Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Patient Case Presentation
Patient Overview
M.J. is a 25-year-old, African American female presenting to her PCP with complaints of fatigue, weakness, and shortness of breath with minimal activity. Her friends and family have told her she appears pale, and combined with her recent symptoms she has decided to get checked out. She also states that she has noticed her hair and fingernails becoming extremely thin and brittle, causing even more concern. The patient first started noticing these symptoms a few months ago and they have been getting progressively worse. Upon initial assessment, her mucosal membranes and conjunctivae are pale. She denies pain at this time, but describes an intermittent dry, soreness of her tongue.
Vital Signs:
Temperature – 37 C (98.8 F)
HR – 95
BP – 110/70 (83)
Lab Values:
Hgb- 7 g/dL
Serum Iron – 40 mcg/dL
Transferrin Saturation – 15%
Medical History
- Diagnosed with peptic ulcer disease at age 21 – controlled with PPI pharmacotherapy
- IUD placement 3 months ago – reports an increase in menstrual bleeding since placement
Surgical History
- No past surgical history reported
Family History
- Diagnosis of iron deficiency anemia at 24 years old during pregnancy with patient – on daily supplement
- Otherwise healthy
- Diagnosis of hypertension – controlled with diet and exercise
- No siblings
Social History
- Vegetarian – patient states she has been having weird cravings for ice cubes lately
- Living alone in an apartment close to work in a lower-income community
- Works full time at a clothing department store
Learn about the nursing care management of patients with anemia .
Table of Contents
What is anemia, classification, hypoproliferative anemia, hemolytic anemia, clinical manifestations, complications, assessment and diagnostic findings, medical management, nursing assessment, planning & goals, nursing interventions, discharge and home care guidelines, documentation guidelines.
Anemia is a condition that is slowly rising in cases across all countries. Every age and every stage can be affected by anemia, and though others may consider this as a simple condition, it could blow out of proportion if left untreated.
- Anemia is a condition in which the hemoglobin concentration is lower than normal.
- Anemia reflects the presence of fever than the normal number of erythrocytes within the circulation.
- Anemia is not a specific disease state but an underlying disorder and the most common hematologic condition.
A physiologic approach classifies anemia according to whether the deficiency in erythrocytes is caused by a defect in their production, by their destruction, or by their loss.
- Hypoproliferative anemias . In hypoproliferative anemias, the marrow cannot produce adequate numbers of erythrocytes.
- Hemolytic anemias . There is premature destruction of erythrocytes that results in the liberation of hemoglobin from the erythrocytes into the plasma ; the released hemoglobin is then converted into bilirubin , therefore bilirubin concentration rises.
- Bleeding anemias . Bleeding anemias are caused by the loss of erythrocytes in the body.
Pathophysiology
The pathophysiology of anemias is drawn according to the cause of the disease.
- Decreased erythrocyte production . There is decreased erythrocyte production, reflected by an inappropriately normal or low reticulocyte count .
- Marrow damage . As a result of marrow damage, inadequate production of erythrocyte occurs due to the medications or chemicals or from a lack of factors.
- Premature destruction . Premature destruction of erythrocytes results in the liberation of hemoglobin from the erythrocytes into the plasma.
- Conversion . The released hemoglobin is converted in large part to bilirubin, resulting in high concentration of bilirubin.
- Erythropoietin production . The increased erythrocyte destruction leads to tissue hypoxia which stimulates erythropoietin production.
- Increased reticulocytes . This increased production is reflected in an increased reticulocyte count as the bone marrow responds to the loss of erythrocytes.
- Hemolysis . Hemolysis is the end result, which can result from an abnormality within the erythrocyte itself or within the plasma, or from direct injury to the erythrocyte within the circulation.
It is usually possible to determine whether the presence of anemia is caused by destruction or inadequate production of erythrocytes on the basis of the following factors.
- Response . The marrow’s response to decreased erythrocytes as evidenced by an increased reticulocyte count in the circulation blood .
- Proliferation . The degree to which young erythrocytes proliferate in the bone marrow and the manner in which they mature as observed in the bone marrow biopsy .
- Destruction . The presence or absence of end products of erythrocyte destruction within the circulation.
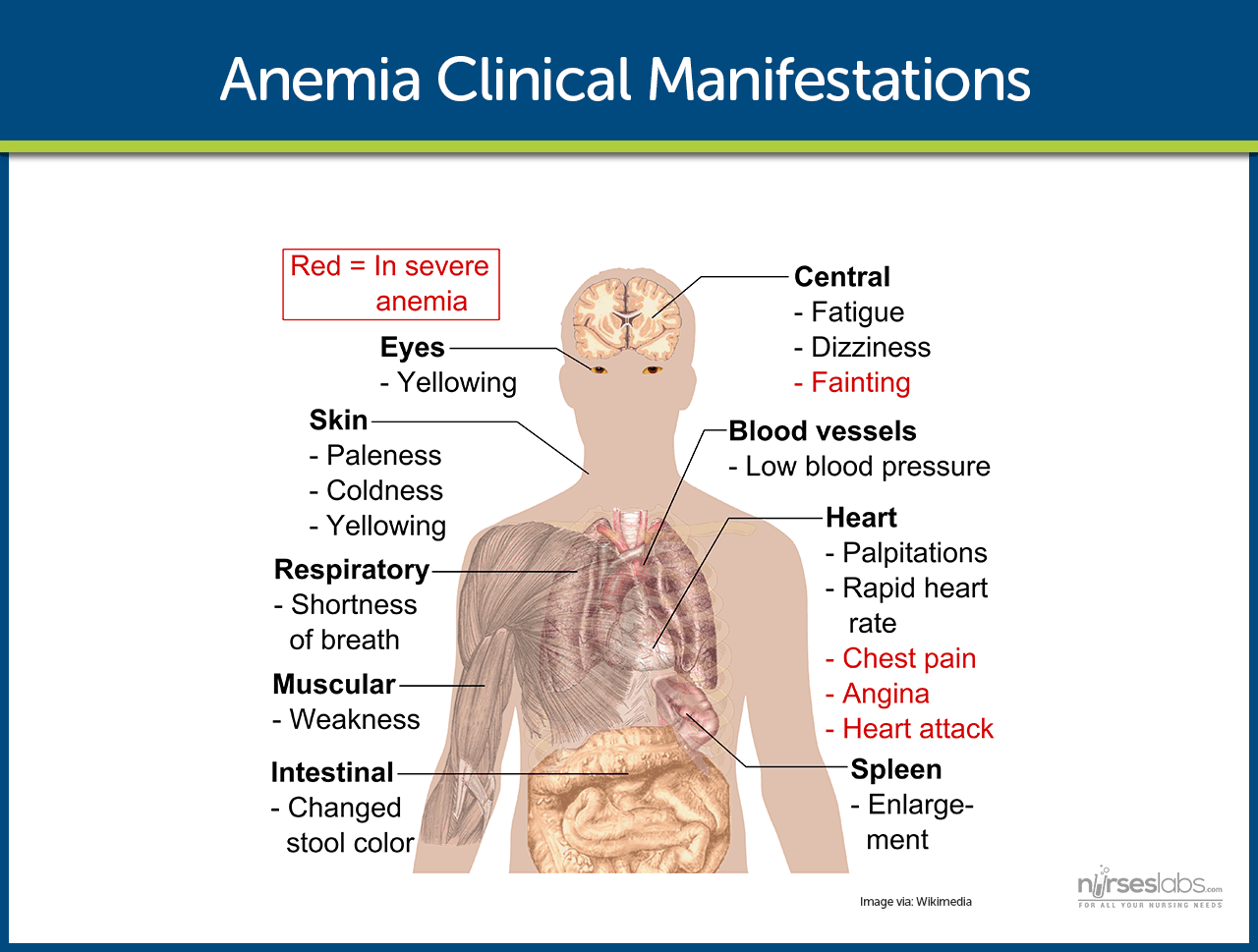
In general, the more rapidly the anemia develops, the more aggressive is its symptoms.
- Decreased hemoglobin . A patient with anemia has hemoglobin levels between 9 to 11 g/dL.
- Fatigue . Fatigue occurs because there is inadequate oxygen levels in the tissues that should have been carried by hemoglobin.
- Tachycardia . The heart compensates for the decrease in oxygen by pumping out more blood so it can reach peripheral tissues in the body.
- Dyspnea . Difficulty of breathing occurs because of the decreased concentrations of oxygen in the blood.
- With decreased hemoglobin that serves as the pigment in the red blood cells, the patient may become pale because of the lack or decrease in the pigment that is hemoglobin.
To prevent anemia, lifestyle modifications must be made.
- Diet rich in iron . Ingestion of iron-rich foods could help prevent anemia because it adds to the hemoglobin in the body.
- Iron supplements . Iron supplements can also be taken to increase the hemoglobin levels in the body.
Anemia has general complications and this includes:
- Heart failure . As the heart compensates by pumping faster than the normal rate, the heart muscles gradually weaken until the muscles wear out and the heart fails to function.
- Paresthesias . Paresthesias develop when the muscles do not have enough oxygen delivered to them.
- Delirium . Insufficient oxygen in the brain results in delirium and is considered a fatal complication of anemia.
A number of hematologic studies are performed to determine the type and cause of anemia.
- Blood studies . In an initial evaluation , the hemoglobin, hematocrit, reticulocyte count, and RBC indices, particularly the mean corpuscular volume and red cell distribution width are taken to assess for the presence of anemia.
- Iron studies . Serum iron level, total iron binding capacity, percent saturation, and ferritin, as well as serum vitamin B12 and folate levels, are all useful in diagnosing anemia.
- CBC values . The remaining CBC values are useful in determining whether the anemia is an isolated problem or part of another hematologic condition.
Management of anemia is directed towards correcting or controlling the cause of anemia.
- Nutritional supplements . Use of nutritional supplements should be appropriately taught to the patient and the family because too much intake cannot improve anemia.
- Blood transfusion . Patients with acute blood loss or severe hemolysis may have decreased tissue perfusion from decreased blood volume or reduced circulating erythrocytes, so transfusion of blood would be necessary.
- Intravenous fluids . Intravenous fluids replace the lost volumes of blood or electrolytes to restore them to normal levels.
Nursing Management
The management of anemia by nurses should be accurate and appropriate so that objectives and goals would be achieved.
The assessment of anemia involves:
- Health history and physical exam . Both provide important data about the type of anemia involved, the extent and type of symptoms it produces, and the impact of those symptoms on the patient’s life.
- Medication history . Some medications can depress bone marrow activity, induce hemolysis, or interfere with folate metabolism.
- History of alcohol intake . An accurate history of alcohol intake including the amount and duration should be obtained.
- Family history . Assessment of family history is important because certain anemias are inherited.
- Athletic endeavors . Assess if the patient has any athletic endeavor because extreme exercise can decrease erythropoiesis and erythrocyte survival.
- Nutritional assessment . Assessing the nutritional status and habits is important because it may indicate deficiencies in essential nutrients such as iron, vitamin B12, and folic acid.
Based on the assessment data, major nursing diagnosis for patients with anemia include:
- Fatigue related to decreased hemoglobin and diminished oxygen-carrying capacity of the blood.
- Altered nutrition , less than body requirements , related to inadequate intake of essential nutrients.
- Altered tissue perfusion related to insufficient hemoglobin and hematocrit.
The major goals for a patient with anemia include:
- Decreased fatigue
- Attainment or maintenance of adequate nutrition.
- Maintenance of adequate tissue perfusion .
- Compliance with prescribed therapy.
- Absence of complications.
Nursing interventions are based on the data assessed by the nurse and on the symptoms that the patient manifests.
To manage fatigue :
- Prioritize activities . Assist the patient in prioritizing activities and establishing balance between activity and rest that would be acceptable to the patient.
- Exercise and physical activity . Patients with chronic anemia need to maintain some physical activity and exercise to prevent the deconditioning that results from inactivity.
To maintain adequate nutrition:
- Diet . The nurse should encourage a healthy diet that is packed with essential nutrients.
- Alcohol intake . The nurse should inform the patient that alcohol interferes with the utilization of essential nutrients and should advise the patient to avoid or limit his or her intake of alcoholic beverages.
- Dietary teaching . Sessions should be individualized and involve the family members and include cultural aspects related to food preference and preparation.
To maintain adequate perfusion:
- Blood transfusion monitoring . The nurse should monitor the patient’s vital signs and pulse oximeter readings closely.
To promote compliance with prescribed therapy:
- Enhance compliance . The nurse should assist the patient to develop ways to incorporate the therapeutic plan into everyday activities.
- Medication intake . Patients receiving high-dose corticosteroids may need assistance to obtain needed insurance coverage or to explore alternative ways to obtain these medications.
Included in the expected patient outcomes are the following:
- Reports less fatigue .
- Attains and maintains adequate nutrition.
- Maintains adequate perfusion.
Health education is the main focus during discharge and for the home care.
- Instruct the patient to consume iron-rich foods to help build-up hemoglobin stores.
- Iron supplements. Enforce strict compliance in taking iron supplements as prescribed by the physician.
- Follow-up. Stress the need for regular medical and laboratory follow-up to evaluate disease progression and response to therapies.
The data to be documented consists the following:
- Baseline and subsequent assessment findings to include signs and symptoms.
- Individual cultural or religious restrictions and personal preferences.
- Plan of care and persons involved.
- Teaching plan.
- Client’s responses to teachings, interventions, and actions performed.
- Attainment or progress toward desired outcome.
- Long-term needs, and who is responsible for actions to be taken.
Posts related to Anemia:
- 6 Sickle Cell Anemia Nursing Care Plans
- Sickle Cell Anemia
- 4 Aplastic Anemia Nursing Care Plans
5 thoughts on “Anemia”
thank youuu
I love love love this thank you
Wow, triple the love—that’s fantastic! 🎉 So thrilled you’re enjoying it. If there’s anything special you loved or something more you’re keen on seeing, don’t hesitate to share. Thank you, Terri!
i appreciated you so much
Hi Geeta, Thanks a bunch! I’m so glad to hear you appreciated the info on anemia care management. If there’s anything more you’d like to know or if you have questions on other health topics, feel free to reach out. Always happy to help!
Leave a Comment Cancel reply
Anemia: Nursing Diagnoses, Care Plans, Assessment & Interventions

Anemia occurs when there are not enough red blood cells or red blood cells do not function properly, resulting in low hemoglobin and a lack of oxygen throughout the body .
Anemia is caused by blood loss, decreased red blood cell (RBC) production, or the destruction of RBCs . There are many types of anemia. While some anemias are mild and temporary, others can be chronic and lifelong. Anemia can develop from a poor diet, a genetic condition, cancer , autoimmune diseases, toxic chemicals, infection, or as a side effect of chronic conditions.
In this article:
- Nursing Process
- Review of Health History
- Physical Assessment
- Diagnostic Procedures
- Nursing Interventions
- Decreased Cardiac Output
- Imbalanced Nutrition: Less Than Body Requirements
- Ineffective Tissue Perfusion
Types of Anemia
The following is a list of anemias the nurse may encounter and treat:
- Iron-deficiency anemia (the most common type of anemia)
- Pernicious anemia
- Megaloblastic anemia
- Sickle cell anemia
- Thalassemia anemia
- Fanconi anemia
- Diamond-Blackfan anemia
- Hemolytic anemia
- Aplastic anemia
- Macrocytic anemia
- Microcytic anemia
- Normocytic anemia
Anemia will likely result from a larger condition, and treatment will depend on the type of anemia and underlying cause. For example, acute anemia may result from blood loss and require volume resuscitation with blood products. On the other hand, Sickle cell anemia is a chronic and severe form of anemia that requires inpatient treatment when a pain crisis occurs, and nurses must understand how to assess and manage it appropriately.
Nursing Assessment
The first step of nursing care is the nursing assessment, during which the nurse will gather physical, psychosocial, emotional, and diagnostic data. In this section, we will cover subjective and objective data related to anemia.
1. Determine the patient’s general symptoms. Check for the following symptoms of anemia:
- General: fatigue, general weakness
- CNS: dizziness , lightheadedness, headaches
- HEENT: pounding or “whooshing” sound in the ear (pulsatile tinnitus)
- Respiratory: dyspnea , tachypnea
- Cardiovascular: fast or irregular heartbeat, palpitations, chest discomfort, chest pain
- Integumentary: pale skin, cool skin, reports of feeling cold, numbness in the hands and feet, brittle nails
2. Review the medical history of the patient. Pay special attention to conditions that affect the bone marrow, like a history of leukemia or other blood cancers, since this is where RBCs are formed. Other chronic conditions like chronic kidney disease or rheumatoid arthritis may also cause anemia.
3. Review medications. The following medications may cause hemolytic anemia:
- Cephalosporins
- Levofloxacin
- Nitrofurantoin
- Penicillins
4. Interview the patient about their activities and possible risk factors. Inquire about the patient’s occupation or hobbies to uncover whether they are exposed to tranquilizers, pesticides, paints, solvents, or hair dyes, as these are possible environmental causes of anemia.
5. For women, identify the gynecological status of the patient. Identify if there is a presence of heavy menstrual bleeding, a recent abortion, or a current pregnancy that may contribute to anemia.
6. Ask the patient about bleeding with bowel movements. Patients must recognize the importance of changes in bowel habits and not ignore blood in the stool. Inquire about dark, tarry stools, blood observed on toilet paper or in the toilet bowl after a bowel movement, diarrhea with bleeding, or hemorrhoids causing bright red bleeding.
7. Identify the patient’s gastrointestinal history. The following gastrointestinal problems commonly cause bleeding and associated anemia:
- Diverticulitis
- Hiatal hernias
- Peptic ulcers
- Gastroenteritis
- Inflammatory bowel disease
8. Determine if the patient has changes in their urine. Ask the patient for any changes in the urine color. Abnormal urine color can indicate active bleeding in the genitourinary system.
9. Assess the patient’s diet. Review the patient’s usual diet. A diet that lacks vitamins and minerals increases the risk of nutritional anemias. Excessive alcohol intake can predispose the patient to conditions causing anemia. Some patients on vegan or vegetarian diets may not consume the correct foods for adequate iron and vitamin B12.
10. Determine the patient’s economic status. If the patient lives in a food desert or is unable to afford quality food, they are at risk for experiencing nutritional anemias.
1. Assess for any nutritional deficiencies. Nutritional deficiencies are often associated with obvious physical symptoms, such as:
- Brittle fingernails
- Tachycardia
- Bleeding gums
- Pale skin or jaundice
- Weight loss
- Muscle weakness
- Inflamed tongue (glossitis)
2. Assess for any obvious bleeding or bleeding disorder. Bleeding disorders like hemophilia, intestinal conditions like ulcers, or medications like aspirin or warfarin may result in bleeding. Monitor for unusual bleeding to the skin, such as purpura, bruising, or petechiae. Assess for signs of obvious trauma or injuries.
3. Perform a neurological assessment. Due to low levels of oxygen-carrying blood to the brain, patients with anemia may display alterations in the nervous system. Monitor closely for vision disturbances, memory loss, poor coordination, headache, irritability, and paresthesias.
4. Examine the patient’s eyes. Low levels of iron may cause the vascular area of the eyes to become pale pink or white. A blue tint to the sclera indicates iron-deficiency anemia.
5. Perform a cardiopulmonary assessment. A low level of circulating RBCs negatively affects the heart and lungs. The patient may experience chest discomfort or dyspnea. Assess for tachycardia, tachypnea, and hypoxia. There is an increased risk of heart failure with anemia.
6. Palpate the lymph nodes. Conduct a thorough examination for any palpable lymph node enlargement that might indicate an infection or neoplasia. Infection and cancer can cause a decrease in RBCs.
1. Draw blood to identify the type of anemia. The following blood tests are used to differentiate the type of anemia:
- Red blood cell count
- Hemoglobin/hematocrit
- Reticulocyte count
- MCV (mean corpuscular volume)
- RDW (red cell distribution width)
- Platelet count
- Iron profile (iron, ferritin, and total iron-binding content)
- Folate and vitamin B12
The following lab tests may aid in diagnosing underlying conditions causing anemia:
- Coagulation screenings (aPTT, PT/INR)
- Lead levels
- Factor assays
- Coombs test
2. Assist with imaging scans. Imaging scans are utilized with acute anemia to determine an underlying cause or complications.
- Ultrasonography offers quick evaluation for intraperitoneal bleeding
- Chest X-rays are useful with severe anemia causing cardiomyopathy
- CT scans of the abdomen detect masses, internal bleeding, or abnormalities with the spleen and other abdominal organs
- Esophagogastroduodenoscopy (EGD) can diagnosis acute upper GI bleeding
- Outpatient colonoscopy may be considered to diagnosis lower GI bleeding
3. Prepare for bone marrow aspiration. While not necessary for most patients with anemia, bone marrow analysis may be required if lab results are inconclusive.
Nursing interventions and care are essential for the patients recovery. In the following section, you will learn more about possible nursing interventions for a patient with anemia.
1. Identify and manage the cause. Anemia results from conditions that affect RBC production or cause RBC destruction. Possible causes of anemia include the following, with each requiring individual interventions:
- Acute blood loss
- Nutritional deficiencies (iron, vitamin B12, and folate)
- Conditions affecting the bone marrow
- Chronic renal disease
- Autoimmune and rheumatological conditions
- Increased red blood cell destruction (faulty mechanical valves, hemolytic anemia, DIC)
- Side effects of medications
2. Administer IV fluids as ordered. IV fluids can increase the intravascular volume in instances of trauma or acute blood loss.
3. Transfuse blood as ordered. Packed red blood cells (RBCs) should only be transfused to actively bleeding patients and those with severe and symptomatic anemia with a hemoglobin level of 7 g/dL or less.
4. Apply oxygen as needed. Since RBCs are the oxygen-carrying components of blood, if the patient is anemic, they may experience hypoxia or dyspnea. Apply supplemental oxygen as needed.
