- Search Menu
- Advance articles
- Editor's Choice
- Graphical Abstracts and Tidbit
- Author Guidelines
- Submission Site
- Open Access
- About American Journal of Hypertension
- Editorial Board
- Board of Directors
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- AJH Summer School
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Clinical management and treatment decisions, hypertension in black americans, pharmacologic treatment of hypertension in black americans.
- < Previous
- Article contents
- Figures & tables
- Supplementary Data
Suzanne Oparil, Case study, American Journal of Hypertension , Volume 11, Issue S8, November 1998, Pages 192S–194S, https://doi.org/10.1016/S0895-7061(98)00195-2
- Permissions Icon Permissions
Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
At physician visit one, Ms. C presented with complaints of headache and general weakness. She reported that she has been taking many medications for her hypertension in the past, but stopped taking them because of the side effects. She could not recall the names of the medications. Currently she is taking 100 mg/day atenolol and 12.5 mg/day hydrochlorothiazide (HCTZ), which she admits to taking irregularly because “... they bother me, and I forget to renew my prescription.” Despite this antihypertensive regimen, her blood pressure remains elevated, ranging from 150 to 155/110 to 114 mm Hg. In addition, Ms. C admits that she has found it difficult to exercise, stop smoking, and change her eating habits. Findings from a complete history and physical assessment are unremarkable except for the presence of moderate obesity (5 ft 6 in., 150 lbs), minimal retinopathy, and a 25-year history of smoking approximately one pack of cigarettes per day. Initial laboratory data revealed serum sodium 138 mEq/L (135 to 147 mEq/L); potassium 3.4 mEq/L (3.5 to 5 mEq/L); blood urea nitrogen (BUN) 19 mg/dL (10 to 20 mg/dL); creatinine 0.9 mg/dL (0.35 to 0.93 mg/dL); calcium 9.8 mg/dL (8.8 to 10 mg/dL); total cholesterol 268 mg/dL (< 245 mg/dL); triglycerides 230 mg/dL (< 160 mg/dL); and fasting glucose 105 mg/dL (70 to 110 mg/dL). The patient refused a 24-h urine test.
Taking into account the past history of compliance irregularities and the need to take immediate action to lower this patient’s blood pressure, Ms. C’s pharmacologic regimen was changed to a trial of the angiotensin-converting enzyme (ACE) inhibitor enalapril, 5 mg/day; her HCTZ was discontinued. In addition, recommendations for smoking cessation, weight reduction, and diet modification were reviewed as recommended by the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). 1
After a 3-month trial of this treatment plan with escalation of the enalapril dose to 20 mg/day, the patient’s blood pressure remained uncontrolled. The patient’s medical status was reviewed, without notation of significant changes, and her antihypertensive therapy was modified. The ACE inhibitor was discontinued, and the patient was started on the angiotensin-II receptor blocker (ARB) losartan, 50 mg/day.
After 2 months of therapy with the ARB the patient experienced a modest, yet encouraging, reduction in blood pressure (140/100 mm Hg). Serum electrolyte laboratory values were within normal limits, and the physical assessment remained unchanged. The treatment plan was to continue the ARB and reevaluate the patient in 1 month. At that time, if blood pressure control remained marginal, low-dose HCTZ (12.5 mg/day) was to be added to the regimen.
Hypertension remains a significant health problem in the United States (US) despite recent advances in antihypertensive therapy. The role of hypertension as a risk factor for cardiovascular morbidity and mortality is well established. 2–7 The age-adjusted prevalence of hypertension in non-Hispanic black Americans is approximately 40% higher than in non-Hispanic whites. 8 Black Americans have an earlier onset of hypertension and greater incidence of stage 3 hypertension than whites, thereby raising the risk for hypertension-related target organ damage. 1 , 8 For example, hypertensive black Americans have a 320% greater incidence of hypertension-related end-stage renal disease (ESRD), 80% higher stroke mortality rate, and 50% higher CVD mortality rate, compared with that of the general population. 1 , 9 In addition, aging is associated with increases in the prevalence and severity of hypertension. 8
Research findings suggest that risk factors for coronary heart disease (CHD) and stroke, particularly the role of blood pressure, may be different for black American and white individuals. 10–12 Some studies indicate that effective treatment of hypertension in black Americans results in a decrease in the incidence of CVD to a level that is similar to that of nonblack American hypertensives. 13 , 14
Data also reveal differences between black American and white individuals in responsiveness to antihypertensive therapy. For instance, studies have shown that diuretics 15 , 16 and the calcium channel blocker diltiazem 16 , 17 are effective in lowering blood pressure in black American patients, whereas β-adrenergic receptor blockers and ACE inhibitors appear less effective. 15 , 16 In addition, recent studies indicate that ARB may also be effective in this patient population.
Angiotensin-II receptor blockers are a relatively new class of agents that are approved for the treatment of hypertension. Currently, four ARB have been approved by the US Food and Drug Administration (FDA): eprosartan, irbesartan, losartan, and valsartan. Recently, a 528-patient, 26-week study compared the efficacy of eprosartan (200 to 300 mg/twice daily) versus enalapril (5 to 20 mg/daily) in patients with essential hypertension (baseline sitting diastolic blood pressure [DBP] 95 to 114 mm Hg). After 3 to 5 weeks of placebo, patients were randomized to receive either eprosartan or enalapril. After 12 weeks of therapy within the titration phase, patients were supplemented with HCTZ as needed. In a prospectively defined subset analysis, black American patients in the eprosartan group (n = 21) achieved comparable reductions in DBP (−13.3 mm Hg with eprosartan; −12.4 mm Hg with enalapril) and greater reductions in systolic blood pressure (SBP) (−23.1 with eprosartan; −13.2 with enalapril), compared with black American patients in the enalapril group (n = 19) ( Fig. 1 ). 18 Additional trials enrolling more patients are clearly necessary, but this early experience with an ARB in black American patients is encouraging.
Efficacy of the angiotensin II receptor blocker eprosartan in black American with mild to moderate hypertension (baseline sitting DBP 95 to 114 mm Hg) in a 26-week study. Eprosartan, 200 to 300 mg twice daily (n = 21, solid bar), enalapril 5 to 20 mg daily (n = 19, diagonal bar). †10 of 21 eprosartan patients and seven of 19 enalapril patients also received HCTZ. Adapted from data in Levine: Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study, in Programs and abstracts from the 1st International Symposium on Angiotensin-II Antagonism, September 28–October 1, 1997, London, UK.
00195-2/2/m_ajh.192S.f1.jpeg?Expires=1715912260&Signature=m2JuurBni9XVjiybM3wXE401VWu4HNWdtD79r0atsyyKUC2aP3ObV-PT7Is78Qblcdrt5EPN3x3KfsCiJGsSTx1mEEBJokzNSQnsRxO6y2rP0wQwOub0kjziZp1wW8sr5aXAZrePCbZcYswK5-Yao-wojv7yn3Z-hiQU2mAD-oiytEMnDwMZft~WXpzxZTF5VOaj1DuXeJ~gldf0LKbtdHDOtvytG7ywcwd4cPMULAVxXSHMeX9JQJAaLqQ2Cr2Q9NefpOeccUKUQU94nY6f0sUAiPI5RlZ93CzskWmJkCf2gEv307Dt~DhaOFE6xPs38RP-HEa285lZ0X1ADKGhcg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Approximately 30% of all deaths in hypertensive black American men and 20% of all deaths in hypertensive black American women are attributable to high blood pressure. Black Americans develop high blood pressure at an earlier age, and hypertension is more severe in every decade of life, compared with whites. As a result, black Americans have a 1.3 times greater rate of nonfatal stroke, a 1.8 times greater rate of fatal stroke, a 1.5 times greater rate of heart disease deaths, and a 5 times greater rate of ESRD when compared with whites. 19 Therefore, there is a need for aggressive antihypertensive treatment in this group. Newer, better tolerated antihypertensive drugs, which have the advantages of fewer adverse effects combined with greater antihypertensive efficacy, may be of great benefit to this patient population.
1. Joint National Committee : The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure . Arch Intern Med 1997 ; 24 157 : 2413 – 2446 .
Google Scholar
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg . JAMA 1967 ; 202 : 116 – 122 .
3. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: II. Results in patients with diastolic blood pressures averaging 90 through 114 mm Hg . JAMA 1970 ; 213 : 1143 – 1152 .
4. Pooling Project Research Group : Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to the incidence of major coronary events: Final report of the pooling project . J Chronic Dis 1978 ; 31 : 201 – 306 .
5. Hypertension Detection and Follow-Up Program Cooperative Group : Five-year findings of the hypertension detection and follow-up program: I. Reduction in mortality of persons with high blood pressure, including mild hypertension . JAMA 1979 ; 242 : 2562 – 2577 .
6. Kannel WB , Dawber TR , McGee DL : Perspectives on systolic hypertension: The Framingham Study . Circulation 1980 ; 61 : 1179 – 1182 .
7. Hypertension Detection and Follow-Up Program Cooperative Group : The effect of treatment on mortality in “mild” hypertension: Results of the Hypertension Detection and Follow-Up Program . N Engl J Med 1982 ; 307 : 976 – 980 .
8. Burt VL , Whelton P , Roccella EJ et al. : Prevalence of hypertension in the US adult population: Results from the third National Health and Nutrition Examination Survey, 1988–1991 . Hypertension 1995 ; 25 : 305 – 313 .
9. Klag MJ , Whelton PK , Randall BL et al. : End-stage renal disease in African-American and white men: 16-year MRFIT findings . JAMA 1997 ; 277 : 1293 – 1298 .
10. Neaton JD , Kuller LH , Wentworth D et al. : Total and cardiovascular mortality in relation to cigarette smoking, serum cholesterol concentration, and diastolic blood pressure among black and white males followed up for five years . Am Heart J 1984 ; 3 : 759 – 769 .
11. Gillum RF , Grant CT : Coronary heart disease in black populations II: Risk factors . Heart J 1982 ; 104 : 852 – 864 .
12. M’Buyamba-Kabangu JR , Amery A , Lijnen P : Differences between black and white persons in blood pressure and related biological variables . J Hum Hypertens 1994 ; 8 : 163 – 170 .
13. Hypertension Detection and Follow-up Program Cooperative Group : Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level: a further analysis . J Community Health 1984 ; 9 : 314 – 327 .
14. Ooi WL , Budner NS , Cohen H et al. : Impact of race on treatment response and cardiovascular disease among hypertensives . Hypertension 1989 ; 14 : 227 – 234 .
15. Weinberger MH : Racial differences in antihypertensive therapy: evidence and implications . Cardiovasc Drugs Ther 1990 ; 4 ( suppl 2 ): 379 – 392 .
16. Materson BJ , Reda DJ , Cushman WC et al. : Single-drug therapy for hypertension in men: A comparison of six antihypertensive agents with placebo . N Engl J Med 1993 ; 328 : 914 – 921 .
17. Materson BJ , Reda DJ , Cushman WC for the Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents : Department of Veterans Affairs single-drug therapy of hypertension study: Revised figures and new data . Am J Hypertens 1995 ; 8 : 189 – 192 .
18. Levine B : Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study , in Programs and abstracts from the first International Symposium on Angiotensin-II Antagonism , September 28 – October 1 , 1997 , London, UK .
19. American Heart Association: 1997 Heart and Stroke Statistical Update . American Heart Association , Dallas , 1997 .
- hypertension
- blood pressure
- african american
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1941-7225
- Copyright © 2024 American Journal of Hypertension, Ltd.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 6: 10 Real Cases on Hypertensive Emergency and Pericardial Disease: Diagnosis, Management, and Follow-Up
Niel Shah; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Diagnostic Evaluation
- Full Chapter
- Supplementary Content
Case 1: Management of Hypertensive Encephalopathy
A 45-year-old man with a 2-month history of progressive headache presented to the emergency department with nausea, vomiting, visual disturbance, and confusion for 1 day. He denied fever, weakness, numbness, shortness of breath, and flulike symptoms. He had significant medical history of hypertension and was on a β-blocker in the past, but a year ago, he stopped taking medication due to an unspecified reason. The patient denied any history of tobacco smoking, alcoholism, and recreational drug use. The patient had a significant family history of hypertension in both his father and mother. Physical examination was unremarkable, and at the time of triage, his blood pressure (BP) was noted as 195/123 mm Hg, equal in both arms. The patient was promptly started on intravenous labetalol with the goal to reduce BP by 15% to 20% in the first hour. The BP was rechecked after an hour of starting labetalol and was 165/100 mm Hg. MRI of the brain was performed in the emergency department and demonstrated multiple scattered areas of increased signal intensity on T2-weighted and fluid-attenuated inversion recovery (FLAIR) images in both the occipital and posterior parietal lobes. There were also similar lesions in both hemispheres of the cerebellum (especially the cerebellar white matter on the left) as well as in the medulla oblongata. The lesions were not associated with mass effect, and after contrast administration, there was no evidence of abnormal enhancement. In the emergency department, his BP decreased to 160/95 mm Hg, and he was transitioned from drip to oral medications and transferred to the telemetry floor. How would you manage this case?
The patient initially presented with headache, nausea, vomiting, blurred vision, and confusion. The patient’s BP was found to be 195/123 mm Hg, and MRI of the brain demonstrated scattered lesions with increased intensity in the occipital and posterior parietal lobes, as well as in cerebellum and medulla oblongata. The clinical presentation, elevated BP, and brain MRI findings were suggestive of hypertensive emergency, more specifically hypertensive encephalopathy. These MRI changes can be seen particularly in posterior reversible encephalopathy syndrome (PRES), a sequela of hypertensive encephalopathy. BP was initially controlled by labetalol, and after satisfactory control of BP, the patient was switched to oral antihypertensive medications.
Hypertensive emergency refers to the elevation of systolic BP >180 mm Hg and/or diastolic BP >120 mm Hg that is associated with end-organ damage; however, in some conditions such as pregnancy, more modest BP elevation can constitute an emergency. An equal degree of hypertension but without end-organ damage constitutes a hypertensive urgency, the treatment of which requires gradual BP reduction over several hours. Patients with hypertensive emergency require rapid, tightly controlled reductions in BP that avoid overcorrection. Management typically occurs in an intensive care setting with continuous arterial BP monitoring and continuous infusion of antihypertensive agents.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- Previous Article
- Next Article
Presentation
Clinical pearls, case study: treating hypertension in patients with diabetes.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Evan M. Benjamin; Case Study: Treating Hypertension in Patients With Diabetes. Clin Diabetes 1 July 2004; 22 (3): 137–138. https://doi.org/10.2337/diaclin.22.3.137
Download citation file:
- Ris (Zotero)
- Reference Manager
L.N. is a 49-year-old white woman with a history of type 2 diabetes,obesity, hypertension, and migraine headaches. The patient was diagnosed with type 2 diabetes 9 years ago when she presented with mild polyuria and polydipsia. L.N. is 5′4″ and has always been on the large side,with her weight fluctuating between 165 and 185 lb.
Initial treatment for her diabetes consisted of an oral sulfonylurea with the rapid addition of metformin. Her diabetes has been under fair control with a most recent hemoglobin A 1c of 7.4%.
Hypertension was diagnosed 5 years ago when blood pressure (BP) measured in the office was noted to be consistently elevated in the range of 160/90 mmHg on three occasions. L.N. was initially treated with lisinopril, starting at 10 mg daily and increasing to 20 mg daily, yet her BP control has fluctuated.
One year ago, microalbuminuria was detected on an annual urine screen, with 1,943 mg/dl of microalbumin identified on a spot urine sample. L.N. comes into the office today for her usual follow-up visit for diabetes. Physical examination reveals an obese woman with a BP of 154/86 mmHg and a pulse of 78 bpm.
What are the effects of controlling BP in people with diabetes?
What is the target BP for patients with diabetes and hypertension?
Which antihypertensive agents are recommended for patients with diabetes?
Diabetes mellitus is a major risk factor for cardiovascular disease (CVD). Approximately two-thirds of people with diabetes die from complications of CVD. Nearly half of middle-aged people with diabetes have evidence of coronary artery disease (CAD), compared with only one-fourth of people without diabetes in similar populations.
Patients with diabetes are prone to a number of cardiovascular risk factors beyond hyperglycemia. These risk factors, including hypertension,dyslipidemia, and a sedentary lifestyle, are particularly prevalent among patients with diabetes. To reduce the mortality and morbidity from CVD among patients with diabetes, aggressive treatment of glycemic control as well as other cardiovascular risk factors must be initiated.
Studies that have compared antihypertensive treatment in patients with diabetes versus placebo have shown reduced cardiovascular events. The United Kingdom Prospective Diabetes Study (UKPDS), which followed patients with diabetes for an average of 8.5 years, found that patients with tight BP control (< 150/< 85 mmHg) versus less tight control (< 180/< 105 mmHg) had lower rates of myocardial infarction (MI), stroke, and peripheral vascular events. In the UKPDS, each 10-mmHg decrease in mean systolic BP was associated with a 12% reduction in risk for any complication related to diabetes, a 15% reduction for death related to diabetes, and an 11% reduction for MI. Another trial followed patients for 2 years and compared calcium-channel blockers and angiotensin-converting enzyme (ACE) inhibitors,with or without hydrochlorothiazide against placebo and found a significant reduction in acute MI, congestive heart failure, and sudden cardiac death in the intervention group compared to placebo.
The Hypertension Optimal Treatment (HOT) trial has shown that patients assigned to lower BP targets have improved outcomes. In the HOT trial,patients who achieved a diastolic BP of < 80 mmHg benefited the most in terms of reduction of cardiovascular events. Other epidemiological studies have shown that BPs > 120/70 mmHg are associated with increased cardiovascular morbidity and mortality in people with diabetes. The American Diabetes Association has recommended a target BP goal of < 130/80 mmHg. Studies have shown that there is no lower threshold value for BP and that the risk of morbidity and mortality will continue to decrease well into the normal range.
Many classes of drugs have been used in numerous trials to treat patients with hypertension. All classes of drugs have been shown to be superior to placebo in terms of reducing morbidity and mortality. Often, numerous agents(three or more) are needed to achieve specific target levels of BP. Use of almost any drug therapy to reduce hypertension in patients with diabetes has been shown to be effective in decreasing cardiovascular risk. Keeping in mind that numerous agents are often required to achieve the target level of BP control, recommending specific agents becomes a not-so-simple task. The literature continues to evolve, and individual patient conditions and preferences also must come into play.
While lowering BP by any means will help to reduce cardiovascular morbidity, there is evidence that may help guide the selection of an antihypertensive regimen. The UKPDS showed no significant differences in outcomes for treatment for hypertension using an ACE inhibitor or aβ-blocker. In addition, both ACE inhibitors and angiotensin II receptor blockers (ARBs) have been shown to slow the development and progression of diabetic nephropathy. In the Heart Outcomes Prevention Evaluation (HOPE)trial, ACE inhibitors were found to have a favorable effect in reducing cardiovascular morbidity and mortality, whereas recent trials have shown a renal protective benefit from both ACE inhibitors and ARBs. ACE inhibitors andβ-blockers seem to be better than dihydropyridine calcium-channel blockers to reduce MI and heart failure. However, trials using dihydropyridine calcium-channel blockers in combination with ACE inhibitors andβ-blockers do not appear to show any increased morbidity or mortality in CVD, as has been implicated in the past for dihydropyridine calcium-channel blockers alone. Recently, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) in high-risk hypertensive patients,including those with diabetes, demonstrated that chlorthalidone, a thiazide-type diuretic, was superior to an ACE inhibitor, lisinopril, in preventing one or more forms of CVD.
L.N. is a typical patient with obesity, diabetes, and hypertension. Her BP control can be improved. To achieve the target BP goal of < 130/80 mmHg, it may be necessary to maximize the dose of the ACE inhibitor and to add a second and perhaps even a third agent.
Diuretics have been shown to have synergistic effects with ACE inhibitors,and one could be added. Because L.N. has migraine headaches as well as diabetic nephropathy, it may be necessary to individualize her treatment. Adding a β-blocker to the ACE inhibitor will certainly help lower her BP and is associated with good evidence to reduce cardiovascular morbidity. Theβ-blocker may also help to reduce the burden caused by her migraine headaches. Because of the presence of microalbuminuria, the combination of ARBs and ACE inhibitors could also be considered to help reduce BP as well as retard the progression of diabetic nephropathy. Overall, more aggressive treatment to control L.N.'s hypertension will be necessary. Information obtained from recent trials and emerging new pharmacological agents now make it easier to achieve BP control targets.
Hypertension is a risk factor for cardiovascular complications of diabetes.
Clinical trials demonstrate that drug therapy versus placebo will reduce cardiovascular events when treating patients with hypertension and diabetes.
A target BP goal of < 130/80 mmHg is recommended.
Pharmacological therapy needs to be individualized to fit patients'needs.
ACE inhibitors, ARBs, diuretics, and β-blockers have all been documented to be effective pharmacological treatment.
Combinations of drugs are often necessary to achieve target levels of BP control.
ACE inhibitors and ARBs are agents best suited to retard progression of nephropathy.
Evan M. Benjamin, MD, FACP, is an assistant professor of medicine and Vice President of Healthcare Quality at Baystate Medical Center in Springfield, Mass.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer
Making Best Practice, Every Day Practice
Case study: The hypertensive patient
Working with patients who are not willing to engage fully with healthcare services is a common occurrence. The process requires patience and a focus on providing the patient with full information about their condition and then allowing them to make decisions about their treatment. Here, Dr Terry McCormack (GP and Cardiovascular Lead, North Yorks) describes the approach of his practice to a man with hypertension.
A 57-year old man Mr ‘Hawk’ Ward attends a routine NHS Health Check with a health care assistant (HCA) in the local surgery. He had had no contact with healthcare for many years and was not keen on any interventions. Repeated blood pressure (BP) measurements showed very high BP of 205/91 mmHg. The assessment also showed:
- A strong family history of CV disease (brother
- Smoker 30/day
- Appearance healthy
- Alcohol intake 100 units/week
The HCA immediately referred him to the GP who had a long discussion with him and was able to persuade him to take a blood test and have home blood pressure monitoring (HBPM) although he declined ambulatory blood pressure monitoring.
He returned to see the practice senior nurse after HBPM and further investigations showed:
- HBPM average of 8 readings (first 2 discounted) 180/95 mmHg
- Total cholesterol 7.2 mmol/L, HDL 1.4 mmol/L, non-HDL 5.8 mmol/L
- QRISK2 36.1
- Liver Function Tests normal
Mr Ward agreed with the senior nurse to stop smoking, excess alcohol intake, adding salt to food, but would not take medication. He reluctantly agreed to make an appointment to see Dr McCormack.
At the GP appointment
- Mr Ward announces that ‘medication is not an option’
- The GP explains all his risks (including the relevance of non-HDL cholesterol and QRISK2 assessment) and then ask him what he would like to do about it.
- Shared, informed decision making explained
- The GP offers ABPM to confirm the diagnosis
After some time spent considering the GPs evidence and advice, the patient decided to accept some medication and was put on amlodipine 5mg.
Current situation
At a later visit Mr Ward’s blood pressure had reduced to 147/84 mmHg. He has cut down on alcohol and was less agitated. He agreed to take atorvastatin 20 mg and is continuing on therapy and has improved his engagement with the practice team. This patient and ongoing approach has produced significant improvements in his condition, lowered his risk of subsequent events and provides promise for ongoing interaction with health care services.

