REVIEW article
The state of music therapy studies in the past 20 years: a bibliometric analysis.

- 1 School of Kinesiology, Shanghai University of Sport, Shanghai, China
- 2 Department of Sport Rehabilitation, Shanghai University of Sport, Shanghai, China
- 3 Department of Sport Rehabilitation Medicine, Shanghai Shangti Orthopedic Hospital, Shanghai, China
Purpose: Music therapy is increasingly being used to address physical, emotional, cognitive, and social needs of individuals. However, publications on the global trends of music therapy using bibliometric analysis are rare. The study aimed to use the CiteSpace software to provide global scientific research about music therapy from 2000 to 2019.
Methods: Publications between 2000 and 2019 related to music therapy were searched from the Web of Science (WoS) database. The CiteSpace V software was used to perform co-citation analysis about authors, and visualize the collaborations between countries or regions into a network map. Linear regression was applied to analyze the overall publication trend.
Results: In this study, a total of 1,004 studies met the inclusion criteria. These works were written by 2,531 authors from 1,219 institutions. The results revealed that music therapy publications had significant growth over time because the linear regression results revealed that the percentages had a notable increase from 2000 to 2019 ( t = 14.621, P < 0.001). The United States had the largest number of published studies (362 publications), along with the following outputs: citations on WoS (5,752), citations per study (15.89), and a high H-index value (37). The three keywords “efficacy,” “health,” and “older adults,” emphasized the research trends in terms of the strongest citation bursts.
Conclusions: The overall trend in music therapy is positive. The findings provide useful information for music therapy researchers to identify new directions related to collaborators, popular issues, and research frontiers. The development prospects of music therapy could be expected, and future scholars could pay attention to the clinical significance of music therapy to improve the quality of life of people.

Introduction
Music therapy is defined as the evidence-based use of music interventions to achieve the goals of clients with the help of music therapists who have completed a music therapy program ( Association, 2018 ). In the United States, music therapists must complete 1,200 h of clinical training and pass the certification exam by the Certification Board for Music Therapists ( Devlin et al., 2019 ). Music therapists use evidence-based music interventions to address the mental, physical, or emotional needs of an individual ( Gooding and Langston, 2019 ). Also, music therapy is used as a solo standard treatment, as well as co-treatment with other disciplines, to address the needs in cognition, language, social integration, and psychological health and family support of an individual ( Bronson et al., 2018 ). Additionally, music therapy has been used to improve various diseases in different research areas, such as rehabilitation, public health, clinical care, and psychology ( Devlin et al., 2019 ). With neurorehabilitation, music therapy has been applied to increase motor activities in people with Parkinson's disease and other movement disorders ( Bernatzky et al., 2004 ; Devlin et al., 2019 ). However, limited reviews about music therapy have utilized universal data and conducted massive retrospective studies using bibliometric techniques. Thus, this study demonstrates music therapy with a broad view and an in-depth analysis of the knowledge structure using bibliometric analysis of articles and publications.
Bibliometrics turns the major quantitative analytical tool that is used in conducting in-depth analyses of publications ( Durieux and Gevenois, 2010 ; Gonzalez-Serrano et al., 2020 ). There are three types of bibliometric indices: (a) the quantity index is used to determine the number of relevant publications, (b) the quality index is employed to explore the characteristics of a scientific topic in terms of citations, and (c) the structural index is used to show the relationships among publications ( Durieux and Gevenois, 2010 ; Gonzalez-Serrano et al., 2020 ). In this study, the three types of bibliometric indices will be applied to conduct an in-depth analysis of publications in this frontier.
While research about music therapy is extensively available worldwide, relatively limited studies use bibliometric methods to analyze the global research about this topic. The aim of this study is to use the CiteSpace software to perform a bibliometric analysis of music therapy research from 2000 to 2019. CiteSpace V is visual analytic software, which is often utilized to perform bibliometric analyses ( Falagas et al., 2008 ; Ellegaard and Wallin, 2015 ). It is also a tool applied to detect trends in global scientific research. In this study, the global music therapy research includes publication outputs, distribution and collaborations between authors/countries or regions/institutions, intense issues, hot articles, common keywords, productive authors, and connections among such authors in the field. This study also provides helpful information for researchers in their endeavor to identify gaps in the existing literature.
Materials and Methods
Search strategy.
The data used in this study were obtained from WoS, the most trusted international citation database in the world. This database, which is run by Thomson & Reuters Corporation ( Falagas et al., 2008 ; Durieux and Gevenois, 2010 ; Chen C. et al., 2012 ; Ellegaard and Wallin, 2015 ; Miao et al., 2017 ; Gonzalez-Serrano et al., 2020 ), provides high-quality journals and detailed information about publications worldwide. In this study, publications were searched from the WoS Core Collection database, which included eight indices ( Gonzalez-Serrano et al., 2020 ). This study searched the publications from two indices, namely, the Science Citation Index Expanded and the Social Sciences Citation Index. As the most updated publications about music therapy were published in the 21st century, publications from 2000 to 2019 were chosen for this study. We performed data acquisition on July 26, 2020 using the following search terms: title = (“music therapy”) and time span = 2000–2019.
Inclusion Criteria
Figure 1 presents the inclusion criteria. The title field was music therapy (TI = music therapy), and only reviews and articles were chosen as document types in the advanced search. Other document types, such as letters, editorial materials, and book reviews, were excluded. Furthermore, there were no species limitations set. This advanced search process returned 718 articles. In the end, a total of 1,004 publications were obtained and were analyzed to obtain comprehensive perspectives on the data.
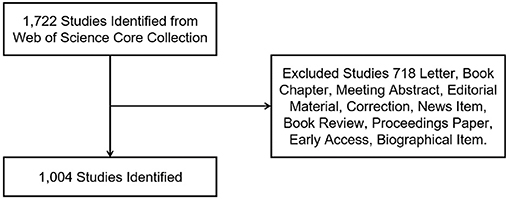
Figure 1 . Flow chart of music therapy articles and reviews inclusion.
Data Extraction
Author Lin-Man Weng extracted the publications and applied the EndNote software and Microsoft Excel 2016 to conduct analysis on the downloaded publications from the WoS database. Additionally, we extracted and recorded some information of the publications, such as citation frequency, institutions, authors' countries or regions, and journals as bibliometric indicators. The H-index is utilized as a measurement of the citation frequency of the studies for academic journals or researchers ( Wang et al., 2019 ).
Analysis Methods
The objective of bibliometrics can be described as the performance of studies that contributes to advancing the knowledge domain through inferences and explanations of relevant analyses ( Castanha and Grácio, 2014 ; Merigó et al., 2019 ; Mulet-Forteza et al., 2021 ). CiteSpace V is a bibliometric software that generates information for better visualization of data. In this study, the CiteSpace V software was used to visualize six science maps about music therapy research from 2000 to 2019: the network of author co-citation, collaboration network among countries and regions, relationship of institutions interested in the field, network map of co-citation journals, network map of co-cited references, and the map (timeline view) of references with co-citation on top music therapy research. As noted, a co-citation is produced when two publications receive a citation from the same third study ( Small, 1973 ; Merigó et al., 2019 ).
In addition, a science map typically features a set of points and lines to present collaborations among publications ( Chen, 2006 ). A point is used to represent a country or region, author, institution, journal, reference, or keyword, whereas a line represents connections among them ( Zheng and Wang, 2019 ), with stronger connections indicated by wider lines. Furthermore, the science map includes nodes, which represent the citation frequencies of certain themes. A burst node in the form of a red circle in the center indicates the number of co-occurrence or citation that increases over time. A purple node represents centrality, which indicates the significant knowledge presented by the data ( Chen, 2006 ; Chen H. et al., 2012 ; Zheng and Wang, 2019 ). The science map represents the keywords and references with citation bursts. Occurrence bursts represent the frequency of a theme ( Chen, 2006 ), whereas citation bursts represent the frequency of the reference. The citation bursts of keywords and references explore the trends and indicate whether the relevant authors have gained considerable attention in the field ( Chen, 2006 ). Through this kind of map, scholars can better understand emerging trends and grasp the hot topics by burst detection analysis ( Liang et al., 2017 ; Miao et al., 2017 ).
Publication Outputs and Time Trends
A total of 1,004 articles and reviews related to music therapy research met the criteria. The details of annual publications are presented in Figure 2 . As can be seen, there were <30 annual publications between 2000 and 2006. The number of publications increased steadily between 2007 and 2015. It was 2015, which marked the first time over 80 articles or reviews were published. The significant increase in publications between 2018 and 2019 indicated that a growing number of researchers became interested in this field. Linear regression can be used to analyze the trends in publication outputs. In this study, the linear regression results revealed that the percentages had a notable increase from 2000 to 2019 ( t = 14.621, P < 0.001). Moreover, the P < 0.05, indicating statistical significance. Overall, the publication outputs increased from 2000 to 2019.
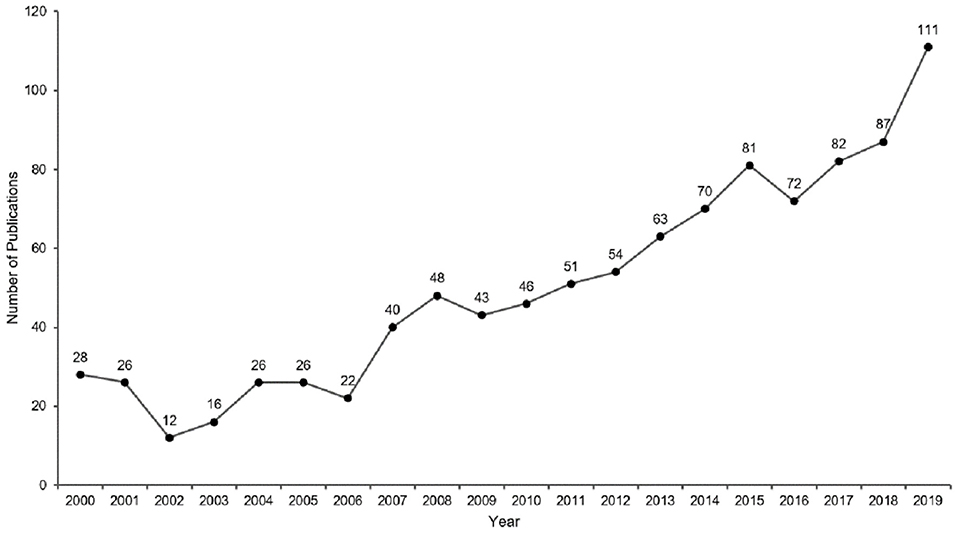
Figure 2 . Annual publication outputs of music therapy from 2000 to 2019.
Distribution by Country or Region and Institution
The 1,004 articles and reviews collected were published in 49 countries and regions. Table 1 presents the top 10 countries or regions. Figure 3 shows an intuitive comparison of the citations on WoS, citations per study, Hirsch index (H-index), and major essential science indicator (ESI) studies of the top five countries or regions. The H-index is a kind of index that is applied in measuring the wide impact of the scientific achievements of authors. The United States had the largest number of published studies (362 publications), along with the following outputs: citations on WoS (5,752), citations per study (15.89), and a high H-index value (37). Norway has the largest number of citations per study (27.18 citations). Figure 4 presents the collaboration networks among countries or regions. The collaboration network map contained 32 nodes and 38 links. The largest node can be found in the United States, which meant that the United States had the largest number of publications in the field. Meanwhile, the deepest purple circle was located in Austria, which meant that Austria is the country with the most number of collaborations with other countries or regions in this research field. A total of 1,219 institutions contributed various music therapy-related publications. Figure 5 presents the collaborations among institutions. As can be seen, the University of Melbourne is the most productive institution in terms of the number of publications (45), followed by the University of Minnesota (43), and the University of Bergen (39). The top 10 institutions featured in Table 2 contributed 28.884% of the total articles and reviews published. Among these, Aalborg University had the largest centrality (0.13). The top 10 productive institutions with details are shown in Table 2 .
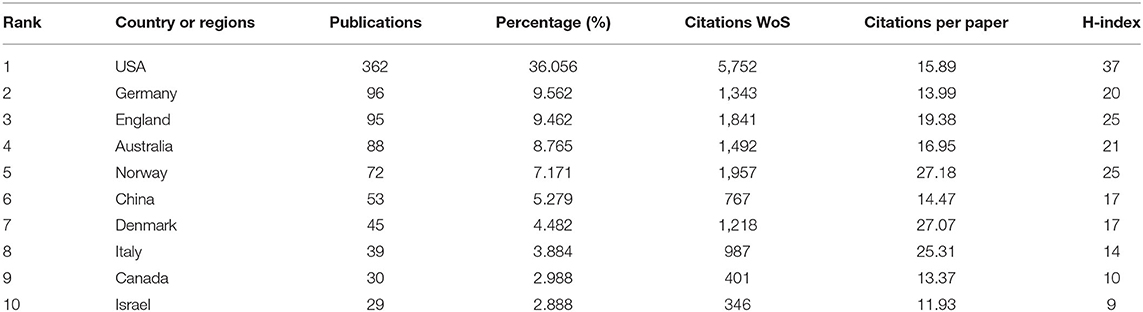
Table 1 . Top 10 countries or regions of origin of study in the music therapy research field.
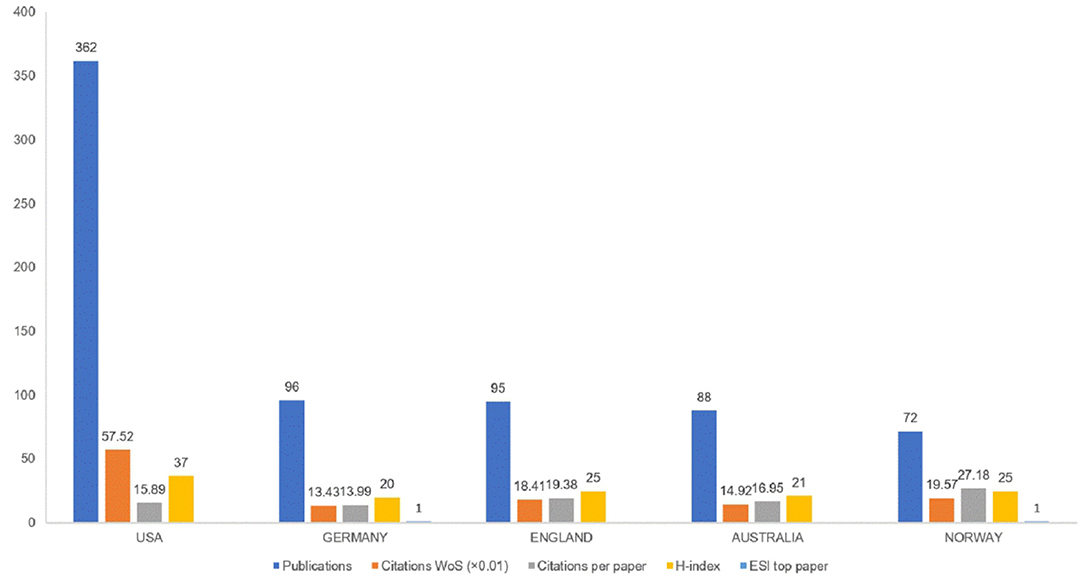
Figure 3 . Publications, citations on WoS (×0.01), citations per study, H-index, and ESL top study among top five countries or regions.
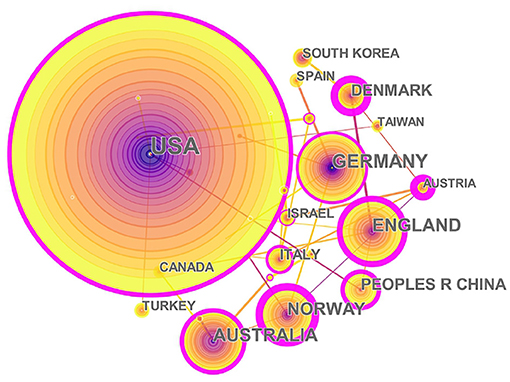
Figure 4 . The collaborations of countries or regions interested in the field. In this map, the node represents a country, and the link represents the cooperation relationship between two countries. A larger node represents more publications in the country. A thicker purple circle represents greater influence in this field.
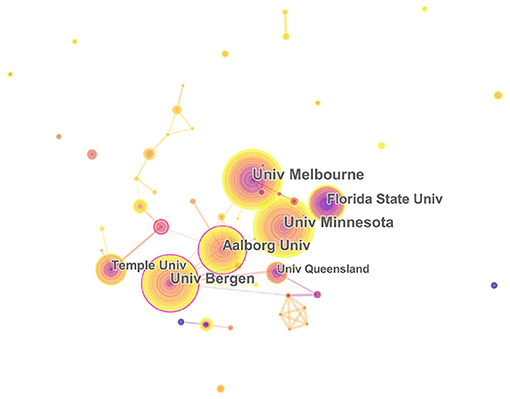
Figure 5 . The relationship of institutions interested in the field. University of Melbourne, Florida State University, University of Minnesota, Aalborg University, Temple University, University of Queensland, and University of Bergen. In this map, the node represents an institution, and the link represents the cooperation relationship between two institutions. A larger node represents more publications in the institution. A thicker purple circle represents greater influence in this field.
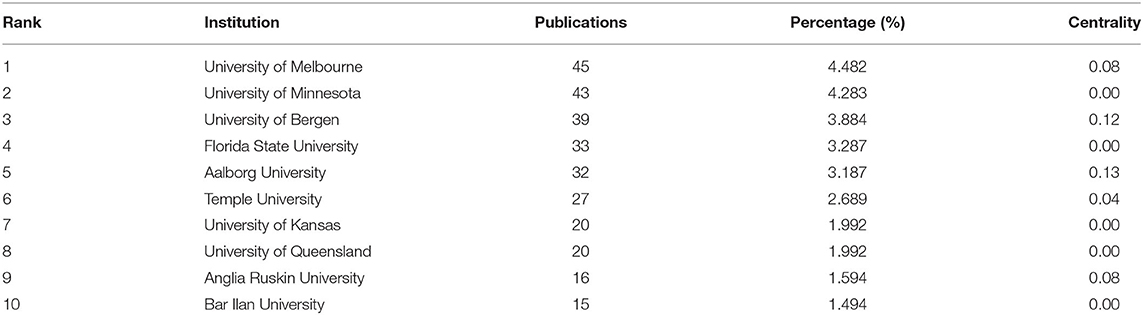
Table 2 . Top 10 institutions that contributed to publications in the music therapy field.
Distribution by Journals
Table 3 presents the top 10 journals that published articles or reviews in the music therapy field. The publications are mostly published in these journal fields, such as Therapy, Medical, Psychology, Neuroscience, Health and Clinical Care. The impact factors (IF) of these journals ranged between 0.913 and 7.89 (average IF: 2.568). Four journals had an impact factor >2, of which Cochrane Database of Systematic Reviews had the highest IF, 2019 = 7.89. In addition, the Journal of Music Therapy (IF: 2019 = 1.206) published 177 articles or reviews (17.629%) about music therapy in the past two decades, followed by the Nordic Journal of Music Therapy (121 publications, 12.052%, IF: 2019 = 0.913), and Arts in Psychotherapy (104 publications, 10.359%, IF: 2019 = 1.322). Furthermore, the map of the co-citation journal contained 393 nodes and 759 links ( Figure 6 ). The high co-citation count identifies the journals with the greatest academic influence and key positions in the field. The Journal of Music Therapy had the maximum co-citation counts (658), followed by Cochrane Database of Systematic Reviews (281), and Arts in Psychotherapy (279). Therefore, according to the analysis of the publications and co-citation counts, the Journal of Music Therapy and Arts in Psychotherapy occupied key positions in this research field.
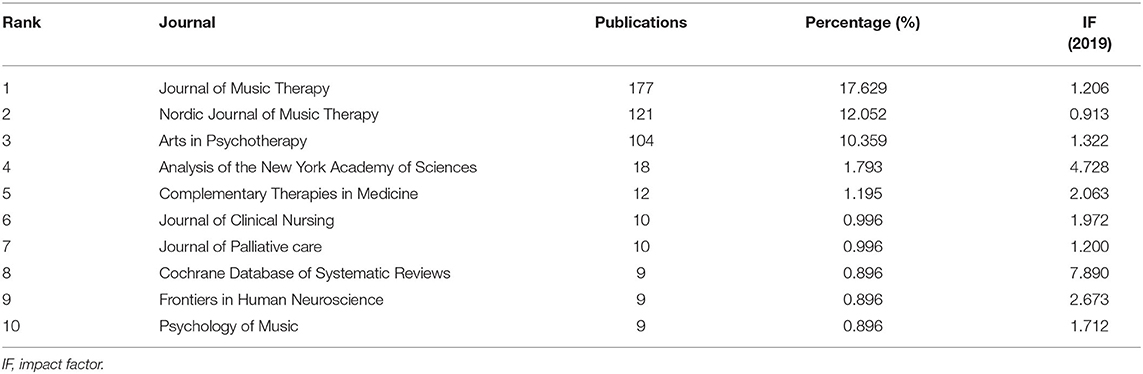
Table 3 . Top 10 journals that published articles in the music therapy field.
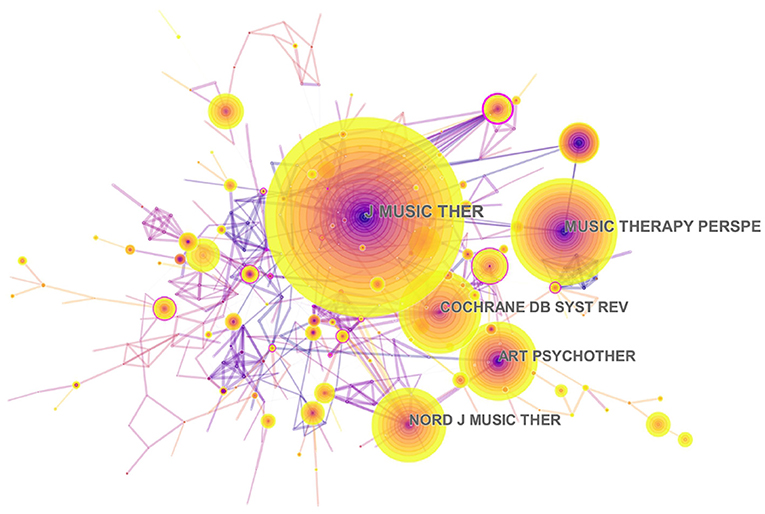
Figure 6 . Network map of co-citation journals engaged in music therapy from 2000 to 2019. Journal of Music Therapy, Arts in Psychotherapy, Nordic Journal of Music Therapy, Music Therapy Perspectives, Cochrane Database of Systematic Reviews. In this map, the node represents a journal, and the link represents the co-citation frequency between two journals. A larger node represents more publications in the journal. A thicker purple circle represents greater influence in this field.
Distribution by Authors
A total of 2,531 authors contributed to the research outputs related to music therapy. Author Silverman MJ published most of the studies (46) in terms of number of publications, followed by Gold C (41), Magee WL (19), O'Callaghan C (15), and Raglio A (15). According to co-citation counts, Bruscia KE (171 citations) was the most co-cited author, followed by Gold C (147 citations), Wigram T (121 citations), and Bradt J (117 citations), as presented in Table 4 . In Figure 7 , these nodes highlight the co-citation networks of the authors. The large-sized node represented author Bruscia KE, indicating that this author owned the most co-citations. Furthermore, the linear regression results revealed a remarkable increase in the percentages of multiple articles of authors ( t = 13.089, P < 0.001). These also indicated that cooperation among authors had increased remarkably, which can be considered an important development in music therapy research.
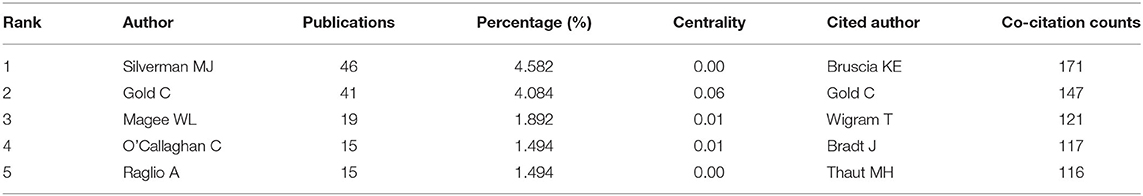
Table 4 . Top five authors of publications and top five authors of co-citation counts.
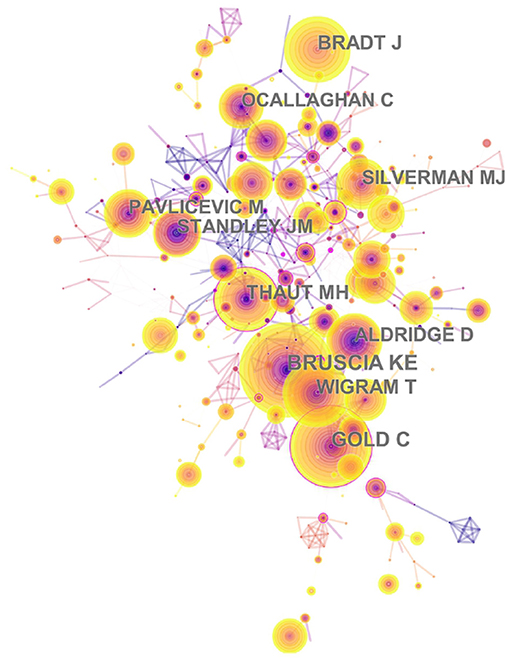
Figure 7 . The network of author co-citaion. In this map, the node represents an author, and the link represents the co-citation frequency between two authors. A larger node represents more publications of the author. A thicker purple circle represents greater influence in this field.
Analysis of Keywords
The results of keywords analysis indicated research hotspots and help scholars identify future research topics. Table 5 highlights 20 keywords with the most frequencies, such as “music therapy,” “anxiety,” “intervention,” “children,” and “depression.” The keyword “autism” has the highest centrality (0.42). Figure 8 shows the top 17 keywords with the strongest citation bursts. By the end of 2019, keyword bursts were led by “hospice,” which had the strongest burst (3.5071), followed by “efficacy” (3.1161), “health” (6.2109), and “older adult” (4.476).
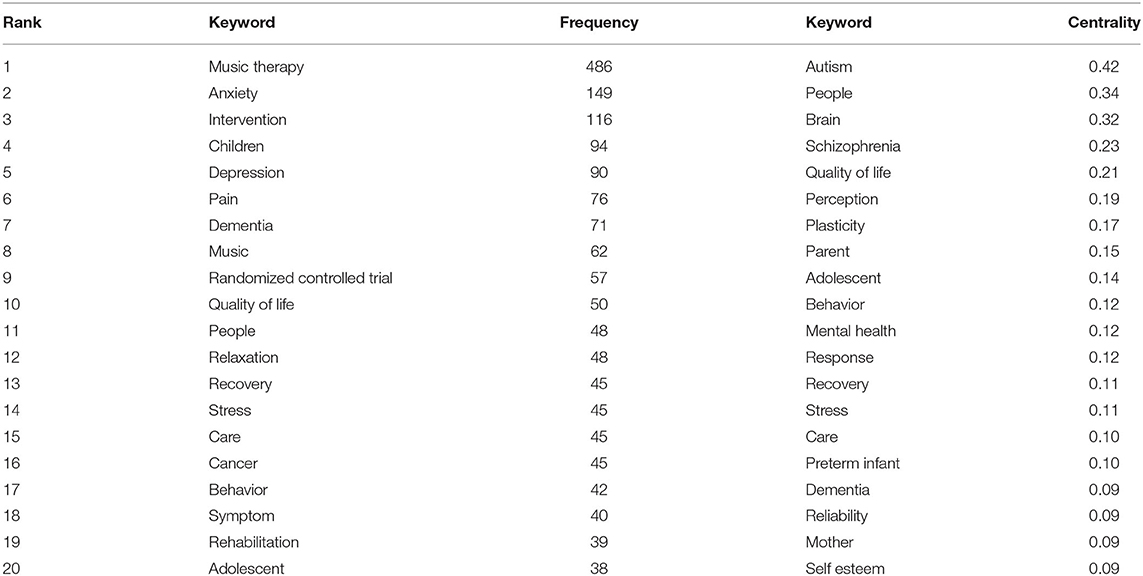
Table 5 . Top 20 keywords with the most frequency and centrality in music therapy study.
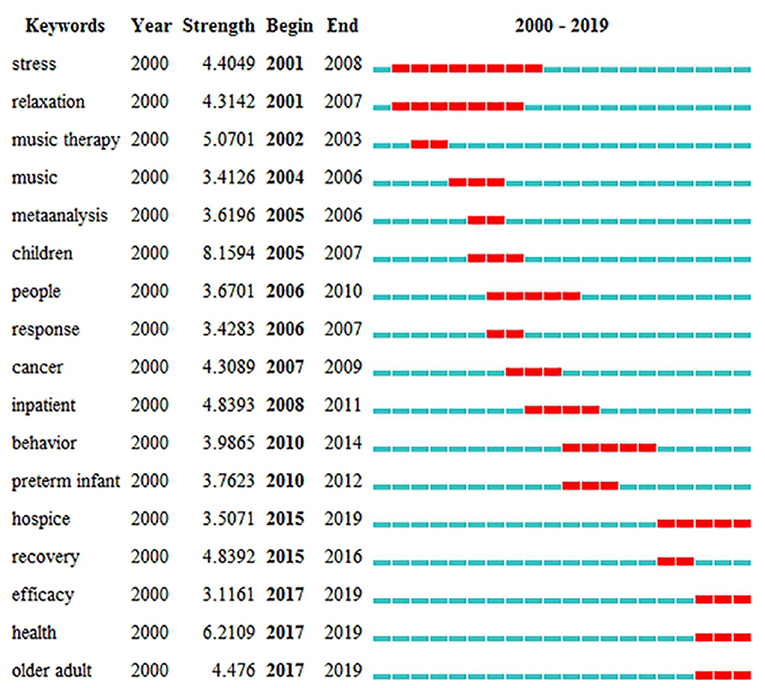
Figure 8 . The strongest citation bursts of the top 17 keywords. The red measures indicate frequent citation of keywords, and the green measures indicate infrequent citation of keywords.
Analysis of Co-cited References
The analysis of co-cited references is a significant indicator in the bibliometric method ( Chen, 2006 ). The top five co-cited references and their main findings are listed in Table 6 . These are regarded as fundamental studies for the music therapy knowledge base. In terms of co-citation counts, “individual music therapy for depression: randomized controlled trial” was the key reference because it had the most co-citation counts. This study concludes that music therapy mixed with standard care is an effective way to treat working-age people with depression. The authors also explained that music therapy is a valuable enhancement to established treatment practices ( Erkkilä et al., 2011 ). Meanwhile, the strongest citation burst of reference is regarded as the main knowledge of the trend ( Fitzpatrick, 2005 ). Figure 9 highlights the top 71 strongest citation bursts of references from 2000 to 2019. As can be seen, by the end of 2019, the reference burst was led by author Stige B, and the strongest burst was 4.3462.
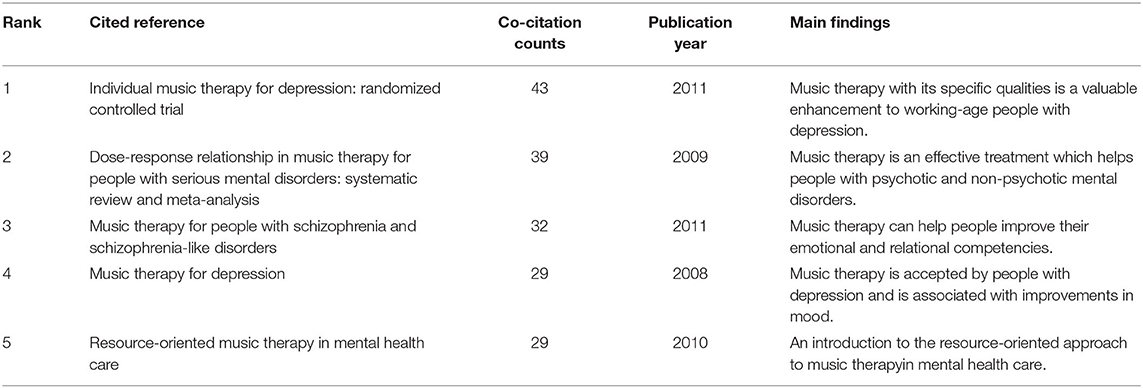
Table 6 . Top five co-cited references with co-citation counts in the study of music therapy from 2000 to 2019.
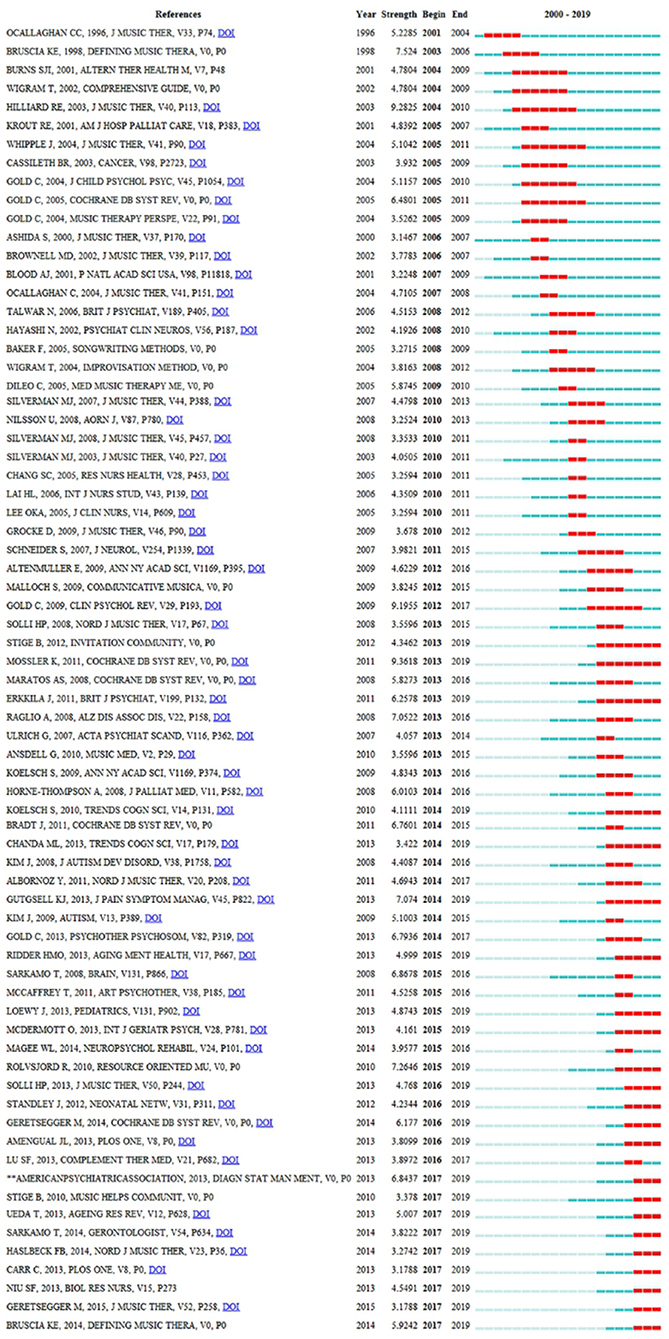
Figure 9 . The strongest citation bursts among the top 71 references. The red measures indicate frequent citation of studies, and the green measures indicate infrequent citation of studies.
Figure 10A presents the co-cited reference map containing 577 nodes and 1,331 links. The figure explains the empirical relevance of a considerable number of articles and reviews. Figure 10B presents the co-citation map (timeline view) of reference from publications on top music therapy research. The timeline view of clusters shows the research progress of music therapy in a particular period of time and the thematic concentration of each cluster. “Psychosis” was labeled as the largest cluster (#0), followed by “improvisational music therapy” (#1) and “paranesthesia anxiety” (#2). These clusters have also remained hot topics in recent years. Furthermore, the result of the modularity Q score was 0.8258. That this value exceeded 0.5 indicated that the definitions of the subdomain and characters of clusters were distinct. In addition, the mean silhouette was 0.5802, which also exceeded 0.5. The high homogeneity of individual clusters indicated high concentration in different research areas.
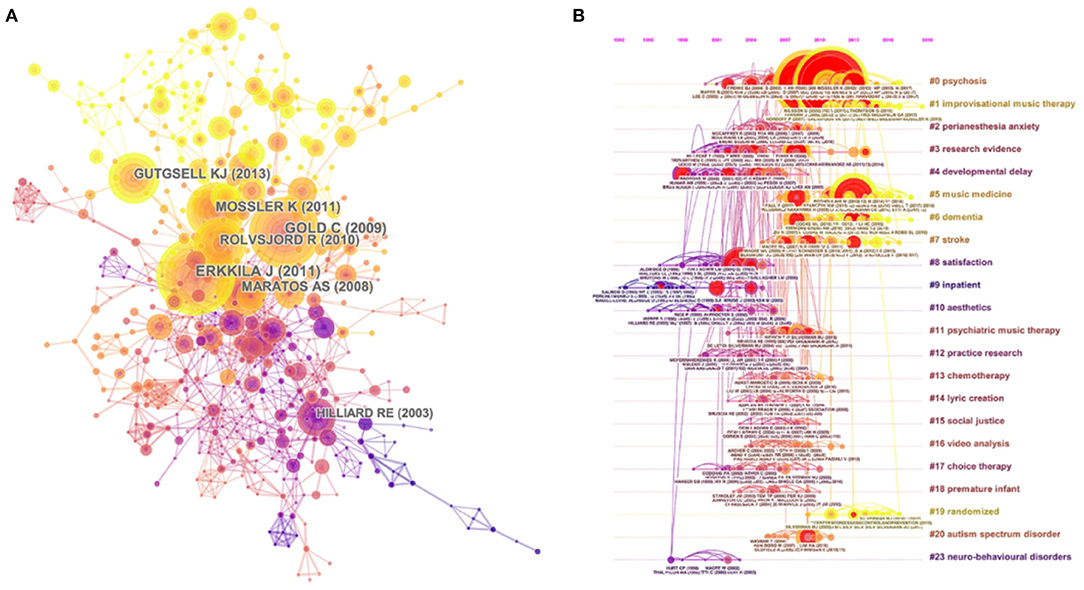
Figure 10. (A) The network map of co-cited references and (B) the map (timeline view) of references with co-citation on top music therapy research. In these maps, the node represents a study, and the link represents the co-citation frequency between two studies. A larger node represents more publications of the author. A thicker purple circle represents greater influence in this field. (A) The nodes in the same color belong to the same cluster. (B) The nodes on the same line belong to the same cluster.
Global Trends in Music Therapy Research
This study conducted a bibliometric analysis of music therapy research from the past two decades. The results, which reveal that music therapy studies have been conducted throughout the world, among others, can provide further research suggestions to scholars. In terms of the general analysis of the publications, the features of published articles and reviews, prolific countries or regions, and productive institutions are summarized below.
I. The distribution of publication year has been increasing in the past two decades. The annual publication outputs of music therapy from 2000 to 2019 were divided into three stages: beginning, second, and third. In the beginning stage, there were <30 annual publications from 2000 to 2006. The second stage was between 2007 and 2014. The number of publications increased steadily. It was 2007, which marked the first time 40 articles or reviews were published. The third stage was between 2015 and 2019. The year 2015 was the key turning point because it was the first time 80 articles or reviews were published. The number of publications showed a downward trend in 2016 (72), but it was still higher than the average number of the previous years. Overall, music therapy-related research has received increasing attention among scholars from 2000 to 2020.
II. The articles and reviews covered about 49 countries or regions, and the prolific countries or regions were mainly located in the North American and European continents. According to citations on WoS, citations per study, and the H-index, music therapy publications from developed countries, such as United States and Norway, have greater influence than those from other countries. In addition, China, as a model of a developing country, had published 53 studies and ranked top six among productive countries.
III. In terms of the collaboration map of institutions, the most productive universities engaged in music therapy were located in the United States, namely, University of Minnesota (43 publications), Florida State University (33 publications), Temple University (27 publications), and University of Kansas (20 publications). It indicated that institutions in the US have significant impacts in this area.
IV. According to author co-citation counts, scholars can focus on the publications of such authors as Bruscia KE, Gold C, and Wigram T. These three authors come from the United States, Norway, and Denmark, and it also reflected that these three countries are leading the research trend. Author Bruscia KE has the largest co-citation counts and is based at Temple University. He published many music therapy studies about assessment and clinical evaluation in music therapy, music therapy theories, and therapist experiences. These publications laid a foundation and facilitate the development of music therapy. In addition, in Figure 11 , the multi-authored articles between 2000 and 2003 comprised 47.56% of the sample, whereas the publications of multi-authored articles increased significantly from 2016 to 2019 (85.51%). These indicated that cooperation is an effective factor in improving the quality of publications.
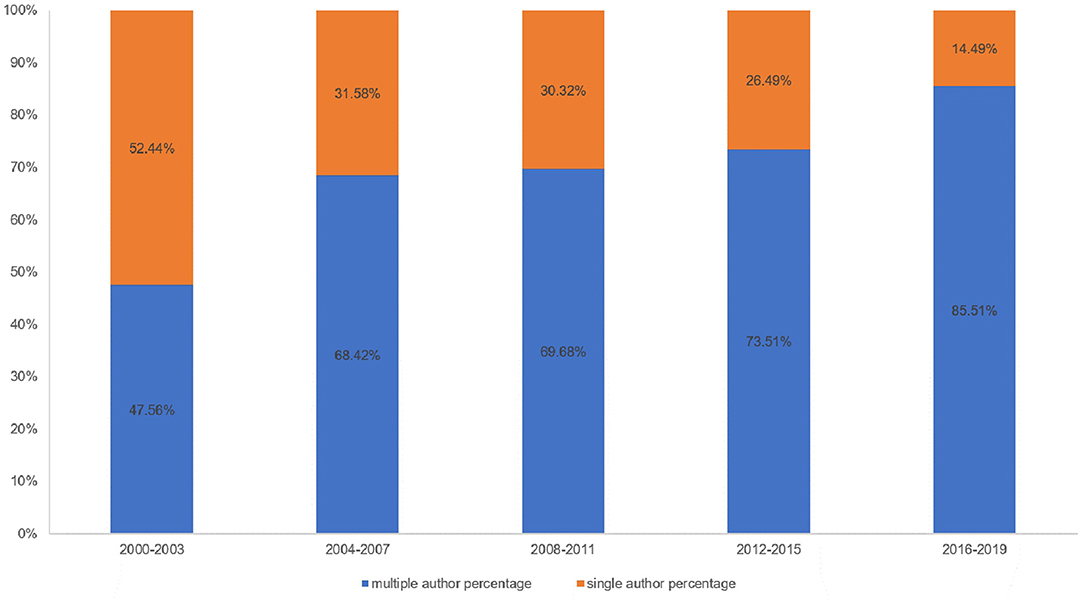
Figure 11 . The percentage of single- vs. multiple-authored articles. Blue bars mean multiple-author percentage; orange bars mean single-author percentage.
Research Focus on the Research Frontier and Hot Topics
According to the science map analysis, hot music therapy topics among publications are discussed.
I. The cluster “#1 improvisational music therapy” (IMT) is the current research frontier in the music therapy research field. In general, music therapy has a long research tradition within autism spectrum disorders (ASD), and there have been more rigorous studies about it in recent years. IMT for children with autism is described as a child-centered method. Improvisational music-making may enhance social interaction and expression of emotions among children with autism, such as responding to communication acts ( Geretsegger et al., 2012 , 2015 ). In addition, IMT is an evidence-based treatment approach that may be helpful for people who abuse drugs or have cancer. A study applied improving as a primary music therapeutic practice, and the result indicated that IMT will be effective in treating depression accompanied by drug abuse among adults ( Albornoz, 2011 ). By applying the interpretative phenomenological analysis and psychological perspectives, a study explained the significant role of music therapy as an innovative psychological intervention in cancer care settings ( Pothoulaki et al., 2012 ). IMT may serve as an effective additional method for treating psychiatric disorders in the short and medium term, but it may need more studies to identify the long-term effects in clinical practice.
II. Based on the analysis of co-citation counts, the top three references all applied music therapy to improve the quality of life of clients. They highlight the fact that music therapy is an effective method that can cover a range of clinical skills, thus helping people with psychological disorders, chronic illnesses, and pain management issues. Furthermore, music therapy mixed with standard care can help individuals with schizophrenia improve their global state, mental state (including negative and general symptoms), social functioning, and quality of life ( Gold et al., 2009 ; Erkkilä et al., 2011 ; Geretsegger et al., 2017 ).
III. By understanding the keywords with the strongest citation bursts, the research frontier can be predicted. Three keywords, “efficacy,” “health,” and “older adults,” emphasized the research trends in terms of the strongest citation bursts.
a. Efficacy: This refers to measuring the effectiveness of music therapy in terms of clinical skills. Studies have found that a wide variety of psychological disorders can be effectively treated with music. In the study of Fukui, patients with Alzheimer's disease listened to music and verbally communicated with their music therapist. The results showed that problematic behaviors of the patients with Alzheimer's disease decreased ( Fukui et al., 2012 ). The aim of the study of Erkkila was to determine the efficacy of music therapy when added to standard care. The result of this study also indicated that music therapy had specific qualities for non-verbal expression and communication when patients cannot verbally describe their inner experiences ( Erkkilä et al., 2011 ). Additionally, as summarized by Ueda, music therapy reduced anxiety and depression in patients with dementia. However, his study cannot clarify what kinds of music therapy or patients have effectiveness. Thus, future studies should investigate music therapy with good methodology and evaluation methods ( Ueda et al., 2013 ).
b. Health: Music therapy is a methodical intervention in clinical practice because it uses music experiences and relationships to promote health for adults and children ( Bruscia, 1998 ). Also, music therapy is an effective means of achieving the optimal health and well-being of individuals and communities, because it can be individualized or done as a group activity. The stimulation from music therapy can lead to conversations, recollection of memories, and expression. The study of Gold indicated that solo music therapy in routine practice is an effective addition to usual care for mental health care patients with low motivation ( Gold et al., 2013 ). Porter summarized that music therapy contributes to improvement for both kids and teenagers with mental health conditions, such as depression and anxiety, and increases self-esteem in the short term ( Porter et al., 2017 ).
c. Older adults: This refers to the use of music therapy as a treatment to maintain and slow down the symptoms observed in older adults ( Mammarella et al., 2007 ; Deason et al., 2012 ). In terms of keywords with the strongest citation bursts, the most popular subjects of music therapy-related articles and reviews focused on children from 2005 to 2007. However, various researchers concentrated on older adults from 2017 to 2019. Music therapy was the treatment of choice for older adults with depression, Parkinson's disease, and Alzheimer's disorders ( Brotons and Koger, 2000 ; Bernatzky et al., 2004 ; Johnson et al., 2011 ; Deason et al., 2012 ; McDermott et al., 2013 ; Sakamoto et al., 2013 ; Benoit et al., 2014 ; Pohl et al., 2020 ). In the study of Zhao, music therapy had positive effects on the reduction of depressive symptoms for older adults when added to standard therapies. These standard therapies could be standard care, standard drug treatment, standard rehabilitation, and health education ( Zhao et al., 2016 ). The study of Shimizu demonstrated that multitask movement music therapy was an effective intervention to enhance neural activation in older adults with mild cognitive impairment ( Shimizu et al., 2018 ). However, the findings of the study of Li explained that short-term music therapy intervention cannot improve the cognitive function of older adults. He also recommended that future researchers can apply a quality methodology with a long-term research design for the care needs of older adults ( Li et al., 2015 ).
Strengths and Limitations
To the best of our knowledge, this study was the first one to analyze large-scale data of music therapy publications from the past two decades through CiteSpace V. CiteSpace could detect more comprehensive results than simply reviewing articles and studies. In addition, the bibliometric method helped us to identify the emerging trend and collaboration among authors, institutions, and countries or regions.
This study is not without limitations. First, only articles and reviews published in the WoS Science Citation Index Expanded and Social Sciences Citation Index were analyzed. Future reviews could consider other databases, such as PubMed and Scopus. The document type labeled by publishers is not always accurate. For example, some publications labeled by WoS were not actually reviews ( Harzing, 2013 ; Yeung, 2021 ). Second, the limitation may induce bias in frequency of reference. For example, some potential articles were published recently, and these studies could be not cited with frequent times. Also, in terms of obliteration by incorporation, some common knowledge or opinions become accepted that their contributors or authors are no longer cited ( Merton, 1965 ; Yeung, 2021 ). Third, this review applied the quantitative analysis approach, and only limited qualitative analysis was performed in this study. In addition, we applied the CitesSpace software to conduct this bibliometric study, but the CiteSpace software did not allow us to complicate information under both full counting and fractional counting systems. Thus, future scholars can analyze the development of music therapy in some specific journals using both quantitative and qualitative indicators.
Conclusions
This bibliometric study provides information regarding emerging trends in music therapy publications from 2000 to 2019. First, this study presents several theoretical implications related to publications that may assist future researchers to advance their research field. The results reveal that annual publications in music therapy research have significantly increased in the last two decades, and the overall trend in publications increased from 28 publications in 2000 to 111 publications in 2019. This analysis also furthers the comprehensive understanding of the global research structure in the field. Also, we have stated a high level of collaboration between different countries or regions and authors in the music therapy research. This collaboration has extremely expanded the knowledge of music therapy. Thus, future music therapy professionals can benefit from the most specialized research.
Second, this research represents several practical implications. IMT is the current research frontier in the field. IMT usually serves as an effective music therapy method for the health of people in clinical practice. Identifying the emerging trends in this field will help researchers prepare their studies on recent research issues ( Mulet-Forteza et al., 2021 ). Likewise, it also indicates future studies to address these issues and update the existing literature. In terms of the strongest citation bursts, the three keywords, “efficacy,” “health,” and “older adults,” highlight the fact that music therapy is an effective invention, and it can benefit the health of people. The development prospects of music therapy could be expected, and future scholars could pay attention to the clinical significance of music therapy to the health of people.
Finally, multiple researchers have indicated several health benefits of music therapy, and the music therapy mechanism perspective is necessary for future research to advance the field. Also, music therapy can benefit a wide range of individuals, such as those with autism spectrum, traumatic brain injury, or some physical disorders. Future researchers can develop music therapy standards to measure clinical practice.
Author Contributions
KL and LW: conceptualization, methodology, formal analysis, investigation, resources, writing—review, and editing. LW: software and data curation. KL: validation and writing—original draft preparation. XW: visualization, supervision, project administration, and funding acquisition. All authors contributed to the article and approved the submitted version.
This study was supported by the Fok Ying-Tong Education Foundation of China (161092), the scientific and technological research program of the Shanghai Science and Technology Committee (19080503100), and the Shanghai Key Lab of Human Performance (Shanghai University of Sport) (11DZ2261100).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
WoS, Web of Science; ESI, essential science indicators; IF, impact factor; IMT, improvisational music therapy; ASD, autism spectrum disorder.
Albornoz, Y. (2011). The effects of group improvisational music therapy on depression in adolescents and adults with substance abuse: a randomized controlled trial. Nord. J. Music Ther. 20, 208–224. doi: 10.1080/08098131.2010.522717
CrossRef Full Text | Google Scholar
Association, A. M. T. (2018). History of Music Therapy . Available online at: https://www.musictherapy.org/about/history/ (accessed November 10, 2020).
Google Scholar
Benoit, C. E., Dalla Bella, S., Farrugia, N., Obrig, H., Mainka, S., and Kotz, S. A. (2014). Musically cued gait-training improves both perceptual and motor timing in Parkinson's disease. Front. Hum. Neurosci. 8:494. doi: 10.3389/fnhum.2014.00494
PubMed Abstract | CrossRef Full Text | Google Scholar
Bernatzky, G., Bernatzky, P., Hesse, H. P., Staffen, W., and Ladurner, G. (2004). Stimulating music increases motor coordination in patients afflicted with Morbus Parkinson. Neurosci. Lett. 361, 4–8. doi: 10.1016/j.neulet.2003.12.022
Bronson, H., Vaudreuil, R., and Bradt, J. (2018). Music therapy treatment of active duty military: an overview of intensive outpatient and longitudinal care programs. Music Ther. Perspect. 36, 195–206. doi: 10.1093/mtp/miy006
Brotons, M., and Koger, S. M. (2000). The impact of music therapy on language functioning in dementia. J. Music Ther. 37, 183–195. doi: 10.1093/jmt/37.3.183
Bruscia, K. (1998). Defining Music Therapy 2nd Edition . Gilsum: Barcelona publications.
Castanha, R. C. G., and Grácio, M. C. C. (2014). Bibliometrics contribution to the metatheoretical and domain analysis studies. Knowl. Organiz. 41, 171–174. doi: 10.5771/0943-7444-2014-2-171
Chen, C. (2006). CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inform. Sci. Technol. 57, 359–377. doi: 10.1002/asi.20317
Chen, C., Hu, Z., Liu, S., and Tseng, H. (2012). Emerging trends in regenerative medicine: a scientometric analysis in CiteSpace. Expert Opin. Biol. Ther. 12, 593–608. doi: 10.1517/14712598.2012.674507
Chen, H., Zhao, G., and Xu, N. (2012). “The analysis of research hotspots and fronts of knowledge visualization based on CiteSpace II,” in International Conference on Hybrid Learning , Vol. 7411, eds S. K. S. Cheung, J. Fong, L. F. Kwok, K. Li, and R. Kwan (Berlin; Heidelberg: Springer), 57–68. doi: 10.1007/978-3-642-32018-_6
Deason, R., Simmons-Stern, N., Frustace, B., Ally, B., and Budson, A. (2012). Music as a memory enhancer: Differences between healthy older adults and patients with Alzheimer's disease. Psychomusicol. Music Mind Brain 22:175. doi: 10.1037/a0031118
Devlin, K., Alshaikh, J. T., and Pantelyat, A. (2019). Music therapy and music-based interventions for movement disorders. Curr. Neurol. Neurosci. Rep. 19:83. doi: 10.1007/s11910-019-1005-0
Durieux, V., and Gevenois, P. A. (2010). Bibliometric indicators: quality measurements of scientific publication. Radiology 255, 342–351. doi: 10.1148/radiol.09090626
Ellegaard, O., and Wallin, J. A. (2015). The bibliometric analysis of scholarly production: How great is the impact? Scientometrics 105, 1809–1831. doi: 10.1007/s11192-015-1645-z
Erkkilä, J., Punkanen, M., Fachner, J., Ala-Ruona, E., Pöntiö, I., Tervaniemi, M., et al. (2011). Individual music therapy for depression: randomised controlled trial. Br. J. Psychiatry 199, 132–139. doi: 10.1192/bjp.bp.110.085431
Falagas, M. E., Pitsouni, E. I., Malietzis, G. A., and Pappas, G. (2008). Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. Faseb J. 22, 338–342. doi: 10.1096/FJ.07-9492LSF
Fitzpatrick, R. B. (2005). Essential Science IndicatorsSM. Med. Ref. Serv. Q. 24, 67–78. doi: 10.1300/J115v24n04_05
Fukui, H., Arai, A., and Toyoshima, K. (2012). Efficacy of music therapy in treatment for the patients with Alzheimer's disease. Int. J. Alzheimer's Dis. 2012, 531646–531646. doi: 10.1155/2012/531646
Geretsegger, M., Holck, U., Carpente, J. A., Elefant, C., Kim, J., and Gold, C. (2015). Common characteristics of improvisational approaches in music therapy for children with autism spectrum disorder: developing treatment guidelines. J. Music Ther. 52, 258–281. doi: 10.1093/jmt/thv005
Geretsegger, M., Holck, U., and Gold, C. (2012). Randomised controlled trial of improvisational music therapy's effectiveness for children with autism spectrum disorders (TIME-A): study protocol. BMC Pediatr. 12:2. doi: 10.1186/1471-2431-12-2
Geretsegger, M., Mossler, K. A., Bieleninik, L., Chen, X. J., Heldal, T. O., and Gold, C. (2017). Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst. Rev. 5:CD004025. doi: 10.1002/14651858.CD004025.pub4
Gold, C., Mössler, K., Grocke, D., Heldal, T. O., Tjemsland, L., Aarre, T., et al. (2013). Individual music therapy for mental health care clients with low therapy motivation: multicentre randomised controlled trial. Psychother. Psychosom. 82, 319–331. doi: 10.1159/000348452
Gold, C., Solli, H. P., Krüger, V., and Lie, S. A. (2009). Dose-response relationship in music therapy for people with serious mental disorders: systematic review and meta-analysis. Clin. Psychol. Rev. 29, 193–207. doi: 10.1016/j.cpr.2009.01.001
Gonzalez-Serrano, M. H., Jones, P., and Llanos-Contrera, O. (2020). An overview of sport entrepreneurship field: a bibliometric analysis of the articles published in the Web of Science. Sport Soc. 23, 296–314. doi: 10.1080/17430437.2019.1607307
Gooding, L. F., and Langston, D. G. (2019). Music therapy with military populations: a scoping review. J. Music Ther. 56, 315–347. doi: 10.1093/jmt/thz010
Harzing, A.-W. (2013). Document categories in the ISI web of knowledge: misunderstanding the social sciences? Scientometrics 94, 23–34. doi: 10.1007/s11192-012-0738-1
Johnson, J. K., Chang, C. C., Brambati, S. M., Migliaccio, R., Gorno-Tempini, M. L., Miller, B. L., et al. (2011). Music recognition in frontotemporal lobar degeneration and Alzheimer disease. Cogn. Behav. Neurol. 24, 74–84. doi: 10.1097/WNN.0b013e31821de326
Li, H. C., Wang, H. H., Chou, F. H., and Chen, K. M. (2015). The effect of music therapy on cognitive functioning among older adults: a systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 16, 71–77. doi: 10.1016/j.jamda.2014.10.004
Liang, Y. D., Li, Y., Zhao, J., Wang, X. Y., Zhu, H. Z., and Chen, X. H. (2017). Study of acupuncture for low back pain in recent 20 years: a bibliometric analysis via CiteSpace. J. Pain Res. 10, 951–964. doi: 10.2147/jpr.S132808
Mammarella, N., Fairfield, B., and Cornoldi, C. (2007). Does music enhance cognitive performance in healthy older adults? The Vivaldi effect. Aging Clin. Exp. Res. 19, 394–399. doi: 10.1007/bf03324720
McDermott, O., Crellin, N., Ridder, H. M., and Orrell, M. (2013). Music therapy in dementia: a narrative synthesis systematic review. Int. J. Geriatr. Psychiatry 28, 781–794. doi: 10.1002/gps.3895
Merigó, J. M., Mulet-Forteza, C., Valencia, C., and Lew, A. A. (2019). Twenty years of tourism Geographies: a bibliometric overview. Tour. Geograph. 21, 881–910. doi: 10.1080/14616688.2019.1666913
Merton, R. K. (1965). On the Shoulders of Giants: A Shandean Postscript . New York, NY: Free Press.
Miao, Y., Xu, S. Y., Chen, L. S., Liang, G. Y., Pu, Y. P., and Yin, L. H. (2017). Trends of long noncoding RNA research from 2007 to 2016: a bibliometric analysis. Oncotarget 8, 83114–83127. doi: 10.18632/oncotarget.20851
Mulet-Forteza, C., Lunn, E., Merigó, J. M., and Horrach, P. (2021). Research progress in tourism, leisure and hospitality in Europe (1969–2018). Int. J. Contemp. Hospit. Manage. 33, 48–74. doi: 10.1108/IJCHM-06-2020-0521
Pohl, P., Wressle, E., Lundin, F., Enthoven, P., and Dizdar, N. (2020). Group-based music intervention in Parkinson's disease - findings from a mixed-methods study. Clin. Rehabil. 34, 533–544. doi: 10.1177/0269215520907669
Porter, S., McConnell, T., McLaughlin, K., Lynn, F., Cardwell, C., Braiden, H. J., et al. (2017). Music therapy for children and adolescents with behavioural and emotional problems: a randomised controlled trial. J. Child Psychol. Psychiatry 58, 586–594. doi: 10.1111/jcpp.12656
Pothoulaki, M., MacDonald, R., and Flowers, P. (2012). An interpretative phenomenological analysis of an improvisational music therapy program for cancer patients. J. Music Ther. 49, 45–67. doi: 10.1093/jmt/49.1.45
Sakamoto, M., Ando, H., and Tsutou, A. (2013). Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int. Psychogeriatr. 25, 775–784. doi: 10.1017/s1041610212002256
Shimizu, N., Umemura, T., Matsunaga, M., and Hirai, T. (2018). Effects of movement music therapy with a percussion instrument on physical and frontal lobe function in older adults with mild cognitive impairment: a randomized controlled trial. Aging Ment. Health 22, 1614–1626. doi: 10.1080/13607863.2017.1379048
Small, H. (1973). Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inform. Sci. 24, 265–269. doi: 10.1002/asi.4630240406
Ueda, T., Suzukamo, Y., Sato, M., and Izumi, S. (2013). Effects of music therapy on behavioral and psychological symptoms of dementia: a systematic review and meta-analysis. Ageing Res. Rev. 12, 628–641. doi: 10.1016/j.arr.2013.02.003
Wang, X. Q., Peng, M. S., Weng, L. M., Zheng, Y. L., Zhang, Z. J., and Chen, P. J. (2019). Bibliometric study of the comorbidity of pain and depression research. Neural. Plast 2019:1657498. doi: 10.1155/2019/1657498
Yeung, A. W. K. (2021). Is the influence of freud declining in psychology and psychiatry? A bibliometric analysis. Front. Psychol. 12:631516. doi: 10.3389/fpsyg.2021.631516
Zhao, K., Bai, Z. G., Bo, A., and Chi, I. (2016). A systematic review and meta-analysis of music therapy for the older adults with depression. Int. J. Geriatr. Psychiatry 31, 1188–1198. doi: 10.1002/gps.4494
Zheng, K., and Wang, X. (2019). Publications on the association between cognitive function and pain from 2000 to 2018: a bibliometric analysis using citespace. Med. Sci. Monit. 25, 8940–8951. doi: 10.12659/msm.917742
Keywords: music therapy, aged, bibliometrics, health, web of science
Citation: Li K, Weng L and Wang X (2021) The State of Music Therapy Studies in the Past 20 Years: A Bibliometric Analysis. Front. Psychol. 12:697726. doi: 10.3389/fpsyg.2021.697726
Received: 20 April 2021; Accepted: 12 May 2021; Published: 10 June 2021.
Reviewed by:
Copyright © 2021 Li, Weng and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xueqiang Wang, wangxueqiang@sus.edu.cn
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The State of Music Therapy Studies in the Past 20 Years: A Bibliometric Analysis
Affiliations.
- 1 School of Kinesiology, Shanghai University of Sport, Shanghai, China.
- 2 Department of Sport Rehabilitation, Shanghai University of Sport, Shanghai, China.
- 3 Department of Sport Rehabilitation Medicine, Shanghai Shangti Orthopedic Hospital, Shanghai, China.
- PMID: 34177744
- PMCID: PMC8222602
- DOI: 10.3389/fpsyg.2021.697726
Purpose: Music therapy is increasingly being used to address physical, emotional, cognitive, and social needs of individuals. However, publications on the global trends of music therapy using bibliometric analysis are rare. The study aimed to use the CiteSpace software to provide global scientific research about music therapy from 2000 to 2019. Methods: Publications between 2000 and 2019 related to music therapy were searched from the Web of Science (WoS) database. The CiteSpace V software was used to perform co-citation analysis about authors, and visualize the collaborations between countries or regions into a network map. Linear regression was applied to analyze the overall publication trend. Results: In this study, a total of 1,004 studies met the inclusion criteria. These works were written by 2,531 authors from 1,219 institutions. The results revealed that music therapy publications had significant growth over time because the linear regression results revealed that the percentages had a notable increase from 2000 to 2019 ( t = 14.621, P < 0.001). The United States had the largest number of published studies (362 publications), along with the following outputs: citations on WoS (5,752), citations per study (15.89), and a high H-index value (37). The three keywords "efficacy," "health," and "older adults," emphasized the research trends in terms of the strongest citation bursts. Conclusions: The overall trend in music therapy is positive. The findings provide useful information for music therapy researchers to identify new directions related to collaborators, popular issues, and research frontiers. The development prospects of music therapy could be expected, and future scholars could pay attention to the clinical significance of music therapy to improve the quality of life of people.
Keywords: aged; bibliometrics; health; music therapy; web of science.
Copyright © 2021 Li, Weng and Wang.
PubMed Disclaimer
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Flow chart of music therapy…
Flow chart of music therapy articles and reviews inclusion.
Annual publication outputs of music…
Annual publication outputs of music therapy from 2000 to 2019.
Publications, citations on WoS (×0.01),…
Publications, citations on WoS (×0.01), citations per study, H-index, and ESL top study…
The collaborations of countries or…
The collaborations of countries or regions interested in the field. In this map,…
The relationship of institutions interested…
The relationship of institutions interested in the field. University of Melbourne, Florida State…
Network map of co-citation journals…
Network map of co-citation journals engaged in music therapy from 2000 to 2019.…
The network of author co-citaion.…
The network of author co-citaion. In this map, the node represents an author,…
The strongest citation bursts of…
The strongest citation bursts of the top 17 keywords. The red measures indicate…
The strongest citation bursts among…
The strongest citation bursts among the top 71 references. The red measures indicate…
The percentage of single- vs.…
The percentage of single- vs. multiple-authored articles. Blue bars mean multiple-author percentage; orange…
Similar articles
- Hotspots, trends, and advice: a 10-year visualization-based analysis of painting therapy from a scientometric perspective. Liang Q, Ye J, Lu Y, Dong J, Shen H, Qiu H. Liang Q, et al. Front Psychol. 2023 May 22;14:1148391. doi: 10.3389/fpsyg.2023.1148391. eCollection 2023. Front Psychol. 2023. PMID: 37284478 Free PMC article. Review.
- Global scientific research on social participation of older people from 2000 to 2019: A bibliometric analysis. Fu J, Jiang Z, Hong Y, Liu S, Kong D, Zhong Z, Luo Y. Fu J, et al. Int J Older People Nurs. 2021 Jan;16(1):e12349. doi: 10.1111/opn.12349. Epub 2020 Sep 20. Int J Older People Nurs. 2021. PMID: 32951349 Free PMC article.
- Bibliometric analysis of recent sodium channel research. Zhao D, Li J, Seehus C, Huang X, Zhao M, Zhang S, Wang W, Ji HL, Guo F. Zhao D, et al. Channels (Austin). 2018;12(1):311-325. doi: 10.1080/19336950.2018.1511513. Channels (Austin). 2018. PMID: 30134757 Free PMC article.
- Global trends and performances of Mediterranean diet: A bibliometric analysis in CiteSpace. Pan C, Jiang N, Cao B, Dong C. Pan C, et al. Medicine (Baltimore). 2021 Sep 24;100(38):e27175. doi: 10.1097/MD.0000000000027175. Medicine (Baltimore). 2021. PMID: 34559106 Free PMC article.
- Bibliometric and Visualized Analysis of 2011-2020 Publications on Physical Activity Therapy for Diabetes. Huang K, Zhu J, Xu S, Zhu R, Chen X. Huang K, et al. Front Med (Lausanne). 2022 Apr 7;9:807411. doi: 10.3389/fmed.2022.807411. eCollection 2022. Front Med (Lausanne). 2022. PMID: 35463021 Free PMC article. Review.
- Research hotspots and nursing inspiration in research of older adults with subjective cognitive decline from 2003 to 2023: A bibliometric analysis. Ding X, Shi J, Wang Q, Chen H, Shi X, Li Z. Ding X, et al. Int J Nurs Sci. 2024 Mar 6;11(2):222-232. doi: 10.1016/j.ijnss.2024.03.003. eCollection 2024 Apr. Int J Nurs Sci. 2024. PMID: 38707682 Free PMC article. Review.
- Effectiveness of music-based interventions for cognitive rehabilitation in Parkinson's disease: a systematic review of randomized controlled clinical trials. Citon LF, Hamdan AC. Citon LF, et al. Psicol Reflex Crit. 2023 Aug 10;36(1):20. doi: 10.1186/s41155-023-00259-x. Psicol Reflex Crit. 2023. PMID: 37561275 Free PMC article. Review.
- Value co-creation in business-to-business context: A bibliometric analysis using HistCite and VOS viewer. Ullah F, Shen L, Shah SHH. Ullah F, et al. Front Psychol. 2023 Jan 11;13:1027775. doi: 10.3389/fpsyg.2022.1027775. eCollection 2022. Front Psychol. 2023. PMID: 36710832 Free PMC article. Review.
- Bibliometric assessment of world scholars' international publications related to conceptual metaphor. Han Y, Peng Z, Chen H. Han Y, et al. Front Psychol. 2022 Nov 22;13:1071121. doi: 10.3389/fpsyg.2022.1071121. eCollection 2022. Front Psychol. 2022. PMID: 36483716 Free PMC article.
- A visualized and scientometric analysis of research trends of weight loss in overweight/obese children and adolescents (1958-2021). Sun G, Li L, Zhang X. Sun G, et al. Front Public Health. 2022 Oct 20;10:928720. doi: 10.3389/fpubh.2022.928720. eCollection 2022. Front Public Health. 2022. PMID: 36339176 Free PMC article.
- Albornoz Y. (2011). The effects of group improvisational music therapy on depression in adolescents and adults with substance abuse: a randomized controlled trial. Nord. J. Music Ther. 20, 208–224. 10.1080/08098131.2010.522717 - DOI
- Association A. M. T. (2018). History of Music Therapy. Available online at: https://www.musictherapy.org/about/history/ (accessed November 10, 2020).
- Benoit C. E., Dalla Bella S., Farrugia N., Obrig H., Mainka S., Kotz S. A. (2014). Musically cued gait-training improves both perceptual and motor timing in Parkinson's disease. Front. Hum. Neurosci. 8:494. 10.3389/fnhum.2014.00494 - DOI - PMC - PubMed
- Bernatzky G., Bernatzky P., Hesse H. P., Staffen W., Ladurner G. (2004). Stimulating music increases motor coordination in patients afflicted with Morbus Parkinson. Neurosci. Lett. 361, 4–8. 10.1016/j.neulet.2003.12.022 - DOI - PubMed
- Bronson H., Vaudreuil R., Bradt J. (2018). Music therapy treatment of active duty military: an overview of intensive outpatient and longitudinal care programs. Music Ther. Perspect. 36, 195–206. 10.1093/mtp/miy006 - DOI
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Europe PubMed Central
- Frontiers Media SA
- PubMed Central
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 June 2021
Mental health and music engagement: review, framework, and guidelines for future studies
- Daniel E. Gustavson ORCID: orcid.org/0000-0002-1470-4928 1 , 2 ,
- Peyton L. Coleman ORCID: orcid.org/0000-0001-5388-6886 3 ,
- John R. Iversen 4 ,
- Hermine H. Maes 5 , 6 , 7 ,
- Reyna L. Gordon 2 , 3 , 8 , 9 &
- Miriam D. Lense 2 , 8 , 9
Translational Psychiatry volume 11 , Article number: 370 ( 2021 ) Cite this article
42k Accesses
21 Citations
73 Altmetric
Metrics details
- Medical genetics
- Psychiatric disorders
Is engaging with music good for your mental health? This question has long been the topic of empirical clinical and nonclinical investigations, with studies indicating positive associations between music engagement and quality of life, reduced depression or anxiety symptoms, and less frequent substance use. However, many earlier investigations were limited by small populations and methodological limitations, and it has also been suggested that aspects of music engagement may even be associated with worse mental health outcomes. The purpose of this scoping review is first to summarize the existing state of music engagement and mental health studies, identifying their strengths and weaknesses. We focus on broad domains of mental health diagnoses including internalizing psychopathology (e.g., depression and anxiety symptoms and diagnoses), externalizing psychopathology (e.g., substance use), and thought disorders (e.g., schizophrenia). Second, we propose a theoretical model to inform future work that describes the importance of simultaneously considering music-mental health associations at the levels of (1) correlated genetic and/or environmental influences vs. (bi)directional associations, (2) interactions with genetic risk factors, (3) treatment efficacy, and (4) mediation through brain structure and function. Finally, we describe how recent advances in large-scale data collection, including genetic, neuroimaging, and electronic health record studies, allow for a more rigorous examination of these associations that can also elucidate their neurobiological substrates.
Similar content being viewed by others

