- Industries Served
- Core Values
- Differentiators
- Employee & Consultant Reviews
- Client Testimonials
- Corporate Social Responsibility
- Quality Assurance
- Regulatory Affairs
- Clinical Operations
- Commissioning, Qualification, and Validation
- Chemistry, Manufacturing, and Controls
- Pharmacovigilance
- Expert Witness
- Consulting Projects
- Staff Augmentation
- FTE Recruitment
- Functional Service Program
- Browse Consultant CVs
- Start a Consultant Search
- Join Our Consulting Team
- Insider Newsletter
- White Papers
- Case Studies
- The Life Science Rundown
- The Passionate Workforce Podcast
- Regulations and Standards
- The Passionate Workforce
17 April 2024

Clinical Investigator Site Audits: A Guide and Checklist
In the last decade, there has been a significant shift in auditing clinical trials towards a risk-based model. Our approach takes it a step further by incorporating a quality management framework into our clinical audit methodology.
During our audits, we prioritize areas of risk that have the potential to impact patient safety, reliability of study data, and ethical considerations. Additionally, we strive to identify any underlying process deficiencies.
By carefully assessing which processes are affected and the resulting deficiencies, we are able to enhance the efficiency of the corrective and preventive action process (CAPA) by addressing the root cause of process breakdown and finding effective ways to mitigate it.
Our quality system evaluation extends to investigator or vendor sites and sponsors. By utilizing the QM approach, we analyze whether the process deficiencies occurred during the planning, execution, or verification stages.
Through this comprehensive approach, we have delivered clear and impactful audit findings, which have resulted in more successful CAPA measures and sustainable improvements at the process level. In this article, we will delve into the numerous benefits that this approach offers.
| Our services include: Our Quality Assurance team is well-versed in both domestic and international markets, ready to align with your specific compliance requirements and development phase. to enhance and execute your audit program. |
The Basics of Clinical Investigator Site Audits
Clinical investigator site audits are a critical component of clinical research, serving as a quality assurance tool to ensure that the rights, safety, and well-being of human subjects are protected, and that the data generated from clinical trials are accurate, reliable, and verifiable. These audits are conducted to assess compliance with the study protocol, Good Clinical Practice (GCP) guidelines, and applicable regulatory requirements.
What are clinical investigator site audits?
Clinical investigator site audits are formal examinations of how clinical trials are conducted at the research sites. They involve a systematic and independent evaluation of the clinical trial processes and procedures to ensure adherence to clinical protocol, regulatory and ethical standards, and data integrity.
The primary reasons for conducting these audits include:
- To protect the rights and welfare of participants.
- To ensure the credibility and reliability of clinical trial data.
- To verify adherence to the approved protocol and amendments.
- To assess the investigators' and site staff's qualifications and abilities to conduct the trial.
- To ensure that the site is following regulatory requirements and GCP standards.
- To identify areas of potential risk and non-compliance.
- To provide feedback and guidance for continuous improvement.
When are they conducted?
Audits can be performed at various stages of a clinical trial:
- Pre-study audits , before the trial commences, to ensure the site is capable of conducting the trial.
- Routine audits , conducted during the trial, to monitor ongoing compliance and data quality.
- For-cause audits , triggered by specific events or concerns that arise during the trial.
- Close-out audits , conducted after trial completion, to review the entirety of the trial conduct and data collection.
How are they performed?
An audit typically involves:
- A review of essential documents, such as the Investigator's Brochure, trial protocol, informed consent forms, and case report forms.
- Interviews with the principal investigator, study coordinators, and other site staff.
- Direct observation of study processes and procedures.
- Verification of data accuracy by comparing source documents (e.g., medical records) with the data reported to the sponsor.
- Assessment of adverse event reporting and handling.
- Evaluation of the storage and handling of investigational products.
What happens after an audit?
The auditor will provide a report detailing findings and observations after an audit. If non-compliance issues or areas for improvement are identified, the site is usually required to respond with a CAPA. Follow-up audits may be conducted to ensure the CAPA is implemented effectively.
How Clinical Study Audits Have Evolved
In the past, clinical audits were performed based on a set cycle and would cover all aspects of a process from beginning to end.
Instead of routine full-process audits, regulators, including the FDA, now recommend a risk-based approach to determine the timing and focus of audits. This shift emphasizes using resources effectively by targeting areas that present the highest organizational risk.
Audit planning now relies on risk assessments that evaluate operational, regulatory, and compliance factors to identify critical areas for review. Auditors concentrate on elements that affect patient safety, ethical considerations, and data integrity, guided by data analysis and risk indicators. This method enhances organizational efficiency by spotlighting areas with the most significant risk potential.
How We're Taking Clinical Study Audits Even Further
We aim to advance risk-based auditing by applying this approach to identifying and reporting audit findings. This method allows us to highlight non-conformances and pinpoint the flawed processes causing these issues.
By linking deficiencies directly to their consequences, we strengthen our case for necessary changes and improvements, facilitating a clearer understanding among stakeholders of the need for action.
Here's an example to illustrate:
| Consider a scenario where a pharmaceutical company consistently encounters data integrity issues during clinical trials. These issues frequently rank as one of the top findings in regulatory inspections and internal audits. A typical audit might reveal that trial data was not recorded in a timely manner, leading to corrective actions focused on immediate data handling practices, such as retraining staff on proper documentation procedures. However, a more insightful approach would be to investigate the underlying processes contributing to these data integrity issues. For instance, it might be discovered that the electronic data capture (EDC) system is not user-friendly, causing delays in data entry. Alternatively, the root cause could be inadequate staffing or a lack of clear data management protocols. By identifying the core process deficiencies—whether they are technological, procedural, or resource-related—the CAPA can be designed to improve the overall quality management system. This could lead to enhancements in the EDC system, revision of data management protocols, or adjustments in staffing models, thereby preventing similar issues across multiple clinical trials and sites. |
The assessment of the QMS at both the investigator site and the sponsor level is crucial for identifying where failures may have occurred throughout the lifecycle of a clinical study.
Here's how an auditor might approach this assessment:
| Was the study set up correctly? If there were issues in the planning phase, such as inadequate training or unclear protocols, this could lead to systemic problems later on. How well was the study executed? Failures here might include incorrect data collection or non-adherence to the study protocol. Did the principal investigator have proper oversight and control mechanisms to catch issues early? A lack of effective monitoring could allow errors to go unnoticed and unaddressed. Were there prompt and effective corrective actions to address identified errors? Failures to act, or ineffective actions, can exacerbate issues and lead to further non-compliance. |
| Were the tools and instructions provided by the sponsor adequate for successful execution? Insufficient guidance can lead to confusion and non-compliance at the study site. Was the sponsor's monitoring of the clinical study site effective? Inadequate monitoring can miss critical issues that compromise data integrity and participant safety Were there performance indicators to identify risks? The absence of such indicators can prevent the early detection of potential problems. How effective were the sponsor's controls to prevent or mitigate risks? Ineffective controls may not adequately protect against the recurrence of issues. |
The Keys to Success
A clinical investigator site audit checklist.
To ensure FDA compliance during clinical trials, firms should have a comprehensive audit checklist. Here's a structured checklist with key areas to review. Keep in mind this is not exhaustive.
| Verify that the Investigator and site staff have adhered to the IRB-approved study protocol. Confirm documentation and on-site storage of all IRB approvals, amendments, and informed consent documents. Review informed consent forms, medical records, and other source documents for completeness and protocol adherence. Check administrative files, correspondence, subject lists, logs, and forms for accuracy and completeness. Ensure informed consent is obtained using IRB-approved forms and that the process is documented. Review financial interest disclosures from investigators and study staff for currency. Validate that electronic systems meet regulatory requirements and staff are trained in their use. Confirm proper receipt, labeling, inventory, storage, and disposal of the drug. Ensure records are stored and retained according to protocol and regulations. Verify submission of all required reports, especially on safety issues or protocol deviations, to the Sponsor. Assess the Investigator's experience, training, and knowledge of GCP and regulatory requirements. Confirm that the Investigator has sufficient qualified staff and facilities to conduct the trial. Ensure trial subjects receive proper medical care and oversight for trial-related decisions. Check for documented IRB approvals for the research application, consent forms, and subject information. Review compliance with randomization and blinding procedures, and documentation for any unblinding. Ensure data reported to the sponsor is accurate, complete, legible, and timely. Confirm submission of research status to the IRB and immediate reporting of serious adverse events to the sponsor. Review the regulatory binder for completeness, including Form FDA 1572, protocol, and IRB correspondence. Verify qualifications, licenses, and training of all study staff. For high-risk trials, review DSMB reports for compliance issues or patterns. Check that all documents and data are organized and stored securely. Ensure procedures are in place for informing subjects, regulatory authorities, and for subject follow-up. Verify that the IRB and regulatory authorities have been informed of the trial's outcome and that all required reports have been submitted. |
The Importance of Independent Auditors
Conducting an independent audit is essential for several reasons. An objective evaluation is chief among these. Independent audits provide a fresh, unbiased perspective on the quality systems of your program, ensuring a thorough and impartial assessment.
Other reasons include:
Avoiding Conflicts of Interest: Audits performed by parties associated with the program may unintentionally overlook or downplay issues due to inherent conflicts of interest.
Regulatory Compliance: Independent audits are critical for uncovering issues proactively, allowing for corrections before regulatory bodies like the FDA identify them during their inspections.
Vendor Compliance: With the significant investment involved in drug development, ensuring that your vendors adhere to quality standards is crucial. Independent audits scrutinize vendor processes to ensure they meet compliance requirements, safeguarding against costly errors that could be flagged by the FDA.
Risk Mitigation: By identifying and addressing gaps in quality systems early, independent audits help mitigate the risk of non-compliance, which can lead to severe consequences such as trial invalidation or mandated remedial actions.
Investment Protection: Independent audits are a proactive step in protecting your drug development program and financial investment by ensuring that all aspects of the program are compliant and on track.
Quality System Development: Firms like ours not only conduct independent audits but also assist in developing robust quality systems and metrics to monitor ongoing compliance, further safeguarding your investment.
Expertise and Consistency: Independent audits are conducted by seasoned professionals who bring expertise and consistency to the audit process, contributing to the reliability and integrity of your compliance efforts.
To ensure comprehensive compliance and protect your drug development program, we always advise using the services of a specialized firm for independent auditing.
The FDA Group has provided expertise and support in maintaining and improving quality systems for ongoing compliance with FDA regulations for hundreds of firms. Contacting a professional audit service can be a crucial step in ensuring the quality and success of your clinical trial and drug development endeavors.
A Few Investigator Site Audit FAQs
Q: How does a Risk-Based Monitoring (RBM) approach affect the audit process of clinical investigator sites?
RBM tailors the audit process to prioritize the most critical and high-risk aspects of clinical trials. In an RBM approach, auditors give precedence to data and processes that are crucial to protecting human subjects and ensuring the reliability of trial results. Although traditional comprehensive audits may still occur, RBM leads to a more efficient allocation of auditing resources, focusing on areas such as informed consent, adherence to the protocol, and the integrity of reported data. Auditors use a combination of on-site and centralized monitoring techniques to identify and mitigate risks throughout the study.
Q: What are the implications of electronic data capture (EDC) systems on site audits?
EDC systems have significantly changed the landscape of clinical data management and, consequently, the audit process. Auditors must now be proficient in validating electronic systems to ensure they are compliant with 21 CFR Part 11 and other relevant regulations. This includes verifying the security of the system, the accuracy of data transfers, and the integrity of electronic records. Auditors must also assess how site personnel are trained on these systems and how data corrections and audit trails are managed.
Q: How are findings from clinical investigator site audits typically communicated to the sponsor and the site?
Audit findings are typically summarized in a formal audit report that is shared with both the sponsor and the site. The report will categorize findings according to their severity, such as critical, major, or minor non-compliance. It will also recommend CAPAs. The site is usually required to respond to the findings, outlining how they will address each issue and prevent its recurrence. The sponsor is responsible for ensuring that the site implements these CAPAs and may conduct follow-up audits to verify compliance.
Q: Can a clinical investigator site fail an audit, and what are the consequences?
Yes. If a site fails an audit and significant non-compliance issues are found that could affect participant safety, data integrity, or violate regulatory requirements, it can have serious consequences. The consequences can range from requiring a response with CAPAs to more severe actions such as suspending the study at the site, disqualifying the investigator, or reporting the findings to regulatory authorities, which can lead to further regulatory acti ons.
Q: What role do auditors play in the continuous improvement of clinical trial processes?
Auditors play a pivotal role in continuous improvement by not only identifying non-compliance and areas for improvement but also by sharing best practices and providing feedback on processes. Their findings can help shape training programs, refine protocols, and improve overall trial conduct. The goal of an audit is not just to find faults but to help the site enhance its processes for future trials.
Q: How are global clinical trials with multiple international sites managed from an auditing perspective?
Global clinical trials present unique challenges due to varying regulatory requirements and cultural differences. Auditors must be knowledgeable about the local regulations of each country involved. Audits may be conducted by local teams with global coordination to ensure consistency. The audit plan for such trials is often developed with a global scope but allows for local flexibility to address specific regional requirements and risks
Need Clinical Investigator Site Audit Support? We Can Help.
When conducting clinical trials on investigational medicinal products or devices, you must show that planning, study conduct, performance, monitoring, auditing, analysis, and reporting all meet the ethical and scientific standards for GCP.
As new technologies transform the way clinical research is carried out around the world, keeping ahead of these trends is no small task. Whether you follow a traditional approach to monitoring or are transitioning to a Risk-Based Monitoring (RBM) system, our quality professionals tailor their auditing plans to accommodate your particular needs.
Our quality professionals closely examine your particular study before planning and executing study-specific GCP audits of protocols, investigator sites, trial master files, pharmacovigilance, databases, and reports.
With the help of experienced industry professionals, you can be confident knowing results are credible and accurate while maintaining quality practices throughout the research.
- Mock BIMO Inspections
- Auditing and document review for SOPs, clinical GCP protocols, and reports
- Audits of submission for ethical approval for GCP clinical trials
- Audits of clinical sites
- Audits of Trial Master Files (TMFs)
- Audits of Contract Research Organizations (CROs) and other vendors
Clinical trial audits are tailored to your particular compliance needs and stage of product development. Our Quality Assurance team has performed audits in a variety of markets both domestic and international.
Contact us to learn more about how we can support your auditing program.
Gap Analysis Remediation: A Guide to Resourcing & Implementation

Topics: GCP
Need clinical site audit support?
Contact us to access the industry's top clinical auditors.
Sign up for updates from our blog.
Proprietary talent selection of former FDA and industry professionals amplified by a corporate culture of responsiveness and execution.
US Toll-Free: 1-833-FDA-GROUP
International: +001 508 926 8330
Advarra Clinical Research Network
Onsemble Community
Diversity, Equity, & Inclusion
Participants & Advocacy
Advarra Partner Network
Community Advocacy

Institutional Review Board (IRB)
Institutional Biosafety Committee (IBC)
Data Monitoring Committee (DMC)
Endpoint Adjudication (EAC)
GxP Services
Research Compliance & Site Operations
Professional Services
Coverage Analysis
Budget Negotiation
Calendar Build
Technology Staffing
Clinical Research Site Training
Research-Ready Training
Custom eLearning
Services for
Sponsors & CROs
Sites & Institutions
BioPharma & Medical Tech
Oncology Research
Decentralized Clinical Trials
Early Phase Research
Research Staffing
Cell and Gene Therapy
Ready to Increase Your Research Productivity?
Solutions for need.
Clinical Trial Management
Clinical Data Management
Research Administration
Study Startup
Site Support and Engagement
Secure Document Exchange
Research Site Cloud
Solutions for Sites
Enterprise Institution CTMS
Health System/Network/Site CTMS
Electronic Consenting System
eSource and Electronic Data Capture
eRegulatory Management System
Research ROI Reporting
Automated Participant Payments
Life Sciences Cloud
Solutions for Sponsors/CROs
Clinical Research Experience Technology
Center for IRB Intelligence
Not Sure Where To Start?
Resource library.
White Papers
Case Studies
Ask the Experts
Frequently Asked Questions
COVID-19 Support

About Advarra
Consulting Opportunities
Leadership Team
Our Experts
Accreditation & Compliance
Join Advarra
Learn more about our company team, careers, and values. Join Advarra’s Talented team to take on engaging work in a dynamic environment.
Critical Steps for Writing an Impactful Clinical Audit Report
The amount of detail required in an audit may vary – ranging from an executive, high-level summary with detailed observations, to an exhaustive, all-inclusive report. A report may only include detailed observations, but it might also provide a list of all the documents reviewed, describing all processes reviewed in detail, along with any audit observations. While it’s critical for the auditor to understand the expectations of whom they are writing the report for, an impactful clinical audit report includes critical information to describe the status of the auditee in a factual way while excluding information that does not add value to the audience.
As defined in ICH E6 (R2), an audit is “a systematic and independent examination of trial-related activities and documents to determine whether the evaluated trial-related activities were conducted, and the data were recorded, analyzed and accurately reported according to the protocol, sponsor’s standard operating procedures (SOPs), good clinical practice (GCP), and the applicable regulatory requirement(s).”
The audit’s output and report are written evaluations of the audit’s results. A typical audit report contains the following sections:
- General information, including who was audited, what was audited, and where the audit occurred
- Executive summary
- Summary of observations (typically in table format)
- What regulations and guidance the audit was conducted against
- Audit scope
- List of staff involved/interviewed in the audit
- Documentation reviewed during the audit
- Narrative section for describing topics covered and facilities reviewed during the audit
- Detailed observations
Industry standards are shifting to focus on building quality into studies and determining critical-to-quality factors (ref. ICH E8 R1 ) and an appropriate risk management approach (ref. ICH E6 R2 ). The audit report should identify how quality and risk management are managed throughout the entirety of the study conduct.
Critical Steps: Executive Summary
The executive summary succinctly describes the audit’s key points. This gives the audience — especially senior management — the key information and audit outcome. It should include whether it is a routine or for-cause audit, site/vendor identification, dates of audit conduct, and if there were any significant concerns or major findings. Research teams need to include a summary of these findings and an overall statement of compliance and acceptability. They should also indicate if the audit was conducted as planned, and if not, it should state the reason for any deviations from the audit plan.
Critical Steps: Observations
Observations are graded relative to the level of non-compliance or deviation. An example of this is formatting observations as critical, major, minor, or recommendation. The definitions of these are usually described in an audit’s SOPs or detailed in the report template. The definitions are based on the impact or potential to subject safety, data integrity, and the protection of human subject rights.
Multiple major audit observations may result in a systemic critical audit observation, even though each of the major observations are not “critical” themselves. Similarly, the same can be said for multiple minor observations, which may result in a major observation. Potential critical observations must be escalated – usually within 24 hours – to a client, so they can take appropriate action right away. Ideally, reports should be reviewed to ensure consistent observation grading and categorization, providing an objective perspective to verify the report is complete and clear.
Observations should be structured clearly. Typically, they start with an overarching statement of the non-compliance, followed by a detailed description of the issue with examples, and references for non-compliance (e.g., applicable regulations, guidelines, SOPs, protocol, or other study-level plans). The details provided must be factual and not based on subjective information.
When describing the critical and major observations, it’s important to also provide an impact statement. This details how the observation potentially impacts patient safety, their rights, data integrity, etc. Critical and major observations require root cause investigation and corrective and preventive action (CAPA), as ICH E6 R2 addendum section 5.20 requires. Minor observations usually only require correction. Observations must stand alone as the auditee will likely receive them separately from the report. The details in the observation must allow for the auditee to understand the observation and enable them to take action to rectify it.
Critical Steps: Trending
In addition to grading observations, observations should also be categorized – and subcategorized if need be – so trending can be performed. Trending is important to understand the organization’s health, giving visibility to repeat or systemic issues. Instead of raising an observation for each individual discrepancy, similar issues should be grouped in one observation wherever possible, instead of surfacing an observation for each individual discrepancy. For example, instead of creating an observation for a missing ethics committee (EC) letter, and another observation for a missing protocol signature page, these can be grouped under investigator site file/essential documents.
Critical Steps: Narrative
The narrative section of the report is where there are differences in the level of detail required by each organization. A best practice is to evaluate what would be value-added for a particular audit and understand the audience who will read the report. Providing too much information may take away from the site’s or vendor’s status. Some examples include:
- For a site audit, it would be relevant to detail the impact of COVID-19, as this could have resulted in missed patient visits or procedures. Facilities also may not have been available for routine patient visits, monitoring visits, or audits
- For a site audit, a detailed description of the facilities and processes relevant to clinical trial’s conduct (e.g., pharmacy, investigational product administration or infusion of investigational product, laboratory sample, and processing) must be included
- For a vendor audit, it may not be practical to describe company background/mergers in detail if the clinical or procurement team can be easily obtained from the internet
- The clinical team may be familiar with the procedures necessary in the protocol; therefore, each step of a procedure does not need to be described in detail, but rather a high-level description would suffice. If any issues with the process or procedure are identified, the narrative references in the observation section rather than including that deviation detail in the narrative
- Noting each reviewed narrative document can distract from the overall activity of the electronic trial master file (eTMF) or investigator site file (ISF) review activity. Staff can note their review for the eTMF and ISF and list any issues in the observation section or on a separate addendum to the report
Providing the correct level of information in an audit is a delicate balance. Critical to successful audit report writing is to understand the report’s audience, the essential information needed for the audience – site or vendor – to execute the plan, as well as sufficient detail allowing for a full understanding and a chance for observation correction.
Tagged in: CRO , fda audits , quality coe , quality management , sponsors
Back to Resources
Ready to Advance Your Clinical Research Capabilities?
Subscribe to our monthly email.
Receive updates monthly about webinars for CEUs, white papers, podcasts, and more.
Advancing Clinical Research: Safer, Smarter, Faster ™
Copyright © 2024 Advarra. All Rights Reserved.
- Privacy Policy
- Terms of Use
- Cookie Policy

- Advanced Features
- Technical Information
- Rapid Study Development
- Intelligent Electronic Data Capture (EDC)
- Streamlined EDC Data Management
- Electronic Patient Reported Outcomes (ePRO)
- Clinical Randomization Technology (IRT) – Clinical Trial Supply Management (RTSM)
- Enterprise Solution
- Registry Solutions
- See ClinicalPURSUIT Live
A Guide to Writing an Impactful Clinical Audit Report
- Clinical Research
- A Guide to Writing an…
From an all-inclusive, exhaustive report to a high-level, executive summary with in-depth observations, the amount of detail required in an audit may vary. While a report may only include a range of observations, it may also provide a list of every document reviewed, describing every process reviewed in detail, as well as any audit observations .
Although it’s important for the auditor to understand the expectations of whom they’re writing the report for, a good clinical audit report comprises critical information to describe the auditee’s status factually while eliminating information that doesn’t add value to the audience.
Here, our clinical trial data management software expert offers a guide to writing an impactful clinical audit report.
The Executive Summary
The executive summary briefly describes the key points of the audit. This gives the audience, for example, the senior management, audit outcome and key information. It should consist of major findings, significant concerns (if any), dates of audit conduct, vendor/site identification, and whether it’s a for-cause or a routine audit . Research teams must include an overall statement of acceptability and compliance as well as a summary of these findings. They should also include if the audit was performed as planned. If not, reasons must be stated as to why it deviated from the audit plan.
Observations

Besides grading observations, observations must be categorized – and if need be, subcategorized. This will help you perform trending. Trending is important as it gives visibility to systemic or repeats issues and helps you understand the organization’s health. Instead of raising an observation for every individual discrepancy, similar groups must be grouped in a single observation wherever possible. For instance, instead of creating an observation for a missing protocol signature page and another observation for a missing EC (ethics committee) letter, these can be grouped under essential documents.
In the narrative section of the report, there are differences in the level of detail required by every organization. Assess what would be value-added for a certain audit and understand the audience who will read the report. Offering too much information may take away from the vendor’s or site’s status.
Clinical PURSUIT offers top-of-the-line clinical trial data management solutions
Whether you’re looking for randomization and drug supply management solutions or electronic patient-reported outcome software, ClinicalPURSUIT can help.
Get in touch with us now for more information!
Related Posts

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.62(2); 2021 Feb
Language: English | French
A practical guide to implementing clinical audit
Clinical audit is a quality improvement tool for evaluating and improving patient care and outcomes. This is achieved by systematically reviewing current practices against explicit criteria and measuring the impact of change(s) introduced to generate improvement. The clinical audit process can be described by “Plan,” “Do,” “Study,” “Act” phases that comprise an audit cycle. The phases are moved through in turn to attempt quality improvement. Clinical audits are widely used in human medicine at both local (individual clinic or hospital) and national (to achieve nationwide improvements in care) levels. Substantial and sustained improvements in patient care have been attributed to the use of clinical audits. Clinical audits have been described in the veterinary literature since the 1990s, but their adoption does not appear widespread. This paper is intended as a practical, “how to” guide to applying clinical audit in veterinary practice.
Résumé
Un guide pratique pour la mise en place d’un audit clinique . Un audit clinique est un outil d’amélioration de la qualité pour évaluer et améliorer les soins aux patients et les résultats. Ceci est obtenu en révisant systématiquement les pratiques actuelles envers des critères spécifiques et en mesurant l’impact des changements introduits pour générer une amélioration. Le processus d’audit clinique peut être décrit par les phases « Planifier », « Exécuter », « Examiner » et « Agir » qu’incluent un cycle d’audit. Le passage en séquence des phases vise une amélioration de la qualité. Les audits cliniques sont utilisés extensivement en médecine humaine à l’échelle locale (clinique individuelle ou hôpital) et nationale (pour atteindre des améliorations des soins à la grandeur du pays). Des améliorations substantielles et soutenues dans les soins aux patients ont été attribuées à l’utilisation des audits cliniques. Les audits cliniques ont été décrits dans la littérature vétérinaire depuis le début des années 1990, mais l’adhésion ne semble pas être répandue. Cet article se veut un guide pratique sur le « comment faire » pour mettre en application un audit clinique en pratique vétérinaire.
(Traduit par D r Serge Messier)
Introduction
Clinical audit is a quality improvement tool that is used to monitor, assess, and improve the quality of care in human and veterinary medicine ( 1 – 7 ). The procedure involves measuring an outcome or process and comparing this to current evidence or best practice, then implementing changes to improve the quality of care ( 8 , 9 ). In human medicine, clinical audit is considered a standard of care ( 2 , 9 , 10 ). For example, The National Hip Fracture Database (UK) has allowed institutions to audit the care they provide to hip fracture patients according to national standards ( 2 ). Through clinical audit, 1 facility was successful in shortening the median time to surgery and discharged more patients to rehabilitation units following a hip fracture ( 2 ). In veterinary medicine, the Royal College of Veterinary Surgeons (RCVS) includes clinical audit in its Practice Standards Scheme, in which approximately 65% of UK practices participate ( 11 ). Performing clinical audit is a requirement for practices accredited as Veterinary Hospitals and encouraged for those accredited as General Practice and Emergency Service Clinics ( 11 ). However, as audits are not frequently published (there is no requirement for publication in the Practice Standards Scheme), it is unclear to what extent clinical audits are being conducted ( 5 ). At the time of writing, the American Veterinary Medical Association (AVMA), and the Canadian Veterinary Medical Association (CVMA) do not appear to provide resources on clinical audit. The aim of this paper is to provide a practical “how-to” guide on performing clinical audit. This guide is supplemented by a fictitious example of a clinical audit ( Appendix , “Antimicrobial use in bacterial cystitis”). Key principles are illustrated with examples, including one based on a clinical audit performed on the subject of postoperative hypothermia in dogs in a large referral hospital ( 4 ).
Antimicrobial use in bacterial cystitis.
| A small animal clinic is looking into performing a clinical audit. The group begins by answering the 3 preparatory questions. After reading the Canadian Veterinary Medical Association recommendations on judicious use of antimicrobials, the veterinary team would like to improve their diagnosis and treatment of bacterial cystitis in dogs ( ). The team agrees to follow the International Society for Companion Animal Infectious Diseases (ISCAID) guidelines ( ). Based on their clinical experience, the team identifies the following points from the ISCAID guidelines as areas that would qualify as improvement ( ): An initial short audit cycle was conducted over a week and identified that very few sporadic cystitis cases were being cultured and that treatment duration was usually 7 to 10 days. Upon further discussion with the staff there was no clear definition for what was considered sporadic cystitis and therefore what length of treatment was required. The staff created a checklist to aid in identifying cases of sporadic cystitis which included the following i) less than 3 episodes of cystitis in the preceding 12 months; ii) healthy non-pregnant females or neutered males; iii) no known urinary tract anatomical or functional abnormalities or co-morbidities. This information was then brought to the Plan stage. |
| The team’s purpose statement was to improve antimicrobial use following the diagnosis and treatment of bacterial cystitis by: To help achieve these goals the RVTs were in charge of filling the prescriptions and confirming the duration of treatment. |
| One RVT was allocated 2 h a week to collect the data. This involved searching the computer database for “cystitis,” verifying the duration of antimicrobial treatment and determining whether a urine culture was performed. |
| After the 2-month period, the team reviewed the data. A bar graph was used to compare the number of cystitis cases against those cultured ( ). Following discussion, the team realized that discrepancies in performing cultures were largely explained by different levels of comfort with collecting urine ultrasound-guided cystocentesis. A run chart was plotted to monitor treatment duration. The team was happy to see a trend towards treating between 3 to 5 days except for 2 astronomical points ( ). On further investigation they realized that this case was from a locum who was not made aware of the practice policy. |
| To improve urine culturing, the clinic elected to support a continuing education day on basic ultrasonography. Once the CE course was completed, a new clinical audit cycle was performed. |
Materials and methods
The process of achieving sustained improvement in a complex system, such as the provision of veterinary care, may not be straightforward ( 12 , 13 ). This is because of the complexity of the system and the habits of the workforce. A successful change in practice is reflected in a measurable improvement that can be maintained ( 7 – 9 , 13 , 14 ). Common to most existing descriptions of clinical audit is the concept that an audit is cyclical, repeated at intervals to track performance. Multiple cycles may be necessary to achieve the desired changes, particularly in complex processes or where the key activities resulting in change are not obvious. While several audit cycle models exist, one which has been widely used in the domains of both business and medicine, is the “Model for Improvement” ( 9 , 13 ). The original model consists of 3 preparatory questions linked to a Plan-Do-Study-Act (PDSA) cycle ( Figure 1 ). “Plan” is identifying the process(es) and outcome(s) to be studied and how data will be collected, “Do” is collecting the data, “Study” is interpreting the collected data, and “Act” brings the current audit cycle to completion by reviewing the results and planning for ongoing improvement. The following is an elaboration of each component of the model.

The audit cycle, showing the 4 necessary steps of a complete audit cycle, from planning an audit (“Plan”), to the collection and analysis of data (“Do” and “Study”) and identifying steps leading towards improvement (“Act”). The cycle is intended to be repeated with the goal of continuous improvement. Adapted from Langley et al ( 13 ).
Preparatory questions
The 3 preparatory questions of the Model for Improvement precede the first step, the “Plan” stage of the PDSA cycle and improve the likelihood of conducting a successful audit ( 13 ). The questions are: 1. “What are we trying to accomplish?” 2. “How will we know that a change is an improvement?” 3. “What changes can we make that will result in an improvement?”
1. “What are we trying to accomplish?”
Identify the aim of the clinical audit. The selected topic may be determined by relevance to an individual practitioner or clinic, with common topics often related to patient/staff safety, clinical practice or finances ( Table 1 ). When choosing a topic, it is essential that staff understand the rationale for the desired improvement, as this will build buy-in and improve compliance with introduced changes. Ideally, the selected topic has an associated set of explicit criteria/guidelines based on current evidence, against which performance can be compared [e.g., the use of physiologic monitors during cardiopulmonary resuscitation ( 15 )]. Where guidelines exist, they should be written in a way that identifies measurable criteria that have been shown to improve the quality of care ( 16 , 17 ). Unfortunately, in veterinary medicine the evidence-base for outcome criteria or the existence of guidelines is often limited, resulting in a reliance on a combination of evidence and expert opinion, such as seen in consensus guidelines ( 15 , 18 ). Where neither evidence-based criteria nor consensus guidelines exist, criteria may be derived from observation of achievements in comparable settings: this is known as benchmarking. For example, the RCVS Knowledge website has a cumulative online database reporting on the outcomes of neutering procedures (spays and neuters in dogs, cats, and rabbits; currently reports outcomes from over 39 000 procedures) ( 19 ). These outcome data can be used as a benchmark for performance and to potentially identify areas for clinical audit/investigation. For example, the current data show that approximately 1% of cat castrations and 10% of dog castrations have a postoperative complication requiring medical treatment ( 19 ). So, if a practice was experiencing a higher incidence of complications requiring medical treatment with their canine neuters, such as 15%, this suggests an area for improvement and a percentage goal to achieve.
Sample subjects for clinical audit.
| Subject | Potential measurement | Associated criteria/guidelines? | Potential target |
|---|---|---|---|
| Staff safety | |||
| Bite wounds | Cat bites that penetrate skin | None | Zero cat bites |
| Patients escaping | Patients escaping kennel, patients loose on walks | None | Zero kennel or walk escapes |
| Finances | |||
| Appointment scheduling | Client wait time beyond scheduled appointment time | None | Within 5 min |
| Emergencies | Returning calls for after hour emergencies | None | Triaging calls within 30 min |
| Clinical practice | |||
| Pre-operative antimicrobials | Antimicrobial administration time and surgical incision time | Within 30 to 60 min of surgery ( ) | Within 60 min |
| Diabetes mellitus management | Appropriate dietary management | American Anima Hospital Association diabetes guidelines ( ) | Achieving and maintaining ideal body mass |
Using our hypothermia example, the response to “What are we trying to accomplish?” would be a reduction in incidence of postoperative hypothermia in dogs. A quick literature search in human and veterinary medicine reveals multiple adverse effects of perioperative hypothermia in humans and a high incidence of postoperative hypothermia in dogs and cats ( 4 , 20 – 23 ). The latter provides indirect support for the perception that the clinic has a high incidence of post-operative hypothermia (an example of benchmarking). The reported incidence of hypothermia in the literature can be used as a performance target, with the goal of providing a similar or better level of care. It is important with this first question that all staff understand the importance of the task identified for improvement. By taking the time to explain the potential adverse effects of hypothermia on patients, staff are encouraged to support the audit and comply with implemented changes. For example, kennel staff members may be more vigilant in monitoring patients’ post-operative temperature if they understand the potential consequences of hypothermia.
2. “How will we know that a change is an improvement?”
It is often easy to introduce a change, but it may not be straightforward, particularly in complex systems, to know if that change has a positive effect. Some form of data collection confirms that a change results in an improvement (and supports future assessments of performance and improves support from staff ). The data collected should provide information relevant to the outcome of interest. In its simplest form, the outcome itself can be measured (e.g., incidence of postoperative hypothermia). However, in complex systems or to better understand weaknesses in a system, it is often helpful to measure processes within a system (e.g., How many cases had active warming applied? Was rectal temperature recorded during surgery?). It is often tempting to focus on outcome measures as these reflect success (or failure). However, focusing on an outcome can be frustrating when it is unclear which processes resulted in an improved outcome. Additionally, if an instituted change does not result in improvement and data collection was limited to an outcome, it is impossible to know if the underlying processes were performed properly or if the right processes were altered, or both [e.g., if the change is to provide active warming during all surgeries and the incidence of hypothermia (outcome measurement) remains unchanged, the cause(s) of failure to generate improvement is unknown]. Similarly, if improvement occurs, the assumption is that this resulted entirely from the introduced change, unless a measure of process(es) is included to ensure that the change was implemented as planned or that other processes were affected/unaffected as predicted (e.g., the incidence of hypothermia drops when active warmers are made available, but perhaps the timing of active warmer use also has an important effect on the incidence of hypothermia). Therefore, including process measurements in an audit provides richer information than focusing exclusively on outcome.
Process measurements relate to specific activities (actions or steps) associated with outcomes. Documenting processes is often more sensitive than measuring outcomes ( 8 , 24 ). Process measurements may be the only feasible option when the outcome of interest is delayed (e.g., time to death or disease development) or the outcome occurs infrequently (e.g., anesthetic death). However, it is not always evident which processes influence outcome and to what extent (not all change in a system will result in improvement) ( 13 ). Ideally, process measurement selection would focus on those with the greatest influence on outcome and amenability to measurement.
Returning to the hypothermia example, focusing on the outcome alone (hypothermia at recovery) could miss processes with a direct and important effect on outcome. These could include, when/if rectal temperatures are recorded in the perioperative period, the use of active warmers (timing of application, temperature setting, availability of warmers), and procedure duration.
3. “What changes can we make that will result in an improvement?”
In veterinary medicine, evidence linking specific activities to beneficial outcomes can be sparse. Methods to help identify items for change (a “needs assessment”) may include conducting initial surveys, receiving feedback from relevant parties, and collecting initial data on performance. In complex systems in which numerous outcomes could be improved, an initial survey of users may help identify which outcomes to initially pursue ( 13 ). For example, with the goal of improved client service, a survey of clients may identify that delays in scheduled appointments are less important than segregated waiting areas for dogs and cats. This information can then be discussed with staff to explore if, and how, suggested changes can be introduced (e.g., feasibility of a screen to provide a visual barrier between cats and dogs), followed by an audit cycle to assess the impact of that change (survey of clients, record of pet density in segregated areas, feedback from staff on effectiveness). When considering a clinical audit, seeking contributions from relevant parties can identify items that may contribute to, or obstruct, the success of an audit (e.g., achieving an outcome of reducing medication errors is more likely to be successful if the number of different concentration preparations is minimized). Performing a short audit cycle, with limited scope, can enable rapid feedback and provide information on the impact of the tested changes. This can be valuable when it is unclear if a change is likely to be successful or there is a financial commitment associated with a change in practice. The resulting information could then be used in a larger scale clinical audit.
In the hypothermia example, it was important to verify the perception that the incidence of postoperative hypothermia was high. An initial, short period of data collection (over 1 wk) showed that 88% of dogs were hypothermic at extubation and that post-operative temperature recording, and warming were inconsistent. Discussing the findings with the registered veterinary technicians (RVTs) revealed that there was no consistent definition of hypothermia applied in the clinic, there was no standard practice for frequency of temperature measurements, and the availability of forced air warmers was limited ( 4 ). This process of acting on the perception that hypothermia was occurring frequently by collecting data to document its incidence and discussing the findings, was effectively a short audit cycle, the outcome of which was to confirm that a problem (hypothermia) existed, and to identify barriers and opportunities for improvement. These findings were incorporated into the “Plan” stage of the larger, more comprehensive, PDSA cycle.
Step 1: “Plan” (preparing for the clinical audit)
The planning stage is critical to the success of the audit cycle and considers: identification of the process(es)/outcome(s) to be studied based upon responses to the 3 preparatory questions (above), identification of the Who, What, When, and Where of the cycle, and preparation for data collection (“Do” phase) ( 8 , 13 ). The 3 preparatory questions should result in a statement of the aim/purpose of the audit cycle ( 1 ). An example of a purpose statement could be: “To improve the management of postoperative hypothermia in dogs presenting for non-urgent procedures.” However, such a statement is vague because no specific target is identified. Should the target be to achieve 0% hypothermia after surgery? This is ideal, but probably unrealistic. A more realistic target might be, “90% of dogs returning to normothermia within 4 h after surgery.” This latter statement recognizes that maintaining normothermia during surgery is difficult, but that management of hypothermia can be improved.
Once the purpose statement has been created, the groups involved and resources required are identified ( 7 ). This allows an appraisal of whether the selected outcome can be realistically manipulated and (hopefully) improved ( 14 ). For the hypothermia example, it is important to ensure that there are sufficient resources (staff and equipment) to support the goal. Similarly, it is important that key parties are invested in the project: presenting the current situation (including the current incidence of hypothermia), the aim of the audit cycle, the reasons why reducing the incidence of hypothermia is important, the planned changes and contributions of staff, are more likely to result in support and eventual success ( 5 ). Absence of staff involvement is a common source of failure or of resistance to bring about change ( 8 , 27 ). Similarly, a key aspect of successful audit is creating an environment in which the goal is improvement rather than placing blame on specific groups or individuals ( 8 ). Finally, an initial timeframe for data collection (the “Do” phase) can be set out. This is determined based upon local constraints but should set a minimum time to have a chance of identifying an improvement (if one were to occur; this could naturally be determined by caseload, for example) and be short enough that lack of success is not unnecessarily prolonged. Visualizing and interpreting data as they are collected (see Step 3: “Study”) can identify when change has occurred and a suitable time to stop data collection.
From this “Plan” stage, the following was described for the hypothermia clinical audit:
- Purpose statement: “to have 90% of dogs return to normothermia within 4 h after surgery.”
- The results of the short data collection period (identifying an 88% incidence of postoperative hypothermia) were presented to the practice, with attendance by the majority of veterinarians, registered veterinary technicians, and technician assistants. An in-person meeting was appropriate for the size of clinic but for larger clinics, or those in which veterinarians work in shifts, more than 1 meeting, or use of e-mail (with a deadline for comments) or posters (for example) could help ensure information was widely communicated.
- A general discussion achieved a consensus to: a. measure rectal temperature hourly when hypothermia was identified at extubation (included in recovery area monitoring by technicians: Who and Where); b. implement a practice-wide target temperature of 37.5°C (What); c. use forced air warmers and continue temperature measurements until the target temperature was achieved; and d. move unused forced air warmers from the surgical floor to the recovery area at the end of the day to ensure equipment availability. Data collection was planned for 1 mo (When) with a view to interpreting the data at this stage (Step 3: “Study”) and deciding the next step(s) (Step 4: “Act”).
Step 2: “Do” (carrying out the plan)
This is the data collection phase. Once the audit is in progress, monitoring the data collection process itself helps ensure that data are being collected properly (staff included in data collection should be appropriately instructed and supported) ( 28 ). Time to collect data should be budgeted into the workload of participants to maximize the likelihood of complete and accurate reporting. There should be the opportunity to record problems encountered as these will help identify causes of audit failure, or limited improvement gains, and can be incorporated in future audit cycles. This could be achieved informally, such as asking for feedback during regular clinic meetings/rounds, or by making available a box in which suggestions can be placed, or providing an e-mail contact (specific person or dedicated e-mail address). Ongoing visualization of data can provide rapid feedback on progress towards achieving a change and serve to motivate participants if goals are set.
In large-scale, multicenter/national audits it can be invaluable to have people dedicated to collecting data, monitoring progress, and providing feedback ( 29 ). This approach facilitates early identification of factors contributing to likely failure to implement change(s), which can then be addressed. Software can also be used to facilitate data collection ( 30 ).
In the hypothermia example, a poster summarizing the changes being implemented was prominently displayed. Additionally, the line in the postoperative record sheet for recording temperature was highlighted. To minimize data loss, a designated person was responsible for inputting data into an electronic spreadsheet weekly.
Step 3: “Study” (data analysis and interpretation)
Following data collection, graphs are often used to visualize and interpret the data. The data should be discussed among colleagues to obtain a wide range of perspectives ( 9 ). This discussion is essential to complete the current audit cycle (moving to the “Act” phase) and prepare for future audits.
A common method of displaying collected clinical audit data, which facilitates tracking of progress, is the run chart ( Figure 2 ) ( 31 ). Run charts are an example of control charts and more sophisticated forms, such as cumulative summation plots, are used in statistical process control, a formal technique to evaluate quality control/improvement ( 3 , 32 , 33 ). Run charts facilitate rapid assessment of the data as they are collected, allowing users to see emerging patterns, including deviations from an audit goal. They are simple and fast to compile, and easy to interpret. The x-axis of a run chart represents a measure of time, such as days or visit/procedure number. The y-axis represents the subject of study e.g., client time in waiting room ( Figure 2 ). Targets to achieve or avoid can be plotted on the y-axis (e.g., Figure 2 shows a desired maximum wait time of 10 min after scheduled appointment time), enabling a rapid assessment of progress and motivation.

Run chart of fictitious data illustrating percentage of clients meeting a goal of 10 min or less (dashed horizontal line) for time spent waiting for appointment to start. The historical median wait time is 15 min (dotted horizontal line). A trend (5 or more consecutive points moving in the same direction) and an astronomical point (deviant data point) are identified. These could result from the knock-on effect of an appointment running late and a cancellation, respectively. The impact of a new DVM requiring longer appointments contrasts with an experienced practitioner (cases 32 onwards).
Beyond subjective observations, several standardized rules can be applied to aid run chart interpretation, including identification of a “trend” and “astronomical point” ( 13 , 31 ). These rules help identify non-random changes in the data and limit the risk of over-interpreting small changes. A trend is identified when 5 (or more) consecutive data points all move in the same direction (either upwards or downwards). Identifying an astronomical point is based on subjective evaluation of the run chart and is indicated by a datum that is striking by its deviation from the adjacent data. More complex interpretations of run charts can also be applied using statistical methods ( 3 , 13 , 31 , 34 ).
For the hypothermia clinical audit, a box plot was used to track the percentage of animals achieving normothermia within 4 h over the 4 wk following the introduction of the temperature management changes ( Figure 3a ). Data were compiled weekly as this fitted in with the work schedule of the person responsible for managing data. A run chart, reflecting rectal temperatures at the target 4-hour time point for individual dogs could also be applied to provide detail at an individual case level ( Figure 3b ).

a — Circles indicate percentage of animals normothermic at 4 h after recovery for 6 days of the week (Monday–Saturday). Box plot (box limits are range, central horizontal line is median: calculated from daily percentage values). The initial positive effects of changes introduced during the audit begin to wane in weeks 3 and 4 (lower median and daily percentages and increased data variability). Tracking performance identifies this change and can be used to trigger a more detailed investigation to understand the basis of the change (e.g., individual case tracking, Figure 3b) or a further audit cycle. b — Run chart showing rectal temperature for sequential cases anesthetized before (cases 1–9) and after (cases 10–28) warming management changes introduced (“Temp mx change”). Changes result in more cases achieving the target temperature and less variability between cases.
The duration of data collection is somewhat arbitrary, often based on a prediction of caseload so that enough cases are collected to be representative. In general, though collecting more data is informative, compliance in maintaining introduced changes and/or continuing data collection is likely to wane over time (especially if data are not visualized on an ongoing basis). In contrast, too short a period of data collection may not provide an accurate reflection of reality and improvements may reflect the Hawthorne effect (a change in behavior as a result of being observed), with a return to previous performance levels once data collection stops ( 35 , 36 ).
Step 4: “Act” (decision for further action based on results)
After data collection and interpretion of results, the current audit cycle is completed by defining and implementing further action to continue improvement (or address identified problems). This could be as simple as intermittent periods of data collection to confirm improvements are maintained. Further audit cycles may be planned, with the goal of continuous improvement (or to test alternative approaches in the case of an unsuccessful outcome). The results of the hypothermia audit were presented to clinic staff, providing the opportunity to reflect on the process and discuss strategies for further improvement (the initial target was achieved but a small number of animals remained hypothermic beyond the 4-hour goal).
Factors associated with failure of clinical audit
Successful audit depends on a careful selection of the audit subject (see preparatory questions) and a supportive environment ( 9 , 27 ). Environment can be considered as structure and culture ( 8 ). Structure refers to ensuring adequate time and resources are available to conduct an audit (from preparation through to data collection and presentation). This could include time to identify relevant guidelines when establishing outcomes/processes to measure and audit targets as well as the time and resources to collect and interpret data. Culture refers to a collective desire to promote and sustain improvement, including supporting openness, so that errors/failures can be identified without blame ( 37 , 38 ). All phases of the audit cycle are more likely to be successful if the process is inclusive, with staff involvement. The extent of involvement varies, from consultation and discussion during the planning phase to participation in data collection and review of results ( 39 ). There is an important distinction between a successful audit cycle, that is, completion of the audit cycle, and success in generating an improvement. Failure to achieve improvement does not necessarily constitute a failed audit process: it may be that the action taken had limited impact on the outcome of interest or was not closely related to the outcome. Failure to achieve improvement still provides useful information to be incorporated in subsequent audit cycles.
Ethical review for clinical audits
The overarching goal of clinical audit is quality improvement, resulting from observing and evaluating processes and outcomes against explicit criteria. Thus, the end result should be an improvement in the quality of care. Understanding the audit cycle process provides a framework for ethical review. It is simplistic to assume that clinical audit does not require ethical review ( 28 , 40 – 43 ). Though clinical audit often differs from prospective clinical research in that animals are not randomized to receive different treatments (with the possibility that a subject receives a less effective/placebo treatment), there are several areas that warrant ethical review: 1. There may be randomization to assess the effect of different interventions in improving standard of care; 2. The change introduced with the goal of improving care may be associated with risk (perceived or actual); 3. Safeguarding of patient data; 4. A radical change in care/practice that could have unforeseen effects; and 5. Re-allocation of resources from other patients as a result of a change in care.
Publishing quality improvement studies
The number of published clinical audits in veterinary medicine is limited, although it is unclear if this reflects the number of audits performed, the selection process of journals or the number of audits submitted for publication ( 5 ). The publication of clinical audits should be encouraged. This is particularly important in veterinary medicine, where evidence of criteria associated with improvement is limited: published audits will disseminate information on the success/failure of changes implemented. Furthermore, as evidence-based guidelines are developed, clinical audit can help evaluate if guidelines are achievable in practice and written in a way that the relationship between process(es) and outcome is clear. To facilitate clinical audit publishing and standardize reporting, reporting guidelines are available: SQUIRE (Standards for QUality Improvement Reporting Excellence) ( 44 , 45 ). These guidelines are also helpful when planning clinical audits, providing a framework of items to consider.
The quality of clinical audit is reflected by completion of the audit (PDSA) cycle, as well as the selection of measurable criteria, reliable and accurate data collection and analysis, and reporting and interpretation of the results ( 8 ).
In conclusion, clinical audit has the potential to promote and maintain high standards of patient care. Available literature shows that clinical audit is being discussed and applied in veterinary medicine ( 1 , 4 , 5 , 7 , 30 , 46 – 48 ), with evidence that complete audit cycles are being performed ( 1 , 3 , 7 , 47 – 49 ). A current barrier to the widespread adoption of clinical audit may be a relative lack of evidence-based guidelines in veterinary medicine. Nevertheless, clinical audit can and should be used to assess performance against widely accepted (best-practice) standards of care. The importance of clinical audit cannot be overstated. With the increase in volume of published literature, a gradual move towards evidence-based veterinary medicine, increased focus on the relationship between human and veterinary medicine (“One Health”), and increasing public awareness, steady improvement of practice standards is a challenging yet critical task. Clinical audit is a useful, accessible, under-utilized tool to achieve this goal.

a — Bar graph of fictitious data showing relationship between weekly cystitis cases and number of cultures performed. b — Run chart documenting duration of antimicrobial prescriptions for fictional cases of cystitis. Upper and lower broken horizontal lines indicate target prescription duration window. Case 17 could be classified as an astronomical point (see text for details), warranting investigation.
Acknowledgments
Funding was provided by a Natural Sciences and Engineering Research Council of Canada (NSERC) Discovery Grant (424022-201). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors thank Dr. Vivian Leung for designing Figure 1 and Dr. Pam Mosedale, Lead Assessor, Royal College of Veterinary Surgeons Practice Standards Scheme, for helpful comments on the sections referring to the Practice Standards Scheme. CVJ
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office ( gro.vmca-amvc@nothguorbh ) for additional copies or permission to use this material elsewhere.
Not a member?
Find out what The Global Health Network can do for you. Register now.
Member Sites A network of members around the world. Join now.
- 1000 Challenge
- ODIN Wastewater Surveillance Project
- CEPI Technical Resources
- UK Overseas Territories Public Health Network
- Global Malaria Research
- Global Outbreaks Research
- Sub-Saharan Congenital Anomalies Network
- Global Pathogen Variants
- Global Health Data Science
- AI for Global Health Research
- MRC Clinical Trials Unit at UCL
- Virtual Biorepository
- Epidemic Preparedness Innovations
- Rapid Support Team
- The Global Health Network Africa
- The Global Health Network Asia
- The Global Health Network LAC
- Global Health Bioethics
- Global Pandemic Planning
- EPIDEMIC ETHICS
- Global Vector Hub
- Global Health Economics
- LactaHub – Breastfeeding Knowledge
- Global Birth Defects
- Antimicrobial Resistance (AMR)
- Human Infection Studies
- EDCTP Knowledge Hub
- CHAIN Network
- Brain Infections Global
- Research Capacity Network
- Global Research Nurses
- ZIKAlliance
- TDR Fellows
- Global Health Coordinators
- Global Health Laboratories
- Global Health Methodology Research
- Global Health Social Science
- Global Health Trials
- Zika Infection
- Global Musculoskeletal
- Global Pharmacovigilance
- Global Pregnancy CoLab
- INTERGROWTH-21ˢᵗ
- East African Consortium for Clinical Research
- Women in Global Health Research
- Global Health Research Management
- Coronavirus
Research Tools Resources designed to help you.
- Site Finder
- Process Map
- Global Health Training Centre
- Resources Gateway
- Global Health Research Process Map
- About This Site
Downloadable Templates and Tools for Clinical Research
Welcome to global health trials' tools and templates library. please note that this page has been updated for 2015 following a quality check and review of the templates, and many new ones have been added. please click on the orange text to download each template., the templates below have been shared by other groups, and are free to use and adapt for your researchstudies. please ensure that you read and adapt them carefully for your own setting, and that you reference global health trials and the global health network when you use them. to share your own templates and sops, or comment on these, please email [email protected]. we look forward to hearing from you.
These templates and tools are ordered by category, so please scroll down to find what you need.
|
|
| |
|
|
| |
|
|
| |
|
| ||
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
| ||
|
| ||
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
|
| |
|
| ||
|
|
| |
|
| ||
|
| ||
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
|
|
|
|
| |
|
| ||
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
|
| |
| /td>< |
| |
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
|
| |
|
| ||
|
| ||
|
| ||
|
|
| |
|
|
| |
|
|
To share your own templates and SOPs, or comment on these, please email [email protected]. We look forward to hearing from you!
- Webinar on community engagement in clinical research involving pregnant women
- Free Webinar: Science, technology and innovation for upskilling knowledge-based economies in Africa
- Open Public Consultation on “Strengthened cooperation against vaccine preventable diseases”
Trial Operations Trial Management Ethics and Informed Consent Resources Trial Design Data Management and Statistics
training
This is Degena Bahrey Tadesse from Tigray, Ethiopia. I am new for this web I am assistant professor in Adult Health Nursing Could you share me the sample/templet research proposal for Global Research Nurses Pump-priming Grants 2023: Research Project Award
I have learned lot..Thanks..
i was wondering why there is no SOP on laboratory procedures ?
Hi, Can you provide me the SOP for electronic signatures in Clinical trial
Do you have an "SOP for Telephonic site selection visit". Kindly Share on my registered mail ID
Thank you for sharing the resources. It is very kind of you.
Hi These tolls are very useful! Thank you
Do you have a task and responsability matrix template for clinical trial managment ? Best
I am very much happy to find myself here as a clinician
Dear Getrude
We have a free 14-module course on research ethics on our training centre; you'll receive a certificate if you complete all the modules and quizzes. You can take it in your own time. Just visit 'Training centre' in the tabs above, then 'short courses'.
Kind regards The Editorial Team
need modules on free online gcp course on research ethics
Estimados: me parece excelente el aporte que han hecho dado que aporta. por un lado a mejorar la transparencia del trabajo como a facilitar el seguimiento y supervisión de los mismos. Muchas gracias por ello
We also have an up to date list of global health events available here: https://globalhealthtrials.tghn.org/community/training-events/
Dear Nazish
Thank you, I am glad you found the seminars and the training courses useful. We list many training events (all relevant to Global Health, and as many of them as possible are either free or subsidised) on the 'community' web pages above. Keep an eye on those for events and activities which you can get involved with. Also, if you post an 'introduction' on the introduction group stating where you are from and your research interests, we can keep you updated of relevant local events.
Thanks so much. These are very helpful seminars. Please let me know any other websites/links that provide free or inexpensive lectures on clinical Research. Appreciate your help.
Hi Nazish, and welcome to the Network. The items here are downloadable templates for you to use; it sounds like you may be seeking lectures and eLearning courses? If so - no problem! You can find free seminars with sound and slides here: https://globalhealthtrainingcentre.tghn.org/webinars/ , and you can find free, certified eLearning courses here: https://globalhealthtrials.tghn.org/elearning . Certificates are awarded for the eLearning courses for those scoring over 80% in the quiz at the end of each course. If you need anything else, do ask! Kind regards The Editorial Team
Hi, I am new to this website and also to the Clinical Research Industry for that matter I only am able to see the PDF of these courses, just wanted to know are these audio lectures and also happen to have audio clips that go with the pdf?
This site is impeccable and very useful for my job!!!!
Thank you for your kind comments.
Fantastic resources
I am delighted you found this website. I earlier introduced it to you because of your prolific interest in health care information and resource sharing....
Please Sign in (or Register ) to view further.
Useful Resources
Related articles.
- PRISMA for Abstracts: Reporting Systematic Reviews in Journal and Conference Abstracts BY Jai K Das
- 5 ways statistics can fool you—Tips for practicing clinicians BY Jai K Das
- How to prepare for a job interview and predict the questions you’ll be asked BY The Editorial Team
- Preparing for and Executing a Randomised Controlled Trial of Podoconiosis Treatment in Northern Ethiopia BY Henok Negussie, Thomas Addissie, Adamu Addissie, Gail Davey
- Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control BY WHO/ TDR
Most popular tags
- Archive (303)
- archive (104)
- data sharing (70)
- sharing (63)
- training (49)
- malaria (30)
- ACT consortium (25)
- informed consent (7)
- data management (6)
- trial management (6)
- careers (5)
- guidelines (5)
- monitoring (5)
- workshop (5)
- administration (4)
- clinical research (4)
You are using an outdated browser. Please upgrade your browser or activate Google Chrome Frame to improve your experience.
- Patient safety and quality improvement
- Conducting a clinical audit
Clinical audit templates
The College have developed a series of online clinical audit templates to support pathologists with revalidation, meeting the standards set for high quality audit by the RCPath.
The audit templates are the same basic layout and have been partially completed demonstrating step by step the process of how to plan and complete a specific clinical audit. These templates focus on methodology, help you chose a topic and ensure audit activities are conducted efficiently with maximum benefit to patient care, whilst helping you to meet the information requirements of revalidation.
Audit templates
An audit of compliance of serological screening tests for coeliac disease against the national institute for health and care excellence (nice) 2015 coeliac disease guidelines.
Dr Melanie York & Dr Ravishankar Sargur May 2019
An audit of best practice for cryoglobulin evaluation
An audit of compliance with published recommendations on the management of c1 inhibitor deficiency.
Dr Elcombe, Dr Stroud & Dr Yong May 2019
An audit of compliance of diagnosis of common variable immunodeficiency disorders (CVID) with the International CONsensus (ICON) or European Society for Immunodeficiencies (ESID) criteria
Dr Susan Tadros & Dr Sorena Kiani May 2019
The use of C1 esterase concentrate prophylaxis in patients with hereditary angioedema
Dr Tasneem Rahman & Dr Sorena Kiani May 2019
An audit of compliance of diagnosis of specific antibody deficiency (SPAD) with the European Society for Immunodeficiencies (ESID) criteria v2.doc
An audit of compliance with british society for allergy and clinical immunology and nice guidelines for the documentation and communication of drug allergy testing outcomes.
Dr Stephen Boag & Dr Catherine Stroud May 2019
An audit of compliance with the British Society for Allergy and Clinical Immunology (BSACI) guidelines for the management of hymenoptera allergy
Dr Catherine Stroud May 2019
Haematology
An audit of compliance with the british society for haematology guideline on the management of iron deficiency in pregnancy.docx, an audit of compliance with the british society for haematology (bsh) guideline on the identification and management of pre-operative anaemia.
August 2020
An audit of compliance with the British Society for Haematology (BSH) guidelines for the diagnosis and treatment of cobalamin and folate disorders
An audit of compliance with the british society for haematology (bsh) guidelines on the management of drug-induced immune and secondary autoimmune haemolytic anaemia.
January 2018
An audit of compliance with the British Society for Haematology (BSH) guideline on the diagnosis and management of primary autoimmune haemolytic anaemia
An audit of compliance with the bsh guideline for the laboratory diagnosis of functional iron deficiency.
Dr Wayne Thomas August 2016
An audit of compliance with the British Committee for Standards in Haematology (BCSH) guideline for management of iron deficiency in pregnancy
Dr Will Lester May 2012
An audit of compliance with the BCSH guideline for the diagnosis and management of hereditary spherocytosis
Dr May-Jean King May 2012
An audit of compliance with the British Committee for Standards in Haematology (BCSH) guideline for the diagnosis of aplastic anaemia
Dr Mari Kilner May 2012
Bleeding and platelet disorders
An audit of compliance with bsh guidelines for diagnosis and management of thrombotic thrombocytopenic purpura (tpp) and other thrombotic microangiopathies (tmas).docx.
February 2024
An audit of compliance with the British Society for Haematology guideline for the diagnosis and management of heparin-induced thrombocytopenia.DOC
September 2024
An audit of clinical and laboratory diagnosis of heritable platelet disorders in adults and children.docx
January 2022
An audit of compliance with the UK Haemophilia Centre Doctors’ Organisation (UKHCDO)/British Society for Haematology(BSH) guideline on the diagnosis and management of von Willebrand disease
An audit of compliance with the british society for haematology (bsh) guideline on patient self-testing and self-management of oral anticoagulation with vitamin k antagonists, an audit of compliance with the guideline on aspects of cancer-related venous thrombosis.
Dr Watson Dr Keeling Prof Laffan Dr Tait Dr Makris May 2015
An audit of compliance with BCSH guidelines for diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies
Dr John-Paul Westwood April 2014
An audit of compliance with the standards for reporting and acting on critical results in haematology - high INR for patients who are on Warfarin
Dr Mike Galloway July 2013
An audit of compliance with the BCSH guideline on the management of haemophilia in the fetus and neonate
Dr Deepa Arachchillage May 2012
An audit of compliance with the BCSH guideline for the investigation and management of adults presenting with a thrombocytosis
Dr Mike Galloway May 2012
An audit of compliance with the British Society for Haematology guideline on laboratory diagnosis of malaria.docx
Audit of bsh/bsbmt/uk clinical virology network guideline on diagnosis/management of respiratory viral infections when undergoing treatment for haematological malignancies or stem cell transplantation.
Fiona Dignan January 2018
An audit of compliance with the British Committee for Standards in Haematology (BCSH) guidelines for laboratory diagnosis of malaria
Michael Wright & Dan Pelling February 2015
An audit of compliance with the BCSH guideline for the prevention and treatment of infection in patients with an absent or dysfunctional spleen
Dr Andy Charlton May 2012
An audit of Richter transformation of chronic lymphocytic leukaemia.docx
An audit of compliance with the bsh on the diagnosis and management of chronic myeloid leukaemia.docx, an audit of compliance with the bsh good practice paper on the management of cardiovascular complications of bruton tyrosine kinase inhibitors.docx, an audit of compliance with the bsh guideline on diagnosis and management of hairy cell leukaemia and hairy cell variant.
February 2021
An audit of compliance with the British Society for Haematology (BSH) 2018 guideline for the treatment of patients with chronic lymphocytic leukaemia (CLL)
Dr Nilima Parry-Jones March 2019
An audit of compliance with the BCSH guideline on the diagnosis and management of acute myeloid leukaemia (AML) in pregnancy
Dr Gail Jones April 2016
An audit of compliance with key aspects of BCSH guidelines on diagnosis, investigation and management of chronic lymphocytic leukaemia
Dr Nilima Parry-Jones March 2014
An audit of compliance with the BCSH revised guidelines for the diagnosis and management of hairy cell leukaemia a hairy cell variant
Dr Mike Galloway November 2012
An audit of compliance with the British Society for Haematology guideline for the management of newly diagnosed large B-cell lymphoma.docx
An audit of compliance with bsh guidelines for diagnosis and management of mantle cell lymphoma (mcl).docx, an audit of compliance with the bsh guideline on the management of mature t-cell and nk-cell lymphomas (excluding cutaneous t-cell lymphoma).docx, an audit of compliance with the british society for haematology good practice paper on the management of castleman disease.docx, an audit of compliance with the british society of haematology (bsh) on the management of post-transplantation lymphoproliferative disorder (ptld) in adult solid organ transplant (sot) recipients, an audit of compliance with the bsh good practice paper on the management of primary mediastinal b-cell lymphoma, an audit of compliance with the british society of haematology (bsh) guideline on the diagnosis and management of primary central nervous system diffuse large b-cell lymphoma, an audit of compliance with the british society for haematology (bsh) guidelines for the investigation and management of nodular lymphocyte predominant hodgkin lymphoma (nlphl), an audit of compliance with the british society for haematology (bsh) good practice paper on the diagnosis and investigation of mantle cell lymphoma, an audit of compliance with the bcsh guidelines for the management of diffuse large b-cell lymphoma (dlbcl).
Dr Simon Stern July 2016
An audit of compliance with the BCSH guideline on the first line management of classical Hodgkin lymphoma (cHL)
An audit of compliance with the bcsh guidelines on the diagnosis and management of waldenström macroglobulinaemia (wm).
Dr Guy Pratt August 2014
An audit of compliance with the BCSH guidelines for the management of adults’ relapsed and refractory Hodgkin’s lymphoma
Dr Kirit Ardeshna July 2014
An audit of compliance with the BCSH guidelines on the investigation and management of newly diagnosed follicular lymphoma
Dr Charlotte Lees May 2012
An audit of compliance with the British Society for Haematology guideline for the management of myelofibrosis.docx
An audit of compliance with the british society for haematology good practice paper on genetic testing of myeloproliferative disorders.docx, an audit of compliance with the bsh guideline diagnosis and evaluation of prognosis of adult myelodysplastic syndromes.docx, an audit of compliance with the bsh on the diagnosis, investigation and initial treatment of myeloma.docx, an audit of compliance with the bsh guideline on the management of adult myelodysplastic syndromes.docx, an audit of compliance with the british society for haematology (bsh) guideline for screening and management of late and long-term consequences of myeloma and its treatment.
Dr Guy Pratt September 2017
An audit of compliance with the British Society for Haematology (BSH) guideline for the use of imaging in the management of patients with myeloma
An audit of compliance with the bcsh guidelines for supportive care in multiple myeloma.
Dr Simon Stern February 2014
An audit of compliance with the BCSH guideline for the use of bisphosphonate therapy in patients with myeloma
Dr Michelle Lannon May 2012
Miscellaneous
An audit of compliance with bsh guidelines for diagnosis and management of the monoclonal gammopathy of undetermined significance (mgus).docx, an audit of compliance with the british society for haematology (bsh) guideline on the management and admission to intensive care of critically ill adult patients with haematological malignancy.
Dr Nilima Parry-Jones June 2021

An audit of compliance with the British Society for Haematology (BSH) guideline for the laboratory diagnosis of G6PD deficiency
September 2020
An audit of compliance with the British Society for Haematology (BHS) guideline for the management of specific situations in polycythaemia vera (PV) and secondary erythrocytosis
Professor Mary Frances McMullin March 2019
An audit of compliance with the British Society of Haematology (BSH) guideline for the investigation and management of a raised serum ferritin (SF)
Dr Savio Fernandes June 2018
An audit of compliance with the BCSH guideline on the management of tumour lysis syndrome (TLS) in adults and children with haematological malignancies
An audit of compliance with the british committee for standards in haematology (bcsh) guidelines on the use of multicolour flow cytometry in the diagnosis of haematological neoplasms.
Mr Michael Wright October 2015
An audit of compliance with the BCSH guideline for the investigation and management of adults diagnosed with (PMF), (post-PV MF) and (post-ET MF)
Dr Joanne Howard September 2015
An audit of compliance with the Guideline on the clinical use of apheresis procedures for the treatment of patients and collection of cellular therapy products
Ms Catherine Howell July 2015
An audit of compliance with the two BCSH guidelines on the diagnosis, investigation and management of patients with AL amyloidosis
Dr Guy Pratt February 2015
An audit of compliance with British Committee for Standards in Haematology guidelines on obtaining consent for systemic anti-cancer chemotherapy
Dr Fiona Clark July 2014
An audit of compliance with the BCSH guidelines for the management of cytomegalovirus (CMV) in haematological malignancy
Dr Andrew Clark February 2014
An audit of compliance with BCSH guidelines for the investigation of newly detected M-proteins and the management of MGUS
Dr Emily Graves May 2012
An audit of compliance with the British Society for Haematology (BSH) guideline on transfusion for fetuses, neonates and older children
An audit of compliance with the british society for haematology (bsh) guideline on management of thrombotic and haemostasis issues in paediatric malignancy.
Dr Keith Richard Sibson March 2018
Sickle cell disease
An audit of compliance with the british society for haematology guideline on the management of sickle cell disease in pregnancy.docx 1, an audit of compliance with the british society of haematology (bsh) guideline on the use of hydroxycarbamide in children and adults with sickle cell disease.
Dr Amrana Qureshi August 2020
Audit of compliance with the BSH guideline for the management of Acute Chest Syndrome in Sickle Cell Disease
Dr Jo Howard May 2017
Transfusion
An audit of acute transfusion reactions, an audit of compliance on the use of irradiated blood components.docx, an audit of compliance with bsh good practice paper on pre-operative patient blood management during the sars-cov-2 pande.docx, an audit of compliance with the british society for haematology (bsh) guideline on haematological management of major haemorrhage, an audit of compliance with the british society for haematology (bsh) guidelines on the management of anaemia and red cell transfusion in adult critically ill patients, an audit of compliance with the updated british society of haematology (bsh) guideline on the use of fresh frozen plasma (ffp) and cryoprecipitate products in patients without major bleeding, an audit of compliance with the british society for haematology (bsh) guideline on the investigation and management of acute transfusion reactions (atrs), an audit of compliance with the british society for haematology (bsh) guideline on red cell transfusion in sickle cell disease (scd). part i: principles and laboratory aspects, an audit of compliance with the british society for haematology (bsh) guideline on red cell transfusion in sickle cell disease (scd). part ii: indications for transfusion.
Dr Jacky Wilson September 2017
An audit of compliance with the British Society for Haematology (BSH) guideline for platelet transfusions in adult patients
Dr Lise Estcourt and Dr Janet Birchall August 2017
Audit of compliance with BCSH/BSBMT guideline on diagnosis and management of veno-occlusive disease following haematopoietic stem cell transplantation
Dr Fiona Dignan January 2014
An audit of compliance with the BCSH/BSBMT guidelines on the diagnosis and management of acute graft-versus-host disease
Dr Mike Galloway & Dr Will Lester July 2013
An audit of compliance with the BCSH/BSBMT guidelines on the diagnosis and management of chronic graft-versus-host disease
An audit of compliance with the bcsh/bsbmt guidelines on the organ-specific management and supportive care with chronic graft-versus-host disease, medical microbiology, antimicrobial choice and stewardship, an audit of antimicrobial stewardship 'start smart - then focus' compliance with national and local recommendations for antimicrobial prescribing.
Dr Marina Morgan December 2012
An audit of antimicrobial choice and administration for neutropenic sepsis
An audit of diagnosis and antimicrobial management of community-acquired pneumonia (cap), an audit of compliance with local and national guidelines for treatment of urinary tract infection, an audit of compliance with local and national guidelines for treatment of urinary tract infection in pregnancy, audit of compliance with the guidelines for prevention and control of group a strep (gas) infection in acute health care and maternity settings in uk, an audit of diagnosis and management of encephalitis, an audit of the management of invasive candidaemia, an audit of the diagnosis and treatment of infective endocarditis, an audit of the diagnosis and management of septic arthritis in adults, clinical biochemistry, an audit of the laboratory investigation of suspected multiple myeloma.
Mr Peter West February 2014
An audit of implementation of NICE guidelines on ovarian cancer in primary care
Dr Roanna George & Dr Soha Zouwail February 2013
An audit of compliance with the RCPath KPIs for the percentage of core investigations from A&E comp within 1 hour of receipt, including out of hours
Mr James Allison & Dr Bernie Croal February 2013
An audit against the All Wales Clinical Biochemistry Audit Group Standards for the Investigation of Porphyria
Dr Annette Thomas February 2013
An audit of the investigation of patients presenting with hyponatraemia and hyperkalaemia
Dr Housley Dr Freedman Dr Mylvaganam Dr Banerjee February 2013
An audit of critical result communication
Miss Helen Turner & Dr Bernie Croal February 2013
An audit of timeliness of responding to requests for clinical advice
Dr Kevin Deans & Dr Bernie Croal February 2013
An audit of the appropriate use of tumour markers
Dr Lance Sandle February 2013
An audit of delayed specimen transport
Dr Allan Dunlop & Dr Bernie Croal February 2013
An audit of the compliance of samples to meet the minimum sample acceptance criteria
Dr Mark Lum & Dr Bernie Croal February 2013
Cellular Pathology
Audit of core biopsy diagnosis of breast lesions.doc 1, an audit of breast cancer grading.
Dr Rahul Deb & Dr David Parham January 2017
An audit of compliance with guidance for the pathological examination of sentinel lymph nodes
Dr Rahul Deb & Dr Pauline Carder January 2017
Bone and soft tissue
Audit of soft tissue sarcoma reporting in resection specimens.
Professor Charles Mangham January 2017
An audit of the histopathological reporting of soft tissue sarcomas
An audit of tissue pathways for bone and soft tissue pathology, cancer of unknown primary malignancy of unknown primary origin, an audit of histopathological reporting of cup and muo.docx, cardiovascular system, central nervous system, an audit of quality of reporting epilepsy surgical resections for non-neoplastic lesions.
January 2021
An audit of quality of reporting muscle biopsies
An audit of quality of reporting peripheral nerve biopsies, an audit of quality of reporting non-neoplastic brain biopsies, an audit of quality of reporting skin biopsies for the diagnosis of small fibre neuropathy, cytopathology, an audit of reporting of thyroid cytology specimens and their correlation with thyroid histology.
December 2022
An audit of the content and format of cytopathology reports
Endocrine system, an audit of histopathological reporting of thyroid cancer.docx.
September 2023
An audit of histopathological reporting of carcinomas of the parathyroid
October 2023
An audit of reporting of ACC and phaeochromocytoma paraganglioma.docx
An audit of uveal melanoma reporting in resection specimens, an audit on quality of reporting of non-neoplastic enucleation specimens, an audit of non-neoplastic ophthalmic pathology specimen reporting turnaround times.
Dr Luciane Irion September 2020
An audit of uveal melanoma reporting in enucleation specimens
Dr Luciane Irion January 2019
An audit of retinoblastoma reporting in enucleation specimens
An audit of conjunctival melanoma reporting in conjunctival specimens.
Dr Hardeep Singh Mudhar October 2013
Gastrointestinal tract
An audit of reporting appendiceal carcinomas and mucinous tumours in resection specimens.docx, an audit of reporting metastatic colorectal carcinoma in liver resection specimens.
November 2022
An audit of reporting primary gallbladder cancer resection specimens
An audit of reporting primary liver cancer resection specimens, 11 an audit of the specimen quality and reporting of medical liver biopsies.
Dr Judy Wyatt June 2021
12 A clinicopathological audit of the effect of medical liver biopsies on patient management
An audit of colorectal carcinoma reporting standards, audit of anal cancer reporting in biopsy specimens.docx, audit of colorectal carcinoma reporting standards.
Dr Maurice Loughrey January 2018
An audit of compliance with recommended sampling and core data items in the Royal College of Pathologists’ dataset for colorectal cancer reporting
Prof Roger Feakins November 2015
An audit of quality of reporting of colorectal mucosal biopsies taken for the diagnosis and assessment of inflammatory bowel disease (IBD)
Prof Roger Feakins October 2013
Gynaecological tract
An audit of quality of reporting vulva cancer resection specimens.
Dr Asma Faruqi, Dr Brian Rous January 2024
An audit on tissue pathways for gynaecological pathology
Audit of quality of reporting placental pathology.
October 2022
An audit of reports of excisional biopsy specimens for the diagnosis of cervical carcinoma
An audit of reports of hysterectomy specimen for the management of cervical carcinoma, audit of endometrial carcinoma reporting in hysterectomy specimens.
Prof Glenn McCluggage January 2018
An audit of reporting of endometrial carcinomas on biopsy specimens
Dr Raji Ganesan January 2018
Head and neck
An audit of quality of reporting of intraoral mucosal biopsies.
December 2023
An audit of reporting intraoral mucosal polypoid lesions
An audit of quality of reporting of nasal biopsies, an audit of quality of reporting of oral cavity resection specimens, an audit of histopathology reports on carcinomas of the oropharynx and nasopharynx.
December 2021
An audit of histopathology reports on laryngeal carcinoma resections (also applies to other head and neck cancer resections)
Dr Tim Helliwell October 2013
An audit of reporting of carcinomas of the larynx, hypopharynx and trachea
Lung and thorax, an audit of reporting quality of non-neoplastic pulmonary pathology, an audit of biopsy/cell pellet reporting for non-small cell lung cancer (nsclc).
Professor Andrew Nicholson January 2017
An audit of reporting mesotheliomas.docx
Lymph node and bone marrow, an audit of peripheral neuroblastic tumours reporting standards, an audit of renal tumours in childhood reporting in resection specimens, post mortem, an audit of compliance with national guidelines for external and internal examination at coronial autopsy.
Dr Michael Osborn January 2017
An audit of compliance with the standards for cancer reporting
Dr Paul Barrett February 2017
An audit of turnaround times for reporting of non-neoplastic dermatopathology specimens.docx
An audit of reporting primary cutaneous lymphoma, audit of primary cutaneous basal cell carcinoma reporting standards.
Dr David Slater April 2019
Audit of primary cutaneous invasive malignant melanoma reporting standards
Audit of primary cutaneous squamous cell carcinoma reporting standards, audit of primary cutaneous invasive merkel cell carcinoma reporting standards, audit of skin biopsies for diagnosis of an inflammatory dermatosis.
Dr Asok Biswas February 2019
Urinary tract and testes
An audit of quality of reporting transurethral resection of bladder tumour specimens, histocompatibility and immunogenetics, clinical audit on hla typing and donor selection for patients receiving an hpc allograft final.pdf, clinical audit on hla typing and donor selection for patients receiving an hpc allograft final.doc, cross-specialty, an audit of compliance with the national minimum retesting intervals in pathology guideline.
Dr Tim Lang, Dr Bernie Croal July 2021
An audit of the post-mortem examination of animals having received chemotherapeutic or radioactive agents
- ICH GCP (De)
- ICH GCP (En)
- ICH GCP (Es)
- ICH GCP (Fr)
- ICH GCP (It)
- ICH GCP (Pt)
- ICH GCP (Ru)
- AUSTRALIA (NHMRC)
- JAPAN (PMDA)
- US Clinical Trials Registry
- EU Clinical Trials Registry
- Pharmaceutical Companies
- Clinical Research Labs
- Service Companies
- Clinical Research Events
- Publications
- Researchers
Planning Of Audits
Before conducting an audit, the auditor (including the auditing department manager) should establish a written audit plan (such as an annual plan, a monthly plan, and a plan specific to each trial or audit) based on the results of the risk assessment according to the written auditing procedures. 5.1 Establishing the Goals of Audits One or more objectives are generally established for a trial audit based on the importance of the trial with regard to submissions to regulatory authorities, the type and complexity of the trial, the level of risk to the trial, and any problem(s) identified previous. The most important part of audit planning is to specify the goal(s) of the audit. By establishing the goal(s) of an audit, the subjects and methods of the audit will be determined and the consistent conduct of the audit will be ensured. One or more objectives may be chosen from the following examples:
Clinical Research News
Upcoming clinical research training and conferences.
Upcoming Clinical Trials
- Center for Innovative Public Health Research University of Miami; Ann and Robert H Lurie Childrens Hospital of Chicago Recruiting Testing a Gender-inclusive HIV Prevention Program HIV Prevention United States
- Takeda Not yet recruiting A Study to Explore Hereditary Angioedema (HAE) Symptoms and Treatment Patterns in Korean People (SPEAKUP) Hereditary Angioedema (HAE)
- Abbott Medical Devices Recruiting Abbott Structural Heart Device Registry (SH-Registry) Heart Diseases | Valvular Heart Disease | PFO - Patent Foramen Ovale | VSD - Muscular Ventricular Septal Defect | PIVSD - Post Infarct Muscular Ventricular Septal Defect | ASD - Atrial Septal Defect France, Germany
- Lisata Therapeutics, Inc. Not yet recruiting LSTA1 Phase 1b/2a Continuous Infusion Trial in mPDAC (FORTIFIDE) Pancreas Adenocarcinoma | Pancreatic Ductal Adenocarcinoma | Pancreas Cancer | Pancreatic Carcinoma | Metastatic Pancreatic Cancer | Unresectable Pancreatic Cancer | PDAC | PDAC - Pancreatic Ductal Adenocarcinoma
- Yonsei University Recruiting ATezolizumab and BEvacizumab With STereotactic Body Radiotherapy for Advanced Hepatocellular Carcinoma (ATBEST) Chemotherapy | Advanced Hepatocellular Carcinoma | Stereotactic Body Radiotherapy Korea, Republic of
- The First Affiliated Hospital with Nanjing Medical... Chinese Medical Association Not yet recruiting Effects of an Information-Based Discharge Service on Preterm Infants, Parents, and Hospitals Infant, Premature | Patient Discharge
- The First Affiliated Hospital with Nanjing Medical... Not yet recruiting Multi-Technology Integrated Total Mesorectal Excision Versus Conventional Total Mesorectal Excision for the Treatment of Middle and Distal Rectal Cancer. Rectal Cancer
- Guangzhou Medical University Recruiting Feasibility and Safety of Remote Robotic Bronchoscopy System in Diagnosis of Peripheral Pulmonary Lesions: a Multicenter, Randomized Controlled, Proof-of Concept Trial Pulmonary Nodule China
- The General Hospital of Western Theater Command Recruiting Clinical Study of Combined Platelet Transfusion Hematologic Diseases China
- Gerd Care Medical Ltd Recruiting Safety and Effectiveness of eGERD Device to Reduce Gastroesophageal Reflux Disease (GERD) Symptoms GERD (Gastroesophageal Reflux Disease) Israel
- Gazi University The Scientific and Technological Research Council of Turkey Recruiting The Effect of Mobile Application Use on Drug Administration Knowledge and Skill Level of Pediatric Nursing Students Nursing Caries | Nurse's Role Turkey
- Duke University Medical University of South Carolina; Eunice Kennedy Shriver National Institute... and other collaborators Not yet recruiting PK/PD of Digoxin in Infants With SVHD Infant, Newborn, Diseases | Infant, Premature, Diseases | Infant Conditions | Single-ventricle United States
Clinical Research Jobs
Sponsors and Collaborators
- Assiut University
- GlaxoSmithKline
- National Cancer Institute (NCI)
- Cairo University
- AstraZeneca
- Assistance Publique - Hôpitaux de Paris
- Mayo Clinic
- M.D. Anderson Cancer Center
- Novartis Pharmaceuticals
- National Institute of Allergy and Infectious Diseases (NIAID)
- Massachusetts General Hospital
- National Taiwan University Hospital
- Boehringer Ingelheim
- Hoffmann-La Roche
- Merck Sharp & Dohme LLC
- Stanford University
- University of California, San Francisco
- Eli Lilly and Company
- Duke University
- View Full List
Medical Conditions
- Breast Cancer
- Hypertension
- Prostate Cancer
- HIV Infections
- Coronary Artery Disease
- Heart Failure
- Diabetes Mellitus, Type 2
- Colorectal Cancer
- Lung Cancer
- Schizophrenia
- Cardiovascular Diseases
- Atrial Fibrillation
Drug Interventions
- Cyclophosphamide
- Carboplatin
- Dexamethasone
- Gemcitabine
- Capecitabine
- Bevacizumab
- Pembrolizumab
- Methotrexate
- Oxaliplatin
- Dexmedetomidine
- Fludarabine
Clinical Researcher
Clinical Study Reports 101: Tips and Tricks for the Novice
Clinical Researcher September 15, 2020

Clinical Researcher—September 2020 (Volume 34, Issue 8)
PEER REVIEWED
Sheryl Stewart, MCR, CCRP
The tenets of Good Clinical Practice (GCP), promulgated by the International Council for Harmonization (ICH), require that investigator-initiated trials (IITs), especially those involving an Investigational New Drug application to the U.S. Food and Drug Administration (FDA), have the principal investigator (PI), the institution, and the study team assume roles of both the sponsor (ICH GCP E6(R2), Section 5) and of the PI (ICH GCP E6(R2), Section 4).{1} If you are part of an IIT team, whether you are the investigator, a clinical research coordinator, or someone working in any of the many other important roles within the team, you may be tasked with authoring a clinical study report (CSR) at one time or another within the course of the study. At the very least, you may be asked to contribute to, or provide peer review of the document before it is submitted for its intended purpose.
The purpose of this review is to provide a framework for study team members, whether it’s for a large team that includes regulatory and administrative support or for smaller teams with only one or two members, for writing and organizing the CSR.
First, is important to understand the definition, requirements, and potential uses of a CSR. The report is a comprehensive look at all the data produced in a clinical study, presented in text, tables, and figure formats. It will often include discussions and conclusions that provide context to the findings regarding the drug, device, biological product, surgical method, counseling practice, or any other type of therapeutic product or practice under study and where it may contribute to an improvement on the state of the art for treating or preventing a particular health condition.
If a study has prespecified endpoints or parameters, the CSR will report the current outcomes and statistical parameters for these endpoints. Key messages will be referred to and highlighted throughout. Key messages are important study findings that support the prespecified endpoints, supply proof of the justification of clinical benefit, or differentiate the study product from others in the therapeutic space.
Most likely you already appreciate the ethical responsibility a clinical study team has to clinical study data transparency, which for that reason alone would make the production of some sort of CSR necessary. Indeed, the preparation and representation of study progress is prescribed in the aforementioned ICH GCP E6(R2) guideline,{1} which states that study sponsors should ensure that clinical trial reports are prepared and provided to regulatory agencies as they are required.
Further, the guideline recommends study sponsors to rely on a subsequent guideline on Structure and Content of Clinical Study Reports (ICH E3).{2} Lastly, adhering to this ethical responsibility and following GCP have become mandated both in the U.S. and in Europe, where study data are expected to be recorded on ClinicalTrials.gov and the EudraCT database, respectively, for the sake of transparency and in support of further scientific inquiry, thus making the organization and preparation of study data in a prespecified format necessary.{3,4}
There are a few different uses for a CSR, though primarily it is utilized either to summarize the data and outcomes at the end of the study, or for marketing authorization. Those two purposes are specifically outlined in ICH E3 and ICH E6.{1,2} However, a CSR may also be written for third-party payer reimbursement purposes, providing details in support of clinical benefit. Because in most cases CSRs will ultimately have a regulatory reviewer, authoring a report that is consistent in formatting and content with what is expected will hopefully not only enable a smooth review, but also will facilitate proper data cleaning, presentation, and timeliness that make the document fit for purpose.
ICH E3 offers a CSR template to guide you in terms of providing the proper data and content in a specified order and format. This guideline can be found either on the ICH website or the FDA website.{2,5}
It is important to note that there are no requirements to follow the template precisely. Not every section is appropriate for every study, and because the overarching purpose of a CSR is to provide proper representation of the study data and any key messages you want to report, flexibility is allowed and encouraged in order to meet those important goals. However, for anyone new to the process of crafting a CSR, this template is a helpful starting point.
Transcelerate Biopharma, a nonprofit organization involved in researching means to increase efficiency and innovation in the pharmaceutical research sciences, also has interpreted the ICH template and has produced a useful tool to improve this reporting.{6} If the instruction and guidance in the ICH or Transcelerate templates do not meet your needs, or you have further questions as to how to properly represent the study data, the CORE reference manual (Clarity and Openness in Reporting E3-based) is another resource. It was produced in 2016 in response to regulatory changes for public disclosure of clinical study data, and can provide direction and interpretation of the ICH E3 template.{7}
For the novice author of a CSR, however, the ICH E3 template, coupled with the Transcelerate template, should provide a strong starting point for the project planning of the report, as well as the document formatting.
Sidebar: Tips and Tricks for Getting Started
|
|
Determining Stakeholders
Once you’ve reviewed the template and created a draft outline of the project, determine the key stakeholders with whom you’ll need to partner to complete this project. Likely you will need input from your clinical study management team, teammates responsible for data entering and cleaning, a biostatistician, any teammate or organization member able to perform literature reviews, those staff qualified to compose patient or adverse event narratives, and those team members who can help determine key messaging in this report. Lastly you will want to determine the group of key stakeholders who will be your final review team for the document—those who will help you finalize the document prior to submission.
Sidebar: Tips and Tricks for Stakeholder and Project Management
|
|
Determining Timelines
Once you have determined your key stakeholders, you will want to determine timelines to ensure steady progress continues to be made on the document. If you’ve chosen to utilize a scope document, you’ll want to include these timelines in it, so the entire team is aware of the project process, the timing requirements, and each gating item (key gating items are summarized in Figure 1).
Figure 1: Preparing, Writing, and Review of the Clinical Study Report—Key Gating Items
| o Data cleaning and query resolution | o Write non-results sections |
| o Plan tables, listings, and figures (TLFs) | o Perform literature review |
| o TLF creation and revisions | o Write results sections |
| o TLF editing | o Cross team/stakeholder review |
| o Data-lock process | o Incorporation of revisions |
| o Final TLF preparation | o Finalize report for submission |
Time management is paramount for clinical trial submissions to regulatory authorities. Attendees at medical writing conferences over the course of a five-year period (2008 to 2013, n=78) were surveyed to determine to how long each step of the CSR process can typically require.{8}
To complete a “moderately complex” CSR for a Phase III study with 200 to 400 participants, the surveyed medical writers responded with a mean answer of 16.9 days from the receipt of the final tables, listings, and figures (TLFs) to delivery of the first draft of the CSR. They estimated a mean of 25.7 days from the first draft to the final draft routed for review. The time from database lock to completion was reported to be on average 83 days.
While there was a wide range for the timelines reported, these data provide the novice CSR author a basic reference point for how long the individual processes can expect to take with experienced medical writers. Fortunately, while TLFs are being crafted, multiple other “Writing and Document Review” tasks from Table 1 can be performed simultaneously.
At Last…the Writing!
Typically, the flow of your CSR will progress under six primary headings or sections, not unlike those used in a research manuscript. On the front end, even before the background and introduction, the document will include a title page, synopsis, table of contents, list of abbreviations, ethics statements, and details on the study’s administrative structure. The primary sections to come after that are highlighted in Figure 2 and summarized in turn below.
Figure 2: Primary Sections
Background, Intro. > Non-Results > Results > Discussion > Conclusion > Exec. Summary
Background and Introduction
When available, utilize any state-of-the-art analysis of the product/therapy from the protocol for your CSR introduction. If not available, you can briefly summarize the study design, objectives, and population and then you’ll need to craft a novel but brief state-of-the-art analysis based on literature review.
Be sure to align with the key messaging of your study and the indications of your study drug, device, or other type of therapeutic product or method. Utilize good literature review practices, such as choosing peer-reviewed publications, editorials from key opinion leaders in the therapeutic area, and studies with large or randomized cohorts, for support. This section will likely be no longer than one page.
Non-Results Section
Whether to cut and paste the procedures and assessments, primary and secondary endpoints, parameters or hypotheses, planned statistical analyses, monitoring plans, adverse event definitions, and assessment rules directly from the protocol or to simply refer to the protocol and the other study documents in an appendix is a topic of debate amongst medical writers of CSRs. Keep in mind that the CSR should be able to stand alone as a document, and thus while it is important to keep the document concise, it must be comprehensive enough for the reader to understand the study design, objectives, endpoints, processes, and intended analyses without having to refer constantly to the protocol. Regardless, in any summary of the study design, processes, and endpoints, be sure to align with any previously utilized language for consistency across study documents.
Results Section
Using the template and your tables as your structure, summarize the data and pull out any signals and trends, aligning with key messaging where possible. Start with patient disposition and demographics as per the template. Note any protocol deviations that may or may not have impacted patient safety or the evaluation of the outcomes.
Assess and evaluate the study outcome results against primary endpoints and secondary endpoints before discussing any additional secondary outcomes. You should not simply restate the data in the tables; however, refer to specifics in the tables when summarizing.
If you find that you cannot make a statement or conclusion given the TLFs you have, or you are consistently having to perform your own math to support your statements, consider asking your biostatistician to create the tables that will represent the data in a way that will better support your statement. For instance, it is acceptable to state that “most” of the patients responded to the study drug if more than 50% did so; however, if you are having to consistently add up percentages in a table to be able to state, for example, that 77% of the patients responded in a certain way and 33% responded in another, then you should have the biostatistician reformat the data output so it represents the percentages you want to report.
Patient narratives are an important source of context for the reader of the CSR. Depending on your study, you may need to collaborate with either your teammates responsible for assessment of adverse events or the study database administrator to help generate patient and/or event narratives for the CSR. If tasked with compiling or editing patient narratives yourself, the ICH E3 guideline prescribes the necessary components of a comprehensive patient safety narrative (Section 12).{2}
Narrative writing advice has also been previously published and would be a helpful source of direction for the novice narrative writer.{9,10} Narratives are suggested for every patient who experienced a safety endpoint event or death during the course of the study. Tie in patient narratives where appropriate when discussing safety events or refer to the patient narrative section when highlighting a particular patient’s data.
Discussions and Conclusions
Discussion and conclusion sections can either be placed after each section or placed at the end of the document. They should not simply restate the previous table summaries, but provide context and align the results with key messaging. Use an evidence-based approach, including literature references to provide more context as to the nature of the study outcomes with respect to the state of the art for the product/therapy, outcomes from alternate approaches, or further justification of clinical benefit with regard to potential disease progression. The conclusion section at the end of the document is often in bulleted format—not only for ease of the reader, but also to clearly highlight the key messaging and important outcomes you wish to impart.
Executive Summary
The executive summary, while placed at the front of the document prior to the introduction, is often easiest to construct last, as an overall summary of the entire document. The key elements of this summary should briefly recap the study design and objectives. Most likely only the primary and secondary endpoints should be included, unless additional outcomes proved compelling and important within the course of the study. Refer to any important literature comparisons as they relate to any conclusions made about the success or outcomes of the trials. Conclude the executive summary in a similar fashion to the overall study conclusion.
Sidebar: Tips and Tricks for the CSR Writing Process
|
|
Review Process
The review process can either facilitate a better document or it can slow down the entire process. The purpose of a cross functional review of a CSR is to confirm accurate key study messaging and data; allow medical review of the patient narratives, outcomes, and conclusionary statements; review the logical flow of ideas; and ensure that the CSR language is consistent across any other study document (i.e., the protocol, statistical analysis plan, etc.).
Sidebar: Tips and Tricks for an Efficient Review Process
CSRs are required by regulatory authorities to report and summarize the outcomes of a clinical study. Pre-project stakeholder determination and timeline planning can help with project management. Templates contained with the ICH E3 guideline can help organize the project as well as help create and finalize a document that is fit for purpose and meets the content expectations of the regulatory reviewer.
- ICH Working Group. 2016. ICH HARMONISED GUIDELINE INTEGRATED ADDENDUM TO ICH E6(R1): GUIDELINE FOR GOOD CLINICAL PRACTICE E6(R2).
- ICH Working Group. 1995. ICH HARMONISED TRIPARTITE GUIDELINE: Structure and Content of Clinical Study Reports E3 .
- U.S. Department of Health and Human Services. 2016. Clinical Trials Registration and Results Information Submission, 42 CFR Part 11. https://www.federalregister.gov/documents/2016/09/21/2016-22129/clinical-trials-registration-and-results-information-submission
- European Commission. 2001. Letter to Stakeholders Regarding the Requirements to provide results for Authortied clinical trials in EUDRACT. In: Article 57(2) Regulation (EC) No 726/2004 and Article 41(2) of Regulation (EC) No 1901/2006. https://eudract.ema.europa.eu/
- U.S. Food and Drug Administration. 2018. ICH Guidance Documents . https://www.fda.gov/science-research/guidance-documents-including-information-sheets-and-notices/ich-guidance-documents
- Transcelerate Biopharma Inc. Clinical Template Suite (CTS), Template, Resources, and Use Guidance. https://transceleratebiopharmainc.com/assets/clinical-content-reuse-assets/
- Hamilton S, Bernstein AB, Blakey G, et al. 2016. Developing the Clarity and Openness in Reporting: E3-based (CORE) Reference user manual for creation of clinical study reports in the era of clinical trial transparency. Research integrity and peer review. 1:4.
- Hamilton S. 2014. Effective authoring of clinical study reports. Medical Writing 23(2).
- Nambiar I. 2018. Analysis of serious adverse event: Writing a narrative. Perspect Clin Res 9(2):103–6.
- Ledade SD, Jain SN, Darji AA, Gupta VH. 2017. Narrative writing: Effective ways and best practices. Perspect Clin Res 8(2):58–62.

Sheryl Stewart, MCR, CCRP, ( [email protected] ) is a Medical Writer working in the medical device industry in southern California.
Sorry, we couldn't find any jobs that match your criteria.

The Industry Shift Toward Decentralized Clinical Trials: Impacts on Quality Management, Participant Outcomes, and Data Management

Insights into the Clinical Research Associate Career Pathway

The Future of Multi-Omics in Cancer Clinical Trials
All Formats
Report Templates
12+ clinical audit report templates – pdf, doc.
Audits can be done for different departments and for various purposes on businesses and organizations. When an investigation or audit is specifically done to businesses and organizations in the health industry or those operating in a clinical setting, a clinical audit report is created. You may also see Health and Safety Report Templates.
Report Template Bundle
- Google Docs
Free Annual Clinical Audit Report Template
Free Clinical Audit & Effectiveness Annual Report
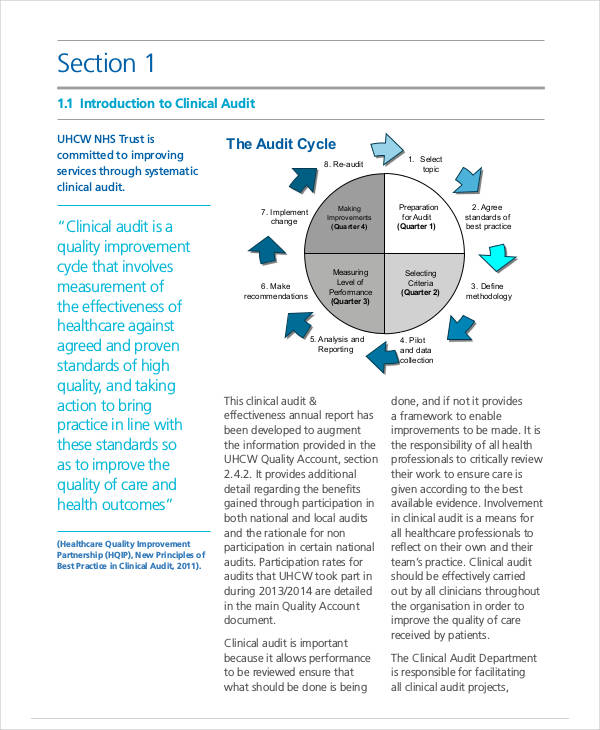
Check Out These Clinical Audit Report Templates
Free printable clinical audit report template.
What is a Clinical Audit Report?
Free blank clinical audit report template.
Free End of Life Clinical Audit Report Template
What to Write in a Clinical Audit Report
1. introduction, 2. audit methodology, free standard clinical audit report template.
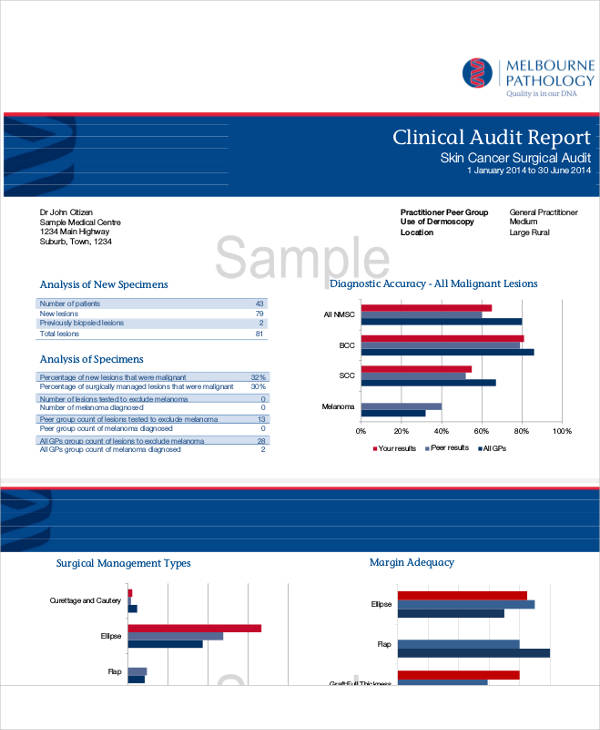
Free Clinical Audit & Patient Experience Facilitator
Free Clinical Audit Report Format
Free Sample Clinical Audit Report Template
3. Audit Results and Discussion
4. conclusions, 5. action plan and recommendations, 6. references and appendices, free clinical audit report example.
Free Clinical Audit Report Template Example
Free Record Keeping Clinical Audit Report Template
It’s Your Turn
More in report templates.
National Nurses Day Flyer Vector Template
National nurses day quote vector template, children clinic business card template, blank doctor id card template, medical booklet template, national dentist's day illustration template, national dentist's day whatsapp post template, national dentist's day website banner template, national dentist's day banner template, national dentist's day drawing vector template.
- How to Create a Financial Audit Report [10+ Templates to Download]
- 40+ Monthly Management Report Templates in PDF | Google Docs | Excel | Apple Pages
- 25+ Non Conformance Report Templates – PDF, Docs, Word, Pages
- 19+ Event Report Templates – Word, PDF, Docs, Pages
- 34+ Report Card Templates- Word, Docs, PDF, Pages
- 23+ Sample Inspection Report Templates- Docs, Word, Pages
- 36+ Weekly Activity Report Templates – PDF, Docs
- 10+ Free Audit Findings Report Templates in PDF | MS Word
- 10+ Audit Exception Report Templates in PDF | MS Word
- 11+ Audit Committee Report Templates in PDF | MS Word
- 6+ Logistics Audit Report Templates in PDF | MS Word
- 11+ Logistic Report Templates in PDF
- 8+ Logistics Monthly Report Templates in PDF | MS Word
- 17+ Internship Student Report Templates
- 64+ Monthly Report Samples
File Formats
Word templates, google docs templates, excel templates, powerpoint templates, google sheets templates, google slides templates, pdf templates, publisher templates, psd templates, indesign templates, illustrator templates, pages templates, keynote templates, numbers templates, outlook templates.

Forms & Templates
The CRCO is actively creating and connecting to forms and templates that promote regulatory compliance and best practices in clinical research. Explore these resources by topic.
- Study Planning
- Study Start-Up
- Recruitment and Enrollment
- Study Conduct
- Study Close-Out
- Feasibility Assessment
- Data Managment
- Informed Consent Process
- Investigational Product (IP) Accountability Standard Operating Procedure and Work Instructions
- Management and Reporting Adverse Events
- Study Start-Up Checklist
- Guidance for Completing a Supervisory Plan for Clinical Research
- PI Supervisory Plan for Clinical Research
- Delegation of Responsibility Log
- Training Log
- Comprehensive Monitoring Plan Template
- Concise Monitoring Plan Template
- Eligibility Checklist Template
- Participant Enrollment Documentation
- Informed Consent Process and HIPAA Authorization Documentation
- Enrollment Log
- Master Subject ID Log
- Good Clinical Practices Checklist
- Protocol/Amendment Tracking Log
- Concomitant Medication/Therapies Worksheet
- Adverse Event Log
- Deviation Log
- Device Accountability Log
- Monitoring Visit Log
- Inventory List for Study Storage Documents
- Close-out Checklist
- Transfer of Subject Checklist
Redirect Notice
Audit requirements.
Certain NIH funding recipients are subject to audit requirements under federal law.
What is an audit?
An audit is a systematic review or appraisal made to determine whether internal accounting and other control systems provide reasonable assurance of the following:
- Financial operations are properly conducted. Financial reports are timely, fair, and accurately
- The entity has complied with applicable laws, regulations, and other grant terms
- Resources are managed and used economically and efficiently
- Desired results and objectives are being achieved effectively.
Requirements
Per federal regulation, NIH recipients or sub-recipients that expend $750,000 or more in federal awards during the fiscal year are subject to an audit requirement. Organizations expending less than $750,000 during the fiscal year are not required to have an annual audit for that year, but must make their grant-related records available to NIH or other designated officials for review or audit.
Audits shall be completed and submitted to the designated offices shown below within a period that is either the earlier of (1) 30 days after receipt of the auditor's report(s), or (2) nine months after the end of the audit period (i.e., the organization's fiscal year).
Federal Audit Clearinghouse Bureau of the Census 1201 East 10th Street Jeffersonville, IN 47132 800-253-0696
For-profit organizations, including for-profit hospitals, and foreign organizations should submit their audit report directly to:
National External Audit Review Center HHS Office of Audit Services 1100 Walnut Street, Suite 850 Kansas City, MO 64106-2197 800-732-0679/816-426-7725

COMMENTS
As such the aim of this 'How To' guide is to provide advice on sharing your clinical audit results, addressing both report writing and designing a presentation. 1. REPORT At UHBristol you will be required to complete a Summary form and an Action Plan form at the end of your project (both are available on the clinical audit website or from ...
Audit findings are typically summarized in a formal audit report that is shared with both the sponsor and the site. The report will categorize findings according to their severity, such as critical, major, or minor non-compliance. ... As new technologies transform the way clinical research is carried out around the world, keeping ahead of these ...
Critical Steps: Observations. Observations are graded relative to the level of non-compliance or deviation. An example of this is formatting observations as critical, major, minor, or recommendation. The definitions of these are usually described in an audit's SOPs or detailed in the report template. The definitions are based on the impact or ...
SEARCH, EXPERIMENTS. ICAL RESEARCH AUDI. N DATEDATE OF REVIEWDISCLAIMERAny articles, templates, or information provided by Smartsheet on th. website are for reference only. While we strive to keep the information up to date and correct, we make no representations or warranties of any kind, express or implied, about the completeness, accuracy ...
Writing a clinical audit report. It is recommended that you structure your audit report in the following way: Title: Give your audit a title that describes what is being audited. Background: Provide rationale for topic selection and include background information that is essential to understanding a process or problem. Aim and objectives: The aim describes what you want to achieve.
Clinical and ranslational Science Awards Program, grant number UL1R0011020S1. www.smartirb.org Harmonied: his document underwent a review and input process from December 2020 to April 2021 and has now been finalied. ONFIDENTIAL SAMPLE AUDIT REPORT TEMPLATE 1 PROTOCOL TITLE: PRINCIPAL INVESTIGATOR: Name Department, School FUNDING SOURCE: DATE OF ...
provided to the DISC Administrator, ADCI, and AD-CRO. Process Auditsprocess audit is a systematic review of the clinical t. ial process and is typically a less detailed r. view than a full audit. Process audits are done on an as needed basis. Process audits are intended to identif.
Introduce themselves and show credentials. Review FDA form 482, notice of inspection, and give the investigator the original form. Review why the study is being inspected. Review the inspection process and what to expect during the audit. Provide a projected timeline for the audit. Start the inspection by reviewing the regulatory binder, then ...
This gives the audience, for example, the senior management, audit outcome and key information. It should consist of major findings, significant concerns (if any), dates of audit conduct, vendor/site identification, and whether it's a for-cause or a routine audit. Research teams must include an overall statement of acceptability and ...
The clinical audit report should: Be simple and clear. Be written in plain English. Use a structured, systematic approach, for example, IMRAD (introduction, method, results and discussion which would include recommendations and an agreed quality improvement plan). Present descriptive statistics graphically where possible.
Introduction. Clinical audit is a quality improvement tool that is used to monitor, assess, and improve the quality of care in human and veterinary medicine (1-7).The procedure involves measuring an outcome or process and comparing this to current evidence or best practice, then implementing changes to improve the quality of care (8,9).In human medicine, clinical audit is considered a ...
Informed consent template for clinical trials. Reviewing and obtaining informed consent SOP. Informed consent template for observational in-patient clinical trials : Informed consent template for interviewing research studies : Informed consent template sampling only : Monitoring informed consent checklist : Subject informed consent log template
a separate clinical and statistical report. Although this CSR Template is mainly developed for the most common efficacy and safety clinical studies (also referred to as clinical trials), the basic principles and structure can be applied to other kinds of studies, such as clinical pharmacology studies (e.g., pharmacokinetic [PK] or biomarker of ...
Clinical audit templates. The College have developed a series of online clinical audit templates to support pathologists with revalidation, meeting the standards set for high quality audit by the RCPath. The audit templates are the same basic layout and have been partially completed demonstrating step by step the process of how to plan and ...
The audit plan should be updated in accordance with progress of the trial or auditing activity. Prior to conducting an audit, the auditors and the auditee will discuss and adapt the audit plan, as necessary. 5.3 Determining the Subject[s], Timing, and Method[s] of an Audit The subject(s) (e.g., a medical institution. CRO, system, clinical trial ...
Supporting Clinical ResearchThe purpose of the NIA Clinical Research Toolbox is to provide a Web-based informational repository for investigators and staff involved in clinical research. The Toolbox contains templates, sample forms, guidelines, regulations and informational materials to assist investigators in the development and conduct of high quality clinical research studies.
Clinical Researcher—September 2020 (Volume 34, Issue 8) PEER REVIEWED. Sheryl Stewart, MCR, CCRP . The tenets of Good Clinical Practice (GCP), promulgated by the International Council for Harmonization (ICH), require that investigator-initiated trials (IITs), especially those involving an Investigational New Drug application to the U.S. Food and Drug Administration (FDA), have the principal ...
An observation which is a deviation and/or deficiency in compliance with applicable regulations and guidelines, the protocol, and/or university policies, or an observation which has the potential to impact patient safety, data integrity and or non-compliance with regulations. Examples may include:
Customizable template that outlines the process for an FDA/OHRP inspection, and describes activities that should be done to facilitate the inspection. Preparing for an FDA Inspection Presentation for Coordinators to prepare for and participate in external audits and what comprises inpection readiness. Cancer Center FDA Inspection Guidance.
PDF. Size: 488 KB. Download Now. This article focuses on the creation of effective clinical audit reports using printable audit report templates that anyone may use. In addition, we have also compiled numerous tips on how to make your organization's or your team's clinical auditing process more efficient. You may also check here Report in PDF.
Guidance on Responding to Audit Findings. The purpose of this document is to provide Overall Principal Investigators and their research teams guidance on responding to audit findings. For an internal audit conducted by the Office for Data Quality (ODQ), any major violation noted in the final audit report requires a formal written response from ...
Guidelines suggest that following the good clinical research practice of monitoring/auditing should be done for the reasons previously stated. That is why, whether you participate in FDA regulated research or not, there should be some local policies and procedures in place for the routine evaluation (i.e, an audit) of a clinical trial.
Study Close-Out. Feasibility Assessment. Standard Operation Procedure/Work Instruction Templates. Data Managment. Informed Consent Process. Investigational Product (IP) Accountability Standard Operating Procedure and Work Instructions. Management and Reporting Adverse Events. Training. FDA Part 11 Epic Certification.
Audits shall be completed and submitted to the designated offices shown below within a period that is either the earlier of (1) 30 days after receipt of the auditor's report(s), or (2) nine months after the end of the audit period (i.e., the organization's fiscal year). Federal Audit Clearinghouse Bureau of the Census 1201 East 10th Street
• CLIA SAPR Review Protocol: The FY 2024 review has been updated from FY 2023. We are updating three documents to improve readability and ease by which SAs may complete the templates: the FY 2024 SAPR Excel Workbook, the FY 2024 Summary Report, and the FY 2024 CLIA SAPR Cover Letter CAP Resp Template.