Quiz 11: Critical Thinking and the Nursing Process
Access For Free
Multiple Choice
A nurse who just moved from an urban area to a sparsely populated rural area understands that certain customs and practices the nurse is familiar with may be quite foreign to the people in the new area. This nurse is practicing which of the attitudes of critical thinking?
A nurse uses an example of divergent thinking, when a client states, "I think I have a tumour", by saying:
A client comes into the clinic with complaints of "extreme" low back pain after helping to move a heavy object. The client is pale and diaphoretic and walks bent at the waist. Before taking vital signs, the nurse projects that the blood pressure as well as heart rate will be elevated. This is an example of which of the following?
A rehab client has a treatment plan for active range of motion exercises to her shoulder following a stroke. The client doesn't like to do these because they are uncomfortable and she has little insight into the treatment. Which of the following demonstrates the critical-thinking component of creativity?
A new graduate nurse learns a quicker way to set up and initiate an IV. This graduate nurse still follows safe practice, but implements changes that help with time management. This nurse is practicing which of the attitudes of critical thinking?
Nurses must use critical thinking in their day-to-day practice, especially in circumstances surrounding client care and wise use of resources. In which of the following situations would critical thinking be most beneficial?
A nurse continues to question the practice of administering rectal suppositories to residents in a long-term care facility at bedtime, rather than earlier in the day. She is told that this is the best time for staff and that's the routine that has been practiced for a long time. The nurse continues to research whether there would be a better time, especially in the best interest of the residents. This nurse is practicing which of the critical-thinking attitudes?
A nurse educator has always believed that lectures with focused outlines are the best way to present theory content in class. A colleague, who teaches the same group of students, but a different subject, utilises group work and in-class activities to teach difficult content and finds that students perform as well, or better, on their tests. The first educator in this situation is starting to rethink her position. This is an example of which of the following?
A client has just been admitted, is complaining of shortness of breath, has no pallor, no cyanosis and no accessory muscle use with respirations. The client's respiratory rate is 16 breaths per minute. The nurse is performing the assessment and continues to ask herself how the client's report and the physical findings conflict. This nurse is using which universal standard of critical thinking?
A nurse is checking over the past charting of the previous shift, paying special attention to how a particular client responded to nursing interventions throughout the day. The nurse is caring for this client and wants to see what has been effective, as well as what didn't work. This nurse is utilising which of the steps of the decision-making process?
A client comes into the emergency department (ED) with a productive cough, audible coarse crackles, elevated temperature of 40.2 °C, high respiratory rate, chills and body aches. The nurse identifies the problem as respiratory compromise. The nurse is using which of the following?
A seasoned nurse works in a busy ICU unit. When a particularly complex client is admitted, the nurse uses past experiences and knowledge gained from those situations to help care for this client. This nurse is practicing which of the attributes of critical thinking?
A nurse is interviewing a client who claims that she refuses to have immunisations because they are harmful. Using Socratic questioning about this assumption, the nurse would state:
A nurse is caring for a client who has unstable cardiac dysrhythmias. The client has orders for medications, one of which is by oral route, the other by IV delivery. The nurse realises that the IV route would be fastest, but is also concerned about the side effects that this drug may produce and the fact that the client has never taken the drug, so any adverse effect is unknown. The nurse is implementing which step of the decision-making process?
An experienced nurse educator senses that a student has been struggling with clinical skills learned in lab. In the clinical area, this student is usually lagging behind and seems to be minimally involved when the other students have opportunities to perform some of the tasks. The educator pairs the student with a particularly outgoing staff nurse who has a number of unique clients with a variety of treatments and cares. The educator is utilising which step in the decision-making process?
A nurse is completing a plan of care for a client. The statement, "Client will be able to walk three metres, twice a day without shortness of breath", is which part of the nursing process (in comparison to the decision-making process) ?
A nurse is taking an admission history from a client who is easily distracted and offers much information about his health and social history. Although careful to document what the client relates, the nurse sorts out the relevant data to determine the best nursing care for this client. This nurse is practicing which attribute of critical thinking?
Nursing in a complex environment requires nurses to be able to think critically. The key to critical thinking is:
Which one of the following is not a trait that nurses must develop for critical thinking?
A student nurse is being taught about how to promote wound healing. As part of critical thinking, this student is being taught about previously learned information as well as new information. Critical-thinking skills are used in various ways, for example:
showing 1 - 20 of 29
Related Quizzes
Historical and Contemporary Nursing Practice
20 Questions
Nurse Education, Research and Evidence-Based Practice
28 Questions
Nursing Theories and Conceptual Frameworks
30 Questions
Legal Aspects of Nursing
Values, Ethics and Advocacy
24 Questions
Health Care Delivery Systems
Community Health
Regional, Rural and Remote Nursing
19 Questions
Health Informatics
26 Questions
29 Questions
Implementing and Evaluating
Documenting and Reporting
Health Promotion
Health, Wellness and Illness
18 Questions
Culture, Nursing and Indigenous Health
Complementary and Alternative Therapies
27 Questions
Concepts of Growth and Development
Promoting Health From Conception Through to Adolescence
Promoting Health in Young and Middle-Aged Adults
Promoting Health in Older Adults
Promoting Family Health
Communicating
25 Questions
Teaching and Learning
32 Questions
Leading and Managing
Vital Signs
Health Assessment
Infection Prevention and Control
Diagnostic Testing
Medications
33 Questions
Skin Integrity and Wound Care
Perioperative Nursing
Sensory Perception
23 Questions
Self-Concept
Spirituality
Stress and Coping
Loss, Grieving and Death
21 Questions
Mental Health Nursing
Activity and Exercise
Pain Management
Urinary Elimination
Faecal Elimination
Oxygenation
31 Questions
Circulation
Fluid, Electrolyte and Acidbase Balance


ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Nursing Process: A Comprehensive Guide
In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse ‘s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
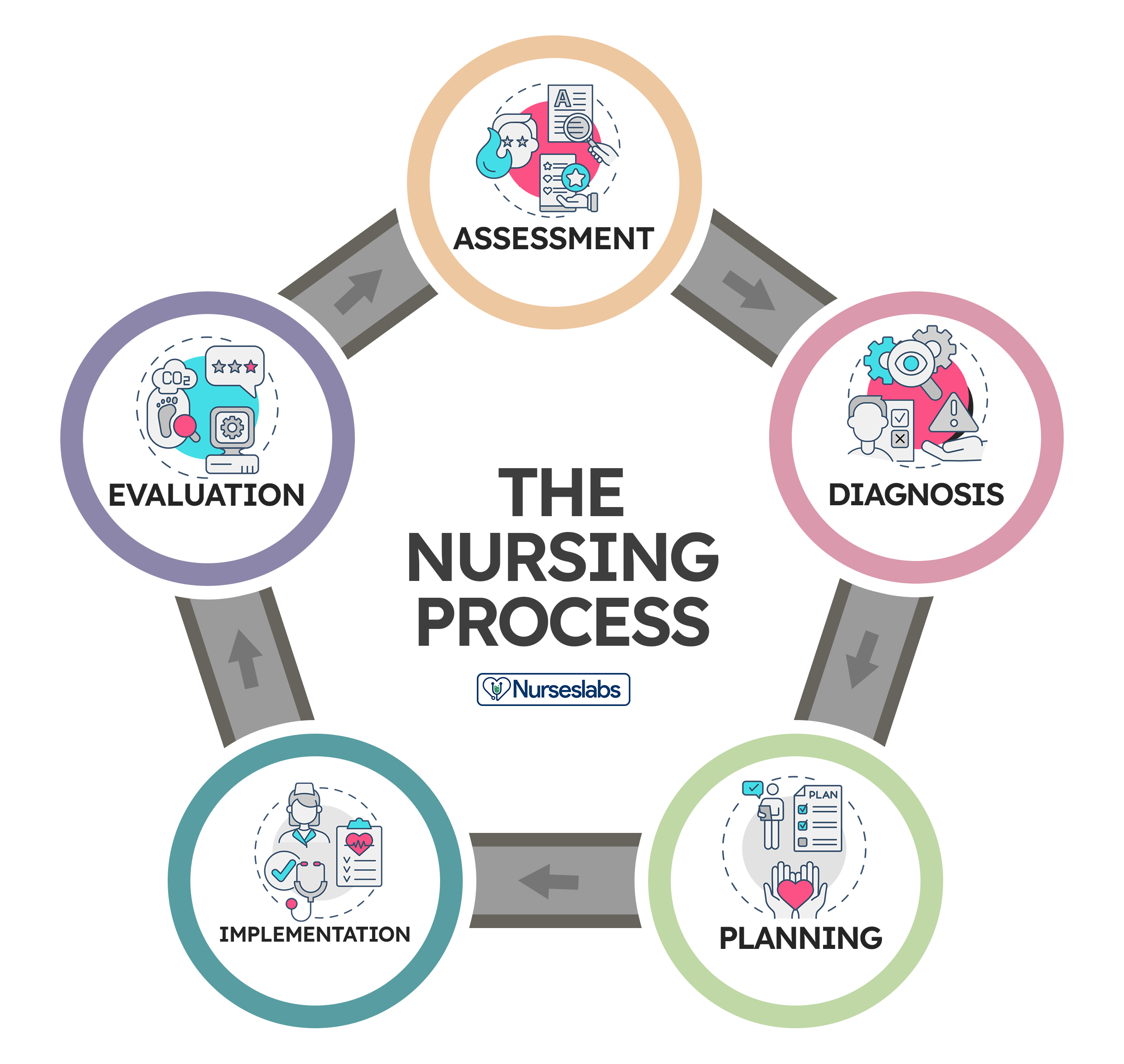
Application of the fundamental principles of critical thinking , client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care .
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation . The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch , smell , or hearing , and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure , vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance , facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members , support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history , which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation .
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste ) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care .
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions . When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement , and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration, educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking , to reduce the patient’s anxiety , anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing , administering an injection, manipulating equipment, bandaging, moving , lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non- RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory, nursing practice , and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan , and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan .
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
39 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
Leave a Comment Cancel reply
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Critical Thinking, Clinical Judgment, and the Nursing Process
9 Critical Thinking, Clinical Judgment, and the Nursing Process Brenda Morris, EdD, RN, CNE OBJECTIVES At the completion of this chapter, the reader will be able to: • Define critical thinking. • Describe the components and characteristics of critical thinking. • Understand the relationship of critical thinking to clinical judgment and the nursing process. • Describe the steps of the nursing process and the relationships among those steps. • Discuss nursing activities associated with each step of the nursing process. • Evaluate the utility of the nursing process as a systematic framework for the delivery of nursing care. • Apply critical thinking in nursing practice situations. The author acknowledges the important foundational work for this chapter developed by Dr. C. Fay Raines in the previous edition of this book. PROFILE IN PRACTICE Elizabeth R. Lenz PhD, RN, FAAN Dean and Professor, College of Nursing, The Ohio State University, Columbus, Ohio Critical thinking: it’s recognizable when someone does it well and certainly evident when it is not happening. During the past 20 years we have talked increasingly about critical thinking in nursing, but that wasn’t always the case. In the early 1960s, when I was entering the profession, serious efforts to change the “handmaiden” image of nursing were only just beginning. Clearly, if one’s role is defined as handmaiden, rather than as colleague or independent decision maker, critical thinking is not deemed particularly important or even desirable. Rather, blind, noncritical obedience is the order of the day. Fortunately, as nursing has become more truly professional and nurses have functioned with increasing autonomy in increasingly complex situations, critical thinking has become a most important and valued competency. What elements converge to produce a good critical thinker? It seems to me that there are several requisites, not the least of which is intelligence. However, even though intelligence is a necessary condition, critical thinking is not guaranteed to occur without training and a nourishing environment as well. We assume that critical thinking is something that can be learned; hence we address it at all levels of nursing curricula. Based on my experience, I believe that two essential types of learning provide the basis for critical thinking. The first is substantive. It is impossible to think truly critically about something you do not understand or about which you possess only partial information. Mastery of the theory and research findings that relate to the problem or issue to be addressed is critical, but this is not something that nurses always take time to achieve. Unfortunately, we have been less successful than other professions (namely, medicine) in socializing our practitioners to value learning as a career-long pursuit; yet pursuit of the most state-of-the-science information is an essential ingredient of critical thinking. The second type of learning involves the process of critical thinking itself. The skills of raising questions, using logic, and comprehensively considering alternative perspectives, explanations, and courses of action can often best be learned experientially within a structure that encourages and, in fact, mandates that kind of thoughtful consideration. The model that comes to mind is the daily medical rounds in which physicians-in-training are challenged to present cases and to lay out their diagnostic reasoning clearly for others to critique. Equally valid as an environment for cultivating critical thinking is that found in many of the social sciences and humanities, where freewheeling debate and open challenge of ideas are encouraged. At first frightened by that kind of candor during my doctoral studies in sociology, I later came to value greatly the critical input of my peers. More of that kind of willingness to challenge one another’s assumptions and ideas within an atmosphere of mutual respect would benefit our profession. For me, the groundwork for critical thinking was laid early in my education. Fortunately, the faculty responsible for the BSN program I attended were forward-thinking and highly committed to the emerging definition of nursing as a true profession, with the requisite obligation to base action on scientific knowledge and clear and logical thinking. Without labeling the goal as such, we were consistently encouraged, groomed, and enabled to be critical thinkers. We were continually challenged by being asked to provide rationales for our decisions, to make explicit all of the alternative approaches and explanations we had considered and rejected, and to explain why. Not inconsequentially, the school was in a small liberal arts institution, where we were exposed on a daily basis to a wide range of points of view and disciplinary perspectives and assumptions. If anything, the nursing students were the “oddballs” whose pragmatism and goal-directedness seemed strange to the arts, sciences, and music majors. I wrestled more than once with how in the world assignments such as dissecting the symbolism in Moby Dick might be relevant to my career in nursing, but I now appreciate the mind-expanding contribution that such activities made to my ability to think critically. The base hopefully having been laid during one’s professional education, critical thinking depends not only on training but also on an environment or context that enables, encourages, and rewards it. Regretfully, today’s employment picture in nursing is typically one with precious little time for contemplation. Downsizing, high proportions of nonprofessional personnel, high levels of acuity, and high productivity requirements may discourage critical thinking. That means every effort must be made to counter the tendency to let critical thinking slide and, instead, to encourage, nurture, and reward it, even if that means bucking the tide and incurring some additional short-term costs. The “community of scholars” type of environment to which top educational institutions aspire should, by definition, be conducive to critical thinking. Nevertheless, even in those settings, time and energy to engage in deliberation, to exchange ideas, and to critique those ideas openly are scarce, and the kind of culture that encourages such scholarly dialogue is relatively rare. When it is in place, it is wonderful. One of my most exciting opportunities to engage in intense and prolonged critical thinking occurred when a group of four colleagues and I were “freed up” from many of our routine responsibilities to plan a doctoral program “from scratch.” In weekly full-day sessions we argued, debated, challenged, cajoled, compromised, and created. We drew on what we knew substantively about nursing, science, philosophy, and the disciplines of our respective doctoral degrees (none of which were in nursing). It was hard work, but invigorating. The ground rules were that no idea was to be belittled or rejected out of hand; all perspectives were heard and considered. We were given time to think with minimal interruption and maximal flexibility; accordingly, the end product was excellent and the process truly energizing. Such time away from the routine is rarely available in today’s environment, but the model is certainly not without merit. Essential are a culture and leadership that permit and encourage critique without recrimination. In clinical settings, time to engage in deliberative critical thinking is even more difficult to attain. Rather, critical thinking seems to be expected to occur routinely without much cultivation. Benner’s model of progression from novice to expert suggests that excellent clinical experience fosters critical thinking that eventually becomes almost automatic and intuitive. However, I assert that the level of critical thinking displayed by clinical experts needs to be developed deliberately and strategically. The clinical environment in which I have seen critical thinking encouraged most effectively was one in which the expectations were explicit, critical thinking was measured routinely in the practice context, relevant learning and growth opportunities were provided, and critical thinking was taken into account in performance evaluation. In other words, the nursing leadership in that academic medical center truly valued critical thinking and was willing to assign it priority. Nursing has reached the point in its evolution in which a consistent and continuous pattern of critical thinking by its practitioners is a mandate—a sine qua non . The assurance that critical thinking will be truly woven into the fabric of our profession will depend on our ability to recruit and retain intelligent, interested, and committed nurses; to provide challenging educational opportunities that develop the requisite competencies; and to provide and sustain the kinds of environments in which critical thinking is valued and demanded. Introduction The ability to process information from multiple sources and make decisions is a fundamental ability of professional nursing practice. Dramatic changes in the health care system and the practice of nursing have occurred during the past decade as a result of an aging population, cost containment efforts, technological advances, increased complexity of clients’ health care needs, decreased average hospital length of stay, and a shift from acute care to community-based care. All of these changes have emphasized the need for professional nurses to think critically in order to provide safe and effective client care to diverse populations. To function effectively in complex, rapidly changing health care environments, nurses must use higher-order thinking skills and apply content knowledge to clinical practice. The critical thinking process provides nurses with the ability to use purposeful thinking and reflective reasoning to examine ideas, assumptions, principles, conclusions, beliefs, and actions in the context of professional nursing practice ( Brunt, 2005 ). Professional nurses must think critically to process complex data from multiple sources and make intelligent decisions in planning, managing, delivering, and evaluating the health care of their clients. Nurses also use their critical thinking skills to reduce health care errors and improve client safety ( Fero, Witsberger, Wesmiller, Zullo, & Hoffman, 2008 ). To become a critical thinker, a nurse must understand the concept of critical thinking; possess or acquire the essential knowledge, skills, and attributes required to think critically; and deliberately apply critical thinking principles in making clinical judgments. This chapter covers both classical and current sources to examine critical thinking, clinical judgment, and the nursing process. Defining Critical Thinking Critical thinking, as a concept, has been examined and presented from a variety of perspectives. An early definition, proposed by Watson and Glaser (1964) , described critical thinking as the combination of abilities needed to define a problem, recognize stated and unstated assumptions, formulate and select hypotheses, draw conclusions, and judge the validity of inferences. A less prescriptive definition was offered by Ennis (1989) , who characterized critical thinking as “reasonable reflective thinking focused on deciding what to believe or do” (p. 4). Paul (1992) stated that critical thinking is a process of disciplined, self-directed rational thinking that “certifies what we know and makes clear wherein we are ignorant” (p. 47). Alfaro-LeFevre (2006) presented critical thinking for nursing as informed, purposeful, and outcome-focused thinking that requires the ability to identify problems, issues, and risks and make judgments based on evidence. Bandman and Bandman (1995) describe critical thinking for nursing as “the rational examination of ideas, inferences, assumptions, principles, arguments, conclusions, issues, statements, beliefs, and actions” (p. 7) and include the following functions: • Discriminating among use and misuse of language • Analyzing the meaning of terms • Formulating nursing problems • Analyzing arguments and issues into premises and conclusions • Examining nursing assumptions • Reporting data and clues accurately • Making and checking inferences based on data • Formulating and clarifying beliefs • Verifying, corroborating, and justifying claims, beliefs, conclusions, decisions, and actions • Giving relevant reasons for beliefs and conclusions • Formulating and clarifying value judgments • Seeking reasons, criteria, and principles that justify value judgments • Evaluating the soundness of conclusions Conclusions are drawn as a result of this reasoning process. In nursing practice, the desired outcome of this reasoning is effective action. Conflicting viewpoints exist regarding whether critical thinking is subject specific or generalizable ( U.S. Department of Education, 1995 ). Most authors agree that the critical thinking processes are not discipline specific but, rather, are generalizable ( Ennis, 1987 ; Facione, 1990 ; Paul, 1992 ; Watson & Glaser, 1964 ). The same critical thinking skills of interpretation, analysis, inference, and evaluation are applied in different subjects. However, the difference lies in how the critical thinking processes are applied to specific disciplines. For example, professional nurses apply critical thinking skills to client care situations in order to make sound clinical judgments, whereas engineers apply critical thinking skills to business or industrial situations in order to make sound decisions. Meyers (1991) and McPeck (1990) believe that mastery of basic terms, concepts, and methodologies must occur before critical thinking skills can be developed. Ennis (1987) agrees that some familiarity with subject matter is necessary for the development of critical thinking; however, some principles of critical thinking bridge many disciplines and can transfer to new situations. An attempt to define critical thinking by consensus was begun in the late 1980s, and the results became known as the Delphi Report. The Delphi research project used an expert panel of theoreticians representing several disciplines from the United States and Canada to develop a conceptualization of critical thinking from a broad perspective ( Facione, 1990 ). The resulting work described critical thinking in terms of cognitive skills and affective dispositions. The outcome was a definition of critical thinking as the process of purposeful, self-regulatory judgments: an interactive, reflective reasoning process ( Facione & Facione, 1996 ). A critical thinker gives reasoned consideration to evidence, context, theories, methods, and criteria to form a purposeful judgment. At the same time, the critical thinker monitors, corrects, and improves the judgment. The Delphi project produced the following consensus definition from its panel of experts: We understand critical thinking (CT) to be purposeful, self-regulatory, judgment which results in interpretation, analysis, evaluation, and inference, as well as explanation of evidential, conceptual, methodological, criteriological, or contextual considerations upon which that judgment is based. … CT is essential as a tool of inquiry. As such, CT is a liberating force in education and a powerful resource in one’s personal and civic life. ( American Philosophical Association, 1990 ) The Delphi participants identified core critical thinking skills as interpretation, analysis, inference, evaluation, and explanation. These critical thinking cognitive skills and subskills are listed in Box 9-1 . BOX 9-1 Critical Thinking Cognitive Skills and Subskills Interpretation Inference Categorization Querying evidence Decoding sentences Conjecturing alternatives Clarifying meaning Drawing conclusions Analysis Explanation Examining ideas Stating results Identifying arguments Justifying procedures Analyzing arguments Presenting arguments Evaluation Self-regulation Assessing claims Self-examination Assessing arguments Self-correction Critical Thinking in Nursing Scheffer and Rubenfeld (2000) replicated the Delphi study with a panel of 55 nurse educators to obtain a consensus definition of critical thinking for nursing. That study resulted in the identification of 17 dimensions of critical thinking and agreement on the definition of critical thinking for nursing as: … an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting and transforming knowledge. (p. 7) Although many areas overlap with the American Philosophical Association’s (1990) Delphi Report definition of critical thinking, some important differences also exist. According to Allen, Rubenfeld, and Scheffer (2004) , the dimensions of creativity, intuition, and transforming knowledge that are so crucial to effective clinical practice were not included in the Delphi Report definition. These dimensions emerged in the consensus definition of critical thinking for nursing. SUMMARY OF DEFINITIONS OF CRITICAL THINKING Although a universally accepted definition of critical thinking has not emerged, agreement exists that it is a complex process. The variety of definitions helps provide insight into the myriad dimensions of critical thinking. Commonalities in definitions include an emphasis on knowledge, cognitive skills, beliefs, actions, problem identification, and consideration of alternative views and possibilities ( Daly, 1998 ). The definitions presented earlier are summarized for comparison in Table 9-1 , and characteristics of critical thinking are listed in Box 9-2 . BOX 9-2 Characteristics of Critical Thinking Involves conceptualization Is rational and reasonable Is reflective Is partially attitudinal Is autonomous Includes creativity Is fair Focuses on what to believe and do From Wilkinson, J. M. (2001). Nursing process: A critical thinking approach (2nd ed.). Upper Saddle River, NJ: Prentice-Hall. TABLE 9-1 Definitions of Critical Thinking Author(s) Definition Watson and Glaser (1964) Combination of abilities needed to define problems, recognize assumptions, formulate and select hypotheses, draw conclusions, and judge validity of inferences Ennis (1989) Reasonable reflective thinking focused on deciding what to believe or do Paul (1992) Process of self-disciplined, self-directed, rational thinking that verifies what we know and clarifies what we do not know The Delphi Report ( American Philosophical Association, 1990 ); Facione, Facione, and Sanchez (1994) Purposeful, self-regulatory judgments resulting in interpretation, analysis, inference, evaluation, and explanation Bandman and Bandman (1995) Rational examination of ideas, inferences, assumptions, principles, arguments, conclusions, issues, statements, beliefs, and actions Alfaro-LeFevre (2006) Informed, purposeful, and outcome-focused thinking that uses evidence to make clinical judgments The activities involved in the process of critical thinking include appraisal, problem solving, creativity, and decision making. The interrelationships among these concepts are illustrated in Figure 9-1 . These activities are embedded in the critical thinking process in both nursing education and nursing practice. FIGURE 9-1 Critical thinking model. (Modified from Strader, M. K., & Decker, P. J. [1995]. Role transition to patient care management. Upper Saddle River, NJ: Prentice-Hall.) CRITICAL THINKING AND THE NURSING PROCESS In nursing, critical thinking has often been portrayed as a rational, linear process that is synonymous with clinical judgment, problem solving, and the nursing process ( Ford & Profetto-McGrath, 1994 ; Huckabay, 2009 ; Jones & Brown, 1993 ; Kintgen-Andrews, 1991 ; Wilkinson, 1996 ). However, some critics believe that the problem-solving emphasis of the nursing process constrains critical thinking because it does not incorporate the creativity and open-mindedness components of critical thinking ( Conger & Mezza, 1996 ; Duchscher, 1999 ; Jones & Brown, 1993 ; Miller & Malcolm, 1990 ). Although critical thinking skills are important components of the nursing process and problem solving, these are not synonymous terms. The nursing process serves as a tool for applying critical thinking to nursing practice. The nurse uses critical thinking throughout the nursing process, by sorting and categorizing data; identifying patterns in the data; drawing inferences; developing hypotheses that are stated in the form of outcomes; testing these hypotheses as care is delivered; and making criterion-based judgments of effectiveness. Therefore critical thinking can distinguish between fact and fiction, providing a rational basis for clinical judgments and the delivery of nursing care. Although an argument can be made that the nursing process constrains critical thinking because of its structured format, general agreement exists that critical thinking skills and subskills are evident throughout the nursing process ( Alfaro-LeFevre, 2006 ). Although the components of the nursing process are described as separate and distinct steps, they become an integrated way of thinking as nurses gain more clinical experience. An overview of critical thinking throughout the nursing process is presented in Table 9-2 . A thorough understanding of the nursing process reveals that critical thinking is indeed an integral part of its most effective use. TABLE 9-2 Overview of Critical Thinking Throughout the Nursing Process Nursing Process Critical Thinking Assessment Observing Distinguishing relevant from irrelevant data Distinguishing important from unimportant data Validating data Organizing data Categorizing data Analysis/diagnosis Finding patterns and relationships Making inferences Stating the problem Suspending judgment Planning Generalizing Transferring knowledge from one situation to another Developing evaluative criteria Hypothesizing Implementation Applying knowledge Testing hypotheses Evaluation Deciding whether hypotheses are correct Making criterion-based evaluations and judgments Modified from Wilkinson, J. M. (2001). Nursing process: A critical thinking approach (2nd ed.). Upper Saddle River, NJ: Prentice-Hall. The Nursing Process The nursing process is a systematic, problem-solving approach used extensively in the United States and Canada for the delivery of nursing care. The nursing process was first described in the literature in 1955 by Lydia Hall. Her approach was built around three interrelated spheres of nursing activity: care, core, and cure. The focus in the care sphere is the body, including assessment and evaluation of the client’s ability to perform basic functions and activities of daily living. The focal point in the core sphere was on the therapeutic use of self in providing nursing care, whereas nursing activities related to the cure sphere centered on the administration of treatments and therapies, as well as supporting the patient and family during the treatment process. Subsequently, many others have described a “nursing process,” but the model that has withstood the test of time is that developed by Yura and Walsh (1988) . They proposed a four-step nursing process model that consisted of assessing, planning, implementing, and evaluating. The current model closely resembles the Yura and Walsh model, but with the addition of a diagnostic component. The five-step nursing process consists of the following elements: • Assessment —gathering and validating client health data, strengths, risks, and concerns • Analysis/diagnosis —processing client data and identifying appropriate nursing diagnoses • Planning —designing strategies to solve identified problems and build on client strengths • Implementation —delivering and documenting the planned care • Evaluation —determining the effectiveness of the care delivered The American Nurses Association (ANA), in its publication Nursing: Scope and Standards of Practice (2004), parallels the steps of the nursing process and supports its use. Outcome identification, which follows the nursing diagnosis phase and precedes the planning phase, is identified as a separate step in the ANA model. The nursing process is sometimes depicted as a systematic, linear model proceeding from assessment through diagnosis, planning, implementation, and evaluation. It is more appropriately conceptualized as a continuous and interactive model ( Figure 9-2 ), thereby providing a flexible and dynamic approach to client care. This model can accommodate changes in the client’s health status or failure to achieve expected outcomes through a feedback mechanism. The interactive nature of the model with its feedback mechanism permits the nurse to reenter the nursing process at the appropriate stage to collect additional data, restructure nursing diagnoses, design a new plan, or change implementation strategies. This model is consistent with the concept of critical thinking as a continuous reflective process. Further examination of the elements of the nursing process reveals the multiple activities embedded in each step. FIGURE 9-2 The interactive nursing process model. (Modified from Christensen, P. J., & Kenney J. W. [1995]. Nursing process: Application of conceptual models [4th ed.], St. Louis: Mosby.) ASSESSMENT In the assessment phase, the nurse deliberately and systematically collects data to determine the client’s health, functional status, strengths, and risk factors ( Carpenito, 2008 ). Data collection centers on the use of multiple sources and types of data, a variety of data collection techniques, and the use of reliable and valid measurement instruments. All these elements are critical to building a comprehensive database. Sources of Data The primary source of data is the client, whether the client is defined as the individual, the family, or the community. Secondary sources of data include written records, other health care providers, and significant others (e.g., family members, friends). To strengthen the overall assessment and validate client data, it is important to use primary and secondary data sources. Data Collection Techniques Assessment techniques include measurement, observation, and interview. Measurement is used to determine the dimensions of a given indicator (e.g., blood pressure) or to ascertain characteristics such as quantity, size, or frequency. Measurement may require the use of specialized equipment (e.g., stethoscope, thermometer) or specialized assessment tools (e.g., pain scale, depression scale) to assess functional, behavioral, social, or cognitive domains. Data collection by observation requires the use of the senses, including visual observation and tactile (palpation) and auditory techniques (auscultation). Observation provides a variety and depth of data that may be difficult to obtain by other methods. A structured or unstructured interview may be used to obtain information such as a health history and demographic data. A structured interview is commonly used in emergency situations when the nurse needs to gather specific information. An unstructured interview is commonly used in situations in which the nurse wishes to elicit information from the client’s perspective or gain insight to the client’s understanding of a problem. The unstructured interview allows the nurse to use active listening skills while building rapport with the client through the use of an open-ended interview format. These communication techniques are discussed in chapter 8 Types of Data To complete a comprehensive assessment, objective and subjective data are obtained. Objective data are factual data, usually obtained through observation or measurement. An example of objective data occurs when the nurse uses an otoscope to assess the client’s tympanic membrane and observes that it is reddened and inflamed. Subjective data are based on the client’s perception of the health problem. An example of subjective data occurs when the client states that he is having pain in his right ear. It is important to collect both objective and subjective data to complete a comprehensive assessment. Care should be taken to record data factually and to avoid personal or biased interpretations. Data Collection Instruments The use of selected data collection measures and instruments can assist the nurse in compiling a comprehensive database and organizing data into meaningful patterns. Assessment usually begins by taking a nursing history and conducting a physical examination. Many clinical areas have developed nursing history and physical forms specific to the type of agency and the clients served. Regardless of the format, the nursing database should include the following categories of information ( Edelman & Mandle, 1994 ): • Demographic data • Current and past medical problems • Family medical history • Surgical and (if appropriate) obstetrical history • Childhood illnesses • Allergies • Current medications • Psychological status • Social history • Environmental background • Physical assessment
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Genetics and Genomics in Professional Nursing
- Intimate Partner Violence as a Health Care Problem
- Ethical Dimensions of Nursing and Health Care
- Theories and Frameworks for Professional Nursing Practice
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Create A Quiz
- Relationship
- Personality
- Harry Potter
- Online Exam
- Entertainment
- Training Maker
- Survey Maker
- Brain Games
- ProProfs.com
Nursing Process Quizzes, Questions & Answers
Welcome to our Nursing Process Quizzes, designed to sharpen your clinical decision-making skills and deepen your understanding of the essential steps in patient care. As a nursing professional or student, mastering the nursing process is crucial for providing safe and effective care to patients. Through a series of thought-provoking multiple-choice questions, we'll explore each step of the nursing process - assessment, diagnosis, planning, implementation, and evaluation. These quizzes will challenge your knowledge and critical thinking abilities, simulating real-life scenarios you may encounter in healthcare settings. Assessment is the foundation of nursing care, and our quizzes will test your ability to gather comprehensive patient data, identify potential health problems, and prioritize care needs. Diagnosis involves formulating nursing diagnoses based on the assessment data, and our quizzes will assess your proficiency in differentiating between actual and potential health issues. Planning encompasses setting achievable and measurable goals for patient care. Our quizzes will challenge your skills in developing appropriate nursing interventions to meet those goals. Implementation involves putting the care plan into action, and our quizzes will explore your knowledge of nursing interventions and your ability to execute them safely and effectively. Whether you're a nursing student preparing for exams, a newly licensed nurse honing your skills, or an experienced practitioner looking to refresh your knowledge, these quizzes offer valuable learning experiences. Happy quizzing, and may your exploration of the nursing process quizzes lead you to become a competent and confident healthcare provider dedicated to delivering the highest quality care to your patients!
Top Trending Quizzes
Popular Topics
Recent quizzes.
What is the Nursing Process?
Characteristics of the nursing process, history of the nursing process.

Understanding the nursing process is key to providing quality care to your patients. The nursing process is a cyclical process used to assess, diagnose, and care for patients as a nurse. It includes 5 progressive steps often referred to with the acronym:
- Planning/outcomes
- Implementation
In this article, we’ll discuss each step of the nursing process in detail and include some examples of how this process might look in your practice.
Find Nursing Programs
The nursing process is a patient-centered, systematic, evidence-based approach to delivering high-quality nursing care. It consists of five steps: assessment , diagnosis , outcomes/planning, implementation, and evaluation.
The Nursing Process (ADPIE)
| Identify patients' health needs and collect about their condition. | |
| Identify any real or potential health problems that the patient is experiencing or may possibly experience. | |
| Develop a nursing plan of care, which outlines the actions that will be taken to meet the needs identified to achieve the desired patient outcomes. | |
| Carry out the plan of care and monitor patients' progress. | |
| Evaluate whether the plan of care was successful. If necessary, the process is then repeated until the patient is discharged or until they reach all their health care goals. |
1. Assessment
To begin the nursing process, assessment involves collecting information about the patient and their health. This information is used to identify any problems, or potential problems, that may need to be addressed while you’re caring for a patient.
Example: If you’re admitting an older patient who is falling and getting injured at home, you’ll want to do a thorough physical and mental health assessment, including a medical history to try and determine why this is happening.
Some important things you’ll want to find out are:
- What medications and over-the-counter products is the patient taking
- History of alcohol and recreational drug use
- Where the person lives and the layout of their home, including scatter rugs they may be tripping over: clutter, pets, stairs, slippery tubs they’re climbing into or out of, fluid or food spills on floors, lighting, mobility aids they use, etc.
2. Diagnosis
The Nursing Diagnosis is the second step in the nursing process and involves identifying real or potential health problems for a patient based on the information you gathered during the assessment.
Example: Using the falls patient example above, you may identify from your assessment that the patient is falling because they’re tripping on things in their environment that they don’t see, like their pet cat lying on the floor and loose scatter rugs.
Based on this, you might form a diagnosis such as “Falls related to poor vision, cluttered environment, unsteady gait, Lt. hip pain due to previous fall.”
3. Outcomes/Planning
Planning or Outcomes is the third step in the nursing process. This step involves developing a nursing care plan that includes goals and strategies to address the problems identified during the assessment and diagnosis steps.
Example: Continuing with the example above, you will likely recommend that the patient keep their environment,
- Free of scatter rugs
- Check to ensure the cat is not underfoot before they mobilize
- Suggest the patient use a walker for support when mobilizing
- Recommending that the patient schedule an eye exam to get their vision checked if they have not had one in the last year or two would also be a good idea or if they’ve noticed any changes in their vision lately.
4. Implementation
As the fourth step of the nursing process, implementation involves putting the plan of care into action.
Example In the above example, this would include:
- Making sure the patient’s environment is free of clutter and tripping hazards while in the hospital or a skilled nursing facility.
- Teaching the patient to wear proper footwear before mobilizing.
- Assisting the patient with mobility as needed, including putting proper footwear on the patient if needed.
- Speaking to the patient and family about removing scatter rugs from the patient’s home, scheduling an eye exam, and ensuring proper footwear is worn for mobilizing at home.
- Discussing with the patient and family about getting the patient a walker to assist with mobility on discharge and providing one while the patient is admitted.
5. Evaluation
The last step of the nursing process is evaluation , which involves determining whether or not the goals of care have been met.
Example Here you would look back at the patient’s medical record to see if the patient has had any further falls since implementing the preventative actions above.
If so, you would repeat the nursing process over and reassess why this is still happening and plan new actions to prevent future falls.
>> Show Me Online MSN Programs
The nursing process is also characterized by the following elements.
1. Dynamic and Cyclic
The nursing process is an evolving process that continues throughout a patient’s admission or illness and ends when the problems identified by the nurse are no longer an issue.
2. Patient-Centered and Goal-Directed
The entire nursing process is sensitive to and responsive to the patient's needs, preferences, and values. As nurses, we need to act as patient advocates and protect the patient’s right to make informed decisions while involving the patient in goal setting and attainment.
3. Collaborative and Interpersonal
This describes the level of interaction that may be required between nurses, patients, families and supports, and the interprofessional healthcare team. These aspects of the nursing process require mutual respect, cooperation, clear communication, and decision-making that is shared between all parties involved.

4. Universally Applicable
As a widely and globally accepted standard in nursing practice, the nursing process follows the same steps, regardless of where a nurse works.
5. Systematic and Scientific
The nursing process is also an objective and predictable process for planning, conducting, and evaluating patient care that is based on a large body of scientific evidence found in peer-reviewed nursing research.
6. Requires Critical Thinking
Most importantly, it’s essential that nurses use critical thinking when planning patient care using the nursing process. This means as nurses, we must use a combination of our knowledge and past experiences with the information we have about a current patient to make the best decisions we can about nursing care.
The nursing process was introduced in 1958 by Ida Jean Orlando. Today, it continues to be the most widely-accepted method of prioritizing, organizing, and providing patient care in the nursing profession.
It’s characterized by the key elements of:
- Critical thinking
- Client-centered methods for treatment
- Goal-oriented activities
- Evidence-based nursing research and findings
Popular Online Master of Science in Nursing (MSN) Programs

At Purdue Global, discover a faster, more affordable way to earn your Nursing degree. Purdue Global is committed to keeping your tuition costs as low as possible and helping you find the most efficient path to your degree.
Enrollment: Nationwide, but certain programs have state restrictions. Check with Purdue for details.
- Accelerated BSN-to-MSN
- MSN - Adult-Gerontology Acute Care NP
- MSN - Psychiatric Mental Health NP
- MSN - Nurse Educator
- MSN - Executive Leader

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
Enrollment: Nationwide
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals. GCU offers a full spectrum of nursing degrees, from a pre-licensure BSN degree to a Doctor of Nursing Practice (DNP) program.
- MSN - Family NP
- MSN - Adult Gerontology Acute Care NP
- MSN - Nursing Education
- MSN - Health Informatics
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MBA & MSN - Nursing Leadership in Health Care Systems
- See more GCU nursing programs

- BSN-to-MSN - Nurse Admin
- BSN-to-MSN - Nurse Educator
- BSN-to-MSN - Nursing Informatics
- BSN-to-MSN - Community Health
- BSN-to-MSN - Health Policy
- The nursing process helps nurses to provide quality patient care by taking a holistic view of each patient they plan care for.
- The nursing process is an evidence-based approach to caring for patients that helps nurses provide quality care and improve patient outcomes.
- Ida Jean Orlando introduced the nursing process in 1958.
- The primary focus of the nursing process is the patient or client. The process is designed to meet the real and potential healthcare needs of the patient/client and to prevent possible illness or injury.

Leona Werezak BSN, MN, RN is the Director of Business Development at NCLEX Education. She began her nursing career in a small rural hospital in northern Canada where she worked as a new staff nurse doing everything from helping deliver babies to medevacing critically ill patients. Learning much from her patients and colleagues at the bedside for 15 years, she also taught in baccalaureate nursing programs for almost 20 years as a nursing adjunct faculty member (yes! Some of those years she did both!). As a freelance writer online, she writes content for nursing schools and colleges, healthcare and medical businesses, as well as various nursing sites.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 6 clinical reasoning, decisionmaking, and action: thinking critically and clinically.
Patricia Benner ; Ronda G. Hughes ; Molly Sutphen .
Affiliations
This chapter examines multiple thinking strategies that are needed for high-quality clinical practice. Clinical reasoning and judgment are examined in relation to other modes of thinking used by clinical nurses in providing quality health care to patients that avoids adverse events and patient harm. The clinician’s ability to provide safe, high-quality care can be dependent upon their ability to reason, think, and judge, which can be limited by lack of experience. The expert performance of nurses is dependent upon continual learning and evaluation of performance.
- Critical Thinking
Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. The American Philosophical Association (APA) defined critical thinking as purposeful, self-regulatory judgment that uses cognitive tools such as interpretation, analysis, evaluation, inference, and explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations on which judgment is based. 2 A more expansive general definition of critical thinking is
. . . in short, self-directed, self-disciplined, self-monitored, and self-corrective thinking. It presupposes assent to rigorous standards of excellence and mindful command of their use. It entails effective communication and problem solving abilities and a commitment to overcome our native egocentrism and sociocentrism. Every clinician must develop rigorous habits of critical thinking, but they cannot escape completely the situatedness and structures of the clinical traditions and practices in which they must make decisions and act quickly in specific clinical situations. 3
There are three key definitions for nursing, which differ slightly. Bittner and Tobin defined critical thinking as being “influenced by knowledge and experience, using strategies such as reflective thinking as a part of learning to identify the issues and opportunities, and holistically synthesize the information in nursing practice” 4 (p. 268). Scheffer and Rubenfeld 5 expanded on the APA definition for nurses through a consensus process, resulting in the following definition:
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, openmindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge 6 (Scheffer & Rubenfeld, p. 357).
The National League for Nursing Accreditation Commission (NLNAC) defined critical thinking as:
the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research 7 (p. 8).
These concepts are furthered by the American Association of Colleges of Nurses’ definition of critical thinking in their Essentials of Baccalaureate Nursing :
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9).
Course work or ethical experiences should provide the graduate with the knowledge and skills to:
- Use nursing and other appropriate theories and models, and an appropriate ethical framework;
- Apply research-based knowledge from nursing and the sciences as the basis for practice;
- Use clinical judgment and decision-making skills;
- Engage in self-reflective and collegial dialogue about professional practice;
- Evaluate nursing care outcomes through the acquisition of data and the questioning of inconsistencies, allowing for the revision of actions and goals;
- Engage in creative problem solving 8 (p. 10).
Taken together, these definitions of critical thinking set forth the scope and key elements of thought processes involved in providing clinical care. Exactly how critical thinking is defined will influence how it is taught and to what standard of care nurses will be held accountable.
Professional and regulatory bodies in nursing education have required that critical thinking be central to all nursing curricula, but they have not adequately distinguished critical reflection from ethical, clinical, or even creative thinking for decisionmaking or actions required by the clinician. Other essential modes of thought such as clinical reasoning, evaluation of evidence, creative thinking, or the application of well-established standards of practice—all distinct from critical reflection—have been subsumed under the rubric of critical thinking. In the nursing education literature, clinical reasoning and judgment are often conflated with critical thinking. The accrediting bodies and nursing scholars have included decisionmaking and action-oriented, practical, ethical, and clinical reasoning in the rubric of critical reflection and thinking. One might say that this harmless semantic confusion is corrected by actual practices, except that students need to understand the distinctions between critical reflection and clinical reasoning, and they need to learn to discern when each is better suited, just as students need to also engage in applying standards, evidence-based practices, and creative thinking.
The growing body of research, patient acuity, and complexity of care demand higher-order thinking skills. Critical thinking involves the application of knowledge and experience to identify patient problems and to direct clinical judgments and actions that result in positive patient outcomes. These skills can be cultivated by educators who display the virtues of critical thinking, including independence of thought, intellectual curiosity, courage, humility, empathy, integrity, perseverance, and fair-mindedness. 9
The process of critical thinking is stimulated by integrating the essential knowledge, experiences, and clinical reasoning that support professional practice. The emerging paradigm for clinical thinking and cognition is that it is social and dialogical rather than monological and individual. 10–12 Clinicians pool their wisdom and multiple perspectives, yet some clinical knowledge can be demonstrated only in the situation (e.g., how to suction an extremely fragile patient whose oxygen saturations sink too low). Early warnings of problematic situations are made possible by clinicians comparing their observations to that of other providers. Clinicians form practice communities that create styles of practice, including ways of doing things, communication styles and mechanisms, and shared expectations about performance and expertise of team members.
By holding up critical thinking as a large umbrella for different modes of thinking, students can easily misconstrue the logic and purposes of different modes of thinking. Clinicians and scientists alike need multiple thinking strategies, such as critical thinking, clinical judgment, diagnostic reasoning, deliberative rationality, scientific reasoning, dialogue, argument, creative thinking, and so on. In particular, clinicians need forethought and an ongoing grasp of a patient’s health status and care needs trajectory, which requires an assessment of their own clarity and understanding of the situation at hand, critical reflection, critical reasoning, and clinical judgment.
Critical Reflection, Critical Reasoning, and Judgment
Critical reflection requires that the thinker examine the underlying assumptions and radically question or doubt the validity of arguments, assertions, and even facts of the case. Critical reflective skills are essential for clinicians; however, these skills are not sufficient for the clinician who must decide how to act in particular situations and avoid patient injury. For example, in everyday practice, clinicians cannot afford to critically reflect on the well-established tenets of “normal” or “typical” human circulatory systems when trying to figure out a particular patient’s alterations from that typical, well-grounded understanding that has existed since Harvey’s work in 1628. 13 Yet critical reflection can generate new scientifically based ideas. For example, there is a lack of adequate research on the differences between women’s and men’s circulatory systems and the typical pathophysiology related to heart attacks. Available research is based upon multiple, taken-for-granted starting points about the general nature of the circulatory system. As such, critical reflection may not provide what is needed for a clinician to act in a situation. This idea can be considered reasonable since critical reflective thinking is not sufficient for good clinical reasoning and judgment. The clinician’s development of skillful critical reflection depends upon being taught what to pay attention to, and thus gaining a sense of salience that informs the powers of perceptual grasp. The powers of noticing or perceptual grasp depend upon noticing what is salient and the capacity to respond to the situation.
Critical reflection is a crucial professional skill, but it is not the only reasoning skill or logic clinicians require. The ability to think critically uses reflection, induction, deduction, analysis, challenging assumptions, and evaluation of data and information to guide decisionmaking. 9 , 14 , 15 Critical reasoning is a process whereby knowledge and experience are applied in considering multiple possibilities to achieve the desired goals, 16 while considering the patient’s situation. 14 It is a process where both inductive and deductive cognitive skills are used. 17 Sometimes clinical reasoning is presented as a form of evaluating scientific knowledge, sometimes even as a form of scientific reasoning. Critical thinking is inherent in making sound clinical reasoning. 18
An essential point of tension and confusion exists in practice traditions such as nursing and medicine when clinical reasoning and critical reflection become entangled, because the clinician must have some established bases that are not questioned when engaging in clinical decisions and actions, such as standing orders. The clinician must act in the particular situation and time with the best clinical and scientific knowledge available. The clinician cannot afford to indulge in either ritualistic unexamined knowledge or diagnostic or therapeutic nihilism caused by radical doubt, as in critical reflection, because they must find an intelligent and effective way to think and act in particular clinical situations. Critical reflection skills are essential to assist practitioners to rethink outmoded or even wrong-headed approaches to health care, health promotion, and prevention of illness and complications, especially when new evidence is available. Breakdowns in practice, high failure rates in particular therapies, new diseases, new scientific discoveries, and societal changes call for critical reflection about past assumptions and no-longer-tenable beliefs.
Clinical reasoning stands out as a situated, practice-based form of reasoning that requires a background of scientific and technological research-based knowledge about general cases, more so than any particular instance. It also requires practical ability to discern the relevance of the evidence behind general scientific and technical knowledge and how it applies to a particular patient. In dong so, the clinician considers the patient’s particular clinical trajectory, their concerns and preferences, and their particular vulnerabilities (e.g., having multiple comorbidities) and sensitivities to care interventions (e.g., known drug allergies, other conflicting comorbid conditions, incompatible therapies, and past responses to therapies) when forming clinical decisions or conclusions.
Situated in a practice setting, clinical reasoning occurs within social relationships or situations involving patient, family, community, and a team of health care providers. The expert clinician situates themselves within a nexus of relationships, with concerns that are bounded by the situation. Expert clinical reasoning is socially engaged with the relationships and concerns of those who are affected by the caregiving situation, and when certain circumstances are present, the adverse event. Halpern 19 has called excellent clinical ethical reasoning “emotional reasoning” in that the clinicians have emotional access to the patient/family concerns and their understanding of the particular care needs. Expert clinicians also seek an optimal perceptual grasp, one based on understanding and as undistorted as possible, based on an attuned emotional engagement and expert clinical knowledge. 19 , 20
Clergy educators 21 and nursing and medical educators have begun to recognize the wisdom of broadening their narrow vision of rationality beyond simple rational calculation (exemplified by cost-benefit analysis) to reconsider the need for character development—including emotional engagement, perception, habits of thought, and skill acquisition—as essential to the development of expert clinical reasoning, judgment, and action. 10 , 22–24 Practitioners of engineering, law, medicine, and nursing, like the clergy, have to develop a place to stand in their discipline’s tradition of knowledge and science in order to recognize and evaluate salient evidence in the moment. Diagnostic confusion and disciplinary nihilism are both threats to the clinician’s ability to act in particular situations. However, the practice and practitioners will not be self-improving and vital if they cannot engage in critical reflection on what is not of value, what is outmoded, and what does not work. As evidence evolves and expands, so too must clinical thought.
Clinical judgment requires clinical reasoning across time about the particular, and because of the relevance of this immediate historical unfolding, clinical reasoning can be very different from the scientific reasoning used to formulate, conduct, and assess clinical experiments. While scientific reasoning is also socially embedded in a nexus of social relationships and concerns, the goal of detached, critical objectivity used to conduct scientific experiments minimizes the interactive influence of the research on the experiment once it has begun. Scientific research in the natural and clinical sciences typically uses formal criteria to develop “yes” and “no” judgments at prespecified times. The scientist is always situated in past and immediate scientific history, preferring to evaluate static and predetermined points in time (e.g., snapshot reasoning), in contrast to a clinician who must always reason about transitions over time. 25 , 26
Techne and Phronesis
Distinctions between the mere scientific making of things and practice was first explored by Aristotle as distinctions between techne and phronesis. 27 Learning to be a good practitioner requires developing the requisite moral imagination for good practice. If, for example, patients exercise their rights and refuse treatments, practitioners are required to have the moral imagination to understand the probable basis for the patient’s refusal. For example, was the refusal based upon catastrophic thinking, unrealistic fears, misunderstanding, or even clinical depression?
Techne, as defined by Aristotle, encompasses the notion of formation of character and habitus 28 as embodied beings. In Aristotle’s terms, techne refers to the making of things or producing outcomes. 11 Joseph Dunne defines techne as “the activity of producing outcomes,” and it “is governed by a means-ends rationality where the maker or producer governs the thing or outcomes produced or made through gaining mastery over the means of producing the outcomes, to the point of being able to separate means and ends” 11 (p. 54). While some aspects of medical and nursing practice fall into the category of techne, much of nursing and medical practice falls outside means-ends rationality and must be governed by concern for doing good or what is best for the patient in particular circumstances, where being in a relationship and discerning particular human concerns at stake guide action.
Phronesis, in contrast to techne, includes reasoning about the particular, across time, through changes or transitions in the patient’s and/or the clinician’s understanding. As noted by Dunne, phronesis is “characterized at least as much by a perceptiveness with regard to concrete particulars as by a knowledge of universal principles” 11 (p. 273). This type of practical reasoning often takes the form of puzzle solving or the evaluation of immediate past “hot” history of the patient’s situation. Such a particular clinical situation is necessarily particular, even though many commonalities and similarities with other disease syndromes can be recognized through signs and symptoms and laboratory tests. 11 , 29 , 30 Pointing to knowledge embedded in a practice makes no claim for infallibility or “correctness.” Individual practitioners can be mistaken in their judgments because practices such as medicine and nursing are inherently underdetermined. 31
While phronetic knowledge must remain open to correction and improvement, real events, and consequences, it cannot consistently transcend the institutional setting’s capacities and supports for good practice. Phronesis is also dependent on ongoing experiential learning of the practitioner, where knowledge is refined, corrected, or refuted. The Western tradition, with the notable exception of Aristotle, valued knowledge that could be made universal and devalued practical know-how and experiential learning. Descartes codified this preference for formal logic and rational calculation.
Aristotle recognized that when knowledge is underdetermined, changeable, and particular, it cannot be turned into the universal or standardized. It must be perceived, discerned, and judged, all of which require experiential learning. In nursing and medicine, perceptual acuity in physical assessment and clinical judgment (i.e., reasoning across time about changes in the particular patient or the clinician’s understanding of the patient’s condition) fall into the Greek Aristotelian category of phronesis. Dewey 32 sought to rescue knowledge gained by practical activity in the world. He identified three flaws in the understanding of experience in Greek philosophy: (1) empirical knowing is the opposite of experience with science; (2) practice is reduced to techne or the application of rational thought or technique; and (3) action and skilled know-how are considered temporary and capricious as compared to reason, which the Greeks considered as ultimate reality.
In practice, nursing and medicine require both techne and phronesis. The clinician standardizes and routinizes what can be standardized and routinized, as exemplified by standardized blood pressure measurements, diagnoses, and even charting about the patient’s condition and treatment. 27 Procedural and scientific knowledge can often be formalized and standardized (e.g., practice guidelines), or at least made explicit and certain in practice, except for the necessary timing and adjustments made for particular patients. 11 , 22
Rational calculations available to techne—population trends and statistics, algorithms—are created as decision support structures and can improve accuracy when used as a stance of inquiry in making clinical judgments about particular patients. Aggregated evidence from clinical trials and ongoing working knowledge of pathophysiology, biochemistry, and genomics are essential. In addition, the skills of phronesis (clinical judgment that reasons across time, taking into account the transitions of the particular patient/family/community and transitions in the clinician’s understanding of the clinical situation) will be required for nursing, medicine, or any helping profession.
Thinking Critically
Being able to think critically enables nurses to meet the needs of patients within their context and considering their preferences; meet the needs of patients within the context of uncertainty; consider alternatives, resulting in higher-quality care; 33 and think reflectively, rather than simply accepting statements and performing tasks without significant understanding and evaluation. 34 Skillful practitioners can think critically because they have the following cognitive skills: information seeking, discriminating, analyzing, transforming knowledge, predicating, applying standards, and logical reasoning. 5 One’s ability to think critically can be affected by age, length of education (e.g., an associate vs. a baccalaureate decree in nursing), and completion of philosophy or logic subjects. 35–37 The skillful practitioner can think critically because of having the following characteristics: motivation, perseverance, fair-mindedness, and deliberate and careful attention to thinking. 5 , 9
Thinking critically implies that one has a knowledge base from which to reason and the ability to analyze and evaluate evidence. 38 Knowledge can be manifest by the logic and rational implications of decisionmaking. Clinical decisionmaking is particularly influenced by interpersonal relationships with colleagues, 39 patient conditions, availability of resources, 40 knowledge, and experience. 41 Of these, experience has been shown to enhance nurses’ abilities to make quick decisions 42 and fewer decision errors, 43 support the identification of salient cues, and foster the recognition and action on patterns of information. 44 , 45
Clinicians must develop the character and relational skills that enable them to perceive and understand their patient’s needs and concerns. This requires accurate interpretation of patient data that is relevant to the specific patient and situation. In nursing, this formation of moral agency focuses on learning to be responsible in particular ways demanded by the practice, and to pay attention and intelligently discern changes in patients’ concerns and/or clinical condition that require action on the part of the nurse or other health care workers to avert potential compromises to quality care.
Formation of the clinician’s character, skills, and habits are developed in schools and particular practice communities within a larger practice tradition. As Dunne notes,
A practice is not just a surface on which one can display instant virtuosity. It grounds one in a tradition that has been formed through an elaborate development and that exists at any juncture only in the dispositions (slowly and perhaps painfully acquired) of its recognized practitioners. The question may of course be asked whether there are any such practices in the contemporary world, whether the wholesale encroachment of Technique has not obliterated them—and whether this is not the whole point of MacIntyre’s recipe of withdrawal, as well as of the post-modern story of dispossession 11 (p. 378).
Clearly Dunne is engaging in critical reflection about the conditions for developing character, skills, and habits for skillful and ethical comportment of practitioners, as well as to act as moral agents for patients so that they and their families receive safe, effective, and compassionate care.
Professional socialization or professional values, while necessary, do not adequately address character and skill formation that transform the way the practitioner exists in his or her world, what the practitioner is capable of noticing and responding to, based upon well-established patterns of emotional responses, skills, dispositions to act, and the skills to respond, decide, and act. 46 The need for character and skill formation of the clinician is what makes a practice stand out from a mere technical, repetitious manufacturing process. 11 , 30 , 47
In nursing and medicine, many have questioned whether current health care institutions are designed to promote or hinder enlightened, compassionate practice, or whether they have deteriorated into commercial institutional models that focus primarily on efficiency and profit. MacIntyre points out the links between the ongoing development and improvement of practice traditions and the institutions that house them:
Lack of justice, lack of truthfulness, lack of courage, lack of the relevant intellectual virtues—these corrupt traditions, just as they do those institutions and practices which derive their life from the traditions of which they are the contemporary embodiments. To recognize this is of course also to recognize the existence of an additional virtue, one whose importance is perhaps most obvious when it is least present, the virtue of having an adequate sense of the traditions to which one belongs or which confront one. This virtue is not to be confused with any form of conservative antiquarianism; I am not praising those who choose the conventional conservative role of laudator temporis acti. It is rather the case that an adequate sense of tradition manifests itself in a grasp of those future possibilities which the past has made available to the present. Living traditions, just because they continue a not-yet-completed narrative, confront a future whose determinate and determinable character, so far as it possesses any, derives from the past 30 (p. 207).
It would be impossible to capture all the situated and distributed knowledge outside of actual practice situations and particular patients. Simulations are powerful as teaching tools to enable nurses’ ability to think critically because they give students the opportunity to practice in a simplified environment. However, students can be limited in their inability to convey underdetermined situations where much of the information is based on perceptions of many aspects of the patient and changes that have occurred over time. Simulations cannot have the sub-cultures formed in practice settings that set the social mood of trust, distrust, competency, limited resources, or other forms of situated possibilities.
One of the hallmark studies in nursing providing keen insight into understanding the influence of experience was a qualitative study of adult, pediatric, and neonatal intensive care unit (ICU) nurses, where the nurses were clustered into advanced beginner, intermediate, and expert level of practice categories. The advanced beginner (having up to 6 months of work experience) used procedures and protocols to determine which clinical actions were needed. When confronted with a complex patient situation, the advanced beginner felt their practice was unsafe because of a knowledge deficit or because of a knowledge application confusion. The transition from advanced beginners to competent practitioners began when they first had experience with actual clinical situations and could benefit from the knowledge gained from the mistakes of their colleagues. Competent nurses continuously questioned what they saw and heard, feeling an obligation to know more about clinical situations. In doing do, they moved from only using care plans and following the physicians’ orders to analyzing and interpreting patient situations. Beyond that, the proficient nurse acknowledged the changing relevance of clinical situations requiring action beyond what was planned or anticipated. The proficient nurse learned to acknowledge the changing needs of patient care and situation, and could organize interventions “by the situation as it unfolds rather than by preset goals 48 (p. 24). Both competent and proficient nurses (that is, intermediate level of practice) had at least two years of ICU experience. 48 Finally, the expert nurse had a more fully developed grasp of a clinical situation, a sense of confidence in what is known about the situation, and could differentiate the precise clinical problem in little time. 48
Expertise is acquired through professional experience and is indicative of a nurse who has moved beyond mere proficiency. As Gadamer 29 points out, experience involves a turning around of preconceived notions, preunderstandings, and extends or adds nuances to understanding. Dewey 49 notes that experience requires a prepared “creature” and an enriched environment. The opportunity to reflect and narrate one’s experiential learning can clarify, extend, or even refute experiential learning.
Experiential learning requires time and nurturing, but time alone does not ensure experiential learning. Aristotle linked experiential learning to the development of character and moral sensitivities of a person learning a practice. 50 New nurses/new graduates have limited work experience and must experience continuing learning until they have reached an acceptable level of performance. 51 After that, further improvements are not predictable, and years of experience are an inadequate predictor of expertise. 52
The most effective knower and developer of practical knowledge creates an ongoing dialogue and connection between lessons of the day and experiential learning over time. Gadamer, in a late life interview, highlighted the open-endedness and ongoing nature of experiential learning in the following interview response:
Being experienced does not mean that one now knows something once and for all and becomes rigid in this knowledge; rather, one becomes more open to new experiences. A person who is experienced is undogmatic. Experience has the effect of freeing one to be open to new experience … In our experience we bring nothing to a close; we are constantly learning new things from our experience … this I call the interminability of all experience 32 (p. 403).
Practical endeavor, supported by scientific knowledge, requires experiential learning, the development of skilled know-how, and perceptual acuity in order to make the scientific knowledge relevant to the situation. Clinical perceptual and skilled know-how helps the practitioner discern when particular scientific findings might be relevant. 53
Often experience and knowledge, confirmed by experimentation, are treated as oppositions, an either-or choice. However, in practice it is readily acknowledged that experiential knowledge fuels scientific investigation, and scientific investigation fuels further experiential learning. Experiential learning from particular clinical cases can help the clinician recognize future similar cases and fuel new scientific questions and study. For example, less experienced nurses—and it could be argued experienced as well—can use nursing diagnoses practice guidelines as part of their professional advancement. Guidelines are used to reflect their interpretation of patients’ needs, responses, and situation, 54 a process that requires critical thinking and decisionmaking. 55 , 56 Using guidelines also reflects one’s problem identification and problem-solving abilities. 56 Conversely, the ability to proficiently conduct a series of tasks without nursing diagnoses is the hallmark of expertise. 39 , 57
Experience precedes expertise. As expertise develops from experience and gaining knowledge and transitions to the proficiency stage, the nurses’ thinking moves from steps and procedures (i.e., task-oriented care) toward “chunks” or patterns 39 (i.e., patient-specific care). In doing so, the nurse thinks reflectively, rather than merely accepting statements and performing procedures without significant understanding and evaluation. 34 Expert nurses do not rely on rules and logical thought processes in problem-solving and decisionmaking. 39 Instead, they use abstract principles, can see the situation as a complex whole, perceive situations comprehensively, and can be fully involved in the situation. 48 Expert nurses can perform high-level care without conscious awareness of the knowledge they are using, 39 , 58 and they are able to provide that care with flexibility and speed. Through a combination of knowledge and skills gained from a range of theoretical and experiential sources, expert nurses also provide holistic care. 39 Thus, the best care comes from the combination of theoretical, tacit, and experiential knowledge. 59 , 60
Experts are thought to eventually develop the ability to intuitively know what to do and to quickly recognize critical aspects of the situation. 22 Some have proposed that expert nurses provide high-quality patient care, 61 , 62 but that is not consistently documented—particularly in consideration of patient outcomes—and a full understanding between the differential impact of care rendered by an “expert” nurse is not fully understood. In fact, several studies have found that length of professional experience is often unrelated and even negatively related to performance measures and outcomes. 63 , 64
In a review of the literature on expertise in nursing, Ericsson and colleagues 65 found that focusing on challenging, less-frequent situations would reveal individual performance differences on tasks that require speed and flexibility, such as that experienced during a code or an adverse event. Superior performance was associated with extensive training and immediate feedback about outcomes, which can be obtained through continual training, simulation, and processes such as root-cause analysis following an adverse event. Therefore, efforts to improve performance benefited from continual monitoring, planning, and retrospective evaluation. Even then, the nurse’s ability to perform as an expert is dependent upon their ability to use intuition or insights gained through interactions with patients. 39
Intuition and Perception
Intuition is the instant understanding of knowledge without evidence of sensible thought. 66 According to Young, 67 intuition in clinical practice is a process whereby the nurse recognizes something about a patient that is difficult to verbalize. Intuition is characterized by factual knowledge, “immediate possession of knowledge, and knowledge independent of the linear reasoning process” 68 (p. 23). When intuition is used, one filters information initially triggered by the imagination, leading to the integration of all knowledge and information to problem solve. 69 Clinicians use their interactions with patients and intuition, drawing on tacit or experiential knowledge, 70 , 71 to apply the correct knowledge to make the correct decisions to address patient needs. Yet there is a “conflated belief in the nurses’ ability to know what is best for the patient” 72 (p. 251) because the nurses’ and patients’ identification of the patients’ needs can vary. 73
A review of research and rhetoric involving intuition by King and Appleton 62 found that all nurses, including students, used intuition (i.e., gut feelings). They found evidence, predominately in critical care units, that intuition was triggered in response to knowledge and as a trigger for action and/or reflection with a direct bearing on the analytical process involved in patient care. The challenge for nurses was that rigid adherence to checklists, guidelines, and standardized documentation, 62 ignored the benefits of intuition. This view was furthered by Rew and Barrow 68 , 74 in their reviews of the literature, where they found that intuition was imperative to complex decisionmaking, 68 difficult to measure and assess in a quantitative manner, and was not linked to physiologic measures. 74
Intuition is a way of explaining professional expertise. 75 Expert nurses rely on their intuitive judgment that has been developed over time. 39 , 76 Intuition is an informal, nonanalytically based, unstructured, deliberate calculation that facilitates problem solving, 77 a process of arriving at salient conclusions based on relatively small amounts of knowledge and/or information. 78 Experts can have rapid insight into a situation by using intuition to recognize patterns and similarities, achieve commonsense understanding, and sense the salient information combined with deliberative rationality. 10 Intuitive recognition of similarities and commonalities between patients are often the first diagnostic clue or early warning, which must then be followed up with critical evaluation of evidence among the competing conditions. This situation calls for intuitive judgment that can distinguish “expert human judgment from the decisions” made by a novice 79 (p. 23).
Shaw 80 equates intuition with direct perception. Direct perception is dependent upon being able to detect complex patterns and relationships that one has learned through experience are important. Recognizing these patterns and relationships generally occurs rapidly and is complex, making it difficult to articulate or describe. Perceptual skills, like those of the expert nurse, are essential to recognizing current and changing clinical conditions. Perception requires attentiveness and the development of a sense of what is salient. Often in nursing and medicine, means and ends are fused, as is the case for a “good enough” birth experience and a peaceful death.
- Applying Practice Evidence
Research continues to find that using evidence-based guidelines in practice, informed through research evidence, improves patients’ outcomes. 81–83 Research-based guidelines are intended to provide guidance for specific areas of health care delivery. 84 The clinician—both the novice and expert—is expected to use the best available evidence for the most efficacious therapies and interventions in particular instances, to ensure the highest-quality care, especially when deviations from the evidence-based norm may heighten risks to patient safety. Otherwise, if nursing and medicine were exact sciences, or consisted only of techne, then a 1:1 relationship could be established between results of aggregated evidence-based research and the best path for all patients.
Evaluating Evidence
Before research should be used in practice, it must be evaluated. There are many complexities and nuances in evaluating the research evidence for clinical practice. Evaluation of research behind evidence-based medicine requires critical thinking and good clinical judgment. Sometimes the research findings are mixed or even conflicting. As such, the validity, reliability, and generalizability of available research are fundamental to evaluating whether evidence can be applied in practice. To do so, clinicians must select the best scientific evidence relevant to particular patients—a complex process that involves intuition to apply the evidence. Critical thinking is required for evaluating the best available scientific evidence for the treatment and care of a particular patient.
Good clinical judgment is required to select the most relevant research evidence. The best clinical judgment, that is, reasoning across time about the particular patient through changes in the patient’s concerns and condition and/or the clinician’s understanding, are also required. This type of judgment requires clinicians to make careful observations and evaluations of the patient over time, as well as know the patient’s concerns and social circumstances. To evolve to this level of judgment, additional education beyond clinical preparation if often required.
Sources of Evidence
Evidence that can be used in clinical practice has different sources and can be derived from research, patient’s preferences, and work-related experience. 85 , 86 Nurses have been found to obtain evidence from experienced colleagues believed to have clinical expertise and research-based knowledge 87 as well as other sources.
For many years now, randomized controlled trials (RCTs) have often been considered the best standard for evaluating clinical practice. Yet, unless the common threats to the validity (e.g., representativeness of the study population) and reliability (e.g., consistency in interventions and responses of study participants) of RCTs are addressed, the meaningfulness and generalizability of the study outcomes are very limited. Relevant patient populations may be excluded, such as women, children, minorities, the elderly, and patients with multiple chronic illnesses. The dropout rate of the trial may confound the results. And it is easier to get positive results published than it is to get negative results published. Thus, RCTs are generalizable (i.e., applicable) only to the population studied—which may not reflect the needs of the patient under the clinicians care. In instances such as these, clinicians need to also consider applied research using prospective or retrospective populations with case control to guide decisionmaking, yet this too requires critical thinking and good clinical judgment.
Another source of available evidence may come from the gold standard of aggregated systematic evaluation of clinical trial outcomes for the therapy and clinical condition in question, be generated by basic and clinical science relevant to the patient’s particular pathophysiology or care need situation, or stem from personal clinical experience. The clinician then takes all of the available evidence and considers the particular patient’s known clinical responses to past therapies, their clinical condition and history, the progression or stages of the patient’s illness and recovery, and available resources.
In clinical practice, the particular is examined in relation to the established generalizations of science. With readily available summaries of scientific evidence (e.g., systematic reviews and practice guidelines) available to nurses and physicians, one might wonder whether deep background understanding is still advantageous. Might it not be expendable, since it is likely to be out of date given the current scientific evidence? But this assumption is a false opposition and false choice because without a deep background understanding, the clinician does not know how to best find and evaluate scientific evidence for the particular case in hand. The clinician’s sense of salience in any given situation depends on past clinical experience and current scientific evidence.
Evidence-Based Practice
The concept of evidence-based practice is dependent upon synthesizing evidence from the variety of sources and applying it appropriately to the care needs of populations and individuals. This implies that evidence-based practice, indicative of expertise in practice, appropriately applies evidence to the specific situations and unique needs of patients. 88 , 89 Unfortunately, even though providing evidence-based care is an essential component of health care quality, it is well known that evidence-based practices are not used consistently.
Conceptually, evidence used in practice advances clinical knowledge, and that knowledge supports independent clinical decisions in the best interest of the patient. 90 , 91 Decisions must prudently consider the factors not necessarily addressed in the guideline, such as the patient’s lifestyle, drug sensitivities and allergies, and comorbidities. Nurses who want to improve the quality and safety of care can do so though improving the consistency of data and information interpretation inherent in evidence-based practice.
Initially, before evidence-based practice can begin, there needs to be an accurate clinical judgment of patient responses and needs. In the course of providing care, with careful consideration of patient safety and quality care, clinicians must give attention to the patient’s condition, their responses to health care interventions, and potential adverse reactions or events that could harm the patient. Nonetheless, there is wide variation in the ability of nurses to accurately interpret patient responses 92 and their risks. 93 Even though variance in interpretation is expected, nurses are obligated to continually improve their skills to ensure that patients receive quality care safely. 94 Patients are vulnerable to the actions and experience of their clinicians, which are inextricably linked to the quality of care patients have access to and subsequently receive.
The judgment of the patient’s condition determines subsequent interventions and patient outcomes. Attaining accurate and consistent interpretations of patient data and information is difficult because each piece can have different meanings, and interpretations are influenced by previous experiences. 95 Nurses use knowledge from clinical experience 96 , 97 and—although infrequently—research. 98–100
Once a problem has been identified, using a process that utilizes critical thinking to recognize the problem, the clinician then searches for and evaluates the research evidence 101 and evaluates potential discrepancies. The process of using evidence in practice involves “a problem-solving approach that incorporates the best available scientific evidence, clinicians’ expertise, and patient’s preferences and values” 102 (p. 28). Yet many nurses do not perceive that they have the education, tools, or resources to use evidence appropriately in practice. 103
Reported barriers to using research in practice have included difficulty in understanding the applicability and the complexity of research findings, failure of researchers to put findings into the clinical context, lack of skills in how to use research in practice, 104 , 105 amount of time required to access information and determine practice implications, 105–107 lack of organizational support to make changes and/or use in practice, 104 , 97 , 105 , 107 and lack of confidence in one’s ability to critically evaluate clinical evidence. 108
When Evidence Is Missing
In many clinical situations, there may be no clear guidelines and few or even no relevant clinical trials to guide decisionmaking. In these cases, the latest basic science about cellular and genomic functioning may be the most relevant science, or by default, guestimation. Consequently, good patient care requires more than a straightforward, unequivocal application of scientific evidence. The clinician must be able to draw on a good understanding of basic sciences, as well as guidelines derived from aggregated data and information from research investigations.
Practical knowledge is shaped by one’s practice discipline and the science and technology relevant to the situation at hand. But scientific, formal, discipline-specific knowledge are not sufficient for good clinical practice, whether the discipline be law, medicine, nursing, teaching, or social work. Practitioners still have to learn how to discern generalizable scientific knowledge, know how to use scientific knowledge in practical situations, discern what scientific evidence/knowledge is relevant, assess how the particular patient’s situation differs from the general scientific understanding, and recognize the complexity of care delivery—a process that is complex, ongoing, and changing, as new evidence can overturn old.
Practice communities like individual practitioners may also be mistaken, as is illustrated by variability in practice styles and practice outcomes across hospitals and regions in the United States. This variability in practice is why practitioners must learn to critically evaluate their practice and continually improve their practice over time. The goal is to create a living self-improving tradition.
Within health care, students, scientists, and practitioners are challenged to learn and use different modes of thinking when they are conflated under one term or rubric, using the best-suited thinking strategies for taking into consideration the purposes and the ends of the reasoning. Learning to be an effective, safe nurse or physician requires not only technical expertise, but also the ability to form helping relationships and engage in practical ethical and clinical reasoning. 50 Good ethical comportment requires that both the clinician and the scientist take into account the notions of good inherent in clinical and scientific practices. The notions of good clinical practice must include the relevant significance and the human concerns involved in decisionmaking in particular situations, centered on clinical grasp and clinical forethought.
The Three Apprenticeships of Professional Education
We have much to learn in comparing the pedagogies of formation across the professions, such as is being done currently by the Carnegie Foundation for the Advancement of Teaching. The Carnegie Foundation’s broad research program on the educational preparation of the profession focuses on three essential apprenticeships:
To capture the full range of crucial dimensions in professional education, we developed the idea of a three-fold apprenticeship: (1) intellectual training to learn the academic knowledge base and the capacity to think in ways important to the profession; (2) a skill-based apprenticeship of practice; and (3) an apprenticeship to the ethical standards, social roles, and responsibilities of the profession, through which the novice is introduced to the meaning of an integrated practice of all dimensions of the profession, grounded in the profession’s fundamental purposes. 109
This framework has allowed the investigators to describe tensions and shortfalls as well as strengths of widespread teaching practices, especially at articulation points among these dimensions of professional training.
Research has demonstrated that these three apprenticeships are taught best when they are integrated so that the intellectual training includes skilled know-how, clinical judgment, and ethical comportment. In the study of nursing, exemplary classroom and clinical teachers were found who do integrate the three apprenticeships in all of their teaching, as exemplified by the following anonymous student’s comments:
With that as well, I enjoyed the class just because I do have clinical experience in my background and I enjoyed it because it took those practical applications and the knowledge from pathophysiology and pharmacology, and all the other classes, and it tied it into the actual aspects of like what is going to happen at work. For example, I work in the emergency room and question: Why am I doing this procedure for this particular patient? Beforehand, when I was just a tech and I wasn’t going to school, I’d be doing it because I was told to be doing it—or I’d be doing CPR because, you know, the doc said, start CPR. I really enjoy the Care and Illness because now I know the process, the pathophysiological process of why I’m doing it and the clinical reasons of why they’re making the decisions, and the prioritization that goes on behind it. I think that’s the biggest point. Clinical experience is good, but not everybody has it. Yet when these students transition from school and clinicals to their job as a nurse, they will understand what’s going on and why.
The three apprenticeships are equally relevant and intertwined. In the Carnegie National Study of Nursing Education and the companion study on medical education as well as in cross-professional comparisons, teaching that gives an integrated access to professional practice is being examined. Once the three apprenticeships are separated, it is difficult to reintegrate them. The investigators are encouraged by teaching strategies that integrate the latest scientific knowledge and relevant clinical evidence with clinical reasoning about particular patients in unfolding rather than static cases, while keeping the patient and family experience and concerns relevant to clinical concerns and reasoning.
Clinical judgment or phronesis is required to evaluate and integrate techne and scientific evidence.
Within nursing, professional practice is wise and effective usually to the extent that the professional creates relational and communication contexts where clients/patients can be open and trusting. Effectiveness depends upon mutual influence between patient and practitioner, student and learner. This is another way in which clinical knowledge is dialogical and socially distributed. The following articulation of practical reasoning in nursing illustrates the social, dialogical nature of clinical reasoning and addresses the centrality of perception and understanding to good clinical reasoning, judgment and intervention.
Clinical Grasp *
Clinical grasp describes clinical inquiry in action. Clinical grasp begins with perception and includes problem identification and clinical judgment across time about the particular transitions of particular patients. Garrett Chan 20 described the clinician’s attempt at finding an “optimal grasp” or vantage point of understanding. Four aspects of clinical grasp, which are described in the following paragraphs, include (1) making qualitative distinctions, (2) engaging in detective work, (3) recognizing changing relevance, and (4) developing clinical knowledge in specific patient populations.
Making Qualitative Distinctions
Qualitative distinctions refer to those distinctions that can be made only in a particular contextual or historical situation. The context and sequence of events are essential for making qualitative distinctions; therefore, the clinician must pay attention to transitions in the situation and judgment. Many qualitative distinctions can be made only by observing differences through touch, sound, or sight, such as the qualities of a wound, skin turgor, color, capillary refill, or the engagement and energy level of the patient. Another example is assessing whether the patient was more fatigued after ambulating to the bathroom or from lack of sleep. Likewise the quality of the clinician’s touch is distinct as in offering reassurance, putting pressure on a bleeding wound, and so on. 110
Engaging in Detective Work, Modus Operandi Thinking, and Clinical Puzzle Solving
Clinical situations are open ended and underdetermined. Modus operandi thinking keeps track of the particular patient, the way the illness unfolds, the meanings of the patient’s responses as they have occurred in the particular time sequence. Modus operandi thinking requires keeping track of what has been tried and what has or has not worked with the patient. In this kind of reasoning-in-transition, gains and losses of understanding are noticed and adjustments in the problem approach are made.
We found that teachers in a medical surgical unit at the University of Washington deliberately teach their students to engage in “detective work.” Students are given the daily clinical assignment of “sleuthing” for undetected drug incompatibilities, questionable drug dosages, and unnoticed signs and symptoms. For example, one student noted that an unusual dosage of a heart medication was being given to a patient who did not have heart disease. The student first asked her teacher about the unusually high dosage. The teacher, in turn, asked the student whether she had asked the nurse or the patient about the dosage. Upon the student’s questioning, the nurse did not know why the patient was receiving the high dosage and assumed the drug was for heart disease. The patient’s staff nurse had not questioned the order. When the student asked the patient, the student found that the medication was being given for tremors and that the patient and the doctor had titrated the dosage for control of the tremors. This deliberate approach to teaching detective work, or modus operandi thinking, has characteristics of “critical reflection,” but stays situated and engaged, ferreting out the immediate history and unfolding of events.
Recognizing Changing Clinical Relevance
The meanings of signs and symptoms are changed by sequencing and history. The patient’s mental status, color, or pain level may continue to deteriorate or get better. The direction, implication, and consequences for the changes alter the relevance of the particular facts in the situation. The changing relevance entailed in a patient transitioning from primarily curative care to primarily palliative care is a dramatic example, where symptoms literally take on new meanings and require new treatments.
Developing Clinical Knowledge in Specific Patient Populations
Extensive experience with a specific patient population or patients with particular injuries or diseases allows the clinician to develop comparisons, distinctions, and nuanced differences within the population. The comparisons between many specific patients create a matrix of comparisons for clinicians, as well as a tacit, background set of expectations that create population- and patient-specific detective work if a patient does not meet the usual, predictable transitions in recovery. What is in the background and foreground of the clinician’s attention shifts as predictable changes in the patient’s condition occurs, such as is seen in recovering from heart surgery or progressing through the predictable stages of labor and delivery. Over time, the clinician develops a deep background understanding that allows for expert diagnostic and interventions skills.
Clinical Forethought
Clinical forethought is intertwined with clinical grasp, but it is much more deliberate and even routinized than clinical grasp. Clinical forethought is a pervasive habit of thought and action in nursing practice, and also in medicine, as clinicians think about disease and recovery trajectories and the implications of these changes for treatment. Clinical forethought plays a role in clinical grasp because it structures the practical logic of clinicians. At least four habits of thought and action are evident in what we are calling clinical forethought: (1) future think, (2) clinical forethought about specific patient populations, (3) anticipation of risks for particular patients, and (4) seeing the unexpected.
Future think
Future think is the broadest category of this logic of practice. Anticipating likely immediate futures helps the clinician make good plans and decisions about preparing the environment so that responding rapidly to changes in the patient is possible. Without a sense of salience about anticipated signs and symptoms and preparing the environment, essential clinical judgments and timely interventions would be impossible in the typically fast pace of acute and intensive patient care. Future think governs the style and content of the nurse’s attentiveness to the patient. Whether in a fast-paced care environment or a slower-paced rehabilitation setting, thinking and acting with anticipated futures guide clinical thinking and judgment. Future think captures the way judgment is suspended in a predictive net of anticipation and preparing oneself and the environment for a range of potential events.
Clinical forethought about specific diagnoses and injuries
This habit of thought and action is so second nature to the experienced nurse that the new or inexperienced nurse may have difficulty finding out about what seems to other colleagues as “obvious” preparation for particular patients and situations. Clinical forethought involves much local specific knowledge about who is a good resource and how to marshal support services and equipment for particular patients.
Examples of preparing for specific patient populations are pervasive, such as anticipating the need for a pacemaker during surgery and having the equipment assembled ready for use to save essential time. Another example includes forecasting an accident victim’s potential injuries, and recognizing that intubation might be needed.
Anticipation of crises, risks, and vulnerabilities for particular patients
This aspect of clinical forethought is central to knowing the particular patient, family, or community. Nurses situate the patient’s problems almost like a topography of possibilities. This vital clinical knowledge needs to be communicated to other caregivers and across care borders. Clinical teaching could be improved by enriching curricula with narrative examples from actual practice, and by helping students recognize commonly occurring clinical situations in the simulation and clinical setting. For example, if a patient is hemodynamically unstable, then managing life-sustaining physiologic functions will be a main orienting goal. If the patient is agitated and uncomfortable, then attending to comfort needs in relation to hemodynamics will be a priority. Providing comfort measures turns out to be a central background practice for making clinical judgments and contains within it much judgment and experiential learning.
When clinical teaching is too removed from typical contingencies and strong clinical situations in practice, students will lack practice in active thinking-in-action in ambiguous clinical situations. In the following example, an anonymous student recounted her experiences of meeting a patient:
I was used to different equipment and didn’t know how things went, didn’t know their routine, really. You can explain all you want in class, this is how it’s going to be, but when you get there … . Kim was my first instructor and my patient that she assigned me to—I walked into the room and he had every tube imaginable. And so I was a little overwhelmed. It’s not necessarily even that he was that critical … . She asked what tubes here have you seen? Well, I know peripheral lines. You taught me PICC [peripherally inserted central catheter] lines, and we just had that, but I don’t really feel comfortable doing it by myself, without you watching to make sure that I’m flushing it right and how to assess it. He had a chest tube and I had seen chest tubes, but never really knew the depth of what you had to assess and how you make sure that it’s all kosher and whatever. So she went through the chest tube and explained, it’s just bubbling a little bit and that’s okay. The site, check the site. The site looked okay and that she’d say if it wasn’t okay, this is what it might look like … . He had a feeding tube. I had done feeding tubes but that was like a long time ago in my LPN experiences schooling. So I hadn’t really done too much with the feeding stuff either … . He had a [nasogastric] tube, and knew pretty much about that and I think at the time it was clamped. So there were no issues with the suction or whatever. He had a Foley catheter. He had a feeding tube, a chest tube. I can’t even remember but there were a lot.
As noted earlier, a central characteristic of a practice discipline is that a self-improving practice requires ongoing experiential learning. One way nurse educators can enhance clinical inquiry is by increasing pedagogies of experiential learning. Current pedagogies for experiential learning in nursing include extensive preclinical study, care planning, and shared postclinical debriefings where students share their experiential learning with their classmates. Experiential learning requires open learning climates where students can discuss and examine transitions in understanding, including their false starts, or their misconceptions in actual clinical situations. Nursing educators typically develop open and interactive clinical learning communities, so that students seem committed to helping their classmates learn from their experiences that may have been difficult or even unsafe. One anonymous nurse educator described how students extend their experiential learning to their classmates during a postclinical conference:
So for example, the patient had difficulty breathing and the student wanted to give the meds instead of addressing the difficulty of breathing. Well, while we were sharing information about their patients, what they did that day, I didn’t tell the student to say this, but she said, ‘I just want to tell you what I did today in clinical so you don’t do the same thing, and here’s what happened.’ Everybody’s listening very attentively and they were asking her some questions. But she shared that. She didn’t have to. I didn’t tell her, you must share that in postconference or anything like that, but she just went ahead and shared that, I guess, to reinforce what she had learned that day but also to benefit her fellow students in case that thing comes up with them.
The teacher’s response to this student’s honesty and generosity exemplifies her own approach to developing an open community of learning. Focusing only on performance and on “being correct” prevents learning from breakdown or error and can dampen students’ curiosity and courage to learn experientially.
Seeing the unexpected
One of the keys to becoming an expert practitioner lies in how the person holds past experiential learning and background habitual skills and practices. This is a skill of foregrounding attention accurately and effectively in response to the nature of situational demands. Bourdieu 29 calls the recognition of the situation central to practical reasoning. If nothing is routinized as a habitual response pattern, then practitioners will not function effectively in emergencies. Unexpected occurrences may be overlooked. However, if expectations are held rigidly, then subtle changes from the usual will be missed, and habitual, rote responses will inappropriately rule. The clinician must be flexible in shifting between what is in background and foreground. This is accomplished by staying curious and open. The clinical “certainty” associated with perceptual grasp is distinct from the kind of “certainty” achievable in scientific experiments and through measurements. Recognition of similar or paradigmatic clinical situations is similar to “face recognition” or recognition of “family resemblances.” This concept is subject to faulty memory, false associative memories, and mistaken identities; therefore, such perceptual grasp is the beginning of curiosity and inquiry and not the end. Assessment and validation are required. In rapidly moving clinical situations, perceptual grasp is the starting point for clarification, confirmation, and action. Having the clinician say out loud how he or she is understanding the situation gives an opportunity for confirmation and disconfirmation from other clinicians present. 111 The relationship between foreground and background of attention needs to be fluid, so that missed expectations allow the nurse to see the unexpected. For example, when the background rhythm of a cardiac monitor changes, the nurse notices, and what had been background tacit awareness becomes the foreground of attention. A hallmark of expertise is the ability to notice the unexpected. 20 Background expectations of usual patient trajectories form with experience. Tacit expectations for patient trajectories form that enable the nurse to notice subtle failed expectations and pay attention to early signs of unexpected changes in the patient's condition. Clinical expectations gained from caring for similar patient populations form a tacit clinical forethought that enable the experienced clinician to notice missed expectations. Alterations from implicit or explicit expectations set the stage for experiential learning, depending on the openness of the learner.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses’ continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
This section of the paper was condensed and paraphrased from Benner, Hooper-Kyriakidis, and Stannard. 23 Patricia Hooper-Kyriakidis wrote the section on clinical grasp, and Patricia Benner wrote the section on clinical forethought.
- Cite this Page Benner P, Hughes RG, Sutphen M. Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 6.
- PDF version of this page (147K)
In this Page
- Clinical Grasp
Other titles in this collection
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. [Int J Nurs Stud. 2007] Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. Funkesson KH, Anbäcken EM, Ek AC. Int J Nurs Stud. 2007 Sep; 44(7):1109-19. Epub 2006 Jun 27.
- Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. [Nurse Educ Today. 2016] Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. Lee J, Lee YJ, Bae J, Seo M. Nurse Educ Today. 2016 Nov; 46:75-80. Epub 2016 Aug 15.
- Combining the arts: an applied critical thinking approach in the skills laboratory. [Nursingconnections. 2000] Combining the arts: an applied critical thinking approach in the skills laboratory. Peterson MJ, Bechtel GA. Nursingconnections. 2000 Summer; 13(2):43-9.
- Review About critical thinking. [Dynamics. 2004] Review About critical thinking. Hynes P, Bennett J. Dynamics. 2004 Fall; 15(3):26-9.
- Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. [Nurse Educ Today. 2010] Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. Levett-Jones T, Hoffman K, Dempsey J, Jeong SY, Noble D, Norton CA, Roche J, Hickey N. Nurse Educ Today. 2010 Aug; 30(6):515-20. Epub 2009 Nov 30.
Recent Activity
- Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinical... Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
NURSING PROCESS AND CRITICAL THINKING
Get better grades with Learn
82% of students achieve A’s after using Learn
Pharmacology and the Nursing Process
Medical Terminology: Learning Through Practice

Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1316 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Thinking Critically About the Quality of Critical Thinking Definitions and Measures

Criticality in Osteopathic Medicine: Exploring the Relationship between Critical Thinking and Clinical Reasoning

A guide to critical thinking: implications for dental education
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
definition of nursing. the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations. nursing process. a systematic process by which nurses plan ...
a document plan for giving patient care and includes the health-care provider's orders, nursing diagnoses, and nursing orders. what is critical thinking. using skillful reasoning and logical thought to determine the merits of a belief or action. what is validating in critical thinking skills. verifying patients information.
1) Define the problem clearly. 2) Consider all possible alternatives as solutions to the problem. 3) Consider all the possible outcomes for each alternative. 4) Predict the likelihood of each outcome occurring. 5.) Choose the alternative with the best chance of success that has the fewest undesirable outcomes.
Quiz 11: Critical Thinking and the Nursing Process. Access For Free. Study Flashcards. Practice Exam. Learn. Question 1. Multiple Choice. A nurse who just moved from an urban area to a sparsely populated rural area understands that certain customs and practices the nurse is familiar with may be quite foreign to the people in the new area. This ...
Chapter 05: Nursing Process and Critical Thinking Cooper: Foundations of Nursing, 8th Edition MULTIPLE CHOICE 1. What best defines the nursing process? a. A method to ensure that the health care provider's orders are implemented correctly. b. A series of assessments that isolate a patient's health problem. c.
Chapter 5: Nursing Process and Critical Thinking. Lesson 5. Explain the use of each of the six phases of the nursing process. List the elements of each of the six phases of the nursing process. Describe the establishment of the database. Discuss the components of a patient problem statement.
CHAPTER 5: NURSING PROCESS AND CRITICAL THINKING. American Nurse9s Association (ANA) definition of nursing: <Nursing is the protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups ...
Establishing and determining new diagnosis for allied health. Developing criteria for collaborative practice between nursing and MD. The planning stage of the nursing process involves: Will reduce his risk of falls by correct use of his walker each time him ambulates. The nurse will teach the patient the to use a walker within 2 days.
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
The nursing process is a sequence of steps that requires critical thinking to provide sound, individualized patient care. Critical thinking makes the nursing process accurate, scientifically sound, appropriate, flexible, and individualized. DIF: Cognitive Level: Comprehension REF: p. 163 OBJ: 4.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse's critical thinking to provide the best care possible to the client.
This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care. 4.2. BASIC CONCEPTS. Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice.
Bandman and Bandman (1995) describe critical thinking for nursing as "the rational examination of ideas, inferences, assumptions, principles, arguments, conclusions, issues, statements, beliefs, and actions" (p. 7) and include the following functions: • Discriminating among use and misuse of language.
Through a series of thought-provoking multiple-choice questions, we'll explore each step of the nursing process - assessment, diagnosis, planning, implementation, and evaluation. These quizzes will challenge your knowledge and critical thinking abilities, simulating real-life scenarios you may encounter in healthcare settings.
6. Requires Critical Thinking. Most importantly, it's essential that nurses use critical thinking when planning patient care using the nursing process. This means as nurses, we must use a combination of our knowledge and past experiences with the information we have about a current patient to make the best decisions we can about nursing care.
1. Describes a patient response (e.g. Ineffective Airway Clearance) 2. May change from day to day as response changes (e.g. impaired gas exchange) 3. Treatable by nurses with scope of nursing practice. 4. Often deals with the patients perception of his/own health state (e.g. Body image disturbance) 5.
The nursing process functions as a systematic guide to client-centered care with 5 sequential steps. These are assessment, diagnosis, planning, implementation, and evaluation. Assessment. Assessment is the first step and involves critical thinking skills and data collection; subjective and objective. Subjective data involves verbal statements ...
Critical Thinking. Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. ... The process of critical thinking is stimulated by integrating the essential ...
Study with Quizlet and memorize flashcards containing terms like Nursing Process definition, The Nursing Process is an..., What is Critical Thinking? and more.
king nurses engage in every day. It must be based on good c1itica. thinking. It determines what the nurse DOES after thinking about a problem.• Good thinking requires attitudes such. as intellectual humility, intellectual autonomy, and intellectual inte. rity.• The clinical judgment process works well with the nur.
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered.