An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts


Case 6–2020: A 34-Year-Old Woman with Hyperglycemia
Presentation of case.
Dr. Max C. Petersen (Medicine): A 34-year-old woman was evaluated in the diabetes clinic of this hospital for hyperglycemia.
Eleven years before this presentation, the blood glucose level was 126 mg per deciliter (7.0 mmol per liter) on routine laboratory evaluation, which was performed as part of an annual well visit. The patient could not recall whether she had been fasting at the time the test had been performed. One year later, the fasting blood glucose level was 112 mg per deciliter (6.2 mmol per liter; reference range, <100 mg per deciliter [<5.6 mmol per liter]).
Nine years before this presentation, a randomly obtained blood glucose level was 217 mg per deciliter (12.0 mmol per liter), and the patient reported polyuria. At that time, the glycated hemoglobin level was 5.8% (reference range, 4.3 to 5.6); the hemoglobin level was normal. One year later, the glycated hemoglobin level was 5.9%. The height was 165.1 cm, the weight 72.6 kg, and the body-mass index (BMI; the weight in kilograms divided by the square of the height in meters) 26.6. The patient received a diagnosis of prediabetes and was referred to a nutritionist. She made changes to her diet and lost 4.5 kg of body weight over a 6-month period; the glycated hemoglobin level was 5.5%.
Six years before this presentation, the patient became pregnant with her first child. Her prepregnancy BMI was 24.5. At 26 weeks of gestation, the result of a 1-hour oral glucose challenge test (i.e., the blood glucose level obtained 1 hour after the oral administration of a 50-g glucose load in the nonfasting state) was 186 mg per deciliter (10.3 mmol per liter; reference range, <140 mg per deciliter [<7.8 mmol per liter]). She declined a 3-hour oral glucose tolerance test; a presumptive diagnosis of gestational diabetes was made. She was asked to follow a meal plan for gestational diabetes and was treated with insulin during the pregnancy. Serial ultrasound examinations for fetal growth and monitoring were performed. At 34 weeks of gestation, the fetal abdominal circumference was in the 76th percentile for gestational age. Polyhydramnios developed at 37 weeks of gestation. The child was born at 39 weeks 3 days of gestation, weighed 3.9 kg at birth, and had hypoglycemia after birth, which subsequently resolved. Six weeks post partum, the patient’s fasting blood glucose level was 120 mg per deciliter (6.7 mmol per liter), and the result of a 2-hour oral glucose tolerance test (i.e., the blood glucose level obtained 2 hours after the oral administration of a 75-g glucose load in the fasting state) was 131 mg per deciliter (7.3 mmol per liter; reference range, <140 mg per deciliter). Three months post partum, the glycated hemoglobin level was 6.1%. Lifestyle modification for diabetes prevention was recommended.
Four and a half years before this presentation, the patient became pregnant with her second child. Her prepregnancy BMI was 25.1. At 5 weeks of gestation, she had an elevated blood glucose level. Insulin therapy was started at 6 weeks of gestation, and episodes of hypoglycemia occurred during the pregnancy. Serial ultrasound examinations for fetal growth and monitoring were performed. At 28 weeks of gestation, the fetal abdominal circumference was in the 35th percentile for gestational age, and the amniotic fluid level was normal. Labor was induced at 38 weeks of gestation; the child weighed 2.6 kg at birth. Neonatal blood glucose levels were reported as stable after birth. Six weeks post partum, the patient’s fasting blood glucose level was 133 mg per deciliter (7.4 mmol per liter), and the result of a 2-hour oral glucose tolerance test was 236 mg per deciliter (13.1 mmol per liter). The patient received a diagnosis of type 2 diabetes mellitus; lifestyle modification was recommended. Three months post partum, the glycated hemoglobin level was 5.9% and the BMI was 30.0. Over the next 2 years, she followed a low-carbohydrate diet and regular exercise plan and self-monitored the blood glucose level.
Two years before this presentation, the patient became pregnant with her third child. Blood glucose levels were again elevated, and insulin therapy was started early in gestation. She had episodes of hypoglycemia that led to adjustment of her insulin regimen. The child was born at 38 weeks 5 days of gestation, weighed 3.0 kg at birth, and had hypoglycemia that resolved 48 hours after birth. After the birth of her third child, the patient started to receive metformin, which had no effect on the glycated hemoglobin level, despite adjustment of the therapy to the maximal dose.
One year before this presentation, the patient became pregnant with her fourth child. Insulin therapy was again started early in gestation. The patient reported that episodes of hypoglycemia occurred. Polyhydramnios developed. The child was born at 38 weeks 6 days of gestation and weighed 3.5 kg. The patient sought care at the diabetes clinic of this hospital for clarification of her diagnosis.
The patient reported following a low-carbohydrate diet and exercising 5 days per week. There was no fatigue, change in appetite, change in vision, chest pain, shortness of breath, polydipsia, or polyuria. There was no history of anemia, pancreatitis, hirsutism, proximal muscle weakness, easy bruising, headache, sweating, tachycardia, gallstones, or diarrhea. Her menstrual periods were normal. She had not noticed any changes in her facial features or the size of her hands or feet.
The patient had a history of acne and low-back pain. Her only medication was metformin. She had no known medication allergies. She lived with her husband and four children in a suburban community in New England and worked as an administrator. She did not smoke tobacco or use illicit drugs, and she rarely drank alcohol. She identified as non-Hispanic white. Both of her grandmothers had type 2 diabetes mellitus. Her father had hypertension, was overweight, and had received a diagnosis of type 2 diabetes at 50 years of age. Her mother was not overweight and had received a diagnosis of type 2 diabetes at 48 years of age. The patient had two sisters, neither of whom had a history of diabetes or gestational diabetes. There was no family history of hemochromatosis.
On examination, the patient appeared well. The blood pressure was 126/76 mm Hg, and the heart rate 76 beats per minute. The BMI was 25.4. The physical examination was normal. The glycated hemoglobin level was 6.2%.
A diagnostic test was performed.
DIFFERENTIAL DIAGNOSIS
Dr. Miriam S. Udler: I am aware of the diagnosis in this case and participated in the care of this patient. This healthy 34-year-old woman, who had a BMI just above the upper limit of the normal range, presented with a history of hyperglycemia of varying degrees since 24 years of age. When she was not pregnant, she was treated with lifestyle measures as well as metformin therapy for a short period, and she maintained a well-controlled blood glucose level. In thinking about this case, it is helpful to characterize the extent of the hyperglycemia and then to consider its possible causes.
CHARACTERIZING HYPERGLYCEMIA
This patient’s hyperglycemia reached a threshold that was diagnostic of diabetes 1 on two occasions: when she was 25 years of age, she had a randomly obtained blood glucose level of 217 mg per deciliter with polyuria (with diabetes defined as a level of ≥200 mg per deciliter [≥11.1 mmol per liter] with symptoms), and when she was 30 years of age, she had on the same encounter a fasting blood glucose level of 133 mg per deciliter (with diabetes defined as a level of ≥126 mg per deciliter) and a result on a 2-hour oral glucose tolerance test of 236 mg per deciliter (with diabetes defined as a level of ≥200 mg per deciliter). On both of these occasions, her glycated hemoglobin level was in the prediabetes range (defined as 5.7 to 6.4%). In establishing the diagnosis of diabetes, the various blood glucose studies and glycated hemoglobin testing may provide discordant information because the tests have different sensitivities for this diagnosis, with glycated hemoglobin testing being the least sensitive. 2 Also, there are situations in which the glycated hemoglobin level can be inaccurate; for example, the patient may have recently received a blood transfusion or may have a condition that alters the life span of red cells, such as anemia, hemoglobinopathy, or pregnancy. 3 These conditions were not present in this patient at the time that the glycated hemoglobin measurements were obtained. In addition, since the glycated hemoglobin level reflects the average glucose level typically over a 3-month period, discordance with timed blood glucose measurements can occur if there has been a recent change in glycemic control. This patient had long-standing mild hyperglycemia but met criteria for diabetes on the basis of the blood glucose levels noted.
Type 1 and Type 2 Diabetes
Now that we have characterized the patient’s hyperglycemia as meeting criteria for diabetes, it is important to consider the possible types. More than 90% of adults with diabetes have type 2 diabetes, which is due to progressive loss of insulin secretion by beta cells that frequently occurs in the context of insulin resistance. This patient had received a diagnosis of type 2 diabetes; however, some patients with diabetes may be given a diagnosis of type 2 diabetes on the basis of not having features of type 1 diabetes, which is characterized by autoimmune destruction of the pancreatic beta cells that leads to rapid development of insulin dependence, with ketoacidosis often present at diagnosis.
Type 1 diabetes accounts for approximately 6% of all cases of diabetes in adults (≥18 years of age) in the United States, 4 and 80% of these cases are diagnosed before the patient is 20 years of age. 5 Since this patient’s diabetes was essentially nonprogressive over a period of at least 9 years, she most likely does not have type 1 diabetes. It is therefore not surprising that she had received a diagnosis of type 2 diabetes, but there are several other types of diabetes to consider, particularly since some features of her case do not fit with a typical case of type 2 diabetes, such as her age at diagnosis, the presence of hyperglycemia despite a nearly normal BMI, and the mild and nonprogressive nature of her disease over the course of many years.
Less Common Types of Diabetes
Latent autoimmune diabetes in adults (LADA) is a mild form of autoimmune diabetes that should be considered in this patient. However, there is controversy as to whether LADA truly represents an entity that is distinct from type 1 diabetes. 6 Both patients with type 1 diabetes and patients with LADA commonly have elevated levels of diabetes-associated autoantibodies; however, LADA has been defined by an older age at onset (typically >25 years) and slower progression to insulin dependence (over a period of >6 months). 7 This patient had not been tested for diabetes-associated autoantibodies. I ordered these tests to help evaluate for LADA, but this was not my leading diagnosis because of her young age at diagnosis and nonprogressive clinical course over a period of at least 9 years.
If the patient’s diabetes had been confined to pregnancy, we might consider gestational diabetes, but she had hyperglycemia outside of pregnancy. Several medications can cause hyperglycemia, including glucocorticoids, atypical antipsychotic agents, cancer immunotherapies, and some antiretroviral therapies and immunosuppressive agents used in transplantation. 8 However, this patient was not receiving any of these medications. Another cause of diabetes to consider is destruction of the pancreas due to, for example, cystic fibrosis, a tumor, or pancreatitis, but none of these were present. Secondary endocrine disorders — including excess cortisol production, excess growth hormone production, and pheochromocytoma — were considered to be unlikely in this patient on the basis of the history, review of symptoms, and physical examination.
Monogenic Diabetes
A final category to consider is monogenic diabetes, which is caused by alteration of a single gene. Types of monogenic diabetes include maturity-onset diabetes of the young (MODY), neonatal diabetes, and syndromic forms of diabetes. Monogenic diabetes accounts for 1 to 6% of cases of diabetes in children 9 and approximately 0.4% of cases in adults. 10 Neonatal diabetes is diagnosed typically within the first 6 months of life; syndromic forms of monogenic diabetes have other abnormal features, including particular organ dysfunction. Neither condition is applicable to this patient.
MODY is an autosomal dominant condition characterized by primary pancreatic beta-cell dysfunction that causes mild diabetes that is diagnosed during adolescence or early adulthood. As early as 1964, the nomenclature “maturity-onset diabetes of the young” was used to describe cases that resembled adult-onset type 2 diabetes in terms of the slow progression to insulin use (as compared with the rapid progression in type 1 diabetes) but occurred in relatively young patients. 11 Several genes cause distinct forms of MODY that have specific disease features that inform treatment, and thus MODY is a clinically important diagnosis. Most forms of MODY cause isolated abnormal glucose levels (in contrast to syndromic monogenic diabetes), a manifestation that has contributed to its frequent misdiagnosis as type 1 or type 2 diabetes. 12
Genetic Basis of MODY
Although at least 13 genes have been associated with MODY, 3 genes — GCK , which encodes glucokinase, and HNF1A and HNF4A , which encode hepatocyte nuclear factors 1A and 4A, respectively — account for most cases. MODY associated with GCK (known as GCK-MODY) is characterized by mild, nonprogressive hyperglycemia that is present since birth, whereas the forms of MODY associated with HNF1A and HNF4A (known as HNF1A-MODY and HNF4A-MODY, respectively) are characterized by the development of diabetes, typically in the early teen years or young adulthood, that is initially mild and then progresses such that affected patients may receive insulin before diagnosis.
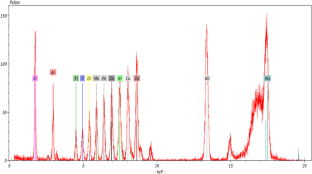
In patients with GCK-MODY, genetic variants reduce the function of glucokinase, the enzyme in pancreatic beta cells that functions as a glucose sensor and controls the rate of entry of glucose into the glycolytic pathway. As a result, reduced sensitivity to glucose-induced insulin secretion causes asymptomatic mild fasting hyperglycemia, with an upward shift in the normal range of the fasting blood glucose level to 100 to 145 mg per deciliter (5.6 to 8.0 mmol per liter), and also causes an upward shift in postprandial blood glucose levels, but with tight regulation maintained ( Fig. 1 ). 13 This mild hyperglycemia is not thought to confer a predisposition to complications of diabetes, 14 is largely unaltered by treatment, 15 and does not necessitate treatment outside of pregnancy.

Key features suggesting maturity-onset diabetes of the young (MODY) in this patient were an age of less than 35 years at the diagnosis of diabetes, a strong family history of diabetes with an autosomal dominant pattern of inheritance, and hyperglycemia despite a close-to-normal body-mass index. None of these features is an absolute criterion. MODY is caused by single gene–mediated disruption of pancreatic beta-cell function. In MODY associated with the GCK gene (known as GCK-MODY), disrupted glucokinase function causes a mild upward shift in glucose levels through-out the day and does not necessitate treatment. 13 In the pedigree, circles represent female family members, squares male family members, blue family members affected by diabetes, and green unaffected family members. The arrow indicates the patient.
In contrast to GCK-MODY, the disorders HNF1A-MODY and HNF4A-MODY result in progressive hyperglycemia that eventually leads to treatment. 16 Initially, there may be a normal fasting glucose level and large spikes in postprandial glucose levels (to >80 mg per deciliter [>4.4 mmol per liter]). 17 Patients can often be treated with oral agents and discontinue insulin therapy started before the diagnosis of MODY. 18 Of note, patients with HNF1A-MODY or HNF4A-MODY are typically sensitive to treatment with sulfonylureas 19 but may also respond to glucagon-like peptide-1 receptor agonists. 20
This patient had received a diagnosis of diabetes before 35 years of age, had a family history of diabetes involving multiple generations, and was not obese. These features are suggestive of MODY but do not represent absolute criteria for the condition ( Fig. 1 ). 1 Negative testing for diabetes-associated autoantibodies would further increase the likelihood of MODY. There are methods to calculate a patient’s risk of having MODY associated with GCK , HNF1A , or HNF4A . 21 , 22 Using an online calculator ( www.diabetesgenes.org/mody-probability-calculator ), we estimate that the probability of this patient having MODY is at least 75.5%. Genetic testing would be needed to confirm this diagnosis, and in patients at an increased risk for MODY, multigene panel testing has been shown to be cost-effective. 23 , 24
DR. MIRIAM S. UDLER’S DIAGNOSIS
Maturity-onset diabetes of the young, most likely due to a GCK variant.
DIAGNOSTIC TESTING
Dr. Christina A. Austin-Tse: A diagnostic sequencing test of five genes associated with MODY was performed. One clinically significant variant was identified in the GCK gene ( {"type":"entrez-nucleotide","attrs":{"text":"NM_000162.3","term_id":"167621407","term_text":"NM_000162.3"}} NM_000162.3 ): a c.787T→C transition resulting in the p.Ser263Pro missense change. Review of the literature and variant databases revealed that this variant had been previously identified in at least three patients with early-onset diabetes and had segregated with disease in at least three affected members of two families (GeneDx: personal communication). 25 , 26 Furthermore, the variant was rare in large population databases (occurring in 1 out of 128,844 European chromosomes in gnomAD 27 ), a feature consistent with a disease-causing role. Although the serine residue at position 263 was not highly conserved, multiple in vitro functional studies have shown that the p.Ser263Pro variant negatively affects the stability of the glucokinase enzyme. 26 , 28 – 30 As a result, this variant met criteria to be classified as “likely pathogenic.” 31 As mentioned previously, a diagnosis of GCK-MODY is consistent with this patient’s clinical features. On subsequent testing of additional family members, the same “likely pathogenic” variant was identified in the patient’s father and second child, both of whom had documented hyperglycemia.
DISCUSSION OF MANAGEMENT
Dr. Udler: In this patient, the diagnosis of GCK-MODY means that it is normal for her blood glucose level to be mildly elevated. She can stop taking metformin because discontinuation is not expected to substantially alter her glycated hemoglobin level 15 , 32 and because she is not at risk for complications of diabetes. 14 However, she should continue to maintain a healthy lifestyle. Although patients with GCK-MODY are not typically treated for hyperglycemia outside of pregnancy, they may need to be treated during pregnancy.
It is possible for a patient to have type 1 or type 2 diabetes in addition to MODY, so this patient should be screened for diabetes according to recommendations for the general population (e.g., in the event that she has a risk factor for diabetes, such as obesity). 1 Since the mild hyperglycemia associated with GCK-MODY is asymptomatic (and probably unrelated to the polyuria that this patient had described in the past), the development of symptoms of hyperglycemia, such as polyuria, polydipsia, or blurry vision, should prompt additional evaluation. In patients with GCK-MODY, the glycated hemoglobin level is typically below 7.5%, 33 so a value rising above that threshold or a sudden large increase in the glycated hemoglobin level could indicate concomitant diabetes from another cause, which would need to be evaluated and treated.
This patient’s family members are at risk for having the same GCK variant, with a 50% chance of offspring inheriting a variant from an affected parent. Since the hyperglycemia associated with GCK-MODY is present from birth, it is necessary to perform genetic testing only in family members with demonstrated hyperglycemia. I offered site-specific genetic testing to the patient’s parents and second child.
Dr. Meridale V. Baggett (Medicine): Dr. Powe, would you tell us how you would treat this patient during pregnancy?
Dr. Camille E. Powe: During the patient’s first pregnancy, routine screening led to a presumptive diagnosis of gestational diabetes, the most common cause of hyperglycemia in pregnancy. Hyperglycemia in pregnancy is associated with adverse pregnancy outcomes, 34 and treatment lowers the risk of such outcomes. 35 , 36 Two of the most common complications — fetal overgrowth (which can lead to birth injuries, shoulder dystocia, and an increased risk of cesarean delivery) and neonatal hypoglycemia — are thought to be the result of fetal hyperinsulinemia. 37 Maternal glucose is freely transported across the placenta, and excess glucose augments insulin secretion from the fetal pancreas. In fetal life, insulin is a potent growth factor, and neonates who have hyperinsulinemia in utero often continue to secrete excess insulin in the first few days of life. In the treatment of pregnant women with diabetes, we strive for strict blood sugar control (fasting blood glucose level, <95 mg per deciliter [<5.3 mmol per liter]; 2-hour postprandial blood glucose level, <120 mg per deciliter) to decrease the risk of these and other hyperglycemia-associated adverse pregnancy outcomes. 38 – 40
In the third trimester of the patient’s first pregnancy, obstetrical ultrasound examination revealed a fetal abdominal circumference in the 76th percentile for gestational age and polyhydramnios, signs of fetal exposure to maternal hyperglycemia. 40 – 42 Case series involving families with GCK-MODY have shown that the effect of maternal hyperglycemia on the fetus depends on whether the fetus inherits the pathogenic GCK variant. 43 – 48 Fetuses that do not inherit the maternal variant have overgrowth, presumably due to fetal hyperinsulinemia ( Fig. 2A ). In contrast, fetuses that inherit the variant do not have overgrowth and are born at a weight that is near the average for gestational age, despite maternal hyperglycemia, presumably because the variant results in decreased insulin secretion ( Fig. 2B ). Fetuses that inherit GCK-MODY from their fathers and have euglycemic mothers appear to be undergrown, most likely because their insulin secretion is lower than normal when they and their mothers are euglycemic ( Fig. 2D ). Because fetal overgrowth and polyhydramnios occurred during this patient’s first pregnancy and neonatal hypoglycemia developed after the birth, the patient’s first child is probably not affected by GCK-MODY.

Pathogenic variants that lead to GCK-MODY, when carried by a fetus, change the usual relationship of maternal hyperglycemia to fetal hyperinsulinemia and fetal overgrowth. GCK-MODY–affected fetuses have lower insulin secretion than unaffected fetuses in response to the same maternal blood glucose level. In a hyperglycemic mother carrying a fetus who is unaffected by GCK-MODY, excessive fetal growth is usually apparent (Panel A). Studies involving GCK-MODY–affected hyperglycemic mothers have shown that fetal growth is normal despite maternal hyperglycemia when a fetus has the maternal GCK variant (Panel B). The goal of treatment of maternal hyperglycemia when a fetus is unaffected by GCK-MODY is to establish euglycemia to normalize fetal insulin levels and growth (Panel C); whether this can be accomplished in the case of maternal GCK-MODY is controversial, given the genetically determined elevated maternal glycemic set point. In the context of maternal euglycemia, GCK-MODY–affected fetuses may be at risk for fetal growth restriction (Panel D).
In accordance with standard care for pregnant women with diabetes who do not meet glycemic targets after dietary modification, 38 , 39 the patient was treated with insulin during her pregnancies. In her second pregnancy, treatment was begun early, after hyperglycemia was detected in the first trimester. Because she had not yet received the diagnosis of GCK-MODY during any of her pregnancies, no consideration of this condition was given during her obstetrical treatment. Whether treatment affects the risk of hyperglycemia-associated adverse pregnancy outcomes in pregnant women with known GCK-MODY is controversial, with several case series showing that the birth weight percentile in unaffected neonates remains consistent regardless of whether the mother is treated with insulin. 44 , 45 Evidence suggests that it may be difficult to overcome a genetically determined glycemic set point in patients with GCK-MODY with the use of pharmacotherapy, 15 , 32 and affected patients may have symptoms of hypoglycemia when the blood glucose level is normal because of an enhanced counterregulatory response. 49 , 50 Still, to the extent that it is possible, it would be desirable to safely lower the blood glucose level in a woman with GCK-MODY who is pregnant with an unaffected fetus in order to decrease the risk of fetal overgrowth and other consequences of mildly elevated glucose levels ( Fig. 2C ). 46 , 47 , 51 In contrast, there is evidence that lowering the blood glucose level in a pregnant woman with GCK-MODY could lead to fetal growth restriction if the fetus is affected ( Fig. 2D ). 45 , 52 During this patient’s second pregnancy, she was treated with insulin beginning in the first trimester, and her daughter’s birth weight was near the 16th percentile for gestational age; this outcome is consistent with the daughter’s ultimate diagnosis of GCK-MODY.
Expert opinion suggests that, in pregnant women with GCK-MODY, insulin therapy should be deferred until fetal growth is assessed by means of ultrasound examination beginning in the late second trimester. If there is evidence of fetal overgrowth, the fetus is presumed to be unaffected by GCK-MODY and insulin therapy is initiated. 53 After I have counseled women with GCK-MODY on the potential risks and benefits of insulin treatment during pregnancy, I have sometimes used a strategy of treating hyperglycemia from early in pregnancy using modified glycemic targets that are less stringent than the targets typically used during pregnancy. This strategy attempts to balance the risk of growth restriction in an affected fetus (as well as maternal hypoglycemia) with the potential benefit of glucose-lowering therapy for an unaffected fetus.
Dr. Udler: The patient stopped taking metformin, and subsequent glycated hemoglobin levels remained unchanged, at 6.2%. Her father and 5-year-old daughter (second child) both tested positive for the same GCK variant. Her father had a BMI of 36 and a glycated hemoglobin level of 7.8%, so I counseled him that he most likely had type 2 diabetes in addition to GCK-MODY. He is currently being treated with metformin and lifestyle measures. The patient’s daughter now has a clear diagnosis to explain her hyperglycemia, which will help in preventing misdiagnosis of type 1 diabetes, given her young age, and will be important for the management of any future pregnancies. She will not need any medical follow-up for GCK-MODY until she is considering pregnancy.
FINAL DIAGNOSIS
Maturity-onset diabetes of the young due to a GCK variant.
Acknowledgments
We thank Dr. Andrew Hattersley and Dr. Sarah Bernstein for helpful comments on an earlier draft of the manuscript.
This case was presented at the Medical Case Conference.
No potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org .
- Open access
- Published: 17 January 2024
Nutrient patterns and risk of diabetes mellitus type 2: a case-control study
- Morteza haramshahi 1 ,
- Thoraya Mohamed Elhassan A-Elgadir 2 ,
- Hamid Mahmood Abdullah Daabo 3 ,
- Yahya Altinkaynak 4 ,
- Ahmed Hjazi 5 ,
- Archana Saxena 6 ,
- Mazin A.A. Najm 7 ,
- Abbas F. Almulla 8 ,
- Ali Alsaalamy 9 &
- Mohammad Amin Kashani 10
BMC Endocrine Disorders volume 24 , Article number: 10 ( 2024 ) Cite this article
1931 Accesses
1 Altmetric
Metrics details
Backgrounds
Although the significance of diet in preventing or managing diabetes complications is highlighted in current literature, there is insufficient evidence regarding the correlation between nutrient patterns and these complications. The objective of this case-control study is to investigate this relationship by analyzing the dietary intake of nutrients in participants with and without type 2 diabetes (T2D).
A case-control study was conducted at the Tabriz Center of Metabolism and Endocrinology to investigate the relationship between nutrient patterns and type 2 diabetes (T2D). The study enrolled 225 newly diagnosed cases of T2D and 225 controls. The dietary intake of nutrients was assessed using a validated semi-quantitative food frequency questionnaire (FFQ). Principal component analysis using Varimax rotation was used to obtain nutrient patterns. Logistic regression analysis was performed to estimate the risk of T2D.
The participants’ mean (SD) age and BMI were 39.8 (8.8) years and 27.8 (3.6) kg/m2, respectively. The results identified three major nutrient patterns. The first nutrient pattern was characterized by high consumption of sucrose, animal protein, vitamin E, vitamin B1, vitamin B12, calcium, phosphorus, zinc, and potassium. The second nutrient pattern included fiber, plant protein, vitamin D, Riboflavin, Vitamin B5, copper, and Magnesium. The third nutrient pattern was characterized by fiber, plant protein, vitamin A, riboflavin, vitamin C, calcium, and potassium. Individuals in the highest tertile of nutrient pattern 3 (NP3) had a lower risk of T2D compared to those in the lowest tertile after adjusting for confounders. The odds ratio was 0.52 with a 95% confidence interval of 0.30–0.89 and a P_trend of 0.039.
This study found that conforming to a nutrient pattern consisting of plant protein, vitamin C, vitamin A, vitamin B2, potassium, and calcium is linked to a lower likelihood of developing T2D.The initial results suggest that following a nutrient pattern that includes these nutrients may reduce the risk of T2D. However, further research is required to confirm the relationship between nutrient patterns and T2D.
Peer Review reports
Type 2 diabetes is a significant concern for public health in developed nations. It leads to high rates of illness and death and places a significant financial burden on healthcare systems [ 1 , 2 ]. In the past few decades, there has been a sharp increase in the occurrence of diabetes, and is expected to continue increasing, with an estimated 693 million people living with the disease by 2045 [ 1 ]. Complications associated with type 2 diabetes can also contribute to premature death. A concerning aspect of the disease is that a significant proportion of cases (40%) go undetected [ 3 ], and there is also an increasing prevalence of prediabetes, which raises the risk of developing type 2 diabetes and other chronic diseases [ 1 ].
The connection between diet and type 2 diabetes has been extensively studied, including the examination of dietary patterns and individual foods or nutrient patterns [ 4 , 5 , 6 , 7 ]. Various sources have suggested that chronic diseases may be influenced by a combination of nutrients [ 8 ]. In the field of nutritional epidemiology, the examination of dietary patterns has emerged as a viable approach to investigate the correlation between diet and disease. This method involves using statistical techniques to combine multiple foods or nutrients into dietary or nutrient patterns, which are believed to provide a more detailed understanding of the connection between diet and disease. It has been suggested that the impact of individual nutrients or foods on chronic disease may be too subtle to detect, but their collective effect within a pattern may be more indicative [ 9 ].
There have been some recent studies examining the effect of nutrient patterns on chronic disease such as, non-alcoholic fatty liver, breast and gastric cancer, Polycystic Ovary Syndrome (PCOs) and metabolic syndrome [ 10 , 11 , 12 , 13 , 14 ]. For example, it was found that a nutrient pattern consisting mainly of protein, carbohydrates, and various sugars was linked to a higher risk of Metabolic Syndrome (MetS) in both men and women, whereas a pattern characterized by copper, selenium, and several vitamins was linked to greater odds of MetS [ 14 ]. A prospective study conducted among participants of the Tehran Lipid and Glucose Study indicates that a nutrient pattern rich in vitamin A, vitamin C, vitamin B6, potassium, and fructose is associated with a reduced risk of insulin-related disorders [ 15 ]. Although there have been limited investigations on the connection between nutrient patterns and the likelihood of developing diabetes, the present study seeks to explore this relationship by analyzing the adherence to different nutrient patterns and its effect on the risk of type 2 diabetes.
Study population
This study utilized a case-control design and involved participants between the ages of 18 and 60 who had been diagnosed with type 2 diabetes within the previous six months based on specific glucose level criteria (FBS levels of ≥ 126 mg/dl and 2 h-PG levels of ≥ 200 mg/dl [ 17 ]). Healthy individuals within the same age range were also included, with specific glucose level criteria (FBS levels of < 100 mg/dl and 2 h-PG levels of < 200 mg/dl [ 17 ]). The study excluded individuals with certain chronic diseases, Type 1 Diabetes, gestational diabetes, those following specific dietary patterns or taking certain medications, pregnant and breastfeeding women, those with a family history of diabetes or hypertension, and those who did not complete the food frequency questionnaire (more than 35 items) or whose reported energy intake was outside of a specific range (range of 800–4200 kcal [ 18 ]).
This study enrolled 450 adult participants, with 225 individuals in the case group and 225 in the control group. The case group was selected using a simple sampling method from patients diagnosed with diabetes at the Tabriz Center of Metabolism and Endocrinology as a referral center affiliated to tabriz University of Medical Sciences from January 2021 to March 2022, as well as through a two-stage cluster sampling method among patients referred to private endocrinologists to enhance the sample’s external validity. Participants in the control group were also selected through a two-stage cluster sampling method from individuals who had undergone blood glucose checkups at the Tabriz Center of Metabolism and Endocrinology, a referral center affiliated with Tabriz University of Medical Sciences, within the past six months. All participants provided informed consent at the beginning of the study. The study was financially supported by Tabriz University of Medical Sciences and is related to project NO. 1400/63,145.
Dietary assessment
To collect dietary intake information, personal interviews and a semi-quantitative food frequency questionnaire (FFQ) consisting of 168 food items were used [ 16 ]. The FFQ asked about the frequency of consumption for each item over the course of one year, with the year before diagnosis for the case group and the year before the interview for the control group. Participants were also asked about the frequency of consumption (per day, week, month, or year) for each type of food. to ensure consistency in measurements, a nutritionist provided instructions on converting the size of reported food items from household measures to grams using four scales. The quantity of food consumed by each individual was calculated based on their intake in grams and reported on a daily basis. The nutrient composition of all foods was derived by using modified nutritionist IV software.
Nutrient pattern assessment
We conducted factor analyses using a comprehensive set of 34 nutrients, encompassing various macronutrients, micronutrients, and other dietary components. These included sucrose, lactose, fructose, fiber, animal protein, plant protein, saturated fatty acids, monounsaturated fatty acids, polyunsaturated fatty acids, cholesterol, as well as an array of vitamins and minerals such as A, D, E, K, C, thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), folate (B9), B12, calcium, phosphorus, iron, zinc, copper, magnesium, manganese, chromium, selenium, sodium, potassium, and caffeine. The dietary intake of these 34 nutrients per 1,000 Kcal of energy intake was computed and utilized as input variables. Subsequently, nutrient patterns (NPs) were derived through principal component analysis (PCA) with varimax rotation, based on the correlation matrix. Factor scores for each participant were then calculated by aggregating the frequency of consumption and multiplying it by the factor loadings across all 34 nutrients. To assess the statistical correlation between variables and evaluate the adequacy of the sample size, we employed the Bartlett test of sphericity ( P < 0.001) and the Kaiser-Mayer-Olkin test (0.71), respectively.
Assessment of other variables
To obtain the participants’ anthropometric measurements, weight and height were measured using a seca scale, and the participants’ BMI was determined by dividing their weight in kilograms by the square of their height in meters. Waist circumference was measured using a metal anthropometric tape, and the participants’ hip circumference was measured using a metal anthropometric tape while standing [ 17 ]. Daily physical activity was measured using a physical activity questionnaire [ 18 ], and personal questioning was employed to gather information on population and socioeconomic characteristics, including marital status, academic degree, and smoking.
Statistical analysis
Statistical analysis was performed using the Statistical Package Software for Social Science, version 21. The normality of the data was assessed using Kolmogorov-Smirnov’s test and histogram chart. The characteristics and dietary intakes of the case and control groups were presented as mean ± SD or median and frequency (percentages). Independent sample t-tests and chi-square tests were used to compare continuous and categorical variables, respectively, between the case and control groups.
The participants’ mean (SD) age and BMI were 39.8 (8.8) years and 27.8 (3.6) kg/m2, respectively. The mean (SD) BMI in the case group was 30.5 ± 4.1, and in the control group, it was 25.2 ± 3.2 kg/m2. The mean (SD) physical activity in the case group was 1121 ± 611 MET/min/week, and in the control group, it was 1598 ± 940 MET/min/week. There were significant differences in BMI and physical activity between the two groups. The mean (SD) waist circumference in the case group was 109.32 ± 10.28 cm, and in the control group, it was 87.25 ± 9.35 cm. The mean (SD) hip circumference in the case group was 107.25 ± 8.61 cm, and in the control group, it was 91.44 ± 6.17 cm. The study identified three primary nutrient patterns (NPs) with eigenvalues greater than 2. Table 1 displays the factor loadings for nutrient patterns, which accounted for 56.11% of the total nutrient variation. The high intake of sucrose, animal protein, phosphorus, zinc, potassium, calcium, vitamin E, vitamin B1 and vitamin B12 were the distinguishing features of the first pattern. The second nutrient pattern was positively associated with copper, magnesium, fiber, vitamin D, B2, B5 and plant protein but had a negative correlation with lactose and saturated fatty acids. On the other hand, the high intake of fiber, vitamin A, B2, vitamin C, plant protein and potassium were the distinguishing features of the third pattern.
The following are the characteristics of T2D patients compared to the control group, as shown in Table 2 : Higher BMI, More likely to be smokers, Lower physical activity levels, higher FBS, HbA1C, Insulin ( p < 0.05). Other variables did not differ significantly between the two groups ( p > 0.05). Additionally, T2D patients had a greater intake of energy and vitamin B3 but consumed less plant protein, vitamin A, vitamin E, vitamin B2, and zinc ( p < 0.05).
Table 3 summarizes the partial correlation coefficient between NPs and food sources, with NP1 showing a strong positive correlation with low-fat dairy, NP2 with refined grains, and NP3 with fruits and vegetables.
Table 4 demonstrates the relationships between NPs and T2D. After adjusting for age and sex, there was no significant link between each nutrient pattern (NP) and T2D. However, when adjusting for other factors such as BMI, physical activity, smoking, and energy intake, individuals in the highest tertile of NP1 and NP2 did not show a significant association with T2D compared to those in the lowest tertile. On the other hand, those in the highest tertile of NP3 had a lower probability of developing T2D than those in the lowest tertile (OR: 0.52, 95%CI: 0.30–0.89, P_trend = 0.039).
In this study, three major NPs were identified. After adjusting for potential confounders, we observed a significant inverse association between the Third NP and the odds of T2D. The high intake of fiber, vitamin A, B2, vitamin C, plant protein and potassium were the distinguishing features of the third pattern.
Dietary patterns, such as healthy, Mediterranean, traditional, and Western dietary patterns, have recently received significant attention in studying the connection between diet and health. When looking at the relationship between nutrients and disease incidence, it is more challenging to evaluate when considering individual foods and the metabolism of all nutrients together [ 19 ]. It is therefore more effective to take a broader view and consider diet as a whole. Dietary and nutrient patterns can have a greater impact on health than specific nutrients or nutritional groups. There is supporting evidence that links high calorie or high glycemic index foods with an increased risk of T2D. The quality of one’s diet is also associated with the risk, progression, and side effects of T2D [ 20 ]. Establishing a desirable food pattern has become a priority in public health efforts to prevent T2D. By studying dietary and nutrient patterns, we can gain a comprehensive understanding of an individual’s overall diet beyond just the consumption of specific nutrients and food groups. Moreover, it is easier for people to understand health recommendations when presented as dietary patterns rather than focusing solely on individual nutrients [ 19 ].
A previous cross-sectional study investigated the relationship between NPs and fasting glucose and glycated hemoglobin levels among apparently healthy black South Africans. The study stratified 2,010 participants by gender and urban/rural status and identified three nutrient patterns per stratum. In rural women, a nutrient pattern driven by starch, dietary fiber, and B vitamins was significantly associated with lower fasting glucose and glycated hemoglobin levels. A nutrient pattern that included vitamin B1, zinc, and plant protein was linked to notable decreases in glycated hemoglobin and fasting glucose levels in rural men. These findings suggest that nutrient patterns that are plant-based are linked to lower levels of fasting glucose and glycated hemoglobin [ 21 ].
Iwasaki et al. found that specific nutrient patterns were associated with lower risks of MetS. One nutrient pattern high in potassium, fiber, and vitamins, while another pattern high in vitamin B2, saturated fatty acids and calcium [ 22 ]. A recent study found that a nutrient pattern characterized by high intake of calcium, potassium, fats, cholesterol, vitamins B2, B12, A, D, K and C was positively linked to MetS [ 23 ]. Salehi-Sahlabadi et al. found that adhering to a nutrient pattern rich in potassium, vitamin A, fructose, vitamin C and vitamin B6 was negatively associated with the likelihood of NAFLD [ 11 ]. A nutrient pattern high in potassium, vitamin A, vitamin B6, vitamin C and fructose was associated with a reduced risk of hyperinsulinemia, IR, and dyslipidemia among participants in Tehran, according to a prospective study [ 11 , 24 , 25 ].
Due to several variations among studies exploring NPs linked to chronic diseases, including differences in the number of nutrients, populations, study designs and outcomes there has been a considerable diversity in the identified NPs, with only a few NPs being replicated across studies. Our study is the first of its kind to explore the correlation between nutrient patterns and T2D in this context.
In our study, there was no association between NPs 1 and 2 and T2D. This lack of correlation may be attributed to the absence of harmful nutrients or food categories linked to diabetes in these NPs. NP3 in this study, unlike other NPs, is positively associated with beneficial food groups such as nuts, fruits, plant oil and vegetables, and negatively associated with unhealthy food groups like red-processed meat, snacks, high-fat dairy and refined grains. A recent systematic review and meta-analysis found that individuals who consumed higher amounts of fruits and vegetables had a lower risk of developing type 2 diabetes [ 26 ]. Moreover, the consumption of vegetables was found to have an inverse relationship with ALT, TC and LDL levels among adults, while fruit consumption was associated with a positive reduction in visceral fat [ 27 , 28 ]. Another study suggested that an increased intake of vegetables and fruits could potentially lower the risk of MetS [ 29 ]. According to a study, greater nut consumption was significantly linked to a reduced prevalence of T2D [ 30 ]. Consuming fruits and vegetables is a crucial component of a healthful dietary pattern that can lower the risk of type 2 diabetes [ 31 ]. On the other hand, Consuming a Western dietary pattern, which primarily consists of fast foods, high-fat dairy, refined grains, soft drinks and processed meat has been found to be correlated with an increased risk of type 2 diabetes [ 31 ].
Several mechanisms have been identified that explain the positive associations between the components of NP 3 and T2D or its risk factors. Vitamin intake has been shown to play a role in the development of T2D through various pathways. Consuming vitamin C has been found to have beneficial effects in reducing the risk of type 2 diabetes mellitus. These effects can be attributed to the following actions of vitamin C: vasodilator, cytoprotective, platelet anti-aggregator and anti-mutagenic. To achieve this, the body increases the production of several substances including prostaglandin E1, PGI2, endothelial nitric oxide, and lipoxin A4. Additionally, the body restores the Arachidonic Acid content to normal levels [ 32 ]. Vitamin A has a multifaceted role in cell regulation beyond its antioxidant function. It contributes to gene regulation, epithelial cell integrity, and resistance to infection. Research suggests that vitamin A also enhances antioxidant enzyme function in the body. Research has indicated a link between vitamin A deficiency and type 2 diabetes mellitus (T2DM), which suggests that vitamin A may have a role in the biology of T2DM [ 33 ]. Moreover, a meta-analysis has found that replacing animal protein with plant protein can lead to minor improvements in glycemic control for individuals with diabetes [ 34 ]. According to a recent meta-analysis, increasing the consumption of fruits, especially berries, yellow vegetables, cruciferous vegetables, green leafy vegetables is associated with a lower risk of developing type 2 diabetes. These results support the recommendation to incorporate more fruits and vegetables into the diet as a way to prevent various chronic diseases, including type 2 diabetes [ 35 ]. A study showed that maintaining adequate potassium intake could regulate insulin secretion and carbohydrate metabolism, leading to the prevention of obesity and metabolic syndrome (MetS) [ 36 ].
A number of research studies conducted in the Western societies have shown that Western dietary pattern including higher intake of red meat, processed meat, and refined grains is significantly associated with increased risk of T2D [ 37 , 38 ]. For example, in the 12-years cohort prospective study, van Dam et al. investigated dietary pattern of 42,504 American white men at the age range of 40–75 years old using the FFQ. After controlling the confounders, the risk of T2D increased 60% in people adherent to the western-like dietary pattern [ 38 ]. The rapid process of change in lifestyle, diets, and physical activity that have been occurred as a result of extended urbanization, improved economic status, change of work pattern toward jobs, and change in the processes of producing and distributing nutrients during the recent years in developing countries have led people to more consumption of fast food and processed foods [ 20 ].
Significant research has been conducted on the impact of nutrient type and sequence on glucose tolerance. Multiple studies have shown that manipulating the sequence of food intake can enhance glycemic control in individuals with type 2 diabetes in real-life situations. The glucose-lowering effect of preload-based nutritional strategies has been found to be more pronounced in type 2 diabetes patients compared to healthy individuals. Moreover, consuming carbohydrates last, as part of meal patterns, has been proven to improve glucose tolerance and reduce the risk of weight gain [ 39 ]. Recent findings on meal sequence further emphasize the potential of this dietary approach in preventing and managing type 2 diabetes [ 40 ].
Several studies have shown that food from a short supply chain has a significant impact on metabolic syndrome. The length of the food supply chain is important in determining the risk of metabolic syndrome in a population [ 41 ]. Research indicates that people who consume food from short supply chains have a lower prevalence of metabolic syndrome compared to those who consume food from long supply chains. Specifically, food from short supply chains is associated with lower levels of triglycerides and glucose, which leads to a reduced occurrence of metabolic syndrome [ 42 ]. Adhering to the Mediterranean diet with a short supply chain is also found to significantly reduce the prevalence of metabolic syndrome. Therefore, these studies provide evidence that food from short supply chains positively affects metabolic parameters and the occurrence of metabolic syndrome [ 41 ].
The study we conducted presented several advantages. It was the first case-control research to investigate the correlation between nutrient patterns and the likelihood of developing type 2 diabetes (T2D). While numerous studies have explored the relationship between dietary patterns and diabetes, there is a scarcity of research specifically focusing on nutrient patterns in individuals with type 2 diabetes. Furthermore, the collection of dietary intake data was carried out through face-to-face interviews conducted by trained dieticians to minimize measurement errors. However, this study also had some limitations. Case-control studies are susceptible to selection and recall biases. Additionally, the use of factor analysis to identify patterns, and the potential influence of research decisions on the number of factors and nutrient factor loadings in each pattern, should be considered. Lastly, despite the use of a validated semi-quantitative FFQ (food frequency questionnaire), there remains a possibility of measurement error due to dietary recall. The study’s findings and limitations contribute to the ongoing discourse on the role of nutrient patterns in the development of T2D and the importance of considering these factors in future research and preventive strategies.
Conclusions
The results of this study indicate that conforming to a nutrient pattern consisting of plant protein, vitamin C, vitamin A, vitamin B2, potassium, and calcium is linked to a lower likelihood of developing T2D. Our investigation did not reveal any significant correlation between other nutrient patterns and T2D risk. However, additional research is necessary to authenticate these initial findings and establish the correlation between nutrient patterns and T2D.
Data availability
Upon reasonable request, the corresponding author can provide the datasets that were produced and analyzed during the current study.
Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL-D, Sacre JW, Karuranga S, et al. IDF Diabetes Atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118.
Article PubMed Google Scholar
Teo ZL, Tham Y-C, Yu M, Chee ML, Rim TH, Cheung N, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128(11):1580–91.
Sugiyama T, Yanagisawa-Sugita A, Tanaka H, Ihana-Sugiyama N, Imai K, Ohsugi M, et al. Different incidences of diabetic retinopathy requiring treatment since diagnosis according to the course of diabetes diagnosis: a retrospective cohort study. Sci Rep. 2023;13(1):10527.
Article CAS PubMed PubMed Central Google Scholar
Hodge AM, English DR, O’Dea K, Giles GG. Dietary patterns and diabetes incidence in the Melbourne Collaborative Cohort Study. Am J Epidemiol. 2007;165(6):603–10.
Jannasch F, Kröger J, Schulze MB. Dietary patterns and type 2 diabetes: a systematic literature review and meta-analysis of prospective studies. J Nutr. 2017;147(6):1174–82.
Article CAS PubMed Google Scholar
Sami W, Ansari T, Butt NS, Ab Hamid MR. Effect of diet on type 2 diabetes mellitus: a review. Int J Health Sci. 2017;11(2):65.
Google Scholar
Miller V, Micha R, Choi E, Karageorgou D, Webb P, Mozaffarian D. Evaluation of the quality of evidence of the association of foods and nutrients with cardiovascular disease and diabetes: a systematic review. JAMA Netw open. 2022;5(2):e2146705–e.
Article PubMed PubMed Central Google Scholar
Salehi-Sahlabadi A, Teymoori F, Jabbari M, Momeni A, Mokari-Yamchi A, Sohouli M, et al. Dietary polyphenols and the odds of non-alcoholic fatty liver disease: a case-control study. Clin Nutr ESPEN. 2021;41:429–35.
Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L, Keshteli AH, Feizi A, Feinle-Bisset C, et al. Nutrient patterns and their relation to general and abdominal obesity in Iranian adults: findings from the SEPAHAN study. Eur J Nutr. 2016;55:505–18.
Panjeshahin A, Salehi-Abargouei A, Ghadiri-Anari A, Rasouli A, Hosseinzadeh M. The Association between nutrient patterns and polycystic ovary syndrome: a case-control study. J Nutr Food Secur. 2022.
Salehi-Sahlabadi A, Teymoori F, Ahmadirad H, Mokhtari E, Azadi M, Seraj SS, et al. Nutrient patterns and non-alcoholic fatty liver disease in Iranian Adul: a case-control study. Front Nutr. 2022;9:977403.
Fereidani SS, Eini-Zinab H, Heidari Z, Jalali S, Sedaghat F, Rashidkhani B. Nutrient patterns and risk of breast cancer among Iranian women: a case-control study. Asian Pac J cancer Prevention: APJCP. 2018;19(9):2619.
CAS Google Scholar
Narmcheshm S, Sasanfar B, Hadji M, Zendehdel K, Toorang F, Azadbakht L. Patterns of nutrient intake in relation to gastric cancer: a case control study. Nutr Cancer. 2022;74(3):830–9.
Khayyatzadeh SS, Moohebati M, Mazidi M, Avan A, Tayefi M, Parizadeh SMR, et al. Nutrient patterns and their relationship to metabolic syndrome in Iranian adults. Eur J Clin Invest. 2016;46(10):840–52.
Teymoori F, Mokhtari E, Salehi P, Hosseini-Esfahani F, Mirmiran P, Azizi F. A nutrient pattern characterized by vitamin A, C, B6, potassium, and fructose is associated with reduced risk of insulin-related disorders: a prospective study among participants of Tehran lipid and glucose study. Diabetol Metab Syndr. 2021;13(1):12.
Esmaillzadeh A, Azadbakht L. Major dietary patterns in relation to general obesity and central adiposity among Iranian women. J Nutr. 2008;138(2):358–63.
Wang J, Thornton JC, Bari S, Williamson B, Gallagher D, Heymsfield SB, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr. 2003;77(2):379–84.
Committee IR. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. http://www.ipaq.ki.se/scoring.pdf ; 2005.
Mandalazi E, Drake I, Wirfält E, Orho-Melander M, Sonestedt E. A high diet quality based on dietary recommendations is not associated with lower incidence of type 2 diabetes in the Malmö Diet and Cancer Cohort. Int J Mol Sci. 2016;17(6):901.
Beigrezaei S, Ghiasvand R, Feizi A, Iraj B. Relationship between dietary patterns and incidence of type 2 diabetes. Int J Prev Med. 2019;10:122.
Chikowore T, Pisa PT, Van Zyl T, Feskens EJ, Wentzel-Viljoen E, Conradie KR. Nutrient patterns associated with fasting glucose and glycated haemoglobin levels in a black South African population. Nutrients. 2017;9(1):9.
Iwasaki Y, Arisawa K, Katsuura-Kamano S, Uemura H, Tsukamoto M, Kadomatsu Y, et al. Associations of nutrient patterns with the prevalence of metabolic syndrome: results from the baseline data of the Japan multi-institutional collaborative cohort study. Nutrients. 2019;11(5):990.
Sadeghi O, Sadeghi A, Mozaffari-Khosravi H, Shokri A. The association between nutrient patterns and metabolic syndrome among Iranian adults: cross-sectional analysis of Shahedieh cohort study. Public Health Nutr. 2021;24(11):3379–88.
Mottaghian M, Salehi P, Teymoori F, Mirmiran P, Hosseini-Esfahani F, Azizi F. Nutrient patterns and cardiometabolic risk factors among Iranian adults: Tehran lipid and glucose study. BMC Public Health. 2020;20:1–12.
Article Google Scholar
Teymoori F, Mokhtari E, Salehi P, Hosseini-Esfahani F, Mirmiran P, Azizi F. A nutrient pattern characterized by vitamin A, C, B6, potassium, and fructose is associated with reduced risk of insulin-related disorders: a prospective study among participants of Tehran lipid and glucose study. Diabetol Metab Syndr. 2021;13(1):1–13.
Halvorsen RE, Elvestad M, Molin M, Aune D. Fruit and vegetable consumption and the risk of type 2 diabetes: a systematic review and dose–response meta-analysis of prospective studies. BMJ Nutr Prev Health. 2021;4(2):519.
Mollahosseini M, Daneshzad E, Rahimi MH, Yekaninejad MS, Maghbooli Z, Mirzaei K. The association between fruit and vegetable intake and liver enzymes (aspartate and alanine transaminases) in Tehran, Iran. Ethiop J Health Sci. 2017;27(4):401–10.
Plaz Torres MC, Bodini G, Furnari M, Marabotto E, Zentilin P, Giannini EG. Nuts and non-alcoholic fatty liver disease: are nuts safe for patients with fatty liver disease? Nutrients. 2020;12(11):3363.
Lee M, Lim M, Kim J. Fruit and vegetable consumption and the metabolic syndrome: a systematic review and dose–response meta-analysis. Br J Nutr. 2019;122(7):723–33.
Muley A, Fernandez R, Ellwood L, Muley P, Shah M. Effect of tree nuts on glycemic outcomes in adults with type 2 diabetes mellitus: a systematic review. JBI Evid Synthesis. 2021;19(5):966–1002.
Beigrezaei S, Ghiasvand R, Feizi A, Iraj B. Relationship between dietary patterns and incidence of type 2 diabetes. Int J Prev Med. 2019;10.
Das UN. Vitamin C for type 2 diabetes mellitus and hypertension. Arch Med Res. 2019;50(2):11–4.
Iqbal S, Naseem I. Role of vitamin A in type 2 diabetes mellitus biology: effects of intervention therapy in a deficient state. Nutrition. 2015;31(7–8):901–7.
Viguiliouk E, Stewart SE, Jayalath VH, Ng AP, Mirrahimi A, De Souza RJ, et al. Effect of replacing animal protein with plant protein on glycemic control in diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2015;7(12):9804–24.
Wang PY, Fang JC, Gao ZH, Zhang C, Xie SY. Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: a meta-analysis. J Diabetes Invest. 2016;7(1):56–69.
Cai X, Li X, Fan W, Yu W, Wang S, Li Z, et al. Potassium and obesity/metabolic syndrome: a systematic review and meta-analysis of the epidemiological evidence. Nutrients. 2016;8(4):183.
van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in US men. Ann Intern Med. 2002;136(3):201–9.
Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004;164(20):2235–40.
Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, et al. Macronutrients, Food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012;35(2):434–45.
Dwibedi C, Mellergård E, Gyllensten AC, Nilsson K, Axelsson AS, Bäckman M, et al. Effect of self-managed lifestyle treatment on glycemic control in patients with type 2 diabetes. Npj Digit Med. 2022;5(1):60.
Santulli G, Pascale V, Finelli R, Visco V, Giannotti R, Massari A, et al. We are what we eat: impact of food from short supply chain on metabolic syndrome. J Clin Med. 2019;8(12):2061.
De Rosa M, Giannotti R, Pascale A, Finelli R, Ilario M, Ciccarelli M, et al. P6280 food of short supply chain impacts metabolism and cardiovascular risk. A survey in Southern Italy. Eur Heart J. 2018;39(suppl1):ehy566. P6280.
Download references
Acknowledgements
The researchers express their gratitude towards all the individuals who volunteered to take part in the study.
This research received no external funding.
Author information
Authors and affiliations.
Faculty of medicine, Tabriz University of medical sciences, Tabriz, Iran
Morteza haramshahi
Department of clinical biochemistry, College of medicine, King Khalid University, Abha, Saudi Arabia
Thoraya Mohamed Elhassan A-Elgadir
Fharmacy Department, Duhok polytechnic, University Duhok, Kurdistan, Iraq
Hamid Mahmood Abdullah Daabo
Department of Medical Services and Techniques, Ardahan University, Ardahan, Turkey
Yahya Altinkaynak
Department of Medical Laboratory Sciences, College of Applied Medical Sciences, Prince Sattam bin Abdulaziz University, Jeddah, Saudi Arabia
Ahmed Hjazi
Department of Management, Uttaranchal Institute of Management, Uttaranchal University, Dehradun, Uttarakhand, India
Archana Saxena
Pharmaceutical Chemistry Department, College of Pharmacy, Al-Ayen University, Thi-Qar, Iraq
Mazin A.A. Najm
College of technical engineering, The Islamic University, Najaf, Iraq
Abbas F. Almulla
College of technical engineering, Imam Ja’afar Al-Sadiq University, Al‐Muthanna, 66002, Iraq
Ali Alsaalamy
Department of Medicinal Chemistry, Faculty of Pharmacy, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
Mohammad Amin Kashani
You can also search for this author in PubMed Google Scholar
Contributions
The study’s protocol was designed by M.K., M.H., and T.E., while H.A., Y.A., and A.H. carried out the research. A.S. analyzed the data and prepared the initial draft of the manuscript. M.N., A.FA., and A.A. interpreted the data and provided critical feedback on the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Correspondence to Mohammad Amin Kashani .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Informed consent was obtained from all participants or their legal guardians. Approval was granted by the Research Ethics Committee of Islamic Azad University of Medical Sciences (Approval number: IR.AUI.MEDICINE. REC.1401.147).
Consent for publication
Not applicable.
Competing interests
The authors declared no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
haramshahi, M., A-Elgadir, T.M.E., Daabo, H.M.A. et al. Nutrient patterns and risk of diabetes mellitus type 2: a case-control study. BMC Endocr Disord 24 , 10 (2024). https://doi.org/10.1186/s12902-024-01540-5
Download citation
Received : 04 November 2023
Accepted : 09 January 2024
Published : 17 January 2024
DOI : https://doi.org/10.1186/s12902-024-01540-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nutrient pattern
BMC Endocrine Disorders
ISSN: 1472-6823
- General enquiries: [email protected]
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
The patient has been treated for hypertension for 10 years, currently with amlodipine 10 mg by mouth daily. She was once told that her cholesterol value was "borderline high" but does not know the value.
She denies symptoms of diabetes, chest pain, shortness of breath, heart disease, stroke, or circulatory problems of the lower extremities.
She estimates her current weight at 165 lbs (75 kg). She thinks she weighed 120 lbs (54 kg) at age 21 years but gained weight with each of her three pregnancies and did not return to her nonpregnant weight after each delivery. She weighed 155 lbs one year ago but gained weight following retirement from her job as an elementary school teacher. No family medical history is available because she was adopted. She does not eat breakfast, has a modest lunch, and consumes most of her calories at supper and in the evening.
On examination, blood pressure is 140/85 mmHg supine and 140/90 mmHg upright with a regular heart rate of 76 beats/minute. She weighs 169 lbs, with a body mass index (BMI) of 30.9 kg/m 2 . Fundoscopic examination reveals no evidence of retinopathy. Vibratory sensation is absent at the great toes, reduced at the medial malleoli, and normal at the tibial tubercles. Light touch sensation is reduced in the feet but intact more proximally. Knee jerks are 2+ bilaterally, but the ankle jerks are absent. The examination is otherwise within normal limits.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

12.3: Case Study- Tailoring Nutrition – Carbohydrates in Diabetes Care
- Last updated
- Save as PDF
- Page ID 465675
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Introduction: In the daily lives of people with diabetes, carbohydrates take on a significance that goes beyond simple nutrition. As a primary energy source, the types and amounts of carbohydrates consumed can have a direct impact on blood glucose control. This case study explores the intimate role dietitians play in guiding patients through the complexities of carbohydrate management.
Scenario: Anna Roberts, a compassionate dietitian at Valley Health Hospital, is sitting down with Mr. Thompson, who has been facing the daily challenges of managing his type 2 diabetes. Together, they are embarking on a journey to adjust his diet. Anna’s goal is not just to inform but to connect with Mr. Thompson on a level that reshapes his relationship with food.
The Role of Carbohydrates in the Human Body: Anna begins by walking Mr. Thompson through the basics. "Think of carbohydrates as your body's fuel," she says. She describes how the body breaks them down into sugars like glucose, which his cells use for energy, and why managing the type of 'fuel' is particularly important for his condition.
Case Study Questions:
- Describe the role of carbohydrates in the human body.
- How can understanding carbohydrates help manage blood sugar levels?
Hands-On Classroom Activities:
1. Carbohydrate Analysis: During the "Carbohydrate Analysis" activity, students will examine and quantify the carbohydrate content found in various food items and then engage in a detailed discussion about how these carbohydrates can affect blood sugar levels in the human body.
Conclusion: For Mr. Thompson, Anna's guidance turns the often-overwhelming information about diabetes into actionable and sustainable dietary choices. Her personalized approach demystifies the science of carbohydrates, making it relevant and manageable within the context of Mr. Thompson’s everyday life. This case study paints a vivid picture of the crucial role dietitians like Anna play in translating the science of nutrition into personalized care plans, helping patients with diabetes take control of their health one meal at a time.

Nutrition Case Study #4: Diabetes
by Kim Rose | Mar 26, 2021 | Uncategorized
One of the most FAQ you will receive as a dietitian practicing in a hospital setting is whether it is safe to feed or not to feet an inpatient. Safely resuming a patient’s diet is more than just looking if the digestive tract is working. GI tolerance and lab work are also important. In today’s video let’s look at what the dietitian should know when treating patients with diabetic ketoacidosis (DKA).
Disclaimer: This video is for educational purposes only and is not intended as medical advice. It should be noted that health recommendations change over time and it is best to contact your primary care provider for more information.
— #dietitian #diabetes #Diabeticketoacidosis
— ► Sign up for a FREE 15 minute nutrition call: https://www.kimrosedietitian.com/nutr … ► music: https://www.bensound.com/royalty-free …

Kim has an active YouTube channel where she shares videos about life as a registered dietitian; solutions to common dietitian, intern, RD-to-be, student problems, and health talks.
“The thing I like the most about Kim’s videos is how knowledgeable and approachable she is. She makes it feel like she is there to support you! I have watched Kim’s videos from the beginning of my internship, to studying for my RD exam, to finding my first job. She felt my virtual cheerleader!”
– Rachel, RDN LD, Clinical and Community Dietitian, Minnesota State University, Mankato
Privacy Overview
Insights into the Age-Dependent Variation in Nutrition-Related Trace Elements in Diabetes Blood Using Total Reflection X-Ray Fluorescence
- Published: 03 June 2024
Cite this article

- Manjunatha 1 ,
- A. S. Bennal 1 ,
- Ramesha Hanumanthappa 2 ,
- S. S. Kulkarni 3 ,
- K. S. Devaraju 2 ,
- U. R. Hallikeri 4 ,
- N. M. Badiger 5 &
- P. B. Gai 3
The prevalence of diabetes has reached alarming levels in India, making it essential to understand the concentration of nutritional-trace elements (Fe, Cu, Zn, Cr. and Se) in blood samples from diabetic adults. In this study, 208 whole blood samples from diabetic ( n = 104) and non-diabetic ( n = 104) adults across various age groups were analyzed using total reflection X-ray fluorescence (TXRF) spectroscopy with a sample dilution method. Statistical analysis was performed to assess descriptive statistics and determine a significant correlation between elemental concentrations in the blood samples of diabetic and non-diabetic adults. The mean concentration of nutritional-related trace elements in diabetic blood was as follows: Fe (46 ± 5) > Zn (1.28 ± 0.14) > Cu (0.10 ± 0.01) > Cr (0.05 ± 0.004) > Se (0.013 ± 0.001) in mg/L, respectively. Additionally, this study investigated the influence of nutrition-related trace element concentrations across various age groups such as 25–40 years (young adults), 41–55 years (middle-aged adults), and 56–70 years (older adults). In this investigation, Zn ( p < 0.001) and Cr ( p < 0.05) concentrations differed significantly between diabetic and non-diabetic adults aged 56–70 years. These findings will help us to understand age-dependent changes in element concentrations, clarify their role in diabetes, and improve risk factor management associated with diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Data Availability
No datasets were generated or analysed during the current study.
Forouhi NG, Wareham NJ (2010) Epidemiology of diabetes. Medicine (Baltimore) 38:602–606. https://doi.org/10.1016/j.mpmed.2010.08.007
Article Google Scholar
Sun H, Saeedi P, Karuranga S et al (2022) IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
Article PubMed Google Scholar
Anjana RM, Unnikrishnan R, Deepa M et al (2023) Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17). Lancet Diabetes Endocrinol 11:474–489. https://doi.org/10.1016/S2213-8587(23)00119-5
Mohan V, Sudha V, Shobana S et al (2023) Are unhealthy diets contributing to the rapid rise of type 2 diabetes in India? J Nutr 153:940–948. https://doi.org/10.1016/j.tjnut.2023.02.028
Article CAS PubMed Google Scholar
Lin Y, Meng L, Guo F et al (2023) Association between whole blood essential trace elements and cognitive function in older adults. Ecotoxicol Environ Saf 261:115114. https://doi.org/10.1016/j.ecoenv.2023.115114
Simić A, Hansen AF, Åsvold BO et al (2017) Trace element status in patients with type 2 diabetes in Norway: the HUNT3 survey. J Trace Elem Med Biol 41:91–98. https://doi.org/10.1016/j.jtemb.2017.03.001
Pyrzynska K, Sentkowska A (2023) Selenium species in diabetes mellitus type 2. Biol Trace Elem Res. https://doi.org/10.1007/s12011-023-03900-z
Article PubMed PubMed Central Google Scholar
Nazari M, Nikbaf-Shandiz M, Pashayee-Khamene F, et al (2023) Zinc supplementation in individuals with prediabetes and type 2 diabetes: a GRADE-assessed systematic review and dose-response meta-analysis. Biol Trace Elem Res. https://doi.org/10.1007/s12011-023-03895-7
Dubey P, Thakur V, Chattopadhyay M (2020) Role of minerals and trace elements in diabetes and insulin resistance. Nutrients 12:1864
Article CAS PubMed PubMed Central Google Scholar
Luan F, Chen Y, Xu Y et al (2022) Associations between whole blood trace elements concentrations and HbA1c levels in patients with type 2 diabetes. Biometals 35:1011–1022. https://doi.org/10.1007/s10534-022-00419-z
Wandt VK, Winkelbeiner N, Lossow K et al (2021) Ageing-associated effects of a long-term dietary modulation of four trace elements in mice. Redox Biol 46:102083. https://doi.org/10.1016/j.redox.2021.102083
Rao NS, Raju GJN, Tiwari MK et al (2022) Serum elemental analysis of type 2 diabetes patients using SRXRF. Biol Trace Elem Res 200:1485–1494. https://doi.org/10.1007/s12011-021-02762-7
Harrington JM, Young DJ, Essader AS et al (2014) Analysis of human serum and whole blood for mineral content by ICP-MS and ICP-OES: development of a mineralomics method. Biol Trace Elem Res 160:132–142. https://doi.org/10.1007/s12011-014-0033-5
Marguí E, Queralt I, García-Ruiz E et al (2018) Energy dispersive X-ray fluorescence spectrometry for the direct multi-element analysis of dried blood spots. Spectrochim Acta Part B At Spectrosc 139:13–19. https://doi.org/10.1016/j.sab.2017.11.003
Article CAS Google Scholar
Martinez T, Lartigue J, Avila-Perez P et al (2004) Determination of trace elements in blood samples by TXRF analysis. J Radioanal Nucl Chem 259:511–514
El-Amri FA, El-Saltani HA, Dogadkin NN, Ashour IA (1994) Determination of trace elements in normal and diabetic whole blood by neutron activation analysis. Biol Trace Elem Res 43:383–388. https://doi.org/10.1007/BF02917339
Klockenkämper R, Von Bohlen A (2014) Total-reflection X-ray fluorescence analysis and related methods. John Wiley & Sons
Book Google Scholar
Mirji S, Badiger NM, Sanyal K et al (2018) Determination of trace elements in normal and malignant breast tissues of different age group using total reflection X-ray fluorescence spectrometer. X-Ray Spectrom 47:432–440
Sathish V, Chandrasekaran A, Manjunatha Bennal AS (2023) Geochemical contamination of heavy metals and health risk assessment of coastal sediments along the North Chennai to Pondicherry, India using total reflection X-ray fluorescence spectroscopy (TXRF). Mar Pollut Bull 197:115722. https://doi.org/10.1016/j.marpolbul.2023.115722
De La Calle I, Cabaleiro N, Romero V et al (2013) Sample pretreatment strategies for total reflection X-ray fluorescence analysis: a tutorial review. Spectrochim Acta Part B At Spectrosc 90:23–54
Marguí E, Jablan J, Gerić M et al (2019) Critical evaluation of the use of total reflection X-ray fluorescence spectrometry for the analysis of whole blood samples: application to patients with thyroid gland diseases. Anal Bioanal Chem 411:1659–1670
Stosnach H, Mages M (2009) Analysis of nutrition-relevant trace elements in human blood and serum by means of total reflection X-ray fluorescence (TXRF) spectroscopy. Spectrochim Acta Part B At Spectrosc 64:354–356
Jablan J, Besalú E, Žarak M et al (2021) Analytical potential of total reflection X-ray fluorescence spectrometry for simultaneous determination of iron, copper and zinc in human blood serum and plasma. Talanta 233:122553. https://doi.org/10.1016/j.talanta.2021.122553
Manjunatha, Bennal AS, Badiger NM et al (2023) Effect of sample carriers on analytical parameters in total reflection X-ray fluorescence-a tool for multi-trace elemental analysis. Spectrosc Lett 57:45–58. https://doi.org/10.1080/00387010.2023.2285912
Borgese L, Dalipi R, Riboldi A et al (2018) Comprehensive approach to the validation of the standard method for total reflection X-ray fluorescence analysis of water. Talanta 181:165–171
Varghese J, James JV, Anand R et al (2020) Development of insulin resistance preceded major changes in iron homeostasis in mice fed a high-fat diet. J Nutr Biochem 84:108441. https://doi.org/10.1016/j.jnutbio.2020.108441
Lynch S, Pfeiffer CM, Georgieff MK et al (2018) Biomarkers of nutrition for development (BOND)—iron review. J Nutr 148:1001S-1067S. https://doi.org/10.1093/jn/nxx036
Swaminathan S, Fonseca VA, Alam MG, Shah SV (2007) The role of iron in diabetes and its complications. Diabetes Care 30:1926–1933
Sun L, Zong G, Pan A et al (2013) Elevated plasma ferritin is associated with increased incidence of type 2 diabetes in middle-aged and elderly Chinese adults. J Nutr 143:1459–1465
Eljazzar S, Abu-Hijleh H, Alkhatib D et al (2023) The role of copper intake in the development and management of type 2 diabetes: a systematic review. Nutrients 15:1655
Fernández-Cao JC, Warthon-Medina M, Hall Moran V et al (2018) Dietary zinc intake and whole blood zinc concentration in subjects with type 2 diabetes versus healthy subjects: a systematic review, meta-analysis and meta-regression. J Trace Elem Med Biol 49:241–251. https://doi.org/10.1016/j.jtemb.2018.02.008
Hennigar SR, Lieberman HR, Fulgoni VL, McClung JP (2018) Serum zinc concentrations in the US population are related to sex, age, and time of blood draw but not dietary or supplemental zinc. J Nutr 148:1341–1351. https://doi.org/10.1093/jn/nxy105
Basaki M, Saeb M, Nazifi S, Shamsaei HA (2012) Zinc, copper, iron, and chromium concentrations in young patients with type 2 diabetes mellitus. Biol Trace Elem Res 148:161–164
Mateo MC, Bustamante JB, Quiros JF, Manchado OO (1975) A study of the metabolism of zinc its metalloenzymes in diabetes mellitus. Biomed Pour l’AAICIG 23:134–136
CAS Google Scholar
Yary T, Virtanen JK, Ruusunen A et al (2016) Serum zinc and risk of type 2 diabetes incidence in men: the Kuopio ischaemic heart disease risk factor study. J Trace Elem Med Biol 33:120–124
Hua Y, Clark S, Ren J, Sreejayan N (2012) Molecular mechanisms of chromium in alleviating insulin resistance. J Nutr Biochem 23:313–319. https://doi.org/10.1016/j.jnutbio.2011.11.001
McIver DJ, Grizales AM, Brownstein JS, Goldfine AB (2015) Risk of type 2 diabetes is lower in US adults taking chromium-containing supplements1, 2, 3. J Nutr 145:2675–2682. https://doi.org/10.3945/jn.115.214569
Rabinovitz F, Leibovitz et al (2004) Effect of chromium supplementation on blood glucose and lipid levels in type 2 diabetes mellitus elderly patients. Int J Vitam Nutr Res 74:178–182
Steinbrenner H, Duntas LH, Rayman MP (2022) The role of selenium in type-2 diabetes mellitus and its metabolic comorbidities. Redox Biol 50:102236
Bleys J, Navas-Acien A, Guallar E (2007) Serum selenium and diabetes in US adults. Diabetes Care 30:829–834
Ruíz C, Alegría A, Barberá R et al (1998) Selenium, zinc and copper in plasma of patients with type 1 diabetes mellitus in different metabolic control states. J Trace Elem Med Biol 12:91–95. https://doi.org/10.1016/S0946-672X(98)80031-X
Ekmekcioglu C, Prohaska C, Pomazal K et al (2001) Concentrations of seven trace elements in different hematological matrices in patients with type 2 diabetes as compared to healthy controls. Biol Trace Elem Res 79:205–219
Download references
Acknowledgements
Dr. A. S. Bennal extends heartfelt appreciation to UGC-DAE CSR, Indore, for their invaluable support in funding the research project, and Mr. Manjunatha expresses sincere gratitude for the financial assistance from National Fellowship for Higher Education of ST Students (NFST), Ministry of Tribal Affairs, Govt. of India. The authors are also thankful to the DST PURSE phase-II programme, Karnatak University Dharwad, for facilitating the TXRF instrument throughout the research work.
This work was supported by the UGC-DAE Consortium for Scientific Research (CRS-ISUM-44/CRS-299 dated 23–05-2023. Author Dr A. S. Bennal has received a research grant from UGC-DAE CSR.
Author information
Authors and affiliations.
Department of Studies in Physics, Karnatak University, Dharwad, Karnataka, India
Manjunatha & A. S. Bennal
Department of Biochemistry, Karnatak University, Dharwad, Karnataka, India
Ramesha Hanumanthappa & K. S. Devaraju
Karnataka Institute for DNA Research (KIDNAR), Dharwad, Karnataka, India
S. S. Kulkarni & P. B. Gai
The Karnatak Cancer Therapy and Research Institute, Hubballi, Karnataka, India
U. R. Hallikeri
School of Advanced Sciences, KLE Technological University, Hubli, Karnataka, India
N. M. Badiger
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Sample collection, preparation, analysis and data collection were performed by Manjunatha, Ramesha Hanumanthappa and Dr. U. R. Hallikeri. The first draft of the manuscript was written by Manjunatha. Authors, S. S. Kulkarni, K. S. Devaraju, N. M. Badiger, P. B. Gai reviewed and commented on previous versions of the manuscript. The manuscript was finally reviewed and draft edited by Dr. A S Bennal. All authors read and approved the final manuscript.
Corresponding author
Correspondence to A. S. Bennal .
Ethics declarations
Ethics approval.
This study was approved by the institutional ethical committee of Karnataka Institute for DNA Research (KIDNAR) Dharwad, Karnataka, India (Ref: KIDNAR/2015/11/14/05 dated 14 November 2015. Wide resolution no. 5 on November 14, 2015).
Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.

Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Manjunatha, Bennal, A.S., Hanumanthappa, R. et al. Insights into the Age-Dependent Variation in Nutrition-Related Trace Elements in Diabetes Blood Using Total Reflection X-Ray Fluorescence. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-024-04253-x
Download citation
Received : 14 March 2024
Accepted : 28 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1007/s12011-024-04253-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Blood sample
- Nutritional trace elements
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 May 2024
Effect of a diabetes-specific formula in non-diabetic inpatients with stroke: a randomized controlled trial
- Juan J. López-Gómez ORCID: orcid.org/0000-0003-3144-343X 1 , 2 , 3 ,
- Esther Delgado García 1 , 2 , 3 ,
- David Primo-Martín 1 , 2 ,
- Mónica Simón de la Fuente 3 ,
- Emilia Gómez-Hoyos 1 , 2 , 3 ,
- Rebeca Jiménez-Sahagún 1 , 2 ,
- Beatriz Torres-Torres 1 , 2 , 3 ,
- Ana Ortolá-Buigues 1 , 2 , 3 ,
- Beatriz Gómez-Vicente 3 , 4 ,
- Juan F. Arenillas-Lara 3 , 4 &
- Daniel A. De Luis Román ORCID: orcid.org/0000-0002-1745-9315 1 , 2 , 3
Nutrition & Diabetes volume 14 , Article number: 34 ( 2024 ) Cite this article
251 Accesses
16 Altmetric
Metrics details
- Pre-diabetes
Background/objectives
In patients with acute stroke, the presence of hyperglycaemia has been associated with higher morbidity and less neurological recovery. The aim of the study was to evaluate the impact of a diabetes specific enteral nutrition (EN) formula on glycaemia, comorbidities and mortality in patients admitted with a first episode of stroke who received complete EN.
This was a prospective randomised controlled trial. Patients with acute stroke did not have diagnosis of diabetes mellitus and required nasogastric tube feeding. This study has been registered with code NCT03422900. The patients were randomised into two arms: an isocaloric isoprotein formula (control group (CG), 27 patients) vs a diabetes-specific formula (low glycaemic index carbohydrates, fibre (80% soluble) and higher lipid content) (experimental group (EG), 25 patients). Pre-EN blood glucose, hyperglycaemia during EN treatment, HbA1c, insulin use, oral route recovery, length of stay (LOS) and mortality at 30 days were collected. The complications of enteral nutrition during admission were collected as well.
52 patients were included, 50% females, with an age of 77.44(11.48) years; 34 (65.4%) had ischaemic stroke, with a Rankin score of 0(0–2), and a National Institute of Health Stroke Scale (NIHSS) of 19 (15–22). In CG, there were more cases of hyperglycaemia on the 5th day post-NE (13(65%) vs7(35%), p < 0.01). CG showed an OR of 7.58(1.49–39.16) ( p = 0.02) for the development of hyperglycaemia. There were no differences in LOS between groups (12(8.5) days vs 14(23) days, p = 0.19) or in the death rate (10(37%) vs 10(40%), p = 0.8), although differences were found in terms of oral route recovery (EG: 11(44%) patients vs CG: 5(18.5%) patients, p = 0.04) (OR (EG): 5.53(1.25–24.47); p = 0.02).
Conclusions
The use of a diabetes-specific enteral formula in non-diabetic patients admitted with acute stroke reduced the risk of developing hyperglycaemia and improved the rate of oral route recovery.
Registered under ClinicalTrials.gov Identifier no. NCT03422900.
Similar content being viewed by others

Effect of early enteral nutrition combined with probiotics in patients with stroke: a meta-analysis of randomized controlled trials
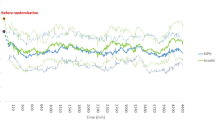
A randomized trial to investigate the efficacy and safety of insulin glargine in hyperglycemic acute stroke patients receiving intensive care

Effect of micronutrient supplementation in addition to nutritional therapy on clinical outcomes of medical inpatients: results of an updated systematic review and meta-analysis
Background and aims.
Stroke is a neurological disorder derived from alterations in vascularisation in the brain. This pathology affects 15 million people year, causes 5.5 million deaths per year and results in the loss of 116 million years of quality of life [ 1 ]. In Spain, incidence of stroke is ~128 cases per 100.000 person years, it is the second cause of global death in the general population, with a mortality rate of 11% [ 2 ]. Stroke is a leading cause of death and disability worldwide [ 3 ].
There is a clear association between diabetes mellitus and vascular diseases [ 4 ]. It is well demonstrated that diabetes mellitus increases the risk of stroke. In addition, patients with diabetes have a double risk of suffering from stroke recurrence and an increase in complications and rehabilitation or functional recovery [ 5 ].
The development of hyperglycaemia after an episode of stroke can be related to a worse evolution of stroke-related damage [ 6 ]. In patients with diabetes mellitus, the hyperglycaemia produces an alteration in the recanalisation associated with a reduced reperfusion, a worse evolution of ischaemic penumbra area and direct damage in the tissues [ 7 ]. This alteration has shown an increase in mortality and a worse functional recovery in patients with ischaemic [ 8 ] or haemorrhagic stroke [ 9 ].
Oropharyngeal dysphagia is a symptom identified in up to 78% of patients in the acute post-stroke phase. This is one of the main causes of post-stroke mortality due to its association with complications such as malnutrition or aspiration pneumonia, which occurs in >20% of patients [ 10 ]. In these patients, medical nutrition therapy is usually required via an enteral route [ 11 ].
In patients with complete enteral nutrition, the incidence of hyperglycaemia can reach 30% [ 12 ]. In a previous study in 158 non-diabetic patients admitted by stroke in our hospital, 33% (52 patients) of non-diabetic patients with stroke and complete enteral nutrition developed stress hyperglycaemia and 19.1% (30 patients) developed hyperglycaemia related to the use of enteral nutrition [ 13 ].
Diabetes-specific formulas were developed as a method to avoid enteral nutrition-related hyperglycaemia in patients with diabetes. These formulas usually have a reduction of energy from carbohydrates and a replacement with energy from lipids or proteins; the use of carbohydrates with a low glycaemic index such as lactose or isomaltulose; and/or an increase in the amount of soluble fibre to decrease glucose absorption [ 14 ]. In addition, some of these formulas are enriched in monounsaturated (MUFA) and polyunsaturated fatty acids (PUFA) to have a benefit in the lipid profile [ 15 ].
Diabetes-specific formulas have shown an improvement in glycaemic control and lipid control in patients with diabetes. In 2005, Elia et al. concluded that the use of diabetes-specific formulas in the short- and long-term was associated with better glycaemic control related to standard formulas [ 16 ]. In 2019, Ojo et al. also showed better glycaemic control and an increase in HDL-cholesterol but no effect in other lipid parameters [ 17 ]. In 2020, Sanz Paris et al. studied diabetes-specific formulas that are high in MUFAs and concluded that these formulas can improve glucose control and metabolic risk factors among patients with diabetes [ 15 ]. Most of these studies are being developed in patients with diabetes and stress hyperglycaemia, but there are few studies that have compared diabetes-specific formulas with standard formulas in patients without diabetes.
In patients without diabetes who suffer a stroke, hyperglycaemia can be caused by several reasons: stress induced-hyperglycaemia, enteral nutrition, and acute treatments for stroke. As a result, medical nutrition therapy must be oriented to avoid this condition of hyperglycaemia. The use of diabetes-specific formulas in patients with stroke has shown an improvement in acute-term glycaemic control in severe acute ischaemic patients with non-insulin dependent diabetes and without diabetes [ 18 ]. However, there is no evidence of the use of these formulas in patients with stroke and no diabetes.
The purpose of this study was to evaluate the effect of a diabetes-specific nutritional formula on the development of hyperglycaemia in non-diabetic inpatients with recent stroke who require complete enteral nutrition through a nasogastric tube, as well as the effect of the use of this formula on the development of comorbidities, mortality and tolerance.
Study design
A randomised controlled clinical trial was developed in patients without diabetes mellitus admitted due to stroke and with an indication for nutritional support by nasogastric tube. We randomly assigned patients to receive either a diabetes-specific enteral formula or a standard formula.
The primary outcome of the study was the development hyperglycaemia associated with enteral nutrition formula during admission. The secondary outcomes were to observe the influence of enteral nutrition formula on comorbidity of stroke (oral route recovery, death, readmission and length of stay) and in complications of enteral nutrition formula.
This study was developed between January 2018 and September 2021 in patients admitted to the Stroke Unit, Department of Neurology of Clinic University Hospital of Valladolid. All patients signed informed consent before recruitment and randomisation.
The study was carried out in accordance with the Declaration of Helsinki and all procedures were approved by the Medical Research Ethics Committee (CEIm) of East Valladolid under code CASVE-NM-17-315. This clinical trial was registered in www.clinicaltrials.gov with code NCT03422900.
Study subjects
Patients with a first-ever ischaemic or haemorrhagic stroke, without history of diabetes mellitus, admitted to the Stroke Unit of our hospital were included in the study. The patients had complete dysphagia and required total enteral nutrition via a nasogastric tube (for at least 7 days). The inclusion criteria were the start of enteral nutrition during the first 72 h after stroke and acceptance by the patient or their legal representative to participate in the study. The main reason to select 72 h was that there is no evidence of the use of early enteral nutrition by nasogastric tube could ameliorate the outcomes and if the patient has no dysphagia could be dangerous [ 3 ]. We select 72 h to ensure the stability of patient and the protocol to confirm dysphagia in these patients in our hospital.
The exclusion criteria were enteral nutrition not feasible; severe gastrointestinal pathology; diagnosed diabetes mellitus; current glycated haemoglobin (HbA1c) >6.5%; allergy or intolerance to ingredients of the formula; pregnant women; patients who required an Intensive Care Unit (ICU) stay; previous neurodegenerative disease; and did not sign the informed consent.
Randomisation was done by a randomisation seed generated by http://www.randomization.com/ with a block assignation AABB, ABAB, ABBA, BAAB, BBAA and BABA.
The investigators were aware of the allocation sequence and treatment allocation. The trial personnel who worked in hospital plant only administrate the enteral nutrition prescribed by investigators. There was no blinding because it was a trial in real clinical practice with the formulas commonly used in the hospital. Nevertheless, the investigator who made the randomization is not involved in the clinical follow-up of the patient. This investigator informed the allocation of treatment to the physician of clinical nutrition services that prescribed the indicated treatment. This physician is not involved in data collection or analysis. At the end of the study the physician who had followed the patient in a multidisciplinary team delivered a report of variables to the investigator that includes it in the database. Another investigator took care of the data analysis. In this way, the investigator who collected and analyzed the variables was not the physician who followed the patient.
There was no predefined stopping rule. In the development of study, we have seen a better glycaemia evolution in patients with diabetes-specific formula. For this reason, we consider the primary outcome was solved and all patients could benefit from the use of diabetes-specific formula.
Medical nutrition therapy
A standard enteral nutrition formula (isocaloric, isoproteic formula without fibre) was compared with a diabetes-specific enteral formula (isocaloric and isoproteic formula with carbohydrates with a lower glycaemic index and the presence of mixed soluble and insoluble fibre) (Table 1 ).
Energy requirements for patients were estimated by Harris Benedict equation with a stress factor of 1.2. The amount of enteral nutrition was calculated in the function of energy density of the formula and energy requirements of the patient.
Enteral nutrition was delivered with a continuous infusion pump for 24 h without rest.
Study variables
Sociodemographic variables : Age (years), gender (male/female).
Clinical variables : Stroke type (ischaemic/haemorrhagic); stroke clinical severity (National Institutes of Health Stroke Scale (NIHSS)); Rankin scale.
Anthropometric Variables : Usual weight (kg); actual weight (kg); height (m); body mass index (kg/m 2 ).
Metabolic variables:
Biochemical: performed with a Cobas c-711 autoanalyser (Roche Diagnostics): glucose (mg/dL); creatinine (mg/dl); albumin (g/dL); C-reactive protein (CRP) (mg/dL), prealbumin (mg/dL); CRP/prealbumin ratio; glycaemia (mg/dL); sodium (mEq/l); potassium (mEq/l); urea (mg/dL); total cholesterol (mg/dL); and triglycerides (mg/dL).
Diagnosis of hyperglycaemia: fasting plasma glucose >126 mg/dl before the beginning of enteral nutrition or glycaemia >180 mg/dl during the administration of the enteral formula.
Capillary blood glucose (Abbott ® Lifestyle Measurer): this was considered the average of capillary glycaemia (mg/dl) every 8 h for 7 days, from the start of enteral nutrition until discharge from hospital.
Gastrointestinal Tolerance : diarrhoea, constipation, gastric emptying, abdominal distension, presence of vomiting. All of these variables were collected daily in the form of a dichotomous variable yes/no by the same investigator.
Complications : length of stay (days); mortality during admission; readmission; presence of pneumonia; dysphagia recovery (negative method of clinical volume-viscosity test (MECV_V)) [ 19 ].
Statistical analysis
The data were stored in a database on the statistical package SPSS 23.0 (SPSS Inc. Il, USA) with an official license from the University of Valladolid. An analysis of normality of the continuous variables was performed with the Kolmogorov-Smirnov test.LIe.
The calculated sample size was 150 patients (75 per branch with 10% loss). The study had to be stopped at 60 patients because the primary aim was achieved, and we could not continue due to ethical considerations, these considerations were to obtain the main outcome in patients with diabetes-specific formula, so all the patients could benefit from the use of diabetes-specific formula.
Continuous variables were expressed as mean (standard deviation), parametric variables were analysed with the unpaired and paired t -Student test, and non-parametric variables with the Friedman, Wilcoxon, K Kruskal, and U -Mann Whitney tests. If it was necessary to compare variables in more than two groups, the ANOVA U test (with the Bonferroni post-hoc test) was used. The analysis of variables at the different times of the study was performed using multivariable analysis of variance (MANOVA).
A multivariable analysis was performed adjusted by variables which show differences between groups in a descriptive analysis and with variables which can influence glycaemia.
Qualitative variables were expressed as percentages (%) and analysed using the Chi-square test (with Fisher and Yates corrections when necessary). A p -value < 0.05 was considered significant.
Sixty patients were assessed for eligibility, 8 patients were excluded, and 52 patients were randomised (25 patients to the intervention group and 27 patients to the control group) (Fig. 1 ).
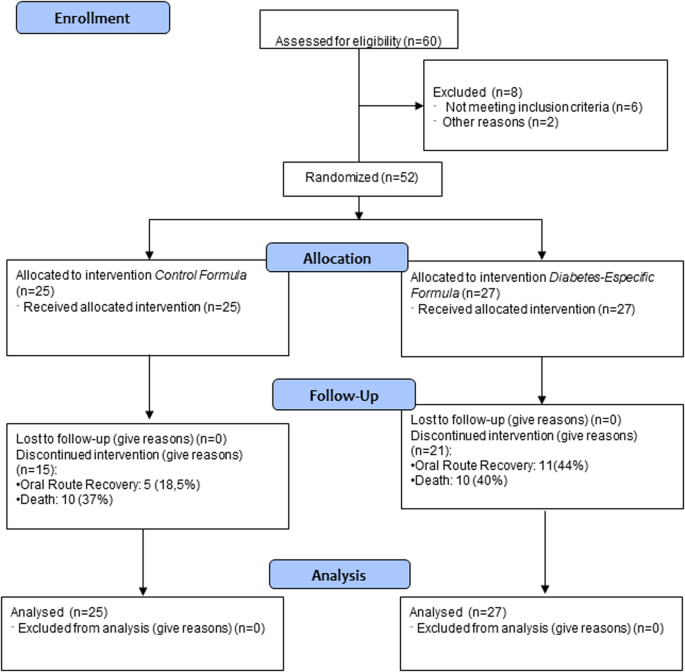
Flow chart.
Sample Description
There were no differences between variables in both groups except for natremia and stroke type (ischaemic/haemorrhagic) (Table 2 ).
Evaluation of glycaemic parameters during the admission
Fasting venous glucose levels after 5 days of enteral nutrition was 133 (118–160.5) mg/dl. The values were significantly higher in the control group (Control (C): 150.5 (132.25–173.5) mg/dl vs. Experimental (E): 121 (113.5–142) mg/dl; p -value = 0.02).
Average capillary blood glucose levels after 7 days of enteral nutrition were 130.58 (22.6) mg/dl. No statistically significant differences were found between the two groups (C: 132.96 (22.56) mg/dl vs. E: 127.79 (22.83) mg/dl; p -value = 0.43).
In addition, the absolute number of participants who developed hyperglycaemia (more than two episodes) after 5 days of enteral nutrition (cut-off point the value of 140 mg/dl and 180 mg/dl) had a higher rate of hyperglycaemia in the control group using the cut-off point 140 (CONTROL: 16 patients (65%); EXPERIMENTAL: 9 patients (35%); p < 0.05) and at the cut-off point 180 mg/dl (CONTROL: 16 patients (64.7%); EXPERIMENTAL: 9 patients (35.3%); p < 0.05).
A multivariable analysis was performed to assess whether the use of the control formula is an independent risk factor for the development of hyperglycaemia ( > 140 mg/dl) after 5 days of enteral nutrition. The use of a control formula was an independent risk factor for the development of hyperglycaemia (OR: 7.58 (1.47–39.16); p -value: 0.02), adjusted by type of stroke, age, use of corticosteroids, NIHSS value and sodium levels (Table 3 ).
The use of subcutaneous basal insulin to reach normal glycaemia during admission was needed in 13 patients (25%) (9 (33%) from the control group vs. 4 (16%) from the experimental group, with no statistical difference between groups).
The evolution of the venous glycaemia of the subjects was compared between groups (Fig. 2 ). It was observed that the glycaemia in the experimental group was lower at the three determined cut-off points (baseline, at 5 days, and at 10 days). On the other hand, capillary glycaemia tended to normalise 14 days after starting enteral nutrition. There were differences in the control group and total sample but there were no differences in the experimental group (Fig. 2 ).
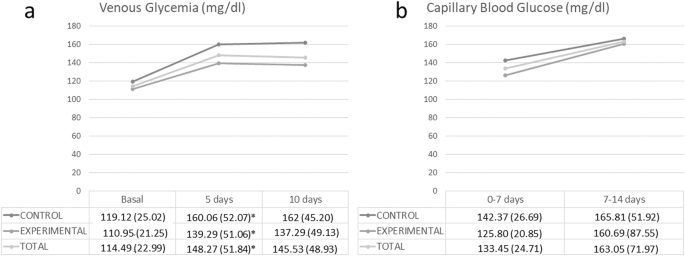
a Basal venous glycaemia, 5 days glycaemia and 10 days glycaemia, and in b average capillary blood glycaemia at 0–7 days and 7–14 days. malization and correction for chance.
It was observed a significant decrease in total cholesterol in both groups 5 days after the start of enteral nutrition (CONTROL: Start: 171.84 (41.44) mg/dL; 5 days: 132.95 (24.21) mg/dL; p < 0.01; EXPERIMENTAL: Start: 170.61 (32.77) mg/dL; 5 days: 135.39 (20.55); p < 0,01); at 10 days after the start of enteral nutrition there was a significant decrease in control group (CONTROL: Start: 171.84 (41.44) mg/dL; 10 days: 135.67 (29.10) mg/dL; p < 0.01; EXPERIMENTAL: Start: 170.61 (32.77) mg/dL; 10 days: 147.95; p = 0.07). The decrease in total cholesterol was more striking in control group (CONTROL: 34.48 (11.63) %; EXPERIMENTAL: 11.33 (23.35) %; p = 0.04). There were no significant differences in level of triglycerides in both groups.
Evaluation of comorbidities
Patients receiving the experimental formula showed greater recuperation of the oral route than the control group. There were no differences in terms of length of hospital stay, readmission or death (Table 4 ).
A multivariable analysis was performed to assess risk factors for the recovery of the oral route at discharge and as independent variables: the use of the experimental formula (diabetes-specific), age and type of stroke. It was observed that the use of a diabetes-specific formula increased the probability of recovery of the oral route at hospital discharge (OR: 6.26 (95% CI: 1.22–32.17); p -value = 0.03) adjusted by NIHSS (OR: 0.89 (95%: 0.79–0.99); p -value < 0.05); age (OR: 0.98 (95% CI: 0.93–1.04); p -value = 0.57) and type of stroke (OR: 2.3 (95%: 0.46–11.59); p = 0.31).
They were evaluated as independent risk factors for mortality: type of formula, age, NIHSS and type of stroke. There was no statistical relationship. On the other hand, the length of stay > 14 days did not show any association with the variables age, type of stroke or type of formula.
Evaluation of complications
The rate of digestive complications was evaluated. There was an increase in the development of diarrhoea in the experimental group. There were no significant differences for the rest of the digestive complications (Table 5 ). No statistically significant differences were observed for other admission complications (Table 5 ).
In non-diabetic patients who are admitted for stroke and require complete enteral nutrition via an enteral route, the use of a diabetes-specific formula decreased the rate of hyperglycaemia associated with enteral nutrition. These patients also showed better glycaemic control during the admission and better recovery of the oral route.
The age of patients ranged from 75–80 years, like the median age of patients with stroke in most studies. The incidence of stroke increased with age with a high rate in older patients [ 20 ]. Most of the patients presented a normal nutritional status at admittance assessed by subjective global assessment; the mean BMI showed an overweight state. These data are like those of other studies which assessed malnutrition in patients with stroke at admission. Sato et al. observed that 57% of patients admitted to a Stroke unit have a normal nutritional status assessed by GLIM criteria [ 21 ]. If we observe functional status prior to stroke in patients, the modified RANKIN scale shows a very slight disability in our sample related to the age of patients; the rate of great disability in our patients were very low.
There was also a difference between the type of stroke, with an increase in ischaemic stroke in the experimental group, these differences could be based on chance and must not influence results because there are no data on differences in the development of hyperglycaemia related to the type of stroke [ 22 ]. Hyperglycaemia and diabetes are related to worse events in patients with ischaemic or haemorrhagic stroke. However, there are no clear effects of hyperglycaemia on differences in events related to the type of stroke [ 22 ].
The use of diabetes-specific formulas have been studied in patients with diagnosed diabetes mellitus with better control in fast glucose and glycated haemoglobin, as Ojo et al. showed in a recent metanalysis [ 17 ]. However, the effect on the development of hyperglycaemia in patients with no previous diagnosis of diabetes is still unclear. Sanz et al. showed that high monounsaturated fatty acid diabetes-specific formulas can ameliorate the glycaemic control in patients with diabetes or stress-induced hyperglycaemia [ 15 ]. Our study has shown that the use of this type of formulas in patients admitted for stroke can decrease the development of hyperglycaemia induced by enteral nutrition. Another similar study by Shao et al. in patients with ischaemic stroke with complete enteral nutrition by nasogastric tube proved that the use of a diabetes-specific formula may improve acute-term glycaemic control in severe acute ischaemic stroke patients, but there were no differences in glycaemic variability control. The main differences with our study were the selection of patients with or without diabetes, except insulin-dependent diabetes [ 18 ]. Our study population only included patients without any type of previous diagnosed or undiagnosed diabetes and the patients can be either ischaemic or haemorrhagic stroke.
Dysphagia is a frequent complication after a stroke. A recent study has estimated that it occurs in >20% of stroke patients and persists in >50%. The severity of the stroke, more than the location, is what determines the appearance of dysphagia. Dysphagia deteriorates nutritional status and increases the risk of aspiration pneumonia in >20% of patients, which causes death in 20% of patients in the year following the stroke [ 23 ]. In our study, patients in the interventional group had an increased probability (OR: 5.53) of recovery of the oral route. As seen in recent studies, the development of hyperglycaemia is related to non-recovery of the oral route in these patients. An intervention which avoid the increase of glycaemia can improve the dysphagia [ 13 ]. Our trial shows that the diabetes-specific formula produces a lower rate of hyperglycaemia and, therefore, greater recovery from the oral route. However, it is necessary to design studies directed to study the oral route recovery to better assess the effect of the control of glycaemia and the use of a diabetes-specific formula.
There were no significant differences in the percentage of deaths in both groups. Hospital mortality due to stroke has decreased from 1970–2008 from 35.9%–19.8%. Some of the factors associated with an increased risk of mortality after a stroke are the following: age, the initial severity of the stroke, gender, race, previous functional status, hyperthermia, hyperglycaemia, high or low blood pressure and previous cardiovascular diseases [ 24 ]. In our trial, mortality was higher, around 40%, due to the extension of stroke that involved the ability to swallow, and the advanced age (77 years) of the patients included in the study. The need for a nasogastric tube is usually linked to a greater clinical severity and/or to the development of severe clinical complications [ 25 ]. There were no differences between groups, although there was better glycaemic control in the experimental group.
An increase in the development of diarrhoea in the experimental group was shown, probably related to the enteral formula. Diarrhoea is the most frequent gastrointestinal complication in patients receiving enteral nutrition. In general, the prevalence is around 30% in hospitalised patients, reaching 80% in those who are in the intensive care unit (ICU) [ 26 ]. The causes of diarrhoea associated with enteral nutrition are varied. The main causes are high osmolarity of the formula and the fibre content. In the experimental group, osmolarity of the formula was lower than in the control group but there was a mixed fibre content with 80% soluble fibre and 20% insoluble fibre. These characteristics may have influenced the development of diarrhoea in the experimental group. In the study by León et al., which compared two specific diabetes enteral formulas (low carbohydrate and high lipids content vs. high carbohydrate diet), the high carbohydrate group showed a significantly higher incidence of diarrhoea, as in our study [ 27 ]. However, another study performed by De Luis et al. showed no differences in diarrhoea between high or low doses of a diabetes-specific formula. This situation can be related to the use of the formula as oral nutritional supplementation and not in a complete route [ 28 ].
The main strength of the study is the type of study as a randomised controlled trial with two different enteral formula. Otherwise, the population selected, as the use of a diabetes-specific formula has mainly been studied in patients with diagnosed diabetes and its prescription in patients with a risk of development of hyperglycaemia has a lack of evidence. On the other hand, in addition to the reported effect on glycaemia, differences were observed in outcome variables such as recovery of the oral route in those fed with the specific formula for diabetes, a condition that could be studied in subsequent trials and well-designed trials.
The main limitations of the study were the different type of stroke studied that could interfere with the results. However, as we have adjusted multivariable analysis with this condition, the type of stroke seems not to influence the main objective of the study on glycaemic control and secondary outcomes as oral route recovery. Another limitation was that the calculated sample size was 150 patients, but the study had to be stopped at 60 because it had accomplished the primary aim, and we could not continue due to ethical considerations. We think that more striking results on p -value must be a better guarantee for reducing possible false positive results. Nevertheless, the use of diabetes-specific formulas has a long experience in control hyperglycaemia in diabetic patients in critic and non-critic condition. There is less experience in non-diabetic patients but as we can see in these patients, the behaviour was similar in glycaemia, and we see secondary aims as oral route recovery in patients with an adequate control of glucose metabolism. These two reasons lead us to plant the use of a more specific formula in all patients. On the other hand, there was no blinding due to the use of usual formulas of the hospital in real clinical practice; we think that these characteristics did not influence the trial result because the use of diabetic enteral formulas is clear in patients with diabetes, but this not so clear in patients with diagnosed diabetes. On the other hand, the separation between investigators who allocated patients to the different groups of study and the physicians that followed the patients in their clinical route avoid the possible bias of not blinding the study.
The main clinical consequences of the development of this study are the planification of use diabetes-specific formulas (enteral formulas with low glycaemic index carbohydrates, monounsaturated fatty acids and mixed fibre) in non-diabetic patients with ischaemic or hemorragic stroke during admission with a low rate of complications.
These formulas have shown a decrease in hyperglycaemia, but it is necessary to develop studies to show whether the use of these formulas can improve the evolution of stroke. These studies can improve the results using continuous glucose monitoring systems to evaluate the glycaemic variability and its relationship with the secondary outcomes of the evolution of stroke. Another point to investigate is the different evolution of stroke by imaging techniques in relation with glycaemia evolution.
The use of a specific-diabetic formula in non-diabetic patients with stroke and complete enteral nutrition by a nasogastric tube showed a lower development of hyperglycaemia episodes compared to an isocaloric isoprotein formula. The use of a diabetes-specific formula produced lower venous and capillary glycaemia compared to the control formula.
In patients treated with a diabetes-specific formula, there was an increased recovery of the oral route, which could be related to the less frequent development of hyperglycaemia. No differences between groups were observed in the mean hospital stay, readmissions or percentage of deaths.
It is necessary to develop new studies on the use of diabetes-specific formulas in non-diabetic patients to assess clinical outcomes of the nutritional intervention. The effect of glycaemic control in patients without diabetes treated with a diabetes-specific formula may help to create some lines of investigation into the effect of glycaemic control using the new continuous glucose monitoring devices. Also, given the results obtained for oral route recovery, it would be interesting to develop studies with this aim as a principal objective.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to confidentiality of clinical records but are available from the corresponding author on reasonable request.
Purroy F, Montalà N. Epidemiology of stroke in the last decade: a systematic review. Rev Neurol. 2021;73:321–36.
CAS PubMed Google Scholar
Sánchez-Larsen Á, García-García J, Ayo-Martín O, Hernández-Fernández F, Díaz-Maroto I, Fernández-Díaz E, et al. Has the aetiology of ischaemic stroke changed in the past decades? analysis and comparison of data from current and historical stroke databases. Neurol Barc Spain. 2016;S0213-4853:30168–2.
Google Scholar
Burgos R, Breton I, Cereda E, Desport JC, Dziewas R, Genton L, et al. ESPEN guideline clinical nutrition in neurology. Clin Nutr Edinb Scotl. 2018;37:354–96.
Article Google Scholar
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SRK, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet Lond Engl. 2010;375:2215–22.
Sharma M, Gubitz GJ. Management of stroke in diabetes. Can J Diabetes. 2013;37:S124–5.
Article PubMed Google Scholar
Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci. 2016;351:380–6.
Article PubMed PubMed Central Google Scholar
Kruyt ND, Biessels GJ, Devries JH, Roos YB. Hyperglycemia in acute ischemic stroke: pathophysiology and clinical management. Nat Rev Neurol. 2010;6:145–55.
Article CAS PubMed Google Scholar
Mi D, Wang P, Yang B, Pu Y, Yang Z, Liu L. Correlation of hyperglycemia with mortality after acute ischemic stroke. Ther Adv Neurol Disord. 2018;11:1756285617731686.
Kruyt ND, Biessels GJ, DeVries JH, Luitse MJA, Vermeulen M, Rinkel GJE, et al. Hyperglycemia in aneurysmal subarachnoid hemorrhage: a potentially modifiable risk factor for poor outcome. J Cereb Blood Flow Metab J Int Soc Cereb Blood Flow Metab. 2010;30:1577–87.
Article CAS Google Scholar
Huppertz VAL, Pilz W, Pilz Da Cunha G, de Groot LCPGM, van Helvoort A, Schols JMGA, et al. Malnutrition risk and oropharyngeal dysphagia in the chronic post-stroke phase. Front Neurol. 2022;13:939735.
Article CAS PubMed PubMed Central Google Scholar
Crary MA, Humphrey JL, Carnaby-Mann G, Sambandam R, Miller L, Silliman S. Dysphagia, nutrition, and hydration in ischemic stroke patients at admission and discharge from acute care. Dysphagia. 2013;28:69–76.
Sanz-Paris A, Álvarez Hernández J, Ballesteros-Pomar MD, Botella-Romero F, León-Sanz M, Martín-Palmero Á, et al. Evidence-based recommendations and expert consensus on enteral nutrition in the adult patient with diabetes mellitus or hyperglycemia. Nutr Burbank Los Angel Cty Calif. 2017;41:58–67.
López-Gómez JJ, Delgado-García E, Coto-García C, Torres-Torres B, Gómez-Hoyos E, Serrano-Valles C, et al. nfluence of hyperglycemia associated with enteral nutrition on mortality in patients with stroke. Nutrients. 2019;11:E996.
Kokubo E, Morita S, Nagashima H, Oshio K, Iwamoto H, Miyaji K. Blood glucose response of a low- carbohydrate oral nutritional supplement with isomaltulose and soluble dietary fiber in individuals with prediabetes: a randomized, single-blind crossover trial. Nutrients. 2022;14:2386.
Sanz-París A, Matía-Martín P, Martín-Palmero Á, Gómez-Candela C, Camprubi Robles M. Diabetes-specific formulas high in monounsaturated fatty acids and metabolic outcomes in patients with diabetes or hyperglycaemia. A systematic review and meta-analysis. Clin Nutr. 2020;39:3273–82.
Elia M, Ceriello A, Laube H, Sinclair AJ, Engfer M, Stratton RJ. Enteral nutritional support and use of diabetes-specific formulas for patients with diabetes: a systematic review and meta-analysis. Diabetes Care. 2005;28:2267–79.
Ojo O, Weldon SM, Thompson T, Crockett R, Wang X-H. The effect of diabetes-specific enteral nutrition formula on cardiometabolic parameters in patients with type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Nutrients. 2019;11:E1905.
Shao Y, Heng W, Li S, Xu Y, Hu G. Tube feeding with a diabetes-specific enteral formula improves glycemic control in severe acute ischemic stroke patients. J Parenter Enter Nutr. 2018;42:926–32.
Clavé P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr Edinb Scotl. 2008;27:806–15.
Zhang Y, Chapman A-M, Plested M, Jackson D, Purroy F. The incidence, prevalence, and mortality of stroke in France, Germany, Italy, Spain, the UK, and the US: a literature review. Stroke Res Treat. 2012;2012:436125.
PubMed PubMed Central Google Scholar
Sato K, Inoue T, Maeda K, Shimizu A, Ueshima J, Ishida Y, et al. Undernutrition at admission suppresses post-stroke recovery of trunk function. J Stroke Cerebrovasc Dis J Natl Stroke Assoc. 2022;31:106354.
Snarska KK, Bachórzewska-Gajewska H, Kapica-Topczewska K, Drozdowski W, Chorąży M, Kułakowska A, et al. Hyperglycemia and diabetes have different impacts on outcome of ischemic and hemorrhagic stroke. Arch Med Sci AMS. 2017;13:100–8.
Sánchez-Sánchez E, Avellaneda-López Y, García-Marín E, Ramírez-Vargas G, Díaz-Jimenez J, Ordonez FJ. Knowledge and practice of health professionals in the management of dysphagia. Int J Environ Res Public Health. 2021;18:2139.
Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355–69.
Nascimento A, Carvalho M, Nogueira J, Abreu P, Nzwalo H. Complications associated with nasogastric tube placement in the acute phase of stroke: a systematic review. J Neurosci Nurs J Am Assoc Neurosci Nurses. 2018;50:193–8.
Pitta MR, Campos FM, Monteiro AG, Cunha AGF, Porto JD, Gomes RR. Tutorial on diarrhea and enteral nutrition: a comprehensive step-by-step approach. JPEN. J Parenter Enter Nutr. 2019;43:1008–19.
León-Sanz M, García-Luna PP, Sanz-París A, Gómez-Candela C, Casimiro C, Chamorro J, et al. Glycemic and lipid control in hospitalized type 2 diabetic patients: evaluation of 2 enteral nutrition formulas (low carbohydrate-high monounsaturated fat vs high carbohydrate). JPEN J Parenter Enter Nutr. 2005;29:21–9.
de Luis DA, Izaola O, de la Fuente B, Terroba MC, Cuellar L, Cabezas G. A randomized clinical trial with two doses of an enteral diabetes-specific suplements in elderly patients with diabetes mellitus type 2. Eur Rev Med Pharm Sci. 2013;17:1626–30.
Download references
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Servicio de Endocrinología y Nutrición, Hospital Clínico Universitario de Valladolid, Valladolid, Spain
Juan J. López-Gómez, Esther Delgado García, David Primo-Martín, Emilia Gómez-Hoyos, Rebeca Jiménez-Sahagún, Beatriz Torres-Torres, Ana Ortolá-Buigues & Daniel A. De Luis Román
Centro de Investigación en Endocrinología y Nutrición (IENVA), Universidad de Valladolid, Valladolid, Spain
Department of Medicine, Universidad de Valladolid, Universidad de Valladolid, Valladolid, Spain
Juan J. López-Gómez, Esther Delgado García, Mónica Simón de la Fuente, Emilia Gómez-Hoyos, Beatriz Torres-Torres, Ana Ortolá-Buigues, Beatriz Gómez-Vicente, Juan F. Arenillas-Lara & Daniel A. De Luis Román
Stroke Program, Department of Neurology, HCUV, Valladolid, Spain
Beatriz Gómez-Vicente & Juan F. Arenillas-Lara
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: JJL, JFA, DAL, data curation: EDG, DPM, MSF, format analysis: JJL, funding acquisition: DAL, JFAL, investigation: JJL, DPM, BGV, MSF, EDG, EGH, RJS, BTT, AOB, methodology: JJL, DAL, JFAL, project administration: JJL, DAL, JFAL; resources: JJL, DAL; software: JJL, DAL, DPM; supervision: JJL, DAL, JFAL; validation: JJL, DAL, JFAL; visualization: JJL, DAL, JFAL, writing-original draft: JJL, MSF; writing-review and editing: JJL, DAL, JFAL.
Corresponding author
Correspondence to Juan J. López-Gómez .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
All patients signed informed consent before recruitment and randomisation. The study was carried out in accordance with the Declaration of Helsinki and all procedures were approved by the Medical Research Ethics Committee (CEIm) of East Valladolid under code CASVE-NM-17-315. This clinical trial was registered in www.clinicaltrials.gov with code NCT03422900.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
López-Gómez, J.J., Delgado García, E., Primo-Martín, D. et al. Effect of a diabetes-specific formula in non-diabetic inpatients with stroke: a randomized controlled trial. Nutr. Diabetes 14 , 34 (2024). https://doi.org/10.1038/s41387-024-00292-4
Download citation
Received : 13 October 2023
Revised : 02 May 2024
Accepted : 08 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1038/s41387-024-00292-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
- Insulin, Medicines, & Other Diabetes Treatments
- Español
Insulin, Medicines, & Other Diabetes Treatments
On this page:
What medicines might I take for diabetes?
What type of diabetes do i have, what are the different types of insulin, what are the different ways to take insulin, what oral medicines treat type 2 diabetes, what other injectable medicines treat diabetes, what should i know about side effects of diabetes medicines.
- What questions should I ask about my diabetes medicines?
Do I have other treatment options for my diabetes?
Clinical trials for insulin, medicines, & other diabetes treatments.
Taking insulin or other diabetes medicines is often part of treating diabetes. In addition to making healthy food and beverage choices, getting physical activity, getting enough sleep, and managing stress, medicines can help you manage the disease. Some other treatment options are also available.
The medicine you take depends on the type of diabetes you have and how well the medicine controls your blood glucose levels, also called blood sugar levels. Other factors, such as any other health conditions you may have, medication costs, your insurance coverage and copays, access to care, and your lifestyle, may affect what diabetes medicine you take.
Type 1 diabetes
If you have type 1 diabetes , you must take insulin because your pancreas does not make it. You will need to take insulin several times during the day, including when you eat and drink, to control your blood glucose level.
There are different ways to take insulin . You can use a needle and syringe , an insulin pen , or an insulin pump . An artificial pancreas —also called an automated insulin delivery system—may be another option for some people.
Type 2 diabetes
Some people with type 2 diabetes can control their blood glucose level by making lifestyle changes. These lifestyle changes include consuming healthy meals and beverages, limiting calories if they have overweight or obesity , and getting physical activity.
Many people with type 2 diabetes need to take diabetes medicines as well. These medicines may include diabetes pills or medicines you inject, such as insulin. Over time, you may need more than one diabetes medicine to control your blood glucose level. Even if you do not take insulin, you may need it at special times, such as if you are pregnant or if you are in the hospital for treatment.
Gestational diabetes
If you have gestational diabetes , you can manage your blood glucose level by following a healthy eating plan and doing a moderate-intensity physical activity, such as brisk walking for 150 minutes, each week. If consuming healthy food and beverages and getting regular physical activity aren’t enough to keep your blood glucose level in your target range, a doctor will work with you and may recommend you take insulin. Insulin is safe to take while you are pregnant.
No matter what type of diabetes you have, taking diabetes medicines every day can feel like a burden sometimes. New medications and improved delivery systems can help make it easier to manage your blood glucose levels. Talk with your doctor to find out which medications and delivery systems will work best for you and fit into your lifestyle.
Several types of insulin are available. Each type starts to work at a different speed, known as “onset,” and its effects last a different length of time, known as “duration.” Most types of insulin reach a peak, which is when they have the strongest effect. After the peak, the effects of the insulin wear off over the next few hours or so. Table 1 lists the different types of insulin, how fast they start to work, when they peak, and how long they last.
Table 1. Types of insulin and how they work 1,2
Another type of insulin, called premixed insulin, is a combination of insulins listed in Table 1. Premixed insulin starts to work in 15 to 60 minutes and can last from 10 to 16 hours. The peak time varies depending on which insulins are mixed.
Your doctor will work with you to review your medication options. Talk with your doctor about your activity level, what you eat and drink, how well you manage your blood glucose levels, your age and lifestyle, and how long your body takes to absorb insulin.
Follow your doctor’s advice on when and how to take your insulin. If you're worried about the cost, talk with your doctor. Some types of insulin cost more than others. You can also find resources to get financial help for diabetes care .
The way you take insulin may depend on your lifestyle, insurance plan, and preferences. Talk with your doctor about the options and which one is best for you. Most people with diabetes take insulin using a needle and syringe, insulin pen, or insulin pump. Inhalers and insulin jet injectors are less common ways to take insulin. Artificial pancreas systems are now approved by the U.S. Food and Drug Administration (FDA). Talk with your doctor to see if an artificial pancreas is an option for you.
Needle and syringe
You can give yourself insulin shots using a needle and syringe . You draw up your dose of insulin from the vial—or bottle—through the needle into the syringe. Insulin works fastest when you inject it in your belly, but your doctor may recommend alternating the spot where you inject it. Injecting insulin in the same spot repeatedly could cause the tissue to harden, making it harder to take shots in that area over time. Other spots you can inject insulin include your thigh, buttocks, or upper arm, but it may take longer for the insulin to work from those areas. Some people with diabetes who take insulin need 2 to 4 shots a day to reach their blood glucose targets. Others can take a single shot. Injection aids can help you give yourself the shots.

An insulin pen looks like a writing pen but has a needle for its point. Some insulin pens come filled with insulin and are disposable. Others have room for an insulin cartridge that you insert and replace after use. Many people find insulin pens easier to use, but they cost more than needles and syringes. You may want to consider using an insulin pen if you find it hard to fill the syringe while holding the vial or cannot read the markings on the syringe. Different pen types have features that can help with your injections. Some reusable pens have a memory function, which can recall dose amounts and timing. Other types of “connected” insulin pens can be programmed to calculate insulin doses and provide downloadable data reports, which can help you and your doctor adjust your insulin doses.

An insulin pump is a small machine that gives you steady doses of insulin throughout the day. You wear one type of pump outside your body on a belt or in a pocket or pouch. The insulin pump connects to a small plastic tube and a very small needle. You insert the plastic tube with a needle under your skin, then take out the needle. The plastic tube will stay inserted for several days while attached to the insulin pump. The machine pumps insulin through the tube into your body 24 hours a day and can be programmed to give you more or less insulin based on your needs. You can also give yourself doses of insulin through the pump at mealtimes.
Another type of pump has no tubes. This pump attaches directly to your skin with a self-adhesive pad and is controlled by a hand-held device. The plastic tube and pump device are changed every several days.

Another way to take insulin is by breathing powdered insulin into your mouth from an inhaler device. The insulin goes into your lungs and moves quickly into your blood. You may want to use an insulin inhaler to avoid using needles. Inhaled insulin is only for adults with type 1 or type 2 diabetes. Taking insulin with an inhaler is less common than using a needle and syringe.
Jet injector
A jet injector is a device that sends a fine spray of insulin into the skin at high pressure instead of using a needle to deliver the insulin. It is used less commonly than a needle and syringe or a pen.
Artificial pancreas
An artificial pancreas is a system of three devices that work together to mimic how a healthy pancreas controls blood glucose in the body. A continuous glucose monitor (CGM) tracks blood glucose levels every few minutes using a small sensor inserted under the skin that is held in place with an adhesive pad. The CGM wirelessly sends the information to a program on a smartphone or an insulin infusion pump. The program calculates how much insulin you need. The insulin infusion pump will adjust how much insulin is given from minute to minute to help keep your blood glucose level in your target range. An artificial pancreas is mainly used to help people with type 1 diabetes.
You may need to take medicines to manage your type 2 diabetes, in addition to consuming healthy foods and beverages and being physically active. You can take many diabetes medicines by mouth. These medicines are called oral medicines.
Most people with type 2 diabetes start with metformin pills. Metformin also comes as a liquid. Metformin helps your liver make less glucose and helps your body use insulin better. This drug may help you lose a small amount of weight.
Other oral medicines act in different ways to lower blood glucose levels. Combining two or three kinds of diabetes medicines can lower blood glucose levels better than taking just one medicine.
Read about different kinds of diabetes medicines (PDF, 2.8 MB) from the FDA.
If you have type 1 diabetes, your doctor may recommend you take other medicines, in addition to insulin, to help control your blood glucose. Some of these medicines work to slow how fast food and beverages move through your stomach . These medicines also slow down how quickly and how high your blood glucose levels rise after eating. Other medicines work to block certain hormones in your digestive system that raise blood glucose levels after meals or help the kidneys to remove more glucose from your blood.
Besides insulin, other types of injected medicines (PDF, 2.8 MB) are available that will keep your blood glucose level from rising too high after you eat or drink. These medicines, known as glucagon-like peptide-1 (GLP-1) receptor agonists, 3 may make you feel less hungry and help you lose some weight. GLP-1 medicines are not substitutes for insulin.
Side effects are problems that result from taking a medicine. Some diabetes medicines can cause hypoglycemia , also called low blood glucose, if you don’t balance your medicines with food and activity.
Ask your doctor whether your diabetes medicine can cause hypoglycemia or other side effects, such as upset stomach and weight gain. Aim to take your diabetes medicines as your doctor instructs you, to help prevent side effects and diabetes problems.
If medicines and lifestyle changes are not enough to manage your diabetes, there are other treatments that might help you. These treatments include weight-loss (bariatric) surgery for certain people with type 1 or type 2 diabetes, or pancreatic islet transplantation for some people with type 1 diabetes.
Weight-loss surgery
Weight-loss surgery are operations that help you lose weight by making changes to your digestive system. Weight-loss surgery is also called bariatric or metabolic surgery.
This type of surgery may help some people who have obesity and type 2 diabetes lose a large amount of weight and bring their blood glucose levels back to a healthy range. How long the improved response lasts can vary by patient, type of weight-loss surgery, and the amount of weight the person lost. Other factors include how long a person had diabetes and whether the person used insulin. Some people with type 2 diabetes may no longer need to use diabetes medicines after weight-loss surgery . 4
Researchers are studying whether weight-loss surgery can help control blood glucose levels in people with type 1 diabetes who have obesity. 5
Pancreatic islet transplantation
Pancreatic islet transplantation is an experimental treatment for people with type 1 diabetes who have trouble controlling their blood glucose levels. Pancreatic islets are clusters of cells in the pancreas that make the hormone insulin. In type 1 diabetes, the body’s immune system attacks these cells. A pancreatic islet transplantation replaces destroyed islets with new islets from organ donors. The new islets make and release insulin. Because researchers are still studying pancreatic islet transplantation , the procedure is only available to people enrolled in research studies.
The NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for insulin, medicines, and other diabetes treatments?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Find out if clinical trials are right for you .
Researchers are studying many aspects of diabetes medicines, including
- new types of insulin
- the most effective times to take diabetes medicines
- new types of monitoring devices and delivery systems
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for insulin, medicines, and other diabetes treatments are looking for participants?
You can view a filtered list of clinical studies on insulin, medicines, and other diabetes treatments covered in this health topic that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank Stuart A. Weinzimer, M.D., Yale University School of Medicine

Diabetes Case Studies : Real Problems, Practical Solutions
- Book Chapters
- Figures & tables
- Supplementary Data
- Peer Review
- Cite Icon Cite
- Get Permissions
Diabetes Case Studies : Real Problems, Practical Solutions Edited by: Boris Draznin, MD, PhD, Cecilia C. Low Wang, MD, FACP, Daniel J. Rubin, MD, MSc, FACE https://doi.org/10.2337/9781580405713 ISBN (print): 978-1-58040-571-3 Publisher: American Diabetes Association
Download citation file:
- Ris (Zotero)
- Reference Manager
Table of Contents
- Notes Open the PDF Link PDF for Notes in another window
- Preface Open the PDF Link PDF for Preface in another window
- Introduction Open the PDF Link PDF for Introduction in another window
- Case 1: Maturity-Onset Diabetes of the Young (MODY) as a Diagnostic Possibility By Suzi Kochar, MD ; Suzi Kochar, MD 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Janice L. Gilden, MS, MD, FCP, FACE Janice L. Gilden, MS, MD, FCP, FACE 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.01 Open the PDF Link PDF for Case 1: Maturity-Onset Diabetes of the Young (MODY) as a Diagnostic Possibility in another window
- Case 2: Diagnosis of Coexistent Maturity-Onset Diabetes of the Young in a Patient with Type 1 Diabetes By Shazli Azmi, MBChB ; Shazli Azmi, MBChB 1 Institute of Human Development, Center for Endocrinology and Diabetes, University of Manchester. 2 Department of Medicine and Manchester Diabetes Center, University of Manchester and Central Manchester NHS Foundation Trust. Search for other works by this author on: This Site PubMed Google Scholar Rayaz A. Malik, MBChB, PhD Rayaz A. Malik, MBChB, PhD 1 Institute of Human Development, Center for Endocrinology and Diabetes, University of Manchester. 2 Department of Medicine and Manchester Diabetes Center, University of Manchester and Central Manchester NHS Foundation Trust. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.02 Open the PDF Link PDF for Case 2: Diagnosis of Coexistent Maturity-Onset Diabetes of the Young in a Patient with Type 1 Diabetes in another window
- Case 3: An Unusual Clinical Presentation of Diabetes Eventually Diagnosed as a Monogenic Form By Vince N. Montes, MD ; Vince N. Montes, MD 1 University of Washington, Division of Metabolism, Endocrinology, and Nutrition, Seattle, WA. Search for other works by this author on: This Site PubMed Google Scholar Alan Chait, MD ; Alan Chait, MD 1 University of Washington, Division of Metabolism, Endocrinology, and Nutrition, Seattle, WA. Search for other works by this author on: This Site PubMed Google Scholar Craig E. Taplin, MD Craig E. Taplin, MD 2 Department of Pediatrics, University of Washington, Seattle Children’s Hospital, Division of Endocrinology and Diabetes, Seattle, WA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.03 Open the PDF Link PDF for Case 3: An Unusual Clinical Presentation of Diabetes Eventually Diagnosed as a Monogenic Form in another window
- Case 4: A Case of Monogenic Diabetes By Robert H. Slover, MD Robert H. Slover, MD 1 Professor of Pediatrics, University of Colorado School of Medicine, Denver, CO; Director of Pediatrics, Barbara Davis Center for Childhood Diabetes; Wagner Family Chair in Childhood Diabetes. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.04 Open the PDF Link PDF for Case 4: A Case of Monogenic Diabetes in another window
- Case 5: Recurrent Ketoacidosis: Lessons from Multiple Clinical Presentations By Eli Ipp, MD ; Eli Ipp, MD 1 Division of Endocrinology, Los Angeles Biomedical Research Institute at Harbor–UCLA Medical Center, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Kristina Djekic, MS Kristina Djekic, MS 1 Division of Endocrinology, Los Angeles Biomedical Research Institute at Harbor–UCLA Medical Center, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.05 Open the PDF Link PDF for Case 5: Recurrent Ketoacidosis: Lessons from Multiple Clinical Presentations in another window
- Case 6: Ketoacidosis in a Patient with Type 1 Diabetes on a Low-Calorie Meal Replacement Diet By Katy Brown, DO ; Katy Brown, DO 1 Fellow in Endocrinology, University of Colorado, School of Medicine, Denver, CO. Search for other works by this author on: This Site PubMed Google Scholar Daniel Bessesen, MD Daniel Bessesen, MD 2 University of Colorado, School of Medicine, Chief of Endocrinology, Denver Health Medical Center, Denver, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.06 Open the PDF Link PDF for Case 6: Ketoacidosis in a Patient with Type 1 Diabetes on a Low-Calorie Meal Replacement Diet in another window
- Case 7: Reevaluation after Ketoacidosis Presentation By Paulina Cruz-Bravo, MD ; Paulina Cruz-Bravo, MD 1 Fellowship in Endocrinology, Diabetes and Metabolism, Division of Endocrinology, Metabolism and Lipid Research, Washington University School of Medicine, St. Louis, MO. Search for other works by this author on: This Site PubMed Google Scholar Janet B. McGill, MD Janet B. McGill, MD 1 Fellowship in Endocrinology, Diabetes and Metabolism, Division of Endocrinology, Metabolism and Lipid Research, Washington University School of Medicine, St. Louis, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.07 Open the PDF Link PDF for Case 7: Reevaluation after Ketoacidosis Presentation in another window
- Case 8: Metabolic Syndrome-Related Comorbidities Typical of Older Adulthood Complicate Diabetic Ketoacidosis in a Youth with Type 2 Diabetes By Kristen Nadeau, MD, MS Kristen Nadeau, MD, MS 1 University of Colorado Denver/Children’s Hospital Colorado, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.08 Open the PDF Link PDF for Case 8: Metabolic Syndrome-Related Comorbidities Typical of Older Adulthood Complicate Diabetic Ketoacidosis in a Youth with Type 2 Diabetes in another window
- Case 9: Not Your Usual Diabetic Ketoacidosis By Ruchi Gaba, MD ; Ruchi Gaba, MD 1 Division of Endocrinology Diabetes and Metabolism, Baylor College of Medicine, Houston, TX. Search for other works by this author on: This Site PubMed Google Scholar Susan L. Samson, MD, PhD ; Susan L. Samson, MD, PhD 2 Department of Medicine, Baylor College of Medicine, Houston, TX. Search for other works by this author on: This Site PubMed Google Scholar Alan J. Garber, MD, PhD, FACE Alan J. Garber, MD, PhD, FACE 3 Departments of Medicine, Molecular and Cellular Biology, Biochemistry and Molecular Biology, Baylor College of Medicine, Houston, TX. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.09 Open the PDF Link PDF for Case 9: Not Your Usual Diabetic Ketoacidosis in another window
- Case 10: Ketosis-Prone Diabetes By David Saxon, MD ; David Saxon, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora CO. Search for other works by this author on: This Site PubMed Google Scholar Neda Rasouli, MD Neda Rasouli, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora CO. 2 Denver Veterans Affairs Medical Center, Denver CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.10 Open the PDF Link PDF for Case 10: Ketosis-Prone Diabetes in another window
- Case 11: From a Total Daily Dose of Insulin of 415 Units to No Insulin: A Case of Ketosis-Prone Diabetes By Caroline T. Nguyen, MD ; Caroline T. Nguyen, MD 1 Keck School of Medicine, Division of Endocrinology, Diabetes, and Metabolism, University of Southern California, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Jorge H. Mestman, MD Jorge H. Mestman, MD 1 Keck School of Medicine, Division of Endocrinology, Diabetes, and Metabolism, University of Southern California, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.11 Open the PDF Link PDF for Case 11: From a Total Daily Dose of Insulin of 415 Units to No Insulin: A Case of Ketosis-Prone Diabetes in another window
- Case 12: The Worst Case Scenario: Severe HHS in a Relatively Young Man By Elizabeth Herman, MD ; Elizabeth Herman, MD 1 Boston University School of Medicine, Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston MA. Search for other works by this author on: This Site PubMed Google Scholar Marie E. McDonnell, MD Marie E. McDonnell, MD 1 Boston University School of Medicine, Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston MA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.12 Open the PDF Link PDF for Case 12: The Worst Case Scenario: Severe HHS in a Relatively Young Man in another window
- Case 13: Unusual Cause of New-Onset Diabetes By Kelsey M. Shikuma, MD ; Kelsey M. Shikuma, MD 1 Keck School of Medicine, Division of Endocrinology, Diabetes and Metabolism, University of Southern California, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Jorge H. Mestman, MD Jorge H. Mestman, MD 1 Keck School of Medicine, Division of Endocrinology, Diabetes and Metabolism, University of Southern California, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.13 Open the PDF Link PDF for Case 13: Unusual Cause of New-Onset Diabetes in another window
- Case 14: What Type of Diabetes? By Anthony L. McCall, PhD, FACP Anthony L. McCall, PhD, FACP 1 University of Virginia School of Medicine and Health System, Charlottesville, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.14 Open the PDF Link PDF for Case 14: What Type of Diabetes? in another window
- Case 15: Type 1 Diabetes versus LADA in a Patient Misdiagnosed with Type 2 Diabetes By Cecilia C. Low Wang, MD Cecilia C. Low Wang, MD 1 Department of Medicine Division of Endocrinology, Metabolism and Diabetes; University of Colorado Anschutz Medical Campus School of Medicine, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.15 Open the PDF Link PDF for Case 15: Type 1 Diabetes versus LADA in a Patient Misdiagnosed with Type 2 Diabetes in another window
- Case 16: Type 1 Diabetes Can Present at Any Age By David S.H. Bell, MB David S.H. Bell, MB 1 Clinical Professor, University of Alabama. Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.16 Open the PDF Link PDF for Case 16: Type 1 Diabetes Can Present at Any Age in another window
- Case 17: Is This Type 2 Diabetes, Type 1 Diabetes, or Late Autoimmune Diabetes in Adults? By Devjit Tripathy, MD, PhD ; Devjit Tripathy, MD, PhD 1 Audie L. Murphy VA Hospital, South Texas Veterans Health Care System, San Antonio, TX. Search for other works by this author on: This Site PubMed Google Scholar Sheila Pinkson, MPAS, PA-C ; Sheila Pinkson, MPAS, PA-C 1 Audie L. Murphy VA Hospital, South Texas Veterans Health Care System, San Antonio, TX. Search for other works by this author on: This Site PubMed Google Scholar Maureen Koops, MD ; Maureen Koops, MD 1 Audie L. Murphy VA Hospital, South Texas Veterans Health Care System, San Antonio, TX. Search for other works by this author on: This Site PubMed Google Scholar Ralph A. DeFronzo, MD Ralph A. DeFronzo, MD 1 Audie L. Murphy VA Hospital, South Texas Veterans Health Care System, San Antonio, TX. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.17 Open the PDF Link PDF for Case 17: Is This Type 2 Diabetes, Type 1 Diabetes, or Late Autoimmune Diabetes in Adults? in another window
- Case 18: A Common Misdiagnosis By Irene E. Schauer, MD, PhD Irene E. Schauer, MD, PhD 1 Department of Medicine, University of Colorado Anschutz Medical Campus School of Medicine, Aurora, CO. 2 Research/Endocrine Sections, Denver Veterans Affairs Medical Center, Denver, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.18 Open the PDF Link PDF for Case 18: A Common Misdiagnosis in another window
- Case 19: Almost All Nonobese Young People with an Acute Onset of Diabetes Have Type 1 Diabetes By David S.H. Bell, MB David S.H. Bell, MB 1 Clinical Professor, University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.19 Open the PDF Link PDF for Case 19: Almost All Nonobese Young People with an Acute Onset of Diabetes Have Type 1 Diabetes in another window
- Case 20: Symptomatic Postprandial Hyperglycemia By Amita Maturu, MD ; Amita Maturu, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Michael McDermott, MD Michael McDermott, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.20 Open the PDF Link PDF for Case 20: Symptomatic Postprandial Hyperglycemia in another window
- Case 21: A Patient with Newly Diagnosed, Asymptomatic Hyperglycemia By Aidan McElduff, MD Aidan McElduff, MD 1 Discipline of Medicine, Sydney University, Sydney, NSW, Australia. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.21 Open the PDF Link PDF for Case 21: A Patient with Newly Diagnosed, Asymptomatic Hyperglycemia in another window
- Case 22: Glucokinase Maturity-Onset Diabetes of the Young and Pregnancy By Jill Apel, MD ; Jill Apel, MD 1 Division of Endocrinology, Rush University Medical Center, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Chung-Kay Koh, MD Chung-Kay Koh, MD 1 Division of Endocrinology, Rush University Medical Center, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.22 Open the PDF Link PDF for Case 22: Glucokinase Maturity-Onset Diabetes of the Young and Pregnancy in another window
- Case 23: Latent Autoimmune Diabetes of the Adult (LADA) in an Elderly Patient By Monica Shah, MD ; Monica Shah, MD 1 Division of Endocrinology, Rush University, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Mahtab Sohrevardi, MD ; Mahtab Sohrevardi, MD 1 Division of Endocrinology, Rush University, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar David Baldwin, MD David Baldwin, MD 1 Division of Endocrinology, Rush University, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.23 Open the PDF Link PDF for Case 23: Latent Autoimmune Diabetes of the Adult (LADA) in an Elderly Patient in another window
- Case 24: A Diagnostic Dilemma in a Patient with Elevated Glycosylated Hemoglobin By Shalini Paturi, MD ; Shalini Paturi, MD 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Janice L. Gilden, MS, MD, FCP, FACE Janice L. Gilden, MS, MD, FCP, FACE 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.24 Open the PDF Link PDF for Case 24: A Diagnostic Dilemma in a Patient with Elevated Glycosylated Hemoglobin in another window
- Case 25: An Unexplained Decline in HbA1c in Spite of Persistent Hyperglycemia By David S.H. Bell, MB David S.H. Bell, MB 1 Clinical Professor, University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.25 Open the PDF Link PDF for Case 25: An Unexplained Decline in HbA1c in Spite of Persistent Hyperglycemia in another window
- Case 26: What to Do with Discrepant HbA1c and SMBG Results? The Utility of Fructosamine and Glycated Albumin By Tatiana Gandrabura, MD ; Tatiana Gandrabura, MD 1 Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Daniel J. Rubin, MD, MSc Daniel J. Rubin, MD, MSc 1 Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.26 Open the PDF Link PDF for Case 26: What to Do with Discrepant HbA1c and SMBG Results? The Utility of Fructosamine and Glycated Albumin in another window
- Case 27: A “Tricky” Low HbA 1c By Chiara Mazzucchelli, MD ; Chiara Mazzucchelli, MD 1 Department of Internal Medicine, University of Genova, Genova, Italy. Search for other works by this author on: This Site PubMed Google Scholar Caterina Bordone, MD ; Caterina Bordone, MD 1 Department of Internal Medicine, University of Genova, Genova, Italy. Search for other works by this author on: This Site PubMed Google Scholar Davide Maggi, MD, PhD ; Davide Maggi, MD, PhD 1 Department of Internal Medicine, University of Genova, Genova, Italy. Search for other works by this author on: This Site PubMed Google Scholar Renzo Cordera, MD Renzo Cordera, MD 1 Department of Internal Medicine, University of Genova, Genova, Italy. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.27 Open the PDF Link PDF for Case 27: A “Tricky” Low HbA<sub>1c</sub> in another window
- Case 28: Use of Insulin U-500 in a Patient with Severe Insulin Resistance By Hussain Mahmud, MBBS ; Hussain Mahmud, MBBS 1 Clinical Assistant Professor of Medicine, Division of Endocrinology, University of Pittsburgh Medical Center, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Mary T. Korytkowski, MD Mary T. Korytkowski, MD 2 Professor of Medicine, Division of Endocrinology, University of Pittsburgh Medical Center, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.28 Open the PDF Link PDF for Case 28: Use of Insulin U-500 in a Patient with Severe Insulin Resistance in another window
- Case 29: Effective Use of U-500 Insulin via Insulin Pump in a Type 2 Diabetes Patient with Severe Insulin Resistance By Vijay babu Balakrishnan, MD ; Vijay babu Balakrishnan, MD 1 Section of Endocrinology, Diabetes and Metabolism, Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Elias S. Siraj, MD Elias S. Siraj, MD 1 Section of Endocrinology, Diabetes and Metabolism, Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.29 Open the PDF Link PDF for Case 29: Effective Use of U-500 Insulin via Insulin Pump in a Type 2 Diabetes Patient with Severe Insulin Resistance in another window
- Case 30: U-500 Insulin Pump Case By Anthony L. McCall, MD, PhD, FACP Anthony L. McCall, MD, PhD, FACP 1 James M. Moss Professor of Medicine, University of Virginia, School of Medicine and Health System, Charlottesville, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.30 Open the PDF Link PDF for Case 30: U-500 Insulin Pump Case in another window
- Case 31: Difficulties in Managing Patients with Insulin Resistance: Alternatives to U-500 Insulin By Narmada Movva, MD ; Narmada Movva, MD 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Boby G. Theckedath, MD, FACE ; Boby G. Theckedath, MD, FACE 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Janice L. Gilden, MS, MD, FCP, FACE Janice L. Gilden, MS, MD, FCP, FACE 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.31 Open the PDF Link PDF for Case 31: Difficulties in Managing Patients with Insulin Resistance: Alternatives to U-500 Insulin in another window
- Case 32: Management Issues in the Syndrome of Autoantibodies to the Insulin Receptor (Type B Insulin Resistance) By Elaine Cochran, MSN, CRNP ; Elaine Cochran, MSN, CRNP 1 National Institutes of Health, National Institute of Diabetes, Digestive, and Kidney Diseases, Diabetes, Endocrine, and Obesity Branch, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Rebecca Brown, MD, MhSc ; Rebecca Brown, MD, MhSc 1 National Institutes of Health, National Institute of Diabetes, Digestive, and Kidney Diseases, Diabetes, Endocrine, and Obesity Branch, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Phillip Gorden, MD Phillip Gorden, MD 1 National Institutes of Health, National Institute of Diabetes, Digestive, and Kidney Diseases, Diabetes, Endocrine, and Obesity Branch, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.32 Open the PDF Link PDF for Case 32: Management Issues in the Syndrome of Autoantibodies to the Insulin Receptor (Type B Insulin Resistance) in another window
- Case 33: Type B Insulin Resistance By Nisha Bincent Jacob, APN, FNP-C, CDE, MBA ; Nisha Bincent Jacob, APN, FNP-C, CDE, MBA 1 University of Texas Southwestern Medical Center, Department of Internal Medicine, Division of Endocrinology and Metabolism, Dallas, TX. Search for other works by this author on: This Site PubMed Google Scholar Hilary Trevino, APN, FNP-C ; Hilary Trevino, APN, FNP-C 1 University of Texas Southwestern Medical Center, Department of Internal Medicine, Division of Endocrinology and Metabolism, Dallas, TX. Search for other works by this author on: This Site PubMed Google Scholar Chanhaeng Rhee, MD, MBA Chanhaeng Rhee, MD, MBA 1 University of Texas Southwestern Medical Center, Department of Internal Medicine, Division of Endocrinology and Metabolism, Dallas, TX. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.33 Open the PDF Link PDF for Case 33: Type B Insulin Resistance in another window
- Case 34: Adhering or Not? That Is the Question: A Case of Glucolipotoxicity and Concentrated Insulin By Sanaa Deshmukh, MD ; Sanaa Deshmukh, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Rino Buzzola, MD ; Rino Buzzola, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Mariana Touza, MD ; Mariana Touza, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Michael Gardner, MD ; Michael Gardner, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar James R. Sowers, MD James R. Sowers, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.34 Open the PDF Link PDF for Case 34: Adhering or Not? That Is the Question: A Case of Glucolipotoxicity and Concentrated Insulin in another window
- Case 35: Cosecreting Adrenal Tumor Causing Severe Insulin Resistance By Kathya Rivera, MD ; Kathya Rivera, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Florida, Gainesville, FL. Search for other works by this author on: This Site PubMed Google Scholar Kenneth Cusi, MD ; Kenneth Cusi, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Florida, Gainesville, FL. 2 Division of Endocrinology, Diabetes and Metabolism, Malcom Randall VAMC, Gainesville, FL. Search for other works by this author on: This Site PubMed Google Scholar Catherine Edwards, MD Catherine Edwards, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Florida, Gainesville, FL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.35 Open the PDF Link PDF for Case 35: Cosecreting Adrenal Tumor Causing Severe Insulin Resistance in another window
- Case 36: Management of Severe Insulin Resistance in a Pregnant Patient with Type 2 Diabetes: The Use of U-500 Regular Insulin via Continuous Subcutaneous Infusion By Tiffany Hor, MD ; Tiffany Hor, MD 1 Division of Endocrinology, Rush University, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar David Baldwin, MD David Baldwin, MD 1 Division of Endocrinology, Rush University, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.36 Open the PDF Link PDF for Case 36: Management of Severe Insulin Resistance in a Pregnant Patient with Type 2 Diabetes: The Use of U-500 Regular Insulin via Continuous Subcutaneous Infusion in another window
- Case 37: Diabetes in Hereditary Hemochromatosis By Donald A. McClain, MD, PhD Donald A. McClain, MD, PhD 1 Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, UT. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.37 Open the PDF Link PDF for Case 37: Diabetes in Hereditary Hemochromatosis in another window
- Case 38: Challenging Insights from Albuminuria Early in the Course of Disease By Cem Demirci, MD ; Cem Demirci, MD 1 Department of Endocrinology, Connecticut Children’s Medical Center, Hartford, CT. Search for other works by this author on: This Site PubMed Google Scholar Vered Lewy-Weiss, MD ; Vered Lewy-Weiss, MD 2 Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Mark A. Sperling, MBBS, FRACP Mark A. Sperling, MBBS, FRACP 2 Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.38 Open the PDF Link PDF for Case 38: Challenging Insights from Albuminuria Early in the Course of Disease in another window
- Case 39: Copresentation of Addison’s Disease and Type 1 Diabetes in a 9-Year-Old Boy By Shideh Majidi, MD ; Shideh Majidi, MD 1 Pediatric Endocrinology Fellow, University of Colorado Denver, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Jennifer Raymond, MD, MCR Jennifer Raymond, MD, MCR 2 Assistant Professor, Pediatric Endocrinology, Barbara Davis Center for Diabetes, University of Colorado Denver, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.39 Open the PDF Link PDF for Case 39: Copresentation of Addison’s Disease and Type 1 Diabetes in a 9-Year-Old Boy in another window
- Case 40: Diagnosis of Addison’s Disease and Type 1 Diabetes in Twin Boys By Andrea Dann Urban, MSN, PNP-BC, CDE ; Andrea Dann Urban, MSN, PNP-BC, CDE 1 Yale Children’s Diabetes Program, Associate Clinical Faculty, Yale University School of Nursing, New Haven, CT. Search for other works by this author on: This Site PubMed Google Scholar William V. Tamborlane, MD William V. Tamborlane, MD 2 Professor of Pediatrics, Department of Pediatrics, Chief, Pediatric Endocrinology, Deputy Director, Yale Center for Clinical Investigation, Director, Children’s Diabetes Program, Yale School of Medicine, New Haven, CT. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.40 Open the PDF Link PDF for Case 40: Diagnosis of Addison’s Disease and Type 1 Diabetes in Twin Boys in another window
- Case 41: New-Onset Type 1 Diabetes, Addison’s Disease, and Hypothyroidism: A Case of Autoimmune Polyendocrine Syndrome Type 2 By Lauren Golden, MD ; Lauren Golden, MD 1 Assistant Professor Clinical Medicine, Naomi Berrie Diabetes Center, Columbia University Medical Center, New York, NY. Search for other works by this author on: This Site PubMed Google Scholar Robin Goland, MD Robin Goland, MD 2 J. Merrill Eastman Professor of Clinical Diabetes, Columbia University Medical Center, New York, NY. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.41 Open the PDF Link PDF for Case 41: New-Onset Type 1 Diabetes, Addison’s Disease, and Hypothyroidism: A Case of Autoimmune Polyendocrine Syndrome Type 2 in another window
- Case 42: The Slow Progression of Type 1 Diabetes as Part of Autoimmune Polyendocrine Syndrome Type 2 By Natalia Pertzeva, MD ; Natalia Pertzeva, MD 1 Dnepropetrovsk Medical Academy, Dnepropetrovsk, Ukraine. Search for other works by this author on: This Site PubMed Google Scholar Boris Mankovsky, MD, PhD Boris Mankovsky, MD, PhD 2 National Medical Academy for Postgraduate Education, Kiev, Ukraine. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.42 Open the PDF Link PDF for Case 42: The Slow Progression of Type 1 Diabetes as Part of Autoimmune Polyendocrine Syndrome Type 2 in another window
- Case 43: Atypical Type 2 Diabetes with Profound Dyslipidemia By Jeremy H. Pettus, MD ; Jeremy H. Pettus, MD 1 Endocrinology Fellow, Division of Endocrinology and Metabolism, University of California, San Diego, CA. Search for other works by this author on: This Site PubMed Google Scholar Robert R. Henry, MD Robert R. Henry, MD 2 Professor of Medicine, Division of Endocrinology and Metabolism, University of California, San Diego, CA; Chief, Section of Diabetes, Endocrinology and Metabolism; Director, Center for Metabolic Research, VA San Diego Healthcare System, San Diego, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.43 Open the PDF Link PDF for Case 43: Atypical Type 2 Diabetes with Profound Dyslipidemia in another window
- Case 44: Patient with Diabetes Who Has Hemiballismus By Miriam Padilla, MD, CDE ; Miriam Padilla, MD, CDE 1 Fellow, Department of Endocrinology and Diabetes at University of Southern California. Search for other works by this author on: This Site PubMed Google Scholar Jorge Mestman, MD Jorge Mestman, MD 2 Professor of Clinical Medicine in the Department of Endocrinology and Diabetes at University of Southern California, Professor of Clinical Medicine in the Department of Obstetrics and Gynecology at University of Southern California. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.44 Open the PDF Link PDF for Case 44: Patient with Diabetes Who Has Hemiballismus in another window
- Case 45: A Case of Diabetic Myonecrosis By Umal Azmat, MD ; Umal Azmat, MD 1 Division of Endocrinology, Diabetes and Metabolism, Ohio State University Wexner Medical Center, Columbus, OH. Search for other works by this author on: This Site PubMed Google Scholar Jason E. Payne, MD ; Jason E. Payne, MD 2 Division of Radiology, Ohio State University Wexner Medical Center, Columbus, OH. Search for other works by this author on: This Site PubMed Google Scholar Kathleen Dungan, MD ; Kathleen Dungan, MD 1 Division of Endocrinology, Diabetes and Metabolism, Ohio State University Wexner Medical Center, Columbus, OH. Search for other works by this author on: This Site PubMed Google Scholar Steven W. Ing, MD Steven W. Ing, MD 1 Division of Endocrinology, Diabetes and Metabolism, Ohio State University Wexner Medical Center, Columbus, OH. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.45 Open the PDF Link PDF for Case 45: A Case of Diabetic Myonecrosis in another window
- Case 46: A Case of Stiff Person Syndrome in a Patient with Type 1 Diabetes By Matthew P. Gilbert, DO, MPH ; Matthew P. Gilbert, DO, MPH 1 Department of Medicine, Division of Endocrinology and Diabetes, University of Vermont College of Medicine, Burlington, VT. Search for other works by this author on: This Site PubMed Google Scholar Muriel H. Nathan, MD, PhD Muriel H. Nathan, MD, PhD 1 Department of Medicine, Division of Endocrinology and Diabetes, University of Vermont College of Medicine, Burlington, VT. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.46 Open the PDF Link PDF for Case 46: A Case of Stiff Person Syndrome in a Patient with Type 1 Diabetes in another window
- Case 47: Stiff Person Syndrome in a Patient with Multiple Autoimmune Diseases By Jing Hughes, MD, PhD ; Jing Hughes, MD, PhD 1 Professor of Medicine, Director, Fellowship in Endocrinology, Diabetes and Metabolism, Division of Endocrinology, Metabolism and Lipid Research, Washington University School of Medicine, St. Louis, MO. Search for other works by this author on: This Site PubMed Google Scholar Janet B. McGill, MD Janet B. McGill, MD 1 Professor of Medicine, Director, Fellowship in Endocrinology, Diabetes and Metabolism, Division of Endocrinology, Metabolism and Lipid Research, Washington University School of Medicine, St. Louis, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.47 Open the PDF Link PDF for Case 47: Stiff Person Syndrome in a Patient with Multiple Autoimmune Diseases in another window
- Case 48: Glycogenic Hepatopathy in an Adolescent with Type 1 Diabetes By Nehama Zuckerman-Levin, MD ; Nehama Zuckerman-Levin, MD 1 Department of Pediatrics, Pediatric Diabetes and Obesity Clinic, Rambam Health Care Campus, Bruce Rappaport Faculty of Medicine, Technion, Haifa, Israel. Search for other works by this author on: This Site PubMed Google Scholar Oz Mordechai, MD ; Oz Mordechai, MD 1 Department of Pediatrics, Pediatric Diabetes and Obesity Clinic, Rambam Health Care Campus, Bruce Rappaport Faculty of Medicine, Technion, Haifa, Israel. Search for other works by this author on: This Site PubMed Google Scholar Naim Shehadeh, MD Naim Shehadeh, MD 1 Department of Pediatrics, Pediatric Diabetes and Obesity Clinic, Rambam Health Care Campus, Bruce Rappaport Faculty of Medicine, Technion, Haifa, Israel. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.48 Open the PDF Link PDF for Case 48: Glycogenic Hepatopathy in an Adolescent with Type 1 Diabetes in another window
- Case 49: Glycemic Control in a Child with Type 1 Diabetes and Autoimmune Hepatitis By Sandro Muntoni, MD, PhD ; Sandro Muntoni, MD, PhD 1 Department of Biomedical Sciences, University School of Cagliari and Centre for Metabolic Diseases and Atherosclerosis, The ME.DI.CO Association, Cagliari, Italy. Search for other works by this author on: This Site PubMed Google Scholar Mauro Congia, MD Mauro Congia, MD 2 Pediatric Gastroenterologic Unity, Microcitemic Hospital, ASL 8, Cagliari, Italy. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.49 Open the PDF Link PDF for Case 49: Glycemic Control in a Child with Type 1 Diabetes and Autoimmune Hepatitis in another window
- Case 50: Dizziness, Lightheadedness, and Syncope in a Patient with Type 2 Diabetes By Shalini Paturi, MD ; Shalini Paturi, MD 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Janice L. Gilden, MS, MD, FCP, FACE Janice L. Gilden, MS, MD, FCP, FACE 1 Endocrinology Division, Department of Medicine, Rosalind Franklin University of Medicine and Science/Chicago Medical School, North Chicago, IL. 2 Endocrinology Section, Department of Medicine, Captain James A. Lovell Federal Health Care Center, North Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.50 Open the PDF Link PDF for Case 50: Dizziness, Lightheadedness, and Syncope in a Patient with Type 2 Diabetes in another window
- Case 51: Growth Hormone Excess-Induced Diabetic Ketoacidosis By Andrew P. Demidowich, MD ; Andrew P. Demidowich, MD 1 Section on Pediatric Diabetes and Metabolism, Diabetes, Endocrinology, and Obesity Branch, NIDDK, National Institutes of Health, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Maya Lodish, MD ; Maya Lodish, MD 2 Heritable Disorders Branch, NICHD, National Institutes of Health, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Kristina I. Rother, MD, MHSc Kristina I. Rother, MD, MHSc 1 Section on Pediatric Diabetes and Metabolism, Diabetes, Endocrinology, and Obesity Branch, NIDDK, National Institutes of Health, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.51 Open the PDF Link PDF for Case 51: Growth Hormone Excess-Induced Diabetic Ketoacidosis in another window
- Case 52: Refractory Angina in a Patient with Type 2 Diabetes By Mikhail Kosiborod, MD Mikhail Kosiborod, MD 1 Professor of Medicine, Saint Luke’s Mid America Heart Institute, University of Missouri-Kansas City, Kansas City, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.52 Open the PDF Link PDF for Case 52: Refractory Angina in a Patient with Type 2 Diabetes in another window
- Case 53: Glycemic Control in a Patient with Type 2 Diabetes Undergoing Cardiac Surgery By M. Kathleen Figaro, MD, MS M. Kathleen Figaro, MD, MS 1 Medical Director, Diabetes Care Center, Endocrinology, Genesis Health Care, Bettendorf, IA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.53 Open the PDF Link PDF for Case 53: Glycemic Control in a Patient with Type 2 Diabetes Undergoing Cardiac Surgery in another window
- Case 54: Inpatient Insulin Management for Complex Enteral Feedings By Anna Beth Barton, MD ; Anna Beth Barton, MD 1 Endocrinology Fellow, Department of Medicine Division of Endocrinology, Metabolism, and Nutrition, Duke University Medical Center, Durham, NC. Search for other works by this author on: This Site PubMed Google Scholar Kathryn J. Evans, DNP, FNP-BC ; Kathryn J. Evans, DNP, FNP-BC 2 Division of Endocrinology, Metabolism and Nutrition, Duke University Medical Center, Durham, NC. Search for other works by this author on: This Site PubMed Google Scholar Lillian F. Lien, MD Lillian F. Lien, MD 3 Medical Director, Duke Inpatient Diabetes Management Associate Professor, Department of Medicine Division of Endocrinology, Metabolism, and Nutrition, Duke University Medical Center, Durham, NC. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.54 Open the PDF Link PDF for Case 54: Inpatient Insulin Management for Complex Enteral Feedings in another window
- Case 55: Glycemic Control in a Patient with Type 1 Diabetes and Severe Burns By R. Matthew Hawkins, PA-C ; R. Matthew Hawkins, PA-C 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Colorado Anschutz Medical Center, Aurora CO. Search for other works by this author on: This Site PubMed Google Scholar Boris Draznin, MD, PhD Boris Draznin, MD, PhD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Colorado Anschutz Medical Center, Aurora CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.55 Open the PDF Link PDF for Case 55: Glycemic Control in a Patient with Type 1 Diabetes and Severe Burns in another window
- Case 56: Combined Effect of Intravenous Insulin Infusion and Subcutaneous Rapid-Acting Insulin for Glycemic Control in Severe Insulin Resistance By Magdalena Szkudlinska, MD ; Magdalena Szkudlinska, MD 1 University of Washington School of Medicine, Division of Metabolism, Endocrinology, & Nutrition, Seattle, WA. Search for other works by this author on: This Site PubMed Google Scholar Irl B. Hirsch, MD Irl B. Hirsch, MD 1 University of Washington School of Medicine, Division of Metabolism, Endocrinology, & Nutrition, Seattle, WA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.56 Open the PDF Link PDF for Case 56: Combined Effect of Intravenous Insulin Infusion and Subcutaneous Rapid-Acting Insulin for Glycemic Control in Severe Insulin Resistance in another window
- Case 57: Therapeutic Hypothermia and Severe Insulin Resistance in Patients with Diabetes and Cardiac Arrest By Stacey Seggelke, RD, MS, CDE ; Stacey Seggelke, RD, MS, CDE 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Boris Draznin, MD, PhD Boris Draznin, MD, PhD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.57 Open the PDF Link PDF for Case 57: Therapeutic Hypothermia and Severe Insulin Resistance in Patients with Diabetes and Cardiac Arrest in another window
- Case 58: Extreme Insulin Resistance Following Heart Transplant By Suruchi Gupta, MBBS, MPH ; Suruchi Gupta, MBBS, MPH 1 Division of Endocrinology, Metabolism and Molecular Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Diana Johnson Oakes, APRN-BC ; Diana Johnson Oakes, APRN-BC 1 Division of Endocrinology, Metabolism and Molecular Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Ashley Therasse, MD ; Ashley Therasse, MD 1 Division of Endocrinology, Metabolism and Molecular Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Amisha Wallia, MD, MS ; Amisha Wallia, MD, MS 1 Division of Endocrinology, Metabolism and Molecular Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Mark E. Molitch, MD Mark E. Molitch, MD 1 Division of Endocrinology, Metabolism and Molecular Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.58 Open the PDF Link PDF for Case 58: Extreme Insulin Resistance Following Heart Transplant in another window
- Case 59: Glycemic Control after Left Ventricular Assist Device Placement in a Patient with Type 2 Diabetes By Gitana Staskus, MD Gitana Staskus, MD 1 Assistant Professor of Medicine, Division of Endocrinology, Metabolism and Diabetes, University of Utah, School of Medicine. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.59 Open the PDF Link PDF for Case 59: Glycemic Control after Left Ventricular Assist Device Placement in a Patient with Type 2 Diabetes in another window
- Case 60: Management of Diabetic Ketoacidosis in a Patient on Hemodialysis By Roopashree Prabhushankar, MD ; Roopashree Prabhushankar, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Sofia Syed, MD ; Sofia Syed, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar James R. Sowers, MD, FACE, FACP, FAHA James R. Sowers, MD, FACE, FACP, FAHA 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. 2 Department of Medical Pharmacology and Physiology, University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. 3 Diabetes and Cardiovascular Center, University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.60 Open the PDF Link PDF for Case 60: Management of Diabetic Ketoacidosis in a Patient on Hemodialysis in another window
- Case 61: New Diabetes Emergency: Acute Rhabdomyolysis Complicating Hyperglycemic Hyperosmolar Coma By Cherie Vaz, MD ; Cherie Vaz, MD 1 Section of Endocrinology, Department of Medicine, Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Ajay Chaudhuri, MD, MRCP Ajay Chaudhuri, MD, MRCP 2 Department of Endocrinology, State University of New York, University at Buffalo and Kaleida Health, Buffalo, NY. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.61 Open the PDF Link PDF for Case 61: New Diabetes Emergency: Acute Rhabdomyolysis Complicating Hyperglycemic Hyperosmolar Coma in another window
- Case 62: Transitioning from Intravenous to Subcutaneous Insulin in a Complicated Patient By Kathryn J. Evans, DNP, FNP-BC ; Kathryn J. Evans, DNP, FNP-BC 1 Division of Endocrinology, Metabolism and Nutrition, Duke University Medical Center, Durham, NC. Search for other works by this author on: This Site PubMed Google Scholar Lillian F. Lien, MD Lillian F. Lien, MD 2 Duke Inpatient Diabetes Management, Department of Medicine, Division of Endocrinology, Metabolism, and Nutrition, Duke University Medical Center, Durham, NC. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.62 Open the PDF Link PDF for Case 62: Transitioning from Intravenous to Subcutaneous Insulin in a Complicated Patient in another window
- Case 63: Failure to Coordinate Diabetes Care between Hospital and Ambulatory Settings: A Threat to Safe and Quality Patient Care By Shawn Peavie, DO ; Shawn Peavie, DO 1 University of Cincinnati College of Medicine; Division of Endocrinology, Diabetes, and Metabolism, Cincinnati, OH. Search for other works by this author on: This Site PubMed Google Scholar Mercedes Falciglia, MD Mercedes Falciglia, MD 1 University of Cincinnati College of Medicine; Division of Endocrinology, Diabetes, and Metabolism, Cincinnati, OH. 2 Cincinnati Veterans Affairs Medical Center, Cincinnati, OH. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.63 Open the PDF Link PDF for Case 63: Failure to Coordinate Diabetes Care between Hospital and Ambulatory Settings: A Threat to Safe and Quality Patient Care in another window
- Case 64: Preventing Readmission: Translating the Hospital Diabetes Regimen into a Home Regimen that Is Safe, Effective, and Easy to Follow By Jane Jeffrie Seley, DNP, MPH, MSN, BC-ADM, CDE, CDTC Jane Jeffrie Seley, DNP, MPH, MSN, BC-ADM, CDE, CDTC 1 New York Presbyterian/Weill Cornell Medical Center, New York, NY. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.64 Open the PDF Link PDF for Case 64: Preventing Readmission: Translating the Hospital Diabetes Regimen into a Home Regimen that Is Safe, Effective, and Easy to Follow in another window
- Case 65: Novel Combination Therapy for Type 2 Diabetes By Donna White, RPh, CDE, BCACP ; Donna White, RPh, CDE, BCACP 1 University of Virginia Health System, Department of Pharmacy, Charlottesville, VA. Search for other works by this author on: This Site PubMed Google Scholar Svetlana Goldman, PharmD Svetlana Goldman, PharmD 1 University of Virginia Health System, Department of Pharmacy, Charlottesville, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.65 Open the PDF Link PDF for Case 65: Novel Combination Therapy for Type 2 Diabetes in another window
- Case 66: Do Many People with Type 2 Diabetes Really Need Insulin? By Stanley S. Schwartz, MD Stanley S. Schwartz, MD 1 Main Line Health System, Wynnewood, PA. 2 University of Pennsylvania, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.66 Open the PDF Link PDF for Case 66: Do Many People with Type 2 Diabetes <em>Really</em> Need Insulin? in another window
- Case 67: Glycemic Control in a Patient with Type 1 Diabetes and Peritoneal Dialysis By Nadir Khir, MD ; Nadir Khir, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Stephen Brietzke, MD ; Stephen Brietzke, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar James R. Sowers, MD James R. Sowers, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.67 Open the PDF Link PDF for Case 67: Glycemic Control in a Patient with Type 1 Diabetes and Peritoneal Dialysis in another window
- Case 68: Insulin Allergy in an Insulin-Requiring Patient By Nestoras Mathioudakis, MD Nestoras Mathioudakis, MD 1 Assistant Professor of Medicine, Division of Endocrinology, Diabetes, & Metabolism, Johns Hopkins University School of Medicine, Baltimore, MD. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.68 Open the PDF Link PDF for Case 68: Insulin Allergy in an Insulin-Requiring Patient in another window
- Case 69: Use of 3-Day Continuous Glucose Monitoring to Investigate Persistent Fasting Hyperglycemia in Type 2 Diabetes By Michelle Griffith, MD ; Michelle Griffith, MD 1 Division of Endocrinology and Metabolism, Department of Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Mary Korytkowski, MD Mary Korytkowski, MD 1 Division of Endocrinology and Metabolism, Department of Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.69 Open the PDF Link PDF for Case 69: Use of 3-Day Continuous Glucose Monitoring to Investigate Persistent Fasting Hyperglycemia in Type 2 Diabetes in another window
- Case 70: Insulin Injections: What You “See” May Not Be What You Get By Robert J. Rushakoff, MD ; Robert J. Rushakoff, MD 1 Division of Endocrinology and Metabolism, University of California, San Francisco, CA. Search for other works by this author on: This Site PubMed Google Scholar Mary M. Sullivan, DNP, RN, ANP-BC, CDE, FAAN ; Mary M. Sullivan, DNP, RN, ANP-BC, CDE, FAAN 2 Department of Nursing, University of California, San Francisco, CA. Search for other works by this author on: This Site PubMed Google Scholar Arti Shah, MD ; Arti Shah, MD 3 Division of Endocrinology and Metabolism, University of California, San Francisco, CA. Search for other works by this author on: This Site PubMed Google Scholar Heidemarie Windham MacMaster, PharmD, CDE Heidemarie Windham MacMaster, PharmD, CDE 4 Department of Pharmaceutical Services, University of California, San Francisco, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.70 Open the PDF Link PDF for Case 70: Insulin Injections: What You “See” May Not Be What You Get in another window
- Case 71: Prolonged Insulin-Free Management of Type 1 Diabetes By Danielle Castillo, MD ; Danielle Castillo, MD 1 Division of Endocrinology & Metabolism, Eastern Virginia Medical School, Norfolk, VA. Search for other works by this author on: This Site PubMed Google Scholar Joseph Aloi, MD, FACE Joseph Aloi, MD, FACE 1 Division of Endocrinology & Metabolism, Eastern Virginia Medical School, Norfolk, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.71 Open the PDF Link PDF for Case 71: Prolonged Insulin-Free Management of Type 1 Diabetes in another window
- Case 72: Delayed Response to NPH Insulin By Mayer B. Davidson, MD Mayer B. Davidson, MD 1 Department of Internal Medicine, Charles R. Drew University, Los Angeles, CA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.72 Open the PDF Link PDF for Case 72: Delayed Response to NPH Insulin in another window
- Case 73: Reversal of Type 2 Diabetes by Weight Loss Despite Presence of Macro- and Microvascular Complications By Carl Peters, MB, ChB ; Carl Peters, MB, ChB 1 Newcastle Magnetic Resonance Centre, Campus for Ageing and Vitality, Newcastle upon Tyne, England. Search for other works by this author on: This Site PubMed Google Scholar Sarah Steven, MB, ChB ; Sarah Steven, MB, ChB 1 Newcastle Magnetic Resonance Centre, Campus for Ageing and Vitality, Newcastle upon Tyne, England. Search for other works by this author on: This Site PubMed Google Scholar Roy Taylor, MD Roy Taylor, MD 1 Newcastle Magnetic Resonance Centre, Campus for Ageing and Vitality, Newcastle upon Tyne, England. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.73 Open the PDF Link PDF for Case 73: Reversal of Type 2 Diabetes by Weight Loss Despite Presence of Macro- and Microvascular Complications in another window
- Case 74: Glycemic Control in Older Adults with Diabetes and Use of New SGLT2 Inhibitors By Carolyn Horney, MD ; Carolyn Horney, MD 1 University of Colorado Health Sciences Center, Division of Geriatric Medicine, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Jeffrey Wallace, MD, MPH Jeffrey Wallace, MD, MPH 1 University of Colorado Health Sciences Center, Division of Geriatric Medicine, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.74 Open the PDF Link PDF for Case 74: Glycemic Control in Older Adults with Diabetes and Use of New SGLT2 Inhibitors in another window
- Case 75: Blood Glucose Control of Patients with Hypertriglyceridemia By Henning Beck-Nielsen, DMSc Henning Beck-Nielsen, DMSc 1 Department of Endocrinology, Odense University Hospital, Odense, Denmark. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.75 Open the PDF Link PDF for Case 75: Blood Glucose Control of Patients with Hypertriglyceridemia in another window
- Case 76: No Effect of Gluten-Free Diet in Prevention of Autoimmune Type 1 Diabetes and Other Autoimmune Disorders in a Child with Celiac Disease By Sandro Muntoni, MD, PhD ; Sandro Muntoni, MD, PhD 1 Department of Biomedical Sciences, University School of Cagliari and Centre for Metabolic Diseases and Atherosclerosis, The ME.DI.CO. Association, Cagliari, Italy. Search for other works by this author on: This Site PubMed Google Scholar Mauro Congia, MD Mauro Congia, MD 2 Pediatric Gastroenterologic Unity, Microcitemic Hospital, Cagliari, Italy. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.76 Open the PDF Link PDF for Case 76: No Effect of Gluten-Free Diet in Prevention of Autoimmune Type 1 Diabetes and Other Autoimmune Disorders in a Child with Celiac Disease in another window
- Case 77: What Does It Take to Keep Glucose Normal? By Lawrence S. Phillips, MD Lawrence S. Phillips, MD 1 Atlanta VA Medical Center, Decatur, GA. 2 Division of Endocrinology and Metabolism, Department of Medicine, Emory University, School of Medicine, Atlanta, GA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.77 Open the PDF Link PDF for Case 77: What Does It Take to Keep Glucose Normal? in another window
- Case 78: Psychosocial Stressors and Management in an Adolescent with Type 2 Diabetes By Radha Nandagopal, MD ; Radha Nandagopal, MD 1 Pediatric Endocrinology, Providence Medical Group, Spokane, WA. Search for other works by this author on: This Site PubMed Google Scholar Kristina I. Rother, MD, MHSc Kristina I. Rother, MD, MHSc 2 Section on Pediatric Diabetes and Metabolism, Diabetes, Endocrinology, and Obesity Branch, NIDDK, National Institutes of Health, Bethesda, MD. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.78 Open the PDF Link PDF for Case 78: Psychosocial Stressors and Management in an Adolescent with Type 2 Diabetes in another window
- Case 79: Suicide, Homicide, or Diabetes-Related Incident? By John N. Carter, BSc (Med), MBBS, FRACP, MD John N. Carter, BSc (Med), MBBS, FRACP, MD 1 Clinical Professor of Endocrinology, Sydney Medical School, University of Sydney, Australia. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.79 Open the PDF Link PDF for Case 79: Suicide, Homicide, or Diabetes-Related Incident? in another window
- Case 80: The Case of an Older Woman with Diabetes on Insulin Pump Therapy, Struggling with Cognitive Decline, Hypoglycemia, and Loss of Autonomy By Jennifer M. Hackel, DNP, GNP-BC, CDE ; Jennifer M. Hackel, DNP, GNP-BC, CDE 1 University of Massachusetts Boston, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Liselle Douyon, MD ; Liselle Douyon, MD 2 University of Michigan, Endocrinology and Metabolism, Ann Arbor, MI. Search for other works by this author on: This Site PubMed Google Scholar Jeffrey B. Halter, MD Jeffrey B. Halter, MD 3 University of Michigan Geriatrics Center, Ann Arbor, MI. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.80 Open the PDF Link PDF for Case 80: The Case of an Older Woman with Diabetes on Insulin Pump Therapy, Struggling with Cognitive Decline, Hypoglycemia, and Loss of Autonomy in another window
- Case 81: Somnambulism (Sleepwalking) Caused by Nocturnal Hypoglycemia By David S.H. Bell, MB David S.H. Bell, MB 1 Clinical Professor of Medicine, University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.81 Open the PDF Link PDF for Case 81: Somnambulism (Sleepwalking) Caused by Nocturnal Hypoglycemia in another window
- Case 82: Hypoglycemic Unawareness By Amita Maturu, MD ; Amita Maturu, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Neda Rasouli, MD Neda Rasouli, MD 1 Division of Endocrinology, Diabetes and Metabolism, University of Colorado, Aurora, CO. 2 Denver Veterans Affairs Medical Center, Denver, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.82 Open the PDF Link PDF for Case 82: Hypoglycemic Unawareness in another window
- Case 83: Successful Use of Plasmapheresis in the Treatment of Hypoglycemia Due to Insulin Antibody Syndrome By Pankaj Sharda, MD ; Pankaj Sharda, MD 1 Section of Endocrinology, Diabetes and Metabolism, Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Thottathil Gopan, MD ; Thottathil Gopan, MD 2 Department of Endocrinology, Diabetes and Metabolism, Cleveland Clinic, Cleveland, OH. Search for other works by this author on: This Site PubMed Google Scholar Robert Zimmerman, MD ; Robert Zimmerman, MD 2 Department of Endocrinology, Diabetes and Metabolism, Cleveland Clinic, Cleveland, OH. Search for other works by this author on: This Site PubMed Google Scholar Elias S. Siraj, MD Elias S. Siraj, MD 1 Section of Endocrinology, Diabetes and Metabolism, Temple University School of Medicine, Philadelphia, PA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.83 Open the PDF Link PDF for Case 83: Successful Use of Plasmapheresis in the Treatment of Hypoglycemia Due to Insulin Antibody Syndrome in another window
- Case 84: Postprandial Hypoglycemia, an Uncommon Presentation of Type 2 Diabetes By Muhammad W. Salam, MD ; Muhammad W. Salam, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar James R. Sowers, MD James R. Sowers, MD 1 Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Missouri, Columbia, MO. 2 Department of Medical Pharmacology and Physiology, University of Missouri, Columbia, MO. 3 Diabetes and Cardiovascular Center, University of Missouri, Columbia, MO. 4 University of Missouri, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.84 Open the PDF Link PDF for Case 84: Postprandial Hypoglycemia, an Uncommon Presentation of Type 2 Diabetes in another window
- Case 85: Factitious Hypoglycemia in a Type 2 Diabetic Patient By Stacey A. Seggelke, MS, RN, CNS, CDE, BC-ADM Stacey A. Seggelke, MS, RN, CNS, CDE, BC-ADM 1 Adult Diabetes Program, University of Colorado Denver, School of Medicine, Denver, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.85 Open the PDF Link PDF for Case 85: Factitious Hypoglycemia in a Type 2 Diabetic Patient in another window
- Case 86: Recurrent Hypoglycemia in a Patient with Type 2 Diabetes By Pavani Srimatkandada, MD ; Pavani Srimatkandada, MD 1 Boston University School of Medicine, Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Marie E. McDonnell, MD ; Marie E. McDonnell, MD 1 Boston University School of Medicine, Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Sonia Ananthakrishnan, MD Sonia Ananthakrishnan, MD 1 Boston University School of Medicine, Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.86 Open the PDF Link PDF for Case 86: Recurrent Hypoglycemia in a Patient with Type 2 Diabetes in another window
- Case 87: Munchausen Syndrome: Hypoglycemia in an Obese Woman with Type 2 Diabetes By R. Paul Robertson, MD R. Paul Robertson, MD 1 Professor of Medicine, University of Minnesota, Professor of Medicine and Pharmacology, University of Washington, President Emeritus and Principal Investigator, Pacific Northwest Diabetes Research Institute. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.87 Open the PDF Link PDF for Case 87: Munchausen Syndrome: Hypoglycemia in an Obese Woman with Type 2 Diabetes in another window
- Case 88: The Use of Medical Technologies for the Reduction of Hypoglycemia in Type 1 Diabetes: Technology for Hypoglycemia Reduction By Viral N. Shah, MD ; Viral N. Shah, MD 1 Barbara Davis Center for Diabetes, University of Colorado Denver, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Aaron W. Michels, MD ; Aaron W. Michels, MD 1 Barbara Davis Center for Diabetes, University of Colorado Denver, Aurora, CO. 2 Departments of Internal Medicine and Pediatrics, School of Medicine, University of Colorado, Denver, Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Satish K. Garg, MD Satish K. Garg, MD 1 Barbara Davis Center for Diabetes, University of Colorado Denver, Aurora, CO. 2 Departments of Internal Medicine and Pediatrics, School of Medicine, University of Colorado, Denver, Aurora, CO. 3 Editor-in-Chief, Diabetes Technology and Therapeutics , Aurora, CO. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.88 Open the PDF Link PDF for Case 88: The Use of Medical Technologies for the Reduction of Hypoglycemia in Type 1 Diabetes: Technology for Hypoglycemia Reduction in another window
- Case 89: Reversal of Insulin-Requiring Type 2 Diabetes and Development of Hypoglycemia in a Morbidly Obese Patient By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.89 Open the PDF Link PDF for Case 89: Reversal of Insulin-Requiring Type 2 Diabetes and Development of Hypoglycemia in a Morbidly Obese Patient in another window
- Case 90: Munchausen-by-Proxy: Hypoglycemia in an Islet Autotransplantation Recipient By R. Paul Robertson, MD R. Paul Robertson, MD 1 Professor of Medicine, University of Minnesota; Professor of Medicine and Pharmacology, University of Washington; President Emeritus and Principal Investigator, Pacific Northwest Diabetes Research Institute. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.90 Open the PDF Link PDF for Case 90: Munchausen-by-Proxy: Hypoglycemia in an Islet Autotransplantation Recipient in another window
- Case 91: Treatment of a Patient with Diabetes and Severe Hypoglycemia By Henning Beck-Nielsen, DMSc Henning Beck-Nielsen, DMSc 1 Department of Endocrinology, Department of Endocrinology, Odense University Hospital, Odense, Denmark. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.91 Open the PDF Link PDF for Case 91: Treatment of a Patient with Diabetes and Severe Hypoglycemia in another window
- Case 92: Hypoglycemia with Use of Glargine Insulin in the Management of Type 2 Diabetes, Occurring with Titration Aimed at Achieving Prebreakfast Glucose Levels <100 mg/dL (5.6 mmol/L) By Saira Adeel, MD ; Saira Adeel, MD 1 Atlanta VA Medical Center, Division of Endocrinology, Emory University School of Medicine, Atlanta, GA. Search for other works by this author on: This Site PubMed Google Scholar Lawrence S. Phillips, MD Lawrence S. Phillips, MD 2 Division of Endocrinology and Metabolism, Emory University, Atlanta, GA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.92 Open the PDF Link PDF for Case 92: Hypoglycemia with Use of Glargine Insulin in the Management of Type 2 Diabetes, Occurring with Titration Aimed at Achieving Prebreakfast Glucose Levels <100 mg/dL (5.6 mmol/L) in another window
- Case 93: Progressive Hypoglycemia Due to Insulinoma in a Patient with Type 2 Diabetes: Treatment with Image-Guided Minimally Invasive Pancreas-Sparing Surgery By Mary-Elizabeth Patti, MD ; Mary-Elizabeth Patti, MD 1 Joslin Diabetes Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Mark P. Callery, MD, FACS ; Mark P. Callery, MD, FACS 2 Institute for HepatoBiliary and Pancreatic Surgery, Beth Israel Deaconess Medical Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Robert M. Najarian, MD ; Robert M. Najarian, MD 3 Department of Pathology, Beth Israel Deaconess Medical Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Mandeep S. Sawhney, MD, MS ; Mandeep S. Sawhney, MD, MS 4 Department of Medicine, Beth Israel Deaconess Medical Center and Dana Farber Harvard Cancer Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Lyle Mitzner, MD ; Lyle Mitzner, MD 1 Joslin Diabetes Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Allison B. Goldfine, MD ; Allison B. Goldfine, MD 1 Joslin Diabetes Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar A. James Moser, MD, FACS A. James Moser, MD, FACS 2 Institute for HepatoBiliary and Pancreatic Surgery, Beth Israel Deaconess Medical Center, Boston, MA. 5 Harvard Medical School, Boston, MA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.93 Open the PDF Link PDF for Case 93: Progressive Hypoglycemia Due to Insulinoma in a Patient with Type 2 Diabetes: Treatment with Image-Guided Minimally Invasive Pancreas-Sparing Surgery in another window
- Case 94: Managing Pain and Paralysis in Chronic Inflammatory Demyelinating Polyneuropathy in Diabetes By Aaron I. Vinik, MD, PhD, FCP, MACP, FACE Aaron I. Vinik, MD, PhD, FCP, MACP, FACE 1 Eastern Virginia Medical School, Strelitz Diabetes Center, Norfolk, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.94 Open the PDF Link PDF for Case 94: Managing Pain and Paralysis in Chronic Inflammatory Demyelinating Polyneuropathy in Diabetes in another window
- Case 95: Neuropathy in Metformin-Treated Type 2 Diabetes By Aaron I. Vinik, MD, PhD, FCP, MACP, FACE Aaron I. Vinik, MD, PhD, FCP, MACP, FACE 1 Eastern Virginia Medical School, Strelitz Diabetes Center, Norfolk, VA. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.95 Open the PDF Link PDF for Case 95: Neuropathy in Metformin-Treated Type 2 Diabetes in another window
- Case 96: A Case of Acute Sensory Neuropathy in Type 1 Diabetes By Andrew J.M. Boulton, MD, DSc, FACP, FRCP Andrew J.M. Boulton, MD, DSc, FACP, FRCP 1 University of Manchester, UK; University of Miami, Miami, FL; Manchester Royal Infirmary, Manchester, UK; President, European Association for the Study of Diabetes, Dusseldorf, Germany. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.96 Open the PDF Link PDF for Case 96: A Case of Acute Sensory Neuropathy in Type 1 Diabetes in another window
- Case 97: Nondiabetic Neuropathy in a Patient with Type 2 Diabetes By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.97 Open the PDF Link PDF for Case 97: Nondiabetic Neuropathy in a Patient with Type 2 Diabetes in another window
- Case 98: Severe Distal Symmetrical and Autonomic Neuropathy in a Patient with a Short Duration of Type 1 Diabetes By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.98 Open the PDF Link PDF for Case 98: Severe Distal Symmetrical and Autonomic Neuropathy in a Patient with a Short Duration of Type 1 Diabetes in another window
- Case 99: Diabetic Amyotrophy and Neuropathic Cachexia By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.99 Open the PDF Link PDF for Case 99: Diabetic Amyotrophy and Neuropathic Cachexia in another window
- Case 100: High GAD Antibody Levels and Cerebellar Atrophy in a Patient with Type 1 Diabetes By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.100 Open the PDF Link PDF for Case 100: High GAD Antibody Levels and Cerebellar Atrophy in a Patient with Type 1 Diabetes in another window
- Case 101: Resolution of Infertility with Diabetes Therapy By David S.H. Bell, MB David S.H. Bell, MB 1 University of Alabama, Birmingham, AL. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.101 Open the PDF Link PDF for Case 101: Resolution of Infertility with Diabetes Therapy in another window
- Case 102: The Initial Pregnancy Visit of a Woman with Type 1 Diabetes and Diabetes Complications By Aidan McElduff, MD Aidan McElduff, MD 1 Discipline of Medicine, Sydney University, Sydney, NSW, Australia. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.102 Open the PDF Link PDF for Case 102: The Initial Pregnancy Visit of a Woman with Type 1 Diabetes and Diabetes Complications in another window
- Case 103: Gastroparesis and Pregnancy By Carl Peters, MB, ChB ; Carl Peters, MB, ChB 1 Newcastle Magnetic Resonance Centre, Campus for Ageing and Vitality, Newcastle upon Tyne, England. Search for other works by this author on: This Site PubMed Google Scholar Roy Taylor, MD Roy Taylor, MD 1 Newcastle Magnetic Resonance Centre, Campus for Ageing and Vitality, Newcastle upon Tyne, England. Search for other works by this author on: This Site PubMed Google Scholar Doi: https://doi.org/10.2337/9781580405713.103 Open the PDF Link PDF for Case 103: Gastroparesis and Pregnancy in another window
- Index Open the PDF Link PDF for Index in another window
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Fats and Cholesterol
When it comes to dietary fat, what matters most is the type of fat you eat. Contrary to past dietary advice promoting low-fat diets , newer research shows that healthy fats are necessary and beneficial for health.
- When food manufacturers reduce fat, they often replace it with carbohydrates from sugar, refined grains, or other starches. Our bodies digest these refined carbohydrates and starches very quickly, affecting blood sugar and insulin levels and possibly resulting in weight gain and disease. ( 1-3 )
- Findings from the Nurses’ Health Study ( 4 ) and the Health Professionals Follow-up Study ( 5 ) show that no link between the overall percentage of calories from fat and any important health outcome, including cancer, heart disease, and weight gain.
Rather than adopting a low-fat diet, it’s more important to focus on eating beneficial “good” fats and avoiding harmful “bad” fats. Fat is an important part of a healthy diet. Choose foods with “good” unsaturated fats, limit foods high in saturated fat, and avoid “bad” trans fat.
- “Good” unsaturated fats — Monounsaturated and polyunsaturated fats — lower disease risk. Foods high in good fats include vegetable oils (such as olive, canola, sunflower, soy, and corn), nuts, seeds, and fish.
- “Bad” fats — trans fats — increase disease risk, even when eaten in small quantities. Foods containing trans fats are primarily in processed foods made with trans fat from partially hydrogenated oil. Fortunately, trans fats have been eliminated from many of these foods.
- Saturated fats , while not as harmful as trans fats, by comparison with unsaturated fats negatively impact health and are best consumed in moderation. Foods containing large amounts of saturated fat include red meat, butter, cheese, and ice cream. Some plant-based fats like coconut oil and palm oil are also rich in saturated fat.
- When you cut back on foods like red meat and butter, replace them with fish, beans, nuts, and healthy oils instead of refined carbohydrates.
Read more about healthy fats in this “Ask the Expert” with HSPH’s Dr. Walter Willett and Amy Myrdal Miller, M.S., R.D., formerly of The Culinary Institute of America
1. Siri-Tarino, P.W., et al., Saturated fatty acids and risk of coronary heart disease: modulation by replacement nutrients. Curr Atheroscler Rep, 2010. 12(6): p. 384-90.
2. Hu, F.B., Are refined carbohydrates worse than saturated fat? Am J Clin Nutr, 2010. 91(6): p. 1541-2.
3. Jakobsen, M.U., et al., Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr, 2010. 91(6): p. 1764-8.
4. Hu, F.B., et al., Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med, 1997. 337(21): p. 1491-9.
5. Ascherio, A., et al., Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ, 1996. 313(7049): p. 84-90.
6. Hu, F.B., J.E. Manson, and W.C. Willett, Types of dietary fat and risk of coronary heart disease: a critical review. J Am Coll Nutr, 2001. 20(1): p. 5-19.
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.

IMAGES
VIDEO
COMMENTS
CHARACTERIZING HYPERGLYCEMIA. This patient's hyperglycemia reached a threshold that was diagnostic of diabetes 1 on two occasions: when she was 25 years of age, she had a randomly obtained blood glucose level of 217 mg per deciliter with polyuria (with diabetes defined as a level of ≥200 mg per deciliter [≥11.1 mmol per liter] with symptoms), and when she was 30 years of age, she had on ...
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes. Case Presentation A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes.
Nutrition Care Process: Case Study A ... Both of his parents have type 2 diabetes. JO's father was forced ... Case Study A: This table demonstrates how the weight loss program addresses JO's nutrition diagnosis, and how that nutrition diagnosis might change over time. Content is organized to present food and nutrition-related history first ...
Deborah Thomas-Dobersen; Case Study: A Woman With Type 2 Diabetes and Severe Hypertriglyceridemia Sensitive to Fat Restriction. Clin Diabetes 1 October 2002; 20 (4): 202-203. ... Kulkarni K: The evidence for the effectiveness of medical nutrition therapy in diabetes management.
Registered dietitians (RDs) who have earned the Board Certified-Advanced Diabetes Manager (BC-ADM) credential hold a master's or doctorate degree in a clinically relevant area and have at least 500 hours of recent experience helping with the clinical management of people with diabetes.1 They work in both inpatient and outpatient settings, including diabetes or endocrine-based specialty ...
Study population. This study utilized a case-control design and involved participants between the ages of 18 and 60 who had been diagnosed with type 2 diabetes within the previous six months based on specific glucose level criteria (FBS levels of ≥ 126 mg/dl and 2 h-PG levels of ≥ 200 mg/dl []).Healthy individuals within the same age range were also included, with specific glucose level ...
CASE. A 47-year-old woman was found to have hyperglycemia at a health fair when a random blood glucose level was 227 mg/dL (12.6 mmol/L). Several days later, a fasting blood glucose value was 147 mg/dL (8.2 mmol/L). She has no previous history of diabetes, is alarmed by the possibility of having this disorder, and seeks your advice.
Dietetic and Nutrition Case Studies. ... 24 Type 1 diabetes mellitus, 106 25 Type 2 diabetes mellitus - Kosher diet, 111 26 Type 2 diabetes mellitus - private patient, 114 27 Gestational diabetes mellitus, 117 28 Polycystic ovary syndrome, 121 29 Obesity - specialist management, 125
Brief Introduction to Diabetes and Gastroparesis: Diet plays an important role in the management of type 2 diabetes, and as such, the main goal of medical nutrition therapy is to promote healthy eating patterns to achieve glycemic goals. People with diabetes are also at increased risk of developing
This case study paints a vivid picture of the crucial role dietitians like Anna play in translating the science of nutrition into personalized care plans, helping patients with diabetes take control of their health one meal at a time. 12.3: Case Study- Tailoring Nutrition - Carbohydrates in Diabetes Care is shared under a not declared license ...
Dietetic and Nutrition Case Studies. Editor(s): Judy Lawrence, Pauline Douglas, Joan Gandy, ... Type 2 diabetes mellitus - private patient (Pages: 114-116) Barbara M. Arora, Juneeshree S. Sangani, ... Case studies' answers. no. Renal - black and ethnic minority (Pages: 221-223) Summary; PDF;
Nutrition Case Study #4: Diabetes. One of the most FAQ you will receive as a dietitian practicing in a hospital setting is whether it is safe to feed or not to feet an inpatient. Safely resuming a patient's diet is more than just looking if the digestive tract is working. GI tolerance and lab work are also important.
This chapter discusses the case of an 18‐year‐old male, Harry who was diagnosed with type 1 diabetes at 7 years of age. Harry has not attended specialist diabetes or dietetic services for several years, with his diabetes care being provided by his GP. Harry is fearful of developing diabetes complications later in life and realises this is a ...
[email protected] m. Abstract. Diabetes mellitus, is a grou p of metabolic disorders that leads to high blood glucose level, resul ting in excessive urination, increased thirst, blurred vi ...
One of the most FAQ you will receive as a dietitian practicing in a hospital setting is whether it is safe to feed or not to feet an inpatient. Safely resumi...
Objective: To investigate the impact of the Nutrition and Culinary in the Kitchen (NCK) Program on the cooking skills of Brazilian individuals with type 2 diabetes mellitus (T2DM). Methods: A randomized controlled intervention study was performed, with intervention and control groups. The intervention group participated in weekly sessions of the NCK Program for six weeks (including two in ...
In a study conducted by Heled et al.,1 three treatments were used to test the hypothesis that exercise training might prevent diabetes in Psammomys obesus (rodent animal models used to study diet-induced type 2 diabetes). The treatments included a high-energy diet, a high-energy diet plus exercise, and a low-energy diet, with protein kinase C ...
Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol. 2013;28:845-58. de Munter JS, Hu FB, Spiegelman D, Franz M, van Dam RM. Whole grain, bran, and germ intake and risk of type 2 diabetes: a prospective cohort study and systematic review.
The presence of metabolic syndrome is significantly more likely to be present in those with type 2 diabetes than in patients diagnosed with LADA or type 1 diabetes. 7 This patient in this case was ...
The prevalence of diabetes has reached alarming levels in India, making it essential to understand the concentration of nutritional-trace elements (Fe, Cu, Zn, Cr. and Se) in blood samples from diabetic adults. In this study, 208 whole blood samples from diabetic (n = 104) and non-diabetic (n = 104) adults across various age groups were analyzed using total reflection X-ray fluorescence (TXRF ...
The aim of the study was to evaluate the impact of a diabetes specific enteral nutrition (EN) formula on glycaemia, comorbidities and mortality in patients admitted with a first episode of stroke ...
In type 1 diabetes, the body's immune system attacks these cells. A pancreatic islet transplantation replaces destroyed islets with new islets from organ donors. The new islets make and release insulin. Because researchers are still studying pancreatic islet transplantation, the procedure is only available to people enrolled in research studies.
Study Identifies Biomarkers in the Breath for Eosinophilic Esophagitis. ... May 23, 2024 / Digestive / Research. Increased Risk of Gastroparesis Associated with GLP-1RA Use in Type 2 Diabetes Patients. Provider vigilance and patient education are key for management. May 22, ... 2024 / Digestive / Case Study.
Open the PDF Link PDF for Case 41: New-Onset Type 1 Diabetes, Addison's Disease, and Hypothyroidism: A Case of Autoimmune Polyendocrine Syndrome Type 2 in another window Case 42: The Slow Progression of Type 1 Diabetes as Part of Autoimmune Polyendocrine Syndrome Type 2
When it comes to dietary fat, what matters most is the type of fat you eat. Contrary to past dietary advice promoting low-fat diets, newer research shows that healthy fats are necessary and beneficial for health.. When food manufacturers reduce fat, they often replace it with carbohydrates from sugar, refined grains, or other starches. Our bodies digest these refined carbohydrates and starches ...