Case study: Nurse COPD assessment

Case study: Painful diabetic peripheral neuropathy

Case study: Statin intolerance in a patient with high cardiovascular risk
Join our community of primary care professionals today, educational partners.

- Open access
- Published: 15 September 2020
Treatment adherence among patients with hypertension: findings from a cross-sectional study
- Fahad M. Algabbani 1 &
- Aljoharah M. Algabbani 2
Clinical Hypertension volume 26 , Article number: 18 ( 2020 ) Cite this article
13k Accesses
33 Citations
Metrics details
Hypertension is a major risk factor for cardiovascular disease, which is the leading cause of mortality globally. Patient’s adherence to treatment is a cornerstone factor in controlling hypertension and its complications. This study assesses hypertension patients’ adherence to treatment and its associated factors.
This cross-sectional study conducted in Riyadh, Saudi Arabia. The study targeted outpatients aged ≥18 years who were diagnosed with hypertension. Participants were recruited using a systemic sampling technique. The two main measurements were assessing adherence rate of antihypertensive medications using Morisky scale and identifying predictors of poor medication adherence among hypertensive patients including socio-economic and demographic data, health status, clinic visits, medication side effects, medications availability, and knowledge. Descriptive and logistic regression analyses were performed to assess factors associated with poor adherence.
A total of 306 hypertensive outpatients participated in this study. 42.2% of participants were adherent to antihypertensive medications. Almost half of participants (49%) who reported having no comorbidities were adherent to antihypertensive medications compared to participants with one or more than one comorbidities 41, 39% respectively. The presence of comorbid conditions and being on multiple medications were significantly associated with medication adherence ( P -values, respectively, < 0.004, < 0.009). Patients with good knowledge about the disease and its complications were seven times more likely to have good adherence to medication ( P < 0.001).
Conclusions
Non-adherence to medications is prevalent among a proportion of hypertensive patients which urges continuous monitoring to medication adherence with special attention to at risks groups of patients. Patients with comorbidities and on multiple medications were at high risk of medication non-adherence. Patients’ knowledge on the disease was one of the main associated factors with non-adherence.
Hypertension is one of the most common chronic diseases in Saudi Arabia and a rising health burden, affecting 26.1% adult population [ 1 ]. Hypertension is a major risk factor for heart failure, myocardial infarction, cerebrovascular disease, and renal failure [ 2 ]. Controlling hypertension reduces the risk of cerebrovascular accident (CVA), coronary heart disease, congestive heart failure, and mortality [ 2 , 3 ]. There are several factors that affect blood pressure control. Patients’ adherence to treatment is one of the major factors in controlling blood pressure and preventing hypertension complications [ 3 ]. The World Health Organization (WHO) defines adherence to long-term therapy as “the extent to which a person’s behavior-taking medication, following a diet, and/or executing lifestyle changes-corresponds with agreed recommendations from a healthcare provider” [ 3 ]. Patients with a high level of medication adherence were found to have better blood pressure control [ 4 ]. Still, adherence to hypertension treatment is challenging, due to the asymptomatic nature of the disease [ 5 ].
Several studies investigated the adherence rate among hypertension patients and sociodemographic factors affecting medication adherence including age, gender, comorbidities, patients’ knowledge about the disease, the number of medications. A study conducted in Saudi Arabia showed that only 34.7% of male hypertensive patients were found to be adherent to their medication [ 6 ]. The study reported a negative association between the presence of comorbidities and the adherence level [ 6 ]. A cross-sectional study on medication adherence among patients with hypertension in Malaysia, found an association between adherence and good knowledge of the medications and disease [ 7 ]. The study also found that the increase in the number of drugs patients taking has a negative effect on medication adherence [ 7 ]. Other studies had similar findings regarding the association between the number of medications and adherence [ 8 , 9 , 10 ]. In a cross-sectional study conducted in Iran, older patients reported high adherence to antihypertensive medication and better knowledge of their disease than younger patients [ 9 ]. However, number of studies reported no significant associations between age and medication adherence [ 8 , 11 ]. Female patients were more likely to adhere to their medication, compared to males [ 12 ]. Another study on the prevalence and predictors of poor antihypertensive reported that male patients were more adherent than female patients [ 13 ]. Some studies reported no relationship between gender and adherence [ 9 , 11 ].
Educational level and health literacy were shown to be associated with medication adherence. A cross-sectional study conducted in Iraq showed that adherence decreased in patients with primary and secondary school education, while no significant difference among patients with higher education and undereducated patients [ 14 ]. Similar results found in a systematic review conducted in hypertension management and medication adherence [ 15 ]. On the other hand, no association between educational level and adherence was found in a study conducted in Saudi Arabia [ 8 ]. However, good health knowledge of hypertension shown to be associated with good adherence to medication treatment in several studies [ 7 , 11 ]. Two cross-sectional studies conducted in Turkey and Algeria showed a significant association between knowledge of complications related to hypertension and good adherence to antihypertensive therapy [ 16 , 17 ].
Hypertension is one of the major health issues in Saudi Arabia; affecting more than a quarter of the Saudi adult population [ 1 ]. Only 37% of hypertensive patients on medication have their blood pressure controlled [ 18 ]. Non-adherence to antihypertensive medications is a potential contributing factor to uncontrolled hypertension. With limited studies conducted to investigate this challenging issue, this cross-sectional study aims to assess the adherence rate among hypertensive patients and associated factors affecting adherence to antihypertensive medications.
Study design and sampling
This cross-sectional study was conducted to determine the adherence rate of antihypertensive medications and the predictors of poor medication adherence among hypertensive patients at primary health clinics (PHCs) in Prince Sultan Medical City (PSMMC) in Riyadh the capital city of Saudi Arabia. Single population proportion formula was used to calculate the sample size based on the prevalence of hypertension in Saudi Arabia (26.1%) [ 1 ]. With a 95% confidence level and a 5% margin of error, a total of 306 randomly selected outpatients with hypertension following up at primary health clinics were included in this study.
Participants recruitment
Participants in this study were recruited using a systemic sampling technique. Every fourth consecutive patient who fits the criteria was included. Arabic speaker patients older than 18 years who have been diagnosed with hypertension for more than three months were included in this study. Patients who do not speak Arabic had mental retardation, secondary hypertension, or who were younger than 18 years old were excluded from the study. The data was collected using a self-administered questionnaire that was distributed in the waiting area of the pharmacy. Illiterate participants were interviewed by a trained data collector. Before participants’ recruitment in the study, informed consent was obtained from all patients after a full explanation of the study. The study was approved and supervised by the institution review board (IRB) of Prince Sultan Medical City.
Measurements
The questionnaire consists of four main sections. The first section assesses participants’ socio-economic factors including age, gender, marital status, occupation, the highest level of education currently attained, occupation, and monthly income. The second section assesses the factors affecting medication adherence including comorbidities, number of medications, number of daily doses, number of clinic visits, the distance to the clinic, medication side effects, medication availability at the pharmacy. The third section aimed to assess patients’ adherence to treatment. The fourth part assesses the patients’ knowledge about hypertension.
Medication adherence was assessed using the 8- items Morisky scale [ 19 ]. Morisky scale has been validated and found to be reliable (α = .83) [ 20 ]. The scale is based on the patients’ self-response and consists of eight questions, seven items with yes or no response, and one item with a 5-point Likert scale response option. The total score ranges from 1 to 8, the patient whose adherence score was six or more is considered adherent. For linguistic validation, questions were translated forward and backward into Arabic by an independent translator.
The participant’s knowledge about hypertension was assessed using nine structured questions. The questions focused on different aspects of hypertension, namely blood pressure target, lifestyle modification effect, complications, treatment, and cure. During analysis, patients who answered < 70% were considered to have low knowledge and patient how answered ≥70% of the questions were considered to have good knowledge. The 70 % cut-off is based on the minimally acceptable level of quality control at PSMMC [ 21 ].
The questionnaire was pre-tested and then a pilot survey was conducted on 20 patients for clarity and feasibility. The questionnaire was also evaluated and reviewed by two independent family medicine consultants at Prince Sultan Medical City for validation.
Data analysis
Frequencies and percentages were used to assess participants’ characteristics. Chi-square analysis was used to determine the association between demographic, socioeconomic, and clinical factors with medication adherence. Logistic regression analysis was performed to assess factors associated with poor adherence. The variables were analyzed collectively using logistic regression to study the potential factors to avoid confounding bias. The association was considered statistically significant if the P -value was less than 0.05. Statistical Package for Social Sciences version 25 and Statistical Analysis System version 9.4 was used for data analysis.
A total of 306 outpatients who have hypertension participated in this study. Approximately 43% of the participants’ ages range was between 56 and 65. The majority of participants were married (92%), employed (61%), and had a high school diploma or above (80%). Most of the participants were middle income in the 5000–10,000 Saudi Riyal range of monthly income. Nearly one-third (28.1%) of the respondents in this study had no comorbidities while two-thirds reported having one or more comorbidities. The demographic, and socioeconomic clinical characteristics of the participants are presented in Table 1 .
Only 13% of the respondents live at a distance of less than half an hour from the clinic. Of the total participants, 14.1% reported visiting the primary health clinic once in the last year, 29.4% twice, 24.2% three times. The majority of participants reported taking less than four medications a day and 31.4% reported taking four or more medications a day. As to antihypertensive medication side effects, 19.6% reported having medication side effects. Only 4.9% of the participants reported that they stop taking their antihypertensive medications when they get sick. Approximately 9% of the participants reported that they stop taking their medications when it is not available at the pharmacy. Findings show that half (50.7%) of the participants were knowledgeable about the disease. The clinical characteristics of the participants are presented in Table 1 .
Figure 1 presents the percentage of participants’ adherence to antihypertensive treatment. Based on Morisky scale test results, 42.2% of the participants in this study were adherent to antihypertensive medications, while 57.8% were not adherent.
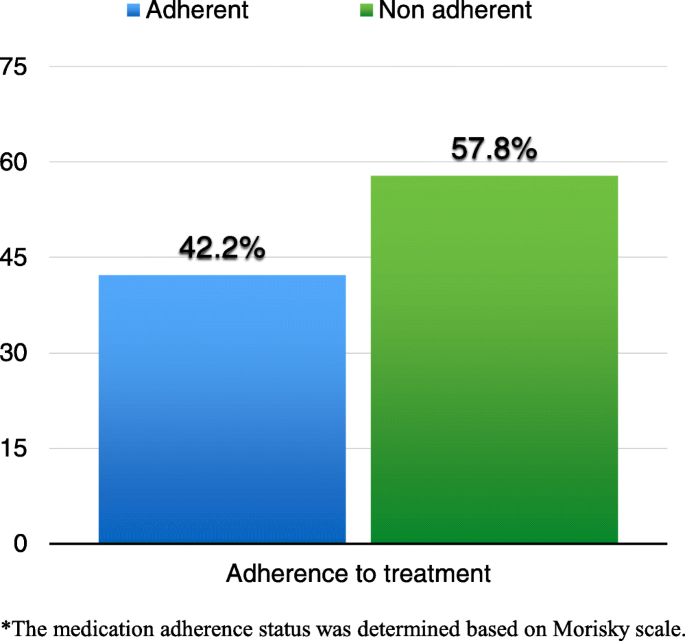
Distribution of patients according to their medication adherence status*
Table 2 presents the adherence rate in relation to the participants’ demographic, socioeconomic, and clinical characteristics. The presence of comorbid conditions is significantly associated with medication adherence ( P < 0.001). Almost half of participants (49%) who reported having no comorbidities were adherent to antihypertensive medications compared to the participants with one or more than one comorbidities 41, 39% respectively. As for the number of medications, the adherence rate was found to be better among patients who were taking less than four medications (47.1%) compared to patients who were taking four or more medications (31.3%). Patients who visited the clinic once in the last year were more adherent than those who visited the clinic more than once ( p < 0.05). No significant association between age, gender, income, educational level, and distance from home to the clinic.
The participants were asked eight questions about hypertension. Table 3 shows the distribution of the correct and incorrect answers giving by the participants. Most participants (64.4%) knew the target blood pressure for hypertensive patients and 40.8% think that hypertension can be cured. The majority (78%) knew that a low salt diet helps in lowering high blood pressure. Only 61% knew that hypertension can affect eyes and 13.4% reported that they stop taking their medication when they feel their blood pressure under control.
Adherence to antihypertensive medications among patients with good and poor knowledge levels about hypertension was assessed based on nine structured questions. Figure 2 shows the adherence to hypertension treatment among patients with good and poor knowledge level. 57.4% of patients with good knowledge levels were adherent compared to 42.6% who were not adherent. The majority (73.5%) of patients with poor knowledge levels were not adherent to treatment.
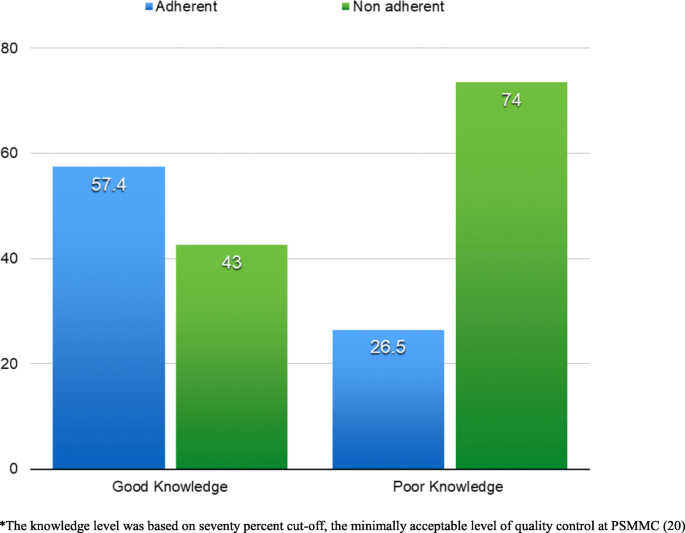
Adherence to hypertension treatment among patients with good and poor knowledge level*
Table 4 presents the factors associated with good adherence. When conducting binary logistic regression, knowledge about the disease was found to be significantly associated with adherence. Patients with good knowledge about the disease were seven times more likely to have good adherence to antihypertensive medications than those with poor knowledge (AOR 7.4 [95% CI: 4.177–13.121], p < 0.001).
Several studies have investigated factors affecting medication adherence. This study shows that the level of adherence to antihypertensive medications is low. In this sample the adherence rate to hypertension treatment was found to be only 42%, which is similar to the study conducted in Al-Khobar and higher than the study conducted in Taif where adherence rate was found to be 47 and 34.7%, respectively [ 6 , 8 ]. Other studies conducted in different countries reported adherence rates ranging from 15 to 88% [ 22 , 23 , 24 , 25 ]. This discrepancy in adherence rate is potentially due to the differences in population characteristics, medication adherence assessment tools, and healthcare systems.
The association between sociodemographic and socioeconomic factors and adherence level has been investigated in several studies. In a study done in Hong Kong, older patients were found to be more adherent. However, in this study, there was no association between age and adherence. In another study done in the United States, female patients were less adherent to hypertension medication compared to male patients [ 13 ]. A study conducted in Malaysia reported that female patients were more adherent than male patients [ 22 ]. Our study showed that there was no significant relationship between gender and adherence. A meta-analysis suggested that the association between age, gender, and adherence level is weak [ 26 ]. The results of our study also demonstrate no significant relationship between marital status and educational level with adherence, which is similar to findings reported by other studies [ 9 , 27 ].
Previous research found that shorter traveling time from residence to the healthcare facility could increase patients’ adherence [ 28 ]. A study in Ethiopia found that the adherence level was lower in patients who lived more than 10 km from healthcare facilities [ 29 ]. A cross-sectional observational study done in Northwest Ethiopia indicated that patients who live less than 10 km from the healthcare facility had an adherence rate of 74% compared to 58% for patients who live far from the healthcare facility [ 29 ]. As the authors attributed this problem to poor infrastructure and lack of transportation in Ethiopia, the study suggested that shorter traveling time from residence to the healthcare facility could increase patients’ adherence [ 29 ]. In this study, distance from home to the clinic was not associated with hypertensive treatment. These differences may be due to the higher level of car ownership in Saudis Arabia which makes it easier to access health care facilities [ 30 ].
Only 8.8% of the participants reported not taking their medication when it is not available at the hospital pharmacy. This low percentage may be explained by the multiple community health centers in Saudi Arabia which provide free health care including medications dispensing. Moreover, the medication cost at private pharmacies in Saudi Arabia is affordable for most patients. According to the published Saudi Hypertension Management Guidelines the prices of the antihypertensive medications ranges between 7 to 118 Saudi Riyal (about 2 to 31 US Dollar) [ 31 ].
Many patients with hypertension will need two or more antihypertensive medications to achieve goal blood pressure [ 2 ]. In this sample significant association was observed between the number of medications and adherence level. The adherence rate among patients taking less than four medications was 47.1% compared to 31.3% to those who take four or more medications. Similarly, other studies reported the negative association between the number of medication and adherence levels [ 29 , 32 ].
Findings indicate that patients with multiple comorbidities were less adherent to antihypertensive medication, which is inconsistent with a previous study done in Taif which showed a negative association between the presence of comorbidity and adherence level [ 6 ]. This may be related to the fact that most patients with multiple comorbidities require taking multiple complex medications.
The result of our study showed that the patient who visited the clinic once in the last year were more adherent than the patient who visited the clinic more than once. This could be explained by that most patients with multiple comorbidities and on multiple medications frequently visit the clinic for issues related to their disease and to refill prescriptions.
Our study demonstrated the positive association between knowledge and adherence levels. Patients who had good knowledge were more adherent to the treatment [ 29 ]. Previous studies showed that patients who know the ideal target blood pressure level were more adherent to their medications [ 16 , 20 ]. In this study, only 64.4% of the participants knew the ideal target of blood pressure and 40.8% of the patients believe that hypertension can be cured. A study conducted in Rajshahi, Bangladesh found that 65.8% of the patients believe that hypertension is curable. Patients how have been educated by their physicians and healthcare providers were more adherents to treatment as they have a better understanding of the disease nature, the ideal target of blood pressure, and the complications of hypertension [ 33 ]. Therefore, patient education in disease nature and management is considered a key factor in the treatment of hypertension.
The study findings were based on self-reported survey. Self-reported data is a common method used in a cross-sectional study. However, self-reported data is subjected to biases such as response and recall biases that can lead to under- or overestimation of findings. On the other hand, adherence in this study was measured based on a validated self-report adherence scale and knowledge was tested based on evaluated and reviewed assessment items by two independent family medicine consultants. Moreover, this study conducted in one of the largest medical cities that serves a large community in the capital city Riyadh. Due to the study design and sampling method, study findings cannot be generalized and temporal relationships cannot be established between risk factors and adherence. Nevertheless, this study provides a snapshot of adherence to antihypertensive medication status and associated determinates among outpatients. Future large scale longitudinal studies will contribute to a better understanding of adherence status and associated factors among hypertensive patients.
Non-adherence to medications is prevalent in proportion of patients with hypertension. Therefore, there is an urge to continually monitor patients’ adherence to antihypertensive medication using a standardized scale. Patients with comorbidities and on multiple medications were at higher risk of non-adherence. There is a need to encourage patients on multiple medications to use adherence aids such as weekly pill organizers and medication alarm devices. Hypertensive patients’ knowledge of the disease and its complications was one of the main factors affecting patients’ adherence to treatment. Implementation of health awareness interventions and education programs intended for hypertensive patients will help improve medication adherence.
Availability of data and materials
The data sets generated during and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
Adjusted odd ratio
Confidence interval
Blood pressure
Prince Sultan Medical City
primary health clinic
institution review board
Cerebrovascular accident
The World Health Organization
Al-Nozha MM, Abdullah M, Arafah MR, Khalil MZ, Khan NB, Al-Mazrou YY, et al. Hypertension in Saudi Arabia. Saudi Med J. 2007;28(1):77–84.
PubMed Google Scholar
Chobanian AV, Bakris GL, Black HR, et al. Prevention, detection, evaluation, and treatment of high blood pressure the seventh report of the joint National Committee on complete report. Natl High Blood Press Educ Progr. 2003;42(6):1206.
CAS Google Scholar
De Geest S, Sabaté E. Adherence to long-term therapies: Evidence for action. Eur J Cardiovasc Nurs. 2003;2:323.
Bramley TJ, Gerbino PP, Nightengale BS, Frech-Tamas F. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. 2006;12(3):239–45.
Saeed AA, Al-Hamdan NA, Bahnassy AA, Abdalla AM, MAF A, Abuzaid LZ. Prevalence, awareness, treatment, and control of hypertension among Saudi adult population: A national survey. Int J Hypertens. 2011, 2011:174135 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21912737 . [cited 2020 May 4].
Elbur AI. Level of adherence to lifestyle changes and medications among male hypertensive patients in two hospitals in taif; kingdom of Saudi Arabia. Int J Pharm Pharm Sci. 2015;7(4):168–72.
Google Scholar
Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–22.
PubMed PubMed Central Google Scholar
Al-Sowielem LS, Elzubier AG. Compliance and knowledge of hypertensive patients attending PHC centres in Al-Khobar, Saudi Arabia. East Mediterr Heal J. 1998;4(2):301–7 Available from: https://apps.who.int/iris/handle/10665/118129 . [cited 2020 May 4].
Hadi N, Rostami-Gooran N. Determinant factors of medication compliance in hypertensive patients of Shiraz, Iran. Arch Iran Med. 2004;7(4):292–6 Available from: https://www.sid.ir/en/journal/ViewPaper.aspx? ID=13626. [cited 2020 May 4].
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics-2012 update: a report from the American heart association. Circulation. 2012;3:125(1).
Goussous LS, Halasah NA, Halasa M. Non - Compliance to Antihypertensive Treatment among Patients Attending Prince Zaid Military Hospital. World Fam Med Journal/Middle East J Fam Med. 2015;13(1):15–9 Available from: https://platform.almanhal.com/Files/2/58839 . [cited 2020 May 4].
Article Google Scholar
Schoberberger R, Janda M, Pescosta W, Sonneck G. The COMpliance praxiS survey (COMPASS): a multidimensional instrument to monitor compliance for patients on antihypertensive medication. J Hum Hypertens. 2002;16(11):779–87.
Article CAS PubMed Google Scholar
Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, KB DS. Prevalence and Predictors of Poor Antihypertensive Medication Adherence in an Urban Health Clinic Setting. J Clin Hypertens. 2007;9(3):179–86 Available from: http://doi.wiley.com/10.1111/j.1524-6175.2007.06372.x . [cited 2020 May 4].
Issa H, Banna A, Mohmed LH. Compliance and knowledge of hypertensive patients attending Shorsh Hospital in Kirkuk Governorate. Iraqi Postgrad Med J. 2010;9(2):145–50.
Klootwyk JM, Sanoski CA. Adherence and persistence in hypertension management. J Clin Outcomes Manag. 2011;18(8):351–8.
Karaeren H, Yokuşoǧlu M, Uzun Ş, Baysan O, Köz C, Kara B, et al. The effect of the content of the knowledge on adherence to medication in hypertensive patients. Anadolu Kardiyol Derg. 2009;9(3):183–8.
Ghembaza MA, Senoussaoui Y, Tani M, Meguenni K. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev. 2014;10(1):41–8.
Elzubier AG, Al-Shahri MA. Drug control of hypertension in primary health care centers-registered patients, Al-khobar, saudi arabia. J Family Community Med. 1997;4(2):47–53 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23008573 . [cited 2020 May 4].
CAS PubMed PubMed Central Google Scholar
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–54.
González-fernández RA, Rivera M, Torres D, Quiles J, Jackson A. Usefulness of a systemic hypertension in-hospital educational program. Am J Cardiol. 1990;65(20):1384–6.
Article PubMed Google Scholar
Brown J, Mellott S. The healthcare quality handbook : a professional resource and study guide; 2016. p. 439.
Mafutha GN, Wright SCD. Compliance or non-compliance of hypertensive adults to hypertension management at three primary healthcare day clinics in Tshwane. Curationis. 2013;36(1):E1–6.
Hussanin S, Boonshuyar C, Ekram A. Non-adherence to antihypertensive treatment in essential hypertensive patients in Rajshahi, Bangladesh. Anwer Khan Mod Med Coll J. 2011;2(1):9–14.
Al-Mehza AM, Al-Muhailije FA, Khalfan MM, Al-Yahya AA. Drug compliance among hypertensive patients; an area based study. Eur J Gen Med. 2009;6(1):6–10 Available from: http://www.ejgm.co.uk/download/drug-compliance-among-hypertensive-patients-an-area-based-study-6685.pdf . [cited 2020 May 4].
Busari OA, Olanrewaju TO, Desalu OO, Opadijo OG, Jimoh AK, Agboola SM, et al. Impact of Patients’ Knowledge, Attitude and Practices on Hypertension on Compliance with Antihypertensive Drugs in a Resource-poor Setting. TAF Prev Med Bull. 2010;9(2):87–92 Available from: www.korhek.org . [cited 2020 May 4].
Fitz-Simon N, Bennett K, Feely J. A review of studies of adherence with antihypertensive drugs using prescription databases. Ther Clin Risk Manag. 2005;1(2):93–106.
Article PubMed PubMed Central Google Scholar
Lee GKY, Wang HHX, Liu KQL, Cheung Y, Morisky DE, Wong MCS. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky medication adherence scale. PLoS One. 2013;8(4):e62775.
Gonzalez J, Williams JW, Noël PH, Lee S. Adherence to mental health treatment in a primary care clinic. J Am Board Fam Pract. 2005;18(2):87–96.
Ambaw AD, Alemie GA, Wyohannes SM, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;12(1):282.
Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access [internet]. J Commun Health. 2013;38:976–93 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23543372 . [cited 2020 May 4].
Saudi Hypertension Management Society. Saudi Hypertension Guidelines. 2018.
Marcum ZA, Gellad WF. Medication Adherence to Multidrug Regimens. Clin Geriatr Med. 2012;28(2):287–300 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22500544 . [cited 2020 May 5].
Neutel JM, Smith DHG. Improving Patient Compliance: A Major Goal in the Management of Hypertension. J Clin Hypertens. 2003;5(2):127–32 Available from: http://doi.wiley.com/10.1111/j.1524-6175.2003.00495.x . [cited 2020 May 5].
Download references
Acknowledgments
Not applicable.
Author information
Authors and affiliations.
Family Medicine Department, Prince Sultan Military Medical City (PSMMC), Riyadh, Riyadh, Saudi Arabia
Fahad M. Algabbani
George Mason University, Fairfax, VA, USA
Aljoharah M. Algabbani
You can also search for this author in PubMed Google Scholar
Contributions
The study design was conceptualized by FA and AA. Data collection was managed by FA and data analysis and interpretation were conducted by FA and AA. All authors participated in writing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Fahad M. Algabbani .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from institution review board (IRB) of Prince Sultan Medical City. Before participants’ recruitment in the study, informed consent was obtained from all participants.
Consent for publication
Competing interests.
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Algabbani, F.M., Algabbani, A.M. Treatment adherence among patients with hypertension: findings from a cross-sectional study. Clin Hypertens 26 , 18 (2020). https://doi.org/10.1186/s40885-020-00151-1
Download citation
Received : 21 May 2020
Accepted : 03 August 2020
Published : 15 September 2020
DOI : https://doi.org/10.1186/s40885-020-00151-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- High blood pressure
- Uncontrolled hypertension
- Nonadherence
Clinical Hypertension
ISSN: 2056-5909
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Case Studies: BP Evaluation and Treatment in Patients with Prediabetes or Diabetes
—the new acc/aha blood pressure guidelines call for a more aggressive diagnostic and treatment approach in most situations..
By Kevin O. Hwang, MD, MPH, Associate Professor, McGovern Medical School, Houston, TX
The following case studies illustrate how the new ACC/AHA guideline specifies a shift in the definition of BP categories and treatment targets.