5. Administer supplements as recommended. Supplements and their prescribed route will depend on the patient’s deficiencies and include:
- Oral/IV iron
- Oral/IM vitamin B12
- Oral/IV/IM folate
6. Educate on oral iron supplementation. For patients to get the most benefit from iron supplements, provide the following education:
- Side effects include gastrointestinal problems such as constipation, black, tarry stools, and metallic taste
- On an empty stomach
- With water or fruit juice (or any source of vitamin C to aid in absorption)
- 1 hour prior or 2 hours after meals (may take with food if GI upset occurs)
7. Administer erythropoietin for patients with renal disease. With renal disease, the kidneys cannot produce enough erythropoietin (EPO), which is necessary to maintain healthy RBCs. Administering synthetic EPO stimulates the production of RBCs.
8. Prepare the patient for possible bone marrow and stem cell transplantation. For those with severe aplastic anemia, healthy stem cells from a donor replace the patient’s destructive bone marrow. Younger patients with a matched donor (usually a sibling) are the best candidates for a stem cell transplant or bone marrow transplant.
9. Refer the patient to a dietitian. Dietitians can assist and educate the patient regarding recommended foods for nutritional deficiencies (iron, vitamin B12, and folate).
10. Advise the patient when to seek immediate medical attention. Advise the patient to consult a healthcare provider if symptoms worsen despite treatments. If any of these signs are present, advise them to go to the nearest emergency department:
- Breathing difficulties
- Lightheadedness
- Chest discomfort
- Bright red bleeding in the stool
Nursing Care Plans
Once the nurse identifies nursing diagnoses for anemia, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for anemia.
Acute pain is a nursing diagnosis specific to sickle cell anemia. This genetic condition causes red blood cells to ‘sickle’ and clump together, decreasing blood flow and perfusion causing a pain crisis.
Nursing Diagnosis: Acute Pain
Related to:
- Sickling of red blood cells occluding blood vessels
- Lack of perfusion and oxygenation to extremities
As evidenced by:
- Intense complaint of pain anywhere in the body
- Pain described as stabbing, sharp, or throbbing
- Reduced activity
- Restlessness
- Distractive behavior (pacing, watching tv, talking on the phone)
Expected outcomes:
- Patient will report a decrease in pain to a level of 2/10 by discharge.
- Patient will verbalize an understanding of behaviors that trigger a pain crisis.
- Patient will adhere to the prescribed pain medication regimen.
Assessment:
1. Assess pain. Perform a complete pain assessment using a numeric or FACES pain scale. Assess character, duration, frequency, precipitating factors, and any interventions.
2. Assess for acute chest syndrome. Acute chest syndrome is vaso-occlusion that occurs in the pulmonary vasculature. It is life-threatening and the most common cause of death in sickle cell patients. Monitor for symptoms of chest pain, fever, dyspnea, and infiltrates on a chest x-ray.
3. Assess pain medication regimen. Many sickle cell pain crises occur due to missed doses of pain medication or an inadequate regimen. Assess the patient’s adherence as well as doses and frequency of pain medication.
Interventions:
1. Provide fluids. IV hydration is a priority for treating a sickle cell crisis. IV fluids will stop or slow the sickling process and reduce pain. Patients should also be encouraged to drink plenty of fluids.
2. Administer analgesics. Sickle cell patients often have a very high pain tolerance and will receive high doses of narcotics. Some patients may be on a PCA pump until their pain is better controlled. The nurse should closely monitor the patient and provide adequate pain control without over-sedating the patient.
3. Administer blood transfusions. Depending on the patient’s hemoglobin level, blood transfusions may be necessary to prevent worsening complications and correct anemia. Some patients may receive long-term transfusions monthly on an outpatient basis.
4. Educate on preventing a sickle cell crisis. Patients should be educated on triggers of a sickle cell crisis to prevent them. Maintaining hydration, preventing infections, avoiding exposure to cold weather, reducing stress , and adhering to medications are necessary to manage sickle cell anemia.
Anemia causes decreased cardiac function (central venous pressure and heart filling), decreasing cardiac output.
Nursing Diagnosis: Decreased Cardiac Output
- Inadequate filling of blood in the heart
- Decreased oxygenated blood to the heart
- Inadequate cardiac muscle contraction
- Low pressure to pump blood
- Difficulty of the heart muscle to pump oxygenated blood
- Increased cardiac workload
- Severe blood loss
- Low red blood cells
- Decreased cardiac output
- Hypertension
- Cardiac arrhythmias
- Diminished pulses
- Patient will demonstrate blood pressure and pulses within normal limits.
- Patient will manifest normal sinus rhythm in ECG.
- Patient will have no complaints of chest pain.
1. Monitor the vital signs. Anemia results in compensatory mechanisms such as increased heart rate and blood pressure. Monitor for possible heart fatigue that can lead to heart failure if tachycardia and hypertension are uncontrolled.
2. Obtain cardiovascular history. Note any histories of cardiovascular diseases that may affect the blood supply. Decreased cardiac output due to cardiovascular diseases and anemia will add strain and workload to the heart.
3. Assess cardiovascular status. Anemia can significantly impact the progression of heart failure (HF) . It causes a decrease in oxygen-carrying and delivery capacity. It compromises blood circulation.
4. Check the RBC count Check the RBC’s volume and quality in size and shape through complete blood count (CBC) and peripheral blood smear. The RBC count and its characteristics may affect the cardiac output and circulating blood in the body.
5. Obtain ECG. Anemia can cause a fast and irregular heartbeat (arrhythmia) that can be seen in ECG. Anemia causes the heart to pump extra blood to compensate for a lack of oxygen.
1. Reduce cardiac stress. Anemia can affect heart performance by increasing the heart rate and stroke volume. It will also reduce blood flow to the kidneys and fluid retention, putting additional strain on the heart.
2. Treat the anemia according to its type. Manage anemia based on its type and cause. It will resume all the organ functions once the circulating volume is within normal limits. The heart will be able to pump acceptable cardiac output.
3. Prepare for a possible blood transfusion. Severe anemia would necessitate a blood transfusion to supplement cardiac output and aid in circulating oxygenated blood throughout the body.
4. Stop the cause of anemia. Anemia can be a result of treatment such as chemotherapy . Discontinue as ordered if the anemia is causing a life-threatening complication for the patient. Allow the heart to rest and be free from treatments or medications to maximize its function to pump quality RBCs.
A lack of oxygen-carrying red blood cells will result in decreased energy and fatigue.
Nursing Diagnosis: Fatigue
- Decreased hemoglobin
- Exhaustion
- Inability to maintain physical activity
- Increased need for rest
- Reported lack of energy
- Lethargy
- Patient will verbalize techniques to conserve energy.
- Patient will report an increase in energy and ability to perform tasks.
1. Monitor CBC. Assess the patient’s complete blood count including red blood count and hemoglobin levels. These will be low in anemic patients.
2. Assess for chronic conditions that worsen anemia. Chronic conditions can cause and contribute to anemia. These include pregnant patients, those with cancer, or autoimmune diseases. Treating the underlying cause of anemia should be a priority.
3. Assess the extent of fatigue in daily life. Inquire about activities the patient can or cannot perform, the effect it has on their responsibilities and roles, and how they manage their symptoms.
1. Instruct on energy conservation. Plan rest periods, delegate tasks to others, cluster activities together, prioritize activities when energy levels are highest.
2. Apply oxygen. Patients being treated for anemia in the hospital may require supplemental oxygen for very low hemoglobin levels.
3. Administer blood transfusions. If a patient is severely anemic or has suffered a blood loss causing anemia, blood transfusions may help with fatigue.
4. Administer erythropoietin injections. Epogen and Procrit are two common injections given that stimulate the bone marrow to produce red blood cells. Patients with cancer, HIV , or kidney disease often have severe anemia and require these injections.
Iron-deficient and vitamin-deficient anemia can occur due to poor dietary intake or an inability to absorb nutrients.
Nursing Diagnosis: Imbalanced Nutrition
- Inability to absorb iron or vitamins
- Lack of vitamin B12 and folate in the diet
- Pregnancy
- Gastric bypass surgery
- Inflammatory bowel diseases
- Vegetarian diet
- Pale skin
- Feeling cold
- Fatigue
- Rapid heartbeat
- Brittle nails
- Hair loss
- Craving ice (pagophagia)
- Headaches
- Patient will display an improvement in iron and B-12 levels through lab testing.
- Patient will add three foods high in iron, B-12, and folic acid to their diet.
- Patient will recognize the signs and symptoms of anemia and when to call their doctor.
1. Assess lab values. Monitor red blood cell count, hemoglobin, hematocrit, ferritin, iron, and total iron-binding capacity for abnormalities.
2. Assess the patient’s usual diet. Assess for nutritional gaps in the patient’s diet by taking a history of foods they normally eat as well as any food allergies they may have.
3. Assess access to healthy foods. Assess if access to food prevents the patient from obtaining nutritionally-balanced foods that are high in vitamins.
1. Instruct on a healthy diet. Iron-rich foods include dark green, leafy vegetables, nuts, and eggs. Foods high in vitamin B-12 include meat and dairy products. Folic acid is found in legumes, citrus juices, and dark green leafy vegetables.
2. Consider supplements. Patients may be prescribed oral supplements of iron or vitamin B-12 (cyanocobalamin) if they cannot get enough from their diet. Patients may also receive vitamin B-12 injections regularly usually administered by a nurse.
3. Encourage prenatal supplements. Pregnant patients should be instructed on the importance of prenatal vitamins which contain iron and folate. These vitamins are essential to support a healthy pregnancy and prevent birth defects.
4. Improve iron absorption. Some patients struggle with absorbing iron and will need instruction on when and which foods to eat to increase absorption. It is easier for the body to absorb meat and seafood iron-containing products. Iron in vegetables, grains, and seeds is more difficult for the body to absorb. Vitamin C can help with the absorption of iron when taken with a meal. Tannins in tea and coffee can inhibit the absorption of iron.
Tissue perfusion requires adequate blood circulation to the tissues. Anemia results in a loss or destruction of RBCs, preventing oxygen from perfusing tissues.
Nursing Diagnosis: Ineffective Tissue Perfusion
- Bone marrow suppression
- Poor diet or deficiency in iron or vitamin B12
- Low supply of oxygenated RBCs
- Impaired transport of oxygen
- Chronic conditions (chronic kidney disease, rheumatoid arthritis, cancer)
- Body attacks own RBCs
- Lightheadedness or dizziness
- Change in mentation
- Cold extremities
- Prolonged capillary refill time
- Shortness of breath
- Low hemoglobin levels
- Patient will demonstrate evidence of perfusion through warm skin and color within the normal range for ethnicity.
- Patient will report relief of shortness of breath, chest pain, and fatigue.
- Patient will demonstrate a hemoglobin level >10.0 g/dL.
1. Determine the patient’s medical and family history. Certain types of anemia may be inherited or can develop as a result of a chronic condition. Identify whether the anemia is acute or chronic by establishing a thorough history. Management will depend on the type and cause of anemia.
2. Perform a physical assessment. Red blood cells are needed in all body processes. Low red blood cells (anemia) lead to decreased levels of oxygenated blood in the tissues, causing hypoxia and decreased bodily functions. Monitor for pale, cold skin, changes in respiration, orthostatic hypotension, tachypnea, and chest pain.