Biological principles for music and mental health

A comprehensive investigation into the genetic relationship between music engagement and mental health
The effects of playing music on mental health outcomes
Introduction.
Music engagement, including passive listening and active music-making (singing, instrument playing), impacts socio-emotional development across the lifespan (e.g., socialization, personal/cultural identity, mood regulation, etc.), and is tightly linked with many cognitive and personality traits [ 1 , 2 , 3 ]. A growing literature also demonstrates beneficial associations between music engagement and quality of life, well-being, prosocial behavior, social connectedness, and emotional competence [ 4 , 5 , 6 , 7 , 8 ]. Despite these advances linking engagement with music to many wellness characteristics, we have a limited understanding of how music engagement directly and indirectly contributes to mental health, including at the trait-level (e.g., depression and anxiety symptoms, substance use behaviors), clinical diagnoses (e.g., associations with major depressive disorder (MDD) or substance use disorder (SUD) diagnoses), or as a treatment. Our goals in this scoping review are to (1) describe the state of music engagement research regarding its associations with mental health outcomes, (2) introduce a theoretical framework for future studies that highlight the contribution of genetic and environmental influences (and their interplay) that may give rise to these associations, and (3) illustrate some approaches that will help us more clearly elucidate the genetic/environmental and neural underpinnings of these associations.
Scope of the article
People interact with music in a wide variety of ways, with the concept of “musicality” broadly including music engagement, music perception and production abilities, and music training [ 9 ]. Table 1 illustrates the breadth of music phenotypes and example assessment measures. Research into music and mental health typically focuses on measures of music engagement, including passive (e.g., listening to music for pleasure or as a part of an intervention) and active music engagement (e.g., playing an instrument or singing; group music-making), both of which can be assessed using a variety of objective and subjective measures. We focus primarily on music engagement in the current paper but acknowledge it will also be important to examine how mental health traits relate to other aspects of musicality as well (e.g., perception and production abilities).
Our scoping review and theoretical framework incorporate existing theoretical and mechanistic explanations for how music engagement relates to mental health. From a psychological perspective, studies have proposed that music engagement can be used as a tool for encouraging self-expression, developing emotion regulation and coping skills, and building community [ 10 , 11 ]. From a physiological perspective, music engagement modulates arousal levels including impacts on heart rate, electrodermal activity, and cortisol [ 12 , 13 ]. These effects may be driven in part by physical aspects of music (e.g., tempo) or rhythmic movements involved in making or listening to music, which impact central nervous system functioning (e.g., leading to changes in autonomic activity) [ 14 ], as well as by personality and contextual factors (e.g., shared social experiences) [ 15 ]. Musical experiences also impact neurochemical processes involved in reward processing [ 10 , 13 , 14 , 16 , 17 , 18 ], which are also implicated in mental health disorders (e.g., substance use; depression). Thus, an overarching framework for studying music-mental health associations should integrate the psychological, physiological, and neurochemical aspects of these potential associations. We propose expanding this scope further through consideration of genetic and environmental risk factors, which may give rise to (and/or interact with) other factors to impact health and well-being.
Regarding mental health, it is important to recognize the hierarchical structure of psychopathology [ 19 , 20 ]. Common psychological disorders share many features and cluster into internalizing (e.g., MDD, generalized anxiety disorder (GAD), posttraumatic stress disorder (PTSD)), externalizing (e.g., SUDs, conduct disorder), and thought disorders (e.g., bipolar disorder, schizophrenia), with common variance shared even across these domains [ 20 ]. These higher-order constructs tend to explain much of the comorbidity among individual disorders, and have helped researchers characterize associations between psychopathology, cognition, and personality [ 21 , 22 , 23 ]. We use this hierarchical structure to organize our review. We first summarize the emerging literature on associations between music engagement and generalized well-being that provides promising evidence for associations between music engagement and mental health. Next, we summarize associations between music engagement and internalizing traits, externalizing traits/behaviors, and thought disorders, respectively. Within these sections, we critically consider the strengths and shortcomings of existing studies and how the latter may limit the conclusions drawn from this work.
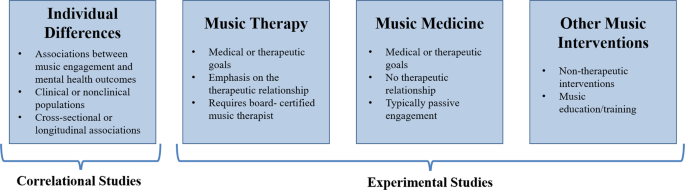
Our review considers both correlational and experimental studies (typically, intervention studies; see Fig. 1 for examples of study designs). We include not only studies that examine symptoms or diagnoses based on diagnostic interviews, but also those that assess quantitative variation (e.g., trait anxiety) in clinical and nonclinical populations. This is partly because individuals with clinical diagnoses may represent the extreme end of a spectrum of similar, sub-clinical, problems in the population, a view supported by evidence that genetic influences on diagnosed psychiatric disorders or DSM symptom counts are similar to those for trait-level symptoms in the general population [ 24 , 25 ]. Music engagement may be related to this full continuum of mental health, including correlations with trait-level symptoms in nonclinical populations and alleviation of symptoms from clinical disorders. For example, work linking music engagement to subjective well-being speaks to potential avenues for mental health interventions in the population at large.
Within experimental studies, music interventions can include passive musical activities (e.g., song listening, music and meditation, lyric discussion, creating playlists) or active musical activities (e.g., creative methods, such as songwriting or improvisation and/or re-creative methods, such as song parody).
The goal of this scoping review was to integrate across related, but often disconnected, literatures in order to propose a comprehensive theoretical framework for advancing our understanding of music-mental health associations. For this reason, we did not conduct a fully systematic search or quality appraisal of documents. Rather, we first searched PubMed and Google Scholar for review articles and meta-analyses using broad search terms (e.g., “review” and “music” and [“anxiety” or “depression” or “substance use”]). Then, when drafting each section, we searched for additional papers that have been published more recently and/or were examples of higher-quality research in each domain. When giving examples, we emphasize the most recent and most well-powered empirical studies. We also conducted some targeted literature searches where reviews were not available (e.g., “music” and [“impulsivity” or “ADHD”]) using the same databases. Our subsequent framework is intended to contextualize diagnostic, symptom, and mechanistic findings more broadly within the scope of the genetic and environmental risk factors on psychopathology that give rise to these associations and (potentially) impact the efficacy of treatment efforts. As such, the framework incorporates evidence from review articles and meta-analyses from various literatures (e.g., music interventions for anxiety [ 26 ], depression [ 27 ]) in combination with experimental evidence of biological underpinnings of music engagement and the perspective provided by newly available methods for population-health approaches (i.e., complex trait genetics, gene–environment interactions).
Music engagement and well-being
A growing body of studies report associations between music engagement and general indices of mental health, including increased well-being or emotional competence, lending support for the possibility that music engagement may also be associated with better specific mental health outcomes. In over 8000 Swedish twins, hours of music practice and self-reported music achievement were associated with better emotional competence [ 5 ]. Similarly, a meta-ethnography of 46 qualitative studies revealed that participation in music activities supported well-being through management of emotions, facilitation of self-development, providing respite from problems, and facilitating social connections [ 28 ]. In a sample of 1000 Australian adults, individuals who engaged with music, such as singing or dancing with others or attending concerts reported greater well-being vs. those who engaged in these experiences alone or did not engage. Other types of music engagement, such as playing an instrument or composing music were not associated with well-being in this sample [ 4 ]. Earlier in life, social music experiences (including song familiarity and synchronous movement to music) are associated with a variety of prosocial behaviors in infants and children [ 6 ], as well as positive affect [ 7 ]. Thus, this work provides some initial evidence that music engagement is associated with better general mental health outcomes in children and adults with some heterogeneity in findings depending on the specific type of music engagement.
Music engagement and internalizing problems
MDD, GAD, and PTSD are the most frequently clustered aspects of internalizing psychopathology [ 19 , 24 , 29 , 30 ]. Experimental studies provide evidence for the feasibility of music intervention efforts and their therapeutic benefits but are not yet rigorous enough to draw strong conclusions. The most severe limitations are small samples, the lack of appropriate control groups, few interventions with multiple sessions, and publications omitting necessary information regarding the intervention (e.g., intervention fidelity, inclusion/exclusion criteria, education status of intervention leader) [ 31 , 32 , 33 ]. Correlational studies, by contrast, suggest musicians are at greater risk for internalizing problems, but that they use music engagement as a tool to help manage these problems [ 34 , 35 ].
Experimental studies
Randomized controlled trials have revealed that music interventions (including both music therapies administered by board-certified music therapists and other music interventions) are associated with reduced depression, anxiety, and PTSD symptoms [ 26 , 27 , 33 , 36 ]. A review of 28 studies reported that 26 revealed significantly reduced depression levels in music intervention groups compared to control groups, including the 9 studies which included active non-music intervention control groups (e.g., reading sessions, “conductive-behavior” psychotherapy, antidepressant drugs) [ 27 ]. A similar meta-analysis of 19 studies demonstrated that music listening is effective at decreasing self-reported anxiety in healthy individuals [ 26 ]. A review of music-based treatment studies related to PTSD revealed similar conclusions [ 36 ], though there were only four relevant studies. More recent studies confirm these findings [ 37 , 38 , 39 ], such as one randomized controlled trial that demonstrated reduced depression symptoms in older adults following musical improvisation exercises compared to an active control group (gentle gymnastic activities) [ 39 ].
This work is promising given that some studies have observed effects even when compared to traditional behavior therapies [ 40 , 41 ]. However, there are relatively few studies directly comparing music interventions to traditional therapies. Some music interventions incorporate components of other therapeutic methods in their programs including dialectic or cognitive behavior therapies [ 42 ], but few directly compare how the inclusion of music augments traditional behavioral therapy. Still other non-music therapies incorporate music into their practice (e.g., background music in mindfulness therapies) [ 43 , 44 ], but the specific contribution of music in these approaches is unclear. Thus, there is a great need for further systematic research relating music to traditional therapies to understand which components of music interventions act on the same mechanisms as traditional therapies (e.g., developing coping mechanisms and building community) and which bolster or synchronize with other approaches (e.g., by adding structure, reinforcement, predictability, and social context to traditional approaches).
Aside from comparison with other therapeutic approaches, an earlier review of 98 papers from psychiatric in-patient studies concluded that promising effects of music therapy were limited by small sample sizes and methodological shortcomings including lack of reporting of adverse events, exclusion criteria, possible confounders, and characteristics of patients lost to follow-up [ 33 ]. Other problems included inadequate reporting of information on the source population (e.g., selection of patients and proportion agreeing to take part in the study), the lack of masking of interviewers during post-test, and concealment of randomization. Nevertheless, there was some evidence that therapies with active music participation, structured sessions, and multiple sessions (i.e., four or more) improved mood, with all studies incorporating these characteristics reporting significant positive effects. However, most studies have focused on passive interventions, such as music listening [ 26 , 27 ]. Active interventions (e.g., singing, improvising) have not been directly compared with passive interventions [ 27 ], so more work is needed to clarify whether therapeutic effects are indeed stronger with more engaging and active interventions.
Correlational studies
Correlational studies have focused on the use of music in emotional self-regulation. Specifically, individuals high in neuroticism appear to use music to help regulate their emotions [ 34 , 35 ], with beneficial effects of music engagement on emotion regulation and well-being driven by cognitive reappraisal [ 45 ]. Music listening may also moderate the association between neuroticism and depression in adolescents [ 46 ], consistent with a protective effect.
A series of recent studies have used validated self-reported instruments that directly assess how individuals use music activities as an emotion regulation strategy [ 47 , 48 , 49 , 50 ]. In adults, the use of music listening for anger regulation and anxiety regulation was positively associated with subjective well-being, psychological well-being, and social well-being [ 50 ]. In studies of adolescents and undergraduates, the use of music listening for entertainment was associated with fewer depression and anxiety symptoms [ 51 ]. “Healthy” music engagement in adolescents (i.e., using music for relaxation and connection with others) was also positively associated with happiness and school satisfaction [ 49 ]. However, the use of music listening for emotional discharge was also associated with greater depression, anxiety, and stress symptoms [ 51 ], and “unhealthy” music engagement (e.g., ‘hiding’ in music to block others out) was associated with lower well-being, happiness, school satisfaction, and greater depression and rumination [ 49 ]. Other work has highlighted the role of valence in these associations, with individuals who listen to happier music when they are in a bad mood reporting stronger ability for music to influence their mood than those who listen to sad music while in a negative mood [ 52 , 53 ].
This work highlights the importance of considering individuals’ motivations for engaging with music in examining associations with well-being and mental health, and are consistent with the idea that individuals already experiencing depression, anxiety, and stress use music as a therapeutic tool to manage their emotions, with some strategies being more effective than others. Of course, these correlational effects may not necessarily reflect causal associations, but could be due to bidirectional influences, as suggested by claims that musicians may be at higher risk for internalizing problems [ 54 , 55 , 56 ]. It is also necessary to consider demographic and socioeconomic factors in these associations [ 57 ], for example, because arts engagement may be more strongly associated with self-esteem in those with higher education [ 58 ].
It is also necessary to clarify if musicians (professional and/or nonprofessional) represent an already high-risk group for internalizing problems. In one large study conducted in Norway ( N = 6372), professional musicians were higher in neuroticism than the general population [ 56 ]. Another study of musician cases ( N = 9803) vs. controls ( N = 49,015) identified in a US-based research database through text-mining of medical records found that musicians are at greater risk of MDD (Odds ratio [OR] = 1.21), anxiety disorders (OR = 1.25), and PTSD (OR = 1.13) [ 55 ]. However, other studies demonstrate null associations between musician status and depression symptoms [ 5 ] or mixed associations [ 59 ]. In N = 10,776 Swedish twins, for example, professional and amateur musicians had more self-reported burnout symptoms [ 54 ]. However, neither playing music in the past, amateur musicianship, nor professional musicianship was significantly associated with depression or anxiety disorder diagnoses.
Even if musicians are at higher risk, such findings can still be consistent with music-making being beneficial and therapeutic (e.g., depression medication use is elevated in individuals with depressive symptoms because it is a treatment). Clinical samples may be useful in disentangling these associations (i.e., examining if those who engage with music more frequently have reduced symptoms), and wider deployment of measures that capture emotion regulation strategies and motivations for engaging with music will help shed light on whether high-risk individuals engage with music in qualitatively different ways than others [ 51 , 57 ]. Later, we describe how also considering the role of genetic and environmental risk factors in these associations (e.g., if individuals at high genetic and/or environmental risk self-select into music environments because they are therapeutic) can help to clarify these questions.
Music engagement and externalizing problems
The externalizing domain comprises SUDs, and also includes impulsivity, conduct disorder, and attention-deficit hyperactivity disorder (ADHD), especially in adolescents [ 20 , 24 , 60 , 61 ]. Similar to the conclusions for internalizing traits, experimental studies show promising evidence that music engagement interventions may reduce substance use, ADHD, and other externalizing symptoms, but conclusions are limited by methodological limitations. Correlational evidence is sparce, but there is less reason to suspect musicians are at higher risk for externalizing problems.
Intervention studies have demonstrated music engagement is helpful in patients with SUDs, including reducing withdrawal symptoms and stress, allowing individuals to experience emotions without craving substance use, and making substance abuse treatment sessions more enjoyable and motivating [ 62 , 63 , 64 ] (for a systematic review, see [ 65 ]). Similar to the experimental studies of internalizing traits, however, these studies would also benefit from larger samples, better controls, and higher-quality reporting standards.
Music intervention studies for ADHD are of similar quality. Such interventions have been shown to reduce inattention [ 66 ], decrease negative mood [ 67 ], and increase reading comprehension for those with ADHD [ 68 ]. However, there is a great amount of variability among children with ADHD, as some may find music distracting while others may focus better in the presence of music [ 69 ].
Little research has been conducted to evaluate music engagement interventions for impulsivity or conduct disorder problems, and findings are mixed. For example, a music therapy study of 251 children showed that beneficial effects on communication skills (after participating in a free improvisation intervention) was significant, though only for the subset of children above age 13 [ 70 ]. Another study suggested the promising effects of music therapy on social skills and problem behaviors in 89 students selected based on social/emotional problem behaviors, but did not have a control group [ 71 ]. Other smaller studies ( N < 20 each) show inconsistent results on disruptive behaviors and aggression [ 72 , 73 ].
Correlational studies on externalizing traits are few and far between. A number of studies examined how listening habits for different genres of music relate to more or less substance use [ 74 , 75 , 76 , 77 ]. However, these studies do not strongly illuminate associations between music engagement and substance use because musical genres are driven by cultural and socioeconomic factors that vary over the lifespan. In the previously cited large study of American electronic medical records [ 55 ] where musicianship was associated with more internalizing diagnoses, associations were nonsignificant for “tobacco use disorder” (OR = 0.93), “alcoholism” (OR = 1.01), “alcohol-related disorders” (OR = 1.00), or “substance addiction and disorders” (OR = 1.00). In fact, in sex-stratified analyses, female musicians were at significantly decreased risk for tobacco use disorder (OR = 0.85) [ 55 ]. Thus, there is less evidence musicians are at greater risk for externalizing problems than in other areas.
Regarding other aspects of externalizing, some studies demonstrate children with ADHD have poor rhythm skills, opening a possibility that working on rhythm skills may impact ADHD [ 78 , 79 ]. For example, music might serve as a helpful scaffold (e.g., for attention) due to its regular, predictable rhythmic beat. It will be important to examine whether these associations with music rhythm are also observed for measures of music engagement, especially in larger population studies. Finally, musicians were reported to have lower impulsiveness than prior population samples, but were not compared directly to non-musicians [ 80 , 81 ].
Music engagement and thought disorders
Thought disorders typically encompass schizophrenia and bipolar disorder [ 20 ]. Trait-level measures include schizotypal symptoms and depression symptoms. Much like internalizing, music interventions appear to provide some benefits to individuals with clinical diagnoses, but musicians may be at higher risk for thought disorders. Limitations of both experimental and correlational studies are similar to those for internalizing and externalizing.
Music intervention studies have been conducted with individuals with schizophrenia and bipolar disorder. A recent meta-analysis of 18 music therapy studies for schizophrenia (and similar disorders) [ 82 ] demonstrated that music therapy plus standard care (compared to standard care alone) demonstrated improved general mental health, fewer negative symptoms of schizophrenia, and improved social functioning. No effects were observed for general functioning or positive symptoms of schizophrenia. Critiques echoed those described above. Most notably, although almost all studies had low risk of biases due to attrition, unclear risk of bias was evident in the vast majority of studies (>75%) for selection bias, performance bias, detection bias, and reporting bias. These concerns highlight the need for these studies to report more information about their study selection, blinding procedure, and outcomes.
More recent papers suggest similar benefits of music therapies in patients with psychosis [ 83 ] and thought disorders [ 84 ], with similar limitations (e.g., one study did not include a control group). Finally, although a 2021 review did not uncover more recent articles related to bipolar disorder, they argued that existing work suggests music therapy has the potential both to treat bipolar disorder symptoms and alleviate subthreshold symptoms in early stages of the disorder [ 85 ].
Much like internalizing, findings from the few existing studies suggest that musicians may be at higher risk for thought disorders. In the large sample of Swedish twins described earlier [ 54 ], playing an instrument was associated with more schizotypal symptoms across multiple comparisons (professional musicians vs. non-players; amateur musicians vs. non-players; still plays an instrument vs. never played). However, no associations were observed for schizophrenia or bipolar disorder diagnoses across any set of comparison groups. Another study demonstrated that individuals with higher genetic risk for schizophrenia or bipolar disorder were more likely to be a member of a creative society (i.e., actor or dancer, musician, visual artist, or writer) or work in a profession in these fields [ 86 ]. Furthermore, musician status was associated with “bipolar disorder” (OR = 1.18) and “schizophrenia and other psychotic disorders” (OR = 1.18) in US electronic health records (EHRs) [ 55 ].
Interim summary
There is promising evidence that music engagement is associated with better mental health outcomes. Music engagement is positively associated with quality of life, well-being, social connectedness, and emotional competence. However, some individuals who engage with music may be at higher risk for mental health problems, especially internalizing and thought disorders. More research is needed to disentangle these contrasting results, including clarifying how “healthy” music engagement (e.g., for relaxation or social connection) leads to greater well-being or successful emotion regulation, and testing whether some individuals are more likely to use music as a tool to regulate emotions (e.g., those with high neuroticism) [ 34 , 35 ]. Similarly, it will be important to clarify whether the fact that musicians may be an at-risk group is an extension of working in an artistic field in general (which may feature lower pay or lack of job security) and/or if similar associations are observed with continuous music engagement phenotypes (e.g., hours of practice). As we elaborate on later, genetically informative datasets can help clarify these complex associations, for example by tested whether musicians are at higher genetic risk for mental health problems but their music engagement mitigates these risks.
Music intervention studies are feasible and potentially effective at treating symptoms in individuals with clinical diagnoses, including depression, anxiety, and SUDs. However, it will be essential to expand these studies to include larger samples, random sampling, and active control groups that compare the benefits of music interventions to traditional therapies and address possible confounds. These limitations make it hard to quantify how specific factors influence the effectiveness of interventions, such as length/depth of music training, age of sample, confounding variables (e.g., socioeconomic status), and type of intervention (e.g., individual vs. group sessions, song playing vs. songwriting, receptive vs. active methods). Similarly, the tremendous breadth of music engagement activities and measures makes it difficult to identify the specific aspects of music engagement that convey the most benefits to health and well-being [ 87 ]. It is therefore necessary to improve reporting quality of studies so researchers can better identify these potential moderators or confounds using systematic approaches (e.g., meta-analyses).
Various mechanisms have been proposed to explain the therapeutic effects of music on mental health, including psychological (e.g., building communities, developing coping strategies) [ 10 , 11 ] and specific neurobiological drivers (e.g., oxytocin, cortisol, autonomic nervous system activity) [ 12 , 13 , 14 ]. However, it will be vital to conduct more systematic research comparing the effects of music interventions to existing therapeutic methods and other types of creative activities (e.g., art [ 88 ]) to quantify which effects and mechanisms are specific to music engagement. Music interventions also do not have to be an alternative to other treatments, but may instead support key elements of traditional interventions, such as being engaging, enjoyable, providing social context, and increasing structure and predictability [ 89 ]. Indeed, some music therapists incorporate principals from existing psychotherapeutic models [ 42 , 90 ] and, conversely, newer therapeutic models (e.g., mindfulness) incorporate music into their practice [ 43 , 44 ]. It is not yet possible to disentangle which aspects of music interventions best synergize with or strengthen standard psychotherapeutic practices (which are also heterogeneous), but this will be possible with better reporting standards and quality experimental design.
To encapsulate and extend these ideas, we next propose a theoretical framework that delineates key aspects of how music engagement may relate to mental health, which is intended to be useful for guiding future investigations in a more systematic way.
Theoretical framework for future studies
Associations between music engagement and mental health may take multiple forms, driven by several different types of genetic predispositions and environmental effects that give rise to, and interact with, proposed psychological and neurobiological mechanisms described earlier. Figure 2 displays our theoretical model in which potential beneficial associations with music are delineated into testable hypotheses. Four key paths characterize specific ways in which music engagement may relate to (and influence) mental health traits, and thus represent key research questions to be addressed in future studies.
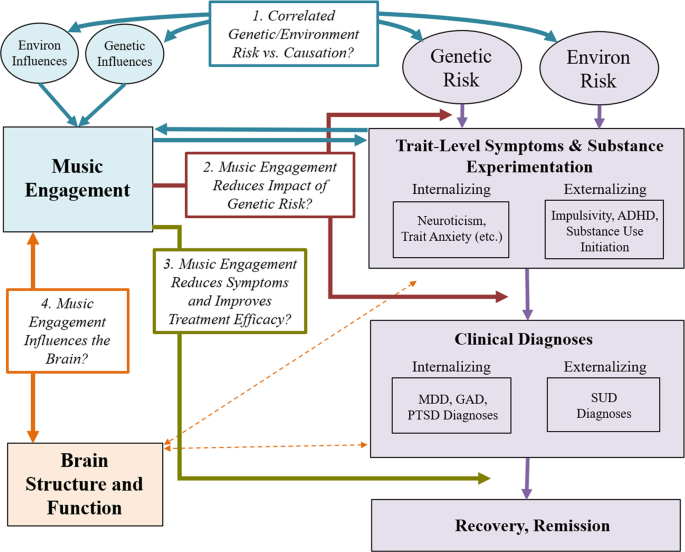
Progression of mental health problems is based on a diathesis-stress model, where genetic predispositions and environmental exposures result in later problems (which can be remedied through treatment). Potential associations with music engagement include (Path 1; blue arrows) correlated genetic/environmental influences and/or causal associations between music engagement and trait-level mental health outcomes; (Path 2; red arrows) interactions between music engagement and risk factors to predict later trait-level or clinical level symptoms; and (Path 3; gold arrow) direct effects of music engagement on reducing symptoms or improving treatment efficacy. Path 4 (orange arrows) illustrates the importance of understanding how these potential protective associations are driven by neuroanatomy and function. MDD major depressive disorder, GAD generalized anxiety disorder, PTSD posttraumatic stress disorder, SUD substance use disorder(s).
Path 1: Music engagement relates to mental health through correlated genetic and environmental risk factors and/or causation
The diathesis-stress model of psychiatric disease posits that individuals carry different genetic liabilities for any given disorder [ 91 , 92 , 93 ], with disorder onset depending on the amount of negative vs. protective environmental life events and exposures the individual experiences. Although at first glance music engagement appears to be an environmental exposure, it is actually far from it. Twin studies have demonstrated that both music experiences and music ability measures are moderately heritable and genetically correlated with cognitive abilities like non-verbal intelligence [ 94 , 95 , 96 , 97 ]. Music engagement may be influenced by its own set of environmental influences, potentially including socioeconomic factors and availability of instruments. Thus, music engagement can be viewed as a combination of genetic and environmental predispositions and availability of opportunities for engagement [ 98 ] that are necessary to consider when evaluating associations with mental health [ 54 ].
When examining music-mental health associations, it is thus important to evaluate if associations are in part explained by correlated genetic or environmental influences (see Fig. 3 for schematic and explanation for interpreting genetic/environmental correlations). On one hand, individuals genetically predisposed to engage with music may be at lower risk of experiencing internalizing or externalizing problems. Indeed, music engagement and ability appear associated with cognitive abilities through genetic correlations [ 3 , 99 ], which may apply to music-mental health associations as well. On the other, individuals at high genetic risk for neuroticism or psychopathology may be more likely to engage with music because it is therapeutic, suggesting a genetic correlation in the opposite direction (i.e., increased genetic risk for musicians). To understand and better contextualize the potential therapeutic effects of music engagement, it is necessary to quantify these potential genetic associations, while simultaneously evaluating whether these associations are explained by correlated environmental influences.
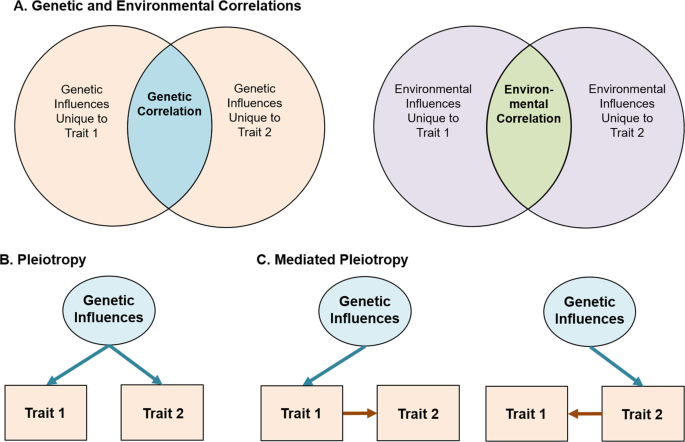
Variance in any given trait is explained by a combination of genetic influences (i.e., heritability) and environmental influences. For complex traits (e.g., MDD or depression symptoms), cognitive abilities (e.g., intelligence), and personality traits (e.g., impulsivity), many hundreds or thousands of independent genetic effects are combined together in the total heritability estimate. Similarly, environmental influences typically represent a multitude of factors, from individual life events to specific exposures (e.g., chemicals, etc.). The presence of a genetic or environmental correlation between traits indicates that some set of these influences have an impact on multiple traits. A Displayed using a Venn diagram. Identifying the strength of genetic vs. environmental correlations can be useful in testing theoretical models and pave the way for more complex genetic investigations. Beyond this, gene identification efforts (e.g., genome-wide association studies) and additional analyses of the resulting data can be used to classify whether these associations represent specific genetic influences that affect both traits equally (i.e., genetic pleiotropy ( B )) or whether a genetic influence impacts only one trait which in turn causes changes in the other (i.e., mediated genetic pleiotropy ( C )). Environmental influences can also act pleiotropically or in a mediated-pleiotropy manner, but only genetic influences are displayed for simplicity.
Beyond correlated genetic and environmental influences, music engagement and mental health problems may be associated with one another through direct influences (including causal impacts). This is in line with earlier suggestions that music activities (e.g., after-school programs, music practice) engage adolescents, removing opportunities for drug-seeking behaviors [ 100 ], increasing their social connections to peers [ 101 ], and decreasing loneliness [ 41 ]. Reverse causation is also possible, for example, if experiencing mental health problems causes some individuals to seek out music engagement as a treatment. Longitudinal and genetically informative studies can help differentiate correlated risk factors (i.e., genetic/environmental correlations) from causal effects of music engagement (Fig. 2 , blue arrows) [ 102 ].
Path 2: Engagement with music reduces the impact of genetic risk
Second, genetic and environmental influences may interact with each other to influence a phenotype. For example, individual differences in music achievement are more pronounced in those who engage in practice or had musically enriched childhood environments [ 97 , 98 ]. Thus, music exposures may not influence mental health traits directly but could impact the strength of the association between genetic risk factors and the emergence of trait-level symptoms and/or clinical diagnoses. Such associations might manifest as decreased heritability of trait-level symptoms in musicians vs. non-musicians (upper red arrow in Fig. 2 ). Alternatively, if individuals high in neuroticism use music to help regulate their emotions [ 34 , 35 ], those who are not exposed to music environments might show stronger associations between neuroticism and later depressive symptoms or diagnoses than those engaged with music (lower red arrow in Fig. 2 ). Elucidating these possibilities will help disentangle the complex associations between music and mental health and could be used to identify which individuals would benefit most from a music intervention (especially preventative interventions). Later, we describe some specific study designs that can test hypotheses regarding this gene-environment interplay.
Path 3: Music engagement improves the efficacy of treatment (or acts as a treatment)
For individuals who experience severe problems (e.g., MDD, SUDs), engaging with music may reduce symptoms or improve treatment outcomes. This is the primary goal of most music intervention studies [ 27 , 33 ] (Fig. 2 , gold arrow). However, and this is one of the central messages of this model, it is important to consider interventions in the context of the paths discussed above. For example, if music engagement is genetically correlated with increased risk for internalizing or externalizing problems (Path 1) and/or if individuals at high genetic risk for mental health problems have already been using music engagement to develop strategies to deal with subthreshold symptoms (Path 2), then may be more likely to choose music interventions over other alternatives and find them more successful. Indeed, the beneficial aspects of music training on cognitive abilities appear to be drastically reduced in samples that were randomly sampled [ 103 ]. Therefore, along with other necessary reporting standards discussed above [ 32 , 33 ], it will be useful for studies to report participants’ prior music experience and consider these exposures in evaluating the efficacy of interventions.
Path 4: Music engagement influences brain structure and function
Exploring associations between music engagement and brain structure and function will be necessary to elucidate the mechanisms driving the three paths outlined above. Indeed, there are strong links between music listening and reward centers of the brain [ 104 , 105 ] including the nucleus accumbens [ 106 , 107 ] and ventral tegmental areas [ 108 ] that are implicated in the reward system for all drugs of abuse [ 109 , 110 , 111 , 112 ] and may relate to internalizing problems [ 113 , 114 , 115 ]. Moreover, activity in the caudate may simultaneously influence rhythmic sensorimotor synchronization, monetary reward processing, and prosocial behavior [ 116 ]. Furthermore, music listening may help individuals control the effect of emotional stimuli on autonomic and physiological responses (e.g., in the hypothalamus) and has been shown to induce the endorphinergic response blocked by naloxone, an opioid antagonist [ 18 , 117 ].
This work focusing on music listening and reward processing has not been extended to music making (i.e., active music engagement), though some differences in brain structure and plasticity between musicians and non-musicians have been observed for white matter (e.g., greater fractional anisotropy in corpus callosum and superior longitudinal fasciculus) [ 118 , 119 , 120 , 121 ]. In addition, longitudinal studies have revealed that instrument players show more rapid cortical thickness maturation in prefrontal and parietal areas implicated in emotion and impulse control compared to non-musician children/adolescents [ 122 ]. Importantly, because the existing evidence is primarily correlational, these cross-sectional and longitudinal structural differences between musicians and non-musicians could be explained by genetic correlations, effects of music training, or both, making them potentially relevant to multiple paths in our model (Fig. 2 ). Examining neural correlates of music engagement in more detail will shed light on these possibilities and advance our understanding of the correlates and consequences of music engagement, and the mechanisms that drive the associations discussed above.
New approaches to studying music and mental health