A 59-year-old man with type 2 diabetes presents with concerns about high blood pressure (BP). At a recent visit to his dentist he was told his BP was high. He was reclining in the dentist’s chair when his BP was taken, but he doesn’t remember the exact reading. He has no symptoms. He has never taken medications for high BP. He takes metformin for type 2 diabetes.
His BP is measured once at 146/95 mm Hg in the left arm while sitting. Physical exam is unremarkable except for obesity. EKG is unremarkable.
BP Measurement
Controlling BP in patients with diabetes reduces the risk of cardiovascular events, but the available data are not sufficient to classify this patient with respect to BP status. The reading taken while reclining in the dentist’s chair was likely inaccurate. A single reading in the medical clinic, even with correct technique, is not adequate for clinical decision-making because individual BP measurements vary in unpredictable or random ways.
The accuracy of BP measurement is affected by patient preparation and positioning, technique, and timing. Before the first reading, the patient should avoid smoking, caffeine, and exercise for at least 30 minutes and should sit quietly in a chair for at least 5 minutes with back supported and feet flat on the floor. An appropriately sized cuff should be placed on the bare upper arm and with the arm supported at heart level. For the first encounter, BP should be recorded in both arms. The arm with the higher reading should be used for subsequent measurements.
It is recommended that one use an average of 2 to 3 readings, separated by 1 to 2 minutes, obtained on 2 to 3 separate visits. Some of those readings should be performed outside of the clinical setting, either with home BP self-monitoring or 24-hour ambulatory BP monitoring, especially when confirming the diagnosis of sustained hypertension. Note that a clinic BP of 140/90 corresponds to home BP values of 135/85. Multiple BP readings in the clinic and at home allow for classification into one of the following categories.
The BP is measured in the office with the correct technique and timing referenced above. The patient is educated on how on to measure BP at home with a validated monitor. He should take at least 2 readings 1 minute apart in the morning and in the evening before supper (4 readings per day). The optimal schedule is to measure BP every day for a week before the next clinic visit, which is set for a month from now. Obtaining multiple clinic and home BP readings on multiple days will support a well-informed assessment of the patient’s BP status and subsequent treatment decisions.
A 62 year old African-American woman with prediabetes presents for her annual physical. She has no complaints. The average of 2 BP readings in her right arm is BP 143/88. Her physical exam is unremarkable except for obesity. She has no history of myocardial infarction, stroke, kidney disease, or heart failure. After the visit, she measures her BP at home and returns 1 month later. The average BP from multiple clinic and home readings is 138/86.
Her total cholesterol is 260 mg/dL, HDL 42 mg/dL, and LDL 165 mg/dL. She does not smoke.
Stage 1 Hypertension
Under the 2017 ACC/AHA guideline, she has stage 1 hypertension (HTN). This guideline uses a uniform BP definition for HTN without regard to patient age or comorbid illnesses, such as diabetes or chronic kidney disease.
In patients with stage 1 HTN and no known atherosclerotic cardiovascular disease (ASCVD) , the new guideline recommends treating with BP-lowering medications if the 10-year risk for ASCVD risk is 10% or greater. With input such as her age, gender, race, lipid profile, and other risk factors, the ACC/AHA Pooled Cohort Equations tool estimates her 10-year risk to be approximately 10.5%.
With stage 1 HTN and 10-year ASCVD risk of 10% or higher, she would benefit from a BP-lowering medication. Thiazide diuretics, angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and calcium channel blockers are first-line agents for HTN because they reduce the risk of clinical events. In African-Americans, thiazide diuretics and calcium channel blockers are more effective for lowering BP and preventing cardiovascular events compared to ACE inhibitors or ARBs.
Patient-specific factors, such as age, comorbidities, concurrent medications, drug adherence, and out-of-pocket costs should be considered. Shared decision making should drive the ultimate choice of antihypertensive medication(s).
Nonpharmacologic strategies for prediabetes and HTN include dietary changes, physical activity, and weight loss. If clinically appropriate, she should also avoid agents which could elevate BP, such as NSAIDs, oral steroids, stimulants, and decongestants.
A goal BP of 130/80 is recommended. After starting the new BP medication, she should monitor BP at home and return to the clinic in 1 month. If the BP goal is not met at that time despite adherence to treatment, consideration should be given to intensifying treatment by increasing the dose of the first medication or adding a second agent.
A 63 year old man with type 2 diabetes has an average BP of 151/92 over the span of several weeks of measuring at home and in the clinic. He also has albuminuria.
Stage 2 Hypertension:
The BP treatment goal patients with diabetes and HTN is less than 130/80. While some patients can be effectively treated with a single agent, serious consideration should be given to starting with 2 drugs of different classes, especially if BP is more than 20/10 mm Hg above their BP target. Giving both medications as a fixed-dose combination may improve adherence.
In this man with diabetes and HTN, any of the first-line classes of antihypertensive agents (diuretics, ACE inhibitors, ARBs, and CCBs) would be reasonable choices. Given the presence of albuminuria, an ACE inhibitor or ARB would be beneficial for slowing progression of kidney disease. However, an ACE inhibitor and ARB should not be used simultaneously due to an increase in cardiovascular and renal risk observed in clinical trials.
He is started on a fixed-dose combination of an ACE-inhibitor and thiazide diuretic. He purchases a validated BP monitor which can transmit BP readings to his provider’s electronic health records system. Direct transmission of BP data to the provider has been shown to help patients achieve greater reductions in BP compared to self-monitoring without transmission of data. One month follow-up is recommended to determine if the treatment goal has been met.
Published: April 30, 2018
- 2. Final Recommendation Statement: High Blood Pressure in Adults: Screening. U.S. Preventive Services Task Force. September 2017.
Does cabg owe its success more to sag--or to mag, dvt treatment: home versus hospital, perioperative thromboembolic complications predict long-term vte risk, coronary plaque in people with well-controlled hiv and low ascvd risk, poor neighborhood, poor mi outcome, stroke risk at age 66 to 74 years—with atrial fibrillation but without other risk factors, using cardiovascular biomarkers to diagnose type 2 mi: yea or nay, cardiac rehabilitation: outcomes in south asian patients.