3. Review the hemoglobin level. Low hemoglobin levels indicate a lack of oxygenated blood available to perfuse organs.
1. Investigate reports of chest pain or palpitations. If the patient reports chest pain or discomfort, obtain an EKG to monitor for arrhythmias.
2. Apply oxygen. A lack of oxygenated RBCs may result in hypoxia. Administer supplemental oxygen to keep SpO2 > 95%.
3. Implement safety precautions. Anemia can affect the central nervous system and cause lightheadedness, dizziness, vision changes, and muscle weakness that could cause fainting and falls. Implement fall and safety precautions for patients experiencing these symptoms.
4. Administer epoetin injections as ordered. Epoetin alfa is a synthetic form of the human hormone erythropoietin and increases RBC production in the bone marrow.
- Anemia. (n.d.). American Society of Hematology. Retrieved February 24, 2022, from https://www.hematology.org/education/patients/anemia
- Anemia – Symptoms and causes. (2023, May 11). Mayo Clinic. Retrieved July 2023, from https://www.mayoclinic.org/diseases-conditions/anemia/symptoms-causes/syc-20351360
- Cleveland Clinic. (2022, September 12). Anemia: Symptoms, types, causes, risks, treatment & management. Retrieved August 2023, from https://my.clevelandclinic.org/health/diseases/3929-anemia#symptoms-and-causes
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2008). Nurse’s Pocket Guide Diagnoses, Prioritized Interventions, and Rationales (11th ed.). F. A. Davis Company.
- Epoetin Alfa (Injection Route) Side Effects. (2022, February 1). Mayo Clinic. Retrieved February 24, 2022, from https://www.mayoclinic.org/drugs-supplements/epoetin-alfa-injection-route/side-effects/drg-20068065?p=1
- Friend A, Girzadas D. Acute Chest Syndrome. [Updated 2021 Jun 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441872/
- Iron. (n.d.). Harvard T.H. Chan School of Public Health. Retrieved February 24, 2022, from https://www.hsph.harvard.edu/nutritionsource/iron/
- Iron-Deficiency Anemia. (n.d.). American Society of Hematology. Retrieved February 24, 2022, from https://www.hematology.org/education/patients/anemia/iron-deficiency
- Maakaron, J. E. (2023, June 13). Anemia workup: Approach considerations, pathogenesis investigation, and blood loss evaluation. Diseases & Conditions – Medscape Reference. Retrieved July 2023, from https://emedicine.medscape.com/article/198475-workup#showall
- Mayo Clinic. (2022, February 11). Anemia – Diagnosis and treatment – Mayo Clinic. Retrieved August 2023, from https://www.mayoclinic.org/diseases-conditions/anemia/diagnosis-treatment/drc-20351366
- Mayo Clinic. (2022, February 11). Anemia – Symptoms and causes. Retrieved August 2023, from https://www.mayoclinic.org/diseases-conditions/anemia/symptoms-causes/syc-20351360
- Sickle Cell Crisis. (2020, September 23). Michigan Medicine. Retrieved February 24, 2022, from https://www.uofmhealth.org/health-library/hw253529
- Turner, J., Parsi, M., & Badireddy, M. (2022, August 8). Anemia – StatPearls – NCBI bookshelf. National Center for Biotechnology Information. Retrieved July 2023, from https://www.ncbi.nlm.nih.gov/books/NBK499994/

Complete Your CE
Course case studies, external link, this link leads outside of the netce site to:.
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
Anemia in the Elderly
Course #99084 - $30-
#99084: Anemia in the Elderly
Your certificate(s) of completion have been emailed to
- Back to Course Home
- Review the course material online or in print.
- Complete the course evaluation.
- Review your Transcript to view and print your Certificate of Completion. Your date of completion will be the date (Pacific Time) the course was electronically submitted for credit, with no exceptions. Partial credit is not available.
CASE STUDY 1
Patient H is a White woman, 89 years of age, who resides in a skilled nursing facility. She is being evaluated due to an Hgb level of 8.1 g/dL. She is ambulatory with a rolling walker, generally alert, and oriented with some mild cognitive impairment. She is compliant with medical treatments and takes medications as prescribed. Her medical history is positive for congestive heart failure, chronic obstructive pulmonary disease (COPD), chronic kidney disease, and osteoarthritis. She is oxygen dependent on 2 L/minute per nasal cannula. She is bright and outgoing and verbalizes multiple vague physical complaints.
During her last hospitalization, one year ago for pneumonia, the nephrologist and pulmonologist told Patient H there was not much else that could be done for her. Despite the poor prognosis, her multiple medical conditions stabilized and she completed a rehabilitation program. She enjoys participating in activities and has developed friendships with some other residents. Over the past year, she has been treated for multiple infections, including bronchitis and multiple urinary tract infections.
Patient H's chief complaint is of feeling tired and short of breath at times. She also complains of arthritic pains in her neck and hands. Review of systems is notable for hearing loss, dentures, glasses, and dyspnea, mostly with exertion. She has occasional palpitations of the heart and orthopnea at times. Her bowel movements are regular, and she has not noticed any blood in the stool. She has 1+ chronic edema of the legs, which is about usual for her. She has not had a mammogram for five years, and she has not had a dual energy x-ray absorptiometry scan, colonoscopy, or other preventive care recently.
Patient H's record indicates an allergy to sulfa drugs and penicillin. She also has completed advance directives (a do not resuscitate order and a living will). She is taking the following medications:
Amlodipine besylate (Norvasc): 5 mg/day
Calcium carbonate (OsCal) with vitamin D twice daily
Polyethylene glycol powder (Miralax): 17 g in 8 oz liquid daily
Furosemide (Lasix): 40 mg/day
Escitalopram (Lexapro): 20 mg/day
Prednisone: 10 mg/day
Omeprazole (Prilosec): 20 mg/day
Cinacalcet (Sensipar): 30 mg/day
Simvastatin (Zocor): 20 mg at bedtime
Tiotropium oral inhalation (Spiriva): 1 cap per inhalation device daily
Vitamin B12: 1,000 mcg twice daily
Enteric-coated aspirin: 81 g/day
Upon physical examination, Patient H appears well-nourished and groomed. She is mildly short of breath at rest but in no apparent pain or distress. She is 5 feet 6 inches tall and weighs 156 pounds. Her vital signs indicate a blood pressure of 132/84 mm Hg; pulse 72 beats/minute; temperature 97.4 degrees F; respirations 20 breaths/minute; and oxygen saturation 94% on 2 L/minute. Her oropharynx is clear, and her neck is supple. There is no lymphadenopathy. The patient is hard of hearing and wears glasses for distance and reading.
Patient H's heart rate is slightly irregular, with a soft systolic ejection murmur. Evaluation of her lungs indicates diminished breath sounds in the bases with no adventitious sounds. The abdomen is soft and non-tender, with active bowel sounds and no signs of hepatosplenomegaly. As noted, Patient H has 1+ pitting chronic edema and vascular changes to lower extremities. There are no active skin lesions. Neurologic assessment shows no focal deficit. Extremity strength is rated 4 out of 5. A mini-mental status exam is administered, and the patient scores 22/30, indicating mild cognitive impairment.
Blood is drawn and sent to the laboratory for CBC and a basic metabolic panel. The results are:
Leukocytes: 5,700 cells/mcL
RBC: 3.02 million cells/mcL
Hgb: 8.1 g/dL
MCH: 26.5 Hgb/cell
RDW-CV: 15.8%
Platelets: 150,000 cells/mcL
Glucose: 82 mg/dL
Blood urea nitrogen (BUN): 34 mg/dL
Creatinine: 1.4 mg/dL
GFR: 38 mL/minute/1.73 m2
Patient H is in no apparent distress at present, but she appears to have anemia, as evidenced by the low Hgb. She has chronic kidney disease (stage 3), which may be contributing to the anemia. Further laboratory evaluation is necessary to determine the etiology of the anemia and to determine if specialty referral to gastroenterologist or hematologist is necessary. The clinician orders an iron profile, vitamin B12 and folate levels, reticulocyte count, and stool for occult blood. The results of this testing are:
Vitamin B12: 1,996 pg/mL
Folate: 9.9 mcM
Ferritin: 20 ng/mL
Serum iron: 26 mcg/dL
Unsaturated iron binding capacity: 216 mcg/dL
Total iron binding capacity: 242 mcg/dL
Transferrin saturation: 11%
Reticulocyte count: 1%
Stool for occult blood: Negative (three samples)
Vitamin B12 is a water-soluble vitamin that is excreted in urine, so a high level is generally not significant. The folate level is sufficient, while the ferritin level is considered low-to-normal. The iron profile shows a low level of iron in the blood; this may be caused by gastrointestinal bleeding or by inadequate absorption of iron by the body. Patient H has medical conditions that can cause elevated cytokines, which would interfere with iron absorption. If her ferritin level was high, which it is not, it would suggest AI/ACD. Therefore, the patient appears to have anemia secondary to chronic kidney disease and possibly inadequate iron absorption and processing.
Prior to initiating treatment with an ESA, the patient is evaluated for a history of cancer, as these agents may cause progression/recurrence of cancer. Before writing the prescription for darbepoetin alfa, the clinician signs the ESA APPRISE Oncology Patient and Healthcare Professional Acknowledgement Form to document discussing the risks associated with darbepoetin alfa with the patient. The lowest dose that will prevent blood transfusion is prescribed.
The multidisciplinary team works with Patient H to develop a treatment plan. It is determined that treating the anemia will improve the patient's quality of life. The patient is prescribed ferrous sulfate 325 mg twice daily. Because vitamin C facilitates iron absorption, the iron can be given with a glass of orange juice or other citrus juice (not grapefruit). Iron must not be given with calcium, milk products, and certain medications as they can interfere with absorption. The patient should be monitored for the development of constipation and the need for stool softeners. In addition, darbepoetin alfa 40 mcg is prescribed, to be administered subcutaneously every week. This requires significant monitoring. Hgb and HCT should be measured on the day patient is to receive the injection, and the drug should be held if the Hgb is greater than 11.5 g/dL. If a current Hgb level is unavailable, the drug should not be given.
Blood pressure should be measured twice daily after treatment with darbepoetin alfa is initiated. Staff must also monitor for symptoms of a deep vein thrombosis and pulmonary embolus (e.g., unilateral edema, cough, and/or hemoptysis). Daily exercise is encouraged to help reduce the risk of a blood clot.
After one month, Patient H has received darbepoetin alfa weekly for four weeks. She is also taking the ferrous sulfate and a stool softener. The review of systems is unchanged from the previous evaluation. The physical examination is also unchanged aside from a 1-pound weight loss. No new complaints or problems are reported. A review of the patient's vital signs shows a blood pressure of 130/80 mm Hg; pulse 78 beats/minute; temperature 97.8 degrees F; and oxygen saturation 97 on 2 L/minute. Her Hgb levels over the last month have improved:
Week 1: 8.4 g/dL
Week 2: 9.2 g/dL
Week 3: 9.6 g/dL
Week 4: 10.1 g/dL
No side effects from darbepoetin alfa have been observed. Patient H's blood pressure remains stable, with no signs or symptoms of a blood clot.
The clinician orders the weekly monitoring of Hgb and HCT to continue with the darbepoetin alfa held if the Hgb is greater than 11.5 g/dL. If the medication is held more than once, the clinician will re-evaluate the dosage and frequency. The patient may only need the injection once or twice a month after the anemia is stabilized. The clinician also reduces the patient's vitamin B12 supplement to daily (rather than twice daily) and reduces her prednisone dose to 5 mg/day.
Patient H's initial complaint was of shortness of breath and fatigue. These symptoms may have been related to the anemia or may have been a chronic complaint secondary to her congestive heart failure and COPD. The decreased hematocrit level is likely contributing to the patient's symptomatic heart failure. By exploring her condition further, it was determined that treating the anemia might improve the patient's quality of life and prevent the necessity for more extreme interventions (e.g., blood transfusion). Patient H was informed of the potential side effects of darbepoetin alfa and agreed to take it to prevent transfer to the hospital for blood transfusion.
The patient's condition was monitored closely, with weekly blood draws for Hgb. Her blood pressure remained stable, and no signs of complications were detected. Her shortness of breath and fatigue improved as the treatment progressed and her Hgb level rose above 10 g/dL. This allowed her to be more active.
For patients with terminal or end-stage conditions, treatment of anemia can restore or preserve their quality of life. Treating problems that could potentially cause suffering, while avoiding futile care, is the goal for patients with a life-limiting condition. Anemia affects the quality of life in elders by causing fatigue, poor endurance, and shortness of breath, and alleviating these symptoms can allow for more activity and comfort.
CASE STUDY 2
Patient P is a White man, 92 years of age, who resides in an assisted living facility. He uses a motorized scooter for mobility but can ambulate short distances with his rolling walker. He requires assistance with medication administration and attends community meals three times a day. His daughter visits once a week and assists with laundry and transports to medical appointments.
Patient P is brought to the primary care clinic by his daughter. She states that he is very fatigued and is not performing his usual daily tasks. He sleeps more than is usual and must be coaxed to attend the community meals. At times, he has refused to take medications that the staff attempt to administer. The patient minimizes his symptoms saying, "What do you expect? I'm 92 years old." Patient P's medical history is positive for Parkinson disease, hypertension, COPD, osteoporosis, compression fracture to the lumbosacral spine, and weight loss. He is a widower and reports no tobacco use and rarely drinking beer or wine. His chief presenting complaints are fatigue, shortness of breath, chronic back and leg pain, and poor appetite.
On review of systems, the patient is noted to be hard of hearing and wearing a hearing aid. Vision is adequate with correction. He wears dentures and denies pain or difficulty with mastication. He has difficulty swallowing large pills, and his caregivers crush his medications. He states his appetite is not good; he has lost 15 pounds over the last year. Patient P denies chest pain, but complains of shortness of breath. This occurs when he exerts himself and often when he lays down. He has a regular bowel movement every one to two days and denies nausea, vomiting, or diarrhea. He has not had dyspepsia but does state he does not seem to be able to eat as much as he used to (early satiety). He complains of nonradiating pain in his lower back. All other review of systems is non-contributory. Patient P has previously been tried on antiparkinsonian medications and osteoporosis medications that were discontinued due to unacceptable side effects. He is currently taking the following medications:
Atenolol (Tenormin): 25 mg twice daily
Vitamin D3: 1,000 units/day
Calcium carbonate: 500 mg three times every day
Vitamin B12: 1,000 mcg/day
Amlodipine (Norvasc): 10 mg/day
Omeprazole: 20 mg/day
Multivitamin daily
Acetaminophen (Tylenol): 650 mg three times daily routinely
Stool softener twice daily
Tramadol (Ultram): 50 mg every six hours as needed
Upon physical examination, Patient P appears frail but well groomed; he is in no apparent distress. He is 5 feet 5 inches tall and weighs 134 pounds. His vital signs indicate a blood pressure of 110/64 mm Hg; pulse 82 beats/minute (regular rate and rhythm); temperature 97.8 degrees F; respirations 22 breaths/minute; and oxygen saturation 91% on room air.
As noted, the patient is hard of hearing with hearing aid and wears glasses. There is no evidence of lymphadenopathy or carotid bruit. His oropharynx is clear. His lungs are clear to auscultations, with diminished air flow in lung bases. The abdomen is soft and non-tender, not distended, with bowel sounds active in four quadrants. There is no hepatosplenomegaly. Extremities are clear of edema. Vascular changes are noted on both legs, and the toenails are thickened. The patient displays dry, flaky skin of lower extremities. Tenderness is noted over the lumbar spine with palpation. Disuse atrophy is noted to the extremities. Chronic skin lesions are also present, with actinic keratoses on the nose and forehead. Neurologic assessment reveals fine resting tremor of both hands and flat affect. Strength is equal bilaterally with strong hand grasps. Gait and balance are unsteady.
The clinician orders Patient P's medical records and diagnostics from previous care providers. She also requests a CBC with differential, a complete metabolic profile, and thyroid studies. A home health care evaluation is also recommended to determine if rehabilitation services would be appropriate. Patient P's laboratory studies indicate:
Leukocytes: 5,400 cells/mcL
RBC: 2.95 million cells/mcL
Hgb: 8.7 g/dL
MCH: 29.4 Hgb/cell
MCHC: 33.3%
RDW-CV: 13.7%
Platelets: 289,000 cells/mcL
Glucose: 77 mg/dL
BUN: 20 mg/dL
Sodium: 139 mEq/L
Potassium: 4.5 mEq/L
Chloride: 104 mmol/L
Carbon dioxide: 27 mmol/L
Creatinine: 0.9 mg/dL
Calcium: 8.8 mg/dL
GFR: Greater than 60 mL/minute/1.73 m2
Thyroid-stimulating hormone: 2.88 mIU/L
The low RBC, Hgb, and HCT indicate that the patient has a normocytic, normochromic anemia. However, blood-loss anemia is not ruled out by lack of microcytosis. If the blood loss is recent, changes to the cells may not yet be evident. The RDW-CV is normal, which may indicate a lack of erythropoietic response. Further laboratory evaluation is indicated.
The clinician requests an iron profile, ferritin level, folate level, vitamin B12 level, reticulocyte count, and stool for occult blood. The results of this testing are:
Vitamin B12: 1,006 pg/mL
Folate: 17.2 mcM
Ferritin: 246 ng/mL
Serum iron: 38 mcg/dL
Total iron binding capacity: 197 mcg/dL
Transferrin saturation: 27%
Reticulocyte count: 1.2%
Stool for occult blood: Negative on two samples, mildly positive on third sample
These findings indicate the patient is not deficient in vitamin B12 or folate. The serum iron is low while the ferritin level is high, suggesting adequate iron stores that are not being utilized by the body. This is a diagnostic indicator of anemia of chronic inflammation. The total iron binding capacity is low, showing that the blood's ability to bind transferrin with iron is reduced. Patient P has signs of a "mixed" anemia, the result of both ACI and gastrointestinal blood loss. Elderly patients often have more than one etiology contributing to the anemia, and all the possible causes should be thoroughly evaluated.
One of the stools for occult blood is positive, which may be representative of intermittent gastrointestinal bleeding. The clinician refers the patient to a gastroenterologist for further diagnostic evaluation. An endoscopy and colonoscopy should be performed if the patient and healthcare surrogate are willing. He is also prescribed a 5% lidocaine patch to be applied to his lower back in the morning and to be removed at bedtime.
Patient P visits a gastroenterologist, who performs an endoscopy and a colonoscopy. He is found to have several polyps in the large intestine, which are removed and biopsied during the colonoscopy. He tolerates the procedures well and has no adverse effects. The polyps are found to be benign.
One month later, Patient P returns to the clinic for follow-up. His review of systems is unchanged, although he reports improvement in his lower back pain. His vital signs are all stable. A CBC is completed to monitor the anemia, and the results are:
Leukocytes: 5,600 cells/mcL
RBC: 3.36 million cells/mcL
Hgb: 9.6 g/dL
MCV: 88.0 fL
MCH: 28.7 Hgb/cell
MCHC: 32.5%
RDW-CV: 14.9%
Platelets: 262,000 cells/mcL
Patient P's RBC, Hgb, and HCT have improved slightly. The RDW-CV has also increased, indicating an improved erythropoietic response. The removal of the colon polyps, which may have been causing some intermittent bleeding contributing to the anemia, appears to have improved the patient's condition. Patient P is instructed to return in one month for additional follow-up.
Patient P is a frail, elderly patient with multiple medical problems. From a primary care perspective, it is important to identify any new or existing medical problems that can be treated and improved. Elderly persons often present with multiple vague complaints that do not point to any one disorder. Laboratory evaluation is crucial to narrow down the diagnostic differential.
Because there is an upward trend in the CBC values, the necessity of a blood transfusion is reduced. However, if the anemia worsens, a hematology consult may be necessary. At 92 years of age, the patient is at risk for myelodysplasia, but if present, lower values of leukocytes, RBCs, and platelets would be expected.
While the use of an ESA might result in an improvement in elderly patients, there are multiple side effects and precautions associated with their use. For Patient P, they should be avoided unless truly necessary to prevent the need for transfusions.
- About NetCE
- Do Not Sell My Personal Information
Copyright © 2024 NetCE · Contact Us
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 6-1: Approach to the Patient with Anemia - Case 1
Jeremy Smith
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Chief complaint, constructing a differential diagnosis.
- RANKING THE DIFFERENTIAL DIAGNOSIS
- MAKING A DIAGNOSIS
- CASE RESOLUTION
- FOLLOW-UP OF MRS. A
- Full Chapter
- Supplementary Content
Mrs. A is a 48-year-old white woman who has had fatigue for 2 months due to anemia.
Figure 6-1.
Diagnostic approach: anemia.

Anemia can occur in isolation, or as a consequence of a process causing pancytopenia, the reduction of all 3 cell lines (white blood cells [WBCs], platelets, and red blood cells [RBCs]). This chapter focuses on the approach to isolated anemia, although a brief list of causes of pancytopenia appears in Figure 6-1 . The first step in determining the cause of anemia is to identify the general mechanism of the anemia and organize the mechanisms using a pathophysiologic framework:
Acute blood loss: this is generally clinically obvious.
Underproduction of RBCs by the bone marrow; chronic blood loss is included in this category because it leads to iron deficiency, which ultimately results in underproduction.
Increased destruction of RBCs, called hemolysis.
Signs of acute blood loss
Hypotension
Tachycardia
Large ecchymoses
Symptoms of acute blood loss
Hematemesis
Rectal bleeding
Vaginal bleeding
After excluding acute blood loss, the next pivotal step is to distinguish underproduction from hemolysis by checking the reticulocyte count:
Low or normal reticulocyte counts are seen in underproduction anemias.
High reticulocyte counts occur when the bone marrow is responding normally to blood loss; hemolysis; or replacement of iron, vitamin B 12 , or folate.
Reticulocyte measures include:
The reticulocyte count: the percentage of circulating RBCs that are reticulocytes (normally 0.5–1.5%).
The absolute reticulocyte count; the number of reticulocytes actually circulating, normally 25,000–75,000/mcL (multiply the percentage of reticulocytes by the total number of RBCs).
The reticulocyte production index (RPI)
Corrects the reticulocyte count for the degree of anemia and for the prolonged peripheral maturation of reticulocytes that occurs in anemia.
Normally, the first 3–3.5 days of reticulocyte maturation occurs in the bone marrow and the last 24 hours in the peripheral blood.
When the bone marrow is stimulated, reticulocytes are released prematurely, leading to longer maturation times in the periphery, and larger numbers of reticulocytes are present at any given time.
For an HCT of 25%, the peripheral blood maturation time is 2 days, and for an HCT of 15%, it is 2.5 days; the value of 2 is generally used in the RPI calculation.
The normal RPI is about 1.0.
However, in patients with anemia, RPI < 2.0 indicates underproduction; RPI > 2.0 indicates hemolysis or an adequate bone marrow response to acute blood loss or replacement of iron or vitamins.
Get Free Access Through Your Institution
Download the Access App: iOS | Android

Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Sickle cell anemia
Best practices for patient-centered care.
GENERAL PURPOSE: To provide information on patient-centered care best practices for treating vaso-occlusive crisis due to SCA. LEARNING OBJECTIVES/OUTCOMES: After completing this continuing-education activity, you should be able to: 1 . Describe the prevalence, financial aspects, incidence, and pathophysiology of SCA. 2 . Summarize patient-centered management strategies for patients with vaso-occlusive crisis due to SCA.
- When describing SCA to a patient, the nurse explains that it
- affects more than 1 million people in the US.
- causes RBCs to have longer life spans.
- is an inherited disorder causing a defect of the hemoglobin molecule in RBCs.
- The annual Medicare cost due to patients with SCA is estimated at
- $10 million.
- $100 million.
- $1 billion.
- The US occurrence rate for SCA is
- 1 out of every 365 births.
- 1 out of every 950 births.
- 1 out of every 1,000 births.
- The case study of Mr. E explains his symptoms when arriving at the ED. After an evaluation, the healthcare providers believe that he's experiencing
- drug-seeking behavior.
- a hypertensive crisis.
- a vaso-occlusive crisis.
- In the case study, the healthcare providers for Mr. E feel that his SCA crisis could be related to
- depression.
- dehydration.
- gastroesophageal reflux disease.
- In the case study, the hospitalist reviews Mr. E's existing medications and then addresses management of his present crisis, which includes providing
- esomeprazole.
- lisinopril.
- In adults with SCA, one of the most common symptoms of vaso-occlusive crisis is
- extremity pain.
- Patients with SCA have blood cells that contain an abnormal form of hemoglobin known as
- hemoglobin C.
- hemoglobin S.
- beta-globin hemoglobin.
- Patients with SCA have misshaped RBCs that cause an inadequate blood and oxygen supply by obstructing blood vessels, which leads to
- heavy bleeding.
- various malignancies.
- The patient with SCA begins to show signs of jaundice. This is the result of rupturing sickle-shaped blood cells releasing hemoglobin into the
- gallbladder.
- bloodstream.
- Darbari identified an intensification of stigma toward patients with SCA, including
- “drug seeking.”
- “hypochondriac.”
- “nonadherence.”
- The patient arrives at the hospital experiencing a vaso-occlusive crisis due to SCA. The standard first-line treatment is initiated, which includes
- an RBC transfusion.
- opioid administration.
- comfort measures and relaxation techniques.
- When a patient with SCA is experiencing a crisis, barriers to receiving care for symptom control in the ED include
- overcrowding.
- overtraining of healthcare providers.
- reduced turnover rates of healthcare providers.
- According to the Expert Panel Report released by the National Heart, Lung, and Blood Institute, the best route of medication administration for vaso-occlusive crisis is I.V. or
- subcutaneous.
- The patient with SCA is experiencing vaso-occlusive pain and asks for meperidine. The healthcare provider explains that this medication
- should be avoided.
- needs to be increased by 25% until the pain is controlled.
- is usually combined with another medication to increase effectiveness.
- Within 30 minutes of triage in the ED, safe and effective relief of vaso-occulusive crisis includes
- strict fluid and food restrictions.
- rapid analgesia administration of opioids.
- avoidance of using heat to the affected area.
- Stat labs for vaso-occlusive crisis would most likely include
- drug toxicology.
- sedimentation rate.
- lactate dehydrogenase.
- After the patient with SCA is treated with first-line therapy for severe pain, a CAM therapy is initiated, which includes
- meperidine.
- cold compresses.
- When using morphine for a vaso-occlusive crisis, it acts by increasing
- adverse reactions and shouldn't be used.
- blood flow to areas with less blood flow.
- the stiff sickle shape of RBCs.
- During treatment for SCA, patients are often
- instructed to restrict fluids.
- provided I.V. fluids due to dehydration.
- comforted with cold compresses on painful areas.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Bullying on the unit, apixaban for a-fib, nurses and smoking cessation: get on the road to success, one hospital's war on diabetes, fine-tuning osteoporosis outcomes.
Iron Deficiency Anemia: 47-Year-Old Male Patient Case Study
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Important questions to help explore patient’s disease symptoms, important questions to help explore the patient’s medical history, abnormal and normal findings in the physical examination, interpretation of diagnostic findings, the disease process for iron-deficiency anemia, nursing care plan.
This paper responds to questions concerning the case study provided. It involves a 47 years old man who visited a clinic with gradual onset of dyspnea on exertion and fatigue. In addition, the patient complained of constant dyspepsia with nausea and occasional epigastric pain. The paper begins by illustrating questions which are pertinent to exploring the patient’s disease symptoms and past medical history. Moreover, it discusses the diagnostic tests carried out and shows pertinent positive and negative findings in the physical examination. This is followed by an interpretation of the findings of the diagnostic tests which in turn gives a green light to discuss the disease process related to the hemolytic system. Finally, all appropriate NANDA nursing diagnoses for anemic patients are provided.
The first step in treating the patient’s condition may involve understanding his family history, history of drug use and amount of alcohol consumed per day (Springhouse, 2006). In addition, the patient should be grilled on any pre-existing mental disorder, metabolic conditions, cardiac problems and medication regimen as well as his sleep patterns. More so, it is wise to ask the patient if he ever suffered any head injury in the past and have him describe his smoking habits. Furthermore, he should be asked to explain the condition he is complaining of (dyspepsia) in relation to meals and the effects of remedies taken. Finally, the practitioner may inquire if the patient is undergoing any stress.
The case presented may warrant a medical practitioner to ask about the patient’s critical diseases history and major hospitalizations. The caregiver should inquire about past hematologic setbacks, past surgeries and liver problems as well as breeding abnormalities (Collins, 2003).
In addition, many want to know the patient’s family history, recent medications and bleeding duration. Furthermore, it is recommended to ask if the bleeding is associated with shock and whether the patient bruises easily. Moreover, caregivers should ask about any case of petechie and renal or splenic disease. Finally, a medical officer may want to know whether the patient is allergic. This is done by considering past treatment using drugs like chloramphenicol which are known to cause allergy (Springhouse, 2006). Then, both physical and diagnostic procedures may be taken.
Physical tests carried out on the patient revealed several abnormal conditions. General physical examination indicated that the patient had a thin pale coloration and he appeared older than the stated age even though he suffered no stress. Furthermore, the patient’s sclera was pale although it lacked icterus and his mouth’s corner had signs of cheilosis. In addition, his nails were brittle and thin in appearance. Finally, abdominal and rectal tests showed the presence of moderate epigastric tenderness and guaiac positive stool. These are the physical manifestation of anemia (Coya & Lash, 2009). Nevertheless, there were some encouraging results.
The patient had a standard body temperature (37° Celsius) and a normal pulse rate (95 beats per min). In addition, respiratory rate was normal (16 breaths per minute) while the blood pressure was typical at 120/72 mmHg (Coya & Lash, 2009). The patient’s pupils were equal, round and reactive to light and his pharynx was clear and without any postnasal drainage. More encouraging results indicated that the patient suffered no cases of thyromegaly, adenopathy, or bruits.
Moreover, the client had good bilateral lung expansion and lungs were clear to auscultation. More so, the heart rate was proved to be all right although there was a grade II/VI systolic murmur at the left sternal border. Any cases of gallops, heaves or thrills were dispelled. In addition, the patient’s abdomen was non-distended and the liver span was 8cm at the midclavicular line. His prostate was healthy and he seemed to have stamina. Finally, he had normal body strength (5/5), intact sensation, normal gait, and he had deep tendon reflexes that were 2+ and symmetric throughout. After the physical tests, diagnostic procedures were carried out and their findings are interpreted below.
The patient’s hemoglobin was shown to be 8 g/dl instead of 13-18g/dl for normal men (Springhouse, 2006). This means that there was less oxygen in circulation. In addition, Mean Corpuscular Volume (MCV) was normal and this condition may exist in a normocytic anemia. Additionally, the patient’s Mean Corpuscular Hemoglobin Content (MCHC) was slightly decreased. This is associated with conditions like microcytic anemia and it is attributed to factors such as iron deficiency, chronic blood loss and thalassemia (Springhouse, 2006). Moreover, the red cell distribution width was markedly increased while the MCV was normal.
This presented possible cases of early stages of iron deficiency, vitamin B deficiency, and early folate deficiency as well as initial stages of the anemic condition. The diagnostic results also showed mixed microcytic/hypochromic and macrocytic/normochromic red blood cells. The findings can be associated with folate and iron deficiencies (Springhouse, 2006). This condition may also be responsible for normal MCV. The appearance of platelets was normal hence their function in blood clotting was not jeopardized. The further result revealed that Prothrombin Time (PT), Partial Thromboplastin Time (PTT), liver function, electrolytes, and amylase were normal.
Normal PPT meant that coagulation factors such as fibrinogen and prothrombin as well as heparin were up to standard amounts. Normal PT implied that there was good interaction of prothrombin groups V, VII, X and fibrinogen which are useful in determining amounts of oral anti-coagulants. Furthermore, serum ferritin levels were decreased and this is attributed to prolonged bleeding of the digestive tract, iron deficiency or deprived iron absorption due to abnormal intestinal conditions (Springhouse, 2006). This may ultimately lead to anemia. Moreover, the patient’s transferrin saturation was decreased and this is also associated with iron deficiency.
Decreased levels of total iron-binding capacity implied that the patient also suffered from anemia of chronic ailments. Folate and cell folate levels were decreased and this shows depletion of folate storage. More so, a bone marrow biopsy showed megaloblastic changes and low iron stores giving more clues to iron deficiency anemia as well as megaloblastic anemia (Coya & Lash, 2009). Finally, an upper endoscopy revealed a 2cm duodenal ulcer with evidence of recent but no acute hemorrhage. This could be attributed to Helicobacter pylori infection and may cause bleeding. All the findings are therefore contributing to iron deficiency anemia.
Iron deficiency anemia is an abnormal body condition whereby there are not enough erythrocytes in the blood (McCance et al, 2010). The condition is brought about by low amounts of iron which then hinder the production of hemoglobin. The rate of iron absorption in the jejunum and duodenum is very low and dietary iron may fail to supply the required amounts when such foods lack heme iron. Non-heme iron has to be converted to ferrous iron before absorption (Coya & Lash, 2009).
