- Research article
- Open access
- Published: 01 May 2020

A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: current challenges and inconsistencies
- Rosie Mansfield ORCID: orcid.org/0000-0002-8703-5606 1 ,
- Praveetha Patalay 2 &
- Neil Humphrey 1
BMC Public Health volume 20 , Article number: 607 ( 2020 ) Cite this article
22k Accesses
47 Citations
18 Altmetric
Metrics details
With an increased political interest in school-based mental health education, the dominant understanding and measurement of mental health literacy (MHL) in adolescent research should be critically appraised. This systematic literature review aimed to investigate the conceptualisation and measurement of MHL in adolescent research and the extent of methodological homogeneity in the field for meta-analyses.
Databases (PsycINFO, EMBASE, MEDLINE, ASSIA and ERIC) and grey literature were searched (1997–2017). Included articles used the term ‘mental health literacy’ and presented self-report data for at least one MHL domain with an adolescent sample (10–19 years). Definitions, methodological and contextual data were extracted and synthesised.
Ninety-one articles were identified. There was evidence of conceptual confusion, methodological inconsistency and a lack of measures developed and psychometrically tested with adolescents. The most commonly assessed domains were mental illness stigma and help-seeking beliefs; however, frequency of assessment varied by definition usage and study design. Recognition and knowledge of mental illnesses were assessed more frequently than help-seeking knowledge. A mental-ill health approach continues to dominate the field, with few articles assessing knowledge of mental health promotion.
Conclusions
MHL research with adolescent samples is increasing. Results suggest that a better understanding of what MHL means for this population is needed in order to develop reliable, valid and feasible adolescent measures, and explore mechanisms for change in improving adolescent mental health. We recommend a move away from ‘mental disorder literacy’ and towards critical ‘mental health literacy’. Future MHL research should apply integrated, culturally sensitive models of health literacy that account for life stage and acknowledge the interaction between individuals’ ability and social and contextual demands.
Peer Review reports
Around 50% of mental health difficulties have their first onset by age 15 [ 1 , 2 ] and are associated with negative outcomes such as lower educational attainment and physical health problems [ 3 ]. Approximately 10–20% of young people are affected worldwide, and many more will experience impairing mental distress at varying degrees across the mental health continuum [ 4 , 5 , 6 , 7 , 8 ]. Adolescence is a critical period of transition, characterised by physical, cognitive, emotional, social and behavioural development [ 9 ]. It has therefore been identified as a particularly important developmental phase for improving ‘mental health literacy’ (MHL) and promoting access to mental health services [ 10 , 11 ]. However, better understanding of the conceptualisation and measurement of MHL in this population is needed.
MHL was first defined as ‘ knowledge and beliefs about mental disorders which aid their recognition, management or prevention’ ( [ 12 ] pp 182) and consisted of six domains: ‘1) the ability to recognise specific disorders or different types of psychological distress; 2) knowledge and beliefs about risk factors and causes; 3) knowledge and beliefs about self-help interventions; 4) knowledge and beliefs about professional help available; 5) attitudes which facilitate recognition and appropriate help-seeking, and 6) knowledge of how to seek mental health information’ ( [ 13 ] pp 396). Domains were later revised to include early recognition, prevention and mental health first aid skills [ 14 ]. The most recent definition comprises four broad domains aligned with current definitions of health literacy: ‘1) understanding how to obtain and maintain positive mental health; 2) understanding mental disorders and their treatments; 3) decreasing stigma related to mental disorders, and 4) enhancing help-seeking efficacy (knowing when and where to seek help and developing competencies designed to improve one’s mental health care and self-management capabilities’ ( [ 15 ] pp 155).
In a review of MHL measurement tools, O’Connor et al. revealed that the most commonly assessed domain was recognition of mental disorders. No studies assessed either knowledge of how to seek information or knowledge of self-help interventions [ 16 ]. The focus on recognition of mental disorders, along with knowledge about risk factors, causes and appropriate treatments, has been criticised for promoting the psychiatric and biogenetic conceptualisation of mental illness [ 17 , 18 ]. Despite being found to reduce blame, biogenetic explanations and attributions can lead to misconceptions about dangerousness and unpredictability and pessimism about recovery [ 19 ]. Early research also suggested that biogenetic causal theories increase a desire for social distance [ 20 , 21 ]. MHL modelled on recognition of psychiatric labels, and diagnostic language such as ‘disorder’, often leads to psychosocial predictors being ignored, and more negative attitudes towards individuals experiencing mental distress [ 22 , 23 ].
These criticisms, in line with broader socio-cultural approaches to literacy [ 24 ] understand MHL as a socio-political practice used to communicate, and make dominant, the psychiatric discourse. This appears to undermine attempts to reduce stigma, the most common outcome of school-based MHL interventions [ 25 ]. In their review of MHL measurement tools, O’Connor et al. excluded all disorder specific scales, claiming that ‘ MHL by definition should encompass knowledge and attitudes relating to a range of mental health disorders and concepts .’ ( [ 16 ] pp 199). Chambers et al. further criticised current MHL definitions for being narrow in focus with a predominantly mental-ill health approach, ignoring the complete mental health state that goes beyond the dichotomy of illness and wellness [ 26 , 27 ]. The difference between literacy about mental disorders and the ability to seek out, comprehend, appraise and apply information relating to the complete mental health state is an emerging point of discussion, and has seen MHL re-defined to include self-acquired knowledge and skills relating to positive psychology [ 28 , 29 ]. This aligns with the World Health Organisation’s (WHO) definition of mental health, which includes subjective wellbeing, optimal functioning and coping, and recognises mental health beyond the absence of disorder [ 30 ].
In response to increasingly inclusive definitions of MHL, Spiker and Hammer presented the argument for MHL as a ‘multi-construct theory, rather than a multi-dimensional construct’ ( [ 31 ] pp 3). The proposal suggested that by stretching the MHL construct, researchers have reduced the consistent use of the definition across studies, resulting in heterogeneous measurement [ 32 ]. Reviews of the psychometric properties of MHL measurement tools support this argument, and conclude that more consistent measurement with valid scales is needed [ 33 , 34 , 35 , 36 ]. Spiker and Hammer also outline problems with construct irrelevant variance [ 31 ], in which measures capture more than they intended to. Furthermore, they note that construct proliferation or the ‘jingle jangle fallacy’ [ 37 ], in which scales may have different labels but measure the same construct, and vice versa, increase problems with discriminant validity. Understanding MHL as a multi-construct theory could help delineate between its broad domains: recognition, knowledge, stigma and help-seeking beliefs, and acknowledge their complexity.
Internationally, there is growing political interest in child and adolescent mental health promotion and education [ 6 , 38 ]. Despite limited evidence, it is suggested that educating the public by improving their ability to recognise mental disorders, and increasing help-seeking knowledge, can promote population mental health [ 39 , 40 ]. Furthermore, a reduction in stigmatising attitudes is consistently reported to improve help-seeking [ 41 , 42 ]. MHL, by definition, includes these interacting domains. However, despite a comprehensive set of reviews that assess the psychometric properties of MHL measurement tools [ 33 , 34 , 35 , 36 ], there is no systematic literature review, to date, that assesses the current conceptualisation and measurement of MHL across adolescent research. Being able to clearly operationalise what is meant by a MHL intervention and meta-analyse their effectiveness, will have implications for the investment in school and population level initiatives. Similarly, being able to conduct time trend analyses that plot possible improvements in adolescents’ MHL against mental health outcomes, will reveal the extent to which population level improvements in MHL promote mental health. First though, we must have a clear picture of the understanding of MHL in adolescent research and how it is currently being measured.
Objectives and research questions
The aim of the current study was therefore to examine the ways in which MHL has been conceptualised and measured in adolescent research to date, and explore the extent of methodological homogeneity in the field for meta-analyses. We set out to answer the following research questions: 1) What are the most common study designs, contexts, and aims? 2) How is MHL conceptualised? 3) What are the most commonly measured domains of MHL, and do these vary by study design and definition usage? 4) To what extent do articles use measures that have evidence of validity for use with adolescent samples? 5) Is there enough methodological homogeneity in the field to conduct meta-analyses?
A protocol was published on PROSPERO in December 2017 (reference: CRD42017082021 ), and was updated periodically to reflect the progress of the review. Relevant PRISMA guidelines for reporting were followed [ 43 ].
Eligibility criteria
Articles were included with adolescent samples aged between 10 and 19 [ 44 ]. Samples with a mean age outside of this range were excluded. If no mean was presented and the age range fell outside of the criterion, articles were only included if results were presented for sub-groups (e.g. 12–17 years from a sample aged 12–25). General MHL and diagnosis-specific literacy research was included. Articles with quantitative study designs and extractable self-report data for at least one time point measurement of any MHL domain were eligible. These criteria ensured that only articles with extractable data from adolescents, who had not yet received any form of intervention were included. At the full text screening phase, articles published before 1997, based on the date of the first MHL definition [ 12 ], and those that did not explicitly use the term ‘mental health literacy’ or a diagnosis-specific equivalent (e.g. ‘depression literacy’) were excluded. By applying this criterion, the current study was able to present the number of articles that measured domains without referring to MHL. Identifying cases where researchers measure the same construct but use different labels is important when considering conceptualisation and meta-analyses.
Only articles available in English were included. Specific populations such as clinical/patient populations and juvenile offenders were excluded, as were university students. In contrast to schools in most countries, universities are not universal, with only a sub-set of young people entering higher education. University samples were therefore not seen as representative and often included participants outside the age criterion. Post-partum and later life neurocognitive disorders (e.g. Alzheimer’s disease) were removed given their limited relevance for this age group. In line with other MHL reviews [ 33 ], articles with a focus on substance abuse were excluded to avoid reviewing a large number of adolescent risk behaviour studies and substance abuse prevention programmes.
Search strategy
The search strategy was developed to include a number of combinations of terms to ensure that literature relating to different domains of MHL were captured. Population terms such as ‘adolescen*’ or ‘young people*’ had to be present and mental health related terms (e.g. ‘mental health’ and ‘mental disorders’) were exploded to capture general MHL and diagnosis-specific studies. Similarly, outcome terms (e.g. ‘health literacy’ and ‘health education’) were exploded, and domain specific terms included (e.g. ‘knowledge’, ‘recogni*’, ‘attitud*’, ‘stigma*’, ‘help-seek*’, ‘prevent*’ or ‘positive*’). See Additional File 1 . for an example search strategy.
Data sources
The following databases were searched from their start date to the search dates (November 2017): PsycINFO, EMBASE, MEDLINE, ASSIA, and ERIC. Key authors were also contacted to identify grey literature. References were harvested from related reviews and all papers identified in the search. Hand searches of key authors’ publication lists were also conducted, and Google Scholar was used to find studies known by the authors but not identified in the database searches.
Article selection
Results from the database searches were saved to Endnote and duplicates were removed. The lead author screened the article titles and abstracts to identify those that met the inclusion criteria. Full texts were then screened and reasons for exclusion were recorded. Any uncertainties were resolved through discussion with other members of the research team. A sub-set of 20 articles were screened at full text stage by the third author, and a strong level of agreement was found (k = .78, p = .001).
Data extraction
Research was assessed on an article level (rather than by study) for the purposes of investigating the conceptualisation of MHL. The fact that authors break MHL down into component parts to write separate articles is support for identifying which domains are more commonly associated with the use of the term. Data on the following methodological factors were extracted from eligible articles using a uniform data extraction form: year of publication, country and setting (community (research conducted outside of the school setting e.g. population level surveys) vs. school-based research), study design (intervention vs. population-based), primary aims, MHL definition and use of the term, general MHL vs. diagnosis-specific literacy, number/types of MHL domains measured, and measurement tools (e.g. vignette, yes/no, Likert scales).
Data analysis
A content analysis was conducted using NVivo 12 to organise articles by their primary aim and understand the conceptualisation of MHL based on the definition presented and use of the term. Frequencies and percentages for each group were calculated and articles coded based on whether they included items related to general MHL or diagnosis-specific literacy. Existing definitions of MHL [ 12 , 13 , 14 , 15 , 28 ] were used to create a coding framework that clearly delineated its broad constituent domains (e.g. recognition, knowledge, stigma and beliefs), the object of these domains (e.g. mental illnesses, mental health prevention and promotion, and help-seeking), and their directionality (e.g. self vs. other) – see Fig. 1 .
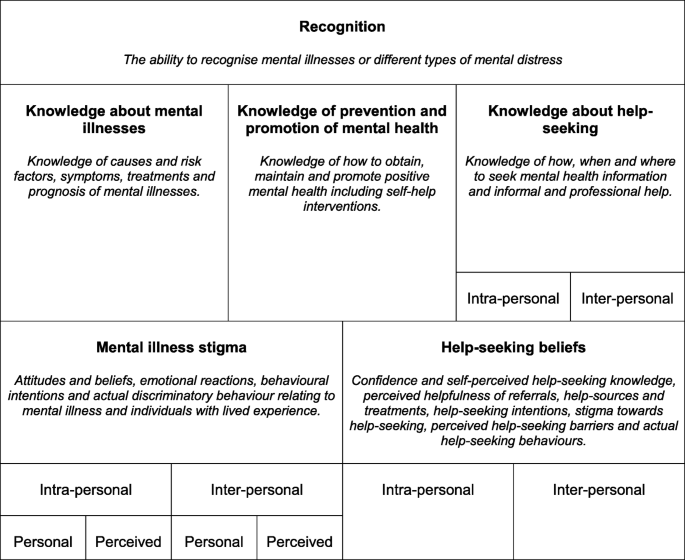
MHL Coding Framework
Mental illness stigma was assessed using existing conceptualisation i.e. personal and perceived stigma relating to self (intra-personal) and others (inter-personal), and broad domains (e.g. attitudes and beliefs, emotional reactions, and social distancing) [ 45 ]. The coding of help-seeking beliefs was informed by the theory of planned behaviour [ 46 ], assessing not only help-seeking intentions but also help-seeking confidence and self-perceived help-seeking knowledge, perceived helpfulness of referrals, help-sources and treatments, help-seeking stigma and perceived help-seeking barriers. A distinction was also made between help-seeking beliefs for self (intra-personal) vs. others (inter-personal). Although not explicitly included in any MHL definition, help-seeking behaviour was also assessed as the term is sometimes confused with help-seeking intentions. Domains were coded at an item level due to many articles presenting this form of data (e.g. % of sample that answered each item correctly as opposed to a scale mean). Frequencies and percentages were produced across all articles and by study design and definition usage.
Assessment of measures
An assessment of all MHL related measurement tools was conducted in order to assess methodological homogeneity across articles, and whether there was evidence that the measures were psychometrically valid for adolescent samples. In order to present instruments with the most comprehensive psychometric assessments, measures were coded based on whether an article existed with the primary aim of establishing its psychometric properties with an adolescent sample.
Article selection and characteristics
In total, 206 articles were identified that presented extractable adolescent data on at least one MHL domain. Of these, 91 articles (44%) used the term ‘mental health literacy’. Those that did not use the term ( N = 115, 56%), were therefore not perceived to have intended to explicitly measure the construct and were not included beyond this point. (see Fig. 2 . for a PRISMA flowchart of articles, Additional File 2 . for the full set of coded articles, and Additional File 3 . for the reference list of included articles).
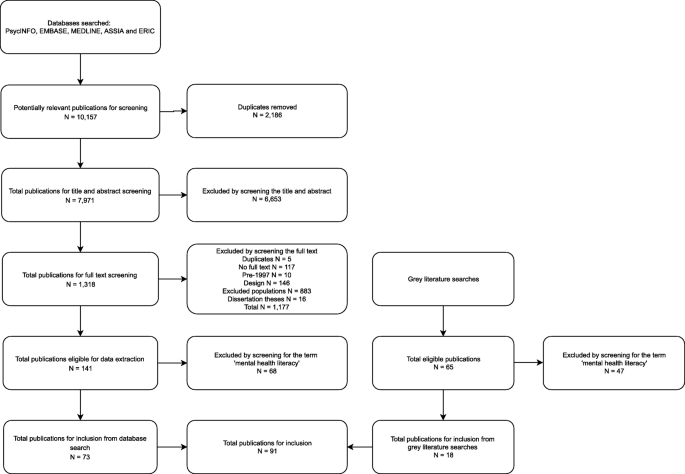
PRISMA Flowchart of Included Studies
Synthesised findings
Design, context and aims.
Figure 3 shows the number of publications by year and country. Australian research dominated the field up until 2013, at which point there was an increase in research being published globally. Australia (34%), USA (15%), Canada (9%), Republic of Ireland (9%) and the UK (8%) have published the majority of research between 2003 and 2017.
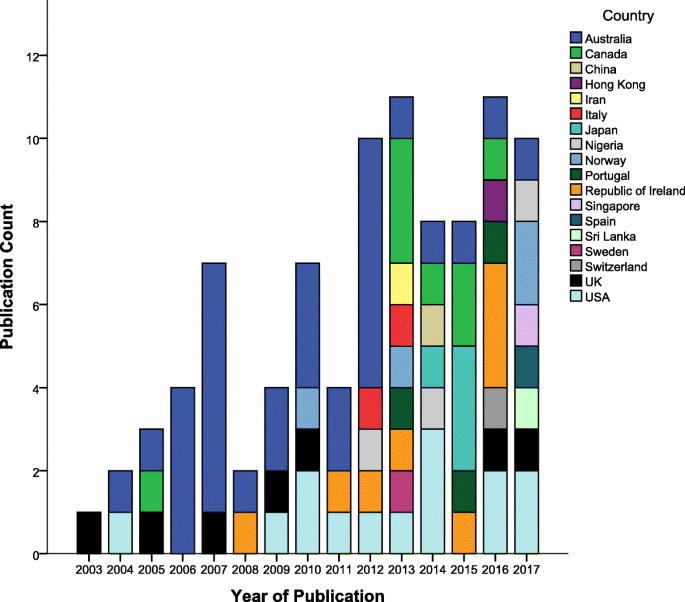
Publication Count by Year and Country
Table 1 presents a summary of articles’ study design, context and primary aim. The majority of articles reported on school-based studies. Articles with the primary aim of describing levels of MHL also included variables such as age, school year, gender, education, socio-economic variables, occupation, urbanicity, mental health status and previous mental health service use.
- Conceptualisation
Of the 91 articles that used the term ‘mental health literacy’, only 41 (45%) defined it. The most common definition, presented by 29 out of 41 (71%) articles, was that coined by Jorm and colleagues [ 12 ]. A further 3 articles (7%) used a simplified or adapted version of this definition [ 47 , 48 , 49 ]. Four articles (10%) defined MHL as related to knowledge only (e.g. ‘knowledge of mental health problems as well as the sources of help available’ ; ( [ 50 ] pp. 485) . The full list of MHL domains presented by Jorm and colleagues [ 13 ], was included in over a third ( N = 14, 34%) of articles that defined the term. However, there was some variation. For example, very few of these articles ( N = 2, 14%) referred to different types of psychological distress as well as mental disorders when presenting the recognition domain. Furthermore, in most cases ( N = 11, 79%), ‘knowledge and beliefs’ was replaced with ‘knowledge’ only, for domains relating to causes and risk factors, self-help strategies and professional help available.
A small number of articles that defined MHL ( N = 5, 12%) presented Jorm’s additional domains relating to mental health first aid skills and advocacy [ 14 ]. Some articles ( N = 4, 10%) provided examples of specific MHL domains, namely recognition of mental disorders and knowledge and beliefs about appropriate help-seeking and treatment, as opposed to presenting a comprehensive list. An emerging group of articles ( N = 5, 12%) either acknowledged mental health promotion as a component of MHL or presented Kutcher and colleagues’ four broad domains including ‘understanding how to obtain and maintain good mental health’ ( [ 15 ] pp 155).
Regardless of whether a definition was provided, approximately one third of identified articles ( N = 31, 34%) referred to MHL as a construct separate to mental illness stigma, with some suggesting that MHL predicts stigma. For example, articles described the measurement of these constructs as separate (e.g. ‘All respondents were then asked a series of questions that assessed sociodemographic characteristics, mental health literacy, stigma …’; ([ 51 ] pp. 941), and referred to or presented a relationship between the two constructs (e.g. ‘Participants with higher MHL displayed more negative attitudes to mental illness’ ; ( [ 52 ] pp. 100) . There were also instances where articles presented MHL as a predictor of help-seeking intentions and attitudes (e.g. ‘Studies indicate that in general, mental health literacy improves help seeking attitudes’ ; [ 53 ] (pp. 2), or used the term MHL to refer only to improved knowledge (e.g. ‘to assess the extent to which the students had learned the curriculum and developed what we called ‘depression literacy’ ; ([ 54 ] pp. 230).
- Measurement
Thirty-nine (43%) articles included items relating to general MHL. The exact terminology varied across studies e.g. mental disorder [ 55 ], mental illness [ 56 ], mental health problem [ 57 ], and mental health issue [ 58 ]. Few articles included items relating to mental health as opposed to mental ill-health. Bjørnsen et al. developed and validated a scale to assess adolescents' knowledge of how to obtain and maintain good mental health [ 28 ]. Kutcher et al. and McLuckie et al. also included an individual knowledge item that assessed an understanding of the complete mental health state (e.g. ‘People who have mental illness can at the same time have mental health’ ) [ 59 , 60 ].
Table 2 . presents the frequency and percentage of articles that assessed different types of diagnosis-specific literacy. In line with this focus, 57 (63%) articles utilized a vignette methodology, basing questions on descriptions, stories and scenarios relating to an individual meeting diagnostic criteria for a given mental disorder. Of these articles, 12 (21%) used comparator vignettes describing individuals with physical health problems (e.g. asthma or diabetes), control characters with good academic attainment, or ‘normal issues’ or mental health problems relating to stressful life events (e.g. the death of an elderly relative or the end of a romantic relationship). Table 3 . presents the frequency and percentage of articles that assessed different domains of MHL.
Measurement tools were too heterogeneous to conduct meta-analyses. As noted in Table 1 , four articles (4%) had the primary aim of validating MHL related measures with adolescent samples [ 28 , 55 , 61 , 62 ]. The scales assessed in Bjørnsen et al. and Pang et al. measured only one broad domain of MHL; knowledge of mental health promotion and mental illness stigma respectively [ 28 , 62 ]. Hart et al. assessed the psychometric properties of a depression knowledge questionnaire and found a one factor general knowledge latent structure to be the best fit to the data [ 61 ]. Campos et al. aimed to provide a more comprehensive assessment of MHL, and by psychometrically assessing a pool of items, developed a 33-item tool with three latent factors: first aid skills and help seeking, knowledge/stereotypes, and self-help strategies [ 55 ]. A further 22 articles (24%), stated that some items or scales had been developed for the purpose of the study.
Thirty-nine articles (43%) stated that they based their items on Jorm and colleagues original MHL survey or later 2006 and 2011 versions [ 12 , 63 ]. Furthermore, two articles (2%) included items from the Mental Health First Aid Questionnaire (MHFAQ) as detailed by Hart et al. [ 64 ]. However, there is no evidence of the validity of these surveys as whole scales, and researchers commonly selected and modified items. The Friend in Need Questionnaire, similar to Jorm and colleagues MHL survey in that it covers multiple MHL domains, was developed by Burns and Rapee to avoid leading multiple-choice answers. Instead, open-ended responses were coded in order to quantify levels of MHL [ 65 ]. Despite finding six articles (7%) that utilised a version of this questionnaire, no published validation paper was found. As part of the Adolescent Depression Awareness Programme (ADAP), an Adolescent Depression Knowledge Questionnaire (ADKQ) was developed and later validated [ 61 ]. Six articles (7%), including the validation paper, presented data using versions of the ADKQ.
Due to the multi-faceted nature of stigma, a range of measurement tools were identified across articles. The Attribution Questionnaire (AQ-27) was originally developed by Corrigan and colleagues [ 66 , 67 ] along with a brief 9-item scale (r-AQ) covering the following emotional reactions: blame, anger, pity, help, dangerousness, fear, avoidance, segregation and coercion. A similar 8-item version (AQ-8-C) was also developed for children [ 68 ]. The r-AQ was adapted by Watson et al. for use with middle school aged adolescents [ 69 ], and a 5-item version was more recently validated by Pinto et al. [ 70 ]. Four articles (4%) identified in this review used variations of the r-AQ.
Link et al. developed the 5-item Social Distance Scale (SDS) [ 71 ], which was later adapted for young people [ 72 ]. This version was more recently validated with a large sample aged 15–25 [ 73 ]. Five articles (5%) cited this version of the SDS. Seven articles (8%) used variations of the World Psychiatric Association’s (WPA) social distance items [ 74 ]; however, no adolescent validation paper was found. This review also found factual and attitudinal WPA scales presented by Pinfold et al. including the Myths and Facts About Schizophrenia Questionnaire. In total, these scales, or modified versions, were used in eight articles (9%), but no validation papers were found. The Reported and Intended Behaviour Scale (RIBS) [ 75 ] was utilised in three articles (3%). This scale has been translated into Japanese and Italian, and there is evidence of its validity with adult and university student samples [ 76 , 77 ]. The evidence of its validity with an adolescent sample was mixed [ 78 ].
The Depression Stigma Scale (DSS) was developed by Griffiths et al. to measure personal and perceived depression stigma [ 79 ]. Yap et al. later validated the DSS and confirmed that personal and perceived stigma were distinct constructs comprised of ‘weak-not-sick’ and ‘dangerous/unpredictable’ factors in a sample aged 15–25 [ 73 ]. Six articles (7%) utilised a version of the DSS, more commonly the items relating to personal stigma. Items from the Opinions about Mental Illness Scale (OMI) were used in two articles (2%). The original scale was cited by both [ 80 ], however, a Chinese version of the OMI has been tested for validity with a sample of secondary school students [ 81 ]. Other validated stigma scales identified included: the Attitudes Toward Serious Mental Illness Scale–Adolescent Version (ATSMI-AV) [ 82 ] ( N = 1, 1%) and the Subjective Social Status Loss Scale [ 83 ] ( N = 1, 1%). Measures of help-seeking attitudes and intentions were often not validated with adolescent samples. Two articles (2%) modified the General Help Seeking Questionnaire (GHSQ), previously validated for use with high school students [ 84 ]. A further two articles (2%) utilised the Self-Stigma of Seeking Help (SSOSH) scale; however, tests of its validity have only been conducted with college students [ 85 ].
The aims of this review were to investigate the conceptualisation and measurement of MHL in adolescent research, and scope the extent of methodological homogeneity for possible meta-analyses. The review clearly shows an increase in school-based MHL research with adolescent samples in recent years. This makes sense given that adolescence is increasingly identified as an important period for improving MHL and access to mental health services [ 6 , 10 , 11 , 38 ]. However, the field is still dominated by research from Western, developed countries and takes a predominantly mental-ill health approach. Furthermore, numerous challenges and inconsistencies have emerged in the field over the past 20 years.
Included articles were required to use the term ‘mental health literacy’ or a diagnosis-specific equivalent. However, by first including all articles that presented data for at least one MHL domain, a large number of articles that measured domains without referring to MHL were revealed. Researchers were measuring the same constructs but providing different labels indicating problems with discriminant validity [ 31 , 37 ]. It must be acknowledged that some of the articles included in the final set may have used the term without intending to measure the whole construct, and some articles were removed that measured multiple domains. For example, 16 intervention studies, previously included in a systematic literature review of the effectiveness of MHL interventions [ 25 ], were excluded from this current review because they did not use the term. Despite the exclusion of some potentially relevant data on a domain level, this criterion was considered most appropriate given one of the aims was to assess the conceptualisation of MHL.
Although under half of the articles identified defined MHL, those that did predominantly used definitions from Jorm and colleagues [ 12 , 13 , 14 ]. However, the various adaptations and interpretations of the original definition has clearly led to a lack of construct travelling in the field, in particular, confusion about the inclusion of beliefs and stigma related constructs as MHL domains. Furthermore, few articles referred to mental health and varying degrees of psychological distress in addition to mental illness, supporting the argument that current MHL definitions take a predominantly mental-ill health approach [ 16 , 26 ].
Although an adolescent specific definition of MHL may not be necessary, definitions frequently adopted by articles in this review were developed for adults. It is important for future research to consider not only cognitive development but also the unique social structures and vulnerabilities of adolescents in the conceptualisation and assessment of MHL. Given that the definition of adolescence in the current study ranges from 10 to 19 years, it is clear that even within this age range, different developmental factors could be considered. Applying integrated models of generic health literacy to MHL that acknowledge the life course and social and environmental determinants should therefore be a future priority [ 86 , 87 ].
Around a third of articles measured recognition of specific mental illnesses, with the majority using open-ended questions such as ‘ What, if anything, do you think is wrong …’, and calculating the % of correct responses. Knowledge of mental illnesses was measured more frequently than knowledge of prevention and promotion, therefore an understanding of the complete mental health state was often neglected [ 27 ]. More research is needed to develop and validate measures that assess the ability to seek out, comprehend, appraise and apply information relating to the complete mental health state as opposed to only assessing literacy of mental disorders. By using measurement tools that predominantly focus on psychiatric labels, there is evidence to suggest that stigma could be increased [ 22 , 23 ]. Given that over three quarters of intervention studies identified in this review included a measure of stigma, future research should consider the way in which mental-ill health approaches to MHL, in terms of intervention content and study measures, may influence stigma related outcomes.
It is perhaps unsurprising that the MHL field continues to be modelled on psychiatric labelling given the influence of Jorm and colleagues early work in Australia that came out of the National Health and Medical Research Council (NHMRC) Social Psychiatry Research Unit [ 12 ]. Kutcher and colleagues MHL definition also has its origins in psychiatry, but more explicitly includes understanding of mental health promotion and stigma reduction [ 15 ]. A growing body of research relating to eating disorders literacy also emphasises the need to distinguish between health promotion, prevention and early intervention initiatives in reducing the population health burden of eating-disordered behaviour and to prioritise mental health promotion programs, including those targeting stigma reduction [ 88 , 89 , 90 ]. This review identified an emerging group of articles that included understanding of how to obtain and maintain good mental health in their conceptualisation of MHL. However, this domain was rarely measured.
Just under half of the articles included items relating to general MHL. However, terminology was varied (e.g. mental illness, mental disorder, mental health problem, mental health issue). Leighton revealed that young people have a lack of conceptual clarity when it comes to these mental health related terms, unsurprising given the lack of consistent definitions in practice [ 91 ]. The range and subjectivity of mental health related terms reduces the meaningfulness of comparisons across MHL studies. Similarly, over half of the articles identified in this review assessed mental illness stigma, but the complexity of the construct caused heterogeneity in measurement. Intentions to seek help were the most commonly measured help-seeking belief; these findings support previous assessments of MHL measurement tools [ 16 ]. Measuring only intentions to seek help, without capturing knowledge of what help is available, will not provide a true picture of actual behaviour change. Findings also suggested that recognition and help-seeking related beliefs may be more directly associated with the MHL construct and, in line with previous literature [ 25 ], mental illness stigma was found to be a common outcome measure in MHL related interventions.
It is worth considering whether the MHL construct should continue to be stretched or whether we should accept that the multiple domains exist in their own right. For example, self-acquired knowledge and skills relating to positive psychology are being investigated, but are only just starting to emerge under the MHL construct [ 28 , 29 ]. Similarly, stigma and help-seeking knowledge and beliefs are assessed as part of, and independently from, the MHL framework. Adopting a multi-construct theory approach to MHL, as suggested by Spiker and Hammer [ 31 ], would see increased focus on developing and validating measures of specific MHL domains in order to better understand the way in which these domains relate to each other.
Developing better MHL theory will help provide clear logic models and theories of change for MHL interventions aiming to improve adolescent mental health, something currently lacking in the field. Although it should be acknowledged that the aims of MHL interventions will vary based on the scope, setting and cultural context, an increased number of validated measures as well as improved MHL theory could inform decisions about the most appropriate domain to measure as the outcome i.e. is the main aim of the intervention to reduce stigma or improve help-seeking. This is particularly important for school-based evaluations of MHL interventions for which respondent burden is often a concern.
We acknowledge that there were some articles in this review that adapted adult measures and tested for face and content validity with child and adolescent mental health professionals, and internal reliability and comprehension with adolescent samples. However, in general there was a lack of psychometric work to assess factor structure of scale-based measures in this age group, with large numbers of articles presenting data on an item level. More research should be conducted like that of Campos et al., working with young people to develop and psychometrically test pools of MHL items to identify latent factors [ 55 ]. This will help to inform future conceptualisation and measurement in this age group.
Even when there was evidence of a measure’s validity for use with adolescents, many articles selected only the items relevant for their study or adapted the scale to fit the cultural context. This may, in part, be an attempt to reduce the number of items and therefore the response burden. However, adaptation to measures based on the cultural discourse around mental health aligns with school-based mental health promotion approaches that account for children’s social, cultural and political contexts [ 92 ]. This raises the important question as to whether we should be trying to test and compare mental health related knowledge across cultures, particularly given the ongoing levels of disagreement amongst mental health professions between and within countries. A previous review of cross-cultural conceptualisations of positive mental health concluded that future definitions should be inclusive and culturally sensitive, and that more work was needed to empirically validate criteria for mental health [ 93 ]. Future research should consider conducting measurement invariance on existing MHL measures across different cultures. A comparison of knowledge items and their pre-defined correct answers, could help understand cultural differences in the discourse around mental health and what it means to be mental health literate across contexts.
Given the increased political interest in mental health promotion and education [ 6 , 38 ], we recommend that MHL research focuses on increasing understanding of ways to promote and maintain positive mental health, including subjective wellbeing, optimal functioning, coping and resilience [ 30 , 94 ]. Examples of knowledge items with true/false responses were identified in the current review and many aligned with a biogenetic conceptualisation of mental illness. Not only could these ‘truths’ cause more negative attitudes towards individuals experiencing mental health difficulties [ 19 ], many mapped directly onto the content of interventions and therefore do not provide any evidence of adolescents’ ability to critically appraise mental health information. To enhance individual and community level critical mental health literacy, the MHL field should apply models of public health literacy that aim to increase empowerment and control over health decisions, and acknowledge the interaction between an individual’s ability and their social and contextual demands [ 86 , 95 , 96 , 97 ]. Given that mental health is a key component of health, it is also worth questioning the usefulness of this separation moving forward; a MHL field that is playing catch up with more developed health literacy approaches could further exaggerate the existing lack of parity of esteem.
MHL research with adolescent populations is on the rise, but this review has highlighted some important areas for future consideration. Increasingly stretched definitions of MHL have led to conceptual confusion and methodological inconsistency, and there is a lack of measures developed and psychometrically tested with adolescents. Furthermore, the field is still dominated by a mental-ill health approach, with limited measures assessing the promotion of positive mental health. We suggest that the MHL field moves away from assessing ‘mental disorder literacy’ and towards critical ‘mental health literacy’. A better understanding of what MHL means for adolescents is needed in order to develop reliable, valid and feasible measures that acknowledge their developmental stage and unique social and contextual demands. In conclusion, by treating MHL as a multi-construct theory, more could be understood about the mechanisms for change in improving adolescent mental health.
Availability of data and materials
Link to PROSPERO review protocol included in the manuscript, example search strategy included as supplementary material.
Abbreviations
- Mental health literacy
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. https://doi.org/10.1001/archpsyc.62.6.593 .
Article PubMed Google Scholar
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder. Arch Gen Psychiatry. 2003;60(7):709. https://doi.org/10.1001/archpsyc.60.7.709 .
Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369:1302–13. https://doi.org/10.1016/S0140-6736(07)60368-7 .
Belfer ML. Child and adolescent mental disorders: the magnitude of the problem across the globe. J Child Psychol Psychiatry Allied Discip. 2008;49(3):226–36. https://doi.org/10.1111/j.1469-7610.2007.01855.x .
Article Google Scholar
Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44(10):972–86. https://doi.org/10.1097/01.chi.0000172552.41596.6f .
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–25. https://doi.org/10.1016/S0140-6736(11)60827-1 .
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry Allied Discip. 2015;56(3):345–65. https://doi.org/10.1111/jcpp.12381 .
Sadler K, Vizard T, Ford T, Marcheselli F, Pearce N, Mandalia D, et al. Mental health of children and young people in England , 2017. London; 2018. Available from https://files.digital.nhs.uk/A6/EA7D58/MHCYP%202017%20Summary.pdf .
Hagell A, Coleman J, Brooks F. Key data on adolescence 2013. London; 2013. Available from http://www.ayph.org.uk/publications/457_AYPH_KeyData2013_WebVersion.pdf .
Neufeld SAS, Dunn VJ, Jones PB, Croudace TJ, Goodyer IM. Reduction in adolescent depression after contact with mental health services: a longitudinal cohort study in the UK. Lancet Psychiatry. 2017;4(2):120–7. https://doi.org/10.1016/S2215-0366(17)30002-0 .
Article PubMed PubMed Central Google Scholar
O’Connell ME, Boat T, Warner KE. Preventing mental, emotional, and behavioural disorders among young people: progress and possibilities. Washington DC: National Academies Press; 2009. Available from https://www.ncbi.nlm.nih.gov/books/NBK32775/pdf/Bookshelf_NBK32775.pdf .
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166:182–6.
Article CAS PubMed Google Scholar
Jorm AF. Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177:396–401. https://doi.org/10.1192/bjp.177.5.396 .
Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–43. https://doi.org/10.1037/a0025957 .
Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present and future. Can J Psychiatr. 2016;61(3):154–8. https://doi.org/10.1177/0706743715616609 .
O’Connor M, Casey L, Clough B. Measuring mental health literacy: a review of scale-based measures. J Ment Health. 2014;23(4):197–204. https://doi.org/10.3109/09638237.2014.910646 .
Gattuso S, Fullagar S, Young I. Speaking of women’s “nameless misery”: the everyday construction of depression in Australian women’s magazines. Soc Sci Med. 2005;61(8):1640–8. https://doi.org/10.1016/j.socscimed.2005.03.020 .
Read J. Why promoting biological ideology increases prejudice against people labelled “schizophrenic”. Aust Psychol. 2007;42(2):118–28. https://doi.org/10.1080/00050060701280607 .
Kvaale EP, Haslam N, Gottdiener WH. The ‘side effects’ of medicalization: a meta-analytic review of how biogenetic explanations affect stigma. Clin Psychol Rev. 2013;33(6):782–94. https://doi.org/10.1016/j.cpr.2013.06.002 .
Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: a review of the “mental illness is an illness like any other” approach. Acta Psychiatr Scand. 2006;114(5):303–18. https://doi.org/10.1111/j.1600-0447.2006.00824.x .
Angermeyer MC, Matschinger H. Causal beliefs and attitudes to people with schizophrenia: trend analysis based on data from two population surveys in Germany. Br J Psychiatry. 2005;186:331–4. https://doi.org/10.1192/bjp.186.4.331 .
Kinderman P, Read J, Moncrieff J, Bentall RP. Drop the language of disorder. Evid Based Ment Health. 2013;16(1):2–3. https://doi.org/10.1136/eb-2012-100987 .
Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, et al. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–52. https://doi.org/10.1111/j.1600-0447.2012.01826.x .
Gee J. Socio-cultural approaches to literacy (literacies). Annu Rev Appl Linguist. 1992;12:31–48.
Wei Y, Hayden JA, Kutcher S, Zygmunt A, McGrath P. The effectiveness of school mental health literacy programs to address knowledge, attitudes and help seeking among youth. Early Interv Psychiatry. 2013;7(2):109–21. https://doi.org/10.1111/eip.12010 .
Chambers D, Murphy F, Keeley HS. All of us? An exploration of the concept of mental health literacy based on young people’s responses to fictional mental health vignettes. Ir J Psychol Med. 2015;32(1):129–36. https://doi.org/10.1017/ipm.2014.82 .
Keyes CLM. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539–48. https://doi.org/10.1037/0022-006X.73.3.539 .
Bjørnsen HN, Eilertsen MB, Ringdal R, Espnes GA, Moksnes UK. Positive mental health literacy: development and validation of a measure among Norwegian adolescents. BMC Public Health. 2017;17(1):717. https://doi.org/10.1186/s12889-017-4733-6 .
Kusan SB. Dialectics of mind, body and place: groundwork for a theory of mental health literacy. SAGE Open. 2013:1–16. https://doi.org/10.1177/2158244013512131 .
World Health Organisation. Mental health: strengthening our response. 2018. Available from: http://www.who.int/mediacentre/factsheets/fs220/en/ .
Spiker DA, Hammer JH. Mental health literacy as theory: current challenges and future directions. J Ment Health. 2018:1–5. https://doi.org/10.1080/09638237.2018.1437613 .
Wacker JG. A theory of formal conceptual definitions: developing theory-building measurement instruments. J Oper Manag. 2004;22(6):629–50. https://doi.org/10.1016/j.jom.2004.08.002 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry. 2015;15(1):291. https://doi.org/10.1186/s12888-015-0681-9 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry. 2016;16(1):297. https://doi.org/10.1186/s12888-016-1012-5 .
Wei Y, McGrath P, Hayden J, Kutcher S. The quality of mental health literacy measurement tools evaluating the stigma of mental illness: a systematic review. Epidemiol Psychiatr Sci. 2017:1–30. https://doi.org/10.1017/S2045796017000178 .
Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of mental health literacy tools measuring help-seeking: a systematic review. J Ment Health. 2017:1–13. https://doi.org/10.1080/09638237.2016.1276532 .
Marsh HW. Sport motivation orientations: beware of jingle-jangle fallacies. J Sport Exerc Psychol. 1994;16:365–80.
Department of Health and Education. Transforming children and young people’s mental health provision: a green paper. 2017. Available from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/664855/Transforming_children_and_young_people_s_mental_health_provision.pdf .
Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(7):1–5.
Google Scholar
Wright A, Jorm AF, Harris MG, McGorry PD. What’s in a name? Is accurate recognition and labelling of mental disorders by young people associated with better help-seeking and treatment preferences? Soc Psychiatry Psychiatr Epidemiol. 2007;42(3):244–50. https://doi.org/10.1007/s00127-006-0156-x .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. https://doi.org/10.1017/S0033291714000129 .
Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10. https://doi.org/10.1186/1471-244X-10-113 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
World Health Organization. Adolescence: a period needing special attention - age-not-the-whole-story. 2014. Available from http://apps.who.int/adolescent/second-decade/section2/page2/age-not-the-whole-story.html .
Corrigan P. A toolkit for evaluating programs meant to Erase the stigma of mental illness. Illinois Inst Technol. 2012. Available from http://www.scattergoodfoundation.org/sites/default/files/EvaluationToolkit__Corrigan.pdf .
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–221.
Leighton S. Using a vignette-based questionnaire to explore adolescents understanding of mental health issues. Clin Child Psychol Psychiatry. 2010;15(2):231–50. https://doi.org/10.1177/1359104509340234 .
Serra M, Lai A, Buizza C, Pioli R, Preti A, Masala C, et al. Beliefs and attitudes among Italian high school students toward people with severe mental disorders. J Nerv Ment Dis. 2013;201(4):311–8. https://doi.org/10.1097/NMD.0b013e318288e27f .
Ojio Y, Yonehara H, Taneichi S. Effects of school-based mental health literacy education for secondary school students to be delivered by school teachers: a preliminary study. Psychiatry Clin Neurosci. 2015;69:572–9. https://doi.org/10.1111/pcn.12320 .
Swords L, Hennessy E, Heary C. Adolescents’ beliefs about sources of help for ADHD and depression. J Adolesc. 2011;34(3):485–92. https://doi.org/10.1016/j.adolescence.2010.06.002 .
Yap MBH, Reavley N, Jorm AF. Young people’s beliefs about preventive strategies for mental disorders: findings from two Australian national surveys of youth. J Affect Disord. 2012;136(3):940–7. https://doi.org/10.1016/j.jad.2011.09.003 .
O’Keeffe D, Turner N, Foley S, Lawlor E, Kinsella A, O’Callaghan E, et al. The relationship between mental health literacy regarding schizophrenia and psychiatric stigma in the Republic of Ireland. J Ment Health. 2016;25(2):100–8. https://doi.org/10.3109/09638237.2015.1057327 .
Attygalle UR, Perera H, Jayamanne BDW. Mental health literacy in adolescents: ability to recognise problems, helpful interventions and outcomes. Child Adolesc Psychiatry Ment Health. 2017;11(38). https://doi.org/10.1186/s13034-017-0176-1 .
Hess SG, Cox TS, Gonzales LC, Kastelic EA, Mink SP, Rose LE, et al. A survey of adolescents’ knowledge about depression. Arch Psychiatr Nurs. 2004;18(6):228–34. https://doi.org/10.1016/j.apnu.2004.09.005 .
Campos L, Dias P, Palha F, Duarte A, Veiga E. Development and psychometric properties of a new questionnaire for assessing mental health literacy in young people. Univ Psychol. 2016;15(2):61–72. https://doi.org/10.11144/Javeriana.upsy15-2.dppq .
Pinto-Foltz MD, Logsdon M, Myers JA. Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Soc Sci Med. 2011;72(12):2011–9. https://doi.org/10.1016/j.socscimed.2011.04.006 .
Dogra N, Omigbodun O, Adedokun T, Bella T, Ronzoni P, Adesokan A. Nigerian secondary school children’s knowledge of and attitudes to mental health and illness. Clin Child Psychol Psychiatry. 2012;17(3):336–53. https://doi.org/10.1177/1359104511410804 .
Livingston JD, Tugwell A, Korf-Uzan K, Cianfrone M, Coniglio C. Evaluation of a campaign to improve awareness and attitudes of young people towards mental health issues. Soc Psychiatry Psychiatr Epidemiol. 2013;48(6):965–73. https://doi.org/10.1007/s00127-012-0617-3 .
Kutcher S, Wei Y, Morgan C. Successful application of a Canadian mental health curriculum resource by usual classroom teachers in significantly and sustainably improving student mental health literacy. Can J Psychiatr. 2015;60(12):580–6. https://doi.org/10.1177/070674371506001209 .
Mcluckie A, Kutcher S, Wei Y, Weaver C. Sustained improvements in students’ mental health literacy with use of a mental health curriculum in Canadian schools. BMC Psychiatry. 2014;14(1):379. https://doi.org/10.1186/s12888-014-0379-4 .
Hart SR, Kastelic EA, Wilcox HC, Beth M, Rashelle B, Kathryn JM, et al. Achieving depression literacy: the adolescent depression knowledge questionnaire ( ADKQ ). School Ment Health. 2014;6:213–23. https://doi.org/10.1007/s12310-014-9120-1 .
Pang S, Liu J, Mahesh M, Chua BY, Shahwan S, Lee SP, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. 2017;7(10):1–12. https://doi.org/10.1136/bmjopen-2017-016432 .
Reavley NJ, Jorm AF. National survey of mental health literacy and stigma. Canberra: Dep Heal Ageing; 2011. Available from https://pdfs.semanticscholar.org/d96a/e351a5b9ecfe6a519c8e4c2dd947873f426e.pdf .
Hart LM, Mason RJ, Kelly CM, Cvetkovski S, Jorm AF. “ teen Mental Health First Aid ”: a description of the program and an initial evaluation. Int J Ment Health Syst 2016;10(3):1–19. doi: https://doi.org/10.1186/s13033-016-0034-1 .
Burns JR, Rapee RM. Adolescent mental health literacy: young people’s knowledge of depression and help seeking. J Adolesc. 2006;29(2):225–39. https://doi.org/10.1016/j.adolescence.2005.05.004 .
Corrigan P, Markowitz FE, Watson A, Rowan D, Corrigan P. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–79.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophr Bull. 2002;28(2):293–309. https://doi.org/10.1093/oxfordjournals.schbul.a006939 .
Corrigan PW, Watson AC, Otey E, Westbrook AL, Gardner AL, Lamb TA, et al. How do children stigmatize people with mental illness? J Appl Soc Psychol. 2007;37(7):1405–17. https://doi.org/10.1177/0020764007078359 .
Watson A, Otey E, Westbrook A, Gardner A, Lamb T, Corrigan P, et al. Changing middle schoolers’ attitudes about mental illness through education. Schizophr Bull. 2004;30(3):563–72. https://doi.org/10.1093/oxfordjournals.schbul.a007100 .
Pinto MD, Hickman R, Logsdon MC, Burant C. Psychometric evaluation of the revised attribution questionnaire (r-AQ) to measure mental illness stigma in adolescents. J Nurs Meas. 2012;20(1):47–58.
Link BG, Bresnahan M, Stueve A, Pescosolido A, Star S. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–33. https://doi.org/10.2105/ajph.89.9.1328 .
Article CAS PubMed PubMed Central Google Scholar
Jorm AF, Wright A. Influences on young people’s stigmatising attitudes towards peers with mental disorders: national survey of young Australians and their parents. Br J Psychiatry. 2008;192(2):144–9. https://doi.org/10.1192/bjp.bp.107.039404 .
Yap MB, Mackinnon A, Reavley N, Jorm AF. The measurement properties of stigmatizing attitudes towards mental disorders: results from two community surveys. Int J Methods Psychiatr Res. 2014;23(1):49–61. https://doi.org/10.1002/mpr.1433 .
Pinfold V, Toulmin H, Thornicroft G, Huxley P, Farmer P, Graham T. Reducing psychiatric stigma and discrimination: evaluation of educational interventions inUK secondary schools. Br J Psychiatry. 2003;182:342–6. https://doi.org/10.1192/bjp.182.4.342 .
Evans-Lacko S, Rose D, Little K, Flach C, Rhydderch D, Henderson C, et al. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011;20(3):263–71. https://doi.org/10.1017/S2045796011000308 .
Pingani L, Evans-Lacko S, Luciano M, Del Vecchio V, Ferrari S, Sampogna G, et al. Psychometric validation of the Italian version of the reported and intended behaviour scale (RIBS). Epidemiol Psychiatr Sci. 2016;25(5):485–92. https://doi.org/10.1017/S2045796015000633 .
Yamaguchi S, Koike S, Watanabe KI, Ando S. Development of a Japanese version of the reported and intended behaviour scale: reliability and validity. Psychiatry Clin Neurosci. 2014;68(6):448–55. https://doi.org/10.1111/pcn.12151 .
Mansfield R, Humphrey N, Patalay P. Psychometric validation of the reported and intended behavior scale (RIBS) with adolescents. Stigma Heal. 2019. https://doi.org/10.1037/sah0000200 .
Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive behavioural therapy interventions on stigmatising attitudes to depression randomised controlled trial. Br J Psychiatry. 2004;185:342–9. https://doi.org/10.1192/bjp.185.4.342 .
Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. J Abnorm Soc Psychol. 1962;64(5):349–60.
Ng P, Chan KF. Sex differences in opinion towards mental illness of secondary school students in Hong Kong. Int J Soc Psychiatry. 2000;46(2):79–88. https://doi.org/10.1177/002076400004600201 .
Watson AC, Miller FE, Lyons JS. Adolescent attitudes toward serious mental illness. J Nerv Ment Dis. 2005;193(11):769–72. https://doi.org/10.1097/01.nmd.0000185885.04349.99 .
Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA, et al. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics. 2001;108(2):1–8. https://doi.org/10.1542/peds.108.2.e31 .
Wilson CJ, Dean FP, Ciarrochi J. Measuring help-seeking intentions: properties of the general help-seeking questionnaire. Can J Couns. 2005;39(1):15.
Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. J Couns Psychol. 2006;53(3):325–37. https://doi.org/10.1037/0022-0167.53.3.325 .
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80.
Bröder J, Okan O, Bauer U, Bruland D, Schlupp S, Bollweg TM, et al. Health literacy in childhood and youth: a systematic review of definitions and models. BMC Public Health. 2017;17(1):1–25.
Bullivant B, Rhydderch S, Griffiths S, Mitchison D, Mond JM. Eating disorders “mental health literacy”: a scoping review. J Ment Health. 2020:1–14. https://doi.org/10.1080/09638237.2020.1713996 .
Mond JM. Optimizing prevention programs and maximizing public health impact are not the same thing. Eat Disord. 2016;24(1):20–8. https://doi.org/10.1080/10640266.2015.1113824 .
Mond JM. Eating disorders “mental health literacy”: an introduction. J Ment Health. 2014;23(2):51–4. https://doi.org/10.3109/09638237.2014.889286 .
Leighton S. Adolescents’ understanding of mental health problems: conceptual confusion. Jounal Public Ment Heal. 2009;8(2):4–14. https://doi.org/10.1108/17465729200900009 .
O’Toole C. Towards dynamic and interdisciplinary frameworks for school-based mental health promotion. Health Educ. 2017;117(5):452–68. https://doi.org/10.1108/HE-11-2016-0058 .
Vaillant GE. Positive mental health: is there a cross-cultural definition? World Psychiatry. 2012;11(2):93–9. https://doi.org/10.1016/j.wpsyc.2012.05.006 .
Srivastava K. Positive mental health and its relationship with resilience. Ind Psychiatry J. 2011;20(2):75–6. https://doi.org/10.4103/0972-6748.102469 .
Freedman DA, Bess KD, Tucker HA, Boyd DL, Tuchman AM, Wallston KA. Public health literacy defined. Am J Prev Med. 2009;36(5):446–51. https://doi.org/10.1016/j.amepre.2009.02.001 .
Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–8. https://doi.org/10.1016/j.socscimed.2008.09.050 .
Pleasant A, Kuruvilla S. A tale of two health literacies: public health and clinical approaches to health literacy. Health Promot Int. 2008;23(2):152–9. https://doi.org/10.1093/heapro/dan001 .
Download references
Acknowledgements
Not applicable
RM’s PhD is part of the Education for Wellbeing Programme funded by the Department for Education, England (grant number: EOR/SBU/2017/015). The views expressed in this article are those of the author(s) and not necessarily those of the Department for Education, England or its arm’s length bodies, or other Government Departments.
Author information
Authors and affiliations.
Institute of Education, University of Manchester, Ellen Wilkinson Building, M13 9PL, Manchester, UK
Rosie Mansfield & Neil Humphrey
Institute of Education and Faculty of Population Health Sciences, University College London, WC1E 6BT, London, UK
Praveetha Patalay
You can also search for this author in PubMed Google Scholar
Contributions
RM designed the systematic literature review and wrote the protocol published on PROSPERO. RM conducted the initial database search and grey literature search and was responsible for all stages of screening and data extraction. Any uncertainties relating to screening and data extraction were resolved through discussion with NH and PP. A sub-set of articles were screened at full text stage by NH to determine levels of agreement. RM wrote the first draft of the manuscript with input from NH and PP. All authors read and approved the submitted version.
Corresponding author
Correspondence to Rosie Mansfield .
Ethics declarations
Ethics approval and consent to participate.
not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
example search strategy.
Additional file 2.
full set of coded articles.
Additional file 3.
full reference list of included articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mansfield, R., Patalay, P. & Humphrey, N. A systematic literature review of existing conceptualisation and measurement of mental health literacy in adolescent research: current challenges and inconsistencies. BMC Public Health 20 , 607 (2020). https://doi.org/10.1186/s12889-020-08734-1
Download citation
Received : 13 December 2019
Accepted : 20 April 2020
Published : 01 May 2020
DOI : https://doi.org/10.1186/s12889-020-08734-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic literature review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
A Narrative Review of Mental Illness Stigma Reduction Interventions Among African Americans in The United States
Affiliations.
- 1 Department of Psychiatry, Carver College of Medicine, University of Iowa. 200 Hawkins Dr, Iowa City, Iowa, 52242, United States.
- 2 Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine, Northwestern University. 446 E. Ontario St, #7-200, Chicago, Illinois, 60611, United States.
- 3 Center for Behavioral Intervention Technologies, Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University. 680 N. Lake Shore Dr, Suite 1400, Chicago, Illinois, 60611, United States.
- 4 Galter Health Sciences Library, Feinberg School of Medicine, Northwestern University. 320 E Superior St, Chicago, Illinois, 60611, United States.
- PMID: 34632464
- PMCID: PMC8496896
- DOI: 10.29245/2578-2959/2021/2.1235
Among African Americans, the chronicity and severity of mental illness correlates with worse health outcomes and widens health disparities. Stigma related to mental illness compounds mental health disparities by creating barriers to help-seeking behavior. We examine the current tools designed to reduce mental illness stigma and promote improved mental health outcomes among African Americans. The authors reviewed the current evidence in the literature for such stigma reduction interventions. The review team developed a focused search across four databases: PubMed, Embase, Scopus, and APA PsycINFO. Initial searches identified 120 articles, from which six studies were included as reporting on mental illness stigma reduction interventions among African Americans. We describe these four quantitative and two qualitative studies. There have been various interventions used among African Americans to reduce mental illness stigma, and the level of efficacy and effectiveness is not well studied. Our review demonstrated a need for more robust studies to yield strong evidence on effectiveness among stigma reduction interventions in this target population. The evidence does support tailoring intervention studies to this population. Effectively engaging and partnering with key stakeholders, including schools, community organizations, and faith-based institutions enhances the acceptance and delivery of stigma reduction interventions.
Keywords: African American; Black People; Intervention; Mental Health; Stigma; Stigma Reduction.
Grants and funding
- UL1 TR001422/TR/NCATS NIH HHS/United States
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The stigmatization of mental illness by mental health professionals: Scoping review and bibliometric analysis
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation School of Applied Psychology, Griffith University, Brisbane, Queensland, Australia
Roles Conceptualization, Data curation, Methodology, Project administration, Supervision, Validation, Writing – review & editing
Affiliations School of Applied Psychology, Griffith University, Brisbane, Queensland, Australia, Department of English and Communication, International Research Centre for the Advancement of Health Communication, Hong Kong Polytechnic University, Hong Kong, China
Roles Conceptualization, Supervision, Validation, Writing – review & editing
- Michael Jauch,
- Stefano Occhipinti,
- Analise O’Donovan

- Published: January 20, 2023
- https://doi.org/10.1371/journal.pone.0280739
- Peer Review
- Reader Comments
Although research suggests that mental health professionals stigmatize mental illness, studies on this topic are relativity new. Little is known about the state of this research and existing literature reviews exhibit multiple limitations. Accordingly, a scoping review was performed on the endorsed stigmatization of mental illness by mental health professionals, with the aim of exploring how research is conducted and whether there are gaps in the literature. Studies were included from any time period if they supplied findings on the endorsed stigmatization of mental illness by mental health professionals. Research was identified through electronic databases (i.e., PsycINFO, Embase, Medline, Scopus) and other sources (i.e., the Griffith University library, Google Scholar, literature reviews). It was found that the research is characterized by a number of limitations, and little progress has been made in this important domain. Among other limitations, there was a lack of comprehensive studies on the relative stigma of mental illness and how the components of stigmatization relate to each other. A bibliometric analysis also found that a large proportion of the research is not connected by references. Recommendations were made with respect to future research in this area.
Citation: Jauch M, Occhipinti S, O’Donovan A (2023) The stigmatization of mental illness by mental health professionals: Scoping review and bibliometric analysis. PLoS ONE 18(1): e0280739. https://doi.org/10.1371/journal.pone.0280739
Editor: Juan Diego Ramos-Pichardo, University of Huelva: Universidad de Huelva, SPAIN
Received: January 26, 2022; Accepted: January 7, 2023; Published: January 20, 2023
Copyright: © 2023 Jauch et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Studies suggest that health professionals can be just as susceptible to stigmatizing attitudes within their respective fields as the general population [ 1 – 3 ]. Researchers have found both that physiotherapists stigmatize individuals who are overweight and physicians stigmatize lung cancer patients [ 2 – 4 ]. Of primary relevance to the current paper, provider-based stigma is of significant concern in the domain of mental health, where mental health professionals have been found to express stigmatizing reactions towards people with mental illness [ 1 , 5 – 7 ]. For example, a study by Servais and Saunders [ 8 ] found that clinical psychologists perceive people with borderline features to be dangerous, and people with schizophrenia to be undesirable. This is troubling considering that the stigmatization of mental illness can have a negative impact on people who suffer from mental illness, and provider-based stigma is associated with negative outcomes for health care recipients [ 3 , 9 – 11 ]. The stigmatizing of mental illness including that by mental health professionals is also increasingly recognized as a public health concern and there are calls for government-based responses in some jurisdictions [ 12 ]. Thus, there is strong impetus for research that can provide insight into how the stigmatization of mental illness by mental health professionals can be mitigated. Surprisingly, studies on mental health professionals stigmatizing mental illness are fairly new and only a relatively limited amount of research has been conducted on this subject [ 1 , 5 – 7 ]. As well, the state of research on mental health professionals stigmatizing mental illness is mostly unknown and extant literature reviews on the topic add little clarity to this and are marked by several limitations [ 1 , 5 – 7 , 13 ]. Therefore, it is timely for the state of research on mental health professionals stigmatizing mental illness to be investigated in a rigorous manner. Accordingly, a scoping review will be undertaken, as this type of literature review serves to describe the state of research in an area, including how studies are conducted and whether there are any gaps in the literature [ 14 – 16 ].
The context
A large number of studies have demonstrated that mental illness is stigmatized by the general population [ 1 , 10 , 11 , 17 ]. Stigmatization is a collective system of negative reactions that are elicited by human attributes [ 18 – 20 ]. The components of stigmatization include negative stereotypes (e.g., incompetence), negative emotions (e.g., anger), and discrimination (e.g., avoidance) [ 18 , 19 ]. One variant of stigmatization is endorsed stigma , referring to expressed agreement with stigmatizing reactions [ 20 ]. When endorsed stigma manifests as discrimination against individuals with mental illness, these people encounter a range of negative consequences [ 1 , 5 , 9 ]. For example, individuals with mental illness experience limited access to housing, unemployment, financial difficulties, health problems, and poor treatment outcomes [ 5 , 10 , 11 , 17 ]. In fact, such consequences are in themselves evidence of structural stigma . Thus, mental illness causes harm directly, but such harm is also potentiated by the negative consequences associated with stigmatization [ 21 ].
Research suggests that in addition to the general population, mental health professionals also stigmatize mental illness, and this has implications for public health and policy [ 1 , 3 , 5 , 6 , 12 ]. Provider-based stigma occurs when occupational groups endorse the stigmatization of the people they are meant to help and is related to negative repercussions for health care recipients [ 3 , 20 ]. In the area of mental health, studies indicate that mental health professionals such as clinical psychologists endorse many of the same negative stereotypes, emotions, and behaviors as the general population [ 22 – 27 ]. This is of concern, as the stigmatization of mental illness is in many ways incompatible with good mental health practice. Given that provider-based stigma can have a negative impact on health care recipients, it is likely that the stigmatization of mental illness by mental health professionals is also linked to negative consequences for those who suffer from mental illness. Recently in Australia, the Productivity Commission exhibited an awareness of these likely negative outcomes in recommending to the government that action be taken towards reducing the stigmatization of mental illness by health professionals, which includes mental health professionals [ 12 ]. This is an example of institutions becoming more conscious of mental health professionals stigmatizing mental illness, and advocating for a change.
Despite the noted importance of research on mental health professionals stigmatizing mental illness, this topic has only more recently garnered attention from the scientific community, and seemingly only a small body of literature has accumulated in this area [ 1 , 5 – 7 , 13 ]. Research on mental health professionals stigmatizing mental illness appears to have emerged in the 2000s, with few studies being conducted prior to this time period [ 1 , 5 – 7 , 13 ]. To our knowledge, by 2014 only about 20 studies had been completed on mental health professionals stigmatizing mental illness [ 7 ]. In comparison to research with mental health professionals, the stigmatization of mental illness by the general population had been investigated in a number of studies prior to the 2000s, with some research being conducted as far back as the 1950s [ 21 , 28 – 30 ]. Further, the state of research on mental health professionals stigmatizing mental illness is currently unknown, as extant literature reviews in this domain mostly summarize findings, and provide little to no information about how research is being conducted and whether there are any gaps in the literature [ 1 , 5 – 7 , 13 ].
Existing literature reviews on mental health professionals stigmatizing mental illness are also limited in ways that have likely caused literature to be overlooked and make it difficult to draw conclusions about the research area [ 1 , 5 – 7 , 13 ]. First, not all of these reviews were conducted with systematic and reproducible methods for identifying relevant studies. Further, the literature reviews that did satisfy this level of rigor, arguably did not use search terms with sufficient detail to capture most of the literature on mental health professionals stigmatizing mental illness. For the most part, the search terms that were used included two or three variants of the terms stigmatization , mental illness , and mental health professional , respectively. Although these terms outline the relevant articles generally, they may exclude studies that are more specific, such as those that could be on particular mental disorders (e.g., schizophrenia, major depression, alcohol use disorder), or particular mental health professions (e.g., psychologists, psychiatric nurses, counselors). There are also several inconsistencies between the literature reviews on mental health professionals stigmatizing mental illness. One inconsistency regards the focus of the literature reviews. Specifically, none of the reviews summarized research on just the endorsed stigmatization of mental illness by mental health professionals (e.g., one review included studies on stigmatization by the general population), and the reviews differed in the extent to which this was the focus. Possibly related to this, there are inconsistencies between some of the literature reviews with respect to the number of articles included on the endorsed stigmatization of mental illness by mental health professionals. For instance, despite Wahl and Aroesty-Cohen [ 1 ] including 17 studies in their review, one year later a review by Ahmedani [ 13 ] only included three studies. The last inconsistency between the literature reviews concerns restrictions placed on time periods. Namely, Wahl and Aroesty-Cohen [ 1 ] did not review studies prior to 2004, Carrara et al. [ 6 ] only reviewed studies between 1992 and 2015, and the other reviews did not restrict searches to any time period.
As there are several inconsistencies between the literature reviews on mental health professionals stigmatizing mental illness, the literature on this topic itself may be inconsistent. Such inconsistencies are highly likely observable in the manner research is executed, and likely to result in multiple gaps in the literature. With respect to the latter, type of mental disorder is one factor that is of particular interest to the current review. This variable is referred to here as the relative stigma of mental illness, or the degree to which mental disorders are stigmatized compared to other mental disorders. Within research on the general population, a number of studies have explored and demonstrated the relative stigma of mental illness with a range of mental disorders [ 21 , 31 – 35 ]. A second variable, or more accurately system of variables, that is salient to this scoping review, is the components of stigmatization as they relate to each other. This has been examined in research with the general population, including studies on how the components relate to each other in a complete framework, with emotions mediating the relationship between stereotypes and discrimination [ 32 , 36 – 39 ]. Understanding the relative stigma of mental illness and how the components of stigmatization relate to each other is crucial to reducing the stigmatization of mental illness generally and in particular among mental health professionals. Knowledge of which mental disorders are stigmatized more than others provides guidance for interventions on which approaches are appropriate for the different mental disorder stigmas, and which stigmas should be prioritized. Moreover, having a grasp of how the components of stigmatization relate to each other is necessary for uncovering the mechanisms of change interventions should target to be effective. Inconsistencies in the literature may also impede the identification of broad findings within the research, and could be due to a lack of referencing connections between articles and research being published in lesser-known journals.
This scoping review aims to examine the state of available research on the endorsed stigmatization of mental illness by mental health professionals. In addition to investigating the state of research broadly, this scoping review aims to more precisely elucidate how studies are being conducted and whether there are gaps in the literature, two common scoping review objectives [ 14 , 15 ]. As well, the current study aims to appraise whether there are any clear findings in the literature on mental health professionals stigmatizing mental illness and explore some of the bibliometric features of the research in this area. Bibliometrics can be defined as the study of referencing patterns amongst the various forms of literature [ 40 , 41 ], and bibliometric analyses are finding increasing use in the field of mental illness stigma [e.g., 42 ]. These analyses will supply an indication of referencing connections between studies and a summary of the types of journals that articles are being published in.
This scoping review was guided by the methodological framework developed by Arksey and O’Malley [ 15 ] and is reported as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guideline ( S16 Appendix ) [ 43 ].
Eligibility criteria
Articles were selected if they provided findings on the endorsed stigmatization of mental illness by mental health professionals. Literature was also included on mental health professionals perceiving the stigmatization of mental illness in other mental health professionals. As this perceived form of stigma likely reflects endorsed stigma, this literature was selected as indirect evidence of the endorsed stigmatization of mental illness by mental health professionals. Articles were only included if the participants were referred to as mental health professionals broadly, or if it was clear that particular professional groups were part of the sample. Providers were considered mental health professionals if they were professionals from the fields of psychology, counseling/psychotherapy, social work, occupational therapy, psychiatric nursing, psychiatry, or general/family/primary care medicine. Participants were also regarded as mental health professionals if they were unspecified physicians working in a primary care setting, or any type of nurse or physician working in a psychiatric facility.
Research was excluded on the stigmatization of individual psychological symptoms (e.g., self-harm, suicide, hallucinations) and subclinical behaviors (e.g., alcohol consumption), as these attributes alone do not constitute mental illness. Similar to this, literature was excluded on diagnostic processes (e.g., a symptom of major depressive disorder is anhedonia), and beliefs regarding society-level decisions about people with mental illness (e.g., involuntary hospitalization) that were not explicitly linked to stigmatization. These phenomena were excluded as they are not necessarily indicative of stigmatization, and rather may reflect an objective assessment. Research was also not included if it was on the psychometric properties of stigmatization scales, if the results combined mostly items irrelevant to stigmatization with comparatively few stigmatization items, and if the analyses compared one sample to a completely different sample. Literature with these characteristics was excluded because such research either does not add to an understanding of mental health professionals stigmatizing mental illness or is not conducive to unambiguous conclusions. See Table 1 for the full inclusion and exclusion criteria.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0280739.t001
Search and information sources
To access relevant studies via electronic databases, a three-part search string was constructed. This search string consisted of variations of the terms stigmatization, mental illness, and mental health professional. In addition to these general terms, specific mental disorders and particular professions were incorporated into the search string, to ensure that articles on specific mental disorders and professions were included in this review. Given the infeasibility of accounting for every classified mental disorder in the search string, only certain mental disorders were listed. These classifications were mood disorder, substance use disorder, anxiety disorder, impulse control disorder, depression, and schizophrenia. The first four of these were included because research suggests that globally these mental disorders are the most prevalent [ 44 ]. Schizophrenia and depression were added based on the observation that these mental disorders are the most commonly specified mental disorders in the literature on mental health professionals stigmatizing mental illness [ 1 , 5 – 7 , 13 ]. Refer to Table 2 for the complete search string in the form of one database search. It is noted that the search string accounts for the inclusion of midwives, despite the decision to only include non-psychiatric nurses if they work in a psychiatric facility. This discrepancy is due to the inclusion criteria being refined after the review process had progressed too far for changes to be made to the search string.
https://doi.org/10.1371/journal.pone.0280739.t002
The search string was entered into a psychology database, two biomedical databases, and a multidisciplinary database. PsycINFO was the psychology database, Embase and Medline were the biomedical databases, and Scopus was the multidisciplinary database. Searches were carried out on the basis of titles, abstracts and keywords, and all searches occurred for the first time on the 29 th of May 2019. These searches were replicated on either the 9 th (PsycINFO, Embase) or 10 th (Medline, Scopus) of December 2019 to identify any articles that had been added to the databases since the first set of searches. The same set of searches were also conducted for a third time on either the 16th (Scopus, Embase) or 17th (Medline, PsycINFO) of September 2021. In addition to the database searches, relevant studies were found through Google Scholar and the Griffith University library. As the full search string could not be entered into Google Scholar or the Griffith University library, a number of different searches had to be performed for these search engines. These searches involved combining terms from each of the three parts of the database search string (e.g., mental health professionals and mental illness stigma), and were executed roughly around the same time as the first database searches. Potentially relevant articles were also screened for in literature reviews on mental health professionals stigmatizing mental illness. These reviews were by Wahl and Aroesty-Cohen [ 1 ], Schulze [ 5 ], Henderson et al. [ 7 ], Carrara et al. [ 6 ], and Ahmedani [ 13 ]. After studies were located through the first set of database searches, search engines, and literature reviews, the reference lists of relevant studies were inspected to find any articles that were not acquired via the primary sources.
Selection of sources of evidence
Relevant literature was identified by screening titles, abstracts, and full texts in a sequential order. In some cases, if the abstracts were either non-existent or too vague, articles were probed further without reading the full text. This phase of the scoping review was conducted by one reviewer. However, to verify that inclusion and exclusion was congruent with the eligibility criteria, an evaluation of inter-reviewer consistency was performed with a second reviewer. This first entailed randomly selecting a quantity of included and excluded literature that corresponded to 10% of the ultimate corpus of relevant articles (not including the second and third database searches). Half of this literature was comprised of included studies from any of the information sources, and the other half covered excluded articles from just the electronic databases. With the eligibility criteria in mind, the second reviewer then chose from this sample the literature that they deemed relevant and irrelevant while being blind to the inclusion and exclusion decisions of the other reviewer. It was found that for 90% of the sampled literature the two reviewers made the same inclusion and exclusion choices, and this level of agreement was considered acceptable. For the remaining 10%, the two reviewers had a discussion about their decisions, and the eligibility criteria was adjusted where necessary. Previous inclusion and exclusion decisions were changed to be consistent with the new eligibility criteria.
Data charting process and data items
As with the selection of sources of evidence, data charting was also executed by one reviewer. Data items were year of publication, countries the studies were conducted in, research methods, analytical approaches, populations sampled, measures of stigmatization, mental disorders included, predictors of stigmatization, component relations, and findings. To clarify, research methods denote the design of the studies, how mental illness was presented and whether an intervention was used, and analytical approaches include either the statistical or qualitative procedures employed to interpret data. Populations sampled refers to the types of mental health professionals that participated in the research, and any irrelevant populations (e.g., the lay population) that were not separated from the mental health professionals in the results. As a final clarification, findings represent the amount of stigmatization exhibited by the mental health professionals, and what factors do or do not account for variation in stigmatization, including interventions. For the bibliometric analysis, data were gathered on how frequently articles were cited in other articles, and on the rank (e.g., Q1) of the journals that the studies were published in.
Synthesis of results and bibliometric analysis
Evidence was summarized via narrative form, tables, and illustrations (i.e., a flow-chart and citation network), and the bibliometric analysis followed Bhandari [ 45 ] and Donthu et al. [ 46 ]. To examine citation links between articles a direct citation analysis was performed with the program VOSviewer [ 47 ]. In order for VOSviewer to access as many articles as possible, several data sources were considered (i.e., bibliographic database files, supported application programming interfaces). Through this process it was established that compared to other sources Scopus provided access to the highest number of studies. As for the analysis itself, literature was read in through Scopus, citation was selected as the type of analysis, and documents were specified as the unit of analysis. This produced a citation network and a list of clusters. Each of the nodes within the citation network were weighted by the number of links to other nodes. Conclusions were drawn based on an inspection of the clusters and nodes. Data on the rank of the journals that the articles were published in were obtained through the webpage www.scimagojr.com , and data were collected by documenting the highest and most recent rank the journals had been given.
The first set of database searches yielded 9310 documents, and 116 articles were identified through other sources (i.e., search engines and literature reviews). These records were then combined, and after removing duplicates the remaining 5938 documents were screened for relevance. Through this, 184 articles were deemed relevant. The reference lists of these studies were then examined, and a further 89 studies were found that met the inclusion criteria. This brought the total number of relevant articles to 273. For the second set of database searches, six new studies were found that fit the inclusion criteria, and for the third set of searches 21 new studies were identified. With these records, the final number of relevant articles was 300 (the complete process of selecting articles is summarized in Fig 1 ). In addition to excluding documents in accordance with the exclusion criteria, many records were excluded as they were either not focused on stigmatization (e.g., the effectiveness of a particular type of treatment, the self-efficacy and knowledge of mental health professionals), they were not about attitudes towards mental illness (e.g., attitudes towards evidence-based practice, attitudes towards people with HIV), or they were on stigmatization by the general population.
https://doi.org/10.1371/journal.pone.0280739.g001
Characteristics of sources of evidence and results of individual sources of evidence
Characteristics of sources of evidence and the results of individual sources of evidence are presented as supporting information.
Synthesis of results
Preliminary findings..
On examining the 300 articles, a proportion were found to contain results that merged mental health professionals with irrelevant populations. This included members of the general population and in most cases non-mental health professionals (e.g., teachers, lawyers, engineers). In some instances, this occurred because non-mental health professionals (e.g., social work students, pharmacists, paramedics) were considered to be mental health professionals by the authors. Study findings that mix mental health professionals with irrelevant populations are problematic for the current review, as it is unclear whether these results truly reflect the mental health professionals sampled. Thus, for the remaining results, findings that merged mental health professionals with irrelevant populations, and article details that corresponded to this were excluded. Consequently, 34.33% of studies were completely excluded, 22% of articles were included but only a subset of the applicable characteristics could be used, and 43.33% of studies were included in full. This meant that 197 out of the original 300 articles were the basis of the following analyses.
Most of the studies were published in the 21 st century, with 32.49% appearing in the 2000s, and 43.65% emerging in the 2010s and 2020s as a whole. Prior to this, 10.66% of articles were published in the 1990s, small quantities of studies appeared in the 1980s, 1970s, and 1960s, and just one article was published in the 1950s. Regarding geographical region, 30.96% of studies were conducted in North America, and most of this was in the United States. In comparison, only a few studies occurred in Brazil, and no other studies were conducted in South America. A further 25.38% of studies occurred in the United Kingdom, the majority of which were conducted in England. A very small number of studies were conducted in Scandinavia (e.g., Denmark, Norway), whereas 15.23% of studies occurred in other European regions (e.g., France, Italy, Germany). For the rest of the studies, 10.66% were conducted in the Middle East (e.g., Israel, Iran, Turkey), 9.14% occurred in Asia (e.g., China, Japan, India), and 7.61% were conducted in Africa (e.g., Nigeria, Ghana, South Africa). Also, 9.14% of studies occurred in Oceania, most of which were conducted in Australia.
Research methods and analytical approaches.
The most common research method by far was the cross-sectional survey. This type of research method was utilized in 68.53% of studies, while only 4.06% and 6.09% of articles reported the use of longitudinal surveys and structured interviews, respectively. Experiments/quasi-experiments were employed in 11.68% of studies, and a few articles acknowledged the use of other quantitative methods (e.g., repertory grid technique, implicit association test, behavioral observation). Additionally, 6.60% of studies explored interventions for reducing stigmatization (e.g., alcoholism training program, Balint groups, educational workshop on borderline personality disorder). It may also be worth noting here that two of these interventions were not examined through the utilization of statistical modelling (e.g., test statistics, confidence intervals). Qualitative methods were considerably less common than quantitative methods. More specifically, 9.64% of articles reported the use of semi-structured interviews, and only a small number of unstructured interviews and focus groups were conducted. There was also one structured interview and four cross-sectional surveys that used open-ended questions to collect qualitative data. Across the research methods, mental illness was presented to participants via labels in 90.86% of studies, and for four more articles labels may have been employed but it was unclear. In contrast to labels, only 21.83% of studies made use of vignettes or some other means of portraying mental illness (e.g., short descriptions, audio recordings). Of these, vignettes were utilized the most, and in one article the mode of representing mental illness was not obvious.
A variety of quantitative analyses were used throughout the studies. Many of these were standard statistical procedures (e.g., correlation analysis, ANOVA, t-test, regression analysis) and some were more rarely applied analyses (e.g., McNemar’s test, Mantel-Haenszel test, Fisher’s exact test). For several articles, the appropriate statistical figures were omitted to some extent, although more noteworthy was the observation that 89.61% of the applicable studies failed at least partially to correct for family-wise error rate. With respect to qualitative analyses, thematic analysis was employed in 51.35% of articles that included qualitative research. To a much lesser degree, a range of other qualitative analyses were utilized (e.g., contextual semantic interpretation, phenomenological analysis, discourse analysis), but not a single study used an analytical approach that involved making connections between themes (e.g., grounded theory). For both quantitative and qualitative analyses, some articles were not completely clear about the types of analyses, and 21.97% of studies that performed analyses were unable to be fully interpreted with the amount of information provided. These two issues occurred mostly for quantitative analyses.
Types of mental health professionals.
Most of the prominent mental health professions were well represented within the corpus of studies. Psychiatrists (including registrars)/psychiatry professionals were in 31.98% of articles, general practitioners/family physicians/primary care physicians participated in 30.46% of studies, and social workers/social work professionals were included in 26.40% of articles. Adding to this, psychologists/psychology professionals were represented in 25.38% of articles, and psychiatric nurses participated in 20.30% of studies. However, counselors/psychotherapists were only included in 7.61% of articles, and occupational therapists/professionals from the field of occupational therapy participated in just 3.05% of studies. There was also one article that included general nurses that work in a psychiatric facility, and another study that included professionals from the field of neurology. To varying degrees, a number of studies were not clear about the types of mental health professionals that participated. Namely, 16.24% of articles included unspecified nurses from psychiatric facilities, 8.63% of studies included unspecified mental health professionals, and a small proportion of articles included unspecified physicians from either primary care or psychiatric settings.
Measures and scales.
A large quantity of different measures were employed to examine stigmatization both across and often within studies. Of the measures, stereotypes were utilized the most, with 77.16% of articles reporting the use of this type of measure. A small amount of studies investigated stereotypes in general (e.g., an aggregate score of multiple stereotypes), but a plethora of specific stereotypes were also included throughout the articles. The five stereotypes that were used the most were about causal attributions (e.g., mental illness is caused by a lack of will power), prognosis (e.g., people with mental illness will not recover), dangerousness (e.g., people with mental illness are a danger to other patients and staff), difficulty (e.g., people with mental illness are difficult to treat), and incompetence (e.g., people with mental illness are incapable). None of the stereotypes took the form of perceived stigma.
Compared to stereotypes, emotions and behaviors were utilized far less to measure stigmatization. This was especially true for emotions, as only 23.35% of studies measured this component of stigmatization, whereas 40.10% of articles included behaviors as a measure of stigmatization. Similar to stereotypes, some studies explored emotions in general, yet a variety of particular emotions were included within the corpus of articles. The four most frequently measured emotions were fear, frustration, sympathy, and anger. For behaviors, general measures were also employed in several studies, although much fewer specific behaviors were examined in contrast to stereotypes and emotions. Avoidance (e.g., best to avoid people with this problem) and segregation (e.g., mental health facilities should be kept out of residential neighborhoods) were the two most commonly measured kinds of discrimination. Almost all of the emotions and behaviors reflected endorsed stigma, while just two articles reported perceived emotions (i.e., sympathy, empathy), and three studies measured perceived behavior (i.e., avoidance). On top of individual components of stigmatization, general stigmatization (e.g., an aggregate score of different components of stigmatization, I dislike people with mental illness) was investigated in 44.16% of articles. Most of these studies measured endorsed and explicit general stigmatization, and perceived and implicit general stigmatization were included in only a few studies. Besides implicit general stigmatization, no other measures of implicit stigma were used in any of the articles (e.g., implicit stereotypes).
Stereotypes, emotions, behaviors, and stigmatization in general were either measured with established scales, or with scales that had not been previously validated. Amongst the studies a range of different established scales were utilized (e.g., Attribution Questionnaire, Medical Condition Regard Scale, Attitude to Personality Disorder Questionnaire) and the two most commonly used scales were the Community Attitudes towards Mental Illness questionnaire, and the Depression Attitude Questionnaire. In addition to the variety of such scales, the same scales were not always scored or computed in a consistent way across the articles (e.g., one study scoring the items on a 7-point Likert-type scale and another study scoring the items on a 4-point Likert-type scale; one article computing scores as a mean of all the items and another article using a total of all the items). Whether established scales were employed or not, there were some instances of measures being unclear (e.g., confirming behavioral responses was all the information provided), and in other cases, not enough information was supplied to interpret the measures in the results (e.g., when the meaning of points in a Likert-type scale were not specified). Further, several measures included items that are irrelevant to stigmatization (e.g., if depressed patients need antidepressants, they are better off with a psychiatrist than a GP), or items that do not match the construct supposedly being measured (e.g., taking care of borderline personality disorder patients can evoke unfamiliar feelings as an item for empathy).
Types of mental illness.
Mental illness in general (e.g., the mentally ill, patients in a mental hospital, a person who has a mental illness) was included as stimuli for 43.65% of articles. Studies in the current review also elicited responses with a multitude of particular mental disorders (e.g., anxiety disorders, personality disorders, eating disorders). However, most of these mental disorders were present in only a small number of articles, and the majority of studies that presented specific categories of mental illness included the same three mental disorders. These were schizophrenia spectrum disorders, depressive disorders, and addiction/substance use disorders, and they were in 28.93%, 26.40%, and 17.77% of articles, respectively. Additionally, some studies included comorbid disorders, and several articles either did not specify the mental disorders or reported that the participants reacted to broad categories of mental illness (e.g., other psychiatric disorders, other clients). Mental disorders that were not present in any of the studies were sexual dysfunctions, sleep-wake disorders, gender dysphoria, and elimination disorders.
Relative stigma, component relations, and other variables.
In contrast to articles on the stigmatization of either mental illness in general or one mental disorder, fewer studies were conducted on stigmatization as it varies with the type of mental illness. In other words, there was a comparatively small amount of research on the relative stigma of mental illness, with just 19.29% of articles exploring this phenomenon. Further, most of the studies on relative stigma did not compare a wide range of mental disorders. Specifically, 55.26% of studies compared two disorders, 23.68% compared three, 18.42% compared four, one article compared six, and one study compared nine. Adding to this, many of the included mental disorders appeared in only a few articles, and a large proportion of the studies included the same two mental disorders, schizophrenia spectrum disorders and depressive disorders. The former was compared to a minimum of one other mental disorder in 65.79% of studies, and the latter was included in 63.16% of articles. Excluding the mental disorders already mentioned at the end of the previous subsection, mental disorders that did not appear in any of the research on relative stigma were somatic symptom disorders, impulse control disorders, and neurocognitive disorders. As a final observation regarding the literature on relative stigma, many of the quantitative studies did not utilize statistical modelling either at all or in the appropriate manner (i.e., performing an ANOVA without following up with multiple comparisons). In 36.36% of the relevant articles, these statistical limitations were apparent for all mental disorder comparisons, and for 12.12% of studies, this occurred for at least one comparison.
Amongst the literature, research on how the components of stigmatization relate to each other was even more scarce than studies on the relative stigma of mental illness, as only 10.66% of articles examined component relations. A number of these studies investigated the effect of stereotypes on emotions and behaviors, whereas there were fewer articles on the relationship between emotions and behaviors. There were also some studies that explored how different stereotypes relate to each other, and one article examined the link between different emotions. However, not one study investigated how the different components of stigmatization relate to each other as a whole in one framework (e.g., a model with emotions mediating the relationship between stereotypes and behaviors). Despite the little amount of research on relative stigma and component relations, a substantial quantity of articles detailed research on other predictors of stigmatization. The proportion of studies that included these other predictor variables was 61.91%. Throughout and frequently within these articles there was an enormous variety of different predictors. The majority of these variables were individual differences (e.g., ethnicity, marital status, trait authoritarianism), while a small number of studies explored situational and other variables (e.g., the use of labels, target sex, target age; media influence). The four most common individual differences were profession, sex, age, and years of professional experience, and the levels of some predictor variables were not specified (e.g., occupational characteristics, professional function). Additionally, although to a lesser extent, several articles that quantitatively examined these other predictors exhibited the same statistical weaknesses present in the research on relative stigma to some degree. Whether relative stigma, component relations, or other predictor variables were being investigated, there were very few studies that did so while explicitly controlling for other variables (i.e., were not merely controlled for as an incidental part of multiple regression analysis).
The state of evidence.
Within the corpus of articles, there was certainly a lot of variability with respect to particular data items. This was especially the case for the measures and variables, and even within categories that ought to be homogeneous, this level of variability was still evident. As a result of this, it was extremely difficult to identify any general findings amongst the literature, and practically impossible to summarize findings for all of the included variables. To increase the feasibility of outlining broad findings, an overview was attempted only for the most prevalent research questions. However, even after narrowing down the research questions, the level of variability between articles was still large enough to hinder the identification of general findings. Further, on examining these studies numerous inconsistencies were found between the articles regarding both the presence and direction of effects.
Bibliometric analysis.
Scopus was unable to access 13 articles, and this meant that 184 or 93.40% of studies were included in the direct citation analysis. Of these articles, VOSviewer identified 57 clusters. 32 of the clusters were individual studies that either did not or were not cited by any other study, and this represented 17.39% of all articles in the direct citation analysis. These articles can be seen in Fig 2 as the individual nodes that form most of the belt of studies surrounding the central structure of articles.
https://doi.org/10.1371/journal.pone.0280739.g002
The belt of studies in Fig 2 also contains small clusters of two or more interconnected articles that are isolated from all other studies. Together, these small, isolated clusters account for 8.15% of articles. The remaining 137 or 74.46% of studies are all contained within the central structure articles (see Fig 3 for a more detailed image of the structure). Although this structure is a dense network of interconnected studies, it also includes clusters of articles that are mostly disconnected from the rest of the network. The best examples of this are the green cluster at the top of the network, and the red, yellow, and blue clusters to the right of the network. As depicted in Fig 3 , these peripheral clusters are only linked to the remainder of the network indirectly via one or a few other articles. The other studies in the central structure of articles make up the clusters that are closest to each other. These clusters contain the three authors that were cited the most within the whole citation network. Beginning with the most references, Nordt et al. [ 23 ] had 27 citations, Jorm et al. [ 48 ] received 22 references, and Lauber et al. [ 49 ] had 19 citations.
https://doi.org/10.1371/journal.pone.0280739.g003
Out of 197 articles, 27 or 13.64% were not found through the scimagojr webpage. For all other studies, the highest and most recent rank in the majority of cases was either Q1 or Q2. In particular, 52.76% of articles were published in Q1 journals, and 34.12% of studies were published in journals with a rank of Q2. In contrast, the highest and most recent rank for 11.76% of articles was Q3, and for 2.36% of studies, it was Q4.
It was imperative that a scoping review was performed with the aim of outlining the state of available research on the endorsed stigmatization of mental illness by mental health professionals. Most of the objectives for this scoping review were concerned with exploring how studies are being conducted, and whether there are any gaps in the research. Of particular importance was the extent to which studies had been carried out on the relative stigma of mental illness and the components of stigmatization as they relate to each other. As part of a bibliometric analysis, this scoping review also investigated how often articles are connected via a citation, and whether research is being published in well-known journals.
Summary and interpretation of the results
Inappropriate samples..
The first major finding of this scoping review was that a substantial proportion of the literature reported results that were based on inappropriate samples. As a result, a subset of the literature was excluded from the subsequent results.
Gaps in the research.
Another key finding of this scoping review was that there are a number of gaps in the literature that constitute weaknesses in the research on mental health professionals stigmatizing mental illness. Several gaps that were particularly salient concerned the relative stigma of mental illness and the components of stigmatization. Many studies examined the stigmatization of either mental illness in general or one mental disorder, and in contrast, much less research was conducted on the relative stigma of mental illness. Adding to this, the construct of relative stigma was often not adequately covered. Most of the studies on relative stigma did not compare a variety of mental disorders, and mainly included schizophrenia spectrum disorders and depressive disorders.
When inspecting the dimensions of stigmatization that were investigated, it was found that the emotional and behavioral components of stigmatization were explored in far fewer studies than stereotypes, and this was especially the case for emotions. This lack of research on emotion is striking when considering there is ample evidence to suggest that emotional processes have a stronger relationship with interpersonal contact than stereotypes [ 50 ]. This is relevant to mental health practice, as contact with others is an integral part of practice within the mental health field. In addition to little research on emotions and behavior, studies on how the components of stigmatization relate to each other were lacking. Although some studies explored the impact of stereotypes on emotions and behavior, again there was less research investigating the effect of emotions on behavior, and not a single study was conducted on how the components of stigmatization relate to each other as a whole.
Rather than examining the relative stigma of mental illness or component relations, a large proportion of the studies on mental health professionals stigmatizing mental illness were on individual differences (e.g., profession, sex, age). Together with the findings of the previous paragraph, this shows that research in this area has moved little beyond mental illness in general, single mental disorders, stereotypes, and individual differences. This suggests that the literature on mental health professionals stigmatizing mental illness is often not informed by existing theory. However, more importantly, the current state of research on this topic does not supply much guidance on how to reduce this stigmatization and improve the related aspects of mental health practice.
Multiple other gaps were found in the literature on the stigmatization of mental illness by mental health professionals. For example, counselors and occupational therapists participated in only a small proportion of studies, indicating that knowledge in this domain is far from complete for these professional groups. Also, none of the qualitative studies in this area employed theory-building analyses (e.g., grounded theory), and most of the research presented mental illness to participants via labels. The literature would likely benefit from qualitative research that can supply guidance on the variables and hypotheses that warrant examination, and studies that use vignettes or something similar.
Other limitations.
On top of the limitations noted in the previous subsections, several other limitations were found within the literature on mental health professionals stigmatizing mental illness. These included issues with construct validity, a lack of clarity surrounding aspects of method and results, statistical weaknesses, and inconsistencies with measures and variables. The diversity of measures and variables is more evidence to indicate that established theory is seldom drawn upon and may suggest that variables are frequently selected ad hoc. However, collectively, these limitations likely make it hard to be confident in and comprehend individual articles and the research in general.
The state of evidence and bibliometric analysis.
Due to the high level of variability and inconsistency of data items, it was deemed mostly infeasible to derive broad findings from the literature on mental health professionals stigmatizing mental illness. As a result, it is unlikely that research on the stigmatization of mental illness by mental health professionals is in a position to direct the reduction of this stigmatization, whether in general or with respect to practice. Additionally, given the nature of studies on mental health professionals stigmatizing mental illness, it would be difficult if not impossible to conduct either systematic reviews or meta-analyses in this domain.
In prior subsections, it was proposed that variability in the literature and research not moving far beyond mental illness in general, single mental disorders, and individual differences, could be accounted for by studies not drawing upon existing theory. Another possible explanation for this could be that research is disconnected, and the authors of articles on mental health professionals stigmatizing mental illness are not considering other studies in the area. Empirical support for the literature being fragmented in this way was obtained via a direct citation analysis, which showed that close to half of the literature is comprised of individual studies and small systems of research that are isolated to some extent from the rest of the literature. Further, clusters of interconnected articles that were either completely or predominantly disconnected from the remainder of the research were often characterized by a theme (e.g., studies on just borderline personality disorder or personality disorders in general). These results may be due to authors not knowing that research on specific mental disorders or professions sits within a broader literature on mental health professionals stigmatizing mental illness. A third potential explanation for the current state of research could be that studies are not being published in well-known journals. However, it was found that a large proportion of the research was published in Q1 and Q2 journals.
Recommendations
Based on the findings of this scoping review, recommendations are made regarding prospective research on the endorsed stigmatization of mental illness by mental health professionals.
To reduce stigmatization and improve the relevant facets of mental health practice, a comprehensive understanding of this type of stigmatization needs to be achieved. Namely, studies must focus on the relative stigma of mental illness, multiple dimensions of stigmatization, and how all three components of stigmatization relate to each other in one framework. Moreover, the construct of relative stigma should be sufficiently covered by addressing a range of mental disorders, and research should include all types of mental health professionals.
In order for conclusions to be easily and confidently drawn from this research, studies need to employ procedures that are standard of all good research. However, the current review has shown that this standard of research is often not reached, and studies are not being conducted with a systematic approach. Thus, to have high-quality research the time has come to address studies on the stigmatization of mental illness by mental health professionals programmatically. In particular, many of the limitations within this area of research can likely be overcome with multisite studies.
Limitations of the current scoping review
While the search string for the current scoping review was far more comprehensive than that of previous literature reviews, a number of studies may have still been overlooked. More specifically, it was impractical to include all classified mental disorders in the search string, and as such articles on mental disorders not in the search string may have been missed in the search. Although, the search string did in fact yield studies on mental disorders that were not part of the search string (e.g., borderline personality disorder, somatic symptom disorder). Another limitation of the current review was that only one reviewer selected the sources of evidence. Consequently, the inclusion and exclusion of articles may not have been entirely consistent with the eligibility criteria. However, an evaluation of inter-reviewer consistency with a second reviewer found a high level of agreement between reviewers, and disagreement led to refinement of the eligibility criteria. A final limitation of the current scoping review pertains to the direct citation analysis. In this analysis, 13 studies were unable to be included due to these articles not being accessible through Scopus. This means that the citation network produced by the direct citation analysis may have looked different with these studies incorporated, though it is unlikely that the overall findings of this analysis would have changed.
Mental health professionals, including clinical psychologists, have been found to endorse stigmatizing reactions towards mental illness [ 5 , 8 , 22 – 24 ]. Despite the importance of research in this domain, the current scoping review found that literature on mental health professionals stigmatizing mental illness is marked by an array of limitations. Notably, multiple gaps were found within the research and the literature has become stagnant. Amongst the gaps in research was a dearth of studies thoroughly exploring the relative stigma of mental illness and how the components of stigmatization relate to each other. As a result of some of these limitations, novel broad findings were unable to be decerned from the literature, and thus research on mental health professionals stigmatizing mental illness is likely not capable of informing the reduction of this stigmatization. It was suggested that several of the limitations in this area may be explained by researchers not drawing on relevant theory and the finding that literature on this topic is partially disconnected. In accordance with the findings of this scoping review, recommendations were proposed for future research on the endorsed stigmatization of mental illness by mental health professionals.
Supporting information
S1 appendix. table notes and abbreviations..
https://doi.org/10.1371/journal.pone.0280739.s001
S2 Appendix. Table A-B.
https://doi.org/10.1371/journal.pone.0280739.s002
S3 Appendix. Table C-D.
https://doi.org/10.1371/journal.pone.0280739.s003
S4 Appendix. Table E-F.
https://doi.org/10.1371/journal.pone.0280739.s004
S5 Appendix. Table G-H.
https://doi.org/10.1371/journal.pone.0280739.s005
S6 Appendix. Table I-J.
https://doi.org/10.1371/journal.pone.0280739.s006
S7 Appendix. Table K-L.
https://doi.org/10.1371/journal.pone.0280739.s007
S8 Appendix. Table M-N.
https://doi.org/10.1371/journal.pone.0280739.s008
S9 Appendix. Table O-P.
https://doi.org/10.1371/journal.pone.0280739.s009
S10 Appendix. Table Q-R.
https://doi.org/10.1371/journal.pone.0280739.s010
S11 Appendix. Table S-T.
https://doi.org/10.1371/journal.pone.0280739.s011
S12 Appendix. Table U-V.
https://doi.org/10.1371/journal.pone.0280739.s012
S13 Appendix. Table W-Z.
https://doi.org/10.1371/journal.pone.0280739.s013
S14 Appendix. Direct citation analysis data.
https://doi.org/10.1371/journal.pone.0280739.s014
S15 Appendix. Journal type and rank data.
https://doi.org/10.1371/journal.pone.0280739.s015
S16 Appendix. PRISMA-ScR fillable checklist.
https://doi.org/10.1371/journal.pone.0280739.s016
- View Article
- Google Scholar
- PubMed/NCBI
- 12. Productivity Commission. Mental health: Productivity commission inquiry report. Canberra: Productivity Commission; 2020.
- 17. Corrigan PW. On the stigma of mental illness: Practical strategies for research and social change. 1st ed. Washington, DC: American Psychological Association; 2005.
- 40. Greenfield T, Greener S. Research methods for postgraduates 3rd ed: John Wiley & Sons; 2016.
- Open access
- Published: 18 January 2021
Review of Australian initiatives to reduce stigma towards people with complex mental illness: what exists and what works?
- Amy J. Morgan ORCID: orcid.org/0000-0003-3784-0540 1 ,
- Judith Wright 1 &
- Nicola J. Reavley 1
International Journal of Mental Health Systems volume 15 , Article number: 10 ( 2021 ) Cite this article
43k Accesses
34 Citations
34 Altmetric
Metrics details
A Correction to this article was published on 05 August 2021
This article has been updated
Australian national mental health policy outlines the need for a nationally coordinated strategy to address stigma and discrimination, particularly towards people with complex mental illness that is poorly understood in the community. To inform implementation of this policy, this review aimed to identify and examine the effectiveness of existing Australian programs or initiatives that aim to reduce stigma and discrimination.
Programs were identified via a search of academic databases and grey literature, and an online survey of key stakeholder organisations. Eligible programs aimed to reduce stigma towards people with complex mental illness, defined as schizophrenia, psychosis, personality disorder, or bipolar disorder; or they focused on nonspecific ‘mental illness’ but were conducted in settings relevant to individuals with the above diagnoses, or they included the above diagnoses in program content. Key relevant data from programs identified from the literature search and survey were extracted and synthesized descriptively.
We identified 61 programs or initiatives currently available in Australia. These included face-to-face programs (n = 29), online resources (n = 19), awareness campaigns (n = 8), and advocacy work (n = 5). The primary target audiences for these initiatives were professionals (health or emergency), people with mental illness, family or carers of people with mental illness, and members of the general population. Most commonly, programs tended to focus on stigma towards people with non-specific mental illness rather than on particular diagnostic labels. Evidence for effectiveness was generally lacking. Face-to-face programs were the most well-evaluated, but only two used a randomised controlled trial design.
Conclusions
This study identified areas of strength and weakness in current Australian practice for the reduction of stigma towards people with complex mental illness. Most programs have significant input from people with lived experience, and programs involving education and contact with a person with mental illness are a particular strength. Nevertheless, best-practice programs are not widely implemented, and we identified few programs targeting stigma for people with mental illness and their families, or for culturally and linguistically diverse communities, Aboriginal and Torres Strait Islander communities and LGBTIQ people. These can inform stakeholder consultations on effective options for a national stigma and discrimination reduction strategy.
Stigmatising attitudes towards people with mental illness are prevalent in Australia [ 1 ]. While there have been some improvements in community understanding of common mental illnesses (particularly depression and anxiety), there is still widespread misunderstanding and ignorance [ 2 , 3 ]. In particular, complex mental illnesses, such as schizophrenia, bipolar disorder and personality disorders, tend to be poorly understood and attitudes are much less positive. The low prevalence of these mental illnesses means that most people do not personally know someone with these illnesses, so they are more likely to rely on stereotypical attitudes. Common stereotypes about people with complex or severe mental illness include are that they are dangerous, unpredictable, lack competence to look after themselves, and have little chance of recovery [ 4 ]. Negative attitudes lead to discriminatory behaviour, primarily avoidance and exclusion, as people seek to avoid the risks of associating with people with mental illness. This can affect a person with mental illness’ opportunities for finding and keeping a job and their relationships with friends, family, and romantic partners [ 5 ]. This discrimination can increase feelings of worthlessness, hopelessness about the future, and suicidality [ 6 , 7 ]. Reducing stigma and discrimination is therefore critical to improving the wellbeing of people with mental illness and their carers.
Reducing stigma towards people with complex mental illness is a key priority area of Australian national mental health policy. The Fifth National Mental Health and Suicide Prevention Plan (the Fifth Plan), released in 2017, focuses on stigma reduction as one of eight priorities for mental health reform [ 8 ]. It outlines the need for a nationally coordinated strategy to address stigma and discrimination and requires that the Australian government build on existing initiatives, including the evidence base of what works in relation to reducing stigma and discrimination. A recent meta-analysis of randomised controlled trials evaluated the evidence of interventions to reduce stigma towards people with severe mental illness (schizophrenia, psychosis or bipolar disorder) [ 9 ]. This found that both contact- and education-based interventions showed small-to-medium immediate reductions in stigma, but there was limited evidence on longer-term effects. There was also little guidance on what components of interventions are needed for effective stigma reduction. Furthermore, only two interventions had been evaluated in Australia, one of which was only available as part of a university experiment. While the review focused on high-quality randomised trial evidence from an international perspective, there is a need to understand what programs and initiatives are currently available in Australia specifically, and whether they have any evidence of effectiveness, even if not from randomised trials. This information is critical to inform options for a national stigma and discrimination reduction strategy as part of implementation of the Fifth Plan in Australia.
The aim of this study was therefore to (1) identify existing programs or initiatives run by Australian lived experience groups and other key non-government organisations that aim to reduce stigma and discrimination and promote positive behaviours towards people with complex mental illness; and (2) examine the evidence of effectiveness for these programs.
In order to review existing Australian stigma and discrimination reduction initiatives and their evidence of effectiveness, we conducted literature searches and surveyed lived experience groups and key non-government organisations (NGOs).
Program inclusion/exclusion criteria
Programs were eligible if they (1) aimed to reduce stigma towards people with complex mental illness, defined as schizophrenia, psychosis, personality disorder, or bipolar disorder; (2) they focused on nonspecific ‘mental illness’ but were conducted in settings relevant to individuals with the above diagnoses (e.g., public mental health services, with mental health nurses); (3) they included the above diagnoses in program content; (4) stigma reduction was explicitly mentioned as a focus, or was implied (e.g. by including a stigma measure as an outcome or by focusing on improving understanding or knowledge of severe mental illness). All kinds of stigma were eligible, including personal or public stigma, perceived stigma, desire for social distance, discrimination, self/internalised stigma, and beliefs about recovery or prognosis.
Programs were ineligible if they (1) focused on common mental disorders (depression or anxiety), suicide, eating disorders, dementia, intellectual disability, PTSD, OCD, substance misuse or dual diagnoses; (2) aimed to improve mental health literacy or promote help-seeking without a specific focus on reducing stigma and discrimination; (3) were not conducted in Australia.
Literature search
A systematic search of the ‘grey’ and academic literature was conducted to identify Australian programs that aim to reduce stigma and discrimination.
Academic databases
For the academic databases we searched PubMed and PsycINFO, limited to studies published since 2009 to ensure that they were relevant to current practice. Literature search strategies were developed using medical subject headings (MeSH) and text words related to stigma and discrimination (see Additional file 1 : Table S1). All study designs were eligible including quantitative (e.g. uncontrolled trials) and qualitative (e.g. participant interviews). A total of 652 studies were screened for eligibility.
These searches were supplemented by screening our results from a previous literature review [ 9 ] to identify any reports that did not meet the inclusion criteria for that review (e.g. due to lack of a control group) but met the inclusion criteria for this review.
‘Grey’ literature
The ‘grey’ literature search was conducted using Google Australia. The purpose of the ‘grey’ literature search was to identify eligible programs and to identify organisations with potential programs to be invited to participate in the survey.
Separate searches were conducted using the following key search terms: bipolar, personality disorder, (schizophrenia OR psychosis), (mental illness OR mental health), (stigma OR discrimination), and Australia. For each search, the first 50 websites were retrieved, and duplicates were excluded. The remaining websites were reviewed for relevant information and any links from these websites were followed when they were thought to contain useful information.
We also systematically searched websites of lived experience advocacy and support groups and other key NGOs to identify programs and evaluation reports. Overall, a total of 267 websites were searched for eligible programs.
Survey of lived experience groups and key NGOs
We conducted an online survey of lived experience advocacy and support groups and key NGOs, inviting them to provide details of their programs and associated evaluation or evidence of effectiveness.
Survey participants
Survey participants comprised key informants in Australian organisations of any type that have programs that aim to reduce stigma and discrimination and promote positive behaviours. These were reached in 4 key ways: (1) An email sent to organisations identified in web searches (see above); (2) Information about the study with a link to the survey included in the following organisations’ newsletters: Mental Health Australia, Mental Health Victoria, and Mental Health Coordinating Council; (3) An email sent to all voting and non-voting members of Mental Health Australia. Mental Health Australia is the peak, national non-government organisation representing the interests of the Australian mental health sector. Its members include national organisations representing consumers, carers, special needs groups, clinical service providers, public and private mental health service providers, researchers and state/territory community mental health peak bodies; (4) Snowball sampling—survey respondents were encouraged to pass on details of the project to other organisations with programs that met the inclusion criteria. In total we invited 177 organisations to participate in the survey.
Survey content
Survey data were collected online using Qualtrics software with both multiple choice and open-ended questions. The survey included information such as location, target audience, type of program, program delivery mechanisms, program reach and source of funding. Organisations were able to provide information about multiple stigma-reduction programs, if relevant. Organisations were asked to provide any available evaluation or evidence of effectiveness. Participants provided informed consent before completing the survey. The survey opened 9th of December, 2019 and closed on 31st of January, 2020.
A concerted effort was made to obtain missing information about programs from those identified in our searches and from completed surveys. Authors of academic papers were emailed to enquire about whether programs were still operating and to obtain information not reported in the scientific literature. Organisations were also sent reminder emails to undertake or finish completing the survey before it was closed.
Data analysis
Key relevant data from programs identified from the literature search and survey were extracted and synthesized descriptively and thematically. Level of evidence for each program was classified on a scale from 1–5, with 1 = no evaluation evidence, 2 = post survey feedback or qualitative interviews, 3 = one or more uncontrolled trials or repeated cross-sectional surveys, 4 = one or more controlled trials, 5 = one or more randomised controlled trials.
Results from our survey of organisations in the mental health sector, grey literature search, and search of academic literature, identified 79 Australian programs or initiatives. These 79 programs were described or evaluated in 108 resources (as some programs were included in multiple academic papers). However, some of the identified programs did not appear to be currently available, based on information from program authors or a web search for further information. Programs that were one-offs conducted in the past, had ceased operating, or were experimental research studies not designed to be ongoing, are included in supplementary material (Tables 2 and 3 ). Excluding these programs left 61 programs currently operating in Australia. See Fig. 1 for a flow chart of the process of identifying eligible programs. These were further broken down into face-to-face programs (n = 29), community awareness campaigns (n = 8), programs or organisations undertaking advocacy for the rights of people with mental illness (advocacy programs, n = 5), and publicly-available online resources (n = 19).
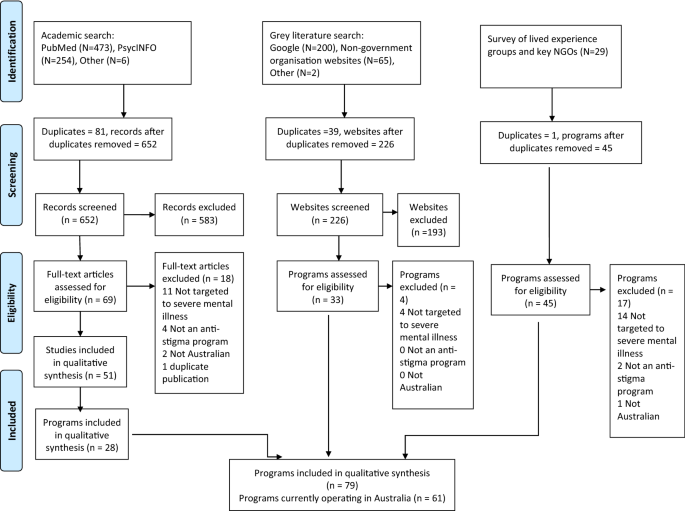
Flow chart for identifying eligible programs
Face-to-face programs
Face-to-face programs were primarily targeted to four types of audiences: (1) Health professionals and health professional students; (2) People with a mental illness; (3) Family of people with a mental illness; (4) Members of the general population (particularly at school, university, or workplaces). See Tables 1 , 2 , 3 and 4 for characteristics of each included program.
About half (55%) of the face-to-face programs focused on stigma towards people with a non-specific mental illness, six (21%) targeted a range of disorders including psychosis, schizophrenia, bipolar disorder or personality disorders, three (10%) specifically focused on psychosis or schizophrenia, two (7%) on ‘severe’ mental illness, and two (7%) specifically on Borderline Personality Disorder.
Three-quarters (76%) of organisations providing anti-stigma programs were classified as not-for-profit or community sector, and the remainder were government (10%), university/tertiary education (10%), or private/for-profit (3%). A majority of organisations (66%) provided a range of services, including some anti-stigma programs, rather than only running anti-stigma programs (34%), and a majority reported running multiple anti-stigma programs (62%). A minority of programs were run in all Australian states and territories (24%), with the largest number run in NSW (31%), followed by Victoria (28%), the ACT (17%), Queensland (14%), South Australia (10%), Tasmania (10%), Northern Territory (10%) and Western Australia (3%)). Programs were also delivered across metropolitan (72%), regional and/or rural areas (62%) and remote communities (31%) with half delivered across multiple geographic areas.
Programs were delivered in a variety of settings, most commonly community settings (e.g. sports or arts organisations, 45%), followed by community health centres (41%). Also common were workplaces (38%), university or tertiary education settings (34%), primary healthcare (17%), and high school (14%). Only 2 were run in primary schools (7%). Programs tended to target adults (59%) or ‘all ages’ (14%). Adolescents were the target age group in four programs (14%) and young adults in two (7%). In addition, one program targeted children 8–18 years old (3%).
Most programs involved people with lived experience in their design (59%) or delivery (76%). Programs often included multiple types of components, but the most common was an education component (66%) followed by face to face contact (62%) or online/video contact (24%). Protest or advocacy was reported in 24% of programs. Only one program included an (optional) hallucination simulation component (3%).
Seven programs did not report a funding mechanism. Of the remainder, there was a variety of funding sources. Funding was sourced most frequently from the Commonwealth government (25% of reported) or from earned income (22%), followed by state government (19%), donations or volunteers (11%), philanthropic (8%), corporate sponsorship (6%), and other means (8%).
Most of the programs were well-established, with half running for more than 10 years (48%), 28% running for 5–10 years, one was 2–5 years old (3%), and one was 6–12 months old (3%). This information was not reported or available for nearly a fifth of programs, however. Information about program reach was not available for seven programs. Of the remainder, ten (45%) had reached up to 1000 people, five (23%) 1000–10,000, four (18%) reached 10,000–100,000, and three programs (14%) had reached over 100,000 people.
The level of evidence for most programs was low. Seven programs (24%) reported no evaluation evidence and a further eight (28%) were evaluated with post program surveys or qualitative interviews only. These surveys tended to focus on satisfaction outcomes rather than impact on stigma. Only two programs (7%) were evaluated with one or more randomised controlled trials, the highest level of evidence. Six programs (21%) had one or more controlled trials, four (14%) were evaluated with one or more uncontrolled trials or repeated cross-sectional surveys, and for two programs the type of evaluation was unclear. Information about program evaluations is available in Table 5 .
Programs targeted the following audiences:
Health professionals, health professional students, emergency workers
Our search identified seven programs that target health professionals, health professional students, or emergency workers. These varied in their approach but often included a focus on the potential for recovery, to counterbalance health professionals’ frequent contact with people when they are most unwell. Two programs target nursing students with contact interventions. One of these, Recovery Camp , is a nursing placement designed to facilitate contact between nursing students and people with lived experience outside an acute setting, where recovery is a focus. The program has run since 2013 and is funded by universities who pay for the placement by students. Two controlled trials found reduced anxiety about mental illness, negative stereotyping, and desire for social distance after the placement compared with traditional nursing placements. A second program, Recovery for Mental Health Nursing Practice , is taught by an academic with lived experience and also focuses on recovery concepts. Two controlled trials found improvements in some attitudes compared to a traditional mental health nursing subject. Pharmacy students are targeted by the Remind Training and Education program , which involves trained mental health consumers participating in pharmacy tutorials as educators. This program has run since 2010 and has reached 2,500 students at the University of Sydney. Evaluations in a controlled trial and an uncontrolled trial found reductions in stigma after the program and up to 12 months later. Of note, we identified one other program targeted to health students in a research study, but it is no longer running. This was a contact intervention for final year medical students to reduce stigma against people with schizophrenia as part of 6 week psychiatry rotation (see Additional file 1 : Table S3).
Two programs target health professionals with education interventions. The Collaborative Recovery Training Program trains professionals in recovery concepts and is offered by the University of Wollongong. An uncontrolled trial found improved attitudes to consumers’ recovery possibilities after the training. The Managing Mental Health Emergencies short course trains rural and remote generalists how to respectfully and effectively manage mental health emergency care. An evaluation found better skills identifying psychosis and improved attitudes towards mental health clients. A third program, no longer running, focused on improving employment outcomes for consumers by funding Vocation, Education, Training and Employment Coordinators within mental health services (see Additional file 1 : Table S2). An evaluation found an improvement in clinicians’ attitudes towards consumer capability of full-time, open employment.
Finally, Mental Health Intervention Team training is delivered to police officers and emergency service communication officers. The training is offered across an intensive 4-day program or 1-day training course. It teaches how to respond effectively during mental health emergencies with education and contact components. It has operated for more than 10 years in the NSW Police Force and Queensland Police Service. While an evaluation of a brief 2-h version for communications officers found no impact on stigma, a second controlled trial evaluating the full training package showed positive effects. Police officers reported increased confidence and understanding of how to deal with jobs involving individuals with a mental health problem or a drug induced psychosis.
People with mental illness
Eight programs target people with a mental illness (see Table 2 ). Most of these focus on reducing self-stigma, but some programs additionally aim to reduce public stigma through consumer participation in the community (i.e. contact). For example, The Station and TasRec both offer recreation programs where consumers engage with community members in a variety of activities. The Station aims to increase social connections and skills for living in people with a mental illness. It has operated since 1998 in South Australia and receives funding from a variety of sources. Interviews with participants found it increased feelings of empowerment and led to a greater belief in oneself. Similarly, TasRec provides recreation activities to help build skills, increase confidence, and reduce isolation. It has operated for more than 5 years in Tasmania by the Richmond Fellowship Tasmania and receives Commonwealth government funding. The Richmond Fellowship Tasmania also runs another program— Residential Accommodatio n, for people with mental illness. The service provides support to tackle stigma, access services, build social networks, and reach greater independence.
Two programs provide the opportunity for people with a mental illness to meet and support each other. The Hearing Voices group is a monthly/fortnightly peer support group for people with schizophrenia, who share stories and coping strategies on living with voices. It is offered in Victoria by Uniting Prahran. The BPD Community Information Nights are a forum for sharing information and support for people with Borderline Personality Disorder. They aim to address stigma and discrimination by focusing on hope and optimism about recovery. They are held three times a year in Victoria, supported by volunteers.
My Recovery is a peer-led education program for people living with mental illness offered in Darwin by Northern Territory Mental Health Coalition. The program aims to support recovery and provide a vocational pathway to people with lived experience. It is facilitated by peers and consists of nine weekly sessions that cover education topics such as stigma and discrimination, advocacy, recovery and skills training in communication, personalised recovery planning and goal setting.
A different sort of contact intervention is offered by Compeer (The Friendship Program) . Community volunteers and people with a mental illness are matched and meet regularly to develop friendships. The ACT branch of this international program has operated since 2009 with 253 participants. An evaluation found lower levels of stigma in volunteers with stronger relationships with their matches and that stigma was not related to the length of the relationship/contact.
Finally, Being Herd by batyr is a workshop for young people with mental illness who are trained how to share their stories to reduce stigma. This 2-day workshop has trained more than 700 people but has not been evaluated for its impact on stigma.
Families of people with mental illness
Three programs target families of people with mental illness (see Table 3 ). These include psychoeducation elements to increase understanding of mental illness and how to cope, and as such, may reduce self-stigma and stigma towards their family member, even though this may not be an explicit aim. The BPD Community Family and Friends Group provides support and psychoeducation. The group meets monthly and has operated in Victoria since 2015 on a volunteer basis. The Journey to Recovery is offered by St Vincent’s Mental Health Service in Victoria and has run since 2009. It is a group psychoeducation program for families and friends of people experiencing early psychosis to assist coping and reduce isolation. An outpatient version runs for 5 × 2-h sessions and an inpatient version is a single session. Two uncontrolled trials found improved knowledge of psychosis and recovery and reduced feelings of isolation in participants. A third program, Kookaburra Kids Camps and Activity Days , targets children of people with a mental illness. The program offers therapeutic recreation camps and activities in most states of Australia. Operating for more than 10 years, it has reached more than 3,000 people. Funding is from government, donations and corporate sponsorships.
Members of the general population
The most frequent target of anti-stigma programs was the general population, as we identified 11 programs of this type (see Table 4 ). Eight of these were training programs delivered in organisations such as schools, universities or workplaces. All programs focus on non-specific mental illness or mental illness including schizophrenia, psychosis, personality disorder, or bipolar disorder, rather than these disorders specifically. These programs are typically quite short, such as around 60 min in length. The exception is Mental Health First Aid training, which is at least 12 h in length. Six programs include both contact and education elements, one includes only contact and one includes only education.
Three programs have been established for more than ten years and have had a wide reach: Mental Health 101 , Mental Health First Aid training, and SANE Australia’s Peer Ambassador Program . Mental Illness Education ACT (MIEACT) has run Mental Health 101 courses for youth and adults in the ACT since 1993 with 8,000 people trained each year. These are 60-min workshops delivering contact and education to schools or workplaces. Consumer educators are guided by the DoNOHarm safe story-telling framework. A controlled trial of Mental Health 101 Youth found increased knowledge about mental illness and reduced stigma after the training. Interviews with the consumer educators showed that participating in the program had an effect on self-stigma but there was also a fear of being stigmatised as a result of presenting.
Mental Health First Aid (MHFA) training was established in 2000 and has trained 800,000 people across Australia. Training focuses on how to support a person developing a mental health problem or crisis and includes contact, education, and (optionally) a hallucination simulation activity. Training is delivered by accredited instructors who choose where to offer the course, such as workplaces, universities, and other organisations. To maintain program fidelity, accredited instructors are required to regularly deliver MHFA courses and undertake continuing professional development. MHFA has been rigorously evaluated in Australia and internationally since its inception with 3 meta-analyses, 16 RCTs, 7 controlled trials, and a number of uncontrolled trials. Meta-analyses show the program leads to a reduction in stigmatising attitudes after training and up to six months later [ 10 ]. Of note, the course has been evaluated in several culturally and linguistic diverse populations in Australia, including Vietnamese, Chinese, ‘multicultural’ communities, and Chinese international students, with positive effects on stigma. It has also been evaluated with health professional students, including nursing students and pharmacy students.
SANE Australia’s Peer Ambassador Program also involves presentations in workplaces and community settings across Australia by people with lived experience. Ambassadors receive training and support to share their personal experiences and also contribute to advocacy projects. This is a long-running program which currently supports 110 Peer Ambassadors, with more than 1000 trained since 1986. However, the program has not been evaluated for its impact on stigma.
Although only operating for 5–10 years, batyr has had already had a significant reach. Batyr run three programs—for schools ( batyr@school ), universities ( batyr@uni ) and workplaces ( batyr@work ). Sessions last 60–90 min and include contact from two people with lived experience as well as education about mental illness. Lived experience speakers are trained in the Being Herd workshop described above. Batyr programs have been delivered to more than 220,000 people and the batyr@school program has been evaluated with an RCT. This evaluation has not been published in the peer-reviewed literature but the authors report that the program reduced stigma towards mental health issues and this lasted for at least 3 months after the program.
Other similar awareness training programs delivered in organisations around Australia include SPEAK UP! Stay ChaTY , LIVINGWell , Mental Health Awareness by Mental Health Partners, and Staff Wellbeing Workshop by Chess Connect (delivered to workplaces in NSW only). SPEAK UP! Stay ChaTY has been evaluated and found participants reported being more comfortable in talking about mental health after the training. The other programs provided no information about evaluations.
Australian Rotary Health and Rotary Clubs hold Mental Health Awareness Forums in communities around Australia. These usually involve a consumer, a carer, and a mental health professional as speakers on mental health. Since 2000, about 5,000 people have participated in these forums. The program was evaluated with post feedback surveys and found improvements in perceptions of knowledge and what can be done to reduce stigma.
The Dax Centre in Victoria offers two complementary anti-stigma initiatives that are different to the programs described above—the Exhibition Program and the Education Program (Mindfields) . These are based around the exhibition of art by people with mental illness. The Exhibition Program educates the general public via the biographies of the artists. It has operated for more than 10 years and has received more than 24,000 visitors. Feedback forms from visitors show that most agree the exhibitions increase sympathy, understanding of mental illness, and appreciation of the creative ability of people with mental illness. The Education program is delivered to secondary and tertiary students and is a structured program including a tour of the exhibition, education and contact with people with lived experience. Another one-off program has also used art by people with lived experience to reduce self-stigma and stigma in the community (see Additional file 1 : Table S3). Art created by young people attending Headspace in regional NSW was exhibited in commercial retail outlets and local community centres. Interviews with retail staff involved in the exhibition reported that the program had brought mental illness out into the open and increased empathic understanding of others’ emotional experiences.
Also of note is a one-off program that was run in Sydney’s Macedonian community to reduce stigma towards people with schizophrenia (see Additional file 1 : Table S2). Fear and Shame was a theatre play about a Macedonian family with a son with schizophrenia. This was a culturally appropriate approach that reached about 1,600 people in the community over six months of staging. An uncontrolled trial of its impact found improved attitudes towards mental illness and a greater willingness to disclose and seek help from health services.
Online resources accessible to the public
The search identified 19 online resources with a focus on reducing stigma towards mental illness that were designed and delivered by Australian organisations (see Table 6 ). These organisations provided a range of services and were not exclusively focused on running anti-stigma programs. Most organisations were not-for-profit or community sector (73%), with the remainder government (13%) and private (7%). Online resources were publicly and freely available by organisations via their websites or their content was uploaded to popular online streaming services such as Apple, Facebook and YouTube.
Most online resources focused on reducing stigma towards non-specific mental illness (26%) and psychosis or schizophrenia (26%), with the remainder focused on ‘complex’ mental illness (16%), bipolar disorder (16%) and personality disorders, primarily borderline personality disorder (16%). The majority of online resources (63%) took a whole of population approach and used text, audio and video content to reduce self-stigma and public stigma. A minority of online resources identified additional targets to the general public; notably, ‘ Let’s Talk’ , a podcast series that also targets rural and remote populations and the #WeSpeakUp campaign, which features a diverse cross-section of people with lived experience, including members of the Aboriginal, LGBTIQ, and CALD communities. The remainder of online resources targeted specific groups such as health professionals (16%) and people with lived experiences (21%). The search identified three online resources for health professionals. These were primarily education based and focused on upskilling clinicians through online training modules and webinars.
Most online resources (84%) were contact-based or involved an element of contact, such as via online videos. Contact involved people with lived experience sharing their insight and stories, except for two that involved people with lived experience as experts in online training for health professionals (e.g., BPD Webinar , Consumer and Carers as Educators ), and one that involved peer-to-peer support (e.g., SANE Forums ). The remaining online resources were education-based or included an educational component.
People with lived experience were usually involved in delivering the content of online resources (89%). Most online resources did not report whether people with lived experience were involved in the design of the resources.
Online resources with notable reach were SANE Forums and specific episodes from television programs produced by national broadcasters— The Feed (SBS) and You Can’t Ask That (ABC). SANE Forums are an online peer-support community used by people living with mental illness and by family and other carers from around Australia. The forums provide a safe, supportive and stigma-free environment for users to build stronger connections with others affected by complex mental illnesses. Seventy-five partner organisations syndicate the Forums on their own websites. In the past 12 months the SANE forums were accessed by 35,000 Australians and gained 4,400 new members. Two episodes of The Feed feature interviews of people sharing their experiences of psychosis, treatment and recovery. These episodes have amassed more than one million views on Facebook. One episode of You Can’t Ask That features eight Australians providing insight into living with schizophrenia and addressing misconceptions of the public. This episode has amassed 65,750 views on Facebook.
The level of evidence for most online resources was low. No evaluation evidence was reported for the majority (79%). Of the remaining, evaluations were in the form of usage data, post-feedback surveys, or qualitative interviews only, and did not report on effects on stigma. Notably, an evaluation conducted on users of SANE Forums identified its value as a supportive online environment free of stigma, where people felt understood by others who had shared similar experiences.
Awareness campaigns
We identified eight community campaigns in Australia with a focus on reducing stigma towards mental illness (see Table 7 ). These are mainly campaigns held annually that last for one day, one week, or one month. Apart from BPD Awareness Week and Schizophrenia Awareness Week , all campaigns focus on non-specific mental illness. All but two are conducted Australia-wide. Three campaigns have existed for more than ten years, two for 5–10 years, two for 2–5 years, and one was unclear. Six campaigns comprise multiple events, activities, promotional material and online/social media activity. There is a strong lived experience involvement in these campaigns, across their design, organisation, and delivery. Many of the events held as part of these campaigns include some form of contact between the public and people with a mental illness, whether that is via face-to-face stories or online video stories. Where reported, these campaigns have a wide reach from tens of thousands to hundreds of thousands each year. Only one campaign, World Mental Health Day , provided information from an evaluation. This was a feedback survey assessing satisfaction with campaign materials and willingness to participate in future, rather than assessing impact on stigma.
Two campaigns take a different approach to those above—Grow’s Odd Socks Day and batyr’s One Sock One Goal . Both involve wearing socks as a way of raising awareness about mental illness and showing support. Odd Socks Day occurs annually on the Friday before World Mental Health Day and One Sock One Goal is ongoing.
Although no longer running, the Napranum Social and Emotional Wellbeing Week was a week-long campaign run in the Cape York community of Napranum (see Table 2 in supplementary material). This was led by a local steering committee with support from Townsville mental health services. The week comprised a variety of activities to reduce the stigma of mental illness, including MHFA courses, live radio shows and concerts, community breakfasts, and consultations with school and community organisations. Campaign feedback was positive and that perceptions of mental illness as frightening had reduced.
Advocacy programs
Five programs were classified as advocacy initiatives (see Table 8 ). All programs focus on non-specific mental illness or mental illness including schizophrenia, psychosis, personality disorder, or bipolar disorder. Being’s Mental Health and Wellbeing Consumer Advisory Group , and Lived Experience Australia , both broadly advocate for improved acceptance of people with mental illness through activities such as participation in committees and media releases. Two programs advocated for change in specific areas—insurance coverage (Beyond Blue’s Insurance Discrimination Project ), and media reporting (SANE’s StigmaWatch ). The Stop Mental Illness Stigma Charter advocates for organisations to reduce stigma by committing to 7 principles. To date, 72 organisations have signed and committed to the charter. This program has existed for 2–5 years and a feedback survey from participating organisations showed 84% said adopting the Charter had made a difference in their organisation.
This review aimed to identify and examine the effectiveness of existing Australian programs or initiatives that aim to reduce stigma and discrimination towards people with complex mental illness that is poorly understood in the community. The broader aim was to inform options for a national stigma and discrimination reduction strategy as part of implementation of the Fifth National Mental Health and Suicide Prevention Plan in Australia.
Our review found 61 programs or initiatives currently available in Australia that had a focus on reducing stigma. These took a variety of stigma-reduction approaches across face-to-face programs, online resources, awareness campaigns, and advocacy work. The primary target audience for these initiatives were professionals (health or emergency), people with mental illness, family or carers of people with mental illness, and members of the general population. Most commonly, particularly for programs with a general public audience, programs tended to focus on stigma towards people with non-specific mental illness rather than on particular diagnostic labels. For some programs there may only have been a small component on poorly understood mental illnesses (i.e. schizophrenia, psychosis, personality disorder, bipolar disorder) and it is unclear whether anti-stigma messaging is diluted for these illnesses.
Evidence for whether programs are effective in reducing stigma is generally lacking. Only half of the face-to-face programs had been evaluated to test whether they had an impact on stigma, with only two programs evaluated with a ‘gold standard’ randomised controlled trial design. Nevertheless, most evaluations suggested positive effects on stigmatising attitudes. We did not find strong evidence of effectiveness for the other types of programs or online resources, noting that some of these are difficult to evaluate effectively.
There was little overlap of the programs identified in this review with those found in a meta-analysis of randomised controlled trials of international anti-stigma programs [ 9 ]. Only two programs were conducted in Australia, Mental Health First Aid training and a research-only program [ 11 ]. Although international programs have not been adopted into the Australian context, it is worth highlighting that most of the international studies did not evaluate ‘named’ programs that could be easily implemented elsewhere.
Strengths in Australian practice
The most well-developed area is Australian face-to-face programs involving education and contact with a person with mental illness. This reflects the findings of a meta-analysis of randomised trials which showed both education and contact interventions were effective in reducing stigma [ 9 ]. It would appear that both approaches are complementary, as education can correct myths and misunderstandings that underpin stereotypes, and lived experience stories about recovery have an emotional resonance that make the impact of mental illness more tangible. Additionally, consumers who share their story of lived experience often receive a benefit of reduced self-stigma related to increased confidence, sense of meaning and connection to similar consumer peers. Consumers who take on this role usually receive training and ongoing support, and this is fairly extensive in some programs (e.g. a 2-day workshop).
Another strength is that most programs or initiatives have significant input from people with lived experience. This input is into program design (e.g. through co-design or acting as project advisors) and program delivery, often covering facilitation or co-facilitation, not just in presenting lived experience stories.
There are several programs that are examples of best practice in Australia, due to being well-established or sustainable and showing reasonable evidence of effectiveness. For the general population these are Mental Illness Education ACT’s Mental Health 101 programs and Mental Health First Aid training. Other best-practice programs are Recovery Camp and the Remind Training and Education program for health professional students, and the Journey to Recovery program for family members of people with mental illness.
Weaknesses in Australian practice
Several weaknesses were identified in current Australian practice. It should be noted that these weaknesses should be considered in light of some potential review limitations. Despite every attempt to reach relevant Australian organisations with our survey, we may have missed some programs as the survey was only open in the busy December/January holiday season. Further caveats are described below where relevant. Notwithstanding these potential limitations, there were very few programs that targeted culturally and linguistically diverse communities, Aboriginal and Torres Strait Islander communities and LGBTIQ people. Two programs that were identified, a culturally-appropriate theatre show for the Macedonian community, and a Social and Emotional Wellbeing campaign for the community of Napranum, were one-off programs that did not appear to be currently available.
Programs for people with mental illness and their carers or family members are not widespread and are generally only available in certain locations, such as particular mental health services or recreation programs provided by not-for-profits. However, it is possible that we did not identify some relevant psychoeducation programs for carers if they did not allude to reducing stigma as a focus. Nevertheless, we could not identify any programs that explicitly focus on reducing self-stigma, such as via psychoeducation, cognitive restructuring or disclosure approaches (e.g. Honest Open Proud 12). Broadening the search to programs that focused on empowerment may have identified further relevant programs for people with mental illness.
While there are some examples of best-practice stigma reduction for health professional students (particularly nursing and pharmacy students), these are not widespread in all Australian education programs. There are also few programs focusing on stigma for health professionals once they are practicing, with the caveat that there may be some continuing professional development resources on stigma that we could not access. The one initiative for mental health professionals that showed improvements in attitudes related to people with mental illness’s capacity to work was not systematically implemented after being defunded.
Finally, we only identified one available program for primary school students, which was a program for children of parents with a mental illness.
Policy implementation recommendations
This review has highlighted the need for extensive consultations with key stakeholder groups to inform options for a national approach to stigma reduction in Australia. In particular, these consultations could address several questions that were unable to be answered in this review and provide guidance on implementation issues. Our review found programs offered to the general population tend to focus on non-specific ‘mental illness’, rather than complex mental illnesses that are poorly understood in the community. Given stigma varies by mental health problem, there is some debate about the merits of taking a generalist ‘mental illness’ approach, versus one that focuses more on specific mental illnesses and the particular issues associated with them [ 3 ]. Internationally, England’s Time to Change anti-stigma program uses non-specific mental illness in its approach and has shown positive effects upon stigma. Yet the authors of an evaluation of the program acknowledge that this may be because the public’s concept of mental illness has widened to include milder issues such as stress and grief, which are less stigmatised [ 13 ]. Consultations with Australian program providers and people with lived experience could explore views on whether existing programs targeted to mental illness should have a greater focus on complex mental illness, whether specific programs should be developed to do this, or whether existing programs should be implemented more widely.
Our review found that effective anti-stigma programs for nursing and pharmacy students exist but are not widespread, and we did not identify any effective programs for medical students. Consultations with health professional peak bodies and education providers could explore the options for development of new programs or sustainable expansion of existing programs that have evidence of effectiveness. Similarly, consultations with health care providers and people with lived experience could consider how to more widely implement into mental health services effective group psychoeducation for carers of people with early psychosis.
Overall, our review identified very few programs that target culturally and linguistically diverse or Indigenous communities. Consultations with these key stakeholder groups could identify communities in which anti-stigma initiatives are a priority, as well as how to support these communities in designing the most culturally appropriate sustainable interventions. There is also a need to expand the reach of programs that focus on reducing self-stigma in people with mental illness, and to identify which policy and funding mechanisms are required to do so.
This study identified areas of strength and weakness in current Australian practice for the reduction of stigma towards people with complex mental illness that is poorly understood in the community. Most programs have significant input from people with lived experience, and programs involving education and contact with a person with mental illness are a particular strength. Nevertheless, best-practice programs are not widely implemented, and we identified few programs targeting stigma for people with mental illness and their families, or for culturally and linguistically diverse communities, Aboriginal and Torres Strait Islander communities and LGBTIQ people. These findings can inform implementation of Australian National mental health policy, with the aim of reducing stigma and discrimination and ultimately supporting social inclusion and recovery.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
05 august 2021.
A Correction to this paper has been published: https://doi.org/10.1186/s13033-021-00490-y
Abbreviations
Australian Capital Territory
Borderline Personality Disorder
Culturally and linguistically diverse
Lived Experience
Lesbian, Gay, Bisexual, Trans and gender diverse, Intersex, Queer and questioning
Mental Health First Aid
Mental Health Intervention Team
Mental Illness Education ACT
Not Reported
Non-government organisations
New South Wales
Obsessive Compulsive Disorder
Posttraumatic Stress Disorder
Randomised controlled trial
South Australia
SANE Australia. A life without stigma: A SANE Report. SANE Australia; 2013.
Reavley NJ, Jorm AF. Stigmatising attitudes towards people with mental disorders: Changes in Australia over 8 years. Psychiatry Res. 2012;197(3):302–6.
Article PubMed Google Scholar
Reavley NJ, Jorm AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian National Survey of Mental Health Literacy and Stigma. Aust N Z J Psychiatry. 2011;45(12):1086–93.
Sheehan L, Nieweglowski K, Corrigan PW. Structures and types of stigma. In: Gaebel W, Rossler W, Sartorius N, editors. The stigma of mental illness - end of the story? Cham: Springer International Publishing; 2017. p. 43–66.
Chapter Google Scholar
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373(9661):408–15.
Farrelly S, Jeffery D, Rüsch N, Williams P, Thornicroft G, Clement S. The link between mental health-related discrimination and suicidality: service user perspectives. Psychol Med. 2015;45(10):2013–22.
Article CAS PubMed Google Scholar
Schauman O, MacLeod AK, Thornicroft G, Clement S. Mental illness related discrimination: The role of self-devaluation and anticipated discrimination for decreased well-being. Stigma and Health. 2019;4(1):11–8.
Article Google Scholar
Department of Health. The Fifth National Mental Health and Suicide Prevention Plan. Canberra, Australia: Commonwealth of Australia; 2017.
Google Scholar
Morgan AJ, Reavley NJ, Ross A, Too LS, Jorm AF. Interventions to reduce stigma towards people with severe mental illness: systematic review and meta-analysis. J Psychiatr Res. 2018;103:120–33.
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: effects on knowledge, stigma, and helping behaviour. PLoS ONE. 2018;13(5):e0197102.
Article PubMed PubMed Central CAS Google Scholar
Giacobbe MR, Stukas AA, Farhall J. The effects of imagined versus actual contact with a person with a diagnosis of schizophrenia. Basic Appl Soc Psychol. 2013;35(3):265–71.
Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Rossi RD, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. 2015;229(1):148–54.
Henderson C, Potts L, Robinson EJ. Mental illness stigma after a decade of Time to Change England: inequalities as targets for further improvement. Eur J Public Health. 2020;30(3):526–32.
Moxham L, Patterson C, Taylor E, Perlman D, Sumskis S, Brighton R. A multidisciplinary learning experience contributing to mental health rehabilitation. Disabil Rehabil. 2017;39(1):98–103.
Moxham L, Taylor E, Patterson C, Perlman D, Brighton R, Sumskis S, et al. Can a clinical placement influence stigma? An analysis of measures of social distance. Nurse Educ Today. 2016;44:170–4.
Patterson C, Moxham L, Brighton R, Taylor E, Sumskis S, Perlman D, et al. Nursing students’ reflections on the learning experience of a unique mental health clinical placement. Nurse Educ Today. 2016;46:94–8.
Patterson C, Perlman D, Taylor EK, Moxham L, Brighton R, Rath J. Mental health nursing placement: A comparative study of non-traditional and traditional placement. Nurse Educ Pract. 2018;33:4–9.
Byrne L, Happell B, Welch T, Moxham LJ. “Things you can’t learn from books”: teaching recovery from a lived experience perspective. Int J Mental Health Nurs. 2013;22(3):195–204.
Byrne L, Platania-Phung C, Happell B, Harris S, Sci DH, Nurs MMH, et al. Changing nursing student attitudes to consumer participation in mental health services: a survey study of traditional and lived experience-led education. Issues Mental Health Nurs. 2014;35(9):704–12.
Happell B, Bennetts W, Harris S, Platania-Phung C, Tohotoa J, Byrne L, et al. Lived experience in teaching mental health nursing: issues of fear and power. Int J Mental Health Nurs. 2015;24(1):19–27.
Happell B, Byrne L, Platania-Phung C, Harris S, Bradshaw J, Davies J. Lived-experience participation in nurse education: reducing stigma and enhancing popularity. Int J Mental Health Nurs. 2014;23(5):427–34.
Nguyen E, Chen TF, O’Reilly CL. Evaluating the impact of direct and indirect contact on the mental health stigma of pharmacy students. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1087–98.
O’Reilly CL, Bell JS, Chen TF. Consumer-led mental health education for pharmacy students. Am J Pharm Educ. 2010;74(9):167.
Article PubMed PubMed Central Google Scholar
O’Reilly CL, Bell JS, Chen TF. Mental health consumers and caregivers as instructors for health professional students: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(4):607–13.
Salgado JD, Deane FP, Crowe TP, Oades LG. Hope and improvements in mental health service providers’ recovery attitudes following training. J Mental Health. 2010;19(3):243–8.
University of Wollongong Australia. Collaborative Recovery Model Wollongong, Australia: University of Wollongong; 2020. https://www.uow.edu.au/social-sciences/research/iimh/collaborativerecoverymodel/ .
Ellis IK, Philip T. Improving the skills of rural and remote generalists to manage mental health emergencies. Rural Remote Health. 2010;10(3):1503.
PubMed Google Scholar
Herrington V, Clifford K, Lawrence P, Ryle S, Pop R. The impact of the NSW Police Force Mental Health Intervention Team: Final evaluation report. Melbourne: Charles Sturt University; 2009.
NSW Police. Mental health: Government of NSW. https://www.police.nsw.gov.au/safety_and_prevention/your_community/mental_health
RiCharde SG. American and Australian communications officers: Mental health stigma and crisis intervention team. Dissertation Abstracts International: Section B: The Sciences and Engineering. 2017;78(5-B(E)):No-Specified.
Taylor J, Jones RM, O’Reilly P, Oldfield W, Blackburn A. The Station Community Mental Health Centre Inc: nurturing and empowering. Rural Remote Health. 2009;10(3):1411.
Sacca R, Ryan C. Relationships between interpersonal contact as a volunteer companion and stigma. Austr Psychiatry. 2011;19(5):439–43.
Uniting Prahran. Hearing voices groups: UnitingCare Prahran Mission; 2020. https://www.unitingprahran.org.au/ourservices/voices-vic/#page_4
Batyr. Being herd. https://www.batyr.com.au/being-herd/ .
Petrakis M, Bloom H, Oxley J. Family perceptions of benefits and barriers to first episode psychosis carer group participation. Social Work Mental Health. 2014;12(2):99–116.
Petrakis M, Laxton S. Intervening early with family members during first-episode psychosis: an evaluation of mental health nursing psychoeducation within an inpatient unit. Arch Psychiatr Nurs. 2017;31(1):48–54.
Petrakis M, Oxley J, Bloom H. Carer psychoeducation in first-episode psychosis: evaluation outcomes from a structured group programme. Int J Soc Psyc. 2013;59(4):391–7.
Day K, Starbuck R, Petrakis M. Family group interventions in an early psychosis program: a re-evaluation of practice after 10 years of service delivery. Int J Soc Psychiatry. 2017;63(5):433–8.
MIEACT. Mental Health 101 - Adult. https://mieact.org.au/workshops/mental-health-101-adult/ .
MIEACT. Mental Illness Education ACT Research Report. 2019.
Read S, Rickwood DJ. Volunteering as a community mental health educator: Positives and negatives for recovery. AeJAMH (Australian e-Journal for the Advancement of Mental Health). 2009;8(2):1–10.
Rickwood D, Cavanagh S, Curtis L, Sakrouge R. Educating young people about mental health and mental illness: Evaluating a school-based programme. Int J Mental Health Promot. 2004;6(4):23–32.
Burns S, Crawford G, Hallett J, Hunt K, Chih HJ, Tilley PJ. What’s wrong with John? a randomised controlled trial of Mental Health First Aid (MHFA) training with nursing students. BMC Psychiatry. 2017;17(1):111.
Jorm AF, Kitchener BA, Fischer JA, Cvetkovski S. Mental health first aid training by e-learning: a randomized controlled trial. Aust N Z J Psychiatry. 2010;44(12):1072–81.
Jorm AF, Kitchener BA, Sawyer MG, Scales H, Cvetkovski S. Mental health first aid training for high school teachers: a cluster randomized trial. BMC Psychiatry. 2010;10:51.
Kelly CM, Mithen JM, Fischer JA, Kitchener BA, Jorm AF, Lowe A, et al. Youth mental first aid: A description of the program and an initial evaluation. Int J Mental Health Syst. 2011;5:1.
Lam AYK, Jorm AF, Wong DFK. Mental health first aid training for the Chinese community in Melbourne, Australia: Effects on knowledge about and attitudes toward people with mental illness. Int J Mental Health Syst. 2010;4:1.
Minas H, Colucci E, Jorm AF. Evaluation of Mental Health First Aid training with members of the Vietnamese community in Melbourne, Australia. Int J Mental Health Syst. 2009;3:1.
Morawska A, Fletcher R, Pope S, Heathwood E, Anderson E, McAuliffe C. Evaluation of mental health first aid training in a diverse community setting. Int J Mental Health Nurs. 2013;22(1):85–92.
Morgan AJ, Fischer J-AA, Hart LM, Kelly CM, Kitchener BA, Reavley NJ, et al. Does Mental Health First Aid training improve the mental health of aid recipients? The training for parents of teenagers randomised controlled trial. BMC Psychiatry. 2019;19: 1.
Reavley NJ, Morgan AJ, Fischer JA, Kitchener B, Bovopoulos N, Jorm AF. Effectiveness of eLearning and blended modes of delivery of Mental Health First Aid training in the workplace: randomised controlled trial. BMC Psychiatry. 2018;18(1):312.
Zhuang XY, Wong DFK, Ng TK, Poon A. Effectiveness of Mental Health First Aid for Chinese-Speaking International Students in Melbourne. Res Soc Work Pract. 2019;2019:1049731519890398.
O’Reilly CL, Bell JS, Kelly PJ, Chen TF. Impact of mental health first aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: a controlled trial. Aust N Z J Psychiatry. 2011;45(7):549–57.
Batyr. Batyr@work https://www.batyr.com.au/batyr-work/ .
Hudson J, Ingram V. Stigma-reduction & help-seeking in australian classrooms: A research report on the batyr@school program. date unknown.
SPEAK Up! Stay ChatTY, Relationships Australia Tasmania. Combined report of sessions evaluated in 2019.
SPEAK Up! Stay ChatTY, Relationships Australia Tasmania. Combined report of sessions from the 6th December 2017 to the 20th October 2019.
LIVIN. Get involved 2019 https://livin.org/pages/get-involved/#programs .
CHESS Connect. Fee Schedule: Mentally health workplace workshops 2019 [Available from: https://www.chessconnect.org.au/wp-content/uploads/2019/02/MHW-Fee-Structure-Document-2019.pdf .
CHESS Connect. Addressing the stigma of mental health in the workplace. 2020.
Koh E. The Cunningham Dax Collection: a unique mental health resource. Austr Psychiatry. 2014;22(1):41–3.
Koh E, Shrimpton B. Art promoting mental health literacy and a positive attitude towards people with experience of mental illness. Int J Soc Psychiatry. 2014;60(2):169–74.
The Dax Centre. Education 2015. https://www.daxcentre.org/education/ .
Australian Rotary Health. Evaluation of the national Mental Health Awareness Campaign.
Invisible intruders - The voices in my head. All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2013.
Linking body and mind. All in The Mind with Lynne Malcom. Australia: ABC Radio National; 2013.
Borderline personality disorder - what works? All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2014.
A roller-coaster of emotion Borderline Personality Disorder. All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2018.
BPD and healing relationships. All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2018.
Borderline Personality Disorder: Stigma to strength. All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2018.
The silence around schizophrenia. All in The Mind with Lynne Malcolm. Australia: ABC Radio National; 2019.
Bipolar Caregivers. Dealing with stigma or discrimination. https://bipolarcaregivers.org/stigma-and-discrimination/ways-to-deal-with-stigma-or-discrimination .
Spectrum BPD. Webinar: What is BPD? : Eastern Health; https://www.spectrumbpd.com.au/health-professionals/virtual-library/webinars/module-1 .
Lived Experience Australia. Resources https://www.livedexperienceaustralia.com.au/resources .
Coming out: Living with bipolar. Earshot. Australia: ABC Radio National; 2015.
Postnatal psychosis: The stigma of mothers with mental illness. The Feed. Australia: SBS; 2018.
Günsberg O. Falling apart behind the scenes. The Feed. Australia: SBS; 2018.
Let's talk rural mental health [Internet]. NSW: Centre for Rural and Remote Mental Health; 2017. Podcast
PANDA Perinatal Anxiety & Depression Australia. Postnatal psychosis recovery stories 2017 https://www.panda.org.au/info-support/postnatal-psychosis/personal-stories-postnatal-psychosis .
Project Air Strategy. Lived experiences Wollongong: University of Wollongong; https://projectairstrategy.org/mpapersonaljourneys/index.html .
Project Air Strategy. Project Air Films Wollongong: University of Wollongong; https://projectairstrategy.org/videos/index.html .
Neami National. Recovery stories: Neami National; [Available from: https://www.neaminational.org.au/get-support/recovery-stories/ .
SANE Australia. SANE Forums: SANE Australia; https://www.sane.org/forums .
SANE Australia. SANE Research Bulletin 19: SANE Forums: online peer support for people living with mental illness and for carers 2015. https://www.sane.org/images/PDFs/rb19_forums.pdf .
'Say no to stigma!' says mental health charity, SANE Australia [press release] [press release]. Aug 21 2013.
SANE Australia. A life without stigma [video on the Internet] 2013. https://www.youtube.com/watch?v=kYoi9RAxzvQ&list=PLl8yqrAao0dzQZwGtRko8Tq6bOjuXJ0ZB&index=4&t=0s .
SANE Australia. Stigma and the media [video on the Internet] 2013. https://www.youtube.com/watch?v=8WWKXyIXZX0&list=PLl8yqrAao0dzQZwGtRko8Tq6bOjuXJ0ZB&index=5 .
SANE Australia. Overcome stigma - get the facts and help you need [video on the internet] 2013. https://www.youtube.com/watch?v=XmyTGJnP8uY&list=PLl8yqrAao0dzQZwGtRko8Tq6bOjuXJ0ZB&index=6 .
SANE Australia. Work, mental illness, and stigma [video on the Internet] 2013. https://www.youtube.com/watch?v=odDVVKzsmc0&list=PLl8yqrAao0dzQZwGtRko8Tq6bOjuXJ0ZB&index=8 .
Orygen. Social anxiety, stigma and early psychosis [video on the internet] 2017 [Available from: https://www.orygen.org.au/Training/Resources/Anxiety/Webinars/Social-anxiety-stigma-and-early-psychosis .
SANE Australia. Building thriving communities through social connection: SANE Australia; https://www.sane.org/images/PDFs/Thriving_Communities_A4_Single.pdf .
Uniting Prahran. Our stories - Voices unplugged: UnitingCare Prahran Mission; 2020 https://www.unitingprahran.org.au/ourservices/voices-vic/#page_8 .
Australian Genetics of Bipolar Study. 2018. https://www.geneticsofbipolar.org.au/ .
Borderline in the ACT. Home - Borderline in the ACT. 2020. https://www.borderlineintheact.org.au/ .
Neami National. #WeSpeakUp campaign aims to increase awareness of mental health issues and reduce stigma https://www.neaminational.org.au/news/wespeakup-campaign-aims-to-increase-awareness-of-mental-health-issues-and-reduce-stigma/ .
Schizophrenia [video on the internet]. You can't ask that. Australia: ABC; 2016.
HelpingMinds. Schizophrenia awareness week 2020 https://helpingminds.org.au/schizophreniaawarenessweek/ .
Lucas F. Odd Socks Day helps to tackle stigma and discrimination around mental health. 2019. https://thesector.com.au/2019/10/03/odd-socks-day-helps-to-tackle-stigma-and-discrimination-around-mental-health/ .
Batyr. One sock one goal https://www.batyr.com.au/one-sock-one-goal/ .
Murray PHN. Stop mental illness stigma 2015 https://www.murrayphn.org.au/stopstigma/ .
Harman G, Heath J. Australian country perspective: The work of beyondblue and SANE Australia. The stigma of mental illness - End of the story? Cham, Switzerland: Springer International Publishing; 2017. p. 289–315.
Download references

Acknowledgements
The authors would like to acknowledge Anthony Jorm for feedback on a draft of the report provided to the funders.
Funding for this research was received from the Commonwealth Department of Health, Australia. The views expressed in this publication are those of the authors and are not necessarily those of the funder.
Author information
Authors and affiliations.
Centre for Mental Health, Melbourne School of Population and Global Health, University of Melbourne, 207 Bouverie Street, Melbourne, VIC, 3010, Australia
Amy J. Morgan, Judith Wright & Nicola J. Reavley
You can also search for this author in PubMed Google Scholar
Contributions
AM, JW and NR designed the study. AM and JW conducted the literature searches and data extraction. JW managed the survey data collection. AM drafted the manuscript and JW and NR read, edited and approved this submission. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Amy J. Morgan .
Ethics declarations
Ethics approval and consent to participate.
Approval for the research was granted by the University of Melbourne Human Research Ethics Committee (ethics ID 1955944).
Consent for publication
Not applicable.
Competing interests
AM and NR collaborate with MHFA Australia on a number of projects, including development and evaluation of training. JW declares she has no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Additional tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Morgan, A.J., Wright, J. & Reavley, N.J. Review of Australian initiatives to reduce stigma towards people with complex mental illness: what exists and what works?. Int J Ment Health Syst 15 , 10 (2021). https://doi.org/10.1186/s13033-020-00423-1
Download citation
Received : 29 July 2020
Accepted : 29 November 2020
Published : 18 January 2021
DOI : https://doi.org/10.1186/s13033-020-00423-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental illness
- Discrimination
- Schizophrenia
- Bipolar disorder
- Personality disorder
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]
- Open access
- Published: 30 May 2024
Barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with psychosis: a scoping review protocol
- Cláudia C. Gonçalves ORCID: orcid.org/0000-0001-6767-0920 1 ,
- Zoe Waters 2 ,
- Shae E. Quirk 1 ,
- Peter M. Haddad 1 , 3 ,
- Ashleigh Lin 4 ,
- Lana J. Williams 1 &
- Alison R. Yung 1 , 5
Systematic Reviews volume 13 , Article number: 143 ( 2024 ) Cite this article
124 Accesses
Metrics details
The prevalence of psychosis has been shown to be disproportionately high amongst sexual and gender minority individuals. However, there is currently little consideration of the unique needs of this population in mental health treatment, with LGBTQA+ individuals facing barriers in accessing timely and non-stigmatising support for psychotic experiences. This issue deserves attention as delays to help-seeking and poor engagement with treatment predict worsened clinical and functional outcomes for people with psychosis. The present protocol describes the methodology for a scoping review which will aim to identify barriers and facilitators faced by LGBTQA+ individuals across the psychosis spectrum in help-seeking and accessing mental health support.
A comprehensive search strategy will be used to search Medline, PsycINFO, Embase, Scopus, LGBTQ+ Source, and grey literature. Original studies of any design, setting, and publication date will be included if they discuss barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with experiences of psychosis. Two reviewers will independently screen titles/abstracts and full-text articles for inclusion in the review. Both reviewers will then extract the relevant data according to pre-determined criteria, and study quality will be assessed using the Joanna Briggs Institute (JBI) critical appraisal checklists. Key data from included studies will be synthesised in narrative form according to the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews.
The results of this review will provide a comprehensive account of the current and historical barriers and facilitators to mental healthcare faced by LGBTQA+ people with psychotic symptoms and experiences. It is anticipated that the findings from this review will be relevant to clinical and community services and inform future research. Findings will be disseminated through publication in a peer-reviewed journal and presented at conferences.
Scoping review registration
This protocol is registered in Open Science Framework Registries ( https://doi.org/10.17605/OSF.IO/AT6FC ).
Peer Review reports
The prevalence of psychotic disorders in the general population has been estimated to be around 0.27–0.75% [ 1 , 2 ], with the lifetime prevalence of ever having a psychotic experience being estimated at 5.8% [ 3 ]. However, rates of psychotic symptoms and experiences are disproportionately high amongst LGBTQA+ populations, with non-heterosexual individuals estimated to be 1.99–3.75 times more likely to experience psychosis than their heterosexual peers [ 4 , 5 , 6 , 7 ]. Additionally, it has been estimated that transgender or gender non-conforming (henceforth trans) individuals are 2.46–49.7 times more likely than their cisgender peers (i.e. individuals whose gender identity is the same as their birth registered sex) to receive a psychotic disorder diagnosis [ 8 , 9 ]. The increased rates of psychotic experiences noted amongst gender and sexual minorities may be explained by evidence indicating that LGBTQA+ people are also exposed to risk factors for psychosis at a far greater rate than members of the general population, such as childhood adversity [ 10 , 11 , 12 ], minority stress [ 13 ], discrimination [ 14 ], and stigma [ 15 , 16 ]. Furthermore, there is added potential for diagnostic biases leading to over-diagnosing psychosis in gender diverse individuals, whose gender expression and dysphoria may be pathologized by mental health service providers [ 8 ].
Despite these concerning statistics, there is very little research examining the experiences of LGBTQA+ people with psychosis, and limited consideration of the unique needs these individuals may have in accessing and engaging with mental health services. While timely access to treatment has consistently been associated with better symptomatic and functional outcomes for people with psychosis [ 17 , 18 ], there are often delays to treatment initiation which are worsened for LGBTQA+ individuals [ 19 , 20 ]. These individuals face additional barriers to accessing adequate mental health support compared to cisgender/heterosexual people [ 19 ] and may need to experiment with several mental health services before finding culturally competent care [ 20 ]. This in turn may lead to longer duration of untreated psychosis. Additionally, there seems to be a lack of targeted support for this population from healthcare providers, with LGBTQA+ individuals with serious mental health concerns reporting higher rates of dissatisfaction with psychiatric services than their cisgender and heterosexual counterparts [ 7 , 14 , 21 ]. However, the extent of these differences varies across contexts [ 22 ], potentially due to improved education around stigma and LGBTQA+ issues within a subset of mental health services.
Nonetheless, stigma remains one of the highest cited barriers to help-seeking for mental health problems, particularly with regard to concerns around disclosure [ 23 ], which can be particularly challenging for people experiencing psychosis [ 24 , 25 ]. Stigma stress in young people at risk for psychosis is associated with less positive attitudes towards help-seeking regarding both psychiatric medication and psychotherapy [ 26 ], potentially partly due to fears of judgement and being treated differently by service providers [ 27 ]. This issue may be compounded for people who also belong to minoritized groups [ 23 , 28 ], particularly as LGBTQA+ individuals have reported experiencing frequent stigma and encountering uninformed staff when accessing mental healthcare [ 7 , 29 ]. Furthermore, stigma-fuelled hesitance to access services may be heightened for trans people [ 30 ] whose identities have historically been pathologized and conflated with experiences of psychosis [ 31 ].
Even when individuals manage to overcome barriers to access support, there are added challenges to maintaining adequate treatment engagement. In a large online study, half of trans and nearly one third of LGB participants reported having stopped using mental health services in the past because of negative experiences related to their gender identity or sexuality [ 20 ]. This can be particularly problematic as experiences of stigma predict poorer medication adherence in psychosis [ 32 ] which subsequently multiplies the risk for relapse and suicide [ 33 ]. While no research to date has explored non-adherence rates in people with psychosis who are LGBTQA+, concerns around suicidality are heightened for individuals who are gender and sexuality diverse [ 34 , 35 , 36 ].
Generally, there is rising demand for mental healthcare that specifically addresses the needs of gender and sexual minority individuals and promotes respect for diversity, equity, and inclusion [ 29 , 37 ]. This is particularly salient as positive relationships with staff are associated with better medication adherence for people with psychosis [ 38 ] and healthcare providers with LGBTQA+-specific mandates have demonstrated higher satisfaction rates for LGBTQA+ individuals [ 20 ]. Mental health services need to adapt treatment options to acknowledge minority stress factors for those with stigmatised identities and, perhaps more importantly, how these intersect and interact to increase inequalities in people from minoritized groups accessing and benefiting from treatment [ 37 , 39 ].
Additionally, gender affirming care needs to be recognised as an important facet of mental health treatment for many trans individuals, as it is associated with positive outcomes such as improvements in quality of life and psychological functioning [ 40 , 41 , 42 ] and reductions in psychiatric symptom severity and need for subsequent mental health treatment [ 8 , 43 ]. While there are additional barriers in access to gender affirming care for individuals with psychosis, this treatment has shown success in parallel with treatment to address psychosis symptom stabilisation [ 19 , 44 ]. The importance of affirmation is echoed by the finding that many negative experiences of LGBTQA+ participants with mental health services could be avoided simply by respecting people’s pronouns and using gender-neutral language [ 20 ].
To ensure timely access to appropriate treatment for LGBTQA+ people with psychosis, there is a need for improved understanding of the factors which challenge and facilitate help-seeking and engagement with mental health support. A preliminary search of Google Scholar, Medline, the Cochrane Database of Systematic Reviews, and PROSPERO was conducted and revealed no existing or planned reviews exploring benefits and/or obstacles to mental health treatment specific to this population. Therefore, the proposed review seeks to comprehensively search and appraise the existing literature to identify and summarise a range of barriers and facilitators to adequate mental health support faced by LGBTQA+ people with experiences of psychosis. This will allow for the mapping of the types of evidence available and identification of any knowledge gaps. Moreover, we hope to guide future decision-making in mental healthcare to improve service accessibility for LGBTQA+ individuals with psychosis and to set the foundations for future research that centres this marginalised population. Based on published guidance [ 45 , 46 , 47 ], a scoping review methodology was identified as the most appropriate approach to address these aims.
Selection criteria
This scoping review protocol has been developed in compliance with the JBI Manual for Evidence Synthesis [ 48 ] and, where relevant, the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) checklist [ 49 ] (see Additional file 1). In the event of protocol amendments, the date, justification, and description for each amendment will be provided.
Due to the limited literature around the topic of this review, any primary original study design, setting, and publication date will be considered for inclusion. Publications written in English will be included, and articles in other languages may be considered pending time and cost constraints around translation. Publications will be excluded if the full text is not available upon request from authors.
The PCC (Population, Concept, Context) framework was used to develop the inclusion criteria for this scoping review:
This review will include individuals of any age who are LGBTQA+ and have had experiences of psychosis. For the purposes of this review, ‘LGBTQA+ individuals’ will be broadly defined as any individual that is not heterosexual and/or cisgender or anyone who engages in same-gender sexual behaviour. Studies may include participants who are cisgender and heterosexual if they separately report outcomes for LGBTQA+ individuals. Within this review, the term ‘psychosis’ includes (i) any diagnosis of a psychotic disorder, such as schizophrenia spectrum disorders, mood disorders with psychotic features, delusional disorders, and drug-induced psychotic disorders, (ii) sub-threshold psychotic symptoms, such as those present in ultra-high risk (UHR), clinical high risk (CHR), or at risk mental state (ARMS) individuals, and (iii) any psychotic-like symptoms or experiences. Studies may include participants with multiple diagnoses if they separately report outcomes for individuals on the psychosis spectrum.
This review will include publications which discuss potential barriers and/or facilitators to mental health help-seeking and/or engagement with mental health treatment. ‘Barriers’ will be operationalised as any factors which may delay or prevent individuals from accessing and engaging with appropriate mental health support. These may include lack of mental health education, experienced or internalised stigma, experiences of discrimination from health services, and lack of inclusivity in health services. ‘Facilitators’ will be operationalised as any factors which may promote timely help-seeking and engagement with sources of support. These may include improved access to mental health education, positive sources of social support, and welcoming and inclusive services. Mental health help-seeking will be broadly defined as any attempt to seek and access formal or informal support to address a mental health concern related to experiences of psychosis (e.g. making an initial appointment with a service provider, seeking help from a friend). Mental health treatment engagement will be broadly defined as adherence and active participation in the treatment that is offered by a source of support (e.g. attending scheduled appointments, taking medication as prescribed, openly communicating with service providers).
This review may include research encompassing any setting in which mental healthcare is provided. This is likely to include formal healthcare settings such as community mental health teams or inpatient clinics as well as informal settings such as LGBTQA+ spaces or informal peer support. Studies will be excluded if they focus exclusively on physical health treatment.
Search strategy
Database searches will be conducted in Medline, PsycINFO, Embase, Scopus, and LGBTQ+ Source. The full search strategy for this protocol is available (see Additional file 2). This strategy has been collaboratively developed and evaluated by a scholarly services health librarian. Searches will include subject headings relevant to each database and title/abstract keywords relating to three main concepts: (i) LGBTQA+ identity, (ii) experiences of psychosis, and (iii) mental health treatment. Keywords for each concept will be combined using the Boolean operator ‘OR’, and the three concepts will be combined using ‘AND’. This search strategy was appropriately translated for each of the selected databases. There will be no limitations on language or publication date at this stage to maximise the breadth of the literature captured. Publications returned from these searches will be exported to EndNote. Searches will be re-run prior to the final analysis to capture any newly published studies.
The database searches will be supplemented by searching the grey literature as per the eligibility criteria detailed above. These may include theses and dissertations, conference proceedings, reports from mental health services, and policy documents from LGBTQA+ groups. Google and Google Scholar will be searched using a combination of clauses for psychosis (Psychosis OR psychotic OR schizophrenia OR schizoaffective), treatment (treatment or “help-seeking”), and queer identity. The latter concept will have three clauses for three separate searches, with one including broad queer identity (LGBT), one specific to non-heterosexual individuals (gay OR lesbian OR homosexual OR bisexual OR queer OR asexual), and one specific to trans individuals (transgender OR transsexual OR transexual OR “non-binary” OR “gender minority”). Additionally, reference lists and citing literature will be manually searched for each paper included in the review to capture any articles and policy documents not previously identified.
Data selection
Search results will be imported into Covidence using EndNote, and duplicates will be eliminated. Titles and abstracts will be screened by the first and second authors according to pre-defined screening criteria, which will be discussed by the authors and piloted prior to screening. These criteria will consider whether the articles included LGBTQA+ participants with experiences of psychosis (as operationalised above) in relation to mental health help-seeking and/or treatment. Full texts of relevant articles will then be obtained and screened by the first and second reviewer in accordance with the full inclusion and exclusion criteria after initial piloting to maximise inter-rater reliability. Decisions on inclusion and exclusion will be blinded and recorded on Covidence. Potential discrepancies will be resolved through discussion, and when consensus cannot be reached, these will be resolved by the supervising author. The process of study selection will be documented using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram [ 50 ].
Data extraction
Data extraction will be performed independently by two reviewers using Covidence. Prior to beginning final extraction, both reviewers will independently pilot the extraction tool using a sample of five included studies and discuss any necessary changes. Information extracted is planned to include the following: title, author name(s), year of publication, country in which the study was conducted, study design, sample size, population of focus (i.e. sexual minorities, gender minorities, or both), sample demographics (i.e. age, gender identity, and sexual orientation), setting (e.g. early intervention service, community mental health team, etc.), psychosis characteristics (e.g. diagnoses included, severity of symptoms, etc.), type of treatment (e.g. cognitive behavioural therapy, antipsychotic medication, etc.), and any barriers and/or facilitators identified according to the aforementioned operationalised definitions. Disagreements will be resolved through discussion between the two reviewers and, when necessary, final decisions will be made by a senior supervisor. Once extracted, information will be recorded in Excel. Lead authors of papers will be contacted by the primary review author in cases where there is missing or insufficient data.
Quality assessment
Due to the expected heterogeneity in the types of studies that may be included in this review (e.g. qualitative studies, randomised controlled trials, case control studies, case reports), the relevant revised Joanna Briggs Institute (JBI) critical appraisal checklists [ 51 ] will be used to assess risk of bias and study quality for each study design. Two reviewers will independently use these checklists to assess each paper that is included following the full-text screening. If there are discrepancies in article ratings, these will be resolved through discussion between the two authors. If no consensus is reached, discrepancies will be resolved by a senior supervisor. In line with the scoping nature of this review, low-quality studies will not be excluded from the synthesis.
Evidence synthesis
Data from included studies will be synthesised using a narrative synthesis approach in accordance with the Guidance on the Conduct of Narrative Synthesis in Systematic Reviews [ 52 ]. A preliminary descriptive synthesis will be conducted by tabulating the extracted data elements from each study alongside quality assessment results and developing an initial description of the barriers and facilitators to (1) accessing and (2) engaging with mental health support that are identified in the literature. This initial synthesis will then be interrogated and refined to contextualise these barriers and facilitators in the setting, population, and methodology of each study to form the basis for an interpretative synthesis.
This review will not use a pre-existing thematic framework to categorise barriers and facilitators as it is expected that the factors identified will not neatly fit into existing criteria. Instead, these will be conceptualised according to overarching themes as interrelated factors, so that potentially complex interactions between barriers and facilitators within and across relevant studies may be explored through concept mapping. If most of the studies included are qualitative, there may also be scope for a partial meta-synthesis. To avoid oversimplifying the concept of ‘barriers and facilitators’ (see criticism by Bach-Mortensen & Verboom [ 53 ]), this data synthesis will be followed by a critical reflection of the findings through the lens of the socio-political contexts which may give rise to the barriers and facilitators identified, exploring the complexities necessary for any changes to be implemented in mental health services.
If the extracted data indicate that gender minority and sexual minority individuals experience unique or different barriers and/or facilitators to each other, these population groups will be analysed separately as opposed to findings being generalised across the LGBTQA+ spectrum. Furthermore, if there is scope to do so, analyses may be conducted to investigate how perceived barriers and facilitators for this population may have changed over time (i.e. according to publication date) as definitions of psychosis evolve and LGBTQA+ individuals gain visibility in clinical services.
The proposed review will add to the literature around mental health treatment for LGBTQA+ people with psychosis. It will provide a thorough account of the barriers and facilitators to accessing and engaging with support faced by this population and may inform future research and clinical practice.
In terms of limitations, this review will be constrained by the existing literature and may therefore not be sufficiently comprehensive in reflecting the barriers and facilitators experienced by subgroups within the broader LGBTQA+ community. Additionally, although broad inclusion criteria are necessary to capture the full breadth of research conducted in this topic, included studies are likely to be heterogeneous and varied in terms of their methodology and population which may complicate data synthesis.
Nonetheless, it is anticipated that the findings from this review will provide the most comprehensive synthesis to date of the issues driving low help-seeking and treatment engagement in people across the psychosis spectrum who are LGBTQA+. This review will likely also identify gaps in the literature which may inform avenues for future research, and the factors identified in this review will be considered in subsequent research by the authors.
Additionally, findings will be relevant to healthcare providers that offer support to people with psychosis who may have intersecting LGBTQA+ identities as well as LGBTQA+ organisations which offer support to LGBTQA+ people who may be experiencing distressing psychotic experiences. These services are likely to benefit from an increased awareness of the factors which may improve or hinder accessibility for these subsets of their target populations. Therefore, results from this review may inform decision-making around the implementation of service-wide policy changes.
The findings of this review will be disseminated through the publication of an article in a peer-reviewed journal and presented at relevant conferences in Australia and/or internationally. Additionally, the completed review will form part of the lead author’s doctoral thesis.
Availability of data and materials
Not applicable for this protocol.
Abbreviations
- At risk mental state
Clinical high risk for psychosis
Joanna Briggs Institute
Lesbian, gay, and bisexual
Lesbian, gay, bisexual, transgender, queer or questioning, asexual or aromantic, and more
Population, Concept, Context
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols
Ultra-high risk for psychosis
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study (GBD) Results. Seattle, WA: IHME, University of Washington. 2020. https://vizhub.healthdata.org/gbd-results/ . Accessed 26 May 2023
Moreno-Kustner B, Martin C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13(4):e0195687. https://doi.org/10.1371/journal.pone.0195687 .
Article CAS PubMed PubMed Central Google Scholar
McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross-national analysis based on 31 261 respondents from 18 countries. JAMA Psychiatry. 2015;72(7):697–705. https://doi.org/10.1001/jamapsychiatry.2015.0575 .
Article PubMed PubMed Central Google Scholar
Chakraborty A, McManus S, Brugha TS, Bebbington P, King M. Mental health of the non-heterosexual population of England. Br J Psychiatry. 2011;198(2):143–8. https://doi.org/10.1192/bjp.bp.110.082271 .
Article PubMed Google Scholar
Gevonden M, Selten J, Myin-Germeys I, De Graaf R, Ten Have M, Van Dorsselaer S, et al. Sexual minority status and psychotic symptoms: findings from the Netherlands Mental Health Survey and Incidence Studies (NEMESIS). Psychol Med. 2014;44(2):421–33. https://doi.org/10.1017/S0033291713000718 .
Article CAS PubMed Google Scholar
Jacob L, Smith L, McDermott D, Haro JM, Stickley A, Koyanagi A. Relationship between sexual orientation and psychotic experiences in the general population in England. Psychol Med. 2021;51(1):138–46. https://doi.org/10.1017/S003329171900309X .
Welch S, Collings SCD, Howden-Chapman P. Lesbians in New Zealand: their mental health and satisfaction with mental health services. Aust N Z J Psychiatry. 2000;34(2):256–63. https://doi.org/10.1080/j.1440-1614.2000.00710.x .
Barr SM, Roberts D, Thakkar KN. Psychosis in transgender and gender non-conforming individuals: a review of the literature and a call for more research. Psychiatry Res. 2021;306:114272. https://doi.org/10.1016/j.psychres.2021.114272 .
Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. 2019;39:1–7. https://doi.org/10.1016/j.annepidem.2019.09.009 .
Schneeberger AR, Dietl MF, Muenzenmaier KH, Huber CG, Lang UE. Stressful childhood experiences and health outcomes in sexual minority populations: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1427–45. https://doi.org/10.1007/s00127-014-0854-8 .
Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y. Childhood trauma and psychosis: an updated review. Child Adolesc Psychiatr Clin N Am. 2020;29(1):115–29. https://doi.org/10.1016/j.chc.2019.08.004 .
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–71. https://doi.org/10.1093/schbul/sbs050 .
Mongelli F, Perrone D, Balducci J, Saccheti A, Ferrari S, Mattei G, et al. Minority stress and mental health among LGBT populations: an update on the evidence. Minerva Psichiatr. 2019;60(1):27–50. https://doi.org/10.23736/S0391-1772.18.01995-7 .
Article Google Scholar
Kidd SA, Howison M, Pilling M, Ross LE, McKenzie K. Severe mental illness in LGBT populations: a scoping review. Psychiatr Serv. 2016;67(7):779–83. https://doi.org/10.1176/appi.ps.201500209 .
Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth. Pediatr Clin North Am. 2016;63(6):985–97. https://doi.org/10.1016/j.pcl.2016.07.003 .
Rüsch N, Heekeren K, Theodoridou A, Müller M, Corrigan PW, Mayer B, et al. Stigma as a stressor and transition to schizophrenia after one year among young people at risk of psychosis. Schizophr Res. 2015;166(1–3):43–8. https://doi.org/10.1016/j.schres.2015.05.027 .
Howes OD, Whitehurst T, Shatalina E, Townsend L, Onwordi EC, Mak TLA, et al. The clinical significance of duration of untreated psychosis: an umbrella review and random-effects meta-analysis. World Psychiatry. 2021;20(1):75–95. https://doi.org/10.1002/wps.20822 .
McGorry PD. Early intervention in psychosis: obvious, effective, overdue. J Nerv Ment Dis. 2015;203(5):310–308. https://doi.org/10.1097/NMD.0000000000000284 .
Peta JL. The Oxford Handbook of Sexual and Gender Minority Mental Health. Oxford (GB): Oxford University Press; 2020. Chapter 11, Schizophrenia spectrum and other psychotic disorders among sexual and gender minority populations; 125-134. Available from: The Oxford Handbook of Sexual and Gender Minority Mental Health - Google Books. Accessed 01 Jun 2023
Simeonov D, Steele LS, Anderson S, Ross LE. Perceived satisfaction with mental health services in the lesbian, gay, bisexual, transgender, and transsexual communities in Ontario, Canada: an internet-based survey. Can J Commun Ment Health. 2015;34(1):31–44. https://doi.org/10.7870/cjcmh-2014-037 .
Avery AM, Hellman RE, Sudderth LK. Satisfaction with mental health services among sexual minorities with major mental illness. Am J Public Health. 2001;91(6):990–1. https://doi.org/10.2105/AJPH.91.6.990 .
Plöderl M, Mestel R, Fartacek C. Differences by sexual orientation in treatment outcome and satisfaction with treatment among inpatients of a German psychiatric clinic. PLoS ONE. 2022;17(1):e0262928. https://doi.org/10.1371/journal.pone.0262928 .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. https://doi.org/10.1017/S0033291714000129 .
Pyle M, Morrison AP. “It’s just a very taboo and secretive kind of thing”: making sense of living with stigma and discrimination from accounts of people with psychosis. Psychosis. 2014;6(3):195–205. https://doi.org/10.1080/17522439.2013.834458 .
Wood L, Burke E, Byrne R, Pyle M, Chapman N, Morrison AP. Stigma in psychosis: a thematic synthesis of current qualitative evidence. Psychosis. 2015;7(2):152–65. https://doi.org/10.1080/17522439.2014.926561 .
Rüsch N, Heekeren K, Theodoridou A, Dvorsky D, Müller M, Paust T, et al. Attitudes towards help-seeking and stigma among young people at risk for psychosis. Psychiatry Res. 2013;210(3):1313–5. https://doi.org/10.1016/j.psychres.2013.08.028 .
Gronholm PC, Thornicroft G, Laurens KR, Evans-Lacko S. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. Psychol Med. 2017;47(11):1867–79. https://doi.org/10.1017/S0033291717000344 .
Rossman K, Salamanca P, Macapagal K. A qualitative study examining young adults’ experiences of disclosure and nondisclosure of LGBTQ identity to health care providers. J Homosex. 2017;64(10):1390–410. https://doi.org/10.1080/00918369.2017.1321379 .
Rees SM, Crowe M, Harris S. The lesbian, gay, bisexual and transgender communities’ mental health care needs and experiences of mental health services: an integrative review of qualitative studies. J Psychiat Mental Health Nurs. 2020;28(4):578–89. https://doi.org/10.1111/jpm.12720 .
Shipherd JC, Green KE, Abramovitz A. Transgender clients: identifying and minimizing barriers to mental health treatment. J Gay Lesbian Ment Health. 2010;14(2):94–108. https://doi.org/10.1080/19359701003622875 .
Hoening J, Kenna JC. The nosological position of transsexualism. Arch Sex Behav. 1974;3:273–87. https://doi.org/10.1007/BF01541490 .
Eliasson ET, McNamee L, Swanson L, Lawrie SM, Schwannauer M. Unpacking stigma: meta-analyses of correlates and moderators of personal stigma in psychosis. Clin Psychol Rev. 2021;89:102077. https://doi.org/10.1016/j.cpr.2021.102077 .
Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114(1):169–79. https://doi.org/10.1093/bmb/ldv017 .
De Lange J, Baams L, van Bergen D, Bos HMW, Bosker RJ. Minority stress and suicidal ideation and suicide attempts among LGBT adolescents and young adults: a meta-analysis. LGBT Health. 2022;9(4):222–37. https://doi.org/10.1089/lgbt.2021.0106 .
Skerrett DM, Kolves K, De Leo D. Are LGBT populations at higher risk for suicidal behaviours in Australia? Research findings and implications. J Homosex. 2015;62(7):883–901. https://doi.org/10.1080/00918369.2014.1003009 .
Strauss P, Cook A, Winter S, Watson V, Toussaint DW, Lin A. Trans Pathways: the mental health experiences and care pathways of trans young people: summary of results. Perth, Australia: Telethon Kids Institute. 2017. trans-pathways-report.pdf (telethonkids.org.au). Accessed 16 June 2023
DeLuca JS, Novacek DM, Adery LH, Herrera SN, Landa Y, Corcoran CM, et al. Equity in mental health services for youth at clinical high risk for psychosis: considering marginalized identities and stressors. Evid Based Pract Child Adolesc Ment Health. 2022;7(2):176–97. https://doi.org/10.1080/23794925.2022.2042874 .
Day JC, Bentall RP, Roberts C, Randall F, Rogers A, Cattell D, et al. Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry. 2005;62(7):717–24. https://doi.org/10.1001/archpsyc.62.7.717 .
Coyne CA, Poquiz JL, Janssen A, Chen D. Evidence-based psychological practice for transgender and non-binary youth: defining the need, framework for treatment adaptation, and future directions. Evid Based Pract Child Adolesc Ment Health. 2020;5(3):340–53. https://doi.org/10.1080/23794925.2020.1765433 .
Baker KE, Wilson LM, Sharma R, Dukhanin V, McArthur K, Robinson KA. Hormone therapy, mental health, and quality of life among transgender people: a systematic review. J Endocr Soc. 2021;5(4):bvab011. https://doi.org/10.1210/jendso/bvab011 .
Hughto JMW, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health. 2016;1(1):21–31. https://doi.org/10.1089/trgh.2015.0008 .
Wernick JA, Busa S, Matouk K, Nicholson J, Janssen A. A systematic review of the psychological benefits of gender-affirming surgery. Urol Clin North Am. 2019;46(4):475–86. https://doi.org/10.1016/j.ucl.2019.07.002 .
Bränström R, Packanhkis JE. Reductions in mental health treatment utilization among transgender individuals after gender-affirming surgeries: a total population study. Am J Psychiatry. 2019;177(8):727–34. https://doi.org/10.1176/appi.ajp.2019.19010080 .
Meijer JH, Eeckhout GM, van Vlerken RHT, de Vries ALC. Gender dysphoria and co-existing psychosis: review and four case examples of successful gender affirmative treatment. LGBT Health. 2017;4(2):106–14. https://doi.org/10.1089/lgbt.2016.0133 .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. https://doi.org/10.1186/s12874-018-0611-x .
Munn Z, Pollock D, Khalil H, Alexander L, McInerney P, Godfrey CM, et al. What are scoping reviews? Providing a formal definition of scoping reviews as a type of evidence synthesis. JBI Evid Synth. 2022;20(4):950–2. https://doi.org/10.11124/JBIES-21-00483 .
Peters MDJ, Marnie C, Colquhoun H, Garritty CM, Hempel S, Horsley T, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263. https://doi.org/10.1186/s13643-021-01821-3 .
Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editors. JBI Manual for Evidence Synthesis. JBI; 2024. https://synthesismanual.jbi.global . https://doi.org/10.46658/JBIMES-24-01
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350: g7647. https://doi.org/10.1136/bmj.g7647 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Barker TH, Stone JC, Sears K, Klugar M, Leonardi-Bee J, Tufanaru C, et al. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid Synth. 2023;21(3):478–93. https://doi.org/10.11124/JBIES-22-00125 .
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. Lancaster University; 2006. https://doi.org/10.13140/2.1.1018.4643
Bach-Mortensen AM, Verboom B. Barriers and facilitators systematic reviews in health: a methodological review and recommendations for reviewers. Res Synth Methods. 2020;11(6):743–59. https://doi.org/10.1002/jrsm.1447 .
Download references
Acknowledgements
The authors would like to acknowledge the support of Ms Olivia Larobina, Scholarly Services Librarian (STEMM) at Deakin University, in the development of the search strategy.
CCG is funded by a Deakin University Postgraduate Research (DUPR) Scholarship. ZW is funded by a University of Western Australia Research Training Program (RTP) Scholarship. AL is supported by a National Health and Medical Research Council (NHMRC) Emerging Leaders Fellowship (2010063). LJW is supported by a NHMRC Emerging Leaders Fellowship (1174060). ARY is supported by a NHMRC Principal Research Fellowship (1136829). The funding providers had no role in the design and conduct of the study, or in the preparation, review, or approval of this manuscript.
Author information
Authors and affiliations.
Institute for Mental and Physical Health and Clinical Translation, Deakin University, Geelong, VIC, 3220, Australia
Cláudia C. Gonçalves, Shae E. Quirk, Peter M. Haddad, Lana J. Williams & Alison R. Yung
Telethon Kids Institute, University of Western Australia, Perth, WA, 6009, Australia
University Hospital Geelong, Barwon Health, Geelong, VIC, 3220, Australia
Peter M. Haddad
School of Population and Global Health, University of Western Australia, Perth, WA, 6009, Australia
Ashleigh Lin
School of Health Sciences, University of Manchester, Manchester, M13 9PL, UK
Alison R. Yung
You can also search for this author in PubMed Google Scholar
Contributions
CCG is the guarantor. CCG conceptualised the review, developed the study design, and drafted the manuscript. CCG, ZW, and SQ collaborated with OL (Scholarly Services Librarian) to develop the search strategy. All authors critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Cláudia C. Gonçalves .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
In the last 3 years, PMH has received honoraria for lecturing from Janssen, NewBridge Pharmaceuticals, and Otsuka and royalties from edited textbooks (Cambridge University Press, Oxford University Press).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. prisma-p 2015 checklist. completed prisma-p checklist for this systematic review protocol., 13643_2024_2566_moesm2_esm.docx.
Additional file 2. Search Strategy. Detailed search strategy for this systematic review, including search terms and relevant controlled vocabulary terms for each included database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gonçalves, C.C., Waters, Z., Quirk, S.E. et al. Barriers and facilitators to mental health treatment access and engagement for LGBTQA+ people with psychosis: a scoping review protocol. Syst Rev 13 , 143 (2024). https://doi.org/10.1186/s13643-024-02566-5
Download citation
Received : 04 July 2023
Accepted : 17 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s13643-024-02566-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Treatment access
- Treatment engagement
- Facilitators
- Clinical high risk
- Ultra-high risk
- Psychotic experiences
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Downloadable Content
Mental Health Help-Seeking Attitudes in Asian American Young Adult College Students: A Scoping Review of the Literature
- Masters Thesis
- Debonis, Judith
- Jacobsen, Jeanna
- Sorrell-Medina, Zayda
- Social Work
- California State University, Northridge
- Dissertations, Academic -- CSUN -- Social Work.
- young adult
- Asian American
- college students
- help-seeking attitudes
- mental health
- http://hdl.handle.net/20.500.12680/bn999f33m
- by Kelly Thi

Items in ScholarWorks are protected by copyright, with all rights reserved, unless otherwise indicated.
Understanding the Stigma Experience of Men Living with HIV in Sub-Saharan Africa: A Qualitative Meta-synthesis
- Substantive Review
- Published: 22 May 2024
Cite this article

- Sarah E. Janek ORCID: orcid.org/0009-0002-1213-2791 1 ,
- Sandy Hatoum ORCID: orcid.org/0009-0002-3618-9733 2 ,
- Leila Ledbetter ORCID: orcid.org/0000-0002-5206-8002 3 &
- Michael V. Relf ORCID: orcid.org/0000-0002-4951-8869 1 , 2
62 Accesses
Explore all metrics
Men living with HIV (MLWH) in sub-Saharan Africa experience poor health outcomes and increased AIDS-related deaths due to stigma influencing testing and treatment uptake and adherence. PRISMA 2020 was used to report a meta-synthesis of the stigma experiences of MLWH in SSA. With the help of an expert librarian, a search of six databases was formulated and performed to examine the available qualitative and mixed method studies with qualitative results relevant to the research question. Studies focused on adult men living with HIV, with five studies specifically examining the HIV experience of men who have sex with men. Study themes were synthesized to describe MLWH’s perceived, internalized, anticipated, enacted, and intersectional stigma experiences. Most studies included masculinity as a key theme that affected both testing and treatment adherence upon diagnosis. Future research is needed to better understand subpopulations, such as men who have sex with men living with HIV, and what interventions may be beneficial to mitigate the disparities among MLWH in SSA.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

“It is not an acceptable disease”: A qualitative study of HIV-related stigma and discrimination and impacts on health and wellbeing for people from ethnically diverse backgrounds in Australia
Overcoming hiv stigma a qualitative analysis of hiv cure research and stigma among men who have sex with men living with hiv, understanding hiv-related stigma among women in the southern united states: a literature review.
Kaiser Family Foundation. The global HIV/AIDS epidemic. KFF. 2022. https://www.kff.org/global-health-policy/fact-sheet/the-global-hivaids-epidemic/ . Accessed 13 Nov 2022.
UNAIDS. Fact sheet—latest global and regional statistics on the status of the AIDS epidemic. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2022. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf . Accessed 23 Oct 2022.
West CA, Chang GC, Currie DW, Bray R, Kinchen S, Behel S, McCullough-Sanden R, Low A, Bissek A, Shang JD, Ndongmo CB, Dokubo EK, Balachandra S, Lobognon LR, Dube L, Nuwagaba-Biribonwoha H, Li M, Pasipamire M, Getaneh Y, Lulseged S, Eshetu F, Kingwara L, Zielinski-Gutierrez E, Tlhomola M, Ramphalla P, Kalua T, Auld AF, Williams DB, Remera E, Rwibasira GN, Mugisha V, Malamba SS, Mushi J, Jalloh MF, Mgomella GS, Kirungi WL, Biraro S, Awor AC, Barradas DT, Mugurungi O, Rogers JH, Bronson M, Bodika SM, Ajiboye A, Gaffga N, Moore C, Patel HK, Voetsch AC. Unawareness of HIV infection among men aged 15–59 years in 13 sub-Saharan African countries: findings from the population-based HIV impact assessments, 2015–2019. JAIDS. 2021;87:S97.
PubMed Google Scholar
UNAIDS. Executive summary—in danger: UNAIDS global AIDS update 2022 [Internet]. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2022. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update-summary_en.pdf . Accessed 23 Oct 2022.
UNAIDS. Addressing a blind spot in the response to HIV—reaching out to men and boys. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2017. https://www.unaids.org/sites/default/files/media_asset/blind_spot_en.pdf . Accessed 23 Oct 2022.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–21. https://doi.org/10.2105/AJPH.2012.301069 .
Article PubMed PubMed Central Google Scholar
Relf MV, Holzemer WL, Holt L, Nyblade L, Caiola CE. A review of the state of the science of HIV and stigma: context, conceptualization, measurement, interventions, gaps, and future priorities. J Assoc Nurses AIDS Care. 2021;32:392–407. https://doi.org/10.1097/JNC.0000000000000237 .
Herek GM. AIDS and stigma. Am Behav Sci. 1999;42:1106–16. https://doi.org/10.1177/00027649921954787 .
Article Google Scholar
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17:1785–95. https://doi.org/10.1007/s10461-013-0437-9 .
Derlega VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. J Health Psychol. 2002;7:415–32. https://doi.org/10.1177/1359105302007004330 .
Article PubMed Google Scholar
Arinaitwe I, Amutuhaire H, Atwongyeire D, Tusingwire E, Kawungezi PC, Rukundo GZ, Ashaba S. Social support, food insecurity, and HIV stigma among men living with HIV in rural southwestern Uganda: a cross-sectional analysis. HIV AIDS (Auckl). 2021;13:657–66. https://doi.org/10.2147/HIV.S316174 .
Mburu G, Ram M, Siu G, Bitira D, Skovdal M, Holland P. Intersectionality of HIV stigma and masculinity in eastern Uganda: implications for involving men in HIV programmes. BMC Public Health. 2014;14:1061. https://doi.org/10.1186/1471-2458-14-1061 .
Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. A scoping review on the role of masculine norms in men’s engagement in the HIV care continuum in sub-Saharan Africa. AIDS Care. 2019;31:1435–46. https://doi.org/10.1080/09540121.2019.1595509 .
Abara WE, Garba I. HIV epidemic and human rights among men who have sex with men in sub-Saharan Africa: implications for HIV prevention, care, and surveillance. Glob Public Health. 2017;12:469–82. https://doi.org/10.1080/17441692.2015.1094107 .
Joshi K, Lessler J, Olawore O, Loevinsohn G, Bushey S, Tobian AAR, Grabowski MK. Declining HIV incidence in sub-Saharan Africa: a systematic review and meta-analysis of empiric data. J Int AIDS Soc. 2021. https://doi.org/10.1002/jia2.25818 .
Nyato D, Kuringe E, Drake M, Casalini C, Nnko S, Shao A, Komba A, Baral SD, Wambura M, Changalucha J. Participants’ accrual and delivery of HIV prevention interventions among men who have sex with men in sub-Saharan Africa: a systematic review. BMC Public Health. 2018. https://doi.org/10.1186/s12889-018-5303-2 .
Hamilton A, Thompson N, Choko AT, Hlongwa M, Jolly P, Korte JE, Conserve DF. HIV self-testing uptake and intervention strategies among men in sub-Saharan Africa: a systematic review. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.594298 .
Hlongwa M, Hlongwana K, Makhunga S, Choko AT, Dzinamarira T, Conserve D, Tsai AC. Linkage to HIV care following HIV self-testing among men: systematic review of quantitative and qualitative studies from six countries in sub-Saharan Africa. AIDS Behav. 2022. https://doi.org/10.1007/s10461-022-03800-8 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021. https://doi.org/10.1136/bmj.n71 .
Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107:863–9. https://doi.org/10.2105/AJPH.2017.303744 .
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021 .
UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf . Accessed 10 June 2023.
UNAIDS. AIDS by the numbers: AIDS is not over, but it can be. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2016. https://www.unaids.org/sites/default/files/media_asset/AIDS-by-the-numbers-2016_en.pdf . Accessed 10 June 2023.
Covidence systematic review software. Veritas Health Innovation. 2022. https://www.covidence.org/ . Accessed 8 Mar 2022.
Kmet LM, Lee RC, Cook LS. HTA initiative #13: standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research. 2004. https://www.ihe.ca/download/standard_quality_assessment_criteria_for_evaluating_primary_research_papers_from_a_variety_of_fields.pdf . Accessed 24 Oct 2022.
Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer Publishing Company; 2007.
Google Scholar
Belay YA, Yitayal M, Atnafu A, Taye FA. Patient experiences and preferences for antiretroviral therapy service provision: implications for differentiated service delivery in Northwest Ethiopia. AIDS Res Ther. 2022;19:1–16. https://doi.org/10.1186/s12981-022-00452-5 .
Hlongwa M, Jama NA, Mehlomakulu V, Pass D, Basera W, Nicol E. Barriers and facilitating factors to HIV treatment among men in a high-HIV-burdened district in KwaZulu-Natal, South Africa: a qualitative study. Am J Mens Health. 2022. https://doi.org/10.1177/15579883221120987 .
Lofgren SM, Tsui S, Atuyambe L, Ankunda L, Komuhendo R, Wamala N, Sadiq A, Kirumira P, Srishyla D, Flynn A, Pastick KA, Meya DB, Nakasujja N, Porta C. Barriers to HIV care in Uganda and implications for universal test-and-treat: a qualitative study. AIDS Care. 2022;34:597–605. https://doi.org/10.1080/09540121.2021.1946000 .
Mandawa MB, Mahiti GR. Factors contributing to loss to follow-up from HIV care among men living with HIV/AIDS in Kibaha District, Tanzania. HIV AIDS (Auckl). 2022;14:503–16. https://doi.org/10.2147/hiv.S381204 .
Mange T, Henderson N, Lukelelo N. ‘After 25 years of democracy we are still stigmatised and discriminated against’ healthcare experiences of HIV-positive older black gay men in a township in South Africa. J Pract Teach Learn. 2022;9:87–100. https://doi.org/10.1921/jpts.v19i1-2.1674 .
Mathenjwa M, Khidir H, Milford C, Mosery N, Rambally Greener L, Pratt MC, O’Neil K, Harrison A, Bangsberg DR, Safren SA, Smit JA, Psaros C, Matthews LT. Acceptability of an intervention to promote viral suppression and serostatus disclosure for men living with HIV in South Africa: qualitative findings. AIDS Behav. 2022;26:1–12. https://doi.org/10.1007/s10461-021-03278-w .
Muwanguzi PA, Nelson LE, Ngabirano TD, Kiwanuka N, Osingada CP, Sewankambo NK. Linkage to care and treatment among men with reactive HIV self-tests after workplace-based testing in Uganda: a qualitative study. Front Public Health. 2022. https://doi.org/10.3389/fpubh.2022.650719 .
Nabikande S, Namutundu J, Nangendo J, Okello T, Agwang W, Tusabe J, Kabwama SN, Katahoire AR. Men’s late presentation for HIV care in Eastern Uganda: the role of masculinity norms. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0277534 .
Ndione AG, Procureur F, Senne JN, Cornaglia F, Gueye K, Ndour CT, Lépine A. Sexuality-based stigma and access to care: intersecting perspectives between health care providers and men who have sex with men in HIV care centres in Senegal. Health Policy Plan. 2022;37:587–96. https://doi.org/10.1093/heapol/czac010 .
Rich C, Mavhu W, France NF, Munatsi V, Byrne E, Willis N, Nolan A. Exploring the beliefs, experiences and impacts of HIV-related self-stigma amongst adolescents and young adults living with HIV in Harare, Zimbabwe: a qualitative study. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0268498 .
Hendrickson ZM, Naugle DA, Tibbels N, Dosso A, Van Lith LM, Mallalieu EC, Kamara D, Dailly-Ajavon P, Cisse A, Ahanda KS, Thaddeus S, Babalola S, Hoffman CJ. “You take medications, you live normally”: the role of antiretroviral therapy in mitigating men’s perceived threats of HIV in Côte d’Ivoire. AIDS Behav. 2019;23:2600–9. https://doi.org/10.1007/s10461-019-02614-5 .
Naugle DA, Tibbels NJ, Hendrickson ZM, Dosso A, Van Lith LM, Mallalieu EC, Kouadio AM, Kra W, Kamara D, Dailly-Ajavon P, Cissé A, Seifert-Ahanda K, Thaddeus S, Babalola S, Hoffman CJ. Bringing fear into focus: the intersections of HIV and masculine gender norms in Côte d’Ivoire. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0223414 .
Tibbels NJ, Hendrickson ZM, Naugle DA, Dosso A, Van Lith LM, Mallalieu EC, Kouadio AM, Kra W, Kamara D, Dailly-Ajavon P, Cisse A, Seifert-Ahanda K, Thaddeus S, Babalola S, Hoffmann CJ. Men’s perceptions of HIV care engagement at the facility- and provider-levels: experiences in Cote d’Ivoire. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0211385 .
Balogun A, Bissell P, Saddiq M. Negotiating access to the Nigerian healthcare system: the experiences of HIV-positive men who have sex with men. Cult Health Sex. 2020;22:233–46. https://doi.org/10.1080/13691058.2019.1582802 .
Mukumbang FC. Leaving no man behind: how differentiated service delivery models increase men’s engagement in HIV care. Int J Health Policy Manag. 2021;10:129–40. https://doi.org/10.34172/ijhpm.2020.32 .
Ogunbajo A, Kershaw T, Kushwaha S, Boakye F, Wallace-Atiapah N-D, Nelson LE. Barriers, motivators, and facilitators to engagement in HIV care among HIV-infected Ghanaian men who have sex with men (MSM). AIDS Behav. 2018;22:829–39. https://doi.org/10.1007/s10461-017-1806-6 .
Okal J, Lango D, Matheka J, Obare F, Ngunu-Gituathi C, Mugambi M, Avina S. “It is always better for a man to know his HIV status”—a qualitative study exploring the context, barriers and facilitators of HIV testing among men in Nairobi, Kenya. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0231645 .
Okoror TA, Falade CO, Walker EM, Olorunlana A, Anaele A. Social context surrounding HIV diagnosis and construction of masculinity: a qualitative study of stigma experiences of heterosexual HIV positive men in southwest Nigeria. BMC Public Health. 2016;16:507. https://doi.org/10.1186/s12889-016-3165-z .
Sileo KM, Reed E, Kizito W, Wagman JA, Stockman JK, Wanyenze RK, Chemusto H, Musoke W, Mukasa B, Kiene SM. Masculinity and engagement in HIV care among male fisherfolk on HIV treatment in Uganda. Cult Health Sex. 2019;21:774–88. https://doi.org/10.1080/13691058.2018.1516299 .
Zissette S, Watt MH, Prose NS, Mntambo N, Moshabela M. “If you don’t take a stand for your life, who will help you?”: men’s engagement in HIV care in KwaZulu-Natal, South Africa. Psychol Men Masc. 2016;17:265–73. https://doi.org/10.1037/men0000025 .
Berner-Rodoreda A, Ngwira E, Alhassan Y, Chione B, Dambe R, Bärnighausen T, Phiri S, Taegtmeyer M, Neuhann F. “Deadly”, “fierce”, “shameful”: notions of antiretroviral therapy, stigma and masculinities intersecting men’s life-course in Blantyre, Malawi. BMC Public Health. 2021. https://doi.org/10.1186/s12889-021-12314-2 .
Mantell JE, Masvawure TB, Mapingure M, Apollo T, Gwanzura C, Block L, Bennett E, Preko P, Musuka G, Rabkin M. Engaging men in HIV programmes: a qualitative study of male engagement in community-based antiretroviral refill groups in Zimbabwe. J Int AIDS Soc. 2019. https://doi.org/10.1002/jia2.25403 .
Misra S, Mehta HT, Eschliman EL, Rampa S, Poku OB, Wang W-Q, Ho-Foster AR, Mosepele M, Becker TD, Entaile P, Arscott-Mills T, Opondo PR, Blank MB, Yang LH. Identifying “what matters most” to men in Botswana to promote resistance to HIV-related stigma. Qual Health Res. 2021;31:1680–96. https://doi.org/10.1177/10497323211001361 .
Mooney AC, Gottert A, Khoza N, Rebombo D, Hove J, Suárez AJ, Twine R, MacPhail C, Treves-Kagan S, Kahn K, Pettifor A, Lippman SA. Men’s perceptions of treatment as prevention in South Africa: implications for engagement in HIV care and treatment. AIDS Educ Prev. 2017;29:274–87. https://doi.org/10.1521/aeap.2017.29.3.274 .
Moyo I, Macherera M, Mavhandu-Mudzusi AH. The lived experiences of men who have sex with men when accessing HIV care services in Zimbabwe. Health SA. 2021. https://doi.org/10.4102/hsag.v26i0.1462 .
Meskele M, Khuzwayo N, Taylor M. Mapping the evidence of intimate partner violence among women living with HIV/AIDS in sub-Saharan Africa: a scoping review. BMJ Open. 2021. https://doi.org/10.1136/bmjopen-2020-041326 .
Tenkorang EY, Asamoah-Boaheng M, Owusu AY. Intimate partner violence (IPV) against HIV-positive women in sub-Saharan Africa: a mixed-method systematic review and meta-analysis. Trauma Violence Abuse. 2021;22:1104–28. https://doi.org/10.1177/1524838020906560 .
Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. What role do masculine norms play in men’s HIV testing in sub-Saharan Africa?: a scoping review. AIDS Behav. 2018;22:2468–79. https://doi.org/10.1007/s10461-018-2160-z .
Naanyu V, Ruff J, Goodrich S, Spira T, Bateganya M, Toroitich-Ruto C, Otieno-Nyunya B, Siika AM, Wools-Kaloustian K. Qualitative exploration of perceived benefits of care and barriers influencing HIV care in trans Nzoia, Kenya. BMC Health Serv Res. 2020. https://doi.org/10.1186/s12913-020-05236-z .
Makoae LN, Seboni NM, Molosiwa K, Moleko M, Human S, Sukati NA, Holzemer WL. The symptom experience of people living with HIV/AIDS in southern Africa. J Assoc Nurses AIDS Care. 2005;16:22–32. https://doi.org/10.1016/j.jana.2005.03.005 .
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2020. https://doi.org/10.1002/jrsm.1411 .
Download references
Acknowledgements
The manuscript was supported by the Fogarty International Center/National Institutes of Health through Award Number R21TW011247 (M. Relf, Contact MPI/L. Nyblade, MPI) and the Duke University Center for AIDS Research (CFAR), an NIH funded program (5P30AI064518). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Research reported in this publication was supported by the Fogarty International Center of the National Institutes for Health under award R21TW012007 and by the Duke Center for AIDS Research, a National Institutes of Health funded program under award number 5P30AI064518. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
School of Nursing, Duke University, 307 Trent Drive, Box 3322, Durham, NC, 27710, USA
Sarah E. Janek & Michael V. Relf
Duke Global Health Institute, Durham, NC, USA
Sandy Hatoum & Michael V. Relf
Medical Center Library, Duke University, Durham, NC, USA
Leila Ledbetter
You can also search for this author in PubMed Google Scholar
Contributions
All authors on this paper meet the four criteria for authorship as identified by the International Committee of Medical Journal Editors; all authors have contributed to the drafting or been involved in revising it, reviewed the final version of this manuscript before submission, and agree to be accountable for all aspects of the work. Specifically, using the CRediT taxonomy, the specific contribution of each author is as follows: Conceptualization & Methodology: S. Janek, L. Ledbetter, M. Relf. Formal Analysis: S. Hatoum, S. Janek, M. Relf. Funding Acquisition: M. Relf. Investigation: S. Hatoum, S. Janek, L. Ledbetter, M. Relf. Methodology: S. Janek, L. Ledbetter, M. Relf. Project administration: M. Relf. Supervision: M. Relf. Verification: S. Hatoum, S. Janek, M. Relf. Writing—manuscript draft: S. Janek. Writing—review & editing: S. Hatoum, S. Janek, L. Ledbetter, M. Relf.
Corresponding authors
Correspondence to Sarah E. Janek or Michael V. Relf .
Ethics declarations
Conflict of interest.
The authors report no real or perceived vested interests related to this article that could be construed as a conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Registration The protocol that guided this meta-synthesis was prospectively registered with Prospero (registration ID: CRD42022315871).
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 35 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Janek, S.E., Hatoum, S., Ledbetter, L. et al. Understanding the Stigma Experience of Men Living with HIV in Sub-Saharan Africa: A Qualitative Meta-synthesis. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04329-8
Download citation
Accepted : 20 March 2024
Published : 22 May 2024
DOI : https://doi.org/10.1007/s10461-024-04329-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Meta-synthesis
- People with HIV
- Sub-Saharan Africa
- Qualitative methodology
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 June 2024
Associations between HIV stigma and health-related quality-of-life among people living with HIV: cross-sectional analysis of data from HPTN 071 (PopART)
- Emily Hall 1 , 2 ,
- Katherine Davis 1 , 2 ,
- Julius Ohrnberger 1 , 2 ,
- Michael Pickles 1 , 2 ,
- Simon Gregson 1 , 2 ,
- Ranjeeta Thomas 3 ,
- James R. Hargreaves 4 ,
- Triantafyllos Pliakas 4 ,
- Justin Bwalya 5 ,
- Rory Dunbar 6 ,
- Tila Mainga 5 , 7 ,
- Kwame Shanaube 5 ,
- Graeme Hoddinott 6 ,
- Virginia Bond 5 , 7 ,
- Peter Bock 6 ,
- Helen Ayles 8 ,
- Anne L. Stangl 9 , 10 ,
- Deborah Donnell 11 ,
- Richard Hayes 12 ,
- Sarah Fidler 13 ,
- Katharina Hauck 1 , 2 &
The HPTN 071 (PopART) study team
Scientific Reports volume 14 , Article number: 12835 ( 2024 ) Cite this article
Metrics details
- Epidemiology
- HIV infections
- Public health
- Quality of life
People living with HIV (PLHIV) report lower health-related quality-of-life (HRQoL) than HIV-negative people. HIV stigma may contribute to this. We explored the association between HIV stigma and HRQoL among PLHIV. We used cross-sectional data from 3991 randomly selected PLHIV who were surveyed in 2017–2018 for HPTN 071 (PopART), a cluster randomised trial in Zambia and South Africa. Participants were 18–44 years, had laboratory-confirmed HIV infection, and knew their status. HRQoL was measured using the EuroQol-5-dimensions-5-levels (EQ-5D-5L) questionnaire. Stigma outcomes included: internalised stigma, stigma experienced in the community, and stigma experienced in healthcare settings. Associations were examined using logistic regression. Participants who had experienced community stigma (n = 693/3991) had higher odds of reporting problems in at least one HRQoL domain, compared to those who had not (adjusted odds ratio, aOR: 1.51, 95% confidence interval, 95% Cl: 1.16–1.98, p = 0.002). Having experienced internalised stigma was also associated with reporting problems in at least one HRQoL domain (n = 552/3991, aOR: 1.98, 95% CI: 1.54–2.54, p < 0.001). However, having experienced stigma in a healthcare setting was less common (n = 158/3991) and not associated with HRQoL (aOR: 1.04, 95% CI: 0.68–1.58, p = 0.850). A stronger focus on interventions for internalised stigma and stigma experienced in the community is required.
Similar content being viewed by others

Relationship of health rating and HIV-related stigma among people living with HIV: a community study
HIV/AIDS stigma accumulation among people living with HIV: a role of general and relative minority status
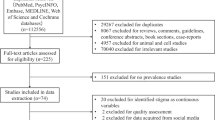
A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action
Introduction.
Life expectancy for people living with human immunodeficiency virus (HIV) has improved substantially 1 . However, people living with HIV still have higher rates of comorbidities, and lower health-related quality-of-life than the general population 2 . Health-related quality-of-life measures a person’s wellbeing across different domains that are directly affected by their health, such as mobility and pain 3 . Concerns about health-related quality-of-life among people living with HIV led to recent suggestions that health-related quality-of-life should be an additional fourth pillar in the Joint United Nations Programme on HIV/AIDS (UNAIDS)’s 90–90-90 targets for HIV testing, treatment, and viral suppression 2 . To improve the health-related quality-of-life of people living with HIV, an understanding of the factors that influence health-related quality-of-life is needed.
It has been proposed that experiencing HIV stigma might make people living with HIV who know their status more likely to experience lower health-related quality-of-life 4 , 5 . HIV stigma refers to the negative behaviours and attitudes directed towards people living with HIV 6 . This stigma remains prevalent in sub-Saharan Africa, with a South African study reporting that 29% of people living with HIV surveyed had experienced discrimination or exclusion because of their status 7 . HIV stigma has been linked to adverse health outcomes including delayed access to healthcare, and reduced treatment adherence, which may lower health-related quality-of-life 8 , 9 , 10 , 11 , 12 , 13 , 14 . Ongoing work to reduce stigma offers an opportunity to improve health-related quality-of-life among people living with HIV in Africa, yet to do so effectively we need to understand the mechanisms by which HIV stigma might affect health-related quality-of-life 15 .
Gaining a comprehensive understanding of the relationship between HIV stigma and health-related quality-of-life in sub-Saharan African settings is challenging, however, as few relevant studies have been conducted in the region 4 , 5 . Furthermore, the limited existing research has often focused exclusively on individuals entering clinical care or on treatment, which does not provide a complete insight into the relationship between stigma and health-related quality-of-life among all people living with HIV in the community 4 , 5 , 8 , 16 , 17 . Use of HIV-specific measures of health-related quality-of-life is also common and makes it hard to compare the effect of stigma on wellbeing among people living with HIV against the effect of other threats to wellbeing among different population groups 4 , 5 , 8 , 16 , 17 . Finally, studies have frequently been small in scale, reducing the precision of the findings 4 , 5 , 8 , 16 , 17 . As a result, there is a lack of robust information on the relationship between HIV stigma and health-related quality-of-life, which constrains efforts to improve the health-related quality-of-life of people living with HIV.
This information is also important for economic appraisals of the benefits of interventions, which often rely on health-related quality-of-life measures 18 . The lack of clarity about the relationship between stigma and health-related quality-of-life may undermine these assessments, complicating economic evaluations of stigma reduction interventions 19 , 20 .
We analysed data from approximately 4,000 people living with HIV who knew their HIV status and participated in the HIV Prevention Trials Network (HPTN) 071 (PopART) trial, to assess the association between HIV stigma and health-related quality-of-life. We aimed to compare health-related quality-of-life profiles between people living with HIV who had and had not experienced HIV stigma; explore associations between three types of HIV stigma and health-related quality-of-life; and examine which domains of health-related quality-of-life are associated with HIV stigma. Our analyses included people living with HIV not on treatment or in care, and the findings provide crucial evidence of the need for interventions to improve the wellbeing of people living with HIV.
Study design
Data were from the HPTN 071 (PopART) study, a three-arm, matched cluster-randomised controlled trial, implemented across 21 urban and peri-urban communities in Zambia (12 communities) and South Africa (9 communities) between 2013 and 2018. Each community was the catchment population for a government clinic, and in total, the study communities had a population of approximately 1 million people. The study measured the effect of a combination prevention package on HIV incidence. Arm A received the full intervention of door-to-door HIV testing plus access to HIV treatment for all PLHIV, Arm B received the intervention but followed national treatment guidelines (universal ART from 2016) and Arm C received standard care. Further details on the trial are available in the supplement (section S1), the trial protocol ( https://www.hptn.org/research/studies/hptn071 ), and are described by Hayes et al. 21
At baseline of the trial, a random sample of households were selected and visited in each community. All adults aged between 18 and 44 years in each household were identified and one selected at random. The selected adults were surveyed by trained research assistants in the respondent’s preferred language using electronic tablets and followed up annually for three years. This analysis used data from the final survey, conducted 36 months after the trial started, between 8th September 2017 and 7th July 2018.
The EuroQoL five dimensions, five levels questionnaire (EQ-5D-5L) was included in the survey to collect health-related quality-of-life data 20 , 22 . To complete the EQ-5D-5L, participants reported if they had problems, on a five-level scale (no problems, slight problems, moderate problems, severe problems or extreme problems/unable to do), in five domains: mobility (ability to walk around), self-care (ability to wash and dress), daily activities (ability to carry out their usual daily activities), pain, and anxiety/depression 22 . In South Africa the certified translation of the EQ-5D-5L was used, whereas in Zambia, members of the study team translated the questionnaire into Zambian dialects because no certified translation was available. Visuals with faces were shown alongside the written words describing each of the five levels to improve understanding of the levels of each domain. Each respondent was asked to indicate their health state against the most appropriate level of problems in each of the 5 dimensions, and the answer was recorded by the research assistant. The EQ-5D-5L has been widely used in the general population and with people living with HIV in high-income countries and low- and middle-income countries (LMICs) 19 , 20 , 23 . It has been shown to be reliable and valid in diverse settings 19 , 23 .
Participants who self-reported being HIV-positive were asked 11 questions about their experience of HIV stigma. These questions captured four composite stigma outcomes: internalised stigma (three questions), stigma experienced in the community in the last year (five questions), stigma experienced in healthcare settings in the last year (three questions) and any stigma experienced (11 questions), as described in section S1 and by Stangl et al. 24 Internalised stigma occurs when people living with HIV apply negative feelings and beliefs associated with HIV to themselves 24 . Wording of the stigma measures was informed by conceptual frameworks 6 .
HIV status was assessed by venous blood testing. Detail on HIV testing is available in section S1.
Statistical analysis
The study population was restricted to participants who self-reported living with HIV, which was confirmed by laboratory testing. Participants with missing data on health-related quality-of-life, stigma or other variables of interest were excluded, but participants did not need to be on treatment or in HIV care (section S2).
Firstly, a binary variable was created to summarise whether participants agreed with feeling any of three manifestations of internalised stigma. Two further binary variables captured whether participants had experienced stigma in a community setting and whether participants had experienced stigma in a healthcare setting. A fourth binary variable was also generated to encapsulate whether participants had experienced any stigma.
We then generated health-related quality-of-life profiles, which described the participants’ responses for each EQ-5D-5L domain 22 . Profiles were generated for two groups: people living with HIV who had never experienced HIV stigma, and people living with HIV who had experienced HIV stigma at least once. Each level of problems was given a quantitative score from one (no problems) to five (unable to/extreme problems), and Wilcoxon rank sum tests were applied to the scores to examine differences in each health-related quality-of-life domain between people living with HIV who had experienced stigma and people living with HIV who had not.
Participants’ responses to the EQ-5D-5L were collapsed into a binary health-related quality-of-life outcome, as suggested in the EQ-5D-5L User Guide, which captured whether they reported problems in any health-related quality-of-life domain 22 . If participants had a quantitative health-related quality-of-life score above one out of five for any of the domains, then they were considered to have problems in a health-related quality-of-life domain.
Logistic regression was used to assess the unadjusted and adjusted association between experiencing any HIV stigma and reporting problems in at least one health-related quality-of-life domain. Potential confounders included age, sex, education, wealth, religion, recreational drug use, tuberculosis status, and marital status. Cluster robust standard errors were computed to account for clustering by community. Wealth was assessed using an index generated from principal components analysis of data on assets owned by participants 6 .
After the variable capturing whether any HIV stigma had been experienced was assessed, the associations between the different types of stigma (community, healthcare setting, and internalised) and reporting problems in at least one health-related quality-of-life domain were examined. Three separate unadjusted models were developed, followed by a single adjusted model. The adjusted model included the three stigma variables and the potential confounders listed above, with cluster robust standard errors.
Finally, we conducted separate unadjusted univariable and separate adjusted logistic regression analyses for each of the health-related quality-of-life domains (mobility, self-care, daily activities, pain, and anxiety/depression) to determine which domains were associated with experiencing any HIV stigma. For each regression, the variable capturing whether any stigma had been experienced was the independent variable of interest and the health-related quality-of-life domain was the dependent variable. Adjusted models controlled for the potential confounders listed above and cluster robust standard errors were used.
All logistic regressions were complete case analyses. Calculated odds are in section S3.
Analyses were performed using R (version 4.0.3) and the package Miceadds 25 , 26 .
Patient and public involvement
The public were involved through-out the HPTN 071 (PopART) research process. Before the trial began, individuals from existing representative structures, including members of community advisory boards from previous studies in the area, local opinion leaders, and government stakeholders, were consulted about study design 27 . A broad-brush survey approach was also used to provide a rapid assessment of the HIV prevention, treatment and care landscapes prior to trial initiation 28 . During the trial, multiple involvement and engagement mechanisms were employed to understand and improve the study, including meetings with community advisory boards for adults and adolescents, and connections with civil society groups 27 . Links with the public were also drawn upon at the end of intervention delivery to understand how results should be disseminated, with the first dissemination round using a community dialogue approach, which focused on what results meant to the communities 29 . Further dissemination of study results, such as those presented here, will continue to involve communities in decision making.
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Ethical approval for the HPTN 071 (PopART) trial was obtained from institutional review boards at London School of Hygiene and Tropical Medicine (LSHTM), the University of Zambia, and Stellenbosch University. Participants provided written informed consent. The study was performed in accordance with relevant guidelines and regulations, including the Declaration of Helsinki.
There were 6,261 participants with laboratory confirmed HIV-positive status, 4,413 of whom self-reported living with HIV. After excluding 422 participants due to missing data on stigma, health-related quality-of-life or other variables, the study sample included 3991 self-reported people living with HIV (section S2).
There were more women (88%) than men (12%) in the sample (Table 1 ). Nearly half of participants (46%) were aged between 30 and 39.
Problems in at least one health-related quality-of-life domain were reported by 515 participants (12%), and 1,034 participants (35%) reported experiencing HIV stigma at least once. The Wilcoxon tests, which analysed problem severity coded as a score from one to five, showed that, for all health-related quality-of-life domains, there was a significant difference in the proportion of people reporting each level of problem severity between people living with HIV who had and had not experienced HIV stigma (Table 2 ). This unadjusted analysis suggested that having experienced stigma was associated with poorer health-related quality-of-life in all five domains.
In univariable regression analyses exploring the association between experiencing any HIV stigma and participants’ health-related quality-of-life, the odds of reporting problems in at least one health-related quality-of-life domain were 2.10 (95% confidence intervals, CI 1.72–2.56, p < 0.001) times higher if a participant experienced HIV stigma at least once, compared to never experiencing HIV stigma (Table 3 ).This finding remained stable on adjusting for confounders and introducing cluster robust standard errors; participants who had experienced any HIV stigma had more than twice the odds of reporting problems in at least one health-related quality-of-life domain compared to those who had not (adjusted odds ratio, aOR 2.08, 95% CI 1.55–2.79, p < 0.001). Using recreational drugs in the last year (OR 1.94, 95% CI 1.00–3.75, p = 0.050), and being diagnosed with tuberculosis in the last year (OR 2.15, 95% CI 1.14–4.04, p = 0.018) were also associated with higher odds of reporting problems in at least one health-related quality-of-life domain.
When the three types of stigma were analysed, HIV stigma experienced in the community was the most frequently reported (17%), followed by internalised stigma (14%) and stigma experienced in healthcare settings (4%) (Table 1 ). In unadjusted analyses of the association between the three different types of stigma and health-related quality-of-life, participants who had experienced internalised stigma, stigma in the community, or stigma in a healthcare setting had higher odds of reporting problems in at least one health-related quality-of-life domain, with unadjusted ORs of 2.29 (95% CI 1.81–2.88, p < 0.001), 1.86 (95% CI 1.48–2.32, p < 0.001), and 1.56 (95% CI 1.00–2.35, p = 0.040), respectively (Table 4 ).
After adjusting for potential confounders and using cluster robust standard errors, the odds of reporting problems in at least one health-related quality-of-life domain were nearly twice as high in those who had experienced internalised stigma compared to those who had not (aOR 1.98, 95% CI 1.54–2.54, p < 0.001). The odds of reporting problems in at least one health-related quality-of-life domain were 51% higher for people living with HIV who had experienced community stigma at least once compared to those who had not (aOR 1.51, 95% CI 1.16–1.98, p = 0.002). There was no association between experiencing healthcare setting stigma and reporting problems in at least one health-related quality-of-life domain after adjustment (aOR 1.04, 95% CI 0.68–1.58, p = 0.850) (Table 4 ).
Unadjusted and adjusted regression analyses of the associations between experiencing any stigma and health-related quality-of-life domains showed that experiencing any HIV stigma was associated with increased odds of reporting problems in all health-related quality-of-life domains (Fig. 1 ). In unadjusted analyses, participants who experienced any type of stigma had higher odds of reporting problems with mobility (OR 2.59, 95% CI 1.67–4.02, p < 0.001), self-care (OR 1.93, 95% CI 1.10–3.30, p = 0.018), performing daily activities (OR 1.95, 95% CI 1.31–2.86, p = 0.001), pain (OR 2.01, 95% CI 1.58–2.55, p < 0.001), and anxiety/depression (OR 3.03, 95% CI 2.24–4.11, p < 0.001) than those who had never experienced HIV stigma. In adjusted analyses, results were similar. The odds of reporting problems among those who had experienced HIV stigma were 2.5 (OR 2.50, 95% CI 1.39–4.50, p = 0.002) times higher for mobility, 97% (OR 1.97, 95% CI 1.18–3.29, p = 0.010) higher for self-care, 94% (OR 1.94, 95% CI 1.30–2.90, p = 0.001) higher for performing daily activities, 2.01 (OR 2.01, 95% CI 1.47–2.77, p < 0.001) times higher for pain, and 3.06 (OR 3.06, 95% CI 1.75–5.35, p < 0.001) times higher for anxiety/depression.

The association between experiencing any HIV stigma and reporting problems in five dimensions of health-related quality-of-life among 3991 people living with HIV from 21 study communities in South Africa and Zambia. Not experiencing any HIV stigma is the base category. An odds ratio greater than one shows those not in the base category are more likely to report “problems” in that health-related quality-of-life domain. Adjusted models include the covariates age, sex, education, wealth index, religion, recreational drug use, tuberculosis status, and marital status, with cluster robust standard errors to account for clustering by community.
This study analysed the association between HIV stigma and the health-related quality-of-life of people who self-reported living with HIV, in 21 urban and peri-urban communities across South Africa and Zambia. 17% of participants reported experiencing HIV stigma in the community, 4% had experienced stigma in healthcare settings, and 14% of participants had internalised stigma. Experiencing internalised stigma or stigma in the community was associated with twice, and one and a half times higher odds, respectively, of reporting worse health-related quality-of-life outcomes. We also found that problems in all domains of health-related quality-of-life contributed to the association between HIV stigma and reduced health-related quality-of-life. Experiencing stigma in a healthcare setting was not associated with reporting worse health-related quality-of-life.
Our findings build on previous studies linking internalised stigma with lower health-related quality-of-life among people living with HIV who knew their status 4 , 16 . Moreover, several studies have found that people living with HIV with internalised stigma have an increased likelihood of developing depression, and our analysis found those who experienced any stigma had three times higher odds of reporting problems with anxiety or depression 30 . Likewise, community stigma has previously been linked to avoidance of healthcare, and poor mental health, supporting our finding that experiencing community stigma is negatively associated with health-related quality-of-life among people living with HIV 31 . Our stigma prevalence values differ slightly from those in previous reports relating to the HPTN 071 (PopART) trial due to the different study sample selected here 6 .
Our finding that experiencing any HIV stigma was associated with increased odds of reporting problems in all the health-related quality-of-life domains aligns with some, but not all previous research. Specifically, our finding mirrors the results of a study in Nigeria, but differs from results of two studies in Ethiopia, wherein associations were only found for some health-related quality-of-life domains 5 , 8 , 17 . The difference between the results of the Ethiopian studies and our study may be due to diversity in participant characteristics, such as age, lifestyle, and perception of personal beliefs 5 . Nevertheless, it should also be recognised that the differences may be a consequence of the use of various health-related quality-of-life and stigma measures, which capture distinct concepts and so may reveal differing associations.
An unexpected finding of our study was that stigma experienced in a healthcare setting was not associated with worse health-related quality-of-life in adjusted analyses. Qualitative stigma data from the HPTN 071 (PopART) trial consistently and strongly indicates concerns about people living with HIV being seen accessing HIV services in healthcare settings, and the role of group identity, spatial layout, client flow, and items that signify HIV, in driving healthcare setting stigma 32 . Thus, the qualitative data does not support this finding. In our study, healthcare setting stigma was the least frequently experienced stigma type, consequently the study may have been underpowered to detect significant effects. Additionally, the EQ-5D-5L is a generic measure of health, so might not be sufficiently sensitive to identify indirect adverse impacts of healthcare stigma, such as altered healthcare-seeking behaviours 9 . The HPTN 071 (PopART) trial was also associated with the healthcare system, which may have led to under-reporting of stigma experienced in healthcare settings. Lastly, the three items used to assess healthcare setting stigma may not have captured less overt stigma, which may be more prevalent in healthcare settings in sub-Saharan Africa, given the long history of stigma reduction efforts 33 . Nonetheless, our finding is potentially important because most current literature on interventions to reduce HIV stigma focuses on healthcare settings 34 . Stigma occurs in many places, with six main settings identified by UNAIDS: the healthcare sector, the education sector, the workplace, the justice system, families and communities, and emergency and humanitarian settings 35 . Our findings provide crucial guidance to policymakers in South Africa and Zambia to refocus stigma reduction policies beyond the healthcare sector.
The main strength of this study is the substantial sample of people living with HIV. Our study is among the largest and most robust analyses of associations between HIV stigma and health-related quality-of-life in Africa. We included nearly 4,000 people living with HIV from 21 communities in two countries. Moreover, while previous studies have often evaluated health-related quality-of-life in people living with HIV who were enrolling into clinical care or on treatment, our data were from people living with HIV in the community 4 , 5 , 8 , 16 , 17 . Approximately one in ten of the included people living with HIV were not in care 20 . This gives a more representative insight into the relationship between stigma and health-related quality-of-life. Additionally, our measures of the core manifestations of HIV stigma and of health-related quality-of-life had been validated previously and self-reported HIV-positive status was confirmed via laboratory testing. Finally, the scope of the PopART trial allowed many confounders, selected based on research in similar populations, to be adjusted for.
Our study had limitations. Males were underrepresented, possibly due to selection bias; the survey was administered during the day, when men may have been more likely to be at work. There are also fewer men than women living with HIV in South Africa and Zambia. This limits the generalisability of our findings to men, particularly as some studies have found gender differences in stigma and health-related quality-of-life 6 , 17 . Additionally, we excluded people living with HIV who did not self-report living with HIV, as they were not asked about HIV stigma. This excluded people living with HIV who did not know their status or chose not to report their status. Excluding people who chose not to report their status may result in sample selection bias, because individuals who have experienced stigma may be less likely to disclose their status, perhaps leading to an underestimation of the prevalence of HIV stigma and its associations with health-related quality-of-life. Moreover, despite CD4 cell count (an indication of immune system health) being identified as a potential confounder, we were unable to adjust for this as data on CD4 cell counts were not collected 19 . Finally, this study focused on experienced and internalised stigma, but did not investigate anticipated stigma. Therefore, future work should explore the role of anticipated stigma. Future work could also examine the impact of the HPTN 071 (PopART) combination prevention intervention on the relationship between stigma and health-related quality-of-life. While previous research has demonstrated that the intervention had no effect on overall stigma or overall health-related quality-of-life, the intervention may have modified the effect of stigma on health-related quality-of-life and this could be explored to complement our findings 36 , 37 .
Over recent years, studies have shown that progress has been made in the design of interventions addressing both stigma experienced in the community and internalised stigma 33 . Interventions to reduce community stigma are often information-based, aiming to educate people living with HIV and the wider community about HIV to improve attitudes 35 . There is existing evidence that these approaches tend to result in some reduction in stigmatising behaviour, however, studies could not always demonstrate quantifiably measurable change 38 . Evidence suggests that interventions combining broad information-based campaigns with strategies targeting community leaders and groups who are influential in setting norms and practices may be more effective 9 . Furthermore, internalised stigma has been successfully addressed through interventions including formal psychological support, treatment buddies, and support groups 9 . Studies have shown that substantial challenges exist in scaling interventions for internalised stigma, especially in LMICs, but this is important as internalised stigma has been linked with poorer viral suppression 39 , 40 . Implementing and evaluating evidence-based interventions to reduce both internalised stigma and stigma experienced in the community should be a priority.
Our analysis demonstrates the use of the EQ-5D-5L, a generic measure of health-related quality-of-life, to detect adverse effects of stigma. In future, this instrument could be employed to assess the benefits of stigma interventions and compare them against a wide range of other health interventions that are assessed with generic measures 41 . For example, the benefit estimates could be used in comparative cost-effectiveness analyses of stigma interventions, to determine the societal value of such interventions against other health interventions 19 , 20 . Eventually, these estimates may be used in comparative cost-effectiveness league tables, such as those used to determine health packages for universal health coverage 41 . This provides invaluable guidance to policymakers navigating constrained health budgets and may inform decisions on funding allocations that stigma interventions receive 19 , 20 .
Conclusions
Our study showed that internalised stigma and stigma experienced in the community were associated with worse health-related quality-of-life, but stigma experienced in healthcare settings was not associated with health-related quality-of-life. These findings indicate that there is a need for research into, and implementation of, cost-effective stigma reduction interventions that focus on internalised stigma and community stigma, in South Africa and Zambia. Efforts to reduce stigma must continue at multiple levels to improve the lives of people living with HIV and achieve the new societal enabler targets for HIV, which are key to reaching global HIV goals by 2030.
Data availability
The data archive is held at Fred Hutchinson Cancer Center, Seattle, WA, USA. Requests can be sent to HPTN‐Data‐[email protected].
Wandeler, G., Johnson, L. F. & Egger, M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: Comparisons with general population. Curr. Opin. HIV AIDS 11 , 492–500 (2016).
CAS PubMed PubMed Central Google Scholar
Safreed-Harmon, K. et al. Reorienting health systems to care for people with HIV beyond viral suppression. Lancet HIV 6 , e869–e877 (2019).
PubMed Google Scholar
Cooper, V. et al. Measuring quality of life among people living with HIV: A systematic review of reviews. Health Qual. Life Outcomes 15 , 220 (2017).
Parcesepe, A. M. et al. Gender, HIV-Related stigma, and health-related quality of life among adults enrolling in HIV care in Tanzania. AIDS Behav. 24 , 142–150 (2020).
Mekuria, L. A., Sprangers, M. A. G., Prins, J. M., Yalew, A. W. & Nieuwkerk, P. T. Health-related quality of life of HIV-infected adults receiving combination antiretroviral therapy in Addis Ababa. AIDS Care 27 , 934–945 (2015).
Hargreaves, J. R. et al. Individual and community-level risk factors for HIV stigma in 21 Zambian and South African communities: Analysis of data from the HPTN071 (PopART) study. AIDS 32 , 783–793 (2018).
Peltzer, K. & Pengpid, S. Prevalence and associated factors of enacted, internalized and anticipated stigma among people living with HIV In South Africa: Results of the first national survey. HIV/AIDS - Res. Palliat. Care 11 , 275 (2019).
Google Scholar
Onu, D. U. Treatment adherence mediates the relationship between HIV-related stigma and health-related quality of life. AIDS Care 33 , 1335–1339 (2021).
Andersson, G. Z. et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV 7 , e129–e140 (2020).
Shubber, Z. et al. Patient-reported barriers to adherence to antiretroviral therapy: A systematic review and meta-analysis. PLOS Med. 13 , e1002183 (2016).
PubMed PubMed Central Google Scholar
Katz, I. T. et al. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J. Int. AIDS Soc. 16 , 18640 (2013).
Ahmed, S. et al. Why do people living with HIV not initiate treatment? A systematic review of qualitative evidence from low- and middle-income countries. Soc. Sci. Med. 213 , 72–84 (2018).
Fuge, T. G., Tsourtos, G. & Miller, E. R. Risk factors for late linkage to care and delayed antiretroviral therapy initiation among adults with HIV in sub-Saharan Africa: A systematic review and meta-analyses. Int. J. Infect. Dis. 122 , 885–904 (2022).
CAS PubMed Google Scholar
Gesesew, H. A. et al. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: A systematic review and metaanalysis. PLoS One 12 , e0173928 (2017).
UNAIDS. Global AIDS Strategy 2021–2026 — End Inequalities. End AIDS. https://www.unaids.org/en/resources/documents/2021/2021-2026-global-AIDS-strategy (2021).
Tsai, A. C. et al. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS Behav. 17 , 427 (2013).
Tesfay, A., Gebremariam, A., Gerbaba, M. & Abrha, H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle Town, northern Ethiopia. Biomed Res. Int. 2015 , 516369 (2015).
A guide to health economic evaluations. Drug Ther. Bull. 48 , 105–108 (2010).
Tran, B. X., Ohinmaa, A. & Nguyen, L. T. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual. Life Outcomes 10 , 132 (2012).
Thomas, R. et al. Differences in health-related quality of life between HIV-positive and HIV-negative people in Zambia and South Africa: a cross-sectional baseline survey of the HPTN 071 (PopART) trial. Lancet Glob. Heal. 5 , e1133–e1141 (2017).
Hayes, R. J. et al. HPTN 071 (PopART): Rationale and design of a cluster-randomised trial of the population impact of an HIV combination prevention intervention including universal testing and treatment - a study protocol for a cluster randomised trial. Trials 15 , 1–17 (2014).
EuroQol Research Foundation. EQ-5D-5L user guide . https://euroqol.org/publications/user-guides (2019).
Wu, A. W. et al. Responsiveness of the MOS-HIV and EQ-5D in HIV-infected adults receiving antiretroviral therapies. Health Qual. Life Outcomes 11 , 42 (2013).
Stangl, A. L. et al. Development of parallel measures to assess HIV stigma and discrimination among people living with HIV, community members and health workers in the HPTN 071 (PopART) trial in Zambia and South Africa. J. Int. AIDS Soc. 22 , e25421 (2019).
Robitzsch, A. & Grund, S. miceadds: Some Additional Multiple Imputation Functions, Especially for 'mice'. R package version 3.16-18. https://CRAN.R-project.org/package=miceadds (2023)
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/ (2022).
Simwinga, M. et al. Implementing community engagement for combination prevention: Lessons learnt from the first year of the HPTN 071 (PopART) community-randomized study. Curr. HIV/AIDS Rep. 13 , 194–201 (2016).
Bond, V. et al. Value and limitations of broad brush surveys used in community-randomized trials in Southern Africa. Qual. Health Res. 29 , 700–718 (2019).
Simwinga, M. et al. Disseminating complex primary outcome results from a community-randomised trial to Zambian communities: lessons learned using a community dialogue approach in the HPTN 071 (PopART) trial. Lancet HIV 9 , e801–e808 (2022).
Ashaba, S. et al. Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Glob. Ment. Heal. 5 , 1–10 (2018).
Yi, S. et al. AIDS-related stigma and mental disorders among people living with HIV: A cross-sectional study in Cambodia. PLoS One 10 , e0121461 (2015).
Bond, V. et al. “Being seen” at the clinic: Zambian and South African health worker reflections on the relationship between health facility spatial organisation and items and HIV stigma in 21 health facilities, the HPTN 071 (PopART) study. Heal. Place 55 , 87–99 (2019).
Stangl, A. L., Lloyd, J. K., Brady, L. M., Holland, C. E. & Baral, S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come?. J. Int. AIDS Soc. 16 , 18734 (2013).
Nyblade, L. et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 17 , 1–15 (2019).
UNAIDS. Evidence for eliminating HIV-related stigma and discrimination — Guidance for countries to implement effective programmes to eliminate HIV-related stigma and discrimination in six settings . https://www.unaids.org/en/resources/documents/2020/eliminating-discrimination-guidance (2020).
Stangl, A. L. et al. The effect of universal testing and treatment on HIV stigma in 21 communities in Zambia and South Africa. AIDS 34 , 2125–2135 (2020).
Davis, K. et al. The effect of universal testing and treatment for HIV on health-related quality of life – An analysis of data from the HPTN 071 (PopART) cluster randomised trial. SSM Popul Health . 23 , 101473 (2023).
Prinsloo, C. D., Greeff, M., Kruger, A. & Khumalo, I. P. HIV stigma experiences and stigmatisation before and after a HIV stigma-reduction community “hub” intervention. Afr. J. AIDS Res. 16 , 203–213 (2017).
Pantelic, M., Steinert, J. I., Park, J., Mellors, S. & Murau, F. ‘Management of a spoiled identity’: Systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Glob. Heal. 4 , e001285 (2019).
Hargreaves, J. R. et al. HIV stigma and viral suppression among people living with HIV in the context of universal test and treat: Analysis of data from the HPTN 071 (PopART) trial in Zambia and South Africa. J. Acquir. Immune Defic. Syndr. 85 , 561–570 (2020).
Bertram, M. Y., Lauer, J. A., Stenberg, K., Ralaidovy, A. H. & Edejer, T. T. T. Progressive Realisation of Universal Health Coverage in Low- and Middle-Income Countries: Beyond the ‘Best Buys’. Int. J. Heal. policy Manag. 10 , 697–705 (2021).
Download references
Acknowledgements
We are grateful to all members of the HPTN 071 (PopART) Study Team and to the study participants and their communities for their contributions to this research. HPTN 071/PopART was sponsored by the National Institute of Allergy and Infectious Diseases (NIAID) under Cooperative Agreements UM1-AI068619, UM1-AI068617, and UM1-AI068613, with funding from the U.S. President's Emergency Plan for AIDS Relief (PEPFAR). Additional funding was provided by the International Initiative for Impact Evaluation (3ie) with support from the Bill & Melinda Gates Foundation, as well as by NIAID, the National Institute on Drug Abuse (NIDA) and the National Institute of Mental Health (NIMH), all part of NIH. The stigma ancillary study was funded by NIMH. EH, KD, JO, MP, SG, and KH acknowledge funding from the Medical Research Council Centre for Global Infectious Disease Analysis (reference: MR/R015600/1), jointly funded by the UK Medical Research Council (MRC) and the UK Foreign, Commonwealth & Development Office (FCDO), under the MRC/FCDO Concordat agreement and is also part of the Second European & Developing Countries Clinical Trials Partnership (EDCTP2) programme supported by the European Union; and acknowledge funding by Community Jameel. KD was also supported by the Wellcome Trust (reference: 220098/Z/20/Z). JH, TP, GH, TM, VB and AS received writing support from the Bill & Melinda Gates Foundation (reference: INV-005239). KH was also partially funded by the National Institute for Health and Care Research (NIHR) Health Protection Research Unit in Modelling and Health Economics, a partnership between Public Health England, Imperial College London and London School of Hygiene and Tropical Medicine (reference: NIHR200908). RH receives funding from the MRC and the FCDO under the MRC/FCDO Concordat agreement and is also part of the EDCTP2 programme supported by the European Union (reference: MR/R010161/1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAID, NIMH, NIDA, PEPFAR, 3ie, the Bill & Melinda Gates Foundation, the NIHR, Public Health England or the UK Department of Health and Social Care. For the purpose of open access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Author information
A list of authors and their affiliations appears at the end of the paper.
Authors and Affiliations
MRC Centre for Global Infectious Disease Analysis, Imperial College London, London, UK
Emily Hall, Katherine Davis, Julius Ohrnberger, Michael Pickles, Simon Gregson & Katharina Hauck
Abdul Latif Jameel Institute for Disease and Emergency Analytics, School of Public Health, Imperial College London, London, UK
Department of Health Policy, London School of Economics, London, UK
Ranjeeta Thomas
Department of Public Health, Environments and Society, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London, UK
James R. Hargreaves & Triantafyllos Pliakas
Zambart, School of Medicine, University of Zambia, Lusaka, Zambia
Justin Bwalya, Tila Mainga, Kwame Shanaube & Virginia Bond
Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Faculty of Medicine and Health, University of Stellenbosch, Cape Town, South Africa
Rory Dunbar, Graeme Hoddinott & Peter Bock
Department of Global Health and Development, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London, UK
Tila Mainga & Virginia Bond
Department of Clinical Research, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK
Helen Ayles
Hera Solutions, Baltimore, MD, USA
Anne L. Stangl
Department of International Health, Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, USA
Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, WA, USA
Deborah Donnell, Lynda Emel, Lisa Bunts, Heather Noble, Megan Baldwin & Erin Hughes
Department of Infectious Disease Epidemiology, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, UK
Richard Hayes
Department of Infectious Disease, Faculty of Medicine, Imperial College London, London, UK
Sarah Fidler
London School of Hygiene & Tropical Medicine, London, UK
James R. Hargreaves, Deborah Watson-Jones, Peter Godfrey-Faussett, Kalpana Sabapathy & Virginia Bond
Imperial College London, London, UK
Katharina Hauck, Peter C. Smith, Anne Cori & Michael Pickles
Desmond Tutu TB Centre, Stellenbosch University, Stellenbosch, South Africa
Nomtha Bell-Mandla, Blia Yang, Anelet James, Redwaan Vermaak, Nozizwe Makola, Graeme Hoddinott, Vikesh Naidoo & Lyn Horn
Zambart, University of Zambia School of Medicine, Lusaka, Zambia
Virginia Bond, Musonda Simwinga, Alwyn Mwinga, Barry Kosloff, Mohammed Limbada, Justin Bwalya, Chepela Ngulube & Albert Mwango
Nuffield Department of Medicine, Oxford University, Oxford, UK
Christophe Fraser
Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, MD, USA
Susan Eshleman, Yaw Agyei, Vanessa Cummings, Denni Catalano, Estelle Piwowar-Manning & Shauna Wolf
HIV Prevention Trials Network Statistical and Data Management Center, Statistical Center for HIV/AIDS Research and Prevention, Seattle, WA, USA
Deborah Donnell
Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD, USA
David Burns & Alain Kouda
FHI 360, Durham, NC, USA
Niru Sista, Ayana Moore, Rhonda White, Tanette Headen, Eric Miller & Kathy Hinson
Yale University, New Haven, CT, USA
Sten Vermund
Ropes & Gray, Boston, MA, USA
Mark Barnes
Mailman School of Public Health, Columbia University, New York, NY, USA
Wafaa el-Sadr
You can also search for this author in PubMed Google Scholar
- James R. Hargreaves
- , Deborah Watson-Jones
- , Peter Godfrey-Faussett
- , Kalpana Sabapathy
- , Katharina Hauck
- , Peter C. Smith
- , Anne Cori
- , Michael Pickles
- , Nomtha Bell-Mandla
- , Blia Yang
- , Anelet James
- , Redwaan Vermaak
- , Nozizwe Makola
- , Graeme Hoddinott
- , Vikesh Naidoo
- , Virginia Bond
- , Musonda Simwinga
- , Alwyn Mwinga
- , Barry Kosloff
- , Mohammed Limbada
- , Justin Bwalya
- , Chepela Ngulube
- , Christophe Fraser
- , Susan Eshleman
- , Yaw Agyei
- , Vanessa Cummings
- , Denni Catalano
- , Estelle Piwowar-Manning
- , Deborah Donnell
- , Lynda Emel
- , Lisa Bunts
- , Heather Noble
- , David Burns
- , Alain Kouda
- , Niru Sista
- , Ayana Moore
- , Rhonda White
- , Tanette Headen
- , Eric Miller
- , Kathy Hinson
- , Sten Vermund
- , Mark Barnes
- , Albert Mwango
- , Megan Baldwin
- , Shauna Wolf
- , Erin Hughes
- & Wafaa el-Sadr
Contributions
K.D. and K.H. developed the research idea, with guidance from R.H., S.F., P.B., H.A., J.R.H., G.H., and V.B. A.S., J.R.H., V.B. and G.H. developed the HPTN 071 (PopART) stigma measures. E.H. and K.D. developed and led the statistical analysis. E.H., K.D., and K.H. took the lead on writing and revising of the article. R.H., S.F., P.B., and H.A. were the principal investigators of the HPTN 071 (PopART) study and led the design and conduct of the HPTN 071 (PopART) study. All other authors contributed to conception or design of the HPTN 071 (PopART) trial, acquisition of data, and interpretation of data for the current work. All authors made substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data, and all authors either drafted the work or revised it critically for important intellectual content. All authors approved the manuscript for submission and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Katherine Davis .
Ethics declarations
Competing interests.
SG declares holding shares in AstraZeneca and GlaxoSmithKline. All other authors declare no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hall, E., Davis, K., Ohrnberger, J. et al. Associations between HIV stigma and health-related quality-of-life among people living with HIV: cross-sectional analysis of data from HPTN 071 (PopART). Sci Rep 14 , 12835 (2024). https://doi.org/10.1038/s41598-024-63216-3
Download citation
Received : 31 August 2023
Accepted : 27 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1038/s41598-024-63216-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
FIND AN AGING LIFE CARE EXPERT
- What is Aging Life Care
- ALCA Partners

Breaking the Stigma: Embracing Mental Health Treatment in Older Adults
By Sam van Kalkeren, MSN, RN, CMC, CDP, CADDCT – Aging Life Care Association ®
Mental health is just as important as physical health for older adults. Let’s break the stigma and prioritize mental well-being. #MentalHealthAwarenessMonth
Many people with mental illness report that the stigma surrounding mental illness is more challenging to deal with than the mental illness itself. Stigma can make reaching out for help difficult, leaving someone feeling judged, alone, or as though no one could understand what they are going through.
Stigma is basically a brand of shame put on a person or group of people. It’s based on negative attitudes and beliefs that aren’t always true. According to the National Library of Medicine , is “characterized by negative stereotypes, prejudice, and discrimination, is a significant impediment in psychiatric care, deterring the timely provision of this care and hindering optimal health outcomes.” Stigma creates perceptions that cause the public to “fear, avoid, and discriminate against people with mental illnesses,” according to a report by the President’s New Freedom Commission on Mental Health.
There is stigma associated with mental illness. This ethics-laden issue is a barrier to individuals seeking or engaging in treatment services.
Mental health stigma can either be public stigma, self-stigma, or a combination of the two. Often, public stigma can create self-stigma (if it doesn’t already exist).

Examples of Mental Illness Stigma
People in the media and even in our communities will refer to someone with a mental illness as “dangerous,” “crazy,” or “incompetent” rather than unwell. There is often an idea that if you ask for help, you are “weak.” These examples cause more people to suffer in silence than realize it is braver to seek help and not struggle alone. There is also significant stigma in the language we use to describe behaviors that we assume are associated with a diagnosis.
Inaccurate stereotypes, labels, and descriptions all contribute to someone’s ability to ask for help. Someone labeled as a “procrastinator” may be struggling with anxiety. Telling them to “try harder” and “get over it” may not motivate them because it’s inaccurate to what’s going on for them. When someone refuses to eat, saying “they should just eat” can cause more harm. Saying someone “committed suicide” is yet another form of hurtful language implying the person “committed” an action, which is often seen as a crime instead of a mental illness. We need to be more aware of the way we add to the stigma against people with mental illnesses.
Stigma creates a barrier to mental health services, which, as a result, can create isolation and avoidance.
The Harmful Effects of Stigma
Some harmful effects of stigma include:
- Feelings of shame, hopelessness, and isolation
- Reluctance to ask for help or to get treatment
- Lack of understanding by family, friends, or others
- Fewer opportunities for employment or social interaction
- Bullying, physical violence, or harassment
- Self-doubt – the belief that you will never overcome your illness or be able to achieve what you want in life.
The most significant consequence of stigma is that people don’t get the treatment they need. Hence, fewer than half of those with a mental health condition get treatment, according to Mental Health America. People are afraid to disclose that they have mental health problems. They fear they will be treated differently.
Reducing Stigma
To reduce stigma, we all must commit to action—and many are very simple. Awareness of our language is one of the most significant changes we can all make, causing us to confront myths and stereotypes and become more open to the challenges someone may face. Becoming educated on different mental health topics allows us to become more aware of our language. Attending seminars and reading the research (including what you’re doing right now) are ways we can be actively engaged in reducing stigma. Understanding also creates empathy, so don’t be afraid to talk about it!
Mental Health Stereotypes
Next, confront negative stereotypes when they come up in conversations. Educate people against negative, inaccurate language to describe someone who might be struggling. Lean into helping them understand how saying they experienced a “panic attack” when maybe it was elevated stress could create harm for someone who struggles with panic. Remember, people are not their illness, so be mindful of describing people with mental illness as someone who “lives with” or “has…” vs. that “they are…”. Share your education with family, friends, and people in your circles. An important reminder when sharing your information or offering someone feedback is to remember they were probably uninformed, so be sensitive in your delivery. This can make all the difference to them leaning in versus rejecting what you share.

Learn About Mental Illness Symptoms
While learning more about mental illnesses, learn how to become a faithful ally —whether within your community, online, or different activist groups. Interacting with people who have mental illness and becoming an ally can also help you better understand some of the struggles they face regularly. Understanding people for who they are rather than their illness is also essential.
If you have ever struggled with stigma or mental health, it’s also vital for you to get the help you need. Reach out to people you trust who can help you find the best services. Don’t be afraid to lead by example by sharing about asking and receiving help when and if you need it. This story could save someone else’s life. Owning your experience helps not only you as well as others. Speaking up can help dispel myths and even empower others to know it is ok for them to get help. Together, we can all help people understand that mental illness is not shameful and can often be helped.
Together, we can all learn how to better offer support and acceptance to family, friends, neighbors, and community members who have mental health challenges. As a result of all of us leaning in to do our part in breaking the stigma, more people will be able to get the actual help they need and, as a result, live more fulfilling, healthier lives.
Mental Health Resources and Support:
Help is available.
Take the initiative to educate yourself about common mental health disorders in older adults, signs and symptoms to watch out for, and appropriate ways to offer support and assistance. Here are some resources you can explore to learn more about aging and mental health.
- National Coalition on Mental Health and Aging
- Resources from the E4 Center of Excellence for Behavioral Health Disparities in Aging
- Resources for older adults from the Substance Abuse and Mental Health Services Administration
- Mental health and aging information from the Center for Disease Control and Prevention
- World Health Organization facts on the mental health of older adults
- Resources from the National Institute of Mental Health on older adults and mental health
- Suicide in Older Adults — and Help for Them
For additional assistance for yourself or a loved one dealing with mental health issues, consider hiring an Aging Life Care Manager to help you navigate care.
This article originally appeared on OConnorPG.com April 2024. It has been edited with permission/approval of the original author for aginglifecare.org.
About the Author:
Sam van Kalkeren , MSN, RN, CMC, CDP, CADDCT is the Director of Aging Services at O’Connor Professional Group. He has been working as a psychiatric RN since 2012 and is a member of the Aging Life Care Association. He is a Care Manager Certified, Certified Alzheimer’s Disease, Dementia Care Trainer, and a Certified Dementia Practitioner through the National Council of Certified Dementia Practitioners. Sam has worked with all age populations, from pediatrics to geriatrics, suffering from mental illness. He has experience working with clients suffering from substance use and co-occurring disorders, complex mental health diagnoses, neurocognitive disorders, and personality disorders. Sam received his Master of Science in Nursing degree, specializing in Leadership and Management, from Aspen University. He invites you to connect with him by visiting the O’Conner Professional Group blog or following Sam on LinkedIn .
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
Comments are closed.

What to Do Before Talking to a Boss About Your Mental Health
When you're tired, stressed, and would rather not be at work..
Posted May 30, 2024 | Reviewed by Gary Drevitch
- What Is a Career
- Find a career counselor near me
- It is essential to understand your own mental health needs before approaching your supervisor at work
- Familiarize yourself with available workplace resources and understand your rights as an employee.
- Pay attention to your workplace culture and communicate your mental health needs clearly.

Mental health, like physical health, exists on a spectrum. Most people experience various levels of anxiety , stress, burnout , and depression depending on the circumstances of their lives. Yet some mental health struggles are easier to discuss openly than others—for example, conversations about burnout tend to be more socially acceptable than those about suicide loss.
When considering whether to talk to your boss about a mental-health concern, first and foremost, it is important to understand your own needs and assess if the life events you are dealing with are interfering with your ability to complete your everyday responsibilities at work. Evaluating the strategies you have tried to reduce the impact of your current problems on your performance will allow for brainstorming other options you might have.
Awareness-building practices such as mindfulness meditation —whether guided through an online app or using a creative writing workbook that also includes breathing exercises and grounding strategies—can aid self-exploration and recognizing patterns (Balan, 2023). Additionally, attention to your diet , including healthy meal choices, minimizing substance use, and getting adequate sleep will help with emotion regulation and improve overall health.
Asking for Help
We are not designed to face life entirely on our own and rely on each other for mental and physical well-being, If you are dealing with a stressful life event that interferes with your day-to-day ability (e.g. divorce ) reaching out to your loved ones or to a trusted colleague for support and guidance will reduce the feeling of isolation.
If stress, sadness, anxiety, or other symptoms are not improving, or are persisting or worsening, consider reaching out to a professional mental health provider. A therapist will be able to assess, diagnose, and treat your symptoms, monitor your progress, as well as communicate any additional support you might need. Connecting with a clinician can be done privately, through your insurance provider, as well as through mental health offerings by your organization.
Know Your Rights
Pay close attention to your workplace culture, how leadership discusses mental health issues, and if there is an atmosphere of support and understanding. If, for example, your company celebrates mental health awareness events, or provides education to managers about communicating and reducing stigma , you will likely have a more pleasant experience (Lu et al., 2022).
Regardless, each business exists for very specific reasons—for profit or not, there is a set of deliverables that must be met. Discussing your own mental health concerns with your boss will be in the context of the laws they must follow, as well as the needs of the organization. Your personal needs are of tertiary concern.
Depending on the size and type of company you work for, federal protections, including the Americans with Disabilities Act (ADA) and the Family Medical Leave Act (FMLA), prevent discrimination due to mental illness, and mandate the protection of your position if you need time off.
Explore what wellness tools your company offers; there may be an Employee Assistance Program (EAP), coaching , childcare options, resources for retreats, and self-care apps. Take time to familiarize yourself with existing policies and procedures that human resources must abide by, and potential options you may have for reasonable accommodations.
Communicate Clearly
After reflecting on your mental health needs, and how they are impacting your work, it’s time to decide what you feel comfortable sharing with your boss. You are not required to share anything you do not want to. It is critical to prioritize your own comfort, well-being, and privacy.

Consider role-playing, or rehearsing what and how you will express yourself and advocate for yourself. Tailor the information so that your boss can clearly understand your situation and direct you to appropriate resources.
If you are working with a clinician, consider speaking with them for guidance based on your needs, as well as a note that outlines recommended workplace accommodations. Your needs may include flexible hours, or meeting schedules to allow for appointments, hybrid work environments to reduce noise or other interruptions, being assigned to another department, or extra time to complete a project.
Be specific about what accommodations you will need, how long they will be necessary, and what they will accomplish.
Document Everything
Keep a record of who you spoke with in your organization, as well as emails and other communications. The purpose is to help you track your progress, what you have tried, and barriers you encountered, as well as successes. Your inherent value to an organization is greater when you are efficient, productive, and competent. It costs systems more to deal with allegations, discriminatory lawsuits, terminating an employee, recruiting, and retraining someone else to replace them.
When business, economic, and employee incentives are aligned, your best efforts to communicate your needs, and the organization’s accommodating response, will likely productively match up (Bondar et al. 2022).
As an informed participant, advocating for yourself, you will experience the support you have earned as an employee, a sense of calm and control at work, while you take care for your mental health needs.
To find a therapist, visit the Psychology Today Therapy Directory .
Balan, D (2023). Re-Write: A Trauma Workbook of Creative Writing and Recovery in Our New Normal . Routledge.
Bondar J, Babich Morrow C, Gueorguieva R, et al. Clinical and Financial Outcomes Associated With a Workplace Mental Health Program Before and During the COVID-19 Pandemic. JAMA Netw Open. 2022; 5(6):e2216349.
Khalid, A, Syed, J. Mental health and well-being at work: A systematic review of literature and directions for future research. Human Resource Management Review. 2024; 34 (1), 100998.
Lu X, Yu H, Shan B. Relationship between Employee Mental Health and Job Performance: Mediation Role of Innovative Behavior and Work Engagement. Int J Environ Res Public Health. 2022; 19(11):6599.

Duygu Balan, LPCC , is a psychotherapist and the co-author of Re-Write: A Trauma Workbook of Creative Writing and Recovery in Our New Normal.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

A Markov Chain Model for Mental Health Interventions
David claudio.
1 Department of Mechanical and Industrial Engineering, University of Massachusetts Lowell, Lowell, MA 01854, USA
Sally Moyce
2 College of Nursing, Montana State University, Bozeman, MT 59717, USA
Tyler Albano
Nick miller, marshall o’leary, associated data.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Poor mental health affects nearly one billion people worldwide and can end in suicide if not treated. Unfortunately, stigma and a lack of mental healthcare providers are barriers to receiving needed care. We developed a Markov chain model to determine whether decreasing stigma or increasing available resources improves mental health outcomes. We mapped potential steps in the mental health care continuum with two discrete outcomes: getting better or committing suicide. Using a Markov chain model, we calculated probabilities of each outcome based on projected increases in seeking help or availability of professional resources. Modeling for a 12% increase in awareness of mental health concerns yielded a 0.39% reduction in suicide. A 12% increase in access to professional help yielded a 0.47% reduction in suicide rate. Our results show that expanding access to professional services has a higher impact on reducing suicide rates than creating awareness. Any intervention towards awareness or access positively impacts reducing suicide rates. However, increased access results in a higher reduction in suicide rates. We have made progress in increasing awareness. Awareness campaigns help to increase recognition of mental health needs. However, focusing efforts on increasing access to care may have a higher impact on reducing suicide rates.
1. Introduction
The World Health Organization (WHO) reported in 2020 that mental disorders affect nearly one billion people worldwide [ 1 ]. According to the same report, one person dies every 40 s by suicide [ 1 ]. The situation has been exacerbated by the COVID-19 pandemic [ 2 , 3 , 4 ].
Many issues can lead to mental disorders, including unemployment, poverty, financial struggles, alcohol or drug abuse, homelessness, uncertainty, isolation, fear, and large-scale movement restrictions [ 3 , 5 , 6 ]. An additional problem is the reluctance of people to seek help when they start experiencing emotional distress, anxiety, or depression [ 7 , 8 , 9 , 10 , 11 ]. Psychiatric intervention for individuals with worsening mental health is critical to treating depression and anxiety and preventing suicide [ 12 , 13 , 14 ].
Two major barriers prevent persons with poor mental health from seeking professional care: stigma and access. Stigma is a complex concept that occurs when an individual deems the need for mental health treatment shameful [ 7 ]. Reluctance to seek formal and informal support is associated with self-stigma [ 7 , 8 , 10 ]. There is a sense of shame that accompanies self-stigma, and the adaptive response to this shame is secrecy; this results in not acknowledging or disclosing mental health problems and not seeking treatment. Access to mental health services is another barrier due to an inability to find a provider or to the high cost of available care [ 15 ]. For example, much of the population in the United States live in a mental health provider shortage area [ 16 ].
In response to the disparities in access to care, recent studies have focused on mental health prevention and treatment programs [ 8 , 9 , 10 , 11 , 12 , 13 , 14 ]. Researchers have used Markov chain models to analyze and evaluate mental health programs in the past, including suicide prevention models. For example, Yip et al. [ 17 ] estimated population suicide risk as a dynamic system to evaluate the effectiveness of suicide prevention programs. They assumed the population remained in equilibrium as births replaced the deceased. While this model was useful for studying the effectiveness of suicide prevention programs, we focused our model on the individual. We aimed to elaborate on the choices individuals can make to determine their state in a Markov chain.
Oskooyee et al. [ 12 ] used real clinical data to model depression severity through Markov transitional matrices. Their Markov chain contains probabilities of moving from one state of depression to another, where state 0 is no depression and state 3 is severe depression [ 12 ]. Through their case study, they demonstrated the effectiveness of professional help with real measured data.
Our research study developed a Markov chain model that details the complicated web an individual enters when dealing with any mental illness (AMI). AMI is defined as a mental, behavioral, or emotional disorder that can range from no impairment to mild, moderate, and even severe impairment [ 18 ]. We developed a transitional matrix that defines the probability of jumping from one attitude or mental state in the Markov chain to another. Throughout the article, we will be answering two main questions:
Q1: What are the probabilities of moving from one mental state to another within our proposed Markov chain?
Q2: Where would the allocation of resources have the most positive impact, increasing awareness (decreasing stigma) so that an individual seeks help, or increasing access to professional resources?
To answer the first question, we performed a literature review to accurately map the cascade effect these probabilities have on the different states within the Markov chain. Consequently, through multiple interpolations, we explored whether resources would be better spent by strengthening the system, which is actively supporting people looking for help, or by increasing the ease of access and awareness of such resources.
Different stages of the potential actions of a person with AMI were mapped through a community-based participatory research process [ 4 , 19 , 20 ]. Members of a community advisory board seeking to reduce poor mental health outcomes created a flowchart to illustrate various stages in the experience of a person with AMI. Figure 1 presents the flowchart as a person moves through recognition of AMI to one of four states: (1) complacency, (2) attempting to remedy the issue alone through healthy behavior, (3) seeking professional help, or (4) electing to participate in unhealthy behavior. For this research, we considered each occurrence in the flowchart as independent of past and future occurrences. In reality, mental health is a constantly evolving state of mind, and an individual may progress through the flowchart many times. We assumed that the end goal was to feel relief from AMI, and we created two discrete outcomes: get better or commit suicide.

Flowchart describing how the actions of an individual determine the potential outcomes.
The flowchart served as a baseline to develop our Markov chain model. A couple of assumptions were made to create the initial Markov chain model. Firstly, the model assumes that doing something beneficial and seeking professional help are mutually exclusive. Individuals could do something beneficial as part of their treatment, but the model differentiates them based on doing something as an individual versus doing something at the recommendation of a professional. Furthermore, actions and individual attempts that are not successful at relieving AMI were not included. For simplicity’s sake, we modeled this as going straight to the final negative outcome (suicide).
Figure 2 displays the generalized Markov chain model for AMI, while Figure 3 displays the generalized transitional matrix of the Markov chain (denoted by P ). Each probability, p ij , represents the probability of transitioning from state i to state j, given that an individual is in state i. One of the most basic assumptions of Markov chains is that the future depends only on the state we are in (current state), not on how we arrived at this state. In other words, the future depends on the present and not on the past [ 21 ].

Markov chain for any mental illness with two absorbing states: get better and commit suicide.

Generalized P matrix for any mental illness (AMI).
Since we looked at each mental health occurrence independently of past and future occurrences, the “get better” state was modeled as an absorbing state. An absorbing state is one which, once entered, cannot be left [ 21 ]. For obvious reasons, the “commit suicide” state was also modeled as an absorbing state.
An absorbing Markov chain with s number of states can be represented by an s × s probability matrix, denoted by P . The canonical form of an absorbing matrix with m absorbing states can be represented with four matrices within P . Figure 4 displays the canonical form of an absorbing Markov chain probability matrix [ 21 ]. The matrix denoted by Q represents the probability of transitioning from a transient state to another, while the R matrix describes the probability of transitioning from a transient state to an absorbing state. The 0 matrix contains only zeroes (0), while I represents an m × m identity matrix created by grouping the absorbing states.

Canonical form of an absorbing Markov chain probability matrix [ 21 ].
The matrix (I-Q) −1 is referred to as the Markov chain’s fundamental matrix, which provides the expected number of visits from one transient state to another before being absorbed. The matrix (I-Q) −1 R provides the probability of eventually ending in an absorbing state from any transient state.
The first task was to answer research question #1 by conducting a literature review to accurately map the probabilities within our Markov chain model. A total of sixteen probabilities needed to be populated (p 11 , p 12 , p 14 , p 15 , p 21 , p 23 , p 25 , p 31 , p 33 , p 34 , p 35 , p 36 , p 41 , p 44 , p 45 , and p 46 ). With these probabilities, we created our current state model to serve as a baseline.
We then conducted a series of experiments in which we increased two factors: awareness of seeking professional help (increased awareness) and access to receiving professional help (increased access). Each factor was increased by 4, 8, and 12% from the current state while the other factors were left constant. We then conducted a third experiment in which both factors were increased 2, 4, and 6% concurrently (which corresponds to a combined increase of 4, 8, and 12%). In all three experiments, we were interested in reducing the overall probability that someone recognizing AMI would eventually commit suicide. With these experiments, we wanted to explore whether resources would be better spent by increasing awareness (p 12 ) or strengthening the system to increase access for those seeking professional help (p 23 ).
3.1. Current State
The review of the literature revealed that the global suicide rate is approximately 1.4% in the general population, but among people with AMI, the rate jumps to 6.5% [ 22 ]. We used the 1.4% rate as the probability of moving from any state into the “commit suicide” state (p 15 = p 25 = p 35 = p 45 = 0.014). As previously stated, suicide is an absorbing state and, therefore, p 55 = 1. We used the 6.5% rate to validate our model with the probability that someone who recognizes any mental illness will eventually commit suicide.
In the U.S., 45% of individuals with a clinical-level mental problem do not seek professional help [ 15 ]. Furthermore, approximately 29% of those individuals who do not seek professional help prefer to manage their challenges on their own or do not think they need mental health treatment or therapy [ 15 ]. This led to setting p 14 = 0.13 (29% of the 45%) and p 11 = 0.32 (45 − 13%). Consequently, the probability of recognizing AMI and seeking help (p 12 ) was estimated as 1 − p 11 − p 14 − p 15 = 1 − 0.32 − 0.13 − 0.014 = 0.536.
Approximately 27.5% of the people not receiving help claim the primary reason as lack of affordability or access [ 15 ]. This led to setting p 21 = 0.124 (27.5% of 45%). This probability represents the chances of ending in state (1,1) given that there is no access or people cannot afford professional help.
In 2020, only 46.2% of adults with AMI in the U.S. received mental health services [ 18 ]; alternatively stated, of the 53.6% of people who seek care, 86.2% successfully accessed it. Therefore, we estimated p 23 = 0.862 to achieve the 46.2% of adults who seek and receive care [ 18 ]. Finally, professional help has an estimated 80% effectiveness rate [ 23 ], and thus p 36 = 0.800. Figure 5 presents the current state Markov chain model with the probabilities found in the literature.

Current state Markov chain model for any mental illness. * Statistic obtained directly from the literature; + Calculated from statistics obtained from the literature.
Some probabilities within our Markov chain lacked current literature and were missing proper data (p 31 , p 33 , p 34 , p 41 , p 44 , p 46 ). They can be classified into one of two major categories: (1) statistics of people who receive professional service with no effect, and (2) statistics regarding what happens to people who decide to do something beneficial on their own. Therefore, these values were inferred and adjusted until we achieved a final probability close to the 6.5% suicide rate for people with mental health problems.
For the probabilities regarding ineffective professional services (p 31 , p 33 , p 34 ), we assumed 10% of the population returns to the initial state of realizing they have AMI (p 31 = 0.100). After removing the chance of committing suicide (0.014), the remaining probabilities were equally divided among the two states (p 33 = p 34 = 0.043).
For the probabilities regarding doing something beneficial (p 41 , p 44 , p 46 ), we assumed that after removing the chance of committing suicide (0.014), the remaining states had an equal chance of being achieved. Therefore, 0.986 was equally divided among the three probabilities (p 41 = p 44 = p 46 = 0.32866). For simplicity, we assigned two probabilities at 0.329 and the third at 0.328. All these probabilities resulted in the P matrix presented in Figure 6 . For convenience, Figure 7 and Figure 8 present the Q and R transient and absorbing state matrices for the current state.

Current state P matrix.

Q matrix (current state).

R matrix (current state).
The fundamental matrix for the current state is found by subtracting the transient matrix from the identity matrix and taking the inverse of the resulting matrix ( Figure 9 ). As seen in Figure 9 , the highest number in the matrix is in recognizing AMI. This number (2.035) means an individual will end up in this state twice before getting better or committing suicide.

Fundamental matrix (current state).
The absorbing matrix for the current state is found by multiplying the fundamental matrix by the R matrix ( Figure 10 ). From the absorbing matrix, we note a probability of 6.39% that an individual who recognizes AMI will eventually commit suicide, which is close to the 6.5% found in the literature [ 22 ].

Absorbing matrix (current state).
3.2. Future State #1: Increasing Awareness of Seeking Professional Help
Increasing awareness of seeking professional help involves increasing the probability of moving from recognizing AMI to seeking professional help (p 12 ). Increasing p 12 results in a decrease in p 11 and p 14 . The changes on p 11 and p 14 were estimated in the same manner as the current state. For example, a 4% increase in seeking professional help results in 41% of the population not seeking help (4% lower than the current state, which was 45%). We continued to assume that 29% of individuals who do not seek professional help prefer to manage their challenges on their own [ 15 ]. This results in p 14 = 11.89% (29% of 41%) and the remainder going to p 11 (41% − 11.89% = 29.11%).
Table 1 presents the new probabilities according to each scenario. Table 2 presents the probabilities that someone who recognizes AMI will eventually commit suicide for each of the proposed scenarios. The table also presents the suicide rate reduction of each scenario against the current state (6.39%) and the additional rate reduction compared to the previous scenario.
Revised probabilities for increasing awareness of seeking professional help.
Results of increasing awareness of seeking professional help.
For example, increasing awareness by 4% from the current state reduces the suicide rate by 0.1419%, whereas increasing awareness from 4% to 8% awareness sees an additional reduction of 0.1278%. The results from Table 2 show that the suicide rate reduces with every scenario, but the reduction slightly weakens as awareness increases.
3.3. Future State #2: Increasing Access to Professional Services
Increasing access to services involves increasing the probability of receiving help for those who seek help (p 23 ). Increasing p 23 only affects p 21 . Table 3 presents the new probabilities according to each scenario, whereas Table 4 presents the results of these experiments. Similar to the previous experiment, the results from Table 4 show that the suicide rate reduces with every scenario, but the reduction weakens as access increases.
Revised probabilities for increasing access to professional services.
Results of increasing access to professional services.
3.4. Future State #3: Increasing Awareness and Access to Professional Services
Increasing awareness and access to professional services involves all the probabilities that changed during the previous two experiments (p 11 , p 12 , p 14 , p 21 , and p 23 ). We decided to increase both factors by 2, 4, and 6%, which corresponds to a combined increase of 4, 8, and 12%. Table 5 presents the revised probabilities for increasing awareness and access to professional services, whereas Table 6 presents the results of increasing awareness and access concurrently in equal proportions.
Revised probabilities for increasing awareness and access to professional services.
Results of increasing awareness and access to professional services.
4. Discussion
While we found relevant statistics related to AMI, suicide rates, and the effectiveness of professional service, our review of the literature revealed a lack of relevant statistics. These statistics can be classified into two major categories: (1) statistics related to ineffective professional services (p 3j ), and (2) statistics regarding people who decide to do something beneficial on their own (p 4j ). For research purposes, these values were estimated and adjusted until we achieved a final probability close to the 6.5% suicide rate for people with AMI. A total of six probabilities in our chain fell into these two classifications, which resulted in the biggest limitation of this study.
We conducted a series of experiments in which we increased two factors: increased awareness and increased access. While the results suggest that increasing either of these factors reduced suicide rates, we found that increasing access resulted in a larger reduction. Interestingly, this reduction was larger than the reduction sought when we combined awareness and access. Figure 11 shows the reductions in suicide rates for each of the three options at different increment levels.

Reductions in suicide rates when increasing awareness, access, and both by 4, 8, and 12%.
With every 4% increase in awareness and/or access, the reduction in suicide rates weakened. Figure 12 shows that increases in awareness result in more diminishing effects than increases in access or increases in both.

Additional improvements in suicide rates for every 4% increase in awareness and/or access.
We believe that increased access to health services resulted in a greater reduction in suicide rates, because access eliminates some of the pathways in the model that lead to “commit suicide.” For example, an increase in p 23 , results in a reduction in p 21 ; therefore, the chances of going through p 21 → p 15 are reduced. There is also a reduction in the chances of taking the p 21 → p 14 → p 45 pathway. Furthermore, assuming an 80% effectiveness of treatment (as found in the literature), increased access would logically result in improvements in AMI. Conversely, increasing awareness without increasing access adds more people to the p 12 → p 23 → p 36 pathway, but not at the same rate as the previous alternative. In addition, it also adds more people to the p 12 → p 21 pathway, which could still lead to the previously mentioned pathways of p 21 → p 15 and p 21 → p 14 → p 45 .
In contrast, the potential effects of increased awareness could be hindered by the percentage that returns to state one (through the p 12 → p 21 pathway). In practice, this finding means that increased awareness can only have a positive outcome if people can find the services they are looking for (access). If we increase awareness without increasing access (via affordability or extra capacity), then it is conceivable that a percentage of the population will loop back to the initial state (state 1). The results also show that when we increased access concurrently with awareness at the same rate, the suicide rate reduced at a steady pace. Studies of attitudes toward seeking professional help reveal that many people who suffer from AMI are confident that they will get better on their own or that their symptoms will eventually disappear [ 24 ]. Others report concerns that seeking professional help will not make a difference [ 25 ]. Therefore, while our results suggest moderate improvement in suicide rates when increasing both awareness and access, other literature suggests interventions that address both aspects may increase mental health professional service utilization overall. Our model did not examine attitudes toward seeking professional help.
These results mathematically display the importance of access to professional services. They also demonstrate the importance of thinking about the benefits of potential intervention plans holistically. For example, rather than spending all our efforts on creating awareness (which might be easier to do than expanding access or improving services), we should perhaps consider spending more than half of our efforts on expanding access for those looking for professional services. Some recommendations for interventions to give people better access to professional help are revoking insurance requirements, consistent online support group attendance, and telehealth recommendations. When our results are extrapolated to the estimated 1 billion persons worldwide with AMI [ 1 ], increasing awareness and access could result in 1.42 to 4.73 million suicides that could be prevented each year.
5. Conclusions and Future Recommendations
This research study developed a Markov chain model that details the complicated web people enter when dealing with AMI. Our literature review found reliable statistics on some aspects related to AMI and suicide, but a lack of statistics related to ineffective professional service and the potential benefits of independent actions taken by those with AMI. We also conducted a series of experiments in which we increased two factors, awareness and access. The results reveal that while intervention does reduce suicide rates, access results in a greater reduction. Strategies aimed at improving access, such as telehealth or financial assistance, could result in reduced suicides.
Additional strategies must address individuals’ reluctance to seek professional services, as simply increasing supply does not increase demand. Potential interventions to improve attitudes toward seeking help may include social media campaigns and tailoring interventions to cultural and socio-economic characteristics [ 26 ].
Future research should focus on understanding the outcomes for the 20% of individuals who have access to professional services but do not find them effective. Additional research could focus on the outcomes for those who decide to do something beneficial on their own. Furthermore, given the widespread mental health impact of COVID-19, the projections we found are likely to change as more research examines these outcomes. Future research should also look at other factors, such as economic status, social support, and access to medication, and the role they might play in suicide rates.
Mental health is a public health crisis, and suicide is a global concern. While recent awareness campaigns have sought to reduce stigma and encourage persons with AMI to seek care, access to professional care remains a barrier. Strategies to develop the mental health workforce and reduce geographical and financial barriers may be effective in increasing access and reducing suicide rates.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, D.C. and S.M.; methodology, D.C., T.A., E.I., N.M. and M.O.; software, T.A.; validation, T.A., E.I., N.M. and M.O.; formal analysis, D.C. and S.M.; investigation, D.C.; resources, D.C.; data curation, T.A., E.I., N.M. and M.O.; writing—original draft preparation, D.C., T.A., E.I., N.M. and M.O.; writing—review and editing, D.C. and S.M.; visualization, D.C.; supervision, D.C. and S.M.; project administration, D.C. and S.M.; funding acquisition, Not Applicable. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
This study did not involve human participants.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
Therefore, this literature review aims to examine the manifestation and impacts of stigma across different cultural contexts, laying the foundation for tailored strategies to combat this healthcare barrier. Review. ... Furthermore, mental illness stigma often intersects with other forms of stigma, such as gender, race, and socio-economic status ...
The purpose of the present literature review is twofold (i) to examine the existing research on the stigma surrounding psychiatry across different cultural contexts and (ii) to identify the ...
Mental illness stigma was assessed using existing conceptualisation i.e. personal and perceived stigma relating to self (intra-personal) and others (inter-personal), and broad domains (e.g. attitudes and beliefs, emotional reactions, and social distancing) [].The coding of help-seeking beliefs was informed by the theory of planned behaviour [], assessing not only help-seeking intentions but ...
A systematic review of barriers and facilitators to mental health help-seeking in young people showed the key barriers to be stigma, confidentiality issues, lack of accessibility, self-reliance, low knowledge about mental health services and fear/stress about the act of help-seeking or the source of help itself (Gulliver et al. Reference ...
anti-stigma campaigns which aim to reduce mental health-related stigma in society. The relevance of this review to the author's development through clinical psychology training is to develop a clearer understanding of the literature around mental health stigma and help-seeking to inform the design of her final year research thesis.
Stigma related to mental illness compounds mental health disparities by creating barriers to help-seeking behavior. We examine the current tools designed to red … A Narrative Review of Mental Illness Stigma Reduction Interventions Among African Americans in The United States ... The authors reviewed the current evidence in the literature for ...
Researchers have long recognized that stigma is a global, multi-level phenomenon requiring intervention approaches that target multiple levels including individual, interpersonal, community, and structural levels. While existing interventions have produced modest reductions in stigma, their full reach and impact remain limited by a nearly exclusive focus targeting only one level of analysis.
The majority of people experiencing mental-health problems do not seek help, and the stigma of mental illness is considered a major barrier to seeking appropriate treatment. More targeted interventions (e.g. at the workplace) seem to be a promising and necessary supplement to public campaigns, but little is known about their effectiveness. The aim of this systematic review is to provide an ...
Although research suggests that mental health professionals stigmatize mental illness, studies on this topic are relativity new. Little is known about the state of this research and existing literature reviews exhibit multiple limitations. Accordingly, a scoping review was performed on the endorsed stigmatization of mental illness by mental health professionals, with the aim of exploring how ...
However, research on initiatives targeting stigma of mental illness among mental health professionals is limited. ... 4.3 Method. A systematic literature review was performed using the databases MEDLINE, CINAHL, PsycINFO, PubMed, Scopus, Google Search engine and Google Scholar. The papers were limited to English language, published in peer ...
A particular issue which requires consideration through such a review is the best way to assess dual stigma. There is no shortage of mental health stigma measures. In a critical review of mental illness stigma measures, over 400 were identified, a situation that has been described as 'overwhelming' (Fox et al., Citation 2018).
Australian national mental health policy outlines the need for a nationally coordinated strategy to address stigma and discrimination, particularly towards people with complex mental illness that is poorly understood in the community. To inform implementation of this policy, this review aimed to identify and examine the effectiveness of existing Australian programs or initiatives that aim to ...
1.2 Literature Review. In the 1950's and 1960's two key conclusions were drawn regarding people. diagnosed with mental illnesses. First, people with mental illnesses were often. socially rejected. Second, mental illness and the label of having a mental illness were. associated with fear, distrust, and dislike.
Community health workers (CHWs) are facilitators between health services and service users, providing essential and effective support to those seeking health care. However, stigmatizing attitudes towards people with mental illness also exist among CHWs and are based on prejudicial and biasedopinions. This integrative review critically assessed evidence regarding CHWs approaches for addressing ...
The proposed review will add to the literature around mental health treatment for LGBTQA+ people with psychosis. ... Laurens KR, Evans-Lacko S. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. ... Harris S. The lesbian, gay, bisexual and ...
This graduate project conducted a scoping review of the literature using published studies from 2018 to the present, to explore the experiences of Asian American young adult college students regarding their help-seeking attitudes toward mental health. Internal and external factors were examined to determine their role in shaping help-seeking.
This meta-synthesis was designed to understand how stigma impacts the coping, mental health, adherence, and engagement in care of men living with HIV in SSA. Methods. Design. ... The extant literature, and this review, would also benefit from additional intersectional research. Additional insight for studies based on age, such as young or older ...
Likewise, community stigma has previously been linked to avoidance of healthcare, and poor mental health, supporting our finding that experiencing community stigma is negatively associated with ...
Examples of Mental Illness Stigma. People in the media and even in our communities will refer to someone with a mental illness as "dangerous," "crazy," or "incompetent" rather than unwell. There is often an idea that if you ask for help, you are "weak." These examples cause more people to suffer in silence than realize it is ...
Khalid, A, Syed, J. Mental health and well-being at work: A systematic review of literature and directions for future research. Human Resource Management Review. 2024; 34 (1), 100998.
Poor mental health affects nearly one billion people worldwide and can end in suicide if not treated. Unfortunately, stigma and a lack of mental healthcare providers are barriers to receiving needed care. We developed a Markov chain model to determine whether decreasing stigma or increasing available resources improves mental health outcomes.