Using our theoretical model as a guide, we next highlight key avenues of research that will help disentangle these music-mental health associations using state-of-the-art approaches. They include the use of (1) genetic designs, (2) neuroimaging methods, and (3) large biobanks of EHRs.
Genetic designs
Genetic designs provide a window into the biological underpinnings of music engagement [ 123 ]. Understanding the contribution of genetic risk factors is crucial to test causal or mechanistic models regarding potential associations with mental health. At the most basic level, twin and family studies can estimate genetic correlations among music ability or engagement measures and mental health traits or diagnoses. Genetic associations can be examined while simultaneously quantifying environmental correlations, as well as evaluating (bidirectional) causal associations, by testing competing models or averaging across different candidate models [ 102 , 124 ], informing Path 1.
By leveraging samples with genomic, music engagement, and mental health data, investigators can also examine whether individuals at higher genetic risk for psychopathology (e.g., for MDD) show stronger associations between music engagement measures and their mental health outcomes (Path 2). As a theoretical example, individuals with low genetic risk for MDD are unlikely to have many depressive symptoms regardless of their music engagement, so the association between depressive symptoms and music engagement may be weak if focusing on these individuals. However, individuals at high genetic risk for MDD who engage with music may have fewer symptoms than their non-musician peers (i.e., a stronger negative correlation). This is in line with recent work revealing the heritability of depression is doubled in trauma exposed compared to non-trauma exposed individuals [ 125 ].
Gene–environment interaction studies using polygenic scores (i.e., summed indices of genetic risk based on genome-wide association studies; GWAS) are becoming more common [ 126 , 127 ]. There are already multiple large GWAS of internalizing and externalizing traits [ 128 , 129 , 130 ], and the first large-scale GWAS of a music measure indicates that music rhythm is also highly polygenic [ 131 ]. Importantly, is not necessary to have all traits measured in the same sample to examine cross-trait relationships. Studies with only music engagement and genetic data, for example, can still examine how polygenic scores for depression predict music engagement, or interact with music engagement measures to predict other study outcomes. Figure 4 displays an example of a GWAS and how it can be used to compute and apply a polygenic score to test cross-trait predictions.
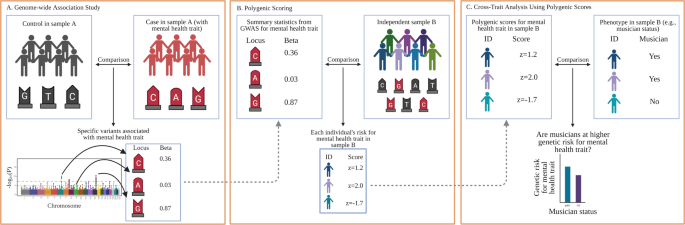
A GWAS are conducted by examining whether individual genetic loci (i.e., single-nucleotide polymorphisms, or SNPs, depicted with G, A, C, and T labels within a sample (or meta-analysis) differentiate cases from controls. The example is based on a dichotomous mental health trait (e.g., major depressive disorder diagnosis), but GWAS can be applied to other dichotomous and continuous phenotypes, such as trait anxiety, musician status, or hours of music practice. Importantly, rather than examining associations on a gene-by-gene basis, GWAS identify relevant genetic loci using SNPs from across the entire genome (typically depicted using a Manhattan plot, such as that displayed at the bottom of A ). B After a GWAS has been conducted on a given trait, researchers can use the output to generate a polygenic score (sometimes called a polygenic risk score) in any new sample with genetic data by summing the GWAS effect sizes for each SNP allele present in a participant’s genome. An individual with a z = 2.0 would have many risk SNPs for that trait, whereas an individual with z = −2 would have much fewer risk SNPs. C Once a polygenic score is generated for all participants, it can be applied like any other variable in the new sample. In this example, researchers could examine whether musicians are at higher (or lower) genetic risk for a specific disorder. Other more complex analyses are also possible, such as examining how polygenic scores interact with existing predictors (e.g., trauma exposure) or polygenic scores for other traits to influence a phenotype or predict an intervention outcome. Created with BioRender.com.
Finally, longitudinal twin and family studies continue to be a promising resource for understanding the etiology and developmental time-course of the correlates of mental health problems. Such designs can be used to examine whether associations between music and mental health are magnified based on other exposures or psychological constructs (gene-by-environment interactions) [ 132 ], and whether parents engaged with music are more likely to pass down environments that are protective or hazardous for later mental health (gene-environment correlations) in addition to passing on their genes. These studies also provide opportunities to examine whether these associations change across key developmental periods. The publicly available Adolescent Brain Cognitive Development study, for example, is tracking over 10,000 participants (including twin and sibling pairs) throughout adolescence, with measures of music engagement and exhaustive measures of mental health, cognition, and personality, as well as neuroimaging and genotyping [ 133 , 134 ]. Although most large samples with genomic data still lack measures of music engagement, key musical phenotypes could be added to existing study protocols (or to similar studies under development) with relatively low participant burden [ 135 ]. Musical questionnaires and/or tasks may be much more engaging and enjoyable than other tasks, improving volunteers’ research participation experience.
Neuroimaging
Another way to orient the design of experiments is through the exploration of neural mechanisms by which music might have an impact on mental health. This is an enormous, growing, and sometimes fraught literature, but there is naturally a great potential to link our understanding of neural underpinnings of music listening and engagement with the literature on neural bases of mental health. These advances can inform the mechanisms driving successful interventions and inform who may benefit the most from such interventions. We focus on two areas among many: (1) the activation of reward circuitry by music and (2) the impact music has on dynamic patterns of neural activity, both of which are likely vectors for the interaction of music and mental health and provide examples of potential interactions.
Music and reward
The strong effect of music on our emotions has been clearly grounded in its robust activation of reward circuitry in the brain, and motivational and hedonic effects of music listening have been shown to be specifically modulated by dopamine [ 16 , 105 , 136 ]. The prevalence of reward and dopaminergic dysfunction in mental illness makes this a rich area for future studies. For example, emotional responses to music might be used as a substitute for reward circuit deficiencies in depression, and it is intriguing to consider if music listening or music engagement could potentiate such function [ 137 , 138 ].
Music and brain network dynamics
The search for neuronally based biomarkers of aspects of mental illness has been a central thrust within the field [ 139 ], holding promise for the understanding of heterogeneity within disorders and identification of common mechanistic pathways [ 140 ]. A thorough review is beyond the scope of this paper, but several points of contact can be highlighted that might suggest neuro-mechanistic mediators of musical effects on mental health. For example, neurofeedback-directed upregulation of activity in emotion circuitry has been proposed as a therapy for MDD [ 141 ]. Given the emotional effects of music, there is potential for using musical stimuli as an adjuvant, or as a more actively patient-controlled output target for neurofeedback. Growing interest in measures of the dynamic complexity of brain activity in health and disease as measured by magnetic resonance imaging or magneto/electroencephalography (M/EEG) [ 142 ] provides a second point of contact, with abnormalities in dynamic complexity suggested as indicative of mental illness [ 143 ], while music engagement has been suggested to reflect and perhaps affect dynamic complexity [ 144 , 145 ].
The caveats identified in this review apply equally to such neuro-mechanistic studies [ 146 ]. High-quality experimental design (involving appropriate controls and randomized design) has been repeatedly shown to be critical to providing reliable evidence for non-music outcomes of music engagement [ 103 ]. For such studies to have maximal impact, analysis of M/EEG activity not at the scalp level, but at the source level, has been shown to improve the power of biomarkers, and their mechanistic interpretability [ 147 , 148 ]. Moreover, as with genetic influences that typically influence a trait through a multitude of small individual effects [ 149 ], the neural underpinnings of music-mental health associations may be highly multivariate. In the longer term, leveraging large-scale studies and large-scale data standardization and aggregation hold the promise of gleaning deeper cross-domain insights, for which current experimentalists can prepare by adopting standards for the documentation, annotation, and storage of data [ 150 ].
Biobanks and electronic health records
Finally, the use of EHR databases can be useful in quantifying associations between music engagement and mental health in large samples. EHR databases can include hundreds of thousands of records and allow for examination with International Statistical Classification of Diseases and Related Health Problems codes, including MDD, SUD, and schizophrenia diagnoses. This would allow for powerful estimates of music-mental health associations, and exploration of music engagement with other health outcomes.
The principal roadblock to this type of research is that extensive music phenotypes are not readily available in EHRs. However, there are multiple ways to bypass this limitation. First, medical records can be scraped using text-mining tools to identify cases of musician-related terms (e.g., “musician”, “guitarist”, “violinist”). For example, the phenome-wide association study described earlier [ 55 ] compared musician cases and controls identified in a large EHR database through text-mining of medical records and validated with extensive manual review charts. This study was highly powered to detect associations with internalizing and thought disorders (but showed null or protective effects for musicians for SUDs). Many EHR databases also include genomic data, allowing for integration with genetic models even in the absence of music data (e.g., exploring whether individuals with strong genetic predispositions for musical ability are at elevated or reduced risk for specific health diagnosis).
EHRs could also be used as recruitment tools, allowing researchers to collect additional data for relevant music engagement variables and compare with existing mental health diagnoses without having to conduct their own diagnostic interviews. These systems are not only relevant to individual differences research but could also be used to identify patients for possible enrollment in intervention studies. Furthermore, if recruitment for individual differences or intervention studies is done in patient waiting rooms of specific clinics, researchers can target specific populations of interest, have participants complete some relevant questionnaires while they wait, and be granted access to medical record data without having to conduct medical interviews themselves.
Concluding remarks
Music engagement, a uniquely human trait which has a powerful impact on our everyday experience, is deeply tied with our social and cultural identities as well as our personality and cognition. The relevance of music engagement to mental health, and its potential use as a therapeutic tool, has been studied for decades, but this research had not yet cohered into a clear picture. Our scoping review and framework integrated across a breadth of smaller literatures (including extant reviews and meta-analyses) relating music engagement to mental health traits and treatment effects, though it was potentially limited due to the lack of systematic literature search or formal quality appraisal of individual studies. Taken together, the current body of literature suggests that music engagement may provide an outlet for individuals who are experiencing internalizing, externalizing, or thought disorder problems, potentially supporting emotion regulation through multiple neurobiological pathways (e.g., reward center activity). Conducting more rigorous experimental intervention studies, improving reporting standards, and harnessing large-scale population-wide data in combination with new genetic analytic methods will help us achieve a better understanding of how music engagement relates to these mental health traits. We have presented a framework that illustrates why it will be vital to consider genetic and environmental risk factors when examining these associations, leading to new avenues for understanding the mechanisms by which music engagement and existing risk factors interact to support mental health and well-being.
Mankel K, Bidelman GM. Inherent auditory skills rather than formal music training shape the neural encoding of speech. Proc Natl Acad Sci. 2018;115:13129–34.
Article CAS PubMed PubMed Central Google Scholar
Swaminathan S, Schellenberg EG. Musical competence is predicted by music training, cognitive abilities, and personality. Sci Rep. 2018;8:9223.
Article PubMed PubMed Central CAS Google Scholar
Mosing MA, Pedersen NL, Madison G, Ullen F. Genetic pleiotropy explains associations between musical auditory discrimination and intelligence. PLos One. 2014;9:e113874.
Weinberg MK, Joseph D. If you’re happy and you know it: Music engagement and subjective wellbeing. Psychol Music. 2017;45:257–67.
Article Google Scholar
Theorell TP, Lennartsson AK, Mosing MA, Ullen F. Musical activity and emotional competence - a twin study. Front Psychol. 2014;5:774.
Article PubMed PubMed Central Google Scholar
Cirelli LK, Trehub SE, Trainor LJ. Rhythm and melody as social signals for infants. Ann N Y Acad Sci. 2018;1423:66–72.
Zentner M, Eerola T. Rhythmic engagement with music in infancy. Proc Natl Acad Sci. 2010;107:5768–73.
Lense MD, Beck S, Liu C, Pfeiffer R, Diaz N, Lynch M, et al. Parents, peers, and musical play: Integrated parent-child music class program supports community participation and well-being for families of children with and without Autism Spectrum Disorder. Front Psychol. 2020;11:11.
Honing H. On the biological basis of musicality. Ann N Y Acad Sci. 2018;1423:51–6.
Maratos AS, Gold C, Wang X, Crawford MJ. Music therapy for depression. Cochrane Database Syst Rev. 2008;1:CD004517.
Ansdell G, Meehan J. “Some Light at the End of the Tunnel”: exploring Users’ evidence for the effectiveness of music therapy in adult mental health settings. Music Med. 2010;2:29–40.
Khalfa S, Bella SD, Roy M, Peretz I, Lupien SJ. Effects of relaxing music on salivary cortisol level after psychological stress. Ann N Y Acad Sci. 2003;999:374–6.
Article PubMed Google Scholar
McKinney CH, Antoni MH, Kumar M, Tims FC, McCabe PM. Effects of guided imagery and music (GIM) therapy on mood and cortisol in healthy adults. Health Psychol. 1997;16:390–400.
Article CAS PubMed Google Scholar
Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013;17:179–93.
Olff M, Koch SB, Nawijn L, Frijling JL, Van Zuiden M, Veltman DJ. Social support, oxytocin, and PTSD. Eur J Psychotraumatol. 2014;5:26513.
Ferreri L, Mas-Herrero E, Zatorre RJ, Ripollés P, Gomez-Andres A, Alicart H, et al. Dopamine modulates the reward experiences elicited by music. Proc Natl Acad Sci. 2019;116:3793–8.
Evers S, Suhr B. Changes of the neurotransmitter serotonin but not of hormones during short time music perception. Eur Arch Psychiatry Clin Neurosci. 2000;250:144–7.
Blum K, Simpatico T, Febo M, Rodriquez C, Dushaj K, Li M, et al. Hypothesizing music intervention enhances brain functional connectivity involving dopaminergic recruitment: Common neuro-correlates to abusable drugs. Mol Neurobiol. 2017;54:3753–58.
Kotov R, et al. The hierarchical Taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017. https://doi.org/10.1037/abn0000258 .
Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychological Sci. 2014;2:119–37.
Whiteside SP, Lynam DR. Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: Application of the UPPS impulsive behavior scale. Exp Clin Psychopharmacol. 2003;11:210–7.
Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. J Abnorm Psychol. 2013;122:1142–53.
Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, et al. Behavioral disinhibition: liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. J Abnorm Psychol. 2009;118:117–30.
Gustavson DE, Franz CE, Panizzon MS, Lyons MJ, Kremen WS. Internalizing and externalizing psychopathology in middle age: Genetic and environmental architecture and stability of symptoms over 15 to 20 years. Psychological Med. 2019;50:1–9.
Google Scholar
Martin J, Taylor MJ, Lichtenstein P. Assessing the evidence for shared genetic risks across psychiatric disorders and traits. Psychological Med. 2018;48:1759–74.
Panteleeva Y, Ceschi G, Glowinski D, Courvoisier DS, Grandjean D. Music for anxiety? Meta-analysis of anxiety reduction in non-clinical samples. Psychol Music. 2017;46:473–87.
Leubner D, Hinterberger T. Reviewing the effectiveness of music interventions in treating depression. Front Psychol. 2017;8:1109.
Perkins R, Mason-Bertrand A, Fancourt D, Baxter L, Williamon A. How participatory music engagement supports mental well-being: a meta-ethnography. Qualitative Health Res. 2020. https://doi.org/10.1177/1049732320944142 .
Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: reflections and directions. J. Abnorm Child Psychol. 2003;31:285–91.
Kendler KS, Myers J. The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychological Med. 2014;44:647–55.
Article CAS Google Scholar
Robb SL, Burns DS, Carpenter JS. Reporting guidelines for music-based interventions. J Health Psychol. 2011;16:342–52.
Robb SL, Hanson-Abromeit D, May L, Hernandez-Ruiz E, Allison M, Beloat A, et al. Reporting quality of music intervention research in healthcare: a systematic review. Complement Ther Med. 2018;38:24–41.
Carr C, Odell-Miller H, Priebe S. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLos One. 2013;8:e70252.
Miranda D, Blais-Rochette C. Neuroticism and emotion regulation through music listening: a meta-analysis. Musica Sci. 2018. https://doi.org/10.1177/1029864918806341 .
Miranda D. The emotional bond between neuroticism and music. Psychomusicology: Music, Mind, Brain. 2019. https://doi.org/10.1037/pmu0000250 .
Landis-Shack N, Heinz AJ, Bonn-Miller MO. Music therapy for posttraumatic stress in adults: a theoretical review. Psychomusicology. 2017;27:334–342.
Schäfer K, Saarikallio S, Eerola T. Music may reduce loneliness and act as social surrogate for a friend: evidence from an experimental listening study. Music Sci. 2020;3. https://doi.org/10.1177/2059204320935709 .
Braun Janzen T, Al Shirawi MI, Rotzinger S, Kennedy SH, Bartel L. A pilot study investigating the effect of music-based intervention on depression and anhedonia. Front Psychol. 2019;10:1038.
Biasutti M, Mangiacotti A. Music training improves depressed mood symptoms in elderly people: a randomized controlled trial. Int J Aging Hum Dev. 2019. https://doi.org/10.1177/0091415019893988 .
Castillo-Pérez S, Gómez-Pérez V, Velasco MC, Pérez-Campos E, Mayoral M-A. Effects of music therapy on depression compared with psychotherapy. Arts Psychother. 2010;37:387–390.
Hendricks CB, Robinson B, Bradley LJ, Davis K. Using music techniques to treat adolescent depression. J Humanist Counseling. 1999;38:39–46.
Chwalek CM, McKinney CH. The use of dialectical behavior therapy (DBT) in music therapy: a sequential explanatory study. J. Music Ther. 2015;52:282–318.
Tang YY, Yang L, Leve LD, Harold GT. Improving executive function and its neurobiological mechanisms through a mindfulness-based intervention: advances within the field of developmental neuroscience. Child Dev. Perspect. 2012;6:361–66.
PubMed PubMed Central Google Scholar
Didonna F. Mindfulness-based interventions in an inpatient setting. In: Clinical handbook of mindfulness. Springer, New York, NY; 2009. p. 447–62.
Chin T, Rickard NS. Beyond positive and negative trait affect: flourishing through music engagement. Psychol Well-Being. 2014;4:25.
Miranda D, Claes M. Personality traits, music preferences and depression in adolescence. Int J Adolescence Youth. 2008;14:277–98.
Fancourt D, Garnett C, Spiro N, West R, Mullensiefen D. How do artistic creative activities regulate our emotions? Validation of the Emotion Regulation Strategies for Artistic Creative Activities Scale (ERS-ACA). PLos One. 2019;14:e0211362.
Saarikallio S. Development and validation of the brief music in mood regulation scale (B-MMR). Music Percept. 2012;30:97–105.
Saarikallio S, Gold C, McFerran K. Development and validation of the healthy-unhealthy music scale. Child Adolesc Ment Health. 2015;20:210–17.
Groarke JM, Hogan MJ. Development and psychometric evaluation of the adaptive functions of music listening scale. Front Psychol. 2018;9:516.
Thomson CJ, Reece JE, Di Benedetto M. The relationship between music-related mood regulation and psychopathology in young people. Musica Sci. 2014;18:150–65.
Shifriss R, Bodner E, Palgi Y. When you’re down and troubled: views on the regulatory power of music. Psychol Music. 2014;43:793–807.
Garrido S, Schubert E. Moody melodies: do they cheer us up? A study of the effect of sad music on mood. Psychol Music. 2013;43:244–261.
Wesseldijk LW, Ullen F, Mosing MA. The effects of playing music on mental health outcomes. Sci Rep. 2019;9:12606.
Niarchou M, Lin G, Lense MD, Gordon RL, Davis LK. The medical signature of musicians: a phenome-wide association study using an electronic health record database. medRxiv. 2020;10:51. https://doi.org/10.1101/2020.08.14.20175109 .
Vaag J, Sund ER, Bjerkeset O. Five-factor personality profiles among Norwegian musicians compared to the general workforce. Musica Sci. 2017;22:434–445.
Fancourt D, Garnett C, Müllensiefen D. The relationship between demographics, behavioral and experiential engagement factors, and the use of artistic creative activities to regulate emotions. Psychol Aesthet Creat Arts. 2020.(advance online publication)
Mak HW, Fancourt D. Longitudinal associations between ability in arts activities, behavioural difficulties and self-esteem: Analyses from the 1970 British Cohort Study. Sci Rep. 2019;9:14236.
West SG, Taylor AB, Wu W. Model fit and model selection in structural equation modeling. In: Hoyle RH, editor. Handbook of structural equation modeling. New York, NY: The Guilford Press; 2012. p. 209–31.
Weiss B, Susser K, Catron T. Common and specific features of childhood psychopathology. J Abnorm Psychol. 1998;107:118–27.
Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personal Individ Differences. 2001;30:1245–159.
Morse S, et al. Audio therapy significantly attenuates aberrant mood in residential patient addiction treatment: putative activation of dopaminergic pathways in the meso-limbic reward circuitry of humans. J Addict Res Ther. 2011;3:2.
Baker FA, Gleadhill LM, Dingle GA. Music therapy and emotional exploration: exposing substance abuse clients to the experiences of non-drug-induced emotions. Arts Psychother. 2007;34:321–330.
Dingle GA, Gleadhill L, Baker FA. Can music therapy engage patients in group cognitive behaviour therapy for substance abuse treatment? Drug Alcohol Rev. 2008;27:190–6.
Hohmann L, Bradt J, Stegemann T, Koelsch S. Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLos One. 2017;12:e0187363.
Swope PM. Effects of learning the drums on inattention, vigilance, and sustained attention in adolescents with ADHD. Spalding University; 2018.
Zimmermann MB, Diers K, Strunz L, Scherbaum N, Mette C. Listening to Mozart improves current mood in adult ADHD: a randomized controlled pilot study. Front Psychol. 2019;10:1104.
Madjar N, Gazoli R, Manor I, Shoval G. Contrasting effects of music on reading comprehension in preadolescents with and without ADHD. Psychiatry Res. 2020;291:113207.
Pelham WE, Waschbusch DA, Hoza B, Gnagy EM, Greiner AR, Sams SE, et al. Music and video as distractors for boys with ADHD in the classroom: comparison with controls, individual differences, and medication effects. J Abnorm Child Psychol. 2011;39:1085–98.
Porter S, McConnell T, McLaughlin K, Lynn F, Cardwell C, Braiden HJ, et al. Music therapy for children and adolescents with behavioural and emotional problems: a randomised controlled trial. J Child Psychol Psychiatry. 2017;58:586–94.
Chong HJ, Kim SJ. Education-oriented music therapy as an after-school program for students with emotional and behavioral problems. Arts Psychother. 2010;37:190–96.
Rickson DJ, Watkins WG. Music therapy to promote prosocial behaviors in aggressive adolescent boys—a pilot study. J. Music Ther. 2003;40:283–301.
Montello L, Coons EE. Effects of active versus passive group music therapy on preadolescents with emotional, learning, and behavioral disorders. J Music Ther. 1999;35:49–67.
Mulder J, Ter Bogt TF, Raaijmakers QA, Gabhainn SN, Monshouwer K, Vollebergh WA. The soundtrack of substance use: Music preference and adolescent smoking and drinking. Subst Use Misuse. 2009;44:514–31.
Mulder J, Ter Bogt TF, Raaijmakers QA, Nic Gabhainn S, Monshouwer K, Vollebergh WA. Is it the music? Peer substance use as a mediator of the link between music preferences and adolescent substance use. J Adolescence. 2010;33:387–94.
Chen MJ, Miller BA, Grube JW, Waiters ED. Music, substance use, and aggression. J Stud Alcohol. 2006;67:373–81.
ter Bogt TF, Gabhainn SN, Simons-Morton BG, Ferreira M, Hublet A, Godeau E, et al. Dance is the new metal: adolescent music preferences and substance use across Europe. Subst Use Misuse. 2012;47:130–42.
Slater JL, Tate MC. Timing deficits in ADHD: insights from the neuroscience of musical rhythm. Front Comput Neurosci. 2018;12:51.
Carrer LR. Music and sound in time processing of children with ADHD. Front Psychiatry. 2015;6:127.
Miksza P. Relationships among impulsivity, achievement goal motivation, and the music practice of high school wind players. Bull Council Res Music Educ. 2009;180:9–27.
Miksza P. Relationships among achievement goal motivation, impulsivity, and the music practice of collegiate brass and woodwind players. Psychol Music. 2010;39:50–67.
Geretsegger M, Mössler KA, Bieleninik Ł, Chen XJ, Heldal TO, Gold C. Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database Syst Rev. 2017;5:CD004025.
PubMed Google Scholar
Volpe U, Gianoglio C, Autiero L, Marino ML, Facchini D, Mucci A, et al. Acute effects of music therapy in subjects with psychosis during inpatient treatment. Psychiatry. 2018;81:218–27.
Pavlov A, Kameg K, Cline TW, Chiapetta L, Stark S, Mitchell AM. Music therapy as a nonpharmacological intervention for anxiety in patients with a thought disorder. Issues Ment Health Nurs. 2017;38:285–8.
Haugwitz, B. (2021). Music therapy in the early detection and indicated prevention in persons at risk of bipolar disorders: state of knowledge and potential. Br J Music Ther. 2021. https://doi.org/10.1177/1359457521997386 .
Power RA, Steinberg S, Bjornsdottir G, Rietveld CA, Abdellaoui A, Nivard MM, et al. Polygenic risk scores for schizophrenia and bipolar disorder predict creativity. Nat Neurosci. 2015;18:953–5.
Fancourt D, Ockelford A, Belai A. The psychoneuroimmunological effects of music: a systematic review and a new model. Brain Behav. Immun. 2014;36:15–26.
Baker FA, Metcalf O, Varker T, O’Donnell M. A systematic review of the efficacy of creative arts therapies in the treatment of adults with PTSD. Psychol Trauma. 2018;10:643–51.
Lense MD, Camarata S. PRESS-Play: musical engagement as a motivating platform for social interaction and social play in young children with ASD. Music Sci. 2020. https://doi.org/10.1177/2059204320933080 .
Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. Psychological Rev. 1997;104:667–85.
Zuckerman M, Riskind JH. Vulnerability to psychopathology: a biosocial model. J Cogn Psychother. 2000;14:407–8.
Trucco EM, Madan B, Villar M. The impact of genes on adolescent substance use: a developmental perspective. Curr Addict Rep. 2019;6:522–531.
Butkovic A, Ullen F, Mosing MA. Personality related traits as predictors of music practice: underlying environmental and genetic influences. Personal Individ Differences. 2015;74:133–8.
Coon H, Carey G. Genetic and environmental determinants of musical ability in twins. Behav Genet. 1989;19:183–93.
Ullén F, Mosing MA, Holm L, Eriksson H, Madison G. Psychometric properties and heritability of a new online test for musicality, the Swedish Musical Discrimination Test. Personal Individ Differences. 2014;63:87–93.
Hambrick DZ, Tucker-Drob EM. The genetics of music accomplishment: evidence for gene-environment correlation and interaction. Psychonomic Bull Rev. 2015;22:112–20.
Wesseldijk LW, Mosing MA, Ullen F. Gene-environment interaction in expertise: the importance of childhood environment for musical achievement. Dev Psychol. 2019;55:1473–9.
Ullen F, Mosing MA, Madison G. Associations between motor timing, music practice, and intelligence studied in a large sample of twins. Ann N Y Acad Sci. 2015;1337:125–9.
Botvin GJ. Substance abuse prevention: theory, practice, and effectiveness. Crime Justice. 1990;13:461–519.
Fredricks JA, Simpkins S, Eccles JS. Family socialization, gender, and participation in sports and instrumental music. In: Developmental pathways through middle childhood. Mahwah, NJ: Psychology Press; 2006. p. 53–74.
Maes HH, Neale MC, Kirkpatrick RM, Kendler KS. Using multimodal inference/model averaging to model causes of covariation between variables in twins. Behav Genet. 2020. https://doi.org/10.1007/s10519-020-10026-8 .
Sala G, Gobet F. When the music’s over. Does music skill transfer to children’s and young ado escents’ cognitive and academic skills? A meta-analysis. Educ Res Rev. 2017;20:55–67.
Salimpoor VN, Zald DH, Zatorre RJ, Dagher A, McIntosh AR. Predictions and the brain: how musical sounds become rewarding. Trends Cogn Sci. 2015;19:86–91.
Loui P, Patterson S, Sachs ME, Leung Y, Zeng T, Przysinda E. White matter correlates of musical anhedonia: Implications for evolution of music. Front Psychol. 2017;8:1664.
Salimpoor VN, van den Bosch I, Kovacevic N, McIntosh AR, Dagher A, Zatorre RJ. Interactions between the nucleus accumbens and auditory cortices predict music reward value. Science. 2013;340:216–9.
Zatorre RJ, Salimpoor VN. From perception to pleasure: music and its neural substrates. Proc Natl Acad Sci. 2013;110:10430–7. Suppl 2
Alluri V, Brattico E, Toiviainen P, Burunat I, Bogert B, Numminen J, et al. Musical expertise modulates functional connectivity of limbic regions during continuous music listening. Psychomusicology. 2015;25:443–54.
Vanyukov MM, Tarter RE, Kirisci L, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 1. Common mechanisms and manifestations. Neurosci Biobehav Rev. 2003;27:507–515.
Volkow ND, Morales M. The brain on drugs: from reward to addiction. Cell. 2015;162:712–25.
Wise RA. Dopamine and reward: the anhedonia hypothesis 30 years on. Neurotox Res. 2008;14:169–83.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Mukherjee S, Coque L, Cao JL, Kumar J, Chakravarty S, Asaithamby A, et al. Knockdown of Clock in the ventral tegmental area through RNA interference results in a mixed state of mania and depression-like behavior. Biol Psychiatry. 2010;68:503–11.
Kaufling J. Alterations and adaptation of ventral tegmental area dopaminergic neurons in animal models of depression. Cell Tissue Res. 2019;377:59–71.
Small KM, Nunes E, Hughley S, Addy NA. Ventral tegmental area muscarinic receptors modulate depression and anxiety-related behaviors in rats. Neurosci Lett. 2016;616:80–5.
Kokal I, Engel A, Kirschner S, Keysers C. Synchronized drumming enhances activity in the caudate and facilitates prosocial commitment-if the rhythm comes easily. PLos One. 2011;6:e27272.
Goldstein A. Thrills in response to music and other stimuli. Physiological Psychol. 1980;8:126–9.
Moore E, Schaefer RS, Bastin ME, Roberts N, Overy K. Can musical training influence brain connectivity? Evidence from diffusion tensor MRI. Brain Sci. 2014;4:405–27.
Imfeld A, Oechslin MS, Meyer M, Loenneker T, Jancke L. White matter plasticity in the corticospinal tract of musicians: a diffusion tensor imaging study. Neuroimage. 2009;46:600–7.
Han Y, Yang H, Lv YT, Zhu CZ, He Y, Tang HH, et al. Gray matter density and white matter integrity in pianists’ brain: a combined structural and diffusion tensor MRI study. Neurosci Lett. 2009;459:3–6.
Schmithorst VJ, Wilke M. Differences in white matter architecture between musicians and non-musicians: a diffusion tensor imaging study. Neurosci Lett. 2002;321:57–60.
Hudziak JJ, Albaugh MD, Ducharme S, Karama S, Spottswood M, Crehan E, et al. Cortical thickness maturation and duration of music training: Health-promoting activities shape brain development. J Am Acad Child Adolesc Psychiatry. 2014;53:1153–61.
Gingras B, Honing H, Peretz I, Trainor LJ, Fisher SE. Defining the biological bases of individual differences in musicality. Philos Trans R Soc B. 2015;370:20140092.
Heath AC, Kessler RC, Neale MC, Hewitt JK, Eaves LJ, Kendler KS. Testing hypotheses about direction of causation using cross-sectional family data. Behav Genet. 1993;23:29–50.
Coleman JRI, Peyrot WJ, Purves KL, Davis KAS, Rayner C, Choi SW, et al. Genome-wide gene-environment analyses of major depressive disorder and reported lifetime traumatic experiences in UK Biobank. Mol Psychiatry. 2020;25:247353–1446.
Domingue BW, Liu HX, Okbay A, Belsky DW. Genetic heterogeneity in depressive symptoms following the death of a spouse: polygenic score analysis of the US Health and Retirement Study. Am J Psychiatry. 2017;174:963–970.
Barcellos SH, Carvalho LS, Turley P. Education can reduce health differences related to genetic risk of obesity. Proc Natl Acad Sci USA. 2018;115:E9765–E9772.
Howard DM, Adams MJ, Shirali M, Clarke TK, Marioni RE, Davies G, et al. Genome-wide association study of depression phenotypes in UK Biobank identifies variants in excitatory synaptic pathways. Nat Commun. 2018;9:1470.
Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat Genet. 2016;48:624–33.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Niarchou M, et al. Unraveling the genetic architecture of music rhythm. https://www.biorxiv.org/content/10.1101/836197v1 . 2019 ; 29:S62.
Purcell S. Variance components models for gene-environment interaction in twin analysis. Twin Res. 2002;5:554–71.
Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev Cogn Neurosci. 2018;32:55–66.
Uban KA, Horton MK, Jacobus J, Heyser C, Thompson WK, Tapert SF, et al. Biospecimens and the ABCD study: rationale, methods of collection, measurement and early data. Dev Cogn Neurosci. 2018;32:97–106.
Mullensiefen D, Gingras B, Musil J, Stewart L. The musicality of non-musicians: an index for assessing musical sophistication in the general population. PLos One. 2014;9:e89642.
Blood AJ, Zatorre RJ. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci. 2001;98:11818–23.
Jenkins LM, Skerrett KA, DelDonno SR, Patrón VG, Meyers KK, Peltier S, et al. Individuals with more severe depression fail to sustain nucleus accumbens activity to preferred music over time. Psychiatry Res Neuroimaging. 2018;275:21–7.
Belfi AM, Loui P. Musical anhedonia and rewards of music listening: current advances and a proposed model. Ann N Y Acad Sci. 2020;1464:99–114.
Insel T, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am Psychiatric Assoc. 2010;167:748–51.
Loo SK, McGough JJ, McCracken JT, Smalley SL. Parsing heterogeneity in attention-deficit hyperactivity disorder using EEG-based subgroups. J Child Psychol Psychiatry. 2018;59:223–31.
Zotev V, Mayeli A, Misaki M, Bodurka J. Emotion self-regulation training in major depressive disorder using simultaneous real-time fMRI and EEG neurofeedback. Neuroimage Clin. 2020;27:102331.
Yang AC, Jann K, Michel CM, Wang DJJ. Editorial: advances in multi-scale analysis of brain complexity. Front Neurosci. 2020;14:337.
Lin C, Lee SH, Huang CM, Chen GY, Ho PS, Liu HL, et al. Increased brain entropy of resting-state fMRI mediates the relationship between depression severity and mental health-related quality of life in late-life depressed elderly. J Affect Disord. 2019;250:270–7.
Bhattacharya J, Lee EJ. Modulation of EEG theta band signal complexity by music therapy. Int J Bifurc Chaos. 2016;26:1650001.
Carpentier SM, McCulloch AR, Brown TM, Faber S, Ritter P, Wang Z, et al. Complexity matching: brain signals mirror environment information patterns during music listening and reward. J Cogn Neurosci. 2020;32:734–45.
Etkin A. A reckoning and research agenda for neuroimaging in psychiatry. Am J Psychiatry. 2019;176:507–11.
Rissling AJ, Makeig S, Braff DL, Light GA. Neurophysiologic markers of abnormal brain activity in schizophrenia. Curr Psychiatry Rep. 2010;12:572–8.
Loo SK, Makeig S. Clinical utility of EEG in attention-deficit/hyperactivity disorder: a research update. Neurotherapeutics. 2012;9:569–87.
Boyle EA, Li YI, Pritchard JK. An expanded view of complex traits: from polygenic to omnigenic. Cell. 2017;169:1177–86.
Sivagnanam S, Yoshimoto K, Carnevale T, Nadeau D, Kandes M, Petersen T, et al. Neuroscience Gateway enabling large scale modeling and data processing in neuroscience research. In: Practice and Experience in Advanced Research Computing. Association for Computing Machinery, Portland, OR, USA ; 2020. p.510–513.
Download references
Acknowledgements
This work was supported by NIH grants DP2HD098859, R01AA028411, R61MH123029, R21DC016710, U01DA04112, and R03AG065643, National Endowment for the Arts (NEA) research lab grants 1863278-38 and 1855526-38, and National Science Foundation grant 1926794. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Endowment for the Arts. The authors would like to thank Navya Thakkar and Gabija Zilinskaite for their assistance.
Author information
Authors and affiliations.
Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
- Daniel E. Gustavson
Vanderbilt Genetics Institute, Vanderbilt University Medical Center, Nashville, TN, USA
Daniel E. Gustavson, Reyna L. Gordon & Miriam D. Lense
Department of Otolaryngology – Head & Neck Surgery, Vanderbilt University Medical Center, Nashville, TN, USA
Peyton L. Coleman & Reyna L. Gordon
Swartz Center for Computational Neuroscience, Institute for Neural Computation, University of California, San Diego, La Jolla, CA, USA
John R. Iversen
Department of Human and Molecular Genetics, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA
- Hermine H. Maes
Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA
Massey Cancer Center, Virginia Commonwealth University, Richmond, VA, USA
Vanderbilt Brain Institute, Vanderbilt University, Nashville, TN, USA
Reyna L. Gordon & Miriam D. Lense
The Curb Center, Vanderbilt University, Nashville, TN, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniel E. Gustavson .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gustavson, D.E., Coleman, P.L., Iversen, J.R. et al. Mental health and music engagement: review, framework, and guidelines for future studies. Transl Psychiatry 11 , 370 (2021). https://doi.org/10.1038/s41398-021-01483-8
Download citation
Received : 23 November 2020
Revised : 03 June 2021
Accepted : 10 June 2021
Published : 22 June 2021
DOI : https://doi.org/10.1038/s41398-021-01483-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Laura W. Wesseldijk
- Miriam A. Mosing
Translational Psychiatry (2023)
Effects of music-based interventions on cancer-related pain, fatigue, and distress: an overview of systematic reviews
- Ana Trigueros-Murillo
- Javier Martinez-Calderon
- Alberto Marcos Heredia-Rizo
Supportive Care in Cancer (2023)
A Systematic Review of Music-Based Interventions to Improve Treatment Engagement and Mental Health Outcomes for Adolescents and Young Adults
- Aaron H. Rodwin
- Rei Shimizu
- Michelle R. Munson
Child and Adolescent Social Work Journal (2023)
Heritability of Childhood Music Engagement and Associations with Language and Executive Function: Insights from the Adolescent Brain Cognitive Development (ABCD) Study
- Srishti Nayak
Behavior Genetics (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Articles on Music therapy
Displaying 1 - 20 of 26 articles.

Music therapy could help manage the pain of bereavement
Lisa Graham-Wisener , Queen's University Belfast and Tracey McConnell , Queen's University Belfast

How music heals us, even when it’s sad – by a neuroscientist leading a new study of musical therapy
Leigh Riby , Northumbria University, Newcastle

How music therapy can help rebuild the lives of refugees
Elizabeth Coombes , University of South Wales

Drawing, making music and writing poetry can support healing and bring more humanity to health care in US hospitals
Marlaine Figueroa Gray , University of Washington

How an African church choir made a difference to care home life in Greater Manchester
Kayonda Hubert Ngamaba , University of York and Cheyann Heap , University of York

What’s your school closures playlist? Why music should be part of parents’ pandemic survival strategy
Ala Krivov , Western University

Anxiety: a playlist to calm the mind from a music therapist

High-tech concert hall measures brain waves and heart rates during performances
Laurel Trainor , McMaster University and Dan J. Bosnyak , McMaster University

Curious Kids: is it OK to listen to music while studying?
Timothy Byron , University of Wollongong

How music therapy can help anxious children

Music therapy improves the health of premature babies and boosts parental bonding

Creative arts therapies can help people with dementia socialise and express their grief
Joanna Jaaniste , Western Sydney University

Groovy findings: Researching how and why music moves you
Tomas Matthews , Concordia University

Singing death: why music and grief go hand in hand
Helen Maree Hickey , The University of Melbourne and Helen Dell , The University of Melbourne

The healing power of hip hop
Alexander Crooke , The University of Melbourne and Raphael Travis Jr. , Texas State University

Understanding the NDIS: how does the scheme view music therapy?
Katrina McFerran , The University of Melbourne

Ageing in harmony: why the third act of life should be musical
Jennifer MacRitchie , Western Sydney University

Songwriting as solace: ‘I live in the same body but it can’t talk to me any more’
Felicity Anne Baker , The University of Melbourne

Questions to ask your teenager about music and mental health

How music can help relieve chronic pain
Don Knox , Glasgow Caledonian University
Related Topics
- Art therapy
- Music education
Top contributors
Senior Lecturer in Music Therapy, University of South Wales
Professor and Head of Music Therapy, The University of Melbourne
Senior Research Fellow, Music Therapy, The University of Melbourne
PhD Candidate, Music and Public Health, Griffith University
Professor of Music Therapy, Berklee College of Music
Senior research fellow in health and wellbeing, University of Sheffield
Reader in health technology assessment, Brunel University London
Senior audio lecturer, Glasgow Caledonian University
Postdoctoral Research Fellow in Music Therapy, The University of Melbourne
Researcher in the Australian Research Council for the History of Emotions, The University of Melbourne
Professor of Social Work, Texas State University
Honorary Research Fellow in the School of Culture and Communication, University of Melbourne, The University of Melbourne
Research Fellow, Social Policy & Social Work, School for Business and Society, University of York
PhD Candidate, Concordia University
Career Development Fellow, Western Sydney University
- X (Twitter)
- Unfollow topic Follow topic
- Introduction
- Conclusions
- Article Information
IV indicates inverse variance; MT, music therapy. Box size corresponds to the weighting of each study in the meta-analysis. Diamonds provided for each subgroup as well as the overall analysis indicate the aggregated mean (middle of the diamond) and 95% CIs (points of the diamonds) of results from appropriate included studies. Total refers to the total number of participants included in analyses at preintervention and postintervention time points.
IV indicates inverse variance; MT, music therapy. Total refers to the total number of participants included in analyses at preintervention and postintervention time points.
IV indicates inverse variance. Total refers to the total number of participants included in analyses at preintervention and postintervention time points.
eTable 1. Articles Excluded After Full-text Review, With Reasons
eTable 2. Reviews Searched for Additional Records in This Meta-analysis
eTable 3. GRADE Quality of Evidence Ratings for Included Studies
eFigure 1. PRISMA Flow Diagram
eFigure 2. Funnel Plot Detailing Distribution of MCS Pre-post Changes
eFigure 3. Funnel Plot Detailing Distribution of PCS Pre-post Changes
eFigure 4. Funnel Plot Detailing Distribution of MCS Changes in Music Plus TAU vs TAU Interventions
eFigure 5. Funnel Plot Detailing Distribution of PCS Changes in Music Plus TAU vs TAU Interventions
eFigure 6. Meta-analysis of Pre-post Changes in MCS Scores, Stratified by Music Plus TAU vs All Other Interventions
eFigure 7. Meta-analysis of Pre-post Changes in PCS Scores, Stratified by Music Plus TAU vs All Other Interventions
eFigure 8. Meta-analysis of MCS Scores in Music vs Meditation Interventions
eFigure 9. Meta-analysis of PCS Scores in Music vs Meditation Interventions
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
McCrary JM , Altenmüller E , Kretschmer C , Scholz DS. Association of Music Interventions With Health-Related Quality of Life : A Systematic Review and Meta-analysis . JAMA Netw Open. 2022;5(3):e223236. doi:10.1001/jamanetworkopen.2022.3236
Manage citations:
© 2024
- Permissions
Association of Music Interventions With Health-Related Quality of Life : A Systematic Review and Meta-analysis
- 1 Institute of Music Physiology and Musicians’ Medicine, Hannover University of Music, Drama and Media, Hannover, Germany
- 2 Prince of Wales Clinical School, University of New South Wales, Sydney, New South Wales, Australia
Question Are music-making and listening interventions associated with positive changes in health-related quality of life?
Findings This systematic review and meta-analysis of 26 studies comprising 779 individuals found that music interventions were associated with statistically and clinically significant changes in mental HRQOL, both preintervention to postintervention as well as when music interventions were added to treatment as usual vs treatment as usual control groups.
Meaning These results suggest that associations between music interventions and clinically significant changes in HRQOL are demonstrable in comprehensive reviews of previous studies.
Importance Increasing evidence supports the ability of music to broadly promote well-being and health-related quality of life (HRQOL). However, the magnitude of music’s positive association with HRQOL is still unclear, particularly relative to established interventions, limiting inclusion of music interventions in health policy and care.
Objective To synthesize results of studies investigating outcomes of music interventions in terms of HRQOL, as assessed by the 36- and 12-Item Health Survey Short Forms (SF-36 and SF-12).
Data Sources MEDLINE, Embase, Web of Science, PsycINFO, ClinicalTrials.gov, and International Clinical Trials Registry Platform (searched July 30, 2021, with no restrictions).
Study Selection Inclusion criteria were randomized and single-group studies of music interventions reporting SF-36 data at time points before and after the intervention. Observational studies were excluded. Studies were reviewed independently by 2 authors.
Data Extraction and Synthesis Data were independently extracted and appraised using GRADE criteria (Grading of Recommendations, Assessment, Development, and Evaluations) by multiple authors. Inverse-variance random-effects meta-analyses quantified changes in SF-36 mental and physical component summary (respectively, MCS and PCS) scores from preintervention to postintervention and vs common control groups.
Main Outcomes and Measures SF-36 or SF-12 MCS and PCS scores, defined a priori.
Results Analyses included 779 participants from 26 studies (mean [SD] age, 60 [11] years). Music interventions (music listening, 10 studies; music therapy, 7 studies; singing, 8 studies; gospel music, 1 study) were associated with significant improvements in MCS scores (total mean difference, 2.95 points; 95% CI, 1.39-4.51 points; P < .001) and PCS scores (total mean difference, 1.09 points; 95% CI, 0.15-2.03 points; P = .02). In subgroup analysis (8 studies), the addition of music to standard treatment for a range of conditions was associated with significant improvements in MCS scores vs standard treatment alone (mean difference, 3.72 points; 95% CI, 0.40-7.05 points; P = .03). Effect sizes did not vary between music intervention types or doses; no evidence of small study or publication biases was present in any analysis. Mean difference in MCS scores met SF-36 minimum important difference thresholds (mean difference 3 or greater).
Conclusions and Relevance In this systematic review and meta-analysis, music interventions were associated with clinically meaningful improvements in HRQOL; however, substantial individual variation in intervention outcomes precluded conclusions regarding optimal music interventions and doses for distinct clinical and public health scenarios.
Health-related quality of life (HRQOL) is a broad concept capturing “an individual’s or group’s perceived physical and mental health over time.” 1 HRQOL is closely related to and frequently used interchangeably with well-being, 1 with the importance of these broad health concepts reflected in their prominence in United Nations Sustainable Development goals: “To ensure healthy lives and promote well-being for all at all ages.” 2
Listening to and making music (eg, by singing or playing instruments) is increasingly advocated, including in a recent World Health Organization report, as a means of improving HRQOL as well as various domains of well-being in clinical and healthy populations. 3 - 7 However, a lack of clarity regarding the magnitude of music effects on HRQOL, particularly compared with other established health interventions, presents clear challenges to the inclusion of music in health policies and care at local, national, and international levels. 8 Additionally, optimal music intervention types and doses for specific scenarios are still unclear, precluding the formulation of evidence-based music prescriptions. 3 , 8
The 36-item Health Survey Short Form (SF-36) HRQOL questionnaire is the most widely used patient-reported outcome instrument in health research, demonstrating strong validity, sensitivity, and reliability across a range of languages, versions (eg, RAND, 9 Medical Outcomes Study 10 ), interventions, and clinical and healthy populations. 9 - 12 Additionally, summary scores from the SF-36 and the reduced 12-item Health Survey Short Form (SF-12) have demonstrated good consistency. 13 - 15 The SF-36 has also been frequently used in studies of music interventions, 3 , 4 providing a means of both quantifying and easily contextualizing the magnitude of music’s association with HRQOL using a broadly valid and applicable instrument. Accordingly, the aim of this study is to quantitatively synthesize and contextualize the associations of music interventions and changes in HRQOL assessed by the SF-36 and SF-12. A secondary study aim is to evaluate these associations relative to specific music intervention types and doses.
The protocol for this systematic review and meta-analysis was prospectively registered with PROSPERO ( CRD42021276204 ) and written following the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline. This study was exempted from ethics review by the central ethics committee of Leibniz University Hannover because it was a secondary synthesis of deidentified data.
Four databases—MEDLINE, EMBASE, Web of Science, and PsycINFO—and 3 clinical trials registries—Cochrane Central Register of Controlled Trials (CENTRAL), ClinicalTrials.gov, and International Clinical Trials Registry Platform (ICTRP)—were searched for peer-reviewed articles, clinical trial registrations, and gray literature reports on July 30, 2021, using the following query: (Music* OR singing OR listening) AND (SF12 OR SF36 OR SF-12 OR SF-36 OR “short form 36” OR “short form 12”) . All related subject headings were included where possible and no limitations on study date or language were imposed. The reference lists of included studies and relevant systematic reviews were also hand searched for additional relevant studies.
Following removal of duplicate records, titles and abstracts of database search results were screened, followed by full-text review of potentially relevant abstracts against inclusion and exclusion criteria. Screening and full-text review were performed independently in duplicate by 2 study authors (J.M.M. and C.K.), with disagreements resolved through discussion.
Inclusion criteria were randomized and nonrandomized studies investigating the association of music-making (eg, instrumental music, singing, active music therapy) and/or music listening (eg, to recorded or live music, receptive music therapy) interventions with HRQOL in adults using the SF-36 or SF-12 (reduced version) questionnaires. No restrictions were made on eligible control groups. Studies that investigated the association of music with HRQOL as either a primary or secondary objective were both eligible for inclusion. Additionally, studies must have reported the SF-36 or SF-12 Mental Component Summary (MCS) score and/or Physical Component Summary (PCS) score, or data enabling the calculation of a MCS and/or PCS score (eg, data from all 8 subscales included in both the SF-36 and SF-12 10 , 13 ), at both preintervention and immediate postintervention time points. Higher MCS and PCS scores indicated better mental and physical HRQOL, respectively. MCS and PCS from the SF-12 and SF-36 have demonstrated good consistency across a range of populations. 15 , 16
MCS and PCS scores are both calculated using norm-based scoring methods including all 8 subscales of the SF-36 and SF-12: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. In calculations of MCS scores, vitality, social functioning, role-emotional, and mental health subscale scores are given the most weight. Conversely, in calculations of PCS scores, physical functioning, role-physical, bodily pain, and general health subscale scores are given the most weight. 17 Ware, Kosinsky, and Keller 17 described MCS and PCS score calculations in further detail, including precise scoring procedures and algorithms. Exclusion criteria were observational and cross-sectional studies and studies that investigated other music-related activities that do not focus on music-making or listening (eg, songwriting).
The quality of evidence supporting review conclusions was appraised using the GRADE system. GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) provides a framework for evaluating the risk of bias of individual studies, as well as the level of certainty supporting specific review results. 18 GRADE was selected for this review because of its broad applicability to different study types and because it has been “designed for reviews…that examine alternative management strategies.” 18
The risk of bias of individual studies was evaluated using the following standard criteria: allocation concealment, masking (of assessors and data analysts), percentage lost to follow-up, intention-to-treat analysis, selective outcome reporting, use of individual randomization, and control for carryover effects (crossover study design). 19 Based on these criteria, an evidence quality rating of high, moderate, low, or very low was assigned to each study using established procedures. 19 All studies were appraised independently by 2 study authors (J.M.M. and C.K.), with any disagreements resolved through discussion. The overall quality and certainty of evidence supporting the results of each meta-analysis was then appraised by the primary author in consultation with the authorship team using the same rating scale. 19
Demographic, music and control intervention, and SF-36 or SF-12 data before and after the intervention were extracted in duplicate by 2 study authors (J.M.M. and C.K.). Data from all available SF-36 and SF-12 subscales were extracted, as well as MCS and PCS summary scores. To maximize consistency of data across studies, MCS and PCS scores were recalculated where possible from underlying subscale data using the methodology of Ware, Kosinsky, and Keller. 17 Missing MCS and PCS standard deviations were imputed from mental health and physical function subscale scores, respectively, or as medians with minimum and maximum or interquartile range data as per established methods. 20 , 21 Authors of studies meeting inclusion criteria but reporting unclear or incomplete SF-36 or SF-12 data were contacted to retrieve compatible MCS and/or PCS data.
Weighted inverse-variance random-effects meta-analyses were conducted to determine the aggregate pre- to postintervention change in MCS and PCS scores. Additionally, inverse-variance random-effects meta-analyses were performed on postintervention MCS and PCS scores in music vs control groups common to at least 3 studies. The presence of statistical heterogeneity, indicating significant variation in the overall effects of music interventions on MCS and PCS scores, was evaluated using the χ 2 test and I 2 statistic. Potential small study or publication biases were evaluated using the Egger test. 22 Sensitivity analyses were performed where possible according to music intervention types (eg, music therapy, singing, music listening) and quality of study evidence (very low and low vs moderate and high). Additionally, exploratory nonparametric Spearman correlation analyses were performed to evaluate potential links between key characteristics of the music intervention “dose” (ie, intervention duration, music session frequency and length) and MCS and PCS scores. Significance was set at α = .05 for all statistical tests except meta-analysis main effects; α = .033 was used for meta-analysis main effects to control for multiplicity of related MCS and PCS outcomes, as per recommendations for meta-analyses aiming to best balance Type I and II error risk. 23 Analyses were conducted in RevMan version 5.4 (Cochrane Collaboration) and SPSS version 26 (IBM Corp).
Finally, published meta-analyses of MCS and PCS scores from established non–pharmaceutical or medical health interventions were retrieved to serve as a basis for comparison with results of the present study. Additionally, changes in MCS and PCS scores were evaluated against a 3-point minimum clinically important difference threshold established by the SF-36 developers. 24 This threshold was designed to be a general benchmark for meaningful change based on a range of longitudinal and cross-sectional data sets from both clinical and healthy populations; accordingly, this threshold was deemed particularly appropriate for the broad scope and heterogeneous literature included in this review. 24
Data from 26 eligible studies and 779 total participants (mean [SD] age, 60 [11] years) were included in the present study (eFigure 1, eTables 1 and 2 in the Supplement ). Included studies were conducted in Australia, 25 Brazil, 26 - 28 China (Hong Kong SAR), 29 Germany, 30 India, 31 Italy, 32 - 34 The Netherlands, 35 , 36 Spain, 37 Sweden, 38 Thailand, 39 Turkey, 40 the United Kingdom, 41 - 45 and the US. 46 - 50 Included studies comprised 22 investigations of clinical populations and 4 of healthy populations (10 investigations examined music listening, 7 music therapy, 8 singing, and 1 gospel music intervention) and 20 randomized clinical trials (RCTs) and 6 single-group studies (8 RCTs included comparisons with a usual treatment control group, 3 RCTs used meditation control groups, and 9 RCTs used a range of other disparate control groups). MCS and PCS scores were available for 25 studies; only MCS data was available in 1 additional study. 49 Evidence quality was high in 5 studies (19%), moderate in 11 studies (42%), low in 7 studies (27%), and very low in 3 studies (12%) (eTable 3 in the Supplement ).
Music interventions were associated with significant increases in both MCS (total mean difference, 2.95 points; 95% CI, 1.39-4.51 points; P < .001) and PCS scores (total mean difference, 1.09 points; 95% CI, 0.15-2.03 points; P =.02) from preintervention values ( Figure 1 and Figure 2 ). Standardized mean differences were 0.25 (95% CI, 0.15-0.36) for MCS scores and 0.15 (95% CI, 0.05-0.26) for PCS scores. MCS scores (including 779 participants) were significantly greater in moderate-quality and high-quality vs very low–quality and low-quality studies and varied significantly across intervention types (χ 2 = 4.56; I 2 = 78.1%; P = .03) ( Figure 1 ). However, changes in MCS scores did not significantly vary across intervention types when the 1 gospel music intervention study 46 was excluded. PCS scores (including 763 participants) did not significantly vary according to study quality or intervention type.
No key characteristics of the music intervention dose (ie, intervention duration, music session frequency and length), nor any combination of these characteristics, were associated with changes in MCS or PCS scores. No significant statistical heterogeneity or evidence of small study or publication bias (eFigures 2 and 3 in the Supplement ) was present in either analysis. Results of these meta-analyses were also judged to be minimally affected by individual study biases but limited by the imprecision of relatively wide confidence intervals. Accordingly, results were appraised to provide moderate-quality evidence, indicating that “the true effect is probably close to the estimated effect.” 18
Adding music interventions to treatment as usual (TAU) was associated with significant increases in MCS scores vs TAU alone (total mean difference, 3.72 points; 95% CI, 0.40-7.05 points) (standardized mean difference, 0.24; 95% CI, 0.02-0.45) ( P = .03) ( Figure 3 ). Differences for PCS scores were not significant ( Figure 4 ). Improved MCS in music plus TAU vs TAU groups did not vary significantly with study quality or music intervention type, and no significant statistical heterogeneity or evidence of small study or publication biases was present in either analysis (eFigures 4 and 5 in the Supplement ). Pre-post intervention changes in MCS and PCS scores associated with music plus TAU interventions did not significantly differ from changes in MCS and PCS scores associated with all other included music interventions (eFigures 6 and 7 in the Supplement ). Results of these meta-analyses were judged to be minimally affected by individual study biases but limited by the imprecision of wide confidence intervals across studies. Accordingly, results were appraised to provide moderate-quality evidence.
No significant differences in MCS or PCS scores in music listening vs meditation intervention studies were present across 3 included studies (eFigures 8 and 9 in the Supplement ). Once again, no significant statistical heterogeneity or evidence of small study or publication biases was present in either analysis. However, results were limited by the small number of studies and wide confidence intervals, and judged to provide low-quality evidence (ie, “the true effect might be markedly different from the estimated effect”). 18
Changes in MCS scores, both pre-post intervention and vs TAU, met or exceeded the proposed 3-point minimum important difference threshold for MCS and PCS scores. 17 Pre-post changes in PCS scores (1.1-point improvement) fell below this threshold.
Changes in MCS scores (pre-post and vs TAU) were similar to changes in PCS scores reported for weight loss in studies of adults with obesity (2.8-point improvement; no significant MCS change). 51 However, mean differences in MCS and PCS scores (pre-post and vs TAU) associated with music interventions were substantially smaller than differences in MCS and PCS scores associated with resistance exercise (ie, strength training) in older adults from mixed clinical and healthy populations vs mixed control groups (standardized mean difference: MCS, 0.54; PCS, 0.50) 52 and mixed modes of exercise in participants with knee osteoarthritis vs inactive or psycho-educational control groups (standardized mean difference: MCS, 0.44; PCS, 0.52). 53
This meta-analysis of 26 studies of music interventions provided clear and quantitative moderate-quality evidence that music interventions are associated with clinically significant changes in mental HRQOL. Additionally, a subset of 8 studies demonstrated that adding music interventions to usual treatment was associated with clinically significant changes to mental HRQOL in a range of conditions. Music interventions were associated with substantially smaller changes in physical HRQOL, which are of potentially equivocal practical importance. 17 The substantial individual variation in responses to music interventions across included studies should be emphasized; this analysis must only be used as a general guide to the associations between music interventions and HRQOL changes.
Included studies presented considerable heterogeneity in study populations and geographic locations, music intervention types and doses, and TAU control groups. However, no statistical heterogeneity or evidence of small study or publication bias was present in any analyses. This suggests that results approximate the true, albeit general, association between music interventions and changes in HRQOL. Further research is still needed to provide guidance regarding optimal music interventions and doses in distinct clinical and public health scenarios.
Associations between music interventions and changes in MCS scores (pre-post and music plus TAU vs TAU) are within the range, albeit on the low end, of changes in MCS and PCS scores associated with established non–pharmaceutical/medical, 51 - 54 as well as pharmaceutical/medical, 55 - 57 health interventions, and thus are likely to be clinically significant. 17 Accordingly, this review quantitatively confirmed narrative syntheses from prior systematic reviews asserting that music interventions are linked to meaningful improvements in well-being and HRQOL. 3 - 6 Of particular interest for future study and health policy is the fact that these benefits are associated with participation in a broadly rewarding activity. 58 While uptake and adherence challenges persist with other non–pharmaceutical/medical interventions (eg, weight loss, exercise), 59 , 60 music is “reliably ranked as one of life’s greatest pleasures.” 61 As such, music interventions may present a more attractive and effective nonpharmaceutical alternative to other health interventions. Further study is required to investigate this hypothesis and clarify the specific utility of music vs other established interventions.
Additionally, targeted research is also needed to provide insights into the mechanisms of music interventions’ association with positive changes in HRQOL—ie, the who, what, when, where, and how underpinning their effectiveness. The absence of any significant differences between music intervention types and doses in the present analyses is intriguing but not definitive; these results could also be simply explained by the diversity of included populations and interventions, even within specific intervention types (particularly clearly demonstrated for music listening interventions in the Table ). Broad confidence intervals of both main and intervention type–specific results in this meta-analysis likely also reflect the diversity of interventions. A 2021 analysis 62 indicated that the mechanisms of music’s impact on health are complex and specific to distinct settings, suggesting that targeted study is required to determine optimal music intervention characteristics in each setting. However, other analyses propose that such targeted research may be able to be rapidly generalized to other settings if foundational physiological mechanisms of music intervention effects can be identified and targeted. 63
This study had several limitations. Review was limited by its broad inclusion criteria that limited conclusions regarding the associations of specific music interventions in particular scenarios with specific HRQOL changes, especially given the diversity of included interventions. Despite this limitation, which would preclude the conduct of many meta-analyses, we contend that our meta-analysis was justified by the demonstrated need for even general quantitative syntheses, which allow music effects to be clearly contextualized. 8 Additionally, standardized mean differences describing the magnitude of pre-post intervention effects have been shown to be prone to bias and must be interpreted with caution. 64 However, the similar effect sizes of changes in MCS scores in pre-post and music plus TAU vs TAU analyses provided additional confidence in the average magnitude of pre-post MCS changes. Finally, this review was ultimately limited to studies evaluating the association of music interventions HRQOL using the SF-36 or SF-12 instruments, a possibly skewed subset of music intervention studies. Statistical homogeneity, the absence of apparent publication or small study biases, and the broad psychometric rigor of the SF-36 and SF-12 15 , 16 suggest that results of this review approximated the true associations between music interventions and HRQOL changes. However, the possibility remains that this subset of studies was not representative of music’s general effects on HRQOL or that the SF-36 and SF-12 instruments do not completely capture the impact of music on HRQOL. This uncertainty is reflected in the moderate quality rating of key review results, indicating that “the true effect is probably close to the estimated effect.” 18
This study provided moderate-quality quantitative evidence of associations between music interventions and clinically significant changes in mental HRQOL. Mean differences in physical HRQOL associated with music interventions were potentially equivocal. Changes in mental HRQOL associated with music interventions were within the range, albeit at the low end, of average effects of established non–pharmaceutical and medical interventions (eg, exercise, weight loss). Substantial individual variation in music intervention effects precluded conclusions regarding music use in specific scenarios. Future research is needed to clarify optimal music interventions and doses for use in specific clinical and public health scenarios.
Accepted for Publication: January 31, 2022.
Published: March 22, 2022. doi:10.1001/jamanetworkopen.2022.3236
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 McCrary JM et al. JAMA Network Open .
Corresponding Author: J. Matt McCrary, Institute of Music Physiology and Musicians’ Medicine, Hannover University of Music, Drama and Media, Neues Haus 1, 30175 Hannover, Germany ( [email protected] ).
Author Contributions : Dr McCrary had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: McCrary, Altenmuller.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: McCrary, Altenmuller, Scholz.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: McCrary, Scholz.
Obtained funding: McCrary, Altenmuller.
Administrative, technical, or material support: Altenmuller, Kretschmer.
Supervision: McCrary, Altenmuller, Scholz.
Conflict of Interest Disclosures: None reported.
Funding/Support: Dr McCrary holds a postdoctoral fellowship from the Alexander von Humboldt Foundation, which directly supported this study.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
The Transformative Power of Music in Mental Well-Being
- August 01, 2023
- Healthy living for mental well-being, Patients and Families, Treatment
Music has always held a special place in our lives, forming an integral part of human culture for centuries. Whether we passively listen to our favorite songs or actively engage in music-making by singing or playing instruments, music can have a profound influence on our socio-emotional development and overall well-being.

Recent research suggests that music engagement not only shapes our personal and cultural identities but also plays a role in mood regulation. 1 A 2022 review and meta-analysis of music therapy found an overall beneficial effect on stress-related outcomes. Moreover, music can be used to help in addressing serious mental health and substance use disorders. 2 In addition to its healing potential, music can magnify the message of diversity and inclusion by introducing people to new cultures and amplifying the voice of marginalized communities, thereby enhancing our understanding and appreciation for diverse communities.
Healing Trauma and Building Resilience
Many historically excluded groups, such as racial/ethnic and sexual minorities and people with disabilities, face systemic injustices and traumatic experiences that can deeply impact their mental health. Research supports the idea that discrimination, a type of trauma, increases risk for mental health issues such as anxiety and depression. 3
Music therapy has shown promise in providing a safe and supportive environment for healing trauma and building resilience while decreasing anxiety levels and improving the functioning of depressed individuals. 4 Music therapy is an evidence-based therapeutic intervention using music to accomplish health and education goals, such as improving mental wellness, reducing stress and alleviating pain. Music therapy is offered in settings such as schools and hospitals. 1 Research supports that engaging in music-making activities, such as drumming circles, songwriting, or group singing, can facilitate emotional release, promote self-reflection, and create a sense of community. 5
Empowerment, Advocacy and Social Change
Music has a rich history of being used as a tool for social advocacy and change. Artists from marginalized communities often use music to shed light on social issues (.pdf) , challenge injustices, and inspire collective action. By addressing topics such as racial inequality, gender discrimination, and LGBTQ+ rights, music becomes a powerful medium for advocating for social justice and promoting inclusivity. Through music, individuals can express their unique experiences, struggles, and triumphs, forging connections with others who share similar backgrounds. Research has shown that exposure to diverse musical genres and artists can broaden perspectives, challenge stereotypes, and foster empathy among listeners especially when dancing together. 7
Genres such as hip-hop, reggae, jazz, blues, rhythm & blues and folk have historically served as platforms for marginalized voices, enabling them to reclaim their narratives and challenge societal norms. The impact of socially conscious music has been observed in movements such as civil rights, feminism, and LGBTQ+ rights, where songs have played a pivotal role in mobilizing communities and effecting change. Music artists who engage in activism can reach new supporters and help their fans feel more connected to issues and motivated to participate. 6

Fostering Social Connection and Support
Music can also serve as a catalyst for social connection and support, breaking down barriers and bridging divides. Emerging evidence indicates that music has the potential to enhance prosocial behavior, promote social connectedness, and develop emotional competence. 2 Communities can leverage music’s innate ability to connect people and foster a sense of belonging through music programs, choirs, and music education initiatives. These activities can create inclusive spaces where people from diverse backgrounds can come together, collaborate, and build relationships based on shared musical interests. These experiences promote social cohesion, combat loneliness, and provide a support network that can positively impact overall well-being.
Musicians and Normalizing Mental Health
Considering the healing effects of music, it may seem paradoxical that musicians may be at a higher risk of mental health disorders. 8 A recent survey of 1,500 independent musicians found that 73% have symptoms of mental illness. This could be due in part to the physical and psychological challenges of the profession. Researchers at the Max Planck Institute for Empirical Aesthetics in Germany found that musically active people have, on average, a higher genetic risk for depression and bipolar disorder.
Commendably, many artists such as Adele, Alanis Morrisette, Ariana Grande, Billie Eilish, Kendrick Lamar, Kid Cudi and Demi Lovato have spoken out about their mental health battles, from postpartum depression to suicidal ideation. Having high-profile artists and celebrities share their lived experiences has opened the conversation about the importance of mental wellness. This can help battle the stigma associated with seeking treatment and support.
Dr. Regina James (APA’s Chief of the Division of Diversity and Health Equity and Deputy Medical Director) notes “Share your story…share your song and let's help each other normalize the conversation around mental wellness through the influence of music. My go-to artist for relaxation is jazz saxophonist, “Grover Washington Jr” …what’s yours?” Submit to [email protected] to get featured!
More on Music Therapy
- Music Therapy Fact Sheets from the American Music Therapy Association
- Music Therapy Resources for Parents and Caregivers from Music Therapy Works
By Fátima Reynolds DJ and Music Producer Senior Program Manager, Division of Diversity and Health Equity American Psychiatric Association
- Gustavson, D.E., et al. Mental health and music engagement: review, framework, and guidelines for future studies. Transl Psychiatry 11, 370 (2021). https://doi.org/10.1038/s41398-021-01483-8
- Golden, T. L., et al. (2021). The use of music in the treatment and management of serious mental illness: A global scoping review of the literature. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.649840
- Schouler-Ocak, M., et al. (2021). Racism and mental health and the role of Mental Health Professionals. European Psychiatry, 64(1). https://doi.org/10.1192/j.eurpsy.2021.2216
- Aalbers, S., et al. (2017). Music therapy for Depression. Cochrane Database of Systematic Reviews, 2017(11). https://doi.org/10.1002/14651858.cd004517.pub3
- Dingle, G. A., et al. (2021). How do music activities affect health and well-being? A scoping review of studies examining Psychosocial Mechanisms. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.713818
- Americans for the Arts. (n.d.). A Working Guide to the Landscape of Arts for Change. Animating Democracy. http://animatingdemocracy.org/sites/default/files/Potts%20Trend%20Paper.pdf
- Stupacher, J., Mikkelsen, J., Vuust, P. (2021). Higher empathy is associated with stronger social bonding when moving together with music. Psychology of Music, 50(5), 1511–1526. https://doi.org/10.1177/03057356211050681
- Wesseldijk, L.W., Ullén, F. & Mosing, M.A. The effects of playing music on mental health outcomes. Sci Rep 9, 12606 (2019). https://doi.org/10.1038/s41598-019-49099-9
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Psychotherapy?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- SMI Adviser
- Annual Meeting
- APA On Demand
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- At the APA Educational Series
- The Virtual Immersive
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2024 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Conference Publications
- Library and Archive
- Member Obituaries
- Practice Guidelines
- Resource Documents
- Member Directory
- Assembly Directory
- Component Directory
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APA/APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- What is Schizophrenia?
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Advocacy and APAPAC
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows
- Share full article
Advertisement
Supported by
How Music Can Be Mental Health Care
In music therapy, clients play and listen to music as treatment for stress, depression and anxiety. Here’s how it works.

By Christina Caron
The therapy session begins when Isobell, 17, picks up a guitar.
Her fingers, adorned with silver rings and black nail polish, are positioned to play the first chord of Lana Del Rey’s “Candy Necklace.”
Listen to This Article
Then she starts to sing, her voice a melancholy, breathy soprano that seems to float across the room.
White noise coming out of my brain Turns off for nothing
Isobell’s therapist, Caitlin Bell, accompanies her on the piano.
Although they are actually sitting in a medical clinic — the Louis Armstrong Center for Music and Medicine at Mount Sinai-Union Square in Manhattan — the space feels more like a musician’s living room, with sheet music on display and wooden bookcases that line the walls, each housing different instruments.
Music therapy, while still a relatively small field, has grown over the last decade . The practice helps people cope with ailments as wide-ranging as stress, chronic pain, limited mobility and hypertension, and is performed in a variety of settings, including psychiatric hospitals, outpatient clinics, senior centers and schools.
Scientific research has begun to explore why music appears to have such a strong effect on health and wellness, particularly mental health, where sounds can serve as a conduit to lift someone’s mood, help them reflect and reduce stress, anxiety and depression.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
American Music Therapy Association
Please enter email. Please enter password.
- Music Therapy Journals & Publications
- Selected Bibliographies
- Researching Music Therapy
- Strategic Priority on Research
- Arthur Flagler Fultz Research Award from AMTA

Follow AMTA on Social Media

- What is Music Therapy?
- Who are Music Therapists?
- AMTA Board of Directors
- What is AMTA?
- Membership in AMTA
- Support Music Therapy
- A Career in Music Therapy
- Schools Offering Music Therapy
- Education and Clinical Training Information
- National Roster Internship Sites
- Find a Job in Music Therapy
- Advertise a Job in Music Therapy
- Scholarship Opportunities for AMTA Members
- Continuing Music Therapy Education
- Advocacy Basics
- Federal Advocacy - for members
- State Advocacy - for members
- AMTA Government Relations Team
- Coalitions & Partnerships - for members
- Advocacy Events - for members
- Find My Legislators
- AMTA Annual Conference
- Special Events & Media
- Sponsor AMTA Events
- Advertising in AMTA Publications
- Publish with AMTA
- Join AMTA/Renew Membership
- Donate to AMTA
- Visit the Bookstore
- Scholarships for AMTA Members
- Official Documents
- AMTA Officials
- News from AMTA Committees & Boards
- Member Toolkit
- Reimbursement Resources
- Online Publications & Podcasts
- AMTA Member Recognition Awards
Music Therapy Journals and Publications
Click to go directly to: Opt-in to Receive Printed Journal Copies! The Journal of Music Therapy Journal of Music Therapy - AMTA Member Access Portal Music Therapy Perspectives Music Therapy Perspectives - AMTA Member Access Portal Steps to Access Your Online Member Subscription to Research Journals Music Therapy Matters Monthly Other Publications from AMTA Imagine, early childhood newsletter 2010, 2011 & 2012 Back Issues of AMTA Journals Music Therapy - 1981-1996 journal Advertising in AMTA Publications
Or scroll down to read about each.
The Journal of Music Therapy
Journal of Music Therapy webpage at Oxford University Press
Journal of music therapy amta member access portal.
A forum for authoritative articles of current music therapy research and theory, including book reviews and guest editorials. An index appears in issue four of each volume. ISSN #0022-2917
Subscriptions to the Journal of Music Therapy are now available for the current and upcoming year. For subscription rate information and to subscribe to the Journal of Music Therapy , please contact AMTA's partner in publishing, Oxford Universtiy Press, https://academic.oup.com/jmt/subscribe
Mission statement.
The Journal of Music Therapy (JMT) is a forum for authoritative articles of current music therapy research and theory, including book reviews and guest editorials. Its mission is as follows:
The Journal of Music Therapy seeks to advance research, theory, and practice in music therapy through the dissemination of scholarly work. Its mission is to promote scholarly activity in music therapy and to foster the development and understanding of music therapy and music-based interventions. To this end, the journal publishes all types of research, including quantitative, qualitative, historical, philosophical, theoretical, and musical, and may include discipline, profession, and foundational research topics. The journal strives to present a variety of research approaches and topics, to promote critical inquiry, and to serve as a resource and forum for researchers, educators, and clinicians in music therapy and related professions.
Journal Content
The Journal of Music Therapy publishes only the very best of what is submitted and includes articles concerning the psychology of music, applied music therapy techniques, perception of music, and effects of music on human behavior. All papers for publication are selected on the basis of their quality and contribution to existing knowledge. About 30% of submitted manuscripts are accepted for publication and include but are not limited to qualitative, quantitative, and mixed methodologies; historical, descriptive, philosophical, or experimental designs; and integrative reviews, meta-analysis or meta-synthesis. Individual case studies or studies with very small numbers of subjects are rarely published; however, an extremely innovative case study may be accepted due to its unique contribution to knowledge. Conversely, articles of any type which do not advance the science and practice of music therapy are not accepted.
Normal 0 false false false EN-US X-NONE X-NONE MicrosoftInternetExplorer4
Journal of Music Therapy Online Member Access
AMTA's journals are available to subscribers and current AMTA members who may access and search the online journals. At times, articles may be published online as open access for a limited number of weeks. For member access to articles that are not open access, go to www.musictherapy.org and log in in the upper right with your current member personal email address and password. Once logged into your personal member account, then go to Research>Music Therapy Journals and Publications and select the "Member Access Portal" link for your desired journal. This is the member portal to AMTA's music therapy journals at Oxford University Press. Just one more click on the link in the access portal and you will be directed to the journal page. Once you are there, you may begin browsing the journals. You will see the unlocked padlocked icon next to articles that you are able to access and the AMTA Members account in the upper right. This means you are logged into your online subscription and are able to browse the journal and its archives. Alternatively (for fewer steps), you can use the Quick Links for each journal on the AMTA home page after you initially log in.
Contributions to the Journal of Music Therapy
Please submit manuscripts and submission letters electronically using AMTA's online submission program at the URL/link below. AMTA's online submission system is ScholarOne located at: http://mc.manuscriptcentral.com/jmt Please review all Instructions for Authors before submitting. Should you have any difficulties with your online submission, please contact via email:
Blythe LaGasse, PhD, MT-BC Editor, Journal of Music Therapy Colorado State University College of Liberal Arts, UCA 145D Fort Collins, CO 80523-1701 [email protected]

AMTA Journals Complaint Resolution Process
- The complaint or concern is raised, preferably in an email to the editorial office, including specific and detailed evidence to support the claim.
- The editor will notify the complainant that they will investigate and communicate the outcome but may not be in regular contact before the conclusion of the investigation.
- The editor will notify the AMTA’s journal business manager and/or CEO, and journal publisher, and work with them to seek out all applicable industry guidelines concerning matters of research integrity and publication ethics (including those of the Committee on Publication Ethics), case examples, and AMTA Bylaws.
- In consultation with the AMTA CEO and the publisher, the editor will review the issue in accordance with industry standards and best practices.
- During the investigation, the editor may consult with relevant experts and/or may form a committee for recommendation. All consultants are expected to maintain the confidentiality of the process and declare any conflicts of interest and, if appropriate, recuse themselves immediately. The editor will make the final decision.
- The editor will provide written explanation of the decision to the complainant. Journal of Music Therapy Email: [email protected]
Music Therapy Perspectives
Music therapy perspectives webpage at oxford university press, music therapy perspectives - amta member access portal, advertising in music therapy perspectives.
Designed to appeal to a wide readership, both inside and outside the profession of music therapy. Articles focus on music therapy practice, as well as academics and administration. ISSN #0734-6875
Subscriptions to Music Therapy Perspectives are now available for the current and upcoming year! For subscription rate information and to subscribe to Music Therapy Perspectives , please contact AMTA's partner in publishing, Oxford University Press, https://academic.oup.com/mtp/subscribe
Music Therapy Perspectives seeks to promote the development of music therapy clinical practice through the dissemination of scholarly work. It publishes all forms of reports that have implications for music therapy practice including clinically-focused research reports, innovative developments, case studies, educational research, and theoretical articles. With a focus on clinical benefits of music therapy, Music Therapy Perspectives strives to serve as a resource and forum for music therapists, music therapy students and educators, and those in related professions.
Music Therapy Perspectives seeks to:
- Speak to the direct clinical and professional experiences of practicing music therapists, and in so doing advance the profession.
- Include information useful to music therapists, music therapy students, and professionals interested in the therapeutic uses of music.
- Address issues related to the supervision of music therapy students and the supervision of music therapists in both professional and advanced practice.
- Include articles addressing the education and training of music therapists.
- Address ethical concepts and issues as they pertain to music therapy education, training, research and professional practice.
Music Therapy Perspectives focuses on scholarly articles in the following areas:
- Music therapy models, methods and practices that reflect broad theoretical perspectives reflective of the AMTA Standards of Clinical Practice (professional and advanced).
- Information useful to clinical training directors, educators and administrators
- Discussions, commentaries and analyses of professional issues related to music therapy practice, such as ethics and licensure.
- Qualitative research consistent with the mission and objectives of the journal.
- Quantitative research, consistent with the mission and objectives of the journal, with small sample sizes that may serve as a foundation for larger research studies suitable for the Journal of Music Therapy and other relevant music therapy journals.
- Pilot projects that reflect new areas of clinical practice.
- Case Studies.
- Analyses of literature that expand clinical practice knowledge.
- Book Reviews.
Music Therapy Perspectives Online Member Access
Contributions to music therapy perspectives.
Please submit manuscripts and submission letters electronically using AMTA's online submission program at the URL/link below. AMTA's online submission system is ScholarOne located at: http://mc.manuscriptcentral.com/mtp Please review all Instructions for Authors before submitting. Should you have any difficulties with your online submission, please contact via email:
Laura Beer, PhD, MT-BC (she, her) Editor, Music Therapy Perspectives Associate Professor, Music Therapy Colorado State University Campus Delivery 1778 Fort Collins, CO 80523-1778 [email protected]
- The editor will provide written explanation of the decision to the complainant. Music Therapy Perspectives Email: [email protected]
Music Therapy
Music Therapy was the official publication of the American Association for Music Therapy (AAMT) and was published annually from 1981 to 1996. The goal of the journal Music Therapy was to reflect a wide diversity of clinical, research and educational issues concerning the profession of music therapy during the years it was published. Now provided here for archival purposes, contributors to Music Therapy were practicing clinicians, music therapy educators, and professionals deeply involved in their organizations and dedicated to the enhancement of the music therapy profession.
Music Therapy Matters Monthly

This e-newsletter is provided to all current AMTA members as a benefit of membership in AMTA and published on the AMTA website under " Latest News ." An abridged version is sent directly to the primary email address of record for each individual member. For information on membership or subscribing, please contact the AMTA National Office at (301) 589-3300 or [email protected] .
Archives of past issues can be found in the AMTA Member Toolkit on the AMTA website . AMTA members joining after a specific issue was e-mailed out may check the Member Toolkit for access to all previous issues.
Music Therapy Matters Monthly Submission Guidelines
Music Therapy Matters is a monthly e-publication that welcomes article submissions from AMTA members.
Article submissions will be reviewed by the Editor and AMTA Executive Director and considered for inclusion based on available space and relevance to the music therapy profession and circulation of Music Therapy Matters Monthly .
Please note that while every effort will be made to include submissions received, they will be published on a space-available basis. Submissions may be edited for content, grammar and length. Publication dates are subject to change, but generally happen around the 15th of each month. To contact the Music Therapy Matters Monthly Editor, please email [email protected] or call 301-589-3300. Currently, Music Therapy Matters Monthly does not accept advertising.
Other Publications
In addition to research journals and newsletters, AMTA publishes a variety of other publications including texts and monographs such as the monograph series Effective Clinical Practice in Music Therapy, Music in Special Education, and Music Therapy and Premature Infants or Music Therapy in Pediatric Healthcare . AMTA also produces videos such as Music Therapy & Medicine: Partnerships in Care . Back issues of music therapy journals are available as well as products and informational brochures about the music therapy profession.
AMTA's complete publications catalog can be found in the AMTA online store. Simply hover over the "Bookstore" menu item above and select "Visit the Bookstore." Then, under "Shop for," choose "Merchandise" and "Select Category," choose "Publications" and click "Go." You'll find a list of all books and publications AMTA offers or click this link to go directly there .
Book Proposals
AMTA welcomes book and publication proposals on music therapy. Music therapy professionals and academics are encouraged to consider donating manuscripts for publication consideration with AMTA. See the menu item Bookstore> Publish with AMTA for more information.
Imagine , early childhood newsletter 2010, 2011 & 2012
Click here to explore and read archived issues.
Browse the imagine archive using an innovative viewing mode. Learn about our AMTA early childhood network opportunities, international perspectives on early childhood music therapy, and the "imagine" editorial team. Be part of future issues by reading the guidelines for authors and submitting your paper.
Back Issues of AMTA Journals
Back issues of any of the Journal of Music Therapy and Music Therapy Perspectives can be found on the respective journal's website and may be downloaded for a fee. Please see link for each journal above and click on "Browse the Archives."
Copyright © 1998-2024. American Music Therapy Association® and its logo are registered trademarks with the U.S. Patent and Trademark office. Information, files, graphics, and other content on this site are the property of the American Music Therapy Association® and may not be used, reprinted or copied without the express written permission of the American Music Therapy Association.
The American Music Therapy Association® is a 501(c)3 non-profit organization and accepts contributions which support its mission. Contributions are tax deductible as allowed by law.

10125 Colesville Road, #136 Silver Spring, MD 20901 Phone: 301.589.3300 Fax: 301.589.5175
- MEMBER LOGIN
- MEDIA RELATIONS
Military Stress

- ASSESSMENTS
- DOCUMENTARIES

An answer to the ongoing mental health crisis in the workplace: Music therapy
- November 10, 2023

Statistics reveal a stark reality: the American Institute of Stress estimates that work-related stress accounts for $300 billion in lost productivity, absenteeism, and increased healthcare costs annually. This staggering figure underscores the urgency of addressing the mental health challenges faced by the American workforce.
The silent struggle: Mental health issues Mental health issues have been a silent but steadily growing concern among American workers. The constant pressure to perform, meet targets, and excel in a competitive environment takes a toll. Many employees silently battle anxiety and depression, fearing stigma or career consequences if they seek help. The isolation and loneliness that can accompany a demanding work schedule further exacerbate these mental health challenges. Employees often find themselves trapped in a cycle of stress, anxiety, and reduced productivity, which can impact not only their job performance but their overall quality of life. And even worse, if they do seek help, traditional methods of support and resources often feel inaccessible and inadequate — and the data shows. Depressive episodes are up 90% in the last decade , 83% of workers report work related stress and only 24% of workers feel their employers care about their well-being.
The helpful harmonies of music Given the demands and stress of the modern workplace, executives and employees alike are constantly seeking ways to improve their mental well-being, productivity and focus. Historically, many have turned to caffeine, exercise, therapy or meditation to help give them a mental boost in their day, though oftentimes these options aren’t as effective, accessible or as culturally relevant as a tool that doesn’t often get the recognition it deserves: music.
Research has shown that listening to music while working can improve cognitive performance , enhance mood , and boost creativity . There is also good evidence to support that music can improve executive function, particularly when it comes to performance on cognitive tasks that involve sustained attention, response inhibition, repetition and flow. All of course very critical when we want to execute tasks efficiently and operate at our best in the workplace.
So, how exactly does music help improve mood and executive function? And what are some best practices for incorporating music into your work routine? Let’s dive in.
Look at the science It’s important to understand the science behind music and the brain. Studies have shown that listening to music can improve negative moods and reduce stress, factors which can significantly decrease executive function and cognitive performance. Conversely, when we’re in a relaxed, positive state, our brains are primed for productivity: we’re better at attending to and focusing on the work at hand and we get more done. Music stands out in this context because it is one of the easiest and most accessible ways to boost mood and decrease stress, particularly while on the job. And it turns out that many employees are already taking advantage of music’s many benefits during their work day, as Nielsen reports that 75% of workers listen to music at work at least once a week.
But there is a tricky part: picking the right music to soundtrack your success. Not all music is created equal, and there’s a lot of nuances to consider, so listen up.
Read more: Do your mental health benefits need an update?
Tip 1: Don’t choose based on genre People often make the mistake of choosing genre as a starting point, believing one specific genre to be more helpful than another. Given there is a lot of structural variance within a genre, it’s better to get more specific than that. As an initial guidepost, you can start with instrumental music to enhance cognitive performance. This is because instrumental music is less distracting than music with lyrics, which can interfere with verbal processing and memory.
Tip 2: Calibrate the tempo and volume Next consider tempo and volume. Up-tempo music can be arousing, which is good, but it’s important to not go too high with the tempo, otherwise you might start a dance party instead of getting down to business. Same with volume — if you go too high the brain will start focusing on the music rather than the task at hand.
Tip 3: Get familiar with music texture Consider texture in the music. This might be a new term for you. Music that is dense in texture will likely be too attention-grabbing to aid in work focus, and music that is too light in texture may not be stimulating enough. Experiment and see what the right balance is for you. This is one factor that tends to be pretty personal for each of us.
Tip 4: Match the music to your mood Music is not one-size-fits-all, and selecting the right music for focus can vary greatly depending on your emotional state, the task you are doing and your environment. A rule of thumb you can leverage from music therapy is called the iso principle , a technique by which music is matched to the mood of a person, then gradually altered to affect the desired mood state. For example, if you’re feeling tired, you might first want to select down-tempo music to match your low energy profile, helping you to acknowledge and embrace your current mood. Then gradually select music that can pull you out of fatigue into a more energized state.
Read more: How Prudential, Walmart, Aflac and PwC support mental health at work
Recognize the significance Unlocking the power of music to boost your brain can be a game-changer in getting your most important work done in your day. This is important to recognize as stress, anxiety, and mental health issues cast a long shadow over productivity and job satisfaction. The cost of this silent suffering is measured in billions of dollars and countless lost opportunities, having a detrimental impact in the workplace.
Music is such a crucial part of our daily lives but isn’t often enough looked at as a solution to major issues such as stress and productivity. Yet its benefits are well-researched and clear.
By incorporating music into the work routine, employers can help reduce stress and improve cognitive performance, leading to increased productivity and job satisfaction, and ultimately a reduction in costs. And for all you workers ready to boost your productivity, with some trial and error, you may discover that music is just the boost you need to level up and ultimately offer some real benefit in your workday.
To see a great podcast from The American Institue of Stress-Music can help you escape stress, click here!
More Articles

The hits keep coming. So how do we fight back against stress?

New Research Sheds Light on the Impact of Stress on Tobacco Users

Four Tools For A Healthier Relationship With Stress

Relax and Unwind: Ways to deal with stress and methods to fall asleep

Stress Awareness Month: Tips for keeping tensions in check

Are Workers Really Rage Quitting? Here’s What To Do Instead

Harnessing Emotional Intelligence: A Key To Reducing Stress At Work

Understanding the relationship between bruxism and stress

Air pollution associated with increased risk of stress and depression, in turn affecting heart health: study

Virtual reality environment for teens may offer an accessible, affordable way to reduce stress

American Psychological Association

The impact of transgender legislation
Psychological science points to an increased risk of suicide and poor mental health amid a record number of bills aimed at restricting the rights of the LGBTQ+ population
APA policy supporting transgender, gender diverse, nonbinary individuals
Membership in APA

APA Community
A new exclusive destination tailored for APA members

Membership benefits
Unlock the tools, discounts, and services included with your membership

Renew your membership
Keep your benefits and access to leading psychological information
Psychology topics spotlight

Misinformation and disinformation

Resources to navigate trauma

Tips to foster a healthy workplace
Science and practice of psychology

Ethics Code

Continuing Education

Grants, Awards, and Funding

Standards and Guidelines
Networks and communities

Network with peers, enhance your professional development, expand your personal growth, and more

APA Divisions

High school teachers

Undergraduate educators

Graduate students

Early career psychologists

Managing your career
Resources to help you throughout your career in psychology, including finding a job, salary data, finances and money management, mentoring and supervision, and training and professional development

Explore career paths

Psychologist profiles

How did you get that job?

Events and training
Featured jobs
Apa publications and products.

Write with clarity, precision, and inclusion
Children’s books
Monitor on Psychology
Newsletters
Reports and surveys
Continuing education
Merchandise

Real Siblings

Jacob's Missing Book

Harper Becomes a Big Sister
Attachment-Based Family Therapy for Sexual and Gender Minority Young Adults and Their Non-Accepting Parents
Dismantling Everyday Discrimination
APA Services

Learn how you can help APA advocate for psychology-informed federal policy and legislation, and support psychological research

APA Services, Inc.
A companion professional organization to APA, serving all members and advocating for psychology
Here’s how you know
- U.S. Department of Health and Human Services
- National Institutes of Health
Complementary, Alternative, or Integrative Health: What’s In a Name?

We’ve all seen the words “complementary,” “alternative,” and “integrative,” but what do they really mean?
This fact sheet looks into these terms to help you understand them better and gives you a brief picture of the mission and role of the National Center for Complementary and Integrative Health (NCCIH) in this area of research. The terms “complementary,” “alternative,” and “integrative” are continually evolving, along with the field, but the descriptions of these terms below are how we at the National Institutes of Health currently define them.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Complementary Versus Alternative
According to a 2012 national survey, many Americans—more than 30 percent of adults and about 12 percent of children—use health care approaches that are not typically part of conventional medical care or that may have origins outside of usual Western practice. When describing these approaches, people often use “alternative” and “complementary” interchangeably, but the two terms refer to different concepts:
- If a non-mainstream approach is used together with conventional medicine, it’s considered “complementary.”
- If a non-mainstream approach is used in place of conventional medicine, it’s considered “alternative.”
Most people who use non-mainstream approaches also use conventional health care.
In addition to the terms complementary and alternative, you may also hear the term “functional medicine.” This term sometimes refers to a concept similar to integrative health (described below), but it may also refer to an approach that more closely resembles naturopathy (a medical system that has evolved from a combination of traditional practices and health care approaches popular in Europe during the 19th century).
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Integrative Health
Integrative health brings conventional and complementary approaches together in a coordinated way. Integrative health also emphasizes multimodal interventions, which are two or more interventions such as conventional health care approaches (like medication, physical rehabilitation, psychotherapy), and complementary health approaches (like acupuncture, yoga, and probiotics) in various combinations, with an emphasis on treating the whole person rather than, for example, one organ system. Integrative health aims for well-coordinated care among different providers and institutions by bringing conventional and complementary approaches together to care for the whole person.
The use of integrative approaches to health and wellness has grown within care settings across the United States. Researchers are currently exploring the potential benefits of integrative health in a variety of situations, including pain management for military personnel and veterans, relief of symptoms in cancer patients and survivors, and programs to promote healthy behaviors.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What is whole person health?
Whole person health refers to helping individuals, families, communities, and populations improve and restore their health in multiple interconnected domains—biological, behavioral, social, environmental—rather than just treating disease. Research on whole person health includes expanding the understanding of the connections between these various aspects of health, including connections between organs and body systems.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Integrative Approaches for Pain Management for Military Personnel and Veterans
- An NCCIH-funded study is developing an innovative, collaborative treatment model involving chiropractors, primary care providers, and mental health providers for veterans with spine pain and related mental health conditions.
- Other NCCIH-funded studies are testing the effects of adding mindfulness meditation, self-hypnosis, or other complementary approaches to pain management programs for veterans. The goal is to help patients feel and function better and reduce their need for pain medicines that can have serious side effects.
- For more information on pain management for military personnel and veterans, see NCCIH’s Complementary Health Practices for U.S. Military, Veterans, and Families webpage.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Integrative Approaches for Symptom Management in Cancer Patients and Survivors
- Massage therapy may lead to short-term improvements in pain and mood in patients with advanced cancer.
- Yoga may relieve the persistent fatigue that some women experience after breast cancer treatment, according to the results of a preliminary study.
- Tai chi or qigong have shown promise for managing symptoms such as fatigue, sleep difficulty, and depression in cancer survivors.
- For more information, see NCCIH’s fact sheet on cancer .
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Integrative Approaches and Health-Related Behaviors
- Preliminary research suggests that yoga and meditation-based therapies may help smokers quit.
- In a study funded by the National Cancer Institute, complementary health practitioners (chiropractors, acupuncturists, and massage therapists) were successfully trained to provide evidence-based smoking cessation interventions to their patients.
- An NCCIH-funded study is testing whether a mindfulness-based program that involves the whole family can improve weight loss and eating behavior in adolescents who are overweight.
- For more information, see the NCCIH Quitting Smoking and Weight Control webpages.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Complementary Health Approaches
Complementary approaches can be classified by their primary therapeutic input (how the therapy is taken in or delivered), which may be:
- Nutritional (e.g., special diets, dietary supplements, herbs, and probiotics)
- Psychological (e.g., mindfulness)
- Physical (e.g., massage, spinal manipulation)
- Combinations such as psychological and physical (e.g., yoga, tai chi, acupuncture, dance or art therapies) or psychological and nutritional (e.g., mindful eating)
Nutritional approaches include what NCCIH previously categorized as natural products, whereas psychological and/or physical approaches include what was referred to as mind and body practices.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Examples of complementary health approaches that fall within the categories: Psychological, Physical, and Nutritional
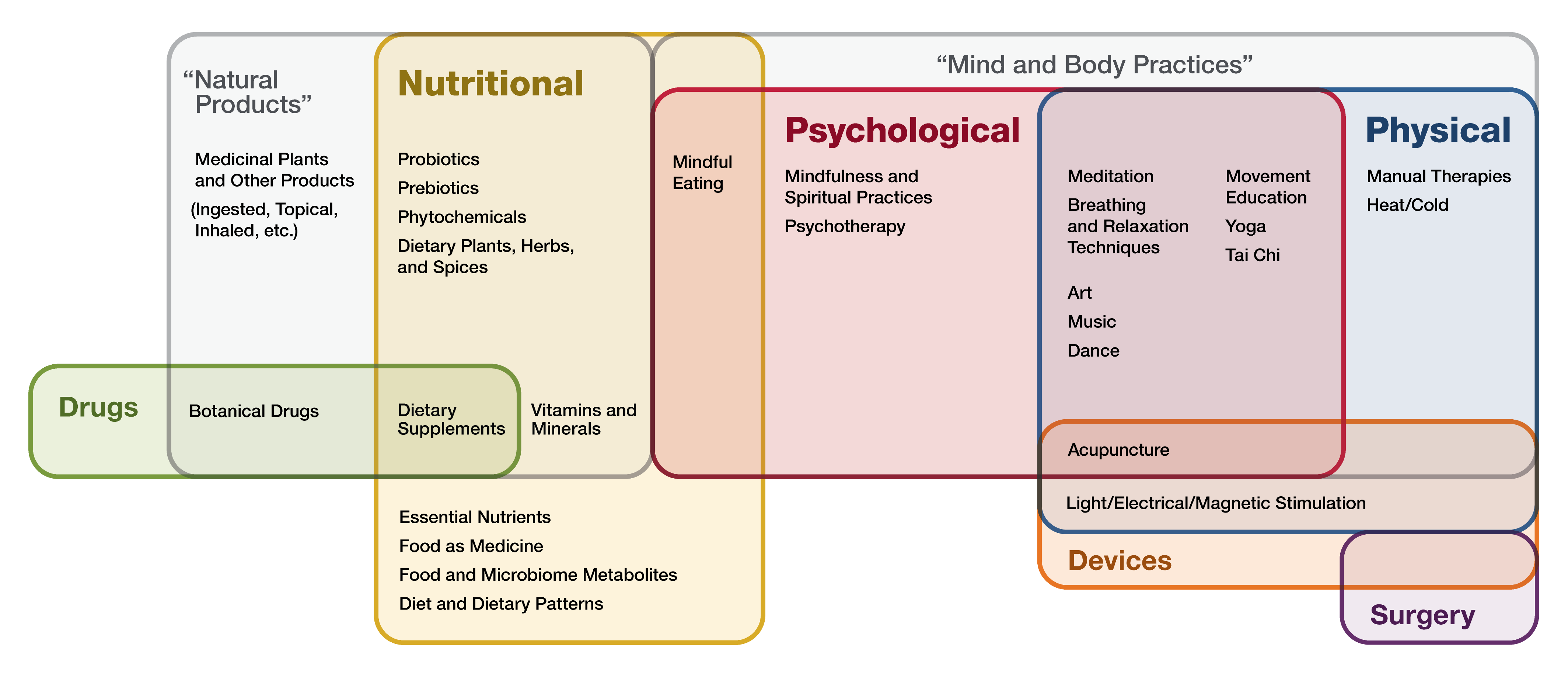
Click image to enlarge
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Nutritional Approaches
These approaches include a variety of products, such as herbs (also known as botanicals), vitamins and minerals , and probiotics . They are widely marketed, readily available to consumers, and often sold as dietary supplements .
According to the 2012 National Health Interview Survey (NHIS), which included a comprehensive survey on the use of complementary health approaches by Americans, 17.7 percent of American adults had used a dietary supplement other than vitamins and minerals in the past year. These products were the most popular complementary health approach in the survey. (See chart.) The most commonly used nonvitamin, nonmineral dietary supplement was fish oil.
Researchers have done large, rigorous studies on a few dietary supplements, but the results often showed that the products didn’t work for the conditions studied. Research on others is in progress. While there are indications that some may be helpful, more needs to be learned about the effects of these products in the human body, and about their safety and potential interactions with medicines and other natural products.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Psychological and Physical Approaches
Complementary physical and/or psychological approaches include tai chi , yoga , acupuncture , massage therapy , spinal manipulation , art therapy, music therapy, dance, mindfulness-based stress reduction, and many others. These approaches are often administered or taught by a trained practitioner or teacher. The 2012 NHIS showed that yoga, chiropractic and osteopathic manipulation , and meditation are among the most popular complementary health approaches used by adults. According to the 2017 NHIS , the popularity of yoga has grown dramatically in recent years, from 9.5 percent of U.S. adults practicing yoga in 2012 to 14.3 percent in 2017. The 2017 NHIS also showed that the use of meditation increased more than threefold from 4.1 percent in 2012 to 14.2 percent in 2017.
Other psychological and physical approaches include relaxation techniques (such as breathing exercises and guided imagery), qigong , hypnotherapy , Feldenkrais method, Alexander technique, Pilates, Rolfing Structural Integration, and Trager psychophysical integration.
Research findings suggest that several psychological and physical approaches, alone or in combination, are helpful for a variety of conditions. A few examples include the following:
- Acupuncture may help ease types of pain that are often chronic, such as low-back pain, neck pain, and osteoarthritis/knee pain. Acupuncture may also help reduce the frequency of tension headaches and prevent migraine headaches.
- Meditation may help reduce blood pressure, symptoms of anxiety and depression, and symptoms of irritable bowel syndrome and flare-ups in people with ulcerative colitis. Meditation may also benefit people with insomnia.
- Tai chi appears to help improve balance and stability, reduce back pain and pain from knee osteoarthritis, and improve quality of life in people with heart disease, cancer, and other chronic illnesses.
- Yoga may benefit people’s general wellness by relieving stress, supporting good health habits, and improving mental/emotional health, sleep, and balance. Yoga may also help with low-back pain and neck pain, anxiety or depressive symptoms associated with difficult life situations, quitting smoking, and quality of life for people with chronic diseases.
The amount of research on psychological and physical approaches varies widely depending on the practice. For example, researchers have done many studies on acupuncture, yoga, spinal manipulation, and meditation, but there have been fewer studies on some other approaches.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Other Complementary Health Approaches
Some complementary approaches may not neatly fit into either of these groups—for example, the practices of traditional healers, Ayurvedic medicine , traditional Chinese medicine , homeopathy , naturopathy , and functional medicine.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} NCCIH’s Role
NCCIH is the Federal Government’s lead agency for scientific research on complementary and integrative health approaches.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} NCCIH’s Mission and Vision
The mission of NCCIH is to determine, through rigorous scientific investigation, the fundamental science, usefulness, and safety of complementary and integrative health approaches and their roles in improving health and health care.
NCCIH’s vision is that scientific evidence informs decision making by the public, by health care professionals, and by health policymakers regarding the integrated use of complementary health approaches in a whole person health framework.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} For More Information
Nccih strategic plan.
NCCIH’s current strategic plan, Strategic Plan FY 2021 – 2025: Mapping a Pathway to Research on Whole Person Health , presents a series of goals and objectives to guide us in determining priorities for future research on complementary health approaches.
NCCIH Clearinghouse
The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature. The Clearinghouse does not provide medical advice, treatment recommendations, or referrals to practitioners.
Toll-free in the U.S.: 1-888-644-6226
Telecommunications relay service (TRS): 7-1-1
Website: https://www.nccih.nih.gov
Email: [email protected] (link sends email)
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your health care provider(s). We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.
Related Topics
NCCIH Strategic Plan FY 2021–2025 Mapping a Pathway to Research on Whole Person Health
Related Fact Sheets
Are You Considering a Complementary Health Approach?
Be an Informed Consumer

How to Cultivate Purpose
A Sense of Purpose Can Improve Life
- Find a Therapist
Verified by Psychology Today
- Psychiatrists
- Treatment Centers
- Support Groups
Professionals
Therapists Sign Up | Login
Psychology Today: Health, Help, Happiness + Find a Therapist
Today’s essentials today’s essential reads.
Sorry, But I Didn’t Recognize You With Your Clothes On
Alan S Brown Ph.D. on June 10, 2024 in The Memory Underground
Have you ever bumped into someone who looks extremely familiar, yet you have no clue who they are or why you know them? While confusing, there is a simple explanation.

Forensic Psychology
The anatomy of public humiliation at work.
Joni E Johnston Psy.D. on June 10, 2024 in The Human Equation
Just how far would some people go to get revenge after being humiliated at work? New research sheds some disturbing answers.

Growth Mindset
Before you bet big, be curious and ask questions.
Jeff Wetzler Ed.D. on June 9, 2024 in Unexpected Breakthroughs
When we feel certain of our conclusions, we fail to think about the consequences if we’re wrong. As they say, when you assume, you make an… well, you know the rest.

The Secret Power of Mind-Wandering
Sebastian Ocklenburg, Ph.D. on June 9, 2024 in The Asymmetric Brain
Mind-wandering is a common phenomenon, but it is not well understood how it affects our emotions. A new meta-analysis sheds some light on this complex question.

Is Your Brain Sad or Sluggish? Maybe It's Your Diet
Susan McQuillan on June 10, 2024 in Cravings
Several new studies confirm that how you eat can positively or negatively affect how your brain ages and functions.

- Relationships
Why Being Comfortable with Silence Is a Superpower
Michele DeMarco Ph.D., Rev on June 10, 2024 in Soul Console
Research shows silence is good for our relationships and well-being—yet many of us still fear silence. Here's why it's healthier to embrace it than fight it.

How Optimism Combats Learned Helplessness in Relationships
Jessica Koehler Ph.D. on June 10, 2024 in Beyond School Walls
Learned helplessness can trap you in a cycle of negativity, impacting your mental health and relationships. Discover how optimism can break the cycle and transform connections.
Music Belongs in the Hospital
Raymond Leone MMT, MT-BC on June 10, 2024 in Music Therapy, Music Musings
A Personal Perspective: Music therapy can be effective for the healing process.

Adverse Childhood Experiences
Child abuse reporting within an institution.
Franne Sippel Ed.D., LP on June 10, 2024 in Don't Shoot the Messenger
Are you aware of the reporting laws in your state and the institution where you work? Important factors to consider as a mandatory reporter.

- Child Development
Adverse Childhood Adaptations: Superpowers and Kryptonite
Annie Wright LMFT on June 10, 2024 in Making the Whole Beautiful
Childhood adaptations can lead to unique strengths in adulthood. Traits viewed as negative can become valuable assets in personal and professional settings.

Hearing Loss Is Challenging at the Doctor's Office
Shari Eberts on June 10, 2024 in Life With Hearing Loss
Personal Perspective: Hearing loss, like many other chronic conditions, is invisible, making it challenging to get assistance in a medical setting without asking for it.

Patient Trust Is Not Just About Care—It’s Also About Caring
Deepak Sirdeshmukh M.S., Ph.D. on June 10, 2024 in Patient Trust Matters
Building and sustaining patient trust depends not just on competence and reliability, but also on demonstrating concern and benevolence.

5 Subtle and Not-So-Subtle Signs of an Unhappy Person
Seth Meyers Psy.D. on June 10, 2024 in Insight Is 20/20
The signs of an unhappy person are often subtle and detectable only when identifying a pattern of several distinct behaviors.

- Neuroscience
A Boost for Infant Brain Development
Suhanee Mitragotri on June 10, 2024 in The Synaptic Connection
The neural mechanisms underlying magnesium sulfate treatment in pregnant individuals expecting a pre-term child.

Mental Illness at Work: To Disclose or Not to Disclose
Andrea Rosenhaft LCSW-R on June 10, 2024 in From Both Sides of the Couch
Personal Perspective: Should you disclose a mental illness to an employer? You may not have to think about it until your illness becomes symptomatic.

Compulsive Behaviors
Managing chronic complainers.
Ilene Strauss Cohen Ph.D. on June 10, 2024 in Your Emotional Meter
Over time, individuals who constantly complain become "addicted" to negativity, attracting more drama and dissatisfaction into their lives.

Do We Ever Fully Heal From Trauma?
Kaytee Gillis, LCSW-BACS on June 10, 2024 in Invisible Bruises
Healing from trauma is not a linear process. It's marked by ups and downs, progress and setbacks, and learning how to manage in the aftermath.

Discovering Meaning Through the Lens of Intuition
Alex Pattakos Ph.D. on June 10, 2024 in The Meaningful Life
This post explores a different way to view the trendy topic of gut health by exploring the gut-brain connection and how to trust your gut with greater confidence.

Assertiveness
What seasonal transitions reveal about negotiation success.
Cindy Watson B.A., LLB, JD on June 10, 2024 in Life as a Negotiation
There's a lot to be learned about negotiation success in preparing for seasonal transitions.

Are You Emotionally Numb?
A Key to Healing

Death Awareness in Clinical Practice
Kirk J. Schneider Ph.D. on June 10, 2024 in Awakening to Awe
Reconnecting clients to their transcendent self, deepening presence with others, and awe in daily life.

Women and Addiction Recovery: The 13th Step
Lindsay Weisner Psy.D. on June 10, 2024 in The Venn Diagram Life
Within the supposed safety of Alcoholics Anonymous meetings, the likelihood of someone new to sobriety becoming sexual prey is very real.

Why Appreciation from Management Matters
Victor Lipman on June 10, 2024 in Mind of the Manager
Appreciation is a critical element in retaining employees.
Freudian Psychology
The psychology of consumer behavior.
Lawrence R. Samuel Ph.D. on June 10, 2024 in Psychology Yesterday
Why do consumers think and act the way they do? Ask Sigmund Freud.

What 'Invisible Work' Looks Like in the 21st Century
Janelle E. Wells, Ph.D., and Doreen MacAulay, Ph.D. on June 10, 2024 in Our (In)visible Work
Learn how invisible work infiltrates 21st-century workplaces. From emotional labor to mentoring and bringing work home, it impacts our well-being. What invisible work do you do?

When People Say They Don't Want Drama, What Do They Mean?
Bruce Y. Lee M.D., M.B.A. on June 10, 2024 in A Funny Bone to Pick
When people preemptively announce "I don't want drama", what does it say about them and their past?

Dromomania: An Uncontrollable Urgency to Travel
Bethany Yeiser BS on June 10, 2024 in Recovery Road
A Personal Perspective: Dromomania is a symptom of some types of schizophrenia and bipolar disorder involving an uncontrollable urgency to travel.

Antidepressant Withdrawal: A Tale of Two Studies
Christopher Lane Ph.D. on June 10, 2024 in Side Effects
After almost four decades of antidepressant prescribing, the incidence, duration, and severity of withdrawal effects is still highly contested.

Havana Syndrome: Exploitation of Medicine for Political Gain
Racheed M Mani M.D. on June 10, 2024 in Brain Bulletin
Neurological symptoms misrepresented as a byproduct of geopolitical warfare through modern-day "Red Scare."

Animal Behavior
Wildlife corridors: conservation, compassion, and freedom.
Marc Bekoff Ph.D. on June 10, 2024 in Animal Emotions
Amy Propen's new book combines empathy with ecology and explains why we must offer wildlife corridors to animals.

Do You Have A “Shame Demon” On Your Shoulder?
Sean Grover L.C.S.W. on June 10, 2024 in When Kids Call the Shots
Shame destroys happiness; here’s how to set yourself free.

The 3 Key Things That Happy People Grasp
Maria Baratta Ph.D., L.C.S.W. on June 10, 2024 in Skinny Revisited
There are three particular learnable behaviors that might help in developing the skill of actualizing happiness

Success and the 4 Universal Outcomes of Therapy
Hope Perlman M.Ed, LMSW on June 10, 2024 in Unmapped Country
Being successful, in the simplest terms, means you are flourishing. But flourishing isn’t something that happens from the outside in; it’s something internal.

Are We in an Estrangement Epidemic?
Jennifer Gerlach LCSW on June 10, 2024 in Beyond Mental Health
With family rifts and loneliness at all-time highs, are we in an estrangement epidemic?
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medicine (Baltimore)
- v.102(24); 2023 Jun 16
- PMC10270468
The effect of music therapy on delirium in patients receiving mechanical ventilatory support in the Intensive Care Unit: A protocol for systematic review and meta-analysis
Changyan zhou.
a Department of Critical Care Medicine, The Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
b Child Intensive Care Unit, The Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, China.
Background:
Delirium is a very common sick syndrome in patients receiving mechanical ventilatory support in the Intensive Care Unit (ICU). Music therapy is a promising non-pharmacological intervention. However, its effect on the duration, incidence and severity of delirium is unknown. So we will perform a systematic review and meta-analysis to evaluate the effect of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU.
This systematic review was registered in the PROSPERO. We will follow the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocol to accomplish the systematic review protocol. Searches of PubMed, EMbase, the Cochrane library, CBM, CNKI and Wanfang databases will be conducted through computer to collect randomized controlled trials (RCTs) on the effects of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU. The search time will be all from database establishment to April 2023. Two evaluators will independently screen the literature, extract information and evaluate the risk of bias of included studies, then data analysis will be performed using Stata 14.0 software.
The results of this systematic review and meta-analysis will be publicly available and published in a peer-reviewed journal.
Conclusion:
This study will provide evidence-based medical evidence for music therapy to control delirium in patients receiving mechanical ventilatory support in the ICU.
1. Introduction
Delirium is an acute, reversible, widespread cognitive disorder psychotic syndrome characterized by fluctuating disorders of consciousness, inattention, disorganized thinking, or changes in level of consciousness. [ 1 , 2 ] Patients receiving mechanical ventilatory support in the Intensive Care Unit (ICU) are at high risk of delirium. [ 3 ] Delirium can be diagnosed when certain psychiatric symptoms are present without abnormal central nervous system function and organic comorbidities. And its main symptoms are relatively acute confusion, restlessness, excitement, hallucinations, and delusions. [ 4 ] The literature reports that the incidence of delirium is generally 5% to 40%, up to 80%, and 50% to 60% in elderly patients. [ 5 ] The risk of iatrogenic pneumonia increases tenfold after delirium, and the incidence of complications such as aspiration, pulmonary embolism, and pressure sores also increases greatly, which may cause accidental extubation, difficulty in weaning ventilators, or reintubation after extubation in mechanically ventilated patients. [ 6 ] Active and effective nursing interventions by nursing staff for ICU patients are very important to avoid and reduce the occurrence of delirium in a timely manner, improve the prognosis of patients, and improve their quality of life.
The pathogenesis of delirium is still unclear, but nurses, as the staff with the longest contact time with ICU patients, have an important influence on the clinical care of delirious patients, and good nursing interventions can effectively improve the patient’s disease outcome and prognosis. Mechanically ventilated patients experience pain and anxiety, which are usually relieved by the tranquillizer independently associated with the onset of delirium. [ 7 – 10 ] Despite the prevalence of delirium, there are no effective pharmacological interventions for delirium. [ 11 ] Previous use of drugs such as haloperidol, ziprasidone, and acetylcholine-lowering drugs has not been superior to placebo. [ 7 ] Therefore, non-pharmacological interventions may be potentially effective interventions for the treatment or prevention of delirium. [ 12 ]
Music therapy is a therapeutic modality in which medical psychology and music are interwoven. With the shift in medical model, music therapy is gradually being used in clinical practice. [ 13 ] It has been reported in the literature that music therapy has a positive effect on preventing and reducing the occurrence of delirium. [ 14 ] Music therapy affects the physiological functions of patients through music, promotes the release of beneficial chemicals such as acetylcholine, which can reduce the psychological reactions of anxiety, depression and fear, stabilize patients’ emotions, slow down their heart rate, dilate blood vessels, reduce cardiac load and enhance blood circulation, which play a role in regulating blood flow and nervous system functions. [ 3 , 13 , 14 ]
The ability of music therapy to improve delirium in patients receiving mechanical ventilatory support in the ICU is currently controversial. [ 11 , 15 – 17 ] Therefore, we will perform a systematic review and meta-analysis to investigate the effect of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU.
2.1. Protocol and registration
This systematic review was registered in the PROSPERO (registration number: CRD42023418303). We will follow the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocol to accomplish the systematic review protocol. [ 18 ] This study is conducted for the secondary collection and analysis of original data; therefore, ethical approval is not required.
2.2. Type of study
A randomized controlled trial (RCT) incorporating the effects of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU.
2.3. Types of participants
Age > 18 years, duration of mechanical ventilatory support in the ICU > 24h, consistent with the indications for the application of mechanical ventilatory support.
2.4. Interventions and comparators
The control group will be given routine ICU care, including basic care, intensive care, specialist care and health education; the experimental group will be given music therapy on the basis of routine ICU care.
2.5. Types of outcome measures
Incidence of delirium, duration of delirium state, severity of delirium, duration of mechanical ventilatory support, length of ICU stay, and in-hospital mortality.
2.6. Search strategy
Computer search of PubMed, EMbase, the Cochrane library, CBM, CNKI, and Wanfang databases will be conducted to collect RCTs on the effect of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU. Only studies published in English and Chinese will be included. The searching strategy in PubMed is shown in Table Table1 1 .
Search strategy for PubMed.
| Number | Search terms |
|---|---|
| #1 | Delirium[MeSH] |
| #2 | Delirium of Mixed Origin[Title/Abstract] |
| #3 | Subacute Delirium[Title/Abstract] |
| #4 | Delirium, Subacute[Title/Abstract] |
| #5 | Deliriums, Subacute[Title/Abstract] |
| #6 | Mixed Origin Delirium[Title/Abstract] |
| #7 | Mixed Origin Deliriums[Title/Abstract] |
| #8 | Subacute Deliriums[Title/Abstract] |
| #9 | OR/1-8 |
| #10 | Intensive Care Units[MeSH] |
| #11 | Care Unit, Intensive[Title/Abstract] |
| #12 | Care Units, Intensive[Title/Abstract] |
| #13 | Intensive Care Unit[Title/Abstract] |
| #14 | Unit, Intensive Care[Title/Abstract] |
| #15 | Units, Intensive Care[Title/Abstract] |
| #16 | OR/10-15 |
| #17 | Music Therapy[MeSH] |
| #18 | Therapy, Music[Title/Abstract] |
| #19 | Music[Title/Abstract] |
| #20 | OR/17-19 |
| #21 | Randomized Controlled Trial [Publication Type] |
| #22 | Randomized Controlled Trial[MeSH] |
| #23 | Random*[Title/Abstract] |
| #24 | OR/21-23 |
| #25 | #9 AND #16 AND #20 AND #24 |
2.7. Data collection and analysis
2.7.1. selection of studies..
Based on the inclusion and exclusion criteria, 2 investigators will independently read the titles and abstracts of the obtained literature, and after excluding trials not meeting the inclusion criteria, the remaining literature will be read in full, screened, and cross-checked. In case of disagreement, the discussion will help to resolve it. The procedures of study selection will be performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis flow chart (as shown in Fig. Fig.1 1 ).

Flow diagram of study selection process. RCTs = randomized controlled trial.
2.7.2. Data extraction and management.
Two researchers will independently screen the literature, extract and cross-check the data. In case of disagreement, discussion will be held to help resolve it. Data extraction will be included: disease type, date of publication, age, sex, study site, sample size, intervention, follow-up time, and mean and standard deviation of continuous indicators for outcome indicators.
2.7.3. Risk of bias assessment.
The quality of the included literature will be independently evaluated independently by 2 investigators, and the results will be cross-checked. The risk of bias will be assessed based on the risk of bias assessment tool for RCTs in the Cochrane Handbook, [ 19 ] including the generation of random sequences, allocation concealment, implementation of blinding, completeness of outcome data, selective reporting of results, and other biases.
2.7.4. Measures of treatment effect.
Stata 14.0 software will be used to calculate the outcome data. We will use 95% confidence intervals and risk ratios to estimate binary data. For continuous outcomes, comparisons will be made using weighted mean differences or standardized mean differences.
2.7.5. Additions of missing data.
If an article has any missing or insufficient data, we will send basic information to the relevant authors via email. If no contact is established or the data is incomplete, the study will be excluded.
2.7.6. Assessment of heterogeneity and data synthesis.
The heterogeneity of included RCTs will be assessed by the Chi-square test. If I 2 ≤ 50% and P ≥ .10, a fixed-effects model will be adopted; Otherwise, a random-effects model will be used for analysis.
2.8. Subgroup analysis
If there is significant heterogeneity in the study data, subgroup analyses will be conducted according to different types of music therapy, different control groups, and duration of intervention.
2.9. Sensitivity analysis
After excluding the low-quality studies, the combined effect sizes will be re-estimated and compared with the results of the meta-analysis before exclusion, thus exploring the effect of the remaining RCTs on the combined effect size and the robustness of the results.
2.10. Reporting bias analysis
When more than 10 studies are included, funnel plots will be depicted to detect publication bias. [ 20 – 22 ]
2.11. Confidence in cumulative evidence
The Grading of Recommendations Assessment, Development, and Evaluation method was conducted to assess the quality of evidence for each outcome. [ 23 ] The quality of evidence will be classified as high, medium, low, or very low.
2.12. Ethics and dissemination
Ethics approval is not required because this is conducted on published data and not on individual patient information. The results will be submitted to a peer-reviewed journal and presented at relevant conferences.
2.13. Amendments
The information will be described in the final report, and if the protocol is modified.
3. Discussion
Delirium is an acute brain failure syndrome, and patients receiving mechanical ventilatory support are at high risk of delirium. [ 24 ] Intubated patients experiencing pain, anxiety, and physiological stress often require treatment with tranquillizer, which are also risk factors for the occurrence of delirium, and in turn, a vicious cycle of pain, anxiety, sedation, and delirium. [ 25 ] Therefore, how to effectively prevent and reduce the incidence of delirium has become a hot topic of clinical research. Previously published RCTs on the effects of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU have reached different conclusions [ 11 , 15 – 17 ] caused by that these studies were limited by small sample sizes. To overcome these limitations, we will perform a high-quality systematic review and meta-analysis to assess the effect of music therapy on delirium in patients receiving mechanical ventilatory support in the ICU.
Author contributions
Conceptualization: Zina Liang, Changyan Zhou.
Data curation: Changyan Zhou.
Formal analysis: Changyan Zhou.
Funding acquisition: Zina Liang.
Investigation: Hong Ma.
Methodology: Hong Ma.
Project administration: Zina Liang.
Resources: Hong Ma.
Software: Hong Ma, Xiaoxue Qi, Chunru Xu.
Supervision: Zina Liang.
Validation: Xiaoxue Qi, Chunru Xu.
Visualization: Xiaoxue Qi, Chunru Xu.
Writing – original draft: Zina Liang, Changyan Zhou.
Writing – review & editing: Zina Liang, Changyan Zhou.
Abbreviations:
This work was supported by the Wenzhou Basic Scientific Research Project (no. Y20210928).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Zhou C, Ma H, Qi X, Xu C, Liang Z. The effect of music therapy on delirium in patients receiving mechanical ventilatory support in the Intensive Care Unit: A protocol for systematic review and meta-analysis. Medicine 2023;102:24(e33956).

IMAGES
VIDEO
COMMENTS
The Journal of Music Therapy is the perfect home for research articles that advance the science and practice of music therapy. Can you contribute your latest work? Read our Author Guidelines. ... Learn about the type of reviews published in the music therapy research literature, including systematic reviews, meta-analyses, scoping reviews, and ...
Music therapy versus music medicine. Research on music therapy is fast-growing (de Witte et al., Citation 2020a). The effects of music listening interventions, such as 'music medicine', are mainly caused by the general influence of music on the stress response, whereas the effects of music therapy may also be explained by the therapeutic ...
The findings provide useful information for music therapy researchers to identify new directions related to collaborators, popular issues, and research frontiers. ... In this study, the CiteSpace V software was used to visualize six science maps about music therapy research from 2000 to 2019: the network of author co-citation, collaboration ...
One new study was found for inclusion. Randomized controlled trials involving adults or children with autism spectrum disorders. Treatment was auditory integration therapy or other sound therapies involving listening to music modified by filtering and modulation. ... Music therapy research in the NICU: an updated meta-analysis: Not SR based on ...
Music therapy was the last thing that Julia Justo, a graphic artist who immigrated to New York from Argentina, expected when she went to Mount Sinai Beth Israel Union Square Clinic for treatment ...
Abstract. Purpose: Music therapy is increasingly being used to address physical, emotional, cognitive, and social needs of individuals. However, publications on the global trends of music therapy using bibliometric analysis are rare. The study aimed to use the CiteSpace software to provide global scientific research about music therapy from ...
Music interventions were also found to be beneficial for communication outcomes following aphasia, with moderate effect sizes of up to .75 standard deviations improvement in the intervention group ( Magee et al., 2017 ). However, the studies reviewed were found to present a high risk of bias, undermining the quality of the evidence ( Magee et ...
To summarize the growing body of empirical research on music therapy, a multilevel meta-analysis, containing 47 studies, 76 effect sizes and 2.747 participants, was performed to assess the strength of the effects of music therapy on both physiological and psychological stress-related outcomes, and to test potential moderators of the ...
Music therapy and emotional exploration: exposing substance abuse clients to the experiences of non-drug-induced emotions. ... (RDoC): toward a new classification framework for research on mental ...
Music Therapy Handbook. New York, New York, USA: Guilford Publications, 2015.] 8. One item that I am not seeing is group therapy versus individual therapy. ... Music in the treatment of affective disorders: an exploratory investigation of a new method for music-therapeutic research. Music Percept. Interdisc. J. 27, 307-316. doi: 10.1525/mp ...
Music therapy could help manage the pain of bereavement. Lisa Graham-Wisener, Queen's University Belfast and Tracey McConnell, Queen's University Belfast. Research suggests that music therapy can ...
Within music therapy research, there is a strong need for research into the effectiveness of different aspects of the therapy, quantifying therapeutic progress and novel ways of evaluating therapeutic processes, as well as developing technology tools that are sensitive to users with complex needs. ... Journal of New Music Research, 46(2), 118 ...
The American Music Therapy Association produces two scholarly journals where research in music therapy is published and shared: The Journal of Music Therapy is published by AMTA as a forum for authoritative articles of current music therapy research and theory. Articles explore the use of music in the behavioral sciences and include book ...
In short, research is a foundational element of the profession and is about: a) the use of research to increase access to quality music therapy services, b) knowing how research affects practice policy, c) an integral professional and association-wide element, d) being good consumers of music therapy research findings, and e) collaborating and ...
Key Points. Question Are music-making and listening interventions associated with positive changes in health-related quality of life?. Findings This systematic review and meta-analysis of 26 studies comprising 779 individuals found that music interventions were associated with statistically and clinically significant changes in mental HRQOL, both preintervention to postintervention as well as ...
Considering the healing effects of music, it may seem paradoxical that musicians may be at a higher risk of mental health disorders. 8 A recent survey of 1,500 independent musicians found that 73% have symptoms of mental illness. This could be due in part to the physical and psychological challenges of the profession.
In music therapy, clients play and listen to music as treatment for stress, depression and anxiety. Here's how it works. Isobell, 17, plays guitar and sings during a music therapy session at ...
In the later part of the twentieth century music therapy research reports using new methods entered the published literature, and references to new methods can be observed (for example, Aigen 1993; Amir 1993a, b; Comeau 1991; Forinash 1992; Forinash and Gonzalez 1989; Langenberg et al. 1993).
The new domains of approach and context are directly linked as they situate music therapy practice for SM within a wider theoretical landscape, in particular the UK-based manualised treatment for SM (Johnson & Wintgens, Citation 2001, Citation 2016) and international research on care pathways for SM (Keen et al., Citation 2008).
Purpose: Music therapy is increasingly being used to address physical, emotional, cognitive, and social needs of individuals. However, publications on the global trends of music therapy using bibliometric analysis are rare. The study aimed to use the CiteSpace software to provide global scientific research about music therapy from 2000 to 2019.
While music has long been recognized as an effective form of therapy to provide an outlet for emotions, the notion of using song, sound frequencies and rhythm to treat physical ailments is a relatively new domain, says psychologist Daniel J. Levitin, PhD, who studies the neuroscience of music at McGill University in Montreal.
Music Therapy. Music Therapy was the official publication of the American Association for Music Therapy (AAMT) and was published annually from 1981 to 1996.The goal of the journal Music Therapy was to reflect a wide diversity of clinical, research and educational issues concerning the profession of music therapy during the years it was published.Now provided here for archival purposes ...
Historically, many have turned to caffeine, exercise, therapy or meditation to help give them a mental boost in their day, though oftentimes these options aren't as effective, accessible or as culturally relevant as a tool that doesn't often get the recognition it deserves: music. Research has shown that listening to music while working can ...
Modern music therapy, starting around the middle of the Twentieth century as an organized profession has traditionally been rooted in concepts of social science. ... As the content of this special Research Topic clearly indicates, driven by new insights from research in music and brain function, a new understanding of the capabilities of music ...
Music is deeply rooted in the human experience as well as a fundamental part of psychedelic-assisted therapies (PAT) and entheogenic ceremonies. Although a large body of research exists highlighting the importance of music from rehabilitative, psychological, neurobiological, anthropological, religious, and sociological contexts, there is limited scientific literature regarding the specific ...
The theory behind sound therapy states that cells have frequencies and bodies have rhythms that respond to sound vibrations. In an interview with Her Agenda, Sara Auster, a world-renowned sound ...
The American Psychological Association (APA) is a scientific and professional organization that represents psychologists in the United States. APA educates the public about psychology, behavioral science and mental health; promotes psychological science and practice; fosters the education and training of psychological scientists, practitioners and educators; advocates for psychological ...
The mission of NCCIH is to determine, through rigorous scientific investigation, the fundamental science, usefulness, and safety of complementary and integrative health approaches and their roles in improving health and health care. NCCIH's vision is that scientific evidence informs decision making by the public, by health care professionals ...
View the latest from the world of psychology: from behavioral research to practical guidance on relationships, mental health and addiction. Find help from our directory of therapists ...
Delirium is a very common sick syndrome in patients receiving mechanical ventilatory support in the Intensive Care Unit (ICU). Music therapy is a promising non-pharmacological intervention. However, its effect on the duration, incidence and severity of delirium is unknown. So we will perform a systematic review and meta-analysis to evaluate the ...