, suicide or low self-esteem may occur. That is why students are advised to carefully choose mental health research paper topics for their paper with the mind reader.
To get mental health topics for research paper, you can use the following sources:
- The WHO website
- Websites of renowned psychology clinics
- News reports and headlines.
However, we have a list of writing ideas that you can use for your inspiration. Check them out!
Top Mental Disorders Research Topics
- Is the psychological treatment of mental disorders working for all?
- How do substance-use disorders impede the healing process?
- Discuss the effectiveness of the mental health Gap Action Programme (mhGAP)
- Are non-specialists in mental health able to manage severe mental disorders?
- The role of the WHO in curbing and treating mental disorders globally
- The contribution of coronavirus pandemic to mental disorders
- How does television contribute to mental disorders among teens?
- Does religion play a part in propagating mental disorders?
- How does peer pressure contribute to mental disorders among teens?
- The role of the guidance and counselling departments in helping victims of mental disorders
- How to develop integrated and responsive mental health to such disorders
- Discuss various strategies for promotion and prevention in mental health
- The role of information systems in mental disorders
Mental Illness Research Questions
- The role of antidepressant medicines in treating mental illnesses
- How taxation of alcoholic beverages and their restriction can help in curbing mental illnesses
- The impact of mental illnesses on the economic development of a country
- Efficient and cost-effective ways of treating mental illnesses
- Early childhood interventions to prevent future mental illnesses
- Why children from single-parent families are prone to mental illnesses
- Do opportunities for early learning have a role in curbing mental diseases?
- Life skills programmes that everyone should embrace to fight mental illnesses
- The role of nutrition and diet in causing mental illness
- How socio-economic empowerment of women can help promote mental health
- Practical social support for elderly populations to prevent mental illnesses
- How to help vulnerable groups against mental illnesses
- Evaluate the effectiveness of mental health promotional activities in schools
Hot Mental Health Topics For Research
- Do stress prevention programmes on TV work?
- The role of anti-discrimination laws and campaigns in promoting mental health
- Discuss specific psychological and personality factors leading to mental disorders
- How can biological factors lead to mental problems?
- How stressful work conditions can stir up mental health disorders
- Is physical ill-health a pivotal contributor to mental disorders today?
- Why sexual violence has led many to depression and suicide
- The role of life experiences in mental illnesses: A case of trauma
- How family history can lead to mental health problems
- Can people with mental health problems recover entirely?
- Why sleeping too much or minor can be an indicator of mental disorders.
- Why do people with mental health problems pull away from others?
- Discuss confusion as a sign of mental disorders
Research Topics For Mental Health Counseling
- Counselling strategies that help victims cope with the stresses of life
- Is getting professional counselling help becoming too expensive?
- Mental health counselling for bipolar disorders
- How psychological counselling affects victims of mental health disorders
- What issues are students free to share with their guiding and counselling masters?
- Why are relationship issues the most prevalent among teenagers?
- Does counselling help in the case of obsessive-compulsive disorders?
- Is counselling a cure to mental health problems?
- Why talking therapies are the most effective in dealing with mental disorders
- How does talking about your experiences help in dealing with the problem?
- Why most victims approach their counsellors feeling apprehensive and nervous
- How to make a patient feel comfortable during a counselling session
- Why counsellors should not push patients to talk about stuff they aren’t ready to share
Mental Health Law Research Topics
- Discuss the effectiveness of the Americans with Disabilities Act
- Does the Capacity to Consent to Treatment law push patients to the wall?
- Evaluate the effectiveness of mental health courts
- Does forcible medication lead to severe mental health problems?
- Discuss the institutionalization of mental health facilities
- Analyze the Consent to Clinical Research using mentally ill patients
- What rights do mentally sick patients have? Are they effective?
- Critically analyze proxy decision making for mental disorders
- Why some Psychiatric Advance directives are punitive
- Discuss the therapeutic jurisprudence of mental disorders
- How effective is legal guardianship in the case of mental disorders?
- Discuss psychology laws & licensing boards in the United States
- Evaluate state insanity defence laws
Controversial Research Paper Topics About Mental Health
- Do mentally ill patients have a right to choose whether to go to psychiatric centres or not?
- Should families take the elderly to mental health institutions?
- Does the doctor have the right to end the life of a terminally ill mental patient?
- The use of euthanasia among extreme cases of mental health
- Are mental disorders a result of curses and witchcraft?
- Do violent video games make children aggressive and uncontrollable?
- Should mental institutions be located outside the cities?
- How often should families visit their relatives who are mentally ill?
- Why the government should fully support the mentally ill
- Should mental health clinics use pictures of patients without their consent?
- Should families pay for the care of mentally ill relatives?
- Do mentally ill patients have the right to marry or get married?
- Who determines when to send a patient to a mental health facility?
Mental Health Topics For Discussion
- The role of drama and music in treating mental health problems
- Explore new ways of coping with mental health problems in the 21 st century
- How social media is contributing to various mental health problems
- Does Yoga and meditation help to treat mental health complications?
- Is the mental health curriculum for psychology students inclusive enough?
- Why solving problems as a family can help alleviate mental health disorders
- Why teachers can either maintain or disrupt the mental state of their students
- Should patients with mental health issues learn to live with their problems?
- Why socializing is difficult for patients with mental disorders
- Are our online psychology clinics effective in handling mental health issues?
- Discuss why people aged 18-25 are more prone to mental health problems
- Analyze the growing trend of social stigma in the United States
- Are all people with mental health disorders violent and dangerous?
Mental Health Of New Mothers Research Topics
- The role of mental disorders in mother-infant bonding
- How mental health issues could lead to delays in the emotional development of the infant
- The impact of COVID-19 physical distancing measures on postpartum women
- Why anxiety and depression are associated with preterm delivery
- The role of husbands in attending to wives’ postpartum care needs
- What is the effectiveness of screening for postpartum depression?
- The role of resilience in dealing with mental issues after delivery
- Why marginalized women are more prone to postpartum depression
- Why failure to bond leads to mental disorders among new mothers
- Discuss how low and middle-income countries contribute to perinatal depression
- How to prevent the recurrence of postpartum mental disorders in future
- The role of anti-depression drugs in dealing with depression among new mothers
- A case study of the various healthcare interventions for perinatal anxiety and mood disorders
What Are The Hot Topics For Mental Health Research Today
- Discuss why mental health problems may be a result of a character flaw
- The impact of damaging stereotypes in mental health
- Why are many people reluctant to speak about their mental health issues?
- Why the society tends to judge people with mental issues
- Does alcohol and wasting health help one deal with a mental problem?
- Discuss the role of bullying in causing mental health disorders among students
- Why open forums in school and communities can help in curbing mental disorders
- How to build healthy relationships that can help in solving mental health issues
- Discuss frustration and lack of understanding in relationships
- The role of a stable and supportive family in preventing mental disorders
- How parents can start mental health conversations with their children
- Analyze the responsibilities of the National Institute for Health and Care Excellence (NICE)
- The role of a positive mind in dealing with psychological problems
Good Research Topics On Refugees Mental Health
- Why do refugees find themselves under high levels of stress?
- Discuss the modalities of looking after the mental health of refugees
- Evaluate the importance of a cultural framework in helping refugees with mental illnesses
- How refugee camp administrators can help identify mental health disorders among refugees
- Discuss the implications of dangerous traditional practices
- The role of the UNHCR in assisting refugees with mental problems
- Post-traumatic Stress Disorder among refugees
- Dealing with hopelessness among refugees
- The prevalence of traumatic experiences in refugee camps
- Does cognitive-behavioural therapy work for refugees?
- Discuss the role of policy planning in dealing with refugee-mental health problems
- Are psychiatry and psychosomatic medicine effective in refugee camps?
- Practical groups and in‐group therapeutic settings for refugee camps
Adolescent Mental Health Research Topics
- Discuss why suicide is among the leading causes of death among adolescents
- The role of acting-out behaviour or substance use in mental issues among adolescents
- Mental effects of unsafe sexual behaviour among adolescents
- Psychopharmacologic agents and menstrual dysfunction in adolescents
- The role of confidentiality in preventive care visits
- Mental health disorders and impairment among adolescents
- Why adolescents not in school risk developing mental disorders
- Does a clinical model work for adolescents with mental illnesses?
- The role of self-worth and esteem in dealing with adolescent mental disorders
- How to develop positive relationships with peers
- Technology and mental ill-health among adolescents
- How to deal with stigma among adolescents
- Curriculum that supports young people to stay engaged and motivated
Research Topics For Mental Health And Government
- Evaluate mental health leadership and governance in the United States
- Advocacy and partnerships in dealing with mental health
- Discuss mental health and socio-cultural perspective
- Management and coordination of mental health policy frameworks
- Roles and responsibilities of governments in dealing with mental health
- Monitoring and evaluation of mental health policies
- What is the essence of a mental health commission?
- Benefits of mental well-being to the prosperity of a country
- Necessary reforms to the mental health systems
- Legal frameworks for dealing with substance use disorders
- How mental health can impede the development of a country
- The role of the government in dealing with decaying mental health institutions
- Inadequate legislation in dealing with mental health problems
Abnormal Psychology Topics
- What does it mean to display strange behaviour?
- Role of mental health professionals in dealing with abnormal psychology
- Discuss the concept of dysfunction in mental illness
- How does deviance relate to mental illness?
- Role of culture and social norms
- The cost of treating abnormal psychology in the US
- Using aversive treatment in abnormal psychology
- Importance of psychological debriefing
- Is addiction a mental disease?
- Use of memory-dampening drugs
- Coercive interrogations and psychology
Behavioural Health Issues In Mental Health
- Detachment from reality
- Inability to withstand daily problems
- Conduct disorder among children
- Role of therapy in behavioural disorders
- Eating and drinking habits and mental health
- Addictive behaviour patterns for teenagers in high school
- Discuss mental implications of gambling and sex addiction
- Impact of maladaptive behaviours on the society
- Extreme mood changes
- Confused thinking
- Role of friends in behavioural complications
- Spiritual leaders in helping deal with behavioural issues
- Suicidal thoughts
Latest Psychology Research Topics
- Discrimination and prejudice in a society
- Impact of negative social cognition
- Role of personal perceptions
- How attitudes affect mental well-being
- Effects of cults on cognitive behaviour
- Marketing and psychology
- How romance can distort normal cognitive functioning
- Why people with pro-social behaviour may be less affected
- Leadership and mental health
- Discuss how to deal with anti-social personality disorders
- Coping with phobias in school
- The role of group therapy
- Impact of dreams on one’s psychological behaviour
Professional Psychiatry Research Topics
- The part of false memories
- Media and stress disorders
- Impact of gender roles
- Role of parenting styles
- Age and psychology
- The biography of Harry Harlow
- Career paths in psychology
- Dissociative disorders
- Dealing with paranoia
- Delusions and their remedy
- A distorted perception of reality
- Rights of mental caregivers
- Dealing with a loss
- Handling a break-up
Consider using our expert research paper writing services for your mental health paper today. Satisfaction is guaranteed!

Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Comment * Error message
Name * Error message
Email * Error message
Save my name, email, and website in this browser for the next time I comment.
As Putin continues killing civilians, bombing kindergartens, and threatening WWIII, Ukraine fights for the world's peaceful future.
Ukraine Live Updates
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Mental health and the pandemic: What U.S. surveys have found
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
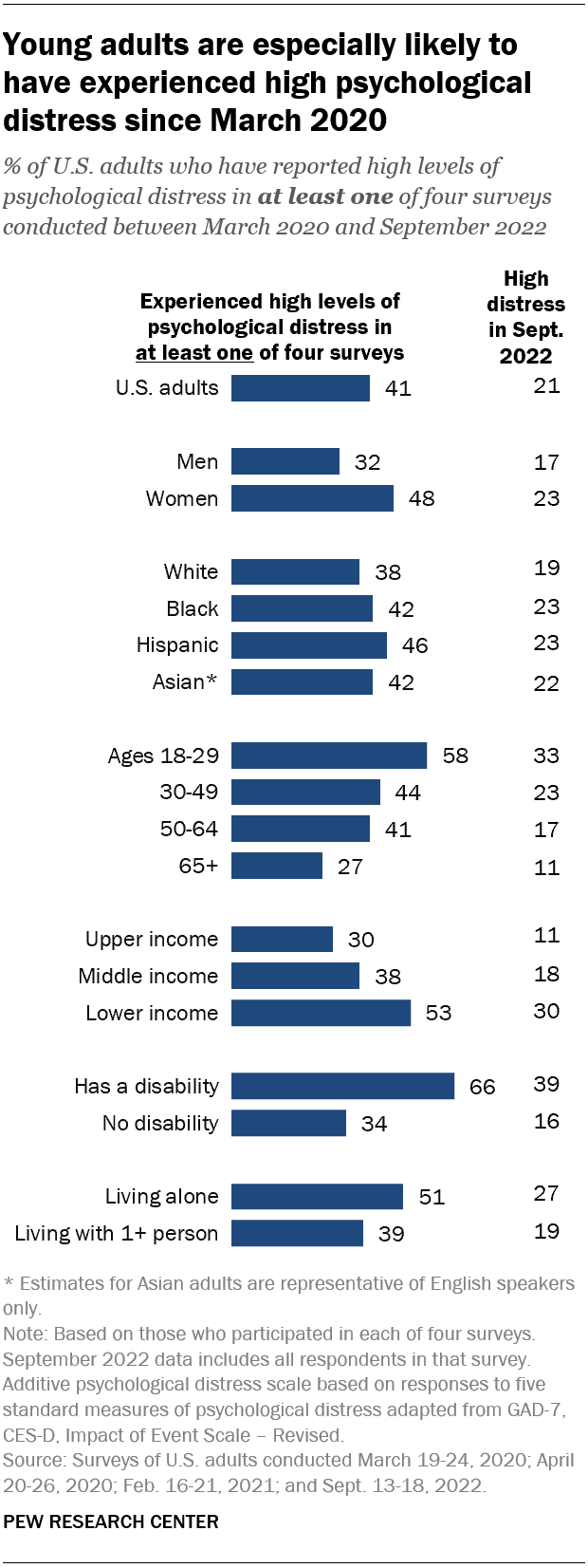
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
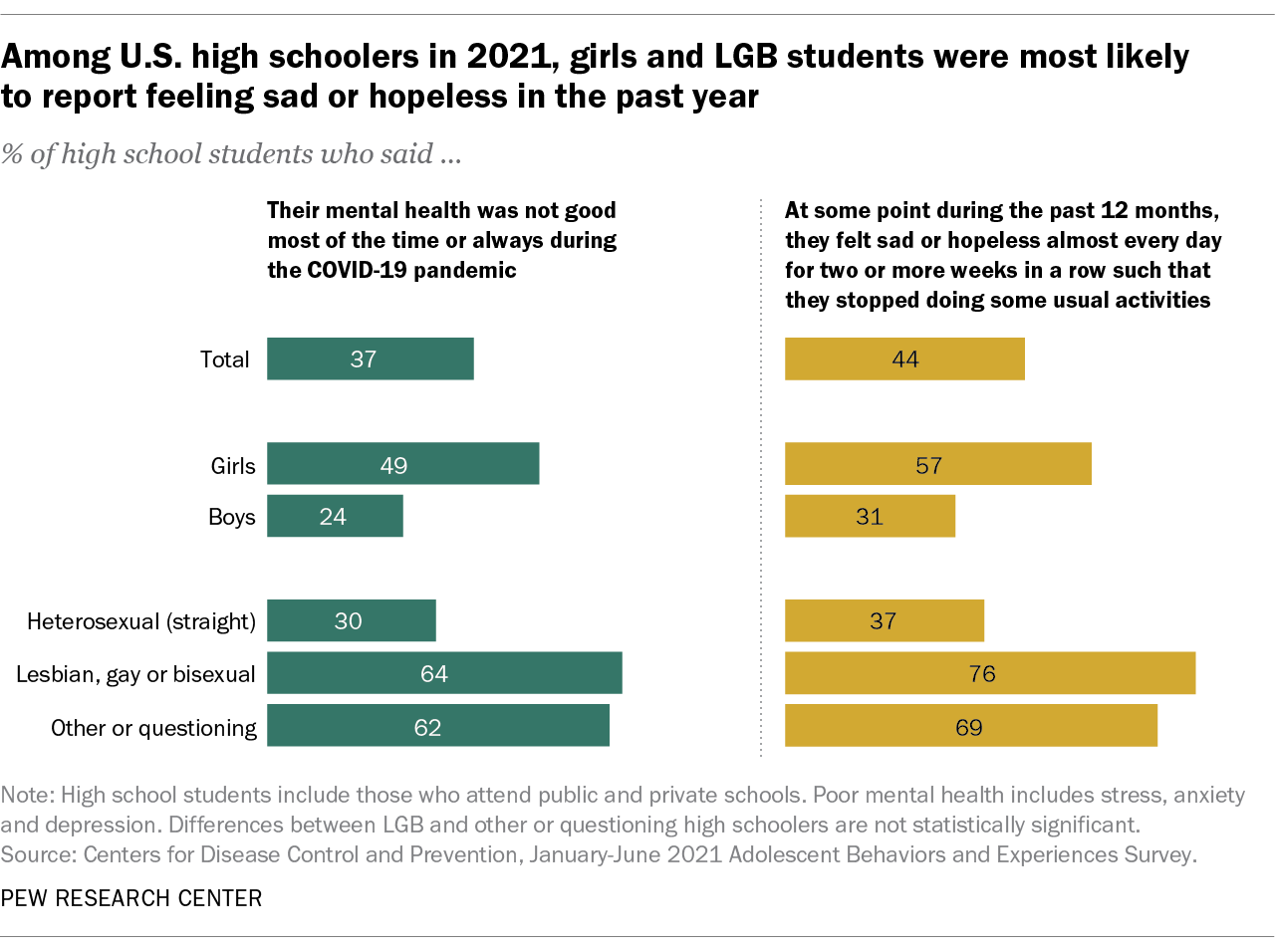
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
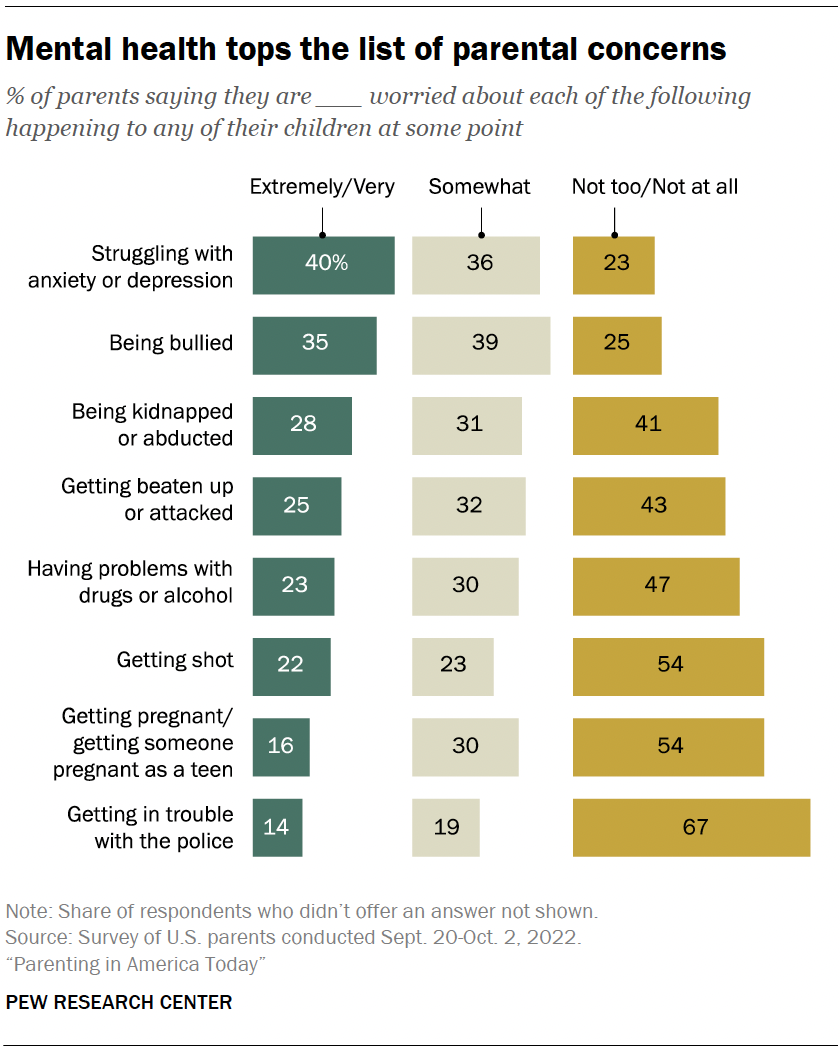
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
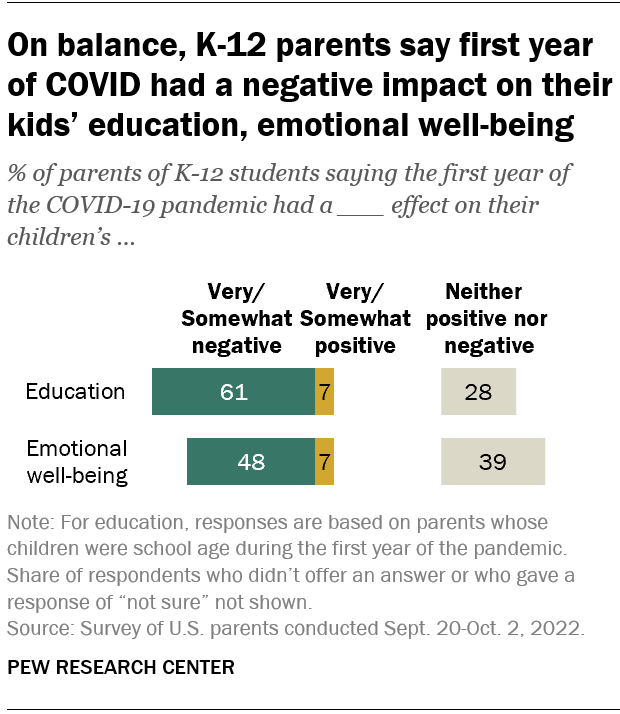
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.
- Coronavirus (COVID-19)
- Happiness & Life Satisfaction
- Medicine & Health
- Teens & Youth

John Gramlich is an associate director at Pew Research Center .
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, economy remains the public’s top policy priority; covid-19 concerns decline again, most popular.
901 E St. NW, Suite 300 Washington, DC 20004 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan, nonadvocacy fact tank that informs the public about the issues, attitudes and trends shaping the world. It does not take policy positions. The Center conducts public opinion polling, demographic research, computational social science research and other data-driven research. Pew Research Center is a subsidiary of The Pew Charitable Trusts , its primary funder.
© 2024 Pew Research Center
72 Mental Health Questions for Counselors and Patients

Is it the same as happiness?
Or is it simply the absence of mental illness?
Whether you are a professional therapist or want to help a friend in need, it helps to have some mental health questions up your sleeve.
You may not be able to diagnose someone who isn’t doing 100%, but with a little insight into their state of mind, you can play a valuable role in supporting them to get the help they need.
In this article, we’ll cover some mental health questions to ask yourself, your clients, or even your students. Read on to learn more.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises will explore fundamental aspects of positive psychology including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
What are mental health questions, mental health questions, 5 examples of common mental health questions for risk assessment and evaluation, 20 mental health interview questions a counselor should ask, 10 mental health questions aimed at students, 7 questions for group discussion, common mental health research questions, 9 mental health questions a patient can ask, 12 questions to ask yourself, 9 self-reflection questions, a take-home message.
Let’s start with a definition of mental health – more precisely, what it isn’t. In the article The Mental Health Continuum : From Languishing to Flourishing , positive psychologist Corey Keyes (2002) is very adamant about not oversimplifying the mental health concept, writing:
“mental health is more than the presence and absence of emotional states.”
Recapping the definition of a syndrome from the clinical literature, he then reminds us of the following:
“[a syndrome is] … a set of symptoms that occur together.”
Finally, Keyes argues that we can challenge the idea that syndromes are all about suffering. Instead, he argues that can we view mental health as:
“a syndrome of symptoms of an individual’s subjective well-being” or “a syndrome of symptoms of positive feelings and positive functioning in life.”
The right questions can give you insight into others’ wellbeing and promote the benefits of mental health .
These questions also help you:
- Show your concern for someone who is struggling
- Open up a dialogue about their mental state
- Trigger them to reflect on their overall wellbeing
- Prompt or encourage them to seek professional help if it is necessary
To get a clearer idea of these questions, let’s consider some examples.

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
Where do you take a mental health conversation once you’ve opened with, “ How are you feeling? ”
For professionals, it might help to screen your client for any disorders or distress. The Anxiety and Depression Detector (Means-Christensen, Sherbourne, Roy-Byrne, Craske, & Stein, 2006) can help you assess depression and anxiety disorders, and it’s only five questions long (O’Donnell, Bryant, Creamer, & Carty, 2008).
You may want to tweak some of these questions to make them more relevant to your client.
- Have you ever experienced a terrible occurrence that has impacted you significantly? Examples may include being the victim of armed assault, witnessing a tragedy happen to someone else, surviving a sexual assault, or living through a natural disaster.
- Do you ever feel that you’ve been affected by feelings of edginess, anxiety, or nerves?
- Have you experienced a week or longer of lower-than-usual interest in activities that you usually enjoy? Examples might include work, exercise, or hobbies.
- Have you ever experienced an ‘attack’ of fear, anxiety, or panic?
- Do feelings of anxiety or discomfort around others bother you?
These are just a few examples, and they are primarily concerned with identifying any potential signs of anxiety and depression. By design, they do not assess indicators of wellbeing, such as flourishing, life satisfaction, and happiness.
If you want to find out more about the latter, we have some great articles about Life Satisfaction Scales , as well as Happiness Tests, Surveys, and Quizzes and mental health exercises .
Open-ended questions are never a bad thing when you’re trying to start a discussion about mental health.
A study by Connell, O’Cathain, and Brazier (2014) suggested that seven quality of life domains are particularly relevant to a counselor who wants to open up dialogue with a client: physical health, wellbeing, autonomy, choice and control, self-perception, hope and hopelessness, relationships and belonging, and activity.
Physical health
Questions of this type were related to feelings such as agitation, restlessness, sleep, pain, and somatic symptoms. Examples of prompts to investigate this domain could include:
- Tell me about your sleeping habits over the past X months. Have you noticed any changes? Difficulty sleeping? Restlessness?
- How would you describe your appetite over the past X weeks? Have your eating habits changed in any way?
Wellbeing (and ill-being)
These questions looked at feelings of anxiety, distress, motivation, and energy. The ‘absence of negative feelings of ill-being,’ was understandably related to a higher perceived quality of life Connell et al., 2014). Sample prompts might include:
- Could you tell me about any times over the past few months that you’ve been bothered by low feelings, stress, or sadness?
- How frequently have you had little pleasure or interest in the activities you usually enjoy? Would you tell me more?
Autonomy, choice, and control
Questions about independence and autonomy were related to quality of life aspects such as pride, dignity, and privacy. Potential questions might include:
- How often during the past X months have you felt as though your moods, or your life, were under your control?
- How frequently have you been bothered by not being able to stop worrying?
Self-perception
Self-perception questions were related to patients’ confidence, self-esteem, and feelings of being capable of doing the things they wanted to do. Counselors might want to use the following prompts:
- Tell me about how confident you have been feeling in your capabilities recently.
- Let’s talk about how often you have felt satisfied with yourself over the past X months.
Hope and hopelessness
These questions ask about the patient’s view of the future, their hopes and goals, and the actions they were taking toward them.
- How often over the past few weeks have you felt the future was bleak?
- Can you tell me about your hopes and dreams for the future? What feelings have you had recently about working toward those goals?

Relationships and belonging
These questions consider how the client felt they ‘fit in with society,’ were supported, and possessed meaningful relationships. Examples include:
- Describe how ‘supported’ you feel by others around you – your friends, family, or otherwise.
- Let’s discuss how you have been feeling about your relationships recently.
The more purposeful, meaningful, and constructive a client perceived their activities to be, the better.
- Tell me about any important activities or projects that you’ve been involved with recently. How much enjoyment do you get from these?
- How frequently have you been doing things that mean something to you or your life?
Read our post on mental health activities to assist clients in this area.
Other mental health questions for counselors
Another useful source of questions can be found on this website by Mental Health America (n.d.a; n.d.b). You’ll find questions about:
Depression – e.g., How bothered have you felt about tiredness or low energy over the past two weeks? How bothered have you felt about thoughts that you’ve let yourself or others down?
Anxiety – e.g., Over the last two weeks, how bothered have you been by feelings of fear or dread, as though something terrible might happen? How often have you been bothered by so much restlessness that you can’t sit still?
Mental health for young people – e.g., How often have you felt fidgety or unable to sit still? Have you felt less interested in school?
Whatever counseling interview questions you choose to ask as a practitioner, you may find that you need to refer your client to a different healthcare provider. You can help others improve their mental health by making them feel supported and ensuring they are aware of their options for continued support.

Bashir (2018) mentions several assessments used to assess mental health, including:
- The Life Skills Assessment Questionnaire (Saatchi, Kamkkari, & Askarian, 2010)
- The Self-Efficacy Scale (Singh & Narain, 2014)
- Mental Health Scale (Talesara & Bano, 2017)
Bashir (2018) found “a positive significant relationship between the mental health of senior secondary school students with life skills and self-efficacy,” suggesting that the two measures together can be used to get an understanding of students’ mental health.
Mental health questions for students
Other self-efficacy and life skills measures could give us a good idea of some example mental health questions for students. The following may help:
Academic self-efficacy questions for students
How much confidence do you have that you can successfully:
- Complete homework within deadlines?
- Focus on school subjects?
- Get information on class assignments from the library?
- Take part in class discussions?
- Keep your academic work organized?
Mental health questions (World Health Organization, 2013)
- Over the last 12 months, how frequently have you felt so worried about something that you were unable to sleep at night?
- Over the last 12 months, how frequently have you felt alone or lonely?
- Over the last 12 months, how often did you seriously consider attempting suicide?
- Over the last 12 months, did you ever plan how you might attempt suicide?
- How many close friends would you say you have?
As with all the other questions in this article, you’ll probably want to tweak and amend these items to suit your audience.
Your mental health questions answered – jacksepticeye
The catch-all term “mental health group” can refer to several different things. Mental health groups may gather together for therapy or may be more informal peer support groups. You may also find yourself part of a group that’s purely for friends, family, and carers of those whose mental health is a concern.
Whatever group you find yourself in, the World Health Organization (2017) has some suggestions that will help you create a safe and productive space.
Mental health group best practices
Everything that is said in therapy should remain confidential; nothing from the discussion should be shared outside of the group setting.
Bear in mind that not everyone in the discussion will be at the same stage. Some may be new, others may be more seasoned or regular visitors.
Recognize that people won’t necessarily get along, but they all are welcome anyway.
Try not to view peer support or group discussions as a panacea for mental conditions. While they may be a great place to get suggestions or clarity, mental health is about feeling good in more than one way. Participants or caregivers may also require coaching, counseling, or medication to feel better.
7 Group questions
What questions can we ask to get some discussion flowing in a mental health group?
You may want to start with a focus for your discussion. Ask someone to share a story, experience, or step in as a facilitator with a video about the theme at hand. If you are discussing the role of social support, for example, you may have a presentation or case study prepared on the importance of friends and family.
Once you’ve opened with your story or resource, try some of these to spark a discussion (Gruttadaro & Cepla, 2014):
- How do you feel about the story you just heard? What was your first reaction? How about as the story unfolded?
- What were your thoughts regarding the signs and symptoms of this mental health issue? Have you experienced any of these yourself or in someone you know?
- How would you react if you noticed these in someone you care about?
- How might taking action benefit you and the person you care about?
- What actions could you take to help someone who is exhibiting these signs and symptoms?
- What do you believe is important for anyone to be aware of if they know someone with this mental health issue?
- What experiences have you had that are related to this story? What was similar? What differed?
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Curious to know the top research questions related to mental health worldwide? Tomlinson et al. (2009) identified some of the key priorities for researchers to look at.
The group came up with 55 questions, and the top three topics included:
- Health policy and systems research topics – e.g., How can health policy and systems research help us create parenting and social skills interventions for early childhood care in a cost-efficient, feasible, and effective way?
- Cost-effective interventions for low-resource settings – e.g., How can affordable interventions be delivered in settings where resources are scarce?
- Questions about child and teen mental disorders – e.g., How effective and cost-effective are school-based mental health treatments for special needs schoolchildren?
Engaging with your mental health practitioner is one of the best ways to get the most out of your check-ups. The healthcare system is changing, and gone are the days when a patient sat passively for a diagnosis or prescription (Rogers & Maini, 2016).
These days, arguably, medical dialogues place more emphasis on helping a client help themselves through information, education, and commitment to a better lifestyle. It’s good news indeed for anyone who wants to get proactive about their mental health. So what should you be asking your practitioner?
Before committing to a mental health practitioner, you’ll need to know a few things about the services they provide. Many therapists can provide psychological treatments but aren’t able to prescribe medication. You’ll need a psychiatrist or physician for that.
Bear this in mind, and consider the following questions when you’re deciding whether a provider is right for you (Association for Children’s Mental Health, n.d.; Think Mental Health, n.d.):
- What is your experience with treating others with my mental health condition?
- Will you be able to collaborate or liaise with my physician on an integrated care plan?
- What does a typical appointment with you look like?
- What treatments or therapies are you licensed to administer?
- Are there benefits or risks that I should know about these therapies?
- What is the general time frame in which most patients will see results?
- How will I know if the treatment is having an effect?
- How long does this type of treatment last?
- What does research say about this type of treatment?

It is an awareness-raising campaign that encourages us to tune in early to the symptoms of mental illness.
But, of course, you can always check in with yourself as regularly as you like.
Example questions about wellbeing
The Canadian Mental Health Association (n.d.) provides some self-report questions that you can start with; these questions cover six areas and require only agree/disagree responses. Try some of these as an example:
- Sense of self questions– e.g., I see myself as a good person. I feel that others respect me, yet I can still feel fine about myself if I disagree with them.
- Sense of belonging questions – e.g., I have others around me who support me. I feel positive about my relationships with others and my interpersonal connections.
- Sense of meaning or purpose questions – e.g., I get satisfaction from the things I do. I challenge my perspectives about the world and what I believe in.
- Emotional resilience questions – e.g., I feel I handle things quite well when obstacles get in my way. I accept that I can’t always control things, but I do what I can when I can.
- Enjoyment and hope questions – e.g., I have a positive outlook on my life. I like myself for who I am.
- Contribution questions – e.g., The things that I do have an impact. My actions matter to those around me.
According to Rath and Clifton (2004), we each possess a metaphorical bucket representing our emotional and mental wellbeing. This imaginary bucket can be empty, full, or anywhere in between, and it undergoes a continuous process of filling (through positive interactions) and emptying (through negative interactions).
We feel energized, happy, and content when our buckets are full. When our buckets run low or empty, we can easily become negative, insecure, and defensive.
Having positive, meaningful interactions and showing kindness not only makes us feel good and fills our buckets but also fills the buckets of those around us. When our bucket is full, we are more inclined to fill the buckets of others.
However, when our bucket is running low or empty, we don’t have anything left to give to ourselves, let alone others. Therefore, it’s important to show kindness and compassion to ourselves to fill our bucket back up before we can service the buckets of others.
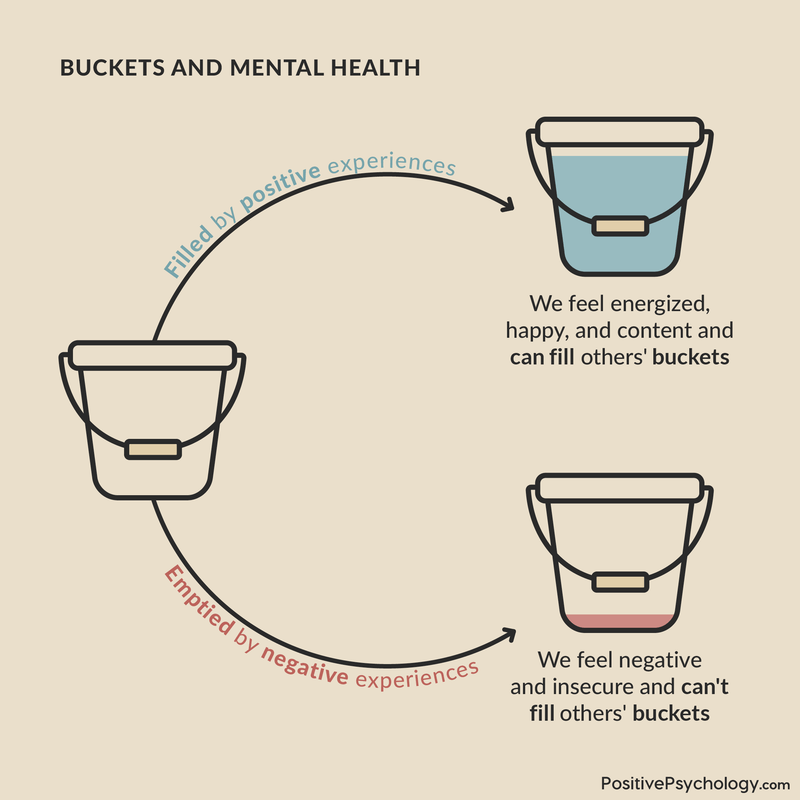
Elsewhere on PositivePsychology.com, we’ve written about the many potential benefits of narrative therapy . If you’re looking for some writing or journal prompts to help you get started, you can try putting your responses to these questions down on paper (Post Trauma Institute, 2019).
- Have my sleeping habits changed? Do I wake up and fall asleep at regular times? When I sleep, how would I describe the quality of my rest?
- How has my appetite increased or decreased recently?
- Am I having trouble focusing at work or school? Can I concentrate on the things I want to do? Do I find pleasure in things that usually make me happy?
- Am I socializing with my friends as much as I usually do? How about spending time with my family? Am I withdrawing or pulling away from those around me who matter?
- Do I feel like I’m maintaining a healthy balance between leisure, myself, my career, physical activity, and those I care about? How about other things that matter to me?
- How relaxed do I feel most of the time, out of 10? Is this the same, more, or less than usual?
- How do I feel most of the time? Happy? Anxious? Satisfied? Sad?
- What are my energy levels like when I finish my day? Are there any significant changes in my tiredness?
- Am I having any extreme emotions or mood swings? Any suicidal thoughts, breakdowns, or panic attacks?
It may help to keep track of your responses over time and take notice of any differences in your answers. It should go without saying that the earlier you seek out any help you may need, the better.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
Mental health is not about the absence of mental illness. When we take the time to ask ourselves and others about our mental states, we can potentially make some crucial steps toward wellbeing.
As Keyes (2002) describes, we can think of our mental health as a continuum, with languishing at one end and flourishing at the other. By starting a dialogue and showing that we care, we can help each other get the help we need and potentially begin to feel better.
What questions have you asked yourself before? And what would you add to our list? Let us know in the comments below!
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
- Association for Children’s Mental Health. (n.d.). Questions to ask your mental health professional about treatment options, medications, and more. Retrieved July 29, 2021 from http://www.acmh-mi.org/get-information/childrens-mental-health-101/questions-ask-treatment/
- Bashir, L. (2018). Mental health among senior secondary school students in relation to life skills and self-efficacy. International Journal of Multidisciplinary Research Review, 3 (9), 587–591. https://www.proquest.com/docview/2618174004?pq-origsite=gscholar&fromopenview=true
- Canadian Mental Health Association. (n.d.). Check in on your mental health. Retrieved from https://mentalhealthweek.ca/check-in-on-your-mental-health/
- Connell, J., O’Cathain, A., Brazier, J. (2014). Measuring quality of life in mental health: Are we asking the right questions? Social Science & Medicine , 120 , 12–20. https://doi.org/10.1016/j.socscimed.2014.08.026
- Keyes, C. L. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43 , 207–222. https://doi.org/10.2307/3090197
- Means-Christensen, A. J., Sherbourne, C. D., Roy-Byrne, P. P., Craske, M. G., & Stein, M. B. (2006). Using five questions to screen for five common mental disorders in primary care: Diagnostic accuracy of the Anxiety and Depression Detector. General Hospital Psychiatry, 28 (2), 108–118. https://doi.org/10.1016/j.genhosppsych.2005.08.010
- Mental Health America. (n.d.a). Questions to ask a provider. Retrieved July 29, 2021, from https://www.mhanational.org/questions-ask-provider/
- Mental Health America. (n.d.b). Mental health screening tools . Retrieved July 29, 2021, from https://screening.mhanational.org/screening-tools
- Gruttadaro, D., & Cepla, E. (2014). Say it out loud: NAMI discussion group facilitation guide. National Alliance on Mental Illness. Retrieved July 29, 2021, from https://www.nami.org/getattachment/Get-Involved/Raise-Awareness/Engage-Your-Community/Say-it-Out-Loud/Say-it-Out-Loud-Discussion-Group-Facilitation-Guide.pdf
- O’Donnell, M. L., Bryant, R. A., Creamer, M., & Carty, J. (2008). Mental health following traumatic injury: Toward a health system model of early psychological intervention. Clinical Psychology Review, 28 (3), 387–406. https://doi.org/10.1016/j.cpr.2007.07.008
- Post Trauma Institute. (2019). How to do a mental health check-up DIY style! Retrieved from https://www.posttraumainstitute.com/how-to-do-a-mental-health-check-up-diy-style/
- Rath, T., & Clifton, D. O. (2004). How full is your bucket? Positive strategies for work and life . Gallup Press. https://www.amazon.com/dp/1595620044/
- Rogers, J., & Maini, A. (2016). Coaching for health: Why it works and how to do it. Open University Press. https://www.amazon.com/dp/B01EI68LMU/
- Saatchi, M., Kamkkari, K., & Askarian, M. (2010). Life skills questionnaire. Psychological Tests Publish Edits, 85 .
- Singh, A. K., & Narain, S. (2014). Manual for Self-Efficacy Scale. National Psychological Corporation.
- Talesara, S., & Bano, A. (2017). Mental Health Scale. National Psychological Corporation.
- Think Mental Health. (n.d.). Questions to ask your GP – What to discuss. Retrieved from https://www.thinkmentalhealthwa.com.au/mental-health-support-services/how-your-gp-can-help/questions-to-ask-your-gp/
- Tomlinson, M., Rudan, I., Saxena, S., Swartz, L., Tsai, A. C., & Patel, V. (2009). Setting priorities for global mental health research. Bulletin of the World Health Organization , 87 (6), 438–446. https://doi.org/10.2471/BLT.08.054353
- World Health Organization. (2013). Global school-based student health survey: 2013 core questionnaire modules. Retrieved July 29, 2021, from https://www.who.int/docs/default-source/ncds/ncd-surveillance/gshs/gshs-core-modules-2013-english.pdf
- World Health Organization. (2017). Creating peer support groups in mental health and related areas: WHO QualityRights training to act, unite, and empower for mental health (pilot version) (No. WHO/MSD/MHP/17.13).
Share this article:
Article feedback
What our readers think.
Thank you so much for this helpful resource. As a masters student for Public Health Nursing, I found these questions helpful ice breakers for me to use for a focus-group collection strategy paper I am writing (questions were modified, of course to my topic). Thank you!
hello Nicole,
Would like to thank the writer of this article. Used some of these questions to design a mental health survey for our website project to raise awareness about early treatment of mental illnesses. Really informative and useful to raise in-depth questions and start meaningful conversations. Thank you so much!
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

High-Functioning Autism: 23 Strengths-Based Daily Worksheets
Autism diagnoses are rising exponentially. A study by Russell et al. (2022) reported a 787% increase in UK diagnoses between 1998 and 2018. Similarly, 1 [...]

Treating Phobias With Positive Psychology: 15 Approaches
Phobophobia is a fear of phobias. That is just one in our list of 107 phobias. Clearly a person suffering from phobophobia has a lot [...]

How to Fuel Positive Change by Leveraging Episodic Memory
Some researchers believe that our memory didn’t evolve for us to only remember but to imagine all that might be (Young, 2019). Episodic memory is [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (22)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (37)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (39)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)
3 Positive Psychology Tools (PDF)
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals
You are here
- Volume 13, Issue 2
- Qualitative Research Methods in Mental Health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Sarah Peters
- Correspondence to : Dr Sarah Peters, School of Psychological Sciences, The University of Manchester, Coupland Building 1, Oxford Road M13 9PL, UK; sarah.peters{at}manchester.ac.uk
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and implementation. However, mental health research has lagged behind many other healthcare specialities in using qualitative methods within its evidence base. Rigour in qualitative research raises many similar issues to quantitative research and also some additional challenges. This article examines the role of qualitative methods within mental heath research, describes key methodological and analytical approaches and offers guidance on how to differentiate between poor and good quality qualitative research.
https://doi.org/10.1136/ebmh.13.2.35
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
The trajectory of qualitative methods in mental health research
Qualitative methodologies have a clear home within the study of mental health research. Early and, arguably, seminal work into the study of mental illnesses and their management was based on detailed observation, moving towards theory using inductive reasoning. Case studies have been long established in psychiatry to present detailed analysis of unusual cases or novel treatments. Participant observation was the principle method used in Goffman's seminal study of psychiatric patients in asylums that informed his ideas about the institutionalising and medicalising of mental illness by medical practice. 1 However, the 20th century saw the ‘behaviourist revolution’, a movement where quantification and experimentation dominated. Researchers sought to identify cause and effects, and reasoning became more deductive – seeking to use data to confirm theory. The study of health and illness was determined by contemporary thinking about disease, taking a biomedical stance. Psychologists and clinical health researchers exploited natural science methodologies, attempting to measure phenomenon in their smallest entities and do so as objectively as possible. This reductionist and positivist philosophy shaped advances in research methods and meant that qualitative exploration failed to develop as a credible scientific approach. Indeed, ‘objectivity’ and the ‘discovery of truth’ have become synonymous with ‘scientific enquiry’ and qualitative methods are easily dismissed as ‘anecdotal’. The underlying epistemology of this approach chimes well with medical practice for which training is predominately in laboratory and basic sciences (such as physics and chemistry) within which the discourse of natural laws dominate. To this end, research in psychiatry still remains overwhelmingly quantitative. 2
Underlying all research paradigms are assumptions. However, most traditional researchers remain unaware of these until they start to use alternative paradigms. Key assumptions of quantitative research are that facts exist that can be quantified and measured and that these should be examined, as far as possible, objectively, partialling out or controlling for the context within which they exist. There are research questions within mental health where this approach can hold: where phenomenon of interest can be reliably and meaningfully quantified and measured, it is feasible to use data to test predictions and examine change. However, for many questions these assumptions prove unsatisfying. It is often not possible or desirable to try and create laboratory conditions for the research; indeed it would be ecologically invalid to do so. For example, to understand the experience of an individual who has been newly diagnosed with schizophrenia, it is clearly important to consider the context within which they live, their family, social grouping and media messages they are exposed to. Table 1 depicts the key differences between the two methodological approaches and core underlying assumptions for each.
- View inline
Comparison of underlying assumptions of quantitative and qualitative research approaches
It should be cautioned that it is easy to fall into the trap of categorising studies as either quantitative or qualitative. The two traditions are often positioned within the literature as opposing and in conflict. This division is unhelpful and likely to impede methodological advancement. Though, undeniably, there are differences in the two approaches to research, there are also many exceptions that expose this dichotomy to be simplistic: some qualitative studies seek to test a priori hypotheses, and some quantitative studies are atheoretical and exploratory. 3 Hence it is more useful to consider research methodologies as lying along a spectrum and that researchers should be familiar with the full range of methodologies, so that a method is chosen according to the research question rather than the researcher's ability.
Rationale for qualitative methods in current mental health research
There are a number of scientific, practical and ethical reasons why mental health is an area that can particularly benefit from qualitative enquiry. Mental health research is complex. Health problems are multifactorial in their aetiology and the consequences they have on the individual, families and societies. Management can involve self-help, pharmacological, educative, social and psychotherapeutic approaches. Services involved are often multidisciplinary and require liaison between a number of individuals including professionals, service-users and relatives. Many problems are exacerbated by poor treatment compliance and lack of access to, or engagement with, appropriate services. 4
Engagement with mental health research can also be challenging. Topics may be highly sensitive or private. Individuals may have impaired capacity or be at high risk. During the research process there may be revelations of suicidal ideation or criminal activity. Hence mental health research can raise additional ethical issues. In other cases scepticism of services makes for reluctant research participants. However, if we accept the case that meaningful research can be based in subjective enquiry then qualitative methods provide a way of giving voice to participants. Qualitative methods offer an effective way of involving service-users in developing interventions for mental health problems 5 ensuring that the questions asked are meaningful to individuals. This may be particularly beneficial if participants are stakeholders, for example potential users of a new service.
Qualitative methods are valuable for individuals who have limited literacy skills who struggle with pencil and paper measures. For example qualitative research has proved fruitful in understanding children's concepts of mental illness and associated services. 6
How qualitative enquiry is used within mental health research
There are a range of types of research question where qualitative methods prove useful – from the development and testing of theory, to the piloting and establishing efficacy of treatment approaches, to understanding issues around translation and implementation into routine practice. Each is discussed in turn.
Development and testing of theory
Qualitative methods are important in exploratory work and in generating understanding of a phenomenon, stimulating new ideas or building new theory. For example, stigma is a concept that is recognised as a barrier to accessing services and also an added burden to mental health. A focus-group study sought to understand the meaning of stigma from the perspectives of individuals with schizophrenia, their relatives and health professionals. 7 From this they developed a four-dimensional theory which has subsequently informed interventions to reduce stigma and discrimination that target not only engagement with psychiatric services but also interactions with the public and work. 7
Development of tools and measures
Qualitative methods access personal accounts, capturing how individuals talk about a lived experience. This can be invaluable for designing new research tools. For example, Mavaddat and colleagues used focus groups with 56 patients with severe or common mental health problems to explore their experiences of primary care management. 8 Nine focus groups were conducted and analysis identified key themes. From these, items were generated to form a Patient Experience Questionnaire, of which the psychometric properties were subsequently examined quantitatively in a larger sample. Not only can dimensions be identified, the rich qualitative data provide terminology that is meaningful to service users that can then be incorporated into question items.
Development and testing of interventions
As we have seen, qualitative methods can inform the development of new interventions. The gold-standard methodology for investigating treatment effectiveness is the randomised controlled trial (RCT), with the principle output being an effect size or demonstration that the primary outcome was significantly improved for participants in the intervention arm compared with those in the control/comparison arm. Nevertheless, what will be familiar for researchers and clinicians involved in trials is that immense research and clinical learning arises from these substantial, often lengthy and expensive research endeavours. Qualitative methods provide a means to empirically capture these lessons, whether they are about recruitment, therapy training/supervision, treatment delivery or content. These data are essential to improve the feasibility and acceptability of further trials and developing the intervention. Conducting qualitative work prior to embarking on an RCT can inform the design, delivery and recruitment, as well as engage relevant stakeholders early in the process; all of these can prevent costly errors. Qualitative research can also be used during a trial to identify reasons for poor recruitment: in one RCT, implementing findings from this type of investigation led to an increased randomisation rate from 40% to 70%. 9
Nesting qualitative research within a trial can be viewed as taking out an insurance policy as data are generated which can later help explain negative or surprising findings. A recent trial of reattribution training for GPs to manage medically unexplained symptoms demonstrated substantial improvements in GP consultation behaviour. 10 However, effects on clinical outcomes were counterintuitive. A series of nested qualitative studies helped shed light as to why this was the case: patients' illness models were complex, and they resisted engaging with GPs (who they perceived as having more simplistic and dualistic understanding) because they were anxious it would lead to non-identification or misdiagnosis of any potential future disease 11 , an issue that can be addressed in future interventions. Even if the insights are unsurprising to those involved in the research, the data collected have been generated systematically and can be subjected to peer review and disseminated. For this reason, there is an increasing expectation from funding bodies that qualitative methodologies are integral to psychosocial intervention research.
Translation and implementation into clinical practice
Trials provide limited information about how treatments can be implemented into clinical practice or applied to another context. Psychological interventions are more effective when delivered within trial settings by experts involved in their development than when they are delivered within clinical settings. 12 Qualitative methods can help us understand how to implement research findings into routine practice. 13
Understanding what stakeholders value about a service and what barriers exist to its uptake is another evidence base to inform clinicians' practice. Relapse prevention is an effective psychoeducation approach that helps individuals with bipolar disorder extend time to relapse. Qualitative methodologies identified which aspects of the intervention service-users and care-coordinators value, and hence, are likely to utilise in routine care. 14 The intervention facilitated better understanding of bipolar disorder (by both parties), demonstrating, in turn, a rationale for medication. Patients discovered new, empowering and less socially isolated ways of managing their symptoms, which had important impacts on interactions with healthcare staff and family members. Furthermore, care-coordinators' reported how they used elements of the intervention when working with clients with other diagnoses. The research also provided insights as to where difficulties may occur when implementing a particular intervention into routine care. For example, for care-coordinators this proved a novel way of working with clients that was more emotionally demanding, thus highlighting the need for supervision and managerial support. 14
Beginners guide to qualitative approaches: one size doesn't fit all
Just as there is a range of quantitative research designs and statistical analyses to choose from, so there are many types of qualitative methods. Choosing a method can be daunting to an inexperienced or beginner-level qualitative researcher, for it requires engaging with new terms and ways of thinking about knowledge. The following summary sets out analytic and data-generation approaches that are used commonly in mental health research. It is not intended to be comprehensive and is provided only as a point of access/familiarisation to researchers less familiar with the literature.
Data generation
Qualitative data are generated in several ways. Most commonly, researchers seek a sample and conduct a series of individual in-depth interviews, seeking participants' views on topics of interest. Typically these last upwards of 45 min and are organised on the basis of a schedule of topics identified from the literature or pilot work. This does not act as a questionnaire, however; rather, it acts as a flexible framework for exploring areas of interest. The researcher combines open questions to elicit free responses, with focused questions for probing and prompting participants to provide effective responses. Usually interviews are audio-recorded and transcribed verbatim for subsequent analysis.
As interviews are held in privately, and on one-to-one basis, they provide scope to develop a trusting relationship so that participants are comfortable disclosing socially undesirable views. For example, in a study of practice nurses views of chronic fatigue syndrome, some nurses described patients as lazy or illegitimate – a view that challenges the stereotype of a nursing professional as a sympathetic and caring person. 15 This gives important information about the education and supervision required to enable or train general nurses to ensure that they are capable of delivering psychological interventions for these types of problems.
Alternatively, groups of participants are brought together for a focus group, which usually lasts for 2 hours. Although it is tempting to consider focus groups as an efficient way of acquiring data from several participants simultaneously, there are disadvantages. They are difficult to organise for geographically dispersed or busy participants, and there are compromises to confidentiality, particularly within ‘captive’ populations (eg, within an organisation individuals may be unwilling to criticise). Group dynamics must be considered; the presence of a dominant or self-professed expert can inhibit the group and, therefore, prevent useful data generation. When the subject mater is sensitive, individuals may be unwilling to discuss experiences in a group, although it often promotes a shared experience that can be empowering. Most of these problems are avoided by careful planning of the group composition and ensuring the group is conducted by a highly skilled facilitator. Lester and colleagues 16 used focus-group sessions with patients and health professionals to understand the experience of dealing with serious mental illness. Though initially participants were observed via focus-group sessions that used patient-only and health professional only groups, subsequently on combined focus groups were used that contained both patients and health professionals. 16 The primary advantage of focus groups is that they enable generation of data about how individuals discuss and interact about a phenomenon; thus, a well-conducted focus group can be an extremely rich source of data.
A different type of data are naturally occurring dialogue and behaviours. These may be recorded through observation and detailed field notes (see ethnography in Table 2 ) or analysed from audio/ video-recordings. Other data sources include texts, for example, diaries, clinical notes, Internet blogs and so on. Qualitative data can even be generated through postal surveys. We thematically analysed responses to an open-ended question set within a survey about medical educators' views of behavioural and social sciences (BSS). 17 From this, key barriers to integrating BSS within medical training were identified, which included an entrenched biomedical mindset. The themes were analysed in relation to existing literature and revealed that despite radical changes in medical training, the power of the hidden curriculum persists. 17
Key features of a range of analytical approaches used within mental health research
Analysing qualitative data
Researchers bring a wide range of analytical approaches to the data. A comprehensive and detailed discussion of the philosophy underlying different methods is beyond the scope of this paper; however, a summary of the key analytical approaches used in mental health research are provided in Table 2 . An illustrative example is provided for each approach to offer some insight into the commonalities and differences between methodologies. The procedure for analysis for all methods involves successive stages of data familiarisation/immersion, followed by seeking and reviewing patterns within the data, which may then be defined and categorized as specific themes. Researchers move back and forth between data generation and analysis, confirming or disconfirming emerging ideas. The relationship of the analysis to theory-testing or theory-building depends on the methodology used.
Some approaches are more common in healthcare than others. Interpretative phenomenological (lPA) analysis and thematic analysis have proved particularly popular. In contrast, ethnographic research requires a high level of researcher investment and reflexivity and can prove challenging for NHS ethic committees. Consequently, it remains under used in healthcare research.
Recruitment and sampling
Quantitative research is interested in identifying the typical, or average. By contrast, qualitative research aims to discover and examine the breadth of views held within a community. This includes extreme or deviant views and views that are absent. Consequently, qualitative researchers do not necessarily (though in some circumstances they may) seek to identify a representative sample. Instead, the aim may be to sample across the range of views. Hence, qualitative research can comment on what views exist and what this means, but it is not possible to infer the proportions of people from the wider population that hold a particular view.
However, sampling for a qualitative study is not any less systematic or considered. In a quantitative study one would take a statistical approach to sampling, for example, selecting a random sample or recruiting consecutive referrals, or every 10th out-patient attendee. Qualitative studies, instead, often elect to use theoretical means to identify a sample. This is often purposive; that is, the researcher uses theoretical principles to choose the attributes of included participants. Healey and colleagues conducted a study to understand the reasons for individuals with bipolar disorder misusing substances. 18 They sought to include participants who were current users of each substance group, and the recruitment strategy evolved to actively target specific cases.
Qualitative studies typically use far smaller samples than quantitative studies. The number varies depending on the richness of the data yielded and the type of analytic approach that can range from a single case to more than 100 participants. As with all research, it is unethical to recruit more participants than needed to address the question at hand; a qualitative sample should be sufficient for thematic saturation to be achieved from the data.
Ensuring that findings are valid and generalisable
A common question from individuals new to qualitative research is how can findings from a study of few participants be generalised to the wider population? In some circumstances, findings from an individual study (quantitative or qualitative) may have limited generalisability; therefore, more studies may need to be conducted, in order to build local knowledge that can then be tested or explored across similar groups. 4 However, all qualitative studies should create new insights that have theoretical or clinical relevance which enables the study to extend understanding beyond the individual participants and to the wider population. In some cases, this can lead to generation of new theory (see grounded theory in Table 2 ).
Reliability and validity are two important ways of ascertaining rigor in quantitative research. Qualitative research seeks to understand individual construction and, by definition, is subjective. It is unlikely, therefore, that a study could ever be repeated with exactly the same circumstances. Instead, qualitative research is concerned with the question of whether the findings are trustworthy; that is, if the same circumstances were to prevail, would the same conclusions would be drawn?
There are a number of ways to maximise trustworthiness. One is triangulation, of which there are three subtypes. Data triangulation involves using data from several sources (eg, interviews, documentation, observation). A research team may include members from different backgrounds (eg, psychology, psychiatry, sociology), enabling a range of perspectives to be used within the discussion and interpretation of the data. This is termed researcher triangulation . The final subtype, theoretical triangulation, requires using more than one theory to examine the research question. Another technique to establish the trustworthiness of the findings is to use respondent validation. Here, the final or interim analysis is presented to members of the population of interest to ascertain whether interpretations made are valid.
An important aspect of all qualitative studies is researcher reflexivity. Here researchers consider their role and how their experience and knowledge might influence the generation, analysis and interpretation of the data. As with all well-conducted research, a clear record of progress should be kept – to enable scrutiny of recruitment, data generation and development of analysis. However, transparency is particularly important in qualitative research as the concepts and views evolve and are refined during the process.
Judging quality in qualitative research
Within all fields of research there are better and worse ways of conducting a study, and range of quality in mental health qualitative research is variable. Many of the principles for judging quality in qualitative research are the same for judging quality in any other type of research. However, several guidelines have been developed to help readers, reviewers and editors who lack methodological expertise to feel more confident in appraising qualitative studies. Guidelines are a prerequisite for the relatively recent advance of methodologies for systematic reviewing of qualitative literature (see meta-synthesis in Table 2 ). Box 1 provides some key questions that should be considered while studying a qualitative report.
Box 1 Guidelines for authors and reviewers of qualitative research (adapted from Malterud 35 )
▶ Is the research question relevant and clearly stated?
Reflexivity
▶ Are the researcher's motives and background presented?
Method, sampling and data collection
▶ Is a qualitative method appropriate and justified?
▶ Is the sampling strategy clearly described and justified?
▶ Is the method for data generation fully described
▶ Are the characteristics of the sample sufficiently described?
Theoretical framework
▶ Was a theoretical framework used and stated?
▶ Are the principles and procedures for data organisation and analysis described and justified?
▶ Are strategies used to test the trustworthiness of the findings?
▶ Are the findings relevant to the aim of the study?
▶ Are data (e.g. quotes) used to support and enrich the findings?
▶ Are the conclusions directly linked to the study? Are you convinced?
▶ Do the findings have clinical or theoretical value?
▶ Are findings compared to appropriate theoretical and empirical literature?
▶ Are questions about the internal and external validity and reflexivity discussed?
▶ Are shortcomings of the design, and the implications these have on findings, examined?
▶ Are clinical/theoretical implications of the findings made?
Presentation
▶ Is the report understandable and clearly contextualised?
▶ Is it possible to distinguish between the voices of informants and researchers?
▶ Are sources from the field used and appropriately referenced?
Conclusions and future directions
Qualitative research has enormous potential within the field of mental health research, yet researchers are only beginning to exploit the range of methods they use at each stage of enquiry. Strengths of qualitative research primarily lie in developing theory and increasing understanding about effective implementation of treatments and how best to support clinicians and service users in managing mental health problems. An important development in the field is how to integrate methodological approaches to address questions. This raises a number of challenges, such as how to integrate textual and numerical data and how to reconcile different epistemologies. A distinction can be made between mixed- method design (eg, quantitative and qualitative data are gathered and findings combined within a single or series of studies) and mixed- model study, a pragmatist approach, whereby aspects of qualitative and quantitative research are combined at different stages during a research process. 19 Qualitative research is still often viewed as only a support function or as secondary to quantitative research; however, this situation is likely to evolve as more researchers gain a broader skill set.
Though it is undeniable that there has been a marked increase in the volume and quality of qualitative research published within the past two decades, mental health research has been surprisingly slow to develop, compared to other disciplines e.g. general practice and nursing, with relatively fewer qualitative research findings reaching mainstream psychiatric journals. 2 This does not appear to reflect overall editorial policy; however, it may be partly due to the lack of confidence on the part of editors and reviewers while identifying rigorous qualitative research data for further publication. 20 However, the skilled researcher should no longer find him or herself forced into a position of defending a single-methodology camp (quantitative vs qualitative), but should be equipped with the necessary methodological and analytical skills to study and interpret data and to appraise and interpret others' findings from a full range of methodological techniques.
- Crawford MJ ,
- Cordingley L
- Dowrick C ,
- Edwards S ,
- ↵ MRC Developing and Evaluating Complex Interventions 2008
- Nelson ML ,
- Quintana SM
- Schulze B ,
- Angermeyer MC
- Mavaddat N ,
- Lester HE ,
- Donovan J ,
- Morriss R ,
- Barkham M ,
- Stiles WB ,
- Connell J ,
- Chew-Graham C ,
- England E ,
- Kinderman P ,
- Tashakkoria A ,
- Ritchie J ,
- Ssebunnya J ,
- Chilvers R ,
- Glasman D ,
- Finlay WM ,
- Strauss A ,
- Hodges BD ,
- Dobransky K
- Dixon-Woods M ,
- Fitzpatrick R ,
- Espíndola CR ,
Read the full text or download the PDF:

Guidance on Conducting Research Involving Mental Health Topics
In human subjects research, many studies utilize questionnaires and assessments that address mental health, behavior or quality of life. These may include questions and assessments of the subject’s intent to harm him/herself or others. As part of its responsibility to protect research subjects, COUHES evaluates the risks and benefits of asking study participants about these topics.
This guidance document is intended to help researchers determine the appropriateness of including mental health topics in their research and considerations in developing acceptable plans for mitigating any potential risk.
Identifying Risk of Harm
Intentional identification.
Studies may be designed to gauge intent to harm self or others. This may be done through assessments such as behavioral evaluations, interviews, surveys or other measures for depression and suicidality.
When using such clinical diagnostic measures, researchers should consider if the study setting and population are appropriate with regards to the safety, risk-benefit ratio, and knowledge to be gained. If these measures identify study participants as clinically at-risk, or the study targets populations at high risk for injury to self or others, the COUHES application must include a a safety plan that describes what actions will be taken to ensure the safety of at-risk participants.
Unintentional Identification
For studies that include quality-of-life assessments or questionnaires that ask about sadness, anxiousness, or stress, the identification of a participant at-risk for harm to self or others may be unintentional. This is because these assessments are not typically designed for diagnostic purposes.
COUHES evaluates if a safety plan is needed for such studies on a case-by-case basis. A plan may be required if responses reveal acute risk (e.g. imminent danger to self or severe low mood) or if the study population is at elevated risk (e.g. receiving mental health treatment for depression, mood, or anxiety disorders).
In-Person vs. Remote Identification
When conducting research related to mental health, researchers should consider the physical environment where the study procedures will take place, and how participants will be adequately protected in that environment. Safety and ethical considerations can differ depending on whether the participants complete the intervention remotely or in-person, and whether the researchers know the identity of the participant or study participation is anonymous.
Creating a Participant Safety Plan
For studies that may identify a participant is at immediate or emerging risk for harming self or others, researchers must develop a safety plan.
The key to a safety plan is an assessment of how imminent is the risk. How this assessment is made can vary depending on: whether study procedures are carried out remotely or in-person; in a clinical, laboratory, or other setting; or whether the information is collected anonymously or not tied to an individual.
The COUHES application must explain:
- How the risk will be assessed;
- When investigators will review a subject’s response to questionnaires and assessments, and the frequency at which this review will occur; and
- By whom the level and immediacy of risk will be assessed.
If participants’ responses will not be individually assessed, the COUHES application should explain why the investigators believe an individually identifiable assessment will not be included.
Any researchers administering the clinical measures and assessments, or reviewing a subject’s responses, should be appropriately qualified to assess the measures and assessments, and be familiar with the safety plan. In particular, individuals that are assessing participants’ risk of harm to self or others must have appropriate training in the assessment and implementation of the safety plan.
Intervention
Safety plans described in a COUHES application may include the follow, as appropriate:
- If participants will be provided mental health or other resources, a copy of the resource referral document, and an explanation of how/when the resources will be made accessible to participants.
- For assessments that determine imminent risk, procedures on transferring the participant to appropriate crisis intervention or de-escalation resources.
- For assessments that determine less than imminent risk, referral or intervention procedures and how this information is communicated to participants.
- For research that gathers anonymous information or where responses are not tied to an individual the plan should provide for a resource referral document to be given to participants that includes mental health resources, crisis intervention services, or hotline information depending on the type of risk.
- Qualifications of researchers and/or clinicians involved in participant interactions, assessments, and safety interventions.
- Confirmation that research staff directly interacting with participants will be adequately trained on the safety plan.
- If participants and parents/legal guardians, as applicable, will be notified of findings.
- If information is reportable under state or federal law, plans for notifying the relevant authorities and/or agencies under mandated reporting requirements.
Consent Process
As part of the consent process, consent forms should:
- Clearly explain to potential participants the sensitive nature of any interviews or questionnaires;
- Describe what will happen if participants acknowledge/disclose harm to self or others;
- Have information on the risks and benefits of participating in this type of research. For example, for research with populations at elevated risk, include that the involvement in the research does not provide participants with “protection” against future harmful behavior, and how potential risk is mitigated; and
- Include any limitations on data confidentiality in the Privacy and Confidentiality section. If information collected during research must be disclosed under mandated reporting requirements, this must be included. Language regarding mandated reporting may be reviewed by MIT Office of General Counsel.
Appendix: Suggested Consent Language
For research that gathers anonymous information and researchers plan only to provide resources, the consent process should not lead participants to think that the researchers will provide immediate assistance. Suggested language to add in the risk section is as follows:
There are no anticipated risks from your participation in this study. However, some people become anxious or upset when answering questions about (behaviors, well-being, mood, views). Your responses will not be individually identified, so we cannot provide you with personal feedback or intervention based on any of your answers. If you are worried about your mood, please refer to the attached resource referral information sheet.
If responses will be individually assessed and can be linked back to participants, the consent form should explain what options the participant will have if they become upset or uncomfortable during study activities. For example:
In the event that you tell the research team you are thinking about harming yourself or others, the research team will provide you resources and may ask you more questions about these thoughts. Based on your responses, the research team may provide you will additional resources or assistance to identify appropriate follow-up. This may include working with you to contact your doctor, contacting a trusted family member or therapist to discuss your thoughts, or working with you on a plan that may include getting you to a hospital for safety.
When using clinical diagnostic or symptom severity measures, participants scores above a pre-defined threshold of the measure should be reported back to the participant with an offer for referrals and/or counseling resources. The threshold for intervention needs to be defined in the COUHES application along with when and how the study findings will be shared with participants. Researchers should be prepared to offer appropriate counseling resources, assistance in making appointments, and/or offering a list of referrals. An example email message is below:
I am part of the team for a research study you recently completed. Based in your responses to some of the questions we asked, you seem to be experiencing (sadness, stress, blue moods, etc.). We provided you some information about mental health resources, but I wanted to follow-up and offer any other information you might want to get help.
To assist investigators with identifying counseling resources, COUHES provides the following:
Conducting Research on Mental Health Topics - Participant Counseling Resources [PDF]
The links below provide additional guidance for engaging participants on the topic of mental health.
- National Institute of Mental Health (NIMH): Conducting Research with Participants at Elevated
- Risk for Suicide: Considerations for Researchers
- NIMH Clinical Research Toolbox
- NIMH Guidance on Risk-Based Monitoring
- FDA Guidance for Industry, Suicidal Ideation and Behavior: Prospective Assessment of Occurrence in Clinical Trials
- FDA Guidance for Industry, Major Depressive Disorder: Developing Drugs for Treatment
- Certificates of Confidentiality
- NIH Policy for Data and Safety Monitoring
- PhenX Toolkit
- Dates & Deadlines
- Members & Staff
- Engaged in Research: Scenarios
- Continuing Review
- Criteria for Acceptance of Studies
- Financial Conflicts of Interest
- Guidance on NIH Genomic Data Sharing (GDS) Policy
- Ongoing Monitoring and Reporting
- Principal Investigator Status
- Record Keeping
- Research at Collaborating Institution
- Review and Approval of Studies
- Sabbaticals and Leaves of Absence
- Training of Research Personnel
- Additional Review (China, Russia or Saudi Arabia)
- Adult Subjects with Cognitive Impairment and Reduced Decision-Making Capacity
- Audiotaping and Videotaping
- COUHES Policy for Using Amazon's Mechanical Turk
- Data Handling When a Subject Withdraws From a Study
- Data Protection
- Data Sharing
- Electronic Consent
- General Data Protection Regulation (GDPR) and Research Activities
- Guidance on Use of Protected Health Information for Research Purposes
- Guidelines for Single IRB
- Guidance for Student Research and Class Projects
- Including Women of Childbearing Potential in Research and Pregnancy Testing
- MIT Students and Lab Members as Subjects
- MRI and Pregnancy
- Non-English Speakers
- Oral History Activities
- Other Vulnerable Subjects
- Passive Parental Consent
- Payment and Costs
- Pregnant Women
- Private Data, Human Specimens and Cells
- Research Involving Deception
- Research Involving Mental Health Topics
- Research Involving Non-MIT Collaborators
- Research that May Affect Privacy of Health Information
- Students as Subjects
- Subjects with Limited Ability to Read, Hear, or See
- Subjects with Limited Comprehension
- Surveys, Questionnaires and Interviews
- Additional Standard Language for Informed Consent
- Basic Elements of Informed Consent
- Waiver or Alteration of Informed Consent or Waiver of Documentation of Informed Consent
- ClinicalTrials.gov Requirements
- Data Safety Monitoring Plan (DSMP)
- GCP Training
- COUHES Connect FAQs
- COUHES Connect Guidance
- Helpful Links
- Department of Defense (DoD) Sponsored or Supported Exempt Research
- HIPAA Guidance Document
- Forms & Templates
- HST Notifications
- HST Reports
- Single IRB Review FAQs
- Announcements
- Frontiers in Public Health
- Public Mental Health
- Research Topics
Advances in Artificial Intelligence Applications that Support Psychosocial Health
Total Downloads
Total Views and Downloads
About this Research Topic
Generative Artificial Intelligence (AI) has an unquestionable influence on the progress of scientific knowledge in psychosocial health, especially in the detection and prevention of common as well as less prevalent health disorders. AI systems are being used to improve the psychosocial well-being of patients with psychologically damaging diseases such as cancer, as they allow for a less invasive approach and improve their prognosis. AI also plays a major role in the field of health interventions. Algorithms created from messages posted on social networks help predict the risk of users suffering from mental health problems or psychopathology. Generative AI also facilitates the inclusion of patients with functional diversity by creating universal communication channels and cognitive stimulation programs, thereby helping to create more humane and friendly environments. Furthermore, they offer the possibility of health education, facilitating adherence to treatment, and making training more accessible to health professionals. This enables them to acquire complex knowledge and train in simulated environments. Since generative AI contains highly sensitive personal information, it is necessary to publish protocols and measures that guarantee security in the handling of this information. This Research Topic aims to provide valuable insights for health professionals, health managers, and other stakeholders, seeking to enhance the quality of life of people by showcasing practical examples and compiling interdisciplinary evidence on the effective integration of AI into health interventions. advances in mental and social health, which are facilitated by the use of generative AI. This includes the use of AI in prevention, diagnosis, intervention, and rehabilitation. Some main topics of interest are: Ways in which AI can be used in research on mental health The use of AI to improve the learning methods of healthcare professionals. The use of AI in decision-making in mental health AI as a tool for predicting adverse effects of treatments AI as a tool to increase patient adherence, as well as to support, accompany and monitor treatments. The use of AI as a tool to make navigating mental health more accessible and inclusive through humanisation Ways in which mental health professionals and policies secure sensitive information utilised by AI
Keywords : Digital health technologies, e-inclusion, health, well-being, digital divide, artificial intelligence
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines.
| Manuscript Summary | |
| Manuscript |
Participating Journals
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

Teens are spending nearly 5 hours daily on social media. Here are the mental health outcomes
Forty-one percent of teens with the highest social media use rate their overall mental health as poor or very poor
Vol. 55 No. 3 Print version: page 80
- Social Media and Internet
- Technology and Design

Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor , compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest users.
Average number of hours a day that U.S. teens spend using seven popular social media apps, with YouTube , TikTok , and Instagram accounting for 87% of their social media time. Specifically, 37% of teens say they spend 5 or more hours a day, 14% spend 4 to less than 5 hours a day, 26% spend 2 to less than 4 hours a day, and 23% spend less than 2 hours a day on these three apps.
[ Related: Potential risks of content, features, and functions: The science of how social media affects youth ]
Percentage of the highest frequency social media users who report low parental monitoring and weak parental relationships who said they had poor or very poor mental health , compared with 25% of the highest frequency users who report high parental monitoring and strong parental relationships . Similarly, 22% of the highest users with poor parental relationships and monitoring expressed thoughts of suicide or self-harm compared with 2% of high users with strong parental relationships and monitoring.
Strong parental relationships and monitoring significantly cut the risk of mental health problems among teen social media users, even among those with significant screen time stats.
Rothwell, J. (October 27, 2023). Parenting mitigates social media-linked mental health issues . Gallup. Survey conducted between June 26–July 17, 2023, with responses by 6,643 parents living with children between ages 3 and 19, and 1,591 teens living with those parents. https://news.gallup.com/poll/513248/parenting-mitigates-social-media-linked-mental-health-issues.aspx .
Rothwell, J. (2023). How parenting and self-control mediate the link between social media use and mental health . https://ifstudies.org/ifs-admin/resources/briefs/ifs-gallup-parentingsocialmediascreentime-october2023-1.pdf .
Recommended reading

Contact APA
You may also like.
- Open access
- Published: 16 September 2024
Children’s and adolescents’ views of health and mental health concepts - A qualitative group interview study
- Sven Hassler 1 ,
- Siri Jakobsson Støre 2 , 3 ,
- Louise Persson 1 &
- Linda Beckman 1 , 4
BMC Public Health volume 24 , Article number: 2506 ( 2024 ) Cite this article
Metrics details
Definitions and perceptions of health and mental health have not remained static over time. This is also true for statistics over Swedish children’s and adolescents’ health and mental health status. The majority of Swedish school-aged children and adolescents report good physical health and good life satisfaction. However, there are some warning signs when it comes to children’s and adolescents’ health and mental health status, for instance, an increased overweight or obesity in children and adolescents, as well as a higher proportion reporting psychological problems and stress. There is also a need for knowing more about the younger population’s voices in this matter. The aim was therefore to explore children’s and adolescent’s conceptualizations and perceptions of health in general, and mental health in particular.
Open semistructured group interviews with 44 Swedish children and adolescents (10–14 years old) recruited from four schools were conducted. The interviews were conducted between April 2022 and January 2023. Data were analyzed with qualitative content analysis.
Children’s and adolescents’ conceptualizations of health included aspects of both the body and the mind, with a focus on the latter. Mental health was expressed as a state of being, illustrated by various lived experiences of emotions, moods, and thoughts. The social world was ever present in their understanding of health, e.g., through the lenses of social and gender norms.
Conclusions
This study revealed children’s and adolescents’ recognition of health terms and their ability to observe nuances between mental health problems and everyday struggles. The participants discussed mental health problems to a greater extent than positive mental health. An implication of this study is the highlighted need to focus more on mental health promotion in future preventive programs. These findings might potentially influence how school staff and student health teams communicate with children and adolescents about these concepts.
Peer Review reports
The majority of school-aged children and adolescents in Sweden have good physical health, and report good life satisfaction. However, around 25% of the 6–10 years old school children are overweight or obese, and far from all are physically active enough [ 1 , 2 ]. Many children and adolescents also experience stress and report psychological problems, painting a complex and elusive picture of their health and well-being [ 3 ]. Common indicators of mental health problems among school-aged children and adolescents include anxiety, worry, sleeping problems, and low mood. A high percentage of children also express feeling stressed by schoolwork, with 15-year-old girls reporting the highest percentage (78%) compared with boys of the same age (51%) [ 3 ].
Further, throughout the 2000s, visits to Child and Adolescent Psychiatry (CAMHS) in Sweden dramatically increased [ 4 ]. However, whether this reflects an actual increase in illness or a shift in demand, diagnostic criteria, and school dynamics remains inconclusive. As discussed in Lindholm and Wickström [ 5 ] and Wickström and Kvist Lindholm [ 6 ], professionals working with children and adolescents note that “crises” once considered normal aspects of maturation and development in children and adolescents risk being increasingly categorized as mental illness [ 7 ]. Life crises and everyday behavior may become medicalized, leading more individuals to seek assistance from CAMHS for issues that were previously addressed within family or social circles, such as relationship breakups ( 8 – 9 ). Moreover, a growing number of children and adolescents present with challenging and complex needs, indicating a diverse demand for assistance [ 4 ]. Thus, a medicalization of everyday challenges seems to have expanded the scope of health and mental health. This development reflects a changing society and a new coping mechanism for emerging realities.
The concept of health and mental health has been discussed in the literature for a long time. WHO have defined health as: “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [ 10 ], and have been criticized for, among other things, being too idealistic, referring to the statement of a complete health [ 11 ]. Children and adolescents’ perceptions of health as a concept have also been scrutinized. Research shows that children and adolescents, instead of defining health in terms of absence of chronic sickness, tend to use psychosocial health and health-related behaviors (such as sports activity, ( 12 – 13 ), being happy, feeling good [ 14 ], diet/healthy food, fruits and vegetables not smoking and sleeping) [ 15 ] as criteria.
Definitions and understandings of mental health - a relatively new concept - have not remained static. A process of reconceptualizing has led to uncertainty in two ends. In one end the functional understanding of the individual, public lay members and in the other the pragmatic use of the concept by policy workers and academia ( 16 – 17 ). Manwell et al. [ 17 ] suggest that the widespread use of the term ‘mental health’ serves as a euphemism for ‘mental illness’ and that the lack of agreement on the subcomponents and factors encompassed by the concept underscores the need for distinct definitions for individual and societal understanding.
As mental health often is used in general conversation but given different meanings in different contexts, a uniform use of key concepts related to mental health has been proposed [ 18 ]. It is notable that positive mental health is represented solely by mental well-being while negative mental health has a multitude of expressions and representations such as mental illness, mental problems, psychiatric conditions, neuropsychiatric impairments and mental illnesses and syndromes [ 18 ].
A mapping by Manwell et al. [ 17 ] of how mental health experts determine core concepts illustrates how different empirical discourses shape mental health definitions. There is the definition proposed in the spirit of health promotion, emphasizing the positive aspects of the concept. Mental health is seen as the capacity for individuals to feel, think, and act in ways that enhance their ability to enjoy life and cope with the challenges, respecting culture, equity, social justice, interconnections, and personal dignity [ 19 ]. The World Health Organization’s (WHO) definition echoes similar positive dimensions: “a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community” [ 20 ]. The criticism of such broad definitions highlights their contributions to the medicalization of society by viewing everyday problems within the scope of mental health [ 16 ]. An argument supported by Graham [ 9 ] who finds that the discourse of wellbeing is underpinned by an individual disease model and as such, is inherently medical in concept [ 9 ].
A previous scoping review [ 21 ] on children and youth’s perceptions of mental health revealed some uncertainty in the understanding of the concept. A shared mental health language would help children clarify distinctions between everyday challenges and issues requiring specialist attention. According to Beckman et al. [ 21 ], highlighting the positive aspects of mental health can increase the understanding that mental health can be improved. Similar conclusions are drawn by Hermann et al. [ 22 ], who emphasize the importance of clear terminology in mental health discussions. They further demonstrated that older adolescents (15–18 years) discuss mental health in holistic terms, indicating their understanding of its complexity despite the use of simplified language.
The various discourses around the concepts of health and mental health raise questions about whether we can expect children and adolescents to understand and communicate about them. Empirically investigating perceptions of health among children and adolescents needs to consider researchers’ presumptions of these concepts. As a response to the biomedical approach, Antonovsky [ 23 ] introduced the salutogenic approach to health, which views health as more than just the absence of risk factors. It focuses on human strengths, viewing health as a continuum rather than a dichotomy. Mental health in a salutogenic perspective refers to the level of health and resources present that can be recognized, utilized, and nurtured. Also acknowledge tension as a normal and necessary feeling for coping and therefore potentially health-promoting [ 24 ]. Consequently, there is a pressing need for more studies involving children and adolescents’ voices to gather their perspectives on the health concept and mental health.
Understanding how health and mental health are perceived and communicated among children and adolescents is crucial in planning interventions and strategies for health and mental health care and support. Therefore, this study aimed to explore children’s and adolescent’s conceptualizations and perceptions of health in general, and mental health in particular. With the explorative approach of the study, we have chosen to stay rather free from newly proposed conceptual frameworks of mental health as our ambition is to empirically add information and shape those frameworks rather than to apply them. Our broad and open approach motivated us to even include health in this conceptual mapping.
We opted for group interviews to gather in-depth information from the participants, foster comfort within their peer groups and peer support [ 25 ], facilitate the exchange of experiences, and enable them to comment on each other’s viewpoints. The interview guide was not followed strictly. According to Leeson [ 26 ], letting the children guide the conversation will help the researchers see what is important to them.
Data and participants
This study involved 44 participants (26 girls and 18 boys) aged 10–14 years from four different schools in Värmland County, Sweden. This age range was chosen because it comprises grades 4 to 8 in Swedish schools, and because children of that age could be considered old enough to discuss these questions and understand what they comply with. Eight mixed-gender group interviews were conducted from April 2022 to January 2023 (see Table 1 for the gender and grade distributions). The interviews took place at the participants’ respective schools.
Procedure and interview guide
The study received approval from the Swedish Ethical Review Authority (No: 2021-06168-01). Central Student Health Services (SHS) assisted in selecting schools and recruiting participants from grades 4–8 at four different schools. Subsequently, the schools were contacted and provided with documents and project information. Participants were recruited from classes through school personnel (principals, school nurses, and school social workers). No specific selection criteria were outlined, except that the participants were required to have their parents’ signed consent at the time of the interview. Children and adolescents interested in participating in a group interview were eligible for the study. Some schools opted to inform the entire class about participation, whereas in other cases, teachers approached specific children. The participating children received both oral and written information about the study, emphasizing its voluntary nature, their right to terminate participation at any time, and the assurance that their responses would remain confidential. Written and oral informed consent was obtained simultaneously with the interviews, which took place approximately two weeks after the first information session. The group interviews were conducted using open-to-semistructured interview techniques, with an interview guide developed on the basis of previous literature, such as Beckman et al. [ 21 ], which focused on amplifying children’s voices on health matters. Slightly different questions were tailored for different age groups so the questions would fit their ages and maturation (Appendix A).
The interviews were conducted by all the authors, with two authors present for each interview, alternating between being the roles of moderator and co-moderator. The moderator posed the questions and followed up with probes such as “Can you elaborate on what you just said?” and “Can you provide an example?”. Before concluding each group interview, participants were invited to share any additional thoughts or highlight any overlooked topics. The interviews were audio recorded digitally and the interviews lasted between 30 and 59 min. The participants were not requested to review the transcripts before analysis because of potential embarrassment or confusion in distinguishing their statements from others in the group [ 27 ]. As the schools were chosen by the school health team manager, the sample could be considered a convenience sample. The socioeconomic status of the schools was assessed as middle to high on the basis of grade points and average income for the district where the school is located.
Data analysis
Data analysis was conducted via the qualitative content analysis described by Graneheim and Lundman [ 28 ] and discussed by Graneheim, Lindgren and Lundman [ 29 ]. In the first step, each group interview was transcribed verbatim, and all the authors read the transcription of each group interview numerous times. Descriptions of health and mental health constituted the unit of analysis. Next, the meaning-carrying units were condensed and abstracted into codes. These codes were then compared and sorted into categories. As the analysis progressed, the categories and subcategories were further clarified and adjusted, resulting in the creation of three categories (Table 2 ). The initial coding of the transcripts were generated by SH, SJS, and LB, each coding different interviews. The data were then collectively examined to construct categories. Comparisons were made with the context in each step to verify the empirical basis of the data. Tentative codes and categories were discussed by all the authors and revised until consensus was reached. In cases of disagreements, we revisited the meaning-carrying unit to ensure the fit with the category or reconsidered the preliminary coding. Reflection and discussion led to agreement on sorting the codes. By including quotations from the transcribed text, similarities within and differences between categories were illustrated [ 28 ]. The quotations were translated from Swedish to English with the help of a native English speaker. The quotations cited in the results are labeled on the basis of school and grade. The current study is reported following the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [ 29 ]. In conducting qualitative studies, it is important to acknowledge an awareness of the researchers’s pre-understanding to minimize its influence on the results and analysis. However, eliminating it entirely is neither possible nor desirable. The challenge is to make clear whose voice is heard: the participants’ voice or the researchers’ interpretation [ 29 ]. According to Alvesson and Sandberg [ 30 ], preunderstanding can broaden the empirical base, generate ideas, formulate research questions, and evaluate the relevance and novelty of knowledge. The authors of this article have diverse backgrounds in social science, public health sciences, and psychology, contributing to - and constraining - the understanding and interpretation of the results.
Trustworthiness
To enhance trustworthiness, each step of the study included discussions concerning credibility, dependability, and transferability [ 28 ]. Credibility was bolstered by including a variety of participants from various schools, striving for diversity in age and gender. Our research team also included members with different backgrounds, allowing for a multifaceted examination of the data. We believe that the choice of group interviews further enhanced the credibility since children may feel a sense of imbalance in power dynamics when meeting an unknown person alone and discussing health and mental health [ 31 ]. Additionally, we developed an interview guide ensuring that the same questions were addressed in all interviews, further bolstering credibility. To reinforce credibility, we included representative quotations from the interviews, and thoroughly discussed the codes and preliminary categories. The research team included experienced interviewers, as well as a licensed Psychologist specializing in clinical child and adolescent psychology (PsyD) (i.e., an expert on mental health), which have contributed to maintaining a safe environment, particularly if the discussion touched sensitive topics such as suicide [ 26 ]. Dependability refers to the stability of data over time [ 28 ]. Seven of the eight group interviews were conducted during late spring and after the summer holiday, with one conducted the following winter. We believe that the gap between the seventh and the eighth interviews likely did not affect the results. While new follow-up questions may have emerged during the later interviews, we did not review the transcripts beforehand. However, we do not consider this a factor contributing to inconsistencies in results but rather a source of greater variation in answers. The description of culture and context, characteristics, and selection process enables readers to assess the transferability of findings to other groups and contexts [ 28 ]. Owing to the nature of the sampling, which is partly adapted to school circumstances and the availability of time and willing teachers, transferability is open to discussion. Nonetheless, by selecting schools from different socioeconomic districts and including boys and girls across grades 4–8, we believe that the sample can be considered transferable within a cultural context comparable to that of Sweden.
The analysis resulted in three categories: (1) Conceptualizations of health (2), Experience-based manifestations of being , and (3) Social norms . Please see Table 2 for an overview of the categories and belonging subcatogories.
Conceptualizations of health
The first category included the subcategories Health - body and mind; The meaning and value of the word and Overlapping concepts. In conceptualizations of health, the participants gave their view of what health, mental health, and similar concepts meant to them.
Health - body and mind
When asked to describe what health is, the participants discussed diet and exercise – especially the younger ones. Good health was associated with the ability to eat nutritious food and essential vitamins, and to generally avoiding eating junk food. Staying “fit”, i.e., maintaining a stable weight was also considered an important aspect of good health. It was evident that some children’s conceptualization of health encompassed mental well-being, and that these children recognized an interconnectedness of the body and the mind:
These factors affect each other. Therefore, if you have positive thoughts and feel good mentally, it might be easier for you to be active and eat well. For some, it could also be that staying active and sleeping well may lead to better thoughts and such. (North School, grade 8b) I would say that they are two completely separate things: one is about how your body feels, and the other is about how you feel mentally. (East School, grade 5)
Although some younger students in Grade 4 were unsure of the meaning of mental health, it was described as “how you feel in your brain”, “that you are happy and energetic”, how you are treated by others, and how you enjoy your surroundings. Mental health was also associated with academic performance and peer relationships. However, understanding someone’s true emotional state was acknowledged as challenging:
For some people, you might think that they’re doing really well, but deep down, they may not always be feeling great. Mental health can encompass many things because much is happening under the surface. (South School, grade 5)
One pupil in Grade 6 described mental illness as unwell in the mind, emphasizing that it involves prolonged feelings of sadness rather than transient emotions. There was a perception that mental health was more important than physical health. Taking care of one’s body through exercise was seen to positively impact mental well-being, and that the two are intricately linked. A fifth-grader illustrated this by emphasizing that you need to work harder to get rid of a state of feeling mentally unwell than being physically sick:
I think there’s more weight in regards to the mental aspect because when you’re feeling mentally unwell, you have to put in extra effort to overcome it. Whereas, if you’re physically unwell, it often tends to pass after a while, such as when you’re sick. (East School, grade 5)
The meaning and value of the word
A call for greater caution was evident in how the concepts related to mental health should be used. The participants expressed concern that mental illness was often trivialized through humor, risking its significance being undermined. With respect to mental health concepts, the participants stated: “One must know what the word means”. One fifth grader provided an example of the non-sarcastically use of a loaded expression:
Sometimes people may joke about being depressed, like saying, “Oh, the game got canceled today; I’m so depressed now.“(East School, grade 5).
The more general expression “feel bad” was described as a collective term that could carry varying degrees of seriousness:
You don’t necessarily have to use it (feel bad) for mental problems; if you have a stomachache, you feel unwell. The weight of the term varies depending on the context in which it is used. (East School, grade 6)
The multiple views of what constitutes mental health indicate the complexity of mental health-related concepts, highlighting the challenges in their usage and understanding across different contexts.
Overlapping concepts
With respect to the concepts related to mental health, the children reported that their perceptions of these concepts frequently overlapped. Concepts such as sadness appeared to be perceived as easier for the children to cope with and worry was perceived as different yet interconnected. The participating children and adolescents disclosed that it was more challenging to feel worried than sad. One reason for this was, “When you are sad, you can cry, but when you are worried, you have to talk.” (East School, grade 6). Dealing with sadness could be perceived as “easier”. Worry, on the other hand, could be experienced as stressful, with stress being described, among other things, as a mixture of feeling sad and worried. Stress was characterized as a sensation that “took over,” but it was acknowledged that there could be both positive and negative forms of stress. Anxiety was seen as an extension of stress, where individuals tend to “overthink” various situations and events:
Anxiety is a combination of stress and feeling a bit down. Homework, negative social circles, exams, and things that weigh you down can lead to a point where you cannot handle it anymore, resulting in a panic attack or something similar. (North School, grade 8a)
Anxiety was described as a sudden and intense feeling that could cause difficulty in breathing. However, older children believed that anxiety was not a term commonly used and was considered “harsher”. Panic attacks were viewed as an escalation of anxiety: “Stress is more common; a panic attack is the peak of anxiety.” (North School grade 8a). During a panic attack, everything could seem to freeze, and there could be a sense of darkness for a while.
Yes, I believe there’s a difference between anxiety and panic attacks. It seems that anxiety is something that lasts for a longer period, possibly transitioning from stress to anxiety. Many different factors can trigger this anxiety. However, when it becomes a panic attack, I think it is more intense and happens closely together. That is what I think. (North School, grade 8a)
When asked to define depression, it was described as feeling unhappy, very low, lacking the motivation to take care of oneself, and struggling to get out of bed. It could involve overthinking, “worrying” and burying oneself. There could also be different versions of depression, where some deny it and go around smiling all day, but then when they get home, they dive into bed and are “completely destroyed”. The children said that everyone feels bad sometimes, but depression is being down for a longer period of time and that it was important to get help.
Experience-based manifestations of being
In contrast to the perhaps more knowledge-driven conceptualizations of health, experienced-based manifestations of being represent answers relating to the inner self and one’s own experience of ill- and well-being. Experience-based manifestations of being include the subcategories Health as a state of being; Negative mental health as an elusive emotion , and Health affected by sources of worries.
Health as a state of being
Health is expressed by the participants as consisting of various expressions of emotions, moods, thoughts, and overall well-being. If conceptualizations of health represent explicit descriptions of concepts, health as a state of being represents hints of ideas originating from one’s own experiences, implicitly relating to health through aspects of being. The spectrum on which these expressions move stretches from concrete expressions regarding physical health and sedentary lifestyles to vague and elusive expressions of being. The former is more often a response to physical health. Feeling fit and alert, being physically active, and sleeping properly were seen as expressions of well-being, whereas inactivity represented mental illness. A fourth grader gives this example:
I think bad health is mostly when you sit all the time and do not do much. (South School, grade 4)
Negative mental health as an elusive emotion
There is an elusiveness that characterizes these perceptions, mostly related to the negative aspects of being or moods, where the participants seemingly do not quite grasp the word that correctly describes the feeling or state of being. An elusiveness in contrast to others, more clear illustrations of mental health such as being happy, in good spirits, or enjoying oneself. However, negative perceptions of mental health manifested as a form of ill-being, often more vaguely expressed as a certain emotion, thought, mood, or gut feeling. Something they carry with them, sometimes for longer periods, as a state of being of the inner self.
It kind of doesn’t feel good. (East School, grade 5) I think it means psychologically, it’s inside, that is when you kind of do not feel good inside and that it is like, it is like that thing with stress, that you do not feel so good inside. (East School, grade 4)
Health affected by sources of worries
Worries are also perceived as something that triggers mental illness and stress and are expressed in different forms and distances from oneself. Worries about the war in Ukraine and Syria or worries that a family member will die or become hurt. However, worries about school and schoolwork were also quite extensively expressed. These worries as expressions of mental illness resemble what was also perceived as stress. When asked how they would describe stress, associations with thoughts were quite common, and they thought of something that made them stressed. Some describe it as overthinking or as a feeling that ends up in the stomach and creates anxiety. School education seems to be the source of much anxiety and stress. Stress about tests, grades, and not learning enough or as a general feeling of being chased and unable to make it. A feeling apparently tangible and overwhelming to the informants but seldom concretized or further described. A sixth grader emphasizes stress when it is too high.
One becomes overwhelmed, you know. You might think, for example, that you have many things to do, such as studying, exercising, and many other things, and it can become a bit too much. (East School, grade 6)
Social norms
The social world was ever-present in children’ understanding of health, either implicitly or explicitly. Social norms included Fitting in and being affirmed , Complexion and self-image , Social life in school and on social media platforms , and Tell , ask , show . The children viewed fun activities with friends as having beneficial health effects because you do something enjoyable (and hence good) for yourself in a shared experience with close ones. However, social relationships are also associated with potential disadvantageous health consequences. “Being normal” was considered vital for health, and it was also evident that beauty standards and gender norms were related to mental health and showing emotions.
Fitting in and being affirmed
Being normal and fitting in were considered essential to health; it is important to look and act like everyone else. If you do not fit in, you are left out:
And it can also be that you feel like, ‘I do not fit in here; everyone else is so cool, and I just come in here suddenly like a little…’. Yeah, it is probably mostly feeling a bit excluded or left out. (South School, grade 5)
Mental health was, in this context, described as being affected by how people view you, what you do, and whether you are liked or not and feeling affirmed.
Yes, I can get sad sometimes, I can think about what people think of me, or you really want to be liked, and sometimes you might just feel that you think you’re really ugly or something and that, yes, you get very depressed. (South School, grade 6)
On the same note, being socially awkward or prone to overanalyzing social situations can be stressful and depressing. Conforming to the group may lead to a sense of belonging, but chasing social affirmation may be compromising your health, e.g., doing things you do not want to do through peer pressure:
You do things you do not want to, as others want it, and so you want to be with them. So instead of saying, ‘No, I don’t want to do this, can’t we do anything else?‘, you do it anyway, so you do not exactly take care of yourself. Additionally, you sit there feeling sad because you did something that made you feel sick or bad. (South School, grade 5)
Complexion and self-image
Mental health is also described with reference to how one feels about how one looks and appears in the eyes of others. There seems to be a definitive link between physical appearance and mental health, and it occurs in both ways. To desire something you do not have, a look or appearance, was one way of describing how mental health could be affected by complexions or one’s self-image. Trends in looks and body shapes are other examples of what could affect mental well-being.
So it could also be that you feel bad, for example, about your appearance or you feel that you are not enough, so then you think that you are mean even though you are not satisfied with yourself, and then it becomes psychological. (South School, grade 5)
The body trends reflected in social media were considered unhealthy, and these beauty standards mostly affected girls - and made them feel worse.
Social life in school and on social media platforms
Well-being and ill-being as a signifier of health were also expressed in social terms, such as how things are going at school and how one handles life. Well-being and ill-being become extensive in the descriptions of children and adolescents; they can be about not feeling as usual, feeling scared, or not being good enough. It was perceived as part of life and an everyday occurrence, appearing to many of the informants not only as a consequence of social situations and encounters in real life, but certainly also on social media platforms. The participants expressed concerns about the ongoing talk but also as incitement around trends and behaviors. The participants’ experiences of social media were described as both positive and negative in terms of being seen and being part of a community, but it also led to more comparisons of oneself to others and more negative feelings. However, at the same time, informants referred to social media and the cell phone as a place to take a break and escape from stress at school, thus facilitating well-being. The children described how they try to act like everyone else on social media. Social media sets standards for how one should look, which can lead to stress and depression:
Social media sort of raises the standard of how one should look and dress. For example, many people Photoshop and tinker with the pictures, whether they want to get a smaller waist or larger biceps or, yes, to make it look better and: This is how a body should look - even if it is not supposed to look like that. (North School, grade 8a) Many have experienced stress or depression because they want to look like those who have been Photoshopped. Yes, so there are also many disadvantages. (North School, grade 8a)
The adolescents and children also spoke about the role that social media has in spreading so-called fake news and, by that, spreading anxiety.
Tell, show, ask
The children and adolescents perceived it to be more of a taboo for boys to cry than for girls. They expressed that boys often abstain from crying to avoid being perceived as weird or non-masculine, even though they emphasized that everyone cries sometimes and that it is necessary to cry occasionally. Girls were described as having more reasons to be sad because they hurt each other more:
I’m not a girl myself, but girls seem to get more hurt by their friends, so it feels like it is quite difficult to be, well if there are three of them, two might hang out together, it can be quite difficult to be the third wheel. However, we guys can be a group of several boys without, well, without any issues, and it works truly well. (North School, grade 8b)
The children attributed these gender differences to society, with one explaining that there’s just this feeling in his head that it is how things work. Additionally, there is an age difference to consider, where it is believed that it is acceptable for young children to cry, but teenagers need to maintain a cool image to a greater extent. Crying in front of others would make you feel weak.
The children emphasized responsibility for others and the importance of asking friends how they are. They value the support of others but noted that it is “not something they usually do in their spare time”. The participants also expressed a risk of rejection when one opens up about how one truly feels, and friends may also recoil when asked about their feelings. It’s also a matter of integrity; you do not have to share everything , and you cannot force another person to share how they are feeling:
It is difficult to share because you do not need to disclose everything that has happened. You only need to share if you’re truly worried about something, like 'This is what I’m most concerned about how they will react and what they will think’. In that case, they can skip that part and share everything they feel comfortable sharing. (South School, grade 4)
Analyzing the data of school children’s views on health and mental health revealed several important information about how they understand these concepts. The results are first discussed in relation to each of the inductive coding categories: Conceptualizations of health , Experience-based manifestations of being , and Social norms . After that, the findings are discussed in relation to implications for practice and future research.
Conceptualizations of health – the children are well aware
When we inquired about health in general, there was a significant emphasis on eating well and doing physical activity, mirroring the findings of another Swedish study that interviewed children between the ages of 9–11 [ 32 ]. Our main findings reveal that health and mental health are not unfamiliar concepts to school-aged children and adolescents, although the youngest children in Grade 4 struggled with mental health, which is consistent with findings from a recent scoping review [ 21 ]. However, mental health was also included in these discussions, and the two concepts - health and mental health - were seen as interconnected, reflecting the relationship between the body and mind. Mental health was sometimes perceived to be even more crucial than physical health.
Mental health was described by the youngest participants as how “one feels in the brain”, which encompasses feelings such as mood, emotions, and overall well-being experienced in the mind. It includes feelings of happiness and energy, findings that are consistent with other qualitative studies with children and adolescents ( 22 , 33 – 34 ). The children also included social relationships and surroundings in their descriptions of mental health, a finding echoed elsewhere ( 33 , 35 – 36 ). Mental health was also described as when nothing goes against you, akin to the feeling of harmony, as reported by Landstedt et al. [ 37 ].
However, mental health is also intertwined with general health, which risks further conceptual ambiguity. Manwell et al. [ 17 ] proposed that the integration of mental and physical health can be defined by the level of autonomy (i.e., the capacity for control over one’s self), whereas the integration of mental and social health can be defined by a sense of ‘us’ (i.e.,the capacity for relating to others). A capacity that was observed in our material as the children associated mental health to peer relationships and how “you enjoy your surroundings”.
Depression, as part of mental health, was understood somewhat distinctly as characterized by not being happy and feeling very bad. The participants emphasized that everyone feels bad sometimes but that depression is feeling down for a longer period of time and that it is important to seek help. Similar findings were reported by Hermann et al. [ 22 ], where depression was viewed as a severe mental health problem and an illness, and by Perre et al. [ 34 ], where the length of time feeling depressed determined the difference between feeling down and being diagnosed with clinical depression. We further found that depression could be used in many situations, although it is not meant to be real clinical depression, and some participants underlined that it is important to use the word right; otherwise, the word will not be taken seriously. Hermann et al. [ 22 ] reported that adolescents’ thought peers commonly self-diagnosed depression without knowing what the condition entails ( 21 – 22 ).
However, there seems to be a lack of agreement on what strengths are most associated with mental health [ 38 ]. In his critical discussion on positive mental health, Vaillant [ 38 ] argues that positive mental health represents the presence of human strengths such as maturity, the dominance of positive emotions, high socioemotional intelligence, subjective well-being or resilience rather than the absence of weaknesses [ 38 ].
Experience-based manifestations of being – an integration of two constructs of mental health?
Children and adolescents struggle to link their cognitive understanding of negative mental health concepts with their limited experiences with mental health issues. Moreover, they partly make use of these concepts when they describe experiences of feeling down or low. An approach to distinguish children and adolescents’ perceptions and articulations of mental health that has been suggested in several relevant studies is the social constructionist perspective on knowledge. A perspective of the history of psychiatry that demonstrates that the talk of lighter mental symptoms has changed over time. The analysis shows how the participants‘s descriptions of mental illness are characterized by the free use of psychological and psychiatric expert language and a normalization of different emotions, such as in contrast to the norms and demands of adult (expert) society [ 21 , 39 ]. The elusiveness of the descriptions of being could very well relate to a constructivist merger of more advanced psychological expressions picked up by the adolescents from their immediate environment and from society at large with a self-reflective understanding of one’s feelings and moods. A perception of mental health that is similar to the dual-factor model [ 40 ]. A model that suggests a conceptualization of mental health consisting of two separate but still related constructs; an integration of subjective well-being with psychopathological symptoms [ 40 ]. The vague and trying expressions of being that our study recognized among the children could represent a sense of doubled awareness of either internalizing or externalizing mental disorders and well-being [ 41 ].
Worries were perceived as triggers of ill-being. Worries, manifested as stress about school and schoolwork, were also quite extensively expressed. It is clear that school seems to be the source of much anxiety and stress, which was confirmed in our interviews and elsewhere [ 3 , 22 ]. In navigating expressions of positive and negative mental health in a school environment, it is interesting to note how Putwain et al. [ 42 ], in their network analysis, identified school-related well-being to be distinct from test anxiety and more serious conditions such as generalized anxiety disorder and panic disorder. Again, the dual-factor model suggests a way of separating but not disconnecting subjective expressions of well-being with psychological distress [ 40 , 42 ].
Moreover, schools are the most common arena for promoting mental health and the most important because there is a possibility to reach children and adolescents who would not have been reached otherwise. An arena for promoting positive mental health but where stigma and negative attitudes are also addressed to encourage appropriate help-seeking for mental health problems. The latter represents more of a deficit approach although meta‐analyses show that multicomponent mental health promotion interventions are more effective when adopting a positive mental health stance rather than focusing exclusively on illness prevention [ 43 ].
Vague and elusive expressions of being presented by the children and adolescents should also be understood from the perspective of the professional. To what extent are we as researchers the cause of this vagueness? A question raised from the perspective that mental health has both a descriptive ( What is ) and a prescriptive ( What should be ) function. Manwell et al. [ 17 ] argue that the differences in how these functions are perceived must be empirically determined. In such an investigation, that we believe partly has been undertaken in this study, Huber et al. [ 16 ] emphasize that we must be aware of the risk of mixing scientific evidence with moral argument. A thought in line with the argument of the early criticisms of health-promoting perspectives, viewing health in positive, normative terms, avoiding a focus on risk and deficit [ 44 ]. The fact that children and adolescents struggle with sorting out the meaning of mental health might just reflect an academic uncertainty.
Social norms – body image, mental health and social media links
Being normal and fitting in were considered essential to health. The results confirmed that it is important to look and act like everyone else. The concept of normality is ubiquitous in the debate on mental illness and mental health. Horowitz [ 45 ] argues that it is impossible to determine what constitutes a mental disorder without delineating what constitutes normal functioning. If everyday challenges increasingly are being medicalized and, as such, represent deviance from normality, this according to Aneshensel [ 46 ], raises the question of whether psychopathology constitutes a disjuncture with normality or is on the same continuum as normality, but at the opposite pole. However, Vaillant [ 38 ] contests the idea of the average being equal to healthy, meaning that at the community level the healthy individuals always mix with various forms of psychopathological presence [ 38 ]. The centrality and normativity of normality have been the subject of critical research [ 47 ]. From being an expression of the probable , it has become burdened with a discriminating power, therefore it has been scrutinized in medicine as well as in the fields of disability studies, gender studies, anthropology, psychiatry, cultural studies, sociology, and critical race studies [ 47 ].
Departing from these definitions, factors relating to the individual and one’s capacity and ability to interact with society can be identified, stressing concepts of agency, autonomy, and control. In the mapping by Manwell et al. [ 17 ] meaningful participation in valued roles such as family and work was recognized as important in understanding mental health. For children and adolescents, this would represent social role-taking in a school environment, but also social aspects such as being able to disconnect by choice, as opposed to being excluded. It is widely recognized that socially excluded adolescents are at increased risk of depression and anxiety [ 48 ]. The participants recognized a link between mental health, body image, and social media. The appearance was thought to influence one’s mental health, and this was exaggerated by Photoshopped influencers on social media. According to Choukas-Bradley et al. [ 49 ], social media constructs a “perfect storm” where idealized images of peers and quantifiable feedback, together with developmental factors and sociocultural gender socialization processes, amplify adolescent girls’ body image concerns. This can later lead to depression symptoms and disordered eating. The importance of social media for children and mental health cannot be emphasized enough, and adults need to raise awareness and be educated on this matter.
Limitations
In this study, we interviewed a small sample of children; therefore, the results may not be directly transferable to other countries or age groups, although our findings are in line with previous research. Although the participants were recruited from different schools, we did not reach the most vulnerable areas; thus, the transferability to multicultural settings and rural areas is limited. Despite employing a nonclinical sample, several participants expressed personal interactions with counselors, doctors, and psychologists regarding mental health concerns, which may have influenced their views. We attempted to steer the discussion away from personal disclosures when these situations arose. Furthermore, the global COVID-19 pandemic and its associated restrictions and isolation for this target group may have affected their views on mental health. However, compared with other countries, Sweden faced fewer restrictions in closing compulsory schools, which might have positively influenced their mental health. Another consideration applies to the recruitment process; in some cases, the schools asked a few selected pupils if they wanted to participate rather than informing the whole class. More verbal and outwardly directed pupils were likely recruited over others. This might have influenced the richness and nuances of the interviews.
We used group interviews to encourage active discussions and enhance interactions by talking to one another, exchanging experiences, and commenting on each other’s points of view. However, the composition of the groups might have contributed to more or less interaction. For example, some participants might not have been comfortable talking in groups with the other sex, as the groups included both boys and girls. This could also be true for age differences within the group. There is also a risk of personal negative emotions toward other children in the group, influencing the dynamics of the discussions. Choosing girls and boys from different schools and of different ages may have enhanced the credibility of the data, as it might have offered a richer variation and understanding of mental health among children with different backgrounds. However, logistical constraints prevented this option from being feasible. We chose not to let the participants read and comment on the transcripts which could be considered a limitation [ 27 ], although we do not believe that this had a great impact on the analysis. Finally, we were two researchers at each interview, which could imply both pros and cons. It is possible that some children felt intimidated by having two adults ask them questions, but this was nothing we sensed was a problem.
Health and mental health might be among the most important concerns for children and adolescents today. In an unstable and rapidly changing world where uncertainty dominates the global landscape, it is natural for individuals to feel worried. Transitioning from childhood to adolescence involves navigating various challenges, including friendships, social media, conformity to societal norms, and self-image, all of which significantly contribute to participants’ mental health, as articulated by them. The influence of social media and gender norms in adolescents’ lives has, according to the participants in our study, considerable effects on their mental well-being. It is imperative for adults to raise awareness and become educated on this matter. The participants’ familiarity with mental health concepts indicates a strong recognition of the terms, albeit not always fully comprehended. They demonstrated the ability to differentiate between mental health problems and everyday struggles more effectively than anticipated. However, how can we expect children’s understanding and expression of mental health and mental illness to match those that science might anticipate when several discourses and presumptions around the concept exist? When definitions and understandings of mental health have not remained stable, we, as researchers, have a great responsibility in finding that common language. Furthermore, it seems that children and adolescents are more aware of the negative side of mental health problems than the mental health-promoting side; thus, there is a need for more focus on positive mental health. We hope that our results will be used in schools by teachers, student health teams, and pupils in the ongoing health and mental health discussions and health promotion. Our results can hopefully support the process of developing a common language between adults and children. Future research should make use of this knowledge when creating health and mental health-promoting interventions and continue to ask children and adolescents about their views on their lives, and a specific focus should be on social media and how that affects their mental health.
Data availability
The collected data have been processed by personal data assistants. Audio files and printouts are stored at a secured server so that no unauthorized person has access to them. All information about the informants is encrypted and data will be saved for at least 10 years. Karlstad University is the responsible research principal and personal data controller. The university’s data protection officer could be reached at [email protected]. To obtain access to the raw data analysed in our study, please contact Sven Hassler at [email protected].
Abbreviations
Child and Adolescent Psychiatry
The World Health Organization
Student Health Services
Sven Hassler (Author)
Siri Jakobsson Støre (Author)
Louise Persson (Author)
Linda Beckman (Author)
Consolidated Criteria for Reporting Qualitative Research
Doctor of psychology
FHM. Statistik om övervikt och fetma hos barn 6–10 år [Statistics on overweight and obesity in 6–10 year olds]. Sweden: 2024 [cited 2024 Aug 24]. https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/mat-fysisk-aktivitet-overvikt-och-fetma/overvikt-och-fetma/statistik-om-overvikt-och-fetma/overvikt-och-fetma-hos-barn-6-10-ar/
FHM. Statistik om fysisk aktivitet och stillasittande [Statistics on overweight and sedentary]. Sweden: 2024 [cited 2024 Aug 24]. https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/mat-fysisk-aktivitet-overvikt-och-fetma/fysisk-aktivitet-och-stillasittande/statistik-om-fysisk-aktivitet-och-stillasittande/
Public Health Agency of Sweden. Skolbarns hälsovanor i Sverige 2021/22 Nationella resultat [Health Behaviour in School-aged children (HBSC), results for Sweden in the 2021/22]. Stockholm: Folkhälsomyndigheten; 2023. [Swedish].
Google Scholar
SKR. Hur mår BUP? En nulägesbeskrivning av barn- och ungdomspsykiatrin i sverige inhämtad av Uppdrag Psykisk Hälsa [How is CAP? A description of the current state of child and youth psychiatry in Sweden obtained by Uppdrag Psykisk Hälsa]. Stockholm: Uppdrag hälsa; 2017. [Swedish].
Lindholm SK, Wickström A. Looping effects’ related to young people’s mental health: how young people transform the meaning of psychiatric concepts. Global Stud Child. 2020;10(1):26–38.
Article Google Scholar
Wickström A, Kvist Lindholm S. Young people’s perspectives on the symptoms asked for in the Health Behavior in School-aged children survey. Childhood. 2020;27(4):450–67.
Public Health Agency of Sweden. Varför Har den psykiska ohälsan ökat bland barn och unga i sverige? Utvecklingen under Perioden 1985 – 2014. [Why have multiple health complaints increased among children and adolescents in Sweden? The development between 1985 and 2014]. Stockholm: Folkhälsomyndigheten; 2018. [Swedish].
Suhr J, Johnson E. First do no harm: ethical issues in pathologizing normal variations in Behavior and Functioning. Psychol Injury Law. 2022;15:1–15.
Graham L. To be well is to be not unwell: the New Battleground Inside our children’s heads. Rethinking Youth Wellbeing: Crit Perspect. 2015;11–33.
World Health Organization. 1948 Constitution of the World Health Organization, 2006.
Larson J. The World Health Organization’s definition of health: Social versus spiritual health. Soc Indic Res. 1996;38:181–92.
Piko B. Health-related predictors of self-perceived health in a student population: the importance of physical activity. J Community Health. 2000;25(2):125–37.
Article PubMed CAS Google Scholar
Piko B, Bak J. Children’s perceptions of health and illness: images and lay concepts in preadolescence. Health Educ Res. 2006;215:643–53.
Onyango-Ouma W, Aargaard-Hansen J, Jensen BB. Changing concepts of health and illness among children of primary school age in Western Kenya. Health Educ Res. 2004;19:326–39.
Pridmore P, Bendelow G. Images of health: exploring beliefs of children using the ‘draw-and-write’ technique. Health Educ J. 1995;54:473–88.
Huber M, Knottnerus JA, Green L, Horst H, v d, Jadad AR, Kromhout D et al. How should we Define Health? BMJ 2011; 343.
Manwell LA, Barbic SP, Roberts K, Durisko Z, Lee C, Ware E, McKenzie K. What is mental health? Evidence toward a new definition from a mixed methods multidisciplinary international survey. BMJ Open. 2015;5(6).
National Board of Health and Welfare. Begrepp inom området psykisk hälsa [Concepts in the field of mental health]. Stockholm. Socialstyrelsen. 2024. [Swedish].
Public Health Agency of Canada. Mental Health promotion. Canada: Government of Canada; 2014 [cited 2023 Oct 24]. https://www.canada.ca/en/public-health/services/health-promotion/mental-health/mental-health-promotion.html
World Health Organization. Promoting mental health: concepts, emerging evidence, practice. Geneva: World Health Organization; 2004.
Beckman L, Hassler S, Hellström L. Children and youth’s perceptions of mental health—A scoping review of qualitative studies. BMC Psychiatry. 2023;23(1):669.
Article PubMed PubMed Central Google Scholar
Hermann V, Durbeej N, Karlsson A, Sarkadi A. Feeling down one evening doesn’t count as having mental health problems’—Swedish adolescents’ conceptual views of mental health. J Adv Nurs. 2023;79(8):2886–99.
Article PubMed Google Scholar
Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promot Int. 1996;11:11–8.
Langeland E, Vinje HF. Applying salutogenesis in Mental Healthcare Settings. In: Mittelmark MB, Bauer GF, Vaandrager L, et al. editors. The handbook of Salutogenesis. 2nd ed. Cham (CH): Springer; 2022. pp. 433–9. January 1.
Chapter Google Scholar
Hill M. Children’s voices on ways of having a Voice: children’s and young people’s perspectives on methods used in research and consultation. Childhood. 2006;13(1):69–89.
Leeson C. Asking difficult questions: exploring research methods with children on painful issues. Int J Res Method Educ. 2013;37(2):206–22.
Mero-Jaffe I. Is that what I said?’ Interview transcript approval by participants: an aspect of ethics in qualitative research. Int J Qualitative Methods. 2011;10(3):231–47.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34.
Alvesson M, Sandberg J, Preunderstanding. An interpretation-enhancer and horizon-expander in research. Organ Stud. 2022;43(3):395–412.
Eder D, Fingerson L. Interviewing children and adolescents. Inside interviewing: New lenses, new concerns. Sage; 2003. pp. 33–53.
Kostmann E, Nilsson L. Children’s perspectives on Health: what makes children feel good according to themselves? Int J Educ. 2012;4(1).
Johansson A, Brunnberg E, Eriksson C. Adolescent girls’ and boys’ perceptions of mental health. J Youth Stud. 2007;10(2):183–202.
Perre NM, Wilson NJ, Smith-Merry J, Murphy G. Australian university students’ perceptions of mental illness: a qualitative study. JANZSSA-Journal Australian New Z Student Serv Association. 2016;24(2).
Svirydzenka N, Bone C, Dogra N. Schoolchildren’s perspectives on the meaning of mental health. J Public Mental Health. 2014;13(1):4–12.
Teng E, Crabb S, Winefield H, Venning A. Crying wolf? Australian adolescents’ perceptions of the ambiguity of visible indicators of mental health and authenticity of mental illness. Qualitative Res Psychol. 2017;14(2):171–99.
Landstedt E, Asplund K, Gillander Gådin K. Understanding adolescent mental health: the influence of social processes, doing gender and gendered power relations. Sociol Health Illn. 2009;31(7):962–78.
Vaillant GE. Positive mental health: is there a cross-cultural definition? World Psychiatry. 2012;11(2):93–9.
Skagius P, Lindgren AL, Nelson KZ. Psykisk ohälsa Eller bara livet? Narrativ Om Psykisk ohälsa i en internetbaserad stödverksamhet organiserad av och för ungdomar [Mental illness or just life? Narratives of mental illness in an internet-based support activity organized by and for young people]. Socialmedicinsk Tidskrift. 2018;95(5):568–76.
Greenspoon PJ, Saklofske DH. Toward an integration of Subjective Well-Being and Psychopathology. Soc Indic Res. 2001;54:81–108.
Moore SA, Widales-Benitez O, Carnazzo KW, Kim EK, Moffa K, Dowdy E. Conducting Universal Complete Mental Health Screening via Student Self-Report. Contemp School Psychol. 2015;19:253–67.
Putwain DW, Stockinger K, von der Embse NP, Suldo SM, Daumiller M. Test anxiety, anxiety disorders, and school-related wellbeing: manifestations of the same or different constructs? J Sch Psychol. 2021;88:47–67.
Renwick L, Pedley R, Johnson I, Bell V, Lovell K, Bee P, Brooks H. Mental health literacy in children and adolescents in low-and middle-income countries: a mixed studies systematic review and narrative synthesis. Eur Child Adolesc Psychiatry. Apr; 2024;33(4):961–85.
Seedhouse D. Health promotion: philosophy, prejudice and practice. 2nd ed. Wiley; 2003.
Horowitz JA, Vessey JA, Carlson KL, Bradley JF, Montoya C, McCullough B. Conducting school-based focus groups: lessons learned from the CATS project. J Pediatr Nurs. 2003;18(5):321–31.
Aneshensel CS, Phelan JC, Bierman A. The sociology of mental health: surveying the field. Handbook of the Sociology of Mental Health. Springer; 2013. pp. 1–19.
Rost M, Favaretto M, De Clercq E, Philosophy. Ethics Humanit Med. 2022;17(1):15.
Hunt X, Shakespeare T, Vilyte G, Melendez-Torres GJ, Henry J, Bradshaw M, et al. Effectiveness of social inclusion interventions for anxiety and depression among adolescents: a systematic review. Int J Environ Res Public Health. 2023;20(3):1895.
Choukas-Bradley S, Roberts SR, Maheux AJ, Nesi J. The perfect storm: a developmental–sociocultural framework for the role of social media in adolescent girls’ body image concerns and mental health. Clin Child Fam Psychol Rev. 2022;25(4):681–701.
Download references
Acknowledgements
We thank all participants and schools for their time. Data and the materials necessary to reproduce the analyses presented here are not publicly accessible, but the analytic code is available from the first author upon reasonable request. The analyses presented here were not preregistered.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Open access funding provided by Karlstad University.
Author information
Authors and affiliations.
Department of Health Sciences, Karlstad University, Karlstad, Sweden
Sven Hassler, Louise Persson & Linda Beckman
School of Behavioural, Social and Legal Sciences, Örebro University, Örebro, Sweden
Siri Jakobsson Støre
Department of Social and Psychological Studies, Karlstad University, Karlstad, Sweden
Department of Health Services Research, Management and Policy, University of Florida, Gainesville, US
Linda Beckman
You can also search for this author in PubMed Google Scholar
Contributions
Sven Hassler (SH) Siri Jakobsson Støre (SJS) Louise Persson (LP) Linda Beckman (LB) criteria. Author Initials Made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; SH, SJS, LP, LB. Involved in drafting the manuscript or revising it critically for important intellectual content; SH, SJS, LP, LB. Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; SH, SJS, LP, LB. Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; SH, SJS, LP, LB.
Corresponding author
Correspondence to Sven Hassler .
Ethics declarations
Ethics approval and consent to participate.
The study has been performed in accordance with the Declaration of Helsinki and has received approval from the Swedish Ethical Review Authority (No: 2021-06168-01). Participating children (oral and written) and their caregivers (written) received information about the study, emphasizing its voluntary nature, their right to terminate participation at any time, and the assurance that their responses would remain anonymous. Informed and written consent was collected from the caregivers beforehand and written and oral consent from the children was obtained simultaneously with the interviews, which took place approximately two weeks after the first information session.
Consent for publication
Not applicable.
Confirmation of manuscript not previously being published
The content of the manuscript has not been published, or submitted for publication elsewhere.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hassler, S., Støre, S.J., Persson, L. et al. Children’s and adolescents’ views of health and mental health concepts - A qualitative group interview study. BMC Public Health 24 , 2506 (2024). https://doi.org/10.1186/s12889-024-20042-6
Download citation
Received : 02 July 2024
Accepted : 10 September 2024
Published : 16 September 2024
DOI : https://doi.org/10.1186/s12889-024-20042-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Content analysis
- Group interviews
- Health literacy
- Health promotion
- Mental health
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Disability, Equity, and Mental Health Research Webinar Series: Transforming Mental Health Disability Research Through Lived Experience Leadership and Co-Production
This webinar introduced a range of approaches to meaningfully integrate individuals with lived experiences of psychiatric disabilities into mental health research.
Nev Jones, Ph.D. , discussed proven methods of integration and co-creation, including co-production, integration, and co-leadership, and highlighted ways in which the National Institute of Mental Health (NIMH) research portfolio would benefit from greater emphasis on and high standards for meaningful inclusion.
Read the transcript .
About the speaker

Dr. Jones is an assistant professor in the School of Social Work at the University of Pittsburgh, and an interdisciplinary mental health services researcher focused on serious mental illness (SMI). Dr. Jones' work is grounded in her personal and family experiences of schizophrenia and associated experiences with public sector mental health services. She has been a steadfast champion of participatory methods and the integration and co-leadership of individuals and families directly impacted by psychiatric disability in research, policy, and implementation. She currently leads studies focused on early psychosis, community-based SMI services, civil commitment, and poverty and unemployment.
About the Office for Disparities Research and Workforce Diversity’s Disability, Equity, and Mental Health Research Webinar Series
The Office for Disparities Research and Workforce Diversity is hosting a Disability, Equity, and Mental Health Research Webinar Series, which focuses on exploring the health disparities experienced by people with disability. These include disparities in mental health outcomes, which can be further compounded for those with intersecting identities. This webinar series brings together researchers, advocates, and people with lived experience to discuss the intersection of disability, mental health, and race and ethnicity. There will be a special emphasis on how disability intersects with other health disparities populations to contribute to mental health outcomes and ways to increase equity, accessibility, and inclusion and reduce disparities. Additionally, the series explores the notion of mental health conditions as a disability and considers the viewpoints of those with lived experience.
Sponsored by
National Institute of Mental Health, Office for Disparities Research and Workforce Diversity
- All health topics
Popular topics
- Communicable Diseases Department
- Vaccine preventable disease
- Department of Healthier Populations and Noncommunicable Diseases (HPN)
- Universal health coverage
- Research and Innovation
- Planning, Monitoring and Evaluation
- Publications
- News releases
- Media Statements
- Feature stories
- Opinion Editorials
- World Health Day 2024
- Emergency Operations
- Country Health Emergency Preparedness & IHR
- Infectious Hazard Management
- Health Emergency Information & Risk Assessment
- Public health Laboratory services
- Regional Strategic Roadmap for Health Security (2023-2027) endorsed by the Regional Committee
- Nepal Earthquake
- Thailand becomes first in SEAR with WHO classified emergency medical team
- Where we work
- Country Strategy and Support
- Regional Director
- Regional Committee
- Seventy-seventh Session of the WHO Regional Committee
- Collaborating Centers
WHO calls for adolescent responsive health systems, emphasizes on triple dividend benefit
The World Health Organization urged countries in South-East Asia Region to ensure health systems are responsive to the unique needs of adolescents, highlighting its ‘triple dividend’ benefit – immediate, future, and intergenerational.
“Adolescence, from 10 to 19 years of age, is a time of distinctive development - cognitive, social, physical, emotional, and sexual. Adolescents require special attention in national health and development policies, due to their unique needs,” said Saima Wazed, Regional Director WHO South-East Asia in her address to the ongoing three-day ‘Regional Meeting to Achieve Universal Health Coverage for Adolescent Population through Adolescent Responsive Health Systems,’ here.
Investments in adolescent health bring triple dividend - immediate benefit through health promoting positive behaviors and by prevention, early detection, treatment, and rehabilitation. Future benefit by helping inculcate healthy lifestyles resulting in reduction in harmful behaviors and morbidity later in adulthood, and intergenerational benefit by promoting healthy practices during adolescence and preventing risk factors for diseases, the Regional Director said.
There is strong evidence of high cost-effectiveness and benefit cost ratios from investing in adolescent health and well-being – for every dollar invested in adolescent health, there is an estimated 5-10 times return from health, social and economic benefits.
Nearly 670 adolescents die in WHO South-East Asia Region every day. There is a high burden of morbidity due to many causes, ranging from adolescent pregnancy, mental health, nutrition, noncommunicable diseases, self-harm, and more.
While most adolescent health issues are preventable or treatable, there is ample evidence that adolescents face multiple barriers in accessing health care and information, and these challenges were amplified during the COVID-19 pandemic.
Over the past decade, our region has observed significant political, technical, and programmatic advances to prioritize adolescent health and well-being. This has led to favorable policies, and national programs and strategies on adolescent health, including school health. However, funding, lack of accountability, fragmented implementation with poor coverage and quality, and unavailability of quality disaggregated data continue to be among the key challenges, the Regional Director said.
“Our health systems have not achieved the same level of ‘adolescent-centricity’ as other age groups. They, along with the health service delivery platforms, are primarily designed for disease management or for other specific age groups such as mothers, children or adults”, the Regional Director said.
Efforts at the institutionalizing adolescent-friendly services have primarily focused on individual facilities, rather than on institutionalizing adolescent-friendly elements into health systems. They have prioritized sexual and reproductive health, and curative services, rather than comprehensive packages of services which include mental health, non-communicable diseases, prevention of violence, and such, she said.
“Designing and creating adolescent-responsive health systems is vital. There is also a need to incorporate the views of adolescents and their families in designing and implementing these health services. We need to ensure their access to high-quality, inclusive, and respectful health services. Adolescents should be able to avail these services anywhere they choose, and without any restrictions, financial or otherwise. This will also strengthen comprehensive primary health care, moving us closer to our Universal Health Coverage goals,” Wazed said.
The Regional Director reiterated WHO’s commitment to investing in the health of women, girls, adolescents, and vulnerable populations, which is one of the five tactical approaches for a healthier, more equitable and sustainable WHO South-East Asia Region.
Media Contacts
Public Information and Advocacy Unit
WHO South-East Asia Regional Office
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rand Health Q
- v.7(3); 2018 Apr

Understanding mental health in the research environment
Short abstract.
This study aimed to establish what is known about the mental health of researchers based on the existing literature. The literature identified focuses mainly on stress in the academic workforce and contributory factors in the academic workplace.
This study aimed to establish what is known about the mental health of researchers based on the existing literature. There is limited published evidence on the prevalence of specific mental health conditions among researchers. The majority of the identified literature on prevalence relates to work-related stress among academic staff and postgraduate students in university settings.
Survey data indicate that the majority of university staff find their job stressful. Levels of burnout appear higher among university staff than in general working populations and are comparable to “high-risk” groups such as healthcare workers. The proportions of both university staff and postgraduate students with a risk of having or developing a mental health problem, based on self-reported evidence, were generally higher than for other working populations. Large proportions (>40 per cent) of postgraduate students report symptoms of depression, emotion or stress-related problems, or high levels of stress.
Factors including increased job autonomy, involvement in decision making and supportive management were linked to greater job satisfaction among academics, as was the amount of time spent on research. Opportunities for professional development were also associated with reduced stress. UK higher education (HE) and research staff report worse wellbeing, as compared to staff in other sectors, in most aspects of work that can affect workers' stress levels.
The evidence around the effectiveness of interventions to support the mental health of researchers specifically is thin. Few interventions are described in the literature and even fewer of those have been evaluated.
The Royal Society and Wellcome Trust are interested in better understanding the mental health needs of researchers, and what interventions could be used to support them. This reflects the recent focus on mental health among undergraduate students in the UK, and the concern that others in the academic and wider research environment may have mental health needs that have not been as well explored and considered. This study aims to establish what is currently known about the mental health of researchers based on the existing literature.
Over 6 million working-age people in England have a mental health condition at a given time. The most common diagnosable difficulties among working age adults are anxiety and depression, each of which includes a number of different conditions. Less common but still widespread mental health diagnoses include personality disorders and psychoses such as bipolar disorder and schizophrenia. Many people will have more than one diagnosis at a time, or receive different diagnoses over time.
The causes and triggers of poor mental health are complex and not fully understood. There is evidence that the vast majority of people who experience poor mental health in adulthood first experienced difficulties as children, often from a young age. Risk factors for poor mental health include having a parent with mental health difficulties, growing up in prolonged poverty and housing insecurity, experiences of abuse, neglect and bullying, and traumatic experiences during childhood. Some groups of people have a heightened risk of poor mental health, including some black and ethnic minority communities, people with long-term physical conditions, lesbian, gay, bisexual and transgender people, and people with disabilities.
There is mixed evidence about the extent to which a person's experiences of work contribute to their having a mental health difficulty. Survey evidence suggests that workplace factors such as bullying, insecurity and a lack of control are major causes of mental ill health among staff. On the other hand, there is also evidence that work helps many people to recover from an episode of poor mental health, and there is clear evidence that unemployment is a major risk factor for mental and physical ill health.
Mental ill health and work-related stress are key issues for the labour market as they affect productivity through absenteeism and presenteeism, and are associated with high economic costs for individuals, employers and the economy at large. It has been estimated that poor mental health costs employers in the UK £26 billion nationwide each year, equivalent to £1,035 for every employee in the workforce ( Centre for Mental Health, 2007 ).
Little is known about how mental health needs vary across working environments, or about how to tailor interventions to address different working populations.
The aim of this study was to assess what is known about mental health in research environments through a literature review, and it focused on the UK and comparable research systems. A better understanding of researchers' mental health needs will enable the design of more effective interventions to address them, while a better understanding of evidence gaps can also help guide future research efforts in this area. The following research questions guided the study:
- How are “mental health” and “wellbeing” understood in the context of research environments?
- What is currently known about researchers' mental health and wellbeing, and does it differ from that of other populations?
- What interventions are used to support researchers, and what evidence is there of their effectiveness?
- What are the strengths and limitations of the evidence base in this area?
How Are “Mental Health” and “Wellbeing” Understood in Research Environments?
Overall, the existing literature offers little insight into what sets the research environment apart from other workplaces, or into how mental health, stress, and wellbeing are defined in these contexts. Rather, the majority of the literature identified focuses on describing the levels of stress amongst the academic workforce and, in particular, identifying contributory factors within the workplace. There is little available evidence based on objective clinical assessment about the prevalence of clinically defined mental health conditions and their treatment in this context. The focus on wellbeing raises the issue that although the presence of common mental health conditions does correlate with some of the wellbeing scales used commonly in the literature, more serious (e.g. psychotic) mental illnesses are not necessarily aligned with measurement of wellbeing.
The literature is also almost exclusively focused on universities, with many studies covering all university staff, which will include both researchers and non-research staff. Some studies focused more specifically on researchers, and a more limited group within that looked at particular groups of researchers—most commonly PhD students, reflecting the wider focus on (typically undergraduate) students in the literature around this topic. The majority of the existing research is based on survey data, which is subject to sampling biases, relies on self-reporting, and was not triangulated with other objective indicators, such as absence data.
What Is Currently Known About Researchers' Mental Health and Wellbeing, and How It Differs from Other Populations?
Evidence on the prevalence of work-related stress and mental health problems.
Despite widely reported anecdotal evidence and press coverage of a “mental health crisis” in academia, there is limited published evidence regarding the prevalence of specific mental health conditions among researchers. The majority of the literature on prevalence identified through this review relates to the experience of work-related stress (and arguably the risk of developing a mental health condition as a result of exposure to identified stressors) among academic staff and postgraduate students in university settings.
- Survey data indicate that the majority of university staff find their job stressful. Levels of burnout appear higher among university staff than in general working populations and are comparable to “high-risk” groups such as healthcare workers.
- The proportions of both university staff and postgraduate students with a risk of having or developing a mental health problem, based on self-reported evidence, were generally higher than for other working populations.
- Large proportions (>40 per cent) of postgraduate students report symptoms of depression, emotion or stress-related problems, or high levels of stress.
UK national statistics indicate that only 6.2 per cent of staff disclosed a mental health condition to their university, though academics have been found to be among the occupational groups with the highest levels of common mental disorders with prevalence around 37 per cent. It should be noted, however, that prevalence may generally be over-reported in surveys of occupational groups.
Personal Factors That Contribute to Mental Health Outcomes in the Research Workplace
Gender was the key personal factor that emerged as a determinant for mental health (or its reporting), with women reporting more exposure to stress than men, as well as greater challenges around work-life balance. There was also evidence that personality and perceived competence affect mental health as self-critical personalities are more susceptible to stress, though it is also possible that they are more aware of it or more willing to report it. However, it was unclear whether stress was a result of working conditions in the research environment, or whether research settings attracted particular types of individuals. The results on whether age affects mental health were inconclusive, partly as age is often difficult to disentangle from discussions about rank and seniority. Other factors such as disability, sexuality and minority status were mentioned in a small number of articles in the sample, and these articles indicated that these personal factors generally increase stress.
Environmental Factors Commonly Considered in Surveys of Mental Health and Wellbeing in Workplaces
Based on the Health and Safety Executive's framework, and evidence from the wider literature, we identify six key aspects of work that can affect workers' stress levels: work demands, job control, change management, work relationships, support provided by managers and colleagues, and clarity about one's role.
- These aspects of the work environment can be sources of stress or they can help counteract it.
- Findings from studies of university staff and researchers were consistent with the wider understanding of factors that contribute to stress in workplaces.
- Factors including increased job autonomy, involvement in decision making and supportive management were linked to greater job satisfaction among academics, as was the amount of time spent on research. Opportunities for professional development were also associated with reduced stress.
UK higher education (HE) and research staff report worse wellbeing in most of the six aspects, as compared to staff in other sectors.
- In large-scale surveys, UK higher education staff have reported worse wellbeing than staff in other types of employment (including education, and health and social work) in the areas of work demands, change management, support provided by managers and clarity about one's role.
- The only area where higher education staff have reported higher wellbeing in large-scale surveys is in job control, though even here results are mixed across studies. Wide variability was seen among respondents in relation to the level of support provided by managers and colleagues.
- Job insecurity (real and perceived) appears to be an important issue for those working in the research environment, and particularly for early-career researchers, who are often employed on successive short-term contracts.
PhD students face similar challenges to other researchers and higher education staff.
- The main factors associated with development of depression and other common mental health problems in PhD students are high levels of work demands and work-life conflict, low job control, poor support from the supervisor and exclusion from decision making.
- Believing that PhD work is valuable for one's future career helps reduce stress, as does confidence in one's own research abilities.
Some studies suggested that changes to the UK higher education system had brought increased job stress.
- These studies discussed changes that had occurred in the UK higher education system from the 1990s onwards, and had resulted in increased emphasis on accountability, efficiency and performance management. Study authors suggested that these changes could have brought about increases in job stress for staff working in this system.
- However, data explicitly linking the changes to an increase in stress are limited, partly due to a lack of comparable data from before the 1990s.
Staff who can devote a large proportion of their working time to research have better wellbeing.
- Studies found that spending a larger percentage of one's time on research was associated with reduced stress, and that research-only staff reported lower levels of work-life conflict and had better wellbeing than other higher education institution (HEI) staff. However, this may be to some extent confounded by other characteristics of such researchers (e.g. they may be more senior).
Research on emotionally challenging topics can put staff wellbeing at risk.
- Studies showed that staff involved in research on sensitive topics, such as trauma or abuse, may be emotionally affected by the material they encounter in their work and should receive greater support to mitigate the negative impacts of this work.
Outcomes Related to Poor Mental Health and Wellbeing
In addition to considering the extent to which individuals in research environments suffer from mental health issues, it is important for employers and institutions to recognise that these issues have further implications:
- Job stress and poor workplace wellbeing can contribute to reduced productivity—both through absence and, more importantly, through presenteeism, where researchers attend work and are less productive.
- They can also lead to lower levels of commitment to their research and to institutions—which can be seen in high levels of turnover and through negative attitudes in the workplace.
- Effects on job satisfaction are less clear because of the satisfaction researchers gain from intrinsic factors such as the intellectual stimulation of their work. Several studies note that high levels of job-related stress can coexist with high levels of job satisfaction.
- Effects can also spill over into personal and family life.
The overall effects of these negative outcomes on the sector have not been fully quantified, but estimates drawing on broader experience suggest that the costs could be high. An estimate from Shutler-Jones et al (2008) which has several caveats and assumptions, suggests that the costs to the UK HE sector could be more than £500 million per year (c. 5 per cent of the sector's total annual income). Costs to the economy and the country more widely could also be significant due to the lost potential for scientific advances and due to impacts on the availability of research talent if PhD students fail to complete their studies or choose to leave research subsequently.
What Interventions Are Used to Support Researchers, and What Evidence Is There of Their Effectiveness?
Though poor mental health at work is often related to difficulties that are not caused by work (e.g. childhood adversity, family life and other stressors), support in the workplace can offer benefits. However, the evidence around the effectiveness of interventions to support the mental health of researchers specifically is thin. Few interventions are described in the literature and even fewer of those have been evaluated. Where evaluations have been conducted, they are often of limited utility, either because of the evaluation design or the length of follow-up.
Interventions typically focus on stress and wellbeing rather than clinical mental health conditions, reflecting the wider focus in the literature as described above. In addition, the majority of interventions identified aim to support researchers to deal with workplace stress, but they may not be effective in addressing the root causes of that stress or stresses relating to life outside work. The interventions identified can be broadly classified into four groups: policy changes, communication activities, training, and health-promotion activities.
Focusing specifically on the UK, a range of interventions were piloted and evaluated (to a limited extent) as part of a wellbeing initiative by the Higher Education Funding Council for England (HEFCE) around 2009–2011. These offer scope for further investigation and potentially evaluation now that more time has elapsed. Additionally, the project, though completed in 2011, has spawned a network that is now managed by the Universities and Colleges Employers Association (UCEA), which may offer a route to identify further ongoing initiatives and potentially a space to pursue and evaluate efforts to address these issues in the HE sector.
What Are the Strengths and Limitations of the Evidence Base in This Area?
The existing evidence base is limited, meaning it is not possible to draw robust conclusions about the mental health status and needs of researchers, and how researchers may differ from other populations in this regard. More work is needed to understand both the mental health needs of researchers and how they can be addressed. Particular gaps include the effectiveness of interventions, prevalence of specific mental health needs (rather than stress) among researchers, and any evidence about researchers outside the academic setting. There are also limitations to the quality and design of many of the studies conducted, such as lack of long-term follow-up and absence of control groups.
Based on the evidence gaps identified and the information available, we suggest the following avenues for further research on this topic:
- Study the prevalence of mental health conditions amongst postdoctoral researchers: Further work on prevalence could use a targeted approach building on the recent work by Levecque et al. (2017) , who used a survey to assess the presence of psychological distress and potential psychiatric disorders in a sample of PhD students and compared the results to those of three other sample populations, and Eisenberg et al. (2007) , who surveyed a sample of undergraduate and postgraduate university students to assess prevalence of depressive and anxiety disorders and took steps to address the issue of non-response bias. In particular, we suggest a similar study focusing on postdoctoral researchers, a group that is particularly poorly addressed in the existing literature.
- Map mental health policies and procedures at UK HEIs: The current standard of mental health policies and procedures in UK research institutions is not well understood. We suggest that a mapping of the current policies in place across institutions could be valuable, and could build on standards such as those set out in the Mindful Employer Charter ( Mindful Employer, 2017 ).
- Evaluate the interventions introduced through the HEFCE wellbeing and engagement initiative: The wellbeing initiative established by the HEFCE and subsequently maintained as a network by UCEA offers a range of interventions for evaluation. In the project reporting in 2011, many of the institutions noted that it was too soon to tell whether their interventions had been effective. Though these initiatives generally focus on wellbeing rather than clinical mental health conditions, there is scope to explore with the relevant institutions whether those interventions have developed over the years, and whether data are now available (or could be collected) to provide more useful evaluation of the interventions introduced.
- Investigate and develop the HSE management standards as a framework for workplace mental health management in research environments: As well as providing a framework for workplace stress used in several important surveys, the Health and Safety Executive (HSE) have also set out management standards that describe an approach to identifying sources of workplace stress and addressing them at an organisational level. It could be useful to work through that approach with a university or a research organisation to identify the mechanisms at play in those environments. Doing so could establish the relevance of the approach in this context, and potentially provide a model that could be used more widely in the sector.
- Conduct more and higher-quality evaluations of mental health interventions and publish their results: Broadly, better-quality evaluations are needed to identify what works in this area. There is a need for high-quality studies to test the effectiveness of interventions.
The research described in this article was prepared for the Royal Society and the Wellcome Trust and conducted by RAND Europe.
- Centre for Mental Health. Mental health at work: Developing the business case. 2007. 2017. http://www.centreformentalhealth.org.uk/Handlers/Download.ashx?IDMF=4c278a50-8bd6-4aff-9cf3-7667c0770288 As of May 30.
- Eisenberg D., Gollust S. E., Golbertstein E., Hefner J. L. “Prevalence and correlates of depression, anxiety, and suicidality among university students.” American Journal of Orthopsychiatry. 2007; 77 (4):534–542. [ PubMed ] [ Google Scholar ]
- Levecque K., Anseel F., De Beuckelaer A., Van der Heydan J. and Gisle L. “Work organization and mental health problems in PhD students.” Research Policy. 2017; 46 (4):868–879. [ Google Scholar ]
- Mindful Employer. “Charter for employers”. 2017. http://www.mindfulemployer.net/charter/ As of June 10, 2017.
- Shutler-Jones K. Improving performance through well-being and engagement. 2011. 2017. http://www.qub.ac.uk/safety-reps/sr_webpages/safety_downloads/wellbeing-final-report-2011-web.pdf As of June 10.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Press Releases
DHS Awards $18 Million to Law Enforcement, Public Health, and Nonprofits in Underserved Communities to Help Prevent Targeted Violence and Terrorism
Today, the Department of Homeland Security (DHS) awarded 35 grants, totaling $18 million, under the Targeted Violence and Terrorism Prevention (TVTP) Grant Program for Fiscal Year 2024 (FY24). The TVTP Grant Program provides financial assistance to eligible applicants to develop sustainable, multidisciplinary targeted violence and terrorism prevention capabilities in local communities, to pilot innovative prevention approaches, and to identify prevention best practices that can be replicated in communities across the country.
"In our current dynamic threat environment, any town, anywhere can be a target,” said Secretary of Homeland Security Alejandro N. Mayorkas . “The Department of Homeland Security’s Targeted Violence and Terrorism Prevention grant awards announced today will help local communities pilot, strengthen, and share evidence-based prevention strategies, significantly expanding our nation’s counterterrorism capacity and making all of us safer.”
Leveraging a public health-informed approach, the Center for Prevention Programs and Partnerships (CP3) brings together behavioral and mental health providers, educators, faith leaders, social service providers, nonprofits, law enforcement, and other state, local, and community partners to address systemic factors that can lead to violence while strengthening protective factors at the local level that support the safety, well-being, and resiliency of communities in the U.S. This focus has also led to an increase in public health organizations applying for the grant program. In FY24, 35 public health entities applied and 7 were selected, compared to 3 applicants and 2 awardees in FY23. Public health organizations receiving an award include:
- Boston Children’s Hospital
- Indiana Family and Social Services Administration, Division of Mental Health and Addiction
- Oakland Community Health Network
- Parents for Peace
- Rhode Island Department of Health
- Safe States Alliance
- University of Nebraska Medical Center
- Weber-Morgan Health Department
- Wood County Alcohol, Drug Addiction, and Mental Service Board
Given widespread concern regarding youth involvement in targeted violence nationally, CP3 selected 20 grantees focused wholly or in part on prevention in youth settings, including grants to improve clinical practice with at-risk youth (Boston Children’s Hospital) and upskilling behavioral threat assessment and management tools for at-risk youth (Safe States Alliance). Awardees include:
- Auburn University
- Board of Regents, Nevada System of Higher Education
- Dillard University
- Elizabeth City State University
- Green River Educational Cooperative
- Independent Production Fund
- Jewish Federation of Greater Pittsburgh
- North Carolina State University
- School Administrative Unit #18
- Southern University
- Southern Illinois University
- The Research Foundation for the State University of New York on behalf of the Rockefeller Institute of Government
- The Research Foundation for the State University of New York on behalf of the University at Buffalo
- Trustees of Indiana University
- University of Southern Maine
DHS prioritizes targeted violence and terrorism prevention in underserved communities and has continued its outreach to these areas in recent award cycles, including FY24. This year, the TVTP Grant Program received 39 applications from, or proposing to do work with, underserved communities. CP3 awarded 8 grants that provide services to underserved populations, including one tribal government, three Historically Black Colleges and Universities (HBCUs), one LGBTQ+ serving institution, one organization serving religious minorities, and two organizations serving rural communities. Awardees include:
- Otoe-Missouria Tribe
CP3’s financial and technical assistance helps grow the TVTP community of practice. The FY24 awards have created approximately 50 new prevention jobs in addition to the dozens of existing positions that will be partially or fully funded by these awards.
Launched in 2020, the program, administered by the DHS CP3 and the Federal Emergency Management Agency (FEMA), is the only federal grant program solely dedicated to helping local communities develop and strengthen their targeted violence and terrorism prevention capabilities in this area. DHS awarded nearly $90 million via 178 awards to organizations working to prevent violence in 41 states plus the District of Columbia.
To date, TVTP grant programs have conducted training sessions that built prevention capacity among 38,250 attendees. This program has also funded projects that directly address and manage cases involving individuals with behavioral indicators for violence. As of August 2024, grantees from FY20-FY23 have opened 1,172 cases and referred them to partners or provided direct mental health counseling, social services, and other services to increase protective factors in these clients.
The anticipated next round of TVTP grant funding will be announced in spring 2025. Additional information about current and previous TVTP grantees, such as programs, tools, resources, accomplishments, closeout reports, award grants, and more can be found on the TVTP Grant Program webpage . These resources support prevention practitioners in advancing their work and reaffirm DHS’s commitment to transparency.
- Preventing Terrorism and Targeted Violence
- Center for Prevention Programs and Partnerships (CP3)
- Grant Funding
- Targeted Violence and Terrorism Prevention (TVTP)
- Targeted Violence and Terrorism Prevention (TVTP) Grant Program

IMAGES
VIDEO
COMMENTS
Research questions about anxiety and depression. Anxiety and depression are two of the most commonly spoken about mental health conditions. You might assume that research about these conditions has already been exhausted or that it's no longer in demand. That's not the case at all. According to a 2022 survey by Centers for Disease Control ...
In the context of increasing prevalence of youth and young adult mental health problems, 1, 2 including university students, 3 concern about mental health in the university setting is mounting and gaining media and public attention. 4 Increasing demand for services on campus has been observed internationally. 2, 3 However, current approaches lack a solid evidence base, 5, 6 and students have ...
Overview: Mental Health Topic Ideas. Mood disorders. Anxiety disorders. Psychotic disorders. Personality disorders. Obsessive-compulsive disorders. Post-traumatic stress disorder (PTSD) Neurodevelopmental disorders. Eating disorders.
The research questions for this study were (1) to map general characteristics of published literature focusing on the young people's experiences of seeking help for mental health problems, and (2) to explore how the previously published theoretical model Lost in Space could be further refined and complemented via an abductive approach ...
In 2021, the Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) published an inventory, which identified over 2000 evidence gaps in mental health1 from the two known international database of evidence gaps: the SBU Evidence Gap database, which is continuously updated, and the former UK Database of Uncertainties about the Effects of Treatments. Within the ...
Sadly, psychological distress among young people seems to be rising. One study found that rates of depression among a nationally representative sample of US adolescents (aged 12 to 17) increased ...
Introduction. Childhood and adolescence are critical periods to promote mental health as more than half of mental health problems start at these stages, and many of these persist throughout adult life (Kessler et al., 2005).Currently, this has become a priority as worldwide data shows an increase in the prevalence of mental health issues in childhood and adolescence (de la Barra M, 2009) and ...
The National Institute of Mental Health (NIMH), part of the National Institutes of Health (NIH), is the lead federal agency for research on mental disorders, supporting research that aims to transform the understanding and treatment of mental illnesses through basic and clinical research. Learn more about NIMH-funded research areas, policies ...
This unique study aims to assess age differences in the reporting of mental health issues using question based computational language assessments (QCLA), which to the best of our knowledge has not ...
The second major priority setting exercise was conducted in 2011, when the Grand Challenges in Global Mental Health initiative identified research priorities for the following 10 years. The main priority was given to research questions that: identify root causes, risks, and protective factors. advance prevention and implementation of early ...
UK university students ( N = 385) submitted 991 questions, categorised into seven themes: epidemiology, causes and risk factors, academic factors and work-life balance, sense of belonging, intervention and services, mental health literacy and consequences. Across themes, respondents highlighted the importance of understanding the experience ...
Conduct disorder among children. Role of therapy in behavioural disorders. Eating and drinking habits and mental health. Addictive behaviour patterns for teenagers in high school. Discuss mental implications of gambling and sex addiction. Impact of maladaptive behaviours on the society. Extreme mood changes.
Education and training regarding psychosocial issues should be provided to health system leaders, first responders, and health care professionals. The mental health and emergency management ...
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health. Mental health tops the list of worries that U.S. parents express about their kids' well-being, according to a fall 2022 Pew Research ...
Common Mental Health Research Questions. Curious to know the top research questions related to mental health worldwide? Tomlinson et al. (2009) identified some of the key priorities for researchers to look at. The group came up with 55 questions, and the top three topics included: Health policy and systems research topics - e.g.,
Mental health. Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community. It has intrinsic and instrumental value and is integral to our well-being. At any one time, a diverse set of individual, family, community and ...
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and implementation.
Social media (Jacobsen & Forste, Citation 2011) and financial difficulty resulting from increased tuition fees (Gani, Citation 2017) have both been suggested but have little research evidence. Most mental health problems develop in early life, with the onset of 75% of lifetime mental disorders occurring by age 25 years (Kessler et al., Citation ...
Impact on mental health. Mental health is defined as a state of well-being in which people understand their abilities, solve everyday life problems, work well, and make a significant contribution to the lives of their communities [].There is debated presently going on regarding the benefits and negative impacts of social media on mental health [9,10].
COVID-19 is a disease caused by a virus named SARS-CoV-2. COVID-19 most often affects the lungs and respiratory system, but it can also affect other parts of the body. Some people develop post-COVID conditions, also called Long COVID . These symptoms can include neurological symptoms such as difficulty thinking or concentrating, sleep problems ...
We provided you some information about mental health resources, but I wanted to follow-up and offer any other information you might want to get help. Resources. To assist investigators with identifying counseling resources, COUHES provides the following: Conducting Research on Mental Health Topics - Participant Counseling Resources [PDF]
Background: Doctors report high rates of workplace stress and are at increased risk of mental health disorders. However, there are few real-world studies evaluating the effectiveness of interventions aimed at addressing workplace risk factors and improving doctors' mental health in a hospital setting. This study was conducted over two years (2017-2019) to assess the effects of a multi ...
Some main topics of interest are: Ways in which AI can be used in research on mental health The use of AI to improve the learning methods of healthcare professionals. The use of AI in decision-making in mental health AI as a tool for predicting adverse effects of treatments AI as a tool to increase patient adherence, as well as to support ...
Topics in Psychology. Explore how scientific research by psychologists can inform our professional lives, family and community relationships, emotional wellness, and more. ... Parenting mitigates social media-linked mental health issues. Gallup. Survey conducted between June 26-July 17, 2023, with responses by 6,643 parents living with ...
The participants discussed mental health problems to a greater extent than positive mental health. An implication of this study is the highlighted need to focus more on mental health promotion in future preventive programs. ... Leeson C. Asking difficult questions: exploring research methods with children on painful issues. Int J Res Method ...
Abstract. Social media platforms are popular venues for sharing personal experiences, seeking information, and offering peer-to-peer support among individuals living with mental illness. With significant shortfalls in the availability, quality, and reach of evidence-based mental health services across the United States and globally, social ...
The Office for Disparities Research and Workforce Diversity is hosting a Disability, Equity, and Mental Health Research Webinar Series, which focuses on exploring the health disparities experienced by people with disability. These include disparities in mental health outcomes, which can be further compounded for those with intersecting identities.
The World Health Organization urged countries in South-East Asia Region to ensure health systems are responsive to the unique needs of adolescents, highlighting its 'triple dividend' benefit - immediate, future, and intergenerational."Adolescence, from 10 to 19 years of age, is a time of distinctive development - cognitive, social, physical, emotional, and sexual. Adolescents require ...
Short abstract. This study aimed to establish what is known about the mental health of researchers based on the existing literature. The literature identified focuses mainly on stress in the academic workforce and contributory factors in the academic workplace. Keywords: Depression, Scientific Professions, Workforce Management, Workplace ...
Leveraging a public health-informed approach, the Center for Prevention Programs and Partnerships (CP3) brings together behavioral and mental health providers, educators, faith leaders, social service providers, nonprofits, law enforcement, and other state, local, and community partners to address systemic factors that can lead to violence ...