An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Med Sci Educ
- v.31(1); 2021 Feb


Teaching Critical Thinking and Problem-Solving Skills to Healthcare Professionals
Jessica a. chacon.
Department of Medical Education, Paul L Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso, TX USA
Herb Janssen
Associated data, introduction.
Determining approaches that improve student learning is far more beneficial than determining what can improve a professor’s teaching. As previously stated, “Lecturing is that mysterious process by which the contents of the note-book of the professor are transferred through the instrumentation of the fountain-pen to the note-book of the student without passing through the mind of either” [ 1 ]. This process continues today, except that the professor’s note-book has been replaced with a PowerPoint lecture and the student’s note-book is now a computer.
In 1910, the Flexner report noted that didactic lectures were antiquated and should be left to a time when “professors knew and students learned” [ 2 ]. Approximately 100 years later, the Liaison Committee on Medical Education (LCME) affirmed Flexner’s comment and suggested that student learning must involve active components [ 3 ]: It seems somewhat obscured that almost 100 years separated these two statements.
Our strategy requires the following: student engagement in the learning process; a curriculum that develops a foundation for each student’s knowledge acquisition; focusing primarily on student learning instead of professor teaching; helping enable students develop critical thinking skills; and encouraging students to develop “expertise” in their chosen discipline.
Six fundamental topics that play a role in the development of a health sciences student’s critical thinking ability will be described. In “Section I,” these topics will be discussed independently, highlighting the importance of each. In “Section II: Proposed Curriculum and Pedagogy to Improve Student Learning,” the topics will be united into a practical approach that can be used to improve student learning, curriculum, pedagogy, and assessment.
Foundation Knowledge
Students use mnemonics to provide a foundation for new information. Although mnemonics help students associate information that they want to remember with something they already know, students learn tads of information that is not placed into a practical, meaningful framework developed by the student [ 4 , 5 ]. This commentary highlights the problem of recalling facts when these facts are presented in isolation. The responsibility for this resides not with the student, but with a curriculum that teaches isolated facts, instead of integrated concepts.
A taxonomy for significant learning presented by Dr. Fink emphasizes the need to develop foundational knowledge before additional information can be learned in an effective manner [ 6 ]. He provides suggestions on developing specific learning goals in given courses. Two of his most important criteria are (1) the development of a foundation of knowledge and (2) helping students “learn how to learn” [ 6 ].
Learning Approaches and Abilities
Howard Gardner introduced the concept of multiple intelligences in the 1980s [ 7 ]. Gardner expanded this idea to include intelligence in the areas of (1) Verbal-linguistic, (2) Logical-mathematical, (3) Spatial-visual, (4) Bodily-kinesthetic, (5) Musical, (6) Interpersonal, (7) Intrapersonal personal, (8) Naturalist, and (9) Existential. He concluded that students gifted in certain areas will be drawn in that direction due to the ease with which they excel. While it is important to recognize these differences, it is crucial to not ignore the need for student development in areas where they are less gifted. For example, students gifted in mathematics who fail to develop intrapersonal and interpersonal skills will more likely become recluse, limiting their success in real-world situations [ 7 , 8 ]. Similar examples can also be found in the medical world [ 7 , 8 ].
Based on Gardner’s work, it seems evident that students admitted to our health sciences schools will arrive with different skills and abilities. Despite this, educators are required to produce graduates who have mastered the competencies required by the various accrediting agencies. Accomplishing this task demands sensitivity to the students’ different abilities. While the curriculum remains focused on the competencies students must demonstrate when training is complete. Creating this transition using a traditional lecture format is difficult, if not impossible.
Active Engagement
In 1910, Flexner suggested that didactic lecture is important; however, it should be limited only to the introduction or conclusion of a given topic [ 2 ]. Flexner stated that students should be given the opportunity to experience learning in a context that allowed them to use scientific principles rather than empirical observations [ 2 ]. Active engagement of the student in their learning process has been recently promoted by the LCME [ 3 ]. This reaffirmation of Flexner’s 1910 report highlights the incredibly slow pace at which education changes.
Critical Thinking
Critical thinking is an active process that, when applied appropriately, allows each of us to evaluate our own activities and achievements. Critical thinking also allows an individual to make minor, mid-course corrections in thinking, instead of waiting until disastrous outcomes are unavoidable.
Educators in Allied Health and Nursing have included critical thinking as part of their curriculum for many years [ 9 ]. Medical educators, on the other hand, have not fully integrated critical thinking as part of their curriculum [ 10 , 11 ].
Bloom’s taxonomy has often been used to define curriculum [ 12 ]. The usefulness and importance of Bloom’s taxonomy is not to be underestimated; however, its limitations must also be addressed. As Bloom and his colleagues clearly stated, their taxonomy describes behavioral outcomes and is incapable of determining the logical steps through which this behavior was developed [ 12 ]. Bloom highlights this shortcoming in his initial book on the cognitive domain. He described two students who solved the same algebra problem. One student does this by rote memory, having been exposed to the problem previously, while the other student accomplishes the task by applying mathematical principles. The observer has no way of knowing which approach was used unless they have prior knowledge of the students’ background [ 12 ]. The importance of this distinction becomes apparent in medical problem-solving.
Contextual Learning
Enabling students to learn in context is critical; however, trying to teach everything in context results in a double-edged sword [ 13 ]. On the one hand, learning material in context helps the student develop a solid foundation in which the new information can be built. On the other hand, the educator will find it impossible to duplicate all situations the student will encounter throughout his or her career as a healthcare provider. This dilemma again challenges the educator to develop a variety of learning situations that simulate real-world situations. It seems that “in context” can at best be developed by presenting a variety of patients in a variety of different situations.
In the clinical setting, the physician cannot use a strict hypothesis-driven study on each patient, but must treat patients using the best, most logical treatment selected based on his or her knowledge and the most reliable information.
Development of Expertise
Several researchers have studied the characteristics required of expert performance, the time required to obtain these traits, and the steps that are followed as an individual’s performance progresses from novice to expert.
Studies involving expert physicians have provided data that can be directly used in our attempt to improve curriculum and pedagogy in the healthcare profession. Patel demonstrated that medical students and entry-level residents can recall a considerable amount of non-relevant data while the expert cannot [ 14 ]. Conversely, the expert physician has a much higher level of relevant recall, suggesting they have omitted the non-relevant information and retained only relevant information that is useful in their practice. Using these methods, the expert physicians produce accurate diagnosis in almost 100% of cases, while the medical students can achieve only patricianly correct or component diagnosis only [ 14 ].
In the healthcare setting, both methods are used. The expert physicians will use forward reasoning when the accuracy of the data allows this rapid problem-solving method. When the patient’s conditions cannot be accurately described using known information, the expert diagnostician will resort to the slower hypothesis-driven, backward reasoning approach. In this manner, the highest probability of achieving an accurate diagnosis in the shortest time will be realized [ 14 ].
Section II: Proposed Curriculum and Pedagogy to Improve Student Learning
The following section will outline several distinct but interrelated approaches to accomplish the six educational principles discussed above. The topics will be highlighted as they apply to the specific topic and each section will be comprised of curriculum, pedagogy, and assessment.
Developing a Knowledge Base Using Active Learning Sensitive to Students’ Abilities
Students admitted into healthcare training programs come from various backgrounds. This is both a strength for the program and a challenge for the educator. The strength is recognized in the diversity the varied backgrounds bring to the class and ultimately the profession. The challenge for the educator is attempting to provide each student with the material and a learning approach that will fit their individual ability and knowledge level. The educator can provide prerequisite objectives that identify the basic knowledge required before the student attempts the more advanced curriculum. Scaffolding questions can also be provided that allow students to determine their mastery of these prerequisite objectives. Briefly, scaffolding questions are categorized based on complexity. Simple, factual questions are identified with a subscript “0” (i.e. 1. 0 , 2. 0 , etc.). Advanced questions have a subscript suggesting the estimated number of basic concepts that must be included/combined to derive the answer.