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 April 2024
Efficacy and safety of a four-drug, quarter-dose treatment for hypertension: the QUARTET USA randomized trial
- Mark D. Huffman 1 , 2 , 3 ,
- Abigail S. Baldridge 3 , 4 ,
- Danielle Lazar 5 ,
- Hiba Abbas 5 ,
- Jairo Mejia 5 ,
- Fallon M. Flowers 5 ,
- Adriana Quintana 5 ,
- Alema Jackson 5 ,
- Namratha R. Kandula 3 , 6 ,
- Donald M. Lloyd-Jones 3 , 7 ,
- Stephen D. Persell 6 , 8 ,
- Sadiya S. Khan 3 , 7 ,
- James J. Paparello 3 , 9 ,
- Aashima Chopra 3 ,
- Priya Tripathi 3 ,
- My H. Vu 3 ,
- Clara K. Chow 10 &
- Jody D. Ciolino 3 , 11
Hypertension Research ( 2024 ) Cite this article
404 Accesses
1 Altmetric
Metrics details
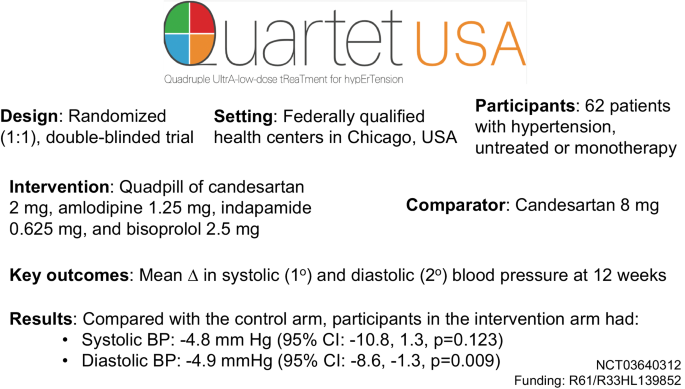
New approaches are needed to lower blood pressure (BP) given persistently low control rates. QUARTET USA sought to evaluate the effect of four-drug, quarter-dose BP lowering combination in patients with hypertension. QUARTET USA was a randomized (1:1), double-blinded trial conducted in federally qualified health centers among adults with hypertension. Participants received either a quadpill of candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg or candesartan 8 mg for 12 weeks. If BP was >130/>80 mm Hg at 6 weeks in either arm, then participants received open label add-on amlodipine 5 mg. The primary outcome was mean change in systolic blood pressure (SBP) at 12 weeks, controlling for baseline BP. Secondary outcomes included mean change in diastolic blood pressure (DBP), and safety included serious adverse events, relevant adverse drug effects, and electrolyte abnormalities. Among 62 participants randomized between August 2019-May 2022 ( n = 32 intervention, n = 30 control), mean (SD) age was 52 (11.5) years, 45% were female, 73% identified as Hispanic, and 18% identified as Black. Baseline mean (SD) SBP was 138.1 (11.2) mmHg, and baseline mean (SD) DBP was 84.3 (10.5) mmHg. In a modified intention-to-treat analysis, there was no significant difference in SBP (−4.8 mm Hg [95% CI: −10.8, 1.3, p = 0.123] and a −4.9 mmHg (95% CI: −8.6, −1.3, p = 0.009) greater mean DBP change in the intervention arm compared with the control arm at 12 weeks. Adverse events did not differ significantly between arms. The quadpill had a similar SBP and greater DBP lowering effect compared with candesartan 8 mg. Trial registration number: NCT03640312.
Similar content being viewed by others
Reduced efficacy of blood pressure lowering drugs in the presence of diabetes mellitus—results from the TRIUMPH randomised controlled trial
Sonali R. Gnanenthiran, Ruth Webster, … on behalf of the TRIUMPH Study Group
Efficacy and safety of esaxerenone (CS-3150) in primary hypertension: a meta-analysis
Ran Sun, Yali Li, … Xiaoxia Guo
Association of intensive blood pressure management with cardiovascular outcomes in patients using multiple classes of antihypertensive medications: a post-hoc analysis of the STEP Trial
Kaipeng Zhang, Qirui Song, … Jun Cai
Introduction
More than 1 billion adults have hypertension globally [ 1 ]. Despite widespread availability of generic blood pressure lowering drugs for decades, hypertension control rates (defined as a blood pressure <140/<90 mm Hg) remain persistently low (<50%) among adults in the United States [ 2 ]. Control rates are even lower (<25%) when accounting for newer, lower blood pressure targets (defined as a blood pressure <130/<80 mm Hg) recommended by national and international clinical practice guidelines [ 3 , 4 , 5 ]. Hypertension is more prevalent in racially and ethnically minoritized individuals, in whom control rates are also lower than other groups [ 6 ]. Most patients with hypertension are initially treated with a single blood pressure lowering drug that is titrated up over multiple, monthly office visits with additional medications added sequentially. Therapeutic inertia contributes to persistently low hypertension control rates and has not improved [ 7 , 8 ]. Thus, a new approach is needed. New strategies are especially important among low-income individuals who seek care within federally qualified health centers, where the burden of hypertension is high and control rates are lower than the general population [ 9 ].
Previous trials of single drug ultra-low dose (i.e., one-quarter of a standard dose) blood pressure lowering therapy demonstrated an average of −4.7 systolic and −2.4 diastolic mm Hg greater blood pressure lowering compared with placebo with no significant difference in adverse events [ 10 , 11 ]. Each additional drug added in a combination (e.g., two-, three-, and four-drug combinations) of quarter-dose blood pressure lowering drugs demonstrated a stepwise gradient of blood pressure lowering. Two- and three-drug single pill combinations have a favorable balance between greater blood pressure lowering effect, tolerability, adherence, and persistence in blood pressure control [ 12 , 13 , 14 ], As a result, major clinical practice guidelines and the World Health Organization recommend single pill combination therapy [ 3 , 4 , 5 ],
The QUARTET trial [ 15 ] in Australia randomized 591 adults with mild to moderate hypertension and demonstrated a mean −6.9/−5.8 mm Hg greater systolic/diastolic blood pressure lowering effect at 12 weeks with initiation of a four-drug, quarter-dose combination of irbesartan 37.5 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg (quadpill) compared with irbesartan 150 mg daily alone. This effect was observed even with add-on amlodipine 5 mg at six-week follow-up in either arm among individuals who were not controlled, defined as a blood pressure of 140/90 mm Hg or greater, while both arms remained blinded to initial treatment allocation. Most (>90%) participants in QUARTET identified as White or Asian. It is uncertain if similar effects would be observed in other race/ethnic groups based on previous reports of differential blood pressure lowering effects of some drug classes by race/ethnicity [ 16 ].
Thus, the objective of the QUARTET USA trial was to evaluate whether treatment with four-drug, quarter-dose combination therapy will have a greater reduction in office-measured blood pressure, and with fewer side effects, compared with standard dose monotherapy in patients with hypertension who receive care at a federally qualified health center network in Chicago, Illinois. We hypothesized that a quadpill would have a greater blood pressure lower effect than standard dose monotherapy without any increase in adverse events.
The Northwestern Institutional Review Board provided oversight and approval for the trial. All study staff completed Good Clinical Practice training. Each participant provided informed consent prior to participation. The Food and Drug Administration approved the study drug for research purposes (Investigational New Drug: 133846), and an independent clinical trial monitor was employed to ensure compliance to Good Clinical Practice principles at the study sites. An independent Data and Safety Monitoring Board reviewed the study materials and provided interim guidance related to the safety, conduct, and analysis of the trial.
The methods for the QUARTET USA trial have been published [ 17 ]. Briefly, the study used a type I hybrid, phase II randomized (1:1), double-blind trial design to evaluate efficacy and safety of a quarter-dose combination of four blood pressure lowering drugs with a corresponding process evaluation to understand factors related to trial implementation and study drug acceptability. The results of the process evaluation have been reported separately [ 18 ].
Study procedures
From August 2019 to May 2022, participants were recruited from two primary care health centers that are part of Access Community Health Network in Chicago, Illinois (ACCESS Ashland Family Health Center or ACCESS Martin T. Russo Family Health Center). Electronic health record data were used to screen potentially eligible participants followed by chart review by trained study staff. Clinicians also identified potentially eligible participants in person. Participants were recruited via telephone, electronic health record portal messaging, or in the health center. Study staff obtained informed consent among eligible individuals before starting study procedures. Data were captured using paper forms and transferred to REDCap, an electronic data capture system that was also used to perform randomization, stratified by clinic site. All investigators, study staff, and study clinicians were blinded except the study biostatistician (JDC) or her back-up team members (AC, MV, SDP).
After providing informed consent, participants reported demographic information and had their blood pressure measured in triplicate by trained study staff after a five-minute, unobserved rest period. Blood pressure was calculated using the mean of the second and third measurements. Staff used an appropriately sized cuff and a validated, automated blood pressure monitoring device (Omron HEM 907 Automated Blood Pressure Monitor). If participants remained eligible based on mean blood pressure measurements, then they completed baseline surveys, provided blood and urine samples, and had an electrocardiogram performed. Once eligibility was confirmed, then participants were randomized, and the study kit, including study drug, was dispensed. Participants who were on monotherapy at baseline were instructed to stop their treatment with no wash-out period.
At six-week follow-up, participants completed additional surveys, and study staff counted their pills, inquired about adverse events, and measured their blood pressure. If the systolic blood pressure was greater than 130 mm Hg or the diastolic blood pressure was greater than 80 mmHg, then participants in either arm were given open label amlodipine 5 mg daily in addition to continuing their blinded study medication.
Participants returned for the final study visit at 12 weeks and completed additional surveys and had their blood pressures measured. During the peak of the COVID-19 pandemic lockdown period, we provided active participants with an Omron Series 3 ( n = 3) or Series 5 ( n = 7) machine and trained them remotely on how to accurately measure their blood pressure in accordance with the principles of the study protocol (Supplementary Materials).
Participants
Inclusion criteria were modified to simplify eligibility criteria during the COVID-19 pandemic and to align with the QUARTET trial in Australia more closely. Participants needed to be adults 18 years or older, English or Spanish speakers, and with mild to moderate hypertension that was either untreated or treated with monotherapy. Clinically measured blood pressure thresholds for inclusion were: 140–179/90–109 mm Hg for untreated participants and 130–159/85–109 mmHg for participants on monotherapy. Participants with contraindications to any of the included medications, prevalent cardiovascular disease, significant proteinuria, and secondary hypertension were not eligible. Women who were pregnant or were breastfeeding were also not eligible. Additional details related to eligibility are outlined in the Supplemental Materials.
Intervention
We created a quarter-dose combination pill using a milling-and-filling approach that included candesartan 2 mg, amlodipine 1.25 mg, indapamide 0.625 mg, and bisoprolol 2.5 mg using Good Manufacturing Practice principles in collaboration with Sharp Clinical Services, which served as the study drug manufacturer. Candesartan was selected instead of irbesartan as in the original QUARTET trial to minimize pill size. Quarter doses are based on the usual maintenance doses outlined in the British National Formulary, Martindale, and Monthly Index of Medical Specialties [ 10 ]. Sharp also manufactured a matching active comparator pill (containing candesartan 8 mg only) and provided add-on amlodipine pills.
The primary outcome was mean change from baseline in systolic blood pressure at 12 weeks, controlling for baseline. We report unadjusted and adjusted analyses that controlled for pre-specified covariates: sex, age, race/ethnicity, prior monotherapy, and limited literacy as defined by the Newest Vital Sign instrument [ 19 ]. Secondary outcomes included mean change in diastolic blood pressure, rates of hypertension control and medication adherence defined as 80% or greater use measured by pill count, and health related quality of life measured by the Patient-Reported Outcomes Measurement Information System (PROMIS) global physical and mental health outcomes.
Safety outcomes included occurrence of serious adverse events based on Good Clinical Practice definitions, relevant adverse drug effects (i.e., adverse events of special interest), and electrolyte abnormalities. Adverse events were collected by study staff during six- and 12-week follow-up visits and from participant contact during their time in the trial. Adverse event severity and relatedness were assessed by the blinded trial safety monitor. All events were coded by independent, blinded, and trained coders using the Medical Dictionary for Regulatory Activities (MedDRA) classification system [ 20 ]. Additional details related to the study outcomes are included in the Protocol and Statistical Analysis Plan (Supplementary Materials).
The primary study analysis used a linear mixed model with fixed study arm, study visit, and baseline outcome value effects and a random participant effect to account for within participant correlation. Secondary and safety analyses used generalized linear mixed modeling methods appropriate to the outcome of interest. For all outcomes, we used the model adjusted Wald type III tests for fixed effects to first evaluate significance of a visit-by-arm interaction at the 5% level of statistical significance. If insignificant at the 5% level, then this interaction term was removed and the model Wald type III test for fixed arm effect evaluated the overall intervention effect in this longitudinal model at the 5% level. Adverse event rates were tabulated overall and by arm, and chi-squared tests or exact methods were used to evaluate the differences across arms in event rates at the participant level.
No interim outcome analyses were planned. At the request of the Data and Safety Monitoring Board, we conducted a conditional power analysis in August 2021 using recruitment data from QUARTET USA trial in August 2021 and published trial data from QUARTET [ 15 ]. These analyses suggested that an analytic sample of 77 participants would provide 90% conditional power to detect a between-group difference of 5 mm Hg change in systolic blood pressure. We halted recruitment in May 2022 due to low recruitment.
Analyses involved the (modified) intention-to-treat (mITT) dataset, whereby all those participants with data at any follow-up time point and baseline were included in analyses according to arm to which they were randomized, regardless of adherence to the study protocol. We also conducted a sensitivity analysis on the per protocol dataset (defined as 80% treatment regimen adherence) since precise estimates of intervention effect (if any) on outcomes are important in a phase II study like this one. We used SAS (version 9.4, The SAS Institute) for all analyses. We defined statistical significance using a two‐sided p < 0.05 and did not include corrections for multiple hypothesis tests. MDH and JDC had full access to all data in the trial and take responsibility for its integrity and the data analysis.
Figure 1 shows the flow of participants throughout the study, including reasons for exclusion. Among 120 participants assessed for eligibility, 62 were randomized, including 32 to the four-drug, quarter-dose combination therapy intervention arm and 30 to the control arm. Two participants in the control arm did not provide any follow-up data and were excluded from analysis.
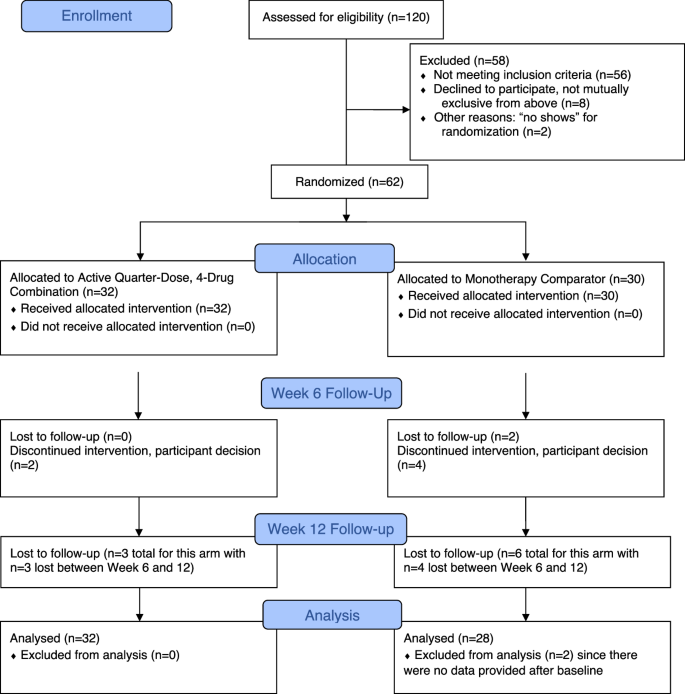
CONSORT flowchart of study participants
Participants’ baseline characteristics are reported in Table 1 and were comparable between randomized arms. Mean (SD) age was 52 (11.5) years, 45% were female, 73% identified as Hispanic, and 18% identified as Black. Nearly half (48%) of participants did not have health insurance, 24% had an education level of less than grade nine, and 65% had an annual household income of $25,000 or less. Baseline mean (SD) systolic blood pressure was 138.1 (11.2) mm Hg, and baseline mean (SD) diastolic blood pressure was 84.3 (10.5) mm Hg. Most (84%) participants were on monotherapy for blood pressure lowering at baseline.
Table 2 shows the primary and selected secondary outcomes, including adjusted systolic and diastolic blood pressures and between-group differences in blood pressure at 12 weeks. At the end of the study period, the intervention arm had an adjusted mean blood pressure of 122 (95% CI: 118, 127)/73 (95% CI: 71, 76) mm Hg compared with the control arm adjusted mean blood pressure of 127 (95% CI: 123, 132)/78 (95% CI: 75, 81) mm Hg. Based on these differences, there was no significant difference in systolic blood pressure change (−4.8 mm Hg [95% CI: −10.8, 1.3, p = 0.123]) and a mean −4.9 mm Hg (95% CI: −8.6, −1.3, p = 0.009) greater diastolic blood pressure lowering in the intervention arm compared with the control arm. These findings were observed despite a substantially lower odds of amlodipine 5 mg add-on at six weeks in the intervention arm compared with the control arm (19% versus 53%, model estimated Odds Ratio = 0.08 [95% CI: 0.02, 0.41], p = 0.003). A higher proportion of participants achieved hypertension control defined as blood pressure <130/<80 mm Hg (66% versus 54%) in the intervention arm compared to the control arm, but the results were imprecise (model estimated Odds Ratio = 2.85 [95% CI: 0.94, 8.59], p = 0.063). Adherence to >80% of study medication was similar between arms (intervention: 66% versus control: 70%, model adjusted Odds Ratio = 0.63 [95% CI: 0.19, 2.08] p = 0.444).
Supplementary Table 1 shows the unadjusted blood pressure results, and Fig. 2 shows temporal changes in systolic and diastolic blood pressure between randomized arms from baseline to six- and 12-week follow-up. Supplementary Fig. 1 a, b shows individual participant level changes in blood pressure. Mean blood pressures declined in both arms with greater declines from baseline to six-week follow-up in the intervention arm compared with the between-group difference observed during six- and 12-week follow-up.
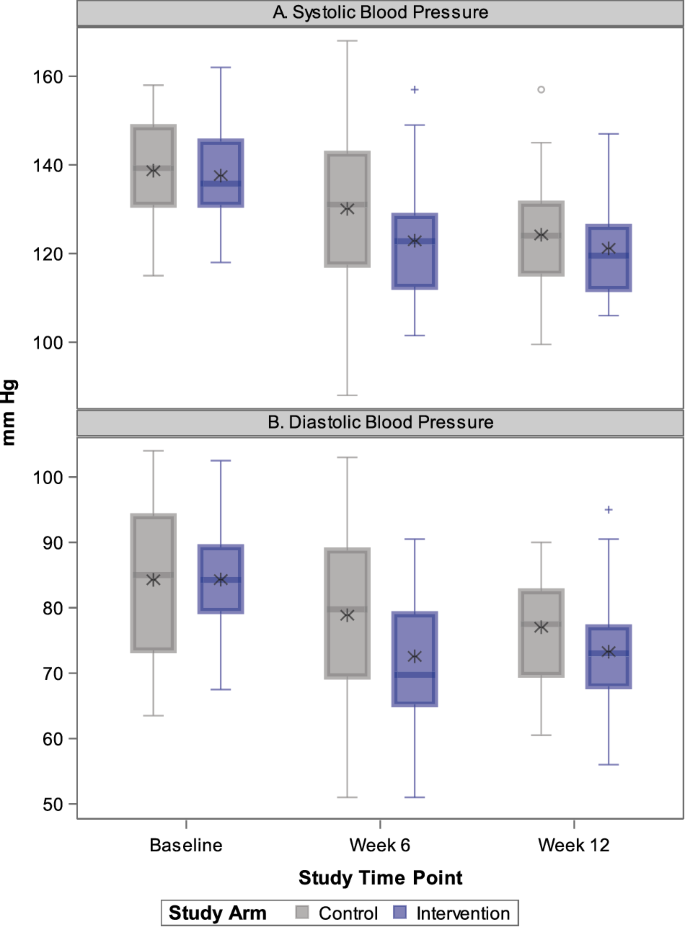
Box plots outlining temporal changes in distribution of systolic blood pressure (SBP) in ( A ) and distribution of diastolic blood pressures (DBP) by study arm in ( B ). Asterisk represents the mean value
Supplementary Fig. 2 shows results of pre-specified subgroup analysis, which do not provide evidence of heterogeneity of treatment effect by subgroups of baseline age, sex, race/ethnicity, baseline literacy level, and baseline monotherapy use.
Table 3 shows results related to adverse events among the study participants. Overall, there were 77 adverse events experienced by 34 participants. A somewhat higher proportion of participants experienced one or more adverse events in the intervention arm compared with the control arm (63% versus 47%, p = 0.210). Adverse events according to Medical Dictionary for Regulatory Activities (MedDRA) coding are shown in Supplementary Table 2 . The proportion of patients who permanently discontinued the study drug due to adverse effects was low (intervention: n = 1 [3%] versus control: n = 3 [10%], exact p = 0.347). There were two serious adverse events, both experienced by participants randomized to the intervention arm, but neither was deemed related to the study drug by the blinded medical monitor. There were no significant between-arm differences in mean serum electrolyte, laboratory, and urine studies (Supplementary Table 3 ) nor health-related quality of life scores (Supplementary Table 4 ).
The QUARTET USA results suggest that a strategy of initiating four-drug, quarter-dose combination therapy is similar in reducing systolic blood pressure and is more effective in lowering diastolic blood pressure than starting with standard dose angiotensin receptor blocker monotherapy at 12 weeks. These results were observed even with a substantially higher rate of add-on calcium channel blocker at six weeks in the control arm (53% versus 19%) among patients who receive care within a federally qualified health center network. The direction and magnitude of effect on systolic blood pressure were similar to the effect of diastolic blood pressure, but the observed effect was not statistically significant.
The four-drug, quarter-dose combination approach was developed to address poor blood pressure control rates, which have been exacerbated with lower treatment targets recommended by clinical practice guidelines [ 3 , 4 , 21 ], Contemporary guidelines increasingly recommend two-drug combination therapy, but this approach is often reserved for patients whose blood pressures are well above their treatment target [ 3 ]. QUARTET USA provides evidence that an ultra-low dose quadpill approach efficiently reduces blood pressure using a single pill as the initial treatment step. The mean blood pressure in the intervention arm at both six weeks (123/73 mm Hg) and 12 weeks (122/73 mm Hg) was below the target level recommended by contemporary clinical practice guidelines (blood pressure <130/ < 80 mm Hg). The upper bounds of the 95% confidence intervals for blood pressure in the intervention arm at 12 weeks (i.e., 126/75 mm Hg) in QUARTET USA suggest that this approach may be far more efficient in achieving lower targets than current approaches. For example, patients randomized in the intervention arm in the Systolic Blood Pressure Intervention Trial (SPRINT) needed three pills and six months to achieve a similar systolic blood pressure, a strategy that reduced the risk of major cardiovascular events by 25% and of all-cause mortality by 27% [ 22 ].
The results of the QUARTET USA trial are consistent with the QUARTET trial [ 15 ] results, which was conducted in Australia. We note some differences between the studies, including in mean baseline blood pressures (138/84 mm Hg in QUARTET USA versus 141/85 mm Hg in QUARTET), proportion of baseline monotherapy use (84% in QUARTET USA versus 46% in QUARTET), study drug adherence (67% at 12 weeks in QUARTET USA versus 76% at 52 weeks in QUARTET), and lower socioeconomic position among participants in QUARTET USA compared with QUARTET. QUARTET also used a higher blood pressure threshold for amlodipine 5 mg add on therapy at six weeks (140/90 mm Hg). Nevertheless, the similar direction and magnitude of effect from two trials with different study populations and drug combinations provides robust and supporting evidence for the overall approach of four-drug, quarter-dose combination therapy.
While there was a somewhat higher rate of adverse events in the intervention arm in the trial, the difference was not statistically significant. However, the rate of study drug discontinuation was lower in the intervention arm (3% vs. 10%). There were only two serious adverse events, and while both occurred among participants in the intervention arm, neither was deemed related to the study drug. Reassuringly, safety measures of electrolyte and serum creatinine levels were not significantly different between groups. The overall rate of discontinuation due to adverse events at 12 weeks was higher in QUARTET USA compared with QUARTET (7% versus 3%). Differences in study populations, sample size, and methods of adverse event ascertainment may have influenced these results. On the other hand, the rates of serious adverse events were low and similar in both trials (3% versus 2%). In aggregate, this suggests a clinically meaningful and favorable risk-benefit balance of a four-drug, quarter-dose combination therapy approach to safely, effectively, and efficiently lower blood pressure to achieve treatment goals.
QUARTET USA enrolled a large proportion of participants who self-identified as Hispanic or Black with low education levels and household income from a federally qualified health center network in Chicago, Illinois. More than 30 million patients receive care in federally qualified health centers in the U.S., which receive federal funding under Section 330 of the Public Health Service Act to care for vulnerable populations [ 23 ]. While patients from minoritized populations are disproportionately affected by hypertension [ 9 ], they are less likely to be included in clinical trials to address this condition [ 24 ]. The design of the QUARTET USA trial is thus responsive to the burden of hypertension in the United States, and the results inform treatment strategies to reduce racial and ethnic and socioeconomic disparities in hypertension control [ 20 , 25 ].
To support wider implementation of a four-drug, quarter-dose combination therapy approach, our study team also conducted an explanatory sequential, mixed methods process evaluation of the trial among patients and healthcare professionals [ 17 ]. This treatment approach was considered acceptable and convenient, despite the tension that patients reported related to necessity and concerns of blood pressure lowering medications. Healthcare professionals expressed some concerns about relative inflexibility of the treatment regimen, which may paradoxically lead to greater therapeutic inertia among patients treated with fixed dose combination therapy [ 26 ]. More importantly, process evaluation participants said that health insurance coverage and limiting out-of-pocket costs for four-drug, quarter-dose combination were essential for future sustainment and scale-up. Our results are generally similar to those from previous process evaluations of combination therapy for prevention and control of cardiovascular diseases [ 27 , 28 ].
QUARTET USA had several strengths, including using a randomized, double-blind trial design and an active, well-tolerated comparator. Blood pressure was measured using rigorous and reliable methods to maximize precision, and the study included participants from diverse backgrounds in a resource-limited context. The trial was also conducted during the COVID-19 pandemic, which had a major impact on clinical and research activities. However, adherence to study procedures was high, and loss to follow-up was relatively low.
Limitations
Despite these strengths, the trial had several limitations, including lower than planned recruitment and study drug adherence, which likely reduced the statistical power to detect an effect on the primary outcome of between-arm difference in systolic blood pressure. There were changes to the study protocol to respond to the COVID-19 pandemic, and some planned outcome measures, such as 24-h ambulatory blood pressure became infeasible to collect. Details of these changes are outlined in the study protocol. Nevertheless, the results add to the body of literature of quarter-dose, four drug combination therapy [ 29 , 30 ], and our team will participate in a pooling of published trials to better characterize effect sizes, including in different contexts, using different combinations, and across subgroups.
Conclusions
The QUARTET USA trial provides evidence of efficacy and safety of a four-drug, quarter-dose combination therapy with a similar reduction in systolic blood pressure and a greater reduction in diastolic blood pressure compared with standard dose angiotensin receptor blocker monotherapy in patients with mild to moderate hypertension receiving care at a federally qualified health center network in Chicago, Illinois. This new approach may be useful in improving blood pressure control among the more than one billion adults with hypertension around the world, especially among vulnerable groups in whom prior research has been limited.
NCD-Risk Factor Collaborators, Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Article Google Scholar
Muntner P, Miles MA, Jaeger BC, Hannon Iii L, Hardy ST, Ostchega Y, et al. Blood pressure control among US adults, 2009 to 2012 through 2017 to 2020. Hypertension. 2022;79:1971–80.
Article CAS PubMed Google Scholar
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison-Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;71:e127–e248.
Article PubMed Google Scholar
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
World Health Organization. Guideline for the pharmacological treatment of hypertension in adults. WHO Report: Geneva; 2021.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation 2023;147:e93–e621.
Chow CK, Gupta R. Blood pressure control: a challenge to global health systems. Lancet. 2019;394:613–5.
Derington CG, King JB, Herrick JS, Shimbo D, Kronish IM, Saseen JJ, et al. Trends in antihypertensive medication monotherapy and combination use among US adults, National Health and Nutrition Examination Survey 2005–2016. Hypertension. 2020;75:973–81.
Olomu A, Khan NNS, Todem D, Huang Q, Bottu S, Qadri S, et al. Blood pressure control in hypertensive patients in federally qualified health centers. Mdm Policy Pr. 2016;1:2381468316656010.
Google Scholar
Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427–31.
Article CAS PubMed PubMed Central Google Scholar
Bennett A, Chow CK, Chou M, Dehbi H-M, Webster R, Salam A, et al. Efficacy and safety of quarter-dose blood pressure-lowering agents: a systematic review and meta-analysis of randomized controlled trials. Hypertension. 2017;70:85–93.
Salam A, Huffman MD, Kanukula R, Prasad EH, Sharma A, Heller DJ, et al. Two‐drug fixed‐dose combinations of blood pressure‐lowering drugs as WHO essential medicines: an overview of efficacy, safety, and cost. J Clin Hypertens. 2020;22:1769–79.
Salam A, Atkins ER, Hsu B, Webster R, Patel A, Rodgers A. Efficacy and safety of triple versus dual combination blood pressure-lowering drug therapy. J Hypertens. 2019;37:1567–73.
Parati G, Kjeldsen S, Coca A, Cushman WC, Wang J. Adherence to single-pill versus free-equivalent combination therapy in hypertension. Hypertension. 2021;77:692–705.
Chow CK, Atkins ER, Hillis GS, Nelson MR, Reid CM, Schlaich MP, et al. Initial treatment with a single pill containing quadruple combination of quarter doses of blood pressure medicines versus standard dose monotherapy in patients with hypertension (QUARTET): a phase 3, randomised, double-blind, active-controlled trial. Lancet. 2021;398:1043–52.
Park IU, Taylor AL. Race and ethnicity in trials of antihypertensive therapy to prevent cardiovascular outcomes: a systematic review. Ann Fam Med. 2007;5:444–452.
Article PubMed PubMed Central Google Scholar
Baldridge AS, Huffman MD, Lazar D, Abbas H, Flowers FM, Quintana A, et al. Efficacy and safety of a quadruple ultra-low-dose treatment for hypertension (QUARTET USA): rationale and design for a randomized controlled trial. Am Heart J. 2022;254:183–93.
Sanuade OA, Jacobson TA, Quintana A, Flowers FM, Abbasi H, Vu MH, et al. Process evaluation of a double blind randomized controlled trial to assess the efficacy and safety of a quadruple ultra-low-dose treatment for hypertension within a federally qualified health center network (QUARTET USA). J Am Heart Assoc. 2024;13:e032236.
Weiss BD. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med. 2005;3:514–22.
Medical Dictionary for Regulatory Activities. International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH). Available from: https://www.ich.org/page/meddra . Accessed January 9, 2024.
Campbell NRC, Burnens MP, Whelton PK, Angell SY, Jaffe MG, Cohn J, et al. 2021 World Health Organization guideline on pharmacological treatment of hypertension: policy implications for the region of the Americas. Lancet Regional Heal - Am. 2022;9:100219.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
National Association of Community Health Centers. America’s health centers fact sheet, August 2022. Available from: https://www.nachc.org/wp-content/uploads/2022/08/Americas-Health-Centers-2022_final.pdf . Accessed January 9, 2024.
Zheutlin AR, Caldwell D, Anstey DE, Conroy MB, Ogedegbe O, Bress AP. Trends in hypertension clinical trials focused on interventions specific for Black adults: an analysis of clinicaltrials.gov. J Am Hear Assoc. 2020;9:e018512.
Mueller M, Purnell TS, Mensah GA, Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? Am J Hypertens. 2014;28:699–716.
Wang, Salam N, Webster A, Silva R, de A, Guggilla R, Stepien S, et al. Association of low-dose triple combination therapy with therapeutic inertia and prescribing patterns in patients with hypertension: a secondary analysis of the TRIUMPH trial. JAMA Cardiol. 2020;5:1219–26.
Laba T-L, Howard K, Rose J, Peiris D, Redfern J, Usherwood T, et al. Patient preferences for a polypill for the prevention of cardiovascular diseases. Ann Pharmacother. 2015;49:528–39.
Wood F, Salam A, Singh K, Day S, Jan S, Prabhakaran D, et al. Process evaluation of the impact and acceptability of a polypill for prevention of cardiovascular disease. BMJ Open. 2015;5:e008018.
Chow CK, Atkins ER, Billot L, Chalmers J, Hillis GS, Hay P, et al. Ultra-low-dose quadruple combination blood pressure lowering therapy in patients with hypertension: The QUARTET randomized controlled trial protocol. Am Heart J. 2021;231:56–67.
Chow CK, Thakkar J, Bennett A, Hillis G, Burke M, Usherwood T, et al. Quarter-dose quadruple combination therapy for initial treatment of hypertension: placebo-controlled, crossover, randomised trial and systematic review. Lancet. 2017;389:1035–42.
Download references
Acknowledgements
We acknowledge the patients and teams at Access Community Health Network. We thank members of the QUARTET USA team, including Ms. Mianzhao (Tracy) Guo, Ms. Alexandra Soriano, Mx. Rolando Serna, Ms. Linda Rosul, Ms. Patricia Helbin, Mr. Edgar Pizarro, Dr. Daneen Woodard, Dr. Natasha Pavlovcik, Dr. Charity Alikpala, Ms. Katherine McKeough, Ms. Sonya Hopkins, and Ms. Eloisa Lopez. We would like to thank the trial Data and Safety Monitoring Board members include Dr. Paul Muntner (chair), Dr. Christopher Lindsell, Dr. Kenneth Jamerson, Dr. Emily Anderson, and Ms. Perla Herrera. We would like to thank members of the QUARTET Australia study team, including Dr. Emily Atkins and Dr. Anthony Rodgers. We would like to thank George Clinical for providing independent clinical trial monitoring and Sharp Clinical Services for study drug manufacturing.
The study was supported by the National Heart, Lung, and Blood Institute (R61/R33HL139852), National Center for Advancing Translational Sciences (UL1TR001422), and Northwestern University Feinberg School of Medicine. The funders were not involved in the development of the study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication. The program officers representing the National Heart, Lung, and Blood Institute participated in Data and Safety Monitoring Board activities ( ex officio , non-voting).
Author information
Authors and affiliations.
Cardiovascular Division and Global Health Center, Washington University in St. Louis, St. Louis, MO, USA
Mark D. Huffman
The George Institute for Global Health, University of New South Wales, Sydney, NSW, Australia
Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Mark D. Huffman, Abigail S. Baldridge, Namratha R. Kandula, Donald M. Lloyd-Jones, Sadiya S. Khan, James J. Paparello, Aashima Chopra, Priya Tripathi, My H. Vu & Jody D. Ciolino
Bluhm Cardiovascular Institute, Northwestern Medicine, Chicago, IL, USA
Abigail S. Baldridge
Access Community Health Network, Chicago, IL, USA
Danielle Lazar, Hiba Abbas, Jairo Mejia, Fallon M. Flowers, Adriana Quintana & Alema Jackson
Division of General Internal Medicine, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Namratha R. Kandula & Stephen D. Persell
Division of Cardiology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Donald M. Lloyd-Jones & Sadiya S. Khan
Center for Primary Care Innovation, Institute for Public Health and Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Stephen D. Persell
Division of Nephrology and Hypertension, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
James J. Paparello
Westmead Applied Research Centre, University of Sydney, Westmead, NSW, Australia
Clara K. Chow
Northwestern University Data Analysis and Coordinating Center, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
Jody D. Ciolino
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mark D. Huffman .
Ethics declarations
Conflict of interest.
MDH has received travel support from the American Heart Association and World Heart Federation and consulting fees from PwC Switzerland. MDH has an appointment at The George Institute for Global Health, which has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy through its social enterprise business, George Medicines. MDH has pending patents for heart failure polypills. CKC has a patent for quarter-dose, quadruple drug combination therapy for blood pressure lowering. SDP receives unrelated research support from Omron Healthcare Co. Ltd. and honoraria for speaking from Omron Healthcare Co. and the National Committee for Quality Assurance. The remaining authors have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental materials, statistical analysis plan, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Huffman, M.D., Baldridge, A.S., Lazar, D. et al. Efficacy and safety of a four-drug, quarter-dose treatment for hypertension: the QUARTET USA randomized trial. Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01658-y
Download citation
Received : 19 January 2024
Revised : 23 February 2024
Accepted : 01 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1038/s41440-024-01658-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Single pill combination
- Randomized trial
- Federally qualified health centers
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Wait! Try this Special Offer
Subscribe now and save 15%, wait – try this special offer.

Plus 2 free gifts

- Facebook . opens in new tab
- Twitter . opens in new tab
- LinkedIn . opens in new tab
- Open Athens/Shibboleth
- Activate Print Subscription
- Create Account
- Renew subscription

Stay Informed, with Concise, Evidence Based Information

Renew today to continue your uninterrupted access to NEJM Journal Watch.
Subscribe or Renew
Sign into your account
Forgot Password? Login via Athens or your Institution
Already a print subscriber? Activate your online access.
- SUMMARY AND COMMENT |
- General Medicine
- Ambulatory Medicine
- Hospital Medicine
April 9, 2024
Managing Elevated Blood Pressure in Hospitalized Patients
Neil H. Winawer, MD, SFHM , reviewing Wilson LM et al. Ann Intern Med 2024 Apr 2
Practice patterns vary for asymptomatic patients, and guidelines for management are lacking.
Management of elevated blood pressure (BP) in hospitalized patients varies widely. In this systematic review of 14 clinical practice guidelines on BP management in adults, researchers examined whether (and how) these guidelines addressed managing hypertension in hospitalized patients, with particular attention to hypertensive urgencies or emergencies. Findings were as follows:
No guideline recommended specific BP targets or provided goals for managing asymptomatic moderately elevated BP in hospitalized patients.
Hypertensive emergency (i.e., BP >180/120 mm Hg with end-organ damage) recommendations consistently included use of intravenous antihypertensive agents in intensive care settings.
Recommendations for managing hypertensive urgency (i.e., BP >180/120 mm Hg without end-organ damage) were inconsistent.
No recommendations addressed management of elevated inpatient BP for transitions from hospital to home. Outpatient treatment with oral medications and follow-up in days to weeks were advised most often.
Unlike inpatient management of elevated BP, outpatient BP goals were defined clearly, varying between 130/80 mm Hg and 140/90 mm Hg.
Clear practice guidelines exist for managing elevated BP for hypertensive emergency or for outpatients, but those strategies are not applicable to treatment of asymptomatic inpatients. In this population, use of parenteral agents often yields adverse outcomes ( NEJM JW Gen Med Mar 15 2023 and J Hypertens 2023; 41:288), and titrating up oral medications can lead to serious adverse events and excess readmissions ( NEJM JW Gen Med Oct 15 2019 and JAMA Intern Med 2019; 179:1528). For asymptomatic hypertensive inpatients, the most prudent approach for hospitalists is communicating BP concerns to primary care clinicians and arranging close outpatient follow-up, rather than treating BP elevations during hospital stays or at discharge.
Wilson LM et al. Management of inpatient elevated blood pressures: A systematic review of clinical practice guidelines. Ann Intern Med 2024 Apr 2; [e-pub]. ( https://doi.org/10.7326/M23-3251 )
Facebook | Twitter | LinkedIn | Email | Copy URL
- Disclosures
Disclosures for Neil H. Winawer, MD, SFHM, at time of publication
Topics hypertension, latest in general medicine.
- Apr 9, 2024
Mixed Connective Tissue Disease: A Large Case Series
Allan S. Brett, MD
Should Patients with COVID-19 Who Are at Standard Risk Take Nirmatrelvir/Ritonavir?
Molly S. Brett, MD
The Role of Imaging in Managing Patients with Gastrointestinal Bleeding
Aaron J. Calderon, MD, FACP, SFHM
- Apr 8, 2024
No Benefit of Beta-Blockers in Revascularized Patients with Normal Ejection Fraction After MI
Frederick A. Masoudi, MD, MSPH, MACC, FAHA
Transcatheter vs. Surgical Aortic Valve Replacement for Low-Risk Patients
David J. Cohen, MD, MSc

Neil H. Winawer, MD, SFHM
Editor-in-Chief
NEJM Journal Watch Hospital Medicine
Stay Informed, with Concise, Evidence-Based Information.
Three-Year Cardiovascular Outcomes of Telmisartan in Patients with Hypertension: An Electronic Health Record-Based Cohort Study
Affiliations.
- 1 Department of Biostatistics, Korea University College of Medicine, Seoul, Republic of Korea.
- 2 Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Republic of Korea.
- 3 Department of Medical Informatics, Korea University College of Medicine, Seoul, Republic of Korea.
- 4 Korea University Research Institute for Medical Bigdata Science, College of Medicine, Korea University, Seoul, Republic of Korea.
- 5 Division of Cardiology, Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Republic of Korea.
- 6 Division of Cardiology, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Republic of Korea.
- PMID: 38285627
- DOI: 10.1093/ajh/hpae012
Background: Telmisartan exhibits superior efficacy in controlling 24-hour blood pressure (BP) compared with other angiotensin receptor blockers (ARBs). However, data on its cardiovascular effects in patients with hypertension are limited. This study aimed to evaluate the cardiovascular outcomes in patients taking telmisartan compared to those taking other ARBs.
Methods: This multicenter retrospective study used data from the Korea University Medical Center database, built from electronic health records. A total of 19,247 patients taking two or more antihypertensive medications were identified. Patients prescribed telmisartan (telmisartan users) were compared with those prescribed an ARB other than telmisartan (other ARB users). The primary outcome was major adverse cardiac events (MACE), a composite of cardiovascular death, myocardial infarction, stroke, and hospitalizations due to heart failure. The adjusted outcomes were compared using 1:1 propensity score (PS) matching.
Results: Overall, 3,437 (17.9%) patients were telmisartan users. These patients were more likely to be younger and male and less likely to have a history of chronic kidney disease, dialysis, or heart failure. In the PS-matched cohort, BP control was similar in both groups; however, telmisartan users exhibited significantly lower visit-to-visit BP variability. The adjusted 3-year MACE rate was similar between telmisartan users (4.6%) and other ARB users (4.7%, log-rank p = 0.75), with comparable safety profiles.
Conclusions: In real-world practice, telmisartan showed cardiovascular outcomes similar to those of other ARBs in patients with hypertension taking two or more antihypertensive drugs.
Keywords: heart failure; mortality; myocardial infarction; stroke; telmisartan.
© The Author(s) 2024. Published by Oxford University Press on behalf of American Journal of Hypertension, Ltd. All rights reserved. For permissions, please e-mail: [email protected].
- Open access
- Published: 11 April 2024
Association between dietary selenium and zinc intake and risk of dilated cardiomyopathy in children: a case-control study
- Maryam Aryafar 1 ,
- Mohammad Mahdavi 1 ,
- Hossein Shahzadi 1 ,
- Yeganeh Rajabpour Ranjbar 2 ,
- Mohammad Hassan Sohouli 3 ,
- Sina Afzal 4 ,
- Asal Neshatbini Tehrani 5 , 6 ,
- Danial Fotros 2 &
- Ghazal Daftari 7 , 8
BMC Pediatrics volume 24 , Article number: 251 ( 2024 ) Cite this article
122 Accesses
1 Altmetric
Metrics details
Dilated cardiomyopathy (DCMP) is characterized by the enlargement and weakening of the heart and is a major cause of heart failure in children. Infection and nutritional deficiencies are culprits for DCMP. Zinc is an important nutrient for human health due to its anti-oxidant effect that protects cell against oxidative damage. This case-control study aimed to investigate the relationship between dietary intake of zinc and selenium and the risk of DCMP in pediatric patients.
A total of 36 DCMP patients and 72 matched controls were recruited, and their dietary intakes were assessed via a validated food frequency questionnaire. We used chi-square and sample T-test for qualitative and quantitative variables, respectively. Logistic regression analysis was applied to assess the relationship between selenium and zinc intake with the risk of DCMP.
After fully adjusting for confounding factors, analyses showed that selenium (OR = 0.19, CI = 0.057–0.069, P trend < 0.011) and zinc (OR = 0.12, CI = 0.035–0.046, P trend < 0.002) intake were strongly associated with 81% and 88% lower risk of pediatric DCMP, respectively.
Conclusions
This study highlights the protective role of adequate dietary intake of selenium and zinc in decreasing the risk of DCMP in children. Malnutrition may exacerbate the condition and addressing these micronutrient deficiencies may improve the cardiac function. Further studies are recommended to detect the underlying mechanisms and dietary recommendations for DCMP prevention.
Peer Review reports

Introduction
Dilated cardiomyopathy (DCMP) is a condition characterized by systolic dysfunction and biventricular or left ventricle dilation in the lack of predisposing factors such as coronary artery disease, hypertension or valvular disorders which cause systolic dysfunction [ 1 ]. DCMP usually begins in the left ventricle by thinning and stretching of the heart muscles resulting in enlargement of heart chambers that impairs the normal contraction and blood pumping [ 2 ]. DCMP presents with orthopnea, heart failure, breathlessness, impaired exercise tolerance, poor feeding, fatigue and sweating [ 3 ]. The prevalence of DCMP is estimated from 1:500 to 1:2500 in general population [ 4 , 5 ]. In children, the incidence rate is about 0.57 per 100,000 population annually and is higher in boys than girls [ 6 ]. In children, the common causes of DCMP is idiopathic, neuromuscular disorders such as Becker and Duchen dystrophies, nutritional deficiencies and inflammation [ 7 ]. Paediatric DCMP is observed to occur after influenza, parvo virus B19, coxsackie, herpes, Ebstein Barr, adeno and human immunodeficiency viruses [ 7 ]. Furthermore, taurine, calcium, zinc and selenium depletion decrease the heart contractility and are implicated in DCMP [ 8 ].
Selenium and zinc, micronutrients found in red meat, grains, nuts and sea foods is an indispensable elements in human health [ 9 ]. Selenium in the form of selenocysteine and as the 21st amino acid is incorporated in the selenoproteins, modulating immunologic, cardiovascular and metabolic functions via anti-inflammatory, anti-cancer and anti-oxidant effects [ 10 ]. Also, selenium is crucial for sperm motility and thyroid function [ 11 ]. Gluthatione peroxidases, iodothyronine deiodinases and thioredoxin reductases are anti-oxidant enzymes depending on selenium [ 12 , 13 ]. Zinc is an important element in apoptosis and cellular membrane stability [ 14 ]. In addition, it is a necessary component of enzymes such as angiotensinogen converting enzyme and carbonic anhydrases that are regulators of acid-base balance and fluid homeostasis [ 15 ]. Zinc is a co-factor of different enzymes that contribute to function of anti-oxidant systems. It stabilizes cellular membrane and protects the cells against oxidative conditions. In addition, zinc inhibits pro-oxidant enzymes and decreases reactive oxygen species production in stress conditions [ 16 , 17 , 18 ].
Several studies have demonstrated that selenium deficiency may contribute to cardiovascular disorders such as Keshan disease, which is an endemic DCMP in China [ 19 ]. It is also indicated that zinc deficiency is culprit of cardiac cellular damage and decreased cardiac function [ 20 , 21 ]. It is suggested that high selenium and zinc intake may reduce the risk of cardiovascular incidence and mortality [ 22 ]. Considering previous studies, little is known about the selenium and zinc intake in children with DCMP, thus we aimed to explore the association of dietary intake of selenium and zinc with DCMP risk in children.
Methods and materials
Study population.
In this case-control study, 45 patients within the age range of 2–17 years old who had been diagnosed with idiopathic DCMP for at least 6 months, were recruited from Rajaie cardiovascular, medical and research center during spring and summer of 2022 in Tehran, Iran. Physical exam, electrocardiogram (ECG), clinical history, echocardiography and chest X-ray had been used for diagnosis.
Inclusion criteria were individuals with signs and symptoms of heart failure such as low exercise tolerance, fatigue, edema and shortness of breath. Exclusion criteria were following: having renal failure, diabetes mellitus, malignancies, infectious disease, pregnancy, valvular, rheumatic, hypertensive and congenital heart diseases and also, life expectancy less than 6 months. Among 45 patients that were initially identified, 9 patients were excluded due to the high risk of mortality. Also, 72 controls were matched according to sex and age. The controls were randomly allocated patients admitted to other wards of the same hospital with no history of cardiovascular diseases, confirmed with echocardiography. It is important to mention that when the cases are selected from hospital, controls from hospital are preferred over community-based control selection. The protocol of this study was approved by Rajaie cardiovascular, medical and research center ethics committee (IR.RHC.REC.1401.016). All the parents / legal guardian of participants were informed about the study and signed the written informed consent form.
Dietary intake assessment
A reproducible and valid food frequency questionnaire (FFQ) [ 23 , 24 , 25 ] was used to collect dietary intake. A trained dietician collected the portion size and frequency of food items based on daily, weekly, monthly or yearly intake. The dietary intakes of participants were checked with their parents to reduce the recall bias. We used Nutritionist IV [ 26 ] to analyse the collected data and The United States Department of Agriculture (USDA) Food Composition Table (FCT) to calculate nutrients and energy contents.
Data collection
Socio-demographic and anthropometric information of the participants were collected by a trained interviewer. Body weight was measured to the nearest 100 g while standing on digital scales (Soehnle, Berlin, Germany). Height was calculated by a non-stretch portable meter to the nearest 0.5 cm. Body mass index (BMI) was measured by dividing of weight in kilograms to square of height in meter.
Statistical analysis
After assessing the normality of the variable’s distribution by Kolmogorov-Smirnov test, independent sample T-test was used to compare quantitative variables between the two groups, as Chi-square was also used for qualitative variables. The baseline characteristics were reported as mean ± standard deviation (SD) for quantitative variables, and number for qualitative variables. The association of selenium/zinc with the odds of cardiomyopathy was assessed by applying logistic regression. The analyses were adjusted for probable confounders, including age, sex, BMI, energy, fiber, Na and K. All analyses were performed using statistical package software for social science (SPSS) 22.0 statistical software, and P -value less than 0.05 was considered statistically significant.
Baseline characteristics
The mean ± SD for the age across case and control groups were 9.83 ± 4.55 and 8.7 ± 1.54 years, respectively. There was a significant difference in the distribution of sex between cases and controls ( p < 0.001), with a higher proportion of males in the control group. However, no significant differences were observed in weight ( p = 0.208) and BMI ( p = 0.702) between the two groups (Table 1 ).
Dietary intakes
The dietary intakes of study participants across the case and control groups are presented in Table 2 . Significant differences were found in the intake of protein, carbohydrate, total fiber, fat, cholesterol, sodium, potassium, vitamin A.RE, vitamin C, iron, vitamin D, vitamin E, folate, B12, magnesium, zinc, and selenium between cases and controls ( p < 0.05 for all). Cases generally exhibited lower intakes of these nutrients compared to controls.
Odds ratios for cardiomyopathy
The odds ratio (ORs) and 95% confidence interval (CIs) for the occurrence of cardiomyopathy based on the tertiles of selenium and zinc intake are reported in Table 3 . In the crude model, selenium and zinc were inversely associated with the lower odds of cardiomyopathy, with an OR of 0.144 and 0.179 for the highest tertile, respectively ( P < 0.05 for trend). Furthermore, after adjusting for age, sex, BMI, energy, fiber, Na and K (in the fully adjusted model), in the highest versus lowest tertile of selenium and zinc, the lower odds of cardiomyopathy remained significant (OR = 0.198, 95% CI: 0.05–0.69; P value = 0.011 for trend and OR = 0.127, 95% CI: 0.03–0.46; P value = 0.002 for trend, respectively).
The present case-control study demonstrated that lower intake of macronutrients and micronutrients such as selenium and zinc is associated with higher risk of DCMP in children, after fully adjusting of confounding factors such as energy, BMI, age, sex, fiber, Na and K.
In our study, dietary intake of macronutrients was significantly lower in cases than controls. Align with our finding Ocal et al. reported that children with malnutrition exhibit cardiovascular disorder including arrythmia, sudden death, heart failure and dilated cardiomyopathy [ 27 ]. Also, gross examination of the myocardium in malnourished children showed a flabby, pale and thin-walled heart [ 28 ]. Nutritional interventions may improve the quality of life and myocardial function. Failure to thrive is one of the most important problems in children with cardiomyopathy. Adequate intake of macronutrients may improve cardiac function and also, specific micronutrients decrease the myocardial abnormalities that occur in cardiomyopathies and heart failure [ 29 ].
There is a vicious circle between malnutrition and DCMP. Poor nutritional status is a cause of DCMP and on the other hand, DCMP leads to malnutrition through metabolic disturbances, chronic inflammation and gastrointestinal malabsorption [ 30 , 31 , 32 ]. The inflammatory condition in most chronic diseases such as DCMP affects the metabolism and results in reduced cardiac muscle function and mass over time [ 33 ]. Different micronutrients deficiency may cause DCMP. Vema et al. reported a 15-month-old child with DCMP caused by hypocalcemia nutritional rickets that responded to vitamin D and calcium supplementation and systolic function normalized after 3 months [ 34 ].
Consistent with our study, Ripa et al. reported that primary or secondary zinc deficiency may result in DCMP and also, reduced plasma level of zinc is an important prognostic and diagnostic marker for DCMP [ 35 ]. In addition, Topuzoglu et al. demonstrated that patients with DCMP have lower plasma level of zinc compared with healthy controls [ 36 ]. Zinc is an important component of various enzymes such as superoxide dismutase. An impairment in superoxide dismutase function leads to reaction of superoxide anions with hydrogen peroxide and production of hydroxide radicals that induce cell damage. Zinc protects the cells against free radicals and thus decreases the cardiovascular disorders. In DCMP and consequently heart failure, activation of atrial natriuretic peptide (ANP) causes high urinary excretion of zinc, concluding to zinc deficiency and impaired cardiac performance [ 37 ]. On the other hand, Chou et al. did not find any association between patients with DCMP and control group [ 38 ]. The differences in reports may be due to sample size, dietary food intake and methodology.
Another micronutrient that is protective in cardiovascular diseases is selenium. Dasgupta et al. reported a 14 years old boy with severe malnutrition, selenium deficiency and heart failure that has been treated with selenium replacement and nutritional support and become completely asymptomatic after four weeks [ 33 ]. In line with our study, Khater et al. demonstrated that pediatric patients with DCMP have reduced plasma level of selenium and this element can prevent myocardial damage [ 39 ]. Frustaci et al. indicated that in patients with intestinal malabsorption, a reversible selenium and zinc DCMP may occur oxidative damages to cell membrane, increased cell autophagy and decreased anti-oxidant activity [ 40 ]. Furthermore, Basil et al. reported that selenium level is significantly lower in patients with DCMP in comparison with control group [ 41 ]. In contrast to our study, Cunha et al. investigated that there is no difference between selenium level in patients with DCMP and control group [ 42 ]. It may be due to different food pattern and sample size. Selenium is a crucial element in inflammation and immunity and improves antioxidant reserve and suppresses production of tumor necrosis factor alfa and interleukins. Selenium deficiency may also play a role in myocardial damage and recovery.
Current study has some strengths including the analysis of various macro and micronutrients and also adjusting the confounding factors to improve the reliability of the study. There are some limitations, due to case-control nature of the study we could not establish a causative relationship between selenium and zinc intake with DCMP and the possibility of recall bias is another issue to consider.
In conclusion, current study concluded that there is an inverse association between macronutrients, selenium and zinc intake with the risk of pediatric DCMP. Further studies are needed to evaluate the amount of selenium and zinc intake to prevent DCMP.
Data availability
The datasets examined in the current study are available from the corresponding author on.
reasonable request.
Abbreviations
dilated cardiomyopathy
electrocardiogram
food frequency questionnaire
the United States department of agriculture
food composition table
body mass index
standard deviation
statistical package software for social science
confidence interval
saturated fatty acid
retinol equivalent
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial diseases. Eur Heart J. 2008;29(2):270–6.
Article PubMed Google Scholar
Ampong I. Metabolic and metabolomics insights into dilated cardiomyopathy. Annals Nutr Metabolism. 2022;78(3):147–55.
Article CAS Google Scholar
Bailer J, Kaufman BD. Nutrition implications of heart failure and heart transplantation in children with dilated cardiomyopathy: a case series. ICAN: Infant Child Adolesc Nutr. 2010;2(6):377–84.
Google Scholar
Weintraub RG, Semsarian C, Macdonald P. Dilated cardiomyopathy. Lancet. 2017;390(10092):400–14.
Article CAS PubMed Google Scholar
Reichart D, Magnussen C, Zeller T, Blankenberg S. Dilated cardiomyopathy: from epidemiologic to genetic phenotypes: a translational review of current literature. J Intern Med. 2019;286(4):362–72.
Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, et al. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006;296(15):1867–76.
Amrita M, Amar T. Dilated cardiomyopathy in children: early detection and treatment. Cureus. 2022;14(11).
Carvajal K, Moreno-Sánchez R. Heart metabolic disturbances in cardiovascular diseases. Arch Med Res. 2003;34(2):89–99.
Rayman MP. Selenium and human health. Lancet. 2012;379(9822):1256–68.
Shan H, Yan R, Diao J, Lin L, Wang S, Zhang M, et al. Involvement of caspases and their upstream regulators in myocardial apoptosis in a rat model of selenium deficiency-induced dilated cardiomyopathy. J Trace Elem Med Biol. 2015;31:85–91.
Rayman MP. The importance of selenium to human health. Lancet. 2000;356(9225):233–41.
Lu J, Holmgren A, Selenoproteins. J Biol Chem. 2009;284(2):723–7.
Reeves M, Hoffmann P. The human selenoproteome: recent insights into functions and regulation. Cell Mol Life Sci. 2009;66:2457–78.
Article CAS PubMed PubMed Central Google Scholar
Wood R, Ronnenberg A, King J, Cousins R, Dunns J, Burk R, Levander O. Modern nutrition in health and disease. Lippincott’s Illustrated Reviews Biochemistry, Lippincott Williams & Wilkins; 2005. pp. 248–70.
Cohen N, Golik A. Zinc balance and medications commonly used in the management of heart failure. Heart Fail Rev. 2006;11:19–24.
Marreiro DDN, Cruz KJC, Morais JBS, Beserra JB, Severo JS, De Oliveira ARS. Zinc and oxidative stress: current mechanisms. Antioxidants. 2017;6(2):24.
Ruz M, Carrasco F, Rojas P, Codoceo J, Inostroza J, Basfi-Fer K, et al. Zinc as a potential coadjuvant in therapy for type 2 diabetes. FoodNutr Bull. 2013;34(2):215–21.
Chasapis CT, Loutsidou AC, Spiliopoulou CA, Stefanidou ME. Zinc and human health: an update. Arch Toxicol. 2012;86:521–34.
Loscalzo J. Keshan disease, selenium deficiency, and the selenoproteome. N Engl J Med. 2014;370(18):1756–60.
McKeag NA, McKinley MC, Woodside JV, Harbinson MT, McKeown PP. The role of micronutrients in heart failure. J Acad Nutr Dietetics. 2012;112(6):870–86.
Prasad AS. Zinc deficiency: has been known of for 40 years but ignored by global health organisations. British Medical Journal Publishing Group; 2003. pp. 409–10.
Kuria A, Tian H, Li M, Wang Y, Aaseth JO, Zang J, Cao Y. Selenium status in the body and cardiovascular disease: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2021;61(21):3616–25.
Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran lipid and glucose study. Br J Nutr. 2012;108(6):1109–17.
Azizi F, Hedayati M, Hosseini Esfahani F, Mehrabi Y, Mirmiran P. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Rezazadeh A, Omidvar N, Tucker KL. Food frequency questionnaires developed and validated in Iran: a systematic review. Epidemiol Health. 2020;42:e2020015.
Article PubMed PubMed Central Google Scholar
Hearst C, First IVD, Nutritionist. IV: diet analysis. San Bruno, CA: First DataBank. 1995.
Öcal B, Ünal S, Zorlu P, Tezic H, Oğuz D. Echocardiographic evaluation of cardiac functions and left ventricular mass in children with malnutrition. J Paediatr Child Health. 2001;37(1):14–7.
Garson A. The science and practice of pediatric cardiology. (No Title). 1998.
Miller TL, Neri D, Extein J, Somarriba G, Strickman-Stein N. Nutrition in pediatric cardiomyopathy. Prog Pediatr Cardiol. 2007;24(1):59–71.
Rahman A, Jafry S, Jeejeebhoy K, Nagpal AD, Pisani B, Agarwala R. Malnutrition and cachexia in heart failure. J Parenter Enter Nutr. 2016;40(4):475–86.
Sciatti E, Lombardi C, Ravera A, Vizzardi E, Bonadei I, Carubelli V, et al. Nutritional deficiency in patients with heart failure. Nutrients. 2016;8(7):442.
Marinescu V, McCullough PA. Nutritional and micronutrient determinants of idiopathic dilated cardiomyopathy: diagnostic and therapeutic implications. Expert Rev Cardiovasc Ther. 2011;9(9):1161–70.
Dasgupta S, Aly AM. Dilated cardiomyopathy induced by chronic starvation and selenium deficiency. Case Reports in Pediatrics. 2016;2016.
Verma S, Khadwal A, Chopra K, Rohit M, Singhi S. Hypocalcemia nutritional rickets: a curable cause of dilated cardiomyopathy. J Trop Pediatr. 2011;57(2):126–8.
Ripa S, Ripa R, Giustiniani S. Are failured cardiomyopathies a zinc-deficit related disease? A study on Zn and Cu in patients with chronic failured dilated and hypertrophic cardiomyopathies. Minerva Med. 1998;89(11–12):397–403.
CAS PubMed Google Scholar
Topuzoglu G, Erbay AR, Karul AB, Yensel N. Concentations of copper, zinc, and magnesium in sera from patients with idiopathic dilated cardiomyopathy. Biol Trace Elem Res. 2003;95:11–7.
Nouraei SM, Ghayemian A, Salehifar E. Serum zinc level in dilated and ischemic cardiomyopathy. J Tehran Univ Heart Cent. 2007;2(3):157–60.
CAS Google Scholar
Chou H, Yang H, Tsou S, Ho R, Pai P, Hsu H. Status of trace elements in patients with idiopathic dilated cardiomyopathy in central Taiwan. Zhonghua Yi Xue Za Zhi = Chinese Medical Journal. Free China ed. 1998;61(4):193–8.
Abdellatif GM, Morsy SM, Khater NM, Ahmed HS. The role of Selenium Deficiency in dilated cardiomyopathy. Zagazig Univ Med J. 2020;26(1):46–52.
Frustaci A, Sabbioni E, Fortaner S, Farina M, del Torchio R, Tafani M, et al. Selenium-and zinc‐deficient cardiomyopathy in human intestinal malabsorption: preliminary results of selenium/zinc infusion. Eur J Heart Fail. 2012;14(2):202–10.
Basil OMS, Lewai SAA, Thair IAB. Selenium status and echocardiographic parameters in Iraqi patients with idiopathic dilated cardiomyopathy. 2007.
Cunha Sd A, Filho FM, Bastos VLFC, Antelo DS. Souza MMd. Thiamin, selenium, and copper levels in patients with idiopathic dilated cardiomyopathy taking diuretics. Arquivos brasileiros de cardiologia. 2002;79:460–5.
Article Google Scholar
Download references
Acknowledgements
Authors have no acknowledgments to declare.
No funding.
Author information
Authors and affiliations.
Rajaei Cardiovascular Medical and Research Center, Iran University of Medical Sciences Tehran, Tehran, Iran
Maryam Aryafar, Mohammad Mahdavi & Hossein Shahzadi
Department of Clinical Nutrition and Dietetics, Faculty of Nutrition Sciences and Food Technology, Research Institute, National Nutrition and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Yeganeh Rajabpour Ranjbar & Danial Fotros
Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Mohammad Hassan Sohouli
Department of Orthopedic and Trauma Surgery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Student Research Committee, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Asal Neshatbini Tehrani
Department of Nutrition, School of Allied Medical Sciences, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Ghazal Daftari
Keshavarz Boulevard, Tehran, Iran
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, M.A; Formal analysis, M.S and D.F; Methodology, M.M, H.S and Y.R; Project administration, M.A and G.D; Writing – original draft, S.A and A.N.T; Writing – review & editing, G.D and S.A. All authors read and approved.
Corresponding author
Correspondence to Ghazal Daftari .
Ethics declarations
Ethics approval and consent to participate.
The protocol of this study was approved by Rajaie cardiovascular, medical and research center ethics committee (IR.RHC.REC.1401.016). All the parents / legal guardian of participants were informed about the study and signed the written informed consent form. All procedures performed in studies involving human participants adhered to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Aryafar, M., Mahdavi, M., Shahzadi, H. et al. Association between dietary selenium and zinc intake and risk of dilated cardiomyopathy in children: a case-control study. BMC Pediatr 24 , 251 (2024). https://doi.org/10.1186/s12887-024-04706-1
Download citation
Received : 16 October 2023
Accepted : 12 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s12887-024-04706-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dilated cardiomyopathy
- Case-control study
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Blood pressure variability is a major predictor of heart attack and stroke risk, finds analysis
C hanges to blood pressure over time could be used to identify patients at greatest risk of heart attack and stroke. These are the findings of a new analysis from the ASCOT study, led by researchers from Imperial College London and published in the European Heart Journal .
It reveals that patients with blood pressure that varies significantly from one doctor's visit to the next may be at greater risk of cardiovascular events compared to those with high blood pressure but low variability, and which is kept under control with medication.
In a group of more than 8,000 UK patients with high blood pressure who were followed up for more than 20 years, researchers found that variation in systolic pressure (the larger of the two numbers used to measure blood pressure) over time was a strong predictor of stroke, heart attack and atrial fibrillation. High variability of blood pressure was also a strong predictor of risk at all levels of average blood pressure from low to high.
The team behind the study is calling for medical guidelines to be changed to focus not only on the measurement of a patient's blood pressure, but how it varies from visit to visit, in order to intervene earlier and reduce risk.
The researchers also highlight that data from the trial show that one blood pressure medication, a drug called amlodipine, was effective in lowering blood pressure variability and could help to reduce risk.
Professor Peter Sever, from the National Heart & Lung Institute at Imperial College London, and senior author of the study, said, "We've long known that high blood pressure increases the risk of heart attacks and stroke, but our latest findings highlight the importance of tracking variability in blood pressure over time as well.
"While a degree of this was known to doctors, without clinical trials it has been difficult to quantify the risk of blood pressure variability over the long term, or the impact of interventions such as calcium blockers to reduce patients' risk."
Hypertension
High blood pressure, or hypertension, is a leading cause of death and disability worldwide—contributing to millions of strokes and heart attacks. An estimated 1.28 billion people have hypertension around the world, affecting one in three adults. Using new definitions for hypertension (blood pressure of more than 130/80 mmHg) this rate increases to almost 50% of all adults. The condition can be well-controlled with medications, including ACE-inhibitors, calcium channel blockers, diuretics and betablockers.
It is well-established that blood pressure can vary over the course of the day. For example, ambulatory blood pressure monitoring requires a patient to wear a device at home to take their average blood pressure levels over a 24-hour period, which can be used by their doctor to help with treatment decisions. But the impact of blood pressure variability over the longer term, from one doctor's visit to the next, has been less clear.
Professor Peter Sever, who leads the ASCOT Legacy trial, added, "We urgently need to explore new practical ways to assess blood pressure variability and are currently studying the possibilities of incorporating data from home blood pressure monitoring into clinical decision-making.
"The low cost and wide availability of digital blood pressure monitors and health apps means people can readily track their blood pressure over time and this could provide invaluable data for doctors to make the best treatment decisions—though we'd urge patients not to be overly concerned, as we would expect a degree of variation in their readings over time.
"Crucially, we need international guidelines for clinicians to be updated to reflect these latest findings and to include blood pressure variability as a major risk factor for heart attack and stroke."
In the latest study, researchers used data from the ASCOT study , which involved more than 1 million measurements of blood pressure in almost 20,000 participants observed for over five years and up to 21 years of follow up data.
From the original ASCOT study, 8,580 participants from England, Wales and Scotland were included in the ASCOT Legacy Study and followed up until 2019, during which period 717 of them died. The majority of patients were male (81%) and the average age was 64 years old at the start of the study, and half were taking a calcium channel blocker called amlodipine to manage their hypertension.
Analyzing blood pressure
In the analysis, the team split the group into thirds, based on their average systolic blood pressure and their blood pressure variability. They found that among patients with an average systolic blood pressure of less than 140 mmHg, the group with the highest variability was at a 16% greater risk for heart attacks, strokes and other cardiovascular events compared with the group with lowest variability.
It also showed that more than half (53%) of all cardiovascular events occurred in patients whose blood pressure was well-controlled with medication and who would not have been considered for additional treatment under the guidelines in place at the time of the trial (i.e. with medication they achieved a systolic blood pressure of <140 mmHg).
Some European guidelines now recommend a lower target for systolic pressure of 130-135 mmHg, but even applying these values those with high blood pressure variability still have a considerable excess of heart attacks and strokes.
The findings indicate that a systolic blood pressure variability of 13 mmHg or more over the course of five years may be associated with significantly increased risk of cardiovascular events.
In the original ASCOT trial, researchers showed that amlodipine-based treatment was better than a betablocker-based treatment strategy for preventing heart attacks and strokes and that this benefit was best explained by the effect of amlodipine on reducing blood pressure variability.
Other studies have now confirmed amlodipine's beneficial effect on blood pressure variability. Of the other classes of blood pressure lowering drugs only thiazide-like diuretics have some beneficial effect on blood pressure variability.
Professor Sever added, "We still don't know what the optimum method for capturing blood pressure variability over time looks like—whether this may incorporate office and home measurements to best inform a patient's health record in the long term—and more research is needed.
"While new trials are necessary to confirm the benefits of drugs which lower blood pressure variability, in the meantime our best evidence is that in patients with high variability, a treatment regimen that includes a long-acting calcium channel blocker such as amlodipine is the sensible option."
More information: Peter S Sever et al, Legacy benefits of blood pressure treatment on cardiovascular events are primarily mediated by improved blood pressure variability: the ASCOT trial, European Heart Journal (2023). DOI: 10.1093/eurheartj/ehad814
Provided by Imperial College London

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medicine (Baltimore)
- v.99(52); 2020 Dec 24
Nursing case management for people with hypertension
To explore the effect of management of nursing case on blood pressure control in hypertension patients.
This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808). Our research includes 200 patients. Patients who meet the following conditions will be included in this experiment: the patients aged 18 to 60 years; the patients had the diagnosis of hypertension; and the urban residents. While patients with the following conditions will be excluded: having renal failure, liver failure, heart and respiratory failure; and known pregnancy. Primary result is blood pressure, while secondary results are treatment compliance, waist circumference, body mass index (BMI), type and number of antihypertensive agents used, and the existence of metabolic and cardiovascular comorbidities.
Table 1 shows the clinical outcomes between the two groups.
Conclusion:
Nursing case management is effective to improve the prognosis of hypertension patients.
1. Introduction
Hypertension is one of the cause of death worldwide, which is preventable. [ 1 , 2 ] It is also a significant risk factor for myocardial infarction, heart failure, stroke, as well as other serious renal and cardiovascular diseases. [ 3 – 5 ] The incidence rate of hypertension rises with the age of adults. It is reported that 36% of the adults aged 40 to 64 suffer from hypertension; among adults aged 65 and above, the proportion has increased to 70%. [ 6 , 7 ] It has become a serious problem of public health. Since the hypertension is asymptomatic, its detection and control remains a challenge. The hypertension patients are managed via the primary health care provider. [ 8 ] Nevertheless, although the progress has been made in the management of chronic diseases, the hypertensive patients who receive regular treatment from primary care providers do not meet their targets of blood pressure.
In recent years, more and more researches begin to pay attention to the significant role of the management of nursing case in treating hypertension. [ 9 , 10 ] It requires a complex care, involving major lifestyle changes such as adherence to medication, reduced salt intake, the measurement of blood pressure and exercise. Nevertheless, the hypertension patients have poor self-management behaviors. The self-care and self-efficacy behavior of uncontrolled hypertension patients are lower. Case management is a kind of healthcare strategy that determines patients at high risk, prevents complications and disease progression, and promotes the patients participation in self-care. Other targets involve caring for the perspectives and needs of patients, developing personalized care programs, improving the quality of health care, and decreasing decentralized patient care. The former researches have suggested that management of case may have a positive effect on hypertension. [ 11 – 13 ] In addition, it can increase the knowledge about the disease; adhere to the treatment plans and help the patients improve their own lifestyle. Although it has achieved positive results in the case management of chronic disease, it has not been applied in patients with hypertension. Hence, we conduct the randomized controlled study protocol to explore the effect of management of nursing case on blood pressure control in hypertension patients.
2. Materials and methods
This is a randomized controlled study which will be carried out from May 2021 to May 2022 at the People's Hospital of Chengyang District. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808) and recorded in research registry (researchregistry6244).
2.1. Inclusion criteria and exclusion criteria
Patients who meet the following conditions will be included in this experiment: the patients aged 18 to 60 years; the patients had the diagnosis of hypertension; and the urban residents. While patients with the following conditions will be excluded: having renal failure, liver failure, heart and respiratory failure; and known pregnancy. All the patients are randomly assigned to the random number through utilizing a random-number table, and the result of distribution is kept in a random envelope and is invisible. All the patients are randomly divided to the control group and study group, and there are 100 patients in each group.
2.2. Nursing case management
The nursing standards of the control group are as follows: renewal of prescriptions in meetings, free distribution of hypertension medication, and the monitor of blood pressure every 2 months, nursing and medical appointments, and consultation with psychologists and nutritionists based on the needs of patients.
In intervention group, patients are given management of nursing case. From the existing management activities, the arrangements are as follows: telephone contacts, nursing consultations, personal health education activities, and home visits. The nursing consultations are implemented every 6 months. The purpose of the consultation is to gather information that can be utilized to draft personal care plans and to set mutually agreed targets. The consultation lasts about an hour, involving the targeted health education, the measurement of waist circumference and blood pressure, and the calculation of BMI. Telephone contact is conducted every 1 month to reassess the healthcare plans of patients and remind the patients to consult the agendas in a timely manner. WeChat is a kind of instant messaging tool, which allows the voice calls through using the mobile phone, and it is also utilized for communication. Each telephone meeting lasts about 10 min. In the process of home visits, the case manager will observe the home environment, for instance, the living conditions and family's interaction. They offer the health education, check the weight of patient and their blood pressure, and then review the targets and medical plans. All the verbal instructions will be recorded and the patients will be provided the copy for consultation if needed. For the home visits, it lasts about 45 min. And the group activities contain the interactive activities and informational lectures. The focus of these activities is to develop healthy habits. The theme of educational activities is selected according to patients’ main needs. The activities of collective health education are carried out in community space. These group activities last about 1 h. Personalized educational activities are offered in the process of nursing consultation, telephone consultation, and home visit. All information acquired in the process of nursing management will be recorded.
2.3. Outcomes
Primary result is blood pressure, while secondary results are treatment compliance, waist circumference, BMI, type and number of antihypertensive agents used, and the existence of metabolic and cardiovascular comorbidities.
2.4. Statistical analysis
The analysis of all the data are conducted with the software of IBM SPSS Statistics for Windows, version 20 (IBM Corp, Armonk, NY). Afterwards, all the data acquired are represented through the appropriate characteristics, for example, standard deviation, and mean, median as well as percentage. And independent t tests and χ 2 -tests are respectively utilized to analyze the categorical variable and continuous variable. P value < .05 indicates that there is statistical significance.
Table Table1 1 shows the clinical outcomes between the two groups.
The clinical outcomes between the two groups.
4. Discussion
Hypertension is the most significant risk factor for disability and death worldwide, which affects more than one billion people and causes ∼9.4 million deaths each year. [ 14 ] On the basis of a report by the World Health Organization, hypertension is the single most significant risk factor, which accounts for 13% of global mortality. Human hypertension may be the result of lifestyle and genetic factors. [ 15 , 16 ] The current evidence-based treatment for the hypertension is a key intervention measure to reduce the incidence rate and mortality of cardiovascular diseases. Researches have determined a variety of barriers to the control of hypertension in routine care that are composed of factors related to patients, physicians, healthcare system, and healthcare services.
People with lower income and education levels are more likely to be insufficiently physically active, which predisposes them to the risk of complications associated with chronic diseases, particularly the hypertension. [ 17 ] In contrast, people with higher educational and economic levels tend to be more effective at controlling the levels of blood pressure. Therefore, it is essential to consider the effect of these variables and then incorporate these variables into the development of nursing planning and educational activities for hypertension patients. Case management can be utilized for this objective by providing a personalized plan based on each person's needs.
5. Conclusion
Author contributions.
Shiqiang Song designs the protocol. Xianhong Li reviews the protocol. Xueling Ning performs the data collection. Chunjing Song finishes the manuscript. All of the authors approved the submission.
Conceptualization: Xianhong Li.
Data curation: Xianhong Li.
Funding acquisition: Shiqiang Song.
Investigation: Xueling Ning.
Methodology: Xueling Ning.
Writing – original draft: Chunjing Song.
Abbreviations: BMI = body mass index, Trial registration = The protocol was registered in Research Registry (researchregistry6244).
How to cite this article: Song C, Li X, Ning X, Song S. Nursing case management for people with hypertension: A randomized controlled trial protocol. Medicine . 2020;99:52(e23850).
Qingdao Health Bureau project (2013-WSZD120).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are publicly available.

- Opsumit shows real-world safety, efficacy for CTD-PAH patients
Treatment mostly given as combination therapy, US drug registry studies find

by Andrea Lobo | April 15, 2024
Share this article:

Most people with pulmonary arterial hypertension (PAH) due to connective tissue disease (CTD) who are using Opsumit (macitenan) do so as part of a combination therapy, according to real-world evidence from two U.S. drug registry studies.
Its safety and effectiveness, in terms of clinical outcomes, for these patients were comparable to people with idiopathic (of unknown cause) or hereditary PAH, more common disease types .
“We show that macitentan [Opsumit] is used in newly diagnosed and prevalent patients with CTD-PAH … as part of a combination therapy regimen in the majority of patients,” the scientists wrote.
The study, “ Macitentan in Pulmonary Arterial Hypertension Associated with Connective Tissue Disease (CTD-PAH): Real-World Evidence from the Combined OPUS/OrPHeUS Dataset ,” was published in the journal Cardiology and Therapy .

Delayed diagnosis common with PAH, multinational survey finds
Opsumit works to widen blood vessels in pah patients.
PAH is characterized by the narrowing of the pulmonary arteries, the blood vessels that supply the lungs, which restricts blood flow and causes high blood pressure. This forces the heart to work harder to pump blood through the body, and can lead to right heart failure.
Opsumit is an oral, once-daily therapy that works to widen the blood vessels of people with PAH, slowing disease progression and lowering patients’ risk of being hospitalized.
“However, patient characteristics, treatment patterns, safety profile, and outcomes of patients with CTD-PAH … newly initiating [Opsumit] are not well understood,” the scientists wrote. CTD refers to disorders affecting the connective tissue — which supports and holds organs together — such as systemic lupus erythematosus or scleroderma .
Researchers in the U.S. analyzed data from two real-world studies of patients newly treated with Opsumit: OPUS (NCT02126943) — the OPsumit USers Registry — and OrPHeUS (NCT03197688) , the Opsumit Historical Users study that was initiated to supplement OPUS registry data. Collected findings covered the years 2013 to 2022.
“Data from both studies provide a unique insight into contemporary real-world clinical practice for the management of a broad range of patients with PAH, including those with CTD-PAH, and report real-life clinical outcomes of these patients, complementing the findings of [randomized, controlled trials] and other registries,” the researchers added.
The combined study population was 5,654 patients, with a majority (81.9%) diagnosed with PAH and having follow-up data. Among this group, 4,459 patients had PAH as the only reason for using Opsumit — most had idiopathic or hereditary PAH (2,498 people, 56%), followed by CTD-PAH (1,192 people, 26.7%). The CTD-PAH group included 708 people with scleroderma, 159 with systemic lupus erythematosus, and 124 with PAH associated with mixed connective tissue disease.
Across all groups, most patients were white (52.6% to 79.7%) and their median age ranged from 49 to 64 years.
Compared to patients with idiopathic and hereditary PAH, those with CTD-PAH at Opsumit initiation were more frequently women (86.2% vs. 73.1%); were more commonly in World Health Organization functional class III/IV (69.3% vs. 61.2%), meaning they had more severe disease symptoms ; and they were less likely to be obese (20.6% vs. 34.1%).
Most CTD-PAH patients using Opsumit as part of a combination therapy
Before starting on Opsumit, 61.4% of idiopathic or hereditary PAH patients and 68.4% of those with CTD-PAH had received at least one previous PAH-specific therapy . The median duration of Opsumit treatment was 14 months for participants with idiopathic/hereditary PAH and 15.8 months for those with CTD-PAH.
A higher proportion of CTD-PAH patients received Opsumit as part of combination therapy (65.2% vs. 58.1%), mainly given with a phosphodiesterase 5 inhibitor. This group of therapies includes Adcirca (tadalafil) and Revatio (sildenafil). In addition, at one and two years of treatment, results showed that patients with CTD-PAH were more likely to escalate from monotherapy to combination therapy, and from double to triple therapy, than were people with idiopathic or hereditary PAH.
Compared with the larger PAH group, “a higher proportion of patients with CTD-PAH initiated [Opsumit] as part of combination therapy and were more likely to escalate therapy up to 2 years after [Opsumit] initiation,” the scientists wrote.
Still, “contrary to guideline recommendations , a considerable proportion remained on monotherapy therapy at follow-up,” they added.
Adverse events were recorded only in the OPUS study, and most patients experienced at least one such event. The most common side effects were shortness of breath, headache, and edema (swelling).
One year into treatment, 60.3% of the patients with idiopathic/hereditary PAH and 59.3% of those with CTD-PAH had no need for hospitalization due to any cause. Moreover, both groups showed a similar survival rate at one year (90.5 vs. 90.6%) and at three years (75.5 vs. 74.3%) of treatment.
“The outcomes of patients with CTD-PAH in our study indicate progress has been made for early diagnosis and improved treatment options, however, outcomes could be further enhanced with increased use of initial combination therapy,” the researchers wrote.
About the Author

Recent Posts
- AKF fellowship to support new research into PH in kidney disease
- PH, transplant, and COVID-19 taught me how to live in isolation
- Winrevair likely to be available soon in US via CVS, Accredo: Merck
- PH raises risk of severe cardiac, respiratory issues in HIV patients
A Conversation With Rare Disease Advocates

Recommended reading
Triple combo therapy boosts heart, lung function in PAH study

Janssen stops Phase 3 trial testing high-dose Opsumit in CTEPH

Janssen seeks approval in Europe for PAH combination therapy tablet
Subscribe to our newsletter.
Get regular updates to your inbox.
- Open access
- Published: 09 April 2024
On-demand mobile hypertension training for primary health care workers in Nigeria: a pilot study
- Joseph Odu 1 ,
- Kufor Osi 1 ,
- Leander Nguyen 2 ,
- Allison Goldstein 1 ,
- Lawrence J. Appel 3 ,
- Kunihiro Matsushita 3 ,
- Dike Ojji 4 ,
- Ikechukwu A. Orji 5 ,
- Morenike Alex-Okoh 6 ,
- Deborah Odoh 6 ,
- Malau Mangai Toma 6 ,
- Chris Ononiwu Elemuwa 7 ,
- Suleiman Lamorde 7 ,
- Hasana Baraya 7 ,
- Mary T. Dewan 8 ,
- Obagha Chijioke 8 ,
- Andrew E. Moran 1 , 2 ,
- Emmanuel Agogo 1 &
- Marshall P. Thomas 1
BMC Health Services Research volume 24 , Article number: 444 ( 2024 ) Cite this article
142 Accesses
Metrics details
Only one out of every ten Nigerian adults with hypertension has their blood pressure controlled. Health worker training is essential to improve hypertension diagnosis and treatment. In-person training has limitations that mobile, on-demand training might address. This pilot study evaluated a self-paced, case-based, mobile-optimized online training to diagnose and manage hypertension for Nigerian health workers.
Twelve hypertension training modules were developed, based on World Health Organization and Nigerian guidelines. After review by local academic and government partners, the course was piloted by Nigerian health workers at government-owned primary health centers. Primary care physician, nurse, and community health worker participants completed the course on their own smartphones. Before and after the course, hypertension knowledge was evaluated with multiple-choice questions. Learners provided feedback by responding to questions on a Likert scale.
Out of 748 users who sampled the course, 574 enrolled, of whom 431 (75%) completed the course. The average pre-test score of completers was 65.4%, which increased to 78.2% on the post-test ( P < 0.001, paired t-test ). Health workers who were not part of existing hypertension control programs had lower pre-test scores and larger score gains. Most participants (96.1%) agreed that the training was applicable to their work, and nearly all (99.8%) agreed that they enjoyed the training.
Conclusions
An on-demand mobile digital hypertension training increases knowledge of hypertension management among Nigerian health workers. If offered at scale, such courses can be a tool to build health workforce capacity through initial and refresher training on current clinical guidelines in hypertension and other chronic diseases in Nigeria as well as other countries.
Peer Review reports
Hypertension in Nigeria
In Nigeria, cardiovascular disease accounts for 9% of all deaths each year [ 1 ]. Hypertension is a major driver of cardiovascular disease burden, with a prevalence between 32.5% and 38.1% among adults in Nigeria [ 2 , 3 ]. However, access to care and treatment for hypertension in Nigeria is inadequate, with only 12.0–33.6% of hypertensive individuals estimated to receive treatment [ 2 , 3 ]. Moreover, blood pressure control rates are extremely low, ranging from 2.8 to 12.4% [ 2 , 3 ]. Several factors contribute to this situation, including poor detection and management of hypertension at primary health centers (PHCs), a shortage of health workers (HWs), limited knowledge among some HWs, and inadequate equipment and supplies at health facilities [ 4 ].
The Nigerian Federal Ministry of Health (FMOH) has established national targets and developed a roadmap to address the rising burden of non-communicable diseases based on the World Health Organization (WHO) HEARTS hypertension control technical package [ 5 , 6 , 7 ]. In collaboration with the National Primary Healthcare Development Agency (NPHCDA), WHO, and Resolve to Save Lives, the FMOH launched the Nigerian Hypertension Control Initiative in 2020 [ 8 ]. The initiative aims to improve population-level blood pressure control by strengthening and scaling up screening, diagnosis, treatment, monitoring, and health education at the primary health care level.
Nigeria Hypertension Control Initiative strategies include standardizing hypertension treatment with a simple treatment protocol and implementing task shifting and task sharing of hypertension service delivery duties. This approach engages all cadres of PHC staff in hypertension management. The government is currently conducting in-person training of HWs in PHCs across the country using Nigeria-specific guidelines. However, traditional in-person training has several limitations.
Current gaps in health worker training
Low- and middle-income countries face significant challenges in establishing and maintaining a skilled health workforce to combat the growing burden of non-communicable diseases and other health challenges [ 9 ]. Conventional HW in-service training methods have not kept up with the rapid evolution of clinical guidelines and best practices [ 10 , 11 ]. Nigeria has over 30,000 PHCs that are staffed by hundreds of thousands of HWs [ 12 ]. Providing in-person training to upskill the entire PHC workforce on new hypertension guidelines would be a costly and logistically challenging endeavor. The system of pre-service HW training is also under strain. Meanwhile, developing countries continue to face severe shortages of HWs, particularly in rural and underserved areas [ 13 ].
The COVID-19 pandemic has further highlighted the need for innovative approaches to HW training. The pandemic significantly disrupted traditional training methods like in-person seminars and workshops [ 14 , 15 ]. Online training is emerging as a viable option to provide health professionals with the flexibility to study at their own pace and from any location while minimizing the risk of the spread of infection [ 14 ].
Present study
Our team previously piloted and evaluated a short, mobile-optimized online infection prevention and control course with HWs in Nigeria [ 15 ]. We found that the course had high completion rates and strong learning gains. Based on the success of the online infection prevention and control course, we applied a similar methodology to train HWs based in PHCs in Nigeria on new national hypertension diagnosis and management guidelines.
Program design informed by learning science
We expanded on the learning approach we developed in previous pilots of an infection prevention and control course in Nigeria [ 15 ]. We used insights from the learning sciences and our understanding of HWs’ learning and technology needs to develop a set of design principles. These include:
Structuring the learning around clinical cases that are directly relevant to HWs’ practice. This approach can boost HWs’ interest and motivation [ 16 ]. It also allows HWs to directly apply experiences and knowledge stored in long-term memory.
Engaging HWs through continuous low-stakes assessments (quiz questions) with constructive feedback. These assessments are intended to promote learning rather than merely evaluate learners [ 17 ]. Each question is accompanied by a brief explanation, which improves learners’ subjective experience [ 18 ].
Developing modules that repeat and expand upon key concepts, harnessing the benefits of spaced repetition to facilitate learning [ 19 ].
Focusing on essential content and eliminating nonessential material, which improves factual retention [ 20 ].
Teaching basic knowledge and skills, which may be more appropriate for online HW training than teaching advanced clinical practices [ 16 ].
Offering short courses, which increases course completion [ 21 ].
Implementing a user-friendly and well-organized learning experience, which reduces frustration and maintains learners’ self-efficacy [ 22 ].
Requiring learners to complete a short “sample” module to enroll in the full course. Some learners who sign up for free online courses do not intend to complete them [ 23 ], so this small commitment helps to ensure that those who enroll are invested in the learning.
Evaluation methodology
To assess short-term knowledge gains we used a pre-/post-test design. The 10-question multiple choice test was given once at the beginning of the course, with the same set of questions given again at the end of the course. Questions were presented in the same order each time, with the order of answers randomized. Although the pre-/post-test emphasized the content taught in the course, the pre-/post-test questions were not repeated in other modules of the course. Learners could only take each of these tests once and no minimum score was required on the test to advance in the course. Learners received minimal feedback (they could see the correct answers but there were no explanations given) after submitting their answers. To evaluate learners’ reactions, HWs answered a short survey at the beginning of the last module of the course. This survey included the net promoter score question, “How likely is it that you would recommend this course to a friend or colleague?” The survey also included two 5-point Likert scale questions assessing learners’ enjoyment of the course and its relevance to their work. Learners provided basic demographic data by answering a short survey at the end of the first (sample) module of the course. We based the survey questions (supplementary file 1 ) on questions we used in previous courses [ 15 ], with some additions and refinements to match the context of this course.
Collaborative course development
The development of the course was a collaborative and coordinated process that involved multiple government stakeholders, academic partners, and non-governmental organizations. These entities included the FMOH, NPHCDA, WHO-Nigeria Office, Johns Hopkins University, the University of Abuja Teaching Hospital’s Hypertension Treatment in Nigeria Project team, and Resolve to Save Lives.
The FMOH coordinated the co-creation of course materials aligned with the National Hypertension Treatment Guideline, developed in 2021. Prior to the pilot study, four hypertension program managers from WHO, NPHCDA, the Hypertension Treatment in Nigeria Project, and RTSL, three FMOH policymakers, and four clinical experts reviewed the course to ensure alignment with local guidelines and cultural context. An example module from the course is provided in supplementary file 2 . After the content was reviewed, the course was built on our learning management system and quality assurance was conducted by the team at Resolve to Save Lives.
Next, we conducted user testing at a PHC in Abuja to ensure the course’s usability and effectiveness. Four HWs from different cadres took part in the testing, including a medical doctor, a nurse/midwife, a community health extension worker (CHEW), and a pharmacy technician. HWs were selected who had a smartphone, an email account, and access to cellular data or Wi-Fi internet at the testing site. We carried out individual user testing sessions with each HW. Throughout these sessions, we offered an overview and context for the online hypertension course, secured consent from the participants, and clarified the procedure for accessing the course. The HW then received a text message with a link to the course and accessed selected modules on their mobile device. They were encouraged to provide feedback on their progress, including difficulties encountered, observations, and suggestions. The results of user acceptance testing were used to improve the course content and navigation for the subsequent pilot.
Course dissemination
Enrollment in the pilot online training was open from February 13 to April 20, 2023. Learners who enrolled had access through May 4, 2023 to ensure that they had enough time to complete the course. The FMOH, NPHCDA, the Hypertension Treatment in Nigeria Project manager, and state non-communicable disease coordinators distributed the link to the online course to HWs at Nigeria Hypertension Control Initiative facilities, hypertension treatment in Nigeria project facilities, and other facilities implementing hypertension control programs. The link was primarily shared via email and WhatsApp. The target audiences included doctors, nurses, and community health workers at PHCs who care for hypertensive patients. Due to task shifting and task sharing, all of these HW cadres contribute to hypertension diagnosis and management in PHCs in Nigeria.
Technologies used
The course was hosted on the LearnWorlds platform [ 24 ]. We optimized LearnWorlds settings to remove any unnecessary buttons or menus, simplify navigation, and maximize readability on mobile devices. Learners were required to answer all questions and move through the course in sequence. LearnWorlds was integrated with another tool, Zapier [ 25 ], to automatically enroll learners in the full hypertension course after they completed a sample module. Support requests were handled over email and learners used WhatsApp to support each other informally and contact program staff for support.
Data analyses
All data were downloaded from the LearnWorlds platform in.csv format. To calculate pre-/post-test scores, we gave each question equal weight. The net promoter score question was presented on an 11-point scale from 0 (not at all likely) to 10 (extremely likely). We calculated net promoter score by subtracting the percentage of detractors (6 and below) from the percentage of promoters (9 and 10) [ 26 ]. Likert scale questions were numerically coded to compute a mean. All data were analyzed in Microsoft Excel. Paired t tests were used to evaluate learning gains.
Enrollment, completion, and learner demographics
748 users entered the first “sample” module of the course. Of these, 574 completed the sample module to enroll in the full course. 75% of enrolled learners ( n = 431) completed the course. The mean pre-test score was 65.4% among learners who completed the course, and 59.6% among learners who did not. Over 99% of enrolled learners reported living in Nigeria, and 75% of them were asked to take the course by a supervisor. 59% of learners reported working in a PHC that was part of an existing hypertension control program in Kano State, Ogun State, or the Federal Capital Territory. The vast majority of learners (89%) reported accessing the course on a smartphone or other mobile device. Almost all learners (98%) reported some work responsibilities related to hypertension diagnosis and management or the administration of hypertension programs (Table 1 ).
70% of learners reported completing training for at least one clinical role (Junior CHEW, CHEW, community health officer, Nurse, Midwife, or Doctor). 54% of learners reported completing some post-secondary schooling (but not a bachelor’s degree), and 34% reported completing a bachelor’s degree.
Learning gains and completion by health worker cadre and education level
Among the 431 learners who completed the course, the pre-test score was 65.4% and the post-test score was 78.2% ( P < 0.001). There was a wide range of scores on both tests (Fig. 1 ).
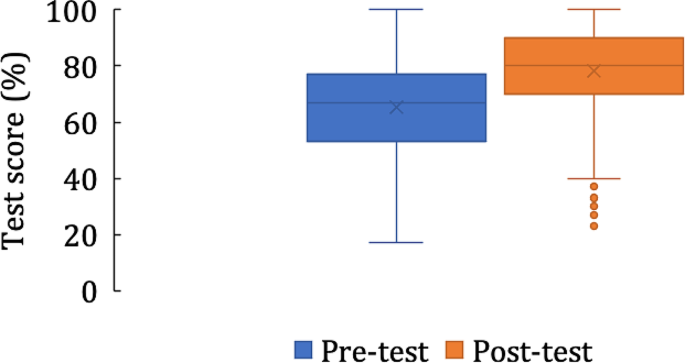
Pre- and post-test scores among learners who completed the course ( n = 431)
There were differences in test scores and course completion by HW cadre (Table 2 ), but learning gains were significant in all cadres. Nurses, midwives, doctors, and those who completed a bachelor’s degree or above in microbiology or biomedical sciences had the largest learning gains. Doctors had the highest pre-test scores of any group, while community health officers had the lowest pre-test scores. CHEWs had the highest completion percentage and doctors had the lowest completion percentage.
Learning gains interact with study time and prior participation in hypertension control programs
Learners who completed all learning activities spent a median time of 160 min working in the course. Those who took longer to complete the course had greater learning gains than those who spent the median amount of time or less (Table 3 ). 59% of the 431 learners who completed the course reported working in a PHC that was part of an existing hypertension control program. These learners had higher pre-test scores and lower learning gains than those who were not working at such PHCs (Table 3 ).
Learner feedback
Of 434 responses to the net promoter score question, the average rating was 9.6/10, corresponding to a net promoter score of + 86. Learners also gave the course high ratings on two Likert-scale questions assessing their enjoyment of the course and its relevance to their work (Table 4 ).
We developed and piloted an online learning approach to train HWs in Nigeria on new national guidelines for hypertension management. The pilot had a high percentage of completion, positive learner feedback, and significant learning gains across different categories of PHC-based HWs. Most importantly, learners significantly gained clinically relevant knowledge regardless of their cadres. Along with our previous work [ 15 ], these results suggest that a mobile, digital, on-demand training approach is effective for training PHC-based HWs in Nigeria on best clinical practices in hypertension management. Future research, ideally randomized controlled trials, will be needed to determine the impact of such training on patient care and health outcomes.
This course had a high percentage of completion compared to industry norms, with 75% of enrolled learners completing the course, in contrast to massive open online courses, in which completion rarely exceeds 25% [ 27 , 28 , 29 , 30 ]. The high percentage of completion of this course is likely due to its endorsement by the FMOH and the encouragement HWs received to take the course from their supervisors. Factors that affect online course completion include endorsement and promotion by employers, the government, trusted sources, and professional networks [ 31 , 32 , 33 ]. Other factors reported to promote uptake of online courses include perceived usefulness and value relative to the effort required [ 29 , 34 , 35 ]. We hypothesize that the case-based nature of the training, its brevity, and its focus on only the most relevant material contributed to its effectiveness, as more than 95% of HWs said the course was relevant to their work, and almost all reported performing at least one work task related to hypertension management.
Learning gains were substantial and statistically significant, indicating that HWs’ knowledge of hypertension management improved upon completing the course in all relevant cadres. However, we observed some heterogeneity of learning gains, with HWs who had completed four or more years of post-secondary education (such as nurses, midwives, and medical doctors) having greater learning gains than cadres of HWs with two or three years of post-secondary schooling (CHEWs and community health officers). This association between level of formal schooling and preparedness to succeed in self-paced and self-directed online learning is in keeping with several previous studies, which reported the importance of self-efficacy, motivation, and digital skills to a participant’s success in online learning [ 33 , 36 , 37 , 38 , 39 ].
HWs who were not staff at PHCs taking part in existing hypertension treatment programs had lower pre-test scores and greater learning gains than those who were. This is at variance with other studies, which suggested that low prior knowledge is associated with poor outcomes in online courses [ 40 , 41 , 42 ]. It may be that those who were not in existing hypertension programs were more motivated to learn hypertension management, thereby leading to the large knowledge gains we observed in this group. Therefore, this mobile training approach might be useful for introducing HWs to new guidelines while also acting as “refresher training” for HWs who have already learned new guidelines.
Learner feedback was overall positive. Responses to two Likert-scale questions indicated that most learners found the course enjoyable and relevant to their work, with higher ratings than similar questions reported in other courses [ 43 , 44 , 45 ]. The net promoter score of this course (+ 86) was high, exceeding the “excellent” benchmark of + 50 and the reported net promoter score of other online courses [ 15 , 46 , 47 ].
On-demand, smartphone-based health worker training has the potential to fill the demand for clinical training efficiently and at lower cost compared with traditional, in-person training in Nigeria and other countries. The Nigeria hypertension training course can be deployed to meet several hypertension control program needs: (1) induction training of workers either en masse at facility activation, or when new workers join primary care teams that were previously trained, or (2) refresher training of workers who were already trained.
Online training for HWs is becoming more widespread globally due to higher demand (more HWs who can access digital training) and increasing supply (more options for those learners). The rapid rise in access to cellular internet and increasing smartphone ownership in Africa [ 48 ] could be a fulcrum that will promote online training in this part of the world. In Nigeria, an estimated 55% of the population is connected to the internet and over 97% of users access the internet with a mobile device [ 49 ]. Most HW cadres that work in PHCs in Nigeria have some post-secondary education, and many have completed bachelor’s degrees, so this group may be among early adopters of technology-enabled learning. It remains unclear whether mobile training applications are best used as an adjunct to traditional in-person group training, or a substitute for in-person training. Finally, rigorous educational and economic evaluations are needed to inform the optimal strategy for primary care health worker training.
Limitations
We only evaluated short-term knowledge gains, and we haven’t yet tested the impact of this training on clinical skills (such as proper blood pressure measurement) or clinical outcomes (such as control of hypertension). Without a comparator group, we can’t be certain that the observed knowledge gains are fully attributable to the online course. All data on learners’ demographics and education levels are self-reported and we did not independently verify the identity of course participants. Many HWs were asked to take the course by their supervisors and were encouraged to complete the course within 14 days, which may have led some HWs to rush through the course to complete it. There was also likely self-selection of HWs with high motivation, access to an internet-connected smartphone, and a certain level of digital literacy and familiarity with navigating through interactive websites.
We found that a simple-to-use, mobile-optimized, case-based online short course can effectively train PHC-based HWs on updated hypertension management guidelines. A high percentage of learners completed the course, learner feedback was very positive, and there were significant learning gains in all cadres of HWs. These results suggest that such training is a scalable way to build health workforce capacity on new clinical guidelines and to refresh knowledge of best clinical practices. Either on its own or in combination with traditional in-person group trainings, this approach could be applied to a variety of topics to improve HWs’ adherence to evidence-based practices in Nigeria and elsewhere.
Data availability
De-identified data are available from the corresponding author upon request.
Abbreviations
community health extension worker
Federal Ministry of Health
health worker
National Primary Health Care Development Agency
primary health center
World Health Organization. https://ncdportal.org/CountryProfile/GHE110/NGA , ncdportal.org. https://ncdportal.org/CountryProfile/GHE110/NGA (accessed May 21, 2023).
Adeloye D, et al. Prevalence, awareness, treatment, and control of hypertension in Nigeria in 1995 and 2020: a systematic analysis of current evidence. J Clin Hypertens. Feb. 2021;23(5). https://doi.org/10.1111/jch.14220 .
Odili AN, et al. Prevalence, awareness, Treatment and Control of Hypertension in Nigeria: data from a Nationwide Survey 2017. Global Heart. Jul. 2020;15(1). https://doi.org/10.5334/gh.848 .
Nelson O. Management of hypertension in Nigeria: the barriers and challenges. J Cardiol Cardiovasc Med. Mar. 2021;6(1):023–5. https://doi.org/10.29328/journal.jccm.1001112 .
World Health Organization., Hypertension, World Health Organization , Mar. 16, 2023. https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed May 21, 2023).
World Health Organization. HEARTS technical package for cardiovascular disease management in primary health care. World Health Organization; 2020.
Federal Ministry of Health, Nigeria., National Multi-sectoral Action Plan for the Prevention and Control of Non-communicable Diseases (2019–2025), 2019.
Resolve to Save Lives. accessed May 21, Resolve to Save Lives: New program announced to lower high blood pressure in unreached communities across Nigeria, resolvetosavelives.org. (2023). https://resolvetosavelives.org/about/press/new-program-announced-to-lower-high-blood-pressure-in-unreached-communities-across-nigeria
Ganju A, et al. Systemic solutions for addressing non-communicable diseases in low- and Middle-Income Countries. J Multidisciplinary Healthc. Jul. 2020;13:693–707. https://doi.org/10.2147/jmdh.s252300 .
Zulu JM, Perry HB. Community health workers at the dawn of a new era. Health Res Policy Syst. Oct. 2021;19. https://doi.org/10.1186/s12961-021-00761-7 .
Nicol E, Turawa E, Bonsu G. Pre- and in-service training of health care workers on immunization data management in LMICs: a scoping review. Hum Resour Health. Dec. 2019;17(1). https://doi.org/10.1186/s12960-019-0437-6 .
Makinde OA, Azeez A, Bamidele S, Oyemakinde A, Oyediran KA, Wura A et al. Development of a Master Health Facility List in Nigeria. Online J Public Health Inf. 2014;6(2).
Puchalski Ritchie LM, Khan S, Moore JE, Timmings C, van Lettow M, Vogel JP et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. Journal of Clinical Epidemiology [Internet]. 2016 Aug [cited 2020 Jan 15];76:229–37. Available from: https://www.sciencedirect.com/science/article/pii/S0895435616001542 .
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A et al. Introduction of Mobile Health Tools to support COVID-19 training and surveillance in Ogun State Nigeria. Front Sustainable Cities. 2021;3.
Thomas MP, Kozikott S, Kamateeka M, Abdu-Aguye R, Agogo E, Bello BG et al. Development of a simple and effective online training for health workers: results from a pilot in Nigeria. BMC Public Health. 2022;22(1). https://doi.org/10.1186/s12889-022-12943-1
Bin Mubayrik HF. Exploring Adult Learners’ Viewpoints and Motivation Regarding Distance Learning in Medical Education. Advances in Medical Education and Practice [Internet]. 2020 Feb 19 [cited 2020 May 25];11:139–46. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7036663/ .
Roediger HL, Karpicke JD. The power of testing memory: Basic Research and implications for Educational Practice. Perspect Psychol Sci. 2006;1(3):181–210.
Article PubMed Google Scholar
Thomas MP, Türkay S, Parker M. Explanations and interactives improve subjective experiences in Online Courseware. Int Rev Res Open Distrib Learn. 2017;18(7).
Kerfoot BP, Fu Y, Baker H, Connelly D, Ritchey ML, Genega EM. Online Spaced Education generates transfer and improves Long-Term Retention of Diagnostic skills: a Randomized Controlled Trial. J Am Coll Surg. 2010;211(3):331–337e1.
Brame CJ. Effective Educational Videos: Principles and Guidelines for Maximizing Student Learning from Video Content. Perez KE, editor. CBE—Life Sciences Education [Internet]. 2016;15(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5132380/#B35 .
Padilla Rodriguez BC, Armellini A, Rodriguez Nieto MC. Learner engagement, retention and success: why size matters in massive open online courses (MOOCs). Open Learning: J Open Distance e-Learning. 2019;1–17.
Simunich B, Robins DB, Kelly V. The impact of Findability on Student Motivation, Self-Efficacy, and perceptions of Online Course Quality. Am J Distance Educ. 2015;29(3):174–85.
Article Google Scholar
Reich J. MOOC Completion and Retention in the Context of Student Intent [Internet]. er.educause.edu. 2014 [cited 2016 Sep 26]. Available from: http://er.educause.edu/articles/2014/12/mooc-completion-and-retention-in-the-context-of-student-intent .
LearnWorlds. Create & Sell Online Courses from Your Own Site. LearnWorldscited. (2023 Jul 26) Available from https://www.learnworlds.com .
Zapier. The easiest way to automate your work. Zapier. Published 2011. (cited. 2023 Jul 26). Available from https://zapier.com/ .
Koladycz R, Fernandez G, Gray K, Marriott H. The net promoter score (NPS) for insight into client experiences in sexual and Reproductive Health clinics. Global Health: Sci Pract. 2018;6(3):413–24.
Google Scholar
Reich J, Ruipérez-Valiente JA. The MOOC pivot. Science. 2019;363(6423):130–1.
Article CAS PubMed Google Scholar
Fu Q, Gao Z, Zhou J, Zheng Y. CLSA: a novel deep learning model for MOOC dropout prediction. Comput Electr Eng. 2021;94:107315.
Gütl C, Rizzardini RH, Chang V, Morales M. Attrition in MOOC: lessons learned from Drop-Out students. Commun Comput Inform Sci. 2014;37–48.
Jordan K. Massive open online course completion rates revisited: Assessment, length and attrition. Int Rev Res Open Distrib Learn. 2015;16(3).
Stark CM, Pope J. Massive Open Online courses: how registered dietitians Use MOOCs for Nutrition Education. J Acad Nutr Dietetics. 2014;114(8):1147–55.
Scott KW, Dushime T, Rusanganwa V, Woskie L, Attebery C, Binagwaho A. Leveraging massive open online courses to expand quality of healthcare education to health practitioners in Rwanda. BMJ Open Qual. 2019;8(4):e000532.
Article PubMed PubMed Central Google Scholar
Magaña-Valladares L, Rosas-Magallanes C, Montoya-Rodríguez A, Calvillo-Jacobo G. Celia Mercedes Alpuche-Arande, Sebastián García-Saisó. A MOOC as an immediate strategy to train health personnel in the cholera outbreak in Mexico. BMC Med Educ. 2018;18(1).
Ma L, Lee CS. Investigating the adoption of MOOCs: a technology-user-environment perspective. J Comput Assist Learn. 2018;35(1):89–98.
Ma L, Lee CS. Drivers and barriers to MOOC adoption: perspectives from adopters and non-adopters. Online Information Review. 2020;ahead-of-print(ahead-of-print).
Barnard L, Paton V, Lan W. Online Self-Regulatory Learning behaviors as a Mediator in the relationship between online course perceptions with achievement. Int Rev Res Open Distrib Learn. 2008;9(2).
Lee Y, Choi J, Kim T. Discriminating factors between completers of and dropouts from online learning courses. British Journal of Educational Technology [Internet]. 2012 Apr 20 [cited 2019 May 26];44(2):328–37. Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/j.1467-8535.2012.01306.x .
Prior DD, Mazanov J, Meacheam D, Heaslip G, Hanson J. Attitude, digital literacy and self efficacy: Flow-on effects for online learning behavior. The Internet and Higher Education [Internet]. 2016 Apr [cited 2019 Apr 19];29:91–7. Available from: https://www.sciencedirect.com/science/article/abs/pii/S109675161630001X .
Wang Y, Baker R. Grit and intention: why do Learners Complete MOOCs? Int Rev Res Open Distrib Learn. 2018;19(3).
Kennedy G, Coffrin C, de Barba P, Corrin L. Proceedings of the Fifth International Conference on Learning Analytics And Knowledge New York: Association for Computing Machinery; 2015. Predicting success: how learners’ prior knowledge, skills and activities predict MOOC performance; pp. 136–140.
Butcher KR, Sumner T. How does prior knowledge impact students’ online learning behaviors? Int J Cyber Behav Psychol Learn. 2011;1(4):1–18.
Bingol I, Kursun E, Kayaduman H. Factors for success and course completion in massive Open Online courses through the Lens of participant types. Open Praxis. 2020;12(2):223.
Meijerman I, Nab J, Koster AS. Designing and implementing an inquiry-based undergraduate curriculum in pharmaceutical sciences. Currents Pharm Teach Learn. 2016;8(6):905–19.
Amini H, Gregory ME, Abrams MA, Luna J, Roland M, Sova LN, et al. Feasibility and usability study of a pilot immersive virtual reality-based empathy training for dental providers. J Dent Educ. 2021;85(6):856–65.
Gable BD, Hommema L. In-Situ Simulation in Interdisciplinary Family Practice Improves Response to In-Office Emergencies. Cureus. 2021.
Jolles MW, Vries M, Hollander MH, Dillen J. Prevalence, characteristics, and satisfaction of women with a birth plan in the Netherlands. Birth. 2019;46(4):686–92.
Palmer K, Devers C. An Evaluation of MOOC Success: Net Promoter Scores. Association for the Advancement of Computing in Education (AACE). 2018;1648–53.
Digital Africa.: Technological Transformation for Jobs [Internet]. [cited 2023 May 18]. Available from: https://www.worldbank.org/en/region/afr/publication/digital-africa .
Digital. 2023: Nigeria [Internet]. DataReportal– Global Digital Insights. 2023 [cited 2023 May 18]. Available from: https://datareportal.com/reports/digital-2023-nigeria .
Download references
Acknowledgements
We would like to thank all of the health workers who participated in the course and shared their feedback.
This study was supported by Resolve to Save Lives. Resolve to Save Lives is funded by Bloomberg Philanthropies, the Bill and Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation. This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation grant award #OPP1175906. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission.
Author information
Authors and affiliations.
Resolve To Save Lives, New York, USA
Joseph Odu, Kufor Osi, Allison Goldstein, Andrew E. Moran, Emmanuel Agogo & Marshall P. Thomas
Columbia University Irving Medical Center, New York, USA
Leander Nguyen & Andrew E. Moran
Welch Center for Prevention, Epidemiology, and Clinical Research, Johns Hopkins University, Baltimore, MD, USA
Lawrence J. Appel & Kunihiro Matsushita
Department of Internal Medicine, Faculty of Clinical Sciences, University of Abuja, Abuja, Nigeria
Cardiovascular Research Unit, University of Abuja Teaching Hospital, Gwagwalada, Abuja, Nigeria
Ikechukwu A. Orji
Federal Ministry of Health, Abuja, Nigeria
Morenike Alex-Okoh, Deborah Odoh & Malau Mangai Toma
National Primary Health Care Development Agency, Abuja, Nigeria
Chris Ononiwu Elemuwa, Suleiman Lamorde & Hasana Baraya
World Health Organization, Abuja, Nigeria
Mary T. Dewan & Obagha Chijioke
You can also search for this author in PubMed Google Scholar
Contributions
JO, KO, LJA, KM, AEM, EA, and MPT designed the project, contributed to course development, and wrote the paper. MPT and JO analyzed the data. LN, AG, DO, IAO, MA-O, DO, MMT, COE, SL, HB, MTD, and OC contributed to project design and course development. All authors reviewed this manuscript and provided critical feedback.
Corresponding author
Correspondence to Marshall P. Thomas .
Ethics declarations
Ethics approval and consent to participate.
This work was reviewed and given expedited committee approval by the National Health Research Ethics Committee of Nigeria (NHREC/01/01/2007) and determined to be exempt human subjects research by the Resolve to Save Lives Research Committee. All participants provided informed consent to participate in the training. All methods were carried out in accordance with relevant institutional guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Odu, J., Osi, K., Nguyen, L. et al. On-demand mobile hypertension training for primary health care workers in Nigeria: a pilot study. BMC Health Serv Res 24 , 444 (2024). https://doi.org/10.1186/s12913-024-10693-x
Download citation
Received : 26 September 2023
Accepted : 07 February 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s12913-024-10693-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Online learning
- Primary health care
- Clinical guidelines
- Mobile technology
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The patient had been in her usual state of health until 18 months before the current admission, when the blood pressure was noted to be 140/90 mm Hg during a routine appointment with her primary ...
Patient Case Presentation. Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without ...
Definitions used in these clinical case scenarios. Definitions Stage 1 hypertension Clinic blood pressure is 140/90 mmHg or higher and. subsequent ambulatory blood pressure monitoring (ABPM) daytime average or home blood pressure monitoring (HBPM) average blood pressure is 135/85 mmHg or higher. Stage 2 hypertension Clinic blood pressure is 160 ...
Case study. Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
The patient had a significant family history of hypertension in both his father and mother. Physical examination was unremarkable, and at the time of triage, his blood pressure (BP) was noted as 195/123 mm Hg, equal in both arms. The patient was promptly started on intravenous labetalol with the goal to reduce BP by 15% to 20% in the first hour.
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
Bosisio et al. describe the case of a patient affected by malignant hypertension. Prior history of hypertension, high mean arterial pressure, significant renal impairment but relatively modest thrombocytopenia, and a lack of severe ADAMTS-13 deficiency (activity <10%) at diagnosis are clues to diagnose malignant hypertension-induced thrombotic ...
diagnosis of hypertension. As the patient's home blood pressure readings were considerably lower at home than those obtained in the clinic, following discussion it was decided that the patient would continue to monitor his blood pressure at home while the dosage of his antihypertensive medication was gradually increased.
From Framingham Heart Study displays, about 17% of women and 19% of men with hypertension had this as their only CVD risk factor, while 32% of women and 30% of men with this hypertension had 3 or more additional risk factors. 9 Therefore, the main goal of this study was to identify those risk factors that lead hypertensive patients to CVD at ...
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
Hypertension is a risk factor for cardiovascular complications of diabetes. Clinical trials demonstrate that drug therapy versus placebo will reduce cardiovascular events when treating patients with hypertension and diabetes. A target BP goal of < 130/80 mmHg is recommended. Pharmacological therapy needs to be individualized to fit patients'needs.
Case Presentation. The patient was a 17-year-old male who was admitted to our hospital in May 2020 due to uncontrolled hypertension for 6 months and weakness of limbs for 20 days. Six months prior to admission, blood pressure of the patient was found to have increased to 200/120 mmHg during the physical examination.
Speakers also present telehealth hypertension case studies. Speakers. Kate Kirley, MD, MS, director, chronic disease prevention, AMA ... So this was before the pandemic, but this particular study looked at patients who have hypertension and they were asked whether a health care professional is recommending that their blood pressure be checked ...
Case Study Topic(s): Cardiovascular, Cardiovascular disease, Heart disease, Heart failure, Hypertension Publication: PCCJ Edition: Volume Number Online 2019. Working with patients who are not willing to engage fully with healthcare services is a common occurrence.
In another study, 4,396 patients aged 65 to 74 years with mild to moderate hypertension were randomly assigned to receive diuretic, β blocker, or placebo. 3 Patients in the treatment group had a 25% reduction in stroke and a 19% reduction in coronary artery events.
Background Hypertension is a major risk factor for cardiovascular disease, which is the leading cause of mortality globally. Patient's adherence to treatment is a cornerstone factor in controlling hypertension and its complications. This study assesses hypertension patients' adherence to treatment and its associated factors. Methods This cross-sectional study conducted in Riyadh, Saudi ...
Ochsner Health System is a nonprofit, academic, multi-specialty, integrated delivery system based in New Orleans, LA, that serves over 700,000 patients a year. Ochsner employs over 1,200 physicians and operates over 90 clinics and 20 hospitals. In 2015, Ochsner launched the Hypertension Digital Medicine program, which provides digitally enabled ...
Stage 1 hypertension (HTN) is now defined as 130-139/80-89. In patients with stage 1 HTN, BP-lowering meds are recommended for those with ASCVD, diabetes, chronic kidney disease, or estimated 10 ...
Methods: Cross-sectional Survey design was used among 30 hypertensive patients (patients with a confirmed diagnosis of hypertension for at least six months or with current blood pressure ≥ 140/ ...
The proportion of patients who permanently discontinued the study drug due to adverse effects was low (intervention: n = 1 [3%] versus control: n = 3 [10%], exact p = 0.347). There were two ...
Outpatient treatment with oral medications and follow-up in days to weeks were advised most often. Unlike inpatient management of elevated BP, outpatient BP goals were defined clearly, varying between 130/80 mm Hg and 140/90 mm Hg. Clear practice guidelines exist for managing elevated BP for hypertensive emergency or for outpatients, but those ...
The patient had a history of hypertension, dyslipidemia, and hypothyroidism. Surgical history included hemiarthroplasty of the right shoulder and arthroplasty of both knees.
Bariatric surgery is effective for hypertension control in patients with grade 1 and 2 obesity, according to a study in the Journal of the American College of Cardiology.. Researchers presented 5-year follow-up data from the randomized, nonblinded GATEWAY (Gastric Bypass to Treat Obese Patients With Steady Hypertension; ClinicalTrials.gov Identifier: NCT01784848) trial, which was conducted at ...
Background: Telmisartan exhibits superior efficacy in controlling 24-hour blood pressure (BP) compared with other angiotensin receptor blockers (ARBs). However, data on its cardiovascular effects in patients with hypertension are limited. This study aimed to evaluate the cardiovascular outcomes in patients taking telmisartan compared to those taking other ARBs.
This case-control study aimed to investigate the relationship between dietary intake of zinc and selenium and the risk of DCMP in pediatric patients. ... hypertension or valvular disorders which cause systolic ... In this case-control study, 45 patients within the age range of 2-17 years old who had been diagnosed with idiopathic DCMP for at ...
The majority of patients were male (81%) and the average age was 64 years old at the start of the study, and half were taking a calcium channel blocker called amlodipine to manage their hypertension.
Abstract. Objective: To explore the effect of management of nursing case on blood pressure control in hypertension patients. Method: This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808).
One year into treatment, 60.3% of the patients with idiopathic/hereditary PAH and 59.3% of those with CTD-PAH had no need for hospitalization due to any cause. Moreover, both groups showed a similar survival rate at one year (90.5 vs. 90.6%) and at three years (75.5 vs. 74.3%) of treatment. "The outcomes of patients with CTD-PAH in our study ...
2.2 Nursing case management. The nursing standards of the control group are as follows: renewal of prescriptions in meetings, free distribution of hypertension medication, and the monitor of blood pressure every 2 months, nursing and medical appointments, and consultation with psychologists and nutritionists based on the needs of patients.
Only one out of every ten Nigerian adults with hypertension has their blood pressure controlled. Health worker training is essential to improve hypertension diagnosis and treatment. In-person training has limitations that mobile, on-demand training might address. This pilot study evaluated a self-paced, case-based, mobile-optimized online training to diagnose and manage hypertension for ...