Iron in the blood system binds to transferrin which conveys it to erythroblast receptors and also to cells in the liver and placenta. The erythroblast mitochondria then convert iron to protoporphyrin and then to heme while transferrin is recycled (McCance et al, 2010). An iron that remains after this process is transported and stored as ferritin and hemosiderin. More iron is recycled from dying erythrocytes by transferrin.
When iron absorption is low, bone marrow stores are diminished so that no red blood cell production occurs hence anemia. Nevertheless, a major cause of this disease is blood loss due to prolonged bleeding from gastrointestinal tracts and extended intravascular hemolysis in men (Springhouse, 2006). Low levels of iron intake may also result from upper small bowel malabsorption or from gastrectomy. There are odd situations when the disease is attributed to undernutrition.
Iron deficiency anemia leads to inadequate hemoglobin levels and thus the low amount of oxygen is circulated. A decreased amount makes an individual feel exhausted, feeble and have shortness of breath as well as pale skin (McCance et al, 2010). As the disease progresses, an individual may have cheilosis and brittle nails and suffer from dysphagia. The disease can be detected through conducting Complete Blood Count (CBC) (Springhouse, 2006). The test is used to ascertain hematocrit and hemoglobin levels. Low levels are a sign of anemia. The test also assesses the amount of leukocytes, erythrocytes and blood platelets.
Unusual results signify a body disorder. Finally, the CBC investigates the MCV and MCHC which give clues to possible causes of anemia. In addition to CBC, blood smears are made to observe the shape of erythrocyte (McCance et al, 2010). Furthermore, reticulocyte count test may be conducted to assess the functionality of bone marrow. Quantity of iron in the body may be determined through testing serum ferritin and iron as well as investigating the concentration of transferrin. Moreover, red blood cell protoporphyrin tests as well as stool occult blood procedures are important in establishing an anemic condition.
Clinical manifestations of this disease include fatigue, black stool, dizziness, dyspepsia and ulcers as well as hometochezia (McCance et al, 2010). Iron deficiency anemia can be cured by first treating the root causes such as hemorrhages and then taking iron supplements like ferrous sulphate (Springhouse, 2006). The supplements may come inform of non heme iron or as heme iron. Supplements can be taken orally or through an injection depending on the patient’s reaction. Other treatments may include taking iron rich foods like fish, eggs and raisins. With such treatment, iron level should normalize within two months (Mosby, 2010). There are no associated complications although the disease may reappear. Therefore, one is advised to take regular medical check ups.
According to Doenges (2010), interpretation of all the collected data may lead to nursing diagnoses. Conditions like exhaustion and weakness, lack of breath on exertion as well as low levels of perseverance during activity are signs of ‘activity intolerance’. As such, care plan 1 in table 1 deals with this condition by determining the desired outcome on the patient so as to achieve endurance. This is achieved through appropriate nursing interventions supported by specific scientific rationales. In addition, care plan 2 in table 2 is aimed at treating malnutrition. This plan is as a result of imbalanced diet- inadequate amount nursing diagnoses which was necessitated by conditions like exhaustion and weakness while performing minor duties.
This plan is important as it aims at ensure proper health through appropriate diet. Finally, the nursing diagnoses in care plan 3 in table 3 deals with risk of infection. This is important as the patient has a lesion on the mouth which may lead to contamination. Furthermore, anemic individuals are prone to cross infections. The care plans aims at protecting the patient from such infections and ensure stability of his immunity.
Table 1. Care Plan 1.
| NANDA Diagnosis 1: Activity Intolerance. | |
| NOC (Nursing Outcome Classification) Label: Endurance. | |
| Expected Client Outcomes: | |
| NIC (Nursing Intervention Classification) Label: Management of energy. | |
| Nursing Interventions/Strategies | Scientific Rationales |
Table 2. Care Plan 2.
| NANDA Diagnosis 2: Lack of balanced diet- Inadequate amounts. | |
| NOC Label: Status of Nutrition. | |
| Expected Client Outcomes: | |
| NIC Label: Nutrition remedy | |
| Nursing Interventions/Strategies | Scientific Rationales |
Table 3. Care Plan 3.
| NANDA Diagnosis 3: Dangers of infection. | |
| NOC Label: Risk management and the situation of immune system. | |
| Expected Client Outcomes: | |
| NIC Label: Shielding the patient from infection. | |
| Nursing Interventions/Strategies | Scientific Rationales with Citations |
It is wise to know the patients personal, family and medical history where anemia is suspected. This should be followed by physical and diagnostic tests like CBC which help to understand the real situation of anemic condition. The disease may be brought about by loss of blood and failure of the body to make use of iron found in meals. Its various symptoms include fatigue and loss of breath among others. Treatment is through iron supplement and dietary changes. This is achieved through proper nursing diagnoses and care plan as well as medical diagnosis.
Collins, D. (2003). Algorithmic Diagnosis of Symptom . Web.
Coya, S., & Lash, A. (2009). Pathophysiology of anemia and nursing care implications. Web.
Doenges, M., Moorhouse, M., & Murr, A. (2010). Nursing Care Plans: Guidelines for Individualizing Client Car across the Life Span . Philadelphia: F. A. Davis Company.
McCance, K.L., Huether, S.E., Brashers, V., & Rote (2010). Pathophysiology: The biologic basis for disease in adults and children (6th Ed.). Maryland Heights, MO: Elsevier Mosby. Web.
Springhouse. (2006). Professional Guide to Signs & Symptoms . (5th Ed.). Lippincott Williams & Wilkins.
- Nursing as a Profession and Career
- The Importance of Nursing Job Satisfaction
- Pernicious Anemia: Medical Analysis
- Anemia: Types, Etiology and Clinical Manifestation
- Prognosis, Diagnosis, and Treatment of Iron Deficiency Anemia
- Nursing Job Satisfaction: Turkey, Australia, Slovenia, Iran
- Hand Washing in Health Care
- Skill Enhancement Lab to Establish Communication Competency
- Evidence-Based Strategies for Palliative Care
- The Assessment and Management of Pain in Nursing Fields
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, March 19). Iron Deficiency Anemia: 47-Year-Old Male Patient. https://ivypanda.com/essays/nursing-case-study-on-iron-deficiency-anemia/
"Iron Deficiency Anemia: 47-Year-Old Male Patient." IvyPanda , 19 Mar. 2022, ivypanda.com/essays/nursing-case-study-on-iron-deficiency-anemia/.
IvyPanda . (2022) 'Iron Deficiency Anemia: 47-Year-Old Male Patient'. 19 March.
IvyPanda . 2022. "Iron Deficiency Anemia: 47-Year-Old Male Patient." March 19, 2022. https://ivypanda.com/essays/nursing-case-study-on-iron-deficiency-anemia/.
1. IvyPanda . "Iron Deficiency Anemia: 47-Year-Old Male Patient." March 19, 2022. https://ivypanda.com/essays/nursing-case-study-on-iron-deficiency-anemia/.
Bibliography
IvyPanda . "Iron Deficiency Anemia: 47-Year-Old Male Patient." March 19, 2022. https://ivypanda.com/essays/nursing-case-study-on-iron-deficiency-anemia/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
Pernicious Anemia HESI RN case study

Get better grades with Learn
82% of students achieve A’s after using Learn
Winningham's Critical Thinking Cases in Nursing
Clinical Reasoning Cases in Nursing
Rationale: Choose matching term 1 The nurse finds that Mr. Baker has a weak, irregular, and rapid pulse and his tongue is inflamed. The nurse decides to perform a neurological assessment because of mild tremoring. His unexpected neurological findings included hyperactive deep tendon reflexes and mild burning and prickling sensations on his feet and hands. He also appears to startle easily, and he has lost about 15% of his weight as compared to his last visit, which was four months ago. During the assessment, the nurse suspects that the client may have pernicious anemia. Which pathophysiological process promotes this condition? 2 3 The pharmacy delivers another vial of cyanocobalamin. The healthcare provider has prescribed subcutaneous vitamin B12 (cyanocobalamin) 100 mcg daily for seven days. How many milliliters (mL) of cyanocobalamin should the nurse draw into a syringe in preparation for administration? (Enter numerical value only. If rounding is required, round to the tenth.) 4 Which action is most important for the nurse to perform before calling the healthcare provider to report the lab values? Don't know?
Medscape.org provides accredited, ad-free, and evidence-based independent education
A Case-Based Look at Recognizing, Diagnosing, and Managing Anemia Earlier in CKD
Join us for a symposium on dialysis-dependent (DD) chronic kidney disease (CKD) anemia designed to encourage the exchange of ideas between leaders in the field and attendees.
All Credits Available
AMA PRA Category 1 Credit(s)™
ANCC Contact Hour(s)
Target Audience and Goal Statement
This activity is intended for nephrologists, primary care physicians, nurses, and other clinicians who treat patients with CKD.
The goal of this activity is for clinicians to be better able to understand the role and use of hypoxia-inducible factor prolyl-hydroxylase inhibitors (HIF PHIs) for the treatment of patients with DD-CKD anemia.
Upon completion of this activity, participants will:
- The safety and efficacy of HIF PHIs for the treatment of DD-CKD anemia
- Use of HIF-PHIs in appropriate patients for the treatment of DD-CKD anemia
Disclosures
Medscape, LLC requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated. Others involved in the planning of this activity have no relevant financial relationships.

Matthew R. Weir, MD
Professor of Medicine University of Maryland School of Medicine Director, Division of Nephrology Department of Medicine University of Maryland Medical Center Baltimore, Maryland
Anne M. Sendaydiego, PharmD
Medical Education Director
Compliance Reviewer/Nurse Planner
Leigh schmidt, msn, rn, cne, chcp.
Associate Director, Accreditation and Compliance, Medscape Education
Accreditation Statements
Developed through a strategic collaboration between KDIGO and Medscape Education.
In support of improving patient care, Medscape, LLC is jointly accredited with commendation by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
For Physicians
Medscape, LLC designates this live activity for a maximum of 0.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Contact This Provider
Awarded 0.50 contact hour(s) of nursing continuing professional development for RNs and APNs; 0.5 contact hours are in the area of pharmacology.
For questions regarding the content of this activity, contact the accredited provider for this CME/CE activity noted above. For technical assistance, contact [email protected] .
Instructions for Participation & Credit
There are no fees for participating in or receiving credit for this online educational activity. For information on applicability and acceptance of continuing education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity online during the valid credit period that is noted on the title page. To receive AMA PRA Category 1 Credit ™, you must receive a minimum score of 75% on the post-test.
Follow these steps to earn CME/CE credit*:
- Read about the target audience, learning objectives, and author disclosures.
- Study the educational content online or print it out.
- Online, choose the best answer to each test question. To receive a certificate, you must receive a passing score as designated at the top of the test. We encourage you to complete the Activity Evaluation to provide feedback for future programming.
You may now view or print the certificate from your CME/CE Tracker. You may print the certificate, but you cannot alter it. Credits will be tallied in your CME/CE Tracker and archived for 6 years; at any point within this time period, you can print out the tally as well as the certificates from the CME/CE Tracker.
*The credit that you receive is based on your user profile.
Supported by an independent educational grant from Akebia Therapeutics, Inc.

THIS ACTIVITY HAS EXPIRED FOR CREDIT
Medscape Education makes these downloadable slides available solely for non-commercial use by you as a reference tool. You may not use these slides for any commercial purpose or provide these slides to any third party for such party’s use for any commercial purpose. Please refer to the Medscape Terms of Use for additional details.
Activity Transcript
Abbreviations, webmd network.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Iran Red Crescent Med J
- v.14(3); 2012 Mar
First Presentation of Sickle Cell Anemia in A 3.5-Year-Old Girl: A Case Report
1 Thalassemia and Hemoglobinopathy Research Center, Ahvaz Jondishapur University of Medical Sciences, Ahvaz, Iran
2 Department of Pediatrics Hematology/Oncology, Ahvaz Jondishapur University of Medical Sciences, Ahvaz, Iran
Dear Editor,
Sickle cell disease is an inherited disorder of hemoglobin synthesis, which affects many individuals worldwide. Vaso-occlusive, aplastic and sequestration crises are common in a sickle cell child.[ 1 ] One of the leading causes of death in children with sickle cell anemia is an acute splenic sequestration crisis.[ 2 ] Children with splenic sequestration disease who have not yet undergone autosplenectomy, as well as older patients with sickle cell disease or S-beta thalassemia, may have sudden, rapid, massive enlargement of the spleen with trapping of a considerable portion of the red cell mass. On physical examination, there may be profound hypotension with cardiac decompensation and massive splenomegaly. The hemoglobin concentration is at least 2 g/dL lower than baseline and is accompanied by a brisk reticulocytosis with increased nucleated red cells and moderate to severe thrombocytopenia.[ 2 ] ACS is an acute illness with lung injury characterized by any combination of chest pain, fever, or respiratory symptoms and accompanied by a new pulmonary infiltrate on a chest radiograph.[ 3 ] Elevated WBC count, dactylitis, and anemia predicted more severe later outcomes in children younger than 4 years.[ 4 ] Dactylitis, often referred to as hand-foot syndrome, is frequently the 1st manifestation of pain in children with sickle cell anemia, occurring in 50% of children by 2 years of age.[ 5 ]
A 3.5-year-old girl from race of Arab reffered to Shafa Hospital with severe anemia, thrombocytopenia, leucocytosis and elevated ESR and LDH. Her parents assigned fever, cough, pallor, weakness and tachypnea from six day ago ( Figure 1 ).

Chest x ray.
Past medical history and familial history of the patient was negative. On physical examination, she had fever with temperature of 39.5°C, severe pallor, pulse rate of 110 per minute, respiratory rate of 32 per minute and blood pressure of 90/60 mmHg. On abdominal examination, she had hepatosplenomegaly. Rales and rhonchi were in both lung fields on respiratory examination while the other systemic examination was essentially normal. Initial laboratory investigations demonstrated hemoglobin of 4.5 gm/dL, white cell count of 19,000/mm(3) (55% neutrophils, 45% lymphocyte), platelet count of 70,000/mm(3) and an erythrocyte sedimentation rate of 45 mm/hour. Renal function tests and urinalysis were normal. A chest radiograph revealed bilateral haziness. For decline of malignancy, bone marrow aspiration was done and discussed reactive bone marrow due to infection.
After one day a dactylitis was present in hands of the patient ( Figure 2 ).

Dactylitis.
In follow up of Hb electrophoresis, Hb s was 80%, Hb F: 18%, and Hb A2: 2%. Finally in peripheral blood smear, sickling of RBC was detected and the patient was diagnosed with sickle cell anemia and acute splenic sequestration crisis which was associated with acute chest syndrome treated with wide spectrum antibiotic (cefotaxim and erythromycin) and transfusion exchange ( Figure 3 ). The patient was discharged with stable clinical state after 8 days.

Prepheral blood smears with sickle cell.
The clinical presentation of our patient is rare and unusual for initial presentation of sickle cell anemia. Also association between acute chest syndrome and splenic sequestration is unusual.
Conflict of interest: None declared.
- Case Reports
Approach to Anemia & case study
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Lorestan University of Medical Sciences
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

IMAGES
VIDEO
COMMENTS
Anemia case study - Student version Nur 170 harding: critical thinking cases in nursing, 6th edition student learning outcomes analyze health assessment. ... Determine how to apply the nursing process for patients with anemia. Identify development principles, prevention and/or early detection of health problems and strategies in order to ...
The level of anemia often depends upon the age and gender of individuals, including lifestyle patterns and altitude of the person's residence. This course introduces a case study at the start and end of the study relative to nursing care. Case Study: Vanessa. The following case study may be seen in the outpatient primary care setting.
Mother alive at 50 years old. Diagnosis of iron deficiency anemia at 24 years old during pregnancy with patient - on daily supplement. Otherwise healthy. Father alive at 52 years old. Diagnosis of hypertension - controlled with diet and exercise. Otherwise healthy.
A number of hematologic studies are performed to determine the type and cause of anemia. Blood studies. In an initial evaluation, the hemoglobin, hematocrit, reticulocyte count, and RBC indices, particularly the mean corpuscular volume and red cell distribution width are taken to assess for the presence of anemia. Iron studies.
Nurse Michael works on an inpatient Medical-Surgical unit and is caring for Hannah, a 26-year-old female with a history of Crohn disease who was admitted for iron deficiency anemia. After settling Hannah in her room, Nurse Michael goes through the steps of the Clinical Judgment Measurement Model to make clinical decisions about Hannah's care ...
Perform a physical assessment. Red blood cells are needed in all body processes. Low red blood cells (anemia) lead to decreased levels of oxygenated blood in the tissues, causing hypoxia and decreased bodily functions. Monitor for pale, cold skin, changes in respiration, orthostatic hypotension, tachypnea, and chest pain.
CASE STUDY 1. Patient H is a White woman, 89 years of age, who resides in a skilled nursing facility. She is being evaluated due to an Hgb level of 8.1 g/dL. ... Anemia affects the quality of life in elders by causing fatigue, poor endurance, and shortness of breath, and alleviating these symptoms can allow for more activity and comfort. CASE ...
Between October 2009 and June 2015, 86 patients were admitted for very severe anemia. Of these, 61 (71%) were women and 25 (29%) were men; eight patients (9.3%) came from nursing homes, one from a prison and the remaining cases were from home. The mean age was 76.8 ± 15.6 (range: 33-100).
Anemia can occur in isolation, or as a consequence of a process causing pancytopenia, the reduction of all 3 cell lines (white blood cells [WBCs], platelets, and red blood cells [RBCs]). This chapter focuses on the approach to isolated anemia, although a brief list of causes of pancytopenia appears in Figure 6-1. The first step in determining ...
Case study. Mr. E, a 22-year-old Black male, presents to the ED with severe pain in his hands and abdomen. Mr. E has a history of anemia, gastroesophageal reflux disease, SCA, hypertension, and depression. He's currently a student at a local university where he studies psychology and plays soccer.
Purpose: To discuss the diagnosis and treatment of severe anemia in an older adult who presents the challenge of declining blood transfusion in a real-world scenario where critical thinking, evidence-based care, and collaboration with other providers must come together to serve this patient's unique needs. Data sources: Extensive review of the ...
Nursing Made Incredibly Easy! 18 (6):p 1, November/December 2020. | DOI: 10.1097/01.NME.0000720280.28438.0b. Free. Metrics. GENERAL PURPOSE: To provide information on patient-centered care best practices for treating vaso-occlusive crisis due to SCA. LEARNING OBJECTIVES/OUTCOMES: After completing this continuing-education activity, you should ...
The disease process for iron-deficiency anemia. Iron deficiency anemia is an abnormal body condition whereby there are not enough erythrocytes in the blood (McCance et al, 2010). The condition is brought about by low amounts of iron which then hinder the production of hemoglobin.
Crystal Siercks NURS 102 Anemia Case Study ANEMIA CASE STUDY Patient Profile D., a 72-year-old male whose wife died six months ago, is brought to the health care provider by his daughter because he is not eating much and has been lethargic and sleeping a lot. He has a history of hyperlipidemia for which he takes niacin/lovastatin (Advicor) 500/20 mg PO daily at bedtime.
A 39-year-old woman was referred to our institution for evaluation of anemia. She was known to have multiple comorbidities and had a baseline hemoglobin concentration of approximately 10.5 g/dL. About 6 months before her referral, the patient began having recurrent episodes of severe anemia, with hemoglobin values as low as 3.5 g/dL.
Abstract. The following fictional case is intended as a learning tool within the Pathology Competencies for Medical Education (PCME), a set of national standards for teaching pathology. These are divided into three basic competencies: Disease Mechanisms and Processes, Organ System Pathology, and Diagnostic Medicine and Therapeutic Pathology.
4.0 (13 reviews) pernicious anemia case study. John Baker is a 45-year-old Caucasian male who was admitted to the medical-surgical unit 6 hours ago from the Emergency Department due to nausea, vomiting, shortness of breath, pallor, weakness, and severe fatigue. John is divorced with no children and has been practicing law for 15 years.
Unfolding reasoning Case study. Sickle Cell Anemia Crisis - Anthony Perkins. sickle cell anemia anthony perkins, 15 years old primary concept perfusion
CASE STUDY ON ANEMIA.pdf - Free download as PDF File (.pdf), Text File (.txt) or read online for free. This case study summarizes the nursing care provided to a 38-week pregnant patient with severe anemia. The patient's hemoglobin levels were very low at admission. The nurse conducted a full physical assessment and documented the patient's medical history, social history, and obstetric history.
Join us for a symposium on dialysis-dependent (DD) chronic kidney disease (CKD) anemia designed to encourage the exchange of ideas between leaders in the field and attendees. ... A Case-Based Look at Recognizing, Diagnosing, and Managing Anemia Earlier in CKD ... Study the educational content online or print it out. Online, choose the best ...
Dactylitis, often referred to as hand-foot syndrome, is frequently the 1st manifestation of pain in children with sickle cell anemia, occurring in 50% of children by 2 years of age. [5] A 3.5-year-old girl from race of Arab reffered to Shafa Hospital with severe anemia, thrombocytopenia, leucocytosis and elevated ESR and LDH.
case study. Dr Abdolkarimi. P ediatric hematologist. Anemia Definition: • Anemia:2SD decrease in Median Hb level base on age &. sex & r ace. • Pediatric CBC iterpretation is age adjusted ...
N527 Theories of Holistic Nursing B Case Study 89: Anemia SCENARIO: G. is a widow who relies on her late Social Security income for all of her expenses. Over the past few years, G. has eaten less and less meat because of her financial situation and the trouble of preparing a meal for She struggles financially to buy medicines for the treatment ...
CASE STUDY on anemia - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. This case study describes the nursing care provided to a 25-year-old pregnant woman, Mrs. Kiran, admitted to the hospital with severe anemia and intrauterine growth restriction (IUGR). Upon examination, she was found to have pale skin and conjunctiva, tachycardia, and edema.