Using technology to provide these individual learning opportunities online allows each student to address his or her own potential deficits. Obviously, those who find their knowledge lacking will need to spend additional time learning this information; however, using technology, this can be accomplished without requiring additional class time. This approach will decrease learning gaps for students, while excluding unnecessarily repeating material known by others.
The curriculum is divided into two parts: (1) content and (2) critical thinking/problem-solving skills. The basic knowledge and factual content can be provided online. Students are expected to learn this by actively engaging the material during independent study. This saves classroom or small-group sessions for interaction where students can actively learn critical thinking/problem-solving skills.
The curriculum should be designed so that students can start at their own level of understanding. The more advanced students can identify the level appropriate for themselves and/or review the more rudimentary information as needed. As shown by previous investigators, experts omit non-relevant information so that they can focus on appropriate problem-solving. Requiring students to learn by solving problems or exploring case studies will be emphasized when possible.
Technology can be used to deliver the “content” portion of the curriculum. Voice-over PowerPoints and/or video clips made available online through WebCT or PodCast will allow each student to study separately or in groups at their own rate, starting at their own level of knowledge. The content delivered in this fashion will complement the handout and/or textbook information recommended to the students. This will provide the needed basic information that will be used as a foundation for the development of critical thinking and problem-solving. The flipped classroom and/or team-based learning can both be used to help facilitate this type of learning. [ 15 ]
Student Assessments
It is imperative for students to know whether they have mastered the material to the extent needed. This can be accomplished by providing online formative evaluations. These will not be used to determine student performance; however, the results will be provided to the educator to determine the class’s progress and evaluation of the curriculum.
Developing Critical Thinking Skills in the Classroom or Small-Group Setting
Critical thinking skills are essential to the development of well-trained healthcare professionals. These skills are not “taught” but must be “learned” by the student. The educator provides learning experiences through which the students can gain the needed skills and experience. Mastery of the content should be a responsibility placed on the student. Information and assistance are given to the students, but students are held accountable for learning the content. This does not indicate that the educator is freed from responsibility. In fact, the educator will most likely spend more time planning and preparing, compared to when didactic lectures were given; however, the spotlight will be placed on the student. Once the learning modules are developed, they can be readily updated, allowing the educators to improve their sessions with each evaluation.
Curriculum designed to help student students develop critical thinking/problem-solving skills should be learned in context. During the introductory portions of the training, this can be accomplished by providing problem-based scenarios similar to what will be expected in the later clinical setting. The transition to competency-based evaluation in many disciplines has made this a virtual necessity. Critical thinking/problem-solving skills should emphasize self-examination. It should teach an individual to accomplish this using a series of steps that progress in a logical fashion, stressing that critical thinking is a progression of logical thought, not an unguided process.
The methods of teaching critical thinking can be traced back to the dialectic methods used by Socrates. Helping the students learn by posing questions remains an effective tool. Accomplishing this in a group setting also provides each student with the opportunity to learn, not only from their mistakes and accomplishments, but from the mistakes and accomplishments of others. Scenario questions can be presented in a manner similar to those found in many board and licensure exams. This exposes students to material in a format relevant to the clinical setting and to future exams. In larger groups, PowerPoint presentation of scenario questions can be used. Team-based learning (TBL) is useful in encouraging individual self-assessment and peer-peer instruction, while also providing an opportunity for the development of critical thinking and problem-solving skills. After the Individual Readiness Assurance Test (iRAT) exam, students work together to answer the Group Readiness Assurance Test (gRAT). Following this, relevant material is covered by clinicians and basic scientists working together and questions asked using an audience response system. This has been useful in encouraging individual self-assessment and peer-peer instruction while also providing an opportunity for the development of critical thinking and problem-solving skills.
Formative assessment of the students will be given in the class session. This can be accomplished using an audience response system. This gives each individual a chance to determine their own critical thinking skill level. It will prevent the “Oh, I knew that” response from students who are in denial of their own inabilities. Summative assessment in the class will be based on the critical thinking skills presented in the classroom or small-group setting. As mentioned earlier, the students will be evaluated on their ability to think critically and to problem-solve. This will by necessity include evaluation of content knowledge—but only as it pertains to the critical thinking and problem-solving skills. This will be made clear through the use of objectives that describe both content and critical thinking.
Enhancing Critical Thinking Skills in Simulation Centers and Clinics
The development of critical thinking skills in healthcare is somewhat unique. In chess, students can start playing using the same tools employed by the experts (the chess board); however, in healthcare, allowing students to make medical decisions is ethically inappropriate and irresponsible. Simulations centers allow students to gain needed experience and confidence without placing patients at risk. Once the students have mastered simulation center experiences and acquired the needed confidence, they can participate in patient diagnosis under the watchful eye of the expert healthcare professional.
The student’s curriculum now becomes the entire knowledge base of each healthcare discipline. This includes textbooks and journal articles. Students are required to come well prepared to the clinics and/or hospital having developed and in-depth understanding of each patient in their care.
Each day, the expert healthcare provider, serving as a mentor, will provide formative evaluation of the student and his/her performance. Mentors will guide the student, suggesting changes in the skills needed to evaluate the patients properly. In addition, standardized patients provide an excellent method of student/resident evaluation.
Summative evaluation is in the form of subject/board exams. These test the student’s or resident’s ability to accurately describe and evaluate the patient. The objective structured clinical examination (OSCE) is used to evaluate the student’s ability to correctly assess the patient’s condition. Thinking aloud had been previously shown as an effective tool for evaluating expert performance in such settings [ 16 ]. Briefly, think aloud strategies require the student to explain verbally the logic they are using to combine facts to arrive at correct answers. This approach helps the evaluator to determine both the accuracy of the answer and if the correct thought process was followed by the student.
If the time required to develop an expert is a minimum of ten years, what influence can education have on the process?
Education can:
- Provide the student with a foundation of knowledge required for the development of future knowledge and skills.
- Introduce the student to critical thinking and problem-solving techniques.
- Require the student to actively engage the material instead of attempting to learn using rote memory only.
- Assess the performance of the student in a formative manner, allowing the lack of information of skills to be identified early, thus reducing the risk of failure when changes in study skills are more difficult and/or occur too late to help.
- Provide learning in a contextual format that makes the information meaningful and easier to remember.
- Provide training in forward reasoning and backward reasoning skills. It can relate these skills to the problem-solving techniques in healthcare.
- Help students develop the qualities of an expert healthcare provider.
Authors’ Contributions
The authors wrote and contributed to the final manuscript.
Data Availability
Compliance with ethical standards.
The authors declare that they have no conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.

Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Help and Feedback
Publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
Critical Thinking in Medicine and Health
- First Online: 01 March 2020
Cite this chapter
- Louise Cummings 2
770 Accesses
1 Citations
This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations. Our cognitive resources are our only bulwark to the misinformation and faulty logic that exists in medicine and health. One resource in particular—reasoning—can counter the flawed thinking that pervades many medical and health issues. This chapter examines how concepts such as reasoning, logic and argument must be conceptualised somewhat differently (namely, in non-deductive terms) to accommodate the rationality of the informal fallacies. It also addresses the relevance of the informal fallacies to medicine and health and considers how these apparently defective arguments are a source of new analytical possibilities in both domains.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Albano, J. D., Ward, E., Jemal, A., Anderson, R., Cokkinides, V. E., Murray, T., et al. (2007). Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute, 99 (18), 1384–1394.
Article Google Scholar
Coxon, J., & Rees, J. (2015). Avoiding medical errors in general practice. Trends in Urology & Men’s Health, 6 (4), 13–17.
Google Scholar
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78 (8), 775–780.
Cummings, L. (2002). Reasoning under uncertainty: The role of two informal fallacies in an emerging scientific inquiry. Informal Logic, 22 (2), 113–136.
Cummings, L. (2004). Analogical reasoning as a tool of epidemiological investigation. Argumentation, 18 (4), 427–444.
Cummings, L. (2009). Emerging infectious diseases: Coping with uncertainty. Argumentation, 23 (2), 171–188.
Cummings, L. (2010). Rethinking the BSE crisis: A study of scientific reasoning under uncertainty . Dordrecht: Springer.
Book Google Scholar
Cummings, L. (2011). Considering risk assessment up close: The case of bovine spongiform encephalopathy. Health, Risk & Society, 13 (3), 255–275.
Cummings, L. (2012a). Scaring the public: Fear appeal arguments in public health reasoning. Informal Logic, 32 (1), 25–50.
Cummings, L. (2012b). The public health scientist as informal logician. International Journal of Public Health, 57 (3), 649–650.
Cummings, L. (2013a). Public health reasoning: Much more than deduction. Archives of Public Health, 71 (1), 25.
Cummings, L. (2013b). Circular reasoning in public health. Cogency, 5 (2), 35–76.
Cummings, L. (2014a). Informal fallacies as cognitive heuristics in public health reasoning. Informal Logic, 34 (1), 1–37.
Cummings, L. (2014b). The ‘trust’ heuristic: Arguments from authority in public health. Health Communication, 29 (10), 1043–1056.
Cummings, L. (2014c). Coping with uncertainty in public health: The use of heuristics. Public Health, 128 (4), 391–394.
Cummings, L. (2014d). Circles and analogies in public health reasoning. Inquiry, 29 (2), 35–59.
Cummings, L. (2014e). Analogical reasoning in public health. Journal of Argumentation in Context, 3 (2), 169–197.
Cummings, L. (2015). Reasoning and public health: New ways of coping with uncertainty . Cham, Switzerland: Springer.
Fowler, F. J., Jr., Levin, C. A., & Sepucha, K. R. (2011). Informing and involving patients to improve the quality of medical decisions. Health Affairs, 30 (4), 699–706.
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499.
Hamblin, C. L. (1970). Fallacies . London: Methuen.
Johnson, R. H. (2011). Informal logic and deductivism. Studies in Logic, 4 (1), 17–37.
Kahane, H. (1971). Logic and contemporary rhetoric: The use of reason in everyday life . Belmont, CA: Wadsworth Publishing Company.
Loucks, E. B., Buka, S. L., Rogers, M. L., Liu, T., Kawachi, I., Kubzansky, L. D., et al. (2012). Education and coronary heart disease risk associations may be affected by early life common prior causes: A propensity matching analysis. Annals of Epidemiology, 22 (4), 221–232.
Saposnik, G., Redelmeier, D., Ruff, C. C., & Tobler, P. N. (2016). Cognitive biases associated with medical decisions: A systematic review. BMC Medical Informatics and Decision Making, 16, 138. https://doi.org/10.1186/s12911-016-0377-1 .
Trowbridge, R. L. (2008). Twelve tips for teaching avoidance of diagnostic errors. Medical Teacher, 30, 496–500.
Walton, D. N. (1985a). Are circular arguments necessarily vicious? American Philosophical Quarterly, 22 (4), 263–274.
Walton, D. N. (1985b). Arguer’s Position . Westport, CT: Greenwood Press.
Walton, D. N. (1987). The ad hominem argument as an informal fallacy. Argumentation, 1 (3), 317–331.
Walton, D. N. (1991). Begging the question: Circular reasoning as a tactic of argumentation . New York: Greenwood Press.
Walton, D. N. (1992). Plausible argument in everyday conversation . Albany: SUNY Press.
Walton, D. N. (1996). Argumentation schemes for presumptive reasoning . Mahwah, NJ: Erlbaum.
Walton, D. N. (2010). Why fallacies appear to be better arguments than they are. Informal Logic, 30 (2), 159–184.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. Western Journal of Medicine, 172 (6), 390–393.
Woods, J. (1995). Appeal to force. In H. V. Hansen & R. C. Pinto (Eds.), Fallacies: Classical and contemporary readings (pp. 240–250). University Park: The Pennsylvania State University Press.
Woods, J. (2004). The death of argument: Fallacies in agent-based reasoning . Dordrecht: Kluwer Academic.
Woods, J. (2007). Lightening up on the ad hominem. Informal Logic, 27 (1), 109–134.
Woods, J. (2008). Begging the question is not a fallacy. In C. Dégremont, L. Keiff, & H. Rükert (Eds.), Dialogues, logics and other strange things: Essays in honour of Shahid Rahman (pp. 523–544). London: College Publications.
Download references
Author information
Authors and affiliations.
Department of English, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Louise Cummings
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Louise Cummings .
Chapter Summary
Medicine and health have tended to be overlooked in the critical thinking literature . And yet robust critical thinking skills are needed to evaluate the large number and range of health messages that we are exposed to on a daily basis.
An ability to think critically helps us to make better personal health choices and to uncover biases and errors in health messages and other information. An ability to think critically allows us to make informed decisions about medical treatments and is vital to efforts to reduce medical diagnostic errors.
A key element in critical thinking is the ability to distinguish strong or valid reasoning from weak or invalid reasoning. When an argument is weak or invalid, it is called a ‘fallacy’ or a ‘fallacious argument’.
The informal fallacies are so-called on account of the presence of epistemic and dialectical flaws that cannot be captured by formal logic . They have been discussed by many generations of philosophers and logicians , beginning with Aristotle .
Historically, philosophers and logicians have taken a pejorative view of the informal fallacies. Much of the criticism of these arguments is related to a latent deductivism in logic , the notion that arguments should be evaluated according to deductive standards of validity and soundness . Against deductive standards and norms, many reasonable arguments are judged to be fallacies.
Developments in logic , particularly the teaching of logic, forced a reconsideration of the prominence afforded to deductive logic in the evaluation of arguments. New criteria based on presumptive reasoning and plausible argument started to emerge. Against this backdrop, non-fallacious variants of most of the informal fallacies began to be described for the first time.
Today, some argument analysts characterize non-fallacious variants of the informal fallacies in terms of cognitive heuristics . During reasoning , these heuristics function as mental shortcuts, allowing us to bypass knowledge and come to judgement about complex health problems.
Suggestions for Further Reading
Sharples, J. M., Oxman, A. D., Mahtani, K. R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A., & Hoffmann, T. (2017). Critical thinking in healthcare and education. British Medical Journal, 357 : j2234. https://doi.org/10.1136/bmj.j2234 .
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. Its aim is to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health.
Hitchcock, D. (2017). On reasoning and argument: Essays in informal logic and on critical thinking . Cham: Switzerland: Springer.
This collection of essays provides more advanced reading on several of the topics addressed in this chapter, including the fallacies, informal logic , and the teaching of critical thinking . Chapter 25 considers if fallacies have a place in the teaching of critical thinking and reasoning skills.
Hansen, H. V., & Pinto, R. C. (Eds.). (1995). Fallacies: Classical and contemporary readings . University Park: The Pennsylvania State University Press.
This edited collection of 24 chapters contains historical selections on the fallacies, contemporary theory and criticism, and analyses of specific fallacies. It also examines fallacies and teaching. There are chapters on four of the fallacies that will be examined in this book: appeal to force; appeal to ignorance ; appeal to authority; and post hoc ergo propter hoc .
Diagnostic errors are a significant cause of death and serious injury in patients. Many of these errors are related to cognitive factors. Trowbridge ( 2008 ) has devised twelve tips to familiarize medical students and physician trainees with the cognitive underpinnings of diagnostic errors. One of these tips is to explicitly describe heuristics and how they affect clinical reasoning . These heuristics include the following:
Representativeness —a patient’s presentation is compared to a ‘typical’ case of specific diagnoses.
Availability —physicians arrive at a diagnosis based on what is easily accessible in their minds, rather than what is actually most probable.
Anchoring —physicians may settle on a diagnosis early in the diagnostic process and subsequently become ‘anchored’ in that diagnosis.
Confirmation bias —as a result of anchoring, physicians may discount information discordant with the original diagnosis and accept only that which supports the diagnosis.
Using the above information, identify any heuristics and biases that occur in the following scenarios:
Scenario 1: A 60-year-old man has epigastric pain and nausea. He is sitting forward clutching his abdomen. He has a history of several bouts of alcoholic pancreatitis. He states that he felt similar during these bouts to what he is currently feeling. The patient states that he has had no alcohol in many years. He has normal blood levels of pancreatic enzymes. He is given a diagnosis of acute pancreatitis. It is eventually discovered that he has had acute myocardial infarction.
Scenario 2: A 20-year-old, healthy man presents with sudden onset of severe, sharp chest pain and back pain. Based on these symptoms, he is suspected of having a dissecting thoracic aortic aneurysm. (In an aortic dissection, there is a separation of the layers within the wall of the aorta, the large blood vessel branching off the heart.) He is eventually diagnosed with pleuritis (inflammation of the pleura, the thin, transparent, two-layered membrane that covers the lungs).
Many of the logical terms that were introduced in this chapter also have non-logical uses in everyday language. Below are several examples of the use of these terms. For each example, indicate if the word in italics has a logical or a non - logical meaning or use:
University ‘safe spaces’ are a dangerous fallacy —they do not exist in the real world ( The Telegraph , 13 February 2017).
The MRI findings beg the question as to whether a careful ultrasound examination might have yielded some of the same information on haemorrhages ( British Medical Journal: Fetal & Neonatal , 2011).
The youth justice system is a slippery slope of failure ( The Sydney Morning Herald , 26 July 2016).
The EU countered with its own gastronomic analogy , saying that “cherry picking” the best bits of the EU would not be tolerated ( BBC News , 28 July 2017).
As Ebola spreads, so have several fallacies ( The New York Times , 23 October 2014).
Removing the statue of Confederacy Army General Robert E. Lee no more puts us on a slippery slope towards ousting far more nuanced figures from the public square than building the statue in the first place put us on a slippery slope toward, say, putting up statues of Hitler outside of Holocaust museums or of Ho Chi Minh at Vietnam War memorials ( Chicago Tribune , 16 August 2017).
We can expand the analogy a bit and think of a culture as something akin to a society’s immune system—it works best when it is exposed to as many foreign bodies as possible ( New Zealand Herald , 4 May 2010).
The Josh Norman Bowl begs the question : What’s an elite cornerback worth? ( The Washington Post , 17 December 2016).
The intuition behind these analogies is simple: As a homeowner, I generally have the right to exclude whoever I want from my property. I don’t even have to have a good justification for the exclusion. I can choose to bar you from my home for virtually any reason I want, or even just no reason at all. Similarly, a nation has the right to bar foreigners from its land for almost any reason it wants, or perhaps even no reason at all ( The Washington Post , 6 August 2017).
Legalising assisted suicide is a slippery slope toward widespread killing of the sick, Members of Parliament and peers were told yesterday ( Mail Online , 9 July 2014).
In the Special Topic ‘What’s in a name?’, an example of a question-begging argument from the author’s recent personal experience was used. How would you reconstruct the argument in this case to illustrate the presence of a fallacy?
On 9 July 2017, the effect of coconut oil on health was also discussed in an article in The Guardian entitled ‘Coconut oil: Are the health benefits a big fat lie?’ The following extract is taken from that article. (a) What type of reasoning is the author using in this extract? In your response, you should reconstruct the argument by presenting its premises and conclusion . Also, is this argument valid or fallacious in this particular context?
When it comes to superfoods, coconut oil presses all the buttons: it’s natural, it’s enticingly exotic, it’s surrounded by health claims and at up to £8 for a 500 ml pot at Tesco, it’s suitably pricey. But where this latest superfood differs from benign rivals such as blueberries, goji berries, kale and avocado is that a diet rich in coconut oil may actually be bad for us.
The article in The Guardian also makes extensive use of expert opinion. Two such opinions are shown below. (b) What three linguistic devices does the author use to confer expertise or authority on the individuals who advance these opinions?
Christine Williams, professor of human nutrition at the University of Reading, states: “There is very limited evidence of beneficial health effects of this oil”.
Tom Sanders, emeritus professor of nutrition and dietetics at King’s College London, says: “It is a poor source of vitamin E compared with other vegetable oils”.
The author of the article in The Guardian went on to summarize the findings of a study by two researchers that was published in the British Nutrition Foundation’s Nutrition Bulletin. The author’s summary included the following statement: There is no good evidence that coconut oil helps boost mental performance or prevent Alzheimer’s disease . (c) In what type of informal fallacy might this statement be a premise ?
Scenario 1: An anchoring error has occurred in which the patient is given a diagnosis of acute pancreatitis early in the diagnostic process. The clinician becomes anchored in this diagnosis, with the result that he overlooks two pieces of information that would have allowed this diagnosis to be disconfirmed—the fact that the patient has reported no alcohol use in many years and the presence of normal blood levels of pancreatic enzymes. By dismissing this information, the clinician is also showing a confirmation bias —he attends only to information that confirms his original diagnosis.
Scenario 2: A representativeness error has occurred. The patient’s presentation is typical of aortic dissection. However, this condition can be dismissed in favour of conditions like pleuritis or pneumothorax on account of the fact that aortic dissection is exceptionally rare in 20-year-olds.
(2) (a) non-logical; (b) non-logical; (c) non-logical; (d) non-logical; (e) non-logical; (f) logical; (g) logical; (h) non-logical; (i) logical; (j) logical
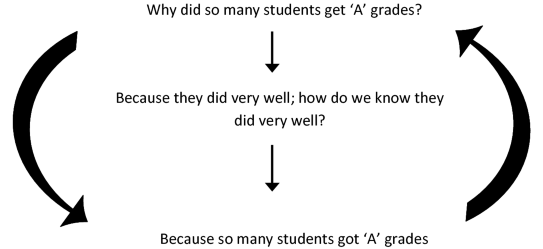
(3) The fallacy can be illustrated as follows. The head of department asks the question ‘Why did so many of these students get ‘A’ grades’? He receives the reply ‘Because they did very well’. But someone might reasonably ask ‘How do we know that they did very well?’ To which the reply is ‘Because so many students got ‘A’ grades’. The reasoning can be reconstructed in diagram form as follows:
The author is using an analogical argument , which has the following form:
P1: Blueberries, goji berries, kale, avocado and coconut oil are natural, exotic, pricey and surrounded by health claims.
P2: Blueberries, goji berries, kale and avocado have health benefits.
C: Coconut oil has health benefits.
This is a false analogy , or a fallacious analogical argument , because coconut oil does not share with these other superfoods the property or attribute < has health benefits >.
The author uses academic rank, field of specialization, and university affiliation to confer authority or expertise on individuals who advance expert opinions.
This statement could be a premise in an argument from ignorance .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cummings, L. (2020). Critical Thinking in Medicine and Health. In: Fallacies in Medicine and Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-28513-5_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-28513-5_1
Published : 01 March 2020
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-28512-8
Online ISBN : 978-3-030-28513-5
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
This article attempts to provide a conceptual analysis of critical thinking with reference to medical education along with measures to foster critical thinking through relevant teaching learning and assessment methods. Key words: Critical thinking, medical education, quality patient care, fostering critical thinking.
Three main conceptions of critical thinking were identified, each of which will be elaborated in greater detail below: biomedical critical thinking, humanist critical thinking, and social justice-oriented critical thinking.
Critical thinking, the ability to think clearly and rationally about what to do or what to believe, is essential for the practice of medicine. Few doctors are likely to argue with this.
Critical thinking skills are essential to the development of well-trained healthcare professionals. These skills are not “taught” but must be “learned” by the student. The educator provides learning experiences through which the students can gain the needed skills and experience.
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes. While problem-solving tends to focus on the identification and resolution of a problem, critical thinking involves asking skilled questions and critiquing solutions.
Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking. It is important to define these skills explicitly, explain their rationales, describe methods of instruction and provide examples of optimal application.
Clinicians today need strong critical thinking skills in order to properly diagnose and treat patients. That’s one reason why it is critical for educators to help medical students cultivate these skills early in their training.
Critical thinking, the capacity to be deliberate about thinking and actively assess and regulate one’s cognition (1–4), is an essential skill for all physicians. Absent critical thinking, one typically relies on heuristics, a quick method or shortcut for problem solving, and can fall victim to cognitive biases .
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors.
1 Citations. Abstract. This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations.